Sir,
A 47-year-old female presented with a history of fever and cough for a duration of four months. The physical examination was unremarkable. Contrast-enhanced computed tomography (CECT) thorax demonstrated a large conglomerate lymph nodal enlargement in the right paratracheal, pretracheal, precarinal, and subcarinal stations [Figure 1]. The nodes appeared hypodense, with areas of central necrosis and demonstrated peripheral rim enhancement. The tuberculin skin test demonstrated an 18 mm induration. Other routine investigations were normal. The patient had been diagnosed with squamous cell carcinoma of the cervix three years previously and had received combination chemotherapy and radiotherapy. Six months following that, inguinal lymph node tumor recurrence occurred, for which external beam radiotherapy was administered. The patient remained asymptomatic subsequently. The current CECT scan of the abdomen and pelvis did not reveal any lymphadenopathy or local recurrence. A possibility of disseminated tuberculosis (TB) was considered.
Figure 1.
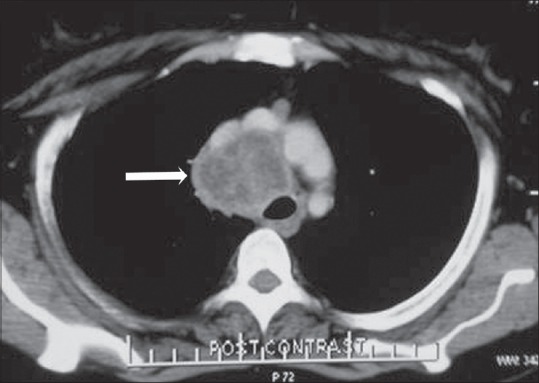
CECT thorax (mediastinal window) axial section demonstrating heterogeneous-appearing mediastinal lymph nodes in the right paratracheal location, demonstrating central necrosis and peripheral rim enhancement
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) was done under conscious sedation using the Olympus BF-UC-180 F EBUS bronchoscope (Olympus Corporation, Japan). On EBUS, enlarged lymph nodes were observed at the right lower paratracheal - size 38.1 mm × 28.4 mm, subcarinal - size 21 mm × 20.4 mm, and left lower paratracheal - size 12 mm × 12 mm, lymph node stations. The right lower paratracheal lymph node had indistinct margins with a heterogeneous echotexure. Rapid-onsite evaluation of the EBUS aspirates demonstrated presence of malignant cells. The acid-fast bacilli (AFB) smear, Gene Xpert test, and mycobacterial cultures of the aspirates were negative. The final cytopathological diagnosis was metastatic squamous cell carcinoma [Figure 2]. The patient was referred to the Radiation Oncology Services for subsequent palliative care.
Figure 2.
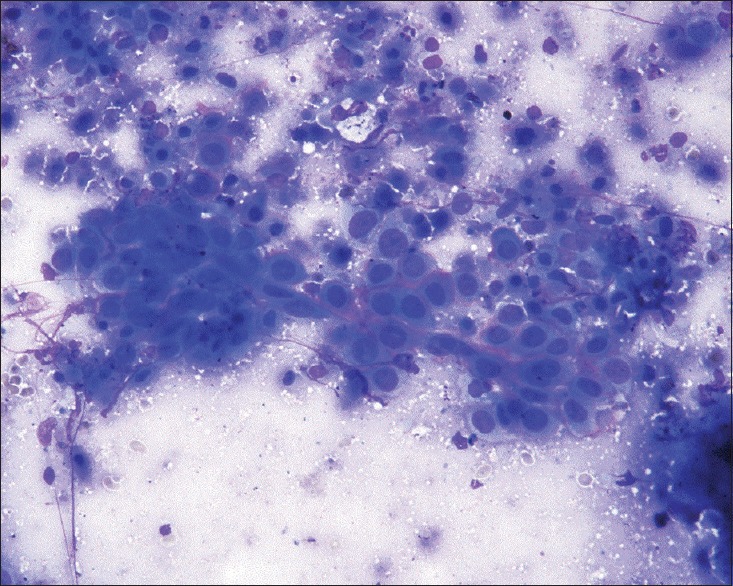
Cytopathological image of the EBUS aspirates demonstrating a cohesive group and few dyscohesive malignant squamous cells exhibiting high nucleo-cytoplasmic ratio and hyperchromasia. MGG stain, 200X
Malignancies that commonly metastasize to mediastinal lymph nodes include carcinoma of the lung, esophagus, stomach, pancreas, testes, breast, and colon. Lymphomas can also present as necrotic mediastinal lymphadenopathy. Intrathoracic metastases have been described in carcinoma of the cervix, more commonly with the histology showing adenocarcinoma. Parenchymal lung nodules are the most common presentation, followed by mediastinal lymphadenopathy with pleural effusion. Isolated lymphadenopathy without effusion is relatively more common with adenocarcinoma.[1] Rare findings include bone metastases (6%), endobronchial obstruction (5%), and lymphangitis carcinomatosis (3%).[2] In one study, approximately 6% of the patients, who were treated for carcinoma cervix, developed pulmonary metastases, with the incidence increasing from 3.2% in stage I to 20.9% in stage IV disease. Ninety-six percent were diagnosed within two years from the initiation of treatment. Eighty-one percent of the patients had local recurrence or other distant metastatic lesions.[3] Isolated mediastinal and hilar lymphadenopathy was uncommon. A previously published report from India described a patient with treated cervical cancer, who developed pulmonary parenchymal metastases, which was treated with chemotherapy. The patient subsequently developed isolated mediastinal lymphadenopathy. Although a tissue diagnosis of the same was not obtained, the patient responded clinically and radiologically to chemoradiotherapy.[4] Metachronous second malignancy should also be considered in a presentation such as the one in our patient and Metachronous bronchogenic carcinoma has been described in patients with carcinoma of the cervix.[5] However, the absence of any primary lung parenchymal lesion, ruled out the same in our patient.
