Abstract
Background:
Residual radiological lesions may persist even after successful treatment of tuberculosis. There is insufficient data as to the nature and magnitude of these opacities in the treated cases of tuberculosis.
Aims and Objectives:
This study evaluates the nature and magnitude of residual radiological opacities and of complete radiological resolution in new successfully treated cases of tuberculosis.
Design:
Four hundred and forty one new cases of pulmonary, pleural or mediastinal tuberculosis were radiologically evaluated by chest x-ray, PA view, at the start and end of a successful treatment, which was as per the World Health Organization (WHO), Revised National Tuberculosis Control Program (RNTCP), and Directly Observed Treatment, Short-Course (DOTS) guidelines. Patients with a previous history of tuberculosis or other lung conditions, treatment failure, retreatment cases, and multidrug tuberculosis (MDR-TB) cases were excluded.
Results:
Residual x-ray lesions were seen in 178 cases of tuberculosis (40.36%). Complete radiological resolution was seen in 263 cases (59.64%). Of the residual lesions, 67.4% were parenchymal were parenchymal in nature, 23.59% were pleural lesions and 8.99% were mediastinal lesions. Out of the 126 sputum-positive cases, 70% (n = 88)had residual lesions on chest x-ray whereas of the 315 sputum-negative cases 28.5%, (n = 99) had radiological residual lesions.
Conclusion:
Residual radiological opacities are seen in a large proportion of treated cases of tuberculosis (40%). Pulmonary lesions show more residual lesions (67%) than pleural (23%) and mediastinal lesions (9%).
KEY WORDS: Antitubercular treatment, fibrosis, post tuberculosis, sequelae
INTRODUCTION
Tuberculosis is a chronic infection that is associated with widespread morbidity and mortality. The WHO estimates the global incidence of TB to be 8.6 million cases each year, with a mortality of 1.3 million.[1] India is among the countries with the highest burden of TB, accounting for one-fifth of the global burden. It is important to understand the pathogenesis of tuberculosis in order to realise what minor and major damages might remain even after proper treatment of the disease. Mycobacterium tuberculosis spreads via the inhalation route. Once in the alveoli, macrophages ingest the bacilli. If these cells are unable to completely eradicate the bacilli, intracellular multiplication occurs and the bacilli spread further toward the regional lymph nodes.[2] In an immunocompetent person, development of specific immunity is generally sufficient to limit multiplication of the bacilli; the host remains asymptomatic and the lesions heal with resorption of caseous necrosis, fibrosis, and calcification. Immunocompromised persons may develop progressive disease with dissemination.[3] Some bacilli can remain dormant and reactivate causing post primary tuberculosis. Therefore, various residual lesions and complications can occur following tubercular infection at any of the points described in the pathogenesis.
A variety of residual lesions and complications can occur in both treated and untreated cases of pulmonary tuberculosis. Kim et al. describes these sequelae and complications under various headings: (a) Parenchymal lesions, which include tuberculoma, cavity, cicatrization, end-stage lung destruction, aspergilloma, and bronchogenic carcinoma; (b) airway lesions, such as, bronchiectasis, tracheobronchial stenosis, and broncholithiasis; (c) vascular lesions: Pulmonary or bronchial arteritis and thrombosis, bronchial artery dilatation, and Rasmussen aneurysm; (d) mediastinal lesions, which include lymph node calcification, fistula of the esophagomediastinum or esophagobronchial, constrictive pericarditis, and fibrosing mediastinitis; (e) pleural lesions, such as, chronic empyema, fibrothorax, bronchopleural fistula, pleural calcification, and pneumothorax; and (f) chest wall lesions, which include rib tuberculosis, tuberculous spondylitis, and malignancy associated with chronic empyema.[4]
In this article, we describe the proportion of residual pleural, parenchymal, and mediastinal lesions, as evidenced on a chest x-ray following treatment of new cases of tuberculosis.
MATERIALS AND METHODS
Study type
It was a retrospective observational study. Chest x-rays of patients who were diagnosed and treated with antitubercular treatment were studied prior to starting the treatment and at the end of their treatment.
Patient characteristics
The records of patients who attended the Outpatient Department of a tertiary care hospital in New Delhi, who were treated for tuberculosis were studied.
