Abstract
Skin is the first line of defense for protecting our bodies against external perturbations, including ultraviolet (UV) irradiation, mechanical/chemical stress, and bacterial infection. Nutrition is one of many factors required for the maintenance of overall skin health. An impaired nutritional status alters the structural integrity and biological function of skin, resulting in an abnormal skin barrier. In particular, the importance of micronutrients (such as certain vitamins and minerals) for skin health has been highlighted in cell culture, animal, and clinical studies. These micronutrients are employed not only as active compounds in therapeutic agents for treating certain skin diseases, but also as ingredients in cosmetic products. Here, the author describes the barrier function of the skin and the general nutritional requirements for skin health. The goal of this review is to discuss the potential roles and current knowledge of selected micronutrients in skin health and function.
Keywords: Skin disease, Skin function, Micronutrient, Therapeutic agent, Cosmetic ingredient
INTRODUCTION
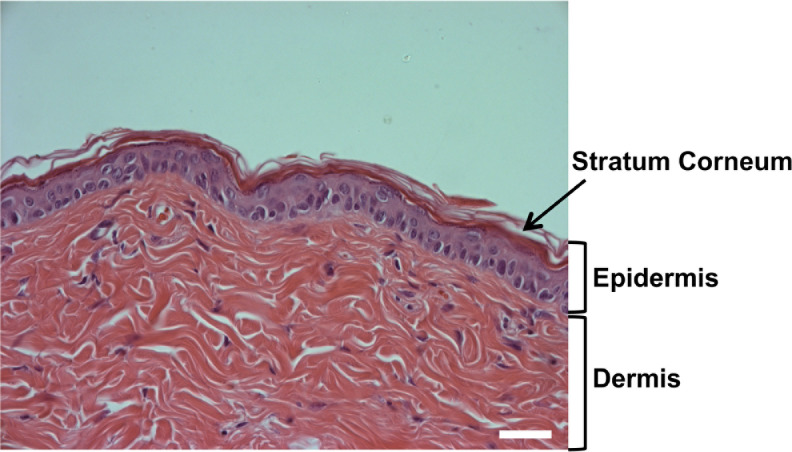
The skin is composed of two primary layers, epidermis and dermis (Fig. 1), and each layer exhibits unique structural and physiological functions (Bouwstra et al., 2006; Thangapazham et al., 2014). Because the epidermis directly faces the external environment, including factors such as UV irradiation, pathogens, and toxic insults, it primarily functions as a barrier (Elias and Feingold, 2006). The dermis that is located below the epidermis contains nerves, blood vessels, connective tissues, hair follicle, and fibroblasts which are required for not only the maintenance of the structural foundation of the skin, but also for provision of important biological functions (Bouwstra et al., 2006; Thangapazham et al., 2014).
Fig. 1.
Structure of mammalian skin. Intact skin of mouse was subjected to hematoxylin and eosin (H&E)-staining. The skin consists of two primary layers, epidermis and dermis. The outermost layer of epidermis is the stratum corneum. Scale bar, 20 μm.
Nutritional status, dependent on both macro and micronutrients, is vital for skin health (Boelsma et al., 2003; Lakdawala et al., 2013). Proper nutritional intake complements endogenous factors in regulating skin barrier function (Boelsma et al., 2003; Lakdawala et al., 2013). Notable examples of nutrients are calcium and vitamin C, which are responsible for the differentiation of keratinocytes, a major cell type in epidermis (Bikle et al., 2001; Uchida et al., 2001). A decrease in nutritional status can alter the structural and biological function of skin, resulting in skin abnormalities, including dry skin (Boelsma et al., 2003; Cosgrove et al., 2007; Lakdawala et al., 2013).
In this review paper, the author will describe briefly various functions of the epidermal barrier with a focus on the role of selected micronutrients in maintaining skin integrity.
SKIN BARRIER FUNCTION
Skin deploys multiple barrier functions; i.e., permeability-(Elias and Friend, 1975), antimicrobial- (Elias, 2007), antioxidant- (Thiele et al., 2001), and UV-barrier (Thiele et al., 2001) (Table 1), to protect our bodies from external perturbants. The permeability barrier prevents loss of excess water from nucleated layers of epidermis and penetration of harmful chemicals, allergens, and pathogens into the epidermis (Elias and Friend, 1975). Of the multiple factors that contribute to the maintenance/improvement of the permeability barrier, a well-known cutaneous lipid, ceramide, serves as a key constituent in epidermal membrane (Uchida and Hamanaka, 2006). Since maintenance of skin pH below 5.5 is vital for suppressing virulent microbial pathogen growth, including Staphylococcus aureus, skin acidification is essential in enhancing the antimicrobial barrier (Elias, 2007). In addition to acidification, antimicrobial barrier function can be improved by the action of antimicrobial peptides, which are expressed in epidermal keratinocytes to kill invaded microbial pathogens (Park et al., 2011; Park et al., 2013b). A number of antioxidant chemicals, including vitamin C, are present in the skin (Thiele et al., 2001). These anti-oxidants maintain skin homeostasis; i.e., protection of proteins/lipids from oxidation (Tyrrell and Keyse, 1990; Thiele et al., 2001). The influence of UV irradiation depends upon the structure of cellular components. Urocanic acid, which is generated from histidine in skin, is a potent, endogenous UV absorbent (Barresi et al., 2011). In addition, exogenous nutrients, such as α-tocopherol, β-carotene, lycopene, and lutein, could contribute to forming the UV barrier via enzymatic and non-enzymatic mechanisms (Thiele, 2001; Eichler et al., 2002; Larsson et al., 2006; Evans and Johnson, 2010).
Table 1.
Cutaneous barrier functions
| Barrier | Roles | Effectors |
|---|---|---|
| Permeability | Prevents excess water loss, harmful chemicals, allergens, and microbial pathogens; Maintains body temperature |
Components of skin structure |
| Antimicrobial | Protects against multiple pathogens, e.g, Gram-positive and Gram-negative bacteria, fungi, and some viruses | Acidic pH (<5.5); Sphingoid bases; Innate immune elements, including antimicrobial peptides |
| Antioxidant | Protects skin from oxidative stress | α-/γ-tocopherol Vitamin C and E Certain flavonoids |
| UV | Protects skin from UV light-mediated DNA damage, and oxidative stress | Urocanic acid Structure components, including sphingolipids |
GENERAL NUTRITION REQUIREMENTS FOR SKIN HEALTH
Glucose is the primary source of energy for most mammalian cells, including keratinocytes (Spravchikov et al., 2001). It provides the carbohydrate backbone for glycosylation of proteins/lipids that comprise the extracellular environment of the skin, suggesting that altered levels of glucose in skin may cause structural changes and abnormal barrier functions (Halprin and Ohkawara, 1966; Van Hattem et al., 2008). High glucose concentration has been reported to increase proliferation in MCF-7 breast cancer cells (Yamamoto et al., 1999), renal cortical fibroblasts (Han et al., 1999), and SV40 transformed human corneal epithelium (McDermott et al., 1998). However, high glucose also has been shown to inhibit proliferation in epidermal keratinocytes (Spravchikov et al., 2001) and dermal fibroblasts (Hehenberger et al., 1998) (Table 2), suggesting that a role for glucose in regulation of cellular proliferation appears to be cell/tissue specific. In studies conducted to evaluate the effects of glucose on differentiation, high levels of glucose significantly enhanced calcium-induced keratinocyte differentiation, while their proliferation was obviously inhibited (Spravchikov et al., 2001) (Table 2). Because a well-balanced proliferation and differentiation process is one of the critical steps in wound healing, high glucose levels might contribute to impaired wound healing in certain diseases, including diabetes (Spravchikov et al., 2001).
Table 2.
