SCIENTIFIC ABSTRACTS
“A ONE-STOP SHOP:” PERCEIVED BENEFITS OF DIABETES GROUP VISITS IN THE SAFETY NET CLINIC SETTINGArshiya A. Baig1; Amanda Benitez1; Amanda Campbell2; Cynthia T. Schaefer3,2; Loretta J. Heuer4,2; Michael T. Quinn1; Deborah L. Burnet1; Marshall Chin1. 1University of Chicago, Chicago, IL; 2MidWest Clinicians’ Network, Lansing, MI; 3University of Evansville, Evansville, IN; 4North Dakota State University, Fargo, ND. (ID #1934849)
BACKGROUND: Diabetes group visits, shared appointments in which patients with diabetes receive self-management education in a group setting and have a medical visit, are an innovative and promising way to deliver diabetes care. The group visit model may be especially promising in safety net clinics where many patients with diabetes in underserved settings receive their care. However, little is known about safety net providers’ perceptions of diabetes group visits in the community health center setting.
METHODS: The research team conducted site visits at community health centers across the Midwest to assess their experiences in providing diabetes group visits. Site visits were conducted at centers that had implemented diabetes group visits in the past or currently had them. Two members of the research team interviewed health center personnel at each site regarding their diabetes group visit program. Health center personnel included chief executive officers, medical and nursing directors, care coordinators, physicians, nurses, physician assistants, diabetes educators, mental health professionals, dietitians, medical assistants, pharmacists, and other recommended staff members who were familiar with the diabetes group visits at the site. Interviewees were asked about the benefits of having diabetes group visits at their site. All interviews were audio-recorded and transcribed. Systematic qualitative analysis techniques were used to identify the range and consistency of opinions and experiences across interviewees.
RESULTS: The research team visited five health center sites across four states in the Midwest and conducted a total of 26 interviews with health center personnel. One site was rural, three were urban, and one was suburban. Health center personnel noted many benefits of group visits to the health center, providers, and patients. The benefits of group visits to the health center included an alignment of the group visit model with the mission of becoming a patient centered medical home, the ability to bill for group visits, and an efficient way to improve guideline-driven care for patients. Provider benefits from group visits included boost to provider morale, opportunities to collaborate with multidisciplinary colleagues, and having more time to focus on other medical concerns during patient’s routine follow-up visits. Patients derived many benefits, including receiving education and medical care in a single appointment, e.g. “the one-stop shop” or “best bang for your buck,” the opportunity to obtain social support and enhanced motivation through peers, and the potential to improve their clinical outcomes by attending group visits.
CONCLUSIONS: Diabetes group visits can offer many unique benefits to safety net clinics by providing patient-centered care, boosting provider morale, increasing multidisciplinary collaboration, and offering patients the convenience of combining an educational session with a primary care appointment. Further studies need to assess best practices in implementing group visits in health centers and assess their impact on patient outcomes.
“A PLACE AT THE TABLE:” EVALUATION OF COMMUNITY MEMBERS’ EXPERIENCES AND EXPECTATIONS FOR ACADEMIC-COMMUNITY PARTNERSHIPS IN HIV/AIDS RESEARCHStella Safo1; Chinazo Cunningham3,2; Alice Beckman2; Joanna L. Starrels3,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY; 3Montefiore Medical Center, Bronx, NY. (Tracking ID #1937992)
BACKGROUND: The foundation of community based participatory research (CBPR) is collaboration between academic researchers and members of a given community. Community advisory boards (CABs) are one mechanism through which academic-community partnerships are formed, but current research about CAB members’ opinions on barriers to collaborations with academics is limited. This qualitative study examined CAB members’ expectations and experiences in working with academic researchers in the field of HIV/AIDS.
METHODS: We conducted 10 semi-structured one-on-one interviews with individuals serving on a CAB for HIV-related research at an urban academic medical center. Participating CAB members were leaders of HIV/AIDS community organizations in Bronx, NY and had at least 5 years of experience working in the field of HIV/AIDS. Interview questions focused on participants’ current and previous experiences with academic research and researchers, trust in these relationships, and best practices for collaboration. Interviews were professionally transcribed and data was analyzed using a grounded theory approach. Transcript data were coded by two independent researchers using NVivo 10 software and analyzed in an iterative process to identify emergent themes.
RESULTS: CAB members described positive aspects of inclusion on a CAB, including improved access to information about current HIV topics and the opportunity to help shape HIV research in their communities. However, CAB members also described negative previous interactions with researchers, and a lack of trust in researchers themselves or in the process of conducting research with academic institutions. A major reason for distrust was that power was perceived as unequal, often resulting in miscommunications that led to lasting negative impressions. For example, several members recounted researchers approaching subjects directly, without informing the home organization about the intended study focus. In addition, CAB members felt that expectations for collaboration were not clearly established. CAB members also shared suggestions for improving the collaborative process, including outlining expectations from the outset of the partnership and holding CAB meetings in the community rather than at the academic center.
CONCLUSIONS: We identified complex interpersonal issues in relationships between CAB members and academic partners, particularly around trust and power-sharing in conducting HIV/AIDS research. Our findings suggest that academic-community collaborations could be enhanced by improving transparency, explicitly addressing issues of distrust from previous negative experiences, and ensuring equitable power-sharing among researchers and community members. Further research should be conducted to determine the best ways to engage and maximize the impact of CABs in the field of HIV/AIDS.
“ARE YOU AFRAID OF PNEUMONIA?” PATIENTS’ FEEDBACK ON THE DEVELOPMENT OF AN EDUCATIONAL VIDEO ABOUT PNEUMOCOCCAL VACCINATIONKenzie A. Cameron; Tiffany Brown; Shira N. Goldman. Northwestern University, Chicago, IL. (Tracking ID #1926320)
BACKGROUND: Invasive pneumococcal disease causes a mortality burden among people age 65 and older. Consequently, the Advisory Committee on Immunization Practices recommends pneumococcal vaccination (PnVx) for these adults. However, national rates of PnVx for those age 65 and older are just over 60 %. Further, racial and ethnic disparities in vaccination remain: 2011 estimates reported 66.5 % vaccination among whites age 65 and older, as compared to only 47.6 % among blacks. Informed by our previous research on perceptions toward PnVx among unvaccinated adults, we developed a 2 min patient education video targeted at unvaccinated 65 and 66 year olds to encourage uptake of PnVx. Our objective was to discuss patient attitudes toward vaccination and beliefs about pneumonia, and obtain feedback regarding suggested revisions for the video.
METHODS: At an academic general internal medicine clinic, we queried the electronic health record to identify 65 and 66 year old black and white patients who had no record of receipt or refusal of PnVx. In early 2013, patients were recruited to participate in race-concordant focus groups. Prior to the start of each group, participants completed a brief demographic survey, which included questions regarding past experience with pneumonia and PnVx. During the audio-recorded focus group, we asked participants to describe pneumonia, tell us what they knew about PnVx, and specify what they would want included in educational messages about the vaccine.
RESULTS: Four white and two black patient focus groups were conducted, with a total of 26 participants. Mean age was 65.9 (3.1), 81 % were female, 88 % had attended college, and 39 % reported receipt of PnVx. Based on our previous research, the video included a strong focus on individual susceptibility to pneumonia, as well as personal testimonial from a black man about his late wife who did not think she needed PnVx. Black patients in particular noted that the testimonial was a persuasive part of the video. Participant response to the video was positive, with some individuals indicating a newly found motivation to consider vaccination (e.g., “Even though I refused the pneumonia vaccine already, next time I see my provider, I’m going to tell her I want to get shot,” and “I’m going to go get my shot now. I didn’t realize how potent and prevalent it is.”). However, some participants felt that the video focused too heavily on severity and fear (e.g., “I find it dire. Very uncomfortable watching it.”). The video included an appeal to consistency and the need for vaccination across the lifespan (“Just as you got vaccinated as a child, you need to receive important lifesaving vaccines as an adult”), which was met with favorable responses from participants. Several participants highlighted the importance of discussing PnVx with their providers and indicated that viewing this video prior to an appointment could provide an opportunity for such discussion (e.g., “I might talk to my doctor. I don’t know if she could persuade me to get it. Maybe she could explain it to me differently”).
CONCLUSIONS: Feedback from the focus group participants led to revisions to the patient education video, specifically with regard to reducing the number of times the severity of pneumonia was stressed. The personal narrative was retained as numerous individuals spoke of its persuasiveness, as was a focus on personal susceptibility to pneumonia and the need for vaccination across the lifespan. The revised video is under 2 min long, has been integrated into our electronic health record system, and is being tested at the point-of-care to assess its effect on receipt of PnVx among patients eligible for vaccination.
“BEYOND OUR CONTROL”: HOW ORGANIZATIONAL CONTEXT IMPACTS PERFORMANCE MEASUREMENTMolly Harrod1; Jane Forman1; Claire Robinson1; Adam Tremblay2,3; Leo Greenstone2,3; Eve A. Kerr1,3. 1VA Ann Arbor Health Care System, Ann Arbor, MI; 2VA Ann Arbor Health Care System, Ann Arbor, MI; 3University of Michigan, Ann Arbor, MI. (Tracking ID #1937968)
BACKGROUND: The Patient Centered Medical Home (PCMH) model requires a shift from a physician centric to a team-based approach to care, as well as improvement in process measures that reflect PCMH goals. As a result, as primary care (PC) providers are learning to work in teams, they also must learn how to change their clinic processes to meet PCMH-specific performance measures. The Veterans Health Administration (VHA) transitioned over 900 PC sites to a PCMH model beginning in 2010 and has implemented national metrics of PCMH success that include same day access and continuity with the patient’s usual provider. One large VHA health system implemented a coaching model to help newly formed PC teams redesign their delivery processes to improve access and continuity measures. This study examines how these PC teams discussed and responded to these measures during their coaching sessions.
METHODS: Nine of 20 PC teams were longitudinally observed during coaching sessions (25+ hours) that entailed discussion of both performance measures and processes to improve measure results. Conversations and interactions were recorded via hand-written field notes. We analyzed data using a grounded approach.
RESULTS: As PC teams reviewed their access and continuity measures, two predominant, and often overlapping, themes emerged: lack of control and lack of consistency across the organization. PC teams felt they did not have control over processes both within and outside PC. For example, a centralized call center with variable understandings of PC redesign continued to refer patients to the Emergency Department even though PC providers had open appointments within their schedules, thus impacting continuity. A lack of consistency across the organization as a whole was apparent given that many of the other departments did not change their patient care processes to align with PCMH goals. For example, inpatient physicians followed a rule that patients discharged from the inpatient setting needed “follow-up with primary care physician in 7–10 days”. Because this 7–10 day mandate meant fewer open slots in a PC provider’s clinic, it decreased same day access. Thus, organizational processes were often working against one another resulting measures that were not reflective of all the changes.
CONCLUSIONS: Improving even straightforward performance measures, like same-day access, requires an understanding of the entire practice context. In our study, measurement results that fell short of goals reflected the organizational inconsistency of processes that impacted individual measures. It is important to develop processes designed to meet PACT goals across the organization rather than within each team or department. As more PC practices become part of Accountable Care Organizations and are assessed using these and other performance measures, a better understanding of what is being measured, how these measures reflect patient-centered care, unintended consequences of measures and other organizational actions, and how to align organizational performance goals is needed so that organizational performance reflects true quality of care and patient-centeredness, and not just performance on individual metrics.
“CODE R”: INTRODUCTION OF A HOSPITAL-WIDE PEER REVIEW PROCESS TO ASSESS RESIDENTS’ POTENTIAL IMPACT ON PATIENT SAFETY AND QUALITYDaniel I. Kim1,3; Lawrence Loo2; Huy Au1,3; Ramiz Fargo1,3; Roger C. Garrison1,3; Gary Thompson1,3; Minho Yu2,3. 1University of California, Riverside, Riverside, CA; 2Loma Linda University Medical Center, Loma Linda, CA; 3Riverside County Regional Medical Center, Moreno Valley, CA. (Tracking ID #1928321)
BACKGROUND: The hospital physician peer review process is a valuable method of reviewing physician competency and safety, but it is rarely used to evaluate residents, who frequently work under indirect supervision. In 2008, our institution introduced “Code R” to our peer review process to highlight the potential resident involvement in cases undergoing peer review. To our knowledge, there are no published studies that utilize a hospital-wide peer review process to evaluate and track residents in training. Our study sought to characterize resident errors using the ACGME’s core competencies to determine whether interns are more prone to errors than senior residents and to see if there were patterns of resident errors by time of day or month of year.
METHODS: The study is a retrospective review of all peer review cases recorded from 2008 to 2011 by the Quality Management department at Riverside County Regional Medical Center, an academic safety net institution. The institutional peer review process spans all the departments within the hospital and reviews the cases involving patient deaths, unexpected adverse outcomes, incident reports, quality measure fallouts and random physician quality reviews. Cases designated a Code R were identified and the following information was collected using a standardized form: peer review level assigned, area of deficiency, resident post-graduate year, originating department, month, and time of day. Care issues were characterized into the five core competencies of patient care, medical knowledge, professionalism, communication/interpersonal skills and systems-based practice. The chi-square and Fisher’s exact tests were used to make comparisons and an a priori statistical level of significance of p value ≤ 0.01 was used to adjust for multiple comparisons.
RESULTS: Between 2008 and 2011, 8052 individual cases were peer reviewed by the medical staff and 258 (or 3.2 %) had “Code R” assigned. Of the total charts initially identified, nine cases were determined to not be resident related, nine charts were unavailable and two cases had incorrect medical record numbers. Two hundred thirty-eight charts qualified for final data analysis. The peer reviewed designations and prevalence in each category were Level 1 (Meets standard)- 13 (5.5 %), Level 2 (Meets standard - opportunity for improvement) −196 (82.4 %), Level 3 (Deviation from standard) −26 (10.9 %), and Level 4 (Unacceptable care) −3 (1.3 %). Compared with the non-Code R, or attending physician cases, there were significantly more errors in all the competencies (5.5 % vs. 89.3 % Level 1 assignments for resident vs. attending physicians). In the Code R cases, 60 % (143/238) of the charts had documentation issues. One-third (79/238) of the charts had deficiencies in patient care issues, which include clinical judgment, decision-making and lack of follow-up. The next most common errors were in the competencies of Systems-based Practice and Interpersonal Communication, 9.2 % and 8.0 % respectively. We did not find any significant differences in resident errors by time of day or calendar year. However, interns (PGY-1) were more prone to errors than senior residents (PGY ≥ 2) (p = 0.002).
CONCLUSIONS: The introduction of “Code R” helped identify cases in which resident involvement potentially impacted patient care and safety. Our analysis of Code R cases suggest specific areas for focused resident supervision and education are needed in the areas of documentation and patient care. This simple peer review process can be readily adopted by other institutions to help improve resident education, facilitate attending supervision, and potentially improve patient safety. Use of this instrument can be used to track the individual resident and attending performance that has not been previously described.
“HAVE YOU THOUGHT ABOUT SENDING THAT AS AN ECONSULT?”: PRIMARY CARE PROVIDERS’ EXPERIENCES WITH ELECTRONIC CONSULTATIONS AT AN ACADEMIC MEDICAL CENTERSara Ackerman1; Gina Intinarelli4; Nathaniel Gleason2; Michael Wang3; Sereina Catschegn2; Delthia McKinney4; Ralph Gonzales2. 1University of California, San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA; 3University of California, San Francisco, San Francisco, CA; 4University of California, San Francisco, San Francisco, CA. (Tracking ID #1936109)
BACKGROUND: Electronic consultations (eConsults) are a recent innovation enabling primary care clinicians to request advice from specialists, via a shared electronic health record (EHR), for lower-complexity clinical problems that do not require an in-person evaluation of the patient by the specialist. Prior studies suggest that eConsults can improve the time-to-access to specialty care and reduce specialty care office visit utilization. Using in-depth interviews, we sought to elucidate primary care providers’ (PCPs) experiences with a recently adopted eConsult program at an academic medical center.
METHODS: We recruited a purposive sample of PCPs from an academic medical center with a recently implemented EHR-based program in which specialists and PCPs receive reimbursement for completed eConsults. Semi-structured interviews were conducted to explore the benefits and limitations of eConsults and their impact on clinical work - including information transfer and clinician-patient and PCP-specialist interactions. Interviews were audiotaped, professionally transcribed, and checked for accuracy. Each interview transcript was reviewed by at least two authors in addition to the interviewer. The constant comparative method was used by the team to collaboratively and iteratively develop themes related to the study objectives.
RESULTS: Nine interviews have been completed to date, with participants representing a range of primary care professions and levels of experience, including faculty physicians, medical residents and nurse practitioners. A total of 20 interviews will be completed by March 2014. We identified three key thematic domains related to eConsult benefits, limitations, and influence on clinical work. 1) Access to expert advice: Most participants reported that eConsults were preferable to the use of informal, or “curbside”, consultations because they offer timely and standardized access to specialist advice without requiring PCPs to call on social networks or ask for favors, and because the consultation is stored in the electronic medical record and is conveniently linked to information about related tests and treatments. As one PCP explained, “I like that it is more formal and that it gets into the patient’s chart and it is recorded and I can refer to it later.” Nonetheless, the occasional use of curbside consultations persisted even among PCPs who routinely use eConsults, and was not seen as incompatible with eConsult use. The perception that an eConsult renders the specialist part of a patient’s care team, while simultaneously obviating the need for an office visit, was also reported as a source of increased patient and PCP satisfaction. 2) Providing better care: The use of eConsults was associated with increased clarity about specialists’ and PCPs’ roles, more transparent and efficient care coordination procedures, and PCPs’ enhanced participation in determining a patient’s follow-up plan. “I just feel like I’m providing better primary care”, said one PCP. Some participants reported that patient management using an eConsult is more time-consuming, and entails greater responsibility on the part of the PCP, than a traditional consultation, but most felt that this was an acceptable tradeoff for the satisfying learning opportunities and increased sense of mastery accompanying the incorporation of eConsults in their workflow. 3) Uneven adoption patterns: A minority of participants was less enthusiastic about eConsults and the frequency of use varied widely among individual providers. Some PCPs described a reluctance to initiate an eConsult because of difficulty with technical aspects of the program, frustration with slower-than-promised responses from consultants, or concern about how and when to communicate with patients regarding a consultant’s recommendations. Others reported “pushback” from patients who wanted in-person advice from a specialist. Most participants reported weighing both clinical and non-clinical factors when deciding when to request an eConsult. “That is why I choose the right patients…”, said a PCP about the need to balance clinical appropriateness and patient preference when deciding between an eConsult and a conventional referral.
CONCLUSIONS: Our results suggest that eConsults present an effective strategy for improving PCPs’ ability to obtain specialist expertise, and that they increase PCPs’ engagement and satisfaction with their clinical work. However, eConsults do not uniformly replace informal “curbside” consultation practices, and decisions about their use are influenced by non-clinical factors such as convenience, usability of the electronic interface, and patient preference. eConsult program designers should elicit continual feedback from providers in order to increase the ease of use and appeal of this mode of consultation.
“IN THE MILITARY, YOUR BODY AND YOUR LIFE AREN’T YOUR OWN:” UNIQUE FACTORS INFLUENCING HEALTH BEHAVIOR CHANGE IN OVERWEIGHT AND OBESE VETERANSMelanie Jay1,3; Katrina F. Mateo1,2; Molly Horne2,1; Allison Squires4,2; Adina Kalet2; Scott Sherman1,3. 1VA NY Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU School of Medicine, New York, NY; 4NYU College of Nursing, New York, NY. (Tracking ID #1920967)
BACKGROUND: Obesity affects 36 % of the Veteran population. The Veterans Affairs (VA) Healthcare System offers an intensive weight management program called MOVE!, but only approximately 10 % of eligible patients attend even one session. Since veterans see their PCPs 3.6 times per year, developing primary care-based weight management interventions may improve MOVE! attendance. To inform intervention development, we conducted a single-center qualitative study to explore unique VA patient 1) attitudes, barriers, and facilitators to healthy behavior change; 2) uses and understandings of goal-setting; and 3) weight management-related experiences with health care providers, technology, and MOVE!.
METHODS: We sent recruitment letters to overweight and obese patients at the New York Harbor VA. Eligibility criteria included Veterans aged 18–75, having a BMI ≥ 30 or ≥ 25 with at least one co-morbidity, and self-reported ability to read and participate in focus groups. We organized patients into focus groups of 6–11 participants, grouped by gender and MOVE! attendance. The interview guide was informed by the Theory of Planned Behavior (TPB). Sessions were audio-recorded, contextually supplemented with field notes, and transcribed by a professional company. Initial codes were determined based on session recollection and field notes. Using an iterative coding approach, two coders separately reviewed segmented transcripts, modified the codebook as new codes emerged, and met to negotiate codes. We utilized NVivo software to assist with coding and subsequent thematic analysis.
RESULTS: We screened 161 patients for eligibility, 77 were scheduled to attend, and 54 attended one of six focus groups (two female and four male). Participants were predominantly male (63 %), African-American (46 %) or White/Caucasian (32 %), college-educated or higher (74 %), and reported having attended MOVE! (61 %). We found that although we attempted to stratify focus groups by MOVE! attendance, the VA electronic health record did not accurately capture this information, and some study participants were confused or unaware of their attendance. Thematic analyses revealed how military service informed participants’ attitudes, social norms, and perceived behavioral control with regards to weight management. Participants described how the structured environment and strict standards of the military motivated them to maintain weight control while enlisted, but that lack of autonomy was a barrier to learning how to manage their health when they left service. The military also influenced their perceived need for more personalized and tailored health counseling. Physical activity was largely considered the predominant method to lose weight, and participants felt the MOVE! program lacked a physical activity-related component. While participants acknowledged the potential usefulness of technology to help identify and achieve weight management goals, they expressed the need to have a knowledgeable person (i.e. health coach, PCP, dietician, etc.) provide guidance and support.
CONCLUSIONS: This study revealed how military service may influence veterans’ intentions to lose weight and their weight management-related experiences. This will guide the development of a computer-assisted intervention to treat obesity within primary care and improve access and quality of weight management services. The implications from this study may be limited as it was conducted at a single site within a specific and a mostly self-selected patient population.
“NONE OF THEM APPLY TO ME:” A USABILITY STUDY OF THE VA’S MOVE!23 ONLINE WEIGHT MANAGEMENT SOFTWARE IN LATINA WOMENHector R. Perez4; Michael W. Nick5; Katrina F. Mateo1,2; Scott Sherman1,3; Adina Kalet2; Melanie Jay1,3. 1VA NY Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU School of Medicine, New York, NY; 4NYU School of Medicine, New York, NY; 5NYU School of Medicine, New York, NY. (Tracking ID #1920971)
BACKGROUND: The obesity epidemic disproportionately affects Latina women, but there are few interventions in this population. The MOVE!23 software program is a publicly available, English-only, online questionnaire used by the Veteran’s Affairs (VA) Administration to facilitate weight management. It evaluates patients’ current behaviors and stage of change and provides computer-generated, individualized advice. Completion of MOVE!23 during an intensive weight management program is associated with greater 6-month weight loss outcomes. Thus, adapting this tool for use in Latina women may be beneficial. However, the MOVE!23 is not specifically tailored for use in non-VA populations and its usability in this population is uncertain. The International Organization for Standardization (ISO) defines usability as “the extent to which a product can be used by specified users to achieve specified goals with effectiveness, efficiency, and satisfaction in a specified context of use.” In order to determine the utility of tailoring the MOVE!23 for Latina women and translating it into Spanish, we conducted usability testing of this software.
METHODS: We recruited English-speaking, adult Latina women. A researcher observed each participant individually as they used the MOVE!23 . Participants were asked to verbalize their thoughts and reactions as part of a “Think-Aloud” protocol. A semi-structured interview followed that elicited reflections on this experience and how it might influence lifestyle behavior change. We utilized ScreenFlow (Version 4.0.3) to capture on-screen interactions, and each session was digitally recorded and professionally transcribed. A coding guide was derived from the ISO definition of usability and focused on positive and negative interactions between four domains (Tool, Task, User, Context). Two researchers reviewed and coded the transcripts independently using the guide and secondary codes were derived inductively. The researchers met to review the codes and resolve discrepancies. NVivo software was used to facilitate data analysis.
RESULTS: Six female Latina participants completed the study (mean age 39, SD = 17); all had lived in the US for more than 20 years. Analysis indicated general satisfaction with tool navigation and the content, sequencing and segmentation of materials. Participants wanted individualized patient handouts to be more accessible and easily available on paper and suggested that images and icons might enhance visual appeal. Significant tool-user interactions included problems with navigation, difficulty understanding questions and answer choices, and sensitivity to the personal nature of the topics. User-context interactions included lack of experience with technology and requests for more support during completion of the questionnaire. In addition, subjects described personal experiences or beliefs while interacting with the materials. The extent to which questions or advice approximated their own experiences influenced the ease with which they were understood.
CONCLUSIONS: This study supports the utility of translating and tailoring the MOVE!23 for use in Latina women and identified several areas for improvement. Findings suggest that task execution may be enhanced when users are able to compare and reconcile the online materials with personal experiences and beliefs, highlighting the need to take these into consideration when tailoring software. Further research will aim to tailor and pilot the MOVE!23 software in populations of Latina women.
“SOMEDAY IT WILL BE THE NORM”: PHYSICIAN PERCEPTIONS OF THE CLINICAL UTILITY OF WHOLE GENOME SEQUENCINGJason L. Vassy1,2; Kurt D. Christensen2; Melody J. Slashinski3; Denise Lautenbach2; Jill Oliver Robinson3; Jennifer A. Blumenthal-Barby3; Lindsay Feuerman3; Robert C. Green2; Amy L. McGuire3. 1VA Boston Healthcare System, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Baylor College of Medicine, Houston, TX. (Tracking ID #1934488)
BACKGROUND: There is excitement that medicine is entering a genomic era, in which knowledge of one’s genetic makeup can guide medical decision-making. Whole genome sequencing (WGS) can identify 3–5 million genetic variants for an individual. However, the clinical significance of most of these variants is currently unknown, and the specific clinical contexts in which WGS might add value to current standards of care have not been identified. The uptake of WGS into medical practice will largely depend on whether and how physicians perceive it to improve patient care.
METHODS: We have enrolled primary care physicians (PCPs) and cardiologists to participate with their patients in the MedSeq Project: a randomized trial of WGS in the clinical care of healthy adult primary care patients and cardiomyopathy patients. We used mixed methods to describe the clinical utility that physicians perceive WGS to have. In a baseline survey on enrollment, we asked physicians to rate on a scale of 1–10 (“Not at all useful” to “Extremely useful”) how useful they thought WGS would be for “managing [their] patients’ health” at two times: now and in the future. We categorized responses as not useful (1–5) or useful (6–10) for analyses. We then conducted in-depth semi-structured interviews to explore whether and in what circumstances physicians might perceive WGS to have clinical utility. Transcribed interviews were consensus-coded with thematic content analysis to identify emergent themes.
RESULTS: Of 17 physicians (mean age 52 years), nine were women, and five were of non-white race. Nine were PCPs, and 11 reported no genetics training “beyond the typical medical school curriculum.” Only 4 (24 %) said that WGS had utility now, but 15 (88 %) predicted it would have future utility for their patients’ care. We identified three major themes influencing physician perceptions of utility. 1) Inevitability: Physicians expected WGS to be widely integrated into medical practice in the near future. When asked his opinion about the routine use of WGS in clinical care, one responded, “That’s like saying, ‘What do I think about getting cholesterol tests on people?’ I mean, it’s a reality, and I think it’s going to happen.” 2) Uncertainty: Physicians perceived WGS results to have too little analytic and clinical validity at present to be useful for patient care. One commented, “It’s like doing a CT scan and finding a nodule and not knowing what it means. And the next thing you know, you have a biopsy, and then you have a complication from the biopsy.” 3) Contexts of utility: In particular, physicians anticipated that WGS may 1 day be useful for nudging patient behavior change, tailoring drug therapy (pharmacogenomics), and efficiently targeting preventive health maintenance. One said, “If it turns out that we don’t have to do colonoscopies every 10 years on 100 % of the people, maybe that will save a lot of money. If we know who we really should be doing PSA’s or mammograms on, instead of doing them on everybody, we can save a lot of money, stop creating a lot of harm and disability.” Physicians often used analogies to current medical testing to describe their perceptions of WGS.
CONCLUSIONS: Physicians are skeptical about the current clinical utility of WGS for general patient care but anticipate a near future when the clinical integration of WGS will be widespread. Evidence that WGS improves health outcomes will likely be necessary to persuade physicians of its utility in patient care.
“WE TORTURE THEM BEFORE THEY DIE, EVEN THOUGH WE KNOW THAT THEY ARE GOING TO DIE:” THE INFLUENCE OF HOSPITAL POLICIES AND CULTURE ON ETHICAL DNR DECISION MAKING IN THE US AND UKElizabeth Dzeng1,2; Michael P. Kelly2; Sydney M. Dy1; Thomas J. Smith1; Martin Roland2; Stephen Barclay2; David M. Levine1. 1Johns Hopkins School of Medicine, Baltimore, MD; 2University of Cambridge, Cambridge, United Kingdom. (Tracking ID #1939234)
BACKGROUND: Physicians face ethical challenges when there are conflicts between autonomy and beneficence, which is defined as acting in the best interest of the patient. Shared decision-making, where the patient and doctor form a partnership to decide on treatment plan, has emerged as a model on the spectrum in between medical paternalism and patient autonomy. In the United States, there are significant variations in hospital policies regarding Do Not Resuscitate (DNR) decision-making. In the United Kingdom, it is standard practice for doctors to make unilateral decisions to institute a DNR order in situations where survival is unlikely. The aim of this study is to explore how doctors in the US and UK balance autonomy and beneficence in decisions regarding DNR status at the end of life and how their ethical values and clinical approach are shaped by their institution’s culture and legal frameworks.
METHODS: Semi-structured in-depth interviews were conducted with 58 internal medicine doctors across four sites (New York, Baltimore, Seattle and Cambridge, England), who were routinely involved in DNR conversations with end of life patients. Participants were purposively sampled by stage of training and medical subspecialty to provide a wide range of perspectives and contribute to understanding emerging patterns and themes. Interviews lasted on average 60 min and were audio-taped and transcribed. Transcripts were analyzed and double coded using thematic analysis with an interpretive approach.
RESULTS: 13–16 doctors participated at each site. Approximately equal numbers of senior faculty, junior faculty, fellows and residents were interviewed. Experienced doctors at all sites generally felt comfortable engaging in shared decision-making and when clinically appropriate, making more paternalistic recommendations against resuscitation. However, there was greater variation amongst residents and fellows that was site specific. At each hospital, there appeared to be a dominant mode of decision-making that impacted trainees’ perspectives on DNR decision-making. Although hospital policies primarily dictate whether patient preferences should be honored, trainees at hospitals with policies that prioritize patient autonomy often interpreted them to mean that they should not provide clinical recommendations. They felt compelled to offer choice even if the chance of successful resuscitation was negligible. In contrast, trainees at hospitals that had policies that encouraged paternalism or shared decision-making, which included the hospital in the UK and one in the US, felt more comfortable expressing clinical judgment against resuscitation when appropriate. Trainees at hospitals that prioritized autonomy more frequently perceived conflict between honoring autonomy and acting with beneficence and recalled more conflicts with patients regarding preferred decision.
CONCLUSIONS: Institutional norms and policies influence how doctors develop their professional attitudes and practices regarding DNR decision-making. Doctors at the American hospital that encouraged shared decision-making, had attitudes and beliefs about DNR decision-making that were more similar to British doctors than doctors at the other American sites. Hospitals characterized by higher levels of shared decision-making and paternalism provided an environment where trainees felt more comfortable withholding resuscitation when success was unlikely and in doing so, experienced fewer patient conflicts.
“WHAT DOES A GOOD LIFESTYLE MEAN TO YOU?” A QUALITATIVE ANALYSIS OF FIRST YEAR MEDICAL STUDENTS’ VIEWSKimberly Clinite1; Alex Garnett1; Shalini Reddy1; Kent DeZee2; Stephanie Kazantsev1; Steven Durning2; Jennifer R. Kogan3. 1University of Chicago, Pritzker School of Medicine, Chicago, IL; 2Uniformed Services University, Bethseda, MD; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA. (Tracking ID #1938451)
BACKGROUND: Medical students consider a specialty’s lifestyle when selecting a career; meeting the physician workforce shortage requires an understanding of how students define a “good” lifestyle. Understanding the lifestyle expectations of entering students may help medical educators guide students towards careers that will fulfill their ambitions and serve the health needs of our society. The purpose of this study was to determine how first year medical students define a good lifestyle.
METHODS: First year medical students at 11 schools were surveyed at matriculation in 2012. The survey included the open-ended question, “When someone says ‘That specialty has a good lifestyle,’ what does that mean to you?” Two investigators performed a directed content analysis of responses. Descriptive statistics of the themes were calculated.
RESULTS: 60 % (1020/1704) of students completed the survey; 934 answered the open-ended question. Responses encompassed four major themes: schedule control (66 % of students), off-time (54.5 % of students), financial aspects (35 % of students), and work-life (21 % of students). Schedule control was described with multiple subthemes (reasonable hours, flexible hours, predictable hours, and limited call). Nine student responses were categorized as disparaging.
CONCLUSIONS: This study has helped establish how matriculating medical students define lifestyle, a known factor in career selection. Matriculating medical students’ definition of lifestyle is largely defined by schedule control, though students’ concept of schedule control varies. Salary associated with a good lifestyle ranged from $175,000–$400,000. Understanding early perceptions of career decision-making may provide a context for medical educators to begin conversations with students about career choice. Additionally, specialties experiencing physician shortages should consider how their specialty will evolve to meet the needs of society while addressing the concerns of trainees. Policies that hope to successfully address the medical workforce shortages must account for students’ desire to have control of their work schedule.
“WHEN YOU ARE OLD, HAVE CANCER AND A STORM IS APPROACHING” -THE EFFECTS OF HURRICANE SANDY ON CANCER PATIENTS AND PROPOSALS ON POTENTIAL INTERVENTIONSMisako Nagasaka1; Hassan Alsabbak1; Zaid Aljuboori2; Koji Sasaki3; Alfred Burger1; Benjamin Levy1. 1Beth Israel Medical Center, New York, NY; 2Bronx Lebanon Hospital, New York, NY; 3MD Anderson Cancer Center, Houston, TX. (Tracking ID #1939110)
BACKGROUND: The estimated loss to the nation’s economy from Hurricane Sandy has climbed to as much as $50 billion, making it one of the nation’s most costly disasters. While data on the economic impact of natural disasters are often reported in a timely manner, very little data exists on the impact of natural disasters to health care, especially in cancer care.
METHODS: A retrospective chart review was performed to examine the impact of Hurricane Sandy and the subsequent blackout in southern Manhattan on emergency room (ER) visits of patients with a diagnosis of cancer. The records of cancer patients who had visited ER during the week of Hurricane Sandy (10/29/2012 to 11/4/2012) were reviewed. For control, ER visits of cancer patients of the same dates 1 year prior (10/29/2011 to 11/4/2011) were reviewed and compared. All data were extracted from the ER and/or inpatient electronic medical records. Collected data included age group, sex, cancer type, chief complaint, ER diagnosis and admission status. The diagnosis of cancer was extracted from the “History of Present Illness” or “Past Medical History” and included solid as well as hematologic malignancies. For patients who were admitted, additional data including metastatic disease, comorbidities, length of stay and mortality were extracted.
RESULTS: During the week of Sandy, 144 ER visits of cancer patients were identified. One hundred eighteen were identified the prior year. In patients over age 70, 84 visits were observed during Sandy, while only 41 visited the previous year (p value: 0.000143). The chief complaint of “shortness of breath (SOB) or asthma” was significant, with 21 ER visits in 2012 and only eight in 2011 (p value: 0.045). Out of the 21 visits of SOB, 10 required continuation of their current therapy (8 requested home oxygen therapy and two requested dialysis), while these requests were unobserved the prior year. During the Sandy week, 77 ER visits resulted in admission, while 64 were admitted the year prior (p value: 0.902). Out of 77, seven expired and from 64, four expired (p value: 0.759). The ER admitting diagnoses of the seven who expired during Sandy included a septic patient with fungating head and neck cancer, a brain cancer patient with respiratory failure, a lung cancer patient with pleural effusion, a sarcoma patient with pneumonia, an ovarian cancer patient with anemia, a melanoma patient with acute coronary syndrome and a lung cancer patient with SOB requesting home oxygen therapy. Corresponding data from the year prior included a lung cancer patient with pancytopenia, a CLL patient with pneumonia, a septic patient with breast cancer and a lung cancer patient with suicidal ideation.
CONCLUSIONS: Although there were no significant increase in the total ER visits of cancer patients during Sandy, there were significantly more ER visits during Sandy in cancer patients over age 70, suggesting increased vulnerability to this cohort. To our knowledge, this is one of the first few studies to evaluate cancer care related to natural disasters. In retrospect, the admission and death of a lung cancer patient with SOB requesting continuation of home oxygen therapy may have been the one potentially preventable. Cancer patients requiring additional medical assistance such as home oxygen therapy and dialysis may benefit from a natural disaster back-up plan. House calls, early and prioritized evacuation of these patient groups may be some options to minimize the effects of an approaching natural disaster.
Top 10 Chief Complaints
| Chief Complaints | 2011 | 2012 | p value |
|---|---|---|---|
| SOB or asthma | 8 | 21 | 0.049 |
| Chest pain or discomfort | 7 | 11 | 0.6 |
| Abd pain | 10 | 10 | 0.8 |
| Fall | 3 | 10 | 0.1 |
| Altered mental status | 4 | 8 | 0.5 |
| Weakness | 4 | 7 | 0.7 |
| Pain in extremeties | 9 | 7 | 0.43 |
| Requesting dialysis | 0 | 6 | 0.034 |
| Nausea and vomiting | 3 | 6 | 0.51 |
| Intoxication | 4 | 6 | 1 |
30 DAY READMISSION RATE FOR PATIENTS DISCHARGED WITH CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD): ANALYSIS OF 1,858,618 ADMISSIONS. WHICH PATIENTS ARE MOST AT RISK?Devin B. Malik; Sourabh Aggarwal. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1939043)
BACKGROUND: COPD is a major cause of morbidity and is associated with a high 30-day re-admission rate (RR) and economic burden on health care. This study was done to determine demographic parameters associated with high 30-day RR secondary to COPD
METHODS: Nationwide Inpatient Sample data was used to extract data of patients discharged with DM with complications for years 2009–2011 using clinical classification software (CCS). NIS represents 20 % of all hospital data in US. All the patients who were discharged with primary diagnosis of COPD and readmitted within 30 days were identified and categorized based on admitting diagnosis. Patients were classified as readmissions secondary to COPD as a primary cause, readmissions with COPD as a secondary cause and non-COPD associated readmissions. Statistical analysis was done using SPSS.
RESULTS: We identified a total of 1,858,618 admissions for COPD nationwide during the study period with total 30-day RR of 21.06 % and RR of 7.22 % secondary to COPD as a primary cause (Table 1). Age group (45–64), males, patients under Medicaid, patients in low median income for zip code and in metropolitan areas had higher 30-day re-admissions secondary to COPD as a primary cause (P < 0.001). Young patients (18–44 years of age), females, patients covered under Medicaid and living in Metropolitan areas had higher 30-day RR secondary to non-COPD related causes.
CONCLUSIONS: Strategies to reduce 30-day readmissions secondary to COPD should be focused on more susceptible population including males, aged 45–64 years old, under Medicaid, having low median income for zip code and staying in metropolitan areas.
A CLUSTER RANDOMIZED CONTROLLED TRIAL OF INTERVENTIONS TO IMPROVE WORK CONDITIONS AND CLINICIAN STRESS: RESULTS FROM THE HEALTHY WORK PLACE (HWP) STUDYMark Linzer1; Sara Poplau2; Ellie Grossman3; Steven H. Yale4; Anita B. Varkey5; Eric Williams6; Lanis Hicks7; Roger Brown8; Jill Wallock5; Diane Kohnhorst4; Michael Barbouche9. 1Hennepin County Medical Center, Minneapolis, MN; 2Hennepin County Medical Center, Minneapolis, MN; 3New York University Medical Center, New York, NY; 4Marshfield Clinic, Marshfield, WI; 5Loyola University Medical Center, Chicago, IL; 6University of Alabama, Tuscaloosa, AL; 7University of Missouri, Columbia, MO; 8University of Wisconsin, Madison, WI; 9Forward Health Group, Inc,, Madison, WI. (Tracking ID #1927618)
BACKGROUND: Work conditions in primary care are associated with stress, burnout, intent to leave the practice and quality of care. Time pressured office visits, lack of control of the workplace, a chaotic work pace, and lack of values alignment between clinicians and leaders contribute to stress and burnout. To determine the best ways to organize clinical practice, we measured the effects of work condition interventions on clinician and patient outcomes. Our goal was to assess if a “healthy workplace” could decrease clinician stress and improve care quality. This abstract reports on clinician outcomes.
METHODS: We performed a cluster randomized controlled trial in 34 rural and urban clinics in the upper Midwest and New York City. Primary care clinicians (general internists, family physicians, nurse practitioners and physician assistants) were studied. Seventeen clinics were randomized to participate in quality improvement interventions (QIIs) to improve worklife. Time pressure, work control, pace of work (chaos) and values alignment with leaders were measured at baseline and approximately 1 year later, along with clinician stress, burnout, satisfaction and intent to leave the practice in 2 years. The 17 clinics randomized to the intervention arm received their baseline data in an Office and Work Life (OWL) summary measure. QIIs were chosen by clinics based upon baseline OWL data, and focused predominantly in three areas: 1) improved communication, 2) changes in workflow and 3) clinical QI projects (e.g., a new prescription-refill telephone line, or a medication reconciliation project). Two level multilevel regression analysis was performed to assess the impact on clinician outcomes of being in the intervention arm. When these analyses did not disclose an overall intervention effect, we then explored whether clinicians who showed improvement in burnout, satisfaction or intent to leave the practice were more likely to be found in intervention clinics. Multivariate modeling determined which types of interventions were associated with improvement in these clinician outcomes.
RESULTS: Within 34 clinics, 166 clinicians were initially studied, and 139 subjects completed the study. Data were analyzable from 32 clinics and 135 clinicians. Burnout was present at baseline in 41 % of clinicians in intervention clinics and in 33 % of controls. While there was no overall effect of all interventions considered together, there were more clinicians with improvement in burnout in intervention vs. control clinics (21.8 % versus 7.1 %, Odds Ratio (OR) of burnout improvement 4.0, p = 0.014). Burnout was almost six times more likely to improve within clinics performing workflow interventions than in control sites (OR 5.9, p = 0.015), and was also more likely to improve in clinics performing clinical QI projects (OR 4.8; p = 0.021). Clinician satisfaction improved more often in the 10 clinics with interventions in the areas of communication and workflow than in control sites (OR 3.1; p = 0.042).
CONCLUSIONS: While these results should be confirmed in future studies, they suggest that organizations can address high rates of burnout by 1) measuring clinician outcomes (satisfaction, stress and burnout), 2) providing feedback on these outcomes to clinicians, clinic managers and staff, and 3) intervening by improving communication and workflow and initiating clinical QI projects.
A COMMUNITY PARTNERED APPROACH TO ENGAGE DIVERSE COMMUNITIES IN STROKE DISPARITIES RESEARCHNazleen Bharmal1; Aziza L. Wright3,2; Stefanie D. Vassar1; Felica U. Jones3; Loretta Jones3,2; Rebekah Wells4; Jason Cienega2; Arleen Brown1. 1University of California, Los Angeles, Los Angeles, CA; 2Charles R. Drew University of Medicine & Science, Los Angeles, CA; 3Healthy African American Families II, Los Angeles, CA; 4University of North Carolina, Greensboro, NC. (Tracking ID #1929958)
BACKGROUND: Racial/ethnic minorities have a higher burden of stroke and worse post-stroke outcomes. Contributors to this disparity include lower awareness of stroke signs and treatment, differences in access to care, mistrust in the healthcare system, and low participation in stroke clinical research studies. Despite emerging evidence that community input into interventions may enhance feasibility and sustainability, few stroke studies have incorporated the community perspective. The Los Angeles Stroke Prevention & Intervention Research Program to Reduce Health Disparities (LA SPIRP) is a center to reduce stroke disparities. The Community Engagement Core of LA SPIRP consists of community and academic co-leaders that review projects and work with investigators to understand community research priorities. To enhance public engagement in stroke research, our community-academic collaborative hosted a one-day symposium in South Los Angeles. The objectives of the symposium were to increase awareness of stroke, share information about and receive feedback on the LA SPRIP research projects, and promote collaboration between researchers and community partners to address stroke disparities.
METHODS: We used a community-partnered participatory research process to conceptualize the symposium. The symposium started with talks that provided information on stroke risk factors, stroke disparities, and the impact of stroke from the perspective of patients and caregivers. Simultaneous translation was available for monolingual Spanish speakers, and printed materials were available in English, Spanish, Korean, and Mandarin. We surveyed participants about stroke knowledge, stroke disparities, and trust in medical researchers. In the afternoon, attendees participated in six facilitated, small group breakout sessions (one conducted in Spanish) that addressed two questions: 1) What can we do as a community to prevent stroke?, and 2) How can we recruit more diverse populations in stroke research studies? Breakout session notes were analyzed using qualitative data analysis: content analysis used to code notes from group and pile-sorting by community and academic attendees to identify themes.
RESULTS: The symposium was attended by 236 community residents; staff from local clinical, social service, and faith-based organizations; and researchers. The survey response rate was 54 %. Over 90 % of the attendees were African American, Latino, or Asian; 40 % had hypertension. The majority of respondents had limited prior knowledge of stroke, and most had learned about stroke from family members, friends, or media. The average increase in knowledge about stroke pre- and post- didactic sessions was 15 %. On average, 21 % of respondents did not trust medical researchers to provide full explanations of research studies or protect participants from harm. Community recommendations for community-based strategies to prevent stroke focused on types of educational efforts (n = 128 quotes), educational content and cultural considerations (79), venues to share information (65), healthy eating efforts (50), partnerships with trusted stakeholders and institutions (34), types of audiences to receive stroke awareness information (30), physical activity efforts (26), and blood pressure screening (14). Community recommendations to enhance minority recruitment into clinical research studies included types of outreach methods (116), communication strategies (72) and partnerships with trusted stakeholders (51) to gain trust, types of incentives for participation (48), and considerations about the relevance and location of the research study for minorities (11).
CONCLUSIONS: Community-academic partnered events are effective ways to obtain community input into stroke research and may build trust and foster collaborations with community members for stroke research. Recommendations from the community stroke symposium will be used to frame future annual symposia, inform current LA SPIRP research, and develop smaller, culturally targeted stroke disparities programs in African-American, Latino, Korean, and Chinese-American communities in Los Angeles.
Recommendations from Breakout Sessions
| Community strategies to address stroke disparities | Commnity strategies to increase diversity in stroke research studies |
|---|---|
| ● Culturally sensitive advertising on risk factor reduction | ● Investigators should partner with community organizations to increase trust in research |
| ● Community participation in media campaigns | ● Have trusted, community-based medical and non-medical personnel recruit for studies |
| ● Use mobile vans to provide access to information and medical treatment | ● Use stories to appeal to community members |
| ● Educate primary and secondary students about stroke risk factors | ● Research that benefits the community |
| ● Make healthy food affordable (e.g., community gardens, local farmers’ markets) | ● Provide non-monetary incentives (e.g., blood pressure monitors) |
| ● Recognize the family’s role in prevention | ● Research takes place in the community |
A COMPARISON OF ACTIVE ADVERSE EVENT SURVEILLANCE SYSTEMS WORLDWIDEJodi B. Segal1,2; Yulin Huang1; Jinhee Moon1. 1Johns Hopkins Bloomberg School of Public Health, Baltimroe, MD; 2Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1930394)
BACKGROUND: Typically, fewer than 5,000 people have been exposed to a drug before marketing, so adverse drug events (ADEs) at low frequency will not have been observed. Drug regulatory agencies and industry are vigorously developing active surveillance systems for drugs, vaccines, and medical devices in order to quickly identify therapies causing harm to exposed patients. We conducted an environmental scan in order to describe the status of active surveillance systems for the detection of ADEs, worldwide.
METHODS: We developed a working definition of active surveillance systems. The key components of the systems that we sought to capture were: Structure—what is the structure, partnership relationships, and funding of existing active surveillance systems? Data—what are the data used in existing surveillance systems, what patient populations are included, and what is the content of these data? Function—what are examples of adverse drug events that have been identified with the active surveillance systems? Paired researchers reviewed published literature, as well as online sources, to identify existing systems. Data was extracted into tables designed to capture the key components of the active surveillance systems. We reviewed and synthesized the information across systems to identify common, and presumably, essential features of active surveillance systems.
RESULTS: We identified 12 active surveillance systems meeting our criteria, meaning that they were designed for post-marketing surveillance of pharmaceutical products (including vaccines), had a goal of generating post-marketing drug safety information, do not require personnel to initiate safety reports (describing individual cases), use real-world data which are generated from routine practice, and involve data from more than a single institution. Three systems are U.S. based - the FDA Sentinel Initiative, the Federal Partners Collaboration, and the Vaccine Safety Datalink; two are Canadian systems—The Canadian Network for Observational Drug Effect Studies (CNODES) and the Vaccine and Immunization Surveillance in Ontario (VISION); and two are European—the EU-Adverse Drug Reaction (ADR) Alliance and the Vaccine Adverse Event Surveillance and Communication (VAESCO). Additionally, there is a Japanese surveillance system called the Medical Information for Risk Assessment Initiative (MIHARI), a trans-Asian system called the Asian Pharmacoepidemiology Network (AsPEN), and one in Shanghai called the Shanghai Drug Monitoring and Evaluative System (SDMES). Two additional systems in the U.K. met our criteria: the Tayside Medicines Monitoring Unit (MEMO) and the Drug Safety Research Unit (DSRU), an independent academic unit that uses diverse European data for pharmacovigilance. The surveillance systems all use administrative claims or electronic medical records for data; some conduct pharmacovigilance explicitly on behalf of a regulatory agency, while others function more independently.
CONCLUSIONS: Active surveillance systems are rare. North America and Europe have the most developed systems and most coverage of the population; although some Asian countries are making good advances. There is no coverage of the patients exposed to medications in India, the Eastern European countries, or the South American and African continents. With the ever increasing availability of electronic data, active ADE surveillance should be increasing feasible. This should translate to more rapid signal detection, timely validation, and then steps to assure that drugs and vaccines are used safely.
A DESCRIPTION OF NEEDS FOR CARE COORDINATION AT A COMMUNITY-BASED GENERAL HOSPITAL IN JAPAN’S SUPER-AGED SOCIETYYukio Tsugihashi. 1Tenri Hospital, Tenri, Japan; 2Tenri Hospital, Tenri, Japan. (Tracking ID #1920518)
BACKGROUND: Japan’s population is aging rapidly because of long life expectancy and a low birth rate. In 2025, it is estimated that the percentage of aged population will increase to 25 %. Furthermore, the standout features of the Japanese healthcare system are “universal insurance scheme” and “unrestricted access to any doctor” which add strain to an already overburdened healthcare system. Therefore, a well-designed collaborative system is essential, one that supports the community healthcare and enables functional differentiation and the establishment of referral/transferal networks among a variety of institutions. The purpose of this study is to investigate 1) a medical service area in a community-based general hospital in Japan, 2) the places where the patients were discharged with professional discharge planning and 3) to estimate the future demographic changes in the number of inpatients.
METHODS: Participants: Inpatients discharged from one community-based general hospital in 2012. Setting: Tenri hospital, Tenri city, Nara, Japan (a total of 1001 beds, 26 departments and over 230 medical doctors) Study design: Retrospective cohort study Outcomes: 1) Mapping the medical service area 2) Specifying the places where the participants were discharged from the hospital that provided professional discharge planning 3) Estimating the changes of inpatient numbers and their age groups in 2012, 2025 and 2035. Analysis: First, we described the medical service area by connecting the participants’ address code and Geographical Information System (GIS). Second, a focus group interview lead by professional physicians was performed to find out which diseases frequently required professional discharge planning. Then, we evaluated the places where these patients were discharged from the hospital. Lastly, we projected the annual change in the number of inpatients and their respective age groups in the major medical service area for 2025 and 2035 respectively.
RESULTS: A total of 17,196 patients were included in this study. The medical service area was wide and included some cities outside Nara prefecture, the established government-designated administrative medical area (Figure). In addition, we highlighted five disease categories that needed professional discharge planning: cerebral stroke, fracture, cancer, infectious disease and heart failure categories. The results of professional discharge planning showed that the patients’ homes were the main place to be discharged to. There were some notable trends found between the places where patients were discharged to and the disease categories (Table). Furthermore, we estimated the change in the number of inpatients living in the top 10 areas to be 12,242 in 2025 (41.2 % of patients being 75 years old or over) and 11,337 in 2035 (42.2 %) compared with 12,088 (30.9 %) in 2012.
CONCLUSIONS: We investigated the medical service area of a community-based hospital in Japan highly reflective of its super-aged society and the needs for care coordination based on the actual practical performance. GIS analysis would help the general hospital to foresee the medical service area more concisely while preparing for the collaborative healthcare network. Additionally, to prepare for the rapid aging of inpatients, general hospitals should develop a collaborative healthcare system and a system for discharge planning appropriate to the medical service area and disease-specific needs for care coordination.
Table. Places where the participants were discharged from that provided professional discharge planning
| Cerebral stroke (N = 325) | Fracture (N = 30) | Cancer (N = 126) | Infection (N = 84) | Heart failure (N = 28) | |
|---|---|---|---|---|---|
| Age* | 74 ± 12 | 82 ± 9 | 72 ± 12 | 82 ± 10 | 82 ± 9 |
| Types of places** | |||||
| Home | 100 (31) | 4 (13) | 74 (59) † | 24 (29) | 7 (25) |
| Rehabilitation hospital | 152 (47) † | 16 (53) † | 4 (3) | 7 (8) | 2 (7) |
| Community hospital | 30 (9) | – | 23 (18) | 30 (36) † | 11 (39) † |
| Chronic care hospital | 29 (9) | – | 14 (11) | 15 (18) | 5 (18) |
| Mental hospital | 1 (0) | – | – | – | – |
| Hospice | – | – | 10 (8) | – | – |
| Nursing home | 13 (4) | 1 (3) | 1 (1) | 8 (10) | 3 (11) |
*mean ± SD, **n (%), †the most frequent place in each disease category
Figure. The medical service area of Tenri Hospital. Each dot represents the density of inpatients’ number living in each specified address code. Thick lines indicate the borders of cities in Nara Prefecture. *Tenri City.
A FAILURE TO COMMUNICATE: CHALLENGES AND SOLUTIONS TO CARE COORDINATION BETWEEN HOSPITALISTS AND PRIMARY CARE PROVIDERS AROUND HOSPITALIZATIONSChristine D. Jones1; Maihan B. Vu2; Christopher O’Donnell3; Mary Anderson1; Snehal Patel3; Eric A. Coleman4; Darren A. DeWalt5. 1University of Colorado, Denver, Aurora, CO; 2University of North Carolina at Chapel Hill, Chapel Hill, NC; 3Duke University School of Medicine, Durham, NC; 4University of Colorado, Denver, Aurora, CO; 5University of North Carolina at Chapel Hill, Chapel Hill, NC. (Tracking ID #1933333)
BACKGROUND: Care coordination (e.g., information exchange, direct communication) between hospitalists and primary care providers (PCPs) is critical to successful care transitions from hospital to home, yet such coordination is frequently lacking. We sought to understand care coordination challenges and potential solutions from the perspective of both hospitalists and PCPs in North Carolina.
METHODS: We conducted a qualitative study with eight focus groups (4 hospitalist groups and four primary care groups, 59 total participants). The team recruited practices from diverse settings; six of the groups shared patients between inpatient and outpatient settings. Interview guides were based on the AHRQ Care Coordination Measurement Framework and included questions about care coordination, information exchange, follow up care, accountability, and medication management. Focus groups were digitally recorded, transcribed verbatim, and analyzed in ATLAS.ti. Two team members independently coded transcripts and resolved differences through discussion. The constant comparison method was used to evaluate differences between hospitalists and PCPs.
RESULTS: Overall, we found that hospitalists and PCPs encounter many similar challenges to care coordination, including: 1) lack of time, 2) difficulty reaching the other provider by telephone, 3) lack of personal relationships with the other provider, 4) lack of clarity about accountability for pending tests and home health orders, and 5) discrepancies between what medications patients are taking and should be taking at home. Specific concerns for hospitalists include: 1) uncertainty about whether PCPs receive information about patient hospitalizations, and 2) difficulty obtaining timely follow up appointments for patients, particularly for after-hours or weekend discharges. Specific concerns for PCPs include: 1) not knowing when their patients are hospitalized, 2) not having records available for post-hospitalization appointments, 3) feeling disrespected by hospitalists when medication changes are made for unclear reasons without their involvement, and 4) difficulty locating important information (e.g., pending tests) in discharge summaries. Hospitalists and PCPs identified common themes to achieving successful care coordination: 1) making extra efforts to coordinate care for “high risk” patient populations (e.g., patients on Warfarin needing INR checks), 2) improving direct telephone access to each other, 3) improved information exchange through sharing EMRs with improved integration of care transitions workflow into EMRs (e.g., enhanced messaging capabilities, scheduling capabilities for follow up), and 4) enhancing personal relationships with clinicians in the other setting.
CONCLUSIONS: Hospitalists and PCPs encounter many similar challenges to care coordination, yet have important experiential differences related to sending and receiving roles for hospital discharges. Challenges that were cited in one setting were often not experienced by clinicians in the other setting. Efforts to improve care coordination between hospitalists and PCPs should aim to understand perspectives of clinicians in each setting. Such solutions include: 1) enhancing direct communication between providers in different settings, 2) clearly defining accountability for tests and home health orders, and 3) building personal relationships between clinicians in each setting.
A HEALTH LITERACY INTERVENTION TO IMPROVE MEDICATION ADHERENCE USING MEDUCATION® TECHNOLOGYLeah L. Zullig; Felicia McCant; S. Dee Melnyk; Susanne Danus; Hayden bOSWORTH. Durham Veterans Affairs Medical Center, Durham, NC. (Tracking ID #1926044)
BACKGROUND: Many Americans are reliant upon medication management for chronic conditions. Medication non-adherence is rampant, leading to increased healthcare cost and worsened health outcomes. Low health literacy is a contributing factor to medication non-adherence. Our objective was to determine whether antihypertensive medication adherence could improve using a Meducation® technology health literacy intervention.
METHODS: We conducted a six-month feasibility study among patients with cardiovascular disease risk factors who received care from hospital-based primary care clinics associated with Durham Veterans Affairs Medical Center (VAMC). To enhance potential benefit and future generalizability, the intervention was integrated into clinics’ practice tailored to address needs of high risk, potentially non-adherent patients. All patients received the intervention, which included a personalized Meducation® calendar. We evaluated changes in medication adherence and clinical outcomes at 6 months. Potential participants were initially identified through an electronic health record data pull. To be eligible for study inclusion, patients must have met all of the following criteria: enrolled in one of three primary care clinics affiliated with the Durham VAMC for at least 1 year; had at least one visit to an affiliated primary care provider in the previous 12 months; an outpatient diagnostic code for hypertension (ICD9 401.1, 401.9) diabetes (ICD9 250.x), and/or hypercholesterolemia (ICD9 272.x); prescribed metoprolol tartrate (beta blocker) and have poor medication adherence for the 12 months prior to baseline (medication possession ratio <80 %); and be prescribed more than nine active medications.
RESULTS: There was a 42 % enrollment rate (n = 23). The sample was predominantly married (57 %), African American (61 %), and male (91 %). Few participants (9 %) completed less than 12 years of school. Forty percent had low health literacy, defined as less than 9th grade reading level. The majority of participants were diagnosed with hypertension (91 %), hyperlipidemia (87 %), or diabetes (61 %). At 3 months self-reported medication adherence improved. There was a 45 % decrease in participants who agreed or strongly agreed that they sometimes forget their heart medications and 58 % fewer participants reported that they agreed or strongly agreed that they were ‘sometimes careless with how they take their medications’. At 6 months, medication possession ratio improved nearly 13 % and there were decreases in patients’ average systolic blood pressure (0.5 mmHg), diastolic blood pressure (1.5 mmHg), and body weight (3.6 lb) (p > 0.05).
CONCLUSIONS: A health literacy intervention is a feasible mechanism to improve cardiovascular-related medication adherence and outcomes. In this sample, 9 % of participants attained less than a high school level of education, yet 40 % had health literacy levels below the 9th grade reading level. This is problematic as much health promotion and medication adherence information is targeted to a tenth grade reading level, which may be inaccessible to many patients. Interventions to improve adherence through health literacy have the potential to require relatively few resources to implement, making them particularly important tools to combat medication non-adherence. Future interventions may target and/or oversample patients at greatest risk for health literacy-related medication non-adherence.
A LONGITUDINAL ANALYSIS OF THE EFFECT OF TOTAL OPIOID ANALGESIC DOSE ON SUBSEQUENT USE AND DURATION OF HOSPITALIZATIONBarbara J. Turner1,3; Benjamin R. Ehler2; Yuanyuan Liang2,3. 1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX; 3University of Texas Health Science Center at San Antonio, San Antonio, TX. (Tracking ID #1937908)
BACKGROUND: High opioid analgesic (OA) doses for chronic non-cancer pain (CNCP) increase the risk of adverse events such as drug overdose and car accidents but it is not known whether these drugs are associated with an increased risk of future all cause hospitalization. Objective: To conduct a population-based study of the association of total dose of filled OA prescriptions (Rxes) in a baseline 6 month interval and patient age with any hospitalization and duration of hospitalization in the next 6 months.
METHODS: For persons enrolled >1 year from 1/2009 to 7/2012 in Aetna’s national HMO (2.1 million), 278,975 persons aged 18 to 64 years were selected if they filled ≥2 Rxes for non-injectable Schedule II or III OAs. From claims and enrollment files for these subjects, a database was developed including demographics, encounters, ICD-9-CM codes, and filled Rxes. For this analysis, we selected persons aged 45–64, no cancer diagnosis (except basal cell) within 6 months of an OA Rx, and no OAs for opioid dependence. Follow-up after the first OA Rx was divided into 6-month intervals until 1/2012 (excluding incomplete intervals). The total morphine equivalent dose (TMED) was calculated from all filled OAs Rxes for each 6-month interval and categorized for analysis as none and approximate quartiles: NO risk (0 days); LOW risk (1–190 TMED); MEDIUM risk (191–450 TMED); HIGH risk (451–1830 TMED); and VERY HIGH risk (>1830 TMED). Days covered by filled Rxes for other drugs used for CNCP—benzodiazepines, zolpidem, and antidepressants—were analyzed per 6-month interval. From ICD-9 codes, we created indicators for five categories of CNCP, mental health conditions, and substance abuse. Repeated measures logistic regression was used for hospitalization (Y/N) and repeated measures Poisson regression was used for inpatient days. All analyses adjust for patient demographic, clinical, and treatment factors. No significant interaction was observed for OA risk and age; therefore, we only report results for OA risk.
RESULTS: The cohort totaled 109,292 persons with a mean age of 53.7 years (SD = 5.5), 54.7 % female, and residence in South (46.9 %), West (16.8 %), Midwest (6 %) and Northeast (30.3 %). In the cohort’s 253,531 six-month follow-up intervals, the proportion hospitalized was 6 % and median hospital days was 4 (IQR = 3–6). For hospitalization, the adjusted odds ratio [95 % CI] for OA risk categories vs. NO risk were: VERY HIGH: 1.45 [1.38, 1.54]; HIGH: 1.15 [1.08, 1.21]; MEDIUM: 0.98 [0.93, 1.04]; LOW: 1.04 [0.98, 1.10]. For inpatient days, the incident rate ratio [95 % CI] for OA risk vs. NO risk were: VERY HIGH: 1.47 [1.34, 1.62]; HIGH: 1.10 [1.01, 1.20]; MEDIUM: 0.87 [0.80, 0.95]; and LOW: 0.95 [0.87, 1.03].
CONCLUSIONS: High or very high total dose of filled OA Rxes in a baseline 6-month interval is associated with an increased risk of subsequent hospitalization and more inpatient days independently of age, pain-related comorbidities, and other prescribed medications commonly used for pain. Reasons for these hospitalizations need to be examined to inform interventions to address this high use of costly inpatient care.
A MIXED METHOD STUDY OF THE QUALITY OF WRITTEN FEEDBACK BY ATTENDINGS OF INTERNAL MEDICINE RESIDENTSCynthia Kay1; Jeffrey L. Jackson2,1; Wilkins Jackson3. 1Medical College of Wisconsin, Milwaukee, WI; 2Zablocki VAMC, Milwaukee, WI; 3University of Wisconsin-Milwaukee, Milwaukee, WI. (Tracking ID #1920218)
BACKGROUND: Residents uniformly criticize the quality of feedback they receive. The purpose of this study was to evaluate the quality of feedback in an internal medicine residency program.
METHODS: Subjects for this retrospective analysis were Medical College of Wisconsin (MCW) internal medicine residents who completed residency training between 2004 and 2012. Over the 8 years, there were 6603 evaluations by 334 attendings. These evaluations followed ACGME guidelines and assessed residents in six domains and included a comment box. From these 6603 written comments, we randomly selected 500 and coded them using grounded theory methods. An initial coding tree was developed by two raters (CK, JLJ). Once the tree was saturated, 25 % of utterances were double coded with good inter-rater reliability (Spearman: 0.94). Utterances were further classified as high, moderate or low quality, also with good inter-rater reliability (Quadratic Kappa: 0.83). Focus groups were also conducted with medicine faculty and housestaff. First written comments were placed on notecards and the groups sorted the cards into high, moderate and low quality feedback. As they did this, they discussed the characteristics that merited this rating. The last few minutes of each focus group was spent reflecting and developing criteria for high, moderate and low quality feedback.
RESULTS: The majority of the attending’s 500 written comments were rated as moderate quality (65 %); 22 % were rated as high and 13 % low. The most common type of feedback (29 %) was nonspecific comments, often about the resident’s personality, 16 % about patient care, 14 % interpersonal communication, 7 % medical knowledge, 6 % professionalism, 4 % each commented on practice based learning or systems based practice. The majority of written feedback comments (88 %) were positive, 8 % were negative and 4 % were neutral; three ABIM domains were more likely to include negative comments (medical knowledge: OR: 3.5, 95 % CI: 2.2–5.6; Practice Based Learning: OR: 2.5, 95 % ci: 1.3–4.8, Systems Based Practice: OR: 4.6, 95 % CI: 2.5–8.3). Nonspecific comments and comments on resident’s attitude or personality were much less likely to include negative comments than the other domains (nonspecific: OR: 0.22, 95 % CI: 0.13–0.39, attitude/personality OR: 0.53, 95 % CI: 0.34–0.82). Focus groups uniformly sorted quality into low, moderate and high quality feedback based on three criteria: specificity, quantitative ratings, actionable, Low quality feedback was nonspecific, moderate feedback had at least some specificity and high quality feedback included specificity plus either some aspect of quantification or was actionable. Despite the uniformity of the criteria espoused by focus groups, the inter-rater reliability between the focus groups was low, (quad kappa: 0.24).
CONCLUSIONS: Written feedback suffers from lack of balance, lack of specificity and lack of actionability. Much of it is focused on personality characteristics of the resident. While the focus groups developed nearly identical criteria for quality, agreement between the groups was low because the groups disagreed as to what constituted specific and actionable feedback. Residents are justified in expressing chagrin at the quality of feedback they are receiving.
A MIXED-METHODS EVALUATION OF A VA PATIENT-CENTERED MEDICAL HOME FOR SPECIALTY CAREMichael Ho2; Catherine Battaglia1; Leah M. Haverhals2; Katherine M. Fagan2; Jackie G. Szarka3; Rebecca Alexander3; George Sayre3; Christian Helfrich3; Susan Kirsh5; David Au3; David Aron6; Julie Lowery4. 1Eastern Colorado Health Care System, Denver, CO; 2Eastern Colorado Health Care System, Denver, CO; 3Puget Sound Health Care System, Seattle, WA; 4Ann Arbor Health Care System, Ann Arbor, MI; 5Case Western Reserve University, Cleveland, OH; 6Louis Stokes VA Medical Center, Cleveland, OH. (Tracking ID #1938016)
BACKGROUND: The Veterans Health Administration (VA) implemented a pilot program called Specialty Care Neighborhood (SCN) to align with the VA’s Patient Centered Medical Home to deliver comprehensive patient-centered care. SCN is a team-based specialty care model, in which teams of specialists engage in proactive and long term collaboration with primary care in order to provide coordinated, optimal care for Veterans with the greatest specialty care needs. SCNs were implemented at 25 VAs in 20 specialties including Heart Failure, Diabetes, Cancer, Pain, Orthopedic Surgery, and HIV. We completed an evaluation of the SCN initiative for the VA Office of Specialty Care (OSC).
METHODS: Findings are presented here from semi-structured interviews and staff surveys. A goal of the evaluation was to identify factors that differentiated four high from two low performing sites as determined by OSC from regular site reports on implementation progress. The evaluation consisted of 27 semi-structured interviews with Primary Care Providers, specialists, and key stakeholders (administrators, chiefs of staff, and facility directors) at the participating sites. Additionally, SCN staff from the six sites returned 39 surveys about their experience with SCN. Interview and survey data were coded using the Consolidated Framework for Implementation Research.
RESULTS: SCNs were viewed positively. Participants from all sites described improved professional relationships and communication as well as improved quality and quantity of specialty services. Interviewees felt improved relationships led to increased job satisfaction and engagement. Participants expressed frustration as to lack of clarity regarding how to implement SCN, and despite this barrier, pulled together to creatively implement SCNs best adapted to meet local needs. In structured ratings of implementation facilitators and barriers, High performing sites, in contrast to low performing sites, engaged leadership, utilized a thoughtful planning process that allowed for ample implementation time, and used systems redesign techniques to streamline processes. Additionally, there were factors from interview data that facilitated implementation at both high and low sites: 1) positive knowledge and beliefs about the program; 2) obtaining patient and provider feedback; 3) recognizing patient needs; 4) active champions; and 5) ability to adapt the program easily. Common barriers included 1) problems with hiring staff, 2) lack of commitment to long-term staff funding, 3) lack of administrative support, 4) insufficient materials for facilitating implementation, and 5) coordination and communication challenges among different providers and services. Interview data and staff survey data were largely congruent. However, survey participants reported high leadership engagement despite interview data suggesting this was less positive among low performing sites.
CONCLUSIONS: The findings were used to identify areas on which to focus attention for improving dissemination of the program. Recommendations were based on factors that distinguished high from low performing sites and included recommendations to overcome barriers: 1) Provide opportunities for sharing best practices across sites; 2) Encourage innovation through site-based flexibility and individualization while limiting micromanaging; 3) Facilitate access to systems redesign expertise; 4) Minimize complexity by utilizing programs in place; and 5) Begin planning process early and involve all key stakeholders.
A MODEL TO PREDICT RISK OF CERVICAL ABNORMALITIES IN PRIMARY CAREMichael B. Rothberg; Bo Hu; Sarah Schramm; Kelly Nottingham; Glen Taksler; Xian W. Jin; Laura Lipold; Andrea L. Sikon. Cleveland Clinic, Cleveland, OH. (Tracking ID #1937479)
BACKGROUND: Cervical cancer screening tests are highly sensitive but have low specificity, resulting in high false positive rates among low-risk women. Although there are known risk factors for cervical cancer, there are no validated tools for assessing risk in primary care. Using data from electronic health records, we derived and validated a risk prediction model for cervical intraepithelial neoplasia grade 2 or higher (CIN2+) lesions.
METHODS: Our dataset included information on all women aged ≥30 years who underwent cervical cancer screening with cytology and human papilloma virus (HPV) testing at 33 physician practices associated with the Cleveland Clinic between 2004 and 2010. Patient risk factors at the time of screening (age, race, marital status, insurance type, smoking history, median income based on zip code and physician practice) were determined by reviewing the electronic health record. Pathology results were obtained from the Cleveland Clinic’s pathology database (for patients who underwent colposcopy with biopsy) or by imputation (for patients with abnormal cytology who did not undergo colposcopy). Imputation was based on observed associations between patient risk factors, HPV and cytology results and CIN2+ status among women who underwent colposcopy. Using CIN2+ as our outcome, we then derived a hierarchical generalized linear model with a logit link that included all patient risk factors available before screening (i.e. not HPV or cytology results) as independent variables. We then stratified patients into tertiles of low, medium and high predicted risk of CIN2+. We then compared the actual rate of CIN2+ (either observed or imputed) in the low-risk tertile to an implied threshold value, which was based on combinations of HPV and cytology results for which colposcopy is typically not recommended. The threshold was 0.20 %, which is equivalent to the rate of CIN2+ among patients with low risk ASCUS and negative HPV. The final model was validated using 100 bootstrap iterations for the entire population and noting the proportion of low risk patients who had CIN2+.
RESULTS: The dataset included 99,388 women. Of these, 574 had pathology findings of CIN2+ and 175 had CIN2+ assigned by imputation (overall rate of CIN2+=0.75 %). The final multivariable model had a c-statistic of 0.73. All factors but race were associated with CIN2+: older age (OR 0.69 per 5 years, 95 % CI 0.66, 0.73), Medicare vs. private insurance (OR 0.51, 95 % CI 0.34, 0.75) and higher income (OR 0.97 per $5 K, CI 0.94, 0.99) were negatively associated, while being single vs. married (OR 1.50, 95 % CI 1.24, 1.82) and smoking (OR 1.66, 95 % CI 1.35, 2.04) were positively associated. Tertiles of predicted risk were 0.20 %, 0.53 %, and 1.51 %, with observed rates of CIN2+ over the same tertiles of 0.19 %, 0.52 %, and 1.53 %. Therefore, before cervical cancer screening, women in the lowest risk tertile had observed CIN2+ risk slightly below that of women with ASCUS and HPV negative (0.20 %). In 100 bootstrap iterations, the observed risk in the lowest tertile ranged from 0.13 to 0.25 % (IQR 0.18 % to 0.22 %).
CONCLUSIONS: A multivariable model based on data derived from the electronic health record was able to risk stratify women across an 8-fold gradient of risk for cervical abnormalities and to identify a large group of women who are at very low risk for cervical cancer and may not require screening. After further validation, use of a similar model could enable more targeted cervical cancer screening.
A NATIONAL SURVEY OF PATIENT CENTERED MEDICAL HOME INITIATIVESSamuel T. Edwards1,2; Asaf Bitton3,4; Johan S. Hong4; Bruce E. Landon4,5. 1Boston VA Healthcare System, Boston, MA; 2Harvard Medical School, Boston, MA; 3Brigham and Women’s Hospital, Boston, MA; 4Harvard Medical School, Boston, MA; 5Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1932105)
BACKGROUND: The reorganization and improvement of primary care through the implementation of the patient-centered medical home (PCMH) is central to healthcare delivery system reform efforts. PCMH initiatives, often organized by health plans, states or multi-stakeholder groups, seek to create the appropriate context to promote transformation of participating primary care practices into medical homes by building learning collaboratives, providing practice coaching, and reforming physician payment to support medical home services. Although there has been expansion of PCMH activity across the country, the current national scope of PCMH initiatives remains undefined. To address this gap, we conducted a nationwide survey of PCMH initiatives. We describe their size, scope, organization and payment methodology and assess their approach to practice transformation and program evaluation.
METHODS: We performed a cross-sectional survey of all PCMH initiatives nationally that included payment reform as an operational feature. We identified initiatives for the survey from existing databases supplemented by formal literature review, internet searches, and by contacting known experts, state Medicaid directors, and representatives from all major national health plans. We included initiatives that were active as of February 1st, 2013 but excluded programs directed solely toward specific medical conditions or serious mental illness. The survey included descriptive questions including initiative start and end dates, numbers of participating practices, physicians and patients, and identity of key stakeholders. We asked about the selection process for practices to enter the initiative, the use of formal PCMH recognition, and payment methods. Finally, we asked about how initiatives facilitated practice transformation and plans for program evaluation. The survey was fielded from February 1st 2013–October 31st 2013 via web or telephone. Respondents were physicians, senior administrators, or senior health policy experts from each initiative. We present descriptive statistics to compare initiatives sponsored by commercial health plans, state Medicaid programs, and multiple payers.
RESULTS: Of 119 identified initiatives, we received 114 responses (96 % response rate). Forty-one programs were small commercial single payer initiatives, 29 were large single payer initiatives, 23 were Medicaid only and 21 were multi-payer. In total, the programs included 63,011 providers caring for 20,389,327 patients nationally. Small commercial programs had a median of 3,896 patients and typically included a small number of practices (median = 4). Large commercial single payer initiatives included a median of 160,000 patients, often covering most or all practices in a specific region or an entire state (median 105 practices). Medicaid initiatives were typically large statewide programs (median 224,040 patients) run directly by state Medicaid agencies. Multi-payer initiatives included a median of six health plans (IQR 4–7) with a median of 187,343 patients, and 68 practices. These initiatives included commercial health plans, Medicare and Medicaid. Formal PCMH recognition was required by 69 % of initiatives. Nearly half of initiatives use practice consultants (46 %) or learning collaboratives (48.7 %), but this was more common in multi-payer initiatives (90.5 % and 95.2 %, respectively). Nearly all initiatives had a formal evaluation plan (92 %). A combination of fee for service payments (FFS) for office visits, a per-member-per month care management fee (PMPM), and pay for performance bonuses was the most common payment structure (55 % of programs). Median PMPM was $4.90 (range $0.25–$60.00), but was higher in multi-payer initiatives (median $7.00). Since 2009, fewer initiatives are time-limited pilots, shared savings programs are more commonly used, and more initiatives are performing formal evaluations (table).
CONCLUSIONS: In this national survey of PCMH initiatives, we demonstrate there has been a large expansion of PCMH activity over the last several years, with 114 initiatives representing over 60,000 providers and nearly 21 million patients in 2013. Initiatives are on average larger, feature more robust transformation efforts, and have higher care management fees. This expansion of PCMH initiatives suggests that the PCMH will continue to play an important role in national delivery reform efforts.
Comparison of PCMH initiatives in 2009 and 2013
| 2009 (N = 26) | 2013 (N = 114) | |
|---|---|---|
| Total patients | 4,971,070 | 20,970,277 |
| Time limited initiatives (%) | 62 % | 20 % |
| Median patients per initiative | 30,000 | 40,986 |
| Number multi-payer initiatives | 9 | 22 |
| Median patients in multi-payer | 39,000 | 146,636 |
| Use Shared Savings | 0 % | 44 % |
| PMPM (range) | $0.50–$9.00 | $0.25–$60.00 |
| Use Learning Collaboratives and Consultants | 15 % | 37 % |
| Performing Program Evaluation | 40 % | 92 % |
A PROFILE OF HOSPITALIZED SMOKERS AND THE CARE THEY RECEIVEEllie Grossman1; Alissa R. Link2; Erin Rogers2,3; Binhuan Wang2; Scott Sherman2,3. 1NYU School of Medicine, New York, NY; 2NYU School of Medicine, New York, NY; 3VA New York Harbor Healthcare System, New York, NY. (Tracking ID #1939163)
BACKGROUND: Identification and treatment of patients who smoke is a priority treatment area for hospitals. Hospitalization can be a ‘teachable moment’ for patients contemplating behavior change, and they may be newly motivated by health consequences. Evidence suggests that appropriate treatment should begin during an inpatient stay and continue for at least four weeks post-discharge. To optimize success, treatment should include both counseling and medications. Patients with mental illness tend to smoke at higher rates than those without, and tend to die earlier of cardiovascular disease, but there is a paucity of evidence about the state of treatment offered to these patients. We aimed to describe the care offered to hospitalized smokers at two urban safety-net hospitals.
METHODS: As part of a randomized controlled trial of smoking cessation interventions focused on the post-discharge time period, we assessed the care for smokers hospitalized at two large public hospitals in New York City. Adult patients were eligible for study inclusion if they: smoked at least one puff of a cigarette in the past 30 days; spoke English, Spanish, or Mandarin; were not incarcerated or in police custody; were not pregnant or breastfeeding, and had a U.S. phone number. At the time of discharge, study staff reviewed participants’ electronic medical records (EMR) for information about type of inpatient unit, history of medical or psychiatric illnesses, and tobacco treatment received during hospitalization and on discharge.
RESULTS: From July 2011 to December 2013, we enrolled 1486 study participants. 511 (35 %) were on psychiatric inpatient units and 934 (65 %) were on medical/surgical units (n = 41 missing). Mean age was 47.9 years, 79 % were male. Of these patients, 17 % had EMR documentation of coronary artery disease, 12 % chronic obstructive pulmonary disease, 14 % asthma, 5 % cerebrovascular disease, 4 % congestive heart failure, 55 % significant alcohol or drug use history, and 10 % schizophrenia or schizoaffective disorder. We found EMR documentation that smoking status was assessed at admission in 1444 (97 %) and bedside counseling was provided in 1294 (87 %). Of those that received counseling, the EMR indicated that 1015 received it from nurses and 145 received it from physicians (for the rest the personnel was not specified). For 647 patients (44 %), physicians ordered smoking cessation pharmacotherapy during hospitalization (36 % NRT patch, 3 % NRT gum, 2 % NRT lozenge, 1 % other). On discharge, 274 patients (18 %) were prescribed cessation medication. Patients on inpatient psychiatric units were more likely to be counseled by their physician regarding smoking cessation (odds ratio (OR) 1.93, 95 % CI 1.20–3.09) and were more likely to be prescribed cessation medication in hospital (OR 3.21, 95 % CI 2.51–4.11) than were patients on non-psychiatric units. There was no association between type of inpatient service (psychiatric vs. non-psychiatric) and likelihood of prescription of smoking cessation medication at discharge.
CONCLUSIONS: At urban safety-net hospitals, patients who smoke have high rates of mental illness and substance use disorders. Although assessment and counseling are provided at relatively high rates, there is much room for improvement in prescribing smoking cessation pharmacotherapy in the hospital and on discharge.
A QUALITATIVE ANALYSIS OF HOSPITAL LEADERS OPINIONS ABOUT PUBLICLY REPORTED MEASURES OF HEALTH CARE QUALITYSarah L. Goff1,2; Tara Lagu2,1; Amy S. Shatz2; Penelope S. Pekow2; Peter K. Lindenauer2,1. 1Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 2Baystate Medical Center, Springfield, MA. (Tracking ID #1937659)
BACKGROUND: Public reports of hospitals’ performance on quality measures are intended to both encourage hospital leaders to stimulate improvement activities and to enable consumers to make more informed decisions about where to seek care. How effective public reporting is at fostering quality improvement may be influenced by whether and to what extent hospital leaders find the measures valid and meaningful. We sought to qualitatively describe hospital leaders’ views regarding quality measures reported on the Centers for Medicare and Medicaid Services’ Hospital Compare website.
METHODS: We mailed or e-mailed a 21-item questionnaire to the chief executive officer and the senior executive responsible for quality at a stratified random sample of U.S. hospitals. Stratification was based upon performance on selected quality measures to achieve a balance of high, average and low performers. While the quantitative portion of the study assessed attitudes regarding publicly reported quality measures, opinions regarding quality measures were elicited using an open-ended prompt at the end of the survey, “Please share your additional thoughts about publicly reported measures of healthcare quality, including strengths or weaknesses of current measures, ideas for new measures, etc.” We qualitatively analyzed responses to this prompt, identifying the presence and frequency of pertinent themes in an iterative process.
RESULTS: Leaders (n = 480) from 380 of the 630 hospitals surveyed (60 %) completed the questionnaire. Of those who completed the questionnaire, 146 leaders from 131 hospitals responded to the open-ended prompt. The majority of respondents to the open-ended prompt were chief executive officers (27 %), chief quality officers or vice presidents of quality (17 %) or chief medical officers (19 %). Half of the responses to the prompt came from leaders at urban hospitals and 68 % were from leaders at non-teaching hospitals. Most respondents were from hospitals that had fewer than 200 beds (41 %), with 23 % from hospitals with more than 400 beds. Forty-one percent of the respondents’ hospitals had performance scores higher than the national average and 27 % scored lower than the national average. Major themes identified included: 1) Positive views of the value of quality measures (12.5 %, e.g., measuring quality can stimulate change and enhance patient engagement); 2) Concerns regarding the validity and utility quality measures (63 %, e.g., measures fail to measure what is important, inadequate risk-adjustment); 3) Challenges to improving quality scores (e.g., inability to impact factors affecting care outside of the hospital, such as patient adherence to prescribed medication); and 4) Recommendations for improving measures (e.g., compare similar hospitals to each other). Many of the positive views expressed were general support for the concept of measuring quality: “Oversight and comparison with peers/standards is necessary and beneficial.” Criticisms of quality measures included concerns about whether doctors can actually influence change in the entities measured: “…the scores for which the doctors are held accountable are subject to profound influence by others besides the doctor to whom the score is attributed.” Challenges described included lack of resources: “Resources are stretched to the limit with meaningful use and data reporting!” Recommendations for improvement in quality measures included an emphasis on the continuous learning cycle, suggesting new targets for quality improvement should be identified as older measures reach acceptable levels of compliance: “…care measures should evolve as compliance becomes ingrained thus continuing the improvement cycle.”
CONCLUSIONS: Among hospital leaders who responded to an open-ended prompt eliciting their views about quality measures some expressed support for the concept of measuring quality, while the majority offered criticisms concerning the validity and utility of current quality measures or described challenges to improving quality. As current quality measures are reassessed and new measures developed, the concerns of those responsible for implementing system changes to address quality should be taken into account.
A QUALITATIVE ANALYSIS OF PATIENT FACTORS ASSOCIATED WITH HOSPITAL READMISSIONColleen M. Rafferty; Tyler Sechrist; Heather Stuckey; Nicole Swallow; Cynthia H. Chuang. Penn State Hershey Medical Center, Hershey, PA. (Tracking ID #1936483)
BACKGROUND: Given the focus on hospital readmissions as a quality indicator, health care organizations nation-wide are interested in finding ways to reduce hospital readmissions. Existing readmission prediction models have relied mainly on clinical and administrative data. A weakness in these methods is that they are not informed by the patient perspective. Exploring patient experiences with readmission may broaden our understanding of what leads to readmission, thereby facilitating a more patient-focused approach to identifying high-risk patients, and enabling institutions to allocate resources to the highest risk patients and to the most cost-effective and efficacious interventions. We conducted qualitative interviews with readmitted patients to identify more precisely the patient-centered factors associated with readmission.
METHODS: We conducted semi-structured interviews with a convenience sample of hospitalized patients readmitted to the Internal Medicine service within 30 days of discharge to home from a previous hospitalization at our institution, a 500-bed tertiary care academic medical center. Patients were eligible if they received their primary medical care within our medical system and were readmitted from June–August 2011 (n = 19). Open-ended interview questions addressed the patients’ perspectives on the medical care they received during the previous admission, access to outpatient care, the patient’s knowledge of his/her medical conditions and treatments, ability to provide self- care, and social support available to them. We also encouraged the patient to discuss from his/her perspective what could have been done differently to help prevent the readmission. The contents of the interviews were transcribed and a thematic analysis was conducted. We also conducted a medical chart review to determine if the patient had a scheduled follow-up appointment that they attended.
RESULTS: We found that the majority of patients had a limited understanding of their medical conditions and their medications. Many patients relied heavily on an advocate (family member or friend) to assist them in their disease management. The vast majority of patients had identified advocates, but we found that not all advocates were effective in providing the needed assistance. Also, most patients did not view their health as under their control, but identified an external locus of control (i.e. the doctors, the disease process, God). All patients identified a primary care physician, and all had been scheduled for follow up appointments within 5–24 day after discharge, but 9 of 19 patients were readmitted prior to their scheduled appointment (8/19 readmitted within 7 day, 10/19 within 10 day). The majority of patients did not feel their readmission was preventable, but attributed it to the disease process, or an issue that was not viewed by the patient as avoidable or predictable.
CONCLUSIONS: These findings suggest potential patient-centered factors that may be used to help identify patients at high risk for readmission: insufficient understanding of medical condition or medications, lack of an effective advocate, a belief that one’s health is not under the one’s own control, and lack of timely access to outpatient follow up care. Early assessment of these risk factors may help target appropriate interventions to high risk patients to help prevent hospital readmission.
A QUALITATIVE ASSESSMENT OF CPOE AND THE EFFECTS OF VARIATION IN DRUG NAME DISPLAYAlexandra Robertson1; Arbor J. Quist1; Thu-Trang Thach1; Lynn A. Volk2; Adam Wright1,3; Shobha Phansalkar1,4; Sarah P. Slight1,5; David W. Bates1,3; Gordon D. Schiff1,3. 1Brigham and Women’s Hospital, Boston, MA; 2Partners HealthCare Systems, Inc., Wellesley, MA; 3Harvard Medical School, Boston, MA; 4Wolters Kluwer Health, Indianapolis, IN; 5The University of Durham, Durham, United Kingdom. (Tracking ID #1938546)
BACKGROUND: Previous work suggests that prescribing errors account for the highest proportion of medication errors (Lisby, 2010) and that one in every four reported in the U.S. can be linked to drug name confusion (Lambert, 1999). Computerized provider order entry (CPOE) has been widely proposed, implemented, and shown to reduce errors associated with traditional, handwritten, medication prescribing. However, CPOE has not fully lived up to its predicted benefits and many attribute these shortfalls to suboptimal design of systems that are “neither interoperable nor easy to use” (Kellerman, 2013, Health Affairs). Given recent calls for CPOE performance testing post-implementation (Thompson, 2010 & Bates, 2013) and the proportion of medication errors which occur during the prescribing phase, we undertook a study to assess drug name design and display issues in CPOE including: look-alike-sound-alike pairs, similar name adjacency errors, font, and visual display to better understand their potential to contribute to medication errors.
METHODS: As part of an FDA Task Order, this qualitative study assessed 10 leading vendor and home-grown CPOE systems in six major U.S. academic medical centers via remote walk-throughs and on-site visits. To standardize assessment, the team developed and iteratively refined a CPOE Assessment Tool (CAT) relating to 18 elements defined by the FDA to systematically test the potential for drug name/identification errors across various stages of the medication ordering process. This tool incorporated specific medication ordering, review, and deletion scenarios used to guide system assessments with a series of “regular” and “expert” users of these systems. Outputs from these evaluations were recorded from each system using screen shots, video and audio transcripts of user and designer comments. Recordings were transcribed, analyzed, and used to inform the content of onsite visits to each medical center to obtain additional system information from medical leadership, IT experts, users, and pharmacists. Inter- and intra-system characteristics were analyzed descriptively for patterns, themes, and variations.
RESULTS: We identified a variety of ways drug names are displayed in CPOE systems that could potentially contribute to medication errors. Recurrent issues and themes that emerged included: (a) Brand versus generic name: Presentation of brand and generic names varied both across and within systems depending on task functionality. In nine of the ten CPOEs assessed, for example, one brand name search (Plavix) yielded results displaying the drug in eight different ways. Some systems used all caps, some only initial caps, some used both. Some were inconsistent in the drug name searched and drug name returned. One system displayed two columns which listed both the brand and generic names, others included only one, and others presented one or the other parenthetically, based on the search term. One system allowed ordering by generic name only. If one searched by brand name, the medication did not appear; we observed end user frustrations resulting from inability to search for and find desired drugs searched non-generically. Systems also used varied methods to display brand and generic options to steer prescribing towards preferred products (typically the generic). (b) Combination products: In most systems, searching for a combination drug often yielded the brand name with the ingredients listed parenthetically. We rarely saw systems provide explanations of ingredient strengths. In some systems, searching the brand name yielded only the brand name, without its generic ingredients. (c) Drug-name modifiers: Across systems, drug modifiers seemed to have some consistency in both representation and display. Drug modifiers appeared primarily at the end of the drug name, in all caps, and were abbreviated (e.g. XR, DS, etc.). They were rarely truncated. (d) Extraneous additions to drug name fields: Across systems, we observed several instances of non-systematically populating (jerry rigging) name fields with additional information ranging from drug indication to which facility the drug could be ordered from. (e) Font, text size, capitalization: These all varied widely with no standardized approaches seen both across and often within systems.
CONCLUSIONS: There is little consistency in the ways that leading CPOE systems search for and present drug names. This lack of standardization was seen both across systems and often within a single system or institution’s CPOE systems. Brand vs. generic, combination products and drug name modifiers were particularly inconsistent, each presenting the potential for user frustration, confusion, and erroneous orders.
A QUALITATIVE STUDY EXPLORING THE VULNERABILITIES OF COMPUTERIZED PHYSICIAN ORDER ENTRY SYSTEMSSarah P. Slight1,2; Tewodros Eguale1,3; Mary Amato1,4; Andrew C. Seger4; Diana L. Whitney5; David W. Bates1,6; Gordon D. Schiff1,6. 1Brigham and Women’s Hospital, Boston, MA; 2Durham University, Stockton on Tees, United Kingdom; 3McGill University, Montreal, QC, Canada; 4MCPHS University, Boston, MA; 5Baylor College of Medicine, Houston, TX; 6Harvard Medical School, Boston, MA. (Tracking ID #1935926)
BACKGROUND: Computerized Physician Order Entry (CPOE) systems can prevent medication errors in both inpatient and outpatient settings. Depending on how they are designed, however, they can fail to optimally prevent various prescribing errors or introduce new errors. The Institute of Medicine report Health IT and Patient Safety: Building Safer Systems for Better Care recommended that specific examples of potentially unsafe processes and risk-enhancing interfaces be identified and shared amongst the health IT community. This study aims to test the vulnerabilities of a wide range of CPOE systems to different types of medication errors, and to develop a more comprehensive understanding of how CPOE human factors design could be improved.
METHODS: As part of a National Patient Safety Foundation-funded project, we examined a range of leading vendor and home grown CPOE systems (e.g., Cerner; Epic; Medi-tech; LMR; BICS; GE Centricity) in diverse organizations in United States and Canada. Typical users at each of 16 sites were asked to enter 13 different orders on test patients based on scenarios of previously reported CPOE errors. Users were encouraged to use both usual practice and, where-needed, workarounds to enter the erroneous orders, as well as reflect on their overall knowledge and experience of using their system. A research pharmacist and research assistant independently observed test users enter each order and rated the ease or difficulty of these entries using standardized operational definitions.
RESULTS: Ease of entry of erroneous orders and the generation of alert warnings in different CPOE systems was highly variable and appeared to depend on a number of factors including how the order information was entered (i.e., in a structured or unstructured way); whether a specific alert functionality (e.g., duplicate-drug checking) was operational in the system; and which drugs or drug combinations were included in the clinical decision support algorithms. Test users found the wording of many of the alert warnings confusing and expressed frustrations with the way irrelevant warnings appeared on the same screen as those more relevant to the current order. The timing of alert warnings also differed across CPOE systems, with dangerous drug-drug interaction warnings displayed, for example, only after both Imdur® (isosorbide mononitrate) and Revatio® (sildenafil) had been entered and the order signed off in two CPOE systems. Alert warnings also varied in their level of severity in different systems even within the same institution (e.g., test user was presented with a hard stop alert warning in the inpatient system after entering Lovenox® (enoxaparin sodium injection) 40 mg subcutaneous daily followed by a second order for Lovenox® 100 mg subcutaneous twice daily, whereas the equivalent outpatient system produced an alert for the same order that was easily overridden). Test users commented on how there may be situations where they needed to prescribe the same drug twice, requiring workarounds such as entering the brand name of the drug for the morning dose and the generic name for the evening dose, to avoid getting duplicate drug alert warnings.
CONCLUSIONS: We found a high degree of variability of vulnerability in ordering and alerting between different CPOE systems. Detailed qualitative analysis of both the observed CPOE functionality and users think-aloud comments provided rich insights into the ways both systems and users were susceptible to ordering errors. System developers and users need to be aware of these vulnerabilities and build in protection strategies to re-engineer their systems to ensure safer prescribing.
A RANDOMIZED TRIAL OF A COMMUNITY HEALTH WORKER LED INTERVENTION TO IMPROVE DIABETES INTERMEDIATE OUTCOMES AMONG LATINOS PATIENTS WITH POORLY CONTROLLED DIABETESOlveen Carrasquillo; Yisel Alonzo; Cynthia Lebron; Natalie Ferras; Ernesto Reyes-Arrechea; Hua Li; Sonjia Kenya. University of Miami, Miami, FL. (Tracking ID #1936786)
BACKGROUND: Diabetes disproportionately impacts Latinos. Community Health Workers (CHWSs) are one approach that may improve health outcomes in this population. However, evidence from rigorous randomized studies is limited.
METHODS: The Miami Health Heart Initiative examined the impact of a comprehensive community health worker (CHW) intervention on diabetes intermediate outcomes of systolic blood pressure (SBP), lipids (LDL) and Hemoglobin A1C (HbA1c). We recruited 300 Latino patients with poorly controlled diabetes (HbA1c>=8.0 %) ages 35–65 from the primary care clinics of Miami-Dade county’s public hospital. Subjects were randomized to usual health care or a comprehensive structured CHW 1 year intervention consisting of home visits, phone calls and group education sessions. The intervention included patient navigation as well as assistance with social and non-medical needs. An RA blinded to group assignment conducted initial and follow-up evaluations at 12 months. We used linear mixed models to statistically test for the impact of our intervention on outcomes using intention to treat analyses.
RESULTS: The mean age of our patients was 56 + 7 years, 55 % were female and mean BMI was 31.6 + 7.4 kg/m2. Over half (55 %) were sedentary (IPAQ) and median daily fruit and vegetable was two (BRFSS). Cubans made up 29 % of our sample with no other Hispanic ethnic subgroup representing over 15 % of the sample; 47 % of respondents scored the lowest possible acculturation score (Marin-Marin). Intervention patients received a median of five home CHW visits and 25 phone calls; 84 % of intervention group participants had at least 12 CHW contacts over the course of the year. Participation at group session was more skewed with 52 % of participants not attending any sessions. Of those that attended at least one session, average attendance was four sessions per participant. At 1 year the retention rate was 72 % and similar in both arms. Data on outcomes by group is shown in Table 1.
CONCLUSIONS: In a heterogeneous Latino population with poorly controlled diabetes, a rigorous CHW intervention resulted in statistically and clinically meaningful changes in HbAIC but not in blood pressure or lipids. The impact of the intervention on the latter two outcomes may have been limited by the fact nearly half of patients were at the SBP and LDL targets prior to the intervention.
Figure 1: Baseline and One Year Outcomes in MHHI
| Usual Care | CHW | ||
|---|---|---|---|
| HbA1C (%)* | Baseline | 9.03 | 9.19 |
| One Year | 9.25 | 8.81 | |
| Change | +0.21 | −0.38 | |
| SBP (mm/Hg) | Baseline | 135 | 131 |
| One Year | 134 | 128 | |
| Change | −1 | −3 | |
| LDL (mg/dl) | Baseline | 108 | 100 |
| One Year | 111 | 99 | |
| Change | +3 | −1 | |
*p = 0.01 for HbA1C NS for SBP and LDL
A REDUCTION IN TELEMETRY ORDER DURATION DOES NOT CHANGE TELEMETRY ORDERING FREQUENCY AND REDUCES UTILIZATIONJoel Boggan1,2; Ann Marie Navar-Boggan4; Ryan D. Schulteis3,2; David Simel6,5. 1Durham Veterans Affairs Medical Center, Durham, NC; 2Duke University Health System, Durham, NC; 3Durham Veterans Affairs Medical Center, Durham, NC; 4Duke University Health System, Durham, NC; 5Duke University Health System, Durham, NC; 6Durham Veterans Affairs Medical Center, Durham, NC. (Tracking ID #1940176)
BACKGROUND: American Heart Association guidelines for appropriate use of telemetry have not decreased inappropriate use of in-hospital cardiac monitoring. We evaluated how changing the default order set for telemetry affected overall telemetry utilization.
METHODS: The computerized ordering system at the Durham VA Medical Center was changed so that the maximum number of hours of cardiac monitoring was reduced by 33 %, from 72 to 48 h, before requiring a renewal order. No other intervention or general education about telemetry appropriateness was done. We compared the frequency of orders/week for telemetry and duration of cardiac monitoring for 12 weeks before through 6 weeks after this intervention. To assess the safety of the intervention, we measured the number of rapid response team (RRT) or code events occurring at any time during the hospital stay of general medical or general surgical patients. We compared event rates on telemetry before and after the intervention.
RESULTS: Over a 4-month period, there were 1051 telemetry orders placed for general medical or surgical patients before the intervention and 450 after. The average number of orders/week did not differ significantly before vs after the reduction in telemetry order duration (88 +/− 10 vs. 75 +/− 22 orders/week, p = 0.11). The mean duration of telemetry was reduced by 32 %, which was the same percent reduction required by the change in policy (mean reduction in telemetry time decreased from 64 +/− 3.1 h/patient to 44 +/− 1.2 h/patient, p < 0.01). The rate of code events and rapid response team events in hospitalized general medical or surgical patients decreased from 2.5 events/week to 2.2 events/week. Only seven RRT/code events occurred in patients on telemetry prior to the intervention, while one RRT/code event occurred in a patient on telemetry after the intervention (p = 0.28).
CONCLUSIONS: A simple change in the default maximum number of hours a provider can prescribe cardiac monitoring before requiring a renewal order led to a dramatic decrease in telemetry utilization. Although the number of orders for patients to receive cardiac monitoring was unchanged, the duration of cardiac monitoring dropped substantially. Even with less monitoring, we found no increase in the rate of adverse events. Similar reductions at other medical centers may reduce telemetry utilization, technologist and nurse staffing requirements, and cost while preserving patient safety.
A RESIDENT INITIATIVE TO INCREASE USE OF NALTREXONE FOR ALCOHOL USE DISORDER AT A SAFETY NET HOSPITALMaria E. Otto1; Jeffrey K. Hom1; Shilpa M. Shah1; Natalie C. Young1; Weston S. Fisher2; Edgar Pierluissi1. 1University of California San Francisco, San Francisco, CA; 2University of California San Francisco, San Francisco, CA. (Tracking ID #1939058)
BACKGROUND: Alcohol use disorder (AUD) is extremely common at San Francisco General Hospital (SFGH), with nearly one in four inpatients on the Medicine service affected. These patients frequently present to the Emergency Department (ED) with alcohol-related falls, seizures, and symptoms of withdrawal. Their 30-day readmission rate is 16 %, above the 13 % for the remainder of the hospital. Hospitalization provides a window of opportunity to help this vulnerable population, as patients are often motivated to make changes following an alcohol-related illness but are frequently without primary care doctors. Despite the effectiveness of naltrexone, an inexpensive, FDA-approved medication for treatment of AUD, it has been underutilized. A pilot intervention in 2011 at SFGH increased prescriptions of naltrexone to eligible patients at discharge, but was not sustained.
METHODS: A resident-led, quality improvement (QI) project was implemented in February 2013 to 1) sustainably increase the prescribing of naltrexone to eligible inpatients with AUD upon discharge and 2) to measure the effect of the intervention on ED visits and readmissions within 30 days. The intervention 1) identified inpatients with AUD via the electronic handoff system, 2) educated providers about naltrexone, 3) prompted providers to prescribe naltrexone to eligible patients at discharge planning rounds, and 4) utilized principles of QI to continuously evaluate and improve the intervention. Data were collected via retrospective chart review to identify patients with AUD and determine eligibility for naltrexone. Among patients with AUD, number of ED visits and readmissions within 30-days of discharge were also obtained.
RESULTS: Among 118 patients with AUD identified between March 1 and April 15, 2013, 43 % (n = 51) were eligible for naltrexone. Following the initial intervention, naltrexone offering increased from 2 to 58 % of eligible patients. This effect was sustained through continuous cycles of improvement, with 67 % of patients offered it most recently. Compared to patients not prescribed naltrexone (n = 31), patients prescribed the medication (n = 20) had 30-day readmission rates and hospital visits that were 74 % and 88 % lower, respectively.
CONCLUSIONS: These results are promising and suggest that an intervention to systematically identify and offer treatment to patients with AUD is important in caring for our patient population and decreasing hospital utilization. Additionally, this QI initiative demonstrates that a deep-rooted problem can be addressed with the commitment of an interdisciplinary team, which can include a rotating group of trainees. By assessing the effect of this intervention on hospital utilization, the project shows that measuring true outcomes, rather than just processes, can help build a business case for sustainability. Next steps include 1) expanding the intervention to other hospital services, 2) ensuring the safe transition of patients on naltrexone from the hospital setting to their outpatient providers, and 3) collaborating with hospital leadership to improve systems to identify and offer treatment to all patients with AUD.
A ROLLING, INTEGRATED EVIDENCED-BASED MEDICINE CURRICULUM’S IMPACT ON EVIDENCE-BASED PRACTICE SKILLS, KNOWLEDGE, BEHAVIOR AND ATTITUDES ON INTERNAL MEDICINE STUDENTS AND RESIDENTS AT THE WASHINGTON, DC VETERANS AFFAIRS MEDICAL CENTERMatthew Tuck; Samantha Mcintosh; David Maron. Department of Veterans Affairs Medical Center, Washington, DC. (Tracking ID #1941446)
BACKGROUND: Teaching evidence-based medicine (EBM) skills to students and residents has become an imperative for medical education. The AAMC made recommendations to incorporate problem-based clinical skills in medical schools’ curricula. Similarly, the Next Accreditation System of the ACGME requires that residency programs train and evaluate residents in practice-based learning and improvement. Developing effective techniques for integrating these practices across the years of medical education remains a challenge for medical schools and residency programs.
METHODS: We developed a rolling EBM curriculum for medical students and residents rotating through the Medical Service of the Washington, DC Veterans Affairs Medical Center (VAMC) that provides repeated opportunities for students and residents to learn, practice, and evaluate their skills within the context of real-time patient care. The curriculum is integrated into morning report over the course of a month-long rotation. Using a patient case on the wards, learners are guided through the process of formulating a PICO question, searching the literature to find an article that answers the question, appraising the validity of the article and applying the literature to the case. The aim of the study was to evaluate the curriculum on learners’ self-reported patient care practices, attitudes and knowledge using validated rubrics. We hypothesized that exposure to the curriculum would improve learners’ EBM-related patient care practices, attitudes and knowledge. Using a before-and-after design, consented learners were given questionnaires. We used validated rubrics on attitudes and behavior as well as a rubric to assess EBM knowledge (the so-called Berlin Questionnaire) at the beginning and end of their rotation at the VAMC. Incentives were provided for completion of the questionnaires. Means, standard deviations, percentages and univariate paired t-tests were calculated for pre- and post-exposure scores. The research was funded by a Medical Education Research Grant awarded by George Washington University.
RESULTS: 231 residents and students were exposed to the curriculum. Sixty-three learners completed the pre-curriculum questionnaire and 21 completed both the pre- and post-curriculum questionnaires. Up to 74 % of respondents had never received formal education on EBM prior to their rotation at the VAMC. Mean scores on attitudinal and belief questions improved after exposure to the curriculum, but to a non-significant level. Similarly, knowledge of EBM, as assessed by the Berlin Questionnaire, improved to a non-significant level (pre-curriculum mean score 4.5, post-curriculum mean score 5.3, p = 0.10). A regression was conducted to determine if the number of days between the pre and post-curriculum assessment predicted improved performance on the Berlin Questionnaire and was non-significant (p = 0.13).
CONCLUSIONS: We successfully implemented a rolling, integrated EBM curriculum for internal medicine students and residents. Attitudinal, behavioral and knowledge scores improved to a non-significant level after the month-long exposure to the curriculum. The lack of significant findings may be in part due to small sample size.
A SALARY EQUITY STUDY: DIFFERENCES BY GENDER AND RACE, DEPARTMENT OF MEDICINE, UNIVERSITY OF MINNESOTAAnne Joseph; Wesley Miller; Jeremiah Menk; Stewart McMullan. University of Minnesota, Minneapolis, MN. (Tracking ID #1938954)
BACKGROUND: Salary inequities for female faculty have been documented in many academic disciplines.
METHODS: The University of Minnesota Department of Medicine (DOM) conducted cross-sectional studies in 2011, 2012, and 2013 with the objective of examining gender equity issues related to salary (n = 165, n = 196, and n = 213 respectively). A pre-specified multivariable linear regression was used to adjust the salary comparison between men and women and Whites and non-Whites. The analysis included the following variables: gender, race, academic rank (and time in rank), leadership roles, degree(s), number of ABIM certifications, time from highest degree to current position, percent clinical effort, and subspecialty.
RESULTS: In 2011, 8 % of women were full Professors compared to 35 % of men. Leadership roles were held by 7 % of women compared to 19 % of men; similar differences in career characteristics were observed across all 3 years. The unadjusted mean salary for women was $69,717–$76,009 lower compared to men depending on the year. In 2011, 2012, and 2013 the adjusted mean comparisons for women vs. men were $-10,513, −$9,377, and −$16,132 respectively. For non-Whites vs. Whites the comparisons were −$9,018, −$741, and −$13,002. R-squared values for the models were between 0.757 and 0.767. As predicted, the model confirmed that the following were associated with increased salary: a PhD or Masters in addition to MD degree, number of ABIM certifications, rank, time variables, and holding a leadership position. For clinicians, procedural subspecialties (cardiology, gastroenterology, pulmonary, renal) conferred higher salaries than hematology-oncology-transplant, endocrinology, rheumatology, infectious disease, general internal medicine (in that order).
CONCLUSIONS: Gender differences persisted over the 3-year period despite preferential salary adjustments for women. Professional accomplishment characteristics do not fully explain faculty salary differences by gender and race. In response, the DOM has formed a Salary Equity Committee to systematically address these differences abiding by principles of transparency, simplicity, value of clinical, educational and research missions, validated benchmarks of productivity, equal access to leadership positions and supplemental income, and sustainability.
Adjusted Mean Comparisons
| 2011 | 2012 | 2013 | |
| R-squared | 0.767 | 0.757 | 0.759 |
| Sex | |||
| Women vs. men | −$10,513 | −$9,377 | −$16,132 |
| Race | |||
| Non-White vs. White | −$9,108 | −$741 | −$13,002 |
A SIMPLE SCREENING METHOD TO DETECT MALIGNANCY USING RED CELL DISTRIBUTION WIDTH (RDW)Hiroaki Wakakuri; Toshihiko Ohara; Makoto Suzaki; Sonoko Kirinoki; Naoko Onodera; Takashi Araki; Hideya Hyodo; Makoto Kawai; Masahiro Yasutake. Nippon medical school, Bunkyoku-sendagi, Japan. (Tracking ID #1928358)
BACKGROUND: RDW is rapidly calculated parameter using an automatic cell counter. Recent studies showed that RDW is strongly associated with prognosis in disorders such as chronic heart failure, idiopathic pulmonary fibrosis, sepsis, various cancer, and chronic kidney disease. However, it is still unclear that the relationship of RDW and diagnosis of malignancy. The aim of this study is to evaluate the usefulness of RDW to screening malignancy at the first visit outpatient clinic.
METHODS: Fifty one consecutive patients diagnosed as malignancy at ER and general internal medicine of our hospital were reviewed in the period between September 2012 and September 2013. Fifty one patients, matching age and sex, with common diseases, including hypertension and dyslipidemia were assigned to control group. The patients complicated severe anemia (Hb < 9.0), chronic heart failure, chronic inflammation disease, with a dosing history of medication that have effect on RDW were excluded from control group. RDW was calculated using an automatic cell counter (Sysmex XE-5000). We also measured Hb, BUN, Cre, TC, albumin and CRP at the same time. The receiver operating characteristic (ROC) curve showed the best cut-off value of RDW for predicting malignancy.
RESULTS: Malignancy group (age 67.8 [24–88], man 27, woman 24) was classified into the digestive organs n 26 (gastric ca, colon ca, cecal ca, vater ca, HCC, GIST), hemopathy n 10 (malignant lymphoma, multiple myeloma, AML), respiratory organs n 6 (lung ca), gynecologic disease n 3 (ovarian ca, uterine ca), urinary organs n 3 (prostate ca, renal pelvic ca), breast cancer n 2, and liposarcoma n 1. Control group (age67.4 [28–86]) included 27 men and 24 women. Malignancy group had lower Hb and alb values than control group, and higher CRP values than control group (Hb: 12.0 [5.0–17.3] vs 13.6 [10.5–16.9], albumin: 3.64 [2.6–4.9] vs 4.21 [3.2–4.8], CRP: 3.33 [0.03–21.3] vs 0.37 [0.01–2.88], P < 0.05). There was no strong correlation between the RDW and other parameters (vs BUN r 0.096, vs Cre r 0.071, vs TC r −0.284, vs CRP r 0.182, vs albumin r −0.437, vs Hb r = −0.537). RDW of malignancy group (14.6 [12.6–25]) was significantly higher than RDW of control group (13.3 [12.2–15.6]), (P < 0.05). Using ROC analysis (AUC = 0.744), RDW of 13.9 % was the best cut-off value for predicting malignancy with a sensitivity of 58.9 % and a specificity of 78.5 %.
CONCLUSIONS: Our result shows that RDW of malignancy group is significantly higher than control group. It is not enough to discriminate patients with malignancy diseases between healthy persons by just RDW value, but an elevated RDW > 13.9 % value is a reliable additional predictor for screening malignancy at the first visit outpatient clinic.
A STRUCTURED REVIEW OF BENEFIT AND HARM DATA IN CANCER SCREENING GUIDELINES AND POINT-OF-CARE CLINICAL RESOURCES: DO CLINICIANS HAVE THE INFORMATION THEY NEED?Tanner Caverly; Elyse Reamer; Rodney A. Hayward; Michele Heisler; Angela Fagerlin. University of Michigan Medical School, Ann Arbor, MI. (Tracking ID #1939040)
BACKGROUND: Data on the absolute benefits and harms of preventive interventions represent essential information for clinicians. Clinicians cannot practice informed or shared decision making if they lack ready access to this information, which is needed to help weigh trade-offs between potential benefits and harms. We might expect that transparent quantification of potential benefits and harms would be provided in prevention guidelines and point-of-care resources (such as UpToDate©), but to date, a systematic assessment of whether these clinical resources provide this important clinical information has not been conducted. We sought to address this gap by conducting a review of current cancer prevention guidelines and point-of-service resources to examine what information they provide on the chance of benefit and the potential for harms.
METHODS: We reviewed all recommendation statements related to cancer prevention and screening from the United States Preventative Services Task Force (USPSTF), excluding statements rated I for insufficient evidence, pediatric and adolescent guidelines, and those only discussing counseling interventions. To capture other non-USPSTF guidelines in the same topic areas, we examined within the National Guidelines Clearing House (NGC) all discrete guidelines developed by US organizations. We also searched two popular point-of-care clinical resources (UpToDate© and Dynamed). A standardized abstraction form was iteratively created. We abstracted basic guideline demographic data and information about how benefits and harms are presented.
RESULTS: We reviewed 11 cancer prevention guidelines from the USPSTF, 19 guidelines from other organizations within the same cancer-prevention areas, 15 related articles from Dynamed and 14 from Up-to-Date. These resources contained 114 separate recommendations, 77 of which described recommendations for the use of the preventive service in at least some sub-populations (positive recommendations). Among the positive recommendations, 31 % (24 out of 77) simply made a recommendation without mentioning any estimate of the chance of benefit. Twenty-seven percent (21 out of 77) presented the benefit as an absolute risk reduction. Regarding the potential for harm inherent in any intervention, 48 % (37 out of 77) of the recommendation statements did not mention any harms and an additional 18 % (14 out of 77) mentioned but did not quantify those harms. Of the 27 % (21 out of 77) that quantified both potential benefits and potential harms, 19 % (4 out of 21) presented benefit as a relative risk reduction (larger number) while presenting harm as an absolute risk increase (smaller number)—a format known as mismatched framing that exaggerates the relative magnitude of the benefit compared with the harm. Only 21 % (n = 16; 10 from guidelines and 6 from point-of-care resources) of the 77 positive recommendations quantified both the potential benefits and harms as absolute risks so that they could be directly compared.
CONCLUSIONS: Guidelines and point-of-care clinical resources for cancer prevention interventions frequently do not provide needed information on the chance of the intervention resulting in patient benefit or the potential of being harmed. The resources we reviewed may not represent all of the resources that clinicians use in daily practice. However, other resources are unlikely to present this information if the resources we reviewed did not. After undertaking the effort to summarize and rate the quality of evidence supporting use of a preventive service, evidence review bodies should also seek to quantify and present the potential benefits and harms of the proposed intervention. A satisfactory way to present this data would be to depict estimates of absolute benefits and harms together in a single table within the guideline—as is promoted by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach.
ACCEPTABILITY AND FEASIBILITY OF HPV SELF-SAMPLING FOR CERVICAL CANCER SCREENING AMONG PATIENTS AND PROVIDERS IN TWO SAFETY-NET INSTITUTIONS IN MIAMIKumar Ilangovan1; Erin N. Kobetz-Kerman2,4; Tulay Koru-Sengul2,4; Erin N. Marcus1; Brendaly Rodriguez3; Yisel Alonzo3; Orieta Fontan2; Valentine Cesar2; Olveen Carrasquillo1,4. 1University of Miami Miller School of Medicine, Miami, FL; 2Sylvester Comprehensive Cancer Center, Miami, FL; 3University of Miami Miller School of Medicine, Miami, FL; 4University of Miami Miller School of Medicine, Miami, FL. (Tracking ID #1931851)
BACKGROUND: Cervical cancer disproportionately impacts minority women. While screening substantially reduces cervical cancer mortality, many women in safety-net settings remain unscreened. System level barriers include limited resources and staffing. Patient barriers include financial (lack of insurance and co-payments), health literacy, and cultural norms. Provider barriers such as visit time constraints also exist. Human Papilloma Virus (HPV) self-sampling, in which women use a cotton swab device to self-collect material for an HPV assay, may be an attractive option in such settings.
METHODS: 1) To measure the acceptability and feasibility of HPV self-sampling among patients, we had two Community Health Workers (CHWs) recruit women from two clinics in Miami-Dade County. One site was a public hospital based clinic primarily serving Hispanics; the other a community based facility serving Haitians. CHWs identified women aged 30–65 years with no Pap smear in the past 3 years and gave a brief description of the study. We offered all eligible women the option of HPV self-sampling or discussing screening through Pap smears with their provider. If HPV self-sampling was selected, instructions on sampler use and assistance with collection was provided by the CHW. Patient attitudes towards HPV self-sampling were assessed using a 12-item survey modeled after existing surveys. Among women in whom the HPV self-sampler option was not chosen, the electronic medical record or paper chart were reviewed to assess if a Pap smear was performed. 2) To measure acceptability and feasibility among clinic staff (medical assistant, nurse, nurse practitioner, and physician), we developed a 9-item survey based on prior studies of provider screening acceptability. Through emails and personal invitations, staff were encouraged to participate in an anonymous online questionnaire.
RESULTS: Of 1725 women assessed, 62 % were not eligible due to having a Pap smear in the last 3 years. Of the 184 study eligible women, 91 % agreed to participate (n = 167). Latinas represented 73 % and Haitians 27 % of the sample; 99 % were uninsured. The HPV self-sampling approach was selected by 67 % of participants. The majority of participants agreed that HPV self-sampling was faster than the Pap smear (86 %), more private (93 %), and easy to use (97 %). Nearly all participants agreed they would use the self-sampler again (97 %) and recommend it to a friend or family member (96 %). Overall, 76 % of participants preferred the self-sampler to the Pap smear. High-risk HPV was detected in 11 % of samples. The CHW provided navigation to Pap smear for all women having high-risk HPV strains. Of those not selecting the self-sampler, 34 % had not yet had a Pap smear at 1 month post-recruitment. Of 178 clinic staff invited to participate in our survey, 16 % (n = 29) completed the survey. Of those completing the survey, 69 % agreed it was difficult to perform a Pap smear because of time constraints and 79 % agreed they would be willing to incorporate HPV self-sampling into their practice.
CONCLUSIONS: HPV self-sampling was both feasible and highly acceptable in the safety-net clinics studied. A low response rate by clinic staff may limit the generalizability of the provider survey results. HPV self-sampling may be an important tool to address barriers to cervical cancer screening in resource limited settings.
ACCESS TO AND PREFERENCES FOR TEXT MESSAGING FOR MEDICAL AND INSURANCE REMINDERS IN A SAFETY NET POPULATIONLeah Zallman1,2; Alex Harsha1,3; Danny McCormick1,3. 1Cambridge Health Alliance, Cambridge, MA; 2Institute for Community Health, Cambridge, MA; 3Harvard Medical School, Boston, MA. (Tracking ID #1934972)
BACKGROUND: Text messaging has been used successfully to deliver health information interventions to underserved communities. Evidence suggests that text message reminders can increase patient appointment and treatment completion, and is a reliable method of communication even in communities with low literacy. Text messaging may offer similar opportunities to reach patients in health care safety net settings who are disproportionately impacted by homelessness or unstable housing, low health literacy and may be lost to follow up. The immediate, direct-to-patient nature of text messaging and the ability to send automated reminders at relatively low cost may help overcome communication barriers between healthcare providers and underserved communities in the US. While the opportunity to improve this communication may exist through text messaging, preferences for text messaging and patient characteristics associated with preferring text messages have not been elucidated
METHODS: Between August and December 2013, we conducted a face-to-face verbally delivered survey regarding preferences for text messaging with 415 patients presenting to three emergency departments at a large integrated safety net health care system in the greater Boston area. We included patients aged 18–64, who had an Emergency Severity Index (ESI) of 2–5 (excluded most severely ill), had only one insurance type and spoke English, Portuguese, Spanish or Haitian Creole. We asked participants about their access to mobile phones with text messaging capability, preferences for receiving specific types of reminders by text (appointment, medication, and expiring insurance), and preferences for text messaging over other forms of communication. We used logistic regression models that controlled for age, gender, race/ethnicity, health insurance type and medical comorbidities to identify predictors of preferring text messages for medical reminders over other forms of communication with medical providers.
RESULTS: Overall, 96.5 % of participants reported having access to mobile phones with text messaging capability. Half reported a preference for text messaging over other forms of communication such as phone, mail or email. Respondents expressed preferences for appointment reminders (77 %), reminders regarding expiring insurance (55 %), and medication reminders (32 %). A minority (17 %) indicated that they preferred not to be text messaged by their healthcare provider. Reasons for not preferring text messaging included: cost of receiving text messages (11 %), privacy (17 %), not liking or understanding text messaging (40 %) and other (31 %). In logistic regression analyses, Hispanic ethnicity (1.68 [1.03–2.75]) and younger age (0.98 [0.96–1.00]) were associated with preferences for medication reminders. Similarly, Hispanic ethnicity (1.93 [1.09–3.43]) and younger age (0.98 [0.95–1.00)) were associated with preferences for expiring insurance reminders.
CONCLUSIONS: In a safety net population, the vast majority of patients have access to text messaging and a high proportion express preferences for text message reminders over other forms of communication. Reminders regarding appointments and expiring insurance were most highly desired. Text messaging may be a promising method to improve healthcare provider communication with underserved communities in the US.
ACCESS TO DEPRESSION CARE SERVICES: A NEEDS ASSESSMENT IN AN URBAN ACADEMIC PRIMARY CARE CLINICLauren Peccoralo; Susan Truong. Mount Sinai Medical Center, New York, NY. (Tracking ID #1937528)
BACKGROUND: Major depressive and anxiety disorders are common and these and other psychiatric conditions are often encountered by primary care practitioners. Urban academic training centers serve patients at high risk for mental health disorders who often have little access to care, yet little is known about the perceived need for mental health services amongst primary care providers in these environments. The US Preventive Services Task Force endorses routine screening of all adults for depression in settings with adequate staff-assisted depression care support to provide appropriate care and follow up. The purpose of this survey was to assess the needs and barriers to depression care services amongst physician primary care providers in an urban academic training practice in the United States prior to the implementation of universal screening and a depression care program.
METHODS: From April through June 2013, we conducted an online survey about the perceptions of barriers to depression care and unmet psychiatric needs in the primary care practice in our clinic. Survey participants included primary care providers (all internal medicine residents and faculty providers) at the resident training clinic practice at the Mount Sinai School of Medicine in New York, New York. The survey was analyzed as descriptive data.
RESULTS: Ninety-two participants responded to the survey (74 resident trainees and 18 attending physicians, 62 % and 78 % response rate, respectively) during the study period. Eighty-three percent of residents and 88 % of attendings are currently caring for a patient(s) with depression. Eighty-six percent of residents and 100 % of attendings believe there are barriers to providing optimal care for patients with depression. The most commonly identified barriers to care are lack of psychiatrists (85 % residents, 94 % attendings), lack of coordination between primary care and psychiatry (83 % residents, 100 % attendings). and lack of patient education (54 % residents, 78 % attendings). Ninety-six percent of residents and 94 % of attendings have at least one patient with an unmet psychiatric need and 18 % of residents and 35 % of attendings have >10 patients with such a need. The most commonly cited psychiatric needs are depression (93 % residents, 100 % attendings), anxiety (74 % residents, 94 % attendings) and substance abuse (45 % residents, 47 % attendings).
CONCLUSIONS: Primary care providers at all levels perceive high need for and multiple barriers to depression and other mental health care. These data support the recommendation that appropriate mental health services should be available in tandem with the initiation of universal depression screening. Further research is needed to determine the impact of implementation of universal screening and depression care program in a primary care training environment.
ACCULTURATION AND MEASURES OF CARDIOVASCULAR RISK AMONG FILIPINA IMMIGRANTSJane Jih1; Alka M. Kanaya1; Maria Rosario G. Araneta2. 1UCSF, San Francisco, CA; 2UCSD, San Diego, CA. (Tracking ID #1938915)
BACKGROUND: Acculturation is a dynamic process that encompasses a broad spectrum of cultural changes, interactions and adaptations that affect health. In immigrant populations, acculturation has been associated with increased prevalence of obesity, diabetes and coronary heart disease (CHD). CHD and its risk factors are highly prevalent among Filipino Americans. However, limited studies have examined acculturation and CHD specifically among Filipino Americans. We used the University of California San Diego (UCSD) Filipino Women’s Health Study to examine the relationship of acculturation and CHD and related risk factors among Filipina immigrants.
METHODS: The UCSD Filipino Women’s Health Study is a longitudinal study of 453 Filipino American women ages 39–86 years recruited from 1995 to 1999 in which the prevalence of and risk factors for CHD, hypertension (HTN), diabetes and obesity was measured. In addition to collecting immigration data, an adapted acculturation scale with three domains [a) functional integration via language use; b) values on preserving culture; c) attitudes on family structure and sex-gender roles] was administered. Outcome variables included prevalence of CHD (defined by ECG, Rose questionnaire and history of myocardial infarction), HTN, diabetes and obesity. We examined several measures of acculturation including length of residence in the United States (US), proportion of life years in the US (years residing in US/age at enrollment) and each domain of the acculturation scale. We used logistic regression, adjusting for age, education and exercise, smoking, alcohol use and body mass index (BMI) for the CHD outcome, to estimate the association of each measure of acculturation to each outcome.
RESULTS: The mean age of Filipina immigrants (n = 446) was 58 ± 9 years old. The mean length of US residence was 16 years (range 0–48). The prevalence of CHD was 21 %, HTN was 51 %, and type two diabetes was 33 %. Mean BMI was 25 ± 3 kg/m2 and 23 % were obese as defined by the World Health Organization (WHO) Asian BMI scale (BMI ≥ 27.5 kg/m2). Measures of acculturation were not associated with CHD, HTN and diabetes outcomes. Length of residence in the US but not proportion of life years or the acculturation scale was associated with obesity defined by the WHO Asian BMI scale. For each additional year of living in the US, Filipina immigrants had a 21 % increase in the odds of obesity (adjusted odds ratio 1.21 (95 % CI 1.01–1.47)).
CONCLUSIONS: Filipina immigrants have a substantial burden of CHD and risk factors. Unlike other immigrant populations, acculturation to life in the US was not associated with CHD, HTN and diabetes prevalence in Filipino women. However, longer duration of residence in the US was associated with increased odds of obesity. Exposure to a westernized lifestyle during the Spanish and US colonization in the Philippines may mitigate the impact of migration on cardiovascular health among Filipina immigrants.
ACCURACY AND GAMING OF THE ACUTE BRONCHITIS ANTIBIOTIC PRESCRIBING PERFORMANCE MEASUREPatrick P. Dempsey1; Harry Reyes Nieva1; Alexandra C. Businger1; Jeffrey A. Linder1,2. 1Brigham and Womens Hospital, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1938252)
BACKGROUND: Acute bronchitis is a cough-predominant illness of less than 3 weeks duration in a patient without chronic lung disease. A national performance measure states that antibiotics are not indicated for acute bronchitis. However, concerns have been raised about the measure’s accuracy and susceptibility to gaming. We compared the performance measure to chart review to assess the accuracy of the performance measure and detect gaming.
METHODS: We assessed 57,766 visits to an academic primary care practice between May 2011 and September 2012. For the chart review, we included patients aged 18–64 and excluded patients with chronic lung disease on the problem list or who made a study clinic visit in the prior 30 days (n = 26,539). Two trained chart abstractors reviewed these notes and coded whether the treating clinician diagnosed the patient with acute bronchitis. We calculated a modified Healthcare Effectiveness Data and Information Set (HEDIS) performance measure by including patients aged 18–64 with ICD-9 diagnosis codes of 466 or 490, excluding patients with chronic lung disease, immunosuppression, and cancer. Using chart review as the gold standard, we calculated the sensitivity, specificity, and positive predictive value of the acute bronchitis performance measure.
RESULTS: There were 31,174 visits which neither the performance measure nor chart review identified as an acute bronchitis visit. According to the performance measure, there were 90 acute bronchitis visits (88 with a diagnosis code of 466 and 2 with a diagnosis code of 490). There were 143 visits identified as acute bronchitis visits by both the performance measure and chart review (n = 41; “true positives”), the performance measure only (n = 49; “false positives”), or chart review only (n = 53; “false negatives”). These patients had a mean age of 48 years old; 77 % women; and 44 % white, 28 % Black, and 17 % Latino. Compared to chart review, the performance measure had a positive predictive value of 46 %, a sensitivity of 44 % and a specificity of >99 %. Of the 49 “false positives,” according to the chart, 10 visits were for other ARIs, seven visits were to other practices, seven the patient had been coughing for more than 3 weeks, five the patient did not have cough, five the patient had chronic lung disease, and 15 the patient had a visit in the prior 30 days. Of the 53 “false negatives”—for which the clinician diagnosed the patient with acute bronchitis in their note—52 did not have an acute bronchitis diagnosis code (most common diagnosis codes were cough, hypertension, upper respiratory infection, and viral infection) and one had a diagnosis code of asthma that was not mentioned in the chart. The antibiotic prescribing rate for true positives was 22 %, for false positives was 4 %, and false negatives was 30 %.
CONCLUSIONS: Compared to chart review, the acute bronchitis performance measure has a sensitivity and positive predictive value of less than 50 %. The performance measure omitted visits with antibiotic prescribing and falsely included visits without antibiotic prescribing, suggesting gaming.
ADAPTIVE RESERVE AT COMMUNITY HEALTH CENTERS: THE CANCER PREVENTION AND CONTROL RESEARCH NETWORK (CPCRN) MULTI-STATE SURVEYShin-Ping Tu1,2; Alan Kuniyuki2; Vicki M. Young3; Maria Fernandez4; Rebecca S. Williams5; Amanda Kimura2. 1Virginia Commonwealth University, Richmond, VA; 2University of Washington, Seattle, WA; 3South Carolina Primary Healthcare Association, Columbia, SC; 4University of Texas at Houston, Houston, TX; 5UNC Chapel Hill, Chapel Hill, NC. (Tracking ID #1936531)
BACKGROUND: Adaptive Reserve comprises intangible elements of a practice’s capacity (i.e., human relationships, teamwork, a learning culture) that provides flexibility, resilience, and enhance positive change. Our objective is to determine the Adaptive Reserve at Community Health Centers (CHCs) in seven states (California, Colorado, Georgia, Missouri, South Carolina, Texas, and Washington).
METHODS: We selected the Patient Centered Medical Home (PCMH) and the Consolidated Framework for Implementation Research to guide this research. Our survey included questions on colorectal cancer screening PCMH best practices and items from the Clinician Staff Questionnaire to examine the practice Adaptive Reserve (PAR) of participating CHC clinics. PAR scores were scaled from 0.00 to 1.00, with higher scores representing greater Adaptive Reserve. In collaboration with Primary Care Associations and CHCs, we recruited a convenience sample of 76 CHC clinics and invited their clinical staff (providers, nurses, and medical assistants) to participate in our CPCRN Community Health Center Survey.
RESULTS: Survey respondents (N = 246) are mostly female (82 %) and non-Hispanic (61 %). Forty-two percent reported their clinic had 7–8 colorectal cancer (CRC) screening PCMH best practices (maximum 8). Preliminary PAR scores in the states ranged from 0.61 to 0.7. In a study on PCMH implementation, 36 practices expected to have significant capability for change had a mean baseline PAR score of 0.69. Our survey indicates higher levels of PAR to be positively associated with CRC screening best practices in the clinics (adjusted OR = 3.62; 95 % CI 1.31, 10.02) and how frequently staff performed the best practices (p = 0.005).
CONCLUSIONS: Evidence from primary care transformation indicates that practices with strong Adaptive Reserve are more successful at incorporating change. With the Affordable Care Act, understanding the Adaptive Reserve of CHC clinics will be timely for the many changes needed to successfully expand primary care at CHCs.
ADVANCE DIRECTIVE INTERVENTION FOR CHRONICALLY HOMELESS PEOPLE: ACCEPTABILITY, FACTORS ASSOCIATED WITH COMPLETION, AND TREATMENT PREFERENCESAlexander Leung1; Dhruv Nayyar1; Manisha Sachdeva1; John Song2; Stephen Hwang1. 1St. Michael, Toronto, ON, Canada; 2University of Minnesota, Minneapolis, MN. (Tracking ID #1933803)
BACKGROUND: End-of-life care planning is relevant for homeless individuals because they experience high morbidity and mortality. A previous study has shown that homeless persons are more likely to complete advance directives with a one-on-one counselor-guided intervention than if the advance directive is self-completed. However, the acceptability of a counselor-guided intervention for the completion of advance directives among chronically homeless individuals has not been investigated. The aim of this study was to determine the acceptability of a counselor-guided intervention for the completion of advance directives among chronically homeless individuals. Secondary objectives were to identify characteristics associated with willingness to complete an advance directive and to characterize treatment preferences in this population.
METHODS: In a single-group intervention study, homeless men residing at a shelter in Toronto, Ontario were recruited from April to June 2013. Recruitment took place among programs that served chronically homeless individuals who were residents in a managed alcohol harm reduction program, a medical respite program that treats individuals with acute or uncontrolled chronic illnesses, and a long-term program for individuals who have been homeless for extended periods of time. Two hundred five homeless men (89.1 % of those approached) participated in the study. Participants completed a survey which obtained information on potential predictors of advance directive completion, including socio-demographic characteristics, health status, health care use, and attitudes towards end-of-life care and death. After completing this survey, all participants were offered an opportunity to complete an advance directive with a trained counselor. The primary outcome was the proportion of participants who completed an advance directive. The characteristics associated with completion of an advance directive were examined.
RESULTS: The duration of homelessness was 12 months or longer in 72.8 % of participants. A total of 103 participants (50.2 %) completed an advance directive. Socio-demographic characteristics, health status, and health care use were not associated with completion of an advance directive. Participants were significantly more likely to complete an advance directive if they reported thinking about death on a daily basis, believed that thinking about their friends and family was important, or reported knowing their wishes for end-of-life care but not having told anyone about these wishes. Of 103 individuals who completed an advance directive, the proportion expressing a preference to receive cardiopulmonary resuscitation in the event of a cardiorespiratory arrest was 94.1 %, 81.3 %, 64.7 %, and 36.3 % if there was a chance of returning to their current state of health or hypothetical health states of moderate dementia, severe dementia, and permanent coma, respectively.
CONCLUSIONS: As the homeless population continues to age, health care professionals will encounter an increase in chronically homeless persons facing complex end-of-life care needs. A single-encounter, one-on-one counselor-guided intervention can achieve a high rate of advance directive completion among chronically homeless individuals. Health care providers should initiate advance care planning discussions with their patients who are homeless. Future research aims to ascertain whether the completion of an advance directive has an effect on subsequent care in homeless individuals.
ADVANCED DIRECTIVE USE IN INTERNAL MEDICINE RESIDENCY CLINICS: A RETROSPECTIVE REVIEWBriana N. Ketterer; Corinne Self; Guadalupe Martinez; Jennifer Gabbard; Macy Whitley; Ellyn Lee. University of Arizona, Tucson, AZ. (Tracking ID #1923316)
BACKGROUND: Advanced directives (AD) allow patients to voice preferences about life sustaining therapies and end-of-life (EOL) care. ADs improve satisfaction, reduce stress, anxiety and depression at EOL. However, this information needs to be discussed and documented to be effective. Resident physicians play a key role as one of the first providers to encounter patients thus, making them an integral hub in the health delivery system. We sought to evaluate Internal Medicine (IM) Residents’ practice habits and assess participation in EOL/AD planning, and documentation of those preferences. This information will serve to address potential weaknesses in the Residency curricula and areas for improvement.
METHODS: Retrospective chart review of patients seen in IM Residency clinics at The University of Arizona Medical Center (UAMC) from July 2011–2013. Inclusion criteria: ≥65 years of age with at least one chronic, debilitating diagnosis associated with morbidity or mortality (dementia, AIDS, cancer, neurodegenerative disease, chronic obstructive pulmonary disease, chronic kidney disease, cerebral vascular accident or transient ischemic attack, liver cirrhosis, coronary artery disease or myocardial infarction, post-transplant) documented in the electronic medical record, AllScripts. Documentation was reviewed and ADs were recorded along with demographics (age, gender), number and type of diagnoses.
RESULTS: Reviewed 1075 charts, 165 met inclusion criteria (M 47 %, F 53 %; average age, 75; average number of problems, 7) with most frequent diagnoses of: cardiovascular disease (52 %), cancer (34 %), CKD (17 %). AD documented in 17 of 165 charts (10 %) which included: AD discussion (2), no specific qualifiers (1), Medical Power Of Attorney (8), DNR/DNI (9), Living Will (4), Hospice (1), and documentation for first responders (4).
CONCLUSIONS: IM Residents at UAMC clinics documented ADs in a mere 10 % of seemingly tenuous patients ≥65 years of age. This represents a cohort who would benefit from AD conversations to preserve their wishes at EOL. Although residents have some training in EOL care and AD, the curricula appears insufficient as the rate of AD documentation is very low and residents feel uncomfortable with those discussions as unpublished data from our group similarly suggests. One way to improve upon this is to implement an educational intervention to enhance training, improve AD discussions, and address all AD components with patients. Improvement in this area is crucial as it would not only fulfill residency competency requirements but also lead to more complete ADs allowing patients greater autonomy in their EOL care.
AGING WITH HIV: SYMPTOM BURDEN AND IMPACT ON QUALITY OF LIFEMeredith Greene1,2; Christine Ritchie1; Jeff Martin4; Joy A. Madamba3; Monica Mattes5; Yinghui Miao2; Steven Deeks3; Victor Valcour1,6. 1University of California San Francisco, San Francisco, CA; 2San Francisco VA Medical Center, San Francisco, CA; 3University of California San Francisco, San Francisco, CA; 4University of California San Francisco, San Francisco, CA; 5University of Central Florida College of Medicine, Orlando, FL; 6University of California San Franscico, San Francisco, CA. (Tracking ID #1932204)
BACKGROUND: As HIV infection has shifted from a life-threatening disease to a chronic illness, the HIV-infected population is aging and often facing multiple co-morbid conditions. Symptom assessment is an important clinical tool in the management of patients with complex chronic disease, yet limited data exists about symptom burden in older HIV-infected adults especially in the modern treatment era. The primary aim of this study was to describe the symptom burden (frequency and severity of symptoms) among HIV-infected adults over age 50 on combination antiretroviral therapy. We also examined factors associated with symptom burden in this population and the association of symptom burden on health related quality of life.
METHODS: We conducted a cross-sectional survey in 2012–2013 of HIV-infected adults over age 50 that had an undetectable viral load (HIV RNA) on antiretroviral therapy and were enrolled in a clinic based cohort at a county medical center in San Francisco. Sixteen symptoms were measured by self-report in a two part question based on the 12 item HIV symptom index:1) yes/no for presence of each symptom in the past week and 2) degree of severity of each symptom (not a problem, mild, moderate, severe, very severe) as judged by symptom frequency, intensity, and duration. Symptom severity was analyzed by examining the number of symptoms rated as moderate, severe, or very severe. Health related quality of life was assessed by a single-item self-report of health as excellent, very good, good, fair or poor. Demographics, HIV related factors, co-morbidities and medications were measured by self-report and verified by chart review. Descriptive statistics were used for data analysis.
RESULTS: 142 participants were enrolled, of which 94 % were male, 63 % were Caucasian, with a median age of 57 (range 50–74). The median CD4 count was 576 (IQR 393–715) and the median length of HIV infection was 22 (IQR 18–25) years. Participants had a median of 4 (IQR 3–6) co-morbid conditions, most commonly hyperlipidemia (61.3 %) and hypertension (52.8 %) and were taking a median of 9 (IQR 5–12) non-antiretroviral medications. Sixty-nine percent of participants reported two or more symptoms, with a median of 3 (IQR 1–5) symptoms reported. Fatigue (n = 72, 51 %), “feeling sad or depressed” (n = 60, 42 %), “pain, tingling, loss of feeling in feet or hands” (n = 54, 38 %) and insomnia (n = 53, 37 %) were the most commonly reported symptoms. Fifty-five percent of participants reported at least one moderate to very severe symptom with a median of 1 (IQR 0–2) moderate to very severe symptom reported. Fatigue (n = 31, 22 %), “feeling sad” (n = 31, 22 %) and insomnia (n = 25, 18 %) were the most frequent severe symptoms. The total number of co-morbid conditions was associated with both the total number of symptoms reported (rs = 0.21, p = 0.01) and symptom severity (rs = 0.27, p < 0.001) and the total number of non-antiretroviral medications was associated with symptom severity (rs = 0.21, p = 0.01). HIV related factors such as CD4 count and length of HIV infection did not have statistically significant correlations with symptom frequency or severity. Both the total number of symptoms and symptom severity were inversely correlated with overall health related quality of life (rs −0.42, p < 0.001; rs −0.47, p < 0.001).
CONCLUSIONS: Among adults age 50 and older with well-controlled HIV-infection, symptom burden was substantial and associated at least in part with co-morbid conditions. Addressing symptom burden during routine clinical encounters merits attention and may improve quality of life as the HIV-infected population ages.
ALLOWING PATIENT CHOICE BETWEEN TWO DIVERSE DIETS DID NOT IMPROVE WEIGHT LOSSWilliam S. Yancy1,2; Cynthia Coffman1,3; Valerie Smith1; Stephanie B. Mayer4; Ronette L. Kolotkin6; Paula J. Geiselman5; Megan McVay1; Eugene Z. Oddone1,2; Corrine Voils1,2. 1VAMC, Durham, NC; 2Duke University, Durham, NC; 3Duke University, Durham, NC; 4Virginia Commonwealth University, Richmond, VA; 5Louisiana State University, Baton Rouge, LA; 6Quality of Life Consulting, Durham, NC. (Tracking ID #1941417)
BACKGROUND: A variety of diet approaches lead to modest weight loss, and dietary adherence is a strong predictor of success. Allowing individuals to choose diet composition after considering their food preferences may improve adherence by increasing autonomy and self-efficacy. In a randomized trial, we examined whether participants who chose a diet experienced greater weight loss than those randomly assigned a diet.
METHODS: Participants were Durham Veterans Affairs Medical Center outpatients aged <75 years with body mass index (BMI) ≥30 kg/m2 and no unstable health problems. They were randomized to the Control or Choice arm, stratified by sex, BMI < or ≥40 kg/m2, and presence of type two diabetes. Control participants were randomly assigned to follow a low-carbohydrate (LCD) or a low-fat/reduced-calorie (LFD) diet. Choice participants were presented individual results from the Geiselman Food Preference Questionnaire, indicating which diet fit their food preferences best, as well as information about the two diets; 1 week later, they were called to elicit their diet choice. All participants then received diet counseling led by a dietitian in groups of 8–19 participants separated by arm and diet approach. In-person group sessions occurred every 2 weeks for 24 weeks, then every 4 weeks for 24 weeks interspersed with one-on-one telephone sessions mid-month from the dietitian focusing on behavioral goal-setting. All participants received literature specific to their diet; a pocket calorie/carbohydrate/fat counting guide; and a recommendation to exercise 150 min per week. At week 12, Choice participants could switch to the other diet if dissatisfied with their initial diet choice. The primary outcome, weight, was measured on a digital scale at the 19 visits in light clothing and no shoes. Secondary outcomes measured every 12 weeks were dietary intake by Block food frequency questionnaire and the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) questionnaire (scale 0–100; higher score indicates higher quality of life). Linear mixed models were fit for these continuous outcomes, and included a common intercept, time effect, time*treatment interaction, randomization stratification variables and random effect to account for group clustering.
RESULTS: A total of 207 participants were enrolled. Mean age was 54 years, 27 % were women, 51 % were White, 43 % were Black, 22 % had diabetes. Mean weight at baseline was 109 kg and mean BMI 36 kg/m2. In the Choice arm, 61 (58 %) chose the LCD and 44 (42 %) chose the LFD; only three LCD and two LFD participants switched diets at 12 weeks. Final measurements were collected in 88 of 102 (86 %) in the Control arm and 87 of 105 (83 %) in the Choice arm. Mean weight loss at 48 weeks was −5.3 % in Control participants and −4.2 % in Choice participants (difference 1.1 %, 95 % CI 0.0 to 2.2, p = 0.06). Dietary adherence was similar in the Control and Choice arms, with mean percent deviation from macronutrient goal differing by 0.6 % (10.1 % vs 10.7 %, respectively) at week 48. Mean IWQOL-Lite total scores were similar at week 48 (Control 82.9, Choice 81.7, difference −1.3, 95 % CI −4.5 to 2.0).
CONCLUSIONS: Educating patients on diet approaches and their food preferences, and then allowing them to choose their diet composition, did not result in greater weight loss compared to random diet assignment. Future research could consider targeting diet to individuals based on metabolic, genetic or other characteristics that might predict improved outcomes.
AN ACHILLES HEEL OF DISPARITIES RESEARCH: MISSING RACIAL DATA IN A STUDY OF MORTALITY AFTER CRITICAL ILLNESSMallika Mundkur1,2; Swapna Abhyankar1; Fiona M. Callaghan1; Clement J. McDonald1. 1National Institutes of Health, Bethesda, MD; 2George Washington University, Washington, DC. (Tracking ID #1936298)
BACKGROUND: Research has consistently demonstrated the presence of racial disparities in care and outcomes across inpatient and outpatient settings. However, studies focused on disparities in the intensive care unit (ICU) have yielded conflicting results, albeit with considerable variation in design and case-mix. Some analyses of ICU outcomes have detected greater mortality for minorities as compared to non-minority populations for conditions such as severe sepsis or trauma (Mayr et al., 2010; Haider et al., 2007), while others have found lower mortality rates for minorities with conditions such as community-acquired pneumonia (Frei et al., 2010). Recently, a retrospective study of 9518 patients in California concluded that in-hospital all-cause mortality for ICU patients was equivalent across race categories after adjusting for socioeconomic status, resuscitation preferences and severity of illness (Erickson et al., 2011). In the study by Erickson et al., patients without known race, equivalent to 10 % of overall study population, were excluded from the analysis—potentially biasing results, but noted to be common practice among other studies of racial disparities (Long, Bamba, Ling, Shea, 2006). We designed our study not only to contribute to the unresolved discourse on disparities in the ICU but also to ensure that patients with missing race would be examined.
METHODS: We performed a retrospective cohort study utilizing the Multiparameter Intelligence Monitoring in Intensive Care (MIMIC-II) research database (Saeed et al., 2011; Lee et al., 2011). MIMIC-II contains de-identified clinical information on 32,425 adult and neonatal ICU patients admitted to Beth Israel Deaconess Hospital in Boston, MA between 2001 and 2008. Our cohort was comprised of adult patients (age >18) admitted to a medical or surgical ICU for at least 4 h for a non-elective admission. For patients with multiple ICU admissions, only the first stay was included. Our primary outcome was 30-day all-cause mortality. Covariates were: race, age, gender, marital status, type of insurance coverage (indicator of socioeconomic status), code status within 2 h of ICU admission, Simplified Acute Physiology Score (SAPS) (severity of illness indicator), admission source (e.g., emergency room vs. transfer) and comorbidities including congestive heart failure, chronic renal failure/end-stage renal disease, chronic liver disease, and cancer. We used demographic data to group patients into the following race categories: White, Black, Hispanic, Asian/Pacific Islander, Other and included an Unknown category for patients without documented race. We used the software package R for all statistical analysis. We used Kruskal-Wallis, Pearson’s chi-squared, and Fisher’s exact tests to assess the unadjusted associations between race and the covariates, log-rank test to detect differences in survival curves, and multivariable logistic regression for our main analysis.
RESULTS: 13, 491 patients met our inclusion criteria and crude mortality rates for the race categories (p < 0.0001) were as follows: 17.6 % for the total population, 17.6 % for the White group, 13.6 % for the Asian group, 6.7 % for the Hispanic group, 14.7 % for the Other category, and 28 % for the Unknown group. Odds ratios for our primary outcome of 30-day mortality are summarized in Table 1. For the Unknown group, 40.2 % of the patients were transfers as compared to 14.6 % for the overall study population (p < 0.0001).
CONCLUSIONS: We were surprised by the finding that all-cause mortality at 30 days was substantially higher for patients with unknown race than for any of the other race categories. Aside from the White group, the unknown group was larger than any of the other race categories. Thus, while the White group appeared to have the greatest mortality among the known race groups, if the unknown group were predominantly Black, Hispanic or another race, the results could have been different. For the Unknown category, we observed a disproportionate number of transfers from other hospitals. Our findings generate questions for those researching healthcare disparities, including why race is unknown for many patients and whether this group is at higher risk of other adverse outcomes. Efforts should be made to include these patients in analyses and reduce the number of patients without documented race to improve our ability to accurately examine and eliminate healthcare disparities.
Table 1. Risk for 30-day Mortality by race based on adjusted multivariable logistic regression
| Race Category | n | 30-day mortality risk OR (95 % CI) | p-value |
| White (reference group) | 9523 | 1.00 | n/a |
| Black | 1244 | 0.66 (0.53, 0.82) | 0.0002 |
| Asian | 331 | 0.56 (0.39, 0.81) | 0.0019 |
| Hispanic | 489 | 0.53 (0.36, 0.78) | 0.0014 |
| Other | 307 | 1.06 (0.73, 1.55) | 0.75 |
| Unknown | 1594 | 1.96 (1.67, 2.29) | <0.0001 |
AN EVALUATION OF “CLINICALLY PROVEN” DIETARY SUPPLEMENTSAlysha Melnyk; Bimal Ashar; April S. Fitzgerald. Johns Hopkins University, Baltimore, MD. (Tracking ID #1939374)
BACKGROUND: The Dietary Supplement Health and Education Act (DSHEA) permits manufacturers to sell products without providing pre-market evidence of safety or efficacy. One fundamental reason for the passage of the DSHEA was to empower consumers to make their own choices. Yet, data suggests that the public is unaware of the limited regulation on product marketing and advertising. Dietary supplements are frequently advertised as being “clinically proven.” Yet, there are not standards in place to determine acceptable use of this term. This study was undertaken to evaluate products that have been advertised as being “clinically proven” in order to determine the availability of data used to make such an assertion.
METHODS: An internet survey for products was performed by using the search the search tems “clinically proven dietary supplements”, “dietary supplements”, “best dietary supplements” in common search engines. Advertisements were then reviewed to see if they contained terms that suggested definitive efficacy. Products whose advertisements contained terms such as “clinically proven”, “scientifically proven”, “clinically supported” were included in the study. Products returned via the search were then categorized for what they were purported to be proven to do. Additionally, the supplement advertisements were analyzed to determine if evidence was readily available to consumers that would support the “clinically proven” label. If evidence supporting the statement was not readily available on their website, companies were contacted to attempt to obtain any information supporting their claim. Descriptive statistics were used to categorize products and determine what percentage of such products had available references to studies supporting their claims.
RESULTS: A total of 99 dietary supplements were found that referenced definitive scientific efficacy. Most of these products (63 %) were advertised as being useful for helping consumers lose weight and/or build muscle. Despite the assertion for efficacy, only 28 made direct reference on their website to any scientific studies. After being contacted, an additional eight companies provided studies and/or links to evidence. The remaining companies (64 %) either had no testing to report (21 %), claimed that they had testing but would not provide it (4 %), claimed that their evidence was all on their website (13 %), did not respond to inquiries (14 %), or had no listed contact information on their internet advertisement (11 %)
CONCLUSIONS: A number of dietary supplements are advertised as being clinically or scientifically proven, yet provide little to no evidence to consumers to substantiate their claims. Truth-in-advertising standards for dietary supplements should define parameters for using such terminology in order to protect the public from potentially misleading claims.
AN EVALUATION OF COMPUTERIZED DRUG-DRUG INTERACTION ALERT OVERRIDES IN AMBULATORY CARESarah P. Slight1,2; Diane L. Seger3; Karen C. Nanji4,5; Insook Cho1,6; Nivethietha Maniam3; Patricia C. Dkyes1,4; David W. Bates1,4. 1Brigham and Women’s Hospital, Boston, MA; 2Durham University, Stockton on Tees, United Kingdom; 3Partners Healthcare Systems, Inc.,, Boston, MA; 4Harvard Medical School, Boston, MA; 5Massachusetts General Hospital, Boston, MA; 6Inha University, Incheon, MA. (Tracking ID #1935807)
BACKGROUND: Computerized physician order entry with clinical decision support (CDS) represents a valuable tool for improving medication safety, quality, and efficiency. CDS systems can provide health care providers with real-time, relevant, patient-specific information and alert them to potential prescribing errors. Providers may choose to override these alerts however, selecting a coded reason in order to proceed with the medication order. It is often unclear whether these particular actions, e.g., will monitor drug levels as recommended, are carried out by the provider or just simply ignored. We evaluated why providers overrode drug-drug interaction (DDI) alerts and what actions they took as a consequence of the alert.
METHODS: This study was a cross-sectional, observational study of DDI alerts generated over a three-year period between January 2009 and December 2011. All Level 2 DDI alert overrides were downloaded with IRB approval from 36 primary care practices affiliated with two Harvard teaching hospitals (total 14,966 overrides, 60.2 % of alerts generated). Any duplicates were removed and replaced. A physician and pharmacist expert panel assessed the appropriateness of these DDI alert overrides. A detailed chart review was conducted for each of the appropriate overrides to ascertain whether the provider had carried out their intended action(s).
RESULTS: Providers appropriately overrode just over two-thirds (338/496) of the DDI alerts and carried out the intended action in less than two-thirds (214/338) of these cases. Eight drugs were responsible for generating approximately three quarters of these alerts. The most common coded reasons for overriding DDI alerts were ‘will monitor as recommended’ (43.9 %, n = 218), ‘will adjust dose as recommended’ (16.9 %, n = 84), and ‘patient has already tolerated combination’ (15.7 %, n = 78). Of the 121 appropriate alert overrides where the provider said they would ‘monitor as recommended’, only 35.5 % (n = 43) actually completed the monitoring. Our study also revealed how only 60 % (n = 21) of providers who indicated that they would ‘adjust the dose as recommended’ actually did. Furthermore, some providers selected the coded reason ‘patient has already tolerated combination’, yet no information was found to suggest that the patient had been taking both drugs together previously.
CONCLUSIONS: We found that providers continue to override important and useful alerts, some of which likely cause serious patient injuries, although we did not measure injuries in this study. A key difference between our study and previous studies1 is that we also reviewed the charts to see whether the provider actually took action as a consequence of the alert. We found that the intended action was carried out in only two-thirds of cases. More research is needed to explore the human factors elements that influence provider behaviour, such as patient demands, workload, and time constraints. References: 1. Shah NR, Seger AC, Seger DL et al. Improving Acceptance of Computerized Prescribing Alerts in Ambulatory Care. JAMIA 2006;13:5–11.
AN EVALUATION OF COMPUTERIZED MEDICATION ALERT OVERRIDE BEHAVIOR IN AMBULATORY CARENivethietha Maniam1; Sarah P. Slight1,3; Diane L. Seger1; Mary Amato1,7; Dustin McEvoy1; Karen C. Nanji4,5; Insook Cho1,6; Patricia C. Dkyes2,4; David W. Bates1,2. 1Partners HealthCare, Cambridge, MA; 2Brigham and Women’s Hospital, Boston, MA; 3The University of Durham School of Medicine, Stockton on Tees, United Kingdom; 4Harvard Medical School, Boston, MA; 5Massachusetts General Hospital, Boston, MA; 6Inha University, Incheon, Republic of Korea; 7Massachusetts College of Pharmacy and Health Sciences University, Boston, MA. (Tracking ID #1939988)
BACKGROUND: While evidence suggests that computerized decision support (CDS) increases safety and quality of care, understanding how physicians respond to CDS alerts is a critical factor in achieving meaningful use of electronic health records. We continue to observe a high level of medication alert overrides for many prescription domains. While some overrides are justified clinically, others are not, and it is important to be able to reach out to those providers who are not prescribing optimally and understand their reasons for overriding alerts.
METHODS: All Level 2 alert overrides that required a coded reason to be provided at the time of prescribing were downloaded between January 2009 and December 2011 in the outpatient primary care setting. We limited our sample to providers who had received 20 or more alerts in each of the prescribing domains (drug-drug interaction, drug-allergy interaction, renal suggestion, age-based, duplicate-drug, and formulary substitution alerts) and the number of times each provider overrode these alerts was calculated. Of the 725 providers eligible, those with a high inappropriate override rate (above 75 % within a specific domain or overall) were targeted for interviews. The sessions were tailored to each provider’s overrides and conducted by a research pharmacist or physician trained in counter-detailing techniques. Graphical material, including performance level data, a list of their inappropriate overrides and supporting evidence-based summaries, was presented to each provider during the discussion. An analysis of the data was carried out and prevalent concepts related to general views on alert functionality and specific prescribing behavior identified.
RESULTS: We conducted 23 interview sessions across primary care clinics affiliated with Brigham and Women’s Hospital and Massachusetts General Hospital. We identified seven high level content categories: clinical satisfaction, clinical utility and relevance, variant user knowledge, impact on clinician reviewing process, patient preferences, current alerting tool challenges, and considerations for the future. Overall, providers were favorable towards the alerts and found them helpful in identifying possible adverse interactions. Many providers, however, found that the clinical relevance of the alerts could be improved by including magnitude of risk, suggested alternate treatments, recent laboratory values, and more up-to-date reference material. Additionally, many participants said they failed to provide a valid override reason because they found the alerts time-consuming and disruptive. Limitations of the existing EHR infrastructure such as inaccurate medication and allergy lists were identified as contributing to unnecessary alerts. Creating a more patient specific alerting tool was recognized as a future area of focus.
CONCLUSIONS: Many providers were unaware of their relatively high rate of overriding and this study allowed providers the unique opportunity of objectively assessing their prescribing behavior. Key issues that emerged from the sessions included the perceived risk to physician autonomy in decision-making, the increase of clinically irrelevant alerts leading to alert fatigue, and the lack of supplementary clinical information. By incorporating provider preferences, customizing alerts to the context of the visit, and offering additional clinical data, providers felt that CDS alerts would be less likely to be overridden providing more effective, efficient, and equitable care.
AN INTERNATIONAL EVALUATION OF DRUG-DRUG INTERACTION ALERTS THAT SHOULD BE NON-INTERRUPTIVE IN U.K. AND U.S. SETTINGSAlexandra Robertson1; Sarah P. Slight1,2; Diane L. Seger3; Sarah K. Thomas4; Jamie Coleman4; David W. Bates1,5; Shobha Phansalkar1,6. 1Brigham and Women’s Hospital, Boston, MA; 2The University of Durham, Durham, United Kingdom; 3Partners HealthCare Systems, Inc., Wellesley, MA; 4The University of Birmingham, Birmingham, United Kingdom; 5Harvard Medical School, Boston, MA; 6Wolters Kluwer Health, Indianapolis, IN. (Tracking ID #1937914)
BACKGROUND: Clinical Decision Support (CDS) has the potential to improve patient safety by providing knowledge and support at the point of prescribing. CDS systems can, however, deliver an overdose of alerts that may result in “alert fatigue,” with providers overlooking clinically significant alerts as well as those considered less critical. In a previous study, Phansalkar et. al. (2012), identified 33 non-critical drug-class and class-class interaction alerts that could be safely made non-interruptive with a goal to reduce alert fatigue. This study aims to establish whether these non-critical drug-drug interaction (DDI) alerts were set as interruptive or non-interruptive in U.K. and U.S. systems, and the rate at which these alerts were generated and overridden.
METHODS: With the necessary ethical approvals, we downloaded all low priority drug-class and class-class DDI alerts generated from January 2009 to December 2011 in three home-grown electronic health records (EHRs) at two academic medical centers: one British inpatient system and one U.S. inpatient and one outpatient system. We defined interruptive alerts as those requiring a provider response or action when generated and non-interruptive alerts as those that did not require a provider response. In the U.K. system we downloaded all level 3 inpatient alerts, which require a box to be ticked to acknowledge receipt of the alert. No override reasons are collected by this system. In the U.S. systems we downloaded all level 2 alerts, which require a coded reason to be provided at the point of prescribing. The number of alerts generated and overridden were downloaded for all three systems. Using this data, we calculated the frequency of alerts generated and override rates for all low priority DDI alerts.
RESULTS: In the U.S. system, 2 of the 33 low-priority drug-class and class-class interactions were set as interruptive; these included niacin and statins, and proton pump inhibitors and imidazoles. These drug-drug combinations triggered a total of 301 alerts in the U.S. outpatient and inpatient systems, which were overridden in 77.7 % of cases (n = 234) during the period assessed. The niacin and statin interaction was triggered most often in both the U.S. inpatient (n = 62) and outpatient (n = 215) systems, and overridden 90.3 % of the time in the inpatient system (n = 56) and 70.2 % in the outpatient system (n = 151). In the U.K. system, 8 of the 33 low priority drug-class and class-class interactions identified were set as interruptive and triggered a total of 2,354 interruptive alerts, which were overridden in 63.5 % of cases (n = 1,495). The most common were: ACE inhibitors and angiotensin II receptor antagonists; anticoagulants and corticosteroids; NSAIDs and β-adrenergic blockers; thiazide-type diuretics and NSAIDs; ACE inhibitors and NSAIDs; and sulfonylureas and ACE inhibitors, with the latter two pairs overridden most often. Sulfonylureas and ACE inhibitors triggered 42.6 % of all class-class alerts (n = 1,002) and were overridden in 63.4 % of cases (n = 645). Of the sulfonylureas and ACE inhibitors, the gliclazide/gliclazide MR and perindopril alerts accounted for almost half of this class-class category (55.4 %, n = 556) and were overridden in 69.9 % (n = 387) of cases. ACE inhibitors and NSAIDs occurred second most often (22.3 %, n = 525) in the U.K system, with an 87.4 % override rate (n = 459). Within this class-class category, ramipril and ibuprofen accounted for more than half (52.4 %, n = 275) and were overridden in 90.1 % of cases (n = 248).
CONCLUSIONS: Our team has previously shown that certain non-critical alerts may be safely made non-interruptive in provider workflows. This study offers assessment of the non-critical alerts previously identified to better understand user response to these alerts. Given the high rates of override amongst those reviewed, we feel this work offers further validation that these alerts may be safely made non-interruptive to minimize alert fatigue and support the patient safety aims of CDS.
AN INTERNATIONAL EVALUATION OF USER PERCEPTIONS OF DRUG-DRUG AND DRUG-ALLERGY INTERACTION ALERTSAlexandra Robertson1; Pamela M. Neri2; Elisabeth Burdick1; Sarah P. Slight1,3; David W. Bates1,4; Shobha Phansalkar1,5. 1Brigham and Women’s Hospital, Boston, MA; 2Partners HealthCare Systems, Inc., Wellesley, MA; 3The University of Durham, Durham, United Kingdom; 4Harvard Medical School, Boston, MA; 5Wolters Kluwer Health, Indianapolis, IN. (Tracking ID #1938373)
BACKGROUND: Electronic medical records (EMR) with integrated clinical decision support (CDS) have the potential to improve patient safety. Increasing adoption, refining the delivery and content of existing CDS, and improving user-centered design are key to meeting core measures for Meaningful Use of EMRs. Override rates of CDS alerts are estimated to be between 49 and 96 %. Limited evidence supports a direct link between the availability of CDS to measurable improvements in patient safety. Among several reasons, poor user acceptance of alerts is widely recognized as a major barrier to realizing the potential impacts of CDS systems on patient safety. Poor alert design and lack of contextual specificity are causes for negative user perceptions about the utility of CDS. In this study, our objective was to evaluate the relationships between user perceptions of Drug-Drug Interaction (DDI) and Drug-Allergy Interaction (DAI) alert volume, content, and user acceptance.
METHODS: We conducted a survey of user perceptions of DDI and DAI alerts using a validated survey tool, developed by Zheng, et al. The purpose of this survey was to understand the relationship between the acceptance of alerts to users’ perceptions of the number and content of these alerts. To increase the generalizability of our evaluation we included a multi-national sample of EMRs, with users of both home-grown and commercially available products, surveying physicians at seven healthcare institutions in two countries. The EMRs evaluated were two commercially available products and four home-grown products. A total of 1,423 internal medicine physicians were invited to participate in the study. The survey questions evaluated providers’ perceptions regarding the volume of alerts they received. Specifically, providers were asked to quantify the DDI/DAI alerts they receive in an average week, read thoroughly, found clinically relevant, changed their prescribing behavior, and overrode. We performed descriptive statistics on the survey responses to establish correlations between perception of alert frequency, alert relevancy, and alert override. We ran the means in three groups based on the number of alerts reported per week; 1–10 alerts per week (group 1), 11–50 (group 2), and greater than 50 (group 3).
RESULTS: Of the 1,423 physicians invited to participate, 342 consented to participate for an overall response rate of 24 %. For both DAI and DDI alerts across all three groups, we found that as the number of perceived alerts increases, the percentage of providers who report reading, finding these alerts relevant, or changing prescribing behaviors based on the information provided decreases while the number of alerts overridden increases (Table 1, 2). Overall, participants estimated receiving a greater number of DDI (22.9) than DAI (13.8) alerts per week, but were more likely to override DAI than DDI alerts, with reported override rates of 83.22 % and 78.5 %, respectively.
CONCLUSIONS: This is the first study to establish an empirical correlation between the perceptions of physicians on alerts to alert acceptance. Physicians who perceive receiving a high number of alerts are less likely to read them, find them clinically relevant, allow them to affect their prescribing behavior, and more likely to override them. Future research should focus on how providers’ perceptions of alert volume can be improved. Decreasing the volume of interruptive alerts may foster a more positive attitude of physicians towards CDS alerting in EMRs.
AN INTERNET-BASED STUDY CHARACTERIZING THE ASSOCIATION BETWEEN PAIN SEVERITY AND THE BURDEN OF FIBROMYALGIA IN THE USElizabeth T. Masters2; Caroline Schaefer1; Rachael Mann3; Joseph C. Cappelleri4; Shoshana Daniel5; Edgar Adams1; Gergana Zlateva2; Heather McElroy6; Arthi Chandran2; Annlouise Assaf4; Michael McNett7; Philip Mease8,9; Stuart Silverman10; Roland Staud11. 1Covance Market Access Services Inc, Gaithersburg, MD; 2Pfizer Inc, New York, NY; 3Covance Market Access Services Inc, San Diego, CA; 4Pfizer Inc, Groton, CT; 5Covance Market Access Services Inc, Conshohocken, PA; 6Covance Market Access Services Pty Ltd, Sydney, NSW, Australia; 7Aurora Pain Program, Milwaukee, WI; 8Swedish Medical Center, Seattle, WA; 9University of Washington, Seattle, WA; 10Cedars-Sinai Medical Center, Beverly Hills, CA; 11University of Florida, Gainesville, FL. (Tracking ID #1922702)
BACKGROUND: Although patients with fibromyalgia (FM) report a variety of symptoms that impact function and quality of life, chronic widespread pain is the hallmark symptom. Pain management in patients with FM is challenging, and the presence of pain contributes to the overall burden. This study characterizes the burden of FM by pain severity in the US.
METHODS: Subjects ≥18 years old with FM were identified during a study to determine the prevalence and burden of FM and chronic widespread pain in a sample of US adults recruited from a national online panel. Given the gender distribution of FM, females were oversampled (80:20). FM confirmation was made by physician evaluation during a site visit among 350 with and 125 subjects without chronic widespread pain. A total of 171 FM subjects subsequently completed an online questionnaire to assess clinical characteristics, patient-reported outcomes (including but not limited to the Revised Fibromyalgia Impact Questionnaire [FIQ-R], Brief Pain Inventory-Short Form [BPI-SF], Medical Outcomes Study Sleep Scale [MOS-SS], and Short Form 12-Item Heath Survey, version 2 [SF-12]), and direct and indirect costs during the past 3 months. Subjects were categorized by pain severity using cutoff scores on the BPI-SF (mild, 0–3; moderate, 4–6; severe, 7–10); statistical significance was evaluated at the 0.05 level across severity levels with ANOVA (continuous variables) and chi-square or Fisher’s exact test (categorical variables).
RESULTS: Mild, moderate, and severe pain were reported by 27 (15.8 %), 57 (33.3 %), and 87 (50.9 %) FM subjects, respectively. Across pain severity levels, age, gender, and race were similar. However, the percentage of subjects employed for pay was lower with increasing pain severity: 70.4 %, 45.6 %, and 23.0 % for mild, moderate, and severe, respectively (P < 0.0001). Among those reporting at least one comorbid condition, greater pain severity was associated with a higher mean ± standard deviation (SD) number of comorbid conditions, from 3.0 ± 2.0 (mild) to 4.5 ± 3.1 (moderate) and 5.8 ± 2.9 (severe) (P < 0.0001). The FIQ-R and its subscales (Function, Overall Impact, and Symptom Intensity) showed progressive worsening with increasing pain severity (all P < 0.0001). The MOS-SS Overall Sleep Problems Index score indicated poorer sleep with increasing pain (P < 0.0001). Pain severity was significantly associated with poorer health status, as indicated on the SF-12 domains (all P < 0.05) as well as the Physical Component Summary (P < 0.0001). Higher total costs during the past 3 months were associated with increasing pain (P = 0.0053), with the highest costs among those with severe pain (mean ± SD:$9,553 ± 9,601) relative to moderate ($6,701 ± 6,477) and mild ($4,143 ± 4,657). Across all severity levels, indirect costs were the primary driver of total costs, and increased as pain increased (P = 0.0063).
CONCLUSIONS: Severe pain was common in a broadly representative sample of FM patients, underscoring the challenges of pain management. Pain severity was significantly associated with sleep, function, and health status, indicating that the burden of FM was greater among subjects with more severe pain. The economic burden of FM was higher with greater pain severity; the highest costs were observed among subjects with severe pain. These findings highlight the importance of comprehensive treatment and the need for effective pain management strategies, especially among those experiencing greater pain levels.
AN OBJECTIVE STRUCTURED TEACHING EXAM DEMONSTRATES THAT CLINICAL FACULTY PERFORM BETTER AT FEEDBACK GIVING WHEN INSTRUCTED TO FOCUS ON FEEDBACK SKILLSSheira Schlair1; Sharon Parish1; Mooseong Heo2; Felise Milan1. 1Albert Einstein College of Medicine/Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1937665)
BACKGROUND: The Objective Structured Teaching Exam (OSTE) is an emerging faculty development and teaching assessment tool. Often the only data available to assess clinical teaching quality are learner evaluations, which are subject to bias. The objectives of this evaluation were to assess faculty’s areas of effectiveness and those needing improvement on simulated clinical teaching encounters.
METHODS: 18 faculty participants (FP), six expert observers (EO) and 10 standardized students (SS) participated in a three-station OSTE at AECOM’s Clinical Skills Center. Cases and checklists were developed by a team of experts and further modified with input from SSs and EOs after a 3-hour training session. FPs participated in three stations: (1) Attending rounds involving a medical error with a team of an intern, resident and sub-intern (“attending rounds”); (2) Bedside teaching of a focused cardiac exam in a patient with chronic atrial fibrillation (“bedside teaching”); and (3) Learner feedback to a medical student with professionalism issues in his clinical work (“feedback”). FPs were assessed by EOs who completed station-specific checklists consisting of core teaching skills, case specific skills, and two global items (communication and teaching skills) using a behaviorally-anchored 5-point scale (1 = poor to 5 = excellent). Inter-station comparisons were performed using a mixed effects linear regression model followed by a Bonferroni correction, and paired t-tests were used to assess the impact of specific teaching domains on overall station performance.
RESULTS: EO assessment of FP performance showed that core teaching skills were significantly different across stations: (1) FPs’ instructional skill scores were higher in the bedside teaching and attending rounds stations as compared to the feedback station (4.11, 3.83, 2.85, p = 0.0340); (2) FPs’ feedback scores were higher in the feedback station (4.00 vs. 2.97 for attending rounds, 3.81 for bedside teaching; p = 0.0358) and the highest rated teaching skills in the entire OSTE; (3) Case specific skills were significantly worse in the feedback as compared with attending rounds and bedside teaching stations (3.12, 4.03 and 4.33, respectively; p = 0.0014). FPs’ feedback skills had a negative impact on bedside teaching and attending rounds’ overall station performance, while it had a significantly positive impact on the feedback station performance.
CONCLUSIONS: Faculty case specific skill performance was stronger in the attending rounds and bedside teaching cases as compared to the professionalism station. However, feedback skills were superior and most highly rated in the feedback station in which feedback was the specific teaching task being evaluated. These findings raise the question of whether feedback can be effectively delivered while concentrating on a clinical task. One possible explanation for is that that when clinical teachers have multiple tasks to juggle, feedback may not be given priority and perhaps may be performed less skillfully. Implications are that feedback to learners may need to be explicitly separated from other tasks in the daily clinical workflow. In addition, these findings might suggest the need for systematic faculty development in feedback-giving in complex clinical environments.
AN OCCULT FINDING IN HEPARIN DRIP ORDER SETDaniel A. Kim2; Ileana L. Ponor1,2; Rajanigandhi Hanumanthu3; Scott Wright2. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins University School of Medicine, Baltimore, MD; 3Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1939349)
BACKGROUND: Order sets in electronic medical records (EMR) have been shown to reduce variation in clinical practice, to increase quality of care, and to reduce costs. However, it is important to continually evaluate the benefit and appropriateness of existing order sets. Some order sets may not be evidence-based, and all need to be periodically reviewed and updated. There have been efforts to reduce, or even eliminate, fecal occult blood test (FOBT) in hospitalized patients. Friedman’s 2010 study asserts that there is no place for FOBT in an acute hospital setting as the test leads to inappropriate clinical decisions with considerable costs. One example of using FOBT in an ill-chosen and ill-timed manner, is the inclusion of FOBT in the heparin drip order set, which occurs at our hospital and others. Our study was conducted to assess the frequency of FOBT ordered and sent, as well as the results, documentation, and change in management among hospitalized patients who are on heparin drip therapy.
METHODS: A retrospective study of 898 adult hospitalized patients, who had heparin drip ordered at a single academic medical center during a 6 month period (from November 2012 to May 2013) was conducted. Demographics, hospital admission information, diagnosis, discharge disposition, laboratory data, and indication for heparin drip were collected. For patients with FOBT sent, further data was gathered and analyzed for FOBT results, documentation, and influence over clinical decision making and management.
RESULTS: During the 6 month period studied, 898 patients had heparin drip ordered through the available order set, which includes a nurse collect lab order for FOBT. A total of 128 (14.3 %) patients had FOBT sent, of which 33 (25 %) came back positive. About half (51.5 %) of these results were documented by a provider either in a progress note (36 %) or discharge summary (36 %). An occult blood test was sent despite the fact that seven patients (21 %) had obvious signs of bleeding. In only one instance, was the heparin drips were stopped as a direct result of the positive test. From all positive tests, 7 (21 %) resulted in a gastroenterology consult, with four of these patients (57.1 %) getting an inpatient endoscopy. These did not change anticoagulation management in a single patient. The endoscopies were unremarkable in three patients (no cause of bleed found) and in one patient adenocarcinoma was diagnosed via a polyp biopsy. Among the 14 patients that were discharged home (n = 14), approximately 43 % were readmitted within 90 days with a diagnosis of GI bleed.
CONCLUSIONS: Regular review of order sets in our EMRs, with careful consideration of the consequences, is essential. While the automatic FOBT order in the heparin drip order set at our hospital seems ineffective, we were surprised to learn that the order is ignored by our nurses recurrently. Because the FOBT results changed management very infrequently, it is probably not indicated to be included in the heparin order set. That said, any positive FOBT that is noted in the hospital should be passed on to the patient and the primary care physician, particularly given the very high 90 day readmission rate for a GI bleed.
ANALYSIS OF 256 CASES OF CLASSIC FEVER OF UNKNOWN ORIGINMasashi Yamanouchi; Toshio Naito; Yuki Uehara; Hirohide Yokokawa; Tomohiro Hosoda; Yukiko Watanabe; Takayasu Shiga; Akihiro Inui; Yukiko Otsuki; Kazutoshi Fujibayashi; Hiroshi Isonuma; Teruhiko Hisaoka. Juntendo University School of Medicine, Tokyo, Japan. (Tracking ID #1937281)
BACKGROUND: Fever of unknown origin (FUO) can be caused by many diseases that vary depending on region and time period. Studies on the causes of FUO in Japan has been small number of cases, often representing regional studies limited to a single hospital. The aim of the present study were <1> Age group, sex, and causes of FUO (%) in all patients. <2> Differences in causes of FUO (%) between patients 65 years old and older, and <65 years old. <3> Differences in causes of FUO (%) between the periods 1994–2003 and 2004–2012. <4> Number of cases requiring 150 days and longer from the time of fever onset for diagnosis.
METHODS: For the present single-institution retrospective observational study, data were extracted from the medical records of patients ≥18 years old who met the criteria for classic FUO and were hospitalized between August 1, 1994, when our department was established, and December 31, 2012. Durack and Street’s criteria for classic FUO were used in this study: fever ≥38 °C at least twice over a ≥3-week period, without a diagnosis after three outpatient visits or 3 days of hospitalization, and no diagnosis of HIV or immunodeficiency prior to the fever.
RESULTS: A total of 256 patients were enrolled in this study, including 131 men and 125 women, with a median age of 55 years (range, 18–94 years). The most frequent age group comprised patients in their 60s. Patients 65 years old and older accounted for 33.2 % (85/256) of all patients. The cause of FUO was infection in 27.7 % of patients (n = 71), Non infectious inflammatory disease (NIID) in 18.4 % (n = 47), malignancy in 10.2 % (n = 26), other in 14.8 % (n = 38), and unknown in 28.9 % (n = 74). The most common single cause was HIV/acquired immunodeficiency syndrome (AIDS) in 17 patients, accounting for 25 % of all infections. Among these, 16 patients were <65 years old. The next leading causes were malignant lymphoma and infective endocarditis in 12 patients each; with these causes, four patients and 10 patients, respectively, were <65 years old. The fourth leading cause was polymyalgia rheumatica in 10 patients; seven were 65 years old and older. In patients 65 years old and older, compared to those <65 years old, percentages of infections (21.7 % vs. 30.6 %) and other causes (7.2 % vs. 18.5 %) were lower, whereas percentages of NIID (27.7 % vs. 13.9 %) and malignancy (14.5 % vs. 8.1 %) were higher. The percentage of unknown causes was the same (28.9 %) in both patients <65 years old and 65 years old and older. The trend in 2004–2012, compared to 1994–2003, was similar to that in the 1990s in an overseas report. In eight of the 256 patients, 150 days and longer were required from the time of fever onset for diagnosis. The longest time was 300 days in a case of adult Still’s disease.
CONCLUSIONS: This study reviewed patients with classic FUO evaluated at our hospital department since it was established. Our study found that together with the increase in HIV patients in Japan, HIV/AIDS is now the most common cause of FUO. In addition, the percentage of unknown causes of FUO has increased, now exceeding 20 % of cases. As the present study collated data from a long period and reviewed the largest number of FUO cases in Japan to date, these findings will serve as a useful reference for the future care of FUO patients.
ANALYSIS OF PREDICTIVE FACTORS OF BACTEREMIA AMONG INPATIENTS OF GENERAL MEDICINESayato Fukui1; Yuki Uehara1; Toshio Naito1; Teruhiko Hisaoka1; Osamu Takahashi2. 1Juntendo University School of Medicine, Tokyo, Japan; 2St. Luke’s Life Science Institute, Tokyo, Japan. (Tracking ID #1937325)
BACKGROUND: Criteria to take blood culture from patients with suspicion of severe infection has not been established, and decision depends on each physician’s opinion. Several report investigated predictive factors for positive blood culture results among ICU patients or aged patients, but analysis of predictive factors among patients hospitalized in department of general internal medicine has not been reported yet. This study was performed in inpatient wards of general medicine of Japanese university hospital to clarify the predictive factors of bacteremia and to identify patients from that blood cultures should be taken.
METHODS: This cross-sectional study was performed at the department of general medicine in Juntendo University Hospital, Tokyo, Japan, from January 2011 to December 2012. All inpatients from that blood cultures were taken were included in this study. The results of blood cultures of the patients were collected from the database of the clinical laboratory, and only the first culture results were used for analysis in each patient if blood cultures were taken repeatedly to check the treatment effects or to deny bloodstream infection. Other clinical information was also extracted by chart review; age, sex, height, weight, admission except from their own houses, type of devices used when blood cultures were taken, antimicrobial use within 2 weeks, surgery within a month, hemodialysis, use of immunosuppressive agents, active malignant diseases and HIV infection. Body temperature, systolic and diastolic blood pressure, pulse rate, white blood cell count with percentages of neutrophils and lymphocytes, blood urea nitrogen, creatinine, glucose and CRP levels just at or before blood culture sampling were extracted from medical charts, as well. Predictive factors of bacteremia were analyzed using t-test or Chi-square test, followed by multivariate logistic regression model.
RESULTS: A total of 223 patients (M:F = 130:93, 64 ± 19 years old) were included in this study and 60 patients (26.8 %) had positive blood culture results. Multivariate logistic regression model showed that older age (OR = 1.5, 95%CI = 1.1–2.0, p = 0.017), higher temperature (OR = 2.7, 95%CI = 1.8–4.1, p < 0.01) and higher neutrophil percentage (OR = 1.1, 95%CI = 1.0–1.1, p < 0.01) were the independent predictors of bacteremia. In contrast, other factors were not predictors of bacteremia; for example, CRP was not associated with bacteremia (p = 0.56). Area under the ROC curve of this model was 0.84 (95%CI = 0.79–0.90) .
CONCLUSIONS: Existence of bacteremia can be highly predicted by fundamental clinical information such as age, body temperature and neutrophil percentage. Our results emphasize the importance of taking blood culture from elderly even though they are not febrile, and the importance of ordering differential count of white blood cell in addition to total cell count. To confirm the patient characteristics that have diagnostic and therapeutic benefits from blood culture, further prospective study should be performed with standard criteria and methods for taking blood culture.
ANNUAL SALARY OR HOURLY WAGE? HOW 4TH YEAR MEDICAL STUDENTS CONSIDER FINANCIAL COMPENSATION WHEN SELECTING A SPECIALTYKent DeZee1,2; Elexis McBee2,1; Nathalie Paolino2,1. 1Uniformed Services University, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD. (Tracking ID #1939766)
BACKGROUND: Financial compensation is a well known consideration in medical student selection of their medical discipline, particularly as it relates to primary care specialties. However, the manner in which students define financial compensation is unclear. The purpose of this study is to determine whether or not 4th year medical students view annual salary and hourly wage as equally important when selecting their specialty in order to help guide future research.
METHODS: The authors conducted a cross sectional survey of 4th year medical students from the University of Chicago, the University of Pennsylvania and all 4th year medical students with a military service obligation in the U.S. during the 2011–2012 academic year. Following the residency match, participants were invited to participate in the study via e-mail. The student’s self-reported specialty choice in the residency match was classified into one of four categories: 1) primary care (PC: internal medicine, family medicine, pediatrics, and internal medicine-pediatrics), 2) non-controllable lifestyle specialties (Non-CL: general surgery, neurosurgery, obstetrics and gynecology, orthopedics, and urology), 3) controllable lifestyle, considered PC (CL-considered PC: all other specialties in which the student listed PC as a secondary choice), and 4) controllable lifestyle, did not consider PC (all other specialties in which the student did not list PC as a secondary choice). Using a five-point Likert-type scale (1 = not important at all; 5 = extremely important), respondents rated the importance of two items related to attending salary when choosing their specialty: 1) annual salary earned by civilian (not military) physicians in their chosen specialty and 2) hourly wage of civilian (not military) physicians in their chosen specialty. In addition, the amount of self-reported educational debt and length of military service obligation were collected. One-way ANOVA was used to compare the mean of the importance of annual salary and hourly wage to the four categories of specialty choice, with a Bonferroni multiple comparison test. Effect sizes were calculated to measure the strength of statistically significant associations. T-tests and stratified analyses were conducted to test for confounding by military service and level of debt.
RESULTS: The response rate for the questionnaire was 46 % (540/1184). Attending physician annual salary was slightly more important than hourly wage when selecting a specialty (mean annual salary 2.6, mean hourly wage 2.4, p < 0.0001, paired T-test). Students selecting PC rated annual salary as less important than all other students (PC mean 2.3, all other students 2.8, p < 0.0001, small effect size of 0.42). When rating attending hourly wage, the importance was different between all four specialty groups (PC mean: 2.2, Non-CL mean: 2.4, CL-considered PC mean: 2.6, CL-did not consider PC mean: 2.8), with a moderate effect size (0.57) between PC and CL-did not consider PC, and a small effect size (0.40) between both PC and CL-considered PC as well as Non-CL and CL-did not consider PC. The results were not affected by educational debt or military service obligation.
CONCLUSIONS: Fourth year medical students placed slightly more importance on annual salary versus hourly wage when selecting their specialty. However, these factors were equally important for students who chose a controllable lifestyle specialty and did not consider primary care. Future studies of specialty choice should select the type of financial compensation question or intervention (annual salary or hourly wage) based on the research goal and the intended specialty type of the student to be studied.
ANTIBIOTIC SUSCEPTIBILITIES OF URINARY ISOLATES IN OLDER ADULTSTheresa A. Rowe; Lee Lindquist; Abel Kho. Northwestern University Feinberg School of Medicine, Chicago, IL. (Tracking ID #1927517)
BACKGROUND: Background: Older adults are at an increased risk for development of multi-drug resistant organisms because of compounded exposure to antibiotics. Clinicians empirically treat suspected urinary tract infections (UTI) in older adults, selecting antibiotics based on guidelines intended for younger patients. No prior studies have examined whether there are age-related differences in UTI antibiotic susceptibility. We sought to identify antibiotic susceptibility patterns of urinary isolates in outpatient older adults and compare them to younger patients over a 3-year period.
METHODS: Retrospective analysis of all adult outpatients with a positive urine culture who received antibiotic treatment for UTI within 3 days. The most common organisms Escherichia Coli (E. Coli) and Klebsiella spp. were tested for resistance to commonly prescribed antibiotics. We compared resistance patterns of adults over the age of 65 to younger adults under the age of 65 using descriptive statistics and chi square analysis.
RESULTS: Urine cultures from 8,659 patients were reviewed. For E. Coli the percentage of resistance for adults ≥65, compared to adults <65 were: Ciprofloxacin (31.97 % in 65 years and older patients vs. 16.85 % in under 65 year old patients; p < 0.01), Trimethoprim/Sulfamethoxazole (30.12 % vs 25.19 %; p < 0.01), Ampicillin/Sulbactam (19.47 % vs 19.36 %), Cefuroxime (5.27 % vs 4.23 %; p < 0.05), Nitrofurantoin (1.80 % vs 1.47 %). For the second most common organism, Klebsiella species: Ciprofloxacin (5.28 % vs 4.99 %), Trimethroprim/Sulfamethoxazole (12.61 % vs 13.59 %), Ampicillin/Sulbactam (6.88 % vs 12.85 %; p < 0.01), Cefuroxime (6.39 % vs 7.91 %), Nitrofurantoin (26.28 % vs 24.36 %)
CONCLUSIONS: Older adults with UTIs have different resistance patterns to microorganisms when compared to younger patients. Current clinical guidelines for treatment may not reflect these differences. Clinicians need to be aware of the resistance patterns unique to older adults so that they can be appropriately treated
ANTICOAGULATION-RELATED PROCESSES OF CARE AND SHORT-TERM OUTCOMES IN ELDERLY PATIENTS WITH ACUTE VENOUS THROMBOEMBOLISMCharlene Insam1; Marie Méan1; Andreas Limacher2; Nicolas Rodondi1; Drahomir Aujesky1. 1Bern University Hospital, Bern, Switzerland; 2University of Bern, Bern, Switzerland. (Tracking ID #1937453)
BACKGROUND: Whether recommended anticoagulation-related processes of care are associated with improved clinical outcomes in elderly patients with acute venous thromboembolism (VTE) remains uncertain.
METHODS: We studied 991 in- and outpatients aged ≥65 years with acute VTE in a prospective multicenter Swiss cohort study (09/2009–03/2012). We assessed the performance of the following processes of care recommended by the American College of Chest Physicians: use of low-molecular-weight heparin or fondaparinux rather than unfractionated heparin in patients with deep vein thrombosis or non-massive pulmonary embolism, parenteral anticoagulation (PAC) ≥5 days, start of oral anticoagulation (OAC) within 24 h of VTE diagnosis, and achievement of an international normalized ratio (INR) ≥2.0 for ≥24 h before stopping PAC. Outcomes were overall mortality, VTE-recurrence, and major bleeding at 6 months and the length of hospital stay. We assessed the association between processes of care and clinical outcomes using Cox regression models, and the association between processes of care and length of hospital stay using the lognormal survival model, adjusting for multiple patient baseline characteristics.
RESULTS: Overall, 9 % of patients died, 2 % had VTE- recurrence, and 7 % had major bleeding at 6 months after the index VTE. The median length of hospital stay was 8.0 days (interquartile range 5.0; 11.0). Starting OAC within 24 h of VTE diagnosis was associated with a lower risk of overall mortality (adjusted hazard ratio [HR] 0.44, 95 % confidence interval [CI] 0.21–0.92) and major bleeding (adjusted HR 0.35, 95 % CI 0.18–0.66) and a decreased length of stay (adjusted time ratio [TR] 0.77, 95 % CI 0.69–0.85). While the use of low-molecular-weight heparin or fondaparinux significantly decreased the length of stay (adjusted TR 0.87, 95 % CI 0.77–0.97), the achievement of an INR ≥2.0 for ≥24 h before stopping PAC increased the length of stay (adjusted TR 1.20, 95 % CI 1.08–1.34). None of the processes of care were associated with VTE recurrence. We found no association between PAC for ≥5 days and outcomes.
CONCLUSIONS: In elderly patients with acute VTE, two out of four recommended processes of care were associated with improved clinical outcomes and/or a decrease in length of hospital stay. These processes should be implemented when treating elderly patients with acute VTE.
ANTIPSYCHOTIC MEDICATION USE AND THE RISK FOR HOSPITAL-ACQUIRED PNEUMONIAShoshana J. Herzig1; Michael B. Rothberg3; Jamey R. Guess1; Long H. Ngo1; Jerry H. Gurwitz4; Edward R. Marcantonio1,2. 1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Cleveland Clinic, Cleveland, OH; 4UMass Memorial Medical Center, Worcester, MA. (Tracking ID #1933568)
BACKGROUND: With the advent of atypical antipsychotic medications, use of antipsychotics has markedly increased in long-term care facilities, often in patients without a psychiatric diagnosis. Both typical and atypical antipsychotics have been associated with pneumonia in community and nursing home settings. However, rates of antipsychotic use in the acute hospital setting and the association between this use and hospital-acquired pneumonia (HAP) are unexplored.
METHODS: We studied an observational cohort of all patients admitted to a large academic medical center in Boston, Massachusetts from 1/2007 to 7/2013, at least 18 years of age, and hospitalized for at least 2 days. We excluded transfers from outside hospitals, patients admitted to the psychiatry service, and patients with a diagnosis of a psychotic disorder. Data were collected from electronic medical information databases at the medical center. We defined antipsychotic use as any pharmacy charge for an antipsychotic medication, subclassified as typical and atypical. The primary outcome was HAP, defined as any ICD-9 for bacterial pneumonia coded as not present on admission. We used a generalized estimating equation logistic regression model to control for repeated admissions and confounders. Our model included 40 variables, chosen based on hypothesized associations with antipsychotic use and/or HAP, including demographics, comorbidities as defined by Elixhauser et al., and concurrent medication use (sedatives, opioids, immunosuppressive agents, acid-suppressive medications). We assessed for effect modification by age using a dichotomous variable where we varied the cutpoint (< versus ≧ 60, 65, 70, 75 years).
RESULTS: Our cohort included 146,680 admissions (median age = 56 years; 39 % male). Antipsychotics were used in 18,047 (12.3 %) admissions (8.0 % typical and 5.8 % atypical, with 1.5 % exposed to both), and HAP occurred in 2,992 admissions (2.0 %). See table for rates of HAP and adjusted odds of HAP by exposure category. Use of each subclass of antipsychotic medication was associated with increased odds of hospital-acquired pneumonia, with highest risk seen in those admissions with exposure to both classes. There was no effect modification by age at any of the chosen cutpoints.
CONCLUSIONS: Antipsychotic use was common during hospitalization, occurring in 12 % of non-psychiatric admissions. Both typical and atypical antipsychotics were associated with increased odds of hospital-acquired pneumonia after extensive adjustment for patient characteristics and concurrent medication exposures. Given their associated risks, further scrutiny is warranted regarding prescribing practices of antipsychotic medications in the acute hospital setting.
Rates of HAP and adjusted odds of HAP by exposure category
| Exposure Status* | n (% of cohort) | HAP n (% of exposure category) | Adjusted OR for HAP [95 % CI] |
|---|---|---|---|
| Neither | 128,633 (87.7) | 1,970 (1.5) | Reference |
| Typical antipsychotic | 9,512 (6.5) | 392 (4.1) | 1.6 [1.4–1.8] |
| Atypical antipsychotic | 6,276 (4.3) | 339 (5.4) | 1.7 [1.5–1.9] |
| Both | 2,259 (1.5) | 291 (12.9) | 2.5 [2.1–2.9] |
*Categories are mutually exclusive
ANTIRETROVIRAL DRUG EXPENDITURE, PRICING AND JUDICIAL DEMAND: AN ANALYSIS OF FEDERAL PROCUREMENT DATA IN BRAZIL FROM 2004–2011Jing Luo1; Claudia Osorio-de-Castro2; Maria Olivera2; Mariana Ramos3; Aurelio Maia3. 1Yale University School of Medicine, New Haven, CT; 2Sergio Arouca National School of Public Health, Rio de Janeiro, Brazil; 3Ministry of Health, Brasilia, Brazil. (Tracking ID #1942220)
BACKGROUND: Previous studies have described expenditures for antiretroviral (ARV) medicines in Brazil through 2005. While prior studies examined overall expenditures, they have not have analyzed drug procurement data in order to describe the role of court litigation on access and pricing.
METHODS: ARV drug procurement from the years 2004–2011 was obtained through the general procurement database of the Brazilian Federal Government (SIASG). Procurement was measured in Defined Daily Doses per 1000 persons-under-treatment. Expenditures and costs were calculated and expressed in US Dollars. Justifications for ARV purchases were examined in order to determine the relationship between health litigation and incorporation into Brazil’s national treatment guidelines.
RESULTS: Drug procurement of ARVs from purchased sources underwent marked expansion in 2005, peaked in 2009, and stabilized to 2008 levels by 2011. Expenditures followed procurement curves. Newer medications were on average four times more expensive than older medications. Judicial actions initially resulted in purchases of newer mediations for a select number of patients in Brazil but ultimately expanded availability to a larger population through incorporation into the national treatment guidelines. ARVs were purchased at the lowest prices through auction, intermediate prices through single suppliers, and highest prices through emergency procurement resulting from judicial action.
CONCLUSIONS: Drug procurement and expenditures for ARVs in Brazil varied between 2004 and 2011. Medications which once represented a large proportion of federal drug expenditures have been largely eliminated due to domestic production. Judicial demand has resulted in the procurement of large quantities of newer, more expensive medications. In order for the AIDS treatment program to remain sustainable, efforts should be pursued to reduce prices through price negotiation and other public health flexibilities.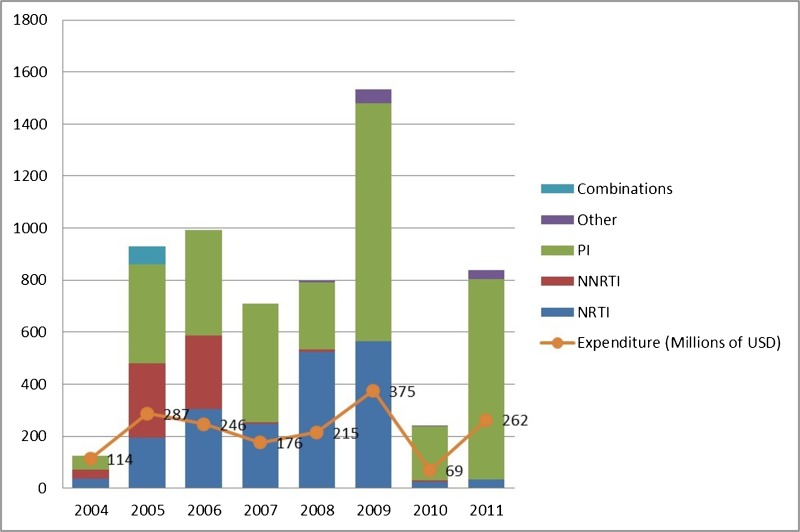
Figure 1. Drug Procurement and total expenditures for antiretroviral medicines in Brazil from 2004 and 2011.
APPROPRIATENESS OF PREVENTIVE CARE FOR ANGIOPATHIC COMPLICATIONS IN OUTPATIENTS WITH DIABETESIdris Guessous1,5; Sophie Excoffier Bottaro1; Manuel R. Blum2; Nicolas Rodondi2; Jacques Cornuz3; Lukas Zimmerli4; Jean-Michel T. Gaspoz1. 1Geneva University Hospitals, Geneva 14, Switzerland; 2Inselspital, University of Bern, Bern, Switzerland; 3University of Lausanne, Lasuanne, Switzerland; 4University Hospital of Zurich, Zurich, Switzerland; 5Institute of Social and Preventive Medicine, Centre Hospitalier Universitaire Vaudois, University of Lausanne, Lausanne, Switzerland. (Tracking ID #1937359)
BACKGROUND: Preventive care of major diabetic angiopathic complications (foot ulcers and retinopathy) is essential. However, data on the prevalence of and factors associated with preventive care of angiopathic complications in outpatients with diabetes are very limited and non-existent within the Swiss context of universal health care coverage. We aimed to determine the prevalence of appropriate preventive care of angiopathic complications in outpatients with diabetes, and to identify factors associated with appropriate preventive care of angiopathic complications.
METHODS: We used data from a retrospective cohort study (the Corif study) that examined recommended preventive care in a random sample of patients aged 50–80 years followed over 2 years (2005–2006) in four Swiss university primary care settings using RAND’s Quality Assessment Tools indicators. We defined appropriateness of preventive care of angiopathic complications using the American Diabetes Association recommendations: annual foot (pallesthesia and visual exam) and ophthalmologic exam. Age-, sex-, center-adjusted regression models were conducted.
RESULTS: Among the 292 outpatients with diabetes included, 59.2 % had appropriate preventive foot care and 55.8 % had appropriate preventive eye care. Only 34.6 % had appropriate preventive care of both foot and eye. Number of GP visits (Odds Ratio = 1.07, 95%CI 1.02–1.11) and Hb1Ac measured at least 2×/year (OR = 2.56, 1.34–4.90) were associated with appropriate foot preventive care. Obesity (OR = 0.37, 0.21–0.65) and hyperlipidemia (OR = 2.47, 1.38–4.43) were associated with appropriate eye preventive care. Hb1Ac measured at least 2×/year (OR = 2.56, 1.34–4.90), obesity (OR = 0.53, 0.29–0.95), and hyperlipidemia (OR = 2.36, 1.23–4.51) were associated with appropriate preventive care of both foot and eye.
CONCLUSIONS: Preventive care of diabetic angiopathic complications is frequently inappropriate among outpatients. Particular attention should be paid to obese patients with diabetes.
ARE PATIENT-CENTERED MEDICAL HOME PRACTICES ASSOCIATED WITH BETTER ACCESS TO PRIMARY CARE SERVICES?Jaya Aysola1; Karin V. Rhodes2; Daniel Polsky1. 1University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA. (Tracking ID #1940136)
BACKGROUND: Patient-centered medical homes (PCMH) have gained prominence as models designed to promote high quality cost effective primary care. An integral component of the PCMH model is providing enhanced access to primary care. However, the potential effect of PCMHs on access to primary care services has not been examined. Our study evaluated whether PCMH practices in ten US states were associated with better access to care, measured using simulated patient (audit) methodology.
METHODS: We conducted a cross-sectional analysis of publically available data on practices recognized as National Committee Quality Assurance (NCQA) patient-centered medical homes (PCMH) before June 2013 and data collected through a simulated patient (audit) study. Our primary predictor was whether or not a practice was a NCQA recognized PCMH. Our primary outcome measure was the ability of the caller (simulated patient) to schedule a new appointment. Trained field staff contacted primary care offices in 10 US states between November 2012 and March 2013 posing as individuals seeking a new patient appointment with varying insurance status (private, Medicaid, or uninsured). All eligible primary care offices were identified using a proprietary database of existing physician clinics (SK&A physician file). Callers contacted a stratified random sample of primary care practices treating non-elderly adults in each state, for a total of 10572 requests for appointments at 7266 practices. We merged detailed practice characteristics (number of sites, number of providers, average patient volume, number of exam rooms) from SK&A physician file, and geographic socioeconomic and health care resource information (county-level percent persons below poverty level, percent minority, percent non-elderly uninsured, number of office based primary care providers, and Health Professional Shortage Area designation) from the Area Resource File, into our audit data. We performed multivariable logistic regression model, adjusting for the caller’s insurance status and race/ethnicity as well as the practice and geographic characteristics listed above, to estimate the association between PCMH status and our outcome variable. We then fitted a multivariable logistic regression model, including interactions of practice PCMH status and caller’s insurance status, adjusting for the same covariates above.
RESULTS: Out of 10572 requests to practices for appointments, 646 (6.1 %) were to NCQA recognized PCMHs. Significant predictors of scheduling new appointments included the caller’s insurance status, number of practice exam rooms, percent minority and percent persons in poverty where the practice was located, and the practice’s NCQA PCMH recognition status. There were no significant interactions between practice PCMH status and caller’s insurance status. Adjusted analysis revealed that calls placed to PCMH practices were significantly more likely to result in scheduled new appointments then calls placed to non-PCMH practices. (Adjusted OR 1.3; 95 % CI 1.0, 1.5; p = 0.02).
CONCLUSIONS: Our findings suggest that practices recognized as patient centered medical homes, after robust adjustment for individual caller, practice, and geographic variables, were associated with better access to new primary care appointments for non-elderly adults, those most likely to gain insurance under the Affordable Care Act.
ARE PATIENTS A RELIABLE SOURCE FOR ADVERSE EVENT REPORTING? SURVEY SAYS…Kristy Deep; Megan Minch. Univ of Kentucky, Lexington, KY. (Tracking ID #1939331)
BACKGROUND: Learning from adverse events is an important way to improve healthcare quality and safety. However, events are underreported by healthcare providers. We sought to determine whether patient comments on the post-discharge Healthcare Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey reliably identify adverse events or errors that occur during the hospital stay.
METHODS: HCAHPS surveys with negative comments returned during a 7 month period were reviewed. Comments that described a specific adverse event or error were then analyzed by two independent raters. The patient’s medical record was reviewed to corroborate the event. A coding scheme was developed iteratively from the data to categorize the types of adverse events reported by patients. One patient comment could receive multiple codes. We assigned a four-tier harm score for each adverse event: significant harm and/or need for additional treatment, potential harm but outcome unknown, emotional distress/inconvenience, and no harm.
RESULTS: Ninety comments were reviewed, 20 of which were adjudicated as complaints which did not identify quality issues leaving 70 comments for analysis. Of these, 29 (41 %) were corroborated in the medical record. An additional 35 (50 %) were not corroborated by the medical record but were deemed credible based on the level of detail within the patient’s report or when the described event was unlikely to be documented (i.e. delays in care). Communication errors were most common and found in 27 events. These included communication between healthcare providers and patients as well as among providers. Other frequent event types were patient education deficits (13), delays in clinical care (13), and medication errors (8). Patients also identified procedural complications (3) and lapses in infection control (2). Ten events (14.2 %) resulted in significant patient harm and/or required additional treatment. Examples include a failure to recognize an abscess resulting in emergent surgery and a patient developing apnea following administration of a medication. Three of these significant harm events were deemed credible but not documented in the medical record. An additional 10 described situations that were potentially harmful but the impact on the patient was unknown. The remainder of the adverse events or errors resulted in either emotional distress/inconvenience (30) or no harm (20).
CONCLUSIONS: Patient comments on the HCAHPS post-discharge survey are a reliable source for insight into the quality of care patients receive. They may also identify significant issues that are not captured by other safety reporting mechanisms.
ARE THERE RACIAL DISPARITIES IN QUALITY OF TREATMENT FOR LOCALLY ADVANCED PROSTATE CANCER?Rajwanth Veluswamy1,3; Rebeca Franco2; Kezhen Fei2; Nina Bickell1,2. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1940153)
BACKGROUND: African American men are more likely to develop and die of prostate cancer than white men. Past studies have shown lower rates of invasive treatment among black men. However, these studies included early-stage disease for which treatments may not be beneficial. We undertook this study to assess the quality of prostate cancer treatment among men with locally advanced cancer who could benefit from active therapies.
METHODS: All black and a random sample of white men with Gleason Scores of 7+, diagnosed at an inner-city academic center between 2007 and 2012, were identified from pathology and charts abstracted for clinical, pathologic and treatment data. A Steering Committee of experts in prostate cancer care created quality measures of treatment for locally advanced prostate cancer. Underuse of definitive treatments (radical prostatectomy and radiotherapy) was identified using these quality measures.
RESULTS: Overall, 290 black and 255 white men were identified. The average age of the entire cohort was 59 years old (standard deviation [sd] = 8.6, range: 32 to 86) and there was no statistical age difference between races. Black men had more comorbidities (30 % vs 9 %; p < 0.001) and higher prostate-specific antigen (PSA) levels prior to biopsy (12.4 vs 6.9; p = 0.0027), but whites were more likely to present with stage three disease (30 % vs 22 %; p = 0.02). Using D’Amico risk criteria, 14 % of patients were found to have intermediate risk, while 86 % were high risk. The distribution of D’Amico risk between race was not statistical different. Black men were less likely than white men to undergo radical prostatectomy (79 % vs 91 %, p < .0001), but more likely to get external beam radiation therapy (EBRT, 13 % vs 5 %; p = 0.0009) or brachytherapy (11 % vs 4 %; p = 0.0037). Of note, 85 % of black and 100 % of white men received the recommended radiotherapy (RT) dose (74Gy). Only 50 % of men undergoing RT received androgen deprivation therapy (ADT), with no racial difference in ADT use. Overall, 5 % of men with locally advanced prostate cancer did not undergo surgery or RT, with no racial difference in underuse. Multivariable analysis using logistic regression showed that patients with intermediate risk were 20 times more likely to experience underuse of definitive treatment as compared to patients with high risk (95 % CI: 7.2-50.3). Additionally, every year increase of age was associated with a 1.06 times higher risk of underuse of definitive treatment (95 % CI: 1.01–1.12). However, even after accounting for potential confounders, race did not play a role in whether patients received definitive treatment according to quality measures.
CONCLUSIONS: The rate of underuse of definitive treatment in men with locally advanced prostate cancer is low and does not appear to be driven by racial differences. However, underuse is significantly associated with patients of intermediate risk and advancing age. We will further investigate why these patients are not receiving active treatment.
ASKING THE PATIENT ABOUT PATIENT-CENTERED MEDICAL HOMESJaya Aysola1,2; Rachel M. Werner1; Judy A. Shea1. 1University of Pennsylvania, Philadelphia, PA; 2Children, Philadelphia, PA. (Tracking ID #1939454)
BACKGROUND: To date the patient perspective is not an integral component of any of the existing patient-centered medical home (PCMH) measurement standards, although upcoming guidelines necessitate patient-reported experience and satisfaction data in evaluations of practice and provider performance. Despite this, patient understanding of PCMH and their perspectives on their role in the evaluation of practices implementing this model is not known. Therefore, we sought to characterize patients’ understanding of the PCMH model, experiences with PCMH practices after transformation, and perceptions on approaches to incorporate patient feedback.
METHODS: We conducted semi-structured interviews of patients from NCQA (National Committee Quality Assurance) recognized PCMH practices at University of Pennsylvania (UPENN). We first surveyed, scored, and ranked all UPENN affiliated PCMH adult primary care practices with three or more providers (n = 23) using a previously validated scale that quantifies the overall degree of PCMH practice transformation. We then identified the practices, representing the four highest and lowest PCMH transforming practices. To determine if the degree of PCMH practice transformation was related to patient responses, participants were recruited from a pool of adult patients with hypertension and/or diabetes from these eight selected practices. We conducted semi-structured, one-on-one telephone interviews with patients consisting of both open- and closed-ended questions about their experiences with care, and perceptions and understanding of key PCMH domains. Interviews were recorded, transcribed, and imported into NVivo 10 for coding and analysis, using a modified grounded-theory approach.
RESULTS: Of the 19 interviews completed, 52 % were from high-transforming practices, 48 % from low. Fifty-seven percent of the sample was African American and the mean age was 61. Responses did not appear to vary between patients from high and low PCMH transforming practices. None of the participants were aware that their clinic was a PCMH, regardless of whether they were from a high- or low-PCMH transforming practice and most did not know what a PCMH was. Of the key aspects of the PCMH, most participants identified a team-based approach and strong patient-provider partnership as more important to them than enhanced access to care. The majority could not identify additional personnel involved in assisting their PCP in their care. Respondents had differing perspectives about their own role in decision making, with many relying on their PCP to make their treatment decisions. Emerging themes included the following: 1) Patients were unaware of what a medical home is and if their practice was one, irrespective of the practices’ degree of PCMH transformation. 2) The patients’ lack of knowledge regarding PCMH concepts did not appear to impact their experiences with care and their uniformly positive relationship with their primary care provider. 3) The PCMH domains patients reported as most important for care delivery in theory did not always relate to their preferences in reality. For example, participants reported team-based care as one aspect of PCMH most important to them, yet when discussing their specific experiences at their practice, the majority could not recall any additional personnel teaming with their provider to participate in their care. The majority of participants also reported a strong patient-provider partnership as the other aspect of primary care delivery most important to them; however, when detailing specific preferences, many were less interested in partnering with their provider to share responsibility in medical treatment decisions.
CONCLUSIONS: Our study aimed to examine patient understanding and perceptions of care within PCMHs and whether their experience varied depending on the degree of PCMH practice transformation. We found that patients uniformly lacked awareness of PCMH concepts and the fact their practice was a PCMH, regardless of the degree of transformation reported by the practice. Moreover, this lack of understanding did not appear to impact their experiences with care or overwhelmingly positive relationships with their providers. As we continue to redesign primary care delivery with an emphasis on patient experience measures as performance metrics, further evaluation is needed to determine what if any aspects of how we structure practices relates to patient experience and satisfaction with care.
ASSESSING CONTENT AND QUALITY OF ADVANCE CARE PLANNING DOCUMENTATION IN AN INTERNAL MEDICINE RESIDENT CLINICKatherine A. Wang1; Jacqueline K. Yuen2,3. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1913261)
BACKGROUND: Despite widespread recognition of the need for advance care planning (ACP), there is a troubling communication gap between patients and physicians. One large multicenter study found that of patients who preferred not to be resuscitated, only 52 % had DNR orders. Primary care physicians, given their longitudinal relationships with patients, are ideally positioned to elicit patients’ values and goals. Meaningful documentation of these conversations is essential to ensure appropriate communication with other health care providers and to guide future decision-making. Educational interventions have been shown to improve residents’ knowledge, skills, and comfort level with ACP and to increase documentation of advance directives, but little data exists about improving the quality of documentation. A novel month-long curriculum was piloted with PGY-2 Internal Medicine (IM) residents from January-June 2013 to improve resident skills with ambulatory ACP discussions and documentation. The objective of this study was to assess the impact of an educational intervention and electronic medical record (EMR) template on the content and quality of documentation of ACP discussions.
METHODS: The setting was an urban academic ambulatory resident clinic. Participants were 41 PGY-2 IM residents who each identified patients with at least one chronic illness and a high likelihood of hospitalization within a year. Residents held visits to address ACP with these patients during the one-month curriculum and documented conversations. An EMR template including prompts for topics introduced in the curriculum (e.g. health care proxy (HCP), disease trajectory, values) was developed for optional use by residents. Investigators conducted a retrospective chart review of all identified patients and measured the frequency of certain discussion elements such as HCP and prognosis. Fisher’s exact test was used to compare the templated and free-text notes. Twenty reviewers from IM and Emergency Medicine will rate the notes for usefulness in clinical decision-making in a hypothetical case scenario using a Likert scale, and a qualitative analysis comparing elements of the most highly-rated notes will be performed.
RESULTS: 41 residents received the ACP curriculum. Twenty-nine residents (71 %) documented a total of 34 ACP discussions (Table). The other 12 residents did not document an ACP discussion because the patient did not show up (n = 2) or for unknown reasons (n = 10). Of the 34 patients, the mean age was 71.8 years (SD 13.0), 65 % were female, and the most common conditions were hypertension (91 %), diabetes (62 %), chronic kidney disease (32 %), CHF (24 %), COPD (18 %), CAD (18 %), and cirrhosis (12 %). Seventy-one percent had a readmit risk score of high or very high (based on number of hospitalizations in last 6 months and certain high risk diagnoses). Of the 34 ACP notes, 6 (18 %) used the template and 28 (82 %) did not. HCP was nearly always addressed (97 % of all conversations), and a signed HCP form was scanned into the chart frequently (56 % of all conversations). Twenty-four percent of notes documented a discussion of goals of care; this was more likely with residents using a template (83 % vs 11 %, p = 0.001). Qualitative analysis results are pending.
CONCLUSIONS: This study assessed the impact of an educational intervention and EMR template on the content and quality of ACP documentation by IM residents. Regardless of template use, certain discussion elements such as HCP were addressed in nearly all ACP notes, while disease trajectory and prognosis were infrequently addressed. However, residents who used the template were significantly more likely to explore goals of care with patients. The limitations of this study are the lack of a control population who did not receive the curriculum and the small number of residents who opted to use the template. Analysis of the clinical usefulness of ACP documentation is still pending and will identify characteristics of notes that are most helpful for future decision-making. Findings will contribute to future iterations of the resident curriculum to improve ACP communication and documentation skills.
Comparison of ACP discussion elements between templated and free-text notes
| Discussion Elements | Template ( n = 6) n (%) | Free-Text ( n = 28) n (%) | P value |
|---|---|---|---|
| HCP discussed | 6 (100) | 27 (96.4) | 1.00 |
| HCP selected | 5 (83.3) | 19 (67.9) | 0.64 |
| HCP form scanned into EMR | 3 (50) | 16 (57.1) | 1.00 |
| HCP involved (or plan to involve) in ACP | 3 (50) | 13 (46.4) | 1.00 |
| Prognosis and/or disease trajectory discussed | 1 (16.7) | 7 (25) | 1.00 |
| Goals of care discussed* | 5 (83.3) | 3 (10.7) | 0.001 |
| Specific medical interventions discussed (including DNR)^ | 4 (66.7) | 9 (32.1) | 0.17 |
| Out of hospital DNR order placed | 1 (16.7) | 3 (10.7) | 0.56 |
* E.g. values, activities, fears, and prior experiences with illness. In the template, prompts include questions such as: “What is important to you in life? What activities or experiences are important for you to live well? What fears or worries do you have about your health?” ^ E.g. code status, artificial nutrition/hydration
ASSESSING LONG TERM OUTCOMES OF A TEACHING COMMUNICATION SKILLS COURSE FOR FELLOWS AND FACULTYSarah B. Merriam; Robert M. Arnold; Carla Spagnoletti. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1936910)
BACKGROUND: The ability to communicate effectively with patients is a key skill for practicing physicians. The importance of effective patient-doctor communication has received increasing attention in the field of medical education. Since 2003, the Clinician Educator Training Program at the University of Pittsburgh has offered a master’s level course entitled “Teaching Communication Skills” designed to provide participants with the skills needed to effectively teach clinicians communication skills. This study’s objective is to evaluate how this course influenced participants’ subsequent teaching of communication skills and related scholarly endeavors.
METHODS: The 65 fellows and faculty who completed the “Teaching Communication Skills” course between 2003 and 2011 were surveyed electronically. The survey assessed participants’ perceived importance and effectiveness of the course and its instructional methods. It also evaluated the use of these teaching skills in their current teaching practice. Demographic characteristics of the respondents as well as their career descriptions and academic productivity were assessed. Descriptive statistics were used to report survey responses.
RESULTS: A total of 53 of 65 course participants completed the survey (response rate 80 %). When asked why they took the course, 38 % indicated that it was highly recommended by peers and 85 % indicated that they anticipated a future role as a clinician educator and thought the course would be helpful in attaining this goal. Almost all (98 %) rated both the course and the individual communication-specific teaching skills taught in the course to be effective in the development of their teaching skills (on a 5-point Likert-type scale where 1 = ineffective and 5 = effective). When participants were asked to list which of the course’s instructional methods were most beneficial in developing their ability to teach patient-doctor communication skills, most frequent responses included: exposure to the “primary teaching method” (a learner-centered small group facilitation method commonly used to teach communication skills; n = 14), the process of direct observation and feedback (n = 22), and small group role play with standardized patients (n = 52). All instructional methods taught in the course were reported to be increasingly utilized in their teaching practice since taking the course, with 77 % using standardized patients, 89 % using small group work, and 83 % using role-play at least annually. Forty-nine (93 %) graduates described their current position as academic. Of those individuals, 72 % described roles as clinician-educators, 11 % as clinician-researchers, and 6 % as clinician-administrators. Since taking the course, 72 % of respondents have either developed or taught in a communication curriculum. Thirteen (25 %) have held a leadership or administrative position directly related to patient-doctor communication. Forty-four (83 %) have since pursued research or other scholarly activity related to communication: 10 obtained grant funding, 28 presented their work at a regional or national conference, and 21 wrote peer-reviewed manuscripts.
CONCLUSIONS: This novel course was highly rated by the fellows and faculty who participated. A majority of course participants went on to design or teach communication curricula. Courses such as this one, designed to instruct educators how to teach communication skills, may be valuable to medical schools and other training programs that want to improve their faculty’s ability to effectively deliver this curricular content to trainees.
ASSESSING PATIENT ATTITUDES AND PRACTICES REGARDING INFORMATION TECHNOLOGY IN A PATIENT CENTERED MEDICAL HOME: ARE WE READY FOR TELEMEDICINE?Jeanne Morley1,2; Daniel J. Coletti1,2; Laura Harrison1; Joseph Conigliaro1,2. 1North Shore LIJ Health Systme, Great Neck, NY; 2Hofstra North Shore-LIJ School of Medicine at Hofstra University, Hempstead, NY. (Tracking ID #1936175)
BACKGROUND: Delivering care in a Patient Centered Medical Home (PCMH) requires an understanding of patient comfort with and access to information technology (IT), as use of that technology in the general population evolves and expands. According to a recent Pew Research Center report, 56 % of Americans owned a smartphone and 34 % used a tablet computer. Nearly 165 million Americans use social media, and as of 2012, one in three cell phone owners reported using their phones to look up health information. While email, text messaging, video chat, and social media have transformed how Americans communicate, most medical practices have failed to keep pace with these changes. Although about one third of Americans prefer getting text messages to phone calls and almost three quarters use email daily, the majority of physician offices still exclusively communicate by telephone with patients to make appointments, review lab results and answer questions. While clearly desirable, implementing new models of patient communication requires an understanding of patient access to technology. This is particularly salient in primary care settings that treat the underserved, who may lack access to novel and expensive forms of technology. The objectives of this investigation were to describe patient patterns of using IT in general, and to examine patient preferences and attitudes to using IT as part of their health care. We also wished to assess whether attitudes were associated with respondent age and sex.
METHODS: We completed a descriptive study as part of a larger feasibility study to prepare for deployment of internet-based patient communications within a large PCMH. The study was approved by our Institutional Review Board. We created a 12-item questionnaire entitled Patient Attitudes to Information Technology (PAIT) to assess the frequency of use of communication modalities such as email, text messaging, video chat, and attitudes towards IT. Our sample included patients seen for routine visits, complete physical exams, and sick calls during July and August of 2013. Questionnaires were completed in the office waiting room prior to a medical appointment. The office is a busy academic primary care practice, and designated Level III PCMH. Our patient population is diverse, and spans a wide range of educational and socioeconomic strata. Roughly half have Medicare or private insurance, and the other half are uninsured or have Medicaid. The questionnaire was offered to all patients on a voluntary basis. No protected health information was collected. Chi-square analyses, T-tests for independent means and Analysis of Variance (ANOVA) were deployed as appropriate to test for differences in attitudes according to demographic variables.
RESULTS: A total of 215 questionnaires were completed. Mean age of the sample was 48.29 years (SD = 18.26, range = 18–90) and was 62.5 % female. On the day of their visit, 50.7 % of the patients surveyed had already used a PC, 55.5 % had used email, 79.2 % made a mobile phone call, 59.9 % had sent or received a text message, and 18.6 % had used a video chat application. When assessment was expanded to the past week, the numbers increased to 78.4 %, 75.9 %, 91.5 %, 72.3 %, and 49.1 % respectively. Patients were also asked to score their agreement with four statements regarding IT on a scale of 0–10. On average, our patients reported moderate-to-high levels of agreement that they “have a lot of experience using smart phones” (mean = 6.01 out of 10), and were “the kind of person who like trying new electronic devices (mean = 6.86 out of 10). We also found high levels of agreement with the statement, “I would be interested in learning more about ways to use information technology…to communicate with my medical team,” (M = 7.0 out of 10). Although patterns of use and comfort with technology were high overall, statistically significant age-related effects were observed across all attitudinal variables (p < .001 for all analyses), with younger respondents more likely to express higher levels of comfort and interest in IT.
CONCLUSIONS: Results from this investigation suggest high levels of both readiness and interest among the patients in our PCMH to use IT to augment current communication with their medical team. Observed age-related effects suggest that older patients, while generally interested in using IT to facilitate healthcare communication, may need additional support to increase their knowledge and comfort level prior to implementing new forms of interaction with their healthcare team. We were particularly surprised and encouraged by the frequent use of video-based applications among our respondents. Using this modality to facilitate more integrated care seems promising and realistic. Areas to explore could be more frequent but remote video monitoring of our high risk patients, extending the range of directly observed therapy, and support for patients involved in modification of high-risk behaviors, such as smoking cessation, ETOH reduction, and substance misuse.
ASSESSING THE IMPACT OF A RESIDENT COORDINATED TRANSITIONAL CARE ROTATION ON RESIDENT ATTITUDES TOWARDS PATIENT TRANSITIONS AND HEALTH MANAGEMENTAlexis Eastman1,3; Elizabeth Chapman1,2; Laury Jensen3; Holly I. Bottoms4; Mary Thompson2; Bennett Vogelman1,2; Amy J. Kind2,3. 1University of WI Hospitals and Clinics, Madison, WI; 2University of Wisconsin, Madison, WI; 3Madison VA Geriatric Research Education and Clinical Center, Madison, WI; 4William S. Middleton Memorial Veterans Hospital, Madison, WI. (Tracking ID #1938974)
BACKGROUND: Although the Accreditation Council for Graduate Medical Education (ACGME) and others have called for improved medical resident education in the area of care transitions, few well-described formal education programs are available in the published literature to accomplish this goal. Pragmatically, instituting a formal transitions training program is challenging due to supervision and site-specific limitations and work hour requirements. Our objective was to evaluate whether Resident Coordinated Transitional Care (RC-TraC), an adaptation of the previously tested phone-based VA Coordinated Transitional Care (C-TraC) program, impacted resident attitudes related to transitional care.
METHODS: In 2009, the University of Wisconsin Internal Medicine residency program established RC-TraC, a phone-based care transitions training experience for residents randomly assigned to VA primary care continuity clinics. Residents with other primary care continuity clinics did not have a formal care transitions training experience. During this rotation, residents act as discharge care managers for hospitalized patients from the resident clinic panel, similar to the RN case manager position in the C-TraC program. Prior to discharge, the RC-TraC residents counsel patients on symptoms that should warrant medical attention. Post-discharge, the RC-TraC residents complete protocolized phone calls weekly for 30 days wherein symptoms are reviewed, medications reconciled and appropriate follow-up appointments are verified. In spring of 2013, all UW internal medicine residents were electronically surveyed to determine their attitudes regarding care transitions, including residents who did (N = 31) and did not experience RC-TraC (N = 56). Responses were collected on a 4-item modified Likert scale (almost never, infrequently, often, almost always). For purposes of analysis, “almost never/infrequently” and “often/almost always” were combined. Frequencies were compared using Chi-squared tests.
RESULTS: Overall survey response rate was 83/87 (95 %), with 29/31 (94 %) RC-TraC and 54/56 (96 %) non-RC-TraC residents responding. Ninety-seven percent of residents who had experienced RC-TraC at least once identified that they had received in-residency transitions training, while only 24 % of non-RC-TraC residents felt they had received transitions training (p < 0.001). When compared to non-RC-TraC residents, RC-TraC residents were more likely to believe patients could “almost always/often” identify their pre-admission meds (45 % RC-TraC versus 18 % non-RC-TraC, p = 0.01), identify their pre-admission diagnoses (55 % vs 35 %, p = 0.08) and know how to contact providers post-discharge (52 % vs 31 %, p = 0.07). Yet, there was no statistical difference between RC-TraC and non-RC-TraC residents’ beliefs on patients’ abilities to identify post-discharge medications and hospital diagnoses.
CONCLUSIONS: Findings suggest that the RC-TraC program is identified by residents as a formal care transitions training experience and that it alters resident perceptions of patients’ baseline capacity for health management. This may suggest that RC-TraC increased residents’ appreciation for a patient’s capacity to participate in their health care. RC-TraC is a feasible care transitions training program, but needs additional testing of its impact on resident knowledge and patient outcomes.
ASSESSING THE UNDERSTANDABILITY AND ACTIONABILITY OF AFTER VISIT SUMMARIES FROM PRIMARY CARE CLINICSAlex Federman1; Christopher Salmon1; Ravishankar Ramaswamy1; Sereena Singh1; Allison L. Russell2; Michael S. Wolf2. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Feinberg School of Medicine, Northwestern University, Chicago, IL. (Tracking ID #1936547)
BACKGROUND: The after visit summary (AVS) is a document given to patients to summarize key elements of the clinical encounter. The AVS has the potential to serve as an organizing and informational tool for patients, and has gained importance as new federal and state health policies, like Meaningful Use, work to advance patient centered care. Despite this, little is known about the AVSs currently in use in ambulatory practices. In this study, we sought to characterize the content and formatting of AVSs from a primary care practices and determine understandability and actionability of the information they provide.
METHODS: We identified National Committee for Quality Assurance (NCQA) accredited level III patient centered medical homes from the NCQA public use database and through snow-ball contacts. A convenience sample of these practices was contacted by email and telephone. Clinic directors or clinician representatives underwent a semi-structured interview about their experience with their practice’s AVS and were asked to email or fax de-identified samples of actual AVSs from their practice. AVS samples were analyzed for content, length, and reading grade level. They were then assessed for understandability and usability using the Patient Education Materials Assessment Tool (PEMAT). Two raters independently evaluated the AVS samples.
RESULTS: We evaluated AVS documents from 18 primary care practices in 14 states. Number of pages ranged from 1 to 9 (median, 2) and the mean and median font size was 10. Content included medication lists (100 %), specific instructions and referrals requested or procedures performed (83 %), diagnoses (72 %), vital signs (67 %), allergies (56 %), appointments (50 %), goals of care (22 %), and immunization history (17 %). On the PEMAT, the average levels of understandability and actionability were 62 % and 80 %, respectively, indicating poor understandability and fair actionability. The median reading grade level was 12 (range 8–19) by the Flesch-Kincaid formula. Interviewed clinicians generally believed that their AVSs were of little use to patients except for the medication lists. None reported providing AVSs in languages other than English.
CONCLUSIONS: After visit summaries may not be achieving their intended purpose of providing patients with accessible and useful information regarding their care, nor meeting Meaningful Use requirements for content, even in NCQA-certified level III patient centered medical homes. Improvements in formatting, wording, and content of AVSs are needed to advance patient-centered care.
ASSESSMENT OF THE “SPEAKING UP” CULTURE: A NEW DOMAIN FOR PATIENT SAFETY CULTURE SURVEYSWilliam Martinez1; Jason M. Etchegaray2; Lisa Lehmann3,5; Eric J. Thomas2; Sigall K. Bell4,5. 1Vanderbilt University Medical Center, Nashville, TN; 2Univesity of Texas Medical School at Houston, Houston, TX; 3Brigham and Women’s Hospital, Boston, MA; 4Beth Israel Deaconess Medical Center, Boston, MA; 5Harvard Medical School, Boston, MA. (Tracking ID #1939052)
BACKGROUND: Despite over a decade focusing on identifying the key components of patient safety culture relevant to healthcare settings, tangible safety progress has been slow. Current safety culture assessments fail to measure an important emerging competency, “speaking up” about patient safety threats, a skill that may be particularly challenging for residents responding to conforming pressures of the medical hierarchy. Thus, we sought to (1) develop and test survey items that measure the speaking up culture in the clinical work environment, (2) examine relationships among speaking up culture, teamwork culture, error disclosure culture and safety culture and (3) establish predictive validity for survey items measuring speaking up culture.
METHODS: All (667) surgical and medical residents from two large academic medical centers were invited to complete an anonymous, electronic questionnaire. The questionnaire asked respondents about personal experience speaking up about threats to patient safety, and contained six items developed by patient safety experts to assess the speaking up culture in the clinical environment. It also included previously validated measures of safety culture including the safety and teamwork dimensions of the Safety Attitudes Questionnaire (SAQ) and the general dimension of the Error Disclosure Scale. Factor analysis was used to test whether the six speaking up items were consistent with the concept of speaking up about threats to patient safety and to create a summary score in order to examine the relationship of speaking up culture to other patient safety domains and compare speaking up culture between groups.
RESULTS: The overall response rate was 52 % (349/667). Factor analysis supported a single 6-item speaking up scale and a scale score was created by summing the 5-point Likert-scale responses to individual items (score range: 5–30, Cronbach α = 0.75). Speaking up culture was a measure unique from safety culture, teamwork culture, and error disclosure culture scales (correlations less than r = 0.85). Speaking up culture predicted residents’ self-reported, personal experience speaking up about patient safety threats during their last inpatient month (OR 1.13, 95%CI 1.05–1.22), while teamwork (OR 1.02, 95%CI 0.91–1.15), error disclosure (OR 0.98, 95%CI 0.92–1.05) and safety culture (OR 0.96, 95%CI 0.92–1.01) did not. Surgical residents perceived their clinical work environment’s culture to be less supportive of speaking up than medical residents (mean scale score: 21.22 vs. 22.19, P = 0.045). Compared to medical residents, fewer surgical residents felt (A) encouraged by colleagues to speak up about patient safety concerns (76 % vs. 62 %; P = 0.006) and (B) that speaking up about patient safety concerns results in meaningful change (67 % vs. 55 %; P = 0.03).
CONCLUSIONS: Our speaking up scale has sound psychometric properties and is a new measure of speaking up culture regarding patient safety threats in the clinical work environment that predicts self-reported speaking up about safety threats among residents. This measure fills an existing gap in assessments of organizational safety by measuring the extent to which the culture within a clinical work environment supports clear, direct, real-time communication between colleagues when a threat to patient safety is identified, a critical aspect of safety culture that is not currently assessed by traditional safety culture instruments. The culture may be less supportive of residents speaking up in surgical environments than in medical environments.
ASSOCIATION BETWEEN AFTER-VISIT CLINICAL SUMMARIES AND CHRONIC DISEASE MANAGEMENTRebecca G. Mishuris1,2; Michael Healey1,2; Endel J. Orav1,2; Jennifer Haas1,2. 1Brigham and Women’s Hospital, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1937817)
BACKGROUND: Electronic health records (EHRs) have been adopted by 72 % of US physicians. The Medicare and Medicaid EHR Incentive Program, or “meaningful use”, incents physicians to adopt EHRs and perform certain tasks with them, including the provision of after-visit clinical summaries following every office visit. These summaries must at least contain the patient’s problem list, medication list, allergies, and recent lab results. It is unknown how these visit summaries, and the written information they provide to the patient, will impact chronic disease management.
METHODS: We used patient data from 14 adult primary care clinics associated with a Boston teaching hospital from October 2010 to October 2013 to determine whether providing after-visit clinical summaries is associated with an improvement in diabetes management, as measured by hemoglobin A1c (HbA1c). After-visit clinical summaries were completely implemented across all clinics by October 2012, which was used as the cut-off time for pre- and post-implementation analysis. After-visit clinical summaries are provided to patients after every clinic visit, either in person, by mail or through an electronic patient portal. Patients were included in the analysis if they were 18 to 74 years of age, seen at one of the clinics at least once and were prescribed an anti-hyperglycemic agent for diabetes management during the period from October 2010 to October 2013. We will perform an interrupted time series analysis with repeated measures to look for a difference in change of HbA1c from the time prior to implementation of the after-visit clinical summaries to the time after the implementation of the after-visit clinical summaries. We will use clustering to account for the effect of the clinic or provider and control for patient characteristics, how the after-visit clinical summary was provided and the number of instances that the after-visit clinical summary was provided.
RESULTS: There were 6935 patients in this cohort; 6281 patients were seen prior to the implementation of the after-visit clinical summary and 5414 patients were seen after the implementation of the after-visit clinical summary. As of October 2013, 94.8 % of physicians were meeting the meaningful use requirement of providing after-visit clinical summaries for greater than 50 % of clinic visits, and patients were provided an after-visit clinical summary for 84.8 % of all clinic visits. Average HbA1c prior to implementation was 7.7, ranging from 3.8 to 18.9. Average change in HbA1c during this period was −0.03, ranging from −12.2 to 13.3. Average percentage change in HbA1c during this period was 1.6 %, ranging from −64.5 to 97.0 %. Average HbA1c after implementation was 7.7, ranging from 4.1 to 18.9. Average change in HbA1c during this period was 0.06, ranging from −13.1 to 8.8. Average percentage change in HbA1c during this period was 3.8 %, ranging from −69.3 to 85.0 %. The study will have a power of 80 % to detect a 0.05 change in HbA1c with 95 % confidence and a power of 95 % to detect a 0.1 change in HbA1c with 95 % confidence.
CONCLUSIONS: After-visit clinical summaries have been successfully implemented in our adult primary care clinics. Average hemoglobin A1c control has not changed from the period preceding implementation of these patient after-visit clinical summaries to the period following implementation. Further analysis is required to determine whether there has not yet been a long enough follow-up period to see a significant change in chronic disease control associated with after-visit clinical summaries or whether there needs to be further emphasis placed on the importance of the information provided in the after-visit clinical summary to effect a change in chronic disease control.
ASSOCIATION BETWEEN BMI AND QUALITY OF CARE AMONG INDIVIDUALS WITH HIV, 2007–2010Erin Fennern1; Somnath Saha1; Stephen Berry2; Rochelle Fu1; Baligh Yehia3; Kelly Gebo2; Allison Agwu2; Philip T. Korthuis1. 1Oregon Health and Science University, Portland, OR; 2Johns Hopkins University School of Medicine, Baltimore, MD; 3University of Pennsylvania, Philadelphia, PA. (Tracking ID #1940304)
BACKGROUND: Prior studies suggest health care providers harbor biased attitudes toward obese patients, which could affect the quality of care received. HIV providers are increasingly encouraged to adhere to quality indicator (QI) performance measures. We sought to assess differences in the care provided to HIV patients by BMI category.
METHODS: We abstracted nine HIV QIs (Table) from medical records of 6,031 patients (10,896 total person-years) age >18 years engaged in care (≥2 clinic visits per calendar year) at seven clinics in the HIV Research Network between 2007 and 2010. Underweight patients were excluded. Patient BMI was categorized as normal (18.5 ≤ 24.9), overweight (25 to 29.9), stage 1 obese (30 to 34.9), stage 2 obese (35 to 39.9), and stage 3 obese (≥ 40). Using generalized estimating equations, logistic regression examined the association between BMI and receipt of each QI, and linear regression examined associations between BMI and the mean percent of QIs received, adjusting for age, race, sex, HIV risk behavior, and number of primary care visits in a year. We used R-squared to assess linear trends in odds ratios (ORs) and beta coefficients across BMI category.
RESULTS: Overall, patients received 65 % of eligible QIs in a given year. Those with stage 3 obesity received slightly lower eligible QIs vs. normal weight patients (64.3 % vs. 65.7 %, adjusted β = −0.04, 95 % CI −0.06, −0.02), with a moderate downward linear trend as BMI increased (R2 = 0.691). With regard to specific QIs, patients with stage 3 obesity received less screening for gonorrhea/Chlamydia (GC) (aOR = 0.76, 95 % CI 0.60 to 0.96) and syphilis (aOR = 0.69, 95 % CI 0.56 to 0.86) relative to normal weight patients. As BMI category increased, linear trends were observed for decreasing syphilis, GC, and HCV screening, and increasing CD4 count monitoring and lipid screening (Table). Receipt of ART, PCP and MAC prophylaxis were comparable across BMI categories.
CONCLUSIONS: Overall, HIV quality of care differed only slightly across BMI categories. Providers prescribed ART regardless of BMI, but performed less sexually transmitted infection screening and more lipid screening as BMI increased, suggesting providers may consciously or unconsciously prioritize some QIs over others in patients with higher BMI. Additional studies are needed to determine the source of these differences.
Adjusted Associations Between BMI Category and Receipt of each QI and Mean Percent QI Received, if Eligible.Adjusted Associations Between BMI Category and Receipt of each QI and Mean Percent QI Received, if Eligible.
| Normal Weight | Overweight | Stage 1 Obese | Stage 2 Obese | Stage 3 Obese | Test of Trend (R2) | |
| Mean% QIs Received | 65.7 % β = 0.00 – | 65.8 % β = −0.01 (−0.02, 0.00) | 65.8 % β = −0.01 (−0.02, 0.00) | 65.8 % β = −0.02 (−0.03, 0.00) | 64.3 % β = −0.04 (−0.06, −0.02) | 0.69 |
| ≥2 CD4 Counts | OR = 1.0 – | OR = 1.20 (1.04, 1.37) | OR = 1.12 (0.93, 1.35) | OR = 1.08 (0.83, 1.42) | OR = 1.44 (1.07, 1.95) | 0.53 |
| ART Therapy | 1.0 – | OR = 0.90 (0.72, 1.12) | OR = 1.08 (0.80, 1.46) | OR = 1.23 (0.80, 1.90) | OR = 0.80 (0.50, 1.30) | 0.00 |
| PCP Prophylaxis | 1.0 – | OR = 0.65 (0.46, 0.92) | OR = 0.63 (0.39, 1.02) | OR = 0.79 (0.41, 1.53) | OR = 1.45 (0.40, 5.22) | 0.24 |
| MAC Prophylaxis | 1.0 – | OR = 0.76 (0.41, 1.40) | OR = 0.81 (0.34, 1.88) | OR = 1.65 (0.51, 5.34) (combined for small n) | 0.39 | |
| Syphilis Screening | 1.0 – | OR = 0.99 (0.89, 1.10) | OR = 0.92 (0.80, 1.05) | OR = 0.84 (0.69, 1.02) | OR = 0.69 (0.56, 0.86) | 0.91 |
| Gonorrhea/Chlamydia Screening | 1.0 – | OR = 1.05 (0.93, 1.18) | OR = 1.00 (0.85, 1.17) | OR = 0.85 (0.68, 1.08) | OR = 0.76 (0.60, 0.96) | 0.78 |
| Lipid Screening | 1.0 – | OR = 1.10 (1.06, 1.37) | OR = 1.24 (1.03, 1.48) | OR = 1.21 (0.92, 1.59) | OR = 1.24 (0.93, 1.66) | 0.79 |
| HCV Screening | 1.0 – | OR = 0.90 (0.77, 1.04) | OR = 0.94 (0.77, 1.15) | OR = 0.86 (0.65, 1.13) | OR = 0.73 (0.53, 1.01) | 0.81 |
| Pneumococcal Vaccination | 1.0 – | OR = 0.96 (0.82, 1.13) | OR = 0.78 (0.63, 0.96) | OR = 0.90 (0.66, 1.23) | OR = 0.91 (0.65, 1.26) | 0.22 |
ASSOCIATION BETWEEN EMERGENCY DEPARTMENT USE AND THE DISCRIMINATION PERCEIVED BY FREQUENT USERSStéphanie Baggio1; Patrick Bodenmann2; Jean-Bernard Daeppen2; Bernard Burnand2; Olivier Hugli2; Ornella Ruggeri2; Jean-Blaise Wasserfallen2; Karine Moschetti2; Philippe Staeger2; Séverine Alary2; Katia Iglesias2; Marina Canepa Allen2. 1Lausanne University, Lausanne, Switzerland; 2Lausanne University Hospital, Lausanne, Switzerland. (Tracking ID #1930263)
BACKGROUND: Frequent Emergency Department (ED) users are often vulnerable patients with many risk factors. Furthermore, they are often perceived as unwelcome patients, causing EDs’ overcrowding, and being time-consuming, “illegitimate” users. However, data are scarce regarding how frequent ED users deal with this perception and particularly regarding their related feelings of discrimination. This study investigated the relationship between frequent ED use and perceived discrimination during such use in Switzerland.
METHODS: Data were part of a baseline assessment of a randomized controlled trial designed to improve frequent users’ quality of care in Lausanne University Hospital, a French-speaking Swiss tertiary care hospital, with over 50,000 annual ED visits. In total, 250 frequent ED users (≥5 attendances during the previous 12 months, ≥ 18 years), were interviewed between May 2012 and July 2013. From a previously published questionnaire, 15 dichotomous sources of discrimination were assessed, and grouped into five dichotomous causes: (i) any cause, (ii) immigration-related, (iii) age/gender, (iv) physical characteristics/sexual orientation, (v) social/economic status. Prevalence rates of perceived discrimination were computed first, then associations between the number of ED attendances and perceived discrimination were assessed with multivariate models (logistic regressions) controlling for socio-demographic characteristics and health-related issues (i.e. age, gender, education, nationality, proficiency in French, health literacy, and somatic-, mental-health-, behavioral-, and social issues).
RESULTS: Participants were 46.2 ± 18.9 years old on average, 57.2 % were men, 47.8 % Swiss, 17.7 % European, and 34.5 % non-European. In total, 11.6 % of the frequent ED users were asylum seekers or undocumented immigrants. Prevalence rates of perceived discrimination showed that 35.2 % reported at least one source of discrimination. Discrimination related to physical characteristics/sexual orientation (20.8 %), social/economic position (16.0 %), and immigration (16.0 %) was more frequent than discrimination related to age and gender (6.8 %). Multivariate models showed that when the number of ED visits increased, frequent users were more likely to feel discriminated against (any cause: odd-ratio [OR] = 1.19, p = 0.023), particularly regarding social/economic status (OR = 1.28, p = 0.011) and physical characteristics/sexual orientation (OR = 1.19, p = 0.023). Contrariwise, discrimination related to immigration and age/gender was not significantly related to the number of ED attendances (p = .803 and p = 0.266).
CONCLUSIONS: Frequent ED users appeared to perceive frequent discrimination (35.2 % compared to 11.1 % of non-frequent ED users hospitalized in another French-speaking Swiss tertiary hospital), associated with an increased number of ED attendances. Moreover, they did not feel discriminated against due to intrinsic characteristics or race-based sources (e.g. age, gender, nationality, or skin color), but rather for social and lifestyle factors (e.g. income, education, physical appearance, or sexual orientation), even if foreigners, asylum seekers, and undocumented immigrants were highly represented in the sample. The conclusions of this study should help health care practitioners and managers to be more cautious about potential discrimination against frequent ED users, as they may be unwittingly perpetuating health care disparities.
ASSOCIATION BETWEEN OFFICE-BASED MEDICAID ACCEPTANCE RATES AND SAFETY-NET SERVICE UTILIZATION BY MEDICAID PATIENTSKimberly Cartmill; Arnab K. Ghosh; Meroe B. Morse; Shawn L. Tyler. New York University, New York, NY. (Tracking ID #1929579)
BACKGROUND: The Patient Protection and Affordable Care Act (ACA) expands Medicaid coverage, which may increase utilization of healthcare safety net facilities such as emergency departments (EDs) and hospital outpatient departments (OPDs). To ease their burden, the ACA raises Medicaid reimbursement rates to encourage primary care physicians to accept Medicaid patients. It is uncertain if an increase in outpatient Medicaid acceptance rates is associated with a decrease in hospital OPD and ED visits among Medicaid patients. This study uses a robust national survey to determine the association between office-based Medicaid acceptance rates and the percent of Medicaid OPD and ED visits.
METHODS: Data from two nationally representative surveys, NAMCS and NHAMCS, were used to measure Medicaid acceptance rates among office-based physicians and percent of Medicaid ED and OPD visits from 2003 to 2010. 231,000 physicians responded to NAMCS. 269,000 OPD visits and 257,000 ED visits were used in NHAMCS. Trends in acceptance rates and percent Medicaid OPD and ED visits were analyzed by year (2003–2010) and across four broad census regions covering the country. Thirty-two point estimates, each representing one region and 1 year, were used to test the relationship between office-based acceptance rates (NAMCS) and hospital-based visits (NHAMCS). Pearson’s correlation coefficient was applied to assess magnitude, direction and significance of the association.
RESULTS: Response rates for the specified questions studied were 97 % for acceptance rates; 94 % for expected method of payment for OPD or ED visits. Nationally, no statistically significant trend in percent of office-based physicians accepting Medicaid was found (adjusted F 2.16, p = 0.62) between 2004 and 2010 (2003 excluded as outlier). These rates did not differ by year within three of the four regions. Percent Medicaid, OPD, and ED visits did not change significantly over the 7-year period nationally or within regions. When Medicaid acceptance rates were compared with percent Medicaid ED visits using point estimates, there was no significant correlation (R2 = 0.05; p = 0.87). However, there is a strong negative correlation between percent office-based Medicaid acceptance and percent Medicaid OPD visits (R2 = −0.59, p < 0.01).
CONCLUSIONS: In nationally representative data sets, office-based physician acceptance rates of Medicaid patients were inversely associated with visits to hospital outpatient departments, but not hospital emergency departments. Hospital outpatient departments may serve as a buffer to prevent emergency department utilization. This requires further investigation with better national surveys to assess the impact of health policy interventions.
ASSOCIATION BETWEEN OUTPATIENT “NO-SHOWS” AND SUBSEQUENT ACUTE CARE UTILIZATIONAndrew S. Hwang1; Steven J. Atlas2; Patrick R. Cronin3; Jeffrey M. Ashburner2; Sachin J. Shah2; Wei He2; Clemens S. Hong2. 1Tufts University School of Medicine, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Boston, MA. (Tracking ID #1934637)
BACKGROUND: To reduce healthcare costs, healthcare systems are focusing on identifying the relatively small percentage of patients who account for a disproportionate share of hospitalizations and emergency department (ED) visits. We hypothesized that primary care patients with a higher propensity for missed outpatient appointments, or “no-shows,” will have higher acute care utilization over the following 3 years.
METHODS: We calculated the “no-show propensity factor” (NSPF) for 140,947 patients seen in an academic primary care practice network from 2007 to 2009 using 5 years (2005–2009) of outpatient appointment data. NSPF transforms a patient’s count of arrivals and no-shows into a score that represents appointment adherence, correcting for patients with few appointments to avoid undue influence on the model. We divided patients into two groups: patients in the highest quartile and patients in the lower 3 quartiles of NSPF, and assessed subsequent hospital and ED utilization over 3 years (2010–2012). We evaluated the association between NSPF and our two continuous outcomes using Poisson regression models adjusting for number of outpatient visits in 5 years (2005–2009). Using a “change-in-estimate” strategy, we included other patient characteristics (age, gender, race, language, insurance, neighborhood median household income, Charlson comorbidity index, diagnosis of depression and alcoholism, and hospitalization and ED visits in 2009) and primary care provider characteristics (gender, years in practice, and whether the provider practiced at a community health center) in the models if they altered the incidence rate ratio (RR) by >5 %. We also ran models adjusting for all patient and provider characteristics and performed a subgroup analysis to examine the association between NSPF and subsequent hospitalization in patients with high-risk chronic illnesses (congestive heart failure, chronic obstructive pulmonary disease, diabetes mellitus, atrial fibrillation, coronary artery and cerebrovascular disease).
RESULTS: Compared to patients in the lower 3 quartiles of NSPF, patients in the highest quartile were significantly (P < 0.001 for all) younger (45 vs. 52 years) and more likely to be male (44 % vs. 42), non-white (37 % vs. 16 %), non-English speaking (17 % vs. 6 %), and insured by Medicaid or uninsured (22 % vs. 9 %), live in neighborhoods with low median household income ($50,612 vs. $63,781) and have higher rates of ED visits (192 vs. 84 visits/1,000 patients) and admissions (94 vs. 68 hospitalizations/1,000 patients) in 2009. In the subsequent 3 years (2010–2012), patients in the highest quartile of NSPF had significantly (p < .0001 for all) higher unadjusted rates of acute care utilization (77 vs. 66 hospitalizations/1,000 patients/year and 153 vs. 73 ED visits/1,000 patients/year) than patients in the lower 3 quartiles. In addition, Poisson regression analysis demonstrated that compared to patients in the lower 3 quartiles of NSPF, eligible patients in the highest quartile had a 19 % increased rate of ED visits in 3 years (adjusted RR 1.19 [1.05–1.34] adjusting for number of outpatient visits, age and ED visits and hospitalizations in 2009), but not a significantly increased rate of hospitalization in 3 years (adjusted RR 1.08 [0.996–1.18] adjusting for number of outpatient visits, age, and ED visits in 2009). Including all variables in the regression models did not change the significance or direction of the findings, and subgroup analysis among patients with high-risk comorbidities (congestive heart failure, chronic obstructive pulmonary disease, diabetes mellitus, atrial fibrillation, coronary artery and cerebrovascular disease) did not reveal a significant association between NSPF and hospitalization.
CONCLUSIONS: NSPF was an independent predictor of subsequent ED utilization. Using NSPF may help primary care delivery systems identify patients at increased risk for frequent utilization of the ED and tailor programs to increase primary care engagement and reduce ED overutilization.
ASSOCIATION BETWEEN OUTPATIENT “NO-SHOWS” AND SUBSEQUENT CLINICAL OUTCOMESAndrew S. Hwang1; Steven J. Atlas2; Patrick R. Cronin3; Jeffrey M. Ashburner2; Sachin J. Shah2; Wei He2; Clemens S. Hong2. 1Tufts University School of Medicine, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Boston, MA. (Tracking ID #1934608)
BACKGROUND: To improve care and achieve performance targets, healthcare systems seek to identify patients at high risk for not achieving preventive cancer screening and chronic disease management goals. We hypothesized that patients with a higher propensity for missed outpatient appointments, or “no-shows,” would have lower colorectal cancer (CRC) screening and low-density lipoprotein (LDL) goal attainment over the following year.
METHODS: We calculated the “no-show propensity factor” (NSPF) for 140,947 patients seen in an academic primary care practice network from 2007 to 2009 using 5 years (2005–2009) of outpatient appointment data. NSPF transforms a patient’s count of arrivals and no-shows into a score that represents appointment adherence, correcting for patients with few appointments to avoid undue influence on the model. We divided patients into two groups: patients in the highest quartile and patients in the lower 3 quartiles of NSPF, and assessed CRC screening completion among patients (52–75 years) without prior colectomy and LDL goal (LDL < 100 mg/dl) attainment in patients with diabetes or coronary artery disease at 1 year follow-up (2010). We evaluated the association between NSPF and our binary outcomes using logistic regression adjusting for number of visits. Using a “change-in-estimate” strategy, we included patient characteristics (age, gender, race, language, insurance, neighborhood median household income, Charlson comorbidity index, and diagnosis of depression or alcohol use disorder) and primary care provider characteristics (gender, years in practice, and whether the provider practiced at a community health center) in the models if they altered the odds ratio by >5 %. We also ran models adjusting for all variables.
RESULTS: Compared to patients in the lower 3 quartiles for NSPF, patients in the highest quartile were significantly (P < 0.0001 for all) younger (45 vs. 52 years) and more likely to be male (44 % vs. 42), non-white (37 % vs. 16 %), non-English speaking (17 % vs. 6 %), lack insurance (7 % vs. 4 %), live in neighborhoods with low median household income ($50,612 vs. $63,781), receive primary care at a community health center (15 % vs. 7 %), have a diagnosis of depression (20 % vs. 11 %) or alcohol use disorder (3 % vs. 1 %), and have higher number of outpatient visits over 5 years (27 vs. 21). Compared to eligible patients in the lower quartiles for NSPF, eligible patients in the highest quartile were significantly more likely to have not completed CRC screening (adjusted OR 1.87 [1.77–1.97] adjusting for number of visits and neighborhood median household income). Compared to patient in the lower quartile for NSPF, eligible patients in highest quartile were significantly more likely to have an above goal LDL (adjusted OR 1.70 [1.57–1.83] adjusting for number of visits and age). Inclusion of all variables in the models did not change the significance or direction of the effect, and the effect changed by less than 6 % for both outcomes.
CONCLUSIONS: NSPF was a strong, independent predictor of subsequent colonoscopy completion and LDL goal attainment. Using NSPF may help healthcare systems identify patients at increased risk for non-adherence to recommended care for targeted interventions to improve care and achieve performance targets.
ASSOCIATION BETWEEN USUAL SOURCE OF CARE AND CHRONIC DISEASE HOSPITALIZATION IN CALIFORNIA MEDICAID PATIENTSHugo A. Torres1; Ed Yelin2. 1Cambridge Health Alliance, Cambridge, MA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1938741)
BACKGROUND: The costs of Medicaid are driven in large part by the prevalence and costs of chronic diseases. Therefore, achieving improved control of chronic diseases by reducing the rates of hospital use associated with them is vital to the future successful expansion of the Medicaid program. Prior research links primary care access, often measured by usual source of care (USOC), with lower rates of hospitalizations for many chronic diseases, called ambulatory care sensitive Conditions (ACSC). Medicaid patients in general have high rates of ER utilization and hospitalization for ACSC relative to the uninsured and privately insured. This study aims to determine if the difference in ACS hospitalizations between Medicaid beneficiaries and low-income privately-insured individuals can be explained by the presence of a USOC.
METHODS: This is a cross-sectional study utilizing the 2009 and 2011 California Health Interview Survey (CHIS). The population studied is respondents to the CHIS, aged 18–64, earning less than 300 % of the Federal Poverty Level (N = 7564). The principal independent variable is Medicaid vs. Private insurance. The outcome is an ED visit or hospitalization for an ACSC. We use logistic regression to control for demographic variables that have been previously shown to affect health access. The analysis determines if Medicaid insurance was associated with rates of ED use or hospitalization; USOC was added to the model, first as an independent variable, then as an interaction term, to determine if the magnitude of the effect of insurance status on chronic disease ED use or hospitalization was altered by primary care access.
RESULTS: Medicaid patients were likelier to be female (60 % vs. 53 %), younger (mean age 43.6 vs. 45.1), in poorer self-rated health, unmarried, and more likely to have children than their counterparts with private insurance (p < 0.05 for all comparisons). They were also more likely to report a disability and to lack a usual source of care (OR = 0.72, 95 % CI 0.54–0.95, p = 0.02). The unadjusted rates of ED use and hospitalization for ACS conditions were 46.8 % vs. 30.9 % for privately insured patients (OR: 1.96, 95 % CI 1.60–2.41, p < 0.0001). The OR adjusted for the above was lower but still significant at 1.54 (95 % CI 1.2–2.0, p < 0.0001). The association remained after controlling for USOC (OR 1.55, p < 0.0001). An interaction term for USOC and Medicaid was positive and significant (OR 1.79, p = 0.05), indicating an increased effect of Medicaid on ED use/hospitalization for ACS conditions.
CONCLUSIONS: This analysis demonstrates a correlation between Medicaid (vs. private) insurance and ED use/hospitalization among people with ACSC, and that possession of primary care access in the form of having a usual source of care did not affect this relationship in the expected pattern; in fact, having a usual source of care increased the association. This is consistent with data from Oregon that found increased primary care use and ED use among Medicaid patients. The explanation for this relationship is likely complex. Medicaid patients may face hardship to access their provider, and are also likelier to have mental health and social issues which complicate their care. This research highlights the need for expanded efforts to understand and treat the causes of poor chronic disease outcomes in Medicaid patients. To do so would be to improve their health status outcomes, decrease ED visits and hospitalizations, and improve quality of life.
ASSOCIATION OF ADHERENCE MEASURES WITH PHYSICAL ACTIVITY OUTCOMES IN AN ONLINE WEIGHT LOSS TRIAL: RESULTS FROM THE OCELOT STUDYBethany Scanlan; Molly B. Conroy; Dana L. Tudorascu; Irina Karpov; Rachel Hess; Gary Fischer; Laurey R. Simkin-Silverman; Kathleen M. McTigue. University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1931481)
BACKGROUND: Lifestyle programs for weight loss and physical activity (PA) promotion have traditionally been delivered in person. Adherence, defined by number of sessions attended, has been shown to correlate with weight loss and PA improvements. With growing use of health information technology, an understanding of adherence to online interventions and the relationship between adherence and PA is needed. We hypothesize that participants adherent to an online intervention will have higher PA levels at 6 and 12 months than those who are non-adherent.
METHODS: The Online Counseling to Enable Lifestyle-focused Obesity Counseling in Primary Care (OCELOT-PC) study is a comparative effectiveness study of three online lifestyle interventions. We recruited 373 primary care patients, 257 of whom were randomized to a 12-month structured online adaptation of the Diabetes Prevention Program’s lifestyle intervention. The remaining patients had access to online resources alone and served as an active control arm. The behavioral online intervention included: lessons; self-monitoring (SM) of weight, eating pattern, and PA; feedback from a lifestyle coach; and links to community resources. We defined a current program user as a participant with a log-in in past 28 days. Non-users are those with no log-in for ≥28 days and no response to either of two weekly phone calls from the coach (initiated after the participant has not logged in for ≥14 days). Adherence was also based on other aspects of program use including: log-in in past week, weight entered in past week, eating pattern and PA SM (including number of days of SM in past week), and number of lessons completed. PA was determined by steps recorded on a pedometer worn for 2 weeks at baseline, 6 months, and 12 month. Adherence measures were correlated with PA outcome using Pearson correlations for continuous variables; means were compared using t-tests.
RESULTS: We were able to calculate program use and other adherence measures for 255 participants who were given access to the structured online intervention. Eighty percent of participants were women, 77 % white, and 62 % had education ≥ college; participants’ average age was 49.2 years. Participants had an average (SD) of 4127 (1918) steps per day and weight of 107.1 (21.6) kg at baseline. At 6 months, patients who were current program users had a mean (SD) of 3955 (2467) steps per day; those who were non-users had a mean of 1888 (1930) steps (p < 0.0001). Those with a log-in in the past week, weight entered in the past week, or any diet or PA SM in the past week also showed statistically significant greater numbers of steps per day compared to those who were non-adherent to these measures (all p < 0.001). Number of lessons completed, mean number of days of dietary SM in past week, and mean number of days of PA SM in past week were positively correlated with PA (r = 0.4; r = 0.37; r = 0.39; all p < 0.0001). Similar trends were observed for PA at 12 months. At 12 months, current program users had a mean (SD) of 4384 (2755) steps; non-users had a mean of 2689 (2348) steps (p < 0.001).
CONCLUSIONS: Participant adherence to the online intervention was associated with PA outcome. Those who were adherent to the tasks of the behavioral online intervention had significantly more steps at 6 and 12 months compared to those who were non-adherent. Further research should focus on which measure of adherence best relates to PA and other behavioral outcomes, as well as mechanisms to increase adherence to online interventions.
ASSOCIATION OF CARDIOVASCULAR HEALTH SCREENING WITH MORTALITY, CLINICAL OUTCOMES, AND HEALTH CARE COSTDong Wook Shin1; Hyejin Lee1; BeLong Cho1; Juhee Cho2; Ju Young Kim1; Eliseo Guallar2. 1Seoul National University Hospital, Seoul, Republic of Korea; 2Bloomberg school of public health, Baltimore, MD. (Tracking ID #1939911)
BACKGROUND: Since several CVD risk factors are modifiable, prevention programs routinely screen for hypertension, diabetes, and dyslipidemia expecting that early detection and treatment of CVD-related health conditions will decrease the burden of CVD. The effectiveness of screening programs for the CVD-related health conditions on health outcomes and healthcare utilization, however, is unclear. In South Korea, a country with universal healthcare coverage, the Korean National Health Insurance (KNHI) Corporation provides a biennial CVD health screening program to all national health insurance members over 40 years of age free of charge. We aimed to determine whether a nationwide CVD health screening program is associated with CVD incidence, mortality, healthcare utilization and costs.
METHODS: We randomly selected a 3 % sample (n = 621 350) of all KNHI members 40 years of age or older as of December 31, 2002. We excluded participants with cancer, diabetes, hypertension, dyslipidemia, or any related CVD including stroke and myocardial infarction (n = 170 490). Study participants were followed-up from January 1, 2005 through December 31, 2010. Propensity score matching was used to improve comparability of screened and non-screened participants. (n = 149 243 matched pairs)
RESULTS: The hazard ratios for CVD mortality, all-cause mortality, and incident myocardial infarction, cerebral infarction, and cerebral hemorrhage during comparing participants who attended a screening exam during 2003–2004 compared to those who did not were 0.55 (95 % CI: 0.50–0.60), 0.63 (95 % CI: 0.61–0.66), 0.85 (95 % CI: 0.76–0.95), 0.82 (95 % CI: 0.77–0.87), and 0.71 (95 % CI: 0.65–0.79). Screening attenders had higher rates of newly diagnosed hypertension and dyslipidemia (p < 0.001), lower inpatient days of stay and cost and lower outpatient cost compared to non-attenders.
CONCLUSIONS: CVD health screening was associated with lower rates of CVD and all-cause mortality and CVD events, higher detection of CVD-related health conditions, and lower healthcare utilization and costs. In the absence of large randomized controlled trials, our findings are suggestive of the effectiveness of CVD screening programs.
ASSOCIATION OF ILLNESS BELIEFS AND END-OF-LIFE TREATMENT PREFERENCES AMONG LUNG CANCER PATIENTSJenny J. Lin; Jessica Lake; Juan Wisnivesky. Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1939176)
BACKGROUND: Patient preferences about end of life care regarding resuscitation and intubation may be influenced by illness beliefs, family/social factors or physician communication. We assessed the association between patient-physician communication and cultural beliefs with patients’ preferences for end-of-life care among recently-diagnosed lung cancer patients.
METHODS: Patients with recently-diagnosed lung cancer were recruited from four medical centers in New York City from 2008 to 2011. Participants were surveyed about beliefs regarding lung cancer and cancer treatment, fatalism, medical mistrust and physician communication regarding treatment, symptoms and needs. Univariate analysis was used to assess which factors were associated with end-of-life preferences.
RESULTS: Of the 352 lung cancer patients enrolled in the study, 168 (48 %) were men; 21 % were black, 20 % were Hispanic and 59 % were white. Overall, 132 (38 %) did not want to be intubated and 88 (25 %) did not want to be resuscitated. Approximately 30 % of the participants did not have a preference regarding either intubation or resuscitation. Overall, 93 % of patients who did not want resuscitation also did not want intubation, while 25 % patients who wanted to be resuscitated did not want to be intubated. Those who were younger or who had lower educational attainment were more likely to want more aggressive care (resuscitation and intubation, p < 0.05 for all comparisons). There was no difference in end-of-life care preferences by lung cancer stage (p > 0.05 for all comparisons). Patients who believed that CPR should always be performed and those who expected their cancer to be cured were more likely to want aggressive care (both resuscitation and intubation, p < 0.04 for all comparisons). Additionally, those who agreed with the statement that “everything that happens is part of God’s plan” (p < 0.01) or who believed there was a >50 % of restarting the heart when in cardiac arrest (p = 0.03) were more likely to want resuscitation. Patients who reported that their physicians discussed issues regarding life sustaining treatment were less likely to want resuscitation, whereas those who reported that their physicians talked about emotional symptoms were more likely to want more aggressive care (p < 0.01 for all comparisons).
CONCLUSIONS: Lung cancer patients’ beliefs about cancer curability, resuscitation efficacy and fatalism impact their preferences about intubation and resuscitation. Physician discussions about life sustaining treatment may facilitate decisions about end-of-life preferences. Clinicians should ensure open conversations about patient beliefs about cancer prognosis and end-of-life care when discussing lung cancer treatment.
ASSOCIATION OF INFLUENZA VACCINATION COVERAGE IN YOUNGER ADULTS WITH INFLUENZA ILLNESS IN THE ELDERLYGlen Taksler1; Michael B. Rothberg1; David M. Cutler2,3. 1Cleveland Clinic, Cleveland, OH; 2Harvard University, Cambridge, MA; 3National Bureau of Economic Research, Cambridge, MA. (Tracking ID #1928183)
BACKGROUND: Older adults suffer the majority of influenza morbidity and mortality, but influenza vaccine effectiveness declines with age. It is unknown whether vaccination of nonelderly adults confers additional disease protection upon the elderly.
METHODS: Using the Behavioral Risk Factors Surveillance System Survey, we estimated countywide influenza vaccination coverage among adults aged 18–64 year in 313 counties comprising 56.5 % of the US population, in each influenza season (Oct–May) of 2002–2010. We linked these data with all Medicare claims for a random sample of 3,090,857 beneficiaries aged ≥65 y residing in these counties, and identified seasonal influenza-like illness (ILI) in each individual during the same years (N = 11,331,129 person-years). Using ICD-9 codes, we identified four types of ILI, from most specific to least specific definition: influenza (primary diagnosis), influenza (primary or secondary diagnosis), pneumonia or influenza, and broader ILI including pneumonia, influenza, bronchitis, cough, or upper respiratory infection. Using logistic regression models, we examined the association between countywide vaccine coverage among adults aged 18–64 year and diagnosis of ILI in Medicare beneficiaries, adjusting for comorbidity, influenza season severity, demographics, countywide health and socioeconomic variables, and dummy variables for influenza season and state of residence. We repeated the analysis for hospitalizations for ILI. Results were stratified by documented receipt of a seasonal influenza vaccine in each Medicare beneficiary. An adjusted odds ratio (AOR) for influenza diagnosis in the elderly that varied inversely with vaccine coverage among nonelderly adults would suggest herd immunity. Additionally, we expected to observe a lower AOR with more specific definitions of ILI than with less specific definitions, and during peak (Dec–Mar) vs. non-peak (Oct–Nov, Apr–May) months of influenza season.
RESULTS: Increases in countywide vaccine coverage among 18–64 year-olds were associated with lower adjusted odds of influenza-like illness in the elderly. Compared with elderly residents of counties with ≤15 % of 18–64 year-olds vaccinated, the AOR for a primary diagnosis of influenza was 0.90 (95 % CI = 0.87–0.94) for elderly residents of counties with 16 %–20 % of 18–64 year-olds vaccinated, 0.84 (95 % CI = 0.81–0.88) for elderly residents of counties with 21 %–25 % of 18–64 year-olds vaccinated, 0.78 (95 % CI = 0.74–0.82) for elderly residents of counties with 26 %–30 % of 18–64 year-olds vaccinated, and 0.77 (95 % CI = 0.73–0.81) for elderly residents of counties with ≥31 % of 18–64 year-olds vaccinated (P for trend <0.001). Weaker associations were observed for less specific definitions of influenza; elderly residents of counties with ≥31 % of 18–64 year-olds vaccinated had an AOR of 0.78 (95 % CI = 0.74–0.81) for a primary or secondary diagnosis of influenza, 0.96 (95 % CI = 0.95–0.98) for pneumonia or influenza, and 0.95 (95 % CI = 0.94–0.96) for the broader definition of ILI, compared with elderly residents of counties with ≤15 % of 18–64 year-olds vaccinated. The association was stronger among vaccinated elderly (AOR for primary influenza in counties with ≥31 % vs. ≤15 % of 18–64 year-olds vaccinated = 0.63, 95 % CI = 0.59–0.68) than for unvaccinated elderly (AOR = 0.84, 95 % CI = 0.79–0.89) (P for difference < 0.001). The association was also stronger in peak months (AOR for primary influenza in counties with ≥31 % vs. ≤15 % of 18–64 year-olds vaccinated = 0.75, 95 % CI = 0.70–0.79) than in non-peak months (AOR = 0.84, 95 % CI = 0.78–0.90) (P for difference = 0.002). For hospitalizations, overall associations were in the expected direction, but trends were not significant due to fewer hospitalizations.
