Abstract
Background
Mindfulness (the ability to attend nonjudgmentally to one’s own physical and mental processes) is receiving substantial interest as a potential determinant of health. However, little is known whether mindfulness is associated with cardiovascular health.
Purpose
The aim of this study is to evaluate whether dispositional mindfulness is associated with cardiovascular health.
Method
Study participants (n=382) were from the New England Family Study, born in Providence, RI, USA, with mean age 47 years. Dispositional mindfulness was assessed using the Mindful Attention Awareness Scale (MAAS). Cardiovascular health was assessed based on American Heart Association criteria. Cross-sectional multivariable-adjusted log binomial regression analyses were performed.
Results
Analyses demonstrated that those with high vs. low MAAS had prevalence ratio (PR) for good cardiovascular health of 1.83 (95 % confidence interval (CI) 1.07, 3.13), adjusted for age, gender, and race/ethnicity. There were significant associations of high vs. low mindfulness with non-smoking (PR=1.37, 95 % CI 1.06, 1.76), body mass index <25 kg/m2 (PR=2.17, 95 % CI 1.16, 4.07), fasting glucose <100 mg/dL (PR = 1.47, 95 % CI 1.06, 2.04), and high physical activity (PR = 1.56, 95 % CI 1.04, 2.35), but not blood pressure, total cholesterol, or fruit/vegetable consumption. Exploratory mediation analyses suggested that sense of control and depressive symptomatology may be mediators.
Conclusion
This study demonstrated preliminary cross-sectional evidence that dispositional mindfulness is positively associated with cardiovascular health, with the associations particularly driven by smoking, body mass index, fasting glucose, and physical activity. If in future research mindfulness-based practices are found to consistently improve cardio-vascular disease risk factors, such interventions may have potential to strengthen effects of cardiovascular health promotion programs.
Keywords: Mindfulness, Cardiovascular health, Epidemiology, Prevention
Introduction
Cardiovascular disease (CVD) remains the primary cause of mortality worldwide [1]. Historically, CVD incidence has typically increased as societies became more industrialized, due in part to creating conditions that foster easier access to palatable, calorie-dense foods, cigarettes, and sedentary life-styles [2]. In these settings, there are concerns with craving and addiction to high caloric palatable foods, sedentary activities (e.g., electronic screen use), and smoking [3-5]. Recent preliminary findings suggest mindfulness may help curb these CVD risk behaviors [5-19].
Mindfulness can be defined as the ability to attend in a nonjudgmental way to one’s own physical and mental processes during ordinary, everyday tasks [20]. “Dispositional mindfulness” has been considered to be an inherent, yet modifiable, trait, where all people have varying capacities to attend and to be aware of what is occurring in the present moment [21]. Dispositional mindfulness is likely influenced by both genetic and environmental factors [22]. Consequently, it is useful to understand associations of this naturally occurring trait with CVD risk. If such associations exist, they would provide the basis for investigating dispositional mindfulness as a target to improve cardiovascular health. Dispositional mindfulness appears to be modifiable, and a number of mindfulness-based interventions have been developed [22]. Mindfulness-based interventions have been shown to be effective in relapse prevention for substance use, including smoking [6, 23]. The interventions may work in part through improving self-regulation and sense of control, where sensations and thoughts are noted but not always acted upon [24]. Mindfulness may help people to take a step back from their thoughts, sensations, and emotions (called reperceiving) and notice that their thoughts, sensations, and emotions (e.g., craving for ice cream or a cigarette) are passing events not needed to act on [24, 25]. Furthermore, it may work in part through improvements in self-awareness (e.g., increased awareness of one’s sedentary lifestyle and its effects on well-being) [24]. In addition, mindfulness may help improve mental health, where depressive symptomatology has been demonstrated in randomized controlled trials (RCTs) to improve using mindfulness-based interventions [26]. Depression itself is a CVD risk marker and may influence CVD behavioral risk factors [27-29].
In measuring CVD risk, the American Heart Association recommended assessing cardiovascular health, where ideal cardiovascular health is defined as healthy levels of seven CVD risk factors, specifically blood pressure, total cholesterol, fasting glucose, body mass index, smoking, diet, and physical activity [30]. This may be a particularly useful construct for measuring cardiovascular effects of mindfulness, as mindfulness may have specific effects on different CVD risk factors, depending on the particular genetics, environment, and personality of each individual. For example, someone who grew up in a household with parents who smoked may have particular use of mindfulness to notice deeply entrenched norms of smoking within themselves and be aware of these thoughts and sensations as they arise, but not act on them to actually initiate smoking. For another person who has a predisposition to toward consumption of sweet, fatty foods, mindfulness may be useful to notice cravings for high caloric palatable foods, and let those thoughts pass. In this way, assessing cardiovascular health evaluates overall cardiovascular effects of mindfulness that may influence multiple CVD risk factors.
Associations of dispositional mindfulness with cardiovascular health to our knowledge have not yet been investigated. Furthermore, potential mediating mechanisms between mindfulness and cardiovascular health, such as sense of control and depression, have not been explored. Consequently, the primary objective of this study was to evaluate whether dispositional mindfulness is associated with cardiovascular health. Secondary objectives were to assess which components of cardiovascular health may be driving any observed associations of mindfulness with cardiovascular health. Further exploratory objectives that are hypothesis generating, given the cross-sectional nature of the data, were to evaluate potential mediators such as sense of control and depressive symptomatology.