Role of macronutrients in skin health and function
| Macronutrient | Function | Mechanism | Reference |
|---|---|---|---|
| Glucose | |||
| High concentration | ↓ Wound healing | ↑ Keratinocyte (KC) differentiation ↓ Proliferation in KC and Fibroblast (FB) |
Spravchikov et al., 2001 Hehenberger et al., 1998 |
| Amino Acid | |||
| Proline | Protect against UV irradiation-induced skin aging | ↑ Collagen synthesis in FB | Karna et al., 2001 |
| Glutamate | |||
| Arginine | ↑ Wound healing | ↑ NO production → ↑ Collagen synthesis in FB | Stechmiller et al., 2005 |
| Ornithine | Shi et al., 2002 | ||
| Mixtures from (Mytilus galloprovincialis & Rapana venosa | Badiu et al., 2010 | ||
| Silk protein (sericin) | Improves AD | ↑ Filaggrin ↓ TEWL |
Kim et al., 2012 |
| Lipid | |||
| Ceramide | ↑ Epidermal | Serve as a key constituent in epidermal membrane | Uchida, 2014 |
| Cholesterol | Permeability | ||
| Fatty acids | Barrier | ||
| Ceramide (toxic levels) | ↑ Apoptosis | High dose UVB → ↑↑ Ceramide → Caspase-independent mechanism | Uchida et al., 2010 |
| Ceramide (Subtoxic levels) | ↓ Apoptosis | Low dose UVB→ ↑ Ceramide → ↑ non-apoptotic metabolites (e.g., Sphingosine-1-Phosphate) | |
| Sphingosine-1-Phosphate | ↑ Innate immunity | NF-κB activation → ↑ Cathelicidin | Park et al., 2013 |
| Ceramide-1-Phosphate | ↑ Innate immunity | STAT1/3 activation → ↑ β-defensin2/3 | Kim et al., 2014 |
UV irradiation has been suggested as a potent force in skin aging (see details in Vitamin C section) (Takema et al., 1996). Collagen is a major constituent of dermis and is necessary to maintain skin structure (Takema et al., 1996); and exposure to excess UV irradiation dramatically decreases dermal collagen content, resulting in skin aging or delayed wound healing (Takema et al., 1996). Several amino acids have been shown to prevent skin aging by their stimulation of dermal collagen synthesis. Proline and its precursors, glutamate, significantly increase collagen synthesis in human dermal fibroblasts (Karna et al., 2001) (Table 2). While nitric oxide (NO) generated by dermal fibroblasts induces collagen synthesis, some amino acids, e.g., arginine (Stechmiller et al., 2005), ornithine (Shi et al., 2002), and amino acid mixtures from Mytilus galloprovincialis and Rapana venosa extracts (Badiu et al., 2010), accelerate wound healing via increased dermal collagen produced by iNOS/NO-dependent mechanisms (Table 2). Moreover, recent studies suggest that dietary silk protein, sericin, improves epidermal hydration in parallel with increased levels of filaggrin in an animal model of atopic dermatitis (AD) (Kim et al., 2012) (Table 2). These results indicate that amino acids not only protect skin against UV irradiation-mediated damages, including skin aging and delayed wound healing, but amino acid supplements might be useful for treatment of certain skin diseases such as AD.
Major epidermal lipids consist of ceramide, cholesterol, and fatty acids (Uchida and Hamanaka, 2006; Uchida, 2014). Particularly, ceramide is a key lipid constituent of the epidermal permeability barrier in the extracellular domain of the stratum corneum (Uchida and Hamanaka, 2006; Uchida, 2014) (Table 2). Ceramide and its metabolites also provide signaling roles in modulating multiple cellular functions, e.g., proliferation, differentiation, and apoptosis in epidermal keratinocytes (Uchida and Hamanaka, 2006; Uchida, 2014). While cellular ceramide production is increased in keratinocytes following UV irradiation, high doses (toxic level) of UVB irradiation induce cell apoptosis/death (Uchida et al., 2010). Whereas, subtoxic levels of ceramide, induced by low dose of UVB irradiation, could be restored to normal levels due to its metabolic conversion into non-apoptotic ceramide metabolites, which contribute to protecting cells against ceramide-induced apoptosis (Uchida et al., 2010) (Table 2). In addition, previous studies showed that decreases in ceramide levels occur in certain skin diseases associated with permeability barrier abnormality; i.e., atopic dermatitis and psoriasis (Yamamoto et al., 1991; Motta et al., 1994). Moreover, our recent studies demonstrated that the key ceramide metabolites, ceramide-1-phosphate and sphingosine-1-phosphate, produced in human keratinocytes in response to subtoxic levels of endoplasmic reticulum (ER) stress stimulate production of major epidermal innate immune elements (beta-defensins and cathelicidin antimicrobial peptide) via STAT1/3- or NF-κB-dependent mechanisms, respectively (Park et al., 2013a; Kim et al., 2014) (Table 2).
IMPORTANCE OF KEY MICRONUTRIENTS IN MAINTAINING SKIN HEALTH
Since Dr. James Lind described the importance of vitamin C in the maintenance of skin health (Bartholomew, 2002), other investigators have studied skin abnormalities/diseases due to vitamin deficiencies, such as scurvy and pellagra, which can be corrected with appropriate oral and/or topical vitamin supplementation.
Vitamin A
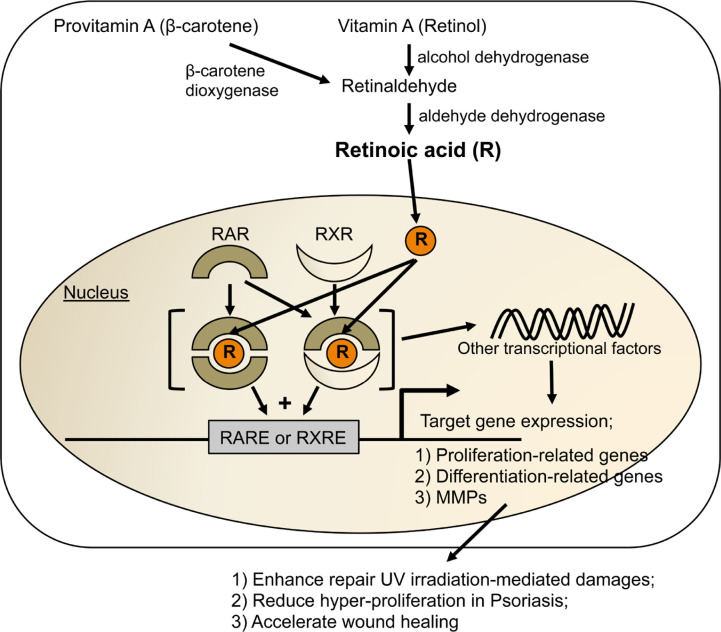
Vitamin A is a group of unsaturated nutritional organic compounds. Vitamin A and its derivatives, e.g., retinoids and carotenoids, play an important role in regulating proliferation, differentiation, and apoptosis of different cell types, including skin cells (Elias et al., 1981; Goodman, 1984; Lee et al., 2009). Retinoids are mostly found in animal sources, whereas provitamin A carotenoids, including β-carotene, are found in plant products (Goodman, 1984). While the beneficial effects of carotenoids are thought to be due to their role as antioxidants, carotenoids first need to be converted to retinoid forms to provide physiological functionalities in skin (Johnson, 2002). Retinoids mainly mediate their function via nuclear hormone receptors (Fig. 2): the retinoic acid receptors (RARs) and the retinoid X receptors (RXRs), each with three isotypes (α, β, and γ) (Elder et al., 1991; Gann et al., 1996). These receptors form heterodimers (RAR/RXR) or homodimers (RXR/RXR) after activation by selective retinoids. These dimers bind consensus DNA regions (called retinoic acid response elements [RARE] or retinoid X response elements [RXRE]), located in the promoter of target genes, which mediate transcriptional regulation (Njar et al., 2006). Since epidermal keratinocytes and dermal fibroblasts express both retinoid receptors (Elder et al., 1991), skin is considered as one of the major retinoid-responsive tissues. Retinoids exert effects in the skin through multiple mechanisms (Fig. 2): 1) regulating expression of epidermal structural and functional genes via direct binding to RARs and/or RXRs (Tomic-Canic et al., 1996; Radoja et al., 1997); 2) modulating skin-related genes by interfering with the signaling of other transcriptional factors after receptor binding (Lee et al., 2005). Previous investigations have shown that retinoids could enhance repair of UV irradiation-damaged skin via following mechanisms (Table 3); i.e., 1) their ability to increase proliferation of epidermal keratinocytes and dermal fibroblasts (Varani et al., 1994); 2) inhibiting the expression of matrix metalloproteinases (MMPs), matrix-degrading enzymes, leading to increased overall protein and extracellular matrix content (Fisher et al., 1997). In contrast, another studies demonstrated that retinoids modulate epidermal proliferation with anti-proliferative potential in hyper-proliferative skin such as psoriasis (van de Kerkhof, 2006; Jean et al., 2011). Hence, the role of retinoids in regulation of epidermal proliferation may be disease/stress specific (normal skin vs. psoriasis) and/or different expression profiles of unknown cofactors required for biological action of retinoids. Moreover, retinoids also have significant potential in the prevention and treatment of other skin diseases, such as ichthyosis (van Steensel, 2007), skin cancer (Niles, 2002), and acne (Kligman, 1997). In particular, topical all-trans-retinoic acid is a safe and effective treatment for mild to moderate acne, while oral 13-cisretinoic acid (isotretinoin) is used to treat severe acne that is resistant to topical therapies (Kligman, 1997; Verfaille et al., 2008). More recent results from clinical studies showed the significantly decreased retinoid concentration and dysregulated retinoid-signaling pathway in the skin of patients with atopic dermatitis (AD) (Mihaly et al., 2011) (Table 4), suggesting that abnormal retinoid activity might contribute to pathogenesis of AD. Vitamin A deficiency is also associated with delayed wound healing (Hunt, 1986) (Table 4). However, prolonged topical/oral treatment with vitamin A can cause unwanted side effects, such as retinoid dermatitis that is characterized by erythema, dryness, scaling, pruritus, and variable degrees of irritation (Voorhees, 1990; Mukherjee et al., 2006).
