Abstract
Based on expectancy theory, adolescents at risk for mental health symptoms, such as those involved in the juvenile court system, may use marijuana due to the belief that use will attenuate anxiety and depressive symptoms. In a diverse sample of youth involved in the Santa Barbara Teen Court system (N = 193), we examined the association between mental health symptoms and marijuana expectancies on marijuana use and consequences. In general, stronger positive expectancies and weaker negative expectancies were both associated with increased marijuana use. Youth that reported more symptoms of both anxiety and depression and stronger positive expectancies for marijuana also reported more consequences. We found that youth experiencing the greatest level of consequences from marijuana were those that reported more depressive symptoms and stronger positive expectancies for marijuana. Findings suggest that these symptoms, combined with strong positive expectancies about marijuana’s effects, have implications for consequences among at-risk youth.
Keywords: at-risk youth, marijuana, expectancies, mental health, depression
Marijuana is the most frequently used illicit drug by adolescents in the United States. A recent large-scale national sample of youth found that 15% of adolescents have tried marijuana by 8th grade and 45% report use by 12th grade (Johnston et al., 2014). Approximately 17% of 10th graders and 23% of 12th graders reported past month use. These data also suggest that rates of use for 10th and 12th graders are increasing, with rates of daily use the highest they have been in the past 30 years. In addition, youth who report marijuana use typically use regularly. For example, among those aged 12 to 17 who reported using in the past year, 64% reported using more than 11 times in the past year (i.e., about once per month or more) and nearly one-third of users reported using more than 100 times in the past year (Substance Abuse and Mental Health Services Administration, 2012).
Adolescent marijuana use is a major public health concern. Use is often associated with consequences such as poor school performance, neuropsychological performance deficits, and further use of other illicit drugs, such as heroin and cocaine (Hall, 2009; Macleod et al., 2004). Marijuana use in adolescence has also been linked with future problems in young adulthood, including increased risk for dependence and difficulties with school (Brook, Adams, Balka, & Johnson, 2002; Ellickson, D'Amico, Collins, & Klein, 2005; Ellickson, Martino, & Collins, 2004; Kandel & Chen, 2000). Marijuana is reported as one of the main substances used by youth when presenting for treatment admissions, emergency room admissions, drug screenings following arrests, and autopsies (Dennis et al., 2004). Further, heavy marijuana use during adolescence may affect the trajectory of normal brain development and these abnormalities may persist beyond one month of abstinence (Ashtari et al., 2009; Jacobus, Bava, Cohen-Zion, Mahmood, & Tapert, 2009; Tapert, Caldwell, & Burke, 2004). Thus, due to the potential for immediate and long-term consequences from adolescent marijuana usage, it is important to examine the correlates of marijuana use and consequences in adolescence to help inform prevention and intervention efforts.
MENTAL HEALTH SYMPTOMS AND AT-RISK YOUTH
Cross-sectional and longitudinal research has found that one of the consequences of adolescent marijuana use is greater risk of future mental health symptoms and disorders (Malone, Hill, & Rubino, 2010; Substance Abuse and Mental Health Services Administration, 2012; van Os et al., 2002). Indeed, although evidence is mixed, there is substantial research linking marijuana use in adolescence with symptoms and diagnoses of depression and anxiety in young adulthood (Crippa et al., 2009; Degenhardt et al., 2013; 2003; Kedzior & Laeber, 2014). There is also substantial evidence examining the correlates of marijuana use with present psychological symptoms in cross-sectional work. For example, youth aged 12 to 17 who reported a major depressive episode in the past year were more likely to report past year marijuana use (26%) than those without a major depressive episode (13%) (Substance Abuse and Mental Health Services Administration: Center for Behavioral Health Statistics and Quality, 2012). Even at levels not meeting clinical significance for a diagnosed anxiety or depressive disorder, adolescents who report anxiety and depressive symptoms tend to report more use of marijuana. For example, the National Center on Addiction and Substance Abuse at Columbia University (National Center on Addiction and Substance Abuse at Columbia University, 2011) found that adolescents who reported depressive symptoms, such as feeling sad (regardless of experiencing a major depressive episode or reporting sub-clinical depressive symptoms) also reported more use of marijuana than adolescents not reporting depressive symptoms. Understanding symptom reporting can help inform intervention efforts to reduce such distress and prevent reliance on the drug for future mood regulation (e.g., learning alternate coping strategies beyond using marijuana to address depressed mood).
Although most research in this area focuses on school-based youth, understanding the association between mental health symptoms and marijuana use is particularly critical for at-risk youth. Adolescents with criminal offense histories are more likely to experience mental health concerns related to depression and anxiety than those without offense histories (Kazdin, 2000), and teenagers involved in the legal system are typically at-risk for more severe mental health symptomatology (Wiesner, Kim, & Capaldi, 2005). Studies have also shown that increased mental health symptoms are often linked with more substance use in adolescence (Armstrong & Costello, 2002; Kaminer, Connor, & Curry, 2007), which could lead to repeated offenses. Indeed there is a reciprocal relationship between substance use and delinquent behavior such that both appear to influence each other (D'Amico, Edelen, Miles, & Morral, 2008). Thus, it is important to better understand the connection between mental health symptoms and marijuana use among at-risk youth with alcohol and drug-related offenses to inform prevention and intervention efforts for this population.
EXPECTANCY THEORY
One mechanism that may explain the connection between mental health symptoms and marijuana use and consequences for at-risk youth is through expectancies, or beliefs, regarding the positive and negative effects of marijuana. Expectancy theory originally sought to explain why individuals drink alcohol (Goldman, Del Boca, Darkes, 1999; Goldman, 1994) and has been applied to adolescent marijuana use as well (Aarons, Brown, Stice, & Coe, 2001; Torrealday et al., 2008). The theory suggests that individuals learn, through observation and experimentation, positive and negative beliefs about how a drug will affect them. These expectancies therefore affect one’s engagement in the behavior. For example, people may expect marijuana to help them relax and when they use it, they may feel relaxation effects, which reinforces the belief that using marijuana will help one feel relaxed. Alternatively, people may expect marijuana to impair cognition (e.g., lead to memory problems) and therefore they may limit use to avoid trouble remembering. For mental health specifically then, if an adolescent believes that using marijuana will help alleviate anxiety and depression, it follows that he or she may be more likely to use it when he/she experiences such symptoms. Indeed, adolescents who report more stressful life events (e.g., family problems) are more likely to use marijuana (Low et al., 2012) and youth report use of marijuana to relieve feelings of anxiety and depression (Bottorff, Johnson, Moffat, & Mulvogue, 2009). Expectancies of marijuana’s effects have been linked to initiation of use, intentions to use, current and future use, reduced motivation to change use, and consequences from use in adolescent samples (Fulton, Krank, & Stewart, 2012; Kristjansson, Agrawal, Lynskey, & Chassin, 2012; Skenderian, Siegel, Crano, Alvaro, & Lac, 2008; Torrealday et al., 2008). In general, this research indicates positive expectancies (e.g., using will reduce stress) serve as risk factors for marijuana use and resulting consequences, while negative expectancies (e.g., using will cause impairment) may lessen risk.
