Abstract
The aim of this retrospective case–control study is to evaluate the incidence of facial nerve injury associated with temporomandibular joint (TMJ) arthroplasty using the endaural approach for the treatment of TMJ pathology. The sample consisted of 36 consecutive patients who underwent TMJ arthroplasty. A total of 39 approaches were performed through an endaural incision. Patients undergoing total joint replacement and/or with preexisting facial nerve dysfunction were excluded from the study. Five patients were lost to follow-up and were excluded from the study. Facial nerve function of all patients was clinically evaluated by resident physicians preoperatively, postoperatively, and at follow-up appointments. Facial nerve injury was determined to have occurred if the patient was unable to raise the eyebrow or wrinkle the forehead (temporalis branch), completely close the eyelids (zygomatic branch), or frown (marginal mandibular branch). Twenty-one of the 36 patients or 22 of the 39 approaches showed signs of facial nerve dysfunction following TMJ arthroplasty. This included 12 of the 21 patients who had undergone previous TMJ surgery. The most common facial nerve branch injured was the temporal branch, which was dysfunctional in all patients either as the only branch injured or in combination with other branches. By the 18th postoperative month, normal function had returned in 19 of the 22 TMJ approaches. Three of the 22 TMJ approaches resulted in persistent signs of facial nerve weakness 6 months after the surgery. This epidemiological study revealed a low incidence of permanent facial nerve dysfunction. A high incidence of temporary facial nerve dysfunction was seen with TMJ arthroplasty using the endaural approach. Current literature reveals that the incidence of facial nerve injury associated with open TMJ surgery ranges from 12.5 to 32%. The temporal branch of the facial nerve was most commonly affected, followed by 4 of the 22 approaches with temporary zygomatic branch weakness. Having undergone previous TMJ surgery did not increase the incidence of facial nerve injury using the endaural approach. This information is important for patients and surgeons in the postoperative period, as a majority of patients will experience recovery of nerve function.
Keywords: temporomandibular joint, arthroplasty, endaural approach, facial nerve injury
Temporomandibular joint (TMJ) arthroplasty is an open surgical procedure typically performed in patients with debilitating TMJ pain and masticatory dysfunction and who have failed noninvasive and minimally invasion treatment modalities. Arthroplasty is the surgery of choice for patients with bony ankylosis, dislocated/damaged articular discs, and severe joint adhesions. Studies have shown that TMJ arthroplasty results in significantly improved incisal opening and range of movement and TMJ-associated pain.1 2 3 Complications are rare but can include wound infection, permanent occlusal changes, relapsing joint pain, life-threatening vascular injuries, and facial nerve injury.4 Intraoperative injury to the facial nerve can result in both functional deficits and poor facial cosmesis and interfere with the expression of emotions and mood.5
To minimize the risk of facial nerve injury, modern open surgical approaches to the TMJ have been specifically designed to avoid and protect this important neural structure. The four basic open approaches used in TMJ surgery are the preauricular, postauricular, submandibular, and endaural.6 The endaural incision, similar to the preauricular incision, provides excellent lateral and posterior exposure with good anterior exposure and has the added advantage of hiding the majority of the scar behind the tragus.7 The endaural incision design and plane of dissection allows for the theoretical avoidance of all five branches of the facial nerve. However, even in the most experienced surgeon's hands facial nerve injury can occur.
A review of the current literature reveals that the incidence of facial nerve injury associated with open TMJ surgery ranges from 12.5 to 32%.3 8 9 10 11 However, in all incidences the facial nerve deficits were transient in nature and typically resolved in 3 to 6 months without long-term sequel. These studies also found that weakness in the forehead region was the most common deficit, and that patients who have undergone previous TMJ surgery are at higher risk of facial nerve injury.5 Most studies consisted of patients who underwent TMJ surgery using the standard preauricular incision.
The evaluation of facial nerve injury following TMJ surgery is often a difficult task given the subjective nature of the physical examination. One way of measuring facial nerve function is using the House–Brackmann facial nerve grading system, which was introduced in 1983 and has since been adopted as the universal standard by the American Academy of Otolaryngology in 1984.12 This grading system uses a gross subjective scale that considers the overall facial function and assigns patients to one of the six descriptive categories based on their degree of facial function both at rest and in motion.12 Although, the House–Brackmann grading system reduces the subjectivity associated with facial nerve function evaluation, it is time-consuming, expensive, and requires special training.13 In clinical practice, a simple bedside estimate of facial weakness is much more efficient and suffices for most intents and purposes.
