Abstract
Tandem two-pore potassium channels (K2Ps) have widespread expression in the central nervous system and periphery where they contribute to background membrane conductance. Some general anaesthetics promote the opening of some of these channels, enhancing potassium currents and thus producing a reduction in neuronal excitability that contributes to the transition to unconsciousness. Similarly, these channels may be recruited during the normal sleep-wake cycle as downstream effectors of wake-promoting neurotransmitters such as noradrenaline, histamine and acetylcholine. These transmitters promote K2P channel closure and thus an increase in neuronal excitability. Our understanding of the roles of these channels in sleep and anaesthesia has been largely informed by the study of mouse K2P knockout lines and what is currently predicted by in vitro electrophysiology and channel structure and gating.
Keywords: K2P channel, Anaesthesia, Sleep, Isoflurane, Halothane, Fluoxetine
K2P channels, sleep and anaesthesia
The contribution of tandem two-pore potassium channels (K2Ps) to background potassium membrane conductance, coupled with their sensitivity to certain anaesthetics, suggests that they may play a role in the effects of anaesthetics on the mammalian conscious state, and by extension, to the mechanisms behind sleep-wake alternation [30]. Franks and Lieb [28] first identified a novel anaesthetic-activated potassium current in the pond snail which was subsequently confirmed to be mediated by a new class of channel, the K2P family, cloned in mammals and snails some years later [4, 45, 50]. Our focus will be on K2P channels with known anaesthetic sensitivities that are expressed in the CNS. The mammalian K2P channel family has 15 mammalian members, separated into six subfamilies by structure and function [33, 41, 54], starting with tandem of P-domains weak inward rectifying K+ channel (TWIK) and the derivatively named TASK, TREK, THIK, TRESK, TRAAK and TALK channels. Various K2P channel subunits heterodimerise so, in addition to the electrophysiological properties and anaesthetic sensitivities of the 15 channel homodimers, there are an unknown number of heterodimers with distinct electrophysiological properties expressed throughout the CNS.
Anaesthetics, particularly halogenated volatile anaesthetics such as isoflurane and halothane, open various K2P channels. What encourages us to think that this opening contributes to the transition into unconsciousness is that mouse K2P knockouts (KOs) have altered behavioural responses after anaesthetics measured as reduction in locomotion, loss of righting reflex (an animal surrogate measure of transition into unconsciousness) and loss of limb withdrawal (deep surgical anaesthesia). Depending on the anaesthetic, this may be for several reasons: first, the K2P channels are the direct target of anaesthetics; second, the channels are recruited downstream of anaesthetic targets; or third, the absence of the channels during development affects neuronal circuitry such that it is less responsive to anaesthesia. With regard to their recruitment downstream of anaesthetic targets, several K2P channels are modulated by G-protein-coupled receptors (GPCRs) for histamine, noradrenaline, acetylcholine and others that make it probable that these channels mediate some of the effects of these neurotransmitters during the sleep-wake cycle. There may also be endogenous signalling molecules, as yet unknown, that directly affect the activity of these channels. Given, the widespread expression of K2P channels in the CNS [78] and varied coupling to receptors, their distribution may help identify which K2P members are involved in sleep circuitry and anaesthesia. CNS expression of the K2P channel family varies both between subtypes (for example, TALK-1 appears to be limited to the pancreas and is not seen in the CNS) and also species [31]. There are some common themes, however: TASK-1, TASK-2, TREK-1, TWIK-1, TRAAK and THIK-1 are all strongly expressed in the cerebellum, hippocampal formation and dentate gyrus which suggest some redundancy in function [2, 78] and may reflect heterodimerisation in these regions [2]. Three of these channels (TREK-1, TASK-1 and TASK-3) are also co-expressed in the adult rodent thalamus, particularly in the intralaminar and reticular nuclei [2, 78], and there is evidence that their recruitment there may be relevant to sleep-wake transitions.
K2P channels regulate diverse aspects of body physiology
Our understanding of how K2P channels are involved in sleep and anaesthesia has relied heavily on mouse KO lines, and it is worth mentioning that these lines display additional phenotypes, reflecting the widespread role of K2P channels in other processes, both in and beyond the brain. Examples include the salt-sensitive hyperaldosteronism observed in TASK-3 KO neonates and TASK-1 KO adults, reflecting the role of these channels in normal kidney function [6, 38]. Meanwhile, out of TASK-3 and TASK-1 knockouts, only TASK-1 KO mice have reduced blood pressure [63] and diminished responses to hypoxia and moderate normoxic hypercapnia [80]. Alterations such as these may interact with sleep-wake behaviour and responses to anaesthetics; for example, the attenuated ventilator response to hypoxia in TASK-1 knockout mice [80] may affect respiratory responses to anaesthesia and this should be borne in mind. Likewise, human variation in K2P channels has already been implicated in several pathologies. Arguably, the most severe example is the single maternally imprinted mutation of TASK-3, which results in Birk-Barel syndrome, characterised by mental retardation and dysmorphism [7]. No other single human K2P mutation has yet been linked to pathology, but single nucleotide polymorphisms (SNPs) and splice variants of K2Ps that have been associated with susceptibility to high blood pressure [42], preterm labour [83] and migraine [48, 65] amongst others. The relationships between K2P channels and human sleep disorders or anaesthetic sensitivity have not yet been investigated.
K2P channel involvement in pain and immobility
The loss of awareness produced by general anaesthetics is part of the functional spectrum of clinical anaesthesia which includes analgesia, anxiolysis, amnesia and suppression of somatic responses to injury that can be motor, cardiovascular and hormonal [71, 72]. Crucial to our discussion is evidence that K2P channels play a role in several of these processes. TREK-1, TRAAK [3, 40, 64], TRESK [48] and TASK-1 [52] have all been implicated in the sensation of pain with knockout animals experiencing heightened pain sensitivity. Given that anaesthetics tend to open these channels, this would predict that the analgesic effect may involve activation of K2P channels. TREK-1 in particular has been highlighted as an important component of pain perception [62] and is expressed in both small sensory neurons of the dorsal root ganglion [3] and in regions like the thalamus that process ascending nociceptive information. Likewise, these channels have been implicated in the suppression of motor function produced by anaesthetics [49, 75]. For example, TASK-like currents have been observed in brainstem motoneurons; the reduction in motoneuronal excitability that accompanies anaesthetic-induced immobility has been attributed to these currents [26, 76]. The involvement of K2P channels in analgesia, muscle relaxation together with loss of awareness should be borne in mind when interpreting ‘loss of pain reflexes’ or ‘immobility’ as an end point for knockout models.
Anaesthetic interaction with K2P channels
The study of the structure of K2P channels has demonstrated that certain intracellular portions of the channel are necessary for halogenated anaesthetics to produce an effect and has given insight into how K2Ps are recruited in cell membrane signalling via the activation of GPCRs. The name ‘tandem two-pore’ comes from a feature that distinguishes K2Ps from other potassium channels. Like all potassium channels, the potassium-selective pore of K2Ps is composed of four-pore-forming (P) domains which contain outer and inner transmembrane helices, a selectivity filter, a signature sequence and a pore helix [60]. In other potassium channels, each channel subunit is expressed with a single P-domain, so functional channels assemble as tetramers. K2Ps, however, are expressed as protomers with four transmembrane domains between which sit two P-domains [60]. The assembly of a functional channel, therefore, requires only a dimer. The N- and C-termini of these dimers are intracellular, and there is an additional feature unique to this member of the potassium channel superfamily: the extended ~55 amino acid extracellular loop between transmembrane domains 1 and 2. In the resolved TWIK-1 and TRAAK channel structures, these loops (which are actually two helices) form an ‘A-frame’ cap directly above the pore selectivity filter [12, 60]. This cap is far enough from the pore that it allows access to potassium ions, but its presence may explain why K2P channels are resistant to certain pore-blocking toxins that affect other potassium channels [12, 60]. This cap feature may be common to all members of the K2P family, though its significance is unknown.