The existing research on marijuana expectancies is generally descriptive, targeted on development of measures, or focused on older adolescent samples (e.g., college students). Little research has examined the association between marijuana expectancies and mental health symptoms to determine how these factors may collectively affect both marijuana use and consequences among adolescents. Furthermore, few studies evaluate this association with at-risk samples of youth. Research with middle school youth suggests that there is a unique association between depressive symptoms and positive expectancies and subsequent marijuana use (Clark, Ringwalt, & Shamblen, 2011). Other work with both clinical and community samples of young adults has found that while social anxiety is positively associated with marijuana use and consequences, this relationship is stronger for those with negative expectancies (Buckner & Schmidt, 2008, 2009). Further research with young adult females has shown that tension reduction expectancies (i.e., marijuana makes me feel carefree and I do not care about my problems as much) mediated the association between anxiety and marijuana use (de Dios et al., 2010). Thus, studies that examine the association between mental health and marijuana use without considering expectancies may miss important qualifying information.
THE PRESENT STUDY
The present study adds to this literature by examining the role of mental health symptoms and expectancies on marijuana use and consequences among at-risk adolescents who reported a first time alcohol or drug offense. We hypothesized that youth who reported more frequent mental health symptoms, stronger positive marijuana expectancies, and weaker negative expectancies would also report greater marijuana use and related consequences. In addition, we hypothesized that the association between mental health symptoms and marijuana outcomes (i.e., use, consequences) would be moderated by positive expectancies, such that those with more frequent mental health symptoms and stronger positive expectancies would use at heavier levels and experience more consequences. We also hypothesized that the association between mental health symptoms and marijuana outcomes would be moderated by negative expectancies, such that those with more frequent mental health symptoms and stronger negative expectancies (e.g., it makes it hard to concentrate) would use at lighter levels and experience fewer consequences compared to those with weaker negative expectancies of marijuana.
MATERIALS AND METHODS
PARTICIPANTS
Participants were part of a randomized controlled trial to pilot the efficacy of a group-based Motivational Interviewing intervention, Free Talk, compared to the current system of care (D'Amico, Hunter, Miles, Ewing, & Osilla, 2013; D'Amico et al., 2012). Participants were youth aged 14 to 18 years old who were referred to the Santa Barbara Teen Court system, a diversion program operated by the Council on Alcoholism and Drug Abuse in Santa Barbara County. Youth are referred to Teen Court because they have committed a first-time alcohol or other drug offense (e.g., possession of alcohol or other drugs, driving under the influence, driving with an open container) and do not warrant more serious intervention. Exclusion criteria included referral to another program, possession of a medical marijuana card, or multiple/more serious offenses. The majority of participants in this study were referred to Teen Court for underage alcohol or illicit marijuana possession, with alcohol use making up 56% of the cases and marijuana making up 38% of cases. The remainder of the youth were cited for concurrent alcohol and marijuana use infractions (4%) or other drug offenses (2%). It is important to note that even about half of the teens may have been referred to Teen Court because of an alcohol possession, marijuana use was reported as the substance of choice by the majority of teens (54%), with 85% reporting lifetime use and 61% reporting past month use. Of those youth eligible and approached (n = 216), 11% were either not interested or unable to participate, leaving a final sample of 193 youth. Participants completed measures prior to their Teen Court hearing. Descriptive information about the sample can be found in Table 1. More detailed information about the pilot efficacy study and the sample can be found elsewhere (D’Amico et al., 2012; 2013).
TABLE 1.
Description of the sample
| Age | M = 16.64 (SD =1.05) | ||
| Sex | 67% male | ||
| Ethnicity | 54% non-Hispanic white | ||
| 45% Hispanic/Latino(a) | |||
| Marijuana use | |||
| Lifetime use | 85% | ||
| Past 30 day use | 61% | ||
| Days used in the past 30 days | M = 3.07 (SD = 2.30) | ||
| Used 5 or more days in past 30 days | 24% | ||
| Used 10 or more times in past 30 days | 19% | ||
| Marijuana consequences | |||
| Composite score | M = 1.23 (SD = 0.44) | ||
| Individual items | |||
| Couldn’t remember what happened when you were using marijuana | M = 1.17 (SD = 0.58) | ||
| Missed school or work because of using marijuana | M = 1.23 (SD = 0.66) | ||
| Did something you later felt sorry for because of using marijuana | M = 1.11 (SD = 0.42) | ||
| Got in trouble at school or home because of using marijuana | M = 1.21 (SD = 0.56) | ||
| Had trouble concentrating on what you were doing because of using marijuana |
M = 1.41 (SD = 0.83) | ||
| Mental health symptoms1 | M = 4.71 (SD = 0.90) | ||
| Positive marijuana expectancies2 | M = 2.47 (SD = 0.72) | ||
| Negative marijuana expectancies3 | M = 2.61 (SD = 0.72) | ||
Mental Health Index-5 (MHI-5); higher scores indicative of better mental health, possible range 1 through 6
higher scores indicative of higher agreement with positive expectancies
higher scores indicative of higher agreement with negative expectancies
PROCEDURE
This cross-sectional study examined baseline data for participants prior to the group-based Motivational Interviewing intervention. Youth were approached by study staff with information about the study before their Teen Court hearing. Parental consent was obtained for youth under age 18 and participants also provided assent (under 18) or consent (18) to participate. Participants received $25 for survey completion. A self-administered survey was completed in a private room at the location where intervention groups were held under supervision of trained field staff. Survey questions were kept confidential. All methods were approved by the institution’s Internal Review Board and a National Institutes of Health Certificate of Confidentiality was obtained to protect participant privacy.
