Abstract
Objective
To describe the proportion of children adhering to recommended physical activity and dietary guidelines, and examine demographic and household correlates of guideline adherence.
Design
Cross-sectional (pre-randomization) data from a behavioral intervention trial designed to prevent unhealthy weight gain in children.
Participants
Four hundred and twenty-one children (ages 5–10 years) at risk for obesity (body mass index percentile 70–95).
Main Outcomes Measured
Physical activity (accelerometry), screen time (parent survey), fruit and vegetable and sugar-sweetened beverage intake (24-hour dietary recall).
Analysis
Proportions meeting guidelines were calculated. Logistic regression examined associations between demographic and household factors and whether children met recommended guidelines for 1) physical activity (≥ 60 minutes/day), 2) screen time (≤ 2 hours/day), 3) fruit/vegetable intake (≥ 5 servings/day), and 4) sugar-sweetened beverage avoidance.
Results
Few children met more than one guideline. Only 2% met all four recommended guidelines, and 19% met none. Each guideline had unique sociodemographic and domain-specific household predictors (i.e. availability of certain food/beverages, media, and active play/exercise equipment).
Conclusions and Implications
Families equipped to promote healthy child behavior patterns in one activity or dietary domain may not be in others. Results have implications for the development of interventions to impact children’s weight-related behaviors and growth trajectories. (200)
Keywords: physical activity, diet, guidelines, child, home environment
INTRODUCTION
Children’s activity patterns and dietary intake are associated with important aspects of their health and well-being. Prior studies suggest that physically active children have stronger cognitive/academic functioning, higher self-esteem, and lower adiposity than less active peers 1–4. Sedentary behaviors (e.g., watching television) have also been associated with overweight/obesity5 and metabolic syndrome markers6,7. Sugar-sweetened beverage intake has been associated with obesity8, and fruit and vegetable consumption has been linked to lower risk of chronic health conditions9,10. Activity and dietary patterns established during childhood often persist into adulthood11, underscoring the importance of identifying who is at risk for maladaptive patterns early on and what modifiable factors may mitigate this risk.
Guidelines for physical activity and healthy eating have been established for obesity prevention in children, and endorsed by the American Academy of Pediatrics12–15. These guidelines include recommendations for minimum levels of moderate-to-vigorous physical activity (i.e., at least 60 minutes per day), limiting screen time (to no more than 2 hours per day), eating at least 5 servings of fruits and vegetables per day, and avoiding sugar-sweetened beverages. Numerous population-based studies have examined demographic correlates of physical activity and dietary intake patterns in children16–20. Some have included rates of adherence to guidelines nationally, with a focus on whether guideline adherence varies as a function of sociodemographic and child characteristics21–23.
Most prior studies have examined guideline adherence in isolation (i.e., a single guideline) or within a single domain (e.g., either activity or dietary intake). A recent parent survey study from a nationally representative dataset21 found 70% of children ages 6–11 met physical activity recommendations and 54% met screen-time viewing guidelines. Older children (9–11) and children who were obese were less likely to meet these guidelines. Rates of adherence to dietary guidelines are much lower. Population-based survey studies estimate that between 16 and 26% of elementary school-aged children meet fruit and vegetable intake guidelines, with obese children showing lower adherence rates23. While sugar-sweetened beverage consumption has decreased over the past decade, a recent study found only 36% of children ages 2–19 met guidelines for sugar-sweetened beverage avoidance22. Demographic factors such as lower levels of parental education and socioeconomic status have been associated with greater consumption of sugar sweetened beverages by children24–26; and other studies have found that soda intake increases with increasing age27–29.
Fewer studies have examined the impact of modifiable household factors and family behavior patterns on children’s adherence to both activity and dietary guidelines. Nonetheless, several studies have examined the role of these factors on children’s weight-related behaviors more generally. Such studies have found that media equipment at home, and specifically in the bedroom, is positively associated with children’s sedentary behavior30–32. Exercise and play equipment availability have been inversely associated with sedentary behavior (e.g., media use), but inconsistently associated with physical activity levels33. Parents’ engagement in physical activity with the child has been inconsistently linked to children’s physical activity and sedentary behavior34. The availability of certain food groups (e.g., fruits and vegetables, sugar-sweetened beverages) in the home has also been associated with children’s intake of these foods35–38, and family behavior patterns such as higher fast food frequency and having the TV on during meals have been associated with lower child intake of fruits and vegetables, and higher intake of unhealthy foods, such as salty snacks and soda39,40. These studies have shown correlations between household factors, family behavior patterns, and children’s dietary/activity levels. However, such studies have not established whether these factors significantly contribute to a meaningful level of engagement in these weight-related behaviors, as reflected by whether or not children are meeting recommended guidelines, and have not examined guideline adherence across physical activity and dietary domains. Identifying household and family behavior patterns that are associated with children’s adherence to both activity and dietary recommendations would support the development of more effective obesity prevention interventions.
This study used data from the Healthy Homes/Healthy Kids Study (HHHK) trial41 to examine the proportion of children meeting dietary and activity guidelines, and associations with demographic and household patterns in a cohort of children ages 5–10 years who are at risk for obesity. In addition to examining adherence to individual dietary and activity guidelines (i.e., objectively-measured moderate-to-vigorous physical activity, screen-time viewing, fruit and vegetable intake, and sugar-sweetened beverage consumption), the proportion adhering to multiple guidelines is also described, to provide a more complete picture of weight-related behaviors within this cohort. To our knowledge, no prior studies have examined adherence to multiple dietary and activity guidelines in this age group. This is a major gap in the literature given that the combined influence of dietary and activity patterns is believed to contribute to childhood obesity risk and often targeted concurrently in interventions42,43. It was hypothesized that overweight children (BMI between the 85th and 95th percentile) would have lower adherence rates to single and multiple guidelines than children at risk for overweight (defined here as 70–84th percentile) and further hypothesized that key household variables (availability of media, exercise/play equipment, and specific food/beverage items), family behavior patterns that comprise the home food, eating, and activity environment (eating fast food, family meals with the TV on, shared parent-child physical activities), and demographic characteristics (child’s age, child’s sex, parent education) would be associated with children’s adherence to these guidelines.