CONCLUSIONS: In a large, nationwide sample of Medicare beneficiaries, influenza vaccination among 18–64 year-olds was inversely associated with influenza-like illness in the elderly.
ASSOCIATION OF LONG-TERM OPIOID AND/OR BENZODIAZEPINE RECEIPT AND MEDICATION COUNT WITH MORTALITY AMONG HIV-INFECTED AND UNINFECTED PATIENTSDaniel Weisberg1; Kirsha S. Gordon2; William Becker3,2; E. Jennifer Edelman3; J. R. Gaither1; Robert D. Kerns1,2; Janet P. Tate2; Amy C. Justice1,3; David A. Fiellin3. 1Yale University, New Haven, CT; 2VA Connecticut Healthcare System, West Haven, CT; 3Yale University, New Haven, CT. (Tracking ID #1936560)
BACKGROUND: In the United States, prescribing of controlled substances, including opioid analgesics and benzodiazepines (BZDs), is on the rise. Opioids and BZDs are known to have synergistic effects on sedation and respiratory depression leading to overdose. Those receiving long-term (LT) opioids and BZDs, older patients and those treated for HIV infection deserve particular attention due to greater exposure, the prevalence of polypharmacy and a diminished capacity for drug metabolism and elimination. We previously demonstrated an association between polypharmacy and mortality among HIV infected and uninfected (HIV+/−) patients. The prevalence and harms of LT opioid and/or BZD receipt beyond polypharmacy in HIV+/− patients are unknown.
METHODS: We used data from the Veterans Aging Cohort Study-Virtual Cohort to analyze the association between opioid/BZD receipt and all-cause mortality. Patients with cancer diagnoses, and HIV+ patients not on anti-retroviral therapy (ART) were excluded. LT medication receipt was defined (using pharmacy fill/refill data) as greater than 90 consecutive days of therapy allowing a 30-day gap. Medication count was determined by average LT concurrent medications over the study period, excluding ART, opioids and BZDs. All-cause mortality was based on the Veterans Health Administration Vital Status File. To account for confounding by indication, propensity scores for opioid/BZD receipt were generated using a logistic regression model including demographics, smoking, pain diagnoses, HIV and HCV status and other medical and psychiatric conditions. Individuals were 1:1 matched by propensity score, using a greedy algorithm. Cox regression was used to generate hazard ratios for all-cause mortality. In sensitivity analysis, separate models were run by HIV status.
RESULTS: From 64,441 eligible individuals, with 14550 opioid and/or BZD recipients, 12,881 pairs were included in the matched sample. The propensity score model had good discrimination (c = .76) and produced a well-balanced sample (Table 1). There were 758 deaths. Both opioid and BZD receipt were associated with a >30 % increase in mortality; patients receiving both had a >50 % increase in mortality. Each additional medication was associated with 4 % higher mortality risk. Results from HIV+/− strata were similar to overall findings (Table 2).
CONCLUSIONS: LT opioid and BZD receipt and average medication count each showed a significant independent risk for mortality, after adjustment for confounding by indication using propensity score matching. The incremental harm associated with opioid and/or benzodiazepine receipt was greater than would be expected due to their contribution to polypharmacy alone. These observational findings suggest the need for designing and testing interventions prioritizing the safe use of opioids and BZDs.
Table 1: Propensity score matching
| Opioid and/or BZD receipt, yes | Opioid and/or BZD receipt, no | P value | |
| Male | 12551 (97.4) | 12551 (97.4) | 1 |
| Age, mean (std dev) | 47.6 (8.2) | 48.0 (9.0) | .0002 |
| White race, n (%) | 6417 (49.8) | 6356 (49.3) | .767 |
| HIV+, n (%) | 2908 (22.6) | 2866 (22.3) | .530 |
| Medication count, mean (std dev) | 5.90 (3.8) | 5.82 (4.0) | .093 |
Table 2: Mortality, Hazard Ratio (95 % Confidence Intervals)
| Overall | HIV − | HIV + | |
| Opioid receipt | 1.38 (1.20–1.59) | 1.25 (1.05–1.50) | 1.46 (1.15–1.87) |
| BZD receipt | 1.33 (1.12–1.58) | 1.34 (1.08–1.66) | 1.28 (.95–1.71) |
| Opioid and BZD receipt | 1.56 (1.24–1.96) | 1.34 (1.00–1.81) | 1.85 (1.29–2.68) |
| Medication count | 1.04 (1.02–1.06) | 1.05 (1.03–1.07) | 1.03 (1.00–1.07) |
ASSOCIATION OF OPIOID USE WITH FALLS AND FRACTURES AMONG OLDER MEN WITH MUSCULOSKELETAL PAINErin E. Krebs1,2; Misti Paudel2; Brent C. Taylor1,2; Douglas Bauer4; Howard A. Fink1,2; Nancy E. Lane3; Kristine E. Ensrud1,2. 1Minneapolis VA Health Care System, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of California at Davis, Sacramento, CA; 4University of California at San Francisco, San Francisco, CA. (Tracking ID #1936417)
BACKGROUND: Older adults are disproportionately affected by painful musculoskeletal conditions and receive more opioid analgesics than younger adults, but insufficient data are available about potential benefits and harms of opioid therapy in older adults. The objectives of this study were to evaluate potential adverse effects of opioid analgesics on prospectively assessed falls and fractures among older men with persistent musculoskeletal pain.
METHODS: This is a secondary analysis of data from the Osteoporotic Fractures in Men (MrOS) study, a longitudinal cohort study of 5994 community-dwelling men age ≥65 years. This analysis includes MrOS participants who reported having back, hip, or knee pain most or all of the time at baseline. Medication exposure and covariate data were collected from participants at baseline and two follow-up visits. Participants were contacted every 4 months to assess fall and fracture outcomes; follow-up contacts were >99 % complete. For falls, the outcome was one or more falls reported during each 4-month period. Fracture outcomes were incident events confirmed with radiographic reports and evaluated in 3 categories: any clinical fracture; major osteoporotic fracture (fractures of the hip, wrist, spine and shoulder); and hip fracture. Propensity scores (PS), representing the conditional probability of receiving opioids, were estimated for each visit using a logistic regression model that included age, BMI, smoking, medical comorbidities, frailty status, activity level, cognitive performance, pain location, and other covariates. To achieve adequate balance of covariates between opioid users and non-users within PS quintiles, men with PS < 0.03 (meaning <3 % conditional probability of receiving opioids) were excluded from the primary analyses. Generalized estimating equations (GEE) were used to model the relationship between repeated measures of opioid use and falls, controlling for time-varying PS quintile. Cox proportional survival analyses were used to model associations between opioid use and incident fractures.
RESULTS: The analytic cohort included 2,732 men with back, hip, or knee pain at baseline. A total of 351 men (12.8 %) reported opioid use at one or more study visits. Over 9.1 (SD 4.0) years of follow-up, 2069 participants reported at least one fall, 318 had any clinical fracture, 149 had a major osteoporotic fracture, and 60 had a hip fracture. In the primary model, the relative risk of falling was 1.10 (95 % CI: 0.97, 1.24) for opioid users compared with non-users. Point estimates for all fracture outcomes were higher for opioid users than non-users, but none of the associations were statistically significant (Table).
CONCLUSIONS: We found non-significantly higher fall and fracture rates for opioid users compared with non-users. This analysis of MrOS data has major advantages over prior studies, including detailed assessment of potential confounders and rigorous prospective ascertainment of fall and fracture outcomes. Study limitations include lack of detailed opioid dose data and infrequent medication assessment. Power was limited for major osteoporotic fracture and hip fracture events, so we cannot exclude a moderate effect of opioid use on these outcomes.
Hazard ratio (HR) of fracture outcomes for opioid users vs. non-users
| Outcome | HR (95 % CI) |
| Any clinical fracture | 1.08 (0.87–1.34) |
| Major osteoporotic fracture | 1.34 (0.88–2.03) |
| Hip fracture | 1.55 (0.80–3.02) |
ASSOCIATIONS BETWEEN INTERNAL MEDICINE RESIDENT SCHOLARSHIP AND CLINICAL PERFORMANCELuke A. Seaburg; Amy T. Wang; Colin P. West; Darcy Reed; Andrew J. Halvorsen; Gregory Engstler; Amy Oxentenko; Thomas J. Beckman. Mayo Clinic, Rochester, MN. (Tracking ID #1936416)
BACKGROUND: The Accreditation Council for Graduate Medical Education requires that resident physicians participate in scholarly activities. Studies have shown that dedicated research time during residency is associated with increased publication, and residents who publish are more likely to select careers in academic medicine and achieve higher academic rank. However, it is unknown whether research productivity among residents is related to broad measures of clinical achievement during residency training. Therefore, we examined associations between the quantity of Mayo Clinic internal medicine residents’ peer-reviewed publications and measures of their knowledge (ABIM certification examination scores), skills (mini-clinical examination scores) and multi-source evaluations of performance.
METHODS: This was a longitudinal study of 312 post-graduate-year three (PGY-3) residents at the Mayo Clinic in Rochester, Minnesota from 2006 to 2012. To quantify scholarship, we identified peer-reviewed articles published in Ovid MEDLINE between July of each resident’s match year and the end of their graduation year. Outcomes included ABIM certification examination scores, mini clinical examination (mini-CEX) scores, and validated multi-source assessments of performance by resident-peers, faculty, and non-physicians. Scores for the clinical performance assessment items were averaged to form an overall score ranging from 1 to 5. Covariates included sex (male/female), medical school (U.S. versus international medical graduate), track (categorical versus clinician-investigator), PhD (yes/no), age at PGY-3 start, and percent correct on PGY-3 ITE examination. Associations between quantity of resident publications and first author status—and ABIM, mini-CEX and clinical performance assessment scores—were determined using multivariate linear regression analysis. The threshold for statistical significance was set at p < 0.01 to account for multiple comparisons.
RESULTS: Of the 312 PGY-3 residents, 199 (63.8 %) were male, 263 (84.3 %) were U.S. medical graduates, 282 (90.4 %) were categorical, and 11 (3.5 %) had PhD degrees. Their average age at PGY-3 start was 29.7 years. The residents published 667 papers, of which 462 were research papers, 204 were case reports, and 288 were first-authored. On adjusted analysis, multi-source evaluations of clinical performance were significantly associated (beta; p-value) with the numbers of research articles (0.013; 0.003), overall publications (0.013; 0.0009), and first-authored articles (0.017; 0.007). There were no statistically significant associations between quantity of publications and ABIM certification examination or mini-CEX scores.
CONCLUSIONS: This may be the first study to demonstrate that, among resident physicians in training, scholarly achievement is associated with clinical performance as determined by observation-based assessments from resident peers, faculty, and non-physicians. Furthermore, performance assessment scores were linked to the publication of journal articles that were first-authored and research-focused. These findings suggest that scholarly productivity may be an indicator of clinical performance during residency training, and underscore the importance of research programs in graduate medical education.
ASSOCIATIONS BETWEEN MEDICAL HOME CHARACTERISTICS AND SUPPORT FOR PATIENT ACTIVATION IN THE SAFETY NET: UNDERSTANDING DIFFERENCES BY RACE, ETHNICITY, AND HEALTH STATUSRobert S. Nocon1; Yue Gao1; Kathryn E. Gunter1; Janel Jin2; Lawrence P. Casalino3; Michael T. Quinn1; Sarah Derrett4; Wm Thomas Summerfelt5; Elbert S. Huang1; Sang Mee Lee6; Marshall Chin1. 1University of Chicago, Chicago, IL; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Weill Cornell Medical College, New York, NY; 4Massey University, Palmerston North, New Zealand; 5Advocate Healthcare, Chicago, IL; 6University of Chicago, Chicago, IL. (Tracking ID #1936110)
BACKGROUND: Few studies have evaluated whether the patient-centered medical home (PCMH) supports patient activation, and existing evidence is mixed. No studies have evaluated whether support for patient activation differs among racial and ethnic groups in a PCMH. This is critical because activation is lower on average among minority patients. We sought to assess the association between clinic PCMH characteristics and patient perception of clinic support for patient activation, and whether that association varies by patients’ self-reported race, ethnicity, and health status.
METHODS: We conducted a cross-sectional analysis of PCMH characteristics and patient-assessed clinic support of patient activation in 24 safety net clinics across five states. PCMH characteristics were measured via surveys of 271 providers and staff. The provider and staff survey produced a 0 (worst) to 100 (best) PCMH score based on a scale created by the authors and described previously in the literature. Clinic scores were created by averaging provider/staff responses. Clinic support of patient activation was measured via surveys of 1,656 patients. The patient survey used the patient activation scale of the Patient Assessment of Care for Chronic Conditions to produce a 0 (worst) to 100 (best) score for clinic support for patient activation. Patient race, ethnicity, and health status were based on self-report in the patient survey. To investigate the relationship between PCMH characteristics and patient activation, while allowing for a clustering effect of patients within clinics, we fitted multivariate models using generalized estimating equation models with an exchangeable correlation structure. We analyzed interactions terms to assess how the association of PCMH characteristics and patient activation varied by race/ethnicity and health status subgroups. We interpret the association in terms of a 10-point change in PCMH score, a difference we found to be operationally meaningful in previous work.
RESULTS: We received 214 (79.0 %) provider and staff survey responses and 735 (44.4 %) patient survey responses. Mean PCMH score among the 24 clinics was 58.7 (SD = 6.4). The mean score for patient perception of clinic support of patient activation was 68.8 (SD = 30.0). Across all patients, a 10-point higher PCMH score was associated with a 5.6-point higher score for patient perception of clinic support for patient activation (95 % CI, 1.3–9.9). The association between PCMH score and patients’ perception of clinic support for patient activation was particularly strong among minority patients in fair or poor health: a 10-point higher PCMH score was associated with a 16.2-point (CI 1.7–30.6) higher score for clinic support of patient activation among Hispanic patients in fair or poor health and a 34.1-point higher score among black patients in fair or poor health (CI 9.1–59.1). The effect of PCMH score on patient activation score among black patients with poor/fair health status was statistically significantly different from the effect seen among non-Hispanic white patients in good or better health.
CONCLUSIONS: In a population of safety net patients, PCMH characteristics showed a moderate, positive association with patients’ perception of clinic support for activation; the magnitude of association was notably larger for minority patients in poor/fair health status. The PCMH may be promising for reducing disparities in patient activation for ill racial and ethnic minority patients.
ATTITUDES TOWARD INTERNAL MEDICINE RESIDENT PROFESSIONALISM TRAININGLaura Nichols; Kathlyn E. Fletcher; Brent Nichols. Medical College of Wisconsin, Wauwatosa, WI. (Tracking ID #1934886)
BACKGROUND: Professional conduct is a core competency of medical practice and residency training. Defining, teaching and evaluating professionalism is challenging and requires collaboration between residents and faculty. In order to facilitate this effort, it is important to understand the beliefs and attitudes of those involved in the process. It was our objective to understand current modalities used, attitudes toward currently utilized curriculum and potential areas for improvement in professionalism training.
METHODS: Two surveys (one for residents and another for program directors) were developed using previously identified methods of teaching and evaluating professionalism. We distributed the survey link via email. Data was analyzed for associations using a chi-squared test.
RESULTS: Sixty-seven program directors and 589 residents completed the respective surveys. The majority (94 %) of residents felt that professionalism education was relevant to their development as physicians. Forty-two percent of programs reported having a formal professionalism curriculum, though the majority of program directors (86.6 %) and residents (87.1 %) felt that residents could be taught professionalism. Residents who reported having a formal professionalism curriculum were significantly more likely to rate the quality of their professionalism training as adequate (27 %) or very good (28 %) (P < 0.0001). Commonly utilized evaluation modalities included faculty evaluation forms (97.0 %) and completion of administrative tasks (85.1 %). Role modeling was the most utilized teaching modality (80.3 %). Residents noted faculty evaluation (66.0 %) and ancillary staff evaluation (61.9 %) to be most effective evaluation methods, while Objective Structured Clinical Examinations (OSCE) and traditional examinations ranked lowest. Role modeling (66 %) and faculty mentorship (48.7 %) were felt by residents to be the most useful methods of teaching professionalism.
CONCLUSIONS: We examined attitudes of residents and program directors toward professionalism curricula to aide in the formation of effective professionalism education. Consistent with previous literature, formal didactics and examinations were noted to be less effective than staff evaluations and role modeling. Less than half of programs reported having professionalism curricula; however, residents who had a formal curriculum were more likely to report high quality professionalism teaching. A multifaceted approach with a focus on faculty and ancillary staff evaluation, role modeling and mentorship is likely to be the most well-received curriculum.
AUTOMATED ELECTRONIC SEPSIS ALERTS: A SYSTEMATIC REVIEWAnil N. Makam1; Oanh K. Nguyen1; Andrew Auerbach2. 1University of Texas Southwestern, Dallas, TX; 2University of California San Francisco, San Francisco, CA. (Tracking ID #1938467)
BACKGROUND: Timely treatment of sepsis, including adequate fluid resuscitation and appropriate antibiotic administration, decreases morbidity and mortality. However, there are diagnostic and therapeutic delays in deploying early-goal directed therapies due to the resource intensive nature of these protocols. To circumvent these delays, automated, electronic sepsis alerts are being implemented to facilitate the delivery of timely and effective care. We sought to systematically evaluate whether automated, real-time electronic sepsis alerts can accurately identify sepsis, and improve process measures and outcomes for patients with sepsis.
METHODS: We systematically searched MEDLINE, Embase, The Cochrane Library, and CINHAL from database inception till August 13, 2013. Two independent reviewers selected studies that empirically evaluated one or both of our prespecified objectives. We excluded studies of bacteremia, nosocomial infections, or rapid response interventions. Two independent reviewers extracted data and assessed the risk of bias. Accuracy of sepsis detection was measured by sensitivity, specificity, positive and negative predictive values and likelihood ratios. Efficacy was assessed by changes in various process measures (i.e. time to antibiotics) and outcomes (length of stay, mortality). Heterogeneity in setting, design, and definitions of the alert precluded a meta-analysis.
RESULTS: We searched 1,091 citations and identified six studies for inclusion, four for the identification of sepsis (n = 34,328) and four for the evaluation of automated, real-time sepsis alerts (n = 6,723). The definition of sepsis alert thresholds varied, but included abnormal systemic inflammatory response syndrome (SIRS) criteria or abnormal SIRS criteria plus organ dysfunction. The accuracy of alerts to identify sepsis varied greatly depending on the clinical setting and the definition of sepsis used for the alert system, with sensitivity ranging from 36.2 to 98.9 %, specificity, 30.7–99.6 %, positive likelihood ratio, 1.4–145.8, and negative likelihood ratio, 0.04–0.86. There was modest evidence for improvement in process measures, such as lactate collection and antibiotic administration, among patients in non-ICU settings; however, without corresponding improvements in mortality or length of stay. We found no studies that reported on overuse and potential harms due to false positive alerts.
CONCLUSIONS: Automated sepsis alerts derived from electronic health records may improve care processes but tend to have poor positive predictive value and do not improve mortality or length of stay. Future efforts should develop and study methods for sepsis alert systems which avoid the potential for alert fatigue while improving outcomes.
AUTOPSY IN THE AGE OF ADVANCED DIAGNOSTIC TECHNOLOGYDavid Chia2; Ali Ershadi1; Majid Sadigh1; Steven I. Aronin2. 1Western Connecticut Health Network, Danbury, CT; 2Yale, Waterbury, CT. (Tracking ID #1928285)
BACKGROUND: Traditionally, the role of autopsy has had many benefits to the healthcare system, including illumination of the exact cause of death, determination of the rate of clinical errors, assurance of the quality of care, and identification of new diseases or changes in preexisting ones. However, autopsy rates have declined worldwide. In the United States, the in-hospital autopsy rate has fallen to 5–10 % from its peak of 70 % in the early 1960s. Furthermore, a heavy reliance on advanced diagnostic technologies have given an impression of diagnostic adequacy that invalidates the present need for autopsy. However, despite these advances in technology, the reported discrepancy between clinical and autopsy diagnoses remains unchanged at 10–30 %.
METHODS: We conducted a retrospective review of all autopsies performed on patients who died in two community hospitals between January 2008 and December 2012. Major discrepancies between clinical and autopsy diagnoses were classified into two categories: significant errors that had the proper diagnosis been made would have changed management and possibly outcome (type I) and significant errors that had the proper diagnosis been made would not have changed management or outcome (type II).
RESULTS: 2,409 deaths occurred during the study period and autopsies were conducted on 284 patients (11 %). Autopsies performed on fetuses, patients who were dead on arrival to the hospital, and those with inadequate documentation were excluded from our study. Major discrepancies were noted in 20 % (33/164) of cases of which 79 % (26/33) were type I errors. The most commonly misdiagnosed conditions included pneumonia (30 %), myocardial infarction (18 %), pulmonary embolism (9 %) and pneumonitis (9 %). Nearly half of patients (17/33) with major discrepancies died under unclear clinical circumstances. Autopsy established the cause of death in 88 % (15/17) of these cases. Major discrepancies occurred mainly because either the diagnosis was not considered on the differential diagnosis (55 %) or the diagnosis was considered, but the result of appropriate diagnostic evaluation was misleading (30 %).
CONCLUSIONS: Despite advances in medical technology, major discrepancies between clinical and autopsy diagnoses continue to occur at relatively high rates. The majority of these discrepancies would have changed management decisions and may have altered outcomes if the proper diagnosis had been made. These discrepancies often occurred because the proper diagnosis was either not considered in the differential diagnosis or the result of appropriate diagnostic testing was misleading. As a result, autopsy should continue to have an important role in the healthcare system, while physicians should maintain broad differential diagnoses and be critical of unexpected results on diagnostic evaluation
AWARENESS OF CENTRAL VENOUS CATHETERS: A PATIENT SAFETY SURVEYRachel E. Thompson1; Natalie Melin1; Vineet Chopra2. 1University of Washington, Seattle, WA; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1938689)
BACKGROUND: Central lines are commonly used in the care of hospitalized patients. Each day a central line is in place the risk of complications such as bloodstream infection rises. Yet central lines often remain in place after they are no longer clinically useful. Preliminary data suggests one obstacle to the timely removal of central lines may be physician being unaware—as was demonstrated in the case of urinary catheters. The goal of this study is to determine the extent of physician awareness of their patients’ central lines.
METHODS: We interviewed intern, resident, and attending physicians on inpatient medical services at an academic hospital. Patients hospitalized on the medicine non-ICU, medicine ICU, cardiology and hospitalist services were included. Physicians were read a list of patients for whom they had direct responsibility and asked whether each had (1) a central venous catheter (CVC) or (2) a peripherally inserted central catheter (PICC). “Yes” or “no” responses were recorded for both types of central line. Physician responses were cross-checked with the hospital’s validated daily central line report for accuracy.
RESULTS: 375 patient records were accessed and their providers interviewed regarding awareness of presence of a CVC or PICC. There were 218 interviews with interns, 264 with senior residents and 347 with attendings. Fifty-two cases had a CVC and 23 a PICC. Of those with either a CVC or PICC, overall provider recall accuracy ranged from 82 to 93 %. On teaching teams, attendings were significantly more likely to miss a central line than residents or interns (p < 0.01). There was no significant difference in missed lines between teaching attendings and hospitalists. Of the ICU attending interviews, lines were present in 36 % compared to only 13 % among non-ICU. Attendings with work that included ICU care were less likely to miss a line (13.9 v 36.1 %, p <0.05). These attendings were also more likely to falsely recall a line when no line was present than the non-ICU attendings (15.4 % v 5.3 %, p < 0.01).
CONCLUSIONS: Our results demonstrate that many physicians are not aware of whether their patient has a central line. Errors in recall occurred in both directions, potentially suggesting a deep-rooted unawareness. The frequency of lines among patients may influence the direction of recall error. The overall greater awareness observed among interns could relate to smaller case-loads. Each day a physician fails to remove an unnecessary line unjustly exposes the patient to an increasing risk of complications. It is important to target awareness of central lines to improve patient safety.
AWARENESS OF PREDIABETES AND ENGAGEMENT IN DIABETES RISK-REDUCING BEHAVIORSAnjali Gopalan1,3; Ilona Lorincz4; Christopher Wirtalla6; Judith A. Long2,3; Steven C. Marcus2,5. 1Philadelphia VA Medical Center, Philadelphia, PA; 2Philadelphia VA Medical Center, Philadelphia, PA; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 5University of Pennsylvania, Philadelphia, PA; 6Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA. (Tracking ID #1933194)
BACKGROUND: Numerous high quality studies have demonstrated the benefit of lifestyle modification, including weight loss, exercise, and a healthy diet, in the prevention of diabetes among those with prediabetes. Almost a third of the U.S. adult population meets criteria for prediabetes and without any intervention, 25 % will develop diabetes within 3 to 5 years. Despite the proven benefits of lifestyle changes and increasing numbers of community-based diabetes prevention programs, only about half of those with prediabetes report engaging in behaviors aimed at preventing the onset of diabetes. One barrier is low patient awareness of being at risk. In this study we aimed to determine whether there is a difference in the performance of diabetes risk-reduction behaviors between individuals who are aware of their prediabetes diagnosis compared to those who are unaware.
METHODS: We conducted a pooled cross-sectional analysis from two consecutive cohorts (2007–2008 and 2009–2010) of the National Health and Nutrition Examination Survey (NHANES). Subjects under age 20, pregnant woman, and those with missing responses to questions relating to diabetes history, physical activity, diet, and weight history were excluded, as were individuals missing all three lab values used to diagnose prediabetes: the hemoglobin A1C (HbA1C), a fasting plasma glucose (FPG), and the two-hour oral glucose tolerance test (OGTT). Patients with a self-reported a history of diabetes were classified as diabetes-aware. The remaining analytic sample was identified using the nationally accepted laboratory criteria to define prediabetes: 5.7 %≤A1C<6.5 %, 100 mg/dL≤FPG<126 mg/dL, and/or 140 mg/dL≤OGTT<200 mg/dL. Patients were classified as prediabetic if they met one of these criteria and did not meet any criteria for diabetes. The prediabetic population was then categorized into prediabetes aware and unaware based on participants’ self-report. We then used multivariate logistic and linear regression to estimate the effect of awareness of prediabetes on the likelihood of the following outcomes: engagement in physical activity, weight-related behaviors, and number of fast food/pizza meals eaten weekly. Any weight related behavior was defined by reported intention to lose weight or maintain weight, while appropriate-weight behavior was defined as an intention to lose weight for those with a BMI ≥ 25 and a desire to maintain weight for those with a BMI < 25.
RESULTS: 34.4 % (3,635/10,556) met criteria for prediabetes. 8.5 % (310) of those meeting these criteria self-reported a diagnosis of prediabetes. Those who were aware of prediabetes differed significantly from those who were unaware by age (55.6 vs 51.7, p < 0.001), but did not differ based on gender, educational attainment, income, or ethnicity. Subjects aware of prediabetes were also more likely to report a regular source of care (94.2 % vs. 85.7 %, p < 0.001), have a family history of diabetes (45.3 % vs. 35.9 %, p = 0,02), have a history of hypertension or hyperlipidemia (58.1 % vs 35.1 %, p < 0.001 and 53.8 % vs. 29.5 %, p < 0.001, respectively), and to report that a physician told them they were overweight or obese (57.2 % vs. 33.3 %, p < 0.001). After adjusting for age, gender, ethnicity, education, number of healthcare visits in the past year, family history of diabetes, being told they were overweight/obese, self-reported limitation on work/activity, BMI, and medications for hypertension and hyperlipidemia, adults who self-reported having prediabetes were significantly more likely to report engagement in any physical activity (any level of intensity) on a weekly basis, adjusted odds ratio (AOR) 1.3, ([95 % CI 1.0–1.7]; p = 0.046) and engagement in moderate or vigorous physical activity, AOR 1.3, ([95 % CI 1.1–1.5]; p = 0.01). Adults with awareness of prediabetes were also significantly more likely to report engaging in any weight-related behavior AOR 1.8, ([95 % CI 1.3–2.5]; p = 0.001) and in appropriate-weight related behavior AOR 1.4, ([95 % CI 1.0–2.0]; p = 0.05). There was no difference noted in number of fast-food/pizza meals eaten weekly based on awareness of prediabetes (1.9 meals vs. 1.6 meals, p = 0.5).
CONCLUSIONS: Adults who were aware of meeting diagnostic criteria for prediabetes were significantly more likely to engage in moderate or vigorous weekly exercise and were more likely to report engagement in appropriate weight-related behaviors. While the cross-sectional nature of the data limits conclusions regarding continued adherence to these risk-reduction efforts, engagement is unarguably the first step toward lifestyle changes. Increasing our patients’ awareness of prediabetes could result in increases in exercise and weight management and, most importantly, to decreases in the incidence of diabetes and improved health outcomes.
AZITHROMYCIN IS ASSOCIATED WITH INCREASED CARDIAC EVENTS BUT LOWER MORTALITY FOR OLDER PATIENTS HOSPITALIZED WITH PNEUMONIAEric Mortensen1,2; Ethan Halm2; Michael J. Fine3; Christopher Johnson1,2; Antonio Anuzeto4. 1VANTHCS, Dallas, TX; 2University of Texas Southwestern Medical Center, Dallas, TX; 3VA Pittsburgh Health Care System, Pittsburgh, PA; 4South Texas Veterans Health Care System, San Antonio, TX. (Tracking ID #1931222)
BACKGROUND: Although clinical practice guidelines recommend combination therapy with macrolides, including azithromycin, as first line therapy for patients hospitalized with pneumonia, recent research suggests that azithromycin may be associated with increased cardiovascular events. The purpose of this study was to examine the association of azithromycin use with all-cause mortality and cardiovascular events for patients hospitalized with pneumonia.
METHODS: We conducted a retrospective national study using Department of Veterans Affairs administrative data of patients hospitalized at any Veterans Administration acute care hospital. We included patients >65 years hospitalized with pneumonia in fiscal years 2002–2012. We included only those who received antibiotic therapy concordant with national clinical practice guidelines. Our outcomes included all-cause mortality, cardiac arrhythmias, heart failure, myocardial infarction, and any cardiac event. We used propensity score matching to control for the possible effects of known confounders with conditional logistic regression.
RESULTS: Out of the 77,972 patients identified, our propensity-matched groups were composed of 34,763 azithromycin-exposed and 34,763 matched unexposed. There were no significant differences in potential confounders between groups after matching. We found that 90-day mortality was significantly lower in those who received azithromycin (exposed- 17.4 % vs. unexposed- 22.8 %, odds ratio [OR] 0.71, 95 % confidence interval [CI] 0.68–0.73). However, we found significant increased odds of any cardiac event (43.2 % vs 42.2 %, OR 1.04, 95 % CI 1.01–1.07), myocardial infarctions (4.9 % vs. 4.2 %, OR 1.17, 95 % CI 1.09–1.26), and cardiac arrhythmias (26.5 % vs. 25.6 %, OR 1.04, 95 % CI 1.002–1.07) but not heart failure (26.1 % vs. 25.8 %, OR 1.02, 95 % CI 0.98–1.05).
CONCLUSIONS: In patients hospitalized with pneumonia we found that although azithromycin is associated with a small increase in cardiac events it is also associated with a significant decrease in all-cause mortality. Our study supports the current clinical practice guidelines that recommend the use of azithromycin as part of empiric combination therapy.
BACTERIAL CONTAMINATION OF RESIDENT IPADS: LAME DUCK OR TROJAN HORSE?Tanu S. Pandey1; Kamaljit Singh2; German E. Giese1; Michael Alebich1; Shubhra Gupta1. 1John H Stroger Hospital of Cook County, Chicago, IL; 2Rush University Medical Center, Chicago, IL. (Tracking ID #1939546)
BACKGROUND: The advent of the Apple iPad, has brought about a revolution in the delivery of medical care. Though clothing, stethoscope and phone contamination has been well documented, to date, no study has examined the bacterial contamination of iPads. Our study aims to establish the rates of bacterial contamination of iPads used by residents in two urban teaching hospitals. We present the findings from one of these institutions.
METHODS: The study was funded by a collaborative research grant from the parent institutions. Twenty four residents from John H. Stroger Jr., Hospital of Cook County who used an iPad for patient care were enrolled into the study. They provided their iPad to the investigators during work hours for culture at random times. A pre-moistened swab was obtained from two 5 cm2 areas of the screen, as well as the “home” button. These swabs were delivered to the microbiology lab promptly and inoculated onto three agar plates for aerobic and anaerobic culture, isolate identification and antibiotic sensitivity. An anonymous questionnaire with demographic information was provided to the residents at time of swab.
RESULTS: All 24 devices were either iPads or iPad mini. There were five PGY-1, eight PGY-2, and eleven PGY-3 residents. Ninety-two percent residents took their device regularly inside patients’ rooms and 67 % placed them on the bed, table or elsewhere. Sixty-three percent carried their device in their hands as opposed to a case or coat pocket. Ninety-six percent used the same device for work and personal reasons and 50 % did not clean them at all. All devices grew multiple skin flora including coagulase negative staphylococcus. One device grew MRSA, three devices grew MSSA, one Acinetobacter and six grew alpha-hemolytic streptococcus. There was no significant statistical difference in contamination between those who cleaned their devices versus those who did not (OR 2.0, 95 % CI 0.3843 to 10.4096, p value = 0.4102).
CONCLUSIONS: The iPad is changing how medicine is practiced; however, no study has examined potential harms afforded by these devices. Our study revealed that the iPad does harbor potentially dangerous pathogens and little regulations guide the decontamination of these devices at the bedside. The relatively low prevalence of organisms is reassuring but further studies in large numbers are needed to establish the role of the iPad in increasing hospital-acquired infections. Based on the behavior of residents in this study, standard precautions for the use of these devices around patients is recommended.
BAR AND NIGHTCLUB INTERVENTION TO DECREASE YOUNG ADULT SMOKING IN NEW MEXICOSara Kalkhoran1; Pamela M. Ling1,2; Jeffrey W. Jordan3. 1University of California, San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA; 3Rescue Social Change Group, San Diego, CA. (Tracking ID #1937993)
BACKGROUND: Over 20 % of young adults in New Mexico are current smokers, which exceeds current national estimates. We evaluated the effect of an anti-tobacco Social Branding intervention on daily and non-daily smoking rates among young adult bar patrons.
METHODS: A series of cross-sectional surveys were collected from adults aged 18–26 in bars and nightclubs popular among young adults in Albuquerque, New Mexico from 2009 to 2013 using randomized time-location sampling. A Social Branding intervention was implemented in Albuquerque during this time. Social Branding is a variant of social marketing using commercial marketing strategies to compete with tobacco marketing by creating a smoke-free brand to promote smoke-free lifestyles within a specific bar subculture. This intervention focused on the “Partier” culture, which was characterized by attendance at large nightclubs, fashion consciousness, valuing physical attractiveness, and achieving high social status by exuding an image of confidence and financial success. Multivariate multinomial regression was used to evaluate differences in rates of daily (smoked on 25–30 of past 30 days) and non-daily (smoked 1–24 of past 30 days) cigarette use between baseline and each of 3 years of follow up, controlling for demographic characteristics, other risk behaviors, and tobacco-related attitudes.
RESULTS: Data was collected from 1066 individuals at baseline, and 767, 1242, and 1231 participants at follow-up years 1, 2, and 3, respectively. Current smoking rates decreased from 47.4 % at baseline to 37.4 % at follow-up year 3 (p < 0.001). In multivariate multinomial regressions, those surveyed at year 3 had significantly lower odds of being either a current daily (OR = 0.41, 95%CI [0.26–0.64]) or non-daily (0.57, [0.41–0.80]) smoker compared to baseline. Factors associated with increased odds of both daily and non-daily smoking included lower education, LGBT sexual orientation, advertising receptivity, binge drinking, and higher trend sensitivity (a measure of social personality traits and frequency/intensity of socializing in bars) (Table 1). Other factors associated with daily and non-daily smoking are shown in Table 1.
CONCLUSIONS: Social Branding interventions aimed at young adult bar patrons may help reduce smoking rates in this population. Bar-based interventions tailored to specific subculture values and lifestyles are an efficient way to address risky behaviors in this hard-to-reach population that continues to have high rates of cigarette smoking.
Predictors of Being a Non-daily or Daily Smoker Among Young Adult Bar Patrons in Albuquerque, New Mexico
| Non-daily smoker | Daily smoker | |
|---|---|---|
| <p align=\"left\">Variable | aOR (95 % CI) | aOR (95 % CI) |
| <p align=\"left\">Age | 0.97 (0.92–1.02) | 0.98 (0.92–1.04) |
| <p align=\"left\">Male Sex | 1.28 (1.06–1.55) | 1.00 (0.78–1.27) |
| <p align=\"left\">Race White Hispanic Other | −1.13 (0.92–1.40) 1.35 (1.02–1.78) | −0.68 (0.52–0.88) 0.80 (0.56–1.13) |
| <p align=\"left\">Education HS only/College dropout In college College graduate (ref) | 1.42 (1.05–1.92) 1.25 (0.98–1.61) − | 2.01 (1.40–2.87) 1.03 (0.75–1.40) − |
| <p align=\"left\">LGBT sexual orientation | 2.17 (1.67–2.83) | 2.16 (1.54–3.02) |
| <p align=\"left\">Study follow-up year Baseline (ref) Year 1 Year 2 Year 3 | −1.00 (0.77–1.31) 1.06 (0.84–1.35) 0.57 (0.41–0.80) | −1.12 (0.82–1.53) 0.91 (0.67–1.23) 0.41 (0.26–0.64) |
| <p align=\"left\">Anti-tobacco industry attitude* | 0.72 (0.66–0.78) | 0.51 (0.46–0.57) |
| <p align=\"left\">Trend sensitivity index | 1.08 (1.05–1.11) | 1.11 (1.07–1.15) |
| <p align=\"left\">Tobacco advertising receptivity | 1.92 (1.55–2.38) | 2.18 (1.69–2.82) |
| <p align=\"left\">Partier peer crowd association** | 0.76 (0.63–0.92) | 0.74 (0.58–0.95) |
| <p align=\"left\">Binge drinking in past 30 days | 2.30 (1.84–2.86) | 3.21 (2.33–4.41) |
| <p align=\"left\">Exposure to smokefree intervention | 1.35 (1.07–1.72) | 1.12 (0.82–1.55) |
*Assessed by agreement with questions regarding support for action against the tobacco industry **Determined by pictures of people with whom the participants were more likely to associated and bars which the participants were more likely to frequent
BARRIERS AND FACILITATORS TO PREVENTIVE CANCER SCREENING AMONG HMONG- AND SPANISH-SPEAKING PATIENTSElizabeth A. Jacobs1,3; Rebecca J. Schwei1; Maichou Lor2. 1School of Medicine and Public Health, University of Wisconsin, Madison, WI; 2School of Nursing, University of Wisconsin, Madison, WI; 3School of Medicine and Public Health, University of Wisconsin, Madison, WI. (Tracking ID #1938836)
BACKGROUND: Language barriers in health care are a large and growing problem in the U.S. Having limited English proficiency (LEP) is a well-recognized risk factor for disparities in health care quality and outcomes. Despite access to high quality interpreter services, LEP patients still experience disparities in preventive cancer screening. We conducted a qualitative study to better understand what factors might contribute to the disparities of cancer screening rates and their reduction among LEP patients seen in primary care.
METHODS: We conducted 28 semi-structured interviews with LEP patients who were eligible for preventive cancer screenings (n = 11 Hmong, n = 10 Spanish) and providers (n = 7 Physician) in a large academic medical system. Patient interviews were conducted in Hmong or Spanish. We interviewed general internal and family practice physicians with varying percentages of LEP patients in their practice. All interviews were audio taped, transcribed verbatim, translated and coded for interpretation. Hmong, Spanish, and provider interviews were coded separately. Themes were developed using content analysis.
RESULTS: Physician recommendation, doctors who care about and respect their patients, gender-concordant doctors, and familial experience with cancer facilitated cancer screening in both Hmong- and Spanish-speaking participants. Physicians identified high quality interpreters, electronic medical record reminders, and educational materials in appropriate language as facilitators to delivering preventive cancer screening to their LEP patients. Two common barrier themes for Hmong- and Spanish-speaking patients were: (1) previous negative health care experiences, which created distrust of health care, and (2) lack of knowledge about cancer, what cancer prevention can do, and how to access community resources. Additional barriers for Hmong patients included poor quality interpreters and the need for health care decisions to be made by the nuclear family. Spanish-speaking patients uniquely identified lack of money or insurance, not enough time, and machismo in men as additional barriers to receipt of preventive cancer screening. Physicians reported that competing social, economic, and health demands of patients, visit time constraints, cultural beliefs of patients, and the nature of the screening tests (e.g. embarrassing) as barriers for LEP patients to seek screening.
CONCLUSIONS: We found that cancer screening is influenced by many different personal, family, interpreter, provider, health care system, and community factors. This study provides insights for addressing cancer health disparities for these two ethnic minority populations in our community. Culturally-tailored community cancer education about prevention and cancer in general, and preventive cancer screenings specifically, is a first step to increasing knowledge and acceptability of preventive cancer screening in Hmong- and Spanish-speaking patients. Additionally, helping providers navigate the barriers that they may face when suggesting preventive cancer services to LEP patients may also increase the rates of preventive cancer screenings in Hmong- and Spanish-speaking patients.
BEARING WITNESS: IMPACT OF A BRIEF INTERVENTION ON RESIDENT ADVERSE EVENT REPORTINGJennifer B. Cowart1,2; Cynthia Peacock2; John Lin2; Addison A. Taylor1,2. 1Houston MEDVAMC, Houston, TX; 2Baylor College of Medicine, Houston, TX. (Tracking ID #1923141)
BACKGROUND: Recent ACGME guidelines require training in quality improvement and patient safety for resident physicians. Prior to the release of these guidelines, it was not clear how much training residents received in incident reporting. We sought to evaluate resident knowledge of hospital incident reporting systems, before and after a brief intervention aimed at increasing residents’ submissions of incident reports.
METHODS: Internal medicine residents at a large academic program were asked to participate in an anonymous survey before and after a brief educational intervention. Invitations for the pre-test survey were sent by email in August 2012. Questions were given in the form of a statement with agreement rated on a 7-point Likert scale (from “strongly disagree” to “strongly agree”). Residents were also asked to enter the number of adverse event reports they had ever submitted. After survey completion, monthly lectures were given during regularly scheduled education time (15 min per month) at each hospital site. Reference guides for the incident reporting systems at each facility were added to the departmental website. Invitations for the post-test survey were sent in May 2013.
RESULTS: 189 residents were invited to participate in the 9-question survey on two occasions (378 total). 138 (73 %) completed all questions in 2012 and 84 (44 %) completed all questions in 2013. There were significant increases in residents’ stated knowledge of mechanisms to report adverse events at two training institutions, with the median response changing from “disagree” to “agree” on a 7-point Likert scale (p = 0.000 for both). Before specific instruction in incident reporting, only 24.1 % of residents stated they had ever reported an adverse event. At the post-survey, 45.3 % of the responding residents stated they had reported one or more adverse events (p = 0.001). A majority of respondents agreed that they worked in a “culture of safety” (76.6 % before, 78.6 % after). There was no significant difference in the proportion of respondents who disagreed with this statement from before and after the intervention (10.2 % vs 9.5 %). The same held true of the proportion of residents who agreed that they were worried about being punished for reporting adverse events both before and after the intervention (27.5 % vs 28.6 %).
CONCLUSIONS: Brief education in adverse event reporting led to an increase in resident awareness of both reporting mechanisms and in self-reported submissions of adverse event reports. The increase in reporting did not correspond with an increase in residents perceiving themselves to be safe from reprisal. Areas for further investigation include identifying barriers to residents’ reporting witnessed events and whether residents’ concerns about reprisal for reporting of adverse events are a significant deterrent.
After education on adverse event reporting, residents were more likely to say they had reported at least one adverse event compared to before education on adverse event reporting.
BEDSIDE INTERPROFESSIONAL ROUNDS: MEDICINE PROVIDERS’ PERCEPTIONS OF BENEFITS AND BARRIERSJed Gonzalo1; Ethan Kuperman2; Erik B. Lehman1; Paul Haidet1. 1Penn State College of Medicine, Hershey, PA; 2University of Iowa, Carver College of Medicine, Iowa City, IA. (Tracking ID #1937728)
BACKGROUND: Interprofessional collaborative care models improve the quality of medical care. On inpatient medicine services, similar conceptualization amongst nurses and physicians regarding the process and goals of interprofessional rounds are required for successful implementation. However, little work has investigated front-line providers’ perceptions regarding bedside interprofessional rounds. We evaluated the perceptions of nursing staff, resident, and attending physicians regarding the benefits and barriers to bedside interprofessional rounds.
METHODS: In June 2013, a cross-sectional survey was sent via email to all medicine nursing staff, resident and attending physicians in our hospital to assess their perceptions regarding the benefits and barriers to bedside interprofessional rounds, defined as “encounters that include the team of providers, at least two physicians plus a nurse or other care provider, discussing the case at the patient’s bedside.” The survey was developed from prior work on bedside rounds and a literature review; 16 items were related to “benefits” and 18 items were related to “barriers” to bedside interprofessional rounds. Descriptive statistics, non-parametric Kruskal-Wallis, and non-parametric correlation statistics were used.
RESULTS: Of 171 surveys sent, data were collected from 149 respondents (87 % response). Highest-ranked benefits to bedside interprofessional rounds were “improves communication between nurses and physicians,” “improves awareness of clinical issues need to be addressed,” and “improves team-building between nurses and physicians;” lowest-ranked benefits were “decreases patients’ hospital length-of-stay” and “improves timeliness of consultations.” Nursing staff reported more favorable ratings compared to both attending and resident physicians for all 16 items (all p-values <0.05); the rank order between respondent groups showed a high degree of correlation (r = 0.92–0.96, p < 0.001). Highest-ranked barriers were “nursing staff have limited time,” “time required for encounters,” and “coordinating the start time of encounters;” lowest-ranked barriers were “patient lack of comfort” and “physicians” lack of bedside skills.” The rank order between respondent groups showed variable correlation (nurse-attending 0.62, nurse-resident 0.76, attending-resident 0.82).
CONCLUSIONS: Nursing staff were more likely to report positive perceptions about the benefits of bedside interprofessional rounds than resident and attending physicians. Overall, the greatest perceived benefits related to improved communication. Standardization of the rounding process and patient inclusion in conversations may allow knowledge assimilation regarding care plans most important to patient care and disposition. Reasons for nurses’ more positive perceptions than physicians are unclear but may reflect their experience with benefits or professional culture of this patient-centered activity. Time was the common theme in the highest-rated barriers, prompting consideration of addressing modifiable systems factors to increase this activity; cost-neutral measures such as tailoring nursing and physician schedules, modifying care coordination rounds, pre-scheduling patient rounding times, and geographic localization of patients and providers may attenuate this barrier. Further investigation into the impact of bedside interprofessional rounds on patient satisfaction and outcomes are necessary to validate widespread dissemination.
BEDSIDE ROUNDS IN THE ERA OF COMPETENCY-BASED EDUCATION: A WORKPLACE-BASED STRATEGY FOR FEEDBACK AND REFLECTIONJed Gonzalo1,2; Brian S. Heist2; Briar Duffy3,2; Liselotte Dyrbye4; Mark J. Fagan5; Gary S. Ferenchick6; Heather Harrell7; Paul Hemmer8; Walter N. Kernan9; Jennifer R. Kogan10; Colleen M. Rafferty1; Raymond Y. Wong11; Michael Elnicki2. 1Penn State College of Medicine, Hershey, PA; 2University of Pittsburgh School of Medicine, Pittsburgh, PA; 3University of Minnesota School of Medicine, Minneapolis, MN; 4Mayo Clinic College of Medicine, Rochester, MN; 5Alpert Medical School of Brown University, Providence, RI; 6College of Human Medicine, Michigan State University, East Lansing, MI; 7University of Florida College of Medicine, Gainesville, FL; 8Uniformed Services University of the Health Sciences, Bethesda, MD; 9Yale University School of Medicine, New Haven, CT; 10Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 11Loma Linda University School of Medicine, Loma Linda, CA. (Tracking ID #1937769)
BACKGROUND: Feedback and reflection are two strategies integral to competency-based medical education and trainee development. These methods are best employed in authentic workplace-based settings, opportunities which are not well described in the literature. Bedside rounds have been highlighted as an ideal venue for observation, feedback, and reflection, and the literature suggests methods for implementing these strategies, but actual strategies used to deliver feedback and team-based reflection by current-day bedside teachers has not been described. We sought to understand the content and timing of feedback and team-based reflection provided by bedside teachers in the context of patient-centered bedside rounds.
METHODS: In 2010, a qualitative thematic analysis of transcripts from digitally recorded, one-on-one telephone interviews with experienced bedside teachers (n = 34) was performed. Co-investigators from 10 U.S. institutions were recruited and asked to identify participants who had: 1) served as inpatient attending physician at least 2 weeks in the prior 2 years, and 2) performed “bedside rounds” while inpatient attending, defined as: “The team of providers, including at least one resident and attending physician, presenting the patient’s history or reviewing one physical exam component, in addition to discussing the diagnosis/management at the bedside in the patient’s presence.” Interviews consisted of closed- and open-ended questions; questions related to feedback were designed from frameworks identified in the literature. For questions related to reflection, defined as “…analyzing an experience for the purposes of learning or improve practice,” no studies were identified, therefore an inductive approach was used. Two investigators analyzed transcripts independently, with regular adjudication sessions to modify the codebook, followed by theme extraction. The study was exempt from review by all Institutional Review Boards.
RESULTS: Participants averaged 14 years of academic experience and 50 % were associate/full professor. Positive feedback about physical exam skills or clinical decision-making occurred during bedside encounters, while positive or constructive team-based feedback occurred immediately following encounters; individualized constructive feedback occurred following rounding sessions in private locations. Team-based reflection occurred immediately following bedside encounters and related to commonplace “teachable moments” more so than less frequent, emotionally-charged events. Three content areas related to team-based reflection were identified: (1) patient characteristics/emotions, (2) trainee actions/emotions, and, (3) attending physician role modeling.
CONCLUSIONS: Bedside teachers use bedside rounds as a workplace-based opportunity to stimulate feedback and team-based reflection with medical trainees. Bedside rounds provide authenticity as bedside activities allow assessments of trainees’ performance and skills in the context of real-time patient encounters. As demonstrated by participants, reflection can be used to promote cognitive and humanistic growth of trainees. Although reflection has been identified in the literature, no prior work has identified a taxonomy of events triggering reflection. Amidst current-day pressures of inpatient medicine, these content and timing-related strategies for feedback and reflection could assist in faculty development efforts geared toward competency-based education.
BEHAVIORAL ECONOMICS-INFORMED INTERVENTIONS TO REDUCE INAPPROPRIATE ANTIBIOTIC PRESCRIBING: A PILOT CLUSTER RANDOMIZED TRIALStephen D. Persell1; Jeffrey A. Linder2; Mark W. Friedberg3,2; Daniella Meeker4; Elisha M. Friesema1; Andrew J. Cooper1; Craig R. Fox5; Noah J. Goldstein5; Jason N. Doctor6. 1Northwestern University, Chicago, IL; 2Brigham and Women’s Hospital, Boston, MA; 3RAND, Boston, MA; 4RAND, Santa Monica, CA; 5UCLA, Los Angeles, CA; 6University of Southern California, Los Angeles, CA. (Tracking ID #1938251)
BACKGROUND: Physicians often use antibiotics for acute respiratory infections (ARIs) when they are not indicated. Interventions to reduce inappropriate prescribing have been only modestly successful.
METHODS: In preparation for a larger, multi-site trial, we performed a pilot cluster-randomized controlled clinical trial with physician as the unit of randomization and office visit as the unit of analysis to evaluate different behavioral economic and social psychological approaches to reduce inappropriate antibiotic prescribing. Physicians and a nurse practitioner at a single large urban academic internal medicine practice were enrolled and randomized within a 2 × 2 × 2 factorial experiment. Qualifying ARI visits triggered each intervention. The interventions were: 1) Accountable Justifications: when prescribing an antibiotic for an ARI, clinicians are prompted to record an explicit justification that appears in the patient electronic health record (EHR); 2) Suggested Alternatives: through computerized clinical decision support, clinicians prescribing an antibiotic for an ARI receive a list of non-antibiotic treatment choices prior to completing the antibiotic prescription; and 3) Peer Comparison: each provider’s rate of inappropriate antibiotic prescribing relative to top-performing peers is provided periodically by email. All providers completed an on-line educational module about ARI treatment at the start of the intervention period. The primary outcome was the rate of antibiotic prescribing for visits with an ARI diagnosis for which antibiotics are not indicated (e.g. acute bronchitis, unspecified upper respiratory infection). Secondary endpoints were prescribing rates for acute sinusitis or pharyngitis, and prescribing rates for all other respiratory infections or symptoms of respiratory infection. We excluded patients with major comorbidities (e.g., COPD, cirrhosis) or a concomitant diagnosis that suggested a non-respiratory-tract bacterial infection (e.g., cystitis). EHR-data was used to measure outcomes during the year prior to and during a 1-year intervention period. We used mixed models to assess intervention effects accounting for fixed effects for patient age and providers’ prior prescription rate and random provider effects.
RESULTS: 28 of 38 providers participated. Antibiotic prescribing fell in the intervention year for non-antibiotic-appropriate ARI diagnoses (from 24.7 to 4.6 %), for sinusitis/pharyngitis (from 45.1 to 35.1 %), and for all other respiratory diagnoses or symptoms of infection (43.5 to 31.5 %; all p < 0.001). There were no significant differences in the primary outcome for any of the interventions. Suggested Alternatives led to a lower odds of antibiotic prescribing for sinusitis/pharyngitis, odd ratio (OR) 0.35, (95 % confidence interval [CI] 0.22–0.58); and for all respiratory visits combined (OR 0.72 [95 % CI 0.54–0.96]). Peer comparisons led to lower odds of antibiotic prescribing for all respiratory visits combined (OR 0.73 [95 % CI 0.53–0.995]). There was no increase in the proportion of total ARI visits within the potentially antibiotic appropriate category or other ARI diagnosis/symptom category.
CONCLUSIONS: The conduct of this study had a large impact on antibiotic prescribing behavior. Given the moderately low baseline rate and the possible Hawthorne effect, the prescribing rate for the primary outcome may have reached a floor below which adding additional interventions could not reduce it further. Since this was a single site, this widespread decline in prescribing may have been due communication between intervention and control group providers that led to attitudinal or cultural changes more broadly within the practice. Evidence of gaming the system (e.g., changing diagnosis codes to make antibiotic prescribing appear more appropriate) was not observed. An ongoing, larger, practice-randomized trial will help elucidate the effects of these interventions on provider behavior.
BETTER INFORMED PATIENTS ARE LESS LIKELY TO CHOOSE PERCUTANEOUS CORONARY INTERVENTION FOR STABLE ANGINAMichael B. Rothberg1; Senthil K. Sivalingam2; Reva Kleppel2; Bo Hu1; Marc Schweiger2. 1Cleveland Clinic, Cleveland, OH; 2Baystate Medical Center, Springfield, MA. (Tracking ID #1937449)
BACKGROUND: Patients with chronic stable angina often believe that percutaneous coronary intervention (PCI) will prevent a myocardial infarction or extend life, even though their cardiologists do not believe this. The extent to which cardiologists contribute to this misperception is unknown. One possibility is that patients do not recieve complete information about the procedure. We reviewed consent conversations to assess the level of informed decision making and its association with choosing to have PCI.
METHODS: Using the Verilogue Point-of-Practice Database, which includes visits with >600 physicians in nine geographic regions throughout the U.S., we searched outpatient/non-acute visit transcripts audio-taped between August 2008 and August 2012 for mention of PCI, cardiac catheterization, angiogram or stent placement. We limited transcripts selected to those that included consent discussions with a cardiologist. Two investigators reviewed each transcript to identify the 7 elements of decision making required for a complex medical decision, using the framework developed by Braddock, et. al. The 7 elements include discussion of the 1) patient’s role in decision making, 2) nature of the decision 3) the alternatives 4) pros and cons of the alternatives 5) uncertainties associated with the decision 6) assessment of the patient’s understanding and 7) exploration of patient preference. We also assessed the cardiologists’ recommendation and the patient’s decision regarding catheterization and PCI (cath/PCI). Because these procedures are usually done at the same time, patients give consent for both procedures at once. We assessed the association between the decision to undergo cath/PCI and specific elements of informed decision making, angina severity, and physician recommendation. Finally, we assessed the association between completeness of informed decision making, defined as the number of elements of informed decision making present in the conversation, and the patient’s decision to undergo cath/PCI in a logistic regression model.
RESULTS: The final dataset included 27 cardiologists in conversations with 60 patients (median two patients per cardiologist, range 1 to 6). Cardiologists were all male, had been in practice for an average of 20.5 years (range 8 to 34), and 2/3 belonged to a private office-based group practice. Mean patient age was 66 years, 70 % were male and 75 % were white. Of the 60 discussions, 4 (7 %) included all 7 elements of informed decision making; 28 % met a more restricted definition of procedure, alternatives and risks. In just over half (52 %) there was some discussion of the patient’s role in decision making. Discussion of the clinical issue was present in 97 % of discussions, but discussion of alternatives (27 %) and uncertainties (10 %) were uncommon. Assessment of patient understanding and exploration of preferences each occurred in 65 % and 73 % cases, respectively. At the end of the visit, 44 (73 %) patients chose to undergo PCI. Physicians made recommendations in 49 cases and patients followed the recommendations in 90 % of cases. In univariate analysis, the proportion of patients choosing cath/PCI was lower when there was discussion of 1) uncertainty associated with the decision (17 % vs. 80 %, p < 0.01), 2) the patient’s role in decision making (61 % vs. 86 %, p = 0.03), and 3) discussion of the alternatives (31 % vs. 89 %, p = <0.01). The proportion choosing cath/PCI was lower, but not statistically so, when the physician assessed patient understanding (67 % vs. 86 %, p = 0.11) and explored patient preference (68 % vs. 88 %, p = 0.13). Anginal symptoms were present in 81 % of patients, but limited activity in only 28 % of patients. Presence of symptoms was not statistically associated with choosing cath/PCI (p = 0.44), but patients whose symptoms limited activity were more likely to choose cath/PCI (94 % vs. 71 %, p = 0.06). In multivariable analysis, better informed patients were more likely to choose not to undergo cath/PCI (OR = 2.7 for each additional element of informed decision making, 95 % CI 1.2 to 6.2, p = 0.02).
CONCLUSIONS: In consent conversations between cardiologists and patients with stable angina, informed decision making is often incomplete. More complete discussions are associated with patients choosing not to undergo cath/PCI. Efforts to involve patients in shared decision making for cath/PCI might also reduce resource utilization.
BLOOD PRESSURE CONTROL IN DIABETIC PATIENTS AT FEDERALLY QUALIFIED HEALTH CENTERS: THE IMPACT OF OFFICE-GUIDELINES APPLIED TO PRACTICE (OFFICE-GAP) PROGRAMAde B. Olomu1; Bikki Gautam1; Bethany Buda1; Wei-Wen Hsu3; Gurpreet Chahal1; David Todem2; Alexis Therman1; Esha R. Kumar1; Margaret Holmes-Rovner4. 1Michigan State University, East Lansing, MI; 2Michigan State University, East Lansing, MI; 3Michigan State University, East Lansing, MI; 4Michigan State University, East Lansing, MI. (Tracking ID #1932917)
BACKGROUND: The most important intervention for preventing death and adverse cardiovascular (CVD) outcomes is adequate control of blood pressure (BP) in diabetic (DM) patients. Unfortunately, diabetic patients with hypertension (HTN) are often not adequately controlled and HTN management is less intensive in patients with DM. HTN is particularly burdensome in low-income groups, where the prevalence of uncontrolled HTN is higher than the general population. Federally Qualified Health Centers (FQHCs) provide care for low income and medically underserved populations. Objectives: 1) to determine the rate and predictors of Blood Pressure (BP) control in patients with DM and HTN in FQHCs. 2) determine the impact of a CVD secondary prevention intervention- Office Guidelines Applied to Practice (Office-GAP) Program on BP control in FQHCs.
METHODS: The Office-GAP study is a two-center intervention and control study designed to improve cardiovascular care for minority and low-income populations in outpatient clinical settings. Intervention included provider training, patient education in a group visit, and use of Office-GAP tools/checklist and patient decision aids during office visits. After a group visit, patients followed up with physician visits using GAP tools. We performed chart abstraction of all patients with HTN, CVD and/or DM from September 2010 to Dec 2012 in 2 FQHCs. Hypertension was defined as Systolic BP > 140 mmHg (>130 mmHg in DM patients) and diastolic BP > 90 mmHg (>80 mmHg in DM patients). Multivariable logistic Regression was used to identify potential predictors of BP control.
RESULTS: Of 242 patients identified, 188 had DM, and 191 had HTN, 146 had HTN and Diabetes. One hundred patients were in the intervention (Office- GAP) arm and 142 in the control arm. At baseline, 32.79 % (60/183) and 26.76 % (38/142) of all patients with HTN without diabetes and HTN patients with DM had their BP controlled respectively. We found that diabetic patients enrolled in the Office GAP Intervention were more likely to have their BP controlled at 6 months (OR = 2.70, p = 0.048) compared to control patients after adjusting for relevant clinical variables. In addition, the logistic regression model revealed that whites (OR 2.6, p = <0.001) and other races (Hispanics, Nepalese, Somali) (OR = 1.685, p = 0.031) were more likely to have their BP controlled compared to black patients. Furthermore, older age (OR 0.98, p = 0.014) and patients with higher Charlson Index (OR 0.85, p = 0.002) were found to be marginally less likely to have their BP controlled.
CONCLUSIONS: We found that the majority of patients attending FQHCs do not have their BP controlled. BP control among diabetics was substantially less frequent than in nondiabetic patients. Black patients were less likely to have their BP controlled compared to other races. The Office-GAP Intervention improved rates of BP control for diabetic patients in FQHCs. The Office-GAP Program could serve as a model for improving care for patients in outpatient clinical settings. Further studies are needed to determine the effectiveness and cost-effectiveness of this approach.
BUILDING COMMUNITY TRUST THROUGH QUALITY ASSURANCE OF MALARIA DIAGNOSIS AND MANAGEMENT AT A RURAL CLINIC IN UGANDASae-Rom Chae1; Toni Biskup2; Sara Heinert2; Janet Lin2,3. 1University of Illinois at Chicago College of Medicine, Chicago, IL; 2University of Illinois at Chicago College of Medicine, Chicago, IL; 3University of Illinois at Chicago School of Public Health, Chicago, IL. (Tracking ID #1933920)
BACKGROUND: At a rural primary care clinic in Uganda, a patient survey indicated that the community members feel it provides a high, trustworthy quality of care. However, no quality assurance studies have been conducted to characterize the quality of care provided. Malaria remains a leading cause of morbidity and mortality in Uganda. Widespread efforts have been made by the public sector to build capacity in diagnosis and treatment of the disease. This study aims to evaluate the quality of care provided by the clinic by examining malaria diagnosis and treatment patterns and assessing the degree of adherence by the clinic staff to national malaria treatment guidelines. Study objectives: 1. Determine how malaria is being diagnosed and consequently managed among a sample of a Ugandan rural clinic patient population. 2. Assess diagnostic methods and appropriate classification of severity of disease. 3. Evaluate malaria treatment regimens as appropriate based on 2012 Ugandan treatment guidelines. 4. Consider the quality of malaria care provided and whether the clinic is providing trustworthy care to the community.
METHODS: A retrospective chart review of patients seen at a rural clinic in Uganda in a 12-month period from June 2012–June 2013 was conducted to determine the rates of appropriate diagnosis and treatment of malaria. All patients with blood smears done on a Monday, Wednesday, or Friday were included. De-identified data on demographics, presenting symptoms, given diagnoses, medications, blood smear results, and notes on management decisions was recorded in a database. Variables were then coded numerically for each record and a second individual re-coded 10 % of the charts for verification. After excluding charts with missing data points, a final sample of 1001 patients was analyzed using SAS and Microsoft Excel.
RESULTS: Of the total 390 positive blood smears, only three patients (0.8 %) were not started on malaria medication. Of patients documented to have a negative smear (572 or 57.1 %), 83 (14.5 %) were started on malaria treatment. 198 (50.8 %) of the positive smears were among adult patients above the age of 17 years, three of which showed hyperparasitemia. Of these, 1 was referred for higher level care, 1 was started on second-line quinine treatment, and the third was started on alternative first-line treatment. Five patients that were documented to have a diagnosis of malaria and a presenting symptom of seizures, qualifying them as severely ill, were not started on parenteral treatment or referred for higher-level care. Of the total 21 patients started on second-line quinine-based treatment, 11 (52.4 %) had a documented and appropriate indication. Of all patients documented to have a positive smear and placed on appropriate malaria treatment, 7 (1.8 %) were concurrently started on an antibiotic (i.e. doxycycline, clindamycin), documented as malaria treatment.
CONCLUSIONS: Overall, clinic staff demonstrate a heightened index of suspicion for malaria infection, appropriate for a highly endemic area. Nearly all patients with positive diagnostic tests were started on treatment. A small number were started on empiric treatment despite a negative test. Investigating the reasons for this would be worthwhile in order to prevent over-treatment. Most of the patients experiencing serious, complicated malarial disease, including those with hyperparasitemia, were not treated according to national guidelines with intravenous quinine. Further training may be needed in identifying and documenting cases of severe malarial illness and the appropriate management sequence. This may significantly impact mortality and morbidity. A knowledge assessment of the staff informed by detailed chart reviews and process mapping in the future may be helpful in delineating where intervention might be the most suitable. Additionally, second-line treatment is being over-prescribed or indications are not adequately documented. If the former is occurring, this may affect drug resistance patterns in an unfavorable manner. Lastly, antibiotic regimens are being prescribed to supplement malaria treatments which warrants additional investigation. Without appropriate indication, this practice may contribute to antimicrobial resistance and unnecessary medication side effects. The national guidelines do not discuss the indications for concurrent antibiotic treatment. In summary, improvement is needed in the areas of classifying severity of malarial illness and consequent management, indications for the various types of treatment, and possible bacterial co-infection with indication for additional treatment.
BUILDING EQUITY IMPROVEMENT INTO QUALITY IMPROVEMENT: REDUCING SOCIOECONOMIC DISPARITIES IN COLORECTAL CANCER SCREENING AS PART OF POPULATION HEALTH MANAGEMENTSeth A. Berkowitz1; Sanja Percac-Lima1; Jeffrey M. Ashburner1; Yuchiao Chang1; Adrian Zai1; Wei He1; Richard W. Grant2; Steven J. Atlas1. 1MGH, Boston, MA; 2Kaiser Permanente, Oakland, CA. (Tracking ID #1921347)
BACKGROUND: Improving colorectal cancer (CRC) screening rates for patients from socioeconomically disadvantaged backgrounds is a recognized public health priority. We tested the hypothesis that implementation of a system-wide screening intervention could increase overall screening rates while also decreasing screening disparities.
METHODS: In June 2011, we implemented the Technology for Optimizing Population Care (TopCare) intervention to improve CRC screening for all eligible patients in our 18-practice primary care network. The TopCare intervention system electronically identifies patients overdue for screening and contacts them by letter or telephone scheduler, with or without physician involvement. Patients identified by automated algorithm as high risk for non-completion are entered into a more intensive program of patient navigation. Using ≤high school (HS) diploma as our marker for socioeconomic disadvantage, we investigated whether baseline differences in CRC screening completion rates between ≤HS diploma vs. >HS diploma patients narrowed after implementation of TopCare. We used an interrupted time series analysis to compare monthly CRC screening completion rate disparities in the 2 years prior to implementation (June 15, 2009–June 14, 2011) and 1 year after implementation (June 15, 2011–June 14, 2012).
RESULTS: At the beginning of the study period, 71 % of 52,011 eligible patients had completed screening, while by the end 74 % of 54,572 eligible patients had completed screening (p < .001). Although CRC screening completion remained higher in >HS diploma vs. ≤HS diploma patients in June 2009 (74 % vs. 66 %, p < .001) and June 2012 (77 % vs. 70 %, p < .001), the difference in screening rates decreased from 8.6 to 7.3 % over this 3-year period (Figure). In our interrupted time series analysis accounting for secular trends, the introduction of TopCare was associated with a significant decrease in the CRC screening disparity (p < .001). The decrease represents approximately 150 more ≤HS diploma patients with complete CRC screening each month than without the intervention, an improvement that would have taken approximately 27 additional months to occur had pre-intervention trends continued.
CONCLUSIONS: A multifaceted population management intervention sensitive to the needs of vulnerable patients narrowed disparities in CRC screening while also increasing overall screening rates. Embedding interventions for vulnerable patients within larger population-based systems represents an effective approach to increasing overall care quality while simultaneously decreasing disparities.
BUILDING THE INFRASTRUCTURE TO SUPPORT ACCOUNTABLE CARE PAYMENT MODELS: LESSONS FROM THE FIELDMaria Han1; M. Susan Ridgely2; Cheryl Damberg2. 1UCLA, Los Angeles, CA; 2RAND, Santa Monica, CA. (Tracking ID #1940916)
BACKGROUND: The accountable care organization (ACO) is a novel payment and delivery system innovation aimed at improving value in health care. As hundreds of healthcare organizations have entered into ACO contracts, they have had to make significant structural and organizational changes, including expanding capabilities to deliver population-based care and forging integrated provider relationships. Despite the scale and complexity of the changes required in transitioning to the ACO model, there is little known or reported about how to optimally design an ACO. Given the substantial investment and risk associated with ACO formation, the future success of the ACO movement will require effectively capturing, disseminating, and replicating the lessons learned by early ACOs. To that end, the objective of this study is to delineate the major types of innovations implemented by provider organizations in their endeavors to become successful ACOs.
METHODS: The accountable care organization (ACO) is a novel payment and delivery system innovation aimed at improving value in health care. As hundreds of healthcare organizations have entered into ACO contracts, they have had to make significant structural and organizational changes, including expanding capabilities to deliver population-based care and forging integrated provider relationships. Despite the scale and complexity of the changes required in transitioning to the ACO model, there is little known or reported about how to optimally design an ACO. Given the substantial investment and risk associated with ACO formation, the future success of the ACO movement will require effectively capturing, disseminating, and replicating the lessons learned by early ACOs. To that end, the objective of this study is to delineate the major types of innovations implemented by provider organizations in their endeavors to become successful ACOs.
RESULTS: One-year following grant funding, eight of the 18 organizations had implemented interventions aimed at redesigning clinical care (the remaining grantees focused on building IT infrastructure). While organizations executed a diversity of interventions in care redesign, most of them focused on delivering care that was increasingly coordinated, team-based, and patient-centered. Almost all (7/8) of the grantees instituted programs to improve care coordination, particularly across patient transitions. Six of the grantees implemented team-based care approaches, including utilization of physician extenders, development of disease-oriented teams, and implementation of the patient-centered medical home model. Finally, all of the organizations emphasized patient-centered care through the promotion of patient education initiatives, group appointments, extended office hours, and social needs assessments.
CONCLUSIONS: Many health systems currently face the challenge of moving the ACO from a theoretical concept to an “on the ground” reality. While “nascent” ACOs have experimented with hundreds of unique approaches to ACO development, this study is one of few reports on their experiences and common themes in implementation. As such, the findings of this study may prove useful in understanding what infrastructure investments will create the right capabilities for delivering accountable care.
BUYING TIME: QUALITY IMPROVEMENT PROJECT TO DECREASE PATIENT CALLS FOR MEDICATION REFILLS IN A RESIDENT RUN CONTINUITY CLINICAmanda Lerner1,2; Shveta Gandhi1,2; Diane Resnick1; John T. Connor1; Rowena Garcia1; Laurie Hudson-Bonner1; Joann Sabados-Carolina1; Andrea Palisi1; Michael P. Carson1,2. 1Jersey Shore University Medical Center, Neptune, NJ; 2Rutgers-Robert Wood Johnson Medical School, Piscataway, NJ. (Tracking ID #1913297)
BACKGROUND: The resident run continuity clinic noted a large volume of calls/faxes for medication refill requests, and we estimated that each required a minimum of 15 min of staff time to complete. In addition, running out of medication poses a potential risk to patient well-being. Objectives: utilize the Plan-Do-Check-Act quality improvement process to quantify and identify Refill Request patterns, develop an education plan, and assess the efficacy of the plan to reduce these requests/improve patient safety.
METHODS: Pre-Education Data: Nurses logged each Refill Request over 3 months noting time since the last office visit, and method of request (patient walking in, patient/pharmacy call to the prescription line vs. main clinic number, pharmacy fax to one of two machines). An action plan was developed and disseminated to the practitioners. Four months later, a second assessment was completed (Post-Education Reassessment).
RESULTS: Pre-Education Data: 17.8 Refill Requests/day (765/43 days). Patients typically return after 12–24 weeks, but 61 % of the requests were received within 8 weeks of a patient’s last visit suggesting physicians were not providing enough refills. Twenty-five percent were due to patients missing visits, and 7 % were to clarify/correct a prescription. Pharmacies generated eight messages per day, and sent 278 faxes. Action Plan: Caregivers were instructed to objectively confirm remaining refills (view pill bottle, or review photocopy of the prior prescription in the chart), and provide enough refills until the next visit plus one extra month (“Month Plus 1” policy). Patients were advised to bring all bottles to each visit, and pharmacies were asked to fax all Requests to a single machine located in our clinic. Reassessment: 3.3 requests/day (110/33 days), an 81 % decrease in the averge volume of daily requests; only 10 % due to physician error and 64 % due to patient issues. Pharmacy calls dropped by 90 % to 33 (~1/day). Patient calls dropped from 3/day to 2/day. As we had 33 observations from the Post-Education phase, a matched analysis required us to use only 33 of the 43 Pre-Education observations. To avoid overestimating the effect, we first compared the 33 lowest Pre-Education data points to the Post-Education values yielding an average decrease of 6.2 requests/day [95 % CI (4,8)]. The analysis using the 33 highest Pre-Education values yielded a decrease of 19 requests/day [95 % CI (12,26)]. Estimating 15 min per Request, this the daily staff workload decreased by at least 1.5, and up to 4.8 h a day.
CONCLUSIONS: A simple caregiver and patient education program facilitated an 81 % decrease in the volume of calls/faxes for medication refills in this resident-run continuity clinic. Patients often told resident physicians they had refills remaining, however not enough to get them to the next visit. Therefore, objectively determining the number of refills and the “Month Plus 1” policy are likely responsible for the majority of the decrease, and they improve patient care by decreasing the chance that a patient will be without their medication. On average, the 14.5 fewer requests/day decreased the time burden on an already limited clinical staff by 3.6 h per day. The staff is satisfied, and a third survey confirmed patients missing visits as the primary reason for Refill Requests. Future efforts will focus on communicating with patients to improve attendance at scheduled visits.
CALLING “DR. GOOGLE”…: DOES TECHNOLOGY FILL THE GAP CREATED BY THE PRENATAL CARE VISIT STRUCTURE?Jennifer Kraschnewski1; Cynthia H. Chuang1; Erika Poole1; Tamara Peyton1; Ian Blubaugh1; Alyssa Feher2; Madhu Reddy1. 1Penn State Hershey Medical Center, Hershey, PA; 2Cumberland/Perry Tapestry of Health, Carlisle, PA. (Tracking ID #1936600)
BACKGROUND: The structure of prenatal care has changed little over the past several decades despite the rapid evolution of technology. Little is known about how pregnant women engage with technologies (e.g. websites, smartphone apps) and the interface between these tools and medical care, especially for women of lower socioeconomic status. We sought to understand the role of technology in pregnancy through a qualitative study with women enrolled in the Women, Infants and Children (WIC) program.
METHODS: We recruited pregnant women ages 18 and older who owned a smartphone at a WIC clinic in central Pennsylvania. Four focus groups were conducted with a total of 25 women. The focus group guide included questions about the positive experiences and challenges women encountered during their current pregnancy, sources of information, and whether they used their smartphones or other technology for pregnancy-related information. Sessions were audiotaped and transcribed. Two members of the research team independently analyzed each transcript, using a thematic analysis approach. Themes related to the topics discussed were identified, for which there was full agreement.
RESULTS: Three major themes emerged. First, the prenatal visit structure was not patient-centered. Women commented that the first visit occurs too late, with too few visits early in pregnancy, when women had the most questions for their doctors: ”…They expected me to wait 13 weeks until I had a conversation with my doctor.” “I know we can’t change the healthcare system… but on your first appointment, they say, ‘We’ll see you in 8 weeks…’ and uh… That’s 2 months! What am I going to do?” Even when women did see their doctor, the materials they received were viewed as unhelpful: “Today they gave me a whole bag of pamphlets and flyers and didn’t explain or go over them with me… and now I have to go home and try to go through them, while I have a kid running around… and when you’re a new mom, that’s overwhelming.” Second, women turned to technology to fill gaps, including using Google and smartphone applications (i.e. Babycenter): “I found myself using Dr. Google, because I couldn’t get an appointment until I was 14 weeks. They just wouldn’t see me.” Turning to technology was viewed to be a generational approach: “It’s interesting cause I think that the generation before us counted a lot on our mom and our sisters to give advice. And now it’s technology…“ Lastly, women reported that technology, although frequently used, was not without limitations: ”… so sometimes you can Google something, like when I was having my round ligament pain for the first time… some things that came up were terrifying… you want to go to the ER right away! You definitely have to be careful and smart about your Google searches.”
CONCLUSIONS: The current prenatal care visit structure is not patient-centered in that it does not allow women to seek advice when they want it the most. A generational shift has occurred, resulting in pregnant women turning to the Internet to fill this gap, which requires significant skills to navigate for useful information. Until systems-based changes are made to the prenatal care visit structure, primary care providers may be called on to assist our patients early in pregnancy seek the information they want and to become better consumers of pregnancy-related information on the Internet.
CAN AN IN-HOSPITAL CARE TRANSITION INTERVENTION IMPROVE PATIENT EXPERIENCE IN THE SAFETY NET? A RANDOMIZED CONTROLLED TRIALBrian Chan1; L. E. Goldman1; Urmimala Sarkar1; Michelle Schneidermann2; Jeffrey Critchfield2; Margot Kushel1. 1UCSF/SFGH, San Francisco, CA; 2UCSF/SFGH, San Francisco, CA. (Tracking ID #1937181)
BACKGROUND: Patient experience measures are important markers of quality, as evidenced by use of the Hospital Consumer Assessment of Healthcare Provider Scores (HCAHPS) and Care Transitions Measures (CTM-3) for hospital value-based purchasing reimbursement. Patient experience scores are lower in safety-net hospitals than non safety-net hospitals; this gap is widening. We assessed the effect of a nurse-led, language concordant, hospital-based care transition intervention on patient experience in older adults hospitalized at a safety-net hospital.
METHODS: We randomized, and stratified by language (English, Spanish or Chinese), 700 inpatients age 55 and older who were inpatients at an academic urban safety-net hospital. The intervention consisted of usual care and 1) inpatient visits by a language concordant nurse that provided individualized post-hospitalization education and 2) post-discharge phone calls by a nurse practitioner to reinforce the care plan and to address acute complaints. Language concordant research assistants, blinded to randomization group, measured HCAHPS nursing, physician, medication, and discharge information domains and CTM-3 scores at 30 days after hospital discharge.
RESULTS: Of 685 participants who survived to 30 days, 90 % (n = 617) completed follow-up research interviews. Mean age was 66 years; 24 % were African American; 19 % were White; 32 % were Asian and 19 % Latino. Over half (61 %) of interviews were conducted in English, 24 % in Chinese and 15 % in Spanish. Over a third of participants noted limited English proficiency, and 51 % met criteria for low health literacy. Study nurses spent an average of 157 min with the intervention participants. There were no statistically significant differences in mean HCAHP domain scores and CTM-3 scores between the intervention and control groups (Table 1); no significant differences were seen between groups when results were stratified by language.
CONCLUSIONS: The failure of a language concordant nurse-led intervention to improve patient experience scores suggests that these measures are difficult to improve using hospital-based interventions. Thus, caution should be exercised when linking hospital-based reimbursement to improved HCAHPS and CTM scores. Further work is necessary to identify interventions that can improve patient experience and care transitions measures.
Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Mean Domain and Care Transitions Measure (CTM-3) Scores assessed at 30 days
| HCAHP domains | Intervention Score out of 100 (standard error) Response number | Usual Care Score out of 100 (standard error) Response number | p-value* |
| Nurse communication | 90.0 (1.0) 291 | 89.0 (1.0) 302 | 0.35 |
| Doctor communication | 91.9 (1.0) 289 | 91.8 (.9) 299 | 0.60 |
| Communication about medicines | 72.3 (2.6) 161 | 75.7 (2.4) 170 | .34 |
| Communication about discharge | 82.9 (1.9) 284 | 78.0 (2.1) 289 | .11 |
| Intervention Score (standard error) Response number | Usual Care Score (standard error) Response number | p-value* | |
| CTM-3 Score | 80.5** (1.1) 286 | 78.5** (1.1) 291 | 0.18 |
| Took preferences into account when I left the hospital | 3.32† (.04) 286 | 3.29† (.04) 291 | .38 |
| Understanding of my responsibility when I left hospital | 3.46† (.04) 291 | 3.37† (.04) 300 | .06 |
| Understood the purpose for each of my medicines | 3.46† (.04) 291 | 3.40† (.04) 300 | .23 |
* wilcoxan rank sum statistic use to generate p-value ** overall CTM-3 score out of 100 † individual CTM-3 question score out of a total of 4
CAN PARTICIPATION IN COMMUNITY ENGAGEMENT ACTIVITIES REDUCE DISTRUST IN MEDICAL RESEARCHERS AMONG DIVERSE COMMUNITIES: RESULTS FROM THE COMMUNITY ENGAGEMENT AND RESEARCH PROGRAM OF THE UCLA CTSINazleen Bharmal1; Li-Jung Liang1; Sitaram Vangala1; Stefanie D. Vassar1; Ibrahima Sankare1; Loretta Jones2; Keith C. Norris1; Martin F. Shapiro1; Arleen Brown1. 1UCLA, Los Angeles, CA; 2Healthy African American Families II, Los Angeles, CA. (Tracking ID #1938942)
BACKGROUND: Racial/ethnic minorities are not adequately represented in medical research studies. One explanation, supported by scientific literature, is that distrust in research and the medical community may impede recruitment of racial/ethnic minorities into medical research studies. Among the goals of the UCLA Clinical and Translational Science Institute’s Community Engagement and Research Program (CERP) are to enhance the community’s trust in health research by promoting knowledge sharing between community and academia and strengthening both community and academic infrastructure for sustainable partnered research. To achieve these goals, the CERP has sponsored or co-sponsored a series of large symposia and smaller workshops on clinical research, public health topics, and community engagement. To assess levels of trust among community members who participate in CERP events, we surveyed attendees at every event held over a 14 month period.
METHODS: Between June 2012 and August 2013, participants at CERP events were asked to respond to four survey items: 1) “If a medical researcher asked you to participate in a medical research study, you trust that he/she would provide you with a full explanation of the study,” 2) “A medical researcher would not ask you to participate in a research study if he/she thought it would harm you,” 3) “If you participate in a medical research study, you trust that the medical researcher will make sure that you fully understand the consent form before you sign it,” and 4) “If you, or people in your community, choose to participate in medical research, do you feel that the medical researcher will always try to protect you from unnecessary risk?” The written items were self-administered in English or Spanish at the end of each event. The response choices, distributed across a 4 point Likert scale, were dichotomized as “strongly agree/agree” vs. “disagree/strongly disagree/don’t know.” We developed a distrust index with a score ranging from 0 to 4 as our main outcome measure. Only participants who responded to at least three of the four questions were assigned a distrust index score. Data from events was aggregated by the quarter of the year during which the event occurred. We compared distrust scores across all quarters using linear mixed-effects regression model, adjusted for participant’s demographic characteristics and accounting for heterogeneity of variance across types of community event. We present the estimated difference between the distrust index scores using model contrast for 2012 Q2 vs. 2013 Q3.
RESULTS: Over 14 Months, we administered 531 surveys; 468 respondents answered at least three of the four questions (response rate 88 %) at nine CTSI/CERP community conferences/workshops. The majority of participants were female (76 %); 49 % were ages 50 years or older; 13 % had a high school education or less; and 53 % were African American, 20 % Latino, 12 % White, 11 % Asian/Pacific Islander, and 4 % other race/ethnicity. The mean distrust score over the timeframe of CTSI/CERP workshops was 1.22 (standard deviation 1.29). The adjusted estimated mean distrust index score (± standard error) decreased from 2.19 ± 0.30 in 2012 Q2 to 1.05 ± 0.26 in 2013 Q3 (p = 0.0035). The estimated change in the distrust index score for African Americans from 2012 Q2 (mean ± SE: 2.34 ± 0.32) to 2013 Q3 (0.82 ± 0.26) was significant (p = 0.0002), but did not reach statistical significance for Latinos (1.56 ± 0.77 vs. 0.69 ± 0.30, p = 0.30), Whites (2.54 ± 0.56 vs. 2.93 ± 0.54, p = 0.62), and Asians (0.90 ± 0.62 vs. 1.23 ± 0.37, p = 0.65).
CONCLUSIONS: The multivariable analyses suggest that CTSI/CERP efforts to increase community engagement in research have been associated with a decrease in distrust in health research, especially among African American participants. These findings are observational and represent ecologic associations; thus our results may be biased by secular trends. Additional qualitative work is needed to better understand reasons for change in levels of distrust over time in these diverse communities as a result of the CTSI/CERP.
CAN THYROID BREAK YOUR HEART? ROLE OF THYROID IN TAKOTSUBO CARDIOMYOPATHY: A SINGLE CENTER RETROSPECTIVE STUDYSourabh Aggarwal; Vishal Gupta. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1940273)
BACKGROUND: Takotsubo cardiomyopathy (TC) is a transient systolic dysfunction of the apical and/or mid segments of the left ventricle that mimics myocardial infarction (MI) but in the absence of obstructive coronary artery disease. The exact etiology of TC is unclear. Few isolated case reports have described association of TC with hyperthyroid state. The exact association of thyroid status and TC has never been studied so far.
METHODS: This was a single center retrospective study. All the patients diagnosed with TC between January 2006 and December 2012 at our hospital were identified retrospectively. Mayo’s revised criteria for TC was used to confirm the diagnosis. Baseline paramenters including demographic profile, cardiac markers, thyroid studies, angiographic and echocardiographic findings were extracted and analysed using SPSSv19.0
RESULTS: Seventy eight patient were identified as diagnosed with TC with 72 females (92.3 %) and six males (7.6 %) with mean age of 66.33 ± 13.37 years (range 23–91). Stressful event precipitating TC was identified only in 19 patients (24.36 %) at the time of admission. Twenty seven patients (34.61 %) had history of hypothyroidism and 25 patients (31.05 %) were on levothyroxine replacement. Thyroid profile was available for 44 patients at the time of admission and five patients (11.36 %) were found to be in a hyperthyroid state based on low TSH and/or high freeT4. During a mean follow up of 2.8 ± 1.5 years, five patients (5.13 %) had episodes of recurrence. Mean length of stay (mLOS) was 4.4 ± 3.9 days (Median 3 days, Range 1–23 days). Both TSH level and ejection fraction had significant independent negative correlation with mLOS (p < 0.05).
CONCLUSIONS: Thyroid status/thyroid hormone replacement may have a significant role in the pathogenesis of TC. In this first retrospective study describing the association of TC with thyroid status, precipitating stress was identifiable in only 24 % patients whereas 35 % of the patients had a history of hypothyroidism with majority on levothyroxine replacement. Additionally, TSH level had an independent negative correlation with mLOS.
CARE FRAGMENTATION AND SURVIVAL FOR PATIENTS WITH STAGE III COLON CANCERTanvir Hussain1,2; Hsien-Yen Chang2; Christine M. Veenstra3; Craig E. Pollack1,2. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3University of Michigan Health Systems, Ann Arbor, MI. (Tracking ID #1939909)
BACKGROUND: Cancer care can be complex and fragmented, spanning many settings and providers. Though the Institute of Medicine cites fragmentation as a priority for improving cancer care, little is known about aspects of fragmentation that affect cancer outcomes. We examine two features which may have different implications for improving care delivery: receiving surgical and medical oncologic care from providers affiliated with different hospitals; and receiving care from a surgeon-oncologist pair who infrequently shares patients with one another. We focus on stage III colon cancer patients as guidelines recommend both surgery and chemotherapy.
METHODS: Patients with stage III colon cancer diagnosed between 2000 and 2005 were identified from SEER-Medicare data. Patients were assigned to their operative surgeon and the medical oncologist who billed for the plurality of their visits in the year following diagnosis. Surgeons and oncologists were linked to the hospital where they billed most for inpatient care. Patients were classified as experiencing “hospital fragmentation” if their surgeon and oncologist were assigned to different hospitals (versus the same hospital). We determined the number of patients each surgeon-oncologist pair shared; patients were classified as having “high patient-sharing” physicians if their oncologist and surgeon shared many patients (top quartile of the shared patients distribution versus lower three). Patient-sharing has been validated as a measure of collaboration and information exchange between physicians. Our primary outcome was all cause mortality (censor date 12/31/2007). Secondary outcomes included timely receipt of chemotherapy (9 months of diagnosis) and cost of care [total claims using MEDPAR (Part A), NCH (Part B), and Outsaf files)] in the 12 months following diagnosis. We used Cox proportional hazard and regression models, adjusted for patient demographics, socioeconomic status, comorbidities, SEER site; surgeon’s yearly procedure volume, oncologist patient panel size; and hospital characteristics (volume; NCI, for-profit, and academic status). Generalized estimating equations and robust standard errors were used to account for hierarchical data and clustering.
RESULTS: Our sample included 7443 patients. Median survival was 3.04 years. One-third (N = 2471) received care from surgeons and oncologists associated with different hospitals. No difference in morality was associated with hospital fragmentation (adjusted HR = 1.00, 95 % CI: 0.93–1.07). We observed an increased risk of death among patients whose surgeons and medical oncologists shared few patients (lower three quartiles of shared patients) compared to those whose doctors were in the top quartile (HR = 1.15, 1.06–1.25). No statistical interaction between the two predictors was noted in the final model (Wald’s test, p = 0.324). Neither hospital fragmentation nor patient-sharing predicted timely receipt of chemotherapy or 12 month costs of care.
CONCLUSIONS: Receiving care from physicians associated with the same hospital did not improve survival for stage III colon cancer patients, whereas receiving care from physicians sharing many patients with another did. These results suggest that efforts to improve care fragmentation need to examine the informal relationships between physicians that may be reflected by patient-sharing. Further, cancer survival, quality, and costs may not be improved by delivery redesign which addresses fragmentation solely by consolidating options for care to one institution.
CAUSES OF SHORT-TERM HOSPITAL MEDICINE READMISSIONS AT AN ACADEMIC MEDICAL CENTERKenton Smitherman; Brian Clay; Leslie Martin-Armstrong. UC San Diego Medical Center, San Diego, CA. (Tracking ID #1927644)
BACKGROUND: Health care continues to undergo significant changes. With the recent creation of the Hospital Readmission Reduction Program (HRRP) by the Centers for Medicare and Medicaid Services (CMS), financial penalties are being assessed to hospitals with high 30-day readmission rates for certain patient groups. Investigating reasons for readmissions could be important in identifying possible patterns and areas for improvement. The objective of this study was to identify the primary contributing cause for each of 341 short-term readmissions (within 7 days of discharge) to ten hospital medicine services at an academic medical center over the ten-month period from 4/1/2011 through 1/31/2012.
METHODS: The UC San Diego Health System includes two hospitals with a combined capacity of 552 beds. Use of a full-spectrum inpatient electronic medical record (EMR) began on February 27, 2011 (a system-wide outpatient EMR was already in place). During the period of April 2011 through January 2012, there were 5,789 admissions to the hospital medicine services. From this total, 341 were readmissions within 7 days. These readmission cases were retrospectively reviewed by two members of the Division of Hospital Medicine to determine the primary factor causing each patient’s readmission. Patient, health system, and physician factors were considered. Patient factors included: (a) exacerbation of chronic illness, (b) new/separate diagnosis, (c) noncompliance with medication or other therapy, (d) noncompliance with outpatient follow up, and (e) patient not responding to reasonable medication or other therapeutic plan. Health system factors were: (a) lack of timely available outpatient follow up appointment, and (b) inability to provide medication or other therapy in the outpatient setting or at a lower level of care. Physician factors included: (a) discharge with inappropriate medications or therapy, (b) incorrect or incomplete diagnosis (excluding cases when further workup in the outpatient setting was planned), and (c) complication of a procedure or therapy instituted during the preceding hospitalization.
RESULTS: Case review showed that most (95 %) short-term readmissions resulted from patient factors: 42 % of cases were due to exacerbations of chronic illness, 29 % were due to new or separate diagnoses, none were shown to be due to noncompliance with follow up (these readmissions were within 7 days of discharge), and 10 % were due to patients not responding to reasonable medication or other therapy. The health system factor of inability to provide medication or other therapy in the outpatient setting or at a lower level of care was deemed the primary cause of readmission in 1 % of cases. Importantly, physician factors were the primary cause of readmission in 13, or 4 %, of the cases: 2 readmissions were due to discharge with inappropriate medications or therapy, 5 readmissions were due to incorrect or incomplete diagnosis, and 6 readmissions were the result of a complication of a procedure or therapy instituted during the preceding hospitalization. Additionally, in this 341 case cohort, 16 % of the readmission cases involved patients with chronic liver disease, and 8 % of the cases involved patients who were homeless.
CONCLUSIONS: Most short-term readmissions to our hospital medicine services are due to patient factors. Health system and physician factors were identified as causes of readmissions in only 5 % of cases. Penalizing hospitals with higher readmission rates may not be a proper tool for decreasing hospital readmissions within 7 days of discharge.
CHALLENGES TO INCREASING ACCESS AND CONTINUITY IN A LARGE ACADEMIC MEDICAL CENTER IMPLEMENTING PCMHClaire Robinson1; Molly Harrod1; Jane Forman1; Ann-Marie Rosland1,2; Adam Tremblay1,2; Eve A. Kerr1,2. 1VA Ann Arbor Health Care System, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1937578)
BACKGROUND: A core goal of the patient-centered medical home (PCMH) model is to increase timely access to primary care while maintaining patient-provider continuity. While definitions of access vary, it is often operationalized as receiving a same-day appointment with the patient’s usual provider. For example, the Department of Veterans Affairs (VA) has implemented a national performance measure examining receipt of same-day appointments with the patient’s usual primary care provider (PCP). Large academic primary care clinics face unique challenges in providing prompt access to a patient’s usual provider, particularly because many of these clinics are staffed by providers and residents who are in the clinic only a few hours each week (‘part-time providers’). We examined factors affecting efforts to increase prompt access and provider continuity in a large VA academic medical center that was in the process of implementing PCMH. Among the medical center’s 78 PCPs, 59 were available in clinic half-time or less. We have previously shown that part-time providers at this medical center were less likely to meet the national access measure.
METHODS: We conducted 20 semi-structured interviews with primary care staff (physicians, residents, registered nurses, licensed practical nurses, and clerks), roughly one and a half years into PCMH implementation. We also observed more than 25 h of coaching sessions designed to help newly formed primary care teams redesign their delivery processes to improve their access and continuity measures. We coded interview transcripts and coaching observation field notes with descriptive, non-hierarchical, grounded codes that emerged from the data and developed findings via group consensus.
RESULTS: We conducted 20 semi-structured interviews with primary care staff (physicians, residents, registered nurses, licensed practical nurses, and clerks), roughly one and a half years into PCMH implementation. We also observed more than 25 h of coaching sessions designed to help newly formed primary care teams redesign their delivery processes to improve their access and continuity measures. We coded interview transcripts and coaching observation field notes with descriptive, non-hierarchical, grounded codes that emerged from the data and developed findings via group consensus.
CONCLUSIONS: The large number of part-time primary care providers and residents combined with the large volume of patients made same-day access with the patient’s usual PCP challenging. Increased flexibility to schedule non face-to-face visits during part-time PCP’s non-clinical duties could help improve access. However, strategies that promote a team approach to access are likely the only long-term solution if we are to improve access while continuing to support providers who choose or need to work part-time. More information is needed on patient needs and preferences for prompt access and continuity in academic environments, so these new strategies can be tailored to patient-centered goals.
CHARACTERISTICS OF PERSISTENT EMERGENCY DEPARTMENT HIGH UTILIZERS IN A LARGE PRIMARY CARE PRACTICE-BASED RESEARCH NETWORKAndrew S. Hwang1; Shan W. Liu2; Carine Yelibi3; Jeffrey M. Ashburner3; Wei He3; Brandon Auerbach3; Steven J. Atlas3; Clemens S. Hong3. 1Tufts University School of Medicine, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Boston, MA. (Tracking ID #1934654)
BACKGROUND: A small percentage of high-utilizing patients account for a disproportionate share of emergency department (ED) visits. Understanding the characteristics of persistent high-utilizers may allow for more effective design of interventions to reduce ED utilization and costs.
METHODS: We performed a cohort analysis to study ED high-utilizers among 161,707 patients receiving care in a large primary care practice-based research network (PBRN) between 2005 and 2007. We identified all PBRN patients who visited the ED ≥4 times in 2007, and divided them into 2 groups: 1) patients who also made ≥4 ED visits between 2005 and 2006 (persistent users) and 2) patients who made <4 ED visits between 2005 and 2006 (non-persistent users). We compared the following characteristics in the two groups: demographic characteristics, chronic conditions, behavioral health problems, count of electronic medication prescriptions (e-prescriptions), and past healthcare utilization (between 2005 and 2007). We used Poisson regression models to assess the association between persistent ED high-utilization and subsequent ED visits and hospitalizations over 5 years (2008–2012) using a “change-in-estimate” strategy, where we included potential covariates (marriage status, insurance, language, chronic conditions, behavioral health problems, count of e-prescriptions, and past healthcare utilization) in the models if they altered the incidence rate ratio (RR) by >5 %.
RESULTS: Among 697 patients with ≥4 ED visits in 2007, 276 (40 %) were persistent users. Compared to non-persistent users, persistent users were significantly (p < 0.01 for all) more likely to be unmarried (80 % vs. 70 %) and English speaking (93 % vs. 87 %), have non-commercial insurance (81 % vs. 68 %), or have a diagnosis of coronary artery disease (26 % vs. 17 %), chronic obstructive pulmonary disease (49 % vs. 38 %), congestive heart failure (50 % vs. 40 %), chronic pain (18 % vs. 10 %), depression (16 % vs. 8 %), bipolar disorder (18 % vs. 11 %), psychosis (44 % vs. 27 %), or alcohol- (34 % vs. 17 %) or drug-related problems (37 % vs. 21 %). Persistent users also received a higher total number of e-prescriptions over 3 years (53 vs. 40) and were more likely to be e-prescribed narcotics (88 % vs. 77 %), benzodiazepines (83 % vs. 69 %), anti-psychotics (55 % vs. 36 %), and medications for depression/anxiety (64 % vs. 50 %) or smoking cessation (24 % vs. 16 %). Compared to non-persistent users, persistent users had higher rates of missed primary care appointments (19 % vs. 14 %), and higher unadjusted rates of acute care utilization (2,685 vs. 1,134 ED visits/1,000 patients/year and 1,822 vs. 934 admissions/1,000 patients/year) in the prior 3 years (2005–2007). Compared to non-persistent users, persistent users also had higher unadjusted rates of acute care utilization (2,030 vs. 1,483 ED visits/1,000 patients/year and 892 vs. 440 admissions/1,000 patients/year) over the subsequent 5 years. Adjusting for prior ED visits and hospitalizations, compared to non-persistent users, persistent users had a higher rate of subsequent hospitalization (adjusted RR 1.33 [1.08–1.65]), but not a higher rate of subsequent ED visits (adjusted RR 1.31 [0.93–1.84]). Including all covariates in the models changed the overall effects by less than 4 % for both outcomes without changing effect direction or significance.
CONCLUSIONS: Compared to non-persistent ED high-utilizing patients, persistent ED high-utilizing patients are more medically and psychosocially complex and have a higher risk of future hospitalization. Persistent ED high-utilizers represent an important target for intervention to improve quality and reduce costs. Such efforts will likely require intensive, multidisciplinary, care management approaches.
CHARACTERIZATION AND LACK OF PLANNING FOR ADVANCED LIFE EVENTS AMONG OLDER ADULTSLee Lindquist1; Priya Sunkara1; Vanessa Ramirez-Zohfeld1; Chris Forcucci2; Megan Huisingh-Scheetz3; Kenzie A. Cameron1. 1Northwestern University Feinberg School of Medicine, Chicago, IL; 2Aging and In-Home Services, Fort Wayne, IN; 3University of Chicago, Chicago, IL. (Tracking ID #1939204)
BACKGROUND: Despite older adults’ wish to remain independent in their own homes, critical health and life events occur that impede their ability to do so. A lack of information exists on what these advanced life events (ALE) entail and the advanced planning older adults perceive is necessary.
METHODS: We conducted focus groups with older adults living in community and independent living facilities in rural, suburban, and urban locales. Subjects were asked to discuss their future living plans and events/experiences that might impact their ability to remain in their own home. Focus group questions also elicited if subjects had planned for, discussed with others (e.g. spouse, offspring), or acted on these plans if one of these advanced life events occurred to them. Content analysis and constant comparative analysis was used to analyze the results.
RESULTS: Across all sites, 68 older adults participated in the focus groups with a mean age of 73.9 years (SD = 6.53); 50 (73.5 %) were female. Analysis revealed older adults perceived several major advanced life events impacted a senior’s ability to remain in their own home: 1) Hospitalization or Serious Illness, 2) Functional Loss 3) Cognitive loss, 4) Spousal death. Subjects voiced experiences with each of these events in multiple forms (e.g. self, spouse, friend, relative). However, very few perceived these events would occur to them, “I’ve decided I’m not going to get Alzheimer’s!” Planning for these events were almost non-existent as many older adult subjects felt that they were too sick or too healthy to look forward. “I’m on borrowed time. So I’m not going to worry about where I’m going to go for my old age because I don’t think I’m going to have one.”,“The new 70 is the old 58!” A number of seniors also felt that offspring would handle it for them although, many subjects stated that they had not discussed current or future needs with their offspring. While many subjects voiced that they had completed end-of-life documentation, including powers of attorney, living wills, obituary/funeral requests, there was a lack of advanced planning for life events that have a high likelihood of occurring to seniors.
CONCLUSIONS: Helping seniors to create plans for Advanced Life Events (e.g. hospitalization, cognitive loss, functional loss) is important as it provides seniors a voice in their future while including key stakeholders (e.g. offspring, spouse). It is well known that these ALEs have a high propensity for occurring with age. Ongoing research will create and test a planning tool that will assist older adults in being prepared for their needs during these events. By planning for—instead of reacting to—ALEs, older adults may be able to remain in their own homes safer and longer.
CHILDREN: A BARRIER TO MATERNAL HEALTH CARE UTILIZATION?Christina Pham2; Johannes R. Kratz1; Danny McCormick2. 1Massachusetts General Hospital, Cambridge, MA; 2Harvard Medical School/Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1936573)
BACKGROUND: Prior studies have demonstrated that women with children are at higher risk for obesity, metabolic syndrome, cardiovascular disease, depression, and all-cause mortality than women without children. No prior studies have examined the impact of having a young child on a mother’s utilization of primary, specialty and preventive care that could mediate these disparities.
METHODS: We analyzed cumulative data from 5 years (2008–2012) of the National Health Interview Survey (NHIS). The NHIS is a representative nationwide sample of households conducted annually by the Centers for Disease Control and Prevention (CDC) though face-to-face in home interviews. The study sample included women age 60 or younger who answered the Family, Person, and Sample Adult surveys (57,746). The NHIS collects data on the number of children under the age of 18 at home, age, income, race/ethnicity, education level, employment status, and health insurance. The primary outcome of this study was having a visit to a primary care physician in the preceding year. Secondary outcomes included visits to a medical specialist or Ob/Gyn in the past year as well as basic health preventative care such as blood pressure checks, cholesterol checks, tetanus shots, mammograms, and Pap smears in the past year. The primary predictor variable was having one or more children under the age of 18 in the home. A total of 27,918 (48.4 %) patients had children under the age of 18; 29,828 (51.6 %) did not. We used multivariable logistic regression models to test associations between predictor and outcome variables while controlling for age, income, race/ethnicity, education level, employment status, and health insurance.
RESULTS: The mean age of the patients was 36.3 and 42.3 for patients with and without children. When adjusted for age, income, race, educational level, employment status, and health insurance, patients who had children under the age of 18 had a 12 % lower odds of having a PCP visit in the preceding year (OR = 0.88 [95 % CI, 0.85–0.92]; P < 0.001) and a 27 % lower odds of having seen a medical specialist (OR = 0.73 [95 % CI, 0.70–0.76]; P < 0.001) in the past year. Patients with children under the age of 18 also had a lower odds of receiving basic health screening such as blood pressure checks (OR = 0.90 [95 % CI, 0.83–0.97]; P = 0.009), cholesterol checks (OR = 0.91 [95 % CI, 0.86–0.96]; P = 0.003), tetanus shots (OR = 0.94 [95 % CI, 0.90–0.97]; P = 0.001), and mammograms (OR = 0.85 [95 % CI, 0.79–0.92]; P < 0.001). In contrast, women with children had a higher odds of visiting an Ob/Gyn (OR = 1.22 [95 % CI, 1.18–1.27]; P < 0.001) and of having received a Pap smear (OR = 1.29 [95 % CI, 1.22–1.37]; P < 0.001) in the past year. Decreased health care utilization was not a function of cost of care: patients with children had a lower odds of reporting needing medical care but not receiving it because of cost (OR = 0.72 [95 % CI, 0.68–0.77]; P < 0.001).
CONCLUSIONS: Women with children younger than 18 years old are less likely to engage in their own primary care and receive important preventive care than women without young children. Current health care delivery system models may not be optimally structured to meet the needs of women with children.
Odds of PCP visit within the previous yearOdds of PCP visit within the previous year
| Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|
| HR | 95 % CI | P value | HR | 95 % CI | P value | ||
| Have children <18 years old | 0.76 | 0.74–0.79 | <0.001 | 0.88 | 0.85–0.92 | <0.001 | |
| Age | |||||||
| ≤20 years old* | |||||||
| >20 and ≤40 years old | 0.99 | 0.92–1.08 | 0.875 | 1.05 | 0.96–1.14 | 0.285 | |
| >40 years old | 1.65 | 1.52–1.79 | <0.001 | 1.53 | 1.40–1.67 | <0.001 | |
| Total Annual Family Income | |||||||
| < $35,000* | |||||||
| ≥$35,000 and <$50,000 | 1.22 | 1.15–1.29 | <0.001 | 1.06 | 1.00–1.11 | 0.065 | |
| ≥$50,000 and <$75,000 | 1.45 | 1.38–1.53 | <0.001 | 1.11 | 1.05–1.17 | <0.001 | |
| ≥$75,000 and <$100,000 | 1.70 | 1.59–1.81 | <0.001 | 1.18 | 1.10–1.26 | <0.001 | |
| ≥$100,000 | 1.86 | 1.76–1.96 | <0.001 | 1.22 | 1.15–1.30 | <0.001 | |
| Race | |||||||
| White* | |||||||
| Hispanic | 0.58 | 0.56–0.61 | <0.001 | 0.86 | 0.82–0.91 | <0.001 | |
| Black | 0.85 | 0.81–0.89 | <0.001 | 1.02 | 0.96–1.07 | 0.552 | |
| Asian | 0.69 | 0.64–0.74 | <0.001 | 0.72 | 0.67–0.78 | <0.001 | |
| Other | 0.95 | 0.80–1.13 | 0.574 | 1.03 | 0.85–1.25 | 0.750 | |
| Education Level | |||||||
| No High School Degree* | |||||||
| High School Degree | 1.39 | 1.33–1.46 | <0.001 | 1.05 | 0.99–1.12 | 0.077 | |
| College Degree | 1.65 | 1.55–1.75 | <0.001 | 1.04 | 0.96–1.11 | 0.348 | |
| Graduate Degree | 1.79 | 1.66–1.92 | <0.001 | 1.01 | 0.93–1.11 | 0.773 | |
| Employed | 1.02 | 0.99–1.07 | 0.126 | 0.86 | 0.83–0.90 | <0.001 | |
| No Health Insurance | 0.28 | 0.27–0.29 | <0.001 | 0.31 | 0.30–0.32 | <0.001 | |
*Baseline comparison group
CHOOSING WISELY: DO PHYSICIANS AND PATIENTS AGREE ON WHAT CONSTITUTES HIGH-VALUE MEDICAL CARE?Ana Sofia Warner1; Neel Shah1,3; Abraham Nick Morse1; Eliyahu Lehmann2; Rie Maurer2; Zoe Moyer2; Lisa Lehmann1,2. 1Harvard Medical School, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1938226)
BACKGROUND: Healthcare delivery systems focus on the concept of value delivery as a way of optimizing patient experience and outcomes while containing costs. Value, patient health outcomes per dollar spent, is a concept that providers, patients and policymakers embrace. Although the Choosing Wisely campaign targets physicians and patients to promote high-value care, there is little data on whether there is concordance between physicians’ and patients’ interpretation of value, particularly for care that has been identified as wasteful, such an unindicated imaging and antibiotic use.
METHODS: To assess physicians’ and patients’ perceptions of the value of care we conducted a cross-sectional survey of 201 primary care patients and 150 primary care physicians at three academic medical centers. The first vignette described a patient with symptoms of a tension headache who is concerned about a brain tumor, but initially denied imaging. The second vignette described a patient with 3 days of symptoms consistent with a viral infection who requests and is denied antibiotics. Respondents rated the care provided in each vignette on a 5-point Likert scale (see Table 1). Descriptive statistics were used to describe frequencies. Chi-square and Fisher’s exact tests were used to compare proportions between patients and physicians. Univariate regression analysis was used to assess predictors of patients’ rating care as high value. Multivariable regression analysis is ongoing.
RESULTS: The response rate was 63 % (201/319) for patients and 53 % (150/283) for physicians. Among patients, 37 % were men, 63 % were white. Physicians more often reported that imaging for a tension headache represented low-value care than patients (77 % vs. 38 %, p < 0.001), and more often reported that denying antibiotics for a viral infection represented high-value care (95 %, vs. 66 %, p < 0.001). Patients improved their rating of care after they were told about the potential harms of radiation, and after receiving information about potential side effects and reasons for not providing antibiotics or imaging (15 % increase in positive ratings for both scenarios). Patients who were concerned about receiving too few tests, treatments and medications were less likely to give a high rating to Part 1 of the headache vignette (OR 0.42 (0.23–0.78) p < 0.006), while patients who rated their own health higher were more likely to rate it favorably (p < 0.01). Patients who had seen their physicians more often were more likely to rate Part 1 of the URI vignette highly (p < 0.03). More educated and white patients were more likely to rate Part 1 of both vignettes highly (p < 0.01).
CONCLUSIONS: There is significant disagreement between physicians’ and patients’ perceptions of the value of care. Patients are more likely to favorably rate care withholding antibiotics than care withholding imaging. Patients are likely to improve their rating of care if they are informed about potential side effects, reasons for not providing antibiotics or imaging, or national guidelines consistent with their doctor’s care. Addressing these topics in clinical settings will be critical to our ability to contain healthcare costs and deliver high value care.
Table 1: Patients and Physicians Ratings of Clinical Vignettes as ‘Very Good’ (4) or ‘Excellent' (5)
CLASSIFICATION OF THEMES HIGHLIGHTS BOTH VARIABILITY AND CONSISTENCY IN PHYSICIAN APPROACHES TO PROFESSIONAL DILEMMASElizabeth C. Bernabeo1; Shiphra Ginsburg2; Eric Holmboe1. 1American Board of Internal Medicine, Philadelphia, PA; 2University of Toronto, Toronto, ON, Canada. (Tracking ID #1940171)
BACKGROUND: Professionalism is grounded in a dynamic system comprised of elements at the individual, social, and societal level. In this view, a physician’s professional behavior is dependent on their personal characteristics, yet also influenced by situational and contextual phenomena arising during learning and practice. Identifying and reflecting on situational context may be difficult for physicians, particularly for physicians in real time professional dilemmas or for whom certain responses have become a personal style or habit.
METHODS: As part of an initiative to develop a self-directed approach to assessment of professionalism, we asked a random sample of general internists and specialists in outpatient and inpatient settings (N = 366) to complete an anonymous web-based survey addressing physician approaches to typical professional challenges. The survey prompted physicians to rate the likelihood of their responding in stated ways, and to rate the importance of a set of contextual factors in their decision making. Physicians also responded to open ended questions prompting alternative responses, additional factors that guided those responses, and what kind of new learning or impact the activity had on themselves personally.
RESULTS: The overall response rate was 132/366 (36.1 %). Qualitative analysis of the open ended comments revealed several themes around which physicians approach professional dilemmas. Physicians were guided by issues of patient welfare (e.g. “I tend to come down on the side of what is best for the patient”), how much they like the patient (e.g. “Decisions are influenced by the level of the relationship with the patient”), policy, ethics, or legal issues (e.g. “I am worried about litigation”), and principles, values or rules (e.g. “I follow my own rules)”. We further identified several personal styles or habits of physicians in responding to professional dilemmas: lenient (e.g. “I am too eager to please”), avoidant (e.g. “I have a great concern about the hassle factor”), and inconsistent (e.g. “I am not consistent with certain patients or behaviors”).
CONCLUSIONS: Physicians were able to reflect on personal approaches and factors listed on the survey, as well as those that were not. The classification of themes that guide physician decisions in professional dilemmas is important, and suggests that despite variability in responses, physicians think about professionalism in systematic and complex ways. Helping physicians explore and identify with their personal reactions to professional dilemmas in a deliberate way can help promote mindfulness and renew interest and commitment to professionalism in practice. Self awareness and reflection are infrequent in medical practice, yet may be powerful agents of change for physicians.
CLASSIFYING PATIENT STATEMENTS ABOUT UNCONTROLLED PAIN IN PRIMARY CAREStephen G. Henry1; Richard L. Kravitz1; Robert A. Bell2. 1University of California Davis, Sacramento, CA; 2University of California Davis, Davis, CA. (Tracking ID #1938853)
BACKGROUND: Physicians frequently cite patient requests for opioids as one reason that visits involving patients on opioids are often frustrating. Past research in this area has focused on “difficult” visits or patients in specialty pain clinics. Little is known about how patients on opioids actually discuss uncontrolled pain during routine primary care visits.
METHODS: Data were derived by coding transcripts of routine primary care visits that were recorded as part of a clinical trial that compared two interventions designed to facilitate patient discussion of depression symptoms. First, we read transcripts to identify patients on chronic opioids (i.e. taking at least 1 dose/day for >90 days). Second, we iteratively reviewed transcripts to develop and apply a coding system to identify strategies patients used to express poorly controlled pain. Our final coding system was adapted from Street’s system for coding patient participation and comprised four types of patient statements: concerns (statements expressing negative emotions about pain), questions, requests for action (e.g. referral), and assertive statements.
RESULTS: We identified 26 eligible transcripts that included patients on opioids for chronic pain. Patient concerns were the most common statement type (n = 84) followed by questions (n = 32), requests for action (n = 22) and assertive statements (n = 16). Approximately 28 % (n = 43) of statements related to pain and suffering in general, 20 % (n = 31) pertained to pain-related functional impairment, 29 % (n = 44) were about non-opioid pain treatments, 19 % (n = 29) related to opioids, and 5 % (n = 7) concerned the underlying pain diagnosis. One patient requested a change from methadone to oxycodone after the physician suggested this change. All other requests for opioid prescriptions involved refills of patients’ existing opioid prescriptions. No direct requests for higher opioid doses were observed.
CONCLUSIONS: Patient were more likely to mention uncontrolled pain indirectly (i.e., through statements of concern and/or questions) rather than through direct requests for action or assertive statements. Statements about opioids comprised a minority of patient statements about uncontrolled pain. Contrary to conventional wisdom, direct patient requests for higher opioid doses appear uncommon in routine primary care visits involving patients on opioids for chronic pain.
CLINICAL CHARACTERISTICS OF PATIENTS ADMITTED FOR ACUTE EXACERBATION OF COPD THAT PREDICT SHORTER LENGTH OF STAYMatthew Cerasale1; Khalil Mroue2; Juan Cesar Fernandez Castillo1; Jennifer Swiderek3; David Paje1. 1Henry Ford Hospital, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Henry Ford Hospital, Detroit, MI. (Tracking ID #1940337)
BACKGROUND: Chronic Obstructive Pulmonary Disease (COPD) exacerbation is a common clinical condition that may lead to frequent hospitalization. However, identifying which patients would be appropriate for a short stay in an observation unit rather than an inpatient admission has not been well established. The aim of this study was to determine which patient characteristics and clinical findings are associated with hospitalizations of <48 h, and thus can be used to guide referral to the observation unit.
METHODS: The study is based on a retrospective review of the medical records of patients who were primarily hospitalized for acute exacerbation of COPD to an 805-bed teaching hospital. Patients were excluded if they were admitted directly to the intensive care unit. Demographic data, baseline history and clinical findings in the emergency department and upon arrival to a hospital unit were abstracted. The occurrence of all-cause death, readmission and revisit to the emergency department within 30 days were also recorded. The clinical characteristics of patients who stayed <48 h were compared to those who stayed longer using independent T-tests for continuous variables and Chi-squared test for categorical variables.
RESULTS: The medical records of 181 patients who were primarily hospitalized for acute exacerbation of COPD between 2009 and 2013 were reviewed. There were 68 (38 %) patients who stayed <48 h (mean length of stay [LOS], 1.63 ± 0.62 days) and 113 (62 %) patients who stayed longer (mean LOS, 3.82 ± 1.99 days). Both groups were similar in terms of age, sex, and racial distribution. They were also similar with regards to smoking status, prior use of inhaled steroids and anticholinergics, intubation within the past year, and hospital admission in the past year. Compared to patients who stayed longer, patients who stayed <48 h had faster initial respiratory rate in the emergency department (23.82 ± 6.05/min vs. 21.42 ± 4.00/min, p = 0.002) and they had higher initial hemoglobin (13.26 ± 1.44 g/dL vs. 12.53 ± 1.89 g/dL, p = 0.007). The rest of the initial clinical findings in the emergency department and upon admission were similar in both groups. The rates of 30-day outcomes were also comparable: revisit to the emergency department within 30 days (22 % vs. 15 %, p = 0.3197), inpatient readmission (18 % vs. 14 %, p = 0.6801) and death from all causes (0 % vs. 2 %, p = 0.7083).
CONCLUSIONS: A significant proportion of patients who are admitted for acute exacerbations of COPD stay less than 48 h. There are no clinically significant differences in baseline characteristics and in initial clinical findings between patients who stay longer and those who stay less than 48 h. Clinical outcomes were also similar in both groups.
CLINICAL EXCELLENCE IN HOSPITAL MEDICINE: INSIGHT GLEANED THROUGH OBSERVATIONSusrutha Kotwal; Eric Howell; Haruka Torok; Regina Landis; Scott Wright. Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1925957)
BACKGROUND: As of July 2010, there were more than 30,000 hospitalists in the United States. The quality of care rendered by hospitalists is not uniform. Although patient satisfaction metrics like Press Ganey attempt to measure service excellence, no empiric research has been performed to characterize or define clinical excellence in hospital medicine.
METHODS: The Chiefs of Hospital Medicine at five different hospitals were emailed and asked to identify the “clinically excellent” hospitalists within their groups. The named hospitalists were invited to participate in the study; those agreeable would be shadowed during routine clinical care of patients. A data extraction sheet was developed and pilot tested to focus the observer’s attention on elements believed to be associated with clinical excellence. Detailed field notes, both quantitative and qualitative, were collected during the observation.
RESULTS: A total of 26 hospitalists were shadowed as they took care of patients. The average age of the physicians was 38 years and their average experience in hospital medicine was 6 years. Each hospitalist was observed for an average of 5 h and they were observed with a mean of seven patients (total number of patient encounters observed = 197). On average, the physicians spent 11 min with each patient; patients were examined for a mean of 100 s. In terms of balance of dialogue, these respected providers spoke on average 71 % of the time during the discourse. The frequency of certain select desirable behaviors observed were as follows: starting encounters with an “open ended” question (76 %); integrating non-medical conversation to connect with patient (30 %); displaying empathy during the encounters (27 %). Each encounter was given a global rating and 14 % were judged to be “clinically excellent”. Several reasons that encounters were judged not to be “clinically excellent” were the lack of non-medical conversation used to connect with patients (70 % of the encounters), doctor neglected to wash hands prior to entering room (24 % of the encounters), doctor did not uncover/disrobe the body part being examined (39 %), and failing to ask permission prior to examining the patient (36 %).
CONCLUSIONS: This study represents a first step in trying to characterize clinical excellence in Hospital Medicine, using both qualitative and quantitative data. Because hospitalists spend only a small amount of time with patients, relative to the time spent in indirect patient care, it is imperative that we make the most of this caring time and strive for clinical excellence consistently during every encounter.
CLINICAL IMPACT OF MEDICAL ASSISTANT HEALTH COACHING IN LOW-INCOME PATIENTS WITH UNCONTROLLED DIABETES, HYPERTENSION, AND HYPERLIPIDEMIA: A RANDOMIZED CONTROLLED TRIALDavid Thom; Rachel Willard-Grace; Danielle Hessler; Denise DeVore; Camille Prado; Thomas Bodenheimer; Ellen Chen. University of California, San Francisco, San Francisco, CA. (Tracking ID #1925738)
BACKGROUND: Medical assistants, part of one of the fastest growing allied health professions, are more likely than clinicians to be culturally and linguistically concordant with patients. Medical assistants trained in health coaching could provide an important resource as members of the primary care team. Previous studies of medical assistant health coaching programs found positive trends in clinical outcomes such as hemoglobin A1c but were not designed as randomized trials, lacked power to find statistically significant differences, and focused on a single condition such as diabetes or hypertension. We conducted a randomized controlled trial to test the effectiveness of clinic-based medical assistant health coaching versus usual care to improve clinical outcomes among low-income patients with uncontrolled type 2 diabetes, hypertension, and/or hyperlipidemia over 12 months.
METHODS: The Health Coaching in Primary Care enrolled low-income patients with uncontrolled diabetes (hemoglobin A1C (HbA1C) > 8.0 %), hyperlipidemia (LDL > 130 mg/dL or >100 mg/dL if diabetic), and/or hypertension (SBP > 140 mmHg) from two safety-net clinics. Patients were randomized to receive usual care or health coaching from a medical assistant who completed health coach training. The primary outcome was a composite measure of being at goal (defined asHbA1c < 8.0 %; LDL < 130 mg/DL or <100 mg/dL if diabetic; and SBP < 140 mmHg) for at least one of the conditions uncontrolled at enrollment. Secondary outcomes were meeting all possible goals and meeting each goal separately.
RESULTS: Of 654 patients determined to be eligible, 441 (67 %) were enrolled; approximately three-quarters from one clinic. Clinical outcome measures at 12 months were available for 94 % (132/144) of patients enrolled with uncontrolled diabetes, 95 % (156/165) of patients enrolled with uncontrolled hypertension, and 83 % (169/203) for patients enrolled with uncontrolled hyperlipidemia. There were no significant differences in participant characteristics by study arm (Table 1). Participants in the health coaching arm were more likely than participants in the usual care arm to achieve both the primary composite measure of one of their clinical goals and the secondary composite measure of reaching all of their clinical goals (Table 2). Almost twice the number of participants in the health coaching arm achieved the goal of HbA1c ≤ 8.0 %. At the largest study site, participants in the health coaching arm were more likely to achieve the specific LDL cholesterol goal compared to usual care (41.8 % vs. 25.4 %, difference 16.4 %, CI 1 %–32 %). There was no significant difference in the proportion of patients who met the treatment goal for hypertension.
CONCLUSIONS: Medical assistants serving as in-clinic health coaches can improve glycemic and cardiovascular health outcomes over usual care for low-income patients with uncontrolled diabetes, hypertension and/or hyperlipidemia
Table 1. Participant characteristics (% or mean (sd))
| Usual care arm (n = 217) | Health coaching arm (n = 224) | |
|---|---|---|
| Age (years) | 52.9 (11.5) | 52.6 (10.7) |
| Gender (female) | 59 % | 52 % |
| Born in the US | 25 % | 26 % |
| Years living in US* | 17.9 (11.9) | 18.5 (10.4) |
| Spanish is primary language | 70 % | 68 % |
| Race/Ethnicity: | ||
| African American | 18 % | 20 % |
| Latino or Hispanic | 71 % | 69 % |
| White non-Hispanic/Asian/Other | 11 % | 11 % |
| Education less than high school | 44 % | 44 % |
| Annual household income <$10,000 | 56 % | 60 % |
| Hemoglobin A1c (%) | 10.0 (1.4) | 9.8 (1.5) |
| Low-density lipoprotein (mg/dL) | 148 (34) | 146 (37) |
| Systolic blood pressure (mmHg) | 160 (17) | 158 (14) |
* For the 328 participants born outside the United States.
Table 2. Percent of participants reaching primary and secondary outcomes at 12 months by study arm
| Health Coaching | Usual Care | Difference | 95 % CI for difference | p-value | |
|---|---|---|---|---|---|
| Composite (primary)* | 46 % | 34 % | 12 % | 2 % to 23 % | .02 |
| Composite (secondary)† | 34 % | 25 % | 9 % | 1 % to 19 % | .05 |
| HbA1c < 8.0 | 49 % | 27 % | 22 % | 5 % to 39 % | .01 |
| LDL < 100 mg/dL | 43 % | 32 % | 11 % | −4 % to 25 % | .15 |
| SBP < 140 mmHg | 24 % | 29 % | −5 % | −9 % to 19 % | .46 |
* Achieved target for control of one or more of specific conditions for which enrolled. † Achieved target for control of all conditions for which enrolled.
CMS PAYMENT REFORM AND THE INCIDENCE OF HOSPITAL-ACQUIRED PULMONARY EMBOLISM OR DEEP VEIN THROMBOSISRisha Gidwani1,2; Jay Bhattacharya3. 1Veterans Health Administration, Menlo Park, CA; 2Stanford University, Stanford, CA; 3Stanford University, Stanford, CA. (Tracking ID #1938121)
BACKGROUND: The Centers for Medicare & Medicaid Services (CMS) has historically provided larger reimbursement to hospitals for inpatient stays in which a patient complication developed post-admission (a hospital-acquired condition). This manner of reimbursement financially rewarded hospitals that may have provided poor-quality care to their patients. In October 2008, CMS stopped reimbursing hospitals for the marginal cost of treating certain preventable hospital-acquired conditions. We evaluated whether CMS’s refusal to pay for hospital-acquired pulmonary embolism (PE) or deep vein thrombosis (DVT) resulted in a lower incidence of these conditions.
METHODS: This analysis employed difference-in-difference regression modeling. Difference-in-difference modeling is a quasi-experimental approach used when it is infeasible to conduct a randomized controlled trial, and when there is one group that is exposed to the intervention, another group that is unexposed to the intervention, and a single start date to the intervention. Comparing pre-post data in the exposed group to pre-post data in the unexposed group serves to remove biases that may be due to systematic differences across the unexposed and exposed groups and well as biases that may be due to larger trends in the environment. In this analysis, the intervention is CMS payment reform, the exposed group is Medicare patients receiving hip or knee surgery, the unexposed group is non-Medicare patients receiving hip or knee surgery, and the outcome of interest is the incidence proportion of PE or DVT. We limited the cohort to Medicare patients aged 65–69 and non-Medicare patients aged 60–64 to minimize the impact of age on developing PE or DVT. A hierarchical regression model was used to account for correlation between discharges within a single hospital. The model was populated using 2007–2009 data from the Nationwide Inpatient Sample, an all-payer database of inpatient discharges in the United States.
RESULTS: There were 136,634 encounters for hip or knee replacement surgery from 2007 to 2009 in patients aged 60–69. At baseline, PE/DVT occurred in 0.81 % of all hip or knee replacement surgeries for Medicare patients aged 65–69. After adjusting for race, sex, hospital region, teaching hospital status, elective admission, rural hospital status, and median houseful income quartile for patient zip code, the CMS policy change was associated with a 32 % reduction, or a 0.26 percentage point reduction, in the incidence proportion of hip or knee encounters with PE or DVT. The incidence of PE or DVT in these orthopedic encounters increased from the pre-intervention to the post-intervention period for non-Medicare patients aged 60–64, while it declined in that same period for Medicare patients aged 65–69. Results were robust to changes in model specification.
CONCLUSIONS: As the U.S. healthcare system increasingly moves from fee-for-service to fee-for-value reimbursement, it becomes important to evaluate whether fee-for-value-based reimbursement has a desired effect. Our administrative-data based analysis of CMS hospital-payment reform indicates payment modification had the desired effect of reducing hospital-acquired PE or DVT amongst patients with hip or knee replacement surgeries. After controlling for other variables, the policy change was independently associated with a 32 % reduction in the incidence of hospital-acquired PE or DVT. While regression models indicate the 0.26 percentage point reduction was statistically significant, it remains the purview of policy makers and clinicians to decide whether a reduction in the incidence of these conditions from 0.81 % to 0.55 % is clinically significant. To our knowledge, this represents the first analysis of the effect of CMS payment reform on the incidence of hospital-acquired pulmonary embolism or deep vein thrombosis.
COGNITIVE REFLECTION AND ANTIBIOTIC PRESCRIBING FOR ACUTE RESPIRATORY INFECTIONSDwan Pineros1; Jason N. Doctor6; Mark W. Friedberg5; Daniella Meeker4; Yelena Kleyner3; Jeffrey A. Linder1,2. 1Brigham and Women’s Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3Partners HealthCare System, Boston, MA; 4RAND, Santa Monica, CA; 5RAND, Boston, MA; 6University of Southern California, Los Angeles, CA. (Tracking ID #1938790)
BACKGROUND: Clinicians frequently prescribe inappropriate antibiotics for acute respiratory infections (ARIs). One contributor to inappropriate antibiotic prescribing may be a tendency toward quick, automatic thinking by clinicians.
METHODS: The Cognitive Reflection Test (CRT) has three questions with intuitive but incorrect answers that respondents tend to reach if they do not consider the question carefully (i.e., incorrect answers that quick, automatic thinking produces). The CRT is scored from 0 to 3, representing the number of correct answers. We administered the CRT to 139 primary care clinicians in June 2013. From billing data and the electronic health record between June 2012 and June 2013, we calculated clinician-level antibiotic prescribing rates for ARIs in 3 categories: all ARIs, antibiotic-appropriate ARIs (e.g., pneumonia, streptococcal pharyngitis, or sinusitis), and non-antibiotic-appropriate ARIs (e.g., colds or acute bronchitis). We used ANOVA to compare CRT scores with antibiotic prescribing rates.
RESULTS: Thirty-three clinicians (24 %) scored 0 points on the CRT; 27 (19 %) scored 1; 45 (32 %) scored 2; and 34 (24 %) scored 3. Antibiotic prescribing rates were 28 % for all ARIs, 50 % for antibiotic-appropriate ARIs, and 17 % for non-antibiotic-appropriate ARIs. For all ARIs, the antibiotic prescribing rates for CRT scores of 0, 1, 2, and 3 were 33 %, 25 %, 26 %, and 29 %, respectively (p = 0.23). For antibiotic-appropriate ARIs, the antibiotic prescribing rates for CRT scores of 0, 1, 2, and 3 were 51 %, 50 %, 50 %, and 50 %, respectively (p = 0.99). For non-antibiotic-appropriate diagnoses, the antibiotic prescribing rates for CRT scores of 0, 1, 2, and 3 were 23 %, 14 %, 14 %, and 17 % (p = 0.01).
CONCLUSIONS: Clinicians who exhibit less reflective thinking may have higher antibiotic prescribing rates for non-antibiotic-appropriate diagnoses, compared to those who are more likely to think reflectively. It is possible that differences in clinicians’ cognitive reflection could contribute to other variations in care.
COLORECTAL CANCER SCREENING RATES 5 YEARS AFTER SWITCHING TO A HIGH-DEDUCTIBLE HEALTH PLAN, OVERALL AND AMONG LOWER-INCOME MEMBERSJames F. Wharam1; Bruce E. Landon2; Robert LeCates1; Fang Zhang1; Steve Soumerai1; Dennis Ross-Degnan1. 1Harvard Medical School, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1940079)
BACKGROUND: The ACA is expected to cause a “seismic shift” in high-deductible health plan (HDHP) enrollment. Colorectal cancer (CRC) screening improves mortality but the increasing prevalence of HDHPs could reduce screening rates, especially among the poor. To protect against this, the ACA requires that health insurers cover CRC screening with no out-of-pocket costs. We studied HDHPs at a large national insurer that similarly has provided generous coverage of CRC screening tests over the last 8 years. No published studies have examined long-term CRC screening patterns after transition to HDHPs or long-term effects on the poor.
METHODS: We studied administrative claims of 28,877 HDHP members age 50–64 insured through a large national insurer between 2004 and 2011. We analyzed screening rates for 1 year before and up to 5 years after their employers mandated a switch from traditional plans to HDHPs, compared with rates among 57,748 contemporaneous propensity score matched controls whose employers chose to remain in traditional plans. Our measure was screening with any of FOBT, flexible sigmoidoscopy, double-contrast barium enema, or colonoscopy. We considered members who received these tests screened for the next 1, 5, 5, and 10 years, respectively. We subtracted monthly screening rates of the control group from those of the HDHP group to generate a before-after differenced trend, then used Joinpoint analysis to determine whether there was a statistically significant inflection point after the HDHP transition. We stratified plots and analyses by geocoded poverty status and fit a linear trend line to the baseline differenced trend to generate a predicted 5-year screening rate. We fit a second-order polynomial trend line to the follow-up rates to estimate an observed 5-year screening rate.
RESULTS: CRC screening rates in the overall HDHP group relative to the control group trended down beginning in the fourth month of the first follow-up year, an estimated −0.176 % per month trend change (p < 0.0001). Both lower- and higher-income HDHP members followed a similar pattern (Figures 1 and 2). HDHP members from lower-income neighborhoods experienced an estimated 2.9 % absolute decrease in CRC screening rates after 5 years (Figure 1), while members from higher-income neighborhoods experienced an estimated 4.3 % absolute reduction (Figure 2).
CONCLUSIONS: HDHPs were associated with reduced CRC screening over 5 years, but the reduction was not greater among members from lower-income neighborhoods. Fully covering CRC screening under HDHPs might protect lower-income members to some degree from substantial reductions in screening. However, health plans and policymakers should consider strategies to broadly promote CRC screening among HDHP members.
Figure 1. Difference in monthly colorectal cancer screening status between higher-income high-deductible and traditional plan members, showing counterfactual trend predicted by the baseline trend and the fitted follow-up trend.
Figure 2. Difference in monthly colorectal cancer screening status between lower-income high-deductible and traditional plan members, showing counterfactual trend predicted by the baseline trend and the fitted follow-up trend.
COMMERCIAL WEIGHT LOSS PROGRAMS - WHICH ONES WORK? A SYSTEMATIC REVIEWRuchi Srivastava1; Kimberly Gudzune1; Zoobia Chaudhry1; Ambereen K. Mehta1; David Jacobs2. 1Johns Hopkins, Baltimore, MD; 2University of Maryland, Baltimore, MD. (Tracking ID #1935829)
BACKGROUND: Commercial weight loss programs are popular among overweight adults, yet a 2005 review found little evidence to support their effectiveness. New studies have since tested these programs. We aimed to determine the weight loss benefits among popular commercial weight loss programs.
METHODS: We selected five programs based on expert recommendations and Internet popularity. We searched MEDLINE from 1/2002 to 6/2013. We included randomized controlled trials (RCTs) among adults that were ≥12 weeks and compared a commercial program to usual care (UC) or lifestyle counseling. We also included trials from the prior review that met these criteria. Paired investigators screened results to assess eligibility, then abstracted data on study design, population characteristics, and weight. We synthesized data qualitatively by program.
RESULTS: Overall, we included 27 RCTs. Weight Watchers (WW): As compared to UC, WW groups had 2.2–10 % greater mean percent weight loss at all time points (8 RCTs). There were inconsistent effects when comparing WW to counseling (2 RCTs). Atkins: As compared to counseling, Atkins groups had 0.8–6.2 % greater mean percent weight loss at 3–6 months (6 RCTs); however, there were no significant between group differences at 12 months or beyond. Jenny Craig (JC): One RCT compared JC to UC, where JC resulted in 7.5 % and 6.4 % greater mean percent weight loss at 6 and 12 months, respectively. Slim-Fast (SF): As compared to UC, SF groups had 6.3–9.7 % greater mean percent weight loss at 3–6 months (4 RCTs). There were inconsistent effects when comparing SF to counseling (3 RCTs). Nutrisystem: One RCT compared Nutrisystem to UC, where Nutrisystem resulted in 6.8 % greater mean percent weight loss at 6 months.
CONCLUSIONS: While commercial weight loss programs can help patients lose weight, these programs may not be superior to counseling. Clinicians may consider these programs when clinic-based options are unavailable.
COMMUNICATION FROM URGENT CARE CENTERS TO EMERGENCY DEPARTMENTSRebekah Gardner1,2; Esther Choo1; Stefan Gravenstein4,2; Rosa Baier2,3. 1Alpert Medical School of Brown University, Providence, RI; 2Healthcentric Advisors, Providence, RI; 3Brown University School of Public Health, Providence, RI; 4Case Western Reserve University, Cleveland, OH. (Tracking ID #1942530)
BACKGROUND: Care transitions occur when patients move from one healthcare setting or provider to another (e.g., when a hospital patient is discharged). Although successful transitions require timely, accurate and sufficient communication of clinical information, such communication is inconsistent and there are few established guidelines outside of the hospital setting. Consistent, high-quality communication is particularly important during and after visits to urgent care centers (UCCs). However, our review of the medical literature revealed no prior investigation on the quality and consistency of communication from UCCs to emergency departments (EDs). Our aim was to assess the quality, consistency and effectiveness of healthcare communication between UCCs and EDs during care transitions.
METHODS: We administered a short anonymous survey to a convenience sample of emergency medicine physicians in Rhode Island. We contacted department chairs at the state’s 13 acute-care hospitals and asked them to distribute the electronic survey to their emergency medicine physicians (MDs or DOs in active practice). The survey asked practitioners to characterize the frequency and completeness of the information they receive from UCCs. We used descriptive statistics to characterize survey respondents, their perceptions about UCC to ED information transfer and their preferences for future communication. We also conducted a qualitative analysis of open-ended questions.
RESULTS: Eleven (84.6 %) ED chairs agreed to distribute the survey. Approximately half (48.7 %) of the 199 emergency medicine physicians at these 11 hospitals responded. Most were attending physicians (62.1 %) and had ≥10 years of experience in the ED (55.7 %). Overall, respondents’ perceptions of the consistency, relevancy and usefulness of the information they receive from UCCs varies widely. For example, despite expressing strong preferences to receive this type of information, respondents report receiving reason for referral 72.0 % of cases and a copy of the chart in 60.6%of cases. Receipt of contact information (52.3 %) and phone calls to the ED (42.0 %) are lower. Conversely, respondents report rarely communicating ED findings back to UCCs (16.7 %). Comments reveal frustration with poor information transfer, particularly when the UCC clinicians are unavailable, and a desire to standardize or formalize communication expectations.
CONCLUSIONS: These data highlight a very real disconnect between the communication and information that emergency medicine physicians believe is necessary for providing care and the information that they receive from UCCs. Additionally, the ED providers’ nearly universal lack of communication back to the urgent care center following treatment of the admitted patient suggests the absence of a closed communication loop between these care settings. Our findings speak to the importance of establishing communication standards and of including UCCs in ongoing initiatives to improve patient care transitions and experiences.
COMMUNITY COLLEGE PATHWAYS TO MEDICAL SCHOOL: EXPLORING THE EXPERIENCES OF LATINO STUDENTSEfrain Talamantes1; Carol Mangione2,3; Karla Gonzalez3; Gery Ryan4; Alejandro Jimenez5; Fabio R. Gonzalez6; Seira Greenwood7; Gerardo Moreno2,8. 1Department of Veteran Affairs and the University of California, Los Angeles, Los Angeles, CA; 2University of California, Los Angeles, Los Angeles, CA; 3University of California, UCLA, Los Angeles, CA; 4RAND Health, Santa Monica, CA; 5University of California, San Francisco, San Francisco, CA; 6San Jose City College, San Jose, CA; 7University of California, Los Angeles, Los Angeles, CA; 8University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1940189)
BACKGROUND: The community college is an essential pathway to medical school for Latino and low-income students, and contributes to a diverse physician workforce. There has been an increase in community college enrollment for the last several decades. The objective of this study was to explore the facilitators and barriers Latino pre-medical students face when they attend a community college.
METHODS: Participants included 48 Latino pre-medical students who were enrolled at or previously attended a California community college, and 20 stakeholders who directly advise and support these students. We conducted five focus groups (4 of undergraduate students who were currently enrolled or previously attended a community college, and 1 of medical school students who attended a community college) and 20 semi-structured interviews with counselors advisors, and teachers based at the community college, and medical school admissions staff and faculty from several California medical schools. Focus groups and interviews were digitally audio-taped, transcribed, and reviewed independently by two coders. Standard qualitative content-analysis methods were used to identify major themes and a third investigator adjudicated disagreements.
RESULTS: Results revealed the following major facilitator themes 1) pre-medical enrichment programs 2) pre-medical specific advising 3) Latino physician mentors and 4) family support for pursuing a pre-medical education. Major barrier themes included: 1) a perception that college was not affordable 2) poor high school academic preparation 3) lack of family support and responsibilities that compete with time to study and 4) limited counseling or advising. The financial burden of attending a community college required many students to take low-paying jobs to pay for tuition, books, housing, and transportation, while taking rigorous science coursework. Enrichment programs such as Math Engineering Science Achievement (MESA) play an important role in providing community college students with academic tutorials and advising, but are not readily accessible to students because of capacity constraints and stringent financial verification requirements. Stakeholders also indicate the need for a more comprehensive and sustainable pre-medical enrichment programs that include financial support and pre-medical counseling for low-income students, many of whom were the first in their family to attend college.
CONCLUSIONS: This is the first qualitative study that explores the role the community college as a pathway to medical school for Latino pre-medical students. We identified a number of potentially mutable barriers for premedical students who attend community college. Enrichment programs and policies that decrease the financial burden of pursuing higher education potentially can mitigate many of these barriers. The significant growth in the number of Latinos at the community college pursuing premedical education represents an important part of the pipeline to increase the diversity of the physician workforce.
COMMUNITY COLLEGE PATHWAYS: IMPROVING THE U.S. PHYSICIAN WORKFORCE PIPELINEEfrain Talamantes1; Carol Mangione2,3; Karla Gonzalez2; Alejandro Jimenez4; Fabio R. Gonzalez5; Gerardo Moreno2,6. 1Department of Veteran Affairs and the University of California, Los Angeles, Los Angeles, CA; 2University of California, Los Angeles, Los Angeles, CA; 3University of California, UCLA, Los Angeles, CA; 4University of California, San Francisco, San Francisco, CA; 5San Jose City College, San Jose, CA; 6University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1939846)
BACKGROUND: Diversity in the physician workforce increases healthcare access for underserved populations, improves culturally and linguistically appropriate care, and better prepares all physicians to serve the needs of a diverse population. How we can achieve that diversity, however, is not well understood. One answer may lie in where students attain the undergraduate training they need before entering medical school. There are no studies that clarify how or if the undergraduate pathway contributes to a diverse physician workforce that is interested in serving underserved communities. Furthermore, the Community College (CC) as a pathway to medical school has not been explored at all.
METHODS: We performed a cross-sectional analyses of the 2012 Association of American Medical Colleges matriculant and applicant files, and the Matriculating School Questionnaire to assess bivariate associations between student characteristics and participation in a CC pathway. We also estimate the association between participation in a CC pathway and acceptance to medical school, intention to practice in underserved areas or work primarily with minority populations using multivariate logistic regression to adjust for confounders.
RESULTS: One third of applicants (N = 40,491) and matriculants (N = 17,518) to U.S. allopathic medical schools used a CC. A higher proportion of Latino matriculants used the CC pathways (34 % vs. 27 %, P < 0.001), compared to Whites. Matriculants who attended a CC after graduating from high school and before transferring to a 4-year university were more likely to have parents without a college education (34 % vs. 13.4 %, P < 0.001), had lower odds of acceptance into medical school (adjusted odds ratio [AOR] = 0.68, 95 % CI 0.61 to 0.75, P < 0.05) and higher odds (AOR = 1.26, 95 % CI 1.04 to 1.53, P < 0.05) of intentions to practice in underserved communities, compared to medical students who never attended a CC, after adjusting for covariates.
CONCLUSIONS: The CC pathways are essential for underrepresented minorities and students who have intentions to practice in underserved communities. While many recruitment and outreach efforts are strictly targeted at 4-year universities, there may be ample opportunities to support students pursuing careers in medicine that use the community college pathways and nurture their desire to ultimately practice medicine in an underserved community.
COMMUNITY HEALTH CENTER PATIENTS’ ATTITUDES AND PREFERENCES REGARDING RECEIVING PREVENTIVE SERVICE OUTREACH MESSAGESTiffany Brown; Shira N. Goldman; Ji Young Lee; Muriel Jean-Jacques; Shreya Shah; Stephen D. Persell. Northwestern University, Feinberg School of Medicine, Chicago, IL. (Tracking ID #1938151)
BACKGROUND: As community health centers (CHC) work to improve their quality of care for clinical preventive services, one possible strategy is outreach to patients who are due for certain services. Multiple studies have evaluated outreach for immunizations and cancer screenings among vulnerable populations. This proactive outreach may be particularly beneficial for CHC patients who may be less likely to have regular preventive service visits and for whom preventive services may be a lower priority if limited clinical encounter time is focused on acute and chronic health issues. However, little is known about CHC patients’ attitudes towards this type of outreach and how they prefer to be contacted with these messages. Our objective was to understand CHC patients’ attitudes and preferences regarding receiving clinical preventive services outreach messages from their CHC. We report interim results from a survey of CHC patients.
METHODS: As part of a larger project evaluating the effectiveness of an outreach intervention to promote the prevention of cardiovascular disease (CVD), we conducted telephone surveys with patients within three CHC systems; two in Chicago, IL and one in Flagstaff, AZ. Patients were eligible if they had been randomized to intervention arm of a randomized controlled trial of mailed and telephone outreach to individuals at increased risk for the development of CVD. Eligibility criteria were: men ≥35 and women ≥45 years old, a 10-year risk of coronary death or myocardial infarction (based on Framingham Risk Score) of at least 10 %, and a visit to CHC within 6 months prior to randomization. The survey was performed 1 year after the intervention was delivered. The survey assessed patient attitudes towards receiving messages about three preventive services: (1) influenza vaccination (2) cancer screenings (3) and primary prevention of CVD. In addition, participants were asked how they preferred to be contacted with these messages. Participants responded to Likert items ranging from 1 (strongly disagree) to 5 (strongly agree). Demographic items were also included.
RESULTS: Among eligible subjects with the recruitment protocol for the survey completed, n = 60 completed interviews (56 % response rate). The majority of participants were male (91.7 %), 48.3 % were black and 38.3 % were white, 68.9 % had a high school degree or higher. Participants expressed agreement with statement that it was a good idea for CHC to let them know when they were due for flu shot (mean 4.3, standard deviation [SD] 1.3), due for cancer screenings (mean 4.7, SD 0.8), and if there were things they could due to lower their risk of developing CVD (mean 4.7, SD 0.7). Patients expressed agreement with wanting to be called by health center staff member (mean 4.1, SD 1.4), and receiving information by mail (mean 4.3, SD 1.3), however they expressed disagreement when asked about receiving a text message (mean 2.5, SD 1.6) or an email message (mean 2.2, SD 1.6). Participants reported strong agreement with preference to come in to discuss recommended services with their provider in person (mean 4.4, SD 1.0).
CONCLUSIONS: CHC patients in our sample report positive attitudes towards receiving outreach messages about their preventive service needs from their clinic. Participants prefer to receive these messages by telephone call or mail as opposed to text message or email. These results may have limited generalizability given specific eligibility criteria and our small, primarily male sample. These data will help inform future outreach efforts to CHC patients to promote important clinical preventive services.
COMPARATIVE EFFECTIVENESS OF A PRACTICE-BASED TRIAL OF BLOOD PRESSURE CONTROL IN BLACKS: IS LESS MORE?Antoinette Schoenthaler1; Jeanne Teresi2; Leanne Luerassi1; Stephanie Silver2; Jian Kong2; Taiye Odedosu1; Gbenga Ogedegbe1. 1New York University School of Medicine, New York, NY; 2The Hebrew Home at Riverdale, Riverdale, NY. (Tracking ID #1929818)
BACKGROUND: The efficacy of interventions targeted at comprehensive therapeutic lifestyle changes (TLC) is well proven in reducing blood pressure (BP) among patients with hypertension (HTN). However their translation to primary care practices is limited, particularly among black patients with HTN, who share a disproportionately greater burden of HTN-related outcomes. More importantly, the comparative effectiveness of single session TLC interventions on BP reduction in primary care practices is unproven. The aim of this vanguard trial was to evaluate the comparative effectiveness of a practice-based comprehensive lifestyle intervention targeted at recommended TLC, delivered through group-based counseling and motivational interviewing (MINT), versus a single session counseling on lifestyle modification (SSC) in reducing BP at 6 months among low-income, blacks with uncontrolled HTN.
METHODS: A total of 194 black patients were randomized to either the MINT-TLC or SSC group. The comprehensive lifestyle intervention (MINT-TLC) was based on established clinical practice guidelines for prevention and treatment of HTN, which recommends weight loss (if overweight), regular physical activity, limiting and/or reducing sodium and alcohol intake, and eating a low-fat diet that is rich in fruit and vegetables. Patients in the MINT-TLC group attended 10 weekly group classes (intensive phase) focused on TLC; followed by 3 monthly individual MINT sessions (maintenance phase) delivered by trained Health Educators. Patients in the SSC condition received a single 30-minute individual counseling session on therapeutic lifestyle changes at the baseline visit by trained study staff. To match the MINT-TLC group for content of intervention material, those in the SSC group also received print versions of the intervention curriculum that was distributed in the group classes. The primary outcome was change in systolic BP and diastolic BP at 6 months assessed with an automated BP monitor (WatchBP). The average of three BP readings was used as the primary outcome measurement, following standard American Heart Association guidelines. The primary analyses examined systolic and diastolic BP separately based on intent-to-treat. A repeated measures mixed model approach was used to account for continuous primary outcomes collected at three waves (baseline, 3 and 6 months), and clustering within primary care providers. The post-treatment values of continuous outcomes were modeled as functions of baseline values, treatment and the interaction of baseline and treatment.
RESULTS: The mean age of all patients was 57 years, 50 % were women, 69 % had income <$20,000/year with mean baseline BP 147.4/89.3 mmHg. Average attendance at the group-based classes in the MINT-TLC condition was 50 %; 35 % of patients completed all three individual MINT sessions. There was non-significant reduction in systolic and diastolic BP for the MINT-TLC compared to the SSC group. The net adjusted reduction in systolic BP by 6 months was 12.9 mmHg for the SSC vs. 9.5 mmHg for the MINT-TLC group. The reduction in diastolic BP was 7.6 mmHg for the SSC vs. 7.2 mmHg for the MINT-TLC group.
CONCLUSIONS: Despite the non-significant between-group difference in BP reduction in the intensive group counseling with multiple office visits versus the single counseling session plus educational material both groups exhibited comparable and clinically meaningful BP reduction. Evaluation of the effectiveness of the interventions in a large Phase 3 trial is warranted in this patient population. Trial Registration: Clinicaltrials.gov NCT01070056
COMPARING CLINICIANS’ PERCEPTION OF THEIR OWN AND THEIR PEERS’ ANTIBIOTIC PRESCRIBING TO ACTUAL ANTIBIOTIC PRESCRIBING FOR ACUTE RESPIRATORY INFECTIONS IN PRIMARY CAREHarry Reyes Nieva1,2; Jason N. Doctor3; Mark W. Friedberg1,4; Caroline Birks2,5; Yelena Kleyner6; Julie Fiskio1; Lynn A. Volk6; Jeffrey A. Linder1,2. 1Brigham and Women, Boston, MA; 2Harvard Medical School, Boston, MA; 3University of Southern California, Los Angeles, CA; 4RAND Corporation, Boston, MA; 5Massachusetts General Hospital, Boston, MA; 6Partners Healthcare System, Boston, MA. (Tracking ID #1941741)
BACKGROUND: Primary care clinicians often prescribe inappropriate antibiotics for acute respiratory infections (ARIs). Inappropriate prescribing may be a result of differences in clinicians’ perceptions of their own antibiotic prescribing rates, perceptions of their peers’ antibiotic prescribing rates, and actual antibiotic prescribing rates.
METHODS: Using a mixed methods approach, we first surveyed 269 primary care clinicians in the Partners Primary Care PBRN about their agreement with antibiotic prescribing guidelines for non-specific upper respiratory infections (URIs), pharyngitis, acute bronchitis, and sinusitis. For each of these diagnoses, the survey asked clinicians to estimate ARI antibiotic prescribing rates for themselves and their peers in five categories: 0 %–20 %, 21 %–40 %, 41 %–60 %, 61 %–80 %, or 81 %–100 %. We then calculated respondents’ actual ARI antibiotic prescribing rates between May 2011–April 2012 using billing and electronic health record data and grouped them using the same five antibiotic prescribing rate categories as the survey. We used the Kruskal-Wallis test to compare respondents’ estimates of their own antibiotic prescribing rates to that of their peers.
RESULTS: 169 of 269 (63 %) primary care clinicians in 23 practices responded to our survey. Mean respondent age was 49 years, 60 % were women, and 85 % were physicians. We linked respondents to 20,025 ARI visits. Clinicians overwhelmingly agreed with antibiotic treatment guidelines for non-specific upper respiratory infections (100 % of clinicians), pharyngitis (95 %), acute bronchitis (92 %), and sinusitis (98 %). For non-specific URIs, the proportion estimating antibiotic prescribing rates in the five categories (i.e., 0 %–20 %, 21 %–40 %, 41 %–60 %, 61 %–80 %, or 81 %–100 %) for themselves was 72 %, 19 %, 7 %, 2 %, and 0 %, respectively, and for their peers was 37 %, 41 %, 17 %, 5 %, and 0 %, respectively (p < 0.001). The actual non-specific URI antibiotic prescribing rate was 34 %; 75 % underestimated and 3 % overestimated their own rate. For pharyngitis, the proportion estimating antibiotic prescribing rates in the five categories for themselves was 81 %, 13 %, 2 %, 2 %, and 1 %, respectively, and for their peers was 63 %, 26 %, 8 %, 3 %, 0 %, respectively (p < 0.001). The actual pharyngitis antibiotic prescribing rate was 59 %; 71 % underestimated and 0 % overestimated their own rate. For acute bronchitis, the proportion estimating antibiotic prescribing rates in the five categories for themselves was 48 %, 31 %, 14 %, 6 %, and 1 %, respectively, and for their peers was 21 %, 40 %, 27 %, 10 %, and 2 %, respectively (p < 0.001). The actual acute bronchitis antibiotic prescribing rate was 76 %; 76 % underestimated and 1 % overestimated their own rate. For sinusitis, the proportion self-reporting antibiotic prescribing rates in the five categories for themselves was 35 %, 41 %, 19 %, 3 %, and 2 %, respectively, and for their peers was 13 %, 40 %, 33 %, 13 %, 1 %, respectively (p < 0.001). The actual sinusitis antibiotic prescribing rate was 88 %; 86 % underestimated and 2 % overestimated their own rate.
CONCLUSIONS: Clinicians agree with ARI antibiotic treatment guidelines. Clinicians think their peers prescribe antibiotics at higher rates than themselves. Clinicians’ estimates of their own and their peers’ prescribing rates are lower than actual prescribing rates. To reduce inappropriate antibiotic prescriptions for ARIs, future interventions might correct clinicians’ misperceptions of their own and their peers’ antibiotic prescribing rates.
COMPARING WARFARIN ANTICOAGULATION MEASUREMENTSZayd A. Razouki1,2; James Burgess3; Shibei Zhao2; Adam Rose1,2. 1Boston Medical Center, Boston, MA; 2Bedford VA Medical Center, BEdford, MA; 3Boston University School of Public Health, Boston, MA. (Tracking ID #1932592)
BACKGROUND: Percent time in therapeutic range (TTR) is a measure of anticoagulation intensity, while INR variability is a measure of anticoagulation stability. Both are valid intermediate measures for warfarin anticoagulation control that predict warfarin associated complications (WAC, i.e. ischemic stroke, major bleeding including fatal bleeding) in patients with atrial fibrillation. However, less is understood about how these two measures complement each other, when used together. This study examines how TTR and INR variability predict WAC, and compares them to a composite measure that combines both of them.
METHODS: We included 40,404 patients anticoagulated for atrial fibrillation, age 65+, within the Veterans Health Administration. We used ICD 9 codes to define WAC as our outcome. For each patient, we calculated TTR using Rosendaal’s method, INR variability using Fihn’s method, and constructed a composite measure (CM) using an equally weighted method, adding standardized TTR to the standardized log-transformation of INR variability. High TTR and low log INR variability represent good anticoagulation. Therefore, we converted the direction of log INR variability to make it consistent with TTR. We divided our sample into quintiles for each measure based on their level of anticoagulation control (i.e. very poor, poor, moderate, good and excellent control). We used Cox regression models to predict WAC; hazard ratios were compared across quintiles of TTR, log INR variability and the intermediate composite measure. The reference group was the quintile of “excellent control”
RESULTS: The composite measure predicted ischemic stroke better than TTR and log INR variability in all quintiles, especially in the first quintile of “very poor control” (HR = 2.43 vs. HR = 2.10 and HR = 1.74, respectively). CM and TTR predicted major bleeding similarly except in the second quintile of “poor anticoagulation” (CM HR = 1.57 vs. TTR HR = 1.35); but both measures were generally better than log INR variability in all quintiles. CM was superior to both TTR and log INR variability when predicting fatal bleeding across all quintiles, especially in the “very poor control” quintile (HR = 3.04 vs.HR = 2.49 vs.HR = 2.18, respectively) and the moderate control quintile (HR = 1.45 vs. HR = 1.19 vs.HR = 1.19 respectively). We were not able to calculate p values to compare whether differences in hazard ratios were statistically significant because individual patients were not distinctly separated across the three studied measures.
CONCLUSIONS: Our composite measure encompasses two aspects of anticoagulation control, namely intensity and stability. Our findings suggest its usefulness in measuring anticoagulation control. It has an advantage in predicting ischemic stroke and fatal bleeding over TTR and log INR variability but it is only better than the log INR variability in predicting major bleeding.
COMPARISON OF EPIGENETIC VERSUS INTENSIVE CHEMOTHERAPY FOR NEWLY DIAGNOSED ELDERLY ACUTE MYELOID LEUKEMIA PATIENTS ≥60 YEARS OLDNeha Gupta1; Shipra Gandhi1; Austin Miller2; Laurie A. Ford3; Elizabeth A. Griffiths3; James E. Thompson3; Meir Wetzler3; Eunice Wang3. 1University at Buffalo, Buffalo, NY; 2Roswell Park Cancer Center, Buffalo, NY; 3Roswell Park Cancer Center, Buffalo, NY. (Tracking ID #1938243)
BACKGROUND: Epigenetic therapy (Epi) with the hypomethylating agents (eg. azacitidine and decitabine) is increasingly being utilized for induction treatment of elderly Acute myeloid leukemia (AML) patients based on studies demonstrating both tolerability and prolonged survival. By contrast, standard intensive chemotherapy (IC) with cytarabine and daunorubicin effectively induces remission in many individuals but is associated with significant toxicity and higher mortality. We compared our institute’s experience with Epi vs. IC for the upfront treatment of newly diagnosed AML patients ≥60 years old.
METHODS: We performed a retrospective chart review of 164 patients ≥60 year old with newly diagnosed AML at Roswell Park Cancer Center between 3/2008 and 2/2013. N = 84 patients received IC, and n = 82 patients received Epi. Kaplan Meier method, log rank test, and multivariate analysis with cox proportional hazard models were used to assess overall survival (OS) and correlation with covariates.
RESULTS: Baseline patient characteristics demonstrated a difference in median age of patients in each group (IC 67 years vs. Epi 75 years; p < 0.01). All other factors were comparable. At our center, older AML patients receiving IC had superior complete response at any time point (CRatp) (43 % vs. 21 %; p < 0.01). IC also resulted in a longer median OS compared to Epi (10.6 vs. 7.9 months; p = 0.01). Thirty-day mortality and leukemia-free survival (LFS) were similar across the two groups (IC 10 % vs. Epi 11 %; p = 0.8; 11.2 vs. 9.3 months; p = 0.47 respectively). Choice of Epi drug (Azacitidine vs. Decitabine) did not impact results. In multivariate Cox regression analysis, older age, higher ECOG score, increased peripheral blasts, and poor-risk cytogenetics were independently associated with inferior survival.
CONCLUSIONS: Our results suggest that IC and Epi represent clinically equivalent approaches for the upfront treatment of older AML patients. In spite of significantly higher complete response (CR) and overall response rate (ORR) in the IC group, our finding of improved OS following IC vs. Epi was not substantiated in multivariate analysis. This finding suggests that difference in response of two agents in univariate analysis may be explained by the comparatively younger age of patients in the IC group. Leukemia-free survival and 30-day mortality were the same for IC vs. Epi-treated patients, as were all response and survival outcomes in the poor-risk cytogenetics subgroup. These data highlight the growing need for prospective clinical trials to conclusively determine the respective roles of IC vs. Epi therapy in older AML patients.
COMPARISON OF READABILITY OF PATIENT DISCHARGE INSTRUCTIONS WITH AND WITHOUT USE OF DISEASE-SPECIFIC TEMPLATESStephanie Mueller; Kyla Giannelli; Robert Boxer; Jeffrey L. Schnipper. Brigham and Women, Boston, MA. (Tracking ID #1937804)
BACKGROUND: In the United States, 21–23 % of the adult population have low literacy, and an additional 27 % have low health literacy (difficulty understanding written health education materials). Written materials are commonly used to communicate with patients at time of discharge, but can vary in readability level. We evaluated the association of the use of templated discharge instructions with readability scores of discharge instructions provided to patients at hospital discharge.
METHODS: We performed a retrospective cohort study of patients discharged from an academic medical center. Data were obtained from electronic medical records. Patients were eligible for inclusion if discharged from any inpatient service to home between October, 2011 and September, 2012, following initiation of a web-based “discharge module,” a quality improvement initiative to improve written communication at discharge, that included optional use of disease-specific templated discharge instructions. We examined the frequency of use of the templated discharge instructions. We then evaluated readability using two common measures: Flesch-Kincaid Grade Level (FKGL) and Flesch Reading Ease Level (FREL) in discharges that provided templated discharge instructions (with or without modification) vs. discharges that provided clinician-derived discharge instructions (where templated instructions were available and not used or were unavailable for the specific discharge diagnosis).
RESULTS: Of the 233 randomly selected patient discharges, 105 (45.1 %) provided templated discharge instructions and 128 (54.9 %) provided clinician-derived discharge instructions (Figure 1). The mean FKGL of templated discharge instructions was grade 5.6 vs. 7.6 for clinician-derived discharge instructions (p < 0.001). The mean FREL of templated discharge instructions was 71 vs. 57.4 for clinician-derived discharge instructions (p < 0.001). In subgroup analysis, FKGL of discharge instructions did not differ significantly when templated instructions were modified versus used without modification (5.8 vs. 5.5, p = 0.15). FREL of modified templated discharge instructions was 69.1 vs. 72.9 for templated instructions without modification (p = 0.02).
CONCLUSIONS: We found that we still lack many disease-specific templated discharge instructions within our “discharge module,” the major reason for clinicians to create discharge instructions themselves. Compared to discharges that used templated instructions, those that did not had significantly lower readability scores (higher FKGL and lower FREL). Modification of templated instructions, which may lead to more customized messages, did not appreciably detract from readability. Our findings suggest that templated instructions are more literacy friendly than clinician-derived discharge instructions.
CONTINUING MEDICAL EDUCATION (CME) PARTICIPANTS’ USE OF SPECIFIC TYPES OF SOCIAL MEDIA (SM) AND ASSOCIATION WITH ATTITUDES FOR USING SM IN CMEAlexander Vengerovsky; Amy T. Wang; Jayawant N. Mandrekar; Nicole P. Sandhu; Christopher M. Wittich; Karen F. Mauck; Thomas J. Beckman. Mayo Clinic, Rochester, MN. (Tracking ID #1939285)
BACKGROUND: Most research on social media (SM) in medicine pertains to issues of professionalism. One recent study found that continuing medical education (CME) course participants who use SM tend to be younger and favor the use of SM for enhancing CME learning. However, the potential link between the specific types of SM and participants’ views on using SM for CME remains unknown. Therefore, we determined what categories of SM are used by CME participants, along with the relationship between categories of SM use and favorable attitudes on using SM for CME.
METHODS: This was a cross-sectional survey of 539 participants at a Mayo Clinic Internal Medicine CME course in 2011. The Social Media Use and Perception Instrument (SMUPI) consisted of 10 items (5-point scales), and has been shown to have strong content, internal structure and criterion validity. Participants were surveyed regarding their demographic characteristics and individual use of SM. We also grouped types of SM into the following categories: professional (LinkedIn, Doximity, or Sermo), social (Facebook, Google+, Myspace, or Twitter), informational (blogs, wikis, podcasts, or StumbleUpon), and media (YouTube, Skype, Picasa, or Flickr). Comparisons of SMUPI scores for users versus non-users of each type of SM, and within categories of SM (professional, social, informational, and media), were calculated using the Wilcoxon Ranked sum test. The threshold for statistical significance was set at p < 0.05.
RESULTS: Of 539 CME participants, 327 (response rate = 61 %) completed the survey and 291 (89 %) reported using SM. CME course participants’ had generally favorable attitudes towards SM (Average SMUPI score 3.12). When comparing users and non-users of specific types of SM, higher SMUPI scores existed for users of Facebook (3.42 vs. 3.00, p < 0.0001), Google + (3.50 vs. 3.08, p < 0.0001), Twitter (3.74 vs. 3.19, p = 0.003), LinkedIn, (3.53 vs. 3.18, p = 0.007), Wikis (3.38 vs. 3.12, p = 0.02), and YouTube (3.32 vs. 3.09, p = 0.02). There were no significant SMUPI score differences for users versus non-users of Skype, blogs, podcasts, and Picasa. Finally, higher SMUPI scores were demonstrated for users versus non-users in the SM categories of professional (3.58 vs 3.17; p = 0.001), social (3.37 vs 2.82; p < 0.0001), and informational (3.35 vs 3.06; p = 0.008).
CONCLUSIONS: We are unaware of previous studies on the relationships between types of SM use and favorable attitudes towards utilizing SM for CME learning. Our results suggest that users of Facebook, Google+, LinkedIn, Twitter, and Wikis had the most positive attitudes regarding the use of SM in CME. Interestingly, these particular types of SM incorporate adult-learning principles of real-time interactivity and adaptability in order to optimize communication and community-building. We suggest that as CME directors increasingly utilize SM, they should focus on incorporating interactive types of SM into their CME courses.
CONTINUITY IN A VA PATIENT-CENTERED MEDICAL HOME REDUCES EMERGENCY DEPARTMENT VISITSKrisda Chaiyachati1,2; Kirsha S. Gordon3; Theodore Long4; Ali M. Khan6; Forrest Levin3,5; Emily M. Meyer2; Amy C. Justice1,2; Rebecca Brienza1,2. 1Yale University School of Medicine, New Haven, CT; 2VA Connecticut Healthcare System, West Haven, CT; 3VA Connecticut Healthcare System, West Haven, CT; 4Yale University School of Medicine, New Haven, CT; 5Evergreen Design, Guilford, CT; 6Iora Health, Brooklyn, NY. (Tracking ID #1922254)
BACKGROUND: One major goal of the Patient Aligned Care Team (PACT), the VA’s Patient-Centered Medical Home (PCMH) model, is to improve continuity of care between patient and provider, partly because poor continuity is believed to contribute to the inappropriate use of healthcare services like the emergency department (ED). Hypothesizing that patients with high continuity of care levels would visit the ED less, we sought to model patient and clinical factors associated with varying continuity levels and assess the association between high levels of continuity and the frequency of ED visits in the year after the initial implementation of PACT teams at Connecticut’s West Haven VA (WHVA).
METHODS: We performed a retrospective analysis of patients with established care at the WHVA primary care clinic from March 1, 2011 to February 29, 2012. We defined continuity as a patient seeing their assigned primary care provider (PCP) or trainee—resident physician or nurse practitioner. Using a multivariable regression model we determined the association between continuity and the frequency of ED visits, controlling for demographics, patient assignment to a trainee, comorbidities, having outside insurance, military service period, and distance from the ED. Additional models analyzed individuals who had at least one continuity visit in the study year to determine the impact of levels of continuity on ED utilization.
RESULTS: Veterans meeting inclusion criteria totaled 13,495 individuals with 42,969 total Clinic visits. Among those, 3185 (24 %) used the WHVA ED for 15,458 total ED visits. After controlling for covariates and potential confounders, continuity with an assigned PCP was independently associated with a 46 % reduction in the odds of using the WHVA ED [adjusted odds ratio (AOR) 0.54; 95 % confidence interval (CI): 0.41–0.71]. In the subset of patients having at least one primary care visit with continuity, those with medium (33–50 % of visits) and high continuity (>50 % of visits) levels were 30 % less likely (AOR 0.70; 95 % CI: 0.54–0.92) and 41 % less likely (AOR 0.59; 95 % CI: 0.25–0.76) to use the ED compared to patients with low continuity (<30 % of visits). Controlling for low (<3 visits/year) versus high (≥3 visits/year) primary care users did not significantly alter the impact of continuity on ED utilization. Patients assigned to a trainee were associated with lower ED utilization (AOR 0.78; 95 % CI: 0.69–0.89).
CONCLUSIONS: Improved continuity of care between patients and providers, including trainees, is associated with decreased ED utilization within the WHVA’s PACT system. To our knowledge, this is the first detailed analysis of continuity within a large PCMH model and assessment of the association between continuity and ED utilization. As outpatient centers and health systems adapt PCMH models to their specific setting, understanding the impact of patient-centered care indicators, like continuity, on healthcare utilization patterns and patient outcomes will be important for understanding PCMH components that may ultimately reduce health system costs.
CONTINUITY VISITS - A MODEL TO IMPROVE RELATIONAL CONTINUITY BETWEEN PATIENTS AND THEIR LONGITUDINAL PHYSICIANS DURING ACUTE HOSPITAL ADMISSIONSRyan Thompson; Chrisanne Sikora; Maria Veo; Keith Jennings; Timothy Ferris. Massachusetts General Hospital, Boston, MA. (Tracking ID #1941793)
BACKGROUND: With the rise of hospital medicine, and professional pressures facing ambulatory-based physicians, fewer patients are seeing the longitudinal physicians they know best when hospitalized. Research has shown that a majority of hospitalized patients feel they receive better care and experience higher levels of trust when cared for by physicians they have known over time. To address this decline in “relational continuity,” we began a pilot program to incentivize physicians identified as having a longitudinal relationship with a patient to make a “Continuity Visit” during the patient’s hospital admission. A secondary aim of the program is facilitate stronger clinical collaboration between hospital and ambulatory physicians based on their unique knowledge of the patient.
METHODS: A Continuity Visit is a brief one-time inpatient visit by a patient’s longitudinal physician with the patient and inpatient care team. Physicians eligible to participate include primary care physicians (PCPs), specialist physicians, and hospitalist physicians (for patients readmitted within 30 days). We provide a small reimbursement to physicians who make a Continuity Visit, and document their visit in the medical record. Physicians are ineligible to participate if they are actively involved in the patient’s current admission, as determined by billing data. PCPs at our institution have received automated electronic notifications of their patients’ Emergency Department visits and hospital admissions for many years. We developed a parallel notification system for specialist physicians by using electronic billing data and an algorithm that identifies longitudinal relationships between patients and specialists. We also began sending hospitalists automated notifications of their 30-day patient readmissions. These electronic “continuity notifications” contain the patient’s admitting diagnosis and hospital location, and a brief outline of the Continuity Visit program, including instructions on how to make and bill for a Continuity Visit. We tracked departmental variation in the number of Continuity Visits made since the launch of the program, and administered an anonymous survey to participating physicians regarding the perceived value of Continuity Visits to their patients and colleagues, and regarding their professional satisfaction with Continuity Visits.
RESULTS: Since the program’s launch in January 2012, 4164 hospitalized patients received a Continuity Visit from a physician with whom they have a longitudinal relationship. Specialists from 12 different departments made and billed for 2916 of these visits (70 %), PCP’s 1100 visits (26 %), and hospitalists 148 visits (4 %). Specialties with the highest volume of Continuity Visits included oncology, obstetrics, and cardiology. Comparing the first quarters of 2012 and 2013, the number of Continuity Visits increased by approximately two-fold among specialists, two-fold among PCPs, and four-fold among hospitalists. We surveyed physicians who made a Continuity Visit to one or more patients during a 3 month period (July–September 2013; n = 182). Of 106 respondents (58 %), 52 were specialists, 43 were PCPs, and 8 were hospitalists. Ninety-seven percent of respondents felt that their Continuity Visit was useful to the patient visited (59 % highly useful, 38 % moderately useful; see Table 1) Eighty percent felt their Continuity Visit was useful to the patient’s inpatient attending physician (37 % highly useful, 43 % moderately useful). Lastly, 96 % of physicians reported personal and/or clinical satisfaction from making the Continuity Visit (61 % highly satisfied, 35 % mostly satisfied; see Table 2).
CONCLUSIONS: Continuity Visits to hospitalized patients by their longitudinal physicians can facilitate stronger relational continuity between patients and physicians, improve collaboration between inpatient and ambulatory physicians, and improve information transfers across transitions of care. We found participating physicians to be highly satisfied with the Continuity Visit model. Further analysis is needed to assess whether the involvement of longitudinal physicians through Continuity Visits has impact on clinical and quality outcomes, including hospital length of stay, readmission rates, and standardized patient experience.
Reasons for Physician-Perceived Usefulness of their Continuity Visit to the Patient Visited (n = 106)
| The patient viewed your visit as an expression of interest in his or her well-being, even though you had no direct clinical responsibility for the care being provided during the hospitalization. | 97.1 % |
| The patient viewed your visit as a \“welcome surprise\”. Though the patient did not expect to see you, s/he was happy to know you were following up on his or her care. | 53.4 % |
| The patient seemed neutral about your visit—h/she expressed neither positive nor negative reaction to your presence. | 0.0 % |
| The patient seemed to view your visit as intrusive, and your involvement in the hospitalization as neither asked for nor desired. | 0.0 % |
* Respondents could check more than one response option
Reasons for Physician-Reported Satisfaction with Continuity Visits (n = 106)
| You were able to informally share clinical insight and information that improved the attending physician’s care of this patient. | 61.2 % |
| You believe that the collaborative relationship between you and the patient was enhanced by the Continuity Visit. | 84.5 % |
| The Continuity Visit you made will improve the transition of care for this patient to the outpatient setting. | 55.3 % |
| You are unsure if the care or treatment of this patient will be affected, positively or negatively, by the Continuity Visit. | 8.7 % |
| You felt the time and effort required to make a Continuity Visit to this patient was not well spent. | 1.9 % |
* Respondents could check more than one response option
CONTRACEPTIVE USE IN WOMEN HAVING BARIATRIC SURGERYRachel S. Casas; Iris Tong; Ghada Bourjeily. Warren Alpert Medical School of Brown University, Providence, RI. (Tracking ID #1936953)
BACKGROUND: Contraceptive counseling in women undergoing bariatric surgery is crucial due to the increased risk of adverse pregnancy and fetal outcomes in the 1 to 2 years following surgery. Women are typically advised to avoid pregnancy during this time period. Oral contraceptive pills (OCPs) are commonly used in the post surgical population, but their effectiveness may be limited by malabsorption. Intrauterine devices (IUDs) and surgical sterilization are the most effective contraceptive options for women not desiring future pregnancy. The aim of this study is to determine if women undergoing bariatric surgery are using and counseled about appropriate contraceptive options.
METHODS: A 36 question survey was sent electronically to pre- and post-surgical patients at the Center for Bariatric Surgery at the Miriam Hospital in Providence, Rhode Island. The survey consisted of questions about demographic data, contraceptive choices, and contraceptive counseling from healthcare providers. The survey did not include any questions containing patient identifying information. Included patients were aged between 18 and 44 years, sexually active with men, pre-menopausal, and lacked a history of hysterectomy or premature ovarian failure.
RESULTS: A total of 35 women completed the survey and met inclusion criteria. Overall, 30 participants (86 %) were counseled about contraceptives and 28 participants (80 %) were counseled to avoid pregnancy in the 1 to 2 years following surgery. Of the 21 women who had bariatric surgery within the last 2 years, 14 women (67 %) were using contraception, and seven women (33 %) were not. Among the seven contraceptive non-users post bariatric surgery, all were counseled to avoid pregnancy 1 to 2 years post surgery, six were counseled about contraceptive choices, and five did not desire pregnancy. Reasons stated for contraceptive nonuse in this subgroup included side effects and lack of regular partner. Of the 21 women who had bariatric surgery within the last 2 years, 11 (52 %) were using OCPs, three (14 %) were using male condoms, two (10 %) were using IUDs, and many women were using multiple forms of birth control. The majority of women chose their contraceptive methods based upon ease of use, ease of accessibility, and recommendation of healthcare provider. No pregnancy was reported following surgery.
CONCLUSIONS: While the majority of women undergoing bariatric surgery were using and counseled about contraceptives, many post surgical women were using less effective forms of contraception. Continued contraceptive counseling with a focus on the most effective methods, the IUD or sterilization for women not desiring future pregnancy, is needed in this population.
COORDINATING CANCER CARE: WHAT ORGANIZATIONS DO TO DELIVER HIGH-QUALITY BREAST CANCER CARE. A FUZZY SET QUALITATIVE COMPARISON ANALYSISNina A. Bickell1; Alexandra Moss2; Ann S. McAlearney2. 1Mount Sinai School of Medicine, New York, NY; 2The Ohio State University, Columbus, OH. (Tracking ID #1938688)
BACKGROUND: Underuse of adjuvant breast cancer treatments delivered by different specialists may be worsened by fragmented care and improved by effective coordination. To improve care coordination and adjuvant treatment delivery, we assessed approaches to coordinate cancer care at hospitals serving predominantly minority breast cancer patients, hospitals historically at higher risk for poorer quality.
METHODS: We interviewed 89 key informants (n = 58 clinical; n = 16 administrative; n = 12 clerical; n = 3 other) from 11 inner-city hospitals with high volumes of minority breast cancer patients to better understand how organizational characteristics might impact coordination of care, implementation and success of the T & F innovation. We used standard techniques to code the data from the key informant interviews and then used fuzzy set Qualitative Comparative Analysis (fsQCA) as the analytical method. For these results we focused our analyses on five conditions that had particular impact on successful implementation of the T&F innovation: handoffs; organizational attention to clinic patients; no-shows; patient-centeredness; and integrated EHRs. We then divided the hospitals into three outcome groups (<10 % underuse, 10–20 % underuse, >20 % underuse), and calibrated each of the conditions for six-value fsQCA using fuzzy set QCA methods.
RESULTS: Five organizational factors appeared particularly salient with respect to impacting coordination of adjuvant breast cancer care. First, with respect to tracking no-shows, the better sites had some way of keeping track of which no-shows actually came back and which no-shows needed to be contacted again; further, this tracking process was someone’s designated job. How organizations managed handoffs in care was also important. Handoffs at the better sites included an exchange of clinical information (e.g., doctors speaking directly to other doctors) as well as a clerical transfer of responsibility (clerks making appointments for patients with other specialties). Handoffs at the less good sites included one or none of these elements. Another key organizational factor involved the level of attention organizations paid to clinic patients. While some sites tolerated hectic, understaffed, and ineffective clinics, the better sites did not. A fifth critical factor was whether sites had an integrated EHR. We found that all the better sites had fully implemented and integrated EHRs, where providers could see what is going on with their patient in other specialties. Some sites had multiple EHRs leaving physicians unable to access needed treatment information. Finally, organizations that appeared to have a culture of patient-centeredness also appeared to have better quality of care. In our study, most of the good sites had a clear focus on trying to make things easy for the patient/the attitude that the hospital works for the patient and not the other way around.
CONCLUSIONS: As care coordination across sites and specialties is encouraged by federal law and regulation, specialty care silos and rigid communication systems still pose barriers to change. Our results suggest that organizational factors can have an important role impacting care coordination for breast cancer care, and highlight five mechanisms that may be truly critical with respect to ensuring good coordination and quality of breast cancer care.
CORRELATES OF SEXUAL SATISFACTION IN MIDLIFE WOMEN: COMMUNICATION IS KEYHolly N. Thomas1,2; Rachel Hess1. 1University of Pittsburgh, Pittsburgh, PA; 2VA Pittsburgh Healthcare System, Pittsburgh, PA. (Tracking ID #1935614)
BACKGROUND: Sex is an essential component of quality of life. While most studies of sex in women focus on sexual dysfunction, sexual satisfaction is just as important. Characteristics related to sexual satisfaction in women are not well-defined and likely change with aging. We used a population-based cohort of midlife and older women to define factors related to sexual satisfaction.
METHODS: The National Survey of Midlife Development in the United States (MIDUS) is a nationally representative cohort study of adults ages 28 to 84. Self-administered questionnaires collected information regarding demographics, psychosocial factors, and physical and mental health. The second wave (2004–2006) included questions about sex. Sexual satisfaction was assessed by: “How would you rate the sexual aspect of your life these days?” with a 0 (worst) to 10 (best) visual analog scale. Women who reported any sexual activity in the prior 6 months were included in the primary analyses. Descriptive statistics were used to compare sexually active and inactive women. Post-stratification weights based on race, age, and education status were used to adjust percentages to the general population. Univariable ordered logistic regression was used to assess the relationship between (1) sociodemographics, (2) relationship characteristics, and (3) physical and mental health of the woman and her partner, and the outcome (sexual satisfaction). Significant (p < 0.05) variables were entered into a multivariable model.
RESULTS: Of the 2647 women in MIDUS, 1345 (63.6 %) were sexually active in the prior 6 months and 531 did not answer the questions regarding sex. The proportion of sexually active women decreased with age. However, among those married or living with a partner, 81.8 % were sexually active overall, and 56.7 % of women 65 and older were sexually active (Table 1). In the multivariable model, better communication with partner, higher frequency of sex, better self-rated mental health, earlier menopausal status, lack of dyspareunia, and no use of antidepressants were related to higher sexual satisfaction at the p < 0.05 level (Table 2). At p ≤ 0.002, only communication and frequency of sex were significant (Bonferroni adjustment for multiple comparisons).
CONCLUSIONS: As long as they have a partner, a large proportion of women are sexually active in midlife and beyond. Neither age nor physical health is significantly related to sexual satisfaction in midlife women. Women who report better communication with their partners have higher sexual satisfaction. Providers caring for women should not assume that sexual satisfaction declines with aging. Improving communication with one’s partner may be a key target in the treatment of sexual problems in women.
Proportion of sexually active women in MIDUS (if married or cohabitating)
| Age | N | % | Weighted % |
| 39 or less | 169 | 97.7 | 96.0 |
| 40–49 | 414 | 92.4 | 90.4 |
| 50–59 | 370 | 86.7 | 87.6 |
| 60–69 | 221 | 71.5 | 69.4 |
| 70–79 | 72 | 48.7 | 42.6 |
| 80 or above | 11 | 44.0 | 36.8 |
Factors associated with higher sexual satisfaction among sexually active women in MIDUS
| Variable | OR (95 % CI) | P-value (Wald) | Overall P-value (LR Chi2) |
| How much can you open up to partner | 0.002 | ||
| A lot | Referent | ||
| Some | 0.64 (0.24, 1.74) | 0.39 | |
| A little | 0.85 (0.14, 5.31) | 0.86 | |
| Not at all | 0.00 (0.00, 0.08) | <0.001 | |
| Frequency of sex | <0.001 | ||
| 2+ a week | 5.22 (1.78, 15.34) | 0.003 | |
| Once/week | 3.13 (0.21, 8.10) | 0.019 | |
| 2–3/month | Referent | ||
| Once/month | 0.06 (0.01, 0.23) | <0.001 | |
| Mental health | 0.031 | ||
| Excellent | Referent | ||
| Very good | 0.64 (0.21, 2.00) | 0.44 | |
| Good | 0.35 (0.11, 1.18) | 0.092 | |
| Fair/poor | 2.46 (0.38, 15.81) | 0.34 | |
| Menopausal status | 0.011 | ||
| Premenopausal | Referent | ||
| Perimenopausal | 0.19 (0.05, 0.73) | 0.016 | |
| Postmenopausal | 1.53 (0.44, 5.27) | 0.50 | |
| Hysterectomy, ovaries intact | 0.34 (0.09, 1.23) | 0.099 | |
| Bilateral oopherectomy | 1.71 (0.49, 5.95) | 0.40 | |
| Pain with intercourse (yes) | 0.39 (0.19, 0.79) | 0.009 | |
| Depression medication (yes) | 0.26 (0.11, 0.64) | 0.003 | |
Adjusted for relationship satisfaction/strain, intimacy, importance of sex, prior sexual satisfaction, age, generation, physical health, chronic diseases, sexual assault, hormone therapy use, BMI, partner status, relationship length, partner disease, partner physical and mental health, difficulty paying bills
COST EFFECTIVENESS COMPARISON OF SCREENING STRATEGIES FOR LATENT TUBERCULOSIS INFECTION AMONG BACILLUS CALMETTE-GUERIN VACCINATED HEALTH CARE WORKERSMehrshid Kiazand1,2; Noor Khan1,2; Kenneth J. Smith2,3. 1UPMC Mercy, Pittsburgh, PA; 2University of PIttsburgh School of Medicine, Pittsburgh, PA; 3UPMC, Pittsburgh, PA. (Tracking ID #1906127)
BACKGROUND: The interferon- gamma release assay (IGRA) is recommended as an alternative to the tuberculin skin test (TST) to detect latent tuberculosis infection (LTBI). IGRA is the preferred test for Bacillus Calmette- Guerin (BCG) vaccine recipients. Despite recommendations, TST is frequently used in many institutions to screen for LTBI, regardless of previous BCG vaccination. We evaluated the cost-effectiveness of alternative strategies for LTBI detection among BCG vaccinated health care workers.
METHODS: We have designed a decision tree to compare three screening strategies in BCG recipients; (1) TST alone; (2) IGRA alone and (3) TST, if positive, then IGRA. In the base case, we assume that LTBI prevalence (assessed by TST among foreign born U.S. residents) is 18 %. In BCG vaccinated populations TST sensitivity and specificity is 71 % and 56 %, while IGRA sensitivity and specificity is 76 % and 96 %. Sixty-three percent of health care workers will accept isoniazid (INH) for LTBI treatment. The cost of TST is $9.79 and IGRA is $33.67. The cost of INH treatment for 9 months is $508.95 and the average cost of managing INH related hepatitis (4 % risk) is $539.74.
RESULTS: In the base case, the IGRA alone strategy cost $23.62 more per person than TST followed by IGRA ($88.87 vs. $62.55), but IGRA alone increased the LTBI absolute detection and treatment rate by 2.5 % (8.6 % vs. 6.1 %). Thus compared to TST then IGRA, IGRA alone cost $1053 per case detected and treated. Compared to IGRA alone, the TST alone strategy is dominated, costing more ($168.89 vs. $88.87, due to more false positives receiving INH) with fewer cases detected and treated. Compared to TST then IGRA, TST alone costs more than $5500 per case. IGRA alone dominates TST alone if IGRA testing costs less than $120. TST alone is no longer dominated and costs less than $1000 per case, if 10 % or less of health care workers agree to INH treatment. Model results were robust to variation of other parameter values.
CONCLUSIONS: TST alone to detect LTBI in BCG vaccinated populations will likely cost more than other strategies and detect fewer cases than an IGRA alone strategy. However, IGRA alone costs more than $1000 per additional case detected and treated compared to TST then IGRA. It is unclear if this cost is acceptable to payers. Although not strongly recommended, IGRA after a positive TST may be more economically reasonable than other strategies in BCG recipients and worthy of future study.
COST-EFFECTIVENESS OF DECISION SUPPORT STRATEGIES FOR SAFELY REDUCING ANTIBIOTIC USE IN ACUTE BRONCHITISConstantinos I. Michaelidis1; Melissa S. Kern2; Kenneth J. Smith3. 1University of Pittsburgh School of Medicine, Pittsburgh, PA; 2Geisinger Health System, Danville, PA; 3University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1929178)
BACKGROUND: A recent clinical trial suggests that printed (PDS) and computer decision support (CDS) strategies can safely reduce antibiotic use in management of acute bronchitis compared to usual care (UC). Yet, little is known about the cost-effectiveness of these strategies. We evaluate the cost-effectiveness of PDS and CDS strategies in safely reducing antibiotic use in management of acute bronchitis.
METHODS: We developed a clinical trial based cost-effectiveness analysis comparing three strategies for acute bronchitis management: UC, PDS and CDS. We assumed a societal perspective, 5 year program duration and 30 day time horizon after each office visit. Our cohort was the U.S. population aged 13–64 years presenting with acute bronchitis in an ambulatory setting. The primary differences between the three strategies were the added intervention costs and reduced likelihood of antibiotic use in the PDS and CDS strategies relative to the UC strategy. Estimated per patient program implementation costs in year 1 were $1.07 in the PDS strategy and $18.11 in the CDS strategy. We performed a base case cost effectiveness analysis and one-way and probabilistic sensitivity analyses in which the primary outcome was the societal cost per antibiotic safely avoided. We assumed that the societal willingness-to-pay (WTP) threshold was $43 per antibiotic safely avoided based on prior estimates of the downstream hidden societal costs of antibiotic resistance attributable to each ambulatory antibiotic prescription.
RESULTS: In the base case analysis, the PDS strategy dominated both the UC and CDS strategies, with lesser total costs (PDS: $2,614, UC: $2,629, CDS: $2,635) and fewer antibiotic prescriptions (PDS: 3.79, UC: 4.60, CDS: 3.95 antibiotic prescriptions) per patient over 5 years. In one-way sensitivity analyses, the PDS strategy dominated the UC strategy across all tested parameter values except when antibiotics reduced the duration of work loss by ≥0.1 days (base case: 0.0 days) or cost ≤$10 (base case: $30). The PDS strategy dominated the CDS strategy across all tested parameter values except when the adjusted odds of antibiotic use during the intervention period relative to baseline was ≥0.64 in the PDS strategy (base case: 0.57) or ≤0.57 in the CDS strategy (base case: 0.64). The PDS strategy cost less than the societal WTP threshold ($43 per antibiotic safely avoided) across all tested parameter values except when antibiotics reduced the duration of work loss by ≥0.5 days (base case: 0.0 days). The analysis was not sensitive to variation in the costs of physician education or patient educational brochures in the PDS and CDS strategies, posters in the PDS strategy or electronic medical programming in the CDS strategy. In a probabilistic sensitivity analysis, varying all parameters simultaneously, the probability of the PDS strategy being preferred at a societal WTP threshold of $43 per antibiotic safely avoided was 66.4 %. The PDS strategy was preferred across all thresholds from $0–$100 per antibiotic safely avoided.
CONCLUSIONS: A printed decision support strategy to safely reduce antibiotic use in ambulatory management of acute bronchitis is likely to be less costly and more effective than usual care and computer decision support strategies. This analysis suggests that even a modestly effective intervention to safely reduce antibiotic prescribing can be economically reasonable when implementation costs are low.
CT SCAN OVERUSE IN FREQUENTLY ADMITTED MEDICAL PATIENTSMina Owlia; Gregory M. Bump; Franziska Jovin; Christopher Deible; Marion Hughes; Lan Yu. University of Pittsburgh Medical Center-Oakland, Pittsburgh, PA. (Tracking ID #1903461)
BACKGROUND: Computed Tomography (CT) is an overused diagnostic tool. Clinicians may have limited understanding of how often CT scans lack clinically important findings. We describe the frequency of CT scan use in patients with frequent medical hospitalizations as well as the frequency of clinically important findings identified on these examinations.
METHODS: We retrospectively reviewed all CT scans done in 130 patients with greater than 7 admissions to medical services between January 1, 2011 and Dec 31, 2011 within an integrated health care system. We calculated the number of CT scans performed, the anatomic site of imaging, the source of ordering (emergency department, inpatient floor, or intensive care unit) and scored all CT scans using a novel scoring system on a 0–4 scale based on the severity of radiographic findings. Higher scores signified more clinically important findings with a score of 0 representing a normal study, a score of 1 showing minimal abnormalities with no need for follow up, score of 2 showing minor abnormalities which likely require followup, a score of 3 showing major abnormalities likely to affect management, and a score of 4 representing a critical or emergent finding.
RESULTS: A total of 795 CT scans were performed with a mean of 6.7 (±SD 5.8) CT scans per patient. Abdominal/Pelvis (39 %), chest (30 %), and head (22 %) CT scans were the most frequently obtained. The most common site of CT scan ordering (53.7 %) was the inpatient floors. Head CTs had the lowest rate of clinically significant findings (4 %), compared to 38.3 % of chest CTs and 31.5 % of abdominal/pelvis CTs (Table 1).
CONCLUSIONS: Patients with frequent medical admissions undergo multiple CT scans that infrequently show findings that change clinical management. In particular, head CTs are rarely associated with significant findings and should be ordered less frequently. Inter-disciplinary measures should be advocated by hospitalists, emergency department physicians, and radiologists to decrease unnecessary imaging in this population.
Distribution and frequency of reconciled scan scores based on type of CT scan
| Scan by modality | Mean # CT scan (SD) per patient | Median $ CT scans per patient | Scores | Total N (%) | ||||
| 0 (n = 90) | 1 (n = 360) | 2 (n = 126) | 3 (n = 200) | 4 (n = 19) | ||||
| Head CT | 2.9 +/− 4.2 | 1 | 64 (37.2) | 95 (55.2) | 6 (3.5) | 3 (1.7) | 4 (2.3) | 172 (21..6) |
| Neck CT | 1.8 +/− 1.3 | 1 | 0 (0) | 5 (31.2) | 4 (25.0) | 4 (25.0) | 3 (18.8) | 16 (2.0) |
| Chest CT | 3.1 +/− 2.4 | 2 | 8 (3.4) | 86 (36.3) | 52 (21.9) | 84 (35.4) | 7 (2.9) | 237 (29.8) |
| Abdominal/Pelvis | 3.2+/− 2.2 | 3 | 11 (3.6) | 141 (45.8) | 59 (19.2) | 92 (29.9) | 5 (1.6) | 308 (38.7) |
| Spine CT | 1.6 +/− 0.8 | 1 | 4 (16) | 18 (72) | 1 (4) | 2 (8) | 0 (0) | 25 (3.1) |
| Total | 6.7 +/− 5.8 | 11.3 % | 45.3 % | 15.9 % | 25.2 % | 2.4 % | 758 | |
CULTURAL COMPETENCE AND PERCEPTIONS OF COMMUNITY HEALTH WORKERS’ EFFECTIVENESS FOR IMPROVING HYPERTENSION OUTCOMES AND REDUCING HEALTH DISPARITIESMeta Mobula1; Mekam T. Okoye1; L. Ebony Boulware2; Kathryn A. Carson1,3; Jill A. Marsteller3; Lisa A. Cooper1,3. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Duke University School of Medicine, Durham, NC; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD. (Tracking ID #1938515)
BACKGROUND: Community Health Worker (CHW) interventions improve hypertension control among ethnic minorities, but health professionals’ perceptions of their effectiveness may impede integration of CHWs into health care delivery systems. Health professionals’ cultural competency has also been identified as a potential strategy to improve health outcomes of patients from diverse social groups. We explored the association between provider and staff self-reported cultural competency and preparedness to deliver cross-cultural care with attitudes towards effectiveness of CHWs in reducing health care disparities and improving clinical outcomes.
METHODS: We administered a questionnaire to providers (physicians and nurse practitioners) and clinical staff (nurses, medical assistants and others) from six urban primary care practices in Maryland to assess their self-reported cultural competence; preparedness to deliver cross-cultural care; and perceptions of a proposed CHW intervention. Cultural competence was assessed in three domains: motivation to learn about other cultures, cultural behavior and power and assimilation. We quantified the associations of cultural competence and preparedness with attitudes towards the effectiveness of CHWs using logistic regression adjusting for respondent age, race, gender, provider/staff status and years at the practice.
RESULTS: We contacted 200 providers and clinical staff, and 119 (60 %) participated. Providers and staff reporting more cultural motivation had higher odds of perceiving CHWs as helpful for improving patient outcomes (OR = 2.56, 95 % CI = 1.32–4.96) and reducing health disparities (OR = 10.05, 95 % CI = 3.55–28.44). Those reporting more frequent culturally competent behaviors also had higher odds of believing CHWs would help improve patient outcomes (OR = 1.96, 95 % CI = 1.02–3.76) and reduce health disparities (OR = 3.59, 95 % CI = 1.62–7.99). Providers’ attitudes towards power and assimilation for socially disadvantaged groups were not associated with their perceptions of CHWs. Cultural preparedness was associated with providers’ perceived utility of CHWs in reducing health disparities (OR = 2.32, 95 % CI = 1.20–4.47), but not significantly associated with improving health outcomes (OR = 1.72, 95 % CI = 0.88–3.35).
CONCLUSIONS: Providers and staff with higher self-assessed cultural motivation, culturally competent behaviors, and cultural preparedness have more positive expectations of CHW interventions to reduce health disparities. The group that self-assesses as more culturally competent may know more about specific challenges faced by underserved patients and thus be more likely to see advantages of involving CHWs to overcome those challenges. Cultural competence training for providers and staff may complement the use of CHWs and support their effective integration into primary care clinics that are seeking to improve health outcomes and reduce disparities.
CULTURAL TAILORING OF STROKE RISK FACTOR REDUCTION AND WALKING PROMOTION COMMUNITY INTERVENTION FOR SOUTH ASIAN OLDER ADULT IMMIGRANTSNazleen Bharmal1; Brian S. Mittman2; Raina Shah3; Catherine Sarkisian2,1. 1UCLA, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA; 3University of California, Irvine, Irvine, CA. (Tracking ID #1933529)
BACKGROUND: South Asians are people with origins from India, Pakistan, Bangladesh, Nepal, and Sri Lanka. They are among the fastest growing U.S. immigrant groups. Epidemiological studies in Western countries have documented disproportionately high prevalence and mortality rates of coronary heart disease and stroke, with much of the excess stroke mortality in South Asians attributed to physical inactivity. Our objectives were to culturally-tailor an existing stroke risk factor reduction/walking promotion intervention and assess the feasibility of implementing the proposed intervention in senior centers for South Asians.
METHODS: We used community-based participatory research (CBPR) and implementation science methods to collect and analyze data from a community advisory board (CAB), focus groups, and stakeholder interviews in an iterative fashion. Community partners included a South Asian community-based organization (CBO) and two senior centers located near ethnic enclaves of low-income, recently immigrated South Asians. The theoretically-grounded intervention curriculum was designed as part of a NIH/NINDS-funded RCT and incorporated elements of moderated small group discussions, scenarios, didactics, goal-setting and reflection over eight sessions. CAB members reviewed the initial curriculum and provided input on the curriculum approach, content, context, and language based on the ecological validity and community-based developmental models to cultural adaptation. Using CAB input on the curriculum, we conducted three focus groups of Hindi-speaking South Asian older adults to identify knowledge and awareness of stroke risk factors and barriers and facilitators to walking. Focus group audio recordings were translated into English and transcribed. Using content analysis, CAB members reviewed the focus group transcripts and generated themes of stroke awareness and walking beliefs, as well as potential curriculum modifications to address these beliefs. We also interviewed key stakeholders to identify general and site-specific factors associated with greater likely effectiveness of the proposed intervention.
RESULTS: During the initial review, CAB members recommended changes to the intervention curriculum to be better received by South Asian seniors (Table 1). The 33 focus group participants had a mean age of 72.8 years. Most were male (55 %), had at least a college degree from India (65 %), had lived in the U.S. for less than 20 years (56 %), and were mostly or very comfortable speaking English (58 %). Participants had been diagnosed with stroke (19 %), hypertension (64 %), and hyperlipidemia (44 %), and engaged in walking (67 %) or yoga (33 %) for physical activity. Themes identified by CAB members from the focus groups to address in the intervention are presented in Table 2. CAB members recommended having 15–20 min of group walking after each small group session. Stakeholder interviews confirmed enthusiasm from both senior centers as intervention sites, CBO interns as potential session moderators, and CBO willingness to provide resources for participant recruitment and follow-up. Two barriers identified were the diversity of South Asian languages spoken by potential participants and participants’ lack of experience in engaging in a long-term intervention, as opposed to a one-time workshop.
CONCLUSIONS: Community-based participatory approaches are effective ways to integrate evidence-based interventions that are systematically and culturally consistent into existing community infrastructure. We found this CBPR approach led to concrete and substantive input on content and delivery, while still allowing for the fidelity of the intervention. Our community-academic partnership resulted in interest about the topic of healthy aging, strong enthusiasm and leadership in shaping the culturally-tailored intervention, and excitement about its implementation by the community partners, CAB, and potential participants. Our next step will be to conduct a pilot intervention in one senior center with the goal of increasing walking steps and beliefs that physical activity is an important part of healthy aging that can reduce stroke risk.
Table 1: Cultural adaptation recommendations by CAB for community-based intervention
| Category | Example of Cultural Adaptation |
| Concept | ● Self-care and modifying one’s fate are new concepts |
| Content | ● South Asian values of Eastern collectivism to include multi-generational families involved in health care decisions ● Ayurvedic medicine and stroke prevention |
| Context | ● South Asian friendly scenarios in terms of dress, activities, food, location ● Most South Asian seniors live with their children and are often restricted by the needs of their children/grandchildren |
| Language | ● Use the word ‘niyam’ or ‘vaada’ to convey the concept of goal-setting ● Use negative language to convey the importance of stroke risk factor reduction (e.g., being sedentary may lead to a stroke and loss of independence or becoming dependent on your children) |
| Persons | ● Social isolation and lack of transportation causes seniors to be home-bound |
| Methods | ● Include photographs of South Asians who have visible signs of stroke |
Table 2: Themes from focus group of South Asian older adults
| Stroke Awareness | Walking Beliefs and Behaviors |
| ● Need for more information as to the nature of stroke, why it occurs (genetic risk?), and what to do if someone is having a stroke | ● Walking groups that have a walking \“leader\” was suggested to increase opportunities for social network as most seniors felt socially isolated |
| ● Stroke knowledge is gained from friends and family, as opposed to healthcare providers | ● Incentives should address social aspects of the activity, such as \“chai\” and biscuits at workshops or after walking |
| ● Ayurvedic and alternative medicine play a role in stroke prevention and treatment | ● There appears to be two extremes: people who walk regularly versus those who are not physically active. This difference impacts walking acceptability and understanding benefits |
| ● Belief in fate and lack of belief that walking can reduce stroke risk may be a barrier to stroke prevention efforts | ● Barriers included family obligations for childcare (grandchildren), not a priority, idea of \“being selfish\” is novel in culture, knee pain, weather. Housework commonly seen as a form of moderate physical activity. |
| ● Stress from obligations to family and family pressure is a significant risk factor for stroke | ● Facilitators included personal stories of how walking prevented more severe disease and/or medical interventions |
CURRENT PRACTICES AND OPPORTUNITIES IN A RESIDENT CLINIC REGARDING THE CARE OF OLDER ADULTS WITH MULTIMORBIDITYNancy Schoenborn; Cynthia M. Boyd; Matthew McNabney; Anushree Ray; Danelle Cayea. Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1936991)
BACKGROUND: Multimorbidity (2 or more chronic conditions) is a common problem that affects more than half of all older adults. Multimorbidity is associated with higher mortality, disability, institutionalization, decreased quality of life, and higher rates of adverse effects from treatments or interventions. Guiding Principles for the care of older adults with multimorbidity were developed and published by the American Geriatrics Society. Clinicians report inadequate training in caring for older adults with multimorbidity but it is not clear what opportunities arise in clinical encounters to apply the Guiding Principles and how clinicians currently practice regarding the Guiding Principles. Our study explores the current practices and opportunities for improvement in a resident clinic regarding the care of older adults with multimorbidity.
METHODS: In this qualitative study, we audio-recorded clinic visits between residents and patients who were ≥65 years old and with ≥2 chronic medical conditions in the General Internal Medicine resident clinic at Johns Hopkins Bayview Medical Center. We explored the resident-patient discussions related to the five domains of the Guiding Principles: Patient Preferences; Interpreting the Evidence; Prognosis; Clinical Feasibility; and Optimizing Therapies and Care Plan. The recordings were transcribed, coded and analyzed using the grounded theory approach, generating themes and sub-themes.
RESULTS: We have recorded visits between 17 residents (6 PGY1s, 6 PGY2s, 5 PGY3s) and 26 patients. Each resident had 1–4 recorded visits. Each patient was recorded once. Patients’ mean age was 74.1 years, with on average 3.5 comorbidities, 12.7 medications, and mean self-rated health score of 68 on the EuroQol visual analog scale. All visits included discussions that were thematically related to the content of at least one of the Guiding Principles, most often Patient Preferences, Clinical Feasibility, and Optimizing Therapies and Care Plan; discussions related to the other two Guiding Principles were less frequent with very rare discussion related to Prognosis: a) The discussions related to Patient Preferences often included patients’ opinions about decisions such as whether to pursue medication changes, procedures, or specialist referrals, but were not often associated with discussions about the expected benefits and harms of these decisions. b) Discussions related to Interpreting the Evidence occurred infrequently, and did not often include consideration of the applicability of the evidence in the context of multimorbidity. c) The discussions related to Clinical Feasibility often considered treatment complexity and feasibility in the context of medications compared to other treatment modalities. d) The discussions related to Optimizing Therapies and Care Plan more frequently involved specific diseases than the interactions among multiple conditions or their treatments. e) A number of opportunities to incorporate Guiding Principles as prompted by patients or patients’ medical conditions were missed by residents.
CONCLUSIONS: During clinic visits with older patients with multimorbidity at a resident clinic, discussions related to some of the Guiding Principles occurred more frequently than others. Medical content of the visits and patient prompts provided regular opportunity to incorporate the Guiding Principles but were not always acted upon, suggesting room for improvement. We will implement an innovative curriculum to teach how to better incorporate elements of the Guiding Principles into clinical visits.
DANCE YOUR WAY TO BETTER HEALTH: EFFECTS OF TANGO DANCE ON MILD COGNITIVE IMPAIRMENT IN OLDEST OLD ADULTSTeresa Ingram1; Madeleine E. Hackney2. 1Emory, Atlanta, GA; 2Emory, Atlanta, GA. (Tracking ID #1941542)
BACKGROUND: With the baby boomer generation in the United States, our elderly population will increase exponentially over the course of the next 30 years. Many oldest-old adults have sensory, motor, and cognitive impairments leading to reduced independence and social isolation. Not only does cognitive impairment causes decline in quality of life, but it also increases morbidity and mortality risk and carries a huge burden on the healthcare economics. Our purpose is to determine the effects of a 12 week course of Tango-adapted dance classes vs. group educational sessions on the cognitive performance in an oldest-old adult population with Mild Cognitive Impairment (MCI).
METHODS: Participants were assigned to 20, 90-min lessons in Tango or Education that took place at six different senior independent living communities. Only one site offered Education; while tango was offered at the other sites. Participants were assessed on the following measures of cognition: Trail Making Test (TMT), with parts A and B, Montreal Cognitive Assessment (MoCA), Timed Up and Go Cognitive, and Brooks Spatial Memory Test prior to and after intervention. Errors and number correct were evaluated.
RESULTS: 74 participants enrolled in the original study (Tango, n = 52; Education, n = 12). For this analysis, criteria for exclusion included anyone under age 80 and completion of less than 5 education or dance sessions which yielded a study population of 41 (Tango, n = 32, Education, n = 9). Within the tango group, there was improvement in Timed Up and Go Cognitive scores (pre-intervention average 19.4, post-intervention average 18.1, change average score of 1.29; p-value 0.07). Timed Up and Go score alone did not improve significantly within the Dance group (change average of 0.75, p-value of 0.37). There was no significant improvement in Timed Up and Go Cognitive scores in the Education group. Alternatively, Brooks spatial scores improved significantly within the Education group (pre-intervention average 59.5, post-intervention average 70.8; p-value 0.007) compared to Dance group (p- value 0.05). There were no statistically significant differences with in MoCA or TMT scores with either intervention.
CONCLUSIONS: Although the Timed Up and Go Cognitive scores within the Dance therapy group were not statistically significant, an improvement within the dual tasking/cognitive portion was evidenced by non-improvement within the motor aspect of the test (Timed and Go). There may be a role for dance and/or exercise in helping to maintain or improve MCI in oldest old adults. It is unclear why there were no improvements within the MOCA or Trail Making Tests which are tests of executive functioning. Further investigation of benefits of educational classes on the effects of spatial memory will be studied. This study is unique because of the focus on adapted Tango as well as having a population group over the age of 80. Limitations include low power, especially in the education group, and significant dropout rate. Also participant knowledge of class assignment could lead to potential bias. Larger population studies that also look into the effect of co-morbities on test performance is warranted.
DEATH AMONG PATIENTS HOSPITALIZED WITH PNEUMONIA; IMPLICATIONS FOR HOSPITAL OUTCOME MEASURESMihaela S. Stefan1,3; Michael B. Rothberg2; Randa Jaber1; Jane Garb1; Janice Fitzgerald1; Peter K. Lindenauer1,3. 1Baystate Medical Center, Springfield, MA; 2Cleveland Clinic, Clevaland, OH; 3Tufts University School of Medicine, Boston, MA. (Tracking ID #1936240)
BACKGROUND: Risk-standardized mortality rates are used to assess the quality of care for patients hospitalized with pneumonia, and were recently added to Medicare’s Value Based Purchasing. The measure includes patients regardless of advanced directives (unless the patient is already in hospice) and those with terminal illnesses for whom pneumonia may play only a minor role in their death. The objective of this study was to assess the proportion of patients included in the CMS pneumonia mortality measure for whom pneumonia was a major contributor to death. In addition, we compared the intensity of care during hospitalization including admission to intensive care unit (ICU) and ventilation management for patients for whom pneumonia was a major contributor to death and those for whom it was not.
METHODS: Retrospective, chart review of adults who died with a principal diagnosis of pneumonia between January 2008 and December 2012 in three hospitals in Western Massachusetts. Determination of pneumonia as a major or minor contributor in the patient death was assessed by two reviewers who used a standardized abstraction form. Results were compared and discussed until the agreement reached 100 % (for a total of 57 charts); thereafter charts were assessed independent by each reviewer. Pneumonia was considered to have been a minor determinant if at admission patient had advanced comorbidities which may have been the major contributor to death (e.g. metastatic cancer). Patients’ characteristics, comorbidities, ventilation management and advance directives were collected and compared between the two groups of patients.
RESULTS: We included 204 pneumonia deaths from three hospitals; 169 from a large academic center and 35 from 2 community hospitals. For the first 30 charts reviewed, inter-rater k agreement coefficient was 0.35. Discrepancies between the reviewers were resolved through discussion; agreement then rose to a k of 0.63 for the next 12 cases and to a k of 1.0 for the next 15 cases. The median age of the study population was 78.5 years, 46 % were male, 98 % had at least one major co-morbidity and majority were white (87 %). During hospitalization, 24 % were intubated and 25 % died in the intensive care unit. Pneumonia was considered to have played a minor role in patients’ death in 167 (80 %) cases. Overall, 51 % of cases had a do-not-resuscitate order (DNR) at admission and 25 % at the time of death. Of those who had their code status changed during hospitalization, the change to DNR or comfort care was made on the day of death in 41 % of the cases.. Compared with patients for whom pneumonia was a major reason to death, patients for whom pneumonia was a minor contributor to death were slightly younger, had more advanced comorbidities (100 % vs 86 %); were less likely to be admitted to ICU (28 % vs 42) and to be mechanically ventilated (22 % vs. 32 %); were less likely to have mechanical ventilator withdrawn before death (78 % vs. 92 %) and were more likely to expire on the medical ward (76 % vs. 53 %).
CONCLUSIONS: Only a small fraction of deaths included in the pneumonia mortality measure are the direct result of pneumonia. The majority of patients who die are frail elderly with advanced non-modifiable conditions, most of whom decide to forego aggressive care at some point during their admission. The deaths of these patients do not necessarily reflect the quality of pneumonia care received. Only half of these patients had DNR orders on admission, and many initially received aggressive care, suggesting opportunities for discussion of end of life care before hospitalization.
DECADE-LONG TRENDS IN MORTALITY AMONG PATIENTS WITH AND WITHOUT DIABETES AT AN ACADEMIC MEDICAL CENTER IN AN ERA OF IMPROVED GLYCEMIC CONTROLNeel M. Butala1; Benjamin K. Johnson3; James F. Dziura3,1; Janis E. Bozzo2; Silvio Inzucchi1; Thomas Balcezak1,2; Leora I. Horwitz1,2. 1Yale School of Medicine, New Haven, CT; 2Yale-New Haven Hospital, New Haven, CT; 3Yale Center for Analyltic Sciences, New Haven, CT. (Tracking ID #1937226)
BACKGROUND: Given the increasing prevalence of diabetes, historically worse outcomes for patients with diabetes when hospitalized, and recent trends toward improving glycemic control in both inpatient and outpatient settings, it is important to understand whether the mortality risk of diabetes during hospitalization has changed over the last decade. The objective of this study was to determine 10-year trends in in-hospital mortality for patients with versus without diabetes and to examine the potential impact of inpatient and outpatient glucose control.
METHODS: We conducted a serial cross-sectional observational study of all adult non-obstetric patients with an inpatient admission between Jan 1, 2000 and Dec 31, 2010 at a major urban medical center. The primary exposure of interest was a diagnosis of diabetes mellitus and the main outcome was in-hospital mortality. Additionally, we looked at measures of inpatient glycemic control (percentage of days with glucose below 70, glucose above 299, and glucose between 70 and 179, and standard deviation of glucose measurements) and hemoglobin A1c, which served as a measure of outpatient glucose control and a proxy for severity of diabetes. We constructed multivariate logistic regression models including time from start of study until admission in years, whether an individual had diabetes, and the interaction between time and diabetes status as well as age, sex, race, payer, diagnosis and comorbidities while stratifying by whether the hospitalization included an intensive care unit (ICU) stay. We then restricted our sample to ICU patients with diabetes and determined the relation between the measures of glucose control and changes in mortality over time using logistic regression.
RESULTS: We included 322,938 patient admissions, of which 54,645 (16.9 %) were ICU patients. 76,758 patients (23.8 %) had diabetes: 26.3 % of ICU patients and 23.2 % of non-ICU patients. Among ICU patients with diabetes, measures of inpatient control were available for 91.5 % and hemoglobin A1c for 34.7 %. The overall mortality rate was 2.4 %, representing 2.7 % of patients with diabetes and 2.2 % of patients without diabetes. However, raw mortality for patients with diabetes decreased from 3.6 % in 2000 to 2.2 % in 2010 while mortality for patients without diabetes decreased from 2.4 to 2.3 % during this interval. Among ICU patients, the 7.8 % reduction in the odds of mortality in each successive year for patients with diabetes (OR = 0.923; 95 % CI: 0.906, 0.940) was significantly greater than the 2.6 % yearly reduction for those without diabetes (OR = 0.974; 0.963, 0.985; p < 0.001 for interaction). However, among non-ICU patients, the 9.6 % reduction in odds of mortality for patients with diabetes (OR = 0.904; 0.879, 0.929) was not significantly different from the 7.5 % reduction for those without diabetes (OR = 0.925; 0.909, 0.940). Among ICU patients with diabetes, a significant decline in mortality persisted after adjustment for measures of inpatient and outpatient glucose control.
CONCLUSIONS: Patients with diabetes in the ICU have experienced a disproportionate reduction in in-hospital mortality that cannot be explained by the quality of inpatient or outpatient glucose control. While improved glycemic control may have other benefits, it does not appear to impact in-hospital mortality. Potential explanations for this interesting trend include improved cardiovascular risk management or advances in therapies for diseases that disproportionately affect diabetics (e.g. coronary stents).
DEEP VEIN THROMBOSIS BELOW THE KNEE: DO WE TREAT AND SHOULD WE TREAT?Anita Pudusseri; Raji Shameem; Robert E. Graham. Lenox Hill Hospital, New York, NY. (Tracking ID #1910852)
BACKGROUND: Below knee DVT is rarely associated with progression to pulmonary embolism (PE). However, patients often receive treatment with novel oral anti-coagulants, with a notable consequence of anti-coagulation being increased risk of bleeding. The current Guidelines for Anti-Thrombotic therapy from Chest 2012 (based upon observational studies and expert opinion) recommend that patients with acute isolated distal DVT of the leg and severe symptoms or risk factors for extension require initial anticoagulation over serial imaging of the deep veins.
METHODS: This was a retrospective review of patients that presented to a community hospital from June 1, 2012 to June 30, 2012 requiring a lower extremity venous doppler for any reason. Information was gathered using the Synapse database. The location of the DVT, which exact vein, the reason for the study, which department, whether the patient was treated and with what form of treatment were all collected. Patients already on anti-coagulation at the time of diagnosis were excluded, including but not limited to atrial fibrillation, stroke prevention, pulmonary embolism, and acute coronary syndrome.
RESULTS: Forty-five patients with lower extremity DVT were included. Of the 45 patients, 28 patients were from the medicine department, 3 from orthopedics, 2 from cardiology and surgery, 1 from obstetrics and 9 from other departments. 80 % (36/45) of patients were treated with anti-coagulation for DVT. Most patients were treated with heparin to warfarin bridge (36 %; 13/36) or enoxaparin to warfarin bridge (42 %; 15/36). Five patients were treated with enoxaparin alone, one patient was treated with heparin to fondaparinux sodium bridge and three patients were treated with warfarin alone. Of the three patients that were not treated with anti-coagulation, one patient had a known DVT and had repeat ultrasound imaging. The other two patients had intramuscular vein thrombosis and thus were not treated. Two of the 45 patients had adverse events of clinically significant bleeding.
CONCLUSIONS: A large majority of our patients were treated with anti-coagulation for a below knee DVT despite the known low risk of progression to PE. Given this data we plan on conducting a prospective study examining the management of a new diagnosis of below knee DVT. One of the outcomes studied will be to determine the extension of DVTs over a period of time using serial imaging.
DEFICITS IN THE TRANSFER OF ADVANCE CARE PLANNING INFORMATION FOR PATIENTS DISCHARGED FROM HOSPITALS TO NURSING HOMESPeggy Leung2,1; Clarke Low1; Anne M. Walling1,2; Neil Wenger1,2. 1University of California, Los Angeles, Los Angeles, CA; 2David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1939638)
BACKGROUND: Prognostic discussions and decisions about aggressiveness of care made in the hospital are often lost when patients transition to nursing facilities. For patients with serious illness and particularly for those for whom decisions have been made not to use cardiopulmonary resuscitation (CPR) and other burdensome treatments, Physician Orders for Life-Sustaining Treatment (POLST) is a legal document that translates patient end-of-life treatment preferences into actionable medical orders that are preserved across venues of care. This tool is widely used in hospitals and nursing homes across California. We aimed to investigate how often patients with do not resuscitate (DNR) orders were discharged from the hospital to a nursing facility without adequate transmission of this information across facilities.
METHODS: We identified all adult discharges from two hospitals to a skilled nursing facility over a three month period in 2013. We developed a medical record abstraction instrument that identified a patient’s resuscitation status during hospitalization and at discharge and whether this was communicated to the nursing home in the discharge summary and whether a POLST was completed. In cases where there was discrepancy between the resuscitation status at discharge and the information communicated, we explored the reasons for the difference.
RESULTS: Of 461 patient discharges (449 unique patients), 347 (75.3 %) patients were “full code” at time of transfer, 89 (19.3 %) patients had a DNR status at the time of transfer, and for 25 (5.4 %) patients there was no “code status” documented on transfer. Of the 347 patients who were full code, 65 (18.7 %) had a POLST indicating this at discharge. Of the 89 patients who had a DNR order at the time of transfer, 29 (32.7 %) had a valid POLST on transfer that contained this information. An additional 23 patients had POLST forms on transfer that were inconsistent with resuscitation decisions at discharge: 13 patients with a “full code” status had a POLST that indicated DNR, five patients with a DNR status on transfer had a POLST that indicated CPR, and five patients had POLST forms with other content inconsistent with decisions made on discharge.
CONCLUSIONS: At two hospitals in one health system, detailed evaluation of medical records for patients discharged to nursing homes demonstrated that even among patients for whom a DNR order was in place at time of transfer, less than one third had POLST documentation of this preference. In the studied hospitals, efforts are needed to improve the transition of resuscitation information from hospital to nursing home.
DEFINING APPROPRIATE USE OF ACID SUPPRESSION AMONG MEDICAL INPATIENTSMatt Pappas1; Sanjay Jolly2; Sandeep Vijan1. 1University of Michigan Health System, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1936603)
BACKGROUND: Proton pump inhibitors (PPIs) are commonly used among medical inpatients, with some studies suggesting that as many as half of all inpatients receive PPIs. Routine use of PPIs is common for symptom relief and, in higher risk patients, to reduce the risk of upper GI bleeding (UGIB). Recent evidence has suggested that PPIs increase the risk of nosocomial infections, including healthcare associated pneumonia (HCAP) and Clostridium difficile infection (CDI). We sought to examine the balance between risks and benefits of PPI use among medical inpatients in various categories of risks of UGIB, HCAP, and CDI.
METHODS: We created a microsimulation model to estimate the risks of UGIB, HCAP, and CDI among medical inpatients. Risks of each of these conditions were generated using published risk models. We then modeled changes in risk associated with PPI use for each of these outcomes, basing our estimates on meta-analyses and observational studies. We examined the overall impact of PPI use on inpatient mortality, including both population level risk and individual thresholds at which PPI use would be beneficial (through reduction in UGIB risk) or harmful (through increases in HCAP and CDI). We examined several scenarios to account for heterogeneity in the strength of the evidence for the causal relationship between PPIs and our modeled outcomes, and conducted both one-way and multivariate sensitivity analyses (using second order Monte Carlo simulation) across all parameters in the model.
RESULTS: In our first scenario, where PPI use was causally linked with changes in risks of all three outcomes (UGIB, HCAP, and CDI), we found that PPI use led to an increase in mortality in over 95 % of hospitalized patients. In our second scenario, with no causal association between PPI use and CDI, we found that PPI use led to an increase in mortality in 86 % of hospitalized patients. Sensitivity analyses showed that even with a low odds ratio for HCAP, PPI use led to increased mortality in 91 % of cases (assuming a causal link with CDI) or 68 % of cases (no causal link with CDI). We then examined percentiles of probabilities for HCAP, CDI, and UGIB to see if we could identify particular cases where benefit from PPI use was likely. However, only at extremes of the distribution were we able to identify patients who may benefit. For example, we modeled a patient at the 10th percentile for probability of HCAP, case fatality of HCAP, risk of CDI, and case fatality of CDI, but at the 90th percentile risk of UGIB risk and fatality. In such a patient, PPIs were neutral, with benefit in about half of such patients and harm in the other half.
CONCLUSIONS: Our study suggests that for the vast majority of medical inpatients, use of PPIs likely leads to an increase in short-term mortality. Even in patients at particularly high risk of UGIB, only those at the very lowest risk of HCAP and CDI should be considered for prophylactic PPI use. Indeed, our estimates suggest that withholding PPI therapy should be considered for most patients upon admission, with the exception of those who are at very high risk of or are hospitalized for UGIB. There are several limitations to our analysis. First, we are reliant on published estimates of the effect of PPI on HCAP, CDI, and UGIB, and for some outcomes, particularly CDI, there remains some controversy on the causality of the observed association. Second, we did not model additional outcomes such as length of stay; however, given the balance of risks and benefits we found, this is more likely to accentuate than alter our finding that PPIs generally lead to harm. Finally, we did not model specific settings such as the ICU or surgical patients. Overall, our findings suggest that PPI use should be avoided in the vast majority of medical inpatients.
Density plot of change in mortality for 100,000 simulations of 100-patient cohorts, assuming increased risk of CDI with acid suppression (red) and no increased risk of CDI (blue).
DELAYS IN ENTERING ABNORMAL TEMPERATURES INTO THE ELECTRONIC MEDICAL RECORDAlvin Rajkomar; S. Ryan R. Greysen. University of California, San Francisco, San Francisco, CA. (Tracking ID #1939063)
BACKGROUND: Newly abnormal vital signs in hospitalized patients often spur additional diagnostic testing and treatment, like evaluation for sepsis in a patient with a fever. Delays between measuring and recording temperatures in the electronic medical record (EMR), functions often performed by nursing staff, can delay timely recognition of conditions like sepsis, especially as clinicians and electronic surveillance tools use EMR data for monitoring. We sought to characterize the frequency and duration of these delays of entering temperature data into the EMR.
METHODS: We identified all temperature readings from adult inpatients admitted to UCSF Medical Center from June 1, 2012 to Dec 5, 2013. For each temperature reading, the location of the patient and the identity of the nurse who took the temperature were obtained. The delay was calculated by the difference between the computer-generated timestamp when the temperature was entered into the EMR and the nurse-generated time of when the vital sign was physically taken. Fever was defined as a temperature greater or equal to 100.4° Fahrenheit. We used descriptive statistics and t-tests to analyze trends in entering temperature values.
RESULTS: There were over 1.3 million temperature readings throughout the study period. The mean delay was 42.6 min for all readings (range: 0 to 720 min, standard deviation: 75.8 min). There were 66,434 readings with a fever, and the mean delay was statistically lower at 36.6 min (p < 0.001). Interestingly, the delay was higher for patients with a new versus a persistent fever: of the 19,619 readings of a new fever, defined as the prior recorded temperature being below 100.4, the mean entry time was 42.3 min. Of the 46,815 readings of a persistent fever, defined as the prior temperature also indicating a fever, the mean delay was lower at 34.2 min. The delay was not only different between different nursing units but also between different nurses within a unit (Figure 1).
CONCLUSIONS: The average delay between obtaining a temperature and entering it into the EMR is greater than 40 min for newly febrile patients, and there is significant variation in delays between nursing units and individual nurses. Hospitals must consider new ways to promote timely entry of data into the EMR of they hope to capitalize on the advent of new sensors and the promise of using big data for real-time electronic surveillance of hospitalized patients.
Figure 1: Median Delay in Entering Temperature into the EMR Each large, numbered rectangle represents a nursing unit, and every colored box represents an individual nurse within that unit. The color of the box is proportional to the median delay in entering temperature data into the EMR by that individual nurse. White indicates a median delay of zero minutes and red indicates a median delay of 60 min or more.
DELIVERING VIDEO PATIENT EDUCATION FROM THE EHR: PROMISES AND PITFALLSShira N. Goldman1; Tiffany Brown1; Stephen D. Persell1; Alpa Patel2; Crystal T. Doan1; Kenzie A. Cameron1. 1Northwestern University, Chicago, IL; 2Northwestern Medical Faculty Foundation, Chicago, IL. (Tracking ID #1926289)
BACKGROUND: Alerts triggered by content in patients’ electronic health records (EHR) are used regularly to prompt providers to improve the quality of care. These alerts can be leveraged to deliver educational content to specific patients at the point of care. We implemented an alert for licensed practical nurses (LPNs) and medical assistants (MAs), prompting them to show an educational video to patients eligible for pneumococcal vaccination (PnVx) while patients waited for their primary care provider (PCP) to enter the exam room. We report on lessons learned from this implementation.
METHODS: The PnVx educational video Best Practice Alert (BPA) was implemented in a large general internal medicine practice at an academic medical center using the Epic EHR. We designed and built the alert using a team of computer programmers, technical support specialists, and clinical and communication experts. We validated the decision rules to ensure the alert only triggered for patients eligible for PnVx who had no documentation of vaccination receipt or refusal in the EHR. PCPs provided consent for their patient panels to be included in this feasibility study. We trained LPNs and MAs to launch the video from within the EHR when the alert appeared, and the PnVx BPA was then activated practice-wide. After 3 months, nurses were invited to participate in individual interviews and PCPs were sent a web-based survey. Patients were asked to participate in a telephone survey to assess their perceptions toward being shown a video at the point-of-care, as well as their thoughts on pneumonia, pneumococcal vaccination (on a Likert scale where 1 = Strongly Disagree and 5 = Strongly Agree).
RESULTS: We encountered technical barriers to successful implementation. These included hardware problems such as the need for uniform monitor resolution and lack of sound capability, and software problems, including failure of the video to function across multiple operating systems. Additionally, to retain the security of Epic and account for the fact that LPNs and MAs had varied workflows within the EHR, the BPA required several decision points, which corresponded to mouse clicks. Upon completion of patient intake, the LPN/MA would secure the patient’s record and launch the video in an external browser. Despite these challenges, overall feedback to the alert was positive. Patients (n = 32) perceived the video as easy to understand (M = 4.71, sd = 0.81) and informative (M = 4.46, sd = 0.58). PCPs (n = 30) did not perceive a negative impact on their workflow, nor did they believe the addition of the alert and video delayed the rooming process. LPNs and MAs (n = 10) had varying responses to the addition of this activity to their workflow; some perceived it to be a minor task benefitting patients, while others reported that it was overly complicated and bothersome.
CONCLUSIONS: At a site using multiple provider-directed alerts, implementing a clinical decision support-triggered patient education video identified unanticipated obstacles. While many of the technical challenges were surmountable, encouraging nurses to act on the alert remains challenging. Challenges include the fact that numerous steps are required to launch the video and the absence of a clinic-wide incentive or policy supporting this effort. Although many nurses responded positively, others did not perceive point-of-care patient education as essential for improving patient care. Further research is needed to determine the best ways to involve the entire medical team in patient care and assess the impact of this point-of-care intervention on uptake of vaccination and other preventive health services.
DENTAL REFERRALS IN A FEDERALLY QUALIFIED HEALTH CENTER: THE LINK BETWEEN ORAL AND SYSTEMIC HEALTHLanna Little; James F. Hanley; Garry Souffrant. University of Texas Health Science Center San Antonio, San Antonio, TX. (Tracking ID #1939712)
BACKGROUND: Oral health and systemic health are intricately connected. The Federally Qualified Health Centers (FQHCs) are uniquely positioned to treat both oral and systemic health as they provide comprehensive medical and dental care. The path for most patients to see the dentist is a referral from a primary care physician. Although the dental referral may be an important link between medical and dental health care, most physicians have little insight on how to optimize this process. Little research has been conducted to characterize the referral process and referral population.
METHODS: Chart review was performed, identifying 420 adult patients who have been seen in the past two years at the FQHC and have received a referral to the dentist. Comorbidities and demographics were recorded for each subject, as was information regarding the dental referral. Data was analyzed using SPSS.
RESULTS: The most common reason for referral was pain, which was cited in 58 % of referrals. In about 40 % of dental referral patients, some sort of dental emergency was reported (pain, abscessed tooth or loose tooth). About one third of patients indicated that seeking dental referral was their primary reason for coming to the clinic. Most patients received only the referral but no treatment by the physician. Only half saw the dentist and half of those were diagnosed with some degree of periodontal disease. Patients with acute complaints such as dental pain or abscess were more likely to see the dentist than those referred for diabetes mellitus. Out of everyone who sought dental referral, 10 % were subsequently screened for and diagnosed with a new condition (diabetes or dyslipidemia).
CONCLUSIONS: Although dental referrals were common in our FQHC and dental pathology was frequent, most physicians provided little treatment prior to the dental visit. Most physicians have both limited experiences and limited knowledge of the management of dental urgencies/emergencies. Implementation of inter-professional education in medical school or primary care residencies could equip physicians to treat the patient properly until they see a dentist, and could also facilitate the referral process. It may be appropriate for FQHCs to develop inter-professional guidelines for physicians and dentists concerning the management of these patients. While dental care is often considered discretionary, urgent dental problems significantly impact patients’ quality of life and poor dental hygiene may impact management of many chronic diseases. Having periodontal disease treated may positively affect these patients’ systemic health. This is especially important for patients with diabetes mellitus. Lastly, it is important to take dental pain patients seriously and use their visit as an opportunity to perform the indicated health screenings.
DEPRESSION IS ASSOCIATED WITH CLINICAL INERTIA IN MANAGEMENT OF HYPERTENSION IN THE PRIMARY CARE SETTINGNathalie Moise1; Karina Davison1,2; William Chaplin1,3; Steven Shea1,4; Ian M. Kronish1. 1Columbia University Medical Center, New York, NY; 2Columbia University Medical Center, New York, NY; 3St. John’s University, Queens, NY; 4Columbia University, New York, NY. (Tracking ID #1926816)
BACKGROUND: Depression is a known risk factor for poor prognosis among patients with cardiovascular disease. Numerous biological and behavioral mechanisms have been proposed. However, few studies have investigated the association between depression and ‘clinical inertia’, or lack of treatment intensification in individuals not at evidence-based goals for care. To address this gap, we assessed whether a diagnosis of depression is associated with clinical inertia in patients with uncontrolled hypertension.
METHODS: A convenience sample of 28 attending primary care providers (PCP) and 158 patients with uncontrolled hypertension was enrolled from two inner-city, academic-hospital based clinics. Eligibility criteria were age ≥18 years, prescribed ≥1 blood pressure (BP) medications, and BP ≥140/90 mmHg (or ≥130/80 mmHg if diabetic or with chronic kidney disease) on at least two consecutive scheduled visits with one’s PCP. Clinical inertia was defined as lack of (1) medication intensification (2) specialist referral or (3) secondary hypertension work-up. Depression diagnosis was based on PCP documentation in the electronic chart. Multilevel modeling accounting for clustering of participants within PCP was conducted to assess the risk of clinical inertia in depressed patients while adjusting for known predictors of clinical inertia. Sensitivity analyses were performed that (1) excluded visits with documentation of at least one controlled clinic or home BP (2) accounted for medication adherence counseling by PCP and (3) excluded diabetics with systolic BP (SBP) ≤140 mmHg.
RESULTS: The mean age (SD) of patients was 64.5 (8.8) years; 74.1 % were women, 79.1 % were Hispanic, 44.9 % was diagnosed with depression and 61.2 % had diabetes. On average, participants had a prior visit SBP of 158.7 (15.7) mmHg, current visit SBP of 154.6 (16.7) mmHg, were taking 2.5 (1.1) BP medications and had 5.3 (2.3) problems addressed during the visit. Clinical inertia was more common amongst depressed than non-depressed patients (70 % vs. 51 %; p = 0.015). Depression diagnosis was associated with clinical inertia in both the adjusted and unadjusted multilevel analyses (RR = 1.40; 95%CI, 1.11–1.74; p = 0.004; adjusted relative risk [ARR] = 1.49; 95%CI, 1.06–2.10; p = 0.021). The relationship remained after excluding those with at least one documented home or clinic visit SBP below goal (ARR = 1.74; 95%CI, 1.07–2.83; p = 0.025), adjusting for adherence counseling (ARR = 1.49; 95 % CI, 1.10–2.04; p = 0.010) and excluding diabetics with SBP ≤ 140 mmHg (ARR = 1.49; 95 % CI, 0.99–2.23 p = 0.057).
CONCLUSIONS: Amongst patients with uncontrolled hypertension, clinical inertia was more likely in those with a diagnosis of depression; this may be one mechanism by which depressed patients have worse cardiovascular outcomes. Research has shown that patients with mental illness receive less intensive medical care, such as coronary revascularization; our study extends this literature by demonstrating differences in clinician behavior with respect to cardiovascular risk factor management in this population. Future studies should explore underlying processes affecting clinician treatment practices. In the meantime, PCPs should be cautious about undertreating cardiovascular risk factors among patients identified as having depression.
DERIVATION OF ICD-10 CODE LISTS FOR NOVEL PATIENT SAFETY INDICATORSWilliam A. Ghali; Danielle Southern; Hude Quan. University of Calgary, Calgary, AB, Canada. (Tracking ID #1896442)
BACKGROUND: Health data coded using the International Classification of Diseases have been widely used to identify the occurrence of adverse events that may be linked to suboptimal safety and quality of care. Some countries record ‘diagnosis timing indicators’, which allow data users to distinguish whether a coded diagnosis or event was present at time of admission as opposed to one that occurred after admission. Using this diagnosis-timing data element, we undertook a multistep process to produce novel patient safety indicators (PSIs).
METHODS: We queried 2,416,413 records in the Canadian national Discharge Abstract Database (DAD) for April 1, 2009 through March 31, 2010. All listed diagnosis codes were compiled, and 2,613 unique diagnoses were found to have a type ‘2’ diagnosis designation, indicating that the diagnosis was not present at time of admission and thus arose after admission. Next, we asked an international panel of experts in patient safety and quality of care to participate in a Modified Delphi review process in which they undertook a two-phase review of all of the identified codes, to determine (using a 9-point scale) the subset of post-admission diagnoses that are highly likely to have a strong link quality of care and/or patient safety. The subset of identified codes were then grouped into clinically-related subgroups, and the frequency of events was determined in a database of all hospitalizations records from the province of Alberta, Canada.
RESULTS: Of the 2,613 diagnosis codes recorded at least once in Canadian data as a diagnosis arising after admission, 640 codes were judged by the expert panel to have a strong link to quality of care and patient safety. These codes were then reviewed by a second group of experts in patient safety to create summary PSI code groupings. These included: a single global PSI for ‘any adverse event’; a smaller grouping of codes for ‘serious adverse event threatening to life or vital organs’; and then a number (n = 17) of other specific code groupings for specific types of events such as ‘cardiac complications, ‘respiratory complications, ‘hospital-acquired infections’, and ‘venous thromboembolic events’. The annual event rates in Alberta provincial data for the global PSI of ‘any adverse event’ ranged from 4.5 % in 2005 to 5.6 % in 2011. The event rate for the ‘serious adverse event’ indicator was 0.8 %. The event rates for the other specific indicators ranged from a high of 2.0 % for ‘Hemorrhagic Events’ to a low of 0.03 % for the ‘obstetrical complications affecting fetus’ PSI.
CONCLUSIONS: The methodological work presented here utilizes the unique potential of diagnosis-timing indicators to produce a clinically-relevant listing of diagnosis codes that can be used to create novel PSIs that overcome some of the shortcomings of existing PSI systems. The resulting work has great potential to inform future approaches to health system monitoring, adverse event surveillance, and quality/safety improvement.
DESCRIBING THE STRUCTURE AND PATTERNS IN THE PHYSICIAN-PATIENT INTERACTIONHarry B. Burke1; Dorothy Becher1; Patrick G. O’Malley1; Jeffrey L. Jackson2; Ronald W. Gimbel1. 1Uniformed Services University of the Health Sciences, Bethesda, MD; 2Zablocki VAMC, Milwaukee, WI. (Tracking ID #1937588)
BACKGROUND: Although there is an extensive literature describing the semantics of physician-patient interactions, i.e., judgments regarding the meaning of participants’ words and individual utterances, little is known about the interactional structures that constitute the physician-patient encounter. Structural units are the categories of verbal interactions that the participants use to achieve their goals (categories are described below). We hypothesized that these structural units would occur in a systematic manner across interactions.
METHODS: The unit of analysis was not the word or the utterance; it was the structural unit. Twenty audio-recorded established (rather than new) patient primary care outpatient physician-patient interactions were coded into structural units in terms of their interactional categories. A structural unit is composed of adjacent sequential utterances of the physician and patient that, taken together, meet one of the eight defined structural categories. The same type of structural unit could occur at various times throughout the interaction and at each occurrence the unit was coded and its location noted. Eight categories of interactional units were sufficient to describe the interactions: NEW, discussing a new medical problem; EXT, discussing an existing medical problem; WEL, discussing wellness and screening; REV, reviewing what had happened to the patient since the last visit including labs and medications; ADM performing administrative tasks such as ordering tests and prescriptions and filling our forms; SUM, summarizing the interaction; AGR, participant agreement; and SOC, discussing social topics.
RESULTS: We coded all pairs of adjacent units. There were 462 pairs across the 20 interactions. The inter-rater category agreement was 94 %. For most pairs we set a threshold of occurrence at 10 %. This analysis focused on the NEW and EXT units. The table below shows the relative frequency of the adjacent unit pairs. Relative frequency is the pair frequency divided by the overall frequency of the target unit. In terms of all the interactional pairs, NEW occurred in 10 % and EXT occurred in 27 % of the pairs. The arrow designates the order of occurrence of the adjacent units. PRIOR TO NEW.....Relative freq.....SUBSEQUENT TO NEW......Relative freq. NEW ⇒ NEW...........0.06..................NEW ⇒ NEW........................0.06 EXT ⇒ NEW............0.15..................NEW ⇒ EXT..........................0.29 REV ⇒ NEW............0.33..................NEW ⇒ EXT..........................0.29 ADM ⇒ NEW...........0.10 .................NEW ⇒ ADM........................ 0.08 SOC ⇒ NEW...........0.21..................NEW ⇒ SOC.........................0.20 PRIOR TO EXT.....Relative freq.....SUBSEQUENT TO EXT.....Relative freq NEW ⇒ EXT.......... 0.11.................EXT ⇒ NEW.......................0.06 EXT ⇒ EXT............0.34.................EXT ⇒ EXT.........................0.34 REV ⇒ EXT............0.21.................EXT ⇒ REV........................0.21 ADM ⇒ EXT...........0.16.................EXT ⇒ ADM.......................0.23 SOC ⇒ EXT...........0.14.................EXT ⇒ SPC........................0.10 It was rare for a new medical problem to be adjacent to a new medical problem (NEW ⇒ NEW = 0.06), but common for an existing medical problem to be adjacent to an existing medical problem (EXT ⇒ EXT = 0.34). Reviews (REV) occurred with the same frequency before and after new problems (NEW), 33 %, 29 % and existing problems (EXT), 21 %, 21 %. Likewise, social topics (SOC) occurred with the same frequency before and after new problems (NEW), 21 %, 20 % and existing problems (EXT), 14 %, 10 %. There was an inverse relationship between new and existing problems in terms of the occurrence of adjacent reviews and social topics.
CONCLUSIONS: Structural units can describe physician-patient interactions. They appear to occur in a systematic manner and they can assist us in understanding of how physicians and patients interact to achieve their goals for the interaction.
DETERMINANTS OF HOSPITAL READMISSIONS AMONG LOW INCOME AND MINORITY OLDER ADULTSUgochi K. Ohuabunwa1,2; Jonathan Flacker1,2; Queenie E. Jordan2. 1Emory University, Atlanta, GA; 2Grady Hospital, Atlanta, GA. (Tracking ID #1942171)
BACKGROUND: Low income and minority seniors constitute a vulnerable group during care transitions. Determinants of failure in transitions of care and rehospitalization in minority and low income populations have not been well defined. Understanding these determinants and consideration of the specific needs of this group of patients is essential in designing a transitional care model that will be effective in this patient population.
METHODS: We evaluated Medicare beneficiaries who were frequently hospitalized at our 953 bed safety net hospital from January to December 2010 by secondary data analysis of hospital administrative data to determine risk factors associated with repeated hospitalizations.
RESULTS: A total of 3790 patients were admitted during this period accounting for 4933 admissions. We classified all patients (n = 189) admitted 2 or more times in a 6 month period as high risk. Our unadjusted all cause readmission rate was 25 %. Factors found to be significantly associated with readmission were female gender (60 %), African American race (94 %), age >75 year, patients residing in the Zip Code areas 30318, 30310 and 30311. The most common presenting diagnoses were congestive heart failure, psychoses, chronic obstructive pulmonary disease, septicemia and renal failure.
CONCLUSIONS: Definition of these determinants will form a basis for further needs assessment and the design of a transitional care model that will be effective in this patient population.
DETERMINING THE ACADEMIC HOSPITALIST SAFE CENSUS: RESULTS FROM A PHYSICIAN SURVEY AND HOSPITALIST SERVICE ANALYSISAmy Baughman2,1; Warren Chuang1; Denisa Gace1; Daniel P. Hunt1. 1Massachusetts General Hospital, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA. (Tracking ID #1940088)
BACKGROUND: Finding the appropriate patient-to-physician ratio is critical for optimizing patient care and physician satisfaction and productivity. Current literature in this area to guide hospitalist models of care is limited. However, it is well established that excessive patient responsibilities and work load can result in worse patient outcomes as well as increased physician burnout and dissatisfaction. Our hospitalist group has grown considerably which enabled our group to study the impact of higher census. In 2009, our service cared for 22 to 68 patients each day; by 2012, we cared for 54 to 127 patients. Despite hiring more staff, the individual physician census also increased. This challenged even our most experienced hospitalists to round on patients and complete discharges and admissions within their twelve-hour shift. When establishing a safe census, programs must consider regionalization of patients, ancillary staff or resident availability, case-mix index and physician characteristics. On our non-regionalized service, an individual hospitalist cares for patients scattered across several floors and buildings. On our regionalized service, however, the complexity of patients is higher. All of our physicians work without ancillary staff such as nurse practitioners or residents and significant physician time is required for administrative tasks, consultant and patient communication, and EHR documentation. Our goal was to determine how many patients a hospitalist physician at a tertiary academic medical center can safely care for during a typical 12 h shift.
METHODS: We describe a survey based method for identifying an optimal and safe census among hospitalists at our tertiary academic medical center. This assessment occurred in 2012 as a quality improvement initiative to gather feedback in several areas including optimal work flow and physician satisfaction. We also separately analyzed the impact of physician census on in-patient quality metrics including hospital readmission rates, length of stay and pre-noon discharges from 2010 to 2013. We then evaluated whether results from the physician survey were consistent with our quality metric outcomes.
RESULTS: Survey results showed that patient census was the most important factor contributing to physician satisfaction (n = 35, Response Rate = 85 %). In that year, daily physician census varied from a low of six to a high of 14. We found that 92 % of physicians felt that the ideal patient-to-physician ratio was 10 or less for providing the highest quality of care. For half of physicians, the maximum patient number for safe care was 12; however the other half reported lower values of 10 or 11 patients. We reviewed monthly readmission rates, length of stay and pre-noon discharge rates from 2010 to 2013 for our hospitalist group. During this time, the monthly physician census ranged from 8.6 to 11.8 patients. We found that the readmission rate was slightly higher when the physician census was more than 11 (P value < 0.05). Average length of stay and the percentage of pre-noon discharges did not change significantly with higher physician census.
CONCLUSIONS: Surveying physicians is a simple and effective method for identifying safe patient-to-physician ratios. For hospitalists at large tertiary medical centers with similar patient complexity, a safe census of ten is ideal for providing the highest quality of in-patient care. Evaluation of readmission rates, a crude measure of quality, supported this finding as readmission rates increased when census increased to more than 11.
DEVELOPING PATIENT-CENTERED DEFINITIONS AND RATINGS OF ENABLING SERVICESRobin Clarke1; Anne Escaron1; Rosy Chang Weir2; Petra Stanton3. 1University of California, Los Angeles, Los Angeles, CA; 2Association of Asian Pacific Community Health Organizations, Oakland, CA; 3California Primary Care Association, Sacramento, CA. (Tracking ID #1938362)
BACKGROUND: Community Health Centers (CHCs) are safety net practices that have a long history of delivering non-medical or “enabling” services intended to reduce the social barriers to care faced by their low-income patients. Enabling services include providing transportation, performing community outreach, and delivering case management. The implementation of the Affordable Care Act offers new opportunities to reimburse these patient-centered services, but limited evidence exists to guide CHCs and other providers in deploying effective services. We sought to begin to address this evidence gap by developing a research framework for analyzing this field of health care services and by starting the initial evaluation of these services.
METHODS: We adapted the RAND/UCLA modified Delphi method typically used to assess appropriateness of medical interventions. Using a community-partnered research team, we had three phases to our project. In the first phase, we used a literature review and an in-person meeting of 17 CHC patients and providers to define broad categories of services, discrete enabling services, and the variable levels of intensity by which a service can be delivered. An example of an intensity variable is: Health education delivered by a licensed personnel vs. by a non-licensed community member. In the second phase, we convened an expert panel composed of 13 CHC patients, providers, community patient advocates, and policy-makers. This panel used the validated RAND/UCLA 1–9 scale and iterative rounds of ratings to rate each enabling service as ineffective, equivocally effective, or effective. Effectiveness was defined as the degree by which a service increases a patient’s access to, use of, and understanding of his or her medical care. In the last phase, we analyzed the ratings to identify the panel’s recommendations by calculating each service’s median effectiveness rating and the level of agreement or disagreement amongst the panelists. We used a Friedman test and a subsequent Wilcoxson Signed Rank test to determine whether effectiveness varied based on level of intensity.
RESULTS: The literature search identified 40 peer-reviewed articles that tested the effectiveness of enabling services. Based on these articles and their own knowledge, the patients and providers in the first group defined six categories: health education & supportive counseling; case management; outreach; interpretation; transportation; and financial counseling & eligibility assistance. Within these categories, 112 unique services were described, of which the expert panel elected to rate 77. Each of these services had between 1 and 4 levels of intensity at which it could be delivered resulting in a total of 181 unique service-variable combinations being rated by the expert panel. Health education & supportive counseling had the lowest median effectiveness rating as a category at 6.6 (out of 9) and outreach the highest at 7.5. Within each category, we identified the services that had a median effectiveness of 8–9 (or 9 for outreach) as the most highly recommended services. Twenty-four services across all categories met this threshold. Lastly, we found that the variable level of intensity had a significant effect on a service’s rated level of effectiveness for some but not all services. For example, licensed professionals were rated significantly higher for developing care plans, whereas community health workers were equally effective in executing that care plan.
CONCLUSIONS: Because of their heterogeneity and the difficulty testing them against clear outcomes, enabling services make up a relatively understudied field of healthcare. In this study, our community-academic research team brought together two patient and stakeholder panels to define three constructs - six broad categories, 112 granular-level services, and various service intensity variables—as a framework for evaluating the effectiveness of these services. While not exhaustive, this list can serve as an important, initial classification scheme to guide further research. For providers and policy-makers, the list of most highly recommended services is the first report of its kind to provide guidance about priority services based on the perspectives of underserved patients and their representatives. In addition, by rating at the level of the service intensity, we identified opportunities to target resources to services where they are most needed to improve effectiveness. In many cases, the highest level of intensity did not necessarily increase perceived effectiveness. This study was limited by the dearth of literature suitable for the expert panel and the small number of experts used to create the recommendations. Nevertheless, given the potential that enabling services have for reducing social barriers to care, the categorization and ratings developed by this study provide a useful framework for further studying these services.
DEVELOPMENT AND APPLICATION OF A CLASSIFICATION SCHEME FOR CARE COORDINATION ACTIVITIES IN AN ACADEMIC PRIMARY CARE SYSTEMNazleen Bharmal1; Robin Clarke1; Paul Di Capua1; Indu Gupta1; Brian Doyle1; Aliza Ali2; Asad Malim3; Brian S. Mittman4,5. 1UCLA, Los Angeles, CA; 2Lake Erie College of Osteopathic Medicine, Bradenton, FL; 3College of Science and Health, Charles R. Drew University, Los Angeles, CA; 4VA Greater Los Angeles Healthcare System, Los Angeles, CA; 5Kaiser Permanente Southern California, Los Angeles, CA. (Tracking ID #1939165)
BACKGROUND: Primary care redesign aims to improve patient experience, improve health, and reduce costs. One opportunity to transform practice care delivery is to introduce supports to enhance primary care team effectiveness. In the field of care coordination, the RN-based case manager model is defined and well-understood; care managers may have a specific group of patients with chronic conditions for whom they develop individualized care plans and/or train in self-management skills. However, one of the limitations of the limited-panel, high-utilizer care manager model is that it may only touch on a small percentage of patients. In our large health system comprised of 28 primary care clinics throughout Los Angeles County, we embedded non-licensed care coordinators (CC) into clinics to integrate with primary care teams. CCs would act as PCP extenders, assess patients’ care needs, coordinate patients’ care with other providers and settings, and connect patients to community resources and social services. To better describe and ultimately analyze the role of CCs in our health system, we developed and applied a classification scheme to categorize CC activities.
METHODS: The first five general internal medicine practices to incorporate a CC were included in the study. CC encounters were defined as any activity performed by a CC that (a) contributed to the development and/or implementation of a plan of care for a patient or family and (b) was documented by the CC in an online Patient Care Coordination System (PCCS) database established to track CC activities. A classification scheme to broadly categorize CC activities was developed iteratively by adapting models cited in a systematic review of care coordination published by the Agency for Healthcare Research & Quality (AHRQ) plus literature on case management, discussions with CCs, and our exploratory review of the PCCS database. Five coders, in total, coded all activities with high inter-rater reliability (kappa 0.89).
RESULTS: The five selected practices represented a diverse group of community and academic practices focused on family medicine, internal medicine, or geriatrics. The PCCS database contained 8,036 CC encounter records entered from June 2012 to July 2013 among the five primary care practices. Our 5-category classification scheme is presented in the table. The proportion of CC activities coded in each category was 38 % for execution of care, 32 % for coordination of transitions, 15 % for link to community resources or self-management support, 10 % for monitor and follow-up, 1 % for patient assessment, and 5 % for no classifiable activity.
CONCLUSIONS: CC documented activities provided evidence to the broad range of potential impact this model can have on patients, including helping patients navigate the health system, improving access and communicating across the care spectrum. CC activities are a vital part of helping primary care practices deliver coordinated, accessible, comprehensive, and patient-centered care; a valid and reliable classification scheme for these activities is an important tool for research and practice. The scheme we developed will be incorporated into CC training and a revised PCCS database and documentation system. The scheme will also facilitate subsequent phases of our research, including an assessment of the impact of CC activities and the degree of CC integration into primary care practices on key outcomes, including patient and provider satisfaction, chronic disease prevention and management, and preventable emergency room utilization.
Care Coordinator Activities by Mutually Exclusive Process Categories
| Category | Definition | Examples of Activities |
| Execution of Care | Executing specific task delegated by PCP or requested by patient/family (with PCP approval) to meet a patient’s needs | ● Medication refills ● Appointment scheduling ● Authorization and/or referrals (e.g., specialists, tests, IV meds, DME) ● Visiting nurse or home health coordination ● Administrative—fax documents (e.g., FMLA, DMV, disability), provider or insurance changes |
| Coordination of Transitions | Managing patient follow-up after a hospitalization or ED visit | ● Schedule post-hospitalization or ED discharge patient for PCP visit within 48 h ● Coordination of referrals and/or tests to be performed post discharge |
| Link to Community Resources or Self-Management Support | Providing patients with resources outside a clinical environment to assist with medical conditions | ● Patient education on urgent care evening hours ● Housing/facility placement (e.g., hospice) ● Caregiver support ● Transportation resources ● Benefit eligibility and financing of medications |
| Monitor and Follow-up | Checking in with patients to ensure proper follow through with medical tasks and maintaining patient-provider communication between clinic visits | ● Scheduling wellness checks ● Notification to PCP and scheduling patients for P4P measures ● Triage patient questions to PCP between visits |
| Patient Assessment | Helping to gather medical information and categorize high-risk patients before PCP visit | ● Referring patients who have high ED utilization to high-risk case management |
| No Activity | Any activity no classifiable under other categories | ● Attempted to contact patient; unable to leave message |
DEVELOPMENT AND EVALUATION OF A PATIENT EMPOWERMENT LETTER IN A PRIMARY CARE SETTINGDan Matlock; Eva M. Aagaard; Adam Abraham; Wagner J. Schorr-Ratzlaff; Nivedita D. Mahidhara; Scott De La Cruz; Lisa Schilling; Brandon Combs; Carmen L. Lewis. University of Colorado, Aurora, CO. (Tracking ID #1939663)
BACKGROUND: Patients often feel disempowered when talking with their physicians. One study noted that patients feared questioning their doctors because they might be dismissed or labeled “difficult.” As part of the Patient Centered Medical Home (PCMH) initiative at the University of Colorado, we developed a letter to be given to patients prior to their clinic appointment to both empower patients and to help them set an agenda. Herein, we describe the development and evaluation of this letter.
METHODS: Development phase: Initially, the idea was to give patients something prior to their visit where they could write down their agenda. The letter was developed iteratively and piloted with patients. Ultimately, it included language designed to empower patients with phrases like “Please don’t feel that we will be upset if you have more questions.” The letter also included several lines for patients to write their “main goals, fears, and worries for the visit that day.” Evaluation phase: All adult patients aged 18–99 seen on one team at an internal medicine clinic over a two-week time period were included. The letter was evaluated using a pre-post design with the first week being the control and the second week including the letter. The primary outcomes were patient empowerment using the low-literacy version of the validated patient activation measure (13 items, 4 point Likert scale, scored 0–100) and patient satisfaction using the hospital mandated patient satisfaction measure (10 items, 5 point Likert scale, scored 0–5). Patients were also given the opportunity to provide open-ended feedback on the letter. Differences between mean scores were tested using t-tests.
RESULTS: We received a total of 171 responses (85 in week one and 86 in week two) from 248 distributed surveys (response rate = 69 %). The sample was 63 % female, 39 % under the age of 55, 37 % had more than 4-year college degree, 76 % Caucasian and 56 % married. There was no difference in the Patient Activation scores between the control and intervention periods (71.4 vs. 68.9/100, p = 0.31). There was a small but statistically significant decrease in satisfaction scores between the control and intervention (4.86 vs. 4.56/5, p < 0.01) and overall satisfaction was very high. Patients had positive things to say about the survey: “Great letter and very impressive that your office is distributing this and indicating the need that every patient should be proactive with their own health and healthcare.” Suggestions on improving the letter including: arranging the key points into a bulleted list, shortening the overall length of the letter (simplifying) and including goals of care in patient print-outs.
CONCLUSIONS: Overall, the letter had no effect on patient activation and there was a small but significant decrease in patient satisfaction scores although overall satisfaction scores were very high. It is possible that satisfaction scores lowered slightly because patients’ agenda written on the letter were not addressed. Overall, the qualitative feedback suggests that the letter was well-received. We are currently working on a shorter version of the letter based on the results of this study.
DEVELOPMENT AND VALIDATION OF THE MEDICAL PROFESSIONALISM BEHAVIOR ASSESSMENT TOOLPreston Reynolds1; James Martindale2. 1University of Virginia, Charlottesville, VA; 2University of Virginia, Charlottesville, VA. (Tracking ID #1940065)
BACKGROUND: Assessment of professionalism behaviors has become a priority with launching of the Milestones Initiative by the Accreditation Council on Graduate Medical Education. The Medical Professionalism Behavior Tool (MPB) was developed by P Reynolds with input from clinician-educators, education researchers, and internal medicine residents beginning in 2008. It is modified from the NBME’s Assessing Professional Behaviors tool with inclusion of behaviors relevant to cultural competency.
METHODS: As part of an annual internal medicine resident seminar series, P Reynolds began introducing the concept of evaluating professional behaviors in 2008. In subsequent years, she reviewed with the residents various behaviors and then a 25-item evaluation tool she developed modified from the NBME’s APB with inclusion of behaviors specific to cultural competency. Based on their feedback, the tool was reduced to 15 items with retention of the cultural competency skills. The MPB was then used by all of the medicine residents in three subsequent annual seminars as part of a self-reflective exercise where they were asked to rate themselves and then discuss with another resident one or two areas they specifically identified as needing improvement. These data were entered into a spreadsheet making the responses anonymous, and then subjected to statistical analysis to determine the degree to which evidence of reliability and validity was present in the MPB as an assessment tool. The MPB was also reviewed by 11 of 13 residency program directors at the University of Virginia for content validity
RESULTS: All of the residency program directors thought the MPB captured behaviors relevant to evaluation of professionalism in clinical medicine. Statistical analysis of the internal consistency (reliability) and construct validity associated with the MPB yielded strong results with Cronbach’s alpha = 0.84 and thus providing good statistical evidence of reliability and validity.
CONCLUSIONS: The strength of the MPB is that it is only 15-items, reflects behaviors central to medical professionalism as described in The Physician Charter, and also incorporates behaviors specific to culturally competent clinical care. Fourteen states now require demonstration of cultural competency as part of medical licensure making the MPB an important assessment tool to shape residency training to include skills training in medical professionalism, and in cultural competency. Additionally, the MPB is a tool that is reliable and valid and thus, can be used in formative and summative assessment.
DEVELOPMENT OF A SCREENING TOOL FOR IDENTIFYING HOUSING-RELATED BARRIERS TO CARE AMONG LOW-INCOME WOMENAmbili Ramachandran1; Samantha Morton2; Naomi Y. Ko3; Kerrie Nelson4; Maria Castano3; Emily Bergling3; Sharon Bak3; Jennifer Cedor3; Wanda Turner3; Tracy A. Battaglia3. 1Boston University School of Medicine, Boston, MA; 2Medical-Legal Partnership | Boston, Boston, MA; 3Boston University School of Medicine, Boston, MA; 4Boston University School of Public Health, Boston, MA. (Tracking ID #1934188)
BACKGROUND: Social determinants of health include access to safe, healthy, and affordable housing. Support services such as patient navigation frequently target and resolve this barrier to care, but vulnerable patients sometimes need legal advice or advocacy to address these housing issues. It is often difficult in a health care setting to appropriately and efficiently determine which patients have housing problems that require legal advice or assistance. We developed a screening tool for use by patient navigators to identify individuals who would benefit from legal advice or assistance regarding housing-related barriers to care.
METHODS: The screening tool was designed in collaboration with Medical-Legal Partnership | Boston (MLP | Boston) and featured questions regarding utility expenses, mortgage and rent payments, foreclosures and evictions, and housing conditions. Dichotomous responses were designated “positive” or “negative” based on current Massachusetts laws protecting tenants, homeowners, utility consumers, and shelter residents, and at least one positive response qualified as a positive screen. After piloting, the screening tool was administered to female patients with public or no health insurance attending a breast health clinic at a safety-net hospital. Performance of the screening tool was validated against a comprehensive, in-person, one-hour legal interview by an attorney followed by a legal evaluation by MLP | Boston, which represented the “gold standard” for detecting housing-related barriers to care. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the screening tool were computed. Descriptive statistics on demographic characteristics were also calculated.
RESULTS: Of 74 eligible women approached, 35 (47 %) of a targeted sample of 50 consented to participate: mean age 42 years, 54 % African-American, 30 % White, 8 % Latina, and 8 % Other Race. Most subjects had state subsidized health insurance (43 %), Medicaid (26 %), or Medicare (11 %), and 83 % of women had incomes under 200 % of the federal poverty level. While 20 % of subjects owned their home, 57 % rented, 17 % stayed with friends or family, and 6 % had other housing arrangements. Almost 40 % of subjects rated their health as fair or poor. Among the 31 out of 35 women who completed full legal evaluation at the time of analysis, the screening tool had a sensitivity of 89 % (17/19), specificity of 42 % (5/12), PPV of 71 % (17/24), and NPV of 71 % (5/7). Based on the legal evaluation, over 60 % of women had housing-related barriers to care. Among owners and renters, the screening tool was most often positive for threatened disconnection of utility services (10/24 or 42 %), of which 3 were false positives among renters only.
CONCLUSIONS: In this population of low-income, predominantly publicly-insured women, housing-related barriers to care were widespread. When compared to the comprehensive legal assessment by the attorneys, our screening tool had acceptable sensitivity, but modest specificity, for identifying housing-related barriers to care that require legal advice or assistance to resolve. After completion of targeted enrollment, future work will refine which screening questions best identify subjects whose housing-related barriers to care are amenable to legal advocacy and which responses trigger the need for access to legal advice or assistance.
DEVELOPMENT OF QUALITY INDICATORS FOR THE CARE OF WOMEN WITH ABNORMAL UTERINE BLEEDINGDonna L. Washington1,2; Marjorie Danz1,3; Kristina M. Cordasco1,2. 1VA Greater Los Angeles Healthcare, Los Angeles, CA; 2University of California, Los Angeles, Los Angeles, CA; 3RAND Corporation, Santa Monica, CA. (Tracking ID #1936245)
BACKGROUND: Abnormal uterine bleeding (AUB) is among the most common gynecologic complaint of reproductive-age women in ambulatory care settings, with up to 30 % of women seeking medical care for AUB during their reproductive years. International consensus recommendations for standardizing the nomenclature and methods for investigating and categorizing potential AUB etiologies (the FIGO classification system for causes of AUB) were recently developed as an approach to improve our understanding and management of AUB. We sought to translate consensus recommendations and evidence-based guidelines for AUB care into quality indicators (QIs) that are measurable from electronic health records (EHRs), with the ultimate goal of applying these QIs to assess variations in clinical management and aid in women’s health education for healthcare providers.
METHODS: To develop QIs, we first performed an extensive literature review to develop a set of potential QIs for the evaluation and management of women with AUB, targeting aspects of care that are within the purview of primary care providers (PCPs). For each potential QI, we specified a numerator, denominator, exclusions, relevant definitions, period of assessment, underlying evidence and data source. We then used a modified Delphi consensus technique based on the RAND/University of California-Los Angeles Appropriateness Method, which consisted of three steps. In step one, nine experts (women’s health PCPs, obstetrician/gynecologists, quality measurement experts, policy stakeholders) independently ranked the indicators using nine-point scales on three metrics: consistency with established guidelines; importance to women’s health; and reliability of measurement from Veterans Health Administration (VHA) EHRs. In step two, we conducted an expert panel tele-conference with internet-based sharing of presentation materials, in which indicators were discussed by the panelists. In the final step, all indicators were independently rated by panelists a second time, using the same nine-point scales. QIs were selected for final inclusion if they had a median score of 7 or higher on all three metrics, and high consistency in their ratings, based on the interpercentile range adjusted for symmetry (IPRAS), using an interpercentile range of 0.3–0.7.
RESULTS: The consensus process resulted in selection of 19 QIs covering multi-dimensional aspects of AUB care, spanning reproductive and post-menopausal life phases, and including profuse vaginal bleeding, and use of hormonal contraception/IUDs. Five QIs relate to documentation of critical aspects of the history; 6 to diagnostic evaluation; and 8 to management. Evaluation QIs highlight the need to recognize pregnancy, need for emergency care, and elevated endometrial cancer risk. Management QIs focus on current profuse bleeding, follow-up of diagnostic studies, and indications for gynecologist referral. Areas of disagreement in panelists’ ratings and discussion related to the acceptable timeframe for completion of different actions, with generalist panelists being more likely to consider the constraints of the ambulatory care setting in their decision-making.
CONCLUSIONS: This project resulted in development of a multi-dimensional set of QIs for primary care AUB evaluation and management, based on published data, consensus recommendations and guidelines, and a modified Delphi process. These QIs are being formulated into an EHR quality of care assessment tool. Once this tool is pilot-tested for feasibility, it will be applied on a larger scale to measure the care quality provided to women with AUB in VHA primary care settings. This rigorously designed set of QIs should facilitate measuring and improving the quality of care for women with suspected AUB. Future work should focus on developing educational programs that are concordant with these QIs and assess potential changes in quality outcomes associated with their implementation.
DEVELOPMENT OF THE IORA WORRY SCORE AND COMPARISON TO SUBJECTIVE PROVIDER WORRY SCORES IN MULTIPLE PRIMARY CARE PRACTICESDaniel P. Croft1; Benjamin Berk2; Whitney Kramer2; Joel Lazar2,3; Rushika Fernandopulle2; Eugene Nelson3. 1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Iora Health, Cambridge, MA; 3The Dartmouth Institute for Health Policy & Clinical Practice, Lebanon, NH. (Tracking ID #1927628)
BACKGROUND: The degree of provider concern for individual patients significantly impacts panel management decisions and subsequent resource allocation within primary care practices. As current decision support tools do not effectively capture provider concern levels, the Iora Worry Score (IWS) was developed to reflect providers’ level of concern for individual Iora Health patients. The primary outcome of interest in this study was the strength of agreement between the IWS and the subjective provider worry score (SPS). This outcome was validated against an established stratification tool, the Milliman Advanced Risk Adjusters (MARA) score. A secondary outcome of interest was the relationship between both worry scores (IWS and SPS) and the average number of primary care visits.
METHODS: Iora Health is a venture-funded health care company based in Cambridge, MA, building a new model of primary care that serves a broad spectrum of patient populations, with a special focus on patients with complex chronic diseases. A patient’s IWS was defined as a provider’s general level of concern for a patient in terms of the anticipated need for team-based review and potential follow-up. The IWS was reported on a scale of 1 (least concern) to 10 (most concern) and was created using 77 evidence-based utilization, clinical, administrative and patient-reported variables. The IWS was applied to 5,773 patients across four Iora Health practices in a retrospective review. Iora Health providers assigned a SPS to each patient within a randomly selected subset of 352 patients for inclusion in the analysis of the primary outcome. The Kendall tau rank correlation coefficient was used to determine the strength of agreement in the analysis of IWS, SPS and MARA score.
RESULTS: The randomly selected cohort of 352 patients accurately represented the demographics of the entire Iora Health system population. Though few significant demographic differences were found across the four practices, there was significant variation in the IWS across practices (p < 0.0001). As the primary outcome, the statistically significant agreement noted between the IWS and the SPS (p < 0.0001; tau = 0.47) was stronger than the agreement between the comparator MARA score and the SPS (p < 0.0001; tau = 0.39). The SPS and the average IWS across all practices both displayed a statistically significant positive relationship with the average number of primary care visits (p < 0.0001, tau = 0.43 and p < 0.0001, tau = 0.44 respectively).