MEASURES
Participants completed items regarding demographic information, marijuana use behavior, marijuana-related consequences, mental health symptoms, and positive and negative expectancies regarding marijuana use. Demographic information included items about age, gender, and race/ethnicity.
MARIJUANA USE AND NEGATIVE CONSEQUENCES
Items regarding marijuana use and related negative consequences were modified from the RAND Adolescent/Young Adult Panel Study (Ellickson, Tucker, & Klein, 2003; Tucker, Orlando, & Ellickson, 2003). We assessed the frequency of marijuana use (i.e., “In the past 30 days before your offense, how many days did you use marijuana [pot, weed, grass, hash, bud, sins]?). Eight response options ranged from 0 days (scored as 1) to 21 to 30 days (scored as 8). Five items assessed marijuana-related consequences (e.g., blacked out, missed school or work, regretted activities, got in trouble, trouble concentrating) (α = 0.77), and response options ranged from “never” (scored as 1) to “3 or more times” (scored as 4). The mean of the five items was calculated to give a composite consequences score. The marijuana frequency of use outcome was also dichotomized into no use (0) and any use (1) in the past 30 days.
MENTAL HEALTH INVENTORY
Mental health symptoms were assessed with the five-item Mental Health Inventory (MHI-5) (Berwick et al., 1991), a measure of general mental health focused on anxiety and depression symptoms in the past month (Rumpf, Meyer, Hapke, & John, 2001; Yamazaki, Fukuhara, & Green, 2005). The scale focuses on symptoms of poor mental health and not diagnosed conditions (e.g., Major Depressive Disorder, Generalized Anxiety Disorder). Participants indicated the frequency to which they experienced five symptoms on mental health on a scale from “1 -- all the time” to “6 -- never”. Symptoms included: (1) anxiety (‘How much of the time have you been a very nervous or anxious person?’), (2) general positive affect (‘How much of the time have you felt calm or peaceful?’), (3) depression (‘How much of the time have you felt downhearted or blue?’), (4) general positive affect (‘How much of the time have you been a happy person?’), and (5) behavioral/emotional control (‘How often have you felt so down in the dumps that nothing could cheer you up?’). The two general positive affect items were reversed coded and summed with the other three items to give a composite score. Higher composite scores indicated better overall mental health. Internal consistency of the MHI-5 composite was good (α = 0.81).
MARIJUANA EXPECTANCIES
Nine items addressed the positive and negative effects of marijuana (Ellickson et al., 2003; Orlando, Ellickson, McCaffrey, & Longshore, 2005). Five positive expectancies (i.e., relaxes you, lets you have more fun, helps you get away from your problems, makes you feel less bored, makes you feel less lonely) and four negative expectancies (i.e., makes it hard to remember things, makes it hard to concentrate, makes you do things you might regret, gets you into trouble) were rated on a scale from 1 “strongly disagree” to 4 “strongly agree.” The five positive expectancies were combined to form a positive expectancies composite (α = 0.82) and the four negative expectancies formed a negative expectancies composite (α = 0.67).
ANALYTIC PLAN
Analyses involved a series of cross-sectional regression analyses to test hypotheses related to marijuana use and marijuana consequences. We used Stata 12 for all analyses. We examined hypotheses in a hierarchical manner in four models to test the unique effects of the positive and negative expectancies composites and their association with mental health symptoms (MHI-5 composite) on use and consequences. In each model, we first examined the association between either positive or negative expectancies and mental health on a specific outcome (marijuana use or consequences) in step 1, followed by an interaction term between either the positive or negative expectancies composite and mental health symptoms in step 2. Next, if we found a statistically significant effect for the MHI-5 composite and expectancies interaction, we followed-up with analyses to look at the individual MHI-5 items to determine which items were influencing the observed effects. For this, we re-ran each series with each of the individual MHI-5 items (anxiety, general positive affect [calm/peaceful], depression, general positive affect [happy], behavioral/emotional control) separately in an analysis. We have used this procedure in a previous article to help determine the unique effects of the 5 MHI items (Pedersen et al., 2013). To interpret the interaction terms, we produced graphs showing the predicted line of best fit for consequences for individuals with high and low expectancy scores. Age, gender, and ethnicity were included as covariates in all analyses. Because of non-normality in the outcome variables (i.e., consequences were positively skewed), we estimated standard errors through bootstrapping (Efron, 1993) with 1000 replications.
RESULTS
MARIJUANA USE
The effect for the MHI-5 was non-significant for the model containing positive marijuana expectancies, whereas the effect for positive marijuana expectancies was positive and significant (estimate = 1.57; p < 0.001; see Table 2). Thus, MHI-5 was not related to use higher positive expectancies were associated with more use. The interaction effect of MHI-5 x positive expectancies was not significantly different from zero. Similarly, for the negative expectancies model, the effect for negative expectancies was negative and significant (estimate= −1.09; p < 0.001). The effects for the MHI-5 and the MHI-5 x negative expectancies interaction were not significant. Because we did not find statistically significant interaction effects, we did not evaluate the specific MHI-5 items in follow-up regression analyses.
TABLE 2.
Hierarchical regression analyses for marijuana use outcome
| Model 1 – Positive Expectancies | Estimate | SE | P-value |
| Step 1: Days used in past 30 days regressed on MHI-5 and positive expectancies | |||
| MHI-5 | 0.03 | 0.17 | 0.840 |
| Positive expectancies | 1.57 | 0.19 | < 0.001 |
| Step 2: Days used in past 30 days regressed on interaction of MHI-5 and positive expectancies | |||
| MHI-5 x Positive expectancies | −0.22 | 0.21 | 0.299 |
| Model 2 – Negative Expectancies | |||
| Step 1: Days used in past 30 days regressed on MHI-5 and negative expectancies | |||
| MHI-5 | −0.13 | 0.18 | 0.473 |
| Negative expectancies | −1.09 | 0.22 | < 0.001 |
| Step 2: Days used in past 30 days regressed on interaction of MHI-5 and negative expectancies | |||
| MHI-5 x Negative expectancies | 0.13 | 0.25 | 0.604 |
Note: MHI-5 = Mental Health Index-5 composite score. Standard errors and p-values estimated from 1000 bootstrap samples. Significant effects are in bold.