Several K2P channels are opened by anaesthetics. Two notable exceptions are TWIK channels which appear insensitive to anaesthetics and THIK channels which are closed by high concentrations of halothane. The gating of all potassium channels is thought to be mediated via two gating mechanisms at distinct sites: an activation site near the intracellular entrance to the channel and an extracellular slow inactivation site at the selectivity filter near the extracellular side [55]. Consistent with this, TASK channel activation by halogenated anaesthetics requires amino acid 159 located on the intracellular side of the transmembrane domain 3 [4, 18]. In addition to this, a six-amino-acid region between transmembrane domain 4 and the C-terminus has also been identified as necessary for TASK channel responses to halogenated anaesthetics [4, 77, 81]. It is unclear whether these six amino acids are directly involved in the activation gate via which anaesthetics open TASK channels or if they are in a site necessary for transduction of the binding signal to the gate [55]. Similarly, the C-terminal domain and site Glu306 is important for anaesthetic effects on TREK-1 [36, 68], although again, this does not confirm that this is where anaesthetics bind. How anaesthetics activate or inactivate other members of K2P channels is currently not fully understood. However, it may be relevant that the two K2P members not opened by anaesthetics, TWIK and THIK, lack conserved glycine residues found in other K2P members and instead have a larger hydrophobic region. These glycine residues in transmembrane domain 2 have been proposed as a hinge for the activating gate in K2Ps and inwardly rectifying potassium channels [16]. Different hinging mechanisms for channel opening could distinguish those K2Ps that are activated by anaesthetics and those that are not. In addition, the structure of the anaesthetic-binding region in K2Ps may differ between species; while rodent and mollusk TASK channels respond differently to anaesthetic enantiomers, human TASK channels do not [4, 44].
GPCRs and K2P channels
As previously mentioned, K2P channels are regulated by a number of GPCRs, which are in turn involved in neurotransmitter systems associated with wakefulness, such as acetylcholine, histamine, serotonin, glutamate and noradrenaline [55]. Briefly, activation of Gαq proteins closes TASK and TREK family channels and opens TRESK channels. Meanwhile, Gi proteins appear to open TREK channels while Gs proteins close TREK channels [55]. Several wake-promoting transmitters such as histamine, acetylcholine, serotonin, glutamate and noradrenaline have receptors that are G-protein coupled, and we can posit that activation of these receptors while awake inhibits K2P channels in distinct neuronal populations making these populations more excitable. For example, all of the abovementioned neurotransmitters have Gαq/11-coupled receptors in the CNS and these proteins inhibit TASK and TREK channels, which would subsequently lead to reduced potassium leak currents and more membrane depolarisation [26], particularly in the thalamus [20]. It is important to note that the effector pathways involving K2P channels are likely to be complicated because K2P channels can exist as heteromers. TASK channels can exist both as functionally distinct homodimers as well as TASK-1/TASK-3 heterodimers [1, 8, 11, 22, 43, 46], even in the same neuronal population. In addition, heterodimerisation between K2P subfamilies TWIK and TASK occurs in cerebellar granule neurons [69], and heterodimerisation between THIK and TASK-1/TASK-3 channels has been predicted in the same population based on expression profiles [2]. Unravelling how these combinations are regulated in situ will advance our understanding of how K2Ps are involved in sleep-wake signalling.
Role of K2P channels in sleep-wake regulation
K2P channel expression in regions associated with sleep-wake transitions, such as the preoptic and superchiasmatic nuclei in the hypothalamus and thalamic relay nuclei [78], suggest that they may be involved in mechanisms promoting transition or maintenance of the two states [21]. Thalamic relay neuronal activity has two distinct activity states: <15 Hz burst activity during sleep and ~40 Hz tonic activity during wakefulness and rapid eye movement sleep (REMS). During normal sleep-wake activity, the switch between these two states is modulated by the ascending brainstem, including cholinergic projections, and other ascending modulatory influences such as serotonergic and glutamateric signalling [20]. These ascending inputs promote closure of K2P channels such as TASK-1/TASK-3 and TREK; the subsequent depolarization of thalamic neurons causes a switch to tonic firing associated with wakefulness and REMS [10, 57–59]. This closure of K2Ps during tonic firing appears to rely crucially on Gαq signalling for the cholinergic input [13] and Gαq/11 signalling for serotonergic and glutamatergic inputs [20, 26]. Conversely, opening of K2Ps when the ascending input is withdrawn and their functional antagonism with hyperpolarisation-activated cyclic nucleotide gated channels (HCN) hyperpolarises thalamocortical neurons and promotes burst firing patterns associated with sleep [21, 82]. Reciprocal regulation of the K2P and HCN current has likewise been observed with application of anaesthetics such as halothane, isoflurane and sevoflurane [14] which also promote hyperpolarisation of the thalamus. Although the main focus has been on the opening of TASK channels mediating this the anaesthetic-induced change in thalamic membrane potential, Budde et al. note a complex effect of halothane on the activation and inhibition of various thalamic K2P channels such as TREK-1, TASK-1, TASK-3 and THIK-2 which overall result in a switch to burst firing [14]. Thalamocortical K2P channels are recruited both during withdrawal of ascending input and after application of anaesthesia but whether or not this recruitment is sufficient to promote unconsciousness is controversial. The thalamus is strongly implicated in the transitions between conscious and unconscious states [82], but as we will discuss, none of the K2P knockouts have so far displayed a compromised ability to transit in and out of consciousness per se. Nevertheless, altered sleep architecture and altered sensitivity to some anaesthetics in these animals suggest that thalamic K2P involvement as well K2Ps in other regions are important.