CONCLUSIONS: When compared to an accepted stratification tool, the IWS had a stronger degree of agreement with subjective provider concern levels. Implementing the IWS electronically through Iora Health’s care collaboration platform can save provider time by automating the triage of patients for team review and increase the responsiveness of Iora Health to concerning changes in individual patient worry scores. Ongoing refinement of the IWS to improve proactive panel management will be an important effort within the overall movement toward improving primary care delivery and patient outcomes.
DIABETES CONTROL IN OLDER PATIENTS IN PRIMARY CARE CLINIC VS. ENDOCRINOLOGY CLINICZoobia Chaudhry; Phil Levin; Lee Bromberger; Hsin-Chieh Yeh. Johns Hopkins School of Medicine, Baltimore, MD. (Tracking ID #1935937)
BACKGROUND: With increasing prevalence of diabetes, the demands for appropriate management by primary care providers as well as endocrinologists have amplified significantly. Although primary care providers see the vast majority of patients with type 2 diabetes, very few studies compared diabetes control in patients seen in primary care setting vs. in endocrinology clinic. A study in early 2000s reported a better quality of care in diabetes clinic than in primary care clinic, but no recent data indicated whether the disparity remained. We therefore conducted a retrospective study to compare HbA1c, blood pressure, and lipids controls in diabetic patients age 65 and older who were all eligible for Medicare coverage.
METHODS: A cross-sectional medical record review for older diabetic patients receiving care in 2010 and 2011 was conducted in a primary care clinic (PCC) and in an endocrinology clinic (EC) located in a close geographic proximity in Baltimore City. Data from the PCC included all older patients seen during the study period (n = 713); data from the EC was a random sample of older patients (n = 100) from medical chart reviews.
RESULTS: Patients seen in the PCC were older (mean age: 75.5 ± 6.7 vs. 73.3 ± 7.0, p = 0.002), were more likely to be black (75 % vs. 14 %, p < 0.0001), had higher body mass index (BMI, 30.9 ± 6.4 vs. 28.2 ± 7.7; p < 0.0001), and were less likely to be on insulin (24 % vs. 38 %, p = 0.004). There was no difference in gender distribution (women 56 % vs. 54 %, p = 0.69). In the univariate analysis, patients seen in the PCC and EC had similar mean HbA1c (PCC 6.93 ± 1.5 %, EC 6.99 ± 1.5 %; p = 0.69), systolic blood pressure (PCC 133 ± 18 mmHg, EC 130 ± 15 mmHg; p = 0.132), and total cholesterol (PCC 166 ± 40 mg/dl, EC 162 ± 36 mg/dl; p = 0.44), but had lower diastolic blood pressure (67 ± 12 mmHg vs.72 ± 10 mmHg; p = 0.0001) and higher HDL-cholesterol (56 ± 19 mg/dl vs. 51 ± 18 mg/dl; p = 0.006). In the multivariable linear regressions adjusting for age, race, sex, BMI, and insulin use, compared to patients seen in PCC, patients seen in EC had a significantly lower mean HbA1c (beta-coefficient: −0.57 %; 95 % confidence interval (CI): −0.94 % to −0.19 %; p = 0.003), but a higher DBP (beta-coefficient: 4.0 mmHg, 95 % CI: 0.88 to 7.14 mmHg; p = 0.012).
CONCLUSIONS: Glycemic control in older patients with type 2 diabetes was better in patients seen in EC as compared to those seen in PCC, partly due to the use of insulin. On the other hand, patients seen in PCC had a better control on diastolic blood pressure. Future research should explore the differences between the primary care clinic and endocrinology clinic on treatment strategies and other aspects of clinical practices such as counseling on lifestyle changes.
DIABETES EMPOWERMENT PROGRAM: CHANGES IN PATIENT SELF-CONFIDENCE, DIABETES SELF-MANAGEMENT, AND HEALTH OUTCOMESMonica E. Peek; Nora Geary; Yue Gao; Daniel J. Rowell; Yolanda O’Neal; Tonya Roberson; Julie L. Whyte; Nyahne Bergeron; Marshall Chin. University of Chicago, Chicago, IL. (Tracking ID #1939499)
BACKGROUND: African-Americans disproportionately suffer from diabetes and its complications. Although culturally tailored education can improve diabetes self-management and health outcomes among this population, little prior work has combined diabetes education with patient/provider communication training to empower African-American patients to better manage their disease.
METHODS: As part of a larger intervention, we developed the Diabetes Empowerment Program, a 10-week program that combined culturally-tailored diabetes education with skills training in patient/provider communication and shared decision-making. The education classes were modeled after the BASICS diabetes curriculum, and were adapted based on principles of health literacy and adult learning theory. Session length was adjusted to reduce the volume of information shared per session and audio visual aids supplemented written materials. The shared-decision making classes focused on building patients’ skills and confidence in asking more questions, giving more information, clarifying/restating what the doctor says, and communicating health care preferences. The classes utilized role-play, narrative, group interaction and problem-solving. Following the 10-week session, patients were invited to join a monthly support group for ongoing learning, skills building and social support. Patients were recruited to participate in the classes from two university clinics and four federally qualified health centers. We utilized in-person surveys to measure the following: 1) patients’ self-confidence about shared decision-making and diabetes self-management (i.e. decision-making empowerment and diabetes self-efficacy), 2) patient’s behaviors regarding diabetes self-management behaviors and shared decision-making (i.e. patients’ perceived involvement in care, blood sugar testing, exercise, healthy eating, and foot care), and 3) intermediate health outcomes (i.e. HbA1c, systolic blood pressure, weight and LDL cholesterol). Data were collected at baseline, immediately following the intervention (post), 3-months, and 6-months post intervention. We used linear mixed models to assess changes between baseline data and three follow-up points, controlling for age, gender, education, health insurance, number of years since diabetes diagnosis, self-reported health status, and co-morbidities (e.g. stroke, asthma, hypertension, hyperlipidemia).
RESULTS: Among the 118 patients (with at least one follow-up data point), the mean age was 57 years, 78 % were female, 97 % were African American and 40 % were uninsured or Medicaid-insured. The average baseline HbA1c was 8.8 %. Patients’ self-confidence about diabetes care significantly improved after program participation in decision-making empowerment and diabetes self-efficacy (Table 1). Significant improvements in diabetes self-management behaviors were also observed after program participation. Patients perceived themselves to be more involved in their care, and reported higher frequencies of exercising, testing blood sugar, and doing foot examinations. No significant findings were observed in healthy eating. After program participation, significant changes in intermediate health outcomes were also observed. There was a significant decrease in HbA1c from baseline, which was sustained at the 6-month follow-up. Additionally, a significant decrease in weight was observed at the 6-month follow-up. No significant changes in LDL or systolic blood pressure values were observed.
CONCLUSIONS: Our findings suggest that combining culturally-tailored diabetes education with skills training in patient/provider communication can be an effective strategy to improve self-confidence and behaviors in self-management and shared decision-making, and also improve diabetes-related health outcomes. Such strategies may serve to reduce diabetes disparities among African-Americans.
Changes in self-confidence, diabetes self-management behaviors, and intermediate health outcomes in the Diabetes Empowerment Program
| Outcome | Time | Adjusted mean (CI) | p-value |
| Decision-making empowerment (a) | baseline post 3-month 6-month | 80.9 (76.8,85.1) 92.2 (87.7,96.7) 89.2 (83.4,95.0) 90.6 (85.1,96.1) | −<0.001 0.002<0.001 |
| Diabetes self-efficacy (a) | baseline post 3-month 6-month | 67.0 (60.6,73.4) 76.6 (69.8,83.5) 69.7 (61.0,78.4) 81.3 (72.9,89.7) | −<0.001 0.47<0.001 |
| Patients’ perceived involvement in care (a) | baseline post 3-month 6-month | 68.0 (58.1,77.9) 77.9 (67.2,88.6) 81.2 (67.6,94.8) 82.8 (69.9,95.6) | −0.03 0.02 0.008 |
| Exercise (b) | baseline post 3-month 6-month | 3.1 (2.3,3.8) 3.5 (2.8,4.3) 3.1 (2.2,4) 4 (3.1,4.9) | −0.10 0.86 0.01 |
| Blood sugar testing (b) | baseline post 3-month 6-month | 4.4 (3.6,5.1) 5.2 (4.4,6) 5 (3.9,6) 5 (3.9,6) | −0.01 0.22 0.24 |
| Foot care (b) | baseline post 3-month 6-month | 4.3 (3.6,4.9) 5 (4.3,5.7) 4.6 (3.7,5.5) 5.1 (4.2,6) | −0.01 0.43 0.03 |
| HbA1c | baseline post 3-month 6-month | 8.8 (8.1,9.4) 8.1 (7.4,8.8) 8.1 (7.3,8.9) 8.1 (7.3,8.9) | −<0.001 0.02 0.04 |
| Weight (pounds) | baseline post 3-month 6-month | 245.6 (226.1,265.1) 246.2 (226.4,265.9) 239.4 (218.6,260.2) 231.4 (209.9,252.9) | −0.85 0.20 0.02 |
(a) Scale from 0 to 100, low to high (b) Number of days per week No significant changes observed in systolic blood pressure, LDL, or healthy eating.
DIABETES PREVENTION: ARE WE TRANSLATING EVIDENCE INTO PRACTICE?Tannaz Moin1,2; Jinnan Li2; O. Kenrik Duru2; Susan Ettner2; Norman Turk2; Robert H. Luchs3; Abigail M. Keckhafer3; Anya Kirvan3; Carol Mangione2. 1VA Greater Los Angeles Healthcare System and HSR&D Center for Healthcare Innovation, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3UnitedHealth Group, Minneapolis, MN. (Tracking ID #1939018)
BACKGROUND: Pre-diabetes is a major health care burden that is associated with an increased risk of type 2 diabetes and related complications. More than 10 years ago, several landmark studies demonstrated that both lifestyle changes and metformin use can significantly reduce the risk of progression to diabetes compared to placebo. Soon after, the safety, tolerability and cost-effectiveness of metformin use in patients with pre-diabetes was also demonstrated. Beginning in 2008, the use of metformin was included in national diabetes prevention guidelines by the American Diabetes Association (ADA). To date, very little is known about the uptake and translation of the evidence supporting metformin use in patients with pre-diabetes. The goal of this analysis was to characterize national patterns of metformin use among patients with pre-diabetes and examine whether a health plan designed specifically for patients with pre-diabetes and diabetes (the “Diabetes Health Plan,” or DHP), which eliminates copayments for metformin and enhances access to care management, could impact the translation of evidence into practice.
METHODS: We conducted a retrospective analysis of claims data from a national commercial health plan between 2009 and 2012. We included patients with pre-diabetes between 19 and 63 years of age with consecutive enrollment over 3 years and compared those who were enrolled in the DHP to those enrolled in a standard medical plan. A diagnosis of pre-diabetes was defined by two or more ICD-9 diagnoses of 790.2× (during an inpatient, outpatient, or ED claim), or last HbA1c value of 5.7–6.4 %, or last Fasting Plasma Glucose (FPG) value of 100–125 ng/dl or last oral glucose tolerance test (OGTT) value of 140–199 ng/dL. We excluded patients with a history diabetes, gestational diabetes, or use of anti-glycemic medications at baseline.
RESULTS: We analyzed data from 23,843 patients with pre-diabetes and compared results among those enrolled in the DHP (n = 935) to those enrolled in standard medical plans (n = 22,908). The prevalence of metformin use among patients with pre-diabetes was similarly low in both groups at baseline (1.9 % in the DHP [n = 18] and 1.7 % in the standard plans [n = 382]). Over the following 2 years we observed minimal change in the proportion of patients with pre-diabetes who were newly prescribed metformin whether or not they were enrolled in the DHP (2.1 % new metformin prescriptions in the DHP plan [n = 19] and 1.2 % in the standard plans [n = 262]).
CONCLUSIONS: Our findings indicate that metformin is rarely used in the management of pre-diabetes, despite a strong evidence base in the literature for over 10 years. This is a concerning gap in the clinical approach to pre-diabetes and potentially impacts up to one third of the U.S. population currently estimated to have pre-diabetes. Enrollment in a pre-diabetes health plan, which eliminates medication and physician visit copays and increases pre-diabetes disease awareness, minimally increased the rates of metformin use among patients with pre-diabetes. Further studies are needed to understand the root causes of this existing gap and possible interventions to help promote the translation of evidence into future practice.
DIAGNOSING AND COUNSELING OBESE PATIENTS IN THE PRIMARY CARE SETTINGAdam J. Balzer; Cynthia Phan; Priya Radhakrishnan. St. Joseph’s Hospital and Medical Center, Phoenix, AZ. (Tracking ID #1938375)
BACKGROUND: The incidence of obesity in the U.S. has expanded to greater than 30 % of the population and is now widely regarded as a national epidemic. Obesity is defined as a body mass index of greater 30 kg/M2. For years, it has been clearly linked to several chronic diseases including coronary artery disease, hypertension, and diabetes mellitus. Studies are also demonstrating that obesity is an independent risk factor for prolonged hospitalizations, increased ambulatory care utilization, and increased healthcare costs. While healthcare providers are very aware of detrimental impact of obesity, a systematic approach to obesity as a disease entity and the implementation of a treatment plan does not occur routinely. With the expansion of electronic health record systems and underlying requirement of “meaning use” rules, BMI must be recorded at each clinic visit. If the BMI is outside parameters, a follow-up visit must be documented.
METHODS: With the transformation into a electronic medical record system in the Internal Medicine, we undertook a quality improvement project. Chart review was performed on patients from May 2012 to June 2012 of patients that had appointments at the Internal Medicine Clinic Health Center. Data was collected and analyzed. We looked at the percentage of patients with a documented body mass index of 30 or greater. A chart review was performed for each patient with a BMI of greater than 30 to see if obesity was diagnosed and if counseling was performed.
RESULTS: From 5/1/2012 to 6/18/2012, 744 encounters were analyzed from both residency clinic and faculty practice. Forty-three percent of 744 encounters had a clinical diagnosis of obesity listed in the problem list. Of these, 60 % of those diagnosed received counseling. Of the 744 encounters, there were 557 patients made up the 744 encounters; 142 patients were seen at least two times and 61 % of those patients were diagnosed with obesity.
CONCLUSIONS: The results of this study demonstrate that BMI is consistently measured and recorded in the EMR, however, obesity is not consistently recorded as a diagnosis in the problem list and treatment options are not routinely documented in the EHR. It is interesting to note that despite having multiple encounters, obesity was consistently not clinically diagnosed in 39 % of the patients. This quality improvement project demonstrates the importance of linking education with meaningful use metrics to make a clinical impact. We hope these findings initiate further research on provider understanding of EHR utilization and potential barriers to recognizing and treating obesity in the primary care setting.
DID THE UNITED STATES PREVENTIVE SERVICES TASK FORCE 2005 GUIDELINES FOR ABDOMINAL AORTIC ANEURYSM SCREENING AFFECT MORTALITY IN THE UNITED STATES POPULATION?Devin B. Malik; Sourabh Aggarwal. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1938931)
BACKGROUND: An abdominal aortic aneurysm (AAA) is defined when infra-renal aortic diameter is at least 3.0 cm. The United States Preventive Services Task Force (USPSTF) made recommendation in 2005 that all men between the age of 65 to 75 years and who have ever smoked should be screened one time for AAA by abdominal ultrasonography. However, the clinical impact of these recommendations are unknown in the American population.
METHODS: We queried Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample (NIS) for AAA and AAA rupture using ICD9 codes 441.4 and 441.3 respectively. The NIS represents 20 % of all hospitals data in US. All the data was extracted for years 2000–2010. The prevalence and in-hospital mortality for pre-screening years (2000–2004) was compared with post-screening years (2006–2010). Chi square was used to find statistical significance.
RESULTS: A total of 527,801 hospitalizations secondary to AAA and AAA rupture were analyzed for the study period. AAA prevalence decreased from 61.72 to 58.77 per 10,000 total hospitalizations with in-hospital mortality decreasing from 3.5 to 2.12 % (p value <0.001). On sub-analysis, the decrease in prevalence was chiefly in 65–84 age group (77.19 to 74.54 per 100 AAA admissions, p < 0.001), with increase in 84+ age group (6.37 to 8.6 per 100 AAA admissions, p < 0.001) and no significant change in 45–64 age group (16.16 to 16.51 per 100 AAA admissions, p value >0.05). Prevalence increased in males (77.84 to 78.13 per 100 AAA admissions, p < 0.001) and decreased in females (22.13 to 21.81 per 100 AAA admissions, p < 0.001). Decrease in mortality was uniform in all age and gender sub-groups. The prevalence of AAA rupture decreased from 9.51 to 7.03 per 10,000 total hospitalizations (p < 0.001). On sub-analysis decrease in prevalence was reciprocated in 65–84 age group (70.08 to 64.94 per 100 AAA rupture admissions, p value <0.001) and males (73.23 to 71.7 per 100 AAA rupture admissions, p value <0.001). However, prevalence of AAA rupture increased in age group 45–64 (14.41 to 15.43 per 100 AAA rupture admissions, p value <0.001), age 84+ (15.21 to 19.2 per 100 AAA rupture admissions, p value <0.001) and females (26.28 to 28.28 per 100 AAA rupture admissions, p value <0.001).
CONCLUSIONS: Our study reveals that post screening recommendations, hospitalizations for AAA decreased significantly with decrease only reciprocated in the age group 65–84 years. Also hospitalizations and in-hospital mortality from AAA rupture decreased in males and age group 65–84, with increase in hospitalizations for the 45–64 and 84+ age group and females. The possible explanation is better screening as outpatient resulted in decreased morbidity with decreased hospitalizations from AAA and AAA rupture in susceptible population. Our study also makes the case to consider extension of recommendations to include other susceptible groups.
DIFFERENCES IN ACCESS TO HEALTH CARE AMONG LESBIAN, GAY, AND BISEXUAL POPULATIONS IN NEW YORK CITYKristin A. Swedish1; Marcus A. Bachhuber2; Viraj V. Patel1. 1Montefiore Medical Center, Bronx, NY; 2University of Pennsylvania, Philadelphia, PA. (Tracking ID #1938935)
BACKGROUND: Lesbian, gay, and bisexual (LGB) groups in the United States experience significant health care disparities across a wide range of conditions. Despite being considered a priority area to target in Healthy People 2020, there is limited nation-wide data available on these populations. Previous research suggests that LGB members of racial or ethnic minorities often face the highest level of health disparities. We examined differences in access to care by self-identified sexual orientation and race/ethnicity in New York City (NYC).
METHODS: We used multi-year pooled data from the 2009–2011 NYC Community Health Surveys, a probability-based survey using a stratified random sampling. The Community Health Survey is based upon the National Behavioral Risk Factor Surveillance System and samples approximately 10,000 adults from all five boroughs of NYC (response rates 37.7–40 % for 2009–2011). We examined two primary outcomes: 1) identifying someone as a primary care provider (PCP) and 2) receiving medical care when needed in the prior 12 months. Self-identified sexual orientation was the primary independent variable, accounting for gender. We conducted descriptive analyses and multivariate logistic regression analyses adjusting for age, race/ethnicity, nativity (US vs. foreign born), education, employment status, insurance status, and primary language spoken at home. All analyses incorporated survey weights.
RESULTS: Survey respondents included 603 gay men, 204 lesbian women, 115 bisexual men, and 133 bisexual women, with mean age 48.9 years (SD 14.9). The majority of LGB individuals were White (59.5 %), college-educated (62.9 %), employed or self-employed (64.9 %), privately insured (57.5 %), and US-born (82 %). Lesbian and bisexual women were significantly less likely than heterosexual women to identify a PCP (adjusted odds ratio [AOR] 0.46, 95 % confidence interval [CI] 0.45–0.47 and AOR 0.66, 95 % CI 0.65–0.68, respectively). Lesbians and bisexual women were also less likely than heterosexual women to have received medical care when needed in the prior 12 months (AOR 0.73, 95 % CI 0.71–0.75 and OR 0.41, 95 % CI 0.40–0.42, respectively). In contrast, when compared to heterosexual men, gay and bisexual men were significantly more likely to have a PCP (AOR 1.09, 95 % CI 1.07–1.11 and AOR 1.22, 95 % 1.18–1.27, respectively). Both gay and bisexual men were also more likely than heterosexual men to have received medical care when needed in the prior 12 months (AOR 1.36, 95 % CI 1.33–1.39 and OR 1.54, 95 % CI 1.47–1.62, respectively). When stratified by race/ethnicity, lesbian and bisexual Black and Hispanic women were significantly less likely than heterosexual white women to have received medical care when needed in the prior 12 months (AOR 0.50, 95 % CI 0.49–0.52 and AOR 0.34, 95 % CI 0.33–0.35, respectively). Gay and bisexual Hispanic men were significantly less likely than heterosexual white men to receive medical care when needed in the prior 12 months (AOR 0.58, 95 % CI 0.56–0.60).
CONCLUSIONS: Lesbian and bisexual women in NYC have worse access to health care when compared with heterosexual women; these disparities are more pronounced in Black and Hispanic women. It is notable that similar disparity is not seen among gay and bisexual men in NYC, apart from the Hispanic subgroup. It is possible that the HIV epidemic may have altered the way gay and bisexual men utilize health care in NYC. It is also possible that lesbian and bisexual women fear greater stigma in the health care setting. Further research is needed to elucidate these disparities. The findings of this study should be used to help public health officials design interventions and policies to increase access to care in LGB populations.
DISCHARGE ROUNDS: IMPLEMENTATION & EFFECTS OF A SYSTEMATIC APPROACH TO EARLY DISCHARGES ON PATIENT THROUGHPUTKrisda Chaiyachati1,2; Andre N. Sofair1,2; Jeremy I. Schwartz1,2; David Chia1,2. 1Yale School of Medicine, New Haven, CT; 2Waterbury Hospital, Waterbury, CT. (Tracking ID #1922266)
BACKGROUND: Patient throughput is an important aspect of hospital medicine. It has effects on patient satisfaction and safe transitions of care from home-to-hospital by decreasing emergency room wait times, time to evaluation by a physician, and time to hospital admission. Early discharges benefit these upstream events by creating bed space and allowing support staff to plan accordingly, setting up a cycle of events necessary for new hospital admissions to begin.
METHODS: In order to improve throughput, our internal medicine residency program systematically instituted daily early morning discharge rounds on the inpatient teaching service on August 1, 2013. Discharge rounds require that each medical team identifies potential discharges and completes the necessary paperwork the day prior to anticipated discharge. The following day, these patients are evaluated early and discharge orders are initiated in real-time. We conducted a retrospective pre-post study to determine whether discharge rounds were effective in changing when discharge orders were initiated and when patients actually left the hospital. To account for changes in practice patterns, we compared the mean time outcomes one month pre- and post-intervention. Moreover, we followed the intervention for two additional months to assess for sustainability.
RESULTS: A total 159 patients in July and 152 in August were discharged by the teaching service. The intervention was associated with earlier discharge order initiation by 59 min (1:07 PM vs. 12:08 PM, p = 0.001). This effect was consistent for patients being discharged to home (12:54 PM vs. 12:03 PM, p = 0.01) and to facility (1:32 PM vs. 12:22 PM, p = 0.05). The percentage of early discharges, namely discharges initiated before 11 AM, increased from 21.4 to 38.8 % (p =< 0.001). The intervention was associated with patients leaving the hospital earlier 50 min (3:21 PM vs. 2:31 PM, p = 0.005). This was significant in patients being discharged to home (2:46 PM vs. 2:05 PM, p = 0.05) but not in those discharged to facility (4:22 PM vs 3:46 PM, p = 0.28). These beneficial effects, however, waned in the subsequent 2 months compared with pre-intervention times. In September and October, the mean discharge order initiation times were 1:00 PM (p = 0.69) and 1:11 PM (p = 0.82), respectively, while the mean discharge times were 3:22 PM (p = 0.94) and 3:42 PM (p = 0.22), respectively.
CONCLUSIONS: The systematic implementation of early discharge rounds significantly decreased the time to initiation of discharge orders and subsequently the time of patient discharge in the immediate period after the intervention. Academic internal medicine services may help improve patient throughput by implementing this intervention. However, as in other quality improvement efforts, consistent reinforcement and reevaluation are likely required for sustainability.
DISCORDANT WEIGHT PERCEPTION AND PHYSICAL ACTIVITY IN OVERWEIGHT AND OBESE WOMEN: IS WEIGHT MISPERCEPTION PROTECTIVE?Nathalie Moise1; Robert Sciacca2; Juviza Rodriguez2; Ian M. Kronish1; Elsa-Grace V. Giardina2. 1Columbia University Medical Center, New York, NY; 2Columbia University Medical Center, New York, NY. (Tracking ID #1926824)
BACKGROUND: One third of U.S. adult women (35.8 %) are obese, placing them at increased risk for cardiovascular disease and mortality. Women are approximately twice as likely to be inactive as men while overweight and obese individuals are less likely to exercise than their normal weight counterparts. Understanding drivers of behavioral change in this population is crucial. Prior studies have suggested that within overweight and obese men, weight underestimation is associated with physical inactivity. However, these studies have relied on self-report, both of weight perception and body mass index (BMI), and have been inconclusive regarding the relationship between weight perception and physical activity in women, whose responses may be particularly influenced by social desirability bias. To address this gap, we assessed whether weight perception measured with a figural rating scale is associated with physical inactivity in overweight and obese women.
METHODS: A cross sectional analysis was conducted on a primary prevention cohort of 580 overweight and obese (BMI ≥ 25 kg/m2) women recruited from the primary care clinics of Columbia University Medical Center. Exclusion criteria were known coronary artery disease, cardiovascular disease, stroke, pregnancy and age ≤18 years. BMI was calculated from measured heights and weights. The outcome variable was based on American Heart Association recommendations of at least 30 min of physical activity on most days, which was subdivided into (a) walking exercise and (b) non-walking exercise. Participants indicated their “self” figure on the Stunkard 9-figure rating scale (FRS), a widely used and validated measure for assessing weight status. Accurate weight perception was determined by comparing participants’ actual BMI with the BMI matched to the selected figure: Underestimators selected underweight or normal weight figures on the FRS and accurate estimators selected overweight or obese figures that matched their BMI. Multivariable logistic regression was used to analyze the relationship between accuracy of weight perception and physical activity after adjusting for age, race, education and BMI.
RESULTS: Mean age was 48 + 14 years; 45.3 % were obese, 65.3 % were Hispanic, 41.6 % had hypertension, 30.7 % had hyperlipidemia, 13.4 % had diabetes mellitus and 28.1 % had 2 or more cardiovascular risk factors. Among participants, 49.2 % correctly perceived their weight and 82.0 % reported they were physically active; 64.6 % reported walking exercise and 41.8 % non-walking exercise. Those who underestimated their weight, compared to accurate estimators, were more likely to be non-Hispanic black (12.9 % vs. 6.7 %, p < 0.0001), Hispanic (70.8 % vs. 60.0 %, p = 0.0001), have 9–12 years of education as opposed to >12 years of education (40.6 % vs. 30.6 %, p = 0.02) and be obese (57.8 % vs. 32.3 %, p =< 0.0001). Those who underestimated their weight reported more physical activity (adjusted odds ratio [AOR] = 1.89, 95 % CI, 1.19–2.99, p = 0.0072) and non-walking exercise (AOR = 1.52, 95 % CI, 1.05–2.21, p = 0.026), but not walking exercise (Table 1).
CONCLUSIONS: Among overweight and obese women, contrary to our hypothesis, those who underestimated their weights were more likely to report increased physical activity. Accurately perceiving oneself as overweight or obese may be a cognitive barrier to physical activity participation. Additionally, we found that obesity, lower educational attainment and minority race were associated with physical inactivity; physicians should continue to focus on these at risk groups. Because we relied on self-report for physical activity, it may be that individuals who underestimate their weight report greater physical activity. Future studies using objective measures of physical activity are needed to better understand the directionality of this association. Notwithstanding this limitation, clinicians should be aware of weight misperception when counseling overweight and obese patients and should be cautious about reinforcing a self-image that is counter to physical activity.
Adjusted Odds Ratios for physical activity, non-walking exercise and walking exercise.
| Physical Activity AOR (95 % CI) | Non-Walking Exercise AOR (95 % CI) | Walking Exercise AOR (95 % CI) | |
| Correct weight perception | Ref | Ref | Ref |
| Misperception | 1.89 (1.19–2.99) * | 1.52 (1.05–2.21) * | 1.31 (0.91–1.88) |
| Age, per year | 1.01 (0.99–1.03) | 0.98 (0.97–0.998)* | 1.01 (1.00–1.03) |
| Race/Ethnicity | |||
| Non-Hispanic White | Ref | Ref | Ref |
| Non-Hispanic Black | 0.71 (0.30–1.68) | 0.54 (0.27–1.08) | 0.81 (0.40–1.63) |
| Hispanic | 0.96 (0.49–1.87) | 0.38 (0.23–0.64)* | 1.09 (0.64–1.86) |
| Education level | |||
| >12 years | Ref | Ref | Ref |
| 9–12 years | 0.98 (0.58–1.67) | 0.62 (0.41–0.95)* | 1.05 (0.68–1.61) |
| <8 years | 1.00 (0.49–2.02) | 0.66 (0.37–1.17) | 0.81 (0.47–1.43) |
| BMI | |||
| Overweight | Ref | Ref | Ref |
| 0.73 (0.47–1.15) | 0.68 (0.47–0.98)* | 1.03 (0.71–1.47) | |
*p < 0.05 AOR = Adjusted Odds Ratio
DISCRIMINATION PERCEIVED BY FREQUENT EMERGENCY DEPARTMENT USERS. IS DISCRIMINATION A RISK FACTOR FOR VULNERABILITY?Stéphanie Baggio1; Jean-Bernard Daeppen2; Bernard Burnand2; Olivier Hugli2; Ornella Ruggeri2; Jean-Blaise Wasserfallen2; Karine Moschetti2; Philippe Staeger2; Séverine Alary2; Katia Iglesias2; Marina Canepa Allen2; Patrick Bodenmann2. 1Lausanne University, Lausanne, Switzerland; 2Lausanne University Hospital, Lausanne, Switzerland. (Tracking ID #1930275)
BACKGROUND: Frequent Emergency Department (ED) users are often vulnerable people with many risk factors and health needs. They are also perceived to be time-consuming, “illegitimate” patients, and thus may feel discriminated against during their hospital visit. Because perception of discrimination, non-adherence to medical treatment, and poorer health status are associated, frequent ED users’ perception of discrimination may constitute an additional risk factor for vulnerability. The aim of this study was to investigate the relationship between perceived discrimination and vulnerability among frequent ED users.
METHODS: Data were part of a baseline assessment of a randomized controlled trial designed to improve frequent users’ quality of care in Lausanne University Hospital, one of the two French-speaking Swiss tertiary care hospitals, with over 50,000 annual ED visits. In total, 250 frequent ED users (≥5 attendances during the previous 12 months; ≥18 years) were interviewed between May 2012 and July 2013. From a previously published questionnaire, 15 dichotomous sources of discrimination, grouped into five causes of discrimination (any cause, immigration-related, age/gender, physical characteristics/sexual orientation, and social/economic status) were assessed. Vulnerability was assessed using health status: objective health status evaluated by health-care practitioners and including somatic-, mental-health-, behavioural-, and social issues (dichotomous variables), and subjective health status self-rated by the frequent ED users, including health-related quality of life (WHOQOL), quality of life (EUROQOL), and satisfaction with care (mean-scores). Associations between perceived discrimination and health status were tested with exact Fischer tests and Mann-Whitney U tests.
RESULTS: Participants were 46.2 ± 18.9 years old on average, 57.2 % were men, 47.8 % Swiss, 17.7 % European, and 34.5 % non-European. A total of 35.2 % reported at least one source of discrimination. Objective health status was not significantly related to perceived discrimination (e.g. 35.8 % of users discriminated against had somatic issues versus 33.8 % of users not discriminated against, p > 0.05, see Table 1). Contrariwise, experiencing discrimination was associated with worse subjective health status (e.g. users discriminated against reported a mean-score of 28.16 for WHOQOL health status, versus 39.44 for users not discriminated against, p < 0.001, see Table 1).
CONCLUSIONS: Perceived discrimination was partially associated with increased vulnerability. Indeed, frequent ED users who experienced discrimination were more likely to self-rate their own health as lower, while health-care practitioners’ rating was not related to perceived discrimination. Therefore, experiencing discrimination was not related to “real” health status, but to subjective health status’s evaluation. Perceived discrimination seemed to be associated with a negative overall picture of their own health and health care services among frequent ED users, even if their health was not really worse. Health-care practitioners should be aware of this phenomenon, and perceived discrimination may also be of concern in improving interventions and providing optimal care to frequent ED users.
Associations between perceived discrimination and health status
| No discrimination reported | Reported discrimination | p-value (a) | |
| Objective health status, % (N) | |||
| Somatic issues | 64.2 % (111) | 35.8 % (62) | 0.776 |
| Mental-health issues | 63.5 % (80) | 36.5 % (46) | 0.693 |
| Behavioural issues | 63.8 % (51) | 36.3 % (29) | 0.887 |
| Social issues | 61.5 % (112) | 38.5 % (70) | 0.101 |
| Subjective health status, mean (SD) | |||
| EUROQOL single index value (0–1) | 0.78 (0.12) | 0.76 (0.11) | 0.331 |
| EUROQOL health status (0–100) | 54.34 (23.99) | 44.52 (23.14) | <0.001 |
| WHOQOL quality of life (0–100) | 51.09 (31.67) | 36.65 (25.97) | <0.001 |
| WHOQOL health (0–100) | 39.44 (28.18) | 28.16 (28.22) | 0.001 |
| Satisfaction (0–10) | 8.93 (1.29) | 7.43 (2.29) | <0.001 |
(a) Objective health status — exact Fischer test; subjective health status — Mann-Whitney U test.
DISPARITIES IN GLYCEMIC AND LIPID CONTROL AMONG DIABETIC PATIENTS IN THE VETERANS ADMINISTRATION: IMPLICATIONS IN THE ERA OF THE AFFORDABLE CARE ACTLeChauncy D. Woodard1; Salim S. Virani1; Laura A. Petersen1; Amber Amspoker1; Tracy Urech1; David Ramsey1; Omolola E. Adepoju1; Praveen Mehta2; Jeffrey A. Murawsky2; Aanand D. Naik1. 1Michael E. DeBakey Medical Center, HSR&D, Houston, TX; 2VISN 12 (Great Lakes), Westchester, IL. (Tracking ID #1931717)
BACKGROUND: Racial and gender disparities in diabetes care are well documented. The Patient Protection and Affordable Care Act offers promise for reducing such disparities by increasing access to care and aligning financial incentives to promote high-quality, comprehensive primary care through delivery models such as the patient-centered medical home (PCMH). Given its widespread transformation to the PCMH model of care, the Veterans Health Administration (VA) serves as an ideal setting in which to examine the impact of universal healthcare access and patient-centered, team-based care on disparities in diabetes outcomes. Thus, we assessed racial and gender disparities in diabetes care among patients receiving care in the VA subsequent to PCMH implementation.
METHODS: We used VA structured clinical data from electronic fields to identify patients with diabetes who received primary care between June 1, 2011 and May 31, 2012, in one Midwestern VA Network encompassing 7 facilities. We assessed differences in glycemic and lipid control between male and female Veterans with diabetes using two VA quality indicators [Hemoglobin (Hb) A1c < 9 %, low-density lipoprotein cholesterol (LDL-C) < 100 mg/dL]. We then used multilevel logistic regression, accounting for facility-level clustering, to determine whether female gender or race was associated with glycemic and LDL-C control.
RESULTS: Of the 203,897 patients who received care during our study interval, we identified 37,644 patients (18.5 %) with diabetes. The majority of patients were male (97.1 %) and white (73.1 %). Male patients were older than female patients (mean age 62.9 vs. 54.4 years, p < 0.0001), and were more likely to have co-existing cardiovascular disease (31.6 % vs. 12.8 %, p < 0.0001) and hypertension (84.5 % vs. 73.5 %, p < 0.0001), but were less likely than female patients to have co-existing depression (21.2 % vs. 38.3 %, p < 0.0001). Compared to men, female patients were less likely to achieve glycemic (84.2 % vs. 81.0 %, p = 0.004) and lipid (72.5 % vs. 57.9 %, p < 0.0001) control. Adjusting for age, illness burden, comorbidities, receipt of care at a teaching facility, number of primary care visits, and provider type, females were as likely as males to achieve glycemic control (OR 1.07; 95 % CI, 0.87–1.33), but were less likely to have controlled LDL-C levels (OR 0.77; 95 % CI 0.65–0.92). Further, white patients had significantly higher odds than non-white patients of achieving both glycemic (OR 1.21; 95 % CI 1.10–1.33) and lipid (OR 1.29; 95 % CI 1.20–1.40) control.
CONCLUSIONS: Despite universal access to care and widespread PCMH implementation within the VA, both gender and racial disparities in diabetes care persist. Of course, these findings could be due to patient preferences or lower cardiovascular risk among females and thus, clinically appropriate. Our findings suggest that additional efforts to adapt the PCMH model of care to diverse populations by accounting for patient characteristics and patient preferences for care may lead to additional gains in eliminating health disparities among chronically ill patients.
DISPARITIES IN THE TREATMENT OF DEPRESSION AMONG LOW-INCOME RACIALLY AND ETHNICALLY DIVERSE PATIENTS WITH TYPE 2 DIABETESCaroline Presley; Ken Wallston; David Schlundt; Chandra Y. Osborn; Sunil Kripalani; Shari D. Barto; Russell L. Rothman. Vanderbilt University Medical Center, Nashville, TN. (Tracking ID #1928731)
BACKGROUND: Comorbid depression among patients with Type 2 Diabetes (T2DM) is common and has been associated with decreased adherence to self-care and worse glycemic control (A1C). There have been few studies examining disparities in the prevalence of depressive symptoms, antidepressant use, and adequacy of treatment among low-income patients with T2DM. Therefore, we examined the prevalence of depression and adequacy of treatment among a low-income, racially and ethnically diverse sample of patients with T2DM.
METHODS: 406 patients with T2DM were enrolled in a randomized controlled trial evaluating a health literacy intervention for diabetes care at 10 Tennessee Department of Health safety net clinics. At enrollment, data on patient characteristics and clinical information were collected via self-report and from the medical record. Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale (CES-D 20, range 0–60), with a score of ≥16 indicating possible depression. Patients were considered to be prescribed an antidepressant if their medication list included an SSRI, an SNRI, a TCA, or an atypical antidepressant. Descriptive statistics characterized the sample and identified prevalence rates. Chi-squared analyses and t-tests were used to examine the bivariate relationships between patient characteristics and the presence of depressive symptoms and, separately, depression treatment status. We performed logistic regression analysis of antidepressant use adjusted for age, gender, race, ethnicity, duration of diabetes, education level, level of depressive symptoms (CES-D score), and study intervention status to evaluate the factors impacting antidepressant use in this patient population.
RESULTS: The sample was on average 51 years old (SD 9.6), 61 % were female, 18 % were African American, and 24 % reported Latino ethnicity. Mean education was 11.1 years (SD 3.4). The majority (88 %) reported no health insurance and annual household incomes <$20,000 (83 %). Mean A1C was 9.2 (SD 2.1). The majority (53 %) had CES-D scores ≥16. There were similar rates of depressive symptoms by race and ethnicity. Despite the high prevalence of depressive symptoms in the overall sample, only 18 % of all patients and 24 % of patients with CES-D scores ≥16 were prescribed an antidepressant. Depressive symptoms were higher among patients prescribed an antidepressant compared to those not prescribed an antidepressant (CES-D score 25 (SD 14.5) vs. 17 (SD 11.9), p < 0.0001). In adjusted analysis, African American/Blacks (AOR 0.25, p = 0.006) and Latinos (AOR 0.16, p = 0.005) were significantly less likely to be on an antidepressant compared to non-Hispanic Whites.
CONCLUSIONS: We found a high prevalence of depressive symptoms among a vulnerable population with T2DM. Only a fraction of patients with possible depression were prescribed an antidepressant. Among patients who were prescribed an antidepressant, there were high rates of depressive symptoms suggesting ineffective treatment. African American and Latino patients were significantly less likely to be treated with an antidepressant even with adjustment for presence of depressive symptoms. These data suggest that depression is often unrecognized and inadequately treated in low-income patients with T2DM, especially racial and ethnic minorities, which may have a negative impact on their diabetes control and outcomes.
DO CANCER PATIENTS FARE WELL IN THE ICU?Vijairam Selvaraj; Jane Garb; James Stewart; Jay Steingrub; Thomas Higgins. Baystate medical center, Springfield, MA. (Tracking ID #1895999)
BACKGROUND: Physicians and patients may have unrealistic expectations about prognosis with cancer, with both over- and under-estimates of mortality. While severity of illness at ICU admission is frequently evaluated using the APACHE (Acute Physiology and Chronic Health Evaluation) system, these scores are designed to assess large cohorts rather than individuals and may help with prognostication, but cannot be used to triage ICU admission in isolation. There is long-standing controversy over “potentially ineffective care” and evidence for a high degree of regional variation in caring for patients with poor prognosis cancer. However, newer studies suggest reduced mortality rates among critically ill cancer patients with the development of newer procedures such as non-invasive ventilation. Our hypothesis is that subgroups of patients with cancer may have APACHE-adjusted outcomes similar to non-cancer patients.
METHODS: A retrospective cross-sectional study of all patients above 18 years admitted to the ICU from May 1, 2009 to April 30, 2013 with chronic health diagnoses of leukemia, lymphoma/myeloma, solid tumor with metastasis and immunosuppression at Baystate Medical Center, Springfield, MA. Exclusion criteria was consistent with APACHE-IV methodology. A control group was selected of patients without an APACHE chronic health diagnosis. Primary outcomes were APACHE-IV score and Standardized Mortality Rates (SMR) during ICU and hospital stay. Secondary outcomes included length of stay in ICU and hospital, and mechanical ventilation on day 1 of admission. Baseline factors in predicting APACHE score were analyzed using multiple regression. Group differences in secondary outcomes were reported descriptively.
RESULTS: 5486 subjects were available for the study: 334 immunosuppressed patients (6 %); 91 leukemia patients (2 %); 50 lymphoma patients (1 %); 162 metastatic cancer patients (3 %); and 4849 non-cancer controls (88 %). All groups were significantly different from controls in Acute Physiology Scores (APS) (p < 0.001), after adjusting for age. Mean APS scores for immunosuppressed were 74.3, leukemia 83.6, lymphoma 83.7 and metastatic cancers 68.6; controls were 60.3 (p < 0.0001). The age-adjusted regression model accounted for 15 % of the variability in APS scores. While APACHE score significantly discriminated diagnosis groups from controls, there were no significant differences between any groups or controls on APACHE-based SMR’s.
CONCLUSIONS: Our study showed patients with cancer or immunosuppression had survival similar to that of non-cancer patients in the ICU; with no difference noted among groups. Because this is a single-site retrospective study, we cannot exclude that triage decisions may be selecting ICU admissions from patients with better prognoses. Further investigation could utilize the national APACHE database to create more generalizeable results. Based on this preliminary work, cancer and immunosuppresed patients do not appear to have a mortality penalty in the context of APACHE severity adjustment. This knowledge can help with ICU resource planning as well as timing for palliative care.
SMR for ICU and Hospital Mortality
DO PHYSICIANS SPEND LESS TIME WITH PATIENTS IN CONTACT ISOLATION? A TIME-MOTION STUDY OF INTERNAL MEDICINE INTERNSCody Dashiell-Earp1; Douglas Bell1; Alexis Ang1; Daniel Uslan2,1. 1University of California, Los Angeles, Los Angeles, CA; 2University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1930419)
BACKGROUND: Studies have shown that isolation precautions used by hospitals to control the spread of resistant organisms may have unintended consequences, including a reduction in time spent with health care providers, lower patient satisfaction and more preventable adverse events.
METHODS: The purpose of this study was to measure the time spent by internal medicine interns in contact with patients in isolation compared to non-isolation hospital rooms. Using RFID tags attached to hospital identification badges, we collected real-time data on the location of 15 internal medicine interns working in our hospital between October 1, 2012 and December 31, 2012. These devices enabled us to record the amount of time spent by interns inside isolated and non-isolated patient rooms. In total, there were 1,156 encounters with isolated patients and 2,467 encounters with non-isolated patients. A mixed model was used to compare the average time spent by each intern with these two patient groups.
RESULTS: Interns visited isolated patients less often (2.3 compared to 2.5 visits per day, P < 0.0001) and spent less time per visit with isolated patients (2.2 compared to 2.8 min per visit, P < 0001). Thus, on average, interns spent 5.2 min per day with each of their isolated patients compared to 6.9 min per day with each of their non-isolated patients (P < 0.0001).
CONCLUSIONS: Internal medicine interns spent significantly less time in the rooms of patients in isolation. This difference was more pronounced for some interns compared to others. Reduced physician contact time may be one of the driving forces behind differences in the quality of care experienced by patients in isolation. Further research is needed, both to better define the patient population for whom the benefits of contact isolation outweigh the risks and to develop strategies to ameliorate those risks for those who must be placed into isolation.
DO PRIMARY CARE PHYSICIANS WHO DELIVER BETTER QUALITY OF CARE ALSO USE LESS HEALTH CARE RESOURCES?Carine Yelibi; Charlotte E. Ward; Yuchiao Chang; Jeffrey M. Ashburner; Clemens S. Hong; Steven J. Atlas. Massachusetts General Hospital, Boston, MA. (Tracking ID #1940237)
BACKGROUND: Access to and a long-term relationship with a primary care provider (PCP) are associated with better health outcomes and decreased rates of acute care utilization and costs. However, it is less clear whether PCPs that deliver higher quality care also reduce utilization and costs. We hypothesized that PCPs delivering higher quality care have lower rates of emergency department (ED) utilization, admissions, and readmissions.
METHODS: We performed a physician-level, retrospective cohort analysis, using data from calendar year 2012 from electronic data repositories, on 173 PCPs and 105,766 patients receiving care in the MGH primary care practice-based research network. A quality composite measure was created using nine individual HEDIS measures at the patient level, where the denominator was the number of measures for which the patient was eligible, and the numerator was the number of measures the patient achieved (e.g. test completion or goal attainment). The composite measure was dichotomized based on whether the patient received 100 % of services that they were eligible for. The nine HEDIS measures included 3 prevention measures: breast, cervical, and colorectal cancer screening; and 6 chronic disease measures: hemoglobin A1c testing in the prior year and proportion with levels >9.0 % in diabetic patients, low-density lipoprotein cholesterol testing in the previous year and proportion with levels <100 mg/dL for patients with diabetes or coronary artery disease. The outcomes of interest were the number of visits to the ED, inpatient services and the number of 30-day readmissions during the calendar year 2012. These were assessed at the PCP level as a rate of visits/100 patients. Ranking for each physician was created based on the log-odds of achieving 100 % of the HEDIS composite measure using logistic regression models controlling for patient age, gender, ethnicity, language, insurance status, Charlson score, and visit frequency. The relationship between physician quality ranking and utilization outcomes was assessed using linear regression. Rankings were also grouped into quartiles and differences between top and bottom quartiles were assessed using a t-test or Wilcoxon Mann-Whitney test.
RESULTS: Of the 173 PCPs eligible for analysis, 55 % were female, and their mean age was 48. We excluded physicians who were in practice for less than 1 year and those who left during the year of analysis. The percent of eligible patients in a PCP’s panel who achieved 100 % of eligible HEDIS measures was 68 % (IQR: 63.6–74.2 %). High physician ranking was predictive of lower ED utilization (p < 0.0001), admissions (p = 0.0001) and 30-day readmissions (p = 0.009). When comparing physicians in the top and bottom quartiles of quality ranking, physicians in the top quartile had significantly lower ED utilization rates (13.1 vs 21.1, p < 0.0001). Physicians in the top quartile also had significantly lower admission rates than physicians in the bottom quartile (7.3 vs 9.8, p = 0.007). There was no significant difference in 30-day readmission rates between top and bottom quartile physicians.
CONCLUSIONS: Among primary care physicians within a large, academic network, we found that physicians with higher performance based on a composite of nine quality of care measures was associated with lower ED utilization, admission rates, and 30-day readmission rates. In addition to access to primary care and having a usual source of care, our study suggests that the patients cared for by PCPs with better performance on quality metrics may have lower rates of ED and hospital utilization. Whether patients of such PCPs also have lower health care costs requires further study.
DO RESIDENT-RN ROUNDS REDUCE CALLS TO THE ONCALL PERSON? (D. R. R. R. O. P.): A QUALITY IMPROVEMENT PROJECT IN THE ICUMaria Yballe1,2; Sehrish Memon1,2; Sandra Kurup1,2; Gen Bahrt1; Jeana Reyes1; Michael P. Carson1,2. 1Jersey Shore University Medical Center, Neptune, NJ; 2Rutgers - Robert Wood Johnson Medical School, Piscataway, NJ. (Tracking ID #1913456)
BACKGROUND: On-call ICU/CCU residents receive many calls from nurses during their overnight shift regarding orders that, in theory, could have been placed by day team residents. These interrupt nursing and physician care, and could distract caregivers from more urgent matters, or contribute to sleep deprivation. The first objective was to determine the number of, and reasons for, calls from nursing to the on-call night resident. The second objective was to identify the most common reasons, modify the process so that the day team would address these orders prior to leaving, and then resample to determine if this educational intervention reduced the number of calls made to on-call residents.
METHODS: Baseline Call Rate: The ICU night resident logged and categorized calls for 20 nights to determine the baseline. Based on the common reasons for calls, we developed a laminated card listing the common issues, distributed it to the nursing and resident staff to use as a reference during end of Day-shift sign-out rounds, and oriented them to the process. Re-Evaluation Call Rate: calls were reassessed 2 weeks later for 10 nights. We coordinated with the ICU nurse manager, nurse educator, and staff nurses. T-test was used to compare the Baseline and Re-Evaluation call rates.
RESULTS: Baseline: 592 calls over 20 nights, Mean 29.6+/−8 calls/night, Range 14–46. The top seven reasons were associated with 81 % of the calls: electrolytes 35 %, medication change 15 %, ventilator change 11 %, order for routine morning labs 11 %, insulin 5 %, diet/NPO 3 %, NG-tube 3 %. Re-evaluation: There were 133 calls over 10 nights; Mean 13+/−4 calls/night (range 5–19) for an average decrease of 16 calls/night. A matched analysis of the 10 lowest nights during the Baseline period vs. the 10 during the Re-evaluation yielded a significant average decline of 10 calls/night [95 % C.I. (4,16)]. Comparing the 10 highest Baseline nights to the 10 Re-evaluation yielded an average decrease of 26 calls/night [95 % C.I. (14,37)]. Calls/night decreased as follows: Electrolytes drop of 3, medication decreased from 4 to 1, routine labs/imaging from 3 to 1.
CONCLUSIONS: A simple program educating the residents to address common orders at the end of the day shift, and nurses to remind the residents to do so, was effective and decreased calls to the night residents by 55 %. This decrease in calls regarding issues that should be addressed by the primary day team was noticed and appreciated by the night resident and nursing staff. The day shift process has been modified, and a repeat survey will be done to assess resident/nursing adherence to this modification. With continued use we anticipate a culture change will result in an additional and sustained decrease in calls for these issues.
DOES RESEARCH TRAINING DURING RESIDENCY PROMOTE SCHOLARSHIP? A CROSS-SECTIONAL ANALYSIS OF A TEN-YEAR COHORT OF THE UCSF-PRIME RESIDENCY PROGRAMMarion Stanley; Jeff Kohlwes; Bridget O’Brien; Rebecca L. Shunk; Denise M. Connor; Patricia A. Cornett; Harry Hollander. VAMC/UCSF, San Francisco, CA. (Tracking ID #1941144)
BACKGROUND: Professional organizations, including the Association of Program Directors in Internal Medicine (APDIM), the Accreditation Council for Graduate Medical Education (ACGME), the Alliance for Academic Internal Medicine Education Redesign Task Force as well as the Carnegie study on medical education call for individualized training approaches to ensure that residents have sufficient experience with the various roles of physicians to make informed career choices. In 2000, the Primary Medical Education (PRIME) track of the University of California, San Francisco (UCSF) categorical residency program implemented a novel clinical outcomes research immersion curriculum to enable residents to experience a research career during residency. In PRIME, residents receive a research training course, mentoring and protected time to complete a project in their area of interest. We examined whether implementation of the PRIME clinical outcomes research track led to increased resident publications, improved mentoring and/or subsequent alumni careers in outcomes research as compared to peers at UCSF.
METHODS: We performed a cross sectional analysis of an email survey of internal medicine residency alumni from the UCSF categorical residency program who graduated from 2001 to 2010. We used Pearson Chi-Square analysis and ANOVA to compare PRIME and non-PRIME alumni on categorical and continuous variables.
RESULTS: From 2001 to 2010, 316 categorical residents became alumni. 211/316 (66 %) responded to the survey. A significantly higher percentage of PRIME alumni published research projects they worked on during residency compared to non-PRIME alumni (64 % vs. 40 %; p = 0.002). A non-significant trend showed PRIME alumni identifying clinical or translational research as their primary career role (35 % of PRIME vs. 29 % non-PRIME) and spending a higher percentage of their professional time conducting research compared to non-PRIME alumni (26 % for PRIME, 21 % for non-PRIME). Process measures that could explain these findings include adequate access to mentors (mean 4.4 for PRIME vs. 3.6 for non-PRIME alumni (p < .001)) on a 5 point Likert scale (strongly disagree to strongly agree) and agreeing that mentoring relationships affected career choice (mean 4.2 for PRIME vs. 3.7 for categorical alumni (p = 0.001)). Finally, 63 % of PRIME alumni agreed that their research experience during residency influenced their subsequent career choice versus 46 % amongst the non-PRIME alumni.
CONCLUSIONS: Our results support that giving residents an opportunity to try out a career in outcomes research during residency enables them to publish their residency-related research more frequently than those who did not have this opportunity. This experience significantly influenced subsequent career choice and may make housestaff more likely to continue doing outcomes research after residency. Implications: Implementation of individualized residency programs tracks that nurture academic interests along with clinical skills will foster important alternative careers within medicine for the graduates who experience them.
EARLY OUTPATIENT FOLLOW-UP AFTER STROKE REDUCES NEIGHBORHOOD SOCIOECONOMIC DISPARITIES IN MORTALITYArleen F. Brown1; Li-Jung Liang1; Stefanie D. Vassar1; Sharon S. Merkin2; Jose J. Escarce1; Bruce Ovbiagele3; W. T. Longstreth4. 1UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA; 3Medical University of South Carolina, Charleston, SC; 4University of Washington, Seattle, WA. (Tracking ID #1939240)
BACKGROUND: Older adults who reside in disadvantaged communities have higher mortality after stroke. We examined whether the timing of post-stroke outpatient visits contributed to previously observed neighborhood disparities in post-stroke mortality.
METHODS: We used data from the Cardiovascular Health Study, a population-based, longitudinal study of adults ≥65 years. Center for Medicare and Medicaid Services (CMS) data were used to obtain the number and dates of outpatient visits and pre-stroke comorbidity. Eligible participants had an incident stroke during the study period, survived through the visit interval (7, 14, 21, or 28 days), were matched to CMS records, and had fee-for-service coverage during the follow up period. Neighborhood socioeconomic status (NSES) was a composite of six census variables (median household income; median value of housing units; % of households with interest, dividend, or rental income; % of residents >25 years with a high school education; % of residents >25 years with a college degree; and % of residents in executive, managerial, or professional specialty occupations). To examine the associations between time to first post-stroke outpatient visit, NSES, and the dependent variable of mortality at 1 year post-stroke, we constructed multilevel Cox proportional hazard models that also included age, sex, race, stroke type, comorbidity score, and an interaction term between time to first visit and NSES. Separate models were constructed for each visit interval.
RESULTS: Among the 495 eligible participants (mean follow up 11.5 years), 17.4 % had an outpatient visit within 7 days, 27.9 % within 14 days, 36.3 % within 21 days, and 43.6 % within 28 days. In adjusted models, the mortality hazard at 1 year after stroke was lower among participants without, compared to those with, an outpatient visit within 7 days (HR = 0.42; 95 % CI = 0.23, 0.79), 14 days (HR = 0.53; 95 % CI = 0.32, 0.85), 21 days (HR = 0.52; 95 % CI = 0.32, 0.83), and 28 days (HR = 0.59; 95 % CI = 0.36, 0.95). NSES was associated with mortality only for models of outpatient visits within 28 days. The visit x NSES interaction was not significant for any models.
CONCLUSIONS: Early follow up after stroke, specifically a visit within the first 3 weeks, was associated with lower mortality at 1 year and appeared to mitigate the association between lower NSES and stroke mortality. For those with later follow up, lower NSES remained independently associated with mortality. Early and appropriate clinical care may play an important role in reducing neighborhood socioeconomic disparities in stroke mortality. These findings suggest a role for community-level interventions to support secondary prevention after stroke.
EARLY PALLIATIVE CARE CONSULTATION IS ASSOCIATED WITH IMPROVED SUPPORTIVE CARE CANCER QUALITY FOR VETERANSAnne M. Walling2,1; Diana Tisnado2; Susan Ettner1; Steven Asch4; Sydney M. Dy5; Philip Pantoja2; Martin Lee2; Sangeeta Ahluwalia3; Hannah C. Schreibeis-Baum2; Karl Lorenz2. 1UCLA, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA; 3Oregon State University, Corvallis, OR; 4VA Palo Alto, Palo Alto, CA; 5Johns Hopkins University, Baltimore, MD. (Tracking ID #1936329)
BACKGROUND: A growing evidence base suggests that palliative care improves outcomes for patients with life-limiting illness including quality of life and bereaved family members satisfaction with end of life care. Less is known about the processes of care influenced by palliative care that lead to these outcomes in real-world settings. We hypothesized that palliative care consultation is associated with improvement in specific processes of supportive care as measured by the Assessing Symptoms Side Effects and Indicators of Supportive Treatment (ASSIST) quality measures.
METHODS: We studied patterns of non-hospice palliative care consultation and the quality of supportive care using ASSIST process of care measures in a retrospective cohort of 719 patients diagnosed with advanced cancer in 2008 over the period of 3 years or until death who received care in the Veterans Affairs Health System (VA) using rigorous chart abstraction methods (inter-rater agreement >90 %). We also studied the association of palliative care consultation and quality of supportive care overall and by domain (information and care planning, pain, non-pain symptoms) using a multivariate regression model. Our main predictor variable was the proportion of time (from diagnosis of metastatic disease to death or end of study) a patient with advanced cancer was exposed to palliative care (range 0–1). Our main outcome variable was a patient-level overall quality score calculated with the scores of 40 process quality measures. To take into account that different patients are eligible for different quality indicators with varying pass-rates, we used an observed minus expected score. Using this methodology, a patient’s observed score is weighed against an average hypothetical patient who was eligible for the same quality indicator pattern. We conducted standard OLS regression controlling for variables pre-specified as important in our conceptual model of quality palliative care. To address the potential for treatment selection, we also conducted a sensitivity analysis using doubly robust propensity score methods and found similar results.
RESULTS: Of 719 patients, all but 54 patients died before the end of the study period and 293 received a palliative care consult at least once during the study period. On average, patients who had involvement of palliative care received their first palliative care consult towards the second half of their disease trajectory between diagnosis and death or end of study. Controlling for other variables, patients who receive a palliative care consult at time of diagnosis receive 7 % higher quality overall (P < 0.001) and 11 % higher quality (p < 0.001) within the information and care planning domain compared to patients who do not receive a consult, with non-significant improvements within the pain and non-pain domains.
CONCLUSIONS: Earlier palliative care leads to a higher process of care quality score in lung, colorectal, and pancreatic cancer, predominantly driven by improvements in the domain of information and care planning. This study supports the effectiveness of early palliative care in three common advanced cancers within the VA.
EARLY WINNERS AND LOSERS IN DIALYSIS CENTER PAY-FOR-PERFORMANCEMilda R. Saunders1; Marshall Chin2. 1University of Chicago, Chicago, IL; 2University of Chicago, Chicago, IL. (Tracking ID #1938490)
BACKGROUND: In 2012, the Centers for Medicare and Medicaid Services (CMS) began the End Stage Renal Disease Quality Incentive Plan (ESRD QIP), a pay-for-performance program for dialysis facilities. Examination of QIP may be instructive as a case-study of the ability of financial incentives both to improve quality and impact disparities. Here we examine the impact of ESRD QIP for dialysis facilities overall, by facility characteristics, neighborhood demographics and region. We also examine how ESRD QIP had its impact by examining changes in its three clinical performance measures over time.
METHODS: Our data sources were the 2012 CMS ESRD QIP Facility Performance File, which contained total performance scores (TPS)—range 1–30—for most CMS certified facilities (n = 5005) in the US, linked to US Census data by zip code. Each facility’s TPS is based on weighted clinical performance measures for dialysis adequacy (urea reduction rate >65) and hemoglobin outside of the targeted range (% of patients with hemoglobin (Hgb)<10 g/dL and % patients with Hgb > 12 g/dL). Per QIP, facilities with a TPS less than 26 (of 30) will have their payments reduced on a sliding scale, ranging from 0.5 to 2 %. We dichotomized the outcomes as ‘any payment reduction’ versus ‘no payment reduction’, and ‘large payment reduction’ (>1.5 %) versus ‘other’ (<1.5 %). We used logistic regression to characterize associations between QIP performance and dialysis facility characteristics, neighborhood demographics, and region. To determine how the QIP impacts facility outcomes, we used linear regression to examine changes in dialysis facility outcomes between 2007 and 2010.
RESULTS: Only 30 % of facilities will have any payment reduction in 2012. In multivariable analysis, dialysis facilities with any payment reductions were more likely to have more dialysis stations (OR 1.02 per station, 95 % CI 1.01, 1.03), longer operation (OR 1.03 per year, 95 % CI 1.02, 1.04) and a greater proportion of African-Americans in the neighborhood (lowest versus highest quartile, OR 1.34, 95 % CI 1.08,1.65) Only a small proportion of facilities (8 %) had a large payment reduction, >1.5 %. Facilities with large payment reductions were less likely to be for-profit (OR 0.69, 95 % CI 0.53, 0.89) and less likely to be in the South and West (OR 0.65, 95 % CI 0.50, 0.85 and OR 0.40, 95 % CI 0.27, 0.59, respectively compared to facilities in the Midwest). Decline in the percentage of patients with a hemoglobin >12 g/dL was largely responsible for improvement in clinical outcomes between 2007 and 2010. For-profit status and increasing proportion of African-Americans in the neighborhood were associated with greater reduction in percentage of patients with hemoglobin above the targeted range (>12 g/dL).
CONCLUSIONS: In the first year of CMS pay-for-performance, a large proportion of dialysis facilities met or exceeded national standards and received no payment reduction. Facilities in African-American communities were more likely to receive a payment reduction despite large improvements in hemoglobin within the targeted range. As the number of outcomes increase and total performance thresholds rise, the quality chasm may widen.
ECONSULTS: CONTENT ANALYSIS OF PCP QUESTIONS, SPECIALIST ADVICE, AND PCP RESPONSESKatherine Wrenn; Nathaniel Gleason; Sereina Catschegn; Marisa Cruz; Ralph Gonzales. University of California, San Francisco, San Francisco, CA. (Tracking ID #1938360)
BACKGROUND: Electronic consults (eConsults) have been proposed as one strategy to help address the excess demand for specialty care, but little is known about the specific types of clinical questions primary care providers (PCPs) are asking through an eConsult program, and how they respond to specialist recommendations. An eConsult service was implemented at the University of California, San Francisco (UCSF) in 2012, in which PCPs can initiate an asynchronous exchange of information with a specialist, posing a clinical question and receiving a response within 3 days, without the need for in-person consultation. The objectives of this study were to describe the types of clinical questions PCPs are asking in eConsults, describe the types of advice specialists are providing, and explore to what extent PCPs implement specialist recommendations.
METHODS: We conducted this study at UCSF, a multi-site academic medical center that includes eight adult primary care practice sites and uses a shared electronic health record (EHR). The following medicine subspecialties participated in the first phase of the eConsult program: Cardiology, Endocrinology, Gastroenterology/Hepatology, Pulmonary Medicine, Rheumatology, and Nephrology. We analyzed the narratives of 98 of the first 158 eConsults completed during the first 2 months of the program. We categorized each eConsult into the following types of questions and responses: “Diagnosis,” “Treatment,” and/or “Monitoring.” The principal investigator (KW) reviewed all 98 eConsults. A second independent reviewer (MC) coded 15 eConsults and specialist responses using coding instructions created by the first reviewer, to check for inter-rater reliability. Kappa statistics ranged between 0.60 (PCP “Diagnosis”) and 1.0 (PCP “Monitoring” and Specialist “Monitoring” categories). Chart abstraction was performed to determine what proportion of specialists’ recommendations PCPs implemented over the 6 months following completion of the eConsult. We report the results of abstractions from the first 50 eConsults.
RESULTS: In our study sample, PCPs asked questions related to diagnosis in 68.4 % of cases, treatment in 49.0 % of cases, and monitoring in 22.4 % of cases. Among specialist responses, 74.5 % related to diagnosis, 66.3 % to treatment, and 36.7 % to monitoring. The types of questions asked by PCPs varied based on the specialty they were consulting. Diagnosis-related questions were dominant (≥80 %) for Cardiology, Nephrology, Pulmonary Medicine, and Rheumatology, whereas treatment-related questions were dominant (>70 %) for Endocrinology. The majority of eConsults included only one type of question posed by the PCP, whereas specialist responses often provided additional recommendations pertaining to more than one category of response (Figure 1). Based on chart review, we found that PCPs ordered 76.5 % of all recommended laboratory tests, 92.3 % of recommended imaging tests or procedures, 66.7 % of recommended new medications, and 85.7 % of recommended medication changes. 24.0 % of eConsult patients had a visit with the specialist during the 6-month period following the eConsult, 4.0 % had an unrelated emergency department (ED) visit, and 8.0 % had a hospitalization, of which 75.0 % were unrelated to the condition in the eConsult.
CONCLUSIONS: We find that eConsults include clinical questions across the spectrum of patient care: diagnosis, treatment, and monitoring of multiple different medical conditions. We also find that PCPs implement specialists’ recommendations in the large majority of cases, and very few patients subsequently require specialty care or ED visits related to the reason for eConsult.
Figure 1. Content of eConsult Questions and Responses.
ED VISITS AFTER MEDICAL HOME IMPLEMENTATION IN VA PRIMARY CARE CLINICSKristina M. Cordasco2; Jean Yoon1; Adam Chow1; Lisa V. Rubenstein2. 1Palo Alto VA, Menlo Park, CA; 2Greater Los Angeles VA, Los Angeles, CA. (Tracking ID #1940650)
BACKGROUND: Implementation of the VA medical home model aimed, in part, to reduce unnecessary acute care by emphasizing access and continuity within primary care-based teams. We assessed for change in number of ED visits, by different varying types of ED visits, after medical home implementation began in the VA system, and we examined the relationships between primary care clinic-level measures of access and continuity and number of ED visits per patient.
METHODS: We obtained a cohort of 75,532 patients using VA care from fiscal years 2010–2012 in 23 clinics based in three VA medical centers. Patient information on demographics, chronic conditions, and VA ED visits were obtained from outpatient and inpatient files and linked to clinic administrative data over the 3-year period. ED visits were categorized, by discharge diagnosis, into non-emergent, primary care treatable, ED care needed but preventable, ED care needed and not preventable, and mental health-related visits, based on the NYU algorithm. We also obtained annual primary care clinic measures of access (percent of patients receiving primary care within 1 day of requested date, waiting time to third next available appointment) and continuity (percent of visits with primary care provider). We compared mean number of ED visits per patient by year and by clinic access and continuity. We conducted multivariable regressions of number of ED visits per patient adjusting for patient and clinic factors with patient random effects using Poisson regression models for each ED visit type.
RESULTS: Although mean clinic measures of access and continuity improved over the 3-year period, ED visits of any categorization increased from 0.55 per patient in 2010 to 0.58 per patient in 2012 among the study cohort (all P < 0.001). In multivariable regressions, clinic measures of higher access predicted significantly fewer ED visits that were both emergent and non-emergent (all P < 0.001) as well as ED visits for psychiatric diagnoses, but was not related to number of ED visits for alcohol and drug use diagnoses. Better clinic continuity predicted fewer ED visits that were non-emergent (P = 0.001) or ED care needed but preventable (P < 0.001), but was not significantly related to mean number of ED visits for any mental health diagnoses.
CONCLUSIONS: Implementation of VA’s medical home was not associated with an overall lower ED visit rate in a primary care cohort although access and continuity measures were reported to be slightly higher by primary care clinics from 2010 to 2012. In adjusted analyses access measures consistently predicted fewer ED visits across types of visits although access did not impact ED visits for substance use diagnoses or for any mental health diagnoses. Clinic continuity was related to fewer ED visits for certain types of ED care but was not related to ED visits for any mental health diagnoses.
EFFECT OF ELECTRONIC HEALTH RECORD IMPLEMENTATION ON INPATIENT WORK PROCESSES OF INTERNAL MEDICINE RESIDENTSMarianne Zachariah1,2; Erin L. Duffy1,2; Michael A. Pfeffer1; Douglas Bell1,2. 1UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA. (Tracking ID #1939481)
BACKGROUND: Electronic health records (EHRs) are rapidly gaining adoption in the U.S. If EHRs increase the time that providers need to spend on documentation and ordering, this might reduce the time available for patient interactions and learning activities. We sought to compare how residents spend their time on inpatient rotations before and after the implementation of a commercial EHR.
METHODS: We shadowed a total of 30 internal medicine residents to observe their usage of time on inpatient general medicine, medical intensive care unit, and coronary care unit rotations, before and after UCLA’s March, 2013 launch of the Epic EHR system. Prior to Epic, most clinical documentation was performed using a home-grown computer system and orders were written on paper. After the launch, nearly all documentation and orders were required to be entered in Epic. Fourteen subjects were shadowed prior to the Epic launch and 27 were shadowed in the period from 30 to120 days after the launch (11 were shadowed both periods). Residents were shadowed only on days when they were not covering another team member or taking morning holdover admissions. Shadowing was performed by trained undergraduate students who recorded the tasks that each resident was conducting each minute between the hours of 7 am and 5 pm. For analysis, certain tasks were grouped together: Write Orders (on paper before Epic, in Epic or on paper afterward); Clinical Documentation (writing admit, discharge and progress notes plus viewing labs, vitals and other patient data); Patient Interaction (time in patient rooms plus hallway conversations with patient or family). Wilcoxon Rank-Sum tests were used to compare time spent on specified task categories.
RESULTS: After Epic implementation, residents spent more time on order writing but not on clinical documentation. The median time spent with patients was 23 % lower after Epic implementation but the difference was not statistically significant. Among residents on general medicine, 6 of 11 (55 %) attended noon conference before Epic vs. 5 of 19 (26 %) afterward, and those who attended spent less time post-Epic (average 51 vs. 26 min.). The median times spent receiving and giving didactic teaching were also lower post-Epic, although the difference was statistically significant only for giving didactic teaching. Time spent in social conversation was higher in the post-Epic period. Median times spent in conversation with nurses and other physicians were also higher post-Epic but the differences weren’t statistically significant. The median time spent in conversation with students was lower post-Epic. Among residents who spent any time talking with a student (12 vs. 13), the average time spent was also lower post-Epic (29.9 vs. 19.5 min.).
CONCLUSIONS: After EHR implementation, residents spent more time writing orders and less on teaching activities, with additional trends toward less time with patients and more time in conversations. However, the residents were observed after only 1–4 months of experience with the system, so these results might not represent their longer-term performance.
Median (IQR) Minutes Spent Before/ After EHR Implementation
| Task Category | Pre N = 14 | Post N = 27 | P-value |
| Write Orders | 18.87 (8.92) | 30.70 (10.25) | 0.001 |
| Clinical Documentation | 109.33 (55.04) | 109.02 (46.53) | 0.946 |
| Patient Interaction | 74.70 (33.08) | 57.17 (33.59) | 0.128 |
| Didactic Receiving | 17.58 (27.08) | 8.50 (21.00) | 0.504 |
| Didactic Giving | 6.04 (13.50) | 1.50 (4.00) | 0.023 |
| Student Conversation | 25.62 (22.63) | 0.00 (12.08) | 0.004 |
| Physician Conversation | 69.72 (84.29) | 82.22 (46.92) | 0.614 |
| Nurse/Staff Conversation | 4.73 (3.33) | 10.54 (24.36) | 0.407 |
| Social | 11.79 (22.88) | 27.83 (30.02) | 0.032 |
EFFECT OF FINANCIAL INCENTIVE FOR COLORECTAL CANCER SCREENING ADHERENCE ON APPROPRIATENESS OF COLONOSCOPY ORDERSThomas B. Morland1; Marie Synnestvedt2; Steven Honeywell2; Feifei Yang2; Katrina Armstrong3; Carmen E. Guerra2. 1Geisinger Medical Center, Danville, PA; 2Hospital of the University of Pennsylvania, Philadelphia, PA; 3Massachusetts General Hospital, Boston, MA. (Tracking ID #1935049)
BACKGROUND: There is some evidence that financial incentives may help physicians achieve higher rates of preventive health screenings among their patients. However, it is unclear whether these incentives affect the appropriateness of screening tests physicians order. In July of 2010 the University of Pennsylvania Health System implemented a performance incentive for general internists based upon achieving target screening adherence rates for several cancers, including colorectal cancer (CRC). Providers were eligible for $1,000 for achieving a 50 % adherence rate and an additional $2,000 for achieving an 80 % adherence rate for all applicable tests. The primary objective of our study was to determine whether implementation of the performance incentive was associated with an increase in potentially inappropriate screening colonoscopy orders for patients with life expectancies <4 years. We also assessed whether providers with high rates of CRC screening adherence had a higher proportion of colonoscopy orders for patients with life expectancies <4 years vs. providers with low rates of screening adherence.
METHODS: Electronic records of visits with participating providers were queried for screening colonoscopy orders during the last year prior to the incentive program (pre-intervention period) and the first year of the incentive program (post-intervention period). Using a previously validated mortality prediction model, orders were classified as “inappropriate” if patients’ 4-year expected mortalities were >50 %. A chi-square test was conducted to compare the proportion of orders that were “inappropriate” during the pre-intervention period vs. the post-intervention period. A t-test was also performed comparing the mean risk scores of patients receiving colonoscopy orders during the pre-intervention period vs. the post-intervention period. Logistic and linear regressions were also performed, controlling for age, race, marital status, and gender. In a second analysis, we compared the proportion of “inappropriate” orders for providers with the highest and lowest proportion of screening colonoscopy orders (defined as the top 20 % and bottom 20 %), respectively.
RESULTS: The study population included screening colonoscopy orders for 1057 patients in the pre-intervention period and 1021 patients in the post-intervention period across 23 providers participating in the financial incentive. Patients were on average 58.03 years of age and 61 % were female. Only 0.6 % (n = 6/1057) of screening colonoscopy orders in the pre-intervention period and 0.6 % (n = 6/1021) of screening colonoscopy orders in the post-intervention period were deemed “inappropriate.” There was no significant difference in the mean risk scores or the proportions of “inappropriate” orders between the pre- and post-intervention periods. Linear regression found no effect of time period upon risk score. There was no significant difference between the proportions of orders that were “inappropriate” among orders by high rate providers vs. low rate providers.
CONCLUSIONS: We found no evidence that a performance incentive based upon colonoscopy adherence rate led to a significant increase in inappropriate orders for screening colonoscopies. Our model is limited in that it only identifies orders that are inappropriate due to patients’ age, functional status, smoking, body mass index, and multiple comorbidities.
EFFECT OF THERAPEUTIC SUBSTITUTION ON MEDICATION RECONCILIATION AT HOSPITAL DISCHARGEJessica S. Wang1; Boback Ziaeian2,3; Osama Abdelghany4; Robert L. Fogerty5,6; Grace Jenq7; Sandhya V. Kanade6; Leora I. Horwitz5,8. 1Yale University School of Medicine, New Haven, CT; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Jonathan and Karin Fielding School of Public Health at UCLA, Los Angeles, CA; 4Yale-New Haven Hospital, New Haven, CT; 5Yale University School of Medicine, New Haven, CT; 6Yale-New Haven Hospital, New Haven, CT; 7Yale University School of Medicine, New Haven, CT; 8Yale-New Haven Hospital, New Haven, CT. (Tracking ID #1927862)
BACKGROUND: Although therapeutic substitution, or the substitution of a chemically different but therapeutically equivalent drug for the one originally prescribed, is widely used by hospitals to control inpatient pharmaceutical costs through hospital formularies, the impact of this practice on patients’ discharge medication regimens has not been adequately studied. We determined the frequency at which inpatient therapeutic substitution led to changes in discharge medications and assessed the extent to which it contributed to medication reconciliation errors.
METHODS: We analyzed data from the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges (DISCHARGE) study, a prospective, observational cohort study of patients 65 years or older admitted to a tertiary care hospital for acute coronary syndrome, heart failure, or pneumonia between May 2009 and April 2010 who were discharged home. We examined patients’ medications from six commonly substituted drug classes: proton pump inhibitors, H2 blockers, HMG-CoA reductase inhibitors, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and inhaled corticosteroids. The occurrence of therapeutic substitution was determined by comparing admission to inpatient medication lists. Medications that were changed to a different drug within the same class at discharge were noted by comparing admission to discharge medication lists. Any medication reconciliation changes at discharge that did not appear intentional based on review of the medical record were classified as suspected errors. We calculated the relative risk of a home medication being switched to a different drug within the same class at discharge among medications that were therapeutically substituted during the hospital stay compared to those that were not. We also calculated the relative risk of a medication reconciliation error between these two groups.
RESULTS: A total of 377 patients enrolled in the DISCHARGE study, collectively taking 2,583 admission medications. We analyzed the 555 (21.5 %) admission medications taken by 303 of the patients (80.4 %) that were within the six drug classes of interest. Of these, 244 (44.0 %) were therapeutically substituted during the hospitalization while the remaining medications were continued unchanged or were held for the duration of the hospital stay. Twenty-eight of the two hundred forty-four therapeutically substituted medications (11.5 %), as compared to 8 of the 311 non-therapeutically substituted drugs (2.6 %), were changed at discharge to a different medication within the same drug class as the patient’s original home medication (relative risk (RR) 4.46, 95 % confidence interval (CI) 2.07–9.61). A total of 41 (7.4 %) of the 555 medications of interest had a suspected medication reconciliation error at discharge. 28 (68.3 %) of these were medications that were therapeutically substituted while inpatient. Suspected medication reconciliation errors were more likely to occur among medications that had been therapeutically substituted than those that had not been (RR 2.75, 95 % CI 1.45–5.19).
CONCLUSIONS: Therapeutic substitution during hospitalization was associated with a significantly higher rate of suspected medication reconciliation errors at discharge as well as a considerable increase in changes to medication type at discharge. This creates a risk for patient misunderstanding and adverse drug events. In light of these findings, the widespread practice of therapeutic substitution may warrant reevaluation.
EFFECTIVENESS OF A BRIEF PEER SUPPORT INTERVENTION FOR VETERANS WITH CHRONIC PAINMarianne S. Matthias; Alan B. McGuire; Marina Kukla; Joanne Daggy; Laura J. Myers; Matthew J. Bair. Roudebush VAMC, Indianapolis, IN. (Tracking ID #1932711)
BACKGROUND: Chronic pain is prevalent, disabling, and costly. Pain reduces quality of life and is associated with emotional distress when it interferes with work, social and recreational activities, and family life. This pilot study tested a peer support program, involving peer delivery of pain self-management strategies, for veterans with chronic pain.
METHODS: This was a pre-test/post-test design with a 4-month intervention period. Measures were administered at baseline and at 4 months. Ten peer coaches and 20 patients were recruited. All had chronic musculoskeletal pain. Peer coaches had participated in a prior chronic pain study involving pain self-management. Patients were recruited from a VA medical center and had at least moderate pain severity, defined by pain ≥5 on a 0 (no pain) to 10 (worst pain imaginable) scale. After a 3-hour training session, peer coaches were each assigned two patients. Coaches and patients were matched on age and pain location to the extent possible and were instructed to meet face-to-face or via phone biweekly for 4 months. Coaches and patients were given a study manual that included sections on chronic pain basics, activity pacing, relaxation skills, and self-care skills. Peer coaches were encouraged to discuss different topics, guided by the manual, at each meeting, as well as to work on goal setting and provide support, motivation, and encouragement as appropriate. Coaches participated in regular supervision calls, which reinforced training, taught additional motivational strategies, and provided a forum to discuss questions or concerns. Pain was the primary outcome and was assessed with the PEG, a 3-item version of the Brief Pain Inventory, and the PROMIS Pain Interference Questionnaire. The following secondary outcomes were assessed: depression (PHQ-9), anxiety (GAD-7), self-efficacy (Arthritis Self-Efficacy Scale), patient activation (PAM), perceived social support (Multi-Dimensional Perceived Social Support Scale), and two measures of negative pain cognitions: pain catastrophizing (Pain Catastrophizing Scale), and pain centrality (Centrality of Pain Scale). A linear mixed model with a random effect for peer coaches was applied to the change scores (post - pre measures). This accounts for the intra-class correlation (patients nested within peer coaches). Outcomes are reported for patients only.
RESULTS: Nine peer coaches and 17 patients completed the study. All were male veterans. Patients’ ages ranged from 35 to 66 (M = 58, SD = 8) years. Peer coaches’ ages ranged from 50 to 71 (M = 60, SD = 7) years. Patients’ pain conditions were as follows: low back (n = 8), neck (6), knees (1), shoulders (1), “everywhere” (1). Patients’ pain improved but did not reach statistical significance (p = .33, ICC = .28, Cohen’s d = −.25 for PEG; p = .17, d = −.35 for PROMIS). Depression showed little improvement (p = .47, d = −.17). Anxiety (p = .11, d = −.36), self-efficacy (p = .16, ICC = .56, d = .60), patient activation (p = .12, ICC = .40, d = .49), perceived social support (p = .11, d = .37), pain catastrophizing (p = .12, d = −.42), and centrality of pain (p = .06, ICC = .32, d = −.62) all improved.
CONCLUSIONS: This study suggests that peers can effectively deliver pain self-management strategies and support to other veterans with pain. Although this was a pilot study with a relatively short intervention period, patients showed improvement in several outcomes. In particular, effect sizes were moderate for improved self-efficacy, patient activation, and pain centrality. Although pain did not significantly improve, there was a modest change in the expected direction, suggesting that a longer intervention, which allows patients more time to adopt and benefit from the self-management strategies learned, may result in a larger effect on pain, as well as greater effects on psychosocial outcomes.
EFFECTIVENESS OF A HEART FAILURE EDUCATION INTERVENTION IN A LOW LITERACY PATIENT POPULATIONShing-Yu Lin; Lori Randall; Mary E. Wiles; Yoo Mee Shin; Michelle Edwards; Diane Wirth; Nurcan Ilksoy; Robin Klein. Emory University, Atlanta, GA. (Tracking ID #1923870)
BACKGROUND: High disease burden and low literacy among patients can make educational interventions important and challenging. The objective was to evaluate the effectiveness of a heart failure education intervention in a low literacy patient population.
METHODS: We conducted a prospective study to evaluate the effectiveness of a heart failure education intervention in a low literacy patient population. Patients completed a pretest prior to the education while inpatient and a subsequent posttest at follow-up clinic visit 1 to 2 weeks later. We included all adult inpatients with new or worsening heart failure newly referred to the Grady Heart Failure Program from November 2012 to April 2013. Outcomes included self-reported education level and employment status, knowledge of and confidence with heart failure self-management, and 30-day and 6 month readmissions.
RESULTS: Fifty-one patients agreed to participate and complete data including pretest and posttest was available for 34 patients. Heart failure education led to a significant increase in patients’ mean knowledge scores (77.6 % to 82.8 %, p = 0.04). Knowledge scores did not correlate with employment status or education level. Confidence scores increased significantly with the educational intervention. Highly confident patients had significantly higher knowledge scores than less confident patients on the pretest and posttest (p = 0.04 and p = 0.01 respectively). There was no significant difference in knowledge or confidence scores between patients readmitted within 30 days or 6 months of discharge and those not readmitted. There was an overall decrease in heart failure readmissions after the implementation of the heart failure program, including the education program.
CONCLUSIONS: Educational intervention geared towards a low literacy population is effective in improving patients’ knowledge of and confidence with managing heart failure. This suggests there is benefit to expanding education programs in patient populations with low literacy and high disease burden.
EFFECTIVENESS OF TARGETED PHONE CALLS TO REDUCE NO-SHOWS IN A HOSPITAL-BASED PRIMARY CARE CLINIC: A RANDOMIZED CONTROLLED TRIALSachin J. Shah1; Clemens S. Hong1; Patrick R. Cronin2; Benjamin I. Bearnot1; Calvin A. Richardson3; Blair W. Fosburgh1; Alexandra Kimball4. 1Massachusetts General Hospital, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Boston, MA; 4Massachusetts General Hospital, Boston, MA. (Tracking ID #1934774)
BACKGROUND: “No-shows”, or missed outpatient appointments, fragment continuity of care, effectively decrease access to primary care for all patients within the practice, and decrease productivity for primary care clinicians. Patient Service Coordinators (PSCs) are the first contact for patients with the office both in person and via phone or electronic communication. They schedule appointments, facilitate referrals, and perform outreach for patients overdue for appointments or screening tests and may be important sources of contact in preventing no-shows. We aimed to assess the effectiveness of a targeted phone call to a population predicted to be at high risk of “no-shows.”
METHODS: We conducted a randomized controlled trial to reduce no-shows at the Internal Medicine Associates (IMA), a large, academic, hospital-based primary care practice staffed by 89 residents and 131 attending physicians. Approximately 320 patients visit the IMA daily. We included all patients older than 18 years old predicted to be at high risk to no-show for an appointment scheduled between April and October 2013. We estimated risk that a patient would no-show using a predictive model that included age, insurance status, prior history of no-shows, appointment type and wait days (days between the scheduling and appointment date) as predictors. We randomized high-risk patients (defined as those with >15 % absolute risk) to usual practice (control) or usual practice plus a phone call from a PSC (intervention) using their medical record number. To encourage patients to arrive for appointments, routine practice for the IMA is to mail a letter 2–6 weeks prior to the appointment and make an automated phone call 3 days prior to the appointment. Patients randomized to the intervention appeared in the queue of an online calling tool 7 days prior to their appointment. PSCs completed calls in the queue daily and recorded outcomes of the call in the online calling tool. Patients would remain in the calling queue until the call was recorded as complete or until the date of their appointment passed. We trained PSC, over 4 weeks, to use the web-based calling tool in both group sessions and one-on-one sessions. PSCs also underwent a brief training in a conversational technique designed to engage patients in concrete planning. We instructed PSCs to remind the patient of the appointment, ask if they will make the appointment and problem solve any barriers that would prevent them from making the appointment. We compared our main outcomes: 1) no-show rate 2) percentage of cancelled appointments slots in which another patient was seen using chi-square test. We performed analyses on an intention-to-treat basis.
RESULTS: We randomized 4055 high-risk patients into intervention (n = 2117) and usual practice (n = 1938) groups. PSC completed 1622 of the 2117 (76.6 %) assigned calls prior to patients’ appointments. In the intervention arm 325 (15.4 %) of 2117 patients no-showed for their appointment, and in the control arm 395 (20.4 %) of 1938 patients no-showed for their appointment (RR 0.75; 95 % CI 0.66–0.86; p < 0.001). The percent of canceled appointment slots in which another patient was scheduled and seen, was no different between the intervention and control groups (24.4 % vs 22.6 %, respectively; RR 1.08; 95 % CI, 0.87–1.33; p = 0.48).
CONCLUSIONS: A targeted program of phone calls from a patient service coordinator designed to engage the patient in concrete planning significantly reduced no-show rates among patients at high risk for no-shows. However, when appointments were canceled, the intervention did not lead to a significantly higher rate of successfully rescheduled appointments. Phone interventions designed to address barriers and reduce no-shows among patients at high-risk, may reduce no-show rates while improving continuity of care, access to primary care, and productivity for primary care clinicians.
EFFECTIVENESS OF USING NON-CLINICIANS IN DELIVERING A BRIEF SMOKING CESSATION INTERVENTION IN THE EMERGENCY DEPARTMENTEllie Grossman1; Maria I. Duenas1; Ashley Colucci2; Renee Fruchter3; Binhuan Wang3. 1New York University, New York, NY; 2New York University, New York, NY; 3New York University, New York, NY. (Tracking ID #1937034)
BACKGROUND: Tobacco remains a leading preventable cause of morbidity and mortality. Prior studies have shown that Emergency Department (ED) patients typically smoke at rates exceeding that of the general population, are interested in quitting, and often have limited access to primary care. However, a busy ED can be a difficult setting to implement preventive-health interventions. In this study, we describe a pilot initiative using non-clinician volunteers to deliver a brief smoking cessation intervention to ED patients who smoke. We focused on providing minimal counseling in the ED and instead encouraging post-visit Quitline contact for high-quality telephone counseling and delivery of cessation medication.
METHODS: We trained a cohort of college-aged volunteers to assess adult patients for use of tobacco products in the Bellevue Hospital ED and proactively refer interested smokers to the NYS Quitline. All patients were offered printed information about resources to help them quit smoking. We collected information about the number of patients approached, the number who reported using tobacco and nicotine products, and acceptance of referral to the NYS Quitline. We collected follow-up reports from the NYS Quitline and also attempted to contact all smokers at least once via phone approximately 1 month after ED visit. These follow-up reports provided information about use of smoking cessation pharmacotherapy, quit attempts, and smoking status. We performed bivariable and multivariable analyses to explore for predictors of quitline referral, successful access of quitline services, and smoking status at 1 month follow-up.
RESULTS: During the two-month intervention period in summer 2013, we screened 1619 adult patients for tobacco use. 428 (26.4 %) had smoked a cigarette in the past 30 days. Mean age was 42.6 years (SD 12.4), and 72 % were male. English (85 %) and Spanish (8 %) were the preferred languages. Other nicotine product use in the past 30 days included electronic cigarettes (8.3 %), cigars (4.6 %), and pipes (1.7 %). Among cigarette users, 40 % reported smoking <5 cigarettes/day, 32 % 5–10 cigarettes/day, 21 % 11–20 cigarettes/day, 5 % 21–30 cigarettes/day, and 3 % >30 cigarettes/day. Two-hundred fifty patients accepted a flyer with information about quit-smoking resources, and 139 (56 % of the smokers with phones) agreed to participate in the Quitline proactive outreach program. The NYS Quitline reported follow-up data for 99 patients, and of these, 25 (25 %) had completed a Quitline telephone encounter. The NYS Quitline reported that 15 (60 %) had already quit smoking, 9 (36 %) wanted to quit smoking, and 2 (8 %) were not ready to quit yet. Our program reached 78 patients for 1-month follow-up, and 25 (32 %) reported abstinence from tobacco for the previous 7 days. Forty-five patients (58 %) reported a quit attempt lasting longer than 24 h since their ED visit, and 11 (14 %) had used a smoking cessation medication. Smokers who smoked more cigarettes per day (11–20 as compared to <5) were more likely to accept quitline referral (OR 2.53, 95 % CI 1.16–5.53); there were no significant associations between age, gender, language, or e-cigarette use and acceptance of quitline referral. Non-English speakers were more likely than English speakers to successfully complete a Quitline outreach call (OR 3.07, 95%CI 1.00–9.42, p = .05). There were no significant associations between age, gender, use of e-cigarettes, or amount of cigarettes smoked and likelihood of successful contact by Quitline. At one-month follow-up, participants who reported smoking 5–20 cigarettes/day at baseline were less likely to have quit than those smoking <5 cigarettes/day (p < .05).
CONCLUSIONS: Trained volunteers are able to deliver a brief smoking cessation intervention in the ED and can feasibly refer patients to the Quitline. This brief intervention, consistent with evidence-based guidelines for tobacco dependence treatment, is acceptable to patients undergoing treatment in a busy urban safety-net hospital ED.
EFFECTS OF 2010 ACGME REGULATIONS ON INTERNAL MEDICINE RESIDENCY PROGRAMS IN THE NORTHEASTOmar Mousa; Rushikesh Shah; Samana Zaidi; Amit S. Dhamoon. SUNY - Upstate Medical University, Syracuse, NY. (Tracking ID #1939563)
BACKGROUND: To study the variables that influence the perceptions of the 2010 Accreditation Council for Graduate Medical Education (ACGME) work hour regulations (WHR) by the housestaff (HS), program directors (PD) and faculty physicians (FP) within the residency training programs of internal medicine.
METHODS: An online questionnaire was distributed among 131 residency training programs in the northeast of the US. Study subjects included the HS, PD and FP in the department of internal medicine. Questionnaires were completed anonymously. Our endpoint focused on analysis of the variables that influence how the 2010 ACGME/WHRs are perceived by HS, PD and FP. Data analysis was conducted using SPSS Statistics v19.
RESULTS: 203 internal medicine HS, PD and FP were included (158 residents, 24 FP, 11 PD). 87.2 % were of ages 20–40 years; 57.1 % Males; 41.9 % US medical graduates (US-MG). Many respondents agreed that the 2010 ACGME/WHR negatively affected the continuity of patient care (48.8 %), and had a positive impact on the residents’ quality of life while not at work (69 %). Among the different levels of training, there was a significant difference in the perceptions regarding patient care (p < 0.05), residency education (p 0.004) and continuity of care (p 0.001). Those of ages >40 years feel that residency education and the care of patients is impacted adversely (p 0.012) compared to their younger colleagues. The younger age groups (<=40 years) were more likely to feel that their programs do not strictly follow the ACGME regulations (p 0.016). However, they were more satisfied with the rules (p 0.033). Compared to international medical graduates (IMG), the US-MGs believe more that residency education (36.5 % vs 28 %) and patient care (40 % vs 30.5 %) worsened. More US-MGs believe that the continuity of care is affected (p 0.011). 58.1 % feel that the residents and interns work under pressure to leave the hospital on time due to the WHRs. Higher rates of IMGs (51.7 %) feel that residents do not work under pressure to leave the hospital on time, while 71.8 % of the US-MG feel that they do (p 0.001). Satisfaction among HS, PD and FP is significantly variable (p 0.003).
CONCLUSIONS: The 2010 ACGME WHRs were implemented to enhance patient safety by improving the quality of life of the resident. Several unintended consequences of this change, including difficulties with continuity of care, patient safety, and residency education have resulted. The perception of these changes is influenced by the age, gender, and previous medical training of the respondents to our survey. These variables should be addressed by the ACGME when future changes to the resident work hour regulations are made. Such changes have a great impact on the current clinical practice.
EFFECTS OF MINIMAL VS. INTENSIVE INTERVENTION TO ENHANCE MOTIVATIONAL INTERVIEWING IN HIV CAREMary Catherine Beach1; Michael B. Laws2; Gary S. Rose1; Debra L. Roter1; Richard D. Moore1; Geetanjali Chander1; Ira Wilson2. 1Johns Hopkins University, Baltimore, MD; 2Brown University School of Public Health, Providence, MA. (Tracking ID #1938857)
BACKGROUND: Behavior change counseling has become an essential component of primary care, but many clinicians lack the skills to counsel patients effectively. Motivational interviewing (MI), a client-centered counseling method of eliciting motivation for change, has been widely endorsed as a framework for clinicians to use in counseling patients. MI may be particularly helpful for clinicians providing HIV care, who counsel patients frequently on issues such as adherence, safe sex, and substance use treatment. As MI programs are rolled out, it is important to evaluate how to efficiently and effectively deliver MI training to busy clinicians. We conducted a randomized trial comparing the effect of two different levels of MI training on clinician communication behaviors and patient experiences.
METHODS: We enrolled 12 HIV clinicians (eight physicians, three nurse practitioners, and one physician assistant) at a single academic medical center. All clinicians attended a one-day workshop with an experienced MI trainer, focusing on behavior change counseling skills. After the workshop, we randomized clinicians to receive (or not) 3 to 5 rounds of personalized one-on-one feedback from the MI trainer, using audio-recordings of the clinician’s own visits with patients as the basis for feedback. We measured clinicians’ attitudes towards and use of MI counseling techniques at baseline and again after completion of the intervention. We also administered post-visit Healthcare Climate Questionnaires assessing patient perceptions of the degree to which the clinician adhered to the spirit of MI. Audio recordings were analyzed using the Roter Interaction Analysis System to evaluate MI-consistent communication behaviors. We compared outcome measures before and after the interventions and between the two intervention groups (workshop alone vs. workshop plus feedback). To assess whether one intervention was more effective than the other, we tested time-by-study arm interactions to determine whether one group improved more than the other. For all analyses, we used generalized estimating equations to account for clustering of patients within clinicians, with Gaussian or negative binomial distributions as appropriate.
RESULTS: Clinicians in both intervention groups reported greater use of MI-consistent behaviors after vs. before the intervention, without differences between groups in the magnitude of the effect. Patients also rated their visits as more MI consistent (6.86 vs. 6.65, p = 0.004), and audio recorded analysis revealed that visits were more patient-centered (1.34 vs. 0.96, p = 0.003), with a more positive patient affect (22.36 vs. 20.84, p < 0.001), after vs. before the intervention, without differences between intervention groups. Analysis of audio-recorded visits revealed increases in clinician behaviors such as empathic statements and asking patient permission, and reductions in disapproval, after vs. before the intervention, again without differences by intervention group. Some clinician behaviors such as asking patient opinions and the ratio of open to closed-ended questions improved to a greater extent in the workshop plus feedback vs. the workshop only intervention arm.
CONCLUSIONS: The workshop alone was as effective as the workshop plus feedback intervention in improving patient experiences and overall communication measures. Certain communication behaviors improved to a greater extent with the more intensive intervention, but these additional improvements may not be substantial enough to warrant the extra financial and logistical resources required.
EHR USABILITY BURDEN AND ITS IMPACT ON PRIMARY CARE PROVIDERS WORKFLOWZia Agha1,2; Alan Calvitti3; Shazia Ashfaq3; Neil J. Farber2; Richard L. Street4; Kristin Bell1; Lin Liu1; Mark Gabuzda1; Yunan Chen5; Barbara Gray3; Steven Rick3. 1VA San Diego Healthcare System, San Diego, CA; 2Univ. of California San Diego, San Diego, CA; 3Veterans Medical Research Foundation San Diego, San Diego, CA; 4Texas A&M, College Station, TX; 5Univ. of California Irvine, Irvine, CA. (Tracking ID #1940994)
BACKGROUND: Electronic Health Records (EHRs) often integrate poorly with clinical workflow and suffer from poor usability. In this paper, we describe how primary care clinicians’ EHR use patterns relate to usability and how these patterns suggest multiple inefficiencies and burdensome workflow for primary care providers.
METHODS: This time-motion study is based on video and EHR activity capture. We observed 21 clinicians and 111 established patients during primary care office visits at 4 Veterans Administration (VA) clinics. Data were coded for specific EHR tasks and clinical workflow. Hierarchical and sequential analysis of EHR clickstream and clinical workflow were integrated to provide objective baseline use patterns.
RESULTS: The 111 outpatient follow-up visits (~60 h of observation) were analyzed in terms of time-at-task in clinical workflow (Figure 1A). Clinicians spent 42 % of visit time with EHR tasks compared to 35 % with patients. We observed a median 158 mouse clicks per visit and for every 100 mouse clicks (Fig 1B), visit duration increases by 6 min (95 % CI = 0.05–0.07, p < 0.0001). Clinicians frequently multitask when using EHRs and navigate across multiple functions (median 19 times per visit). Notes (40 %) and Orders (27 %) were the most frequently used functions. Menu and form driven functions like Consultation (15.8 clicks/unit), imaging (14.5 clicks/unit), and medication orders (9.4 clicks/unit) required burdensome user input.
CONCLUSIONS: EHR activity consumes a majority of visit time and shifts the clinician’s focus away from the patient. EHRs also introduce multitasking, which has been associated with medical errors, clinician dissatisfaction, and missed opportunities for physician-patient communication. While some time-and-motion studies have reported little or no change in visit duration for EHR-based versus paper-based visits, we observed that higher EHR activity is associated with longer visits. These associations while not conclusive, provide partial validation of physicians’ concerns that poorly designed and implemented EHRs can lower clinical productivity. Our study highlights unintended inefficiencies introduced in clinical work due to poorly designed EHR user interfaces and emphasizes the need to address EHR usability as a key area for improvement to support meaningful use.
ELECTRONIC HEALTH RECORDS IMPROVE CLINICAL NOTE QUALITYHarry B. Burke1; Albert Hoang1; Dorothy Becher1; Paul Fontelo2; Ronald W. Gimbel1. 1Uniformed Services University of the Health Sciences, Bethesda, MD; 2National Library of Medicine, Bethesda, MD. (Tracking ID #1938123)
BACKGROUND: Electronic health records (EHR) are being adopted throughout the United States yet it is not known whether they improve the quality of clinical notes. We hypothesized that electronic health records would improve the quality of clinical notes.
METHODS: This five and one-half year blinded longitudinal, retrospective multicenter study compared the quality of handwritten and electronic outpatient clinical notes for the same cohort of 100 patients with type II diabetes mellitus at three time points: 6 months prior to the introduction of the EHR (before-EHR), 6 months after the introduction of the EHR (after-EHR), and 5 years after the introduction of the EHR (5-years-EHR). QNOTE is a quantitative validated instrument that assesses the quality of outpatient clinical notes. (JAMIA online 1/2/14) Its 12 evaluative elements are: chief complaint, history of present illness, problem list, past medical history, medications, adverse drug reactions & allergies, social & family history, review of systems, physical findings, assessment, plan of care, and follow-up information. QNOTE scores can range from a low of 0 to a high of 100. Sixteen primary care physicians with active practices used QNOTE to determine the quality of the 300 clinical notes (100 patients with 3 notes each).
RESULTS: All 12 element quality scores significantly improved in the interval between before-EHR and 5-years-EHR. The grand mean QNOTE scores were: 6 months before the introduction of the EHR (handwritten), 52.0 (SD 18.4), 6 months after EHR, 61.2 (SD 16.3), and 5 years after EHR, 80.4 (SD 8.9). The grand mean QNOTE scores significantly improved after the introduction of the EHR, comparing before-EHR to after-EHR, p < 0.0001, and before-EHR to 5-years-EHR, p < 0.0001.
CONCLUSIONS: The introduction of the electronic health record significantly improved the quality of clinical notes.
QNOTE scores (mean, SD)
| Elements | Before-EHR | 5-years-EHR | Before vs. 5-years |
| Chief complaint | 62.5 (28.3) | 78.2 (23.7) | 25 % (<0.0001) |
| History of present illness | 63.2 (26.1) | 84.7 (18.3) | 34 % (<0.0001) |
| Problem list | 24.0 (28.9) | 59.6 (31.2) | 144 % (<0.0001) |
| Past medical history | 29.4 (36.4) | 84.7 (24.0) | 188 % (<0.0001) |
| Medications | 59.0 (39.0) | 90.8 (17.7) | 54 % (<0.0001) |
| Drug reaction & allergies | 69.1 (33.7) | 79.3 (29.4) | 15 % (<0.05) |
| Social & family history | 25.4 (27.9) | 72.7 (26.0) | 186 % (<0.0001) |
| Review of systems | 30.7 (33.3) | 80.4 (23.8) | 162 % (<0.0001) |
| Physical findings | 66.3 (27.6) | 85.8 (16.5) | 29 % (<0.0001) |
| Assessment | 65.5 (24.4) | 86.6 (14.5) | 32 % (<0.0001) |
| Plan of care | 65.4 (24.6) | 85.3 (15.3) | 31 % (<0. 0001) |
| Follow-up information | 63.5 (27.0) | 81.7 (20.5) | 29 % (<0.0001) |
| Grand mean | 52.0 (18.4) | 80.4 (8.9) | 55 % (<0.0001) |
ELECTRONIC RESOURCE USE AND PRIMARY CARE CAPACITY AS INSURANCE COVERAGE EXPANDSRenuka Tipirneni1,2; Hwajung Choi1,2; Matthew M. Davis3,1. 1University of Michigan, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI; 3University of Michigan, Ann Arbor, MI. (Tracking ID #1934522)
BACKGROUND: As millions of Americans gain health insurance coverage offered by the Patient Protection and Affordable Care Act (ACA), newly insured individuals will face the challenge of finding a primary care physician (PCP). Given the limited supply of PCPs in the U.S., state and local health planners must consider how to increase PCPs’ capacity to accept new patients. Use of electronic resources, or “meaningful use”, has been widely viewed as providing potential savings in practice costs and time. However, it remains unclear whether electronic resource use can improve practice efficiency and, ultimately, expand capacity of primary care physicians to accept the newly insured into their panels. We examine whether increased use of electronic resources is associated with change in primary care capacity.
METHODS: We analyzed data from the Center for Healthcare Research & Transformation 2012 Survey of Michigan Physicians, a cross-sectional survey of Michigan PCPs conducted between October and December 2012. Surveys were mailed to 1500 PCPs, 500 from each of three specialties (pediatrics, internal medicine and family medicine). Survey items included questions about the primary predictor variable, PCPs’ use of electronic resources; this variable was operationalized for each of several resources individually (electronic health records, patient registry, electronic prescribing, web portal for appointment scheduling or prescription refills, reminder system, care improvement registry and electronic access to admitting hospital records) and in aggregate (total count of electronic resources in use). The primary outcome was PCPs’ assessment of their future capacity (yes/no) to accept new patients overall, and by payer (e.g. private insurance, Medicaid, and Medicare). We conducted bivariate analyses between primary predictors and outcomes. We then performed multivariable logistic regression analysis to examine the relationship between use of electronic resources and primary care capacity, after controlling for physician characteristics (gender, specialty, number of years in practice, panel volume; all by self-report), practice factors (practice size, current insurance payer mix; all by self-report), and urbanicity of the PCPs’ practice setting (urban vs. suburban vs. rural county; by linking Federal Information Processing Standard county codes obtained from self-reported zip code to the U.S. Department of Agriculture Economic Research Service 2013 Urban Influence Codes).
RESULTS: The study sample included 739 physicians (response rate = 49 %). Overall, 83 % of PCPs reported they would have capacity to accept new patients in the future. The most common electronic resource in use at the time of the survey was electronic prescribing (89 % of PCPs); the least common resource in use was a web portal for patients to schedule their own appointments (21 %). In aggregate, PCPs had a mean of 5.1 electronic resources in their practices. In bivariate analyses, with each incremental increase in the number of electronic resources in use, there were significantly lower odds of future primary care capacity (OR = 0.87, 95%CI 0.78–0.97). After adjusting for physician-, practice- and community-level covariates, incrementally greater numbers of electronic resources in use remained significantly inversely associated with anticipated capacity (adjusted OR = 0.86, 95%CI 0.76–0.97). Among individual electronic resources examined, electronic health records (EHR) were the only resource significantly associated with anticipated capacity (adjusted OR 0.53, 95%CI 0.30–0.94). In analyses of future capacity by payer type, increased use of electronic resources overall (adjusted OR = 0.87, 95%CI 0.77–0.98), and use of EHR specifically (adjusted OR = 0.50, 95%CI 0.29–0.88), were associated with significantly decreased capacity to accept privately insured patients. There were no associations with future capacity to accept Medicaid or Medicare patients.
CONCLUSIONS: In this study of primary care capacity in a large state in the era of insurance coverage expansion, PCPs who were most likely to implement EHR and use a greater number of electronic resources were significantly less likely to accept new patients. The implication of these findings for patients obtaining coverage under the ACA is that access to primary care may be somewhat impeded, rather than facilitated, by factors associated with electronic resource implementation.
ELEMENTS OF TEAM-BASED CARE IN A PATIENT-CENTERED MEDICAL HOME ARE ASSOCIATED WITH LOWER BURNOUT AMONG VA PRIMARY CARE EMPLOYEESChristian Helfrich1; Joseph Simonetti1; Robert Reid6; Sandra Joos3; Bonnie J. Wakefield4; Ian A. Randall1; Gordon Schectman5; Richard Stark5; Stephan D. Fihn2,1; Henry B. Harvey1; Karin M. Nelson1. 1VA Puget Sound Health Care System, Seattle, WA; 2Veterans Health Administration, Seattle, WA; 3Department of Veterans Affairs, Portland, OR; 4Department of Veterans Affairs, Iowa City, IA; 5Veterans Health Administration, Washington, DC; 6Group Health, Seattle, WA. (Tracking ID #1938477)
BACKGROUND: A high proportion of the US primary care workforce reports burnout, which is associated with negative consequences for clinicians and patients. Many protective factors from burnout are characteristics of patient-centered medical home (PCMH) models, though even positive organizational transformation is often stressful. The existing literature on the effects of PCMH on burnout is limited, with most findings based on small-scale demonstration projects with data collected only among physicians, and the results are mixed. To determine if components of PCMH related to team-based care were associated with lower burnout among primary care team members participating in a national medical home transformation, the VA Patient Aligned Care Team (PACT).
METHODS: We conducted a web-based, cross-sectional survey linked to administrative data from May 2012. A total of 4,539 VA primary care personnel from 588 VA primary care clinics. The dependent variable was burn-out, and the independent variables were measures of team-based care: team functioning, time spent in huddles, team staffing, delegation of clinical responsibilities, working to top of competency, and collective self-efficacy. We also included administrative measures of workload and patient comorbidity.
RESULTS: Overall, 39 % of respondents reported burnout. Participatory decision making (OR 0.65, 95 % CI 0.57, 0.74) and having a fully staffed PACT (OR 0.79, 95 % CI 0.68, 0.93) were associated with lower burnout, while being assigned to a PACT (OR 1.46, 95 % CI 1.11, 1.93), spending time on work someone with less training could do (OR 1.29, 95 % CI 1.07, 1.57) and a stressful, fast-moving work environment (OR 4.33, 95 % CI 3.78, 4.96) were associated with higher burnout. Longer tenure and occupation were also correlated with burnout. Neither spending time on work for which one has too little training, nor measures of workload were associated with burnout.
CONCLUSIONS: Lower burnout may be achieved by medical home models that are appropriately staffed, emphasize participatory decision making, and increase the proportion of time team members spend working to the top of their competency level. Ensuring that primary care team members are tasked with appropriately challenging work appears to be a greater issue for burnout than work that exceeds one’s training or the overall workload.
EMPATHY, CAREER INTERESTS, AND FACTORS INFLUENCING CAREER CHOICE AMONG MEDICAL STUDENTSEmma C. Jeffries; Charlotte E. Ward; Marya J. Cohen. Massachusetts General Hospital, Boston, MA. (Tracking ID #1938468)
BACKGROUND: An initial study indicates that high levels of physician empathy correlate with positive patient outcomes. However, in previous literature, medical student empathy scores have been shown to drop over the course of education despite increasing exposure to patient care, particularly in the inpatient setting. Empathy scores in students exposed to mentorship, educational opportunities, and longitudinal patient care in the outpatient setting have not been studied. At the Crimson Care Collaborative (CCC), five student-faculty collaborative practices across the Harvard teaching hospitals, students have the opportunity to care for and develop long-term relationships with primary care patients. Our goal was to examine the relationship between student empathy, future career interests, and factors influencing career choice.
METHODS: Prior to joining CCC, Harvard Medical School (HMS) students completed a survey about career interests, and factors important in career choice. Empathy was evaluated using the Jefferson Empathy Scale, a validated 20-question survey. A single empathy composite score was then generated for each respondent. The relationship between career interest and career choice factors, and empathy, was assessed using generalized linear models, controlling for year in medical school, gender, race, marital status, undergraduate major (science vs. non-science vs. both), and hometown type (rural vs. urban vs. suburban).
RESULTS: The study population included 166 students who completed both an initial survey and the Jefferson Empathy Scale. The average score was 118.8 (range 89–140). Out of 166 students, 75 % were first year medical students, 59 % were female, 60 % were white, and the average age was 25. Students who were interested in general medicine had a higher empathy score than those who were not (120.3 vs. 114.8; p = 0.04). Students who prioritized working with the under-served had higher empathy scores than those who did not (120.5 vs. 114; p = 0.0003). Students who prioritized future income had a lower empathy score than those who did not (117.4 vs. 120.2; p = 0.004). Students who prioritized the ability to work part-time had higher empathy scores than those who did not (122 vs. 117.3; p = 0.02). Students who wanted to teach students and residents had higher empathy scores than those who did not (120 vs. 115.8; p = 0.0003).
CONCLUSIONS: Among medical students participating in a student-faculty collaborative practice, higher empathy scores were correlated with interest in general medicine, working with the under-served, the ability to work part-time, and teaching. The importance of income was negatively correlated with empathy score. In the future, we hope to examine empathy scores of students before and after participation in the Crimson Care Collaborative. Further research is needed on the extent to which empathy levels can be changed in medical students and what experiences might influence empathy levels. Findings around empathy and career choice may have implications for medical school admissions and primary care recruitment.
EMR-BASED PHYSICAL ACTIVITY COUNSELING AND REFERRAL IN PRIMARY CARE: AN EVALUATION STUDYJulien J. Dedier1; Julie A. Wright2; Timothy Heeren3; Robert H. Friedman1. 1Boston University, Boston, MA; 2University of Massachusetts, Boston, MA; 3Boston University, Boston, MA. (Tracking ID #1939345)
BACKGROUND: Physical activity (PA) is beneficial in the prevention and management of several diseases, and linking primary care patients to effective PA programs may improve health outcomes for exercise-responsive conditions such as diabetes, hypertension and obesity. The purpose of this study was to evaluate the implementation of an electronic medical record (EMR) tool designed to help primary care providers conduct PA counseling and refer patients to an automated telephone PA coach.
METHODS: Content of the EMR PA tool was based on the 5A’s approach to PA counseling and elements of motivational interviewing. Providers reviewed a prototype of the tool, and their feedback was used to design the final version. The tool was publicized at business meetings and by e-mail announcements. Providers could use the tool to do 1 or more of the following: (1) determine the patient’s current level of PA and motivation to increase PA, and counsel accordingly; (2) create an exercise prescription; and (3) refer patients to use an automated telephone PA coach (TLC-PA). TLC-PA was developed by our group, and was shown to significantly increase self-reported PA of moderate-or-greater intensity in an RCT of hypertensive primary care patients. Patients referred to TLC-PA were scheduled to receive 12 weekly calls of roughly 10 min each. We collected implementation information from providers and patients. We captured the electronic footprint providers created whenever they used the tool, and surveyed users’ opinions of the tool each time they used a new feature. We surveyed a random subset of non-users to determine their reasons for non-use. We also surveyed patients who were referred to TLC-PA on their impressions of the referral encounter.
RESULTS: 50 unique providers accessed the EMR tool at least once and were sent a survey about its functions. Of respondents (n = 13), most agreed or strongly agreed the 3 EMR tool functions were easy to use (66 %–88 %), increased the quality of PA counseling they provided (72 %–88 %), were worth the time spent to use them (57 %–75 %), and should be made a permanent part of the EMR (82 %–100 %). Providers accessed the exercise prescription function most often (104 instances), then the stage-based counseling function (62 instances), followed by the TLC-PA referral function (36 instances). Providers’ greatest reservation about PA referral was not knowing enough about the Coach to confidently refer their patients. Among non-user survey respondents (n = 24), only 37.5 % had heard of the EMR PA tool. Ninety-two percent were not sure how to access it. Seventy-eight percent of patients selected for exercise counseling or referral had an exercise-responsive diagnosis of obesity, DM, PVD, or CAD. Fourteen of the 36 patients referred to use TLC-PA completed a survey about the office referral encounter. All recalled discussing PA and TLC-PA, and 86 % recalled receiving printed information about TLC-PA. All referred patients went on to use TLC-PA.
CONCLUSIONS: PA interventions such as our automated PA coach have been shown to increase PA. We successfully linked a PA counseling and referral intervention to the EMR. Primary care providers and their patients considered it helpful, but low-intensity advertising of the tool resulted in only modest use. Comprehensive implementation efforts are required to fully assess the feasibility of linking PA interventions to the EMR in primary care settings.
ENGAGING VETERANS IN CONVERSATIONS ABOUT HEALTH: A COMMUNITY PARTNERSHIP AND ASSESSMENT TO PROMOTE VETERAN HEALTHAnita D. Misra-Hebert1,2; Laura Santurri3; Richard DeChant4; Brook Watts5; David Aron5. 1Cleveland Clinic, Cleveland, OH; 2Louis Stokes Cleveland Veterans Affairs Medical Center, Cleveland, OH; 3Weber State University, Ogden, UT; 4Cuyahoga Community College, Cleveland, OH; 5Louis Stokes Cleveland Veterans Affairs Medical Center, Cleveland, OH. (Tracking ID #1923869)
BACKGROUND: As veterans of recent conflicts in Iraq and Afghanistan return to civilian life, and as veterans of previous conflicts continue to age, the importance of health promotion as related to chronic disease prevention and management in the veteran population will be a required area of focus for clinical providers. The high prevalence of mental health disease in veterans of recent military conflicts may affect risk for chronic disease development and the self-efficacy/coping mechanisms required for optimal chronic disease management. Veteran students pursuing higher education may be particularly motivated to engage in health promotion. The study objective is to explore motivations to improve health and to assess health among student veterans, using a shared forum, through partnership between a Veterans Affairs (VA) medical center and a community college.
METHODS: This study utilized a sequential mixed methodological design with an equally weighted approach for the qualitative and quantitative portions. The study participants were student veterans enrolled at a community college in October 2012–April 2013. Veteran students were recruited to participate in focus groups. Participants discussed views of health, motivations to improve health, and perceptions of medical care. Discussions were audio-recorded and transcribed. Other students then participated in a cross-sectional health assessment survey. Qualitative data analysis utilized a conventional content analysis approach to coding and thematic development. Survey data analysis included descriptive and logistic regression analyses.
RESULTS: A total of 17 veteran students participated in 6 focus groups. Emergent themes included changing views of health after transition from active duty, generational differences among veterans, barriers to accessing health services, and health care costs. Concerns about basic needs such as job/ housing and providing/caring for family, stigma and privacy, and preferences related to health communication were also important themes. The motivation to improve health for many of our study participants was perceived as secondary to the need to obtain stable housing or work, and concerns about privacy and stigma were identified as possible barriers to seeking healthcare. Two hundred four students (21 % response rate) participated in the health assessment survey. Physical and emotional limitations (45 % and 35 %, respectively), and pain interfering with work (42 %) were reported. Self-reported depression and unhealthy behaviors were high.
CONCLUSIONS: Engaging veteran students in conversations about health and conducting a health assessment survey identified factors influencing motivation to improve health and priority areas to inform interventions for chronic disease prevention. The impact of social determinants on health is substantial in this group. A significant proportion of student veterans are limited in daily activities as a result of physical as well as emotional issues and specifically from pain. A partnership between a VA medical center and a community college integrates primary care with public health as a step to improving the health of veteran students in the community.
ENGAGING YOUTH THROUGH A SPOKEN WORD TYPE 2 DIABETES PREVENTION SOCIAL MARKETING CAMPAIGNElizabeth A. Rogers1,2; Sarah Fine4; Margaret A. Handley3,4; Purba Chatterjee4; James Kass5; Dean Schillinger3,4. 1University of Minnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of California San Francisco, San Francisco, CA; 4University of California San Francisco, San Francisco, CA; 5Youth Speaks, San Francisco, CA. (Tracking ID #1939606)
BACKGROUND: Type 2 diabetes (DM2) prevalence is rising among minority young adults. There is an unmet need to engage youth in identifying solutions to decrease this risk. Some media campaigns such as the successful truth® antismoking campaign used a socio-environmental perspective to shift social norms, and this approach may be one avenue toward engagement around DM2. Objective: To evaluate the effectiveness and reach of The Bigger Picture, a youth-generated, youth-targeted DM2 prevention social marketing campaign.
METHODS: Campaign Development: Through a partnership between UCSF and Youth Speaks, a youth spoken-word nonprofit, we used a participatory approach engaging youth poets to create 11 video public service announcements (PSAs) addressing the socio-environmental conditions that increase DM2 risk. Our dissemination focus was regional low-income and minority-serving high schools identified through collaboration with school districts, and we developed a scripted assembly and a writing workshop. We created a campaign website (www.thebiggerpicture.org) with information, PSA videos, and informational toolkit, and used Facebook and Twitter social media. Evaluation: Using the RE-AIM framework, we evaluated the campaign through efficacy measures capturing changes in knowledge and attitude, and those that characterized the reach of the campaign. We gathered data using audience response system handheld devises distributed to students (up to 80 per assembly) to answer 3 questions gauging knowledge and attitude embedded at the beginning and end of the assembly, and through paper pre/post surveys (closed- and open-ended questions) of all students in the workshops. To assess change, we used McNemar’s chi-square test and a mixed model (adjusted for demographics) accounting for clustering at the school level. We employed counts, means, and proportions of state-reported school data and web analytics to assess reach of the school-based dissemination and web-based media.
RESULTS: PSA themes included the association of DM2 with the built environment, industry advertising, and racial and socioeconomic disparities. In 13 high schools over 6 months, 1900 students participated in the poet-led assemblies and 263 in the workshops. The participating schools enrolled on average 982 students, 66 % of whom qualified for free or reduced lunches. Seven hundred eighty-one students responded to assembly surveys. Fifty-six percent were female with an average age of 15.7 years, and 28 % were Latino, 27 % Asian, 18 % African American, and 14 % multi-ethnic. Ninety-two percent agreed that DM2 is preventable after the assembly compared to 70 % before (McNemar’s p < 0.001, adjusted mixed model OR 5.3), and 83 % after identified environmental factors in addition to individual behaviors as influencing DM2 risk compared to 34 % before (p < 0.001, OR 13.1). Using a Likert scale, 59 % after responded “I care a lot” about preventing DM2 compared to 29 % before (p < 0.001, OR 9.1). In the workshops, students identified the DM2 epidemic as a social justice issue. To date, the 11 web-based video PSAs combined had 72,232 views. The campaign’s Facebook page has 383 “likes” and the Twitter account has 342 followers.
CONCLUSIONS: A youth-targeted, youth-generated social marketing campaign improves short-term knowledge and attitudes about DM2 risk. Through high schools, we reached our target population, and web-based media has potential for extending this reach. This type of campaign may be one avenue toward engaging diverse, high-risk youth to change the conditions that increase DM2 risk.
EREFERRALS AND ECONSULTS: DOWNSTREAM IMPACT ON ACCESS, UTILIZATION, AND COST IN A FEE-FOR-SERVICE SETTINGNathaniel Gleason1; Jennifer J. Monacelli6; Chanda Ho2; Sara Ackerman3; Priya A. Prasad4; Michael Wang5; Don Collado1; Delthia McKinney5; Ralph Gonzales1. 1UC San Francisco, San Francisco, CA; 2UC San Francisco, San Francisco, CA; 3UC San Francisco, San Francisco, CA; 4UC San Francisco, San Francisco, CA; 5UCSF Medical Center, San Francisco, CA; 6Michigan State University, Grand Rapids, MI. (Tracking ID #1939845)
BACKGROUND: Demand for specialty care services exceeds supply at many academic referral centers. Delays in access to specialty care are common, and are anathema to patient-centered care. Electronic referrals (eReferrals) and non-face-to-face consultations (eConsults) are mechanisms associated with significant improvements in the specialty care referral process in integrated delivery systems with aligned incentives. Translating these innovations to academic medical centers (AMCs) has been challenging; reimbursement remains largely fee-for-service, and Medicare and most commercial payers do not pay for eConsults. With support from the Medicaid waiver program (DSRIP), UCSF Medical Center implemented a new referral platform. The system is designed to improve information exchange at the point-of-referral and to provide an eConsult option, allowing PCPs to request timely input from specialists for data-oriented referral problems that the PCP does not perceive to require in-person evaluation of the patient by the specialist. In this study, we analyzed the downstream impact of this program on PCP referral rate, specialty care access, and costs.
METHODS: eReferral/eConsult Platform: In May 2012, UCSF introduced a structured referral platform within the electronic health record (EHR) (Epic Systems) with over 90 problem-specific, structured templates providing clinical decision support at the point-of-referral. An eConsult option was added in September 2012. The expected eConsult response time is 3 business days. Upon review, if the specialist determines the case is not appropriate for eConsult, the specialist converts the eConsult to a standard new-patient visit. Specialists receive a payment corresponding to 0.5 wRVU per completed eConsult. PCPs receive 0.5 wRVU credit toward productivity targets. in recognition of the fact that the PCP maintains management responsibility for the referral problem. Study populations: The program included 8 primary care sites and 12 medicine subspecialty practices. The study population includes all eligible PCPs (n = 178) and all referrals to participating practices for patients assigned to an eligible PCP during baseline (9/1/11–8/31/12) and study periods (9/1/12–4/30/13) (n = 13,738 referrals representing 11,597 unique patients). (To account for seasonal effects on ED visits and hospitalizations, we used baseline and intervention periods of Oct–April 2012 vs Oct–April 2013 for the utilization and cost analysis). We obtained data on referral rates from the EHR scheduling database. Data on utilization and costs were obtained from the University Health System Consortium. Analysis: We calculated the total referral rate per 100 primary care visits per month, and the proportion of these sent as eConsults. To compare the trends in referral rate, we modeled the effect of time using a linear spline analysis with two knots to determine whether there were differences in the trajectory following the introduction of the structured referral system and eConsults. To measure impact on access to specialty care, the proportion of UCSF primary care patients who received specialty care input (office visit or eConsult) within 14 business days in the baseline and eConsult periods were compared using chi-square tests. Mean monthly ambulatory, emergency department, hospital utilization and professional fee costs occurring within 120 days following each referral or eConsult were log transformed to minimize effects of outlier data. Average costs were compared between baseline (n = 6 months) and eConsult (n = 6 months) periods with unpaired t-tests.
RESULTS: Of eligible PCPs, 69 % placed at least one eConsult. Based on the spline analysis, the referral rate declined from 12.42 per 100 primary care visits during the baseline period to 10.66 per 100 primary care visits in August 2012 (11 % decrease; p = 0.011). eConsults were added as an option in September 2012, and the referral rate remained stable though the remainder of the study. eConsults were used for 8.2 % of total referrals. The proportion of patients who received specialty care input (office visit or eConsult) within 14 business days improved from 39 to 49 % (p = 0.001) across all participating specialties. Specialties with greatest improvements were pulmonary (from 20 to 50 % (p = 0.004)), GI (from 19 to 40 % (p = 001)) and nephrology (from 50 to 74 % (p = −.05)). The proportion of referrals with an ED visit during the 120-day period following referral or eConsult decreased from 9.8 to 8.6 %, and there was a significant reduction in total ED pro-fee costs (p ss 0.016). Mean ambulatory and hospital pro-fees did not change between periods.
CONCLUSIONS: This combined eReferral (enhanced referral platform) and eConsult program showed robust adoption and had significant impact on referral rate and specialty care access time. The significant impact on ED costs may represent a downstream benefit of improved access to care.
ESTABLISHING GUIDELINES FOR REFERRAL TO ORTHOPAEDIC SPECIALTY CARE: CONSENSUS USING THE MODIFIED DELPHI METHODMaria E. Otto; Carlin Senter; Christy K. Boscardin; Ralph Gonzales; Nathaniel Gleason. University of California San Francisco, San Francisco, CA. (Tracking ID #1939439)
BACKGROUND: Standardized electronic referrals can improve physician communication, provider experience, and wait times. The Council for Subspecialty Societies, sponsored by the American College of Physicians, defines the features of high-quality care coordination between primary care and specialty care in a Patient Centered Medical Home-Neighborhood (PCMH-N). Specifically, high-quality referrals in the PCMH-N are defined as referrals that facilitate effective transfer of clinical information, elicit a clinical question, convey expectations about management roles, and ensure appropriate and timely consultation. The University of California San Francisco (UCSF) implemented an eReferral system, integrated into the Electronic Health Record, in which structured templates facilitate referrals to specialty care that are in keeping with PCMH-N recommendations and provide decision support at the point-of-care. Expanding this program to orthopaedics, we found limited available guidelines for orthopaedic problems regarding referral timing, management steps to be taken prior to referral, imaging in advance of referral, and clinical questions for which a non-face-to-face visit (eConsult) with an orthopaedist might be appropriate. This study describes our experience using the modified Delphi method to inform development of standardized orthopaedic referral guidelines by identifying consensus between referring PCPs and orthopaedic clinicians on specific recommendations.
METHODS: To represent a broad range of expertise, all UCSF Physicians, Physician Assistants, and Nurse Practitioners who provide care to adult patients in the UCSF orthopaedic clinic were asked to participate (Foot & Ankle n = 2, Hand = 3, Sports = 5, Arthoplasty = 6, Spine = 8). Primary care providers (PCPs) volunteered in response to a recruitment email sent to all 8 UCSF adult primary care practices (n = 22 volunteers). The expert panel completed two rounds of anonymous electronic surveys over a period of 4 weeks. PCPs answered all questions, while clinicians in the orthopaedic practice answered only questions related to the joints each treated in practice. Surveys were composed of clinical scenarios followed by questions about appropriate pre-referral evaluation, conservative management, and the utility of a non-face-to-face consultation (eConsult) with an orthopaedist. Scenarios were written for the most commonly referred orthopaedic diagnoses and constructed to differ by one variable at a time (e.g. chronic vs. acute, a sedentary vs. athletic patient). The degree of importance for each possible intervention was ranked on a 5-point Likert scale (strongly disagree to strongly agree). The second round survey included the median response for each group (PCPs and orthopaedic clinicians) from the first round for each question, allowing panelists to factor in these initial responses when re-visiting the scenarios in round two. Consensus was defined as ≥70 % of PCPs and orthopaedic clinicians giving a score of 1–2 or 4–5.
RESULTS: All 22 PCPs completed the Round 1 & 2 surveys. Nineteen orthopaedic clinicians completed Round 1 and 17 completed Round 2 (Response Rate: 79 % & 70 % respectively). Consensus was reached in 142 of 214 items. Most notably, PCPs and orthopaedists agreed that 1) X-ray should be performed in advance of referral for most clinical scenarios while pre-referral MRI is recommended in select scenarios: acute knee pain concerning for ligamentous injury and/or meniscal tear, spinal stenosis, chronic neck pain with arm pain in a dermatomal distribution, and intractable neck pain. 2) Pre-referral physical therapy is recommended for the following conditions: Achilles tendinitis, groin pain concerning for labral tear or impingement in a patient ≥65 years old, trochanteric bursitis, osteoarthritis of the hand, shoulder, and knee, meniscal tear in a patient ≥65 years old patellofemoral knee pain, shoulder impingement syndrome, frozen shoulder, medial and lateral epicondylitis, and spinal stenosis. 3) PCP management guided by electronic consultation by an orthopaedist, in place of a patient visit, could be appropriate for the following conditions: chronic pain after ankle sprain, plantar fasciitis, stress fracture of the foot, osteoarthritis of the hand, shoulder, knee, and hip, trochanteric bursitis, degenerative meniscal tear, patellofemoral pain, shoulder impingement syndrome, medial epicondylitis, intractable low back and neck pain.
CONCLUSIONS: This consensus is the first step in improving the quality of orthopaedic referrals. Through this effort, we hope to have established meaningful referral guidelines that represent the collective opinions of experts with the premise that ‘pooled intelligence’ enhances individual judgment. Our future efforts will aim to measure whether or not standardized referral templates developed using the Delphi method in consultation with a panel of experts and following the current PCMH-N guidelines improve referral efficiency and quality.
ESTIMATING TOBACCO-, ALCOHOL-, AND DRUG-ATTRIBUTABLE DEATHS AND THEIR CONTRIBUTION TO MORTALITY DISPARITIES AMONG HOMELESS ADULTSTravis P. Baggett1,2; Yuchiao Chang1; Bianca Porneala1; Jessie M. Gaeta2,3; James J. O’Connell2,1; Nancy A. Rigotti1. 1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Boston Health Care for the Homeless Program, Boston, MA; 3Boston University School of Medicine, Boston, MA. (Tracking ID #1939356)
BACKGROUND: Homeless individuals have a high prevalence of substance use disorders and experience excess mortality rates in comparison to non-homeless people. Our objective was to estimate the burden of deaths attributable to tobacco, alcohol, and drug use in a large cohort of homeless adults, and to assess the contribution of substance-attributable mortality to the disparity in all-cause mortality with the general population.
METHODS: We assembled a cohort of 28,033 adults aged ≥18 years who were seen at Boston Health Care for the Homeless Program in 2003–08. We used probabilistic methods to cross-link this cohort with Massachusetts mortality files spanning the same years. For decedents, we based causes of death on ICD-10 underlying cause codes in the death occurrence files. We used accepted epidemiologic methods to estimate population attributable fractions (PAFs) for causes of death that high-quality studies have demonstrated to be causally related to the use of tobacco, alcohol, or drugs. For each cause of death, the PAF represents the proportion of these deaths that would not have occurred in the absence of tobacco, alcohol, or drug use. We used Monte Carlo simulation methods to generate 95 % confidence intervals for our PAF estimates. For each condition, we multiplied the PAF by the count of deaths to estimate the number of deaths attributable to tobacco, alcohol, or drug use. For conditions related to more than one substance, we used standard methods to account for overlapping attribution. We divided the number of attributable deaths by the person-time at risk to generate attributable rates. As a basis for comparison, we used the same methods to estimate substance-attributable mortality rates for the 2003–08 Massachusetts general population.
RESULTS: Of 1302 deaths, 236 (95 % CI 215–254) were tobacco-attributable, 215 (95 % CI 199–232) were alcohol-attributable, and 286 (95 % CI 285–287) were drug-attributable. After accounting for overlap, about 52 % (N = 676, [95 % CI 655–698]) of all deaths were attributable to any of these substances. Drug use was the predominant contributor to substance-attributable deaths under the age of 50 years (63 %), while tobacco use was the major contributor to substance-attributable deaths over the age of 50 years (55 %). In comparison to the Massachusetts general population, age- and sex-stratified mortality rates in the homeless cohort were 3–4 times higher for tobacco-attributable causes, 6–12 times higher for alcohol-attributable causes, 8–17 times higher for drug-attributable causes, and 5–11 times higher for all substance-attributable causes combined. Disparities in substance-attributable deaths accounted for nearly 60 % of the age- and sex-standardized mortality rate difference between the homeless cohort and the Massachusetts general population.
CONCLUSIONS: Over half of all deaths among homeless people are attributable to tobacco, alcohol, or drug use. Substance-attributable deaths are a major contributor to mortality disparities between homeless adults and the general population, but they do not fully explain the mortality gap between these groups of people. Efforts to reduce mortality among homeless individuals should focus on the expansion of substance abuse treatment services in conjunction with comprehensive health care and social policy interventions to address non-addiction sources of excess mortality in this vulnerable population.
EVALUATING INPATIENT HOSPITAL CHARGE VARIABILITY USING LOCAL HEALTH AND MARKET FACTORSJames D. Park1; Edward Kim2; Rachel M. Werner3. 1Rutgers, Robert Wood Johnson Medical School, New Brunswick, NJ; 2The College of New Jersey, Ewing, NJ; 3Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. (Tracking ID #1937089)
BACKGROUND: In May 2013, the Center for Medicare and Medicaid Services released previously undisclosed information about the price of hospital care. Within a diagnosis related group, inpatient hospital charges to Medicare demonstrated a wide range of charges across US hospitals. This variation in hospital charges remains unexplained, and this study examines its relationship to the local market environment in which hospitals operate.
METHODS: This descriptive study evaluated the CMS Inpatient Provider Charge data of over 3000 US hospitals using clustered, multivariate linear regression. This analytic approach examined how county health, socioeconomic, and market factors relate to hospital charges. Six common inpatient conditions—cellulitis, chronic obstructive pulmonary disease, congestive heart failure, myocardial infarction, orthopedic surgeries, and pneumonia—were chosen for the analysis. Related DRGs for each condition were grouped together, and a weighted average charge for each hospital was calculated based on the proportion of discharges per DRG. Based on a conceptual model, a common set of covariates was used to create a single regression model for each condition. The analysis used various county-level measures of health status (years of potential life lost per 100,000 population, percent of adults who report fair or poor health, percent days reported as mentally unhealthy per month, diabetes prevalence, obesity prevalence); health behavior (prevalence of smoking, no leisure time activity, or heavy alcohol drinking); clinical access and quality (prevalence of uninsured status, preventable hospital stays rate, percent of diabetics who received a hemoglobin A1c test, number of primary care physician per 100,000 population); socioeconomics status (percent of a 9th grade cohort that graduates in 4 years, prevalence of unemployment, of children living in poverty, and of children living in single-parent homes, median household income, violent crime rate per 100,000 population); the built environment (number of accessible recreational facilities per 100,000 population); demographics (percent of the population that is African American, Asian, Latino, or other race, and percent of the population over the age of 65); and the hospital market (for-profit status, proportion of hospital discharges within the county) from every US county and hospital. All analyses controlled for other market factors such as the hospital wage index, disproportionate share hospital index, hospital cost-to-charge ratio, and the county-level Herfindahl-Hirschman Index. Covariates were extracted from multiple datasets including the US Census Bureau, Behavioral Risk Factor Surveillance System, National Center for Chronic Disease Prevention and Health Promotion, CMS Impact, CMS Provider of Service, County Business Patterns, American Community Survey, Dartmouth Atlas of Health Care, Bureau of Labor Statistics, Small Area Income and Poverty Estimates, Federal Bureau of Investigation Uniform Crime Reporting, National Center for Health Statistics, and the National Center for Educational Statistics. All regression analyses were clustered by county, and statistical testing was deemed significant with p-values <0.05.
RESULTS: The mean number of hospitals included across six regressions was 2603. Across all six conditions, hospital charges were associated with uninsured status and resulted in $210.28–$623.26 higher charges for every 1 % increase in the prevalence of uninsured status (p < 0.01). In addition, hospital charges were associated with for-profit hospital status across all six conditions and resulted in $1230.47–$7772.10 higher charges than not-for-profit status (p < 0.05). In all conditions except myocardial infarction, hospital charges were associated with unemployment status and resulted in $295.83–$752.53 higher charges for every 1 % increase in unemployment prevalence (p < 0.05). Health behavioral factors such as smoking, physical inactivity, and excessive alcohol consumption, or health status factors such as premature death, fair or poor health status, poor mental health days, or diabetes were largely unassociated with hospital charges. Of all health factors utilized in this study, only obesity was repeatedly associated with hospital charges in four of the six conditions, resulting in $232.57–$513.92 higher charges for every 1 % increase in obesity prevalence (p < 0.05).
CONCLUSIONS: Non-health related factors, such as uninsured, unemployment, and for-profit hospital status, were consistently associated with higher hospital charges. In contrast, nearly all health factors had no association to inpatient hospital charges. This research raises concerns about a regressive pricing strategy that is indifferent to health status but charges vulnerable and uninsured populations higher prices.
EVALUATING THE UTILITY OF OSTEOPOROSIS SCREENING TOOLS (OST, FRAX) AND VIDEO EDUCATION IN HOSPITALIZED PATIENTSEve Thau; Eileen Hennrikus. Penn State Milton Hershey Medical Center, Hershey, PA. (Tracking ID #1938794)
BACKGROUND: Approximately eight million women and two million men in US suffer from osteoporosis, with the cost of fragility fractures an estimated $10–15 billion annually. To calculate osteoporotic fracture risk, the FRAX (Fracture Risk Assessment Tool), takes into account age, weight, height, gender, parental fractures, tobacco and alcohol use and secondary causes for osteoporosis. A simpler risk assessment measurement is the OST (Osteoporosis Self-Assessment Tool), a calculation using only age and weight. We proposed that osteoporosis risk assessment and education can be accomplished in patients hospitalized on the inpatient internal medicine service. Our objectives include (1) assess if OST compared to FRAX is a useful tool to screen inpatients for osteoporosis, (2) determine if osteoporosis video education is well received and (3) determine if patients hospitalized for other illnesses will act upon knowledge and education for a preventive health measure.
METHODS: Three days per week for 2 months, an OST was calculated on all internal medicine inpatients >60 years old. One hundred twelve patients with an OST > 2, deemed not at risk for osteoporotic fracture then had a FRAX calculated by chart review. The 72 patients with an OST < 2, deemed at risk for osteoporotic fracture, were consented for further study. Patients were excluded if they were not interested in participating, had altered mental status or were too sick to participate. Fifteen eligible patients were excluded. Patients were given the FRAX questionnaire, a 7-question osteoporosis pre-test, followed by an NIH-sponsored educational osteoporosis video, and the same test post-video. Afterwards, patients were asked their opinion of the video education, and if they would take any new measures following hospital discharge to help improve bone strength and prevent osteoporosis.
RESULTS: 184 patients were evaluated, mean age 73 years old, and mean weight 91 kg. Causes for admission were primarily cardiovascular, pulmonary, and renal disease with only two patients admitted with bone fractures. Forty percent of internal medicine inpatients were found to be at osteoporotic fracture risk by the OST calculation. Of those 72 patients, 68 (94 % p = 0.001) were also found to be at risk for both major fracture and hip fracture by FRAX calculation. Of the 112 patients not found to be at risk by OST, 92 (84 %, p = 0.01) correlated with FRAX risk. Of the 20 patients where the FRAX found risk and the OST did not, 10 (50 %) had an obvious secondary cause for osteoporosis such as a history of chronic renal failure or prednisone usage. Of the other 10 patients who did not have a secondary cause for osteoporosis, eight of them were women over the age of 68, median age 74 years old. 30 % (22) of the at risk patients had been previously counseled by their physician for osteoporosis, and 40 % (29) of these patients were already taking calcium supplements, vitamin D and 12 % (9) were taking bisphosphonates before hospital admission. 36 % (26) patients previously had a DEXA screen before participation in the study. With regards to patient education, we found an improvement of 20.6 % when comparing quiz scores conducted before and after exposure to the NIH-sponsored educational video p = 0.001. Patients found this video very helpful in learning more about osteoporosis and preferred it to written material. After being informed of their risk, and after watching the video, 28 % (20) patients said that they would address osteoporosis, 16 would make mild lifestyle changes and only four planned to speak with their doctor and pursue treatment. Patients who opted to not alter lifestyle or seek further medical advice regarding osteoporosis noted that they were too sick or too old.
CONCLUSIONS: The OST is an effective risk assessment tool for osteoporosis. OST does not capture those patients with obvious secondary causes for osteoporosis. Of those patients at risk, 60 % had not had osteoporosis addressed by their primary care physician. Video education was well received in the hospital and revealed a significant improvement in knowledge about osteoporosis. However, after being informed of their fracture risk and receiving education only 28 % of patients would pursue treatment. A significant number of patients were found to be at risk and untreated for osteoporosis. Although the education was well received, preventive measures for osteoporosis were not a priority compared to the acute issues for which patients are hospitalized. Optimally, screening should be done in the outpatient setting, but perhaps inpatient screening and education can be useful if translated to the primary care physician to address when acute issues recede.
EVALUATION OF AN ELECTRONIC HEALTH RECORD PROMPT FOR HEPATITIS C ANTIBODY SCREENING OF BABY BOOMERS IN PRIMARY CARE - A CLUSTER RANDOMIZED CONTROL TRIALKatherine Krauskopf1; Natalie Kil1; Anastasia Sofianou2; Wilma Toribio1; Joanne Lyons3; Mark Singer3; Joseph Kannry1; Bryce Smiith5; David B. Rein4; Alex Federman1. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai Health System, Huntington, NY; 4NORC at University of Chicago, Atlanta, GA; 5Centers for Disease Control and Prevention, Atlanta, GA. (Tracking ID #1938222)
BACKGROUND: The CDC recommends one-time hepatitis C virus (HCV) testing for all persons born between 1945 and 1965 (birth cohort testing). Electronic Heath Records (EHR) may represent an effective tool to increase testing uptake. We sought to assess use and acceptance of an EHR alert to promote birth cohort testing in primary care, and determine subsequent prevalence of positive HCV tests among previously undiagnosed individuals.
METHODS: We conducted a cluster randomized controlled trial of three adult primary care practices (teaching and faculty) within the Mount Sinai Medical System, NY, beginning 4/2013 and ongoing to 3/2014. Ten clusters were identified based on provider type, geography, and patient population, and randomized to intervention (EHR screening prompt) or control (usual care). A member of the research team gave a brief intro to all physicians (MD), nurse practitioners (NP), medical assistants (MA), and registered nurses (RN), regardless of study arm assignment, about HCV, birth cohort testing recommendations, and the study. In intervention clusters, the EHR (Epic Systems, Madison, WI) triggered a screening prompt when eligible patients (those without prior HCV antibody [Ab] testing or HCV diagnosis born during 1945–1965) registered for a visit. When the MA/RN opened the electronic chart before the MD/NP, the EHR generated a prompt to pend an HCV Ab order for the MD/NP to discuss with the patient, then sign or delete. When the MD/NP opened the chart first, the EHR generated an alert to suggest HCV testing, and provided an HCV Ab order for acceptance or deletion. At study completion, differences in characteristics of intervention and control providers, and among the patients seen in intervention vs. control clusters, will be measured using t test and X2 test. We will compare testing and HCV positivity prevalence between intervention and control arms, as well as process outcomes, using generalized estimating equations.
RESULTS: After 6 months of data collection, 146 of 154 MD/NP (95 %) approached have consented to participate, as have 73 of 78 (93 %) RN/MA. There have been 10,857 eligible intervention-arm visits and 7,372 control-arm visits. Of these, 2,176 HCV Ab tests were ordered in the intervention arm (20 %) versus 225 ordered in the control arm (3 %). There were 20 positive tests in the intervention arm (0.9 % of those tested) versus five in the control arm (2.2 % of those tested).
CONCLUSIONS: Preliminary data show that the EHR intervention results in a higher rate of testing and consequently finds more cases than usual care. While targeted methods of usual care detect a higher prevalence, testing occurs too infrequently to match the aggregate case detection of the EHR prompt. Although successful in detecting more cases, only 20 % of eligible patients were tested via the intervention, suggesting that modification of the intervention may be needed to achieve HCV testing among all birth cohort adults.
EVALUATION OF STEPPED CARE FOR CHRONIC PAIN (ESCAPE) IN VETERANS OF IRAQ AND AFGHANISTAN: A RANDOMIZED TRIALMatthew J. Bair1,2; Dennis Ang4; Jingwei Wu5; Samantha D. Outcalt1; Christy Sargent1; Amanda Gerwig1; Arlene Schmid6; Teresa Damush1,3; Zhangsheng Yu5; Louanne W. Davis7; Kurt Kroenke1,3. 1VA HSR&D Center for Health Information and Communication, Indianapolis, IN; 2Indiana University School of Medicine, Indianapolis, IN; 3Regenstrief Institute, Inc, Indianapolis, IN; 4Wake Forest School of Medicine, Winston-Salem, NC; 5Indiana University School of Medicine, Indianapolis, IN; 6Colorado State University, Fort Collins, CO; 7Roudebush VA Medical Center, Indianaplis, IN. (Tracking ID #1937595)
BACKGROUND: Despite the prevalence and substantial functional, psychological, and economic impact of chronic musculoskeletal pain on military personnel and veterans, there have been few intervention studies to treat chronic pain in these populations. We conducted a randomized controlled trial to determine if a stepped-care intervention is more effective than usual care in reducing pain-related disability, pain interference, and pain severity.
METHODS: We recruited patients from post-deployment and five general medicine clinics at a Veteran Affairs Medical Center. Participants included 242 Operation Enduring Freedom and Operation Iraqi Freedom Veterans with chronic, disabling musculoskeletal pain of the cervical or lumbar spine or extremities (shoulders, knees, and hips). The intervention involved 12 weeks of analgesic treatment and optimization according to an algorithm coupled with pain self-management strategies (Step 1) followed by 12 weeks of brief cognitive behavioral therapy (Step 2). All aspects of the intervention were delivered by nurse care managers. The primary outcome was pain-related disability (Roland Morris Disability Scale) at 9 months. We also assessed pain interference (Brief Pain Inventory) and pain severity (Graded Chronic Pain Scale). The primary analysis compared the change from baseline to 9 months between study groups. To estimate treatment effects, we used random-effect linear regression adjusted for age, sex, severity of pain, and baseline value of outcome measure. Analyses were conducted with SAS version 9.13.
RESULTS: There were no significant baseline differences between stepped-care intervention and usual care arm. The mean age of ESCAPE participants was 36.7 years (range = 21 to 73 years) and 88.4 % were men. In terms of racial mix, 77.7 % were white, 13.0 % were black, and 9.2 % classified as other. The primary site of pain was the low back (57 %) followed by knee pain (21.6 %), neck pain (7.5 %), shoulder pain (7.1 %), and hip pain (6.6 %). Two-thirds (66.4 %) had been in the Army, 74.9 % had been deployed to Iraq, 8.8 % deployed to Afghanistan, and 16.3 % deployed to both conflicts. One hundred twenty-one intervention participants and 120 usual care participants were included in the primary analysis. At 9 months, the mean decrease from baseline in the Roland Morris Disability Scale score was 1.6 points (95 % confidence interval [CI] 0.72–2.6) in the usual care group and 3.4 points (95 % CI 2.5–4.3) in the stepped-care intervention group (between group difference of −1.8 points, −3.1 to −0.51; p = 0.0063). The mean decrease from baseline in the Brief Pain Inventory interference score was 0.86 points in the usual care group and 1.6 points in the intervention group (between group difference of −0.69 points, −1.3 to −0.12; p = 0.0170). The Graded Chronic Pain Scale severity score was reduced by 7.1 % (95 CI’s 2.7 % to 11.5 %) and 20.4 % (95 % CIs 14.3 % to 26.6 %), respectively (between group difference 13.3 %, 11.6 % to 15.1 %; p = 0.0013).
CONCLUSIONS: A stepped-care intervention that combined analgesics, self-management strategies, and brief cognitive behavioral therapy resulted in a significant reduction in pain-related disability, pain interference, and pain severity in Veterans of Iraq and Afghanistan with chronic, disabling musculoskeletal pain of the spine and extremities.
EVALUATION OF THE MODIFIED HEART SCORE IN PREDICTING OUTCOMES IN PATIENTS WITH LOW-RISK CHEST PAINCarlos Calle-Muller; David Paje; Matthew Cerasale; Iani Patsias. Henry Ford Hospital, Detroit, MI. (Tracking ID #1940326)
BACKGROUND: The HEART (History, ECG, Age, Risk factors and Troponin) score was recently shown to be potentially useful in identifying patients presenting with chest pain with a very low pretest probability of acute coronary syndrome (ACS) and where further testing may not be beneficial. However, all of the previous studies relied on the investigators’ retrospective appraisal of the patient’s chest pain history and used a nonstandard definition for classifying chest pain. We adopted the American Heart Association’s clinical classification of chest pain to modify the HEART score and prospectively evaluated its ability to predict outcomes in patients with low-risk chest pain.
METHODS: Patients presenting with chest pain were considered at low risk for ACS and were referred to the observation unit of an 805-bed hospital if they had none of the following features: ongoing chest pain, dynamic ST-segment changes and cardiac troponin I ≥ 0.20 ng/mL. As part of the initial evaluation, clinicians filled out a standard data collection tool that included clinical variables necessary to calculate the modified HEART Score (Table 1). The occurrence of the composite endpoint of death from any cause, acute myocardial infarction and coronary revascularization within 30 days of the visit were recorded through follow-up phone call and medical records review. Sensitivity, specificity, and positive and negative predictive values were calculated.
RESULTS: Of the 420 patients that were enrolled, 298 (71 %) had complete follow-up data and were included in the analysis. The composite endpoint occurred in 9 (3 %) patients within 30 days (1 died, 3 had nonfatal acute myocardial infarction and 5 had significant disease requiring coronary revascularization). A cardiac endpoint occurred in 3 of 155 (1.9 %) patients with a HEART score 0 to 3, and in 6 of 143 (4.2 %) with a score of >3 (p = 0.25). The sensitivity, specificity, and positive and negative predictive values of a HEART score >3 in predicting a cardiac endpoint are shown in Table 2.
CONCLUSIONS: The incidence of significant coronary events is very low among patients presenting with chest pain who do not have ongoing chest pain, dynamic ST-segment changes or abnormal cardiac troponin. The modified HEART score does not appear to be useful in further identifying those who are at very low risk.
EVALUATION OF THE MODIFIED NORTH AMERICAN CHEST PAIN RULE TO IDENTIFY PATIENTS AT VERY LOW RISK OF ACUTE CORONARY SYNDROMEMatthew Cerasale; David Paje; Carlos Calle-Muller; Iani Patsias. Henry Ford Hospital, Detroit, MI. (Tracking ID #1940296)
BACKGROUND: The North American Chest Pain Rule (NACPR) was developed to identify patients presenting with chest pain who are at very low risk for a cardiac event and who may be suitable for discharge from the emergency department without additional investigations. However, this tool defines chest pain as typical for acute coronary syndrome based on the judgment of the attending emergency physician, which makes it difficult to standardize. We adopted the American Heart Association’s definition of typical angina to modify the chest pain component of the NACPR and we prospectively evaluated its ability to predict outcomes among patients with low-risk chest pain.
METHODS: Patients were considered to have low-risk chest pain and were referred to the observation unit of an 805-bed hospital if they had no ongoing chest pain, no dynamic ST-segment changes and no abnormal cardiac troponin value. During their initial evaluation, clinicians filled out a standard data collection tool that included clinical variables necessary to capture the components of the modified NACPR (Table 1). Primary outcome was the composite of all-cause mortality, acute myocardial infarction and coronary revascularization within 30 days of the visit. Follow-up was done through phone call and medical records review. Test characteristics of the modified rule were calculated.
RESULTS: Baseline data was recorded on 419 patients, one patient was excluded because of ST-segment elevation in the initial ECG. A total of 298 patients had complete follow-up data (72 % with phone follow-up) and were included in this analysis. The composite endpoint occurred in 9 (3 %) patients within 30 days (1 died, 3 had nonfatal acute myocardial infarction and 5 had significant disease requiring coronary revascularization). All 9 events occurred in patients that had at least one component of the modified NACPR. The sensitivity, specificity, and positive and negative predictive values of the presence of any component of the modified NACPR in predicting the primary outcome are presented in Table 2.
CONCLUSIONS: The modified NACPR appears useful in identifying chest pain patients who are at very low risk of acute coronary syndrome and who may benefit from early discharge from the emergency department.
EXAMINING PERCEIVED BARRIERS TO GOOD NUTRITION IN A SUBSET OF HOMELESS WOMEN IN URBAN BIRMINGHAM, ALABAMASandhya L. Kumar1; Jeremey B. Walker1; Dennis J. Pillion2; Amanda Willig2; April Agne2; Andrea Cherrington2. 1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama at Birmingham, Birmingham, AL. (Tracking ID #1939137)
BACKGROUND: The relationship between homelessness and poor health is well-recognized. Many of today’s food-insecure homeless suffer from obesity-related complications, including hypertension and diabetes. Homeless individuals who regularly access meals provided by charitable services are at the mercy of well-meaning food-providers. The lack of control over quality and quantity of meals is often viewed as an insurmountable barrier, and can be particularly frustrating for patients and their health educators/providers as they attempt to discuss dietary modifications as an avenue for chronic disease management. The resulting apathy further perpetuates disregard for nutrition. In this study, we used a mixed-methods approach to further explore the various factors that influence dietary choice in the homeless population. In partnership with three community organizations, we interviewed and surveyed women who sought services from an urban Birmingham charitable meal program with the aim of exposing the perceptions and attitudes they held regarding good nutrition, as well as to assess if any relationships existed between factors such as health status, extent and accuracy of nutrition knowledge, food security, and determinants of healthy food choices.
METHODS: A convenience sample of 49 women was recruited over a 6 week period (Summer 2013) based on participation in meal services provided by a partner agency’s charitable organization. In this mixed-methods study, 11 women in a transitional housing program took part in a semi-structured interview focused on perceived barriers to good nutrition and an 83-item questionnaire on demographics, health status, extent and accuracy of nutrition knowledge, food security, and determinants of healthy food choices. Another 38 women recruited from the same institution’s “Day Center” participated in the survey alone. Quantitative analysis was performed using SPSS. Qualitative content analysis was conducted to identify major categories and substantive themes.
RESULTS: Mean age category was 41–50 years. Diabetes and hypertension prevalence were 20 % and 53 %, respectively. Sixty-three percent of participants express a desire for a “special diet”, 81 % citing for health concerns. Thematic analysis of interview scripts reveals food concepts (good versus bad foods, utility versus consequences), desired nutrition knowledge (food budgeting, how to shop, components of food), and influences on food choices (availability, access, competing demands, social reciprocity).
CONCLUSIONS: This subset of homeless experiences a high rate of hypertension and diabetes. Many in the homeless population display an interest in learning more about nutrition and having more control over dietary intake as a way of health management. However, for those on the streets or in temporary housing, meeting immediate physiological needs is the highest priority and dietary control is a secondary or tertiary concern. For these individuals, it seems most appropriate to impact diet by increasing the dietary adequacy and nutrition density of charitable meals. Nutrition-based education and lifestyle modification is a more practical and a desired avenue of chronic disease prevention and management in the transitional population. Individuals in transitional programs are focused on conquering higher order needs, such as security of employment, housing, and health. Given this consideration, this group seems the most amenable to productive discussion of dietary choices and nutrition education. Permanent incorporation of nutrition-based life-skills classes that focus on practical application of nutrition knowledge (i.e. food budgeting, how to shop, etc.) is a long-term investment that will help redefine concepts of food and benefit health status, financial status, and future generation’s health-promoting behaviors.
EXAMINING THE POTENTIAL FOR CPOE SYSTEM DESIGN AND FUNCTIONALITY TO CONTRIBUTE TO MEDICATION ERRORSArbor J. Quist1; Alexandra Robertson1; Thu-Trang Thach1; Lynn A. Volk2; Adam Wright1,2; Shobha Phansalkar1,3; Sarah P. Slight1,4; David W. Bates1,5; Gordon D. Schiff1,5. 1Brigham and Women’s Hospital, Boston, MA; 2Partners HealthCare, Wellesley, MA; 3Wolters Kluwer Health, Indianapolis, IN; 4University of Durham School of Medicine, Durham, United Kingdom; 5Harvard Medical School, Boston, MA. (Tracking ID #1937921)
BACKGROUND: The Institute of Medicine has estimated that at least 1.5 million people are harmed by medication errors each year, thus efforts to reduce medication errors are an essential component to improving patient safety. While computerized prescriber order entry (CPOE) systems have reduced medication errors by creating legible and structured prescriptions and incorporating effective clinical decision support, they have also introduced new types of errors and must be optimally designed if medication errors are to be minimized. The FDA Brigham and Women’s Hospital Computerized Prescriber Order Entry Medication Safety Project is an FDA-funded study conducted to better understand 10 CPOE systems, their functionality, features, interfaces, and safety, at 6 sites.
METHODS: We examined 10 different CPOE systems that varied in providers, vendors, and care settings across 6 different healthcare facilities. CPOE functionality data were collected through usability testing and detailed interviews with key CPOE system users and managers at each site. Test patients were created in each system and a CPOE Medication Safety Assessment Tool was developed to assist in eliciting and collecting structured information regarding the systems and their functions. These interviews and system evaluations were recorded, transcribed, and organized to highlight the similarities and differences between functionality in the systems.
RESULTS: We found a high level of inconsistency in the functionality of the CPOE systems evaluated, both within and across systems. Differences were found based on the system, care setting, care provider, and user role. Inpatient and outpatient systems at the same site were often unable to communicate, causing confusion and burdening clinicians. Users with different roles, such as physicians, nurses, and pharmacists, were found to have different system capabilities. Differences in workflow and medication prescribing across specialties led to some CPOE functionality that varied according to specialty. We found variation in discharge modules, override reasons, and hard stops. In searching institutional “paper trails” for CPOE system change reasons, we found a lack of system documentation of modifications and features. Some unanticipated findings included frequent user unawareness of obvious screen items and features as well as the surprising degree of local customization of various vendor-based systems (including customized interfaces, clinical decision support, order capabilities, and drug name presentation). We found studying CPOE system design features and rationale to be challenging as we attempted to connect the local patient safety logs. We observed differences in the mental models between CPOE system designers and users, complications with creating and using test patients to evaluate functionality, and difficulties in sharing and comparing useful, but proprietary, information. For example, it was often difficult or impossible to create test patients that were pregnant to simulate scenarios that would trigger pregnancy-related alerts.
CONCLUSIONS: A detailed and comprehensive understanding of the functionality of CPOE systems is important in building better systems that will reduce errors due to inefficiencies and inconsistencies in CPOE systems. Design features and tracking of issues arising from experience with these systems need to be more systematically catalogued. To more effectively prevent CPOE frustrations and errors, functionality needs to be improved through more standardized and less confusing interfaces and design features.
EXCESSIVE PERSPIRATION IS A PREDICTIVE FACTOR FOR AGGRAVATION OF RHABDOMYOLYSISMasaki Tago1; Naoko E. Furukawa3,1; Yuka Naito1; Akiko Eiri1; Hiroki Aihara1; Motoshi Fujiwara1; Jun Tokutomi1; Motosuke Tomonaga1; Yuta Sakanishi2; Tsuneaki Yoshioka1; Norio Fukumori2; Masaki Hyakutake1; Itaru Kyoraku1; Takashi Sugioka2; Shu-ichi Yamashita1. 1Saga Medical School Hospital, Saga, Japan; 2Saga Medical School, Saga, Japan; 3Saga Medical School, Saga, Japan. (Tracking ID #1912342)
BACKGROUND: Rhabdomyolysis is a serious syndrome in which skeletal muscle fibers are damaged and release breakdown products such as creatinine kinase, or myoglobin into circulation. Some of the products are harmful and may lead to acute kidney injury, multiple organ failure, and even death. However, which factors are valuable in predicting the prognosis of this condition remains to be clarified. The objective of the study was to elucidate the predictive factors for the prognosis of this syndrome.
METHODS: We analyzed consecutive 53 cases of rhabdomyolysis hospitalized at the department of general medicine of the Saga University Hospital in Japan by retrospective chart review from 2006 to 2013. The diagnosis of rhabdomyolysis was made by the presence of increased amount of serum creatinine kinase (CK) (>200 IU/L). At first, we divided the patients into two groups, one with serious consequences of death or acute kidney injury requiring blood purification therapies such as hemodialysis (HD) or continuous hemodialysis and filtration (CHDF) (Group A) and the others without ones (Group B). Then, we compared the characteristics of the patients of both groups about age, sex, number of days from onset to admission, main reason of admission, symptoms and signs (fever, muscle rigidity, extrapyramidal signs, the state of consciousness, excessive perspiration, dehydration), blood chemistry on admission (CK, blood urea nitrogen, creatinine, albumin, sodium and potassium), and maximum levels (CK, blood urea nitrogen, creatinine).
RESULTS: All of the 53 patients who were enrolled were Japanese (men, 60.4 %; women, 39.6 %; age 58.6 +/− 17.2). Group A consisted of 5 cases, in which 2 cases required blood purification therapies (HD/CHDF), and 4 cases deceased. According to univariate analysis, sex, age, fever, muscle rigidity, consciousness, CK, creatinine level on admission, and maximum level of CK were not significantly related to serious consequences. Only the finding of excessive perspiration on admission was related to the serious consequences (odds ratio 31.33, 95 % confidence interval 2.17–450.07, p-values < 0.05).
CONCLUSIONS: The presence of excessive perspiration on admission is a useful factor to predict the serious prognosis of the patients who are admitted because of rhabdomyolysis.
EXPENSIVE DREAMS: SLEEP DURATION AND INCOME LEVELS IN GENEVA, SWITZERLANDIdris Guessous2,1; Cédric Gubelmann1; Jean-Marc Theler2; José Haba-Rubio3; Jean-Michel T. Gaspoz2; Pedro Marques-Vidal4. 1Lausanne University Hospital, Lausanne, Switzerland; 2Geneva University Hospitals, Geneva 14, Switzerland; 3Center for Investigation and Research in Sleep, Lausanne University Hospital, Lausanne, Switzerland; 4Institute of Social and Preventive Medicine (IUMSP), Lausanne, Switzerland. (Tracking ID #1935443)
BACKGROUND: Sleep has been shown to depend on socioeconomic status (SES), but the associations remain controversial. We aimed to assess associations between sleep duration and several markers of SES (education, monthly income, and nationality).
METHODS: Adults of a representative sample of the Geneva population were recruited. Self-reported sleep duration was assessed by questionnaire, where the participants indicated the usual time they went to bed and they woke up.
RESULTS: The analysis included 3853 adults (50 % women, 51.7 ± 10.9 years). After adjusting for survey year, sleep duration was higher among elderly subjects (adjusted mean ± SE: 7.67 ± 0.02, 7.82 ± 0.03 and 8.41 ± 0.04 h/day for age groups [35–50], [50–65] and [65+ years, respectively, p < 0.001), and lower in participants who were foreigner (7.77 ± 0.03 vs. 7.92 ± 0.03 h/day for Swiss nationals, p < 0.001), with higher education (7.92 ± 0.02 for non-university vs. 7.74 ± 0.03 h/day for university, p < 0.001) or higher income (8.10 ± 0.04, 7.84 ± 0.03 and 7.70 ± 0.03 h/day for <5′000 SFr; 5′000–9′500 SFr and >9′500 SFr, respectively, p < 0.001). Similar associations were found for prevalence of sleep <8 h/day or after multivariate adjustment, except that the association with education was borderline significant (p = 0.065). Finally, no significant trend was found both for reported sleep time (7.7 ± 1.1 in 2005 vs. 7.8 ± 1.1 h/day in 2011, p = 0.36) or the prevalence of sleep <8 h/day, and no interaction was found between SES markers and study year.
CONCLUSIONS: Income, more than education, is negatively and positively associated with sleep duration and short sleep in the Geneva population. No change in sleep duration and short sleep was observed from 2005 to 2011.
EXPLORING THE ASSOCIATION BETWEEN PATIENT-CENTERED MEDICAL HOME TEAM-BASED CARE ELEMENTS AND EMPLOYEE JOB SATISFACTION AT THE VHAIan A. Randall1,2; Henry B. Harvey2; David Mohr3,4; Emily D. Dolan1,2; Karin M. Nelson1,5; Paul Hebert1,5; Stephan D. Fihn5,6; Christian Helfrich1,2. 1University of Washington, Seattle, WA; 2VA Puget Sound Healthcare System, Seattle, WA; 3VA Boston Healthcare System, Boston, MA; 4Boston University, Boston, MA; 5VA Puget Sound Healthcare System, Seattle, WA; 6Veterans Health Administration, Seattle, WA. (Tracking ID #1938409)
BACKGROUND: The Veterans Health Administration (VHA) implemented a patient-centered medical home (PCMH) model, termed Patient Aligned Care Teams (PACT), in 2010. We explored how various team-based care elements of this organization-wide implementation and other employee- and clinic-level covariates were associated with employee job satisfaction.
METHODS: We analyzed a cross-sectional, web-based survey of VHA employees from May 2012 and VHA administrative data. Overall job satisfaction was scored on 5-point scale from “Not at all satisfied” to “Very satisfied” and modeled using multivariate linear regression. PACT team-based care elements that are characteristic of either the presence or absence of an implemented PCMH model were tested for associations with employee job satisfaction.
RESULTS: 4,565 VHA primary care employees, including primary care providers (physicians, physician assistants and nurse practitioners), nurse managers, clinical assistants and clerks from 536 different primary care clinics responded to the survey. Results presented below are coefficients representing the estimated linear change on the 1–5 job satisfaction outcome scale (e.g., a β of 0.5 represents an estimated job satisfaction outcome that is 0.5 points higher). Among PACT characteristics, participatory decision-making (i.e., giving PACT team members a voice in decisions about how the team operates) was associated with higher job satisfaction (s = 0.36, 95 % CI: 0.21, 0.52), while a chaotic or stressful work environment (β = −0.49, 95 % CI: −0.59, −0.40) and spending time on tasks someone with less training could do (β = −0.15, 95 % CI: −0.24, −0.05) were associated with lower job satisfaction. Among employee-level covariates, being a Team Leader (β = 0.13, 95 % CI: 0.04, 0.21), Supervisor (β = 0.36, 95 % CI: 0.16, 0.55) or Manager (β = 0.57, 95 % CI: 0.39, 0.76) were associated with higher job satisfaction compared to having no supervisory responsibility. Being a nurse (β = 0.17, 95 % CI: 0.06, 0.28), clinical associate (β = 0.46, 95 % CI: 0.34, 0.57), or administrative clerk (β = 0.22, 95 % CI: 0.08, 0.35) were associated with higher job satisfaction compared to PCPs. Spending more than 80 % of one’s time in primary care (β = −0.21, 95 % CI: −0.39, −0.03) was associated with lower job satisfaction. Having VA tenure of 1–2 years, 2–5 years, 5–10 years, 10–15 years, 15–20 year or more than 20 years was associated with lower job satisfaction, compared to having VA tenure less than 6 months. Among clinic-level covariates, working in a clinic with a higher mean patient comorbidity (as measured by mean DCG score) was associated with higher job satisfaction (β = 0.14, 95 % CI: 0.06, 0.22), while working in a VA Medical Center-affiliated clinic was associated with lower job satisfaction (β = −0.11, 95 % CI: −0.20, −0.03).
CONCLUSIONS: Some PACT characteristics hypothesized to correlate with job satisfaction were associated with overall job satisfaction after adjusting for employee- and clinical-level covariates. Participatory decision-making was associated with higher job satisfaction while working in a chaotic or stressful environment and working below one’s competency were associated with lower job satisfaction. Results indicated that job satisfaction may be lower among PCPs, longer-tenured VA employees and primary care personnel, posing potential long-term challenges to the sustainability of the PACT model and retention of key personnel.
EXTENT AND PREDICTORS OF TRAINING IN OFFICE-BASED TREATMENT OF OPIOID ADDICTION IN U.S. RESIDENCY PROGRAMS: A NATIONAL SURVEY OF PROGRAM DIRECTORSLello Tesema; Jeffrey Marshall; Rachel Hathaway; Christina Pham; Camille Clarke; Genevieve Bergeron; James Yeh; Michael Soliman; Danny McCormick. Cambridge Health Alliance and Harvard Medical School, Cambridge, MA. (Tracking ID #1938929)
BACKGROUND: Opioid addiction (OA) is a public health epidemic and is associated with a high mortality rate. Highly effective pharmacotherapies to treat OA exist, but less than 15 % of those in need of treatment receive it. While methadone and buprenorphine are the gold standard treatments for OA, buprenorphine alone can be prescribed in office-based settings, potentially providing greater access. Prescription of buprenorphine in ambulatory medical practice is uncommon, however, potentially due to limited instruction of physicians during residency training. However, little is known about the extent to which residency programs provide training in the prescribing of buprenorphine or the treatment of OA.
METHODS: We conducted an email based survey of all U.S. residency program directors (RPD) in Family Medicine, Internal Medicine and Psychiatry that were listed on the website of the American College of Graduate Medical Education (ACGME). Survey items assessed the extent of program training in the use of buprenorphine, in addictions medicine generally, and whether or not residents were required or encouraged to obtain a Drug Enforcement Administration buprenorphine waiver (required to prescribe this medication). We also assessed program directors’ views and attitudes regarding the use of buprenorphine and potential barriers to buprenorphine training. We produced descriptive statistics for all items and also compared responses of RPD across the three program types. We also examined the relationship between RPD views of the value of buprenorphine and the extent of program training in buprenorphine by calculating odds ratios of 95 % confidence intervals.
RESULTS: Of the 947 RPD we surveyed, 471 responded (49 % response rate). The majority of RPD report that their residents frequently manage patients with opioid addiction (77 %), believe buprenorphine is an important treatment option for opioid dependence (88 %), and believe increased residency training in buprenorphine would expand access to care for OA patients (73 %). Yet a minority of programs train residents in the use of buprenorphine (36 %), require or encourage residents to obtain a waiver (23 %) or dedicate greater than 12 h (over 3 years) to formal training to addiction medicines (23 %), although psychiatry programs were more likely to do so (data not shown) A minority also believed that prescribing buprenorphine should be a core competency (37 %) of their discipline. We also found that RPD belief that buprenorphine is an important treatment option for OA was associated with a greater odds of the program providing training in buprenorphine (3.5 [CI95% 1.6–7.4)]. The most frequently cited barriers to implementing buprenorphine training in residency programs included: shortage of licensed preceptors (77 %), competing curricular priorities (64 %), and lack of support services (54 %).
CONCLUSIONS: Most residency programs frequently care for OA patients and most RPD believe in the effectiveness of buprenorphine and its ability to expand access to treatment for OA. Yet only a minority of training programs offer formal training in the treatment of OA generally, or with buprenorphine specifically. Increasing the exposure of physicians during residency training to ambulatory treatment of OA using buprenorphine could promote greater access to this treatment option.
EXTERNAL VALIDATION OF A SCORING SYSTEM THAT PREDICTS READMISSION OF PATIENTS WITH ACUTE PANCREATITIS TO THE HOSPITAL WITHIN THIRTY DAYS OF DISCHARGEMohammed Aljasmi; Aymen Bukannan; Yathreb Alaali; Ahmed Saeed; Gregory Buran. Henry Ford Hospital, Detroit, MI. (Tracking ID #1939127)
BACKGROUND: Acute pancreatitis (AP) is one of the medical conditions that cause a heavy financial burden on the American health care system, in addition to causing significant morbidity to patients. Studies have estimated that the average cost of hospitalization for acute pancreatitis ~$10 k, and acute pancreatitis is responsible for about $2.2 billion in US health care expenditure annually. Studies have shown that the rate for early readmission for acute pancreatitis was found to be close to 20 %. Our aim was to validate a recently published scoring system to predict readmission of patients with acute pancreatitis to the hospital within 30 days of discharge.
METHODS: A Retrospective review of patients with AP admitted to Henry Ford Hospital from October 2008 to December 2010. Inclusion and exclusion criteria reflected that of the original study. Diagnosis of AP required two of the following: characteristic abdominal pain, serum amylase/lipase more than or equal to three times the upper limit of normal, or CT of the abdomen within the first 7 days of hospitalization demonstrating changes consistent with AP. Factors of the scoring system were analyzed at time of discharge including eating less than solid diet; GI symptoms; pancreatic necrosis; antibiotics; pain. Results were analyzed using Logistic regression modeling and a ROC curve to evaluate the strength and performance of the scoring system.
RESULTS: There was 380 patient admitted during the study period with 47 being readmitted within the 30 day period for a readmission rate of 12 %. An odd ratio of 1.381 (p-value <000.1) indicate that each single unit increase in the risk score corresponds to approximately a 1.381 times increase in the likelihood of 30-day readmission within both settings. The resulting ROC curve areas 0.66 indicate that the risk score is a moderate predictor of 30-day readmission.
CONCLUSIONS: Our findings suggest that the “SNNAP” scoring system was predictive of 30-day readmission.
Comparison in 30 day readmission in patients who are low, moderate and high risk for readmission
| Readmission with 30 days | N | |
| Risk Score <2 | 24 (8 %) | 287 |
| Risk Score 2–3 | 7 (15 %) | 47 |
| Risk Score ≥4 | 16 (35 %) | 46 |
| 47 (12.4 %) | 380 |
ROC Curve to predict readmission within 30 days
FACTORS ASSOCIATED WITH LOSING AT LEAST 75 % OF GESTATIONAL WEIGHT GAIN BY EARLY POSTPARTUM IN WOMEN WITH RECENT GESTATIONAL DIABETESJacinda M. Nicklas1,2; Chloe A. Zera3; Sue E. Levkoff4,5; Ellen W. Seely2. 1University of Colorado School of Medicine, Aurora, CO; 2Brigham and Women’s Hospital, Boston, MA; 3Brigham and Women’s Hospital, Boston, MA; 4Brigham and Women’s Hospital, Boston, MA; 5University of South Carolina, Columbia, SC. (Tracking ID #1937893)
BACKGROUND: Women with gestational diabetes (GDM) have a 30–70 % risk for developing type 2 diabetes (T2DM) later in life. Postpartum weight retention is highly predictive for future obesity, and further increases risk for T2DM. We sought to identify factors associated with losing at least 75 % of gestational weight gain by early postpartum in women with recent GDM.
METHODS: We recruited women with GDM during pregnancy or just after delivery. Pre-pregnancy weight was self-reported at recruitment; gestational weight gain, mode of delivery, and insulin use were extracted from medical records. At a mean of 7.2 (±2.1) weeks postpartum we measured weight, height, and administered questionnaires, including: demographics, breastfeeding, sleep, Edinburgh Postnatal Depression Scale, Harvard Food Frequency, and the International Physical Activity Questionnaire. After conducting an analysis of univariates, we used backward selection to fit a multivariable logistic regression model for univariates with p < .2 to identify factors associated with losing 75 % or more of gestational weight gain by early postpartum.
RESULTS: Our study included 75 women (mean 33 ± 5 years; pre-pregnancy BMI 31.4 (±5.6) kg/m2; 57 % White, 29 % African-American, 15 % Asian, with 20 % identifying as Hispanic and 34 % low income). Mean pregnancy weight gain was 12.5 kg (±7.8). Fifty-two percent of participants lost at least 75 % of their pregnancy weight gain by the study visit. Dietary composition, fiber intake, added sugars, and glycemic index were similar between those who demonstrated early weight loss and those who did not, and consequently were not included in the multivariate model. Physical activity, sedentary time, race/ethnicity, education, income, mode of delivery, postpartum depressive symptoms, and breastfeeding were also similar between groups and not included in the model. In a multivariate model adjusting for weeks postpartum, only increased age (OR 1.31; 95 % CI 1.06 to 1.76 per year) and less gestational weight gain (OR 0.63; 0.48 to 0.76 per kg) were associated with at least 75 % early postpartum weight loss. Insulin use, nulliparity, and sleep were not retained in the model.
CONCLUSIONS: A substantial proportion of women with recent GDM lost at least 75 % of their gestational weight gain by early postpartum. Older women and those who had gained less weight during pregnancy were significantly more likely to have lost at least 75 % of gestational weight. Limiting gestational weight gain may help women with GDM return to pre-pregnancy weight quickly during the postpartum period.
FACTORS ASSOCIATED WITH PATIENT’S VIEW ABOUT DISAPPEARENCE OF THEIR CHRONIC PAINMichel P. Kossovsky1; Valerie Piguet2; Christine Cedraschi1; Anne-Francoise Allaz1. 1Geneva University Hospitals, Geneva, Switzerland; 2Geneva University Hospitals, Geneva, Switzerland. (Tracking ID #1935509)
BACKGROUND: Chronic pain is a frequent complaint among internal medicine patients. One important aspect in the care of such patient is to understand how they apprehend the manifestation of the pain and what they expect for the future. The aim of our study was to investigate the variables associated with chronic pain patients’ expectations about the possibility of pain disappearance.
METHODS: A self-administered questionnaire was given to all patients referred to our pain centre over a 2 year period. Patients were asked about the likelihood of pain disappearance (dichotomic answer: possible/probable vs. unlikely/impossible). Multivariate logistic linear regression analysis evaluated which variables were associated with the likelihood of pain disappearance. The model was controlled for age and gender, the presence of depression (evaluated with the Beck Depression Inventory), anxiety (evaluated by the Hospital anxiety and depression scale), present pain intensity (evaluated on a visual analog scale (0–10 cm)), duration of chronic pain, attribution of pain origin (extrinsic, intrinsic or undetermined) and perceived level of illness on a 4 level scale (from considerably to not at all).
RESULTS: We collected information on 437 patients. Mean age was 53; women were 284 (65 %). Table represents the odds-ratios associated with patients’ estimation of the likelihood of pain disappearance.
CONCLUSIONS: Neither age nor sex were associated with likelihood of pain disappearance according to patients. Interestingly, pain intensity, anxiety or causal attribution were not either associated with likelihood of pain disappearance. Depression, a longer duration of chronic pain and a higher perceived level of illness were significantly associated with a reduced likelihood of pain disappearance. Practitioners confronted with chronic pain patients should be aware that these three variables are linked with patients’ views about the future of their pain and taken into account when planning the treatment.
FACTORS ASSOCIATED WITH THE DECISION TO UNDERGO CONTRALATERAL PROPHYLACTIC MASTECTOMY AT THE TIME OF A BREAST CANCER DIAGNOSISKyungsuk Jung1,2; Kala Visvanathan2. 1Presence Saint Francis Hospital, Evanston, IL; 2Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD. (Tracking ID #1921712)
BACKGROUND: Increasing number of breast cancer patients are electing for contralateral prophylactic mastectomy (CPM) to prevent contralateral breast cancer. CPM was shown to be associated with a survival advantage in women with BRCA1/2 mutation carriers, thus at high risk of developing breast cancer with a life expectancy gain of 0.6–2.1 years. This study sought to identify factors that may affect the decision of breast cancer patients to undergo CPM.
METHODS: A cohort of >1200 women who are at high risk of developing breast cancer were recruited primarily from the high risk clinic. Women with either positive family history of breast or ovarian cancer, positive BRCA1/2 gene or <40 years of age were eligible for inclusion. From this cohort, 370 women diagnosed with breast cancer were identified. All study participants had completed a Questionnaire that included—demographic, disease history, surgical history, lifestyle factors extensive family history of cancer, and genetic testing. Pearson’s χ2 test, univariable analysis and multivariable analysis were used to compare characteristics in both groups.
RESULTS: 81/370 patients with unilateral breast cancer, chose to have a CPM. Univariable analyses showed that younger patients were significantly more likely to undergo CPM (OR, 0.93; 95 % CI, 0.91–0.96). Patients were also significantly more likely to under go CPM if they had bilateral oophorectomy (OR, 2.18 95 % CI, 1.22–3.87), deleterious result from BRCA test (OR, 1.87, 95 % CI, 1.00–3.49), had breastfeeding experience (OR, 2.96, 95 % CI, 1.28–3.20) and had a positive family history of breast cancer in 1st and 2nd degree relative (OR, 2.75, 95 % CI, 1.22–6.17). Multivariable logistic regression analysis with significant variables from the above outcome revealed that patients who were younger (OR, 0.92, 95 % CI, 0.89–0.97), had bilateral oophorectomy (OR, 2.63, 95 % CI, 1.18–5.89), had a positive family history of breast cancer in 1st & 2nd degree relative (OR, 4.36, 95 % CI, 1.40–13.60) were more like to choose to undergo CPM. BRCA testing, BRCA test result, marital status, menopausal status and breastfeeding experience were not significantly associated with the use of CPM.
CONCLUSIONS: Younger age is the strongest determinant of undergoing CPM in women at high risk for breast cancer which is consistent with their higher risk of a second breast cancer. For women with family history of breast cancer, it is important to identify their genetic risks to help with their decision. History of oophorectomy was also associated with CPM. However, oophorectomy is reported to be a negative factor on the risk of developing CBC. Evidence-driven models are needed to better inform patients.
FACTORS ASSOCIATED WITH UNCONTROLLED HYPERTENSION IN AN URBAN ACADEMIC PRIMARY CARE CLINIC POPULATIONYaakov Y. Liss; Jonathan Arend; Georgia Giebel; Lauren Peccoralo. Mount Sinai School of Medicine, New York, NY. (Tracking ID #1922682)
BACKGROUND: Despite innumerable anti-hypertensive medication treatment options, only 70 % of Americans receiving treatment have controlled hypertension. Emerging data demonstrates that using a panel-based approach can dramatically improve hypertension control for a clinic population. However, little data exists on factors associated with uncontrolled hypertension within an urban academic primary care clinic population. Identifying such factors is crucial for designing a hypertension panel management program that will succeed in improving hypertension control for this population. This pilot study aims to identify factors related to uncontrolled hypertension in an urban academic primary care clinic population including patient demographics, co-morbid disease status, specific medication use, and disease control measures, as well as to identify visit specific factors that may contribute to hypertension control.
METHODS: Data included in this study is from a convenience sample of all patients with a diagnosis of hypertension seen in an urban academic primary care clinic on October 1, 2013. Data was obtained using the reporting workbench function of the clinic’s Electronic Medical Record (EMR) system. Predictor variables included patients’ sex, ethnicity, race, age, preferred language, marital status, last blood pressure, BMI, presence of diabetes, CHF, CAD, or asthma, ace inhibitor use, beta blocker use, hemoglobin A1C, LDL, and GFR. The outcome variable of uncontrolled hypertension was dichotomized and defined as uncontrolled if the last blood pressure reading performed in an ambulatory setting exceeded 140/90. For categorical non-numeric predictor variables, a chi square test was used to determine an association with blood pressure control, and for continuous predictor variables, a one-way anova test was used. Using the same methods as above, data for all hypertensive patients (>5000) seen in the clinic over a 1-year period will be recorded and analyzed. Additionally, a chart review was performed of 32 randomly selected patients with uncontrolled hypertension to identify the management plan. Eventually, 200 charts will be reviewed by two investigators, with a 3rd investigator to resolve discrepancies.
RESULTS: Based on the convenience sample described above, 261 patients were identified, 40 % of whom had uncontrolled hypertension. Baseline demographic data of the 261 patients identified can be found in Table 1. There was a statistically significant association with gender and uncontrolled hypertension (73 % males uncontrolled versus 27 % females uncontrolled, p = 0.0001), and with race-ethnicity and uncontrolled hypertension (Non-Hispanic African American descent versus Hispanic Non-African American descent versus Non-Hispanic Non-African American Descent, 51 % versus 35 % versus 25 %, p = 0.008). There were no other statistically significant associations. The results of the chart review demonstrated seven common scenarios and management plans (or lack thereof) during the visit when the last (uncontrolled) blood pressure measurement was taken. These are described and quantified in Table 2.
CONCLUSIONS: This study demonstrated significantly worse hypertension control in African American patients and male patients, results that differ significantly from recent national trends where Hispanic and female patients were noted to have worse hypertension control. It is unclear why this discrepancy exists and whether these results are specific to this clinic population or are reflective of a broader trend in urban academic primary care clinics. Additionally, the identification of seven management plans occurring during the patient-doctor interaction presents several different possibilities of interventions that may improve overall hypertension control in this clinic population. Among these are instituting a policy encouraging providers to schedule patients with uncontrolled hypertension for follow up within 1 month; EMR alerts to a patient’s primary doctor when an elevated blood pressure is recorded by a consultant; and a system to remind patients of upcoming appointments.
Table 2. Patient Doctor Interaction Scenarios
| BP Management Plans | Number of Occurrences | Percentage |
| BP normal or near normal- no need for intervention | 6/32 | 19 % |
| BP elevated, meds adjusted, Pt pending f/u within 1 month | 3/32 | 9 % |
| BP elevated, meds adjusted, Pt referred for f/u >1 month | 5/32 | 16 % |
| BP elevated, meds adjusted, Pt referred for f/u within 1 month, Pt never came in | 8/32 | 25 % |
| Elevated BP recorded during consultant visit- BP not addressed during visit | 6/32 | 19 % |
| Elevated BP recorded during urgent visit for other reason at primary care clinic- BP not addressed during visit | 2/32 | 6 % |
| Elevated BP recorded during regularly scheduled primary care visit- BP not addressed during visit. | 2/32 | 6 % |
BP = blood pressure; f/u = follow up; Pt = patient
Table 1. Patient Demographics. Total 261 Patients.
| Sex | Male 29 % | Female 71 % | |
| Race/ Ethnicity | Hispanic Non-AA 45 % | Non-Hispanic AA 40 % | Non-Hispanic Non-AA 15 % |
| Age | Range 33–96 | Mean 63.9 |
AA = African American
FACTORS INFLUENCING MEDICAL STUDENT USE OF ELECTRONIC HEALTH RECORDS: A NEEDS ASSESSMENTDylan Sherry; Megan S. Mcnamara. Case Western Reserve University, Cleveland, OH. (Tracking ID #1934496)
BACKGROUND: Physicians are increasingly using Electronic Health Records (EHRs) in their daily practice, but there is a lack of formalized training about EHRs in most medical school curricula. Education in the use of EHRs for medical students has typically been unofficial “on the job” training by superiors or “how-to” online modules which focus on how to accomplish a specific task using the EHR, such as documenting a history and physical, or writing a progress note. These narrow approaches may lead students to consider the EHR as merely a repository of information, rather than a system which can potentially improve physician workflow and patient care. In order to design effective curricula for medical students, we conducted a needs assessment to understand how students are currently using the EHR and what factors influence their use.
METHODS: We developed a seven-item electronic questionnaire which surveyed students about how they would use the EHR in a particular clinical scenario. Each item was associated with a list of potential responses, and students were asked to justify their choice through a written explanation. The clinical scenarios were developed using the RIME educational framework (Reporter-Interpreter-Manager-Educator) approach to EHR education. We mapped each question to both a RIME category and to ACGME core competencies. For example, a question about whether or not a student might copy and paste a previous day’s progress note to save time would be mapped to the RIME category “Reporter” and to the ACGME core competency “Professionalism.” In order to ensure content validity we sent the questionnaire to 10 national informatics experts for recommendations and made suggested changes. All Case Western Reserve University students were eligible for participation and were recruited via email invitation.
RESULTS: The questionnaire was sent to 495 medical students (Preclinical, Core Clerkships, Elective/Acting Internship) with a 39 % return rate. Using a framework analysis approach we identified 11 specific factors which influence students’ use of the EHR. These included efficiency, communication tool, accuracy of documentation, influence on physician/patient communication, trusting the EHR, intrusive, role modeling, familiarity with the EHR, habit, advancing learning, and impediment to learning. For example, efficiency was a factor that drove students to use templates or copy and paste. Influence on physician/patient communication was a factor which determined how, if at all, the EHR was used during a clinical encounter. These factors could be broadly grouped into how students view the positive and negative aspects of the EHR as it relates to patient care, how students learn about the EHR, and how the EHR influences their medical education overall. The following exemplar quotes help to illustrate why medical students chose to use the EHR in certain ways: “Flipping through fill-in-the-blanks is fastest, but it makes me feel like a robodoctor. I would rather write it out to really make myself learn it, but when you don’t have much time, [templates] are the best.” Core Clerkship Student “I like to be able to shape my differential in my head without a pre-conceived notion of what is important. When I am entering it [in the EHR] afterwards, I am happy that there are templates available so I can be reminded of what I may have missed.” Core Clerkship Student “I [copy and paste] for efficiency in tracking the patient, not just to save time. I like having my note in the same essential format from 1 day to the next so that my eye can scan quickly to pertinent changes. I can quickly see how many days an antibiotic has been taken, which consults have returned recommendations, etc. If I wrote each note from scratch I would have to read the entire thing the next day to find what I wanted to know.” Core Clerkship Student “Copy/pasting is dangerous and can lead to incorrect information in the chart. Always start from scratch and you’ll never be inaccurate. Reference old notes to ensure you’re not missing anything, but don’t copy paste.” Elective/Acting Internship Student
CONCLUSIONS: Medical students are quite aware of the positive and negative impacts that the use of EHRs can have on patient care and on medical education. These factors could be used as a springboard for EHR education. Alongside the current how-to focus, education could be enhanced by addressing student’s concerns about the potential negative impacts of the EHR, such as copy and pasting or interrupting the clinical encounter. Student decision-making regarding EHR use suggests that future EHR education should be placed more in the context of clinical medicine to help students learn to mitigate negative effects on medical education and on patient care.
FACULTY PERCEPTIONS OF COMPETENCY-BASED EVALUATION OF MEDICAL STUDENTSElizabeth Karwowski1,2; Elizabeth Sandman2; Jane M. Liebschutz1; Bruce Fraser3; Jay D. Orlander2,1. 1Boston University Medical Center, Boston, MA; 2Boston VA Healthcare System, Boston, MA; 3Boston University School of Education, Boston, MA. (Tracking ID #1938972)
BACKGROUND: The Accreditation Council for Graduate Medical Education (ACGME) transitioned to competency-based evaluation with its Outcome Project in 1999. The Liaison Committee on Medical Education (LCME) adopted the same core competencies to evaluate medical students: medical knowledge, patient care, interpersonal communication, professionalism, practice-based learning and improvement, and systems-based practice. In May 2012 Boston University School of Medicine changed all student clerkship evaluation forms to a standardized, competency-based format. Little is known about faculty perception of the use of the core competencies to evaluate medical students or their process of student evaluation.
METHODS: Semi-structured, one-on-one interviews were conducted with Department of Medicine physician faculty. Eligibility criteria included evaluating six or more third and/or fourth year clerkship students per year in any clinical setting. Interview questions explored types of faculty interaction with students, faculty attitudes toward student evaluation, and faculty attitudes towards evaluating medical students using the ACGME core competencies. All interviews were transcribed verbatim. Co-investigators reviewed transcripts and identified common themes using Grounded Theory. Two separate investigators coded interviews and achieved consensus on the themes present, resolving discrepancies through discussion. The remaining three co-investigators, with more qualitative experience, checked the final coding schemes for accuracy.
RESULTS: Twelve faculty members with a range of clinical responsibilities (primary care, hospitalist, specialist) and experience participated in the study. All faculty acknowledged that their evaluations were limited due to a lack of direct observation for many competencies. The majority primarily observed case presentations and used these as a proxy for areas they were unable to observe. One faculty commented: “the majority of my evaluation is gonna be based on how they presented the patient to me… so, even if I’m not observing how they’re getting the data, if they come back and they’ve got pretty good data… I can technically check these off [evaluation questions on global assessment form].” For competencies, such as systems based practice, faculty had few, if any, objective or measurable activities to evaluate. Faculty identified multiple barriers to student evaluation including time, other learners, patient care responsibilities, and lack of training in evaluation methods. Faculty expressed significant tension over the evaluation process. They contrasted a sense of inadequacy in their ability to reliably evaluate students with a heightened awareness of the significance of their evaluations in determining student grades. In particular, faculty felt they could identify and evaluate students at the extremes of performance but struggled with discriminating between students in the middle. One faculty commented: “I feel like… there’s not enough ability to distinguish [between students], just using this scoring system. And… presumably, that’s the intent.” The purpose and ramifications of medical student evaluation were not well understood: does evaluation certify that a student is competent or does it provide a means of stratification between students? Often this resulted in self-reported grade inflation.
CONCLUSIONS: Competency-based evaluation on the clinical clerkships presents a challenge to many experienced faculty members. Faculty development around student evaluation that explicitly addresses student milestones and expectations, purpose of evaluation, and feedback on an individual’s grading practices may be beneficial in improving the process. Given the frequency at which it seems to occur, further work needs to elucidate the association of presentation skills as a proxy for other clinical skills.
FAILING TO CHOOSE WISELY: LACK OF TREATMENT DE-INTENSIFICATION IN OLDER PATIENTS WITH DIABETESEve A. Kerr1,2; Rob Holleman1; Mandi L. Klamerus1; Sameer D. Saini1,2; Lillian Min1,2; Sandeep Vijan1,2; Jeremy Sussman1,2; TImothy Hofer1,2. 1VA Center for Clinical Management Research, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1936536)
BACKGROUND: It is increasingly recognized that efforts to intensively improve hemoglobin A1c (A1c) and blood pressure (BP) control in patients with diabetes sometimes unintentionally result in overtreating patients who are unlikely to benefit. Recent guidelines and initiatives like Choosing Wisely recommend less aggressive treatment for older patients with limited life expectancy (LE), since such treatment is unlikely to improve outcomes and may cause harm. This suggests that medication de-intensification is indicated among many patients with limited LE. Yet, we know little about how often providers decrease treatment intensity among patients who are unlikely to benefit. We examined how often the number or dose of medications are decreased in older patients with diabetes and lower than recommended levels of A1c or BP, and whether medication de-intensification is more common in patients with lower LE.
METHODS: Using the Veterans Health Administration’s (VHA) Corporate Data Warehouse, we identified all patients with diabetes, age 70 and older, receiving primary care in VHA during 2012. We then identified the patients’ last A1c and BP during 2012, and their prescribed medications at the time of this index A1c or BP. Patients with A1c < 6.5 % and on hypoglycemic medications (other than metformin alone) were considered eligible for de-intensification. Patients with BP < 130/65 and on BP medications (other than low dose angiotensin converting enzyme inhibitor (ACEI) alone or low dose angiotensin receptor blockade (ARB) alone) were similarly eligible. We determined the proportion of patients who had medications discontinued or had the dose decreased in the 6 months after the index A1c or BP. Using logistic regression, we examined the association between limited LE, based on the Charlson comorbidity index, and de-intensification, controlling for number of medications the patient was taking at the time of the index A1c or BP.
RESULTS: 500,742 patients with diabetes, age 70+, were receiving primary care in VHA during 2012. Among the 114,411 with A1c < 6.5 %, 51 % were on no medications, 15 % were on metformin only, 8 % were on insulin only, 14 % were on sulfonylureas only, and 12 % were on other or combination therapy. Among the 36,686 eligible for de-intensification, 8,466 (23 %) were de-intensified within 6 months. Patients with LE < 5 years were modestly more likely to be de-intensified than those with LE > 10 years (predicted probability 29 % vs 19 %, p < 0.001). Among the 66,750 patients with a BP < 130/65, 10 % were on no medications, 6 % were on low dose ACEI or ARB only, 22 % were on 1 BP medication, and 62 % were on 2 or more BP medications. Among those eligible for de-intensification, 9,883 (21 %) were de-intensified. Patients with LE < 5 years were somewhat more likely to be de-intensified than those with LE > 10 years (predicted probability 24 % vs 17 %, p < 0.001).
CONCLUSIONS: Despite increasing awareness that overtreatment of diabetes may be harmful in older adults, less than one quarter of patients treated to levels significantly lower than recommended had medications de-intensified. While patients with limited LE were more likely to be de-intensified than those in good health, the majority of eligible older patients, even those with limited LE, continued to receive care that is of low value or potentially harmful. Future initiatives that seek to help patients and providers choose wisely will need to address this significant clinical inertia for de-intensification of treatment.
FEAR OF INDEPENDENCE LOSS (FOIL): OLDER ADULT PERCEPTIONS ON REFUSAL OF HOME CAREVanessa Ramirez-Zohfeld1; Kenzie A. Cameron1; Priya Sunkara1; Chris Forcucci2; Megan Huisingh-Scheetz3; Lee Lindquist1. 1Northwestern University, Chicago, IL; 2Aging and In-Home Services of Northeast Indiana, Fort Wayne, IN; 3University of Chicago, Chicago, IL. (Tracking ID #1935965)
BACKGROUND: Remaining in one’s own home is often one of the highest priorities of older adults. As their physical, functional, cognitive, and social needs increase, older adults may require more care in their home which they may illogically refuse. We sought to understand seniors’ perceptions, in particular fears that they faced related to the potential loss of independence and refusal of accepting care in the home.
METHODS: We conducted eight focus groups with older adults (age 65 and older) living in rural, suburban and urban areas. Following a semi-structured interview guide, participants discussed advanced planning, decision-making, barriers, and resources that might have an impact on their ability to remain in their own home. We elicited participant’s thoughts regarding losing independence. Three independent coders used content and constant comparative analysis to interpret results.
RESULTS: Sixty-eight older adults participated in the focus groups with a mean age of 73.9 years (SD = 6.53); 50 (73.5 %) were female. Several major themes related to fear of independence loss (FOIL) as well as strategies to overcome FOIL emerged. FOIL was associated with loss of control, resentment of depending on others, annoyance with working around other people’s schedules, as well as guilt of being burdensome. One participant stated: “I had to depend on friends and neighbors to fix food or shop or do anything, and I thought, I don’t want to be in that position.” A feeling of burden, especially related to their children was a prominent theme across the focus groups with one participant stating: “I don’t want to be a hinder. I don’t want to stop their living. Because I have enjoyed my life and I want them to enjoy their life.” Lack of trust in others and concerns about being exploited were also identified as reasons for FOIL: “At times, it seems like trying to get across a mine field avoiding exploitation from caregivers, from relatives and it is very disconcerting. Who can you trust?” Conversely, multiple participants re-framed the concept of independence and saw the actions as more inter-dependent. Someone noted that even if one becomes more limited over time, the recognition that one is still contributing something meaningful to society is important to overcoming FOIL: “I think we forget what the other person is contributing… the person who is able to see his grandchildren to smile at them; I mean he’s giving them something as well.” Another strategy presented to overcome FOIL was recognition that others may engender positive emotions by helping someone who is in need once they are less able to do so themselves: “When I’m on the receiving end, I’ve got to remember that that’s giving somebody else some joy.”
CONCLUSIONS: Older adults perceive fear of independence loss, which can impact their willingness to accept help. Addressing and promoting strategies to overcome this fear may aid in understanding how to assist seniors to obtaining and accepting needed home care, enabling them to remain safely in their own homes.
FINANCIAL BARRIERS TO CARE AMONG THE INSURED IN MASSACHUSETTS AFTER HEALTH CARE REFORM: DISPARITIES BY RACE, INCOME, AND HEALTH STATUSSonali Saluja1,2; Leah Zallman4,2; Steffie Woolhandler3; David Himmelstein3; David Bor2,1; Danny McCormick2,1. 1Harvard Medical School, Boston, MA; 2Cambridge Health Alliance, Cambridge, MA; 3City University of New York School of Public Health, New York, NY; 4Institute of Community Health - Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1936234)
BACKGROUND: Massachusetts’ 2006 Health Care Reform, the model for the Affordable Care Act (ACA), aimed to increase coverage and access to health care by making care more affordable, particularly for minorities, persons with low incomes and persons in poor health. Little is known about the post-reform prevalence of financial barriers to care among the insured in Massachusetts.
METHODS: We analyzed data from Massachusetts Behavioral Risk Factor Surveillance System, a representative statewide cross-sectional population-based survey of adults, pre-reform (2004–2005) and post-reform (2009–2010). The sample included adults ages 18 to 65 who reported having health insurance (2004–2005: N = 11,876; 2009–2010: N = 21,782). We considered respondents to have a financial barrier to care if they indicated that within the last 12 months they needed to see a doctor but could not because of cost. We compared rates pre and post-reform, overall and for racial/ethnic, income and health status groups. We used multivariate logistic regression models to assess the independent effect of race and income on financial barriers to care after adjusting for other covariates. Finally we examined the association between financial barriers to care and potential markers of need for care and utilization of care.
RESULTS: Among all non-elderly insured adults in Massachusetts, the proportion reporting a financial barrier to care did not change after state health care reform (pre-reform:5.8 %, post-reform:6.0 %; p = 0.60). However, the proportion citing such a barrier rose 37.9 % (from 9.5 to 13.2 %; p = 0.004) among low-income individuals (incomes $15,000–$34,999)—many of whom acquired subsidized insurance requiring copayments for physician visits under the reform. Post-reform, financial barrier rates varied by race and income group—with the highest rates in low-income minority individuals. Among persons with incomes below $15,000, 24.9 % of Blacks and 24.2 % of Hispanics reported financial barriers vs. 9.8 % of Whites (p = 0.011). In multivariate analyses, lower income individuals reported more financial barriers than those with incomes over $50,000 (<$15,000: OR = 5.68 95%CI = 5.61–5.74, $15,000–$34,999: OR = 4.91; 95%CI = 4.87–4.95, $35,000–$49,999: OR = 3.43; 95%CI = 3.40–3.47) as did minorities compared to Whites (Black: OR = 1.18; 95%CI = 1.16–1.19, Hispanic: OR = 1.45; 95%CI = 1.43–1.46). Individuals reporting financial barriers were less likely to have a primary care provider (RR = 0.91; 95%CI = 0.86–0.95) and to have a routine health care visit in the last year (RR = 0.89; 95%CI = 0.83–0.95), but were more likely to have two or more chronic health conditions (RR = 1.26; 95%CI = 1.10–1.44) and much more likely to be in poor or fair health (RR = 3.13; 95%CI = 2.63–3.77).
CONCLUSIONS: After full implementation of health reform in Massachusetts, financial barriers to care among Black, Hispanic and low-income residents are common and strongly related to worse health status. These findings raise concern about the likely persistence of financial barriers to care nationwide after implementation of the ACA.
FINANCIAL INCENTIVES FOR COMPLETION OF FECAL OCCULT BLOOD TESTS AMONG VETERANS: A 2-STAGE PRAGMATIC CLUSTER RANDOMIZED, CONTROLLED TRIALJeffrey T. Kullgren1; Tanisha N. Dicks2; Xiaoying Fu2; George L. Tzanis2,3; Martin Tobi2,3; Steven C. Marcus2,3. 1Ann Arbor VA Healthcare System and University of Michigan, Ann Arbor, MI; 2Philadelphia Veterans Affairs Medical Center, Philadelphia, PA; 3University of Pennsylvania, Philadelphia, PA. (Tracking ID #1940020)
BACKGROUND: Rates of primary care patient completion of prescribed fecal occult blood tests (FOBTs) are often low. A promising tool for improving rates of FOBT completion is financial incentives, which capitalize on insights from behavioral economics that suggest patients disproportionately weight near-term relative to distant costs and benefits. The objective of this study was to identify the dose and design of modest financial incentives that could increase rates of initial completion of prescribed FOBTs among Veterans Health Administration (VHA) primary care patients.
METHODS: We conducted a 2-stage pragmatic cluster randomized, controlled trial in the primary care clinics of the Philadelphia Veterans Affairs Medical Center. All 1,549 patients who were prescribed an FOBT during the study period were enrolled (i.e., there were unique samples of 713 patients in stage 1 and 836 patients in stage 2). In stage 1, patients were assigned to usual care or $5, $10, or $20 for FOBT completion within 30 days. In stage 2, different patients were assigned to usual care or $5, a 1 in 10 chance of $50, or a $500 raffle for FOBT completion within 30 days. The primary outcome was FOBT completion within 30 days. Secondary outcomes included time to FOBT completion and, among patients who had failed to complete a prescribed FOBT in the previous year, 30-day FOBT completion and time to FOBT completion.
RESULTS: In stage 1, $5 (40.4 %, 95 % CI, 30.4 % to 51.3 %; P = 0.96), $10 (44.9 %, 95 % CI, 37.6 % to 52.3 %; P = 0.44), and $20 (45.3 %, 95 % CI, 38.4 % to 52.4 %; P = 0.38) did not lead to a statistically significant increase in FOBT completion compared to usual care (40.7 %, 95 % CI, 33.3 % to 48.6 %). In stage 2, a 1 in 10 chance of $50 led to a statistically significant increase (47.8 %, 95 % CI, 39.5 % to 56.3 %; P = 0.002) but $5 (38.9 %, 95 % CI, 29.5 % to 49.3 %; P = 0.15) and a $500 raffle (41.5 %, 95 % CI, 32.4 % to 51.2 %; P = 0.05) did not lead to a statistically significant increase in FOBT completion compared to usual care (30.7 %, 95 % CI, 25.0 % to 37.0 %). In each stage there were no significant differences in time to FOBT completion and, among patients who had failed to complete a prescribed FOBT in the previous year, no significant differences in 30-day FOBT completion or time to FOBT completion.
CONCLUSIONS: Fixed payments of $5, $10, and $20 did not increase rates of VHA patient completion of prescribed FOBTs within 30 days. However, when we tested 3 different financial incentive designs that shared a common upfront per patient allocation of $5, we found that a 1 in 10 chance of $50 was effective at increasing rates of FOBT completion within 30 days. Our finding serves as an example of a low-cost, scalable intervention that can improve health care quality by promoting patient adherence to a high-value clinical preventive service and adds to a growing evidence base supporting the effectiveness of financial incentives in improving health behaviors among VHA patients.
FINANCIAL ISSUES AND ADULT IMMUNIZATION: MEDICARE COVERAGE AND THE AFFORDABLE CARE ACTLaura Hurley1,2; Megan C. Lindley4; Mandy Allison1,5; Lori A. Crane1,6; Michaela Brtnikova1; Brenda Beaty1,3; Megan Snow1; Carolyn Bridges4; Allison Kempe1,5. 1Children’s Hospital Colorado, Aurora, CO; 2Denver Health, Denver, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4Centers for Disease Control and Prevention, Atlanta, GA; 5University of Colorado Anschutz Medical Campus, Aurora, CO; 6Colorado School of Public Health, University of Colorado, Denver, CO. (Tracking ID #1935920)
BACKGROUND: Financial barriers are often reported for adult vaccinations. The Affordable Care Act addresses some of these barriers; most notably by mandating private health plans to cover Advisory Committee on Immunization Practices recommended vaccinations with first-dollar coverage when delivered by in-network providers. The law does not change coverage of vaccines by Medicare: Medicare Part D, a pharmaceutical benefit, covers some vaccines, and Medicare Part B, a medical provider office-based benefit, covers others. Medicare part D has been seen as a barrier to physician-based vaccination. Our objectives were to assess among general internists (GIM) and family physicians (FM): 1) how often vaccines are deferred or refused by adult patients for financial reasons 2) how often physicians reported not recommending an adult vaccine for financial reasons 3) knowledge of Medicare coverage of vaccines, and 4) awareness of vaccine specific provisions of the Affordable Care Act.
METHODS: We administered an Internet and mail survey from June to October 2013 to a national network of 438 GIM and 401 FM physicians representative of the American College of Physicians and American Academy of Family Physicians memberships. Descriptive analyses were performed.
RESULTS: Response rates were 72 % (317/438) for GIM and 59 % (236/401) for FM. Depending on the vaccine, 2–23 % of GIM and 5–30 % of FM reported adult patients defer or refuse vaccines due to financial reasons the majority of the time. The vaccines most commonly deferred or refused by patients for financial reasons were zoster and human papillomavirus vaccine for both specialties. Physicians in many instances reported they do not recommend vaccines when they thought a patient could not afford it (GIM 4 % ‘frequently’, 16 % ‘sometimes;’ FM 5 % ‘frequently’, 20 % ‘sometimes’), when they thought a patient’s insurance would not cover the vaccine (GIM 9 % ‘frequently’, 24 % ‘sometimes’; FM 12 % ‘frequently’, 24 % ‘sometimes’) and when they thought a patient could receive a vaccine more affordably elsewhere (GIM 9 % ‘frequently’ 30 % ‘sometimes’; FM 11 % ‘frequently’, 26 % ‘sometimes’). The table shows physicians’ knowledge regarding Medicare coverage for vaccines. Over a third of physicians were unaware of provisions in the Affordable Care Act that promote vaccinations (GIM-39 %, FM-34 %) and one-fifth were only ‘a little aware’ (GIM-20 %, FM 17 %) of these provisions.
CONCLUSIONS: Patients are refusing and physicians are not recommending adult vaccinations for financial reasons. Increased knowledge of Medicare coverage would better enable physicians to direct older patients to the best venue to receive vaccines, particularly if their practice does not bill Medicare Part D. Heightened awareness of the favorable financial implications of the Affordable Care Act on vaccinations might result in physicians being more likely to recommend them.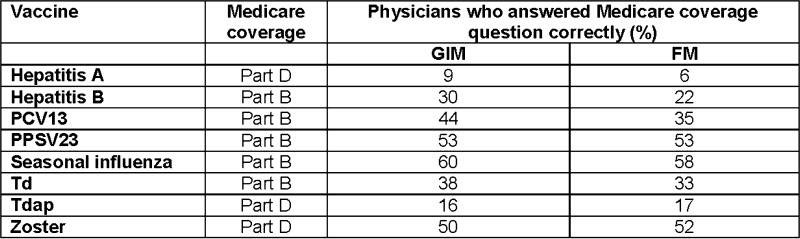
FIRST YEAR EXPERIENCE OF HCV SCREENING OF 2,765 BABY BOOMERS ADMITTED TO A SAFETY NET HOSPITAL IN SOUTH TEXASBarbara J. Turner2,1; Barbara S. Taylor1,2; Joshua T. Hanson1,2; Mary E. Perez2; Ludivina Hernandez2. 1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX. (Tracking ID #1935853)
BACKGROUND: Baby boomers account for over 75 % of the 3 to 5 million HCV-infected persons in the U.S., and 75 % of these HCV-infected persons are undiagnosed. The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force now both endorse one-time testing of all baby boomers (born 1945 to 1965) for hepatitis C virus (HCV) infection. Objective: To implement a baby boomer HCV screening and linkage to care program in the largest safety net hospital in South Texas.
METHODS: The program has 4 key features: 1) Education in English and Spanish about HCV screening of baby boomers using posters throughout the hospital and flyers in admission packets that offer an opt out option; 2) Electronic medical record algorithm that identifies eligible baby boomers and, for most, places an order for HCV antibody (HCV Ab) with a reflex HCV RNA test for positive HCV Ab [exclusion criteria: record of prior HCV test or diagnosis, poor prognosis (e.g. metastatic cancer), psychiatric admission]; 3) Personalized counseling for HCV Ab+ patients by a bilingual inpatient counselor who reviews a mobile app-based HCV educational program in English and Spanish that was developed by our team; and 4) Navigation by a bilingual community health worker to facilitate follow-up primary and HCV specialty care after hospital discharge by addressing barriers to care, poor health literacy, substance abuse, and lack of social support.
RESULTS: From 12/1/2012 to 11/30/2013, 5,572 unique baby boomers were hospitalized of whom 45 % were women, 59 % Hispanic, median birth year 1956, and 46 % uninsured. Of these, over 1,400 patients had a prior HCV test or diagnosis and were excluded. Of 2,765 unique baby boomers screened for HCV infection, 230 (8.3 %) tested HCV Ab+. HCV Ab+ was more likely for men (75 % vs. 55 % of HCV Ab negative, p < .001) but did not differ by birth year, Hispanic ethnicity, or insurance status. Follow-up HCV RNA testing was performed for 205 (89 %) of HCV Ab+ patients. 125 (61 %) were HCV RNA+ while 80 (39 %) were HCV RNA negative. HCV RNA positive and negative patients did not differ by birth year, gender, Hispanic ethnicity, or insurance status. Of the 125 patients diagnosed with chronic HCV infection, 110 (88 %) have been counseled, 100 (80 %) have had follow-up ambulatory care addressing HCV and 43 (34 %) have received HCV specialty care.
CONCLUSIONS: To our knowledge, this is the first baby boomer HCV screening program that has been broadly implemented in a civilian, safety-net hospital. The 8.3 % HCV Ab+ prevalence in persons without evidence of prior HCV testing or diagnosis supports the public health value of screening in similar inpatient settings. This program has newly identified 125 patients with chronic HCV infection and linked the majority to follow-up ambulatory care. The high rate of apparent clearance of HCV (39 %) needs to be confirmed by repeat HCV RNA testing after 3–6 months. If confirmed, cost-effectiveness models may need to be adjusted to account for a lower proportion of HCV Ab+ baby boomers with persistent infection.
FOLLOW-UP OF ABNORMAL CT RESULTSLinda J. Canty1; Paul Visintainer1; Mihaela S. Stefan1; Philip Henneman1; Sean Stanhope1; Reva Kleppel1; Annie Lagoy1; Jessilia Santiago1; Michael B. Rothberg2. 1Tufts University School of Medicine / Baystate Medical Center, Springfield, MA; 2Cleveland Clinic, Cleveland, OH. (Tracking ID #1939790)
BACKGROUND: CT scans often include abnormal findings, and follow-up is frequently recommended. However, when a CT scan ordered in the emergency department (ED) or the inpatient unit contains an abnormal finding, it may not always be followed up by the primary care provider. Mechanisms in place to ensure the appropriate follow-up of tests may miss these types of handoffs. The objective of this study was to quantify the proportion of abnormal findings with follow-up and to assess factors associated with timely follow-up.
METHODS: We conducted a retrospective cohort study to assess the proportion of abnormal findings that had documented follow-up. The CT scans were performed at three hospitals within Baystate Health, a large health system in western Massachusetts. For the two community hospitals, we looked at all scans performed in 2010 on patients who also had a visit during 2010 to the primary care office associated with the hospital. For the academic medical center, we used a sample of two-thirds of the scans from January to mid-July 2010 performed on patients who had a visit during 2010 to one of six nearby primary care practices. All providers in the system have access to radiology readings through a shared electronic health record, but only for scans ordered in outpatient settings does the ordering provider receive the scan results in their electronic medical record inbox. CT scans involved the chest (including angiograms,) abdomen, pelvis or a combination of these. An abnormal result was defined as any finding for which the radiologist’s dictated final report recommended follow-up using wordings such as “recommend,” “suggest,” or “should be” followed, or cited guidelines outlining a timeframe for follow-up. For each of these findings, we used the electronic health record to assess whether the patient received appropriate follow-up, defined as either adherence to the radiologist’s suggestion or documentation that the finding was discussed and a conscious decision was made not to pursue the finding further. We compared the proportion of findings that received follow-up if they were ordered by outpatient providers to those ordered in the ED and inpatient wards.
RESULTS: We reviewed 1922 scans performed on 1524 patients. Overall, there was documentation of follow-up within the recommended time period in 176 out of 236 findings (75 %.) Of these, documentation of follow-up was seen in 41 of 64 (64 %) ED findings, 37 of 52 (71 %) inpatient findings, and 98 of 120 (82 %) outpatient findings. Follow-up was more common for findings on CT scans ordered by outpatient providers than for those ordered in the ED (p = 0.01.) Findings on inpatients were not statistically more likely to be followed when compared to either the ED or the outpatient setting. Radiologists stating in the dictated report that the results were “communicated” was not associated with greater follow-up (44 of 56 findings; 79 %) compared to when this was not in the report (132 of 180 findings; 73 %; p = 0.49.)
CONCLUSIONS: Abnormal findings on CT scans ordered in the outpatient setting were more likely to have documentation of follow-up than those ordered through the emergency department. For patients scanned in the ED, more than 1/3 of abnormal findings went without evidence of timely follow-up. Improved communication systems appear needed for radiological handoffs between the ED and the outpatient setting.
FOLLOW-UP PRIMARY CARE VISITS IN A RESIDENT PRACTICE AFTER HOSPITAL DISCHARGE - HOW ARE WE DOING?Sanjai Sinha1; Thomas Uttaro3; Daniel M. Stein2; Amanda S. Carmel1. 1Weill Cornell Medical College, New York, NY; 2Weill Cornell Medical College, New York, NY; 3Weill Cornell Medical College, New York, NY. (Tracking ID #1935099)
BACKGROUND: Patients cared for in internal medicine teaching clinics often have poor primary care follow up after hospital discharge. Such discontinuity can result in medical errors, suboptimal care, and re-hospitalization. In a Medicare study, more than half of patients who were re-admitted within 30 days of hospital discharge had not had an outpatient encounter between admissions. Based on a 6-week period of inpatient and emergency department (ED) discharges from New York Presbyterian/Weill Cornell Medical Center (NYP/WCMC), we aimed to assess the percentage of Weill Cornell Internal Medicine Associates (WCIMA) patients that completed a post discharge appointment at WCIMA within 30 days of discharge. Secondarily, we examined the percentage of patients who utilized the hospital or ER more than once in the study period, and who saw their PCP for follow up.
METHODS: WCIMA is a large internal medicine practice affiliated with Weill Cornell Medical College in New York City. It is the main practice site for 33 faculty physicians and 136 internal medicine residents. Through data extraction of our electronic health records, we identified all WCIMA discharges from NYP/WCMC from 9/1/2013 to 10/12/2013. Information for each discharge including basic patient identifiers, age, payer, hospital department/ service, assigned primary care provider, completed visit date and provider were obtained. Interval between discharge and the follow up visit were calculated. The unit of analysis was a hospital discharge event, some patients had multiple hospitalizations and ED/urgent care visits. IBM SPSS software version 22 procedures for data manipulation and descriptive statistics were used for data analysis. IRB approval is pending.
RESULTS: We identified 1,908 unique discharges for 1,513 WCIMA patients from NYP/WCMC during the study period. Two hundred ninety-three patients (19.4 %) had more than one discharge. In WCIMA patients discharged from a Medicine admission, 51.2 % (N = 259/506) had a post discharge visit at WCIMA, 37.2 % (N = 188/506) had the visit within 30 days of hospital discharge, and 37.7 % (N = 190/506) saw their assigned PCP. In WCIMA patients discharged from the ED/Urgent care, 35.8 % (N = 375/1,047) had a post discharge visit at WCIMA, 24.1 % (N = 242/1,047) had the visit within 30 days of discharge, and 19.2 % (N = 201/1,047) saw their PCP. The mean follow up interval was 23.01 days (SD 22.360) after a Medicine discharge and 25.40 days (SD 23.619) after ED/Urgent care. The mean age of all discharged patients was 52.62 years (SD 18.468). Patients who completed post-discharge appointments were significantly older than those who did not (57.2 vs. 49.3 years, P < 0.001), however, this difference was lost when examining Medicine patients alone.
CONCLUSIONS: Only half of WCIMA patients discharged from Medicine during the study period, and fewer from the ED/Urgent care had a WCIMA follow up visit, indicating significant missed opportunities to coordinate care from hospital to home. Fewer than half had visits within 30 days or saw their assigned PCP. Overall, older patients were more likely to follow up. Other resident teaching practices likely have similar challenges in hospital-outpatient continuity. We have designed an intervention using a transitions registrar and care manager to ensure timely and appropriate post discharge care. We hope the intervention will identify one strategy to improve follow up rates and clinical outcomes among patients of a large internal medicine teaching clinic.
FOOD INSECURITY AND COST-RELATED MEDICATION UNDERUSE ARE INDEPENDENT BARRIERS TO DIABETES CONTROL: RESULTS FROM THE MEASURING ECONOMIC INSECURITY IN DIABETES (MEND) STUDYSeth A. Berkowitz1; James B. Meigs1; Steven J. Atlas1; Darren A. DeWalt4; Hilary K. Seligman3; Deborah J. Wexler2. 1MGH, Boston, MA; 2MGH, Boston, MA; 3UCSF, San Francisco, CA; 4UNC, Chapel Hill, NC. (Tracking ID #1934690)
BACKGROUND: Food insecurity, cost-related medication underuse (CRMU), and housing instability may be significant, yet modifiable, barriers to diabetes management. However, whether these barriers are independently associated with poor diabetes control, accounting for other aspects of low socioeconomic status and comorbidity, is unclear. To inform future population management interventions, we tested the hypothesis that they are independently associated with poor diabetes control.
METHODS: We contacted a stratified random sample of adult (age >20 years) diabetes patients in 4 clinic sites (2 community health centers, 1 academic internal medicine practice, and a diabetes center) from June 15-Sept 15th 2013. Participants completed validated instruments assessing food insecurity, CRMU, and housing instability, in English or Spanish. We also collected information on other social circumstances, including educational attainment, limited English proficiency (LEP), health literacy, and nativity, along with age, gender, race/ethnicity, insurance, diabetes duration, Charlson comorbidity score, diabetes medications, Hemoglobin A1c (HbA1c) tests/year and number of outpatient visits. The primary outcome was poor diabetes control (most recent HbA1c > 9.0 % or LDL cholesterol >100 mg/dL). We estimated prevalence using inverse probability weighting. We performed multivariable logistic regression analysis with generalized estimating equations to account for clustering by clinic, and used pseudo-R2 statistics to evaluate explained variation in diabetes control.
RESULTS: Overall, 412 patients were included (response rate: 62 %). Of these, 19 % reported food insecurity, 28 % CRMU, and 11 % housing instability. Patients reporting food insecurity were more likely to be younger (mean age 56 vs. 63 years, p = .01), non-white (35 % vs 22 %, p = .01), and have Medicaid (22 % vs. 11 %, p = .03). In unadjusted analyses, the prevalence of poor diabetes control was higher in those with, vs. without, food insecurity (53 % vs. 28 %, p = .01), CRMU (53 % vs. 22 %, p = .01) and housing instability (56 % vs. 30 %, p = .01). Those with, vs. without, food insecurity, CRMU, or housing instability had similar comorbidity and HbA1c tests/year (an indicator of engagement with care), but more outpatient visits/year (Table 1). In a multivariable regression analysis, adjusted for the covariates listed above, food insecurity and CRMU were associated with worse diabetes control (Table 2). Using Pseudo-R2 statistics, our model explained 28 % of the variation in diabetes control; food insecurity, CRMU, and housing accounted for 4 % of total variation. By comparison, education, health literacy, LEP, and nativity (other indicators of social disadvantage) together explained only 2 %.
CONCLUSIONS: Food insecurity and CRMU are common, and independently identify patients at increased risk of poor diabetes control despite similar comorbidity and engagement with care. Because these patients already have higher healthcare utilization, interventions targeting food insecurity and cost-related medication underuse may have greater utility than increasing usual care.
Table 1
| Food Insecure | Food Secure | p-value | Cost-related Medication Underuse | No Cost-related Medication Underuse | p-value | Unstable Housing | Stable Housing | p-value | |
| Charlson Score Median (IQR) | 4 (3–7) | 4 (2–7) | .44 | 4 (3–6.5) | 4 (2–7) | .84 | 3.5 (2–6) | 4 (3–7) | .11 |
| HbA1c tests/year Median (IQR) | 2.5 (1.8–3.0) | 2.5 (1.9–3.0) | .90 | 2.4 (1.9–3.1) | 2.5 (2.0–3.0) | .94 | 2.9 (2.1–3.4) | 2.5 (1.9–3.0) | .08 |
| Outpatient Visits/year Median (IQR) | 8 (5–11) | 6 (4–10) | .01 | 8 (5–11) | 7 (4–10) | .048 | 9 (6–13) | 7 (4–10) | .01 |
Table 2
| Adjusted Odds Ratio (95 % CI) | |
| Food Insecurity | 1.62 (1.18–2.23) |
| Cost-related Medication Underuse | 2.59 (1.41–4.75) |
| Housing Instability | 0.82 (0.28–2.40) |
FOOD INSECURITY IS ASSOCIATED WITH DIABETES SELF-CARE BEHAVIORS AND GLYCEMIC CONTROLWilliam J. Heerman1; Ken Wallston2; Chandra Y. Osborn3; David Schlundt4; Shari D. Barto1; Russell L. Rothman1. 1Vanderbilt University Medical Center, Nashville, TN; 2Vanderbilt University Medical Center, Nashville, TN; 3Vanderbilt University Medical Center, Nashville, TN; 4Vanderbilt University, Nashville, TN. (Tracking ID #1928444)
BACKGROUND: Food insecurity is the “limited or uncertain availability of nutritionally adequate and safe foods,” and has been associated with worse glycemic control among patients with type 2 diabetes (T2DM). Less is known about food insecurity’s relationship with diabetes self-care behaviors, and whether its effects on glycemic control can be attributed to that relationship. Therefore, we examined the relationships between food insecurity, self-care, and glycemic control, and whether any effect on glycemic control was due to relationships with self-care.
METHODS: We conducted a cross-sectional analysis of baseline data from patients with T2DM enrolled in a randomized trial evaluating a health literacy-focused diabetes intervention at 10 county health departments across middle Tennessee. Food insecurity was assessed with 3 items from the U.S. Household Food Security Survey and patients who answered “sometimes” or “often” to at least one of these items were considered “food insecure.” Diabetes self-care behaviors were assessed with the Summary of Diabetes Self Care Activities Scale (SDSCA), Personal Diabetes Questionnaire (PDQ-11), and Adherence to Refills and Medication Scale (ARMS). Glycemic control was assessed with A1C, collected prospectively unless available in medical record within 4 weeks of study enrollment. Student’s t-tests or Wilcoxon rank-sum tests were used to evaluate the bivariate relationships between food insecurity and each self-care behavior, food insecurity and A1C, and each self-care behavior and A1C. Significant bivariate relationships were re-examined using linear regression models adjusted for gender, ethnicity, education, and income. Mediational analyses were performed as appropriate.
RESULTS: The sample consisted of 401 participants, of whom 61 % were female, 57 % self-identified as non-Hispanic White, 17 % as non-Hispanic Black, 24 % as Hispanic, and 2 % as non-Hispanic other. The majority (88 %) were uninsured, and 37 % had less than a high school education. Nearly three-quarters (73 %) reported some level of food insecurity. Food insecurity was significantly associated with self-care behaviors (Table) including less adherence to a general diet (p = 0.03), routine physical activity (p = 0.05), and medications (p = 0.01), and a greater occurrence of poor eating (p = 0.02) and skipping meals (p = 0.03). Food insecurity was also associated with worse glycemic control (adjusted β co-efficient 0.6, p = 0.015). The median A1C for food insecure participants was 9.8 % (IQR 8.2, 11) compared to 9.3 % for food secure participants (IQR 7.7, 10.6). There was no relationship between any of the self-care behaviors assessed and A1C, so tests for mediation were not performed.
CONCLUSIONS: There was a high rate of food insecurity in this sample of diabetes patients with low socioeconomic status. Food insecurity was associated with less adherence to recommended self-care behaviors, a greater occurrence of undesirable behaviors, and worse glycemic control. Further work is needed to understand the mechanisms by which food insecurity impacts self-care, including behaviors not directly related to food (e.g., physical activity and medication adherence) as well as the mechanisms by which it also impacts glycemic control. While our measures of self-care were not associated with A1C, limiting our ability to explore self-care as a mechanism, other more sensitive measures of behavior may hold promise. Nonetheless, our findings contribute to a limited literature on the relationship between food insecurity and diabetes behaviors.
Food Insecurity and Diabetes Self-Care Behaviors
| All Participants (n = 401) | Food Secure (n = 109) | Food Insecure (n = 292) | p-value | |
| Summary of Diabetes Self Care Activities (range 0–7) | Mean (SD) | Mean (SD) | Mean (SD) | |
| General Diet | 3.5 (2.3) | 3.9 (2.5) | 3.3 (2.2) | 0.03 |
| Specific Diet | 3.4 (1.7) | 3.4 (1.8) | 3.5 (1.6) | 0.77 |
| Exercise | 2.7 (2.3) | 2.7 (2.1) | 2.7 (2.3) | 0.76 |
| Blood Glucose Testing | 4.6 (2.7) | 4.3 (2.7) | 4.7 (2.6) | 0.2 |
| Foot Care | 4.1 (2.5) | 4.1 (2.7) | 4.2 (2.4) | 0.74 |
| Personal Diabetes Questionnaire | ||||
| Poor Eating Behavior (range 0–18) | 7.0 (3.4) | 6.4 (3.3) | 7.2 (3.4) | 0.02 |
| Use of Data to Modify Diet (range 0–18) | 5.2 (4.7) | 5.1 (4.8) | 5.2 (4.6) | 0.7 |
| Skipped Meals (range 0–6) | 1.4 (1.7) | 1.1 (1.6) | 1.5 (1.7) | 0.03 |
| Reduced Portion Size (range 0–6) | 2.0 (1.8) | 1.8 (1.8) | 2.1 (1.7) | 0.1 |
| Routine Physical Activity (range 0–6) | 2.8 (1.4) | 3.0 (1.4) | 2.7 (1.4) | 0.05 |
| Stage of Change for Weight Management (range 0–5) | 2.2 (1.4) | 2.1 (1.3) | 2.3 (1.4) | 0.4 |
| Stage of Change for Exercise (range 0–5) | 2.2 (1.3) | 2.3 (1.2) | 2.1 (1.3) | 0.1 |
| Non-Adherence to Refills and Medication Scale (range 12–48) | 17.6 (3.7) | 16.9 (3.1) | 17.8 (3.9) | 0.01 |
t-test with unequal variance
FOOD INSECURITY, COPING STRATEGIES, AND GLYCEMIC CONTROL IN LOW-INCOME PATIENTS WITH DIABETESVictoria L. Mayer1; Kevin H. McDonough1; Hilary K. Seligman2; Judith A. Long1,3. 1Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 2University of California San Francisco, San Francisco, CA; 3Philadelphia Veterans Affairs Medical Center, Philadelphia, PA. (Tracking ID #1933037)
BACKGROUND: In the U.S., people who are food insecure (lack sufficient food for an active and healthy life) have a higher prevalence of diabetes and worse diabetes control. However, the mechanisms underlying these associations are not well understood. In this study we evaluate the relationship between food insecurity and coping strategies hypothesized to worsen glucose control in a population of low-income diabetics.
METHODS: We performed a cross-sectional telephone survey among low-income adults with diabetes seen at a large, urban medical center. We interviewed people within 8 weeks of having a hemoglobin A1c (HbA1c) evaluation and characterized individuals as having poor glycemic control (HbA1c ≥ 8.0) or adequate glycemic control (HbA1c < 8.0). The main independent variable was a dichotomous measure of food insecurity (18-item U.S. Department of Agriculture Household Food Security Survey Module). We assessed the use of coping strategies including a diet low in fruits and vegetables and high in added sugars (using the California Health Interview Survey Dietary Screener), foregone medications, foregone medical care, use of food assistance programs (including the Supplemental Nutrition Assistance Program - SNAP) and emergency food programs, and overeating in times of adequacy. Additional independent variables included socio-demographic and clinical covariates. In bivariate analyses, we compared glucose control and use of coping strategies in the food insecure and food secure groups. We developed logistic regression models to evaluate the association between food insecurity and glucose control, with adjustment for covariates and coping strategies. Finally, we assessed the role of interactions between food insecurity and coping strategies.
RESULTS: Of 413 respondents (response rate 51 %), 40.4 % were food insecure. The food insecure group had a higher proportion of patients with poor glycemic control (68.3 % vs. 53.3 %, p = 0.002). There were no significant differences between the food insecure and food secure groups in daily intake of fruits, vegetables, or added sugars. A significantly higher percentage of patients in the food insecure group reported foregone medications, foregone medical care, participation in food assistance programs and use of emergency food programs. Food insecure patients were also more likely to report overeating at times when food is adequate. However, these coping strategies were not significantly associated with glucose control. In the adjusted model without interaction terms, when compared to food secure individuals, food insecure individuals were more likely to have poor glucose control (OR 2.83, 95 % CI 1.47–5.44). However, there was a significant interaction between food insecurity and receipt of SNAP: food insecure individuals receiving SNAP benefits were less likely to have poor glucose control (OR 0.28, 95 % CI 0.09–0.90), while food insecure individuals not receiving SNAP were more likely to have poor glucose control (OR 7.41, 95 % CI 2.41–22.77).
CONCLUSIONS: Food insecurity was associated with higher risk of poor glucose control. While more prevalent among patients who were food insecure, many coping strategies previously thought to underlie this relationship were not significantly associated with poor glucose control. However, receipt of food assistance among food insecure individuals was associated with better diabetes control, suggesting that in addition to helping individuals afford food, such programs may also play a role in improving health.
FORGET ME NOT: A RANDOMIZED TRIAL OF THE DURABILITY OF HOSPITAL-BASED EDUCATION ON INHALERS FOR PATIENTS WITH COPD OR ASTHMAValerie G. Press1; Vineet Arora2; Kristin L. Constantine3; Edward T. Naureckas4; Steven R. White4; Jerry Krishnan5. 1University of Chicago, Chicago, IL; 2University of Chicago, Chicago, IL; 3University of Michigan, Ann Arbor, MI; 4University of Chicago, Chicago, IL; 5University of Illinois at Chicago, Chicago, IL. (Tracking ID #1934140)
BACKGROUND: As part of a nationwide strategy to reduce readmissions for chronic diseases, hospitals are increasingly using the inpatient setting as a “teachable moment” to train patients in important self-management techniques to improve both patient-centered outcomes as well as to avoid preventable re-hospitalizations. Inpatient education is particularly salient for patients with COPD, which is the 3rd leading cause of readmission among Medicare patients, who are often not aware how to use their preventive and rescue inhaler medications correctly. While hospital-based education is not new, it is unclear how durable it is and when reinforcement may be needed. The objective of this two-center randomized clinical trial was to test the short-term effectiveness and longer-term retention of a guideline-based, patient-centered approach, called teach-to-goal (TTG) compared to a brief intervention (BI) of simple verbal instructions to teach inhaler technique to inpatients with COPD or asthma.
METHODS: Patients were randomized to TTG or BI, stratified by level of health literacy (high/low/unknown [due to insufficient vision]). Use of metered-dose inhaler (MDI) and Diskus® devices was assessed using step-by-step checklists. Misuse was defined as <75 % of steps correct. TTG participants received cycles of inhaler demonstration followed by re-assessment of technique (“teach-back”). BI participants received verbal instructions without demonstration. Participants returned at 30-days and 3 months post-hospital discharge. Significance was tested using Chi square and Fishers exact tests.
RESULTS: Between September 2011–October 2012, 120 participants were enrolled from two urban hospitals and were randomized to either the TTG (n = 62) or BI (n = 58) interventions. The majority were female (73 %) and African-American (90 %), with a mean age of 47 years. Two-thirds (66 %) had been hospitalized at least once in the last year and nearly half (49 %) had a near-fatal event (ICU admission and/or intubation) in their lifetime. Fifteen percent had insufficient vision, 19 % had low health literacy. Eighty-nine percent of participants returned at 30-days and 86 % returned at 3 months. There were no baseline differences between groups (TTG vs. BI) in the baseline prevalence of misuse for either MDI or Diskus. Immediately after education, misuse was less common in TTG vs. BI for MDI (11 vs. 60 %, p < 0.001) and Diskus devices (5 vs. 61 %, p = 0.001). At 30-days there were no significant differences in misuse for either MDI (53 vs. 70 %, p = 0.09) or Diskus (53 vs. 59 %, p = 0.73). Despite the lack of significant 30-day findings, MDI misuse was significantly less likely at 3 months in the TTG vs. BI group (48 vs. 76 %, p = 0.003). A similar result at 3 months for the Diskus device was not seen (p = 0.2). Stratifying the results by level of health literacy did not produce any clear patterns [Table]. There were no differences between TTG and BI for any health literacy group at 30 days; those with adequate health literacy were less-likely to misuse MDI at 3 months in TTG vs. BI group (p = 0.02). Participants were less-likely to misuse Diskus if they received TTG vs. BI for those with adequate health literacy (p = 0.006) or less-than-adequate health literacy (p = 0.048), but not for those with insufficient vision (p > 0.99). There were no differences between TTG and BI for any health literacy group at 30-days or 3 months for the Diskus device.
CONCLUSIONS: Although patient-centered TTG education can improve self-management skills among inpatients with asthma or COPD, the effects of hospital-based education wane over time. This suggests that in order to improve patient-reported outcomes and potentially decrease re-admissions, post-discharge educational reinforcement is likely necessary for long-term mastery of chronic disease self-management. Further, data are needed about the effectiveness of hospital-based education on subsequent clinical outcomes for hospitalized patients with COPD or asthma in the short-term and long-term after hospital discharge.
Proportion of Misuse
| MDI | DISKUS | |||||
| TTG | BI | p-value | TTG | BI | p-value | |
| Baseline | 92 | 84 | n/a | 75 | 89 | n/a |
| Post-education | 11 | 60 | <0.001 | 5 | 61 | <0.001 |
| 30-days | 54 | 70 | 0.112 | 53 | 59 | 0.73 |
| 3 months | 48 | 76 | 0.003 | 38 | 63 | 0.157 |
TTG: Teach To Goal; BI: Brief Intervention
FROM FLIPPING THE CLASSROOM TO FLIPPING THE HOMEWORK: A LEARNER-CENTERED APPROACH TO ADVANCE PREPARATION ASSIGNMENTSPaul Haidet; Klara Papp; Daniel R. Wolpaw. Penn State College of Medicine, Hershey, PA. (Tracking ID #1939412)
BACKGROUND: The commonly used convention for preparing learners to participate in active classroom learning is to assign them pre-readings or similar materials. We have found that such published resources do not always align well with educational objectives. Further, pre-reading assignments often present information according to the teacher’s organizational schema, rather than allowing students to identify learning needs and incorporate material according to their own emerging conceptual frameworks. We sought to develop a method for advance preparation that addresses these issues.
METHODS: We designed a 2-hour session on “introduction to educational concepts” for junior faculty enrolled in a 12-month faculty development fellowship. The in-class portion used the Team-Based Learning method to foster active learner participation. However, rather than assign specific readings for the pre-session preparation, we gave learners a list of 27 educational terms (e.g., ‘Bloom’s Taxonomy’, etc.) and instructed them to research unfamiliar terms and reflect on their own assumptions and beliefs regarding teaching. We performed internet searches using the terms to review information that our learners might access. We distributed a post-session survey containing three open-ended questions that addressed how the assignment: 1) affected learning about educational concepts, 2) differed from typical reading assignments, and 3) influenced levels of enjoyment during completion. We performed a thematic analysis of learner responses to the open-ended questions.
RESULTS: Nineteen learners (33 % women) participated in the session and returned surveys (100 % response). Forty-eight percent of learners were clinically focused in their scholarly work, 28 % educationally focused, and 24 % research focused. For our session, several themes emerged from the responses about the advance preparation assignment. First, some learners struggled with uncertainty and a need to find the “right” answer, particularly when they found conflicting information. A few learners viewed uncertainty as an opportunity to deepen understanding, because it forced them to critically appraise information, identifying knowledge gaps during the process. Second, learners generally perceived more active engagement as compared to typical reading assignments; however, this effect was tempered for learners who focused on collecting definitions at the expense of understanding concepts. Finally, the majority of learners expressed enjoyment with the assignment and appreciated the ability to allocate preparation time according to their own needs.
CONCLUSIONS: Using a learner-directed approach for advance preparation merits further exploration. Learner experiences suggested more active, critical thinking, and may represent more efficient and deeper learning of course concepts, and better preparation for subsequent learning in the classroom. Future work should more rigorously test these outcomes, and explore additional methods of fostering learner-centeredness in advance preparation assignments.
FULFILLING UNMET NEEDS: INTEGRATING WOMEN’S HEALTH INTO THE INTERNAL MEDICINE RESIDENCY PROGRAM CURRICULUMSneha Shrivastava; Abby Spencer. Allegheny General Hospital, Pittsburgh, PA. (Tracking ID #1941879)
BACKGROUND: National guidelines and the American Board of Internal Medicine (ABIM) have highlighted key areas of women’s health that are critical to the training of an internal medicine resident. The federated council for Internal Medicine (FCIM), who sets the core knowledge curriculum for IM residency programs, argues that all general internists should be competent in conditions that are “unique to, more common in or more serious in women or that have manifestations, risk factors, or interventions that are different in women”. Our objective is to improve the women’s health curriculum in a large academic community Internal Medicine residency program.
METHODS: A 147-item anonymous online survey was sent to PGY1&2 residents to assess their comfort, perceived knowledge, perceived importance, and exposure to 28 Women’s Health topics identified as critical to the training of an internist. Topics were selected based on a thorough literature review, curricular recommendations by ABIM, FCIM, and the NIH Women’s Health Congress. We used descriptive statistics to determine and rank comfort, exposure, perceived knowledge, and perceived importance of the topics. We then analyzed the In-Training exam results from the last 3 years and compared the performance of our residents to national data on topics related to women’s health. Based on our survey results and ITE review, we designed a new longitudinal interactive women’s health curriculum to meet critical learning needs of our residents. Curricular methods included problem-based learning (PBL) workshops on osteoporosis, multi-disciplinary case conferences on depression and anxiety during pregnancy traditional didactics, and STD jeopardy. Our interprofessional panel experts during case conferences included faculty from internal medicine, psychiatry, and obstetrics-gynecology Pre-post surveys were conducted after problem-based learning (PBL) and multi-disciplinarycase conferences. The Wilcoxon signed-rank test was used to compare resident knowledge and comfort before and after case conferences.
RESULTS: Response rate on the initial survey was 63 % (38/60). Non-responders were similar to responders in gender and pgy-year. 13/28 topics were identified as having the highest perceived importance to our IM residents. Of these, residents felt they had insufficient clinical exposure in prescribing contraception, evaluating breast symptoms, managing menopause, performing pap smears and pelvic exams, and diagnosing or managing polycystic ovarian syndrome (PCOS). Lower clinical exposure in these areas correlated significantly with lower comfort and lower perceived knowledge. Osteoporosis was identified by residents as their single greatest learning need; this topic was rated as highly important and residents had low knowledge and comfort with it. While residents reported a low perceived knowledge on several women’s health topics, their performance on the In-Service exam was on par with that of the national average. . After an interactive PBL conference on osteoporosis, 95.1 % of the residents felt knowledgeable and comfortable in this topic as compared to 37,9 %% who were knowledgeable and comfortable before the case discussion (p = 0.0003). After the multi-disciplinary case discussion on anxiety and depression during pregnancy, 80.1 % of the residents felt more comfortable in this topic as compared to only 36.4 % who were comfortable before the case discussion (p = 0.0009). Additionally, 94.7 % of the residents preferred PBL conference and 88.9 % of the residents preferred multi-disciplinary conference to a standard noon conference lecture. All the residents (100 %) agreed that PBL cases and multi-disciplinary conferences are extremely effective methods of learning.
CONCLUSIONS: Our study highlighted significant gaps in our women’s health curriculum. Additionally, there is a concerning perception among residents that many topics critical to the health of women and the education of IM residents are not very important. Based on our findings, we are redesigning our didactic and experiential women’s health curriculum to augment knowledge, comfort, importance of, and exposure to areas in need. Problem based learning and multi-disciplinary case discussions are effective educational tools to achieve this. Enhancing education and increasing clinical exposure to fundamental women’s health issues will produce better residents and promote higher quality care for women.
GENDER AND RACIAL DIFFERENCES IN CONTROL OF CARDIOVASCULAR DISEASE RISK FACTORS AMONG VETERANSKaren M. Goldstein1,3; S. Dee Melnyk1,4; Leah L. Zullig1,5; Karen Stechuchak1; Eugene Z. Oddone1,3; Lori A. Bastian6,7; Susan Rakley2,3; Maren Olsen1,8; Hayden Bosworth1,9. 1Durham Veterans Affairs Medical Center, Durham, NC; 2Durham Veterans Affairs Medical Center, Durham, NC; 3Duke University, Durham, NC; 4University of North Carolina, Chapel Hill, NC; 5University of North Carolina, Chapel Hill, NC; 6University of Connecticut Health Center, Farmington, CT; 7VA Connecticut Healthcare System, West Haven, CT; 8Duke University, Durham, NC; 9Duke University, Durham, NC. (Tracking ID #1934589)
BACKGROUND: Female Veterans are the fastest growing Veterans Administration (VA) patient population, nearly doubling in the past decade. Compared with non-Veteran females, Veteran women have higher rates of cardiovascular disease (CVD) risk factors, such as smoking and obesity, which put them at significant risk for long-term cardiovascular morbidity and mortality. Recent findings suggest that black female Veterans are more likely to have a diagnosis of hypertension, diabetes, and obesity compared with white female Veterans. However, there is little information about CVD risk factor control between male and female Veterans, particularly by race. We sought to address the following: 1) Is there a significant difference in CVD risk factor control between men and women Veterans at high risk for CVD, defined as poor control of blood pressure (mmHg), hemoglobin A1c, and LDL cholesterol (mg/dL)?; and 2) Is there a significant difference in CVD risk factor control between African-American and White Veterans by gender, defined as blood pressure (mmHg), hemoglobin A1c, and LDL cholesterol (mg/dL)?
METHODS: We used analysis of variance, adjusting for age, to compare gender and racial differences in three risk factors that predispose to CVD (i.e. diabetes, hypertension, and hyperlipidemia) in a cohort of Veterans who were eligible for enrollment in a clinical trial. To be eligible for the trial, individuals had to be enrolled at the Durham VA Medical Center and have a diagnosis of hypertension, hyperlipidemia, or both. Means provided were estimated from our ANOVA model that adjusted for age. Our sample included 23,955 men (33.9 % black and 54.0 % white) and 1,010 women (54.8 % black and 39.3 % white).
RESULTS: LDL values were higher in female than male Veterans with hyperlipidemia with age-adjusted estimated mean values of 111.7 mg/dl vs 97.6 mg/dl (p < 0.01). There was no difference in LDL values between black and white women. There was a small but significant difference between black and white male Veterans with hyperlipidemia, specifically 99.6 mg/dl vs 95.8 mg/dl respectively (p < 0.01). Systolic blood pressures were similar between male and female Veterans with hypertension, though there was a significant difference in diastolic blood pressures of 79.0 mmHg vs 76.8 mmHg (p < 0.01) respectively. Blood pressures were higher among black than white female Veterans with hypertension with age-adjusted estimated mean systolic blood pressures of 136.3 mmHg versus 133.5 mmHg, respectively (p < 0.01), and diastolic blood pressures of 82.4 mmHg versus 78.9 mmHg (p < 0.01); a similar pattern between black and white male Veterans was also seen. There was no difference in hemoglobin A1c between male and female Veterans with diabetes. Age-adjusted estimated mean hemoglobin A1cs for African-American and White men were 7.5 and 7.3 (p < 0.01), respectively. Age-adjusted estimated mean hemoglobin A1cs for African-American and White women were 7.6 and 7.1 respectively, though this was not significant.
CONCLUSIONS: Among this Veteran population at high-risk for CVD, we found that female Veterans had worse control of hyperlipidemia than male Veterans. This difference was observed despite the fact that female Veterans in this cohort on average were almost 10 years younger than male Veterans. In addition, we found that African-American women and men had worse blood pressure control than white women. Further examination of CVD gender and racial disparities in this population may help to develop targeted treatments and strategies applicable to the general population.
GENERAL MEDICINE CAREER INTEREST, PRIMARY CARE KNOWLEDGE AND MENTORSHIP AFTER PARTICIPATING IN A STUDENT-FACULTY COLLABORATIVE PRACTICECharlotte E. Ward; Emma C. Jeffries; Marya J. Cohen. MGH, Boston, MA. (Tracking ID #1938150)
BACKGROUND: It is becoming increasingly difficult for patients to find primary care physicians (PCPs) in the United States. The Medicaid expansion will extend coverage to 30 million new patients, many of whom will likely need a PCP. It is important therefore, to attract a greater number of medical students to the field of primary care and to better understand factors that contribute to student career interests. The Crimson Care Collaborative (CCC), a series of five student-faculty collaborative practices, aims to give students hands-on practical experience in understanding innovation in primary care clinics across the Harvard Medical School network. We surveyed medical students before and after participating in CCC. Our goal was to examine whether knowledge and understanding of primary care-related constructs, and interest in general medicine as a career, increased after participating in CCC. A secondary aim was to examine whether influential factors, such as mentorship and peer and faculty support for primary care, also increased over time.
METHODS: All Harvard Medical School (HMS) students who joined CCC as student-volunteers and participated for a minimum of one semester were administered pre- and post-participation surveys. The surveys focused on assessing career interest, attitudes toward and knowledge about primary care, and presence of faculty mentoring. Pre- and post-survey responses were compared using logistic regression.
RESULTS: The study population included 225 HMS students who filled out a survey prior to participating in CCC and 61 HMS students who filled out a post-survey; 31 students completed both a pre- and post-survey. Students who completed a post-survey were more likely to report having interest in or having decided upon a career in general medicine compared to students who completed a pre-survey (Pre: 38.9 %, Post: 59 %, p = 0.01). Post-survey respondents were more likely to report feeling comfortable with their knowledge of chronic disease management (Pre: 24.9 %, Post: 52.5 %, p < 0.001), understanding the role of coordination of care (Pre: 55.6 %, Post: 73 %, p = 0.01), and understanding the roles of non-MD clinicians on a patient care team (Pre: 49.3 %, Post: 73.8 %, p = 0.03) compared with students who completed a pre-survey. Students who completed a post-survey were more likely to report having heard positive comments about primary care from residents (Pre: 11.8 %, Post: 23 %, p = 0.04), students (Pre: 33.5 %, Post: 36.1 %, p = 0.65) and faculty (Pre: 31.1 %, Post: 34.4 %, p = 0.58) compared to pre-survey respondents. Post-survey respondents were also more likely to agree with the positive comments that they heard about primary care compared to pre-survey respondents (Pre: 84.1 %, Post: 93.3 %, p = 0.07). Finally, post-survey respondents were more likely to report knowing an HMS faculty member whose career in general medicine is one they would like to emulate (Pre: 37.2 %, Post: 50.8 %, p = 0.14).
CONCLUSIONS: For a group of medical students who participated in a primary-care based student-faculty collaborative clinic, rates of knowledge and interest in general medicine increased. Factors that would be influential in student interest and knowledge, such as mentorship and peer support, also increased from pre- to post-survey administration. Further research is needed in order to assess what factors predict general medicine or primary care career interest.
GRAND-PARENTING EXPERIENCES AMONG ADULTS WITH A HISTORY OF DEPRESSION: A MIXED-METHODS STUDYAdriana Izquierdo1; Jeanne Miranda1; Elizabeth Bromley1,2; Cathy Sherbourne3; Gery Ryan3; David Kennedy3; Kenneth B. Wells1. 1University of California Los Angeles, Los Angeles, CA; 2West Los Angeles VA Healthcare Center, Desert Pacific Mental Illness Research, Education, and Clinical Center (MIRECC), Los Angeles, CA; 3RAND, Santa Monica, CA. (Tracking ID #1923290)
BACKGROUND: Grand-parenting is an important social role but how adults with a history of depression experience grand-parenting is unknown; we describe grand-parenting experiences reported by an ethnically-diverse sample of adults with a history of depression.
METHODS: Mixed-methods study using semi-structured interviews of adults at 10-year follow-up and quantitative data collected over 9 years from 280 systematically-sampled participants from a longitudinal, multi-site trial of quality-improvement interventions for depressed primary care patients; of 280, 110 reported noncustodial grand-parenting experiences.
RESULTS: Of 110 adults reporting grand-parenting experiences, 90 (82 %) reported any positive experience such as special joy; 57 (52 %) reported any stressful experience such as geographic separation; 27 (34 %) reported mixed experiences. Adults with chronic or recent depression were significantly more likely than their respective counterparts to report any stressful experience (p < 0.05). There was no significant association between depression status and reporting a positive experience.
CONCLUSIONS: Grand-parenting was a highly salient and positive experience as reported by ethnically-diverse adults 10 years after being identified as depressed in primary care. Depression status was associated with reporting stressful but not positive experiences. Specific themes underlying positive and stressful experiences may have implications for developing strategies to enhance quality of life for adults with a history of depression who are grandparents.
GRASSROOTS REFORM OF DISCHARGE SUMMARIES - ASSESSING HOUSE STAFF ATTITUDESMadeline R. Sterling1; Mallory Otto1; Brian Eiss2; Eugenia Siegler2. 1New York Presbyterian - Weill Cornell, New York, NY; 2New York Presbyterian - Weill Cornell, New York, NY. (Tracking ID #1927328)
BACKGROUND: With more transitions of care in the era of hospitalist-based medicine, a greater focus must be placed on handoffs to preserve patient safety. Discharge summaries (dsumms) are a prime example. Research has identified many flaws with current dsumms; outpatient practitioners are dissatisfied with the quality of dsumms, and medication reconciliation errors made in dsumms lead to readmission. However little is known about the attitudes of the primary authors of these documents at academic institutions, namely interns, residents, and physician assistants (PAs). This study aims to address this gap.
METHODS: Surveys were administered to 79 of 135 residents (PGY 1–3) and 10 PAs at a large academic medical center in New York City. The survey was developed using resident focus groups and was internally validated via review by an expert committee. Using Likert scale analysis, dichotomous relationships, and open-ended questions, the survey sought to measure the attitudes of residents and PAs (house staff) toward authoring dsumms. Surveys were voluntarily completed and anonymous. Results were calculated and stratified by level of training or PA. Comparisons of interns (PGY1) vs. residents (PGY2 and PGY3) and of MDs (PGY1, PGY2, and PGY3) vs. PAs were also conducted for relevant questions and assessed using Fishers exact test. This study was approved by the institutional review board.
RESULTS: Of 89 respondents, 38 (42.7 %), 21 (23.6 %), 20 (22.5 %), and 10 (11.2 %) were PGY1, PGY2, PGY3, and PAs, respectively. Eighty-four percent reported to authoring and using dsumms frequently, and 77.2 % reported that quality dsumms are useful for primary care practitioners. Compared to upper level residents however, interns have less experience in using the discharge summary in the outpatient setting (23.7 % vs. 63.4 %, P < 0.001). Interns were also less comfortable authoring dsumms for patients who were not their primary responsibility, compared to their resident colleagues (47.4 % vs. 24.4 %, P = 0.038). While over three-quarters of housestaff reported having received formal teaching at least once on authoring dsumms, 54.8 % of interns surveyed reported never receiving feedback from their senior resident or attending on their dsumms, and no PAs reported ever received feedback from attendings. Furthermore, the majority of interns and 90 % of PAs responded that further formal teaching would be helpful.
CONCLUSIONS: This study demonstrates a gap in translating theory into practice. While greater than three-quarters of house staff identified the importance of a dsumm in the transfer of care, interns especially admit that they are not comfortable authoring discharge summaries for patients they may not have cared for during the duration of their hospital stay, a rather common practice for MDs on rotational schedules. Furthermore, they welcome further teaching. The interns’ discomfort in authoring dsumms for patients they do not know well likely speaks to their lack of experience in general, and thus targeted teaching sessions and/or feedback, especially from their residents who report more comfort in this arena, may be most appropriate at this level. Future studies could further characterize the effect formalized feedback and or teaching sessions have on house staff attitudes toward dsumms.
GRATEFUL PATIENT PHILANTHROPY: A QUALITATIVE STUDY OF PATIENTS WHO GIVE BACK TO THEIR DOCTORSSean Tackett1; Rosalyn W. Stewart2; Leah Wolfe1; Scott Wright1. 1Johns Hopkins Bayview Medical Center, Baltimore, MD; 2Johns Hopkins Hospital, Baltimore, MD. (Tracking ID #1935909)
BACKGROUND: Philanthropy is a vital source of financial support for academic medical centers, and grateful patients are the single most important source for substantive philanthropic gifts. The factors surrounding patients’ decisions to make financial donations have not been empirically studied.
METHODS: Individual structured interviews were conducted with 20 patients who were identified by the Johns Hopkins Medicine development office as having made significant financial contributions to Johns Hopkins Medicine. An interview guide was developed to elicit patients’ initial motivations for giving, how patients became aware of the need for financial support, how their gifts may have affected their care or relationships with treating physicians, and the elements of stewardship that were most effective. Interviews were transcribed verbatim. Content analysis was performed by two investigators using an editing analysis style.
RESULTS: Informants were on average 65.1 years old (range 45–87 years) and had affiliations with Johns Hopkins Medicine for a mean of 22.3 years (range 3–64 years). Most (13/20, 65 %) were men. Estimated personal financial donations ranged from a few thousand dollars to over $15 million (median $500,000), and most (11/20, 55 %) also supported the institution in other ways (e.g. serving on a board). Their donations were directed in various ways, including unrestricted gifts to individual physicians, support for specific research projects that relate to illnesses of interest (e.g. those affecting donors themselves or donors’ loved ones), endowed chairs, and institutional gifts directed to new construction. While some donations were made after the first clinical encounter, others came after decades of exposure to Johns Hopkins physicians. Five themes emerged from the analysis that shed light on this content area: (i) excellence in patient care was an activating provocation that stimulated patients to consider making donations, (ii) patients welcomed learning about, and were comfortable discussing, specific ways in which they could direct donations, (iii) gifts were often intended to support the work and effort of physicians whom patients had come to respect and admire, (iv) patients felt satisfied knowing their gift could make things better for future patients, and (v) stewardship and explanations about how gifts were being used further encouraged and activated donors. Additionally, while most patients sensed that they now receive “VIP” treatment, they maintained that they did not expect special treatment as a result of their gifts. Similarly, none felt that their gift impacted the doctor-patient component of their relationship, and none believed that there were ethical issues associated with their giving.
CONCLUSIONS: This study of patients that have made philanthropic contributions to our institution suggests that the best way to attract significant donations is to make exceptional patient care routine. Patients with significant means who are grateful for the care they have received appreciate knowing how they can contribute and feel gratified from giving back.
GUYS GET PAP TESTS TOO: DEVELOPING CERVICAL CANCER SCREENING PATIENT OUTREACH MATERIALS FOR FEMALE-TO-MALE TRANSGENDER PATIENTSIda M. Bernstein1,2; Sarah M. Peitzmeier3; Sari L. Reisner2,4; Jennifer Potter1,5. 1Harvard Medical School, Boston, MA; 2Fenway Health, Boston, MA; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4Harvard School of Public Health, Boston, MA; 5Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1938176)
BACKGROUND: The American College of Obstetricians and Gynecologists recommends that female-to-male (FTM) transgender patients with a cervix follow the same cervical cancer screening guidelines as non-transgender women. However, there are unique barriers to screening for transgender men, including a disconnect between biological sex and gender identity, a high frequency of trauma histories, and a high likelihood of being nulliparous, among others. We have found that even at Fenway Health, an urban health clinic with expertise working with lesbian, gay, bisexual and transgender (LGBT) populations, FTM patients are significantly less likely to be up-to-date on Pap tests and 10 times more likely to have an inadequate Pap than non-transgender women (in press). Targeted interventions are needed to improve Pap utilization among FTM patients, including improved patient outreach materials. This study seeks to develop novel community-driven cervical cancer screening outreach materials for FTM patients.
METHODS: In-depth interviews (IDI) and an open-ended online survey administered on LimeSurvey® software were conducted with individuals who were 21 or older, born with a cervix, and self-identified on the FTM spectrum. Participants were purposively recruited through advertisements on social media, the Fenway Health website, and local trans community listservs. Topics explored in the IDIs and survey included participant experiences with Pap tests and preferences for a patient outreach campaign. Text and images of a brochure on cervical cancer screening for FTM patient outreach were developed from qualitative analysis of interview transcripts and survey responses. Existing community-driven cervical cancer screening education materials were reviewed and compared to participant feedback. A team of clinicians, patient outreach and transgender healthcare specialists reviewed and edited the brochure.
RESULTS: We performed 32 IDIs (Mean age 33.3 (SD = 10.6), 18.8 % racial/ethnic minority) and received 65 completed online survey responses (Mean age 33.4 (SD = 8.98), 13.8 % racial/ethnic minority). Some of the key themes identified from participant feedback and incorporated in designing the brochure text include: (1) FTM patients and their providers should jointly customize the Pap test to fit varying patient needs and comfort levels; (2) a need for gender-neutral language and presentation of Pap tests and associated health information; and (3) feeling in control during the exam and having confidence in provider competency in trans care are priorities for many trans men. Participant feedback informing the selection of images for the brochure included a desire for representation of diversity in age, gender expression, and race/ethnicity of the FTM community as well as exclusion of images of women, medical equipment, and anatomical diagrams.
CONCLUSIONS: The experiences with Pap tests and preferences regarding patient outreach materials reported in this study reflect the unique barriers to adequate cervical cancer screening faced by the trans masculine community. However, the diversity of acceptability of and comfort with Pap tests that was observed across participants suggests that presenting options for customization of the exam and strategies to increase comfort and control during screening may be an effective outreach tool. A brochure was developed from participant feedback that will be further evaluated by community member focus groups to ensure it is effectively tailored to the needs of FTM individuals.
HAS CARDIOVASCULAR DIAGNOSTIC TESTING BECOME THE SIXTH ‘VITAL SIGN’ IN THE EMERGENCY DEPARTMENT? NHAMCS 2009–2010Anil N. Makam; Oanh K. Nguyen. University of Texas Southwestern Medical Center, Dallas, TX. (Tracking ID #1939616)
BACKGROUND: Current cardiology guidelines are increasingly discouraging cardiovascular diagnostic testing among low-risk ambulatory populations. Routine use of electrocardiograms (ECGs) on hospital admission has also been long discouraged due to low diagnostic utility. However, little is known about the extent of cardiovascular testing among low-risk populations in acute care settings such as the emergency department (ED). We hypothesize there is a high prevalence of cardiovascular diagnostic testing even among individuals who present to the ED without risk factors, signs or symptoms of cardiovascular disease.
METHODS: We analyzed data from the 2009–2010 National Hospital Ambulatory Medical Care Surveys (NHAMCS), a probability sample of ED visits in the US. Our primary outcome was the collection of cardiovascular tests (ECG and/or cardiac enzymes) during ED visits in adults (≥18 years) who were subsequently hospitalized. We estimated the adjusted probabilities of cardiovascular testing in the ED in low risk, average risk, and high risk scenarios using multivariate logistic regression adjusting for patient, visit and ED characteristics.
RESULTS: This study included 8,089 visits, representing 15.1 million ED visits per year by adult patients who were subsequently hospitalized. Of these visits, 52 % (95 % CI, 50 %–54 %) had symptoms potentially attributable to cardiovascular disease, and 59 % (95 % CI, 56 %–61 %) had a cardiovascular admitting diagnosis. Overall, 69 % of individuals (95 % CI, 66 %–71 %) had cardiovascular diagnostic testing, with 59 % (95 % CI, 57 %–62 %) having an ECG and 47 % (95 % CI, 43 %–51 %) with cardiac enzymes collected. In a low-risk scenario (25th percentile for age = 44 years, female, no cardiovascular symptoms, normal vital signs, no comorbidities, no cardiovascular admission diagnosis, disposition to a non-ICU bed, no/mild pain, normal mental status, non-emergent triage, and 0–5 other tests or services performed), 21 % (95 % CI, 18 %–25 %) of individuals had cardiovascular diagnostic testing (Table). In an average risk-scenario (50th percentile for age = 59 years and holding all other covariates at their mean values), 72 % (95 % CI, 69 %–74 %) had cardiovascular diagnostic testing. In a high-risk scenario (75th percentile of age = 76 years, male, cardiovascular symptom(s) present, abnormal vital sign(s), 2–4 comorbidities, cardiovascular admission diagnosis present, disposition to an ICU bed, moderate/severe pain, abnormal mental status, emergent triage, and >10 other tests or services performed), 99 % (95 % CI, 99 %–100 %) had cardiovascular diagnostic testing.
CONCLUSIONS: There is excessive cardiovascular diagnostic testing among low-risk individuals and highly prevalent testing among average-risk individuals in the emergency department. Our findings suggest more attention is needed to develop strategies for more targeted use of cardiovascular diagnostic tests among individuals presenting to the ED for care.
Table: Adjusted Probability of Cardiovascular Testing in the ED Among Subsequently Hospitalized Individualsa
| Scenario | |||
| Low risk (95 % CI) | Average risk (95 % CI) | High risk (95 % CI) | |
| <div align=\"left\">Age | 21.3 (17.6–24.9) | 72.0 (69.3–74.2) | 99.2 (98.6–99.9) |
| <div align=\"left\">Sex | |||
| <div align=\"left\"><p style='padding-left : 10px'>Female | 21.3 (17.6–24.9) | 68.9 (65.9–71.9) | 99.1 (98.3–99.9) |
| <div align=\"left\"><p style='padding-left : 10px'>Male | 23.4 (19.6–27.3) | 71.5 (68.6–74.4) | 99.2 (98.6–99.9) |
| <div align=\"left\">Cardiovascular symptomsb | |||
| <div align=\"left\"><p style='padding-left : 10px'>No | 21.3 (17.6–24.9) | 66.0 (62.9–69.1) | 98.9 (98.0–99.8) |
| <div align=\"left\"><p style='padding-left : 10px'>Yes | 28.0 (23.4–32.7) | 73.7 (70.8–76.6) | 99.2 (98.6–99.9) |
| <div align=\"left\">Vital signsc | |||
| <div align=\"left\"><p style='padding-left : 10px'>Normal | 21.3 (17.6–24.9) | 68.4 (64.9–71.9) | 99.1 (98.3–99.9) |
| <div align=\"left\"><p style='padding-left : 10px'>Abnormal | 23.4 (19.4–27.4) | 71.0 (68.3–73.7) | 99.2 (98.6–99.9) |
| <div align=\"left\">Cardiovascular comorbiditiesd | |||
| <div align=\"left\"><p style='padding-left : 10px'>0 | 21.3 (17.6–24.9) | 67.4 (64.4–70.4) | 98.6 (97.4–99.8) |
| <div align=\"left\"><p style='padding-left : 10px'>1 | 26.2 (21.1–31.3) | 73.2 (70.2–76.2) | 98.9 (98.0–99.9) |
| <div align=\"left\"><p style='padding-left : 10px'>2–4 | 32.7 (24.8–40.7) | 79.0 (73.9–84.0) | 99.2 (98.6–99.9) |
| <div align=\"left\">Cardiovascular admission diagnosis e | |||
| <div align=\"left\"><p style='padding-left : 10px'>No | 21.3 (17.6–24.9) | 57.9 (54.3–61.5) | 98.0 (96.3–99.7) |
| <div align=\"left\"><p style='padding-left : 10px'>Yes | 40.9 (34.9–46.9) | 78.1 (75.4–80.7) | 99.2 (98.6–99.9) |
| <div align=\"left\">Disposition | |||
| <div align=\"left\"><p style='padding-left : 10px'>Non-ICU | 21.3 (17.6–24.9) | 69.3 (66.6–72.0) | 98.9 (98.0–99.9) |
| <div align=\"left\"><p style='padding-left : 10px'>ICU | 27.2 (21.0–33.4) | 75.8 (71.2–80.4) | 99.2 (98.6–99.9) |
a Estimated using logistic regression adjusting for listed covariates plus race/ethnicity, payer, mental status, pain, triage status, number of other tests and services performed, length of visit and ED characteristics (region, metropolitan status, owner).
b Defined by ‘reason for visit’ fields.
c Abnormal vital signs defined as ≥1 of the following: heart rate ≥100 or <60 beats/min, systolic blood pressure ≥160 or <90 mmHg, diastolic blood pressure ≥100 or <60 mmHg, respiratory rate <10 or >20 breaths/min, or oxygen saturation <90 %.
d Diabetes, CHF, cerebrovascular disease, or ESRD on dialysis.
e ≥1 ‘ED provider diagnosis’ fields coded as a disease of the circulatory system per the AHRQ Clinical Classification Software.
HEALTH ACCESS INDICATORS AND ER USE AMONG LATINO MEDICAID BENEFICIARIESHugo A. Torres1; Ed Yelin2. 1Cambridge Health Alliance, Cambridge, MA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1939978)
BACKGROUND: The Medicaid program is a major source of health insurance for the Latino population. The purpose of this study is twofold: first, to measure the association between health access indicators and insurance type in the Latino population, comparing Medicaid to private insurance. The second is to assess chronic disease care by measuring differences in ER and hospital usage for ambulatory-care-sensitive conditions (ACSC) between Medicaid and privately-insured Latinos.