Methods
Sample
Study participants were from the New England Family Study (NEFS), which includes 17,921 offspring of pregnant women in the Collaborative Perinatal Project (CPP), born at the Providence, RI, and Boston, MA, sites (USA) between 1959 and 1974 [31]. The current NEFS sub-study, named the Longitudinal Effects on Aging Perinatal (LEAP) Project, was composed of Providence-born participants. Participants were assessed during 2010–2011. There were 1,400 participants randomly selected with preference for racial/ethnic minorities, of which 796 participants were eligible for assessment (i.e., not deceased, not incarcerated, had assessments taken at age 7 years, and were located and lived within 100 mi of the clinical assessment site). Of the 796 eligible participants, we were unable to establish contact with 274 (34 %) of participants within the relatively brief 13-month data collection period, leaving 522 participants who were contacted and invited to participate in the study. Of the 522 participants, 19 % (n=95) refused to participate in the study, and a further 5% (n=27) agreed to participate but were unable to schedule assessments within the data collection period. This left 400 participants on whom assessments were made. In this sample (n=400), 23 % (n=122) of participants were non-white (95 black participants, 13 Native American, and 14 other race/ethnicity). We excluded nine participants who did not complete the Mindful Attention Awareness Scale (MAAS), eight missing data for the covariate educational attainment, and five missing information on sense of control, resulting in a total of 18 participants excluded. Accordingly, the sample size was 382 participants, which represented 48 % of the eligible population. Of the 400 participants assessed, included (n=382) participants were similar to excluded (n=18) participants for the MAAS score (4.7 vs. 5.0, respectively), good cardiovascular health (24.4 vs. 22.2 %, respectively), and covariates including age, sex, depressive symptomatology, education, smoking, total cholesterol, diabetes, systolic blood pressure, diastolic blood pressure, body mass index (BMI), fruit/vegetable consumption, and physical activity (p>0.05). There was evidence of differences between included (n=382) vs. excluded (n=18) participants for race/ethnicity (66.5 vs. 35.5 % white race/ethnicity, respectively, p=0.004). Analyses comparing included participants (n=382) with the 1,400 participants randomly selected from the original CPP study showed significantly higher female participants in the included sample (57 vs. 52 %; p=0.02) but no differences in race/ethnicity or age (p>0.05). The study protocol was approved by the institutional review boards at Brown University and Memorial Hospital of Rhode Island.
Independent Variable
The MAAS is a 15-item questionnaire of dispositional mindfulness in which respondents indicate, on a six-point Likert-type scale (1=almost always to 6=almost never), their level of awareness and attention to present events and experiences [21]. Sample MAAS items include “I find it difficult to stay focused on what’s happening in the present,” “I break or spill things because of carelessness, not paying attention, or thinking of something else,” and “I could be experiencing some emotion and not be conscious of it until some time later” [21]. The MAAS has been shown to have a single factor structure [21] and appears to emphasize an element related to dissociation and absent-mindedness [32]. A mean score is calculated (range 1.00–6.00), where higher scores reflect greater self-reported attention and awareness, or “dispositional mindfulness.” The scale exhibits good internal consistency (Cronbach’s α=0.82–0.87) and high test-retest reliability over a 1-month period (intraclass correlation=0.81, p<0.0001) [21, 32]. The MAAS score has been shown to be positively related to long-term meditation experience, where Zen meditators were shown to have higher MAAS scores than age- and sex-matched community members [21], and Thai monks showed higher MAAS scores than Thai or American students [33]. A systematic review and meta-analysis showed randomized controlled trials that evaluate impacts of mindfulness training on self-reported mindfulness scores, including the MAAS, show overall improvements in self-reported mindfulness in relation to wait-list control groups, but not in relation to active control groups [34]. The convergent and discriminant validity of the MAAS has been evaluated, and it appears to tap a single construct where higher scorers on the MAAS tend to be more aware of and receptive to inner experiences and are more mindful of their overt behavior [21]. High MAAS scorers are more aware of their emotional states and able to alter them and are more likely to fulfill basic psychological needs [21]. Furthermore, higher MAAS scorers are less likely to be self-conscious, socially anxious and ruminative than low scorers [21]. Questions about the defining characteristics of mindfulness continue be discussed between scientists and traditional mindfulness practitioners, some who feel current definitions do not fully reflect the classical intent of mindfulness practices [35]. However, the MAAS is one of the most commonly used and accepted mindfulness measures at this time [22].
Dependent Variable
Ideal cardiovascular health was defined by the American Heart Association as the absence of clinically manifest CVD and simultaneous presence of optimal levels of all seven health behaviors (smoking avoidance, physical activity, lean body mass, healthy diet) and health factors (untreated total cholesterol <200 mg/dL, untreated blood pressure <120 mmHg systolic/<80 mmHg diastolic, untreated fasting blood glucose <100 mg/dL) [36]. Measurement of cardiovascular health in this study was designed to be similar to the American Heart Association definition and included the following ideal level definitions: smoking, never smoker or quit >12 months ago; BMI, <25 kg/m2; total cholesterol, <200 mg/dL and no cholesterol medication; fasting glucose, <100 mg/ dL and no diabetes medication; blood pressure, systolic <120 and diastolic <80 mmHg and no antihypertensive medication; fruit/vegetable consumption, ≥5 servings of fruit and/or vegetables per day; and physical activity, International Physical Activity Questionnaire category “high.” A dichotomous cardiovascular health score was created based on American Heart Association criteria [30], where good cardiovascular health was defined as ≥4 cardiovascular health components at the ideal levels described above, and poor CV health was <4 cardiovascular health components at ideal levels. Summing the number of cardiovascular health components at ideal levels is a standard approach for studies on cardiovascular health [37]. The percent of participants who had 0, 1, 2, 3, 4, 5, 6, or 7 cardiovascular health components at ideal levels was 7, 18, 27, 23, 16, 7, 2, and 0 %, respectively. Providing a cut-point of ≥4 cardiovascular health components at ideal levels represented 25 % of participants, providing adequate statistical power for analyses.