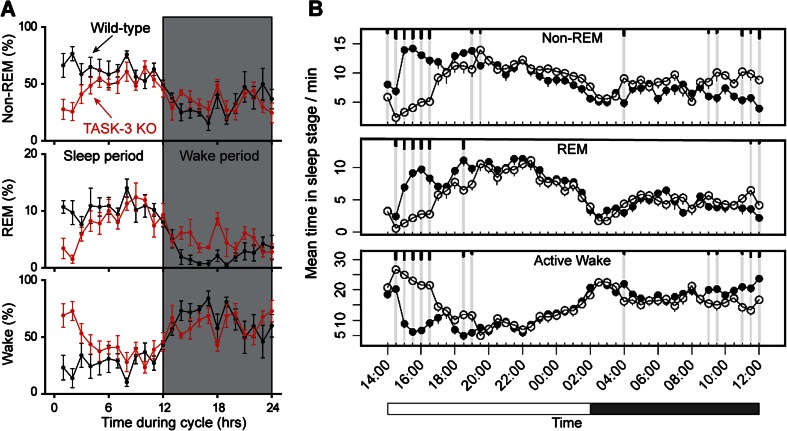
So far, the only K2P channel mouse knockout with a characterised sleep phenotype is the TASK-3-deficient line [17, 34, 53, 67]. TASK-1 knockout mice were assessed for sleep-wake behaviour and found to be indistinguishable from controls [57]. Whilst the proportion of time TASK-3 knockout mice spend in wakefulness, non-rapid eye movement sleep (NREMS) and REMS is similar to littermates, the distribution of these states and their EEG quality varies. The REMS episodes of TASK-3 mice show clear oscillatory fragmentation, and the mice have enhanced wake activity [67] as well as an overall increase in the amplitude of sleep architecture [34, 53]. The locomotor activity within the wake period of these mice is 2–3-fold increased above that of littermates [34, 53]; these results were replicated on independently generated TASK-3 KO lines. The two key phenotypes that have emerged from TASK-3 KOs, fragmented REMS and exaggerated wake activity, draw interesting parallels with the effects of drugs that suppress TASK-3 activity (Fig. 1). A recently developed TASK-3 antagonist, compound 23, produces a significant elevation in wake simultaneous with REMS and NREMS suppression in wild-type mice [17]; this effect on the sleep-wake is similar to the TASK-3 KO phenotype (Fig. 1). The elevation in wakefulness in both these cases may be mediated by disinhibition of cortico-thalamic processes, although why this effect is restricted to the light phase is not clear (in the case of the antagonist this is simply the phase in which the animals were dosed, so it may be a trivial parallel). An alternative explanation for the wake-promoting compound 23 effect and the TASK-3 knockout phenotype is that the inhibition of TASK-1/TASK-3 channels in arousal nuclei, such as the noradrenergic neurons in the locus coeruleus [52, 75], increases the excitability of these arousal nuclei and thereby promotes arousal. Given that locus coeruleus firing is associated with alert and attentive behaviour [9], an overactive locus coeruleus may produce hyperactivity in the ‘active’ nocturnal part of the sleep-wake cycle [34, 53]. Disinhibition of this arousal nucleus may also explain the REMS phenotype of the TASK-3 mice. During normal REMS, neurons in the locus coeruleus are silent [27], so an aberrantly active locus coeruleus may interfere with maintenance of this sleep state. Meanwhile, the REMS-suppressing effect of the TASK-3 antagonist appears to be TASK-3-specific because it cannot be replicated if the TASK-3 antagonist is administered to the TASK-3-deficient mice [17]; it is controversial whether this is because the baseline REMS is already impaired in these animals. Notably, the REMS-suppressing effect of the antidepressant fluoxetine on wild-type mice also cannot be replicated in TASK-3-deficient mice [34]. The majority of antidepressants are also REMS-suppressants, so it is interesting that the ‘REMS-impaired’ TASK-3-deficient mice have an ‘antidepressant phenotype’ [34]. In addition, TREK-1-deficient animals also show an antidepressant phenotype [39, 56], although there is some dispute over this [61]. Given that TREK-1 channels are robustly blocked under most experimental conditions by the application of the selective serotonin reuptake inhibitors (SSRIs) fluoxetine, norfluoxetine, paroxetine and sipatrigin [24, 26, 84], it would be interesting to see if TREK-1-deficient animals have impaired REMS and are also resistant to the REMS-suppressing effects of fluoxetine. A recent review has questioned whether antidepressant suppression of REMS preferentially suppresses some aspects of the sleep state (motor inhibition) over others [25]. Studying the apparent resistance of K2P knockouts to SSRI effects on REMS may shed light on this question.
Fig. 1.
Similarity between TASK-3 KO ‘sleep phenotype’ mice and how TASK-3 antagonist drugs affect the sleep-wake cycle in mice. a TASK-3 KO animals (red traces) have elevated wake in the light period with concurrent reductions in both REMS and NREMS compared to wild-type mice [67]. b Similarly, mice dosed with 100 mg/kg TASK-3 antagonist ‘compound 23’ (open circles) have elevated wake in the light period with concurrent reductions in REMS and NREMS compared to mice dosed with vehicle (closed circles) (modified from Coburn et al. [17])
Role of K2P channels in anaesthesia
General anaesthetics, whatever their various effects on analgesia, amnesia and muscle relaxation, all have in common their ability to suspend consciousness to some degree, depending on the drug dose administered. It is therefore crucial to study their relationship with putative targets in whole animal or clinical paradigms. The study of K2P channels and anaesthesia has, so far, therefore consisted of two necessary branches of research: electrophysiology to determine which anaesthetics directly open/close K2P channels, and the testing of anaesthetics on K2P channel-deficient mouse strains to determine whether the end point of hypnosis, sedation or loss of pain reflexes can still achieved by the same dose of drug. There is a third emerging branch that investigates indirect modulation of K2P s during anaesthesia. For example, the α2 adrenoceptor agonist and sedative drug dexmedetomidine is not likely to open K2P channels, nor to act through Gq/11, the G-protein associated with TASK channels, and yet TASK-1-deficient mice are less sensitive to low sedative doses of dexmedetomidine [52], suggesting an indirect mechanism of action. Many K2P channels are also closed by local anaesthetics [47], but as these drugs do not suspend consciousness, these interactions will not be discussed here.
Five of the six subfamilies of K2P channels are directly sensitive to general anaesthetics, with the exception being weak inward-rectifier TWIK-1 and TWIK-2 channels. Notably, TWIK-1 channels can still be closed by local anaesthetics such as bupivacaine [31]. Because enhancement of background potassium current is a plausible mechanism for producing anaesthesia [30, 44], THIK channels that are inhibited by high concentrations of halothane are implausible candidates for mediating anaesthetic mechanisms. In contrast, based on in vivo mouse studies, TASK-1, TASK-3 and TREK-1 channels are strong candidates for a likely role in anaesthesia. Table 1 summarises the K2P channel knockout lines and whether or not they have a reported change in anaesthetic sensitivity. It is important to note that these assessments were made in adult animals. Anaesthetic sensitivity changes with rodent age, with adult animals having a much lower minimum alveolar concentration for halogenated anaesthetics than juveniles [66]. This change in sensitivity may rely in part on significant K2P channel CNS expression changes CNS during development [2, 5]. The various studies use different end points to assess different aspects of anaesthetic effects on the conscious state: reduction in movement (a surrogate measure of sedation), loss of righting reflex (a surrogate measure of unconsciousness in animals) and loss of paw or tail withdrawal to painful stimuli, which is normally assumed to be unconsciousness coupled with immobility. These different end points usually reflect the effects of increasing doses of drug, e.g. low doses of halothane are sedative and high doses cause loss of surgical reflexes, but do not necessarily mean an escalation of the same mechanism or recruitment of identical receptor populations in the CNS.
Table 1.