METHOD
Participants
Baseline (pre-randomization) data were used from a behavioral intervention trial (HHHK) designed to prevent unhealthy weight gain among children who were overweight or at-risk for becoming overweight. The study recruited families scheduled for a well-child visit at clinics in the Minneapolis-St. Paul area. Eligible children were ages 5–10 years with BMI percentiles between 70th and 95th for age and gender; parents were English speaking, and willing to complete measures and participate in a parent-targeted intervention. Children with a history chromosomal abnormality, chronic medical conditions, consistent use of steroid medication, or participation in other child health research were excluded. Parent informed consent and child assent were obtained. Study protocol and procedures were approved by the Institutional Review Board. Further details of the trial are described elsewhere41.
Dependent Variables
Physical activity guidelines
Children were asked to wear ActiGraph GT1M accelerometers (ActiGraph LLC, Pensacola, FL) for 7 full days during waking hours to measure physical activity. The devices were placed on elastic belts and fitted on the right hip. Children were included in analyses if they recorded at least 4 valid monitoring days, defined as 10 or more hours of wear time per day (77%). Non-wear time was defined as a string of ≥ 60 minutes of zero-counts, allowing for a 2-minute interruption interval of 100 counts or less. To estimate minutes spent in moderate-to-vigorous activity (MVPA), data were aggregated into 1-minute epochs. Cutpoints were developed using the Evenson et al. 44 equations and dichotomized to reflect those who were meeting (≥ 60 minutes MVPA, coded 1) or not meeting guidelines (<60 minutes, coded 0).
Screen time guidelines
Parents reported the amount of time in hours that children spent watching TV and playing video or computer games or using a computer for purposes other than schoolwork on an average weekday and weekend day 45. Response options were 0 hours (coded as 0), less than 1 hour (0.5), 1 hour (1), 2 hours (2), 3 hours (3), 4 hours (4), and 5 or more hours (5) per day. Total time per day spent watching TV or using a computer was calculated as the sum of the weekday TV and computer/videogame time estimates multiplied by 5 and the weekend estimates multiplied by 2, divided by 7. Children were then classified as meeting (≤ 2 hours, coded 1) or exceeding (> 2 hours, coded 0) recommendations for daily screen time.
Dietary guidelines
Child intake was assessed using a single multi-pass 24-hour recall administered by staff trained and certified to use the Nutrition Data System for Research (NDSR, Nutrition Coordinating Center, NCC, University of Minnesota, Minneapolis, MN). Parents reported whether the child ate a typical amount on the day of the recall, and recalls in which the parent or child could not recall one or more meals were flagged as unreliable. Only “typical” and “reliable” daily intake recalls were included in the analyses (94%). Recalls were analyzed using NDSR version 2011. Total energy intake, and servings of whole fruit, vegetables, and sugar-sweetened beverages were used in analyses. White potatoes and 100% fruit juice were excluded from the fruit and vegetable count to be consistent with intervention approaches to prevent unhealthy weight gain 46,47. Fruit and vegetable servings were summed and dichotomized into meeting (≥ 5 servings, coded 1) or not meeting guidelines (coded 0). Sugar sweetened beverages included: sugar-sweetened flavored milk and waters; sweetened soft drinks, fruit drinks (<100% juice); sweetened sports drinks and supplements (e.g., Gatorade, Powerade, Red Bull); and sweetened tea. Sugar sweetened beverage consumption was dichotomized into meeting guidelines (no sugar-sweetened beverage consumption, coded 1) versus any sugar-sweetened beverage consumption (not meeting guidelines, coded 0).
Predictor Variables
Sociodemographic characteristics
Parents reported their child’s and their own sociodemographic characteristics, such as age, sex, ethnicity, race, and educational attainment.
Anthropometry
Child height and weight were measured in the family home by trained staff using a Seca 217 stadiometer and Seca 876 flat scale (Seca Corp., Hanover, MD). Children were measured without shoes and heavy clothing. Height was measured to the nearest 0.1 cm and weight to the nearest 0.1 kg. Measurements were performed twice, and repeated a third time if the first two differed by more than 1.0 cm for height or more than 0.2 kg for weight. Child BMI was calculated as weight in kilograms/height in meters2, and BMI percentile derived using the CDC 2000 Growth Charts Study 48.
Household food availability
Food availability was assessed from lists of items within five food and beverage categories (fruits, vegetables, salty snacks, sweet snacks, and beverages) developed from the Food Frequency Questionnaire49,50. Parents selected items available in their home within the last week. A count variable was created for each category to indicate the number of different types of items from that category available in the home. Unhealthy snacks (e.g., cheese puffs/doodles, sweetened or full fat popcorn, chips) were aggregated and reported together (7 possible items). Fruit (e.g., apples, bananas) and vegetable (e.g., string and green beans, celery, broccoli) availability were combined and reported together (24 possible items). All sugar-sweetened beverages (e.g., soda, sports-drinks, fruit-drinks <100% juice) were also combined (5 possible item types).
Household media and play equipment availability
Parents reported household availability of play and media equipment for their child using a 47-item inventory 51. Play equipment was categorized as: active play equipment (a count of 34 possible items; e.g., soccer ball, playhouse, gym shoes), active/exercise media (a count of two possible items: active videogames, exercise-related media), and non-active/exercise media (a count of 11 possible items; e.g., computer, digital TV recorder, handheld videogame player). A count variable was created for each category to indicate household availability.
Child’s fast food intake
Parents reported the number of times during the past week that their child ate something from a fast food restaurant (e.g., McDonald’s, Taco Bell, etc.) using a single item based on a modification of Boutelle 52. Based on the distribution of this variable, response options (“Never,” “1–2 times,” “3–4 times,” “5–6 times,” and “7+ times”) were dichotomized to compare any fast food intake (ate out ≥1 times during the past week) to none (“never ate out”).
Media in the child’s bedroom
Presence of media (i.e., a television, computer or laptop, video game console) in the child’s bedroom was assessed with three questions modified from the Dennison survey53. Parents who endorsed having any one of these items in their child’s bedroom were categorized as having media in the child’s bedroom.