Current smoking and past history of smoking were assessed via self-report. Glucose and total cholesterol were measured enzymatically in plasma samples at CERLab (Harvard Medical School, Boston, MA) with the Roche P Modular system using reagents and calibrators from Roche Diagnostics (Indianapolis, IN), described elsewhere [38, 39]. These assays are approved by the Food and Drug Administration for clinical use. CERLab is certified by the Centers for Disease Control and Prevention/National Heart, Lung, and Blood Institute Lipid Standardization Program. At cholesterol concentrations of 132.8 and 280.4 mg/dL, the day-to-day reproducibility (CV), was 1.7 and 1.6 %, respectively. Glucose at the concentrations of 90 and 312 mg/dL showed day-to-day variability (CV) of 1.7 and 1.6 %, respectively. Systolic and diastolic blood pressures were assessed by certified research nurses using mercury sphygmomanometers, in seated participants with arms at heart level, resting 5 min prior to assessment, consistent with American Heart Association guidelines [40]. The mean of the second and third blood pressure readings was used. Due to a lack of micronutrient data for elaborate diet measures, we used fruit and vegetable consumption to assess diet as it is an established determinant of cardiovascular disease; we utilized standard criteria for a minimum of ≥5 fruit and/or vegetables consumed per day for the ideal category [41]. Self-reported physical activity during the previous week was assessed using the International Physical Activity Questionnaire Short Form with validation described elsewhere [42, 43]. This questionnaire codes high physical activity as having ≥1 of the following: (a) vigorous-intensity activity ≥3 days and accumulating ≥1,500 metabolic equivalent of task (MET)-min/week; (b) ≥7 days of any combination of walking, moderate-intensity or vigorous intensity activities achieving ≥3,000 MET-min/week.
Covariates
Age was directly assessed via date of birth (recorded directly in this birth cohort), subtracted from clinic visit date. Sex was self-reported. Race/ethnicity was self-reported in adulthood. In rare cases that it was missing (n=11), race/ethnicity obtained prenatally from mother was used. Depressive symptomatology was computed as the sum of responses from the ten-item Center for Epidemiologic Studies Depression Scale (CES-D) (range 0–30) and dicohotomized based on previously described scores of <10 vs. ≥10 [44]. Education was categorized as ≤high school vs. >high school. Sense of control was assessed via the Pearlin and Schooler Mastery Scale (range 7–35) with good internal consistency (Cronbach’s α=0.71) and categorized as > vs. ≤the median score of 14, where higher scores represent lower sense of control [45].
Analytic Methods
Multivariable-adjusted regression analyses evaluated associations of MAAS score with cardiovascular health. Analyses prioritized calculating multivariable-adjusted prevalence ratios utilizing log-binomial regression described elsewhere, given the data were cross-sectional and outcome prevalence was >10 % [46]. Primary analyses utilized a categorical exposure variable, called “MAAS score level.” Participants were likely to report fairly high mindfulness levels, where the number of participants with MAAS score of 1.00–2.00, 2.01–3.00, 3.01–4.00, 4.01–5.00, and 5.01–6.00 was 7 (1.8 %), 17 (4.5 %), 57 (14.9 %), 127 (33.3 %), and 174 (45.6 %), respectively. Consequently, we utilized MAAS score-driven cut-points to allow for analyses to evaluate associations of low (MAAS score<4; n=77) and medium MAAS levels (MAAS score 4–5; n=131), in relation to high MAAS levels (MAAS score >5, n=174), all with reasonable sample sizes to allow for adequate statistical power. Sensitivity analyses were performed using MAAS score quartiles and tertiles. The dependent variable was dichotomous “good” vs. “poor” cardiovascular health, described above. Statistical tests of a product term between mindfulness and sex, and mindfulness and race/ethnicity, demonstrated no significant effect measure modification (p=0.50 and 0.82, respectively); consequently, analyses were pooled by sex and race/ethnicity.
Multivariable regression analyses were adjusted for age, sex, and race/ethnicity. We further assessed whether depressive symptomatology, sense of control, and education were potential mediators in the association between mindfulness and cardiovascular health using formal mediation methods based on the counterfactual framework, which allows for decomposition of a total effect into direct and indirect effects, even in models with interactions and nonlinearities [47]. The indirect effect is the part of the total effect that operates through a particular mediating pathway. Examining indirect effects provides evidence of whether mindfulness may exert its effects uniquely through any of the potential mediators examined in this study. Percentile based 95 % confidence intervals were estimated via bootstrapping with 1,000 samples with replacement. Due to common issues of log-binomial models not converging for mediation analyses [47], we utilized linear regression analyses evaluating associations of MAAS level and each potential mediator, with number (range 0–7) of ideal cardiovascular health components. Analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Descriptive unadjusted characteristics demonstrated significant associations of MAAS level with age, depressive symptomatology, sense of control, smoking, and physical activity (Table 1). Further descriptive characteristics are shown for covariates stratified by cardiovascular health status in Table 2. These findings demonstrated significant associations of cardiovascular health status with sex, race/ethnicity, depressive symptomatology, sense of control, and education.
Table 1.