Sensitivity of K2P knockout mice to anaesthetics and sedatives
| Channel KO | Reduction in movement | Loss of righting reflex | Loss of pain reflex |
|---|---|---|---|
| TASK-3 | dex—no change hal (low dose)—↓ |
iso—no change prop—no change cyc—no change etom—no change hal—↓ |
iso—controversial; both no change and ↓ have been shown etom—no change hal—↓ |
| TASK-1 | win—no change zolp—no change barb—no change dex—↓ flur—↑ diaz—↑ gab—↑ (females only) prop—⬆ (males only) preg—↑ (males only) |
iso—controversial. both no change and ↓ have been shown hal—no change prop—↑ (extended duration of LORR) barb—↑ (extended duration of LORR) |
hal—↓ iso—no change |
| TASK-1/-3 | hal (low dose) –↓ | iso—no change hal—↓ |
iso—↓ hal—↓ |
| TASK-1/TASK-3 in cholinergic cells only | hal (low dose) –↓ | hal—no change | iso—↓ hal—↓ |
| TASK-2 | Not tested | Not tested | iso—no change hal—no change desf—no change |
| TREK-1 | Not tested | iso—↓ hal—↓ sevo—↓ desf—↓ prop—no change |
Not tested |
| TRESK | Not tested | Not tested | iso—no change hal—no change desf—no change sevo—no change* |
| KCNK7 | Not tested | Not tested | iso—no change hal—no change desf—no change |
Downwards arrows (↓) indicate that knockout animals were less affected by anaesthetic on that measure; conversely, upwards arrows (↑) indicate that knockout animals were more affected than controls by anaesthetic on measure indicated
iso isoflurane, hal halothane, sevo sevoflurane, desf desflurane, chlor chloroform, prop propofol, etom etomidate, dex dexmedetomidine, cyc cyclopropane, barb pentobarbital, win WIN55212-3, flur flurazepam, diaz diazepam, zolp zolpidem, preg pregnenalone, gab gaboxadol [15, 32, 36, 39, 49, 51–53, 86]
*Increased mortality after anaesthetic exposure
Despite the caveats of compensation, especially given that K2P channels such as TASK-3 have been implicated in mouse CNS development [5], and TASK-1 KO mice have upregulated GABAA receptor function [51], K2P channel-deficient mouse lines have yielded some interesting insights into anaesthetic processes. To date, there are mouse knockouts of TASK-1, TASK-2, TASK-3, TREK-1, TRAAK, KCNK7 and TRESK channels, as well as a TASK-1/TASK-3 double knockout [1, 11, 15, 32, 39, 49, 80, 86]. In addition, there is a TASK-1/TASK-3 channel knockout restricted to cholinergic cells that is substantially less sensitive to isoflurane and halothane-induced loss of righting reflex [49]. For anaesthesia using halogenated anaesthetics (isoflurane, halothane, sevoflurane, desflurane and chloroform), loss of specific K2P channel expression generally results in a reduction, but not complete loss, of anaesthetic sensitivity. However, even within this class, there are differences. Halothane, for example, requires TASK-1 and TASK-3 for loss of pain reflex and TREK-1 for loss of righting reflex but does not require the TRESK channel [15, 39, 49, 52, 53, 67]. On the other hand, isoflurane-induced loss of pain reflex is diminished when both TASK-1 and TASK-3 are absent [49] but it is unclear whether single knockouts of TASK-3 channels have a diminished sensitivity for pain reflex [49, 67] or if TASK-1 channels are involved in isoflurane-induced loss of righting reflex [49, 67] the way that TREK-1 channels appear to be [39]. Other classes of anaesthetics have also been tested in K2P knockouts, although not comprehensively. TASK-1 mice are more sensitive to GABAA receptor ligands and modulators propofol, pentobarbital, and benzodiazepines as it takes them longer to recover from the anaesthetised state [51]. This may be related to the increased expression of GABAA receptors in these animals. No such extended recovery time was seen in TREK-1 channel knockouts, which recover the same as controls from pentobarbital anaesthesia [39]. Propofol was tested on TASK-3 knockouts, but recovery time was not reported, so while the animals are certainly not less sensitive, it is not clear if they would take longer to recover from the anaesthetic dose [53]. Opposing changes in sensitivity to halogenated and non-halogenated anaesthetics such as those seen in TASK-1 channel knockouts highlights the importance of testing several classes of anaesthetics on each knockout model because generalising between channels or between anaesthetics is problematic. Given that knockout lines of six of the eight anaesthetic-sensitive K2P channels are available, comprehensive testing of propofol, pentobarbital, halothane, isoflurane and others using a range of anaesthetic end points to make the studies comparable might be informative. In any case, the K2P knockout mouse studies have shown that K2P are plausible targets for the actions of certain volatile and gaseous agents; however, they are not the only targets and other receptors and ion channels play a role—particularly certain populations of GABAA receptors [29, 73, 79, 85].
In the absence of a comprehensive testing paradigm, there are still published in vitro sensitivities that could be followed up in vivo. So far, the translation from electrophysiology to animal behaviour has been complex and likely to be affected by compensatory mechanisms during development. For example, TASK-2 channels are opened by clinically relevant concentrations of isoflurane in vitro [35], but TASK-2 deficient mice lose pain reflexes at the same dose of isoflurane anaesthesia as wild-types [32]. It is possible that TASK-2-deficient mice would show differences in loss of righting reflex and reduction in locomotion, but these have not been reported. Given the difficulty in predicting knockout sensitivity, it is crucial to test each drug by experiment. Another question that can now be addressed following the development of specific K2P channel blockers [17, 19, 56, 70] is whether K2P channel blockers can, to some degree, reverse general anaesthesia. As discussed above, TASK-3 channel antagonists are wake-promoting in rodents [17], so it is at least plausible that administration of such an agent during anaesthesia would produce some degree of reversal. So far, it appears that such agents do not reverse anaesthesia. In a recent study of rat respiration during isoflurane anaesthesia, administration of TASK antagonists, whilst stimulating breathing, did not affect anaesthetic depth [19]. Quantified support for this important observation is necessary, ideally using the same anaesthetic end points as those in the mouse knockout studies.
Conclusions and future directions
The focus on K2Ps as putative mediators of anaesthetics has been to understand how these drugs produce a loss of consciousness and painful sensation. There are two key motivations for this research: to understand how currently used anaesthetics exert their effects and to identify novel targets and develop better sedatives and anaesthetics. K2P channels are likely to be necessary for the mechanism of action of halogenated anaesthetics and may or may not mediate the effects of some others. It is a curious phenomenon that in K2P knockout mice loss of consciousness in response to one drug can remain intact while others are less potent. Work on these channels may also help us dissect out the pathways responsible for desirable effects of anaesthesia from their side effects. For example, TREK-1 may contribute to the neuroprotective effect of the anaesthetic xenon [23, 37]. Conversely, while TWIK-1 channels are so far not implicated in the transition to unconsciousness in the CNS, they may be recruited in phenobarbital-mediated hepatotoxicity [74] and as such are undesirable targets. It may be no coincidence that the K2P channels implicated in thalamocortical regulation, TASK and TREK, are also those deficient in anaesthetic-resistant knockout mouse lines. The same channels are sensitive to REMS manipulating fluoxetine, and the TASK-1 channel knockout is less sensitive to sedative doses of dexmedetomidine, suggesting it may also be a downstream effector of this distinct class of anaesthetic. Thus, drugs that manipulate sleep architecture such as fluoxetine and sedatives, such as low dose dexmedetomidine, may have common K2P targets with general anaesthetics.
A key question is whether K2P channels are recruited in physiological sleep-wake regulation. With regard to REMS and its pharmacological suppression, it is crucial to see if the interaction between K2P channels and the REMS suppressor fluoxetine is limited to this molecule or whether it is a common mechanism of many other REMS suppressants. Because thalamocortical rhythms involve background potassium currents, K2P channels may be necessary for physiological sleep-wake regulation [21]. Support for this comes from the altered sleep phenotype and inability to sustain coherent REMS oscillations in TASK-3 knockout mice [67]. On the other hand, sleep-wake transitions and time spent in arousal states are still intact in TASK-3 knockouts, but this may be because other thalamic (or non-thalamic) K2Ps can buffer the loss of TASK-3. This emphasis on K2Ps in the thalamocortical circuits would predict that channel knockouts of TASK-1 and TREK-1 and possibly TREK-2 (all found in the thalamus) may have a similar sleep phenotype to TASK-3 knockouts and that double knockouts may produce a more severe phenotype. In addition, this hypothesis also predicts that selective disruption of thalamic K2P channels in vivo may produce a similar sleep phenotype to that seen in the TASK-3 global knockout. In comparison to the study of K2Ps and sleep, the study of K2P channels in anaesthesia has advanced much further. The emerging trend is that both TASK and TREK-1 channels are both necessary for the full effects of halogenated anaesthetics, but exactly which neuronal networks is only beginning to be revealed [63]. Much still remains to be understood about the roles these K2P channels play in the regulation of the natural sleep-wake cycle.
Acknowledgments
EAS holds a BBSRC CASE award. Work in our laboratory is supported by the Medical Research Council, UK (G0901892, N.P.F., S.G. and W.W.; G0800399, W.W.), and the BBSRC (G021691 and BB/K018159/1, N.P.F., S.G. and W.W.). We would like to thank E.C. Harding for his critical reading of the manuscript.
