Abstract
Purpose
High levels of reactive oxygen species (ROS) are a leading cause of male factor infertility. Measurement of ROS has been hampered by a lack of standardisation and confounding variables including choice of controls and sample selection. This study aimed to determine a reference range for ROS in human semen.
Methods
Semen samples were obtained from men attending for routine semen analysis who gave informed consent for the study. Samples were assigned groups: Group 1 (N = 94) normal semen parameters, no leucocytospermia; Group 2 (N = 100) abnormal semen parameters, no leucocytospermia; Group 3 (N = 41) any semen parameters with leucocytospermia. ROS levels were assayed in fresh neat semen using a chemiluminescence assay measured in a single tube luminometer. Data are reported in relative light units (RLU)/sec/106 sperm
Results
ROS levels were significantly different between Groups 1, 2 and 3 (19.75 ± 8.12, 95.03 ± 33.63, 890.17 ± 310.23 RLU/sec/106 sperm respectively; p < 0.001). Group 3 gave the highest value confirming this group as the optimum choice for positive controls. The reference range < 24.1 RLU/sec/106 sperm was determined by ROC analysis that differentiates a reference population (Group 1) from a positive control group (Group 3), optimising the sensitivity and specificity (80.5 and 87.2 % respectively) of the test.
Conclusions
We have determined a reference range for ROS in human semen and identified a patient population that falls outside the normal range. This simple, cost effective assay can be incorporated into routine diagnostic testing to aid in the diagnosis of male infertility, especially with regard to unexplained infertility.
Keywords: Reactive oxygen species, Oxidative stress, Chemiluminescence, Human semen, Male infertility
Introduction
Almost 50 % of infertility may be associated with a male factor [1, 2]. Although a semen analysis has classically been used as the gold standard for determining a man’s fertility [3], this test alone cannot accurately predict infertility since between 6 and 27 % men with normal semen parameters are infertile [1, 4]. One explanation is that a semen analysis is unable to detect abnormalities at the molecular level that may contribute to unexplained cases [5]. Oxidative stress resulting from excessive production of reactive oxygen species (ROS) can have a profound effect on the sperm plasma membrane and subsequent functional integrity of the sperm [6–10]. Elevated ROS levels are cytotoxic, resulting in a loss of sperm motility and vitality [11–15]. In addition, they impair crucial events required for fertilisation [11, 14, 16] including capacitation [17] the acrosome reaction [18] and sperm-oocyte fusion [12, 19], as well as initiating DNA strand breaks [6, 8, 14, 19], adversely affecting pronuclear and blastocyst development and negatively affecting pregnancy rates after in vitro fertilisation (IVF) [6, 19–22]. They are also correlated with an increased time to natural conception and recurrent miscarriage [23].
Infertile men demonstrate significantly increased ROS levels with a reduction in antioxidant capacity compared with fertile controls, irrespective of semen parameters [24–29]. Thus determination of ROS levels would clearly contribute valuable diagnostic information to standard male fertility investigation. ROS assays tend to focus on ROS production by isolated spermatozoa since they are a source of ROS, and there are published protocols for the measurement of ROS levels using washed sperm cell suspensions [3]. Assessing ROS levels in sperm preparations is fraught with artefacts, as centrifugation and other manipulation triggers significant ROS production [30–34]. Conversely removal of seminal plasma during the washing process removes natural antioxidant pathways that would naturally protect sperm from ROS attack [31, 33–36]. Although this technique may be valuable for assessing ROS exposure during assisted conception as sperm are washed prior to IVF, it does not reflect the physiological environment of the sperm that may contribute to infertility in vivo.
Oxidative stress in the reproductive tract cannot be attributed to ROS production from sperm cells alone. By far the major source of ROS is derived from polymorphonuclear leucocytes (PMN) in semen [13, 25, 35–38]. Furthermore, sperm may be exposed to a plethora of other factors in the testes, epididymis and male accessory gland fluid that are responsible for the regulation of ROS generation [39–42]. Measurement of physiological ROS levels must therefore take into account the dynamic state of both ROS generation and neutralisation by antioxidant pathways in the male reproductive environment.
For determination of oxidative stress in diagnosing infertility, measuring ROS in unwashed, whole semen is most appropriate. It more accurately and reliably reflects the physiological level of oxidative stress that the sperm are exposed to [27, 36], taking into account both the pro- and anti-oxidant status of the sperm microenvironment, and is therefore more relevant to our understanding of male infertility. Assessing ROS in whole semen is less time consuming and more cost effective than measuring it in washed sperm samples. Another advantage for measuring ROS in whole semen is that ROS values decline with time after ejaculation [43, 44], so it is imperative to measure levels as soon as possible, ideally soon after liquefaction in order to obtain a true reading. The ROS assay measuring chemiluminescence in a single tube luminometer, has recently been validated [44], demonstrating it is a highly reliable and accurate diagnostic test. In the present study, we have determined a reference range in whole semen as the sample of choice for determining potentially damaging levels to sperm that may contribute to infertility.
Materials and methods
Semen samples
Samples were obtained from 227 men attending the Andrology Laboratory for routine semen analysis between December 2009 and 2013. All men had given informed consent to use the remainder of their sample prior to inclusion in the study and it was approved by the institutional quality management board. Ethical approval was not deemed necessary. The age of the men ranged from 18 to 62 years. Men were asked to provide only one sample for the study. Semen samples were produced on site by masturbation after 2 to 5 days sexual abstinence. Samples were maintained for approximately 20 min at 36 ± 1 °C to liquefy. Semen analysis was performed on all samples according to WHO guidelines [3]. Morphology was assessed on Papanicolaou stained slides using Kruger strict criteria [3]. If the round cell count was equal to or exceeded 1 million/ml, polymorphonuclear leucocytes (PMN) were identified using a kit that differentiates round cells on the basis of their peroxidase content (LeucoScreen™; Microm, UK; CE marked, demonstrating it conforms with the relevant essential requirements in the European Union Directives, and that it is fit for its stated, intended purpose). Samples containing less than 1 million/ml sperm were excluded from the study as ROS measurement is inaccurate and unreliable when the sperm concentration falls below this value [45].