Unadjusted participant characteristics for the entire sample (overall) and stratified by Mindful Attention Awareness Scale (MAAS) level
| Overall | MAAS levela |
p valueb | |||
|---|---|---|---|---|---|
| Low (n=77) | Medium (n=131) | High (n=174) | |||
| Cardiovascular health components | |||||
| Smoking, % ideal | 61 (56, 66) | 49 (38, 61) | 60 (52, 69) | 66 (59, 73) | 0.01 |
| BMI, % ideal | 23 (19, 27) | 13 (5, 21) | 27 (19, 34) | 24 (18, 31) | 0.11 |
| Total cholesterol, % ideal | 47 (42, 52) | 45 (33, 56) | 44 (36, 53) | 49 (42, 57) | 0.42 |
| Diabetes status, % ideal | 51 (45, 56) | 40 (28, 52) | 51 (41, 61) | 56 (47, 64) | 0.05 |
| Blood pressure, % ideal | 34 (29, 39) | 38 (27, 49) | 34 (26, 42) | 32 (25, 39) | 0.34 |
| Fruit/vegetable consumption, % ideal | 14 (11, 18) | 13 (5, 21) | 12 (6, 17) | 17 (11, 23) | 0.30 |
| Physical activity, % ideal | 40 (35, 45) | 27 (17, 38) | 41 (32, 50) | 45 (37, 52) | 0.02 |
| Confounders | |||||
| Age, years | 47.0 (46.8, 47.1) | 46.8 (46.4, 47.1) | 46.8 (46.5, 47.0) | 47.2 (46.9, 47.5) | 0.03 |
| Sex, % female | 57 (52, 62) | 65 (54, 76) | 57 (49, 66) | 53 (45, 60) | 0.08 |
| Race/ethnicity, % white | 66 (62, 71) | 68 (57, 78) | 71 (63, 79) | 63 (55, 70) | 0.29 |
| Potential mediators | |||||
| Depressive symptoms, % CESD ≥10 | 30 (26, 35) | 65 (54, 76) | 34 (25, 42) | 12 (7, 17) | <0.001 |
| Sense of control, % with score >14 | 48 (43, 54) | 74 (64, 84) | 50 (41, 58) | 36 (29, 43) | <0.001 |
| Education, % ≤high school | 70 (66, 75) | 73 (63, 83) | 70 (62, 78) | 70 (63, 76) | 0.66 |
Point estimates represent means or percentages (95 % confidence intervals)
BMI body mass index, CESD Center for Epidemiologic Studies Depression Scale
MAAS levels represent the following MAAS scores (range 1–6): low, <4; medium, 4–5; high, >5
p values derived from ANOVA for continuous variable and chi-squared tests for categorical variables
Table 2.
Participant characteristics of confounders and potential mediators, stratified by ideal cardiovascular health status
| Cardiovascular health statusa |
p valueb | ||
|---|---|---|---|
| Not good (n=289) | Good (n=93) | ||
| Confounders | |||
| Age, years | 47.0 (46.8, 47.2) | 46.8 (46.4 ,47.1) | 0.11 |
| Sex, % female | 53 (47, 59) | 68 (58, 77) | 0.01 |
| Race/ethnicity, % white | 63 (58, 69) | 76 (67, 85) | 0.02 |
| Potential mediators | |||
| Depressive symptoms, % CESD ≥10 | 34 (29, 40) | 18 (10, 25) | 0.002 |
| Sense of control, % with score >14 | 52 (46, 58) | 39 (29, 48) | 0.03 |
| Education, % ≤high school | 76 (71, 81) | 52 (42, 62) | <0.001 |
Point estimates represent means or percentages (95% confidence intervals)
CESD Center for Epidemiologic Studies Depression Scale
Good cardiovascular health represents having ≥4 ideal cardiovascular health components
p values derived from unpaired t test for continuous variable and chi-squared tests for categorical variables
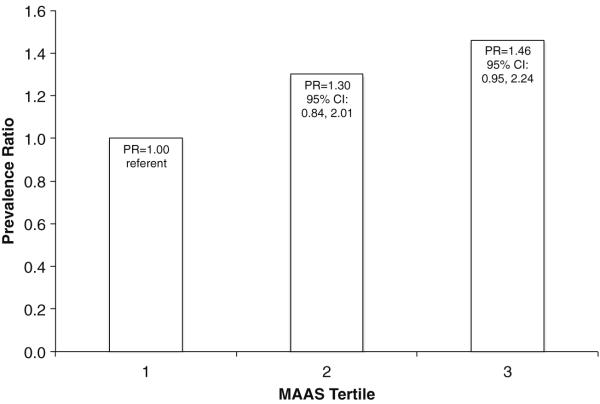
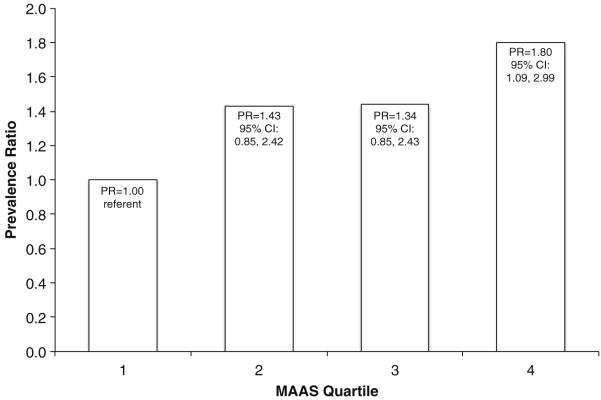
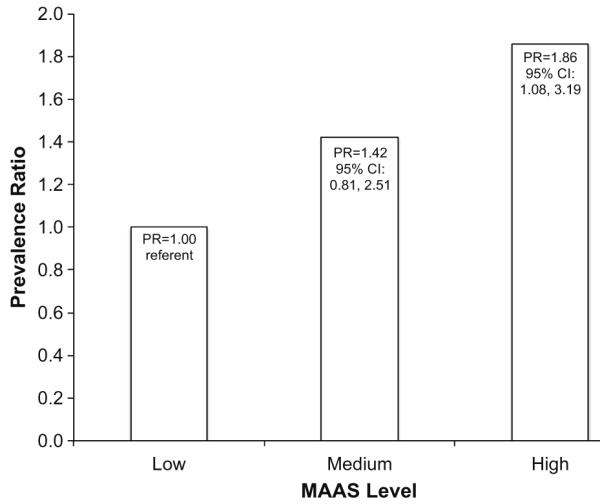
Multivariable adjusted log-binomial regression analyses demonstrated prevalence ratio (PR) of 1.86 (95 % confidence interval (CI) 1.08, 3.19) for associations of high vs. low MAAS level with good cardiovascular health, adjusted for age, sex, and race/ethnicity (Fig. 1). Similar associations were found in analyses using MAAS quartiles or tertiles, where prevalence ratios were 1.80 (95 % CI 1.09, 2.99) or 1.46 (95 % CI 0.95, 2.24), respectively (Appendix Figs. 2 and 3).
Fig. 1.