Fig. 2.
Signaling of vitamin A to alter cellular functions in epidermal keratinocytes and dermal fibroblasts. RAR, retinoic acid receptor; RXR, retinoid X receptor; RARE, retinoic acid response element; RXRE, retinoid X response element; MMPs, matrix metalloproteinases.
Table 3.
Role of key micronutrients in skin health and function
| Micronutrients | Roles |
|---|---|
| Vitamin A |
|
| Vitamin C |
|
| Vitamin D |
|
| Vitamin E |
|
| Zinc |
|
| Copper |
|
| Selenium |
|
Table 4.
Skin disorders associated with micronutrient deficiencies
| Deficiency | Skin disorders |
|---|---|
| Vitamin A | Atopic dermatitis (Mihaly et al., 2011); Delayed wound healing (Hunt, 1986) |
| Vitamin C | Thickening of the stratum corneum, subcutaneous bleeding and delayed wound healing in scurvy (Hodges et al., 1971) |
| Vitamin D | Atopic dermatitis (Mesquita Kde et al., 2013; Peroni et al., 2011) |
| Vitamin E | Skin ulcerations (Machlin et al., 1977); Changes in skin collagen cross-linking (Igarashi et al., 1989) |
| Zinc | Epidermolysis bullosa (Fine et al., 1989); Atopic dermatitis (Ewing et al., 1991) |
| Copper | Steely-hair syndrome (Menkes, 1988) |
| Selenium | Psoriasis (Juhlin et al., 1982; Naziroglu et al., 2012); Epidermolysis bullosa (Fine et al., 2008); Certain skin cancer (McKenzie, 2000) |
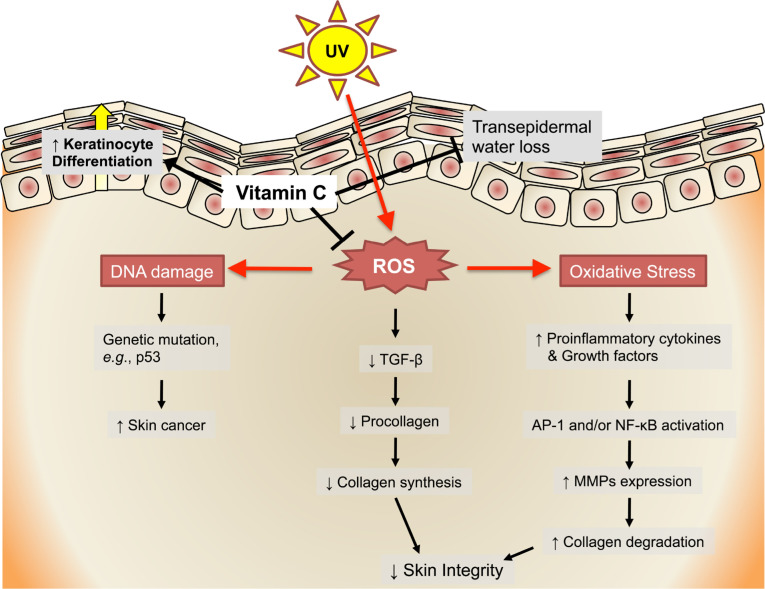
Vitamin C
Exposure to excess UV irradiation induces oxidative stress, impacting the genetic integrity of a living organism, including the skin (Chen et al., 2012). While UVB (wavelengths 280–310 nm) directly damages DNA, UVA (320–400 nm) causes indirect DNA mutations by generating reactive oxygen species (ROS) such as superoxide anion and hydrogen peroxide (Double et al., 2002; Chen et al., 2012) (Fig. 3). Excessive exposure to UV irradiation is associated with photoaging and the development of skin cancer (Chen et al., 2012). UV irradiation triggers the production of pro-inflammatory cytokines and growth factors (Chen et al., 2012). These mediators increase expression of MMPs (MMP-1, -3, -8 and -9) via either activation protein-1 (AP-1) and/or NF-κB activation, resulting in degraded collagen and elastin in the skin (Sardy, 2009; Chen et al., 2012) (Fig. 3). Moreover, UV irradiation-induced ROS have been shown to suppress expression of transforming growth factor (TGF)-β, which is a signaling mediator to promote collagen formation (Walraven et al., 2014) (Fig. 3). These results indicate that an increase in production of ROS following exposure to UV irradiation could degrade the structural integrity of skin by altering the collagen and elastin components in the dermis, causing skin aging characterized by deep wrinkles, coarse textures, telangiectasia, and pigmentation. In addition, UV irradiation-induced ROS have been suggested as a mutagen in certain skin cancer; e.g., squamous cell carcinoma (SCC) (Halliday, 2005). ROS induces mutation of p53 gene, driving precursor lesions to malignancy (Halliday, 2005). But the mechanistic connection between ROS and SCC is still unclear. In this regard, vitamin C is a water-soluble, powerful antioxidant that has been shown to attenuate UV irradiation-mediated damages in the skin (Stewart et al., 1996; McArdle et al., 2002). Vitamin C significantly suppresses the UV light-triggered production of free radicals, protecting cells from oxidative stress (McArdle et al., 2002) (Fig. 3). It has an additional role in wound healing by increasing pro-collagen and collagen synthesis (Peterkofsky, 1991; Fisher et al., 1996), which stimulate the formation of the skin barrier (Table 3). In efficacy studies on human skin, vitamin C significantly increased epidermal moisture content, improving skin hydration (Campos et al., 2008) (Table 3). As noted earlier, scurvy is a disease caused by lack of vitamin C. Symptoms of scurvy in the skin include a thickening of the stratum corneum and spots of small subcutaneous bleeding (Hodges et al., 1971). In addition, cutaneous wound healing is delayed due to the scurvy-mediated decrease in mature collagen (Ross and Benditt, 1962) (Table 4).
Fig. 3.
Vitamin C attenuates UV irradiation-mediated damages in Skin. AP-1, activation protein-1; MMPs, matrix metalloproteinases.