Population study groups
To perform a routine laboratory test for ROS measurement in clinical samples, it is essential to establish an accurate reference range for the levels of ROS in semen. As ROS performs an important physiological role in sperm function, low levels of ROS would be expected in all semen samples and it is this level that should constitute the reference range.
Group 1: Normal semen parameters (reference group)
Criteria for selection of the reference population were demonstration of semen parameters within the WHO (2010) reference range [3]. Crucially, all of the semen samples contained less than 1 million/ml PMN. From the 227 men who randomly provided semen samples for the ROS validation, a total of 94 men aged between 22 and 51 years, had semen parameters that fell within the WHO reference range [3].
Group 2: Abnormal semen parameters
This group was selected based on semen parameters that fell outside of the normal range [3] but with low levels of PMN defined as <1 million/ml. One hundred men were included in this group with an age range of 18 to 50 years.
Group 3: High polymorphonuclear leucocytes (PMN) (positive test group)
This group was selected based only on the concentration of PMN in the semen and represented the positive test group. Forty one semen samples contained PMN concentrations of ≥ 1 million/ml. Within this group, 9 samples had normal semen parameters and the remainder had one or more abnormal parameters. The age range of these men was 31 to 62 years
ROS assay
All 227 semen samples were assessed for ROS levels between 10 and 30 min after ejaculation. ROS levels diminish with time post ejaculation (44), so it was important to capture the signal as soon as possible. Samples were therefore assessed as soon as possible after liquefaction, beginning at 10 min but no later than 30 min. The general methodology is reviewed elsewhere [46]. Briefly, a sperm count was performed for each semen sample. Negative and positive controls were run for each semen sample assay. Negative controls contained 400 μl phosphate buffered saline (PBS) with 10 μl of a luminol (5-amino-2,3-dihydro-1,4-phthalazinedione; Sigma-Aldrich, UK) working solution (5 mM luminol prepared in dimethylsulphoxide (DMSO)). Positive controls contained 395 μl PBS, 5 μl 30 % H202 (VWR UK) and 10 μl of 5 mM luminol working solution. For measuring ROS in semen, 10 μl luminol working solution was added to 400 μl liquefied whole semen. All samples were mixed gently immediately.
Measurement of chemiluminescence
ROS were measured using luminol, which is oxidised in the presence of ROS, resulting in chemiluminescence. The luminescence generated by this reaction was measured using a CE marked single tube luminometer (Turner Biosystems Instrument Modulus Model no. 9200–001, Sunnyvale, California, USA). This luminometer is economical compared to a multiple-tube luminometer or plate analyser, and the chemiluminescence assay is uncomplicated to perform. Chemiluminescence was reported as Relative Light Units per second (RLU/sec). RLU/sec were measured at 1 min intervals after addition of luminol, over a total period of 10 min and then averaged for each sample. To eliminate any variation, the mean control value was subtracted from the mean semen value to give the true value of the test sample. This value was adjusted for sperm concentration and ROS were reported as RLU/sec/106 sperm.
Statistical analysis
Group comparisons with respect to categorical variables were performed with Fisher’s exact test or chi-square test. Due to the expected non-normality of quantitative variables in this study, group comparisons with respect to quantitative variables were performed with Kruskal-Wallis test for 3-group comparisons, or Wilcoxon rank sum test for pairwise group comparisons. These nonparametric tests were used for age, volume of semen, sperm concentration/ml, total motility, progressive motility, morphology, PMN concentration and ROS values. In all cases, p values < 0.05 were considered to be statistically significant. Sensitivity and specificity were determined for different cut-off values of ROS to aid in the determination of reference values. Receiver operating characteristic curves (ROC) were used to demonstrate the sensitivity and specificity, and to identify the cut-off value yielding the maximum sum of the sensitivity and specificity. Analyses were performed using R version 3.0.1 [47].
Results
Distribution of semen parameters between groups
Table 1 shows the distribution of semen parameters within the 3 selection groups. The average age of Group 1 was not significantly different from Group 2 or 3. However, men in Group 3 were significantly older than men in Group 2 (p = 0.008). For all groups together, ROS levels were independent of age as the values were not significantly different between men younger than 40 (n = 159) compared to men of 40 or over (n = 76). Sperm count, total motility, progressive motility and normal morphology were significantly lower in the abnormal Groups 2 and 3, compared with the normal Group 1 (p < 0.001 for all parameters). As expected, these parameters were lower in Group 2 compared with Group 3 parameters, as Group 2 men were specifically selected for these abnormal semen parameters. However this difference was only significant for morphology between Groups 2 and 3 (p = 0.019). Men were only included in Groups 1 and 2 with less than 1 million/ml PMN. The mean PMN level in semen samples in these groups was slightly higher in Group 1 compared with Group 2 (p = 0.031), however, the mean PMN level in Group 3 was approximately 10 times higher than both groups (p < 0.001 vs Group 1 or Group 2).
Table 1.