Abbreviations
- CNS
Central nervous system
- GPCR
G-protein-coupled receptor
- HCN
Hyperpolarisation-activated cyclic nucleotide-gated channels
- K2P or KCNK
Tandem two-pore potassium channel
- KO
Knockout mouse model
- NREMS
Non-rapid eye movement sleep
- REMS
Rapid eye movement sleep
- SSRI
Selective serotonin reuptake inhibitor
- TWIK
Tandem of P-domains weak inward rectifying K+ channel (TWIK-1 (KCNK1), TWIK-2 (KCNK6), TWIK-3 (KCNK7))
- TREK
TWIK-related K+ channel (TREK-1 (KCNK2), TREK-2 (KCNK10))
- TASK
TWIK-related acid-sensitive K+ channel (TASK-1 (KCNK3), TASK-3 (KCNK9), TASK-5 (KCNK15))
- TRAAK
TWIK-related arachidonic acid-activated K+ channel (KCNK4)
- TALK
TWIK-related alkaline-sensitive K+ channel (TALK-1 (KCNK16), TALK-2 (KCNK17))
- THIK
TWIK-related halothane-inhibited K+ channel (THIK-1 (KCNK13), THIK-2 (KCNK12))
- TRESK
TWIK-related spinal cord K+ channel (KCNK18)
References
- 1.Aller MI, Veale EL, Linden AM, Sandu C, Schwaninger M, Evans LJ, Korpi ER, Mathie A, Wisden W, Brickley SG. Modifying the subunit composition of TASK channels alters the modulation of a leak conductance in cerebellar granule neurons. J Neurosci. 2005;25:11455–11467. doi: 10.1523/JNEUROSCI.3153-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aller MI, Wisden W. Changes in expression of some two-pore domain potassium channel genes (KCNK) in selected brain regions of developing mice. Neuroscience. 2008;151:1154–1172. doi: 10.1016/j.neuroscience.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Alloui A, Zimmermann K, Mamet J, Duprat F, Noel J, Chemin J, Guy N, Blondeau N, Voilley N, Rubat-Coudert C, Borsotto M, Romey G, Heurteaux C, Reeh P, Eschalier A, Lazdunski M. TREK-1, a K+ channel involved in polymodal pain perception. EMBO J. 2006;25:2368–2376. doi: 10.1038/sj.emboj.7601116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andres-Enguix I, Caley A, Yustos R, Schumacher MA, Spanu PD, Dickinson R, Maze M, Franks NP. Determinants of the anesthetic sensitivity of two-pore domain acid-sensitive potassium channels: molecular cloning of an anesthetic-activated potassium channel from Lymnaea stagnalis. J Biol Chem. 2007;282:20977–20990. doi: 10.1074/jbc.M610692200. [DOI] [PubMed] [Google Scholar]
- 5.Bando Y, Hirano T, Tagawa Y. Dysfunction of KCNK potassium channels impairs neuronal migration in the developing mouse cerebral cortex. Cereb Cortex. 2014;24:1017–1029. doi: 10.1093/cercor/bhs387. [DOI] [PubMed] [Google Scholar]
- 6.Bandulik S, Tauber P, Penton D, Schweda F, Tegtmeier I, Sterner C, Lalli E, Lesage F, Hartmann M, Barhanin J, Warth R. Severe hyperaldosteronism in neonatal Task3 potassium channel knockout mice is associated with activation of the intraadrenal renin-angiotensin system. Endocrinology. 2013;154:2712–2722. doi: 10.1210/en.2013-1101. [DOI] [PubMed] [Google Scholar]
- 7.Barel O, Shalev SA, Ofir R, Cohen A, Zlotogora J, Shorer Z, Mazor G, Finer G, Khateeb S, Zilberberg N, Birk OS. Maternally inherited Birk Barel mental retardation dysmorphism syndrome caused by a mutation in the genomically imprinted potassium channel KCNK9. Am J Hum Genet. 2008;83:193–199. doi: 10.1016/j.ajhg.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berg AP, Talley EM, Manger JP, Bayliss DA. Motoneurons express heteromeric TWIK-related acid-sensitive K+ (TASK) channels containing TASK-1 (KCNK3) and TASK-3 (KCNK9) subunits. J Neurosci. 2004;24:6693–6702. doi: 10.1523/JNEUROSCI.1408-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berridge CW, Schmeichel BE, Espana RA. Noradrenergic modulation of wakefulness/arousal. Sleep Med Rev. 2012;16:187–197. doi: 10.1016/j.smrv.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bista P, Meuth SG, Kanyshkova T, Cerina M, Pawlowski M, Ehling P, Landgraf P, Borsotto M, Heurteaux C, Pape HC, Baukrowitz T, Budde T. Identification of the muscarinic pathway underlying cessation of sleep-related burst activity in rat thalamocortical relay neurons. Pflugers Arch. 2012;463:89–102. doi: 10.1007/s00424-011-1056-9. [DOI] [PubMed] [Google Scholar]
- 11.Brickley SG, Aller MI, Sandu C, Veale EL, Alder FG, Sambi H, Mathie A, Wisden W. TASK-3 two-pore domain potassium channels enable sustained high-frequency firing in cerebellar granule neurons. J Neurosci. 2007;27:9329–9340. doi: 10.1523/JNEUROSCI.1427-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brohawn SG, del Marmol J, MacKinnon R. Crystal structure of the human K2P TRAAK, a lipid- and mechano-sensitive K+ ion channel. Science. 2012;335:436–441. doi: 10.1126/science.1213808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broicher T, Wettschureck N, Munsch T, Coulon P, Meuth SG, Kanyshkova T, Seidenbecher T, Offermanns S, Pape HC, Budde T. Muscarinic ACh receptor-mediated control of thalamic activity via G (q)/G (11)-family G-proteins. Pflugers Arch. 2008;456:1049–1060. doi: 10.1007/s00424-008-0473-x. [DOI] [PubMed] [Google Scholar]
- 14.Budde T, Coulon P, Pawlowski M, Meuth P, Kanyshkova T, Japes A, Meuth SG, Pape HC. Reciprocal modulation of I (h) and I (TASK) in thalamocortical relay neurons by halothane. Pflugers Arch. 2008;456:1061–1073. doi: 10.1007/s00424-008-0482-9. [DOI] [PubMed] [Google Scholar]
- 15.Chae YJ, Zhang J, Au P, Sabbadini M, Xie GX, Yost CS. Discrete change in volatile anesthetic sensitivity in mice with inactivated tandem pore potassium ion channel TRESK. Anesthesiology. 2010;113:1326–1337. doi: 10.1097/ALN.0b013e3181f90ca5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatelain FC, Bichet D, Feliciangeli S, Larroque MM, Braud VM, Douguet D, Lesage F. Silencing of the tandem pore domain halothane-inhibited K+ channel 2 (THIK2) relies on combined intracellular retention and low intrinsic activity at the plasma membrane. J Biol Chem. 2013;288:35081–35092. doi: 10.1074/jbc.M113.503318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coburn CA, Luo Y, Cui M, Wang J, Soll R, Dong J, Hu B, Lyon MA, Santarelli VP, Kraus RL, Gregan Y, Wang Y, Fox SV, Binns J, Doran SM, Reiss DR, Tannenbaum PL, Gotter AL, Meinke PT, Renger JJ. Discovery of a pharmacologically active antagonist of the two-pore-domain potassium channel K2P9.1 (TASK-3) ChemMedChem. 2012;7:123–133. doi: 10.1002/cmdc.201100351. [DOI] [PubMed] [Google Scholar]