The aim of this retrospective study is to evaluate the incidence of facial nerve injury associated with TMJ arthroplasty using the endaural approach for the treatment of temporomandibular pathology. The study includes patients treated by oral and maxillofacial surgeons at the Hospital of University of Pennsylvania.
Patients and Methods
The patient sample consisted of 36 adult patients (33 females and 3 males) who underwent TMJ arthroplasty using an endaural approach for the treatment of various TMJ-associated pathologies (Table 1). The study includes surgical procedures performed by the Department of Oral and Maxillofacial Surgery at the Hospital of the University of Pennsylvania between January 2008 and January 2013. The mean age was 40 with a range of 18 to 99 years. A total of 39 endaural approaches (21 left, 12 right, and 3 bilateral) were completed by various residents and attending surgeons as the method to gain access to the TMJ. Patients undergoing total joint replacement and/or with preexisting facial nerve dysfunction were excluded from the study.
Table 1. Summary of the 36 patients who were included in this study.
| Patient (n) | Age (y) | Gender | Pathology | Surgical procedure | Side | Previous surgery | POD1 | Facial nerve weakness (follow-up) |
|---|---|---|---|---|---|---|---|---|
| 1 | 52 | F | Internal derangement | Lt LOA | L | No | Temporal | Yes (8 wk), no (3 mo) |
| 2 | 42 | F | Internal derangement | Rt LOA | R | No | No | No |
| 3 | 73 | F | Internal derangement | Lt disc plication | L | No | No | No |
| 4 | 18 | M | Ankylosis | Lt gap arthroplasty, coronoidectomy | L | No | Temporal/zygomatic | Yes (8 wk), no (6 mo) |
| 5 | 41 | F | Internal derangement | Lt disc plication | L | No | No | No |
| 6 | 31 | F | DJD | Rt osteophyte removal, condylectomy | R | Arthrocentesis | Temporal | No (1 wk) |
| 7 | 36 | F | Internal derangement | Lt disc plication | L | No | No | No |
| 8 | 44 | F | Ankylosis | Lt gap arthroplasty | L | Arthrocentesis | Temporal/mandibular | Yes (24 mo) |
| 9 | 26 | F | Internal derangement | Rt disc plication, Lt injection | R | No | No | No |
| 10 | 18 | F | Internal derangement | Lt disc plication, Rt condylectomy | RL | Arthrocentesis | Rt temporal | Yes (3 wk), no (12 mo) |
| 11 | 35 | F | DJD | Rt discectomy with silastic implant | R | Disc plication Rt, arthroscopy Lt | Rt temporal | No (9 mo) |
| 12 | 49 | F | Synovial chondromatosis | Lt excision of lesions | L | No | No | No |
| 13 | 23 | F | Internal derangement | Lt disc plication | L | No | No | No |
| 14 | 47 | F | DJD | Lt discectomy with fat graft | L | Multiple | Temporal | No (12 mo) |
| 15 | 38 | F | Internal derangement | Rt discectomy with silastic implant | R | Arthroscopy | Temporal/mandibular | No (9 mo) |
| 16 | 31 | F | Synovial chondromatosis | Lt excision of lesions | L | No | All branches | No (9 mo) |
| 17 | 18 | F | Internal derangement | L discectomy with silastic implant | L | No | Temporal | No (9 mo) |
| 18 | 41 | F | DJD | Rt LOA | R | Rt arthroplasty | No | No |
| 19 | 53 | M | Ankylosis | Lt discectomy with silastic, coronoidectomy | L | Scope | Temporal | No (3 mo) |
| 20 | 41 | F | DJD | b/l discectomy with silastic implant | RL | b/l arthroplasty, arthrocentesis | Lt temporal | No (1 wk) |
| 21 | 21 | F | DJD | Lt discectomy with costasis | L | No | No | No |
| 22 | 56 | F | Synovial chondromatosis | Rt excision of lesions | R | No | Temporal/zygomatic | Yes (12 wk), no (18 mo) |
| 23 | 51 | F | DJD | L discectomy with silastic implant | L | Scope 4/10 | Temporal/zygomatic | Yes (12 wk), no (6 mo) |
| 24 | 22 | F | DJD | Lt LOA | L | No | Temporal | Yes (2 wk), no (3 mo) |
| 25 | 20 | F | Ankylosis | Rt discectomy with silastic implant | R | No | Temporal | Yes (12 wk), no (3 mo) |
| 26 | 42 | F | Internal derangement | Lt discectomy | L | Arthrocentesis | No | No |
| 27 | 24 | F | Internal derangement | Lt LOA | L | Scope | Temporal | Yes (6 mo) |
| 28 | 60 | F | Internal derangement | Lt discectomy with silastic | L | Arthroscopy | No | No |
| 29 | 55 | F | Internal derangement | b/l discectomy | RL | No | b/l temporal and buccal | Yes (6 mo) |
| 30 | 50 | F | Internal derangement | Lt discectomy | L | Lt arthroscopy | Temporal/mandibular | No (4 wk) |
| 31 | 75 | F | Internal derangement | Rt discectomy | R | Arthroscopy 4/12 | No | No |
| 32 | 20 | F | Internal derangement | Rt discectomy | R | Arthroscopy 6/12 | No | No |
| 33 | 99 | F | Internal derangement | Lt disc plication | L | Arthroscopy/arthrocentesis | Temporal | Yes (1 wk), no (3 mo) |
| 34 | 24 | F | Internal derangement | Rt discectomy | R | Arthroscopy | No | No |
| 35 | 34 | M | Internal derangement | Lt discectomy | L | No | Temporal | No (2 wk) |
| 36 | 46 | F | Internal derangement | Rt discectomy | R | Arthroscopy 7/12 | No | No |
Abbreviations: b/l, bilateral; DJD, degenerative joint disease; F, female; Lt, left; LOA, lysis of adhesions; M, male; POD, postoperative day; Rt, right.