Comparison of semen parameters between men grouped according to WHO 2010 reference range
| Semen Parameters | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Number men | 94 | 100 | 41 |
| Age | 37.70 ± 0.64 (22;33.25;37;41.75;51) |
36.72 ± 0.52 (18;34;37;39.25;50) |
40.39 ± 1.15a
(31;36;39;43;62) |
| Volume (ml) | 3.54 ± 0.16 (1.5;2.4;3.35;4.2;11.1) |
3.61 ± 0.15 (0.5;2.5;3.5;4.53;7) |
3.74 ± 0.28 (1.3;2.4;3.6;4.6;10.2) |
| Sperm Count (x 106) | 71.43 ± 5.34 (17;37.25;57;94.25;331) |
32.76 ± 3.76b
(0.8;5.57;18.5;46.5;177) |
41.83 ± 8.44b
(1;8.4;15;54;230) |
| Total motility (%) | 69.17 ± 1.01 (44;63;69;77;89) |
47.70 ± 2.27b
(0;32.75;52;65.25;88) |
53.80 ± 3.44b
(2;36;60;69;87) |
| Progressive motility (%) | 58.52 ± 1.26 (32;51;60;66;84) |
36.00 ± 2.16b
(0;17.75;37.5;52;74) |
43.71 ± 3.40b
(1;24;49;59;80) |
| Normal forms (%) | 8.65 ± 0.34 (4;6;8;10;20) |
2.73 ± 0.32b
(0;1;2;3;14) |
3.78 ± 0.51b,c
(0;2;3;6;14) |
| PMN (x 106) | 0.36 ± 0.03 (0;0.1;0.3;0.6;0.9) |
0.28 ± 0.03e
(0;0.01;0.2;0.46;0.9) |
3.54 ± 0.70b,d
(1;1.3;2.4;4;28.1) |
Group 1 - normal semen parameters; Group 2- abnormal parameters with < 1 million/ml PMN; Group 3 – any parameters, but ≥ 1 million/ml PMN
*Quantitative variables summarized as mean ± SEM and (minimum;25th%;median;75th%;maximum)
aSignificantly different from Group 2; p = 0.008 bSignificantly different from Group 1; p < 0.001
cSignificantly different from Group 2; p = 0.019 dSignificantly different from Group 2; p < 0.001
eSignificantly different from Group 1; p = 0.031
ROS levels in whole semen
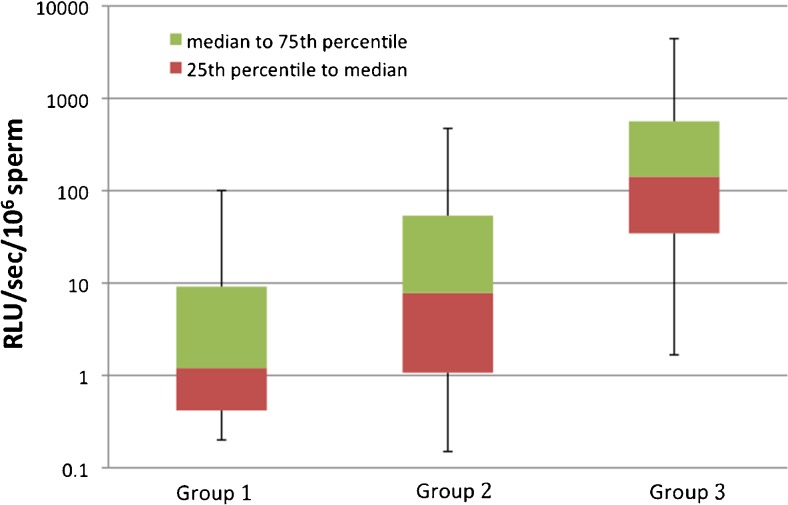
Figure 1 shows the box and whisker plots for the median and interquartile ranges for the three groups. The data emphasise the non-parametric distribution and the differences between groups. Groups 2 and 3 showed a considerably higher range of ROS values compared to samples from men in Group 1. There was no overlap between Group 1 and 3 boxes. The upper quartile for the reference parameter group was determined as 9.1 RLU/sec/106 sperm (N = 74; 75.5 %). Only 12.2 % (N = 5) of samples with high PMN (Group 3) had ROS levels below 9.1 RLU/sec/106sperm. These are likely to represent PMNs that have been previously activated and are no longer viable. Samples with abnormal semen parameters and low PMN (Group 2) were equally distributed above and below this ROS value (N = 51, 51 % and N = 48, 48 % respectively). There were 12 anomalous values that fell outside the upper adjacent value for Group 1, 14 for Group 2 and 8 for Group 3, although the maximum RLU values were considerably less in Group 1 than in the other 2 groups. There are no anomalies on the lower side of the data, due to the large number of patients with low ROS levels in all groups.
Fig. 1.
Box and whisker plots for Group 1, Group 2 and Group 3 data showing the median to interquartile ranges. Group 1 - normal semen parameters; Group 2- abnormal parameters with < 1 million/ml leucocytes; Group 3 - any parameters but ≥ 1 million/ml leucocytes. Lower whisker = 5th percentile; Upper whisker = 95th percentile. Data are shown on a logarithmic scale. All pairwise group differences were significant with p < 0.001 according to Wilcoxon rank sum tests
Table 2 shows the descriptive parameters for ROS values for semen samples from men in each of the study groups. The distribution of ROS values for Groups 2 and 3 rise from a minimum of 0 and 0.1 to 3041.4 and 10980.3 RLU/sec/106sperm respectively. Values for Group 1 ranged from 0 to 170 RLU/sec/106sperm, with only one outlier at 724.6 RLU/sec/106sperm. Samples from men with abnormal semen parameters or high PMN had significantly higher mean ROS levels compared with those from samples with normal parameters (Table 2; p < 0.001 for all groups). The mean seminal ROS value for men in Group 3 was approximately 9.4 times higher than that of Group 2 and 45 times higher than that of Group 1. The range of RLU values is a non-parametric distribution as there is a considerable difference between the mean and median values in all groups. A considerable difference in the maximum value, variance and standard deviation was observed between the three groups. The interquartile range for ROS levels in semen from men with normal semen parameters is established as 0.4–9.1 RLU/sec/106 sperm, while for Groups 2 and 3 the range is 1.0–54.8 and 30.3–538.3 RLU/sec/106 sperm respectively.