Vitamin D
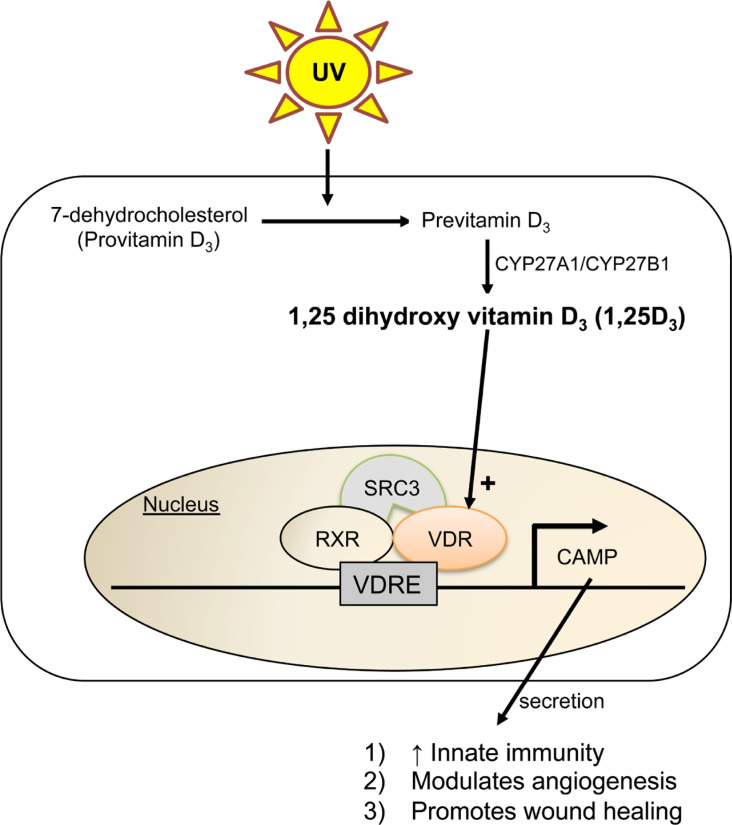
Vitamin D is synthesized from 7-dehydrocholesterol by two key enzymes, 25-hydroxylase (CYP27A1) and 25-hydroxyvitamin D3 1-α-hydroxylase (CYP27B1), in human skin following UVB irradiation (Bikle et al., 2004; Park et al., 2013b). Combined activity of both enzymes is critical in forming active vitamin D, 1,25 dihydroxy vitamin D3 (1,25D3). In particular, CYP27B1, which is expressed in keratinocytes, is under the control of signals that occur in bacterial infection or injury (Bikle et al., 2004; Bikle et al., 2010). Activated 1,25D3 binds to the vitamin D receptor (VDR) to recruit transcriptional coactivator proteins such as steroid receptor coactivator (SRC) 3 (Bikle et al., 2007; Bikle et al., 2010) (Fig. 4). A primary biological role of 1,25D3 in skin is the stimulation of antimicrobial defense through increasing levels of cathelicidin antimicrobial peptide (CAMP), an innate immune element (Gombart et al., 2005) (Fig. 4). In both cell culture and animal systems, treatment with 1,25D3 significantly increases CAMP expression via VDR-dependent mechanism, stimulating innate immunity (Gombart et al., 2005) (Table 3). In addition to antimicrobial activity, vitamin D3 significantly inhibits the proliferation of keratinocytes (Bikle, 1995). As such, topical treatment with 1,25D3 has been used to treat skin diseases linked to hyper-proliferation of keratinocytes, including psoriasis (Abramovits, 2009) (Table 3). Vitamin D appears to modulate inflammation, angiogenesis, and wound healing through regulation of CAMP production (Frohm et al., 1997; Koczulla et al., 2003). Moreover, recent studies have shown significantly lower levels of vitamin D in patients with mild AD compared with those with moderate or severe AD, indicating that vitamin D deficiency might be related to the severity of AD (Peroni et al., 2011; Mesquita Kde et al., 2013) (Table 4).
Fig. 4.
Vitamin D modulates innate immunity, angiogenesis, and wound healing in skin via VDR-dependent mechanism. CAMP, cathelicidin antimicrobial peptide; VDR, vitamin D receptor; RXR, retinoid X receptor; VDRE, vitamin D response element.
Vitamin E
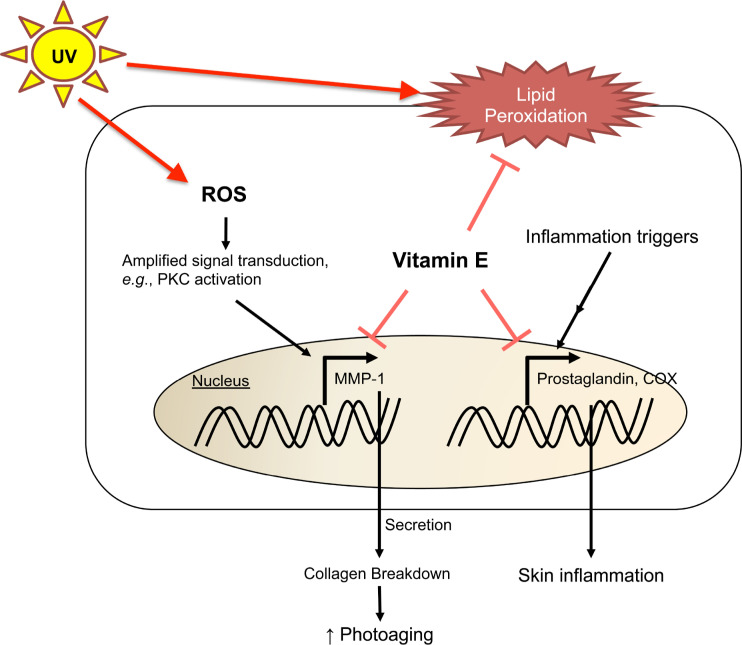
Vitamin E is a lipid-soluble, membrane-bound antioxidant in multiple tissues (Burke, 2007). Since the level of vitamin E can be depleted even after exposure to a single dose of UV irradiation, it is a sensitive oxidative stress maker in human skin (Thiele et al., 1998). A number of studies have shown that vitamin E treatment modulates UV irradiation-mediated free radical damages in skin; e.g., lipid peroxidation (Lopez-Torres et al., 1998), photoaging (Bissett et al., 1990; Jurkiewicz et al., 1995), immunosuppression (Steenvoorden and Beijersbergen van Henegouwen, 1999), and photocarcinogenesis (Burke et al., 2000). Vitamin E significantly suppresses collagen breakdown by inhibiting MMP-1 expression (Ricciarelli et al., 1999) (Fig. 5). Interestingly, topical application of vitamins C (15%) with E (1%) showed a synergistic protective effect from UV irradiation-induced erythema, compared with either vitamin alone (Lin et al., 2003). In addition to antioxidant properties, vitamin E could downregulate features of skin inflammation; i.e., attenuating production of inflammatory prostaglandin, pro-inflammatory cytokines, cyclooxygenease-2, and NADPH oxidase (Meydani et al., 1990; Wu et al., 2008), suggesting the use of vitamin E as an anti-inflammatory agent in skin (Fig. 5 and Table 3). Vitamin E deficiency in animal has been reported to cause skin ulcerations (Machlin et al., 1977) and changes in skin collagen cross-linking (Igarashi et al., 1989) (Table 4).
Fig. 5.
Vitamin E protects skin from photoaging and inflammation. MMP-1, matrix metalloproteinase-1; PKC, protein kinase C.
Minerals
Minerals, including zinc, copper, and selenium, also have an important role in maintaining skin health. Zinc is an essential cofactor of numerous metalloenzymes. Its main function is to protect the skin against photodamage by absorbing UV irradiation, limiting penetration of radiation into skin (Mitchnick et al., 1999). Co-treatment with zinc and vitamin C exhibits antimicrobial activity that helps to clear bacteria in acne (Mitchnick et al., 1999) (Table 3). Moreover, zinc deficiency has been reported in patients with epidermolysis bullosa (Fine et al., 1989) (Table 4). Although patient with AD also showed a significant decreased level of zinc, zinc supplementation does not result in clinical improvement of AD (Ewing et al., 1991) (Table 4).
Like zinc and vitamins C and E, copper with peptides also serves as an antioxidant, protecting skin from damage that is caused by an UV light-induced increase in free radical levels (Pickart et al., 2012). Furthermore, copper is known to stimulate the maturation of collagen, thus is critical in improving skin elasticity and thickness (Pickart, 2008) (Table 3). While it also plays a role in melanin synthesis enables pigmentation of skin and hair, steely-hair syndrome (white and silver hair) is a severe multisystemic disease caused by copper deficiency/abnormal copper metabolism (Menkes, 1988) (Table 4).
Lastly, selenium protects the skin from UV irradiation-induced oxidative stress by stimulating the activities of the selenium-dependent antioxidant enzymes, glutathione peroxidase and thioredoxin reductase, that are present in the plasma membrane of epidermal keratinocytes (Balagopalakrishna et al., 1997; Rafferty et al., 1998). Selenium also has been considered for treatment of psoriasis, which shows decreased glutathione peroxidase levels (Juhlin et al., 1982; Naziroglu et al., 2012). Results from human studies showed that selenium supplementation lead to an increase in levels of glutathione peroxidase in patients with psoriasis, resulting in disease improvement (Juhlin et al., 1982) (Table 3). Since selenium deficiency has been detected in patients with recessive dystrophic epidermolysis bullosa, the level of selenium is one marker in this disease (Fine et al., 2008) (Table 4). Moreover, its deficiency is associated with an increased risk of skin cancer (McKenzie, 2000) (Table 4).