Patients who presented with symptoms of cough or fever, hemoptysis, weight loss or loss of appetite and other chest complains such as, chest pain and breathlessness were all evaluated with a chest x-ray. Those who were suspected of pulmonary tuberculosis based on history or a chest x-ray were subjected to at least two sputum examinations for acid fast bacilli. Patients were diagnosed as suffering from tuberculosis either based on history and sputum examination positive for acid fast bacilli or based on history and radiological lesions. Treatment regimens were oral medications according to the Revised National Tuberculosis Control Program of India (RNTCP) recommendations.[5] All patients who were declared cured, as evidenced by their records citing stopping treatment after an adequate duration due to improvement of symptoms and sputum conversion in case of sputum-positive tuberculosis, were included in the study. Patients with a previous history of antitubercular treatment or those who had a radiological picture suggestive of previous tuberculosis-like pleural calcification or parenchymal calcification were excluded from the study list. Also, those who did not respond to initial anti-tubercular treatment and required further workup for treatment failure and multidrug-resistant tuberculosis were excluded from the study. Patients presenting with other concomitant respiratory diseases, such as, chronic obstructive pulmonary diseases, interstitial lung disease, and bronchiectasis were excluded from the study.
Methods
Radiological lesions were classified into parenchymal, pleural, and mediastinal, depending on the dominant x-ray picture visualized on a posterior-anterior plain x-ray film. At the end of the treatment, the chest x-rays were studied for the remaining sequelae and categorized into pleural, parenchymal, and mediastinal.
The severity of the lesion was classified on a chest x-ray using the classification of the National Tuberculosis and Respiratory Disease Association of the USA, into four groups:[6]
Minimal lesion
Moderate
Moderately advanced
Far Advanced.
RESULTS
A total of 441 new cases of pulmonary, pleural, and mediastinal tuberculosis were included in the study. Males comprised of 63.8% of the total and females, 36.2% of the total cases. One hundred and twenty-six cases (28.6%) were sputum-positive and 315 cases (71.4%) were sputum-negative tuberculosis.
Residual x-ray lesions were observed in 178 cases of tuberculosis. They formed 40.36% of the total cases. Complete radiological resolution was seen in 263 cases (59.64%); 67.41% of the residual lesions were parenchymal in nature, 23.59% of total were pleural lesions, and 8.99% were mediastinal lesions [Figure 1].
Figure 1.
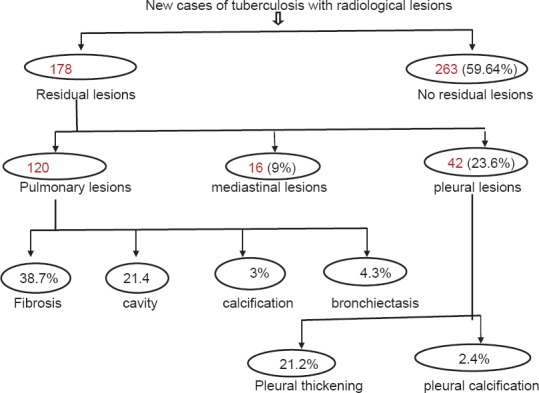
Flow diagram depicting the findings of the study
Out of a total 120 cases with residual pulmonary lesions, we observed that 38.7% were suggestive of fibrosis, 21.4% were cavity-related, 3% were pulmonary calcifications, and 4.3% were cases of bronchiectasis [Figure 2].
Figure 2.
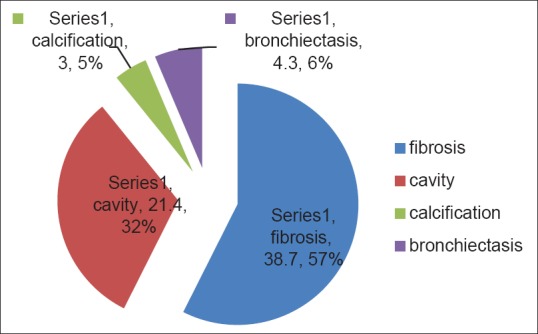
Proportion of parenchymal residual lesions
Forty-two cases (23.59%) had residual pleural lesions; 21.2% of these consisted of pleural thickening, and 2.4% consisted of pleural calcification.
Mediastinal opacities were observed in 16 (8.99%) of the total cases, with residual lesions that consisted of partially resolved mediastinal lymphadenopathy.
Out of 126 sputum-positive cases, 70% had residual lesions, comprising of a total of 88 cases with residual lesions on their chest x-rays [Figure 3].
Figure 3.