Table 2.
Descriptive parameters for ROS levels in semen samples
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| N | 94 | 100 | 41 |
| Mean | 19.75 | 95.0 | 890.2 |
| Standard error | 8.12 | 33.6 | 310.2 |
| Variance | 6203.4 | 113081.6 | 3945854.8 |
| Standard deviation | 78.8 | 336.3 | 1986.4 |
| Sum | 1876.6 | 9503.2 | 36496.8 |
| Minimum | 0.0 | 0.0 | 0.1 |
| 5th percentile | 0.2 | 0.15 | 1.67 |
| Lower quartile | 0.4 | 1.0 | 30.3 |
| Median | 1.2 | 7.8 | 142.1 |
| Upper quartile | 9.1 | 54.8 | 538.3 |
| 95th percentile | 91.15 | 419.1 | 3868.4 |
| Maximum | 724.6 | 3041.4 | 10980.3 |
| Interquartile range | 8.7 | 53.8 | 508.0 |
| Lower adjacent value | 0.0 | 0.0 | 0.0 |
| Upper adjacent value | 22.1 | 135.4 | 1300.4 |
Group 1 - normal semen parameters; Group 2- abnormal parameters with < 1 million/ml leucocytes; Group 3 - any parameters but ≥ 1 million/ml leucocytes
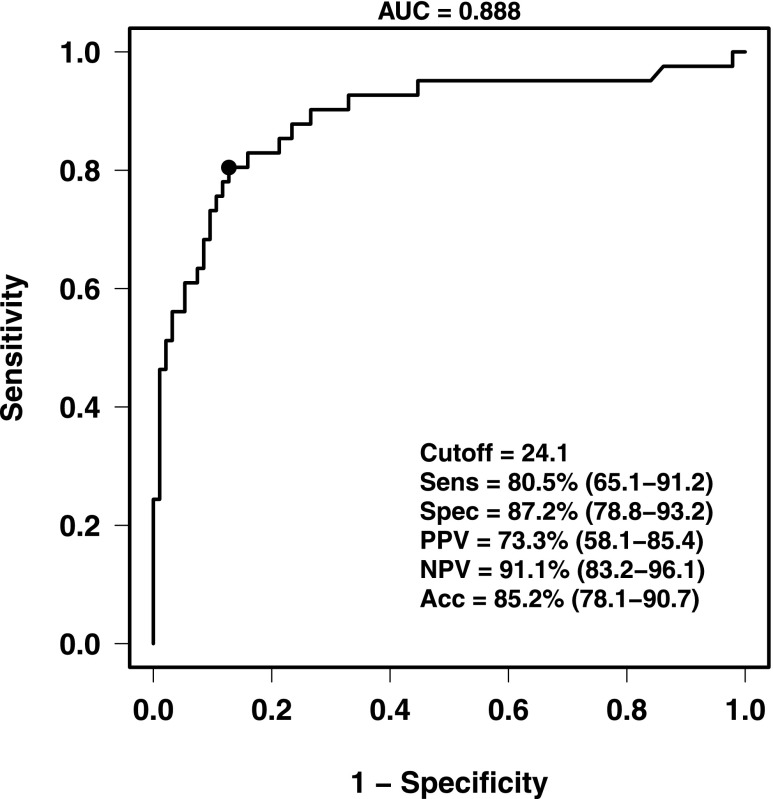
Sensitivity and specificity of the ROS assay
The data from the receiver operating characteristic curve analysis suggests an optimal reference value for high ROS levels at approximately 24.1 RLU/sec/106 sperm based on its ability to differentiate between those with normal semen parameters and those with high PMN in the semen (Figure 2). This value shows the maximum sum of sensitivity and specificity of the test. Both specificity (87.2 %) and sensitivity (80.5 %) are high. A ROS cut-off value of 24.1 RLU/sec/106 sperm will capture approximately 87.2 % of the ROS values among samples with normal sperm parameters, defining typical ROS levels among normal samples. Values below 24.1 probably represent basal physiological ROS production in semen. On the other hand, 80.5 % of men with high PMNs should be captured using this cut-off value for ROS.
Fig. 2.
Receiver operating characteristic curve. Data showing the area under the curve in men with normal semen parameters, abnormal semen parameters and those with > 1 million/ml seminal PMN. AUC = area under the curve; Sens = sensitivity; Spec = specificity; PPV = positive predicted value; NPV = negative predicted value; ACC = accuracy. Values in parentheses are the 95 % confidence intervals
Discussion
High levels of ROS are a leading cause of male factor infertility, contributing to poor semen parameters, reduced sperm vitality, impaired sperm function and fertilisation, and DNA damage [6, 7, 10]. While the detrimental effects of ROS are well accepted, there is a lack of standardisation of methodology for ROS determination and inconsistencies in establishing a reference range. We have determined a reference range for ROS levels in human semen that demonstrates both high sensitivity and specificity. The test is sensitive over a wide range of RLU values for semen samples obtained from a random group of men attending for semen analysis. Mean ROS levels are significantly higher in semen of men with abnormal parameters compared to the reference group by 4.8 fold, and particularly in semen from men containing 1 million/ml or more PMN representing a 45 fold increase from those with normal semen parameters. These findings are consistent with previous studies [35, 36] which showed higher seminal ROS in samples with abnormal semen parameters compared to samples with normal parameters, and an even higher level correlated with the presence of PMN. Another study demonstrated significantly higher ROS levels in fertile patients who had PMN in their semen compared to those without [25].