Prevalence ratios (95 % confidence intervals) of good cardiovascular health according to mindfulness level, adjusted for age, sex, and race/ethnicity. Point estimates represent prevalence ratios of having ≥4 ideal cardiovascular health components per Mindful Attention Awareness Scale (MAAS) level. MAAS levels represent the following MAAS scores (range 1–6): Low, <4 (n=77), Medium, 4–5 (n=131), High, >5 (n=174)
Fig. 2.
Prevalence ratios (95 % confidence intervals) of good cardiovascular health according to mindfulness tertile, adjusted for age, sex, and race/ethnicity. Point estimates represent prevalence ratios of having ≥4 ideal cardiovascular health components per Mindful Attention Awareness Scale (MAAS) tertile. Tertiles 1 and 3 represent the lowest and highest MAAS tertile, respectively. Sample sizes for tertiles 1, 2, and 3 are 128, 123, and 131, respectively
Fig. 3.
Prevalence ratios (95 % confidence intervals) of good cardiovascular health according to mindfulness quartile, adjusted for age, sex, and race/ethnicity. Point estimates represent prevalence ratios of having ≥4 ideal cardiovascular health components per Mindful Attention Awareness Scale (MAAS) quartile. Quartiles 1 and 4 represent the lowest and highest MAAS quartile, respectively. Sample sizes for quartiles 1, 2, 3, and 4 are 94, 91, 103, and 94, respectively
Mediation analyses provided evidence of depressive symptomatology and sense of control, but not education, as mediators. In these analyses, effect sizes represent regression beta estimates for high or medium vs. low MAAS level, in relation to number (range 0–7) of ideal cardiovascular health factors. The total effect of high vs. low MAAS level on cardiovascular health was 0.69 (95 % CI 0.32, 1.05) additional ideal cardiovascular health factors, adjusted for age, race/ethnicity, and gender (Table 3). Indirect effects for depressive symptomatology, sense of control, and education were 0.26 (95 % CI 0.05, 0.48), 0.24 (95 % CI 0.08, 0.44), and 0.04 (95 % CI −0.04, 0.14), respectively, additional ideal cardiovascular health factors for high vs. low MAAS level. This demonstrated that 0.26, 0.24, and 0.04 of the 0.69 total effects may be mediated through depressive symptomatology, sense of control, and education, respectively.
Table 3.
Mediation analyses showing direct and indirect effects of sense of control, depressive symptomatology, and education for associations of Mindful Attention Awareness Scale (MAAS) level with ideal cardiovascular health
| MAAS levela |
|||
|---|---|---|---|
| High (n=174) | Medium (n=131) | Low (n=77) | |
| Total effect model | 0.69 (0.32, 1.05) | 0.38 (−0.02, 0.77) | 0 (ref) |
| Direct effect models | |||
| Depressive symptoms | 0.42 (0.02, 0.78) | 0.21 (−0.19, 0.62) | 0 (ref) |
| Sense of control | 0.45 (0.07, 0.83) | 0.23 (−0.14, 0.60) | 0 (ref) |
| Education | 0.63 (0.30, 0.94) | 0.34 (−0.01, 0.73) | 0 (ref) |
| Indirect effect models | |||
| Depressive symptoms | 0.26 (0.05, 0.48) | 0.17 (0.03, 0.35) | 0 (ref) |
| Sense of control | 0.24 (0.08, 0.44) | 0.15 (0.04, 0.29) | 0 (ref) |
| Education | 0.04 (−0.04, 0.14) | 0.03 (−0.09, 0.15) | 0 (ref) |
Effect sizes (95 % confidence intervals) represent regression beta estimates for high or medium vs. low MAAS level, in relation to number (range 0–7) of ideal cardiovascular health components. All analyses are adjusted for age, race/ethnicity, and gender
ref referent category
MAAS levels represent the following MAAS scores (range 1–6): low, <4; medium, 4–5; high, >5
In order to evaluate if there were specific CVD risk factors that may be particularly important for the observed associations of mindfulness with cardiovascular health, log-binomial regression analyses evaluated associations of MAAS score level with each of the seven cardiovascular health components, adjusted for age, sex, and race/ethnicity. Analyses demonstrated significant associations of high vs. low mindfulness with ideal levels of smoking (PR = 1.37, 95 % CI 1.06, 1.76), BMI (PR = 2.17, 95 % CI 1.16, 4.07), fasting glucose (PR = 1.47, 95 % CI 1.06, 2.04), and physical activity (PR = 1.56, 95 % CI 1.04, 2.35; Table 4). There were no significant associations of mindfulness with blood pressure, total cholesterol, or fruit/vegetable consumption (Table 4).
Table 4.