- 18.Conway KE, Cotten JF. Covalent modification of a volatile anesthetic regulatory site activates TASK-3 (KCNK9) tandem-pore potassium channels. Mol Pharmacol. 2012;81:393–400. doi: 10.1124/mol.111.076281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cotten JF. TASK-1 (KCNK3) and TASK-3 (KCNK9) tandem pore potassium channel antagonists stimulate breathing in isoflurane-anesthetized rats. Anesth Analg. 2013;116:810–816. doi: 10.1213/ANE.0b013e318284469d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coulon P, Kanyshkova T, Broicher T, Munsch T, Wettschureck N, Seidenbecher T, Meuth SG, Offermanns S, Pape HC, Budde T (2010) Activity modes in thalamocortical relay neurons are modulated by G(q)/G(11) family G-proteins—serotonergic and glutamatergic signaling. Front Cell Neurosci 4:132. doi: 10.3389/fncel.2010.00132 [DOI] [PMC free article] [PubMed]
- 21.Coulon P, Budde T, Pape HC. The sleep relay—the role of the thalamus in central and decentral sleep regulation. Pflugers Arch. 2012;463:53–71. doi: 10.1007/s00424-011-1014-6. [DOI] [PubMed] [Google Scholar]
- 22.Czirjak G, Enyedi P. Formation of functional heterodimers between the TASK-1 and TASK-3 two-pore domain potassium channel subunits. J Biol Chem. 2002;277:5426–5432. doi: 10.1074/jbc.M107138200. [DOI] [PubMed] [Google Scholar]
- 23.Dickinson R, Franks NP. Bench-to-bedside review: molecular pharmacology and clinical use of inert gases in anesthesia and neuroprotection. Crit Care. 2010;14:229. doi: 10.1186/cc9051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eckert M, Egenberger B, Doring F, Wischmeyer E. TREK-1 isoforms generated by alternative translation initiation display different susceptibility to the antidepressant fluoxetine. Neuropharmacology. 2011;61:918–923. doi: 10.1016/j.neuropharm.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 25.Ellenbogen JM, Pace-Schott EF Drug-induced sleep: theoretical and practical considerations. Pflugers Arch 463:177–86 [DOI] [PubMed]
- 26.Enyedi P, Czirjak G (2009) Molecular background of leak K+ currents: two-pore domain potassium channels. Physiol Rev 90:559–605. doi: 10.1152/physrev.00029.2009 [DOI] [PubMed]
- 27.Eschenko O, Magri C, Panzeri S, Sara SJ. Noradrenergic neurons of the locus coeruleus are phase locked to cortical up-down states during sleep. Cereb Cortex. 2012;22:426–435. doi: 10.1093/cercor/bhr121. [DOI] [PubMed] [Google Scholar]
- 28.Franks NP, Lieb WR. Volatile general anaesthetics activate a novel neuronal K+ current. Nature. 1988;333:662–664. doi: 10.1038/333662a0. [DOI] [PubMed] [Google Scholar]
- 29.Franks NP, Lieb WR. Molecular and cellular mechanisms of general anaesthesia. Nature. 1994;367:607–614. doi: 10.1038/367607a0. [DOI] [PubMed] [Google Scholar]
- 30.Franks NP, Lieb WR. Background K+ channels: an important target for volatile anesthetics? Nat Neurosci. 1999;2:395–396. doi: 10.1038/8054. [DOI] [PubMed] [Google Scholar]
- 31.Gabriel A, Abdallah M, Yost CS, Winegar BD, Kindler CH. Localization of the tandem pore domain K+ channel KCNK5 (TASK-2) in the rat central nervous system. Brain Res Mol Brain Res. 2002;98:153–163. doi: 10.1016/S0169-328X(01)00330-8. [DOI] [PubMed] [Google Scholar]
- 32.Gerstin KM, Gong DH, Abdallah M, Winegar BD, 2nd Eger EI, Gray AT. Mutation of KCNK5 or Kir3.2 potassium channels in mice does not change minimum alveolar anesthetic concentration. Anesth Analg. 2003;96:1345–1349. doi: 10.1213/01.ANE.0000056921.15974.EC. [DOI] [PubMed] [Google Scholar]
- 33.Goldstein SA, Bayliss DA, Kim D, Lesage F, Plant LD, Rajan S. International Union of Pharmacology. LV. Nomenclature and molecular relationships of two-P potassium channels. Pharmacol Rev. 2005;57:527–540. doi: 10.1124/pr.57.4.12. [DOI] [PubMed] [Google Scholar]
- 34.Gotter AL, Santarelli VP, Doran SM, Tannenbaum PL, Kraus RL, Rosahl TW, Meziane H, Montial M, Reiss DR, Wessner K, McCampbell A, Stevens J, Brunner JI, Fox SV, Uebele VN, Bayliss DA, Winrow CJ, Renger JJ. TASK-3 as a potential antidepressant target. Brain Res. 2011;1416:69–79. doi: 10.1016/j.brainres.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gray AT, Zhao BB, Kindler CH, Winegar BD, Mazurek MJ, Xu J, Chavez RA, Forsayeth JR, Yost CS. Volatile anesthetics activate the human tandem pore domain baseline K+ channel KCNK5. Anesthesiol. 2000;92:1722–1730. doi: 10.1097/00000542-200006000-00032. [DOI] [PubMed] [Google Scholar]
- 36.Gruss M, Bushell TJ, Bright DP, Lieb WR, Mathie A, Franks NP. Two-pore-domain K+ channels are a novel target for the anesthetic gases xenon, nitrous oxide, and cyclopropane. Mol Pharmacol. 2004;65:443–452. doi: 10.1124/mol.65.2.443. [DOI] [PubMed] [Google Scholar]
- 37.Harris K, Armstrong SP, Campos-Pires R, Kiru L, Franks NP, Dickinson R. Neuroprotection against traumatic brain injury by xenon, but not argon, is mediated by inhibition at the N-methyl-D-aspartate receptor glycine site. Anesthesiology. 2013;119:1137–1148. doi: 10.1097/ALN.0b013e3182a2a265. [DOI] [PubMed] [Google Scholar]
- 38.Heitzmann D, Derand R, Jungbauer S, Bandulik S, Sterner C, Schweda F, El Wakil A, Lalli E, Guy N, Mengual R, Reichold M, Tegtmeier I, Bendahhou S, Gomez-Sanchez CE, Aller MI, Wisden W, Weber A, Lesage F, Warth R, Barhanin J. Invalidation of TASK1 potassium channels disrupts adrenal gland zonation and mineralocorticoid homeostasis. EMBO J. 2008;27:179–187. doi: 10.1038/sj.emboj.7601934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heurteaux C, Guy N, Laigle C, Blondeau N, Duprat F, Mazzuca M, Lang-Lazdunski L, Widmann C, Zanzouri M, Romey G, Lazdunski M. TREK-1, a K+ channel involved in neuroprotection and general anesthesia. EMBO J. 2004;23:2684–2695. doi: 10.1038/sj.emboj.7600234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heurteaux C, Lucas G, Guy N, El Yacoubi M, Thummler S, Peng XD, Noble F, Blondeau N, Widmann C, Borsotto M, Gobbi G, Vaugeois JM, Debonnel G, Lazdunski M. Deletion of the background potassium channel TREK-1 results in a depression-resistant phenotype. Nat Neurosci. 2006;9:1134–1141. doi: 10.1038/nn1749. [DOI] [PubMed] [Google Scholar]
- 41.Honore E. The neuronal background K2P channels: focus on TREK1. Nat Rev Neurosci. 2007;8:251–261. doi: 10.1038/nrn2117. [DOI] [PubMed] [Google Scholar]