The median and interquartile ranges for ROS determined for samples with normal semen parameters and less than 1 million/ml PMN has been established as 1.2 (0.4, 9.1) RLU/sec/106sperm. From the ROC analysis of the data, the reference range was determined as < 24.1 RLU/sec/106 sperm. This cut-off value gives high specificity (87.2 %) and sensitivity (80.5 %) using semen samples with high PMN as the positive ROS group, demonstrating the robustness of the test. Recently, Kashou et al. [48] established a normal ROS range of < 20 RLU/sec/million sperm, which is remarkably similar to our determined range. Earlier studies determining ROS reference ranges reported ROS values in counted photons per minute, generally per 20 million sperm, whereas only more recent studies have used RLU. Venkatesh et al. [33] reported a median and interquartile range of 0.03 (0.014, 0.068) x 104 RLU/min/20 million sperm in normozoospermic fertile volunteers, while Fingerova et al. [36] reported a median and interquartile range of 0.26 (0.12, 0.55) RLU x 103 /min/20 million sperm for fertile volunteers, although it is unclear whether all these volunteers were normozoospermic. Like this study, Venkatesh et al. [33] and Fingerova et al. [36] used single tube luminometers, however, it is difficult to compare results as the luminometers were from different manufacturers which may have different specifications and sensitivity. Furthermore, their data was reported as RLU/min whereas the Modulus luminometer used in this study presents data as RLU/second. However, we have found that ROS values measured on one machine (luminometer) are similar on other machines of the same make and model using similar protocols and reagents when using the same semen sample.
Differences in results may be attributed to laboratory variation and differences in inclusion for reference groups. Our criteria for normal semen parameters were based on WHO 2010 guidelines [3], whereas previous studies relied on WHO 1999 guidelines [49], hence samples which they considered to be in the normal range may have been excluded using more up-to-date criteria. Other studies frequently determined reference values based on samples from fertile men [33, 36]. Conversely, our reference values were based solely on samples with normal semen parameters without leucospermia with no determination of fertility status.
The selection of appropriate negative and positive reference groups is an important determinant for an accurate and reliable reference range. It could be argued that it is more appropriate to select fertile and infertile men to determine a reference range for the ROS assay. However, these criteria have limitations. While fertile men tend to have low ROS and infertile patients have higher ROS levels [26, 28, 29], this is not always the case. We also considered groups of men with normal and abnormal semen parameters as our reference and positive controls. Although the mean ROS levels in the men with abnormal semen parameters are significantly higher than those in semen from men with normal parameters, there is considerable overlap between ROS values for these two groups. This may be explained by factors other than ROS that may contribute to abnormal semen parameters [1]. Indeed, there are a higher number of semen samples with abnormal parameters that have ROS levels within the reference range of < 24.1 RLU/sec/106 sperm compared with those above the range (64 % below; 36 % above). This agrees with previous findings [50, 51] and indicates that semen parameters are not directly correlated with ROS.
While studies have shown that ROS is elevated in infertile men [29, 33, 46, 52], it is the presence of PMN in the semen that is the prime source of ROS [25, 35–37], contributing up to one thousand fold more ROS than the contribution of the sperm [12, 53]. For these reasons, samples with elevated PMN were chosen as the positive control group and samples with negligible PMN as the reference range. As abnormal semen parameters are likely to be associated with increased ROS, our reference group samples were further selected for normozoospermia. In this study, ROS was elevated in over 80 % of samples with high PMN (Group 3) compared with the reference group (Group 1), whereas only 36 % of samples with abnormal semen parameters (Group 2) had elevated ROS. This confirms that the group of men with elevated PMN (Group 3) is not only a valid alternative to infertile controls, but is by far the optimum ROS positive reference group compared to men with abnormal semen parameters. The data provide further evidence that PMN are a major source of ROS generation.
ROS assessment is clearly valuable in the diagnosis of infertility, as it is a far more powerful predictor than semen analysis [54]. ROS have far reaching consequences, not only in terms of peroxidation of sperm membrane and intracellular lipids and proteins, but also as the major etiological factor resulting in DNA damage [10]. Such broad spectrum damage results in a significant reduction in fertility [19–23]. Because of its powerful association with infertility, ROS measurement is particularly relevant as it may serve to identify a cause of infertility in hitherto unexplained cases, irrespective of their semen parameters, which could not be identified by performing WHO semen analysis alone. A significant number of men with normal semen parameters are infertile and have significantly higher seminal ROS levels compared to those with normal parameters who are fertile [52]. Although we have not delineated between fertile and infertile men within our patient groups, 12.8 % men with normal semen parameters had high seminal ROS and it is likely they represent individuals with unexplained infertility. Measurement of ROS levels is of considerable benefit, since it would provide more insight into the causes of infertility and warrant further investigation. The value of ROS testing is further justified as in many cases, factors that contribute to increased ROS can be addressed with a change in lifestyle [55], oral antioxidant treatment [55–57], antibiotics [58], or varicocoele repair [59] to significantly reduce ROS levels and DNA damage, restore fertility and improve pregnancy rates. Initiatives to reduce ROS can be assessed by undertaking a second test 3 months later.