CONCLUSIONS
Micronutrients, including vitamins and minerals, are not only essential components of skin structure, but they also modulate multiple biological functions. Although the importance of these micronutrients has been widely characterized, therapeutics utilizing such nutrients have been limited to antioxidants and stimulating wound healing. Like findings which show the novel role of vitamin D in stimulating a major epidermal antimicrobial peptide, cathelicidin, thus stimulating innate immunity (Gombart et al., 2005), further studies are required to better understand previously-undefined roles of micronutrients in order to develop potential therapeutic agents and/or cosmetic products to treat skin diseases and improve barrier function.
Acknowledgments
The author thanks Ms. Joan Wakefield (NCIRE-VA Medical Center, University of California, San Francisco) and Dr. Shivtaj Mann (College of Medicine, Nova Southeastern University, FL, USA) for superb editorial assistance. The author gratefully acknowledges Drs. Yoshikazu Uchida (NCIRE-VA Medical Center, University of California, San Francisco) and Yong-Moon Lee (College of Pharmacy, Chungbuk National University, Cheongju, South Korea) for numerous critical discussions.
REFERENCES
- Abramovits W. Calcitriol 3 microg/g ointment: an effective and safe addition to the armamentarium in topical psoriasis therapy. J Drugs Dermatol. 2009;8:s17–22. [PubMed] [Google Scholar]
- Badiu DL, Luque R, Dumitrescu E, Craciun A, Dinca D. Amino acids from Mytilus galloprovincialis (L.) and Rapana venosa molluscs accelerate skin wounds healing via enhancement of dermal and epidermal neoformation. Protein J. 2010;29:81–92. doi: 10.1007/s10930-009-9225-9. [DOI] [PubMed] [Google Scholar]
- Balagopalakrishna C, Bhunia AK, Rifkind JM, Chatterjee S. Minimally modified low density lipoproteins induce aortic smooth muscle cell proliferation via the activation of mitogen activated protein kinase. Mol Cell Biochem. 1997;170:85–89. doi: 10.1023/A:1006840927835. [DOI] [PubMed] [Google Scholar]
- Barresi C, Stremnitzer C, Mlitz V, Kezic S, Kammeyer A, Ghannadan M, Posa-Markaryan K, Selden C, Tschachler E, Eckhart L. Increased sensitivity of histidinemic mice to UVB radiation suggests a crucial role of endogenous urocanic acid in photoprotection. J Invest Dermatol. 2011;131:188–194. doi: 10.1038/jid.2010.231. [DOI] [PubMed] [Google Scholar]
- Bartholomew M. James Lind’s treatise of the scurvy (1753) Postgrad Med J. 2002;78:695–696. doi: 10.1136/pmj.78.925.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bikle D, Teichert A, Hawker N, Xie Z, Oda Y. Sequential regulation of keratinocyte differentiation by 1,25(OH)2D3, VDR, and its coregulators. J Steroid Biochem Mol Biol. 2007;103:396–404. doi: 10.1016/j.jsbmb.2006.12.063. [DOI] [PubMed] [Google Scholar]
- Bikle DD. 1,25(OH)2D3-regulated human keratinocyte proliferation and differentiation: basic studies and their clinical application. J Nutr. 1995;125:1709S–1714S. doi: 10.1093/jn/125.suppl_6.1709S. [DOI] [PubMed] [Google Scholar]
- Bikle DD, Chang S, Crumrine D, Elalieh H, Man MQ, Choi EH, Dardenne O, Xie Z, Arnaud RS, Feingold K, Elias PM. 25 Hydroxyvitamin D 1 alpha-hydroxylase is required for optimal epidermal differentiation and permeability barrier homeostasis. J Invest Dermatol. 2004;122:984–992. doi: 10.1111/j.0022-202X.2004.22424.x. [DOI] [PubMed] [Google Scholar]
- Bikle DD, Ng D, Tu CL, Oda Y, Xie Z. Calcium- and vitamin D-regulated keratinocyte differentiation. Mol Cell Endocrinol. 2001;177:161–171. doi: 10.1016/S0303-7207(01)00452-X. [DOI] [PubMed] [Google Scholar]
- Bikle DD, Teichert A, Arnold LA, Uchida Y, Elias PM, Oda Y. Differential regulation of epidermal function by VDR coactivators. J Steroid Biochem Mol Biol. 2010;121:308–313. doi: 10.1016/j.jsbmb.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissett DL, Chatterjee R, Hannon DP. Photoprotective effect of superoxide-scavenging antioxidants against ultraviolet radiation-induced chronic skin damage in the hairless mouse. Photodermatol Photoimmunol Photomed. 1990;7:56–62. [PubMed] [Google Scholar]
- Boelsma E, van de Vijver LP, Goldbohm RA, Klopping-Ketelaars IA, Hendriks HF, Roza L. Human skin condition and its associations with nutrient concentrations in serum and diet. Am J Clin Nutr. 2003;77:348–355. doi: 10.1093/ajcn/77.2.348. [DOI] [PubMed] [Google Scholar]
- Bouwstra JA, Pilgram GSK, Ponex M. Structure of the skin barrier. In: Elias PM, Feingold KR, editors. Skin Barrier. Taylor & Francis; New York: 2006. pp. 65–96. [Google Scholar]
- Burke KE. Interaction of vitamins C and E as better cosmeceuticals. Dermatol Ther. 2007;20:314–321. doi: 10.1111/j.1529-8019.2007.00145.x. [DOI] [PubMed] [Google Scholar]
- Burke KE, Clive J, Combs GF, Jr, Commisso J, Keen CL, Nakamura RM. Effects of topical and oral vitamin E on pigmentation and skin cancer induced by ultraviolet irradiation in Skh:2 hairless mice. Nutr Cancer. 2000;38:87–97. doi: 10.1207/S15327914NC381_13. [DOI] [PubMed] [Google Scholar]
- Campos PM, Goncalves GM, Gaspar LR. In vitro antioxidant activity and in vivo efficacy of topical formulations containing vitamin C and its derivatives studied by non-invasive methods. Skin Res Technol. 2008;14:376–380. doi: 10.1111/j.1600-0846.2008.00288.x. [DOI] [PubMed] [Google Scholar]
- Chen L, Hu JY, Wang SQ. The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67:1013–1024. doi: 10.1016/j.jaad.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Cosgrove MC, Franco OH, Granger SP, Murray PG, Mayes AE. Dietary nutrient intakes and skin-aging appearance among middle-aged American women. Am J Clin Nutr. 2007;86:1225–1231. doi: 10.1093/ajcn/86.4.1225. [DOI] [PubMed] [Google Scholar]
- Double KL, Ben-Shachar D, Youdim MB, Zecca L, Riederer P, Gerlach M. Influence of neuromelanin on oxidative pathways within the human substantia nigra. Neurotoxicol Teratol. 2002;24:621–628. doi: 10.1016/S0892-0362(02)00218-0. [DOI] [PubMed] [Google Scholar]
- Eichler O, Sies H, Stahl W. Divergent optimum levels of lycopene, beta-carotene and lutein protecting against UVB irradiation in human fibroblastst. Photochem Photobiol. 2002;75:503–506. doi: 10.1562/0031-8655(2002)075<0503:DOLOLC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Elder JT, Fisher GJ, Zhang QY, Eisen D, Krust A, Kastner P, Chambon P, Voorhees JJ. Retinoic acid receptor gene expression in human skin. J Invest Dermatol. 1991;96:425–433. doi: 10.1111/1523-1747.ep12469889. [DOI] [PubMed] [Google Scholar]
- Elias PM. The skin barrier as an innate immune element. Semin Immunopathol. 2007;29:3–14. doi: 10.1007/s00281-007-0060-9. [DOI] [PubMed] [Google Scholar]
- Elias PM, Feingold KR. Stratum corneum barrier function: Definitions and broad concepts. In: Elias PM, Feingold KR, editors. Skin Barrier. Taylor & Francis; New York: 2006. pp. 1–4. [Google Scholar]