Multivariable-adjusted regression analyses evaluating associations of the Mindful Attention Awareness Scale (MAAS) score with subcomponents of cardiovascular health
| Ideal cardiovascular health component | PR (95 % CI) | p value |
|---|---|---|
| Smoking (never smoker or quit >12 months ago) | ||
| High mindfulness | 1.37 (1.06, 1.76) | 0.01 |
| Medium mindfulness | 1.23 (0.95, 1.61) | 0.12 |
| Low mindfulness | 1.00 | |
| Body mass index (<25 kg/m2) | ||
| High mindfulness | 2.17 (1.16, 4.07) | 0.02 |
| Medium mindfulness | 2.09 (1.11, 3.95) | 0.02 |
| Low mindfulness | 1.00 | |
| Total cholesterol (TC <200 mg/dL and no cholesterol medication) | ||
| High mindfulness | 1.14 (0.85, 1.53) | 0.38 |
| Medium mindfulness | 0.99 (0.73, 1.36) | 0.97 |
| Low mindfulness | 1.00 | |
| Fasting glucose (<100 mg/dL and no diabetes medication) | ||
| High mindfulness | 1.47 (1.06, 2.04) | 0.02 |
| Medium mindfulness | 1.28 (0.90, 1.81) | 0.16 |
| Low mindfulness | 1.00 | |
| Blood pressure (SBP <120 and DBP <80 mmHg and no AH) | ||
| High mindfulness | 0.91 (0.66, 1.26) | 0.58 |
| Medium mindfulness | 0.84 (0.60, 1.18) | 0.31 |
| Low mindfulness | 1.00 | |
| Fruit/vegetable consumption (≥5 fruit and vegetable servings per day) | ||
| High mindfulness | 1.35 (0.70, 2.63) | 0.37 |
| Medium mindfulness | 0.92 (0.44, 1.94) | 0.83 |
| Low mindfulness | 1.00 | |
| Physical activity (IPAQ category “high”) | ||
| High mindfulness | 1.56 (1.04, 2.35) | 0.03 |
| Medium mindfulness | 1.53 (1.00, 2.33) | 0.05 |
| Low mindfulness | 1.00 | |
Point estimates (95 % confidence intervals) represent prevalence ratios (PRs) for likelihood of having ideal level of each cardiovascular health component per MAAS level. Treatment goals are as follows: total cholesterol, <200 mg/dL; diabetes, <100 mg/dL; blood pressure, SBP<120 and DBF<80 mmHg
MAAS levels represent the following MAAS scores (range 1–6): low, <4; medium, 4–5; high, >5
AH antihypertensive medication, CI confidence interval, DBP diastolic blood pressure, IPAQ International Physical Activity Questionnaire, PR prevalence ratio, SBP systolic blood pressure, TC total cholesterol
Discussion
Results from these cross-sectional analyses provided preliminary evidence that dispositional mindfulness is positively associated with cardiovascular health. Findings suggested that sense of control and depressive symptomatology may be mediators. Furthermore, smoking, BMI, fasting glucose, and physical activity appeared to be the most important cardiovascular health components responsible for observed associations of dispositional mindfulness with cardiovascular health. These findings, due to their cross-sectional nature, should be interpreted with caution. Future longitudinal studies and mindfulness interventions will provide stronger evidence on whether mindfulness influences cardiovascular health. However, to our knowledge, no longitudinal data that can answer this question currently exist; consequently, these findings are an early indication of possible associations.
Prior Literature
This study’s findings showing positive associations of dispositional mindfulness with cardiovascular health to our knowledge are completely novel. Findings that demonstrated mindfulness was associated with several of CV health subcomponents are in general agreement with the limited amount of scientifically rigorous literature to date.
With regard to smoking, a recent systematic review found evidence that mindfulness-based interventions were associated with significantly lower smoking outcomes in three of four studies [6]. One of the most methodologically rigorous randomized controlled trials to date demonstrated a 31 % smoking abstinence rate for those randomized to mindfulness training vs. 6 % in the active control group at 17 weeks follow-up (p=0.012) [7]. Another study showed that a mindful attention intervention reduced self-reported craving to smoking images and reduced neural activity in a craving-related region of subgenual anterior cingulate cortex [48]. These intervention findings are supported by a recent meta-analysis of 11 observational studies that showed significant inverse associations between dispositional mindfulness and smoking (aggregate r=−0.14; p<0.001) [49] consistent with findings in the current study.
With regard to obesity, to our knowledge, this is the first study to evaluate associations of dispositional mindfulness with directly assessed BMI. However, a number of studies evaluated impacts of mindfulness interventions on weight loss. A recent systematic review stated that nine of ten mindfulness-based intervention studies demonstrated weight loss or stabilized weight; however, the review included studies with and without control groups [5]. Another systematic review demonstrated weight loss in all six mindfulness interventions that used control groups; however, effects were often not statically significant, likely in part due to small sample sizes and low statistical power for most studies (n=27–108) [8]. There is evidence of potential floor effects of interventions, where effects may be greatest in participants of higher weight [12] and in participants who are currently attempting to lose weight [9, 11]. These preliminary findings of mindfulness interventions associated with weight loss are consistent with the current study that showed inverse associations of dispositional mindfulness with BMI.
For diabetes, although associations of dispositional mindfulness with fasting glucose or diabetes have, to our knowledge, not been evaluated, a number of studies evaluated impacts of mindfulness interventions on diabetes control. Studies found evidence of an effect of acceptance and commitment therapy (ACT) on likelihood to have HbA1c in the target range (HbA1C<7 %) [14], but no evidence of effect of mindfulness-based stress reduction (MBSR) or mindfulness-based cognitive therapy (MBCT) on diabetes control [15]. The current study adds to the small amount of literature on this topic evidence that dispositional mindfulness may be positively associated with ideal fasting glucose levels.
Very little is known about associations of mindfulness with physical activity. One cross-sectional study in 266 participants demonstrated dispositional mindfulness was positively associated with being more successful at maintaining an exercise program at a YMCA [50]. The current study adds evidence to this limited field of knowledge that mindfulness may be positively associated with physical activity.
With regard to the lack of association found in our study of mindfulness with blood pressure, lipids and fruit and vegetable consumption, this study adds to the literature showing mixed findings with blood pressure [17-19] and lipids [16], and to our knowledge, no previous findings on associations of mindfulness with fruit and vegetable consumption.
Mechanisms
We explored three potential mediators of the association between mindfulness and cardiovascular health, specifically sense of control, depressive symptomatology, and education.
The current study found evidence of mediation for sense of control. It has been suggested that mindful, compared to less mindful, people have greater awareness of their behavioral routines and precursors driving behavior, and that because they pay greater attention to their behaviors, they have improved abilities to initiate or prevent the behavior itself [21, 51-53]. For example, a prospective study found that participants with greater dispositional mindfulness were more likely to enact their physical activity intentions than those with lesser dispositional mindfulness [51]. With regard to depressive symptomatology, both dispositional mindfulness and mindfulness interventions are related to more positive affect including reduced anxiety and depression [21, 25, 26]. Negative affect, such as depressive symptomatology, is one of the main risk factors for maintaining addictive behaviors such as cigarette smoking [27] and is negatively related to CVD behavioral risk factors such as adhering to dietary changes, smoking cessation recommendations, antihypertensive regimens, and glycemic control recommendations [28]. Depression is itself a risk marker for CVD [29]. The current study findings demonstrated evidence of depressive symptomatology as a mediator between mindfulness and CVD risk. As mindfulness interventions have been shown to improve test scores [54], education is a risk marker for CVD [55], and measures of socioeconomic position such as education often have important impacts on study findings, we felt it was worthwhile to evaluate education as a potential mediator. Results showed that mindfulness was not associated with education, and there was no evidence of mediation by education in analyses.