MARIJUANA CONSEQUENCES
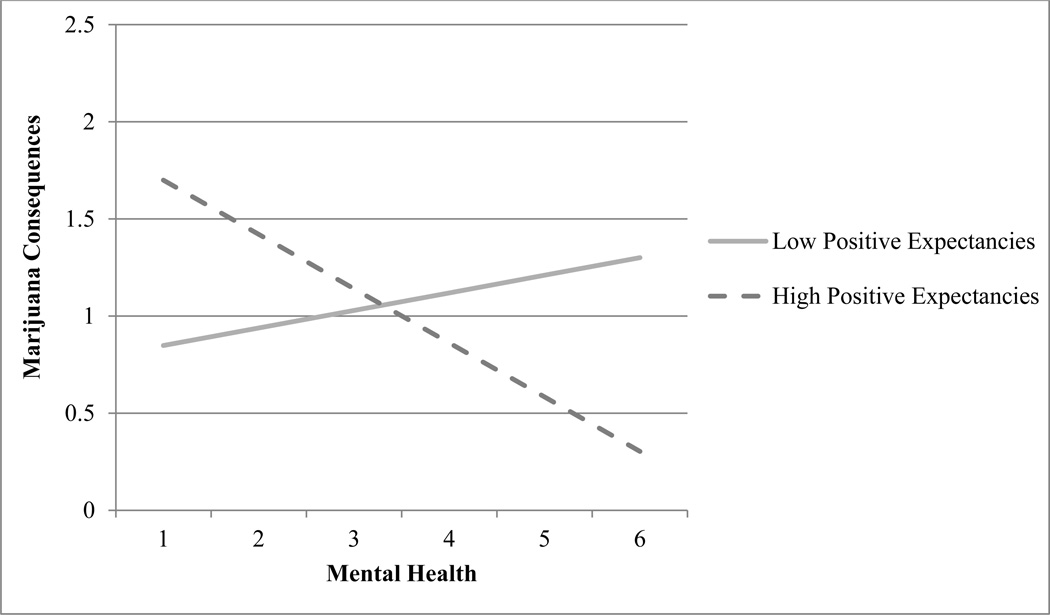
Table 3 contains results from the hierarchical regression analyses for marijuana consequences. For the model containing positive expectancies, the effect for the MHI-5 in step 1 was statistically significant and negative, with an estimate of 0.10 (p = 0.004), indicating that reports of more frequent mental health symptoms were associated with reports of more marijuana consequences. There was also a significant and positive effect for positive expectancies, 0.18 (p < 0.001), with greater agreement with positive expectancies associated with more marijuana consequences. In step 2, the interaction effect between expectancies and the MHI-5 was also statistically significant, with an estimate of −0.12. Interpretation of multiplicative interaction terms is sometimes challenging (Miles, 2001); thus, we graphed the interaction in Figure 1. The greatest risk for consequences was evident among participants who reported both high agreement with positive expectancies and more frequent mental health symptoms; that is, when positive expectancies were low, the association between mental health and consequences was reduced and negative. For the model with negative expectancies as the predictor, the effect for the MHI-5 was statistically significant and negative with an estimate of −0.12 (p = 0.001); however, the effects for negative expectancies and the MHI-5 x negative expectancies interaction did not reach statistical significance.
TABLE 3.
Hierarchical regression analyses for marijuana consequences outcome
| Model 1 – Positive Expectancies | Estimate | SE | P-value |
| Step 1: Frequency of consequences in past 30 days regressed on MHI-5 and positive expectancies | |||
| MHI-5 | −0.10 | 0.04 | 0.004 |
| Positive expectancies | 0.18 | 0.05 | < .001 |
| Step 2: Frequency of consequences in past 30 days regressed on interaction of MHI-5 and positive expectancies | |||
| MHI-5 x Positive expectancies | −0.12 | 0.05 | 0.014 |
| Model 2 – Negative Expectancies | |||
| Step 1: Frequency of consequences in past 30 days regressed on MHI-5 and negative expectancies | |||
| MHI-5 | −0.12 | 0.04 | 0.001 |
| Negative expectancies | −0.03 | 0.03 | 0.284 |
| Step 2: Frequency of consequences in past 30 days regressed on interaction of MHI-5 and negative expectancies | |||
| MHI-5 x Negative expectancies | 0.02 | 0.04 | 0.508 |
Note: MHI-5 = Mental Health Index-5 composite score. Standard errors and p-values estimated from 1000 bootstrap samples. Significant effects are in bold.
FIGURE 1.
Positive expectancies moderate the relationship between mental health (MHI-5 composite score) and marijuana consequences.
Note: higher values on the X-axis indicate better mental health (i.e., less distress). Solid and dotted lines within the axes represent the line of best fit for an individual with low (score = 1) and high (score = 4) positive expectancies.