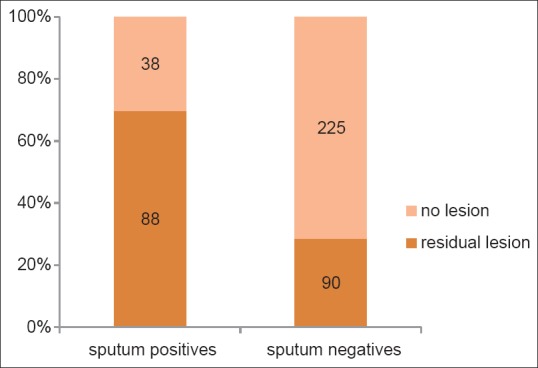
Proportion of sputum-positive and sputum-negative with residual lesions
Out of 315 sputum-negative cases 28.5%, that is, a total of 90 had radiological residual lesions [Figure 3].
Using the National TB and Respiratory Disease Association of the USA classification to grade the severity of the lesion on chest x-ray, 55.7% of the patients had minimal residual lesions, 22.8% had moderate, 15.2% had moderately advanced cases, and 6% had a far advanced lesion. Fifteen percent had overlap lesions (either parenchymal and pleural or parenchymal mediastinal or mediastinal, pleural, and parenchymal).
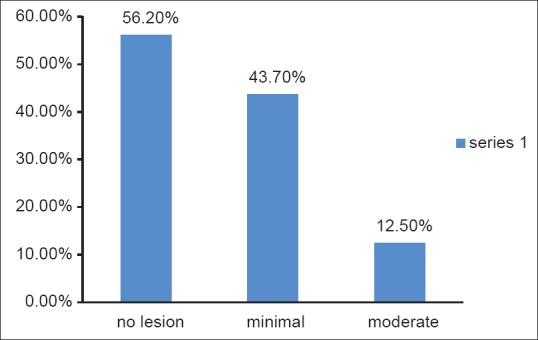
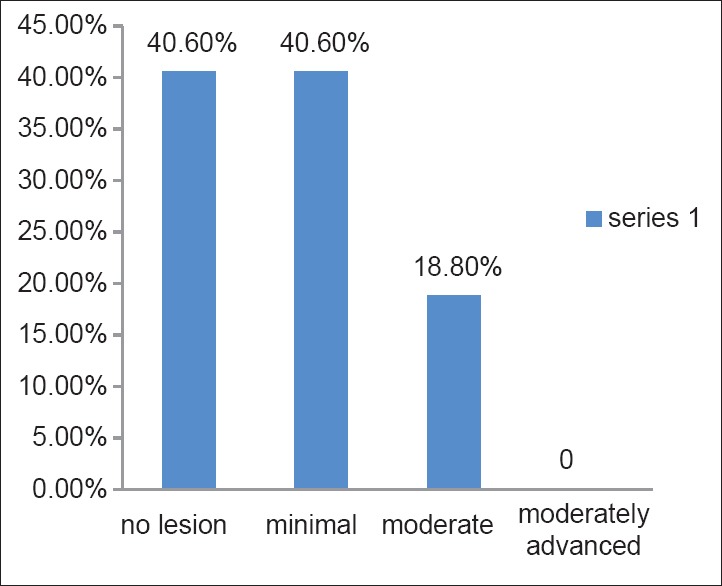
Figure 4 depicts the radiological progression of a minimal lesion before ATT to a different severity after ATT. Likewise, Figure 5 depicts the radiological progression of a moderate lesion. Figure 6 shows the progression of a moderately advanced lesion, and Figure 7 depicts the radiological progression of a far advanced lesion.
Figure 4.
Radiological progression of the minimal lesion after ATT
Figure 5.
Radiological progression of a moderate lesion, after ATT, to a different severity
Figure 6.
Radiological progression of a moderately advanced lesion after ATT
Figure 7.

Radiological progression of a far advanced lesion after ATT
DISCUSSION
In this study, we observed that despite adequate chemotherapy and adequate clinical response in new cases of tuberculosis, a large proportion of patients are left with residual radiological sequelae.
Pulmonary tuberculosis with parenchymal involvement is the most common form of tuberculosis.[1] Therefore, it is not surprising to observe that the maximum number of cases in our study have been with parenchymal involvement, and so it forms the maximum number with residual lesions. Up to 40% of the patients with post primary tuberculosis have a marked fibrotic response, which manifests as atelectasis of the upper lobe with retraction of the hilum, compensatory lower lobe hyperinflation, and a mediastinal shift toward the fibrotic lung.[7,8] Similar findings were observed in our study where 38.7% of the patients with pulmonary involvement had shadows suggestive of fibrosis.