METHODS: This is a cross-sectional study utilizing the 2009 California Health Interview Survey (CHIS). The population studied is Latino respondents, aged 18–64, with private or Medicaid insurance (N = 5005). The principal independent variable is health coverage. For the first objective, the outcome is presence of a usual source of care (USOC) and interruption in health insurance in the past year. For the second objective, the analysis was limited to patients with conditions that have been documented to be ambulatory-care sensitive (ACSC); the outcome variable is ED visit or hospitalization for an ACSC. We use logistic regression to control for age; gender; rural location; education; English-speaking ability; presence of children; and self-reported health, chronic disease, and disability status.
RESULTS: There were 5,005 survey respondents that met the inclusion criteria, of whom 28.4 % were Medicaid recipients. Medicaid recipients were more likely to be female, younger, Spanish-speaking, and have children in the household. Medicaid recipients also had a lower level of education and mean income than the privately-insured respondents of the survey. Significantly more Medicaid recipients reported fair/poor health status (68.8 % vs. 52.5 %), and disability due to a physical or emotional condition (31.2 % vs. 21.0 %). 67.0 % of Medicaid recipients reported having a USOC, compared to 85.5 % of privately-insured patients (OR 0.34, p < 0.0001). The proportion of Medicaid recipients who were uninsured at any time in the past year is 25.6 %, compared to 6.5 % of privately-insured people (OR 2.9, p = 0.002). After adjustment with logistic regression, Medicaid recipients were half as likely to report having a USOC (OR = 0.52, 95%CI 0.37–0.73, p < 0.0001) and three times more likely to report having been uninsured in the past year (OR 3.0, 95%CI 2.0–4.5, p < 0.0001). Among patients with chronic disease, there was a trend toward more Medicaid respondents reporting use of the emergency department or being hospitalized in the past year: 13.0 % of Medicaid recipients used the ER in the past year for their chronic condition, compared to 6.8 % of privately-insured patients, (OR = 2.04, p = 0.082). This association became statistically significant after adjustment for the covariates (OR = 2.2, p = 0.03).
CONCLUSIONS: This study demonstrates that Latinos with Medicaid report worse health access and have a greater chance of going to the emergency room with a chronic condition than those with private insurance, even when controlled for demographic variables and health status. In light of the importance of having a usual source of care and continuous insurance in the prevention of adverse health outcomes, these findings point to a need to ensure that a robust primary care system and education on how to access it support Medicaid patients. This is particularly true of patients with chronic disease, where strong primary care supports can prevent unnecessary emergency room visits or hospital stays.
HEALTH AND FINANCIAL HARMS OF 25 STATES’ DECISION TO OPT OUT OF MEDICAID EXPANSIONDavid Himmelstein2; Samuel L. Dickman1; Danny McCormick1,3; Steffie Woolhandler2. 1Harvard Medical School, Boston, MA; 2City University of New York, School of Public Health, New York, NY; 3Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1929214)
BACKGROUND: As of December 2013, 25 states have chosen to opt out of expanding Medicaid coverage for low-income adults following the Supreme Court ruling that they are not required to do so. Salutary effects of previous Medicaid expansions have been observed in several states. We quantified the health and financial consequences of states’ decision to opt out.
METHODS: We categorized states as opting in or opting out of Medicaid expansion using data from the Kaiser Family Foundation. We used data from the 2013 Current Population Survey to project the number of persons in each state who will remain uninsured after implementation of the Affordable Care Act (ACA) and to analyze the number of people whose health and financial circumstances would improve if states opting out of Medicaid expansion were to opt in. We used data from the Oregon Health Insurance Experiment to predict the effects of Medicaid expansion on cervical and breast cancer screening, pharmacotherapy for diabetes mellitus, catastrophic medical expenditures and positive depression screening. We used two prior studies of the impact of insurance on death rates (Wilper et al., 2009 and Sommers et al., 2012) to project excess mortality associated with opt-outs.
RESULTS: Of the 47.95 million people who were uninsured in 2012, 32.20 million will remain so after implementation of the ACA, 7.78 million of whom would have been covered had all states expanded Medicaid. Medicaid expansion in opt-out states would have resulted in between 7,115 and 17,104 fewer deaths, 712,037 fewer persons screening positive for depression, 240,700 fewer persons suffering catastrophic medical expenditures, 422,533 more diabetics receiving medication, 195,492 more indicated mammograms and 443,677 additional indicated pap smears.
CONCLUSIONS: Many low-income adults will forego health and financial benefits that would be expected had their states opted to expand Medicaid coverage.
HEALTH INSURANCE PLAN KNOWLEDGE IN MASSACHUSETTS: A COMPARISON OF CONSUMERS OBTAINING INSURANCE FROM A HEALTH EXCHANGE, NON-EXCHANGE SOURCE OR MEDICAIDRachel Nardin1,3; Leah Zallman1,2; Assaad Sayah1,3; Danny McCormick1,3. 1Cambridge Health Alliance, Cambridge, MA; 2Institute for Community Health, Cambridge, MA; 3Harvard Medical School, Cambridge, MA. (Tracking ID #1935010)
BACKGROUND: Like the Affordable Care Act, the 2006 Massachusetts health care reform law (fully implented by 2008) expanded Medicaid coverage and created a state health insurance exchange offering publicly subsidized private health insurance plans (called Commonwealth Care (CWC)) to low income residents. Informed decision-making by those seeking insurance coverage requires that the application process, as well as the cost and coverage features of plans, be comprehensible. Limited understanding of plan features could adversely affect utilization of care and could undermine the consumer-driven competition between plans that is expected to be a key driver of health plan affordability. However, little is known about health plan knowledge among those obtaining Medicaid or a subsidized health plan via a health insurance exchange.
METHODS: Between August and December 2013, we conducted face-to-face structured interviews with a convenience sample of 681 patients presenting to three emergency departments at a large safety net health care system in the Boston area. We confirmed respondents’ insurance type using a statewide database updated daily. We included patients age 18–64 who had only one type of insurance and spoke English, Portuguese, Spanish or Haitian Creole. We excluded severely ill patients. We examined subjects’ responses to questions about the application process for their current insurance, about their knowledge of their current plan’s costs and benefits and about whether the extent of their knowledge affected their utilization of care. Comparisons across insurance types were made using the chi-square test.
RESULTS: Of the 681 participants, 16 % were uninsured, 14 % had CWC, 42 % had Medicaid and 28 % had private insurance. Overall, 21 % of respondents reported not understanding features of their coverage, including costs, and 34 % reported not being confident in their knowledge; this did not vary by insurance type. Among those who were not confident, 33 % delayed medical care due to this uncertainty. Overall, 24 % of respondents found it difficult to apply for their current insurance; this was significantly worse for those with publicly subsidized than for those with private insurance (Medicaid 25 %, CWC 35 %, private 14 %, p = 0.03). Similarly, more respondents reported difficulty completing the application process for Medicaid (39 %) and CWC (37 %) than for private insurance (16 %, p = 0.003). Overall, 41 % of respondents said the information provided regarding plan choices was hard to understand, 17 % said they did not have all the information they needed about costs when signing up for a plan and 38 % reported difficulty submitting the paperwork necessary to keep their insurance active; these measures did not vary by insurance type.
CONCLUSIONS: A high proportion of safety-net patients in Massachusetts report knowledge deficits about their insurance plan features and the application process, often resulting in delayed medical care due to this uncertainty. Those obtaining Medicaid and subsidized insurance though the state exchange reported the greatest difficulties. New federal and state insurance exchanges created under the Affordable Care Act should provide information about health plans and the application process in a format that is readily understandable to consumers. Relying on informed consumer choice to maximize competition in insurance exchanges may be premature.
HEALTH LITERACY AND USABILITY OF PATIENT EDUCATION DOCUMENTSRaman Singhal1; Katya Ostrow2; Calie Santana1. 1Montefiore Medical Center, Bronx, NY; 2Sackler School of Medicine, Tel Aviv, Israel. (Tracking ID #1929654)
BACKGROUND: In 2003, the National Assessment of Adult Literacy found that 36 % of the population has basic or below basic health literacy and 41 % of Bronx County adults lack basic literacy skills. With the advent of electronic medical records (EMRs), the dissemination of patient education materials has become increasingly feasible and required as part of the meaningful use federal incentive program. It remains largely unknown, however, if patients can understand and act on the information presented. We sought to determine the literacy level and usability of patient handouts, which document characteristics should be improved upon to increase usability, and how documents from different vendors perform on a usability scale.
METHODS: We analyzed 35 patient education documents in English from four vendors (A–D) and pertaining to six medical conditions (3 acute, 3 chronic) using the Suitability Assessment of Materials (SAM) tool. Vendors A and D provide easy-to-read (“basic”) as well as regular (“standard”) versions of documents—we analyzed 11 basic and 9 standard documents. The SAM tool assesses a document’s usability in six domains: content, literacy demand, graphics, layout/typography, learning stimulation, and cultural appropriateness. The literacy demand domain incorporates the reading grade level of the document’s text, which was calculated manually. Documents were printed in black-and-white, and were randomly numbered. Two researchers (RS and KO), blinded to each other’s scores and vendor, reviewed each document. For each document, we calculated a usability score, defined as the average SAM score—usability is categorized as not suitable (SAM < 40 %), adequate (40–70 %), or superior (>70 %). We also calculated the average score for each domain; because of the disparate weighting of each domain within the SAM score, domain scores were converted to percentages.
RESULTS: Usability ranged from 36.3 to 76.2 %–25 documents (71 %) were adequate, six were superior, and four were not suitable. Figure 1 shows this distribution and the relationship between usability and reading grade level. All not-suitable documents were written at or above the 9th grade reading level and all superior documents were written between the 4th and 7th grade level. The 11 basic documents had an average reading grade level of 5.7 (range 4–7), 1 (9 %) had superior usability, and zero were not suitable. The 9 standard documents averaged a 9.3 reading grade level (range 6–14), zero had superior usability, and 3 (33 %) were not suitable. As expected, average scores in all domains of the SAM tool trended up with increasing usability; the highest correlation was with literacy demand and the lowest with layout/typography. By domains, literacy demand achieved the highest average score across all documents at 75.3 %, while graphics achieved the lowest at 30.7 %. Documents from vendor A had an average usability score of 56.4 %, vendor B 70.3 %, vendor C 61.9 %, and vendor D 52.9 %. Vendors A (25 %) and D (75 %) produced all not-suitable documents, and vendor B produced 66 % of the superior documents.
CONCLUSIONS: The majority of patient education handouts available to us are acceptable by health literacy standards. Literacy demand had the highest correlation with usability, however, our study highlights that it is just one factor in creating a superior document. As an example, the literacy differences between basic and standard documents are muted when these documents are scored for usability. While several documents have mastered the literacy domain, the next area to improve is graphics—this domain had the second highest correlation with usability, but the lowest average score. As we aim to always choose usable documents, our results show that vendor B produced a majority of the superior documents. B’s documents achieved the highest average score in 4 domains, excelling by the greatest absolute magnitude in the graphics domain. As we increase the use of printed materials in our daily practice, we must continue to critically appraise their value and quality to ensure that they are useful for our patients.
HEALTHCARE FRAGMENTATION IN A MAJOR U.S. CITYLisa M. Kern1; Zachary Grinspan1; Jason Shapiro2; Rainu Kaushal1. 1Weill Cornell Medical College, New York, NY; 2Mount Sinai School of Medicine, New York, NY. (Tracking ID #1939540)
BACKGROUND: American healthcare is fragmented, with patients routinely seeking care from multiple providers in different practices and health systems. Healthcare fragmentation is thought to be particularly common in cities with multiple academic medical centers. Healthcare fragmentation is important, because it can lead to fragmentation of clinical information (that is, clinical information that is needed by healthcare providers but which is missing at the point of care because of gaps in communication across providers). Previous studies have estimated that such gaps occur frequently, with relevant clinical information missing in one of every seven ambulatory visits, potentially contributing to adverse events and readmissions. The degree to which healthcare fragmentation is contributing to this problem of information fragmentation has not been measured. In the absence of data on the amount of healthcare fragmentation, healthcare providers and policy makers may underestimate the actual degree of fragmentation and may, thus, underestimate the value of interventions designed to address it. Our aim was to derive a quantitative estimate of the amount of healthcare fragmentation in New York City.
METHODS: We conducted a longitudinal study using data from 2010 to 2011. We obtained the data from a health information exchange (HIE) organization previously called the New York Clinical Information Exchange (NYCLIX); it subsequently merged with another HIE organization and is now part of Healthix. We selected data from NYCLIX because it had detailed information on individual patient encounters with health care. The NYCLIX data included emergency department (ED) and inpatient visits for patients who sought care at six hospitals in Manhattan: Beth Israel Medical Center, Mount Sinai Medical Center, New York-Presbyterian Hospital, New York University Medical Center, Roosevelt Hospital, and St. Luke’s Hospital. For each patient who sought ED or inpatient care at one of the six hospitals, we determined whether that patient had been seen in a different hospital in the previous 12 months. This analysis allowed the specific 12-month window to vary from patient to patient, fixing time zero as the date of that patient’s encounter in 2011. The purpose of this analysis was to calculate the rate of encounters for which a patient’s clinical information could be missing if data were not exchanged across providers.
RESULTS: We identified 566,907 patients who were seen in the ED or inpatient settings in the six participating hospitals in 2011. We found that each of the six hospitals shared patients with every other hospital. For the entire group of patients, we found that there were 74,196 ED visits for which clinical information could have been missing, because the patient had been seen elsewhere in the previous 12 months. This is equivalent to 10.0 % of ED visits having potentially missing clinical information. Similarly, we found that there were 31,967 inpatient admissions for which clinical information could have been missing, because the patient had been seen elsewhere in the previous 12 months. This is equivalent to 9.1 % of inpatient admissions having potentially missing clinical information. The risk of potentially missing clinical data varied slightly by institution, but all institutions were affected. Depending on the institution, between 6.8 % and 16.9 % of ED visits had clinical data potentially missing. Similarly, between 6.6 % and 26.5 % of inpatient admissions had clinical data potentially missing, depending on the institution.
CONCLUSIONS: Healthcare fragmentation in New York City is extensive. All six participating hospitals were affected by healthcare fragmentation, with each hospital having its patients seen at each of the other five hospitals in a single year. It was very common for patients to seek care at the ED or inpatient setting of one hospital and have had previous care within the past 12 months at another hospital; this affected 10 % of all ED visits and 9 % of all inpatient admissions. This puts both patients and hospitals in a risky situation, in which relevant clinical information may be missing at the point of care. Interventions designed to decrease healthcare fragmentation are needed. In addition, interventions such as electronic health information exchange are needed, as they can potentially facilitate the efficient sharing of clinical data across providers and minimize the impact of healthcare fragmentation.
HEALTHCARE PROFESSIONALS’ ATTITUDES, PERCEPTIONS AND PRACTICES REGARDING BREAST SELF-EXAMINATIONKah Poh Loh1; Eng Keong Tan1; Owolabi Ogunneye1; Jennifer Friderici1; Reva Kleppel1; Mihaela S. Stefan1; James Stewart2. 1Baystate Medical Center/Tufts University, Springfield, MA; 2Baystate Medical Center/Tufts University, Springfield, MA. (Tracking ID #1934250)
BACKGROUND: n 2009, the United States Preventive Service Task Force (USPSTF) published a revised guideline for breast cancer screening. Specifically for breast self-examination (BSE), USPSTF recommends against teaching breast self-examination, as opposed to the previous guideline stating “insufficient evidence to suggest for or against SBE”. The objectives of this study is to assess healthcare professionals’ knowledge, perception and attitude in BSE as well as their adherence to the newly revised USPSTF guideline in BSE. We hypothesized that the knowledge and adherence of healthcare providers to the USPSTF newly revised guidelines is poor.
METHODS: A cross-sectional survey study was carried out in five medical and gynecogical practices affiliated with a large academic teaching hospital in Western Massachusetts. The survey was populated and e-mailed to all attendings, residents, advanced practitioners (APs), physician assistants (PAs) and nurses working in these medical practices. The first part of the survey contains demographic data including gender, age, residency program, job position, previous experience in medical practice in years and medical school they graduated from. The second part of the survey will enquire their awareness and perceptions of the 2009 USPSTF guidelines in BSE and clinical breast examination by physician, followed by their practices in BSE and the reasons why they do or do not teach BSE and whether any of their patients detected any breast lumps through BSE. Characteristics associated with adherence and knowledge were compared using Fisher’s Exact test and univariable logistic regression analysis. Characteristics associated with adherence and knowledge were compared using Fisher’s Exact test and univariable logistic regression analysis.
RESULTS: The survey completion rate was 50.7 % (104/205). Respondents were primarily female (64.4 %, a median (IQR) age of 31 years (29, 43)). Fifty-one percent of the responders were residents, 26.0 % were attending MDs and 23.1 % were APs, PAs and nurses. Fewer than half of respondents correctly perceived the 2009 USPSTF guidelines for BSE (41.4 %, 95 % CI 31.7 %, 51.0 %). Most (70.2 %, 95 % CI 61.3 %, 79.1 %) teach patients to perform BSE. The most frequent reason cited for teaching BSE was “early detection of cancer (48.0 %), and to “empower woman”, (37.0 %). In univariable analyses, recommendation for BSE was significantly associated with female gender (OR 2.64, 95 % CI 1.11, 6.29). Other characteristics which showed an association without reaching statistical significance were: ≥5 years of practice (OR 2.11, 95 % CI 0.84, 5.30); non physician practitioner (OR 3.5, 95 % CI 0.82, 14.93); US Med School (OR 2.20, 95 % CI 0.84, 5.75); ever detecting a lump in a patient (OR 2.95, 95 % CI 0.80, 10.87) and belief that BSE reduces morbidity and mortality (OR 2.12, 95 % CI 0.84, 5.37). Among 35 respondents who stated they were aware of USPSTF guidelines, surprisingly approximately half (48.6 %) taught BSE frequently or occasionally.
CONCLUSIONS: Knowledge of, and adherence to, the 2009 USPSTF guidelines related to BSE is relatively low. Several personal and professional characteristics may be associated with adherence. Despite being aware of the guidelines, some health professionals still taught BSE. Greater efforts should be made to educate healthcare professionals about the 2009 USPSTF guidelines.
HEALTHCARE PROVIDERS’ KNOWLEDGE OF DIFFERENT DIETS AND DIETARY ADVICE PROVIDED TO PATIENTSSonali Arora1,2; Auras R. Atreya2; Reva Kleppel2; Jennifer Friderici3; Tara Lagu2; Michael B. Rothberg4. 1Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 2Baystate Medical Center/ Tufts University School of Medicine, Springfield, MA; 3Baystate Medical Center, Springfield, MA; 4Cleveland Clinic, Cleveland, OH. (Tracking ID #1938959)
BACKGROUND: Therapeutic lifestyle changes, including diet and exercise, are considered first line therapy for patients at risk of coronary heart disease (CHD). It is unknown what dietary advice healthcare providers offer to patients and whether they tailor that advice to specific risk factors. Similarly, healthcare providers’ knowledge of the evidence supporting various diets has not been assessed. Our objective was to determine which diets physicians recommended to patients, as well as their beliefs about the evidence behind those recommendations.
METHODS: We surveyed attending physicians, fellows, residents, nurse practitioners and physician assistants in internal medicine, cardiology, endocrinology and family medicine at multiple practices within Baystate Health, a large integrated health system in Western Massachusetts. The 22-question survey was devised by the investigators to determine physicians’ dietary recommendations for patients with diabetes mellitus (DM), hypertension (HTN), dyslipidemia, obesity and CHD; and to test healthcare providers’ knowledge regarding published evidence for various diet recommendations. Knowledge scores were constructed based on number of correct responses to questions about evidence for the benefits of various diets. Average knowledge scores were compared according to provider characteristics using one-way analysis of variance.
RESULTS: The overall response rate was 57 % (115/203); and 13 questionnaires were excluded from the knowledge calculation for incomplete knowledge scores. Among 102 remaining responses, 40 (39 %) were attending physicians, 46 (45 %) house staff and 16 (16 %) advanced practitioners. The majority (n = 88, 86 %) were from primary care specialties and 76 (75 %) worked in an academic practice. Seventy-nine percent (79 %) of healthcare providers felt it was important for patients to follow a healthy diet, but only 27 % offered dietary advice to all patients. Instead, 66 % gave dietary advice to high-risk patients or those who asked for advice. The top dietary recommendation for HTN was a low salt diet (79 %), for uncontrolled DM a low carbohydrate diet (65 %), for obesity a low calorie diet (75 %), for CHD and for dyslipidemia a low saturated fat diet (64 % and 74 % respectively). Only 9 % of healthcare providers recommended the same diet for all conditions. Providers believed that their 58 % of their incorrect diet recommendations were supported by randomized trial evidence. The most common misconceptions were that randomized trial evidence existed that low carbohydrate diet helps control DM (58 % of providers) and that Mediterranean diet increases life expectancy (51 % of providers). Respondents’ overall knowledge of randomized trial evidence for dietary interventions was low (Mean/SD knowledge score 32 %/13 %, range 0 % to 58 %). Knowledge scores of attending physicians were significantly higher than those of house staff (+6.0 percentage points, p = 0.02) and advanced practitioners (+11.0 percentage points, p = 0.006). Knowledge scores did not vary significantly between specialties (32 % primary care vs. 30 % other, p = 0.72) or practice type (30 % academic practice vs. 35 % non-academic, p = 0.10).
CONCLUSIONS: Physicians and advanced practitioners report recommending different diets depending on specific risk factors and generally believe that their recommendations are evidence based. However, there remain substantial gaps between their knowledge and the randomized trial evidence regarding diet in disease prevention. Apart from increased provider education regarding diets (through medical school curricula, residency training and CME), guidelines could take a more comprehensive approach to cardiovascular risk reduction, rather than focusing on single specific macronutrients for individual risk factors.
HIGH VALUE CARE BY US INTERNAL MEDICINE RESIDENTS: USING EXAM VIGNETTES TO ASSESS PRACTICEKira L. Ryskina1,2; Deborah Korenstein3; Arlene Weissman3; Philip Masters3; Patrick C. Alguire3; Cynthia D. Smith3. 1University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3American College of Physicians, Philadelphia, PA. (Tracking ID #1940181)
BACKGROUND: Unsustainably high healthcare spending in the US has lead to calls to incorporate high value care (that balances benefits of tests or treatments against potential harms and costs) as a competency for internal medicine residents. However, objective evaluation of resident practice of high value care (HVC) is a challenge for educators. In this study, we describe the development of an assessment of HVC resident practice using a set of clinical vignettes from the Internal Medicine In-Training Examination (IM-ITE).
METHODS: HVC concepts were broadly discussed with IM-ITE authors prior to and during question development. After the exam was finalized, three physicians independently reviewed each of the 340 questions for selection in the HVC subscore and categorized each selected question according to six specific HVC rationales. We measured inter-observer agreement across reviewers for (1) question selection, and (2) the HVC rationale, using Fleiss’ kappa statistic. Exam questions were included in the HVC subscore if, after discussion, the reviewers reached a consensus about both the item and the associated rationale. The IM-ITE exam from which the HVC subscore was defined was administered in October 2012. Using descriptive statistics, we characterized residents’ HVC subscore performance according to their year of training, medical school location, residency program track, career plans, overall ITE performance, and the Dartmouth Atlas’ hospital care intensity (HCI) index of the training hospital. We used multivariate linear regression with clustering at the program level to identify resident and program characteristics associated with hypothetical practice of HVC, adjusting for overall exam performance and other potential confounders.
RESULTS: Thirty-eight questions were included in the HVC subscore. Initial inter-observer agreement was moderate for question selection (kappa = 0.56, 95 % CI 0.51–0.58, p < 0.001), and fair for HVC rationale (kappa = 0.25, 95 % CI 0.16–0.26, p < 0.001). Of the 18,102 US residents who completed the exam and had a measurable subscore, 34.1 % were PGY1, 34.6 % were PGY2, and 31.3 % were PGY3. About one in five (20.3 %) planned to pursue a career in general internal medicine. The mean HCI index of participants’ hospitals was slightly higher than the national average (1.12 vs. 1.0, p < 0.001). The average percent correct was lower for the HVC subscore compared to the overall exam (60.1 % vs 63.1 %, p < 0.001). The HVC subscore correlated strongly with the overall exam score (Pearson correlation coefficient 0.73, p < 0.001). The mean HVC subscore was lower for interns compared to senior residents (20.1 vs. 24.0, p < 0.001) and slightly higher for residents who trained at a hospital with below average HCI index compared to those who trained at a hospital with above average HCI index (22.6 vs 22.0, p < 0.001). The difference in mean HVC subscores between residents trained at high vs. low HCI index hospitals was more pronounced for residents in lower quintiles of overall exam performance (Table). After adjusting for resident and program characteristics and overall test performance, the HVC subscore was negatively associated with the HCI index of the training hospital (beta coefficient −0.31, p = 0.02, 95 % CI −0.57 −0.05).
CONCLUSIONS: The process used to develop an HVC subscore of the IM-ITE exam had face validity and resident scores varied slightly based on their home institution’s level of healthcare utilization. Although alone it is likely inadequate, this measure may assist in evaluation of resident practice of HVC and may also motivate program directors and residents to focus their learning and curriculum more on high value care principles.
Mean Subscore by Quintile of HCI and Overall Performance
| Quintile of overall performance | Mean Subscore for Lowest HCI Index Quintile (SD) | Mean Subscore for Highest HCI Index Quintile (SD) | P-value |
| Lowest | 18.5 (4.0) | 17.5 (3.9) | <0.0001 |
| 2nd | 20.9 (3.7) | 20.2 (3.8) | 0.0005 |
| Middle | 22.7 (3.7) | 22.0 (3.6) | 0.0002 |
| 3rd | 24.2 (3.5) | 23.8 (3.4) | 0.047 |
| Highest | 26.6 (3.5) | 26.3 (3.2) | 0.15 |
HOME-BASED PRIMARY CARE IS ASSOCIATED WITH REDUCED AMBULATORY CARE SENSITIVE HOSPITALIZATIONS IN VETERANS WITH DIABETESSamuel T. Edwards1,2; Julia Prentice3,4; Steven R. Simon1,5; Steven D. Pizer3,6. 1VA Boston Healthcare System, Boston, MA; 2Harvard Medical School, Boston, MA; 3VA Boston Healthcare System, Boston, MA; 4Boston University, Boston, MA; 5Brigham and Women’s Hospital, Boston, MA; 6Northeastern University, Boston, MA. (Tracking ID #1927327)
BACKGROUND: Intensive primary care and home-based services have the potential to reduce the likelihood of hospitalization of elderly patients with multiple chronic diseases. We examined the relationship between enrollment in Home Based Primary Care (HBPC), a national home care program operated by the US Department of Veterans Affairs (VA) and ambulatory care sensitive condition (ACSC) hospitalizations among elderly Veterans with diabetes.
METHODS: We performed a national cohort study of Veterans over age 67, who were traditional Medicare beneficiaries, had a diagnosis of diabetes mellitus and one other chronic disease, and had at least one hospitalization in 2005 or 2006. Our primary exposure was enrollment in HBPC, defined as a minimum of 3 HBPC encounters. Our main outcome was hospitalization due to an ambulatory care sensitive condition, as measured by the Agency for Healthcare Research and Quality Prevention Quality Indicators. Our data consisted of VA records supplemented by Medicare claims. Patients were followed from January 1st 2006 or 2007 (end of baseline year) through December 31st, 2010. Outcomes were analyzed using a two-stage discrete time survival model with distance from the Veteran’s residence to a VA facility that provides HBPC serving as an instrumental variable to control for selection. Patients were censored after enrollment in Medicare Advantage or death.
RESULTS: We identified a total of 56,502 Veterans with a total of 2,049,838 person-months of follow up for analysis. Of these patients, 1,872 enrolled in HBPC and 54,630 did not. HBPC patients were older (mean 79.1 years vs. 77.1 years), and more often black (20.8 % black among HBPC patients vs. 10.9 % black among non-HBPC patients). HBPC patients had higher diabetes severity (Young’s Diabetes Severity Index mean 4.8 vs. 4.2), and had more co-existing conditions such as CHF (59.2 % vs. 53.5 %). HBPC patients also had a higher prevalence of mental illness including psychosis (24.6 % vs. 13.7 %) and depression (32.6 vs. 18.3 %). Multivariate predictors for HBPC enrollment included paralysis (OR 2.12, 95 % CI 1.63–2.76), depression (OR 2.03, 95 % CI 1.73–2.40), CHF (OR 1.37, 95 % CI 1.17–1.59) and distance from HBPC providing VA (10–30 miles vs. <5 miles, OR 0.58, 95 % CI 0.49–0.70). After controlling for selection, HBPC enrollment was associated with a 22.5 % relative reduction in the probability of experiencing one or more ACSC hospitalizations in one year (table), corresponding to an absolute reduction in risk of ACSC hospitalization of 7 %, from 27 to 20 %.
CONCLUSIONS: HBPC enrollment is associated with decreased risk of ACSC hospitalization among elderly Veterans with diabetes. Programs like HBPC may play an important role in the management of elderly patients with multiple chronic diseases in accountable care models.
Change in probability of one or more ACSC hospitalization in 1 year associated with HBPC and other comorbidites
| Relative change in probability | p | |
| HBPC | −22.5 % | <0.01 |
| CHF | 42.4 % | <0.01 |
| COPD | 36.0 % | <0.01 |
| Pulmonary Circulatory Disorder | 15.9 % | <0.01 |
| Fluid/Electrolyte Imbalance | 12.6 % | <0.01 |
| Depression | 10.8 % | <0.01 |
| Diabetes Severity Index (per unit) | 2.6 % | <0.01 |
HOSPITAL TO HOME HEALTH CARE TRANSITIONS: A GAP ANALYSIS OF TARGETS FOR QUALITY IMPROVEMENTChristine D. Jones1; Julia E. Clemons1; Ethan U. Cumbler1; Benjamin Honigman2; Darren A. DeWalt4; Eric A. Coleman3; Robert Burke5; Heidi Wald1,3. 1University of Colorado School of Medicine, Aurora, CO; 2University of Colorado School of Medicine, Aurora, CO; 3University of Colorado School of Medicine, Aurora, CO; 4University of North Carolina at Chapel Hill, Chapel Hill, NC; 5Department of Veterans Affairs Medical Center, Eastern Colorado Health Care System, Denver, CO. (Tracking ID #1933651)
BACKGROUND: Adequate information exchange is critical to high-quality care transitions, yet little is known about the quality of information transfer from hospitals to home health care services. To evaluate perceptions of completeness and timeliness of medical information transferred from a tertiary care University Hospital to home health care agencies, we performed a cross-sectional survey of home health care clinicians and staff.
METHODS: During the fall of 2013, we submitted a web-based 34-question survey to 30 individuals from two health agencies that provide the highest volume post-hospitalization home health care for the hospital’s discharged patients. The survey explored various aspects of care coordination, including access to medical records in a timely fashion and adequacy of information provided. Respondents could select answers from a 4- or 5-point Likert scale as well as enter free-text comments.
RESULTS: 24 of 30 home health representatives responded to the survey (80 % response rate). Among 24 respondents, 46 % identified as client services managers, 38 % were clinical managers, and 17 % held other positions (e.g., administration, liaison, marketing, etc.). We found that 38 % of respondents indicated having “occasional” or “rare” access to sufficient information from the hospital about a patient’s discharge medical conditions and management. In addition, 23 % of respondents indicated encountering problems related to not having adequate information about a patient “often” to “almost always.” The most common insufficient aspects of discharge communication were: advanced directives/code status (55 %), how to contact the appropriate hospital clinician with questions (55 %), and the appropriate clinician (e.g., primary care provider, hospital clinician) to contact with questions (50 %). Altogether, 86 % of respondents found it “somewhat difficult” or “difficult” to reach the appropriate physician with questions after discharge. Additionally, respondents indicated having insufficient access to information on care plans related to: physical or occupational therapy issues (45 %), follow up plans for labs or imaging studies pending at the time of discharge (33 %), and indication and planned duration for lines or catheters (33 %). Most respondents (86 %) indicated that internet-based access to the hospitals electronic medical record (EMR) would be important to help manage patients.
CONCLUSIONS: In this study, we performed a unique survey of home health care organizations in which we identified perceptions of quality gaps in the completeness of medical information provided to home health care clinicians and staff. As a next step, these individuals will be provided with internet-based access to the hospital EMR. We plan to repeat this survey 6 months following implementation of internet-based EMR access to determine which components of information exchange improve with this intervention and which require alternative interventions to drive improvement.
HOSPITALIST CAREER DECISIONS AMONG INTERNAL MEDICINE RESIDENTSJohn Ratelle1; Denise Dupras2; Patrick C. Alguire3; Philip Masters3; Arlene Weissman3; Colin P. West4,5. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN; 3American College of Physicians, Philadelphia, PA; 4Mayo Clinic, Rochester, MN; 5Mayo Clinic, Rochester, MN. (Tracking ID #1904482)
BACKGROUND: Since its inception in the mid-1990s, hospital medicine (HM) has grown into a distinct field of medical practice including more than 30,000 physicians, most of whom are trained in Internal Medicine. Despite its growth, little is known about internal medicine residents’ decisions to pursue careers in HM. To meet this knowledge gap, we sought to identify which internal medicine residents choose a career in HM and how that choice changes over the course of their training.
METHODS: We conducted an observational cohort study of postgraduate year 3 (PGY-3) residents who completed the annual Internal Medicine In-Training Examination (IM-ITE) in 2009–2011. Survey questions addressed self-reported career plans, and linkage to National Board of Medical Examiners (NBME) records allowed analysis by program type (categorical or primary care), sex, and medical school location (United States or international). Results were linked to each resident by unique identifiers to allow analysis of changes in career plan across postgraduate years 1, 2, and 3.
RESULTS: We analyzed data from the 16,781 PGY-3 residents who completed the IM-ITE survey, representing 77.7 % of the 21,608 PGY-3 internal medicine residents in training in the 2009–2010, 2010–2011, and 2011–2012 academic years. 1552 (9.3 %) of these 16,781 PGY-3 residents reported HM as their ultimate career choice. Categorical residents were more likely than primary care track residents to report a hospitalist career plan in PGY-3 (9.8 % vs. 3.5 %, adjusted odds ratio (aOR) 3.19, 99 % CI 2.11–4.83, p < 0.001). Men were more likely than women to report a hospitalist career plan (9.8 % vs. 8.5 %, aOR 1.16, 99 % CI 1.01–1.33, p = 0.007). Among categorical residents, hospitalist career plans did not differ for United States and international medical graduates (9.8 % in both groups), while among primary care track residents, United States medical graduates were more likely to report a hospitalist career plan (5.7 % vs. 1.8 %, aOR 3.64, 99 % CI 1.59–8.31, p < 0.001). Among the 9501 residents completing the survey in all 3 years of training, only 276 (2.9 %) indicated a hospitalist career plan during the PGY-1 year, compared with 450 (4.7 %) in PGY-2, and 951 (10.0 %) in PGY-3. Among these 951 PGY-3 residents, 128 (13.5 %) originally made this decision in PGY-1, 192 (20.2 %) in PGY-2 and 631 (66.4 %) in PGY-3. Only 87 (9.1 %) of these residents maintained a career decision in HM during all 3 years of training. Overall, 148 (53.6 %) of the 276 residents with a hospitalist career plan during PGY-1 reported a different career plan during PGY-3. Of these residents who changed career plans away from HM, 74 (50.0 %) planned a general medicine career and 64 (43.2 %) reported a subspecialty career. For the 823 residents with a hospitalist career plan during PGY-3, but not during PGY-1, 221 (26.9 %) had planned to be general medicine physicians and 445 (54.1 %) had previously reported a subspecialty plan.
CONCLUSIONS: Hospital medicine is a reported career choice for a significant proportion of graduating internal medicine residents. However, most residents do not finalize this decision until their final year of training. Additionally, the majority of residents who indicated HM as a career interest during PGY-1 indicate plans for an alternative career path by PGY-3. Further study is required to understand the reasons for these career plan shifts and to inform the best educational structures for hospitalist training.
HOSPITALIZATION-ASSOCIATED DISABILITY IN OLDER ADULTS IN A SAFETY NET HOSPITALAnna H. Chodos1; David Guzman3; S. Ryan R. Greysen4; Jeffrey Critchfield2; Urmimala Sarkar3; L. E. Goldman3; Margot Kushel3; Edgar Pierluissi1,2. 1UCSF, San Francisco, CA; 2UCSF, SFGH, San Francisco, CA; 3UCSF, SFGH, San Francisco, CA; 4UCSF, San Francisco, CA. (Tracking ID #1938146)
BACKGROUND: Hospitalization-associated disability (HAD) affects one-third of adults over 70 years old and predicts future disability and death. Adults cared for at safety net hospitals may be at risk of HAD at younger ages given the higher prevalence of risk factors for premature disability, such as low socioeconomic status. We measured the incidence of HAD by age group and examined associated risk factors in hospitalized adults at a safety net hospital.
METHODS: We measured functional outcomes of 548 patients 55 years and older who spoke English, Spanish, or Chinese, and were admitted to the San Francisco General Hospital, a safety net hospital. Participants’ functional status at baseline (2 weeks prior to admission) and 30 days post- discharge was ascertained by self-report of ADL function. The outcome measure was new or additional disability in 1 or more ADL. Functional outcomes by age group were compared using chi-square tests. Logistic regression was used to identify associated risk factors for new or additional disability at 30 days.
RESULTS: Most participants were functionally independent at baseline. HAD was common in all age groups but it was the lowest in the middle age group, 65–69 years old, and significantly higher in the oldest group compared to all others. (See Table).
CONCLUSIONS: In adults at a safety net hospital, HAD at 30 days post-hospitalization occurred in almost as many adults 55–59 years old as 70–79 (30 %), which is similar to the proportion in the general population among adults 70 and older. Risk for HAD was significantly higher in the oldest group, ≥80, compared to all other groups. In safety net hospitals, aggressive interventions that prevent and modify disability are needed and should also target adults younger than 65.
Hospitalization-Associated Disability at 30 Days by Age Group
| Age, years | No Baseline Disability N (Row %) | Incidence of HAD at 30 days Row % | P-value for HAD at 30 days* | Odds Ratio for HAD at 30 days** (95 % CI) |
| 55–59 | 97 (73.5 %) | 25.8 % | p = 0.151 | 1.80 (0.81, 4.01) |
| 60–64 | 155 (80.7 %) | 22.4 % | p = 0.342 | 1.28 (0.59, 2.75) |
| 65–69 | 71 (87.7 %) | 17.3 % | reference | 1.0 |
| 70–79 | 61 (66.3 %) | 29.4 % | p = 0.063 | 1.28(0.55, 2.97) |
| ≥80 | 27 (52.9 %) | 62.8 % | p < 0.001 | 4.96 (1.98, 12.41) |
*Chi-square test. **Controlled for sex, any baseline ADL disability, ADL disability at admission (categories), any IADL disability at admission, cognitive impairment, Charlson score, Creatinine ≥1.5
HOW AN INTERVENTION TO HELP PREGNANT WOMEN USE PUBLICLY AVAILABLE PEDIATRIC QUALITY DATA AFFECTS THEIR TRUST IN THE INTERNET AS A SOURCE FOR THESE DATAYara Youssef1,2; Penelope S. Pekow1,2; Peter K. Lindenauer1,4; Jasmin L. Roberts1; Katharine O. White1,5; Kathleen M. Mazor2,3; Sarah L. Goff1,4. 1Baystate Medical Center, Springfield, MA; 2University of Massachusetts Amherst, Amherst, MA; 3University of Massachusetts Medical School/Meyers Primary Care Institute, Worcester, MA; 4Tufts University School of Medicine/CTSI, Boston, MA; 5Baystate Medical Center, Springfield, MA. (Tracking ID #1935060)
BACKGROUND: IDEAS for a Healthy Baby is a randomized trial that examines whether helping pregnant women use publicly available pediatric quality data impacts their choice of pediatrician. Women randomized to the intervention group received an information session with a trained patient navigator who assisted them in using a website that reports pediatric quality data. Women randomized to the control group received a pamphlet that explained what quality data is, why it is important, and that included the web-address for the website used in the intervention.
METHODS: English-speaking women ages 16–50 between 20 and 34 weeks of gestation who attended a prenatal clinic that serves a low income population were enrolled between May and December 2013. As part of the baseline survey, participants were asked to rate how much they trust various sources of health quality information (e.g., friends, family, coworkers, the internet, social media) using a four-point Likert scale. Trust was again measured after the intervention to determine if changes in trust had occurred in the intervention and control groups. Health literacy was assessed using the Newest Vital Sign. Responses were collapsed into “high” and “low” trust. Wilcoxon matched-pairs signed-ranks test were used to assess changes in trust in sources of health quality information from baseline to follow-up.
RESULTS: Among participants with complete baseline and follow-up data (n = 189; 102 intervention/87 control), the median age was 25; 57 % were Hispanic, 25.6 % White, and 18.9 % Black. 33.5 % of women had completed <12 years of education; 34.1 % earned <$20,000/year; 76.2 % scored in the “possible” to “likely” limited health literacy range. There was no baseline difference in the level of trust in the internet between the intervention and control groups (40.8 % vs. 43.1 %, p = 0.10). There was a significant increase in trust in the internet in the intervention group (40.8 % vs. 52.8 %, p < 0.05); there was no change in trust in the internet in the control group (43.1 % vs. 40 %, p = 0.81). A substantial proportion of participants in both the intervention and control groups reported a high level of trust in family as a source of information about health care quality (88.3 % and 87.4 %) with fewer participants reporting high levels of trust in friends (68.2 % and 64.9 %) or co-workers (43.5 % and 46.5 %) at baseline. There were no significant changes in levels of trust for these other sources after the intervention.
CONCLUSIONS: Participation in an intervention to enable use of publicly reported pediatric quality data was associated with an increase in trust in the internet as a source of health quality information. A pamphlet that provided information about health quality information and a link to the website did not have the same effect. Trust in other sources such as friends, family and coworkers did not significantly change in either the intervention or control groups. The greater increase in trust in information found on the internet in patients who viewed the information with a patient navigator compared to patients who only received written information about the website may indicate a role for facilitated review of this information for low-income, low health-literacy populations.
HOW CAN EHEALTH TECHNOLOGY ADDRESS MULTIMORBIDITY CHALLENGES? PERSPECTIVES FROM PATIENTS WITH MULTIPLE CHRONIC CONDITIONSDonna M. Zulman1,2; Emily Jenchura4; Danielle Cohen2; Eleanor Lewis1; Thomas Houston3; Steven Asch1,2. 1VA Palo Alto Health Care System, Menlo Park, CA; 2Stanford University, Stanford, CA; 3Bedford VA Medical Center, Bedford, MA; 4Arizona State University, Tempe, AZ. (Tracking ID #1937094)
BACKGROUND: eHealth technology such as personal health records, web-based disease management programs, and mobile applications can support patient self-management and health care navigation. These tools, however, are frequently disease-specific in design. Optimization of eHealth tools for patients with multiple chronic conditions requires an understanding of challenges and technology needs specific to multimorbidity.
METHODS: We conducted a qualitative needs assessment of patients with multiple chronic conditions from an academic medical center and a Veterans Affairs facility. A screening questionnaire was used to identify 330 patients with ≥3 chronic conditions and with experience using health-related technology. We used purposive sampling to construct 10 groups of 3–8 patients, grouping individuals by age, sex, primary health care setting, and a common chronic condition to facilitate discussion. A trained facilitator moderated the focus groups using a semi-structured guide based on the Fit between Individual, Task, and Technology (FITT) framework to elicit discussion about 1) challenges that patients face when they have multiple chronic conditions, and 2) patients’ use of technology—and opportunities to enhance technology—to address these challenges. Standard content analysis methods were used to code textual data from focus group transcripts. Three investigators generated preliminary codes based on the FITT framework, and two investigators independently read and coded all transcripts using ATLAS.ti software. Emergent themes were reviewed with all collaborators, and final themes and representative quotes were validated through a follow-up survey with a sample of focus group participants.
RESULTS: Among focus group participants (n = 53), the mean (SD) number of chronic conditions was 5(2) with the most common including hypertension (75 %), chronic pain (64 %), arthritis (49 %), diabetes (34 %), and depression (40 %). Patients described using technology most frequently to search for health information (96 %), communicate with health care providers (92 %), track medical information (83 %), track medications (77 %), and support decision-making about treatment (55 %). Focus group discussions yielded three overarching themes about multimorbid patients’ challenges that may be amenable to eHealth technology support: 1) Needing to serve as expert and advocate because of a unique combination of health issues (“You have to be your own advocate and research everything you can because sometimes you will be more cutting-edge than your doctor”); 2) Managing a high volume of information, visits, and self-management tasks (“I can save myself easily 15 or 20 visits a year just by messaging my primary or my neurologist”); and 3) Coordinating, synthesizing, and reconciling information from different providers and about different conditions (“My illness crosses so many specialty boundaries…I am always playing tag between one of four doctors”). Several desirable eHealth tools emerged from discussions, including resources that retrieve and synthesize information about multiple conditions and medications, applications that manage tasks and health records across multiple healthcare systems, tools that facilitate communication with multiple providers, and social media that connects patients with similar conditions.
CONCLUSIONS: Patients with multiple chronic conditions have holistic, rather than condition-specific, needs from eHealth technology, and desire tools that reconcile information about different conditions and enhance communication across providers and systems.
HOW DO PATIENTS PERCEIVE BREAST DENSITY? A QUALITATIVE STUDYErin N. Marcus1,4; Monica Yepes2,4; Noella Dietz3,4. 1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL; 3University of Miami Miller School of Medicine, Miami, FL; 4University of Miami Miller School of Medicine, Miami, FL. (Tracking ID #1939566)
BACKGROUND: Breast density is a radiologic term denoting the degree of opacity of breast tissue on mammographic imaging. Mammography is less sensitive in women with dense breasts. Supplemental ultrasound can help detect additional cancers in these women, but it also results in a significant increase in biopsies and imaging of noncancerous lesions. Some patient groups have urged that all women be told about their breast density and advised to consider additional testing for cancer. More than a dozen states now require that breast centers convey density findings to individual patients in writing with mammogram results. Little is known about women’s baseline understanding of the concept of breast density and about optimal ways to convey this information.
METHODS: Focus groups are being conducted with women who underwent screening mammography at a high volume academic medical center in 2013 and were found to have dense breasts with no suspicious lesions. The center routinely includes breast density information in the result letters it sends to patients, even though Florida state law does not require this. Women ages 40–69 with no history of breast cancer are eligible. All women meeting eligibility criteria were sent post cards providing them with the choice of opting out of a recruitment call. At least 3 attempts have been made to all women who did not opt out. Content analysis using a grounded theory approach is ongoing.
RESULTS: Thus far, 27 English-speaking women have participated in 4 groups. Participants’ ages range from 42 to 67. Ten women self-identified as Hispanic, 8 as Black, 5 as white non-Hispanic, and 4 as Asian. Repeated themes include confusion about the term “dense breasts” and the benefits of additional testing, as well as a fear that increased density is associated with a higher risk of cancer. Women liked print materials that included mammogram images showing normal, heterogeneous, and extremely dense breast tissue. Women stated they wanted a clear explanation of the potential financial costs of additional testing. Two more English and two Spanish focus groups are planned.
CONCLUSIONS: Simply adding language about density to patient result notification letters is inadequate to ensure these findings are communicated effectively. Our results suggest a need for tools to improve breast density understanding so that women can make an informed decision about additional breast imaging. Policymakers should keep in mind potential public confusion about this complex topic when crafting future density notification laws.
HOW DOES THE NUMBER OF BARRIERS TO CARE AFFECT TIMELINESS OF FOLLOW-UP AMONG WOMEN WITH ABNORMAL CANCER SCREENING TESTS IN THE PATIENT NAVIGATION RESEARCH PROGRAM?Ambili Ramachandran1; Frederick R. Snyder2; Elizabeth Calhoun3; Donald J. Dudley4; Steven R. Patierno5; Tracy A. Battaglia6; On behalf of the Patient Navigation Research Program7. 1Boston University School of Medicine, Boston, MA; 2NOVA Research Company, Bethesda, MD; 3University of Illinois at Chicago, Chicago, IL; 4University of Texas Health Science Center, San Antonio, TX; 5The George Washington University, Washington, DC; 6Boston University School of Medicine, Boston, MA; 7Patient Navigation Research Program, Rockville, MD. (Tracking ID #1931236)
BACKGROUND: Patient navigation (PN) programs were designed to address barriers to cancer care among underserved populations in order to improve access to timely care. While there is widespread dissemination of PN programs nationwide, there is a paucity of research examining the association of barriers and clinical outcomes within navigation programs. Better understanding of this relationship would help to guide improvements and adaptations of PN programs.
METHODS: We conducted a secondary analysis of the multicenter Patient Navigation Research Program (PNRP) using data from the intervention arms of seven sites that navigated women for abnormal breast or cervical cancer screening tests from 2006 to 2010. The independent variable was barriers to care documented by navigators during encounters with subjects. Barriers were characterized by quantity (0, 1, 2, 3+) and specific type. The dependent variable was median number of days to diagnostic resolution, defined by the time interval from index screening event to definitive diagnosis of cancer or no cancer, estimated using Kaplan-Meier cumulative incidence curves. Breast (n = 2600) and cervical (n = 1387) subjects were analyzed separately. Using chi-square tests, we compared subjects with and without barriers by socio-demographic characteristics. We then conducted descriptive statistics to examine specific barrier types and to describe the association of barrier quantity and navigation efforts (total number of encounters and total time spent by the navigator). Using log-rank tests, we compared median days to resolution by barrier quantity.
RESULTS: In both screening groups, compared to women without barriers, those with at least one barrier were more likely to be of minority race, non-English language speakers, and uninsured (p < 0.0001). The most common barriers identified were health insurance (24 %), system problems scheduling care (23 %), language (18 %), and fear (18 %). As the number of barriers increased, total number of encounters and total time spent by the navigator increased significantly (p < 0.0001). Breast subjects were more likely than cervical subjects to have at least one barrier to care (74 % vs. 55 % respectively, p < 0.0001). For both breast and cervical subjects, women with an intermediate number of barriers (1 or 2) had the longest time to resolution, while those with none or many (3+) had the shortest time to resolution. Among breast subjects, median time to resolution for those with 0 barriers or 3+ barriers was 52 days (95 % CI 45,62) and 60 days (95 % CI 54,68); whereas women with 1 or 2 barriers had median time to resolution of 83 (95 % CI 65,104) and 81 days (95 % CI 60,97). The median time to resolution among cervical subjects for those with 0 barriers or 3+ barriers was 75 days (95 % CI 69,80) and 69 days (95 % CI 62,80), while women with 2 barriers had longer time to resolution [102 days (95 % CI 84,139)].
CONCLUSIONS: In a multicenter study of patient navigation, those with barriers were among the most vulnerable. For both breast and cervical subjects, we found that women with the most barriers resolve cancer screening abnormalities as quickly as women with no barriers. However, women with an intermediate number of barriers experience a longer delay until definitive diagnosis. Future analyses will explore if this pattern may be explained by intensity of navigation or types of barriers.
HOW INPATIENT MEDICINE TEAMS MAKE SENSE OF THEIR PATIENTS AND TASKS: ROUNDING PATTERNS, PATIENT DISCUSSIONS, AND CLINICAL OUTCOMESLuci Leykum2; Hannah Chesser1; Carla Pezzia1; Holly Lanham1; Jacqueline Pugh2; Ray Palmer1; Jamie Kohn5; Heather S. Reisinger3; Michael Agar4. 1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2STVHCS/UTHSCSA, San Antonio, TX; 3Iowa City VA/Univ Iowa, Iowa City, IA; 4Ethknoworks, Santa Fe, NM; 5Kenan-Flagler Business School, UNC Chapel Hill, Chapel Hill, NC. (Tracking ID #1934905)
BACKGROUND: Recent literature explores how relationships among providers influence patient outcomes. Relationships may influence providers’ ability to engage in sensemaking, or how they come to understand what is happening with their patients and act based on their understanding. We examined sensemaking among inpatient medical teams, assessing patterns of team sensemaking and their association with patient outcomes of unnecessary length of stay (ULOS) and complication rates.
METHODS: We observed 11 inpatient teams in 2 teaching hospitals over 2 to 4 week periods, rounding with them daily. We took detailed field notes regarding team activities and audiotaped rounds. We assessed sensemaking in two ways: first, by how the team made sense of what they needed to do on rounds, and second, by how they made sense of individual patients’ clinical courses. To assess how teams made sense of their rounding tasks, we examined the order in which they rounded. We categorized rounding order as: “gravity,” starting at the highest floor and moving down; “geography,” starting on a particular unit and then moving to the next units; “intern by intern,” rounding on one intern’s patients first and then the other’s; “running the board,” sitting in the team room and rounding; and “patient-driven,” rounding based on patients’ clinical needs. We assessed the number of rounding patterns per team, hypothesizing that use of a greater number of patterns indicated that the team was better able to make sense of their clinical tasks and round accordingly. To assess sensemaking of individual patients, we listened to audiotaped discussions of 4 patient encounters. Two encounters were of complex patients on post-call days, and 2 were of patients who had complications. Complications were defined as the development of a new problem, or a clinical deterioration after at least 24 hours of stability. We used Charlson Comorbidity Score and presenting symptoms to sample post-call discussions, and Charlson and type of complication to sample patients with complications. We then applied the situation, task, intent, concern, calibrate (STICC) framework, assessing whether patient discussions included each of these elements. We gave each team a score from 0 to 4 for each STICC element, reflecting whether we heard the element in each of the 4 patient encounters. We then summed the scores from each element to obtain a total “STICC Score.” We assessed the association between number of rounding patterns, STICC score, and ULOS and complications using regression analysis. All analyses were adjusted for Charlson score, mental illness, and team workload.
RESULTS: Teams who used a higher number of rounding patterns and whose patient discussions reflected Intent had significantly lower ULOS (p = 0.01 and 0.04). Use of more rounding patterns was associated with fewer complications (p = 0.02), as were use of task, intent, and total STICC score in patient discussions (p = 0.02, <0.001, 0.01.).
CONCLUSIONS: Inpatient teams differ in how they round and discuss individual patients, and these differences are associated with patient outcomes. A shared understanding of the intent of the treatment plan may be particularly important for effective patient care, as may consideration of patient needs in rounding order. Improving sensemaking among clinical teams may be an important strategy for improving patient outcomes.
HOW OFTEN ARE CATHETER-ASSOCIATED URINARY TRACT INFECTIONS THAT ARE IDENTIFIED FOR NATIONAL HEALTHCARE SAFETY NETWORK SURVEILLANCE REPORTING ALSO NOTED AS DIAGNOSES IN CLAIMS DATA?Jennifer Meddings; Heidi Reichert. University of Michigan, Ann Arbor, MI. (Tracking ID #1939737)
BACKGROUND: Since 2008, claims data descriptions of urinary tract infections are used to determine whether the condition is a payable comorbidity, or is one of certain hospital-acquired conditions (such as catheter-associated urinary tract infection, CAUTI) for which hospitals no longer receive additional payment. Hospital CAUTI rates from claims data were publicly reported on Medicare’s ‘Hospital Compare’ website from 2011 and 2013. Since January 2012, hospitals have been required to collect CAUTI data for patients in intensive care units (ICUs) using criteria from the Center’s for Disease Control and Prevention and National Healthcare Safety Network (NHSN); these NHSN CAUTI events are publicly reported on ‘Hospital Compare.’ Our objective was to assess how often ICU patients with CAUTI events reported for NHSN surveillance were also noted to have a CAUTI diagnosis in the discharge claims data (which includes diagnoses from ICU and non-ICU days during hospitalization).
METHODS: We first performed a retrospective analysis of 6 months of patient-level infection control data for all adult and pediatric ICU patients from one large academic tertiary care hospital, to identify patients with at least one NHSN CAUTI event reported as acquired while in the ICU. We next performed a retrospective analysis of the discharge claims data that was submitted for payment for these patients’ hospitalizations. We identified claims data cases of CAUTI by having the ICD-9-CM diagnosis code 996.64 (infection or inflammation due to an indwelling urinary catheter); cases of UTI without catheter-association were identified by having at least one of 10 potential ICD-9-CM UTI codes listed among all diagnoses in the claims data without the 996.64 code.
RESULTS: Of the 4,522 adult and pediatric ICU patients admitted between January 1, 2012 and June 30, 2012, 56 patients were identified as having one or more CAUTI events during the ICU stay according to the infection control NHSN data. By claims data, 5 (9 %) of these 56 patients were identified as having a hospital-acquired CAUTI by the diagnosis code 996.64; 37 (66 %) were identified as having a UTI without catheter-association, of which 25 UTIs were noted as hospital-acquired. Of the 56 patients with NHSN CAUTI events, 14 (25 %) were not identified in claims data as having either CAUTI or UTI events.
CONCLUSIONS: CAUTI events reported by the CDC’s National Healthcare Safety Network as hospital-acquired infections for comparing hospital performance are rarely identified as CAUTI diagnoses in claims data, which requires an accurate description of the UTI to identify it as a payable or non-payable comorbidity. NHSN CAUTI events (identified by infection preventionists using laboratory data and symptoms as documented in the medical record) may not be listed as diagnoses in claims data (generated by hospital coders based upon descriptions of UTIs in physician notes) because physicians may not recognize and/or document the UTIs as catheter-associated, or because physicians apply different criteria for clinical diagnosis of CAUTI compared to the NHSN surveillance definitions. Consequently, hospitals may be receiving additional comorbidity payment for hospital-acquired CAUTI events being reported to the NHSN surveillance system, because two mandatory and resource-intensive data collections (NHSN data and claims data) for identifying hospital-acquired conditions are occuring in parallel, without communication between them.
HOW WELL DOES MEDICARE’S VTE-1 CORE MEASURE CAPTURE HOSPITAL PERFORMANCE FOR VENOUS THROMBOEMBOLISM PROPHYLAXIS?Claire Griffiths1; Marc Moote1; Carol Becker1; Julie Wietzke1; Amy N. Brant1; Daniel Nielsen1; Steven J. Bernstein1,2; Scott A. Flanders1. 1University of Michigan, Ann Arbor, MI; 2US Department of Veterans’ Affairs, Ann Arbor, MI. (Tracking ID #1928904)
BACKGROUND: Venous thromboembolism (VTE), including pulmonary embolism and deep-vein thrombosis, is an important cause of preventable morbidity and mortality, and commonly occurs in the setting of hospitalization. Pharmacologic and mechanical prophylaxis are effective at preventing VTE and it is recommended that all patients admitted to the hospital be screened for VTE risk and given prophylaxis when indicated. The Centers for Medicare and Medicaid Services (CMS) has accordingly developed a set of 6 Core Measures of hospital performance for the prevention of VTE. The first of these measures, VTE-1, assesses whether at least 1 dose of pharmacologic prophylaxis or use of mechanical prophylaxis was provided to patients during hospital day 1 or 2 when indicated. However, the administration of a single dose of prophylaxis is not necessarily an accurate measure of hospital VTE prophylaxis performance as high performing hospitals should accurately assess risk, capture contraindications to pharmacologic prophylaxis, and deliver appropriately dosed VTE prophylaxis throughout the duration of a patient’s hospital stay. The Michigan Hospital Medicine Safety Consortium (HMS), a multi-hospital quality collaborative, collects detailed data regarding VTE prophylaxis provided during hospitalization, allowing a comparison of hospital performance by the current CMS VTE-1 measure to a more rigorous definition developed by HMS.
METHODS: Data were collected from 21 participating hospitals from January to June, 2013. For VTE-1, CMS requires that each hospital randomly sample medical records of non-ICU patients >18 years old and report the rate at which patients receive any dose of pharmacologic or mechanical prophylaxis on day 1 or 2 of hospitalization or have a documented reason why prophylaxis was not given. CMS data were collected from an average of 229 patients per hospital (range 201–292), and CMS VTE-1 performance for each hospital was determined by using the average of monthly rates over the 6 month study period. HMS data were collected by trained medical record abstractors from an average of 369 non-ICU, non-surgical patients per hospital (range 324–401). Appropriate VTE prophylaxis by HMS criteria was defined as receipt of appropriately dosed pharmacologic prophylaxis on hospital day 1 or 2 for patients at high risk of VTE as determined by Padua risk score. High risk patients with contraindications to pharmacologic prophylaxis not receiving anticoagulants required an order for mechanical prophylaxis on day 1 or day 2. Hospitals were first placed into performance quartiles based on CMS VTE-1 rates of prophylaxis, and were then re-ranked by performance quartile based on the HMS appropriate prophylaxis definition.
RESULTS: Using the CMS VTE-1 performance measure, a mean of 92.1 % of patients (hospital performance range: 71.6 % to 99.6 %) met CMS core measure criteria for adequate VTE prophylaxis at all hospitals. The mean rate of prophylaxis and ranking of each hospital by performance quartile is shown in Fig 1. Using the HMS definition, only 72.5 % of patients (hospital performance range: 41.1 % to 90.5 %) received appropriate prophylaxis. Of the 5 hospitals in the top-performing quartile for the CMS measure, 2 hospitals (40 %) shifted to a lower quartile using the HMS performance criteria, 1 of which dropped to the bottom quartile. Of the 6 lowest performing hospitals by CMS criteria, 3 hospitals (50 %) moved out of the bottom quartile when ranked by the HMS performance criteria. In all, 13 hospitals (62 %) moved by 1 or more quartiles using the more rigorous HMS criteria (Fig 2).
CONCLUSIONS: Comparisons of hospital performance for VTE prophylaxis vary considerably based on the definition used for appropriate prophylaxis. A more rigorous, guideline-based definition of appropriate prophylaxis resulted in a shift of performance quartile for over 60 % of hospitals. As hospitals are increasingly being rewarded and penalized based on their performance by these measures, more effort is needed to better understand and address the limitations of existing measures.
Figure 2: HMS VTE Performance
HYPERTENSION IN WESTERN ALASKA NATIVE PEOPLE: THE WESTERN ALASKA TRIBAL COLLABORATIVE FOR HEALTH (WATCH) STUDYStacey E. Jolly1; Kathryn R. Koller2; Jesse Metzger2; Scarlett Hopkins3; Bernadette Boden-Albala4; Bert Boyer3; Sven O.E. Ebbesson3; Barbara V. Howard5; Jason G. Umans5. 1Cleveland Clinic, Cleveland, OH; 2Alaska Native Tribal Health Consortium, Anchorage, AK; 3University of Alaska-Fairbanks, Fairbanks, AK; 4Mount Sinai Hospital, New York, NY; 5MedStar Research Institute, Washington DC, DC. (Tracking ID #1918808)
BACKGROUND: Hypertension (HTN) is a common and an important risk factor for cardiovascular diseases (CVD), such as stroke, heart disease, and heart failure. Estimates of HTN among Alaska Native people are lacking from national surveys, yet CVD is increasing in this population; thus we assessed the prevalence of HTN, risk factors, awareness and treatment among western Alaska Native people.
METHODS: This cross-sectional analysis from the Western Alaska Tribal Collaborative for Health (WATCH) study, comprised of four epidemiologic cohort studies from 2000 to 2010, includes Alaska Native adults ≥18 years of age from the Norton Sound and Yukon- Kuskokwim regions of Alaska. Participants were categorized as having HTN if they had systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, were taking blood pressure medication at the time of entry into the study, and/or had a diagnosis of HTN in their medical record. Covariates examined were age, body mass index (BMI), glycemic status, smoking (current/former vs. never), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C). Obesity was defined as a BMI ≥30 kg/m2. Diabetes and impaired fasting glucose were defined using 2010 American Diabetes Association criteria. High TG and low HDL-C were defined using 2002 National Cholesterol Education Program guidelines for metabolic syndrome. HTN awareness was by self-report, HTN treatment was defined by use of prescribed blood pressure medication, and HTN control was a baseline blood pressure <140/85 mmHg with concurrent use of blood pressure medication. U.S. General Population estimates are from NHANES.
RESULTS: Of the 4,569 participants, 54 % (n = 2,453) were women. Mean age was 41 years (SD +/− 16). One quarter, 25 % (n = 1,138) had prevalent HTN; U.S. general population prevalent HTN is about 33 %. Women (27 %) had more HTN than men (23 %); HTN increased with age with 50 % of participants aged 55–64 years and nearly 70 % of those 65 years and older having HTN. The prevalence of HTN in the Yukon-Kuskokwim region was 28 % vs. 21 % in the Norton Sound region. Prevalent diabetes was 5 % (n = 219) and impaired fasting glucose was 23 % (n = 1,047); 71 % (n = 3,222) were current/former smokers. In multivariate analysis, age obesity, elevated triglycerides, and impaired fasting glucose were independently associated with HTN prevalence (see table). Of the people with HTN, 64 % (n = 731) were aware of their condition. Of the 700 participants with HTN and for whom medication data was available, 61 % (n = 428) were on blood pressure medication, and 39 % (n = 273) were controlled. Among U.S. general population, 52 % have controlled HTN.
CONCLUSIONS: HTN in western Alaska Native people was less prevalent than in the U.S. general population and efforts to understand the protective factors are needed. Important correlates of risk for HTN were age, obesity, and high triglycerides. Data on awareness, treatment and control suggest the need for programs to better control HTN among those with it and stem the tide of rising cardiovascular disease.
Multivariate Regression Analysis of Independent Risk Factors for Prevalent HTN among Western Alaska Native People
| Odds Ratio (95 % Confidence Interval) | |
| Sex (Female vs Male) | 0.95 (0.80–1.13) |
| Age (referent is 18–34 years) 35–44 | 2.41 (1.89–3.08) |
| 45–54 | 4.23 (3.30–5.42) |
| 55–64 | 11.41 (8.72–14.94) |
| 65+ | 27.12 (20.12–36.51) |
| Region (referent is Yukon-Kuskokwim) Norton Sound | 0.51 (0.42–0.61) |
| Body Mass Index (>=30 vs <30) | 2.31 (1.93–2.78) |
| Impaired Fasting Glucose | 3.29 (2.30–4.71) |
| Prevalent Diabetes | 1.11 (0.92–1.34) |
| Current/Former Smoker | 0.74 (0.61–0.88) |
| Triglycerides (>=150 vs <150) | 2.19 (1.76–2.72) |
| Low HDL (<40 for men; <50 for women) | 0.89 (0.71–1.12) |
IDENTIFYING AND DISCOURAGING OVERUSE IN AMBULATORY CARE: THE SWISS LESS IS MORE PROJECTKevin Selby1; Joana Le Boudec1; Jean-Michel T. Gaspoz2; Arnaud Perrier2; Meier A. Christoph3,2; Andreas Zeller4; Nicolas Rodondi5; Stefan Neuner-Jehle6; Jacques Cornuz1. 1University of Lausanne, Lausanne, Switzerland; 2University of Geneva, Geneva, Switzerland; 3Triemli Hospital, Zurich, Switzerland; 4University of Basel, Basel, Switzerland; 5University of Bern, Bern, Switzerland; 6University of Zurich, Zurich, Switzerland. (Tracking ID #1929778)
BACKGROUND: There is a growing movement in several countries to identify and list low-value healthcare activities so as to discourage their use, with the goal of reducing waste and avoiding harm to patients. In 2012, the Swiss Society for General Internal Medicine launched a process to create a list of activities to be avoided in Swiss primary care. Given differences in practice patterns between countries and the potential controversies surrounding such a list, a transparent process was needed to adapt international lists to the local context.
METHODS: A literature review of similar initiatives was performed to identify low-value healthcare lists in the US, UK et Australia. Recommendations with little relevance to ambulatory internal medicine were excluded. A panel of experts from throughout Switzerland participated in an online, modified Delphi process to rank international recommendations and propose additional low-value health care activities commonly performed in Switzerland.
RESULTS: 1090 recommendations were identified. Nine hundred thirty-two recommendations were excluded because they were not relevant to primary care and 91 were excluded because they were poorly substantiated or were recommendations of activities ‘to do’, leaving 38 unique recommendations relevant to ambulatory general internal medicine. Thirty-five Swiss experts ranked items based on their agreement with each statement, and suggested 12 new recommendations using a modified Delphi process. The average agreement score of the 50 items was 8.52/10 (SD = 0.80). In a third round, the top 18 recommendations were re-ranked based on perceived frequency, costs and potential harms to patients. To ensure that an initial ‘do not do’ list would have a potential large impact on primary care, the top 10 items based on frequency were identified (table).
CONCLUSIONS: Amongst Swiss experts, there is generally a high level of agreement with international recommendations to avoid low-value care. A score based on frequency, costs and potential harms can provide a transparent way to measure the potential impact of recommendations.
Low-value healthcare activities to be avoided, ranked by frequency encountered in Swiss primary care
| Rank | Recommendation | Agreement Score (0–10) | Impact Score (96–288) | Frequency Score (32–96) |
| 1 | Do not obtain imaging studies in patients with non-specific low back pain | 9.56 | 212 | 94 |
| 2 | Do not prescribe antibiotics for uncomplicated upper respiratory tract infections (URIs) | 9.40 | 201 | 92 |
| 3 | Do not perform the Prostate Specific Antigen (PSA) test to screen for prostate cancer without a discussion of the risks and benefits | 9.59 | 211 | 90 |
| 4 | Do not perform lab testing in patients with a clinical diagnosis of an uncomplicated upper respiratory tract infection (URI) | 9.03 | 168 | 87 |
| 5 | Do not continue pharmacological treatment of gastroesophageal reflux disease (GERD) with long-term acid suppression therapy without titrating to the lowest effective dose | 9.50 | 196 | 82 |
| 6 | Do not routinely prescribe antibiotics for acute mild-to-moderate sinusitis | 9.50 | 186 | 81 |
| 7 | Do not use antimicrobials to treat bacteriuria in immunocompetent older adults | 9.16 | 180 | 80 |
| 8 | Do not routinely obtain radiographic imaging for patients who meet diagnostic criteria for uncomplicated acute rhinosinusitis. | 9.91 | 190 | 78 |
| 9 | Do not obtain preoperative chest radiography in the absence of a clinical suspicion | 9.26 | 168 | 77 |
| 10 | Do not use dual-energy x-ray absorptiometry (DEXA) screening for osteoporosis in women younger than 65 or men younger than 70 | 9.16 | 169 | 72 |
Bold: New recommendations proposed by Swiss experts.
Impact Score = Frequency + Cost + Harms
IDENTIFYING BARRIERS AND FACILITATORS TO IMPROVING THE IMPLEMENTATION OF WEIGHT MANAGEMENT SERVICES WITHIN A PATIENT-CENTERED MEDICAL HOMEMelanie Jay1,3; Sumana Chintapalli2,1; Kathryn Oi2,1; Allison Squires4,2; Scott Sherman1,3; Adina Kalet2. 1VA NY Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU School of Medicine, New York, NY; 4NYU College of Nursing, New York, NY. (Tracking ID #1920970)
BACKGROUND: The Veterans Affairs (VA) Healthcare System uses Patient-Aligned Care Teams (PACT) as part of its patient-centered medical home model. “Teamlets” often consist of an RN, an LPN, a program assistant, and a PCP who are tasked with screening for obesity, providing brief interventions, counseling patients, and advising eligible patients to attend MOVE!, an intensive weight management program. While every VA hospital has a MOVE! Program to address the high prevalence of overweight and obesity among Veterans, less than 10 % of eligible patients attend even one session. Since Veterans visit PACT 3.6 times per year, there are opportunities to improve counseling and service coordination. A single-center, qualitative research study of healthcare team members assessed attitudes and practices as well as elicited barriers and facilitators to care implementation for overweight and obese patients.
METHODS: We recruited healthcare team members for individual key informant interviews using a combination of convenience and snowball sampling. We used a semi-structured interview guide with questions informed by the Theory of Planned Behavior. Interviews lasted 30–60 min and were conducted by a general internist in a private office while a research assistant took field notes. The interviews were audio recorded and transcribed by a transcription company. Research assistants reviewed transcripts to correct mistakes and de-identify content. Analysts then used an iterative and directed coding approach, facilitated by NVivo software and structured by an initial coding guide developed from field notes and recollections. The primary coder segmented and coded each transcript, allowing additional codes to emerge. A second researcher then independently coded each segment. The researchers met frequently to harmonize codes and synthesize themes that emerged from coded transcripts.
RESULTS: There were 25 participants in the study (11 MD or NP, 5 RN, 2 RD, 5 LPN, 2 Other, with 6 holding an additional managerial role); 80 % were female, 48 % identified as White, 28 % African American, 16 % Asian, and 8 % Hispanic. Emerging themes included: system constraints, patient barriers, and perceived role responsibility. We found that performance measures and reminders motivate and shape current practices by the PACT teamlets. Barriers to treating patients included time, competing demands, and lack of understanding about what happens in the MOVE! Program. Facilitators included having received training in motivational interviewing (MI) and having a personal interest in nutrition and physical activity. Perceptions about role responsibility varied, with some RNs, LPNs, and MDs perceiving that they play important roles in weight management counseling, while others stated that it was the role of other team members. Similarly, perceived counseling competency varied within and between the different professions. For instance, some RNs and PCPs described in great detail how they used MI to counsel patients around weight, while others questioned whether they had adequate time and training.
CONCLUSIONS: These data allowed us to identify several approaches to improve weight management by the PACT teamlets and will inform the design of PACT-based weight management interventions. Findings, however, may be organization-specific, so replication of the study at other sites is necessary to determine common implementation issues.
IDENTIFYING PROVIDER FACTORS ASSOCIATED WITH PSA SCREENING AMONG ELDERLY VETERANSVictoria Tang1,2; Ying Shi1,2; Kathy Fung1,2; Roxanne Espaldon1,2; Jessica E. Tan1,2; Louise Walter1,2. 1SFVAMC, San Francisco, CA; 2UCSF, San Francisco, CA. (Tracking ID #1926332)
BACKGROUND: Despite guidelines recommending against prostate-specific antigen (PSA) screening in elderly men with limited life expectancy, screening is common. PSA screening is heavily dependent upon the health care provider; however, little is known about the provider-level determinants of PSA screening in elderly men with differing life expectancy. We sought to identify provider characteristics that are associated with PSA screening rates in elderly men with limited life expectancy and those with favorable life expectancy.
METHODS: We conducted a cross-sectional study of 636,413 men age 65+ years eligible for PSA screening and had laboratory tests performed at a VA in 2003. Men with limited life expectancy were defined as men age 85+ with Charlson score ≥1 or age 65+ with Charlson score ≥4. Men with favorable life expectancy were defined as men age 65–74 with Charlson score = 0. We identified providers who ordered these patients’ index screening PSA test or ordered the majority of their lab tests in 2003. The primary outcome was the percentage of men who had a screening PSA at a VA in 2003. The primary predictors were provider characteristics, including provider type, training level, gender, and specialty. We performed log-Poisson regression models for the association between each provider characteristic and PSA screening among men with limited life expectancy and favorable life expectancy, adjusting for patient characteristics (age, race, marital status, income, and education) and provider clustering.
RESULTS: Among 96,644 (15 %) men with limited life expectancy 42 % received PSA screening. Among 127,769 (20 %) men with favorable life expectancy 68 % received PSA screening. Higher PSA screening in men with limited life expectancy was associated with the following provider characteristics: training level (46 % for attendings versus 30 % for residents/fellows, P < 0.001), provider type (48 % for physician assistants versus 46 % for attending physicians and nurse practitioners, P = 0.002), gender (44 % women vs 43 % men, P < 0.001) and specialty (43 % Medicine vs 40 % Surgery, P = 0.007). The same provider characteristics were associated with higher PSA screening in men with favorable life expectancy. All provider characteristics remained independently predictive of PSA screening in multivariate analyses except specialty, which was no longer predictive among men with limited life expectancy.
CONCLUSIONS: A significant percentage of men with limited life expectancy are receiving PSA screening. Practicing clinicians have substantially higher PSA screening rates than trainees regardless of patient life expectancy. Interventions to reduce PSA screening in elderly men with limited life expectancy should be targeted to high screening providers.
ILLICIT BUPRENORPHINE USE, AND ACCESS TO AND INTEREST IN BUPRENORPHINE TREATMENTAaron Fox1,2; Adam Chamberlain2; Taeko M. Frost3; Chinazo Cunningham1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY; 3Washington Heights CORNER Project, New York, NY. (Tracking ID #1927780)
BACKGROUND: In the United States, the opioid addiction epidemic is escalating; however, there is a large gap (nearly 1.5 million persons) between those in need of treatment and those who receive treatment. Primary care physicians have the opportunity to address this treatment gap by offering buprenorphine maintenance therapy (BMT), but access to treatment may not be adequate to meet the current demand. Recently, diversion of buprenorphine has received major media attention, where concerns were raised about illicit buprenorphine use to get high; however, qualitative studies have suggested that opioid users may use illicit buprenorphine to “self-treat” their opioid addiction, especially if they experience barriers to BMT. This study investigated illicit buprenorphine use among syringe exchange participants, a group with high needs for opioid addiction treatment, and explored whether illicit use was associated with access to BMT and interest in initiating BMT.
METHODS: Syringe exchange participants were recruited from the offices of a harm reduction agency in New York City. Computer-based interviews were conducted to determine: 1) prior use of buprenorphine (illicit and prescribed); 2) access to BMT (perceived barriers); and 3) interest in BMT (overall interest in BMT and likelihood of initiating treatment). Overall interest was measured using a 5-point Likert scale; those rating their level of interest as 4 or 5 were considered to be interested in BMT. Access to and interest in BMT were compared between illicit buprenorphine users and non-users using chi square or t-tests.
RESULTS: Of 102 opioid users, 57 had used illicit buprenorphine (34 with illicit buprenorphine use only; 23 with illicit and prescribed buprenorphine use). Nine participants had used prescribed buprenorphine only. Overall, 45 % of participants were interested in BMT. Regarding access, the most common barrier to BMT was, “did not know where to get treatment,” which was reported by 51 % of participants. Other common barriers were costs (33 %) and transportation (28 %). Compared to those who had never used illicit buprenorphine, not knowing where to get treatment was more common among illicit buprenorphine users (64 % vs. 36 %, p < 0.01), overall interest in BMT was greater among illicit buprenorphine users (mean ± SD; 3.37 ± 1.29 vs. 2.80 ± 1.34, p = 0.03), and more illicit buprenorphine users reported they would be likely to initiate BMT if it were easily accessible (82 % vs. 50 %, p < 0.01).
CONCLUSIONS: Illicit buprenorphine use was common. A majority of illicit buprenorphine users were interested in BMT and reported that they would be likely to initiate treatment, but nearly two-thirds of illicit users did not know where to access BMT. Therefore, relatively simple interventions that address barriers to BMT (e.g. linking illicit buprenorphine users to practices that offer BMT or initiating BMT onsite at harm reduction agencies) could reduce illicit buprenorphine use, narrow the treatment gap, and diminish the tragic consequences of opioid addiction.
IMPACT OF A BEHAVIORAL ECONOMICS INTERVENTION ON CONTROL OF HYPERTENSION AMONG VERY POOR, PREDOMINANTLY MINORITY ADULTS: A RANDOMIZED TRIALMartin F. Shapiro1,6; Suzanne B. Shu2; Noah J. Goldstein2,3; Craig R. Fox2,3; Estivali S. Villa1; Martiniano Flores1; Sitaram Vangala1; Chi-Hong Tseng1; Braden Mogler7,8; Stewart B. Reed9; Ronald G. Victor4,5; Jose J. Escarce1,6. 1UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA; 3UCLA, Los Angeles, CA; 4Cedars-Sinai Health System, Los Angeles, CA; 5Cedars-Sinai Health System, Los Angeles, CA; 6UCLA, Los Angeles, CA; 7UCLA, Los Angeles, CA; 8Charles R. Drew University of Medicine and Science, Los Angeles, CA; 9Columbia University, New York, NY. (Tracking ID #1936163)
BACKGROUND: Effective hypertension (HTN) control requires timely diagnosis, appropriate therapy, and long-term adherence. Poor HTN control contributes substantially to cardiovascular risk and racial/ethnic health disparities. We conducted a randomized trial of two interventions to improve blood pressure (BP) control among poor Latino and African American adults attending Federally Qualified Health Clinics in Los Angeles: provision of a home BP monitor and monthly BP checks to the control group, vs. provision of contingent payments and an “identity intervention” to the intervention group in addition to the control treatments.
METHODS: Consenting adults with BPs ≥149 mm systolic (SBP) and/or ≥94 mm diastolic (DBP) on two consecutive visits to the clinic, using a standardized measurement protocol, were randomized into control (CONT) or intervention (INT) conditions. Research staff did not interact with clinicians caring for subjects regarding BP control. Both groups were given educational materials on HTN and home BP monitors and training in their use. CONT received $20 at each of months 1–6 if they returned for BP checks. INT were administered a survey to identify potential reasons to stay healthy or live longer (e.g. people in their lives, responsibilities to others, life goals and activities they enjoy) and were given personalized calendars with pictures of loved ones or representations of their activities/goals. They received $10 at months 1–6 for returning, but an additional $5 per item if they brought their calendar and BP monitor to a visit, and up to 3 lottery tickets at each visit (expected value: $7 per ticket) if they 1) recorded HTN medication use on the calendar most days, 2) measured BP on most days, and 3) if BP was normal or improved from the previous visit. Finally, at each visit through 6 months, INT received contingent payments of $2 per mm of SBP and DBP improvement up to normalization of BP (139/89), to a maximum of $50 per visit; if BP was normalized, minimum payment was $30. A research associate also spent time with INT at months 1–6 discussing what improved BP would mean for their loved ones, goals, and activities. Both groups received $20/visit for coming in for BP checks at 9 and 12 months. Summary statistics (mean, median, standard deviation and frequency distribution) were generated for demographic, social, behavioral and clinical characteristics. Repeated measurement analyses were carried out using logistic mixed effects models for the primary endpoints of change in control of SBP and DBP at 6 and 12 months.
RESULTS: Of 207 subjects randomized, 83 % completed 6 months follow-up and 75 % completed 12 months. Analyses including or excluding those lost to follow-up and with or without covariates other than baseline BP yielded similar results. Subjects were mean age 53.7 years, 51 % male, 59 % <12 years education, 21 % employed, 75 % household income <$10,000, 64.8 % Latino and 33.2 % Black, 59 % born outside the US, 41 % diabetic, 69 % with ≥1 major chronic disease other than HTN; 41 % had recently gone without health care because they needed money for food, clothing or housing; 22 % had gone without food, clothing or housing because they needed money for health care. Experimental groups did not differ in these characteristics. Mean baseline BP was 162.3(SD 14.5)/91.6(14.2) mm in INT and 161.8(14.1)/88.7(12.8) mm in CONT. At 6 months, mean BP was 141.9(16.6)/81.1(13.9) mm in INT and 146.1(18.9)/80.4(15.0) mm in CONT. In multivariable analysis controlling for baseline BP, age, gender, education, race/ethnicity, born in US and diabetes, SBP control was achieved at 6 months in 57.1 % of INT and 40.2 % of CONT (p = .033) . By 12 months, 39.5 % of INT and 35.0 % of CONT had normal range SBPs (p = .729). DBP fell by lesser amounts: nearly half were normal at baseline and over 70 % at 6 and 12 months. There was a trend toward greater DBP control at 6 months in intervention subjects (p = .080), but not at 12 months. At 6 months, INT improved relative to CONT in HTN medication adherence (Morisky Score) (p = .027) and in 2 measures of social support (someone to help with chores, and number of close friends with whom they felt at ease, both p < .04). Groups did not differ in patient activation scores. There was a trend toward more improvement in physical health (SF-12) in INT (p = .058).
CONCLUSIONS: We observed a 17 percentage point greater improvement in SBP control at 6 months in the group receiving contingent payments and the identity intervention compared to those receiving home BP monitors and monthly BP checks alone. This very encouraging result was not sustained once the intervention ended. Further research is needed to determine which component(s) of the intervention contribute to improvement, which characteristics predict benefit, and whether extending one or both interventions would sustain the improvement seen in this study, as well as to identify additional measures to further improve BP control in this highly disadvantaged population.
IMPACT OF CONFLICT OF INTEREST POLICIES ON PHYSICIAN PRESCRIBING OF ANTIPSYCHOTICS 2008–2011Timothy Anderson1; Haiden A. Huskamp2; Andrew Epstein3; Colleen Barry4; Aiju Men5; Ernst R. Berndt6; Marcela Horvitz-Lennon8; Sharon-Lise Normand2,7; Julie M. Donohue5. 1UPMC, Pittsburgh, PA; 2Harvard Medical School, Boston, MA; 3University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA; 4Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 5University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA; 6MIT Sloan School of Management, Cambridge, MA; 7Harvard School of Public Health, Boston, MA; 8RAND Corporation, Pittsburgh, PA. (Tracking ID #1938503)
BACKGROUND: The impact of restrictive conflict of interest (COI) policies on physician prescribing behavior is poorly understood. It is unknown how academic prescribing trends compare with community settings where there has been less focus on regulating COI. We compared trends in physician prescribing of heavily promoted antipsychotic among physicians in academic medical centers and among physicians in two non-academic settings: a tightly regulated integrated delivery system with stringent COI policies and more loosely regulated community settings.
METHODS: We conducted difference-in-difference analyses of antipsychotic prescriptions filled in outpatient pharmacies between 2008 and 2011. We examined changes in prescribing of heavily promoted, new, and reformulated antipsychotics among 2,464 physicians in 101 academic medical centers stratified by exposure to COI policies compliant with American Association of Medical Colleges (AAMC) guidelines (defined as adopting 7 of 9 recommendations) as well as two comparison groups of 186 Kaiser Permanente physicians, and 11,201 community physicians.
RESULTS: 15 % of academic physicians were in AAMC compliant institutions throughout the study period, 23 % were in institutions that attained AAMC compliance, and 61 % were in institutions never reached compliance. The shares of prescriptions for heavily promoted antipsychotics were no different across the academic, Kaiser, and community physician groups (range: 65–66 % in 2008 and 65–68 % in 2011). There were no statistically significant differences in the differences in the share of prescribing for heavily promoted antipsychotics over time across physician groups. Shares of prescriptions for new and reformulated antipsychotics more than doubled among academic physicians (from 2.4 to 6.2 % in AAMC compliant institutions, 2.9 % to 7.7 % in institutions attaining compliance, and 3.3 % to 7.0 % in non-compliant institutions). There were no statistically significant differences in the rate of increase between academic groups. In contrast, Kaiser physicians only increased their prescribing for heavily promoted and new antipsychotics from 1.7 % in 2008 to 2.6 % in 2011 for an increase that was 2 % lower than that of academic physicians in non-AAMC compliant institutions (95 % CI −0.04–0.00, p = 0.02). Community physicians increased their prescribing of new and reformulated products from 4.6 % of antipsychotic prescriptions to 9.8 % from 2008 to 2011, for a change that was 2 % higher than academic physicians (95 % CI 0.01–0.02, p < 0.001).
CONCLUSIONS: Prescribing of heavily promoted antipsychotics was virtually identical among academic physicians, and those practicing in an integrated health system and the community. However, there were differences in prescribing of new and reformulated antipsychotics across settings. The adoption of AAMC recommendations on physician-industry interactions appears to have had little impact on prescribing of a costly and widely used medication class.
IMPACT OF EMERGENCY DEPARTMENT COPAYMENTS IN MEDICAIDMona Siddiqui; Craig E. Pollack. Johns Hopkins University School of Medicine, Arlington, VA. (Tracking ID #1939342)
BACKGROUND: The number of individuals enrolling in Medicaid has increased over the past several years due both to the recent recession which resulted in high levels of unemployment and the federal Deficit Reduction Act (DRA) of 2005 which enabled states to modify and expand the criteria for Medicaid eligibility. In an attempt to offer states more flexibility in administering their Medicaid programs while containing costs, the DRA allowed states discretion in instituting sliding scale premiums and copayments for Medicaid beneficiaries when accessing covered services. While some states had copayments for emergency department (ED) visits prior to 2005, the DRA granted states the ability to enforce cost-sharing. While prior studies show that cost-sharing can reduce health care utilization, the impact of the DRA on ED co-payments remains poorly understood. The objective of this study was to evaluate the impact of ED copayments on overall ED utilization among Medicaid beneficiaries following the DRA.
METHODS: We used the Medical Expenditure Panel Survey (MEPS), a nationally representative and longitudinal sample derived from the National Health Interview Survey, which oversamples African Americans and Hispanics. The study cohort consisted of individuals ages 19–64 who were on Medicaid. State linked data from 2001 to 2010 was used to compare ED use among patients in Washington, Florida, Minnesota, South Carolina, Kentucky, Ohio, Montana, Michigan and Pennsylvania that had instituted ED copayments during the study period against patients in Georgia, Virginia, Maryland Louisiana, North Carolina, Connecticut, Tennessee, Colorado and Texas that had a zero copayment throughout. We used interrupted time series analysis with a Zero Inflated Poisson regression to assess differences between the pre-policy period (2001–2005) and the post-policy period (2007–2010), controlling for gender, race, age, education, marital status, income relative to federal poverty level, self-reported health and state fixed effects. Additional analyses examined changes in primary care office visits and inpatient length of stay.
RESULTS: The study cohort consisted of 3514 adult Medicaid recipients in states with copayments and 6766 adult Medicaid recipients in states with no copayments. Patients in states with copayments were significantly more likely (p < 0.01) to be non-white, single, below the federal poverty level, and to have poor self-reported health. When controlling for these variables and state fixed effects, the study demonstrated that the enforcement authority of the DRA led to no significant differences in ED use in states with copayments when compared to states without copayments (OR: 1.06, 95 % CI: 0.94–1.18, p > 0.3). Contrary to our expectations, office based provider visits decreased (OR: 0.90, 95 % CI: 0.88–0.92, p < 0.01) and inpatient length of stay increased (OR: 1.19, 95 % CI: 1.12–1.27, p < 0.01) in states with copayments when compared to zero copayment states.
CONCLUSIONS: The results of this study demonstrate no significant difference in ED utilization in states with copayments following the enforcement authority granted in the DRA. Although this policy has not impacted ED use, states continue to impose burdensome copayments on this vulnerable Medicaid population. States should consider other options to reduce ED utilization and promote primary care provider visits among Medicaid beneficiaries.
IMPACT OF EMR IMPLEMENTATION ON DIABETES PERFORMANCE MEASURESCalie Santana; Yuming Ning. Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1933136)
BACKGROUND: Montefiore Medical Center (MMC) is a large urban Accountable Care Organization in Bronx, NY with an integrated primary care network. Previous work demonstrated wide variation in diabetes performance measures by clinic type. Non-teaching sites with more Medicaid- or Medicare-insured patients (mixed payer) have the lowest performance, followed by mixed payer teaching sites, while non-teaching sites serving commercially-insured patients had the highest quality of care as measured by HEDIS measures. Although federal policy (e.g. Meaningful Use) incentivizes the implementation of electronic medical records (EMRs), the impact of EMRs on diabetes performance measures in previous studies has been mixed. We carried out this study to answer: (1) Did EMR implementation improve diabetes performance? and (2) Does EMR implementation impact different clinic types differently?
METHODS: We studied 20 sites during EMR implementation (2009–2011). We treated implementation as a natural stepped-wedge experiment since a group of clinics went ‘live’ with the EMR roughly every 4 months. Our performance measures included: HbA1c ≦ 8 %, LDL ≦ 100 mg/dL, BP ≦ 140/80, and microalbumin checked in the last 12 months. We queried our clinical database for the most recent value of each measure during each 4-month period, as well as the last baseline value in 2008 and the last post-EMR value in 2012. We restricted our analysis to patients who had a value documented during the baseline period and a value at least 8 months post-EMR to allow clinicians enough time to get acquainted with the EMR’s diabetes management features (e.g. reminders for missing labs). The stepped-wedge model included EMR status (yes/no) during each time period for the site where each patient belongs as the main independent variable and a time period variable. We adjusted for baseline patient-level value, and patient-level age, sex, race/ethnicity, insurance. The clinic was included as a random effect.
RESULTS: Our sample included 8,375–16,202 patients depending on the measure. EMR implementation was not associated with a significant change in performance. The odds of post-EMR measures meeting the nationally accepted benchmarks compared to pre-EMR were: 0.94 for HbA1c control (p = 0.13), 1.03 for LDL control (p = 0.47), 0.93 for BP control (p = 0.13), and 0.97 for microalbumin checks (p = 0.54). One clinic (Commercial) significantly improved in A1c and LDL control (OR 1.17, (p − 0.01) and OR 1.12 (p = 0.01), respectively). Five clinics improved in BP control while 4 had significantly worse control including the Commercial site that improved in A1c and LDL. All three site types were represented among both groups. There were no sites that significantly changed in microalbumin checks compared to their pre-EMR performance.
CONCLUSIONS: We found no association between EMR implementation and a change in diabetes care as measured by nationally endorsed performance measures. We also did not find a pattern where certain site types were more likely to change in performance post-EMR than other site types. Given the baseline heterogeneity by teaching status and payer mix among our sites, we had hypothesized that the EMR could serve as a large resource investment that could help equalize performance. However, the implementation of a Meaningful Use-compliant EMR did not result in a significant improvement in diabetes control. Although there might be other benefits from the EMR not captured in these performance measures, our network must look to other interventions that may improve the effectiveness of diabetes care.
IMPACT OF GEOGRAPHIC ROUNDING AND MULTI-DISCIPLINARY ROUNDS ON COORDINATION OF CARE AND DISCHARGE TIMESCathryn Caton; Kristin R. Wise; Rogers Kyle; Kim Curnell-Pean; Patty J. Iverson. Medical University of South Carolina, Charleston, SC. (Tracking ID #1915824)
BACKGROUND: Initial studies demonstrate that locating the majority of a physician’s patients on a designated unit (geographic rounding) can enhance physician efficiency and facilitate physician nurse communication. Further benefits can include better patient satisfaction, improved patient outcomes and streamlined hospital throughput. Literature also supports the use of multi-disciplinary rounds to improve coordination of care and teamwork. We sought to evaluate the effects of geographic rounding for hospitalists’ patients and multi-disciplinary rounds on coordination of care and discharge times at our academic medical center.
METHODS: At our institution, we implemented geographic rounding for two non-teaching hospitalist teams (PHS) on a designated unit of the main hospital. We determined that 80 % of all PHS patients should be located on this unit. We initiated multi-disciplinary rounds to include hospitalists, nurses, case managers, physical and occupational therapists with a goal of increasing patient discharges prior to 3 pm. On a monthly basis, we tracked every aspect of the discharge process from the time orders were written to the time patients left the hospital. These discharge times were compared to those prior to project initiation. Physicians and nurses assigned to the designated unit completed a validated survey to assess their perceptions of care decisions before and 5 months after geographic rounding began.
RESULTS: Initial and repeat survey response of physicians and nurses were similar - 98 % and 93 % respectively. Of respondents, 83 % were female, 55 % were nurses and the majority was between ages 29–46. Fifty percent had community based practice experience. Matched analysis was performed on survey data finding improvements in 5 of 6 domains (p < 0.05). Respondents agreed that there was better communication and coordination between physicians and nurses about patient care decisions and plans. The percentage of patient discharges prior to 3 pm increased from 15 to 54 %.
CONCLUSIONS: The initiation of geographic rounding and multi-disciplinary rounds increased communication and coordination of patient care between physicians and nurses. With the implementation of both initiatives, we increased the percentage of patients discharged prior to 3 pm.
IMPACT OF HEALTH COACHING ON PATIENT TRUST IN THEIR PRIMARY CARE PROVIDER: A RANDOMIZED CONTROLLED TRIALDavid Thom; Danielle Hessler; Rachel Willard-Grace; Thomas Bodenheimer; Adriana Najmabadi; Christina Araujo; Ellen Chen. UCSF, San Francisco, CA. (Tracking ID #1928972)
BACKGROUND: In primary care, there has been a move to share tasks and responsibilities traditionally reserved for the primary care provider (PCP) with other members of the patient care team, including medical assistants, nurses, pharmacists, patent educators and coaches. Concern has been raised regarding the impact of the ‘team approach’ on the quality of the patient-provider relationship. We analyzed data from a randomized controlled trial comparing health coaching to usual care to assess the impact of health coaching on patients’ relationship with their primary care provider (PCP).
METHODS: Randomized controlled trial comparing health coaching with usual care. Participants were low-income English or Spanish speaking patients age 18 to 75 with poorly controlled type 2 diabetes, hypertension and/or hyperlipidemia. Health coaches were certified medical assistants who attended 40 h of health coach training over 6 weeks using a curriculum developed by the study team that included instruction in using active listening and non-judgmental communication; helping with self-management skills including creation of action plans, and providing social and emotional support. Patient trust in their primary care provider measured by the 11-item Trust in Physician Scale, converted to a 0 to 100 scale. Patient satisfaction with their PCP was assessed by a single item, “How likely would you be to recommend your doctor to your friend or relative?” with a response scale from 1 = ‘definitely not recommend’ to 5 = ‘definitely recommend’. Data were analyzed using linear mixed modeling. P-values were two-tailed.
RESULTS: A total of 441 patients were randomized to receive 12 months of health coaching (n = 224) vs. usual care (n = 217). At baseline, there were no significant differences in participant characteristics between the two study arms, including trust in their PCP (Table 1). At 12 months, trust and satisfaction were reported by 203 patients (91 %) in the health coaching group and 175 of patients (81 %) in the usual care group. Both the mean level of patients’ trust in their PCP and the percent of patients who would definitely recommend their primary care provider to family or friends increased significantly more in patients receiving health coaching (Table 2). These differences remained significant after adjustment for number of PCP visits during the study.
CONCLUSIONS: Health coaching does not appear to lower, and in fact may increase, patients’ trust in their primary care providers. Clinicians should be reassured that working with health coaches does not appear to compromise, and may in fact enhance, their relationships with their patients.
Table 1. Participant characteristics at enrollment by study arm (% or mean (sd))*
| Characteristic | Health coaching arm (n = 224) | Usual care arm (n = 217) |
| Age (years) | 52.6 (10.7) | 52.9 (11.5) |
| Gender (female) | 52 % | 59 % |
| Born in the US | 26 % | 25 % |
| Years living in US** | 18.5 (10.4) | 17.9 (11.9) |
| Spanish is primary language | 68 % | 70 % |
| Race/Ethnicity: | ||
| African American | 20 % | 18 % |
| Latino or Hispanic | 69 % | 71 % |
| White non-Hispanic/Asian/Other | 11 % | 11 % |
| Education less than high school | 44 % | 44 % |
| Annual household income <$10,000 | 60 % | 56 % |
| Trust score | 72.4 (12.4) | 72.7 (12.7) |
| Would definitely recommend PCP | 57 % | 59 % |
* There were no statistically significant differences by study arm. ** For participants born outside the United States
Table 2. Change in patient trust in and satisfactions with the primary care provider (PCP) and number of visits to the PCP from baseline to 12 months
| Outcome | Change in health coach group | Change in usual care group | Difference in change | 95 % CI | p-value | Adjusted p-value |
| Patient Trust score (mean) | + 3.8 | +1.4 | 2.4 | 0.03 to 4.8 | .047 | .033* |
| Definitely recommend PCP (%) | +16.3 % | +4.0 % | 12.3 % | 5 % to 24 % | .002 | .015* |
*Adjusted for number of visits to PCP during 12 month intervention.
IMPACT OF HIGH-DEDUCTIBLE HEALTH PLANS ON DIABETES MONITORING AND OUTCOMESJames F. Wharam; Fang Zhang; Emma Eggleston; Steve Soumerai; Dennis Ross-Degnan. Harvard Medical School, Boston, MA. (Tracking ID #1939979)
BACKGROUND: The Affordable Care Act is expected to dramatically increase high-deductible health plan enrollment. Hemoglobin A1C monitoring improves diabetes outcomes but the expansion of high-deductible health insurance could reduce secondary preventive care. No studies have examined the impact of high-deductible health plans on intermediate outcomes such as diabetes control.
METHODS: We studied administrative claims representing 13,974 baseline person years of patients with diabetes. Members were continuously enrolled for 2 years through a large national insurer between 2004 and 2012. To minimize selection bias, we included members who could choose only one health plan in their follow-up year. We analyzed monthly hemoglobin A1C testing rates for 1 year before and after subjects’ employers mandated a switch from traditional low-cost-sharing plans to high deductible plans, compared with rates among a contemporaneous 2:1 propensity score matched control cohort. We also examined mean monthly hemoglobin A1C values among a subset of members with laboratory value data. We subtracted monthly measurement rates of the control group from those of the HDHP group to obtain a before-after differenced trend, then used an autoregressive correlation structure in a generalized least squares model containing the covariates of time in months, an indicator for follow-up versus baseline period, and time in months in the follow-up period. We included all covariates in the model regardless of statistical significance.
RESULTS: Hemoglobin A1C testing rates in the high deductible group relative to the control group did not change significantly from the baseline to the follow-up year (level and trend changes of −0.0005 in month 13, [95 % C.I., −0.0040 to 0.0031] and 0.0001 per month, [−0.0004 to 0.0007], respectively, Figure 1). Hemoglobin A1C levels also did not change (level and trend changes of 0.038, [−0.146 to 0.222] and 0.000, [−0.027 to 0.026], Figure 2).
CONCLUSIONS: Switching from traditional health plans to high-deductible health plans did not change hemoglobin A1C testing or levels after 1 year. Initial results might be reassuring to policymakers overseeing the expansion of high-deductible health insurance, but our pending analyses will examine 3 follow-up years as well as key subgroups such as the poor and sick.
Figure 1. Monthly rates of hemoglobin A1C testing before and after transition to high-deductible insurance.
Figure 2. Monthly hemoglobin A1C values before and after transition to high-deductible insurance.
IMPACT OF HOSPITALIST WORKLOAD ON PATIENT OUTCOMES: AN ANALYSIS OF 2 ACADEMIC MEDICAL CENTERSHenry J. Michtalik1,2; Nowella Durkin3; Eric Howell2,4; Amy Deutschendorf3; Jason D. Miller3; Daniel Brotman1,3. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Armstrong Institute for Patient Safety and Quality, Baltimore, MD; 3Johns Hopkins Hospital, Baltimore, MD; 4Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1931177)
BACKGROUND: Front-line hospitalists report that excessive hospitalist workload adversely affects quality of patient care. However, there is a paucity of research examining the direct impact of variation in workload on patient outcomes. We determined the association between individual hospitalist workload at 2 academic medical centers and length of stay, readmission, and hospital-acquired conditions.
METHODS: Using administrative and billing data for standard daytime shifts, we examined all non-observation inpatient admissions to the hospitalist service for fiscal year 2013 at 2 academic medical centers. One site has a fixed hospitalist unit of 17 beds and the other site maintains a census cap of 12 patients per hospitalist. We defined daily hospitalist workload as the number of patient encounters billed by each hospitalist on a given day. For each patient admitted, we then calculated the average workload of all treating hospitalist providers during the respective patient’s entire hospital course. For example, a patient hospitalized for 2 days and cared for by a hospitalist who saw 8 patients on Day 1 and another hospitalist who saw 12 patients on Day 2 would have an average hospitalist workload of 10. We determined the association between average provider workload and odds of exceeding the expected length of stay, having a 30-day all-cause readmission, and developing a Maryland hospital-acquired condition. Using multiple logistic regression, we adjusted for patient demographics (age, race, sex), severity of illness (All Patient Refined Diagnosis Related Group Severity of Illness score; range 1–4), observed length of stay, percentage of weekdays, number of treating hospitalists, and hospital site.
RESULTS: There were 5068 inpatient admissions from July 2012 to June 2013. The average hospitalist workload was 7.7 (SD ± 2.2) encounters per day, and patients were treated by 2 different hospitalists [IQR: 1, 3]. Patients had a median age of 60 years [IQR: 49, 74] and severity of illness score of 2 [IQR: 2, 3]. Sixty-two percent of patients were Caucasian and 54 % were female. Median length of stay was 3 days [IQR: 2, 5] and on average, weekdays accounted for 80 % of the hospitalization. The readmission rate was 15.5 % and 137 patients developed at least one hospital-acquired condition. Average hospitalist workload was not a statistically significant predictor for exceeding the expected length of stay, being readmitted, or developing a hospital-acquired condition. Hospitalizations exceeding the expected length of stay occurred with lower patient severity of illness and percentage of weekdays, and increased length of stay (all p < 0.01). For readmissions, only age (OR: 0.92 per 10 additional years; 95 % CI: 0.88, 0.96) and severity of illness (OR: 1.44 per category increase; 95 % CI: 1.29, 1.61) were significant predictors. For hospital-acquired conditions, severity of illness (OR: 2.86; 95 % CI: 2.15, 3.81) and length of stay (OR: 1.07 per additional day; 95 % CI: 1.04, 1.09) significantly increased the odds of occurrence.
CONCLUSIONS: When hospitalist workload was measured across the entire patient hospitalization, variation in workload did not impact length of stay, readmission, and hospital-acquired conditions; only severity of illness was a consistent statistically significant predictor of these outcomes. Our results suggest that in the setting of workload control strategies (fixed number of hospitalist beds, census caps), workload variation may not be associated with worsened patient outcomes. Larger studies with greater variation in workload at the individual physician level and higher patient volumes are needed to better understand workload’s potential impact on patient outcomes. Multi-center, randomized-controlled studies may also determine the effectiveness of different workload control strategies in managing workload variation, facilitating patient flow, and optimizing patient outcomes.
IMPACT OF INTRODUCTION OF ABUSE-DETERRENT OXYCONTIN ON OPIOID OVERDOSE RATESMarc Larochelle; Fang Zhang; Dennis Ross-Degnan; James F. Wharam. Harvard Medical School, Boston, MA. (Tracking ID #1937010)
BACKGROUND: Opioid overdose and overdose deaths are increasing in the United States. An abuse-deterrent formulation of OxyContin, a frequently abused opioid, was introduced in August 2010. Reports from opioid abusers suggest a decreased preference for OxyContin and increased preference for heroin following the formulation change; however, the impact on overdose rates is unknown.
METHODS: We analyzed an open cohort of commercially insured enrollees aged 18–64 years from a large national United States health insurer claims database. We used an interrupted times series design to analyze quarterly outcomes from 2003 to 2012 divided into three periods: pre formulation change, Q1 2003-Q2 2010; formulation change phase-in period, Q3 2010; and, post formulation change, Q4 2010-Q4 2012. Outcomes were rates of overdose due to any opioid, overdose due to a prescription opioid, and heroin overdose. We identified overdose from inpatient or emergency department claims with ICD-9 diagnosis codes for opioid poisoning. We standardized rates to gender, age, region, and race of Q2 2010 enrollees. We used segmented linear-regression to: a) predict expected post formulation change overdose rates based on Q1 2003-Q2 2010 trends; and b) model the observed Q4 2010-Q4 2012 trend. We used multivariate delta methods to estimate the effect of the formulation change at 2 years.
RESULTS: We analyzed claims for 31.3 million enrollees with a median enrollment of 17 months and 13,654 opioid overdoses from 2003 to 2012. Two years following introduction of abuse-deterrent OxyContin, the observed overall overdose rate was an estimated 5.7 per 100,000 enrollees per quarter, lower than the predicted rate of 6.1 per 100,000 enrollees per quarter (relative change −7.2 %; 95 % CI, −13 % to −1.9 %). The estimated overdose rate due to prescription opioids decreased from an expected 4.1 to 3.2 per 100,000 enrollees per quarter (relative change −21 %; 95 % CI, −25 % to −16 %). However, the estimated heroin overdose rate increased from an expected 0.7 to 1.3 per 100,000 enrollees per quarter (relative change +91 %; 95 % CI, 53 % to 130 %; Figure).
CONCLUSIONS: Two years after introduction of abuse-deterrent OxyContin, overall opioid overdose decreased to a small degree, but heroin overdose nearly doubled. Substitution of alternative opioids may limit the effectiveness of abuse-deterrent formulations on the opioid overdose epidemic.
Age, gender, region, and race standardized rates of opioid overdose before and after introduction of abuse-deterrent OxyContin.
IMPACT OF LOSS OF INTERPERSONAL CONTINUITY ON PATIENT EXPERIENCE OF CARE AND AMBULATORY QUALITY OF CAREAshok Reddy1,4; David A. Asch2,3; Anne Canamucio2; Rachel M. Werner2,3. 1University of Pennsylvania, Philadelphia, PA; 2VISN 4 Center for Evaluation of PACT, Philadelphia, PA; 3Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, PA; 4Robert Wood Johnson Clinical Scholar Program, University of Pennsylvania, Philadelphia, PA. (Tracking ID #1938406)
BACKGROUND: Continuity remains a core tenet of primary care. Several studies link a more continuous PCP-patient relationship with higher patient satisfaction, higher preventive service use, and lower hospitalizations rates. Continuity is often defined as having three components: interpersonal (having a continuous personal physician-patient relationship), longitudinal (having a medical home in which patients receive the majority of their care), and informational (having a patient’s medical records available at the time a doctor sees the patient). While prior work demonstrates the importance of continuity on patient care outcomes, it is uncertain which component of continuity matters most. Our study focuses on isolating the impact of interpersonal continuity in the setting of stable informational and longitudinal continuity. In the setting of the Veterans Health Administration (VHA), we conduct an analysis of patients who experienced a loss of the interpersonal relationship (primary care provider turnover) but continue to receive care at the VHA (stable longitudinal and informational continuity). We then measure the impact of turnover on patient care experience and ambulatory quality of care.
METHODS: We included all patients enrolled in primary care at the Veterans Health Administration (VHA) between 2010 and 2012 who were also included in one of two national datasets used to measure our outcome variables: the Survey of Healthcare Experiences of Patients (SHEP; used to measure patient experience of care) and the External Peer Review Program (EPRP; used to measure ambulatory quality of care). Both datasets include a random sample of veterans receiving outpatient care in the VHA. We measured primary care provider (PCP) turnover in the 2 years prior to measuring patient experience and quality of care using VHA primary care encounter data. A linear probability model was used to test whether PCP turnover was associated with changes in patient experience of care and ambulatory quality of care, adjusting for patient-level covariates (age, gender, race, income and DCG risk score) and clinic-level fixed effects, and clustering standard errors at clinic level.
RESULTS: Our analyses include SHEP responses from 639,011 patients (9 % of who experience PCP turnover) and EPRP data from 361,627 patients (10 % experiencing PCP turnover). A majority of respondents reported positive experiences of care in 3 out of 5 domains: How well doctor/nurse communicate (53 %), rating of personal doctor/nurse (71 %), and overall rating of VHA healthcare (59 %). In addition, patients had high rates of completion of testing for retinal preventive care (90 %), control of hypertension (79 %) and colon cancer screening (82 %). In our primary analysis, PCP turnover was associated with a decrease in all 5 domains of patient care experience. For example, PCP turnover was associated with a 3.7 percentage point (p < 0.05) lower response in how well a patient communicates with his or her provider. However, we found no association between PCP turnover and ambulatory quality of care measures.
CONCLUSIONS: With increasing primary care turnover, interpersonal continuity in medical care continues to diminish. Our study shows that loss of interpersonal continuity is a common experience and is associated with a small but significantly worse patient experience of care. However, this loss of interpersonal continuity does not impact the quality of preventive services for common ambulatory conditions. These findings demonstrate that health care systems with robust informational and longitudinal continuity could mitigate the impact of a loss of any one provider on a person’s healthcare.
IMPACT OF MEDICAID INELIGIBILITY FOR INCARCERATED INDIVIDUALS ON INSURANCE EXPANSION UNDER THE AFFORDABLE CARE ACT: A BLIND SPOT OF REFORMElisabeth Poorman1; Anne Spaulding2. 1Cambridge Health Alliance, Cambridge, MA; 2Rollins School of Public Health, Atlanta, GA. (Tracking ID #1939132)
BACKGROUND: The Patient Protection and Affordable Care Act (ACA) aimed to expand Medicaid coverage to individuals with incomes below 138 % of the federal poverty level. However, inmates of prisons and jails, many of whom have low incomes and high levels of disease burden, have been prohibited from receiving Medicaid since its inception. When previous recipients of Medicaid are freed, they typically have a long lag time before re-enrollment. This prevents connection to care during the early post-release period, a time which has been demonstrated to have high mortality. Little is known about the impact of making incarcerated individuals temporarily ineligible for Medicaid, or what the impact will be on the success of Medicaid expansion.
METHODS: Using the most recently available national surveys of prison and jail inmates from the Bureau of Justice Statistics, this study calculates the expected number of admissions to US prisons and jails in 2014 and the number of these that would have been eligible for Medicaid under the ACA had they not been incarcerated. Using estimates for the number of Americans age 18–64 who will qualify for Medicaid under the ACA in 2014 from the Kaiser Family Foundation, we calculate the percentage of all individuals that would otherwise qualify for Medicaid who will spend part of 2014 in jail or prison.
RESULTS: The total number of adults in prison at year’s end in 2011 was 1,598,780. Adding the total released, subtracting the number of those released predicted to recidivate in 1 year, assuming incarceration rates remain static, we estimate that 2.2 million people will be imprisoned in 2014. Discounting new admissions, most of whom pass through jail, we calculate 1.5 million people who will spend part of the year in prison but not jail. One in three prisoners reports a pre-arrest monthly income below 138 % of the poverty line, and slightly more than 98 % of this population is between the ages of 18 and 65. Therefore, 491,300 prisoners would have been eligible for Medicaid in 2014. The number of unique yearly admissions to jail is calculated to be 8.28 million, derived from total admissions (11.6 million in 2012) divided by 1.4 average admissions per person. Close to 99 % of jail inmates are between 18 and 65, and approximately two out of three jail inmates reports a monthly income below 138 % of the poverty level, resulting in 5.1 million jail inmates who would be Medicaid eligible. According to the Kaiser Family Foundation, the total number of people between 18 and 65 below 139 % of the poverty level is close to 87 million. We therefore calculate that 7.6 %, or one in thirteen people, who meet income eligibility for Medicaid under the Affordable Care Act will be incarcerated in 2014.
CONCLUSIONS: A substantial number of low income individuals will fail to benefit from the Medicaid expansion under the ACA due to the ban on Medicaid coverage for inmates of prisons and jails. Pro-actively enrolling this population upon release is key to ensuring that large numbers of poor Americans are connected to care at a time when they are most vulnerable.
IMPACT OF OBESITY ON HEART RATE RESPONSE DURING TREADMILL EXERCISECindy Wang; Daniel Spevack. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939767)
BACKGROUND: Prior works have found attenuated exercise heart rate response in obese subjects. These studies, however, have compared subjects in terms of peak heart rate achieved. We aimed to compare the exercise heart rate response between obese and non-obese subjects in terms of the heart rate achieved at a fixed level of exercise.
METHODS: Echocardiography reports were reviewed from 4,497 patients referred for treadmill maximal exercise testing using the Bruce protocol between 1/1/2010 and 6/30/2012. Patients were excluded if they had resting HR > 90 bpm (n = 421), performed <6 min of exercise (n = 809), abnormal left ventricular wall motion either before (n = 47) or after (n = 145) exercise. Heart rate response was compared between subjects using the heart rate achieved at 6 min into the Bruce protocol.
RESULTS: The 3,075 patients in the study group were 52 ± 12 years, 56 % female, BMI 29 ± 6, resting HR 70 ± 10 bpm and resting BP 141 ± 19 mmHg. Patients exercised for 8.9 ± 2 min, achieving HR 133 ± 19 bpm at 6 min and 158 ± 19 bpm at peak. Peak BP was 160 ± 23 mmHg. At 6 min exercise, HR change from rest was greater in the obese group (66 ± 17 vs 61 ± 19 bpm, p < 0.001). Obese subjects exercised for shorter duration (8.4 ± 8 vs 9.3 ± 2 min, p < 0.001), but had no difference in the maximum HR achieved compared to non-obese subjects (158 ± 17 vs 157 ± 20, p = 0.2). While BMI directly correlated with HR achieved at 6 min in obese subjects (beta 0.94, p < 0.001), this was not the case in non-obese subjects (beta 0.19, p = 0.2), Figure. Using multiple linear regression, increased age (beta −0.08), female sex (beta −0.94), body mass index (beta −0.09) and HR at 6 min (beta −0.04) were each independently associated (p < 0.001 for all) with reduced maximal exercise duration.
CONCLUSIONS: Obesity is associated with accelerated heart rate response with exercise. Obesity and HR achieved at 6 min of Bruce protocol were independent predictors of reduced exercise capacity.
The Relationship Between Heart Rate and Body Max Index at Six Minutes of Treadmill Exercise Stress Testing
IMPACT OF THE AFFORDABLE CARE ACT ON PATIENTS’ OUT-OF-POCKET BURDENKevin Riggs1,2; Christine Buttorff3; G. Caleb Alexander1,3. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Berman Institute of Bioethics, Baltimore, MD; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD. (Tracking ID #1931572)
BACKGROUND: Out-of-pocket (OOP) spending caps under the Patient Protection and Affordable Care Act (PPACA) are designed to limit the financial toll of high health care costs for individuals and their families. Individuals and families who obtain private insurance outside of health insurance exchanges will have uniform OOP caps, equal to the cap for Health Savings Account qualified plans ($6350 for individuals and $12,700 for families for 2014). In contrast, OOP caps are income-based for those who purchase private insurance through health care exchanges, such that patients with lower incomes have lower OOP caps. The goal of this study was to estimate the proportion of Americans who have OOP costs greater than the OOP spending caps.
METHODS: We used the 2011 Medical Expenditure Panel Survey, a large nationally representative longitudinal panel survey designed by the National Center for Health Statistics, to examine OOP costs for medical care and prescription drug utilization. We limited our analyses to adults age 18–64 with private health insurance. The primary outcome was the proportion of individuals whose spending exceeded the uniform OOP cap for insurance purchased outside of health insurance exchanges. To examine the effect of OOP caps for individuals with varying incomes, we categorized individuals’ incomes relative to the federal poverty limit (FPL). We then estimated the proportion of individuals who would exceed OOP caps under the hypothetical scenario where the income-based OOP caps available through the exchanges are applied to everyone with private insurance. Costs were inflated to 2014 dollars. Lastly, we examined how self-reported cost-related access problems (unable to obtain medical care or prescription drugs for reasons “could not afford” or “insurance would not cover”) varied by OOP costs.
RESULTS: There were 12301 insured adults in the survey, representing a weighted population of over 136 million individuals. Median household income was $77,755. The proportion of individuals with OOP costs greater than the uniform cap was 0.93 %, and the proportion exceeding the cap decreased with increasing family income (2.10 % of those <100 % of FPL, and 0.84 % of those >400 % of FPL). Applying the income-based caps (and assuming those <100 % FPL would be granted a reduced cap, which they would not actually be able to obtain through the exchange), the proportion with OOP costs greater than the cap was 2.29 %. Specifically, 3.75 times as many individuals <400 % FPL would benefit from the income-based caps, compared with the uniform caps. Self-reported cost-related access problems was low (1.99 % overall), although there was an inverse gradient, with problems decreasing as income increased (5.21 % for <100 % FPL and 1.02 % for >400 % FPL).
CONCLUSIONS: Individuals with lower income experience greater self-reported cost-related access problems, and they are more likely to have high OOP costs. The uniform OOP spending caps under PPACA will impact a modest proportion of individuals, with those in the lowest income categories most likely to benefit. However, extending the income-based spending caps to include insurance purchased outside of the exchanges would have a much larger impact.
IMPACT OF VA HEALTH INFORMATION EXCHANGE UPON THE QUALITY OF DIABETES CAREDavid Haggstrom1,2; Laura J. Myers1,2; Dustin D. French3; Jeff Barnd1; Marc Rosenman4; Joseph Kesterson5; Alan Zillich1,7; Deming Mi6; Susan Perkins6. 1VA Health Services Research and Development, Indianapolis, IN; 2Indiana University School of Medicine, Indianapolis, IN; 3VA Health Services Research and Development, Hines, IL; 4Indiana University School of Medicine, Indianapolis, IN; 5Regenstrief Institute, Indianapolis, IN; 6Indiana University School of Medicine, Indianapolis, IN; 7Purdue University, Indianapolis, IN. (Tracking ID #1931393)
BACKGROUND: Like most health care systems, the VA often has patients who receive some portion of their care outside the VA. Due to the lack of interoperability among electronic health record systems, providers caring for veterans who are receiving services outside the VA may not have timely access to important information about their patients. Health information exchange (HIE) advocates believe that greater interoperability will improve the quality of care. In this study, measures of ambulatory care quality were chosen that an expert panel suggests may be sensitive to the effect of HIE, and feasible for electronic data capture.
METHODS: Intervention: A regional VA-HIE demonstration program was conducted through a national initiative called the Virtual Lifetime Electronic Record (VLER). The VA-HIE performed secure, bi-directional health information exchange between the VA and community partners organized together through the Indiana Network for Patient Care. Health care providers inside and outside the VA were able to access exchanged data. Patients were enrolled in the VA-HIE program on-site at the Indianapolis VA in outpatient clinics or through the release-of-information office. Study design: A pre-post cohort evaluation of the VA-HIE program was performed, with a concurrent control group. For the evaluation, data on care received by patients inside and outside the VA were obtained for 1 year before, and 1 year after, the index date of patient enrollment. To allow for program implementation lag time and enable providers to become accustomed to using HIE data, the first study patients were enrolled in the cohort 3 months after VA-HIE implementation. All control patients were enrolled 3 months after VA-HIE implementation. Population: Patients with diabetes (at least 2 diagnoses) were included in the evaluation. Patients were included if they had at least 1 clinical encounter at the Indianapolis VA over a 1-year period prior to the index date. Overall, 9,612 patients diagnosed with diabetes were followed: 1,768 enrolled in the VA-HIE intervention and 7,844 in the control group. Measures/Analyses: For hemoglobin A1c (HgA1c), both the mean lab values and the proportion of diabetics with HgA1c <9 % were measured. For LDL, the mean lab values, and the proportions of diabetics with LDL < 130 and LDL < 100 were measured. Multivariable regression models were constructed as a function of VA-HIE intervention status, time, and baseline covariates (race/ethnicity, insurance, marital status, Charlson comorbidity index, and service-connected disability).
RESULTS: The mean age (62.4 years) and race (27 % non-white) were no different between intervention and control groups. However, there were statistically significant differences between the VA-HIE intervention and control groups in the proportion insured (66 % vs. 64 %), married (63 % vs. 58 %), comorbidity index (0.62 vs. 0.39) and with service-connected disability (85 % vs. 82 %). The sources of the diabetes diagnostic information were the VA (80 %), community partners (3 %), or both (16 %) electronic data systems. Among the diabetes population, the VA-HIE had no significant effect over time on the mean HgA1c value or the proportion of patients with HgA1c <9 %. For all of the LDL measures, there were significant effects of both the VA-HIE intervention and time (Figure 1), but the interaction effect was not significant.
CONCLUSIONS: Providers of patients enrolled in the VA-HIE had better access to data residing in non-VA health care systems. About 1 in 5 veteran patients had data identifying diabetes diagnoses in non-VA electronic data systems. The VA-HIE program had no measureable effect upon the quality of diabetes care. Possible reasons for the lack of effect may be that HIE does not influence these types of care management processes, the amount of data shared with the VA was not sufficient to affect care quality, or the evaluation was performed early in the implementation or diffusion of the VA-HIE.
Adjusted means of LDL for fitted regression model
IMPLEMENTATION OF A TRIAGE-STAFF INITIATED ROUTINE HIV SCREENING PROGRAM IN AN INNER CITY PRIMARY CARE CENTER IN A HIGH HIV PREVALENCE AREANatasha Travis; Jennifer Spicer; Heather Freiman. Emory University, Atlanta, GA. (Tracking ID #1938815)
BACKGROUND: Both the U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Preventive Services Task Force (USPSTF) have issued recommendations for routine HIV testing for individuals 13–64 years of age in all healthcare settings in the United States. However, many primary care centers (PCCs) still have not implemented routine HIV screening. The objective of this analysis is to describe the implementation of a routine HIV screening program in a PCC in a high HIV prevalence area.
METHODS: In July 2013, a routine triage-staff initiated HIV screening program was instituted in the PCC of an inner-city safety-net hospital in a high HIV prevalence area. Triage staff, comprising nurses and medical assistants, was instructed to complete HIV screening for all eligible PCC patients using an electronic medical record based HIV Screening Tool. Patients were eligible to receive a test offer if they were: at least 18 years old, capable of consent, and did not have HIV test results in the last 6 months. Eligible patients were offered an HIV test using opt-out language. If the patient did not opt-out, an HIV test was ordered by the triage staff and the patient was instructed to go to the outpatient laboratory for the test. A retrospective chart review was performed to assess initiation of the Screening Tool and HIV test offer, uptake, and completion rates.
RESULTS: There were 22,372 visits to the PCC between July 9 and November 30, 2013, and the Screening Tool was initiated at 11,774 visits (52.6 %). In October and November 2013, the Screening Tool was initiated at 4,809 visits; of these visits: 3,198 patients were eligible for test offer (66.5 %); 3,173 eligible patients were offered a test (99.2 %), and 1,608 patients (43.5 %) who were offered a test did not opt-out. Of those patients who did not opt-out of HIV testing, 922 (57.3 %) have had the test completed.
CONCLUSIONS: This analysis describes the implementation of a triage-staff initiated routine HIV screening program using laboratory-based HIV tests rather than rapid tests. Implementation of routine screening increased HIV testing by 200 %: in the two months prior to initiation of the routine HIV screening program, 3.5 % of patients received an HIV test (315 tests/9,000 visits) compared to 10.5 % of patients in October and November 2013 (922 tests/8,771 visits). Approximately 60 % of patients who accepted HIV screening in October and November 2013 have already completed the test and many patients will likely complete their test before their next visit. HIV test offer rates were consistent with previous outpatient HIV screening programs using rapid HIV tests and were significantly higher than the 0.4 % to 20 % offer rates reported in previous literature for provider-initiated screening. Although rapid HIV tests have been used in earlier studies because of their convenience, rapid tests require more up-front costs and staff training These data indicate a benefit to coupling non-rapid HIV testing with other tests ordered in PCC’s. Future studies should focus on identifying and addressing patient barriers to accepting routine HIV screening.
IMPLEMENTATION OF THE PATIENT CENTERED MEDICAL HOME (PCMH) IN THE VETERANS HEALTH ADMINISTRATION (VHA); ASSOCIATIONS WITH CLINICAL OUTCOMES, PATIENT SATISFACTION, PROVIDER BURNOUT AND UTILIZATIONKarin M. Nelson1; Christian Helfrich1; Haili Sun1; Paul Hebert1; Chuan-Fen Liu1; Emily D. Dolan1; Leslie Taylor1; Edwin Wong1; Charles Maynard1; Susan Hernandez1; William J. Sanders1; Idamay Curtis1; Ian A. Randall1; Gordon Schectman3; Richard Stark3; Stephan D. Fihn2,1. 1VA Puget Sound Health Care System, Seattle, WA; 2Veterans Health Administration, Seattle, WA; 3Veterans Health Administration, Washington, DC. (Tracking ID #1938591)
BACKGROUND: In 2010, the Veterans Health Administration (VHA) began implementing the patient centered medical home (PCMH) at all clinical sites. The Patient-Aligned Care Team (PACT) initiative aims to improve experiences and health outcomes through team-based primary care, improved access and care management for over 5 million Veterans. To evaluate progress and outcomes throughout the system, we sought to create a measure of PCMH implementation and relate variation in implementation to key outcomes.
METHODS: We conducted an observational study using: (1) VHA clinical and administrative data for >5.6 million Veterans who received primary care at 913 VHA hospital- and community-based clinics; (2) 75,101 responses to a national patient survey that included the Consumer Assessment of Health Plans (CAHPS)-PCMH module and was administered to a weighted, random sample of Veterans who received outpatient care from June–December 2012; and (3) 5,404 responses to a survey distributed to all VHA primary care providers and staff in June 2012. Composite scores were constructed for 8 core domains: access, continuity, care coordination, comprehensiveness, self-management support, patient-centered care and communication, shared decision-making and team-based care. Our main outcome measures were patient satisfaction (defined by a provider rating from 0 to 100), provider burnout (defined by the Maslach Burnout Inventory - MBI), utilization (hospitalization and emergency room use), and VHA clinical performance measures.
RESULTS: 53 items were included in the PACT Implementation Progress Index (Pi2). Among the 77 sites achieving the most effective implementation (i.e., Pi2 score in the top decile), measures of patient satisfaction, provider burnout, and hospitalization and emergency room utilization were all significantly more favorable than among 87 clinics with Pi2 scores in lowest decile. Patient satisfaction was meaningfully higher among sites that had effectively implemented PACT than those that had not (mean rating for satisfaction with provider 9.33 vs. 7.53, p < 0.001). A similarly favorable pattern was observed for provider burnout measured by the MBI emotional exhaustion subscale (2.29 vs. 2.80 respectively, p < 0.05). Emergency department encounters were significantly lower at sites with more rather than less effective implementation (188 encounters/1000 patients vs. 246, respectively, p < 0.001). Among sites with PI2 scores in the highest decile, there was an estimated average reduction of 13.4 % from baseline in admissions for ACSCs per 1,000 patients under age 65 attributable to PACT compared with a 3.0 % decrease among sites with less effective implementation of PACT. Twenty-three of 50 clinical performance measures were significantly associated with PI2 scores, of which 21 were more favorable at sites with PI2 scores in the top decile. Overall, 43 of the 50 measures were higher at sites with the highest PI2 scores (p < 0.0001), including foot exams and A1c <9 % among patients with diabetes (90.0 vs. 85.6 % and 84.0 vs. 81.8 %, respectively), blood pressure <140/90 mmHg among hypertensive patients (82.0 vs. 78.0 %), influenza immunization (68.5 vs. 64.2 %), cervical cancer screening (92.8 vs. 86.7 %) and offering medications for tobacco cessation (96.2 vs. 93.4 %).
CONCLUSIONS: The PI2 was highly associated with important outcomes for both patients and providers and will be used to track PACT implementation within VHA.
IMPROVING ANTIBIOTIC PRESCRIBING FOR ACUTE RESPIRATORY INFECTIONS USING BEHAVIORAL ECONOMIC PRINCIPLES: A CLUSTER RANDOMIZED TRIALJeffrey A. Linder1,2; Daniella Meeker3; Mark W. Friedberg2,3; Stephen D. Persell4; Craig R. Fox5; Noah J. Goldstein5; Alan F. Rothfeld6,7; Joel Hay7; Jason N. Doctor7. 1Brigham and Women’s Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3RAND, Santa Monica, CA; 4Northwestern University Medical School, Chicago, IL; 5University of California, Los Angeles, Los Angeles, CA; 6COPE Health Solutions, Los Angeles, CA; 7University of Southern California, Los Angeles, CA. (Tracking ID #1939232)
BACKGROUND: Acute respiratory infections (ARIs) are the most common reason for inappropriate antibiotic use. Inappropriate antibiotic prescribing for nonbacterial infections increases the costs of care, the prevalence of antibiotic-resistant bacteria, and adverse drug events. Standard approaches to behavior change have had limited success in reducing inappropriate antibiotic prescribing. Interventions that apply behavioral economic and social psychology principles may be more effective. In a large, multisite randomized trial, we evaluated the effectiveness of behavioral economic interventions to reduce inappropriate antibiotic prescribing for ARIs.
METHODS: We randomized 49 Boston and Los Angeles primary care practices in a 2 × 2 × 2 factorial design and enrolled 342 clinicians to receive up to three interventions for 18 months: 1) Suggested Alternatives: Through computerized clinical decision support, clinicians attempting to prescribe antibiotics for ARIs received a list of non-antibiotic treatment choices prior to completing the antibiotic prescription; 2) Accountable Justifications: When attempting to prescribe antibiotics for ARIs, clinicians were prompted to record an explicit justification that appeared in the electronic health record as a separate “Antibiotic Justification Note”; and 3) Peer Comparison: Clinicians received periodic email feedback with their inappropriate antibiotic prescribing rate and were informed if they were a “Top Performer”—in the top 10 %—or they were “Not a Top Performer.” We used logistic regression to assess the primary outcome, antibiotic prescribing for non-antibiotic-appropriate ARIs (e.g., colds, acute bronchitis, and influenza), adjusted for clinician-level pre-intervention prescribing rates.
RESULTS: To date—the study is over 90 % complete, finishing in Spring 2014—there have been 26,783 ARI visits to the 342 participating providers. Patients had a mean age of 49.0 years old and were 33 % male. The antibiotic prescribing rates for non-antibiotic-appropriate diagnoses from the pre-intervention to the intervention period were, respectively, 38.7 % and 29.6 % for control clinicians; 45.3 % and 36.0 % for suggested alternatives; 29.1 % and 17.7 % for accountable justifications; and 30.7 % and 19.8 % for peer comparison. Suggested alternatives were not associated with a significant decrease in the primary outcome (odds ratio [OR], 1.02; 95 % confidence interval [CI], 0.80 to 1.31). There was a significant decrease in antibiotic prescribing for non-antibiotic-appropriate ARIs for accountable justifications (OR, 0.66; 95 % CI, 0.56 to 0.79) and peer comparison (OR, 0.71; 95 % CI, 0.55 to 0.92). There were no significant interactions between suggested alternatives, accountable justifications, or peer comparison.
CONCLUSIONS: In this ongoing cluster randomized trial, accountable justifications and peer comparison were associated with decreased antibiotic prescribing for non-antibiotic-appropriate ARIs.
IMPROVING BLOOD PRESSURE MEASUREMENT AMONG CLINICAL STAFFLauren Block1,2; Romsai T. Boonyasai3; Sarah J. Flynn4; Caroline Lentz5; Tammie Hull5; Lisa A. Cooper3. 1Hofstra North Shore-LIJ School of Medicine, New Hyde Park, NY; 2Bloomberg School of Public Health, Baltimore, MD; 3Johns Hopkins University School of Medicine, Baltimore, MD; 4University of Maryland School of Medicine, Baltimore, MD; 5Johns Hopkins Community Physicians, Baltimore, MD. (Tracking ID #1936977)
BACKGROUND: Blood pressure (BP) measurement in office settings is frequently performed incorrectly, with consequent over- and under-treatment of hypertension. Reasons for this problem include decay in knowledge and drift in skills related to correct technique. We designed a concise online training program in accurate blood pressure measurement for an interdisciplinary group of clinical staff. We sought to evaluate whether this training program improved knowledge and attitudes, as well as performance of recommended techniques among staff.
METHODS: This training program was designed to provide continuing education within a long-term multimodal hypertension quality improvement (QI) project focused on reducing disparities in BP control. As part of the QI project, all medical assistants (MAs), registered nurses (RNs), and licensed practical nurses (LPNs) at six ambulatory internal medicine practices were trained and certified as proficient in BP measurement techniques at the beginning of the intervention, 18–24 months earlier. The training program consisted of a 30-minute online didactic module designed to refresh knowledge of recommended techniques. Topics included the rationale behind BP measurement; importance of a rest period, patient positioning, and taking multiple measurements; key features of the automated device; troubleshooting device errors; and measuring BP in emergency settings and special populations. Participants completed a 20 question pre- and post-test of knowledge and attitudes immediately before and after watching the training video. Trained research assistants performed direct observation of BP measurement at each clinical site for 3 months prior to and subsequent to rollout of the training modules in order to assess use of recommended techniques. Differences in responses to pre- and post-module knowledge and attitudes questions as well as direct observation data were analyzed using chi-square tests and simple logistic regression analysis.
RESULTS: All 88 clinical staff invited to participate viewed the module and completed the pre- and post-test (response rate = 100 %). Most participants were female medical assistants; 68 % were in their current job at least 3 years. LPNs were more likely to answer questions correctly than MAs and RNs, as were those in their current job at least one year. Demographic factors including age, gender, and race/ethnicity were not associated with higher scores. Baseline knowledge was lowest at the site with the largest underserved patient population, but no differences were found between the 3 sites with predominantly underserved populations and the other 3 sites. The total number of questions answered correctly improved following module completion (79.9 % vs. 93.1 %, p < 0.01) as did the average score per participant (80.4 % vs. 93.4 %, p < 0.01). Knowledge scores improved significantly among staff from all job types. Greatest improvement was seen in questions pertaining to patient positioning, measuring BP in patients wearing long sleeves, handling device errors, measuring BP in obese patients, and selecting the appropriate cuff size. Attitudes towards correct BP measurement did not improve significantly. One hundred twenty two direct observations were completed prior to training (20 per site) and 88 subsequent to training (15 per site). Direct observation data revealed no improvement in positioning. Following training, staff at the three sites with underserved patient populations were less likely to support the arm (84 % vs. 67 %, p = 0.03) and place the arm at heart level (96 % vs. 67 %, p < 0.01). However, subsequent to training, participants at all sites were more likely to explain the protocol to patients (60 % vs. 80 %, p < 0.01), offer a rest period prior to measurement (66 % vs. 85 %, p < 0.01), and record the average of three measurements (63 % vs. 95 %, p < 0.01).
CONCLUSIONS: We found baseline knowledge gaps in basic techniques in BP measurement among active clinical staff, revealing the need for ongoing training and assessment. Knowledge of correct BP measurement technique improved significantly following a brief online module. Direct observation data revealed improved adherence to multiple measurements but not to elements of patient positioning. Supervised clinical training may be more effective in changing attitudes and behaviors in accurate blood pressure measurement. Differential approaches may be needed based on characteristics of the clinical site and patient population served.
IMPROVING INTERNAL MEDICINE RESIDENT PREPAREDNESS TO DIAGNOSE AND TREAT SUBSTANCE USE DISORDERS; EVALUATING THE IMPACT OF AN ENHANCED ADDICTION CURRICULUMSarah E. Wakeman1; Genevieve Pham-Kanter2; Meridale Baggett1; Eric Campbell1,3. 1Massachusetts General Hospital, Boston, MA; 2University of Colorado Anschutz Medical Campus, Denver, CO; 3Mongan Institute for Health Policy, Boston, MA. (Tracking ID #1938278)
BACKGROUND: Substance use disorders (SUD) are the number one public health problem facing America, accounting for more morbidity and mortality than any other preventable health condition and affecting 16 % of the population. Despite providing care for large numbers of patients with addiction, a majority of internal medicine residents feel unprepared to treat SUDs and rate the quality of SUD instruction during training as fair or poor.
METHODS: This prospective study evaluated the impact of an enhanced SUD curriculum at Massachusetts General Hospital on internal medicine residents’ self-perceived preparedness to diagnose and treat SUDs, their ratings of the quality and quantity of SUD education, and their basic knowledge of SUDs. The intervention was a didactic curriculum designed by a collaborative group of internists and psychiatrists with addiction expertise, incorporated into the inpatient noon conference, resident report, and ambulatory lecture series over the course of one academic year. Core topics included the neurobiology of addiction; motivational interviewing; SUD screening and diagnosis; withdrawal management; pharmacotherapy for alcohol and opioid use disorders; opioid overdose prevention and management; physician addiction; care for the hospitalized patient with addiction; and exposure to patients in recovery.
RESULTS: Following the intervention, 86 % of residents reported feeling prepared to diagnose addiction and 58 % of residents reported feeling prepared to treat addiction as compared to 74 % and 37 % respectively in the baseline survey. Three quarters of residents rated the overall quality of instruction as good or excellent and 98 % of residents reported that formal residency curriculum had a positive impact on their self-perceived preparedness to provide care to addicted patients. However, 39 % of residents still reported feeling unprepared to treat addiction. Residents who reported receiving an adequate amount of SUD instruction were more likely to feel prepared to diagnose and treat addiction. Nearly one third of residents (31 %) still rated the overall amount of instruction in addictions as too little. Additionally, the majority of residents reported issues with insurance or cost of care (88 %) and access to addiction treatment (80 %) had a negative impact on their self-perceived preparedness to provide care for patients with SUDs. Nearly all residents (96 %) noted time constraints also negatively impacted preparedness. The intervention did not significantly improve residents’ answers to knowledge questions.
CONCLUSIONS: An enhanced didactic SUD curriculum for internal medicine residents resulted in improved self-perceived preparedness to diagnose and treat SUDs and higher quality ratings for SUD instruction. However, there was no significant change in knowledge. Limited access to addiction treatment negatively impacts resident self-perceived preparedness which highlights the need for overall policy changes related to SUD treatment in addition to educational reform. Given the complexity of SUDs, a comprehensive training model beginning in medical school, incorporating clinical experiences, and comparable to other chronic disease curricula is needed to adequately impact knowledge and clinical care.
IMPROVING PATIENT SATISFACTION THROUGH PHYSICIAN EDUCATION, FEEDBACK, AND INCENTIVESGaurav Banka1; Sarah Edgington1; Namgyal Kyulo2; Tony Padilla2; Virgie Mosley2; Nasim Afsarmanesh1; Gregg Fonarow1; Michael Ong1. 1UCLA, Los Angeles, CA; 2UCLA Health System, Los Angeles, CA. (Tracking ID #1936408)
BACKGROUND: Patient satisfaction has been associated with improved outcomes and become a part of reimbursement. Physician communication skills should be taught during residency and individualized feedback is an effective way to allow physicians to track their progress over time and compared to their peers. We aimed to evaluate an intervention to improve patient satisfaction focused on resident physicians and included education, frequent patient feedback, and incentives. We hypothesized that this intervention program would significantly improve Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores.
METHODS: This was a non-randomized pre-post study that took place from 2011 to 2012 at a large tertiary academic medical center. The intervention group was composed of internal medicine (IM) resident physicians and their patients. The control group was the rest of the hospital and the rest of the nation participating in the HCAHPS survey. The intervention implemented in 2012 provided IM resident physicians with patient satisfaction education through a one-hour conference, weekly real-time feedback on individualized patient satisfaction scores, departmental recognition and nominal ($20 value) prizes for outstanding scores, and a $100 incentive program for residents with >90 % of their patients reporting effective communication. We measured the post-intervention change in patient satisfaction on physician-related and overall satisfaction questions on the HCAHPS survey. For our analysis, we focused on the results involving communication with doctors and overall recommendation of the hospital. Our analysis focused on the following specific questions: Would you recommend this hospital to your friends and family? During this hospital stay, how often did doctors: 1) treat you with courtesy and respect? 2) listen carefully to you? 3) explain things in a way you could understand? Responders that did not answer all of the above questions were excluded. We adjusted for perceived patient health, admission through ER, age, race, patient education level, ICU stay, length of stay, and gender with a difference-in-differences regression analysis.
RESULTS: Our sample included 957 IM patients and 2028 non-IM adult control patients from the first two quarters of 2011 and 2012. The percentage of patients that responded positively to all three physician-related HCAHPS questions increased by 8.3 % in the IM and 1.3 % in the control cohorts (absolute difference 7.0 %, p = .04). The percentage of patients that would definitely recommend this hospital to friends and family increased by 6.5 % in the IM and 1.4 % in the control cohorts (absolute difference 5.1 %, p = .04). The national average for the HCAHPS outcomes studied improved by no more than 2.5 %. There was no significant change between cohorts in the percentage of patients that responded positively (choosing “always”) to each of the three individual physician-related HCAHPS questions after introduction of the $100 financial incentive.
CONCLUSIONS: Our intervention was associated with improvement in patient satisfaction with physician-patient communication and overall recommendation of the hospital. The $100 financial incentive that was implemented was not associated with further improvement in patient satisfaction. This intervention can serve as a model for academic hospitals to improve patient satisfaction and avoid revenue loss in the era of Hospital Value-Based Purchasing, and to train the next generation of physicians on providing patient-centered care.
INCIDENTAL FINDINGS ON PRE-VENTRICULAR ARRHYTHMIA ABLATION IMAGING. WAS FOLLOW UP RECOMMENDED?Chelsea K. Ngongang1; David Spragg1,2. 1Johns Hopkins Bayview Medical Center, Baltimore, MD; 2Johns Hopkins Hospital, Baltimore, MD. (Tracking ID #1939549)
BACKGROUND: Pre procedural imaging with computed tomography angiography (CTA) and/or magnetic resonance imaging (MRI) for ventricular arrhythmia ablation is routine in some settings to see the anatomy of the heart and its vessels. With this imaging being done, there are risks of incidental findings and the need of further workup of those findings. Discharge summaries have an important role in the communication of a patient’s “in hospital” course to transition smoothly to resuming primary care. This study looks at the rate of incidental imaging findings and how often physicians document in the discharge summaries these findings and the need for follow up on them with the patient’s primary care doctor.
METHODS: This is a retrospective study of 106 patients who received ablation for ventricular tachycardia, ventricular fibrillation, or premature ventricular complexes. The patient’s procedures were done at Johns Hopkins Hospital during the time period of 2008–2013. Seventy-five were male, average age 54 years old and 31 females, average age 48 years old. Patient’s information were obtained from physician procedure logs and were researched on the electronic medical record by the patient’s medical record number. Only imaging from a maximum of 2 days before the procedure were used to evaluate. All other imaging were not considered a part of pre-procedure time course. The imaging modalities reviewed were, computed tomography angiography (CTA) and magnetic resonance imaging (MRI) of the chest radiology reports for each patient.
RESULTS: There were 32 of the 106 patients that had incidental findings on imaging (30.1 %). There were 35 total radiographic findings in the 32 patients. These included pulmonary nodules (18), pericardial effusions (4), a hiatal hernia (1), breast calcifications (1), liver lesions (5), aortic aneurysms (2), an esophageal mass (1), lymphadenopathy (2), and rough endocardium (1). Interventions were done on 5 patients due to incidental radiographic findings including; cardiac catheterization (1), tissue biopsies (3), and a PET scan (1). Radiologist final reports recommended follow up imaging or evaluation for 26 of the 32 patients (81.2 %) with incidental findings. The discharging physician recommended follow up or mentioned the incidental finding in the discharge summaries for 7 of the 26 incidental finding patients with radiologist specific documentation for recommended follow up (26.9 %). All of the 5 patients who later underwent inventions due to their incidental findings on imaging had documentation in their discharge summary of the imaging and need for follow up.
CONCLUSIONS: This retrospective study shows that incidental findings are quite common in pre procedural imaging for patients undergoing ventricular arrhythmia ablation. These incidental findings often require follow up imaging and/or evaluation that that may lead to interventions being done. Unfortunately these incidental findings are less often mentioned in the discharge summaries the primary care doctor may receive after the procedure that describes the patient’s hospital course. It is important for primary care doctors to be aware of pre procedure imaging and obtain the results, because necessary follow up is not always communicated in discharge information.
INCREASED ACCESS TO PROFESSIONAL INTERPRETERS IN THE HOSPITAL ENHANCES LIMITED ENGLISH PROFICIENCY PATIENTS’ UNDERSTANDING OF PROCEDURAL AND SURGICAL CONSENTLeah S. Karliner; Crawford H. Michael; Steven Gregorich; Adrienne Green; Sunita Mutha; Anna M. Napoles; Eliseo J. Perez-Stable. UCSF, San Francisco, CA. (Tracking ID #1939646)
BACKGROUND: Limited English proficient (LEP) patients are at risk for poor communication leading to errors and adverse events. Professional interpreters improve communication, appropriate resource use and patient satisfaction. However, access to professional interpreters in the acute hospital is challenging due to the frequent and brief nature of many interactions, time pressures, the need for advance scheduling of in-person interpreters, and the around the clock nature of hospital care. We evaluated the impact of the bedside interpreter intervention-placement of a dual-handset telephone with 24-hour access to professional interpreters at the bedside of every patient-on LEP patients’ understanding of procedural and surgical consent.
METHODS: In order to evaluate the impact of access to professional interpreters on communication sensitive outcomes, we recruited two cohorts of hospitalized Chinese and Spanish speaking LEP patients from the cardiovascular, orthopedic, and general surgical floors of an urban academic medical center: one cohort before (pre-group) and one cohort after (post-group) implementation of the bedside interpreter intervention. We interviewed patients in each cohort in-person during their hospitalization. If the patient did not pass a cognitive screener or felt too ill to participate, we recruited a family surrogate. Among those participants who reported that they were awaiting or had already had a major procedure (e.g. cardiac catheterization) or surgery (e.g. CABG), we compared the two cohorts according to participants’ report of having signed a consent form, whether they had all of their questions answered, and how well they understood the reason and the risks of the procedure/surgery.
RESULTS: : Among the 214 participants, two-thirds were Chinese and one-third Spanish speakers; 56 % were women, average age was 70 (range 45–95), 88 % reported speaking English ‘not a at all’ or ‘not well’ and the remainder reported speaking English ‘well’ but preferred Chinese or Spanish for their medical care; there were no demographic difference between pre- and post- intervention groups. The majority (57 %) of participants both pre- and post- intervention were recruited from the cardiovascular floor, 28 % from general surgery and 15 % from orthopedics. At the time of the interview a total of 152 (84 pre- and 68 post- intervention) participants were either awaiting a procedure/surgery or had already had one. Among those 152 participants, post-intervention participants were more likely than pre-intervention participants to remember signing a consent form (93 % vs. 82 %; p = .06). More participants in the post-intervention group reported that they had all of their questions answered about the procedure/surgery (99 % vs. 89 %; p = .02). Likewise, post-intervention participants reported significantly better understanding of the reason for and risks of the procedure/surgery (table).
CONCLUSIONS: Placing a dual-handset telephone with 24-hour interpreter access at every bedside is associated with better understanding of the reasons for and risks of major procedures and surgeries for LEP patients. Implementation of systems changes such as the bedside interpreter intervention to improve communication with LEP patients in the hospital may help to increase patient engagement in their own care, and avert errors and adverse events.
| How well do you understand the reason you need the procedure/surgery… | Not at all | Not well | Well | Very well | p-value* |
| Pre- Post- | 3 (4 %) 0 (0 %) | 7 (8 %) 1 (2 %) | 37 (44 %) 15 (22 %) | 37 (44 %) 52 (76 %) | <.001 |
| How well do you understand the risks of the procedure/surgery… | Not at all | Not well | Well | Very well | p-value |
| Pre- Post- | 3 (4 %) 0 (0 %) | 7 (8 %) 5 (7 %) | 43 (51 %) 24 (35 %) | 31 (37 %) 39 (57 %) | .04 |
*Fisher’s exact test
INDIVIDUALIZED RISK COMMUNICATION AND LAY OUTREACH FOR THE PRIMARY PREVENTION OF CARDIOVASCULAR DISEASE IN COMMUNITY HEALTH CENTERS: PRELIMINARY RESULTS OF A RANDOMIZED CONTROLLED TRIALShreya Shah; Tiffany Brown; Ji Young Lee; Muriel Jean-Jacques; Namratha R. Kandula; Stephen D. Persell. Northwestern University, Feinberg School of Medicine, Chicago, IL. (Tracking ID #1937875)
BACKGROUND: Statin use for primary prevention of cardiovascular disease (CVD) has been shown to reduce CVD and all-cause mortality, yet fewer than half of high-risk individuals are treated with statins. CVD is the largest contributor to disparities in premature death by race and socioeconomic status; yet, rates of statin use among certain racial/ethnic and socioeconomic groups remain suboptimal. Data within electronic health records (EHR) can be used to identify individuals with CVD risk that is sufficiently high to warrant statin therapy. Lay outreach and individualized risk education could lead at-risk patients to seek and obtain treatment. We conducted a randomized controlled trial (RCT) at federally qualified health centers (CHCs), with a high proportion of minority and lower-income patients, to determine if a population health management intervention, compared to usual care, resulted in higher rates of documented statin treatment discussions. We report interim primary outcome results.
METHODS: This RCT was conducted within three CHC networks in Illinois and Arizona. Patients were identified systematically using EHR queries. Patients (men ≥35 and women ≥45 years old) with 10-year risk for myocardial infarction or coronary death of at least 10 % or greater, based on the Framingham Risk Score (FRS), with a visit to CHC within the past year, and no currently prescribed statin medication or previously diagnosed CVD or diabetes were included. The intervention consisted of a mailed letter providing individualized cardiovascular risk scores for each patient and encouraging patients to schedule a visit to discuss CVD prevention. The letter was followed by telephone outreach by CHC non-clinician care managers. Eligible patients from three waves separated in time were randomly assigned to receive the intervention immediately, or after a 1-year delay. The primary outcome was statin or cholesterol treatment discussion with a doctor or other primary care clinician within 6 months. This outcome was measured by chart review (inter-observer agreement, kappa = 0.77) and included a composite of: (a.) statin prescription, (b.) statin recommendation, (c.) patient refusal of statin, or (d.) documented discussion about cholesterol treatment with no clear statin recommendation. Reviewers were blind to the study group assignment. An intention to-treat-approach was used and statistical significance was determined using an unadjusted chi-square test.
RESULTS: Of the 662 patients included in the study, 478 (72.2 %) patients have completed the 6 month observation period and are included in the interim analysis (89.5 % male, mean age 60.6 ± 9.4 years, mean LDL 133.1 ± 25.0 mg/dL, mean FRS 15.3 ± 5.2). Two hundred forty-four were randomized to intervention and 234 to control. Intervention group patients were more likely to have a documented statin or cholesterol treatment discussion within 6 months (23.8 % vs. 10.3 %, OR 2.73, 95 % CI 1.63–4.57, p < 0.001). Among patients in the intervention arm that met criteria for the primary outcome: 6.1 % had a statin prescription, 0.8 % had a statin recommendation without a prescription, 2.9 % had a patient refusal of statin, and 13.9 % had a discussion about cholesterol treatment with no clear statin recommendation. There was a significant difference in discussions about cholesterol treatment with no clear statin recommendation (13.9 % vs. 6.0 %, OR 2.54, 95 % CI 1.33–4.88, p = 0.004), but no significant difference in the other 3 categories. Intervention group patients were more likely than controls to have a CHC office visit within 6 months (70.5 % vs. 52.6 %, OR 2.16, 95 % CI 1.48–3.14, p < 0.001).
CONCLUSIONS: An individualized risk communication and lay outreach intervention targeted towards CHC patients at moderate to high risk for CVD led to a moderately large increase in statin or cholesterol treatment discussions between patients and their clinicians. Most discussions, however, did not result in the patient receiving a statin prescription. Possible explanations include: physician reluctance to prescribe, patient reluctance to take medication, or a greater emphasis by patients and providers placed on cholesterol levels rather than CVD risk levels. Patient interviews and longer-term follow up of prescribing and laboratory results will help elucidate these factors further.
INFORMAL CAREGIVERS’ EXPERIENCES OF SUPPORTING VETERANS THROUGH ANTIVIRAL TREATMENT FOR HEPATITIS CRendelle Bolton1; Jeffrey Solomon1; Jack Clark1; Karen Steinhauser4,5; Eric Dieperink2; Kelly McMaken3; Keith McInnes1. 1Edith Nourse Rogers Memorial Veterans Hospital, Bedford, MA; 2Minneapolis Veterans Health Care System, Minneapolis, MN; 3Minneapolis Veterans Health Care System, Minneapolis, MN; 4Durham VA Medical Center, Durham, NC; 5Duke University School of Medicine, Durham, NC. (Tracking ID #1938568)
BACKGROUND: Hepatitis C (HCV) is the most common blood-borne virus in the United States and disproportionately affects the Veteran population, with sequalae including chronic liver disease, cirrhosis, and hepatocellular cancer. Antiviral treatment for HCV is complex and imposes significant burdens for patients, including substantial emotional and physical side effects. Little is known about the role of informal caregivers during antiviral treatment or how treatment impacts the relationship in the veteran-caregiver dyad. This study characterizes informal caregivers’ experiences of supporting veterans during treatment for HCV, with emphasis on caregiving activities, experienced burden, attributes of the veteran-caregiver relationship, and areas of need.
METHODS: Semi-structured interviews were conducted with 13 veteran-caregiver dyads from two VA hospitals. All veterans were undertaking antiviral treatment for HCV. Participants were queried about treatment experiences, caregiver roles, interactions with clinicians, and resources and needs related to treatment and caregiving. Interviews were audio recorded, transcribed verbatim, and uploaded into NVivo 10 software to organize coding and analysis. Adapting principles of grounded theory, a codebook was iteratively developed by an interdisciplinary team until saturation was reached. Transcripts were coded to consensus by two trained researchers who met weekly. Data from veteran-caregiver dyads were then systematically compared and thematic domains related to caregiving activities, the veteran-caregiver relationship, burden, and areas of need were identified.
RESULTS: SAMPLE: Approximately half of the veteran-caregiver dyads were marital or intimate partners; the remaining caregivers included friends, siblings, and adult children of the veterans. All patients were male, while most caregivers were female. (1) CAREGIVING ACTIVITIES: Caregivers provided instrumental support, including transportation and assistance with housework and shopping; emotional support through listening to veterans’ difficulties and providing encouragement; and informational support by helping veterans recall and understand medical information given to them at appointments. (2) VETERAN-CAREGIVER RELATIONSHIP: Emotional interactions were complicated; while many dyads reported increased tension, some also experienced greater closeness and fulfillment within the relationship. Caregivers’ support was appreciated, yet it could also threaten veterans’ feelings of self-sufficiency and independence as they struggled with limitations secondary to side effects and their commitments to complete their course of treatment. (3) BURDEN: Caregivers experienced both emotional and logistical burdens. The primary source of burden was veterans’ depression, irritability, and fatigue caused by antiviral therapy. Awareness of the stigma associated with HCV was also present, and several caregivers worried about the future should treatment fail. Among intimate couples, challenges to sexual intimacy secondary to veterans’ fatigue and anemia were also present. Logistically, for some caregivers, employment limited their ability to engage in caregiving activities. (4) NEEDS: Caregivers’ needs encompassed both informational and emotional support. While some caregivers attended the veterans’ medical appointments regularly, many only received second-hand information about HCV from veterans and wished they knew more so that they could better understand and support veterans. Finally, few had adequate sources of personal support and often felt alone through the treatment process, particularly if the veteran was an intimate partner.
CONCLUSIONS: Caregivers can play a vital role supporting veterans through antiviral treatment for HCV, yet many in this sample felt under-informed, under-supported, and burdened. Clinicians should consider engaging informal caregivers as partners in the treatment of HCV, and ensure that caregivers receive increased informational and emotional support so that they may in turn better support veterans. Continued systematic study of informal caregiver roles in HCV treatment is needed and directions for future research will be discussed.
INFORMATION AND COMMUNICATION MEDIA USE BY FEMALE RESIDENTS OF PUBLIC HOUSINGShivani M. Reddy1,2; Lisa Quintiliani1,3; Deborah J. Bowen3. 1Boston University School of Medicine, Boston, MA; 2VA Boston Healthcare, Boston, MA; 3Boston University School of Public Health, Boston, MA. (Tracking ID #1936988)
BACKGROUND: Obesity is associated with many chronic diseases and disproportionately affects individuals of lower socioeconomic status (SES), particularly among women. Information and communication technologies (ICT) offer an opportunity to provide obesity-related interventions widely with cost-effectiveness. Evidence suggests that internet, mobile, or social media based-interventions may promote obesity-related behavior change. However, the uptake of ICT among low-SES individuals is unclear. In this study, we examine the frequency of ICT use among a subgroup of low-SES individuals, female public housing residents, and also examine if ICT use varies across demographic, health, or obesity-specific variables.
METHODS: We examined socio-demographic variables collected at the baseline assessment of a cluster randomized obesity intervention designed for mothers/caregivers and their daughters. (n = 211) The majority were Hispanic or Latino (64 %), Spanish-speaking (64 %), non-United States born (66 %), and had a high school education or less (64 %). Nearly 50 % were obese, a third overweight, and over 80 % sedentary. Mean age was 38.1 (SD 7.6). A subset of 158 subjects were surveyed on email, internet, social media (SM), mobile, and health information seeking (HI) internet use. We adapted the Pew Research Center typology of ICT users, defining a “user” as daily use or use within the last day. Comparisons between users and non-users and among users were made with student t-tests, chi square tests, and fisher’s exact tests.
RESULTS: The majority accessed the internet in the past year (84 %), 75 % in the last day; accessed a SM site (85 %), 70 % in the last day; made one daily cell phone call (97 %); and sent at least one daily text message (84 %). ICT users were younger, more educated, US-born, and primary English speakers. For example, email users (vs. non-users) were 37 years old (vs. 39), and 43 % were English speakers (vs. 17 %). Email, internet, or multiple media users were more often White or Black (p = 0.84, p = 0.03, p = 0.39, respectively). However, SM users and HI internet users were more like to be Spanish speakers (58 % vs. 50 % for both, p = 0.6 and 0.1) and Hispanic (p = 0.84, p = 0.21 respectively). There were no significant differences in obesity, or physical activity.
CONCLUSIONS: ICT use is common among low-SES female public housing residents, with mobile use for calls and texts most prevalent. Our findings of differential socio-demographics among users vs. non-users and among users themselves suggests that future public health interventions should consider targeting messages according to the cultural background of the targeted audience.
INPATIENT HEALTHCARE UTILIZATION AMONG PATIENTS WHO REQUIRE INTERPRETER SERVICESJane Njeru1; Paul Takahashi1; Jon Ebbert4,1; Jennifer St. Sauver2; Debra Jacobson3; Chun Fan3; Mark L. Wieland1. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Rochester, MN; 4Mayo Clinic, Rochester, MN. (Tracking ID #1928126)
BACKGROUND: More than 9 % of the US population has limited English proficiency (LEP). LEP is associated with multiple health disparities and suboptimal health outcomes. While LEP is a barrier to effective healthcare, it has been associated with increased outpatient healthcare utilization. However, its association with inpatient healthcare utilization remains unclear. The objective of this study was to determine the association between LEP and inpatient healthcare utilization among adult patients.
METHODS: Design: This was a retrospective cohort study comparing emergency department (ED) visits and hospitalizations between patients requiring interpreter services (IS) and a cohort of age-matched English-proficient patients (non-IS patients). Setting and Participants: The study was set in a large multisite primary healthcare network in a medium-sized US city. The participants were adult patients who were actively empanelled to physicians in this practice for primary care. Measures and analytic procedures: Emergency Department visits and hospitalizations in 2012 were obtained from billing records of the 3 inpatient facilities in the county. Chart reviews were performed for all the study participants with at least 1 hospitalization or ED visit to confirm the event and review the associated diagnoses. Demographic data were obtained from registration information, while medical complexity data (summarized using the Charlson comorbidity index) was obtained from billing records. The total number of ED visits and hospitalizations during the 12-month period was compared by IS status, using a χ2 test. Proportional hazard regression was used to assess the association between IS status and first ED visit or hospitalization, and results were presented as hazard ratios (HRs) with 95 % CIs. Multivariable models were used to adjust for the effect of age, sex, Charlson comorbidity index, and number of outpatient visits.
RESULTS: The cohort included 3,784 patients (1,892 per group). Patients who required interpreter services had significantly more total ED visits (841 vs 620; P < .001) and hospitalizations (408 vs 343; P < .001) than the non-IS patients. Regression analysis showed that the risk of a first ED visit were 60 % higher for IS patients than non-IS patients (unadjusted hazard ratio [HR], 1.6; 95 % CI, 1.4–1.9; P < .05), and risk of a first hospitalization were 50 % higher (unadjusted HR, 1.5; 95 % CI, 1.2–1.8; P < .05). These findings remained significant after adjusting for age, sex, medical complexity, and outpatient healthcare utilization. The reasons for the first ED visit and hospitalization differed between IS patients and non-IS patients; hospitalizations due to infectious, gastrointestinal, mental health, and genitourinary diagnoses were more common among IS patients than non-IS patients. Similarly, for ED visits, these same categories were also more common among IS patients, along with ear-nose-throat (ENT), ophthalmologic, dermatologic, dental, and trauma or assault diagnoses. Conversely, hospitalizations for musculoskeletal diagnoses were higher among non-IS patients, but this difference was explained almost entirely by elective joint arthroplasties.
CONCLUSIONS: Patients who required IS had higher rates of inpatient healthcare utilization compared with non-IS patients. Further research is required to understand factors associated with increased use of the ED and to develop sociolinguistically tailored interventions to facilitate appropriate healthcare in this population.
INSTITUTIONAL PREDICTORS OF MEDICAL STUDENTS’ INTERACTIONS WITH THE PHARMACEUTICAL AND MEDICAL DEVICE INDUSTRIESJames Yeh1; Kirsten Austad1; Jessica Franklin1; Susan Chimonas2; Eric Campbell3; Jerry Avorn1; Aaron Kesselheim1. 1Brigham and Women’s Hospital and Harvard Medical School, Boston, MA; 2Columbia University College of Physicians and Surgeons, New York, NY; 3Massachusetts General Hospital and Harvard Medical School, Boston, MA. (Tracking ID #1921316)
BACKGROUND: Medical students frequently interact with pharmaceutical and medical device industries. Students receive biased information from these interactions, which may lead to non-evidence-based prescribing. Thus, medical schools have designed industry interaction policies regulating students’ contacts with the industry. Professional societies have developed metrics to evaluate the strength of these policies. We compared metrics from two prominent professional societies and investigated which aspects of industry interaction policies were most closely associated with student outcomes. We also considered whether certain characteristics of medical schools were associated with their students’ behavior and attitudes towards pharmaceutical marketing.
METHODS: A national sample of 1610 first- and fourth-year medical students answered survey questions on acceptance of gifts from the industry, interaction with sales representatives, and perceived adequacy of faculty and industry separation. We used hierarchical logistic regression models to determine the association between these reported outcomes with their schools’ strength of industry interaction policies. The strength of the policies was measured using the American Medical Student Association (AMSA) PharmFree Scorecard and the Institute on Medicine as a Profession’s (IMAP) Score. The model included adjustments for year in training, medical school size, and the level of National of Institute of Health (NIH) funding received by the medical school. We also performed LASSO logistic regression models to determine which policy domains were best associated with students’ reported outcomes.
RESULTS: IMAP Score had a lower median value (1.75, interquartile range [IQR]:2–2.45) than the AMSA Score (2.18, IQR:1.5–2). The policy dimensions shared by AMSA and IMAP were not well-correlated (gift policies r = 0.28, 95 % confidence interval [CI]:0.11–0.44); sales representative access policies r = 0.51, 95 % CI:0.36–0.63). Students from schools with the highest-ranked industry interaction policies were less likely to accept gifts (AMSA Score odds ratio [OR]:2.65, 95 % CI:1.38–5.07; IMAP Score OR:2.19, 95 % CI:0.96–5.03) and less likely to interact with sales representatives (AMSA Score OR:2.99, 95 % CI:1.43–6.27; IMAP Score OR:2.71, 95 % CI:1.05–6.97) than students from schools with lowest-ranked policy scores. The association became non-significant when fully adjusted for NIH funding. Policies governing receipt of gifts (OR:1.01–1.30), meals (OR:1.13), and speaking bureaus (OR:1.02–1.13) were best associated with students’ reported behavior of gifts receipt and sales representatives interaction. By contrast, policies regulating industry’s role in educational activities (e.g., CME, travel compensation, and scholarship) were best associated with outcome of perceived adequate separation between faculty and industry (OR:1.01–1.32).
CONCLUSIONS: Policies restricting gifts had significant impact on students’ behavior in reducing the receipt of industry gifts, sales representative interactions, and increased perception of adequate separation among the faculty and industry. Medical schools’ strength of industry interaction policy, as determined by AMSA or IMAP scores, was associated with student reported behavior. However, this relationship was confounded by the level of NIH funding. As medical schools revise their industry interactions policies, limitation on the receipt of gifts should be emphasized and greater attention paid to less research-intensive schools.
INTENTIONAL AND INCIDENTAL SCREENING FOR ABDOMINAL AORTIC ANEURISMS IN OUTPATIENT PRIMARY CARE CLINICSAllison L. Ruff1; Bo Hu2; Kathryn Teng1; Michael B. Rothberg1. 1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH. (Tracking ID #1933802)
BACKGROUND: In 2005, The U.S. Preventive Services Task Force (USPFTF) recommended one-time abdominal aortic aneurysm (AAA) ultrasound screening for men aged 65 to 75 who ever smoked. Reported screening rates have been 12.9 % to 26 %. CT, MRI, and non-aortic abdominal ultrasound all provide adequate visualization of the aorta, but may not be considered AAA screening by providers; therefore, screening rates may be higher than previously reported. The objective of our study was to evaluate rates of screening performed intentionally and incidentally (with other abdominal imaging), rates of redundant screening, and patient and physician characteristics associated with screening.
METHODS: Cross sectional study of 2 years of patient encounters (2007 and 2012) to determine AAA screening trends at the Cleveland Clinic. Data were collected from the electronic health record. We included all patients who were eligible for screening according to the USPSTF guidelines and were seen in a primary care office in the calendar year. For each study year, we evaluated rates of screening by patient age, smoking status (current or former), family history, and completion of other routine screenings including lipid panel, pneumonia vaccination, and colonoscopy. Patients were considered to have been screened for AAA if they underwent a CT, MRI, or ultrasound that visualized the aorta. We examined the rates of screening for patients of 861 primary care physicians. For physicians with at least 20 eligible patients in our data set, we created a multivariate model to assess patient and physician characteristics associated with screening.
RESULTS: There were 15,122 patients eligible for screening in 2007 and 11,068 in 2012. Most screening was completed incidentally by imaging for other indications. When considering all imaging that included the aorta, screening rates were 31 % in 2007 to 45 % in 2012. Screening rates with designated ultrasounds were 2.5 % for 2007 and 7.2 % for 2012, lower than previously reported. Of 1176 screening ultrasounds, 549 (47 %) were performed on patients who had already been screened via another imaging modality. Of 861 physicians, 211 had at least 20 eligible patients in the data set. Rates of any AAA screening by individual physicians ranged from 9 % to 81 % (median = 40.9 %, IQR = [33.3 %, 51.3 %]), and rates of ultrasound screening ranged from 0 to 65 % (median = 10.5 %, IQR = 2.8 %, 20.3 %). Physician characteristics positively associated with screened patients included female sex (OR = 1.47 [1.11, 1.96], p = 0.01), younger age (OR = 1.10 [1.03, 1.18] per 5-years, p = 0.01) and specialty (Internal Medicine vs. Family Medicine, OR = 1.72 [1.30, 2.28], p < 0.001). Patients that were up to date on other age-appropriate screening were more likely to have AAA screening performed. Former smokers were just as likely to have a screening performed as were current smokers (37 % vs. 38 %, p = 0.59). Patients with a positive family history of AAA were more likely to have a screening (55 % vs. 37 % p = 0.001). Patients older than 70 were more likely than patients 65–69 to have a screening (42 % vs. 36 %, p < .001).
CONCLUSIONS: AAA screening rates remain below 50 %, but are improving over time. Screening rate by individual physicians vary 9-fold, indicating substantial opportunity for educational interventions. Most AAA screening is completed incidentally, and some patients later undergo unnecessary ultrasound screening. Before ordering screening, physicians and EMR-based reminder tools should ensure that the aorta has not been previously visualized.
INTER-HOSPITAL TRANSFER STUDY (IHTS): HOW AN UNSTRUCTURED PROCESS IMPACTS PATIENT OUTCOMESMichael G. Usher; Christine Fanning; Karen Balonze; Di Wu; Dana Herrigel; Amay Parikh. Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1939238)
BACKGROUND: Inter-hospital transfers are an important yet understudied area in transitions of care. Timing of transfer, incompatible information systems, geographical distance, and patient acuity combine to create considerable obstacles to safe and efficient patient care. There are few studies that show how the process of triage, information transfer, and patient hand-off when moving patients between facilities impact clinical outcomes; therefore no consensus to standardize the process of coordinating inter-facility transfers exists. This study aims to fill that gap.
METHODS: This retrospective observational study reviewed the medical records of patient transfers from outside hospitals to three ICUs (medical, surgical, and cardiac) during December 2011 to December 2012. We gathered data about each patient’s transfer including time of initiation, acceptance, and arrival. We analyzed the information that came with these patients for completeness using a standardized scoring system with two independent reviewers. Outcomes focused on adverse events, including in-hospital mortality, central line placement, transfusion, intubation, vasopressor initiation, ICU readmission, initiation of renal replacement. We used multivariate logistic regression to identify predictors of high-risk inter-hospital transfers.
RESULTS: 328 patients were transferred from 37 outside hospitals between December 2011 and December 2012. On average, patients were admitted for 4.24 days prior to transfer, and took 9.6 h to be relocated to RWJ once initial call was placed to transfer center. Adverse events occurred in 42 % of patients within 24 h of arrival, with an overall mortality of 18 %. Important predictors of adverse events were critical labs on admission (p < 0.001), MPM/ApacheII score (p < 0.0001), MICU admission (vs SICU/CCU) (p = 0.002). Surprisingly, there was no correlation in severity of illness and the duration it took to complete the patient transfer. Patient arrival followed a bimodal distribution with peak arrival times at 6:00 pm (within 1 hour of shift change) and at 2:00 am. When controlling for MPM and transfer score, arrival during the night shift (50 % of the transfer population) was associated with an increase in adverse events (p = 0.006), and a non-significant trend toward increased mortality (p = 0.17).
CONCLUSIONS: Patients are often transferred between facilities in unstable condition or at inopportune times, associated with an increase in adverse events. We initially hypothesized that higher acuity transfers would be transferred more quickly; however, this is not the case. This suggests the relocation of critically ill patients may often be driven by administrative bottlenecks such as bed availability, causing a large proportion of patients to arrive at night at an increased adverse event rate. Improving the transfer process, including triage of patients based on severity of illness and physician staffing patterns, may improve clinical outcomes.
INTER-HOSPITAL TRANSFER STUDY (IHTS): INFORMATION HAND-OFF AND CLINICAL OUTCOMES OF CRITICALLY ILL PATIENTSMichael G. Usher; Christine Fanning; Karen Balonze; Di Wu; Dana Herrigel; Amay Parikh. Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1936900)
BACKGROUND: Transitions of care, whether within or between institutions, are an important source of medical errors, inefficiency, and unnecessary cost. Multiple studies demonstrate that improving the information quality of patient hand-offs during care transitions is associated with more efficient, less costly care, improved outcomes, and improved patient satisfaction. However, transitions of care involving patients transferred between facilities remains understudied. Inter-hospital transfers face multiple unique challenges, including uncertainty of timing, differing information systems, and geographical distance, which is compounded by patient acuity and complexity. This study is designed to investigate whether the quality of patient hand-off impacts outcomes for patients transferred between facilities.
METHODS: We conducted a retrospective observational study of consecutive patients transferred to the MICU, SICU, and CCU from December 2011 through December 2012. Patient records were scored for the presence and completeness of discharge summary, history and physical, progress notes, consultations, images, and medication reconciliation (0 points if absent, 1 point if incomplete, 2 points if complete). The final transfer score was a percentage of the total possible points following two independent reviews. The primary outcome was in-hospital mortality. Secondary endpoints were adverse outcomes and a measure of over-utilization (that included transfer to another service within 24 h and duplicated labor). Severity of illness was adjusted by MPM0-III, and statistical significance was inferred with p < 0.05 by multivariate logistic regression.
RESULTS: 328 patients were transferred to three ICUs from 37 facilities during the study period. Patients were transferred with documents containing an average of 66 pages and a median transfer score of 60 out of a possible 100. There was no correlation between the length of the transfer documents and the transfer score (p = 0.57). When controlling for severity of illness, patients transferred with higher transfer scores had significantly lower mortality (p = 0.022, 95 % CI −2.73 to −0.21). Similarly, higher transfer scores were associated with decreased adverse events within 24 h (p < 0.001, 95 % CI −3.60 to −1.41) and over-utilization (p = 0.001, 95 % CI −3.18 to −0.80). These results remained significant for all three ICUs separately. Of the individual components of the transfer score, multivariate logistic regression showed that by itself, the transfer of images was an independent predictor of in-hospital mortality (p = 0.017).
CONCLUSIONS: We show patients are frequently transferred with incomplete information, which leads to higher mortality and increased resource utilization. This correlation was significant across a highly variable patient population admitted to three distinct ICUs, demonstrating how the lack of a standardized approach to patient hand-offs can worsen outcomes for high risk patients. Currently, there are no guidelines detailing how to coordinate information during inter-hospital transfers. Systematic improvement of the hand-off process in these cases has the potential to improve patient important outcomes and provide higher value care.
INTEREST IN SMOKING CESSATION AND PRIOR CESSATION ATTEMPTS AMONG PATIENTS RECEIVING OFFICE-BASED BUPRENORPHINE TREATMENTPooja A. Shah1; Shadi Nahvi2,3; Mia Brisbane3; Oni J. Blackstock2,3; Chinazo Cunningham2,3. 1UCSF, San Francisco, CA; 2Albert Einstein College of Medicine, Bronx, NY; 3Montefiore Medical Center, Bronx, NY. (Tracking ID #1940824)
BACKGROUND: Tobacco use and tobacco-related disease are more prevalent among opioid-dependent patients than the general population. Despite this high tobacco burden, smoking cessation treatment is limited among opioid-dependent individuals. Office-based buprenorphine maintenance treatment (BMT) provides an important opportunity to offer smoking cessation treatment to opioid-dependent patients in a primary care setting. To our knowledge, interest in cessation and prior cessation attempts have not been described among buprenorphine-treated patients. To improve smoking cessation among BMT patients, we must first understand patterns of smoking, interest in smoking cessation and prior cessation attempts. Therefore, we sought to describe prevalence of cigarette smoking and patterns of prior cessation attempts among patients receiving office-based BMT.
METHODS: We interviewed 68 patients receiving BMT at a primary care clinic in the Bronx, NY. Physicians referred patients who were currently receiving BMT to the study. Participants were administered a questionnaire using audio computer-assisted self-interview technology in English or Spanish. Questionnaire domains included: socio-demographic characteristics, substance use, buprenorphine maintenance treatment, nicotine dependency, history of smoking cessation attempts, and attitudes about cessation. We report simple frequencies to describe smoking and smoking cessation in this population.
RESULTS: Of 68 participants, the mean age was 47 years; 69.1 % were male, 67.6 % Hispanic and 55.9 % had a high school diploma or equivalent. The participants’ median duration of BMT was just over 3 years. Overall, 95.6 % had ever smoked cigarettes, 87.7 % reported currently smoking, and 83.1 % of those who had ever smoked had tried to quit. Among current smokers, 43.9 % had a Fagerstrom Test for Nicotine Dependence score greater than 6, which corresponds to high dependency. Participants rated quitting smoking as important and were confident in their ability to quit smoking (on a scale from 1 to 10, with 1 = least important/confident and 10 = most important/confident, median importance score = 9, IQR = 7,10 and median confidence score = 6, IQR = 4,8). Of those who had ever tried to quit smoking, 78.5 % reported a prior medication-assisted quit attempt; the most common medications used were nicotine patch (63.1 %), nicotine gum (47.7 %) and varenicline (29.2 %). The most common non-pharmacologic methods of quit attempts were quitting cold turkey (40.0 %) and gradually cutting down the number of cigarettes smoked (32.3 %). In addition, 15.4 % reported use of electronic cigarettes to quit smoking.
CONCLUSIONS: Among opioid-dependent patients receiving BMT in a primary care setting, cigarette smoking was highly prevalent and an overwhelming majority of smokers had tried to quit unsuccessfully. Despite high levels of prior quit attempts, use of pharmacotherapy for smoking cessation and importance ascribed to quitting, most remained actively smoking. These results illustrate the need to develop better strategies to facilitate smoking cessation among patients receiving office-based BMT, and can be used to guide cessation strategies.
INTERHOSPITAL TRANSFER STUDY (IHTS): UNINSURED PATIENTS AND THE POTENTIAL FOR A MEDICAL LIMBOChristine Fanning; Michael G. Usher; Di Wu; Karen Balonze; Dana Herrigel; Amay Parikh. Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1936827)
BACKGROUND: Insurance coverage is an important contributor to health disparities. Uninsured patients are less likely to be hospitalized, receive less intense care overall, and have increased mortality among the critically ill. This occurs despite EMTALA, which mandates patient stabilization and treatment regardless of insurance coverage, and is designed to prevent premature transfer between facilities for financial reasons. EMTALA is balanced by recent privatization of medical care, which may increase incentive to transfer patients without insurance to other facilities as early as possible. This study aims to determine whether insurance status impacts the inter-hospital transfer process and outcomes in the current healthcare climate.
METHODS: We conducted a retrospective study evaluating consecutive patient transfers from outside hospitals to three ICUs (medical, surgical, and cardiac) during December 2011 through 2012. We compared insurance status of patients admitted from outside hospitals against those transferred from the wards or ED. Outcomes included in-hospital mortality, adverse events, and a measure of over-utilization (that included patients being transferred to another service within 24 h and duplicated labor); severity of illness was adjusted using MPM0-III. Outcomes and insurance status were compared by two tailed ANOVA and Fisher’s Exact test, with statistical significance inferred by p < 0.05.
RESULTS: 328 patients were admitted to three ICUs from 37 outside facilities versus 3706 patients transferred from the wards or ED between December 2011 and December 2012. Self-pay or charity care patients were underrepresented in the inter-hospital transfer group (8 %) when compared with those transferred from the wards or ED (14 %, p = 0.005). Patients with insurance were conversely over-represented in the cohort transferred from outside hospitals (p = 0.06). This was not explained by differences in patient demographics or regional variations in insurance rates. Of the cohort transferred from outside hospitals, uninsured patients had a reduced length of stay at the prior hospital (P < 0.0001, 95 % CI −2.786 to −1.189) and had a reduced severity of illness (p < 0.0001) when compared against patients with insurance. Severity adjusted outcomes including in-hospital mortality, adverse events, and over-utilization were similar between groups.
CONCLUSIONS: These data illustrate the complex effect of insurance status on a patient’s likelihood of being transferred between facilities. Uninsured patients are transferred earlier and are of lower acuity than their insured counterparts, reflecting a motivation to move patients who cannot pay to other hospitals. On the other hand, the under-representation of uninsured patients who are actually transferred reflects hospitals’ lack of desire to accept the uninsured. This creates the potential for a medical “limbo,” in which insurance status complicates disposition in patients requiring specialized care, potentially exacerbating health disparities in underserved populations.
INTERHOSPITAL TRANSFERS: PATIENT CHARACTERISTICS AND OUTCOMESCecelia N. Theobald1,2; Stephan Russ3; Jesse Ehrenfeld4; Sunil Kripalani2. 1VA Tennessee Valley Healthcare System, Nashville, TN; 2Vanderbilt University, Nashville, TN; 3Vanderbilt University, Nashville, TN; 4Vanderbilt University, Nashville, TN. (Tracking ID #1939070)
BACKGROUND: The transfer of inpatients between hospitals is often necessitated by differential expertise and capacity among facilities. At some institutions, interhospital transfers constitute nearly 20 % of all inpatient admissions and there is concern they may experience poorer outcomes. Much of the literature to date has examined small subpopulations of interhospital transfers (such as ICU, trauma, and burn patients) without evaluating the characteristics of transfer patients as a population. Our objective was to compare the arrival characteristics and outcomes of interhospital transfer patients with those of patients directly admitted to a large academic medical center.
METHODS: We conducted a retrospective cohort study of patients transferred into an academic medical center and compared these with patients directly admitted during an 18 month period. Patients were excluded if they were transferred into the Emergency Department, Labor and Delivery, or admitted to burn or trauma services. Admission characteristics studied included demographics, site of admission (ICU vs. non-ICU), severity of illness (measured using the modified Elixhauser comorbidity index, range of possible scores −14 to 60), admitting service, and time of arrival. Outcome measures included length of stay, ICU length of stay, in-hospital mortality, and timeliness of initial inpatient care. Transfer patients were compared with non-transfer patients using simple univariate analysis.
RESULTS: Transferred and non-transferred patients had similar rates of ICU admission (46.5 % vs. 47.4 %, p = 0.53) but transferred patients had higher severity of illness (mean modified Elixhauser score 12.0 vs. 9.3, p < 0.001). Nearly two thirds, or 65 % of interhospital transfers arrived during overnight hours (6 PM to 7 AM), vs. only 56.2 % of non-transferred patients (p < 0.001). Transferred patients waited on average 18 min longer for admission orders (p < 0.001) and 15 min longer for non-PRN medication orders (p < 0.001). Furthermore, transferred patients experienced significantly longer length of stay (6.0 vs. 3.1 days, p < 0.001) and ICU length of stay (4.4 days vs. 2.5 days, p < 0.001). Finally, transferred patients had over twice the in-hospital mortality of non-transferred patients (10.9 % vs. 4.9 %, p < 0.001).
CONCLUSIONS: Interhospital transfer patients as a population have an increased severity of illness and experience longer length of stay, delays in initial inpatient care, and higher in-hospital mortality when compared with non-transferred patients. Hospitals may want to focus specific resources on this unique high-risk population.
Table: Comparison of transfer and non-transfer population
| Characteristic | Transfers ( n = 1715) | Non-transfers ( n = 6176) | p value |
|---|---|---|---|
| Age, mean (SD) | 55.3 (16.6) | 57.7 (16.9) | <0.0011 |
| Male % | 48.6 % | 56.3 % | <0.0012 |
| ICU admission (%) | 46.5 % | 47.4 % | 0.532 |
| Modified Elixhauser index, mean (SD) | 12.0 (10.5) | 9.3 (9.6) | <0.0011 |
| Service Medicine Surgery Neurology OB/Gyn | 55.7 % 34.1 % 8.8 % 1.5 % | 63.6 % 29.7 % 6.0 % 0.6 % | <0.0012 |
| Time of arrival Day shift (07:00–17:59) Night shift (18:00–06:59) | 35.2 % 64.8 % | 43.8 % 56.2 % | <0.0012 |
| Time to in minutes, median (IQR) Admission order entry Non PRN medication order Antibiotic order | 46 (19–90) 28 (12–61) 199 (81–505) | 28 (3.5–70) 13 (0–41) 190.5 (35–615) | <0.0013<0.0013 0.00113 |
| Length of stay, median (IQR) Total hospital ICU | 6.0 (3.2–11.3) 4.4 (2.3–8.9) | 3.1 (1.8–6.3) 2.5 (1.3–5.0) | <0.0013<0.0013 |
| In-hospital mortality % | 10.9 % | 4.9 % | <0.0012 |
Statistical tests used: 1 T-test 2 Chi-square 3 Wilcoxon rank-sum
INTERN REFLECTIONS ON TRANSITIONS OF CARE EDUCATIONAL EXPERIENCE: INSIGHTS GAINED FROM PARTICIPATION IN POST HOSPITAL DISCHARGE HOME VISIT AND SKILLED NURSING FACILITY VISITRachel K. Miller1; Zachary Smith1; Shimrit Keddem1; Samuel P. Katz1; Karen B. Hirschman2. 1University of Pennsylvania, Philadelphia, PA; 2School of Nursing- University of Pennsylvania, Philadelphia, PA. (Tracking ID #1939559)
BACKGROUND: Transitions of care, particularly for the elderly and medically complex patient, are a high risk period of time. Through enacted legislation and proposed insurance payment changes, care transitions are under increased scrutiny. Given the importance of recognizing and improving the current care transition system and ACGME competencies and milestones focusing on transitional care, medicine residences are increasing formal education on this topic. Our goal was to provide interactive post-hospitalization transitions of care learning experiences for interns and to determine key intern perspectives and insights gained from the curriculum.
METHODS: The 2012–13 UPenn internal medicine intern class participated in both post-hospitalization home visits with a visiting nurse (HVs) and skilled nursing facility (SNF) transitions experience with geriatric faculty member. Interns were asked to write a reflection essay on each experience with the following questions: “How has this visit changed your perception of discharge?, How will this experience change the way you care for patients?, Did anything in particular surprise you on the visit? The responses were entered into NVivo 10 for analysis. We used a modified grounded theory approach to the analysis. Codes were generated by the team based on the research question and the content of the data. Coders applied these codes to each line of text. A subset of narratives were double-coded for inter-rater reliability. Coding discrepancies were resolved by consensus.
RESULTS: Of the 46 interns, 36 and 34 completed the reflection essays on their HV and SNF experiences, respectively. Two overarching themes arose: the need to create more comprehensive yet articulate discharge instructions and a better appreciation of the patient’s post-hospital care personnel (namely nurses and pharmacists). Additional themes included awareness of need to improve the post-hospital medication reconciliation and importance of assessing a patient’s living situation and social support system before discharge. Interestingly, very few residents placed blame on the patients for any perceived breakdowns in care; most identified barriers to care were a lack of social support, difficult living circumstances, or messy and inadequate discharge instructions including misperceptions or gaps surrounding follow-up care and medication management.
CONCLUSIONS: The intern transitions of care curriculum, out of the hospital, and into the homes and skilled nursing facilities of discharged patients, sought to teach key elements of safer discharge in an interactive format. The reflection essays revealed that the interns gained insights into the importance of effective communication (accurate and informative medication reconciliation, comprehensive discharge summaries/instructions), the roles of interprofessionals in faciliating safe discharges, and the need for in-hospital teams to elicit potential health care challenges. Future goals will be using these to inform and improve specific parts of the discharge process and to determine whether there is a long-term impact in intern actions in discharge planning and patient outcomes.
INTERNAL MEDICINE RESIDENTS’ EXPERIENCE OF CONTINUITY IN OUTPATIENT CARE: A QUALITATIVE STUDYElisabeth Ihler. Montefiore Medical Center, New York, NY. (Tracking ID #1937099)
BACKGROUND: Provider continuity in ambulatory care has been shown to improve patient outcomes. However, maintaining patient continuity in outpatient care is difficult for internal medicine residents who work primarily in the inpatient setting. The effect of this conflict on residents’ experience is unknown.
METHODS: Residents in the categorical internal medicine program at Montefiore Medical Center participated in a series of one-hour focus groups led by the investigator during their monthlong ambulatory rotations. A semi-structured questionnaire was used to guide the conversation. A total of 30 residents participated in 6 focus groups between December 2012 and October 2013, representing all 3 postgraduate years. A qualitative coding scheme was developed from the results of pilot focus groups and was applied to the transcribed interviews using commercial coding software.
RESULTS: Four major thematic domains emerged from the interviews. Residents highly valued the continuity relationship, particularly for its educational benefit. However, they reported great difficulty maintaining continuity with patients, primarily due to conflicting demands on their time and competing educational priorities. They also noted downsides to the continuity experience, including difficulty gauging how much effort to put into non-continuity visits with patients. In addition, residents used a number of strategies to manage their workload and the competing demands on their time, including keeping personal lists of patients, phone/email, overbooking, and use of urgent care slots for routine care.
CONCLUSIONS: Residents have complex perceptions of their experience of continuity in the ambulatory clinic, which are sometimes in conflict. They see significant value in the continuity experience as a whole both for themselves and for patients, but frequently regard it as impinging on their other work. Residents were particularly divided in how to manage visits with patients for whom they were not the primary care physician. They have developed a number of strategies to manage their ambulatory experience, some of which may have negative effects on overall clinic function.
INTERPROFESSIONAL COLLABORATIVE CARE: FACTORS ASSOCIATED WITH BEDSIDE INTERPROFESSIONAL ROUNDSJed Gonzalo; Daniel R. Wolpaw; Erik B. Lehman; Cynthia H. Chuang. Penn State College of Medicine, Hershey, PA. (Tracking ID #1937760)
BACKGROUND: Care delivery in hospital-based medicine units requires collaboration between nursing staff and physicians to optimize care delivery. Although bedside interprofessional rounds is one method to promote interprofessional collaboration between nurses and physicians, this activity has not been well studied. We examined the incidence of bedside interprofessional rounds on medicine teaching services in one academic institution. We hypothesized resident and attending physicians with more experience, smaller team census size, and weekdays would be associated with higher occurrence of bedside interprofessional rounds.
METHODS: From November 2012–June 2013, an observational descriptive study of internal medicine faculty serving as inpatient attending physicians with house staff was performed. Each attending physician (n = 3/day) was sent a daily electronic survey following rounding sessions to assess characteristics of rounds. Bedside interprofessional rounds were defined as “Encounters including the team of providers—at least two physicians plus a nurse or other care provider—discussing the case at the bedside with the patient.” Primary outcomes were: (1) incidence of bedside interprofessional rounds, and, (2) factors associated with increased occurrence of bedside interprofessional rounds. Covariates included resident level-of-training, attending physician years’ of experience, census size, and call day. Descriptive, Kruskal-Wallis, and multivariable logistic regression statistics were used.
RESULTS: Of 549 rounding sessions, 412 surveys were collected (75 % response) from 25 attending physicians. Bedside interprofessional rounds occurred with 64 % of patients (median 8.0 min/encounter), differing by unit (intermediate care 81 %, medicine-specific general medicine 63 %, multispecialty 57 %, p < 0.001). Factors independently associated with increased occurrence of bedside interprofessional rounds were PGY-3/PGY-4 resident (OR 2.67, CI 1.75–4.06, vs. PGY–2), weekdays (OR 1.74, CI 1.13–2.69), team census size ≤11 (OR 2.36, CI 1.37–4.06), and attending physicians with ≤4 years’ experience (OR 2.15, CI 1.31–3.55).
CONCLUSIONS: The occurrence of bedside interprofessional rounds exceeded 50 % for all patients, with significantly more in medicine-based nursing units. Published numbers in recent years suggest bedside rounds infrequently occur, with <25 % of encounters occurring at the bedside. Our increased frequencies likely reflect our hospital’s initiatives to promote bedside interprofessional rounds (e.g. rounding lights designating the start of rounds, email reminders, education, etc.). As hypothesized, smaller team census size, weekdays, and teams with more experienced residents were associated with higher occurrence of bedside interprofessional rounds. Surprisingly, teams with less experienced attending physicians were also more likely to perform bedside interprofessional rounds. Reasons for this finding merit further study, but may relate to attending physicians’ desire to validate house staff decisions or sensitivity to leadership-directed initiatives. Systematic changes to census size caps, resident scheduling, and attending physician education and staffing may be required to increase the occurrence of bedside interprofessional rounds.
INVESTIGATION OF FIRST YEAR MEDICAL STUDENTS’ CAREER PREFERENCESKimberly Clinite1; Stephanie Kazantsev1; Shalini Reddy1; Jennifer R. Kogan2; Steven Durning3; Kent DeZee3. 1University of Chicago, Pritzker School of Medicine, Chicago, IL; 2Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 3Uniformed Services University, Bethseda, MD. (Tracking ID #1938518)
BACKGROUND: The United States physician shortage has been widely publicized, with primary care (PC) accounting for nearly half of estimated shortages. The shortage of PC physicians is further exacerbated by medical students increasingly choosing non-PC and controllable-lifestyle (CL) residencies and specialty fellowships. The process of specialty selection is complex and begins early in medical training. The purpose of this study is to describe the career considerations of 1st year medical students to better understand the initial phases of career selection and to identify demographic factors predictive of specialty interests.
METHODS: This is a cross-sectional survey of 1st year medical students from 11 allopathic medical schools during the first 4 months of the 2012–2013 academic year. Schools were geographically diverse and represented public and private schools with varied social mission rankings. Site coordinators at each institution invited all 1st year medical students to participate via e-mail in the survey by completing an on-line questionnaire. Two reminders were sent before closing the survey at 6 weeks. The 31-item questionnaire was developed after review of current literature and modified based on discussion with the target population, experts, and testing of items for clarity. Students were asked to indicate their most likely specialty choice if they “had to choose today.” If this specialty choice was family medicine, internal medicine (general), or pediatrics, the student was classified as PC. If the specialty choice was PC, general surgery, internal medicine (sub-specialty), medicine-pediatrics, neurosurgery, OB-GYN, orthopedics, or urology, the student was additionally classified as selecting a non-controllable lifestyle (non-CL) specialty. All remaining specialties were classified as CL. Further items asked about demographic factors and educational history. Comparisons were made with chi square.
RESULTS: Overall response rate for the questionnaire was 60 % (1020/1704). PC was the first choice for 24 % (242/1006) of students. Women were more likely to select PC than men (30 % vs. 17 %, p < 0.01). CL specialties were the first choice for 31 % (311/1006) of students. More men than women selected a CL specialty (35 % vs. 27 %, p = 0.01), as did never married versus married/currently engaged/domestic partner students (32 % vs. 23 %, p = 0.03). Students with no anticipated medical school debt, as compared to students with any anticipated debt, were less likely to choose PC (17 % vs. 26 %, p < 0.01) and more likely to select a CL specialty (37 % vs. 29 %, p = 0.04). Age, time off between undergraduate education and medical school, having at least one physician parent, premedical debt, and scholarships were not associated with specialty choice.
CONCLUSIONS: Given the projected significant shortage of PC physicians, future studies should investigate reasons for the minority (24 %) of MS1 students expressing interest in PC specialties. Men and never married students were more likely than women and married/currently engaged/domestic partner students to select CL specialties. This may warrant further investigation into students’ considerations of lifestyle factors. Additionally, scholarships and smaller debt were not associated with selection of PC, suggesting that financial incentives during medical school may not be effective at increasing interest in PC as has recently been proposed in the literature.
IS A PHYSICIAN SCORECARD FOR DIABETES MANAGEMENT POSSIBLE?Ameena Madan Paramasivan; Eric Brown; Ari Robicsek; Liana K. Billings; Chad Konchak; Barry Barrios; Christopher Masi. NorthShore University HealthSystem, Evanston, IL. (Tracking ID #1934156)
BACKGROUND: Physicians play an important role in helping diabetics manage their disease. However, studies suggest that physician-level factors are associated with minimal variance in glycosylated hemoglobin (HbA1c). In contrast, patient-level factors, including age, race/ethnicity, duration of diabetes, number of comorbidities, and body mass index (BMI) appear to account for almost all of the variance in HbA1c. Although the extent of physician influence on glucose control is unclear, scorecards evaluating diabetes management are becoming increasingly popular. Not surprisingly, physicians want assurance that such tools include appropriate risk adjustment (i.e., sufficiently account for patient-level factors that affect glucose control). The goals of this study were to develop a physician scorecard for diabetes management and evaluate the ability of this scorecard to identify physicians who are performing better or worse than expected after accounting for relevant patient characteristics.
METHODS: Using electronic health record (EHR) data from a large, integrated health system, we developed three logistic regression models to assess physician-level effects on diabetes control, defined as HbA1c < 8 %. Model 1 predicts whether HbA1c is greater than or equal to 8 % and produces an area under the curve (AUC) based upon which physician a patient sees. In this unadjusted model, the intercept varies by physician and patient-level data are excluded. Model 2 predicts the same outcome and produces an AUC based upon 40 relevant patient-level factors, including age, race/ethnicity, duration of diabetes, number and type of co-morbidities, insurance type, marital status, and BMI. Using hierarchical logistic regression, Model 3 predicts HbA1c by nesting patient-level data according to physician. Using the unadjusted Model 1, we initially ranked each physician according to the proportion of patients whose most recent HbA1c was greater than or equal to 8 % (i.e., the observed proportion of uncontrolled diabetics). We then used the adjusted Model 3 to re-rank each physician based upon the difference between observed and expected (computed from Model 2) proportions of patients with uncontrolled diabetes.
RESULTS: A query of our EHR indicated that 16,850 (9.3 %) of 181,805 primary care patients aged 18 to 75 years have either type 1 or type 2 diabetes. Of these, the most recent HbA1c was greater than or equal to 8.0 % among 3,089 (18.3 %). All diabetic patients are cared for by 203 primary care physicians (PCPs), yielding an average panel size of 77. The AUC for Model 1 was 0.63, suggesting that the likelihood of having an HbA1c greater than or equal to 8 % is significantly associated with the physician that each patient sees. The AUC for Model 2 is 0.71, indicating that the model which includes only patient-level data is better at predicting uncontrolled diabetes than the model which includes only physician data. Model 3 provides 95 % confidence intervals for each physician’s deviation from expected performance. Using this model, we found that 18 of 203 (8.9 %) PCPs performed better than expected and 14 of 203 (6.9 %) performed worse than expected based upon his or her patients’ risk profiles and after adjusting for patient characteristics. In addition, physician ranking from the adjusted model differed from the unadjusted model such that half of the physicians initially in the top 5 % for diabetes control dropped out after risk adjustment.
CONCLUSIONS: Our results indicate that differences exist among physicians in the proportion of patients who have uncontrolled diabetes. These differences persist after adjusting for multiple patient covariates. Physician performance in diabetes management can be ranked without considering patient-level covariates. However, adjusting for these characteristics using HLM produces a different ordering of physicians and permits identification of physicians who perform better or worse than expected. This approach is replicable across health systems and can serve as the foundation for quality improvement strategies which include identification of best practices, as well as education and up-training of underperforming physicians. We conclude that a physician scorecard for diabetes management is possible with appropriate risk adjustment.
IS EXERCISE USED AS MEDICINE? ASSOCIATION OF FUNCTIONAL LIMITATIONS WITH MEETING STRENGTH TRAINING GUIDELINES AMONG OLDER US ADULTSChristopher Sciamanna1; Jennifer Kraschnewski1; Joseph Ciccolo2; Liza S. Rovniak1; Carolina Candotti1; Noel Ballentine1. 1Penn State Hershey, Hershey, PA; 2Columbia University, New York, NY. (Tracking ID #1936308)
BACKGROUND: For many older adults, the loss of independence is considered a fate worse than death. Unfortunately, functional limitations increase predictably with age due to loss of muscle mass and strength. Many of these functional limitations, however, can be reversed or even prevented by strength training. As a result, the American Heart Association and American College of Sports Medicine guidelines recommend that all adults participate in strength training activities at least twice each week. Further, these organizations launched the “Exercise is Medicine” initiative, in which doctors are encouraged to recommend physical activity to their patients as they would recommend any other effective treatment or preventive service. It remains unknown whether older adults with functional limitations, those with the most to gain, are participating in strength training. The aim of this investigation is to understand the association between functional limitations and meeting strength training guidelines, to understand whether exercise is being used as a medicine.
METHODS: Data from the 2011 National Health Interview Survey were analyzed. Frequency of strength training was assessed using the following question: “How often do you do leisure-time physical activities specifically designed to strengthen your muscles, such as lifting weight or doing calisthenics?” Responses were categorized to signify whether the individual performed these activities at least twice each week, consistent with guidelines. Functional limitations were assessed using 9 self-reported questions that asked whether the individual had difficulty performing a range of common activities (ex. walking a quarter of a mile, push or pull large objects). A composite variable was created by summing the number of functional limitations per individuals, with 0 reflecting no difficulty performing any activity and 9 reflecting difficulty performing all activities. The composite variable was then divided into tertiles. Covariates included demographics variables and past medical history, consistent with variables shown to be associated with strength training in other studies. Analysis was limited to adults of 65 years or older. Mutlitivariate analysis was conducted using multiple logistic regression analysis, with the dependent variable being meeting or not meeting strength training guidelines.
RESULTS: Overall, 16.1 % of adults 65 and older reported doing strength training activities consistent with guidelines. After adjusting for demographic covariates, those without limitations and 1–4 limitations had 1.92 times (95 % CI; 1.51, 2.41) and 1.39 times (95 % CI; 1.08, 1.80) the odds of meeting strength training guidelines, respectively, compared to those reporting 5–9 limitations. This pattern remained when demographic and past medical history variables (i.e. hypertension) were added to the model.
CONCLUSIONS: Our results show a consistent and troubling pattern; those with functional limitations were less likely to meet strength training guidelines. This suggests there is great potential for using strength training to improve the public’s health and alternative strategies are needed to engage older adults, particularly those with functional limitations. Without a change in approach, unfortunately, the profound beneficial effects of strength training will continue to be used least by those who need it most, threatening the best intentions of “Exercise is Medicine.”
IS GREATER ACCULTURATION ASSOCIATED WITH AN INCREASED PREVALENCE OF CARDIOVASCULAR RISK FACTORS AMONG HISPANIC IMMIGRANTS IN SOUTH FLORIDA?Aileen Chang; Kumar Ilangovan; Hua Li; Olveen Carrasquillo. University of Miami, Miami, FL. (Tracking ID #1939054)
BACKGROUND: Acculturation is the process of adapting to a new culture. Among immigrants living in the In the United States, some studies suggest that increased acculturation is associated with a higher prevalence of cardiovascular risk factors (CVDRFs). We examine the association of acculturation with physiologic and behavioral CVDRFs in Hispanics having poorly controlled diabetes in Southern Florida.
METHODS: We performed a cross sectional analysis of baseline data collected as part of larger randomized clinical trial of 300 Latino patients with poorly controlled diabetes (HbA1c>=8.0 %) recruited from the primary care clinics of Miami-Dade county’s public hospital. We grouped subjects into acculturation tertiles using the Marin Short Acculturation Scale. Correlations between acculturation and physiologic measures including hemoglobin A1C (A1C), low density lipoprotein (LDL), systolic blood pressure (SBP), and body mass index (BMI) we examined using ANOVA. Correlations with behavioral measures including smoking status, physical activity (IPAQ), fruit and vegetable intake (BRFSS), and alcohol abuse (AUDIT-C) were examined using Chi-square comparisons.
RESULTS: The mean age of our patients was 56 +/− 7 years, 55 % were female, and Cubans made up 29 % of our sample with no other Hispanic ethnic subgroup representing over 15 % of the sample. Nearly all of the Latinos in the study (85 %) had been living in the US for over 10 years, yet 47 % had the lowest possible acculturation score. However, acculturation scores were positively correlated with length of time in the US (p < .01). Of the eight outcomes examined only smoking status was associated with increased acculturation; 12 % of Latinos in the two lowest acculturation groups were current smokers versus 25 % in the highest acculturation group (p = 0.02). In contrast to our original hypothesis, we observed a non-significant trend of increased acculturation being associated with increased physical activity, increased fruit and vegetable intake, and lower alcohol use. We found no association between acculturation and AIC, LDL, SBP, or BMI.
CONCLUSIONS: With the exception of smoking, our data do not support a link between increased acculturation and higher prevalence of CVDRFs. Although our study sampled a diverse Latino population, our findings may not be generalizable to Latinos in other parts of the country, recently arrived immigrants or to those without diabetes. Studies examining factors leading to increased smoking among more acculturated Latino immigrants may help guide smoking cessation and prevention efforts in this population.
IS HEALTHCARE PROVIDERS’ RESPECT FOR PATIENTS ASSOCIATED WITH COMMUNICATION BEHAVIORS IN CLINICAL ENCOUNTERS?Tabor E. Flickinger1; Somnath Saha2,3; Debra L. Roter4; Philip T. Korthuis3; Victoria L. Sharp5; Jonathan A. Cohn6; Richard D. Moore4; Mary Catherine Beach4. 1University of Virginia, Charlottesville, VA; 2Portland VA Medical Center, Portland, OR; 3Oregon Health and Science University, Portland, OR; 4Johns Hopkins University, Baltimore, MD; 5St. Luke’s Roosevelt, New York, NY; 6Wayne State University, Detroit, MI. (Tracking ID #1935661)
BACKGROUND: Communication training of health professionals emphasizes the acquisition of skills, yet attitudes towards patients may influence how healthcare providers interact. We aimed to investigate whether provider-reported respect for patients was associated with communication behaviors during clinical encounters.
METHODS: We analyzed audio-recordings of routine follow-up visits between 413 adult HIV-infected patients and 45 primary providers in 4 sites across the United States. The primary independent variable was provider-reported respect for that particular patient assessed immediately following the encounter with the item, “Compared to other patients, I have a great deal of respect for this patient” (strongly agree - strongly disagree). Responses were dichotomized to compare those who strongly agreed/agreed (higher respect) with those who were neutral or disagreed (lower respect). The outcomes were provider and patient communication behaviors assessed by the Roter Interaction Analysis System (RIAS). Covariates included patient and provider demographics and length of relationship. To examine associations between provider respect and communication, we performed negative binomial regressions with generalized estimating equations to account for clustering of patients within providers and adjusted for practice site and patient/provider characteristics.
RESULTS: Patients were predominantly male (66 %) and African-American (57 %), while providers were predominantly female (58 %) and white (71 %). Providers strongly agreed that they had a great deal of respect for 155 (38 %) patients, agreed for 182 (44 %), neutral for 66 (16 %), disagreed for 8 (2 %), and strongly disagreed for 2 (1 %). Patients who were non-white, not actively using drugs, and who were known less than 5 years were more highly respected than others. Younger and non-white providers reported more respect for patients than other providers. Providers’ respect for patients was not associated with provider gender, or with patient age or gender. In multivariable analysis, providers with higher respect had a more positive emotional tone [IRR 1.10 (1.06–1.14)], engaged in more social chit chat [IRR 1.78 (1.11–2.84)], and more positive talk [IRR 1.20 (1.04–1.39)]. Patients of providers with higher respect had more positive emotional tone [IRR 1.05 (1.03–1.07)], engaged in more social chit chat [IRR 2.03 (1.16–3.56)], more positive talk [IRR 1.22 (1.08–1.39)], and gave more psychosocial information to their providers [IRR 1.60 (1.26–2.04)]. Encounters between patients and providers with higher respect were characterized by less verbal dominance [IRR 0.87 (0.78–0.96)] and more patient-centeredness [IRR 1.38 (1.12-1.71)].
CONCLUSIONS: Respectfulness is associated with a host of positive and patient-centered communication behaviors during medical encounters that are voiced by both providers and patients. The study results underscore the highly reciprocal nature of communication and suggest that interventions that enhance provider attitudes of respect may help improve communication and care quality.
IS STRENGTH TRAINING ASSOCIATED WITH MORTALITY BENEFITS? A 15 YEAR COHORT STUDY OF US OLDER ADULTSChristopher Sciamanna; Jennifer Kraschnewski; Liza S. Rovniak; Erik B. Lehman. Penn State Hershey, Hershey, PA. (Tracking ID #1936358)
BACKGROUND: Guideline-concordant aerobic activity has consistent and powerful relationships with future mortality. Specific recommendations regarding strength training have come only more recently; in 2007 the American Heart Association (AHA) and American College of Sports Medicine (ACSM) recommended all adults participate in such activities at least twice each week. Although several smaller clinical studies have observed that greater amounts of muscle strength are associated with lower risks of death, few have studied the relationship between strength training behavior and mortality in a large national sample over an extended time period. We undertook this investigation to understand the association between meeting strength training guidelines and future mortality.
METHODS: Data from the 1997–2001 National Health Interview Survey (NHIS), linked to death certificate data found in the National Death Index, were analyzed. The main independent variable, guideline-concordant strength training, was assessed using the following question: “How often do you do leisure-time physical activities specifically designed to strengthen your muscles, such as lifting weight or doing calisthenics?” Responses were categorized to signify whether the individual performed these activities at least twice each week, consistent with guidelines. Covariates included demographics variables, past medical history (i.e. diabetes, hypertension, coronary artery disease, and non-skin cancer), and other health behaviors (i.e. body mass index, physical activity, alcohol use and smoking status), consistent with variables shown to be associated with strength training in other studies. Analysis was limited to adults of 65 years or older. Mutlitivariate analysis was conducted using multiple logistic regression analysis, with the dependent variable being all-cause mortality.
RESULTS: Overall, 9.6 % of NHIS adults age 65 and older (N = 30,162) reported doing strength training consistent with guidelines and 31.6 % died during the follow-up period. After adjusting for demographic covariates, those who reported guideline-concordant strength training had 46 % lower odds of all-cause mortality than those who did not (adjusted odds ratio: 0.64; 95 % CI: 0.57, 0.70; p < 0.001). This association remained when adjusting for past medical history and health behaviors.
CONCLUSIONS: Guideline-concordant strength training is significantly associated with decreased overall mortality in older US adults. Unfortunately, only a minority of adults currently meet recommendations of strength training at least twice each week. This suggests we are far from engaging patients in the “Exercise is Medicine” campaign launched by the AHA/ACSM, where doctors are encouraged to recommend physical activity to patients as they would any other effective treatment. Identifying interventions to successfully engage older adults in guideline-concordant strength training has the potential to significantly reduce all-cause mortality in this population.
IS THERE AN ASSOCIATION BETWEEN CONTINUITY OF CARE AND DIABETES QUALITY MEASURES IN AN URBAN INTERNAL MEDICINE RESIDENT CLINIC?Georgia Giebel; Yaakov Y. Liss; Lauren Peccoralo. Mount Sinai Medical Center, New York, NY. (Tracking ID #1939209)
BACKGROUND: Continuity of care (COC) between patients and trainee providers in academic primary care clinics can be challenging. With poor COC, adhering to the growing number of quality metrics seems daunting. A few recent studies demonstrate that better COC can reduce hospitalizations, reduce cost, and improve glycemic control in diabetic patients. However, few studies have investigated whether improvements in COC can also improve adherence to quality measures in Internal Medicine (IM) resident primary care clinics. We sought to evaluate the association between resident provider continuity and diabetes management and adherence to diabetes related quality measures in an urban IM resident clinic. Primary outcomes included glycemic, blood pressure, and cholesterol control, as well as indicated diabetic screening tests. Secondary outcomes included the association between demographics and continuity, as well as correlations between eye and foot exams in individual patients.
METHODS: This study was conducted at Mount Sinai’s Internal Medicine Associates (IMA) clinic, an urban (New York City) academic IM resident primary care clinic. A retrospective chart review was performed by abstracting data from the electronic medical records (EMRs) of 104 patients. Subjects were randomly selected from a convenience sample of diabetic patients seen in the clinic in December 2013. Selection criteria included patients who: 1) were seen for ≥3 scheduled visits with IM residents between 1/1/2013 and 12/31/13, 2) had a diagnosis of type II diabetes mellitus for >1 year, and 3) had been followed at our resident clinic for >1 year. Data regarding age, gender, rate of eye and foot exams documented for 2013, most recent blood pressure, most recent A1c, most recent LDL, ACE/ARB and statin use, and diagnosis and management of proteinuria (whether microalbumin was measured in 2013, the microalbumin/creatinine value, and use of ACE/ARB therapy) were recorded. Continuity for patients was calculated using the modified, modified continuity index (MMCI), a validated measure of patient-physician continuity that is independent of the specific primary care doctor (index results range from 0 to 1, with 1 being perfect continuity). Statistical analysis assessed the correlation between the MMCI score and diabetes process outcomes and quality measures (using Chi-squared test for two categorical variables, Pearson’s or Spearman’s Correlations for two continuous variables).
RESULTS: The average MMCI for the selected patients was 0.51. There were no significant associations between continuity, as measured by the MMCI, with the rate of eye exams, foot exams, blood pressure control, diabetes control, LDL level, or evaluation and management of proteinuria for patients. Analysis demonstrated that patients who were up to date with ophthalmologic screening were significantly more likely to be up to date with foot exams than those without ophthalmologic screening (75 % vs. 52 %, p = 0.029). There were no clinically important associations with age or gender and continuity.
CONCLUSIONS: Unlike previous reports, our study did not show a correlation between better continuity and improved diabetes outcomes or adherence to quality measures. It is possible that other changes in our clinic related to our patient-centered medical home (PCMH), such as care coordination and physician-directed best practice advisories, helped improve physician adherence to quality metrics, and may have negated any impact of continuity. The correlation between foot and eye exams may indicate that motivated patients are more likely to follow up with all types of referrals. Some limitations of our study are the small sample size and focus on only one institution, as well as the lack of comparison to patient outcomes prior to the implementation of the PCMH initiatives. Given our findings, it is important to continue to investigate the impact of continuity on other important metrics, such as patient and physician satisfaction. In addition, our results suggest that there may be other factors that can help improve the quality of care in an urban academic primary care setting.
IS THERE GLUTTONY IN THE TIME OF STATINS? DIFFERENT TIME TRENDS OF CALORIC AND FAT INTAKE BETWEEN STATIN-USERS AND NON-USERS AMONG US ADULTSTakehiro Sugiyama1,2; Yusuke Tsugawa3,4; Chi-Hong Tseng5; Yasuki Kobayashi1; Martin F. Shapiro5,6. 1The University of Tokyo, Tokyo, Japan; 2National Center for Global Health and Medicine, Tokyo, Japan; 3Harvard Interfaculty Initiative in Health Policy, Cambridge, MA; 4St Luke, Tokyo, Japan; 5David Geffen School of Medicine at UCLA, Los Angeles, CA; 6UCLA Fielding School of Public Health, Los Angeles, CA. (Tracking ID #1932359)
BACKGROUND: Guidelines recommend both diet therapy and statin use as treatments of high blood cholesterol. As the statin use has become prevalent, however, diet among statin-users may have relaxed due to changing regarded importance of diet therapy among continuing statin-users and secular change in the characteristics of newly prescribed statin-users. No study has shown whether the time trend of dietary intake among statin-users is different from that among non-users, although the increase in caloric intake among general population is reported to have plateaued in the last decade. We aimed to examine the difference in the time trends of caloric and fat intake between statin-users and non-users among US adults during the time while the statin use has widened quickly.
METHODS: We conducted a repeated cross-sectional study using a nationally representative US sample of the National Health and Nutrition Examination Survey from 1999 to 2010. Study populations were non-pregnant adults. Caloric and fat intake was measured through 24-hour dietary recall, while statin use was determined through in-person interview. Generalized linear models with interaction term between survey cycle and statin use were constructed to investigate the time trends of intake for statin-users and non-users after adjusted for possible confounders. We calculated model-adjusted caloric and fat intake using these models, and examined if the time trends differ by statin use. Body mass index was also modeled and estimated for each survey cycle and statin use adjusted for possible confounders.
RESULTS: The proportion of statin-users more than doubled from 7.5 to 16.5 % over the decade of observation. Main analyses comprised 27,886 participants. In 1999–2000, the caloric intake was less for statin-users compared with non-users (2,000 vs. 2,179 kcal/day, p = .007). The difference between the groups became smaller as time went by, and there was no statistical difference after 2005–2006. Among statin-users, caloric intake in 2009–2010 was 9.6 % higher (95 % confidence interval (CI): 1.8 to 18.1, p = .02) than that in 1999–2000. In contrast, no significant change was observed among statin non-users during the same period. Statin-users also consumed significantly less fat in 1999–2000 (71.7 vs. 81.2 g/day, p = .003). Fat intake increased 14.4 % in statin-users (95 % CI: 3.8 to 26.1, p = .007) while not changing in non-users. Body mass index also increased more in statin-users (1.3 kg/m2) than non-users (0.4 kg/m2) in the adjusted model (p = .02).
CONCLUSIONS: Our results indicate that statin-users no longer consume fewer calories and less fat than non-users. Efforts aimed at dietary control may be becoming less intensive among continuing statin-users. The characteristics of newly prescribed statin-users may also have changed; those who initiated statin use in later study periods may have consumed more calories and fat than those who started in earlier study periods. Although the repeated cross-sectional study design precluded us from disentangling the mechanisms, our results indicated that caloric and fat intake among statin-users in 2009–2010 was significantly greater than in 1999–2000. We may need to reemphasize the importance of dietary modification for statin-users. At the same time, the relative roles of diet and statins may need to be revaluated based on additional evidence and further discussion from multiple perspectives including effectiveness, cost-effectiveness and ethics.
IS TRAINING IN A PRIMARY CARE INTERNAL MEDICINE RESIDENCY PROGRAM ASSOCIATED WITH A CAREER IN PRIMARY CARE MEDICINE? A CROSS SECTIONAL ANALYSIS OF A 10-YEAR COHORTMarion Stanley; Bridget O’Brien; Rebecca L. Shunk; Sharad Jain; Katherine Julian; Robert Baron; Jeff Kohlwes. University of California, San Francisco, San Francisco, CA. (Tracking ID #1941668)
BACKGROUND: Multiple professional and governmental organizations including the Health Resources and Services Administration (HRSA) and the Council on Graduate Medical Education (COGME) have long endorsed primary care residency programs in order to promote a workforce that would ideally be composed of at least 40 % primary care physicians. In internal medicine, where the vast majority of residency graduates select medical subspecialties, primary care programs are intended to increase the number of graduates selecting and maintaining primary care careers. There is a paucity of data, however, as to whether primary care residency programs are associated with careers in primary care. Our study examines whether enrollment in a primary care internal medicine residency is associated with a career in primary care.
METHODS: We performed a cross-sectional analysis of all internal medicine residency alumni from 2001 to 2010 at a single large academic center via a 27-question survey. Residents at our institution during this period trained in either a traditional categorical internal medicine track, or one of two primary care internal medicine tracks. We used Chi-Square analysis to compare the career outcomes of primary care and categorical residents.
RESULTS: We were able to contact 481 reachable individuals out of a total of 511 living alumni, of which there were 322 respondents (67 % response rate) to the survey. We compared 106 responses from primary care residents to the 169 responses from categorical residents and excluded all self-identified current fellows as well as graduates from the basic science residency track. A significantly higher percentage of primary care residents agreed that the majority of their current work is in primary care medicine (54 %) as compared to categorical residents (20 %) (p < 0.001). A significantly higher percentage of primary care residents also agreed that the majority of their current work is with underserved populations (54 %) as compared to categorical residents (27 %) (p < 0.001). While 92.5 % of primary care residents agreed or strongly agreed that they were interested in a career in primary care medicine prior to starting residency, only 63 % agreed or strongly agreed that they were interested in a career in primary care after residency. Notably, 30 of the 34 residents (88 %) who lost interest in a primary care career during residency agreed or strongly agreed that their ambulatory experience during residency influenced their career choice.
CONCLUSIONS: More primary care internal medicine residents practice a primary care career and work with underserved populations than categorical internal medicine residents. This study demonstrates the effectiveness of primary care tracks in internal medicine programs in meeting national workforce goals. A number of primary care residents, however, lose interest in primary care during their residency training. Improving outpatient clinical experiences may be an important factor to further primary care residents’ interest in primary care careers.
JAPANESE INTERNATIONAL MEDICAL GRADUATES: A QUALITATIVE STUDY OF THEIR MOTIVATIONS FOR AND REFLECTIONS ON U.S. TRAINING, AND RELATIONSHIP TO THE ADVANCEMENT OF JAPANESE MEDICAL EDUCATIONBrian S. Heist1; Haruka Torok2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Johns Hopkins University, Baltimore, MD. (Tracking ID #1930414)
BACKGROUND: Most IMGs have trained in English in their home country and are motivated to pursue U.S. clinical training, in part, by improved financial status and job opportunities. The influences of societal expectations and a culture of migration within the home country have also been described. Japanese physicians, by contrast, face a major language barrier, have low financial incentive and limited prospects of improved job opportunity after U.S. clinical training, and have a modest tradition of migration abroad. Japanese post-graduate medical education is in a state of flux, with fundamental teaching and standardization lacking compared to the United States, which may serve as motivation for foreign training. This study sought to explore Japanese IMGs’ motivations for U.S. clinical training, their impressions of American versus Japanese post-graduate clinical training, and their relationship to the advancement of Japanese medical education.
METHODS: Using purposeful sampling of Japanese professional society memberships and interviewees’ personal connections to identify participants with diverse career paths, two investigators conducted 23 semi-structured individual digitally recorded interviews of Japanese IMGs 1–15 years out from U.S. clinical training. Interviews were conducted in English. Through closed- and open-ended questions, we explored motivations to pursue U.S. training, impressions of American versus Japanese postgraduate clinical training, and endeavors subsequent to U.S. training including participants’ relationships to the advancement of Japanese medical education. Interview transcripts were coded using an inductive thematic analysis to identify emerging themes that influenced subsequent interviews in an iterative fashion.
RESULTS: Of 12 participants working in Japan, there were 7 internists (4 subspecialists), 4 family physicians, and 1 pediatrician. Of 11 participants working in the U.S., there were 7 internists (5 subspecialists), and 1 physician each from family practice, transplant surgery, pediatrics, and pathology. Participants represented academic and non-academic settings. Post-graduate year upon starting U.S. training ranged from 1 to 13 years, with a median of 4 years. Duration since completing U.S. clinical training was 1–13 years with a median of 6 years. Emergent themes from the interviews included the following. (1) Motivations: A. Initial personal exposure to U.S. training methods. B. Scholarly pursuits to improve clinical skills, become better educators, or develop specific clinical expertise. C. No financial incentive; conversely there was financial sacrifice. (2) Impressions of U.S. versus Japanese post-graduate training: A. U.S. provides superior standardization, evaluations, feedback, mentoring, and teaching of clinical reasoning. B. More rigorous Japanese training schedule affords more continuity of care and deeper understanding of pathology. C. Japanese trainees and attending physicians seem more dedicated. (3) Relationship to advancement of Japanese medical education: A. Mentoring and teaching Japanese trainees or eager to do so. B. Publishing narratives of their U.S. training experiences. C. Confronting cultural and linguistic barriers to assimilation back into Japanese academia and implementation of Western educational methodologies within Japan. D. Building networks of marginalized Japanese IMGs and like-minded physicians to advance Japanese medical education.
CONCLUSIONS: Japanese IMGs commonly describe interest in U.S. clinical training originating in personal exposures to U.S. educational methods, with subsequent motivation to develop better clinical skills, become better educators, or develop specific clinical expertise. In reflecting on their U.S. clinical training, they admire the superior infrastructure, but perceive decreased dedication that appears related to duty hour limits not instituted in Japan. They demonstrate intense dedication to improving medical education in Japan, and through networks of Japanese IMGs and like-minded physicians, are surmounting cultural and linguistic barriers. This study deepens understanding of the relationship between Japanese and U.S. medical education, and the IMG landscape and, in turn, has implications for the advancement of medical education in Japan and elsewhere internationally.
KNOWING IS HALF THE BATTLE: HOSPITALIZED PATIENTS WITH ADVANCED CHRONIC KIDNEY DISEASE DO NOT CORRECTLY SELF-IDENTIFYMilda R. Saunders1; Nisha N. Patel2; David Meltzer1. 1University of Chicago Medicine, Chicago, IL; 2University of Chicago Medicine, Chicago, IL. (Tracking ID #1939552)
BACKGROUND: Pre-renal replacement therapy (RRT) patient education leads improved clinical outcomes due in part to reduced central venous catheter use, increased uptake of peritoneal dialysis, and greater access to transplant for patients with end-stage renal disease (ESRD). Yet many patients with advanced chronic kidney disease (CKD) do not receive this important education due to lack of identification or understanding of their kidney disease. The hospital is an important, often overlooked, site for patient education and linkage to nephrology care for patients with advanced CKD. Many patients with advanced CKD are hospitalized in the 3 months prior to dialysis initiation, which represents an opportunity to identify existing CKD and to use a multidisciplinary approach to preventative care, patient education, patient-provider planning for future RRT needs. We sought to determine how often patients with ICD-9 coded CKD correctly identified themselves as having kidney disease.
METHODS: Using data from the University of Chicago Hospitalist Project, a large-scale study of inpatient physicians and patient outcomes, we examined data on 1,234 general medicine patients discharged between January 1, 2012 and March 31, 2012 with an ICD-9 code for chronic kidney disease, end-stage renal disease or transplant (585.0–585.9, 996.81) in their first 20 admission diagnoses. We linked this data with Hospital Project patient surveys in which patients selected their chronic medical conditions from a list and were specifically asked if they had “kidney problems.” Finally, we used logistic regression to determine what clinical and demographic characteristics are associated with patients with physician-identified CKD correctly self-identifying as having kidney disease.
RESULTS: In our sample of urban adult hospitalized general medicine patients, the mean age of 60.8 with 54 % females. Over 86 % of patients identified as African American and 4.2 % reported Hispanic ethnicity. Of the 125 patients with Stage 3 (moderate CKD, eGFR 30–59), only 25 % of patients reported having kidney problems. Of the 108 patients with advanced CKD, 60 % of patients with Stage 4 (eGFR 15–29) and 67 % of patients with Stage 5 (eGFR < 15) reported having kidney problems. The largest proportion of patients with CKD were coded as having CKD unspecified stage (535/1234). Of those, only 29 % reported having kidney problems. Factors significantly associated with the patients correctly self-identifying as having kidney problems include increasing CKD stage (OR 1.29, 95 % CI 1.17, 1.43), race other than African American (OR 1.38, 95 % CI 1.06, 1.80), all p < 0.05. Every 1 year increase in age was associated with an decreased likelihood of patients with CKD correctly self-identifying (OR 0.98, 95 % CI 0.98, 0.99). In multivariable analysis, CKD stage, non-African American race and younger age remained significantly associated with accurately reporting kidney problems, all p < 0.05.
CONCLUSIONS: In this urban, hospitalized sample, patient awareness of chronic kidney disease was low, even among patients with advanced chronic kidney disease (Stage 4 and 5). The hospital provides an important, underutilized opportunity to identify, educate and refer patients with advanced chronic kidney disease in order to increase their knowledge of their renal replacement options and, ultimately, to improve patient outcomes.
KNOWLEDGE, ATTITUDES, AND PRACTICES OF PHYSICIANS-IN-TRAINING RELATING TO COSTS OF CARECeline Goetz1; Kira L. Ryskina2; Tara F. Bishop3,4. 1New York-Presbyterian Hospital - Weill Cornell Medical Center, New York, NY; 2University of Pennsylvania, Philadelphia, PA; 3Weill Cornell Medical College, New York, NY; 4Weill Cornell Medical College, New York, NY. (Tracking ID #1935846)
BACKGROUND: Given the rising costs of health care, various medical societies have issued guidelines on cost-effective care. The concept of cost awareness has been incorporated into the System-Based Practice Core Competency for internal medicine residents. The purpose of this survey study was to investigate residents’ perceptions about costs of care, as well as their knowledge and practice patterns as related to overuse guidelines.
METHODS: We conducted a survey of internal medicine residents in an urban academic medical center. The survey collected the following information: demographics, attitudes about overuse and cost-consciousness practice, knowledge of overuse guidelines, and self-reported frequency of use of services addressed in overuse guidelines. We pilot tested the survey with three out-going residents and revised it based on their feedback. Residents were asked to fill out the survey during a morning academic conference.
RESULTS: The response rate was 80 % (100/125). Among respondents, 24 % were PGY1, 36 % were PGY2, and 35 % were PGY3. The majority of residents (80 %) reported anticipating fellowship training in a specialty, rather than directly entering practice in primary care or hospital medicine (20 %). A large majority (94 %) of residents strongly agreed or somewhat agreed that “overuse is an important problem in medicine.” Similarly, 87 % strongly agreed or somewhat agreed that “Doctors should know how much the tests and procedures s/he orders financially burden his/her patients”, and 91 % strongly agreed or somewhat agreed that “Trying to contain the cost of medical care is the responsibility of every physician.” In regards to overuse guidelines, 93 % reported no familiarity with the Good Stewardship Campaign, 78 % reported no familiarity with Choosing Wisely campaign, 60 % reported no familiarity with the American College of Physicians Back Pain Algorithm. However, 62 % of residents reported that they were “very familiar” with United States Preventative Services Task Force Guidelines. The majority of residents (62 %) disagreed or somewhat disagreed with the statement “I know how to find the costs of the tests and procedures I order” and 56 % of surveyed residents disagreed or somewhat disagreed with the statement “I know how much my patients have to pay out-of-pocket for medications I prescribe.” Only a third of residents (31 %) agreed or somewhat agreed with the statement “During my residency training, I am receiving sufficient instruction on efficient use of health care resources.” In terms of self-reported practice, 81 % reported that they never or rarely ordered baseline EKGs on an asymptomatic, low-risk patients and 76 % never or rarely ordered DEXA screening for women under age 65 or men under age 70 without risk factors. For back pain, 76 % reported never or rarely imaging for low back pain within first 6 weeks of symptom onset. The most common reason for ordering this type of imaging was that the supervising attending physician requested it. Only 32 % reported never or rarely ordering a blood chemistry panel at a preventative visit of an asymptomatic patient. Almost a third of residents (27 %) reported ordering medical tests at least once in a month because of patient requests even though they did not feel it was indicated. Almost half (40 %) reported getting contacted at least once in a month by an insurance company questioning clinical necessity of a test ordered. The majority of residents (70 %) strongly agreed or somewhat agreed with statement “My patients think that the quality of their care is higher if I order more medical tests.”
CONCLUSIONS: We found that internal medicine residents believe that overuse is a problem in medicine, but are largely unfamiliar with overuse guidelines and feel their training on this topic has been insufficient. Interestingly, self-reported practice patterns appear to be largely in-line with overuse guidelines but requests by supervising attending physicians seem to be a reason why residents order non-recommended tests. Future work should look at attitudes, knowledge, and practice of cost-conscious care in other training programs and in other specialties. Residency programs may need to educate residents and supervising attendings in order to encourage cost-conscious practice.
LAPSES IN MEDICAL PROFESSIONALISM: A LACK OF CONSENSUS ON APPROPRIATE SANCTIONSBhavika Kaul1; Cayla R. Teal2; Stephen B. Greenberg3. 1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3Baylor College of Medicine, Houston, TX. (Tracking ID #1935269)
BACKGROUND: With recent literature increasingly citing strong associations between disciplinary actions taken against practicing physicians and prior unprofessional behavior observed in medical schools, the teaching of professionalism has received renewed attention. However, relatively little research has focused on methods for responding to professionalism lapses when identified. The goal of this study was to examine differences in perspective between medical students and faculty regarding appropriate consequences for lapses in medical professionalism - views we predicted would vary with level of training. We sought answers to three primary questions: was there consensus regarding sanction assignment within each cohort? How did views change with level of training? Were there scenarios that respondents felt were not remediable and thus meriting immediate expulsion?
METHODS: A cross-sectional sample of medical students (preclinical vs. clinical) and Internal Medicine faculty at Baylor College of Medicine were asked to assign sanctions (no sanction, verbal warning, written warning, probation, expulsion) to 25 scenarios involving first-time lapses in professionalism. For each scenario, respondents were asked to comment on reasons for sanctions assigned. A mixed methods (quantitative and qualitative) analysis of the data was conducted.
RESULTS: 513 medical students and 37 faculty members completed the survey. There was a lack of homogeneity in sanction assignment within cohorts. On average, there was a significant decrease (p < 0.001) in the severity of sanctions applied between preclinical and clinical years. The faculty were more like preclinical students in their pattern of sanction assignment. Clinical students were less likely to choose “expulsion” than their preclinical counterparts (p < .001); however, no group had >35 % of respondents selecting expulsion. Text responses suggested that preclinical students were more “policy-oriented,” clinical students more “context-oriented” and faculty more “morality-oriented” in their justifications.
CONCLUSIONS: There were significant differences between preclinical and clinical students and between clinical students and faculty in the severity of sanctions applied but no significant differences between preclinical students and faculty on these measures. However, all cohorts favored sanctions with opportunity for remediation suggesting that, short of expulsion, there is a lack of consensus between students and faculty regarding appropriate consequences for lapses in medication professionalism. The hidden curriculum may play a significant role in sanction assignment and much of the variability seems to be guided by preservation of self. We must thus find ways to reconstruct the framework in which learners and faculty see themselves.
LAY HEALTH LEADERS’ EXPERIENCES LEADING A CHURCH-BASED DIABETES SELF-MANAGEMENT INTERVENTION FOR LATINOSArshiya A. Baig3; Helio Zapata1; Cara A. Locklin2. 1Pritzker School of Medicine, University of Chicago, Chicago, IL; 2University of Illinois, Chicago, IL; 3University of Chicago, Chicago, IL. (Tracking ID #1934872)
BACKGROUND: Lay health leaders have been effective in leading diabetes self-management interventions for Latinos. However, little is known regarding lay leaders’ experiences leading these interventions, especially in the church setting. Our objective was to assess lay leaders’ perceived challenges and satisfaction with leading a church-based diabetes self-management intervention in an urban Mexican American community.
METHODS: Our project was based in a low-income, Mexican American neighborhood of Chicago with high rates of diabetes morbidity and mortality. Lay health leaders were selected by the study’s Community Advisory Board to undergo a 3-day training led by diabetes experts and community leaders. Lay leaders were trained to lead weekly 90-minute diabetes education classes at partnering churches as a part of a pilot study testing the impact of a church-based diabetes self-management intervention. We conducted qualitative semi-structured interviews with lay leaders after completion of the training and 1 year post training. We queried respondents regarding: 1) their motivations for joining the project; 2) strengths and weakness of the training they received; 3) perceived challenges and satisfaction with leading the classes; and 4) important characteristics of lay health leaders.
RESULTS: A research assistant interviewed lay leaders who completing training to lead the diabetes education classes as a part of a larger church-based self-management intervention. Interviews were conducted with three of four lay leaders at baseline and with two of three active leaders one-year post-training. All lay leaders were of Mexican descent, spoke English and Spanish, and were involved in their respective church communities. Reasons for wanting to be involved in the diabetes program included either knowing someone affected by diabetes or having diabetes themselves, wanting to learn more about the disease, and to give back to their community. Most participants had doubts about teaching the diabetes education classes due to the belief they had insufficient diabetes knowledge before the training. The training was well received and participants stated they gained a lot of knowledge about diabetes. However they wanted more hours of training and wanted a person with diabetes to share their experiences during the training. Reflecting on their year of teaching, class leaders were comfortable leading class sessions on their own and enjoyed teaching the lessons and interacting with the people in the classes. Lay leaders even noted healthy behavioral changes they made as a part of the class and the motivation they were able to give and receive from the participants. Lay leaders expressed comfort in discussing faith in class if participants mentioned it. They believed that future lay health leaders must be familiar with the Spanish language and the community that they are serving, be empathetic and open, and be very familiar with diabetes but not necessarily have diabetes themselves.
CONCLUSIONS: Lay leaders had many positive experiences teaching diabetes education classes, including learning more about diabetes, having an opportunity to give back to the community, supporting people with diabetes in managing their disease, and being motivated to make healthier lifestyle changes themselves. Future diabetes self-management interventions may consider measuring the impact of health interventions on lay leader health behaviors and impact of lay leader satisfaction on patient outcomes.
LAYERS OF DISADVANTAGE: SICKLE CELL DISEASE AND DISPARITIES IN THE QUALITY OF HEALTH CAREMary Catherine Beach; Carlton Haywood; Sophie Lanzkron; Jennifer Haythornthwaite. Johns Hopkins University, Baltimore, MD. (Tracking ID #1938901)
BACKGROUND: Persons with sickle cell disease (SCD) are anecdotally known to experience deficiencies in the quality of the interpersonal care, but it is unclear how widespread these negative experiences are or whether these experiences are attributable to their predominantly African American race, to their health status, or to some other factors. Our objective was to assess potential disparities in the quality of healthcare provider communication experienced by African-Americans with and without sickle cell disease (SCD) in the United States.
METHODS: We assessed poor communication with healthcare providers using the Provider Communication subscale of the Consumer Assessment of Healthcare Providers and Systems survey, which asks respondents to assess the quality of their communication with providers over the previous 12-month period. Respondents are asked to indicate (never, sometimes, usually, or always) how often did doctors or other health providers listen carefully to you, explain things in a way you could understand, show respect for what you had to say, and spend enough time with you? For analysis, the response options were dichotomized, with “never” or “sometimes” denoting poor provider communication. The SCD sample data was obtained from adult patients participating in a cohort study at academic medical centers in two cities. The national sample African-American data was obtained from published national estimates. Differences between the proportion of poor communication reported by SCD participants and the expected proportion from the corresponding national sample were compared using the binomial test. To assess the effects of poorer health, we also conducted stratified analyses by patient-reported health status.
RESULTS: Two-hundred sixty four African-American adults with SCD in total were included in this analysis. Slightly over half (54.2 %) were female, 75 % were between the ages of 18 and 44, and approximately 48 % perceived their health status as being poor or fair. The SCD sample was more likely than the national sample to report poor communication on each of 4 studied communication domains: Listening (22.3 % vs. 11.5 %, p < 0.0001); Explaining (18.2 % vs. 11.6 %, p < 0.002); Showing Respect (26.1 % vs. 9.5 %, p < 0.0001); and Spending Enough Time (38.3 % vs. 16.2 %, p < 0.0001). Poorer health status seemed to account for some of these differences: among those reporting the worst levels of perceived health (“poor” or “fair”), a greater proportion of SCD patients reported poor provider communication in 3 of the 4 domains, whereas among those with better perceived health, a greater proportion of the SCD sample reported poor provider communication in 2 of the 4 domains.
CONCLUSIONS: Persons with SCD in the U.S. are subject to disparities in the quality of the healthcare they receive that are not reducible to their predominantly African-American race or to their poorer health status generally. This patient population appears to be subject to other sources of disadvantage that negatively impacts the quality of the healthcare they receive.
LEARNING NEEDS OF VHA WOMEN’S HEALTH PROVIDERSJessica Zuchowski1; Alison B. Hamilton1,2; Donna L. Washington1,3; Kristina M. Cordasco1,3. 1US Dept of Veterans Affairs, North Hills, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA. (Tracking ID #1936186)
BACKGROUND: Although a growing number of women Veterans are using Veteran Health Administration (VHA) services for their health care, they are still a minority within the VHA patient populations. Many VHA providers have had historically small caseloads of women patients and therefore may need to supplement their current knowledge and skills in topics specific to caring for women Veterans. In primary care, new women patients are now preferably assigned to designated women’s health primary care providers (PCPs) in an effort to concentrate female caseloads. Potential learning needs of these women’s health PCPs have not been previously assessed. We explored the learning needs of VHA women’s health PCPs.
METHODS: Using mixed methods, we conducted semi-structured telephone interviews with 10 VHA women’s health PCPs in Southern California and Oklahoma. Interviewees were asked about their learning needs relevant to women’s health. All interviews were audio recorded, professionally transcribed, and summarized. A summary template was used to capture key points within each domain of the interview guide. Summaries were analyzed for specific women’s health topics that participants frequently identified as being of interest. We additionally administered 16 e-mail surveys to PCPs, 8 of whom were interviewees, and 8 have not yet been interviewed. Survey respondents were asked to rate their interest in getting additional education on a list of women’s health topics using a four point Likert scale (“not at all interested,” “mildly interested,” “moderately interested,” “very interested”). The topics are shown in the table. For each topic, we assessed the percentage of respondents that rated it as “very interested.” Additional data collection is in progress.
RESULTS: Interviewees most frequently expressed interest in the topic of chronic pain management. Interviewees also frequently expressed interest in the following women’s health topics: the impact of military service on women (e.g. military sexual trauma); abnormal uterine bleeding; medications during pregnancy and lactation. Other topics mentioned, but less frequently, included: dyspareunia; intimate partner violence; abnormal Papanicola smears; contraception; and caring for transgender patients. Interviewees also frequently mentioned a desire to receive updates on changing guidelines for best practice. Among survey respondents, topics with the highest percentage indicating that they are “very interested” were: management of abnormal Pap smear (67 %); contraception counseling (63 %); and evaluation of abnormal uterine bleeding (63 %). Topics with the lowest percentage of respondents indicating they are “very interested” were: intimate partner violence screening (13 %); screening for military sexual trauma (13 %); and emergency contraception (19 %).
CONCLUSIONS: VHA women’s health PCPs express a wide range of learning needs. A fuller assessment of these learning needs, as well as the best ways in which PCPs’ learning needs can be met, is needed. VHA should work with medical education and women’s health experts, both within VHA and at affiliated universities, to continue assessing and addressing these learning needs so that VHA’s women’s health PCPs are equipped to provide optimal care to women Veterans. With the growing population of women Veterans, educational programs on the impact of military service on women will likely have relevance for PCPs both within and outside VHA.
Survey Topics
| Contraception Emergency contraception Infertility Abnormal cervical path Amenorrhea Abnormal uterine bleeding Uterine fibroids Chronic pelvic pain Preconception counseling Initial tests in pregnancy Pharmacology in preg/lact Post-partum depression | Depression mgmt. Menopause mgmt. Abnormal mammogram Breast mass Breast pain Fibromyalgia Connective tissue disease Incontinence Interpersonal violence Military sexual trauma Osteoporosis diagnosis Osteoporosis mgmt. |
LENGTH OF STAY AND IMPLEMENTATION OF GEOGRAPHIC STRUCTURED INTERDISCIPLINARY ROUNDINGMadison Paddock; Alex Montero; Adam Wolk; Elizabeth Moroni; Amarin Sangkharat; Dara Ambrose; Michael Catalino; Alan Chung; Michael Adams. Medstar Georgetown University Hospital, Washington, DC. (Tracking ID #1936784)
BACKGROUND: Geographic localization consists of the co-localization of physician providers and their patients on the same inpatient units. Structured Interdisciplinary Rounding (SIDR) consists of daily, template-driven interdisciplinary rounding on patients among care providers. Both geographic localization and SIDR have been proposed as methods to optimize interdisciplinary communication and work efficiency. Among medicine inpatients, adoption of geographic localization of Hospitalist teams has been associated with increased provider productivity but a possible increase in length of stay (LOS). In a setting where geographic localization of medicine inpatients was already in place, adoption of SIDR had no impact on length of stay. The impact of concurrent implementation of geographic localization and SIDR on LOS has not been studied. In October 2012, the Department of Internal Medicine at MedStar Georgetown University Hospital (MGUH) concurrently implemented geographic localization and structured interdisciplinary rounding (GSIDR) on all teaching service patients. The purpose of this study is to assess the impact of implementation of GSIDR at MGUH on length of stay.
METHODS: A prospective cohort, pre/post intervention study design was employed. All patients admitted to the medicine teaching service 6 months prior to the implementation of GSIDR and up to 6 months after the implementation of GSIDR were eligible. The primary outcome was length of stay. The independent variable was GSIDR Status (before/after implementation of GSIDR). Covariates collected included demographics, case mix index, source of admission, and insurance payer status. LOS was log transformed to account for the non-normal distribution of LOS. Univariate analyses were carried out with student t-tests for categorical covariates and general linear models for continuous covariates. Multivariable analyses were carried out utilizing ANOVA. All analyses were carried out utilizing SAS.
RESULTS: 1470 patients were admitted to the teaching service in the 6 months prior to implementation of GSIDR. 2006 patients were admitted to the teaching service in the 6 months after implementation of GSIDR. In univariate analyses, implementation of GSIDR was associated with an increased LOS of 0.4 days (p < 0.001). In multivariable analyses, there was no difference in LOS.
CONCLUSIONS: Concurrent implementation of geographic rounding and structured interdisciplinary rounding had a neutral impact on LOS. Surrogates of provider work efficiency did improve with an approximately 60 % drop in resident pages and 50 % decrease in daily resident provider miles walked documented in local, ancillary studies related to this GSIDR intervention. However, a significant rise in overall teaching service census (approximately 30 %) was noted in the GSIDR intervention period. A similar increase in census was noted in a prior study of the impact of geographic localization on LOS. Hence, it may be that improvement in work efficiency due to the implementation of GSIDR was attenuated by a concurrent rise in census.
GSIDR Baseline Characteristics: Hospital Medicine Discharges from GSIDR Floors Only
| Pre-GSIDR 4/1/12–10/1/12 (n = 1470) | Post-GSIDR 10/2/12-4/1/13 (p = 2006) | P value | |
| Female Sex | 53.2 % | 51.4 % | .30 |
| Age | 58.5 % | 57.8 % | .27 |
| Race -White -AA -Other | 34.3 % 41.1 % 24.6 % | 31.7 % 44.9 % 23.4 % | .26 |
| Insurance -Medicare -Medicaid -Other | 45.7 % 11.1 % 43.2 % | 43.82 % 10.02 % 46.16 % | .34 |
| ER Admit | 83.7 % | 80.66 % | .02 |
| CMI | 1.37 | 1.52 | .001 |
| Avg Hospitalist Daily Census | 66.3 | 82.8 | .01 |
Length of Stay Multivariable Analysis
| Covariate | Coefficient | P value |
| Insurance (Medicare vs other) | 0.18 | .02 |
| Race (white vs AA) | .05 | .02 |
| CMI | 0.3 | <.0001 |
| Age | .003 | <.0001 |
| ER | .34 | <.0001 |
| GSDIR | .04 | .13 |
LIFE CHAOS AND HIGH-RISK HEALTH BEHAVIORS IN ADOLESCENTSAvik Chatterjee1; Matthew W. Gillman1; Mitchell D. Wong2. 1Harvard Pilgrim Health Care Institute/Harvard Medical School, Boston, MA; 2UCLA, Los Angeles, CA. (Tracking ID #1934803)
BACKGROUND: Life chaos—physical and social disorder in one’s life—is associated with increased psychological distress in children. Life chaos may also be associated with undesirable health behaviors like smoking, drinking, drug use, and sexual activity in adolescents, but data are lacking.
METHODS: We analyzed cross-sectional data among 933 high-school students, aged 13–19 years, who in 2010–2011 took part in the Reducing Health Inequities through Social and Educational Change Study, of how school environments influence health behaviors among low-income, minority adolescents. The students completed a 90-minute interview assessing their demographics, substance use, sexual activity and other personal, familial, and psychosocial characteristics, including the 14 yes/no questions assessing Chaos, Hubbub and Order Scale (CHAOS). Possible score on CHAOS ranges from 0 to 14. In preliminary analysis we examined associations of CHAOS score in four groups (0, 1–2, 3–4, 5–14) with engaging in any of 4 risky health behaviors—any smoking, any drinking, or use of any illegal drugs in the previous 30 days, or having sexual intercourse in the previous 90 days. Because there was evidence of a threshold between 0 and the other 3 categories, we did all further analyses comparing 0 v. 1–14. We ran logistic regression analysis, adjusted for personal, psychosocial, and family-level variables that confounded the associations (changed estimates by >20 %). In an additional model, we added possible mediators to examine the extent of attenuation.
RESULTS: Mean (SD) age of the 933 students was 16.4 (1.3) years, 516 (55 %) were female, and 784 (84 %) were Latino. CHAOS score was 0 among 165 (18 %) students, 1–2 among 303 (32 %), 3–4 among 207 (22 %), and 5–14 among 258 (28 %). Prevalence of any risky behavior was 458 (49 %), including 87 (9.4 %) for smoking, 309 (34 %) for drinking, 206 (22 %) for drug use, and 247 (27 %) for having had sex. In unadjusted analysis, non-zero chaos score was associated with higher odds of participating in any risky health behavior (OR 1.9 [95 % CI 1.4, 2.8]) (Table). After adjustment for age, depression (Center for Epidemiologic Studies Depression Scale score > 16), parenting style (neglectful, indulgent, authoritarian, authoritative, or average), family drug problems, family alcohol problems, and parent smoking, the OR was 1.5 (95 % CI 1.0–2.2). Including the possible mediators of cutting school, spending less time on homework, and choosing peers who engage in risky behaviors attenuated the adjusted OR to 1.3 (95 % CI 0.8–2.0). Examining each risk behavior separately, we found no independent association with having had sex (Table).
CONCLUSIONS: Non-zero CHAOS score among high school students was associated with higher odds of a composite outcome of smoking, drinking, use of any illegal drugs, or sexual activity. Cutting school, spending less time on homework, and choosing peers with poor health behaviors partially explained how life chaos might result in increased participation in undesirable health behaviors. If these findings are replicated in prospective studies, school- or home-based interventions to decrease life chaos may reduce risky health behaviors in adolescents. These behaviors have significant effects on chronic adult diseases and life expectancy and it is important to understand modifiable factors that might deter initiation of these behaviors, which typically begin during adolescence.
Cross-Sectional Associations of the Presence of Life Chaos With 4 Risk Behaviors among 933 Adolescents age 13–19 years
| Unadjusted | Adjusted for Confounders1 | Adjusted for Confounders and Possible Mediators2 | |
| Odds ratio (95 % CI) for CHAOS score 1–14 v. 0 | |||
| Smoking in past 30 d | 5.5 (2.1, 14.4) | 2.4 (0.9, 6.2) | 2.0 (0.7, 5.2) |
| Drinking in past 30 d | 3.5 (2.2, 5.5) | 1.9 (1.2, 2.9) | 1.6 (1.0, 2.6) |
| Illegal drugs in past 30 d | 2.0 (1.3, 3.3) | 1.4 (0.8, 2.3) | 1.2 (0.7, 2.1) |
| Sex in past 90 d | 1.5 (1.0, 2.3) | 0.9 (0.6, 1.4) | 0.7 (0.5, 1.2) |
| Any of the 4 risk behaviors | 2.6 (1.7, 3.9) | 1.5 (1.0, 2.2) | 1.3 (0.8, 2.0) |
1Age, depression, parenting style, family smoking (for smoking), family alcohol use (for alcohol), family drug problems (for drugs) 2Additionally adjusted for cutting school, time spent on homework, peer smoking (for smoking), peer alcohol use (for alcohol), peer drug use (for drugs), peer sexual activity (for sex)
LIMITED ASSOCIATION BETWEEN HOSPITAL FINANCIAL PERFORMANCE AND QUALITY OF CAREOanh K. Nguyen; Anil N. Makam. University of Texas Southwestern Medical Center, Dallas, TX. (Tracking ID #1938018)
BACKGROUND: Increasing attention has been given to the role of hospital profits in contributing to the excessive cost of U.S. health care. However, little is known about the relationship between hospital financial performance and quality of care. We hypothesize that robust hospital financial performance is associated with higher quality of care, through ongoing investments in infrastructure, quality improvement and improved reputation through publicly reported quality measures.
METHODS: We merged data from the 2011 Hospital Annual Financial Data File from the Office of Statewide Health Planning and Development (OSHPD) in the State of California and the 2011 Hospital Compare web site. We included all general acute care hospitals for adults with both 1) comparable financial data and 2) data on 30-day risk-standardized mortality (RSMR) or readmission rates (RSRR) reported for at least one of the following: acute myocardial infarction (AMI), congestive heart failure (CHF) or pneumonia (PNA). We defined hospital financial performance as net revenue from operations (total operating revenue minus total operating expense). We performed a companion analysis using operating margin (net revenue from operations divided by total operating revenue) as an alternate measure of financial performance. Thirty-day RSMR and RSRR for AMI, CHF, and PNA were estimated from Medicare enrollment and claims data, risk-adjusted for age, sex, comorbid conditions, and indicators of patient frailty. We used linear regression to estimate the relationship between hospital financial performance and outcomes, adjusting for hospital characteristics and accounting for clustering of hospitals by owner. We performed a sensitivity analysis excluding 10 extreme outlier hospitals by financial performance (3 underperformers and 7 overperformers).
RESULTS: Of 280 hospitals, 23 (8 %) were teaching, 57 (20 %) were rural, 130 (46 %) were medium size (100–299 beds), 95 (34 %) were large size (≥300 beds), 147 (53) were associated with a hospital system, and 157 (56 %) were non-profit. Median net revenue from operations was $3.8 million (IQR −1.7–17.6, range −185.3–227.2). After adjustment, we observed a weak trend towards decreased AMI mortality, PNA mortality and AMI readmission with increasing net revenue from operations (Table). However, after excluding 10 outliers, the observed decrease in AMI and PNA mortality rates were no longer statistically significant, but the relationship for AMI readmissions persisted. For each $50 million increase in net revenue there was a 0.8 % decrease in the 30-day AMI readmission rate (p = .001). There was no relationship between operating margin and 30-day mortality or readmissions for AMI, CHF, and PNA.
CONCLUSIONS: There is a limited association between hospital financial performance and 30-day readmissions and mortality for AMI, CHF, and PNA. The improvement in mortality for AMI and PNA for hospitals with increasing net revenue from operations was largely driven by a small number of outlier hospitals, and was not associated with a hospital’s operating margin. Outcomes for acute myocardial infarction may be more sensitive to financial performance due to increased availability of costly infrastructure (i.e., catheterization labs) among hospitals with more robust finances.
Table - Relationship Between Hospital Financial Performance and 30-Day Mortality and 30-Day Readmission Ratesa
| N | Median % (IQR) | Adjusted % change (95 % CI) per $50 million increase in net revenue from clinical operationsb | ||
| Overall | Outliers excludedc | |||
| <div align=\"left\">Acute myocardial infarction (AMI) | ||||
| <div align=\"left\"><p style='padding-left : 10px'>Mortality rate | 212 | 15.2 (14.2–16.1) | −0.2 (−0.4 to −0.05)d | −0.4 (−0.8 to 0.04) |
| <div align=\"left\"><p style='padding-left : 10px'>Readmission rate | 186 | 19.4 (18.5–20.3) | nonlinear (significant)e | −0.8 (−1.3 to −0.3)d |
| <div align=\"left\">Congestive heart failure (CHF) | ||||
| <div align=\"left\"><p style='padding-left : 10px'>Mortality rate | 261 | 11.1 (10.0–12.1) | −0.03 (−0.3 to 0.2) | nonlinear (non-significant)f |
| <div align=\"left\"><p style='padding-left : 10px'>Readmission rate | 266 | 24.5 (23.5–25.6) | nonlinear (non-significant)g | −0.5 (−1.0 to 0.09) |
| <div align=\"left\">Pneumonia (PNA) | ||||
| <div align=\"left\"><p style='padding-left : 10px'>Mortality rate | 270 | 11.6 (10.3–13.1) | −0.3 (−0.6 to −0.06)d | −0.2 (−0.8 to 0.4) |
| <div align=\"left\"><p style='padding-left : 10px'>Readmission rate | 270 | 18.2 (17.3–19.1) | −0.02 (−0.2 to 0.2) | 0.2 (−0.2 to 0.6) |
Abbreviations: IQR, interquartile range; CI, confidence interval
a 30-day outcomes are risk-standardized for age, sex, comorbidity count, and indicators of patient frailty.
b Adjusted for teaching status, metropolitan status (urban/rural), bed size, safety net hospital status, hospital ownership, and Medicare caseload, counting for clustering of hospitals by owner.
c 10 hospitals were identified as outliers with respect to net revenue from operations (3 underperformers and 7 overperformers).
dp < .05 for the Wald statistic.
e Net revenue from clinical operations was modeled as a cubic spline function. The overall adjusted F-statistic was 5.6 (p < .001).
f Net revenue from clinical operations was modeled as a cubic spline function. The overall adjusted F-statistic was 2.1 (p = .08).
g Net revenue from clinical operations was modeled as a cubic spline function. The overall adjusted F-statistic was 2.4 (p = .051).
LOCAL PATIENTS, LOCAL STORIES: A LATINO CULTURAL COMPETENCY TRAINING PROGRAM FOR HEALTHCARE PROVIDERSArshiya A. Baig1; Amanda Benitez1; Anghela Z. Paredes2; Yue Gao1; Lisa Monnot3; Kathy Brazda3; Michael T. Quinn1. 1University of Chicago, Chicago, IL; 2University of Illinois College of Medicine, Rockford, IL; 3Taller de Jose, Chicago, IL. (Tracking ID #1934879)
BACKGROUND: Although cultural competency training programs exist for healthcare personnel, these trainings may not focus on providers’ local patient populations, address the use of racial stereotypes, or provide information on local patient resources. Additionally, hearing stories of patients who are from the community may not only increase provider awareness of the challenges and successes of their Latino patients but may improve their effectiveness in managing their patients with diabetes.
METHODS: We designed a cultural competency training program for healthcare providers and staff that incorporated local patient stories, exercises on self-awareness of the use of stereotypes, skill building on patient-centered communication, and information on local patient resources. To tell the stories of local patients, we produced a video that included photographs taken by local patients with diabetes and their stories of challenges and successes in diabetes management. The hour-long training was led by a research team member. A community resource center presented information about local resources for diabetes patients. The trainings were conducted at community health centers with groups of providers and staff members in adult primary care, including physicians, residents, physician assistants, nurse practitioners, and registered nurses. We assessed the impact of the training on provider cultural sensitivity, self-awareness of stereotyping, awareness of Latino cultural and health beliefs, knowledge of the local community, awareness of local patient resources, and self-rated effectiveness in caring for Latino patients using a survey administered pre- and immediately post-training.
RESULTS: Trainings were conducted with four groups of providers and staff at two urban community health centers. Of the 37 providers and staff who participated in the trainings, six (16 %) were family medicine physicians, three (8 %) were internal medicine physicians, one (3 %) was an obstetrician/gynecologist, five (14 %) were family medicine residents, eight (22 %) were physician assistants, three (8 %) were advanced practice nurses, and 11(30 %) were registered nurses. The majority of participants were female (89 %), the average age of respondents was 37 ± 11 years, 39 % reported being of Hispanic ethnicity, and 11 % lived in the community. From pre-test to post-test, providers significantly increased their cultural sensitivity score from 33.6 ± 4.7 to 34.7 ± 5.0 (p = 0.03). Provider awareness of their own stereotypes/biases concerning their patients increased from 3.7 ± 0.8 to 4.2 ± 0.7 (p < 0.001). Awareness of Latino cultural and health beliefs increased from 14.4 ± 4.9 to 15.6 ± 4.8 (p = 0.04). Knowledge of the local community increased from 1.3 ± 1.0 to 3.7 ± 1.1 (p < 0.001) and awareness of local patient resources increased from 2.8 ± 1.0 to 4.0 ± 0.8 (p < 0.001). There was no change in self-rated effectiveness in caring for Latino patients from pre- to post-test. Thirty-six (97 %) respondents agreed the training would help them better care for their Latino patients with chronic conditions.
CONCLUSIONS: A cultural competency training program that included local patient stories, taught self-awareness of the use of stereotypes and patient-centered communication, and provided information on local patient resources has promise in improving awareness of the use of stereotypes and knowledge of Latino cultural and health beliefs and local patient resources. Further research needs to assess the impact of this type of training on patient outcomes.
LONGITUDINAL FOLLOW UP OF A PATIENT SAFETY AND TRANSITIONS OF CARE CURRICULUM - MEDICAL STUDENTS’ CONFIDENCE AND ATTITUDESSara M. Bradley1,2; Dennis Chang2; ERic Barna2; Reena Karani3,1. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1938241)
BACKGROUND: The AAMC recognized patient safety and transitions of care as key components of high quality patient care and noted that there is a critical unmet need for medical education in these areas. This study sought to longitudinally evaluate a patient safety and transitions of care curriculum that was added to a third year Medicine -Geriatrics Clerkship using a survey of fourth year medical students during their Sub-internship. The objectives of the survey were to assess if students utilized skills taught by the patient safety and transitions of care curriculum in third year and subsequently in fourth year and whether they had increased confidence performing those skills following the curriculum. Additionally, the survey sought to evaluate fourth year students’ attitudes about learning these topics, opinions on when during medical school such a curriculum is most useful, and suggestions for additional instruction related to patient safety and transitions of care.
METHODS: All fourth year medical students enrolled in a internal medicine or pediatrics Sub-internship during the first 6 months of the 2013–14 academic year were invited to participate in filling out a 20 item anonymous survey.
RESULTS: 28 students completed the survey. 65.5 % reported using skills from the patient safety and transitions of care curriculum Frequently or Almost Always. The percentage of students who were Quite or Extremely Confident in their ability to assess a patient’s health literacy was 55.2 %, to provide education regarding medications was 53.6 %, and to identify topics to review on follow-up to ensure a safe transition was 44.8 %. Students felt it was Quite or Extremely Important for medical students to learn about discharge planning (100 %), how to complete a discharge summary (96 %), how to assess a patient’s health literacy (92.9 %), transitions of care (89.3 %), patient safety (85.7 %), and how to do a medication reconciliation (85.7 %). Students felt the topics of patient safety, medication reconciliation, discharge planning, transitions of care, how to complete a discharge summary, and how to work with a social worker should be taught during the third year of medical school, but that health literacy should be taught prior to the clinical clerkship years.
CONCLUSIONS: Students utilized skills taught during a patient safety and transitions of care curriculum subsequently in third and fourth year. Students felt these topics were important for medical students to learn and were appropriate to teach in the third year, including how to complete a discharge summary. Students felt health literacy should be taught earlier in the pre-clinical years.
LOOKING BEYOND THE PROSTATE: DETERMINANTS AND IMPACT OF NOCTURIA IN MIDDLE-AGED AND OLDER WOMENAmy Hsu1; Sanae Nakagawa2; Louise Walter1; Stephen K. Van Den Eeden3; Jeanette S. Brown2; David Thom2; Sei Lee1; Alison J. Huang2. 1San Francisco VA Medical Center, San Francisco, CA; 2University of California San Francisco, San, CA; 3Kaiser Permanente Division of Research, San, CA. (Tracking ID #1926776)
BACKGROUND: Nocturia is a common complaint in middle-aged and older adults presenting to primary care, and is linked to poor sleep quality, decreased mental and somatic health, falls and fractures. Among older men, nocturia is widely considered to be a consequence of prostate-related outflow obstruction. In contrast, the determinants of nocturia in older women are poorly understood and little is known about why some women suffer from nocturia but not others.
METHODS: We conducted a cross-sectional study of 2016 community-dwelling women, aged 41 to 83 years, from four racial/ethnic groups (White, Black, Asian and Latina), and enrolled in a group health delivery plan in Northern California. During home-based study visits, interviewers asked women about nocturnal voiding frequency, as well as bother and interference associated with this symptom. Other participant characteristics were examined by questionnaire, medical record abstraction, or physical examination and performance testing. Multivariable models were developed to assess for factors associated with nocturia, defined as waking two or more times to void at night. Potential predictors included demographics, gynecologic history, chronic medical conditions, medication use, and physical and mental functional status.
RESULTS: Of the 2016 participants, mean (SD) age was 56 (9) years, and over half were racial or ethnic minorities (22 % Black, 20 % Asian, 23 % Latina). Thirty-four percent reported waking to urinate at least two times per night, and 15 % reported waking to urinate at least four times per night. Of those with nocturia, 39 % reported being at least “moderately” bothered by this symptom, and 15 % reported that nocturia affected their day-to-day activities. Factors associated with nocturia in multivariable analysis included older age (OR 1.18, CI: 1.10–1.27 per 5 year increase), Black race (OR 1.86, CI: 1.39–2.50), Latina ethnicity (OR 1.36, CI: 1.02–1.83), hysterectomy (OR 1.85, CI: 1.13–3.05), vaginal estrogen use (OR 1.48, CI: 1.02–2.14), decreased mobility (OR 1.29, CI: 1.05–1.58 per 5-second increase in the Timed Up and Go test), and depression (OR 1.09, CI: 1.05–1.13 per 1-point increase on the Hospital Anxiety and Depression Scale score). The strongest predictor of being bothered by nocturia was greater frequency of nocturia (OR 2.63, CI: 2.08–3.31 per each additional nocturnal voiding episode), although 26 % of women who voided 4 or more times per night were only “slightly” or not at all bothered by this symptom.
CONCLUSIONS: Over a third of middle-aged and older community-dwelling women experience nocturia, and nearly 40 % of those with nocturia are significantly distressed by it. A variety of demographic, gynecologic, and geriatric factors are associated with nocturia in women, which suggests that a comprehensive evaluation of the patient is necessary to evaluate the risk for nocturia and tailor management to the individual.
LOW HEALTH LITERACY PREDICTS OUTCOMES AFTER SURGERYSunil Kripalani; Jesse Ehrenfeld; Warren S. Sandberg; Yaping Shi; Catherine M. Bulka; Jonathan S. Schildcrout. Vanderbilt University, Nashville, TN. (Tracking ID #1934807)
BACKGROUND: Prior studies have shown that health literacy can affect medical outcomes, but the impact of health literacy on postoperative outcomes is not well studied. We previously implemented routine health literacy assessment at our academic medical center, in which patients are administered a 3-item Brief Health Literacy Screen (BHLS). We determined the effect of health literacy on likelihood of hospital admission, postoperative hospital length of stay (LOS), and 30-day readmission following a wide range of surgical procedures.
METHODS: This retrospective cohort study included adult patients who completed the BHLS between 2010 and 2012 and subsequently underwent a non-emergent surgical procedure. BHLS scores ranged from 3 to 15, with lower scores indicating potential health literacy limitations. Outcomes included hospital admission after surgery, postoperative hospital LOS among admitted patients, and 30-day readmission rate. Multivariable models included adjustment for demographic characteristics, procedure type, and American Society of Anesthesiologists Physical Status Classification (ASA status).
RESULTS: A total 22,843 patients were analyzed, who had BHLS scores <9 (9 %), 9–11 (18 %), 12–14 (22 %), or 15 (51 %). Patients with a low level of health literacy were more likely to be older, male, less educated, covered by Medicare, and have higher ASA status. In unadjusted analyses, lower BHLS scores were associated with a greater likelihood of hospitalization (e.g., 65 % for BHLS<9 vs. 43 % for BHLS of 15; p < 0.001); longer hospital LOS (e.g., 6.1 days for BHLS<9 vs. 4.1 days for BHLS of 15, p < 0.001); and higher 30-day readmission rates (e.g., 11 % for BHLS<9 vs. 7 % for BHLS of 15, p < 0.001). In adjusted analyses, lower BHLS scores remained significantly associated with likelihood of hospitalization and LOS, but not readmission rates.
CONCLUSIONS: Lower health literacy is associated with multiple indicators of poorer post-operative outcomes. Interventions aimed at improving surgical outcomes and health care utilization should consider the role of health literacy in patients’ recovery.
Postoperative outcomes by BHLS score
| 3–8 | 9–11 | 12–14 | 15 | All | p-value | |
| Hospitalization, N (%) | 1313 (65 %) | 2298 (55 %) | 2962 (59 %) | 5027 (43 %) | 11600 (51 %) | <0.001 |
| LOS, days (10th, 90th percentile) | 6.1 (2.1, 17.2) | 5.4 (1.4, 17.0) | 4.8 (1.8, 14.0) | 4.1 (1.3, 12.1) | 4.7 (1.4, 14.2) | <0.001 |
| 30-day readmission, N (%) | 230 (11 %) | 379 (9 %) | 500 (10 %) | 852 (7 %) | 1961 (9 %) | <0.001 |
LOW PATIENT TRUST IN THEIR PRIMARY CARE PROVIDER PREDICTS MEDICATION NON-ADHERENCE 12 MONTHS LATERDanielle Hessler; David Thom; Rachel Willard-Grace; Thomas Bodenheimer; Denise DeVore; Camille Prado; Ellen Chen. University of California, San Francisco, San Francisco, CA. (Tracking ID #1934204)
BACKGROUND: Patients’ trust in their provider has been associated with medication adherence in cross-sectional studies. We examined the association between patients’ trust in their primary care providers (PCPs) and medication non-adherence, in a prospective study of patients enrolled in health coaching vs. usual care.
METHODS: Participants were 441 low-income English or Spanish-speaking patients age 18 to 75 with poorly controlled type 2 diabetes, hypertension and/or hyperlipidemia at two urban federally qualified health centers. The predictor variable was patient trust in their PCP measured by the Trust in Physician Scale. Outcome measures were medication non-adherence measured by the Hill-Bone Scale (scoring range from 1 to 4, with higher score indicating greater non-adherence) and patient-reported number of days in past week medication not taken. Multivariate modeling adjusted for age, gender, language and race/ethnicity in all models. Twelve month outcome analyses adjusted for baseline adherence and intervention group.