Parent-child shared physical activities
Frequency and type of parent-child shared physical activities was assessed using a 2-item questionnaire developed for this study. Parents reported the number of times they had been physically active with their child over the past week. Response options were: “Never, “1 time,” “2 times,” “3 times,” “4 times,” “5–7 times,” “8–10 times,” and “11+ times.” Based on the distribution of this variable, responses were dichotomized to compare parents who were more frequently active with their child (≥ 3 times, coded 1) with those who were less active (< 3 times, coded 0). Parents then selected the type of physical activity they had participated in with their child from a list of 22 possibilities (e.g., swimming, walking, biking) and asked to write in any not included. Open-ended responses were coded into 3 additional activity types (horseplay, chores, and other). The total number of different physical activities (0–25 categories) was used in analyses.
Family meals with the TV on
Parents rated the frequency of watching television during family meals during the past week using 1 item, adapted from McGarvey et al. 54. Response options were: “Never (0)” “1–2 times (1)” “3–4 times (2)”, “5–6 times (3)” and “7+ times (4).” Based on the distribution of this variable, response options were dichotomized to compare families who ate meals with the TV on (≥ 1 time in the past week) to those who did not (never in the past week).
Statistical Analysis
Data were analyzed with SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY). Descriptive statistics characterize the sample. Logistic regression examined associations between demographic and household factors and whether children met recommended guidelines for physical activity, screen time, fruit and vegetable intake, and sugar-sweetened beverage consumption. Simple logistic regression models included children with: valid accelerometry (n=322) when predicting adherence to physical activity guidelines, valid NDSR (n=396) when examining fruit and vegetable and sugar-sweetened beverage guideline adherence, and complete screen time survey (n=410) when the dependent variable was screen time guideline adherence. All continuous predictors were mean-centered. Household and family behavior pattern variables that were significant in simple logistic models were included in multivariate models in which key demographic characteristics (child age (years), sex (male versus female), parent education (at least college educated versus less than college), race/ethnicity (non-Hispanic white versus Hispanic and/or not-white)) and child weight (BMI percentile) were included as covariates. In analysis of adherence to dietary guidelines, child energy intake (total kcals from NDSR) was included as a covariate. As total kcals were significantly associated with sex and age (i.e., boys had higher energy intakes than girls; older children had higher energy intakes than younger children consistent with expectations in the literature), we centered kcals around the mean for each child’s age and sex and then divided by 100 to ease interpretation in regression analysis. Interactions between sociodemographic and household factors were tested and if significant (p < .05) included in the multivariate model.
RESULTS
Participant Characteristics
Sociodemographic characteristics, household factors, and behavior patterns of parent-child dyads are presented in Table 1. The majority of parents were college educated, and children were predominantly white/non-Hispanic. There were low rates of media present in children’s bedrooms (25%) and nearly half (41%) had no exercise/active media available at home. While more than half (66%) had consumed fast food at least 1–2 times within the past week, few consumed fast food with higher levels of frequency (i.e., 3 or more times; 3.6%).
Table 1.
Participant sociodemographics, weight-related behaviors, and household characteristics
| Sociodemographic | ||
|---|---|---|
| n | ||
| Age at randomization (years), M (SD), range 5–10 years | 421 | 6.6 (1.7) |
| BMI percentile, M (SD) | 421 | 84.9 (6.9) |
| Parents with at least college education (%) | 418 | 71.0% |
| Child, Hispanic ethnicity | 419 | 6.9% |
| Child race | 421 | |
| White (%) | 71.5% | |
| Black or African American (%) | 10.5% | |
| Multi-racial (%) | 11.6% | |
| Asian (%) | 3.3% | |
| American Indian/Alaskan Native | 0.5% | |
| Unknown | 2.6% | |
| Sex of child; Females (%) | 421 | 49.4% |
| Physical activity and dietary intake | ||
| Screen time (hours/day), M (SD) | 418 | 2.4 (1.3) |
| Moderate-vigorous physical activity (minutes/day), M (SD) | 322 | 53.6 (30.9) |
| Sugar-sweetened beverage consumption (servings/day), M (SD) | 396 | 0.8 (1.1) |
| Fruit-vegetable consumption (servings/day), M (SD) | 396 | 2.8 (2.4) |
| Household | ||
| Fruit & vegetables available (range: 0–24), M (SD) | 420 | 13.7 (3.9) |
| Unhealthy snacks available (range: 0–4), M (SD) | 420 | 1.8 (1.8) |
| Sugar-sweetened beverages available (range: 0–4), M (SD) | 420 | 1.5 (1.2) |
| Active play equipment available (range: 0–34), M (SD) | 420 | 19.3 (6.0) |
| Active/exercise media available (range: 0–2), M (SD) | 420 | 0.7 (.59) |
| Non-active/exercise media available (range: 0–11), M (SD) | 420 | 5.5 (2.2) |
| TV/computer/videogames in child’s bedroom (%) | 420 | 25% |
| Family behavior patterns | ||
| Family meals with TV on | 417 | |
| 0 times, past week (%) | 48.2% | |
| 1–2 times, past week (%) | 21.4% | |
| 3–4 times, past week (%) | 13.9% | |
| 5–6 times, past week (%) | 9.8% | |
| 7+ times, past week (%) | 6.7% | |
| Frequency of parent physical activity with child | 416 | |
| 0 times, past week (%) | 12.3% | |
| 1–2 times, past week (%) | 32.2% | |
| 3–4 times, past week (%) | 33.7% | |
| 5–7 times, past week (%) | 16.6% | |
| 8+ times, past week (%) | 5.2% | |
| Eating fast food | 419 | |
| 0 times, past week (%) | 33.7% | |
| 1–2 times, past week (%) | 62.8% | |
| 3–4 times, past week (%) | 3.3% | |
| 5–6 times, past week (%) | 0.2% | |
| Number of parent-child physical activities (range: 0–25), M (SD) | 420 | 3.0 (2.6) |
Meeting Physical Activity, Screen Time, and Dietary Intake Guidelines
Proportions of children meeting aggregate diet and physical activity guidelines were calculated among the 302 children with valid accelerometry, reliable dietary recalls, and complete screen time survey data (72%). Children with sufficiently complete data to calculate diet and activity guidelines were more likely to be white/not-Hispanic (75% versus 55%, p < .01) and their parents more likely to be college-educated (75% versus 64%, p < .05) than children without complete data. However, these groups did not differ on age, sex or child BMI percentile.