- 42.Jung J, Barrett PQ, Eckert GJ, Edenberg HJ, Xuei X, Tu W, Pratt JH. Variations in the potassium channel genes KCNK3 and KCNK9 in relation to blood pressure and aldosterone production: an exploratory study. J Clin Endocrinol Metab. 2012;97:E2160–E2167. doi: 10.1210/jc.2012-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang D, Han J, Talley EM, Bayliss DA, Kim D. Functional expression of TASK-1/TASK-3 heteromers in cerebellar granule cells. J Physiol. 2004;554:64–77. doi: 10.1113/jphysiol.2003.054387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keshavaprasad B, Liu C, Au JD, Kindler CH, Cotten JF, Yost CS. Species-specific differences in response to anesthetics and other modulators by the K2P channel TRESK. Anesth Analg. 2005;101:1042–1049. doi: 10.1213/01.ane.0000168447.87557.5a. [DOI] [PubMed] [Google Scholar]
- 45.Ketchum KA, Joiner WJ, Sellers AJ, Kaczmarek LK, Goldstein SA. A new family of outwardly rectifying potassium channel proteins with two pore domains in tandem. Nature. 1995;376:690–695. doi: 10.1038/376690a0. [DOI] [PubMed] [Google Scholar]
- 46.Kim D, Cavanaugh EJ, Kim I, Carroll JL. Heteromeric TASK-1/TASK-3 is the major oxygen-sensitive background K+ channel in rat carotid body glomus cells. J Physiol. 2009;587:2963–2975. doi: 10.1113/jphysiol.2009.171181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kindler CH, Yost CS, Gray AT. Local anesthetic inhibition of baseline potassium channels with two pore domains in tandem. Anesthesiology. 1999;90:1092–1102. doi: 10.1097/00000542-199904000-00024. [DOI] [PubMed] [Google Scholar]
- 48.Lafreniere RG, Cader MZ, Poulin JF, Andres-Enguix I, Simoneau M, Gupta N, Boisvert K, Lafreniere F, McLaughlan S, Dube MP, Marcinkiewicz MM, Ramagopalan S, Ansorge O, Brais B, Sequeiros J, Pereira-Monteiro JM, Griffiths LR, Tucker SJ, Ebers G, Rouleau GA. A dominant-negative mutation in the TRESK potassium channel is linked to familial migraine with aura. Nat Med. 2010;16:1157–1160. doi: 10.1038/nm.2216. [DOI] [PubMed] [Google Scholar]
- 49.Lazarenko RM, Willcox SC, Shu S, Berg AP, Jevtovic-Todorovic V, Talley EM, Chen X, Bayliss DA. Motoneuronal TASK channels contribute to immobilizing effects of inhalational general anesthetics. J Neurosci. 2010;30:7691–7704. doi: 10.1523/JNEUROSCI.1655-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lesage F, Guillemare E, Fink M, Duprat F, Lazdunski M, Romey G, Barhanin J. TWIK-1, a ubiquitous human weakly inward rectifying K+ channel with a novel structure. EMBO J. 1996;15:1004–1011. [PMC free article] [PubMed] [Google Scholar]
- 51.Linden AM, Aller MI, Leppa E, Rosenberg PH, Wisden W, Korpi ER. K+ channel TASK-1 knockout mice show enhanced sensitivities to ataxic and hypnotic effects of GABA (A) receptor ligands. J Pharmacol Exp Ther. 2008;327:277–286. doi: 10.1124/jpet.108.142083. [DOI] [PubMed] [Google Scholar]
- 52.Linden AM, Aller MI, Leppa E, Vekovischeva O, Aitta-Aho T, Veale EL, Mathie A, Rosenberg P, Wisden W, Korpi ER. The in vivo contributions of TASK-1-containing channels to the actions of inhalation anesthetics, the alpha (2) adrenergic sedative dexmedetomidine, and cannabinoid agonists. J Pharmacol Exp Ther. 2006;317:615–626. doi: 10.1124/jpet.105.098525. [DOI] [PubMed] [Google Scholar]
- 53.Linden AM, Sandu C, Aller MI, Vekovischeva OY, Rosenberg PH, Wisden W, Korpi ER. TASK-3 knockout mice exhibit exaggerated nocturnal activity, impairments in cognitive functions, and reduced sensitivity to inhalation anesthetics. J Pharmacol Exp Ther. 2007;323:924–934. doi: 10.1124/jpet.107.129544. [DOI] [PubMed] [Google Scholar]
- 54.Lotshaw DP. Biophysical, pharmacological, and functional characteristics of cloned and native mammalian two-pore domain K+ channels. Cell Biochem Biophys. 2007;47:209–256. doi: 10.1007/s12013-007-0007-8. [DOI] [PubMed] [Google Scholar]
- 55.Mathie A, Al-Moubarak E, Veale EL. Gating of two pore domain potassium channels. J Physiol. 2010;588:3149–3156. doi: 10.1113/jphysiol.2010.192344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mazella J, Petrault O, Lucas G, Deval E, Beraud-Dufour S, Gandin C, El-Yacoubi M, Widmann C, Guyon A, Chevet E, Taouji S, Conductier G, Corinus A, Coppola T, Gobbi G, Nahon JL, Heurteaux C, Borsotto M. Spadin, a sortilin-derived peptide, targeting rodent TREK-1 channels: a new concept in the antidepressant drug design. PLoS Biol. 2010;8:e1000355. doi: 10.1371/journal.pbio.1000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meuth SG, Aller MI, Munsch T, Schuhmacher T, Seidenbecher T, Meuth P, Kleinschnitz C, Pape HC, Wiendl H, Wisden W, Budde T. The contribution of TWIK-related acid-sensitive K+-containing channels to the function of dorsal lateral geniculate thalamocortical relay neurons. Mol Pharmacol. 2006;69:1468–1476. doi: 10.1124/mol.105.020594. [DOI] [PubMed] [Google Scholar]
- 58.Meuth SG, Budde T, Kanyshkova T, Broicher T, Munsch T, Pape HC. Contribution of TWIK-related acid-sensitive K+ channel 1 (TASK1) and TASK3 channels to the control of activity modes in thalamocortical neurons. J Neurosci. 2003;23:6460–6469. doi: 10.1523/JNEUROSCI.23-16-06460.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Meuth SG, Kanyshkova T, Meuth P, Landgraf P, Munsch T, Ludwig A, Hofmann F, Pape HC, Budde T. Membrane resting potential of thalamocortical relay neurons is shaped by the interaction among TASK3 and HCN2 channels. J Neurophysiol. 2006;96:1517–1529. doi: 10.1152/jn.01212.2005. [DOI] [PubMed] [Google Scholar]
- 60.Miller AN, Long SB. Crystal structure of the human two-pore domain potassium channel K2P1. Science. 2012;335:432–436. doi: 10.1126/science.1213274. [DOI] [PubMed] [Google Scholar]
- 61.Mirkovic K, Palmersheim J, Lesage F, Wickman K. Behavioral characterization of mice lacking Trek channels. Front Behav Neurosci. 2012;6:60. doi: 10.3389/fnbeh.2012.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Moha ou Maati H, Peyronnet R, Devader C, Veyssiere J, Labbal F, Gandin C, Mazella J, Heurteaux C, Borsotto M (2011) A human TREK-1/HEK cell line: a highly efficient screening tool for drug development in neurological diseases. PLoS One 6(10):e25602. doi: 10.1371/journal.pone.0025602 [DOI] [PMC free article] [PubMed]