RESULTS: Patient trust at enrollment predicted medication non-adherence at 12 months by the Hill-Bone scale (adjusted β = −.15, p = .004) and by patient-reported days missed taking medication in past week (adjusted β = −0.17, p = .005). At 12 months, patients who were in the lowest trust quartile at baseline reported missing medications in the past week twice as often as those in the highest trust quartile (mean = 1.7 days vs. 0.8 days). Patients in the usual care group with lower trust at baseline were more likely to be non-adherent, by the Hill-Bone scale, than patients with higher baseline trust. In contrast, patient trust at baseline was not associated with non-adherence at 12 months for patients who received health coaching (p = .002 for test for interaction).
CONCLUSIONS: Patients with low trust in their provider are more likely to be non-adherent to medications up to 1 year later. Health coaching appears to attenuate the association between low trust in the PCP and non-adherence.
LOW-COST PROGRAM WITH SUSTAINED SEVEN-YEAR WEIGHT LOSS THAT CAN HELP OVERWEIGHT AND OBESE PATIENTSNia S. Mitchell1,2; Brenda Beaty3,4; Ariann F. Nassel5; James O. Hill1,2. 1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado Anschutz Medical Campus, Aurora, CO; 5University of Alabama School of Public Health, Birmingham, AL. (Tracking ID #1938648)
BACKGROUND: Obesity continues to be a major problem that is difficult to treat, and there are few effective options for long-term weight loss for patients. While numerous behavioral weight loss interventions have produced significant results in RCTs in the short term, many individuals regain most of that weight within 1 year. Similarly, commercial weight loss programs have shown significant weight loss at 1 year and some weight regain at 2 years; however, their costs are also a barrier to widespread utilization. In both cases, longer term, real-world data are lacking. Take Off Pounds Sensibly (TOPS) is a low-cost, nonprofit, peer-led weight loss program available throughout the United States. The program costs about $90 per year, and TOPS provides educational and administrative materials. Local “chapter” meetings are held weekly, and participants are weighed privately, followed by group educational programming on topics such as healthy eating, physical activity, and behavior modification. Participants’ weights are sent to the TOPS national database when they join the program and at the time they renew their annual memberships. The goals of this study were to determine the annual retention, weight change, and percentage of participants who lost a clinically significant amount of weight among TOPS members with consecutive annual renewals for up to 7 years.
METHODS: This is a non-concurrent prospective cohort analysis of longitudinal weight change of “completers” in the TOPS national database. Study participants were those aged 18 and over who joined TOPS from Jan. 1, 2005 to Dec. 31, 2011 and who consecutively renewed their annual memberships for at least 1 year. There were 213,048 potential participants, and 80,208 were included in the analysis. Retention was calculated by dividing the number of individuals who renewed their membership at a specific time point (“actual participants’) by the number of potential participants who were eligible to renew their membership at that time point. Weight change was calculated using mixed-effects repeated measures models with individual random intercepts. The percentage of participants who lost 5 % or more of their initial weight was also calculated.
RESULTS: The average initial weight of “actual participants” was 99.3 kg; the average age was 58 years; and 93 % of participants were women. The results for the “actual participants” with consecutive annual renewal are depicted in the table below. It includes the annual retention, mean cumulative weight change from initial weight, and percentage of participants who lost ≥5 % of initial weight for all years. The retention rate was inversely proportional to the number of years of consecutive annual renewal. The one-year retention rate was 38 % and the seven-year retention rate was 6 %. The mean cumulative weight change from initial weight was directly proportional to the number of years in the program. The mean weight change for participants in the first year was −5.6 %. For those participants who remained in the program for 7 years, their mean cumulative weight change was −8.2 %. Between 47 and 62 % of participants lost ≥5 % of initial weight over the seven-year study period.
CONCLUSIONS: Long-term weight loss is challenging, and internists must find ways to partner with community resources to help patients manage their weight. Individuals who participated in TOPS for at least 1 year lost a clinically significant amount of weight; and those who remained in the program maintained the weight loss for up to 7 years. The weight loss in TOPS is comparable to more expensive commercial weight loss programs, and the retention rate is higher than other programs. TOPS is an effective community-based resource to which internists can refer their overweight and obese patients for weight management.
Retention, mean cumulative weight change, and percentage of people who lost ≥5 % of inital weight.
| Years of eligibility (N) | Potential participants (N) | Actual participants (N) | Retention rate (%) | Mean cumulative weight change (%) | Percentage with ≥5 % weight loss (%) |
|---|---|---|---|---|---|
| 1 | 213,048 | 80,208 | 38 | −5.6 | 47 |
| 2 | 189,268 | 42,651 | 23 | −6.7 | 53 |
| 3 | 161,884 | 25,864 | 16 | −6.9 | 56 |
| 4 | 131,460 | 15,983 | 12 | −7.1 | 57 |
| 5 | 101,343 | 9,751 | 10 | −7.5 | 59 |
| 6 | 70,678 | 5,487 | 8 | −7.9 | 61 |
| 7 | 36,699 | 2,346 | 6 | −8.2 | 62 |
MAKING HOUSING FIRST HAPPEN: ORGANIZATIONAL ACTIONS THAT AFFECT SUCCESS AMONG VA MEDICAL CENTERS IN ENDING HOMELESSNESSStefan Kertesz1,2; Sally Holmes4,3; Bert White3; David E. Pollio2; Erika L. Austin1,2; Joseph E. Schumacher2; Carol VanDeusen Lukas4,3. 1Birmingham VA Medical Center, Birmingham, AL; 2University of Alabama, Birmingham, AL; 3Boston VA Medical Center, Boston, MA; 4Boston University, Boston, MA. (Tracking ID #1929873)
BACKGROUND: In 2009, the Veterans Administration (VA) proposed to end veteran homelessness by 2015. VA has pursued this by asking VA Medical Centers (VAMCs) to advance an evidence-based housing method, Housing First, using community-based rental vouchers. Housing First (HF) prioritizes the most vulnerable individuals and expedites their placement into permanent housing without requirements for sobriety or treatment success. A massive expansion of vouchers to house ~60,000 veterans, coupled with the novel HF approach, calls on VAMCs to execute an ambitious social endeavor. This study examines organizational actions that facilitate or hinder implementation of this initiative. The study was initiated in response to VA’s desire for formative feedback, and was designed in partnership with VA homeless program leaders, and other homelessness experts. VAMCs’ efforts to implement HF were evaluated with the Organizational Transformation Model (OTM), which identifies key drivers of organizational change: 1) impetus for change, 2) leadership engagement, 3) management structures and processes to foster alignment and integration of efforts and sustainability. The purpose of this qualitative study was to identify variation in organizational practices and to determine if these coincided with variations in fidelity to the HF approach.
METHODS: Two expert panels, a HF site visit and literature review were used to devise scoreable constructs for OTM elements and HF fidelity. A multidisciplinary team conducted over 100 confidential interviews with VAMC leadership, middle managers, and front-line staff at 8 VAMCs. Structured narratives and consensually-derived scores (ranging from 1: not present to 4: fully present) were used to assess HF and OTM constructs at each study site. The relationship between OTM and HF scores was explored with an X-Y plot across the 8 sites.
RESULTS: There was substantial variation in HF fidelity, (mean scores ranging 2.2 to 3.2 (on a 4-point scale) and in mean OTM scores (range 2.5 to 3.7). The X-Y plot of these scores demonstrated that HF fidelity was consistently higher where OTM scores were higher, indicating that greater presence of OTM-defined organizational practices aligned with greater fidelity to HF (Figure). Examples of stronger organizational practices include: 1. Greater involvement of senior leaders in program operations; for example, support for new permanent supervisory positions and multidisciplinary teams to assure success of the HF initiative 2. Planning for sustainability of efforts; for example, transparent discussions between VAMC leadership and mid-level managers to plan services 1–2 years in advance of anticipated reductions in funding. 3. Formal process improvement exercises to overcome barriers and improve speed of placement. These were undertaken in collaboration with non-VA partners, and entailed mapping out all steps required to house a new veteran, flagging typical hitches and inefficiencies, and systematically working to remove them. Such work typically drew on Lean Management and related quality improvement principles. 4. Efforts to integrate disparate homeless initiatives to improve coordination among, for example, case management, primary care, mental health and substance abuse programs. Examples of weaker organizational practices seen in lower HF fidelity sites included: 1. Allowing program execution to become highly dependent on specific high-performing mid-level managers with few formalized linkages from VAMC senior leaders to assure material support, training, and guidance. 2. Lack of influence or collaboration between VAMC senior leadership and non-VA community partners. As is common in large organization endeavors, simple numeric performance metrics figured as important, including “percentage of units leased up” and “percentage of units going to chronically homeless veterans.” We found these played a dual role, helpfully focusing attention and creating impetus, but at times obscuring the underlying complexity of the housing endeavor itself.
CONCLUSIONS: This analysis found variations in HF fidelity that were associated with differences in the organizational practices of medical centers engaged in changing and improving the housing process for homeless veterans. These findings suggest the necessity of both strong mid-level program management together with oversight and participation by senior leadership to drive the success of a critical initiative demanding significant changes in program scope, philosophy and delivery.
MALIGNANT HYPERTENSION-INDUCED THROMBOTIC MICROANGIOPATHY: CAN IT BE DISTINGUISHED FROM THROMBOTIC THROMBOCYTOPENIC PURPURA?Sumit Dahal1; Smrity Upadhyay2; Nabin Khanal2; Vijaya R. Bhatt3. 1Institute of Medicine, Kathmandu, Nepal; 2Creighton University Medical Center, Omaha, NE; 3University of Nebraska Medical Center, Omaha, NE. (Tracking ID #1923879)
BACKGROUND: Malignant hypertension is a common entity which affects approximately 1 % of hypertensive adults or 500,000 Americans. Albeit uncommon, it can present with microangiopathic hemolytic anemia, thrombocytopenia, and renal dysfunction (thrombotic microangiopathy, TMA), thus mimicking thrombotic thrombocytopenic purpura (TTP). While a strong clinical suspicion of TTP mandates urgent initiation of plasmapharesis, malignant hypertension is managed with antihypertensive agents. The rarity of malignant hypertension-induced TMA prohibits our understanding of this condition.
METHODS: We reviewed reports of malignant hypertension-induced TMA published in English-language and pubmed-indexed by 30th November 2013. This included a newly diagnosed case from our institution. Articles without adequate patients’ information were excluded.
RESULTS: Our review included ten patients including five men, with a median age of 33 years at diagnosis. The history of hypertension was known in 50 %. All the patients had elevated blood pressure at diagnosis, with a mean arterial pressure of 159 mmHg on an average (range 123–190 mmHg). The most common presenting symptoms were neurological symptoms such as headache (80 %), blurry vision (50 %), or dizziness (20 %); or gastrointestinal symptoms such as nausea/vomiting (50 %), or abdominal pain (20 %). None of the patients had fever. In addition to significant hemolytic anemia with schistocytes (mean hemoglobin of 8.6 g/dL, range 3.8-12.6 g/dL), and elevated lactate dehydrogenase (mean of 1209 IU/L, range 135–4000 IU/L), all the patients had prominent renal dysfunction (mean creatinine of 4.3 mg/dL, range 2.4–7.6 mg/dL). However, thrombocytopenia was relatively modest (mean platelet count of 58 × 103/uL, range 12–131 × 103/uL) and reported cases (n = 4) had preserved ADAMTS-13 activity level (mean 69 %, range 57–83 %). All the patients received antihypertensive treatment while 40 % of them also received plasmapheresis. Of the cases that reported the particular antihypertensive agent used (n = 8), 87 % started with intravenous agent followed by oral agent, while 13 % used oral agent alone. Following the control of blood pressure, the majority had a significant improvement in presenting symptoms (100 %), and platelet counts (90 %), however, only 60 % of the patients had significant improvement in renal function. Half of the patients needed hemodialysis. At discharge or follow up (n = 6), the mean platelet count was 242 × 103/uL (range 110–350 × 103/uL) and the mean creatinine level was 2.4 mg/dL (range 1.1–4.2 mg/dL). None of the patients died or had any other complication.
CONCLUSIONS: Malignant hypertension can be managed with antihypertensive agents alone without plasmapharesis. Apart from persistent renal impairment, malignant hypertension portends overall favorable outcomes, compared to TTP. Hence, it is important to be able to differentiate between the two conditions. The presence of prior history of hypertension, hypertensive end-organ damage and significantly elevated mean arterial pressure at presentation are important clues to diagnose malignant hypertension. The greater degree of renal impairment at diagnosis, relatively modest thrombocytopenia and preserved ADAMTS-13 activity can further differentiate malignant hypertension from TTP. These findings should be prospectively validated.
MAMMOGRAPHY FACILITY CHARACTERISTICS ASSOCIATED WITH TIMELY FOLLOW-UP OF ABNORMAL MAMMOGRAMSLeah S. Karliner; Celia P. Kaplan; Lin Ma; Karla Kerlikowske. UCSF, San Francisco, CA. (Tracking ID #1934230)
BACKGROUND: Delays in follow-up of abnormal mammograms are common, particularly for minority women. Delays can contribute to anxiety and women being diagnosed and treated for breast cancer at more advanced stages. We investigated whether mammography facilities vary in their timeliness of follow-up and if facility characteristics are associated with length of follow-up times.
METHODS: We examined time to follow-up of abnormal mammograms collected from 2005 to 2011 for 12 facilities participating in the San Francisco Mammography Registry (SFMR). We categorized facilities based on the proportion of exams without follow-up. For abnormal mammograms with a Breast Imaging Reporting and Data System (BI-RADS) 0 assessment, we categorized facilities with <=15 % without imaging follow-up at 60-days as ‘short’ follow-up and >15 % as ‘long’ follow-up. For abnormal BI-RADS 4/5 assessments, we categorized facilities with <=25 % without biopsy follow-up at 30-days as ‘short’ follow-up and >25 % as ‘long’ follow-up. For the BI-RADS 4/5 analysis, we excluded four facilities for which the SFMR does not have complete capture of biopsy data. We then examined facility characteristics pertaining to access and staffing, communication, and population served.
RESULTS: There were 70,393 BI-RADS 0 assessments and 17,750 BI-RADS 4/5 assessments. For BI-RADS 0 assessments, the facilities in the ‘short’ follow-up group completed diagnostic imaging for 95.5 % of examinations at 60-days compared to 74.7 % for the ‘long’ follow-up group (p < .0001). For the BI-RADS 4/5 assessments, the ‘short’ follow-up group completed biopsies for 81.6 % of examinations at 30-days compared to 60.7 % for the ‘long’ follow-up group (p < .0001). For both BI-RADS 0 and 4/5 abnormal mammogram follow-up, the ‘short’ follow-up facilities had higher screening and diagnostic mammography volume, more radiologists’ FTE reading mammography, and shorter times to scheduling diagnostic tests compared to the ‘long’ follow-up facilities. More ‘short’ follow-up facilities contacted women directly about their abnormal result. Additionally, ‘long’ follow-up facilities served more vulnerable populations, including a higher proportion of minority, limited English proficient, and less educated women compared to ‘short’ follow-up facilities.
CONCLUSIONS: Clinically significant differences in follow-up of abnormal mammograms exist. Facilities serving more vulnerable populations have longer and less adequate follow-up completion that is likely related to availability of resources. Providing mammography facilities serving vulnerable populations with additional resources may decrease disparities in abnormal mammogram follow-up, and in turn timely diagnosis and treatment of breast cancer.
MAMMOGRAPHY RATES 3 YEARS AFTER THE USPSTF GUIDELINES CHANGESJames F. Wharam1; Bruce E. Landon2; Fang Zhang1; Xin Xu1; Steve Soumerai1; Suzanne Fletcher1; Dennis Ross-Degnan1. 1Harvard Medical School, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1939213)
BACKGROUND: In November 2009, the United States Preventive Services Task Force (USPSTF) changed from recommending mammography every 1–2 years among women age ≥40 to (1) recommending personalized screening decisions for women age 40–49 and (2) recommending screening every 2 years for women age 50–74. Our objective was to determine the impact of the updated USPSTF guidelines on mammography rates.
METHODS: We performed a retrospective before-after time-series analysis, comparing mammography rates in 2012 to those predicted based on 2005–2009 trends. The sample included 1.71–2.08 million women annually age 40–64 from a large US health plan. We assessed annual and biennial mammography rates, examining for the relative change between observed and predicted rates in 2012.
RESULTS: Among women age 40–49, adjusted annual mammography rates increased from 40.7 to 44.4 % between 2005 and 2009 then declined to 42.3 % by 2012 (Figure 1), an estimated 9.55 % reduction (95 % CI, −10.10 % to −8.99 %) relative to the rate predicted by 2005–9 trends. Black women age 40–49 experienced a lesser decrease of 3.27 % (−5.22 % to −1.28 %, Figure 2). Yearly mammography rates among women age 50–64 increased from 48.7 to 51.3 % from 2005 to 2009 but then declined by 5.87 % (−6.32 % to −5.42 %) to 49.7 % by 2012. For biennial screening, adjusted rates in 2005–6, 2008–9, and 2011–12 among women age 40–49 were 66.4 %, 68.1 %, and 64.7 %, respectively, a 7.86 % relative reduction (−8.49 % to −7.22 %). White, Hispanic, and Asian women age 40–49 experienced similar relative reductions of −8.69 % (−9.41 % to −7.97 %), −7.33 % (−9.35 % to −5.27 %), and −9.24 % (−12.40 % to −5.98 %), respectively, whereas black women experienced a nonsignificant reduction (−1.75 %, [−3.89 % to 0.44 %]). Biennial mammography rates among women age 50–64 were 73.4 %, 74.0 %, 72.0 % in 2005–6, 2008–9, and 2011–12, respectively, a 4.39 % relative reduction (−4.89 % to −3.88 %) that was similar among white, Hispanic, and Asian women. Black women age 50–64 experienced a small increase in biennial mammography (2.90 %, [1.24 % to 4.58 %]).
CONCLUSIONS: After publication of the 2009 USPSTF guidelines, annual and biennial mammography rates declined by 4–17 % among women who were not black. Black women generally experienced lesser decreases. Reductions in biennial mammography might be an unintended consequence of the updated guidelines.
Figure 1. Annual mammography rates by age group before and after publication of the 2009 USPSTF guidelines.
Figure 2. Annual mammography rates among black women by age group before and after publication of the 2009 USPSTF guidelines.
MANAGEMENT OF ATRIAL FIBRILLATION: A COST COMPARISONTadeo A. Diaz Balderrama1; Caroline Pace3; Jennifer Wright2; Shivtej Kaushal1; Alexandria Goldin3. 1Medical College of Wisconsin, Milwaukee, WI; 2Medical College of Wisconsin, Milwaukee, WI; 3Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1926389)
BACKGROUND: Atrial fibrillation (AF) is estimated to affect 2.7 to 6.1 million people in the United States and accounts for 350,000 hospitalizations and 276,000 emergency department (ED) visits per year. Forty-four percent of the estimated annual $6.65 billion spent treating AF is due to inpatient care. While various methods have been used to manage AF in the ED to avoid unnecessary admissions, there is no universal standard for such management. Initial management of AF in the ED setting, with outpatient coordination of care, could decrease the number of unnecessary inpatient stays.
METHODS: All admissions to our institution from January 1, 2010 through December 31, 2010 with AF as a primary diagnosis were identified. An algorithm was created based on prior studies and current guidelines and retrospectively applied to identify the patients eligible for outpatient management. The potential cost savings were calculated by quantifying the diagnostic tests, imaging tests, inpatient days of stay and the consults which were documented during the patients stay.
RESULTS: Fifty-seven out of 120 patients would have qualified for ED management. Patients who qualified for ED management were younger (59 years vs 70.8 years, p < 0.0001), had presenting complaints of palpitations (p < 0.05) and had lower CHADS2 (p < 0.0001) and CHA2DS2VASc scores (p < 0.0001). Patients mean length of stay in the hospital was 2.33 days and after factoring inpatient and ED costs along with potential outpatient follow up costs, the mean cost savings per patient was estimated at $2495.65.
CONCLUSIONS: An algorithm to guide ED management of AF in appropriate patients may reduce the need for hospital admissions and likely result in overall healthcare cost savings. Further evaluation of outpatient costs of care for the patients who qualify for outpatient management will help determine the feasibility of such an approach.
Management Algorithm
MASSACHUSETTS HEALTH CARE REFORM REDUCED RACIAL/ETHNIC DISPARITIES IN ELECTIVE PERCUTANEOUS CORONARY INTERVENTION AND CORONARY ARTERY BYPASS GRAFT SURGERYAmresh D. Hanchate1,2; Steven M. Bradley3,4; Alok Kapoor2; Danny McCormick5; Karen E. Lasser2; Chen Feng2; Nancy R. Kressin1,2. 1VA Boston Healthcare System, Boston, MA; 2Boston University School of Medicine, Boston, MA; 3VA Eastern Colorado Healthcare System, Denver, CO; 4University of Colorado, Denver, Denver, CO; 5Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1937646)
BACKGROUND: Percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG), arguably the most commonly examined surgical procedures in the literature on racial and ethnic disparities, are documented to be used less often among racial/ethnic minorities. The differences in use have been associated with factors other than clinical need. Large-scale insurance coverage expansions, such as the Massachusetts (MA) reform of 2006 and the Affordable Care Act of 2010, have the potential to reduce disparities in access to health care, particularly outpatient care. Thus, they provide an unique quasi-experimental setting to examine the causal impact of insurance coverage expansion on disparities in use of elective PCI and CABG.
METHODS: We applied a difference-in-differences design to estimate the impact of MA reform on use of elective and non-elective PCI and CABG among adults aged 40 to 64 (those most at risk for these procedures among the target beneficiaries of reform) by race/ethnicity (Whites, Blacks and Hispanics). We estimated population rates of procedure use (# procedures per 100,000 census population) during the 2 years prior to the start of reform (7/1/2006) and the 2 years following coverage expansion (1/1/2008). To isolate the impact of reform, we adjusted for secular changes unrelated to reform based on a comparison of the pre-post change in the target subpopulation (MA residents aged 40 to 64) with corresponding changes among (a) residents of three comparison states (New Jersey, New York and Pennsylvania) aged 40 to 64, and (b) residents of MA aged 65 and older. We obtained comprehensive counts of elective and non-elective PCI and CABG procedures from 2004 to 2010 state discharge data files. Population counts were obtained from the census data files. Stratifying the population by race/ethnicity, age and sex, we estimated Poisson regression models with fixed effects for state and time.
RESULTS: During the pre-reform period the total combined numbers of elective PCI and CABG procedures, by race/ethnicity, were: 11,919 (Whites), 227 (Blacks) and 251 (Hispanics). Pre-reform procedure rates (# procedures per 100,000) were significantly lower among Blacks (71) and Hispanics (80) compared to Whites (139). There was a secular decrease in overall rates of elective PCI and CABG, with a larger decrease among the target cohort of MA residents aged 40 to 64 (−41 %) than among comparison-state residents aged 40–64 (−28 %) and MA residents aged 65 and older (−32 %). Adjusted for secular trends, MA reform was associated with an increase in elective procedures among Blacks (7 %, 95 % confidence interval [CI] = [3 %, 11 %]) and Hispanics (4 %, 95 % CI = [2 %, 6 %]), but a decrease among Whites (−7 %, 95 % CI = [−8 %, −6 %]). For non-elective PCI and CABG procedures, MA reform was associated with no change among Whites, Blacks and Hispanics.
CONCLUSIONS: MA health reform may have increased the use of elective PCI and CABG among Blacks and Hispanics, thereby indicating possible improved access to outpatient care and reduction of disparities. Despite a sizable secular decrease in procedure use among all subpopulations, procedure use may have increased among minority groups with previously unmet need or with newly identified need. While this finding might suggest similar potential for ACA nationwide, the role of other facilitating factors, such as adequate provider availability, also need to be taken into account.
MASSACHUSETTS HEALTH REFORM WAS ASSOCIATED WITH MOVEMENT OF INPATIENT CARE FROM SAFETY-NET TO NON-SAFETY-NET HOSPITALS AMONG FREQUENTLY HOSPITALIZED PATIENTSKaren E. Lasser2,4; Chieh Chu2; Danny McCormick3; Amresh D. Hanchate1,2; Nancy R. Kressin1,2. 1VA Boston Healthcare System, Boston, MA; 2Boston Medical Center/Boston University School of Medicine, Boston, MA; 3Cambridge Health Alliance/Harvard Medical School, Cambridge, MA; 4Boston University, Boston, MA. (Tracking ID #1928396)
BACKGROUND: Quality of care may be higher at non-safety-net (non-SNH) hospitals relative to safety-net hospitals (SNH), and non-SNHs may thus be more attractive to patients with freedom to choose where they receive care. Massachusetts (MA) health reform enabled previously uninsured patients the choice to transfer their care from SNH to non-SNH. Prior studies have not examined the effect of MA health reform on individual patient movement from SNH to non-SNH for inpatient care. We hypothesized that changes in patient movement toward non-SNHs would be greater in MA than in comparison states without expanded insurance coverage.
METHODS: We used 2004–2009 inpatient discharge data from MA, New York (NY), and New Jersey (NJ), examining adult hospitalizations for all causes (except obstetrical diagnoses). Defining pre-reform (9/1/2004 to 6/30/2006) and post-reform (1/1/2008 to 9/30/2009) periods, our study examined adult patients with >=2 hospitalizations in each period. In each state, we identified a cohort of patients as “SNH users,” patients for whom all hospitalizations during the pre-reform period were at a SNH. We compared movement from SNH to non-SNH (defined as >=1 hospitalization in a non-SNH in the post-reform period) among patients age 18–64 (those most affected by health reform) and those age >= 65 in MA to movement among patients age 18–64 and those age >=65 in comparison states. We also analyzed movement rates according to race/ethnicity among patients age 18–64, to assess disparities in such changes. We used a difference-in-differences design to identify the post-reform change in MA, adjusted for secular changes unrelated to reform, and adjusted for the effects of factors known to affect SNH use, including race/ethnicity, income, insurance, and nearest hospital type.
RESULTS: In MA, of 10,308 patients, 6924 remained at a SNH in the post-reform period, and 3384 (32.8 %) moved to a non-SNH. In comparison states, of 30,242 patients, 18,584 remained at a SNH in the post-reform period, and 11,658 (38.5 %) moved to a non-SNH. The difference in movement from SNH to non-SNH was greater among MA adults age 18–64, relative to MA elderly adults, than between non-elderly adults and elderly adults in comparison states (difference-in-difference adjusted odds ratio [AOR] 1.11, 95 % confidence interval [CI], 1.0–1.2, p = 0.04). In MA, there was a significant increase in movement to non-SNH for patients with a diagnosis of pneumonia (AOR 1.8, 95 % CI 1.1–3.0), but not for CHF, CAD, asthma, or diabetes. Relative to whites, there was a trend towards less movement to non-SNH for MA Hispanics relative to Hispanics in comparison states (AOR 0.8, 95 % CI 0.7–1.0, p = 0.06). Relative to patients with private insurance, patients who were self-pay (in any state) were less likely to move to a non-SNH (AOR 0.4 95 % CI 0.3–0.4).
CONCLUSIONS: Coverage expansion in MA was associated with increased movement from SNH to non-SNH among a subset of 3384 very sick patients. While anticipation of such movement has been used to justify funding cuts to SNH in MA, other studies that have examined the universe of inpatient care utilization have found very little net shift in inpatient volumes between SNH and non-SNH.
MATCH RATES IN PRIMARY CARE SPECIALTIES FOR MEDICAL STUDENTS WHO PARTICIPATED IN A STUDENT-FACULTY COLLABORATIVE PRACTICECharlotte E. Ward1; Emma C. Jeffries1; Marya J. Cohen1; Rebecca Berman2. 1MGH, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA. (Tracking ID #1938257)
BACKGROUND: It is becoming increasingly difficult for patients to find primary care physicians (PCPs) in the United States. The Medicaid expansion will extend coverage to 30 million new patients, many of whom will likely need a PCP. It is important, therefore, to attract a greater number of medical students to the field of primary care and to better understand factors that contribute to student career interests. The Crimson Care Collaborative (CCC), a series of 5 student-faculty collaborative practices, aims to give students hands-on practical experience in understanding innovation in primary care clinics across the Harvard Medical School network. Since the opening of CCC in 2010, we have had 500 students participate in CCC, including 70 who have since graduated. The aim of our study was to compare primary care residency match rates of CCC students to those who did not participate in CCC.
METHODS: Harvard Medical School (HMS) residency match lists from 2010 to 2013 were compared to CCC rosters over the same time period. Internal medicine, primary care, OB/GYN, family medicine and pediatrics match rates of CCC participants were compared to those of non-CCC participants using Chi-square tests.
RESULTS: Out of 500 students who participated in CCC, 70 students graduated during 2010–2013. During the same time period, 556 non-participants in CCC graduated. Internal medicine match rates were higher among CCC participants compared with non-CCC participants (32.9 %, vs. 19.4 %, p = 0.009). Match rates for internal medicine programs with a focus on primary care were higher among CCC participants compared with non-CCC participants (8.6 %, vs. 3.2 %, p = 0.05). Family medicine match rates were higher among CCC participants compared with non-CCC participants (8.6 %, vs. 3.6 %, p = 0.05). OB/GYN match rates were lower among CCC participants compared with non-CCC participants (2.9 %, vs. 4.7 %, p = 0.49). Pediatrics match rates were lower among CCC participants compared with non-CCC participants (8.6 %, vs. 9.2 %, p = 0.87). Among all five primary care fields combined, match rates were higher among CCC participants compared with non-CCC participants (61.4 %, vs. 40.5 %, p = 0.0008).
CONCLUSIONS: Among a group of medical students who participated in a primary care based student-faculty collaborative clinic, primary care residency match rates were higher in comparison to those who did not participate. As the demand for primary care services grows, so does the need for programs such as CCC that are designed to expose greater numbers of medical students to primary care careers. We plan to continue data evaluation to see whether this residency match trend strengthens over time.
MEDICAL DECISION MAKING IN A PRIMARY CARE CLINICJeffrey L. Jackson1,2; Patrick G. O’Malley2; Dorothy Becher2. 1Zablocki VAMC, Milwaukee, WI; 2Uniformed Services University, Bethesda, MD. (Tracking ID #1921916)
BACKGROUND: Shared medical decision is a goal of most health care delivery systems. Our purpose was to develop a tool to assess patient desire for shared medical decision making and the impact of patient assessment of shared decision making on patient outcomes.
METHODS: In a pilot study, we asked patients to rate the type of shared decision making they desired on a visual analog scale prior to their visit. One end was anchored by a desire for the provider to make all the decisions, in the middle was equal decision making between patients and providers and at the other end was a desire for the patient to make all the decisions. Immediately after the encounter, patients and providers were asked to rate the shared decision making that occured using this same scale. Patient outcomes included trust (Trust-7), satisfaction (Rand-9), adherence (pill count). Additional measures included health literacy, functional status, depression (PHQ-9) and somatization (PHQ-15). Visits were audiotaped and coded using RIAS.
RESULTS: Among 120 ambulatory patients, most expressed a desire for equal decision making (58 %), 19 % wanted the provider to be more dominant and 23 % wanted the patient to be more dominant. At the extremes, only 3 % wanted the provider to make all the decisions and 2 % wanted to personally make all decisions. After the encounter, patients reported 57 % of decision-making in encounters were equally shared, 31 % had provider dominance and 12 % patient dominance. When the patient desires and patient ratings of encounters were compared, 19 % reported more patient dominance than desired, 51 % reported perfect match between the degree of shared decision making experienced and desired; 30 % reported more provider dominance. However, there was no relationship between discordance of decision making and satisfaction, trust or medication adherence. Providers reported some degree of dominance in 50 % of encounters, equal decision making in 26 % and patient dominance in 24 %. There was little agreement between patient and provider perception of dominance during the encounters; providers reporting twice as much patient dominance as reported by patients. There was also no relationship between the difference in perception by patients and doctors about shared medical decision making and patient trust, satisfaction or adherence. Finally, objective assessment with RIAS found no relationship between patient or provider perception of the degree of shared decision making and provider dominance during the encounter.
CONCLUSIONS: About half of encounters had a good match between the patient’s expressed desired style of decision making and the decision making style they experienced. Patients reported that a third of encounters had greater provider dominance than desired, consistent with provider reports of dominating decision making in nearly half of encounters. Providers reported twice as much patient decision making dominance as reported by patients. Interestingly, there was no relationship between desired or perceived style of decision making and patient outcomes, including trust, satisfaction and medication adherence. In addition, there was a lack of agreement between RIAS dominance assessment and either patient or provider dominance ratings.
MEDICAL SCHOOL CHARACTERISTICS AND STUDENT DESIRE TO WORK WITH THE UNDERSERVEDAlex Montero1,2; Rebecca Brown2,3; Tracy V. Fulton2,1; Nicole Szabo4; Thaidra Gaufin4; Sadhana Rajamoorthi4; Eileen Moore1,2. 1Georgetown University Hospital, Washington D.C., DC; 2Georgetown University School of Medicine, Washington D.C., DC; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Georgetown University, Washington D.C., DC. (Tracking ID #1939627)
BACKGROUND: Physician shortages among urban, underserved patient populations are a pressing and complex problem. These populations often have large low-income, minority and immigrant populations in great need of medical services. Prior literature suggests that the shortage of physicians in urban underserved areas is due to complex factors including structural aspects of these communities (barriers to medical access, poverty, race, and cultural barriers) and determinants of medical student career choice in regards to primary care (i.e. debt burden). In response to the declining numbers of medical students entering primary care, there has been increased effort by medical schools to stimulate student interest in both serving the underserved and pursuing primary care careers with mixed success. The aim of this study was to explore possible associations between students interested in serving vulnerable urban populations and medical school characteristics (both curricular and non-curricular) which may increase interest in working with the urban underserved.
METHODS: Design: Cross sectional survey. Methods: We sent an on-line survey to 40 U.S. medical schools in close proximity to urban populations. The survey was sent to medical school deans, relevant student club leaders, and social contacts of the authors known to be at the eligible schools. Approximately 4,000 students were eligible to take the survey. Our response rate was 1,012 medical students. The survey queried students about demographic information, relevant school curricular elements, and their opinions about underserved urban populations; our independent variables were constructed from these domains. A priori, we constructed two main outcome variables: 1) “any interest”—students with any career interest in working the underserved; 2) “strong interest”—students with clear career goals of working with the underserved. We conducted univariate and multivariate analyses with both outcome variables.
RESULTS: With regard to “any interest” students, univariate analysis revealed significant associations with school year (more interest in pre-clinical students, p = 0.01), presence of student free clinic (more interest in schools with student free clinics, p = 0.00), and presence of required community service curriculum (more interest in schools with community service curricula, p = 0.06). Of note, race/ethnicity was not significant. In regards to “strong interest” students, univariate analyses revealed significant associations with political affiliation and race/ethnicity. With regard to “any interest” students, multivariable analyses revealed that only the presence of a student free clinic remained significantly associated with the outcome variable. With regard to “strong interest” students, multivariable analyses revealed that political affiliation and school year remained significantly associated with the outcome variable.
CONCLUSIONS: Student run free clinics (SRFC) are an informal, non-required curricular element present in the majority of US medical schools. However, our study indicates that SRFC are the only medical school characteristic that is independently associated with students having any interest in working with the underserved. For more committed students, other non-curricular elements are independently associated with a desire to work with the underserved.
Student and Medical School Characteristics (n = 1012)
| Number (%) | |
| Male | 468 (46.2 %) |
| Average Debt | $161,273 |
| Race -American Indian -Asian -Black -Hispanic -White -Multiracial | 2 (2.7) 149 (14.4) 66 (6.4) 42 (4.1) 677 (65.3) 73 (7.0) |
| Hometown -Rural -Suburban -Urban | 129 (12.4) 661 (63.7) 210 (20.3) |
| Politics -Conservative -Moderate -Liberal -Other | 132 (12.7) 333 (32.1) 487 (47.0) 66 (6.4) |
| School Characteristics -School based community service -Community service requirement -Health disparities curriculum -Student run free clinic | 771 (76.6) 294 (29.2) 737 (73.2) 878 (87.2) |
MEDICAL STUDENTS’ ENGAGEMENT IN COLLABORATIVE COMMUNICATION DURING AN INTERPROFESSIONAL STANDARDIZED PATIENT ENCOUNTERSandra K. Oza; Maria A. Wamsley; Christy K. Boscardin; Joanne Batt; Karen E. Hauer. University of California, San Francisco, San Francisco, CA. (Tracking ID #1939640)
BACKGROUND: Effective and collaborative communication is essential for the provision of high-quality patient care. As members of healthcare teams, medical students frequently interact with a variety of health professionals while providing patient care. However, the nature of medical students’ communication with other health professionals has not been widely studied. We explored medical students’ engagement in collaborative communication with another health professional during a simulated patient care encounter.
METHODS: We developed a conceptual framework of collaborative communication based on theoretical explanations of collaboration and the empirical research on nurse-physician communication. This framework included constructs related to role identification, information exchange, decision-making, and interpersonal exchanges. We then applied this framework to an analysis of a purposive sample of 60 medical students. The study setting was an objective, structured clinical examination (OSCE) case in which students communicated with a standardized nurse (SN) and standardized patient. Using directed qualitative content analysis, we analyzed medical student dialogue with the SN for the elements of collaborative communication included in our framework. We examined differences in collaborative communication by student performance level as defined by the SN global satisfaction rating.
RESULTS: We found that across encounters, medical students engaged in all elements of collaborative communication in our framework. All students in our sample exchanged interpersonal comments with the SN, and all but one identified their role to the SN. Students who received higher global satisfaction ratings by the SN were more engaged in bidirectional information exchange with the SN (the student both sought information from the SN and shared information with the SN) and joint decision-making with the SN (the student sought the SN’s input into a care plan for the standardized patient).
CONCLUSIONS: We found that medical students engaged in all of the communicative elements that comprised our conceptual framework of collaborative communication in a simulated encounter. Highly rated students were more likely to engage in bidirectional information exchange and joint decision-making, suggesting that these communication elements may be particularly important for collaborative communication. Our study provides support for the further development and use of this conceptual framework of collaborative communication for assessing students’ collaboration with interprofessional colleagues. These study findings suggest that curriculum development in interprofessional collaborative communication could be framed around this conceptual framework, with emphasis on information exchange and joint decision-making with other healthcare professionals.
MEDICATION ACCURACY AND ADOPTION OF A COMPUTERIZED PHYSICIAN HANDOFF TOOLAlex Montero; Millicent Yee. Georgetown University Hospital, Washington, DC. (Tracking ID #1940222)
BACKGROUND: Communication failures and suboptimal patient handoffs are major factors contributing to adverse patient safety events. Unstructured, non-standardized physician handoffs in inpatient settings have been shown to be associated with medical errors and adverse patient safety events. Manually populated, templated written handoffs have been show to frequently contain medication errors of omission and addition of high risk medications such as anticoagulants and narcotics. Computerized physician handoff tools (CHTs) have been widely adopted to optimize patient handoffs but remain understudied with regard to patient safety outcomes, and no study has assessed the impact of CHT on the medication accuracy of written physician handoffs. In June of 2013, a multiphase implementation of a CHT (CORES Smart Handoffs) was started on house staff teaching services throughout Georgetown University Hospital (GUH). We report on the impact of the adoption of a CHT on medication accuracy of physician handoffs on at an academic medical center.
METHODS: Design: prospective observational cohort study. Methods: On June 1st, 2013 CORES Smart Handoffs was implemented on four of six resident teaching teams at GUH. Implementation of CORES on two resident teaching teams was delayed by 6 weeks. Written signouts of all teaching teams was collected on randomly selected days for 6 weeks starting on June 1st, 2013. Medication lists from written sign-outs were compared to “gold standard” lists obtained from GUH’s clinical information systems to ascertain the accuracy of each medication listed on the written sign-outs. Medication errors per written sign-out were quantified and characterized as omissions/additions and according to a standardized severity scale. The error rate of CORES generated medication lists was compared with the error rate of manually populated medication lists. The main outcome was the medication error rate per written signout. The independent variable was the source of the medication list (CORES medication lists vs. manually populated medication lists). Student t-test analysis was employed for all analysis.
RESULTS: Results: The mean rate of medication errors was significantly lower for both omissions and additions for CORES generated written sign-outs. This was true for both high risk and low risk medications. The average number of medications per written sign-out went up significantly with the CORES generated sign-outs.
CONCLUSIONS: Medications listed on a CHT generated written sign-outs were clearly more accurate than those listed on a manually populated and templated written sign-outs. However, the marked increase in medications listed on a CHT written sign-out was concerning for a “clutter” effect that may limit the positive impact of more accurate medication lists on patient safety. The impact of the adoption of a CHT on preventable medication errors needs to be assessed to confirm the safety benefit of more accurate medication lists on CHT generated written sign-outs.
Rate of Omission Errors on Written Sign-outs
| Mean per patient sign-out | P Value < 0.0001 | |
| CHT Generated Sign-outs | 0.2 | |
| Non-CHT Generated Sign-outs | 2.197 |
Rate of Comission Errors on Written Sign-outs
| Mean per Patient Sign-iout | P Value < 0.005 | |
| CHT Generated Sign-outs | 0.148 | |
| Non-CHT Generated Sign-outs | 0.299 |
MEDICINE ATTENDING ROUNDS: FREQUENCY OF OBSERVED TEACHING BEHAVIORS AND LEARNERS’ PERCEPTIONSFrank W. Merritt1; Allan V. Prochazka1,2; Eva M. Aagaard1; Chad Stickrath1,3. 1University of Colorado School of Medicine, Denver, CO; 2Denver Veterans’ Affairs Medical Center, Denver, CO; 3Denver Veterans’ Affairs Medical Center, Denver, CO. (Tracking ID #1938268)
BACKGROUND: Daily rounds with the attending physician are a central component of medical education for both residents and students in teaching hospitals. However, time for education in this setting can limited by the demands of patient care. Little is known about the frequency and effectiveness of teaching behaviors on rounds in the current era.
METHODS: We performed a cross-sectional study of attending rounds on general medicine inpatient wards at 4 teaching hospitals. Trained observers accompanied teams on rounds and recorded frequency of educational activities performed by attendings. Students and residents present on the observed day were asked to rate the attending using a Likert scale (1 = strongly disagree to 4 = strongly agree) in response to the statement “Overall, effective teaching occurred on rounds today.” The effectiveness of 9 specific teaching behaviors was similarly assessed. We compared the frequency of the specific teaching behaviors with their perceived efficacy. In addition, we grouped attendings into tertiles based on perceived overall teaching effectiveness. Then, we compared the frequency of each observed teaching behavior amongst the three tertiles of attendings using the Kruskal Wallis test.
RESULTS: Overall, 90 rounding episodes were observed including 83 attendings, 279 trainees, and 807 patient encounters. The highest-scoring tertile of attendings scored an average of 3.6 on overall teaching effectiveness, the middle 2.2, and the lowest-ranked 1.2. The highest-ranked attendings performed an average of 2.4 teaching behaviors per patient encounter versus 1.5 in the lowest-scoring group. Significant differences also occurred in the frequency of addressing questions about the patient care plan (77.6 % vs 65.9 % vs 47 %, p = 0.003), providing feedback (31.5 % vs 10 % vs 0.5 %; p = 0.001), and teaching about learner-identified topics (8.0 % vs 2.2 % vs 1.9 %; p = 0.018). There was no significant difference in the frequency of teaching general medical topics, specific evidence-based medicine literature, history-taking, physical examination, or oral presentation skills. The average rounding time per patient was approximately 13 min in all 3 groups.
CONCLUSIONS: We found a range of learner satisfaction with teaching from medicine attendings, which may be partially explained by variations in the number and types of teaching behaviors performed. Importantly, the best-ranked teaching attendings performed almost twice as many total teaching behaviors per patient without spending more time rounding. Furthermore, the teaching behaviors that distinguished the highest from the lowest performing attending groups were patient-oriented, such as addressing questions about the patient care plan, and learner-centered, such as giving feedback and teaching about learner-identified topics. In the future, investigators should assess how top-rated attendings are able to perform more teaching behaviors in the same amount of time per patient and whether faculty development efforts aimed at increasing the frequency of patient-oriented and learner-centered teaching behaviors result in better teacher ratings.

Tertiles of attendings are grouped by student and resident rankings of teaching effectiveness (on the particular rounding day the was observed). The boxes represent 25 %–75 % with the thick middle line representing the median. The mean is included in the text but not pictured.
METABOLIC RISK FACTORS AND GENETIC RISK PARTIALLY MEDIATE THE RISK OF TYPE 2 DIABETES CONFERRED BY PARENTAL DIABETES HISTORY IN THE FRAMINGHAM HEART STUDYSridharan Raghavan1,2; Bianca Porneala1; Josée Dupuis3; James B. Meigs1,2. 1Massachusetts General Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3Boston University School of Public Health, Boston, MA. (Tracking ID #1925986)
BACKGROUND: Family history of type 2 diabetes mellitus (T2D) is a strong determinant of an individual’s risk of developing the disease. The effect of parental history is typically divided into genetic heritability and the influence of familial environment; the advent of genetic testing for chronic disease risk has made it possible to assess the exchangeability of measurable indices of environmental and genetic risk for directly ascertained family history. Recent work suggests that only 15–20 % of the risk of T2D associated with parental history is mediated by the combination of common genetic markers associated with diabetes and lifestyle factors including diet and physical activity. We examined whether metabolic risk, as represented by indices of beta-cell function and insulin resistance, could further explain familial T2D risk. We hypothesized that metabolic risk factors substantively mediate T2D risk associated with parental diabetes history.
METHODS: Metabolic risk was estimated using corrected insulin response (CIR, Table 1) to represent beta-cell function, and homeostatic model assessment—insulin resistance (HOMA-IR, Table 1) and a score of 0 to 4 metabolic syndrome components (MSS; one point each for increased waist circumference, elevated systolic or diastolic blood pressure, elevated triglycerides or low high-density lipoprotein, and impaired fasting glucose) to represent insulin resistance. We studied initially non-diabetic participants of the Framingham Offspring Study and tested risk across 0 (n = 1965), 1 (n = 370), or 2 (n = 26) parents with T2D using logistic regression of incident T2D (265 incident cases over median follow-up of 13 years) in models that accounted for sibling correlation and adjusted for age, sex and a count of 62 common T2D genetic risk alleles. The proportion of T2D risk mediated by metabolic factors was estimated by comparing the logistic regression coefficients for parental history with and without adjustments for CIR, HOMA-IR, and MSS (% mediated = 1 − βadj / βunadj).
RESULTS: HOMA-IR and MSS, but not CIR, were statistically significantly correlated with a greater number of parents with T2D at baseline (Table 1). The combination of metabolic risk factors and common T2D genetic risk alleles mediated 18.7 % of incident T2D risk associated with parental history of diabetes, corresponding to a reduction in the odds ratio for incident diabetes from 2.13 to 1.84 per diabetic parent after inclusion of metabolic and genetic covariates (Table 2). After adjusting for genetic risk, metabolic factors mediated 11 % of parental history independent of genetic risk (odds ratio reduction from 1.99 to 1.84; Table 2).
CONCLUSIONS: Similar to prior work examining lifestyle factors and BMI, metabolic factors and genetic risk substantively but partially mediate T2D risk due to family history. A significant proportion of familial T2D risk, however, remains unexplained by metabolic and genetic factors. We conclude that ascertainment of family history remains an important aspect of diabetes risk assessment.
| Parental History | ||||
|---|---|---|---|---|
| None (N = 1965) | Single (N = 370) | Both (N = 26) | p-value | |
| CIR1 | 8.41 (7.60, 9.23) | 8.34 (6.78, 9.90) | 4.47 (−0.48, 9.42) | 0.1718 |
| HOMA-IR2 | 6.79 (6.65, 6.92) | 7.37 (7.07, 7.65) | 7.44 (5.66, 9.21) | 0.0019 |
| Metabolic syndrome score | 1.40 (1.35, 1.46) | 1.59 (1.48, 1.70) | 1.97 (1.59, 2.34) | 0.0016 |
1CIR = Insulin120 / Glucose120*(Glucose120 - 70) [uses 120 min post-oral-glucose challenge values in mg/dL] 2HOMA-IR = Glucose*Insulin / 405 [uses fasting insulin and glucose values in mg/dL]
| Total effect (OR [95 % CI]) | Direct effect (OR [95 % CI]) | Proportion mediated3 (%) | |
|---|---|---|---|
| Mediators: CIR, HOMA-IR, MSS, genetic risk | 2.13 (1.62, 2.79) | 1.84 (1.35, 2.50) | 18.7 |
| 4Mediators: CIR, HOMA-IR, MSS | 1.99 (1.51, 2.63) | 1.84 (1.35, 2.50) | 10.9 |
3proportion mediated = [1 − log ORdirect / log ORtotal] * 100 4Total and direct effects derived from models adjusted for genetic risk
MINDFULNESS BASED COGNITIVE THERAPY VERSUS A HEALTH ENHANCEMENT PROGRAM FOR TREATMENT RESISTANT DEPRESSION: A RANDOMIZED CONTROLLED TRIALMitchell D. Feldman1; Erin P. Gillung2; Kevin Delucchi3; Stuart J. Eisendrath4. 1UCSF, San Francisco, CA; 2UCSF, San Francisco, CA; 3UCSF, San Francisco, CA; 4UCSF, San Francisco, CA. (Tracking ID #1927292)
BACKGROUND: Major depressive disorder (MDD) is the leading cause of disability in the developed world, yet broadly effective treatments remain elusive. Up to 40 % of patients are unresponsive to at least two trials of antidepressant medication and are thus labeled as having treatment-resistant depression (TRD). There is an urgent need for cost-effective, non-pharmacologic, evidence-based treatments for TRD. Prior research has demonstrated that Mindfulness-Based Cognitive Therapy (MBCT) is an effective treatment for major depression, but it has not been previously studied in patients with TRD. MBCT is based on a combination of mindfulness meditation with elements of cognitive behavior therapy. The purpose of this study was to evaluate whether (MBCT) is an effective augmentation of antidepressants for adults with MDD who failed to respond to standard pharmacotherapy.
METHODS: Randomized controlled trial of MBCT versus an active comparator condition, the Health-Enhancement Program (HEP), comprised of physical fitness, nutrition and music therapy. Participants were age 18 years and older with TRD who had failed to respond to two or more antidepressant trials. All participants were taking antidepressants at the time of enrollment. One hundred seventy three participants were recruited from primary care and other settings and randomly assigned to 8 weekly group sessions of MBCT or HEP. Treatment response and depression remission rates were assessed at weeks 4 and follow-up weeks 8, 24, 36 and 52 using the clinician-rated Hamilton Depression Severity Rating Scale (HDRS). HDRS response and remission rates and mean HDRS total scores were compared between treatment conditions using a GEE-based repeated measures model accounting for clustering by cohort. The models included treatment condition, assessment point, and their interaction.
RESULTS: Significant improvement was seen in rates of response (p = <.001), remission (p < .01), severity (p < .001) and percent reduction in severity score (p < .01). No significant differences between treatment groups were found. A significant condition-x-time interaction was observed for both the severity score and percent reduction indicating that the MBCT continued to improve at Week 8 while the improvement in the HEP condition leveled off.
CONCLUSIONS: Both MBCT and HEP produced improvement in patients with treatment-resistant depression over 8 weeks. While the differences between conditions were not statistically significant, differences in course of improvement suggests differences in long-term follow-ups (underway) may be significant.
Clinical Characteristics of Adults with Treatment-Resistant Depression Receiving Mindfulness-Based Cognitive Therapy (MBCT) or the Health Enhancement Program (HEP)
| MBCT (N = 87) | HEP (N = 86) | |||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | ||
| Age at depression onset | 18.8 | 10.9 | 3.5 | 13.2 | ||
| Total # depressive episodes (months) | 3.6 | 2.6 | 78.5 | 2.4 | ||
| Length of current depressive episode (months) | 84.4 | 119.5 | 17.4 | 93.5 | ||
| HAM-D Score | 18.3 | 3.4 | 3.5 | |||
| Single episode (%) | 20.7 | 22.1 | ||||
| ≥3 lifetime episodes | 62.2 | 58.0 | ||||
| Previous treatment for depression (%) | ||||||
| Hospitalization | 16.1 | 18.6 | ||||
| Suicide Attempt | 19.0 | 20.5 | ||||
| Recruitment Source % | ||||||
| GIM | 34.5 | 36.1 | ||||
| Psychiatry Clinic | 43.7 | 39.5 | ||||
| Community | 24.4 | 24.4 | ||||
HAM-D = Hamilton Depression Rating Scale
Depression Outcomes over Time for Adults with Treatment-Resistant Depression Receiving Mindfulness-Based Cognitive Therapy (MBCT) or the Health Enhancement Program (HEP)
| MBCT Group (N = 87) | HEP Group (N = 86) | |
|---|---|---|
| Outcome Variable | Mean ± SD | Mean ± SD |
| HAM-D Mean Score | ||
| Baseline | 18.3 ± 3.4 | 17.4 ± 3.5 |
| Week 4 | 13.8 ± 4.7 | 12.8 ± 4.3 |
| Week 8 | 11.4 ± 4.9 | 12.5 ± 5.0 |
| HAM-D Percent Reduction | ||
| Week 4 | 0.23 ± 0.20 | 0 .24 ± 0.24 |
| Week 8 | 0.36 ± .25 | 0.25 ± 0.27 |
HAM-D = Hamilton Depression Rating Scale. Reduction rates were calculated as mean percent change from baseline to weeks 4 and 8.
MISSED OPPORTUNITIES: A THOROUGH CHART REVIEW OF NEWLY DIAGNOSED HIV POSITIVE PATIENTS IDENTIFIED THROUGH ROUTINE SCREENING IN THE PRIMARY CARE SETTINGNatasha Travis; Jennifer Spicer; Heather Freiman. Emory University, Atlanta, GA. (Tracking ID #1938902)
BACKGROUND: In 2006, the Centers for Disease Control and Prevention (CDC) recommended routine one-time HIV screening for everyone aged 13 to 64 years in healthcare settings. However, these recommendations have not been widely adopted and missed opportunities for HIV diagnosis continue to exist. The objectives of this analysis were to describe the characteristics of newly diagnosed HIV-infected patients identified through a routine HIV screening program and to determine whether missed opportunities for earlier diagnosis still exist in the era of routine HIV screening.
METHODS: In July 2013, a routine HIV screening program was instituted in the primary care center of an inner-city hospital located in a high HIV prevalence area in the South. All newly diagnosed HIV-infected patients were identified and a retrospective chart review was performed to describe patient demographics, CD4 count at diagnosis, previous HIV tests and results, prior access of the healthcare system, and any indications for earlier HIV testing.
RESULTS: In the first 6 months of the screening program (July–December 2013), 2,814 patients were tested for HIV. There were 20 patients with reactive HIV antibody tests: 14 patients were confirmed to be HIV positive via Western Blot and 5 patients were false positive (0.18 %). Eight of the fourteen HIV positive patients were newly diagnosed HIV positive (0.28 % new positive diagnosis), and a chart review was conducted for those eight patients. All newly diagnosed HIV patients were African American and six (75.0 %) were female. The average age at diagnosis was 48 years (range: 33–59 years). Five patients (62.5 %) were diagnosed during a routine office visit and had no HIV-related symptoms. Four patients (50.0 %) had at least one previous negative HIV test (range: 2–5 tests), and the mean number of months since most recent negative HIV test was 28 months (range: 13–37 months). All patients had healthcare visits in the emergency or primary care center within the previous 19 months yet had not been screened for HIV. Two (25.0 %) of the patients had no obvious risk-based indication for an HIV test observed in the medical chart. The mean CD4 count of the patients with a previous negative HIV test was 437 cells/uL (range: 332–542 cells/uL) versus 86 cells/uL (range: 64–107 cells/uL) for those with no previous HIV test.
CONCLUSIONS: All patients newly diagnosed with HIV through our primary care HIV screening program had been seen in our healthcare system within 19 months prior to diagnosis, but only half had a previous HIV test documented despite the 2006 CDC recommendation for routine screening. Half of the patients had at least one previous negative HIV test indicating that repeat HIV screening is likely needed to identify all patients with HIV; however, more studies are needed to determine the appropriate time interval for repeat testing to make it cost-effective. The average CD4 count for patients who had a previous negative HIV test was significantly higher than those with no previous HIV test indicating that repeat HIV screening is effective at detecting HIV at an earlier stage.
MISTRUST, MISPERCEPTIONS, AND MISCOMMUNICATION: A QUALITATIVE STUDY OF PREFERENCES ABOUT KIDNEY TRANSPLANTATION AMONG AFRICAN-AMERICANSMelissa W. Wachterman1,2; Ellen P. McCarthy3,4; Edward R. Marcantonio3,5; Mary Ersek6,7. 1VA Boston Healthcare System, Jamaica Plain, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Harvard Medical School, Boston, MA; 5Beth Israel Deaconess Medical Center, Boston, MA; 6School of Nursing, Philadelphia, PA; 7Philadelphia VA Medical Center, Philadelphia, PA. (Tracking ID #1939528)
BACKGROUND: There are significant racial differences in the rates of kidney transplantation in the United States, with lower rates among African-Americans with end-stage renal disease (ESRD) than among Whites. Well-documented racial disparities in access to transplantation explain only some of these differences, and prior survey-based research found that African-American dialysis patients are also less likely than Whites to desire transplantation. Our primary objective was to explore African-American dialysis patients’ preferences about kidney transplantation. A secondary objective was to compare patients’ expectations about transplantation with their actual status on the transplant list.
METHODS: We conducted semi-structured interviews with African-American patients receiving chronic hemodialysis (HD) at one urban dialysis center. We asked patients about their preferences about transplantation, experience with the transplant evaluation process, and sense of transplant candidacy. After the interview, we reviewed the transplant list to determine which patients were listed for transplant. We analyzed the interviews using the constant comparative method of qualitative data analysis. Transcripts were coded independently by two investigators and consensus on dominant themes was achieved. Interviews were conducted until thematic saturation.
RESULTS: We interviewed 16 African-American patients (63 % men, median age 52.5, median time since HD initiation 2.8 years). From our semi-structured interviews about kidney transplantation, six major themes were identified: 1) Varied patient preferences—transplant was central goal for some, while others were ambivalent or uninterested because they feared transplant rejection or did not find dialysis burdensome. 2) Mistrust of organ allocation system—including specific concerns with inequities in the quality of cadaveric kidneys. 3) Fear of risking a living donor’s health. 4) Barriers to transplantation—most commonly the extensive pre-transplant evaluation, which some felt exists as an intentional barrier to transplantation. 5) “God will heal my kidneys”—led to denial of need for transplantation. 6) Fear that they might assume the donor’s personality. Only two of the 16 participants were active on the transplant list, and, in five cases, the patient’s understanding of his/her listing status was discordant with actual status on the transplant list.
CONCLUSIONS: African-American HD patients have nuanced beliefs and preferences about kidney transplantation. Religious faith, concerns about risking a living donor’s health, and the feeling that dialysis is not burdensome play a role in preferences against transplantation. The misperception that a transplant recipient can take on the personality of the donor is a particularly unexpected finding. However, the strongest underlying theme is mistrust of the allocation process. Thus, addressing both racial disparities in access and lack of trust in the system are critical to affecting preferences. The discordance between patients’ perceptions of status on the transplant list and actual status also suggests important gaps in communication between African-American HD patients and their nephrologists. Additional research should be focused on validating these findings in a larger, geographically-diverse sample and examining factors that influence the development and maintenance of these beliefs and preferences.
MONEY NOT WELL SPENT: ALCOHOL-RELATED HOSPITALIZATIONS IN HOUSED AND HOMELESS PATIENTS AT A PUBLIC HOSPITALTimothy Poore1,2; Rachel Heidt2; Jeffrey A. Tice1; William Huen2. 1University of California at San Francisco, San Francisco, CA; 2San Francisco General Hospital, San Francisco, CA. (Tracking ID #1934291)
BACKGROUND: Alcohol is a well-known cause of morbidity and mortality worldwide. In the United States, there are approximately 80,000 alcohol-related deaths and $223.5 billion in healthcare costs annually. This burden disproportionately affects the homeless, with alcoholism affecting up to 73 % of homeless adults. This study aims to better characterize alcohol-related hospitalizations at San Francisco General Hospital (SFGH), comparing homeless and housed patients on service use, hospitalization costs, and frequency of specific alcohol-related diagnoses.
METHODS: This descriptive study analyzed hospitalization data from SFGH between January 1, 2009 and December 31, 2012. We extracted demographic and service use data from the University Health Consortium Database and the SFGH Electronic Medical Record. We included all patients discharged with an alcohol-related primary diagnosis using ICD-9 codes.
RESULTS: During the study period, there were a total of 1345 hospitalizations of 901 patients (560 housed, 325 homeless, and 16 unknown) with primary alcohol-related diagnoses. Of those patients, 56 % were white, 23 % Hispanic, and 11 % black. Males made up 86 % of the population, and the average age was 48 years (range 14 to 84). The most common diagnosis was alcohol withdrawal (67 %), followed by alcoholic liver cirrhosis and acute alcoholic hepatitis. Ten percent of the patients accounted for 40 % of the costs. Average cost per patient was higher in the homeless than the housed ($20,068 versus $16,018, p = 0.0015), with homeless patients having more admissions during the study period (1.72 versus 1.37 admissions, p = 0.0002). Days in the ICU, length of stay, and cost per visit did not differ significantly between the two groups (p = .023, 0.13, and 0.49 respectively).
CONCLUSIONS: Among patients discharged from SFGH with a primary alcohol-related diagnosis, alcohol withdrawal was the most common diagnosis, and homeless patients cost significantly more than housed patients. Interventions focused on reducing alcohol withdrawal admissions in the homeless could significantly reduce alcohol-related costs at SFGH.
MONITORING DKA & HHS WITH URINE DIPSTICK: A STICKY SITUATIONAlan Hathcock1; Suneeta Ganji2; Ishani Pathmanathan1; Helene Hedian3; Anjali Niyogi1. 1Tulane Medical Center, New Orleans, LA; 2George Washington University, Washington, DC; 3University of Maryland, Baltimore, MD. (Tracking ID #1897136)
BACKGROUND: Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are major causes of morbidity and mortality worldwide. Standard treatment protocols require serum blood glucose monitoring that is relatively expensive and largely unavailable in resource-limited settings. Thus, urine glucose is at times substituted in these situations to monitor and treat patients with DKA and HHS. There has yet to be a study looking at the use of urine glucose and its association to serum glucose in the setting of DKA/HHS.
METHODS: We designed a prospective observational study of patients with DKA or HHS presenting to a single academic center emergency department. After consent and foley placement, serum electrolytes, urine glucose and ketones were obtained at 4-hour intervals until blood glucose was less than or equal to 250 mg/dL or time elapsed greater than 8 hours.
RESULTS: Thirteen patients were enrolled over 1 year, 8 with DKA and 5 with HHS. A total of 40 urine samples were collected. Urine glucose greater than 250 mg/dL was associated with serum glucose greater than 250 mg/dL in 10 of 13 patients (77 %) and in 27 of 30 total samples (90 %). Stratifying for patients with HHS, this relationship was associated in 100 % of samples. Three patients with DKA had urine glucose greater than 250 mg/dL but serum glucose less than 250 mg/dL, representing 10 % of the total samples of urine glucose greater than 250 mg/dL (3 of 30). Urine glucose greater than or equal to 500 mg/dL predicted serum glucose greater than 250 mg/dL in 11 of 13 patients (85 %) and 27 of 29 total samples (93 %). Urine glucose greater than 1000 mg/dL was associated with serum glucose greater than 250 mg/dL in all 13 patients (100 %) and 25 of 26 samples (96 %). Urine glucose less than or equal to 100 mg/dL was associated with serum glucose less than 250 mg/dL in all patients (n = 8). Of note, serum glucose greater than 250 mg/dL was associated with urine glucose greater than or equal to 250 mg/dL in all patients and samples (100 %). High urine glucose (>250 mg/dL) variably predicted high serum glucose (>250 mg/dL) but was accurate approximately 90 % of the time in patients with DKA and 100 % of time in patients with HHS. Moreover, very high (>1000 mg/dL) and very low (≤100 mg/dL) urine glucose were more consistently associated with high and low serum values, respectively.
CONCLUSIONS: Serum and urine glucose appear positively associated at high levels of serum glucose but without a clear pattern. If this trend is corroborated by future studies, urine glucose greater than 250 mg/dL in DKA/HHS likely predicts serum glucose over 250 mg/dL, thus indicating further insulin and fluid administration. This appears especially applicable for patients’ with HHS. Likewise, urine glucose less than 100 mg/dL may signal an endpoint for aggressive insulin administration. In non resource-limited settings, serum blood glucose measurements should still be considered the standard of care for treatment of DKA/HHS.
MULTIPLE TOBACCO PRODUCT USE AMONG YOUNG ADULT BAR PATRONSSara Kalkhoran1; Pamela M. Ling1,2. 1University of California, San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1937807)
BACKGROUND: Use of non-cigarette tobacco products (e.g., hookah, cigarillos, smokeless tobacco, snus) is common and e-cigarette use is increasing among young adults. We aimed to identify what additional tobacco products young adult bar patrons use with cigarettes, and to describe multiple product users.
METHODS: We collected 4,067 cross-sectional surveys from young adults aged 18–26 in bars in Albuquerque, New Mexico using randomized time-location sampling between 2009 and 2013 as part of an evaluation of an intervention to reduce cigarette use among young adults (N = 1066 in 2009–2010, 720 in 2010–2011, 1136 in 2011–2012, and 1145 in 2012–2013). Participants reported past 30-day use of cigarettes, snus, dip, cigarillos, hookah, and electronic cigarettes (not all products were reported in each year of the survey), demographics, and tobacco-related attitudes. Chi-squared tests were used to determine changes in product consumption during the 4 years, and logistic regression was used to determine predictors of poly-use (i.e. use of cigarettes and at least one other tobacco product in the past 30 days) in the pooled sample.
RESULTS: The percentage of study participants reporting cigarette smoking decreased from 47.5 % in 2009 to 37.4 % in 2013 (p = <0.001). The overall rates of poly-use were 56.5 % for non-daily (smoked on 1–24 of the past 30 days, N = 945) and 56.2 % for daily smokers (smoked on 25–30 of the past 30 days, N = 527), which were not significantly different. Among all poly-users, use of e-cigarettes increased from 42.1 % in 2011–2012 to 71 % in 2012–2013, while use of other tobacco products decreased during the time of study. Poly-users most frequently reported using e-cigarettes and hookah (65.8 %), followed by cigarillos (35.7 %), dip (31.6 %), and snus (19.7 %) in 2013. Figure 1 shows the percentage of product use among poly-users who are non-daily cigarette smokers and Figure 2 shows the percentage of product use among poly-users who are daily smokers. The odds of being a poly-user (versus a cigarette-only user) were higher in those who were younger (OR = 3.2, 95%CI [2.1–4.7]), less educated (1.9, [1.4–2.6]), and male (2.5, [2.0–3.1]). Those who reported at least one episode of binge drinking in the preceding 30 days also had greater odds of being a poly-user (1.9, [1.5–2.4]).
CONCLUSIONS: Poly-tobacco use is frequent among young adult bar patrons in Albuquerque, New Mexico, where the majority of cigarette smokers reported currently using at least one other tobacco product. While we observed a decrease in cigarette smoking (which may have been due to the anti-smoking intervention taking place during the study), the use of e-cigarettes increased significantly, exceeding use of hookah, snus, dip, and cigarillos among poly-users in 2013. Clinicians seeing young adult patients should assess use of other tobacco products in addition to cigarettes, particularly e-cigarettes.
NATURAL EXPERIMENT TO EVALUATE PATIENT CENTERED MEDICAL HOME INTERVENTION ON DIABETES OUTCOMESEdwin Young1; Naa-Abia Casely-Hayford1; Nancy Sohler2; Brenda Matti - Orozco1; Jeanine Albu1. 1Mount Sinai Health System, New York, NY; 2City University of New York, New York, NY. (Tracking ID #1941683)
BACKGROUND: The patient-centered medical home (PCMH) emphasizes care coordination and communication. Among the tools for care coordination, registries of high risk patients enable PCMH practices to efficiently use rare resources, such as certified diabetes educators (CDE) and endocrinologists. However, it is often difficult to identify those interventions that produce meaningful outcomes. In this study, we used a natural experiment, comparing two clinics in which PCMH was implemented at different times, to evaluate the effect of the PCMH on diabetes outcomes. Our hypothesis was that the mean A1C would be reduced in the PCMH clinic.
METHODS: We compared two clinics in New York City. In Clinic 1, the treatment group, a PCMH approach was implemented in July 2011 with 580 diabetics. The PCMH used registries of patients with A1C greater than 9, and monthly meetings with providers, staff and CDEs to develop individualized patient improvement plans. In Clinic 2, standard care was provided to 303 diabetics. The following data was obtained from the Electronic Health Record (eClinicalworks) for each patient: Clinic Facility, Date of Birth, Gender, Language, Race, Ethnicity, Encounter Date, A1C Value, BMI, and Assessments at each visit (from which was calculated a Carlson Index of comorbid diseases). Results were analyzed using R statistical software. Missing data was imputed to the mean or the mode for each variable, for continuous and categorical variables respectively. We included a flag for missingness as a variable. Propensity for being in the treatment group was calculated for each patient using age, gender, language, race, ethnicity, BMI, Carlson Index and missingness. The mean A1C values were weighted using the Inverse Propensity for Treatment. The weighted mean A1C for each patient in the first 6 months was compared to the weighted mean A1C in the second 6 months of 2011. To illustrate the effect of the intervention in the treatment clinic, we displayed the data as a time series, interrupted at the time of the intervention, with regression lines before and after.
RESULTS: The overall change in weighted mean A1C for clinic 1 was −0.2709455; for clinic 2, −0.4830450, p-value = 0.2298. Alternative hypothesis: true difference in means is not equal to 0; 95 % confidence interval: −0.1346132 0.5588123. For only those patients whose A1C in the first 6 months was above 9, the change in weighted mean A1C for clinic 1 was −1.6139261; for clinic 2, −0.4496943, p-value = 0.01523. Alternative hypothesis: true difference in means is not equal to 0; 95 % confidence interval: −2.0981380–0.2303256.
CONCLUSIONS: For the general diabetic patients in our study, being affiliated with a PCMH did not significantly affect the mean A1C value. But, for those patients with a mean A1C above 9, our model of the PCMH produced significant benefits. This is consistent with the intervention, which was targeted at patients with A1C above 9. Natural experiments analyzed using Inverse Probability of Treatment Weighted (IPTW) outcomes and interupted time series can identify those interventions that produce significant improvements in selected patient populations.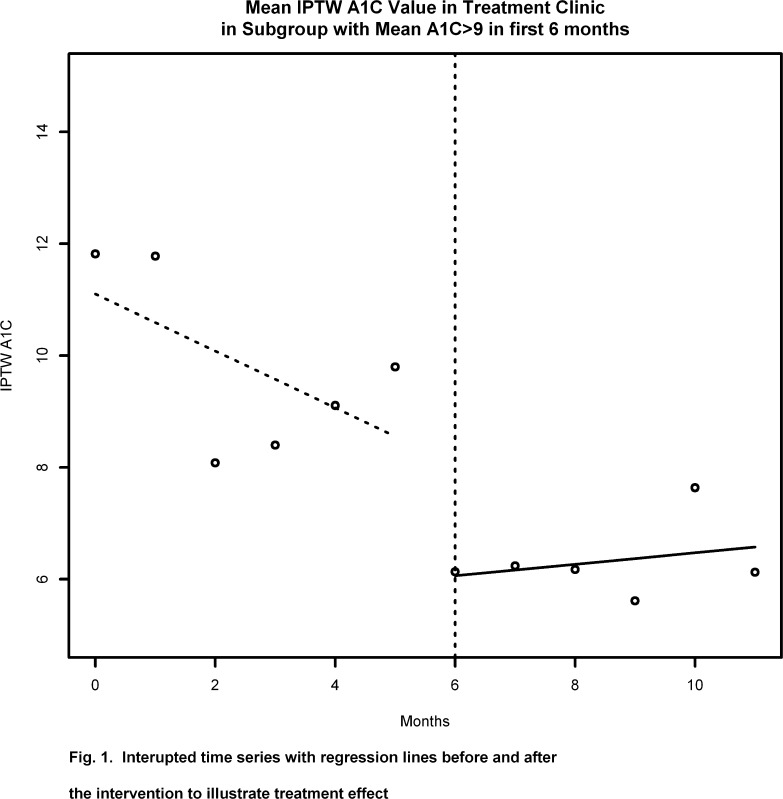
NEGOTIATING EMERGENCY DEPARTMENT ADMISSION HANDOFFS: EXPERIENCES, BELIEFS, AND PERCEPTIONS OF ADMITTING AND EMERGENCY PHYSICIANSChristopher J. Smith; Denise H. Britigan; Nathan Anderson; Elizabeth Lyden; Tedd Welniak; Michael C. Wadman. University of Nebraska Medical Center, Omaha, NE. (Tracking ID #1936119)
BACKGROUND: Transfer of care between healthcare providers is a vulnerable time for patient safety, and ED admission handoffs are subject to unique structural and contextual challenges. The ED admission process involves changes in provider, department, and physical location. It also occurs early in a patient’s evaluation when the clinical trajectory is uncertain. Despite these challenges, there is relatively little research on ED admission handoffs. To better understand the barriers to effective handoff communication, we surveyed admitting and emergency physicians about their experiences, beliefs, and perceptions.
METHODS: A cross-sectional survey was conducted at a 627-bed tertiary-care teaching hospital. Questions were created to examine five domains: clinical content, interpersonal perceptions, expectations, organizational factors, and patient safety. Surveys were distributed to residents, fellows, and faculty physicians from emergency medicine (EM) and six medical admitting services, which account for two-thirds of ED admissions. Data was analyzed using SPSS software. Fisher’s Exact Test was used to compare dichotomized responses between EM and admitting physicians. Non-dichotomized distribution was analyzed using the Mann-Whitney Test. Examples of adverse outcomes related to handoff were categorized independently by two physicians with disagreements settled by consensus. Based on preliminary survey results, a supplemental study was designed to determine the frequency in which 8 pieces of handoff information were communicated: working diagnosis, relevant past medical history, relevant physical exam findings, results of relevant diagnostic studies, therapeutic interventions initiated, trend in the patient’s clinical condition, patient’s clinical condition at the time of handoff, and pending diagnostic studies. Prospective data was collected by a hospitalist immediately following oral handoff and was documented as communicated without prompting, communicated with prompting, or not communicated.
RESULTS: A total of 117 admitting (67 %) and 32 EM (86 %) physicians completed the survey. There was significant disagreement between EM and admitting physicians across multiple domains. Admitting physicians reported communication of clinical information occurred less frequently than EM physicians (p-value <0.05 for all eight content areas). Nearly all EM physicians felt they had to defend their decisions and face-to-face communication was rare. Sixty-three percent of respondents could not identify who was responsible for patients “boarding” in the ED. Competing clinical duties frequently distracted physicians during handoff, but environmental factors more commonly distracted EM physicians (p = 0.007). Sequential handoffs occurred regularly and were felt to have negative impact on patient care. Adverse outcomes related to handoff communication were reported by 30 % of respondents, most of whom reported multiple events. Thirty examples of adverse events were reported. Final categorization is under way, but errors in communication, assignment of responsibility, and boarding were common. Prospective data from 89 admission handoffs were collected. The frequency in which specific clinical information was communicated varied from 35 to 95 % and prompting from the admitting physician was common (73 % of admissions). The content areas least frequently communicated were treatments initiated in the ED (71.9 %), trend in the patient’s clinical condition (57.3 %), and pending studies (34.8 %).
CONCLUSIONS: These results highlight several barriers to the safe transfer of patients from the ED. Admitting and EM physicians had vastly different perceptions about communication of clinical information, although most information was communicated regularly. Inter-disciplinary biases, differing expectations, and egocentric anchoring likely play a role in this discrepancy. The frequency of prompting during handoff suggests that dialogue between EM and admitting physicians was common, but lack of standardized communication may have also contributed. In addition to inconsistent transfer of information, handoffs were further compromised by sequential handoffs, lack of face-to-face communication, distractions, and lack of clearly delineated responsibilities. These results demonstrate the complex interplay of factors that impact admission handoffs. Successful improvement efforts will need to address the dynamic quality of content, institutional culture and policies, environment, and organizational factors. Collaborative interventions may include interdisciplinary team-building, expanded handoff training, implementation of bedside handoffs, and better leveraging of the electronic health record.
NEW YORK CITY GREEN CARTS: IS THE PROGRAM ALLEVIATING FOOD DESERTS?Kathleen Y. Li1,2; Ashley Fox2; Ellen K. Cromley3,4; Carol Horowitz2. 1University of California, San Francisco School of Medicine, San Francisco, CA; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3University of Connecticut School of Medicine, Farmington, CT; 4Lund University, Lund, Sweden. (Tracking ID #1936558)
BACKGROUND: As the proportion of overweight and obesity nears 70 % in the United States, local public health departments are using their authority to implement programs to tackle this growing epidemic. Limited access to fresh fruits and vegetables in low-income neighborhoods is believed to contribute to high rates of obesity. To address the high rates of obesity and related illnesses in its low-income neighborhoods, in 2008, New York City established a fruit and vegetable street vendor program (NYC Green Carts) to promote healthier eating in neighborhoods with the lowest reported rates of fruit and vegetable consumption. Carts are free to move anywhere within designated neighborhoods, which can be large and often border wealthier neighborhoods. We aimed to study whether carts locate in areas that enable them to reach the low-income “food desert” populations they were designed to serve.
METHODS: We obtained a list of Green Cart locations from the New York City Department of Health and information on census tract level demographic and food environment data from the census bureau and Esri Business Analyst Desktop. We identified “healthy” food stores, namely supermarkets, independent grocers, and fruit and vegetable specialty stores according to North American Industry Classification System codes as well as bodegas with evidence of selling fresh produce on Google Maps Street View. We then defined a food desert as a lack of healthy food stores within a ¼ mile. Using ArcGIS software, we mapped the existing Green Carts and generated a list of potential Green Cart locations. Within designated Green Cart areas, the intersection closest to the geographic center of each census tract without a Green Cart was coded as a candidate site. We then analyzed census tract characteristics for actual and candidate Green Carts to determine how they differed with regards to population, income, percent below the poverty level, distance to subway stops, the number of large employers, and the number of healthy food stores at both a ¼-mile and ½-mile distance from each location.
RESULTS: Our team identified 265 Green Carts and 644 candidate locations without Carts. As compared with potential Green Carts sites (see table), Green Carts were significantly more likely to be within a quarter of a mile of supermarkets, grocery and fruit & vegetable stores. Over 1/3 of candidate intersections with no Green Carts were situated in food deserts compared to fewer than 1/10 of Green Carts. Green Carts were positioned in tracts with significantly larger population sizes, tended to be closer to a subway stop, and were more likely to be within a ¼ mile of large employers, though Green Cart tracts had a lower median family income compared to tracts with candidate sites. Some (22) Green Carts were located outside the officially designated Green Cart areas, and these census tracts had significantly higher income and higher access to fruits and vegetables than those within Green Cart boundaries.
CONCLUSIONS: Compared with potential Green Cart locations, census tracts with Carts tended to be located in areas with large numbers of potential customers, namely population centers and areas with more pedestrian traffic (close to subway stops and large businesses), perhaps to increase market share and profitability. However, Green Carts were rarely situated in food deserts. This suggests that many already underserved neighborhoods are still not reached by this initiative. A market-driven imperative to locate near larger numbers of potential customers may be in tension with the objective of the Green Carts program to increase access to fresh fruits and vegetables in regions with lower access to supermarkets and fresh produce. However, we also identified a number of candidate locations where foot traffic is likely to be high but where Green Carts were not located. Since people usually shop close to where they live, the Green Carts program should consider introducing added incentives for Green Cart vendors to locate in high need census tracts to ensure adequate coverage of actual food deserts.
Table. Average Characteristics of Green Cart vs Candidate Sites
| Variable | Green Cart Site | Candidate Site | p value |
|---|---|---|---|
| Tract population | 5,004 | 3,706 | <0.00001 |
| Tract median income | $37,213 | $42,740 | 0.000284 |
| Percent of tract below poverty level | 30.1 % | 25.6 % | <0.00001 |
| Distance to nearest subway stop (ft) | 793 | 3,079 | <0.00001 |
| # large employers within ¼ mi | 0.457 | 0.085 | <0.00001 |
| # supermarkets within ¼ mi | 1.6 | 0.81 | <0.00001 |
| # other stores carrying fruits and vegetables within ¼ mi | 2.09 | 0.84 | <0.00001 |
| # large employers within ½ mi | 1.185 | 0.402 | <0.00001 |
| # supermarkets within ½ mi | 4.72 | 2.86 | <0.00001 |
| # other stores carrying fruits and vegetables within ½ mi | 5.4 | 3.1 | <0.00001 |
NONINVASIVE MECHANICAL VENTILATION USE IN THE ELDERLY: APPROPRIATENESS OF THERAPY, ADEQUACY OF ASSESSMENT, AND EVENTUAL OUTCOMESTarak Rambhatla; Adam Bierzynski. Lenox Hill Hospital, New York, NY. (Tracking ID #1934152)
BACKGROUND: NIPPV has long been shown to be an effective therapy in selected patients with acute respiratory failure as an alternative to endotracheal intubation. Many studies have been done to assess predictors of failure for this therapy, but our search of the literature did not show any studies that assessed the efficacy and application of NIPPV therapy specifically in the elderly. As this population is the most likely to present with acute respiratory failure, it is important to know how effective NIPPV therapy is in this group and whether it is being used appropriately. Our objective is to analyze the appropriateness of the application of non-invasive positive pressure ventilation (NIPPV) at our institution, by comparing patient selection for NIPPV and the difference in outcomes between the elderly and younger patient populations.
METHODS: Retrospective study of all NIPPV ordered for medical patients over a two-month period at a single center university-affiliated teaching hospital. One hundred twenty-seven patients ordered for NIPPV identified by respiratory therapy records and a retrospective chart review with the use of MAR to collect data on each patient prior to and during the course NIPPV therapy.
RESULTS: Group 1 was defined as elderly with ages 70 years or older and group 0 below 70. Chronic obstructive pulmonary disease and congestive heart failure accounted for less than 50 % of admission diagnoses in either group. There was no significant difference in echocardiographic evaluation (63 % vs. 57.4 %, p = 0.586), or cardiac function (19.7 % vs. 11.5 %, p = 0.429). 59.1 % of the elderly group had an arterial blood gas (abg) performed prior to ordering NIPPV (vs. 32.8 %, p = 0.003). There was no significant difference in acid-base status amongst the groups nor was there a significant difference in patients that had a repeat abg while being treated with NIPPV (30.3 % vs. 23.0 %, p = 0.424). Group 1 had NIPPV therapy ordered for a longer duration of time (5.82 days vs. 4.95 days, p = 0.045) and total length of use was longer (5.38 days vs. 4.61 days, p = 0.06). Group 1 was more likely to have a pulmonary infiltrate (66.7 % vs. 45.9 %, p = 0.021) and more likely to be treated with antibiotics (72.7 % vs. 47.5 %, p = 0.006). The elderly population had 13 patients that required escalation of care while 4 patients in the younger population required an escalation of care (19.7 % vs. 6.6 %, p = 0.026).
CONCLUSIONS: We found NIPPV was consistently being ordered for conditions not proven to benefit from NIPPV and there was an inadequate assessment of oxygenation/ventilation status prior to and during the course of NIPPV therapy for all ages. We also found the elderly population, despite not showing a significant difference in cardiac function or oxygenation/ventilation status were being treated with NIPPV for longer periods of time, had more lung infiltrates, use of antibiotics, and had more patients requiring escalation of care. Further investigation into NIPPV use in elderly patients may help identify which factors predict an adverse outcome in this patient population.
| Group 1 (70 years or older) | Group 2 (less than 70 years) | |
|---|---|---|
| Duration NIPPV ordered (days) | 5.82 | 4.95 (p = 0.045) |
| Length of use of NIPPV (days) | 5.38 | 4.61 (P = 0.06) |
| Patients with pulmonary infiltrate (%) | 66.7 | 45.9 (p = 0.021) |
| Patients being treated with antibiotics (%) | 72.7 | 47.5 (p = 0.006) |
| Patients requiring escalation of care (%) | 13 | 4 (p = 0.026) |
NOT ALL INTERNS ARE CREATED EQUAL: UNDERSTANDING MEDICAL SCHOOL EXPERIENCES PRIOR TO STARTING INTERNAL MEDICINE RESIDENCY TRAININGLuke Cunningham; Chirayu Shah; Steffanie Campbell; Anoop Agrawal; Kaushal Patel; Nainesh Shah; Prathit Kulkarni; Richard J. Hamill. Baylor College of Medicine, Houston, TX. (Tracking ID #1941642)
BACKGROUND: As new residents start their Internal Medicine training in July, many studies have raised concerns about patient safety associated with inexperienced residents, also termed the “July effect.” The clinical experiences and curriculum to prepare graduating medical students for internship can vary between medical schools. The purpose of this study was to characterize medical school training in skills required for incoming Internal Medicine interns to provide safe patient care.
METHODS: Prior to Internal Medicine orientation at Baylor College of Medicine, 44 categorical interns, 16 preliminary interns, and 8 medicine-pediatric interns (total of 68 interns) were sent a survey to complete about their training and skills during medical school.
RESULTS: The response rate for the survey was 100 % (68/68). Of the 68 interns, only 53 % had participated in a fourth year medical school course geared towards preparing for intern year. Of the 29 medical schools represented within the intern class, 12 (41 %) offered an internship preparation course. There were 26 interns (38.2 %) that never worked an overnight shift or taken overnight call during their Internal Medicine rotations. Only 35 % of interns reported any formal training about patient handoffs. Forty-four interns (64.7 %) reported no experience in providing cross coverage for patients not admitted to them. In terms of procedural experience, 15 % had performed a thoracentesis, 31 % had placed a central line, 47 % had performed a paracentesis, 48 % had done an arterial blood gas, 81 % had placed peripheral IV access, and 88 % had drawn blood. In addition, 66 % of interns had participated in a live code blue situation. When asked about intern orientation, 98.5 % expected to learn about their clinical responsibilities and 97.1 % expected training in skills needed for intern year.
CONCLUSIONS: There is significant variability in the experience and skills of interns starting their residency training in Internal Medicine. Although internship preparation courses during the end of medical school training may play a role in improving intern skills, these courses are not available across all medical schools. The results of this study suggest that incoming interns may not be adequately prepared for starting residency training. Incoming interns expect some skills training during their orientation. With the adoption of Internal Medicine residency milestones, residency programs need to invest in a training curriculum and milestone-based evaluations for incoming interns prior to starting their clinical duties.
OBESITY IN PRIMARY CARE: KNOWLEDGE OF HEALTH RISKS AND DESIRE TO LOSE WEIGHTKatherine H. Saunders; Erica Phillips; Keith Roach. NewYork-Presbyterian Hospital, New York, NY. (Tracking ID #1928350)
BACKGROUND: Research has shown that many patients do not accurately classify their weight status category. This misperception is a strong predictor of weight loss attitudes and behavior. In addition, most obese and overweight patients have been diagnosed with at least one obesity-associated health condition; however, there has been limited data on patients’ knowledge of which medical conditions are linked to obesity. This study evaluates patients’ perception of their weight category, their awareness of the impact of obesity on a variety of health conditions, and their desire and action to lose weight.
METHODS: Through an anonymous questionnaire, adult patients were surveyed using convenience sampling at a hospital-based primary care practice staffed by attendings and residents. Surveys were distributed in the waiting room on different days of the week, at different times of day. Participation was voluntary and no incentive was provided.
RESULTS: Of 904 patients approached, 652 (72 %; 65.6 % female, 34.3 % male, mean age 53.0 years, range 18–91 years) completed the questionnaire. The mean self-reported BMI (calculated from self-reported height and weight) was 28.4 (range 12.8–66.1, 8.0 % obese, 42.0 % overweight, 37.6 % normal weight). Only 43.3 % of self-reported obese or overweight participants consider their weight to be a health problem and only 30.9 % recall a that a physician or health professional told them in the past year that they were obese or overweight. The most commonly diagnosed health condition was hypertension (41.7 % of participants) followed by dyslipidemia (39.8 %), asthma (22.0 %), osteoarthritis (21.6 %) and type 2 diabetes (20.6 %). Approximately 85 % of participants cited hypertension, dyslipidemia and type 2 diabetes as obesity-related health conditions, whereas only 69.7 % and 56.0 % cited osteoarthritis and asthma respectively as conditions related to obesity. Interestingly, 68.2 % of all participants would like to weight less and 64.7 % have tried to lose weight or taken action to prevent gaining weight during the past year.
CONCLUSIONS: Preliminary findings indicate that 85 % of participants are able to associate common health conditions to obesity yet only 43 % of obese and overweight participants consider their weight to be a health problem for themselves and only 30 % recall a healthcare professional addressing their obesity/overweight. Furthermore, almost 70 % of participants would like to weigh less despite only 50 % of patients considering themselves obese or overweight. Based on these initial data, there appear to be motivating factors other than health driving patients’ desire to lose weight. Future research should focus on identifying these other factors motivating weight loss as well as training healthcare professionals to counsel patients accordingly. Finally, the healthcare community should place more of an emphasis on the association between health risks and weight status on an individual level.
OBESITY, DISORDERED EATING BEHAVIORS, AND DIFFICULTY MAKING DIETARY CHANGES AMONG PRIMARY CARE PATIENTS WITH MODERATE TO SEVERE OBESITYSara A. Chacko1,2; Sarah N. Chiodi1,2; Christina C. Wee1,2. 1Beth Israel Deaconess Medical Center, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1935987)
BACKGROUND: Disordered eating behaviors are prevalent among obese patients seeking weight loss treatment and may impact their ability to make clinically recommended dietary changes. However, few studies have characterized these behaviors among obese patients in primary care or whether these behaviors adversely impact patients’ ability to lose weight. Therefore, we aimed to determine the prevalence of disordered eating behaviors in primary care patients with obesity and identify patients at risk. We also examined how eating behaviors are related to patients’ reported difficulty with making dietary changes.
METHODS: We interviewed by telephone 337 primary care patients (58 % response rate) with BMI > 35 kg/m2 at 4 diverse primary care clinics in Greater-Boston. We measured cognitive restraint, uncontrolled eating, and emotional eating using the Three-Factor Eating Questionnaire R-18 (TFEQ-R18) (Scores 0–100). We characterized scores >50 as “high” indicating that respondents answered ‘definitely true’ or ‘mostly true’ more than 50 % of the time in response to a series of maladaptive eating behaviors. We measured dietary self-efficacy using four questions assessing difficulty in making dietary changes (Scores 0–10). Respondents were asked to rate on a scale of 0–10, where 0 is not at all difficult and 10 is extremely difficult, how difficult it is to limit the portion size, total amount of calories, fat in diet, and the amount of carbohydrates in food. We categorized scores ≥7 as “high difficulty” in making dietary changes. We developed multivariable-adjusted models to examine the relationship between disordered eating and difficulty making dietary changes. Models were adjusted for age, race, sex, education, study site, and BMI.
RESULTS: 49.2 % of patients reported scores >50 for emotional eating (mean = 48.0); 27.9 % reported scores >50 for uncontrolled eating (mean = 37.6). After adjustment, women reported significantly higher scores on emotional eating [β = 18.55 ± 3.91 (p < 0.0001)] than men. Compared to Caucasians, African Americans reported lower scores on emotional eating [β = −20.02 ± 4.84 (p < 0.0001) and uncontrolled eating [β = −18.94 ± 3.49 (p < 0.001)]. As expected, higher BMI was associated with higher scores on uncontrolled eating. Patients who reported emotional eating were more likely to report high difficulty (>7 of 10 on difficulty scale) with reducing portion sizes [OR = 2.74 (2.00, 3.80)], calories [OR = 2.12 (1.55, 2.89)], fats [OR = 2.13 (1.52, 2.99)], and carbohydrates [OR = 3.75 (2.58, 5.43)].
CONCLUSIONS: The prevalence of disordered eating behaviors is high among obese primary care patients and disproportionately affects women and Caucasians. These maladaptive eating behaviors may impact patients’ ability to make dietary changes and limit the success of weight loss treatments. Primary care clinicians should consider screening for and intervening on disordered eating in their patients.
OBSERVATION UNITS AS SUBSTITUTES FOR HOSPITALIZATION OR HOME DISCHARGESaul Blecker; Keith Goldfeld; Joseph Ladapo; Stuart Katz. NYU School of Medicine, New York, NY. (Tracking ID #1936943)
BACKGROUND: Observation units have been associated with quality care at relatively low cost. However, studies of the economic impact of observation units have compared their cost to hospitalization without considering an alternative disposition following an emergency department (ED) visit, i.e., discharge to home. There is evidence from other clinical interventions that increased availability of services can increase overall utilization even in the absence of improvements in quality. This same supply-induced demand may shift patients who would otherwise be discharged home to be admitted to observation units following an ED visit. To determine the potential for alternative post-ED dispositions for these patients, we studied ED visits for chest pain that resulted in discharge to observation units.
METHODS: We identified all ED visits for chest pain in 2009–2010 from the National Hospital Ambulatory Medical Care Survey, a nationally representative sample of ED visits in the United States. First we developed a predictive model for likelihood of hospitalization versus discharge to home for visits to hospitals without an observation unit. Variables considered as predictors for the model included demographic characteristics, comorbid conditions, vital signs, and ED characteristics. The model was validated among patients with chest pain who were cared for at hospitals with observation services and subsequently either hospitalized or discharged. Probability of hospitalization was categorized as: hospitalization likely (p(hospitalization >0.75)), discharge likely (p(hospitalization)<0.25)), and intermediate (0.25<p(hospitalization)<0.75) to reflect clinical uncertainty. These categories were then applied to patients who were admitted to an observation unit to predict likely disposition if observation services had not been not available.
RESULTS: This study included 2,071 ED visits for chest pain, representing 8,257,881 ED visits in the United States. Of these visits, 31.7 % resulted in hospitalization while 13.4 % led to an observation unit admission; 51.9 % of visits were at facilities with available observation services. In the final prediction model, a number of variables were significantly associated with subsequent hospitalization, including age, use of oxygen, history of heart failure, and recorded urgency at triage. The model had fair discrimination in both the training (c-statistic = 0.77) and validation (c-statistic 0.73) datasets. The positive predictive value for hospitalization was 80 % while the predictive value for discharge was 85 % (71 % and 84 %, respectively, for the validation dataset). Among visits subsequently admitted to the observation unit, the model predicted 7 % as hospitalization likely, 32 % as discharge likely, and 61 % as intermediate.
CONCLUSIONS: One third ED visits for chest pain that resulted in an observation unit admission were for patients who would have been discharged to home had the observation unit not been available. Economic evaluations of observation units must consider the potential cost of increased utilization related to patients who otherwise may have been discharged. Policies such as Medicare’s recently adopted “Two Midnight Rule”, which was implemented to curb payment for short stay hospitalizations and will likely result in an increased number of hospital observation unit beds, may have the unintended consequence of increasing the total number of patients treated in the hospital following an ED visit.
OLDER ADULTS’ ATTITUDES ABOUT RECEIVING TEXT MESSAGES RELATED TO COLORECTAL CANCER SCREENINGNancy M. Denizard-Thompson1; Kathryn E. Weaver2; Shellie D. Ellis3; Donna Kronner2; David P. Miller1. 1Wake Forest School of Medicine, Winston-Salem, NC; 2Wake Forest School of Medicine, Winston-Salem, NC; 3University of North Carolina, Chapel Hill, NC. (Tracking ID #1933666)
BACKGROUND: Over 70 % of American adults now send text messages on a regular basis. This technology could be a valuable tool to support primary care patients, particularly as they prepare for cancer screening services. To determine whether older adults would value or access text messages from their physician’s practice, we conducted a qualitative study examining the utility of text messages to support colorectal cancer (CRC) screening.
METHODS: We recruited English-speaking patients aged 50–74 years from 3 community-based practices affiliated with a large academic medical center. One practice served a primarily socioeconomically disadvantaged population. We queried electronic health records to identify two patient groups for mail recruitment: those with a recent colonoscopy and those with no colonoscopy in the past 10 years. We screened patients by telephone and invited eligible patients to attend one of 4 focus groups in community settings. A trained moderator led all groups, following a semi-structured interview guide. Topics included perceived barriers and facilitators to CRC screening, personal use of electronic communications, and attitudes/beliefs about the utility of receiving medical text messages. We also elicited feedback about a series of text messages regarding specific CRC screening tests. Text messages were shared with participants either via their cellphones or by color screenshots.
RESULTS: A total of 27 adults participated in 1 of the 4 focus groups. Participant age ranged from 50 to 73 years (mean = 57 years). Two-thirds of participants were female (17/27) and Black (17/27). Over 25 % had low health literacy (8/27) or were overdue for CRC screening (7/27). Participants reported the main barriers to CRC screening were distaste for the prep solution, fear of the procedure, and fear of bad results. Some stated they were not aware of any screening option other than colonoscopy. Attitudes about receiving text messages from a physician’s office were mixed. Main concerns included confidentiality (fear that someone else would read their texts), intrusiveness (text messages could come at inconvenient times), depersonalization of the patient-physician relationship, and lack of confidence or dislike of texting (for those who did not text currently). Despite these concerns, participants reacted positively to many of the sample text messages. Participants particularly liked text messages that were affirming (“I’m glad you decided to do the stool blood test”), supportive (“Hang in there. I know the prep and clear diet can be challenging”), and informative (“Remember you will need to have someone take you to the test tomorrow”). Participants also favored texts that included their first name, which confirmed the message was intended for them. Participants did not like text messages which asked them to reply back with specific information such as the date of their planned colonoscopy. In general, participants felt providing a choice of communication modalities was important, such as offering texts, e-mails, or phone calls.
CONCLUSIONS: Text messages may be a feasible way to provide CRC screening reminders to older adults; however, it is important to offer other communication options such as email for non-texters. Older adults liked text messages that were positive in tone and contained key information. Health systems should address patients’ concerns about text message confidentiality if they plan to use this communication modality.
ONCE-DAILY TIOTROPIUM RESPIMAT® DECREASES THE RISK OF EXACERBATIONS, INDEPENDENT OF BASELINE CHARACTERISTICS, IN PATIENTS WITH SYMPTOMATIC SEVERE ASTHMA WITHOUT EVIDENCE OF CHRONIC OBSTRUCTIVE PULMONARY DISEASEJonathan Corren1; Kevin R. Murphy2; Gregory Bensch3; Ronald Dahl4; Pierluigi Paggiaro5; Michael Engel6; Petra C. Moroni-Zentgraf6; Hendrik Schmidt7; Huib A. Kerstjens8. 1University of California, Los Angeles, CA; 2Boys Town National Research Hospital, Boys Town, NE; 3Bensch Research & Associates, Stockton, CA; 4Odense University Hospital, Odense, Denmark; 5University of Pisa, Pisa, Italy; 6Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany; 7Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach an der Riss, Germany; 8University Medical Center Groningen, Groningen, Netherlands. (Tracking ID #1939993)
BACKGROUND: All patients (pts) with asthma are at risk of exacerbations, which are potentially life-threatening, adversely affect long-term disease outcomes, and place considerable burden on pts and healthcare systems. In pts with severe symptomatic asthma despite therapy with inhaled corticosteroids (ICS) and long-acting β2-agonists (LABAs), addition of once-daily tiotropium Respimat® (TioR) provides bronchodilation and reduces exacerbations (Kerstjens et al. NEJM 2012;367:1198–207). Secondary analyses may determine whether this effect is limited to subgroups of pts defined by baseline characteristics.
METHODS: Baseline characteristics were investigated and subgroup analyses performed using data from 2 replicate Phase III, randomized, double-blind, placebo (PBO)-controlled studies of once-daily TioR in pts with symptomatic asthma despite high-dose ICS (≥800 μg budesonide equivalent) + LABA, in addition to other therapies (Kerstjens et al. NEJM 2012;367:1198–207). Eligibility criteria included: 18–75 years of age; asthma diagnosis before age 40; ≥5-year history of asthma; 7-question Asthma Control Questionnaire (ACQ-7) score ≥1.5; at least 1 asthma exacerbation in the previous year; life-long non-smokers or ex-smokers (≤10 pack-years) who quit smoking ≥1 year before study enrollment. Pts with chronic obstructive pulmonary disease (COPD) or other lung disease were excluded. Time to first severe exacerbation (defined as asthma deterioration necessitating initiation or doubling of systemic glucocorticosteroids) after 48 weeks was a co-primary endpoint. Secondary endpoints included time to first episode of asthma worsening (defined as either progressive increase in symptoms and/or a decline of ≥30 % in the best morning peak expiratory flow for ≥2 consecutive days). Subgroup analyses of time to first severe exacerbation were performed by baseline characteristics, including age, allergic status, smoking status, and reversibility (Figure).
RESULTS: 912 pts were randomized: 456 received TioR 5 μg and 456 received PBO Respimat® once daily for 48 weeks. Mean age: 53.0 years; 37.6 % of pts were aged ≤50 years. Mean age at diagnosis of asthma: 22.7 (range 0–44) years. Median asthma duration: 28.0 (range 5–72) years, with 76.5 % of pts having asthma for ≥20 years before enrollment. Most pts (75.9 %) were non-smokers; 24.1 % were ex-smokers with a median number of pack-years of 5.0. Mean ACQ-7 score: 2.6 (range 1–5); mean IgE: 1210 μg/L; mean pre-bronchodilation forced expiratory volume in 1 s (FEV1): 1.5 ± 0.5 L; mean FEV1 bronchodilation response to salbutamol: 15.2 ± 15.7 % (all values baseline ± SD). Time to first severe exacerbation was increased by addition of TioR versus PBO (risk reduction 21 %; hazard ratio 0.79; p = 0.03). Time to first episode of asthma worsening increased with TioR versus PBO (risk reduction 31 %; hazard ratio 0.69; p < 0.0001). Subgroup analyses showed that neither time to first severe exacerbation (Figure) nor time to first episode of asthma worsening was dependent on baseline characteristics (no significant interactions). The 24-hour bronchodilatory effect of TioR was demonstrated by lung function data obtained in a subset of pts. Adverse events were well balanced between TioR and PBO; no deaths occurred.
CONCLUSIONS: The increase in time to first severe exacerbation and first episode of asthma worsening in patients receiving tiotropium Respimat® was not limited to specific subgroups. Age of onset, symptom duration, lack of smoking, allergic status, and bronchodilation response provide reasonable certainty that the patients enrolled had asthma and not COPD. Features compatible with COPD were thus more likely to reflect effects of long-standing severe persistent asthma than the alternative diagnosis. Once-daily tiotropium Respimat® add-on reduces risk of exacerbations in patients with asthma who remain symptomatic and experience exacerbations despite ICS+LABA.
Figure: Analysis of time to severe asthma exacerbation by baseline characteristics (final analysis set)
ONLINE COUNSELING TO ENABLE LIFESTYLE-FOCUSED OBESITY TREATMENT IN PRIMARY CAREKathleen M. McTigue1,2; Laurey R. Simkin-Silverman2; Molly B. Conroy1,2; Dana L. Tudorascu1; Rachel Hess1; Gary Fischer1; Cindy L. Bryce3. 1University of Pittsburgh, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1931309)
BACKGROUND: More than one third of US adults are obese. The USPSTF recommends that primary care providers (PCPs) screen for obesity and offer or refer obese patients to intensive, multicomponent behavioral interventions; however, such treatment is rarely accessible in the primary care setting. Online counseling can provide convenient behavioral support in the setting in which lifestyle choices are made. Our prior work has shown that primary care patients find it to be a satisfactory approach for delivering intensive behavioral interventions.
METHODS: We facilitated the delivery of preventive counseling by using information technology to translate an evidence-based intensive lifestyle intervention into diverse primary care settings, and conducted a randomized controlled trial comparing the effectiveness of three online approaches for integrating behavioral lifestyle treatment with primary care medicine. Obese primary care patients were referred by their PCPs for an online weight loss intervention and randomized into 1 of 3 arms. Each participant received an in-person lifestyle counseling session plus 1 year of access to either (1) comprehensive online intervention with standard coaching (COI-S), (2) comprehensive online intervention with modulated coaching (COI-M) or (3) online goals and resources (OGR) alone. Both COI interventions included online lessons adapted from the proven Diabetes Prevention Program’s lifestyle intervention, interactive workbook exercises, asynchronously delivered advice and support from a lifestyle coach, self-monitoring tools with automated feedback, and links to reputable community resources. For COI-M participants, coaches had an electronic tool that helped identify patients in need of counseling, and modulated their counseling intensity to reflect participant need (i.e., no notes were sent unless a potential concern was identified). We measured weight change and used electronic surveys to assess covariates and potential confounders at baseline, 6 months and 12 months. Fisher exact and Chi-square tests were used for our comparisons.
RESULTS: 373 obese patients were recruited from 6 primary care practices in western Pennsylvania from April to December, 2010. On average participants were age 49.4 (SD 12.6), and weighed 106.1 kg (SD 20.7). Of the sample, 76 % were female and 20 % were African American. All study arms lost weight at 6 months, with the largest estimated difference seen in the COI-M group [−3.36, 95 % confidence interval (CI): −4.70,−2.02], the smallest estimated difference seen in the OGR arm [−1.91 (CI: −2.89,−0.94)] and an intermediate estimated difference seen for the COI-S arm [−2.44 (CI: −3.39,−1.48)]. Weight loss was sustained at 12 months in each study arm, with point estimates for weight further declining in the COI-M and OGR arms over the second half of the interventions (see Figure). At each time point, there was no significant difference in weight loss between groups. Survey data indicated that the use of non-study resources for weight loss differed by study arm at 6 months of enrollment with more OGR participants using such resources than did COI-M or COI-S participants (14.4 %, 6.3 %, and 3.4 %, respectively; p = 0.015).
CONCLUSIONS: All three interventions led to weight loss over 1 year of follow-up and weight regain was not seen in any group. While we found no statistically significant difference in the estimated differences between the three groups, the estimated weight change in each group suggests that the intensive intervention with as-needed coaching had the most clinically relevant results. The greater weight loss in the OGR (active control) group than anticipated from the literature may reflect a larger use of participants’ personal resources for lifestyle management. These findings suggest that online lifestyle support can be implemented in coordination with primary care medicine.
OPPORTUNITIES FOR IMPROVING COLORECTAL CANCER SCREENING IN COMMUNITY HEALTH CENTERS - IMPACT OF ELECTRONIC HEALTH RECORD SYSTEMS: A CROSS-SECTIONAL SURVEYAllison Cole1; Shin-Ping Tu2; Maria Fernandez3; William A. Calo3. 1University of Washington, Seattle, WA; 2Virginia Commonwealth University, Richmond, VA; 3University of Texas, Houston, TX. (Tracking ID #1935924)
BACKGROUND: Community Health Centers (CHCs) are important sources of primary care for medically underserved populations. Adoption of electronic health records (EHRs) has increased in CHCs. EHRs represent an important tool for improving quality of preventive care including implementation of evidence based approaches for cancer control. However, to successfully implement evidence-based approaches to cancer screening, EHR data must be reliable and there must be effective systems in place for using EHR data to improve practice. The objectives of this study were to describe the proportion of CHCs reporting specific EHR functionalities important for implementation of evidence based approaches to colorectal cancer screening in CHCs and to describe the ease with which CHCs are able to complete specific colorectal cancer screening tasks using EHR systems.
METHODS: This cross-sectional study analyzed results of the Cancer Prevention Control Research Network’s (CPCRN) Community Health Center survey. The CPCRN is a national network of academic, public health, and community partners who work together to reduce the burden of cancer. Institutional Review Boards at each CPCRN site as well as the Coordinating Center at the University of North Carolina at Chapel Hill and the Centers for Disease Control and Prevention approved all study procedures. We described the characteristics of responding CHCs, calculated the proportions of CHCs using EHR data to measure and improve colorectal cancer screening and estimated the perceived accuracy of EHR reported colorectal cancer screening rates.
RESULTS: The survey was completed by 50 of 75 CHCs in 7 states for a 67 % response rate. We found that 90 % of respondent CHCs have adopted EHRs. Of those with EHRs, 82 % report being able to use EHR data to measure colorectal cancer screening, but only 27 % of CHCs perceive EHR colorectal cancer screening data as very accurate. Though the majority of respondent CHCs with EHRs are able to use EHR systems to identify patients overdue for colorectal cancer screening, only 47 % report it is very easy to do these activities using EHR systems.
CONCLUSIONS: Despite widespread adoption of EHRs, the majority of CHCs do not perceive colorectal cancer screening data from EHRs as accurate. Few CHCs report that use of EHR systems to measure and improve colorectal cancer screening is either “easy” or “very easy”. Poor EHR data quality and cumbersome EHR systems may be significant barriers to implementation of evidence-based approaches to colorectal cancer screening and other preventive services in CHCs. Improvement of EHR functionality in CHCs is a key to reducing disparities in colorectal cancer screening affecting the minority and low income populations served by CHCs.
OPTIMISM, RISKS, AND PERCEPTIONS OF HEALTH FOR EVALUATION OF UNDERLYING SENTIMENT (ORPHEUS)Stephanie A. Rose1; Bharat Kumar1; Brett Capel1; Nicholas Jackson1; Brittany P. Fenner1; Sarah Schuetz1; Dominique Zephyr2; David Rudy1. 1University of Kentucky, Lexington, KY; 2University of Kentucky, Lexington, KY. (Tracking ID #1940331)
BACKGROUND: Interest in the relationship between personality characteristics and health has increased substantially in recent years. One measure correlated with physical health is dispositional optimism, defined as the general expectation that good things will happen. However, the relationship between dispositional optimism and risk perception by patients remains largely unexamined. In this study, we aim to assess the correlation between objective disease risk and perception of disease risk in diabetes (DM). We hypothesize that increased levels of optimism are negatively correlated with perceptions of risk as well as with objectively measured risk.
METHODS: Patients in a university-based internal medicine clinic completed a quantitative survey assessing their level of dispositional optimism via the Revised Life Orientation Test (LOT-R), and their risk perception (RP) of developing DM. We performed chart reviews to obtain laboratory, demographic, and anthropometric data to calculate each patient’s diabetes risk score based on validated risk calculators.
RESULTS: Patients (n = 28) were 96.4 % white, 35.7 % male, mean age 54.52 years (SD 11.92), 18 % were overweight (BMI 25–29.9 kg/m2), 39 % were obese (BMI ≥30), and 3 patients (10 %) had a diagnosis of DM. Mean LOT-R score was 16.2 (SD 5.67) (range 0 low to 24 high). Of patients not already diagnosed with DM (n = 25), mean RP of developing DM was 2.63 (SD 1.49) (range 1 low to 7 high). Mean objective health risk of developing DM was 3.33 (SD 1.98) (range 1 low to 6 high). There was a positive correlation between RP of developing DM and optimism (r = 0.077, p = 0.354). There was a positive correlation between optimism and objective risk of developing diabetes (r = 0.465, p = 0.007).
CONCLUSIONS: There was no significant correlation between optimism and risk perception of developing DM. However, surprisingly, increasing optimism was significantly correlated with increasing objective risk of developing diabetes. Limitations to this analysis include small sample size. Future goals include increasing sample size and assessing the correlation between RP, optimism, and objective risk.
OPTIMIZING EVIDENCE-BASED MEDICINE SEARCHES: PATTERNS OF VISITATION TO A MEDICAL REFERENCE WEBSITE FROM GOOGLEAlex Montero1; Timothy Plante1; David J. Iberri2; Emily Coderre3. 1Georgetown University Hospital, Washington D.C., DC; 2Stanford Hospitals and Clinics, Stanford, CA; 3Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1939872)
BACKGROUND: Evidence-based medicine (EBM) experts cite Google as a comprehensive search engine useful for locating articles which have received significant press and media coverage. Google is not cited as a resource for finding high quality, pre-appraised evidence. Wiki Journal Club (WJC) is an independent, open-access, collaborative, medical reference website with editorial support by resident trainee physicians (the authors). The site provides standardized summaries of Internal Medicine trials in an evidence-based/journal club format similar to established sources of high quality, pre-appraised evidence. Importantly, summaries are titled by the consensus derived colloquial name of the trial. Little is known about the relationship of Google searches for individual clinical trials and traffic flow to sources of high quality, pre-appraised medical evidence websites. Google Analytics is a website analytics platform providing user visitation data. We report on a descriptive analysis of Google search visitor and query trends to WJC over a 36 week block.
METHODS: Visitor data was downloaded to Google Analytics for a 36 week period. Percentage of total weekly visitation for 4 hour and daily blocks was calculated and query specific data was analyzed for the last 92 days of the study period. Statistical analyses were performed with Google Analytics, Google Spreadsheets, and R Gui 64 bit v3.0.1. Of note, mobile application user data was excluded from this analysis.
RESULTS: From January 4, 2013 to September 12, 2013 there were 53,626 visitors to WJC who viewed 141,022 pages. Search engines contributed more than two thirds of all visitors, 95.1 % of whom were from Google. The mean weekly increase of visitation from Google was 5.7 % (2.05 to 9.32; P = 0.003; Table 2). Most of these visitors were from the US. Most Google visitors used a computer running Windows or Macintosh operating systems with 11.5 % using mobile platforms. Google visitors were on almost 5,000 different networks, the largest owned by American commercial telecommunication firms. The top 15 medical group-associated networks contributed 5.5 % of Google visitors. In regards to query data analyses, total impressions for WJC (the amount of times a google query returned WJC in its result) during the study time frame was 146,511. Queries with the most clicks were “wiki journal club,” “affirm trial,” and “accord trial.” Finally, of 1,669 possible queries that would result in an average position <10 for WJC on a Google search, 1330 included either “wiki,” “journal,” or “club.”
CONCLUSIONS: Our analysis supports WJC’s relative success despite the lack of any formal advertising program. Additionally, we infer from our analyses that users search employing a trial’s colloquial name adjoined to “Wiki” and/or “Journal Club” rather than constructing an entire PICO format EBM search. We suspect the term “journal club” connotes some evidence-based pre-appraisal of the trial, and “wiki” connotes the collaborative nature of the content. In comparison, established sources of high quality pre-appraised evidence such as ACP Journal Club, DARE, and Bandolier do not employ any of these strategies. Not surprisingly, none of these sources appear on the first page of any of the top 20 most visited trials on WJC. As advocates and teachers of EBM, we acknowledge that WJC is not equivalent to an established source of high quality, pre-appraised evidence such as ACP Journal Club. However, we see the search factors underpinning WJC success as relevant to these established online sources of high quality EBM, and more direct collaboration and linkage with these sites is planned in WJC’s future.
Wiki Journal Club Traffic Over 36 Weeks
| Visitors (% returning) | Mean weekly visitor growth (95 % Confidence Interval)* | Pageviews | |
|---|---|---|---|
| All | 53,626 (27.0 %) | 5.7 % (−0.12 to 11.5; P = 0.054) | 141,022 |
| 35,251 (24.8 %) | 5.7 % (2.05 to 9.32; P = 0.003) | 90,550 |
Technology used by Google Visitors
| Operating System | |
|---|---|
| Windows | 65.3 % |
| Macintosh | 22.7 % |
| iOS (iPhone, iPad) | 7.7 % |
| Android | 3.4 % |
| Other | 0.5 % |
| Device Type | |
| Desktop | 88.4 % |
| Smartphone | 7.6 % |
| Tablet | 3.9 % |
OPTIONS IN THE HOSPITAL: MEASURING INPATIENT INVOLVEMENT IN DECISION MAKINGZackary Berger; Mary Catherine Beach. Johns Hopkins School of Medicine, Baltimore, MD. (Tracking ID #1937967)
BACKGROUND: Shared decision-making (SDM) has become a goal of many patients and providers in contemporary health care, for humanistic reasons and in order to increase patient satisfaction. However, the implementation of SDM is still inconsistent and of unclear effectiveness. Little is known about SDM in inpatient settings.
METHODS: We conducted a study of patient-doctor communication on an inpatient medicine hospitalist service. A research assistant digitally recorded and transcribed daily doctor-patient dialogue on walk rounds and daily semi-structured interviews with patients and doctors separately. We audio-recorded 24 patient-doctor dialogues, representing 18 separate patient hospitalizations, as well as 24 corresponding interviews with hospitalists and 24 interviews with patients. The total recording time was 558 min. We used the OPTION-12 score, an instrument validated in the outpatient setting, to measure inpatient involvement in decision making in the hospital setting. One reviewer (ZB) used the instrument to score characteristics of shared decision-making in transcripts of audio-recorded patient-physician dialogues. The instrument was completed based on the completeness with which any one of 12 behaviors were found in any dialogue associated with the patient’s hospitalization. Any of these behaviors need only have been found once in any dialogue for it to be noted as present for that hospitalization.
RESULTS: The average OPTION-12 score per encounter was 5.3, compared to the mean of 16.9 in the original validation study by Elwyn et al. done in an outpatient setting. The minimum score was 2, and the maximum was 18. The mode was 4. The behavior among the OPTION-12 questions most commonly found in dialogue was giving the patient an opportunity to ask questions, found in 16 of 18 hospitalizations. Other common behaviors included the clinician’s asking the patient about their expectations or ideas about the management of the problem 12 of 18 hospitalizations), and asking the patient whether they understood the information given (13 of 18 hospitalizations). The behavior least often found was eliciting the patient’s preferred level of involvement in decision-making, which was not demonstrated in any hospitalization. Other uncommon behaviors included the clinician’s acknowledging that there was more than one legitimate management option (equipoise), and acknowledging the need to revisit the decision in the future (each found in 2 of 18 hospitalizations).
CONCLUSIONS: Patient involvement in decision making in the hospital setting varies and seems less common than in the outpatient setting. Further work should consider whether the domains measured by the OPTION are relevant to the inpatient setting, and if so, further explore their prevalence across inpatient settings and develop mechanisms to enhance patient involvement.
ORGANIZATIONAL FACTORS ASSOCIATED WITH MEDICATION ADHERENCE AFTER PATIENT CENTERED MEDICAL HOME TRANSFORMATIONNicholas Meo1; Edwin Wong2; Christopher L. Bryson2,1; Haili Sun2; Idamay Curtis2; Indra Gupta2; Adam Batten2; Stephan D. Fihn3,1; Karin M. Nelson2,1. 1University of Washington, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA; 3Veterans Health Administration, Seattle, WA. (Tracking ID #1938637)
BACKGROUND: Medication adherence is a complex process involving patient, medication, provider and health care delivery system. Primary care clinics throughout the Veterans Health Administration (VHA) adopted the patient-center medical home model, termed Patient Aligned Care Teams (PACT) in 2010. We wondered whether adopting a team-based model of care would be associated with changes in adherence to medications for chronic disease. Objective: To compare clinic level adherence to oral hypoglycemic agents amongst veterans with diabetes at VHA primary care clinics nationally after implementation of PACT and to identify organizational correlates of adherence.
METHODS: Design: Retrospective cohort study. Participants: Patients with diabetes treated with oral hypoglycemic agents seen in VA hospital or community based primary care clinics in April to June 2012. Main Measures: 1 year refill based medication possession ratios (MPR) were calculated at the patient level. Clinic level adherence was defined as the proportion of patients within a clinic with >80 % MPR. Risk adjustment was performed to account for patient level demographic and comorbidities differences between clinics. A VHA-PACT Team Based Care survey and the Consumer Assessment of Healthcare Providers and Systems-Patient Centered Medical Home survey (CAHPS-PCMH) were used to identify organizational factors associated with OHA adherence. Multivariate linear regression was then performed on the results of clinic level survey data to identify organizational factors associated with clinic level adherence.
RESULTS: 440,971 patients with diabetes were included in the analysis at 757 primary care clinics (154 hospital based clinics and 614 community based clinics). Patients per clinic ranged from 100 to 5011. The overall average clinic level adherence was 58.56 %. Organizational factors associated with higher clinic-level adherence included provider continuity (Sβ = .16, P < .001), increased telephone based encounters (Sβ = .13, P < .001), regular medication reconciliation (Sβ = .10, P < .05), patient self report of enough time spent during encounters (Sβ = .19, P = .005), and delegation of tasks to a nursing care coordinator (Sβ = .26, P < .005).
CONCLUSIONS: Amongst a national cohort of veterans with diabetes, organizational characteristics central to the patient-centered medical home, including access, continuity, team-based care, patient-centered care, and care coordination were associated with better adherence to oral hypoglycemic therapy.
OUTCOMES OF A MULTI-DISCIPLINARY FALLS ASSESSMENT CLINICVishal Reddy2,1; Anne Vanderbilt1; Barbara J. Messinger-Rapport1. 1Cleveland Clinic Foundation, Cleveland, OH; 2University of North Carolina, Chapel Hill, NC. (Tracking ID #1927947)
BACKGROUND: Falls create substantial morbidity and cost within a Patient Centered Medical Home (PCMH). The American and British Geriatric Society 2010 Guideline recommends screening for fall risk, and describes a multi-disciplinary assessment of older adults identified as at risk. The Guideline identifies interventions supported by Levels A & B evidence to reduce the risk of fall and fall-related injury. Typically, the evaluation process requires time and skills not available in the practitioner office at the time of the visit.
METHODS: The Cleveland Clinic PCMH developed a pilot Falls Clinic (FC) to provide a structured, 90-minute multidisciplinary assessment of adults 50 years and over. Assessment included screens for balance, strength, vision, fear of falling, cognition, mood, nutrition, and polypharmacy. The FC was staffed by a physical therapist (PT) and an advance practice nurse (APN). Cognitive screening was performed by a geriatric-trained nurse or medical assistant. The APN could initiate some referrals independently (such as home care, physical therapy or low vision occupational therapy) as well as testing (e.g. bone densitometry) and limited medication changes (vitamin D, for example). More substantive referrals, testing, or recommendations had to go through the PCMH practitioner. The PCMH practitioners were encouraged but not required to refer, and patients could self-refer. The Electronic Health Record (EHR) was used to collect demographic and clinically relevant information on FC clients prior to and after the FC visit. A follow-up phone call 3–6 months after the visit was used to gather additional clinical data not available in the EHR. Primary outcomes included recommendations and follow-through. Secondary outcomes included number of falls per patient and number of fallers before and after the intervention. Analysis was descriptive. The protocol was approved by the IRB.
RESULTS: Of the 74 new FC patients between June 2012 and May 2013, there were 42 whose data could not be included in the final data set either because the minimum 3 months past the visit had not occurred, or because after 3 tries we were unable to reach the patient or care partner by phone. Of the 32 new FC patients for whom a complete data set was available, the average age (sd, range) was 79.3(8.4, range 66–93) years. Average number of medications (sd, range) was 11.2(4.8, 2–25). We compared demographic and clinical information with the FC patients who could not be included in the final data set and there were no significant differences. The average number of falls per patient prior to the FC (sd, range) was 3.0 (2.81, 0–12). The most common recommendations and the percent of patients who followed through are listed in the Table. 23/32 attendees of the FC had fewer falls in the 6 months after the appointment than prior including 16 patients eliminating falls completely. Of the 4/32 patients without falls prior to their appointment, none fell after their appointment. Of the 28/32 patients who fell prior to the FC visit, only 12/28 fell after the FC visit. The average number of falls in the 6 months prior to the appointment was 2.97 versus 0.28 in the 6 months following the appointment.
CONCLUSIONS: A multidisciplinary, guideline driven falls clinic can support a PCMH to offer evidence based interventions to reduce the risk of falls. Future steps involve efforts to improve compliance with recommendations and expanding referrals via care pathways in the PCMH.
Recommendations from the Falls Clinic
| INTERVENTION | FREQUENCY RECOMMENDED n(%) | FREQUENCY OF FOLLOW-THROUGH n(%) |
|---|---|---|
| Physical Therapy | 26 (81.3 %) | 16 (61.5 %) |
| Exercise | 23 (71.9 %) | 11 (47.8 %) |
| Vitamin D | 15 (46.9 %) | 11 (73.3 %) |
| Ophthalmology | 15 (46.9 %) | 8 (53.3 %) |
OVARIAN CANCER TREATMENT AND SURVIVAL TRENDS OVER PAST DECADEJenny J. Lin1; Natalia Egorova2; Rebeca Franco2; Nina A. Bickell1,2. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1939426)
BACKGROUND: While death rates from ovarian cancer appear to be decreasing and five-year survival rates are increasing, it is unclear whether overall survival is improving among women with advanced ovarian cancer. We undertook this study to assess trends of overall survival, cancer recurrence and treatment patterns among women with advanced stage ovarian cancer.
METHODS: Using SEER-Medicare claims data from 2000 to 2009, we identified a cohort of women age 65+ years with Medicare diagnosed with stage III and IV epithelial ovarian cancer. Recurrent cancer was identified using claims for chemotherapy, hospice or secondary cytoreductive surgery following a 6 month treatment-free window after primary treatment for ovarian cancer. Persistent cancer was defined as receipt of treatment (surgery or chemotherapy) without a treatment-free window of at least 6 months. Optimal treatment was defined as surgery within 120 days of diagnosis followed by chemotherapy within 120 days of initial surgery. Survival time was calculated from time of diagnosis. Parametric and semi-parametric multivariate survival analyses were used to assess comparative treatment survival rates and factors affecting survival and recurrence.
RESULTS: Of the 46,004 women with ovarian cancer, 6,814 met the study criteria. Of these, only 3,413 women (50 %) underwent primary debulking surgery and chemotherapy in an optimal time frame, 970 (14 %) received surgery alone and 1,799 (26 %) received chemotherapy alone, 214 received no treatment and 418 did not receive surgery and chemotherapy in an optimal time frame. During the past decade, overall median survival time remained relatively constant, although the time to first recurrence increased by 260 days and the probability of having a recurrence grew from 2000 to 2004 and stabilized during 2005–2009. Ovarian cancer was the cause of death for 85 % of women diagnosed in 2000 and 72 % for those who diagnosed in 2008. Optimal treatment was associated with longer survival time (p < 0.001, median survival 1,411 days), a lower proportion of persistent cancers and higher proportion of patients with recurrences (see figure). Survival of patients receiving optimal treatment improved over the decade, while for those who received chemotherapy or surgery alone, survival probability did not change. However, the proportions of women who received optimal treatment versus other treatments did not vary over time. Multivariate survival models controlling for patient demographics, cancer type and comorbidities showed that patients who received optimal primary treatment or who had multiple recurrences had longer survival but there were not substantial changes in overall survival during the last decade. Propensity analyses are underway.
CONCLUSIONS: Among elderly women diagnosed with advanced stage ovarian cancer, patterns of overall survival and treatment types have not changed in the past decade. Optimal cancer treatment is associated with improved survival time. Further work should evaluate barriers to receipt of optimal treatment among this group of patients.
OVER A DECADE OF DUTY HOURS: WHO DO PATIENTS SAY IS MOST INVOLVED IN THEIR HOSPITAL CARE?Vineet Arora; Micah Prochaska; Jeanne M. Farnan; David Meltzer. University of Chicago Medical Center, Chicago, IL. (Tracking ID #1938094)
BACKGROUND: Internal medicine residency training is grounded in experiential learning, or having residents assume care for a set of patients. With implementation of residency duty hours over the past decade, many believe that attending physicians are responsible for a greater portion of patient care and resident education has suffered. Studies to date have largely ignored the patient perspective. Changes over time in hospitalized patients’ perceptions of who is most involved in their hospital care may provide a useful measure of whether roles of resident and attending physicians have changed since implementation of successive duty hour restrictions over the past 12 years.
METHODS: From 2001 to 2013, all general medicine inpatients cared for on the housestaff teaching service at a single academic center were approached for an admission interview and a 30 days post-discharge phone interview. Each patient had a primary team consisting of an intern, resident (PGY2 or 3), and attending physician. Thirty-days after discharge, patients were asked to answer, “Who was most involved in their hospital care?” and were given the options of attending, resident, intern, medical student, nurse, other, or I don’t know. Routine demographics (age, gender, race) were obtained from chart review. Time periods were categorized by duty hour restrictions as pre-2003, post2003-pre2011, and post-2011. Chi square tests were used to assess associations between demographics, duty hour period, and whom patients named as involved in their care. Multinomial logistic regression was used to test the proportional odds of naming a specific person compared to the attending during the duty hour periods controlling for patient demographics and whether inpatient attending was a hospitalist or not.
RESULTS: From July 2001 to June 2013, 39,469 patients were admitted to the teaching service at a single academic medical center. Of these, 22,750 (58 %) could be reached by phone 1 month after discharge. Overall, 29 % did not know who was most involved, followed by 28 % listed the attending, 11 % resident and 6 % intern. The percentage of patients who identified their attending as most involved in their care increased with increasing duty hours restrictions (pre2003 20 %, post2003-pre2011 29 %, post2011 37 %, p < 0.001). With successive duty hour restrictions, the percentage of patients who listed an intern declined in each period (pre2003 9 %, post2003pre2011 6 %, post2011 3 %, p < 0.001) as did the percentage who named any housestaff (resident or intern) (pre2003 20 %, post2003pre2011 17 %, post2011 12 %, p < 0.001). The percentage of patients who responded “I don’t know” decreased with restricted duty hours decreased after 2011 (pre2003 32 %, post2003pre2011 30 %, post2011 22 %, p < 0.001). These associations were not affected by whether the inpatient attending was a hospitalist or not, and they remained significant in multinomial logistic regression.
CONCLUSIONS: The percentage of patients on general medicine teaching services who listed their attending as most involved in their care has more than doubled with successive resident duty hour restrictions over the past 12 years. Given the importance placed on achieving progressive levels of independence in assuming responsibility for patient care during residency, efforts should be undertaken to understand the implications for these findings for residency competence and patient care.
OVERDOSE EDUCATION AND NALOXONE PRESCRIBING FOR PATIENTS ON CHRONIC OPIOIDS: A QUALITATIVE STUDY OF HEALTH CARE PROVIDERSIngrid A. Binswanger1,2; Steve Koester3,4; Shane Mueller1,3; Edward M. Gardner2; Kristin Goddard5; Jason M. Glanz5. 1University of Colorado School of Medicine, Denver, CO; 2Denver Health Medical Center, Denver, CO; 3University of Colorado Denver, Denver, CO; 4University of Colorado Denver, Denver, CO; 5Kaiser Permanente Colorado, Denver, CO. (Tracking ID #1928545)
BACKGROUND: Fatal unintentional poisonings from pharmaceutical opioids have increased nearly four-fold in the last decade. Naloxone is an effective, Food and Drug Administration approved opioid antidote usually administered by first responders to reverse respiratory depression due to opioid poisoning. Increasingly, community-based programs have provided naloxone to heroin users for potential overdose reversal. Patients on chronic pharmaceutical opioids for pain could also benefit from overdose education and naloxone prescription, but there are significant barriers to these practices in routine clinical care. This qualitative study was designed to assess the knowledge, attitudes and beliefs about overdose prevention and naloxone prescription among primary care and HIV clinicians, pharmacists and clinic administrators.
METHODS: We conducted focus groups in two primary care internal medicine and two infectious disease/HIV clinics from a university and a safety net health system in Colorado, a state which passed legislation to permit naloxone prescriptions in 2013. A focus group guide was developed using domains from the Theory of Planned Behavior and the Health Belief Model. Each focus group was led by two experienced qualitative interviewers. Focus groups were recorded and transcribed, coded using ATLAS.ti® qualitative software, and analyzed using a team-based constant comparative method of inductive analysis.
RESULTS: We enrolled 10 (40 %) physicians, 6 (24 %) nurses, 4 (16 %) pharmacists, 3 (12 %) nurse practitioners, 1 (4 %) administrator, and 1 (4 %) counselor into focus groups. Fourteen (56 %) participants were female and participants had a mean age of 42 years (range 26–58 years). Eighteen (72 %) were white, 3 (12 %) were Hispanic or Latino, 2 (8 %) were African American, and 2 (8 %) were Asian. Participants described opioid overdoses among their patients and several formal and informal opioid prescribing policies and guidelines, but little prior knowledge and uptake of overdose education and naloxone prescribing in clinical practice. We identified the following themes from the transcripts (see Table for illustrative quotations): 1) A wide spectrum of patients could be targeted for naloxone prescription, including patients with concomitant mental health problems, impulsivity, and poorly controlled pain; 2) Barriers and challenges to implementation of a naloxone prescription fell into two major categories: attitudinal and practical. Providers were concerned about giving mixed messages about opioid safety (attitudinal) and adding training to administer naloxone to an already busy clinic schedule (practical). 3) The benefits of naloxone prescribing were perceived as significant. They included direct benefits such as preventing accidental overdose, as well as indirect benefits, such as alerting patients and their significant others to the overdose potential of opioids and enhancing medication safety.
CONCLUSIONS: Health care providers had limited awareness about naloxone for take-home use but were receptive to prescribing it to a broad range of patients on opioids for pain. Providers also identified a number of potential safety benefits to naloxone prescribing. However, efficiency concerns and ambivalence about prescribing opioids to patients who could overdose limited enthusiasm for naloxone. To address opioid overdose risk in clinical practice, future efforts should enhance provider knowledge on overdose education and naloxone prescription, reduce implementation barriers, and improve opioid safety messaging for patients on chronic opioids.
Emerging themes and illustrative quotations about overdose education and naloxone prescribing in clinical practice
| Patients to target for naloxone | \“I think the patients on the maximum dose are a good place to start, but I think that’s not… those aren’t the only people at risk for overdose and in fact those are probably the most tolerant of all our patients…I had a patient whose daughter accidentally overdosed on her meds…so, I’m wondering, shouldn’t we be offering it more broadly…?\” |
| Practical barriers to naloxone prescribing | \“But the idea that you teach the person that’s taking the narcotics and relying on them to teach the other person is kind of a limiting factor in how successful it is…\” \“…but I do think it would be tough in sort of a general…to have all the providers in this clinic learn about naloxone and teach it during their regular clinic hours.\” |
| Attitudinal barriers to naloxone prescribing and reservations about naloxone | \“It seems kind of intuitive, like glucagon for insulin. It’s kind of intuitive.... But it just feels a little uncomfortable. You know, it just feels a little uncomfortable where glucagon just doesn’t… It seems like it may have merit. On some level it also makes me feel likes it’s sort of putting our head in the sand just a little bit, you know. If you feel like, my God, this patient is going to kill themselves. Maybe the solution is to not have them on opioids.\” |
| Benefits of naloxone | \“I was sort of hoping that if we implement a good program where even at initiation, we talk about overdose prevention and naloxone that it will bring, you know, the safety concerns to the forefront and then it might actually help people understand that these are potentially lethal medications and I feel like that might be one of the things that might be most beneficial from it is just re-setting of like the culture around these medications as much as, you know, potentially saving someone’s life from overdose.\” |
PANEL MANAGEMENT IN PRIMARY CARE: A SYSTEMATIC REVIEWAshley E. Jensen3; Nicole Skursky3; Matthew Beyrouty3; Katelyn Bennett1,3; Mark D. Schwartz1,2; Scott Sherman1,2. 1VA New York Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU School of Medicine, New York, NY. (Tracking ID #1937511)
BACKGROUND: Panel management is a set of processes and tools for proactively preventing and managing chronic illness in populations of patients, at the level of the primary care panel. It is widely promoted as a component of the patient-centered medical home model. Panel management strategies are still being developed and tested, and have not yet been widely adopted in primary care in the United States. We sought to review the range of panel management strategies tested and assess the effectiveness of panel management interventions in improving primary care processes and clinical outcomes. We used this review to establish a research agenda to advance our understanding of panel management in primary care.
METHODS: A systematic review was conducted utilizing data sources from Ovid Medline, PubMed, Web of Science, and CINAHL from 1990 through January 2014. Study selection included English language trials and longitudinal observational studies that met our criteria for panel management (proactive outreach, conducted in primary care, and use of clinical data). The core search strategy used in each database was (“Population Management” OR “Panel Management”) AND “Primary Care.” We extracted data on study design, population, interventions, outcomes, cost, and risk of bias. Two investigators independently abstracted the data to enhance reliability. In the case of disagreement a third author reviewed the study in question to reach consensus. Using the Cochrane tool, a risk of bias assessment was conducted to verify the studies’ results and to determine if the level of bias was adequate (low) or not adequate (high) across 6 domains.
RESULTS: A total of 87 articles describing unique studies were identified, of which 27 met the inclusion criteria. Of these 27 studies, 17 were randomized controlled trials and 10 were controlled cohort studies, targeting a range of illnesses (e.g. diabetes, various cancers, and heart disease), both primary and secondary prevention, and various care processes (e.g. screenings, labs, appointments) through a variety of panel management approaches (e.g. provider focused, mailed reminders, adding team members). All studies reported significant improvements over usual care or comparison groups, though effect sizes were modest. For instance, 3 out of 4 diabetes studies reported significant improvements in glycemic control (HbA1c) for panel management intervention groups with decreases ranging from 0.3 to 1.07 % over controls and Colorectal cancer screening rates increased significantly (11.0 % to 19.0 % over control) with panel management in all 5 studies reporting screening rates. Only 5 studies undertook any cost-effectiveness analysis; of these 2 reported annual costs per patient ranging from $24 to $464, 2 reported net cost savings (3.6 % to 11 % per patient), and 1 reported no significant savings. The risk of bias was low among the 17 RCTs across most domains, with the predominant risks stemming from the lack of blinding of group assignment and insufficient evidence to determine if there was selective outcome reporting.
CONCLUSIONS: Panel management holds promise for prevention and management of chronic illness within the patient-centered medical home. However, current evidence is insufficient to determine the effects on clinical and economic outcomes. While many of the studies have shown a modest benefit, their heterogeneity to date prevents a definitive conclusion about effect size or ideal approach. This emerging and potentially disruptive innovation in primary care practice needs further research to clarify terms and to cohere around effective and efficient models.
PAP VS. HPV VS CO-TEST FOR CIN2+ DETECTION: A RETROSPECTIVE STUDY OF PERFORMANCE AND COSTAndrea L. Sikon1; Xian W. Jin1; Laura D. Lipold2; Sarah Schramm3; Kelly Nottingham3; Bo Hu4; Michael B. Rothberg1,3. 1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH. (Tracking ID #1936679)
BACKGROUND: Existing cervical cancer screening guidelines allow for two options for women aged 30 and older: pap every 3 years (with reflex testing for HPV when cytology shows ASCUS) or pap and HPV co-testing every 5 years. Some is known about the performance of these two strategies but comparisons of cost are even more limited. To understand the performance of existing as well as a novel strategy (i.e. initial HPV screening with reflex pap if positive,) we compared the expected costs per case of cervical intraepithelial neoplasia 2 or worse (CIN2+) detected by these strategies amongst a large cohort of women.
METHODS: A retrospective chart review was performed of all women 30 years or older who had primary screening with both HPV and cervical cytology (i.e. co-testing) during the same encounter at the Cleveland Clinic from 2004 to 2010. A pathology database was utilized to identify biopsy-proven CIN2+ cases. Information on age, race, marital status, insurance type, and smoking history was also collected. For women who had abnormal screening tests but did not have documented colposcopy results, we performed data imputation based on co-testing results. Sensitivity, specificity, positive and negative predictive values were estimated for 3 strategies: Pap with reflex HPV, HPV with reflex pap and co-testing. For each strategy we calculated costs based on the number of HPV tests, pap tests and colposcopies that would be performed.
RESULTS: The dataset included 99,549 women who had simultaneous cytology and HPV collected during the study period. Subjects were mostly white (78.4 %), married/domestic partner (70.7 %), nonsmokers (61.3 %) and with private insurance (86.1 %). Overall, 5121 subjects (5.14 %, 95 % CI = [5.01 %, 5.28 %]) were infected with HPV and 6115 (6.14 %, 95 % CI = [5.99 %, 6.29 %]) had cytology that demonstrated ASCUS or worse. Of these, 1,347 underwent colposcopy, and 605 subjects (0.61 %; 95 % CI = [0.56 %. 0.66 %]) had CIN2+. An additional 709 women had a combination of HPV+ and ASCUS or higher on cytology but did not have documented colposcopy results. Of these women, 183 had CIN2+ assigned by imputation, for an overall expected incidence rate of CIN2+ of 0.79 % (95 % CI = [0.74 %. 0.85 %]). Sensitivity for CIN2+ was 89.9 % for cytology, 94.0 % for HPV and 97.7 % for co-testing; specificity was 97.7 % for cytology, 98.3 % for HPV and 97.7 % for co-testing. The negative predictive value was 99.92 % for cytology alone, 99.95 % for HPV alone and 99.98 % if both tests were negative. Pap with reflex HPV was least expensive, costing $31.6 M and detecting 708 cases of CIN2+ , with 2965 colposcopies per 100,000 women screened. HPV with reflex pap would detect an additional 33 cases of CIN2+, and require 508 fewer colposcopies, at a marginal cost of $11.3 M, or $342 K per additional case detected. Compared to HPV with reflex pap, co-testing would detect an additional 29 cases, and require an additional 570 colposcopies, at a marginal cost of $21.2 M or $732 K/case. The marginal cost per case would be higher in lower risk populations and vice versa.
CONCLUSIONS: Screening women using HPV initially rather than pap could detect slightly more cases of CIN 2+ at a marginal cost of $342 K/case in this large cohort. Co-testing all patients could detect even more cases, but at a marginal cost of $732 K/case. Acceptable thresholds of additional cost per case to capture a relatively small number of additional cases are currently lacking and further cost effectiveness studies should be considered. In this era of value based care and personalized health care, considerations of varied screening strategies according to individual risk as well as to cost per case is necessary. More sophisticated assessment of risk may help to better modify recommended screening methods and intervals and allow for concentration of more costly resources on those at highest risk while still providing sound screening for those at lower risk.
PARATHYROID HORMONE SUPPRESSION AND INCIDENT HEART FAILUREDerar Albashaireh1; Kawanjit Sekhon4; Mona Hassan1; Laila Shiekh Sroujieh1; Meghan G. Liroff2; Waqas Qureshi3. 1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Wake Forest University, Winston-Salem, NC; 4Wayne State University, Detroit, MI. (Tracking ID #1934393)
BACKGROUND: Secondary hyperparathyroidism is frequently common in patients with chronic kidney disease. Suppression with medications is frequently attempted to prevent accelerated bone loss. However, it is not known if this can decrease the incidence of heart failure.
METHODS: An incident case - control study was performed with cases defined as Stage 3–5 chronic kidney disease (CKD) patients with parathyroid hormone (PTH) levels managed within target levels per National Kidney Foundation guidelines for at least 3 years (CKD stage 3; 35–70 pg/ml, stage 4; 70–110 pg/ml, stage 5; 150–300 pg/ml). Controls were age, gender and race matched and defined as Stage 3–5 CKD patients with <50 % of the times, PTH levels managed within target levels as given above. Conditional multivariate analysis was performed to evaluate the differences between incidences of heart failure. Time to event analysis was performed for heart failure admissions. Echocardiographic evaluation prior to enrollment in the study and after at least 3 years of control in the study were evaluated to define systolic heart failure (left ventricular ejection fraction <50 %) and diastolic heart failure defined based on American society of echocardiography definition.
RESULTS: There were 243 cases (mean age 66.3 ± 13 years, women 60.3 %, whites 58.2 %) and 243 controls. Cases were similar in proportion of hypertension, diabetes, previous history of myocardial infarction, There were 38 systolic heart failure (EF <50 %) and 59 diastolic heart failure in controls, while there were 23 systolic heart failure and 76 diastolic heart failure in cases over a period of 6.3 ± 2.4 years of follow up. Cases were more likely to develop incident systolic and diastolic heart failure (p < 0.01). Predictors of incident heart failure include previous history of diastolic dysfunction (OR 2.45; 95 % CI 1.33–2.95, p = 0.0008), diabetes mellitus (OR 1.45; 95 % CI 1.12–1.84, p = 0.005), and previous history of myocardial infarction (OR 1.94; 95%CI 1.28–2.53, p = 0.007).
CONCLUSIONS: In conclusion, maintaining parathyroid hormone within target limits was associated with decrease in incident heart failure in our study. This may be explained by known role of parathyroid hormone in pathophysiology of heart failure.
PARTICIPATION OF MEDICAL STUDENTS IN TRANSITIONS OF CARE: A NEEDS ASSESSMENTLauren Block1,2; Melissa Morgan-Gouveia3,4; Danelle Cayea4. 1Hofstra North Shore-LIJ School of Medicine, New Hyde Park, NY; 2Bloomberg School of Public Health, Baltimore, NY; 3Christiana Care Health System, Newark, DE; 4Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1936831)
BACKGROUND: As residents are expected to be competent in transitions in care, training in effective transitions must begin in medical school. The Liaison Committee on Medical Education (LCME) cites effective communication and care across the continuum as key skills for trainees. However, medical students report knowledge gaps related to the discharge process. While several medical schools offer curricula on safe transitions of care, formal education on this topic is not universal. We sought to understand the frequency of participation, learning, and independence in transitions in care among third and fourth year medical students.
METHODS: We conducted a cross-sectional survey of third and fourth year students at four medical schools in the mid-Atlantic region. Private, public, and military schools were represented. Students were invited to participate in an electronic survey regarding participation in patient discharges on their medicine clerkship, teaching about discharge skills, independence completing discharge tasks, and additional training desired. IRB approval was obtained at all institutions.
RESULTS: A total of 358 students from the four medical schools completed the survey (response rate = 44 %). 110 (31 %) were third year and 246 (69 %) were fourth year students. 246 (69 %) reported having completed at least one sub-internship. Most students reported participating in discharge tasks with the majority of their patients, including educating patients at discharge (87 %), reconciling medications at discharge (81 %), collaborating with a multidisciplinary team (73 %), identifying barriers to discharge (73 %), and writing discharge instructions (69 %). Fewer students reported writing discharge summaries (66 %) and communicating with the primary care physician (29 %) regularly. Fourth year students were more likely than third year students to report identifying barriers to discharge (76 % vs. 64 %, p = 0.02), reconciling medications at discharge (94 % vs. 85 %, p < 0.01), educating patients at discharge (90 % vs. 81 %, p = .02), reviewing discharge instructions with patients (58 % vs. 46 %, p = 0.03), communicating with the primary care physician (35 % vs. 17 %, p < 0.01), and collaborating with the multidisciplinary team (80 % vs. 56 %, p < 0.01) with the majority of patients. Most students (96 %) reported that residents taught them these skills; only 28 % were taught by attending physicians, and 49 % reported being self-taught. Most students reported independence in reviewing discharge instructions with patients (58 %) and collaborating with the multidisciplinary team (50 %), but fewer than 50 % reported independence in the remaining discharge skills. Students who completed at least one sub-internship reported higher levels of independence in all skills except writing discharge summaries. Students who learned these skills from attending physicians reported more independence in identifying barriers to discharge, writing discharge instructions and summaries, communicating with primary care physicians, and collaborating with multidisciplinary teams. Ninety-seven percent of students reported that additional training in discharge skills would be helpful for their education.
CONCLUSIONS: In a multi-institution sample, most students reported participation in discharge tasks with their patients on the medicine clerkship. Many educational programs prioritize teaching these skills during a subinternship or internship. However, the majority of 3rd year students are involved in tasks related to discharge. Students did not feel fully independent completing these tasks, and the majority reported that additional training would be helpful. While students who learned discharge skills from attending physicians were more likely to report independence in some of these skills, students were more likely to report learning these skills from residents than from faculty, suggesting that formal teaching may be valued by students. Students reported communicating with primary care physicians and reviewing discharge instructions with patients less frequently than other tasks, indicating priority areas for future curricula.
PATIENT ACTIVATION INTERVENTION IMPROVED EVIDENCE-BASED MEDICATION USE IN DIABETIC AND HEART DISEASE PATIENTS IN FEDERALLY QUALIFIED HEALTH CENTERS: THE OFFICE GUIDELINES APPLIED TO PRACTICE PROGRAMAde B. Olomu1; Bikki Gautam1; Bethany Buda1; Wei-Wen Hsu3; Gurpreet Chahal1; Janaki Samaraweera1; Haritha Machavarapu1; Wendy Uwaje1; David Todem2; Margaret Holmes-Rovner4. 1Michigan State University, East Lansing, MI; 2Michigan State University, East Lansing, MI; 3Michigan State University, East Lansing, MI; 4Michigan State University, East Lansing, MI. (Tracking ID #1933143)
BACKGROUND: Many studies have documented suboptimal treatment for cardiac outpatients, especially for minority and low-income population. Despite the well documented efficacy of aspirin, Beta Blockers, statins and angiotensin—converting enzyme inhibitors (ACEIs), appropriate use and adherence to these therapies remains a concern in patients attending Federally Qualified Health Centers (FQHCs). Patient activation/engagement is an increasingly important component of strategies to improve outcomes for patients and reform health care. Objectives: 1) determine the impact of a patient activation intervention on guidelines based medication use for diabetic and heart disease patients in FQHCs 2) determine the predicators of medication use.
METHODS: The Office Guidelines Applied to Practice (Office-GAP) study is a two-center study designed to improve cardiovascular care for minority and low-income populations in outpatient clinical settings. Clinics were assigned to intervention or control arm by tossing the coin. Office-GAP intervention included: 1) Patient activation /engagement intervention during a group visit 2) Physician training for patient activation/engagement and 3) Decision support/Checklist intervention (DSI) used in real time in the office. After a group visit, patients followed up with 2 physician visits using GAP tools. We performed chart abstraction of all enrolled patients with cardiovascular disease (CVD) and Diabetes Mellitus (DM) from September 2010 to Dec 2012 in 2 FQHCs. Logistic Regression analysis was used to examine change over time in the proportion of patients using Aspirin/Plavix, ACEIs /ARBs, beta-blockers and statins.
RESULTS: Of 242 patients studied, 100 patients were in the intervention (Office-GAP) arm and 142 in the control arm. The control group showed no difference between baseline and 6 months medication use, while the intervention group showed the use of ACEIs/ARBs as (58.62 % vs. 63.22 %); Aspirin/Plavix (67.74 % vs. 96.77 %), Beta-blocker (60.00 % vs 71.43 %) and statin (62.78 % vs. 80.52 %) respectively. Longitudinal logistic regression revealed Office-GAP intervention significantly increased the use of ACEIs/ARBs for all eligible patients at 3 months (OR 3.93, p = 0.001), Aspirin/Plavix (OR 2.43, p = 0.046) at 6 months compared to control. Predictors of medication use included age, {ACEIs/ARBs (OR = 1.03, p = <0.001), Aspirin/Plavix (OR = 1.04, p = <0.001), Beta Blocker (OR = 1.02, p = 0.042) and statins (OR = 1.03, p = <0.001)} and Charlson Index {ACEIs/ARBs (OR = 1.28, p = <0.001), ASA/Plavix (OR = 1.4, p = <0.001), Beta Blocker (OR = 1.84, p = <0.001) and statins (OR = 1.38, p = <0.001) }. Whites were more likely to be on ASA/Plavix at baseline, 3 months and 6 months compared to Blacks (OR = 1.78 p = 0.011). Furthermore, patients that completed all 3 Office- GAP visits were more likely to be on ASA/Plavix (OR = 1.73, p = 0.022) compared to patients that completed only one or two Office-GAP visits.
CONCLUSIONS: This Patient Activation Program led to increased use of guidelines based medications for patients with CVD and DM in FQHCs. We found that white patients were more likely to be on aspirin. Age and higher comorbidity predicted increased medication use. The Office-GAP program could serve as a model for implementation of guideline-based care for chronic diseases in outpatient clinical settings. Further study is needed to establish reach, effectiveness, and cost-effectiveness.
PATIENT ACTIVATION MEASURE AND CARE TRANSITIONS AMONG SOCIOECONOMICALLY VULNERABLE ADULTSDevan Kansagara2,3; Molly McClain1,5; Honora Englander2; Dawn Peters1; Cynthia D. Morris4. 1Oregon Health & Science University, Portland, OR; 2Oregon Health & Science University, Portand, OR; 3Portland VA Medical Center, Portland, OR; 4Oregon Health & Science University, Portland, OR; 5University of New Mexico, Albuqurque, NM. (Tracking ID #1937165)
BACKGROUND: The Patient Activation Measure (PAM) quantifies patients’ confidence, skills, and knowledge in regards to managing their own health. Higher levels of activation have been linked to improved health behaviors and health outcomes, and lower health care utilization. Little is known, however, about the use of the PAM during times of care transitions, or in socioeconomically disadvantaged adults, many of whom face poverty and other barriers to accessing care after hospital discharge. We performed this study to explore 1) whether baseline patient activation predicted readmission risk, and 2) whether an intervention that improved patients’ access to care and ability to self-manage care post-discharge might impact patient activation scores.
METHODS: The study is a secondary analysis of data collected in the Care Transitions Innovation (C-TraIn) study. C-TraIn included 382 uninsured and low-income publicly insured adults admitted to general medicine or cardiology inpatient services at a single urban academic medical center in Portland, Oregon. Participants resided in one of three Portland metro area counties, had access to a working phone (friend or shelter phone was okay), spoke English, and had no disabling mental illness (defined as active psychosis or active suicidal ideation). Participants were randomized to receive usual care, or usual care plus C-TraIn, which included (1) transitional nurse coaching and education, often including home visits for highest risk patients; (2) pharmacy care, including provision of 30 days of medications after discharge for those without prescription drug coverage; (3) post-hospital primary care linkages, including establishing new outpatient linkages for those without a usual source of care; and (4) systems integration and continuous quality improvement. Participants were enrolled early in hospitalization and completed a baseline survey with blinded researchers that included the Patient Activation Measure (PAM). The survey was repeated by phone 30 days after discharge. Readmission data for all participants, including the uninsured, were obtained using a hospital administrative database that includes admissions from all Oregon and southwest Washington hospitals We used regression analysis to determine 1) if PAM scores assessed early in hospitalization predicted 30-day readmission, and 2) if there was a difference in PAM scores among C-TraIn compared to control patients We hypothesized that low baseline PAM scores would be associated with higher readmission rates. To measure this, baseline PAM scores were dichotomized as “low” (PAM levels 1 and 2, scores 1–55.1), and “high” (PAM levels 3 and 4, scores of 55.2–100). Odds of readmission comparing low and high baseline PAM were calculated using univariable logistic regression, followed by multivariable logistic regression controlling for clinically relevant covariates, including race, gender, trouble taking medication, depression, illness severity (Charlson index) and social support. We included an interaction between allocation group and baseline PAM score to allow for the possible differential effect of the C-TraIn intervention on the relationship between baseline PAM scores and readmission. We also hypothesized that the C-TraIn intervention would improve patient activation relative to usual care. We compared the 30-day mean change in PAM score between the allocation groups using Student’s t test and followed this by linear regression analysis adjusted for the same covariates as above.
RESULTS: 382 patients enrolled in the C-TraIn study; 209 were allocated to the intervention group and 173 to the control. All 382 completed baseline surveys. 293 (74 %) completed 30-day post-discharge survey, and of these, 254 had complete baseline and post-discharge PAM surveys. Multivariable logistic regression modeling revealed the odds of 30-day readmission was roughly 40 % less for those with high PAM scores [OR: 0.57, 95 % CI: 0.34–0.96, P-value: 0.04] compared to those with low PAM scores. This association was adjusted for race, gender, severity of illness, depression, and social support. Multivariate linear regression modeling, controlling for the same covariates, demonstrated that participation in the Care Transitions Innovation did not affect a change in PAM scores compared to the control group [B-coefficient: −1.06, 95%CI: −4.36–2.11, P-value: 0.52].
CONCLUSIONS: Low baseline PAM scores were associated with higher rates of 30-day readmission, suggesting PAM may be useful in predicting risk of readmission in socioeconomically vulnerable adults. However, PAM scores did not improve in participants who received an intervention that improved transitional care quality and enhanced access to post-discharge care.
PATIENT AND PROVIDER PERCEPTIONS OF THE PATIENT CENTERED MEDICAL HOME: AGREEMENT AND TENSIONSShreya Kangovi1,2; Katherine Kellom4; Christopher Sha5; Sarah Johnson6; Casey Chanton2; Tamala Carter1,4; Judith A. Long3,1; David Grande1,7. 1University of Pennsylvania, Perelman School of Medicine, Phialdelphia, PA; 2University of Pennsylvania Health System, Philadelphia, PA; 3Philadelphia Veterans Affairs Medical Center, Philadelphia, PA; 4University of Pennsylvania, Philadelphia, PA; 5University of San Francisco, San Francisco, CA; 6Johns Hopkins Hospital, Baltimore, MD; 7University of Pennsylvania, Philadelphia, PA. (Tracking ID #1939665)
BACKGROUND: Six years into the movement of Patient-Centered Medical Home (PCMH)-driven primary care redesign, the evidence for its impact on patient and caregiver experience is mixed. Our objective was to explore areas of agreement and tension between the perceptions of high-risk patients and their practice staff on PCMH principles and implementation strategies.
METHODS: We conducted qualitative in-depth, semi-structured interviews with chronically-ill, uninsured or Medicaid patients from low-income Philadelphia ZIP codes (n = 21), and their primary care practice staff (n = 30). We included patients and staff of three practices (two academic and one federally qualified health center).
RESULTS: We observed three key findings. First, while staff were enthusiastic about enhancing access through strategies like online communication and open access scheduling, low-income patients viewed these as access barriers and preferred telephone encounters. Second, both patients and staff described a common tradeoff: timely care from an unfamiliar provider versus delayed access to their personal physician. Participants viewed small, multi-disciplinary teams as a potential strategy for reconciling the tension between access and continuity. Third, practices have re-engineered appointment systems to create slots for unscheduled acute care. Yet, they lacked capacity to manage higher acuity conditions that tended to fill these appointments. As a result, these patients were frequently referred to the emergency room.
CONCLUSIONS: High-risk patients and primary care staff highlighted tensions raised by the PCMH principles and suggested approaches to reconcile those tensions.
PATIENT EXPERIENCES OF AND PREFERENCES FOR ACCESS AND CONTINUITY OF CARE IN A PATIENT-CENTERED MEDICAL HOMEJane Forman1; Molly Harrod1; Claire Robinson1; Ann-Marie Rosland1,2; Leo Greenstone1,2; Adam Tremblay1,2; Eve A. Kerr1,2. 1VA Ann Arbor Healthcare System, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1938328)
BACKGROUND: Two central measures of success of a patient-centered medical home are increasing timely access to primary care (PC) and continuity of care with the patient’s primary care provider (PCP). Compliance with the National Committee for Quality Assurance PCMH and the Centers for Medicare & Medicaid ACO quality standards require practice-level evaluation of access and continuity measures. In its medical home initiative, Patient Aligned Care Teams (PACT), the Department of Veterans Affairs (VA) has emphasized improving access and continuity, and set key metrics for same-day requests with the patient’s assigned PCP (access), and the proportion of encounters completed with the patient’s assigned PCP (continuity). Although measures of access and continuity are built on assumptions about patient preferences, little is known about these preferences and patient experiences. We conducted in-depth qualitative interviews of PC patients in a large VA academic medical center to identify factors that affect where patients choose to seek same-day care (in PC or urgent care), and what influences whether patients prioritize continuity with their usual PCPs vs. short-term access to any PCP.
METHODS: We conducted 25 semi-structured interviews between April and October 2013 with patients who had had at least two visits with their PCP in the 6 months prior to recruitment into the study, and had requested a same-day appointment in the year prior. Interviews were audio-recorded and transcribed. Data were analyzed inductively using grounded theory techniques.
RESULTS: Patient assumptions about whether they could gain same-day access to their PCP (or to PC in general) affected whether they sought care from PC or directly from the site’s urgent care center. Many patients preferred to see a provider in PC if they thought they could get an appointment. Assumptions about access to PC were based largely on prior experiences, including previous success in obtaining same-day PC access, the perception that their provider was “booked up,” experience with a part-time provider who was often unavailable, and experiences with PC clinic processes that necessitated long lead-times to get a routine appointment. Most patients preferred to see their own PCP for acute issues related to a chronic condition, but were willing to see any PCP for unrelated acute issues. Further, patients were willing to see alternate PCPs if they thought that their electronic medical record gave these PCPs adequate information, or if they accepted that their part-time PCP was often unavailable. Some patients were willing to use alternate modes of access such as a telephone visit or secure electronic communication with their PCP, or a visit with the nurse on their team.
CONCLUSIONS: Previous experiences with the PC clinic is a main driver of where patients choose to seek care for urgent issues, and current patterns of care-seeking may not reflect patient preferences in some cases. As clinics make significant changes in access, it will be important to educate patients about the availability of PC appointments, and new ways to get care (e.g., through non face-to-face care or with their team nurse). Clinics will want to move toward aligning triage processes with patient preferences. In constructing access and continuity metrics that allow clinics to meet the needs of patients, policy-makers should consider measuring performance at a team, rather than an individual PCP level, and including modes of care other than face-to-face visits with PCPs.
PATIENT OUTCOMES AFTER GRADUATION OF RESIDENT PRIMARY CARE PHYSICIANS: DOES ACUTE CARE UTILIZATION INCREASE?Sonja Solomon1; Holly Gooding2,3; Harry Reyes Nieva2; Jeffrey A. Linder2. 1Brigham and Women’s Hospital, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3Boston Children’s Hospital, Boston, MA. (Tracking ID #1937542)
BACKGROUND: When residents graduate, their primary care patients are at risk for fragmentation of care, and may be at increased risk of adverse health outcomes and acute care utilization.
METHODS: We examined patients cared for in our hospital-based teaching practice by residents who graduated in 2010, 2011, and 2012. A patient was defined as belonging to a resident’s primary care panel if the patient had seen the resident two or more times in the previous 2 years and had seen that resident more than any other provider in the clinic during that interval. For each year, we identified a transitioning patient cohort, whose residents were graduating, and a non-transitioning patient cohort, whose residents were not graduating. We measured clinic visits, emergency department (ED) visits, and hospitalizations in the 4 months before and after resident graduation. We calculated incident rates and used multivariable negative binomial regression to model the risk of clinic visits, emergency department visits, and hospitalizations by patient transition, adjusting for patient factors, resident factors, and clustering.
RESULTS: Our study population included 90 residents and 4018 unique patients who made up 5988 resident-patient pairs that transitioned (n = 3136) or did not transition (n = 2852) between 2010 and 2012. Patients had a mean age of 50 years old; were 67 % women; 43 % Black, 26 % Latino, and 24 % Non-Latino White; and 78 % spoke English and 13 % spoke Spanish. The clinic visit rate for transitioning patients was 129 per 100 patients in the 4 months before transition and 102 per 100 patients in the 4 months after transition; for non-transitioning patients, the clinic visit rate was 119 per 100 patients and 94 per 100 patients for the same time periods (difference-in-differences, p = 0.13). For transitioning patients, the ED visit rate was 29 per 100 patients before transition and 26 per 100 patients after transition; for non-transitioning patients, the ED visits rate was 28 per 100 patients and 25 per 100 patients for the same time periods (p = 0.49). For transitioning patients, the hospitalization rate was 14 per 100 patients before transition and 13 per 100 patients after transition; for non-transitioning patients, the hospitalization rate was 15 per 100 patients and 12 per 100 patients for the same time periods (p = 0.20). In multivariable modeling there was no increased risk for transitioning patients for clinic visits (adjusted rate ratio [aRR], 1.03; 95 % confidence interval [CI], 0.97 to 1.10), ED visits (aRR, 1.05; 95 % CI, 0.92 to 1.20), or hospitalizations (aRR, 1.04; 95 % CI, 0.83 to 1.31).
CONCLUSIONS: Acute care utilization and clinic visits did not increase or decrease in the 4 months after graduation of resident physicians. However we observed a high rate of acute care utilization in all time periods examined. Residents care for a population at high risk of acute care utilization, and interventions to improve ambulatory continuity of care should be employed throughout the academic year.
PATIENT PERCEPTIONS OF INTENTIONAL MEDICATION DISCONTINUATIONAmy Linsky1,2; Steven R. Simon1,3; Barbara G. Bokhour4,5. 1VA Boston Healthcare System, Boston, MA; 2Boston University School of Medicine, Boston, MA; 3Brigham and Women’s Hospital, Boston, MA; 4ENRM Veterans Affairs Medical Center, Bedford, MA; 5Boston University School of Public Health, Boston, MA. (Tracking ID #1938173)
BACKGROUND: Adverse outcomes from inappropriate medication use, whether measured as adverse clinical events, increased health care costs or decreased quality of life, are pervasive, even within an integrated health care system such as the Veterans Health Administration (VA). While medication adherence and medication reconciliation receive considerable attention, there has been less focus on improving intentional, proactive discontinuation of medications that may no longer be necessary or whose benefits no longer outweigh associated risks. Although discontinuation is often a provider decision, patient perspectives of such discontinuation are important to understand. Therefore, our objective was to identify patient beliefs and attitudes associated with intentional medication discontinuation.
METHODS: We conducted 30–60 min semi-structured qualitative interviews with 20 Veterans and two 60–90 min focus groups with another 7 Veterans. All patients received Primary Care at a VA Medical Center and were taking five or more medications. Patients were asked about their experiences with and attitudes toward taking multiple medications, preferences about taking fewer medications, communication with their clinical providers about medications, and actual or hypothetical response to their provider suggesting to stop a medicine. Fully transcribed interviews were analyzed based on the principles of grounded theory, including open coding, theme development and constant comparative analysis of cases.
RESULTS: The study participants (22 male, 5 female; 22 white, 5 black) had varying exposure to care within the VA and care in non-VA settings. We identified five domains related to Veterans’ perceptions of medication taking and potential discontinuation. 1) Knowledge - Understanding medications’ indications, as well as whether they provided symptom relief, influenced patients’ interest in continuing medication regimens. 2) Internal conflict - Nearly all Veterans expressed their preference not to take any medications, yet because they were recommended for their health, they continued to “follow doctors’ orders.” 3) Communication - Many patients were selective in the information they shared with their providers. Concomitantly, there was a general interest in receiving a rationale from providers when given a recommendation to cease taking a medication. 4) Experience with medication discontinuation - Few Veterans recalled instances of proactive medication discontinuation. 5) Multiple care providers- Many patients had care from multiple providers, leading to differences in which provider’s recommendations to accept, as well as the factors influencing that decision. Overall, Veterans seemed generally interested in taking fewer medications, yet did not voluntarily share these preferences with their providers. Rather, they assumed that the clinician was prescribing what is necessary for their health and did not feel they were in a position to question the provider’s opinion.
CONCLUSIONS: Veterans express a variety of opinions related to medication taking and potential medication discontinuation. For those patients who have a preference to take fewer medicines but do not share their beliefs with providers, there is opportunity to improve the engagement of patients as active players in their health care and enhance communication between patients and providers. Further, while others have noted that providers may believe a patient will feel abandoned by discontinuation of a medication therapy, our findings demonstrate that many patients would welcome such a reduction in pill burden. Future investigation into the full range of patient beliefs will enable development and implementation of targeted interventions that eliminate overuse of potentially inappropriate medications.
PATIENT PREFERENCES FOR CONSENT FOR SECONDARY USES OF ELECTRONIC HEALTH INFORMATIONDavid Grande1,2; Nandita Mitra3,2; Fei Wan3; Anand Shah4,5; David A. Asch1,6. 1University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3University of Pennsylvania, Philadelphia, PA; 4UT Southwestern Medical Center, Dallas, TX; 5PCCI, Dallas, TX; 6Philadelphia VA Medical Center, Philadelphia, PA. (Tracking ID #1938322)
BACKGROUND: The widespread adoption of EHR systems has markedly increased the availability of patient-level electronic health information. This information has substantial value across a range of uses from biomedical research to commercial marketing leading to debate around the role patient consent should play. The federal government has proposed new regulations that would relax requirements for consent for information-based research that poses minimal risk. Because consent for information use has been central to current policies on data use, but new proposals subordinate the role of consent, we examined public perceptions of the importance of consent for health information use.
METHODS: We performed a national experimental survey of 3,064 people (reflecting a 65 % response rate) from a nationally representative panel (GfK Knowledge Networks), structured as a randomized controlled trial, to examine perceptions of different uses of electronic health information under different consent arrangements. We randomized individuals to 2 of 8 vignettes describing the use of electronic health information reflecting the rate and predictors of use of a pharmacologic treatment. The 8 vignettes were identical except, in a 2 × 2 × 2 design, they systematically varied along three dimensions: patient consent (obtained vs. not obtained), use (research vs. commercial marketing), and the framing of how the findings would be or were used (abstract vs. specific benefits). Participants rated the appropriateness of each vignette on a 1–10 scale (1 = not at all appropriate; 10 = very appropriate).
RESULTS: Mean participant ratings ranged from a low of 3.90 for the scenario describing a marketing use when consent was not obtained and the framing was a past and specific use to a high of 6.95 for the scenario describing a research use when consent was obtained and the framing was a past and specific use. Participants rated scenarios where consent was obtained as more appropriate compared to scenarios where consent was not obtained (+1.02; P < 0.001). Participants rated scenarios where the use was marketing as less appropriate compared to when the use was research (−1.88; P < 0.001). Participants rated the scenarios with different framing equally (−0.03; P = 0.86 for future abstract benefits vs. past specific benefits). Overall, the effect of use was greater than the effect of consent on participants’ ratings of appropriateness (1.88 vs. 1.02; P < 0.001). Minority respondents rated the consent arrangements similarly (consent* African American interaction: −0.19, P = 0.54; consent*Hispanic interaction: 0.10, P = 0.73).
CONCLUSIONS: As more electronic health information is available, the potential uses will grow. Clear policies are needed to guide stewardship of information. Our study shows that although the effects of both consent and use were measurable, use was a more important factor than whether consent was obtained. Respondents preferred the use of personal health information for research purposes even without consent over its use for marketing purposes even with consent. These views about research uses and consent policies were consistent regardless of race and ethnicity. Our study suggests we may need to focus more attention on the social value of information use and perhaps apply different standards of consent across uses. Such an approach contrasts with current policies where research uses of this information are often subjected to the strictest standards of consent.
PATIENT SAFETY IMPLICATIONS OF SHARED VISIT NOTES: TRAINEE AND PRECEPTOR VIEWSBradley Crotty2,1; Sigall K. Bell1; Melissa Anselmo1; Lydia A. Flier1; Suzanne Leveille1; Roanne Mejilla1; Jan Walker1. 1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1940605)
BACKGROUND: Safety experts seek ways to reduce medical errors in ambulatory care. OpenNotes, an innovation that invites patients to see their doctors’ notes online, may promote patient safety through increased transparency, but may also “expose” errors previously unseen by patients. We explored trainee and preceptor perceptions about errors in trainee notes and the anticipated effects of shared visit notes on patient safety.
METHODS: Three focus groups with trainees and preceptors from various departments discussing: anticipated effects of shared notes on safety, clinician concerns, anticipated patient reactions to errors, and suggestions). Sessions were recorded and professionally transcribed. We analyzed transcripts using established qualitative methods.
RESULTS: Focus group participants generally agreed that shared notes may improve patient safety, through: 1) increased medication and health maintenance adherence; 2) familiarity with facts, allergies, and review of visits/instructions; and 3) opportunity for patients to catch mistakes and update family history. Some specialists worried that shared notes may harm some patients, and lead doctors to document less, restricting MD-MD communication (“I want to make sure I can communicate this to the referring physician without sugar-coating it.”) Trainees wrestled with what constitutes an error, which mistakes would bother patients (wrong side/gender documentation, wrong diagnosis, misquoting), and “who holds the truth” when patients and doctors disagree. Most believed patients would appreciate transparency, and welcomed corrections that prevented chart propagation of mistakes; others worried patients may lose faith in their doctors. Some added “too much honesty” (like a suspected wrong sponge count) could “freak someone out.” A few had anxiety about medical-legal risk, and thought patients might “scour” the notes. Trainees needed help responding to errors. They advocated education, enhanced professional dictation proofing, note disclaimers (re: dictation errors), preceptor feedback, triage support for patient calls, and enhanced editing capability instead of note addenda to fix mistakes. Preceptors struggled with tensions between supervision, time pressure, and educational goals—conceding that they, (and trainees), may just sign notes to keep up. Some were particularly concerned about liability: “Open sesame, look what they wrote.“ Preceptors underscored increased vigilance to catch errors, and system fixes requiring a cosignature before trainee notes are available to patients.
CONCLUSIONS: Trainees and preceptors generally agree that shared notes have the potential to improve patient safety. Trainees worried about patients finding trivial and real errors in their notes, (and how to handle these), signaling the need for education and support systems. Preceptors were most concerned about liability and time/system constraints for adequate oversight and teaching. Note transparency may expose safety vulnerabilities and errors otherwise unseen, providing opportunities to engage patients in safety, address workload constraints, enhance trainee feedback, and reinforce culture of safety principles.
PATIENT-CENTERED MEDICAL HOME IMPLEMENTATION AND PROVIDER JOB TURNOVERPhilip W. Sylling1; Edwin Wong1,4; Chuan-Fen Liu1,4; Susan Hernandez1,4; Adam Batten1; Christian Helfrich1,4; Karin M. Nelson1,2; Stephan D. Fihn3,5; Paul Hebert1,4. 1VA Puget Sound Healthcare System, Seattle, WA; 2VA Puget Sound Healthcare System, Seattle, WA; 3University of Washington, Seattle, WA; 4University of Washington, Seattle, WA; 5Veterans Health Administration, Seattle, WA. (Tracking ID #1938371)
BACKGROUND: The aim of this study was to examine the relationship between the implementation of a patient-centered medical home (PCMH) model and primary care provider (PCP) job turnover. The Veterans Health Administration (VHA) began implementing a PCMH through its Patient Aligned Care Team (PACT) initiative in April 2010. Although elements of PACT have been individually associated with greater PCP job satisfaction, the magnitude of organizational change required by PACT’s restructuring of primary care may result in higher provider turnover, at least in the short-term. Existing literature has not specifically examined the effect of PCMH on PCP turnover.
METHODS: We applied an interrupted time series model using VHA administrative data. PCP turnover was defined by providers’ dropping out of the primary care workforce for two or more consecutive quarters. We constructed discrete-time longitudinal data from PCPs employed by the VHA anytime from 2003 to 2012 with the unit of analysis at the PCP-quarter level. PCPs included physicians, nurse practitioners, and physician assistants. We estimated the association between PACT and provider turnover using logistic regression and adjusted for seasonality and secular trend, provider and job characteristics, and the local area unemployment rate. For adjusted analysis, we calculated average marginal effects (AMEs), which reflected the change in PCP turnover probability associated with unit increases in the explanatory variables. To examine differential effects of PACT across providers, we interacted a PACT indicator variable with PCP demographics.
RESULTS: The unadjusted quarterly rate of PCP turnover was 3.06 % prior to PACT and 3.38 % after PACT. In adjusted analysis, PACT was associated with higher provider turnover (AME = 0.004, p = 0.004). The association between PACT and PCP turnover was significantly different across age groups and experience levels. PACT was associated with a −0.0008 (p = 0.711), 0.0046 (p = 0.011), and 0.0069 (p = 0.002) percentage point increase in turnover probability for providers under age 45, age 45 to 55, and over age 55, respectively. Compared to PCPs with 5 years of experience (AME = 0.0019, p = 0.239), the estimated effect of PACT on turnover was higher for PCPs with 20 years of experience (AME = 0.0106, p < 0.001). Provider type was also associated with baseline provider turnover. Nurse practitioners (AME = 0.0055, p < 0.001) and physician assistants (AME = 0.0084, p < 0.001) had higher baseline turnover than physicians.
CONCLUSIONS: PCMH implementation in VHA primary care required providers to adopt a team-based model of care as well as utilize new patient-centered forms of care delivery. This transition represented substantial organizational change which may have increased job stress among some providers. Our results suggest that PCMH implementation was associated with higher initial provider job turnover, particularly among older and more experienced providers. From a policy perspective, health system decision makers should consider the potential short-term impact of increased PCP turnover when implementing PCMH models, which could adversely impact quality of patient care delivery. Also, health systems implementing PCMH may maximize resources by focusing retention efforts on older and more experienced providers.
PATIENTS WHO SHARE TRANSPARENT VISIT NOTES WITH OTHERS: CHARACTERISTICS, RISKS AND BENEFITSSara L. Jackson1; Roanne Mejilla2; Jonathan Darer5; Natalia Oster1; James Ralston3; Suzanne Leveille4; Jan Walker2; Tom Delbanco2; Joann G. Elmore1. 1University of Washington, Seattle, WA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 3Group Health Cooperative, Seattle, WA; 4University of Massachusetts, Boston, MA; 5Geisinger Health System, Danville, PA. (Tracking ID #1936331)
BACKGROUND: Inviting patients to read their primary care visit notes may improve communication and help them engage more actively in their health care. Little is known about how patients will use the opportunity to share their visit notes with family members or caregivers, or what the benefits might be.
METHODS: The OpenNotes study invited patients to access their primary care providers’ visit notes in Massachusetts, Pennsylvania, and Washington. Pre- and post-intervention surveys assessed patient demographics, standardized measures of patient-doctor communication, sharing of visit notes with others during the study, and specific health behaviors reflecting the potential benefits and risks of offering patients easy access to their visit notes.
RESULTS: Fifty-five percent of the 4,516 participants who reported viewing at least one visit note would like the option of letting family members or friends have their own access to their visit notes, and 980 (22 %) reported sharing their visit notes with someone during the study year. Participants who shared their visit notes were more likely to report they took better care of themselves and did better with taking their medications as prescribed, after adjustment for age, gender, employment status, and study site. Men, and those retired or unable to work, were significantly more likely to share visit notes, and sharers were neither more nor less concerned about their privacy than were non-sharers.
CONCLUSIONS: One in five OpenNotes patients shared a visit note with someone, and sharers reported better adherence to self-care and medications. As health information technology systems increase patients’ ability to access their medical records, facilitating access to caregivers may improve health behaviors.
PATIENTS’ PERCEPTIONS OF ELECTRONIC SYSTEM MESSAGING WITH PHYSICIANSNeil J. Farber; Lisa J. Wastila; John Fontanessi. University of California, San Diego, La Jolla, CA. (Tracking ID #1913265)
BACKGROUND: Although electronic messaging has been used to improve the medical care of patients in various studies, there are concerns by physicians about the appropriate use of messaging. Concerns by physicians include the possibility of urgent medical problems not being addressed in a timely manner. There is also the concern of the inappropriate use of e-mail for sensitive issues or those requiring face-to-face communication. Recent studies assessed only those patients who have e-mailed about all issues rather than the total with medical problems. In addition, there are no prior studies assessing patient who have not yet signed on to such systems. We therefore conducted a survey of patients who signed on, and have not yet signed on, to a messaging system as to their perceptions about its use.
METHODS: A survey was developed which uses hypothetical scenarios in which patients might use electronic messaging vs. the telephone to communicate with their physicians. The survey was validated among 20 General Internal Medicine faculty, and then pretested in 30 patients in a university faculty practice. The survey instrument asks how likely they would send an e-mail message via the electronic messaging system to their physician in 12 different scenarios. The hypothetical scenarios vary according to the urgency and seriousness of the symptoms and possible underlying diagnoses, with 2 of the scenarios deemed acceptable for patients to e-mail their physicians, and 10 deemed as unacceptable for electronic messaging to be used to communicate the problem. A total of 500 patients in a university faculty practice completed the questionnaire. The total number of correct responses to scenarios was calculated and used to compare electronic messaging users and non-users via student T tests. The total number of scenarios that were deemed as a correct response was used as an independent variable in analyses of the impact of demographic variables via multiple regression analyses.
RESULTS: Of the 500 responses, 33 had no access to e-mail of any kind and were therefore eliminated from the analysis. The respondents were largely well educated, with about 2/3 having signed up for the electronic messaging system. A large portion of respondents incorrectly used electronic messaging in the hypothetical scenarios, with 7 % and 26 % indicating they would not use electronic messaging in the two situations which were deemed appropriate for electronic messaging, and 27–59 % likely to use it in the 10 situations which were deemed inappropriate. Patients who had signed up for electronic messaging were significantly more likely to appropriately use electronic messaging than those who had not signed up for it (p < 0.001) and female patients were more likely to correctly use electronic messaging than male patients (p < 0.001).
CONCLUSIONS: Patients may have inaccurate perceptions of the appropriateness of using electronic messaging for relating symptoms of an urgent nature and receiving test results which should be conveyed in person. Those patients who have not signed up for electronic messaging, and therefore have not received guidelines about its use, are particularly at risk for misperceptions about using the system. All patients who use electronic messaging should be educated about its appropriate use.
PATIENTS’ VS. PHYSICIANS’ VIEWS ON HOSPITALIZATIONS AVOIDABLE THROUGH OUTPATIENT MANAGEMENTSang Been N. Hong; Nirav Vakharia; James Pile; Erik Howell; Kristen Boyer; Kelly Nottingham; Jacqueline Fox; Neha R. Pidatala; Michael B. Rothberg. Cleveland Clinic, Cleveland, OH. (Tracking ID #1940155)
BACKGROUND: There is increasing pressure and incentive for hospitals to reduce avoidable admissions. One potential way to reduce admissions is through better outpatient management. Understanding the patient perspective on what is preventable is important for developing successful outpatient management strategies. However, patients’ views on the nature of their admissions are poorly described.
METHODS: We reviewed 322 serial admissions to a general medicine service at an academic medical center in December 2013. For each admission, the attending physician was asked to determine whether the admission was preventable, defined as the presence of any factor during the 2 weeks prior to admission which, if addressed in the outpatient setting, could have prevented the hospitalization. For each admission deemed preventable, the physician selected one primary and any number of secondary factors that led to the hospitalization from a pre-formed list (including an “other” option). The list was categorized into system, clinician, and patient factors. Every sixth patient with a preventable admission was approached for an open-ended interview. If the patient was unavailable, the next available patient was chosen for interview. Patients unavailable for interview included those who were discharged, confused, or impaired and unable to communicate appropriately. Patients were asked to identify any actions that might have been taken by the patient or outpatient physician in the 2 weeks prior to admission to prevent the current hospitalization, and to identify any barriers to those actions.
RESULTS: Of 122 admissions deemed preventable by an inpatient attending physician, 39 patients were approached for interview, and a total of 20 patients (16 %) were interviewed. Overall, patients were less likely than physicians to identify their admissions as preventable (30 % vs 100 %, p < 0.01). Physicians attributed 50 % of admissions primarily to patient factors, 25 % to system factors, and 25 % to clinician factors. In contrast, patients were equally as likely to identify patient factors (10 %) as they were system and clinician factors (10 % each) as primary contributing factors to hospitalization. Of 12 patients (60 %) who were identified by physicians as having a patient factor contributing in some way—primarily or secondarily—to the admission, none identified the same primary contributing factor as the physician. Patient factors commonly identified by the physicians were secondary gain (42 %), non-adherence (42 %), unreasonable expectations or demands (33 %), and mental health or substance abuse (25 %). In contrast, patients primarily attributed their admissions to a fear of hospitals and doctors that prevented timely access to care, inappropriate inpatient management at an outside hospital, and inadequate pain management by the health system—none of which were factors recognized by the physicians. In only one case did the patient and physician identify the same factor—homelessness--as contributing to the admission. Similarly, of 12 patients (60 %) identified by physicians as having system or clinician factors that led to admission in some way, only one identified the same primary factor—an unaddressed problem from the last admission—as did the physician.
CONCLUSIONS: Patients frequently disagree with physicians as to whether their admissions are preventable through better outpatient management. Disagreement may be most pronounced regarding those things deemed by the physician to be within the patient’s control. This patient perspective will need to be considered when devising interventions to reduce preventable admissions. Further studies of patients’ understanding of the roles of inpatient care, outpatient care, and patient responsibility are needed to inform patient education efforts.
PATTERNS AND PREDICTORS OF MEDICATION DISCREPANCIES IN PRIMARY CAREDaniel J. Coletti1,2; Hara Stephanou2; Nissa Mazzola3; JoAnne Gottridge2; Joseph Conigliaro2; John M. Kane1. 1The Zucker Hillside Hospital, Glen Oaks, NY; 2North Shore-Long Island Jewish Health System, Great Neck, NY; 3St. John’s University, Jamaica, NY. (Tracking ID #1929866)
BACKGROUND: It has been estimated that having patients take a correctly prescribed medication, as prescribed, would result in a savings of $290 billion in avoidable medical costs (constituting 13 % of US healthcare expenditures). Extensive research has documented the impact of patient adherence on medication regimens as well as pervasive problems establishing and maintaining accurate and effective patient medication lists across time and settings of care. Research examining the relations between medication discrepancies and patient adherence to treatment, however, is limited. The primary objective of this investigation was to explore relationships between patient-reported adherence and the presence of patient-provider medication discrepancies in primary care. We sought to examine relations between medication discrepancies, attitudes to health and medication, and perceived physical and emotional well being. We also tested the hypothesis that patient-reported non-adherence would be associated with the presence of medication discrepancies.
METHODS: Eligible participants were enrolled patients in a large, hospital-affiliated patient-centered medical home serving a socioeconomically and culturally diverse catchment area. Participants completed several questionnaires assessing attitudes to health, treatment adherence, emotional and physical functioning, patient activation, and health literacy. Medication discrepancies were examined by comparing each patient’s self-reported medication list for the previous week to all active medications recorded in the patient’s electronic health record at the time of their visit. Discrepancies were categorized as involving a) over-the counter medications and/or supplements, b) time-limited prescriptions, c) medications prescribed to be taken as needed (PRN), d) topic/external agents, and e) an active, daily prescription medication treatment. Electronic record review was conducted by two trained raters using a standardized review algorithm. Multivariate logistic regression was used to identify variables associated with an active medication treatment discrepancy.
RESULTS: A total of 328 patient-participants (217 women and 111 men, mean age = 49.23 years, SD = 15) were taking one or more medications and had a subsequent medical encounter during which medication reconciliation practices could be examined. Participants’ self-assessment of their medication regimens suggested relatively high rates of adherence, with the obtained ASK-12 mean score of 23.69 (SD = 7.22) indicating fewer adherence barriers than the mean of 27.5 (SD = 7.20) obtained in a published validation sample (t = 9.69, df = 323, p < .001). However, a significant difference was obtained between number of medications reported by patients (M = 3.79, SD = 3.13) and the number of active medications in the medical record (M = 4.83, SD = 3.96, t = 6.62, df = 327, p < .001). At least one discrepancy was identified in most patient records (294/328 or 89.6 %). Full or partial medication reconciliation during the medical encounter occurred in only 62/294 (21.1 %) of patients with discrepancies. Additional analyses were completed on a subgroup of 189 patients with one or more discrepancies involving an active, daily, prescribed medication treatment. The presence of one or more daily prescribed treatment discrepancies was associated with lower levels of health literacy, lower subjective well being and patient activation, higher levels of functional impairment, and poorer adherence to the regimen patients believed they had been prescribed. Multivariate analysis, however, indicated that the most significant predictors of medication discrepancies were the number of medication orders in the patient’s medical record, and subjective well being.
CONCLUSIONS: Results from this investigation indicate significant rates of non-concordance between patient representations of their medication regimens and their primary care medical record. Working towards patient-provider agreement on the desired medication regimen, therefore, is likely to be a necessary first step before making valid attempts to address patient adherence. Findings suggest a positive relation between patient non-adherence and the presence of patient-medical record discrepancies. Multivariate results, however, suggest that closing these gaps might best be accomplished by addressing patients’ emotional state as well as making attempts to simplify medication regimens when possible. Observed associations between medication discrepancies and multiple cognitive, functional, emotional, and behavioral patient variables suggests that medication review and reconciliation interventions should combine information about medication with behavioral, emotional, and problem solving supports to help patients understand, coordinate, maintain, and adhere to their medication regimen.
PAYMENT REFORM IN MASSACHUSETTS: EFFECT OF GLOBAL PAYMENT ON HEALTH CARE SPENDING AND QUALITY 4 YEARS INTO THE ALTERNATIVE QUALITY CONTRACTZirui Song1,2; Dana G. Safran3,4; Bruce E. Landon1,5; Sherri Rose1; Matthew Day3; Michael E. Chernew1,2. 1Harvard Medical School, Boston, MA; 2National Bureau of Economic Research, Cambridge, MA; 3Blue Cross Blue Shield of Massachusetts, Boston, MA; 4Tufts University School of Medicine, Boston, MA; 5Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1939467)
BACKGROUND: Slowing the growth of health care spending while improving quality of care remains a national priority. Global payment within accountable care organizations has received increasing attention as a potential way to control spending while improving quality. In 2009, Massachusetts began moving away from fee-for-service with the Blue Cross Blue Shield of Massachusetts Alternative Quality Contract (AQC). The AQC pays provider organizations a global budget that covers the entire continuum of care, while rewarding up to 10 % of the budget in additional quality bonuses. In the ensuing years, membership in the AQC has grown. We evaluated the effect of the AQC on spending and quality after 4 years.
METHODS: We used claims and quality data in a difference-in-differences design to assess the association between the AQC and changes in spending and quality. For the 2009 AQC cohort, the pre-intervention period was 2006–2008, while the post-intervention period was 2009–2012. In addition to basic unadjusted analysis, we used propensity-weighted linear regression models at the enrollee level adjusting for demographics, health status, secular trends, and plan benefit design. We conducted a number of sensitivity analyses, consistent with our prior work. We decomposed the AQC effect by year, as well as by type of care, site of care, health status, risk contracting experience, and price versus utilization effects.
RESULTS: The 2009 AQC cohort comprised about 500,000 unique enrollees across the study period whose primary care physicians belonged to organizations that entered the AQC in 2009. Building on prior work demonstrating AQC-associated savings of 1.9 % in year-1 and 3.3 % in year-2, preliminary analyses show that the AQC continued to slow medical spending in years 3 and 4, on average exceeding 5 % in these years. Medical savings were larger than the sum of budget surpluses and quality payments. Accounting for shared savings and quality bonuses, total health care spending growth after 4 years was lower than the targeted state economic growth of 3.6 %. Savings were larger among organizations without prior risk contracting experience. Changes in both prices (through referral pattern changes) and volume helped explain the results, which were evident in imaging, tests, and procedures. Achievement of quality in chronic care management improved from 79 % in 2007 to 86 % in 2012; adult preventive care from 74 to 82 %; and pediatric care from 79 to 85 %. Analogous results for subsequent cohorts were broadly consistent.
CONCLUSIONS: After 4 years, the AQC was associated with a slowing of spending growth and improved quality. Combining global budgets with pay-for-performance for accountable care organizations may be a successful model for slowing spending and improving quality. Global payment may be able to encourage greater price competition without threatening quality. The AQC could be informative for Medicare in both its Shared Savings and Pioneer ACO programs, as well as for other commercial insurers across the country engaged in payment reform.
PEER SUPPORT FOR CHRONIC PAIN SELF-MANAGEMENT: A QUALITATIVE STUDY OF PEER COACHES’ EXPERIENCESMarianne S. Matthias; Marina Kukla; Alan B. McGuire; Matthew J. Bair. Roudebush VAMC, Indianapolis, IN. (Tracking ID #1937546)
BACKGROUND: Chronic pain is prevalent, disabling, and costly. Pain reduces quality of life and is associated with emotional distress when it interferes with work, social and recreational activities, and family life. In this study we elicited the experiences of peer coaches who participated in an intervention to support patients’ chronic pain self-management.
METHODS: The intervention lasted 4 months. Ten peer coaches with chronic musculoskeletal pain who had participated in a prior pain self-management study participated. Peer coaches attended a 3-hour group training session, which included instruction on goal-setting, motivational interviewing, and role playing. Coaches participated in regular supervision calls with the study psychologist during the intervention, which reinforced training, taught additional motivational strategies, and provided a forum to discuss questions or concerns. Each coach was assigned two patients with musculoskeletal pain, matched, to the extent possible, on age and pain location. Pairs were asked to meet or talk via telephone at least biweekly for 4 months, guided by a study manual on pain self-management. Coaches were asked to discuss different topics in the manual at each meeting, while also providing encouragement, support, and motivation. After the intervention, coaches and patients were asked open-ended questions about their experiences with the intervention. Interviews were audio-taped, transcribed, and checked for accuracy. We used constant comparative methods to analyze the data.
RESULTS: Nine peer coaches completed the study; ages ranged from 50 to 71 (M = 60, SD = 7) years. All were male veterans. Although the intervention targeted patients, peer coaches described benefitting from the study in three key ways: 1) establishing an interpersonal connection with other veterans with pain, 2) putting their own problems in perspective, and 3) strengthening their own pain self-management practices. Each theme is described below. Theme 1: Interpersonal Connections. Coaches valued the human connection they made with another person: “Getting to know them…their private life, situation… the interpersonal contact… that’s fun, rewarding” (P106). Another coached echoed these sentiments: “The most important part was the opportunity to engage someone else… we learn about each other and…I profit from that, too.” (P112) Theme 2: Putting Problems into Perspective. For some peer coaches, participating in the intervention made them realize their own problems were relatively small. One coach stated, “You think you’ve got…problems, and then you talk to somebody that has real…problems, it sort of grounds you.” (P104) For another coach, talking to his assigned patients, as well as to many of his friends, “makes me appreciate that although I have my own little problems, my problems are much smaller…I feel lucky.” (P107) Theme 3: Strengthening Self-Management Practices. For many coaches, discussing pain self-management with their partners served as an important reinforcement of their own pain self-management practices. One coach described helping his patients learn stretching exercises, which he also committed to do with them. As a result, “it actually got me into a stretching routine that was good” and “strengthened my resolve and ability to deal with my own pain.” (P106) Another coach noted that the intervention “showed me that I needed to work on my pain a little bit more, and maybe my attitude. You know, get motivated a little bit more.” (P102)
CONCLUSIONS: Peer coaches described several benefits of participating in a peer support intervention for chronic pain self-management. Additional research is needed to better understand the benefits of peer support for both patients and peer coaches with chronic pain.
PERCEPTIONS OF INTERNAL MEDICINE RESIDENTS ON SUDDEN DISRUPTIONS TO THEIR TRAINING: A STUDY OF HURRICANE SANDYShaun K. Yang1; Yixin Fang2; Patrick M. Cocks1. 1New York University School of Medicine, New York, NY; 2New York University School of Medicine, New York, NY. (Tracking ID #1927669)
BACKGROUND: The effect of natural disasters on medical residency training remains largely unstudied. Hurricane Sandy made landfall on October 29, 2012 and forced the subsequent evacuation and closure of the three teaching hospitals of the New York University (NYU) internal medicine residency program. To minimize the disruptive effects from the storm, NYU internal medicine residents were deployed to nearby medical centers to resume their residency training with the support of neighboring internal medicine residency programs. The objective of this study was to describe the effect of Hurricane Sandy on medical residency training based on the reported experiences of NYU internal medicine residents.
METHODS: All 148 residents of the NYU internal medicine residency program were absorbed by 13 hospitals across New York City. Residents were deployed to offsite general medicine ward rotations for three months in the form of independent ward teams along side the host residency programs. Seven months after Hurricane Sandy, we conducted a cross-sectional survey of all NYU internal medicine residents. Residents were contacted by email and responded via an anonymous electronic survey. Respondents were asked, “What impact has Hurricane Sandy had on your clinical training?” and the 5-point scale ranged response options from “substantially positive impact” to “substantially negative impact” and included the option of “really hard to say”. Respondents were asked to elaborate on their answer with a follow-up free response question. Surveys were fielded and data de-identified by a third party independent of the residency program. Free responses were categorized into common themes. Descriptive statistics were used to summarize the responses. A chi-squared analysis examined the association between the perceived impact on training and the year of residency.
RESULTS: Eighty-six residents completed the questionnaire (58 % response rate). Respondents consisted of 35 first-year residents (41 %), 30 second-year residents (35 %) and 21 third-year residents (24 %). Only five residents (6 %) reported that Hurricane Sandy had a “substantially negative impact” on their clinical training, 44 residents reported a “slightly negatively impact” (51 %), 15 residents reported “slightly positive impact” (17 %), 1 resident reported “substantially positive impact” (1 %), 10 residents reported “no real impact” (12 %), and 11 residents reported the impact of Hurricane Sandy as “really hard to say” (13 %). There was no association between the perceived impact on training and the year of residency (p = 0.251). Frequently cited reasons among residents who reported a slightly or substantially negative impact included missed critical care rotations (26 %), fewer educational activities (19 %), lower patient volume (16 %), lower case acuity (13 %), missed general medicine floor rotations (13 %), learning a new hospital system (8 %), commuting (6 %), and credentialing (3 %). Common reasons among residents who reported a slightly or substantially positive impact included the exposure to other hospital systems and residency programs (23 %), exposure to disaster medicine (5 %), and increased time for education (5 %).
CONCLUSIONS: Natural disasters have the potential to impede the training of medical residency programs and our data suggest strategies to minimize the negative consequences by including specialized rotations and increased educational activities. Observational studies using competency-based assessments could help to determine the sustained effects of natural disasters. Finally, strategies to maintain residency programs should be considered in regional policies for disaster preparedness and response.
PERI-OPERATIVE USE OF MEDICAL CONSULTANTS AND 30-DAY MORTALITY RATESLena M. Chen; Adam S. Wilk; Edward C. Norton; Mousumi Banerjee; John D. Birkmeyer. University of Michigan, Ann Arbor, MI. (Tracking ID #1931367)
BACKGROUND: Use of medical consultants for surgical inpatients varies widely, but its association with mortality is unknown. Therefore, we sought to describe the association between peri-operative medical consult use and mortality.
METHODS: We conducted an observational, retrospective cohort study of fee-for-service Medicare beneficiaries 65 years of age or older, who underwent colectomy or total hip replacement (THR) from 2007 to 2010 at an acute care hospital. We fit two-stage least squares models to estimate the association between inpatient consult use and mortality, controlling for patient-level and hospital-level covariates (i.e., gender, age group, race/ethnicity, 29 Elixhauser co-morbidities, number of beds, teaching status, nurse staffing, urban location, profit status, and region). We used an instrumental variable—average consult use within a patient’s hospital referral region in the prior year—to minimize confounding. Our two primary predictors were total number of inpatient consults and use of at least one inpatient consult. Our primary outcome was 30-day, all-cause, risk-adjusted mortality.
RESULTS: There was considerable variation in the use of inpatient medical consults (for colectomy, median of 5, IQR: 0 to 14; for THR, median of 2, IQR: 0 to 4). Sixty-nine percent (63 %) of colectomy (THR) patients had at least one consult. Unadjusted 30-day mortality rates were 5.7 % after colectomy and 0.4 % after THR. Use of one additional consult was associated with a 0.01 percentage point increase (or 0.02 pp increase) in mortality rates for colectomy (or THR), but this finding was not statistically significant (p = 0.71 and p = 0.25, respectively). Use of at least one consult was associated with a 0.6 percentage point decrease (or 0.05 pp increase) in mortality rates for colectomy (or THR); this finding too was not statistically significant (p = 0.49 and p = 0.44, respectively).
CONCLUSIONS: We found no association between peri-operative medical consult use, and 30-day, risk-adjusted mortality rates after hospitalization for colectomy or THR.
PERSISTENCE OF DIAGNOSTIC DELAY IN 2013: A BIBLIOMETIC STUDYClaudia L. Campos; James L. Wofford. Wake Forest University, Winston-Salem, NC. (Tracking ID #1934783)
BACKGROUND: Previous studies of diagnostic delay have been few, inconsistent in methodology, and tentative in defining the amount of delay for specific diagnoses. The emerging field of diagnostic error deserves an update, as diagnostic delay should have decreased over time with more sophisticated diagnostic tools and greater awareness.
METHODS: We conducted a bibliometric search of the MEDLINE database using the free text phrase “diagnostic delay” and restricting our search to publications in year 2013. Abstract review allowed categorization of abstracts by country of origin, study type, and disease category. The degree of diagnostic delay was determined for most common diseases and with disease registries as the study population.
RESULTS: Of the 135 citations, most citations came from institutions in the USA (9) and UK (19), but 35 countries were represented in the search results. 12 % (17/135) of citations were from developing countries. Study type was not discernible from the abstract with 7 citations. Study types included case-reports or case-series (37), discussions/literature reviews (22), registries/clinical networks (17), physician interviews (2). There were 3 prospective studies with the remaining studies retrospective or cross-sectional in design. Disease categories were most often infection (25/135, 19 %), cancer (20), neurologic (15), rheumatologic (10), or vascular (8). The most common specific diagnoses were tuberculosis (13), ALS (4), endometriosis (3), oral cancer (3), ocular cancer (3) but other diagnoses were represented no more than twice among the citations. Disease registries offered the largest number of patients (mean 6564, range 100–56462), and specific duration of DD were offered in 16 of 17 studies. No studies of systematic approaches to diagnostic error were evident with this search strategy.
CONCLUSIONS: Diagnostic delay is alive and well in the medical literature. Compared with previous studies of diagnostic delay, findings from disease registries offer larger sample sizes and more confidence in defining duration of delay.
PERSPECTIVE OF THE GRADUATING MEDICAL STUDENT: THE IDEAL CURRICULUM FOR THE 4TH YEAR OF UNDERGRADUATE MEDICAL EDUCATIONMary Andrews2,1; Nathalie Paolino2,1; Brian Hemann1,2; Lynn Byars1,2; Steven Durning1,2; Kent DeZee1,2. 1Uniformed Services University, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD. (Tracking ID #1937644)
BACKGROUND: Undergraduate medical education has undergone much reform in the past decade, but the final year has received little attention thus far. The aim of this study is to determine which experiences graduating medical students feel are the most important in designing a fourth year curriculum, as there are no large scale studies from the student’s perspective.
METHODS: This is a cross-sectional survey study, conducted to assess the relative importance of possible experiences during the final year of medical school. A literature review was conducted to identify common educational activities that US medical schools offer in the final year. Using rigorous survey design methodology, a 24-item survey was developed based on this review. Twenty-one of the questions related to the value of various educational activities. Three questions assessed the percent of the final year respondents felt should be allocated to direct patient care, electives, and dedicated to the desired specialty of the student. Students rated each educational activity using a 5-point Likert scale (1 = not important at all; 5 = extremely important). All U.S. medical students graduating in 2012 with a military training obligation were eligible to participate. Students were invited to participate via email 2–3 months prior to graduation. The importance of the experiences was ranked by the mean.
RESULTS: The response rate was 40 % (376/942). The most important experiences were rotation opportunities at other institutions under consideration for residency training (mean 4.4, sd 0.8), clinical rotation opportunities in desired specialty (mean 4.3, sd 0.8), opportunity to solidify clinical skills in preparation for internship (mean 4.2, sd 0.9) and allotted time for residency interviews (mean 4.0, sd 1.0). The least important experiences were learning business skills for running a practice after residency (mean 2.6, sd 1.2), opportunities to conduct research (mean 2.6, sd 1.1), the opportunity to conduct a rotation outside the United States (mean 2.7, sd 1.3) and expanding basic science knowledge (mean 2.7, sd 1.0). Students felt the 4th year should be 69 % (sd 20) direct patient care experience, 68 % (sd 17) electives, and 38 % (sd 17) in the student’s desired specialty. The length of military commitment (4 years or less versus 5 years or more) did not meaningfully change any of the results.
CONCLUSIONS: This study seems to demonstrate that students appear to be more focused on the immediate concerns of residency selection and on solidifying clinical skills in their desired specialty, but place less importance on skills that will not be soon applied. Those designing final year curricula might use these data as a general needs assessment, in particular for anticipating the activities that will likely have student support and those that might have less student engagement.
PERSPECTIVES OF LIFESTYLE FACTORS ON SPECIALTY CHOICE IN 4TH YEAR MEDICAL STUDENTSElexis McBee2,1; Shalini Reddy3; Lynn Byars1,2; Charles D. Magee1,2; Jennifer R. Kogan5; Douglas Maurer4; Steven Durning1,2; Kent DeZee1,2. 1Uniformed Services University, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD; 3University of Chicago Pritzker School of Medicine, Chicago, IL; 4Madigan Army Medical Center, Tacoma, WA; 5Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA. (Tracking ID #1938616)
BACKGROUND: A specialty’s lifestyle is known to be an important factor in specialty selection. It is unclear, however, whether 4th year students consider the lifestyle of a resident or attending in determining the factors most important to their specialty choice. The aim of this study is to determine if 4th year students weigh lifestyle factors differently based on the stage of their future career when considering a specialty.
METHODS: The authors conducted a cross sectional survey of 4th year medical students from the University of Chicago, the University of Pennsylvania and all 4th year medical students with a military service obligation in the United States during the 2011–2012 academic year. Using a five-point Likert-type scale (1 = not important at all; 5 = extremely important), respondents rated the importance of 14 lifestyle factors related to anticipated life as a resident physician versus anticipated life as an attending physician in choosing their specialty. The lifestyle factors surveyed related to the themes of schedule control, off time from work, and quality of the work life, as previously described in the literature. The mean of each lifestyle factor for anticipated life as both a resident and as an attending was calculated and compared using a paired t-test. Since multiple comparisons were made, a two-sided p-value of <0.01 was considered statistically significant. Effect size for each bivariate association was also calculated. Regression analysis controlling for type of medical school, presence of military obligation, and type of specialty choice was conducted for bivariate associations with a p-value <0.01.
RESULTS: The response rate for the questionnaire was 46 % (540/1184). For all 14 lifestyle factors, the level of importance for anticipated life as a resident was statistically different than anticipated life as an attending (p < 0.01, paired t-test). The factors with the highest rated importance when considering anticipated lifestyle as both a resident and attending physician were 1) job satisfaction (resident mean: 4.6, attending mean: 4.7), 2) how enjoyable the work day will be (resident mean: 4.3, attending mean: 4.5) and 3) collegiality of coworkers (resident mean: 4.1, attending mean: 4.2,). The effect size for each of these factors was 0.13, 0.26 and 0.17 respectively, indicating trivial to small differences between anticipated resident and attending life. The factors with the lowest rated importance were 1) working fewer hours (resident mean: 1.9; attending mean: 2.4), 2) minimizing the number of emergencies that affect the daily work schedule (resident mean: 2.2, attending mean: 2.8), and 3) frequency of overnight call (resident mean: 2.3, attending mean: 3.2). The effect size for each of these factors was 0.53, 0.65, and 0.80, respectively, indicating moderate to large differences. Regression analysis of each factor, controlling for type of specialty, military obligation, and type of medical school, did not alter the results.
CONCLUSIONS: When considering anticipated lifestyle related to choice of specialty, quality of work life was the most important consideration for 4th year medical students, with no meaningful differences between anticipated life as a resident and attending physician. In contrast, 4th year medical students seem to place less importance on their anticipated lifestyle as a resident compared to an attending in the constructs of schedule control and off time from work. Future studies of lifestyle and specialty choice should emphasize anticipated lifestyle as an attending physician and not anticipated lifestyle as a resident, with the exception of work life.
PHYSICAL ACTIVITY AND RISK OF BLEEDING IN ELDERLY PATIENTS TAKING ANTICOAGULANTSPascal Frey; Marie Méan; Andreas Limacher; Nicolas Rodondi; Drahomir Aujesky. Bern University Hospital, Bern, Switzerland. (Tracking ID #1937351)
BACKGROUND: Although the possibility of bleeding as a result of anticoagulant treatment may limit patients from taking part in physical activity, the association between physical activity and anticoagulation-related bleeding is uncertain.
METHODS: In a Swiss prospective multicenter cohort study of 988 in- and outpatients aged ≥65 years receiving anticoagulants for acute venous thromboembolism (09/2009–04/2013), we assessed patients’ self-reported physical activity level (low, medium, or high) at baseline using a previously established standard question. The primary outcome was the time to a first major bleeding, defined as fatal bleeding, symptomatic bleeding in a critical site, or bleeding causing a fall in hemoglobin or leading to transfusions. The secondary outcome was the time to a first clinically relevant non-major bleeding. We examined the association between physical activity level and the time to a first bleeding using competing risk regression, accounting for death as a competing event. We adjusted for known bleeding risk factors, including age, female gender, overt pulmonary embolism, history of major bleeding, recent major surgery, cerebrovascular disease, cardiac disease, diabetes mellitus, arterial hypertension, active cancer, chronic liver disease, chronic renal disease, risk of falls, polypharmacy, anemia, low platelets, concomitant antiplatelet therapy, and periods of anticoagulation as a time-varying covariate.
RESULTS: During a mean follow-up of 22 months, patients with a low (n = 367), moderate (n = 310), and high (n = 311) physical activity level had an incidence of major bleeding of 11.6, 6.3, and 3.1 events per 100 patient-years, and an incidence of clinically relevant non-major bleeding of 14.0, 10.3, and 7.7 events per 100 patient-years, respectively. Compared to a low physical activity level, a moderate (adjusted sub-hazard ratio [SHR] 0.72, 95 % confidence interval [CI] 0.45–1.13) and high physical activity level (adjusted SHR 0.40, 95 % CI 0.22–0.72) were associated with a lower risk of major bleeding. There was no association between physical activity and clinically-relevant non-major bleeding.
CONCLUSIONS: Increasing levels of physical activity are associated with a decreased risk of major bleeding in elderly patients receiving anticoagulant therapy, indicating that physical activity is safe when taking anticoagulants.
PHYSICIAN PERSPECTIVES OF INTERDISCIPLINARY CARE IN THE MANAGEMENT OF PATIENTS WITH DIABETESNissa Mazzola1,2; Daniel J. Coletti3,2; Joseph Conigliaro2. 1St. John’s Univerisity College of Pharmacy and Health Sciences, Queens, NY; 2North Shore University Hospital, Great Neck, NY; 3The Zucker Hillside Hospital, Glen Oaks, NY. (Tracking ID #1936039)
BACKGROUND: Evidence from controlled longitudinal trials suggests that effective management of Type 2 diabetes requires an interdisciplinary approach with close collaboration between team members. Prior research has described physician perceptions of barriers to effective diabetes management, but studies that describe physician insights regarding interdisciplinary teams are lacking. New efforts to integrate the services of a Certified Diabetes Educator (CDE) and Health Psychologist into a hospital-based patient-centered medical home (PCMH) offered an opportunity to evaluate physician attitudes toward interprofessional collaboration around diabetes management. Our primary objective was to compare attitudes toward diabetes management between the PCMH’s medical staff and a second internal medicine practice site without an interdisciplinary diabetes team. We also sought to test for attitudinal differences toward interdisciplinary diabetes care between board-certified internists and Internal Medicine residents.
METHODS: Eligible participants for this IRB-approved study included attending physicians and residents practicing at one of two ambulatory care sites within a large, suburban, socioeconomically diverse academic medical center. A 19-item anonymous paper survey was developed to examine the perceived importance of different components of diabetes treatment and education, as well as physician perceptions of the referral process for accessing members of the diabetes team. We used 10-point Likert scale item responses. Practice site directors distributed the questionnaire to all resident and attending physicians between January and March of 2013. T-tests for independent means were deployed to examine differences in mean item scores between the two practice sites, and between residents and attending physicians.
RESULTS: A total of 90 physicians completed the survey (25 attending physicians and 65 residents; 54 at the larger PCMH and 36 at the second IM practice site). Physicians from both sites endorsed positive attitudes to referring patients for additional education when initiating insulin therapy (M = 9.17 out of 10 and M = 9.64 out of 10, respectively). Respondents at both sites were significantly less confident, however, that they understood the specific roles and activities of the CDE (M = 5.8/10 and 5.36/10, respectively). Physicians practicing in the PCMH site perceived fewer barriers to referring their patients for diabetes education (t = 4.83, df = 84, p < .001) and were more likely to feel that their patients were seen for adjunctive services in a timely manner (t = 3.88, df = 85, p < .001). Providers in the PCMH site were more inclined to endorse the facilitation of behavior change as a component of diabetes self management education than the comparison site (t = 2.27, df = 84, p < .05). Analysis of attending-resident patterns of response suggested that residents were more likely to be influenced by concerns about consistent patient adherence than attendings in making a recommendation for insulin therapy (t = 2.01, df = 87, p < .05).
CONCLUSIONS: Results suggest that the diabetes support professionals are seen as valuable team members, and physicians are interested in learning more about their specific roles and activities. The integration of non-physician team members into the PCMH is associated with more positive attitudes around access and efficiency. The finding that residents were more influenced by concerns about patient adherence in recommending insulin therapy than attendings suggests that experience and training may lead to more confidence supporting patients in initiation of insulin. Alternatively, this finding might be related to different barriers to adherence among patients treated by attending physicians vs. patients seen by residents and warrants further investigation. Study findings are limited by the relatively small sample size, obtained within a single health system. Although the anonymous nature of the survey may have facilitated more honest sharing of perceptions about treatment and team services, it also limited the ability to inquire into more detailed information about the respondents. Our findings, however, support the feasibility of integrating diabetes support team services, the acceptability of diabetes-related behavioral interventions within a PCMH, and increased efforts at supporting resident physicians in facilitating patient adherence.
PHYSICIAN PERSPECTIVES ON INTER-HOSPITAL TRANSFERSStephanie Mueller; Jeffrey L. Schnipper. Brigham and Women, Boston, MA. (Tracking ID #1937827)
BACKGROUND: The transfer of patients between acute care hospitals (inter-hospital transfer, IHT) is becoming increasingly common. However, lack of evidence-based guidelines to direct high quality patient transfer creates variability in the quality of the transfer process, potentially leading to poor patient outcomes. Therefore, a better understanding of problematic aspects of the transfer process from frontline providers is a crucial first step to inform development of interventions to improve the quality of IHT.
METHODS: We surveyed residents and inpatient attendings from Internal Medicine, Neurology, and Surgery at a large urban tertiary referral hospital who are involved in accepting and caring for transferred patients. Subjects were asked about the frequency with which they encountered various issues related to quality in caring for transferred patients, and whether they felt these scenarios affected the safety of the transfer process, using 5- and 3-point likert scales respectively. Reponses were then dichotomized into “sometimes or frequently” vs. “rarely or never”.
RESULTS: Overall response rate was 51 % (145/284) with highest response rates from Internal Medicine and Neurology residents and attendings. Responses to survey questions are shown in Figures 1 and 2. The majority of survey respondents reported that they frequently encountered transferred patients arriving without necessary transfer records, greater than 24 h after being accepted, with unrealistic expectations of care, and not requiring specialized care. In addition, survey respondents identified availability of transfer records and time of day of patient arrival as frequently contributing to the safety of the transfer process.
CONCLUSIONS: This survey identifies quality and safety issues frequently encountered by frontline providers involved in the receiving end of the transfer process, providing potential targets for improvement of the IHT process. Further research is needed to identify quality and safety issues from transferring institutions, patients’ and families’ perspectives, and associations with patient outcomes.
PHYSICIAN REPORTED USE OF STRATEGIES TO IMPROVE ADULT IMMUNIZATIONLaura Hurley1,2; Megan C. Lindley4; Mandy Allison1,5; Lori A. Crane1,6; Michaela Brtnikova1; Brenda Beaty1,3; Megan Snow1; Carolyn Bridges4; Allison Kempe1,5. 1Children’s Hospital Colorado, Aurora, CO; 2Denver Health, Denver, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4Centers for Disease Control and Prevention, Atlanta, GA; 5University of Colorado Anschutz Medical Campus, Aurora, CO; 6Colorado School of Public Health, University of Colorado, Denver, CO. (Tracking ID #1926742)
BACKGROUND: Adult immunization rates are low nationally. Several strategies have been shown to increase immunization rates, but little is known regarding their use by physicians who serve adults. In 2013, the National Vaccine Advisory Committee approved standards for adult immunization practices that included incorporating immunization needs assessment into every visit and documenting vaccinations in immunization information systems (IIS). Our objectives were to assess among general internists (GIM) and family physicians (FM): 1) practices regarding assessing immunization status; 2) strategies used to improve immunization rates and 3) factors that interfere with and characteristics associated with assessing immunization status at every visit.
METHODS: We administered an Internet and mail survey from June to October 2013 to a national network of 438 GIM and 401 FM physicians representative of the American College of Physicians and American Academy of Family Physicians memberships. In addition to descriptive analysis, we performed multivariable logistic modeling for the specialties combined to examine associations between assessing immunization status at each visit and demographic and practice characteristics and strategies used to improve adult immunization.
RESULTS: Response rates were 72 % (317/438) for GIM and 59 % (236/401) for FM. Thirty-nine percent of GIM and 42 % of FM reported assessing vaccination status at every visit. The top 2 factors that interfere “a great deal” with assessment at each visit were acute problems taking precedence over vaccinations (GIM-37 %, FM-32 %), and not having an electronic questionnaire for patients to help determine immunization status (GIM-17 %, FM-19 %). The table shows GIM and FM physicians’ practices regarding strategies used to improve vaccination rates. Characteristics associated with assessing immunization status at every visit included working at a community/hospital based clinic (OR-1.88, 95 % CI 1.26–2.78), using standing orders for at least for some ACIP recommended vaccines (OR 1.87, 95 % CI 1.26–2.78), and having an electronic clinical decision support system (CDSS) to help determine vaccine needs (OR 1.83, 95%CI 1.23–2.72).
CONCLUSIONS: Most physicians serving adults are not assessing immunization needs at each visit and cite competing demands predominately interfering with this practice. Physicians reported limited use of strategies that have been shown to improve immunization. Incorporation of these strategies could increase the likelihood of assessment of immunization status at each visit and thereby result in higher vaccination rates.
PHYSICIAN VISITS AND SURVEILLANCE TESTING AMONG BREAST CANCER SURVIVORS IN TAIWANYong A. Wang1,2; An-Chen Feng2; Patricia Ganz1. 1UCLA Jonsson Comprehensive Cancer Center, Los Angeles, CA; 2Koo Foundation Sun Yat-Sen Cancer Center, Taipei, Taiwan. (Tracking ID #1933474)
BACKGROUND: The resource demands from the expanding cancer survivor population pose a significant challenge to health care systems worldwide. Guidelines recommend regular history, physical examination and mammography, but against routine surveillance imaging for detecting distant metastasis in survivors of breast cancer treated with curative intent. Studies of health services utilization of cancer survivors in Asia are limited. We examined patterns of physician visits and surveillance testing in a major cancer center in Taiwan, and assessed their relationship to various patient and physician factors and trends over time.
METHODS: All stage 0, I, II breast cancer cases were identified from the Taiwan Cancer Registry that were treated in the cancer center during 2002 to 2009. After excluding cases with recurrence, cases and institutional claims data were merged to measure the number of outpatient visits, breast imaging, and surveillance tests for detecting metastatic recurrence including serum tumor markers, abdominal imaging, chest X-ray, bone scan and PET, during the disease-free follow-up period from 13 to 60 months after initiation of breast cancer treatment. Poisson regression and logistic regression analyses were used to examine factors contributing to physician visits and testing, and separate analyses were conducted to look at individual patient cohorts from years 2002 to 2008 where sufficient follow up was available.
RESULTS: A total of 3,488 women ages 19 to 88 were identified from the registry. The number of breast cancer-specific physician visits in the 48-month follow up period (mean 18.7 per patient, SD 8.5) and the rates of surveillance testing to detect distant metastasis were greater than those recommended by ASCO/NCCN guidelines. Variables predicting the number of physician visits included age, cancer stage, year of treatment, hormonal therapy, chemotherapy, radiotherapy, whether the patient had seen psychiatry or medical subspecialties other than oncology, and the primary physician/specialty following the patient for breast cancer. After adjusting for covariates, the number of visits was highest among patients primarily followed by medical oncologists and lowest among those followed by breast surgeons (Figure 1). The adjusted 48-month visit rates decreased progressively from the 2003 cohort (mean 22.7) to the 2008 cohort (mean 17.7), related to an institutional effort in care coordination for breast cancer survivors. There was a significant decrease in the adjusted rate of tumor marker testing from the 2002 cohort (99.7 %) to the 2008 cohort (38.0 %) associated with the change in the institutional guideline (Figure 2). Greater number of visits was correlated with more frequent testing. Patients primarily followed by medical oncologists had the highest adjusted testing rates for tumor markers, bone scan, and abdominal imaging.
CONCLUSIONS: Early stage breast cancer survivors in Taiwan had high utilization of physician visits and surveillance testing for distant metastasis. This might be improved by greater coordination of care among breast cancer specialists. Implementation of an evidence-based guideline regarding the number of visits, imaging and tumor marker testing may be necessary to reduce the overutilization of testing.
PHYSICIANS’ INABILITY TO ESTIMATE MEDICAL COSTS: A MULTISITE SURVEYDavid P. Miller1; Dominic Johnson1; Luke Kohan3; Michael Manogue4; Larry D. Case2; Hal Atkinson1. 1Wake Forest School of Medicine, Winston-Salem, NC; 2Wake Forest School of Medicine, Winston-Salem, NC; 3University of Virginia, Charlottesville, VA; 4Emory University, Atlanta, GA. (Tracking ID #1937002)
BACKGROUND: Practicing cost-effective medicine assumes that physicians know the cost of tests and treatments they order. Although physicians routinely order tests and procedures, it is unclear if they know how much these items cost. This uncertainty is particularly relevant given the increasing attention federal and commercial insurers have placed on cost containment and cost-effective medicine. To determine whether physicians are aware of common diagnostic and therapeutic costs, we conducted a survey at two large academic medical centers in the Southeast.
METHODS: Over a 2-month period (June–July 2013), we distributed surveys to all internal medicine residents and clinical faculty at Wake Forest University (Winston-Salem, North Carolina) and the University of Virginia (Charlottesville). We administered surveys in paper and electronic forms. The survey gathered basic demographic data, but to maintain confidentiality, no personal identifiers were collected. The survey included a mixture of multiple-choice and Likert scale items that assessed respondents’ prior experience learning about and obtaining the costs of tests/procedures. We then asked respondents to estimate the cost of 20 commonly ordered diagnostic tests and procedures (i.e., Basic Metabolic Profile, CT Head without contrast, Transthoracic Echocardiogram) for both Medicare patients and commercially insured patients. Lastly, we asked them to estimate the cost of a hospital admission for a COPD exacerbation and a CHF exacerbation. For Medicare costs, we defined the true cost as its Medicare allowable charge.
RESULTS: Overall, 285 of 614 physicians completed the survey (180 faculty and 105 residents; response rate 46 %). Two-thirds of physicians (193/285) stated they had never been given a price list for tests they commonly ordered. Additionally, two-thirds (193/285) reported they were “not at all confident” they could determine the cost of a test before they ordered it, and this lack of confidence did not differ between faculty and residents (p = 0.25). Only 5 % of residents (5/105) thought their attendings knew the costs of test/procedures “very well”, and only 1 % of attendings (2/179) thought their residents knew costs “very well.” The most commonly reported sources of information about costs were personal experience (64 %) and word of mouth (58 %). In contrast, CME programs and medical school curricula were rarely cited as sources of cost information (21 % and 7 % respectively). Individual estimates for commonly ordered tests and procedures varied greatly. Very few physicians could estimate the cost of a test to within 25 % of its actual Medicare allowable charge. On average, residents achieved this benchmark only 7.9 % of the time compared to 10.7 % for faculty (p = 0.02). Only one-third of physicians (35 %) could correctly identify the cost for more than 2 of the 22 surveyed items.
CONCLUSIONS: Physicians have little understanding of the true costs of the medical tests and procedures they order. Additionally, they report little confidence that they could determine the cost of a test before ordering it, and they rarely learn cost information from traditional sources of medical education. Without knowing this cost information, physicians are unable to make cost-benefit decisions. Efforts to improve the cost-effectiveness of medical care should include strategies for making cost information easily accessible to physicians.
POLYPHARMACY AND PHYSIOLOGIC FRAILTY IN HIV-INFECTED VETERANSMinhee Sung1; Kirsha S. Gordon2; E. Jennifer Edelman3,2; Amy C. Justice2. 1Yale University School of Medicine, New Haven, CT; 2VA Connecticut Healthcare System, West Haven, CT; 3Yale University School of Medicine, New Haven, CT. (Tracking ID #1936987)
BACKGROUND: HIV-infected (HIV+) patients are exposed to polypharmacy, the use of multiple medications concurrently, more frequently and at younger ages than their uninfected counterparts. While antiretroviral therapy (ART) sustains life for HIV+, non ART medication benefits are less clear and may contribute to frailty. Clinical research outside of HIV has found associations between polypharmacy and outcomes of frailty like fragility fractures, falls, and cognitive decline. Yet little research demonstrates the associations between polypharmacy and frailty in HIV+. We hypothesized that polypharmacy would be associated with increased risk of frailty among HIV+ veterans.
METHODS: We conducted a cross-sectional analysis of data from October 2009 to September 2010 from the Veterans Aging Cohort Study (VACS), which prospectively collects demographic, pharmacologic, and clinical data on HIV-infected patients receiving care through the Veterans Health Administration (VHA) system. The sample was restricted to HIV+ on ART for at least 12 months. Active long-term medication use (defined as >90 days, allowing for 30 day gap between fill/refill) was determined using electronic pharmacy fill/refill data. Physiologic frailty was determined from self-reported survey items capturing physical shrinking, exhaustion, low physical activity, and slowness, and was categorized as pre-frail/frail vs. not frail. A logistic regression was used to assess the association between average long-term medication count and frailty after adjusting for demographics, VACS Index Score (a validated predictor of all-cause mortality), common medical comorbidities (including chronic obstructive pulmonary disease (COPD), diabetes mellitus, gastroesophageal reflux disease, hypertension, and osteoarthritis), substance use disorders (based on ICD-9 codes for alcohol and drug abuse and dependence), and mental illness.
RESULTS: The sample of 2281 HIV+ was predominately male (98 %), with a mean age of 55 years, and was racially/ethnically diverse (67 % black, 24 % white, 8 % Hispanic). The number of patients who were pre-frail or frail was 723 and not frail was 1558. The mean non ART medication count was 4 and the median and interquartile range was 3 (2,6). Each additional long-term non ART medication conferred a greater odds of being frail/pre-frail (OR [95 % CI] = 1.15 [1.12, 1.18]) compared to not frail. This relationship persisted in the adjusted model (OR [95 % CI] = 1.11 [1.07, 1.15]). Non ART medication count was the strongest predictor of being pre-frail/frail and osteoarthritis was the second strongest predictor (OR 2.23 [1.50, 3.33]). In addition, COPD was associated with being pre-frail/frail vs. not frail (OR = 2.54[1.46,4.42]).
CONCLUSIONS: After adjusting for severity of illness among HIV+ on ART, for every additional long-term non ART medication the risk of being pre-frail or frail increases 11 % after adjustment for severity of illness. Average long-term non ART medication count was the single best predictor of pre-frailty/frailty. Future studies must consider whether particular additional medications do more harm than good among HIV+ on ART.
POST-HOSPITAL DISCHARGE DELIRIUM AMONG OLDER ADULTSPriya Sunkara; Vanessa Ramirez-Zohfeld; Kenzie A. Cameron; Lee Lindquist. Northwestern University Feinberg School of Medicine, Chicago, IL. (Tracking ID #1938704)
BACKGROUND: As older adults are discharged from hospitals, they must remember intricate instructions on medications, follow-up appointments, and dietary changes. It is not surprising that seniors are frequently readmitted in the 30 day period following a hospitalization. Prior research has shown that cognition among seniors is impaired at discharge but improves the month following. We sought to determine how mentation changed in the 48 h following a hospitalization among older adults with mild cognitive impairment.
METHODS: Adults ages 65 and older who were admitted to the hospital acute medicine services for a non-cognitive related diagnosis. Older adults diagnosed with baseline mild cognitive impairment but were able to provide consent were included. Surveys were performed at hospital discharge and 48 h post hospitalization. The Montreal Cognitive Test (MOCA), Mini-Mental Status Examination (MMSE) were administered to evaluate cognition at baseline and 48 h following discharge. The Confusion Assessment Method (CAM) was used to assess delirium. Subjects were excluded if they had a positive screening Confusion Assessment Method during the day of discharge.
RESULTS: Baseline information was collected for 50 older adult subjects with mild cognitive impairment (mean age = 81.2) on day of hospital discharge. Mean cognition testing for subjects on day of hospital discharge was 21.2 MMSE and 15.22 MOCA. Subjects did not have positive CAM on day of discharge. Follow-up interviews were conducted 48 h following discharge, with five repeat attempts for each subject. Two subjects were re-hospitalized, and four subjects could not be reached within the 48 h follow-up window. At 48 h post-hospital discharge, 34 % (15/44) subjects were positive on the CAM and found to have delirium.
CONCLUSIONS: At 48 h following hospital discharge, about 34 % of older adults with mild cognitive impairment were found to have delirium. As delirium waxes and wanes, it is difficult to discern when the true onset of delirium occurred in the 48 h period following hospital discharge. Experiencing delirium after being discharged from a hospital is tremendously concerning. Older adults frequently are discharged home alone and expected to perform self-care functions (including medical management) following hospital discharge. It is unlikely that an older adult with active delirium would be able to reliably manage their self-care. Further research is needed to examine hospital and patient factors that contribute to the onset of post-hospital discharge delirium as well as interventions to support seniors with delirium following hospitalization. Transitional care interventions that focus on surrogates and increasing cognitive support during the post-hospitalization phase may be helpful for recently discharged older adults with mild cognitive impairment.
POTENTIAL IMPACT OF THE PADUA RISK ASSESSMENT MODEL ON THE USE OF VENOUS THROMBOEMBOLISM PROPHYLAXIS IN A TERTIARY MEDICAL CENTER IN THE UNITED STATESBronwyn Small; Alexander Weick; David Paje; Muhammad Usman; Jainil Shah. Henry Ford Hospital, Detroit, MI. (Tracking ID #1918465)
BACKGROUND: The Joint Commission’s core measures of hospital inpatient quality currently mandate that all patients receive prophylaxis against venous thromboembolism (VTE) unless there is a documented reason why it cannot be given. However, the most recent guidelines from the American College of Chest Physicians (ACCP) endorse the use of risk stratification tools such as the Padua Risk Assessment Model (PRAM) to identify who would likely benefit from pharmacologic or mechanical prophylaxis. PRAM was developed and validated in a university hospital in Padua, Italy, where 40 % of acute but not critically ill medical patients were found to be at high risk for VTE. We sought to determine the potential impact of the PRAM on the use of VTE prophylaxis among medical patients in an urban tertiary teaching hospital in the United States.
METHODS: Physicians were asked to complete a standard data collection tool during their initial evaluation of patients admitted to the general medical units of an 805-bed teaching hospital. The tool captured baseline demographic data and clinical variables included in the Padua Risk Assessment Model (PRAM). To assess mobility status, physicians were asked whether they anticipate reduced mobility for at least 3 days that is limited to no more than bed rest with bathroom privileges. A PRAM score of ≥4 was considered high-risk for VTE. The mode of VTE prophylaxis ordered was also recorded for each patient.
RESULTS: A total of 351 patients were enrolled in the study, 41 (11.7 %) were ordered therapeutic anticoagulation for other indications and were excluded from further analysis. Of the remaining 310 patients, 259 (83.5 %) were ordered pharmacologic prophylaxis and 29 (9.3 %) had mechanical prophylaxis ordered, but only 129 (41.6 %) were considered high-risk for VTE based on a PRAM score of ≥4. Of the high-risk patients, 121 (93.8 %) had some kind of prophylaxis ordered, while 167 (92.3 %) of the low-risk patients had prophylaxis against VTE. If the PRAM was applied, 58 % (167/288) of the currently ordered prophylaxis would be considered unnecessary.
CONCLUSIONS: The proportion of acutely ill medical patients admitted to an urban tertiary hospital in the United States that are considered high-risk for VTE based on the Padua Risk Assessment Model is similar to the 40 % reported in the Italian cohort. Applying the PRAM to our population may result in a significant reduction in the use of venous thromboembolism prophylaxis. Future prospective validation of this tool should look at its impact on the clinical outcomes of thrombosis, bleeding and mortality.
PREDICTING MEDICAL SCHOOL AND INTERNSHIP SUCCESS: DOES THE QUALITY OF THE RESEARCH AND CLINICAL EXPERIENCE MATTER?Nathalie Paolino3,1; Kent DeZee1,3; Anthony R. Artino2; Ting Dong2; Steven Durning1. 1Uniformed Services University, Bethesda, MD; 2Uniformed Services University, Bethesda, MD; 3Walter Reed National Military Medical Center, Bethesda, MD. (Tracking ID #1938339)
BACKGROUND: Selecting students for medical school admission remains a high-stake decision for applicants, schools, and society. Unfortunately, only a few applicant characteristics, such as the medical college admission tests (MCAT) and pre-matriculation grade point average (GPA), predict performance in medical school and subsequent clinical practice. This paper explores specific aspects of self-reported clinical and research experience on performance in medical school and graduate medical education (GME), hypothesizing that more experience will be associated with better performance.
METHODS: This is a retrospective cohort study from 7 consecutive classes at the Uniformed Science University (USU) in Bethesda, MD. The American Medical College Application Service (AMCAS) application was used to discern each student’s self-reported clinical and research experience. Two authors (NP and KJD) developed a coding scheme for clinical experience (8 categories) and research experience (3 categories) by reviewing and classifying experiences reported by students until saturation was achieved. Both authors independently applied the coding scheme to all students’ experiences and achieved excellent agreement (kappa >0.9 for both variables). Pre-matriculation GPA was obtained from transcripts. Study outcomes included years 1–2 GPA, years 3–4 GPA, cumulative medical school GPA, USMLE steps 1 and 2 scores, and PGY1 expertise and PGY1 professionalism scores (the latter two obtained from the student’s program director after medical school graduation). A linear regression analysis was conducted for each outcome to determine the predictive validity of clinical exposure and research exposure while controlling for pre-matriculation GPA. Effect sizes were used to assess the strength of significant associations.
RESULTS: Data were retrieved on 1,020 matriculants who had a mean pre-matriculation GPA of 3.41 (SD 0.3). There were several statistically significant, but small differences when comparing the various categories of clinical experience with no clinical experience across all 7 evaluated outcomes. The technician level group of clinical experience, which were students who worked in the healthcare field but did not have jobs requiring significant decision making opportunities regarding patient care (e.g., licensed practicing nurses, laboratory technicians, radiology technicians, orderlies and administrators) appeared to perform slightly worse during medical school with a decrease of 0.1 in cumulative GPA (based on a 4-point scale) in comparison to students without self-reported clinical experience (p = 0.004), but the effect size (0.27) was small. This group also performed 5 points lower on the USMLE step 2 than students who did not report a clinical experience (p = 0.013), but again the effect size (0.26) was small. Research experience quality appeared to have no significant predictive value for success in medical school and GME. Students who performed research, but did not produce a publication performed slightly better on USMLE Step 1 by 2.8 points (p = 0.012) compared to students without research experience; however, the effect size (0.17) was trivial.
CONCLUSIONS: This retrospective study indicates that clinical and research experiences only weakly predict global and knowledge based outcomes in medical school and GME. Other variables besides pre-matriculation GPA and MCAT need to be examined to further risk stratify future students in their ability to be successful in medical school and clinical practice.
PREDICTORS OF ENGAGEMENT IN AN INTERNET SUPPORT GROUP FOR TREATING MOOD AND ANXIETY DISORDERS IN PRIMARY CAREEmily Rosenberger1; Kaleab Abebe2,1; Bea Herbeck Belnap2; Jordan F. Karp3,1; Bruce L. Rollman2,1. 1University of Pittsburgh, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1937516)
BACKGROUND: Internet support groups (ISGs) that enable individuals with similar conditions to exchange information and support are emerging as an important self-help resource. Evidence suggests that ISG participants may experience less psychological distress, be more confident in their knowledge about their health and feel less socially isolated. Building an engaged ISG community is believed to be critical for an ISG’s success, yet little is known about patient characteristics that predict engagement in an ISG for a mental health condition. We examined this issue using data collected as part of an ongoing NIMH-funded trial of online collaborative care for treating mood and anxiety disorders in primary care.
METHODS: Primary care providers from 26 Pittsburgh-area practices referred their depressed and anxious patients aged 18–75 to our trial in response to an electronic medical record system prompt generated during the office encounter. Protocol-eligible patients with Internet access who scored PHQ-9 and/or GAD-7 ≥10 were randomized to one of three groups, including one permitting access to our password-protected ISG. The ISG consists of: (1) moderated discussion boards where patients can pose questions and share treatment information and experiences; (2) links to reliable consumer health information, crisis hotlines, ask-an-expert, pharmacies and other resources; and (3) access to a proven-effective computerized cognitive behavioral therapy program. Patients were encouraged to login and participate via weekly email reminders and updates, quarterly contests to promote ISG discussions and the potential to earn status indicators for participating on discussion boards. We collected baseline data on mood (PHQ-9) and anxiety (GAD-7) symptoms, Internet use and sociodemographics, and we analyzed ISG server logs to measure user logins and creation of new discussion board posts and comments. We investigated predictors of ISG engagement, defined by a new post or comment, using zero-inflated Poisson regression to account for the sizeable proportion of patients who never engaged with the ISG.
RESULTS: Between 8/1/12–9/30/13, we randomized 175 patients to have ISG access. Their mean age was 43 (SD: 14), 82 % were female, 84 % were white, and their mean PHQ-9 and GAD-7 were 14.0 (4.7) and 12.7 (4.6), respectively. Overall, 77 % logged-in at least once (median: 5, range: 0–76) and 47 % made at least 1 post or comment. Those with higher levels of ISG engagement were more educated (RR > high school vs. ≤high school, 5.55, 95 % CI: 4.15–7.43; p < 0.001); had received prior treatment for anxiety or depression (1.72, 1.24–2.38; p = 0.001) including pharmacotherapy (2.75, 1.84–4.11; p < 0.001); lacked social anxiety (4.94, 3.91–6.23; p < 0.001) or PTSD (3.15, 2.05–4.83; p < 0.001); and acknowledged having searched online about alternative medical treatments (1.30, 1.09–1.55; p = 0.003). Furthermore, whereas higher levels of mood symptoms were associated with decreased engagement (RR each 5-point increase in PHQ-9 score, 0.56, 0.51–0.62; p < 0.001), higher levels of anxiety symptoms were associated with increased engagement (RR each 5-point increase in GAD-7 score, 1.34, 1.20–1.49; p < 0.001).
CONCLUSIONS: Certain characteristics can identify depressed and anxious primary care patients who are more likely to engage with an ISG. Our trial is ongoing and will inform whether patient access to an ISG provided as part of a collaborative care intervention improves treatment outcomes.
PREDICTORS OF OPIATE PRESCRIPTION FOR LOW BACK PAIN IN OUTPATIENT AND EMERGENCY CARE SETTINGSJessica Taff; Joanna Loewenstein; Linda Wang; Kate Schwartz; David Wei. New York University, New York, NY. (Tracking ID #1938837)
BACKGROUND: Low back pain (LBP) is a significant problem in both the outpatient and emergency department setting, costing the United States approximately 20–70 billion dollars per year. Opioids are commonly prescribed for the treatment of back pain, and their prescription has increased approximately 100 % from 1997 to 2006. The purpose of this study was to determine common predictors for opiate prescription in the outpatient and emergency department settings.
METHODS: We examined patient visits in the data from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Surveys for the years 2006–2010 for diagnosis of LBP. The primary outcome of interest was prescription of opioids for mechanical low back pain at a particular visit. Predictor variables of interest included insurance type, geographic region, healthcare setting (Emergency Department, Hospital based Outpatient Department, Ambulatory Care), and ethnicity. We performed multivariate logistic regression analysis to determine the relationships between these independent variables and opioid prescriptions for LBP.
RESULTS: We analyzed 12,355 patient visits for LBP in the emergency department [odds ratios (OR): 2.83, 95 % confidence intervals (CI): 2.36–3.38] and those from the south (OR: 1.41, 95 % CI: 1.04–1.91) or west (OR: 1.53, 95 % CI: 1.14–2.05) had increased likelihood of receiving opioid prescription for LBP. Additionally, patients of hispanic (OR: 0.62, 95 % CI: 0.48–0.80) and other (non-black/white) (OR: 0.57, 95 % CI: 0.35–0.93) ethnicities had decreased likelihood of receiving opioid prescriptions compared to white patients. There was no statistically significant relationship between insurance type and receipt of opioids.
CONCLUSIONS: Patients seen in emergency departments were more likely to receive opioids for low back pain; whites were more likely to receive them, and these effects were independent of insurance coverage. The prescriber practices based on location may be related to available resources, differences in presentation acuity, or differences in training based on setting. The racial discrepancies noted are also consistent with past studies. These findings may be reflective of differences in the provider-patient relationship among ethnic groups or the subjective expression of pain. We were surprised to find that insurance type is not a predictor of opioid prescription. Previous studies show that socioeconomic status (SES) is a predictor of opiate prescription. However, we were unable to control directly for SES as mean income was not included in the survey. Findings from our study contradict other recent studies from the same database that illustrate decreased opioid prescriptions with private insurance. This difference in result may reflect the imperfection of using insurance status as a proxy for SES. Data is also limited by confounders such as depression, other chronic comorbid conditions, and absence of imaging results in the workup for back pain. Despite these constraints, our results suggest clear and significant differences in opioid prescription practices among health care setting, geographic region, and ethnicity that need to be better explored in future studies.
PREPAREDNESS FOR DISCHARGE: A COMPARISON OF TWO MEASURES IN PREDICTING READMISSIONAmanda Salanitro1,2; Kathryn M. Goggins2; Samuel K. Nwosu3; Jonathan S. Schildcrout3; Sunil Kripalani2. 1VA Tennessee Valley Healthcare System, Nashville, TN; 2Vanderbilt University, Nashville, TN; 3Vanderbilt University, Nashville, TN. (Tracking ID #1931231)
BACKGROUND: Reducing hospital readmissions has been the focus of much attention recently. Patients who are readmitted may have been ill-prepared for discharge. One measure of preparedness, the Care Transition Measure, has been endorsed by the National Quality Forum; however, other measures of preparedness have been developed. We sought to determine which measure of preparedness better predicts readmission.
METHODS: The Vanderbilt Inpatient Cohort Study (VICS) is an ongoing prospective study that seeks to better define the relationship of social determinants of health with patient outcomes after hospitalization. The study population includes adults hospitalized with acute coronary syndromes (ACS) and/or acute decompensated heart failure (ADHF). Following hospital discharge, patients completed a phone interview that included two measures of preparedness for discharge: Care Transition Measure-3 (CTM-3, range 0–100) and Brief PREPARED (B-PREPARED, range 0–22). Readmission during the 90 days following hospital discharge was analyzed as a binary outcome, as well as time in days to first readmission. We examined the correlation between the preparedness measures, preparedness and rate of readmission, and time to readmission, as well as the discriminative ability of the preparedness measures in predicting readmission.
RESULTS: Among 805 patients, the mean age was 60.3 (+12.6) years. The median preparedness was a score of 78 on the CTM-3 (interquartile range (IQR) 67–100) and 20 on the B-PREPARED (IQR 18–22). The CTM-3 and B-PREPARED measures were moderately correlated (Spearman’s rho 0.4). In the 90 days following hospital discharge, readmission rates were significantly different by category of preparedness (Tables 1 and 2). Additionally, days to readmission were significantly different across categories of CTM-3 (p = 0.000) and B-PREPARED (p = 0.016) scores. In separate time-to-event models, CTM-3 and B-PREPARED scores each predicted readmission within 90 days (hazard ratios 0.735 and 0.785, respectively). Finally, the ability of B-PREPARED to discriminate between patients readmitted and those who were not was slightly better than CTM-3 (Somers’ D 0.108 vs. 0.094). Inclusion of both measures increased the model’s discriminative ability (Somers’ D 0.128).
CONCLUSIONS: In this population 27–55 % of cardiac patients were readmitted within 90 days of hospital discharge, depending on their level of preparedness for discharge. As preparedness for discharge increased, readmission rates and days to readmission decreased. The B-PREPARED measure performed better than the CTM-3 in discriminating patients who are and are not readmitted within 90 days of hospital discharge.
Table 1. Rate of readmission by category of CTM-3 score
| CTM score | N | Number of readmissions | % readmitted |
|---|---|---|---|
| 0–56 | 62 | 25 | 40.3 |
| 57–78 | 354 | 123 | 34.7 |
| 79–100 | 389 | 105 | 27.0 |
Table 2. Rate of readmission by category of B-PREPARED score
| B-PREPARED score | N | Number of readmissions | % readmitted |
|---|---|---|---|
| 0–11 | 49 | 27 | 55.1 |
| 12–17 | 127 | 45 | 35.4 |
| 18–22 | 629 | 181 | 28.8 |
PRESCRIPTION DRUG UTILIZATION UNDER THE AFFORDABLE CARE ACT: WILL ESSENTIAL HEALTH BENEFITS ENSURE ACCESS TO MEDICINES IN “CLASSES OF CLINICAL CONCERN?”Joshua A. Rolnick. Stanford School of Medicine, Palo Alto, CA. (Tracking ID #1940206)
BACKGROUND: Under the Affordable Care Act (ACA), all new insurance plans sold through the health exchanges will be required to provide prescription drug coverage. Plans are not required, however, to include all drugs on their formularies. Under the final ACA regulations, each plan must offer at least as many different drugs in each treatment class (e.g. antihypertensives or antipsychotics) as the model, or “benchmark,” plan chosen by each state to define minimum coverage requirements. The Center for Medicaid and Medicare Services (CMS) chose not to require broader coverage for medications in any “classes of clinical concern.” In contrast to the ACA, CMS requires Medicare drug plans to cover “all or substantially all” drugs in six special classes: antidepressants, anticonvulsants, antineoplastics, antipsychotics, antiparkinson agents, and immunosuppressants. CMS selected these classes for special treatment due to concern that they contain drugs that are not easily substitutable and because patients may depend on continued access to their specific medications when switching insurance plans. Although this decision sparked significant public debate, little is known about utilization of protected class medications among would-be exchange enrollees.
METHODS: This study used data on prescription drug utilization and expenditures from the Medical Expenditures Panel Survey, a nationally representative survey of medical expenditures, demographics, and insurance characteristics. Data was used from the 102,767 respondents to the 2008–2010 survey. Subjects were respondents enrolled in small group or individual plans, combined with uninsured, as these are anticipated to supply the majority of exchange plan enrollees. Utilization was analyzed among nonelderly adults (age 18–64) with income >= 138 % of the federal poverty line enrolled in small group plans, individual plans, or no insurance (uninsured) for at least 6 months of the year. Patterns in utilization and expenditures on drugs overall and in the classes of clinical concern were analyzed.
RESULTS: There were a weighted total of 37,900,000 individuals with small group insurance, 5,462,750 with individual insurance, and 28,269,384 uninsured. Under their current insurance state, these respondents had an average of 6.9 prescription fills per year, spending an average $170 out-of-pocket per year on prescription drugs. Fifty-four percent filled at least one prescription drug per year. Classes of clinical concern accounted for a substantial percentage of expenditures. Antidepressants were used by 14,200,000 (8.5 % of population, 7.9 % of drug fills), anticonvulsants were used by 6,147,986 (3.7 % of population, 3.2 % of fills), antineoplastics by 1,437,719 (1.2 % of population, 0.8 % of fills), and antipsychotics by 1,437,719 (0.9 % of population, 0.7 % of fills). (The last two classes were utilized by too small a percentage to tabulate.) Thus, antidepressants, anticonvulsants, and antineoplastics were used by more than 1 % of the population and together accounted for 14 % of all annual drug fills. Utilization in protected classes was further analyzed by tabulating the number of drugs used in the three most common classes: anticonvulsants, antidepressants, and antipsychotics. Subjects used a total of 18 different anticonvulsants, 18 different antidepressants, and 34 different antipsychotics. In each case, the four most common medications accounted for less than 40 % of total drug fills. Of all medications, immunosuppressive agents was the most expensive class, with an average total expenditures of $4,628 per fill and $318 out of pocket. A second protected class, antipsychotics, was fourth most expensive, with an average $1,518 per fill and $171 out-of-pocket.
CONCLUSIONS: Among those eligible and likely to enrolle in the exchange plans, 54 % fill at least one prescription per year. HHS chose not to follow the Medicare part D rules and require plans to cover all or nearly all medications in any specific classes, including the “classes of clinical concern.” However, among potential enrollees, medications in these classes account for a sizable minority (14 %) of all fills. Enrollees further use a variety of medications in each class, and the classes of concern include some of the most expensive medications available. If exchange plans offer formularies with only a limited number of medications, many enrollees may be unable to obtain coverage for their current medications in these classes. Limitations of this study include the fact that exchange plan enrollees may not be representative of current small group and individual enrollees or the uninsured. Nevertheless, this study contains the most detailed data to date on an important question in prescription drug coverage under the Affordable Care Act.
PREVALENCE OF MENTAL HEALTH CONDITIONS AND ASSOCIATED PATTERNS OF HEALTH CARE UTILIZATION AMONG HIGH COST VA PATIENTSDonna M. Zulman2,4; Grace Hunter1; Jean Yoon3,2; Daniel Blonigen2; Steven Asch2,4. 1Stanford University School of Medicine, Stanford, CA; 2VA Palo Alto Health Care System, Menlo Park, CA; 3VA Palo Alto Health Care System, Stanford, CA; 4Stanford University, Stanford, CA. (Tracking ID #1937115)
BACKGROUND: Mirroring national trends, the most costly 5 % of patients in the Veterans Administration (VA) system account for almost half of total health expenditures. These patients have complex health care needs; the vast majority have at least two coexisting chronic conditions and almost half have at least one diagnosed mental health (MH) condition. While several studies have shown that MH conditions are associated with higher utilization of health services, very little research has focused on the role of these conditions among high-cost patients. The aim of this study was to investigate the influence of MH conditions on health care utilization patterns among high-cost VA patients.
METHODS: We obtained total VA health care costs and utilization by source (inpatient, outpatient, pharmacy, and non-VA contract care) for the costliest 5 % of patients (N = 261,699) who received care within the VA in fiscal year 2010. We used ICD-9 diagnostic codes to assign each patient to one of five mutually exclusive groups based on a hierarchy of MH diagnoses: 1) No MH Condition; 2) Serious Mental Illness (SMI); 3) Substance Use Disorder (SUD); 4) Post-Traumatic Stress Disorder (PTSD); and 5) Depression. We used multivariable linear regression to examine the association between the MH diagnostic group and: 1) hospital admissions and length of stay; 2) outpatient utilization (number of visits for primary, specialty, emergency, and mental health care); 3) costs for inpatient services (MH, residential/domiciliary, medical/surgical, and long term care); and 4) costs for outpatient services (MH, medical/surgical, diagnostic, and pharmacy) after adjusting for patient age, sex, race/ethnicity, marital status and documented homelessness. Finally, for each cohort we calculated the proportion of costs generated by MH care.
RESULTS: Compared with the patients without a diagnosed MH condition, patients with one or more MH diagnoses were statistically significantly younger in age and more likely to be female, not married, without supplemental insurance, and homeless. Among patients with MH conditions, patients in the PTSD and Depression groups had higher rates of most chronic conditions and had a higher level of multimorbidity than patients in the SMI and SUD groups. Compared to patients with SMI and SUD, patients in the PTSD and Depression groups had higher numbers of primary and specialty care visits and longer medical/surgical lengths of stay. In contrast, patients in the SMI and SUD groups had higher MH utilization (e.g., MH visits, behavioral length of stay (LOS), and residential/domiciliary LOS) than the PTSD and Depression groups. These utilization patterns translated to a greater proportion of costs generated by MH care among patients in the SMI and SUD groups (41 % and 31 %, respectively) compared to patients in the PTSD and Depression groups (18 % and 11 %, respectively).
CONCLUSIONS: Among high-cost VA patients with MH conditions, utilization and cost patterns indicate that patients with SMI and SUD incur a greater proportion of care and costs related to their MH conditions, when compared to patients with PTSD or Depression. These findings can help inform patient stratification algorithms and service delivery for intensive primary care programs focusing on high-cost patients.
PREVALENCE OF PRESCRIPTION OPIOID ABUSE/OVERUSE AMONG CHRONIC OPIOID THERAPY (COT) PATIENTS: USE OF NATURAL LANGUAGE PROCESSING (NLP) WITH VALIDATION REVIEW TO IDENTIFY OPIOID ABUSE IN ELECTRONIC MEDICAL RECORD CLINICAL NOTESMichael VonKorff1; David Carrell1; David Cronkite1; Roy Palmer2; Timothy R. Hylan2; Kathleen Saunders1; David E. Gross1. 1Group Health Cooperative, Seattle, WA; 2Pfizer Inc., New York City, NY. (Tracking ID #1938636)
BACKGROUND: A review of studies in unrepresentative patient populations enrolled in clinical research reported that only 0.27 % of 2613 chronic non-cancer pain patients who received opioids for at least 6 months became addicted to opioids or used opioids inappropriately. More recent studies in community practice settings have reported much higher rates of prescription opioid addiction and abuse, with prevalence rates ranging from 4 to 26 %. It is not known whether chronic opioid therapy (COT) patients who become addicted to, or overuse, medically prescribed opioids can be identified through review of clinical notes in electronic medical records. Use of natural language processing (NLP) to efficiently identify patients with prescription opioid addiction, abuse or overuse has potential applications for epidemiologic research on risks of prescription opioid addiction in community practice, for patient monitoring in clinical care, and for quality assurance.
METHODS: Among 22,143 Group Health chronic non-cancer pain patients receiving COT in 2006–12 (defined as 70+ days supply of opioids in a 90 day interval), we developed an NLP system using a custom dictionary of 792 terms to identify mentions of opioid addiction, abuse and overuse in clinical notes. For COT patients with documents that were NLP positive, we manually reviewed up to four positive records per patient with a computer-assisted chart review tool highlighting relevant text to validate the presence of opioid addiction, abuse or overuse. The inter-rater reliability for 100 independently reviewed records was kappa = 0.86, with 97 % agreement on validation status.
RESULTS: Among 3663 NLP positive records, 77 % were manually validated as indicating opioid addiction, abuse or overuse. Among NLP positive records, 75 % documented current or very recent opioid addiction or abuse, 14 % documented opioid overuse only, and 11 % recorded only a diagnostic label or code. Among NLP positive records that were not validated, common reasons for non-validation were non-recent history of opioid abuse (41 %), documentation of discussion of potential addiction risks (35 %), “boilerplate” text that mentioned addiction or abuse risks without reference to the patient (9 %), and reference to opioid abuse by a family member (6 %). Among 22,143 patients who received chronic opioid therapy for at least one quarter in 2006–12, 6.8 % had NLP identified and validated documentation of prescription opioid addiction, abuse or overuse. The prevalence rate was 7.5 % among those receiving COT for at least 6 months (N = 17,062). The prevalence rates for opioid addiction, abuse or overuse were similar for males and females who received COT for at least 6 months, but differed by age (12.3 % for persons age 18–44, 5.8 % for persons age 45–64, and 2.8 % for persons age 65+).
CONCLUSIONS: Efficient identification of clinician documented prescription opioid addiction, abuse and overuse was feasible using NLP techniques that were further enhanced with computer-assisted manual validation. Clinician recognized prescription opioid addiction, abuse or overuse was common among COT patients, with the highest rates observed among younger patients, but with notable risks among middle aged and older COT patients. Extensions of this research will use NLP to identify clinical indicators of opioid addiction (e.g. opioid craving and hazardous use).
PREVENTABLE ADMISSIONS ON A GENERAL MEDICINE SERVICE: PREVALENCE AND CAUSESNirav Vakharia; James Pile; Erik Howell; Sang Been N. Hong; Kristen Boyer; Kelly Nottingham; Jacqueline Fox; Neha R. Pidatala; Michael B. Rothberg. Cleveland Clinic, Cleveland, OH. (Tracking ID #1935775)
BACKGROUND: Rates of preventable admissions will soon be publicly reported and used in calculating performance-based payments. The current method of assessing preventable admissions, the AHRQ Ambulatory Care Sensitive Conditions (ACSC) admission rate, is drawn from claims data and was originally designed to assess population—not patient—level access to care. It has not been validated for assessing the performance of individual healthcare organizations. Specific causes of preventable admissions have not been well studied.
METHODS: We examined 322 serial admissions to a general medicine service at an academic medical center in December 2013. For each admission, the attending physician was surveyed regarding preventability of the admission, defined as the presence of any factor during the 2 weeks prior to admission which, if addressed in the outpatient setting, could have averted the hospitalization. Demographics, principal diagnosis ICD-9 code, and readmission status were gathered from the electronic medical record. Prior to the study, a list of preventability factors drawn from past research and categorized by system, clinician, and patient factors was adapted with input from hospitalist, primary care, and emergency physicians. For admissions deemed preventable, the physician selected a factor from the list which most contributed to the hospitalization and rated the feasibility of prevention on a 4 point scale (very easy to very difficult). For the same admissions, the AHRQ ACSC methodology was applied to determine the claims-derived preventable admission rate for admission.
RESULTS: Of the 322 admissions, 63 (20 %) were readmissions. Physicians rated all 322 admissions and classified 122 (38 %) as preventable, of which 31 were readmissions. Application of the AHRQ ACSC methodology identified 75 (23 %) preventable admissions. Thirty-one admissions (10 %) were classified as preventable by both methods, and the majority of admissions considered preventable by the AHRQ ACSC method (44/78) were not considered preventable by physician assessment. Compared to our method, the AHRQ ACSC method’s sensitivity was 25 % and specificity was 78 %. Of the 122 preventable admissions, physicians chose patient factors in 52 (43 %), specifically non-adherence (17 %), mental health/substance abuse (8 %), poor health literacy (5 %), secondary gain from hospitalization (3 %), and poor home support (1 %). System factors were chosen in 34 (28 %), specifically inpatient management easier than outpatient (11 %), inadequate care at a nursing facility (5 %), inability to access outpatient providers (2 %), and complication from previous admission (1 %). The remaining 36 (30 %) were assigned to clinician factors, including threshold for admission too low (9 %), inadequate follow-up (8 %), inappropriate diagnosis/treatment (7 %). Of the 122 preventable admissions, 63 (52 %) were considered very or somewhat easy to prevent. Preventable admissions for which clinician factors were chosen were considered the easiest to prevent, with 67 % assigned very or somewhat easy; whereas those for which patient factors were chosen were considered the most challenging, with 38 % assigned very or somewhat easy to prevent.
CONCLUSIONS: A large proportion of admissions to a general medicine service appeared preventable, and only a small percentage of these were readmissions. Patient factors were most commonly cited, and these were also rated the most difficult to address. AHRQ’s Ambulatory Care Sensitive Conditions rate showed poor sensitivity and moderate specificity as compared to our method of direct physician assessment. These findings warrant further evaluation of the ACSC rate for use in pay for performance programs, and additional investigation into the factors implicated in preventable admissions.
PRIMARY CARE PATIENTS’ USE OF MOBILE HEALTH (MHEALTH) TOOLSAmy Bauer1; Tessa Rue2,3; Gina A. Keppel3,4; Allison Cole3,4; Laura-Mae Baldwin4; Wayne Katon1. 1University of Washington, Seattle, WA; 2University of Washington, Seattle, WA; 3University of Washington, Seattle, WA; 4University of Washington, Seattle, WA. (Tracking ID #1925955)
BACKGROUND: Mobile health (mHealth) has emerged rapidly as a multibillion dollar industry with tens of thousands of consumer smartphone health applications (apps) available, most of which have not been subject to scientific study or regulatory approval. The potential for mHealth tools to represent an important advancement in chronic disease care (i.e., via education about chronic illness, appointment reminders, monitoring disease control, facilitating behavior change) has been recognized. Although primary care is the setting where most chronic disease care occurs, the patterns of mHealth use among primary care patients have not been documented. This study aimed to determine the prevalence of mHealth use among primary care patients and examine demographic and clinical correlates.
METHODS: All adult patients who presented to one of 6 primary care clinics located in 4 states (Washington, Wyoming, Alaska, Montana) in a practice-based research network during a 2-week period received an anonymous survey that assessed mobile phone ownership, mHealth use including frequency and characteristics of use, sociodemographic characteristics (age, gender, race/ethnicity, health literacy), chronic medical conditions, and current depressive symptoms (PHQ-2). Data analysis employed descriptive statistics and multivariate mixed logistic regression.
RESULTS: 918 patients responded to the survey (estimated response rate: 67.4 %). Mobile phone ownership was nearly ubiquitous (91 %), with the majority of patients (55 %) owning a smartphone. Mobile health use was common (70 % of smartphone owners; 39 % of all patients). Most mHealth users were seeking health information (92 %) and many were using mHealth applications (57 %) or tracking a health condition (54 %). Compared to young adults (ages 18–24), smartphone ownership and mHealth use were each less common among adults in every age group over 45 years (adjusted ORs 0.07–0.39, ps<=0.001). Health literacy, chronic medical conditions, and depression were not associated with mHealth use. Most mHealth users were infrequent users and most (61 %) reported using an app for a short period of time then stopping, often (48 %) because it was too time-consuming. The most popular types of apps were general health apps (36 %) followed by fitness (15 %) and diet (10 %) apps, with very few patients (3 %) using apps for chronic disease management. Fewer than 10 % of mHealth users learned about mHealth apps from their healthcare provider, with 69 % reporting that it was ‘not at all’ or only ‘a little bit’ important for their providers to know about their use of health apps. However, patients rated appointment reminders as the most useful potential feature, followed closely by medication reminders, general health information, and health tracking.
CONCLUSIONS: Smartphone ownership and mHealth use are common among primary care patients. Adoption lags among older adults, however patients with limited health literacy and chronic conditions use mHealth technologies at similar rates as their counterparts, supporting the potential role of mHealth in improving disease management among certain groups in need. Few patients believe it is important for healthcare providers to know about their mHealth use; however, providers who do discuss mHealth use with patients may be able to elicit important information about patients’ self-management activities, which may help these providers to be more adept in the support they offer for chronic disease care.
PRIMARY CARE PHYSICIANS’ READINESS TO PROVIDE ACCOUNTABLE CARE AND ACHIEVE THE TRIPLE AIMPetra W. Rasmussen; Shreya Patel; Anne-Marie J. Audet; Michelle M. Doty. The Commonwealth Fund, New York, NY. (Tracking ID #1938208)
BACKGROUND: Little is known about the extent to which primary care practices are implementing accountable care strategies to provide enhanced access, care management and outreach to individual patients and panel populations; coordinated care among various providers within and outside the practice; engage patients in their care; and track and monitor quality and utilization. This study provides a snapshot of current readiness of primary care physicians to provide accountable care and discusses whether payment incentives and additional practice redesign resources can foster transformation.
METHODS: Data come from the 2012 Commonwealth Fund International Health Policy Survey of Primary Care Physicians administered to a nationally representative sample of 1,012 primary care physicians in the United States. We use 30 items to create composite scores to assess whether physicians have capacity in five domains that are essential for accountable care: 1) providing enhanced access; 2) collecting actionable data to manage individual patients and patient populations; 3) collecting and using quality of care data; 4) managing and coordinating patient care within and outside their practice; 5) patient outreach. We then looked at three aspects of practices to see if certain attributes and activities led to increased provision of accountable care: 1) organization; 2) technical assistance; 3) payment.
RESULTS: Primary care physicians who were part of integrated delivery systems were more likely to report coordinating and managing the care for their patient populations, including the care provided by physicians outside of their practice. Practice size also affected the provision of care across all domains, with larger practices being more likely to report accountable care functionalities. Having formal arrangements to share quality improvement consultants and/or technical support for clinical information systems was also an important predictor of a practice’s capacity to provide accountable care. Practices that were eligible to receive targeted financial incentives for activities such as making home visits and non-face-to-face interactions with patients were more likely to manage and coordinate patient care within and outside of their practice, provide patient outreach, and be able to access and review quality of care data.
CONCLUSIONS: Significant gaps are currently observed in primary care physicians’ readiness to meet functionalities that will be required to be fully accountable for the quality of care, health outcomes and resource use for their panel of patients. The results from the study will inform policy makers and stakeholders as they develop performance targets, technical assistance programs, and new payment models in order to help guide practices as they transform into models of accountable care. Our findings also indicate that increased attention must be paid towards the organization and coordination of delivery systems, and technical assistance. These elements will be essential in fostering a culture of effective partnerships among providers to ensure patients receive coordinated services according to their needs and the successful implementation of best practices for engaging patients in the management of their health.
Practice Profile by Accountable Care Capacity, U.S. Primary Care Physicians, 2012 (Adjusted Percentages)
| Enhanced Access | Electronically Generated Data to Manage Individual Patient | Electronically Generated Data to Manage Patient Population | Availability and Use of Quality of Care Data | Managing and Coordinating Care Provided Within Practice | Managing and Coordinating Care with Providers Outside of Practice | Patient Outreach | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted n | Total Unadjusted Percent | Mean % | Odds Ratio | Mean % | Odds Ratio | Mean % | Odds Ratio | Mean % | Odds Ratio | Mean % | Odds Ratio | Mean % | Odds Ratio | Mean % | Odds Ratio | |
| Practice Size | ||||||||||||||||
| ref=Solo | 238 | 25 % | 28 % | 39 % | 34 % | 33 % | 42 % | 15 % | 26 % | |||||||
| Small (2 to 9) | 485 | 47 % | 28 % | 1.02 | 52 % | 1.78** | 51 % | 2.11** | 41 % | 1.48* | 54 % | 1.72** | 20 % | 1.47 | 32 % | 1.39 |
| Medium (10 to 19) | 99 | 9 % | 32 % | 1.21 | 64 % | 2.91** | 52 % | 2.14** | 48 % | 2.06** | 59 % | 2.15** | 22 % | 1.62 | 42 % | 2.21** |
| Large (20+) | 145 | 14 % | 32 % | 1.22 | 58 % | 2.27** | 56 % | 2.52** | 59 % | 3.53** | 61 % | 2.36** | 34 % | 3.03** | 56 % | 4.01** |
| Part of an Integrated Delivery System | ||||||||||||||||
| ref=No | 721 | 72 % | 28 % | 50 % | 48 % | 39 % | 48 % | 21 % | 31 % | |||||||
| Yes | 276 | 27 % | 32 % | 1.22 | 50 % | 0.99 | 46 % | 0.92 | 56 % | 2.31** | 65 % | 2.08** | 24 % | 1.20 | 48 % | 2.17** |
| Formal Arrangements with other practices/groups to share quality improvement consultants or support and/or technical support for clinical information systems | ||||||||||||||||
| ref=No | 580 | 58 % | 25 % | 44 % | 42 % | 39 % | 48 % | 19 % | 33 % | |||||||
| Yes, either | 112 | 11 % | 29 % | 1.22 | 50 % | 1.27 | 43 % | 1.07 | 39 % | 1.02 | 57 % | 1.55 | 29 % | 1.84* | 34 % | 1.02 |
| Yes, both | 264 | 25 % | 35 % | 1.66* | 62 % | 2.15** | 60 % | 2.15** | 56 % | 2.24** | 63 % | 1.95** | 25 % | 1.51 | 42 % | 1.53* |
| Formal arrangements with other practices/groups to share clinical staff | ||||||||||||||||
| ref=No | 767 | 76 % | 28 % | 52 % | 49 % | 44 % | 53 % | 22 % | 35 % | |||||||
| Yes | 202 | 20 % | 31 % | 1.15 | 44 % | 0.70 | 43 % | 0.77 | 43 % | 0.99 | 48 % | 0.79 | 23 % | 1.07 | 37 % | 1.07 |
| Eligible for targeted financial incentives | ||||||||||||||||
| ref=No | 673 | 67 % | 29 % | 51 % | 48 % | 38 % | 47 % | 19 % | 33 % | |||||||
| Yes | 322 | 32 % | 29 % | 1.01 | 50 % | 0.99 | 48 % | 1.00 | 55 % | 2.25** | 65 % | 2.19** | 26 % | 1.56** | 42 % | 1.52** |
| Physician Payment | ||||||||||||||||
| ref=Fee-for-service based | 474 | 47 % | 34 % | 50 % | 45 % | 41 % | 52 % | 21 % | 37 % | |||||||
| Salary based | 373 | 37 % | 21 % | 0.51** | 55 % | 1.28 | 51 % | 1.27 | 46 % | 1.23 | 52 % | 0.97 | 23 % | 1.13 | 33 % | 0.84 |
Notes: Statistically different from reference category: *p ≤ 0.05, **p ≤ 0.01
PRIMARY CARE PROVIDER EXPERIENCE WITH A NEW HEALTH INFORMATION TECHNOLOGY TOOL TO FACILITATE BETWEEN VISIT MEDICATION MANAGEMENTRichard W. Grant3; Leila H. Borowsky1; Jeffrey M. Ashburner1; Michael Jernigan2; Steven J. Atlas1. 1Massachusetts General Hospital, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Kaiser Permanente, Oakland, CA. (Tracking ID #1937532)
BACKGROUND: Lack of timely medication intensification and inadequate medication safety monitoring are two prevalent and potentially modifiable barriers to effective and safe care for chronic conditions. We developed a novel health information technology tool (Medication Metronome) designed to support non-visit based medication management. Integrated into an existing electronic medical record, this tool enabled primary care physicians (PCPs) to schedule future laboratory monitoring when ordering medication changes (initiation or dose adjustment) for diabetes, hypertension, and/or hyperlipidemia management. We hypothesized that scheduling follow-up laboratory monitoring (e.g. HbA1c 3 months after starting metformin) would reduce delays in further medication titration by obviating the need for a return visit solely to obtain laboratory tests.
METHODS: Forty-four PCPs from two practices within an academic primary care network were randomized to usual care (control group) or to use the Medication Metronome tool. For scheduled laboratory orders, Medication Metronome automatically sent the patient a letter with a lab slip 1 week prior to the lab due date. If the test was not performed, a second letter and lab slip were sent 1 week after the lab due date. The PCP received an alert in the results management section of the electronic health record 3 weeks after the lab due date if it still had not been performed. We report here the results of PCP surveys administered at the end of the 1-year study assessing medication management workflow during the study period. Responses from intervention and control physicians were compared using Fisher’s exact test.