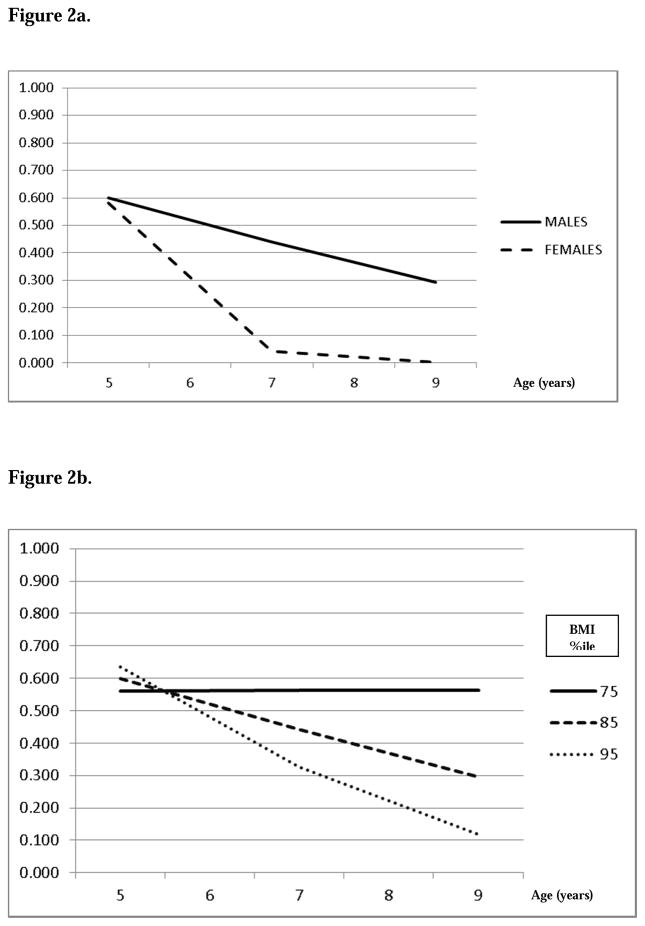
Figure 1 displays the percentage of children meeting recommended guidelines for physical activity, fruit and vegetable intake, screen time viewing, and avoidance of sugar-sweetened beverages for those who provided valid accelerometry, reliable diet recall and complete screen time surveys. Approximately 36% of this sample met recommended guidelines for physical activity and fewer than half (48%) met screen time guidelines. Only 17% met guidelines for both physical activity and screen time. Even fewer children met guidelines for 5 servings per day of fruit and vegetables (14%); however, 42% met sugar-sweetened beverage guidelines. Only 8% met both dietary guidelines. Examination of adherence rates across all four guidelines showed that although 81% of children met at least one guideline, only 31% met two guidelines, 11% met three guidelines and 2% met all four guidelines. Nineteen percent of children met none of these guidelines. There were no differences (all p values > .05) in the proportions of overweight (BMI between the 85th and 95th percentile n=156) and at-risk for overweight (BMI between the 70th and 84th percentile n=146) children adhering to physical activity (X2(1) = .19), screen time (X2(1) = .19), or dietary guidelines (sugar-sweetened beverages, X2(1) = .26; fruit/vegetables, X2(1) =.27), nor were there differences in the proportion meeting none, one, or more than one guideline (X2(4) = 2.39).
Figure 1. Percentage of children meeting recommended dietary and activity guidelines.
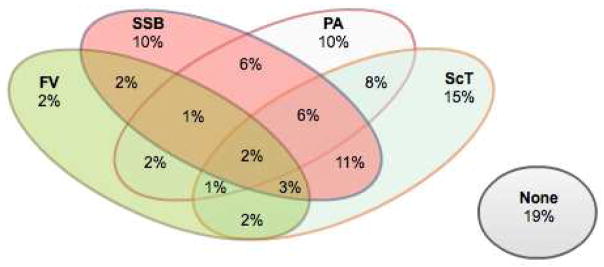
Note: FV= fruit/vegetable intake; SSB = sugar-sweetened beverage intake; PA = physical activity; ScT = screen time; None = meeting none of these activity and dietary guidelines. Figure includes those who provided valid accelerometry, reliable dietary intake, and screen time surveys (n=302).
Factors Associated with Adherence to Physical Activity and Screen Time Guidelines
Associations between availability of exercise/play equipment, non-exercise media availability, having a TV in the child’s bedroom, and parent engagement in physical activity with the child were simultaneously examined as predictors of adherence to physical activity and screen time guidelines (Table 2).
Table 2.