- Elias PM, Friend DS. The permeability barrier in mammalian epidermis. J. Cell Biology. 1975;65:180–191. doi: 10.1083/jcb.65.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias PM, Fritsch PO, Lampe M, Williams ML, Brown BE, Nemanic M, Grayson S. Retinoid effects on epidermal structure, differentiation, and permeability. Lab Invest. 1981;44:531–540. [PubMed] [Google Scholar]
- Evans JA, Johnson EJ. The role of phytonutrients in skin health. Nutrients. 2010;2:903–928. doi: 10.3390/nu2080903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing CI, Gibbs AC, Ashcroft C, David TJ. Failure of oral zinc supplementation in atopic eczema. Eur J Clin Nutr. 1991;45:507–510. [PubMed] [Google Scholar]
- Fine JD, Johnson LB, Weiner M, Suchindran C. Gastrointestinal complications of inherited epidermolysis bullosa: cumulative experience of the National Epidermolysis Bullosa Registry. J Pediatr Gastroenterol Nutr. 2008;46:147–158. doi: 10.1097/MPG.0b013e31812f5667. [DOI] [PubMed] [Google Scholar]
- Fine JD, Tamura T, Johnson L. Blood vitamin and trace metal levels in epidermolysis bullosa. Arch Dermatol. 1989;125:374–379. doi: 10.1001/archderm.1989.01670150064009. [DOI] [PubMed] [Google Scholar]
- Fisher GJ, Datta SC, Talwar HS, Wang ZQ, Varani J, Kang S, Voorhees JJ. Molecular basis of sun-induced premature skin ageing and retinoid antagonism. Nature. 1996;379:335–339. doi: 10.1038/379335a0. [DOI] [PubMed] [Google Scholar]
- Fisher GJ, Wang ZQ, Datta SC, Varani J, Kang S, Voorhees JJ. Pathophysiology of premature skin aging induced by ultraviolet light. N Engl J Med. 1997;337:1419–1428. doi: 10.1056/NEJM199711133372003. [DOI] [PubMed] [Google Scholar]
- Frohm M, Agerberth B, Ahangari G, Stahle-Backdahl M, Liden S, Wigzell H, Gudmundsson GH. The expression of the gene coding for the antibacterial peptide LL-37 is induced in human keratinocytes during inflammatory disorders. J Biol Chem. 1997;272:15258–15263. doi: 10.1074/jbc.272.24.15258. [DOI] [PubMed] [Google Scholar]
- Gann AA, Gates PB, Stark D, Brockes JP. Receptor isoform specificity in a cellular response to retinoic acid. Proc Biol Sci. 1996;263:729–734. doi: 10.1098/rspb.1996.0109. [DOI] [PubMed] [Google Scholar]
- Gombart AF, Borregaard N, Koeffler HP. Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly up-regulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J. 2005;19:1067–1077. doi: 10.1096/fj.04-3284com. [DOI] [PubMed] [Google Scholar]
- Goodman DS. Vitamin A and retinoids in health and disease. N Engl J Med. 1984;310:1023–1031. doi: 10.1056/NEJM198404193101605. [DOI] [PubMed] [Google Scholar]
- Halliday GM. Inflammation, gene mutation and photoimmunosuppression in response to UVR-induced oxidative damage contributes to photocarcinogenesis. Mutat Res. 2005;571:107–120. doi: 10.1016/j.mrfmmm.2004.09.013. [DOI] [PubMed] [Google Scholar]
- Halprin KM, Ohkawara A. Glucose and glycogen metabolism in the human epidermis. J Invest Dermatol. 1966;46:43–50. doi: 10.1038/jid.1966.9. [DOI] [PubMed] [Google Scholar]
- Han DC, Isono M, Hoffman BB, Ziyadeh FN. High glucose stimulates proliferation and collagen type I synthesis in renal cortical fibroblasts: mediation by autocrine activation of TGF-beta. J Am Soc Nephrol. 1999;10:1891–1899. doi: 10.1681/ASN.V1091891. [DOI] [PubMed] [Google Scholar]
- Hehenberger K, Heilborn JD, Brismar K, Hansson A. Inhibited proliferation of fibroblasts derived from chronic diabetic wounds and normal dermal fibroblasts treated with high glucose is associated with increased formation of l-lactate. Wound Repair Regen. 1998;6:135–141. doi: 10.1046/j.1524-475X.1998.60207.x. [DOI] [PubMed] [Google Scholar]
- Hodges RE, Hood J, Canham JE, Sauberlich HE, Baker EM. Clinical manifestations of ascorbic acid deficiency in man. Am J Clin Nutr. 1971;24:432–443. doi: 10.1093/ajcn/24.4.432. [DOI] [PubMed] [Google Scholar]
- Hunt TK. Vitamin A and wound healing. J Am Acad Dermatol. 1986;15:817–821. doi: 10.1016/S0190-9622(86)70238-7. [DOI] [PubMed] [Google Scholar]
- Igarashi A, Uzuka M, Nakajima K. The effects of vitamin E deficiency on rat skin. Br J Dermatol. 1989;121:43–49. doi: 10.1111/j.1365-2133.1989.tb01398.x. [DOI] [PubMed] [Google Scholar]
- Jean J, Soucy J, Pouliot R. Effects of retinoic acid on keratinocyte proliferation and differentiation in a psoriatic skin model. Tissue Eng Part A. 2011;17:1859–1868. doi: 10.1089/ten.tea.2010.0463. [DOI] [PubMed] [Google Scholar]
- Johnson EJ. The role of carotenoids in human health. Nutr Clin Care. 2002;5:56–65. doi: 10.1046/j.1523-5408.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- Juhlin L, Edqvist LE, Ekman LG, Ljunghall K, Olsson M. Blood glutathione-peroxidase levels in skin diseases: effect of selenium and vitamin E treatment. Acta Derm Venereol. 1982;62:211–214. [PubMed] [Google Scholar]
- Jurkiewicz BA, Bissett DL, Buettner GR. Effect of topically applied tocopherol on ultraviolet radiation-mediated free radical damage in skin. J Invest Dermatol. 1995;104:484–488. doi: 10.1111/1523-1747.ep12605921. [DOI] [PubMed] [Google Scholar]
- Karna E, Miltyk W, Wolczynski S, Palka JA. The potential mechanism for glutamine-induced collagen biosynthesis in cultured human skin fibroblasts. Comp Biochem Physiol B Biochem Mol Biol. 2001;130:23–32. doi: 10.1016/S1096-4959(01)00400-6. [DOI] [PubMed] [Google Scholar]
- Kim H, Lim YJ, Park JH, Cho Y. Dietary silk protein, sericin, improves epidermal hydration with increased levels of filaggrins and free amino acids in NC/Nga mice. Br J Nutr. 2012;108:1726–1735. doi: 10.1017/S0007114511007306. [DOI] [PubMed] [Google Scholar]
- Kim YI, Park K, Kim JY, Seo HS, Shin KO, Lee YM, Holleran WM, Elias PM, Uchida Y. An endoplasmic reticulum stress-initiated sphingolipid metabolite, ceramide-1-phosphate, regulates epithelial innate immunity by stimulating beta-defensin production. Mol Cell Biol. 2014;34:4368–4378. doi: 10.1128/MCB.00599-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kligman AM. The treatment of acne with topical retinoids: one man’s opinions. J Am Acad Dermatol. 1997;36:S92–95. doi: 10.1016/S0190-9622(97)70049-5. [DOI] [PubMed] [Google Scholar]
- Koczulla R, von Degenfeld G, Kupatt C, Krotz F, Zahler S, Gloe T, Issbrucker K, Unterberger P, Zaiou M, Lebherz C, Karl A, Raake P, Pfosser A, Boekstegers P, Welsch U, Hiemstra PS, Vogelmeier C, Gallo RL, Clauss M, Bals R. An angiogenic role for the human peptide antibiotic LL-37/hCAP-18. J Clin Invest. 2003;111:1665–1672. doi: 10.1172/JCI17545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakdawala N, Babalola O, 3rd, Fedeles F, McCusker M, Ricketts J, Whitaker-Worth D, Grant-Kels JM. The role of nutrition in dermatologic diseases: facts and controversies. Clin Dermatol. 2013;31:677–700. doi: 10.1016/j.clindermatol.2013.05.004. [DOI] [PubMed] [Google Scholar]