RESULTS: Among PCPs, 86 % (19 of 22) in the control group and 91 % (20 of 22) in the intervention group completed surveys. The proportion of PCPs who reported spending more than 20 min during a typical half-day session on medication management was greater for intervention vs. control PCPs (60 % vs 47 % for diabetes management; 60 % vs. 42 % for hypertension; and 60 % vs. 42 % for hyperlipidemia), although these differences did not reach statistical significance (p > 0.05). The proportion of PCPs who reported improvement in their ability to start or change medications for a patient outside of the context of an office visit was 35 % in the intervention group compared to 26 % in the control group (p = 0.86). Among intervention group PCPs, 30 % indicated that Medication Metronome improved their ability to provide timely medication management, with the remaining 70 % reporting no change. Most intervention group PCPs (80 %) reported barriers to using the Medication Metronome module including poor alignment with current visit-based reimbursement practices.
CONCLUSIONS: Implementation of a novel tool to support non-visit based follow-up after medication changes had only a modest impact on PCP workflow. Despite consenting and enrolling in the clinical assessment trial, most intervention PCPs did not take full advantage of the tool. Among reported barriers to wider use was the misalignment of visit-based reimbursement and productivity requirements with a non-visit based model of care. Health policy and reimbursement changes that support overall quality of management and that recognize non-visit care might encourage greater adoption of innovative tools to support visit-independent medication management.
PRIMARY PREVENTION OF CARDIOVASCULAR DISEASE: ARE WE TARGETING THE RIGHT PATIENTS?Kevin Selby1; David Nanchen1; Pedro Marquez-Vidal1; Reto Auer1; Baris Gencer2; Giulio G. Stefanini3; Lorenz Räber3; Roland Klingenberg4; Jacques Cornuz1; Pierre Vogt1; Peter Jüni3; Christian M. Matter4; Stephan Windecker3; Thomas Lüscher4; François Mach2; Nicolas Rodondi3. 1University of Lausanne, Lausanne, Switzerland; 2University of Geneva, Geneva, Switzerland; 3University of Bern, Bern, Switzerland; 4University Hospital Zurich, Zurich, Switzerland. (Tracking ID #1929718)
BACKGROUND: Guidelines for the primary prevention of cardiovascular disease (CVD) are based on the identification of high-risk patients who are most likely to benefit from medications such as aspirin and statins. Several cardiovascular risk calculators are used in Europe, but their ability to identify those who will develop CVD has not always been demonstrated in external validation cohorts. Furthermore, the implementation of primary prevention guidelines for statin and aspirin prescription is less well studied.
METHODS: We collected baseline information regarding cardiovascular risk factors and medication use for 3,848 consecutive patients admitted with acute coronary syndrome (ACS) between 2009 and 2013 to four university hospitals in Switzerland. Ten-year cardiovascular mortality was computed using the European Systemic COronary Risk Evaluation (SCORE) from the European Society of Cardiology (ESC) guidelines; 10-year fatal and non-fatal risk of CVD using the American College of Cardiology/American Heart Association (ACC/AHA) guidelines; and 10-year fatal and non-fatal risk of coronary heart disease using the Swiss Society for Atherosclerosis (AGLA) guidelines. Use of aspirin and statins before hospitalization was stratified by risk level and compared with recommended use of ESC, ACC/AHA and AGLA guidelines.
RESULTS: 2,810 (73 %) patients had no previous history of CVD. Using ESC guidelines, 771 (20 %) had a 10-year CVD mortality risk below 1 %, compared to 1091 (28 %) with a 10-year CVD risk below 5 % using the ACC/AHA guidelines, and 1331 (35 %) with a 10-year CHD risk below 10 % with AGLA guidelines. Only 1150 (30 %) were taking a statin and 1278 (33 %) aspirin before hospitalization for ACS. The additional proportion of patients in whom a statin would have been indicated reached 50 % using ESC, 46 % using ACC/AHA, and 38 % using the Swiss AGLA guidelines (Figure).
CONCLUSIONS: Among patients presenting with ACS to Swiss hospitals, one-fifth to a third are classified as low risk using risk calculators. The use of statins and antiplatelet medications before hospitalization is low in patients presenting with ACS. This is in contrast with the large number of patients for whom a statin would have been recommended with full compliance to primary prevention guidelines.
Figure: Patients taking a statin on arrival, those with a clear statin indication, those for whom a statin should be considered, and those with no statin indication using different guidelines (n = 3848). AGLA: Swiss Society of Atherosclerosis. ACC: American College of Cardiology. AHA: American Heart Association. ESC: European Society of Cardiology.
PRIORITIZING CONCEPTS OF CLINICAL REASONINGJohn Musgrove1; Jason L. Morris1,2; Ryan Kraemer1,2; Carlos Estrada2,1. 1University of Alabama at Birmingham, Birmingham, AL; 2Birmingham VAMC, Birmingham, AL. (Tracking ID #1928091)
BACKGROUND: The field of cognitive psychology has informed our understanding of how physicians think and make decisions. However, little is known about prioritizing clinical reasoning concepts for teaching. We aim to prioritize commonly described clinical reasoning concepts to facilitate the teaching of clinical problem solving skills.
METHODS: Consensus development. First, two authors compiled an extensive list of clinical reasoning concepts from seminal narrative reviews. Second, seven clinical educators reviewed the list for additions and voted items for inclusion in a systematic review; items with <5 votes were excluded. Third, eight clinical educators ranked the remaining items (most important concept first, least important concept last) using a card-sort method. This technique represents a robust means of measuring opinion enhanced by a visual-motor cognitive dimension. For analysis we used the rank-order centroid method for assigning weights based on ordinal preference (order in card sort). For example, if three items are ranked as 1st, 2nd, and 3rd; their relative weights are 0.61, 0.28, and 0.11. The main outcome was the sum of weights assigned to each clinical reasoning concept by each clinical educator.
RESULTS: Of 49 clinical reasoning concepts identified, 24 received <5 votes and five were deemed synonyms. The remaining 20 clinical reasoning concepts and the percent of total weight assigned to each concept are shown in the Table (sum of weights = 100 %). The top four concepts were problem representation, diagnosis, dual-process thinking, and illness scripts. Excluded concepts were: cognitive load, feedback loops, patient story, test interpretation, deliberate practice, concept maps, prior probability, mental simulation, hypothetico-deductive model, decision analysis, coaching, Bayesian reasoning, and dynamic model.
CONCLUSIONS: Through a systematic consensus development, we prioritized a list of commonly described clinical reasoning concepts for inclusion in a systematic review.
| Item | Weigth | Item | Weight |
|---|---|---|---|
| Problem representation | 11 % | Slowing down | 5 % |
| Diagnosis | 8 % | Cognitive error | 4 % |
| Dual-process thinking | 8 % | Framing | 3 % |
| Illness scripts | 8 % | Premature closure | 3 % |
| System 1 (non-analytic) | 7 % | Bias | 3 % |
| System 2 (analytic) | 6 % | Anchoring | 2 % |
| Hypothesis generation/ refinement | 6 % | Naturalistic decision-making | 2 % |
| Problem categorization | 6 % | System error | 2 % |
| Flexibility | 6 % | Context specificity | 2 % |
| Metacognition | 5 % | Overconfidence | 1 % |
PROACTIVE OUTREACH OF TOBACCO CESSATION TREATMENT TO DISADVANTAGED SMOKERS AFTER A PRIMARY CARE VISIT: A RANDOMIZED CONTROLLED TRIALJeffrey A. Linder1,3; Jennifer Haas1,3; Nancy A. Rigotti2,3; Elyse R. Park2,3; Emily Kontos4,5; Irina Gonzalez1; Elissa Klinger1; Lucas Marinacci1; Phyllis Brawarsky1; Stella St. Hubert1. 1Brigham and Women’s Hospital, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Harvard Medical School, Boston, MA; 4Harvard School of Public Health, Boston, MA; 5Lung Cancer Disparities Center, Boston, MA. (Tracking ID #1923076)
BACKGROUND: Low socioeconomic status (SES) and minority smokers have less access to tobacco treatment. Proactive outreach to these smokers after a primary care (PC) visit, using interactive voice response (IVR) technology, telephone counseling and free nicotine replacement (NRT), might promote treatment access and smoking cessation. In a RCT, we compared this tobacco treatment program for low SES and minority smokers to usual care.
METHODS: African-American, Hispanic, or white adults with a recent PC visit to a large health care delivery system were eligible if they were documented as smokers in the electronic health record and lived in a low-moderate income census tract. The IVR system made up to 15 proactive calls per person to confirm smoking status and offer study participation. Enrollees were randomized to usual care or IVR-mediated intervention (up to 4 calls with a bilingual tobacco treatment specialist, 6 weeks of free NRT, and referral to community resources to reduce life stressors). The primary outcome was self-reported past 7-day smoking status 9 months after randomization, with patients not reached counted as smokers. Multivariate regression was used to test whether the intervention was more effective in any subgroup.
RESULTS: The IVR system attempted to contact 8547 patients, of whom 116 (1 %) were ineligible because they reported not smoking, 5553 (65 %) were not reached by IVR, 2170 (25 %) declined participation, and 708 (8 %) consented and were randomized. To date, 542 have completed outcome assessment (70 % response rate). Participants had a median age of 50 year. (range 19–82); 23 % were African American and 17 % were Hispanic; 34 % had no more than a high school education. At 9-month follow-up, self-reported quit rate was 8.6 % in the control group and 14.9 % in the intervention group (p = 0.02). Hispanics were more likely to quit than whites (p = 0.008).
CONCLUSIONS: An integrated program using IVR outreach and offering centralized telephone smoking cessation counseling, free NRT, and linkage to community resources may be an effective treatment strategy for engaging disadvantaged populations of smokers, particularly Hispanic smokers.
PROFILING MEDICAL SCHOOL LEARNING ENVIRONMENTS ACROSS CULTURES USING ONE NEW SCALESean Tackett1; Hamidah Abu Bakar2; Nicole A. Shilkofski3; Niamh Coady4; Krishna Rampal3; Scott Wright1. 1Johns Hopkins Bayview Medical Center, Baltimore, MD; 2Cyberjaya University College of Medical Sciences, Sepang, Malaysia; 3Perdana University Graduate School of Medicine, Serdang, Malaysia; 4Perdana University Royal College of Surgeons in Ireland School of Medicine, Serdang, Malaysia. (Tracking ID #1928927)
BACKGROUND: In many countries, there is growing interest in improving medical school learning environments; however accurately assessing learning environments is a challenge. As international partnerships in medical education become more common, ensuring that effective learning environments are translated across borders will become more relevant. The goal of this study was to test the ability of a new learning environment assessment tool, the Johns Hopkins Learning Environment Scale (JHLES), to detect differences in pre-clerkship learning environments at 4 medical schools. Two schools are new international partnerships in Malaysia: (i) Perdana University Graduate School of Medicine (PUGSOM)—a graduate-entry program run by Johns Hopkins University School of Medicine (JHUSOM), and (ii) Perdana University-Royal College of Surgeons in Ireland School of Medicine (PU-RCSI)—a school-leaver program run by RCSI. Perdana schools matriculated their first students in the fall of 2011. The other two medical schools were Cyberjaya University College of Medical Sciences (CUCMS), a school-leaver program in Malaysia, and JHUSOM a graduate-entry program in Baltimore, MD.
METHODS: Both first and second year students responded anonymously to surveys at the end of the academic year. All surveys included the JHLES, a 28-item survey using 5-point Likert scale response options. During development at JHUSOM, factor analysis resulted in 7 domains (listed with respective Cronbach’s α): (1) community of peers (α = 0.91), (2) faculty relationships (α = 0.80), (3) academic climate (α = 0.86), (4) engagement (α = 0.82), (5) mentorship (α = 0.74), (6) acceptance and safety (α = 0.58), and (7) physical space (α = 0.66). Surveys at the 3 Malaysian medical schools also included the Dundee Ready Educational Environment Measure (DREEM), the most widely-used method to assess learning environments internationally. DREEM is a 50-item survey using 5-point Likert scale options, with items grouped by its developers into 5 categories, which have not isolated as discrete factors in previous factor analyses. Categories are: (1) perception of teachers, (2) perception of teaching, (3) academic self-perception, (4) perception of atmosphere, and (5) social self-perception. Kruskall-Wallis tests assessed domain differences across schools, and two-tailed t-tests were used for pairwise comparisons. Significance was set at p < 0.05 after Bonferroni correction for multiple comparisons.
RESULTS: Complete surveys were collected with the following response rates: 51/55 (93 %) PUGSOM, 97/134 (72 %) PU-RCSI, 221/240 (92 %) CUCMS, and 189/240 (79 %) JHUSOM students. Total JHLES scores were higher at JHUSOM than PU-RCSI, with no differences in other pairwise comparisons. JHLES detected statistically significant differences between schools in 6/7 (86 %) domains, all except “academic climate.” Differences did not follow a uniform pattern: JHUSOM and PUGSOM rated “acceptance and safety” higher than CUCMS and PU-RCSI, JHUSOM and CUCMS rated “mentorship” higher than PUGSOM and PU-RCSI, and CUCMS had the highest rating for the “community of peers” domain. Comparing only Malaysian medical schools, a difference was only seen in 1/5 (20 %) DREEM categories (CUCMS rated “perception of teachers” lower than PU-RCSI and PUGSOM) and there were no differences in DREEM total scores. By comparison, JHLES detected significant differences in 5/7 (71 %) domains when only data from Malaysian schools were analyzed. Total JHLES score was highly correlated with the total DREEM score (rho = 0.80), and it was more strongly correlated than DREEM to students’ global rating of the learning environment (rho = 0.56 vs. 0.44).
CONCLUSIONS: JHLES can discriminate between discrete learning environment factors across a range of cultural and educational settings. This results in each school having a unique learning environment profile. Interpretation of these profiles may allow schools to understand how they are currently supporting trainees and to identify areas needing attention.
PROGRESS OR STALEMATE IN ACADEMIC GENDER DISPARITIES? 15 YEAR FOLLOW UP OF THE NATIONAL FACULTY SURVEYKaren Freund1,2; Anita Raj3; Norma Terrin1,2; Samantha Kaplan4,5; Tracy Urech2; Subash Pathak2; Phyllis Carr6. 1Tufts University School of Medicine, Boston, MA; 2Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston, MA; 3University of California, San Diego, San Diego, CA; 4Boston University School of Medicine, Boston, MA; 5Boston Medical Center, Boston, MA; 6Massachusetts General Hospital, Boston, MA. (Tracking ID #1931176)
BACKGROUND: Our prior research found that women compared to men received lower compensation, published fewer articles, and did not advance at the same rate despite similar grant funding productivity. Efforts over the past 20 years have sought to reduce such inequities, but long-term gender differences on these outcomes over the course of the academic career remain unknown. The objective of our current research is to assess gender differences in rank, productivity, compensation and career satisfaction among a national cohort of medical faculty followed from 1995 to 2012.
METHODS: We conducted a follow-up of the 1995 National Faculty Survey cohort, which was drawn from a representative sample of 24 US medical schools, and oversampled generalists as well as underrepresented minority faculty and senior women. We supplemented on line survey responses with publically available data on publications, rank, and leadership on grants. We compared unadjusted median and mean responses on variables between men and women. We adjusted analyses by duration of time in academic career and academic department type (categorized as basic science, medical specialty, surgical specialty or generalist).
RESULTS: We report on 288 men and 301 women. At the time of the follow up survey 62 % of women and 77 % of men reached the rank of full professor (p < .0002). Women had fewer median peer-reviewed publications than men (unadjusted median 43 versus 68, p = .0001), with a 15 publication deficit after adjustment for duration of the academic career and department type (Wald 95 % confidence interval (CI) 6–25, p < .005). The proportion of faculty with funded grants in the prior 2 years was similar between men and women (50 % versus 47 %, p = .39). Women had an unadjusted $26,060 lower mean income compared with men ($169,190 versus $195,250, p < .003) which was reduced to $18,830 after adjustment. The difference in a 4 item career satisfaction measure (scale ranged from 4 to 20) was statistically significant, but was a relatively small effect (women, mean = 14.7, standard deviation (SD) = 3.9 versus men, mean = 15.6, SD = 3.5, p < .0001). Adjustment for years in academics and department type explained some but not all gender differences.
CONCLUSIONS: Women report similar satisfaction with academic careers, similar grant funding productivity but lower peer-reviewed publication productivity. Women across the course of their careers continue to report lower compensation, and to be less likely to achieve the rank of professor. These findings parallel the status of this group of women compared with their male counterparts in 1995, indicating that rank and compensation gaps remain over the course of the academic career, despite decades to address these disparities.
| Variable | Analysis Adjusted for Duration in Academics and Department Type | Women versus Men | 95 % CI and p-value |
|---|---|---|---|
| Number of Peer-Reviewed Publications | Adjusted mean number of publications | −15 | 95 % CI −25, −6; p = .002 |
| Leadership on Grants | Adjusted OR | .98 | 95 % CI .69, 1.39; p = .9 |
| Achieving Rank of Professor | Adjusted OR | .56 | 95 % CI .36, .88; p = .01 |
| Career Satisfaction | Adjusted parameter estimate | −.81 | 95 % CI −1.40, −0.22; p = .008 |
| Compensation | Adjusted annual compensation | −$18,830 | 95 % CI −$35,647, −$2,013; p = .03 |
PROJECT BUENA SALUD: EVALUATION OF AN ENHANCED PRIMARY CARE PROGRAM FOR LOW-INCOME HISPANIC PATIENTS WITH TYPE 2 DIABETESSarah L. Goff1,2; Lorna Murphy1,2; Peter K. Lindenauer2; Paul Visintainer3. 1Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 2Baystate Medical Center, Springfield, MA; 3Baystate Medical Center, Springfield, MA. (Tracking ID #1939386)
BACKGROUND: Hispanic patients have a nearly two-fold risk for developing type 2 diabetes (T2DM) compared to their white non-Hispanic peers. Team-based care is increasingly being implemented in the U.S. in an effort to improve management of chronic diseases such as T2DM. This study aimed to assess the impact of enrollment in Buena Salud (BS), a team-based enhanced primary care program, on changes in diabetes control, compliance with target blood pressure and lipid management, and markers of health care utilization for low-income Hispanic patients with T2DM.
METHODS: BS is a pilot intervention initiated in 2011 by Health New England (HNE) a local health insurance company. The program is designed to augment usual primary care by providing individual and group support for chronic disease management for Medicaid Managed Care patients. The bilingual BS team is comprised of 2 nurses, 2 community outreach workers and a social worker. This team offers home visits, interpreter services for specialist visits, diabetes education and other as-needed services for patients enrolled in BS. In this retrospective cohort study, eligible patients were aged 18–64, had been enrolled in BS for at least 15 months, had a least one visit with their primary care provider in the 12 months before enrollment and has had at least 1 visit in the 15 months following their enrollment date. We reviewed the medical records of all patients enrolled in BS between 8/1/2011 and 2/28/2012. Data extracted included pertinent laboratory results (HbA1c, fasting lipids), blood pressure values, and health care utilization markers (unplanned hospitalizations, emergency room visits). Baseline values were collected for up to 3 years prior to enrollment; 15 months following enrollment was considered the intervention phase. Potential confounders included age, gender, primary spoken language, and comorbid illnesses. The control group consisted of T2DM patients who are patients at the study site health center but were not enrolled in the BS program. The controls were matched (3:1) with intervention patients based on having a visit at the health center in the same month each intervention patient was enrolled. We compared the change in HbA1c, diastolic and systolic blood pressure, LDL, number of hospital admissions and number of emergency room visits between the baseline period and the end of the intervention period among patients in BS and controls.
RESULTS: 67 T2DM patients and 194 controls were included in the study. There were no differences between the groups in any of the variables measured in the baseline period. BS patients had 0–23 contacts (phone and in-person) with the BS team during the intervention (mean = 2.7, sd = 4.0) Over the intervention period BS patients had an increase in HbA1C of 0.33 compared to a decrease in of 0.12 in controls (p = 0.05). BS patients had a decrease of −5.59 mm/Hg in mean systolic blood pressure compared to an increase of 2.16 mm/Hg in the controls (p = 0.007). There were no differences in changes in DBP, LDL, the number of hospital admissions or number of emergency room visits between BS patients and controls. The frequency of contact with care team members was not associated with changes in HbA1c, diastolic and systolic blood pressure, LDL, number of hospital admissions and number of emergency room visits.
CONCLUSIONS: Diabetic control worsened slightly for patients enrolled in an enhanced primary care program while blood pressure was modestly improved. This study did not take into account what the nature of the contact between patients and the BS team, which may have a modifying effect on individual patient outcomes. It is also possible that unmeasured factors contributed to the differences observed. Although enrollment in the BS program was not associated with improved control of diabetes it is possible that 15 months is insufficient to see an effect on the outcomes measured and that longer exposure to the intervention may be associated with different outcomes. A randomized controlled trial to compare the effectiveness of usual care compared to enhanced primary care for low-income Hispanic diabetics may better assess the intervention’s impact.
PROMOTING POSITIVE CHANGE IN THE RESIDENCY EXPERIENCE THROUGH DISCOVERY OF RESIDENT VALUESStephanie A. Rose; Nicholas Jackson; Brittany P. Fenner; Brett Capel; David Rudy. University of Kentucky, Lexington, KY. (Tracking ID #1940299)
BACKGROUND: Residency is a trying experience. This study aims to find constructive means of improving of our Internal Medicine Residency program. Previous attempts to improve our residency program focused on eliminating negative aspects. This study utilized Appreciative Inquiry to identify positive aspects of the current program with the aim to expand upon those ideas and incorporate new suggestions.
METHODS: We conducted appreciative interviews on 27 current Internal Medicine residents. Subjects were asked to answer a series of questions while reflecting on their time as a resident. The questions focused on points such as what he/she expected upon beginning residency, what was his/her high point in residency, what fosters a collaborative and engaged work environment and what actions can be taken to achieve a more engaged staff. The answers were analyzed for thematic categories independently through qualitative methods by three reviewers. Discrepancies were resolved via consensus.
RESULTS: Residents initially sought to improve their medical knowledge, work towards autonomy and gain experience. However, as residents continued in their training they valued the support and respect of their superiors and peers while working as part of a collaborative unit. Residents shifted their focus from academic improvement to fostering better patient relationships and seeing results of the care they provided. When asked what they would do to improve the program, many responded with improving team dedication and communication as well as a more open academic environment.
CONCLUSIONS: While very important, knowledge acquisition may not be what residents’ value most in their training. In fact, it was discovered that residents desired to improve their ability to work as part of a medical team, in both leadership and subordinate roles. Residents feel the program is most effective when support, communication and respect as part of a collaborative environment are held at highest regard. Helping resident accomplish these positive aspirations may help make residency a positive experience.
PROVIDER CULTURAL COMPETENCE AND RACIAL DISPARITY IN DOCTOR-PATIENT RELATIONSHIPSSomnath Saha1,2; Melissa S. Gatchell2; Maya O’Neil2; Jeffrey T. Bates3; Howard S. Gordon4; Judith A. Long5; Donna L. Washington6; Martha Gerrity1. 1Portland VA Medical Center, Portland, OR; 2Portland VA Medical Center, Portland, OR; 3Michael E. DeBakey VA Medical Center, Houston, TX; 4Jesse Brown VA Medical Center, Chicago, IL; 5Philadelphia VA Medical Center, Philadelphia, PA; 6Greater Los Angeles VA Healthcare System, Los Angeles, CA. (Tracking ID #1939867)
BACKGROUND: Provider cultural competence (CC) has been widely endorsed as a means to improve the quality of doctor-patient relationships for minority patients and reduce racial disparities in healthcare quality. CC, however, is multidimensional, and few studies have empirically examined which dimensions, if any, are associated with better relationships and greater equity across racial/ethnic groups.
METHODS: We previously developed a self-administered instrument for primary care providers (PCPs), consisting of 6 scales representing different CC dimensions: Perceived Cultural Aptitude, Perceived Cross-Cultural Efficacy, Awareness of Racial Disparities, Valuing Diverse Perspectives, Support for Accommodating Patient Diversity, and Patient-Centered Orientation. In the current study, PCPs at 4 geographically diverse VA Medical Centers completed our CC instrument. We surveyed white and African American patients from participating PCPs’ panels, and administered validated instruments to measure patients’ global ratings of PCPs, their experience with PCPs’ communication and interpersonal style, and their trust in the PCP. We tested associations to determine which CC dimensions were associated with higher ratings of PCPs among minority patients. For CC dimensions positively associated with minority patient ratings, we tested interactions between provider CC and patient race, to determine whether CC dimensions were associated with reduced disparity in outcome measures. We used GEE-based linear regression for all analyses, adjusting for clinic site and patient age, and accounting for clustering of patients within providers.
RESULTS: We recruited 96 PCPs and 998 of their patients. PCPs were predominantly white (49 %) and Asian (27 %), while patients identified mainly as African American (62 %) and white (31 %), reflecting our sampling strategy. The CC dimension most consistently associated with higher minority patient ratings was Valuing Diverse Perspectives. PCPs scoring above the median on this scale received higher ratings from African American patients on communication quality and interpersonal style (Table 1). Higher VDP was not significantly associated with white patients’ ratings. We found significant provider VDP-patient race interactions for all outcome measures, indicating that providers placing higher value on diverse patient perspectives received more equal ratings from minority and nonminority patients. For all outcome measures, we observed racial disparities among PCPs with lower VDP scores but no significant disparities among those with higher VDP scores (Table 2).
CONCLUSIONS: Providers rating themselves higher on Valuing Diverse Perspectives—a construct similar to the concept of cultural humility—received higher ratings from African American patients and had less racial disparity in the quality of their relationships with patients. VDP may be an important target, and intermediate outcome measure, for CC interventions aimed at reducing racial disparities in health care quality.
PROVIDER RESPONSE TO ONLINE SELF-MANAGEMENT SUPPORT FOR OBESITY INTEGRATED WITH PRIMARY CAREKathleen M. McTigue1,2; Molly B. Conroy1,2; Laurey R. Simkin-Silverman2; Dana L. Tudorascu1; Rachel Hess1,2; Gary Fischer1; Cindy L. Bryce3,1. 1University of Pittsburgh, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1937944)
BACKGROUND: Less than half of obese US adults report that their physician has advised them to lose weight and numerous barriers including time constraints, cost and limited physician training make lifestyle counseling in the clinical setting difficult. Health information technology is considered a promising avenue for addressing gaps in care and providing patient-centered, yet affordable, health care services. For widespread implementation, such tools must be acceptable to providers and smoothly integrated with care.
METHODS: We evaluated physician response to a year-long intervention providing self-management support for weight loss to 373 obese primary care patients. Physicians referred patients to the structured behavioral online program. They then received feedback from each participant’s online lifestyle coach over the course of the year. We surveyed physicians at the 6 participating primary care practices representing a range of practice settings (e.g., academic, private, urban, rural) regarding their responses to the program. Each provider was emailed survey links on multiple occasions, and paper surveys were distributed at practice meetings and resident seminars. Cross-sectional analyses examined sample demographics, compared attitudes towards obesity counseling among adopting and non-adopting providers, and quantified impressions of how smoothly the referral model of obesity treatment was integrated with clinical workflow.
RESULTS: Of 185 providers, 67 (36 %) completed surveys; 99 % were physicians, 46 % were female, 5 % were Hispanic and 2 % were African American. Among respondents, 49 (73 %) had referred patients to the program. When we compared referring providers (“adopters”) with non-referring providers (“non-adopters”), the two groups did not differ in sex or race/ethnicity, but varied in training status with 71 % of the non-referring providers and 12 % of referring providers being resident physicians (p < 0.001). Among adopters, most agreed that the referral approach to enrollment (94 %) and the process for providing 1-year follow-up reports (80 %) integrated smoothly with their normal workflow. Compared with adopters, non-adopters were more likely to report preferring counseling on healthy eating and exercise patterns themselves rather than referring for counseling (29 % versus 8 %; p = 0.040). Non-adopters reported sufficient time during clinic visits to counsel patients adequately on diet, physical activity and obesity more often than did adopters (29 % versus 8 %; p = 0.026). Non-adopters more often reported that their patients were generally not interested in using internet-based lifestyle counseling (47 % versus 22 %; p = 0.007), were likely to have minimal computer skills (76 % versus 35 %; p = <0.001), or were likely to lack internet access (64 % versus 32 %; p = 0.04). Both adopters and non-adopters noted that their patients would benefit from advice to lose weight through lifestyle change. However, 20 % of all respondents felt that their patients were generally not interested in receiving counseling for diet, physical activity and weight loss and 20 % reported that obesity should be managed outside the clinical setting. Most respondents agreed that they find it useful to refer patients to community counseling resources for promoting healthy lifestyles (42 % somewhat agreed and 39 % strongly agreed).
CONCLUSIONS: A referral model is able to smoothly integrate online self-management support into routine primary care practice. The adoption of online self-management support tools may be most likely among PCPs with limited available time for counseling, those without a strong preference for personally delivering preventive behavioral counseling, and those who have completed residency training. PCP perception that their patients lack internet access, skills, or interest can inhibit adoption of online counseling tools.
PROVIDERS’ PERSPECTIVES ON ESSENTIAL FUNCTIONS FOR CARE MANAGEMENT IN THE TREATMENT OF HYPERTENSION: THE P.A.R.T.N.E.R. FRAMEWORKTanvir Hussain1,2; Allyssa Allen4,2; Jennifer Halbert2; Cheryl A. Anderson3; Romsai T. Boonyasai1,2; Lisa A. Cooper1,2. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Center to Eliminate Cardiovascular Health Disparities, Baltimore, MD; 3University of California, San Diego School of Medicine, San Diego, CA; 4University of Maryland, Baltimore County, Baltimore, MD. (Tracking ID #1939802)
BACKGROUND: The provision of comprehensive services for chronic illness care in primary care is limited by a lack of physician time and tools. Care management (CM) has become a popular strategy to address this challenge. CM typically involves non-physician care managers working with patients between encounters with primary care providers (PCPs) in order to improve clinical care, enhance care coordination, and reduce health care utilization. To our knowledge, however, PCPs’ perspectives on CM activities that will improve patient care have not been examined, jeopardizing the potential for successful collaboration between care managers and PCPs. We aim to identify functions of CM most valuable to PCPs in hypertension treatment.
METHODS: Six focus groups were conducted. Thirty-nine of the 47 PCPs from six community-based clinics within a large physician group practice in the greater Baltimore metropolitan area participated. PCPs were racially diverse (51 % White, 23 % Black, and 21 % Asian), were in practice on average 17 years, and 69 % worked in an underserved site. Questions and prompts about hypertension treatment and CM in primary care were standardized and pilot tested. Focus groups were audio recorded and transcribed verbatim. Recurring themes were identified by: reviewing the transcripts from three focus groups; reviewing the coding scheme with the research team before analysis; and periodically refining the scheme as new themes emerged during analysis until thematic saturation was reached. Initially, themes for CM included: existing hypertension care support available to PCPs, essential functions for CM, and challenges to CM success. To further refine the breadth of comments under essential CM functions, a second stage of coding was performed independently by two physician-researchers.
RESULTS: We identified 74 statements that fell within seven domains of essential CM functions. Inter-rater agreement on coding of essential functions was 92 %. The most commonly cited functions for care management, each 20 % of total annotations, belonged to the domains of “providing education” and “identifying and resolving barriers to adherence.” Using these data, we created the P.A.R.T.N.E.R. framework, which reflects the activities providers find essential to effective care management: Partner with the patient, providers, and the community; Assess response to the treatment plan & Arrange follow-up care; Resolve barriers to adherence & Recalibrate the treatment plan; Track patient progress; Navigate the health care system with the patient; Educate the patient & Engage the patient in self-management; Relay information between the patient and/or provider. The framework also lists a “scope of activities,” or a range of possible tasks satisfying each function. Based on PCPs’ perspectives, all P.A.R.T.N.E.R. functions should be represented in an optimal care management program, though the specific tasks to fulfill each function may vary across clinical settings.
CONCLUSIONS: The P.A.R.T.N.E.R. framework is the first to offer a comprehensive list of CM functions that may be useful in clinical practice based on primary data collection from PCPs. This perspective has not yet been documented, though PCP buy-in is essential to the success of team-based care models. Future research should examine the reliability and validity of this framework in various settings and for diverse patient populations affected by chronic diseases.
PROVISION OF FAMILY PLANNING TO WOMEN WITH CARDIOVASCULAR RISK FACTORSShivani M. Reddy1,2; Ambili Ramachandran1; Howard Cabral4; Lewis Kazis3. 1Boston University School of Medicine, Boston, MA; 2VA Boston Healthcare, Boston, MA; 3Boston University School of Public Health, Boston, MA; 4Boston University School of Public Health, Boston, MA. (Tracking ID #1936950)
BACKGROUND: Cardiovascular risk factors (CVRFs) in reproductive-aged women can lead to pregnancy complications and fetal anomalies. Family planning in this population is not well studied.
METHODS: We performed a cross-sectional analysis using data from the National Ambulatory Medical Care Survey for the years 2009–2010. The study sample consisted of visits by reproductive-aged women with CVRFs of diabetes, hypertension, hyperlipidemia, obesity, or tobacco use. The comparison group was visits with no chronic disease. Primary outcome measure was family planning action, defined as counseling, medication, or procedure.
RESULTS: Among 223,407,070 ambulatory visits by non-pregnant reproductive-aged women, 30.8 % were associated with at least one CVRF, and 17.2 % had at least one family planning action. There was no increased frequency of family planning for visits by women with CVRFs. In the multivariable model, the odds ratio of receiving family planning with presence of a CVRF was 1.2 (95 % CI 0.9–1.5). Visits for preventive care (OR 2.3, 95 % CI 1.8–3.1), as well as gynecologic and sexual health care (OR 2.6, 95 % CI 1.9–3.7), were significantly associated with increased odds of family planning.
CONCLUSIONS: There are low rates of family planning in visits by reproductive-aged women overall, with no significant difference for visits by women with CVRFs. Comprehensive preventive visits in primary care may especially benefit women of reproductive age with CVRFs, reducing risk of poor pregnancy outcomes.
PUBLICATION RATES OF MEDICAL EDUCATION ABSTRACTS PRESENTED AT THE SOCIETY OF GENERAL INTERNAL MEDICINE 2009 ANNUAL MEETINGAdam Sawatsky; Thomas J. Beckman; Amy T. Wang. Mayo Clinic, Rochester, MN. (Tracking ID #1939341)
BACKGROUND: A recent meta-analysis revealed that 44.5 % of abstracts presented at national meetings were subsequently published in peer-reviewed journals. Two studies have revealed lower publication rates for medical education research abstracts (33 % and 35 %). Previous research has shown that quality of medical education research is a predictor of manuscript acceptance. However, it is unknown whether the quality of medical education abstracts is associated with subsequent publication in peer-reviewed journals. Our goals were to determine: 1) journal publication rates of medical education abstracts presented at a Society of General Internal Medicine (SGIM) Annual Meeting, 2) if abstract quality was associated with subsequent publication, and 3) if there were differences in publication rates and quality of medical education abstracts submitted as scientific abstracts versus ‘innovations in medical education’ (IME).
METHODS: This was a retrospective study of abstracts accepted to the SGIM 2009 Annual Meeting. The 2009 meeting was chosen to allow sufficient time for abstracts to be published. We included all scientific abstracts that described medical education research and all IME abstracts. To identify subsequent publication in a peer-reviewed journal, we searched PubMed, ISI Web of Knowledge and Google Scholar for full-text publications through December 2013 using a combination of first, second, and last authors’ names, as well as keywords from the title. The title, authors, methodology, and results of the published article were compared to the original abstract to confirm matches. We abstracted data on the type of research (quantitative versus qualitative), study population (undergraduate [UME], graduate [GME] or continuing medical education [CME]), submission category, and time to publication. To identify study quality for the abstracts using quantitative methods, we used the Medical Education Research Study Quality Instrument (MERSQI), a previously validated instrument with strong content, criterion, and predictive validity evidence. The MERSQI contains 10 items (overall score range 5–18) within 6 domains of study quality: study design, sampling, data type, validity of assessments, data analysis, and outcomes. Three authors rated 5 abstracts independently, resolved differences by consensus, and reached satisfactory agreement. One author scored the remaining abstracts. We utilized the Chi-squared test to calculate odds ratios to determine if abstract MERSQI scores were associated with subsequent publication; a MERSQI score of >10 was used to define high quality research. We utilized the Fisher’s exact test to compare publication rates and two-sample t-tests to compare MERSQI scores of scientific versus IME abstracts. The threshold for statistical significance was set at a p < 0.05. This study was deemed exempt by the Mayo Clinic Institutional Review Board.
RESULTS: Of 651 scientific abstracts reviewed, 143 met criteria for medical education scholarship. Overall, 62 (43 %) medical education abstracts presented at SGIM were subsequently published in indexed medical journals. The mean time to publication was 21.5 months. The majority of abstracts were quantitative (119, 83 %) and involved GME (75, 52 %) and UME (43, 30 %), with only a minority involving CME (7, 5 %) or mixed populations (18, 13 %). The average MERSQI score for all medical education abstracts was 9.2 (SD, 1.76; range 5–14). Higher quality medical education abstracts (MERSQI ≥ 10) were more likely to be published than lower quality abstracts (MERSQI <10; OR 3.18; 95 % CI, 1.47–6.89; p = 0.003). Scientific abstracts, as compared to IME abstracts, had higher publication rates (53 % v. 33 %, p = 0.02) and higher MERSQI scores (9.8 v. 8.4, p < 0.001). Furthermore, scientific abstracts scored significantly higher than IME abstracts in the following MERSQI domains: sampling (number of institutions studied and response rate), validity of evaluation instrument (content and internal structure), and data analysis (appropriateness and complexity of analysis).
CONCLUSIONS: The journal publication rate of medical education abstracts presented at the SGIM 2009 Annual Meeting was similar to previously demonstrated publication rates for biomedical research abstracts, but was higher than publication rates of medical education abstracts presented at other scientific meetings. Furthermore, this may be the first study to demonstrate an association between a validated measure of abstract quality and subsequent journal publication. These findings suggest that attention to measures of quality, such as those found in the MERSQI, may optimize the likelihood that medical education abstracts will be published in peer-reviewed journals. These findings also indicate that education innovation projects might be improved by utilizing study designs that incorporate multiple institutions, utilize validated evaluation instruments, and apply appropriate statistical analyses.
PULMONARY HYPERTENSION PREVALENCE IN AN AFRICAN-AMERICAN END-STAGE RENAL DISEASE POPULATION ON HEMODIALYSISBronwyn L. Small1; Camelia Arsene2; Irfan Omar2. 1Henry Ford Hospital, Detroit, MI; 2Sinai-Grace Hospital, Detroit Medical Center, Detroit, MI. (Tracking ID #1939103)
BACKGROUND: The development of peritoneal and hemodialysis (HD) have changed kidney failure from a fatal disease to a treatable condition. The overall five-year survival, however, remains relatively low: 39 % in African-Americans compared to 32 % in Caucasians. Cardiac and cardiovascular causes of death continue to be the most common causes of mortality in the prevalent end-stage renal disease (ESRD) population, co-morbid conditions including Pulmonary Hypertension (PH), threaten to further shorten the lifespan of ESRD patients. Recent investigations have shown a high prevalence of PH in HD patients from 26 to 52 %. It has also been found that the presence of PH has led to significantly lower survival rates as compared to those without PH; in addition, PH has been found to be an independent predictor of all-cause mortality in ESRD patients.
METHODS: A prevalence study was undertaken; recruiting patients with ESRD who were undergoing treatment with HD for >3 months, at a teaching hospital or outpatient HD clinic in Detroit, MI. Inclusion in the study required the completion of a short demographics questionnaire, physical examination and permission for researchers to access hospital/clinic records for laboratory values, medical history and imaging results. The questionnaire documented demographics, medical history and presence or absence of various risk factors for PH. A search was conducted within the patients’ medical record for transthoracic echocardiogram (TTE) results within the past year, in addition to recent laboratory values.
RESULTS: Of the 99 patients enrolled in the study, 46 of these patients were found to have a TTE completed within the last year and were included in the study. All participants in the study were African-American. Forty-one patients (89 %) were found to have an RVSP ≥ 25 mmHg, indicating the presence of PH based on TTE findings. The PH patients were also found to have a high prevalence of HTN (97.6 %), CAD (61 %), CHF (58.5 %), COPD/ Asthma (34.2 %). No significant correlations were found between RVSP and Ejection Fraction, Urea reduction ratio, PTH or Calcium-Phosphate product.
CONCLUSIONS: PH appears to be highly prevalent in the ESRD population on HD, particularly in this African-American community. There are likely multiple etiologies of PH in these individuals due to the high incidence of comorbid heart and lung diseases. Further investigations should be completed to determine if the early diagnosis and treatment of PH in these individuals, could help improve survival rates in the ESRD population.
QUALITY OF HYPERTENSION CARE IN A STUDENT-RUN FREE CLINIC: A PILOT STUDYNeil Pathak; Peter Ellis; Rachel J. Perry; Kristina Talbert-Slagle. Yale University, New Haven, CT. (Tracking ID #1928117)
BACKGROUND: Student-run free clinics have become an important source of medical care to underserved populations. Thus, it is critical to determine the quality of medical care delivered in such settings. Few studies have evaluated quality of care in student-run free clinics that serve a predominantly Hispanic population. In this study, we assessed the quality of hypertension care offered by a weekly student-run free clinic, supervised by clinical faculty, that provides care to a mainly Hispanic underserved population.
METHODS: An IRB approved retrospective chart review was performed on all patients who were seen at the clinic between January 2012 and January 2013. Inclusion criteria were that the patient must have been seen for at least two visits following the visit at which hypertension was first recorded. Demographic factors, body mass index (BMI), blood pressure measurements across visits, prescribed medications, alcohol and tobacco use, and comorbidities were collected. Healthy People 2020 and the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) were used as national standards to assess the quality of hypertension care. Fisher’s exact test was used to determine associations between hypertension control and each of the following variables: stage of hypertension; comorbidities; obesity; alcohol use; tobacco use.
RESULTS: Twenty patients (9 females, 11 males) met the inclusion criteria and were included in our pilot study. 18 (90 %) patients were Hispanic, mean age was 46.9 (SD = 13.4), and mean BMI was 27.8 (SD = 3.3). 17 (85 %) had Stage 1 hypertension and 3 (15 %) had Stage 2 hypertension at the visit when hypertension was first recorded. Hydrochlorothiazide was the most commonly prescribed medication (65 %); calcium channel blockers (5 %) and angiotensin-converting enzyme inhibitors (5 %) were used infrequently. The remaining 25 % of patients were solely given lifestyle modification training. It was found that 14 (70 %) patients achieved goal blood pressure (as defined by JNC 7) at the most recent visit. 3 (15 %) patients had dyslipidemia and 1 patient (5 %) had diabetes. 6 (30 %) patients reported using both alcohol and tobacco, 3 (15 %) reported using only tobacco, and 3 (15 %) reported using only alcohol. We found an association between uncontrolled hypertension at the most recent visit and each of the following variables: Stage 2 hypertension diagnosis; simultaneous alcohol and tobacco use (p < 0.05). There was no association between hypertension control and the following variables: sole alcohol use; sole tobacco use; comorbidities; obesity (p > 0.05).
CONCLUSIONS: The percentage of patients in this pilot study who achieved goal blood pressure (70 %) met objectives specified by Healthy People 2020 (61.2 %). Prescribed therapies chosen to treat hypertension met recommended guidelines defined by JNC 7. Simultaneous alcohol and tobacco use as well as initial Stage 2 hypertension diagnosis was found to be linked to uncontrolled hypertension; it therefore may be advisable for medical students to pay more attention to these patients, especially with regard to using multi-drug combinations. This pilot study suggests that a student-run free clinic is able to provide the appropriate pharmacotherapy and/or lifestyle modification training to achieve goal blood pressure in a middle aged, uninsured Hispanic population. Such initiatives may be a potential solution to treating hypertension among some patients in underserved areas.
QUALITY OF LIFE AS AN INDEPENDENT MEASURE IN PATIENTS WITH SYSTEMIC LUPUS ERYTHEMATOSUSAliya Sarmanova1,2; Saule Abisheva1; Gulvira Magzumova2; Rysgul Aytzhanova3. 1Astana Medical University, Astana, Kazakhstan; 2No2 Municipal Hospital, Astana, Kazakhstan; 3The Republican Diagnostic Center, Astana, Kazakhstan. (Tracking ID #1937303)
BACKGROUND: Health-related quality of life (HRQoL) represents patient’s overall perception of the illness, symptoms severity and treatment impact on physical, emotional, and social functions and became an important complementary source of information in patients with Systemic Lupus Erythematosus (SLE). Older age, disease duration and higher scores of activity and damage seems to greatly influence the reduction of HRQoL, but according to many scientific researches, this data is still controversial. The objective of our study was investigation of the HRQoL and its relationship with clinical and demographic data in patients with SLE.
METHODS: in our study we included consecutive patients, fulfilling the 1997 ACR Classification Criteria for SLE. Quality of life was evaluated using patient self-assessment questionnaire of Medical Outcomes Survey Short Form-36 (SF-36, version 2). Disease activity was measured using Systemic Lupus Erythematosus Disease Activity Index (SLEDAI), and organ damage assessed by the Systemic Lupus International Coordinating Clinics/American College of Rheumatology Damage Index (SLICC/ACR-DI). Associations between eight QoL domains and age, disease duration, disease activity, and damage were explored using Spearman’s correlation coefficients (rs).
RESULTS: The study group comprised 30 lupus patients. All of them were women, 86.7 % Asians and 23.3 % Caucasians with mean age of 32.67 years (95 % CI 28.26;37.07) and mean duration of the disease 6.87 years (95 % CI 4.11;9.63). Mean SLEDAI score was 14.57 points (SD ± 8.26). Mean SDI was 1.03 with damage in 53.3 %. There were correlation between SDI score and disease duration (rs = 0.567, p = 0.001) and SLEDAI score (rs = 0.469, p = 0.009). The clinical characteristics of the patients are shown in Table 1. Age and disease duration did not show any significant relationship with the HRQOL scores in any of the domains. Similarly, there were no statistically significant correlations between the scores of the SF-36 domains and scores of SLEDAI and SLICC/ACR-DI (Table 2).
CONCLUSIONS: From obtained results we concluded that there is no clinically important associations between the all domains of the SF-36 and clinical or demographic variables. This suggests that disease activity, accumulated damage, and HRQoL remain an important independent outcome measures in the assessment of health status and full impact of the disease on social functioning. It should be recommended for evaluation in SLE patients.
Clinical and laboratory characteristics of the patients (n = 30)
| Descriptor | Present, % (n = 30) |
|---|---|
| Neurological disorder | 53.3 |
| Renal disorder | 60 |
| Arthritis | 26.7 |
| Mucocutaneous disorder | 66.7 |
| Serositis | 20 |
| Fever | 16.7 |
| Fatigue | 83.3 |
| Leucopenia | 20 |
| Lymphopenia | 43.3 |
Spearman correlation between SLEDAI, SLICC/ACR-DI and SF-36 scores
| SH-36 scores | SLEDAI | SLICC/ACR-DI | ||
|---|---|---|---|---|
| rs | p | rs | p | |
| PF | −0.085 | 0.656 | −0.051 | 0.787 |
| RP | −0.142 | 0.455 | −0.218 | 0.246 |
| BP | −0.352 | 0.056 | −0.206 | 0.276 |
| GH | −0.196 | 0.299 | −0.163 | 0.388 |
| VT | −0.033 | 0.864 | −0.150 | 0.428 |
| SF | 0.059 | 0.755 | 0.297 | 0.112 |
| RE | −0.012 | 0.951 | −0.039 | 0.838 |
| MH | −0.208 | 0.270 | −0.261 | 0.164 |
| PCS | −0.321 | 0.084 | −0.229 | 0.224 |
| MCS | −0.112 | 0.556 | −0.238 | 0.204 |
PF, physical function; RP, role—physical; BP, bodily pain; GH, general health; VT, vitality; SF, social function; RE, role—emotional; MH, mental health; PCS, Physical Component Summary; MCS, Mental Component Summary.
QUANTIFYING THE CONTRIBUTION OF DEFENSIVE MEDICINE TO PRIMARY CARE COSTSAndrei Brateanu; Sarah Schramm; Bo Hu; Kristen Boyer; Kelly Nottingham; Glen Taksler; Stacey E. Jolly; Kenneth Goodman; Anita D. Misra-Hebert; Nirav Vakharia; Aaron Hamilton; Robert Bales; Mahesh Manne; Abhishek Deshpande; Amanda Lathia; Michael B. Rothberg. Cleveland Clinic, Cleveland, OH. (Tracking ID #1918689)
BACKGROUND: Defensive medicine is one contributor to waste in health care. Studies that measure its cost have produced conflicting results. The goal of this study was to directly measure the proportion of primary care costs attributable to defensive medicine.
METHODS: We enrolled primary care physicians (PCP) from 4 outpatient practices in a 6-week prospective study. PCPs completed attitude surveys with information on whether they had been sued, knew anyone who had been sued, and how much they feared being sued. In addition, on 3 distinct days, PCPs were asked to rate each order placed the day before on the extent to which it represented defensive medicine, using a 5-point scale from 0 (not at all defensive) to 4 (entirely defensive). Two scores were calculated: the order defensiveness score for each order (the defensiveness/4) and the physician defensive score (the mean of the defensiveness scores for all orders). Costs were assigned based on Medicare reimbursement rates. Each order was assigned a weighted defensiveness cost by multiplying the cost of that order by its defensiveness score. The proportion of total cost attributable to defensive medicine was defined as the ratio of the weighted cost of defensive orders to the total cost of all orders. A logistic regression model with random effects was used to examine physician and patient factors associated with the defensive medicine score. The model was adjusted for demographic variables, including gender, years in practice, previous malpractice litigation (yes/no), fear of future malpractice litigation, US vs. foreign medical school, and academic vs. community hospital training.
RESULTS: Of 50 eligible PCPs, 23 agreed to participate; 21/23 (91.3 %) returned the surveys and rated 1234 individual orders on 347 patients. Physicians wrote an average of 3.6 ± 1.0 orders/patient/visit with an associated cost of $72.60 ± 18.5 per order. Of the 1,234 orders, 89.8 % were reported as not defensive at all, 9.5 % were reported as somewhat defensive (1–2 on the scale), and 0.8 % were reported as mostly defensive (3–4 on the scale). Across physicians, the median physician defensive score was 0.018 (IQR = [0.008, 0.049]) and the proportion of total costs attributable to defensive medicine was 3.1 % (IQR = [0.5 %, 7.2 %]). PCPs with total defensive scores above compared with those below the median had a higher proportion of total costs attributable to defensive medicine (6.1 %, IQR = [2.4 %, 9.8 %] vs. 1.5 %, IQR = [0.1 %, 2 %], P = 0.004), but similar number of orders (3.38 ± 0.86 vs. 3.74 ± 1.07, P = 0.41) and total costs ($239.9 ± 93.2 vs. $243.9 ± 61.0, P = 0.91), per patient per visit. Physicians were more likely to have high defensive scores if trained in community hospitals vs. academic centers (AOR, 4.29; 95 % CI, 1.55 to 11.86; P = 0.01). Gender, experience, previous malpractice litigations and fear of being sued were not significantly associated with defensiveness.
CONCLUSIONS: This study provides a new method to directly quantify the cost of defensive medicine. Defensive medicine appears to have minimal impact on primary care costs.
QUESTIONING THE VALIDITY OF CONSIDERING LEFT ATRIAL ENLARGEMENT ON EKG AS AN ABNORMAL FINDING IN YOUNG ATHLETESTatvam T. Choksi1; Martin O’Riordan2. 1Mercy Catholic Medical Center, Darby, PA; 2Mercy Catholic Medical Center, Darby, PA. (Tracking ID #1938664)
BACKGROUND: The current ‘Seattle Criteria’ for electrocardiographic interpretation in athletes consider left atrial enlargement as an abnormal finding that requires further investigation. Others have looked into the criteria by involving predominantly Caucasian athletes and it showed around 13 % prevalence of abnormal EKG findings, but very few of them had abnormal 2D-Echo. Given the prevalence of Hypertrophic Obstructive Cardiomyopathy [HOCM] is more in African American than Caucasians; we performed a study on African American athletes of urban Philadelphia.
METHODS: In 2013, we studied a cohort of 55 young athletes aged between 12 and 25 years. All athletes were screened with 12-lead EKG. Electrocardiographic interpretation was based on 2012–13 Seattle criteria for athletes and those with abnormal findings per the criteria underwent 2D-Echo for further evaluation.
RESULTS: Of 55 athletes, 100 % were African American and majority [80 %] were males. None [0 %] reported family history of sudden cardiac death or any cardiovascular symptoms. Athletes were trained in different sporting modalities and trained for an average of 17 h per week. Out of 55 athletes, 7 [12.72 %] had left atrial enlargement and met abnormal EKG findings as per the Seattle Criteria. These athletes underwent echocardiographic evaluation and none [0 %] of them had any structural or functional abnormalities on 2D-Echo.
CONCLUSIONS: Our study showed expected prevalence of left atrial enlargement on EKG in athletes and it did not show any echocardiographic abnormalities. Isolated left atrial enlargement on EKG in young athletes is a common finding that hasn’t shown to predict underlying cardiomyopathies and may be just reflective of benign physiologic adaptation in athletes. Exclusion of left atrial enlargement as an abnormal finding in those without abnormal physical exam findings or family history of sudden cardiac death may increase the cost effectiveness of the pre-participation screening programs. Other study involving Caucasian athletes has highlighted the same point. Given this, it would be reasonable to say that this observation can be applied to young athletes in general and it would be practical to revise the criteria, though our sample size was small.
RACIAL AND ETHNIC DIFFERENCES IN SCREENING FOR DIABETES MELLITUS: NATIONAL HEALTH AND NUTRITION EXAMINATION SURVEY 2005–2012Meghan M. Kiefer1,2; Julie B. Silverman1,2; Karin M. Nelson1,2. 1University of Washington School of Medicine, Seattle, WA; 2VA Puget Sound Healthcare System, Seattle, WA. (Tracking ID #1936714)
BACKGROUND: Nearly 1 in 5 persons with diabetes in the US is undiagnosed, despite the importance of early detection and treatment. Racial disparities in the prevalence and morbidity of diabetes exist; African-Americans are more likely to have worse glycemic control, higher rates of complications, and higher diabetes-associated mortality. Often, patients with diabetes already have complications from their disease at time of diagnosis. Screening is key to detection of diabetes; however, recent population-based estimates of screening prevalence in the US have not been established.
METHODS: We analyzed the 2006–2012 National Health and Nutrition Examination Survey (NHANES) data. Using a nationally representative, cross-sectional sample of non-pregnant US adults, we estimated diabetes screening prevalence according to age, race/ethnicity, and appropriateness of screening status. We then performed multivariate logistic regression, examining the association between race/ethnicity and screening self-report when adjusted for socio-demographic factors. Statistical analysis was conducted using Stata survey procedures to account for the complex sampling design of NHANES.
RESULTS: Forty-three percent of all US non-pregnant adults reported being screened for diabetes in the preceding 3 years. Amongst those who should be screened per American Diabetes Association (ADA) guidelines, only 49.6 % reported screening (95 % CI, 48.2–51.0.), with only 42.0 % of high-risk adults 45 and younger reporting screening. After adjusting for age, gender, sex, BMI, self-reported hypertension, dyslipidemia, physical inactivity, insurance status, poor healthcare access, and survey cycle, Hispanics were more likely to report screening than whites (OR 1.82, p < 0.001) as were non-Hispanic blacks (OR 1.34, p = 0.100.). Among those who reported being screened, the proportion considered appropriate were 87.9 % of non-Hispanic blacks, 88.3 % of whites, 80.4 % of Hispanics, and only 70.0 % of those of other racial/ethnic backgrounds who reported screening were considered appropriate.
CONCLUSIONS: In a nationally representative sample of US adults, fewer than half of those who meet ADA screening guidelines are being screened for diabetes. After adjusting for multiple factors, non-white populations in the US are more likely to report diabetes screening in the preceding 3 years. This suggests that screening inequality is unlikely to account for racial/ethnic disparities in diabetes outcomes. Further efforts to increase appropriate screening, while also reducing unnecessary screening, are needed.
RACIAL AND ETHNIC DISPARITIES IN CONTRACEPTIVE USE AMONG SEXUALLY-ACTIVE WOMEN WHO DESIRE NO MORE CHILDRENCynthia D. Grady1; Christine Dehlendorf2; E. Bimla Schwarz3; Sonya Borrero3,4. 1University of Pittsburgh School of Medicine, Pittsburgh, PA; 2UCSF School of Medicine, San Francisco, CA; 3University of Pittsburgh, Pittsburgh, PA; 4VA Center for Health Equity Research and Promotion, Pittsburgh, PA. (Tracking ID #1934078)
BACKGROUND: There are significant racial/ethnic disparities in contraceptive use among US women. Whether disparities persist among women who explicitly state that they are finished with childbearing is unknown. This analysis examined the relationship between race/ethnicity and contraceptive use among a cohort of women who stated that they do not desire any (more) children.
METHODS: We conducted an analysis of nationally-representative, cross-sectional data from the 2006–2010 National Survey of Family Growth. Our sample consisted of women aged 15–44 who had sexual intercourse with a man in the past 3 months, had no history of infertility, were not currently pregnant, and reported that they did not want (more) children. Our key independent variable was self-reported race/ethnicity. Outcomes included use of any contraceptive method at last heterosexual intercourse and type of contraceptive method used among women who used a method. Methods were categorized as highly effective (male or female sterilization, IUD, implant), moderately effective (injection, pill, patch, ring), or least effective (barrier and behavioral methods). Covariates included socio-demographic characteristics (age, religion, marital status, income, education, insurance), reproductive characteristics (parity, prior unintended pregnancy), and an indicator of healthcare utilization (receipt of any reproductive health services in the past 12 months). We conducted multivariable logistic regression to assess the independent effect of race/ethnicity on our outcomes after adjusting for all covariates.
RESULTS: Our cohort included 2,913 women: 66.1 % were white, 12.3 % black, and 16.3 % Hispanic. The vast majority of women (91.2 %) used a contraceptive method at last intercourse, although this varied by race/ethnicity with 93.3 % of whites reporting use of any method, compared to 84.7 % of blacks and 90.6 % of Latinas (p < 0.01). In adjusted analysis, compared to whites, blacks were significantly less likely to use any contraception (OR:0.43; 95 % CI:0.25–0.72), while there was no significant association for Latinas (OR:0.93; 95 % CI:0.52–1.67). With regard to type of method used at last intercourse, 59.3 % of women used a highly-effective method of contraception, 18.8 % used a moderately-effective method, and 21.9 % used a least-effective method. Type of method varied by race/ethnicity in bivariate analysis with 80.8 % of whites, 75.2 % of blacks, and 73.4 % of Latinas women using a highly- or moderately-effective method (p < 0.01). In the adjusted model, when compared to white women, black and Hispanic women trended toward a lower likelihood of using a highly- or moderately-effective method versus a least-effective method, although these associations did not reach statistical significance (OR:0.70; 95 % CI:0.46-1.05 and OR:0.76; 95 % CI:0.52-1.12, respectively).
CONCLUSIONS: Among a nationally-representative cohort of women at risk for unintended pregnancy who report that they do not desire (more) children, black women were significantly less likely than white women to use any contraception at last intercourse. Future research should explore other factors, beyond socioeconomic status and differential healthcare utilization, that may contribute to observed racial disparities in contraceptive use, including cultural norms, contraceptive knowledge, and patient-provider relationships.
RACIAL DISPARITIES IN GASTROINTESTINAL STROMAL TUMOR CLINICOPATHOLOGIC FEATURES AND SURVIVAL OUTCOMESRaji Shameem1; Muhammad S. Hamid2; Niket Sonpal1; Arvind Randhawa3; Nakul Singhal1; Kevin Sullivan3. 1Lenox Hill Hospital, Dix Hills, NY; 2Detroit Medical Center, Detroit, MI; 3Lenox Hill Hospital, New York, NY. (Tracking ID #1940057)
BACKGROUND: Gastrointestinal Stromal Tumors (GIST) are the most common mesenchymal malignancies of the gastrointestinal tract. In 2002, the tyrosine kinase inhibitor Imatinib was approved as a treatment for unresectable and metastatic GIST. Imatinib has been shown to improve survival in certain patients. Currently little is known of the clinicopathologic features and survival outcomes for different racial groups prior to and after the introduction of Imatinib
METHODS: Patient information from 1988 to 2008, were extracted using Surveillance, Epidemiology, and End Results (SEER) database. Clinicopathologic features that were classified included age at diagnosis (<45 years, 45–60 years, 60–75 years, >75 years), tumor size (<5 cm, 5–10 cm, >10 cm) anatomic location (esophagus, stomach, small intestine, large intestine, rectum), radiation, and surgical intervention). A descriptive analysis and age-adjusted survival rates were calculated using univariate Cox-regression hazard models for non-Hispanic whites (NHW), Hispanics, Blacks, and Asian/ Pacific Islanders (API) races using SPSS 21.0. Difference amongst proportions and groups were calculated using Z-scores and Kurskal-Wallis test respectively.
RESULTS: A total of 4,386 patients were included in our study. Regarding tumor location, compared to NHW, gastric tumors were significantly more common in Blacks (77.8 % vs 52.1 %; p = 0). Gastric tumors were also more common in Hispanics (53.6 %) and API (56.5 %), however no significant difference was seen (p > 0.05). For Blacks, Hispanics and API, the most common non-gastric location was the small intestine (p = 0.01). GIST was significantly more common in female Blacks (51.9 % vs 45.2 %; P = 0.004), whereas it was more common in males in all other groups. Age at diagnosis occurred earlier in Hispanics (57 ± 15.75 years) with the greatest proportion (33.3 %), presenting in the 45–60 age group, compared to 60–75 in all the other races. For all races, age greater than 60 year was associated with decreased survival (P < 0.05), while cancer directed surgical intervention was associated with increased survival (P < 0.05). For API and NHW, radiation therapy (HR: 2.1 and HR: 2.1; P < 0.05) and tumor size >10 cm (HR: 3.72 and HR: 2.07, P < 0.05) respectively, were associated with worse outcomes. Regarding tumor location in NHW, decrease survival was observed in tumors presenting in the splenic flexures (HR: 4.588, p < 0.05). In the post-Imatinib era (after 2002), increased survival was seen in NHW (HR: 0.51, P = 0), Blacks (HR: 0.56, P < 0.05), and API (HR: 0.64, P < 0.05), however no significant difference was seen in Hispanics (HR: 0.80, P = 0.23).
CONCLUSIONS: To our knowledge this is the most up to date SEER analysis of the clinicopathologic features and survival outcomes of GIST tumors among different racial groups. Previous literature has commented that the most common anatomic location is the stomach. Our results support the regularity of gastric GIST but also demonstrate that it is seen more commonly in Blacks compared to NHW. Also Blacks, unlike other races were seen to have significantly higher number of females diagnosed with GIST. Our study was the first to analyze the SEER database for survival outcomes of large tumors (>10 cm), which were associated with poor prognosis. Age greater than 60 years also showed decreased survival. Interestingly, tumors located at the splenic flexures were associated with the worst prognosis in NHW. The introduction of Imatinib as a treatment for GIST has shown impressive results in improving overall survival in patients, which was seen in our analysis for NHW, Blacks, and API. However, Hispanics did not show improved outcomes in the post-Imatinib era despite having the earliest age at diagnosis. This suggests that Hispanics have more aggressive GIST compared to other races.
RACIAL DISPARITIES IN THE PRIMARY CARE OF PATIENTS WITH CHRONIC KIDNEY DISEASE (CKD)Raquel Greer1; Lisa A. Cooper1; Yea-Jen Hsu1; Kathryn A. Carson1; Bernard G. Jaar1; Jill A. Marsteller1; Lawrence J. Appel1; L. Ebony Boulware2. 1Johns Hopkins Medical Institutions, Baltimore, MD; 2Duke University School of Medicine, Durham, NC. (Tracking ID #1938904)
BACKGROUND: African Americans are disproportionately affected by advanced CKD and risk factors for CKD progression. Primary care providers (PCP) care for most patients with CKD and are well-positioned to treat CKD risk factors. However little is known about racial differences in the provision of primary care related to CKD management.
METHODS: We conducted a cross-sectional study of 1800 patients (765 African American, 1035 White) with an estimated glomerular filtration rate between 15 and 59 ml/min/1.73 m2 to quantify racial differences in CKD management. Using electronic medical record data from 6 Baltimore area primary care clinics (n = 49 PCPs), we obtained information on patient race/ethnicity and receipt/achievement of CKD care goals recommended by clinical practice guidelines during a 12 m period (4/12–3/13). We also obtained information on patient age; sex; CKD severity; presence and control of diabetes, hypertension, or CVD; and number of PCP visits during the 12-month study period. We performed random-effects multivariable logistic regression to account for clustering of patients within physicians.
RESULTS: Compared to Whites, African Americans were younger, had greater CKD severity, greater prevalence of hypertension and diabetes, and more frequent utilization of primary care (Table 1). Among patients with diabetes, African Americans were more likely to receive a hemoglobin A1c test compared to Whites (96 % vs. 90 %, respectively, p = 0.004). There were no statistically significant differences in patients’ receipt of other recommended care, including serum creatinine, urine protein, lipid profile, or hemoglobin assessments. African Americans were less likely than whites to achieve a BP goal of <140/90 (63 % vs. 72 %, p = 0.002) and an LDL goal of <100 (54 % vs 64 %, p < 0.001). There was no racial disparity in achieving a hemoglobin A1c goal of <7 among patients with diabetes.
CONCLUSIONS: Compared to Whites, African Americans with CKD were less likely to achieve recommended management goals for blood pressure and cholesterol. Further studies are needed to understand the reasons for these disparities in achievement of CKD management goals and their impact on subsequent clinical outcomes.
Table 1: Patient Characteristics
| Patient Characteristics | African American (n = 765) | White (n = 1035) | P value |
|---|---|---|---|
| n (%) | n (%) | ||
| Age | <0.001 | ||
| 18–44 years | 15 (2.0) | 8 (0.8) | |
| 45–59 years | 99 (12.9) | 79 (7.6) | |
| 60–74 years | 296 (38.7) | 379 (36.6) | |
| 75+ years | 355 (46.4) | 569 (55.0) | |
| Female | 491 (64.2) | 599 (57.9) | 0.007 |
| Hypertension | 671 (87.7) | 828 (80.0) | <0.001 |
| Diabetes | 403 (52.7) | 359 (34.7) | <0.001 |
| Cardiovascular Disease | 432 (56.5) | 642 (62.0) | 0.017 |
| Baseline CKD Stage | 0.019 | ||
| Stage 3a | 434 (56.7) | 605 (58.5) | |
| Stage 3b | 237 (31.0) | 344 (33.2) | |
| Stage 4 | 94 (12.3) | 86 (8.3) | |
| Number of PCP visits in study period | 0.003 | ||
| 1–2 visits | 191 (25.0) | 339 (32.8) | |
| 3–6 visits | 409 (53.5) | 503 (48.6) | |
| 9–11 visits | 93 (12.2) | 120 (11.6) | |
| >11 visits | 72 (9.4) | 73 (7.1) |
Table 2: Achievement of CKD Care Goals among African American and White Patients
| Achievement of Recommended CKD Care Goals (%) | ||||
|---|---|---|---|---|
| Total | African American | White | P value* | |
| Assessment Goals | ||||
| Creatinine | 88.1 | 88.5 | 87.8 | 0.89 |
| Urine protein quantification | 25.1 | 30.7 | 20.9 | 0.69 |
| Lipids | 70.5 | 71.9 | 69.5 | 0.38 |
| Hemoglobin | 67.8 | 67.1 | 68.3 | 0.24 |
| Hemoglobin A1c** | 93.4 | 96.0 | 90.5 | 0.004 |
| Management Goals | ||||
| BP < 140/90 | 68.5 | 63.2 | 72.4 | 0.002 |
| LDL < 100 | 59.7 | 54.0 | 64.1 | <0.001 |
| Hemogloblin A1c < 7** | 57.2 | 56.1 | 58.5 | 0.19 |
*Adjusted for age, sex, hypertension, diabetes, cardiovascular disease, baseline eGFR, PCPs volume of CKD patients, and number of PCP visits during study period, **Assessed only among patients with diabetes
RACIAL/ETHNIC DIFFERENCES IN PALLIATIVE CARE CONSULTATION FOR INPATIENTS WITH ADVANCED CANCERRashmi K. Sharma1; Kenzie A. Cameron1; Jamie Von Roenn1; Joan S. Chmiel1; Holly G. Prigerson2; Frank Penedo1. 1Northwestern University, Chicago, IL; 2Cornell Medical College, New York City, NY. (Tracking ID #1926304)
BACKGROUND: Racial/ethnic minorities with advanced cancer are less likely to receive palliative care and hospice services than non-Hispanic whites (NHW) and more likely to receive intensive, non-curative treatment at the end of life, yet little is known about racial/ethnic differences in rates of inpatient palliative care consultation (PCC). We sought to evaluate the association between race/ethnicity and PCC for advanced cancer patients.
METHODS: We used the electronic medical record (EMR) to identify all patients with metastatic cancer hospitalized between January 1, 2009 and December 31, 2010 at an urban academic medical center. Patient-level multivariable logistic regression was used to evaluate the association between race/ethnicity and PCC.
RESULTS: 6288 advanced cancer patients (69 % NHW, 19 % African American (AA), 6 % Hispanic) were hospitalized during the study period of which 1086 patients had a PCC. More AA (22 %) and Hispanic patients (20 %) received an inpatient PCC compared to NHW patients (16 %) (p < 0.001). In univariate analyses, AA race/ethnicity (OR 1.49, 95 % CI 1.27–1.74), Hispanic ethnicity (OR 1.33, 95 % CI 1.01–1.74), and insurance [Medicaid (OR 1.87, 95 % CI 1.48–2.36) and Medicare (OR 1.24, 95 % CI 1.07–1.42), each vs. private insurance] were associated with higher odds of PCC. Greater severity of illness (measured using the APR-DRG severity of illness score) was linearly associated with higher odds of PCC (trend test p < 0.001). After adjusting for insurance status, race/ethnicity, prior hospitalization, and severity of illness, AA and Medicaid patients had higher odds (OR 1.28, 95 % CI 1.08–1.52, and OR 1.60, 95 % CI 1.23–2.09) of inpatient PCC than NHW and private insurance patients, respectively.
CONCLUSIONS: Hospitalized AA patients with advanced cancer were more likely to receive a PCC than NHW patients, even after adjusting for insurance status and severity of illness, although rates of PCC remained low. Our findings of increased receipt of PCC among AA patients in the hospital appear contrary to studies reporting decreased access to palliative care services by racial/ethnic minorities in the outpatient setting. Better understanding of the factors that are driving higher rates of inpatient PCC rates for AA patients with advanced cancer may thus help to inform the development of interventions to improve access to palliative care for AA patients across other settings.
Factors associated with inpatient palliative care consultation for patients with advanced cancer
| Variables | Bivariate Analysis | Multivariate Analysis* | ||
|---|---|---|---|---|
| OR | 95 % CI | OR | 95 % CI | |
| Race | ||||
| Non-Hispanic White (reference) | ||||
| African American | 1.49 | 1.27–1.74 | 1.28 | 1.08–1.52 |
| Hispanic | 1.33 | 1.01–1.74 | 1.20 | 0.91–1.60 |
| Insurance | ||||
| Private (reference) | ||||
| Medicaid | 1.87 | 1.48–2.36 | 1.60 | 1.23–2.09 |
| Medicare | 1.24 | 1.07–1.42 | 1.03 | 0.89–1.20 |
| Other | 0.92 | 0.63–1.36 | 0.95 | 0.63–1.43 |
| APR-DRG Severity of illness | ||||
| 1: Minor severity (reference) | ||||
| 2: Moderate severity | 2.00 | 1.56–2.58 | 1.80 | 1.39–2.33 |
| 3: Major severity | 3.97 | 3.10–5.08 | 3.38 | 2.62–4.37 |
| 4: Extreme severity | 7.55 | 5.73–9.95 | 7.19 | 5.39–9.59 |
* Adjusted for race, insurance, severity of illness, and prior hospitalization during the study period
RANDOMIZED CONTROLLED TRIAL OF A CULTURALLY ADAPTED, AUTOMATED TELEPHONE EXERCISE COACH TO IMPROVE PHYSICAL ACTIVITY AMONG HYPERTENSIVE AFRICAN-AMERICANSJulien J. Dedier1; Julie A. Wright3; Robert H. Friedman1; Timothy Heeren2. 1Boston University, Boston, MA; 2Boston University, Boston, MA; 3University of Massachusetts, Boston, MA. (Tracking ID #1939226)
BACKGROUND: Regular physical activity (PA) of moderate or greater intensity (MOD+PA) can reduce blood pressure (BP). However, hypertensive urban minority patients may face logistical obstacles to participation in brick-and-mortar PA programs. Automated PA programs delivered by telephone can mitigate these obstacles. We conducted an RCT to test the ability of an automated, interactive, culturally adapted telephone exercise coach to (1) increase PA and (2) lower BP in urban African-Americans (AA) with poorly controlled hypertension (HTN).
METHODS: Subjects were sedentary, hypertensive, AA adult primary care patients at an urban safety net hospital or 2 affiliated health centers. Potential subjects were identified in the electronic medical record database and sent an invitation letter from the practice. Study staff called patients to confirm eligibility and enroll them. The intervention was Telephone-Linked Care for PA (TLC-PA)—a computerized system that ‘converses’ with patients by telephone using pre-recorded human speech. It helps patients set PA goals, devise a plan to meet them, monitors their progress toward these goals, and helps patients overcome barriers that arise. Guided by Social Cognitive Theory and the Transtheoretical Model of behavioral change, TLC-PA conversations were tailored to the user’s level of behavior and motivation. Content was also culturally adapted to aspects of PA relevant to urban AA in Boston. Patients randomized to TLC-PA were schedule to receive 12 weekly TLC-PA calls of roughly 10 min each. Control participants received usual primary care and an educational brochure on HTN. The primary study outcomes were (1) change in minutes of MOD+PA from baseline to 3 months; and (2) change in SBP from baseline to 3 months. PA was measured using 2 validated surveys: (1) the 7-question PA set from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) survey; and (2) the 7-Day Physical Activity Recall (PAR).
RESULTS: 253 patients completed the baseline assessment (123 TLC-PA, 130 control). Mean age was 58 years. Seventy-three percent were female and 20 % partnered. Eighty-three percent reported highschool/GED-level education. Twenty-eight percent were employed full- or part-time, and the median annual household income was $10 K–$20 K. Baseline BP in the TLC-PA and control groups were 136.4/83.5 mmHg and 138.9/81.5 mmHg, respectively. Among patients who completed the final 3-month assessment, self-reported minutes of MOD+PA/week increased significantly more in the TLC-PA group than controls from baseline to 3 months on both the BRFSS survey (143.2 min. TLC-PA vs. 110.2 min. controls, p = .007) and the 7-day PAR (55.1 min. TLC-PA vs. 28.1 min. controls, p = .022). The odds of meeting the national recommendation of ≥150 min/week of MOD+PA at 3 months was statistically greater in the TLC-PA group than in controls on the BRFSS (OR 2.9, p = .001), but not on the PAR (OR 1.7, p = .098). Despite these increases in MOD+PA, change in SBP from baseline to 3 months did not differ significantly between experimental groups.
CONCLUSIONS: TLC-PA was associated with a significant increase in self-reported MOD+PA compared to usual primary care alone. Patients also rated TLC-PA highly on content, convenience and user-friendliness. Given their convenience, scalability, and ability to deliver tailored messages, automated telecommunications systems can promote PA self-management in urban African-Americans with HTN.
RANDOMIZED TRIAL OF TELEPHONE NURSE CASE CO-MANAGEMENT OF DIABETES AND HYPERTENSION IN COMMUNITY PRACTICEDavid Edelman1,2; Cynthia J. Coffman3,2; Rowena Dolor1; Jennifer H. Lindquist2,1; Katherine C. Pereira4; Bradi B. Granger5,4; Alice M. Neary1; Amy C. Harris2,1; Hayden Bosworth1,2. 1Duke University Medical Center, Durham, NC; 2Durham VA Medical Center, Durham, NC; 3Duke University Medical Center, Durham, NC; 4Duke University Medical Center, Durham, NC; 5Duke University Medical Center, Durham, NC. (Tracking ID #1935667)
BACKGROUND: Several trials have demonstrated the efficacy (best-case potency) of nurse telephone case management for diabetes (DM) and hypertension (HTN). However, these trials were performed in academic or vertically-integrated systems. The extent to which these clinical improvements translate to “real world” practices is unknown. Our objective was to assess the effectiveness (real-world potency) of nurse-run behavioral co-management of blood sugar and blood pressure among patients with both diabetes and HTN.
METHODS: The study was a patient-level randomized, controlled trial among 9 practices in a practice-based research network of community primary care practices. Patients were age >=21, had both type 2 DM and HTN, had to have inadequately controlled DM (Hemoglobin A1c (A1c) >= 7.5 %) but could have well controlled HTN. All patients were called by a nurse with experience in DM and HTN management every two months for two years, for a total of 12 calls. Intervention arm patients received DM- and HTN- focused behavioral content; the content was targeted to individuals’ needs (eg, only sedentary subjects received physical activity advice, only smokers received smoking cessation advice). Content was informed by motivational interviewing and attempted to identify and resolve specific barriers to healthful behaviors (eg, healthful eating, physical activity, medication adherence). Medications were not managed. Control patients received non-tailored, non-interactive information regarding health issues unrelated to DM and HTN (eg, skin cancer prevention) at the same frequency as intervention calls. Systolic blood pressure (SBP) and A1c were co-primary outcomes; diastolic blood pressure (DBP), weight and self-efficacy (by Perceived Competence scale, PCS, scale 0–4) were also measured. Subjects were assessed at baseline, 6, 12, and 24 months; 12 months was the primary outcome. Analyses were performed by linear mixed modeling, adjusting for statistical clustering by practice.
RESULTS: 377 subjects were enrolled; 193 randomized to the intervention, 184 to control. The number of subjects per practice ranged from 16 to 104. Subjects were 55 % female, 50 % white; their mean age was 59 (SD =11) years and mean BMI was 36.3 (SD = 7.7) kg/m2. Mean baseline A1c was 9.0 % (SD = 1 %) and mean SBP was 142 mmHg (SD = 20). Intervention patients received 78 % of nurse calls; control patients, 81 %. Eighty-two percent of all data points were obtained; 80 % of intervention patients and 76 % of control patients reached the 12 month time point. Expressing differences as (intervention - control), at 12 months, intervention patients had similar A1c [diff = −0.2 %, 95%CI (−0.6, 0.1), p = 0.23] and SBP [diff = −1.3 mmHg, 95%CI (−5.6, 3.0), p = 0.54] to control patients. DBP (diff = 1.0 mmHg, p = 0.36) and weight (diff = 1.1 kg, p = 0.21) were likewise similar between control and intervention patients. Self-efficacy was slightly worse among intervention patients (diff = −0.25, p = 0.006). Results were similar at the 6 and 24 month time points. Analyses of patients who completed at least 10 encounters were not different from the primary analyses.
CONCLUSIONS: In 9 community, fee-for-service practices, telephonic nurse case management did not lead to improvement in A1c or SBP. The lack of impact on completers suggests that this lack of potency is not due to dropout. Gains seen in telephonic, behavioral self-management interventions in optimal settings may not translate to all primary care settings.
READINESS FOR INTERPROFESSIONAL LEARNING AMONG MEDICAL, NURSING, AND PHYSICIAN ASSOCIATE STUDENTS AT AN AMERICAN UNIVERSITYJaideep S. Talwalkar1,2; Deborah B. Fahs3; Gerald Kayingo1; LInda H. Pellico3. 1Yale School of Medicine, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Yale School of Nursing, New Haven, CT. (Tracking ID #1937558)
BACKGROUND: The Liaison Committee on Medical Education recently adopted a new standard for interprofessional curricular experiences citing the importance of collaborative education and practice for improved patient outcomes, safety, and quality of care. Currently at our university there are few opportunities for medical, nursing, and physician associate students to collaborate. A curricular redesign is in progress that will provide robust interprofessional learning opportunities for students from the start of training longitudinally through graduation. The aim of this study was to determine baseline perceptions among first year health professions students at one American university towards collaborative learning and practice.
METHODS: First year students in three professional programs [medical (n = 101), nursing (n = 81), and physician associate (n = 35)] were sent an anonymous online survey in January 2012 which included six items related to demographic information, as well as the 19-item Readiness for Interprofessional Learning Scale (RIPLS). This validated, widely-utilized scale measures the readiness of healthcare students for shared learning. Scores on the RIPLS and its four subscales were compared among the three groups of students using SAS 9.3 by the general linear model.
RESULTS: Surveys were completed by 70 (69 %) medical, 71 (88 %) nursing, and 25 (71 %) physician associate students. Scores on the RIPLS indicated that all three groups of students scored in the high range, indicating readiness for shared learning. Female students, those with advanced degrees, and those with healthcare experience prior to enrollment in health professional school had significantly higher scores than their counterparts. After controlling for differences in demographic factors, nursing students scored significantly higher (83.06) than physician associate (76.84, p < 0.0001) and medical (76.41, p < 0.0001) students. There was no difference between physician associate and medical student total scores.
CONCLUSIONS: Health professions students from three training programs within an American university demonstrated readiness for interprofessional learning early in their academic programs, however nursing students demonstrated greater readiness than medical and physician associate students. Our findings are similar to those reported in studies from Canada and New Zealand, but different than reports from the United Kingdom and Singapore. Previous work suggests that entering nursing students think collaboratively, in contrast to medical students who think in individualistic terms. It is possible that students with an interest in or a skill set suited for team-based case are attracted to the nursing profession. In contrast, physician associate students learn in the medical model, and the scores of these two groups of learners were similar. In order to optimize the value of curricular innovations that emphasize interprofessional education, it may be necessary to create learning groups that balance predictive features of readiness for interprofessional learning, such as program type, gender, and prior healthcare experience or graduate degree. Extrapolation of predictive features across countries may not be appropriate.
READMISSION REDUCTION INITIATIVE (RRI): CHARACTERIZING THE 30-DAY READMISSION POPULATION AND IDENTIFYING PREDICTORS OF PREVENTABILITYShone Almeida; Edward Ha; Ashley Busuttil; Nasim Afsarmanesh. Ronald Reagan Medical Center at UCLA, Los Angeles, CA. (Tracking ID #1916190)
BACKGROUND: Prior studies have estimated that one in five patients is re-hospitalized within a 30-day period. We sought to characterize the 30-day readmission population at a major academic medical center, the Ronald Reagan Medical Center at the University of California, Los Angeles (RRUCLA). This study also assesses the root cause and preventability of each readmission with the aim of finding potential predictors of preventable readmissions.
METHODS: From 1/1/2012 to 1/16/2013, 3,848 cases of 30-day readmissions were identified. Chart abstractions were performed by physicians, medical students, and nurses. Documentation review was limited to the history and physical (H&P) and discharge summary for the index admission and readmission event.
RESULTS: To date, 611 chart abstractions have been completed, of which 67.4 % were found to be not preventable (NP), 23.5 % potentially preventable (PP), and 9.1 % preventable (P). The majority of readmissions were due to relapse, or worsening of chronic illness, accounting for approximately 44.5 % of cases; another 30.4 % were due to a new, unrelated event. Planned admissions, medication or procedure adverse events, and inadequate discharge planning accounted for 11.3 %, 6.5 %, and 4.1 % respectively. Quality of care during the index admission and access to care issues together accounted for just over 3.1 % of abstracted cases.
CONCLUSIONS: The data shows that the number of unpreventable admissions far outnumbers preventable ones. Trends point to high utilization of the ER, new anticoagulation starts, discharge medication reconciliation, and effective post-discharge follow-up as potential targets of future intervention. However, the current sample size is too small to draw any definite conclusions regarding predictors of preventability.
RECEIPT OF ALCOHOL-RELATED ADVICE AND QUALITY OF CARE AMONG VETERAN OUTPATIENTS WITH UNHEALTHY ALCOHOL USEJoseph Simonetti1,3; Gwen T. Lapham4,2; Emily Williams2,3. 1University of Washington, Seattle, WA; 2Seattle-Denver HSR&D COIN, VA Puget Sound, Seattle, WA; 3University of Washington, Seattle, WA; 4Group Health Research Institute, Seattle, WA. (Tracking ID #1938960)
BACKGROUND: Brief intervention, including advice to reduce or abstain from drinking, is widely recommended for primary care patients with unhealthy alcohol use, but rarely implemented. One cited barrier to implementation is providers’ assumptions that patients do not want to discuss their drinking or may react negatively to such interventions. However, among primary care patients with unhealthy alcohol use who participated in an intervention trial to address their drinking, those who reported receipt of alcohol-related advice rated their care as higher quality than those not reporting advice. It is unknown whether a similar association exists among a more general sample of outpatients. Our aim was to determine whether receipt of alcohol-related advice was associated with perceptions of quality of care among a general sample of Veteran outpatients who screened positive for unhealthy alcohol use and responded to a mailed survey.
METHODS: This retrospective, cross-sectional study included Veteran outpatient respondents to the VA Survey of Healthcare Experiences of Patients (Fiscal Year 2010, response rate 53 %) who screened positive for unhealthy alcohol use on the 3-item Alcohol Use Disorders Identification Test (AUDIT-C) included in the survey (score >3 for women, >4 for men), responded to a question regarding receipt of alcohol-related advice from a VA provider in the past year (yes/no), and to two questions assessing patient ratings of their VA provider and overall VA health care. We used logistic regression to assess the association between receipt of alcohol-related advice and two patient-reported outcomes: patient ratings of their VA provider and their overall VA health care (range 0–10, dichotomized ≥9 to indicate high quality). Models were adjusted for age, gender, race, education, and self-reported health status and were clustered to account for correlation of outcomes at the facility level.
RESULTS: Among 21,912 Veterans who completed the 2010 survey, 3,760 screened positive for unhealthy alcohol use and had complete data. Overall, the mean age of the study sample was 64.4 years; 96.3 % were male, 79.7 % were non-Hispanic White, 91.8 % completed high school and 28.3 % reported their health status as very good or excellent. Nearly half (44.3 %) of the study sample reported receiving alcohol-related advice in the past year, and 68.8 % and 56.2 % of respondents rated their providers and VA health care as high quality, respectively. In adjusted models, patients who reported receipt of alcohol-related advice were more likely than those who did not to rate their provider (OR 1.38; 95 % CI 1.16–1.64) and VA health care (OR 1.29; 95 % CI 1.11–1.51) as high quality.
CONCLUSIONS: Results from this cross-sectional analysis among Veterans with unhealthy alcohol use demonstrate that receipt of alcohol-related advice—a key component of efficacious brief intervention—is associated with patient-reported indicators of high quality care. These findings are consistent with those of a previous study in a more limited population, and are in opposition to provider concerns that delivering such advice may adversely affect patients’ perceptions of their care.
RECENT TRENDS AND REGIONAL VARIATION IN OPIOID ANALGESIC EXPOSURE IN THE VETERANS HEALTH ADMINISTRATIONWilliam Becker1,2; Jian Gao3; E. Jennifer Edelman2; Eileen Moran3; David A. Fiellin2; Robert D. Kerns1,2. 1VA Connecticut Healthcare System, West Haven, CT; 2Yale University, New Haven, CT; 3Veterans Health Administration, Washington, DC. (Tracking ID #1939112)
BACKGROUND: Given data demonstrating modest efficacy and potential for serious harms—including addiction, diversion, overdose and death—opioid analgesic prescribing for non-cancer pain has become increasingly controversial. Within the Veterans Health Administration (VHA), multiple efforts including clinical practice guideline updates, policy changes and educational efforts, have promoted safe opioid prescribing. Risk of harm has been linked to both dose and duration of opioid therapy, which, when considered together, can be defined as opioid exposure. We sought to characterize recent trends and regional variation in opioid analgesic exposure in the VHA, the largest integrated health system in the U.S.
METHODS: Using the VHA Decision Support System’s Pharmacy National Data Extracts we identified all outpatient, oral or transdermal opioid prescriptions for veterans without a cancer diagnosis from 2005 to 2013. Opioids for the treatment of addiction were excluded. We calculated opioid exposure by first converting each prescription to a standard morphine equivalent dose, then multiplying by pill quantity extrapolated over the number of days supplied. Multiple co-occurring prescriptions for the same patient were added together. To calculate per capita data, we aggregated opioid exposure for the entire health system by year and divided it by the total number of patients in the system (exposure per capita) and then by prescription recipient (exposure per recipient). For 2013 only, we then calculated exposure per capita and exposure per recipient for each of VHA’s 140 facilities to assess regional variation; the catchment areas for these facilities are non-overlapping and encompass the entire U.S.
RESULTS: Over 9 years, approximately 54.1 million prescriptions written for nearly 2.7 million veterans met the inclusion criteria. Exposure per capita increased 18 % nationally from 986 mg in 2005 to 1,159 mg in 2013, while exposure per recipient increased 14 % from 5,337 mg in 2005 to 6,088 mg in 2013. Both exposure metrics peaked in 2012 and were slightly lower in 2013. The analysis by facility revealed a nearly 3.2-fold variation in exposure per capita from the mean of the lowest quintile (605 mg) to the mean of the highest quintile (1,931 mg); and a 2.2-fold variation in exposure per recipient from the mean of the lowest quintile (3,927 mg) to mean of the highest quintile (8,629 mg).
CONCLUSIONS: Recent trends in per capita and per recipient opioid exposure indicate stabilization in the use of opioids for non-cancer pain in VHA which may reflect successful dissemination and uptake of practice guidelines, policies and education. Further research is needed to explain and ameliorate marked regional variation in the use of opioids in non-cancer pain.
RECTAL CANCER: CHARACTERISTICS AND SURVIVAL RATES OF YOUNG VS. OLDShams Mistry; Charles Andrew T. Chacko; Harish Madala; Logrono AlMarieGrace; Jill Gernand; Radhika Kakarala. Mclaren Regional Medical Center, Flint, MI. (Tracking ID #1921544)
BACKGROUND: Rectal cancer is detected at a later stage in younger patients (YP) (< 50) due to lack of screening in this age group. There has been an increased incidence of rectal cancer in YP, but they are underrepresented in research studies. The aim of our study is to compare characteristics of rectal cancer and survival outcome in YPs (18–49 years) vs older patients (50+) using the Surveillance, Epidemiology, and End Results (SEER) database.
METHODS: We analyzed a retrospective cohort of patients diagnosed with rectal cancer in the SEER national cancer registry from 1991 to 2010. This National Cancer Institute database is a cancer registry covering approximately 26 % of the US population across several geographic regions. It is the largest publicly available domestic cancer database. Using the SEER database, we reviewed patients >18 years of age with rectal adenocarcinoma from 1991 to 2010. Continuous and categorical variables are reported using mean (SD), proportions, and percentages. Univariate analysis was done using T-test and Chi-square tests respectively. Multivariate Cox regression analysis was used to evaluate risk adjusted outcomes and to predict the hazard of dying. Kaplan Meier method was used to estimate the survival function.
RESULTS: We included 102,167 patients in our study. YPs with rectal carcinoma were more likely to be African American (11.9 % vs 8.8 %; p < 0.001), Hispanic (13.3 % vs 8.3 %; p < 0.001) and Asian (10.9 % vs 8.3 %; p < 0.001) as compared to the older age group. YPs were more likely to present with distant metastasis (16.7 % vs 13.4 %; p < 0.001) and had more poorly differentiated tumors (13.3 % vs 12.1 %; p < 0.001). YPs also received more cancer directed surgery (84 % vs 80 %; p < 0.001) and post-operative radiation (52 % vs 39.8; p < 0.001) compared to their older counterpart. In contrast to previous studies the 5 year survival was better for younger patients (74.3 % vs 70.7 %; p < 0.001{Table 1}). After controlling for gender, race, marital status, grade, stage, cancer specific surgery and post-operative radiation, multivariate Cox regression analysis revealed that age is an independent predictor of death, and younger patients with rectal cancer had a lower risk of dying (HR 0.693; p < 0.001)
CONCLUSIONS: In previous studies younger patients with rectal cancer were found to have poorer or equivalent survival compared to older patients. In contrast, our study shows that young patients less than 50 years of age, have advanced stage rectal cancer at diagnosis but have better survival.
Table 1: Five-year relative survival for rectal cancer patients
| Stage of rectal cancer | Young (< 50 year) N = 12,268 | Older (≥ 50 years) N = 83,232 | P- VALUE |
|---|---|---|---|
| Localized | 280 (93.3 %) | 3,837 (87.7 %) | <0.001 |
| Regional | 792 (74.2 %) | 6,201 (66.6 %) | <0.001 |
| Distant | 1,324 (17.3 %) | 7,110 (13.4 %) | <0.001 |
| OVERALL | 2,516 (74.3 %) | 18,802 (70.7 %) | <0.001 |
RECURRENT VENOUS THROMBOEMBOLISM IS ASSOCIATED WITH AN IMPAIRED LONG-TERM QUALITY OF LIFE IN THE ELDERLYMarie Méan1; Andreas Limacher2; Drahomir Aujesky1. 1Bern University Hospital, Bern, Switzerland; 2University of Bern, Bern, Switzerland. (Tracking ID #1928105)
BACKGROUND: In patients with acute venous thromboembolism (VTE), long-term health-related quality of life (QOL) is substantially influenced by the development of chronic complications, such as the post-thrombotic syndrome. However, whether acute complications, such as recurrent VTE or major bleeding, impair long-term QOL after an index VTE is uncertain.
METHODS: In a prospective multicenter Swiss cohort study, we enrolled consecutive patients aged ≥65 years with an acute VTE between 09/2009 and 08/2011. Generic QOL was assessed at baseline and at 3, 12, and 24 months using the Physical Component Score and the Mental Component Score of the SF-36 questionnaire. Disease-specific QOL was assessed using the VEINES-QoL/Sym questionnaire in patients with deep vein thrombosis and the PEmb-QoL questionnaire in patients with pulmonary embolism. We examined the effect of VTE recurrence and major bleeding on change in QOL over a 24-month follow-up period using repeated measures linear regression analyses based on multiply imputed data, adjusting for age, gender, baseline QOL, time of QOL assessment, education, living status, smoking status, physical activity, risk of falls, body mass index, overt pulmonary embolism, provoked VTE, recent immobilization, recent major surgery, prior varicose vein surgery, cancer, cardiovascular comorbidities, hemi/paraplegia, chronic lung disease, chronic renal disease, diabetes mellitus, polypharmacy (>4 drugs), and the occurrence of the postthrombotic syndrome during follow-up.
RESULTS: Of 745 patients with acute VTE (median age 75 years), 68 (9 %) experienced recurrent VTE and 82 (11 %) a major bleeding within 24 months. Twelve patients (2 %) had an intracranial bleeding. On average, generic and disease-specific QOL scores improved during follow-up (Figure). Patients who developed a VTE recurrence or a major bleeding had lower QOL scores and less improvement in QOL. Adjusted repeated measures analyses showed that patients with recurrent VTE had significantly less increase in disease-specific QOL during follow-up (Table), whereas patients with major bleeding experienced less increase in generic mental QOL.
CONCLUSIONS: Elderly patients with acute VTE who experience recurrent VTE have significantly less improvement in disease-specific QOL, whereas patients who develop major bleeding have significantly less improvement in mental QOL. Acute complications, such as recurrent VTE or major bleeding, impair long-term QOL after an index VTE.
Type of complication and quality of life within 24 months
| Type of complication | QOL measure | Adjusted difference in the average change of score points | P-value |
|---|---|---|---|
| (95 % confidence interval) | |||
| VTE recurrence | SF-36 Physical Score Component | −1.67 (−3.43 to 0.1) | 0.06 |
| SF-36 Mental Score Component | 1.31 (−1.05 to 3.68) | 0.27 | |
| VEINES-QoL/Sym | −2.82 (−5.26 to 0.38) | 0.02 | |
| PEmb-QoL | −5.04 (−9.43 to −0.65) | 0.03 | |
| Major bleeding | SF-36 Physical Score Component | −1.36 (−3.56 to 0.84) | 0.22 |
| SF-36 Mental Score Component | −3.45 (−6.20 to 0.70) | 0.02 | |
| VEINES-QoL/Sym | −1.80 (−5.54 to 1.95) | 0.33 | |
| PEmb-QoL | 0.22 (−4.29 to 4.73) | 0.92 |
REFINED APPROPRIATENESS CRITERIA FOR URINARY CATHETERS IN HOSPITALIZED PATIENTSJennifer Meddings1; Sanjay Saint1,2; Karen E. Fowler2; Elissa Gaies2; Sarah L. Krein1,2; Steven J. Bernstein1,2. 1University of Michigan, Ann Arbor, MI; 2VA Ann Arbor Healthcare System, Ann Arbor, MI. (Tracking ID #1933401)
BACKGROUND: Interventions to reduce inappropriate urinary catheter use are implemented using lists of appropriate and inappropriate criteria (e.g., CDC’s 2009 catheter-associated urinary tract infection guideline), informed by limited evidence without substantial multidisciplinary input. Implementation is challenging due to broad interpretations of indications (e.g., “critical illness”) and common catheter uses not addressed in lists (e.g., patient request). The objective of our project was to refine criteria for “appropriate” use (i.e., benefits outweigh risks) of Foley catheters, intermittent straight catheters (ISC), and external “condom” catheters in hospitalized adults on medical services.
METHODS: Using the RAND/UCLA Appropriateness Method, the literature was systematically reviewed to summarize risks, benefits, and potential catheter indications. A 15 member multi-disciplinary panel of physicians, nurses, and infection preventionists assessed 299 catheter indications (e.g., urinary retention, urine collection to diagnose/monitor, etc.) on a scale of 1 (highly inappropriate) to 9 (highly appropriate). Scenarios accounted for incontinence, illness severity, difficulty turning, and catheter placement issues. Catheter use was assessed by median scores, as inappropriate (1–3), appropriate (7–9) or uncertain (4–6 or having 5 appropriate and inappropriate ratings, regardless of median [termed “disagreement”]).
RESULTS: Overall, 253 (85 %) ratings were scored as appropriate (88) or inappropriate (165); 46 (15 %) were uncertain. Catheter appropriateness of each catheter type was summarized in algorithms for clinical use as illustrated in the Figure.
CONCLUSIONS: Refined appropriateness criteria will inform small and large-scale efforts focusing on avoiding placement and prompting removal of unnecessary catheters. The algorithms further refine indications and non-indications for Foleys, in addition to appropriateness for ISCs and condom catheters as alternatives in each clinical scenario.
REGIONAL CORRELATION IN BRAND-NAME PRESCRIPTION DRUG USE AMONG VA AND MEDICARE PART D PATIENTS WITH DIABETESTimothy Anderson1; Julie M. Donohue2; Nancy E. Morden3; Xinhua Zhao4; Maria Mor4; Carolyn Thorpe4,5; Chester Good4,6; Michael J. Fine4,6; Walid F. Gellad4,6. 1UPMC, Pittsburgh, PA; 2University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA; 3Geisel School of Medicine at Dartmouth, Dartmouth, NH; 4VA Pittsburgh Healthcare System, Pittsburgh, PA; 5University of Pittsburgh School of Pharmacy, Pittsburgh, PA; 6University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1938573)
BACKGROUND: Older adults with diabetes covered by Medicare Part D are substantially more likely to receive brand-name drugs than those who receive care within the VA Healthcare System. There is substantial geographic variation in brand-name use in both systems. However, no prior studies have examined whether regions with high brand-name use in Medicare are also high in the VA. Our aim was to identify whether such regional correlation exists, which might suggest that local practice patterns affect prescribing independent of insurance benefit structures.
METHODS: Using a retrospective cohort study design, we assessed prescription use across 306 U.S. hospital referral regions (HRRs) for 1,061,095 Medicare Part D beneficiaries and 510,485 Veterans receiving care in the VA who were >65 and had a diagnosis of diabetes in 2008. We examined the percentage of patients who filled brand name drugs for oral hypoglycemics, statins, and angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs) and the percentage of patients taking long-acting insulin who filled analogue prescriptions, in order to examine medications with and without restricted access on the VA formulary (the brand name oral medications and analogue insulins, respectively). We calculated correlations between Medicare and VA brand name use within HRRs for each drug class. Second, we examined potential sources of regional correlation between VA and Medicare, including state laws requiring mandatory generic substitution and requiring patient consent for substitution, physician and specialist availability and presence of a medical school or VA Medical Center within the HRR, by comparing these variables between regions in the highest quintile of brand use in both Medicare and VA and regions in the lowest quintile in both systems. We adjusted all brand-name use for individual-level socioeconomic and health-status differences across HRRs using logistic regression models.
RESULTS: The correlation in brand-name use between Medicare Part D and VA at the HRR-level varied by drug class, with the strongest correlation in use of long-acting insulin analogues (r = 0.31, p < 0.001), modest correlation of 0.20 (p < 0.001) for oral hypoglycemics and 0.18 (p < 0.001) for statins, and no significant association for ACE/ARBs (r = 0.03, p = 0.63). Within the subset of 77 HRRs containing both a medical school and VA Medical Center, the correlation between systems was higher for statins (r = 0.27, p < 0.001) but similar in the other three drug classes. Of HRRs in the highest quintile of brand statin use in Medicare, 38 % were also in the highest quintile in VA (‘high-high’ regions). ‘High-high’ regions for brand statin use had on average more cardiologists (8.2 vs 4.9), more endocrinologists (1.8 vs 0.9) and fewer family physicians (21.2 vs. 33.4) per 100,000 residents than ‘low-low regions.’ Generic substitution laws did not differ between high-high and low-low regions.
CONCLUSIONS: We found modest regional correlations in brand name use of oral hypoglycemics, statins and insulin analogues but not ACE/ARBs between the VA and Medicare. Patterns of prescribing were more similar between VA and Medicare for medications with fewer VA formulary access restrictions. These results suggest that a regional ‘culture’ impacts prescribing, beyond the health status of individuals and the health system in which they are treated.
RELATIONSHIP BETWEEN DEPRESSIVE SYMPTOMS, ANTIDEPRESSANT USE, AND PATIENT ATTITUDES AND BEHAVIORS AMONG LOW-INCOME PATIENTS WITH TYPE 2 DIABETESCaroline Presley; Ken Wallston; David Schlundt; Chandra Y. Osborn; Sunil Kripalani; Shari D. Barto; Russell L. Rothman. Vanderbilt University Medical Center, Nashville, TN. (Tracking ID #1934768)
BACKGROUND: This study aimed to evaluate the impact of depressive symptoms and antidepressant use on patients’ attitudes and self-care behaviors in a low-income, racially and ethnically diverse sample of patients with Type 2 Diabetes (T2DM).
METHODS: 406 patients with T2DM were enrolled in a randomized trial evaluating a health literacy intervention for diabetes care at 10 Tennessee Department of Health safety net clinics. At enrollment, data on patient characteristics and clinical information were collected via self-report and from medical records. Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale (CES-D 20, range 0–60), with a score of ≥16 indicating possible depression. Patients were considered to be on an antidepressant if their medication list included an SSRI, SNRI, TCA, or atypical antidepressant. Patient self-care behaviors and attitudes were assessed with these validated scales: Perceived Diabetes Self-Management Scale (PDSMS, range 8–40); Diabetes Treatment Satisfaction Questionnaire (DTSQ, range 0–36), Summary of Diabetes Self-Care Activities (SDSCA) and Personal Diabetes Questionnaire (PDQ); and Adherence to Refills and Medications Scale (ARMS, range 12–48, higher scores signify non-adherence). We performed one-way ANOVA tests between patient-reported attitudes and behaviors and the presence of possible depression and/or antidepressant use. We then performed adjusted regression analyses examining the relationship between each behavioral outcome and depression, antidepressant use, study status, age, gender, ethnicity, education level, duration of diabetes and interaction between depression and antidepressant use.
RESULTS: The sample was on average 51 years old (SD 9.6), 61 % were female, 18 % were African American, and 24 % were Latino. Mean education was 11.1 years (SD 3.4). Most reported no health insurance (88 %) and annual household incomes <$20,000 (83 %). Mean A1C was 9.2 (SD 2.1). The majority (53 %) had CES-D scores >16. Only 18 % were prescribed an antidepressant. The relationships between possible depression, antidepressant use, and patients’ attitudes and behaviors are seen in the Table. Patients on an antidepressant without possible depression had the highest reported self-efficacy. In adjusted analyses, patients with possible depression had less medication adherence, lower self-efficacy, and decreased treatment satisfaction. No significant differences were seen in diet and exercise adherence, blood glucose monitoring, foot care, or glycemic control (A1C). There was no significant interaction between depression status and antidepressant use in any of the models.
CONCLUSIONS: The presence of possible depression negatively impacts self-efficacy, treatment satisfaction, and medication adherence. In this study, antidepressant use was only present in 18 % of the population despite a high rate of depressive symptoms, and use was not significantly associated with most outcomes. Treatment of depression may be important in improving diabetes related self-care behaviors; however additional research is needed on the optimal use of antidepressants to improve outcomes.
| Depressive Symptoms | Absent (CES-D <16) | Present (CES-D ≧16) | ||||
|---|---|---|---|---|---|---|
| Antidepressant Use | No (n = 173) | Yes (n = 22) | No (n = 160) | Yes (n = 51) | P value | Adjusted P value |
| Treatment Satisfaction, DTSQ Score | 29.73 (5.42) | 26.77 (6.85) | 27.35 (6.75) | 25.88 (8.10) | 0.0002 | 0.0023 |
| Medication Adherence, ARMS Score | 16.72 (3.15) | 17.95 (3.48) | 18.07 (4.08) | 18.90 (4.09) | 0.0003 | 0.004 |
| Self-Efficacy, PDSMS Score | 25.82 (5.58) | 27.13 (6.17) | 23.44 (5.51) | 23.23 (6.05) | 0.0001 | 0.0002 |
| Exercise Score | 3.04 (2.31) | 2.06 (2.21) | 2.44 (2.16) | 2.38 (2.13 | 0.0311 | 0.0977 |
| Diet Score | 6.62 (3.44) | 7.64 (3.40) | 7.06 (3.28) | 8.05 (3.16) | 0.0448 | 0.1804 |
RELATIONSHIP BETWEEN LOCAL AREA UNEMPLOYMENT AND PREVENTABLE HOSPITALIZATIONSEdwin Wong1; Paul Hebert1; Susan Hernandez2; Adam Batten1; Philip W. Sylling1; Stephan D. Fihn3; Chuan-Fen Liu1. 1Dept of Veterans Affairs, Seattle, WA; 2University of Washington, Seattle, WA; 3Dept of Veterans Affairs, Seattle, WA. (Tracking ID #1938277)
BACKGROUND: Comprised of over 900 facilities nationwide, the Veterans Health Administration Affairs (VHA) provided care to over 5 million veterans in fiscal year (FY) 2012. Veterans with service connected disabilities or financial means below national thresholds receive higher priority. Prior studies have found greater utilization of VA outpatient health services among veterans residing in areas with higher local unemployment. We sought to determine whether local area unemployment among veterans enrolled in VA was associated with hospitalization for ambulatory care sensitive conditions (ACSCs), defined as 14 medical conditions for which outcomes are thought to be modifiable with optimal outpatient care. We also examined whether the relationship between local unemployment and ACSC hospitalization differed by race/ethnicity.
METHODS: Using VA administrative data from FY2010 and FY2011, we identified a random sample of 437,630 veterans using VA primary care services and responded to the national VA Survey of Healthcare Experiences of Patients (SHEP). Using VA and Medicare inpatient encounter records, we constructed a binary measure indicating whether veterans were hospitalized for any ACSC in a VA or FFS Medicare facility during the 12 months prior to completion of the SHEP. Local area unemployment rates were defined as the 12-month average in clinic’ VA planning sector, the smallest unit of geography used by VA. We used Chamberlain’s random effects probit model, to address unobserved sector-level heterogeneity, while controlling for patient demographics, behavioral characteristics and health status. We stratified analyses by age group (under 65 and 65+) to account for potential differences due to Medicare eligibility.
RESULTS: In the under age 65 group, 1.2 %, 1.9 % and 1.5 % of white, black and other race veterans were hospitalized for ACSCs, respectively. Among the age 65+ group, 4.5 %, 5.3 % and 4.5 % of white, black and other race veterans were hospitalized for ACSCs, respectively. In adjusted analyses, local area unemployment rates were not associated with ACSC hospitalization among under age 65 veterans. For age 65+ veterans, a one percentage point increase in the local area unemployment rate was associated with a 9.8 % (p = 0.022), 11.8 % (p = 0.003) and 10.3 % (p = 0.025) increase in the probability of ACSC hospitalization.
CONCLUSIONS: Higher local area unemployment rates were associated with a higher likelihood of ACSC hospitalization among age 65+ veterans of all races. Our findings suggest that assessment of hospital quality should also consider the context of the local economy.
RELATIONSHIP BETWEEN OBESITY AND COMORBIDITIES AND WEIGHT LOSS MOTIVATIONStephanie A. Rose1; Sarah Schuetz1; Chrisanthi Masero1; Dominique Zephyr2; Kevin Real3; Kelly H. Webber4. 1University of Kentucky, Lexington, KY; 2University of Kentucky, Lexington, KY; 3University of Kentucky, Lexington, KY; 4University of Kentucky, Lexington, KY. (Tracking ID #1940277)
BACKGROUND: Physicians perceive obese patients and those with obesity-related comorbidities as unmotivated and unable to lose weight, and cite these as obstacles to counsel patients regarding weight loss. Greater autonomous (internal), as opposed to controlled (external) motivation (AM vs. CM) is correlated with increased weight loss success. We evaluated the relationship between weight loss motivation and obesity severity and related comorbidities. We hypothesized that higher BMI and greater number of comorbidities (COM) would be associated with higher AM and lower CM to lose weight.
METHODS: Patients and providers in a university-based internal medicine clinic were enrolled in a six-month lifestyle intervention aimed at improving patient outcomes and patient and provider self-efficacy in obesity. Baseline data included the Treatment Self-Regulation Questionnaire to assess motivation, height, weight, and obesity-related comorbidities (HTN, hyperlipidemia, DM, and CV disease). A one-way ANOVA was performed to assess the relationships between BMI and AM/CM and COM and AM/CM.
RESULTS: 65 patients completed the survey (33 obesity class III (BMI ≥ 40 kg/m2), 12 class II (BMI 35–39.9), 20 class I (BMI 30–34.9)). Mean AM was 5.53, (1 (low) to 7 (high)) (Class III = 5.49, II = 5.63, I = 5.52) and mean CM was 2.20 (1 (low) to 7 (high)) (Class III = 2.34, II = 2.17, I = 2.15). AM and CM did not differ significantly across BMI categories (AM: F = 0.06, p = 0.94 and CM: F = 0.21, p = 0.81). Nineteen patients had 0–1, 17 had 2, and 28 had 3 or 4 COM related to obesity. Mean AM for 0–1 COM = 5.39, 2 COM = 6.02, 3–4 COM = 5.34 and mean CM for 0–1 COM = 2.23, 2 COM = 2.34, 3–4 COM = 2.09. Increasing number of COM did not have a significant association with AM or CM (AM: F = 2.00, p = 0.14; CM: F = 0.30, p = 0.74).
CONCLUSIONS: Neither increasing BMI nor increasing number of COM was correlated with increasing AM or decreasing CM. However, we found consistently high AM and consistently low CM among all BMI categories and all numbers of COM. Our findings suggest that all classes of obese patients with differing numbers of COM are consistently motivated to lose weight. Further work is needed to assess the link between increasing BMI and increasing number of COM and associated motivation. Physicians should address weight loss with all patients with all levels of obesity and its related comorbidities.
RELATIONSHIP OF MENTAL ILLNESS AND AMBULATORY CARE SENSITIVE CONDITION (ACSC)-RELATED HOSPITALIZATIONS AMONG VETERANS SEEN IN VA PRIMARY CARERanak Trivedi1,2; Philip W. Sylling2; Edwin Wong2; Chuan-Fen Liu2; Paul Hebert2; Dan Kivlahan2; Edward P. Post2; Andrew Pomerantz2; Stephan D. Fihn3; Karin M. Nelson2. 1Dept of Veterans Affairs, Palo Alto, CA; 2Dept of Veterans Affairs, Seattle, WA; 3Dept. of Veterans Affairs, Seattle, WA. (Tracking ID #1938340)
BACKGROUND: In previous studies, Veterans with a mental health condition had higher hospitalization rates for ambulatory care sensitive conditions (ACSCs) compared to those without a mental health condition. ACSCs are medical conditions thought to be the most sensitive to the receipt of high quality primary care. The Veterans’ Health Administration (VHA) has had an established program for integrated mental health services within Primary Care and implemented a patient centered medical home model, termed Patient Aligned Care Teams (PACT), in April 2010. We assessed ACSCs among cohorts of Veterans with depression and post-traumatic stress disorder (PTSD) before and after PACT to determine the influence of PACT on the rate of ACSC-related hospitalizations.
METHODS: We examined VHA’s corporate data warehouse to identify Veterans who were seen in VHA primary care from 2003-Quarter 4(Q4) to 2012-Q3. ICD9 codes were used to determine a diagnosis of depression or PTSD. To account for temporal trends, facility-cohort level trends for hospitalization were modeled from 2003-Q4 to 2012-Q3. We defined facility-cohort-level ACSC rate as the total number of ACSC-related hospitalizations among Veterans with each diagnosis assigned to a clinic divided by the number of clinic patients with each diagnosis. We compared changes in ACSC hospitalizations after PACT among Veterans with PTSD or depression to Veterans at each clinic without a diagnosis of that mental illness. Changes in ACSC rates were estimated using interrupted time series analyses with the unit of observation set at the facility-cohort-quarter level. Initial and medium-term changes in ACSCs were measured using PACT indicators corresponding to 4/1/2010 (2010-Q2) and 4/1/2011 (2011-Q2). Models were adjusted for seasonality, secular trends in hospitalizations, patient age, sex, health risk, facility size, and facility area economic climate. Regression models were estimated using random effects Poisson models, which allowed intercept and time trend parameters to differ by facility and cohort. We calculated changes in ACSC hospitalizations as the difference between the observed rate of admissions and the predicted rate of admissions that would have occurred had PACT not been implemented. Due to significant utilization of non-VHA care for Veterans ≥65, we estimated separate models for Veterans under and over 65 years of age. Models for PTSD and depression cohorts were performed separately.
RESULTS: 8,068,030 Veterans were included in this study. Veterans with depression had higher ACSC hospitalization rates (5.34 % for <65 y and 16.19 % for ≥65 y) compared with Veterans without a diagnosis of depression (2.68 % for <65 y and 4.48 % for ≥65 y). Likewise, ACSC rates for patients with PTSD (4.59 % for <65 y and 9.95 % for ≥65 y) were higher than for those without PTSD (3.10 % for <65 y and 5.04 % for ≥65 y). After PACT was implemented, Veterans with depression had a significantly lower ACSC-hospitalization rate than projected (with a decrease by 9.74 % and 8.77 % for Veterans <65 y and ≥65 y, respectively). This compared to a 5.77 % reduction among non-depressed cohort <65 y (Fig 1) and a 2.28 % increase among non-depressed Veterans ≥65 y. Veterans <65 y with PTSD had 10.57 % fewer ACSC hospitalizations compared to projected trend (Fig 2), while Veterans with PTSD ≥65 had a 9.55 % reduction.
CONCLUSIONS: Rates of ACSC admission for Veterans with depression or PTSD are high. Since the inception of PACT, Veterans with either depression or PTSD have shown significant decreases in ACSC-related hospitalizations, especially among those <65 y of age.
RESIDENT BINGE DRINKING: PREVALENCE AND IMPLICATIONS FOR PATIENT CAREMagdelena Greene1; Aaron Johnson2; J. Paul Seale2; George A. Tindol3; Kristy B. Le1; David P. Miller1. 1Wake Forest Baptist Health, Winston-Salem, NC; 2Medical Center of Central Georgia, Macon, GA; 3Memorial Health University Physicians, Savannah, GA. (Tracking ID #1936311)
BACKGROUND: According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), approximately one-fourth of American adults engage in binge drinking (consuming more than three or four standard drinks in one day), with highest rates among 18–34 year olds. Given this high prevalence of binge drinking, the United States Preventive Services Task Force recommends that primary care physicians screen all adults for hazardous drinking and perform a brief behavioral counseling intervention when at-risk drinking is identified. Prior studies have found that physicians who are obese or smoke are less likely to counsel patients on these respective topics; however, it is unknown how many resident physicians binge drink or whether personal binge drinking affects the likelihood they will screen and intervene with hazardous drinkers.
METHODS: To determine the prevalence of at-risk drinking and its effect on screening and interventions, we surveyed all internal medicine residents at two academic medical centers in the Southeast. The confidential survey included items about personal alcohol consumption, residents’ current practices with screening and intervening for hazardous drinking, and attitudes and beliefs about addressing substance misuse. We defined at-risk drinking according to the NIAAA definition: consuming more than three standard drinks for women or more than four standard drinks for men.
RESULTS: A total of 103 of 141 residents completed the survey (response rate 73 %). Over half of residents (57/103 or 55 %) reported binge drinking at least once in the prior year. Only 38 % of residents who engaged in binge drinking felt confident they could identify at-risk drinking in their patients, compared to 65 % of residents who did not binge drink (p < 0.01). When residents did identify at-risk drinking in their patients, fewer residents who engaged in binge drinking advised patients to cut down or quit compared to residents who did not binge drink, but the difference was not statistically significant (63 % vs. 74 %, p = 0.25). Regardless of whether residents engaged in binge drinking or not, few residents felt they had been successful helping patients cut down or quit alcohol in the past (14 % vs. 28 %, p = 0.08).
CONCLUSIONS: At-risk drinking is very common among internal medicine residents, most of who are in the age cohort with the highest rates of binge drinking. Residents who binge drink are less confident they can identify hazardous alcohol use in their patients, and those residents may be less likely to advise patients to cut down or quit. Regardless of personal drinking history, most residents lack confidence they can help patients reduce their alcohol use. To help residents identify and successfully intervene with the one-fourth of Americans who are at-risk drinkers, there is a great need for additional training. Such training should also address the high prevalence of at-risk drinking among medical residents.
RESIDENT BURNOUT: IDENTIFICATION AND RAMIFICATIONSKate Jennings1,2; Ravi K. Gopal1,2; Chad Stickrath1,2. 1Veterans Affairs Administration, Denver, CO; 2University of Colorado Denver School of Medicine, Aurora, CO. (Tracking ID #1939602)
BACKGROUND: Burnout is a response to work related stress characterized by depersonalization, emotional exhaustion and a sense of loss of personal efficacy. Burnout affects 30–60 % of all physicians and 67 % of internal medicine residents. Currently, physician burnout is assessed by self-report. No prior study has sought to objectively identify burnout. The objectives of this study were to: 1) generate a list of observable behaviors that may aid in the identification of burned out medicine residents and, 2) identify behaviors of burned out residents that may compromise patient care.
METHODS: Internal medicine clinician educators at the University of Colorado were asked to describe behaviors that burned out residents might demonstrate on rounds. These responses were used to develop items for inclusion in an annual internal medicine resident survey. The survey questions asked residents to identify specific behaviors exhibited by burned out residents during direct patient care and while participating on medicine rounds.
RESULTS: There were 166 residents invited to complete the survey and 108 residents participated (response rate 65.1 %). Among 16 potential behaviors that burned out residents display on rounds, 88.9 % of residents selected at least one behavior (average number of behaviors selected 5.8). Rounding behaviors that subjects felt may signal when a resident is burned out include: leaving the room before completion of team discussion (44.9 %); not knowing the recommendations of consultants (31.5 %); not knowing the recommendations of ancillary staff (34.8 %); and frequently interrupting the presenter (23.6 %) or patient (34.8 %). When evaluating 15 potential behaviors of burned out residents that may impact patient care, 82.4 % of residents identified at least one behavior (average number of behaviors identified 3.8). Burnout behavior that may result in patient harm include, poor hands offs (61.5 %); not “tucking” patients prior to shift change (61.5 %); incomplete physical exams (44.8 %); cursory medication reconciliations (24.0 %); and neglect of daily conferences (75.0 %) and medical student education (70.8 %).
CONCLUSIONS: Burned out residents display behaviors that can be observed while on rounds. In addition, burned out residents may engage in behaviors that can adversely affect patient care. Clinician educators and leaders may be able to utilize these behaviors to identify residents who are burned out and ensure that areas of potential patient harm are monitored by other members of the care team.
RESIDENT PERCEPTIONS OF TEAM BASED CARE IN THEIR CONTINUITY CLINICTacara N. Soones2; Katherine Julian1; Bridget O’Brien1. 1University of California- San Francisco, San Francisco, CA; 2University of California- San Francisco, San Francisco, CA. (Tracking ID #1927140)
BACKGROUND: Interprofessional teams are becoming an integral part of addressing our society’s complex healthcare needs. Yet, the structure and goals of residency can make it difficult for physicians in training to learn to work within ambulatory teams to enhance their current and future practice. Furthermore, little is known about residents’ experiences working in continuity clinic teams and the impact of these teams on their education.
METHODS: Eleven focus groups were conducted with categorical and primary care internal medicine residents at the University of California San Francisco’s three continuity clinic sites: 3 at a veteran’s hospital, 4 at a safety net hospital, and 4 at a university-based clinic. Focus groups were conducted during regularly scheduled conference times and included PGY1, PGY2, and PGY3 residents depending on the clinic site. A total of 78 residents participated and focus groups were conducted until thematic saturation was reached. A general inductive approach was used to analyze themes.
RESULTS: As residents identified factors that aligned with the 4 domains in Reeves’ model of interprofessional collaboration (relational, processual, organizational and contextual), this framework was employed to organize study results. Residents with positive perceptions of team based care, defined as those who expressed feeling like they were part of a team or gave positive examples of interprofessional collaboration, were more likely to cite positive relational factors (stable relationships with their team members and knowledge of team member roles), processual factors (useful huddles), and contextual factors (culture of shared responsibility). Residents with negative perceptions, defined as those who did not feel like they were members of a team, were more likely to cite negative relational factors (high team member turnover and lack of role clarity), processual factors (poor communication through the electronic health record and insufficient clinic time over the course of residency), organizational factors (limited staffing resources) and contextual factors (a culture of the resident being responsible for all patient care). Residents with positive perceptions were more likely to be third year residents or have clinic at the Veteran’s Affairs clinic site. Residents believed the interprofessional model provided more patient support and allowed team members to operate at their highest level of training, but rarely believed working in teams was intrinsically of high educational value.
CONCLUSIONS: Residents’ perceptions of the utility of their interprofessional teams were most affected by their integration into a stable team structure within the continuity clinic site and the opportunity to leverage professional relationships to coordinate patient care. While resident continuity clinics have innate scheduling challenges, high functioning teams can emerge when resources are invested in relational and processual elements of team development.
RESIDENT PRIORITIES IN AMBULATORY TRAINING: NEED FOR IMPROVED EDUCATION AND TRANSITION TO PATIENT-CENTERED MEDICAL HOMETheodore Long1; Ian Halim2; Krisda H. Chaiyachati1; Bradley G. Richards1; Peter Moyer1; John P. Moriarty1. 1Yale University School of Medicine, New Haven, CT; 2Harvard Extension School, Boston, MA. (Tracking ID #1923616)
BACKGROUND: As patients now receive the majority of their chronic disease and preventive care in the ambulatory setting, medical education in ambulatory settings has evolved to begin to address these demands. However, graduating internal medicine residents continue to feel uncomfortable managing common chronic conditions. Studies have shown that inadequate infrastructure and a lack of a team-based system are often prevalent in ambulatory resident training, but there is a paucity of data regarding the perspectives of residents on their priorities for ambulatory education. Especially as the patient-centered medical home is being viewed as a potential intervention to improve the infrastructure and teamwork environment in ambulatory training, elucidating and understanding the priorities of internal medicine residents relating to ambulatory training will help align their priorities and the health system’s goals.
METHODS: We sent an anonymous online survey to all Traditional Internal Medicine, Primary Care Internal Medicine, Combined Internal Medicine and Pediatric, and Pediatric residents at Yale-New Haven Hospital. A survey instrument with open-ended questions was developed from pilot interviews and existing literature targeted at examining educational priorities and structural components of ambulatory training. Two members of our interdisciplinary research team independently applied codes to the responses. We developed our code structure based on grounded theory, applying a systematic and inductive approach to generate insights from the responses of the residents. The research team then met to resolve disagreement and reach consensus on the final coding structure. The final codes were arranged into five main themes.
RESULTS: We received 43 completed surveys (22 % response rate). The responses were grouped into five main themes: inadequate resources, balance of inpatient versus outpatient training, need for improved role clarity and team-based care, issues with patient continuity and scheduling, and a desire for increased didactics with an outpatient emphasis. Specifically focusing on priorities in medical education, residents described wanting further didactic teaching during ambulatory blocks, as well as feeling challenged to meet both inpatient and continuity clinic responsibilities while on inpatient blocks. With respect to the structural aspects of ambulatory training, residents noted several areas needing improvement that are consistent with moving toward a patient-centered medical home: need for role clarity, improved continuity, and a need for establishing team-based care.
CONCLUSIONS: Internal Medicine and Pediatric residents want dedicated outpatient didactics and training that are more evenly balanced and prioritized with respect to inpatient responsibilities. They also identify several components of the patient-centered medical home (improved continuity, role clarity, team-based care) as important structural changes when redesigning ambulatory training.
RESIDENT USE OF A READMISSIONS PREDICTION MODEL DECREASES TIME TO FOLLOW-UP AND IMPACTS TRUE READMISSION RATESRyan D. Schulteis1,2; Thomas W. LeBlanc2; Eugene Z. Oddone2; David Simel1,2. 1Durham VA Medical Center, Durham, NC; 2Duke University Medical Center, Durham, NC. (Tracking ID #1924494)
BACKGROUND: Validated readmission prediction tools could allow targeted interventions towards patients at the highest risk of rehospitalization. We evaluated the validity of a previously derived readmission prediction tool and examined the relationship between a patient’s predicted readmission rate and time to the first scheduled follow-up visit. Most physicians believe that early follow-up prevents readmissions, so we also quantified the impact of the timing of scheduled post-hospitalization clinic visits on a patient’s probability of readmission within 30 days of hospital discharge.
METHODS: At hospital discharge, resident physicians used a calculator to prospectively estimate and record the predicted readmission rate (within 30 days of discharge). In addition to the predicted readmission rates, actual 30-day readmission rates and the time from discharge to the first scheduled follow-up visit were obtained from the electronic medical record.
RESULTS: Over 2 years, discharge summaries from 4568 distinct discharged patients were retrieved. The mean patient age was 66 years, 95 % were male Veterans, and 20 % of patients were readmitted within 30 days. The readmission prediction tool c-statistic, a measure of discriminatory power, was 0.60 (p < 0.001). The predicted readmission rate was significantly correlated with the median time to scheduled follow-up; for every 9.6 % increase in the predicted probability of readmission, patients were scheduled for follow-up 1 day sooner (p < 0.001, Figure 1). In all possible pairs of patients matched for the same predicted probability of readmission (n = 546426 pairs), the patient scheduled for an early follow-up visit was 37 % more likely to be readmitted (p < 0.001) than the patient scheduled for later follow-up (Figure 2).
CONCLUSIONS: Patients with higher predicted rates of readmission were scheduled for earlier follow-up visits. Being scheduled for earlier rather than later follow-up was not associated with a lower risk of readmission. Instead, patients scheduled for early follow-up have a substantially higher risk of readmission that may account for over 1/3 of readmissions.
Figure 1: Time to follow-up decreases as the probability of readmission increases. The probability of readmission is inversely correlated with the scheduled time to follow-up. Error bars represent the interquartile range for that group.
Figure 2: Readmission rates are increased in patients scheduled for early follow-up Within groups of patients with similar predicted readmission rates, we evaluated all possible pairs of patients. Within each pair, the patient scheduled for an earlier follow-up appointment was designated “early” and the other designated “late”. In every group, the patient seen earlier was more likely to be readmitted than the patient seen later. The readmission rate in those seen early was 37 % higher than those seen later (relative risk 1.37, 95 % CI 1.35 to 1.39).
RESIDENTIAL CARE FACILITIES’ ABILITY TO COMMUNICATE WITH HOSPITALSRobert Burke1,2; Christine D. Jones2; Cari Levy4; Adit Ginde3. 1Denver VA Medical Center, Denver, CO; 2University of Colorado, Denver, CO; 3University of Colorado, Denver, CO; 4University of Colorado, Denver, CO. (Tracking ID #1940104)
BACKGROUND: Older adults in residential care facilities (RCFs) are vulnerable to a cycle of hospitalization and institutionalization leading to substantial decrements in their health and functional ability. Prior research indicates a major barrier hospitals and care facilities experience in providing adequate care to these patients is incomplete transfer of information between the two sites. Improved information exchange between facilities and hospitals may decrease errors and potentially improve patient outcomes. We sought to understand the ability of RCFs to generate computerized discharge or transfer summaries, and to electronically exchange information with hospitals.
METHODS: Data were drawn from the 2010 National Survey of Residential Care Facilities (NSRCF), a nationally-representative probability sample survey of United States RCFs conducted by the Center for Disease Control’s National Center for Health Statistics (n = 2302). Eligible facilities had to be licensed, registered, or otherwise regulated by the state, have four or more licensed beds with at least one resident living in their facility at the time of the survey, and at a minimum provide 24 h a day supervision and personal care to the residents, in addition to two meals per day. Facilities that serve mentally ill or developmentally disabled populations were excluded. We compared facilities with and without these capabilities (as reported by the facility director) using Chi-Square tests and multiple logistic regression.
RESULTS: 21.4 % of facilities (n = 493) could produce computerized discharge and transfer summaries; 5.5 % (n = 127) were able to exchange information electronically with hospitals. Bivariate and multivariate analysis resulted in similar findings: larger (OR 1.71, 95 % CI 1.12–2.61 versus 10 beds or less), more expensive (1.63, 1.15–2.31 versus lowest cost), non-profit and government facilities (OR 1.63, 1.17–2.25 versus for-profit), and facilities with skilled nursing services (1.52, 1.15–2.04 versus those without) were significantly more likely to be able to generate computerized discharge and transfer summaries; RCFs with longer waitlists (2.31, 1.29–4.15 versus shorter waitlists) and skilled nursing services (1.92, 1.18–3.13) were more likely to have electronic information exchange capabilities.
CONCLUSIONS: Few RCFs have advanced capabilities for information exchange with hospitals. These findings have substantial patient safety implications given more than one-third of RCF residents visited the ED in the year prior to the survey, and nearly a quarter were hospitalized. Enhancing and standardizing information transfer capabilities may lead to better outcomes for this high-risk population of residents, but substantial financial, legal, and technological barriers to implementation exist.
RESIDENTS’ PERSPECTIVES ON THE VALUE OF IPADS AND POINT-OF-CARE RESOURCES IN THE DELIVERY OF QUALITY CARE AND EVIDENCE-BASED MEDICINE AT THE BEDSIDEAlfredo Sardinas; Kathleen V. Carter; Alexander Bullen Clarke; James F. Hanley. UTHSCSA, Harlingen, TX. (Tracking ID #1941613)
BACKGROUND: There has been an evolutionary change in the delivery of care with the advent of mobile devices. Tablets and smartphones have brought both the medical record and point-of-care (POC) information resources to the patient (bedside or clinic). The utility of this change requires an assessment of both the platform and the resources. It was reported in one small study that only 45 % of medicine-based residents surveyed agreed that iPads facilitated better patient care. There is very little information on the utility of mobile POC information resources, specifically on preference. Although, it is presumed that POC resources will bring the best evidence for making clinical decisions at the bedside there are other factors such as ease of use, accuracy, quantity, current information and timely results that are important when selecting a clinical decision support tool. These factors contribute to a physician’s overall satisfaction with the product. As part of our resident-led evidenced-based curriculum, we questioned our resident perspective on the value of iPads for patient care. We also examined their selection of POC information resources and if that determination was dependent upon the type of clinical question being answered. Finally, during this study the ACP released Smart Medicine, a POC tool. This had face validity, linked easily to the evidence, and was free to its members. We compared Smart Medicine to other information resources to answer clinical questions that were raised during check-in rounds or morning report.
METHODS: iPads were issued to all residents, with access to EMRs and POC resources. At 6 months, residents were surveyed on both the clinical and educational utility of their iPads and their usage of POC resources to answer clinical questions. Subsequently, residents were asked to answer eight clinical questions comparing Smart Medicine to other POC resources. Residents then chose the resource which performed best in the following categories: accuracy, quantity, current information, timeliness, ease-of-use and overall satisfaction.
RESULTS: Residents reported that the iPad was used frequently on rounds (94 %). All residents reported that using the iPad increased efficiency (100 %) and 87 % agreed it facilitated better patient care. UpToDate was the preferred POC resource, but others were often used for specific types of clinical questions. UpToDate was the preferred comparator to Smart Medicine (88.7 %). For accuracy of information, Smart Medicine 19.3 % vs. other resources at 53.2 %; quantity of information, Smart Medicine 12.9 % vs. other resources 64.5 %; current information, Smart Medicine 22.5 % vs. other resources 51.6 %; speed of resource, Smart Medicine 17.7 % vs. other resources 64.5 %; usability, Smart Medicine 21.0 % vs. other resources 59.7 %; and overall satisfaction, Smart Medicine 22.5 % vs. other resources at 51.6 %.
CONCLUSIONS: Our residents felt that their iPads improved clinical efficiency. The iPads facilitated accessing the EMR and answering clinical questions. This was aided by a favorable IT environment that was compatible with EMR and POC apps. There was a strong preference for UpToDate, but other POC resources were selected. Smart Medicine, despite its appealing characteristics, was not well received when compared to other resources. Feedback indicated that this was due to several factors including familiarity with certain resources (cognitive inertia), technical problems (usability issues), and the need for a search engine leading to a broader database of clinical information. Mobile devices and POC resources are interdependent and together show great promise as both educational and clinical tools. Challenges will arise with integration and teaching their use to facilitate clinical practices. The assessment of POC resources will require a more disciplined approach to understanding their value and limitations. High quality clinical care requires that best practices for implementation be developed for successful integration of mobile technology.
RESULTS OF POPULATION-BASED, PROACTIVE OUTREACH TO NON-TREATMENT SEEKING PRIMARY CARE PATIENTS AT HIGH RISK FOR AUD IN THE CHOICE TRIALKatharine Bradley1; Gwen T. Lapham1; Julie E. Richards1; Joseph Merrill4; Emily Williams2; Amy K. Lee1; Erika Holden1; Laura Chavez3; Daniel Kivlahan5. 1Group Health Research Institute, Seattle, WA; 2VA Puget Sound HSR&D COIN, Seattle, WA; 3Department of Health Services University of Washington, Seattle, WA; 4Department of Medicine, University of Washington, Seattle, WA; 5Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA. (Tracking ID #1938738)
BACKGROUND: Clinicians often fail to recognize alcohol use disorders (AUDs), and most patients with AUDs never receive treatment. Population-based, proactive outreach and chronic care management may be a way to engage primary care (PC) patients at high risk for AUD in alcohol-related care. However, little is known about the needs of patients with alcohol misuse who might be recruited by such an approach. We describe results of proactive outreach to PC patients at high risk for AUD for the CHOICE trial—a randomized controlled “encouragement” trial that offers intervention patients alcohol-related collaborative care from a chronic care nurse. Specifically, we report the proportion of potentially eligible patients enrolled over the first 2 years, how they compare to potentially eligible patients who were not enrolled, and describe the AUD severity and readiness to change of enrolled patients.
METHODS: The study sample was recruited from 3 VA PC clinics. Patients were potentially eligible if they screened positive for alcohol misuse (AUDIT-C ≥3 women, ≥4 men) and they were 21–75 years old. Patients were eligible if they: 1) reported frequent heavy episodic drinking at phone screening (≥4 and ≥5 drinks for women and men respectively, ≥ 2× weekly on average); 2) were not in AUD treatment in the prior 90 days, 3) were medically and psychiatrically stable based on chart review (e.g. no acute psychosis) and 4) planned to continue receiving PC from the VA. Baseline interviews assessed: the prevalence and severity of DSM-5 AUD; the number of common mental health (MH) conditions (0–5 based on validated measures for depression, generalized anxiety, panic, PTSD, or drug use disorders); and patient-reported importance, readiness, and confidence in changing their drinking (based on readiness rulers).
RESULTS: Of 2,702 potentially eligible patients, 375 (14 %) patients were eligible at phone screening and agreed to attend baseline enrollment interviews. Of those, 219 (58 %) consented and enrolled in the trial (29 % declined participation; 12 % were ineligible e.g. had decreased drinking, planned to move, etc.). Compared to the potentially eligible patients who did not enroll, those who enrolled were more likely to be men (90 % vs. 85 %; p = 0.05) and had higher AUDIT-C scores (7.2 vs. 6.5 points, p < 0.0001). The first 210 enrolled patients whose baseline interview data were available for analysis at this time represented a range of severity and complexity: 88 % met criteria for DSM-5 AUD (31 %, 27 %, and 30 %, with mild, moderate, and severe, respectively); and 64 % had one or more MH conditions (24 %, 13 %, and 27 % had 1, 2, and 3 or more of the 5 conditions assessed, respectively). About three quarters (73 %) of enrolled patients noted that changing their drinking was somewhat to very important, 72 % reported they were somewhat to very ready to change, and 80 % were somewhat to very confident that they could change their drinking.
CONCLUSIONS: Proactive outreach using population-based alcohol screening engages patients with a range of alcohol misuse severity, MH complexity and readiness to change alcohol use. Programs that engage patients in this way will need to be prepared to offer care that addresses a range of AUD severity, psychiatric comorbidity and readiness to change their drinking.
REVISITING DISPARITIES IN QUALITY OF CARE AMONG U.S. ADULTS WITH DIABETES IN THE ERA OF INDIVIDUALIZED TARGETS, NHANES 2005–2010Neda Laiteerapong; Paige Fairchild; Chia-Hung Chou; Marshall Chin; Elbert S. Huang. University of Chicago, Chicago, IL. (Tracking ID #1940849)
BACKGROUND: Health disparities in diabetes care have been traditionally characterized using universal goals for glycemic, blood pressure, and cholesterol control. In 2008, evidence from major diabetes trials found that intensive glycemic control may cause worse outcomes among older patients with cardiovascular disease and high comorbidity. Since the publication of these trials, diabetes guidelines have made specific recommendations for individualized glycemic goals based on age, duration of disease, and complications. These individualized goals may have important implications for assessments of disparities in diabetes quality of care because minorities differ from non-Hispanic whites on a number of variables that are the basis for individualization. We reassess disparities in diabetes care using new individualized care goals in order to determine 1) the degree to which diabetes recommendations differ by race/ethnicity and 2) if diabetes disparities are altered with new care goals.
METHODS: We analyzed a nationally-representative sample of non-Hispanic whites (W), non-Hispanic blacks (B), and Mexican American/Hispanic (MA) adults with self-reported diabetes aged ≥20 years in the National Health and Nutrition Examination Survey (NHANES), 2005–2010 (N = 1840; weighted N = 16.5 million). Individualized glycemic goals (A1C <6.5 %, <7 %, or <8 %) were specified based on age (20–44, 45–64, 65–75, or >75 years), duration (<= 10 vs. >10 years), self-reported complications, and comorbidity, defined using the weighted combined Charlson Comorbidity Index. Individualized cholesterol goals (LDL <100 or <70 mg/dL) were identified based on cardiovascular history. We assigned participants individualized glycemic goals and compared the proportions assigned to each individualized glycemic goal by race/ethnicity. Then we compared the proportions who had met their individualized glycemic, cholesterol, and comprehensive care goals (glycemic, cholesterol, blood pressure (<140/80 mmHg), and non-smoking) by race/ethnicity.
RESULTS: Blacks and Mexican Americans were younger than Whites (B: 58, MA: 55, W: 61 years, p < .001). Mexican Americans had fewer complications than blacks and whites (MA: 33 %, B: 47 %, W: 45 %; p = .01). The population-wide distribution of individualized glycemic goals differed for Mexican Americans (p < .001), but not blacks (p = .55), compared to whites. Nearly one in five (17 %) Mexican Americans should be recommended an A1C < 6.5 % compared to one in ten (10 %) whites and blacks; 43 % of Mexican Americans should be recommended an A1C < 7 % compared to 31 % of whites and 34 % of blacks. Fewer Mexican Americans (55 %, p < .001) and blacks (60 %, p = .004) had adequate individualized glycemic control compared to whites (70 %). In contrast, using a universal glycemic target of <7 %, Mexican Americans (46 %, p = .01), but not blacks (50 %, p = .12) were less likely to have adequate control, compared to whites (56 %). Blacks were less likely to have comprehensive individualized quality of care compared to whites (4 % vs. 17 %, p < .001), a difference which approached significance for Mexican Americans (10 %, p = .06).
CONCLUSIONS: Compared to universal goals, individualized goals for diabetes care actually accentuate disparities in diabetes care, especially for blacks. Individualized glycemic goals are necessary in evaluating disparities in quality of care, otherwise disparities will be underappreciated and worse diabetes outcomes will persist for blacks and Mexican Americans. Significant disparities exist in individualized glycemic, cholesterol, and comprehensive quality of care.
RISK FACTORS FOR POTENTIALLY AVOIDABLE READMISSION IN CANCER PATIENTSJacques Donze1,2; Stuart R. Lipsitz1,2; Jeffrey L. Schnipper1,2. 1Brigham and Women, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1897611)
BACKGROUND: Cancer patients are particularly at risk for being readmitted within 30 days after discharge. However, many of these readmissions are either related to elective chemotherapy or are not avoidable. In order to identify the cancer patients who might benefit from more intensive discharge interventions, we aim to identify the risk factors associated with 30-day potentially avoidable readmission in cancer patients.
METHODS: We included all consecutive discharges from the oncology division of an academic tertiary medical center in Boston between July 1, 2009 and June 30, 2010. Potentially avoidable 30-day readmissions to the index hospital or two other hospitals within its network were then identified using a validated computerized algorithm based on administrative data (SQLape). We performed a multivariable logistic regression in which the final model included variables that were found to be significantly associated with the outcome in bivariable testing.
RESULTS: Among the 2,916 patient discharges during the study period, 1,086 (37.3 %) were followed by a readmission within 30 days. Of these, 341 (31.4 % of all readmissions, 11.7 % of all discharges) were identified as being potentially avoidable. In a multivariable analysis, the following risk factors were associated with a significantly higher potentially avoidable readmission risk (Table): number of admissions in the previous 12 months, non-elective index admission, and hematological neoplasm.
CONCLUSIONS: Cancer patients have a high risk of readmissions. The main risk factors associated with 30-day potentially avoidable readmission in this population are a higher number of prior admissions, a non-elective index admission, and a hematological neoplasm. Interventions at discharge may be prioritized to the cancer patients with these risk factors.
Multivariate analysis of risk factor for 30-day potentially avoidable readmission in cancer patients *
| Variable | Odds Ratio (95%CI) | P value |
|---|---|---|
| Length of stay, per 1 day increase | 1.01 (1.00–1.02) | 0.06 |
| Elective index admission | 0.45 (0.35–0.58) | <0.001† |
| Number of admissions in the previous 12 months | 1.05 (1.02–1.08) | 0.004† |
| Total number of medications at discharge | 1.00 (0.98–1.02) | 0.86 |
| Opiate medication at discharge | 1.04 (0.86–1.25) | 0.70 |
| Anticoagulation therapy at discharge | 1.14 (0.93–1.41) | 0.20 |
| Elixhauser comorbidity score, per 1 unit increase | 1.00 (1.00–1.01) | 0.37 |
| Congestive heart failure | 1.10 (0.80–1.51) | 0.57 |
| Liver disease | 1.20 (0.79–1.81) | 0.40 |
| Hematological neoplasm | 1.49 (1.13–1.97) | 0.005† |
| Metastatic neoplasm | 1.04 (0.76–1.41) | 0.82 |
| Ovarian neoplasm | 1.49 (0.94–2.37) | 0.09 |
| Hemoglobin, per one unit increase | 1.00 (1.00–1.02) | 0.82 |
| Sodium level, per one unit increase | 1.00 (0.98–1.02) | 0.99 |
*Includes all variables significantly associated with potentially avoidable readmission risk in bivariable testing †Statistically significant (P value < 0.05)
RISK FACTORS FOR RECURRENTCLOSTRIDIUM DIFFICILEINFECTION: A SYSTEMATIC REVIEW AND META-ANALYSISAbhishek Deshpande1; Vinay Pasupuleti2; Priyaleela Thota2; Chaitanya Pant3; David D. Rolston4; Adrian V. Hernandez5,1; Curtis J. Donskey6,2; Thomas Fraser7. 1Cleveland Clinic, Cleveland, OH; 2Case Western Reserve University, Cleveland, OH; 3Kansas University Medical Center, Kansas City, KS; 4Geisinger Medical Center, Danville, PA; 5Universidad Peruana de Ciencias Aplicadas, Lima, Peru; 6Cleveland VA Medical Center, Cleveland, OH; 7Cleveland Clinic, Cleveland, OH. (Tracking ID #1931651)
BACKGROUND: The risk of acquiring Clostridium difficile infection (CDI) during a hospital admission is estimated to be 1 in 100 patients with a 10 % risk of in-hospital death. In the past 2 decades, the prevalence of hospital-acquired CDI has more than doubled in the United States. CDI therapy is initially effective for most patients, but an estimated 20–30 % of patients develop symptomatic recurrence within 2 weeks of successful completion of therapy. While the mechanism of recurrence has not been elucidated, a variety of risk factors have been suggested. Our aim was to evaluate current evidence on the risk factors for recurrent CDI (rCDI).
METHODS: We searched MEDLINE, Web of Science, Cochrane library, and SCOPUS databases for the following search terms: CDI, risk factor, predictor, marker, relapse, recurrence and recurrent. All studies that investigated the risk factors of rCDI using multivariate methods were considered eligible. Information on assessed risk factors was collected and data were combined by means of a random-effects model. Pooled odds ratios (ORs) and 95 % CIs were calculated.
RESULTS: Of the 310 citations identified, 31 studies (n = 16,280 patients) met the inclusion criteria. The most frequent risk factors associated with rCDI were advanced age, antimicrobial therapy and use of proton pump inhibitors (PPI). Age (per year increase) and ≥65 years were associated with an increased risk of rCDI (OR 1.02, 95%CI 1.01–1.02, P < 0.001and OR 1.63, 95%CI 1.22–2.17, P < 0.001 respectively), as was additional non-CDI antibiotic therapy after treatment (OR 2.18, 95%CI 1.63–2.93, P < 0.00001). Risk was also greater for patients who were prescribed fluoroquinolones before the initial occurrence of CDI (OR 1.48, 95%CI 1.19–1.83, P = 0.0004) and patients taking a PPI during CDI treatment (OR 1.80, 95%CI 1.17–2.77, P = 0.007).
CONCLUSIONS: Advanced age, additional antimicrobial therapy during follow up and use of PPI during CDI treatment were associated with a greater risk of developing recurrent CDI. In older patients with a history of CDI, judicious use of antibiotics and PPIs might help reduce CDI recurrence.
RISK FACTORS FOR RECURRENT SPONTANEOUS EPISTAXISVictor Abrich1; Annabelle Brozek2; Timothy R. Boyle3; Steven H. Yale1. 1Marshfield Clinic - St. Joseph’s Hospital, Marshfield, WI; 2Marshfield Clinic - St. Joseph’s Hospital, Marshfield, WI; 3Marshfield Clinic - St. Joseph’s Hospital, Marshfield, WI. (Tracking ID #1939670)
BACKGROUND: Epistaxis is a common medical and surgical otolaryngological condition, accounting for approximately 1 in 200 emergency room visits in the United States. Most episodes of epistaxis are self-limited and few patients seek medical attention. However, a subset of patients will experience frequent recurrent episodes which may be severe enough to warrant medical attention. Although many putative risk factors have been described for a single episode of epistaxis, it is unknown which factors are responsible for recurrent episodes. This study was designed to identify risk factors associated with spontaneous recurrent events.
METHODS: This was a retrospective case-control study assessing patients within the Marshfield Clinic system diagnosed with epistaxis between January 1st 1991 and January 1st 2011. Cases were defined as having at least two episodes of epistaxis requiring medical care separated by a minimum of 3 months within a 36-month period, whereas controls had one episode in the same time period. An episode of epistaxis consisted of a cluster of non-traumatic nosebleeds including the incident event, subsequent care, and follow-up. Controls (n = 916) were 2:1 frequency-matched to cases (n = 458). Episodes were manually adjudicated in the medical record. Data on demographics, social history, treatment, comorbidities, medications, lab values, and adverse outcomes were electronically and manually abstracted for each event. For controls, the second point of data collection was taken from a three-month period corresponding to a case’s second epistaxis episode. Fisher’s Exact Test was used in the statistical analysis to derive p-values. Odds ratios were calculated for each risk factor.
RESULTS: Males were more likely to have recurrent epistaxis compared to females (OR = 1.35, 95 % CI 1.08–1.70, p = 0.0087). A documented history of smoking was found to confer an increased risk of epistaxis recurrence (OR 1.36, 95 % CI 1.07–1.73, p = 0.0119). Warfarin use was higher in cases compared to controls (27 % vs. 19 %, p = 0.0006) without any appreciable difference in the level of anticoagulation when considering INR ranges <2.0, 2.0–3.0, and >3.0. No significant difference was observed between the proportions of cases and controls taking aspirin, clopidogrel, NSAIDS, or antidepressants. Also, no differences were observed between cases and controls for many common co-morbidities including hypertension, diabetes mellitus, coronary artery disease, stroke, and chronic kidney disease; however, cases were more likely than controls to have congestive heart failure (OR = 1.62, 95 % CI 1.25–2.11, p = 0.0004). Most striking was the finding that within 30 days of an epistaxis event, cases had a decreased risk of myocardial infarction (OR = 0.07, 95 % CI 0.03–0.12, p < 0.0001) and stroke (OR = 0.11, 95 % CI 0.06–0.21, p < 0.0001).
CONCLUSIONS: Risk factors for recurrent epistaxis found in this study include male gender, smoking history, warfarin use, and a history of congestive heart failure. Patients with recurrent epistaxis appear to be protected from myocardial infarction and stroke, which may be due to the continued use of antiplatelet medications in the setting of nosebleeds. The opposite may be true for patients who choose to stop such medications temporarily after developing epistaxis. These results demonstrate the importance of promoting medication compliance despite the occurrence of recurrent epistaxis to prevent major adverse cardiovascular events.
RISK PERCEPTION, SELF-EFFICACY, AND OBJECTIVE HEALTH RISKStephanie A. Rose1; Brett Capel1; Bharat Kumar1; Nicholas Jackson1; Brittany P. Fenner1; Chrisanthi Masero1; Dominique Zephyr2; David Rudy1; Kevin Real3. 1University of Kentucky, Lexington, KY; 2University of Kentucky, Lexington, KY; 3University of Kentucky, Lexington, KY. (Tracking ID #1940365)
BACKGROUND: Risk perception and self-efficacy can predict success in health related changes. However, patients may not appropriately perceive their objective risk of disease. We aimed to evaluate the correlation between patient risk perception and self-efficacy and objective patient risk as defined by the Diabetes risk score developed by Bang et al. We hypothesized that higher levels of risk perception and self-efficacy would be associated with lower objective risk of disease.
METHODS: Patients in a university-based internal medicine clinic completed a quantitative survey assessing risk perception (RP) of developing and self-efficacy (SE) of avoiding the development of diabetes (DM) using validated survey tools. We performed chart reviews to obtain laboratory, demographic, and anthropometric data to calculate each patient’s diabetes risk score based on validated risk calculators.
RESULTS: Patients (n = 28) were 96.4 % white, 35.7 % male, mean age 54.52 years (SD 11.92), 18 % were overweight (BMI 25–29.9 kg/m2), 39 % were obese (BMI ≥30), and 3 patients (10 %) had a diagnosis of DM. Of patients not already diagnosed with DM (n = 25), mean SE for avoiding developing DM was 4.55 (SD 2.18) (range 1 low to 7 high), and mean RP of developing DM was 2.63 (SD 1.49) (range 1 low to 7 high). Mean objective health risk of developing DM was 3.33 (SD 1.98) (range 1 low to 6 high). There was a negative correlation between SE and objective risk (r = −0.507, p = 0.005) and a negative correlation between RP and objective risk (r = −0.119, p = 0.281).
CONCLUSIONS: Conclusions: We found a non-significant correlation between patient RP of developing DM and their actual risk; however, we observed a significant negative correlation between SE in stopping the development of the disease and a patient’s objective risk. Although patient understanding of risk may promote an initial desire to improve one’s health, self-efficacy or one’s confidence in avoiding development of diabetes may play a more significant role in influencing a patient’s actual risk of DM. Further goals include increasing sample size; assessing the correlation between RP, SE, and actual risk of developing heart disease and lung cancer; as well as developing tools to help physicians improve perceived risk and self-efficacy.
ROLES DESIRED BY CAREGIVERS OF PATIENTS WITH HEART FAILURE: IMPLICATIONS FOR CLINICIANSRobert Burke1,2; Jacqueline Jones3; David Bekelman4,2. 1Denver VA Medical Center, Denver, CO; 2University of Colorado, Denver, CO; 3University of Colorado, Denver, CO; 4Denver VA Medical Center, Denver, CO. (Tracking ID #1940148)
BACKGROUND: Heart failure (HF) often results in significant burden to patients, their caregivers, and the health care system. A significant contributor to the morbidity and mortality associated with HF is poor adherence to self-management of the disease. Caregivers play a major role in HF management. However, few studies have assessed the roles caregivers desire in interacting with the person they care for and the health care system. Understanding these desired roles is important because doing so may lessen caregiver burden, improve the ability of patients and caregivers to manage their illness at home, and improve the efficacy of the clinicians caring for these patients leading to improved outcomes.
METHODS: Two interviewers with experience in qualitative methods conducted in-depth, semistructured, 60- to 90-minute interviews with 33 diverse patients with New York Heart Association class II to IV HF (confirmed by a cardiologist) and 20 of their family caregivers. The interviews explored specific domains including symptoms, psychosocial issues, decision-making, and the future of illness. Caregivers were identified by asking patients, “Can you think of the one person beside a healthcare provider who helps you the most with your heart condition?” We used the method of constant comparison derived from grounded theory for analysis, using participant triangulation (comparing perspectives of both patients and caregivers) to identify roles caregivers desired and those they perceived were assigned to them.
RESULTS: Caregivers desire different roles than the ones they perceive are assigned to them by the health care system and the person they care for. First, many caregivers express a desire for a role working on behalf of the health care system to carry out HF care at home, but desire more information to be able to do so. Second, most caregivers want a role that is valued when interacting with the health care system, and want to be invited to participate in interactions between the person they care for and the health care system. Third, the majority of caregivers wish for a role moderating communication between the person they care for and the health care system as they frequently observe poor bidirectional communication. Fourth, many caregivers desire a more passive role in communicating at home than the one they feel is assigned to them, and would welcome help discussing difficult topics with the person they care for.
CONCLUSIONS: This study has several important implications for clinicians caring for patients with HF who have supporting caregivers. First, many caregivers, when included in the care plan and supported with relevant information, are eager to facilitate home care for patients with HF. Second, clinicians should solicit the input of caregivers, as many caregivers feel they have important insights that may not be identified otherwise. Third, clinicians should ask patients with HF if they have a caregiver and arrange visits so the caregiver can attend. Fourth, clinicians should inquire about whether the caregiver and patient with HF are communicating about difficult topics, including goals of care, burden, and psychological adjustment to the illness, and offer help to surmount barriers in communication. These changes are may result in more accurate assessment of patients with HF, improved management of the disease at home, and improved quality of life for the patient and caregiver.
ROUNDLY DEBATED: BUILDING BEST PRACTICES FOR ATTENDING ROUNDS AT A TEACHING HOSPITALNader Najafi; Bradley Monash; Michelle Mourad; Yile Ding; Marcia Glass; Gregory Burrell; James D. Harrison. UCSF, San Francisco, CA. (Tracking ID #1938419)
BACKGROUND: Attending rounds, defined as ward rounding with an attending physician, take place every day at teaching hospitals around the country with remarkably little consensus around best practices. At our institution, there is also no clear standardization of rounds from one team to the next. The rounding literature suggests that there is room for improvement in areas such as communication with patients and nurses, efficiency in workflow, and teaching at the bedside. Thus, we set out to identify best practices for attending rounds.
METHODS: The study took place between January and April 2013. We solicited the opinions of six care provider groups that were significant stakeholders in the process of attending rounds: residents, attendings, medical students, case managers, pharmacists, and nurses. A qualitative approach to data collection was undertaken, including one-on-one interviews, group meetings, and e-mail surveys with open-ended questions. Data were transcribed and de-identified and content analysis was performed. This involved at least two reviewers independently coding stakeholder practice recommendations. Consensus for a practice was designated when a majority of one stakeholder group or two or more groups recommended the same practice.
RESULTS: In total, 60 care providers participated in an interview, group meeting, or responded via e-mail, including 23 attendings, 24 housestaff, seven medical students, two medicine team pharmacists, and four nurses. A list of the 15 consensus best practices for rounds is listed in Table 1. We organized these recommendations into four major categories: patient-centered care, interdisciplinary team, education, and efficiency/productivity.
CONCLUSIONS: This study provides concrete, actionable best practice recommendations for standardizing rounds at a teaching hospital. The successful implementation of these best practices requires deliberate training and systems changes, especially for significant interventions such as patient-centered rounds and real-time order writing.
SATISFACTION WITH AND AFFORDABILITY OF HEALTH INSURANCE FOLLOWING MASSACHUSETTS HEALTH CARE REFORM: VIEWS OF SAFETY NET PATIENTSLeah Zallman1,2; Rachel Nardin1,3; Assaad Sayah1,3; Danny McCormick1,3. 1Cambridge Health Alliance, Cambridge, MA; 2Institute for Community Health, Cambridge, MA; 3Harvard Medical School, Boston, MA. (Tracking ID #1935029)
BACKGROUND: Like the Affordable Care Act (ACA), the 2006 Massachusetts (MA) health reform law (fully implanted by 2008) expanded Medicaid coverage and created a health insurance exchange offering publicly subsidized private health insurance plans called Commonwealth Care (CWC). Low income residents were eligible for one of three CWC plans, with different cost sharing requirements, based on income. Prior studies raise concerns about affordability—in particular the calibration of cost sharing with income—of insurance post-reform but neither the affordability of nor satisfaction with specific insurance types has been directly compared previously. .
METHODS: Between August and December 2013, we conducted face-to-face structured interviews with 681 patients presenting to three emergency departments at a large integrated safety net health care system in the greater Boston area. We confirmed insurance type using a statewide database that is updated daily. We included patients aged 18–64, who spoke English, Portuguese, Spanish or Haitian Creole. We excluded severely ill patients. The survey assessed patients’ views of the affordability of care and satisfaction with their insurance in order to understand whether cost sharing was well calibrated to income. Medicaid and CWC 1 plans were available for people with incomes <133 and 150 % of the federal poverty level (FPL), respectively and required no premiums and modest copays for medications only. CWC 2 and 3 plans were available for people with incomes 150–300 % FPL and required monthly premiums and had significant co-pays for most services; these were combined for our analysis (CWC 2 + 3). We used chi-square tests to compare outcomes by insurance type.
RESULTS: Of the 681 participants (81 % response rate), 16 % were uninsured, 5 % had CWC 1, 9 % had CWC 2 + 3, 42 % had Medicaid and 28 % had private insurance. Patients insured by CWC 2 + 3 (71 %) and private insurance (78 %) were less likely to agree that their insurance is affordable than those insured by Medicaid (95 %) and CWC 1 (97 %) (p < 0.001). Patients insured by CWC 2 + 3 (79 %) were less likely to report overall satisfaction with their plan, as compared to those insured by Medicaid (95 %), privately (90 %) and CWC 1 (98 %) (p = 0.003). Satisfaction with services covered was also lower among those insured by CWC 2 + 3 (79 %) and among the privately insured (85 %) as compared to those insured by Medicaid (91 %) and CWC 1 (95 %), though this was of borderline significance (p = 0.057). Uninsured patients (40 %) and those insured by CWC 1 (22 %) and CWC 2 + 3 (19 %) were more likely to report having delayed any care due to cost than were those insured by Medicaid (14 %) and the privately insured (16 %) (p < 0.001). Uninsured (46 %) and privately insured patients (34 %) were more likely to have unpaid medical bills as compared to those insured by CWC1 (24 %), Medicaid (23 %) and CWC 2 + 3 (24 %) (p = 0.0002).
CONCLUSIONS: Affordability and satisfaction with insurance in post-reform MA differs significantly by insurance type. Those insured under public or subsidized plans with minimal cost-sharing plans reported substantially higher rates of satisfaction and affordability of care compared with subsidized private insurance with higher cost-sharing or unsubsidized private insurance. Careful calibration of cost-sharing to income is likely to be important in maximizing afforadability and satisfaction with insurance products offered to low to middle income individuals through health insurance exchanges under the ACA.
SCHEDULE II NARCOTIC USE, ABUSE AND CORRELATION WITH SAFETY MEASURES IN AN ACADEMIC PRIMARY CARE SETTING PRIOR TO THE INITIATION OF FORMAL OPIATE SAFETY POLICIES: A RETROSPECTIVE CHART REVIEWPeter Barkett. Henry Ford Hospital, Detroit, MI. (Tracking ID #1941248)
BACKGROUND: Since the late 1990’s both prescriptions for opioids and opioid-related overdoses have increased three-fold. In 2009, 15,000 people died of opioid-related drug overdoses. The following year there were nearly half a million emergency room visits for non-medical use of opioids, and in 2011, 34 million americans had used opioids at some time in their lives. The vast majority of opioids used in the United States are obtained through prescriptions, and nearly half of these prescriptions originate from primary care providers. Patients using excessive doses of opioids or obtaining prescriptions from multiple sources are much more likely to overdose. As well as initiating a uniform safety policy, our academic primary care clinic in urban Detroit studied who was receiving opioids, why they needed them, how frequently we were using identified “safety measures” and what association (if any) these safety measures had on opioid abuse.
METHODS: A retrospective chart review was performed by five investigators working in close collaboration. Inclusion criteria consisted of adult patients with non-malignant chronic pain prescribed a schedule II narcotic by a primary care physician in our clinic between the dates of March 1 and June 30, 2013. Exclusion criteria included history of malignancy, non-filling of the prescription, use of methadone for non-pain purposes and recent surgery. In addition to recording demographic information we recorded the presence or absence of perceived “safety measures” (use of an opioid risk screening tool, urine toxicology screen, pain contract, reassessment in clinic, referral to pain clinic). Aberrant behavior was considered early refills or multiple providers of opioids. Information was collected from our electronic medical record system and a state-wide electronic narcotic prescription tracking system. Data was analyzed by a professional statistician using Wilcoxon rank sum, Chi-square and Fisher exact testing methods.
RESULTS: 510 patients were assessed for eligibility; 200 excluded: 63 for having malignant pain, 82 for not being prescribed opioids at our internal medicine clinic or being on methadone. Of the 310 left, 85 patients were in the aberrant behavior group and 225 in the non-aberrant group. The most common pain complaint was back pain (32.6 %). In summary, a statistically significant difference between the aberrant and non-aberrant behavior patients have been detected for random urine toxicology status (28.2 % vs 16.9 %, p < 0.026), pain clinic referral (35.3 % vs 24.4 %, p < 0.056), re-evaluation of pain tapering (72.9 % vs 60.9 %, p < 0.048), the safety measures score (2.1 vs. 1.5, p < 0.008) and the ED/clinic visit variable (3.3 vs. 2.2, p < 0.001).
CONCLUSIONS: Compared with other studies of chronic pain patients in the primary care setting, our patients had a similar distribution of age and pain complaints. We did have a significantly higher proportion of African American patients, consistent with our overall patient demographics. Our results suggest that the safety measures identified in this study are not sufficient to eliminate early prescription refills or “doctor shopping.” Possible explanations of the positive correlation between safety measures and aberrant behavior includes identification of at-risk patients by the primary care provider. An alternative explanation would be that poorly controlled pain could cause both “aberrant behavior” (e.g. early refills or seeking out a different provider) and additional “safety measures (e.g. visit to the ED where a urine toxicology screen is standard prior to pain medication prescription). Further research is planned to follow these patients after implementation of uniform policies at the clinic.
SCREENING FOR HEPATITIS C VIRUS IN THE BABY BOOMER POPULATION: AN URBAN CLINICAL EXPERIENCE BEFORE AND AFTER CDC RECOMMENDATIONSSarah Fishman; Robert E. Graham. Lenox Hill Hospital, New York, NY. (Tracking ID #1940069)
BACKGROUND: Hepatitis C Virus (HCV) chronically infects approximately 150 million people worldwide and 2 % of the US population. Prior to the screening of donated blood, HCV was transmitted through transfusion, and now is most commonly spread by exposure to contaminated needles shared by IV drug abusers. As many as 15 % of HCV patients may have acquired HCV infection via sexual contact. HCV infection is the leading indication for liver transplantation in the US, and in 2011 the average cost of healthcare expenses in a lifetime for an HCV infected individual was estimated at $64,490. In May of 2013, the Centers for Disease Control (CDC) issued new recommendations regarding the screening of all patient born between 1945 and 1965, the so called “baby boomers” for HCV, noting that 75 % of chronically infected adults were born in those years. The CDC estimates that universal screening of adults born in this time period will prevent more than 120,000 deaths. We are investigating the impact of this recommendation on the rate of HCV screening in our urban (New York City), resident-physician staffed primary care clinic.
METHODS: We used our clinical scheduler program to identify patients born between 1945 and 1965 that were seen at least twice in our clinic between 8/7/2012 and 9/6/2013. We reasoned that it could take a few months for the news of the CDC recommendations to become common knowledge to practitioners in this clinic. Electronic laboratory records were further queried to identify those patients who were tested for HCV antibodies and/or HCV RNA. The paper charts of those patients were then manually curated to identify potential triggers for HCV testing. In the second phase of this investigation, we will identify a similar cohort of patients seen in the period from 9/7/2013 through 10/8/2014 and again examine the rate and triggers for HCV screening.
RESULTS: 849 patients were seen in our clinic within the designated time frame and met inclusion criteria for age. Of those, 26 (3.1 %) were tested for either HCV antibody or HCV RNA. Six (26.1 %) patients were found to be positive for both HCV antibody and viral RNA, and all six reported a history of active HCV infection. An additional five patients reported a history of HCV infection, hepatitis, or liver disease, but were found to be negative for HCV RNA. Two of these patients had antibody positivity, suggesting a cleared infection. All patients reporting a history of HCV infection were treatment naïve at the time of testing. Of the 15 (57.7 %) patients who were tested for HCV and did not report prior HCV infection or liver disease history, four were tested for HCV in the context of requesting testing for sexually transmitted diseases (STDs) and HIV. One patient was tested for HCV antibody due to unexplained liver enzyme abnormalities found on routine labs, and nine patients were tested without apparent reason to suggest possible HCV infection at the time of initial presentation to the clinic. No patient was found to be positive for HCV antibody or viral RNA who did not report a history of HCV infection.
CONCLUSIONS: Prior to the CDC recommendation for routine screening for HCV infection in the baby boomer population, HCV testing was infrequently performed, and was most often performed in the context of reported history of HCV infection and STD screening. HCV testing revealed a rate of 26.1 % prevalence among those tested, but did not uncover any new cases of HCV in this cohort. This investigation is ongoing to assess the impact of the CDC recommendations on the rate of HCV screening and prevalence of HCV infection. Interventions are planned to increase practitioner awareness of HCV screening recommendations and to identify patients who qualify for screening.
SCREENING FOR HEPATOCELLULAR CARCINOMA IN CHRONIC LIVER DISEASE: A SYSTEMATIC REVIEWAmirala Pasha2; Devan Kansagara1,2; Joel Papak1,2; Maya O’Neil1; Michele Freeman1; Rose Relevo1; Ana Quinones2; Makalapua Motu’apuaka1; Janice H. Jou1,2. 1Portland VA Medical Center, Portland, OR; 2Oregon Health and Science University, Portland, OR. (Tracking ID #1939197)
BACKGROUND: Hepatocellular carcinoma (HCC) incidence and mortality has increased over the past four decades abroad and in the United States, with localized tumors accounting for most of the increase guidelines recommend routine surveillance for hepatocellular carcinoma (HCC) in high-risk patients. However, recommendations for HCC screening remain controversial in part because of concerns over the quality and paucity of existing evidence, and because there have been concerns raised about overdiagnosis and patient harms in other cancer screening programs. We conducted a systematic review of the published literature to better understand the incremental benefits and harms of routine HCC screening compared to clinical diagnosis, and of treating HCC found as a result of screening.
METHODS: We searched Medline, PsycInfo, and Cochrane databases to March 2013; clinical trial registries; reference lists; and technical advisors. We included clinical trials and observational studies comparing screening to no screening, and clinical trials comparing different screening intervals. We also included clinical trials and observational studies comparing active to conservative treatment in patients with early-stage HCC. Mortality and adverse events were the main outcomes of interest. Because there were few comparative studies on treatments other than transarterial chemoembolization (TACE), we also examined noncomparative observational studies. The quality of studies and the overall strength of evidence were dual-reviewed using published criteria.
RESULTS: Of 11,321 citations, 264 were reviewed at the full-text level. Thirty-six studies contained primary data relevant to the efficacy of HCC screening or treatment of early-stage HCC and met our inclusion criteria. We also examined two systematic reviews of treatment modalities. Two trials and 16 observational studies provide very low strength evidence on the effects of screening on mortality because of methodologic flaws and issues of lead- and length-time bias. Moderate strength evidence from two trials shows no advantage of shorter screening intervals (3–4 months compared to 6–12 months). None of the included screening studies reported harms of screening. Low strength evidence from a meta-analysis of 8 studies found a risk of needle-track seeding from liver biopsy of 2.7 %. One recent systematic review of the diagnostic accuracy of imaging for HCC screening and diagnosis found very few studies reporting harms data: one study found contrast-enhanced CT was associated with adverse events in 13–15 % of patients, while another found mild-moderate adverse events in 25 % patients receiving gadoxetic acid-enhanced MRI. We found no studies evaluating the psychologic harms of screening. No studies specifically enrolled patients with screen-detected HCC, so we examined studies of patients with early-stage HCC as a way of approximating screen-detected disease. Overall, there is little evidence with which to draw conclusions about the net benefits of actively treating early-stage HCC compared to conservative treatment. Observational studies show that patients selected for treatment with OLT, resection, or RFA had good long-term survival that was substantially higher than patients not selected for such therapy, but it is unclear whether such effects reflect a true effect of treatment or reflect confounding by indication. Serious harms occurred in 3–20 % of patients, depending on the intervention.
CONCLUSIONS: There is very low strength evidence from which to draw conclusions about the effects of HCC screening on mortality in high-risk patients with chronic liver disease. Screening tests can identify early stage HCC and patients who are selected for surgical treatment often have good long-term survival, but some treatments may be associated with substantial harms. There is very limited evidence to draw firm conclusions about the incremental benefits of using routine screening to identify HCC and treat HCC found as a result of routine screening. Trials examining the balance of benefits and harms of HCC screening in patients with chronic liver disease should be considered.
SEEING IS BELIEVING: VISION-RELATED QUALITY OF LIFE AMONG HOSPITALIZED PATIENTSMadeleine I. Shapiro1; Vineet Arora2; Esther Schoenfeld3; Allison J. Louis1; Alisha S. Ranadive1; Gavin W. Hougham4; Seenu M. Hariprasad5; David Meltzer4; Valerie G. Press4. 1University of Chicago, Chicago, IL; 2University of Chicago, Chicago, IL; 3University of Chicago, Chicago, IL; 4University of Chicago, Chicago, IL; 5University of Chicago, Chicago, IL. (Tracking ID #1934168)
BACKGROUND: Impaired vision may be a risk factor for poor health outcomes during hospitalization, including falls and delirium. Additionally, hospitalized patients with poor vision may be unable to read critical documents such as consent forms. Vision also has large implications for quality of life, including the ability to interact with others and accomplish daily tasks both in and out of the hospital. Our previous work has shown that nearly one-third of hospitalized patients fail an inpatient vision screening. As such, the hospital may represent a missed opportunity to address poor vision and its quality of life (QOL) implications. Therefore, our study set out to examine the prevalence and effect of poor vision on vision-related QOL among hospitalized patients.
METHODS: Hospitalized adult general medicine inpatients at the University of Chicago were enrolled in an ongoing study of resource-allocation and quality-of-care. Eligible patients (English speaking, cognitively intact) were given a vision screening (Snellen Eye Chart); those who had 20/50 or better visual acuity in at least one eye were classified as having sufficient vision. Health literacy was measure using the Rapid Estimate of Adult Literacy in Medicine Revised (REALM-R). Vision-related QOL was measured using the validated National Eye Institute 25-item Visual Functioning Questionnaire (VFQ, scale of 0–100) which covers vision health (near and far sight), social functioning (e.g., visiting people), and mental health (composite of being embarrassed, frustrated, having less control and worrying about vision problems), among other domains.
RESULTS: Of the 405 participants who completed the vision screening, the majority were female (57 %) and African American (77 %) with a mean age of 54 years. Among the participants, half (49 %) had ≤ a high school degree, about one-quarter (n = 92, 23 %) had insufficient vision, and 35 % had poor health literacy. On the single item health screen, participants with insufficient vision were more likely to say they had less than or equal to good health than participants with sufficient vision (86/92, 93 % vs. 259/313, 83 % p = 0.01). Those with insufficient vision were also more likely to report increased dependency on others (p < 0.001), trouble with activities requiring near-vision (p < 0.001), trouble with activities requiring far-vision (p = 0.001), decreased social functioning (p < 0.001) and decreased mental health (p < 0.001). Participants under 65 had lower vision-related mental health than their older counterparts (81.9 vs. 86.6, p = 0.045).
CONCLUSIONS: Given the high prevalence of poor vision and its relationship to diminished vision-related QOL among inpatients, the hospital may represent an important setting to identify patients with poor vision. Future work to test interventions to improve vision and related quality-of-life for inpatients are needed, especially for younger patients who may have the most to benefit.
SEEING THE LIGHT: EXAMINING VISION AMONG INPATIENTS WITH DIABETES (ENVISIONED STUDY)Madeleine I. Shapiro1; Vineet Arora2; Allison J. Louis1; Victoria I. Moreira3; Alisha S. Ranadive1; Gavin W. Hougham4; Seenu M. Hariprasad5; David Meltzer4; Valerie G. Press4. 1University of Chicago, Chicago, IL; 2University of Chicago, Chicago, IL; 3University of Georgia, Athens, GA; 4University of Chicago, Chicago, IL; 5University of Chicago, Chicago, IL. (Tracking ID #1934153)
BACKGROUND: Almost 3 million patients discharged from US hospitals annually have diabetes and more than one-quarter of older patients with diabetes are readmitted to the hospital within three months of discharge. Our prior work has shown that more than one-quarter of general medicine inpatients fail a vision screening test. However, to date, no data have specifically evaluated vision among inpatients with diabetes. Diabetic patients with poor vision may have difficulty performing self-care tasks related to their diabetes, such as injecting insulin. As such, the hospital setting may be a missed opportunity to screen for poor vision and improve access to diabetes related vision care; in-hospital interventions may improve patient self-management on discharge and decrease readmissions. In this pilot project, we aim to evaluate the prevalence of poor vision and characterize access to vision care for inpatients with diabetes.
METHODS: Hospitalized adult general medicine inpatients were enrolled in an ongoing study of resource-allocation and quality of care. Vision was tested using the Snellen eye chart; sufficient vision was defined as at least 20/50 in at least one eye. Health literacy was measured using a set of three verbal screening questions known as the brief health literacy screen (BHLS). Diagnosis of diabetes was determined based on self-report. Participants completed a survey about access to vision care. Descriptive statistics were used to determine means and proportions. Chi-squared tests were used for categorical comparisons.
RESULTS: Vision screenings were completed in 705 participants, the majority of whom were female (55 %) and African-American (77 %), with a mean age of 54. Among the participants, 34 % had diabetes (mean HbA1c 8.37, range 4.7–17.4), 30 % had poor health literacy, and 25 % had insufficient vision. Participants with diabetes were more likely than those without diabetes to have insufficient vision (74/239, 31 % vs. 101/466, 22 %; p = 0.007). Participants with diabetes were also more likely to have poor health literacy (35 % vs. 27 %, p = 0.002). Significantly more participants with diabetes reported that they “think that they need to see an eye doctor” (76/114, 67 % vs. 110/202, 54 %, p = 0.03). While the majority of participants in both groups had ever seen an eye doctor (115/120, 94 % vs. 198/210, 96 %, p = 0.54), participants with diabetes tended to be less likely to have seen one within the last two years (76/100, 41 % vs. 110/156, 59 %, p = 0.3). Further, more participants with diabetes were told that they have eye disease (49/115, 43 %, vs. 56/203, 64 %, p = 0.006). As this is a pilot study, data collection is ongoing.
CONCLUSIONS: Early data from our pilot study demonstrate that the prevalence of poor vision is higher among inpatients with diabetes than those without diabetes. Additionally, the data suggest that access to vision care for patients with diabetes may be inadequate. The hospital setting may be an important opportunity to identify inpatients with diabetes and refer them for guideline-recommended care. Future work should address possible hospital-based interventions to reduce this disparity and improve vision-related transition care for patients with diabetes after discharge home.
SELF-REPORTED HEALTH STATUS PREDICTS OTHER-CAUSE MORTALITY IN MEN WITH LOCALIZED PROSTATE CANCERRichard Hoffman1,9; Tatsuki Koyama2; Peter Albertsen3; Michael Goodman4; Ann S. Hamilton5; Janet Stanford6; Nan Stroup7; Arnold Potosky8; David Penson2. 1Albuquerque VA Medical Center, Albuquerque, NM; 2Vanderbilt University, Nashville, TN; 3University of Connecticut, Farmington, CT; 4Emory University, Atlanta, GA; 5University of Southern California, Los Angeles, CA; 6Fred Hutchinson Cancer Center, Seattle, WA; 7University of Utah, Salt Lake City, UT; 8Georgetown University, Washington, DC; 9University of New Mexico, Albuquerque, NM. (Tracking ID #1937690)
BACKGROUND: Prostate cancers detected by PSA testing are often indolent. Guidelines recommending against screening and treating men with limited life expectancy have had only limited impact on clinical practice. One problem is that physicians have difficulty accurately estimating life expectancy. We used data from the population-based Prostate Cancer Outcomes Study (PCOS) to develop a nomogram to predict 10- and 15-year other-cause mortality among a cohort of men with localized prostate cancer.
METHODS: The PCOS enrolled patients with prostate cancer diagnosed between October 1994 and October 1995. The study cohort for the current analysis was comprised of the men diagnosed with a localized cancer. Baseline measures included demographics, socioeconomic status, comorbidity, tumor characteristics, treatment, quality of life, and a single-item on self-reported health status, with response options ranging from excellent to poor. We used Surveillance, Epidemiology, and End Results program and National Death Index data to determine date and cause of death through December 2010. We estimated other-cause mortality with a proportional hazards survival analysis accounting for competing risks. We then developed a nomogram for predicting risk for other-cause mortality based on age and self-reported health status at time of diagnosis.
RESULTS: The study cohort comprised 2,695 men, of whom 74 % underwent aggressive therapy (47 % surgery). At baseline, 18 % reported excellent health, 36 % very good health, 31 % good health, and 15 % fair/poor health. Healthier men were younger, more likely to be white, have private insurance, more years of education, and undergo surgery. By 15 years after diagnosis, 44 % of the cohort had died; 78 % of the deaths were from causes other than prostate cancer. Self-reported health status strongly predicted other-cause mortality; for men reporting excellent, very good, good, fair/poor health the cumulative incidences of other-cause mortality were 20 %, 29 %, 40 %, and 53 %, respectively, P < 0.001. The competing-risks survival model with age and self-reported health status as the covariates and other-cause death as the outcome had a C-index of 0.72. The Figure shows the nomogram for predicting other-cause mortality based on age and self-reported health status. Increasing age and poorer self-reported health status were associated with increased risk for other-cause mortality. For example, a 69-year-old man reporting fair/poor health status had just over a 30 % chance of other-cause mortality after 10 years and a greater than 50 % chance of other-cause mortality after 15 years. Meanwhile, the corresponding risks for a 69-year-old man reporting excellent health were about 18 % and 28 %, respectively.
CONCLUSIONS: A one-item self-reported health status measure significantly predicted other-cause mortality 15 years after diagnosis with a localized prostate cancer. Men reporting fair/poor health had substantial risks for other-cause mortality suggesting limited benefit for undergoing aggressive treatment. Self-reported health status can be considered in supporting informed decision making about prostate cancer screening and treatment.
Nomogram for predicting other-cause death based on age and self-reported health status
SEX, GENDER, SOCIOECONOMIC STATUS AND ACCESS TO CARDIAC CATHETERIZATION IN THE CONTEXT OF UNIVERSAL HEALTHCARE COVERAGEGabriel E. Fabreau2,1; Alexander A. Leung5,3; Danielle Southern3; John Z. Ayanian4,1; William A. Ghali3,4. 1Harvard Medical School, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3University of Calgary, Calgary, AB, Canada; 4University of Michigan, Ann Arbor, MI; 5University of Calgary, Calgary, AB, Canada. (Tracking ID #1939475)
BACKGROUND: Sex and gender disparities have been described in cardiac care and outcomes following acute coronary syndromes (ACS). Socioeconomic status (SES) may additionally affect medical care and health outcomes, partly through barriers in timely access to cardiac catheterization. In Canada, a universal healthcare system may reduce barriers related to sex/gender and SES. We sought to determine whether sex/gender and SES interact to modify the receipt of cardiac catheterization and mortality following an ACS in a universal healthcare system.
METHODS: Using a provincial multicenter cardiac registry, we assembled a cohort of 14,012 patients admitted with an ACS to any cardiology service in the southern health zones of Alberta, Canada between April 18, 2004 and December 31, 2011 by linking census, vital statistics and clinical registry data. SES was estimated using residential neighbourhood median household income from the 2006 Canadian census. We compared the odds of receiving a cardiac catheterization within 1 and 30 days after admission, and the odds of death within 30 days and 1 year after admission according to income quintiles and stratified by sex. Using multivariable logistic regression we controlled for age, geography, cardiac risk factors and clinical comorbidities to estimate the adjusted odds ratios (ORs) of receiving cardiac catheterization and of death.
RESULTS: Unadjusted rates of cardiac catheterization were higher for men compared to women (41 % vs. 31 % at one day, and 68 % vs. 59 % at 30 days, p < 0.001 for both time points), and in this context, men had lower mortality rates (2 % vs. 2.8 % at 30 days, and 5.2 % vs. 7.4 % at 1 year, p < 0.001 for both time points). In models adjusting for SES, women were less likely to receive cardiac catheterization within 1 day (OR 0.79, 95 % confidence interval [CI], 0.71–0.87) and 30 days (OR 0.73, 95 % CI, 0.62–0.86) of admission with an ACS. When examined across quintiles of SES, adjusted models revealed differing relationships among variables for men vs. women: each incremental decrease in income quintile was associated with a 7 % lower odds of receiving cardiac catheterization for women (p = 0.005) vs. a smaller 3 % decrement in odds for men (p = 0.03). Additionally, among women, each decrease in income quintile was associated with a 13 % higher odds of 30-day mortality (p = 0.02) vs. a 4 % higher odds of 30-day mortality for men (p = 0.39). No SES differences were seen in the adjusted 1-year odds of death for either men or women, nor between them.
CONCLUSIONS: The relationships between socioeconomic status and use of cardiac catheterization and mortality after ACS are different for men vs. women, with women seemingly more vulnerable to the detrimental associations of low income. These findings were present despite a universal healthcare system that does not have any patient user fees. This suggests that factors other than insurance status and/or ability to pay are at play, and that elements of sex and/or gender are effect modifiers. Care protocols designed to improve access to care and improve outcomes in women, especially low SES women, are required.
SHARING TRAINEE NOTES WITH PATIENTS: ANTICIPATED EFFECTS OF OPENNOTES ON GRADUATE MEDICAL EDUCATIONBradley Crotty1,2; Melissa Anselmo2; Deserae Clarke3; Lydia A. Flier2; Jamie Green4; Suzanne Leveille2; Roanne Mejilla2; Rebecca Stametz3; Jan Walker2; Sigall K. Bell2. 1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Geisinger Health System, Danville, PA; 4Geisinger Health System, Danville, PA. (Tracking ID #1937097)
BACKGROUND: OpenNotes is a national initiative inviting patients to read visit notes through a secure patient portal. Although HIPAA gives patients legal access to their medical records, the process can be prolonged and costly, limiting its use. Patients and PCPs report positive experiences with OpenNotes, but little is known about the potential impact of open notes on trainee education and practice.
METHODS: We conducted 7 focus groups with 24 medical and surgical residents and 12 faculty preceptors during 2013 at 2 hospitals prior to OpenNotes implementation. An expert facilitator led each session, discussing attitudes about OpenNotes, concerns, potential benefits, and educational implications. Sessions were recorded and transcribed. We analyzed transcripts using methods established by Crabtree and Miller.
RESULTS: Transcripts revealed 3 central themes: 1) Anticipated effects of transparency (including making clinician thought process “visible” to patients, uncertainty about how much to share, teaching trainees about note nuance, the “power of print” to motivate or offend patients, and “inversion of trust,” where doctors now need to trust their patients); 2) Ideology of a note (including questions about notes’ inherent educational value, purpose, and ideal audience), and 3) concerns about time pressures (including trainee fatigue, responding to patient calls/questions, and faculty overburden limiting proofing, teaching, and timely note turnaround). Participants voiced the following additional concerns: note errors compromising patient trust, note editing capabilities, documentation becoming more vague, ambiguity about documenting sensitive information, notes being hurtful to some patients and inaccessible to others—potentially leading to information access disparities. Potential benefits, included spearheading innovation, improved patient engagement and safety, increased preceptor feedback/supervision, more open discussions with patients, improved note quality (stemming of copy/paste and judgmental language), and possible patient feedback as an educational tool. Participants believed educational interventions should focus on medical students. Trainees emphasized patient education and expectation-setting. Both groups felt that if faculty were sharing notes, trainees should too.
CONCLUSIONS: Trainees and preceptors agree that trainees should be included in OpenNotes, despite concerns about potential effects on the patient-doctor relationship, preceptor oversight requirements, and the sweeping issue of workload. Note transparency may expose existing imperfections in healthcare delivery and “force” confrontation of challenging issues like adequate supervision, time, and supports for trainees, preceptors, and patients—but also may offer innovative educational opportunities and patient care benefits.
SLEEP HABITS, QUALITY OF LIFE AND SATISFACTION WITH ACADEMIC SUCCESS IN SECOND YEAR MEDICAL STUDENTSKay Johnson1,2; Nancy Simon1; Mark Wicks1; Doug Schaad1; Karen P. Barr1; Kim O’Connor1. 1University of Washington School of Medicine, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA. (Tracking ID #1938934)
BACKGROUND: Pre-clinical medical students’ sleep is not yet determined by call schedules or patient care workload, but rigorous academic demands, high aspirations, and sometimes anxiety about their future may impact students’ ability to protect time for sleep and other vital activities. Sleep deprivation can negatively impact efficiency and performance, but may also be associated with depression, anxiety, and poor quality of life. Little has been published about medical students’ sleep habits, which may be a modifiable variable in student wellness. We surveyed second year medical students about their sleep habits to determine whether quantity of sleep is associated with perceived quality of life and academic success.
METHODS: Second year medical students at a large public university responded anonymously to a written questionnaire in the Spring quarters of 2011 and 2012 regarding several components of sleep, including their average amount of sleep on weeknights, weekends, and nights prior to a quiz or an exam, as well as their perception of their personal sleep needs. Other previously validated questions explored burn out, depression and perceived stress. Satisfaction with their quality of life and academic success was also assessed, as well as their perceived efficiency of study and retention of information.
RESULTS: Three hundred seven medical students completed the survey (response rate 68 %). Mean age was 26.4 years. When asked, “In general, how many hours of sleep does your body require for you to function optimally?” the mean response was 7.68 h; 90 % reported needing at least 7 h of sleep. Seventy-one percent said they get significantly less sleep than ideal during the academic year. On typical weeknights, the mean reported number of hours of sleep was 6.9 (range 4–10), with 6.4 on nights prior to a quiz (range 2–10) and 5.7 on nights prior to an exam (range 0–9). In the past academic year, 93 students (30 %) had “pulled an all-nighter” and twenty-five students (8.3 %) reported nodding off while driving. More sleep on weeknights was associated with a lower risk of screening positive for burnout (p= 0.04) or depression (p = 0.01), higher reported satisfaction with quality of life (p = 0.0001), and higher satisfaction with academic success (p = 0.0043). More weeknight sleep was not associated with perceived efficiency of study or retention of information.
CONCLUSIONS: Chronic sleep deprivation was common among the second year students participating in this study. Little sleep was frequently reported prior to exams, when high performance was most desired. Over 8 % of students have nodded off while driving during this academic year. Though a causal relationship could not be confirmed based on this study, higher levels of weeknight sleep were associated with less burnout and depression, and higher quality of life. Though students may assume they must sacrifice their sleep to achieve academic success, more sleep was actually associated with higher satisfaction with academic success. Research on effectiveness of educational and/or behavioral interventions to increase medical student sleep is needed, and evaluation of medical school curriculum reform efforts should take sleep variables into account.
SMARTPHONE-REPORTED STRESS AND DRUG EVENTS AND DAY-END PERCEIVED STRESS, HASSLES, AND MOOD IN METHADONE-MAINTAINED INDIVIDUALSKarran A. Phillips; David H. Epstein; Michelle L. Jobes; Kenzie L. Preston. NIDA/NIH, Baltimore, MD. (Tracking ID #1939477)
BACKGROUND: The consistent finding that there is an overlap in the neural circuitry affected by stress and drug use and animal behavior studies showing that acute stressors (e.g., tail pinching, etc.) increase the likelihood of drug-seeking behavior support the causal role of stress in addiction and relapse. Human self-report and laboratory studies also suggest that stress is a clinically significant precipitant of relapse. We sought to determine relationships among drug use and stressful events (reported in real time) and day-end reports of perceived stress and hassles utilizing smartphones.
METHODS: Opioid-dependent methadone-maintained individuals in a 12-month natural-history study carried smartphones for up to 36 weeks to provide Ecological Momentary Assessment (EMA) data. They initiated event-contingent entries whenever they used drugs or experienced a stressful event, and completed a day-end assessment every night, including 5 items from the Perceived Stress Scale (PSS), 32 hassle items from the Hassles and Uplifts (HS) Scale, and a brief mood assessment.
RESULTS: Participants (n = 102: 76 men, 26 women) reported 1,016 stress events, of which 613 (60 %) had corresponding day-end assessments, and 1,171 drug-use events, of which 832 (71 %) had corresponding day-end assessments. Compared to days on which no stress events were reported, stress-report days had higher day-end PSS scores (mean ± D, none 6.2 ± 3.3 vs. stress 6.5 ± 3.7, p = 0.04) and higher day-end HS scores (mean ± SD, none 2.2 ± 3.6 vs. stress 3.6 ± 4.5, p < 0.005). Compared to days on which no drug use was reported, drug-use days had higher day-end PSS scores (mean ± SD, none 6.1 ± 3.4 vs. drug 7.3 ± 3.2, p < 0.05) and higher day-end HS scores (mean ± SD, none 2.2 ± 3.6 vs. drug 2.9 ± 4.4, p < 0.005). On days on which a stress event was reported, individuals more often rated their mood at the end of the day as angry/annoyed/afraid (p < 0.005) and sad (p = 0.006) and less often as content (p < 0.005). On days on which drug use was reported, individuals more often rated their mood at the end of the day as sad (p = 0.005) and less often as happy (p = 0.003).
CONCLUSIONS: Using smartphones and EMA to collect real-time in-the-field data, we found that both drug and stress events are associated with higher day-end perceived stress, perceived hassles, and negative mood among opioid-dependent individuals in methadone maintenance. In addition to focusing on reducing drug use, addiction treatment should include education on stress, hassles, and mood management.
STANDARDIZING THE DEFINITION OF REDUCED MOBILITY WHEN ASSESSING THE PATIENT’S RISK OF VENOUS THROMBOEMBOLISMAlexander Weick; David Paje; Bronwyn Small; Muhammad Usman; Jainil Shah. Henry Ford Hospital, Detroit, MI. (Tracking ID #1916252)
BACKGROUND: Immobilization is known to be an important contributing factor to venous thromboembolism (VTE). However, the currently available risk assessment models for VTE in hospitalized medical patients use variable definitions of reduced mobility that are difficult to standardize and to apply prospectively. We sought to evaluate the physician’s ability to determine at the time of admission whether a patient will have reduced mobility for at least 3 days.
METHODS: Physicians were asked to complete a standard data collection tool during their initial evaluation of patients admitted to the general medical units of an 805-bed teaching hospital. The tool captured baseline demographic data and clinical variables included in the Padua Risk Assessment Model (PRAM). To assess mobility status, physicians were asked whether they anticipate reduced mobility for at least 3 days that is limited to no more than bed rest with bathroom privileges. This was later compared to the patient’s actual ability to ambulate independently on the 3rd hospital day as determined by the patient’s nurse.
RESULTS: Of the 351 patients enrolled in the study, 123 (35 %) were expected to have reduced mobility by their admitting physician and 154 (44 %) were considered high-risk for VTE based on a PRAM score of ≥4. Among those high-risk for VTE, 111 (72 %) were expected to have reduced mobility, while only 12 (6 %) of those who were low-risk were anticipated to be immobile (p < 0.0001). The physician’s prediction at the time of admission of the patient’s reduced mobility during hospitalization had a sensitivity of 76 % (95 % Confidence Interval [CI], 66 % to 84 %) and a specificity of 81 % (95%CI, 75 % to 86 %). The positive and negative predictive values were 62 % (95%CI, 52 % to 71 %) and 89 % (95%CI, 84 % to 93 %), respectively.
CONCLUSIONS: The physician’s anticipation of patient’s reduced mobility is fairly reliable in predicting actual mobility during hospitalization. This may be used to standardize the operational definition of reduced mobility when assessing the patient’s risk of VTE.
STATE FIREARM LEGISLATION AND NONFATAL FIREARM INJURIESJoseph Simonetti1,2; Ali Rowhani-Rahbar3,5; Douglas Zatzick3,6; Bessie Young7,2; Frederick Rivara3,4. 1University of Washington, Seattle, WA; 2School of Public Health, University of Washington, Seattle, WA; 3University of Washington, Seattle, WA; 4University of Washington, Seattle, WA; 5School of Public Health, University of Washington, Seattle, WA; 6University of Washington, Seattle, WA; 7Northwest Center of Excellence, VA Puget Sound, Seattle, WA. (Tracking ID #1938977)
BACKGROUND: Stricter state firearm legislation has been shown to be associated with lower rates of fatal firearm injuries. However, less is known regarding nonfatal firearm injuries (NFI), which are more common than fatal injuries, and differ in several ways, including age of the injured, intent, and type of firearm involved. The aim of this study was to determine whether stricter state firearm legislation is also associated with lower rates of NFI.
METHODS: We performed a cross-sectional, ecological analysis using available retrospective data from 17 states collected through the 2010 Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases, which include information on more than 95 % of all discharges from community hospitals. We defined each case of hospitalized NFI as a patient discharged alive with an External Cause of Injury Code (E-code) for firearm injury (Assault [E965.0–.4], intentional self-inflicted [E955.0–.4], unintentional [E922.0–.3, .8, .9], or undetermined [E985.0–.4]). The primary predictor of interest was the Brady Score, a measure of state firearm legislative strength based on 2009 scorecards created by the Brady Campaign to Prevent Gun Violence. Scores are based on laws related to firearm trafficking, background checks, child safety, and restrictions on military-style assault weapons and firearms in public places. The Brady Score ranges from 0 to 28, with higher scores indicating more stringent laws, which we categorized into quartiles. The primary outcome was total hospitalized NFI. Secondary outcomes were assault-related, self-inflicted and unintentional hospitalized NFI. We calculated age-adjusted total hospitalized NFI rates for each participating state and used Poisson regression with clustered robust sandwich standard error estimates to determine if states in the highest quartile of legislative strength had fewer total, assault-related, self-inflicted and unintentional hospitalized NFI than states in the lowest quartile. Using data from the 2010 U.S. Census, we adjusted each model for the following state characteristics: age distribution, gender composition, racial/ethnic composition, population density, percentage with a college degree, percentage living below the federal poverty line, and unemployment rate.
RESULTS: The median Brady Score in 17 HCUP-participating states was 7 (interquartile range 4–16). Rates of total hospitalized NFI ranged from 1.7 (Hawaii) to 12.0 (Maryland) per 100,000 individuals. In unadjusted analyses, compared to states in the lowest quartile of legislative strength, those in the highest quartile of legislative strength had lower rates of self-inflicted (incident rate ratio [IRR] 0.33; 95 % confidence interval [CI] 0.27–0.41) and unintentional (IRR 0.53; 95 % CI 0.43–0.66) hospitalized NFI. In multivariable models, states in the highest quartile of legislative strength had lower rates of total (IRR 0.42; 95 % CI 0.34–0.50), assault–related (IRR 0.44; 95 % CI 0.35–0.57), self-inflicted (IRR 0.26; 95 % CI 0.22–0.31), and unintentional (IRR 0.27; 95 % CI 0.22–0.32) hospitalized NFI.
CONCLUSIONS: Findings of this cross-sectional, ecological study indicate that stricter state firearm legislation is associated with lower rates of all types of hospitalized nonfatal firearm injuries.
STATIN PRESCRIBING FOR PRIMARY PREVENTION: WHAT MIGHT THE 2013 ACC/AHA GUIDELINES ACHIEVE?Harb Harb1; Michael B. Rothberg1; Brian Wells2; Bo Hu2. 1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH. (Tracking ID #1937737)
BACKGROUND: The Adult Treatment Panel III guidelines for cholesterol testing and treatment in primary prevention were based on cardiovascular risk factors and LDL cholesterol targets. In contrast, the new American College of Cardiology/American Heart Association (ACC/AHA) 2013 guideline focuses exclusively on cardiovascular risk, with statins recommended for all patients with a 10-year risk of >7.5 % using a new population-based risk calculator. One concern is that the ACC/AHA guidelines may lead to initiation of statin therapy for more patients, including many who would have been considered to be lower risk by the earlier criteria. In contrast, the previous focus on LDL may have led to overprescribing for patients with high LDLs and low risk, or underprescribing for those with low LDLs but high risk. The objective of this study is to quantify the potential change in statin prescribing patterns using the ACC/AHA guidelines compared to current practice for patients without CHD equivalents.
METHODS: We conducted a retrospective cross sectional study of patients aged between 30 and 75 years old who received a first outpatient primary care visit at the Cleveland Clinic between January 1, 2005 and December 31, 2012. Patients with incomplete data, contraindications to lipid lowering medications (history of statin induced rhabdomyolysis, myositis or myopathy, transaminitis, statin allergy); lipid-lowering agent(s) prescribed at their first encounter (implying that they were already taking lipid lowering therapy); and patients with CHD or CHD equivalents (CVD, PVD, Diabetes) were excluded. For each patient we collected the following information from the time of their first lipid panel: age, sex, and race; as well as total, HDL and LDL cholesterol, smoking status, systolic blood pressure and whether they were treated with an antihypertensive medication. Patients were then stratified according to 10-year cardiovascular risk into 3 groups—low (<5 %), intermediate (5–15 %) and high (15 %)—based on the Framingham equation. We then compared the number of patients in each stratum who actually received statins to the number in that same stratum that would be recommended to receive statins based on the ACC/AHA guidelines (i.e. those with a 10-year risk of >7.5 % based on the new risk calculator). We then calculated the number of cardiac events prevented over 10 years under current practice to those that could have been prevented by following the ACC/AHA guidelines using the formula: E = N * R * RRR where E is the number of events prevented, N is the number of patients taking statins, R is the average Framingham risk of the patients taking statins, and RRR is the relative risk reduction related to statin use. We estimated the risk reduction to be 27 %, based on a Cochrane Review of statins for primary prevention.
RESULTS: Of 98,136 patients who had an initial visit (with LDL measured) during the study period, 85,079 (87 %) patients met inclusion criteria. Of these, 41,376 (49 %) were low risk, 30,135 (36 %) intermediate risk, and 12,768 (15 %) high risk based on their Framingham risk scores. Mean patient age was 48 years, 42 % were male, 79 % were white, 37 % were smokers and 27 % were taking medication for hypertension. The comparison of statin use appears in the Table. The total number of patients treated with statins under current practice was 13,896; 31 % of these were high risk and 22 % were low risk. Under the ACC/AHA guidelines, 17,294 patients would qualify for treatment; 70 % would be high risk and 1.4 % low risk. Assuming that statins reduce the risk of a major cardiac event by 27 %, then the total number of events currently being prevented is 510 per 10 years, with NNT = 27. Under ACC/AHA criteria the number of events prevented would be 1034, with NNT = 17.
CONCLUSIONS: Compared to current practice, following the ACC/AHA guidelines would increase the total number of patients on statins. However, it would decrease use among low and intermediate risk patients, while markedly increasing use among high risk patients, thereby decreasing the total number of major cardiac events as well as number needed to treat.
Statin prescriptions by CHD risk
| Framingham 10-year CHD risk | All Patients | Statins Under Current Practice | Statins Under ACC/AHA Guidelines | p-value |
|---|---|---|---|---|
| N (%) | N (%)* | N (%)* | ||
| Low (<5 %) | 41,376 (49 %) | 3000 (7 %) | 234 (0.6 %) | <0.001 |
| Medium (5–15 %) | 30,135 (36 %) | 6441 (21 %) | 4973 (17 %) | <0.001 |
| High (>15 %) | 12,768 (15 %) | 4317 (34 %) | 12087 (95 %) | <0.001 |
*Row percentage
STIGMA AND THE UTILIZATION OF SERVICES FOR MENTAL HEALTH ISSUES IN MEDICAL STUDENTSGwen Thompson1; Rosanne McBride2; Colin P. West1; Gwen W. Halaas2. 1Mayo Clinic, Rochester, MN; 2University of North Dakota, Grand Forks, ND. (Tracking ID #1938859)
BACKGROUND: There is a high prevalence of depression and burnout among medical students. While medical students are taught that mental health issues are disease processes with treatment options, there is still an underutilization of services in this population. This study explores the utilization of services for mental health issues and the stigma perceived regarding this health issue among medical students at the University of North Dakota School of Medicine and Health Sciences (UNDSMHS).
METHODS: A cross-sectional study was used to survey 253 students at UNDSMHS with a survey response rate of 63.6 %. The Maslach Burnout Inventory Human Services Survey was used to evaluate burnout. Depression was assessed using the Patient Health Questionnaire. Additional items pertaining to demographic information, the diagnosis and treatment of depression, the cause of depression and 27 stigma statements regarding depression were also included in the survey. These additional items were adopted with permission from the authors of a previous study.
RESULTS: Of the total respondents, 17.0 % (26 of 153, 95 % CI [11.0 %, 23.0 %]) were experiencing moderate to severe depression and 48.5 % (64 of 132, 95 % CI [40.0 %, 57.0 %]) were experiencing burnout. Of the moderately to severely depressed, 80.8 % (21 of 26, 95 % CI [65.7 %, 95.9 %]) were not diagnosed and 84.6 % (22 of 26, 95 % CI [70.7 %, 98.5 %]) were not being treated for depression. When asked why depression develops, 22.6 % (35 of 155, 95 % CI [16.0, 29.2]) responded that it was due to an inability to cope. No students replied that is was solely attributed to a neurotransmitter abnormality. Among the 27 stigma statements, those who had moderate to severe depression differed in their responses compared to those who had no or mild depression on 12 statements. For example, students with moderate to severe depression were more likely to agree that seeking help for depression would make them feel less intelligent as a medical student (p < 0.01, OR 7.9, 95 % CI [2.8, 22.1]), telling a counselor would be risky (p = 0.04, OR 3.5, 95 % CI [1.2, 10.3] and depression is a sign of personal weakness (p = 0.03, OR 5.9, 95 % CI [1.3, 25.8]).
CONCLUSIONS: Students at the UNDSMHS have rates of depression and burnout similar to those of medical students across the nation. The majority of students at the UNDSMHS were not diagnosed and underutilized treatment services. Despite medical training that mental health is a disease process, more than one fourth of medical students stated that depression develops due to an inability to cope. Medical students also still endorse statements of stigma regarding mental health issues. This is particularly true for students who are categorized as moderately to severely depressed. It is unknown if the stigma perceived by those suffering from mental health issues is amplified by their disease process or if those who are suffering from mental health issues have experienced the negative effects of this stigma first-hand and are therefore able to better comment on it. Investigating the etiology of this perceived or real stigma and addressing the source is an important next step in successfully helping medical students help themselves.
STRONG MEDICAL SCHOOL INDUSTRY INTERACTION POLICIES HAVE NO PROTECTIVE EFFECT ON STUDENTS’ BEHAVIOR AS RESIDENTS: RESULTS OF A NATIONAL SURVEYJames Yeh1; Kirsten Austad1; Jessica M. Franklin1; Susan Chimonas2; Eric Campbell3; Jerry Avorn1; Aaron Kesselheim1. 1Brigham and Women’s Hospital and Harvard Medical School, Boston, MA; 2Columbia University College of Physicians and Surgeons, New York, NY; 3Massachusetts General Hospital and Harvard Medical School, Boston, MA. (Tracking ID #1923322)
BACKGROUND: Medical students at schools with strong industry interaction policies are less likely to receive gifts and meet with sales representatives, and are more likely to have increased perception of adequacy of separation between faculties of their medical school and the industry when compared to students from schools with weak policies. However, it is unknown whether these behaviors and attitudes persist after graduation to residency training. We sought to determine whether there was an association between third-year residents’ openness to meeting with and accepting gifts from pharmaceutical sales representatives and the strength of the industry interaction policies in place at the medical school they had attended. We also considered whether certain demographic or professional characteristics were associated with their behavior.
METHODS: We administered a mailed survey to 1714 third-year residents randomly identified from U.S.-based medical schools (15 graduates from each school). Survey asked about interactions with and acceptance of gifts from pharmaceutical sales representatives, as well as attendance of industry-sponsored educational events, that had occurred in the past 6 months of their residency training. We used hierarchical logistic regression models to determine the association between these outcomes and the strength of their medical schools’ industry interaction policies measured by the Institute on Medicine as a Profession 3 years prior to the administration of the survey. In the final model, we adjusted for medical school class size, decision to enter primary care, plan to conduct translational research, and residents’ concern about their medical school loan debt level.
RESULTS: Among 739 respondents (43.1 %), residents who graduated from medical schools with the strongest industry interaction policies had no statistically significant differences in the main outcomes when compared to graduates of medical schools with the weakest policies: there was no difference in the odds of receiving gifts (unadjusted odds ratio [OR] 0.77; 95 % Confidence Interval [CI] 0.31–1.96; p = 0.59), accepting meals paid for by the industry (unadjusted OR 0.81; 95 % CI 0.28–2.29; p = 0.69), interacting with sales representatives (unadjusted OR 1.11; 95 % CI 0.44–2.80; p = 0.82), or attending educational events sponsored by the industry (OR 1.81; 95 % CI 0.69–4.76; p = 0.23). These statistically non-significant results did not change substantially in the fully-adjusted model.
CONCLUSIONS: Residents’ behavior toward industry sales representatives was not associated with the strength of the industry interaction policies at the medical school they previously attended. These results suggest that residents adapt to the marketing interaction norms at their training hospitals. Any “protective effect” from strong industry interaction policies in insulating students from pharmaceutical marketing during medical school did not carry over to the next stage of their clinical training. Industry interaction policies may be less common, or less stringently enforced, in the hospitals and outpatient clinics in which medical trainees work during their residency. Increased attention should be paid to managing industry interactions throughout medical training.
STUDENT GOALS FOR SUB-INTERNSHIPS; A STUDY OF TWO INSTITUTIONSBeth Liston1; Deepti Rao2. 1The Ohio State University, Columbus, OH; 2Univeristy of New Mexico, Albuquerque, NM. (Tracking ID #1938454)
BACKGROUND: As residency programs adapt curricula to the ACGME milestones, the fourth year of medical school will play an important role in preparing students to meet the minimum competencies for entering interns. Organizations are trying to define learning outcomes for these students. However, there is little written on what knowledge and skills students themselves hope to gain in their sub-internship rotations. Clearly this is important data as incongruous institutional and student goals will lead to failed programming efforts.
METHODS: Students doing a sub-internship between April 2010 and April 2012 at University of New Mexico and between July 2012 and July 2013 at Ohio State University wrote their own rotation objectives. The students at the University of New Mexico completed an internal medicine sub-internship whereas at the Ohio State University students completed either an internal medicine, family medicine, pediatrics, general surgery, neurology, urologic surgery or neurosurgery rotation with the majority choosing internal medicine, family medicine or pediatrics. At both institutions, no didactic examination contributed to the student’s grade. The objectives were grouped into themes and coded by the authors. The numbers of students giving each goal were tabulated.
RESULTS: There were 40 students at the University of New Mexico. Each student was allowed to write unlimited goals. There were 175 students at Ohio State University. Each student was asked to write three goals. The goals most often written at the University of New Mexico were increasing skills in patient management (29), efficiency (18), note writing (17) and dictation (15) and least often written were knowledge of pain management (1), wanting experience with being on call (1), using the lab (1) and gaining skill in listening to heart murmurs (1). The goals most often written at the Ohio State University were increasing skills with patient management (71), increasing medical knowledge of pulmonary problems (67), increasing medical knowledge of renal problems (44), and procedures and least often written were increasing skills with cardiac exam/heart murmurs and assessing residency program
CONCLUSIONS: This two-institution study suggests that (1) learning clinical care (ACGME competency Patient Care) during the sub-internship was perceived as an important goal by students at both medical schools, but the importance of acquiring of medical knowledge (ACGME competency Medical Knowledge) varied considerably among medical students at the two schools; and (2) improving physical examination skills and learning procedures (ACGME competency Patient Care) was not an objective for the vast majority of students at both schools. Students individual objectives for their learning may inform institutional curricula. National efforts to standardize sub-internship experiences should take this into account.
STUDENTS LEAD THE WAY FOR LIFESTYLE MEDICINE INTEGRATION INTO MEDICAL EDUCATIONCamille Clarke1,5; Ingrid Edshteyn2,3; Colin Zhu4. 1Cambridge Health Alliance, Cambridge, MA; 2Columbia University, New York, NY; 3Griffin Hospital, Derby, CT; 4Robert Wood Johnson Medical School, Freehold, NJ; 5Harvard Medical School, Boston, MA. (Tracking ID #1939725)
BACKGROUND: Lifestyle practices profoundly influence short-term and long-term health along with overall quality of life. The majority of chronic diseases are preventable and significantly influenced by poor lifestyle choices. Practice guidelines for chronic disease prevention and management recommend that treatment begin with evidence-based lifestyle medicine interventions as the primary modality. Physicians, however, cite inadequate confidence and lack of knowledge and skill as the major barriers to counseling patients about lifestyle interventions. A change is imminent in addressing this gap and health professional trainees have begun to proactively implement lifestyle medicine initiatives. The past 3 years has seen a rise in student-led interest groups for lifestyle medicine, however the motivation, goals, facilitators, and impediments for these developments remain largely unknown. The purpose of this study was to evaluate the perceptions of lifestyle medicine student interest group leaders on the importance and inclusion of lifestyle medicine in their medical school curricula, their motivation for starting the group, the major lifestyle medicine topics of interest as well as barriers in starting and maintain the groups on their campuses.
METHODS: A 10 question online survey was distributed to eight student leaders of six medical school lifestyle interest groups. Their participation was voluntary, stating the intent of developing standardized lifestyle medicine resources for student groups. Results were reported anonymously and grouped for the final analysis.
RESULTS: Seven medical student leaders responded to the survey. While all stated that it is either important (57 %) or very important (43 %) to include training in Lifestyle Medicine within medical education, the majority (85 %) stated that their medical school equipped students to provide only some (43 %) or very little (29 %) lifestyle recommendations for patients. All cited personal interest as motivation for starting their interest groups along with lack of content in medical curriculum (57 %) and lack of content in other interest groups (71 %). All respondents stated that lack of educational or supportive resources as the primary barrier in starting the medical school group, and it remained the greatest barrier (83 %) in maintaining the interest group. Nutrition, physical activity, stress management, and clinical lifestyle medicine practice models were ranked as the four most important lifestyle medicine topics in their interest groups.
CONCLUSIONS: National guidelines assert the importance of lifestyle counseling by physicians in addressing the preventable chronic disease epidemic. Our results show a growing number of medical student leaders have taken the initiative with a proactive approach in establishing lifestyle medicine interest groups to address the current gap in medical school curricula. Personal interest, lack of content in curricula and lack of content in other interest groups are cited as the main reasons for beginning these groups. The major initial and continuing impediment is a lack of educational or supportive resources. It will be our nation’s imperative to strengthen and enable these lifestyle medicine student interest groups and medical school curricula for treating the cause of both preventable and chronic disease.
SUBCLINICAL THYROID DYSFUNCTION AND FRACTURE RISK: AN INDIVIDUAL PARTICIPANT DATA ANALYSIS OF PROSPECTIVE COHORTSManuel R. Blum1; Douglas Bauer2; Bruno R. da Costa3; Christina D. Wirth1; Anne R. Cappola4; Robin P. Peeters5; Bjørn O. Åsvold6; Howard A. Fink7,8; Wendy P. den Elzen9; Robert N. Luben10; Misa Imaizumi11; Arnulf Langhammer6; Alexandra P. Bremner12; Apostolos Gogakos13; Richard Eastell14; Elsa S. Strotmeyer15; Erin Wallace16; Mari Hoff6,17; Kay-Tee Khaw10; Graziano Ceresini18; Fernando Rivadeneira5; Luigi Ferrucci19; André Uitterlinden5; Graham R. Williams13; Rudi G. Westendorp20; John P. Walsh21,22; Jacobijn Gussekloo9; Drahomir Aujesky1; Nicolas Rodondi1. 1Inselspital, Bern University Hospital, Bern, Switzerland; 2University of California, San Francisco, CA; 3University of Bern, Bern, Switzerland; 4University of Pennsylvania School of Medicine, Philadelphia, PA; 5University of Rotterdam, Rotterdam, Netherlands; 6Norwegian University of Science and Technology, Trondheim, Norway; 7University of Minnesota School of Medicine, Minneapolis, MN; 8VA Medical Center, Minneapolis, MN; 9Leiden University Medical Center, Leiden, Netherlands; 10University of Cambridge, Cambridge, United Kingdom; 11Radiation Effects Research Foundation, Nagasaki, Japan; 12University of Western Australia, Crawley, WA, Australia; 13Imperial College London, London, United Kingdom; 14University of Sheffield, Sheffield, United Kingdom; 15University of Pittsburgh, Pittsburgh, PA; 16University of Washington, Seattle, WA; 17Nord-Trøndelag Hospital Trust, Levanger, Norway; 18University Hospital of Parma, Parma, Italy; 19National Institute on Aging, National Institutes of Health, Baltimore, MD; 20Leiden University Medical Center, Leiden, Netherlands; 21University of Western Australia, Crawley, WA, Australia; 22Sir Charles Gairdner Hospital, Nedlands, WA, Australia. (Tracking ID #1930001)
BACKGROUND: Subclinical thyroid dysfunction is common, particularly with increasing age. Controversy persists as to whether screening and treatment of subclinical thyroid dysfunction are warranted, as current evidence about the risks and effects of treatment is limited. Data from several prospective cohorts on the association between subclinical thyroid dysfunction and fracture events are conflicting. These conflicting results might be attributed to differences in age, gender, thyrotropin (TSH) levels, power and varying cut-offs of the studies.
METHODS: After a systematic literature review, we performed an individual participant pooled data analysis from all available prospective cohorts of adults with measurement of baseline thyroid function and fracture outcomes. We examined hip, non-spine, clinical spine and any fractures. We defined euthyroidism as TSH 0.45–4.49 mIU/L, subclinical hyperthyroidism as TSH < 0.45 mIU/L with normal free thyroxine (FT4) levels and subclinical hypothyroidism as TSH ≥ 4.50–19.99 mIU/L with normal FT4 levels.
RESULTS: Among 13 prospective cohort studies with 69,795 participants during 757,219 person-years of follow-up, 4044 (5.8 %) participants had subclinical hypothyroidism and 2091 (3.0 %) had subclinical hyperthyroidism. During follow-up, 2901 participants (among 12 studies) had a hip fracture, 2018 (8 studies) had non-spine fractures, 320 (7 studies) had spine-fractures, and 2600 (9 studies) had any fracture. In age and gender-adjusted analyses, the overall hazard ratio (HR) for individuals with subclinical hyperthyroidism of any cause compared to euthyroidism was 1.39 (95 % confidence interval, 1.10–1.76) for hip fracture, 1.16 (0.95–1.41) for non-spine fracture, 1.54 (0.96–2.47) for spine fracture, and 1.28 (1.07–1.54) for any fracture. The risk of fracture increased with lower TSH levels for every fracture outcome (all p for trend ≤0.02). Compared to euthyroid participants, HRs for those with TSH < 0.10 mIU/L were 1.67 (1.21–2.30) for hip fracture, 1.72 (1.11–2.68) for non-spine fracture, 3.57 (1.88–6.78) for spine fracture, and 2.01 (1.49–2.71) for any fracture. Risks were similar after further adjustment for known osteoporotic fracture risk factors such as BMI and smoking. The attributable risk for subclinical hyperthyroidism was 28 % for hip fracture and 22 % for any fracture. Endogenous subclinical hyperthyroidism (no use of thyroid hormone) was associated with increased fracture risk for all fracture outcomes, with HR of 1.56 (1.20–2.02) for hip, 1.27 (1.02–1.59) for non-spine, 1.74 (1.01–2.99) for spine and 1.42 (1.16–1.74) for any fracture. Subclinical hypothyroidism was not associated with fracture risk. HRs for participants on thyroid medication (N = 2737) vs. untreated euthyroid participants were 1.36 (1.15–1.61) for hip, 1.31 (1.08–1.59) non-spine, 1.34 (0.87–2.07) for spine and 1.24 (1.04–1.47) for any fracture.
CONCLUSIONS: Pooled individual data from 13 prospective cohorts confirm that subclinical hyperthyroidism is associated with an increased risk of hip and other fractures, particularly in those with a TSH concentration <0.10 mIU/L. Subclinical hypothyroidism is not associated with fracture risk, but treatment with thyroxine is associated with increased fracture risk. Our study cannot address whether treatment of subclinical hyperthyroidism reduces fracture risk, but our results indicate that trials of subclinical hyperthyroidism treatment are needed to identify optimal management strategies in these individuals.
Age and gender-adjusted risks associated with subclinical hyperthyroidism (vs. euthyroidism)
| No. outcomes / participants | TSH <0.45 mIU/L vs. euthyroidism: HR (95 % CI) | TSH 0.10–0.44 vs. euthyroidism: HR (95 % CI) | TSH <0.10 vs. euthyroidism: HR (95 % CI) | P for trend * | |
|---|---|---|---|---|---|
| Hip fracture | 2′616 / 58′106 | 1.39 (1.10–1.76) | 1.37 (0.99–1.90) | 1.67 (1.21–2.30) | 0.002 |
| Non-spine fracture | 1′846 / 22′651 | 1.16 (0.95–1.41) | 1.03 (0.81–1.30) | 1.72 (1.11–2.68) | 0.02 |
| Clinical spine fracture | 292 / 21′312 | 1.54 (0.96–2.47) | 1.19 (0.65–2.20) | 3.57 (1.88–6.78) | < 0.001 |
| Any fracture | 2′378 / 27′041 | 1.28 (1.07–1.54) | 1.11 (0.89–1.39) | 2.01 (1.49–2.71) | < 0.001 |
CI, confidence interval; HR, hazard ratio; TSH, thyroidea-stimulating hormone * P for trend across TSH categories (euthyroidism 0.45–4.49 mIU/L, TSH 0.10–0.44 mIU/L, and TSH <0.10 mIU/L)
SUBCLINICAL THYROID DYSFUNCTION AND THE RISK OF FRACTURES: A META-ANALYSISChristina D. Wirth1; Manuel R. Blum1; Bruno R. da Costa2,3; Tinh-Hai Collet4; Marco Medici5; Robin P. Peeters5; Drahomir Aujesky1; Douglas Bauer6; Nicolas Rodondi1. 1Inselspital, Bern University Hospital, Bern, Switzerland; 2University of Bern, Bern, Switzerland; 3University of Bern, Bern, Switzerland; 4University Hospital of Lausanne, Lausanne, Switzerland; 5Erasmus Medical Center, Rotterdam, Netherlands; 6University of California, San Francisco, CA. (Tracking ID #1920246)
BACKGROUND: The prevalence of subclinical thyroid dysfunction is high and increases with age. Data on the association between subclinical thyroid dysfunction and fractures are conflicting. We aimed to assess the risk of hip and non-spine fractures associated with subclinical thyroid dysfunction among prospective cohort studies.
METHODS: Medline and Embase (1946 to May 2013) and reference lists of retrieved articles were searched without language restriction. Two reviewers screened articles and selected prospective cohort studies that measured thyroid function and followed participants to assess hip and non-spine fracture outcomes. Data were extracted using a standardized abstraction form. Adjusted estimates for hip and non-spine fractures from each study were pooled using a random effects model. For heterogeneity between studies, we assessed the Q statistic with a conservative p-value of 0.1 and the I2 statistic (I2 > 50 % indicating at least moderate statistical heterogeneity).
RESULTS: Among 1052 screened articles, we identified eight studies that met eligibility criteria. All eight were population-based cohorts and included a total of 53,181 participants with 2278 hip fractures and 6085 non-spine fractures. In random-effects models, the pooled adjusted hazard ratios (HRs) of participants with subclinical hyperthyroidism vs. euthyrodism were 1.27 (95 % confidence interval, 0.99–1.62) for hip fractures and 1.16 (1.00–1.34) for non-spine fractures. Pooled estimates for a TSH cutoff ≤0.1mIU/l increased the HR for hip fractures to 2.04 (1.50–2.79) and the HR for non-spine fractures to 1.99 (1.54–2.57). After excluding one study that only included participants taking thyroid hormone and did not measure free thyroxine level, the HRs for subclinical hyperthyroidism were 1.43 (1.03–1.97) for hip fractures and 1.20 (0.98–1.49) for non-spine fractures. For participants with subclinical hypothyroidism, pooled HRs were 1.22 (0.93–1.60) for hip fractures and 1.21 (0.85–1.71) for non-spine fractures, both with heterogeneity across studies (p < 0.10 and I2 > 50 %). In two studies of subclinical hypothyroidism with only thyroxine users, the HRs were 1.69 (1.24–2.29) and 1.77 (1.36–2.30), respectively.
CONCLUSIONS: Our systematic review indicates that subclinical hyperthyroidism may be associated with an increased risk of hip and non-spine fractures, particularly in those with a TSH concentration of 0.1mIU/l or less. Oversubstitution may explain the observed increased fracture risk for subclinical hypothyroidism among thyroxine users. Given the high prevalence of both osteoporosis and subclinical thyroid dysfunction in our aging populations, our findings have public health implications.
SUBSTITUTION OF VITAMINS AND SUPPLEMENTS FOR PRESCRIPTION MEDICINE AMONG VETERANSJennifer N. Goldstein1; Doris Arevalo2; Judith A. Long1; Jun Mao1. 1University of Pennsylvania, Philadelphia, PA; 2University of Illinois, Urbana-Champaign, IL. (Tracking ID #1936713)
BACKGROUND: Previous research suggests that patients may substitute vitamins and supplements for their prescriptions when medications are unaffordable. Since recent evidence has questioned the efficacy and safety of nutritional supplements, it is important to understand whether patients are using ineffective and potentially harmful products because conventional care is unaffordable. This study sought to determine the prevalence of substitution of vitamins and supplements for prescription medications among veterans and whether substitution is associated with prescription rationing due to cost.
METHODS: We conducted a cross sectional survey study among veterans at primary care clinics at the Philadelphia VA Medical Center. Substitution was measured by asking “in the past 3 months have you taken a dietary supplement to treat or prevent a health problem or condition instead of taking a prescription drug?” Prescription rationing was measured by asking “in the past 3 months have you ever taken less of any medication than prescribed by your doctor because of cost?” Both questions were obtained from the National Health Interview Survey from the CDC. We performed bivariate and multivariate analyses with substitution as the dependent variable to determine the relationship between substitution and prescription rationing. Other variables included in the multivariate model were age, sex, race, educational level, and copay-exempt status at the VA.
RESULTS: Among the 275 veterans who completed surveys, 206 (75 %) used vitamins, supplements and herbs, and of those, 46 (22 %) substituted. Hyperlipidemia, back pain/arthritis and anxiety/depression were the most common conditions for which substitution was performed (See Figure). In the multivariate logistic regression, veterans who rationed their prescriptions due to cost were more likely to substitute (AOR 3.57, 95 % CI 1.38–9.25).
CONCLUSIONS: Veterans who ration prescriptions due to cost are more likely to substitute vitamins and supplements for prescription medications. This raises concerns that in spite of the low cost or free prescriptions provided by the VA, veterans may still experience financial strain and make treatment choices that could negatively impact their health. Since most Americans do not receive highly subsidized health care, our findings likely underestimate the magnitude of substitution due to cost within the general population.
Conditions for which Veterans use Vitamins and Supplements Instead of Prescription Medication
SUCCESS OF A FACULTY DEVELOPMENT PROGRAM FOR REMEDIATING CLINICAL TEACHERSThomas J. Beckman; Staci Lee; Mark Lee; Darcy Reed; Andrew J. Halvorsen; Elie Berbari; Furman S. McDonald. Mayo Clinic, Rochester, MN. (Tracking ID #1935708)
BACKGROUND: The remediation of medical learners has been widely studied, but there has been limited research on the remediation of clinical teachers. The objective of this study was to determine whether a faculty development program could improve the evaluations of underperforming clinical teachers in an internal medicine residency program.
METHODS: 123 teachers completed faculty development at the Mayo Clinic from 2009 to 2012. The faculty enhancement and education development program (FEED) consists of six one-hour sessions that are taught by experienced Mayo Clinic faculty. These sessions address the following competencies: asking questions, diagnosing learners, giving feedback, utilizing teaching frameworks, recognizing learning styles, and providing clinical supervision. Resident-of-faculty Mayo teaching effectiveness (MTE) scores have previously demonstrated content, internal structure and criterion validity. Teachers were grouped into the top 80 % or the bottom 20 %, according to baseline MTE scores. Scores from the all the MTE items were combined to form an overall score ranging from 1 to 5. Mixed linear models were used to compare these groups regarding changes in MTE scores after completion of FEED. Results were adjusted for teacher age, gender, medical specialty, academic rank, and teaching awards.
RESULTS: Of the 123 faculty members in this study, most (N,%) were males (82, 67) in non-procedural specialties (88, 72), and they averaged 9 years on faculty and 45.4 years of age. A small proportion of faculty members had received major teaching awards (12, 10), and only a minority held advanced ranks of associate professor or professor (29, 24). For all faculty combined, the adjusted MTE scores (mean; standard error) improved from baseline (3.80; 0.04) to completion of the FEED intervention (3.93; 0.04; p < 0.0001). However, the bottom 20 % of teachers had a significantly greater improvement in scores than the top 80 % (score-change difference = 0.166; p < 0.0001). In multivariate models, there were significant associations (β; p-value) between changes in scores after exposure to FEED and the following variables: bottom 20 % versus top 80 % of teachers (0.166; p < 0.0001), age (−0.007; p < 0.0001), procedural versus non-procedural specialty (−0.119; p < 0.0001), academic rank (β range: −0.166–0.263; p < 0.0001), and receiving a teaching award (0.074; p < 0.0001). There were no significant associations for years on faculty (tenure) or gender.
CONCLUSIONS: We describe a faculty development initiative that was effective at remediating underperforming clinical teachers in internal medicine. These findings have implications for improving the quality of graduate medical education programs.
SUFFERING BURNOUT: THE INTERNAL MEDICINE RESIDENT’S QUALITATIVE EXPERIENCEKate Jennings1,2; Chad Stickrath1,2; Ravi K. Gopal1,2. 1Veterans Affairs Administration, Denver, CO; 2University of Colorado Denver School of Medicine, Aurora, CO. (Tracking ID #1939433)
BACKGROUND: Burnout is a response to work related stress characterized by depersonalization, emotional exhaustion and a sense of loss of personal efficacy. Burnout affects approximately 67 % of internal medicine residents. Prior studies have detailed the impact of burnout on the professional, personal and social lives of physicians. The literature has not provided examples of how residents experience burnout in their daily lives. We sought to describe how burnout influences the experience of Internal Medicine (IM) residents and how it impacts their view of themselves, their relationships and their patient care.
METHODS: As a part of an end-of-year survey, IM residents were asked to free list the most common behaviors that occur when they or one of their fellow residents are burned out. Residents were allowed to list up to three behaviors and were not limited by space or characters. Through a qualitative content analysis of responses, we derived a codebook using both deductive and inductive code development. Deductive codes were derived using two systematic reviews of burnout in medical residents. To capture the nuances within the codes, we used inductive code development to expand the original deductive codes. The final definitions of the deductive and inductive codes and subcodes were tested using portions of the dataset. A second researcher (KJ) read through the responses and further revised the codebook. The final codebook was applied to the entire qualitative dataset and major themes were derived.
RESULTS: Among the 166 residents that were invited to participate, 108 (65.1 %) subjects completed the survey. Of the respondents, 86 % listed at least one behavior and 49 % listed 3 behaviors. Two hundred sixty-five individual responses were collected. “Attitudes and behaviors” was the most common theme, with the subcode of “negative state of being” as the most frequent (13.2 %) with responses such as “negative, bitter, angry, bad attitude and irritable”. The “interactions with colleagues” theme with the subcodes of “negative behavior” (12.8 %) was frequent, and responses detailed “arguing with other residents, talking negatively about other residents, becoming ‘mean’ towards peers, and aggressive pimping”. A theme of “patient care” (9.8 %) emerged with residents stating that burnout causes “neglectful care, negative attitudes towards patients and insufficient time spent with patients.” The idea of poor patient care was followed by themes of “cutting corners” (9.4 %) with behaviors including “shoddy work, missing details, not prepared for rounds, mistakes in orders, and poor medical decision making.” Additional themes of the resident responses detailed the impact of burnout on “teaching and learning”, “self-evaluation” and “career satisfaction”.
CONCLUSIONS: Burnout is very common among IM residents and influences their experiences during residency. Burnout negatively impacts a resident”s sense of well-being, their relationships with other residents and the perception of the care they provide. Further, residents correlate burnout with cutting corners in patient care, demonstrating specific ways that patient safety and outcomes may be adversely affected by the internal medicine resident’s experience of burnout.
SUPPORT FOR A SINGLE PAYER NATIONAL HEALTH INSURANCE PROGRAM SIX YEARS AFTER MASSACHUSETTS HEALTH CARE REFORM: VIEWS OF SAFETY NET PATIENTSSonali Saluja1,2; Leah Zallman4,1; Rachel Nardin2; David Bor2,1; David Himmelstein3; Steffie Woolhandler3; Danny McCormick2,1. 1Harvard Medical School, Boston, MA; 2Cambridge Health Alliance, Cambridge, MA; 3City University of New York School of Public Health, New York, NY; 4Institute of Community Health - Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1936229)
BACKGROUND: Prior to health care reform, polls showed broad support for a universal, government-run national health insurance program (NHI), sometimes called a “single payer” system. In 2006, the state of Massachusetts implemented health insurance reform that became the model for the Affordable Care Act (ACA). It included a Medicaid expansion, an insurance exchange offering subsidized and unsubsidized private health insurance and individual and employer mandates for coverage. The MA reform was fully implemented by 2008. Little is known, however, about which financing system is preferred by Massachusetts residents after 6 years of experience with the reform.
METHODS: Between August 5, 2013 and December 19, 2013, we conducted face-to-face structured interviews with a sample of 867 patients presenting to three emergency departments at safety net health providers in the greater Boston, Massachusetts area. We included patients aged 18–64 who had only one insurance type and spoke any of the four major local languages—English, Portuguese, Spanish or Haitian Creole. We excluded the most severely ill patients—those with an Emergency Severity Index of 1 (1 to 5 point scale). The overall survey response rate was 82.4 %. We asked respondents whether they supported the current insurance system in Massachusetts or an alternative NHI system run by the government and paid for by taxes. In addition to collecting demographic information, we asked respondents about their knowledge, satisfaction and concerns about affordability with their current health plan. We calculated the overall proportion of respondents supporting NHI, and evaluated predictors of such support using chi square tests.
RESULTS: Overall, 73.0 % (548/751) of survey participants preferred NHI to the reformed MA health system (p < 0.0001). Preference for NHI did not vary significantly by age, race, education or income group, although women (76.1 % [328/431]) were more likely to support it than men (68.6 % [218/318]; p = 0.02). Uninsured respondents were the most supportive of single payer NHI (84.0 %), followed by the privately insured (71.7 %) and the publically insured (70.7 %; group p-value = 0.02). Among insured respondents, 87.8 % of those who were dissatisfied overall with their plan supported NHI compared to 70.1 % of those who were somewhat or very satisfied (p = 0.009). Similarly, 82.5 % of respondents who were dissatisfied with their plan’s affordability supported NHI, compared with 69.8 % of those who were satisfied (p = 0.03). Patients who experienced a delay in any medical care due to cost were more likely to favor NHI (81.0 % versus 70.8 %; p = 0.01).
CONCLUSIONS: A majority of Massachusetts safety-net hospital patients, a group encompassing key populations targeted by the reform, favor NHI over the existing system. Current national health care financing debates among politicians and health policy experts focus almost exclusively on the ACA. Our findings from Massachusetts suggest there is a potential disconnect between the preferences of individuals who have experienced health reform and the narrow debate focused on the ACA - implying a broader discourse that includes a single payer health system is warranted.
SUPPORTING COORDINATION OF MEDICAID HOME- AND COMMUNITY-BASED SERVICES: A DEFINITIONAL FRAMEWORK FOR INDIVIDUAL ASSESSMENTS FOR SENIORS AND PERSONS WITH DISABLING CONDITIONS USING NON-INSTITUTIONAL LONG-TERM CARELhasa Ray1; Kathleen H. Wilber4; Robert Newcomer5; Debra Saliba2,3. 1University of California, Los Angeles, Los Angeles, CA; 2University of California, Los Angeles, Los Angeles, CA; 3Greater Los Angeles Veterans Affairs, Los Angeles, CA; 4University of Southern California, Los Angeles, CA; 5University of California, San Francisco, San Francisco, CA. (Tracking ID #1938056)
BACKGROUND: For low-income seniors and people with disabling conditions, Medicaid-funded home and community-based services (HCBS) ideally function in tandem with medical services to support independent living, enhance quality of life and reduce institutionalization. Too often, however, HCBS are provided through a disjointed array of programs that require multiple, redundant eligibility determination and service allocation processes. This lack of coordination is burdensome for recipients and inefficient for payers and service providers. For this reason, a number of states across the U.S. have initiated efforts to implement eligibility and care plan assessment processes that are integrated across Medicaid and state-funded HCBS programs. Despite increased recognition of the importance of creating standardized assessment systems for HCBS, no formal definitional framework for the components of assessment has been proposed. This project aimed to support the state of California’s efforts to develop uniform assessment processes for its Medi-Cal HCBS programs by developing a definitional framework based on literature review and input from experts in the field.
METHODS: To develop a definitional framework that codifies the essential components of standardized assessment for Medicaid HCBS, the project team reviewed the peer-reviewed and grey literature. We also examined Medicaid waiver and state-plan documents for 5 states with developed standardized assessment systems identified by California program leads as potential learning models for California. From this initial work we constructed a preliminary framework that we further refined using a group process with 8 departmental leaders within California’s Department of Health Care Services, Department of Social Services and Department of Aging who are familiar with existing Medicaid and state-funded HCBS systems in the state. Next, we used the framework to gather information about the components of evaluation and enrollment currently in use through key informant interviews with departmental leaders in the 5 comparator states (Michigan, New York, Pennsylvania, Texas, and Washington). Based on these interviews and feedback, we refined the framework further so that it provided clear and consistent nomenclature to describe practices in use by states.
RESULTS: Review of the peer and grey literature failed to identify an existing recognized framework. The subsequent framework development process resulted in the identification of a series of relatively sequential stages of comprehensive assessment for program eligibility, service needs, and implementation of the plan of care. The final framework we developed is provided in the table.
CONCLUSIONS: This framework provides stages and definitions that can assist state leaders, policymakers, and others involved in designing, refining, or evaluating standardized assessment systems for Medicaid HCBS. This common framework can also improve communication among stakeholder groups and facilitate program or state comparisons by defining a nomenclature that can be applied across settings. Standardized assessment of an individual’s program eligibility, need for services, and care plan adequacy is a fundamental tool for bringing coherence and efficiency to an often fragmented system for long term services and supports. Standardized assessment is compelling for several reasons. Coordinated assessment systems can facilitate consistent and reliable identification of an individual’s met and unmet need for HCBS. At the program and provider level, uniformity could enhance information exchange across providers and programs, improving efficiency and promoting partnership between multidisciplinary teams. At the state level, a common set of assessment stages across departments and programs offers the potential to better understand the populations requesting services, to ensure resources are equitably distributed, and to improve planning across programs. Finally, standardized systems could contribute to better monitoring of quality and health outcomes. Standardizing HCBS delivery systems requires that fundamental definitions for system components are formalized. This framework provides the basis for designing and evaluating service delivery systems that maximize efficiency, communication, and coordination for Medicaid and state-funded HCBS.
< Components of Comprehensive Assessment/b>
| Stage | Definition |
| Preliminary screen | Initial contact with applicant seeking to gain entry into an eligibility process or waiting list. Identifies who will go on to a more in-depth assessment. |
| Eligibility Determination | Determination that eligibility criteria for a specific program(s) are met. A needs assessment is typically accomplished as part of this stage in assessment. Results may also determine prioritization of care or position on program waiting lists. |
| » Functional Eligibility | For HCBS 1915(c) waiver programs, establishes that nursing home level of care criteria are met. Sometimes referred to as the \“level of care determination. |
| » Financial Eligibility | Establishes that financial criteria are met. |
| Needs Determination | Identification of specific service needs. |
| Care Planning | Development of a plan of service delivery that takes into account an individual’s needs and goals of care, existing sources of care and support, and resources available through a range of formal programs and informal supports. |
| Service Authorization | Establishing a budget or allocating service hours. May be generated by algorithms that rely upon information gathered during needs assessment or through the development of the care plan, or may be accomplished through a separate process. |
| Service Coordination, Case Management | Determination that services prescribed by the care plan match identified needs and services delivered, and that service delivery is timely. |
| Quality Monitoring | Includes reviews of completed assessments or aggregated data, as well as practices that ensure that data collection is consistent across assessors. |
| Reassessment | Repeated assessments accomplish one or more functions: (1) To verify continued eligibility (functional and/or financial), (2) To verify effectiveness of the care plan, and (3) To assess changing needs. Reassessments are typically conducted quarterly to annually or when there is a change in status. |
SURGICAL AND MEDICAL HOSPITALIZATIONS: CAN THE SAME STRATEGIES BE USED TO DETECT THEIR PHYSIOLOGICAL DETERIORATION?Santiago Romero Brufau; Matthew G. Johnson; James M. Naessens; Bruce W. Morlan; Joel A. Hickman; Jeanne M. Huddleston. Mayo Clinic Rochester, Rochester, MN. (Tracking ID #1940758)
BACKGROUND: It is estimated that about 150,000 cardiorespiratory arrests (CRA) occur in US hospitals every year, with a survival to discharge less than 20 %. But patients usually show signs and symptoms of deterioration hours or days before. Rapid Response Systems (RRS) were designed to improve the detection and intervention upon a deteriorating patient, and their acceptance and use has increased in recent years. They rely on accurate detection of acute physiological deterioration (APD). Published Early Warning Scores (EWS) have been proposed to help in the detection of APDs and have been evaluated in heterogeneous populations, but the same score is calculated for all patients irrespective of their frailty or whether they are surgical or medical. Predictive capacity of EWS may be different in medical vs surgical, or in frail vs non-frail patients.
METHODS: We created a time-stamped database including all discharges from January 2010 to December 2011 from two tertiary hospitals in Minnesota totaling approximately 1,500 general care (non-ICU) beds. Patients were categorized as surgical or medical based on whether they had been to the operating room during their hospitalization, and as frail or non-frail based on their Braden score. Outcomes were unscheduled transfers to the intensive care unit (ICU), activation of the RRS, and calls for cardiorespiratory resuscitation (code). Alerts that would have been issued using the published early warning scores were considered accurate if they predicted an outcome in the following 12 h. Predictive capacity of the most widely used Early Warning Scores (NEWS, ViEWS, MEWS, GMEWS, SEWS, Worthing and Kirkland) was calculated this way and compared between different groups of patients according to their Braden score and whether they were considered medical or surgical.
RESULTS: Our final dataset included more than 6,000,000 data points from 34,898 unique patients. There were 57 % surgical hospitalizations, and a total of 3,328 patients had a Braden score of 12 or less. There were There were 3,517 outcome events: 1,865 RRS activations, 203 codes and 1,449 unscheduled transfers to the ICU. All evaluated scores performed better (higher positive predictive value and sensitivity) on medical than on surgical patients. All scores had a positive predictive value below 25 %. Grouping the patients by Braden score had a heterogeneous effect on the predictive performance of the evaluated EWS.
CONCLUSIONS: Evaluated EWS show a higher predictive performance in medical than in surgical patients. Having different scores for medical and for surgical patients may allow for the improvement of their predictive performance. This suggests that different strategies should be used for the detection of acute physiological deterioration in surgical and medical patients.
SURROGATE MARKERS, COMPOSITE END-POINTS, DISEASE-SPECIFIC MORTALITY, OR ALL-CAUSE MORTALITY? A SURVEY TO UNDERSTAND THE RELATIVE VALUE CLINICIANS PLACE ON DIFFERENT OUTCOMESTanner Caverly1; Allan V. Prochazka2; Rodney A. Hayward1; Daniel Matlock2. 1University of Michigan Medical School, Ann Arbor, MI; 2University of Colorado, Aurora, CO. (Tracking ID #1939177)
BACKGROUND: When weighing the importance of a risk reduction found in a clinical trial, clinicians and patients need to consider the clinical significance of what was reduced. Improvements in surrogate and composite outcomes, for example, do not necessarily imply meaningful improvement in patient-oriented outcomes. Improvement in all-cause mortality is ideal, since it reflects the overall effect of therapies on mortality, but most trials are not large enough to assess this outcome. We conducted a survey that varied the type of benefit observed in hypothetical drug trials to evaluate the extent to which clinician perceptions changed based on the outcome evaluated. We hypothesized that perceptions would be relatively insensitive to the type of outcome reported in the hypothetical trials.
METHODS: Our survey consisted of 4 scenarios that were identical except for differences in the type of outcome: surrogate, composite, disease-specific mortality, or all-cause mortality (Table 1). Each participant received all 4 scenarios which were separated by unrelated questions in order to minimize direct comparisons. They were asked to rate the extent to which each scenario provided proof that the new drug might help people. Answers were on a 1–10 risk perception scale (ranging from 1 = no proof to 10 = good proof). Surveys were distributed during educational conferences to 3rd and 4th year medical students at a single academic institution, to internal medicine residents at two institutions, and to faculty in the division of general internal medicine at one institution. In addition, a national group of clinician-researchers with evidence based medicine expertise took an online version of the survey. We analyzed the distribution of responses for the 4 scenarios in two ways: 1) using analysis of variance to identify differences in the mean response between scenarios and 2) using simple descriptive statistics to evaluate how participants rated each question relative to their responses on the other 3 questions. We also used analysis of variance to examine how differences between mean responses on the all-cause mortality question and the disease-specific mortality question varied by level of training.
RESULTS: We received 546 completed surveys for analysis (response rate: 87 % for medical students [273/313]; 80 % for internal medicine residents [148/185]; 67 % for general medicine faculty [118/175]; and 41 % for the group of experts [7/17]). On average, participants rated the composite outcome as more valuable than the other types of outcomes (Table 1). Overall, 51 % rated improvement in a surrogate marker as equal to or more valuable than an improvement in all-cause mortality, and 79 % rated improvement in a composite outcome containing a surrogate marker as equal to or more valuable than improvement in all-cause mortality. Eighty percent rated improvement in stroke-related mortality as equal to or more valuable than an improvement in all-cause mortality. Mean differences in responses on the all-cause mortality question and the disease-specific mortality question varied by level of training (medical students rated improvement in stroke mortality an average of 1.5 points higher than improvement in all-cause mortality; residents 1.2 points higher; general medicine faculty 0.6 points higher; and experts 1.7 points lower).
CONCLUSIONS: Many clinicians in our sample over-value improvement in surrogate and composite outcomes and under-value improvement in all-cause mortality. This raises concerns that clinical decisions may not reflect the actual value of the intervention, especially if clinicians are exposed to information that emphasizes clinically less important outcomes.
SUSTAINABLE PATIENT-CENTERED MEDICAL HOME TRANSFORMATION IN SAFETY-NET CLINICS: LESSONS LEARNED FROM THREE CASE STUDIESReshma Gupta1; Edward Wagner2; Katie Coleman2. 1University of Seattle, Washington, Seattle, WA; 2McColl Center of Health Care Innovation, Group Health, Seattle, WA. (Tracking ID #1933680)
BACKGROUND: Although only 6 years have passed since the Patient-centered Medical Home (PCMH) was first proposed to reinvigorate primary care, thousands of practices have engaged in transformation activities. However, practice transformation has proven to be difficult and requires wholesale changes to the practice. The Commonwealth Fund sponsored a 5 year demonstration project, the Safety Net Medical Home Initiative (SNMHI), to help clinics become PCMHs. Despite the high level of support made available to each practice, practices varied widely in their transformation success. More intensive study of three successful SNMHI practices confirmed lessons learned in the larger project about: what motivates practices to demolish old ways of organizing and delivering care; what changes enable practices to see a better future and sustain the effort; and how do successful practices go about making changes?
METHODS: The goal of the SNMHI was to develop and test a replicable model for supporting PCMH transformation among 65 safety net practices in five states. Participating practices in each state were supported by a Regional Coordinating Center (RCC) that employed medical home facilitators (MHFs) who worked closely with individual clinics. Transformation was guided by an explicit PCMH model that consisted of eight high level areas for change process (Wagner). Measurement of the transformation process involved multiple instruments including the Patient-centered Medical Home Assessment (PCMH-A), a 33 item self-assessment (Daniels). To study the transformation process more intensively, we selected three practices of different sizes, geographic locations, and organizational structures among those that had made major progress in becoming PCMHs as measured by change in PCMH-A scores. The sites selected included clinic A (an urban FQHC in Oregon), clinic B (a small single-site rural clinic in Colorado), and clinic C (multi-site urban and rural FQHC in Idaho). Data collected included bi-annual PCMH-A and Key Activity Checklists, MHF bi-annual evaluation, PCC narrative reports about each practice, and clinical data from each site. To gain a deeper understanding of the transformation process, we identified individuals at each practice who played key roles in practice transformation. We then conducted semi-structured one hour long qualitative interviews either in person or by phone during February and March, 2013 with these practice leaders. We addressed domains including motivation to change, initial approach to change, role of leadership, key beneficial approaches to change, key barriers to change, and reflection on change process. Data analysis involved coding transcriptions of interviews and identifying themes within and across cases.
RESULTS: The mean overall PCMH-A score across the 65 sites rose from 7 to 9 (out of 12) over 3 years. The scores for clinics A, B, and C rose from 7.0 to 9.0, 5.3 to 10.0, and 6.9 to 9.3, respectively. Prior to the SNMHI, Clinic A had a long history of practice transformation initiatives, but progress had stalled. Clinics B and C had not previously been engaged in practice transformation. Following involvement in the SNMHI all three clinics generated the will or motivation to change, found attractive ideas to guide change, and developed a strategy and infrastructure that facilitated the execution of system changes. Medical and administrative leaders made transformation an organizational priority and visibly drove change. Intrinsic motivators such as concerns about quality of care or community reputation had greater impact on these clinics than extrinsic motivators such as external payments and meeting recognition standards. Ideas for change came primarily from exposure to faculty and other sites in SNMHI learning sessions, or visiting other clinics farther along in the transformation process. We found that practices were able to execute sustained transformation once their leaders were committed to the transformation process, and a trusted performance measurement system and an explicit approach to studying and testing changes in work processes were in place. The sequence with which clinics made the changes to become a PCMH was important. Clinics that hadn’t formally linked patients with specific providers or established well-functioning practice teams found it difficult to provide optimal coordinated care.
CONCLUSIONS: Practice transformation is challenging; however, we hope that it will help to describe how high-performing clinics developed and used will, ideas, and execution to transform themselves. The will for becoming a PCMH must be felt among staff at all levels, and the ideas motivating change were expedited by involvement with transformation initiatives and exposure to more advanced practices. The execution of successful practice transformation built upon a foundation of engaged leaders, available performance measures, and an explicit strategy for testing and implementing changes.
SYMPTOM BURDEN IN PATIENTS HOSPITALIZED FOR DECOMPENSATED HEART FAILURERabeea Khan1; Shelli L. Feder3; Nathan Goldstein2; Sarwat Chaudhry1. 1Yale School of Medicine, New Haven, CT; 2Mount Sinai School of Medicine, New York City, NY; 3Yale University School of Nursing, New Haven, CT. (Tracking ID #1930389)
BACKGROUND: Heart failure is one of the most common reasons for hospitalization among older adults, and is the leading cause of readmissions within 30 days after hospital discharge. Consequently, there is great interest in developing strategies to reduce hospital utilization in this large and growing patient population. Aside from the classic heart failure symptoms of dyspnea and fatigue, other symptoms that have been reported in patients with heart failure include pain, decreased appetite, anxiety, as well as difficulty sleeping. These symptoms may be amenable to treatment, and as such, patients hospitalized with heart failure may benefit from intensive symptom management in the form of palliative care. However, there is limited data in the heart failure population about symptom burden both during hospitalization and shortly after hospital discharge, as well as patients’ perceptions of palliative care.
METHODS: Patients hospitalized with a primary diagnosis of decompensated heart failure at Yale-New Haven Hospital were enrolled in this prospective cohort study. Exclusion criteria included non-English speaking, severe cognitive impairment, and ongoing hemodialysis. Patients were interviewed about their symptom burden using the Edmonton Symptom Assessment System (ESAS) and the Patient Health Questionnaire (PHQ-8) during their hospital admission (“baseline interview”). A follow-up telephone interview was conducted seven to days after hospital discharge, assessing symptom burden using the same standardized instruments. Patients were also questioned about their existing knowledge of palliative care, and then—after a brief, standardized explanation of the goals of palliative care—patients were queried about their interest in receiving palliative care services.
RESULTS: Thirty-five patients were enrolled in the study from September–December 2013. Their mean age was 71.3 years (SD 13.5 years) 54 % were female, and 71.4 % had NYHA class III or IV heart failure. The most frequent symptoms reported during the baseline interview were tiredness (82.9 %), drowsiness (82.9 %), shortness of breath (62.9 %), anxiety (57.1 %) and pain (45.7 %). The most frequent symptoms reported in the follow-up interview were tiredness (93.9 %), drowsiness (81.8 %) shortness of breath (81.8 %), anxiety (57.6 %) and pain (57.6 %). While only 14.3 % of patients had heard of the term “palliative care,” after a brief, standardized explanation of what palliative services are designed to do, 45.7 % were interested in receiving palliative care services while in the hospital.
CONCLUSIONS: Patients hospitalized for heart failure experience a high burden of symptoms, including not just dyspnea and fatigue but also anxiety and pain. These symptoms are common during hospitalization, but the majority of patients experience troublesome symptoms shortly after discharge as well. Given that symptoms frequently drive health care utilization, integration of palliative care into routine heart failure management is a promising strategy to reduce hospital utilization.
TACKLING HEALTH EQUITY: LEADERSHIP’S PERCEPTIONS OF HEALTH CARE PERSONNEL AND ORGANIZATIONSBrooke A. Cunningham1; Pamela J. Johnson1,2; Todd Rockwood3. 1Medica Research Institute, Minnetonka, MN; 2University of Minnesota School of Public Health, Minneapolis, MN; 3University of Minnesota School of Public Health, Minneapolis, MN. (Tracking ID #1938695)
BACKGROUND: Demographic shifts, health care reform, value-based reimbursement, and increased interest in population health are encouraging health systems to act on equity. Although Minnesota ranks high nationally for overall health care quality, it also has high levels of health disparities. This study uses survey methods to examine the perceptions of health care leaders regarding the engagement of health care personnel and delivery systems with health equity.
METHODS: Six health systems in Minnesota invited their senior leaders to a health equity forum in the summer of 2013. As part of the program evaluation, invitations to complete a web-based survey were sent to those who registered for the conference. Respondents were asked to rate senior leaders, mid-level managers, and front-line providers’ and staff’s awareness of health inequities, engagement in addressing health disparities, and sense of “safety” discussing racial and ethnic disparities. They were also asked to rate the factors that contribute to health disparities and the effectiveness of their organizations in addressing those factors. Paired t-tests were used to compare respondents’ perceptions of the engagement of employee groups and health care organizations respectively with health disparities.
RESULTS: The response rate was 41 % (n = 37). Most respondents were white (89 %), female (59 %), had graduate training (86 %), and attended the health equity forum (95 %). Respondents perceived senior leaders to be significantly more informed about health equity, more engaged with addressing disparities, and to feel safer discussing racial/ethnic disparities than mid-level managers and front-line providers and staff respectively. Regarding health system priorities, addressing disparities ranked last, behind 1) reducing medical error; 2) reducing costs/improving customer service; and 3) improving performance measures. Respondents perceived social determinants to be a significantly larger contributor to disparities than any other factor (i.e., individual behavior, health care systems, health insurance, and access barriers). However, compared to these other factors, they reported health systems to be least effective at addressing social determinants of health.
CONCLUSIONS: Leaders from six health systems in Minnesota perceived organizational engagement with health equity to vary by occupational tier. They perceived social determinants of health to be the greatest contributor to disparities but reported that health systems were least effective at addressing them. This data suggests that health system leaders may need to further promote health equity goals with their mid-level managers and front-line providers and staff. This will require identifying and reducing barriers to the uptake of health equity as an organizational priority. If health care leaders highlight how health equity intersects with other organizational goals, promoting health equity may be seen as facilitating the achievement of, rather than competing with, other priorities.
TARGETED IMPROVEMENTS IN HIV COUNSELING AND TESTING SERVICES ON A LARGE UNIVERSITY CAMPUS IN DURBAN, SOUTH AFRICABenjamin I. Bearnot1,2; Nomonde Magantolo3; Ayesha B. Kharsany2. 1Massachusetts General Hospital, Boston, MA; 2University of KwaZulu Natal, Durban, South Africa; 3University of KwaZulu Natal, Durban, South Africa. (Tracking ID #1923142)
BACKGROUND: HIV counseling and testing (HCT) is a requisite gateway to evidence-based prevention and treatment strategies. Despite high levels of knowledge about HIV and modes of transmission, many individuals in South Africa remain untested. In a 2009 report from the South African Higher Education HIV & AIDS Programme, 58 % of higher education students in the South African province of KwaZulu Natal (KZN) have never been tested for HIV. On one flagship university campus, HCT had fallen to just a 312 students at the campus clinic in 2011, approximately 1 % of the student body. With the high prevalence of HIV in the overall KZN community and low levels of HIV status knowledge by university students in KZN, this implementation science project was designed to increase the number of individuals accessing HCT in a tertiary education setting, and to help identify subsequent health services they require.
METHODS: The University of KwaZulu Natal HIV/AIDS Programme provides an integrated package of counseling, testing, and treatment services for university students and staff on all UKZN campuses. In 2012, we designed and implemented a multi-faceted improvement project to encourage students and their networks of friends to get tested for HIV on the Howard College UKZN campus. This included implementation of drop-in testing not requiring an appointment, peer educator sessions led by university students on student requested topics, and a Value in Prevention (VIP) communications campaign organized around weekly HIV testing events in the centrally-located campus center. The study protocol was approved by the Biomedical Research Ethics Committee of the Nelson R. Mandela School of Medicine, Faculty of Health Sciences, UKZN.
RESULTS: In the first 14 weeks of this program, 1,279 students and faculty received HCT services at 3 separate locations on campus. This represents a 4-fold increase in the number of individuals tested on the university campus in the whole of 2011. Twenty-seven individuals were newly diagnosed with HIV (seroprevalence 2.1 %). Of a sample of 298 students surveyed, 252 (85 %) were seen by a counselor in less than 15 min after arriving, and 298 (100 %) received HIV testing after pre-test counseling. Ninety-five individuals (31.8 %) were referred to HCT by a friend. The most common requests for further services were for contraception/pregnancy testing, further STI testing and treatment, and medical male circumcision.
CONCLUSIONS: HIV testing uptake spiked dramatically when HCT services were implemented in a manner that was driven by student preferences. HIV prevalence was found to be low in this community, representing an important site for scaling up of HIV prevention interventions. As a result of this preliminary work, the university has committed to employ counselors to provide drop-in HCT at the campus clinics and HIV Support Units at each of the university’s undergraduate and graduate campuses. Further work is needed to harness peer-recruitment strategies and social networks to bring higher risk students and their sexual partners for HIV prevention and testing.
TC/HDL AND LDL/HDL RATIOS ARE BETTER MEASURES FOR CHOLESTEROL MONITORING ASSESSMENTOsamu Takahashi1,2; Sachiko Ohde1; Gautam A. Deshpande1. 1St. Luke’s Life Science Institute, Tokyo, Japan; 2St. Luke’s International Hospital, Tokyo, Japan. (Tracking ID #1940025)
BACKGROUND: Cholesterol screening is important to identify those at risk of cardiovascular disease. Little information is available on subsequent monitoring including frequency and timing of re-screening and optimal measure to use. We aimed to estimate the long-term between-person variation (“signal”) and short-term within-person variation (“noise”) of the different lipids measures and evaluate the best measure and the optimal interval for lipid re-screening.
METHODS: We conducted a retrospective cohort study from 2005 to 2008. We enrolled all people consecutively admitted to our Centre for Preventive Medicine for the health checkup program at St. Luke’s International Hospital in Tokyo, Japan. Annual measurement of the serum total cholesterol (TC), low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, non-high-density lipoprotein (non-HDL) were measured, calculating TC/HDL and LDL/HDL ratios. We estimated the ratio of “signal” to “noise” for each measure adjusting for age, gender, and body mass index (BMI) using random-effect model.
RESULTS: 15,810 apparently healthy Japanese adults not taking cholesterol-lowering medications at baseline had annual check-ups over 4 years. The mean age of participants was 49.3 years old (SD: 12.2, range: 21 to 92) and 53 % of patients were male; mean BMI was 22.5 kg/m2 (SD: 3.2). Average TC level at baseline was 204 mg/dl (SD, 34 mg/dl). Short-term within-person variations of TC, LDL, non-HDL, HDL, TC/HDL, and LDL/HDL were 186 (coefficient of variation (CV), 6.7 %), 137 (CV: 10 %), 154 (CV: 8.8 %), 27 (CV: 8.3 %), 0.09 (CV: 8.5 %) and 0.06 (CV: 12 %), respectively. The ratio of signal to noise at 3 years was largest for TC/HDL (1.1), followed by LDL/HDL (1.1), non-HDL (0.86), LDL (0.70), TC (0.65), and HDL (0.53), suggesting that cholesterol ratios are more sensitive for re-screening than single measures.
CONCLUSIONS: The signal-to-noise ratios of standard single lipid measures (TC, LDL, non-HDL and HDL) are weak over 3 years and decisions based on these measures are potentially misleading. The ratios, TC/HDL and LDL/HDL, appear to be better measure for monitoring assessments. The lipid re-screening interval should be greater than 3 years for those not on cholesterol-lowering drugs.
TEAM HUDDLES AS WORKPLACE LEARNING OPPORTUNITIES: AN OBSERVATIONAL STUDYBridget OBrien1; Terry Keene2; Rebecca L. Shunk1,3. 1Univ of California, San Francisco, San Francisco, CA; 2San Francisco VA Medical Center, San Francisco, CA; 3San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1939002)
BACKGROUND: Team huddles, or brief meetings at the beginning of clinic among team members, are recommended as a key element of high functioning primary care teams. Huddles seem like a straightforward communication process to coordinate patient care, but as a hub for teamwork they require many of the same complex interpersonal and communication skills associated with teamwork in other contexts. In an era when much emphasis is place on training for interprofessional collaboration and team-based care, we identified team huddles as a potential site for workplace learning related to teamwork. In this study, we identify and describe learning opportunities afforded by team huddles.
METHODS: We conducted an observational study of five academic primary care teams in a San Francisco VA primary care clinic from July to December, 2013. Team huddles include an internal medicine resident, nurse practitioner student, registered nurse (RN), licensed vocational nurse (LVN), clerk, and, on some teams, a psychologist, pharmacist, or social worker. A huddle coach (an MD or NP preceptor) also attends the huddle on a regular basis. Huddles are scheduled for 15 min once or twice per week. One investigator conducted all 52 observations and documented verbal and non-verbal communication in each huddle. The study team analyzed the data using a grounded theory approach. During the open coding phase, we independently identified examples of learning opportunities (content and who initiated the opportunity) and then discussed these to achieve consensus understanding. After reviewing and discussing 5 notes, we reviewed a consolidated list of all learning opportunities and developed a set of categories which we then used to code all notes. In the axial coding phase we looked for patterns within and across teams as well as over time.
RESULTS: We found learning opportunities in six content areas: people (learning about colleagues and patients), clinical (disease and diagnostic processes, medications), relationships (skills such as support, negotiation), team process (schedules, how to communicate, leadership), systems (how things get done), and the organization (how things work in the VA). Most of these opportunities occurred unintentionally and spontaneously, through routine huddle dialogue initiated by various team members such as raising questions, explaining a process or situation, and problem solving. The main exception was coaches. Coaches tended to create intentional, explicit learning opportunities by providing feedback to the team, modeling communication strategies, and raising questions that prompted discussion / clarification among the team. The majority of the content focused on systems issues. Earlier in the year, when residents and NP students were newer to clinic, this content prompted explanations by the coach or RN. As the year progressed, some teams shifted toward problem-solving discussions of systems issues that afforded more collaboration among the team.
CONCLUSIONS: Team huddles offer a rich array of learning opportunities related to systems issues and teamwork. While much may be learned implicitly, simply by participating in a huddle, coaches can enhance the learning opportunities by providing feedback and suggestions on team communication and team process.
TEAM INTERACTIONS DURING COACHING SESSIONS: A WINDOW INTO TRANSFORMATION TO A PCMH TEAM-BASED CARE MODELMolly Harrod1; Jane Forman1; Claire Robinson1; Adam Tremblay2,3; Leo Greenstone2,3. 1VA Ann Arbor Health Care System, Ann Arbor, MI; 2VA Ann Arbor Health Care System, Ann Arbor, MI; 3University of Michigan, Ann Arbor, MI. (Tracking ID #1938830)
BACKGROUND: The Patient Centered Medical Home (PCMH) model of care delivery requires transformation from physician-centric to team-based care. This transformation requires fundamental changes in staff roles and relationships. Although prior research has looked extensively at team functioning and effectiveness, little has been done to understand the process of becoming a team. This study looks at a training approach (i.e. coaching sessions) that is being used in a large Veterans’ Health Administration primary care clinic to educate and support teams in the redesign of their work in order to meet PCMH goals (e.g., open access, continuity, and care coordination). We documented changes in how team members interacted and related to one another during coaching sessions in order to gain insight into the process of these transformations.
METHODS: Coaching sessions were conducted with individual teams, which consisted of a physician(s), a nurse case manager, a licensed practical nurse and a medical clerk, and was led by an assigned primary care provider who was not the provider on the team being coached. Each team was required to meet 1–2 times a month for a total of two hours per month. Nine out of 20 health care teams were longitudinally observed during their coaching sessions (25+ hours) from May 2013 to December 2013. Conversations and interactions (including nonverbal body language) were recorded via hand-written field notes. A grounded approach was used to analyze the data focusing on the interactions between team members. Codes were then categorized into themes.
RESULTS: Over the period of observation, team members began to relate to one another in new ways that included understanding one another’s developing role within the team, advocating for one another, and affirming to one another that they were doing a good job in the midst of complex primary care redesign. In addition, non-physician team members taught physicians about organizational processes that affected PACT implementation, and physicians openly admitted that they needed help from other team members to figure out how to improve team processes and functioning. These elements of relationship-building indicated a flattening of the existing physician-centric hierarchy. As a result, team members gradually shifted to a more team-based identity in the midst of building new work processes and identifying their roles within these processes.
CONCLUSIONS: We observed that teams engaged in relationship-building during coaching sessions while participating in practice redesign to meet PCMH goals such as open access and increased continuity. Understanding how team members interact and construct these relationships is important so that this aspect of PCMH transformation can be facilitated and supported. Teams need the time to interact in order to create the shared meanings that will define them as a team, and to facilitate their ability to redesign work processes to improve provision of patient-centered care
TELEPHONE MEDICINE IN AN URBAN AMBULATORY INTERNAL MEDICINE RESIDENT CLINIC: A NEEDS ASSESSMENTKatherine A. Wang1; Andrew Coyle1; Linda DeCherrie1,2. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1930440)
BACKGROUND: In the age of the patient-centered medical home, triage and management of urgent and chronic conditions by telephone are essential components of comprehensive care that limits unnecessary ED visits and hospitalizations. For both primary care physicians and specialists, the ability to evaluate a patient without the benefit of face-to-face interaction is an essential skill. At Mount Sinai Hospital, Internal Medicine (IM) residents on ambulatory rotations respond to patient phone calls. Common calls include urgent overnight complaints, lab alert values, medication refills and visiting nurse reports. While many of these complaints can be managed safely over the phone, residents receive minimal training in telephone medicine. The objective of this study was to assess perceived gaps in resident training and attitudes about telephone medicine.
METHODS: A 16-question online survey to assess resident comfort level and attitudes toward telephone medicine was offered to 139 Internal Medicine residents (PGY1-3), all of whom respond to patient telephone calls while on ambulatory rotations. A parallel 11-question survey was offered to 21 ambulatory IM attending physicians who supervise resident telephone calls. Both surveys included Likert-scale and open-ended questions addressing themes of 1) confidence, 2) quality, 3) attitudes, and 4) communication with faculty and patients (via MyChart, an online communication portal for patients). Participation was voluntary and no compensation was offered to respondents. Results are reported as descriptive data.
RESULTS: 50 residents (19 PGY1, 17 PGY2, and 14 PGY3, with a 36 % response rate) and 6 attending physicians (29 % response rate) completed the survey online. Reported urgent patient calls included abnormal lab values, elevated blood pressure, and symptoms such as chest pain, bleeding, and diarrhea. Fifty-eight percent of residents stated they had never received any telephone medicine training. The majority of residents (68 %) endorsed feeling confident managing patient care over the phone and most (62 %) felt they have adequate resources and support for handling patient calls. Despite this, 50 % of residents disagreed or strongly disagreed with the statement “I feel I am able to provide good care over the phone.” All faculty respondents felt that residents provide high quality care over the telephone and agreed with resident management “most of the time.” Residents reported conflicting attitudes about telephone medicine; the majority (76 %) note that being available by telephone at night is important for patient care, yet only 34 % feel that providing telephone care is rewarding. Regarding communication, 52 % of residents who cover overnight calls did not feel comfortable contacting faculty overnight. However, 83 % of attendings reported that residents do not contact them enough and no attendings reported being contacted too frequently. All faculty reported providing feedback to a resident; however, only 18 % of residents reported ever receiving feedback. Although 74 % of residents feel that MyChart is a good way to communicate with some patients, only 8 % use it. The most commonly cited reasons for not using it were 1) lack of training, 2) concerns about patient interest and access, and 3) barriers with resident schedules. Areas identified by both residents and faculty for improvement include clarification about resident responsibilities, training about responses to common calls, basic telephone communication and triage skills, improved resident-faculty communication, and MyChart training.
CONCLUSIONS: This study assessed resident and faculty attitudes toward and training gaps in IM resident telephone medicine training. While most residents feel that telephone medicine is an important facet of patient care and feel confident about managing telephone complaints, there are gaps in training and weaknesses in the current system. Both residents and faculty identified a desire for increased communication overnight, more feedback, and strict criteria prompting an attending call or ED referral. Limitations of this study are the fairly low response rate and that many of the expressed attitudes may be specific to this resident clinic. The lack of training and perceived inability to deliver high quality care reveal the need for a revised, standardized approach to telephone medicine training in an IM resident ambulatory clinic.
TEXT MESSAGING HOTLINE: AN INNOVATIVE AND EFFECTIVE WAY TO COMMUNICATE SEXUAL HEALTH INFORMATION TO TEENAGERSMolly A. Fisher1; Kate E. Lucey2; Steven Federico3; E. Bimla Schwarz1. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Northwestern University, Chicago, IL; 3University of Colorado, Aurora, CO. (Tracking ID #1936897)
BACKGROUND: Many teens lack access to reliable information about sexual health. As text messaging is the most utilized form of communication among teens, we examined Colorado teenagers’ use of a texting hotline, In Case You’re Curious (ICYC), which provides evidence-based responses to sexual health questions.