Multivariate logistic regression models for adherence to physical activity and dietary intake guidelines
| Screen time (≤ 2 hours/day) | |||
|---|---|---|---|
| OR | 95% CI | p-value | |
| Child’s age | 0.99 | 0.85–1.13 | .80 |
| Child’s race/ethnicity (1=non-Hispanic white) | 0.86 | 0.50–1.51 | .61 |
| Child’s sex (1=female) | 1.22 | 0.78–1.89 | .37 |
| Child’s BMI %ile | 1.00 | 0.97–1.04 | .85 |
| Parent education (1=college) | 1.60 | 0.96–2.68 | .07 |
| Media availability at home | 0.65 | 0.57–0.74 | <.001 |
| Active play/exercise availability at home | 1.12 | 1.07–1.18 | <.001 |
| Frequency of parent physical activity with child | 1.35 | 0.86–2.10 | .19 |
| Media in child’s bedroom (1 = yes) | 0.65 | 0.37–1.12 | .12 |
| Physical activity (≥ 60 minutes/day) | |||
| Child’s race/ethnicity (1=non-Hispanic white) | 0.51 | 0.27–0.97 | .04 |
| Parent education (1=college) | 1.59 | 0.84–3.01 | .16 |
| Age*Sex | <.001 | ||
| Age, Males | 0.73 | 0.34–1.56 | |
| Age, Females | 0.18 | 0.08–0.38 | |
| Age*Child BMI %ile | .02 | ||
| Age, 75%ile BMI | 1.00 | 0.98–1.03 | |
| Age, 85%ile BMI | 0.73 | 0.71–0.75 | |
| Age, 95%ile BMI | 0.53 | 0.51–0.54 | |
| Number of parent-child shared physical activities | 1.03 | 0.93–1.15 | .53 |
| Fruit/vegetable intake (≥ 5/day) | |||
| Child’s age | 1.25 | 1.05–1.49 | .01 |
| Child’s race/ethnicity (1=non-Hispanic white) | 1.71 | 0.80–3.63 | .17 |
| Child’s sex (1=female) | 0.54 | 0.29–1.00 | .05 |
| Child’s BMI %ile | 1.01 | 0.97–1.06 | .54 |
| Parent education (1=college) | 1.02 | 0.50–2.11 | .95 |
| Child energy intake: Total kcals | 1.06 | 1.01–1.12 | .03 |
| Fruit and vegetable availability at home | 1.11 | 1.01–1.21 | .02 |
| Avoiding sugar-sweetened beverages (0/day) | |||
| Child’s age | 0.85 | 0.75–0.97 | .02 |
| Child’s race/ethnicity (1=non-Hispanic white) | 1.35 | 0.82–2.20 | .24 |
| Child’s sex (1=female) | 0.66 | 0.43–1.02 | .06 |
| Child’s BMI %ile | 0.99 | 0.96–1.02 | .49 |
| Parent education (1=college) | 2.46 | 1.46–4.13 | .001 |
| Child energy intake Total kcals | 0.93 | 0.89–0.97 | .002 |
| Sugar-sweetened beverage availability at home | 0.74 | 0.62–0.90 | .001 |
BMI indicates Body Mass Index. Child energy intake derived from Nutrition Data Systems for Research.
Note: multivariate logistic regression was used to examine associations between sociodemographic characteristics, household factors, family behavior patterns and children’s adherence to dietary and physical activity guidelines.
Screen time
In the multivariate model, children who met screen time viewing guidelines were more likely to have greater amounts of exercise/active play equipment available at home (OR = 1.12 95% CI 1.07–1.18) and fewer non-exercise media items available (OR = 0.65, 95% CI 0.57–0.74). Demographic covariates were not significantly related to adherence to screen time guidelines.
Physical activity
As illustrated in Figures 2a and 2b, respectively, interactions between child age and sex, and between age and BMI percentile, were significant. Although males and females were equally likely to meet guidelines in the younger years, females were much less likely to meet guidelines than males at older ages (≥ 6 years of age). Children with higher BMI percentiles (≥ 85th) were also much less likely to meet guidelines at older ages. Household variables were not significantly related to adherence to physical activity guidelines.
Figure 2.
Figure 2a. Percentage of children meeting recommended guidelines for physical activity as a function of age and sex
Figure 2b. Percentage of children meeting recommended guidelines for physical activity as a function of age and BMI percentile
Factors Associated with Adherence to Dietary Intake Guidelines
Total energy intake, home availability of food/beverage items (i) fruits/vegetables, (ii) unhealthy snacks, (iii) sugar-sweetened beverages), and family behavior patterns (i.e., eating fast food, family meals with the TV on) were examined as predictors of dietary guideline adherence (Table 2).
Fruit and vegetables
Children who met guidelines for fruit/vegetable consumption were more likely to be older (OR 1.25, 95% CI 1.05–1.49), and to consume more total calories (NDSR total Kcal, OR 1.06, 95% CI 1.01–1.12). Greater availability of fruits and vegetables in the home was also positively associated with guideline adherence (OR 1.11, 95% CI, 1.01–1.21) in the multivariable model. Females were less likely to meet fruit and vegetable guidelines (OR 0.54, 95% CI, 0.29–.099).
Sugar-sweetened beverages
Children who met guidelines for sugar-sweetened beverage avoidance were more likely to be younger (OR 0.85, 95% CI 0.75–0.97), to have parents with at least a college education (OR = 2.46, 95% CI 1.46–4.13), and to consume fewer overall calories (OR=.93, 95% CI .89–.97). Home availability of sugar-sweetened beverages was inversely associated guideline adherence (OR = 0.74, 95% CI 0.61–0.90).
DISCUSSION
This study examined rates of adherence to multiple physical activity and dietary intake guidelines in a cohort of children ages 5–10 years at risk for obesity but not yet obese. Subgroups having poor adherence to dietary and activity guidelines were identified, and risk factors for poor adherence were described. Only 1/3 of children in this sample met physical activity recommendations, and fewer than half met screen time recommendations. These findings are similar to previous studies with regards to screen time viewing, but lower than recent population-based estimates of physical activity guideline adherence21. Differences in adherence rates between this sample and population estimates are likely influenced by variations in measurement methods (i.e., accelerometry versus survey) and the BMI range of this cohort. Although 42 percent of children in this sample met guidelines for sugar-sweetened beverage avoidance, the proportion adhering to fruit and vegetable guidelines was smaller, generally consistent with estimated US population trends (e.g., 16–26% for fruit/vegetable consumption and 36% for sugar sweetened beverage avoidance)23,55,56. Contrary to predictions, no differences were observed in guideline adherence between children who were overweight and those at risk for overweight, likely due to the restricted range of BMI within this cohort. Qualitatively, overall rates of guideline adherence in this sample appear more similar to adherence rates among obese and overweight children than the general population of similarly aged children per se, particularly in regards to screen time viewing21 and fruit and vegetable consumption23.
This is the first study of 5 to 10 year old children at risk for obesity to present adherence rates across multiple dietary and physical activity guidelines, an approach that is necessary to provide a more complete picture of weight-related behaviors that may contribute to a child’s obesity risk. Of interest, few children met more than one guideline. Only 2% of children met all four of these guidelines, and a significant portion (19%) met none of the recommended guidelines. There was little overlap between screen time and physical activity guideline adherence with only 17% of children meeting both guidelines. Given that others have observed physical activity and sedentary behavior to be independent57, these findings are not unexpected, although there continues to be controversy as to whether screen time displaces physical activity58. There was also little overlap between children meeting fruit/vegetable and sugar-sweetened beverage guidelines, with only 8% meeting both guidelines.