Patients were treated for the following TMJ-associated pathological conditions: internal derangement (21 patients), degenerative joint disease (8 patients), ankylosis (4 patients), and synovial chondromatosis (3 patients) (Fig. 1). Surgical procedures consisted of discectomy with and without implant (18 approaches), lysis of adhesions (5 approaches), disc plication (7 approaches), excision of lesion (3 approaches), condylectomy (2 approaches), coronoidectomy (2 approaches), and gap arthroplasty (2 approaches). A total of 19 patients had undergone previous TMJ surgery and 17 patients had no previous surgery. Previous surgeries included arthrocentesis, arthroscopy, disc plication, and discectomy with an implant. General anesthesia was administered to all the patients.
Fig. 1.
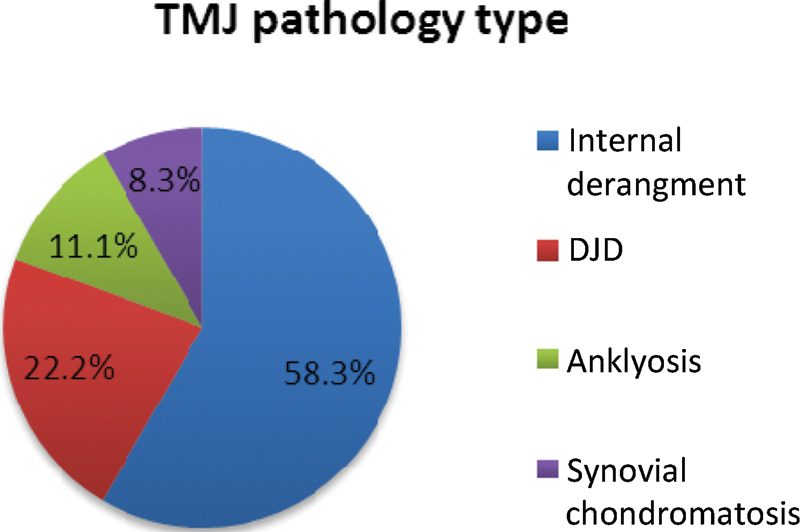
Types of temporomandibular joint pathology in the study patients.
Facial nerve function of all patients was clinically evaluated by resident physicians preoperatively, immediate postoperatively, and at follow-up appointments. Facial nerve injury was determined to have occurred if the patient was unable to raise the eyebrow or wrinkle the forehead (temporalis branch), to completely close the eyelids (zygomatic branch), or to frown symmetrically (marginal mandibular branch). No surgery or medication was used to treat the facial nerve injury.
Results
Twenty-one of the 36 (58.3%) patients or 22 of the 39 (56.4%) approaches showed signs of facial nerve dysfunction following TMJ arthroplasty. This included 12 of the 19 patients (12 of the 21 approaches) who had undergone previous TMJ surgery. Nine of the 17 patients (10 of the 18 approaches) who had TMJ surgery for the first time had a facial nerve injury immediately following TMJ surgery. The most common facial nerve branch injured was the temporal branch, which was dysfunctional in 21 of the 21 patients (Fig. 2). A Fisher exact test revealed that there was no significant difference in the incidence of facial nerve injury among patients with previous TMJ surgery and those having surgery for the first time, 57.1% as compared with 55.6%, respectively (p = 0.55).
Fig. 2.