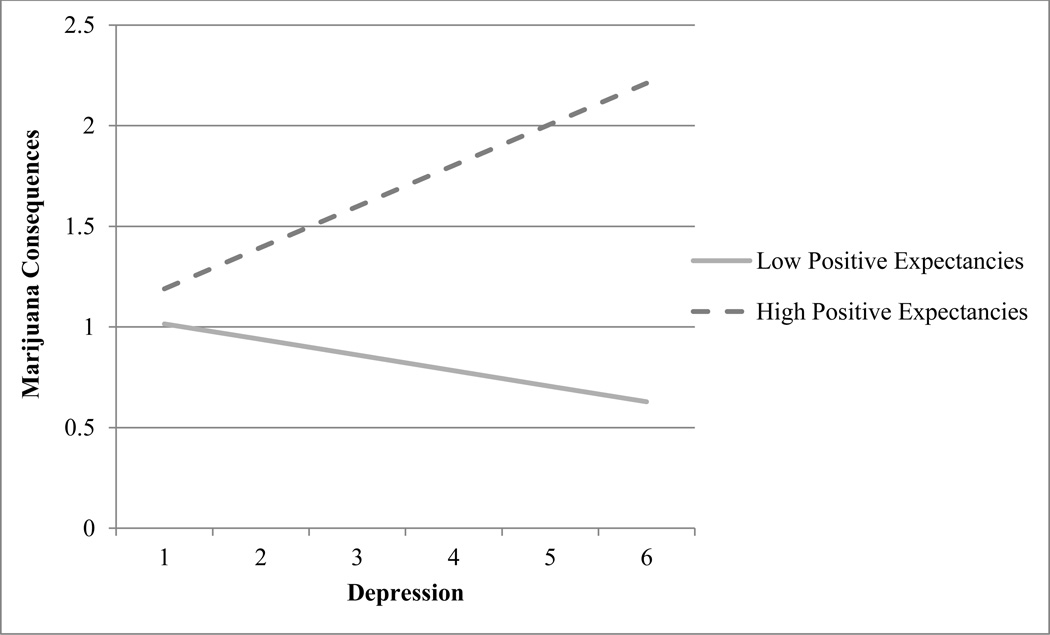
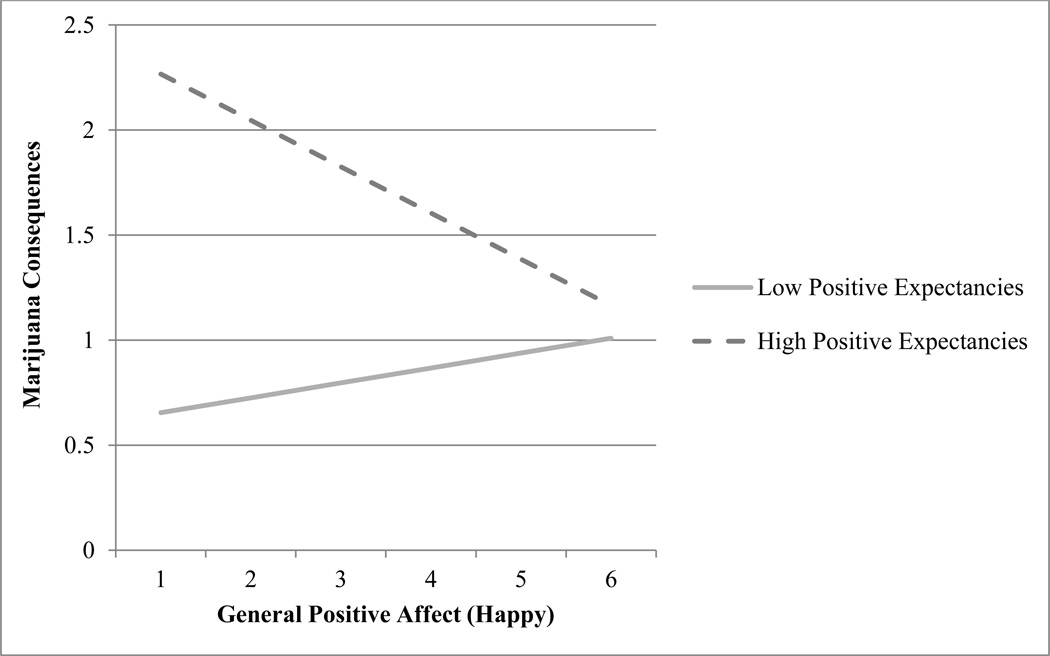
Because the MHI-5 x positive expectancies interaction was significant, we evaluated the unique effects of each of the MHI-5 items that refer to specific mental health symptoms (i.e., anxiety, general positive affect [calm/peaceful], depression, general positive affect [happy], behavioral/emotional control), positive expectancies, and their interaction on marijuana consequences in 5 separate models (see Table 4). In each model, the effect of positive expectancies in step 1 was statistically significant (p < 0.001) with estimates ranging from 0.18 to 0.20. In step 1, the coefficients for the anxiety, depression, general positive affect (happy), and emotional/behavioral control items all achieved statistical significance in the predicted direction. Statistically significant interaction effects were found for the depression and general positive affect (happy) items (marginal p = .05 for the latter symptom). Youth that reported higher levels of depressive symptoms and higher positive marijuana expectancies experienced the most consequences (see Figure 2). Regarding general positive affect (happy), those who reported less happiness and higher positive expectancies also reported more consequences from marijuana (see Figure 3).
TABLE 4.
Follow-up hierarchical linear regression analyses for marijuana consequences outcome
| Estimate | SE | P-value | ||
|---|---|---|---|---|
| Anxiety |
Step 1: Frequency of consequences in past 30 days regressed on MHI-5 (anxiety) and positive expectancies |
|||
| MHI-5 (anxiety) | 0.05 | 0.02 | 0.005 | |
| Positive expectancies | 0.19 | 0.05 | < .001 | |
|
Step 2 Frequency of consequences in past 30 days regressed on interaction between MHI-5 (anxiety) and positive expectancies | ||||
| MHI-5 (anxiety) x Positive expectancies | 0.07 | 0.04 | 0.066 | |
| General positive affect (calm/peaceful) |
Step 1: Frequency of consequences in past 30 days regressed on MHI-5 (calm/peaceful) and positive expectancies |
|||
| MHI-5(calm/peaceful) | −0.03 | 0.02 | 0.169 | |
| Positive expectancies | 0.19 | 0.04 | < 0.001 | |
|
Step 2 Frequency of consequences in past 30 days regressed on interaction between MHI-5 (calm/peaceful) and positive expectancies |
||||
| MHI-5 (calm/peaceful) x Positive expectancies | −0.08 | 0.04 | 0.062 | |
| Depression |
Step 1: Frequency of consequences in past 30 days regressed on MHI-5 (depression) and positive expectancies |
|||
| MHI-5 (depression) | 0.07 | 0.03 | 0.004 | |
| Positive expectancies | 0.19 | 0.04 | < 0.001 | |
|
Step 2 Frequency of consequences in past 30 days regressed on interaction between MHI-5 (depression) and positive expectancies | ||||
| MHI-5 (depression) x Positive expectancies | 0.09 | 0.04 | 0.032 | |
| General positive affect (happy) |
Step 1: Frequency of consequences in past 30 days regressed on MHI-5 (happy) and positive expectancies |
|||
| MHI-5 (happy) | −0.08 | 0.03 | 0.011 | |
| Positive expectancies | 0.18 | 0.05 | < 0.001 | |
|
Step 2 Frequency of consequences in past 30 days regressed on interaction between MHI-5 (happy) and positive expectancies | ||||
| MHI-5 (happy) x Positive expectancies | −0.10 | 0.05 | 0.052 | |
| Emotional/ behavioral control |
Step 1: Frequency of consequences in past 30 days regressed on MHI-5 (emotional/behavioral control) and positive expectancies |
|||
| MHI-5 (emotional/behavioral control) | 0.06 | 0.02 | 0.004 | |
| Positive expectancies | 0.20 | 0.05 | < 0.001 | |
|
Step 2 Frequency of consequences in past 30 days regressed on interaction between MHI-5 (emotional/behavioral control) and positive expectancies | ||||
| MHI-5 (emotional/behavioral control) x Positive expectancies |
0.07 | 0.04 | 0.070 | |
Note: MHI-5 = Mental Health Index-5. Standard errors and p-values estimated from 1000 bootstrap samples. Significant effects are in bold.