Sociodemographic and household correlates of adherence to physical activity and screen time guidelines were specific to each domain. That is, lower levels of non-exercise media at home and higher levels of active play equipment were associated with screen time guideline adherence, but not with adherence to physical activity guidelines. Age, gender, and BMI were strongly associated with physical activity, but not screen time. Although 5-year-old girls and boys were equally likely to meet guidelines for physical activity, at 6–7 years of age, girls were significantly less likely to meet activity guidelines than boys, a pattern that continued through the upper age range of the cohort. While some studies have shown that physical activity levels tend to drop more sharply for girls compared to boys during adolescence59, these findings are consistent with other studies suggesting that gender differences in physical activity may be observed much earlier60,61, warranting early intervention to promote girls’ physical activity, particularly for those at risk for overweight and obesity.
Sociodemographic and household factors associated with fruit/vegetable and sweetened beverage adherence were also guideline specific, with the exception of child’s age. Older children were more likely to meet fruit and vegetable guidelines, but less likely to avoid sugar-sweetened beverages. Children who are older may have more exposure to sugar-sweetened beverages through increasing peer group influences and activities outside the home, which may facilitate consumption27, and be more willing to consume vegetables than their younger counterparts as prior studies have suggested55. As in other studies, children of parents who had at least a college education were more likely to meet guidelines for sugar-sweetened beverage consumption26. However, parental education was not associated with fruit and vegetable consumption. The low numbers of children meeting guidelines for fruit and vegetable consumption in this cohort (14%) may have reduced our ability to document associations between parental education and fruit and vegetable consumption. Household variables associated with dietary guideline adherence corresponded directly to specific guideline content, with availability of fruits and vegetables and sugar-sweetened beverages strongly associated with adherence, consistent with prior studies35,36. While significant at the univariate level, family behavior patterns, including fast food frequency and the frequency of eating family meals with the TV on, were not associated with adherence to dietary guidelines in multivariate models, likely due to the relatively low frequencies of these behaviors within this cohort. Frequency and number of parent-child shared physical activities were also not associated with guideline adherence.
Study results must be understood within the context of potential limitations. The study sample consisted of children with BMI percentiles between 70 and 95 whose parents agreed to participate in an obesity prevention intervention, and is not representative of the general population of children in this age range. Also limiting generalizability is the fact that the sample, while large, is predominantly white and well-educated. Due to time and budgetary constraints, this study used a single 24-hour dietary recall (as opposed to the three recall gold standard), which may not be representative of usual intake. Despite quality assurance efforts for administering and reviewing dietary recalls, parental under or over-reporting may have occurred. Given that other studies have shown that higher BMI tends to be associated with underreporting62,63 it is possible that the actual daily intakes of fruits/vegetables and sugar-sweetened beverages could have been underestimated. The home food availability measure had a restricted range of response options for families. Other factors potentially associated with both home availability and consumption (e.g., household income, child food preferences) and the accessibility of foods in the home (e.g., ready-to-eat carrots in a plastic bag) were not measured. Finally, given the cross-sectional nature of these data, conclusions about a causal role of demographic or household factors in children’s adherence to dietary and activity guidelines cannot be made. Nonetheless, these findings extend our understanding of factors that influence adherence to dietary and activity guidelines in children at risk for obesity.
IMPLICATIONS FOR RESEARCH AND PRACTICE
Understanding determinants of health-related behavior, particularly modifiable home environmental factors, can inform the development of interventions to impact children’s weight-related behavior and growth trajectories. In particular, the role of modifiable home environmental factors in adherence to dietary and activity guidelines has clear importance for obesity prevention efforts. Little overlap was found in adherence to guidelines for child physical activity, fruit and vegetable intake, screen time viewing, and avoidance of sugar sweetened beverages in this cohort of children who are overweight or at risk for overweight, which could suggest that families who are equipped to promote healthy child behavior patterns in one domain may not be so in others. Furthermore, each guideline had unique domain-specific predictors. Taken together, these findings suggest that interventions designed to promote adherence to dietary and activity guidelines for obesity prevention in children should be tailored to address the particular environmental factors relevant to the behavior of interest, and with sufficient flexibility to ensure that families work on the areas from which they would most benefit.