- 63.Muhammad S, Aller MI, Maser-Gluth C, Schwaninger M, Wisden W. Expression of the kcnk3 potassium channel gene lessens the injury from cerebral ischemia, most likely by a general influence on blood pressure. Neuroscience. 2010;167:758–764. doi: 10.1016/j.neuroscience.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 64.Noel J, Zimmermann K, Busserolles J, Deval E, Alloui A, Diochot S, Guy N, Borsotto M, Reeh P, Eschalier A, Lazdunski M. The mechano-activated K+ channels TRAAK and TREK-1 control both warm and cold perception. EMBO J. 2009;28:1308–1318. doi: 10.1038/emboj.2009.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nyholt DR, LaForge KS, Kallela M, Alakurtti K, Anttila V, Farkkila M, Hamalainen E, Kaprio J, Kaunisto MA, Heath AC, Montgomery GW, Gobel H, Todt U, Ferrari MD, Launer LJ, Frants RR, Terwindt GM, de Vries B, Verschuren WM, Brand J, Freilinger T, Pfaffenrath V, Straube A, Ballinger DG, Zhan Y, Daly MJ, Cox DR, Dichgans M, van den Maagdenberg AM, Kubisch C, Martin NG, Wessman M, Peltonen L, Palotie A. A high-density association screen of 155 ion transport genes for involvement with common migraine. Hum Mol Genet. 2008;17:3318–3331. doi: 10.1093/hmg/ddn227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Orliaguet G, Vivien B, Langeron O, Bouhemad B, Coriat P, Riou B. Minimum alveolar concentration of volatile anesthetics in rats during postnatal maturation. Anesthesiology. 2001;95:734–739. doi: 10.1097/00000542-200109000-00028. [DOI] [PubMed] [Google Scholar]
- 67.Pang DS, Robledo CJ, Carr DR, Gent TC, Vyssotski AL, Caley A, Zecharia AY, Wisden W, Brickley SG, Franks NP. An unexpected role for TASK-3 potassium channels in network oscillations with implications for sleep mechanisms and anesthetic action. Proc Natl Acad Sci U S A. 2009;106:17546–17551. doi: 10.1073/pnas.0907228106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Patel AJ, Honore E, Lesage F, Fink M, Romey G, Lazdunski M. Inhalational anesthetics activate two-pore-domain background K+ channels. Nat Neurosci. 1999;2:422–426. doi: 10.1038/8084. [DOI] [PubMed] [Google Scholar]
- 69.Plant LD, Zuniga L, Araki D, Marks JD, Goldstein SA. SUMOylation silences heterodimeric TASK potassium channels containing K2P1 subunits in cerebellar granule neurons. Sci Signal. 2012;5:ra84. doi: 10.1126/scisignal.2003431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Putzke C, Hanley PJ, Schlichthorl G, Preisig-Muller R, Rinne S, Anetseder M, Eckenhoff R, Berkowitz C, Vassiliou T, Wulf H, Eberhart L. Differential effects of volatile and intravenous anesthetics on the activity of human TASK-1. Am J Physiol Cell Physiol. 2007;293:C1319–C1326. doi: 10.1152/ajpcell.00100.2007. [DOI] [PubMed] [Google Scholar]
- 71.Ries CR, Puil E. Ionic mechanism of isoflurane’s actions on thalamocortical neurons. J Neurophysiol. 1999;81:1802–1809. doi: 10.1152/jn.1999.81.4.1802. [DOI] [PubMed] [Google Scholar]
- 72.Ries CR, Puil E. Mechanism of anesthesia revealed by shunting actions of isoflurane on thalamocortical neurons. J Neurophysiol. 1999;81:1795–1801. doi: 10.1152/jn.1999.81.4.1795. [DOI] [PubMed] [Google Scholar]
- 73.Rudolph U, Antkowiak B. Molecular and neuronal substrates for general anaesthetics. Nat Rev Neurosci. 2004;5:709–720. doi: 10.1038/nrn1496. [DOI] [PubMed] [Google Scholar]
- 74.Saito K, Moore R, Negishi M. Nuclear receptor CAR specifically activates the two-pore K+ channel Kcnk1 gene in male mouse livers, which attenuates phenobarbital-induced hepatic hyperplasia. Toxicol Sci. 2013;132:151–161. doi: 10.1093/toxsci/kfs338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sirois JE, Lei Q, Talley EM, Lynch C, 3rd, Bayliss DA. The TASK-1 two-pore domain K+ channel is a molecular substrate for neuronal effects of inhalation anesthetics. J Neurosci. 2000;20:6347–6354. doi: 10.1523/JNEUROSCI.20-17-06347.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sirois JE, Lynch C, 3rd, Bayliss DA. Convergent and reciprocal modulation of a leak K+ current and I (h) by an inhalational anaesthetic and neurotransmitters in rat brainstem motoneurones. J Physiol. 2002;541:717–729. doi: 10.1113/jphysiol.2002.018119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Talley EM, Bayliss DA. Modulation of TASK-1 (Kcnk3) and TASK-3 (Kcnk9) potassium channels: volatile anesthetics and neurotransmitters share a molecular site of action. J Biol Chem. 2002;277:17733–17742. doi: 10.1074/jbc.M200502200. [DOI] [PubMed] [Google Scholar]
- 78.Talley EM, Solorzano G, Lei Q, Kim D, Bayliss DA. Cns distribution of members of the two-pore-domain (KCNK) potassium channel family. J Neurosci. 2001;21:7491–7505. doi: 10.1523/JNEUROSCI.21-19-07491.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thompson SA, Wafford K. Mechanism of action of general anaesthetics—new information from molecular pharmacology. Curr Opin Pharmacol. 2001;1:78–83. doi: 10.1016/S1471-4892(01)00013-3. [DOI] [PubMed] [Google Scholar]
- 80.Trapp S, Aller MI, Wisden W, Gourine AV. A role for TASK-1 (KCNK3) channels in the chemosensory control of breathing. J Neurosci. 2008;28:8844–8850. doi: 10.1523/JNEUROSCI.1810-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Veale EL, Kennard LE, Sutton GL, MacKenzie G, Sandu C, Mathie A. G(alpha)q-mediated regulation of TASK3 two-pore domain potassium channels: the role of protein kinase C. Mol Pharmacol. 2007;71:1666–1675. doi: 10.1124/mol.106.033241. [DOI] [PubMed] [Google Scholar]
- 82.Ward LM. The thalamic dynamic core theory of conscious experience. Conscious Cogn. 2011;20:464–486. doi: 10.1016/j.concog.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 83.Wu YY, Singer CA, Buxton IL. Variants of stretch-activated two-pore potassium channel TREK-1 associated with preterm labor in humans. Biol Reprod. 2012;87:96. doi: 10.1095/biolreprod.112.099499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xi G, Zhang X, Zhang L, Sui Y, Hui J, Liu S, Wang Y, Li L, Zhang Z. Fluoxetine attenuates the inhibitory effect of glucocorticoid hormones on neurogenesis in vitro via a two-pore domain potassium channel, TREK-1. Psychopharmacology (Berlin) 2011;214:747–759. doi: 10.1007/s00213-010-2077-3. [DOI] [PubMed] [Google Scholar]
- 85.Yanovsky Y, Schubring S, Fleischer W, Gisselmann G, Zhu XR, Lubbert H, Hatt H, Rudolph U, Haas HL, Sergeeva OA (2012) GABAA receptors involved in sleep and anaesthesia: beta1- versus beta3-containing assemblies. Pflugers Arch 463(1):187–99. doi: 10.1007/s00424-011-0988-4 [DOI] [PubMed]
- 86.Yost CS, Oh I, Eger EI, 2nd, Sonner JM. Knockout of the gene encoding the K (2P) channel KCNK7 does not alter volatile anesthetic sensitivity. Behav Brain Res. 2008;193:192–196. doi: 10.1016/j.bbr.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]