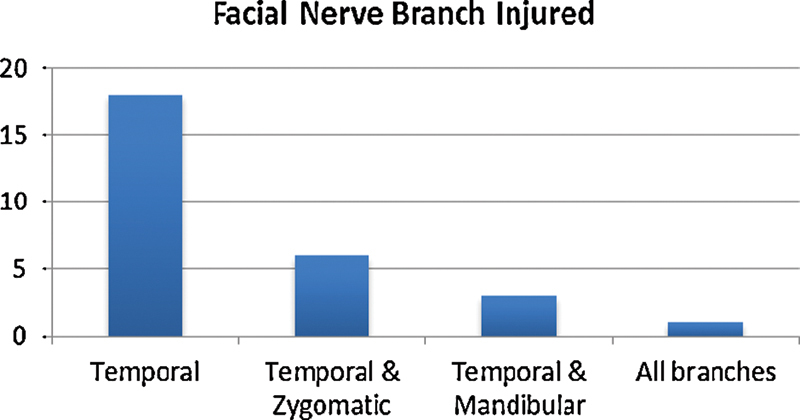
Branch of facial nerve injured from arthroplasty procedure.
By the 18th postoperative month, normal function had returned in 19 of the 22 (86.4%) TMJ approaches (Fig. 3). Five patients were lost to follow-up ranging from 1 week to 3 months, all with facial nerve dysfunction at that time. Only 3 of the 22 TMJ approaches resulted in persistent signs of facial nerve weakness 6 months after the surgery.
Fig. 3.
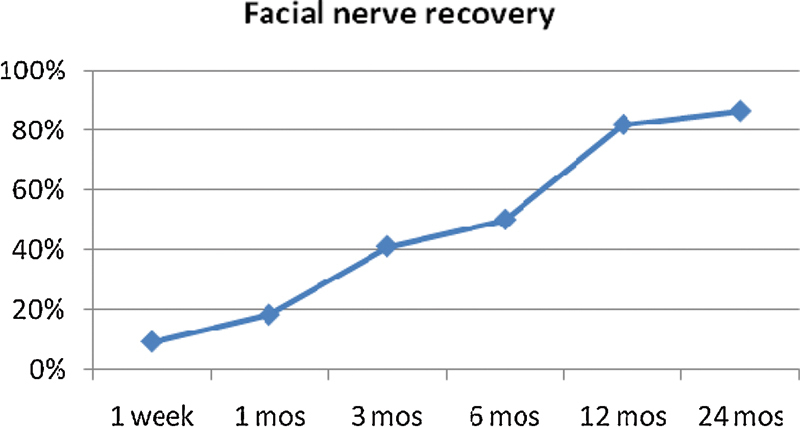
Recovery of facial nerve injury relative to time postprocedure.
Discussion
Various approaches have been described for open surgery of the TMJ including the preauricular, postauricular, submandibular, and endaural.6 Although they differ in design, they share a common objective, which is the adequate exposure of joint structures with maximum protection of the facial nerve. This objective is achieved by meticulous surgical dissection and a thorough understanding and awareness of the regional anatomy.9 In our study, we utilized the endaural incision, which provides excellent lateral and posterior exposure with good anterior exposure and has the added advantage of hiding the majority of the scar behind the tragus.7 The endaural incision design and plane of dissection allows for the theoretical avoidance of all five branches of the facial nerve.
In our study, we found that 21 of the 36 (58.3%) patients or 22 of the 39 (56.4%) approaches showed signs of facial nerve dysfunction immediately following TMJ arthroplasty. Consistent with previous studies,5 9 the most common facial nerve branch injured was the temporal branch, which was dysfunctional in 21 of the 21 patients. The temporal branch of the facial nerve is more vulnerable during TMJ surgery due to their course and close proximity to the incision.14 As the temporal branches cross the lateral surface of the zygomatic arch, they course along the undersurface of the temporoparietal fascia. In their classic article, Al-Kayat and Bramley showed that the temporal branch crosses the zygomatic arch at varying location in different individuals, and may be located anywhere from 8 to 35 mm (20 mm average) anterior to the external auditory canal.15 The design of the endaural approach used in our patients is based on this information, with the thought that the temporal branches of the facial nerve can be protected by incising through the superficial layer of the temporalis fascia no more than 8 mm in front of the anterior border of the external auditory canal.14
By the 18th postoperative month, normal function had returned in 19 of the 22 (86.4%) TMJ approaches. This finding is consistent with previous studies, which found that facial nerve injury typically resolved in without long-term sequel. The transient nature of paralysis suggests that the main cause of injury in our series was due to compression and/or stretching of nerve fibers caused by excessive or heavy-handed retraction. This resulted in neuropraxia which is temporary in nature.