Hatipoglu et al. observed that bronchiectasis is seen in 30 - 60% of the patients with active post primary tuberculosis and in 71 - 86% of the patients with inactive disease, on high-resolution CT.[9] In contrast, we found only a small proportion had bronchiectasis as a sequelae (4.3%). However, one reason may be that we assessed the sequelae only with a chest x-ray and not with computed tomography, which has a greater sensitivity. Bronchiectasis and residual cavities are sequelae usually found in the upper lobes.
The incidence of mediastinal lymphadenopathy is the highest during childhood and it decreases with increasing age.[10] This could be one of the reasons for our observation of a mediastinal residual lesion forming the lowest proportion, as our patients consisted of an age group of 18 to 60 years. It is observed that with anti-tubercular treatment, the nodes may either disappear or form a residual mass composed of fibrotic tissue and calcifications.[11] A residual mediastinal lesion in our patients was a partially resolved mediastinal widening (lymphadenopathy).
Tuberculous pleuritis usually resolves completely even in the absence of treatment.[12] However, in some patients, chronic complications occur during the healing of the tuberculosis lesions or appear as late sequelae. Pleural residual lesions in the form of pleural thickening, pleural calcification, and fibrothorax have been described post tuberculsosis.[13] Kwon and colleagues observed that at the end of antituberculous medication for pleural effusion, the incidence of residual pleural opacity was 68.3% (40 out of 60 cases) on CT.[14] In our study pleural residual lesions formed 23.6% of the total.
A delay in the time period from the onset of symptoms to treatment initiation might contribute to a greater spread and progression of lung lesions leading to more residual damage.[15] Furthermore, it is possible that some patients mount a more severe inflammatory response in an attempt to control the foreign organism, thereby leading to more destruction of self-tissues. How much do hosts or environmental factors contribute to the development of residual sequelae remains to be explored.
In addition we observed that a greater proportion of sputum-positive tuberculosis had a residual lesion, as compared to sputum-negative cases. Seventy percent of the sputum-positive cases were left with residual lesions, whereas, 28.5% of the sputum-negative cases had residual lesions. This could be because of a higher bacterial load in the sputum-positive cases, which caused more damage.
It is possible that in those cases that did not have any residual lesion on chest x-ray after treatment, the lesions healed before necrosis developed.[15]
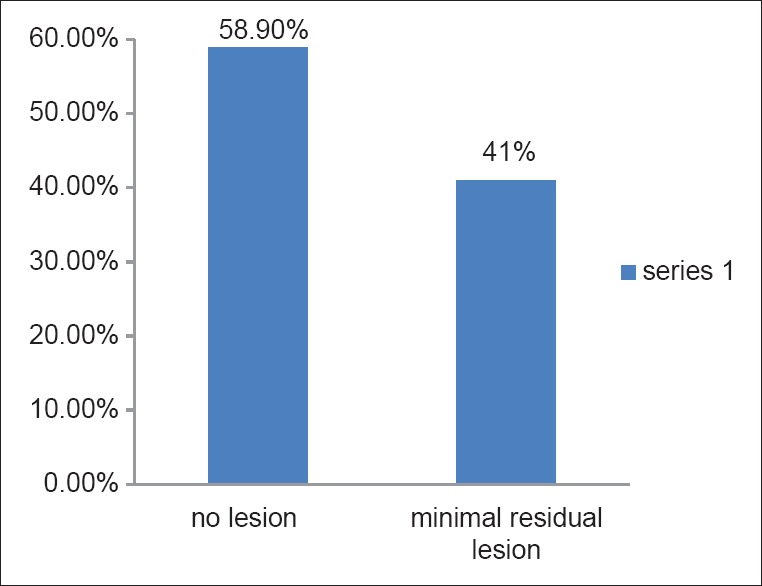
Despite the fact that severe lesions at the start of ATT might lead to severe lesions after completion, it was not the case in this study. Minimal, moderate, and moderately advanced lesions, as seen before ATT led to no residual lesions in the maximum number of the cases. No residual lesions were seen in 58.9% of the cases after ATT from among those that began with a minimal lesion before ATT, no residual lesion was seen in 56.2% of those that began with a moderate lesion, and no residual lesion after ATT was seen in 40.6% of those that began with a moderately advanced lesion. An exception was seen in the far advanced lesion before ATT. In this group, the proportion of a severe x-ray was larger than the proportion with no residual lesion; 30.8% had moderately advanced lesions compared to 23% that formed the group with no residual lesion.
Limitations
We did not measure the time that lapsed between symptom presentation and treatment initiation. This could have been compared among those who had residual lesions and those who did not have lesions.