Conclusion
It is important to emphasise that this study has attempted to define physiological levels of ROS that occur in semen, rather than determining levels that would be linked to infertility. We propose that the reference value of < 24.1 RLU/sec/106 sperm is acceptable for seminal ROS measurement using techniques described in this study. Additional studies would be required to determine whether this cut-off value is directly correlated with fertilisation capacity in vitro, sperm viability and DNA integrity. However, as it is well established that raised ROS levels have a considerable effect on all of these parameters [10] any efforts to reduce ROS should be beneficial. While ROS signals generated by different luminometers cannot be accurately compared between instruments, our study demonstrates that ROS measurement in an individual clinical fertility laboratory can be standardized very effectively and a reference range of seminal ROS values calculated in their own group of patients while using their own instrument and reagents. As the Modulus single tube luminometer is very cost efficient and simple to use, it has the potential to be used in a large number of Andrology laboratories. We recommend this test should ideally be offered in conjunction with a comprehensive semen analysis as it will benefit interpretation of the ROS result. The availability of this test for oxidative stress provides a welcomed addition as an aid in the diagnosis and management of male infertility [6, 54, 60]. We envision it will be particularly relevant to men with unexplained infertility and whose partners have experienced a long time to pregnancy, multiple assisted conception treatment failures or miscarriages
Acknowledgments
The authors would like to thank Jeffrey Hammell for support with statistical analysis
Footnotes
Capsule A reference range for reactive oxygen species in human semen has been determined using a chemiluminescence assay measured in a single tube luminometer.
References
- 1.Irvine DS. Epidemiology and etiology of male infertility. Hum Reprod. 1998;13(Suppl 1):33–44. doi: 10.1093/humrep/13.suppl_1.33. [DOI] [PubMed] [Google Scholar]
- 2.McLachlan R, de Kretser D. Male infertility: the case for continued research. MJA. 2001;174:116–117. doi: 10.5694/j.1326-5377.2001.tb143180.x. [DOI] [PubMed] [Google Scholar]
- 3.WHO . WHO laboratory manual for the examination and processing of human semen. 5. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- 4.Moghissi KS, Wallach EE. Unexplained infertility. Fertil Steril. 1983;39:5–21. doi: 10.1016/s0015-0282(16)46750-6. [DOI] [PubMed] [Google Scholar]
- 5.Pizzol D, Ferlin A, Garolla A, Lenzi A, Bertoldo A, Foresta C. Genetic and molecular diagnostics of male infertility in the clinical practice. Front Biosci (Landmark Ed) 2014;19:291–303. doi: 10.2741/4208. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol. 2008;59:2–11. doi: 10.1111/j.1600-0897.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 7.Tremellen K. Oxidative stress and male infertility – a clinical perspective. Hum Reprod Update. 2008;14:243–53. doi: 10.1093/humupd/dmn004. [DOI] [PubMed] [Google Scholar]
- 8.Mahfouz RZ, Sharma R, Thiyagarajan A, Kale V, Gupta S, Sabanegh E, et al. Semen characteristics and sperm DNA fragmentation in infertile men with low and high levels of seminal reactive oxygen species. Fertil Steril. 2010;94:2141–6. doi: 10.1016/j.fertnstert.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 9.Henkel R. Leukocytes and oxidative stress: dilemma for sperm function and male fertility. Asian J Androl. 2011;13:43–52. doi: 10.1038/aja.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aitken RJ, Smith TB, Jobling MS, Baker MA, de Iuliis GN. Oxidative stress and male reproductive health. Asian J Androl. 2014;16:31–38. doi: 10.4103/1008-682X.122203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alvarez JG, Touchstone JC, Blasco L, Storey BT. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. J Androl. 1987;8:338–348. doi: 10.1002/j.1939-4640.1987.tb00973.x. [DOI] [PubMed] [Google Scholar]
- 12.Plante M, de Lamirande E, Gagnon C. Reactive oxygen species released by activated neutrophils, but not by deficient spermatozoa, are sufficient to affect normal sperm motility. Fertil Steril. 1994;62:387–393. doi: 10.1016/s0015-0282(16)56895-2. [DOI] [PubMed] [Google Scholar]
- 13.De Lamirande E, Gagnon C. Impact of reactive oxygen species on spermatozoa: a balancing act between beneficial and detrimental effects. Hum Reprod. 1995;10:15–21. doi: 10.1093/humrep/10.suppl_1.15. [DOI] [PubMed] [Google Scholar]
- 14.Aitken RJ, Curry BJ. Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal. 2011;14:367–381. doi: 10.1089/ars.2010.3186. [DOI] [PubMed] [Google Scholar]
- 15.Shi T-Y, Chen G, Huang X, Yuan Y, Wu X, Wu B, et al. Effects of reactive oxygen species from activated leucocytes on human sperm motility, viability and morphology. Andrologia. 2011;44:696–703. doi: 10.1111/j.1439-0272.2011.01252.x. [DOI] [PubMed] [Google Scholar]
- 16.Chen SJ, Allam JP, Duan YG, Haidi G. Influence of reactive oxygen species on human sperm functions and fertilizing capacity including therapeutical approaches. Arch Gynecol Obstet. 2013;288:191–9. doi: 10.1007/s00404-013-2801-4. [DOI] [PubMed] [Google Scholar]