FIGURE 2.
Positive expectancies moderate the relationship between depressive symptoms and marijuana consequences.
Note: higher values on the X-axis indicate greater frequency of depressive symptoms. Solid and dotted lines within the axes represent the line of best fit for an individual with low (score = 1) and high (score = 4) positive expectancies.
FIGURE 3.
Positive expectancies moderate the relationship between general positive affect (happy) and marijuana consequences
Note: higher values on the X-axis indicate greater frequency of general positive affect. Solid and dotted lines within the axes represent the line of best fit for an individual with low (score = 1) and high (score = 4) positive expectancies.
DISCUSSION
The current paper adds to the literature by examining associations between concurrent mental health, expectancies, marijuana use, and marijuana consequences among a diverse and at-risk sample of youth. Positive marijuana expectancies and endorsement of more frequent mental health symptoms were both associated with experiencing more consequences from using marijuana. Youth with both depressive symptoms and beliefs about marijuana’s positive effects were at the greatest risk for consequences. Interestingly, although we found mental health symptoms were associated with consequences from use, we did not find an effect for mental health symptoms on actual marijuana use. This could potentially be explained by the manner in which marijuana may be used in this at-risk sample. For example, these adolescents had a first time offense for alcohol or drug use and may be using socially with peers. However, youth with more mental health symptoms may be using marijuana to cope with underlying symptomatology and thus they may experience more severe social and personal consequences from use compared with an adolescent only using socially or experimentally. Indeed, youth involved in the legal system may already be at-risk for mental health concerns (Kazdin, 2000; Wiesner et al., 2005), and using marijuana to relieve depression and anxiety may exacerbate both symptoms and create other problems such as missing school or engaging in other risk behavior that they might regret. Further longitudinal work is needed to better understand the long-term associations between mental health, expectancies, and use and consequences.
Expectancy findings extend previous work in this area (Kristjansson et al., 2012; Torrealday et al., 2008) and suggest that similar to school-based and young adult samples, at-risk youth may use marijuana because they believe it will lead to positive effects. They may also use less because they want to avoid the negative effects. Incorporating a discussion of expectancies into counseling sessions within the juvenile court system may help youth to better understand how their positive beliefs affect their use (D'Amico et al., 2012). This discussion could highlight alternative strategies for obtaining positive feelings and coping with negative affect without using marijuana. Change in use may be facilitated through reinforcing negative expectancies (e.g., presenting objective information on marijuana’s effects on cognition – likely an undesirable effect for teenagers) while also discussing positive expectancies (e.g., sharing balanced placebo studies on marijuana) (Metrik et al., 2012; Metrik et al., 2009). This could be done through the use of Motivational Interviewing strategies, like reflections of ambivalence (e.g., “You like the feeling you get when you’re high, and you’ve heard that when you’re high, it’s hard to remember things like your school work). It is important to note that it may be difficult to reduce marijuana use through expectancy challenge alone because youth with depression and anxiety symptoms who use heavily tend to report more positive (e.g., it enables relaxation) and less negative (e.g., it leads to anxious mood) expectancies than non-users and occasional users (Plancherel et al., 2005). Thus, a teenager who is more depressed and believes using marijuana will alleviate that depression may find that the subjective high they expect from marijuana actually does alleviate undesirable symptoms. Therefore, these individuals may need further cognitive behavioral skills to cope with negative affect (Bonn-Miller, Vujanovic, Feldner, Bernstein, & Zvolensky, 2007; Kristjansson et al., 2012; Marlatt, 2005). Motivational enhancement interventions for youth that include a personalized discussion of both positive and negative expectancies have shown promise (D'Amico et al., 2013; D'Amico, Miles, Stern, & Meredith, 2008; Lee, Neighbors, Kilmer, & Larimer, 2010; Martin & Copeland, 2008; Stein et al., 2011; Walker et al., 2006; Walker et al., 2011).
LIMITATIONS
The generalizability of this study is limited by its use of cross-sectional data with a unique at-risk sample. In addition, we focused on depressive and anxiety symptoms among a non-clinical sample and findings might differ for adolescents diagnosed with a depressive or anxiety disorder. Indeed our sample overall was in good mental health (i.e., mean MHI-5 scores indicated limited distress frequency) and results might be different with a clinical population; or perhaps youth with repeated and more serious offenses. Regarding expectancy items, we only assessed the degree to which participants agreed or disagreed with the expectancies and did not assess valence (i.e., did they think the outcome would be good or bad). For example, it is unknown if the “negative expectancies” conceptualized were viewed as such by participants. It has been suggested that young adults with social anxiety may view theoretically negative marijuana expectancies (e.g., marijuana slows thinking and actions) positively (Buckner & Schmidt, 2009), though few studies have addressed the issue of valence in substance use expectancy research (Fromme & D'Amico, 2000; Fromme, Stroot, & Kaplan, 1993; Fulton et al., 2012).
CONCLUSION
In sum, we found that mental health symptoms and positive expectancies about marijuana combined to promote the greatest risk for consequences from use among an at-risk sample of youth. Results expand on prior research suggesting positive expectancies and mental health are independently indicated in the experience of marijuana-related consequences. Expectancy challenges, decisional balance, and relapse prevention skills may be particularly helpful in reaching these at-risk youth.
Acknowledgments
The current study was funded by a grant from the National Institute of Drug Abuse (R01DA019938; PI: Elizabeth J. D’Amico).