CONCLUSION
There are very limited studies on the residual lesions of tuberculosis. Even more sparse is the availability of literature on residual lesions following successful treatment of tuberculosis. Further studies are needed to explore the genetic and environmental factors that make an individual susceptible to residual lesions as compared to another.
Footnotes
Source of Support: The authors would like to declare that there was no help, either financial or for equipment, from any source
Conflict of Interest: The authors declare no conflict of interests.
REFERENCES
- 1.World Health Organisation. Global Tuberculosis Report 2013. Geneva: WHO; 2013. p. 1. [Google Scholar]
- 2.Leung AN. Pulmonary tuberculosis: The essentials. Radiology. 1999;210:307–22. doi: 10.1148/radiology.210.2.r99ja34307. [DOI] [PubMed] [Google Scholar]
- 3.Bass JR, Farer LS, Hopewell PC, Jacobs RF, Snider DE., Jr Diagnostic standards and classification of tuberculosis. Am Rev Respir Dis. 1990;142:725–35. doi: 10.1164/ajrccm/142.3.725. [DOI] [PubMed] [Google Scholar]
- 4.Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH. Thoracic sequelae and complications of tuberculosis. Radiographics. 2001;21:839–60. doi: 10.1148/radiographics.21.4.g01jl06839. [DOI] [PubMed] [Google Scholar]
- 5.Chauhan LS, Agarwal SP. The Revised National Tuberculosis Control Programme (RNTCP) In: Chauhan LS, Agarwal SP, editors. Tuberculosis Control in India. New Delhi: Directorate General of Health Services Ministry of Health and Family Welfare; 2005. pp. 23–34. [Google Scholar]
- 6.Falk A, O’Connor JB, Pratt PC. Classification of pulmonary tuberculosis. In: Falk A, O’Connor JB, Pratt PC, Webb J A, Wier J A, Wolinsky E, editors. Diagnostic Standards and Classification of Tuberculosis. Vol. 12. New York, N.Y: National Tuberculosis and Respiratory Disease Association; 1969. pp. 68–76. [Google Scholar]
- 7.Van Dyck P, Vanhoenacker FM, Van den Brande P, De Schepper AM. Imaging of pulmonary tuberculosis. Eur Radiol. 2003;13:1771–85. doi: 10.1007/s00330-002-1612-y. [DOI] [PubMed] [Google Scholar]
- 8.Palmer PE. Pulmonary tuberculosis-usual and unusual radiographic presentations. Semin Roentgenol. 1979;14:204–43. doi: 10.1016/0037-198x(79)90007-5. [DOI] [PubMed] [Google Scholar]
- 9.Hatipoðlu ON, Osma E, Manisali M, Uçan ES, Balci P, Akkoçlu A, et al. High resolution computed tomographic findings in pulmonary tuberculosis. Thorax. 1996;51:397–402. doi: 10.1136/thx.51.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agrons GA, Markowitz RI, Kramer SS. Primary tuberculosis in children. Semin Roentgenol. 1993;28:158–72. doi: 10.1016/s0037-198x(05)80105-1. [DOI] [PubMed] [Google Scholar]
- 11.Moon WK, Im JG, Yeon KM, Han MC. Mediastinal tuberculous lymphadenitis: CT findings of active and inactive disease. AJR Am J Roentgenol. 1998;170:715–8. doi: 10.2214/ajr.170.3.9490959. [DOI] [PubMed] [Google Scholar]
- 12.Fraser RS, Müller NL, Colman N, Pare PD. Fraser and Pare's Diagnosis of Diseases of the Chest. (4th ed) 1999;Vol. 4:2743–50. [Google Scholar]
- 13.Choi JA, Hong KT, Oh YW, Chung MH, Seol HY, Kang EY. CT manifestations of late sequelae in patients with tuberculous pleuritis. AJR Am J Roentgenol. 2001;176:441–5. doi: 10.2214/ajr.176.2.1760441. [DOI] [PubMed] [Google Scholar]
- 14.Kwon JS, Cha SI, Jeon KN, Kim YJ, Kim EJ, Kim CH, et al. Factors influencing residual pleural opacity in tuberculous pleural effusion. J Korean Med Sci. 2008;23:616–20. doi: 10.3346/jkms.2008.23.4.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Long R, Maycher B, Dhar A, Manfreda J, Hershfield E, Anthonisen N. Pulmonary tuberculosis treated with directly observed therapy: Serial changes in lung structure and function. Chest. 1998;113:933–43. doi: 10.1378/chest.113.4.933. [DOI] [PubMed] [Google Scholar]