Strengths and Limitations
As study participants were born in Providence, RI, findings may pertain more to urban-born participants of the northeast region of the USA. Future larger, representative study samples will provide more generalizable information. Additionally, the independent variable, mediators, and dependent variable were measured based on cross-sectional study design, as such analyses could not rule out associations between the exposure, mediators, and outcome being due to reverse causation. Future longitudinal observational studies and mindfulness randomized controlled trials will provide stronger evidence for causal inference. A further limitation is that the assessment of mindfulness is without a gold standard, and there is current debate on the accuracy of self-reported mindfulness [56, 57]. All scales, including the MAAS, imperfectly measure the constructs at which they aim. The developers of the MAAS consider it a tool of a developing science, not a finished product [56] (please see the “Methods” section for a summary of MAAS construct validity). Finally, findings using self-reported physical activity should be interpreted with caution as the validity of self-reported assessments are substantially less than direct assessments of physical activity [43]. Strengths of the study include accurate measurement of biological measures (e.g., lipids, glucose, blood pressure, and BMI), using substantial internal and external quality control protocols. Furthermore, novel causal mediation methods based on the counter-factual framework were used [47].
Conclusion
This study demonstrated that mindfulness is positively associated with cardiovascular health and that sense of control and depressive symptomatology may be mediating mechanisms. Furthermore, smoking, body mass index, fasting glucose, and physical activity appeared to be the most important drivers of observed associations of mindfulness with cardiovascular health. These preliminary cross-sectional findings on associations of dispositional mindfulness with cardiovascular health are hypothesis generating, and suggest that there would be benefits of performing longitudinal research studies that evaluate whether mindfulness-based interventions consistently improve cardiovascular risk factors and outcomes with clinically relevant effect sizes.
Acknowledgments
Funding for this study was provided by NIH/NIA grant 1RC2AG036666.
Footnotes
Ethical Standards All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
Conflict of Interest Eric Loucks, Willoughby Britton, Chanelle Howe, Charles Eaton and Stephen Buka declare that they have no conflict of interest.
References
- 1.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. World Health Organization; Geneva: 2011. [Google Scholar]
- 2.Ezeamama AE, Viali S, Tuitele J, McGarvey ST. The influence of socioeconomic factors on cardiovascular disease risk factors in the context of economic development in the Samoan archipelago. Soc Sci Med. 2006;63(10):2533–45. doi: 10.1016/j.socscimed.2006.06.023. doi:10.1016/j.socscimed.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 3.Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1–2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. doi:10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brand M, Young KS, Laier C. Prefrontal control and internet addiction: a theoretical model and review of neuropsychological and neuroimaging findings. Front Hum Neurosci. 2014;8:375. doi: 10.3389/fnhum.2014.00375. doi:10. 3389/fnhum.2014.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–61. doi: 10.1111/obr.12156. doi:10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carim-Todd L, Mitchell SH, Oken BS. Mind-body practices: an alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug Alcohol Depend. 2013;132(3):399–410. doi: 10.1016/j.drugalcdep.2013.04.014. doi:10.1016/j.drugalcdep.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brewer JA, Sinha R, Chen JA, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Subst Abus. 2009;30(4):306–17. doi: 10.1080/08897070903250241. doi:10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204. doi: 10.1016/j.eatbeh.2014.01.005. doi:10.1016/j.eatbeh.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. doi:10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 10.Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52(2):396–404. doi: 10.1016/j.appet.2008.11.012. doi:10.1016/j. appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Mantzios M, Giannou K. Group vs. single mindfulness meditation: exploring avoidance, impulsivity, and weight management in two separate mindfulness meditation settings. Appl Psychol Health Well-Being. 2014 doi: 10.1111/aphw.12023. doi:10.1111/aphw.12023. [DOI] [PubMed] [Google Scholar]
- 12.Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:651936. doi: 10.1155/2011/651936. doi:10.1155/2011/651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hebert JR, Ebbeling CB, Olendzki BC, et al. Change in women’s diet and body mass following intensive intervention for early-stage breast cancer. J Am Diet Assoc. 2001;101(4):421–31. doi: 10.1016/S0002-8223(01)00109-2. doi:10.1016/S0002-8223(01)00109-2. [DOI] [PubMed] [Google Scholar]
- 14.Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–43. doi: 10.1037/0022-006X.75.2.336. doi:10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 15.Hartmann M, Kopf S, Kircher C, et al. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-study) Diabetes Care. 2012;35(5):945–7. doi: 10.2337/dc11-1343. doi:10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel C, Marmot MG, Terry DJ, Carruthers M, Hunt B, Patel M. Trial of relaxation in reducing coronary risk: four year follow up. Br Med J (Clin Res Ed) 1985;290(6475):1103–6. doi: 10.1136/bmj.290.6475.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hughes JW, Fresco DM, Myerscough R, van Dulmen M, Carlson LE, Josephson R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom Med. 2013;75:721–8. doi: 10.1097/PSY.0b013e3182a3e4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blom K, Baker B, How M, et al. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the harmony randomized controlled trial. Am J Hypertens. 2013 doi: 10.1093/ajh/hpt134. doi:10. 1093/ajh/hpt134. [DOI] [PubMed] [Google Scholar]