Acknowledgments
The Healthy Homes/Healthy Kids 5-10 Study is supported by the National Institute of Diabetes and Digestive and Kidney Diseases [R01DK084475 to N.E.S and R.L.L.] and is registered at www.clinicaltrials.gov (No. NCT01084590).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Medicine and science in sports and exercise. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Sibley BA, Etnier JL. The relationship between physical activity and cognition in children: a meta-analysis. Pediatric Exercise Science. 2003;15(3) [Google Scholar]
- 3.Brage S, Wedderkopp N, Ekelund U, et al. Features of the Metabolic Syndrome Are Associated With Objectively Measured Physical Activity and Fitness in Danish Children The European Youth Heart Study (EYHS) Diabetes care. 2004;27(9):2141–2148. doi: 10.2337/diacare.27.9.2141. [DOI] [PubMed] [Google Scholar]
- 4.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. British journal of sports medicine. 2011 doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- 5.Rey-Lopez JP, Vicente-Rodríguez G, Biosca M, Moreno LA. Sedentary behaviour and obesity development in children and adolescents. Nutrition, Metabolism and Cardiovascular Diseases. 2008;18(3):242–251. doi: 10.1016/j.numecd.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Hardy LL, Denney-Wilson E, Thrift AP, Okely AD, Baur LA. Screen time and metabolic risk factors among adolescents. Archives of Pediatrics & Adolescent Medicine. 2010;164(7):643–649. doi: 10.1001/archpediatrics.2010.88. [DOI] [PubMed] [Google Scholar]
- 7.Laurson KR, Eisenmann JC, Welk GJ, Wickel EE, Gentile DA, Walsh DA. Combined influence of physical activity and screen time recommendations on childhood overweight. The Journal of pediatrics. 2008;153(2):209–214. doi: 10.1016/j.jpeds.2008.02.042. [DOI] [PubMed] [Google Scholar]
- 8.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. The Lancet. 2001;357(9255):505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 9.Hung H-C, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease. Journal of the National Cancer Institute. 2004;96(21):1577–1584. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 10.van’t Veer P, Jansen M, Klerk M, Kok FJ. Fruits and vegetables in the prevention of cancer and cardiovascular disease. Public health nutrition. 2000;3(1):103–107. doi: 10.1017/s1368980000000136. [DOI] [PubMed] [Google Scholar]
- 11.Hancox RJ, Milne BJ, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. The Lancet. 2004;364(9430):257–262. doi: 10.1016/S0140-6736(04)16675-0. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics Council on Communications and Media. Policy statement: Children, adolescents, and the media. Pediatrics. 2013;132(5):958–961. doi: 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- 13.Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006 Feb;117(2):544–559. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 14.Active healthy living: prevention of childhood obesity through increased physical activity. Pediatrics. 2006 May;117(5):1834–1842. doi: 10.1542/peds.2006-0472. [DOI] [PubMed] [Google Scholar]
- 15.US Department of Agriculture Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7. Washington, DC: US Department of Agriculture; 2010. [Google Scholar]
- 16.Bergman P, Grjibovski AM, Hagströmer M, Bauman A, Sjöström M. Adherence to physical activity recommendations and the influence of socio-demographic correlates–a population-based cross-sectional study. BMC Public Health. 2008;8(1):367. doi: 10.1186/1471-2458-8-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butcher K, Sallis JF, Mayer JA, Woodruff S. Correlates of physical activity guideline compliance for adolescents in 100 US cities. Journal of Adolescent Health. 2008;42(4):360–368. doi: 10.1016/j.jadohealth.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dolinsky DH, Brouwer RJN, Østbye T, Evenson KR, Siega-Riz AM. Peer Reviewed: Correlates of Sedentary Time and Physical Activity Among Preschool-Aged Children. Preventing chronic disease. 2011;8(6) [PMC free article] [PubMed] [Google Scholar]
- 19.Cutler GJ, Flood A, Hannan P, Neumark-Sztainer D. Multiple sociodemographic and socioenvironmental characteristics are correlated with major patterns of dietary intake in adolescents. Journal of the American Dietetic Association. 2011;111(2):230–240. doi: 10.1016/j.jada.2010.10.052. [DOI] [PubMed] [Google Scholar]
- 20.Pabayo R, Spence JC, Cutumisu N, Casey L, Storey K. Sociodemographic, behavioural and environmental correlates of sweetened beverage consumption among pre-school children. Public health nutrition. 2012;15(08):1338–1346. doi: 10.1017/S1368980011003557. [DOI] [PubMed] [Google Scholar]
- 21.Fakhouri TH, Hughes JP, Brody DJ, Kit BK, Ogden CL. Physical Activity and Screen-Time Viewing Among Elementary School–Aged Children in the United States From 2009 to 2010. JAMA pediatrics. 2013;167(3):223–229. doi: 10.1001/2013.jamapediatrics.122. [DOI] [PubMed] [Google Scholar]
- 22.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013 Jul;98(1):180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lorson BA, Melgar-Quinonez HR, Taylor CA. Correlates of fruit and vegetable intakes in US children. Journal of the American Dietetic Association. 2009;109(3):474–478. doi: 10.1016/j.jada.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 24.Yeh M-C, Ickes SB, Lowenstein LM, et al. Understanding barriers and facilitators of fruit and vegetable consumption among a diverse multi-ethnic population in the USA. Health Promotion International. 2008;23(1):42–51. doi: 10.1093/heapro/dam044. [DOI] [PubMed] [Google Scholar]
- 25.Van der Horst K, Kremers S, Ferreira I, Singh A, Oenema A, Brug J. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health education research. 2007;22(2):295–304. doi: 10.1093/her/cyl080. [DOI] [PubMed] [Google Scholar]
- 26.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. Journal of the Academy of Nutrition and Dietetics. 2013;113(1):43–53. doi: 10.1016/j.jand.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.French SA, Lin B-H, Guthrie JF. National trends in soft drink consumption among children and adolescents age 6 to 17 years: prevalence, amounts, and sources, 1977/1978 to 1994/1998. Journal of the American Dietetic Association. 2003;103(10):1326–1331. doi: 10.1016/s0002-8223(03)01076-9. [DOI] [PubMed] [Google Scholar]
- 28.Striegel-Moore RH, Thompson D, Affenito SG, et al. Correlates of beverage intake in adolescent girls: the National Heart, Lung, and Blood Institute Growth and Health Study. The Journal of pediatrics. 2006;148(2):183–187. doi: 10.1016/j.jpeds.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 29.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 30.Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. Int J Behav Nutr Phys Act. 2012;9:88. doi: 10.1186/1479-5868-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Granich J, Rosenberg M, Knuiman MW, Timperio A. Individual, social, and physical environment factors associated with electronic media use among children: sedentary behavior at home. Journal of physical activity & health. 2011;8(5) doi: 10.1123/jpah.8.5.613. [DOI] [PubMed] [Google Scholar]