A study by do Egito Vasconcelos et al showed that patients who have undergone previous TMJ surgery are at higher risk of facial nerve injury, 25% as compared with 6.5%.5 The increased incidence of facial nerve injury in patients who have undergone previous TMJ surgery may be explained by the fact that surgical scarring leading to fibrosis and distortion of the fascial layers and significantly increases the difficulty of establishing precise tissue plans during the dissection.9 However, our results contradict these findings, and showed no significant difference in the incidence of facial nerve injury among patients with previous TMJ surgery and those having surgery for the first time, 57.1% as compared with 55.6%, respectively. This finding can possibly be explained by the design advantage of the endaural incision, which allows for an easier development of the tissue flap and the plane of dissection. Based on these findings, the endaural approach might benefit patients undergoing repeat open TMJ procedures.
In summary, this epidemiological study revealed a low incidence of permanent facial nerve dysfunction. The temporal branch of the facial nerve was most commonly affected. Having undergone previous TMJ surgery did not increase the incidence of facial nerve injury using the endaural approach. This information is important for patients and surgeons in the postoperative period, as a majority of patients will experience recovery of nerve function.
References
- 1.Katsnelson A, Markiewicz M R, Keith D A, Dodson T B. Operative management of temporomandibular joint ankylosis: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2012;70(3):531–536. doi: 10.1016/j.joms.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Miloro M, Henriksen B. Discectomy as the primary surgical option for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 2010;68(4):782–789. doi: 10.1016/j.joms.2009.09.091. [DOI] [PubMed] [Google Scholar]
- 3.Hall H D, Indresano A T, Kirk W S, Dietrich M S. Prospective multicenter comparison of 4 temporomandibular joint operations. J Oral Maxillofac Surg. 2005;63(8):1174–1179. doi: 10.1016/j.joms.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Fonseca R J, Marciani R D, Turvey T A. St Louis, MO: Elsevier; 2009. Oral and Maxillofacial Surgery. [Google Scholar]
- 5.do Egito Vasconcelos B C, Bessa-Nogueira R V, da Silva L C. Prospective study of facial nerve function after surgical procedures for the treatment of temporomandibular pathology. J Oral Maxillofac Surg. 2007;65(5):972–978. doi: 10.1016/j.joms.2006.06.280. [DOI] [PubMed] [Google Scholar]
- 6.Kreutziger K L. Surgery of the temporomandibular joint. I. Surgical anatomy and surgical incisions. Oral Surg Oral Med Oral Pathol. 1984;58(6):637–646. doi: 10.1016/0030-4220(84)90027-6. [DOI] [PubMed] [Google Scholar]
- 7.Nishioka G J, Van Sickels J E. Modified endaural incision for surgical access to the temporomandibular joint. J Oral Maxillofac Surg. 1987;45(12):1080–1081. doi: 10.1016/0278-2391(87)90171-6. [DOI] [PubMed] [Google Scholar]
- 8.Nogueira R V, Vasconcelos B C. Facial nerve injury following surgery for the treatment of ankylosis of the temporomandibular joint. Med Oral Patol Oral Cir Bucal. 2007;12(2):E160–E165. [PubMed] [Google Scholar]
- 9.Weinberg S, Kryshtalskyj B. Facial nerve function following temporomandibular joint surgery using the preauricular approach. J Oral Maxillofac Surg. 1992;50(10):1048–1051. doi: 10.1016/0278-2391(92)90488-l. [DOI] [PubMed] [Google Scholar]
- 10.Hall M B, Brown R W, Lebowitz M S. Facial nerve injury during surgery of the temporomandibular joint: a comparison of two dissection techniques. J Oral Maxillofac Surg. 1985;43(1):20–23. doi: 10.1016/s0278-2391(85)80008-2. [DOI] [PubMed] [Google Scholar]
- 11.Dolwick M F, Kretzschmar D P. Morbidity associated with the preauricular and perimeatal approaches to the temporomandibular joint. J Oral Maxillofac Surg. 1982;40(11):699–700. doi: 10.1016/0278-2391(82)90141-0. [DOI] [PubMed] [Google Scholar]
- 12.House J W, Brackmann D E. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 13.Reitzen S D, Babb J S, Lalwani A K. Significance and reliability of the House-Brackmann grading system for regional facial nerve function. Otolaryngol Head Neck Surg. 2009;140(2):154–158. doi: 10.1016/j.otohns.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 14.Ellis E, III, Zide M F. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. Surgical Approaches to the Facial Skeleton. [Google Scholar]
- 15.Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg. 1979;17(2):91–103. doi: 10.1016/s0007-117x(79)80036-0. [DOI] [PubMed] [Google Scholar]