- 17.Morielli T, O’Flaherty C. Oxidative stress impairs function and increases redox protein modifications in human spermatozoa. Reproduction. 2015;149:113–23. doi: 10.1530/REP-14-0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ichikawa T, Oeda T, Ohmori H, Schill WB. Reactive oxygen species influence the acrosome reaction but not acrosin activity in human spermatozoa. Int J Androl. 1999;22:37–42. doi: 10.1046/j.1365-2605.1999.00145.x. [DOI] [PubMed] [Google Scholar]
- 19.Aitken RJ, Gordon E, Harkiss D, Twigg JP, Milne P, Jennings Z, et al. Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod. 1998;59:1037–1046. doi: 10.1095/biolreprod59.5.1037. [DOI] [PubMed] [Google Scholar]
- 20.Zorn B, Vidmar G, Meden-Vrtovec H. Seminal reactive oxygen species as predictors of fertilization, embryo quality and pregnancy rates after conventional in vitro fertilization and intracytoplasmic sperm injection. Int J Androl. 2003;26:279–285. doi: 10.1046/j.1365-2605.2003.00424.x. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal A, Allamaneni SS, Nallella KP, George AT, Mascha E. Correlation of reactive oxygen species levels with the fertilization rate after in vitro fertilization: a qualified meta-analysis. Fertil Steril. 2005;84:228–31. doi: 10.1016/j.fertnstert.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 22.Ghaleno LR, Valojerdi MR, Hassani F, Chehrazi M, Janzamin E. High level of intracellular sperm oxidative stress negatively influences embryo pronuclear formation after intracytoplasmic sperm injection treatment. Andrologia. 2014;46:1118–27. doi: 10.1111/and.12202. [DOI] [PubMed] [Google Scholar]
- 23.Imam SN, Shamsi MV, Kumar K, Deka D, Dada R. Idiopathic recurrent pregnancy loss: role of paternal factors; a pilot study. J Reprod Infertil. 2011;12:267–276. [PMC free article] [PubMed] [Google Scholar]
- 24.Aitken RJ, Baker MA. Oxidative stress, sperm survival and fertility control. Mol Cell Endocrinol. 2006;250:66–9. doi: 10.1016/j.mce.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Athayde KS, Cocuzza M, Agarwal A, Krajcir N, Lucon AM, Srough M, et al. Development of normal reference values for seminal reactive oxygen species and their correlation with leukocytes and semen parameters in a fertile population. J Androl. 2007;28:613–20. doi: 10.2164/jandrol.106.001966. [DOI] [PubMed] [Google Scholar]
- 26.Moein MR, Dehghani VO, Tabibnejad N, Vahidi S. Reactive oxygen species (ROS) level in seminal plasma of infertile men and healthy donors. Iran J Reprod Med. 2007;5:51–55. [Google Scholar]
- 27.Desai N, Sharma R, Makker K, Sabanegh E, Agarwal A. Physiologic and pathologic levels of reactive oxygen species in neat semen of infertile men. Fertil Steril. 2009;92:1626–1631. doi: 10.1016/j.fertnstert.2008.08.109. [DOI] [PubMed] [Google Scholar]
- 28.Guz J, Gackowski D, Foksinski M, Rozalski R, Zarakowska E, Siomek A, et al. Comparison of oxidative stress/DNA damage in semen and blood of fertile and infertile men. PLoS One. 2013;8:e68490. doi: 10.1371/journal.pone.0068490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kullisaar T, Türk S, Kilk K, Ausmees K, Punab M, Mändar R. Increased levels of hydrogen peroxide and nitric oxide in male partners of infertile couples. Andrology. 2013;1:850–8. doi: 10.1111/j.2047-2927.2013.00123.x. [DOI] [PubMed] [Google Scholar]
- 30.Aitken RJ, Clarkson JS. Significance of reactive oxygen species and antioxidants in defining the efficacy of sperm preparation techniques. J Androl. 1988;9:367–376. doi: 10.1002/j.1939-4640.1988.tb01067.x. [DOI] [PubMed] [Google Scholar]
- 31.Agarwal A, Ikemoto I, Loughlin KR. Effect of sperm washing on levels of reactive oxygen species in semen. Arch Androl. 1994;33:157–162. doi: 10.3109/01485019408987819. [DOI] [PubMed] [Google Scholar]
- 32.Shekarriz M, DeWire DM, Thomas AJ, Jr, Agarwal A. A method of human semen centrifugation to minimise iatrogenic sperm injuries caused by reactive oxygen species. Eur Urol. 1995;28:31–35. doi: 10.1159/000475016. [DOI] [PubMed] [Google Scholar]
- 33.Venkatesh S, Shamsi MB, Dudeja S, Kumar R, Dada R. Reactive oxygen species measurement in neat and washed semen: comparative analysis and its significance in male infertility assessment. Arch Gynaecol Obstet. 2011;283:121–6. doi: 10.1007/s00404-010-1645-4. [DOI] [PubMed] [Google Scholar]
- 34.Li Z, Zhou Y, Liu R, Lin H, Liu W, Xiao W, et al. Effects of semen processing on the generation of reactive oxygen species and mitochondrial membrane potential of human spermatozoa. Andrologia. 2012;44:157–163. doi: 10.1111/j.1439-0272.2010.01123.x. [DOI] [PubMed] [Google Scholar]
- 35.Allamaneni SSR, Agarwal A, Nallella KP, Sharma RK, Thomas AJ, Jr, Sikka SC. Characterization of oxidative stress status by evaluation of reactive oxygen species levels in whole semen and isolated spermatozoa. Fertil Steril. 2005;83:800–803. doi: 10.1016/j.fertnstert.2004.05.106. [DOI] [PubMed] [Google Scholar]