- Larsson P, Ollinger K, Rosdahl I. Ultraviolet (UV)A- and UVB-induced redox alterations and activation of nuclear factor-kappaB in human melanocytes-protective effects of alpha-tocopherol. Br J Dermatol. 2006;155:292–300. doi: 10.1111/j.1365-2133.2006.07347.x. [DOI] [PubMed] [Google Scholar]
- Lee B, Vouthounis C, Stojadinovic O, Brem H, Im M, Tomic-Canic M. From an enhanceosome to a repressosome: molecular antagonism between glucocorticoids and EGF leads to inhibition of wound healing. J Mol Biol. 2005;345:1083–1097. doi: 10.1016/j.jmb.2004.11.027. [DOI] [PubMed] [Google Scholar]
- Lee DD, Stojadinovic O, Krzyzanowska A, Vouthounis C, Blumenberg M, Tomic-Canic M. Retinoid-responsive transcriptional changes in epidermal keratinocytes. J Cell Physiol. 2009;220:427–439. doi: 10.1002/jcp.21784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JY, Selim MA, Shea CR, Grichnik JM, Omar MM, Monteiro-Riviere NA, Pinnell SR. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866–874. doi: 10.1067/mjd.2003.425. [DOI] [PubMed] [Google Scholar]
- Lopez-Torres M, Thiele JJ, Shindo Y, Han D, Packer L. Topical application of alpha-tocopherol modulates the anti-oxidant network and diminishes ultraviolet-induced oxidative damage in murine skin. Br J Dermatol. 1998;138:207–215. doi: 10.1046/j.1365-2133.1998.02062.x. [DOI] [PubMed] [Google Scholar]
- Machlin LJ, Filipski R, Nelson J, Horn LR, Brin M. Effects of a prolonged vitamin E deficiency in the rat. J Nutr. 1977;107:1200–1208. doi: 10.1093/jn/107.7.1200. [DOI] [PubMed] [Google Scholar]
- McArdle F, Rhodes LE, Parslew R, Jack CI, Friedmann PS, Jackson MJ. UVR-induced oxidative stress in human skin in vivo: effects of oral vitamin C supplementation. Free Radic Biol Med. 2002;33:1355–1362. doi: 10.1016/S0891-5849(02)01042-0. [DOI] [PubMed] [Google Scholar]
- McDermott AM, Kern TS, Murphy CJ. The effect of elevated extracellular glucose on migration, adhesion and proliferation of SV40 transformed human corneal epithelial cells. Curr Eye Res. 1998;17:924–932. doi: 10.1076/ceyr.17.9.924.5133. [DOI] [PubMed] [Google Scholar]
- McKenzie RC. Selenium, ultraviolet radiation and the skin. Clin Exp Dermatol. 2000;25:631–636. doi: 10.1046/j.1365-2230.2000.00725.x. [DOI] [PubMed] [Google Scholar]
- Menkes JH. Kinky hair disease: twenty five years later. Brain Dev. 1988;10:77–79. doi: 10.1016/S0387-7604(88)80074-3. [DOI] [PubMed] [Google Scholar]
- Mesquita Kde C, Igreja AC, Costa IM. Atopic dermatitis and vitamin D: facts and controversies. An Bras Dermatol. 2013;88:945–953. doi: 10.1590/abd1806-4841.20132660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meydani SN, Barklund MP, Liu S, Meydani M, Miller RA, Cannon JG, Morrow FD, Rocklin R, Blumberg JB. Vitamin E supplementation enhances cell-mediated immunity in healthy elderly subjects. Am J Clin Nutr. 1990;52:557–563. doi: 10.1093/ajcn/52.3.557. [DOI] [PubMed] [Google Scholar]
- Mihaly J, Gamlieli A, Worm M, Ruhl R. Decreased retinoid concentration and retinoid signalling pathways in human atopic dermatitis. Exp Dermatol. 2011;20:326–330. doi: 10.1111/j.1600-0625.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- Mitchnick MA, Fairhurst D, Pinnell SR. Microfine zinc oxide (Z-cote) as a photostable UVA/UVB sunblock agent. J Am Acad Dermatol. 1999;40:85–90. doi: 10.1016/S0190-9622(99)70532-3. [DOI] [PubMed] [Google Scholar]
- Motta S, Monti M, Sesana S, Mellesi L, Ghidoni R, Caputo R. Abnormality of water barrier function in psoriasis. Role of ceramide fractions. Arch Dermatol. 1994;130:452–456. doi: 10.1001/archderm.1994.01690040056007. [DOI] [PubMed] [Google Scholar]
- Mukherjee S, Date A, Patravale V, Korting HC, Roeder A, Weindl G. Retinoids in the treatment of skin aging: an overview of clinical efficacy and safety. Clin. Interv. Aging. 2006;1:327–348. doi: 10.2147/ciia.2006.1.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naziroglu M, Yildiz K, Tamturk B, Erturan I, Flores-Arce M. Selenium and psoriasis. Biol Trace Elem Res. 2012;150:3–9. doi: 10.1007/s12011-012-9479-5. [DOI] [PubMed] [Google Scholar]
- Niles RM. The use of retinoids in the prevention and treatment of skin cancer. Expert Opin Pharmacother. 2002;3:299–303. doi: 10.1517/14656566.3.3.299. [DOI] [PubMed] [Google Scholar]
- Njar VC, Gediya L, Purushottamachar P, Chopra P, Vasaitis TS, Khandelwal A, Mehta J, Huynh C, Belosay A, Patel J. Retinoic acid metabolism blocking agents (RAMBAs) for treatment of cancer and dermatological diseases. Bioorg Med Chem. 2006;14:4323–4340. doi: 10.1016/j.bmc.2006.02.041. [DOI] [PubMed] [Google Scholar]
- Park K, Elias PM, Oda Y, Mackenzie D, Mauro T, Holleran WM, Uchida Y. Regulation of cathelicidin antimicrobial peptide expression by an endoplasmic reticulum (ER) stress signaling, vitamin D receptor-independent pathway. J Biol Chem. 2011;286:34121–34130. doi: 10.1074/jbc.M111.250431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park K, Elias PM, Shin KO, Lee YM, Hupe M, Borkowski AW, Gallo RL, Saba J, Holleran WM, Uchida Y. A novel role of a lipid species, sphingosine-1-phosphate, in epithelial innate immunity. Mol Cell Biol. 2013a;33:752–762. doi: 10.1128/MCB.01103-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park K, Lee S, Lee YM. Sphingolipids and antimicrobial peptides: function and roles in atopic dermatitis. Biomol Ther. 2013b;21:251–257. doi: 10.4062/biomolther.2013.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peroni DG, Piacentini GL, Cametti E, Chinellato I, Boner AL. Correlation between serum 25-hydroxyvitamin D levels and severity of atopic dermatitis in children. Br J Dermatol. 2011;164:1078–1082. doi: 10.1111/j.1365-2133.2010.10147.x. [DOI] [PubMed] [Google Scholar]
- Peterkofsky B. Ascorbate requirement for hydroxylation and secretion of procollagen: relationship to inhibition of collagen synthesis in scurvy. Am J Clin Nutr. 1991;54:1135s–1140s. doi: 10.1093/ajcn/54.6.1135s. [DOI] [PubMed] [Google Scholar]
- Pickart L. The human tri-peptide GHK and tissue remodeling. J Biomater Sci Polym Ed. 2008;19:969–988. doi: 10.1163/156856208784909435. [DOI] [PubMed] [Google Scholar]
- Pickart L, Vasquez-Soltero JM, Margolina A. The human tripeptide GHK-Cu in prevention of oxidative stress and degenerative conditions of aging: implications for cognitive health. Oxid Med Cell Longev. 2012;2012:324832. doi: 10.1155/2012/324832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radoja N, Diaz DV, Minars TJ, Freedberg IM, Blumenberg M, Tomic-Canic M. Specific organization of the negative response elements for retinoic acid and thyroid hormone receptors in keratin gene family. J Invest Dermatol. 1997;109:566–572. doi: 10.1111/1523-1747.ep12337483. [DOI] [PubMed] [Google Scholar]
- Rafferty TS, McKenzie RC, Hunter JA, Howie AF, Arthur JR, Nicol F, Beckett GJ. Differential expression of selenoproteins by human skin cells and protection by selenium from UVB-radiation-induced cell death. Biochem J. 1998;332(Pt 1):231–236. doi: 10.1042/bj3320231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricciarelli R, Maroni P, Ozer N, Zingg JM, Azzi A. Age-dependent increase of collagenase expression can be reduced by alpha-tocopherol via protein kinase C inhibition. Free Radic Biol Med. 1999;27:729–737. doi: 10.1016/S0891-5849(99)00007-6. [DOI] [PubMed] [Google Scholar]