Endobronchial ultrasound-guided transbronchial needle aspiration is a minimally invasive procedure that allows real-time sonographic visualization and needle aspiration from the mediastinal lymph nodes. The utility of EBUS-TBNA is well-established in mediastinal lymph node enlargements of both benign as well as malignant etiology, including TB and also in the TB-endemic populations.[6,7] However, the Indian literature on EBUS-TBNA is limited. Mediastinal lymph node tuberculosis is one of the most common etiologies for radiologically necrotic mediastinal lymphadenopathy, especially in highly tuberculosis (TB)-prevalent settings. On account of the relative difficulty in obtaining the pathological samples, diagnosis and management is frequently done based on the clinicoradiological profile, especially in resource-limited settings. Other than tuberculosis, other infections like histoplasmosis can also lead to mediastinal lymphadenopathy. However, a cytological study of the aspirates did not reveal any fungal morphology in our patient. Also, apart from the slide examination of the obtained aspirates during EBUS-TBNA; the lymph node tissue core can also be obtained, which can be subjected to detailed histopathological analysis, which is clinically relevant in situations such as lymphomas.[8]
In the clinical context of our patient (background history of cancer, post chemoradiotherapy status, necrotic mediastinal lymphadenopathy, and a positive tuberculin test), a strong clinical suspicion of TB had been considered, especially considering the fact that the patient had been symptom-free for the primary malignancy in the preceding two years. EBUS-TBNA helped in establishing a correct diagnosis of metastatic squamous cell carcinoma in our patient, thus preventing this patient from a delay in receiving further appropriate treatment for the same and prevented inappropriate administration of antituberculous medications. Our report highlights that in a cancer patient, when extrathoracic malignancy is under remission with no evidence of local recurrence, other etiological possibilities for isolated mediastinal lymphadenopathy should also be entertained. In these circumstances, a histopathological diagnosis becomes imperative. A positive tuberculin skin test must be interpreted with caution, as it is known to be frequently positive in patients who have received Bacille de Calmette et Guérin (BCG) vaccination or in those with latent TB infection. Inappropriate reliance on supportive investigations without a definitive histopathological confirmation of the diagnosis may be associated with serious consequences.
REFERENCES
- 1.Sostman HD, Matthay RA. Thoracic metastases from cervical carcinoma: Current status. Invest Radiol. 1980;15:113–9. doi: 10.1097/00004424-198003000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Shin MS, Shingleton HM, Partridge EE, Nicolson VM, Ho KJ. Squamous cell carcinoma of the uterine cervix. Patterns of thoracic metastases. Invest Radiol. 1995;30:724–9. doi: 10.1097/00004424-199512000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Imachi M, Tsukamoto N, Matsuyama T, Nakano H. Pulmonary metastasis from carcinoma of the uterine cervix. Gynecol Oncol. 1989;33:189–92. doi: 10.1016/0090-8258(89)90549-0. [DOI] [PubMed] [Google Scholar]
- 4.Kesarwani R. Lymph node metastases in carcinoma of cervix. Indian J Cancer. 2013;50:45. doi: 10.4103/0019-509X.112320. [DOI] [PubMed] [Google Scholar]
- 5.Aggarwal AN, Behera D. Metachronous bronchogenic carcinoma in a patient treated for cervical cancer. Indian J Chest Dis Allied Sci. 1998;40:213–6. [PubMed] [Google Scholar]
- 6.Madan K, Mohan A, Ayub II, Jain D, Hadda V, Khilnani GC, et al. Initial experience with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) from a tuberculosis endemic population. J Bronchology Interv Pulmonol. 2014;21:208–14. doi: 10.1097/LBR.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 7.Navani N, Molyneaux PL, Breen RA, Connell DW, Jepson A, Nankivell M, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: A multicentre study. Thorax. 2011;66:889–93. doi: 10.1136/thoraxjnl-2011-200063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madan K, Guleria R. Endobronchial ultrasound needle biopsy with and without aspiration: The “Core” issue. Chest. 2013;143:281–2. doi: 10.1378/chest.12-2239. [DOI] [PubMed] [Google Scholar]