- 32.Cillero IH, Jago R. Sociodemographic and home environment predictors of screen viewing among Spanish school children. Journal of public health. 2011;33(3):392–402. doi: 10.1093/pubmed/fdq087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maitland C, Stratton G, Foster S, Braham R, Rosenberg M. A place for play? The influence of the home physical environment on children’s physical activity and sedentary behaviour. International Journal of Behavioral Nutrition and Physical Activity. 2013;10(1):99. doi: 10.1186/1479-5868-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Medicine and Science in Sports and Exercise. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Spurrier NJ, Magarey AA, Golley R, Curnow F, Sawyer MG. International Journal of Behavioral Nutrition and Physical Activity. International Journal of Behavioral Nutrition and Physical Activity. 2008;5:31. doi: 10.1186/1479-5868-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reinaerts E, de Nooijer J, Candel M, de Vries N. Explaining school children’s fruit and vegetable consumption: the contributions of availability, accessibility, exposure, parental consumption and habit in addition to psychosocial factors. Appetite. 2007;48(2):248–258. doi: 10.1016/j.appet.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 37.Ezendam NP, Evans AE, Stigler MH, Brug J, Oenema A. Cognitive and home environmental predictors of change in sugar-sweetened beverage consumption among adolescents. British journal of nutrition. 2010;103(05):768–774. doi: 10.1017/S0007114509992297. [DOI] [PubMed] [Google Scholar]
- 38.Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Preventive medicine. 2003;37(3):198–208. doi: 10.1016/s0091-7435(03)00114-2. [DOI] [PubMed] [Google Scholar]
- 39.Coon KA, Goldberg J, Rogers BL, Tucker KL. Relationships between use of television during meals and children’s food consumption patterns. Pediatrics. 2001 Jan;107(1):E7. doi: 10.1542/peds.107.1.e7. [DOI] [PubMed] [Google Scholar]
- 40.Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113(1):112–118. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 41.Sherwood NE, Levy RL, Langer SL, et al. Healthy Homes/Healthy Kids: A randomized trial of a pediatric primary care-based obesity prevention intervention for at-risk 5–10 year olds. Contemporary clinical trials. 2013;36(1):228–243. doi: 10.1016/j.cct.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flodmark C-E, Marcus C, Britton M. Interventions to prevent obesity in children and adolescents: a systematic literature review. International journal of obesity. 2006;30(4):579–589. doi: 10.1038/sj.ijo.0803290. [DOI] [PubMed] [Google Scholar]
- 43.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short-and long-term beneficial effects of a combined dietary–behavioral–physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115(4):e443–e449. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 44.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. Journal of Sports Sciences. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 45.Schmitz KH, Harnack L, Fulton JE, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. Journal of School Health. 2004;74(9):370–377. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]
- 46.Klerman JA, Bartlett S, Wilde P, Olsho L. The Short-Run Impact of the Healthy Incentives Pilot Program on Fruit and Vegetable Intake. American Journal of Agricultural Economics. 2014:aau023. doi: 10.3945/ajcn.115.129320. [DOI] [PubMed] [Google Scholar]
- 47.Wojcicki JM, Heyman MB. Reducing childhood obesity by eliminating 100% fruit juice. American Journal of Public Health. 2012;102(9):1630–1633. doi: 10.2105/AJPH.2012.300719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Statistics NCfH, Control CfD. 2000 CDC Growth Charts: United States. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2003. [Google Scholar]
- 49.Raynor HA, Polley BA, Wing RR, Jeffery RW. Is dietary fat intake related to liking or household availability of high- and low-fat foods? Obesity research. 2004 May;12(5):816–823. doi: 10.1038/oby.2004.98. [DOI] [PubMed] [Google Scholar]
- 50.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. 1990 Jan;1(1):58–64. doi: 10.1097/00001648-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 51.Sherwood NE, Crain AL, Martinson BC, et al. Keep it off: a phone-based intervention for long-term weight-loss maintenance. Contemporary clinical trials. 2011 Jul;32(4):551–560. doi: 10.1016/j.cct.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boutelle KN, Fulkerson JA, Neumark-Sztainer D, Story M, French SA. Fast food for family meals: relationships with parent and adolescent food intake, home food availability and weight status. Public health nutrition. 2007 Jan;10(1):16–23. doi: 10.1017/S136898000721794X. [DOI] [PubMed] [Google Scholar]
- 53.Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004 Feb;158(2):170–176. doi: 10.1001/archpedi.158.2.170. [DOI] [PubMed] [Google Scholar]
- 54.McGarvey E, Keller A, Forrester M, Williams E, Seward D, Suttle DE. Feasibility and Benefits of a Parent-Focused Preschool Child Obesity Intervention. Am J Public Health. 2004 Sep 1;94(9):1490–1495. doi: 10.2105/ajph.94.9.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim SA, Moore LV, Galuska D, et al. Vital Signs: Fruit and Vegetable Intake Among Children—United States, 2003–2010. MMWR Morbidity and mortality weekly report. 2014;63(31):671–676. [PMC free article] [PubMed] [Google Scholar]
- 56.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. Journal of the Academy of Nutrition and Dietetics. 2012;112(5):624–635. e626. doi: 10.1016/j.jand.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leatherdale ST, Wong S. Peer Reviewed: Association Between Sedentary Behavior, Physical Activity, and Obesity: Inactivity Among Active Kids. Preventing chronic disease. 2009;6(1) [PMC free article] [PubMed] [Google Scholar]
- 58.Biddle SJ, Gorely T, Marshall SJ, Murdey I, Cameron N. Physical activity and sedentary behaviours in youth: issues and controversies. The Journal of the Royal Society for the Promotion of Health. 2004;124(1):29–33. doi: 10.1177/146642400312400110. [DOI] [PubMed] [Google Scholar]
- 59.Kimm SY, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. New England Journal of Medicine. 2002;347(10):709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 60.Finn K, Johannsen N, Specker B. Factors associated with physical activity in preschool children. The Journal of pediatrics. 2002;140(1):81–85. doi: 10.1067/mpd.2002.120693. [DOI] [PubMed] [Google Scholar]
- 61.Hinkley T, Crawford D, Salmon J, Okely AD, Hesketh K. Preschool children and physical activity: a review of correlates. American journal of preventive medicine. 2008;34(5):435–441. e437. doi: 10.1016/j.amepre.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 62.Savage JS, Mitchell DC, Smiciklas-Wright H, Symons Downs D, Birch LL. Plausible reports of energy intake may predict body mass index in pre-adolescent girls. Journal of the American Dietetic Association. 2008;108(1):131–135. doi: 10.1016/j.jada.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Singh R, Martin BR, Hickey Y, et al. Comparison of self-reported and measured metabolizable energy intake with total energy expenditure in overweight teens. The American journal of clinical nutrition. 2009;89(6):1744–1750. doi: 10.3945/ajcn.2008.26752. [DOI] [PMC free article] [PubMed] [Google Scholar]