- Ross R, Benditt EP. Wound healing and collagen formation. II. Fine structure in experimental scurvy. J Cell Biol. 1962;12:533–551. doi: 10.1083/jcb.12.3.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardy M. Role of matrix metalloproteinases in skin ageing. Connect Tissue Res. 2009;50:132–138. doi: 10.1080/03008200802585622. [DOI] [PubMed] [Google Scholar]
- Shi HP, Fishel RS, Efron DT, Williams JZ, Fishel MH, Barbul A. Effect of supplemental ornithine on wound healing. J Surg Res. 2002;106:299–302. doi: 10.1006/jsre.2002.6471. [DOI] [PubMed] [Google Scholar]
- Spravchikov N, Sizyakov G, Gartsbein M, Accili D, Tennenbaum T, Wertheimer E. Glucose effects on skin keratinocytes: implications for diabetes skin complications. Diabetes. 2001;50:1627–1635. doi: 10.2337/diabetes.50.7.1627. [DOI] [PubMed] [Google Scholar]
- Stechmiller JK, Childress B, Cowan L. Arginine supplementation and wound healing. Nutr Clin Pract. 2005;20:52–61. doi: 10.1177/011542650502000152. [DOI] [PubMed] [Google Scholar]
- Steenvoorden DP, Beijersbergen van Henegouwen G. Protection against UV-induced systemic immunosuppression in mice by a single topical application of the antioxidant vitamins C and E. Int J Radiat Biol. 1999;75:747–755. doi: 10.1080/095530099140096. [DOI] [PubMed] [Google Scholar]
- Stewart MS, Cameron GS, Pence BC. Antioxidant nutrients protect against UVB-induced oxidative damage to DNA of mouse keratinocytes in culture. J Invest Dermatol. 1996;106:1086–1089. doi: 10.1111/1523-1747.ep12339344. [DOI] [PubMed] [Google Scholar]
- Takema Y, Hattori M, Aizawa K. The relationship between quantitative changes in collagen and formation of wrinkles on hairless mouse skin after chronic UV irradiation. J Dermatol Sci. 1996;12:56–63. doi: 10.1016/0923-1811(95)00467-X. [DOI] [PubMed] [Google Scholar]
- Thangapazham RL, Darling TN, Meyerle J. Alteration of skin properties with autologous dermal fibroblasts. Int J Mol Sci. 2014;15:8407–8427. doi: 10.3390/ijms15058407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiele JJ. Oxidative targets in the stratum corneum. A new basis for antioxidative strategies. Skin Pharmacol Appl Skin Physiol. 2001;14(suppl 1):87–91. doi: 10.1159/000056395. [DOI] [PubMed] [Google Scholar]
- Thiele JJ, Schroeter C, Hsieh SN, Podda M, Packer L. The antioxidant network of the stratum corneum. Curr Probl Dermatol. 2001;29:26–42. doi: 10.1159/000060651. [DOI] [PubMed] [Google Scholar]
- Thiele JJ, Traber MG, Packer L. Depletion of human stratum corneum vitamin E: an early and sensitive in vivo marker of UV induced photo-oxidation. J Invest Dermatol. 1998;110:756–761. doi: 10.1046/j.1523-1747.1998.00169.x. [DOI] [PubMed] [Google Scholar]
- Tomic-Canic M, Day D, Samuels HH, Freedberg IM, Blumenberg M. Novel regulation of keratin gene expression by thyroid hormone and retinoid receptors. J Biol Chem. 1996;271:1416–1423. doi: 10.1074/jbc.271.3.1416. [DOI] [PubMed] [Google Scholar]
- Tyrrell RM, Keyse SM. New trends in photobiology. The interaction of UVA radiation with cultured cells. J Photochem Photobiol B. 1990;4:349–361. doi: 10.1016/1011-1344(90)85014-N. [DOI] [PubMed] [Google Scholar]
- Uchida Y. Ceramide signaling in mammalian epidermis. Biochim Biophys Acta. 2014;1841:453–462. doi: 10.1016/j.bbalip.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida Y, Behne M, Quiec D, Elias PM, Holleran WM. Vitamin C stimulates sphingolipid production and markers of barrier formation in submerged human keratinocyte cultures. J Invest Dermatol. 2001;117:1307–1313. doi: 10.1046/j.0022-202x.2001.01555.x. [DOI] [PubMed] [Google Scholar]
- Uchida Y, Hamanaka S. Stratum corneum ceramides: function, origins, and therapeutic applications. In: Elias PM, Feingold KR, editors. Skin Barrier. Taylor & Francis; New York: 2006. pp. 43–65. [Google Scholar]
- Uchida Y, Houben E, Park K, Douangpanya S, Lee YM, Wu BX, Hannun YA, Radin NS, Elias PM, Holleran WM. Hydrolytic pathway protects against ceramide-induced apoptosis in keratinocytes exposed to UVB. J Invest Dermatol. 2010;130:2472–2480. doi: 10.1038/jid.2010.153. [DOI] [PubMed] [Google Scholar]
- vande Kerkhof PC. Update on retinoid therapy of psoriasis in: an update on the use of retinoids in dermatology. Dermatol Ther. 2006;19:252–263. doi: 10.1111/j.1529-8019.2006.00082.x. [DOI] [PubMed] [Google Scholar]
- Van Hattem S, Bootsma AH, Thio HB. Skin manifestations of diabetes. Cleve Clin J Med. 2008;75:772, 774, 776–777. doi: 10.3949/ccjm.75.11.772. passim. [DOI] [PubMed] [Google Scholar]
- van Steensel MA. Emerging drugs for ichthyosis. Expert Opin Emerg Drugs. 2007;12:647–656. doi: 10.1517/14728214.12.4.647. [DOI] [PubMed] [Google Scholar]
- Varani J, Perone P, Griffiths CE, Inman DR, Fligiel SE, Voorhees JJ. All-trans retinoic acid (RA) stimulates events in organ-cultured human skin that underlie repair. Adult skin from sun-protected and sun-exposed sites responds in an identical manner to RA while neonatal foreskin responds differently. J Clin Invest. 1994;94:1747–1756. doi: 10.1172/JCI117522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verfaille CJ, Borgers M, van Steensel MA. Retinoic acid metabolism blocking agents (RAMBAs): a new paradigm in the treatment of hyperkeratotic disorders. J Dtsch Dermatol Ges. 2008;6:355–364. doi: 10.1111/j.1610-0387.2007.06541.x. [DOI] [PubMed] [Google Scholar]
- Voorhees JJ. Clinical effects of long-term therapy with topical tretinoin and cellular mode of action. J Int Med Res. 1990;18(Suppl 3):26c–28c. [PubMed] [Google Scholar]
- Walraven M, Gouverneur M, Middelkoop E, Beelen RH, Ulrich MM. Altered TGF-beta signaling in fetal fibroblasts: what is known about the underlying mechanisms? Wound Repair Regen. 2014;22:3–13. doi: 10.1111/wrr.12098. [DOI] [PubMed] [Google Scholar]
- Wu S, Gao J, Dinh QT, Chen C, Fimmel S. IL-8 production and AP-1 transactivation induced by UVA in human keratinocytes: roles of D-alpha-tocopherol. Mol Immunol. 2008;45:2288–2296. doi: 10.1016/j.molimm.2007.11.019. [DOI] [PubMed] [Google Scholar]
- Yamamoto A, Serizawa S, Ito M, Sato Y. Stratum corneum lipid abnormalities in atopic dermatitis. Arch Dermatol Res. 1991;283:219–223. doi: 10.1007/BF01106105. [DOI] [PubMed] [Google Scholar]
- Yamamoto M, Patel NA, Taggart J, Sridhar R, Cooper DR. A shift from normal to high glucose levels stimulates cell proliferation in drug sensitive MCF-7 human breast cancer cells but not in multidrug resistant MCF-7/ADR cells which overproduce PKC-betaII. Int J Cancer. 1999;83:98–106. doi: 10.1002/(SICI)1097-0215(19990924)83:1<98::AID-IJC18>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]