METHODS: ICYC was created as an anonymous sexual health texting hotline, and marketed to adolescents in Denver, Colorado. Local health education organizations distributed business cards and other marketing tools to teens who participated in after school programming and attended community clinics. Text messages sent to the hotline were received by a third party website, which assigned an identification number to each phone number so that the users would remain anonymous. The questions were then answered by a college-educated health educator, using a database of thousands of medically-accurate 160 character responses. The questions in the database were developed from teen question and answer websites and refined by focus groups. The responses were developed by medical students and reviewed by a physician. The hotline was available 24 h per day, 7 days per week. We used a web-based tool to collect data regarding text questions and responses sent between September 2010 and October 2012. Descriptive statistics were used to assess the number of text messages received per month, the types of questions users submitted, the number of users who submitted questions, and the average number of text questions per user.
RESULTS: During the study period, ICYC received 3,777 text messages from 1,121 users. Between the program’s first and second year, the number of text messages increased from 1,092 to 2,656. During the first year, an average of 2.76 text messages were sent per day, compared to 6.69 text messages per day the second year. More text messages were sent during the school year (317/month) than during the summer months (208/month), and more were sent during weekdays (594/day) than weekends (403/day). Almost half (48 %) of users texted more than one question to the hotline. The most frequent texted questions were about definitions, risk, and consequences of sexual acts (21 %), pregnancy (15 %), sexually transmitted infections (STIs) (11 %), Birth control (10 %), female body/puberty (9 %), male body/puberty (9 %), sexual orientation (6 %), masturbation (5 %), relationships (2), and safety (1 %). The remaining 25 % were about clinic referrals among other topics. ICYC’s response time improved over time; responses were generally provided in less than 4 h, and always within 24 h.
CONCLUSIONS: Texting hotlines offer an innovative and actionable way to provide teens with timely access to evidence-based sexual health information on an as needed basis.
THE ASSOCIATION OF FOOD INSECURITY AND DIABETES CONTROL AMONG LOW-INCOME INDIVIDUALSJulie B. Silverman1,2; Jim Krieger3,4; Meghan M. Kiefer2,1; Paul Hebert1,2; Nathan Drain3; June Robinson3; Leslie Taylor3; Janet Kapp3; Karin M. Nelson1,2. 1VA Puget Sound Healthcare System, Seattle, WA; 2University of Washington, Seattle, WA; 3Seattle King County Public Health, Seattle, WA; 4University of Washington, Seattle, WA. (Tracking ID #1937147)
BACKGROUND: Food insecurity is defined as the lack of dependable access to adequate, safe and nutritious foods necessary for a healthy and active life. Although there is an abundance of literature examining the relationship between diet and health, research on the health consequences of food insecurity is surprisingly limited. Only a few studies have demonstrated an association between food insecurity and glycemic control. The objective of this study was to evaluate the relationship between food insecurity and glycemic control among individuals with diabetes and to explore potential mediators of this association.
METHODS: We conducted a secondary analysis of baseline data from 287 low-income patients with poorly controlled type 2 diabetes (HbA1c >=8 %) who were enrolled in the Peer Support for Achieving Independence in Diabetes (Peer-AID) trial, a randomized controlled study evaluating a diabetes self-management intervention delivered by community health workers. We evaluated the differences in socio-demographic and clinical characteristics, including glycemic control, between food-secure individuals and those struggling with food insecurity (based on the USDA’s 6-item Food Security Survey Module). We used multivariable linear regression to model the relationship between glycemic control and food insecurity, adjusting for age, gender, race, language, education, marital status and BMI. Diabetes-related distress (moderate distress defined by a score of 2 or more on Polonsky’s Diabetes Distress Scale), depression (depression defined by a score of 5 or more on the PHQ-8) and medication adherence (low medication adherence defined by a score of less than 6 on the Morisky Scale) were evaluated as potential mediators.
RESULTS: The prevalence of food insecurity was 47.4 %. Compared to food-secure participants, participants with food insecurity were more likely to be female (59.6 % vs. 39.1 %, p = 0.001), non-white (66.9 % vs. 44.4 %, p < 0.001), speak only English at home (59.6 % vs. 46.4 %, p = 0.025), be unmarried or single (68.4 % vs. 45.7 %, p < 0.001) and be obese (68.4 % vs. 50 %, p = 0.001). Food-insecure participants utilized the health care system more frequently in the past year, with increased physician visits (10.7 vs. 7.3, p < 0.001) and a higher percentage using the emergency department (42.7 % vs. 31.1 %, p = 0.04). Although all subjects had poor glycemic control, food-insecure individuals had significantly higher hemoglobin A1c levels (9.4 vs. 8.8, p = 0.003 unadjusted; 9.4 vs. 8.8, p = 0.002 adjusted). They also had a higher incidence of hypoglycemic episodes in the past year (57.7 % vs. 45.2 %, p = 0.04). Forty percent of the food-insecure individuals who experienced hypoglycemia attributed it to not being able to afford food, compared to none of the food-secure individuals. Food-insecure participants had increased distress regarding their diabetes care (55.1 % vs. 33.7 %, p < 0.001), a greater prevalence of depression (74.1 % vs. 35.6 %, p < 0.001) and lower medication adherence (52.9 % vs. 37.2 %, p = 0.02). After adjusting for these potential mediators, the A1c levels of food-insecure individuals remained significantly higher than those of food-secure individuals (9.4 vs. 8.7, p = 0.002).
CONCLUSIONS: Food insecurity is associated with poorer glycemic control among low-income individuals with diabetes. Given that 1 in 6 households was food insecure during 2012, food insecurity is not an inconsequential concern. Assessing food security status and addressing patients’ food needs may be an effective, non-pharmacological intervention to improve glycemic control in low-income individuals with poor diabetes control.
THE BURDEN OF PRE-DIABETES AMONG OBESE VETERANS: UNDERSTANDING THE PREVALENCE OF DISEASE AND MERITS OF ROUTINE SCREENING PROGRAMSTannaz Moin1,2; Fatima Makki3; Jane E. Weinreb2; Nanette Steinle4,5; Charles J. Billington6,7; Kathryn Havens8; William Yancy9,10; Mathew L. Maciejewski9,10; Laura Damschroder3; Caroline R. Richardson11,12. 1VA Greater Los Angeles HSR&D Center for Healthcare Innovation, Los Angeles, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA; 3Ann Arbor VA Center for Clinical Management Research, Ann Arbor, MI; 4VA Baltimore Healthcare System, Baltimore, MD; 5University of Maryland, Baltimore, MD; 6Minneapolis VA Healthcare System, Minneapolis, MN; 7University of Minnesota, Milwaukee, MN; 8Zablocki VA, Milwaukee, WI; 9Duke University Medical Center, Durham, NC; 10Durham VA, Durham, NC; 11VA Diabetes QUERI, Ann Arbor, MI; 12University of Michigan, Ann Arbor, MI. (Tracking ID #1939081)
BACKGROUND: Type 2 Diabetes is a preventable disease. Individuals with pre-diabetes can reduce their risk of developing diabetes substantially by improving their diet, increasing their daily physical activity and losing a modest amount of weight. VA/DoD Clinical Practice Guideline (CPG), Centers for Disease Control (CDC), and American Diabetes Association (ADA) all recommend screening for diabetes in high risk patients, and the same tests used to screen for diabetes can also be used to detect pre-diabetes. Veterans with a BMI > 30 or >25 with other cardiovascular risk factors, many of whom have already been diagnosed with diabetes, are eligible to participate in a group lifestyle program called MOVE! The MOVE! program does not directly address diabetes prevention. While not all veterans who may have pre-diabetes are eligible for MOVE!, those who are referred to MOVE! represent a high risk group. Targeting these veterans for screening may be an efficient way to identify a significant number of veterans with pre-diabetes. Because of the lack of systematic screening, the incidence of pre-diabetes among veterans referred to the MOVE! program is not known. In an effort to decrease incident diabetes among veterans, the Diabetes Quality Enhancement Research Initiative (QUERI) partnered with the VHA National Center for Health Promotion and Disease Prevention (NCP) and clinical investigators from 3 VA sites to implement systematic screening for pre-diabetes, to estimate the prevalence of pre-diabetes among veterans referred to MOVE!, and to test the feasibility of delivering diabetes prevention focused lifestyle change programs to veterans with pre-diabetes.
METHODS: The VA Diabetes Prevention Clinical Demonstration Project (VA DPP) was implemented at three geographically dispersed medical centers beginning in January 2012. All veterans referred to MOVE! or presenting for a MOVE! orientation session who did not already have a diagnosis of diabetes were encouraged to complete a screening hemoglobin A1c (HbA1c) test. Patients were classified as pre-diabetic if their HbA1c value was between 5.7 and 6.4 % with no known history of diabetes and no use of anti-glycemic medications including metformin. All patients were informed of their HbA1c test results and pre-diabetic patients were systematically assigned to either a MOVE! group class or to a diabetes prevention group class.
RESULTS: Prior to the demonstration, diabetes screening was inconsistent across the 3 clinical sites. None of the sites were routinely conducting diabetes screening for obese Veterans referred to MOVE!. Automated screening programs were subsequently implemented to ensure screening tests were conducted consistently across the sites in accordance with national recommendations. A total of 1528 obese Veterans were referred to MOVE! between August 2012-November 2013 across the sites. Among these, 23 % (n = 358) had a HbA1c value that was consistent with pre-diabetes. Veterans with pre-diabetes had a mean age of 58.6 years (SD 10.2) and BMI of 34.1 (SD 5.7).
CONCLUSIONS: Almost one quarter of veterans referred to the VA MOVE! program have pre-diabetes and are at high risk for developing diabetes. To our knowledge this is the first study to examine screening practices and the prevalence of pre-diabetes among Veterans in multiple VA sites. Screening veterans referred to MOVE! can efficiently identify a significant number of veterans with pre-diabetes. However, the high prevalence of diabetes among MOVE! patients suggests that by waiting until veterans have been referred to MOVE! to screen for pre-diabetes, we may be missing the opportunity to intervene early enough to prevent diabetes in many veterans. While these veterans already have access to a lifestyle change program, it is not a program that specifically addresses diabetes prevention. Optimizing MOVE! for veterans with pre-diabetes or alternatively providing diabetes prevention specific interventions for these veterans may significantly reduce incident diabetes among veterans.
THE CARE TRANSITIONS INNOVATION (C-TRAIN) FOR SOCIOECONOMICALLY DISADVANTAGED ADULTS, RESULTS OF A CLUSTERED RANDOMIZED CONTROLLED TRIALHonora Englander1; LeAnn Michaels3; Benjamin Chan2; Devan Kansagara4,1. 1Oregon Health & Science University, Portand, OR; 2Oregon Health & Science University, Portland, OR; 3Oregon Health & Science University, Portland, OR; 4Portland VA Medical Center, Portland, OR. (Tracking ID #1935654)
BACKGROUND: Despite growing emphasis on transitional care to reduce costs and improve quality, few studies have examined transitional care improvements in socioeconomically disadvantaged adults. It is important to consider these patients separately as many are high-utilizers, have different needs, and may have different responses to interventions. We performed the Care Transitions Innovation (C-TraIn) study to evaluate the impact of a multi-component transitional care improvement program on 30-day readmissions, emergency department (ED) use, transitional care quality, and mortality.
METHODS: We performed a clustered randomized controlled trial conducted at a single urban academic medical center in Portland, Oregon. We enrolled 382 hospitalized low-income adults admitted to general medicine or cardiology who were uninsured or had public insurance. Participants resided in one of three Portland metro area counties, had to have access to a working phone (friend or shelter phone was okay), spoke English, and had no disabling mental illness (defined as active psychosis or active suicidal ideation). Control patients received usual care, which consisted of: (1) a routine inpatient nurse intake; discharge patient education was performed by inpatient nurses and physicians. (2) medication reconciliation performed by treating physicians. Uninsured patients were financially responsible for post-discharge medications. (3) There was no systematic approach to securing post-discharge follow-up. Patients without a usual source of care were often given a list of 14 area safety-net clinics, which have limited capacity for uncompensated care. Prior work showed that uninsured—and to a lesser degree Medicaid—patients have difficulty establishing primary care and frequently cannot access appointments or navigate the complex system. Any coordination of post-discharge services was performed by inpatient care managers, social workers and treating physicians with no formal community linkages. C-TraIn patients received a multi-component intervention which was delivered in addition to usual care, and included (1) transitional nurse coaching and education that started early in hospitalization and lasted for 30 days post discharge, often including home visits for highest risk patients; (2) pharmacy care, including medication reconciliation, low health literacy education, and provision of 30 days of medications after discharge for those without prescription drug coverage; (3) post-hospital primary care linkages, including establishing new outpatient linkages for those without a usual source of care; and (4) systems integration and continuous quality improvement that convened a multidisciplinary team across in- and outpatient care. Primary outcomes included 30-day inpatient readmission and ED use. Readmission data for all participants, including the uninsured, were obtained using a hospital administrative database that includes admissions from all Oregon and southwest Washington hospitals. Secondary outcomes included quality (3-item Care Transitions Measure) and mortality. Research staff administering questionnaires and assessing outcomes were blinded.
RESULTS: Of the 2290 patients screened, 522 were eligible and 382 enrolled (209 to intervention, 173 control). Of those enrolled, 293 (76.7 %) completed a follow-up phone survey 30 days after index discharge. Intervention and control groups were well matched and there were no significant differences between the groups. Among intervention patients, 49.7 % (104/209) received a home visit and 92.8 % (194/209) received an inpatient pharmacy consultation. New primary care linkages were established in 42.1 % of patients (88/209), including 68.7 % (68/100) uninsured and 16.8 % (20/119) publicly uninsured patients. There was no significant difference in 30-day readmission between C-TraIn (30/209, 14.4 %) and control patients (27/173, 16.1 %); p = 0.644 or in ED visits between C-TraIn (51/209, 24.4 %) and control (33/173, 19.6 %); p = 0.271. C-TraIn was associated with improved transitional care quality and mortality. 47.3 % (71/150) of C-TraIn patients reported a high quality transition compared to 30.3 % (36/119) control patients; odds ratio 2.17 (95 % CI 1.30–3.64). Zero C-TraIn patients died in the 30-day post-discharge period compared with 5 in the control group (p = 0.019).
CONCLUSIONS: C-TraIn did not reduce 30-day inpatient readmissions or repeat ED use; however, it improved quality and was associated with improved mortality. Our findings raise questions as to the preventability of readmissions through traditional bridging transitional care improvements among socioeconomically vulnerable adults, many of whom had limited access to care prior to hospitalization. Most health systems interested in transitions of care are seeking a business case. While reducing readmissions is often the centerpiece, care quality and patient experience are important to consider.
THE CHAOTIC PRACTICE ENVIRONMENT IN VA PRIMARY CARE CLINICS: NATIONAL SURVEYMark D. Schwartz1,2; Danielle Rose3; Katelyn Bennett1,2; Elizabeth M. Yano3,4. 1VA New York Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3VA Greater Los Angeles Healthcare Center, Sepulveda Campus, Los Angeles, CA; 4UCLA, Los Angeles, CA. (Tracking ID #1938465)
BACKGROUND: A chaotic practice environment may adversely impact physicians and diminish the quality of care they provide. As part of the VA Clinical Practice Organizational Survey (CPOS), designed to assess organizational traits of VA facilities, we sought to determine the pace of work at VA primary care (PC) clinics and compare the characteristics of clinics percieved as chaotic versus non-chaotic.
METHODS: The 2007 CPOS surveyed the PC Directors at all VA PC clinics with 4,000 or more patients and 20,000 or more annual outpatient visits. The questionnaire asked practice leaders to describe the pace of their PC practice environment on a 5-point scale where 1 = calm; 3 = busy but reasonable; and 5 = hectic or chaotic. We defined clinics rated as 4 or 5 as “chaotic.” In addition to practice pace, the CPOS also assessed organizational practice characteristics including resources, staff, and performance barriers. Data on clinic-level characteristics were collected from CPOS 2007: e.g., VA Medical Centers (VAMC) or community-based outpatient clinics (CBOC), and % minority patient population; and area-level characteristics were collected from the Area Resource File (2008): i.e., urban vs. rural location, and % in poverty. In bi-variate logistic regressions, we tested for associations between chaotic clinics with organizational characteristics of practice stress level, patient flow bottlenecks (7-item scale); use of computerized reminders in the medical record (15-item scale); perceived barriers to improving facility performance (12-item scale); sufficient PC staff (10-item scale); sufficient PC resources and space (9-item scale); and unfilled vacancies (4-item scale). We also tested for associations between chaotic clinics with clinic and area level characteristics.
RESULTS: 225 (90 %) of 250 VA PC clinics surveyed responded. 130 (57.8 %) reported their practice environment as chaotic. Sixty percent of chaotic clinics were described as having high overall stress vs. 9 % of calm or busy clinics (p < 0.001). The associations of chaotic clinics with practice characteristics are summarized in Table 1.
CONCLUSIONS: Most VA PC Directors describe their practice environment as chaotic and under high stress. Chaotic clinics are more likely to have high stress levels, patient flow bottlenecks, barriers to improving performance, fewer computerized reminders, insufficient staff and resources, and more unfilled vacancies. Clinic chaos was not linked to facility type, patient demographics or clinic location. Clinic chaos may serve as a simple measure of the health of a practice, a measure of distress among clinic staff, and a marker for a vulnerable practice. Future studies should evaluate how chaotic clinics effect patient experience and outcomes as well as staff outcomes. Since this study, VA has transformed PC clinics into medical homes (Patient Aligned Care Teams, PACT), which has the potential to reduce chaos and stress. Further research is needed to understand how the implementation of the VA PACT model has impacted chaos in PC clinics and how chaos has influenced PACT implementation.
Table 1: Characteristics of Chaotic VA PC Clinics
| Practice Characteristics | Odds Ratio | 95 % Confidence Interval | P Value |
|---|---|---|---|
| Organizational Characteristics | |||
| Practice stress level | 2.05 | 1.31, 2.78 | <0.0001 |
| Bottlenecks to patient flow | 1.21 | 1.11, 1.34 | <0.0001 |
| Computerized clinical reminders | 0.92 | 0.84, 0.99 | 0.05 |
| Barriers to improving performance | 1.12 | 1.06, 1.17 | <0.0001 |
| Sufficient staff | 0.92 | 0.88, 0.96 | <0.0001 |
| Sufficient resources | 0.92 | 0.89, 0.95 | <0.0001 |
| Unfilled vacancies | 1.10 | 1.03, 1.18 | 0.006 |
| Clinic-level characteristics | |||
| 153 VAMC (vs. 97 CBOC) | 1.15 | 0.67, 1.98 | 0.61 |
| Minority patients | 20.28 | 0.85, 481.31 | 0.06 |
| Area-level characteristics | |||
| Metropolitan location (urban) | 0.91 | 0.61, 1.36 | 0.65 |
| Percent in poverty | 1.02 | 0.95, 1.08 | 0.64 |
THE COLOR PURPLE: MAINTAINING PATIENTS’ WISHESAdam Lammly; Vishal Patel; Nicholas Merritt. Christiana Care Health System, Newark, DE. (Tracking ID #1934758)
BACKGROUND: In 2007, the Society of Hospital Medicine published a study on the lack of standardization of DNR (do not resuscitate) practices across the country. Of the 127 nursing executives, 75 of the respondents recalled situations of confusion pertaining to patient care when “do not resuscitate” (DNR) orders were involved. At our institution, during a 6 month period there were two code blues called and performed on hospital inpatients with a DNR order on their charts in the hemodialysis unit and Gastroenterology (GI) lab. This highlights that miscommunication when patients are transferred or handed off can lead to serious medical errors, poor patient outcomes, and increased unnecessary costs—all deviating from patient-centered care.
METHODS: A multidisciplinary task force was created to standardize the system to identify DNR status for inpatients when transferred to other units. Initially begun in the hemodialysis unit, the task force first met with nursing supervisors and also surveyed all the hemodialysis staff to determine how they determined patients’ DNR status. Concurrently, an educational seminar was provided to all staff members about DNR status/implications. The primary intervention proposed was placing a purple sticker on the top of the hemodialysis flow sheet upon initiation of the dialysis for that day if the patient had a DNR order listed in the electronic medical record. This flow sheet/purple sticker is visible by all staff especially if standing in the middle of the unit. Once implemented, there was a 2 week chart audit period to ensure the validity of this process.
RESULTS: During the initial study of 31 dialysis sessions over 2 weeks, 380 charts were reviewed and the staff correctly identified all 10 patients with DNR status. This program has continued for the past 9 months, with an average of 20 patients with DNR status receiving inpatient hemodialysis each month. This program has now been adopted by the GI lab and another hemodialysis unit at another hospital in the health care system. Since implementing this program, there have been zero code blues on patients with DNR status in these units. In addition, the flow sheet has be redesigned to include a specific area for this sticker, providing another reminder to verify patients’ code status.
CONCLUSIONS: This study showed that a small, inexpensive intervention can reduce inappropriate care and unnecessary health care costs, and more importantly, increase adherence to patients’ end of life decisions. Collaborating with multiple disciplines within the institution provided the foundation to enact change. A simple process of correctly identifying patients’ end of life wishes with a purple sticker on the patients’ bedside paperwork is now being tested in all other ancillary services (imaging departments, rehabilitation services) in hopes of having ZERO inappropriate codes for all patients with DNR orders.
THE DIFFERENCE OF THE CHARACTERISTICS OF NEW PATIENTS VISITING A JAPANESE EMERGENCY HOSPITAL BETWEEN AT NIGHT AND DAYTIME: A CROSS-SECTIONAL STUDYNorio Fukumori1; Hitoshi Eguchi2,3; Jun Tokutomi3; Yuka Naito3; Yuta Sakanishi1; Shu-ichi Yamashita3; Takashi Sugioka1. 1Community Medical Support Institute, Faculty of Medicine, Saga University, Saga, Japan; 2Saga Memorial Hospital, Saga, Japan; 3Saga University Hospital, Saga, Japan. (Tracking ID #1942113)
BACKGROUND: Medical services have been changed to accommodate the needs of patients with increased diversity of life styles by changing the system such as prolongation of office hours. Although prolongation of office hours may facilitate the visit of younger patients, the actual influence of it remains to be investigated. In this study we investigate the difference of the characteristics of new patients visiting a Japanese emergency hospital between at night (N) and daytime (D).
METHODS: 3,341 of new patients visited the department of internal medicine of Saga memorial hospital, an emergency hospital in Japan on 2010. Five hundred patients were randomly selected from all new patients. The characteristics of the patients including sex, age, the date of the visit, specialties of the doctors, with/without of referral from other medical clinics, to be taken by ambulance car or not, the chief complaint and main diagnosis were reviewed from the medical charts. The chief complaint and main diagnosis of the patient were classified by the ICD-10 code. The difference of characteristics of patients were examined by t-test for continuous variables and chi-square test for dichotomous variables. All statistical analyses were performed using Stata SE version 12.0.
RESULTS: The mean age (SD) of the group D and N were 49.3 (), 33.9 (), respectively (p < 0.001 ). The patients D were referred by other clinics more often and visited to the secondary examination of their health check-up. The number of disease associated with pediatrics and orthopedics were larger in the group N. Infectious diseases were most popular in both groups, 56.5 % of which were in the group N.
CONCLUSIONS: The new patients who visited an emergency hospital at night, were younger and tended to have infectious, pediatrics, and orthopedics disease more often. Physician of internal and emergency medicine need versatile ability of medical care not only internal medicine but also pediatrics or orthopedics to care new patients who visit emergency hospital at night.
THE EFFECTIVENESS OF A CASE-BASED CURRICULUM ON INTERNAL MEDICINE RESIDENTS’ PERCEPTIONS REGARDING APOLOGY FOR MEDICAL ERRORSStephen A. McCullough; Meridale Baggett; Victor Chiappa; Hasan Bazari; Paul F. Currier. Massachusetts General Hospital, Boston, MA. (Tracking ID #1930628)
BACKGROUND: The 1999 Institute of Medicine report To Err Is Human focused attention on the importance of medical error disclosure and apologies. Current data support that though medical errors are common, trainees frequently do not disclose or apologize for mistakes. To date, no curriculum to teach internal medicine (IM) residents how to apologize for medical errors has been reported in the literature. A teaching program on apology for medical errors was developed and instituted. A study was undertaken to determine the effect of the curriculum on the perceptions of IM residents.
METHODS: A 3 h curriculum consisting of an introductory lecture and three simulated case scenarios on apology for medical errors was administered to PGY-2 IM residents. A 14-question survey was administered directly pre and post-session to assess (1) resident comfort in apologizing to patients and (2) specific behaviors addressed during the curriculum that residents believe may warrant an apology. The post-session survey contained 8 additional questions regarding the effectiveness of the curriculum. Data were compared using students’ two-tailed t test.
RESULTS: 21 PGY-2 internal medicine residents (52 % female) completed the curriculum and 20 (95.2 %) completed both surveys. On a 5-point Likert scale, residents rated agree to strongly agree that the curriculum was relevant (4.6 ± 0.26), helpful (4.35 ± 0.35), informative (4.35 ± 0.35), and that the cases were realistic (4.45 ± 0.32.) Residents rated agree that the curriculum helped them analyze situations in which an apology may be necessary (4.4 ± 0.26), determine the appropriate setting to apologize (4 ± 0.5), obtain patients’ perceptions regarding their illness (4 ± 0.42), apologize to patients (4.35 ± 0.29), and navigate difficult emotional situations (4.2 ± 0.26.) Before and after the curriculum residents rated neutral to agree they were comfortable apologizing (3.76 vs 3.95), and they rated agree to strongly agree that there is value in apologizing (4.6 vs 4.7) and that apologizing strengthened the doctor-patient relationship (4.14 vs 4.25.) Residents rated disagree that they feared apologizing (2.85 vs 2.6), and they rated disagree to strongly disagree that apologizing was beyond the scope of their responsibility (1.33 vs 1.45.) Lastly, the curriculum increased the number of residents who would apologize for not maintaining sterile technique during a procedure (19 % vs 65 %, p = 0.002) and for administering the wrong dose of a medication (80.9 % vs 100 %, p = 0.04), though there were no differences in other specific behaviors.
CONCLUSIONS: (1) IM residents believe apologizing to patients is largely beneficial, though our curriculum did not change those beliefs. (2) IM residents believe a case-based curriculum on apology is relevant, helpful, and valuable. (3) A curriculum on apology can modify specific resident behaviors.
THE EFFECTS OF A MULTI-FACETED MEDICATION RECONCILIATION QUALITY IMPROVEMENT INTERVENTION ON PATIENT SAFETY: PRELIMINARY RESULTS OF THE MARQUIS STUDYJeffrey L. Schnipper1,2; Sunil Kripalani4; Jason Stein5; Tosha B. Wetterneck6; Peter Kaboli3; Stephanie Mueller1,2; Amanda Salanitro7; Jacquelyn A. Minahan1; Nyryan V. Nolido1; Elisabeth Burdick1. 1Brigham and Women’s Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3Iowa City VA Medical Center, Iowa City, IA; 4Vanderbilt University Medical Center, Nashville, TN; 5Emory University, Atlanta, GA; 6University of Wisconsin, Madison, WI; 7Vanderbilt University, Nashville, TN. (Tracking ID #1938437)
BACKGROUND: Unintentional medication discrepancies during hospitalization can contribute to adverse drug events, resulting in patient harm. Discrepancies can be reduced by performing medication reconciliation; however, effective implementation of medication reconciliation has proven to be challenging. The goals of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS) are to operationalize best practices for inpatient medication reconciliation, test their effect on potentially harmful unintentional medication discrepancies, and understand barriers and facilitators of successful implementation. This analysis focuses on the quantitative results of the two sites that have completed the intervention to date.
METHODS: Five U.S. hospitals are participating in this quality improvement mentored implementation study. Each hospital collected at least 6 months of baseline data (N = 488 patients) on the primary outcome: the number of potentially harmful unintentional medication discrepancies per patient. This was determined by a trained on-site pharmacist taking a “gold standard” medication history on a random sample of approximately 25 medical-surgical inpatients per month and then comparing this history to their admission and discharge medication orders. Discrepancies were categorized as intentional (based on documentation and by questioning the medical team as needed), those due to errors in the medical team’s preadmission medication history, and those due to reconciliation errors (i.e., incorrect orders despite correct medication histories). Trained physician adjudicators at each site then determined the potential for harm of all unintentional discrepancies. With the guidance of trained mentors and using standard quality improvement principles, each site then began to implement one or more of 11 best practices to improve medication reconciliation. Sites were provided with an implementation manual describing these interventions in detail as well as supplementary materials such as instructional videos and slide presentations. Mentors conducted monthly phone calls with local site leaders and made two site visits during the two-year intervention period. Analyses were then conducted to compare discrepancies per patient in patients exposed to any interventions with both pre-intervention controls and concurrent controls using Wilcoxon rank sum test.
RESULTS: The first site to complete the intervention initially chose several interventions to implement, including provider training in taking a “best possible medication history,” assessment of patient risk for medication errors, and provision of intensive discharge counseling in high-risk patients. This site also expanded the use of pharmacy technician “medication reconciliation assistants” (MRAs) to take medication histories on admitted patients while still in the emergency department. Towards the end of the study, this site adopted “measure-vention” techniques (where defects in care are identified and corrected in real time) to ensure that patients who hadn’t received appropriate interventions subsequently received them while still hospitalized. The rate of discrepancies per patient was 4.49 during the pre-intervention period (N = 126), 5.24 among 119 concurrent controls, and 3.44 among 127 intervention patients (p < 0.001 for comparison with both control groups combined). Similarly, rates of potentially harmful discrepancies were 0.25 per patient pre-intervention, 0.32 for concurrent controls, and 0.09 for intervention patients (p = 0.003 for comparison with both controls). The second site to complete the study chose a similar initial set of interventions to adopt. They did not have an MRA program but obtained institutional support to start one in the future with guidance from the first site. Discrepancy rates were 2.04 during the pre-intervention period (N = 119) and 2.37 among 93 intervention patients during the first 6 months of the intervention (p = 0.11). However, discrepancies then rose to 3.81 among 166 patients after adoption of a commonly used electronic medical record (EMR) that actually made it more difficult to document preadmission medications, diffused provider accountability, and made discharge medication instructions less clear (p < 0.001 for comparison with pre-EMR groups). Similarly, rates of potentially harmful discrepancies per patient rose from 0.35 before to 1.10 after EMR implementation (p < 0.001).
CONCLUSIONS: Adoption of a multi-faceted medication reconciliation quality improvement initiative using a mentored implementation model has the potential to reduce potentially harmful medication discrepancies. However, external factors, such as EMRs that are not designed and/or implemented optimally, can have adverse effects on these types of patient safety initiatives.
THE EFFECTS OF AGING ON SICKLE CELL DISEASE AND IDENTIFICATION OF POSSIBLE MARKERS FOR INCREASED SURVIVORSHIPSusanna Curtis1; Zipora Etzion2; Neeraja Danda2; Henny H. Billett2. 1Montefiore Medical Center, Bronx, NY; 2Montefiore Medical Center, Bronx, NY. (Tracking ID #1938717)
BACKGROUND: As our understanding of the pathophysiology of sickle cell disease (SCD) has improved, so has our ability to prevent early mortality. Because elderly SCD patients are a relatively new population, little is known about how SCD affects the normal aging process or how aging affects SCD. This study seeks to examine changes in laboratory and clinical parameters associated with aging in SCD and to identify markers of longevity.
METHODS: We used our electronic medical record (EMR) to identify all patients with SCD seen at our facilities in 2012. Patients were identified as having SCD if hemoglobin (Hb) electrophoresis demonstrated sickle hemoglobin (HbS), fetal hemoglobin (HbF) and Hb A2 but no HbA. Patients were divided into two groups, ages 18–39 and 40–89 and demographics noted. The earliest results starting from 1/1/2012 for each of the laboratory and weight parameters were used for assessment. Health care utilization over the entire year was calculated. Life-time prevalence of end organ damage was evaluated. Since our EMR has >10 years data, additional analyses were performed using patients’ own matched laboratory values from 9 to 11 years previously. Two-tailed t-tests with unequal variances were used to compare different aged cohorts and two-tailed paired t-tests compared patients to their approximately 10-year younger selves.
RESULTS: In the year 2012, 439 patients with SCD were seen at our institution ranging in ages from 18 to 87; of those, 129 (29 %) were over the age of 40. The older group was more anemic (Hb 8.0 g/dl vs 8.5 g/dl, p < .005), had lower absolute reticulocyte counts (228.5 × 109/L vs 289.2 × 109/L, p < .00005) and had less ‘dense’ cells as demonstrated by MCHC (33.9 g/dl vs 34.4 g/dl, p < .001). In agreement with the decreased red cell density, indirect bilirubin levels in the over 40 year cohort were significantly lower (2.0 mg/dl vs 3.1 mg/dl, p < 2.4 × 10−6). ALT and AST tests were not significantly different. Neither absolute nor % HbF were significantly different (8.7 % vs 7.3 %, p = .21), though the older cohort was less likely to be on hydroxyurea (29 % vs 42 %, p < .008). Platelet counts and white blood cell counts were lower in the older cohort (platelet count: 318.9 × 109/L in the older vs 375.9 × 109/L in the younger group, p < .00003, and WBC: 11.0 × 109/L vs 12.5 × 109/L, p < .02 respectively). Serum Cr levels were higher (Cr 1.17 mg/dl vs 0.79 mg/dl, p < .00001) while weight was not statistically different. Older patients had, as expected, a higher prevalence of end organ damage with more leg ulcers (22 % vs 8 %, p < .001) and more documented renal failure (15 % vs 4 %, p < .002) though they had a lower prevalence of acute chest syndrome (35 % vs 51 %, p < .001). When health care utilization in 2012 was examined, older patients were more likely to go to clinic, (8.6 vs 5.7 visits, p < .02) and less likely to go to the emergency room (3.6 vs 5.8 visits, p < .02) or be admitted (1.7 vs 2.4 admissions, p < .02) Of the 439 patients in the 2012 cohorts, 223 (51 %) of them also had laboratory data in the years 2001–2003. Over the decade, patients significantly lowered their Hb levels (Hb delta: −2.6, p < 2.4 × 10−13), and lowered their MCHC (MCHC delta: −4.7, p < 3.8 × 10−7). Their %HbF decreased (HbF delta: −10.0 %, p < .0003) As patients aged, hemolytic parameters increased as evidence by increases in absolute reticulocyte count (delta: +15.5, p < 3.8 × 10−7) and indirect bilirubin levels (delta: +0.13, p < .05) with no significant change in direct bilirubin. They were also shown to increase Cr levels (delta: +0.13 p < .01). A significant change in WBC or platelets was not seen. To assess whether the older group had a survival advantage because they resist the ‘natural decline’, we examined the degree of change in the older vs the younger cohorts. No significant differences were seen
CONCLUSIONS: Older SCD patients demonstrate significant differences in laboratory and clinical parameters from both younger sickle cell patients and from themselves approximately 10 years earlier. They are more anemic and have fewer dense cells. They also appear to be accumulating end organ damage, with increasing Cr levels, more renal failure and an increased prevalence of leg ulcers. They have fewer ER visits and fewer admissions and they utilize the clinic more. However, while our entire cohort increased their indirect bilirubin levels and reticulocyte counts over 10 years, the older group in 2012 still had lower indirect bilirubin and reticulocyte counts. In agreement with this is our data demonstrating that, while the entire cohort decreased their HbF levels over a decade, the older group in 2012 had HbF levels equal to the younger group despite being less likely to be on hydroxyurea. We conclude that even minor changes in HbF levels, coupled with less dense cells and what appear to be lower markers of hemolysis, may confer mortality benefit and might be used to predict late mortality in SCD patients.
THE EFFECTS OF FATIGUE ON DRIVING SAFETY: A COMPARISON OF BRAKE REACTION TIMES IN NIGHT-FLOAT AND POST-CALL PHYSICIANS IN TRAININGTheodore Long1; Paul G. Talusan2; Andrea Halim2; Laura Guliani3; Nicole Carroll3; John Reach2. 1Yale School of Medicine, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Boston College, Boston, CT. (Tracking ID #1931264)
BACKGROUND: Duty hour changes for resident physicians have fostered a great deal of discussion about post-shift fatigue and driving impairment. Other studies have found a high incidence of motor vehicle collisions among post-call trainees. Using a driving simulator, trainees on heavy call rotations have also been found to have similar impairment to trainees on light-call rotations with a blood alcohol concentration of 0.04 to 0.05 g%. Under current duty hour regulations, moving to night-float systems instead of traditional 28-hour call has been implemented in an effort to improve safety among intern and resident trainees. However, it remains unknown whether night-float systems improve the driving safety of trainees.
METHODS: Internal medicine and orthopaedic surgery trainees were enrolled during a traditional 28-hour call shift or at the beginning of a night-float shift. We defined night-float trainees as those that had worked at least one consecutive night prior to the current night shift, in an effort to study the effects of contiguous night shifts in a row. Brake reaction times were tested using a Vericom driving simulator at the time of enrollment and following their shifts. We calculated average reaction times for each participant, and conducted matched pair t-tests of the pre- and post-shift averages. We also had participants complete the Epworth Sleepiness Scale, and we performed the Wilcoxon Signed Rank test to detect differences pre- and post-shift.
RESULTS: From June 2013 to July 2013, 61 pre-shift simulations were conducted, and 58 post-shift simulations were conducted (28 orthopaedic surgery, 30 internal medicine). Three simulations were excluded from the analysis because no post-shift responses were recorded. We included 24 trainees on night-float rotations (41 %) and 34 trainees on traditional 28-hour call shifts (59 %). The average reaction times for internal medicine trainees were not significantly changed pre- and post-shift (p = 0.763). There was an increase in reaction times for orthopaedic trainees (p= 0.007). For trainees on night-float rotations, there was no significant difference pre- and post-shift (p = 0.65). However, there was an increase in reaction times among trainees on traditional 28-hour call rotations (p = 0.011).
CONCLUSIONS: In our study of internal medicine and orthopaedic surgery interns and residents, trainees on traditional 28-hour call rotations had worse brake reaction times post-shift, and trainees on night-float rotations had no difference in reaction times post-shift. While the results of our study suggest that driving safety may be improved through the use of a night-float system, this conclusion should not be taken in isolation of other considerations such as educational tradeoffs and increased hand-offs.
THE FINANCIAL COSTS OF IMPLEMENTING ELECTRONIC HEALTH RECORDS IN HOSPITALSSarah P. Slight1,2; Casey Quinn3; Anthony J. Avery4; David W. Bates2,5; Aziz Sheikh2,6. 1Durham University, Stockton on Tees, United Kingdom; 2Brigham and Women’s Hospital, Boston, MA; 3PRMA Consulting Ltd., Hampshire, United Kingdom; 4The University of Nottingham, Nottingham, United Kingdom; 5Harvard Medical School, Boston, MA; 6The University of Edinburgh, Edinburgh, United Kingdom. (Tracking ID #1932616)
BACKGROUND: Electronic health record (EHR) systems hold the promise of improving the safety, quality and efficiency of health care.(1) Despite this promise, U.K. hospitals have been slow to implement and adopt such systems.(2) This is due, in part, to the inhibitory cost of EHRs and the uncertainty in relation to whether they can achieve a return on investment. With more and more health care institutions considering implementation of EHR systems worldwide, this study aimed to categorize the costs associated with implementation and the factors that can influence these costs.
METHODS: We conducted a qualitative study to explore the views and perspectives of a diverse range of relevant staff and members of the implementation team at 12 hospitals planning to implement three centrally procured applications i.e., iSOFT’s Lorenzo Regional Care, Cerner’s Millennium, and CSE’s RiO. After obtaining ethical approval, we conducted 41 semi-structured interviews between February 2009 and January 2011. A workable list of main- and sub-themes was developed inductively and applied systematically to these data with the aid of the computerized qualitative data analysis software QSR N-Vivo.
RESULTS: We identified four overarching cost categories associated with implementing EHR systems, namely: infrastructure (e.g., hardware and software), personnel (e.g., project management and training teams), estates or facilities (e.g., furniture and fittings), and other (e.g., consumables and training materials). Many factors were felt to impact on these costs, with different hospitals choosing varying amounts and types of infrastructure. This infrastructure was dependent on the stage of hardware maturity within the hospital; the requirements of the software application being implemented; the products currently available on the market; the budget (if predetermined); and the physical requirements of the wards or office rooms. The amount of resource spent on training clinicians and administrative staff to use the new EHR system depended on the number of users at each site; the training methods employed; the decision to backfill staff; and the level of support provided to clinical users.
CONCLUSIONS: We found that organizations faced hard compromises relating to cost, e.g., the infrastructure implemented may not satisfy the demands of ward staff at peak times, and should therefore consider devoting specific attention to these areas in the planning phase. With cost considered one of the most significant barriers to EHR adoption, it is important for hospitals and governments to be clear from the outset as to the categories of costs involved and the factors that may impact on these costs. References: 1. UK Clinical Research Collaboration Select Committee on Health. 2007. 2. Crosson JC, Ohman-Strickland PA, Cohen DJ, Clark EC, Crabtree BF. Typical electronic health record use in primary care practices and the quality of diabetes care. Ann Fam Med. 2012;10(3):221–7.
THE FREQUENCY OF PHLEBOTOMY AND THE INCIDENCE OF HOSPITAL-ACQUIRED ANEMIA AND WORSENING ANEMIA DURING HOSPITALIZATIONDaniel A. Kim; Sonali Palchaudhuri; Anthony Accurso. Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1931990)
BACKGROUND: Hospital-acquired anemia (HAA) is associated with worse health status, higher hospitalization rates, increased length of stay, need for blood transfusions, greater medical costs, lower quality of life, and higher mortality. Amount and frequency of phlebotomy has been shown to be associated with HAA. Therefore, there has been a strong focus on HAA as it can potentially be prevented. HAA is defined as patients who present without anemia, and subsequently developing anemia by hospital discharge. Studies in patients who present with anemia have not been studied. It is hypothesized that if phlebotomy can cause HAA, then it should also affect patients who present to the hospital with anemia, which is a significant portion of hospitalized patients according to our prior awareness study. This study was conducted to find the incidence of worsening anemia, and to assess if it associated with phlebotomy as HAA has been shown in the past.
METHODS: A retrospective study of 762 adult hospitalizations in March of 2013 in a single academic medical center was conducted. Demographics, hospital information (location, length of stay, transfusion requirements), and laboratory data, including daily hematocrit levels, hemoccult (fecal occult blood) results if obtained, initial and discharge creatinine, were analyzed using administrative data. Patients with positive hemoccults, acute kidney injury (indicating hypovolemia and possible hemoconcentration), and who received blood transfusions were excluded from the study. HAA was defined as absence of anemia on admission, but development of anemia at discharge, and further categorized as severe (Hct ≤27.0 %), moderate (Hct 27.1 to 33.0 %), or mild (Hct 33.0 to 36.0 %). Worsening anemia was defined by a transition to a higher severity category of anemia, ie mild to moderate, or moderate to severe anemia by discharge.
RESULTS: In patients who presented with normal Hct, there was a 31.4 % and 12.3 % incidence of overall HAA and mod-severe HAA, respectively. For HAA, there was a statistically significant difference between subjects who developed HAA and those who did not develop HAA for initial hematocrit (38.0 vs 40.7, p < 0.0001), hospital length of stay (4.05 vs 3.34, p = 0.03), and total phlebotomy frequency (4.33 vs 3.40, p = 0.007). In patients presenting with mild to moderate anemia, almost half (49.0 %) had worsening anemia from admission to discharge. A statistically significant difference in the total number of blood draws was seen between those that developed worsening anemia and those that did not (4.70 vs 3.45 blood tests per hospitalization, p = 0.02). Unlike HAA, patients with worsening anemia did not have significant difference in creatinine, length of stay, initial hematocrit than those that did not have worsening anemia.
CONCLUSIONS: Our findings suggest that hospital-acquired anemia as well as patients whose anemia worsens during hospitalization occurs frequently in our hospital. As seen in prior studies, HAA is associated with phlebotomy frequency and hospital length of stay. Similar to HAA, worsening anemia during hospitalization is significantly associated with higher frequency of phlebotomy. Although HAA has been well studied, to our knowledge, worsening anemia during hospitalization has not been examined. Further studies are needed to determine the clinical significance of worsening anemia; however, it is likely to be significant considering that HAA has been shown to be associated with worse health outcomes, increased hospitalization, and higher mortality to name a few. This study also implicates the possibility of targeting phlebotomy frequency to reduce the incidence of worsening anemia in the hospital, and not only for HAA.

THE HUNT FOR DIABETES: CHARACTERISTICS AND RISK FACTORS ASSOCIATED WITH UNDIAGNOSED DIABETES AND PREDIABETES IN NHANESMichael E. Bowen1,2; Lei Xuan2; Ethan Halm1,2. 1UT Southwestern Medical Center, Dallas, TX; 2UT Southwestern Medical Center, Dallas, TX. (Tracking ID #1937085)
BACKGROUND: Over 7 million people with diabetes (DM) and 73 million people with prediabetes (preDM) in the US are undiagnosed. Although characteristics of individuals with diagnosed DM and preDM are well described, those with undiagnosed disease are less well characterized. Understanding risk factors and characteristics of individuals with undiagnosed DM and preDM are essential to successful case-identification strategies.
METHODS: Non-pregnant adults without self-reported DM and preDM in the 2005–2009 NHANES survey were analyzed. Using A1C and fasting glucose, participants were classified as normal (A1C < 5.7 % and fasting glucose <126 mg/DL), undiagnosed preDM (A1C 5.7–6.5 % or fasting glucose 100–125 mg/dL), or undiagnosed DM (A1C ≥6.5 % or fasting glucose ≥126 mg/dL). Patient characteristics and risk factors were obtained from interview and exam survey components. Associations between risk factors and undiagnosed preDM and DM were examined using logistic regression with the normal glucose group as a reference. We present results weighted to national estimates.
RESULTS: Of the 13,792 participants without diagnosed DM, 65 % had normal glucose, 32 % had undiagnosed preDM, and 3 % had undiagnosed DM. Forty-four percent of individuals with undiagnosed DM and 54 % of those with undiagnosed preDM reported not being screened for DM in the past 3 years—potential screening or diagnostic failures. In univariate analyses, undiagnosed DM and preDM were associated with: older age, BMI ≥ 25, non-white race, hypertension, hyperlipidemia, and a family history of DM (p < 0.001; Table 1). Having less than a high school education (DM OR = 2.0, p < 0.001; preDM OR = 1.6, p < 0.001) and Medicare insurance (DM OR = 5.3, p < 0.05; preDM OR = 2.3, p < 0.001) were also associated with undiagnosed disease. Those with undiagnosed disease were more likely to have ≥2 MD visits in the past year (undiagnosed DM OR = 1.4, p = 0.02; undiagnosed preDM OR 1.3, p < 0.001). Individuals satisfying ADA and USPSTF screening criteria were more likely to have undiagnosed DM (ADA OR = 15.6; USPSTF OR = 4.8, P < 0.001 for both) and preDM (ADA OR = 5.2; USPSTF OR = 2.5, p < 0.001 for both) than those with normal glucose. The strongest single predictor of undiagnosed DM was a single random glucose ≥100 mg/dL (OR = 74.1, p < 0.001). A single random glucose ≥100 mg/dL (OR = 4.5, p < 0.001) was a better predictor of undiagnosed preDM than USPSTF (OR = 2.5, p < 0.001) but inferior to ADA guidelines (OR = 5.2, p < 0.001). After multivariate adjustment for age, gender, race, BMI, hypertension, hyperlipidemia, cardiovascular disease, and family history of DM, random glucose ≥100 mg/dL remained a robust predictor of undiagnosed DM (OR 51.3, p < 0.001).
CONCLUSIONS: Risk factors included in ADA and USPSTF guidelines are associated with undiagnosed DM and preDM. However, a single RBG ≥ 100 mg/dL is the best single predictor of undiagnosed DM and superior to either national guideline. Those with undiagnosed disease are routinely engaged with the healthcare system and greater attention to abnormal RBG values may improve identification of undiagnosed DM and preDM.
Table 1. Patient Characteristics Associated with Undiagnosed Prediabetes and Diabetes
| Characteristic | Undiagnosed Prediabetes | Undiagnosed Diabetes |
|---|---|---|
| Age ≥45 | 3.5 (3.1, 3.9) | 6.8 (5.3, 8.8) |
| BMI ≥ 25 kg/m2, (SE) | 2.3 (2.1, 2.6) | 6.5 (4.5, 9.4) |
| Non-white Race, % (SE) | 1.2 (1.1, 1.4) | 1.5 (1.2, 2.0) |
| Family History Diabetes | 1.4 (1.2, 1.5) | 1.9 (1.5, 2.4) |
| Hypertension | 2.5 (2.2, 2.7) | 4.8 (3.8, 6.0) |
| Hyperlipidemia | 2.0 (1.8, 2.2) | 2.4 (2.0, 3.0) |
| Cardiovascular Disease | 2.5 (2.1, 3.1) | 4.7 (3.5, 6.3) |
| ADA guidelines | 5.2 (4.5, 5.9) | 15.6 (8.1, 29.8) |
| USPSTF Guidelines | 2.5 (2.2, 2.7) | 4.8 (3.8, 6.0) |
| Random glucose ≥100 mg/dL | 4.5 (3.9, 5.1) | 74.1 (53.1, 103.4) |
Data presented as weighted Odds Ratio (95 % CI); p < 0.001 for all values BMI: Body mass index ADA: American Diabetes Association USPSTF: US Preventative Services Task Force
THE IMPACT OF A COMMUNITY HEALTH CENTER PATIENT NAVIGATION PROGRAM ON ABNORMAL MAMMOGRAPHY FOLLOW-UPSanja Percac-Lima1,2; Jeffrey M. Ashburner2; Sorbarikor Piawah3; Anne Marie McCarthy1,2; Steven J. Atlas2. 1Massachusetts Genral Hospital, Chelsea, MA; 2Massachusetts General Hospital, Boston, MA; 3Harvard Medical School, Boston, MA. (Tracking ID #1939688)
BACKGROUND: Despite advances in screening, diagnosis and treatment of breast cancer, patients continue to present with advanced disease. This is especially true for racial and ethnic minorities, underinsured, low income, and limited English proficiency patients. Patient navigation has been shown to improve screening and follow-up after abnormal results, particularly among disadvantaged women. We evaluated the impact of a patient navigation (PN) program as part of usual care at a community health center (CHC) on follow-up of abnormal mammograms.
METHODS: At a CHC serving predominately disadvantaged patients, all women with an abnormal mammogram were referred to PN to help them obtain appropriate follow-up care. In this retrospective study, we compared women from the CHC who had an abnormal screening mammogram (Breast Imaging-Reporting and Data System (BI-RADS 0,3,4,5) referred for PN between 2007 and 2010 with disadvantaged women (non-White, non-English speakers, or with Medicaid/Free care or no insurance) who had an abnormal screening mammogram during the same time period and received care in other practices within the same primary care network that did not have PN. The primary outcome was time to follow-up and the proportion of women who received appropriate follow-up between the two groups. Appropriate follow-up was defined: BI-RADS 0: follow-up within 3-months, BI-RADS 3: follow-up within 9-months and BI-RADS 4/5: biopsy within 3-months. Women with BI-RADS 0 who received a follow-up mammogram with BI-RADS 3,4, or 5 were reclassified into the higher BIRADS category. Patient characteristics between groups were compared using t-tests or chi-squared tests. We used logistic regression and Cox proportional hazards modeling to compare the receipt of and time to appropriate follow-up care between groups adjusting for patient age, race, primary language, number of clinic visits, and whether or not the patient was linked with a specific primary care physician (PCP).
RESULTS: Over the four-year period, there were 146 women with total 168 abnormal mammograms in the CHC with PN and 223 women with 239 abnormal mammograms in the practices without PN. Women from the CHC with PN were more likely to be Latina, linked to a specific PCP, less likely to speak English, and had more clinic visits over the prior 3-years. There were no significant differences by age or insurance status between groups. In the CHC with PN, 151 of 168 (89.9 %) abnormal mammograms received appropriate and timely follow-up compared to182 of 239 (76.2 %) in the other practices (adjusted p = 0.006). Most women with BI-RADS 0 received appropriate follow-up in both groups (90.0 % vs. 86.7 % in control, p = 0.55). In women with BI-RADS 3, more navigated women (85.4 %) received appropriate follow up than women from practices without PN (52.3 %, p = 0.003). Among women with BI-RADS 4/5, 92.9 % of women from the CHC with PN received appropriate follow-up compared with 82.0 % of women in control practices (p = 0.19). Time to follow-up was similar between groups following BI-RADS 0 (adjusted hazard ratio (HR), 95 % CI: 1.16 [0.88–1.53]). Women from the CHC with PN received follow-up care sooner than patients from other practices following BI-RADS 3 (HR [95 % CI]: 2.34 [1.37–4.02]) and BI-RADS 4/5 (HR [95 % CI]: 1.46 [0.93–2.30]).
CONCLUSIONS: Disadvantaged women receiving care in a CHC with PN were more likely to receive appropriate follow-up after an abnormal mammogram than disadvantaged women seen in practices without PN. Expanding PN to include all disadvantaged women within primary care networks should be further evaluated as a way to improve equity in cancer care.
THE IMPACT OF A DIABETES-SPECIFIC HEALTH PLAN ON ED AND INPATIENT HOSPITAL USETannaz Moin1,2; Neil Steers2; Susan Ettner2; O. Kenrik Duru2; Norman Turk2; Charles Chan3; Robert H. Luchs3; Anya Kirvan3; Sam Ho3; Carol Mangione2. 1VA Greater Los Angeles Healthcare System and HSR&D Center for Healthcare Innovation, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3UnitedHealth Group, Minneapolis, MN. (Tracking ID #1938946)
BACKGROUND: In the U.S., diabetes-related care accounts for approximately 1 in every 5 health care dollars. Timely and appropriate ambulatory care can help prevent diabetes-related complications that often lead to costly ED visits and/or hospital admissions. The Diabetes Health Plan (DHP) is the first disease-specific health plan for patients with diabetes and pre-diabetes. The DHP provides pharmacy and office visit financial incentives to enhance access to routine care, as well as additional resources for chronic disease management. This study examined changes in annual adjusted rates of ED and inpatient hospital utilization associated with employers’ purchase of the DHP, using employers who did not purchase the DHP as concurrent control groups.
METHODS: We conducted a retrospective, employer-level, intent-to-treat analysis, which included aggregate insurance claim and laboratory data from all employees and dependents with diabetes and pre-diabetes between 19 and 63 years of age, whether or not they were enrolled in the DHP. The 3-year consecutive study window included an initial 12 months of pre-period data (to conduct a baseline assessment and define the study sample) and 24 months of follow-up data (at 1 and 2 years post-DHP implementation). Inverse propensity score weighting was used to adjust for differences in employer level variables including mean age, education level, income, number of chronic medical conditions, proportion of female employees, proportion of employees from different demographic groups, proportion of employees with diabetes and pre-diabetes, and baseline rates of ED and inpatient hospital use between the DHP and control employers. Estimates were used to calculate the average treatment effect on the treated (ATET), or the difference between predicted rate of ED and inpatient hospital use among employer groups offering the DHP and their predicted rates if they had not offered the DHP.
RESULTS: Our results included 3 years of data from 9 employer groups who offered the DHP and 185 control employer groups who did not offer the DHP. Unadjusted rates of ED use were similar at baseline (DHP 7.64 %, control 8.60 %) but ED use decreased at 2 years in DHP groups (DHP 4.50 %, control 9.43 %). Our ATET analysis showed no evidence of significant reduction in ED use at 1 year post DHP but did show a 3.8 percentage point predicted reduction (p = 0.015) in the mean rates of ED use at 2 years post-DHP implementation, representing a 46 % decrease relative to the predicted baseline rate of 8.3 % ED use. No evidence was found of any significant association with predicted inpatient hospital use at 1 and 2 years post-DHP implementation.
CONCLUSIONS: We found that employers who offered the DHP had a 46 % reduction in the adjusted mean rates of ED use at 2 years post-implementation compared to the predicted mean rates of ED use had they not offered the DHP. Longer-term studies may be needed to observe any significant impact on inpatient hospital use. These findings suggest that health insurance benefit designs that decrease out of pocket costs for medications and preventive care can play an important role in decreasing the cost for more resource intensive services such as ED use for persons with diabetes and pre-diabetes.
THE IMPACT OF A PATIENT-CENTERED MEDICAL HOME ON VETERANS WITH DIABETES MELLITUSSivasubramanium Bhavani1,2; Andrew Spiegelman2; Utpal Ghosh1,2; Madhuri M. Vasudevan1,2. 1Baylor College of Medicine, Houston, TX; 2Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX. (Tracking ID #1938167)
BACKGROUND: Over five million veterans receive primary care from the Veteran Health Administration (VHA), making it the nation’s largest integrated health care delivery system. The VHA has launched the Patient Aligned Care Team (PACT) initiative to provide a patient-centered medical home for this sizable population. This paper examines the effect of the PACT in the management of diabetes mellitus in veterans receiving care at the Houston Michael E. DeBakey VA Medical Center (MEDVAMC).
METHODS: All subjects with diabetes mellitus enrolled in primary care clinics at the MEDVAMC were included in this retrospective pretest/posttest design study. Data was collected over a 2 year period consisting of a 1 year pre-PACT period and a 1 year post-PACT period. For each subject, the most recent HbA1c, LDL-C, blood pressure, and BMI were collected from the pre-PACT and post-PACT period. If any of these values were absent, the subject was excluded from the study. A paired student’s t-test was used to compare the subjects’ mean HbA1c, LDL-C, blood pressure, and BMI in the pre-PACT and post-PACT periods, with each subject serving as his/her own control. Sub-group analysis was performed with subjects divided into the following groups based on the subjects’ pre-PACT HbA1c: < 7 %, 7.0–9.0 %, and >9 %. In addition to the pretest/posttest design, an interrupted time series design was used: all available HbA1cs in the pre-PACT and post-PACT periods were collected and grouped together by month relative to PACT implementation. A linear regression trend line was used to plot the trend of average HbA1c in the pre-PACT and post-PACT periods.
RESULTS: 7,105 subjects in 23 primary clinic clinics were identified. The mean HbA1c was 7.6 % in the pre-PACT period and 7.5 % in the post-PACT period (p < 0.001). The mean LDL-C was 87.6 in the pre-PACT period and 84.4 in the post-PACT period (p < 0.001). The mean blood pressure in the pre-PACT and post-PACT period was 130/73 (p = 0.398 for systolic, p = 0.124 for diastolic). The mean BMI in the pre-PACT and post-PACT period was 32.5 (p = 0.839). The linear regression trend line of the pre-PACT HbA1c revealed an average increase of 0.01 % every month (p = 0.009). The linear regression trend line of the post-PACT HbA1c revealed an average decrease of 0.01 % every month (p = 0.023). For patients designated to the pre-PACT HbA1c >9 % group, the mean HbA1c was 10.6 % in the pre-PACT period and 9.1 % in the post-PACT period (p < 0.001).
CONCLUSIONS: The PACT focuses on employing a team-based approach to providing care, improving access to care, providing coordinated care, and forming partnerships with veterans. In the first year of PACT implementation, there has been a favorable change in HbA1c and LDL-C in the veteran population. This study confirms earlier studies demonstrating that a PCMH provides a viable system for management of chronic conditions; furthermore, this study demonstrates the viability of a medical home in the nation’s largest health care delivery system.
THE IMPACT OF AN ACTIVE PERSONAL HEALTH RECORD IN PATIENTS WITH HIGH CARDIOVASCULAR RISK: A PRAGMATIC RANDOMIZED CONTROLLED TRIALRachel Hess1; Sunday Clark2; Gary Fischer1; Melissa Weimer1; Sarah M. Sullivan1; Mark S. Roberts1. 1University of Pittsburgh, Pittsburgh, PA; 2Weill Cornell Medical College, New York City, PA. (Tracking ID #1940097)
BACKGROUND: Chronic diseases that contribute to the development of cardiovascular disease are common. Efforts to improve disease management by increasing rates of guideline-recommended care delivery have focused on clinician-centered solutions and modifying systems of care. Personal health records (PHRs) provide patients with a secure view into their electronic health records (EHRs). We examined the impact of an active PHR, compared to a standard PHR, on patients’ receipt of recommended care related to cardiovascular risk and 10-year cardiovascular risk.
METHODS: We recruited participants from 73 Western Pennsylvania primary care practices between June 2010 and September 2011 to participate in this pragmatic randomized controlled trial. Individuals were eligible to participate if they had (1) coronary artery disease, (2) congestive heart failure, (3) diabetes mellitus, or (4) hypertension or hyperlipidemia and were taking a medication that required routine laboratory monitoring. In addition individuals had to be willing to use the PHR. Participants in the intervention group received an active PHR that was designed in conjunction with standard PHR users. It allowed participants to view Health Maintenance topics, as in the standard PHR, and also included active reminders that notified participants when they had prevention gaps. The reminders included all services due within the next 3 months and were delivered in cycles of up to three weekly messages, with the final message accompanied by a post letter. Participants in the control group received the standard PHR. Participants completed questionnaires at baseline, 6-, and 12-months. Outcome data were abstracted from the EHR. Practices were ranked based on percent of patients receiving recommended care related to cardiovascular risk. We used Chi-square and Fischer’s exact tests, as appropriate, to compare 1-year change in receipt of recommended care (low-density lipoprotein, creatinine, A1C, and potassium testing) and t-tests to compare change in 10-year cardiovascular risk (based on Framingham risk score) from baseline in the active versus standard PHR. In secondary analyses, we examined the outcomes based on the quartile rank of the participant’s primary care practice for delivery of recommended care.
RESULTS: Of the 1,169 enrolled participants, 1,112 (95 %) had complete EHR data and are included in these analyses. Participants were 58.3 years old, 47 % were male, 15 % were non-white race, 38 % had diabetes, and 9 % were current smokers. At baseline 74 % of participants received A1C, 81 % low-density lipoprotein, 87 % creatinine, and 88 % potassium testing. Baseline 10-year cardiovascular risk was 11 %. At 1-year, we found no difference between the active and standard PHR groups in receipt of recommended care or 10-year cardiovascular risk. In the practices in the lowest quartile for delivery of recommended care, participants in the active PHR arm had higher rates of receipt of low-density lipoprotein (57 % vs. 43 %, p = 0.01), creatinine (56 % vs. 44 %, p = 0.02), and A1C (61 % vs. 39 %, p = 0.047) testing versus standard PHR. There was no difference in potassium testing.
CONCLUSIONS: In this 1-year study of an active versus passive PHR, we found no difference in the receipt of recommended care or change in 10-year cardiovascular risk overall. While we estimated that 60 % of patients would already be receiving recommended care at baseline, we found that over 80 % received recommended care. Amongst participants seen in the practices in the lowest quartile for delivery of recommended care, we found an improvement in three of four recommended tests. Future work should explore the potential of this low-intensity intervention to improve care for patients in lower-performing practice settings.
THE IMPACT OF JOB BURNOUT ON MEASURES OF PROFESSIONALISM IN FIRST-YEAR INTERNAL MEDICINE RESIDENTS AT A LARGE URBAN ACADEMIC MEDICAL CENTERJason Kwah; Robert Fallar; Jennifer P. Weintraub; Jonathan Ripp. Mount Sinai School of Medicine, New York, NY. (Tracking ID #1937527)
BACKGROUND: Internal Medicine (IM) residents commonly develop job burnout, which may lead to self-perceived sub-optimal patient care, depression, needle stick injuries and motor vehicle accidents. It remains uncertain what impact burnout has on professional behavior in this population. We hypothesize that first-year IM residents with burnout are more likely to demonstrate decreased levels of professionalism as compared with their burnout-free counterparts.
METHODS: We administered surveys to first-year IM residents at the Icahn School of Medicine at Mount Sinai twice between June 2011 and July 2012. Our survey, which has been previously reported, measured job burnout, sleepiness and other characteristics. Burnout was measured using the Maslach Burnout Inventory and defined by a high score on either the depersonalization or emotional exhaustion domain, in keeping with the most widely used convention. We subsequently gathered data on the following 3 measures of professional behavior for the same residents during the same time period: 1) Percentage of inpatient discharge summaries completed within 48 h of patient discharge, 2) Percentage of outpatient clinic charts completed within 3 days of patient encounter, and 3) Average time to review of outpatient test results ordered during patient encounters, specifically laboratory and imaging reports. The data were analyzed using SAS statistical software to identify relationships between job burnout and these measures of professionalism.
RESULTS: Of 54 eligible first-year IM residents, 53 (98 %) completed the initial survey and 32 (59 %) completed the year-end survey. Nineteen (36 %) of the 53 residents who completed the survey prior to the start of residency met criteria for job burnout. When comparing burnt out residents at the start of training with their burnout-free colleagues, there were no significant differences in timely discharge summary completion (84.5 % vs. 83.5 %; P = 0.64), timely outpatient clinic chart completion (91.4 % v. 96.1 %; P = 0.11), and average time to review of test results. (53.9 min. vs. 393.4 min; P = 0.23) Of the 32 residents who completed the year-end surveys, 24 (75 %) met criteria for burnout. When comparing burnt out residents with their burnout-free colleagues at year end, there were no significant differences in timely discharge summary completion (84.2 % vs. 84.1 %; P = 0.98), timely outpatient clinic chart completion (93.6 % vs. 93.7 %; P > 0.99), and average time to review of test results. (72.3 min vs. 26.89 min; P = 0.28)
CONCLUSIONS: Our study found that job burnout did not correlate with certain measures of professional behavior in a single group of first-year IM residents. Furthermore, residents maintained high levels of professionalism, by our measurement, despite burnout being quite common in their cohort. These findings could be explained by a number of reasons, including the possibility that burnout has no impact on professional behavior or that the measures we chose did not adequately assess the impact of burnout on professionalism. Given that interpersonal relations are central to the professional role of the physician and depersonalization is a domain of burnout, future study should perhaps be directed at measuring the influence of burnout on other aspects of professional behavior.
THE IMPACT OF JOB BURNOUT ON MEDICATION PRESCRIPTION ERRORS IN FIRST-YEAR INTERNAL MEDICINE RESIDENTSJennifer P. Weintraub; Robert Fallar; Jason Kwah; Jonathan Ripp. Mount Sinai School of Medicine, New York, NY. (Tracking ID #1937580)
BACKGROUND: Job Burnout has been increasingly recognized as common among internal medicine (IM) residents. Several studies have found that residents with burnout are more likely to self-report suboptimal patient care than those who are burnout free. Few studies have objectively measured the correlation between resident burnout and medical errors. We hypothesize that residents with burnout are more likely to commit medication prescription errors than their burnout-free counterparts.
METHODS: We administered a survey containing the Maslach Burnout Inventory to first-year IM residents at the Icahn School of Medicine at Mount Sinai twice between June 2011 and June 2012. Burnout was defined by a high score on either the depersonalization or emotional exhaustion domain, in keeping with the most widely used convention. Subsequently, data on all medication orders placed by these residents during the same 1 year period were collected. Based on pharmacy annotations, prescriber orders with the potential to cause adverse drug events (e.g. drug interactions, incorrect dosing) were identified and measured as a rate of errors per 100 prescriptions. Individual burnout scores and prescription error rates were linked using anonymous identifiers and analyzed for correlations using SAS statistical software.
RESULTS: Of the 54 eligible first-year residents, 53 (98 %) completed an initial survey and 32 (59 %) completed a follow-up survey. Burnout prevalence was 36 % (19/53) at the beginning of intern year and 75 % (24/32) at year’s end. Burnt-out residents had a significantly lower rate of pharmacy interventions compared with their burnout-free counterparts in both the initial survey (0.558/100 vs. 0.752/100; p = 0.005) and the year-end survey. (0.553/100 vs. 0.780/100; p = 0.007)
CONCLUSIONS: Burnt-out residents committed fewer prescription errors when compared with their burnout-free colleagues. This finding was contrary to our initial hypothesis and inconsistent with previously published findings based on self-report. Given the low error rate and the uncertain clinical significance of a correlation between burnout and decreased prescriber errors, further research is necessary to evaluate the link between job burnout and patient care in IM residents.
THE IMPACT OF PATIENT-CENTERED MEDICAL HOME TRANSFORMATION WITHIN VETERANS HEALTH ADMINISTRATION ON PATIENT EXPERIENCE OF CAREAshok Reddy1,4; Anne Canamucio2; Rachel M. Werner2,3. 1University of Pennsylvania, Philadelphia, PA; 2VISN 4 Center for Evaluation of PACT, Philadelphia, PA; 3Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, PA; 4Robert Wood Johnson Clinical Scholar Program, University of Pennsylvania, Philadelphia, PA. (Tracking ID #1938552)
BACKGROUND: The patient-centered medical home (PCMH) is an innovative primary care health delivery model that places an emphasis on delivering ‘patient-centered’ healthcare. However, there is little known regarding whether medical home transformation improves patients’ experience of care. In 2010, the Veterans Health Administration (VHA) began implementing its own medical home model, termed Patient Aligned Care Teams (PACT), across all primary care clinics nationwide. Our study takes place in one mid-Atlantic region of the Veterans Health Administration (VISN 4), which includes 56 primary care sites providing care for over 300,000 veterans. We evaluate the impact of adoption of the medical home model on patience experience of care.
METHODS: Patients were selected from the VHA quality improvement assessment program, the Survey of Healthcare Experiences of Patients (SHEP). For our study cohort, we identify patient survey respondents between July 2010 and October 2012. Our primary outcomes include 5 composite measures of patient care experience: how well doctors/nurses communicate, rating of personal doctor/nurse, getting needed care, overall rating of VA healthcare, and getting care quickly. We examine the effect of PACT implementation on these outcomes using two sources of variation—the timing and the effectiveness of PACT implementation across study sites. To do so, we first obtained the date when each primary care provider (PCP) became a PACT provider. Second, based on qualitative site-level interviews, we developed two types of site-level measures of PACT effectiveness: 1) nine indicators for structural changes supporting the PACT model and 2) a scale variable measuring the quality of PACT implementation. For our analysis we use a repeated cross-sectional design to evaluate the impact of the medical home transformation on patient experience of care. We conduct patient-level analyses, with patients clustered within PCPs and sites of care to test whether changes in health care delivery in the VHA under the PACT transformation led to changes in patient experience of care. Our linear probability models are adjusted for age, sex, race, income, and risk-based DCG scores and include PCP-level fixed effects.
RESULTS: Our analyses include SHEP responses from 28,041 patients who were associated with 568 physicians. The median age of respondents was 68 and most were male (96 %) who self-identified as white (91 %). A majority of respondents had a positive experience of care in 3 domains: how well doctor/nurse communicate (59 %), rating of personal doctor/nurse (77 %), and overall rating of the VHA (65 %). Over the study period the percentage of PCPs who were part of the PACT increased from 8.2 % in the first time period to 81.1 % in the last time period. Similarly, we observe an increase the implementation of PACT structural changes and the quality of that implementation. For example, the use of high-risk registries increased from 6.9 % in the first time period to 64.2 % in the last. In our primary analysis, we found no association between medical home transformation and patient experience of care using any of the three measures of PACT implementation. For example, patients assigned to a PACT provider had a 0.51 % (p = 0.66) higher response in how well they communicate with their provider compared to patients not assigned to a PACT provider and to patients in the pre-PACT period.
CONCLUSIONS: While the medical home model is increasingly adopted, in part to improve patient experience of care, we did not see an improvement in patient care experience in the VHA.
THE IMPORTANCE OF TRAINING IN THE IMPLEMENTATION OF AN OUTPATIENT DEPRESSION SCREENING AND TREATMENT PROTOCOLDanielle F. Loeb1; Janet Corral3; Amber Sieja1; Nichole Zehnder1; Mary McCord1; Donald E. Nease2. 1University of Colorado Denver, Aurora, CO; 2University of Colorado School of Medicine, Aurora, CO; 3University of Colorado School of Medicine, Aurora, CO. (Tracking ID #1938911)
BACKGROUND: Patients in primary care settings have a high prevalence of depression and these patients often have worse outcomes for chronic medical conditions. Systematic approaches to the identification and management of depression, such as the stepped care approach, improve the management of depression within the primary care setting. These team-based models of care have gained broad acceptance as the preferred approach to caring for patients with chronic disease. However, implementing these new approaches to care in “real world” settings presents both new opportunities and challenges.
METHODS: From 2012 to 2013 we implemented the Depression Protocol at two academic internal medicine primary care clinics associated with one academic medical center. Providers were offered a one-hour training in the rationale for the protocol and in the care processes associated with the protocol. The Depression Protocol utilizes a stepped-care treatment algorithm based on Patient Health Questionnaire (PHQ) 9 scores. The primary protocol procedures are: 1) The Medical Assistant (MA) administers the PHQ-2 on all patients at new patient or annual visits. 2) The MA gives a paper PHQ-9 to patients with a positive PHQ-2. 3) The provider documents the PHQ-9 into the Electronic Medical Record (EMR). 4) The provider treats the patient based on the PHQ-9 score and their clinical judgment. 5) Patients with positive PHQ-9 scores are reassessed in person in 1–3 months depending on score and treatment strategy. 6) The PHQ-9 is administered at the follow-up visit. 7) When a psychotropic medication is started or changed, the provider initiates a 1–2 week follow-up call by a member of the provider’s team (MA or nurse). We performed a retrospective analysis of provider documentation of protocol processes: 1) documentation of PHQ-9 at visits for patients with positive PHQ-2 s and 2) PHQ-9 monitoring at subsequent visits for patients with positive PHQ-9 s. We utilized both descriptive and logistic regression analysis to assess the association between in-person training attendance and provider performance of the protocol. We employed a generalized estimating equation to control for correlation between documentation within the same provider. We also administered a survey to assess provider comfort with protocol procedures (Procedures), provider perception of impact of training on their competency in managing depression (Competency). Two scales were developed corresponding to the Procedures and Competency questions. We calculated a Cohen’s d effect size for the effect of training on the outcomes.
RESULTS: Clinic 1 (C1) had 32 resident and 26 faculty providers; Clinic 2 (C2) had 21 and 18, respectively. Average documented PHQ-9 s for positive PHQ-2 s for C1 residents, C1 faculty, C2 residents, and C2 faculty was 70.6 %, 66.6 %, 48.8 % and 60.9 %, respectively; and average patients with a repeated PHQ-9 were 27.4 %, 31.4 %, 20.0 %, and 37.0 %, respectively. Logistic regression analysis (see table) showed training attendance was positively associated with documentation of PHQ-9 after a positive PHQ-2 [OR = 2.4 (1.3–4.3)] and repeated documentation of a PHQ-9 after a positive PHQ-9 [OR = 2.5 (1.1–5.3)]. In the provider survey, there was a moderate effect size (d = 0.4) of training attendance on the Procedures outcome. There was no significant effect on provider Competence outcome (d = 0.04).
CONCLUSIONS: That training was associated with increased odds of compliance with protocol procedures, and a moderate effect size for comfort with protocol procedures, points to the importance of practical training in the implementation of practice change in the primary care setting. The movement toward team-based care has been adopted on a national policy level through incentives in the Affordable Care Act for primary care practices to adopt the Patient-Centered Medical Home (PCMH) model. Healthcare administrators and researchers need to consider multifaceted approaches, which incorporate practical training, as they implement these new models of care in the primary care setting. In order to improve provider compliance with the Depression Protocol, an online training module was developed in October 2013, making training accessible to all resident and attending providers in the two clinics.
Multiple Logistic Regression for PHQ-9 documented for Positive PHQ-2 and Repeated PHQ-9 for Positive PHQ-9
| Characteristic | * Adjusted OR | Confidence Interval |
|---|---|---|
| Documented PHQ-9 for Positive PHQ-2 | ||
| Provider (Attending) | 0.8 | 0.5–1.5 |
| Clinic (Lowry) | 0.6 | 0.3–1.2 |
| Training (Attended) | 2.4 | 1.3–4.4 |
| Repeated PHQ-9 for Positive PHQ-9 | ||
| Provider (Attending) | 1.2 | 0.6–2.3 |
| Clinic (Lowry) | 1.2 | 0.7–2.1 |
| Training (Attended) | 2.5 | 1.1–5.3 |
*Repeated documentation by providers have been accounted for using the GEE model. All the variables (provider type, clinic type, and training attendance) were added simultaneously as covariates.
THE JOHNS HOPKINS INDEX OF OVERUSE: A PROOF OF PRINCIPLE THAT REGIONAL OVERUSE IS MEASUREABLEJodi B. Segal1,2; Hsien-Yen Chang2; Najlla Nassery1,2; Eva Chang2; Kitty Chan2; Jonathan Weiner2; John Bridges2. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD. (Tracking ID #1930508)
BACKGROUND: Healthcare quality is frequently described with composite measures representing the overall performance. Despite growing attention to overuse in healthcare, there is little experience with composite measures of overuse. Overuse can be defined as use of a service in the absence of a clear medical basis for its use, or when the risk of harm exceeds its likely benefit. Our goal was to create a composite measure of overuse useable with claims data. We therefore aimed to identify a set of potentially overused medical procedures (indicators), operationalize these to be measureable with administrative claims, aggregate these indicators into a single indicator of overuse, and test whether the index is associated with higher costs and worse clinical outcomes, which would be the proof of principle that the measure is detecting regional overuse.
METHODS: This was an observational study, using 5 % of Medicare claims from 2008 (Parts A and B), of older patients in the U.S. receiving healthcare services in hospitals or outpatient settings. Via an environmental scan, we identified published descriptions of overused procedures. We assessed each procedure’s feasibility for measurement with claims data and developed algorithms for occurrences of procedures in patients unlikely to benefit. We calculated summary statistics to illustrate variance in use across hospital referral regions (HRRs) and selected 20 for inclusion in the Johns Hopkins Index of Overuse (JHOI). We started with an initial analysis of each of the 20 indicators (denote by P). As such, we regressed Pijk as P ijk = βXi + Φjk + εijk where Xi is a vector of patient specific factors, Φjk is a set of regional fixed effects for j procedures across the k HRRs. From this model, the Φjk is a risk-adjusted measure indicating if region k overuses procedure j more or less than expected. The JHOIk was estimated as an average of the Φjk. Thus, in this version of the JHOI each indictor contributes equally to the index. With Spearman’s correlation, we assessed the correlation of this regional measure, presumptively a measure of systematic overuse, with regional measures of total costs, risk-adjusted mortality, 30-day mortality, and total mortality.
RESULTS: 613 procedures were identified as overused. Twenty had abundant frequency and variance to be possible measures of systematic overuse, including 13 diagnostic tests, 2 tests for screening, 1 for monitoring, and 4 therapeutic procedures. Usage varied markedly across HRRs. Among 1,451,142 beneficiaries, 14 % had at least one overuse event. The index was positively correlated with 30-day inpatient mortality (r = 0.27, p = <0.0001), and positively correlated with total costs (r = 0.39, p < 0.0001). It was similarly positively correlated with inpatient days (0.22, p < 0.0001) and intensive care unit days (r = 0.32, p < 0.0001), but not with total mortality.
CONCLUSIONS: We identified a set of overused procedures that demonstrate significant variance in their usage. This study provides proof of principle that systematic overuse exists and is measurable. We need to identify the best combination of indicators for the index, which may require inclusion of procedures prevalent in younger people, and to validate the index when applied to panel data.
THE MEANINGFUL USE OF ELECTRONIC HEALTH RECORDS AND HEALTHCARE UTILIZATIONLisa M. Kern; Alison M. Edwards; Rainu Kaushal. Weill Cornell Medical College, New York, NY. (Tracking ID #1937856)
BACKGROUND: Since 2011, the federal government has been investing $20 billion in incentives for adoption and meaningful use of interoperable electronic health records (EHRs). The effect of “Meaningful Use” (MU) of EHRs on health care utilization is not known. We sought to determine the effects of MU on health care utilization, compared to typical use of EHRs without MU.
METHODS: We conducted a longitudinal cohort study of primary care physicians in the Hudson Valley region of New York over 2 years (2010–2011). We divided physicians, all of whom were using EHRs, into 2 study groups, based on whether they had achieved MU in 2011 or not. We used negative binomial regression to determine associations between study group and 7 different utilization outcomes (primary care visits, specialist visits, laboratory tests, radiology tests, emergency department visits, hospital admissions and 30-day readmissions), adjusting for 11 physician characteristics (membership in an independent practice association, gender, age, degree, specialty, rural county, practice size, Patient-Centered Medical Home status, panel size, case mix and plan mix).
RESULTS: We included 213 physicians and 127,353 patients. Of the physicians, 107 (50 %) had achieved MU and 106 (50 %) had not. For every 100 patients whose physicians achieved MU, there were 17 fewer primary care visits and 61 fewer laboratory tests, compared to patients whose physicians did not achieve MU (p < 0.05 for each adjusted comparison). There were no significant differences for the other outcomes.
CONCLUSIONS: Achieving Stage 1 MU was associated with a decrease in primary care visits and laboratory tests. This suggests that effects of MU on health care utilization are distinct from the effects of typical EHR use without MU.
THE MEDICATION METRONOME: A HEALTH IT SYSTEM TO IMPROVE MEDICATION MANAGEMENT AND LABORATORY MONITORING FOR CHRONIC DISEASESSteven J. Atlas1; Michael Jernigan1; Jeffrey M. Ashburner1; Jaime Chang1; Leila H. Borowsky1; Yuchiao Chang1; Richard W. Grant2. 1Massachusetts General Hospital, Boston, MA; 2Kaiser Permanente Northern California, Oakland, CA. (Tracking ID #1938604)
BACKGROUND: Lack of timely medication intensification and inadequate safety monitoring are two prevalent and potentially modifiable barriers to effective and safe chronic care. To test a model of chronic disease management in which medication initiation or dose adjustment orders are explicitly and immediately linked to future planned laboratory monitoring, we developed a novel health information technology (IT) tool (Medication Metronome) designed to support non-visit based medication management. Integrated into an existing electronic health record (EHR), the tool enabled primary care physicians (PCPs) to schedule future laboratory monitoring when initiating or adjusting doses of medications for diabetes, hypertension, and/or hyperlipidemia management. We hypothesized that scheduling follow-up laboratory monitoring (e.g. HbA1c 3 months after starting metformin) would support a cycle of laboratory monitoring and iterative medication dose adjustment resulting in more effective and safer chronic disease care.
METHODS: Physicians from two sites within a primary care network were randomized to intervention (n = 22) or control (n = 22) groups. During a 1-year intervention, PCPs allocated to the intervention had an additional feature in their electronic medication prescription interface that enabled them to schedule future laboratory tests when ordering new prescriptions or adjusting doses to treat type 2 diabetes, hypertension, or hyperlipidemia. This process initiated automated patient reminders that included a mailed letter and lab slip 1 week before the test was due and (if necessary) a second letter and lab slip 1 week after the test due date if no result was found. Notification of persistently overdue lab results (>3 weeks after due date) was added to a physician “Watchlist” of test results within the EHR. Control physicians had access to the same EHR but without the added Medication Metronome interface. Efficacy labs were defaulted to order, while safety monitoring needed to be actively turned on by intervention physicians. The primary effectiveness outcome was the percentage of follow-up time that a patient was at or below risk factor goal (HbA1c ≤7 % among diabetics prescribed hypoglycemic agents; LDL-cholesterol ≤130 mg/dl for patients with hyperlipidemia without cardiovascular risk and ≤100 mg/dl for patients with cardiovascular risk) using a mixed effects model. The primary safety outcome was the percentage of safety monitoring laboratory tests (creatinine after initiating drugs for hypertension and diabetes, and liver function testing after initiating statins) completed within 4 weeks of the medication order using logistic regression models. Models accounted for clustering by PCP and adjusted for patient age, gender, race/ethnicity, primary language spoken and baseline lab value.
RESULTS: During the study period, there were 2991 eligible medications orders among 2031 patients of intervention PCPs and 2420 orders among 1590 patients of control PCPs. In the intervention group, 659 prescriptions (22 %) used the Metronome interface to initiate laboratory follow-up (521 [79 %] efficacy, 138 [21 %] safety). Patient characteristics were similar among intervention and control groups except slightly more intervention patients were non-Hispanic whites (84.3 % vs. 80.5 %, p = 0.02) and spoke English (95.4 % vs. 92.8 %, p = 0.001), and had lower LDL levels (118.2 vs. 125.6 mg/dl, p = 0.002). The adjusted percentage of time that a patient was at or below the effectiveness outcome goal over 3 months after a medication order did not differ among patients of intervention and control PCPs for diabetes (30.9 % vs. 29.1 %, p = 0.72) or hyperlipidemia (51.6 % vs. 46.7 %, p = 0.2) (see Table). Similarly, the performance of safety monitoring labs within 4 weeks of a medication order for hypertension, diabetes or hyperlipidemia did not differ among intervention or control groups (data not shown).
CONCLUSIONS: A visit-independent, health IT tool to support a cycle of laboratory monitoring and iterative medication dose adjustment following the initiation or change of chronic disease medications during an office-based visit did not increase goal attainment or safety monitoring rates compared to usual care. New models for reimbursing providers for health care services may be needed before adoption of innovative tools that support visit-independent medication management.
Mean proportion of time at or below goal in intervention and control groups
| Intervention | Control | |||||
|---|---|---|---|---|---|---|
| N | Adjusted Mean % | N | Adjusted Mean % | Difference | 95 % CI | |
| Diabetes: HbA1c ≤7 | 308 | 30.9 % | 268 | 29.1 % | 1.8 % | −8.4–12.1 % |
| Intervention group limited to those with Metronome order | 120 | 32.5 % | 268 | 29.1 % | 3.5 % | −8.6–15.5 % |
| Hyperlipidemia: LDL at goal | 674 | 51.6 % | 391 | 46.7 % | 4.9 % | −1.6–11.4 % |
| Intervention group limited to those with Metronome order | 227 | 53.0 % | 391 | 46.7 % | 6.3 % | −1.4–14.0 % |
THE QUALITY AND IMPORTANCE OF FEEDBACK IN PROFESSIONAL DEVELOPMENT OF INTERNS AND RESIDENTSRyan Graddy; Panagis Galiatsatos; Colleen Christmas. Johns Hopkins Bayview Medical Center, 913 Baylis Street, MD. (Tracking ID #1939327)
BACKGROUND: The receipt of high quality feedback during medical education is likely a key component of learner development of professional skills, knowledge, and identity. Available literature demonstrates that physicians are often poor at self-assessing their own strengths and weaknesses as clinicians and educators, suggesting that receipt of outside feedback throughout one’s career is crucial to continuing professional development. Nonetheless, a paucity of data exists on learner attitudes toward feedback as both recipient and provider.
METHODS: We conducted a structured online survey of internal medicine residents and interns at a moderate-sized academic residency program (Johns Hopkins Bayview Medical Center) to assess the perceived role and importance of feedback in trainees’ professional development. Survey questions were developed with a Likert scale model that focused on self-assessed value of several modes of teaching including directed feedback, confidence in giving feedback to individuals at varying levels of training, and importance assigned to feedback giving and receipt in one’s future career path.
RESULTS: 19 interns and 15 upper level residents completed the survey. 89.4 % (17) of interns deemed one-on-one feedback with faculty members as “useful” or “very useful” for professional development; over 50 % of respondents rated this as “very useful.” Teaching on rounds, small group sessions, online reference materials, teaching conferences, a module-based internet learning center, and self-directed learning all received lower ratings. In contrast, residents rated online reference materials most consistently as “useful” or “very useful” (100 %, 15), while 73.6 % (11) of upper level residents rated one-on-one feedback as such. Both interns and residents rated a module-based internet learning resource as the least useful tool in their development. Interns consistently reported a high degree of confidence in providing feedback to students (73.7 % agreed or strongly agreed), but generally felt less confidence in providing feedback to fellows and faculty (36.8 % each). Residents felt confident in providing feedback to medical students and interns in 73.3 % of cases (11 for each), but only 13.3 % (2) felt confident providing feedback to fellows and 26.7 % (4) to attending physicians. Across the board, the importance of giving and receiving feedback during one’s future career was greatly valued; 73.7 % (14) of interns and 80.0 % (12) of residents strongly agreed that receipt of high quality feedback is important to the doctor they aspire to be in 10 years, while 57.9 % (11) of interns and 71.4 % (10) of residents strongly agreed that giving high quality feedback is important to the doctor they aspire to be.
CONCLUSIONS: High quality feedback is consistently recognized as playing an important role in professional development among interns and residents, particularly during intern year. While trainees are highly confident in providing feedback to more junior learners, they report low confidence in providing feedback to more senior team members, suggesting that navigation of the cultural hierarchy of medicine remains challenging. Given the importance of feedback to lifelong professional development, further efforts are needed to improve resident training in this skill area.
THE RELATION BETWEEN ANTIHYPERTENSIVE MEDICATION AND SEXUAL FUNCTION IN WOMEN: BASELINE DATA FROM THE SPRINT STUDYHolly N. Thomas1,2; Gregory W. Evans3; Dan Berlowitz4,5; Denise E. Bonds6; Glenn M. Chertow7; Molly B. Conroy1; Capri Foy8; Stephen Glasser9; Cora E. Lewis9; William T. Riley10; Laurie Russell8; Olubunmi Williams11; Rachel Hess1. 1University of Pittsburgh, Pittsburgh, PA; 2VA Pittsburgh Healthcare System, Pittsburgh, PA; 3Wake Forest University, Winston-Salem, NC; 4Bedford VA Hospital, Bedford, MA; 5Boston University School of Medicine, Boston, MA; 6University of Virginia School of Medicine, Charlottesville, VA; 7Stanford University School of Medicine, Palo Alto, CA; 8Wake Forest University School of Medicine, Winston-Salem, NC; 9University of Alabama at Birmingham School of Medicine, Birmingham, AL; 10National Institute of Mental Health, Bethesda, MD; 11Emory University, Atlanta, GA. (Tracking ID #1937990)
BACKGROUND: Treatment of hypertension results in substantial reductions in cardiovascular risks, yet patients often discontinue antihypertensive medications due to side effects. Studies have suggested an association between antihypertensives and sexual dysfunction in men, but the relationship between these medications and sexual dysfunction in women is less well understood. We used a cross-sectional cohort of older women to examine the relations among different classes of antihypertensives and sexual function.
METHODS: The Systolic Blood Pressure Intervention Trial (SPRINT) is a randomized controlled trial of high-risk (presence of cardiovascular disease, chronic kidney disease, or 10-year Framingham risk score ≥15 %) individuals aged 50 and older comparing the effect of standard (systolic <140 mmHg) and lower (systolic <120 mm Hg) blood pressure control targets on a variety of clinical outcomes. Baseline data were used for this analysis. A randomly selected subset of participants completed questionnaires on quality of life (QoL), including sex. Self-reported sexual function was assessed using a modified version of the Female Sexual Function Index (FSFI), a validated instrument. A score of <27 indicates sexual dysfunction. Antihypertensive class was defined by medications participants were taking at the start of the trial. Only women who enaged in any kind of sexual activity in the prior 4 weeks were included in the analysis (FSFI scores cannot be calculated in inactive women). Descriptive statistics were used to compare sexually active and inactive women. A multivariable linear regression model including class of medication and potential confounding variables (demographic factors, level of blood pressure, and comorbidities) was used to examine the relation between medication class and FSFI score while adjusting for other variables. Two-mean comparison tests were used to determine the power our sample had to detect at least a moderate clinical difference in FSFI score (Cohen’s d = 0.5) for women taking a given medication versus women not taking that medication.
RESULTS: Of 690 women who participated in the QoL portion of SPRINT, 183 (26.5 %) were sexually active. Inactive women were more likely to be older, less educated, live alone, and have medical comorbidities. The mean age for sexually active women was 63.4 (SD 9.1) and 41.5 % were white. Among sexually active women, FSFI scores were low overall, with the mean (25.3) falling below the cutoff for dysfunction. Scores were similar for different antihypertensive classes (Table 1). The mean FSFI was significantly higher for women not taking any antihypertensives (28.0, unadjusted P = 0.041), but this difference did not persist in multivariable analysis (P = 0.35). Neither class of medication, nor any of the potential confounders, was significantly associated with FSFI score on multivariable analyses (Table 2). This analysis had 82.6 % (85.4, 92.0, 90.2) power to detect a moderate difference in FSFI scores between beta-blocker (calcium-channel blocker, diuretic, angiotensin converting enzyme inhibitor/angiotensin receptor blocker) users and non-users.
CONCLUSIONS: Similar to prior studies of older women, FSFI scores were overall low in this cohort. We found no association between any antihypertensive class and sexual dysfunction in women in this cross-sectional sample. Larger, longitudinal studies are necessary to fully understand the relation between antihypertensive medications and sexual function in women.
FSFI scores among sexually active women in SPRINT
| N (%) | Mean FSFI score | SD | |
|---|---|---|---|
| All sexually active women | 183 (100.0) | 25.3 | 6.0 |
| Women on no antihypertensives | 19 (10.4) | 28.0 | 4.7 |
| Beta-blocker users | 45 (24.6) | 24.6 | 6.7 |
| Calcium channel blocker users | 50 (27.3) | 25.4 | 6.4 |
| Diuretic users | 95 (51.9) | 24.8 | 6.5 |
| ACE/ARB users | 115 (62.8) | 24.9 | 5.7 |
ACE/ARB = angiotensin-converting enzyme inhibitor/angiotensin-receptor blocker
Multivariable predictors of FSFI score among sexually active women in SPRINT
| Baseline characteristic | Fully adjusted beta for FSFI score (95 % CI) | P-value |
|---|---|---|
| Not taking antihypertensives (vs. any) | 1.83 (−2.02, 5.68) | 0.35 |
| Beta-blocker use (vs. not) | −0.58 (−2.77, 1.62) | 0.61 |
| Calcium channel blocker use (vs. not) | 0.2 (−1.8, 2.2) | 0.84 |
| Diuretic use (vs. not) | −1.39 (−3.3, 0.52) | 0.153 |
| ACE/ARB use (vs. not) | −0.99 (−2.86, 0.87) | 0.29 |
| Systolic blood pressure (per 10 mm Hg increase) | 0.07 (−0.73, 0.87) | 0.86 |
| Diastolic blood pressure (per 10 mm Hg increase) | 0.67 (−0.47, 1.81) | 0.25 |
| Presence of chronic kidney disease (vs. not) | 0.07 (−2.34, 2.48) | 0.95 |
| Presence of hyperlipidemia (vs. not) | 1.13 (−0.7, 2.96) | 0.22 |
| Presence of cardiovascular disease (vs. not) | 0.0 (−2.77, 2.76) | 1.00 |
Adjusted for age, race, education status, living with others, use of antidepressants, use of hormone therapy
THE RELATIONSHIP BETWEEN ATTRIBUTES OF PATIENT-CENTERED MEDICAL HOMES, PATIENT ENGAGEMENT, AND OUTCOMES OF CARE AMONG INDIVIDUALS LIVING WITH DIABETESAllyson G. Hall1; Fern J. Webb2; David Wood2; Jeffrey S. Harman1. 1University of Florida, Gainesville, FL; 2University of Florida, College of Medicine, Jacksonville, FL. (Tracking ID #1937694)
BACKGROUND: Successful diabetes management requires coordination of multiple modalities, support for patients’ participation in self-management activities, and paying attention to diverse cultural attitudes and beliefs. Patient-centered medical homes (PCMHs) are a conceptualization of how to provide care to individuals living with diabetes. How primary care sites implement key attributes of the medical home may be directly associated with how patients with diabetes experience care, engage in their care, and ultimately their health outcomes. This study examines: 1) how experiences with care and patient engagement (as measured by the Patient Activation Measure (PAM)) varies across four PCMHs; 2) the relationship between patients’ ratings of their medical homes and level of engagement in their care; and 3) the relationship between patient engagement and self-reported outcomes of care.
METHODS: 1,300 randomly selected adult patients with diabetes seen at 4 National Committee for Quality Assurance Level 3 accredited academic primary care practices participated in a telephone survey. Survey items included the PAM and questions on experiences with their medical home. Ordered logistic regression analysis (controlling for race/ethnicity, marital status, education, health status, and age) was used to determine the relationship between a medical home practice and the extent to which patients were more engaged in their care; the relationship between patient ratings of their medical home and their PAM score; and relationship between their PAM score and the degree to which patients report following their diet as prescribed, and whether they check their feet for cracks and calluses. In-depth interviews with staff provided information on how each clinic operated.
RESULTS: The qualitative interviews showed that despite all 4 clinics achieving NCQA accreditation, there are differences in the manner in which key components of the PCMH model are implemented. For example, clinicians at site A had undergone intensive specialized training in diabetes care and provided a comprehensive disease management program to its patients. The survey showed that a higher proportion of patients at location A reported positive experiences with care. Ordered logistic regression analysis confirmed that patients at Location A were significantly more likely to have higher PAM scores compared to patients at the other three clinics. Regression analysis also demonstrated that patients with higher medical home domain ratings were more likely to have higher PAM scores; and that higher PAM scores are associated with reports of following their diet as prescribed and checking feet for cracks and calluses.
CONCLUSIONS: Despite receiving similar NCQA ratings, how medical homes offer and provide services can vary. This variation may lead to differing patient experiences with care and ultimately a difference in how patients can perceive their ability to manage and engage in their care.
THE RELATIONSHIP BETWEEN NEIGHBORHOOD FOOD ACCESS AND FOOD INSECURITY IN AN URBAN ENVIRONMENTVictoria L. Mayer1; Amy Hillier2; Marcus A. Bachhuber1,3; Judith A. Long1,3. 1Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 2School of Design, University of Pennsylvania, Philalephia, PA; 3Philadelphia Veterans Affairs Medical Center, Philadelphia, PA. (Tracking ID #1939936)
BACKGROUND: Approximately 17.6 million households are estimated to be food insecure in the United States, meaning they do not have enough food for an active, healthy life. Programs to augment food access (i.e., neighborhood availability of healthy foods) are increasingly widespread, but the relationship between food access and food insecurity is unknown.
METHODS: We analyzed the 2008, 2010, and 2012 Southeastern Pennsylvania Household Health Survey. Our outcome was food insecurity, defined by skipping or reducing meal size because of budget. Logistic regression models included food access variables, including ease of finding fruits and vegetables and perceived quality of grocery stores in the neighborhood, as well as individual and neighborhood level covariates.
RESULTS: Of 11,599 respondents, 16.7 % of respondents reported food insecurity. Of those who reported food insecurity, 79.4 % found it easy or very easy to find fruits and vegetables and 60.6 % reported excellent or good quality grocery stores in their neighborhood. In the fully adjusted model, compared to those who reported very easy access to fruits and vegetables, those who reported easy, difficult or very difficult access were more likely to report food insecurity (OR 1.18: 95 % CI 1.00–1.38, 2.21: 95 % CI 1.70–2.88, and 3.57: 95 % CI 2.50–5.09). Compared to those who reported excellent stores, those who reported good, fair, and poor quality stores were more likely to report food insecurity (OR 1.35: 95 % CI 1.12–1.62, 1.87: 95 % CI 1.50–2.37, and 2.32: 95 % CI 1.69–3.19).
CONCLUSIONS: Neighborhood food access plays a role in food insecurity. However, many food insecure individuals already have local access to healthy foods. Interventions aimed at improving diet in communities with a high prevalence of food insecurity should focus not only on availability, but also on affordability.
THE RELATIONSHIP BETWEEN TELEPHONE VISITS AND USE OF OUTPATIENT CARE DURING THE VA MEDICAL HOME INITIATIVEDavid A. Katz1,2; Kimberly McCoy1; Mary Vaughan Sarrazin1. 1University of Iowa, Iowa City, IA; 2University of Iowa Carver College of Medicine, Iowa City, IA. (Tracking ID #1939083)
BACKGROUND: Increased use of telephone visits and other non-face-to-face contacts is widely advocated as a key strategy for VA medical homes to improve access and efficiency. The objective of this study is to determine whether telephone visits are associated with fewer in-person primary care visits and fewer ED visits during the Patient Aligned Care Team (PACT) initiative.
METHODS: We conducted a cross-sectional analysis of VA outpatients with at least one chronic condition (HTN, DM, COPD, CAD, CHF, depression/anxiety) who were assigned to a VA primary care provider (PCP) and had at least one primary care visit each year with physicians or physician extenders during FY2010-13 (N = 100,383). To do this, we linked data in the 2010 Patient Care Management Module (PCMM) to VA outpatient data; patients of resident providers, nursing home residents, and those who received home telehealth were excluded. Clinic stop codes were used to identify telephone visits with nurses and providers, primary care visits, and ED visits, which were tabulated during FY2012-13. We used generalized estimating equations (GEE) with overdispersed Poisson models to assess number of primary care visits, and multivariable logistic regression models to predict any ED use. In a longitudinal analysis, we assessed whether patients who received telephone visits during the 6 months following the initial clinic visit in FY2012 (months 0–6) were more likely to visit the primary care clinic and the ED during the subsequent 3 month period (months 7–9), compared to patients who did not receive any telephone visits during months 0–6. All regression models controlled for demographics, disability status, 22 chronic medical and psychiatric conditions [Romano, 1993; Abrams, 2009], as well as number of primary care clinic visits and prior VA hospitalization (all calculated from baseline FY2010-11 data); robust sandwich variance estimates were used to account for clustering at the level of patients’ usual site of care.
RESULTS: During FY2012-13, study patients had a mean of 4.8 primary care visits and 19 % had visited the ED; 44 and 2 % received at least one telephone visit from a primary care nurse and a PCP, respectively. In multivariable models, patients who received 1 and 2+ nurse telephone visits had greater use of primary care visits: IRR (95 % CI) = 1.10 (1.07, 1.13) and 1.30 (1.23, 1.37), respectively. Patients who received 1 and 2+ nurse telephone visits were also more likely to visit the ED during follow-up: OR (95 % CI) = 2.5 (1.8, 3.5) and 4.5 (2.8, 7.2), respectively. In longitudinal analysis, patients who received nurse telephone visits during 6-month follow-up had more primary care visits and were more likely to visit the ED during the subsequent 3 months than those who did not receive telephone visits from a nurse: IRR (95 % CI) = 1.16 (1.11, 1.20) and OR (95 % CI) = 1.7 (1.3, 2.2), respectively. Similar results were observed for providers, except that the results for ED use were not statistically significant.
CONCLUSIONS: Although the use of telephone visits is an important strategy for improving access to care, telephone visits have the potential to generate more outpatient visits and ED referrals, as previously unrecognized problems are brought to the attention of primary care team members. More effective telephone care strategies may obviate the increased need for face-to-face visits.
THE ROLE OF EVOLUTIONARY CONCEPTS IN MEDICAL EDUCATION, 10 YEARS LATERBrandon H. Hidaka1; Anila Asghar3; Randolph M. Nesse5; Katelyn Bennett4,2; Matthew Beyrouty2,4; Nicole Skursky2,4; Mark D. Schwartz2,4. 1University of Kansas Medical Center, Kansas City, KS; 2NYU School of Medicine, New York, NY; 3McGill, Montreal, QC, Canada; 4VA New York Harbor Healthcare System, New York, NY; 5Arizona State University, Tempe, AZ. (Tracking ID #1938046)
BACKGROUND: Understanding evolutionary biology deepens medical knowledge and expands our explanatory models for research, education, and practice. A 2003 survey revealed how, and why, little evolution is taught in medical school. The current survey assessed the current situation and changes since the prior study.
METHODS: We surveyed curriculum deans of all 153 Canadian and US medical schools. Respondents rated the curricular coverage (4-point scale from not covered to covered in depth) and importance (4-point scale from not important to essential) of 12 core evolutionary principles (e.g. somatic selection in cancer, tradeoffs, hygiene hypothesis, and antibiotic resistance). We described the gap between importance and coverage of these principles and compared coverage in 2003 and 2013. We measured the association between mean coverage with school characteristics, resources devoted to teaching evolution, potential controversy, and mean importance. Respondents rated the usefulness of 13 teaching resources that could facilitate teaching evolution. Open-ended questions sought further insight into benefits of and barriers to infusing evolution into medical education. Qualitative responses were sorted into themes by three independent researchers.
RESULTS: Of the 60 (39 %) responding schools, 90 % were from the US, 62 % were public, 27 % from the top NIH quartile, 42 % placed high priority on training future researchers, and 48 % felt that teaching evolution could arouse controversy among students, faculty, legislators, or donors. Schools reported a median (IQR) of 0 (0–2) faculty with a PhD in Evolution, 0 (0–2) faculty doing research based in evolution, 6 (4–16) hours teaching evolutionary topics in the curriculum, and 5 (2–15) hours teaching applications of evolutionary principles to specific medical problems. Figure 1 illustrates the proportion of importance and coverage of the 12 evolutionary principles. Table 1 compares current survey results with those from the 2003 survey. A school’s mean coverage of evolution principles was associated with the number of faculty with a PhD in evolutionary biology (r = 0.29, p = 0.07), the number of faculty whose research is based in evolutionary biology (r = 0.38, p = 0.02), having an evolutionary medicine student interest group (p = 0.04), and the school’s mean rating of importance of evolutionary topics (r = 0.75, p < 0.0001). The 3 teaching resources ranked as most useful were: model test questions and answers with explanations, case studies with facilitator guides, and model curricula for adding evolution content to existing courses and rotations. Qualitative responses revealed barriers to teaching evolution in medical school: competition in already overfull curricula, anticipated religious controversy, low perceived value, and lack of resources, especially faculty.
CONCLUSIONS: North American medical schools have increased the content of evolutionary principles in their curriculum over the past decade. Curriculum deans view many evolutionary principles as important, but report minimal coverage of many topics ranked as important. Their responses suggest that bridging the gap will best be accomplished by bolstering faculty expertise in evolutionary biology, and developing education resources that can augment their effectiveness in teaching the basic principles of evolutionary biology that are useful in medicine.
Table 1
| 2003 survey | 2013 survey | Difference | |
|---|---|---|---|
| % Having evolutionary biologist on faculty | 16 | 49 | +33 |
| % Devoting any curriculum hours to teaching evolution | 80 | 92 | +12 |
| % Reporting coverage of… | |||
| Antibiotic resistance | 94 | 98 | +4 |
| Environmental mismatch | 30 | 94 | +64 |
| Pathogen virulence | 83 | 92 | +9 |
| Tradeoffs | 26 | 90 | +74 |
| Aging/Life-history theory | 19 | 82 | +63 |
| Defense regulation | 20 | 80 | +60 |
| Levels of selection | 51 | 70 | +19 |
| Anatomical flaws from path dependence | 17 | 67 | +50 |
| Proximate vs. evolutionary explanations of disease | 5 | 57 | +52 |
THE ROLES OF COST AND QUALITY INFORMATION IN MEDICARE ADVANTAGE PLAN ENROLLMENT DECISIONSRachel O. Reid1; Partha Deb4; Benjamin L. Howell2; William Shrank3. 1Brigham and Women’s Hospital, Boston, MA; 2Center for Medicare & Medicaid Services, Baltimore, MD; 3Brigham and Women’s Hospital, Boston, MA; 4Hunter College, New York, NY. (Tracking ID #1933518)
BACKGROUND: To facilitate informed decision making in the Medicare Advantage marketplace, the Centers for Medicare & Medicaid Services publishes information about Medicare Advantage plans via the Medicare Plan Finder website, including costs, benefits, and quality ratings provided on a 1-to-5 star scale. Little is known about how beneficiaries weigh costs versus quality when making enrollment choices. In this study, we assess the variation in Medicare Advantage enrollment attributable to plan attributes and willingness to pay for quality.
METHODS: We conducted a nationwide, beneficiary-level cross-sectional analysis of the 2011 Medicare Advantage and Prescription Drug (MAPD) plan choices of beneficiaries enrolling in Medicare Advantage for the first time ever in 2011 who were not eligible for the low-income subsidy. Matching beneficiaries with their choice-sets of MAPD plans by county, we used conditional logistic regression to estimate associations between plan attributes and enrollment, to assess both the proportion of explained enrollment variation attributable to plan attributes and willingness to pay for quality. The model accounted for 5-star quality ratings, costs (premiums and average estimated out-of-pocket costs), benefits (plan structure; deductibles; coinsurance; hearing, vision, dental benefits; and prescription gap coverage), and lagged county-level sponsor organization (i.e., brand) market share. Because willingness to pay for quality may vary at different rating levels, the model included both the 5-star quality rating itself and its quadratic transform. We assessed differential willingness to pay by beneficiary characteristics (age, sex, race, and urban versus rural residence) by interacting these covariates with quality and cost covariates.
RESULTS: The study cohort included 847,069 first-time Medicare Advantage enrollees who selected an eligible MAPD plan in 2011. Relative to the total variation explained by the model, market share accounted for 35.3 % of variation in plan choice, premiums for 25.7 %, estimated out-of-pocket costs for 11.6 %, and 5-star quality ratings for 13.6 %. Mean cumulative willingness to pay for a plan in total annual combined premiums and out-of-pocket costs varied from $4,154.93 for a 2.5-star plan to $5,698.66 for a 5-star plan. Increases in willingness to pay diminished at higher 5-star quality ratings: $549.27 (95 % CI $541.10 to $557.44) to go from a 2.5-star plan to a 3-star plan and $68.22 (95 % CI $61.44 to $75.01) to go from a 4.5-star plan to a 5-star plan. Beneficiaries aged 64–65 years were more willing to pay for plans with higher quality ratings than other age groups; black and rural beneficiaries were less willing to pay for plans with higher quality ratings.
CONCLUSIONS: Medicare Advantage enrollees prefer plans with higher quality ratings and lower costs; however, market share’s contribution to plan choice suggests that word-of-mouth and brand recognition are also influential. Key subgroups’ differential willingness to pay for quality and market share’ influence argue for continued efforts to advance communication of plan attributes to improve marketplace efficiency. If increased enrollment in plans with the highest quality ratings is a goal, the diminishing marginal utility for quality observed supports policy interventions to make achievement of the highest ratings desirable for insurers and enrollment in the highest-rated plans attractive and accessible to beneficiaries.
THE USE OF PANEL MANAGEMENT ASSISTANTS TO IMPROVE SMOKING CESSATION AND HYPERTENSION MANAGEMENT BY VA PRIMARY CARE TEAMS: A CLUSTER RANDOMIZED CONTROLLED TRIALMark D. Schwartz1,2; Ashley E. Jensen1,2; Binhuan Wang1,2; Katelyn Bennett1,2; Anne Dembitzer1,2; Shiela Strauss3; Antoinette Schoenthaler2; Colleen Gillespie2; Scott Sherman1,2. 1VA New York Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU College of Nursing, New York, NY. (Tracking ID #1937793)
BACKGROUND: Panel Management (PM), a set of tools and processes applied to populations of patients, can expand prevention and chronic illness management beyond the office visit, but there is limited evidence for its effectiveness or guidance on how to incorporate it into clinical practice. To test the effectiveness of incorporating PM into clinical practice, we randomly assigned Panel Management Assistants (PMAs) to primary care teams with and without panel management education.
METHODS: We conducted an 8-month, cluster-randomized controlled trial at two campuses of the VA New York Harbor Healthcare System. A total of 20 primary care (PC) teams were randomized, which consisted of 51 physicians and 18 nurses serving 8,153 patients with hypertension and/or smoking. Twelve teams were randomized to receive support from a PMA, a college graduate with no clinical training who underwent a one-month orientation that covered basic clinical issues in hypertension and smoking, skill development in panel management, VA’s electronic medical record and administrative tools, and motivational interviewing and Brief Action Planning. PMAs systematically reviewed panel data for their assigned teams to identify patients with specific gaps in care. They joined biweekly team meetings to review lists of identified patients and propose PM strategies using a toolkit developed for the study and then conducted patient outreach by phone and mail. Six of the 12 intervention teams also received PM education consisting of five, 20-minute PM education sessions during team meetings. These case-based sessions addressed working in multidisciplinary teams, practicing PM, and leveraging the clinical microsystem. The eight control teams received only monthly data on their smoking and hypertensive patients. Primary outcomes were assessed from the medical record and by patient survey: mean systolic and diastolic blood pressure (BP), proportion of patients with controlled BP, self-reported quit attempts, nicotine replacement therapy (NRT) prescriptions, and referrals to disease management services. PC staff was surveyed before and after the intervention.
RESULTS: Regression analysis, controlling for baseline BP and clustering, revealed no significant differences among study arms in mean systolic or diastolic BP values post-intervention. Following the intervention, 90 % of smokers reported quitting for at least 1 day and 64 % reported quitting for at least a week. However, there were no significant differences in smoking rates or quit attempts by study group. Patients on intervention teams were more likely to receive NRT for smoking (OR = 1.4; 95 % CI 1.2–1.6), to enroll in the VA’s weight management (OR = 1.2; 95 % CI 1.1–1.6) or, Telehealth programs (OR = 1.7, 95 % CI 1.4–2.1), than patients on control teams. Most staff (80 %) assigned to an intervention team felt the PMA was a useful resource for their team and 73 % wanted to continue working with a PMA. Only 26 % said the PMA took too much of their time. Only 40 % said they would continue using PM strategies when the PMA left the team.
CONCLUSIONS: PM support and education for PC teams improved process, but not outcomes among veterans with hypertension and smoking. This study has important limitations, as it included only veterans, implementation lasted only 8 months with post-intervention data collection interrupted by Hurricane Sandy, and primary care teams were newly formed at study outset. However, incorporating PMAs into PC teams was feasible and highly valued by the clinical staff, and warrants further study.
THE VALUE OF STUDENT-RUN CLINICS FOR THE PREMEDICAL STUDENT: A MULTI-INSTITUTIONAL STUDYKaylin Pennington1; Ian Tong1; Cindy Lai2; Patricia S. O’Sullivan2; Leslie Sheu2. 1Stanford University, Stanford, CA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1938624)
BACKGROUND: Over 40,000 students apply to US medical schools each year. While the majority of premedical students participate in clinical experiences prior to medical school matriculation, the skills and abilities gained from these widely variable experiences are not well known. In student-run clinics (SRCs), premedical students take on authentic roles in patient care—acting as interpreters, patient navigators, patient advocates, and health educators. While research has shown that SRCs are ideal experiential learning arenas for medical students, the subjective benefit of SRCs on premedical students has not yet been explored. This study is a first attempt to characterize the impact of the SRC experience on the premedical student who later matriculates to medical school.
METHODS: We conducted a retrospective cohort study involving first-year medical students at five California medical schools. Participants completed an anonymous one-time online survey that included demographic information, premedical activities, and Likert scale questions (from not (1) to extremely (4) important) related to SRC participation. We calculated descriptive statistics and used chi-squared and t-tests to compare groups. We used SPSS for all tests and set significance at 0.05.
RESULTS: Two-hundred eighty-seven responses were collected between September and November 2013 (48.2 % response rate, ranging from 30 to 71 % by school). Across all five schools, 50 students in total (17.4 % of respondents) reported volunteering in an SRC and 24 students served as leaders. For those participating in SRCs, major activities included taking patient histories and vital signs; serving as interpreters, patient advocates, or receptionists; case management; and supporting operational activities. Students’ greatest motivations to volunteer were a desire to work with patients and underserved populations (means 3.88 (SD 0.39) and 3.84 (SD 0.37), respectively), and students believed that they gained the most skills in these areas (means 3.67 (SD 0.63) and 3.74 (SD 0.57), respectively). Most students (56 %) found one or more mentors through their SRC experience; 67.8 % identified medical student mentors. Students found their SRC experience to be among their most meaningful premedical experiences (mean score 8.60 out of 10 (SD 1.36)), with those students who served in leadership positions or identified mentors finding the experience more meaningful than those who did not (p < 0.02).
CONCLUSIONS: Nearly one-fifth of first-year medical students surveyed volunteered in SRCs prior to their medical school matriculation. Students identified SRCs as meaningful venues for developing leadership, teamwork, and patient interaction skills. Medical schools could build on the skills these students have as part of a systems-based practice curriculum. One major limitation to our study is our low survey response rate, which may introduce bias to our results. Nevertheless, we hope that this attempt to understand premedical clinical experiences will serve as fertile ground for future research including comparing premedical SRC experiences to other clinical experiences and understanding how premedical SRC experiences may meet early competency milestones (particularly patient care, interpersonal and communication skills, and systems-based practice).
THE VARYING IMPACT OF CHRONIC DISEASES ON PHYSICAL AND MENTAL HEALTH-RELATED QUALITY OF LIFE: IMPLICATIONS FOR A NOVEL MEASURE OF MULTIMORBIDITYMelissa Y. Wei1,2; Ichiro Kawachi3; Olivia Okereke4,2; Kenneth Mukamal1. 1Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, MA; 2Harvard School of Public Health, Boston, MA; 3Harvard School of Public Health, Boston, MA; 4Brigham and Women, Boston, MA. (Tracking ID #1928886)
BACKGROUND: More adults have multimorbidity, the coexistence of two or more chronic conditions, than have one chronic disease. Multimorbidity is associated with decreased health-related quality of life (HRQOL) and greater healthcare utilization and cost. However, heterogeneity in the impact of chronic conditions is not well-characterized and has limited consistent and systematic efforts to study multimorbidity. We aimed to 1) quantify the impact of a broad range of individual chronic diseases on both physical and mental HRQOL, and 2) determine whether a multimorbidity index of diseases weighted by their associated HRQOL differs from a simple count of the number of diseases.
METHODS: The Nurses’ Health Study (NHS) is a prospective cohort of 121,700 female nurses aged 30–55 years when data collection began in 1976. In 2000, participants completed a questionnaire on 50 physician-diagnosed chronic diseases and conditions and the Short Form (SF)-36, including its Physical Component Summary (PCS) and Mental Component Summary (MCS). These summary scores are scaled 0–100 from lowest to highest functioning, and differences of 5–10 points (0.5–1 standard deviations) are typically considered clinically meaningful. We used multiple linear regression to measure the effect of individual morbidities on HRQOL after adjusting for age and other morbidities.
RESULTS: Of 94,839 women who returned questionnaires on chronic disease, we included 61,206 women who also completed the SF-36. Their mean age was 70 years (SD 7.1). The mean PCS score was 46.5 (SD 10.7), and mean MCS score was 54.6 (SD 7.7), close to general population norms. The most common chronic diseases were hypercholesterolemia, hypertension, osteoarthritis, benign breast disease, cataracts, and others shown in Table 1. The impact of common conditions on either PCS or MCS varied widely (PCS: median −1.31, range −6.89 to 0.64; MCS: median −0.80, range −7.24 to 0.33). Osteoarthritis had the greatest adverse impact on PCS, while atrial fibrillation and diabetes also reduced PCS by 2–4 points. While hypercholesterolemia was most prevalent, its impact on PCS was small and non-significant. Diseases with the greatest adverse impact on PCS were multiple sclerosis, Parkinson’s disease, ALS, osteoarthritis, rheumatoid arthritis, lung cancer, emphysema, and congestive heart failure, respectively, but with the exception of osteoarthritis were generally less prevalent (0.03 % for ALS to 3.7 % for rheumatoid arthritis). The conditions with the largest adverse effect on MCS were depression, Parkinson’s disease, lung cancer, inflammatory bowel disease, interstitial cystitis, lupus, hip fracture, and stroke. Although PCS and MCS were not meaningfully correlated across individuals (Pearson’s correlation coefficient r = 0.02), the magnitude of impact of various conditions on PCS was positively correlated with that on MCS (r = 0.26). A multimorbidity index of the most common conditions weighted by their impacts on PCS was positively but far from uniformly correlated with a simple corresponding count of diseases (r = 0.67).
CONCLUSIONS: In this study of over 60,000 women who reported both comorbidities and HRQOL, individual conditions varied widely in their effects on HRQOL, with some conditions associated with several-fold greater impact than others. Even common conditions varied widely in their associations with HRQOL. Across conditions, the impact on physical HRQOL correlated positively but moderately with mental HRQOL. Our results suggest that simple counts of diseases for multimorbidity are unlikely to capture their true impact on health, and that methods weighted to HRQOL or other validated measures are both feasible and promising.
Table 1. Change in Physical Component Summary and Mental Component Summary scores for the most prevalent chronic diseases and conditions in the Nurses’ Health Study in 2000
| Physical Component Summary | Mental Component Summary | ||||||
|---|---|---|---|---|---|---|---|
| Chronic disease or condition | Prevalence, % | Change in PCS | Standard error | P-value | Change in MCS | Standard error | P-value |
| Elevated cholesterol | 36.0 | −0.012 | 0.08 | 0.88 | −0.28 | 0.07 | <0.0001 |
| High blood pressure | 35.0 | −1.79 | 0.08 | <0.0001 | −0.06 | 0.07 | 0.43 |
| Osteoarthritis | 25.6 | −6.89 | 0.09 | <0.0001 | 0.85 | 0.07 | <0.0001 |
| Fibrocystic/benign breast disease | 19.4 | 0.46 | 0.09 | <0.0001 | −0.009 | 0.08 | 0.91 |
| Cataract | 19.0 | −0.82 | 0.10 | <0.0001 | −0.14 | 0.08 | 0.09 |
| Osteoporosis | 14.7 | −0.23 | 0.11 | 0.03 | −0.55 | 0.09 | <0.0001 |
| Depression | 8.6 | −2.60 | 0.13 | <0.0001 | −7.24 | 0.11 | <0.0001 |
| Basal cell cancer | 7.6 | 0.64 | 0.14 | <0.0001 | 0.33 | 0.12 | 0.005 |
| Atrial fibrillation | 7.2 | −2.29 | 0.14 | <0.0001 | −0.32 | 0.12 | 0.007 |
| Diabetes mellitus | 5.9 | −4.11 | 0.16 | <0.0001 | −0.56 | 0.13 | <0.0001 |
PCS: Physical Component Summary; MCS: Mental Component Summary
THINKING OUTSIDE THE BOX: MEDICAL TRAINEE PERSPECTIVES ON THE SOCIAL DETERMINANTS OF HEALTHMaggie K. Benson1; Thuy Bui1; Janet Arida2; Paula Leslie2; Martha Terry2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1931771)
BACKGROUND: The social, political, environmental and economic contexts of peoples’ lives tremendously impact their health. Research shows that factors such as housing, education, income, neighborhood safety, transportation, food availability and social support are strongly correlated with health outcomes and contribute to overall health status more than traditional medical care. The World Health Organization is focusing attention on the “social determinants of health” (SDH) and is challenging governments, providers, and community leaders to do likewise. Medicine has traditionally focused on a biological model emphasizing pathophysiology and discreet medical and surgical interventions to improve health and prevent disease. However, physicians are increasingly called upon to investigate and act upon the social factors impacting their patients’ health. Literature exists on training in health advocacy, cultural competence, communication and health literacy, but little is known about how the SDH are approached in education or how trainees conceptualize the SDH in the context of patient care. We sought: 1. To understand how medical trainees conceptualize the SDH; 2. To explore how medical trainees believe the SDH relate to the care that physicians provide to patients; 3. To identify how medical education approaches the SDH.
METHODS: We conducted focus group discussions with third and fourth year medical students and second and third year internal medicine residents at an urban academic medical center. Participants were recruited via the medical school and residency email lists. Focus groups were stratified by training level: two groups with medical students and two with internal medicine residents. The focus groups were guided by a facilitator experienced in qualitative methodology. Seven open-ended questions were developed by the investigative team to probe how participants conceptualize the SDH and how participants learned about them during their medical education. Each focus group was held over a 60 min period with 4–6 participants. Discussions were audio-recorded and transcribed. Two coders independently read and coded each transcript to elicit primary themes.
RESULTS: In qualitative analysis, the following themes emerged: 1. Medical trainees conceptualize the “social determinants of health” to include a broad range of patient characteristics and experiences. Trainees mentioned socioeconomic status, cultural background, education attainment and health literacy, a history of adverse life events as well as prior personal and family member experience with the healthcare system as elements of the SDH. One student defined the SDH broadly as “everything outside your exact biology.” 2. Medical trainees believe the SDH relate to the care that physicians provide to patients both positively and negatively. Trainees described experiences where physician consideration of the SDH positively impacted the care provided to patients by allowing health care providers to be more mindful of the cost of interventions or transportation difficulties. Conversely, they also discussed experiences where patients’ care was negatively impacted by providers’ preconceptions about a patient based on his socioeconomic status. 3. Trainees have learned about the SDH through both formal and informal educational interventions, however there was agreement that clinical experiences were more meaningful than classroom didactics. Trainees stated that learning about the SDH in the context of “real” patients either through the care of patients in clinical settings or inviting patients to speak in more formal settings made a greater and more lasting impact. Trainees acknowledged that while simulated exercises have good intention in raising awareness about the SDH, they felt such activities could be perceived as “insulting to the real problems actually faced” by patients. There was a strong belief that currently, learning about the SDH “has to be sought out” by those interested, and might not be of interest to all medical trainees. They expressed concern that until the SDH are considered a routine and essential part of traditional medical care, it will be a challenge for medical educators to address it successfully amongst a broad range of medical trainees.
CONCLUSIONS: This is the first study that sought to ask medical trainees about their perceptions and preferred learning strategies related to the social, political, economic and environment factors that impact health. Participants expressed that educational experiences in this domain need to be factored in across the continuum in a clinical context and not as separate modules or “electives” that only serve those already interested and knowledgeable. In this focus group study, medical trainees provided valuable input as to why SDH training is important, where it fails and how to address it more successfully in the future.
TIME IN TRAINING AND CLINICAL SKILLS AS MEASURED BY UNANNOUNCED STANDARDIZED PATIENTSColleen Gillespie; Kathleen Hanley; Lisa Altshuler; Adina Kalet; Jaclyn Fox; Sondra Zabar. NYU SoM, New York, NY. (Tracking ID #1937691)
BACKGROUND: The ACGME’s Next Accreditation System uses outcomes to determine readiness to practice, reflecting growing awareness that simply completing required years of training may not guarantee competence. Measuring those outcomes, however, continues to be a challenge for Residency Programs. Unannounced Standardized Patient visits—standardized clinical scenarios played by highly trained actors integrated, incognito, into providers’ clinical schedule—represent a very promising method for assessing “true” competence. In the context of exploring time—vs competency-based determination of physician preparation, we report on the relationship between time in training and clinical skills as assessed by USPs in a sample of Primary Care Internal Medicine Residents.
METHODS: 4 USP cases were developed to represent common primary care challenges: Educating a patient about her diagnosis (Education); Teaching a patient to take medications correctly (Medication); Assessing underlying reasons for a non-specific complaint (Tiredness); and Counseling on health maintenance and behavior change (Health Promotion). Visits were fielded with Primary Care residents in a small residency program (n = 24) over 5 years. Thirty-five residents treated the “Education” USP (22 PGY1, 6 PGY2, 7 PGY3); 34 residents treated the “Medication” USP (22 PGY1, 5 PGY2, 7 PGY3); 35 treated the “Tiredness” case (18 PGY1, 9 PGY2, 8 PGY3); and 36 residents treated the “Health Promotion” case (20 PGY1, 7 PGY2, 9 PGY3). Behaviorally anchored checklists were used by USPs to rate performance in: Communication, assessment, physical examination, education/counseling, management plan, and patient activation (4–11 items/domain). Scores were calculated as % items rated well done (vs. not or partly); internal consistency was >.70 for all. Time in training was assessed by PGY and as cumulative months of training. Independent samples Kruskal-Wallis tests were used to determine if the distribution of competence scores differed by PGY; correlations assessed the relationship between months of training and competence scores; and hierarchical regressions explored the influence of months of training after controlling for residents’ scores on a PGY1 OSCE (baseline competence).
RESULTS: The distribution of competence scores did not consistently differ by PGY for any of the 4 USP visits (Kruskal-Walllis tests p > .05). Only 4/24 possible correlations between time in training (months) and competence score (4 cases × 6 domains) were significant (Pearson’s r; p < .05): In the Medication case, assessment and physical exam scores were negatively correlated with time in training (r = −.58 and −.41); patient activation scores were positively correlated with time in training in the Tiredness (r = .42) and Education (r = .28) cases. Similar results were obtained after controlling for “baseline” (PGY1) OSCE performance: Months of training accounted for small amounts of variance in assessment scores for the Medication and Health Promotion case (R2 range .09–.16; Std Betas = −.27 and −.34); in exam scores for the Medication case (R2 = .17; Std Beta = −.32); and in Patient Activation scores for the Tiredness and Education cases (R2 range .08–.12; Std Betas = .20 and .25).
CONCLUSIONS: If USP visits are valid and reliable assessments of “true” clinical competence, then time in training does not appear to be a good indicator of competence. However, our exploratory study was powered to detect only fairly substantial effects. In addition, our checklist may be subject to expertise reversal effects as evidenced by negative associations between training and assessment and examination, where highly skilled physicians may omit less relevant information gathering. Our results, however, do suggest that clinical competence is not simply a product of time in training.
TIME PREFERENCE, OBESITY, AND RESPONSE TO CALORIE LABELINGKelly A. Kyanko; Brian Elbel. NYU School of Medicine, New York, NY. (Tracking ID #1936183)
BACKGROUND: Behavioral economics, or applying psychological insights to traditional economic decision making, suggests that individuals do not always make choices that maximize their long-term well-being. Few studies have addressed how these principles may influence food choice and obesity. In particular, time preference, how once values the immediate want to consume healthy food versus the more distant potential health consequences, could be particularly important. We sought to explore the relationship between time preference in obesity and one policy approach meant to influence obesity, calorie labeling.
METHODS: Data were collected from a random digit dial telephone survey of 2926 adults in two cities: one that implemented menu calorie labeling (Philadelphia) and one that did not (Baltimore), both before and after labeling began. Two measures of time preference were used: The choice of a lottery payout of $1000 now or $1500 a year from now measured present bias or time discounting, and financial planning horizon (a few months or greater than a few months) measured planning ability and self-control. Multivariable logistic regression was used to assess factors related to self-reported obesity and the whether the respondent reported noticing and being influenced by calorie labeling, adjusting for age, sex, race, education, income, and health status.
RESULTS: Obese individuals were more likely than non-obese to have a short financial planning horizon (OR = 1.33, 95 % CI: 1.11–1.60), but did not demonstrate differences in time discounting compared to non-obese individuals. Though obesity was predictive of being influenced by calorie labeling (OR obese vs. under or normal weight = 3.29, 95 % CI: 1.86–5.82; OR severely obese vs. under or normal weight = 2.57, 95 % CI: 1.40–4.70), measures of time discounting and financial planning were not.
CONCLUSIONS: Differences in planning ability are associated with and may play a role in the development of obesity. While behavioral economics principles may help target obesity interventions, in this study time preference did not change individuals’ behavior in response to menu calorie labeling.
TIME TRENDS OF CLINICAL OUTCOME AND SPENDING OF CARE FOR ACUTE MYOCARDIAL INFARCTION HOSPITALIZATIONS IN THE UNITED STATES, 2001–2011Takehiro Sugiyama1,2; Kohei Hasegawa3,4; Osamu Takahashi5; Tsuguya Fukui5; Yusuke Tsugawa6. 1The University of Tokyo, Tokyo, Japan; 2National Center for Global Health and Medicine, Tokyo, Japan; 3Massachusetts General Hospital, Boston, MA; 4Harvard Medical School, Boston, MA; 5St. Luke’s International Hospital, Tokyo, Japan; 6Harvard Interfaculty Initiative in Health Policy, Cambridge, MA. (Tracking ID #1932307)
BACKGROUND: The incidence of acute myocardial infarction (AMI), particularly ST-elevation AMI (STEMI), has decreased in the US during the last decade. The in-hospital mortality due to AMI has also decreased. However, it is unclear whether the time trend of in-hospital mortality differs by cardiovascular intervention performed during hospitalization, percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), and by type of AMI, STEMI and non-STEMI (NSTEMI). Additionally, little is known about the time trend of AMI-associated healthcare spending by intervention performed during hospitalization and type of AMI. We aimed to investigate the time trends in in-hospital mortality and hospital charge and cost per discharge for AMI hospitalization, by intervention performed during hospitalization and type of AMI in the US.
METHODS: We performed a serial cross-sectional study using the Nationwide Inpatient Sample from 2001 to 2011. We included all hospital discharges for those who hospitalized with the primary diagnosis of AMI aged 30 years or older. Primary outcome measures were in-hospital mortality as well as hospital charge and cost per discharge adjusted for inflation. We classified AMI hospitalizations into 6 subgroups: by intervention performed during hospitalization (no PCI/CABG, PCI without CABG, and CABG with or without PCI) and by type of AMI (STEMI and NSTEMI). We investigated time trends of outcomes for each subgroup, adjusting for patient characteristics, patient comorbidities, and hospital characteristics. We used logistic regression for in-hospital mortality, whereas we used linear regressions for log-scale hospital charge and cost, estimating percent changes of geometric means.
RESULTS: Between 2001 and 2011, we identified a total of 1,504,462 discharges of AMI in the US, corresponding to a weighted estimate of 7,373,282 discharges. The rate of AMI hospitalizations decreased from 4.6 per 1,000 populations in 2001 to 3.3 per 1,000 populations in 2011. Adjusted in-hospital mortality decreased, particularly in NSTEMI without interventions (OR of 2011 with reference to 2001: 0.59, 95%CI: 0.53–0.66) and NSTEMI with CABG (OR of 2011 with reference to 2001: 0.39, 95%CI: 0.26–0.60). By contrast, hospital charge per discharge increased during 11 years in all subgroups ranging from a 38.5 % (95%CI: 30.1 %–47.4 %) increase in NSTEMI without interventions to an 82.5 % (58.2 %–110.6 %) increase in STEMI with CABG. Hospital cost per discharge increased during 11 years in all strata, ranging from 8.2 % (3.2 %–13.5 %) increase for NSTEMI without interventions to 32.2 % (21.3 %–44.2 %) increase for STEMI with CABG.
CONCLUSIONS: In nationally representative samples, we found that in-hospital mortality for AMI hospitalizations decreased significantly during the last decade. By contrast, hospital charge and cost per discharge increased in all subgroups; the time trends of hospital charge and cost differed by intervention performed during hospitalization and type of AMI. While we succeeded in improving clinical outcomes of AMI in the US in the last decade, the spending of care especially for those who underwent interventions has been increasing substantially.
TIMING IS EVERYTHING: STUDYING INSULIN ADMINISTRATION IN THE INPATIENT SETTINGValentina Rodriguez; Benjamin Levin; Joseph Mermelstein; Marelle Yehuda; Robert E. Graham. Lenox Hill Hospital, Manhattan, NY. (Tracking ID #1939304)
BACKGROUND: Hyperglycemia in hospitalized patients is a common, serious, and costly health care problem that is dependent on multiple factors including food consumption, exercise, and types of insulin used. Variables in insulin action (e.g., onset, peak, and duration) must be considered. Most diabetes experts have recommended checking finger stick glucose level, administering rapid acting insulin, and starting a meal all within 30 min. We have evaluated the timing of these intervals to assess for adherence to these recommendations.
METHODS: At an academic hospital in an urban setting, the times between finger stick glucose testing, rapid acting insulin administration, and meal delivery for general internal medicine patients were directly observed and recorded over the course of several weeks between June and August 2013. Inclusion criteria included any medicine inpatient receiving rapid acting insulin (not limited to diabetic patients). Patients who were NPO, receiving tube feeds, or who refused finger stick checks or insulin, were excluded. To account for variation and volume of staff, data was collected on separate weekdays (including weekends); in addition, 2 separate general medical floors were observed. In order to directly observe nursing staff collection of finger stick glucose levels, administration of insulin, and delivery of meals, 4 residents and 2 medical students participated in data collection.
RESULTS: Of the 122 patients studied, 6 were NPO and thus excluded. Of the remaining 116 patients, only 44 patients (38 %) received their meal within 30 min of their finger stick glucose check. Sixty-one of the 116 patients (53 %) required pre-meal insulin; of these patients, only 16 of the patients (26 %) received insulin within 15 min of their meal. Eleven patients (18 %) received insulin within 30 min of having their finger stick glucose checked.
CONCLUSIONS: For a large percentage of patients, the times from finger stick glucose check to meal and from meal to insulin were each in excess of 30 min. It is clear from our data that we are not adhering to current recommendations. In addition, our hospital as well as similar institutions would likely benefit from staff education. While not examined in this study, this deficiency has the potential to result in hypo/hyperglycemic events and affect patient satisfaction.
TO BUY OR NOT TO BUY: USE OF EXTRAMURAL AMBULATORY CARE CURRICULA AMONG PEDIATRIC, INTERNAL MEDICINE, & MED-PEDS PROGRAMSJaideep S. Talwalkar1,2; D’Juanna Satcher3; Teri Turner3,4; Stephen Sisson5; Ada M. Fenick2. 1Yale School of Medicine, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Baylor College of Medicine, Houston, TX; 4Baylor College of Medicine, Houston, TX; 5Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1929225)
BACKGROUND: The sharing of curricular resources is becoming an increasingly common phenomenon among medical educators, as residency programs implement “extramural curricula,” those which have been developed by other institutions for the purpose of sharing. Existing extramural curricula have been designed to improve education on important topics in ambulatory care for children and adults. Current rates of implementation among pediatric, internal medicine, and combined med-peds training programs are unknown. The purpose of this study was to assess the usage rates of extramural ambulatory care curricula among pediatric, internal medicine, and combined med-peds residency programs.
METHODS: Two independent surveys designed to characterize various aspects of the continuity clinic experience were sent to pediatric and combined med-peds program directors respectively in the spring of 2012. Each survey contained an item asking respondents about their use of extramural ambulatory care curricula. No similar recent data were available for internal medicine. In order to determine current usage rates among internal medicine programs, we queried the editors of the Yale Office Based Medicine Curriculum and the Johns Hopkins Internet Learning Center Internal Medicine Curriculum, the two extramural curricula commonly known to be widely used by internal medicine training programs. To verify the accuracy of this data collection method for comparison purposes to the survey data from pediatric and med-peds programs, we also collected subscription rate information for the Yale Primary Care Pediatrics Curriculum and Johns Hopkins Pediatrics Ambulatory Care Curriculum through direct query. Data were analyzed with SAS 9.3 to conduct the two-proportion tests. Significance was defined as p < 0.05.
RESULTS: Surveys were returned by 111 of 198 (56 %) pediatric and 63 of 79 (80 %) med-peds programs. Of the med-peds survey respondents, 60 answered the item related to extramural ambulatory care curricula. Responses from pediatric programs indicated that 48 of 111 (43 %) were using an extramural curriculum, compared with 39 of 60 (65 %) med-peds programs (p = 0.007). Most pediatric programs utilizing an extramural curriculum indicated using the Yale (23/48, 48 %) or Johns Hopkins (22/48, 46 %) curricula. One program indicated utilizing both curricula. The editors of the Yale Primary Care Pediatrics Curriculum and Johns Hopkins Pediatrics Ambulatory Care Curriculum indicated that 42 and 48 pediatric residency programs had active subscriptions in 2012, collectively representing 45 % of the 201 pediatric programs in the ERAS database. The editors of the Yale Office Based Medicine Curriculum and Johns Hopkins Internal Learning Center Internal Medicine Curriculum indicated that 130 and 170 internal medicine residency programs had active subscriptions in 2012, collectively representing 75 % of the 402 categorical internal medicine programs in the ERAS database. Numbers of med-peds program subscriptions were unavailable from all curricular editors. The collective subscription rate of internal medicine programs was greater than the subscription rate of pediatric programs (p < 0.001).
CONCLUSIONS: Training programs in pediatrics, internal medicine, and combined med-peds utilize extramural curricula to guide education in ambulatory care, but internal medicine and med-peds programs employ these curricula at greater rates than pediatric programs. The difference in utilization rates among these parallel training environments has not been previously identified. Given the similarities in training structure, pediatric programs may wish to look to educational solutions that have been used successfully for internal medicine training. Combined training programs may be in a unique position to bring educational solutions to their categorical counterparts. Our future research will examine the factors that impact subscription decisions among program types.
Extramural ambulatory care curriculum utilization
| Pediatrics | Med-Peds | Medicine | p | |
|---|---|---|---|---|
| Survey respondent indicating use of extramural ambulatory care curriculum | 48/111 (43 %) | 39/60 (65 %) | NA | 0.007 |
| Subscription query of curriculum editors | 90/201 (45 %) | NA | 300/402 (75 %) | <0.001 |
TOTAL TIME SPENT WITH PHYSICIANS IN OFFICE-BASED SETTINGS BY HISPANIC AND NON-HISPANIC WHITE INDIVIDUALS ANNUALLY IN THE UNITED STATESLyndonna M. Marrast1; Leah Zallman2,1; David Bor1; David Himmelstein3; Steffie Woolhandler3; Danny McCormick1. 1Cambridge Health Alliance, Cambridge, MA; 2Cambridge Health Alliance, Cambridge, MA; 3City University of New York at Hunter School of Public Health, New York, NY. (Tracking ID #1939259)
BACKGROUND: Hispanics in the U.S. experience worse healthcare outcomes across a wide range of conditions and settings compared with non-Hispanic whites (subsequently referred to as “whites”). During outpatient visits, physicians must form partnerships with patients, address complex medical and psychosocial problems, ensure informed decision making that respects patients’ needs and preferences and, for primary care physicians, provide preventive care and coordinate care with specialists. Prior studies have indicated that more time spent with a physician during an outpatient visit is associated with better quality of care for some measures, better medication adherence and higher levels of patient satisfaction; however little is known about the total amount of time that Hispanics spend with physicians in the U.S. annually.
METHODS: We analyzed data from the 2010 National Ambulatory Medical Care Survey (NAMCS) and used Census Bureau figures as population denominators to estimate rates. The NAMCS is an annual visit-based cross-sectional survey that provides nationally representative estimates of visits to office-based physicians. It collects data on visit duration, patient demographics and health conditions. We used the NAMCS to estimate the mean visit duration and the average number of office visits annually for Hispanic and white patients. We estimated the frequency of visits for each group by dividing the number of visits by the corresponding U.S. population estimate. We calculated the total annual average number of minutes spent in office visits for each group by multiplying visit duration by visit frequency. We also compared visit duration and frequency as well as total time spent with providers according to specialty. In addition, to partially account for potential differences in need for time spent with a physician, we compared total annual time spent with a physician after age standardization.
RESULTS: The average age of patients making outpatient visits was 34.6 years for Hispanic and 49.0 years for white individuals. Most visits made by Hispanics occurred in the West and South while most visits by whites were made in the South and Midwest. Overall mean visit duration was 6.4 % longer for Hispanic than white individuals (20.5 min vs. 21.5 min). Hispanic-white differences in visit duration varied substantially by physician specialty, with Hispanic individuals having shorter visit duration than whites for psychiatric visits (28.3 vs. 33.3 min respectively) but longer visit duration for primary care visits (24.3 vs. 19.7 min). Whites made 732 million visits to outpatient practices while Hispanics made 114 million visits. Overall, Hispanics made 35.1 % fewer visits to physicians than whites (2.4 vs. 3.7 per person per year) and spent 32.6 % fewer total minutes per person per year than whites (50.5 vs. 74.9 min per person). Age standardization had little impact on these findings.
CONCLUSIONS: While Hispanic individuals have slightly longer visits with physicians, the mean annual total time spent with a physician is markedly lower for Hispanics than whites, even after accounting for differences in age. Reducing these disparities in visits to and minutes with providers might help decrease Hispanic-white disparities in clinical outcomes.
TRANSITIONAL CARE INTERVENTIONS TO PREVENT READMISSIONS FOR PEOPLE WITH HEART FAILURE: A SYSTEMATIC REVIEW AND META-ANALYSISCynthia K. Feltner1,2; Christine D. Jones3; Crystal W. Cene1; Zhi-Jie Zheng4; Carla A. Sueta1; Marina Arvanitis1; Kathleen N. Lohr4; Jennifer C. Middleton2; Daniel E. Jonas1,2. 1University of North Carolina- Chapel Hill, Chapel Hill, NC; 2UNC, Cecil G. Sheps Center for Health Services Research, Chapel Hill, NC; 3University of Colorado, Denver, CO; 4RTI International, Research Triangle Park, NC. (Tracking ID #1937563)
BACKGROUND: Up to 25 % of patients hospitalized with heart failure (HF) are readmitted within 30 days. To reduce rehospitalization of Medicare patients, CMS recently began lowering reimbursements to hospitals with excessive risk-standardized readmission. This policy incentivizes hospitals to develop transition programs to reduce readmission rates. Despite advances in the quality of acute and chronic HF disease management, knowledge gaps remain about effective interventions to support the transition of care for people with HF. The purpose of this review is to assess the comparative effectiveness of transitional care interventions to reduce early readmissions and mortality for adults hospitalized with HF.
METHODS: We searched MEDLINE®, Cochrane Library, CINAHL®, and clinical trial registries (January 1, 1990 to late October, 2013). We required that studies recruit subjects during or within 1 week of an index hospitalization for HF and compare a transitional care intervention with another eligible intervention or with usual care. We required that interventions include one or more of the following components: education to patient or caregiver (or both), discharge planning, appointment scheduling before discharge, planned outpatient clinic visits (primary care, multidisciplinary HF), home visits, telemonitoring, telephone support, or interventions to increase provider continuity. We required studies to report a readmission rate, mortality rate, or the composite outcome (all-cause readmission or mortality). We included outcomes occurring no longer than 6 months following an index hospitalization. Two investigators independently selected, extracted data from, and rated risk of bias of included studies. We grouped studies of similar interventions for our evidence synthesis based on the mode and environment of delivery. We used random-effects models to estimate pooled effects. We stratified analyses for each intervention category by outcome timing. We calculated the number needed to treat (NNT) for readmission and mortality outcomes when appropriate. We graded strength of evidence (SOE) based on established guidance.
RESULTS: We included 47 trials. Most included people with moderate to severe HF; mean ages were in the 70s. Few trials reported 30-day readmission rates. At 30 days, high intensity home-visiting programs reduced all-cause readmission and the composite endpoint (all-cause readmission or death) (low SOE). Over 3 to 6 months, home-visiting programs reduced all-cause readmission, HF-specific readmission, and the composite endpoint (moderate SOE). Multidisciplinary (MDS)-HF clinic interventions reduced all-cause readmission (moderate SOE). Structured Telephone Support (STS) interventions reduced HF-specific readmission (moderate SOE) but not all-cause readmissions (moderate SOE). Home-visiting programs, MDS-HF clinic and STS interventions produced a mortality benefit. Neither telemonitoring nor primarily educational interventions reduced readmissions or mortality.
CONCLUSIONS: Home-visiting programs and MDS-HF clinic interventions reduced all-cause readmission and mortality; STS reduced HF-specific readmission and mortality. These interventions should receive the greatest consideration by systems or providers seeking to implement transitional care interventions for people with HF.
TRANSLATING A HEART DISEASE LIFESTYLE INTERVENTION FOR USE IN SOUTH ASIAN IMMIGRANT COMMUNITIES: PRELIMINARY RESULTS OF A PILOT RANDOMIZED CONTROLLED TRIALNamratha R. Kandula1; Swapna S. Dave1; Yasin Patel1; Paola E. Seguil1; Peter John D. De Chavez2; Santosh Kumar3; Himali Barucha3; David W. Baker1; Bonnie Spring2; Juned Siddique2. 1Northwestern University, Chicago, IL; 2Northwestern University, Chicago, IL; 3Metropolitan Asian Family Services, Chicago, IL. (Tracking ID #1937567)
BACKGROUND: South Asians (Asian Indians and Pakistanis) are the second fastest growing ethnic group in the United States (US) and have an increased risk of atherosclerotic cardiovascular disease (ASCVD) compared to other populations. Although lifestyle interventions have shown effectiveness at reducing ASCVD risk in non-Hispanic Whites, evidence suggests that program reach has been limited in South Asian populations. Over 90 % of US South Asians are immigrants, and there is often a mismatch between the conceptual underpinning of most lifestyle interventions and South Asians’ social and cultural context. Through a community-academic partnership, we pilot-tested a culturally-salient, community-based healthy lifestyle intervention and compared it with print health education materials to reduce ASCVD risk factors in a medically underserved South Asian immigrant community.
METHODS: South Asians in Chicago, 30–59 years, were recruited through a community organization that provides social services to medically underserved South Asians. Participants received community-based screening, and those with at least one ASCVD risk factor (hypertension, hypercholesterolemia, pre-diabetes, type 2 diabetes, or overweight/obesity) were randomized into the South Asian Heart Lifestyle Intervention (SAHELI) study and followed for 6 months. The SAHELI intervention group (n = 31) attended 6 interactive group sessions that incorporated the deep (values, beliefs, explanatory models) and surface (language) structures of South Asian culture. Classes were led by trained, multilingual health educators and focused on simple health messages, skills-building and self-monitoring related to increasing physical activity, eating a healthful diet, portion control, and stress management and coping. Intervention participants also received biweekly support using motivational interviewing via telephone. The control group (n = 32) received translated print education materials containing standard clinical information about ASCVD risk factors and healthy behaviors. Both groups were referred to primary care providers. Outcomes, including weight, blood pressure, cholesterol, hemoglobin A1c, health behaviors, knowledge, coping, and exercise confidence were measured at baseline and 3, and 6 months.
RESULTS: Participants’ average age was 50 (SD ± 8) years, 63 % were female, 46 % had less than or equal to a high school education, one-third were limited English proficient, and two-thirds had no health insurance. At baseline, mean BMI was 30 kg/m2 (SD ± 4.9), hemoglobin A1c 6.3 (SD ±1.2), total cholesterol 185 (SD ± 32), and systolic blood pressure 129 (SD ± 17). Compared to the control group, the SAHELI intervention group lost significantly more weight (−3.2 lb, p-value = 0.04) and had a greater sex-adjusted decrease in hemoglobin A1c (−0.43 %, p-value <0.01) at 6 months. Changes in blood pressure and cholesterol did not differ between the treatment groups. We also observed a significant increase in both intervention and control groups’ knowledge and coping.
CONCLUSIONS: A lifestyle intervention incorporating the socio-cultural context of underserved South Asian immigrants and delivered in a community setting was more effective at improving ASCVD risk factors than print health education materials. Analyses of accelerometer and 24-hour dietary recall data are underway. A future study will evaluate the long-term effect of SAHELI in a larger sample of US South Asians.
TRANSLATION INTO PRACTICE OF COMPARATIVE EFFECTIVENESS OF DEPRESSION MEDICATIONS: THE DEPRESSION MEDICATION CHOICE DECISION AID TRIALAnnie LeBlanc1; Nilay Shah1; Jeph Herrin2; Megan Branda1; Mark Williams1; Jonathan Inselman1; Victor M. Montori1. 1Mayo Clinic, Rochester, MN; 2Yale University, New Haven, CT. (Tracking ID #1940132)
BACKGROUND: Depression care often demands primary care clinicians’ and patients’ discerning among medication regimens of different efficacy, safety, cost, and burden to the patient, as documented in comparative effectiveness research (CER). Decision aids, shared decision making tools, offer CER evidence in a format that is accessible to both patients and their clinicians such that a treatment decision can be made that best fits both the clinical situation, and patient’s values, preferences, and goals. The objective of the study was to determine the effectiveness of a decision aid to translate CER on antidepressants into practice.
METHODS: We used a patient-centered participatory action research approach involving a multidisciplinary team and stakeholders to develop Depression Medication Choice, a decision aid for use during clinical encounters. We then conducted a clustered, practice-based randomized trial in 10 rural, suburban, and urban primary practices, enrolling clinicians and their patients suffering from moderate or severe depression, to assess the impact of the use of Depression Medication Choice in clinical encounters on clinician and patient involvement in decision-making, decision making quality, and patient measures of medication adherence and mood outcomes, compared to usual depression care. Measures of patients’ and clinicians’ decision making quality (decisional conflict, knowledge, and satisfaction) were completed following the encounter whereas patient involvement in decision-making was assessed through the review of video-recordings of the encounters. Six-month medication adherence was assessed through a composite of pharmacy records, survey, and review of patient electronic records. Mood outcome was measured using the Patient Health Questionnaire (PHQ-9) at the initial visit and at 6 months post visit.
RESULTS: Twenty four stakeholders from 12 organizations (patients, health systems, buyer action groups, psychiatrists, care managers, family physicians) contributed to the development of the decision aid, that is comprised of issue cards that organize information on antidepressants around cost, weight change, sleep, sexual dysfunction, discontinuation syndrome, information patients should know, and particular considerations. We then enrolled 10 primary care practices, 117 clinicians and 301 patients [67 % women; age, mean (SD): 44 (15); PHQ-9, mean (SD):15 (4)] in the trial. The use of the decision aid (DA), compared to usual care (UC), was shown to significantly improve patients decision making quality (decisional conflict: DA = 20 % vs. UC = 25 %, p = .02; knowledge: DA = 64 % vs. UC = 56 %, p = .03; satisfaction: DA = 78 % vs. UC 60 %, p = .002), clinicians decision making quality (decisional conflict: DA = 20 % vs. UC 32 %, p = .01; satisfaction: DA = 87 % vs. UC = 67 %, p < .001), and patient involvement: DA = 47 % vs. UC = 33 %, p = <.001. There was no difference in 6-months medication adherence (average percent days covered: DA = 50 vs. UC = 58, P = 0.16). Patients in the DA arm had significantly higher 6 month response rate (defined as >50 % improvement in PHQ-9) compared to usual care (DA = 51 % vs. UC = 32 %, p = .04) in their mood outcomes.
CONCLUSIONS: Through this trial, we were able to successfully engage patients, clinicians, and stakeholders in the development and evaluation of the Depression Medication Choice, a shared decision making tool translating CER of antidepressants, and designed for use by patients and clinicians during clinical encounters. Compared to usual care, patients participating in encounters using Depression Medication Choice decision aid were more comfortable with their decision, were more knowledgeable and satisfied with the information sharing, were more engaged in the decision making process, and showed greater improvement in their depression outcomes. Thus, we have developed and evaluated the efficacy of the decision aid Depression Medication Choice as a novel patient-centered translational tool for CER in depression treatment that can help patients and their clinicians identify and implement the kind of effective treatment that best fits patient’s values, preferences, and goals, a true path to high quality healthcare.
TRENDS IN USE OF MECHANICAL VENTILATION BY OLDER PATIENTS WITH AND WITHOUT DEMENTIATara Lagu1,2; Jennifer Tjia4; Marya Zilberberg3; Penelope S. Pekow1,5; Meng-Shiou Sheih1; Mihaela S. Stefan1,2; Peter K. Lindenauer1,2. 1Baystate Medical Center, Springfield, MA; 2Baystate Medical Center, Springfield, MA; 3EviMed Research Group, LLC, Goshen, MA; 4University of Massachusetts Medical School, Worcester, MA; 5University of Massachusetts Medical School, Amherst, MA. (Tracking ID #1934944)
BACKGROUND: Patients with dementia receiving invasive mechanical ventilation (IMV) are at high risk for delirium, functional decline, and excess mortality, but the number of elderly patients with dementia who receive IMV is unknown. We aimed to examine temporal trends in IMV use by older patients with and without dementia and to predict future use.
METHODS: We used data from the 2001–2011 Nationwide Inpatient Sample, which contains a 20 % stratified sample of short-term, non-federal, and non-rehabilitation hospitals. We included hospitalizations for patients aged ≥65 years who received IMV (ICD-9 CM procedure code: 96.70; 96.71; 96.72). Within this group, we examined admissions with and without a diagnosis code for dementia. Primary outcomes included changes in the number of hospitalizations receiving IMV over time. Using population estimates from the US Census Bureau, we calculated age- and sex-specific rates of IMV for 2001 through 2011. We used linear regression to estimate a trend for each age-sex group and then used population estimates for 2015 and 2020 to project the number of cases ventilated per year nationally to 2020.
RESULTS: We identified a total of 4,855,452 (standard deviation [SD] = 81,349) hospitalizations in patients ≥65 who received IMV; of these, 452,390 (SD = 9354) had a diagnosis of dementia. We observed a steady increase of almost 30 % in the number of hospitalizations of older patients who received IMV, rising from 386,364 (SD = 8,079) in 2001 to 497,496 (SD = 12,929) in 2011 at an annual growth rate of 2.9 % per year. Notably, the percentage of these admissions for patients 85 years or older remained relatively constant from 2001 to 2011 and is expected to decrease over time, from 16 % of all ventilated admissions over 65 years in 2001 to 10 % in 2020. The occurrence of dementia diagnoses among ventilated patients 65 years or older grew at a rate of 11.4 % per year, increasing from 6.4 to 13.8 % between 2001 and 2011. By 2020, we estimate that there will be 671,986 (SD = 19,922) admissions in patients ≥65 requiring IMV, of whom 20 % will have a diagnosis of dementia (Figure).
CONCLUSIONS: The use of IMV by populations ≥65 is expected to double between 2001 and 2020, and growth in hospitalizations for IMV patients with dementia is outpacing, by a factor of 4, those for IMV patients without dementia. Unless changes are made to temper current trends, our health care system faces an upcoming shortage of critical care resources. As general internists, we must promote earlier discussions about end-of-life goals in subpopulations of patients (e.g., patients over 85 years; patients with advanced dementia) who are least likely to benefit from IMV and other critical care therapies.
Projected growth in use IMV by patients ≥65 with and without dementia
UNDER-UTILIZATION OF THE ONLINE-PRESCRIPTION DRUG MONITORING PROGRAM (PDMP) IN MASSACHUSETTSLaila Khalid1; Leonard Young2; Karen E. Lasser1,3; Ziming Xuan3,4; Christopher W. Shanahan1; Allison Lange1; Orlaith Heymann1; Jane M. Liebschutz1. 1Boston Medical Center, Boston, MA; 2Massachusetts Department of Public Health, Boston, MA; 3Boston University School of Public Health, Boston, MA; 4Boston University School of Public Health, Boston, MA. (Tracking ID #1938186)
BACKGROUND: State Prescription Drug Monitoring Programs (PDMPs) are designed to decrease controlled prescription drug misuse by allowing prescribers to identify patients who are going to multiple prescribers and/or multiple pharmacies and thus make better informed prescribing decisions. However, PDMP is only effective if the information is made available to providers and they in turn utilize it. This prompted a 2012 Massachusetts (MA) law requiring all prescribers to join and utilize the MA online-PMP before each controlled substance prescription. There is lack of research on utilization of state PMPs by providers. We examined the frequency and professional designations of prescribers utilizing the MA online PDMP to understand patterns of use prior to the law’s implementation.
METHODS: We analyzed 2011 and 2012 reports of prescriber logins from the MA PMP database. Prescribers included physicians, mid-level providers (nurse practitioners and physician’s assistants), podiatrists and dentists. We tabulated the number of log-ins of each enrolled prescriber and defined prescribers in the highest quartile of logins as high frequency users. We also analyzed data according to physician specialty.
RESULTS: There was an increase in the number of prescribers utilizing the PMP in 2012. Among physicians utilizing the PMP, emergency medicine physicians (37.9 % in 2011, 29.3 % in 2012) made up the largest proportion followed by internal medicine (29.7 % in 2011, 31.6 % in 2012) and family medicine physicians (17.3 % in 2011, 18.8 % in 2012). Emergency medicine physicians made up the largest proportion (59.7 % in 2011, 48.3 % in 2012) of high-frequency utilizers followed by internal medicine (19.4 % in 2011, 21.6 % in 2012) and family medicine physicians (9.0 % in 2011, 10.9 % in 2012).
CONCLUSIONS: Enrollment and utilization of the MA online MA PDMP remained low in 2011 and 2012 with under 60 % of the enrollees actually logging on and searching patients. Reasons for low utilization of the PDMP, such as lack of integration with the electronic health records (EHR), and lack of time should to be explored further. Utilization data should be matched to PDMP data longitudinally to identify possible effects of utilization on rates of doctor/pharmacy shopping and other prescribing patterns.
UNDERDIAGNOSIS OF HYPERTENSION IN ADULTSEmeka C. Anyanwu1; David Kaelber1,2. 1Case Western Reserve University, Cleveland, OH; 2MetroHealth, Cleveland, OH. (Tracking ID #1897047)
BACKGROUND: Nearly a third of adults in the US are known to be hypertensive. Even after diagnosis, many go on to develop sequalae of hypertension in multiple organ systems. We posit there exists a sizable population of adults that meet the criteria of diagnosis for hypertension that remain undiagnosed despite already having presented with qualifying blood pressure measurements. For these adults complications of hypertension are likely to occur if they continue to go undiagnosed. Furthermore we suspect that there are sociodemographic characteristics that predispose one to go undiagnosed. The objective of this study is to determine the rate of underdiagnosis of hypertension in adults as well as the patient characteristics associated with the underdiagnosis of adult hypertension.
METHODS: We examined all blood pressures in our electronic health record (EpicCare, Epic Corporation, Verona, WI) from patients 18 years and older seen at least two times for a primary care or specialty care outpatient visit between 2010 and 2012 at large academic urban medical system in northeast Ohio. Patients were considered hypertensive, as per the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, if the average of at least two blood pressures on two separate visits was greater than 130 mmHg systolic or greater than 90 mmHg. Patients were considered to be undiagnosed if they did not have an ICD-9 code associated with hypertension (401.xx - essential hypertension, 402.9 - elevated blood pressure reading without diagnosis of hypertension and 997.91 - hypertension) in their EHR problem list, past medical history, or encounter diagnoses list during the study period. Patient age, gender, self-reported ethnicity, insurance type, height, weight were also obtained.
RESULTS: 48,712 patients met inclusion criteria for blood pressures consistent with hypertension. Of these only 32,328 (66.3 %) had a diagnosis of hypertension. Logistical regression demonstrated that patients with commercial insurance (OR 1.71 CI 1.65–1.79), of majority ethnicity (Caucasian) (OR 1.88 CI 1.81–1.96), and non-English-speaking (OR 1.13 CI 1.07–1.19) were all more likely to have undiagnosed hypertension, based on blood pressures recorded in their EHR. In contrast, the prevalence of undiagnosed hypertension decreased per 1-y increase over age 18 (OR 0.95 CI 0.95–0.95), with each elevated blood pressure reading (OR 0.79 CI 0.78–0.79), and with each visit during the two year study period (OR 0.96 CI 0.96–0.96). Gender, height, and weight were not associated with an increase or decrease in hypertension diagnosis.
CONCLUSIONS: Up to a third of adults with hypertension, based on data in EHRs, have not had their hypertension diagnosed. Disparities in the underdiagnosis of hypertension exist based on age, insurance, and ethnicity. This study highlights demographics for whom physicians might provide better diagnosis and treatment.
UNDERSTANDING TRIAGE CHOICES FOR PATIENTS WITH DIABETIC KETOACIDOSIS ADMITTED FROM EMERGENCY DEPARTMENTS IN NEW YORKIsabel Preeshagul1; Gargi Bajpayee1; Hannah Wunsch3; Colin R. Cooke4; Hayley B. Gershengorn2. 1Beth Israel Medical Center, New York, NY; 2Montefiore Medical Center, Bronx, NY; 3New York Presbyterian/ Columbia, New York, NY; 4University of Michigan, Ann Arbor, MI. (Tracking ID #1939581)
BACKGROUND: There are no known guidelines directing where in the hospital to admit patients with diabetic ketoacidosis (DKA)—either the general medicine ward or the intensive care unit (ICU). Large variation exists across New York State (NYS) hospitals in how often patients are triaged to the wards versus the ICU. One possible explanation for this variation may be substantial differences in protocols for care and staffing of hospital beds across institutions. We sought to determine the factors that influence emergency department (ED) providers’ decisions to triage DKA patients to the general hospital wards as opposed to an ICU.
METHODS: We created a survey consisting of 11 multiple choice questions pertaining to the management and triage practices for patients with DKA. Surveys were developed to be available by email and as a scripted phone survey. We obtained Institution phone numbers via internet search. The same investigator (IP) phoned each hospital and requested answers to the scripted survey from either an ED physician director, charge nurse, ED physician or ED nurses. These providers are responsible for making triage decisions, therefore were presumed to be most knowledgeable about protocols. Standard summary statistics were used to quantify survey results. We targeted hospitals in New York for which risk-adjusted rates of ICU utilization for patients with DKA are known.
RESULTS: We identified and attempted to survey 146 hospitals. For each site, multiple calls were made and we obtained a total of 23 responses (15.8 %).Of the 23 hospitals providing data, nearly all (82 %) had a protocol for DKA management in the ED. Most (82 %) used continuous intravenous (IV) insulin infusions for the mainstay of therapy with a bolus, as opposed to exclusively bolus administration for treatment. All hospitals permitted continuous IV infusions of insulin in the ED and in the ICU. The majority (59 %) of the surveyed institutions had step down units, but less than half of these institutions (41 %) permitted continuous IV insulin infusions in these units. Only 9 % of hospitals surveyed permitted insulin infusions on a telemetry unit and 5 % on general hospital wards. The greater part of the hospitals (55 %) had a protocol for triage of DKA patients. The majority of institutions (64 %) held patients in the ED until closure of their anion gap.
CONCLUSIONS: Our data provides useful insight into the triage and management of DKA patients statewide. Of the institutions surveyed, most had a protocol for DKA triage. The majority did not allow patients to be admitted to non-ICU locations prior to closure of the anion gap. Our data suggest that many EDs indiscriminately triage patients with DKA to the ICU despite prior data suggesting that care for patients with DKA outside of the ICU is safe. Future research examining DKA triage from the ER to the hospital is warranted to understand how to optimize triage protocols, improve resource allocation and most importantly enhance care for DKA patients on the general wards.
UNDERSTANDING VARIATION IN PCP REFERRAL PATTERNS IN A LARGE MULTISPECIALTY PRACTICE GROUPMIchael L. Barnett1; Thomas D. Sequist1,2. 1Brigham and Women’s Hospital, Boston, MA; 2Partners Healthcare System, Boston, MA. (Tracking ID #1937624)
BACKGROUND: Primary care physicians (PCPs) generate the vast majority of specialty referrals, and the decision to refer directly impacts health care quality, patient experiences, and spending. We analyzed referral rates among PCPs to characterize the relative contribution of patient and physician characteristics to the probability of referral, as well as the long term impact on utilization among PCPs with high rates of referral.
METHODS: We analyzed electronic health record data within a large multispecialty group practice that requires electronic referral orders. We enrolled 78,485 patients 18 years and older who visited 142 PCPs during a baseline referral rate measurement period (2005–2006), and then analyzed subsequent specialist referrals among these patients from 2007 to 2011. We collected information on patient age, gender, race, Charlson comorbidity score (2005–2006), and number of subsequent specialist appointments (2007–2011). To calculate PCP referral rates, we estimated a mixed effects logistic regression model using 2005–2006 data adjusted for patient characteristics, using a random intercept term to account for correlation within individual PCPs. We calculated the ratio of the PCP’s adjusted referral rate estimated from the fitted random intercept over the expected referral rate estimated with the same model without the random intercept. We multiplied this ratio by the average referral rate in the entire cohort to calculate the case-mix adjusted referral rate for each PCP. We used the c-statistic to assess the relative contribution of patient and physician characteristics in this model. We next categorized PCPs according to their quintile of adjusted referral rate and examined the characteristics of the PCPs and their patient panels, testing for trends using logistic regression. In the period from 2007 to 2011, we estimated the adjusted probability with logistic and negative binomial models that patients with PCPs in the different referral quintiles received any specialty referral, the average number of referrals per patient, and the average number of specialty visits.
RESULTS: From 2007 to 2011, the PCPs placed 102,276 referral orders, representing 74 % of the total referrals for this cohort (additional referrals came from urgent care physicians). The five most commonly referred specialties were orthopedic surgery (23 %), dermatology (15 %), otorhinolaryngology (9 %), gastroenterology (9 %), and general surgery (8 %). Physicians with more female, non-white and younger patients as well as those with fewer comorbidities were more likely to be in the highest referral quintile, as were physicians with fewer patient encounters and smaller panels (all p < 0.001, Table). The c-statistic for a logistic regression model to predict referrals using patient characteristics alone was 0.56, while the mixed effects model with a physician-level random intercept alone had a c-statistic of 0.68, which was unchanged after incorporating patient characteristics into the model. The adjusted average rate of referral per 100 patient visits was 5.2, 16.3, 21.0, 25.6, and 36.2 by quintile of referral rate among PCPs, with an overall average of 17.4. Adjusting for age, sex, race, and comorbidities, the average patient with a PCP in the highest quintile of referral rate had a 77 % (95 % CI 76–78) probability of receiving a referral and had 2.2 (95 % CI 2.1–2.3) referrals on average from 2007 to 2011, compared to a 36 % (95 % CI 35–37) chance of receiving a referral and 0.59 (95 % CI 0.57–0.61) average number of referrals in lowest quintile. From 2007 to 2011, in the 12 months subsequent to a referral, patients of PCPs in the highest referral quartile experienced an average of 3.6 (95 % CI 3.4–3.8) follow-up specialist visits versus 0.53 (95 % CI 0.51–0.56) visits among patients of PCPs in the lowest referral quartile.
CONCLUSIONS: We observe wide variation among PCPs in specialty referral rates, which is explained in large part by physician characteristics as opposed to patient characteristics. This variation has substantial long-term implications, with patients seen by PCPs in the highest quintile of referral rates experiencing dramatically more specialist visits over time. Our analyses suggest that physician-level interventions are needed to address this variation which may be due to physician subjectivity in the decision to refer patients.
UNNECESSARY LABS AND IMAGING PERCEIVED BY THIRD YEAR MEDICAL STUDENTS DURING THE INTERNAL MEDICINE CLERKSHIPAmit K. Pahwa1; Reena Karani2; Amanda Bertram1; Bimal Ashar1; Danelle Cayea1. 1Johns Hopkins University, Baltimore, MD; 2Mt Sinai, New York, NY. (Tracking ID #1939257)
BACKGROUND: From 1990 to 2007, hospital expenditures increased an average of 7.2 % per year. Medicare fee for service inpatient spending totaled $114 billion in 2009. While major procedures, evaluation, and management services only increased by approximately 30 % from 2000 to 2009, both imaging and tests increased by 85 % during that same period. Because of this, the AAMC recommends that clinical skills curricula train medical students to select, justify, and interpret clinical tests and imaging. Despite this educational imperative, 60 % of medical students rate their education in medical economics to be inadequate annually. It is likely that students experience this inadequacy not because of poorly executed curriculum but because the curriculum to address these skills is lacking. Currently only 15 % of IM residency programs have a formal curriculum in high value cost-conscious care. To date there has been no assessment of undergraduate medical education in high value cost conscious care and exposure to both high value cost conscious care and unnecessary testing.
METHODS: We conducted a multi institutional study by distributing a survey to third year medical students upon completion of their internal medicine clerkship to assess their exposure to high value cost conscious care and unnecessary care. Questions focused on the frequency of perceived unnecessary testing, reason for unnecessary testing and environmental factors that may lead to unnecessary testing.
RESULTS: To date 28 medical students from two institutions have completed the survey. Seventy eight percent (22 students) noticed at least one instance when labs or imaging tests were ordered that seemed unlikely to impact patient care. Eighty percent (16 students) felt that their patients had unnecessary labs at least once or twice per week. The most common reason unnecessary testing occurred was either physicians practicing defense medicine (65 % or 13 students) or house staff wanting to investigate a potentially rare diagnosis (60 % or 12 students). Most students (50 %) witnessed discussion of costs during work rounds or attending rounds at most twice a month. More often (70 % witnessed at least once or twice per week) teams members were guided to order more testing rather than be praised (50 % were praised at least once or twice week) for not ordering an unnecessary test. However only 30 % of students feel comfortable bringing unnecessary testing to the attention of their supervising house staff or attending.
CONCLUSIONS: This data suggest that medical students are exposed to a fair amount of unnecessary testing on their patients but feel very uncomfortable bringing it to the attention of their supervisors. As faculty we must be more cognizant of how our interventions are perceived by learners. We must also create an environment where learners can feel rewarded for being parsimonious with testing and safely question the value in testing. Limitations include a low sample size but as the year passes, more students will complete the survey. Because third year medical students are developing clinically it is difficult to ascertain if those instances of unnecessary testing were truly unnecessary.
US DECENNIAL CENSUS DATA NO LONGER ACCURATELY PREDICTS INCOME FOR CONTEMPORARY HEALTH DISPARITIES RESEARCHRachel J. Stern1; Hilary K. Seligman1,2; David Guzman2; Melanie Levy3. 1UCSF, San Francisco, CA; 2San Francisco General Hospital, San Francisco, CA; 3University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1939573)
BACKGROUND: When individual-level income data is not available, for example with large, administrative datasets, investigators devise proxy measures to approximate income. In health disparities research, the most common income proxy measure is derived by linking zip code with US Census data for average income. We examined the performance of multiple proxy measures of income (US Census, American Community Survey (ACS) or Internal Revenue Service (IRS)) because 1) there is not clear consensus on the most accurate one (eg, economists use IRS data as a gold-standard proxy), and 2) the US Census stopped collecting income data in 2000.
METHODS: We determined individual-level, self-reported income and health measures for a population-based sample of >40,000 non-institutionalized Californians using the 2003 and 2009 California Health Interview survey (CHIS). We chose two health measures which historically have shown clear income gradients: self-reported health status (very good/excellent vs all other) and current smoking. Using multivariate logistic regression adjusted for age, sex, and race, we examined whether proxy measures of income (US Census 2000, ACS 2009, and IRS 2000 & 2009), linked by patient zip code to the CHIS dataset, replicated gradients observed using individual-level income from CHIS. We divided income into quintiles (common practice in health disparities research) and compared the lowest quintile with each of the measures using kappa statistics for agreement and Spearman’s Rank Correlation.
RESULTS: Comparing proxy variables to the CHIS’ individual income measurement, the Census 2000 income proxy and IRS 2000 income proxy were weakly correlated with individual income in 2003 (kappa 0.24 for both; no ACS available). Proxy income in ACS 2009 (kappa 0.24) and IRS 2009 (0.25) was weakly correlated with individual income in CHIS 2009, but better correlated than Census 2000 (0.22, p < 0.01) was with CHIS 2009. IRS variables performed incrementally better than census and ACS both years (IRS vs census 0.36 vs 0.34 in 2003, 0.36 vs 0.33 in 2009). In the health outcomes analysis, IRS and Census data both replicated the income gradient in smoking prevalence, but IRS better replicated the income gradient in self-reported health status (Figure 1).
CONCLUSIONS: All proxy measures of income commonly used show only poor to fair correlation with individual income, reinforcing their inferiority to individual-level measures. Differences in the performance of the various proxy meaures were small. However, Census 2000 performance deteriorated over time and failed to demonstrate known relationships between income-sensitive health conditions and income by 2009. Census 2000 data should no longer be used to estimate income in contemporary health disparities research. When proxy measures of income are necessary, IRS- or ACS-derived measures of income are superior.
US PHYSICIANS’ EXPOSURE TO, KNOWLEDGE AND PRACTICE OF HIGH VALUE CARE DURING TRAINING: RESULTS FROM A NATIONAL SURVEY OF INTERNAL MEDICINE RESIDENTSKira L. Ryskina1,2; Cynthia D. Smith3; Arlene Weissman3; Jason Post4; Constance J. Dine5; KeriLyn Gwisdalla6; Deborah Korenstein3. 1University of Pennsylvania, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3American College of Physicians, Philadelphia, PA; 4Mayo Clinic, Rochester, MN; 5University of Pennsylvania, Philadelphia, PA; 6Banner Good Samaritan Medical Center, Phoenix, AZ. (Tracking ID #1939258)
BACKGROUND: US healthcare costs continue to be unsustainably high, which has lead to calls to incorporate cost consciousness and high value care training (that balances benefits of tests or treatments against potential harms and costs) into graduate medical education. In this study, we report findings from a national survey of internal medicine residents about their exposure to costs of care as well as knowledge and practice of high value care during training.
METHODS: A two-page paper survey was administered to all residents taking the Internal Medicine In-Training Examination (ITE) in October 2012. The survey included questions regarding knowledge and practice of high value care, exposure to costs of care during training as well as career plans. Residents from programs outside of the United States were excluded from analysis. Residents were characterized according to their year of training, gender, medical school location, residency program track, career plans, and the Dartmouth Atlas’ hospital care intensity (HCI) index of the training hospital. Descriptive statistics were used to report residents’ self-reported knowledge and practice of high value care during training. Multivariate logistic regression with clustering at the program level was used to identify resident and program characteristics associated with self-reported practice of high value care (e.g., discussing costs of care with patients or incorporating costs into clinical decisions) during residency.
RESULTS: Of the 21,617 US internal medicine residents, 18,102 (84 %) completed the survey. Of the sample, 34.1 % were PGY1, 34.6 % were PGY2, and 31.3 % were PGY3. Forty-four percent were women. Half of residents (50.9 %) reported that the issues of balancing benefits and harms with costs was the topic of teaching conferences or rounds at least a few times a month. Residents reported receiving education in this area as part of grand rounds (50.8 %), resident lectures (49.1 %), and intern/resident report (45.7 %). Nearly one in seven residents (14.0 %) reported not receiving any education on providing care that balances the benefits with costs and harms. Residents who trained at a hospital with above average HCI index were more likely to know where to find estimated costs of tests and treatments compared to those who trained at a hospital with below average HCI index (28.0 % vs 24.2 %, p < 0.001), but were less likely to report incorporating the costs of tests and treatments into clinical decisions (44.9 % vs. 47.4 %, p = 0.001), or incorporating patients’ values and concerns into clinical decisions (86.9 % vs. 89.6 %, p < 0.001). Residents who trained at a hospital with an above average HCI index were less likely to report discussing costs when caring for patients (OR = 0.83, p = 0.002, 95 % CI 0.74–0.93) or incorporating costs into clinical decisions (OR = 0.86, p = 0.001, 95 % CI 0.78–0.94).
CONCLUSIONS: A large proportion of residents received some instruction about balancing benefits, harms, and costs, but less than a third of residents know where to find cost information and less than half incorporate costs into clinical decisions. Residents trained at hospitals associated with high levels of healthcare utilization were less likely to report discussing costs with patients and practicing high value care concepts, though differences were small.
USE OF A PATIENT DECISION AID IN ROUTINE CARE: WHAT IMPACT DOES IT HAVE ON DECISION MAKING ABOUT PROSTATE CANCER SCREENING?Leigh H. Simmons1,2; Sandra Feibelmann1; Karen R. Sepucha1,2; Lauren Leavitt1. 1Massachusetts General Hospital, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1937662)
BACKGROUND: Decision aids (DAs) are educational tools that present information about treatment options and outcomes and help patients reflect on goals and treatment preferences. Randomized controlled trials of DAs have been shown to increase patients’ knowledge and involvement in treatment decisions, and reduce decisional conflict. However, less is known about the impact of these tools in routine care. The aim of this study was to assess the effectiveness of a prostate cancer screening DA when used in primary care.
METHODS: The DA used is a 20-minute DVD and booklet produced by the Informed Medical Decisions Foundation and Health Dialog. All primary care providers in practices affiliated with Massachusetts General Hospital are able to order the DA through the electronic medical record. The DA is then mailed with a questionnaire to the patient. One reminder phone call or post card was sent to increase survey response rates. The questionnaire asked patients to indicate their screening intentions before and after watching the program, rate the importance of different goals on a scale from 0 (not at all) to 10 (extremely) important, complete 5 multiple choice knowledge items, and evaluate the DA.
RESULTS: From March 2010-November 2013, 2,588 PSA DAs were mailed to patients and 616 completed the questionnaire (response rate 23.8 %). The respondents were 83.4 % white, 58.4 years old (SD 8.1 years), and 55.3 % reported a college education or more. About half (47.6 %) had never had a PSA test, 44.2 % had a prior PSA test, and 8.3 % did not answer. Most respondents watched all or most of the program (75.8 %), slightly fewer read all or most of the booklet (60.4 %). Men’s screening intentions changed after watching the DA. After viewing the DA, fewer men were not sure about testing (33.6 % unsure pre-viewing vs. 17 % unsure post viewing, p = <.001) and more men did not intend to have a PSA test (32 % pre-viewing vs. 51 % post viewing, p < 0.001). Men who were leaning toward having a PSA test felt it was more important to find cancer early (8.4 vs. 5.0 out of 10, p < 0.001) and to have peace of mind from a negative result (8.2 vs. 4.9 out of 10, p < 0.001) compared to men who were leaning toward not having PSA test. Patients’ mean knowledge score was 89.4 %, (SD 21.7 %). A majority understood that most men with prostate cancer die of something other than prostate cancer (84.4 %) and that a higher than normal PSA test result does not always mean the man has prostate cancer (87.3 %). Most respondents found the DA very or extremely useful in helping them understand what a PSA test is (77.5 %), deciding whether or not to have a PSA test (78.2 %), and preparing to talk with their provider about the PSA test (71.3 %).
CONCLUSIONS: Although the response rate was low, the DA helped men clarify preferences about screening, be well informed, and prepare to discuss PSA screening with primary care providers. These results provide evidence of the effectiveness of DAs in supporting shared decision making in clinical practice.
USE OF A WEB-BASED MODULE FOR FACULTY DEVELOPMENT IN COMMUNICATION AND CHRONIC OPIOID PRESCRIBINGAnna K. Donovan1; Gordon J. Wood2; Doris Rubio1,3; Patrice Gibbs3; Hollis Day1; Carla Spagnoletti1. 1University of Pittsburgh School of Medicine, Pittsburgh, PA; 2Northwestern Lake Forest Hospital, Midwest Palliative & Hospice CareCenter, Glenview, IL; 3University of Pittsburgh, Center for Research on Health Care, Data Center, Pittsburgh, PA. (Tracking ID #1940095)
BACKGROUND: As prescription opioid use and its complications reach epidemic proportions, internists must effectively communicate with patients with chronic non-malignant pain (CNMP). However, few published curricula focus on communication surrounding opioid prescribing. Results of an informal survey of the internal medicine faculty at the University of Pittsburgh School of Medicine (UPSOM) called for faculty development in “communicating with patients about opioid use”. As such, we implemented a web-based curriculum entitled Collaborative Opioid Prescribing Education-Risk Evaluation and Management Strategy (COPE-REMS®), which was developed at the University of Washington School of Medicine. We hypothesized that this curriculum would increase faculty participants’ communication skills knowledge and confidence level, as well as self-reported and actual use of these skills with patients who have CNMP.
METHODS: Eligible participants were the clinician-educator faculty affiliated with the UPSOM Internal Medicine Residency Program. Participants were also required to care for outpatients given the focus of the module. Of note, this study had an IRB exemption. Funding for this study was provided by the Thomas Nimick, Jr. Competitive Research Fund. Faculty were asked to complete the curriculum, along with pre and post electronic surveys to assess their knowledge, attitudes, and reported use of skills between May and June 2013. A follow-up survey was administered to all participants in December 2013, to assess delayed attitudes and reported uses of skills. Analysis of survey items included summary statistics and repeated measures ANOVA between pre, post, and 6 month responses to survey questions. We used the Bonferroni correction for posthoc analysis. All statistical analysis was done using Stata 13. In addition, 23 of the eligible faculty members were randomly selected to participate in a pre and post-module Observed Structured Clinical Exam (OSCE) during this time to assess change in actual communication skills. Each OSCE was scored with a 16-item checklist completed by one of four standardized patients (SPs) in real time and by a communication expert (CE) who viewed recorded encounters in a blinded fashion. Paired t-tests were used for statistical analysis comparing pre and post-module scores on the knowledge-based test and OSCE.
RESULTS: A total of 62 % (33/53) of eligible participants, with a mean of 16.1 years of post-training clinical practice experience, completed the curriculum. They rated their overall baseline physician-patient communication skills as 7.9 (scale 1–10 where 1 = poor and 10 = outstanding). All reported at least some prior faculty-level training in both physician-patient communication and management of patients with CNMP. Participants felt the curriculum was clear (mean 4.7; scale 1–5 were 1 = strongly disagree and 5 = strongly agree) and met its stated learning objectives (mean 4.7). Most felt that the time it took to complete the module was too long (mean 4.5); some faculty reported spending greater than 3 h on completing the module while one participant spent only 24 min. The 25-item knowledge-based test scores improved with completion of the curriculum (pre 75 % vs. post 90 %, p < 0.001). Compared to the pre-curriculum scores, participants reported improved comfort in managing patients both immediately post-curriculum and at 6 months (3.6 vs. 4.0 vs. 4.1 at pre, post, and 6 month time points respectively, p = 0.0184; scale 1–5 where 1 = totally uncomfortable and 5 = totally comfortable), prescribing opioids (3.3 vs. 3.8 vs. 3.9, p = 0.0061), and conducting a conversation about discontinuing opioids (2.8 vs. 3.5 vs. 3.9, p < 0.001). Additionally, repeated measures ANOVA between the three timepoints demonstrated an improvement in faculty comfort with teaching residents about managing patients with CNMP (3.5 vs. 3.9 vs. 4.0 for pre, post, and 6 months respectively, p < 0.0016). Of the 23 faculty randomized to the OSCE, the OSCE participation rate was 57 % (13/23); an additional 4 faculty volunteered to complete at least one OSCE to maximize utilization of the funded SP encounters. When rated by the SPs, the mean pre-OSCE score was 74 % vs. post 82 % (p = 0.0344). When rated by the CE, the scores were 65 % and 71 % respectively (p = 0.0767). The inter-rater reliability between the CE and each of the four SPs was fair to moderate (k = 0.28 to 0.66).
CONCLUSIONS: The COPE-REMS® curriculum was feasible to implement among clinician-educator faculty. Despite rating their baseline communication skills highly, this seasoned group of clinicians had improvement in their knowledge and comfort with managing patients with CNMP after participating in the curriculum. Improvement in actual skill was also achieved, and was statistically significant when rated by SPs during the OSCE component of the study. A web-based curriculum such as the COPE-REMS® may be useful for other programs looking to improve their faculty’s comfort and skill in managing patients with CNMP.
USE OF ELECTRONIC PATIENT PORTALS - DISPARITIES IN AGE, GENDER, AND RACESaira Varghese; Ruchira Sengupta; Javier Rodriguez Sanchez; Juan Pablo Domecq Garces; Sudeep D. Thapa; Kimberly Baker-Genaw. Henry Ford Hospital, Detroit, MI. (Tracking ID #1926444)
BACKGROUND: Just as the essentials of daily living have become more readily available via electronic access, so should the access to our own personal health records. Electronic patient portals are online applications that allow patients to electronically access their personal health information and communicate directly with their healthcare providers. Electronic access to health information will empower patients to become more involved in their own health management. In order for such a system to be successful, it must be readily available and offered to every patient, regardless of their age, sex, or ethnicity. It is important to identify barriers that prevent these portals from being used—whether it be on the part of the provider to offer access, or the patient to initiate access. In addition, use of electronic portals satisfies one of the meaningful use criteria as set by the Centers for Medicare & Medicaid Services (CMS) Incentive Programs, leading to further reimbursement. We analyzed the use of MyChart, the electronic portal implemented at Henry Ford Hospital, with respect to patient activation, usage, and rejection of these electronic portals, across different genders, age groups and ethnicities. Our analysis will help us to improve the implementation of electronic health portals, and also help identify patient populations that need more recruitment.
METHODS: The EPIC clarity database was used to obtain MyChart activation and demographics for four resident-operated Internal Medicine clinic sites, namely Main Campus, Sterling Heights, Grosse Pointe and Fairlaine. This was an observational retrospective descriptive study.
RESULTS: Our results revealed that there was no significant difference between males and females across the four sites with respect to activating MyChart accounts. In contrast, when analyzing across ethnic groups we find that the Caucasian population across all clinic sites, were more likely to active rather than not use or decline their activation codes. More importantly, it was noted that the African-American population were universally less inclined to activate or use MyChart across all sites when compared to all other ethnicities. As for disparities among different age groups, it was noted that the elderly above age 65 were less likely to use or activate MyChart when compared to their middle-aged and younger counterparts.
CONCLUSIONS: Electronic patient portals are an excellent means to improve communication between patients and their physicians, allow patients to have increased autonomy over their own personal health records, and improve overall health care delivery and workflow. However before such portals can be used effectively, it is important to not only to identify which patient populations would be the most active users, but also to elucidate the barriers and reasons why certain other groups may not be able to engage in their healthcare management via these portals. Our study set out to specifically focus on whether there were differences between different age groups, genders and ethnicities in terms of their activation or use of MyChart at certain Henry Ford Clinic sites. Our analysis reveals that it may be worthwhile to focus our attention on the elderly and African American patient populations, as these groups appear to be the least involved in using their electronic health records. Albeit this study has a number of limitations, the overall results are impressive and do warrant a closer look into how certain factors such as socio-economic status, education, and environmental factors correlate with participation in electronic healthcare and in turn would help us to improve the way we offer these tools to certain patient populations to encourage their involvement. Ultimately, the goal of electronic portals is to make it easier for every patient to access, take interest and have a better understanding of their own healthcare and using the results of this study, we hope to improve the use of electronic patient portals, particularly MyChart at HFH, so that more patients can enjoy these benefits.
USE OF EMERGENCY ROOM AFTER MEDICALLY COMPLICATED PREGNANCY: A MEDICAID CLAIMS ANALYSISAshley M. Harris1; Hsien-Yen Chang2; Lin Wang5; Martha Sylvia, PhD,3; Donna Neale4; David M. Levine1; Wendy L. Bennett1. 1Johns Hopkins Hospital, Baltimore, MD; 2Johns Hopkins School of Public Health, Baltimore, MD; 3Johns Hopkins, Baltimore, MD; 4Johns Hopkins Hospital, Baltimore, MD; 5Johns Hopkins HealthCare, Glen Burnie, MD. (Tracking ID #1938772)
BACKGROUND: Frequent interaction with the healthcare system in pregnancy and postpartum provides opportunity for engagement in primary care and risk factor modification. Low income women, however, cite multiple barriers to postpartum primary care and studies suggest they may utilize the emergency room (ER) for care. Women with pregnancies complicated by gestational diabetes (GDM) and hypertensive disorders of pregnancy including gestational hypertension, pre-eclampsia, and eclampsia (HDP) are at increased risk of future diabetes, hypertension and cardiovascular disease. The objectives of this study were to: 1) determine if women with pregnancies complicated by GDM or HDP would be more likely to use the ER in the 6 months postpartum than women with uncomplicated pregnancies, and 2) to determine other risk factors for ER use in the 6 months postpartum.
METHODS: This is a retrospective population based cohort study using 2003–2009 administrative claims data from one Maryland Medicaid Managed Care Organization. Claims data were linked with 2000 U.S. Census data by zip code, to obtain neighborhood characteristics. The sample included pregnant women age 12–45, with more than 100 days Medicaid coverage during pregnancy, and at least 90 days postpartum coverage. The primary outcome was one or more ER visits in the 6 months postpartum. To examine the association between ER visits and pregnancies complicated by GDM or HDP, we used logistic regression models that adjusted for maternal age, race, non-pregnancy related co-morbidities (chronic hypertension, type II diabetes, obesity, asthma, substance abuse, mental health disorders), duration of coverage, prenatal care, pregnancy or postpartum primary care use, and neighborhood socioeconomic characteristics.
RESULTS: We identified 26,074 pregnancies of which 20 % (n = 5,340) were complicated by GDM or HDP, and 80 % (n = 20,734) were not. In the first 6 months postpartum, 24 % of women had one or more ER visits, ranging from 0 to 40 total visits per woman. In unadjusted analyses, 27 % of women with GDM and/or HDP visited the ER compared with 24 % of women without (p < 0.0001). In adjusted analyses, women with GDM or HDP were significantly more likely to have at least one ER visit compared to women without these conditions (OR = 1.17, p < 0.0001, 95 % CI = 0.0800902, 0.2359954). Non-pregnancy related medical co-morbidities were also strongly related to ER use. Women with other medical comorbidities had significantly more ER visits as compared of women without: 33 % vs 20 % respectively (p < 0.0001), and an OR = 1.65 in adjusted analyses (p < 0.0001, 95 % CI = 0.4288324, 0.5676198). Finally, women who attended at least one primary care visit postpartum were more likely to use the ER (OR = 1.49, p < 0.0001, 95 % CI = 0.3301632, 0.4717708).
CONCLUSIONS: Nearly 25 % of women used the ER regardless of pregnancy complication, but those with recent GDM or HDP pregnancy had higher use. These results highlight the importance of targeting women with a history of GDM or HDP, and non-pregnancy related medical co-morbidities, for postpartum outreach.
USE OF HEALTH-RELATED INFORMATION & COMMUNICATION TECHNOLOGY (ICT) AMONG PREGNANT AND POSTPARTUM WOMEN: THE TECHMOM STUDYNymisha Chilukuri1; Meredith West1; Wendy L. Bennett1,2. 1Johns Hopkins University, Baltimore, MD; 2Johns Hopkins University, Baltimore, MD. (Tracking ID #1939249)
BACKGROUND: Pregnancy and the post-partum period provide opportunities to promote health behavior change in women but providers often miss these opportunities. Understanding how low-income, underserved women utilize Internet and Communication Technology (ICT) could inform technology-based interventions to promote behavior change. We examined differences in ICT usage by race/ethnicity and English proficiency to inform the tailoring of ICT-based interventions.
METHODS: The TechMom Study was a cross-sectional survey of 247 women who were pregnant or within one-year post-partum from 4 Johns Hopkins outpatient pediatric and obstetric clinical sites. Descriptive statistics were used to characterize participants. Multivariate logistic regression was performed to determine differences in cell phone/texting, email/internet and social networking usage by race/ethnicity and English proficiency, adjusting for age, income, marital and insurance status.
RESULTS: Most women were pregnant (83.8 %). Proportions of Latino, African-American, Caucasian and women of other races were 28 %, 40 %, 23 % and 9 %, respectively. 51.8 % had Medicaid or Medical Assistance and 59.5 % reported having a PCP. Latinas were more likely to have limited English proficiency compared with non-Latinas (83.8 % vs.1.13 %, p = 0.000). We did not detect any statistically significant differences in cell phone or text messaging use between Latino, Caucasian or African American racial/ethnic groups. Latinas (OR 0.30, p = 0.03) were less likely to use e-mail/internet, but there was no statistically significant difference in use among Caucasians, compared with the reference group of African Americans. Among the Latinas who used the Internet, they were equally as likely to report using social networks as the other racial/ethnic groups (OR 1.409, p = 0.692). Latinas were less likely to prefer receiving health information via cell phone (OR 0.37, p = 0.07), equally likely via Internet (OR 0.804, p = 0.742), and more likely via social networking sites (OR 6.8, p = 0.002) as African-Americans. Women with limited English proficiency were equally likely to use cell phone (OR 1.1, p = 1.0) but less likely to use e-mail/Internet (OR 0.18, p = 0.002) as women with English proficiency. If using these tools, women with limited English proficiency were less likely to prefer receiving health information via a cell phone (OR 0.34, p = 0.05), but had equal desire for receipt via Internet (OR 0.40, p = 0.20), and an increased desire for receipt via social network sites (OR 3.0, p = 0.11).
CONCLUSIONS: In urban, hospital-based outpatient obstetric and pediatric practices, pregnant and post-partum Latinas were equally likely to use texting and cell phones but less likely to use e-mail/internet compared with African-Americans and Caucasians. Women with limited English proficiency were equally likely to use cell phone/texting. These findings support the development of culturally-appropriate health promotional text-messaging focused on improving women’s and family’s health behaviors to reach out to women of all racial/ethnic groups.
USE OF TEXT MESSAGING TO MOTIVATE EXERCISE IN LATINOS WITH ONE OR MORE ATHEROSCLEROTIC RISK FACTORS: TWO PILOT STUDIESTracie C. Collins1; Fanglong Dong1; Elizabeth Ablah1; Deborah Parra-Medina4; Paula Cupertino2; Nicole Rogers3; Carolyn Ahlers-Schmidt5. 1KU School of Medicine - Wichita, Wichita, MN; 2KU School of Medicine - Kansas City, Kansas City, KS; 3Wichita State University, Wichita, KS; 4University of Texas Health Science Center, San Antonio, TX; 5KU School of Medicine Wichita, Wichita, KS. (Tracking ID #1938248)
BACKGROUND: Text messaging offers an innovative approach to motivate behavior change and improve control of atherosclerotic risk factors in adult Latinos. We conducted two pilot studies: 1) to determine cell phone and text message usage among Latinos with one or more atherosclerotic risk factors (e.g. age 50–69 years with diabetes mellitus or a history of smoking; hypertension, or hyperlipidemia) and 2) to determine the efficacy of a motivational counseling script, delivered via text messaging, to improve the use of exercise among Latinos with one or more atherosclerotic risk factors.
METHODS: We administered a 15-item survey to Latino adults with one or more atherosclerotic risk factors. For an additional sample of Latino adults with one or more atherosclerotic risk factors, we conducted a six-week, pre- and post-trial intervention. As part of the six-week trial, we ascertained stage of readiness to engage in exercise, which is a component of the original motivational script -Patient-centered Assessment and Counseling for Exercise (PACE) protocol - and exercise behavior scores (Exercise Behavior Questionnaire). Stage of readiness to exercise is based on the Transtheoretical Model and participants receive a score of one for precontemplation, a score of two to four for contemplation, and a score of five to eight for action/maintenance. Based on a participant’s stage of readiness to exercise score, he/she received text messages. Text messages were sent once per day, 5 days per week for 6 weeks.
RESULTS: Among the 82 persons who completed the survey, (mean age 49.2, SD 12.0 years), 96.3 % owned a cellphone, 91.3 % had texting capacity on their cellphones, and 82.1 % had unlimited text messaging. More than 90 % received and sent text messages daily. Further, of those with text messaging capability, 89.2 % received at least one text message daily, and 52.7 % received five or more text messages daily, For the six-week trial, the mean age of the 13 participants was 49.2 years (SD 11.9). All 13 participants received their text messages. At baseline, the mean PACE score was 2.64 (0.67) out of a maximum score of 8 and this increased to 5.36 (0.81) at 6 weeks (P < 0.001). At baseline, the mean exercise behavior score was 55.91 (55.76) minutes of exercise per week and this increased to 201.82 (61.61) minutes of exercise per week at 6 weeks (P < 0.0003)
CONCLUSIONS: Use of cell phones and text messaging is common among Latinos with one or more atherosclerotic risk factors. Further, delivering a behavioral change intervention via text messaging is feasible and potentially efficacious to improve stage of readiness to engage in exercise as well as exercise behaviors among Latinos with one or more atherosclerotic risk factors.
USING A POSITIVE APPROACH TO IMPROVE PATIENT SATISFACTION IN PRIMARY CAREBrittany P. Fenner; Stephanie A. Rose; Brett Capel; Nicholas Jackson; Bharat Kumar; David Rudy. University of Kentucky, Lexington, KY. (Tracking ID #1940244)
BACKGROUND: Optimizing patient satisfaction is an important goal in healthcare today. Patient satisfaction is measured in several domains and results are utilized to develop strategies for improvement. These commonly involve quality improvement methods where deficits are identified and interventions for correction are initiated. Another method is to discover positive aspects of patient satisfaction and build upon these strengths. To this end we used Appreciative Inquiry to identify positive aspects of patient care in our university-based internal medicine primary care clinic.
METHODS: We conducted appreciative interviews of 50 patients or their family members in our clinic. Subjects were asked to tell a story of a time in their clinic experience that stood out for them when they received, saw, or were part of excellent patient care, who were the individuals involved, what were the positive characteristics of those individuals, and the aspects of the clinic that contributed to this experience Responses were recorded on a response form. The texts were analyzed for thematic categories independently through qualitative methods by three reviewers. Discrepancies were resolved via consensus.
RESULTS: The predominant themes were: personal attention given by the staff, superior bedside manner, efficient care, patient-staff relationship, consistency in care, and educational environment. Personal attention and bedside manner were overwhelmingly the most common responses, with approximately 60 % of patients citing each of these aspects and every patient mentioning at least one of these two themes.
CONCLUSIONS: Patient responses parallel domains commonly utilized to measure patient satisfaction. Improvements in patient satisfaction me be frame in a positive light such as in the present study or deficits in patient satisfaction may be presented in a “blame and shame” fashion. We believe that presenting providers, staff, and administration with what patients value in their interactions with the health care system and asking for mechanisms to propagate these positive aspects may be an effective means of increasing patient satisfaction. We plan to present our data to all involved in the clinic and seek their input on how to accentuate these positive aspects. Patient satisfaction data will be followed longitudinally.
USING LEARNING STYLE ASSESSMENTS FOR INCOMING INTERNSLuke Cunningham; Chirayu Shah; Steffanie Campbell; Richard J. Hamill. Baylor College of Medicine, Houston, TX. (Tracking ID #1937866)
BACKGROUND: General Internists are increasingly becoming the experts in teaching both inpatient and outpatient skills to residents. With duty hour restrictions for resident training and increasing patient care demands, there is increasing need to optimize learning. Moving towards a learner-centered approach, it is important to understand the learning preferences of the housestaff. We attempted to assess learning style preferences of incoming interns and compare the results to their perceived learning style. In addition, we assessed the impact of this exercise during orientation.
METHODS: During the Department of Medicine orientation at Baylor College of Medicine in June 2013, a paper-based VARK (Visual, Auditory, Read/Write, Kinesthetic) instrument was given to all incoming interns. On a voluntary and anonymous basis, the interns submitted a separate page that included their scores and additional survey questions. Studying strategies were discussed for each of the learning styles and the interns received a handout about how to incorporate their learning style. All analysis was done using descriptive statistics.
RESULTS: There were 97 interns at orientation. The response rate was 90 % (87/97). Two responses were removed because of incomplete information. 56.5 % of interns had a multimodal learning style. The interns’ perceived learning preference was 54 % visual, 21 % auditory, 53 % read/write, and 51 % kinesthetic. The VARK learning preferences were 62 % kinesthetic, 60 % read/write, 55 % auditory, and 54 % visual. When comparing their perceived learning style to the results of the VARK, 21 % were the same, 68 % with partial matches, and 11 % with completely different results. The interns reported this exercise was either very helpful or somewhat helpful by 93 % (79/85). 53 % (45/85) were going to try another learning strategy based on the results of their VARK assessment.
CONCLUSIONS: The majority of interns have multimodal learning preferences with the predominant being kinesthetic and read/write. General Internists should evaluate their current teaching methods to determine if a multimodal approach is being used. Offering the VARK assessment to learners will help attendings tailor their teaching based on the learner’s preferences. In addition, the VARK assessment tool was considered a helpful exercise by most interns and over half planned to utilize a different learning strategy guided by the results. Learning style assessments should be considered for incoming trainees during orientation.
USING PATIENT FEEDBACK TO EXPLORE AND IMPROVE DIABETES CONTROL COMMUNICATIONAnjali Gopalan1,2; Kevin H. McDonough4; Katherine Kellom5; Marilyn M. Schapira1,3. 1Philadelphia VA Medical Center, Philadelphia, PA; 2Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 3Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 4University of Pennsylvania, Philadelphia, PA; 5Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA. (Tracking ID #1937786)
BACKGROUND: Only 25 % of patients with diabetes accurately understand the meaning of hemoglobin A1C values (A1C). This is of concern given that an understanding of diabetes management targets, specifically glycemic goals, is associated with better disease outcomes. However, A1C may not be how patients assess their current diabetes control. The purpose of this study was to learn about the metrics patients with diabetes use to gauge whether or not they are meeting their diabetes management goals, and to explore alternative communication formats that might be more effective at conveying information on glycemic control to patients.
METHODS: We conducted semi-structured interviews with patients with diabetes seen at University of Pennsylvania internal medicine practices. The first part of interviews covered the following: basic demographics, personal diabetes history, the participant’s understanding of diabetes and diabetes control, diabetes-related goals, assessment of personal control, and a review of the A1C value and barriers to understanding this value. In the second part of the interview participants reviewed alternative formats designed to communicate glycemic control. Potential alternative communication formats were designed based on information presentation in other contexts and theories regarding the visual presentation of quantitative information. The initial field of 10 tested formats included color-based “traffic light” scales (red/yellow/green), comparisons to averages or norms, A1C trajectory depictions as well as modifications of current medical terminology (i.e., changing the name of the test). Each participant reviewed between 4 and 7 formats, depending on time. For each format reviewed, participants were shown three versions depicting differing levels of control—poor, moderate, and good. We sought both general impressions of these alternative communication formats as well as ratings of format clarity and assessments of participants’ ability to rank the depicted levels of control accurately. The interviews were audio-recorded, transcribed and reviewed by two independent coders to identify themes and analyzed using nVivo software. Based on participant feedback the individual formats were revised and the field of formats narrowed towards the goal of identifying two formats to test more rigorously in a future study.
RESULTS: We completed 25 interviews. The mean age of participants was 56.8 years (range 26–82 years), 17 were women, the majority was African-American, and 9 of the 25 reported education beyond high school. While most participants mentioned the A1C without interviewer prompting and generally understood its relationship to diabetes control and disease outcomes, actual understanding of the measure was poor and stated ideal A1C values were often erroneous, with some stating goal A1C values as low as 3 %. Common reasons participants cited for poor understanding of the A1C were personal denial of disease seriousness and lack of effort. In the second part of the interview, formats associated with both accurate ranking of control levels and high ratings of clarity: 1) employed the colors red, yellow and green; 2) included actual numbers on top of pictorial representation of control; 3) indicated directionality (low = better); and 4) provided clear targets/goals. While participants generally felt graphs were difficult to understand, they frequently led to accurate identification of control and, for those who stated they felt comfortable with graphs, they were preferred over more simple formats. Synthesizing all participant feedback, two final formats have been selected for further study: both of which include the four identified qualities (images of the final formats are included below).
CONCLUSIONS: In this group of patients with diabetes, there was high value placed on being given a numbers in the evaluation of diabetes control and, in spite of poor understanding of the A1C, its relationship to disease outcomes was clear to most. Several common attributes of the designed communication formats were well received by participants and based on their feedback two final formats have been selected. Future studies will focus on evaluating their impact on increasing patient understanding of their diabetes control, improving patient satisfaction with provider communication, and altering diabetes-related behaviors and outcomes.
UTILIZATION OF SURVEY TO IDENTIFY HAND-OFF RELATED NON-ROUTINE EVENTSJessica Kuester1,2; Bambi Wessel2,1; Matthew Doers1; Tessa Damm1; Jennifer Carnahan2,1; Kinsey Nattinger1; Kathlyn E. Fletcher2,1. 1Medical College of Wisconsin, Milwaukee, WI; 2Zablocki VA, Milwaukee, WI. (Tracking ID #1936654)
BACKGROUND: Resident work hour regulations have led to increased periods of time in which hospitalized patients are cared for by covering residents. Previous research has found that such cross-coverage can lead to potentially preventable adverse events. We utilized a facilitated survey to specifically identify hand-off related non-routine events (NREs), a proxy for patient safety. Hand-offs occur when patient information and responsibility for care are passed from one clinician to another.
METHODS: Utilized a 14 question yes/no survey on 44 post-call residents (PGY 1,2,3) on the inpatient medicine wards at an academic medical center to attempt to identify hand-off related non-routine events. Example questions include: “Were any of the patients sicker than you expected?” “Was there any written or verbal information provided by the prior team that was incorrect, missing, and/or misleading?” A “yes” response was a positive screen for all questions except number 7 which asked “As your shift unfolded, were your expectations about these patients realized?”
RESULTS: Approximately 80 % of residents surveyed (35/44) identified at least one NRE occurring on their shift. Forty-five percent (20/44) of the residents reported that something happened to a patient that was unexpected, unusual, notable, or surprising during the cross-cover period. Thirty-two percent of residents (14/44) found patients to be sicker than expected. Fifty-seven percent (25/44) had to perform an unanticipated or unplanned action while caring for the other teams’ patients. Nearly 30 % (13/44) found that there was written or verbal information provided by the prior team that was incorrect, missing, and/or misleading. While, 32 % (14/44) could identify that there was at least one deviation from ideal/preferred care during their patient coverage. Fisher’s test was utilized to calculate two-tailed p values between PGY1 and PGY2-3 responses. There were no statistically significant differences between PGY1 and PGY2-3 responses for each of the 14 questions.
CONCLUSIONS: We were able to demonstrate that the majority of residents were able to identify at least one NRE during their cross-coverage period that was associated with a poor quality hand-off. Plans for future research include evaluating if improvement in written sign-out documents decrease the number of NREs and thus increase patient safety.
UTILIZING ITERATIVE CASE PRESENTATION TO DEMONSTRATE CONCEPTS OF CLINICAL REASONINGJohn Musgrove1; Ryan Kraemer1,2; Jason L. Morris1,2; Carlos Estrada2,1. 1The University of Alabama at Birmingham, Birmingham, AL; 2Birmingham VAMC, Birmingham, AL. (Tracking ID #1928099)
BACKGROUND: Clinical problem solving (CPS) exercises have emerged as a means of exploring the nuances of clinical reasoning. In this format, a case is iteratively presented with interposed commentary from an expert clinician. We aim to characterize the clinical reasoning concepts of published CPS exercises as an initial step towards incorporating such exercises into clinical reasoning curricula.
METHODS: Literature review and text analysis in three steps: First, dentified CPS exercises (table of contents review, 4 journals; Jan 2010–May 2013). Second, compiled a list of clinical reasoning concepts from seminal narrative reviews (seven educators voted from a list of 49 concepts; items with <5 votes were excluded). Third, utilized a regular expression search engine to identify specific mentions of clinical reasoning concepts (including synonyms) in each CPS exercise via automated, batched searches. Search engine compatible text files created using a custom JavaScript function in Acrobat® X. Superfluous text (titles and references) was redacted with regular expression text editing software. Electronic search results concordant with word-by-word article reviews. The primary outcome was the presence of each clinical reasoning concept in each article. Differences between journals were examined with the Chi-square test.
RESULTS: We identified 79 CPS exercises: 41 (52 %) in the N Engl J Med, 22 (28 %) J Hosp Med, 11 (14 %) J Gen Int Med, and 5 (6 %) Am J Med Sci. Six concepts were mentioned in >10 % of the articles: diagnosis 79 (100 %), context 20 (25.3 %), bias 13 (16.5 %), illness script 11 (13.9 %), problem representation 10 (12.7 %), hypothesis 9 (11.4 %). Concepts mentioned in ≤5 % of the articles were cognitive error, framing, dual process, flexibility, metacognition, system error, overconfidence, and naturalistic decision making. Differences between journals were observed on all but five concepts (all p ≤ 0.005, data not shown).
CONCLUSIONS: CPS exercises represent an accessible learning tool capable of detailing expert clinical reasoning while simultaneously addressing the nuances of core clinical reasoning concepts. This study helps to characterize relevant clinical reasoning concepts which have been discussed in CPS exercises.
VALIDATION OF NON-SMOKING STATUS BY SPOUSE FOLLOWING A CESSATION INTERVENTIONRaul Mejia1; Eliseo J. Perez-Stable2; Sandra Braun1; L. Peña1; Steve Gregorich2. 1Hospital de Clinicas, Universidad de Buenos Aires, Benos Aires, Argentina; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1938644)
BACKGROUND: Following cessation interventions self-report of smoking abstinence with biochemical verification is the defined as the “gold standard” outcome. Because obtaining biochemical verification is challenging and costly in community studies, we compared self-reported cessation among participants completing treatment to the smoking status reported by the spouse or proxy.
METHODS: Participants in this study were smokers who had reported quitting 12 months after the cessation intervention. Participants had either attended a smoking cessation clinic based at a university hospital primary care program or they were patients seen by private practice physicians who had participated in tobacco cessation training in Buenos Aires. A subsample of spouses of these participants was then interviewed by telephone to ask about their partner’s smoking status. We compared the participants’ responses to those from the spouses.
RESULTS: At 12 months 346 of 1423 smokers had quit; 161 non-smokers were called and 140 proxies (spouses) of these participants were interviewed. They had an average age of 51 years, 69 % were women, and 49 % had >12 years of education. Mean number of cigarettes per day was 20.1 (SD = 9.9) and the average number of quit attempts was 2.4 (SD = 1.2). Cessation methods used were medical advice or behavioral change only (21 %), bupropion treatment (56 %), nicotine replacement therapy (20 %), and/or varenicline (3 %). At 12 months, of the 140 spouses interviewed, only 10 (7.1 %) reported that their partners continued to be smokers. The agreement between self-response and proxy report was 92.9 % Kappa = 0.9286
CONCLUSIONS: These results suggest that proxy-reported data on smoking status could be used to validate self-reported results in smoking cessation trials in low-resource countries in place of biochemical verification.
VARIABILITY IN ADHERENCE TO OPIOID PRESCRIPTION GUIDELINES AMONG ADULT PRIMARY CARE PROVIDERSAllison Lange1; Karen E. Lasser1,2; Ziming Xuan3; Laila Khalid1; Donna Beers1; Orlaith Heymann1; Christopher W. Shanahan1; Julie Crosson1; Jane M. Liebschutz1. 1Boston Medical Center, Boston, MA; 2Massachusetts Department of Public Health, Boston, MA; 3Boston University School of Public Health, Boston, MA. (Tracking ID #1936182)
BACKGROUND: In order to reduce prescription opioid misuse, clinical guidelines recommend that primary care providers (PCPs) use opioid treatment agreements and urine drug screens to monitor patients on opioid therapy for chronic non-cancer pain, with risk for medication misuse informing monitoring intensity. Little is known about variability among individual PCPs in adherence to opioid management guidelines and whether guideline non-adherence by PCP is associated with greater misuse of opioids.
METHODS: We examined 12 months (September 2011–August 2012) of electronic health record (EHR) data from adult primary care clinics at two community health centers and one urban safety net hospital. Patients age 18–89 were included if they had received >3 opioid prescriptions for chronic pain within a six-month period and were not receiving active cancer treatment. PCPs were included if they had >4 eligible patients. Binary outcome variables were evidence of guideline adherence through (1) EHR documentation of an opioid treatment agreement (OTA) ever, and (2) Urine Drug Screen (UDS) in the past 12 months. Evidence of misuse was a binary outcome of 2 or more early opioid refills (>2 prescriptions written 7–25 days after the previous prescription for the same medication). Covariates were patient demographics, number of primary care visits (past year), number of Emergency Department visits (past year), number of patient risk factors for opioid misuse (age <45, drug use disorder, alcohol use disorder, tobacco use, and mental health disorder), morphine equivalent daily opioid medication dose (MDD) >50 mg/day, PCP type (attending, resident, nurse practitioner), and site of care. We used odds ratios to examine the correlations among patient-level binary outcomes, and Pearson correlations to examine the relationships among PCP-level aggregates of outcomes across patients within PCPs. Further, we used multi-level modeling to account for patient clustering within PCP and examine substantive variance attributable to PCP characteristics.
RESULTS: Sixty-seven PCPs prescribed opioids to 1,546 patients (mean patients per PCP: 23, median: 14, range: 4–95). No PCP met 100 % of guideline practices, and PCPs showed wide variability in adherence. PCPs had a mean of 48 % of patients with OTA (median: 50 %, range: 0–100 %). PCPs had obtained >1 UDS for a mean of 56 % of patients (median: 59 %, range: 0–100 %). Among the three outcomes, the PCP-level variance for OTA and UDS were greater compared to the variance for early refill. The variance for UDS decreased from 1.75 to 0.87 after adjustment for covariates and site (p < 0.001). Step-wise adjustment of the variance for UDS evaluated which portion of the adjustment led to the difference in variance. Adjustment for patient-level covariates decreased variance from 1.75 to 1.14 (p < 0.001); further adjustment for PCP type did not decrease the variance (p < 0.001). Adjustment by site decreased the variance substantially to 0.88 (p < 0.001), reflecting differences in UDS prevalence across the sites (24 %, 37 % vs. 67 %). At the patient level, the presence of >50 mg/day MDD was associated with increased odds of early refill (OR = 2.92, 95 % CI 2.30–3.70), of UDS (OR = 2.65, 95 % CI 2.06–3.41), and of an OTA (OR = 1.93, 95 % CI 1.53–2.44). OTA was associated with UDS (OR = 8.46 95 % CI 6.65–10.75) and early refill (OR = 1.56, 95 % CI 1.27–1.93), and early refill was associated with UDS (OR = 1.76, 95 % CI 1.42–2.18). PCPs with higher aggregates of MDD among their patients tend to have greater proportions of patients with early refills (r = 0.38, p = 0.002) and UDS (r = 0.46, p < 0.0001). PCPs with greater proportions of patients with UDS tend to have greater proportions of patients with OTA (r = 0.34, p = 0.005) and with early refills (r = 0.27, p = 0.03).
CONCLUSIONS: PCPs practicing with an urban underserved population show substantial heterogeneity in adherence to opioid prescription guidelines, with only half of patients getting recommended procedures. PCP use of urine drug screens, but not use of agreements, appears to be heavily influenced by the practice environment. Although high daily doses of opioid are associated with increased monitoring, they are also associated with evidence of greater misuse. Examining the time dependent relationship between monitoring and multiple early refills could help distinguish whether monitoring practices help prevent potential opioid misuse or are a reaction to it.
VARIATION IN OBESITY AND DIABETES PREVALENCE AMONG ASIAN ETHNIC GROUPSAllison Diamant; Susan Babey; Joelle Wolstein. UCLA, Los Angeles, CA. (Tracking ID #1933269)
BACKGROUND: The growing epidemics of diabetes and obesity threaten to dominate health care resources and worsen quality of life. Little is known about the prevalence of diabetes and obesity among Asian groups as researchers rarely disaggregate data on Asians. To inform the development of effective interventions we studied the variation in prevalence of diabetes and obesity among nine Asian ethnic groups. Methods: We used data from four waves of the California Health Interview Survey (CHIS), a large population-based telephone survey with over-sampling of Asian households and interviews conducted in five Asian languages. Using combined samples from 2001/2003 and 2007/2009, we assessed the prevalence of diabetes and obesity by Asian groups controlling for sociodemographic characteristics.
METHODS: We used data from four waves of the California Health Interview Survey (CHIS), a large population-based telephone survey with over-sampling of Asian households and interviews conducted in five Asian languages. Using combined samples from 2001/2003 and 2007/2009, we assessed the prevalence of diabetes and obesity by Asian groups controlling for sociodemographic characteristics.
RESULTS: In 2001/03 Japanese (8.4 %) had the highest and Koreans (2.1 %) had the lowest prevalence of obesity, while in 2007/09 Filipinos (12.2 %) and Japanese (11.7 %) had the highest rates, while Chinese (3.4 %) had the lowest prevalence. In 2001/2003 the overall prevalence of diabetes among Asians was 5.7 %, but was most prevalent among Japanese (11.3 %) and significantly less prevalent among South Asians (3.4 %), Chinese (4.1 %), Koreans (4.8 %) and Vietnamese (5.4 %). By 2007/2009 diabetes prevalence had increased to 7.1 % overall, with significant increases among Chinese, Koreans, Filipinos, and South Asians. In multivariate analyses we found significant variation by Asian ethnic group for obesity and diabetes. All single Asian groups are less likely than Whites to be obese, but Filipinos, Japanese, and South Asians are more likely than Chinese to be obese. Regarding diabetes Filipinos (OR 2.0, 95 % CI 1.3, 2.9), Koreans (OR 2.1, 95 % CI 1.4, 3.0) and South Asians (OR 3.1, 95 % CI 2.1, 4.5) are more likely than whites to have diabetes.
CONCLUSIONS: The prevalence of obesity and diabetes varies significantly by Asian ethnic group. The development and implementation of culturally appropriate interventions are needed to address these growing problems. Where possible, research on diabetes, obesity and other chronic conditions should examine variation by Asian ethnic groups and include sufficient sample sizes to enable such analyses, rather than relying on a summative measure of all Asians.
WALKING THE TALK TO IMPROVE ERROR REPORTINGChaitanya Mandapakala1,2; Diane L. Levine2. 1John D Dingell VA Medical Center, Detroit, MI; 2Detroit Medical Center, Detroit, MI. (Tracking ID #1938661)
BACKGROUND: The Institute of Medicine’s landmark report, “To err is human; building a safer health system” highlighted the importance of discussing medical errors in healthcare. Since then, quality and safety organizations have recommended incident reporting. Learning from adverse events or even latent errors is crucial for quality improvement and patient safety. Yet under reporting remains a continuing problem, especially among physicians. The Internal Medicine (IM) residency program at Detroit Medical Center has over 100 residents who rotate at multiple clinical sites including a Veterans Medical Center (VAMC). Residents rotate at the VAMC for 0–3 months per year. Intermittent rotation and lack of continuity makes it challenging to implement patient safety initiatives, such as improving the incident reporting among residents. In addition, residents have to learn to use a different kind of electronic reporting system at each of their clinical sites. Baseline reporting information provided by the VAMC Patient Safety officer (PSO) showed that between July 2012 and June 2013 residents reported only 2 incident reports. The objective of this quality improvement initiative was to improve error reporting at VAMC by IM residents by understanding the barriers to reporting and implementing changes using Plan-Do-Study-Act (PDSA) cycles to achieve change.
METHODS: Residents completed a pre-intervention questionnaire on the first day of their IM rotation at VAMC to see if they were aware of, and knew how to use, the Electronic Patient Incident Reporting (EPIR) system. Root cause analysis (RCA) was performed and multiple barriers to incident reporting were identified. Based on the information obtained, interventions were developed and implemented by the Chief Resident for Quality Improvement and Patient Safety (CRQS) in PDSA cycles. Information on the number of incidents reported by medicine residents was provided monthly by the PSO. Interventions implemented through PDSA cycles have been summarized in Table 1.
RESULTS: The number of incidents reported over time have also been shown in Table 1. Incidents reported were plotted over time in an XmR control chart (with upper and lower control limits at 3σ) to understand the impact made by our interventions. On review of the baseline data from July 2012 to July 2013, if things were allowed to continue as they were, there was a 99 % probability that the number of incidents reported would be 0–1 per month. Current data over 5 PDSA cycles (32 incidents from August 2013 to December 2013) suggests that if our efforts continue to show similar results, there is a 99 % probability that the number of incidents reported would be 0–19 per month.
CONCLUSIONS: RCA and PDSA cycles allowed us to identify and overcome barriers that prevented resident error reporting. Education (talking) alone was insufficient to increase error reporting. Walk rounds (walking) in conjunction with reinforcing education (talking) allowed us to increase error reporting. Discussion of potential events for reporting at the point-of-care increased error reporting. Walk rounds are effective but time intensive (1–1.5 h per day). To further develop the culture of safety the next PDSA cycles will focus on identifying resident champions from each year of training who will encourage and help their peers identify and report incidents (peer-to-peer coaching) to allow for sustainability and transportability to other clinical sites in our training program.
Table 1: Incidents reported over time with PDSA based interventions
| Time | Intervention | Incidents reported by residents |
|---|---|---|
| July 2012–Dec 2012 | None (baseline data) | 1 |
| Jan 2013–June 2013 | None (baseline data) | 1 |
| July 2013 | None (RCA initiated to identify barriers) | 0 |
| Aug 2013 | PDSA cycle 1: 1-hour orientation lecture (Education) to educate residents on EPIR (Talking) | 1 |
| Sep 2013 | PDSA cycle 2: Education + Daily Patient Safety Walk Rounds ie., CRQS made his own rounds and asked residents 2 questions: a) Have you come across any incident (adverse events or near misses) that you think needs to be reported? b) What can I do to help you report this incident? | 4 |
| Oct 2013 | PDSA cycle 3: Education + Daily Patient Safety Walk Rounds + Observing rounding teams daily to aid in identifying errors and encouraging a culture of reporting | 13 |
| Nov 2013 | PDSA cycle 4: Education + Articles posted on resident website showing importance of reporting, screenshots of how to use the electronic system and process after reporting + Weekly Patient Safety Walk Rounds | 8 |
| Dec 2013 | PDSA cycle 5: Same as PDSA 4 | 6 |
RCA = Root Cause Analysis; PDSA = Plan Do Study Act; CRQS = Chief Resident for Quality Improvement and Patient Safety
WARFARIN THERAPY AMONG PATIENTS NEWLY DIAGNOSED WITH CANCER: EXAMINING CONTROL AND OUTCOMES BY INDICATION FOR THERAPYDaniel B. Ambrus1,2; Adam Rose1,2; Joel Reisman1. 1Bedford VHA, Bedford, MA; 2Boston Medical Center, Boston, MA. (Tracking ID #1938651)
BACKGROUND: While extensive guidelines have been published regarding the management of warfarin for non-valvular atrial fibrillation (AF) in a variety of settings, the problem of a new cancer diagnosis adds significant complexity and uncertainty. Furthermore, there seems to be a significant gap in the literature regarding patients on warfarin for AF rather than for prophylaxis or treatment of venous thromboembolism (VTE) in the setting of cancer.
METHODS: We started with 122,875 veterans who had been receiving warfarin for at least 6 months from a Veterans’ Health Administration Medical Center (VAMC) from October 1st, 2006 through September 30th, 2008. We identified patients with incident cancer during that time by ICD-9 codes. Patients with a history of cancer prior to the study period were excluded from the analysis. To examine adherence to warfarin by indication for anticoagulation, we compared the mean time spent in therapeutic range (TTR) between the baseline period (the six months prior to diagnosis) and up to a year following diagnosis. To examine outcomes, we first compared crude all-cause mortality, major bleeding and stroke rates in the 6 months following cancer diagnosis between patients anticoagulated for VTE and AF. To enhance validity, we then constructed propensity-matched samples of patients with VTE and AF, with matching for presence of metastasis, recent major hospitalization, highly toxic chemotherapy, socioeconomic status and access to care, as well as significant non-cancer comorbidities. Patients receiving low-molecular weight heparins were excluded. Cox models were used to obtain hazard ratios for all-cause mortality, major bleeding and stroke. A similar but separate propensity matching analysis was also performed to examine adjusted outcomes for patients who did and did not continue warfarin following cancer diagnosis, regardless of indication.
RESULTS: Among patients with any cancer (N = 1,936), TTR decreased by an average of 6.5 % in the AF group and by 6.1 % in the VTE group between the baseline period and the first 6 months after diagnosis. There was no difference in average TTR between baseline and months 7–12 for either indication. During the six-month follow up period after cancer diagnosis, crude rates of all-cause mortality (8.0 %, 9.0 %), major hemorrhage (5.2 %, 5.7 %), or stroke (2.6 %, 2.4 %) did not significantly differ between AF and VTE, respectively. Propensity matched analysis for a diagnosis of AF as indication showed that AF (as compared to VTE) was associated with improved survival [(HR = 0.80),(p = 0.01)], a non-significant trend toward decreased hazard of stroke [(HR = 0.38),(p = 0.06)], and no apparent effect on major hemorrhage [(HR = 1.13),(p = 0.69)]. Propensity matched analysis for persistence with warfarin after cancer diagnosis (as compared to patients who did not persist) showed significantly improved survival regardless of indication [(HR = 0.75),(p < 0.001)], with non-significant trends toward lower hazard of stroke [(HR = 0.60),(p = 0.07)] and major bleeding [(HR = 0.86),(p = 0.29)].
CONCLUSIONS: In patients already receiving warfarin, a new diagnosis of cancer conferred poorer anticoagulation control regardless of indication for therapy, and outcome measures 6 months after diagnosis were similar between indications, though slightly favoring AF in the adjusted analysis. Clinical guidelines, which currently address anticoagulation therapy for treatment or prevention of VTE in the setting of cancer, should also explicitly address how to treat patients anticoagulated for AF who are newly diagnosed with cancer.
WATER IS GOOD FOR HEALTH? NOT IN ALL PATIENTSSourabh Aggarwal; Vishal Gupta. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1940229)
BACKGROUND: There is a lot of ambiguity on ideal daily water intake (DWI) requirements especially in patients with underlying cardiovascular symptoms. There is no literature to date that has studied impact of regulated water intake in patients with cardiac symptoms. The average DWI recommended by various societies lack any concrete scientific evidence. The present quality improvement study was designed to identify influence of intensive patient education and effective communication on DWI restriction and its impact on clinical outcomes in patients with cardiovascular symptoms and unregulated water intake.
METHODS: This was a prospective pilot study conducted at our cardiovascular clinic. All patients who presented to our clinic with symptoms of shortness of breath (SOB), chest pain, dizziness, palpitations and peripheral edema were asked for DWI. The patients whose DWI was greater than 2 L/day and were optimally medically managed were included in this study. Patients with underlying systolic heart failure, left ventricular ejection fraction ≤45 % and chronic kidney disease were excluded from the study. The patients were weighed at baseline, their fluid intake recorded. Extensive water intake education was given to patients and were advised to restrict DWI. Primary outcome to be measured was symptomatic improvement in abovementioned symptoms. Patients were followed every 3–6 months in our clinic and importance of fluid restriction re-iterated with extensive patient education at follow up visits. Symptoms were noted and weight measured at each follow up visit. SPSS was used for statistical analysis, p < 0.05 was considered statistically significant
RESULTS: 65 patients (42 females, 23 males) were enrolled in the study with mean age of 55.16 ± 12.44 years and mean follow up of 1.92 ± 0.56 years (range 0.85 to 3.36 years). The average fluid intake decreased from 2.82 ± 1.93 L/day to 1.48 ± 0.95 L/day, with mean decrease of 1.34 ± 0.21 L/day (p < 0.001). The mean weight decreased from 219.2 ± 7.4 lb to 203.5 ± 6.9 lb with mean weight loss of 15.8 ± 3.2 lb (p = 0.06) At end of study, 71.43 % patients reported improvement in shortness of breath (p < 0.001), 38.47 % reported improvement in chest pain (p = 0.09), 25 % patients reported improvement in dizziness (p = 0.77), 74.36 % patients reported improvement in leg edema (<0.001), 77.28 % patients reported improvement in palpitations (p < 0.001) and 42.86 % patients reported improvement in leg pain (p = 0.24). The improvement in symptomatology was reciprocated in both genders individually with significant decrease in shortness of breath, peripheral edema and palpitations.
CONCLUSIONS: This is first study to date which analyzed the impact of fluid restriction in symptomatic patients with unregulated water intake. This shows that non-pharmacologic intervention of fluid restriction was associated with significant improvement in SOB, palpitations and peripheral edema in patients. Also, patient education on water restriction led to significant reduction in DWI and was associated with weight loss in these patients.
WE NEED TO TALK: PCP COMMUNICATION IN THE ERA OF A SHARED EMRLeslie Sheu; Kelly A. Fung; Michelle Mourad; Sumant Ranji; Ethel Wu. University of California, San Francisco, San Francisco, CA. (Tracking ID #1933345)
BACKGROUND: Shared electronic medical record (EMR) systems can facilitate effective communication between inpatient and outpatient providers to ensure safe transitions from hospital to home. We surveyed primary care physicians (PCPs) in the Department of General Internal Medicine at our academic medical center 1 year after inpatient EMR implementation to assess satisfaction with discharge communication and the desired content of communication at discharge.
METHODS: We administered an anonymous 17-question electronic survey about patients discharged from the inpatient Medicine service to resident and attending PCPs (n = 124) at our academic medical center. The survey was designed to determine: 1) overall PCP satisfaction with current communication practices from the inpatient team at patient discharge, 2) perceived adequacy of automatic discharge notifications, and 3) perception of the types of patients and hospitalizations requiring additional high-though communication at discharge.
RESULTS: Seventy-five of 124 (60 %) providers completed the survey. Thirty-nine (52 %) PCPs were satisfied or very satisfied over communication at patient discharge. While most reported receiving automated discharge notifications (71 %), only 39 % felt that the notifications plus the discharge summaries were adequate communication for safe transitions of care. The PCPs surveyed felt that for patients with complex hospitalizations, additional email or verbal communication was needed in addition to the discharge summary (Figure 1), however, only 31 % reported receiving such communication. When asked about the content of additional communication, PCPs reported many elements to be important, most notably 1) medication changes, 2) follow-up actions for the PCP, and 3) active medical issues.
CONCLUSIONS: Shared EMR systems afford new opportunities for communication and record sharing between inpatient and outpatient providers. However, our PCPs reported the need for additional communication to ensure safe transitions of care. Our survey suggests that for complex hospitalized patients, there are opportunities for further standardization of communication around transitions of care. Next steps at our medical center include focused surveys and interviews of PCPs whose patients were recently discharged, creating templates/guidelines for PCP communication at discharge, and implementing an inpatient-wide initiative to improve discharge communication.
Patient characteristics and desired mode of communication
WEATHERING THE STORM: THE IMPACT OF HURRICANE SANDY ON PRIMARY CARE PRACTICE AT THE NEW YORK VA MEDICAL CENTERMark D. Schwartz1,3; Ashley E. Jensen2,1; Matthew Beyrouty2,1; Katelyn Bennett1,2; Scott Sherman1,3; Joseph Leung1,2; Neil Shapiro1,2. 1VA NY Harbor Healthcare System, New York, NY; 2NYU School of Medicine, New York, NY; 3NYU School of Medicine, New York, NY. (Tracking ID #1937759)
BACKGROUND: Superstorm Sandy dramatically disrupted primary care (PC) services at the Manhattan campus of the VA New York Harbor Healthcare System (NY Harbor). The hospital was evacuated and closed on October 28, 2012, and remained closed for 6 months to undergo major repairs. Previous research of the impact of natural disasters on PC utilization is limited, but Hurricane Katrina in New Orleans highlighted the value of quickly establishing flexible “medical homes” following a disaster. In 2010 the VA established its own medical home model (Patient Aligned Care Teams, PACT), which includes strategies for panel management and expanding health care beyond the in-person encounter. During 6 months of displacement, NY Harbor staff provided PC services remotely by telephone, secure messaging, and walk-in access clinics at other VA facilities throughout New York City. The storm abruptly accelerated the need for panel management and remote care strategies, creating a unique opportunity to study how PC staff and patients coped with these changes.
METHODS: In this observational study, 48 PC staff that care for approximately 16,000 veterans were surveyed 2 months following the storm (Displacement), and 6 months after returning to the hospital (Return) about the impact of the storm on their practice, stress, satisfaction, and perceived impact on patient care. Staff responded to a 7-item measure of panel management self-efficacy (11-point scale, Cronbach’s α = 0.9, maximum score of 70 ), and a 3-item scale of confidence in providing remote care (11-point scale, α = 0.8, maximum score of 30. Using VA administrative data, PC service use including visits, telephone encounters, and secure messages was tracked to compare utilization patterns before the storm, during Displacement, and after Return. We also compared the proportions of each providers’ hypertensive patients with blood pressure (BP) >140/90, and diabetic patients with hemoglobin A1c >9.0 % before and after the storm. We tested the correlation between clinicians’ panel management self-efficacy and the proportions of their patients with uncontrolled BP and A1c values.
RESULTS: Of the 36 respondents at Displacement (77 % response rate), 27 % had to evacuate their homes during the storm, 72 % lost power for >24 h, and 31 % reported damage to their property. During Displacement, 35 % felt that patients were well cared for, but upon Return this increased to 78 % (p < 0.001). During Displacement, 77 % said that when they return to the hospital, patients will need to be seen in person less often, 67 % would provide more care by telephone, and 52 % would use more secure messaging. Upon Return, only 48 % of staff reported that they believed patients need to be seen in person less often (p = 0.04), however 70 % said they provide more care by phone and 67 % said they use more secure messaging than before the storm. From Displacement to Return, the proportion with greater work stress (compared to before the storm) decreased from 51 to 45 % (p = 0.80), while job satisfaction increased from 45 to 75 % (p = 0.05). The staffs’ panel management self-efficacy increased from a mean (SD) of 34.9 (10.9) during Displacement to 44.0 (15.1) on Return (26 % increase, p = 0.002). Staff confidence in providing remote care also trended 8.5 % higher (p = 0.18). Provider’s with higher self-efficacy scores for panel management had fewer diabetic patients with out of range A1c readings for the 3 months immediately following the storm (r = −0.47, p = 0.03) and 6 months following the storm (r = −0.52, p = 0.02), but not prior to the storm; while the proportion of hypertensive patients with out of control BP was not correlated with panel management self-efficacy (r = 0.36, p = 0.59).
CONCLUSIONS: Following Hurricane Sandy, PC staff at the NY Harbor were forced to innovatively accelerate the deployment of panel management and remote care strategies, through which they successfully maintained access to care for their patients. This experience has had an impact on the PACT PC model, with substantially increased self-efficacy in panel management (linked to better diabetes control), and improved confidence in providing remote care. Growth in remote care was sustained upon return to the hospital. These results argue for expanding the training of medical home teams in panel management and remote care strategies. These findings thus have implications for disaster planning as well as for advancing medical home models.
Average Monthly Primary Care (PC) Encounters and Outcomes Before and After Hurricane Sandy
| Before Storm (May–Oct. 2012) | Displacement (Nov. 2012–Apr. 2013) | Return (May–Oct. 2013) | |
| Total # of PC of Encounters | 6,356 | 5,251 | 5,643 |
| % of encounters by phone | 25.2 | 45.5 | 28.4 |
| Total # of secure messages | 350 | 561 | 577 |
| % of hypertensive patients with BP > 140/90 | 23.6 | 28.1 | 28.3 |
| % of diabetic patients with A1c >9 % | 23.8 | 25.1 | 28.2 |
WEIGHT GAIN AFTER ART AND ASSOCIATION WITH SURVIVAL IN 4315 HIV INFECTED MEN AND WOMENBianca F. Yuh1; Janet P. Tate1,2; Amy C. Justice1,2. 1Yale School of Medicine, New Haven, CT; 2VA Connecticut Healthcare System, West Haven, CT. (Tracking ID #1934619)
BACKGROUND: With increasing prevalence of overweight and obesity among HIV infected patients, providers need to understand implications of weight gain. Although the association between overweight/obesity with multiple co-morbid conditions and excess mortality is well-established in the general population, the relationship of weight gain and disease burden in HIV infected patients in the modern ART era remains unclear. Therefore, we evaluated weight gain in the 12 months following ART initiation and its association with subsequent mortality.
METHODS: Patients from the Veterans Aging Cohort Study who initiated ART between 2000 and 2008, with recorded weight at baseline and 1 year later were included and followed another 5 years for mortality. BMI was classified as underweight (<18.5), normal (18.5–24.9), overweight (25–29.9) and obese (≥30). Mortality rates were determined as a function of weight gain, stratified by initial BMI. We used logistic regression to identify predictors of weight gain.
RESULTS: The sample of 4188 men and 127 women had mean age of 48; 55 % were black. Only 6 % were underweight at ART initiation, but 30 % were overweight and 12 % were obese. After 12 months of ART, mean weight gain was 8.2 lb, but 902 (21 %) patients gained ≥20 lb. Higher weight gain, up to about 20 lb, was associated with lower mortality regardless of initial BMI, but there was no survival advantage to greater gains (Fig. 1). In fact, mortality increased with weight gain >20 lb in those with normal initial BMI. In those with initial BMI ≥25, mortality rates increased with weight gain >15 lb. After adjustment for initial BMI, both CD4 < 100 cells/ml [OR = 3.2, (95 % confidence interval 2.8–3.8)] and hemoglobin <12 g/dL [2.9 (2.5–3.5)] were strongly associated with weight gain and new obesity.
CONCLUSIONS: In general, weight gain after ART initiation was associated with lower mortality especially among initially underweight and normal weight patients. However, mortality increased with excess weight gain. Based on these findings, providers should counsel all patients to avoid weight gain >20 lb; Overweight and obese patients should limit weight gain to 15 lb. This is consistent with recommendations made to pregnant women where optimum weight gain depends on starting BMI. Patients with low CD4 and/or low hemoglobin should be especially cautious.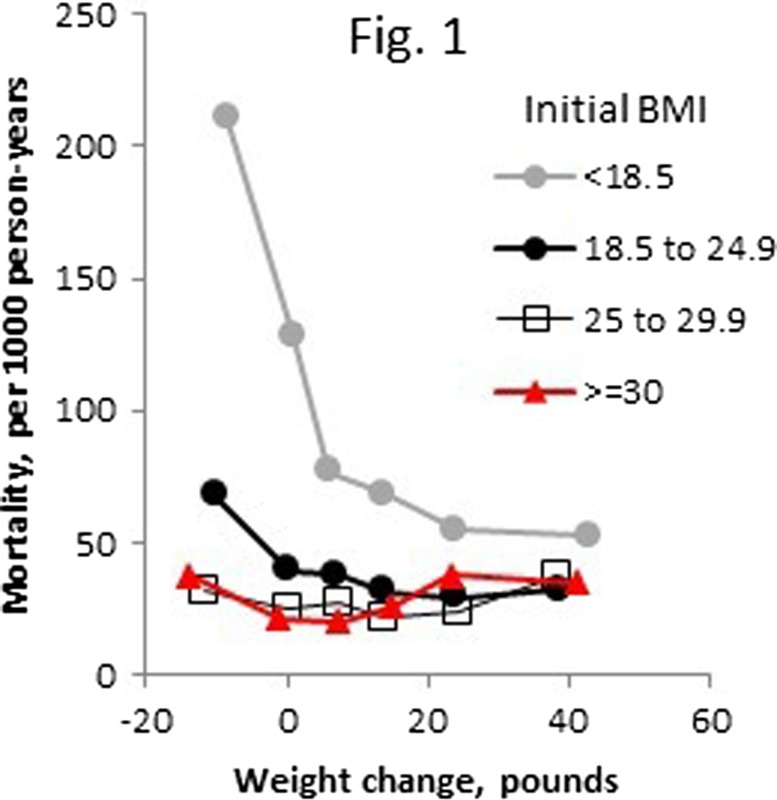

WEIGHT LOSS ASSOCIATED WITH CHOLINESTERASE INHIBITORS IN PATIENTS WITH DEMENTIA IN A NATIONAL HEALTHCARE SYSTEMMeera Sheffrin; Yinghui Miao; W. John Boscardin; Michael A. Steinman. UCSF and the San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1931500)
BACKGROUND: Cholinesterase inhibitors are a commonly used therapy for dementia. Conflicting data from randomized trials suggest cholinesterase inhibitors may lead to weight loss, which is of concern as weight loss in older adults has been associated with increased mortality. Because the selected patient populations in clinical trials may not reflect drug effects in real-world clinical settings, we sought to determine if initiation of cholinesterase inhibitors is associated with clinically significant weight loss in patients with dementia in a national healthcare system.
METHODS: Using national data from the Veterans Affairs health system from 2007 to 2010, we identified patients aged 65 or older with dementia who were new users of cholinesterase inhibitors, and a control group of patients who were new users of other chronic medications (non users). Patients with a diagnosis of heart failure or cancer or unstable weight during a one-year baseline period were excluded. Patients were matched using a propensity score model with baseline clinical and demographic characteristics including initial weight and weight trajectory. The primary outcome was risk of 10 lb weight loss, defined by the first recorded weight>=10 lb lower than the baseline weight. A secondary confirmatory outcome was mean change in weight over 12 months. In secondary analyses, we evaluated outcomes in an on-treatment analysis, matching users and non-users by treatment duration.
RESULTS: Of 6,504 patients that met study criteria, 1190 new users of cholinesterase inhibitors were matched to 2247 non-users. The propensity-matched cohorts were well balanced on baseline covariates; mean age was 78 years, 98 % were male, and mean weight at baseline was 175 +/− 35 lb. Of patients who started cholinesterase inhibitors, 58 % were prescribed donepezil, 41 % rivastigmine, and 1 % galantamine. Overall, 78 % of patients started on cholinesterase inhibitors were still taking using the drug at 12 months. Patients initiated on cholinesterase inhibitors had a higher risk of weight loss compared to non-users over 12 months (HR 1.29, 95 % CI 1.12 - 1.49). At 12 months, 31 % of patients on cholinesterase inhibitors had experienced>=10 lb weight loss compared 25 % of non-users (number needed to harm = 18 over 1 year). The number of weight measures in the follow-up period was similar between the two groups (p = 0.99). In secondary analyses of mean weight change, there was a mean weight loss of 1.9 lb/year in patients on cholinesterase inhibitors, compared to a mean weight loss of 1.6 lb/year in non-users (p = 0.002). To see if there were clinically important subgroups in which cholinesterase inhibitors were associated with greater risk of weight loss, we analyzed data stratified by age, comorbid burden, and initial weight. There were no significant differences in the impact of cholinesterase inhibitor use on weight loss across age groups, levels of comorbid burden, or levels of baseline weight.
CONCLUSIONS: Patients with dementia started on cholinesterase inhibitors had a substantially higher risk of clinically significant weight loss over a 12 month period compared to matched controls, with a number needed to harm of 18 over 1 year. Clinicians should consider the risk of weight loss when deciding whether to prescribe cholinesterase inhibitors in patients with dementia, and consider these medications as possible culprits if substantial weight loss occurs.
WHAT ARE CANCER CENTERS ADVERTISING TO THE PUBLIC? A CONTENT ANALYSIS OF PRINT AND BROADCAST MEDIALaura B. Vater1; Julie M. Donohue3; Robert M. Arnold2; Douglas B. White4; Edward Chu5; Yael Schenker2. 1University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA; 3University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA; 4University of Pittsburgh, Pittsburgh, PA; 5University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1924475)
BACKGROUND: Critics have expressed concerns that advertising by cancer centers exaggerates the benefits of cancer treatment and drives inappropriate demand for clinical services. To date, there has been no empirical examination of the content of cancer center advertisements. We aimed to characterize the informational and emotional content of advertisements placed by these centers.
METHODS: We conducted a systematic content analysis of all cancer center advertisements for clinical services placed in top consumer magazine (N = 269) and television networks (N = 44) in 2012. Using previously defined criteria for classifying health care advertisements, our multidisciplinary team developed a codebook with four domains: (1) types of clinical services promoted; (2) description of risks, benefits, indications, alternatives, and costs of advertised services; (3) use of emotional advertising appeals; and (4) use of patient testimonials and disclaimers. Two coders independently assessed all advertisements using ATLAS.ti. Kappa values for our main findings ranged from 0.77 to 1.0, indicating excellent inter-rater reliability.
RESULTS: One-hundred and two cancer centers placed 409 advertisements for clinical services in top media markets in 2012. The majority (61/102) of these centers were for-profit; 16 % (16/102) were National Cancer Institute-designated cancer centers. Eighty-five percent (87/102) of cancer centers placed clinical advertisements on television, 27 % (28/102) placed clinical advertisements in magazines, and 13 % (13/102) advertised in both media markets. The average number of unique clinical advertisements per institution was 3 (range 1–18) for magazines and 4 (range 1–45) for television. Advertisements most commonly promoted cancer treatments (359/409), often described using vague terms (e.g. “we offer you our most aggressive treatment plan”). Benefits of advertised therapies were discussed more often than risks (27 % (109/409) vs. 2 % (7/409)) but rarely quantified (2 %; 8/409). Over half (235/409) of advertisements indicated the type of cancer targeted, 9 % (38/409) indicated the stage, and 2 % (7/409) mentioned an alternative to an advertised therapy. Costs or insurance coverage were rarely mentioned (5 %; 21/409). Eighty-five percent (347/409) of advertisements included emotional appeals, most frequently evoking hope for survival (61 %; 248/409), describing cancer treatment as a fight or battle (41 %; 167/409), and evoking fear (30 %; 123/409). Medical miracles were described in 6 % (24/409) of advertisements. Nearly half (181/409) of advertisements included patient testimonials, usually focused on survival or cure (79 %; 143/181). Testimonials rarely included disclaimers (15 %; 27/181) and never described the results a typical patient might expect.
CONCLUSIONS: Advertising by cancer centers frequently promotes cancer therapy using emotional appeals that evoke hope and fear while providing scant information about risks, benefits, or costs. Further work is needed to understand how cancer center advertisements influence patient understanding and expectations of benefit from cancer treatments.
WHAT ARE INTERNS REALLY DOING POST-CALL? AN OBSERVATIONAL STUDY OF POST-CALL INTERN ACTIVITIESLuci Leykum1; Albert Lee2; Kathlyn E. Fletcher3; Carla Pezzia2; Holly Lanham2; Jacqueline Pugh1. 1STVHCS / UTHSCSA, San Antonio, TX; 2UT Health Science Center at San Antonio, San Antonio, TX; 3Medical College of Wisconsin / Milwaukee VAMC, Milwaukee, WI. (Tracking ID #1935961)
BACKGROUND: While an increasing literature describes resident work activities in the hospital, no data focus on the post-call day. On this day, residents are responsible for managing diagnostic and treatment plans for a large group of new patients, making it one of their busiest periods. Understanding post-call activities may provide insights into potential patient safety concerns, or strategies for improving care and intern efficiency.
METHODS: We observed 18 interns on 11 different inpatient medicine teams for one to two hour-long periods after attending rounds on their post-call day, for a total of 29 h. We focused on interns as the “front line” of the medicine team. Observations occurred at the 2 primary teaching hospitals of the UT Health Science Center at San Antonio. We wrote field notes to describe all interactions and activities, timing the duration of each. We then described their activities and categorized their interactions.
RESULTS: Interns were seated in the team room at their computers the majority of the time. They spent almost 50 % of their time in documentation in the electronic health record (EHR) (27.6 min, range 2.8 to 51.4 min). They spent an average of only 3 min, or 5 % percent of time, outside of the team room (range 0–22 %). Interns had on average 26.2 interactions during the hour of observation (range 8–46). The number of interactions was not directly correlated with the number of patients being cared for (r = .3). The average duration of each interaction was 71.3 s (range 34.2 to 260.5 s). The majority of these interactions were verbal (81.6 %, range 62.5–100 %). The remainder were electronic, typically orders to nursing or pharmacy. Most communication occurred within the interns’ teams (64.6 %). The groups outside of the team with whom they most frequently interacted were ancillary staff, including ward or diagnostic service clerks (41.6 %), physicians outside of the team (25.4 %), and nurses (19.7 %). Verbal interactions with these groups were usually by telephone instead of face-to-face. We observed interns interacting with patients in 37.9 % of observation periods. In comparison with interactions with other groups, only 13.4 % of outside-team interactions were with patients, but these interactions were much longer, averaging 10.0 mins in duration (2.3–25 mins). Interns initiated interactions 69.1 % of time (range 54.2–89.4 %). The remainder of interactions, on average 7.9 per hour, were initiated by others, most frequently by the resident.
CONCLUSIONS: Interns spent most of their time in their team rooms, documenting in the EHR, and managing a great number of interactions. Most interactions took place within their team. Interactions outside of their teams were by typically by telephone or through the EHR, and were brief. They rarely interacted with patients, though when they did they spent more time. Others initiated interactions almost 8 times an hour, interrupting interns’ work, and raising concern for potential errors. Given that the post-call day is often considered a time of rapid clinical evolution for newly admitted patients, it is surprising that interns spent little time at the bedside. It is also notable that most of the interactions interns had outside of the team were with clerks and other ancillary staff, rather than with nursing or other specialties. Our findings suggest that interns are primarily accomplishing work tasks during the post-call period.
WHAT ARE WE TELLING OUR STUDENTS? A NATIONAL SURVEY OF CLERKSHIP DIRECTORS’ ADVICE FOR STUDENTS APPLYING FOR INTERNAL MEDICINE RESIDENCYKatherine C. Chretien1,2; Laura R. Willett3; Meenakshy K. Aiyer4; Diane L. Levine5; Alwin Steinmann6; Michael Elnicki7. 1Washington DC VAMC, Washington, DC; 2George Washington University, Washington, DC; 3Robert Wood Johnson Medical School, New Brunswick, NJ; 4University of Illinois College of Medicine at Peoria, Peoria, IL; 5Wayne State University, Detroit, MI; 6Exempla Saint Joseph Hospital, Denver, CO; 7University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1936487)
BACKGROUND: Little is known about the advice fourth year medical students planning to apply to categorical internal medicine residencies receive from their faculty advisors regarding their fourth year schedules. The objective of this study was to determine how advisors believe students should structure their fourth year in preparation for an internal medicine residency and how this may differ based on faculty’s experience with advising.
METHODS: In June 2013, Clerkship Directors in Internal Medicine conducted its annual, online, confidential, national survey of its 124 member third-year internal medicine clerkship directors (CDs). One survey section dealt with student advising. Clerkship directors (CDs) were asked whether they advised fourth year students applying for categorical internal medicine residencies, and if so, how likely they would recommend certain courses during the fourth year. Analysis included descriptive statistics and Wilcoxon rank sum tests to examine associations between recommendations and length of time advising as well as number of students advised per year. In a free text question, CDs were asked why they might advise students to take an “away rotation.” Responses were analyzed using an inductive, iterative process involving two independent coders and periodic discussions for consensus. Discrepancies were resolved through discussion or by involving a third author. The Institutional Review Board at Case Western Reserve University determined that the protocol did not fit the definition of human subjects’ research per 45 CFR 46.102.
RESULTS: Seventy-six percent (94/123) responded. Of these, the majority advised fourth year medical students (83/94; 88 %). CDs had advised for a mean of 12.2 years (range 1–45; SD 8.58); 45.3 % advised an average of >20 students a year. CDs most encouraged students to take a medicine sub-internship (Likert scale mean 4.84, SD 0.61, with 1 = strongly discourage and 5 = strongly encourage), critical care (4.38; SD 0.79); medicine specialty clinical rotation (4.01; SD 0.80); and emergency medicine (3.75; SD 0.97). They were least likely to encourage a research rotation (2.92; SD 0.80), a non-clinical rotation (2.54; SD 0.81), and a non-medicine sub-internship (2.44; SD 0.96). An intern preparatory course was encouraged or strongly encouraged by 40.3 % of CDs, required by 11.3 % of schools and not offered at 12.5 % of schools. There was no difference in fourth year course recommendations between CDs who advised fewer versus more students, or for CDs who had advised for shorter versus longer amounts of time. For students who were interested in subspecialty fellowship training, CDs tended to encourage (Likert scale mean 3.39; SD 0.78) students to take a rotation in that subspecialty, with those CDs advising more students (>20), less likely to recommend this (p = 0.01). CDs believed students should spend a mean of 6.6 months doing clinical rotations during their fourth year (range 1–10; SD 1.91). In response to the free-text question asking why CDs might advise medical students to take an “away” rotation, 75 respondents generated 127 evaluable comments. The comments fell into 3 major themes: broadening the student’s educational experience (32 % of responders); allowing a student to become more knowledgeable about a particular program or city (56 % of responders); or attending a program of interest with the expressed or implied possibility that it might improve the student’s chances of matching at that program (69 % of responders). Some CDs responded to the question by stating that they did not recommend away rotations.
CONCLUSIONS: Internal medicine clerkship directors who advise fourth year students applying to internal medicine residencies encourage certain courses during the fourth year and believe the majority of the fourth year should be spent doing clinical work. These recommendations can help inform students planning internal medicine careers, other faculty advisors, educational administrators, and internal medicine program directors.
WHAT BRINGS YOU IN? THE CAUSE OF HOSPITALIZATIONS AMONG YOUNG ADULTSAnna Volerman1; Sonal Parasrampuria2; Valerie G. Press1; David Meltzer1. 1University of Chicago Medicine, Chicago, IL; 2Columbia University, New York City, NY. (Tracking ID #1934624)
BACKGROUND: Although generally considered a healthy population, young adults age 16 to 30 years old account for more than one million hospitalizations in the United States every year. Among young adults, there is an increasing sub-population afflicted with chronic diseases that put them at high risk for hospitalization and at times repeated hospitalizations. In order to better understand the high utilizers among young adults, we undertook a secondary data analysis. Our objective was to identify the most common causes for hospitalization among young adults and to determine what diagnoses were associated with frequent hospital admission in this population.
METHODS: We performed a cross-sectional analysis of three data sets that provide information on all-payer inpatient care as part of the Healthcare Cost and Utilization Project (HCUP). The 2010 California State Inpatient Database (SID) was used to determine the causes of hospitalization among young adults. We also examined the causes of multiple hospital admissions for the same patient in a given year using the patient identifiers within the SID. To assess the generalizability of our results to the broader young adult population in the United States, we created a national database for this target population by combining data from the 2009 Kids’ Inpatient Database (KID) for ages 16 to 20 and the 2010 Nationwide Inpatient Sample (NIS) for ages 21 to 30. Both of these databases contain de-identified data. We examined the causes of hospitalization among young adults in the United States and compared it to the SID data. Frequencies and percentages were calculated with data stratified by age, gender, race, income quartile and payer.
RESULTS: The 2010 California SID contained 373,640 young adults with a total of 574,780 hospitalizations. The mean age at the time of hospital admission was 23.44 years. The average hospital length of stay was 4.94 days. The most common reason for hospital admission was a diagnosis related to pregnancy, childbirth or postpartum care, regardless of payer. When obstetric-related diagnoses were excluded, 194,893 young adults were included in the data analysis, with an equal percentage of males and females. The majority of young adults in the SID were hospitalized once during the year (82 %); nearly one in five patients was admitted more than one time. When obstetric-related diagnoses were excluded, 30 % (n = 59,012) of young adults had more than one hospital admission during the year. The most common diagnoses for young adults with multiple admissions in a year were chronic illnesses, infections and mental disorders. The most common chronic diseases resulting in multiple hospital admissions included: Hereditary Hemolytic Anemia, Diabetes Mellitus, Hypertensive Chronic Kidney Disease, Epilepsy and Recurrent Seizures and Diseases of Pancreas. Among young adults hospitalized with one of these five diseases, 67 % had multiple hospitalizations in a year (ranging from 90 % for Hereditary Hemolytic Anemias and 49 % for Epilepsy). These chronic conditions mirror the list of chronic illnesses leading to hospitalization among young adults in the United States based on the NIS and KID databases.
CONCLUSIONS: Our study demonstrates that a substantial fraction of hospitalization among young adults unrelated to childbirth is due to a set of young adults with chronic disease, mental illness and infections, who are also at high risk for multiple hospital admissions. Thus, the successful management of chronic diseases is a key target in efforts to decrease inpatient utilization among young adults. New models of care are necessary for young adults with chronic disease to successful engage them in their disease during a time of rapid social, emotional and physical change. Evaluating the effect of such interventions on current and future health care utilization and outcomes for young adults should be considered an important research priority.
WHAT DO PATIENTS WANT? A SERIES OF QUALITATIVE INTERVIEWS WITH READMITTED PATIENTSTheodore Long1,2; Sheila Antony1,2; Alexander Pine1,2; Amish Desai1,2; Alexandra Norcott1,2; Cali Luco1,2; Emily M. Meyer1,2; Rebecca Brienza1,2. 1VA Connecticut Healthcare System, West Haven, CT; 2Yale University School of Medicine, New Haven, CT. (Tracking ID #1938293)
BACKGROUND: With an increasing emphasis on patient-centered outcomes, there is a need to understand what aspects of care are most prioritized by patients. While studies in primary care have demonstrated that patient-centered practice is associated with decreased healthcare utilization, and more recently that patient-centered care may reduce cardiovascular mortality, the adoption of such practices is inconsistent. This study sought to determine the elements of patient-centered care that are valued by Veterans who have high levels of interaction with the hospital system, as demonstrated through recent hospital readmissions.
METHODS: As part of an ongoing study, a total of n = 4 semi-structured interviews were conducted with Veterans at the West Haven Veterans Affairs Medical Center (WHVA) who were on a current 30 day readmission. The interview guide was informed by pilot interviews and studies in the area of patient-centered care. Researchers conducted in-depth interviews (approximately 45 min to 1 h per encounter) with patients regarding their healthcare priorities; confidentiality was maintained per VA protocol using patient identification reference numbers stored by study investigators. ATLAS.ti was used to facilitate coding, theme generation, and quote management. Specifically, interview transcripts were topic-analyzed by an interdisciplinary team who developed codes both iteratively and inductively, capturing insights from participating Veteran patients. Tenets of Grounded Theory were used to guide analysis and organize final code structures and predominant themes.
RESULTS: Four major patient care priority themes emerged during this exploratory analysis: (1) the importance of setting the agenda for primary care visits, (2) the necessity of being listened to by clinicians, (3) the desire to feel independent and manage one’s own care at home, and (4) the ability to manage medical problems with outpatient clinicians to avoid admission. Patients stated that they valued their independence and wanted to seek out medical care on their own terms by setting the visit agenda. They were appreciative of the coordination of care in the outpatient setting and wanted further follow up, with the commonly stated goal of remaining at home and avoiding admission.
CONCLUSIONS: Veterans with increased hospital utilization value setting the agenda for their health care, especially in primary care, and prioritizing their independence by self-managing their conditions at home. These Veterans concluded that being listened to was one of the most important aspects of patient care, and consistently stated that they valued outpatient care and prioritized avoidance of hospital admission.
WHAT HAPPENS WHEN AFRICAN ANCESTRY PATIENTS LEARN THEY HAVE A GENETICALLY INCREASED RISK FOR A CHRONIC DISEASE? WHAT DO THEIR DOCTORS THINK?Carol Horowitz1; Kadija Ferryman2,1; Rennie Negron1; Mayra Rodriguez1; Erwin Bottinger1; Saskia Sanderson1; Randi Zinberg1. 1Mount Sinai School of Medicine, New York, NY; 2New School, New York CIty, NY. (Tracking ID #1939516)
BACKGROUND: Few genetic markers are reliably associated with chronic disease risk and thus few non-theoretical studies have examined how patients and doctors view such risk testing. A recently-discovered variant in the APOL1-gene is associated with a five-fold risk of end-stage renal disease (ESRD) among hypertensives. This variant, which originated in Africa to protect against trypanosomiasis, occurs in 15 % of persons with self-reported African Ancestry (black/African American) vs. <1 % of Whites. We conducted in-depth interviews to explore patients’ views on genetic testing and their reactions to receiving APOL1 genetic test results and risk information. We also interviewed primary care physicians to assess their attitudes about using genomic risk information to assess ESRD risk and communicating this risk as part of clinical care for their Black patients.
METHODS: Eligible patients have participated in a bio-repository, self-identify as Black or African American and have hypertension, but no diabetes or kidney disease. After informed consent, patients were tested for the APOL1 gene variation and then met with a genetic counselor who returned their results. We conducted in-depth interviews at baseline (pre-testing), and immediately and 30 days after they received genetic risk results. We also used purposive sampling to identify and interview primary care providers from a large teaching hospital and a network of health centers. All interviews were audiotaped, transcribed, and our team coded transcripts and developed themes using ATLASti and grounded theory.
RESULTS: We recruited 26 Black adult patients with a mean age of 56 years, 73 % had the high risk APOL1 gene risk variation, 73 % were female, 69 % had a yearly income <$30,000 and 27 % had < high school education. We also recruited 15 physicians with a mean age of 39 years; 60 % female, 13 % Black; 50 % in practice >5 years. At baseline, patients had low knowledge of genomics and of kidney disease and their risk for it, but most perceived an inherent benefit to knowing their genetic risk status. After return of results, patients with high-risk alleles felt the information they received was useful, empowering, made them more aware of their health risks, motivated them to better control their hypertension and general health, and planned to share the results with their providers. Patients without increased genetic risk were relieved and most stated they were more conscious of the importance of blood pressure control. Patients reported that the connection between their race and genetic risk was enlightening, made sense, could explain disparities in a way that did not blame patients, were aware other ethnic groups also had unique genetic risks, and they showed little concern about abuse of this information. Physicians felt poorly prepared to test or discuss genetic test results with patients, reported no genetics education since medical school, but were interested in learning to use it as part of patient care, if evidence-based guidelines show such tests can improve patient outcomes. They wanted time-efficient ways to be trained and to share information with patients, including electronic clinical-decision and patient support materials. Some physicians were concerned about using genetic testing for an allele that is associated with African Ancestry.
CONCLUSIONS: Hypertensive patients with African Ancestry had a generally positive reaction to receiving chronic disease genetic risk information, and doctors were interested in, but unsure of how to provide them with this information. Future research should explore whether diverse patients and their providers can use such information to improve healthcare, behaviors and outcomes.
WHEN LESS IS MORE: RESULTS OF A RANDOMIZED CONTROLLED TRIAL ON ASSISTING AND ARRANGING SOCIAL NETWORKS FOR WALKING IN SEDENTARY ADULTSLiza Rovniak1; Jennifer Kraschnewski2; Christopher Sciamanna2; Ding Ding3; Melissa Bopp4; Daniel George5; James Sallis6; Melbourne F. Hovell7. 1Penn State College of Medicine, Hershey, PA; 2Penn State-Hershey Medical Center, Hershey, PA; 3University of Sydney, Sydney, NSW, Australia; 4Pennsylvania State University, State College, PA; 5Pennsylvania State University, Hershey, PA; 6University of California, San Diego, San Diego, CA; 7San Diego State University, San Diego, CA. (Tracking ID #1938319)
BACKGROUND: Epidemiological research suggests that social networks are critical for adopting and sustaining regular physical activity (PA). However, little is known about how best to “engineer” online or in-person social networks to increase PA among sedentary adults. The 5A Model of Behavior Change predicts that “arranging” social networks for PA would be more effective than simply “assisting” participants to build social networks for PA. However, no study to our knowledge has tested this hypothesis.
METHODS: We randomly assigned 308 sedentary adults to three groups: (1) Arranging Networks: weekly feedback on online and in-person social network interactions for walking, and access to an online social networking site for PA, plus 12-week evidence-based walking program and weekly social networking tips for PA; (2) Assisting Networks—High Dose: 12-week evidence-based walking program and weekly social networking tips only; (3) Assisting Networks—Low Dose: weekly social networking tips only. Ongoing process evaluations were conducted to ensure treatment fidelity. In-person assessments were conducted at baseline, post-program, and 6-month follow-up. Differences between groups were analyzed using ANCOVA, adjusted for demographics and baseline scores.
RESULTS: At baseline, participants were 61.6 % female, 83.4 % overweight/obese, and 8.1 % non-White, with a mean age of 50.3 years; 87 % and 83 %, respectively, completed the post-program and 6-month assessments. The Assisting Networks-Low Dose group demonstrated a greater increase in accelerometer-measured light/lifestyle PA from baseline to 6-months (14.1 mins/day), relative to the Assisting Networks-High Dose (−9.2 mins/day) and Arranging Networks (−3.0 mins/day) groups (p < .05). There were no significant between-group differences at post-program or 6-months in accelerometer-measured moderate/vigorous PA or in objectively-measured aerobic fitness, body mass index (BMI), and waist circumference. Within-group analyses indicated that all groups either maintained, or significantly improved, their accelerometer-measured moderate/vigorous PA, BMI, and waist circumference from baseline to 6-months. Qualitative analyses indicated that many of the study’s middle-aged participants lacked interest in visiting online social networking sites for PA. Many participants reported that it was easier to walk alone than to schedule walks with others.
CONCLUSIONS: Unexpectedly, “assisting” sedentary adults to build social networks for PA with weekly tips yielded slightly better objectively-measured outcomes than “arranging” social networks with online networking sites and weekly follow-up. These findings suggest that more needs to be learned about the best strategies for engineering social networks for PA. Future research should explore if study findings replicate among more diverse populations, and how to further improve outcomes. The low-dose, cost-effective intervention to “assist” social networks for PA could easily be replicated and disseminated as part of automated physician-delivered PA interventions.
WHERE DO CURRENT COMPUTERIZED PHYSICIAN ORDER ENTRIES (CPOES) STAND IN AVERTING/FACILITATING MEDICATION ERRORS IN THE UNITED STATES AND CANADA?Tewodros Eguale1,2; Mary Amato4,1; Sarah P. Slight3; Andrew C. Seger1; Diana L. Whitney5; David W. Bates1,2; Gordon D. Schiff1,2. 1Brigham and Women’s Hospital, Boston, MA; 2Harvard Medical School, Boston, MA; 3The University of Durham, Durham, United Kingdom; 4Massachusetts College of Pharmacy and Health Sciences, Boston, MA; 5Baylor College of Medicine, Houston, TX. (Tracking ID #1938527)
BACKGROUND: Computerized Prescriber Order Entry (CPOE) has long been considered and demonstrated to be a high-leverage tool for preventing medication errors and incentives’ are being provided to accelerate its adoption. However, there is a growing awareness and increasing documentation of concerns that CPOE can also introduce or facilitate new errors. Recently, an in depth analysis of USP MEDMARX medication error reporting database resulted in the creation of ‘test cases’ to evaluate the vulnerability of CPOEs in facilitating or averting medication errors in inpatient and outpatient settings. The outpatient test cases include allergy, drug-drug interaction, disease-drug interaction, omission errors, too high doses, duplicate drugs, wrong units, wrong dispensed amount, adjacency errors, and wrong dose for indication. The objective of the study was to evaluate the extent to which leading CPOEs systems in US and Canada handle erroneous outpatient test case scenarios.
METHODS: Sixteen (11 US and 5 Canada) CPOE systems were selected for evaluation and typical users were recruited to enter the erroneous orders on test patients. Outcome was measured using a Likert scale ranging from 1 to 5, where 1 represent ‘easy’ to enter the erroneous order and scales 2–4 represent increasing degree of difficulty and 5 represents ‘impossible’ to enter the erroneous order. To compare the test cases, mean scores and proportions were calculated and radar plot was used to facilitate comparison of test cases.
RESULTS: Scores for US and Canada were combined since there is no statistically significant difference between the CPOEs tested in the two countries. The figure shows the mean scores for the 13 test cases. The tested CPOEs performed worst in averting drug-disease interaction error (pioglitazone was accepted for congestive heart failure patients). The CPOEs performed poorly in detection of look-alike-sound-alike errors (penicillamine vs. penicillin), wrong frequency for the drug form error (Cardizem CD 120 mg PO QID), and wrong dose for the indication error (Methotrexate 15 mg PO daily for rheumatoid arthritis). The CPOEs performed better in averting too high doses, drug-drug interactions, and omission of strength of a drug and in allergy situations. Overall, 52.8 % of the erroneous orders passed through easily or with minor workaround and in 19.2 %, it was not possible to complete these orders. Moreover, only 29.2 % of the orders generated warnings.
CONCLUSIONS: Current CPOEs are generally vulnerable in facilitating potential medication errors. Developers and users need to be aware of this potential for error, and should build strategies to protect patients by improving the safety of CPOE systems.
Radar plot showing mean score for each test scenario across all tested CPOEs in difficulty of entering erroneous orders. The red line ideally should occupy the most outer grid (score 5), i.e. impossible to enter any erroneous orders.