- 36.Fingerova H, Oborna I, Novotny J, Svobodova M, Brezinova J, Radova L. The measurement of reactive oxygen species in human neat semen and in suspended spermatozoa: a comparison. Reprod Biol Endocrinol. 2009;7:118–123. doi: 10.1186/1477-7827-7-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henkel R, Kierspel E, Stalf T, Mehnert C, Menkveld R, Tinneberg HR, et al. Effect of reactive oxygen species produced by spermatozoa and leukocytes on sperm functions in non- leukocytospermic patients. Fertil Steril. 2005;83:635–642. doi: 10.1016/j.fertnstert.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 38.Mupfiga C, Fisher D, Kruger T, Henkel R. The relationship between seminal leukocytes, oxidative status in the ejaculate, and apoptotic markers in human spermatozoa. Syst Biol Reprod Med. 2013;59:304–11. doi: 10.3109/19396368.2013.821540. [DOI] [PubMed] [Google Scholar]
- 39.Ochsendorf FR. Infections in the male genital tract and reactive oxygen species. Hum Reprod Update. 1999;5:399–420. doi: 10.1093/humupd/5.5.399. [DOI] [PubMed] [Google Scholar]
- 40.Sakamoto Y, Ishikawa T, Kondo Y, Yamaguchi K, Fujisawa M. The assessment of oxidative stress in infertile patients with varicocele. BJU Int. 2008;101:1547–52. doi: 10.1111/j.1464-410X.2008.07517.x. [DOI] [PubMed] [Google Scholar]
- 41.Kothari S, Thompson A, Agarwal A, du Plessis SS. Free radicals: their beneficial and detrimental effects on sperm function. Indian J Exp Biol. 2010;48:425–35. [PubMed] [Google Scholar]
- 42.Lavranos G, Balla M, Tzortzopoulou A, Syriou V, Angelopoulou R. Investigating ROS sources in male infertility: a common end for numerous pathways. Reprod Toxicol. 2012;34:298–307. doi: 10.1016/j.reprotox.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi H, Gil-Guzman E, Mahran AM, Sharma RK, Nelson DR, Thomas AJ, Jr, et al. Quality control of reactive oxygen species measurement by luminol-dependent chemiluminescence assay. J Androl. 2001;22:568–574. [PubMed] [Google Scholar]
- 44.Vessey W, Perez-Miranda A, Macfarquhar R, Agarwal A, Homa S. Reactive oxygen species (ROS) in human semen: validation and qualification of a chemiluminescence assay. Fertil Steril. 2014;102:1576–1583. doi: 10.1016/j.fertnstert.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 45.Agarwal A, Allamaneni SS, Said TM. Chemiluminsecence technique for measuring reactive oxygen species. Reprod Biomed Online. 2004;9:466–468. doi: 10.1016/S1472-6483(10)61284-9. [DOI] [PubMed] [Google Scholar]
- 46.Saleh RA, Agarwal A. Oxidative stress and male infertility: from research bench to clinical practice. J Androl. 2002;23:737–752. [PubMed] [Google Scholar]
- 47.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2013; URL http://www.R-project.org/.
- 48.Kashou AH, Sharma R, Agarwal A. Assessment of oxidative stress in sperm and semen. Methods Mol Biol. 2013;927:351–361. doi: 10.1007/978-1-62703-038-0_30. [DOI] [PubMed] [Google Scholar]
- 49.WHO . WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- 50.Agarwal A, Sharma RK, Nallella KP, Thomas AJ, Jr, Alvarez JG, Sikka SC. Reactive oxygen species as an independent marker of male factor infertility. Fertil Steril. 2006;86:878–885. doi: 10.1016/j.fertnstert.2006.02.111. [DOI] [PubMed] [Google Scholar]
- 51.Desai NR, Mahfouz R, Sharma R, Gupta S, Agarwal A. Reactive oxygen species levels are independent of sperm concentration, motility and abstinence in a normal, healthy, proven fertile man: a longitudinal study. Fertil Steril. 2010;94:1541–3. doi: 10.1016/j.fertnstert.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 52.Pasqualotto FF, Sharma RK, Kobayashi H, Nelson DR, Thomas AJ., Jr Oxidative stress in normospermic men undergoing infertility evaluation. J Androl. 2001;22:316–322. [PubMed] [Google Scholar]
- 53.Aitken RJ, West K. Relationship between reactive oxygen species generation and leukocyte infiltration in fractions isolated from the human ejaculate on Percoll gradients. Int J Androl. 1990;13:433–451. doi: 10.1111/j.1365-2605.1990.tb01051.x. [DOI] [PubMed] [Google Scholar]
- 54.Deepinder F, Cocuzza M, Agarwal A. Should seminal oxidative stress measurement be offered routinely to men presenting for infertility evaluation? Endocr Pract. 2008;14:484–491. doi: 10.4158/EP.14.4.484. [DOI] [PubMed] [Google Scholar]
- 55.Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2014;28:684–703. doi: 10.1016/j.rbmo.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 56.Showell MG, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2011;19(1) doi: 10.1002/14651858.CD007411.pub2. [DOI] [PubMed] [Google Scholar]
- 57.Gharagozloo P, Aitken RJ. The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy. Hum Reprod. 2011;26:1628–1640. doi: 10.1093/humrep/der132. [DOI] [PubMed] [Google Scholar]
- 58.Vicari E. Effectiveness and limits of antimicrobial treatment on seminal leukocyte concentration and related reactive oxygen species production in patients with male accessory gland infection. Hum Reprod. 2000;15:2536–44. doi: 10.1093/humrep/15.12.2536. [DOI] [PubMed] [Google Scholar]
- 59.Hamada A, Esteves SC, Agarwal A. Insight into oxidative stress in varococele-associated male infertility: part 2. Nat Rev Urol. 2013;10:26–37. doi: 10.1038/nrurol.2012.198. [DOI] [PubMed] [Google Scholar]
- 60.Ramya T, Misro MM, Sinha D, Nandan D. Sperm function and seminal oxidative stress as tools to identify sperm pathologies in infertile men. Fertil Steril. 2010;93:297–300. doi: 10.1016/j.fertnstert.2009.05.074. [DOI] [PubMed] [Google Scholar]