- 19.Abbott RA, Whear R, Rodgers LR, et al. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J Psychosom Res. 2014;76(5):341–51. doi: 10.1016/j.jpsychores.2014.02.012. doi:10.1016/j.jpsychores.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 20.Epstein RM. Mindful practice. JAMA. 1999;282(9):833–9. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 21.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–48. doi: 10.1037/0022-3514.84.4.822. doi:10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 22.Park T, Reilly-Spong M, Gross CR. Mindfulness: a systematic review of instruments to measure an emergent patient-reported outcome (PRO) Qual Life Res. 2013;22(10):2639–59. doi: 10.1007/s11136-013-0395-8. doi:10.1007/s11136-013-0395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bowen S, Witkiewitz K, Clifasefi SL, et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2013.4546. doi:10.1001/jamapsychiatry. 2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6(6):537–59. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 25.Sedlmeier P, Eberth J, Schwarz M, et al. The psychological effects of meditation: a meta-analysis. Psychol Bull. 2012;138(6):1139–71. doi: 10.1037/a0028168. doi:10.1037/a0028168. [DOI] [PubMed] [Google Scholar]
- 26.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–68. doi: 10.1001/jamainternmed.2013.13018. doi:10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: contrasting affective and physical models of dependence. J Consult Clin Psychol. 2002;70(1):216–27. [PubMed] [Google Scholar]
- 28.Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58(3):175–89. doi: 10.1016/j.biopsych.2005.05.001. doi:10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241–9. doi: 10.1001/jama.2011.1282. doi:10. 1001/jama.2011.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 31.Niswander K, Gordon M. The women and their pregnancies: the Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. National Institutes of Health; Washington DC: 1972. [Google Scholar]
- 32.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. doi:10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 33.Christopher MS, Christopher V, Charoensuk S. Assessing “Western” mindfulness among Thai Theravada Buddhist monks. Ment Health Relig Cult. 2009;12(3):303–14. [Google Scholar]
- 34.Visted E, Jollestad J, Nielsen MB, Nielsen GH. The impact of group-based mindfulness training on self-reported mindfulness: a systematic review and meta-analysis. Mindfulness. 2014 doi:10. 1007/s12671-014-0283-5. [Google Scholar]
- 35.Rapgay L, Bystrisky A. Classical mindfulness: an introduction to its theory and practice for clinical application. Ann N Y Acad Sci. 2009;1172:148–62. doi: 10.1111/j.1749-6632.2009.04405.x. doi:10.1111/j.1749-6632.2009.04405.x. [DOI] [PubMed] [Google Scholar]
- 36.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–220. doi: 10.1161/CIR.0b013e31823ac046. doi:10.1161/CIR. 0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245. doi: 10.1161/CIR.0b013e31828124ad. doi:10.1161/CIR. 0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20(4):470–5. [PubMed] [Google Scholar]
- 39.Sacks D. Carbohydrates. In: Burtis C, Ashwood E, editors. Tietz textbook of clinical chemsitry. Saunders; Philadelphia: 1999. pp. 750–808. [Google Scholar]
- 40.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. doi:10.1161/01.CIR.0000154900.76284. F6. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization . Fruit and vegetables for health: Report of a joint FAO-WHO workshop. Kobe, Japan: 2004. [Google Scholar]
- 42.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. doi:10.1249/01.MSS. 0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 43.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQSF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115. doi:10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CESD (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 45.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 46.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 47.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–50. doi: 10.1037/a0031034. doi:10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, Tindle HA. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Soc Cogn Affect Neurosci. 2013;8(1):73–84. doi: 10.1093/scan/nsr076. doi:10.1093/scan/nsr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Karyadi KA, VanderVeen JD, Cyders MA. A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug Alcohol Depend. 2014 doi: 10.1016/j.drugalcdep.2014.07.014. doi:10.1016/j.drugalcdep.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ulmer CS, Stetson BA, Salmon PG. Mindfulness and acceptance are associated with exercise maintenance in YMCA exercisers. Behav Res Ther. 2010;48(8):805–9. doi: 10.1016/j.brat.2010.04.009. doi:10.1016/j.brat.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 51.Chatzisarantis NL, Hagger MS. Mindfulness and the intention-behavior relationship within the theory of planned behavior. Pers Soc P sychol Bull. 2007;33(5):663–76. doi: 10.1177/0146167206297401. doi: 10.1177 / 0146167206297401. [DOI] [PubMed] [Google Scholar]
- 52.Chambers R, Lo BCY, Allen NB. The impact of intensive mindfulness training on attentional control, cognitive style, and affect. Cogn Ther Res. 2008;32(3):303–22. doi:10.1007/S10608-007-9119-0. [Google Scholar]
- 53.Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cogn Affect Behav Neurosci. 2007;7(2):109–19. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- 54.Mrazek MD, Franklin MS, Phillips DT, Baird B, Schooler JW. Mindfulness training improves working memory capacity and GRE performance while reducing mind wandering. Psychol Sci. 2013;24(5):776–81. doi: 10.1177/0956797612459659. doi:10.1177/0956797612459659. [DOI] [PubMed] [Google Scholar]
- 55.Manrique-Garcia E, Sidorchuk A, Hallqvist J, Moradi T. Socioeconomic position and incidence of acute myocardial infarction: a meta-analysis. J Epidemiol Community Health. 2011;65(4):301–9. doi: 10.1136/jech.2009.104075. doi:10.1136/jech.2009.104075. [DOI] [PubMed] [Google Scholar]
- 56.Brown KW, Ryan RM, Loverich TM, Biegel GM, West AM. Out of the armchair and into the streets: measuring mindfulness advances knowledge and improves interventions: reply to Grossman (2011) Psychol Assess. 2011;23(4):1041–6. doi:10.1037/A0025781. [Google Scholar]
- 57.Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re) invention of mindfulness: comment on Brown (2011) Psychol Assess. 2011;23(4):1034–40. doi: 10.1037/a0022713. [DOI] [PubMed] [Google Scholar]