REFERENCES
- Aarons GA, Brown SA, Stice E, Coe MT. Psychometric evaluation of the marijuana and stimulant effect expectancy questionnaires for adolescents. Addictive Behaviors. 2001;26(2):219–236. doi: 10.1016/s0306-4603(00)00103-9. [DOI] [PubMed] [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70(6):1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Ashtari M, Cervellione K, Cottone J, Ardekani BA, Sevy S, Kumra S. Diffusion abnormalities in adolescents and young adults with a history of heavy cannabis use. Journal of Psychiatry Research. 2009;43(3):189–204. doi: 10.1016/j.jpsychires.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Medical care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Feldner MT, Bernstein A, Zvolensky MJ. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. Journal of Traumatic Stress. 2007;20(4):577–586. doi: 10.1002/jts.20243. [DOI] [PubMed] [Google Scholar]
- Bottorff JL, Johnson JL, Moffat BM, Mulvogue T. Relief-oriented use of marijuana by teens. Substance Abuse Treatment Prevention and Policy. 2009;4 doi: 10.1186/1747-597X-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Adams RE, Balka EB, Johnson E. Early adolescent marijuana use: risks for the transition to young adulthood. Psychological Medicine. 2002;32(1):79–91. doi: 10.1017/s0033291701004809. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Marijuana effect expectancies: Relations to social anxiety and marijuana use problems. Addictive Behaviors. 2008;33(11):1477–1483. doi: 10.1016/j.addbeh.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Social Anxiety Disorder and Marijuana Use Problems: The Mediating Role of Marijuana Effect Expectancies. Depression and Anxiety. 2009;26(9):864–870. doi: 10.1002/da.20567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark HK, Ringwalt CL, Shamblen SR. Predicting adolescent substance use: the effects of depressed mood and positive expectancies. Addictive Behaviors. 2011;36(5):488–493. doi: 10.1016/j.addbeh.2011.01.018. [DOI] [PubMed] [Google Scholar]
- Crippa JA, Zuardi AW, Martin-Santos R, Bhattacharyya S, Atakan Z, et al. Cannabis and anxiety: a critical review of the evidence. Humam Psychopharmacology. 2009;24:515–523. doi: 10.1002/hup.1048. [DOI] [PubMed] [Google Scholar]
- D'Amico EJ, Hunter SB, Miles JN, Ewing BA, Osilla KC. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment. 2013;45(5):400–408. doi: 10.1016/j.jsat.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- D'Amico EJ, Osilla KC, Miles JN, Ewing B, Sullivan K, Katz K, Hunter SB. Assessing motivational interviewing integrity for group interventions with adolescents. Psychology of Addictive Behaviors. 2012;26(4):994–1000. doi: 10.1037/a0027987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Edelen MO, Miles JNV, Morral AR. The longitudinal association between substance use and delinquency among high-risk youth. Drug and Alcohol Dependence. 2008;93(1–2):85–92. doi: 10.1016/j.drugalcdep.2007.09.006. [DOI] [PubMed] [Google Scholar]
- de Dios MA, Hagerty CE, Herman DS, Hayaki J, Anderson BJ, Budney AJ, Stein M. General Anxiety Disorder Symptoms, Tension Reduction, and Marijuana Use Among Young Adult Females. Journal of Womens Health. 2010;19(9):1635–1642. doi: 10.1089/jwh.2010.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Coffey C, Romaniuk H, Swift W, Carlin JB, et al. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction. 2013;108:124–133. doi: 10.1111/j.1360-0443.2012.04015.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98:1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Funk R. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. New York: Chapman & Hall; 1993. [Google Scholar]
- Ellickson PL, D'Amico EJ, Collins RL, Klein DJ. Marijuana use and later problems: When frequency of recent use explains age of initiation effects (and when it does not) Substance Use & Misuse. 2005;40(3):343–359. doi: 10.1081/ja-200049356. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Martino SC, Collins RL. Marijuana use from adolescence to young adulthood: Multiple developmental trajectories and their associated outcomes. Health Psychology. 2004;23(3):299–307. doi: 10.1037/0278-6133.23.3.299. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Tucker JS, Klein DJ. Ten-year prospective study of public health problems associated with early drinking. Pediatrics. 2003;111(5 Pt 1):949–955. doi: 10.1542/peds.111.5.949. [DOI] [PubMed] [Google Scholar]
- Fromme K, D'Amico EJ. Measuring adolescent alcohol outcome expectancies. Psychology of Addictive Behaviors. 2000;14(2):206–212. doi: 10.1037//0893-164x.14.2.206. [DOI] [PubMed] [Google Scholar]
- Fromme K, Stroot EA, Kaplan D. Comprehensive effects of alcohol: Development and psychometric assessment of a new expectancy questionnaire. Psychological Assessment. 1993;5(1):19–26. [Google Scholar]
- Fulton HG, Krank MD, Stewart SH. Outcome expectancy liking: a self-generated, self-coded measure predicts adolescent substance use trajectories. Psychology of Addictive Behaviors. 2012;26(4):870–879. doi: 10.1037/a0030354. [DOI] [PubMed] [Google Scholar]
- Goldman MS, Del Boca FK, Darkes J. Alcohol expectancy theory: The application of cognitive neuroscience. In: Leonard KE, Blane HT, editors. Psychological Theories of Drinking and Alcoholism. New York: Guildford Press; 1999. pp. 203–246. [Google Scholar]
- Goldman MS. The alcohol expectancy concept: Applications to assessment, prevention, and treatment of alcohol abuse. Applied and Preventive Psychology. 1994;3(3):131–144. [Google Scholar]
- Hall W. The adverse health effects of cannabis use: what are they, and what are their implications for policy? The International journal on drug policy. 2009;20(6):458–466. doi: 10.1016/j.drugpo.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Jacobus J, Bava S, Cohen-Zion M, Mahmood O, Tapert SF. Functional consequences of marijuana use in adolescents. Pharmacology Biochemistry and Behavior. 2009;92(4):559–565. doi: 10.1016/j.pbb.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975–2013: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research: The University of Michigan; 2014. p. 84. [Google Scholar]
- Kaminer Y, Connor DF, Curry JF. Comorbid adolescent substance use and major depressive disorders: a review. Psychiatry (Edgmont) 2007;4(12):32–43. [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Chen K. Types of marijuana users by longitudinal course. Journal of Studies on Alcohol. 2000;61(3):367–378. doi: 10.15288/jsa.2000.61.367. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Adolescent development, mental disorders, and decision making of delinquent youths. In: Grisso Thomas, Schwartz Robert G., editors. Youth on trial: A developmental perspective on juvenile justice. Chicago, IL: University of Chicago Press; 2000. pp. 33–65. [Google Scholar]
- Kedzior KK, Laeber LT. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population--a meta-analysis of 31 studies. BMC Psychiatry. 2014;14:136. doi: 10.1186/1471-244X-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjansson SD, Agrawal A, Lynskey MT, Chassin LA. Marijuana expectancies and relationships with adolescent and adult marijuana use. Drug and Alcohol Dependence. 2012;126:102–110. doi: 10.1016/j.drugalcdep.2012.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Kilmer JR, Larimer ME. A brief, web-based personalized feedback selective intervention for college student marijuana use: a randomized clinical trial. Psychology of Addictive Behaviors. 2010;24(2):265–273. doi: 10.1037/a0018859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low NCP, Dugas E, O'Loughlin E, Rodriguez D, Contreras G, Chaiton M, O'Loughlin J. Common stressful life events and difficulties are associated with mental health symptoms and substance use in young adolescents. BMC Psychiatry. 2012;12 doi: 10.1186/1471-244X-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macleod J, Oakes R, Copello A, Crome L, Egger M, Hickman M, Smith GD. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–1588. doi: 10.1016/S0140-6736(04)16200-4. [DOI] [PubMed] [Google Scholar]
- Malone DT, Hill MN, Rubino T. Adolescent cannabis use and psychosis: epidemiology and neurodevelopmental models. British Journal of Pharmacology. 2010;160(3):511–522. doi: 10.1111/j.1476-5381.2010.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Donovan DM. Relapse Prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 2005. [Google Scholar]
- Martin G, Copeland J. The adolescent cannabis check-up: randomized trial of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2008;34(4):407–414. doi: 10.1016/j.jsat.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Metrik J, Kahler CW, Reynolds B, McGeary JE, Monti PM, Haney M, Rohsenow DJ. Balanced placebo design with marijuana: pharmacological and expectancy effects on impulsivity and risk taking. Psychopharmacology. 2012;223(4):489–499. doi: 10.1007/s00213-012-2740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Rohsenow DJ, Monti PM, McGeary J, Cook TA, de Wit H, Kahler CW. Effectiveness of a marijuana expectancy manipulation: Piloting the balanced-placebo design for marijuana. Experimental and Clinical Psychopharmacology. 2009;17(4):217–225. doi: 10.1037/a0016502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles JNV, Shevlin M. Applying regression and correlation. London: Sage; 2001. [Google Scholar]
- National Center on Addiction and Substance Abuse at Columbia University. Adolescent substance use: America’s #1 public health problem. New York, NY: CASA; 2011. Available at http://www.casacolumbia.org/upload/2011/20110629adolescentsubstanceuse.pdf. [Google Scholar]
- Orlando M, Ellickson PL, McCaffrey DF, Longshore DL. Mediation analysis of a school-based drug prevention program: Effects of Project ALERT. Prevention Science. 2005;6(1):35–46. doi: 10.1007/s11121-005-1251-z. [DOI] [PubMed] [Google Scholar]
- Pedersen ER, Miles JN, Hunter SB, Osilla KC, Ewing BA, D'Amico EJ. Perceived norms moderate the association between mental health symptoms and drinking outcomes among at-risk adolescents. Journal of Studies on Alcohol and Drugs. 2013;74(5):736–745. doi: 10.15288/jsad.2013.74.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plancherel B, Bolognini M, Stephan P, Laget J, Chinet L, Bernard M, Halfon O. Adolescents' beliefs about marijuana use: a comparison of regular users, past users and never/occasional users. Journal of Drug Education. 2005;35(2):131–146. doi: 10.2190/DMDW-X35X-P6AV-6F4L. [DOI] [PubMed] [Google Scholar]
- Rumpf HJ, Meyer C, Hapke U, John U. Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Research. 2001;105(3):243–253. doi: 10.1016/s0165-1781(01)00329-8. [DOI] [PubMed] [Google Scholar]
- Skenderian JJ, Siegel JT, Crano WD, Alvaro EE, Lac A. Expectancy change and adolescents' intentions to use marijuana. Psychology of Addictive Behaviors. 2008;22(4):563–569. doi: 10.1037/a0013020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LA, Lebeau R, Colby SM, Barnett NP, Golembeske C, Monti PM. Motivational interviewing for incarcerated adolescents: effects of depressive symptoms on reducing alcohol and marijuana use after release. Journal of Studies on Alcohol and Drugs. 2011;72(3):497–506. doi: 10.15288/jsad.2011.72.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration: Center for Behavioral Health Statistics and Quality. Results from the 2011 National Survey on Drug Use and Health: Summary of national findings HHS Publication No. SMA 12-4713, NSDUH Series H-44. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- Substance Abuse and Mental Health Services Administration: Center for Behavioral Health Statistics and Quality. Results from the 2011 National Survey on Drug Use and Health: Mental Health Findings NSDUH Series H-45, HHS Publication No. (SMA) 12-4725. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- Tapert SF, Caldwell L, Burke C. Alcohol and the adolescent brain: Human studies. Alcohol Research & Health. 2004;28(4):205–212. [Google Scholar]
- Torrealday O, Stein LA, Barnett N, Golembeske C, Lebeau R, Colby SM, Monti PM. Validation of the Marijuana Effect Expectancy Questionnaire-Brief. Journal of Child & Adolescent Substance Abuse. 2008;17(4):1–17. doi: 10.1080/15470650802231861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Orlando M, Ellickson PL. Patterns and correlates of binge drinking trajectories from early adolescence to young adulthood. Health Psychology. 2003;22(1):79–87. doi: 10.1037//0278-6133.22.1.79. [DOI] [PubMed] [Google Scholar]
- van Os J, Bak M, Hanssen M, Bijl RV, de Graaf R, Verdoux H. Cannabis Use and Psychosis: A Longitudinal Population-based Study. American Journal of Epidemiology. 2002;156(4):319–327. doi: 10.1093/aje/kwf043. [DOI] [PubMed] [Google Scholar]
- Walker DD, Roffman RA, Stephens RS, Wakana K, Berghuis J, Kim W. Motivational enhancement therapy for adolescent marijuana users: a preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens R, Roffman R, Demarce J, Lozano B, Towe S, Berg B. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: a further test of the teen marijuana check-up. Psychology of Addictive ehaviors. 2011;25(3):474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner M, Kim HK, Capaldi DM. Developmental trajectories of offending: Validation and prediction to young adult alcohol use, drug use, and depressive symptoms. Development and Psychopathology. 2005;17(1):251–270. doi: 10.1017/s0954579405050133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazaki S, Fukuhara S, Green J. Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health and Quality of Life Outcomes. 2005;3:48. doi: 10.1186/1477-7525-3-48. [DOI] [PMC free article] [PubMed] [Google Scholar]