WHO ARE YOU GONNA CALL? A STUDY OF HOW RESIDENTS MANAGE UNCERTAINTY WHEN CARING FOR CLINIC PATIENTSAudrey L. Tanksley1; Julie Oyler1; Shana Ratner2; Laura Ruth Venable1; Vineet Arora1. 1University of Chicago, Chicago, IL; 2University of North Carolina, Chapel Hill, NC. (Tracking ID #1938642)
BACKGROUND: One third of Internal Medicine training occurs in the ambulatory setting, yet evidence suggests we are not adequately preparing trainees for outpatient practice. With the changing healthcare system there is a growing need for assessment of outpatient education, and a substantial interest in improving the quality of this training. While the literature to date has highlighted effective strategies for attending supervision in the inpatient setting, few have evaluated the ambulatory setting. The aim of this study is to describe resident satisfaction with clinic supervision and management of uncertainty with clinic issues.
METHODS: From 2010 to 2013, Internal Medicine residents at an academic center completed an end-of-year survey on satisfaction with supervision during their continuity clinic experience and how they dealt with uncertain clinical situations. Trainees were asked to rate overall satisfaction with availability, continuity, amount of supervision during and outside of clinic for the faculty preceptor. They were also asked to select the strategies they use to manage uncertainty when faced with a clinical issue for their patients outside of clinic hours. They were asked to report on a 5-point likert scale how frequently they contacted the attending, asked a resident they knew, read about the topic, asked the on service resident, waited until next visit, asked chief resident or other. Trainees were divided by postgraduate year into two groups consisting of interns and upper level residents. T-tests were used to evaluate associations between postgraduate year and frequency of strategy for management of uncertainty.
RESULTS: From 2010 to 2013 categorical and med-peds residents were required to complete an end of year survey, response rate was 90 % (n = 343). While 78 % of residents were satisfied with availability of their clinic preceptor outside clinic, only half (56 %) were satisfied with continuity of clinic preceptor. In addition, while 90 % were satisfied with amount of supervision during clinic, only 63 % were satisfied with amount of supervision outside clinic. When trainees were asked how they managed uncertainty for clinic issues outside of clinic, 84 % reported reading about the topic, 42 % asked a resident they know, 26 % asked the on service resident, 22 % contacted the preceptor, 14 % waited until the next visit to address the clinical issue. When comparing upper residents to interns, residents were more likely to report contacting the faculty preceptor (PGY1 mean = 2.48, PGY2+ mean = 2.81 p = 0.018) while interns were more likely to ask the on-service resident (PGY1 mean = 3.36, PGY2+ mean = 2.45 p = 0.0001). Residents commented, “The preceptors are all fantastic—more continuity would probably be helpful.”
CONCLUSIONS: When residents are faced with a clinic patient issue outside of clinic hours for which they are uncertain, they utilize the “hierarchy of assistance” by consulting the literature and asking colleagues before contacting the attending. Interestingly, upper level residents reported contacting the faculty preceptor for uncertainty more than interns, and interns contacting on-service residents more frequently than upper level residents. This could reflect in part a reluctance of interns to contact the attending or a greater familiarity and comfort with advanced residents for contacting the attending. Regardless, previous studies have described the implication of this step up approach in the inpatient setting and how it can lead to delay of care and patient harm. Further studies are needed to define when clinic attending supervision is warranted, and the most effective ways to improve continuity of the preceptor.
WHO IS PERFORMING INVASIVE BEDSIDE PROCEDURES AT AN ACADEMIC MEDICAL CENTER, AND WHY?Cynthia Kay1; Jeffrey L. Jackson2; Dai Takahashi1. 1Medical College of Wisconsin, Milwaukee, WI; 2Clement J. Zablocki Veterans Affairs Medical Center, Milwaukee, WI. (Tracking ID #1923968)
BACKGROUND: The performance of most procedures are no longer required as part of medicine residency training. However, residents and internists practicing in hospitals often care for patients requiring certain procedures. Our mixed-method study’s aims were to assess the procedure practice patterns at an academic medical center, explore patient characteristics that may affect service performing these procedures, and assess factors influencing residents’ decision making regarding procedures.
METHODS: The yearlong study began February 2013 at the Medical College of Wisconsin. We prospectively collected data on adults admitted to resident or hospitalist services who underwent a thoracentesis, paracentesis, or lumbar puncture. Data included procedural characteristics (procedure; service performing the procedure; primary team), patient characteristics (age; gender; comorbidities; BMI; anticoagulation use; INR; antibiotic use; delirium) and admission characteristics (day of week; time of admission). Two approaches were used to explore residents’ decision making. We conducted resident focus groups and also invited residents to complete a survey each time their patient had a listed procedure. The Likert-scaled survey assessed six potentially important factors: time, patient comorbidities, supervision, attending’s comfort, personal experience, and comfort with the procedure. The study was approved by our institution’s IRB. All residents provided informed consent.
RESULTS: Over a 9-month period, 307 procedures were performed, with 213 on the resident teams and 94 on the hospitalist service. Thoracentesis was most common (44 %), followed by paracentesis (41 %), and lumbar punctures (15 %). Most procedures (n = 253, 72 %) were referred, either to radiology (n = 179, 58 %) or to the Hospital Procedure Service (n = 74, 24 %). Only 54 (18 %) were done by residents. Hospitalists performed few procedures (3 %), significantly less (3 %, p < 0.0005) than residents. There was no difference in likelihood of referral by type of procedure (p = 0.43), day of week, time of admission or other patient characteristics. Focus groups identified six themes that contributed to the likelihood of referral: time, attending’s comfort, supervision, resident’s comfort, patient comorbidities, and experience. Among survey respondents (n = 81), 52 % were interns and 48 % residents; the response rate was low (27 %). Factors cited as important in the decision to refer included lack of training (RR: 6.3, 95 % CI: 2.1–19.3), level of resident comfort (RR: 3.8, 95 % CI: 1.9–7.6), available supervision (RR: 2.4, 95 % CI: 1.2–4.9) and attending’s comfort (RR: 1.9, 95 % CI: 1.1–3.4). Unimportant factors included lack of time (RR: 1.4, 95 % CI: 0.8–2.9) and patient comorbidities (RR: 0.8, 95 % CI: 0.4–1.6). On multivariable modeling, independent predictors of referral included lack of training (RR: 6.9, 95 % CI: 1.7–28.3) and resident’s lack of comfort (RR: 4.3, 95 % CI: 1.4–13.6).
CONCLUSIONS: Most procedures are referred. While focus groups identified time, supervision, comfort with procedure, and comorbidities as important factors in the decision to refer, the resident survey found that time and patient-specific characteristics (such as age and comorbidities) were not important. Factors cited for referral included lack of training, supervision and comfort with the procedure (both for resident and attending). If a goal is to prepare residents to perform procedures when needed, then better training or supervision may be required. Further research is necessary to determine if and how these procedural practice patterns affect residents, patients, and health care.
WHY AREN’T MORE PRIMARY CARE RESIDENTS GOING INTO PRIMARY CARE? STUDYING PROGRAM FACTORS THROUGH QUALITATIVE INTERVIEWS WITH PRIMARY CARE RESIDENTSTheodore Long1; Olatunde Bosu2; Krisda H. Chaiyachati1; Bradley G. Richards1; Nicole Krenitsky2; Leslie Curry3; John P. Moriarty1; Stephen J. Huot1. 1Yale School of Medicine, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3Yale School of Public Health, New Haven, CT. (Tracking ID #1936518)
BACKGROUND: Nearly two-thirds of primary care internal medicine residents report that they do not plan to have a career in primary care or general internal medicine. As we face a potential shortage of up to 44,000 adult care generalists by the year 2025, it is crucial to understand why residents who demonstrate interest in primary care by virtue of entering into primary care residency programs are choosing to not enter the primary care workforce. Others have examined resident satisfaction, indebtedness, and specialty consideration among residents, but it remains largely unknown how these factors contribute and whether other factors that have not been explored are also contributing to the decision to pursue another specialty. We seek to understand programmatic factors that may influence career choices among primary care residents using qualitative interviews.
METHODS: One interviewer completed in-depth 1 h interviews with second and third year residents in the Yale Internal Medicine Primary Care Program using an instrument developed from pilot interviews and existing literature. Two members of the research team independently coded the transcripts and then met to go over coding and resolve differences. The code structure was developed in stages based on grounded theory, using a systematic and inductive approach to generate insights from the comments of the study participants. Using the constant comparative method, the research team then identified emerging themes and refined codes. ATLAS was used for coding, audit trails, and pulling quotes.
RESULTS: To date eight interviews have been completed. Analysis revealed six themes of program-related experiences emerging from the coding. We characterized three of these themes as having potentially negative impact and three as having potentially positive impact on trainee decision to pursue a career in primary care. The themes related to potential negative impact were: mismatch between trainee expectations and actual experience with the practice of primary care; challenges with disjointed care including interruption of continuity by inpatient rotations; and inadequate communication between practice teams and subspecialists. Residents commonly entered training with the ideal of caring for the underserved, but were challenged by limited resources to meet the full range of needs of this population. Themes related to potential positive impact on trainee decision to pursue a career in primary care were: culture of like-mindedness amongst colleagues including comfort with change; positive reflections on outpatient curriculum; and appreciation of exposure to various models of primary care.
CONCLUSIONS: Our results suggest that residents enrolled in primary care programs identify experiences in training that may negatively or positively impact their decision to enter into a career in primary care. Addressing those aspects of training that potentially negatively impact this decision (continuity, adequate resources to address the spectrum of needs of an underserved population, communication with specialists) and strengthening those aspects of training that may positively impact this decision (creating a culture that supports and encourages primary care, having a robust ambulatory curriculum, and providing exposure to a range of primary care delivery models) may increase the proportion of residents enrolled in primary care training programs who pursue a career in primary care. Recognizing the limitations of a single program study, we are broadening these initial findings by undertaking interviews with trainees enrolled in two other differently structured primary care residency programs.
WILLINGNESS TO PARTICIPATE IN CANCER CLINICAL TRIALS AMONG PROSTATE CANCER PATIENTS: THE RELATIONSHIP WITH RACE/ETHNICITY AND HEALTH LITERACYCelia P. Kaplan1,2; Anna Napoles1,2; Steven Gregorich1; Tung T. Nguyen1,2; Jennifer Livaudais-Toman1; Eliseo J. Perez-Stable1,2; Eric J. Small1,2; Mack Roach2,3. 1University of California San Francisco, San Francisco, CA; 2University of California San Francisco, San Francisco, CA; 3University of California San Francisco, San Francisco, CA. (Tracking ID #1935608)
BACKGROUND: Clinical trials provide the foundation for advances in cancer diagnostics and therapeutics and are the major channel for translating treatment-related discoveries in cancer care into clinical practice. To ensure that the benefits and burdens of this research are distributed fairly among all cancer patients and that research findings are generalizable, it is important that minorities participate in clinical trials. However, enrollment of African Americans and Latinos remains lower than that of non-Latino whites. Limited health literacy, more common among minorities than whites, is a key barrier to clinical trial recruitment. We sought to examine the association between race/ethnicity, health literacy and stated willingness to participate in clinical trials among prostate cancer patients.
METHODS: Potential participants consisted of men diagnosed with prostate cancer in 2008 between the ages of 18 and 75, recruited through the California Cancer Registry, living within 60 miles of a site offering access to one or more clinical trials in eight California counties: Alameda, Contra Costa, Marin, Monterey, San Francisco, Santa Clara, Santa Cruz and Los Angeles Counties. Between November 2011 and November 2012, we identified all cases of prostate cancer in African American, Latino and Asian American patients and a random sample of prostate cancer cases in white men. Participants completed a 30-minute telephone interview in English, Spanish or Chinese (Mandarin or Cantonese) to assess their attitudes, knowledge and willingness to participate in prostate cancer clinical trials. Health literacy was assessed with a 3-item previously validated scale that asked about comfort reading hospital materials, filling out medical forms, and understanding written information (scale scores ranged from 1 to 5, dichotomized as <3.5 = low literacy, ≥3.5 = medium-high literacy). In multivariable analyses, logistic regression was used to estimate effects of ethnicity and health literacy on willingness to participate. We estimated odds ratios [OR] and 95 % confidence intervals [CI].
RESULTS: A total of 1,869 men were contacted and the final sample included 855 men for a response rate of 46 %. More than half (52 %) were age 65 years or older. The ethnically diverse sample included white (42 %), Latino (24 %), African American (19 %) and Asian American men (15 %). More than 50 % completed college. Nearly 70 % were born in the U.S. The majority of men (98 %) were insured and 81 % had medium to high health literacy (composite score ≥3.5). Only 17 % believed that “clinical trials are beneficial” but 75 % believed that “clinical trials are important”, while only 38 % expressed a willingness to participate in clinical trials. Bivariate and multivariable analysis results are presented in Table 1.
CONCLUSIONS: Among men with prostate cancer, African American and Latino men expressed a greater willingness to participate in prostate cancer clinical trials than non-Latino white men. Health literacy was not associated with willingness to participate. Given lower rates of clinical trial participation in these racial/ethnic groups, our findings suggest that factors other than willingness to participate affect actual participation and need to be explored.
Table 1. Bivariate and multivariable analyses: Willingness to participate in prostate cancer clinical trials
| Willing to participate % | OR (95 % CI) | aOR* (95 % CI) | |
| Race/Ethnicity | |||
| Non-Latino white | 34 % | Ref | Ref |
| African American | 44 % | 1.31 (0.89–1.92) | 1.69 (1.01–2.82)° |
| Asian | 30 % | 0.85 (0.55–1.32) | 0.86 (0.46–1.61) |
| Latino | 55 % | 2.21 (1.55–3.14)° | 1.75 (1.01–3.05)° |
| Health Literacy | |||
| Low (score <3.5) | 48 % | Ref | Ref |
| Medium to High (score ≥3.5) | 39 % | 0.75 (0.53–1.07) | 1.34 (0.77–2.34) |
*Analysis is also adjusted for age, marital status, education, nationality, employment, health insurance, prior research participation, knowledge of clinical trials, attitudes towards clinical trials, and Gleason score. p < 0.05
WOMAN CLINICAL SCHOLARS: “SOMETIMES YOU NEED TO CLIMB OUT A WINDOW, AND SCALE THE FIRE LADDER, TO GET TO THE PLACE YOU WANT TO BE.”Adina Kalet1; Jennifer Rockfeld1; Nina Bickell2; Kathlyn E. Fletcher3; Kate Schwartz1. 1NYU School of Medicine, New York, NY; 2Mount Sinai School of Medicine, NY, NY; 3Medical College of Wisconsin, Milwaukee, NY. (Tracking ID #1939410)
BACKGROUND: To effectively build the next generation of academic physicians, we will need to understand factors that enable fellowship-prepared women to thrive in academia. To describe and explore the complexity and challenges of creating work/life satisfaction in academic medicine we studied woman graduates of the Robert Wood Johnson Clinical Scholars Program (CSP, Class of 1976–2011).
METHODS: We surveyed every woman graduate of the CSP graduate up through 2011 (n = 360) by both email and post. The survey instrument (12 prompts requiring open text responses) was designed to explore current work situation, personal definitions of success and accomplishments, job negotiations, career regrets or disappointments, predominant feelings about work life, and advice for others. All data was de-identified and 4 independent readers coded overlapping subsets of the data. A coding scheme fit to the data was refined through discussion and applied to the data by two analysts using Dedoose™ qualitative analysis software.
RESULTS: After 5 reminders 104/360 (29 %) of the cohort responded, mean age 45 (range 32 to 65), 6 % single, 85 % partnered, and 8 % divorced/separated, 87 % have children (average number of children 2.15, range 1 to 5). Preliminary analysis revealed the following major theme categories: Work, Balance, Mentoring, Home/Family, Managing Change, Flexibility, Negotiation, Collaboration, Definitions of Success, and Advice. Respondents endorsing being very satisfied were more likely to describe work as personally and locally meaningful, having the needed scheduling flexibility to care for family, egalitarian spousal support, mentoring and other supportive relationships at work and home and were conducting collaborative research on teams. Less common themes include: issues of self care or neglect, painful regrets, leaving academia, being childless by choice. Work hours, financial constraints and availability of mentoring were among the issues, which differed by clinical discipline. Strategies to manage work-life balance were specific to stage of career and age of children. Younger women emphasized both setting boundaries while home and working from home. Senior women described “atypical” paths through and away from academia with career transitions resulting from discordance among work, need for schedule flexibility and institutional values including gender based discrimination, spousal career changes, and/or need for better career-fit. The majority of these women were highly satisfied and passionate about their work, even those early career women uncertain the effort will be worthwhile. Remaining flexible and open to opportunities, mentoring, building teams to do multi-disciplinary collaborative research work, valuing supportive relationships and seeking ongoing meaningful work in later life were significant themes for experienced academic women. Detailed advice about how to survive tough times was shared.
CONCLUSIONS: These CSP graduates are largely satisfied with and passionate about their work and family life and feel, proud and grateful to have pursued meaningful work despite the challenges and uncertain future. Thriving in academic medicine involved remaining flexible and managing change and chaos. Although, currently generalizability is limited we are establishing reliability of coding, conducting subgroup analysis, validating findings through member-checking, and increasing response rates.
WOMEN VETERANS’ EXPERIENCES AND PREFERENCES WITH VA PRIMARY CARE: A QUALITATIVE STUDYAlicia A. Bergman1; Richard M. Frankel2; Alison B. Hamilton1; Elizabeth M. Yano1. 1Greater Los Angeles VA Healthcare System, North Hills, CA; 2Indiana University School of Medicine, Indianapolis, IN. (Tracking ID #1939722)
BACKGROUND: The growing presence of women Veterans in Veterans Administration (VA) healthcare settings has prompted greater attention to improving women’s health (WH) primary care needs. VA policy now recommends that women patients be seen by primary care providers (PCPs) with specialized WH training/experience, who see them for both primary and gender-specific care in the context of a single visit. However, more information is needed regarding the perceptions and preferences of women Veteran patients themselves. The goal of this qualitative study was to develop a better understanding of the experiences and challenges women Veteran patients face as they navigate VA primary care.
METHODS: Semi-structured interviews were conducted with 30 women Veteran patients at the Indianapolis VA Medical Center. All participants visited a PCP in one of five primary care or community based outpatient clinics within the past year. Permission was obtained from 15 PCPs to invite their patients, and purposive sampling was used for sample diversity.
RESULTS: Qualitative thematic analysis of the interviews revealed four major themes: 1) preference for one-stop-shop approach, 2) improving access, 3) the importance of being proactive, and 4) perceived differences in care. A majority of patients expressed their preference for the comprehensive and integrated one-stop-shop approach to primary care for women Veterans; instead of making separate appointments for women’s health related care (e.g., pap smears, breast exams, contraceptive counseling) in the Women’s Clinic or with an private gynecologist, seeing one WH-PCP for everything offered several perceived benefits for patients, including convenience, familiarity and comfort, not having to repeat information, and receiving consistent approaches to treatment and therapy. Many patients also discussed their desire for better access to VA primary care services, such as quicker access to appointments (including more user-friendly phone and/or computer systems to make appointments), reduced waiting times after arriving to the clinic, and flexibility in accommodating patients’ work schedules. The third theme relates to the sentiment of many women that although there is good primary care in the VA, it is necessary to be proactive and take charge of one’s own healthcare in order to receive it. Being proactive included requesting changes in PCPs when one is dissatisfied, doing front-end research before appointments, writing out lists and presenting them to PCPs, taking the initiative to coordinate same-day appointments, and calling PCPs to give them reminders. Finally, many women Veteran patients cited perceived differences in care as compared to what they believed male veterans received, such as perceptions that male Veterans in general get preferential treatment (“I can read faces and I can read lips—‘Oh shit, another female’.” [pt 4]”, not feeling recognized as a woman Veteran (e.g., letters addressed to “Mr.”), and not having symptoms taken as seriously.
CONCLUSIONS: Gaining in-depth knowledge about women Veterans’ preferences with VA primary care is an essential step in successfully implementing an integrated and comprehensive care model that improves their care experiences. Important implications for clinical practice from this study include specific strategies for how PCPs can approach and communicate with women Veteran patients.
WOMEN’S HEALTH INFORMATION IN WOMEN’S MAGAZINES: OFTEN MISINFORMINGAkeira Johnson1; Julie L. Mitchell1; Kathryn Havens2. 1Medical College of Wisconsin, Milwaukee, WI; 2Clement Zablocki Veterans Hospital, Milwaukee, WI. (Tracking ID #1939532)
BACKGROUND: Patients frequently receive health information from non-medical sources. In 1995, Woodford found that health messages were present in 22 % of 11 popular magazines, but little is known about women’s health content in lay periodicals, and more importantly, its quality. We sought to evaluate the quantity and accuracy of information available to women in the most popular lay periodicals that are predominantly viewed by a female audience.
METHODS: Using 2012 data from the Pew Research Foundation, we selected the top ten magazines marketed to women with the largest circulation. These magazines reach >7 million persons annually. Two authors independently: 1) reviewed these magazines for text and ads pertinent to women’s health, 2) recorded the amount of information in increments of 1/4 of a magazine page, 3) placed items into 1 of 10 categories, and 4) evaluated for untruthful or misleading information defined as claims not supported by scientific evidence and/or overtly false statements. When there was disagreement in the independent reviewer assessment, a re-review resulted in an easy consensus in most cases. The third author was consulted when agreement was not easy.
RESULTS: Results: Overall, 6 % of the magazines’ space was devoted to women’s health (WH) content. Some of the magazines had more WH information than others, ranging from 2 to 13 %. Most of the information was presented in the form of advertisements: 58 % of all WH content. Gender-specific health topics (items such as osteoporosis, dieting and fibromyalgia) were the most discussed (19 % of all WH content). Pregnancy prevention and bladder function were the second and third most discussed WH topics at 15.0 and 14.0 % respectively. The least covered subjects were menstruation and obstetrics (6 %), followed by breast health (0 %). We found 12 of 89.5 (13 %) items contained misleading information, 50 % of these misleading items were in advertisements and 50 % in magazine text. Examples of misleading items included advertisements promoting supplementation for addressing weight gain in postmenopausal women and topical agents to prevent the development of stretch marks and an article promoting the benefits of human growth hormone on youthful appearance and improved sexual function. Each magazine had at least one misleading item.
CONCLUSIONS: Women are commonly reading magazines that contain women’s health information, although the overall fraction of women’s health content is small. This information is in both text and ads and 13 % of all items misinform the lay population. In their approach to female patients, healthcare providers need to be cognizant that women’s health misinformation is easily available, and perhaps even accessible in their waiting rooms. Approachable demeanor and open-ended questioning should be employed in exploring patient’s baseline knowledge in women’s health topics, particularly with regards to weight loss and menopausal topics.
WORSENING TRENDS IN THE AMBULATORY MANAGEMENT OF HEADACHEJohn N. Mafi1; Samuel T. Edwards2; Nigel Pederson3; Roger B. Davis1; Ellen P. McCarthy1,4; Bruce E. Landon1,5. 1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Veterans Affairs Boston Healthcare System, Boston, MA; 3Beth Israel Deaconess Medical Center and Massachusetts General Hospital, Boston, MA; 4Harvard Medical School, Boston, MA; 5Harvard Medical School, Boston, MA. (Tracking ID #1930868)
BACKGROUND: Headache is a universal complaint and among the most common reasons for visiting a physician. Despite numerous headache practice guidelines published over the past decade, little is known about the extent to which U.S. physicians adhere to recommended therapies or how this has changed over time. In this context, we sought to characterize trends in the management and treatment of headache from 1999 to 2010.
METHODS: Using nationally representative data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey we examined ambulatory visits for headache. Our primary outcomes included use of advanced imaging, referrals to other physicians, and use of opiates/barbiturates (guideline discordant indicators), as well as physician counseling on headache prevention and use of preventative therapies including verapamil, topiramate, amitriptyline, or propranolol (guideline concordant indicators). Other outcomes included abortive medications such as non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen (APAP) and triptans/ergot alkaloids. We excluded visits with “red flags,” such as neurologic deficit, cancer, or trauma. We used logistic regression models for each outcome focusing on a linear trend for each two-year interval, and adjusted for age, sex, race/ethnicity, insurance, symptom duration, geographic region, urban location, and whether the healthcare professional was the primary care physician (PCP), and weighted results to reflect U.S. population estimates. Additionally, we stratified findings by migraine versus non-migraine, acute versus chronic presentations, and visits to PCPs versus non-PCPs.
RESULTS: We identified 9,110 visits for headache, which represented an estimated 139 million visits from 1999 to 2010. Nearly three-quarters of patients were female and mean age remained stable at approximately 46 years. Our Table summarizes unadjusted use over time. Use of advanced imaging (computed tomography or magnetic resonance imaging) rose from 7.6 % in 1999–2000 to 14.1 % in 2009–2010 (unadjusted p < 0.001) and referrals to other physicians increased from 7.7 to 12.9 % (p = 0.009). In contrast, physician counseling for headache prevention declined from 22.5 % in 1999–2000 to 17.3 % in 2009–2010 (p = 0.034). Use of preventative medications increased from 8.3 to 15.0 % (p = 0.003) while opiates/barbiturates remained unchanged at approximately 18 %. Adjusted trends (Figure) were similar as were results after stratifying by migraine versus non-migraine, acute versus chronic presentations, and visits to PCPs versus non-PCPs, with one important difference being that non-PCPs more frequently ordered advanced imaging (p < 0.001).
CONCLUSIONS: Contrary to numerous headache practice guidelines, physicians are increasingly ordering advanced imaging and referring to other physicians and less frequently offering first-line headache prevention counseling to their patients. Worsening adherence to headache guidelines represents an area of particular concern for our healthcare system and stands out as an important opportunity to improve the value of U.S. healthcare.
Table. Unadjusted Use over Time (% of Visits)
| Year (sample n) | 1999–2000 (n = 1,287) | 2001–2002 (n = 1,694) | 2003–2004 (n = 1,647) | 2005–2006 (n = 1,453) | 2007–2008 (n = 1,515) | 2009–2010 (n = 1,514) | P-value |
| Advanced Imaging (CT/MRI) | 7.6 | 7.3 | 8.0 | 10.7 | 13.5 | 14.1 | <0.001 |
| Referrals to Other Physicians | 7.7 | 9.8 | 11.7 | 10.7 | 13.5 | 12.9 | 0.009 |
| Headache Prevention Counseling | 22.5 | 21.8 | 23.2 | 18.8 | 15.6 | 17.3 | 0.034 |
| Medications | |||||||
| NSAIDs/APAP | 16.2 | 22.9 | 18.0 | 15.9 | 19.6 | 17.2 | 0.58 |
| Triptan/Ergot | 8.4 | 11.1 | 13.7 | 16.3 | 12.2 | 13.5 | 0.054 |
| Preventative | 8.3 | 9.3 | 9.9 | 10.5 | 11.6 | 15.0 | 0.005 |
| Opiate/Barbiturate | 18.3 | 16.5 | 18.9 | 17.2 | 21.2 | 18.4 | 0.63 |
Abbreviations: NSAIDs/APAP: non-steroidal anti-inflammatory drugs or acetaminophen; CT/MRI: computed tomography or magnetic resonance imaging; Preventative: propranolol, verapamil, amitriptyline, or topiramate.
Figure. Adjusted Physician Counseling, Referrals to Physicians, and CT/MRI Use for Headache Over Time
YOGA FOR URINARY INCONTINENCE IN MIDDLE-AGED AND OLDER WOMEN: RESULTS OF A PILOT RANDOMIZED TRIALAlison J. Huang1; Hillary Jenny2; Margaret A. Chesney1; Michael Schembri1; Leslee L. Subak1. 1University of California San Francisco, San Francisco, CA; 2Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1926774)
BACKGROUND: Nearly one-third of middle-aged and older women suffer from urinary incontinence. Existing treatments for incontinence are associated with side effects or other limitations that reduce their accessibility and usefulness, particularly in older women. Yoga can be used to improve awareness of and control over pelvic floor muscles; decrease anxiety, stress, and associated autonomic imbalance; and improve overall physical conditioning, all of which may help improve bladder control. We examined the feasibility, efficacy, and safety of teaching middle-aged and older women to practice yoga to improve incontinence.
METHODS: We conducted a pilot randomized trial in ambulatory women 40 years and older with at least 7 stress or urgency incontinence episodes per week. Women were randomized to a 6-week yoga therapy program designed by an expert yoga panel, consisting of twice weekly group classes and once weekly home practice sessions (“yoga therapy”; N = 10), or to wait 6 weeks before receiving gift certificates for local yoga classes (“control”; N = 9). All participants also received written patient-oriented pamphlets about standard behavioral management techniques for incontinence, consistent with usual first-line care. Changes in incontinence frequency were measured using validated 7-day voiding diaries.
RESULTS: Mean [+SD] age was 61.4[+8.2] years, and mean baseline incontinence frequency was 2.5[+1.3] episodes/day. After 6 weeks, total incontinence frequency decreased by 70 % in the yoga therapy group (1.8 + 0.9 fewer episodes/day), versus 16 % in controls (0.3 + 1.7 fewer episodes/day, p = 0.049). Yoga participants also reported an 83 % decrease in stress incontinence frequency (0.7 + 0.8 fewer episodes/day), versus an 19 % increase in controls (0.2 + 1.1 more episodes/day). Changes in urgency incontinence frequency did not differ significantly between groups (1.0 + 1.0 versus 0.5 + 0.5 fewer episodes/day, p = 0.20). All yoga group participants completed at least 90 % of group classes and 100 % of home practice hours. Two women in each group reported adverse events unrelated to treatment.
CONCLUSIONS: Findings provide preliminary evidence to support the feasibility, efficacy, and safety of a group-based yoga therapy intervention to improve urinary incontinence in middle-aged and older women. When taught in a standardized way with attention to patient safety, yoga may offer a cost-effective, community-based management strategy for urinary incontinence.
YOUR PATIENT’S SUGAR IS TOO HIGH!: RESIDENT PHYSICIAN INTER-PROFESSIONAL PHONE COMMUNICATION SKILLSJennifer Adams; Lisa Altshuler; Jaclyn Fox; Sienna Kurland; Kathleen Hanley; Colleen Gillespie; Adina Kalet; Sondra Zabar. NYU School of Medicine, New York, NY. (Tracking ID #1937994)
BACKGROUND: Inter-professional collaboration (IPC) is essential for effective and safe practice, especially in new models of team-based patient care. Understanding physicians’ competence in communicating with team members over the phone is a critical first step to designing targeted curricula and workplace learning experiences. This study sought to assess internal medicine residents’ baseline IPC phone competence.
METHODS: Inter-professional phone skills were assessed in a 10-minute case with a “Standardized Nurse” (SN) as part of the annual 11-station OSCE for Primary Care Residents (PGY1-3, n = 23). This outpatient case called for the physician, speaking on the phone with the RN played by a trained actor (SN), to develop a treatment plan to address their patient’s recent increase in Hemoglobin A1c and creatinine, which required the discontinuation of metformin and insulin adjustment. In addition, residents were expected to recognize two errors made by the nurse. A checklist was created to assess widely accepted IPC, general communication and case specific skills. The IPC items (9) included: clarifying roles; eliciting full information using check-back technique to clarify; using C.U.S. to state Concern, feeling Uncomfortable, and that issue was about Safety; respect (valuing team member information and assessments); and teamwork (developing a plan, delegation). “SNs” were frame-of-reference trained to complete the checklists. Item response options were: not done, partly done and well done, each with descriptive behavioral anchors. Summary scores were computed for IPC and Communication items within the IPC case and communication items for the overall OSCE as % of items rated well done (all Cronbach’s alphas >0.71). Residents were also surveyed after the OSCE about how prepared they felt and to self-assess performance. Frequencies are reported for specific items and means for summary scores.
RESULTS: Only 2/23 residents introduced themselves using their full name and title and no residents confirmed the identity of patient (name, MR # and DOB). 15/23 residents did not perform check-back technique for medications and dosages. 8/23 identified that metformin should be stopped and explained to the nurse using CUS. Eight residents partially or fully recognized the nurse’s mistake in suggesting a change in blood pressure medicine. Almost all residents (21) made some type of interdisciplinary plan with the nurse. The mean IPC Summary Score was 27 % well done. While the overall mean communication score for all 11 cases in the OSCE was 74 %, the mean communication score specific to the IPC case was 37 %. While most residents found the case particularly challenging and complex, 87 % (16) of residents felt prepared, 7 thought they could have done better. 4.3 % (n = 1) received a “not recommend”, 30 % (n = 7) received “recommend with reservations”, 43.5 % (n = 10) received a “recommend” and 21.7 % (n = 5) received a “highly recommend” rating based on their overall professionalism and ability to work as a member of an inter-professional team.
CONCLUSIONS: Residents vary in their IPC phone skills and therefore Residency IPC curriculum can be targeted and tailored to address demonstrated IPC skills deficits. Given these skills are critical to safe and effective team based patient care, attention needs to be paid to developing feasible, valid assessment techniques to monitor competence in this area.
YOUTUBE AS A SOURCE OF INFORMATION FOR ATRIAL FIBRILLATIONRakshita Chandrashekar; Sourabh Aggarwal; Mark Loehrke. Western Michigan school of medicine, Kalamazoo, MI. (Tracking ID #1939085)
BACKGROUND: Internet has become an easy source for healthcare information. In recent years, websites including Google and YouTube have become increasingly popular for searching for all possible queries. It is necessary to monitor the information, especially scientific facts, being disseminated from these open-access sites which will assist in keeping check on and further, in developing strategies to prevent spread of false information. This study analyzed how information related to Atrial Fibrillation was portrayed in video clips available on YouTube.
METHODS: YouTube (www.youtube.com) was searched on December 1, 2013 using the search terms keyword “Atrial Fibrillation”. First 50 videos displayed were analyzed for the purpose of this study with the theory that a layman does not usually go beyond initial videos during random search. Videos were viewed and classified as useful, misleading and news update by 2 different viewers. Data analyses were conducted for duration of videos, number of viewers and appropriateness of videos by reliability score, content score and global quality score. Statistical analysis done by SPSS.
RESULTS: A total of 50 videos were included in analysis. Mean duration of videos was 642 s (Median 254 s), mean viewership was 22893 views (Median 2992 views, range 12–394554 views) and mean length for video posted on YouTube was 717 days (Median 591 days, range 104–2428 days). Forty three vides (86 %) were classified as useful, 5 as patient views (10 %) and 2 as misleading (4 %). Most of the videos, 26 (52 %) were uploaded by university channels, followed by independent users 17(34 %) and for-profit-companies 4(8 %). Most of the videos 22 (44 %) were focused on patient education in laymen language, followed by medical and scientific education 14 videos (28 %) and personal experience 11 videos (22 %). Two videos (4 %) were focused on drug advertisement and 1 video (2 %) discussed alternate non-approved forms of treatment. On a scale of 1–5, the mean reliability score was 3.26 ± 1.04 (Median 4), mean content score was 3.08 ± 1.06 (Median 3) and mean global quality score was 3.12 ± 1.09 (Media 3.5)
CONCLUSIONS: The results demonstrate that there is a wide variety of information on YouTube regarding Atrial Fibrillation. Though most of the videos are useful, with appropriate content form, there are elements of misleading and inappropriate information available on free internet websites. Viewers can be misled to false information which can have grave implications. As a result, public health professionals should be more vigilant in recognizing videos containing misleading information on health related issues and physicians should counsel and educate patients against inappropriate use of online videos for medical purposes. More studies are however needed for information on YouTube for other more common diseases.
CLINICAL VIGNETTES “I AM ALWAYS IN THE HOT SHOWER.” CANNABINOID HYPEREMESIS SYNDROME - A CASE REPORTTanu S. Pandey; Tanuja Salim. John H Stroger Hospital of Cook County, Chicago, IL. (Tracking ID #1939636)
LEARNING OBJECTIVE 1: Marijuana is the most commonly used illicit drug in the United States. The 2010 National Survey on Drug use and Health recorded 17.4 million past month users of Marijuana. However, relatively few cases of cannabinoid hyperemesis syndrome (CHS) are diagnosed correctly and there exists a distinct lack of knowledge of this syndrome. We present a classic case of CHS in a young man with extensive use of marijuana in an effort to understand it better, especially in current times of legalization of its use across United States.
CASE: A 33 year old man with poorly controlled diabetes mellitus due to non-adherence to treatment and 18 years of marijuana use was admitted with intractable vomiting for 2 days. This was preceded by a week of nausea, abdominal discomfort and early morning vomiting. His symptoms were relieved by taking hot showers and he admitted to taking 10–20 showers in a day. His first such episode was in 2005. Since then he had multiple episodes of the same symptoms and frequent ER admissions. Vomiting was consistently relieved by taking hot showers. Severe episodes in this patient were associated with increase in the amount of marijuana used. On physical examination he had dry oral mucosa with sinus tachycardia. Abdominal exam was unremarkable. Investigational labs was consistent with diabetic ketoacidosis and he was treated successfully with return of blood glucose to normal and improvement in acidosis. However, he continued to be symptomatic with recurrent vomiting and persistent nausea and abdominal discomfort. He was witnessed by the medical team to be in the shower >10 times daily. The patient first presented to this hospital in 2011 followed by repeated admissions for the same problem. Initially, these episodes were attributed to diabetic ketoacidosis and later cyclic vomiting syndrome. Taking into account his chronic marijuana use and relief with hot showers, he was finally diagnosed with cannabinoid hyperemesis syndrome and treated conservatively, with recommended abstinence from marijuana use.
DISCUSSION: This case illustrates the classical symptoms of cannabinoid hyperemesis syndrome which include early morning emesis, a pre-emetic phase consisting of nausea and abdominal discomfort as well as symptomatic relief with hot showers. It also depicts the delay associated with the diagnosis of this syndrome and the possibility of under-diagnosis in the general population. Given the high prevalence of cannabinoid use and its legalization in several states, it is important to raise awareness amongst physicians on the side effects of cannabinoids.
“HEAVY” BREATHING: A CASE OF CEMENT PULMONARY EMBOLISMJustin Skrzynski1; Saad Sahi2; Arati K. Kelekar1. 1William Beaumont Hospital, Royal Oak, MI; 2Oakland University School of Medicine, Rochester, MI. (Tracking ID #1936202)
LEARNING OBJECTIVE 1: Recognize and diagnose a potentially clinically significant sequela of vertebroplasty.
CASE: Our patient is a 53 year old man presenting with dyspnea and cough. He had a complicated medical course since receiving kyphoplasty 6 months prior to admission, and was intermittently hospitalized for recurrent pneumonia and COPD exacerbation. Due to high suspicion of pulmonary embolism at presentation, contrast CT of the chest was obtained which revealed multiple nonocclusive densities in the right pulmonary artery system as well as opacities in the right middle and lower lobe. Patient later corroborated a history of bone cement embolism following his procedure. He was admitted to the intensive care unit and treated for multifactorial respiratory failure with antibiotics, diuretics, steroids and nebulizers. Despite aggressive treatment, on the ninth day of his admission he developed sudden bradycardia and expired. Autopsy was performed with final pathology results pending.
DISCUSSION: Kyphoplasty and vertebroplasty are common procedures in the treatment of vertebral compression fracture in which bone cement is injected percutaneously into a vertebral body to restore height and integrity. While the incidence of local leakage of cement into adjacent spaces can be high (up to 80–90 %), intravasation is less common (24 %) and embolization of cement less common still (4.6–6.8 %). The vast majority of cement emboli are asymptomatic and long term or serious sequelae, including death, are rarely reported. In our patient, the exact role of his cement emboli thus far remains uncertain. While our patient demonstrated no peripheral eosinophilia, he did have persistent bronchospasm which was resistant to steroids and nebulizers; we hypothesize that the long term presence of foreign material in the lungs may have caused a chronic hypersensitivity reaction. Though he had right sided opacities on imaging, he was afebrile and the differential for this finding could include pulmonary hemorrhage. Unfortunately, the patient expired before bronchoscopy could be performed. At this time, autopsy has been performed and initial pathology did demonstrate cement material in the right pulmonary artery system. The vast majority of reported cement emboli were asymptomatic, but our patient’s clinical course clearly deteriorated significantly following his kyphoplasty. Currently no consensus exists in the treatment of this condition, with attempted therapies ranging from antibiotics to anticoagulation to mechanical extraction. The exact effect of bone cement on vascular or lung tissue remains to be determined and to our knowledge no pathologic examination of cement pulmonary embolus exists in the literature. Identifying this effect as well as the true incidence of cement embolization may help in reducing morbidity and mortality for kyphoplasty and vertebroplasty in the future.
“KISSING DISEASE” OF THE LIVERAnuhya Gampa; Maya Srikanth; Jordan Dale; Anupama Ananth. Rush University Medical Center, Chicago, IL. (Tracking ID #1897930)
LEARNING OBJECTIVE 1: Diagnose acute infectious mononucleosis secondary to EBV despite a negative heterophile antibody test, or Monospot, early in the disease course.
LEARNING OBJECTIVE 2: Recognize that clinical presentations of infectious mononucleosis may vary with age as EBV hepatitis is more likely in older adults.
CASE: A 46 year-old healthy man presented with 2 weeks of right upper quadrant pain and 1 week of a sore throat associated with fevers, malaise, jaundice, weight loss and night sweats. He visited another clinic at the onset of symptoms and was found to have an elevated AST (163), ALT (315), ALP (585), and total bilirubin (4.4). RUQ ultrasound showed a fatty liver and a mildly dilated common bile duct (0.6 cm). His labs were also notable for negative EBV IgG (EBV IgM not tested), HIV, and acute hepatitis serologies. His CMV IgG was positive, however IgM was negative. A rapid strep test was also negative. Additionally, he had a mild leukocytosis with a lymphocytic predominance. On presentation to our institution 2 weeks later, he also acknowledged odynophagia and his exam was remarkable for jaundice, with mild RUQ tenderness, anterior cervical lymphadenopathy, and tonsillar exudates. Liver enzymes remained elevated: AST (163), ALT (315), ALP (585), total bilirubin (5.2), conjugated bilirubin (3.5), mild leukocytosis (11.7), with lymphocytosis and atypical lymphocytes noted on the differential. Another extensive workup was done and an initial Monospot test was negative. CT abdomen/pelvis was done due to the concern for lymphoma and revealed a nonenhancing 1.2 cm hypodensity in the medial right hepatic lobe and a left periaortic soft tissue mass. Liver and periaortic soft tissue mass biopsies were performed. Further EBV testing returned positive days later: EBV DNA (16,828 copies) and positive IgM antibodies. His periaortic mass biopsy was found to be metastatic seminoma while his liver biopsy was negative for malignancy and pathologic examination supported EBV hepatitis. His symptoms were self-limited and spontaneously resolved over the next few weeks. He was discharged with the diagnosis of EBV hepatitis and an incidental finding of metastatic seminoma for which he underwent an orchiectomy and chemotherapy as an outpatient after his liver function studies normalized.
DISCUSSION: Although the constellation of clinical symptoms suggestive of infectious mononucleosis was present in our patient, the diagnosis was delayed by an initially negative monospot (heterophile antibody) test without the support of known EBV IgM serologies. However, EBV IgM can be negative for days despite acute infection, so it is unclear if EBV IgM testing at the time of his initial presentation at the outside clinic would have provided diagnostic benefit in this case. The longer the duration of symptoms, the greater reliability of titers for IgM antibodies directed at the viral capsid of EBV. Atypical lymphocytosis in the setting of consistent clinical symptoms can support a diagnosis of infectious mononucleosis, despite negative serologic testing. Our case underlines the importance of understanding that the sensitivity of the Monospot test is only 85 % while specificity approaches 100 %. Further viral serologies, including EBV IgM and IgG titers, should be used to confirm the diagnosis if the monospot test is negative yet clinical suspicion remains high. Thus, the Monospot test is inessential to the final clinical diagnosis of EBV infection. Symptomatic EBV hepatitis is rare and self-limited. Transaminitis associated with lymphadenopathy, fever and pharyngitis should raise concern for EBV hepatitis. Mild transaminitis is common in infectious mononucleosis without acute EBV hepatitis. However, hepatitis from EBV can present prior to classic mononucleosis symptoms. In case studies, only 5 % of patients with infectious mononucleosis initially presented with jaundice, right sided abdominal pain and transaminitis, supporting that this presentation is uncommon, but still possible. Patients with mononucleosis need not present classically prior to developing hepatitis. Case studies show only 12 % of EBV hepatitis patients (all in their 20s) had classic mononucleosis symptoms, while 75 % who presented solely with transaminitis were older than 40. EBV hepatitis is self-limited but should be considered in evidence of transaminitis and cholestasis, especially in older adults, regardless of initial titers and symptoms.
A “TWO-HIT” HYPOTHESIS: PNEUMOCYSTIS PNEUMONIA AND DIGEORGE SYNDROMEWeiyi Tan. UCLA, Los Angeles, CA. (Tracking ID #1939645)
LEARNING OBJECTIVE 1: Recognize that Pneumocystis Pneumonia in non-HIV patients is a disease that carries high morbidity and mortality.
LEARNING OBJECTIVE 2: Consider the use of prophylaxis against Pneumocystis jirovecii in patients with multiple sources of immunosuppression.
CASE: A 20 year-old male with DiGeorge syndrome (DGS) and history of an orthotopic heart transplant in 2010 presented with fever and shortness of breath for 1 day. The patient had a history of recurrent pneumonias. He was on minimal immunosuppression with tacrolimus and mycophenolate mofetil. He had a known IgG2 subclass deficiency, but did not have a diagnosis of complete DGS (severe immunodeficiency). Physical exam showed normal vitals and oxygen saturation of 98 % on room air. Lung sounds were diminished, particularly on the left side, with left-sided egophony. The rest of the exam was normal. Chest x-ray showed a nodular opacity in the left lower lobe. A subsequent non-contrast chest CT showed left perihilar upper lobe and lower lobe confluent airspace infiltrates and consolidation with air bronchograms suggestive for pneumonia. He was initially started on vancomycin, meropenem, levofloxacin, and ganciclovir. Rapid RSV and influenza tests were negative. He then underwent bronchoscopy with bronchoalveolar lavage (BAL) for further diagnostic testing. The BAL studies were positive for Pneumocystis jirovecii via direct fluorescent-antibody testing. His respiratory viral panel via nasal washing was positive for rhinovirus/enterovirus. His regimen was then narrowed to IV trimethoprim-sulfamethoxazole after the BAL studies resulted. Further immunologic studies showed low IgG2 levels and a low absolute CD4 count of 234, and thus intravenous immunoglobulin was administered. He slowly decompensated over the next 7 days, even on therapy. He developed hyponatremia from SIADH and IV trimethoprim-sulfamethoxazole administration. He also developed hypercarbic respiratory failure and was intubated on hospital day seven. He suffered from an ileus as well, and his antibiotic regimen was switched to IV pentamidine. After 2 days of ventilatory support, he was successfully extubated. His serum sodium improved as well and he was discharged home on oral trimethoprim-sulfamethoxazole.
DISCUSSION: This case highlights an atypical presentation of PCP pneumonia, and demonstrates the fact that patients with non-HIV PCP pneumonia have higher rates of morbidity and mortality than those who have HIV, which stresses the importance of a detailed history and a high index of suspicion for this disease. Furthermore, given his immunosuppressed state from his heart transplant and DiGeorge syndrome, the use of prophylactic antibiotics for PCP could be considered in future cases similar to this patient with a “double hit” to the immune system.
A (RING) ENHANCED APPROACH TO HIV AND CENTRAL NERVOUS SYSTEM LESIONSAlexandra Wells; John Moscona. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925933)
LEARNING OBJECTIVE 1: Understand approach to ring enhancing lesions
LEARNING OBJECTIVE 2: Recognize ADEM as a cause for CNS disease in HIV patients
CASE: A 44 year old man with history of HIV presented with 3 weeks of progressive right upper and lower extremity weakness. Symptoms initially began with parasthesias of the fingers and progressed to weakness of right upper extremity and proximal right lower extremity. He endorsed an upper respiratory infection several weeks prior, but denied fevers, neck stiffness, or recent vaccinations. Vitals were temperature 98 F, heart rate 83, and blood pressure 130/80 mmHg. Patient was oriented to person, place, and location. Pupils were equal and reactive, with a midline, and supple neck. Strength was 3/5 throughout the right upper extremity, and 4/5 throughout the right lower extremity. There was decreased sensation to light touch and vibration of both the right upper and lower extremity. Reflexes were 3+ throughout, and Hoffman sign was positive on right hand. Plantar reflexes were down-going bilaterally. CD4 count was 426. Cerebral spinal fluid contained 10 WBC with 92 % lymphocytes, and 1 RBC. All serology was negative including VDRL, cryptococcus, JC virus, and toxoplasma. All cultures and gram stains were also negative including AFB and fungal. An MRI revealed three riing-enhancing lesions in the right frontal and parietal lobes along with the left centrum semiovale. MRI also displayed enhancement within the cervical spinal cord.
DISCUSSION: HIV is encountered commonly in internal medicine. Although rates of CNS disease have decreased with antiretroviral therapy, neurologic complications occur in over 40 % of HIV positive patients. The man described above was found to have multiple, ring-enhancing lesions on MRI despite numeric immunocompetence. With enhancing lesions, it is useful to divide the differential diagnosis into 3 categories, which include infection, neoplasm, and demyelination. Further stratifying infection risk based on CD4 will help direct serum and CSF workup. Additional imaging, and even biopsy, may be required for oncologic and demyelinating diagnoses. Imaging and CSF findings in the above case were consistent with a demyelinating process and lead to the diagnosis of acute demyelinating encephalomyelitis (ADEM). ADEM is an inflammatory demyelinating disorder of the CNS usually preceded by an infectious disease or vaccination. ADEM is estimated to occur in 1 per 125,000 people in the US with higher prevalence in children. However, ADEM has been associated with HIV infection. The hypothesis is that the HIV virus causes neuronal damage leading to an inflammatory response with consequent demyelination. Acutely, these lesions will enhance on MRI with contrast as seen in the man described above. His CSF studies revealed a lymphocytosis that was also consistent with ADEM. After ruling out major infectious causes, he was initiated on corticosteroids and was able to return to near baseline level of functioning. Given the potential for recovery with prompt treatment, it is important for the internist to incorporate ADEM into his or her differential when evaluating HIV positive patients with neurologic symptoms.
A CASE OF ACUTE HEPATITIS B-INDUCED POLYARTERITIS NODOSA IN A PATIENT PRESENTING WITH FEVER OF UNKNOWN ORIGIN AT BELLEVUE HOSPITALArnab K. Ghosh; Karin Warltier. NYU, New York, NY. (Tracking ID #1920727)
LEARNING OBJECTIVE 1: 1. Recognize the clinical reasoning involved in assessing a patient with fever of unknown origin.
LEARNING OBJECTIVE 2: 2. Recognize the association between polyarteritis nodosa and acute hepatitis B in a patient presenting.
CASE: A 50 year old Malian man presented with a 1 month history of fevers, fatigue and anorexia. He was in his usual state of good health until 1 month prior to his presentation when he underwent evaluations at other hospitals and was diagnosed with upper respiratory tract infections. He was prescribed antibiotics and ibuprofen but his symptoms persisted. The patient immigrated to the US in 2005, worked as a freelance photographer and had recently travelled to Texas, Rhode Island and Long Island. He was previously in a monogamous relationship with a woman but denies any current sexual activity. He has smoked 3 cigarettes daily for the past 20 years, but denies other toxic habits. Physical examination was remarkable for a diaphoretic male in no acute distress with a temperature of 101.6oF, heart rate of 118, blood pressure of 124/73 and oxygen saturation of 97 % on room air. A 1 cm non tender lymph node was palpated in the anterior chain of his left neck. The remainder of his physical examination was unremarkable. Laboratory tests revealed a white cell count of 15,900/L (79.7 % neutrophils, 10.1 % monocytes), hemoglobin of 11 g/dL, platelet count of 401,000/L, c-reactive protein of 217U/mL, lactate dehydrogenase 3236 U/mL, AST 86U/L, ALT 97U/L, ALP 185U/L. HIV test was negative. Chest x-ray showed bilateral perihilar radio-opacities. The patient underwent a contrast CT of the chest, neck, abdomen and pelvis, showing edema and inflammatory soft tissue changes involving bilateral carotid and retropharyngeal spaces and severe narrowing (70 %) of the right internal carotid artery, consistent with vasculitis. This was confirmed on CT angiography of the neck. Further workup showed evidence of hepatitis B (core antigen positive, core antibody IgM nonreactive, surface antigen positive, surface antibody nonreactive, viral load 3660 IU/mL, genotype E). The patient was started on tenofovir 300 mg and prednisone 60 mg daily. A temporal artery biopsy was performed, showing no evidence of vasculitis. He responded well to both steroids and tenofovir.
DISCUSSION: Our patient’s course presented as a case of fever of unknown origin. His radiological imaging was concerning for vasculitis affecting both large and medium sized vessels. Differential diagnoses include giant cell arteritis, Takayashu’s arteritis, polyarteritis nodosa and Kawasaki’s disease. Given this patient’s epidemiology, and the finding of hepatitis B, our presumptive diagnosis was acute hepatitis B complicated by polyarteritis nodosa. Ideally a biopsy result is required for confirmation, which in this patient was negative. A well-known extra-hepatic manifestation of the hepatitis B virus is polyarteritis nodosa (PAN) [1,2]. Described as ‘secondary’ PAN, its etiology is not well understood, but thought to be from immune complexes causing systemic inflammation. It may affect upwards of 30 % of patients with active hepatitis B [3]. Occurring within 6 months of contracting the infection [4], hepatitis B related PAN presents with non-specific symptoms such as fever, arthalgias, muscle disease and fatigue. It may present with skin symptoms (tender erythematous nodules, purpura or ulcers), renal insufficiency, mononeuritis multiplex (70 %) gastrointestinal symptoms, and coronary artery disease [1,3].
A CASE OF ACUTE MINDFULNESS TREATMENT FOR ANXIETY FACILITATED BY ON SITE PSYCHOLOGIST IN A VA PRIMARY CARE CLINICDavid Bittleman1,2; Joshua Ruberg1,2. 1VA San Diego, San Diego, CA; 2University of California at San Diego, San Diego, CA. (Tracking ID #1921623)
LEARNING OBJECTIVE 1: Recognize when an acute mindfulness exercise may help a patient in distress.
CASE: A 27 year old male veteran presented to a primary care internal medicine clinic for an initial evaluation. The patient was suffering from an undifferentiated psychotic disorder, possibly bipolar disorder, post-traumatic stress disorder (PTSD), and was known to self-medicate with marijuana. His medications included Buspirone 10 mg three times daily, Citalopram 20 mg daily, folic acid 1 mg daily, Risperidone 1 mg in the morning , 4 mg in the evening, Thiamine 100 mg daily and Trazodone 50 mg at bedtime as needed for insomnia. From the moment the patient entered the exam room, he appeared upset and withdrawn. The veteran was frustrated with both the military and Veteran’s Administration system. In particular, he felt betrayed and was worried that his disability rating would be reduced and that his disability payments would be discontinued. He sat rocking back and forth saying that he was hearing voices whispering that he should kill himself. At that point, the internist contacted the on staff psychologist and he came immediately to assess the veteran. The internist was considering sending the patient directly to the emergency department for assessment and possible psychiatric admission. The psychologist found the patient future oriented with a desire to get better and to spend time with his daughter. Yet, he was described as despondent, looking at the floor and shaking. At that point the psychologist invited the veteran as well as the primary care internist to participate in a mindfulness breathing exercise. The patient reported that following the exercise he felt less anxious, but was still worried and hearing voices. He appeared more at ease and made a bit of eye contact. He was further assessed and felt not to be an imminent risk to himself and he agreed to call the crisis line or present to the emergency department if his symptoms worsened. Plans were made to connect him with ongoing therapy and continued medication treatment. The internist felt less anxious as well following the breathing exercise and was relieved that the veteran did not need to go immediately from the office to the emergency department.
DISCUSSION: The Department of Veterans Affairs (VA) has pioneered the development of a particular kind of patient-centered medical home, the Patient Aligned Care Team (PACT). The PACT allows for seamless cooperation between primary care providers and mental health professionals (1). This case illustrates this model in action. Assessing which patients are at risk for suicide is difficult (2). The mention of suicidal ideation may cause the provider to recommend emergency room evaluation for possible psychiatric admission to the hospital. Close proximity of an onsite psychologist allowed for timely evaluation and intervention. A repeat emergency room visit was avoided. In addition, the brief mindfulness exercise helped calm the veteran as well as the internist. 1. Kearney LK, Post EP, Zeiss A, Goldstein MG, Dundon M. The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med. 2011 December; 1(4): 624–628. [PMCID: PMC3717670] 2. Haney EM, O’Neil ME, Carson S, Low A, Peterson K, Denneson LM, Oleksiewicz C, and Kansagara D. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. VA-ESP Project #05-225; 2012.
A CASE OF ADULT LEAD POISONINGTao Liu1,2; Anne Hyson1; Susan T. Langerman1. 1VA Connecticut Healthcare System, West Haven, CT; 2Yale-New Haven Hospital, New Haven, CT. (Tracking ID #1938010)
LEARNING OBJECTIVE 1: Recognize adult lead poisoning
LEARNING OBJECTIVE 2: Manage adult lead poisoning in a primary care setting
CASE: A 49 year-old Veteran who works as a painter presented to the primary care clinic for a new patient visit. The patient, who had been working for 3 months to restore a historical home, became concerned about lead exposure, and requested lead level testing. Past medical history was unremarkable. Review of systems was positive for two-month history of bilateral shoulder and lower back pain. Vital signs were normal. Physical exam was significant for decreased range of motion of the shoulders. Basic labs and lead levels were ordered. Lead level was 156 mcg/dL. Both the patient and Connecticut Poison Control Center were promptly contacted. The patient was asked to return immediately for evaluation, and was referred to hematology, neurology and Yale Occupational and Environmental Medicine Program. Repeat lead level, which was obtained 6 days after the first level, was 95 mcg/dL. Chelation therapy was deemed not needed, given that the lead level fell rapidly and the patient subsequently changed his occupation. We recommended that the patient obtain a monthly lead level and CBC to ensure that the lead level decreases by 50 % each month.
DISCUSSION: This case illustrates the presentation and management of adult work-related lead poisoning. Occupations associated with lead poisoning include those in smelting and refining industries, brass/bronze foundries, rubber products, plastic industries, battery manufacturing, soldering, painting and construction [1]. Adverse effects of lead include anemia, suppressed immunity, neuropathy, renal failure, hypertension and gout [2]. In the history, it is important to ask about previous occupations, exposures to fumes, dust and toxic substances, protective equipment, and eating and drinking habits in the work areas. On exam, signs of lead poisoning can include pallor, lead line on the gingiva and neurological abnormality. In addition to lead level, one can also obtain zinc protoporphyrin level which reflects lead absorption over the preceding 3 to 4 months and is a better indicator of body lead burden [3]. Primary care physicians should consider referring adult patients with lead level above 20 mcg/dL to occupational medicine specialists, and consider chelation therapy for patients with lead level above 50 mcg/dL, especially for patients with significant symptoms [4]. The decision for chelation therapy should be made in consultation with specialists. For the patient in the current case, chelation therapy was not recommended, because he did not exhibit significant symptoms and his lead level fell quickly. References 1. Toxicological profile for lead, U.S. Department of Health and Human Services, http://www.atsdr.cdc.gov/toxprofiles/tp13.pdf. Retrieved December 7, 2013. 2. Brown MJ, Margolis S. Lead in drinking water and human blood lead levels in the United States. MMWR Surveill Summ. 2012 Aug 10;61 Suppl:1–9. Review. 3. United States Department of Labor Occupational Safety & Health Administration Regulation (Standards - 29 CFR). http://www.osha.gov. Retrieved December 8, 2013. 4. Kosnett MJ, Wedeen RP, Rothenberg SJ, Hipkins KL, Materna BL, Schwartz BS, Hu H, Woolf A. Recommendations for medical management of adult lead exposure. Environ Health Perspect. 2007 Mar;115(3):463–71. Epub 2006 Dec 22. Review.
A CASE OF DAPSONE-INDUCED HYPERSENSITIVITY PNEUMONITIS IN A PATIENT BEING TREATED FOR LEPROSY AT BELLEVUE HOSPITALArnab K. Ghosh; Rachel M. Bond; Richard E. Greene. NYU, New York, NY. (Tracking ID #1920702)
LEARNING OBJECTIVE 1: 1. Recognize the adverse effects of dapsone, including hypoxemic respiratory failure secondary to hypersensitivity pneumonitis.
CASE: The patient is a 40 year old Chinese female previously well who is admitted with a 1 week history of malaise, anorexia, shortness of breath and a dry cough. She was diagnosed with leprosy by biopsy 2 months prior to presentation, and was started on dapsone, thalidomide and minocycline. She migrated from China to the United States in 2004. Physical examination revealed a slender female using accessory muscles of respiration, unable to speak in complete sentences, with a temperature of 103.1o F, heart rate 103, blood pressure 119/73 and respiratory rate 34, saturating at 85 % on room air. Examination also showed dry inspiratory crepitations throughout both lung fields, a papular rash on the knees and thighs with an erythematous plaque on her left elbow consistent with previously diagnosed Hansen’s Disease. Labs were significant for white cell count of 700/uL with no neutrophils, hemoglobin of 11.3 g/dL and platelets 165,000/uL. Lactate dehydrogenase 1300. Liver function tests were within normal limits. Arterial blood gas on room air showed pH 7.43/CO2 32.7/O2 49.4/Lactate 1.2/SaO2 85.2 %. Chest X-ray showed bilateral interstitial infiltrates. CT Chest showed bilateral hilar and mediastinal lymphadenopathy with diffuse bilateral septal thickening and small bilateral pleural effusions. The patient was started on broad spectrum antibiotics including trimethoprim-sulfamethazole and high dose steroids for presumed Pneumocytis jiroveci. All anti-leprosy medication was stopped and a bronchoscopy was performed. Blood cultures were negative, and atypical pneumonia screen was negative. Her clinical picture improved after 3 days, whereupon her Pneumocystis stain returned negative. Bactrim was stopped, the steroid dose was decreased. She completed the course of broad spectrum antibiotics Repeat imaging of her lungs revealed improvement.
DISCUSSION: Our patient’s presentation, with worsening shortness of breath, a rash, combined with negative pneumonia workup and radiological pattern was consistent with a drug-induced pneumonitis. The patient further reported these symptoms beginning after starting dapsone. Dapsone is used for its antibiotic and anti-inflammatory properties, and as the first line therapy in the treatment of leprosy [1], a disease caused by Mycobacterium leprae, which infects both skin and nervous tissue. Dapsone has been implicated in a number of adverse drug reactions, involving different organ systems. Rarely, it has been associated with a drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) [2]. DRESS syndrome typically involves a long latency period (upwards of 8 weeks) after exposure to the offending agent (80 % of cases are due to medications), with high fevers, morbilliform rash and associated lymphadenopathy. Often there are hepatic manifestations (60–80 % have abnormal LFTs) and renal dysfunction (10–30 % suffer interstitial nephritis). More rarely does interstitial pneumonitis occur, although case reports exist in the literature [3,4]. Treatment involves rapid recognition of the illness and stopping the medication. In patients with pulmonary symptoms, high dose steroids are recommended. In our patient, after stopping the offending agent, and treating her with steroids, the patient improved, as evidenced by improving radiology.
A CASE OF DISSEMINATED RETROPERITONEAL PLASMACYTOMA WITH RENAL INVOLVEMENTNaba R. Mainali; Leena Jalota; Ranjan Pathak; Shashank Jain. Reading Health System, West Reading, PA. (Tracking ID #1934062)
LEARNING OBJECTIVE 1: To describe the importance of biopsy and immunohistochemistry to confirm the diagnosis of Extra-Medullary Plasmacytoma (EMP).
LEARNING OBJECTIVE 2: To describe the treatment options available for disseminated retroperitoneal plasmacytoma.
CASE: Introduction: Extramedullary plasmacytoma (EMP) is a neoplastic proliferation of plasma cells in non-osseous sites without the involvement of bone marrow and usually occurs in the head and neck region. Herein we report a rare case of disseminated EMP that presented as a diagnostic challenge especially because of its atypical presentation and location. Case Report: A 65-year-old woman with history of retroperitoneal EMP with complete remission after radiotherapy presented with progressively worsening abdominal pain, generalized weakness and weight loss for 1 month. On examination, distension and fullness in left flank region was noted without palpable mass or organomegaly. Her laboratory results were normal except for hemoglobin 10.4 g/dl. Urinalysis revealed no Bence-Jones protein. CT abdomen and chest showed 10 × 16 cm left paraspinal soft tissue mass at the level of left renal hilum with hydronephrosis and 6.1 × 4.6 cm left pulmonary hilar mass respectively. Bone marrow biopsy revealed normocellularity with trilineage hematopoiesis and less than 10 % plasma cells, thus ruling out multiple myeloma. Fine needle aspiration cytology of the mass was positive for plasmacytoma. Her serum IgA level was elevated at 1150 g/L with normal IgG and IgM levels. Immunohistochemistry was positive for CD138 and CD38 but negative for CD45, CD19 and CD20. She did not respond well to chemotherapy with dexamethasone and lenalidomide. Radiotherapy was offered because of the large size and presence of lung metastases. She was therefore placed on comfort measures.
DISCUSSION: Retroperitoneal EMP involving kidney is an extremely rare condition and difficult to diagnose because of its unusual location and absence of symptoms until advanced stage. Definitive diagnosis of EMP requires histopathological examination and immunohistochemistry work up. EPM is highly radiosensitive; it is usually treated with combined radiotherapy and surgery or chemotherapy depending on the stage.
A CASE OF DUODENAL DIEULAFOY’SRandy Chung1,2; Jeffrey T. Bates1,2. 1Baylor College of Medicine, Houston, TX; 2Michael E. DeBakey VA Medical Center, Houston, TX. (Tracking ID #1939031)
LEARNING OBJECTIVE 1: Recognize that an extragastric Dieulafoy’s lesion, though rare, is an important and likely underreported cause of upper gastrointestinal bleeding
LEARNING OBJECTIVE 2: Manage a bleeding duodenal Dieulafoy’s lesion with therapeutic endoscopy
CASE: The patient is a 69-year-old Caucasian male with a history of coronary artery disease and mitral valve replacement, compliant on warfarin therapy, who was admitted for melena and new-onset anemia. He was in his usual state of health until 4 days prior to admission, when he began having three episodes a day of maroon-colored stools and lightheadedness. He denied hemoptysis, hematemesis, or other overt bleeding. He did not have fever, chills, nausea, vomiting, abdominal pain, or diarrhea. In addition to warfarin, the patient also takes aspirin 81 mg daily but denied any other NSAID use. There were no significant findings on physical examination apart from positive orthostatics and mild pallor. Initial laboratory studies revealed a hemoglobin of 7.7 g/dL (compared to 13.8 g/dL 4 months prior), a prothrombin ratio (INR) of 2.28, a normal activated partial thromboplastin time (aPTT), a normal platelet level, and normal liver function tests. The patient was started on a pantoprazole drip. He received a blood transfusion with an appropriate rise in his hemoglobin level. Esophagogastroduodenoscopy and push enteroscopy were performed, which found a bleeding Dieulafoy’s lesion in the second portion of the duodenum. Hemostasis was achieved with the placement of two endoclips. The patient had no further episodes of melena following the procedure and his hemoglobin level remained stable. He was transitioned to oral pantoprazole and restarted on warfarin.
DISCUSSION: A Dieulafoy’s lesion (DL) is an uncommon and likely underrecognized cause of upper gastrointestinal bleeding in which hemorrhage occurs from a tortuous submucosal arterial lesion. The lesion is most often found in the proximal stomach within 5 cm of the gastroesophageal junction. Duodenal DLs are rare, accounting for about 15 % of all DLs, but have been identified more frequently in recent years because of increased awareness of the condition. The diagnosis is inherently difficult because of the small size and obscure location of the lesion, and it is most often made during episodes of active bleeding. As with our patient, people who bleed from DLs are typically men with multiple comorbidities, including cardiovascular disease, hypertension, and diabetes mellitus. Therapeutic endoscopy is the modality of choice for the treatment of DLs. The use of vascular clips has been reported to be an effective and safe method of hemostasis in DLs, especially in thin walled organs like the duodenum. Our patient’s duodenal DL bleed was effectively controlled with hemoclipping. In conclusion, clinicians should consider a Dieulafoy’s lesion in any patient presenting with an upper gastrointestinal bleed, and recognize that early endoscopy during a bleeding episode is essential for accurate diagnosis and proper treatment.
A CASE OF EXTENSIVE TAKAYASU ARTERITIS IN A YOUNG AFRICAN AMERICAN FEMALEMohammed W. Imam; Hiba Hadid; Mona Hassan. henry ford health system, Detroit, MI. (Tracking ID #1939229)
LEARNING OBJECTIVE 1: The main objective is to highlight the importance of performing a thorough physical examination as an easy and inexpensive means of diagnosing takayasu’s arteritis. This case report also highlights the epidemiological features, diagnostic criteria, and main treatment modalities of this rare disease.
LEARNING OBJECTIVE 2: This case report also highlights the epidemiological features, diagnostic criteria, and main treatment modalities of this rare disease.
CASE: We report a case of Takayasu arteritis in a 38-year old African American female who presented with discrepancies in radial pulses and inability to get a blood pressure reading in the left arm. CT angiography of head, chest, abdomen and pelvis showed multiple areas of significant narrowing in multiple major vessels, including vertebral arteries, left subclavian artery, basilar artery, and bilateral internal iliac arteries.
DISCUSSION: Takayasu arteritis, also known as idiopathic medial aortopathy or pulseless disease, is a rare chronic condition characterized by granulmamtous vasculitis of unknown etiology. Women are affected in the majority of cases with the greatest prevalence in Asians. In the United States, its incidence is 1–3 new cases per year per million population. Takayasu’s arteritis predominantly affects the aorta and its major branches, with the pulmonary vessels and abdominal aorta affected in over 50 % of cases. The pathogenesis of Takayasu’s is poorly understood, but cell-mediated autoimmune mechanisms are thought to play a major rule.
A CASE OF FEVER AND ABDOMINAL PAIN IN A YOUNGER GENTLEMANJocelyn A. Carter A. Carter. Massachusetts General Hospital, Boston, MA. (Tracking ID #1940068)
LEARNING OBJECTIVE 1: To recognize the clinical manifestations and pathophysiology of Ehlers-Danlos syndrome Type IV in the setting of an acute vascular presentation
LEARNING OBJECTIVE 2: To review evidence-based management for Ehlers-Danlos syndrome Type IV
CASE: A 31 year old gentleman without significant previous medical history presented with severe abdominal pain that started suddenly in his right and left upper abdomen. On arrival to the emergency room, the gentleman was noted to have several episodes of bilious emesis and multiple episodes of brown, watery diarrhea. A mild leukocytosis with left shift was observed along with a fever of 101.5 F and stable hemodynamics. Concerns were raised for diverticulitis or colitis and a CT abdomen/pelvis was performed demonstrating a left common and external iliac dissection (with evidence of prior extravasation without active leak) as well as bilateral renal infarcts, a small L common iliac aneurysm (1.7 cm) and a question of bilateral renal artery aneurysms. A vascular surgery consultation was placed and a CT head/neck/chest was performed without additional concerning findings. Due to concerns for the presence of possible renal artery aneurysms, anti-coagulation was initiated with intravenous heparin. Renal artery duplex was unhelpful and a renal angiogram was planned but delayed by emergent cases. On hospital day (HD) 2, additional low grade fevers were also noted. Blood cultures drawn on admission remained negative. On HD 3, after additional questioning, the patient remembered further medical history including prior bilateral inguinal herniorrhaphies in a setting of playing sports as an adolescent and multiple bilateral spontaneous shoulder dislocations. A focused exam revealed very pale skin, periorbital hyperpigmentation, talipes equinovarus and exaggerated joint laxity. Concerns for connective tissue disease were raised. Rheumatology was consulted on HD 3 and recommended a genetics consultation to rule out connective tissue disease. Renal angiogram performance was then scheduled for early afternoon the following day (HD 4). On HD 4, the genetics fellow saw the patient just prior to the patient’s transfer to the operating room for renal angiogram performance. After a discussion with the genetics attending, the genetics fellow contacted the primary team with a likely diagnosis of Ehlers-Danlos syndrome Type IV and a request for expedited cancellation of the renal angiogram, a procedure that could result in massive dissection/obliteration of arterial vasculature in an Ehlers-Danlos syndrome Type IV patient. The procedure was cancelled just moments prior to the start of the procedure. Collagen vascular disease markers were sent for testing as a part of the genetics work-up. All rheumatologic and hypercoagulability testing returned negative. An angiotensin-converting enzyme inhibitor was initiated as standard therapy. Genetics testing later returned positive for Ehlers-Danlos syndrome Type IV.
DISCUSSION: Ehlers-Danlos syndrome Type IV is a rare inherited connective tissue disorder (one of six types of Ehlers-Danlos syndromes) caused by a mutation in type III procollagen (Col3A1). It may be seen in 1/25,000 people. The diagnosis is made by identifying clinical criteria and testing positive for the type II procollagen genetic mutation. The clinical features include a characteristic narrow facies with periorbital hyperpigmentation, pale skin with visible subcutaneous vessels, easy bruisability and history of arterial/digestive tract rupture. Obstetric complications may also be seen in women. Arterial complications including aneurysm rupture and dissection as well as gastrointestinal rupture can be fatal and occur in 80 % of these patients prior to reaching age 40. While there is no active reversal of this condition, medical management with optimal blood pressure control via an angiotensin-converting enzyme inhibitor with anti-TGF properties, anticoagulation (indicated in the setting of aneurysm formation) and avoidance of contact sports/strenuous activity is generally recommended. Although surgery may be performed in a setting of trauma, invasive procedures should typically be avoided. Taking a careful history and understanding the underlying clinical pathophysiology of Ehlers-Danlos syndrome Type IV as well as standard management and therapy are integral to delivering evidence-based care and avoiding catastrophic events in this population.
A CASE OF ISCHEMIC DIGITS AND PAINFUL MUSCLESSagar Y. Patel; Matt Blackwell; Lesile Pack. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1901937)
LEARNING OBJECTIVE 1: Discuss the diagnosis, prognosis, and treatment of calcific uremic arteriolopathy
LEARNING OBJECTIVE 2: Differentiate calcific uremic arteriolopathy from other rheumatologic disorders
CASE: A 60-year-old man on dialysis with atrial fibrillation on warfarin presented with bilateral digital necrosis and progressive lower extremity myalgias. Two weeks prior to presentation, he noticed a small lesion on his left 2nd finger that was treated with Keflex. He gradually developed numbness and ulcerative lesions on multiple digits bilaterally which progressed to dry gangrene. He also had a nine-month history of progressively worsening myalgias and weakness for which he was empirically treated with prednisone. The prednisone alleviated his pain but his weakness persisted. Multiple attempts to taper his prednisone were unsuccessful due to increasing pain. On exam, he had palpable pulses throughout, but his digits were cool with multiple necrotic, gangrenous lesions bilaterally. He had considerable muscle wasting and tenderness of his lower extremities. Strength was 4+/5 in all upper and lower extremity muscles groups. A MRI of his legs revealed diffuse muscle edema. His labs revealed an albumin of 2.2 g/dL, calcium of 8.2 mg/dL, phosphate of 7.9 mg/dL and parathyroid hormone level of 196 pg/mL. Rheumatologic labs (including ANA, anti-PR3, anti-MPO, CPK, Aldolase, Cryoglobulins, C3 and C4) were negative. Coagulopathy work-up (including Antiphospholipid Antibody, SPEP, Factor II, V, VIII, X) was also negative. A transesophageal echocardiogram revealed moderate diastolic dysfunction but no definitive embolic source. Hand x-ray showed severe calcific vasculopathy. EMG revealed diffuse myopathic changes without fibrillation. A muscle biopsy showed moderate type II muscle fiber atrophy. Arteriograms demonstrated widely patent but severely calcified bilateral subclavian, axillary, and brachial arteries as well as severely stenotic bilateral radial and ulnar arteries. Bilateral balloon angioplasty provided pain relief and some recovery of sensory function. Inflammatory myopathy was felt to be unlikely, and steroid taper was initiated, resulting in excruciating pain. Intravenous sodium thiosulfate was started, but unfortunately our patient developed progressive digital ulcerations bilaterally with associated dry gangrene (images included), mottling of both thighs, and early signs of toe ulcerations. His condition worsened with the development of ischemic bowel and ileus. At that point, the patient and his family pursued comfort care, and he passed away shortly thereafter.
DISCUSSION: This case was felt to be an unusual example of calcific uremic arteriolopathy (i.e. calciphylaxis) - a rare complication most commonly seen in dialysis patients that is associated with significant morbidity and mortality. It is often characterized by extra-osseous calcification of the small vessels leading to ischemia with subcutaneous necrosis in areas of greatest adiposity. Less commonly, patients will present with digital ischemia, livedo reticularis, and ischemic myopathy. Labs may or may not reveal elevated parathyroid hormone levels and increasing calcium-phosphate product. Diagnosis is typically based on clinical judgment and findings of the characteristic necrotic eschars, ulcerations, indurated nodules, and dry gangrene. Biopsy of lesions can be done but, as in our case, is sometimes avoided due to concerns of poor wound healing and infection. If biopsy is performed, histologic analysis may reveal small vessel mural calcification, endovascular fibrosis, extravascular calcification, and thrombotic vaso-occlusion. Potential risk factors include female sex, obesity, hypercoagulable state and hypoalbuminemia as well as medications such as warfarin, calcium-based binders, vitamin D analogues and systemic corticosteroids. Given our patient’s clinical presentation, exam findings, risk factors, key laboratory results and radiologic findings, calcific uremic areteriolopathy was felt to best explain his progressively diffuse necrosis and severe myalgias. His muscle wasting was attributed to long-term steroids. This atypical presentation of calcific uremic arteriolopathy has significant overlap with presentations of inflammatory myopathies, vasculitides and coagulopathies. Our case highlights the importance of considering this diagnosis in high risk patients. The poor prognosis of this disorder makes early recognition critical because the sooner treatment is initiated the better the chance of recovery. Treatment is a multifaceted approach with focus on correcting underlying electrolyte abnormalities, discontinuation of contributing medications, adequate dialysis, aggressive wound care and proper pain management. Parathyroid hormone levels can be reduced with cinacalet or, in refractory cases, via parathyroidectomy. Some studies have shown improvement of skin lesions with hyperbaric oxygen chambers as well as intravenous sodium thiosulfate, an antioxidant and cation chelator.
A CASE OF ISOTRETINOIN-INDUCED ACUTE RHABDOMYOLYSISSara Flores; Habtamu A. Asrat; Manish Jain. Presence St. Francis Hospital, Evanston, IL. (Tracking ID #1934868)
LEARNING OBJECTIVE 1: Distinguish between benign elevation of creatine phosphokinase (CPK) and acute rhabdomyolysis.
LEARNING OBJECTIVE 2: Recognize some of the possible side effects for the systemic retinoid, isotretinoin (Accutane).
CASE: An eighteen-year-old female with no medical history presented with three days of calf cramping, generalized weakness, and cola-colored urine. There was no recent trauma or change in exercise activity. She denied smoking cigarettes, drinking alcohol, using street drugs and engaging in sexual activity. Family history was negative for rheumatologic, metabolic and myopathic disease. Oral Accutane was her only medication and was started 3 weeks prior to presentation. Vitals were normal. She was well nourished and had bilateral calf tenderness. There were no rashes. CMP and CBC were normal, but total serum CPK was 8,554 and rose to 17,116 over 12 h. Serum myglobin was high. C-reactive protein, ESR, TSH, free T4, free T3, ANA, ASO, anti Jo-1, RF, myeloperoxidase Ab, thyroid peroxidase Ab, ANCA proteinase 3, HIV, hepatitis B and C and urine toxicology were negative. Serum creatinine was 0.67. AST and ALT were 215 and 59 respectively. Urine dipstick was positive for blood, but no red blood cells were visible on microscopic analysis. No imaging was done. Electrocardiogram showed normal sinus rhythm, normal axis and no ST- or T-wave changes. The diagnosis was acute rhabdomyolysis. Normal saline at 125 cm3/h was administered and CPK decreased over next 24 h to 12,078. Serum Cr remained approximately 0.57. Patient’s symptoms resolved within 48 h, and patient was discharged in stable condition.
DISCUSSION: Muscle pain, generalized weakness, myoglobinuria and elevated serum CPK characterize acute rhabdomyolysis. However, diagnosis requires only acute neuromuscular symptoms or asymptomatic dark urine, plus acute elevation in serum CPK five times the upper level of normal in the absence of brain or cardiac injury. Many causes exist, including muscle trauma, drugs, infections, strenuous exercise, seizures and metabolic myopathies. Although the instigation may vary, the events preceding cellular destruction are the same. Increase in intracellular calcium activates proteases, which degrade proteins within the myocyte. Reduction of ADP to ATP by the electron transport chain may also be impaired. ATP deficiency leads to malfunction of cellular membrane channels and pumps. Cellular death ensues, and calcium, potassium, phosphate and myoglobin are released. Urine dipstick cannot differentiate hemoglobin from myoglobin. Visualization of red blood cells during microscopic analysis confirms hematuria, whereas their scarcity confirms myoglobinuria. Myoglobin is rapidly excreted through the renal tubules and causes tea-colored urine at levels ranging from 100 to 300 mg/dL. As concentration increases, accumulation and blockage within renal tubules may occur, leading to acute tubular necrosis. Copious hydration is necessary to prevent acute kidney injury. Elevation of serum aminotransferases are common but do not correspond to hepatic injury. Accutane is a systemic retinoic acid that inhibits sebum production, which prevents clogging of pores and inhibits colonization by Propionibacterium acnes. Since retinoid receptors are ubiquitous throughout the body, Accutane has several potential complications, including xerosis, nausea, anorexia, transaminitis, suicidal ideation, hypertriglyceridemia and hypercholesterolemia. Craniofacial, central nervous system and thymic birth defects may occur if a woman becomes pregnant while taking oral isotretinoin. These devastating birth defects prompted the FDA to establish I-Pledge, a national registry for regulating all those having access to isotretinoin within the United States. Every patient is regulated to ensure use of two forms of birth control in female patients and monthly blood testing, including lipid panel and liver function testing. Elevation of serum creatine kinase was first reported in the 80’s and 90’s as a benign side effect. In the largest reported series consisting of 442 patients, elevated CPK was reported in 37.3 % of patients, but only 1.58 % had CPK levels >5000 U/L, along with symptoms. Only four cases report muscle pain or weakness, five-fold increase in serum CPK levels and myoglobinuria occurring simultaneously, 6–8 with one having a fatal outcome. Most cases are associated with vigorous exercise during treatment and describe resolution of symptoms and normalization of CPK values within days to weeks after Accutane is discontinued. Our case is the fifth reporting acute rhabdomyolysis with use of Accutane. Our patient had exercised prior to developing symptoms, but her workout was no more strenuous than usual, and there was no evidence in history or laboratory investigation of metabolic, immunologic or rheumatologic disease. Prompt recognition of the symptoms and signs of acute rhabdomyolysis was important for prevention kidney injury in a patient at otherwise low risk.
A CASE OF MYCOBACTERIUM MUCOGENICUM BACTEREMIA-DECIDING TREATMENT AND DURATION OF THERAPYGagan Preet; Deepak Garg. WMU, Kalamazoo, MI. (Tracking ID #1937148)
LEARNING OBJECTIVE 1: To learn the management of Mycobacterium bacteremia.
CASE: 42 year old female presented with fever along with chills and rigors, malaise and nausea over past 7 days. Patient was recently diagnosed with breast cancer and had undergone bilateral mastectomies and subsequent subcutaneous implantable port (mediport) placement for the administration of chemotherapy. Her last chemotherapy was 2 weeks prior to admission. Social history was non-contributory. On physical examination patient was found to be hypotensive (BP 100/50), tachycardiac (HR 118/min), and febrile (Temp 102 F). Otherwise rest of the examination was unremarkable. Initial labs showed WBC 17000 cells/mm3, Hb 11.2 mg/dl, Plt 371. Differential showed absolute neutrophilia. Comprehensive Metabolic Panel, UA and CXR were unremarkable. After 4 days 1 out of 2 sets of blood cultures from the mediport came back positive for acid fast bacilli (AFB). Peripheral blood cultures were negative. Subsequently patient was started on Amikacin and Clarithromycin empirically. Mediport was removed and mediport cultures also grew AFB. Both Mycobacterium isolates were finally identified as Mycobacterium mucogenicum. Based on the sensitivities, Amikacin was changed to oral TMP/SMX after 7 days. All subsequent blood cultures were negative for any growth. Patient improved and was discharged to complete therapy with Clarithromycin and TMP/SMX for 1 month.
DISCUSSION: Rapid growing mycobacteria (RGM) are ubiquitous organisms and in recent years have emerged as an important cause of Central line associated blood stream infections (CLABSI). RGM can also present as wide spectrum of clinical syndromes including respiratory tract, skin infections, osteomyelitis, disseminated infections. Since there are no clear guidelines on how to manage such infections, it can be challenging for the physicians to treat them. Experts report using two active agents empirically and consideration should be given to include Amikacin in initial regimen, as most of RGM are sensitive to Amikacin. But often identification and susceptibility takes more than seven days and use of Aminoglycosides may cause renal toxicity, limiting the use of Aminoglycosides as primary empiric therapy. As from our literature review most of rapid growing mycobacteria are sensitive to Macrolides and TMP/SMX, whether these agents can be used as primary oral empiric regimen needs more evidence. Other management issues including search for disseminated disease, central venous catheter removal, timing of placement of new catheter, duration of therapy and optimal definitive regimen needs more understanding.
A CASE OF PECTUS EXCAVATUM AND NEW ONSET ATRIAL FIBRILLATIONIsabel Preeshagul; Gargi Bajpayee; Preety Chawla; Shamit Patel. Beth Israel Medical Center- Mount Sinai Division, New York, NY. (Tracking ID #1940140)
LEARNING OBJECTIVE 1: To recognize the association between new onset Atrial Fibrillation and Pectus excavatum
LEARNING OBJECTIVE 2: Review the value of cardiac imaging in patients with severe Pectus Excavatum
CASE: A 24 year old African American woman with a history of tricuspid regurgitation, and ligament laxity presented to the emergency department, ED, complaining of sudden onset of palpitations and dizziness for 1 day. Her EKG upon arrival demonstrated atrial fibrillation, AF, with rapid ventricular response at a rate of 158. She was cardioverted and started on a heparin drip for 48 h. Post cardioversion EKG revealed normal sinus rhythm at a rate of 74, right atrial enlargement and ventricular hypertrophy. Her cardiac exam was significant for pectus excavatum, palpable loud P2, and grade four pan systolic murmur at the left lower sternal border. Her musculoskeletal exam revealed long thin extremities and joint hypermobility. The remainder of her exam was normal including laboratory testing. Further evaluation with a transthoracic echo demonstrated redundant tricuspid valve leaflets, moderate tricuspid regurgitation and extrinsic compression of the right ventricle with an ejection fraction of 35 %. She then underwent a cardiac MRI to evaluate for arrhythmogenic right ventricular dysplasia that confirmed severe pectus excavatum with a pectus severity index (PSI) of four. The PSI is measured by dividing the transverse diameter of the chest by the anterior-posterior diameter on MRI. She was evaluated by cardiothoracic surgery and in 1 month will undergo the Nuss procedure- a minimally invasive surgery involving the temporary insertion of a metal bar beneath the chest wall, forcing the sternum outward.
DISCUSSION: Our case highlights the significance of recognizing the correlation of pectus excavatum in patients with new onset AF. Further investigating the underlying etiology of this cardiac arrhythmia with echo and cardiac MRI can aid in diagnosis, expediting a patient’s time to corrective surgery and ultimately preserve cardiac and lung function. Our case is relevant as pectus excavatum is present in one out of every 400 births, often associated with connective tissue disorders such as Marfan and Ehlers-Danlos Syndrome and cardiac arrhythmias. The anterior positioning of the right ventricle permits compression from the depressed sternum, which increases right ventricular pressure, dilates the right atrium and potentiates conduction abnormalities. There appears to be a relationship between lone AF and pectus excavatum as demonstrated in a retrospective analysis of 545 patients with pectus excavatum. This study compared the PSI of 220 patients with lone AF to 225 patients without lone AF. The data revealed that the mean PSI was higher in those with lone AF (P < .001). This indicates that the severity of a patients’ pectus excavatum may influence their propensity to develop AF. Recognizing this correlation and the importance of cardiac imaging to evaluate the underlying cause of the arrhythmia is crucial, as it may alter a patient’s future quality of life.
A CASE OF PERSISTENT ANTERIOR MEDIASTINAL MASS IN A PATIENT WITH GRAVES’ DISEASERie Ueno1; Misako Nagasaka1; Koji Sasaki2. 1Beth Israel Medical Center, New York, New York, NY; 2The University of Texas MD Anderson Cancer Center, Houston, TX. (Tracking ID #1934438)
LEARNING OBJECTIVE 1: Identify the association of anteior mediastinal mass with Graves’ Disease
LEARNING OBJECTIVE 2: Recognize the variable clinical course of anterior mediastinal mass and understand the importance of close radiological follow up
CASE: A 23-year-old Chinese woman with a 5-year history of Graves’ disease (GD) was admitted for a newly diagnosed ovarian tumor. During workup for the tumor, computed tomography (CT) of the chest incidentally showed a large homogeneous anterior mediastinal opacity, 8.6 × 3.1 × 7.4 cm. Physical examination revealed a diffusely enlarged thyroid gland. Thyroid stimulating immunoglobulins were elevated at 468 %, TSH < 0.03 mU/mL, elevated free T4 3.1 ng/dL. Mediastinal biopsy showed immature T cells, negative for primary malignancy or metastases. She was started on treatment with methimazole for hyperthyroidism, underwent salpingo-oophorectomy and was discharged with adjuvant chemotherapy for stage Ic ovarian papillary cystadenocarcinoma. Her free T4 returned to normal within 2 months after optimization of methimazole treatment. Chest CT showed that the mediastinal mass had decreased to 2.4 × 1.2 × 2.3 cm at that time. However, despite maintenance of her euthyroid status, repeat CT 6 months after treatment revealed that the homogeneous mediastinal mass had increased to 5.2 × 3.1 × 7.2 cm. The patient was referred to cardiothoracic surgery for consideration of thymectomy secondary to failure of regression of the mass with medical management of her hyperthyroidism.
DISCUSSION: Thymic hyperplasia in patients with Graves’ Disease (GD) was first reported by Halsted in 1914. Although Michie and Gunn have reported that up to 38 % of patients with thyrotoxicosis have histologic changes in the thymus gland, these findings are usually minimal. Radiologically detectable thymic enlargement as an anterior mediastinal mass has been infrequently reported. Several cases describe that these anterior mediastinal mass often represent benign thymic hyperplasia and regress within a few months after treatment of hyperthyroidism. However, unnecessary surgical interventions have been performed in half of these cases due to a small, yet true concern for neoplasms such as thymoma. A recent review recommends surgical intervention if the size of the mass does not decrease in spite of the patient being euthyroid for several months. In our case, the size of the anterior mediastinal mass significantly increased in a 6-month follow-up despite maintenance of the euthyroid status and thus she was referred to surgery. The literature on the management of patients with GD presenting with a mediastinal mass is limited and the true risk of mediastinal neoplasms remains unknown. Our case suggests the importance of further accumulation of long-term follow up data on patients who present with mediastinal mass with GD to better understand the clinical course and the optimal timing of surgical intervention.
A CASE OF PULMONARY BENIGN METASTATIC LEIOMYOMA (BML) PRESENTING AS MULTIPLE PULMONARY NODULES (MPN)Marcia Ciccone1; Agustin A. Garcia2. 1University of Southern California, Keck School of Medicine, Los Angeles, CA; 2University of Southern California, Keck School of Medicine, Los Angeles, CA. (Tracking ID #1928903)
LEARNING OBJECTIVE 1: Consider BML in a female with MPN
LEARNING OBJECTIVE 2: Recognize clinical features of BML
CASE: A 34 year-old female presented with MPN noted incidentally on chest X-ray performed for a positive PPD. She denied pulmonary symptoms or signs of systemic disease. Past medical history was significant for a seven-year history of menorrhagia and uterine leiomyomata. Family history included a maternal grandmother with uterine cancer. She is a non-smoker and a nurse. Physical exam was unremarkable. Computerized tomography (CT) of the chest showed multiple bilateral non-calcified lung nodules measuring between 3 and 19 mm. Positron emission tomography showed increased metabolic activity in the largest nodule, a uterine mass, a large extra-uterine mass, and enlarged hypermetabolic para-aortic and common-iliac nodes. She underwent a total hysterectomy without oophorectomy. Surgical findings included multiple leiomyoma involving the uterus, parametria, peritoneum, and left para-aortic region. Pathology showed no evidence of necrosis, atypia, or increased mitotic activity. Lesions were described as best fitting BML. Repeat CT scan 5 months later showed increase size of the nodules. CT-guided core lung biopsy demonstrated a metastasizing smooth muscle tumor; diagnosis of BML was confirmed by direct comparison of lung biopsy and uterine pathology. Treatment with leuprolide 22.5 mg IM every 3 months was started. Subsequent CT scans showed decreased size of the largest nodule and resolution of the remaining masses.
DISCUSSION: Our patient presented with MPN. Work-up of these should include a thorough history and physical examination. It is essential to distinguish between benign and malignant nodules. Multiple nodules larger than 1 cm are likely due to metastatic disease from a distant primary tumor. The most common malignancies to manifest as MPN include tumors of testes, ovaries, kidneys, and breast as well as melanomas and sarcomas. Benign causes of MPN include infections, non-infectious inflammatory conditions, arteriovenous malformations, and pneumoconiosis. Our patient lacked findings to suggest these entities. A biopsy was done establishing the diagnosis of BML. BML is a rare condition of well-differentiated, extra-uterine smooth muscle tumors. The etiology is unknown. Over 150 cases have been documented, most in women with prior surgery for uterine leiomyomata. As in our case, the patient may be asymptomatic and diagnosis is incidental; however, it may also present with dyspnea and respiratory distress and has been known to cause pneumothorax and pleural effusion. The most common site of metastases is the lungs; other sites are lymph nodes, deep soft tissues, the omentum and mesentery, bones, nervous system, and the heart. In contrast to leiomyosarcoma, BML has an indolent course and is differentiated histologically by having fewer than 5 mitoses per high power field in the absence of necrosis and cytologic atypia. The mainstay of treatment is primary tumor resection and medical and/or surgical oophorectomy. Other pharmacologic interventions include aromatase inhibitors, raloxifen, tamoxifen, and progestins. Or, BML may be expectantly managed with serial imaging. This case illustrates the importance of considering gynecological conditions in women with MPN. Specifically, BML should be considered in women with history of uterine fibroids. Physicians should be aware that there is no standard treatment and management must be individualized.
A CASE OF TOXIC SHOCK SYNDROME ASSOCIATED WITH THE USE OF THE NUVARINGJack C. Naggar; Nicole Adler. NYU, New York, NY. (Tracking ID #1897155)
LEARNING OBJECTIVE 1: Recognize the clinical features and risk factors of toxic shock syndrome
CASE: A 21-year-old woman with a history of bulimia presented with 1 day of fever to 104.0, diffuse rash, myalgias and abdominal pain. The patient was sexually active with men, and used condoms regularly. She used the NuvaRing for contraception. Her last menstrual period was approximately 3 weeks prior to presentation, and the vaginal ring was inserted two and a half weeks prior to presentation. She reported following instructions for appropriate use of the vaginal ring. Her last sexual encounter was 1 day prior to presentation. On physical examination she was febrile to 104.8, tachycardic and hypotensive. Her exam was notable for diffuse erythroderma. She had conjunctival injection and dry cracked lips. Abdominal exam revealed mild tenderness in the upper quadrants. Vaginal exam demonstrated edematous labia bilaterally, and a thin non-malodorous yellow discharge. The NuvaRing was removed. Laboratory data was notable for a leukocytosis, bandemia and thrombocytopenia. Chemistries obtained showed lactic acidosis, and normal renal and liver function. A pregnancy test was negative. Urinalysis was positive for Leukocyte Esterase, and there were 235 WBC/high powered field. Urine culture grew pan-sensitive Staphylococcus Aureus. The same organism was isolated from vaginal cultures as well. Blood cultures were without growth. The patient was admitted to the intensive care unit with a diagnosis of toxic shock syndrome secondary to NuvaRing. She had intermittent episodes of hypotension that were responsive to fluid resuscitation. She was treated with vancomycin, clindamycin, and aztreonam. The patient improved clinically and was discharged on hospital day four to complete a course of cefadroxil.
DISCUSSION: The Centers for Disease Control and Prevention defines toxic shock syndrome as an illness with six clinical findings. If all six are present the diagnosis is confirmed. A probable diagnosis requires five of the six clinical features. They include: fever, erythroderma, desquamation, hypotension, negative body fluid cultures (other than staph aureus, including viral serologies), and multisystem involvement. Toxic shock syndrome is described as menstrual and non-menstrual related. The non-menstrual cases occur most often post-operatively, or as a result of sinusitis, mastitis or cutaneous staphylococcal infections. Toxic shock syndrome is listed under the possible adverse effects of the NuvaRing. There are however, no case reports documenting such an association. This patient suffered from a probable case of toxic shock syndrome. While impossible to prove a causal relationship between vaginal contraceptive rings and toxic shock syndrome, this patient had no other risk factors for non-menstrual toxic shock syndrome. To our knowledge this is the first report of toxic shock syndrome associated with appropriate NuvaRing use.
A CASE REPORT OF ALTERED MENTAL STATUS FROM A PARATHYROID CARCINOMANanase Honda; Christine Kwan. Teine Keijinkai Medical Center, Sapporo, Japan. (Tracking ID #1935458)
LEARNING OBJECTIVE 1: Recognize the possibility of parathyroid carcinomas (CA), not just adenomas, in patients with primary hyperparathyroidism
LEARNING OBJECTIVE 2: Treat with en-block resection with preoperative suspicion of parathyroid CA
CASE: An 80-year-old Asian woman presents with unwitnessed loss of consciousness. Her son finds her lying on the floor after an unknown period. She denies other neurological symptoms in addition to all other review of systems. Her past medical history includes hypertension for which she takes amlodipine; she has no allergies. She smokes 1 pack/day × 50 years but does not drink alcohol nor use recreational drugs. Her family history is unremarkable. On examination, the patient is alert/oriented to person and time (baseline). Her temperature is 36 °C, blood pressure 160/75, pulse 65, respiratory rate 18, and O2 saturation 97 % room air. Head/neck exam reveals a non-tender, hard, mobile, 2 cm mass in the right thyroid lobe; no lymphadenopathy. The rest of the examination is unremarkable. Laboratory testing, including complete blood counts and chemistry, is significant for serum calcium (Ca) = 16.3 mg/dL, albumin = 3.1 g/dL, corrected Ca = 17.2 mg/dL, and intact parathyroid hormone (PTH) = 432 pg/mL. Neck ultrasound shows a 3 cm heterogeneous mass in the right lower thyroid lobe, and sestamibe scan demonstrates focal retention of tracer over the right lower pole of the thyroid. During this time, the patient has been receiving normal saline, calcitonin, and bisphosphonate with improvement of her mental status, and she is scheduled for a parathyroidectomy for suspicion of parathyroid adenoma. In the operating room, however, a large, stone-hard mass adherent to the inferior pole of the patient’s right hemithyroid is discovered; it is surrounded by a dense, fibrous, and grayish-white capsule suggestive of parathyroid malignancy. En-block resection, including the ipsilateral thyroid lobe and paratracheal lymphatic tissue, is done. Pathology results confirm the diagnosis of parathyroid CA with local invasion of contiguous soft tissue and muscle. Postoperatively, the patient’s Ca decreases to 8 mg/dL, and her Ca and PTH levels are followed up as an outpatient. No further surgical treatment is currently planned because recurrent or metastatic disease has not been identified.
DISCUSSION: Parathyroid adenomas represent a common endocrine problem whereas parathyroid CA very rarely occur as they are one of the rarest human cancers. They cause hyperparathyroidism in ~.02–5 % of cases although many case series report this entity to account for <1 % of patients with primary hyperparathyroidism. Parathyroid CA are hyperfunctional unlike other endocrine tumors that become less hormonally active when malignant. Its clinical features are caused primarily by the effects of the tumor’s excessive PTH secretion rather than by tumor cells’ infiltration of vital organs. Preoperative suspicion and intraoperative recognition of parathyroid CA is critical to achieve a favorable outcome. Nonsurgical therapies such as radiation and chemotherapy have yielded poor results in the treatment of parathyroid CA. In this case, the patient’s clinical features consistent with parathyroid CA include a hard, palpable neck mass, hypercalcemia >14 mg/dL, high PTH >2× normal, and severe hypercalcemia symptoms. Given preoperative suspicion of parathyroid CA, en-bloc resection with avoidance of capsular violation or tumor spillage should be performed.
A CASE REPORT OF B-CELL FOLLICULAR LYMPHOMA IN AN ASYMPTOMATIC WOMAN WITH VIRCHOW’S NODETakako Akimoto; Christine Kwan. Teine Keijinkai Medical Center, Sapporo, Japan. (Tracking ID #1933912)
LEARNING OBJECTIVE 1: Recognize that asymptomatic, while uncommon, lymphadenopathy can be caused by lymphoma
LEARNING OBJECTIVE 2: Recognize that Virchow’s node occurs not only from abdominal/thoracic malignancies
CASE: A 68 year-old Asian woman presents with 2 weeks’ history of gradual swelling in her left supraclavicular fossa that is not painful/erythematous/itchy. She denies fever, chills, weight/appetite change, night sweats, and fatigue, in addition to all other review of systems. Her past medical history includes gastric cancer status post (s/p) resection (6 years ago), hypertension, mitral valve stenosis s/p replacement, and sick sinus syndrome s/p pacemaker. She takes carvedilol, candesartan, torsemide, verapamil, and warfarin; she has no allergies. She does not use tobacco, alcohol, or recreational drugs. Her family history is significant for lung cancer in her brother. Physical examination shows blood pressure 136/86, pulse 65, respiratory rate 18, O2 saturation 98 % room air, and temperature 36.4C. Head/neck exam reveals pale conjunctiva and 3 hard, nontender, 1 × 1 cm, fixed supraclavicular lymph nodes; no axillary or inguinal lymphadenopathy. The rest of the exam shows no irregularities. Laboratory testing, including complete blood counts and chemistry, is significant for hemoglobin (Hgb) = 11.4 g/dL, lactate dehydrogenase (LDH) elevation (331U/L), and PT INR (2.64). Neck ultrasound shows 3–16 mm, lobular, heterogeneous lymph nodes, and biopsy reveals malignant B-cell follicular lymphoma (FL) with left supraclavicular fossa involvement. Chest/abdominal computed tomography shows lymphadenopathy in the left supraclavicular, mediastinal, abdominal paraaortic, and mesenteric lymph nodes (<3 cm); positron emission tomography reveals hot spots in the above corresponding areas. Bone marrow biopsy and immunohistochemistry shows (+) CD10/20/23 and BCL2. The patient is then started on rituximab.
DISCUSSION: Unexplained lymphadenopathy in the general population occurs in only 0.6 % annually. In a study with 2556 patients presenting to their family physician with unexplained lymphadenopathy, only 3 % requires a biopsy while 1 % has a malignancy; the prevalence of malignancies in lymph node biopsies is 40–60 %. Abdominal/thoracic malignancies can metastasize to the supraclavicular lymph nodes, Virchow’s sentinel node, as seen in the above patient. In this patient, however, while she has a history of gastric adenocarcinoma, her lymphadenopathy is actually from malignant lymphoma, not an abdominal/thoracic malignancy. While no specific study about the prevalence of Virchow’s node has been conducted, one study has shown that malignancies originating in the pelvis/abdomen are more likely to metastasize to the left supraclavicular lymph node and that the primary site/types of malignancies involved in the left supraclavicular lymph node are different from the right. Only ~10 % of those patients with positive nodes have a diagnosis of leukemia, non-Hodgkin’s, or Hodgkin’s disease. Patients with FL generally present with asymptomatic lymphadenopathy for years, and <20 % of patients present with B symptoms. The above patient likewise denies any B symptoms. Her FL International Prognostic Index = 4 points (>60 years, Hgb < 12 g/dL, elevated LDH, and Ann Arbor stagIVA) indicating poor survival. Regardless, this case illustrates that Virchow’s node can asymptomatically occur in settings besides abdominal/thoracic malignancies. 1) Fijten GH, Blijham GH. Unexplained lymphadenopathy in family practice. An evaluation of the probability of malignant causes and the effectiveness of physician’s workup. J Fam Pract. 1988;14:53–60 2) Motyckova, G. Steensma, D. “Why dose my patient have lymphadenopathy or splenomegaly?” Hematol oncol clin N Am; 26 2012 395–408 3) Cervin JR, Silverman JF, Loggie BW, Geisinger KR Virchow’s node revisited. Analysis with clinicopathologic correlation of 152 fine-needle aspiration biopsies of supraclavicular lymph nodes. Arch Pathol Lab Med. 1995 Aug; 119(8):727–30. 4) Lee Y, Terry R, Lukes RJ Lymph node biopsy of diagnosis: a statistical study. J surg Oncol.1980; 14:53–60 5) Annual clinical updates in hematological malignancies: A continuing medical education series. Follicular lymphoma:2012 update on diagnosis and management. Freedman A. American Journal of Hematology 2012:988–995
A CASE REPORT OF COLONOSCOPY’S CAUSING CARDIAC ARRESTMasayuki Ohta; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1929230)
LEARNING OBJECTIVE 1: Recognize that colonoscopies may cause takotsubo cardiomyopathy with resultant ventricular fibrillation
CASE: An 84-year-old Asian woman presents with 5 days’ history of gradual-onset, worsening dyspnea that improves with sitting up and worsens with lying down and exercise. She also reports nausea, decreased appetite, diaphoresis, fatigue, wheezing, orthopnea, and bilateral lower extremity edema; no fever, chills, other upper/lower respiratory, or cardiac symptoms. All other review of systems shows no abnormalities. Of note, she has undergone a routine screening colonoscopy 5 days ago. She has a history of thyroid papillary carcinoma with lobectomy, gastritis, dyslipidemia, and constipation and takes levothyroxine, famotidine, ecabet, pravastatin, and senna; she has no known allergies. Her social and family history demonstrates no risk factors. On physical examination, her temperature = 36.4 °C, pulse = 52, blood pressure = 144/72, respiratory rate = 18, and O2 saturation = 97 % room air. She sits comfortably; alert/oriented ×3. Her head/neck and heart exams show no abnormalities, but jugular venous pressure = 12cmH2O. Her breath sounds are decreased throughout but no wheezing or crackles. She has bilateral lower extremity pitting edema up to mid-shins. On labs, her blood counts, electrolytes, and thyroid function are all within normal limits except for blood urea nitrogen = 19.8 mg/dL, creatinine = 1.03 mg/dL (baseline 0.7 mg/dL), creatine kinase (CK) = 255 U/L, CK-MB = 11.7 ng/ml, and BNP = 2115 pg/ml. Chest x-ray shows bilateral dull cardiopulmonary angles with cardiothoracic ratio = 65 %. Electrocardiogram (ECG) reveals 2:1 atrioventricular block (AVB) and T wave inversions in V1-V6. Transthoracic echocardiogram shows an akinetic wall in the apex and mid-left ventricle (LV); ejection fraction = 51 %. Given the patient’s diastolic congestive heart failure, carperitide (alpha-human atrial natriuretic peptide) is given. Meanwhile, her T wave inversions increase in size while still maintaining 2:1 AVB. Eventually, she worsens to ventricular fibrillation but is successfully resuscitated with external pacemaker placement. Angiography shows right coronary artery with 75 % stenosis. LVgram shows depressed contractile function in the mid/apical segments of the LV and hyperkinetic basal wall consistent with takotsubo cardiomyopathy. With furosemide, she slowly recovers and is discharged after 1 month with permanent pacemaker placement.
DISCUSSION: Although the risk of serious complications following colonoscopy is low, ~2.8/1000 exams, they include bleeding, perforation, infection, and cardiopulmonary events. Only 3 acute cardiac failures have been reported in ~3 million colonoscopies in Japan. Takotsubo, or stress-induced, cardiomyopathy is known to be associated with emotional (30 %) or physical (41 %) stress, which includes anesthesia, surgery, gastrointestinal endoscopy, infection, and strokes. Colonoscopies comprise <1 % of all causes. Takotsubo cardiomyopathy generally has a good prognosis, but fatal arrhythmias may occur. T-wave inversions are a common ECG change (38 %) with particularly distinctive giant ones that can lead to prolonged QT. High-degree AVB occurs only rarely (1 %), but in the above case, it may have predisposed the patient to develop torsades de pointes. Although the mortality rate related to colonoscopies is only <1 %, physicians should be aware of the possibility of fatal arrhythmias.
A CASE REPORT OF NECROTIC FINGER FROM PYODERMA GANGRENOSUMYugo Soga; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1948669)
LEARNING OBJECTIVE 1: Recognize that pyoderma gangrenosum (PG) can also occur in the fingers
CASE: A 36 years old Asian man presents with 3 weeks’ abrupt onset, right middle finger skin necrosis along with swelling/redness for which he is initially diagnosed with purulent sore and prescribed cefazolin and incision and drainage ×2 with minimal improvement. The rest of his review of systems shows no abnormalities. His past medical history includes right leg and gluteal necrotizing soft tissue infection 3 years ago and massive gastrointestinal (GI) bleed from nonsteroidal anti-inflammatory drug use last year. He has no allergies and takes no medications. He quit tobacco and alcohol 9 months ago; prior 30 pack-years and 750 mL shochu/day ×20 years. He is an unemployed bartender and sexually active with 1 female partner but no condom use. His family history includes diabetes, alcoholism, and liver disease in his father and alcoholism in his brothers. On exam, vital signs show temperature 36.6, heart rate 90, blood pressure 105/74, O2 saturation 99 % room air, and respirations 14. Generally, he is in no acute distress; alert/oriented ×3. His right middle finger has ulceration with necrosis from the metacarpal to distal interphalangeal joint. The rest of his exam shows no irregularities. Significant lab results reveal white blood cell 14,000/μL, platelets 63 × 103/μL, partial thromboplastin time 34 s, and fibrinogen 645 g/dL; blood cultures are negative. X-ray of the right finger shows no irregularities. Given suspicion of severe necrotizing soft tissue infection and osteomyelitis, cefepime and vancomycin are given. On further chart review before elective right metacarpal bone amputation, however, last year’s colonoscopy is found to show possible inflammatory bowel disease (IBD). Repeat colonoscopy reveals swelling and redness of the entire large bowel and cobble-stone appearance in the sigmoid colon; biopsy shows neutrophilic infiltration and crypt abscesses at the lamina propria consistent with IBD (probably ulcerative colitis (UC)). Given this diagnosis, his finger necrosis is most likely PG. Mesalamine is initiated, and epidermization is performed after 3 weeks with improvement of his finger.
DISCUSSION: PG is a rare (3–10/million/year), chronic, often destructive inflammatory skin disease in which a painful nodule/pustule breaks down to form a progressively enlarging ulcer with a raised, tender, undermined border. Lesions present either in the absence of any apparent underlying disorder (40–50 %) or in association with a systemic disease, such as IBD. PG occurs in 2–12 % of IBD patients (UC > Crohn’s) and can precede colitis or occur at any stage of the disease, even after colectomy. In most patients, symptoms of UC precede PG, and exacerbations of the bowel disease frequently correlate with worsening of the skin lesions. It, however, may not be closely related to the activity of colitis and may persist for long periods while bowel disease is quiescent. PG mostly occurs in the lower limbs (47 %) and trunk (16 %), less commonly in the hand (13 %). Few other case reports demonstrate its occurrence in the upper extremities, so it usually gets misdiagnosed as repetitive infections or skin carcinomas. To avoid misdiagnosis, therefore, one should consider PG in cases of recurrent skin necrosis. REFERENCES Callen JP. Pyoderma gangrenosum. Lancet 1998; 351: 581–585. Holmlund DEW, Wahlby L. Pyoderma gangrenosum after colectomy for inflammatory bowel disease. Acta Chir Scand 1987; 53: 73–74. Ilter N, Adi4en E, Gurer MA, Kevlekci C, Tekin O, Sayin A. Dermatitis artefacta masquerading as pyoderma gangrenosum. Int J Dermatol 2008;47: 975–977. Steven B. Huish et al. Pyoederma gangrenosum of the hand: a case series and review of the literature. The Journal of Hand Surgery 2001; Volume 26, Issue 4, 679–685. Pyoderma gangrenosum: the great pretender and a challenging diagnosis. J Cutan Med Surg. 2011 Nov-Dec;15(6):322–8. Review.
A CASE REPORT OF POLYARTERITIS NODOSA-ASSOCIATED ACUTE AORTIC DISSECTIONTomonao Hashimoto; Christine Kwan. Teine Keijinkai Medical Center, Sapporo, Japan. (Tracking ID #1929118)
LEARNING OBJECTIVE 1: Recognize that polyarteritis nodosa (PAN) can affect large vessels, such as the aorta, leading to dissections
CASE: A 54 year-old Asian woman presents with sudden onset, stabbing, continuous, non-radiating substernal chest/thoracic back pain ×30 min that awakens her from sleep. She also complains of diffuse, continuous abdominal pain and constipation ×4 days. She denies all other review of symptoms. The patient’s medical history includes uterine myoma, hypertension (HTN), and rheumatoid arthritis but no medications; she has undergone Caesarian section. She has no drug allergies and has quit smoking 5 years ago; prior 29 pack-years. She drinks 1 can of beer/night. Her family history is not significant. Physical examination shows blood pressure (BP) 135/76 right and 137/87 left, pulse 55, respiratory rate 28, O2 saturation 97 % room air, and temperature 36.4C. She is lying in bed in pain but alert/oriented ×3. The rest of the exam demonstrates no abnormalities. Laboratory testing, including complete blood counts, chemistry, cardiac/liver enzymes, and hepatitis panel, is all within normal limits. Electrocardiogram shows normal sinus rhythm, Q wave in III, and T wave inversions in V1 and V2. Chest X-ray shows no irregularities. Plain computed tomography (CT) reveals stool in the ileum and ascending/sigmoid colon. Meanwhile, her symptoms spontaneously improve, and she is discharged with a diagnosis of constipation and given a laxative. Nine days later, however, she presents with severe abdominal pain and syncope. Enhanced CT then shows Stanford type B aortic dissection with multiple aneurysms in the hepatic/gastric arteries. Abdominal angiography reveals left hepatic artery rupture for which transarterial embolization is performed. Further questioning reveals unintentional 6 kg weight loss in 8 months and diastolic BP >100 mmHg ×2 years. She is thus diagnosed with PAN and started on prednisolone; follow-up angiography 2 weeks later confirms improvement of aneurysms. Her aortic dissection is medically managed with candesartan and bisoprolol.
DISCUSSION: Acute aortic dissections (AAD) usually present with abrupt onset, sharp, and “tearing” chest/back pain, like the above patient, and risk factors include HTN, atherosclerosis, preexisting aortic aneurysm, vasculitis, and collagen diseases. Diagnosis can be made by chest CT with contrast, but the above patient, however, only receives non-contrast CT on initial evaluation. Treatment of Stanford type A dissections includes surgery while type B includes medical management, like the above patient. PAN, a vasculitis involving small-/mid-sized arteries, typically presents with systemic symptoms, such as fever, weight loss, and hypertension. The American College of Rheumatology’s classification criteria can be used to help in diagnosis although the most definitive technique is biopsy; an alternative includes the presence of microaneurysms on angiography. In the above patient, while she does have a history of untreated HTN and rheumatoid arthritis, her newly-found aneurysms from PAN have most likely caused her AAD. Only 1 other case report shows AAD caused by PAN; autopsy reveals necrotizing vasculitis in the vasa vasorum of the aorta, which the authors conclude to have caused AAD. Other studies have also shown a possible alternative mechanism of AAD involving the vasa vasorum. Given this possible link, PAN can, therefore, involve large vessels, like the aorta.
A CASE SERIES OF AN EMERGING INFECTION IN THE UNITED STATES: INVASIVE KLEBSIELLA PNEUMONIAELinnea S. Amesur1,2; Daniel I. Kim1,2; Jon Persichino1,2; Made Sutjita1,2; Armen Eskandari1,2; Vida Jahangiri1,2. 1University of California, Riverside, Riverside, CA; 2Riverside County Regional Medical Center, Moreno Valley, CA. (Tracking ID #1935091)
LEARNING OBJECTIVE 1: Recognize the emergence of invasive Klebsiella pneumoniae in non-Asian populations in the United States
LEARNING OBJECTIVE 2: Diagnose and treat invasive Klebsiella pneumoniae in a timely fashion for better patient outcomes
CASE: We present a case series of 10 patients with invasive community acquired Klebsiella pneumoniae infections at a county hospital from 2010 to 2013. The data for this study was collected retrospectively. Charts were reviewed for the patients’ hospitalizations. Data collected included age, gender, race, recent travel, country of origin, type of infection, and evidence of dissemination. We gathered information about medical conditions and co-morbidities that may be risk factors for invasive infection, including diabetes mellitus, cancer, steroid use, recent chemotherapy, recent radiation therapy, lung disease, liver disease, alcohol use, kidney disease, and central line or catheter use. In our results, the age range of patients was between 24 and 75 years of age, with a median age of 51. Most of the patients were male (7). The ethnicities of the patients were five Latino, two Caucasian, two Asian, and one African-American. Four were born in the United States (2 Caucasian, 1 Latino, 1 African-American). Four were born in Mexico (all were Latino), and the remainder two patients were born in Asia (Laotian and Cambodian). One had travel history within the past 10 years to South East Asia, and another patient had travel history within the past 2 years to Mexico. The types of infections most commonly seen were liver abscesses (5), followed by soft tissue infections (3), pelvic abscess (1), and pyelonephritis (1). Of the soft tissue infections, one patient had Fournier gangrene, one had neck abscess, and one had necrotizing fasciitis. Seven of the patients showed evidence of disseminated disease including bacteremia (4), urinary tract infection (4), and lung involvement (2). Most patients were septic on presentation and seven patients had elevated liver enzymes. The most common risk factors associated with invasive K. pneumoniae infections were diabetes (40 %), followed by renal failure (30 %) and history of cancer (20 %). All 10 of our patients survived after treatment with appropriate antibiotics.
DISCUSSION: Klebsiella pneumoniae, a member of the Enterobacteriaceae family, is a common human bacterial pathogen that can cause urinary tract infections, pneumonias, bacteremia, and intra-abdominal infections. It is recognized as a highly pathogenic organism that causes disease in the community and nosocomial settings. Invasive K. pneumoniae was first described in the early 1980’s in Taiwan as the cause of pyogenic liver abscess. Since then, its emergence is most notable in Asian countries causing not only liver abscess but also pneumonia, urinary tract infection, brain abscess, endophthalmitis, pyogenic meningitis, empyema, septic pulmonary emboli, and osteomyelitis. Over the last decade, there is an increasing rise of this syndrome in the United States, emphasizing the importance of early recognition, diagnosis, and treatment. Most of these invasive infections are caused by the hypermucoviscous serotypes K1 and K2 and genotypes magA and rmpA. Hypermucoviscosity increases the virulence of K. pneumoniae, making it resistant to phagocytosis. The phenotype is identified in the laboratory using the “string test.” Patients with liver abscesses typically present with fever, chills, and abdominal pain. However, patients with invasive K. pneumoniae may present with leukocytosis, thrombocytopenia, abnormal liver function tests, and increased glucose in the blood. Diabetes mellitus appears to be the most prevalent risk factor at 29 %. Hospital mortality rate has been reported between 9 and 11 %. Antibiotics are given based on culture and sensitivity results, although ceftriaxone has proven effective in most liver abscesses. While invasive K. pneumoniae infections are common and well reported in Asia, they are rare in the United States. There are few case reports published and only one small case series described in California which reports infections affecting mostly patients of Asian descent. Previous cases in the United States occurred in primarily patients of Asian descent while our case series displayed a higher occurrence in Latino patients, which may indicate a different predisposition than previously reported for invasive infections in the United States. The emergence of K. pneumoniae in the United States, and most significantly in the Latino population, emphasizes the importance of recognizing invasive K. pneumoniae as the cause of liver abscesses, soft tissues infections, and other invasive diseases in non-Asian populations.
A CATASTROPHIC SCENARIO OF A HEART DEFECTSamian Sulaiman; Salih Samo; Muhammed Sherid; Husein Husein; Shahriar Dadkhah; Ahmet A. Oktay; Nadia El Hangouche; Muhammad Shahreyar; Ana Inashvili; Addis Asfaw; Preethi Subramanian. St. Francis Hospital. Evanston, evanston, IL. (Tracking ID #1939294)
LEARNING OBJECTIVE 1: Patent Foramen Ovale (PFO) occurs in 25 to 30 % of the general population. It should be considered a normal anatomic variant and not a pathological finding in the absence of possible paradoxical embolism or other specific clinical conditions. Testing for PFO is indicated in patients with paradoxical thrombo-embolic events or cryptogenic stroke (defined as stroke of undetermined pathogenesis). PFO is more common in patients with cryptogenic stroke than in the general population (approximately 50 % to 60 % vs. 20 % to 25 %)
CASE: 40 year-old male who presented with left leg pain that started half an hour prior to presentation. The pain was dull, 10/10 in severity and was associated with tingling. In the Emergency department, absent pulses were noticed in the left dorsalis pedis and posterior tibialis arteries. The left foot was colder and paler as compared to the right side. The Rest of physical exam was normal. His past medical history was insignificant. He was a non-smoker and was drinking alcohol only occasionally. Urine toxicology was positive for cocaine and amphetamine. The rest of labs were normal. Left lower extremity CT angiography showed complete occlusion of the femoral artery starting at above the knee segment of the popliteal artery and extending into the anterior and posterior tibial and peroneal arteries. Heparin infusion was started. Patient underwent left trans-femoral embolectomy under general anesthesia and he was intubated. Next day, he developed tachycardia and acute hypoxemic respiratory failure. CT chest with contrast showed bilateral large pulmonary emboli. Given his venous and arterial emboli, suspicion of paradoxical embolism was raised. Trans-esophageal echocardiography with agitated saline was performed and showed Patent Foramen Ovale with right to left shunt. Despite the full dose of anticoagulation, patient developed left thalamic embolic stroke 4 days after admission. An Inferior Vena Cava filter was placed. Patient was finally extubated and he was referred to another facility for percutaneous closure of the defect.
DISCUSSION: Anatomic closure of the PFO occurs later in infancy in the majority of the population, but autopsy and detailed contrast echocardiographic studies demonstrate that anatomic closure is incomplete in approximately 1 of every 4 adults. Transesophageal echocardiography with agitated saline contrast enables shunt identification in PFO. An incidentally detected PFO generally requires no follow-up or treatment. If a PFO is deemed likely to be causally related to an embolic event, as is the case in this patient, therapeutic options for secondary stroke or other embolic event are controversial. These therapeutic options include medical therapy with antiplatelet agents or anticoagulation, and surgical or percutaneous closure of the defect.
A CEREBROVASCULAR ACCIDENT: ORAL CONTRACEPTIVE PILLS AND PATENT FORAMEN OVALEDavid Linz1; Harish Jasti2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1929275)
LEARNING OBJECTIVE 1: To counsel women about the risk of thrombotic stroke with estrogen containing oral contraceptive pills (OCP).
LEARNING OBJECTIVE 2: To appraise the evidence for device closure of patent foramen ovale (PFO) to prevent recurrent neurological events.
CASE: A 34 year-old woman presented to the ER 1 h after experiencing difficulty speaking. The patient was talking on the telephone when, all of a sudden, she felt as if she could not get her thoughts out. She could laugh, and could speak one or two words at a time, but could not communicate in full sentences. Her husband witnessed her difficulty speaking and asked her to write out her thoughts, but she could not. She had no facial asymmetry, muscle weakness, or altered sensation. She had no significant past medical history. Her medications included a combination oral contraceptive pill containing 20 μg of ethinyl estradiol. She had no family history of cardiovascular disease, hypercoagulable disorders, or malignancies. Examination was notable for an NIH stroke scale of 2, for moderate to severe expressive aphasia. The rest of her neurological exam was normal. Laboratory analysis was remarkable for a hemoglobin A1c of 5.4 and a fasting LDL of 103. A comprehensive hypercoagulable screen was negative. EKG and 48-hour telemetry showed normal sinus rhythm without any irregular activity. MRI of the brain showed a left frontal infarct and MRA showed a corresponding thrombosis of a small mid sylvian arcade vessel. Transthoracic echocardiogram showed normal heart function, without any valvular abnormalities or mural thrombi; however, a PFO was detected by intravenous contrast injection. Bilateral lower extremity ultrasound and CT venography of the pelvis did not detect any venous thrombosis.
DISCUSSION: Stroke is among the leading causes of morbidity and mortality, and nearly 25 % of the 795,000 strokes that occur each year in the US are recurrent attacks. Diagnosis of the stroke etiology is critical for directing efforts for the prevention of recurrent stroke. This patient had no clear identifiable source, such as a cardioembolism, large artery atherosclerosis, or small artery disease. Furthermore, she had no family history of hypercoaguable disorders and blood analysis did not detect any hypercoaguable states. However, her estrogen containing OCP increased the risk of arterial or venous thromboemboli, which can paradoxically cross her PFO. In a 15-year Danish historical cohort study, women were 1.3 to 2.3 times more likely to have an arterial thrombosis if they were taking a combination oral contraceptive pill with 30 to 40 μg ethinyl estradiol, and 0.9 to 1.7 times more likely if they were taking a pill with 20 μg, compared to non-users. The difference amongst progestin type was minimal and progestin-only products, including the levonorgestrel-releasing IUD and subcutaneous implants, did not significantly increase the risk of thrombotic stroke. The authors estimated that among 10,000 women who use OCPs containing 20 μg for 1 year, 2 will have arterial thromboses and 6.8 will have venous thromboses. Secondary prevention of stroke is especially important in patients with PFO because the estimated rate of recurrence is 25 % within a 4-year period. To date, there have been three randomized controlled trials evaluating the effectiveness of percutaneous closure of PFO, and none of these trials has shown a statistical benefit in preventing recurrent neurological events as compared to medical therapy with antiplatelets or anticoagulants. These studies were limited by low enrollment, lower-than-expected event rates, relatively short follow-up, and modest statistical power. A recent meta-analysis does suggest that device closure may have a beneficial effect with an overall reduction in the hazard for a recurrent neurological event of 33–39 %. The safety of the devices was comparable to medical therapy with a low incidence of serious adverse events, the most common being atrial fibrillation. In conclusion, this patient should be counseled that taking an estrogen containing OCP increases her risk of thrombotic stroke, and that the benefit of percutaneous closure of her PFO compared to medical therapy to prevent recurrent neurological events is uncertain.
A COMPLEX CASE OF ATYPICAL PHEOCHROMOCTYOMAJessica Thibault1; Kelly Menachof2; David Saxon1; Ingrid Lobo1,2. 1University of Colorado Hospital, Aurora, CO; 2University of Colorado, Denver School of Medicine, Aurora, CO. (Tracking ID #1933750)
LEARNING OBJECTIVE 1: Recognize both typical and atypical presentations of pheochromocytoma.
LEARNING OBJECTIVE 2: Diagnose and treat pheochromocytoma.
CASE: A 48 year-old previously healthy Caucasian male presented to an outside hospital complaining of several months of gradually progressive dyspnea on exertion. Chest CT revealed bilateral sub massive pulmonary emboli (PE) and an incidental large, incompletely visualized right suprarenal mass. A dedicated abdominal CT showed a 10 cm right adrenal mass. He was discharged on anticoagulation and a CT guided needle biopsy was done 3 weeks later. The day after his biopsy, he was admitted to the same hospital with altered mental status and shortness of breath. He was found to have an ischemic right sided thromboembolic CVA, new acute systolic heart failure with an ejection fraction of 25 %, and bilateral pleural effusions. He was also noted to have episodic hypertension, tachycardia, and fevers with nausea and vomiting. He denied any chest pain, orthopnea, PND, diaphoresis, headaches, palpitations, or fevers prior to admission. Patient also denied a family history of cardiac disease or neuroendocrine tumors. He was started on appropriate medical therapy for heart failure, PE, and CVA and transferred to us for further evaluation and treatment. On presentation he was thin but well appearing, with a blood pressure of 93/60 and otherwise normal vitals. He was oriented with no focal findings. He had JVD of 10 cm, an S4, decreased breath sounds in the bases and fine crackles in the mid lung fields bilaterally. His exam was otherwise normal. A nuclear stress test showed global hypokinesis and a prior infarct in the left circumflex distribution. Repeat CT scans confirmed the adrenal mass without evidence of malignant spread. Laboratory studies were remarkable for urine metanephrines and normetanephrines of 9870 (0–300) and 3174 (0–400), plasma metanephrines and normetanephrines of 14.9 (0–0.49) and 9.95 (0–0.89), normal 24 h urine cortisol levels, and elevated TSH (6.4) and low free T4 (0.7). The final pathology from his biopsy was consistent with a pheochromocytoma. During the patient’s hospitalization, he was hypotensive to the 80s/40s without episodic hypertension. We diuresed him aggressively and continued treatment for his heart failure, PE, and CVA. Given the complexity of this case, Endocrinology, Surgery, Neurology, Cardiology, Oncology, and Anesthesiology were consulted to prepare for surgical Resection. Alpha and beta blockade was started with prazosin 1 mg TID and metoprolol 6.25 mg BID. The patient’s systolic blood pressures were consistently in the low 80s and further titration was not possible. He underwent right adrenalectomy 2 weeks later. The surgery and postoperative course were complicated by hypotension requiring 3 vasoactive medications. By post-op day 3, he was weaned from these medications. He was discharged on post-op day 7 with stable blood pressures. Pathology confirmed pheochromocytoma confined to the fibrous capsule and no morphologic evidence of malignancy. To date, the patient’s cardiac function has not improved with an ejection fraction of 12 %. The patient’s urine metanephrines, while decreased from prior, remain elevated, concerning for residual pheochromocytoma vs paraganglioma. He is scheduled for an MIBG scan to evaluate this further.
DISCUSSION: The World Health Organization defines pheochromocytoma as a tumor arising from chromaffin cells in the adrenal medulla. Pheochromocytomas are rare tumors that often cause symptoms due to secretion of catecholamines including norepinephrine, epinephrine, and dopamine. The classic triad of symptoms described in the literature include episodic diaphoresis, headache, and tachycardia. Patients are often found to have episodic or sustained hypertension. However, up to 10–15 % of patients may present with normal blood pressure and up to 50 % may be asymptomatic. Other presenting signs and symptoms may include cardiomyopathy, hyperglycemia, orthostatic hypotension, anxiety, and weight loss. The diagnosis is suspected by elevated urine and/or serum metanephrines greater than 2 times the normal limit in combination with either MRI or CT showing an adrenal or extra-adrenal mass suspicious of pheochromocytoma. It is ultimately confirmed by tissue diagnosis, usually at the time of resection as biopsy is risky and can precipitate adrenergic storm. Approximately 10 % of pheochromocytomas are malignant at the time of diagnosis. Treatment involves high risk surgical resection with pre-operative therapy, typically with a combination of alpha and beta blockade, to prevent hypertensive crisis. Risk is increased in patients with cardiomyopathy, as our case illustrated. Given the low incidence of pheochromocytomas and the myriad of possible presenting symptoms, some of which are very atypical, clinicians must maintain a high level of suspicion for this disease.
A CRUNCHING COLDLisa Lee; David Dayan-Rosenman; Geeta Laud. Montefiore Medical Center, Bronx, NY. (Tracking ID #1937565)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of spontaneous pneumomediastinum associated with alveolar rupture.
LEARNING OBJECTIVE 2: Understand the management of asthma-induced spontaneous pneumomediastinum.
CASE: A 25 year-old woman with history of well controlled mild-persistent asthma presents with a chief complaint of a day of cough, rhinorrhea and difficulty breathing consistent with asthma exacerbation followed by the sudden onset of sharp retrosternal pleuritic chest pain associated with increased shortness of breath. The pain is devoid of radiation and worsens with bending down. Vital signs on presentation were significant for heart rate of 103, respiratory rate of 22, saturation of 88 % on ambient air and Peak Flow of 160 L/min (from a baseline of at least 340 L/min). Physical exam revealed a thin, young woman in pain breathing rapidly but without help of accessory muscles, able to speak in full sentences in a normal voice; Heart sounds were distant and regular, without rubs, murmurs, or gallops. Crepitus was heard over the precordium with each heartbeat. There was no jugular venous distention and the trachea was not deviated. There were minimal diffuse end-expiratory wheezes. An electrocardiogram showed sinus tachycardia. Serum chemistries were significant for a leukocyte count of 7.5 k/uL and normal cardiac enzymes. Chest X-ray showed right upper lateral pneumothorax and pneumomediastinum. Subsequent chest CT showed pneumomediastinum extending into the neck and hila associated with a small right pneumothorax along the fissures. A diagnosis of pneumomediastinum secondary to alveolar rupture in context of asthma exacerbation was made and the patient was admitted for observation. The patient improved clinically and did not require surgical intervention. She was discharged home 2 days later after repeat imaging showed resolution of the pneumomediastinum.
DISCUSSION: Spontaneous pneumomediastinum (SPM) should be considered in patients with lung disease presenting with chest pain and dyspnea. SPM occurs when high alveolar pressures cause alveolar rupture and dissection of air into adjoining structures, spreading through the perivascular and peribronchial space into the mediastinum. The most common presenting symptoms are chest pain and dyspnea. The most sensitive sign of SPM is crepitus heard over the neck or precordial area. The most specific sign is a crunching sound that is synchronous with the heartbeat—termed Hamman’s sign and resulting from the heart beating against mediastinal emphysema. Spontaneous PMD reported incidence falls between 1 in 800 and 1 in 42,000 hospital admissions and affects predominantly young, thin males. A history of asthma is reported in up to half the cases, chronic interstitial lung disease is also common in older patients. The radiographic findings are distinct and X-ray is the first-line modality for evaluation. SPM can be identified in the frontal view by lucency surrounding mediastinal structures including outlining of the superior aspect of the diaphragm and elevation of the heart. In lateral view, lucency can surround the ascending aorta, the aortic arch, the retrosternal, precardiac, periaortic, and peritracheal areas. CT scan is more sensitive than X-ray though it is unclear whether it is helpful as most of the additional cases identified may be too small to be clinically significant. SPM is usually benign condition that is managed conservatively with analgesia, supplemental oxygen and avoidance of maneuvers that increase intrathoracic pressure such as coughing or straining. It usually resolves spontaneously within 2 weeks and recurs in less than 5 % of cases. Surgical treatment SPM with mediastinotomy is reserved for the extremely rare cases when SPM leads to cardiopulmonary decompensation. Important related conditions to rule out are tension pneumothorax and esophageal rupture.
A CURIOUS CASE OF NEFARIOUS NODULES: ANTIGEN AND CULTURE NEGATIVE PULMONARY HISTOPLASMOSISMichael G. Nanna; Varidhi Nauriyal. Yale-New Haven Hospital, New Haven, CT. (Tracking ID #1936389)
LEARNING OBJECTIVE 1: To review the presentation of histoplasmosis.
LEARNING OBJECTIVE 2: To review the appropriate workup & briefly, the treatment for histoplasmosis.
CASE: A 41 year old otherwise healthy immunocompetent gentleman presented with a two week history of dyspnea, non-productive cough, fevers, chills and pleuritic chest pain. He recently moved to Connecticut eight months prior to presentation and had chickens while living in Puerto Rico. Admission physical examination was notable for bilateral crackles and tenderness over the right costochondral area. Chest radiograph on admission revealed multiple pulmonary nodules along with hilar adenopathy concerning for an infectious, inflammatory or neoplastic process. A chest computed tomography (CT) scan demonstrated scattered dense bilateral pulmonary nodules, some with central cavitation. The patient clinically decompensated with fever to 102.2° Fahrenheit, leukocytosis to 14,600, tachycardia and tachypnea. Broad spectrum antibiotics were initiated and a repeat CT scan revealed a large loculated right sided empyema, for which a chest tube was placed. The patient went for bronchoscopy, right decortication and right upper lobe wedge resection. A complete infectious, inflammatory and neoplastic workup including blood, pleural fluid, tissue and bronchoalveolar cultures, did not reveal the diagnosis. Histoplasma urine antigen was negative. Lung tissue pathology demonstrated necrotizing granulomas. The patient was extubated on post-operative day two and discharged with presumptive diagnosis of bacterial pneumonia complicated by empyema and lung abscess. A fungal stain from the wedge resection following discharge demonstrated yeast forms consistent with Histoplasma capsulatum located within a granuloma. We initiated the patient on itraconazole therapy and referred him for infectious disease follow up.
DISCUSSION: The differential diagnosis of lung nodules and fever can be separated into malignant, inflammatory and infectious categories. Histoplasmosis is an important potential diagnosis in this group of patients and represents the most common endemic mycosis in the United States. The prevalence of histoplasmosis is highest in the states along the Ohio and Missipipi River valleys, as well as Puerto Rico, Central and South America. Histoplasmosis is most frequently classified as primary pulmonary or disseminated in nature. Pulmonary histoplasmosis can present acutely or chonically with cough, dyspnea and constitutional symptoms, with clinical severity ranging from asymptomatic to critically ill. Disseminated histoplasmosis usually occurs in patients who are immunosuppressed, pediatric or elderly and may present with fatigue, weight loss and fever, as well as an assortment of more specific symptoms depending on the potential organ system involved. The appropriate workup should include blood cultures, chest radiograph, computed tomography, urine antigen, serum antigen, antibody assays, cytology and histopathology. Notably, negative antigen testing does not rule out significant disease burden, particularly in immunocompetent individuals as seen with this clinical vignette. Urine antigen testing is 99 % specific, 92 % sensitive in patients with disseminated histoplasmosis and 75–80 % sensitive in patients with acute pulmonary histoplasmosis, while lung histopathology only provides 50 % sensitivity. The appropriate treatment regimen depends on the host and disease severity, with amphotericin B and itraconazole the anti-fungal agents of choice.
A CURIOUS CASE OF SMALL CELL CARCINOMAAnishka D’Souza1; Stanley K. Dea2; Deepthi Karunasiri3. 1Olive View- UCLA Medical Center, Sylmar, CA; 2Olive View- UCLA Medical Center, Sylmar, CA; 3Olive View-UCLA Medical Center, Sylmar, CA. (Tracking ID #1937065)
LEARNING OBJECTIVE 1: Recognize the importance of performing a complete physical exam when evaluating a patient.
LEARNING OBJECTIVE 2: Recognize that the differential diagnosis of a young male with painful rectal bleeding extends beyond hemorrhoidal disease.
CASE: A 24-year-old Caucasian male with no significant past medical history presented to the emergency department with a 1 year history of intermittent rectal bleeding and 1 month of worsening anorectal pain. The patient had been evaluated by an outside clinic several weeks prior to admission, where he had been told that his symptoms were secondary to hemorrhoids. No rectal exam was performed there. On presentation, he denied fevers, chills, weight loss, or abdominal pain. He also denied any history of sexually transmitted infections or family history of colorectal cancer. Physical examination was significant for a firm mass on digital rectal exam, as well as a firm, non-mobile, 2 cm right inguinal lymph node. Labs were significant for iron deficiency anemia, with a normal-range CEA and negative HIV. CT scan of the abdomen and pelvis showed circumferential wall thickening of the rectum extending to the anus with bilateral inguinal and perirectal lymphadenopathy. Flexible sigmoidoscopy revealed a circumferential ulcerated mass in the distal rectum. Biopsy of the mass revealed a poorly-differentiated neuroendocrine carcinoma. Based on pathology, disease was felt to be most consistent with small cell carcinoma. A fine needle aspiration of the right inguinal node was positive for metastatic disease. CT of the chest and MRI of the brain showed no distant metastases. PET showed intense FDG uptake in the rectal mass and regional lymph nodes with no abnormal tracer uptake in the chest or abdomen. The patient was started on cisplatin and etoposide for Stage IIIB disease with referral for possible radiation after completing six cycles.
DISCUSSION: Small cell carcinoma is a neuroendocrine malignancy most commonly associated with cancer of a pulmonary origin. Extrapulmonary small cell carcinoma is a rare occurrence, accounting for about 2.5 % of all small cell carcinomas. While gastrointestinal origin accounts for 23 to 33 % of extrapulmonary cases, primary anal involvement is extremely rare with only a handful of cases documented in the literature. Chemotherapy is the mainstay of treatment. Given the paucity of clinical literature on this disease, drug regimens traditionally have been based on those for pulmonary small cell carcinoma, namely, platinum-based drugs with etoposide. Unfortunately, the disease tends to follow an aggressive course with a generally poor prognosis despite treatment. This case illustrates the importance of performing a careful rectal exam when symptoms dictate. The differential diagnosis of a young male with painful rectal bleeding extends beyond hemorrhoidal disease and a careful physical examination may have led to an earlier diagnosis in this patient.
A CURIOUS CAUSE OF A NON-HEALING ULCERAnna Maria Affan; Praveena N. Iruku; Keyvan Ravakhah. St Vincent Charity Medial Center, Cleveland, OH. (Tracking ID #1936840)
LEARNING OBJECTIVE 1: Diagnosis and management of a non tuberculous mycobacterial skin infection.
CASE: This is a 35 year old male presented with a chief complaint of severe back pain. His recent hospitalization was for a laminectomy for L4 spondylosis with herniated nucleus pulposus. The patient was discharged a few days after the procedure and he did well, including going on a cruise with his wife. In addition to the pain, he reported intermittent serous discharge at the site for approximately 2 weeks. Review of systems was unremarkable. Preceding his visit to our institution, the patient visited another hospital with the same complaints and was prescribed ciprofloxacin for 7 days. Initially there was some improvement in the wound but it soon regressed. His past medical history was significant for hypertension controlled on lisinopril. He had a laminectomy in 1997 after a stress fracture. His family history was noncontributory and his social history was positive for smoking a pack per day with alcohol use occasionally. On examination he appeared comfortable. Vital signs were stable. Back examination revealed a tender, non-erythematous wound. The upper portion of the wound had superficial dehiscence and was soft suggesting some fluid in the sub epidermal area. The lower aspect of the wound had a slight area of dehiscence with superficial scab formation and minimal tenderness. The mid portion of the wound appeared largely intact and was firm suggesting healing. There was no purulent drainage. Examination was otherwise unremarkable. Laboratory results were remarkable only for a creatinine of 1.3. MRI of the lumbar spine was done but did not reveal neither subcutaneous fluid collection nor bony infection. The wound was debrided and tissue sample sent for culture. It was positive for Mycobacterium fortuitum (M. fortuitum). The patient was placed on several antibiotics pending sensitivity which took several weeks to arrive. The organism was found to have sensitivity inclusive of, but not limited to Ciprofloxacin and linezolid. These antibiotics were used orally for 6 weeks. The patient returned 2 months after initial presentation with another wound dehiscence while on the aforementioned therapy. Again imaging of the back was done which showed no deep infection. The wound although superficial was debrided, and cultures sent. M. fortuitum persisted. Trimethoprim-sulfamethoxazole was added to current regimen in light of initial sensitivities. The patient responded well after 4 months of therapy with no current untoward event.
DISCUSSION: M. fortuitum is a nontuberculous mycobacterium (NTM). It is described as a rapidly growing mycobacterium and is ubiquitous in soil and water. Surgical-site infections due to M. fortuitum infection have been documented where the patient may develop a nonhealing but nonspreading wound or skin ulcer. Commonly the source is contamination of the wound, directly or indirectly, with colonized water. Recall that our patient went on a cruise subsequent to his surgery. The prevalence of NTM in both pulmonary and extrapulmonary pathology is increasing. A recent study in 2013 reported M. fortuitum complex as the most common cause of skin and soft tissue infection due to rapidly growing mycobacteria in a patient selection in Korea. NTM are resistant to conventional antituberculous drugs. Susceptibility typically is seen to amikacin, linezolid and moxifloxacin which was noted in our patient. However, susceptibility testing does not guarantee clinical success as was seen in this case. No specific treatment guidelines exist, however a multidrug regimen combined with surgical debridement is often used for therapy Prolonged antibiotic therapy is generally required with increased preference for two antimicrobials. The duration of therapy to prevent relapse remains unclear.
A CURIOUS MANIFESTATION OF AMOXICILLIN-INDUCED DRESS SYNDROMEMusa A. Sharkawi; Noormuhammad Abbasakoor; Sarju Ganatra. Lahey Hospital & Medical Center, Burlington, MA. (Tracking ID #1923654)
LEARNING OBJECTIVE 1: Recognize the diverse clinical features of DRESS syndrome
LEARNING OBJECTIVE 2: Manage a patient with life-threatening DRESS syndrome
CASE: A 19-year-old Caucasian male presented to the emergency department with high-grade fevers, a morbiliform rash, adenopathy, hepatitis, thrombocytopenia and eosinophilia 14 days after being started on amoxicillin for symptoms of sinusitis. His symptoms quickly deteriorated during the first 24 h of hospitalization to involve respiratory compromise requiring intubation and meeting criteria for acute respiratory distress syndrome. Diffuse bilateral pulmonary infiltrates were seen on chest X-ray [Figure 1] which was clear on admission. A chest CT scan was remarkable for diffuse pulmonary edema with prominent air bronchograms [Figure 2]. A bronchoscopy and bronchoalveolar lavage revealed a bloody aspirate and pulmonary eosinophilia indicating diffuse alveolar hemorrhage. Extensive workup for autoimmune disorders, bacterial, viral, fungal and parasitic infections was unrevealing. A punch biopsy of the skin was compatible with a hypersensitivity reaction as it showed superficial perivascular dermatitis with eosinophils. DRESS syndrome was diagnosed with rapid regression of symptoms after treatment with high dose methylprednisone was initiated. The patient made a full recovery and was discharged home on day 13 of hospitalization with a very slow steroid taper.
DISCUSSION: Drug rash with eosinophilia and systemic symptoms (DRESS) is an idiosyncratic and potentially life-threatening syndrome. It is a type of delayed hypersensitivity reaction which usually presents 2–8 weeks after the initiation on the offending agent. The main culprits are allopurinol, aromatic anticonvulsants and sulfonamides, even though 50 Drugs can induce DRESS [1]. It has been described as “the great clinical mimicker” as it masquerades as acute severe sepsis. It presents with fever, cutaneous drug eruption, hematological abnormalities, and systemic manifestations including adenopathy and a wide array of internal organ involvement. There has only been a handful of cases of DRESS syndrome as a consequence of amoxicillin. In our case, the most life-threatening manifestation was diffuse alveolar hemorrhage and eosinophilic pneumonitis causing acute respiratory distress syndrome. Pulmonary involvement is present in only 5 % of cases of DRESS [1]. Use of the Naranjo adverse drug reaction probability scale indicated a “probable” relationship (score of 5) between the patient’s development of DRESS syndrome and treatment with amoxicillin. The Scoring System for Classifying DRESS Cases developed by Kardaun et al. was used and a “definite” score gave us the diagnosis [2]. DRESS can be associated with human herpes virus 4, 6, and 7 infections; thus, serology of these viruses should be checked. The main treatments of DRESS are withdrawal of culprit drug and a very slow corticosteroid taper. Diagnosing DRESS is challenging due to the diversity of cutaneous manifestations and organs involved and as such, there should be a high clinical suspicion for this disease if the introduction of a new drug is followed by a rash, eosinophilia and a sepsis-like syndrome. References: 1- Cacoub P, Musette P & Descamps V, et al. The DRESS syndrome: a literature review, Am J Med. 2011 Jul;124(7):588–97 2- Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms. Br J Dermatol. 2007;156:609–611.
A DEADLY SORE THROATJoshua T. Hanson. 1University of Texas Heath Sciences Center, San Antonio, San Antonio, TX; 2South Texas Veterans Health Care System, San Antonio, TX. (Tracking ID #1939321)
LEARNING OBJECTIVE 1: Recognize the need for an expanded differential diagnosis in acute pharyngitis.
LEARNING OBJECTIVE 2: Recognize the features of Lemierre’s syndrome.
CASE: A 26-year-old man presented to the emergency department with complaints of sore throat, mild fevers, and odynophagia. Symptoms had begun 1 week prior to presentation, but worsened significantly with the presence of trismus in the preceding 3 days. Given tonsillar asymmetry on examination, a bedside needle aspiration of the peritonsillar space was attempted without return of purulent material. Subsequently, the patient began to experience rigors and became febrile to 38.3 ° C with a pulse of 138 beats per minute. A complete blood count demonstrated a white-cell count of 27,500 per microliter and a platelet count of 62,000 per microliter. The sodium was 125 millimoles per liter. The patient was admitted for systemic inflammatory response syndrome with a concern for sepsis. Broad-spectrum antibiotics and resuscitative fluids were initiated. The next morning the patient’s clinical condition had stabilized, biochemical assessment, including white blood cell count, had begun to normalize, and both sets of blood cultures drawn the previous day grew gram negative rods and gram positive cocci. Broad-spectrum antibiotics were continued while speciation of the organisms revealed Fusobacterium necrophorum and β-hemolytic, group C streptococci. In response to the presence of F. necrophorum bacteremia, the patient underwent ultrasonography of the neck, which revealed no thrombus, and computed tomography of the chest with contrast, which revealed multiple scattered soft tissue and ground glass nodular opacities throughout the lung parenchyma. These findings were consistent with septic emboli. Antibiotic therapy was changed to continuous penicillin infusion. The patient was discharged with outpatient intravenous antibiotic therapy for 2 weeks followed by a four-week course of oral therapy with amoxicillin. The patient presented to follow-up with no lasting effects.
DISCUSSION: For the internist, sore throat is a very common presenting complaint. Acute pharyngitis accounted for 12.5 million office visits in 2006 and the infectious causes of pharyngitis are varied. Taken all together, viruses account for roughly 50 % percent of cases. Rhinovirus, coronavirus, influenza, parainfluenza, and adenovirus are all common culprits. Less common viral causes of acute pharyngitis include cytomegalovirus, EBV, HSV-1, HSV-2 and HIV. Streptococcus pyogenes accounts for 5 to 15 % of all cases of acute pharyngitis and is the typical cause of acute bacterial pharyngitis and Groups C and G streptococci cause a minority of streptococcal cases. Other bacteria, including N. gonorrheae, C. pneumoniae, C. diptheriae, and F. necrophorum can cause acute bacterial pharyngitis. F. necrophorum is an anaerobic, Gram-negative pleomorphic rod-shaped bacterium and the putative cause of Lemierre’s syndrome, first described in 1900 by Courmont and Cade. However, Lemierre described postanginal sepsis (tonsillitis followed by thrombophlebitis and complications, including metastatic disease and septic emboli) with such precision that subsequent authors have used his name. Despite longstanding recognition, there remains no formal case definition for the syndrome. There is variation in published case series as to the source of the infection, as well as whether internal jugular vein thrombosis is a requirement. Some authors omit this requirement, permitting pulmonary emboli as a sign. In a literature review, Riordan suggests a formal case definition with three components, namely: 1. History of anginal illness or compatible clinical findings, 2. Evidence of either metastatic lung lesions or metastatic lesions in other sites, and, 3. Either evidence of internal jugular vein thrombophlebitis or isolation of F. necrophorum or Fusobacterium sp. from blood cultures or a normally sterile site. Lemierre’s syndrome is rare; studies estimate a yearly incidence rate of 0.8 to 1.5 cases per one million people. A review of case series indicates 89 % of patients were aged 10 to 35 years. There are no true time trends available, however case reports and case series of the syndrome were numerous in the early half of the 20th century, declined during the 1950s through 1970s, and increased during the 1980s. Some authors suggest the decline was due to widespread use of antibiotics and the current increase due to changes in antibiotic prescribing patterns. In the modern era, one study estimates under 5 % case fatality in appropriately diagnosed cases. Co-infection with streptococcal species is common. This case highlights the need for clinicians to remain vigilant for all of causes of acute pharyngitis. It is of particular importance among adolescents and young adults presenting with acute pharyngitis lasting longer than is usual with features of systemic disease. While Lemierre’s syndrome is rare, the incidence may be rising, is life threatening, and is Treatable.
A DIAGNOSIS MISSED UNTIL A MEDICAL STUDENT GOT INVOLVEDAdam Kost; Alda Maria Gonzaga. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1934160)
LEARNING OBJECTIVE 1: Recognize the features and generate a differential diagnosis for platypnea-orthodeoxia syndrome.
LEARNING OBJECTIVE 2: Consider a right-to-left shunt or shunt physiology as etiology of hypoxia in instances where there is hypoxia that is difficult to correct with supplemental oxygen.
CASE: An 85-year-old female with a history of dementia, paroxysmal atrial fibrillation and orthostatic hypotension presented to the emergency department (ED) after a syncopal episode associated with hypoxia. During a brief walk, she developed shortness of breath and lightheadedness. She sat down and felt better after a brief rest; however, her symptoms recurred with walking. After sitting again, she had a 5-minute episode of unresponsiveness without any abnormal movements, incontinence, cyanosis or diaphoresis. She had regained consciousness by the time paramedics arrived but her oxyhemoglobin saturation by pulse oximetry was only 69 %. On arrival to the ED, she required 15 liters (L) of supplemental oxygen via a non-rebreather mask. An arterial blood gas obtained while she was saturating 88 % on 15 L of oxygen revealed: pH 7.42, pCO2 39, pO2 56, HCO3 25 with a base excess of 1. Shortly thereafter however, she was weaned to room air and maintained normal saturation levels. Other labs including blood counts, a complete metabolic profile, d-dimer, troponin and BNP were all within normal limits. While hospitalized, she was mostly asymptomatic with oxygen saturations nearing 100 % while breathing ambient air. An EKG revealed normal sinus rhythm with normal intervals and axes. A chest x-ray was unremarkable, as was a spiral CT scan of the chest to evaluate for pulmonary embolism. An MRI of the brain showed evidence of chronic small vessel ischemic disease but no acute intracranial disease. She was briefly transferred to the ICU after a desaturation event where she again required supplemental oxygen nearing 100 % FiO2 (fraction of inspired oxygen) but did not require intubation or positive-pressure ventilation. She had an electroencephalogram (EEG) that did not reveal any epileptiform discharges. A transthoracic echocardiogram (TTE) was within normal limits. She returned to the general hospital wards. While walking with a medical student to assess her functional status, she again desaturated, which corrected quickly when she returned to a supine position. This raised suspicion for platypnea-orthodeoxia syndrome. A second TTE with bubble study revealed a right-to-left (R->L) shunt suggestive of a patent foramen ovale (PFO) or atrial septal defect (ASD) that was later verified to be a PFO by cardiac MRI. She underwent closure of her PFO and had resolution of her symptoms.
DISCUSSION: The platypnea-orthodeoxia syndrome is characterized by dyspnea (platypnea) and desaturation (orthodeoxia) in the upright position. It requires an anatomic and functional component. The anatomic component is a R->L shunt that may be intra-cardiac (e.g. PFO, ASD) or intra-pulmonary (e.g. arterio-venous malformation or AVM). The functional component allows for intermittent shunting preferentially in the upright position. In the case of ASD/PFO, there are alterations of the atria and/or septum such that R->L blood flow across the shunt, which is minimal in the recumbent position, becomes augmented due to positional alterations (i.e. standing) favoring R->L blood flow. The differential diagnosis of platypnea-orthodeoxia syndrome includes cardiac causes (PFO, ASD, pericardial effusion, constrictive pericarditis), pulmonary causes (emphysema, pulmonary AVM) and GI causes (hepatic cirrhosis, hepatopulmonary syndrome). The treatment is aimed at correcting the source of shunting. One concerning aspect of this case was the extensive work-up that was pursued prior to arrival at a diagnosis that could have been deduced from history and examination. The presence of a R->L shunt was suggested by hypoxemia that was difficult to correct even with supplemental oxygen approaching 100 % FiO2. While both V/Q mismatch and shunt physiology will cause hypoxemia, the hypoxemia in V/Q mismatch will generally correct more easily with supplemental oxygen. In shunt physiology, which may be due to true R->L shunts (e.g. PFO/ASD, pulmonary AVMs) or pulmonary airspace disease with perfusion of unventilated lung (e.g. pneumonia, pulmonary edema), the hypoxemia may require higher percentages of supplemental oxygen or fail to correct even with 100 % FiO2. In this case, the patient had saturation levels of only 88 % during a desaturation episode despite being on 15 L of oxygen. The other features of her presentation, particularly the moment-to-moment changes in symptoms and oxygen requirement, made other causes of shunt physiology, like true airspace filling disease, unlikely. Since a shunt was not considered earlier, her initial standard TTE was a missed opportunity; PFOs and ASDs are often not structurally apparent on a standard TTE unless a bubble study is also done to demonstrate the presence of a shunt.
A DRAMATIC PRESENTATION OF EOSINOPHILIC ESOPHAGITISSaad M. Emhmed Ali. Presence Saint Francis Hospital, Chicago, IL. (Tracking ID #1940150)
LEARNING OBJECTIVE 1: Importance of maintenance of high degree of suspicion for eosinophilic esophagitis as a cause of dysphagia.
LEARNING OBJECTIVE 2: importance of detailed analysis of patient dietary habits in identifying eosinophilic esophagitis associated food allergy.
CASE: A 26-year-old man presented to the emergency department with complaints of dysphagia, nausea and substernal discomfort for 3 h. His symptoms began while he was eating a boneless piece of chicken and he had had the feeling of “food is stuck in my chest.” The patient had a history of food impaction in his esophagus 2 years ago and food particles were removed endoscopically. Otherwise, he did not have a significant past medical or surgical history and he was not on any medications. He had no known allergies and his family history was unremarkable. On physical examination he appeared anxious and was in mild distress. His vital signs were within normal limits except elevated blood pressure (184/107 mmHg). Physical examination was unremarkable otherwise. The initial laboratory tests included CBC with differentiall, basic metabolic panel and liver function tests and all of the parameters were within normal limits. The patient was admitted to general medicine floor for further diagnostic workup. Shortly after admission, he vomited and disimpacted food particles and his symptoms resolved. Esophagogastroduodenoscopy was performed and showed some linear furrows and multiple mucosal nodularities on the upper and mid esophagus without reflux esophagitis. No foreign body was observed. The stomach and duodenum appeared normal. Biopsy specimens from the upper and mid esophagus showed intense eosinophilic infiltration in the esophageal mucosa while biopsy specimens from the stomach and duodenum were normal. Diagnosis of eosinophilic esophagitis (EoE) was made based on the history and endoscopic and histological findings. On further questioning he reported previous episodes of dysphagia with eating chicken. The patient was started on proton pump inhibitors and he was told to strictly avoid chicken or chicken containing food. On discharge, he was referred to an allergist for food allergy testing.
DISCUSSION: In conclusion, EoE is clinicopathologic disorder diagnosed by taking into consideration both clinical and pathologic information without either of these parameters interpreted in isolation. EoE is defined by the following criteria: symptoms related to esophageal dysfunction (i.e., dysphagia, food impaction or regurgitation), eosinophil-predominant inflammation on esophageal biopsy (characteristically consisting of a peak value of >15 eosinophil per high-power field), mucosal eosinophilia isolated to the esophagus and persistence of these findings after a PPI trial and exclusion of secondary causes of esophageal eosinophilia. A response to treatment (dietary elimination; topical corticosteroids) supports, but is not required for, diagnosis When approaching a patient with dysphagia, it is essential to keep EoE in the differential diagnosis. Detailed history plays an important role in timely diagnosis and appropriate management.
A FAMILY AFFAIR: CHOOSING CONTRACEPTION FOR WOMEN AT RISK OF THE PROTHROMBIN MUTATIONHeidi J. Schmidt. University of California, San Francisco, San Francisco, CA. (Tracking ID #1928453)
LEARNING OBJECTIVE 1: Make informed decisions about whether to screen asymptomatic women with a family history of the prothrombin mutation
LEARNING OBJECTIVE 2: Risk stratify contraception choices for asymptomatic carriers of the prothrombin G20210A mutation
CASE: A 25 year-old woman with no past medical history presents to her primary care doctor for a well woman exam. Her sister was recently diagnosed with the prothrombin G20210G >A mutation as a result of a peri-partum DVT. Her only medication is a combined oral contraception pill. She is a non-smoker and has no personal history of thrombosis. Given concern for increased thrombophilia in this young woman taking combined oral contraception, she underwent and screened positive for the prothrombin mutation. Contraception was changed to the levonorgestrel-realeasing intrauterine system to reduce the risk of thrombotic events.
DISCUSSION: The prothrombin mutation has an estimated prevalence of 1–3 % (heterozygotes) in the United States and is most common in Caucasians [1]. This guanine to adenosine mutation in the noncoding region of the pro-thrombin gene is inherited in an autosomal dominant fashion and leads to increased levels of prothrombin, which is then converted to the pro-coagulant thrombin. The prevalence of venous thromboembolism (VTE) in asymptomatic individuals who are heterozygous for the prothrombin mutation AND have a first-degree relative with VTE is 5–7 % [2]. However, the risk of VTE increases 16–59 fold in prothrombin heterozygotes who use oral contraceptives [3]. Given this increased risk, it has been suggested that women with a first degree relative with a prothrombin mutation should be screened in order to inform birth control choices. However, it may also be reasonable to advise alternative forms of birth control WITHOUT testing for thrombophilias given that their risk may be elevated even if testing for thrombophilias is negative [4]. The costs of screening and patient-specific characteristics need to be weighed individually until more data is available. Unopposed oral progestin contraception does NOT increase the risk of VTE in young women [1]. Similarly, the levonorgestrel-releasing intrauterine device does NOT increase the risk of VTE, leading to the consensus that it is also a safe contraceptive option in women with inherited thombophilias including the prothrombin mutation [5, 6]. Women who have a first-degree relative with the prothrombin mutation should use unopposed progestin contraception (or a barrier device) regardless of whether they themselves have been screened for the pro-thrombin mutation. REFERENCES: [1] Varga, E. A., & Kujovich, J. L. (2012). Management of inherited thrombophilia: guide for genetics professionals. Clinical genetics, 81(1), 7–17. [2] Martinelli I, et al. The risk of venous thromboembolism in family members with mutations in the genes of factor V or prothrombin or both. British journal of Haematology 111.4 (2000): 1223–1229. [3] Martinelli I, Taioli E, Bucciarelli P, Akhavan S, Mannucci PM. Interaction between the G20210A mutation of the prothrombin gene and oral contraceptive use in deep vein thrombosis. Arterioscler Thromb Vasc Biol 1999: 19 (3): 700–703. [4] Baglin T, et al. Clinical guidelines for testing for heritable thrombophilia. British journal of haematology 149.2 (2010): 209–220. [5] Van Hylckama Vlieg A, Helmerhorst FM, Rosendaal FR. The risk of deep venous thrombosis associated with injectable depot-medroxyprogesterone acetate contraceptives or a levonorgestrel intrauterine device. Arterioscler Thromb Vasc Biol 2010: 30 (11): 2297–2300. [6] Trenor CC, Chung RJ, Michelson AD et al. Hormonal contraception and thrombotic risk: a multidisciplinary approach. Pediatrics 2011: 127 (2): 347–357.
A GONOCOCAL CONUNDRUM: THE ETHICS AND LIMITS OF PARTNER NOTIFICATION IN CONNECTICUTSheila M. Quinn; Julie R. Rosenbaum. Yale School of Medicine, New Haven, CT. (Tracking ID #1933356)
LEARNING OBJECTIVE 1: Understand and describe the process of reporting sexually transmitted infection (STI) diagnoses to the state Department of Health (DOH).
LEARNING OBJECTIVE 2: Weigh the ethical considerations regarding disclosure when diagnosing a patient with a (STI)
CASE: A 29-year-old male presented with dysuria and penile discharge and was subsequently diagnosed with gonococcal urethritis. Having acquired the STI from an isolated extra-marital encounter, he did not want to tell his wife. We explained the risk to his wife’s health, and encouraged him to disclose the information to her. However, given his continued refusal, we urged him to ensure she received medical care promptly, and felt reassured by our belief in the DOH’s system of partner notification of STIs. However, we learned that our state’s process for contact tracing was different than we expected, and the wife would likely not be notified.
DISCUSSION: In Connecticut, new cases of reportable conditions are sent directly to the state DOH lab. For STI’s there are defining qualifications that prioritize the identification and contact tracing of index patients (Figure 1)*. These currently include any cases of syphilis, the presence of HIV co-infection, men who have sex with men, individuals less than 20 years old, and residents of “core” (high-prevalence) geographic areas. Even among these priority cases, the only patients that currently trigger automatic partner notification services without a physician request are those involving syphilis. High priority cases are contact-traced with the ultimate goal of notifying and treating partners. Non-priority cases are rarely traced unless a physician request is submitted. With our patient’s case not prioritized for partner notification through the DOH, more pressure was placed on us, his providers, to encourage him to disclose, or for us to tell his wife directly. We employed the Four Box method (Figure 2)* to help make our decision. We weighed the risk to the patient’s wife out of our duty to prevent harm, against our duty to our patient’s confidentiality and autonomy. We strongly encouraged the patient to disclose, and in doing so, we preserved his autonomy. The wife had an appointment with a gynecologist, where she ultimately received appropriate care. This case raises the concern that providers may be misinformed about the logistics of partner notification and contact tracing. Providers must understand the legal processes and the accompanying ethical concerns in order to make appropriate disclosure recommendations when contact tracing may not occur. *Figure 1: An algorithmic depiction of the state DOH partner notification system for 2008–2013. *Figure 2: The Four-Box Method of Ethical Analysis
A HYPERCALCEMIC CRISIS OF EPIC (PTH-RP) PORTIONSThomas Wong; Cawin Wong-Mizuba; Kuo-Chiang Lian. University of Hawaii: John A. Burns School of Medicine, Honolulu, HI. (Tracking ID #1935357)
LEARNING OBJECTIVE 1: Recognize the classic constellation of signs and symptoms of hypercalcemic crisis.
LEARNING OBJECTIVE 2: Diagnose and clinically manage patients with humoral hypercalcemia of malignancy (HHM).
CASE: A 65-year-old woman with a past medical history significant for endometrial hyperplasia, diagnosed 6 years prior and treated exclusively by naturopathic medicine, presented to the emergency department with severe abdominal pain, rated 10 out of 10 and lasting for several hours. The patient stated that she had been experiencing similar cramping pain, albeit not as intense, for the past 4 months. She had not had a bowel movement in the past 10 days. The patient had also been experiencing pain in her coccyx making it excruciatingly painful to sit or lay supine. A review of systems was significant for increased frequency of urination, a forty-pound weight loss in the past 4 months, and diffuse muscle weakness in her extremities such that she had difficulty ambulating without the assistance of a walker. Upon evaluation, physical examination revealed a slightly distended abdomen with hypoactive bowel sounds, which was diffusely tender to palpation with multiple palpable firm masses. There was also a fixed, firm, peri-umbilical soft tissue mass consistent with the Sister Mary Joseph nodule. Computer tomography scan of the abdomen revealed a large heterogenous mass within the uterine cavity with extensive metastasis to the peritoneum, sacrum, and right iliac bone. There was no evidence of bowel obstruction. Laboratory results were significant for an elevated calcium level of 15.5 mg/dL. Alkaline phosphatase was normal. Based on the patient’s constellation of signs and symptoms, the patient was diagnosed with hypercalcemic crisis secondary to stage IV endometrial cancer. The patient was admitted to the telemetry unit for monitoring of possible cardiac arrhythmia. EKG revealed normal QTc, and she had no events on monitor. Aggressive hydration with normal saline was administered. Once the patient was fluid replete, furosemide was initiated on the second hospital day. A serum Parathyroid hormone related protein (PTH-rP) level was ordered to: 1) diagnose a component of humoral hypercalcemia of malignancy (HHM) responsible for the patient’s high serum calcium given normal alkaline phosphatase; and 2) help guide therapy since studies have shown zoledronic acid to be more effective than other bisphosphonates in lowering calcium levels in HHM. The PTH-rP returned elevated at 77 pg/dL. Over the course of hospitalization, the patient’s calcium level returned to normal and the patient’s symptoms improved. In accordance with the patient’s wishes, a palliative care plan was instituted for discharge.
DISCUSSION: This case is a classic example of hypercalcemic crisis, which when recognized promptly can lead to early interventions that prevent the life-threatening consequences of elevated serum calcium. Moreover, as a review of the current literature suggests, this patient suffered from a rare example of humoral hypercalcemia of malignancy due to advanced endometrial cancer. THe PTH-rP responsible for this paraneoplatic syndrome has been recognized as a product of hyperplastic endometrial cells. Serum PTH-rP levels, in addition to its diagnostic value can play a role in guiding therapeutic options for hypercalcemia of malignancy. Furthermore, research interest continues to grown in the potential role of PTH-rP as a tumor marker and as a prognostic indicator of median survival time and response to bisphosphonate therapy. Hopefully, the knowledge gained from these studies will help guide future management of such challenging oncologic cases.
A MASS OF MUCORDevika Nair; Sarah Moore; Deepa Bhatnagar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924929)
LEARNING OBJECTIVE 1: Recognize that Mucormycosis should be suspected in patients with diabetic ketoacidosis, sinusitis, and evidence of thrombosis.
LEARNING OBJECTIVE 2: Discuss the management and complications associated with Mucormycosis
CASE: A 21-year-old man with Type 1 diabetes presented with a four-day history of unilateral blurry vision and rhinorrhea. Vital signs consisted of a temperature of 97 F, heart rate of 118 beats/min, respirations of 22/min, blood pressure of 166/108 mmHg, and oxygen saturation of 98 % on room air. He had proptosis of his left eye and a fixed and dilated left pupil. Extra-ocular movement testing showed a palsy of cranial nerves two, three, four, and six of his left eye. The patient also exhibited tenderness over his sinuses bilaterally. Right eye movement was normal. Laboratory findings were suggestive of diabetic ketoacidosis with a glucose above 500, pH of 7.0 and an elevated anion gap. MRI of the brain with and without contrast revealed cavernous sinus thrombosis as well as thrombi of the left ophthalmic vein and artery. Given the presence of cavernous sinus thrombus in the setting of diabetic ketoacidosis, invasive fungal infections were chief on the differential. The patient was started on fluids, heparin, and insulin, and intravenous amphotericin B, followed by debridement of the infected tissue. Pathology confirmed invasive mucormycosis caused by Mucor. On hospital day three, the patient experienced a hemorrhagic stroke, likely due to septic emboli. Due to this complication, anticoagulation had to be withheld. Despite further treatment and optimization of medical management, the patient passed away due to complications of his stroke.
DISCUSSION: Diabetes is one of the most common illnesses in the United States, and patients with Type 1 diabetes are more prone to developing diabetic ketoacidosis. Acidosis and hyperglycemia have been shown to impair phagocyte function. Moreover, acidosis disrupts the ability of transferrin to bind iron, a growth factor for many bacteria. Malignant otitis externa, bacterial sinusitis, and invasive fungal infections are some of the most common head and neck infections that occur in diabetic patients. However, the presence of carotid artery occlusion or cavernous sinus thrombosis suggests the presence of an invasive fungal infection. In such patients, fungal infections can present as rapidly-progressive rhino-orbital-cerebral disease, most commonly caused by Rhizopus, Absidia, or Mucor. Prompt diagnosis is imperative, as overall mortality ranges from 30 to 70 %. Treatment consists of intravenous amphotericin B and surgical debridement. Our patient experienced one of Mucor’s most feared complications: spread to the cavernous sinus causing thrombosis. Current practice supports the early use of antifungals. Anecdotal evidence points to a benefit of corticosteroids to reduce orbital inflammation, but the risks of this must be weighed in the setting of sepsis. The decision to anti-coagulate is more controversial, as septic emboli are an important cause of mortality. Case reports suggest that anticoagulation is most beneficial in earlier stages of the disease. All studies indicate that early recognition is paramount to treatment, and our case highlights a number of the challenges in management.
A MASSIVE DVT IN A PATIENT WITH ULCERATIVE COLITIS ON ADALIMUMABReuben Abraham; Craig Gluckman; Todd B. Linden. Beth Israel Medical Center, New York, NY. (Tracking ID #1934956)
LEARNING OBJECTIVE 1: Recognize that venous thromboembolic disease may be an adverse effect seen in patients treated with adalimumab for ulcerative colitis
CASE: We present a 61 year old female with a massive DVT, which was first appreciated approximately 2 weeks after beginning therapy with adalimumab for steroid refractory ulcerative colitis (UC). The patient has a history of UC for the past 9 years. She had none of the co-morbid risk factors seen in most reports of DVT in IBD. Her physical exam was normal except for marked swelling of her right lower extremity to above the knee. A CT scan of the chest was negative for PE but her abdominal/pelvic CT showed an intraluminal thrombus within the right deep and superficial femoral veins which propagated superiorly into the IVC. Colonoscopy showed pancolitis which was severe on the left and mild in the proximal colon.
DISCUSSION: While thrombo-embolic events are a widely recognized complication of inflammatory bowel disease, they are rare in the absence of overt risk factors. Although the package insert for adalimumab does list “thrombosis leg” in the section “Less Common Adverse Reactions in Rheumatoid Arthritis Clinical Studies” and “deep vein thrombosis” in the section “Post marketing Experience”; the incidence of these events appears to be exceedingly low. The US FDA Adverse Events Reporting System lists 325 “adalimumab related thrombosis adverse events”. Seventy-eight were in patients with Crohn’s and 13 were in patients with UC. Published data on adalimumab in Crohn’s and UC in IBD do not describe any DVT in 6944 patients (12,925 patient-years). Data from adalimumab use in multiple trials of different autoimmune disease did not report DVT in 23,458 patients. The finding of a DVT in a patient with Ulcerative Colitis on adalimumab has not been previously described in the literature. There are 13 reports in the FDA adverse events database but none have been published. Our patient did not have any of the overt risk factors that are almost always associated with thromboembolic disease in IBD. In addition, the temporal association of an approximately 10 day lag between initiation of adalimumab therapy and onset of lower extremity edema is highly compelling. We recommend that although the incidence of this complication must be vanishingly small, clinicians be aware that it is a possibility that should be considered if appropriate symptoms appear after initiation of therapy with adalimumab.
A MIMIC OF A RHEMATOID ARTHRITIS FLAREPaul Koffer; Zachary D. Horne; Benjamin Lloyd. Reading Hospital, West Reading, PA. (Tracking ID #1938324)
LEARNING OBJECTIVE 1: Recognize the potential for polyarticular septic arthritis in a patient with rheumatoid arthritis
CASE: A 63 year old women with a past medical history of severe Rhematoid Arthritis (RA) with bilateral metacarpal (MCP) prostheses on chronic prednisone presented to the emergency department with pain, stiffness, and warmth of her 1st and 2nd MCP joints of the left hand, the 3rd through 5th MCP joints of the right hand, and left ankle. The patient had complained of subjective fevers and chills over the past 2 days and stated the symptoms were similar to her previous RA flares. Her temperature was 37.3° Fahrenheit, heart rate was 90 beats/min, and she had a white blood cell count of 7.5 (nl: 4.8–10.80 cmm). On physical exam, she had warmth, erythema, swelling, and mildly decreased range of motion of the 1st and 2nd MCP joints of the left hand, the 3rd through 5th MCP joints of her right hand as well as swelling and warmth around the medial malleolus of the left ankle. The patient had been seen earlier in the day by her rheumatologist who took an aspiration of her 1st left MCP joint and increased her prednisone dose for a presumed RA flare. The patient was given 125 mg IV solumedrol in the emergency department for presumed RA flare and started on Vancomycin until septic arthritis could be ruled out. The left MCP joint aspiration grew Methicillin Sensitive Stapholococcus Aureus (MSSA) as did blood cultures and the patient was switched to Cefazolin. The patient’s left ankle was aspirated during her hospitalization which was also positive for MSSA. Patient was also found to have bilateral paraspinal abscesses on MRI of the lumbar spine during the hospital admission. The paraspinal abscesses were drained and cultures were positive for MSSA. The patient was discharged home after her hospitalization to complete a 42 day course of antibiotics.
DISCUSSION: This case demonstrates the potential for polyarticular septic arthritis superimposed on chronic RA. It is critical to keep your clinical suspicion for septic arthritis high in the setting of patients with RA even when the initial clinical presentation is suggestive of an RA flare, as the mortality of polyarticular septic arthritis in patients with RA has been reported to be as high as 50 % (1). Fifteen percent of all patients with septic arthritis have involvement of two or more joints and case series suggest that more than 50 % of patient with polyarticular septic arthritis suffer from underlying RA (1). Other factors predisposing patients to polyartcicular septic arthritis are bacteremia from a secondary cause, immunosuppression, and prosthetic joints and clinical suspicion should be raised in these patient populations. (1) Dubost, J. J., I. Fis, P. Denis, R. Lopitaux, M. Soubrier, J. M. Ristori, J. L. Bussiere, J. Sirot, and B. Sauvezie. “Polyarticular septic arthritis.” Medicine 72, no. 5 (1993): 296.
A MISLEADING PRESENTATION OF HYPERSENSITIVITY PNEUMONITISNadia D. Ali; Darlene LeFrancois. Montefiore Medical Center, New York City, NY. (Tracking ID #1928197)
LEARNING OBJECTIVE 1: Review the utility of measuring serum troponin and creatine kinase levels in the diagnosis of acute myocardial infarction as well as other cardio-pulmonary etiologies.
LEARNING OBJECTIVE 2: Diagnose hypersensitivity pneumonitis based on a collection of history, physical and radiographic data.
CASE: A 51 year old female with a history of seasonal allergic rhinitis, no known chronic respiratory or cardiac disease presented with progressive dyspnea, chest tightness, and post-tussive emesis for 1 day. Patient reports severe shortness of breath and multiple episodes of post-tussive emesis that began several hours prior to admission. On arrival she was found to be hypoxic to 88 %, tachypneic and moderately hypertensive. Troponin T levels were elevated to 1.38 ng/ml with concordant CK-MB to 36.7 mg/ml. Mild kidney injury with creatinine elevated to 1.6 mg/dl up from 1.1 1 year ago. No EKG changes. Cardiac exam was remarkably normal with no volume overload. V/Q scan and echocardiogram were normal. Lung exam was significant for crackles halfway up both lung fields that remained unchanged after administration of IV furosemide. Throughout her stay serum troponin and CK-MB remained elevated. A CT thorax showed diffuse bilateral centrilobular ground glass pulmonary nodules with focal ground glass and small patchy bilateral alveolar infiltrates as well as small mediastinal lymph nodes. Further history indicated that patient had progressive worsening dyspnea on exertion for the past 1–2 months. Notably patient’s place of employment was under construction to rebuild after hurricane Sandy. Pulmonary function tests revealed mild restrictive disease with no bronchodilator response and a reduced DLCO of 36 %. A transbronchial lung biopsy revealed chronic inflammation with a proliferation of lymphocytes, plasma cells, histiocytes, eosinophils and type II pneumocytes hyperplasia consistent with hypersensitivity pneumonitis. On day five following bronchoscopy patient was started on high dose, slow prednisone taper and discharged. Patient followed up outpatient continued to improve clinically and on repeat pulmonary function testing.
DISCUSSION: Serum biomarkers including troponins and creatine kinase - MB are used to confirm the diagnosis of a suspected acute myocardial infarction. Two criteria are important to fulfill, an elevation above the 99th percentile of normal and a rise or fall in troponins in at least two serum levels 6 h apart. Troponin levels begin to rise 2–3 h after infarction, peaking in 1–2 days depending on the size of the infarct followed by a reliable downward trend. A persistent elevation in troponins without evidence of a rise or fall and lack of EKG or echocardiogram abnormalities indicates the need for further work to explain the troponemia. Multiple disease processes have been described with an inexplicable rise in troponins. One theory is that troponin release in the absence of necrosis may occur in conditions that produce increased myocyte membrane permeability. There are 3 ways to classify non-ACS tropinemia: Myocardial damage related to 1) secondary myocardial ischemia (i.e. pulmonary embolism, heart failure); 2) non-ischemic causes (i.e. kidney disease and inflammatory syndromes such as sepsis, myocarditis and hypersensitivity pneumonitis); or 3) multifactorial causes. Hypersensitivity pneumonitis (HP) is a well described disease with a broad spectrum of clinical presentation and severity. The classic clinical finding is progressive cough and shortness of breath with exposure to an offending antigen which can be acute, sub-acute or chronic. Diagnosis is based on history, clinical exam and either bronchoscopy or high resolution CT thorax. Although it is primarily a pulmonary disease it is an inflammatory disorder and can be mistaken for a primary cardiac etiology.
A NIGHT OF EXCESS LEADS TO A NEAR DEATH EXPERIENCEYoo Mee Shin. Emory University, Atlanta, GA. (Tracking ID #1938877)
LEARNING OBJECTIVE 1: Review the physiology of Wolff-Parkinson-White syndrome and its associated risk of tachyarrhythmias.
LEARNING OBJECTIVE 2: Recognize that recreation drug abuse is associated with arrhythmias.
CASE: 38 year old male was brought to the emergency department after being found unresponsive by his wife. EMS found the patient unresponsive and in ventricular tachycardia at his house. He underwent cardiac defibrillation and returned to sinus rhythm. He was given naloxone and was transported to the emergency department. He denied chest pain, palpitations, or shortness of breath prior to the event. Medical history was negative and social history was notable for a new, unknown recreational drug that he took prior to the event. Blood pressure was 144/81, heart rate was 100, respiratory rate was 6–12 breaths/min and oxygen saturation was 100 % on nonrebreather mask. Patient was somnolent but oriented. He had regular rate and rhythm with no murmurs or gallops. The rest of the physical examination was unremarkable. Initial venous blood gas showed respiratory acidosis with pH of 7.17 and PCO2 of 76 mmHg. Urine drug screen was positive for opiates and cocaine. Troponin levels were normal. EKG showed sinus tachycardia and an accessory pre-excitation pathway. He underwent an electrophysiology study that confirmed Wolff-Parkinson-White (WPW) syndrome and had a successful ablation procedure.
DISCUSSION: Wolff-Parkinson-White syndrome (WPW) is a pre-excitation syndrome that develops from the presence of an abnormal accessory pathway between the atria and ventricles. It is most classically known to increase the risk of developing an atrioventricular reentrant tachycardia as the accessory pathway is utilized in the origination and propagation of the arrhythmia. The incidence of WPW is between 0.1 % and 0.3 % in the general population. Albeit rare, it is associated with sudden cardiac death due to tachyarrhythmias with an incidence of less than 0.6 %. In our case, ventricular tachycardia as a presenting arrhythmia in a healthy person without structural heart disease would be highly unusual, even in the presence of WPW. However, recreational drug use likely contributed to this patient’s presentation. Cocaine induces a hyperadrenergic state and blocks sodium channels blockade which can lead to ventricular arrythmias. Cocaine induces a hyperadrenergic state and blocks sodium channels blockade which can lead to ventricular arrythmias. Narcotics increase parasympathetic activity, reduce sympathetic activity, and release histamine from mast cells. This produces bradycardia and enhanced automaticity which can precipitate an increase in ectopic activity, atrial fibrillation, or ventricular tachyarrhythmias. In turn, WPW significantly increases this patient’s arrhythmogenic potential due to the presence of the accessory pathway and localized ion channel blockade. Our case illustrates two important points. First, recreation drug use is associated with cardiac arrhythmias via multiple mechanisms. Second, WPW increases the risk for other arrhythmias beyond supraventricular tachycardias. The dual-hit of drug overdose and WPW can potentiate the risk for serious arrhythmias and sudden cardiac death.
A NON-HEALING WOUND THAT IS NOT SKIN CANCER!Maen Abdelrahim1,2; Glynda Caga-anan1,2. 1Baylor College of Medicine, Houston, TX; 2Michael E. Debakey VA Medical Center, Houston, TX. (Tracking ID #1938953)
LEARNING OBJECTIVE 1: Recognize that cutaneous metastases from hepatocellular carcinoma (HCC) can be the first clinical sign of HCC
LEARNING OBJECTIVE 2: Recognize the different cutaneous manifestations of hepatocellular carcinoma
CASE: Mr. W is a 66 y.o. white man who presented with a 6 month history of a rapidly growing abdominal wound and abdominal pain. He has a history of myeloproliferative disease (MPD) and had a prior ventral hernia repair in 2001, which was complicated by an infected mesh later removed in 2004, with the abdominal wound allowed to heal by secondary intention. His wound persisted since but eventually decreased to approximately 4 cm × 4 cm in size. Over the past 6 months, the wound progressively enlarged, associated with new purulent drainage and worsening right upper quadrant abdominal pain. Exam showed an obese, soft abdomen, with tenderness at the right upper quadrant. A 14 × 14 cm supraumbilical wound was present, with mild bleeding and purulent discharge. Laboratory data showed leukocytosis (30,000/cmm) and thrombocytosis (993,000 /cmm) which were greatly above Mr. W’s chronically elevated baseline levels due to his underlying MPD. Alkaline phosphatase was also elevated at 270 IU/L. CT abdomen showed multiple hypodense, poorly defined liver lesions, concerning for hepatic abscesses versus metastatic squamous cell skin cancer (SCC), seeding from the wound. Broad spectrum antibiotics were begun. The fine needle aspiration of the liver masses were consistent with hepatocellular carcinoma (HCC), an unexpected finding in this patient who does not have a history of cirrhosis, viral hepatitis, or past alcohol abuse. Liver mass cultures remained negative. The abdominal wound pathology showed metastatic poorly differentiated carcinoma, with similar morphology to the liver findings. His carcinoembryonic antigen (CEA) was 1.55, and alpha fetoprotein (AFP) was 1.4. The wound culture grew pseudomonas aeruginosa, treated with 14 days of meropenem. After a multidisciplinary tumor board discussion, the conclusion was made that the morphological and immunohistochemistry aspect of the liver biopsy and abdominal wound biopsy were more likely consistent with poorly differentiated, metastatic hepatocellular carcinoma, with Mr. W’s future treatment to include sorafinib.
DISCUSSION: Hepatocellular carcinoma (HCC) most often metastasizes to the lungs, abdominal lymph nodes, or bone (1). Cutaneous metastases from HCC are very rare but can be the first clinical sign of HCC (6,8). Prior reports have described these skin lesions to be rapidly growing, firm, painless, nonulcerative, 1–2.5 cm nodules, found mostly on the face, scalp, chest, and shoulders (1,2). These lesions may appear singly or in multiples. Some lesions have a pyogenic granuloma-like or a hemangiomatous character (1,3). In one study (4), skin metastases were shown to account for only 2.7 % of cirrhotic HCC’s with no cases found in noncirrhotic HCC (like our case). There have been reports of cutaneous metastases due to direct implantation from a procedure, such as a biopsy or ablation of HCC. One report (5) described a nodule presenting at the injection site of a percutaneous ethanol injection therapy performed 3 months previously. Here, we report HCC metastasizing to a chronically unhealed abdominal wound. Usually, a non-healing wound transforms into squamous cell skin cancer. The possibility of skin metastases should be considered in patients with HCC who present with new skin nodules or non-healing wounds, with diagnosis later confirmed by biopsy. In our review of the literature, this is the first reported case of metastatic HCC to a non-healing skin wound.
A NOVEL CASE OF CRYPTOCOCCAL IMMUNE RECONSTITUTION INFLAMMATORY RESPONSE SYNDROME IN A PATIENT WITH MULTIPLE SCLEROSISHeena A. Birbal Jain; Jacquilene Fischer; Saurabh K. Bansal. University of illinois college of Medicine at Peoria at Saint Francis Medical center., Peoria, IL. (Tracking ID #1901785)
LEARNING OBJECTIVE 1: Recognition of Cryptococcal Immune Reconstitution Inflammatory Response Syndrome associated with natalizumab
CASE: A 49 year male, on natalizumab the past 2 years for multiple sclerosis, presented with progressive weakness, headache and vomiting. Magnetic resonance imaging (MRI) of the brain revealed chronic multiple sclerosis-consistent findings without change since prior study. Cerebrospinal fluid (CSF) analysis showed white blood cells (WBC) 12/mm3 (67 % lymphocytes), protein 63 mg/dl and positive cryptococcal antigen. Both CSF and blood cultures grew Cryptococcus neoformans. CSF was negative for JC virus, West Nile virus and herpes simplex 1 and 2. Serum HIV and hepatitis serologies were negative. A diagnosis of cryptococcal meningitis was made. The meningitis was felt related to the immune suppressant effects of natalizumab. Natalizumab was discontinued and a 28 day course of amphotericin and flucytosine was given. Substantial clinical improvement occurred and the patient was discharged to home on daily oral fluconazole. At discharge, CSF cryptococcal antigen titer was 1:512. One month later the patient was rehospitalized with unilateral ptosis, left sided facial droop and transient dysarthria. MRI brain showed new areas of enhancement in the perivascular spaces, right occipital lobe, right calcarine gyrus, left occipito-parietal confluence, and leptomeninges. CSF cryptococcal titre had decreased to 1:128 but both the CSF protein (85 mg/dl) and WBC (35/mm3) had increased. The patient was diagnosed with immune reconstitution inflammatory response syndrome (IRIS) associated cryptococcal meningitis; the IRIS being attributed to the recent discontinuation of natalizumab. Treatment with methylprednisolone, amphotericin and flucytosine was given and the patient’s clinical symptoms improved. At the completion of this second treatment course, CSF cryptococcal antigen titer had fallen to 1:64.
DISCUSSION: Immune reconstitution inflammatory syndrome (IRIS), first described in the early 1990s, is seen most classically in HIV patients following initiation of highly active antiretroviral therapy (HAART). HAART-related immune recovery may result in a heightened inflammatory host response toward any harbored pathogens. Natalizumab is a humanized antibody against alpha-4 integrin receptors and is FDA approved for multiple sclerosis and Crohn’s disease. We believe our patient experienced IRIS upon the discontinuation of his natalizumab. Despite the successful initial treatment of our patient’s cryptococcal meningitis, he was rehospitalized with progressive cryptococcal disease as evident by worsening neurologic, CSF, and imaging findings. Because the CSF cryptococcal titer at this time had fallen, we feel that natalizumab-discontinuation IRIS best explains the clinical features seen. To our knowledge, ours is the first reported case of cryptococcal meningitis as associated with natalizumab-discontinuation IRIS. Review of the literature revealed no cases of cryptococal meningitis or cryptococcal IRIS as associated with natalizumab. Data from the phase III randomized trial of natalizumab safety and efficacy in relapsing remitting MS (AFFIRM) yielded no information about cryptococcal meningitis as an adverse event of treatment.
A PARADOXICAL MANIFESTATION OF BACLOFEN TOXICITYRachel Jantea. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1939449)
LEARNING OBJECTIVE 1: Recognize an unusual sign of baclofen toxicity
LEARNING OBJECTIVE 2: Identify patients at increased risk of renal insufficiency, and therefore baclofen toxicity
CASE: An 84 year old Caucasian male presented to his PCP with new onset neck pain, for which he was prescribed acetaminophen 1 g orally three times daily, in addition to as-needed diclofenac 75 mg orally up to twice daily and baclofen 10 mg orally up to twice daily for neck pain. The patient proceeded to take all three medications in a scheduled manner. Three days later, he was brought to the emergency department by his daughter with complaint of confusion and abnormal movements. On exam, the patient was hemodynamically stable. He was slightly confused and oriented only to person. His neck was supple but mildly tender to palpation of the paraspinal muscles. He exhibited irregular involuntary purposeless jerking movements of the face, mouth, neck, shoulders, and upper extremities, characterized by repeated flexion and extension of the arms and neck, head turning, and shoulder shrugging. He did not have increased tonicity on passive movement of the extremities, and the remainder of the neurologic exam was unremarkable. CT head and MRI brain were unremarkable, and basic labs revealed acute renal insufficiency with a BUN/Cr of 38/2.2 (GFR 26 by Modification of Diet in Renal Disease formula) up from his baseline of 14/1.1. Diclofenac and baclofen were both discontinued, and acetaminophen was continued for pain control. He was given IV fluids for hydration in the setting of renal insufficiency. Over the next 3 days, the patient’s renal insufficiency resolved, his mental status returned to baseline, and the abnormal movements diminished and subsequently disappeared.
DISCUSSION: Baclofen is a GABA-agonist used as a muscle relaxant to treat spinal spasticity among other things. Baclofen withdrawal has widely been associated with dyskinesias and other neurologic manifestations. However, baclofen toxicity has only rarely been reported to result in movement disorders, a peculiar effect for a muscle relaxant. Usual signs of baclofen toxicity include central nervous system depression, confusion, hypotonia, ataxia, and hypotension. The present case was characterized by the more typical altered mental status, but also exhibited the unusual and paradoxical manifestation of dyskinesia. Movement disorders secondary to baclofen toxicity have rarely been reported in the literature, and when reported, have mostly been associated with intrathecal baclofen treatment of complex regional pain syndrome and/or dystonia. This case was unique in that it occurred with use of oral baclofen and in a previously neurologically normal patient. Baclofen is 90 % renally excreted, and toxicity when reported, has largely occurred in the context of renal insufficiency. Most case reports of baclofen toxicity in the setting of renal failure involve patients with known chronic kidney disease on or off hemodialysis. The patient in the present case had a previously normal GFR, and was found to have acute renal insufficiency secondary to NSAID-induced nephropathy at the time of presentation. There is one report of oral baclofen toxicity in a patient with partial spinal cord injury occuring in the setting of ibuprofen-induced renal insufficiency. However, the manifestations were more typical, including altered mental status and hypotension, and again, this occurred in a patient with a prior neurologic disorder. This unusual presentation of baclofen toxicity illustrates the importance of recognizing that baclofen is renally excreted, and renal function should be assessed prior to initiating this drug. Furthermore, it should be used cautiously in patients with chronic renal insufficiency or patients at increased risk of renal insufficiency, especially geriatric patients and patients using nephrotoxic drugs, such as NSAIDs. This is an especially important point, in treating patients with spinal musculoskeletal symptoms, when baclofen and NSAIDs are commonly co-prescribed, as in this case.
A PATIENT WITH PRURITIS, EOSINOPHILIA, AND A PAINFUL RED EARMorgan Soffler; Christopher Sankey. Yale New Haven Hospital, New Haven, CT. (Tracking ID #1939267)
LEARNING OBJECTIVE 1: 1. Establish a differential for pruritus and eosinophilia.
LEARNING OBJECTIVE 2: 2. Understand the diagnostic strategy for cutaneous T-cell lymphoma. 3. Recognize polychondritis as a potential manifestation of hematologic malignancy.
CASE: Mr. F is an 84 year-old man with a history of atrial fibrillation and stroke who presented with a 2-month history of failure-to-thrive and pruritus. Mr. F reported poor appetite accompanied by a 10-lb weight loss. He had not been taking his medications, which included Coumadin and aspirin. His pruritus began 2 months prior to presentation and was associated with an erythematous rash on his chest and back, though the pruritus was diffuse. He tried steroid cream and Benadryl without effect. A review of systems was otherwise notable for fatigue, global weakness, and depressive symptoms. His exam was notable for a temp of 96.1 F, heart rate of 84, BP of 112/76, respiratory rate of 14 with an O2 sat of 95 % on room air. He was cachectic with temporal wasting. His abdomen was scaphoid without organomegaly. Lymph node examination revealed a 1-cm, non-tender, mobile, left-sided axillary lymph node. Neurologic exam revealed diffuse weaknes. On skin exam there was an erythematous, non-blanching, maculopapular rash on his chest and back. Initial lab results revealed WBC 4.6 with 19 % eosinophilia, hematocrit 25, MCV 105, platelets 250, creatinine 0.7, ESR > 120, ferritin 1350 and prealbumin 3.3. Urinalysis was bland. Blood smear revealed macrocytosis with increased eosinophils. On repeat CBC, eosinophilia increased to 30 %. His rash had resolved prior to biopsy, however, an area of inflammation on his forearm was biopsied which showed non-specific inflammation. Work-up for eosinophilia included a negative stool O&P, negative strongyloides antibody, and mildly elevated IgE level. A bone marrow biopsy revealed hypercellular myeloid-predominant marrow with eosinophilia. T cell lymphocytes ratios revealed CD4+/CD8+ elevated at 22. There were no monoclonal T cells or T-cell re-arrangements. Given the elevation in CD4+/CD8+ ratio, a presumptive diagnosis of Cutaneous T Cell Lymphoma (CTCL) was made. Several days into hospitalization, Mr. F developed a painful, swollen, left ear with sparing of the ear lobe. On further history, he reported he had swelling of his ears on and off for several months, suspicious for relapsing polychondritis.
DISCUSSION: Mr. F’s presentation was highly concerning a systemic catabolic and inflammatory process such as malignancy. In formulating a differential diagnosis for this patient, pruritis and eosinophilia were findings useful in directing our work-up. The approach to the differential diagnosis of eosinophilia (defined as a eosinophils >500cells/microL) involves broad categorizations including infection, allergic disorders, hematologic malignancies, and rheumatologic disorders. A negative parasite work-up eliminated infection as our primary suspicion. A mildly elevated IgE and low tryptase level made an allergic process less likely. An ANA of <1:40 was inconsistent with rheumatologic disease. Hematologic malignancy was left as the likely cause of Mr. F’s wasting syndrome, inflammatory process, and eosinophilia. An elevated CD4+/CD8+ gave rise to the concern of a T-cell lymphoma. Cutaneous T-cell lymphoma is a form of non-Hodgkin’s lymphoma that is caused by a mutation of T cells that migrate to the skin. Pruritis is the most common presenting symptom. Other clinical signs of CTCL include lymphadenopathy and visceral involvement. Pathologic features can be found in skin biopsy, lymph node biopsy, and peripheral blood. Skin biopsy findings are often non-specific but include T-cell inflammation and clonality of TCR gene rearrangement. Lymph nodes can show anything from non-specific reactive changes to frank lymphoma. “Sezary cells” on blood smear are described as large atypical mononuclear cells with grooved nuclei. TCR gene rearrangement clonality is also suggestive of CTCL. Diagnosis is based on clinical, pathologic, and hematologic factors. Recurrent red swollen ears raised suspicion for Relapsing Polychondritis (RP). Relapsing polychondritis is an immune-mediated condition associated with inflammation of cartilage, most often within the ear. Approximately 1/3 of RP cases are associated with a systemic process. The association between RP and CTCL has been examined in the literature, though the more common hematologic process associated with RP is myelodysplastic syndrome. CONCLUSION: In patients with pruritus and eosinophilia with evidence of systemic inflammation, hematologic malignancies such as CTCL should be considered. In cases with diagnostic uncertainty, a thorough history may reveal symptoms, as in our case evidence of polychondritis, which may further support the clinical suspicion of hematologic malignancy.
A PUZZLING CASE OF HYPOCALCEMIA!Venu M. Ganipisetti; Hitu Khaira; Samaneh Dowlatshahi; Pratyusha Bollimunta; Sanjolee Mangat; Erica Sinsheimer. Presence Saint Francis Hospital, Evanston, IL. (Tracking ID #1927988)
LEARNING OBJECTIVE 1: Recognize that Pseudohypoparathyroidism can present with life-threatening complications like seizures and bronchospasm, due to severe hypocalcemia. Hence, early diagnosis and treatment are warranted.
LEARNING OBJECTIVE 2: Recognize that bilateral basal ganglia calcification is one radiological feature that can be associated with pseudohypoparathyroidism.
CASE: A 24-year-old Hispanic male presented to our Emergency Department with multiple syncopal episodes over a period of 2 days. Witnesses reported that he was violently shaking all his limbs during the episodes, which lasted about 20 s each. Patient had no recollection of any of these events. No postictal confusion, bowel or bladder incontinence, or tongue-biting were reported. His past medical and family histories were noncontributory. He reported a three-year history of difficulty lifting heavy objects along with pain and cramping in his hands and arms with repetitive use. Initial labs revealed severe hypocalcemia (calcium level-5.6, ionized calcium-0.55) and hyperphosphatemia (phosphorus levels-6.1). Remaining lab tests including urine toxicology and alkaline phosphatase were normal. Physical exam was normal except for reportedly positive Trosseau and Chvostek signs. A CT of the head revealed bilateral, symmetric and diffuse calcification in the basal ganglia and the dentate nucleus of cerebellum, otherwise negative. A further workup showed elevated PTH (157), low 25-OH Vitamin D (15.5), and low 24-hour urine calcium. He received a preliminary diagnosis of pseudohypoparathyroidism with a coexisting Vitamin D deficiency. Patient was started treatment on both IV and PO supplemental calcium, and ergocalciferol. Despite ongoing supplementation of calcium, he continued to experience these seizure-like episodes for the next few days. The sleep deprived and extended EEGs were negative. Calcitriol and Keppra were later added to the treatment plan. The patient stopped having any further episodes on day 10 of admission, and his calcium levels reached the near normal range.
DISCUSSION: The main differential diagnoses for hypocalcemia in our patient were a Vitamin D deficiency and PTH resistance. With normal alkaline phosphatase, elevated phosphorus levels, and a lack of symptoms associated with osteomalacia, a Vitamin D deficiency was unlikely the sole cause of hypocalcemia. The presence of hyperphosphatemia, hypocalcemia and elevated PTH with normal morphologic features, points more to a diagnosis of PHP type 1b or type 2. Also, bilateral basal ganglia calcification is one radiological feature that can be associated with pseudohypoparathyroidism and might suggest that he had this condition for a long time. Pseudohypoparathyroidism (PHP) is a rare, heterogeneous group of disorders characterized by hypocalcemia, hyperphosphatemia, and increased PTH. This condition is caused by a dysfunctional Gs protein at the receptor level, conferring resistance to the biologic activity of PTH. There are three known subtypes of PHP—types 1a, 1b, and 2. Type 1a is characterized by morphologic abnormalities, whereas the other two subtypes are not. In this condition, hypocalcaemia can often present with life threatening complications like seizures, bronchospasms, laryngospasms, and arrhythmias. Hence, early diagnosis and prompt treatment are essential. The treatment usually consists of maintaining calcium levels to near normal with supplemental elemental calcium, along with an active form of Vitamin D analogue. A close outpatient monitoring of calcium levels is recommended.
A RARE CASE OF ATAXIA AND RAPIDLY PROGRESSING DEMENTIASara Patrawala1; Maryam Soltani1; Mara Zulauf2. 1UCSD, San Diego, CA; 2VA Healthcare System, San Diego, CA. (Tracking ID #1934106)
LEARNING OBJECTIVE 1: Recognize Creutzfeldt-Jakob Disease (CJD) and its variant forms
LEARNING OBJECTIVE 2: Counsel and assist in end-of-life care in fatal neurodegenerative diseases
CASE: A 69-year-old male veteran with a history of diabetes and cardiovascular disease presented to the hospital with a several week history of slurred speech and imbalance and was admitted to the neurology service for an acute stroke evaluation. Vital signs were normal. Neurologic exam revealed decreased attention, left-sided pronator drift, abnormal coordination, peripheral neuropathy and an unsteady, broad-based gait. CT head and basic laboratory results were unremarkable. The patient’s presenting symptoms improved with hydration and he was discharged home. Two weeks later, he returned to the hospital with perceived left-sided weakness, multiple falls, confusion and word-finding difficulties. His examination revealed impaired language output, a child-like affect and truncal ataxia. Reversible causes of dementia and polyneuropathy including vitamin and mineral deficiencies, HIV infection, multiple myeloma and auto-immune diseases were ruled out. The neurology consultants were concerned for a heritable ataxia and recommended outpatient genetic testing. Three weeks later, the patient presented to the hospital with altered mental status and uncontrollable jerking. Neurologic exam revealed significant decline in speech production with inability to communicate within several days, and startle myoclonus in response to sound and touch. Electroencephalography (EEG), cerebrospinal fluid (CSF) testing for infectious etiologies and pan-CT imaging were unrevealing. An MRI was unable to be performed due to the presence of a pacemaker. His hospitalization was complicated by respiratory failure, myocardial infarction, arrhythmia, sepsis and progressive neurologic decline. In accordance with his family’s wishes, he was transitioned to comfort care and passed away just over 2 months after his initial presentation. Given the sub-acute decline in the patient’s neurologic status with startle myoclonus and an otherwise unremarkable work-up, a diagnosis of CJD was suspected. Prion disease was later confirmed when 14-3-3 and tau proteins were discovered in his CSF. Final autopsy results are pending.
DISCUSSION: CJD is a fatal neurodegenerative disease caused by the accumulation of pathologic prion proteins in neuronal tissue with a prevalence of one case per million population. Classically, patients present with progressive dementia accompanied by startle myoclonus and mood lability with eventual progression to akinetic mutism and death. Most cases are sporadic but familial and iatrogenic cases do occur. Although cerebellar findings are common, a small subset of patients may present with an isolated cerebellar syndrome with cognitive decline seen weeks to months later. Some patients may even present with psychiatric symptoms prior to developing dementia and neurologic decline. Sporadic CJD is usually characterized by older age, periodic sharp wave complexes on EEG, an abnormal MRI signal in the putamen and head of the caudate, and positive 14-3-3 proteins on CSF analysis. In the variant forms of CJD, patients are typically younger, EEG changes are only seen in the later stages, CSF 14-3-3 proteins are not consistently present, and MRI may show signal hyper-intensity in the pulvinar nuclei of the thalamus. Recognizing nuances in presentation and testing is important when considering a diagnosis of CJD. As there is no known cure or intervention to slow the progression of this disease, early recognition is crucial so that internists may provide patients and their families with counseling and resources to allow for appropriate expectations of disease progression. With this prognostic information, families and patients may choose to pursue palliative and hospice care in efforts to reduce hospitalizations and potentially uncomfortable or harmful procedures at the end of a patient’s life. In our patient’s case, higher suspicion of CJD initially may have led to earlier discussion with him of his likely progressive neurologic deterioration and allowed for him to express his end-of-life wishes while he was still able, to his family.
A RARE CASE OF BACTEREMIA WITH SPHINGOMONAS PAUCIMOBILIS IN A PATIENT WITH ALLOGENIC STEM CELL TRANSPLANTATIONVikas Singh. SUNY Upstate medical university, Syracuse, NY. (Tracking ID #1936954)
LEARNING OBJECTIVE 1: Sphingomonas paucimobilis, is a yellow-pigmented, aerobic, non fermentative, gram negative motile bacillus. S. paucimobilis which is widely found in nature and hospital environments rarely cause serious or life threatening infections. In this report, a case of bacteremia with S. Paucimobilis secondary to line infection in a patient with stem cell transplant and immunosuppression is presented.
CASE: This is a 43 yo M with h/o AML complex cytogenetics s/p matched unrelated donor allogenic peripheral blood stem cell transplant with fludarabine/melphalan preparatory regimen, 5 months ago, who was admitted with bacteremia. Pt recently went to see his primary oncologist for a follow up visit. His subclavian central line (Hohn catheter) was found to be uncapped and hence blood cultures were drawn from the line. The prelimnary culture showed gram variable rods most likely corynebacterium species, with final culture eventually showing Sphingomonas Paucimobilis in the aerobic bottle. The anaerobic culture bottle didn’t show any growth. He was hospitalized, re-culutred at our facility (Upstate Medical University Hospital) treated with IV vancomycin and Zosyn (total for 5 days) till final cultures came back as Sphingomonas Paucimobilis. Fortunately, patient remained asymptomatic during the entire course of hospitalization. His central line was removed and discharged to home with Amoxicillin for 10 days.
DISCUSSION: This case is reported to emphasize that S. paucimobilis should be kept in mind as a infectious agent in patients with immunosuppression and long term vascular access lines. Central venous catheter infections in hematopoietic SCT recipients may be associated with the development of bacteremia, septic complications, and death, particularly in neutropenic. Cure of such infections requires not only the administration of appropriate antibiotic therapy but also the early removal of the infected intravascular catheters
A RARE CASE OF COMPLETE HEART BLOCKXuanjing Zhou1; Nicholas S. Amoroso2. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1901894)
LEARNING OBJECTIVE 1: Recognize the potential for cardiac involvement in patients with neurodegenerative disorders in the absence of cardiac risk factors.
CASE: A 56 year old white male with hereditary spastic paraplegia and depression reports acute shortness of breath that awoke him from sleep. The wife reports that for the past 2 days, the patient appeared to have some difficulty breathing while lying down. The patient denies a history of chest pain, fever, cough, nausea, diaphoresis, recent infection, toxic ingestions or family history of cardiac disease. Upon arrival to the emergency room, the patient was AAO×3, normotensive, with a heart rate of 26, and saturating 95–98 % on 2 l nasal cannula. The physical exam revealed prominent weakness and spasticity of the lower extremities with clonus and bilateral babinski. The initial electrocardiogram showed complete heart block with a ventricular rate of 25 beats per minute and nonspecific intraventricular conduction delay. His serum electrolytes were within normal limits and cardiac enzymes were negative. B-type natriuretic peptide was 9.7 pg/ml. Chest x-ray showed clear lungs without pulmonary edema or evidence of calcification. Atropine 0.5 mg IVP was given without change in ventricular rate. A transthoracic echocardiogram revealed mildly reduced left ventricular systolic function but was otherwise unremarkable. The patient was admitted to the coronary care unit where a temporary transvenous pacemaker was placed. The patient had 100 % paced rhythm, so a dual lead permanent pacemaker was placed the following day.
DISCUSSION: Hereditary spastic paraplegia (HSP) is a clinical diagnostic designation for those neurological syndromes in which bilateral lower extremity weakness and spasticity are the dominant manifestations and for which gene mutation is the major causative factor. It is well known that cardiac involvement is typical in neuromuscular diseases such as Duchenne muscular dystrophy and myotonic dystrophy. However, it has not been described in HSP. This case illustrates the potential for cardiac involvement in HSP patients in the absence of ischemic symptoms, known ischemic history or other cardiac risk factors. The pathogenesis that explains this cardiac involvement is unknown but endocardial biopsy of patients with similar neurodegenerative disorders have shown interstitial fibrosis of the right atrium and ventricle, as well as electron microscopical findings of myosin filament loss, and mitochondrial and Z-band alterations in degenerated myocytes (Takahashi et al. 2006, Roos et al. 2009). This suggests that an organic or functional lesion in the atrium, ventricle, or anywhere along the atroventricular conduction system may contribute to a common pathway. Although the complete heart block seen in this patient is rare, it is a possible non-neurologic manifestation of HSP. Early recognition of this syndrome is critical to institution of appropriate monitoring and therapy.
A RARE CASE OF GROUP B STREPTOCOCCAL SEPTIC ARTHRITIS WITH A FLARE OF GOUTPhillip Aleksiejuk; Emily R. Haggerty. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1939376)
LEARNING OBJECTIVE 1: Recognizing Streptococcus Agalactiae as an infrequent cause of septic arthritis in the elderly.
CASE: A 73 year-old man with multiple medical comorbidities presented with severe left knee pain of 3 days duration. He has a history of bilateral knee osteoarthritis and gout affecting his wrists and ankle joints. He denied any recent trauma to the knee, fever or additional joint pain. The physical exam revealed an exquisitely tender, warm, swollen left knee, without erythema. Labs were significant for a WBC of 13.5, CRP 21.8, ESR 116, and Uric acid of 9.2. Left knee xray demonstrated degenerative changes and a large effusion. Synovial fluid analysis showed a leukocytosis of 53000, with a moderate amount of monosodium urate crystals. Blood and synovial cultures returned positive for group B streptococcus (GBS). The patient was diagnosed with acute on chronic gout flare with superimposed septic arthritis secondary to GBS. He was treated with Ceftriaxone, Prednisone and Colchicine because of poor baseline renal function. The knee was irrigated and debrided several times to prevent recurrent infection. The remainder of the patient’s hospital course was uneventful, and his condition improved thereafter with many hours of physical therapy.
DISCUSSION: This case illustrates the unique presentation of GBS induced septic arthritis in the setting of an acute gouty flare in an elderly patient. Literature shows an increasing incidence of GBS, and remains a serious cause of morbidity and mortality in nonpregnant adults. It is therefore crucial that clinicians maintain a high index of suspicion for GBS not only in pregnant females, but also in the elderly patient with multiple comorbidities. Increasing the awareness of GBS infection of septic arthritis will not only hasten diagnosis, but will improve clinical outcomes and the quality of life in the geriatric population.
A RARE CASE OF PRIMARY CARDIAC LYMPHOAJason Sayanlar1; David DeMaria1; Ana Barac2. 1Georgetown University Hospital, Washington, DC; 2Medstar Washington Hospital Center, Washington, DC. (Tracking ID #1942107)
LEARNING OBJECTIVE 1: To understand the impact of Primary Cardiac Lymphoma as a rare but clinically important extranodal manifestation of Non-Hodgkin Lymphoma limited to the heart and pericardium.
LEARNING OBJECTIVE 2: To highlight the mainstays of therapy for Primary Cardiac Lymphoma
CASE: A 66 year-old female with no past medical history initially presented to her physician with unilateral facial swelling. A CT scan revealed a stone within the parotid gland, as well as the incidental finding of a pericardial effusion. A transthoracic echocardiogram was done, which demonstrated a large effusion with minimal right ventricle (RV) systolic collapse as well as left ventricle (LV) borders “suspicious for sarcoma”. The patient underwent a pericardial window and ultimately a pericardiectomy, after the fluid re-accumulated. Pathological specimens obtained were initially negative for malignancy. Four months later, the patient again presented with recurrent dyspnea and fatigue. A cardiac MRI showed an infiltrating epicardial mass extending from the anterior base of the left ventricle into the lateral wall. The patient underwent a cardiac biopsy, which was consistent with large B-cell lymphoma. The patient was diagnosed with stage IIE cardiac lymphoma and was started on a chemotherapy regimen consisting of etoposide, prednisone, oncovin, cyclophosphamide, and doxarubicin (EPOCH) with rituximab. An MRI after her first round of chemotherapy showed a significant reduction in tumor size.
DISCUSSION: Primary cardiac lymphoma (PCL) is a rare manifestation of Non-Hodgkin Lymphoma (NHL) characterized by extranodal lymphoma limited to the heart and pericardium. PCL represents approximately 1 % of all cardiac tumors and only 0.5 % of all extranodal lymphomas.4 Most cardiac tumors are metastases, followed by myxomas, which make up 75 % of primary cardiac tumors. Among malignant primary cardiac tumors, sarcomas are approximately 20 times more common than lymphomas. Patients with PCL typically present in the sixth decade of life, with a 3 to 1 male predominance. Sixty-nine percent of all PCL cases involve the right sided chambers of the heart, with the right atrium being the most common site of incidence. Left heart involvement is exceedingly rare and is usually limited to tumors extending from the right side of the heart. Bone marrow and superficial lymph nodes are free of lymphoma in nearly all cases. Symptoms are non-specific, therefore most patients are diagnosed incidentally or after advanced clinical presentation. Idiopathic recurrent pericardial effusion is a common feature of many PCL cases. Biopsy is the gold standard for diagnosis, but is usually accompanied by preceding echocardiography and/or cardiac MRI. If a pericardial effusion is present, a sample should be sent for immunohistochemistry. Therapeutic options include chemotherapy, radiation and surgical resection. Many cases include a combination of chemotherapy and radiation, however, treatment is case-specific and largely depends on the anatomic characteristics and biologic features of the tumor. In extremely rare cases, heart transplant has also been performed. Stem cell therapy may prove to be a treatment option for refractory cases. Like the treatment of other lymphomas, chemotherapy for PCL typically consists of EPOCH or CHOP (cyclophosphamide, hydroxydaunorubicin, oncovin, prednisone) and rituxamab. Given its cardiotoxicity, the use of doxorubicin is controversial, but has not shown to decrease survival. Prognosis is variable and depends on the progression of disease at the time of diagnosis, as well as the patient’s response to chemotherapy. For cases with advanced disease secondary to diagnostic delay, the median survival is 7 months.
A RARE CASE OF PROXIMAL MUSCLE WEAKNESSRonak Shah; Reena Agarwal. Montefiore Medical Center, New York, NY. (Tracking ID #1930431)
LEARNING OBJECTIVE 1: Distinguish Lambert-Eaton Myasthenic Syndrome [LEMS] from its differential diagnosis of proximal muscles weakness.
LEARNING OBJECTIVE 2: Recognize the clinical presentation of LEMS and the importance of early diagnosis because of its high rate of association with malignancy.
CASE: A 60 year-old man presented with 8 months of progressive weakness. Initially, he had significant difficultly getting up from his chair and walking up a hill. His symptoms slowly progressed to having a hard time washing his hair and swallowing solid foods. He denied any muscular pains, tingling or numbness. But he did have dry mouth, erectile dysfunction and mild constipation. He had left eye ptosis, which did not worsen with sustained upward gaze and ocular movements were normal with no signs of fatigue. The strength of all his muscle groups was 5/5, except for the deltoids and hip flexors, which were 4/5 bilaterally. Patient had diminished to absent deep tendon reflexes and struggled to stand up from his chair. Initial laboratory studies revealed a creatine phosphokinase [CPK] of 124 U/L [normal range 20–200 U/L]. He underwent electromyography and nerve conduction studies [EMG / NCS], which were consistent with Lambert-Eaton Myasthenic Syndrome [LEMS]. The patient also had positive voltage gated calcium channel [VCGG] antibodies and a negative acetylcholine receptor antibody, which confirmed the diagnosis of LEMS. CT of the thorax, abdomen and pelvis did not reveal any masses. The patient was given 5 days of IV immune globulin [IVIG] and started on high dose prednisone and pyridostigmine daily. With this treatment, his symptoms of proximal muscle weakness, swallowing and dry mouth slowly resolved. The patient remains free of any evidence of malignancy.
DISCUSSION: Weakness is a common complaint in the outpatient setting. It is often confused with functional limitation due to pain or stiffness. After objectively identifying true weakness, the key in finding the underlying lesion or etiology is figuring out the pattern of distribution. Proximal muscle weakness is particularly important as it narrows the differential to neuromuscular junction disorders like myasthenia gravis [MG] or LEMS, inflammatory myopathies, such as polymyositis or dermatomyositis, and certain motor neuron diseases, like amyotrophic lateral sclerosis. Lambert-Eaton Myasthenic Syndrome is a rare neuromuscular autoimmune disease with an annual incidence of 0.48 per million that is thought to be caused by auto-antibodies against VGCC. The VGCC antibodies block the influx of calcium in the pre-synaptic membrane, which leads to a reduction in the acetylcholine that is released. The classic symptoms of LEMS are proximal muscle weakness, diverse autonomic features such as dry mouth [most common], erectile dysfunction, constipation, and decreased or absent reflexes. EMG studies show an increase muscle action potential after brief isometric exercise, known as post-exercise stimulation. The post-exercise stimulation helps differentiate between LEMS and MS as it has 84–96 % sensitivity and a 100 % specificity for LEMS. Therefore, the clinical signs, positive VGCC antibodies and EMG studies all help in diagnosing LEMS. Early recognition and diagnosis of LEMS is paramount because nearly 50 % of patients with LEMS have an associated malignancy, mostly commonly small cell lung cancer [SCLC]. Clinical symptoms of LEMS are usually present before SCLC is detected, making it important to distinguish LEMS from other disease entities that cause proximal muscle weakness. Myasthenia gravis is the most common etiology that is confused with LEMS, especially when the oculobulbar muscles are involved. But MG patients usually show oculobulbar symptoms first, in contrast to LEMS patients, who initially present with lower extremity weakness. In addition, most MG patients do not have autonomic symptoms or absent reflexes. And unlike inflammatory myopathies, patients with LEMS do not have pain or elevated CPKs. Management of LEMS must incorporate an aggressive screening process for SCLC. Additional treatment consists of symptomatic relief with medications, such as 3,4-diaminopyridine [3,4-DAP] and pyridostigmine that increase the acetylcholine at the post-synaptic membrane. For more refractory or significant symptoms, a trial of IV immune globulin [IVIG] and/or other immunosuppressive agents, like high-dose prednisone or azathioprine, is usually considered. Reference: Titulaer, M et al. Lamber-Eaton myasthenic syndrome: from clinical characteristics to therapeutic strategies. Lancet Neurology. 2011: 10; 1098–1107.
A RARE CASE OF TOXIC EPIDERMAL NECROLYSIS (TEN) ASSOCIATED WITH THE USE OF AZITHROMYCINSteve M. Antoine; Emerald Banas; Shane Keogh. Upstate Medical University, Syracuse, NY. (Tracking ID #1934683)
LEARNING OBJECTIVE 1: Recognize a rare presentation of Steven Johnson Syndrome/Toxic epidermal necrolysis
LEARNING OBJECTIVE 2: Distinguish when to use and not to use systemic steroids
CASE: A 19 year old previously healthy male presented with fever, dyspnea, productive cough, sore throat, oral blisters, diffuse maculopapular and bullous skin lesions. He sought medical consult a week prior for coryza and a productive cough, for which he was prescribed azithromycin. He denied taking any other over-the-counter drugs. Two days later, he woke up with dysphagia and odynophagia at which time he stopped taking the azithromycin. His symptoms progressively worsened; he experienced increased difficulty with swallowing and talking and also began to notice swelling of his tongue and painful blisters inside of his mouth. He then started developing diffuse maculopapular skin lesions over his face, torso and upper extremities, was subsequently rushed to the hospital. Past medical history was significant only for past allergic drug reaction to amoxicillin, which resulted in swelling of his lips. On arrival, he was noted to be febrile (40.5C), tachycardic at 106 bpm and tachypneic. Examination of the skin showed diffuse maculopapular skin lesions from his face down to his upper thighs encompassing approximately 40 % of total body surface area as well as smaller vesiculobullous lesions which showed separation of the epidermis from the dermis. Head and neck exam revealed significant conjuctival injection, severe oropharyngeal swelling and blistering of lips, oral mucosa, and tongue. Routine chemistry studies were unremarkable. Hematologic studies was significant for leukocytosis at 12,600/mm3 with neutrophilic predominance; Chest xray didn’t show any evidence of pneumonia. Patient was admitted to the medicine service for management of suspected SJS/TEN. He received supportive care with IV fluids, topical antibiotics, viscous lidocaine and prednisolone eye drops. Punch biopsy showed epidermal acantholysis with instraspinous and suprabasal keratinocyte separation without immunoglobulin or complement deposition, consistent with SJS/TEN. Ophthalmology determined that his conjunctival injection was consistent with ocular manifestations of SJS/TEN. The use of systemic corticosteroids was discussed, as suggested by many specialist consulted on the case; however we opted not to as there is limited evidence supporting it, and at that point, an infectious trigger was still being debated. The patient’s oropharyngeal and mucocutaneous lesions slowly resolved with conservative care and topical antibiotics. All cultures came back negative. He was eventually transferred to the burn management team and discharged home on hospital day number 12.
DISCUSSION: Stevens-Johnson and toxic epidermal necrolysis (SJS/TEN) represent a spectrum of severe mucocutaneous reactions triggered usually by medications, leading to desquamation, skin necrosis and sometimes death. Multiple medications have been associated with SJS/TEN. There are only 2 reports in the literature associating SJS/TEN with azithromycin. SJS/TEN is associated primarily with medications, secondarily with infections. A thorough investigation has to be conducted to rule out the latter, which can alter treatment. In this case, azithromycin was the most likely culprit, given the onset immediately after use and lack of an identifiable source of infection. The use of steroids in SJS/TEN has been debated and remains controversial. Although it can slow down disease progression, it can be detrimental if infection control is a major concern. Furthermore, in our patient the large exposed lesions provided an accessible site of infection, thus the risks of systemic steroid outweighed the potential benefits.
A RARE CASE: PULMONARY BLASTOMA WITH FOCAL MELANOCYTIC DIFFERENTIATIONAlexandre Zaharia. Allegheny General Hospital, Pittsburgh, PA. (Tracking ID #1940190)
LEARNING OBJECTIVE 1: Recognize the rare but highly aggressive form of primary lung malignancy that are pulmonary blastomas and thereby establish a prompt diagnosis.
LEARNING OBJECTIVE 2: Appreciate the heterogeneity in presentation and histopathology of pulmonary blastomas.
CASE: An 81 year old male with history of chronic obstructive pulmonary disease (COPD) and longstanding cigarette smoking, presented to the emergency department with new-onset dyspnea and atypical chest pain. An extensive work-up was undertaken, with computed tomography (CT) revealing a new right lower lobe 8.3 cm × 7.2 cm necrotic mass with underlying COPD. After stabilization of his symptoms, the patient underwent CT-guided core biopsy, revealing poorly-differentiated adenocarcinoma without further classification. Positron emission tomography (PET) showed absence of distant metastasis. Given these findings, the patient underwent video-assisted thoracoscopic surgery (VATS) and right lower lobectomy with mediastinal lymph node sampling. Intraoperative specimens sent for pathology were consistent with pulmonary blastoma composed of fetal adenocarcinoma and primitive blastematous stroma, with additional foci of squamous differentiation, with staining pattern suggestive of melanoma, yielding the final designation of PB with melanocytic differentiation. With no nodal metastasis found, adjuvant chemotherapy was opted against. In the meantime, the patient was discharged home. A surveillance CT at 3 months showed no evidence of disease recurrence. Unfortunately, the patient presented again with dyspnea 6 months post-surgery. A CT obtained then showed progressive metastatic PB with a new massive right pleural effusion and suspected liver metastases. In consultation with the patient and his family, the patient was made comfort measures only and transferred to hospice, where he expired shortly thereafter.
DISCUSSION: Pulmonary blastomas (PB) are rare (0.25–0.5 % of all lung malignancies) primary malignant epithelial lung tumors consisting of immature lung components that arise in young adults (median age = 35.5 years old). They constitute a form of sarcomatoid adenocarcinoma (2004 WHO classification) and are further subdivided into two histopathological subtypes: 1) well-differentiated fetal adenocarcinomas (WDFA) that contain epithelial components only and 2) classic biphasic pulmonary blastomas (CBPB) that contain both epithelial and mesenchymal components. There exists no current consensus with regards to risk factors or presenting symptomatology. PB are highly aggressive and carry a poor prognosis (5 year survival = 16 %). Presently, complete early surgical resection is the favored treatment approach. However, further modalities such as chemotherapy and/or radiotherapy have not yet been defined. The above case displays PB of the CBPB subtype in an elderly male with early relapse following prompt surgical resection. PB are an uncommon, perhaps underdiagnosed, lung tumor subtype. This case presents two additional atypical variants that have seldom been reported - 1) the melanocytic component noted on pathology and 2) the well-advanced age at time of presentation - and that speak to PB’s heterogeneity. Lastly, it bears witness to the aggressiveness of PB and suggests surgical resection, albeit the current consensus treatment option, does not constitute an effective curative modality.
A RARE CAUSE OF GASTROENTERITISMalav P. Parikh; Venu M. Ganipisetti; Sathish kumar Krishnan; Venu Pararath Gopalakrishnan; John Vainder. Saint Francis Hosptal, Evanston, IL. (Tracking ID #1935674)
LEARNING OBJECTIVE 1: Eosinophilic gastroenteritis (EG) is a rare condition of unclear etiology. It is characterized by gastrointestinal (GI) symptoms, peripheral eosinophilia and eosinophilic infiltration of the bowel to a variable extent and.
CASE: An 83 year old female presented with brownish, watery diarrhea, weight loss of 5 lbs and dull lower abdominal pain for about 2 weeks. The patient reported 7–8 episodes of diarrhea in a day, not associated with blood or mucous. She denied any fever, vomiting, recent travel, sick contact, antibiotic exposure or food intolerance. Patient had a colonoscopy 2 years ago, which was reported as normal. Laboratory studies showed white blood cell count of 21 k/mm3 and absolute eosinophil count of 4180 cells/ mm3 (19 %). Stool studies were negative for clostridium difficile, ova and parasites. Colonoscopy showed diverticulosis of the colon and biopsy was consistent with marked eosinophilic infiltration of the colonic and illeal mucosa. Total IgE level was elevated to 159 Ku/L (normal: 2–114 Ku/L). Patient improved clinically with intravenous fluids and was discharged after 24 h. Steroids or antibiotics were not used. She remained asymptomatic at a follow up visit after 1 month.
DISCUSSION: EG is an uncommon cause of gastroenteritis. Symptoms of EG depend upon the layers of bowel affected by eosinophilic infiltration. Mucosal involvement results in nausea, non-specific abdominal pain, diarrhea, and malabsorption. Muscle layer involvement causes symptoms of intestinal obstruction, whereas subserosal infiltration causes eosinophilic ascites. Diagnosis of EG is confirmed by endoscopic biopsy and/or eosinophilic ascitic fluid. It is very important to rule out intestinal parasitic infection. Irritable bowel syndrome can present with similar clinical presentation and is one the important differential diagnosis. Currently, treatment of EG is empiric and based upon severity of disease. Patients with mild and sporadic symptoms can be managed with reassurance and expectant observation. Patients with severe GI symptoms and malabsorption can be treated with systemic glucocorticoids. Sodium cromolyn, ketotifen and elimination diet may be useful in patients with history of allergic disorders. Surgical intervention is reserved for patients with obstructive symptoms.
A RARE CAUSE OF HEADACHE: SCEDOSPORIUM IN THE SINUSAliza Norwood. UCSF, San Francisco, CA. (Tracking ID #1934629)
LEARNING OBJECTIVE 1: Identify the “red flag” headache symptoms that require imaging
LEARNING OBJECTIVE 2: Recognize fungal sinus infection as an uncommon cause of headache
CASE: A 55 year old woman with a past medical history of depression and no personal or family history of migraine presented with 3 months of a worsening “vice-like” headache. She reported constant left fronto-temporal pain and pressure. Her headache occasionally woke her from sleep and interfered with her ability to work. She denied fevers, chills, night sweats, vomiting, lacrimation, pulsatile sensations, or photophobia and she had no HIV risk factors. Her only medication was Celexa 10 mg by mouth daily. On physical exam, she appeared to be in acute pain, and was rubbing her right temple. Her vital signs were within normal limits. She had no papilledema or nuchal rigidity. Her neurological exam—including speech, cranial nerves, reflexes, strength, and gait—was normal. CBC and TSH were normal. A head CT was obtained and demonstrated ethmoid and sphenoid chronic sinusitis with recommendation for a dedicated sinus CT. CT of the sinuses revealed an interval increase in size of a soft tissue mass within the left sphenoid sinus. The patient underwent endoscopic sinus surgery and was found to have a left sphenoid and posterior ethmoid mycetoma (“fungus ball”), for which she underwent left total ethymoidectomy and sphenoidotomy. Pathology showed Scedosporium apiospermum.
DISCUSSION: Headache is a common primary care complaint, and it is important to determine when it may be treated conservatively and when more aggressive work up is needed. CT or MRI is indicated in patients who present with one or more “red flag” symptoms, which include the following: a new or different headache, a severe headache often referred to as the patient’s “worst headache of their life”, symptoms of systemic illness, seizures, or as in the case of this patient, onset of headache after the age of 50 and disabling headache. Key features on exam that suggest a secondary cause of headache include papilledema, nuchal rigidity, or focal neurological signs. A sphenoid mycetoma is a fungal sinus process and can be a rare cause of headache. The pathophysiology is thought to be due to deficient mucociliary clearance leading to sinus colonization and a chronic inflammatory response. Most cases of non-invasive sphenoid mycetoma are in immunocompetent older women. Patients with this condition usually presents with unilateral fronto-orbital headaches. Rhinological symptoms, including nasal congestion, post-nasal drip, cough, headache or facial pain, occur in 20 % or patients. Approximately 15 % of patients with this condition are asymptomatic and the mycetoma is found during routine tests. Sphenoid mycetomas can lead to recurrent secondary bacterial infections and central nervous system complications but only in a minority of patients. Two thirds of patients have symptomatic improvement after surgery and this is considered the definitive therapy.
A RARE COMPLICATION OF A COMMON CONDITION: WHEN LYMPHEDEMA GETS WORSEThomas Weart1,2; Sean M. Lockwood2,1. 1University of Kentucky Medical Center, Lexington, KY; 2VAMC, Lexington, KY. (Tracking ID #1940099)
LEARNING OBJECTIVE 1: Review the epidemiology of lymphangiosarcoma and the Stewart-Treves syndrome
LEARNING OBJECTIVE 2: Describe the common clinical manifestations, treatment, and prognosis
CASE: A 46 year-old male with a history of congenital pelvic arteriovenous malformations (AVMs) resulting in chronic left lower extremity lymphedema presented with 1 week history of slowly progressive weakness, fatigue, and intermittent fevers with increased lower extremity edema. His past medical history was significant for multiple complications of his AVMs including high output heart failure and chronic gluteal skin wounds. Physical examination revealed normal vital signs, diffuse edema of his left lower extremity with chronic venous stasis changes but no new discrete skin lesion. Bilateral inguinal lymphadenopathy was present with the largest node measuring 2 × 3 cm. Laboratory studies revealed a white blood cell count of 3.0 k/uL, hemoglobin 11.8 g/dL, and platelet count 175 k/uL. Complete metabolic panel was normal. CT imaging revealed extensive lymphadenopathy of the pelvis and retroperitoneum. Excisional lymph node biopsy of the largest inguinal node revealed high-grade angiosarcoma. In a patient with chronic lymphedema, this finding is consistent with Stewart-Treves syndrome. The patient was enrolled in a clinical trial for experimental chemotherapy on recommendation of a multi-disciplinary tumor board. Repeat imaging after initial treatment is suggestive of a positive response to therapy.
DISCUSSION: Stewart-Treves syndrome refers to angiosarcoma arising in the setting of chronic lymphedema. This condition was first described in 1948 in a case series of six patients who developed lymphedema following mastectomy. Overall, the incidence of Stewart-Treves remains low with approximately 400 cases reported in the literature. Only 0.3 % of patients 10 years status post mastectomy develop this condition. The incidence of lower extremity Stewart-Treves Syndrome is even rarer. The pathogenesis is believed to be due to the disruption of immunocompetent cell movement to the affected region while collateral lymph vessels and angiogenesis proliferate in a dysregulated manner. The typical time course for development of this malignancy is 5–16 years after radical mastectomy and/or the onset of lymphedema. Clinicians should consider Stewart-Treves Syndrome when a patient with chronic lymphedema presents with worsening swelling, lymphadenopathy or new skin changes in the affected area. These patients often have atrophic skin with chronic edema and erysipelas being common. However the lesions associated with angiosarcoma may begin as dark or purplish areas mimicking Kaposi’s sarcoma. It may also present as a wound which bleeds easily or fails to heal. Lymphadenopathy is often a late and ominous finding. Early diagnosis is particularly important because the most effective treatment is surgical excision prior to proximal spread which may require amputation. Mean survival is 5–8 months without treatment. Chemotherapy and radiation therapy offer little benefit to overall survival with mean survival up to 20 months with maximal treatment. The need for early diagnosis underscores the importance for internists to recognize this rare but potentially treatable cancer in a patient with the common condition of lymphedema.
A RARE GLIMPSE WITH MULTIMODALITY CARDIAC IMAGING INTO AN EXPANDING LEFT VENTRICULAR OUTFLOW PSEUDOANEURYSM FROM ENDOCARDITISJon N. Quach1,2; Katharine M. Borthwick2; Jeffery Gordon2; John Moriarty3; Murray Kwon4; Paul Finn3; Eric H. Yang2. 1University of California, Los Angeles Olive View Medical Center, Sylmar, CA; 2University of California, Los Angeles Medical Center, Los Angeles, CA; 3University of California, Los Angeles Medical Center, Los Angeles, CA; 4University of California, Los Angeles Medical Center, Los Angeles, CA. (Tracking ID #1935025)
LEARNING OBJECTIVE 1: Recognize the incidence and clinical features of left ventricular outflow tract (LVOT) pseudoaneuryms (PSAs) after endocarditis
LEARNING OBJECTIVE 2: Assess left ventricular outflow tract (LVOT) size and appropriate management using multimodality cardiac imaging (ie echocardiography, MRI, CT)
CASE: A 56-year-old Chinese female with a history of bicuspid aortic valve, underwent an aortic root replacement and mitral valve repair (21 mm CryoLife homograft, CryoLife Inc., Kennesaw, GA) and 32 mm Medtronic Future Band annuloplasty ring (Medtronic, Minneapolis, MN) for Enteroccocus faecalis endocarditis secondary to a longstanding intrauterine device. The patient also received coronary artery bypass graft (CABG) with saphenous vein grafts of all three of her native coronary arteries. Intraoperatively the patient was noted to have a PSA in the LVOT but given the concern for friable and unstable myocardial tissue in light of her recent infection and thus suboptimal surgical repair, the decision was made to conservatively manage and monitor her PSA. A postoperative TTE and multidetector cardiac computed tomography (MDCT) confirmed the presence of her LVOT PSA (Figure 1A and B). The patient was subsequently lost to follow up from our hospital, with interim development of acute occlusion of one of her saphenous vein grafts requiring percutaneous coronary intervention She also was found on outside testing to have exercise induced ischemia on stress echocardiography. The patient once again reestablished care at our hospital 10 months after her initial surgery. Multimodality imaging, including transthoracic and transesophageal echocardiography, MDCT, and cardiac magnetic resonance imaging performed at that time was significant for progression of her LVOT PSA. (Figures 1C-D, Figure 2) Given the rapidly progressing size of the patient’s LVOT PSA, the patient underwent open surgical repair. Her aortic root was redone with a customized-made valve conduit utilizing a 19 mm Edwards Magna Ease pericardial tissue valve (Edwards Lifesciences, Irvine, CA). She also underwent a re-do CABG of her native coronary arteries. Repeat imaging confirmed surgical closure of the LVOT PSA and patent grafts. The patient did well and was discharged with outpatient follow up.
DISCUSSION: A left ventricular psuedoaneursym occurs when cardiac rupture is contained by surrounding pericardium or scar tissue [1]. Left ventricular outflow tract (LVOT) psuedoaneursyms (PSAs) are related primarily to MI, however other common causes include surgical aortic root repair and mitral valve repair. Primarily, patients present with symptoms of heart failure, chest pain, and shortness of breath; however >10 % of patients remain asymptomatic. The diagnosis of LVOT pseudoaneursym remains difficult, however angiography is considered the best available diagnostic test. 2D Transthoracic echocardiogram remains a viable and less invasive option, but results in a definitive diagnosis in only 26 % of patients. With optimal medical management, LVOT PSA has a 35-40 % risk of rupture as well as a 50 % mortality rate [2]. Early identification and surgical repair is essential to improving patient outcomes. Patients generally do well after surgical repair, however perioperative risk of death is approximately 30 % [3]. There is some evidence suggesting that PSA can be conservatively managed with optimal medical therapy, but these results may be skewed by publication bias [4]. Our case shows the significant spatial resolution and ability to reconstruct 3-dimensional aspects of a cardiac PSA using sophisticated modern imaging techniques in evaluating the progression in size of a LVOT PSA. It highlights the importance of early detection and repair in this uncommon sequelae of infective endocarditis utilizing the advantages of multimodality cardiac imaging. 1. Dachman AH, Spindola-Franco H, Solomon N. Left ventricular pseudoaneurysm. Its recognition and significance. JAMA 1981;246:1951–3. 2. Frances C, Romero A, Grady D. Left Ventricular Psuedoaneurysm, JACC 1998:557–61; 3. Eren E, Bozbuga N, Toker ME, Keles C, Rabus MB, Yildirim O, Guler M, Balkanay M, Isik O Yakut C Surgical treatment of post-infarction left ventricular pseudoaneurysm: a two-decade experience. Tex Heart Inst J. 2007;34:47–51. 4. Yeo TC, Malouf JF, Oh JK, Seward JB. Clinical profile and outcome in 52 patients with cardiac pseudoaneurysm. Ann Intern Med 1998; 128:299.
A RARE OCCURRENCE: GRAVE’S OPTHALMOPATHY IN A PATIENT WITH HASHIMOTO’S THYROIDITISMohammed W. Imam; Hiba Hadid; Rashim Gupta; Yogin Patel; Mona Hassan. henry ford health system, Detroit, MI. (Tracking ID #1938559)
LEARNING OBJECTIVE 1: Through this case report, we hope to shed light on the importance of recognizing the possibilities of Grave’s disease and Hashimoto’s thyroiditis occurring consecutively or simultaneously.
LEARNING OBJECTIVE 2: We also aim to highlight the importance of recognizing Grave’s opthalmopathy with vision compromise as an opthalamologic emergency that requires immediate intervention.
CASE: We report a case of a 55-year old male with a medical history significant for Hashimoto’s disease for 13 years and type I diabetes mellitus, presenting with severe exopthalamus, eye swelling, near complete vision loss, and pretibial myxedema. Orbital CT imaging, revealed severe optic nerve compression. Steroids were promptly initiated and the patient was emergently taken to the OR for orbital decompression.
DISCUSSION: The development of hypothyroidism after Grave’s disease is well documented in the literature. However, the occurrence of Grave’s disease after chronic thyroiditis is rare. Patients may become hypothyroid, euthyroid, or hyperthyroid and the occurrence of each is determined by the balance between the stimulating and blocking antibodies, and by the functional state of the thyroid gland. The interval between the onset of these two disease states could range from weeks to decades. There are only a few cases reported in the literature in which Grave’s disease follows hypothyroidism. Through this case report, we hope to shed light on the importance of recognizing the possibilities of these two diseases occurring consecutively or simultaneously. We also aim to highlight the importance of recognizing Grave’s opthalmopathy as an opthalamologic emergency that requires immediate intervention, when vision is compromised.
A RASH DECISIONShara I. Epstein1,2; Sheira Schlair1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1936875)
LEARNING OBJECTIVE 1: Recognize various dermatological manifestations of strongyloidiasis
LEARNING OBJECTIVE 2: Distinguish signs and symptoms of acute versus chronic strongyloidiasis
CASE: A 39 year-old woman presented with a rash on her right buttock recurrent for two and a half years. She initially presented with a non-painful, non-pruritic rash on her left shoulder 3 months ago and a new rash on her breast, abdomen and legs. On physical exam she had mild erythema of the upper chest and erythematous plaques without scaling of the medial breasts. There was streaky erythema at the waistline. The left shoulder and the right buttock revealed annular, atrophic, non-scaling erythematous plaques as well. The bilateral medial buttocks were noted to have multiple track-like lesions. The right shin had two more plaques. Past labs were notable for a white blood cell count of 5.3, with 0.3 eosinophils (upper end of normal). She was initially treated with ketoconazole for disseminated tinea versicolor, with no improvement. The patient remembered spending some time in upstate New York and a concern for lyme disease developed. She was treated empirically with a 4 week trial of doxycycline, without any improvement. A shave biopsy of the left shoulder revealed peri-infundibular, superficial perivascular and interstitial dermatitis with eosinophils. Ultimately, laboratory tests revealed a positive Lyme antibody titer but with negative western blot. A strongyloides titer was ordered in light of the biopsy’s eosinophils and found to be positive. On further questioning, patient stated that she had lived in Greece in the past and takes yearly trips to rural villages there. She was treated with albendazole with complete resolution of the rash.
DISCUSSION: General internists see many types of rashes in their practice and should consider the epidemiology of various eosinophilic rashes, especially for travelers. It is estimated that 30–100 million people are infected with Strongyloides worldwide via fecal-oral contamination, on all continents except Antarctica, and especially in the tropics. Typical presentation is with nonspecific symptoms that span a wide spectrum from abdominal pain and bloating to arthritis and rash, which may appear immediately following exposure or years later. Acute strongyloidiasis is characterized by a pruritic rash at the location of skin penetration followed by other non specific symptoms. Chronic strongyloidiasis, as this patient had, is usually asymptomatic, but can eventually manifest with either gastrointestinal or cutaneous symptoms. Strongyloides can complete its entire lifecycle in the human. The filariform larvae can penetrate the skin and it is often during this phase that they cause the larva currens rash, the pathognomonic rash of strongyloidiasis. However, various other rashes have been described. A diffuse purpuric and petechial rash can occur in disseminated strongyloidiasis, especially in immunocompromised patients. Other allergic type rashes have been seen, more rarely, as was likely the case in this patient with her eosinophil predominant rash. For cutaneous manifestations, treatment is one to two doses of ivermectin or albendazole twice daily for 7 days, while ivermectin is the preferred treatment for intestinal strongyloidiasis. Our patient received albendazole with full recovery. In conclusion, general internists are the first line for many patients with rashes, and it is always important, especially in a practice with patients frequently traveling internationally to rural areas, to consider parasitic causes for their rashes, especially those that are found to be eosinophil-predominant.
A RASH ON THE PALMS AND SOLES—AND EVERYWHERE IN BETWEENNavya Nambudiri3; Vinod E. Nambudiri1,2; Sandy Tsao2. 1Brigham and Women, Brookline, MA; 2Massachusetts General Hospital, Boston, MA; 3Cochin Medical College, Cochin, India. (Tracking ID #1936592)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of guttate psoriasis and the features which distinguish it from other cutaneous eruptions.
LEARNING OBJECTIVE 2: Treat and counsel patients diagnosed with guttate psoriasis.
CASE: A 23-year-old previously-healthy man presented for evaluation of a new rash. He had moved from France to the United States 8 weeks earlier. One week after arriving in the United States, he noted a sore throat associated with pain on swallowing as well as mild subjective fevers. The sore throat resolved after 10 days. Two weeks later, he noted the development of a papular eruption that started on his hands and feet as “many small pink spots.” He denied any arthralgias, myalgias, pruritus, pain or other systemic symptoms with the rash. He had previously been in a monogamous relationship with his girlfriend in France and had a recent negative HIV test. He took no medications, had no known allergies, and no close contacts with a similar rash. There was no family history of a similar eruption. He was evaluated at an outside urgent care provider 1 week following the onset of the eruption. The rash was noted to be predominantly on the palms and soles and was spreading to involve the arms and legs. Titers for Rocky Mountain Spotted Fever (RMSF) as well as Coxsackie virus were sent. He was treated empirically for RMSF with 7 days of doxycycline without improvement. Over the next 2 weeks, the rash progressed to involve the body diffusely. He presented to our institution for further evaluation when he noted the eruption was spreading to his face and becoming mildly pruritic. Titers for both RMSF and Coxsackie virus had returned as negative. He continued to deny fever, chills, or systemic symptoms. On examination, hundreds of 2–3 mm pink papules with silvery scale were noted on the face, arms, chest, back, legs, feet and hands, to the point of coalescence on the palms. Koebnerization of lesions in an area of linear excoriation on the upper arm was appreciated. Anti-Streptolysin-O titer was elevated at 695 IU/mL (normal <530) and Anti DNAse-B titer was markedly elevated at 706 IU/mL (normal <300). A skin biopsy demonstrated psoriasiform hyperplasia, confirming the clinical diagnosis of guttate psoriasis. He was treated with topical triamcinolone acetonide 0.1 % cream with good effect.
DISCUSSION: Guttate psoriasis is a benign inflammatory skin eruption characterized by numerous individual papules and plaques distributed over the trunk and extremities. The name ‘guttate’ is derived from the Latin term ‘gutta’ - meaning ‘a drop’—as the clinical appearance is of individual raindrop-like skin lesions that present in an eruptive manner. While it may occur at any age, guttate psoriasis is more common in children and young adults. The cutaneous lesions may begin as thin pink plaques which develop increasing scale, reflective of the epidermal hyperplasia and hyperkeratosis seen on skin biopsy. Koebnerization—the development of skin lesions in sites of trauma—is a characteristic finding in psoriasis and was noted in this patient’s clinical presentation. This finding helps distinguish guttate psoriasis from differential diagnoses such as an acute viral exanthem, eczema, morbilliform drug eruption, or pityriasis rosea. Guttate psoriasis is unique among other forms of psoriasis as it is often associated with preceding streptococcal infection. Family history of psoriasis and stressful life events have also been associated with the disease’s onset in case-control studies. The classic history is of a streptococcal pharyngitis preceding the onset of the eruptive rash by a few weeks, consistent with our patient’s history. The elevated Anti-Streptolysin-O and Anti-DNAse B seen in our patient confirm a streptococcal cause for his recent sore throat symptoms. Epidemiologic studies suggest patients in whom the development of guttate psoriasis is associated with a streptococcal infection have more rapid and more long-term clearance of the skin than those without evidence of associated streptococcal infection. Treatments for guttate psoriasis remain an ongoing area of investigation in the medical literature. Studies do not suggest any benefit of anti-streptococcal treatments for skin clearance in individuals with guttate psoriasis. Commonly reported treatments for guttate psoriasis include topical corticosteroids (as in our patient), topical Vitamin-D analogues, and ultraviolet-B phototherapy. The prognosis of guttate psoriasis is generally favorable with a self-limited disease course, though a substantial percentage of individuals ultimately develop chronic plaque psoriasis. Clinicians should suspect guttate psoriasis in patients who present with a new eruptive rash following a recent pharyngitis.
A RETRO COLLECTIONTalal Hilal; Andrew Hoellein. University of Kentucky, Lexington, KY. (Tracking ID #1937688)
LEARNING OBJECTIVE 1: Identify the possible etiologies of retroperitoneal fibrosis
LEARNING OBJECTIVE 2: Outline medical management of retroperitoneal fibrosis
CASE: A 58 year-old woman reported 6 weeks of dull, bilateral flank and lower back pain along with progressive fatigue and weakness. She noted anorexia and weight loss over the past 4 weeks and intermittent subjective fever and chills. She has a history of coronary disease requiring stenting over 10 years ago and peripheral arterial disease requiring aortobifemoral bypass grafting 4 years ago. She is a smoker with a 100 pack-year history. Her family history is unremarkable. Physical exam found a thin lady, normal vital signs, tenderness over the flanks, and palpable kidneys. Her metabolic panel revealed BUN 114 mg/dL, creatinine 11 mg/dL, potassium 5.7 mEq/L and bicarbonate 12 mEq/L. A CT of the abdomen and pelvis found severe bilateral hydronephrosis with dilatation of the ureters to the level of the iliac arteries. The patient underwent bilateral percutaneous nephrostomy tube placement with subsequent post-obstructive diuresis. Her BUN and creatinine trended down to 29 mEq/L and 3.3 mEq/L, respectively. It was felt that the bilateral proximal ureteral obstruction was secondary to retroperitoneal fibrosis related to aortobifemoral bypass grafts. Surgical correction of the strictures was not an option due to the close proximity of the grafts and the risk of graft infection and/or fistulization. She was discharged with nephrostomy tubes in place and follow-up was arranged for further outpatient management.
DISCUSSION: Retroperitoneal fibrosis is a slowly progressive condition characterized by deposition of fibro-inflammatory tissue in the retroperitoneal space, usually covering the infrarenal abdominal aorta, and extending into the ureters. Symptoms are usually vague including dull, non colicky pain in the lower back, flank and lower abdomen, and patients tend to present late with complications. Most cases are idiopathic (60–70 %), while a minority appear to be secondary to regional inciting events such as malignant disease, surgery, radiation and chronic inflammatory conditions. Principles of treatment involve suppressing the inflammatory process and preserving renal function. Patients with ureteral obstruction should have emergent relief of the obstruction by percutaneous nephrostomy but long-term pharmacologic therapy should be instituted once diagnosis is confirmed. This is usually in the form of corticosteroids with or without immunosuppressive agents (azathioprine, cyclophosphamide and mycophenolate), or tamoxifen. A prospective study comparing a corticosteroid taper with tamoxifen for maintenance therapy concluded that the relapse rate with tamoxifen was significantly higher at 8 months compared to corticosteroids. The addition of mycophenolate to corticosteroids has shown significant benefit in long-term stabilization of disease in a small sample of patients, but randomized controlled trials to define optimum treatment are lacking. The duration of therapy for most taper regimens is 2 years with patients sometimes requiring further treatment. Patients who do not respond to medical therapy may require surgical intervention to treat ureteral obstruction. A multidisciplinary approach needs to be instituted to manage not only the disease but the complications that tend to coexist. Follow-up is essential and prognosis is usually good.
A STRONG MAN POWERLESS: A PERPLEXING CASE OF GENERALIZED WEAKNESSNivedita Gunturi; David C. Demoise; Brian S. Heist. UPMC Presbyterian Shadyside, Pittsburgh, PA. (Tracking ID #1938353)
LEARNING OBJECTIVE 1: To recognize cervical intervertebral disc herniation in the absence of typical symptomatology
LEARNING OBJECTIVE 2: To manage cervical disc herniation with early imaging and prompt referral for surgical intervention
CASE: A 54 year old obese African American man with poorly controlled type 2 diabetes mellitus and hypertension presented to our clinic with generalized weakness and fatigue progressive over the previous 1–2 months. The patient worked as a sanitation worker and bus driver, and reported his symptoms prevented him from performing daily tasks. Medications consisted of long standing amlodipine, hydrochlorothiazide, lisinopril, metformin, glyburide, and aspirin. He had a 30 pack year smoking history and did not use alcohol or recreational drugs. Physical examination revealed a large obese and muscular man (weight 148 Kg, BMI 44) with blood pressure of 160/100 and was otherwise unremarkable. Laboratory data included hemoglobin A1C of 6.8 % and normal complete blood count, comprehensive metabolic panel, and thyroid stimulating hormone level. He was advised to exercise, improve his diet, and monitor blood pressure and blood glucose. The patient returned 4 weeks later perseverating on loss of power, and with new complaint of diffuse myalgias, but no focal pain. He denied other neurological symptoms including tremors or urinary/fecal incontinence. He denied mood instability, anxiety and depression. Physical exam was remarkable for perceived diffuse 5-/5 strength, though assessment was compromised by his large physique. Sensation to pain and light touch was intact in bilateral upper and lower extremities, but plantar sensation was absent on monofilament testing. Gait was normal. To check for polymyositis and polymyalgia rheumatica, ESR and CPK were obtained and were within normal limits. Per instruction, a week later the patient again returned to clinic. He appeared fatigued and reported nearly collapsing upon rising from his waiting room chair. On physical exam, sensation exam was unchanged, prepatellar reflexes were mildly increased, and upper extremity reflexes were normal. Proprioception testing was normal. Strength testing results were unchanged, though patient felt he was weaker. Based on suspicion of axonal neuropathy and possible neuromuscular junction disorder, nerve conduction studies were performed and showed evidence of sensory motor polyneuropathy of upper and lower extremities. Cervical magnetic resonance imaging (MRI) showed large C3–C4 disc herniation with significant myelomalacia and cord displacement and a smaller disc herniation at C6–C7. MRI brain, obtained per neurology recommendation, showed no acute changes. A methylprednisolone taper was prescribed, with no symptomatic improvement. The patient was then referred to neurosurgery, and underwent C3–C4 anterior cervical discectomy with bony fusion and plating. On 4 week post-operative follow up, patient reported significant symptomatic improvement. He started physical therapy and 2 weeks later demonstrated further improvement of weakness and imbalance. He plans to continue physical therapy for another month and then return to work.
DISCUSSION: This case demonstrates a unique presentation of cervical disc herniation and myelomalacia, which can be difficult to diagnose due to myriad modes of presentation. Symptoms of cervical disc herniation may be mistaken for those of diabetic neuropathy, rheumatological conditions or cerebrovascular accident, among others. As there are no pathognomonic features that can direct diagnosis, the astute physician must be aware of subtle symptomatology that may point to disc herniation, including gait abnormality and unilateral or bilateral hyperreflexia, and obtain appropriate imaging early in the clinical course. Failure to recognize signs and symptoms of cervical disc herniation may delay early surgical intervention, which is associated with significant changes in neurological prognosis, including spastic paraparesis. The risk of spinal cord injury with minimal trauma is also higher in patients with cervical myelopathy, which is of particular concern in this patient, whose occupation requires extensive manual labor. The clinician’s ability to suspect cervical spondylopathy due to disc herniation, diagnose with appropriate imaging and make an early referral for surgical intervention will serve to provide rapid symptomatic relief and avoid further complications, as seen in the case of this patient.
A SUPRATHERAPEUTIC INR FROM AN UNCOMMON INTERACTIONEiran A. Warner; Christopher Taurani; Kristen Coffey; ZuJun Li. Beth Israel Medical Center, New York, NY. (Tracking ID #1939669)
LEARNING OBJECTIVE 1: Recognizing that cisplatin can interact with patients on warfarin
LEARNING OBJECTIVE 2: Understanding the mechanism of cisplatin and warfarin interaction
CASE: A 65 male with locally advanced oropharyngeal squamous cell carcinoma and a history of deep vein thrombosis, on long-term warfarin, was referred to the emergency room (ED) by his oncologist for an INR level of 10. The patient had an INR of 3.7 2 weeks earlier for which his daily warfarin dose of 5 mg was stopped for 2 days and restarted at 5 mg daily for 6 out of 7 days a week. One week prior to ED arrival the patient had started radiation therapy and was given a single dose of cisplatin 40 mg per square meter. Baseline hemoglobin was 13.3 g/dl and serum creatinine was 1.0 mg/dl. Prior to receiving his second weekly dose of cisplatin, the patient’s INR was noted to be 10, with a creatinine of 3.7 mg/dl, a hemoglobin of 11.4 g/dl and normal liver function tests. The patient’s blood pressure was 88/52. He admitted to having several episodes of epistaxis over the previous few days but denied easy bruising, melena or hematochezia. Other medications included fluticasone/salmeterol, tiotropium bromide, lansoprazole and ondansetron, the latter started with the cisplatin. The patient denied any over the counter supplements or change to his diet of 4 cans of Jevity per day via PEG tube. Vitamin K 2 mg iv and 2 L normal saline were given prior to transport to the ED. The patient was given a further 5 mg IV vitamin K in the ED (repeat INR was 8.8) and was admitted. There were no further bleeding episodes and INR returned to under 2 within 72 h of admission. With hydration during hospital stay, the patient’s creatinine returned to baseline. The patient was discharged on his usual dose of 5 mg warfarin daily and after discussion with his oncologist cisplatin was discontinued.
DISCUSSION: Long term anticoagulation is the standard of care for patients with conditions such as recurrent deep vein thrombosis or atrial fibrillation. Warfarin is the anticoagulant traditionally used with a target INR of 2 to 3. Cisplatin is a chemotherapy drug with activity against a wide range of malignancies. It is very commonly used either as a single agent radiosensitizer or as part of combination chemotherapy in the adjuvant, neoadjuvant and palliative treatment settings. Because both cancer and conditions that require anticoagulation are more common in older adults, and because recurrent thromboses are a complication of many malignancies, the prescription of cisplatin for a patient already on chronic warfarin therapy is likely a fairly common occurrence. The acutely elevated INR observed in our patient on a previously stable dose of warfarin is not traditionally recognized as a side affect of cisplatin. Warfarin consists of a racemic mixture of 2 enantiomers (R and S forms). Cyp3A4 and CYP2C9 are involved in the metabolism of R- warfarin and S-warfarin respectively with the latter playing the larger role in warfarin’s metabolism. Recent evidence in vivo suggests that cisplatin has CYP2C9 inhibitory activity. Several recent case studies have, as well, suggested a possible interaction between cisplatin and warfarin. These case studies involved a combination of chemotherapy drugs in addition to cisplatin, with the latter implicated as it was the only drug common to all cases. The fact that our patient only received cisplatin removes any confounding factors and greatly increases the likelihood that the cisplatin-warfarin interaction is real. Our patient’s other medications were all long-standing with the exception of ondansetron. Although ondansetron is a weak CYP2C9 inhibitor, it is unlikely to have been the cause of the acutely elevated INR as the patient continued to take ondansetron during his hospital stay and after discharge with return of his INR to baseline. Moreover, ondansetron is used more commonly than cisplatin and no case of a clinically significant interaction with warfarin has ever been reported. Nevertheless, a small contribution of the ondansetron in this case cannot be excluded. The fact that the interaction between warfarin and cisplatin has not been reported more often based on the expected frequent co-prescription of these drugs, suggests that susceptibility to this interaction may be a function of individual pharmacogenetics and occurs only in patients who have inherited alleles with reduced CYP2C9 activity. Patients on concurrent warfarin and cisplatin should have their INR carefully monitored. If an equally suitable chemotherapeutic drug cannot be substituted, a switch to another anticoagulant such as a low molecular weight heparin should be made at the first sign of a rise in INR.
A SURPRISING CAUSE OF ACUTE KIDNEY INJURY IN A HEALTHY YOUNG MALEHalis K. Akturk. Creighton University Medical Center, Omaha, NE. (Tracking ID #1926128)
LEARNING OBJECTIVE 1: Recognize rare causes of acute kidney injury.
LEARNING OBJECTIVE 2: Diagnose fecal impaction and treat immediately.
CASE: A 19-year-old man presented with abdominal pain and decreased urine output. He also mentions that he has been constipated for about 10 days. The patient was afebrile, tachycardic and tachypneic. He was in acute distress due to severe pain. Physical exam revealed lower abdominal tenderness and palpable abdominal mass. Lab work showed signs of acute kidney injury with increased creatinine of 3.4 mg/dL and blood urea nitrogen of 44 mg/dL. Other routine blood tests were normal. Urine output was less than 10 cm3/h. Urine analysis was unremarkable and urine drug screen was positive for Tetrahydrocannabinol (THC). Computed tomography revealed rectal mass measuring approximately 13 × 10 × 19 cm (Anteroposterior × Transverse × Craniocaudal). There is noticeable mass effect on the bladder with near total collapse of the bladder without hydronephrosis. The patient was not on any medications and there was no previous or family history of severe constipation. He had no underlying disease and no history of abdominal surgery. Patient was admitted to hospital and treated with intravenous hydration, mineral oil enema and several manual disimpactions. After treatment, kidney function returned to normal dramatically.
DISCUSSION: Fecal impaction is a solid bulk of stool, mostly develops in the rectum due to severe constipation. Risk factors are age, chronic narcotic use, immobility and Hirschsprung’s Disease. Massive fecal ball, Fecaloma is a rare entity that may cause mass effect to adjacent structures. A few case reports have been reported that fecaloma caused hydronephrosis in elderly population with mass effect. Fecaloma can cause obstruction, ulceration and perforation and rarely mass effect to adjacent structures. Fecal ball should be considered in the differential diagnosis of patients who have a history of constipation and present with decreased urine output and abdominal mass.
A SWEET RHYTHMDavid Kitchell1; Helen Tsai2; Eugenia Tsai1. 1Montefiore Medical Center, Bronx, NY; 2St. George’s University, True Blue, Grenada. (Tracking ID #1936455)
LEARNING OBJECTIVE 1: Recognize etiologies of hyperkalemia
LEARNING OBJECTIVE 2: Identify EKG changes in hyperkalemia
CASE: A 52 year old gentleman with hypertension, diabetes mellitus type 2 (hemoglobin A1c 11) and obesity presented with weakness, nausea and vomiting for 2 days. Home medications included enalapril and canigliflozin, a new antidiabetic agent which he recently started. Initial vitals were significant for hypotension (BP 90/58 mmHg), bradycardia (HR 46–52 bpm) and hyperglycemia (fingerstick glucose 450 mg/dl). Serum chemistry was notable for potassium of 7.5 meQ/L, glucose of 231 mg/dL, BUN of 56 mg/dL and creatinine of 1.8 mg/dL (reported baseline of 1.5 mg/dL 2 weeks prior to presentation). Complete blood count was unremarkable. Initial electrocardiogram (EKG) revealed junctional rhythm (HR 49 bpm). The patient was treated for hyperkalemia with polystyrene sulfonate, insulin and sodium bicarbonate. Clinical symptoms rapidly resolved with treatment; a repeat serum chemistry showed improvement of hyperkalemia (K+ 5.2 meQ/L) and a repeat EKG showed normal sinus rhythm. Canigliflozin was discontinued during the hospital course and replaced with long-acting insulin for diabetes management. Serum creatinine returned to baseline within 2 days and the patient had no further episodes of hyperkalemia.
DISCUSSION: Canagliflozin (Invokana) is a relatively new antidiabetic agent that works as a sodium-glucose cotransporter 2 (SGLT2) inhibitor. It blocks glucose transport at the level of the proximal tubule in the nephron thereby increasing glucose excretion in the urine. Clinical trials have demonstrated canagliflozin as non-inferior to glimepiride. Studied side effects include urinary tract infection, postural dizziness, orthostatic hypotension and less frequently, syncope. Commonly reported side effects include renal insufficiency and hyperkalemia. Hyperkalemia, defined as serum potassium (K+) >5.5 meQ/L, is a commonly encountered clinical problem. Clinical manifestations may be nonspecific and include neuromuscular complaints such as weakness, generalized fatigue or fasciculations. GI symptoms such as abdominal cramping, nausea, and vomiting, or cardiac symptoms such as slow, weakened or absent pulse may also occur. Due to the lack of characteristic symptoms, hyperkalemia can be easily and dangerously overlooked. Maintaining a high clinical suspicion for hyperkalemia and recognizing associated EKG changes, particularly in those with renal dysfunction or with history of medication and supplement use, is thus vital. The majority of hyperkalemia cases result from impaired urinary excretion as a result of acute or chronic kidney failure. Hyperkalemia can also be caused by the redistribution of potassium from intracellular to extracellular space, as observed in metabolic acidosis, uncontrolled diabetes, rhabodymolysis, hemolysis, burns or trauma. Importantly, iatrogenic causes such as the use of ACE inhibitors, NSAIDS, potassium-sparing diuretics and other medications can precipitate hyperkalemia by affecting renal excretion of potassium. In addition to evaluating a patient’s risk factors, EKG findings can clue in a hyperkalemia diagnosis. Hyperkalemia can present with cardiac arrhythmias such as sinus bradycardia, sinus arrest, ventricular tachycardia, ventricular fibrillation and even asystole. Conduction abnormalities may also be seen and can include right or left bundle branch block, bifascicular block and advanced atrioventricular block. Rapid onset hyperkalemia is more likely to demonstrate EKG changes. These changes often correlate with serum potassium concentration. Classic narrow, tall peaked T waves are often seen with mildly elevated K+ (5.5–6.5 mEQ/L). This is due to the extracellular potassium effects on the repolarization phase of the cardiac action potential. Loss of the P wave and widening of the QRS complex can be seen with K+ >6.5 mEQ/L. This reflects the greater sensitivity of the atrial tissue than the sinoatrial node to elevated serum K+. The sinoatrial node maintains function as the pacemaker of the heart but directly stimulates ventricular depolarization. At K+ >8 meQ/L, a sine wave pattern (fusion of the QRS complex and peaked T wave) can be seen, which can quickly develop into ventricular fibrillation. Nevertheless, a normal EKG does not exclude hyperkalemia. Hyperkalemia is a condition frequently encountered by the general internist. Severe hyperkalemia (K+ ≥7.0 meQ/L) can lead to arrhythmias and conduction abnormalities thus must be quickly identified and treated to prevent fatal complications.
A SWING AND A MISS: HEPARIN INDUCED THROMBOCYTOPENIA (HIT) WITH AN INITIALLY NEGATIVE ANTIBODY SCREENKirtan Nautiyal1,2; Jeffrey T. Bates1,2. 1Baylor College of Medicine, Houston, TX; 2Michael E. DeBakey VA Medical Center, Houston, TX. (Tracking ID #1939797)
LEARNING OBJECTIVE 1: Apply the “4 Ts” clinical scoring system to estimate the pre-test probability of Heparin-induced Thrombocytopenia (HIT) in a patient prior to serologic testing
LEARNING OBJECTIVE 2: Recognize that HIT can occur despite the ELISA for the HIT antibody initially returning negative.
CASE: A 54-year-old male with diabetes mellitus, hypertension, hyperlipidemia, and peripheral arterial disease was admitted for cellulitis. On the second hospital day, Doppler ultrasound could no longer identify a pulse in the patient’s left dorsalis pedis artery. CT runoff showed acute thrombosis of the left superficial femoral artery extending into the popliteal, anterior tibial, and peroneal arteries; platelet count at this time was normal. He was started on IV heparin and was taken to the operating room 6 days later, where he underwent a left femoral-popliteal bypass. A completion angiogram in the operating room showed a patent graft and the heparin was re-started post-procedurally. On the first post-operative day, the patient again lost distal pulses in his left foot. He was taken back to the OR, where he was found to have complete thrombotic occlusion of his vascular graft. By this time, 7 days following the initiation of heparin, the patient’s platelets had fallen 30 % from their peak. Though an immediate ELISA for the HIT antibody returned negative, the patient was switched from heparin to bivalirudin due to the continued high clinical suspicion for HIT and was subsequently bridged to warfarin. A repeat ELISA was sent 8 days after the first negative result and this time returned positive, thus confirming the diagnosis of HIT.
DISCUSSION: HIT is an immune-mediated thrombocytopenia associated with heparin therapy typically caused by the development of IgG antibodies to the complex of unfractionated heparin (UFH) and platelet factor 4 (PF4). These antibodies subsequently bind to platelets, causing their activation and aggregation and leading to the clinical manifestations of the disorder. The pre-test probability of a HIT diagnosis prior to serologic testing can be estimated using the “4 Ts” clinical scoring system, in which patients are assigned zero, one, or two points in each of four categories—degree of thrombocytopenia, timing of platelet fall, thrombosis, and absence of other causes of thrombocytopenia. Our patient had a “4Ts” score of six (one point for 30–50 % drop in platelet count, two points for the platelets falling between 5 and 10 days after the initiation of heparin, two points for a clinically apparent thrombosis, and one point for the recent surgery being an alternative cause of thrombosis), thus giving him a high pre-test probability for HIT. The ELISA-based screening assay typically used has a very high sensitivity (95–100 %) but a lower specificity (~80 %), thus this testing is best performed on patients with a high pre-test probability (greater than six points) to minimize the risk of a false positive result. The serotonin release assay, which is much more specific than the ELISA screen, is still not widely available in hospitals without specialized coagulation laboratories. In patients such as ours, the pre-test probability is high enough that a single negative HIT antibody ELISA is not enough to rule out the condition. There are several scenarios in which a patient may initially have a negative ELISA but still experience HIT. First, as seen in our case, the assay, though extremely sensitive, may not be able to detect the low antibody titers very early in the disease course. Second, a small subset of patients experience clinical HIT due to anti-IL8 or anti-neutrophil activating peptide antibodies, rather than usual anti-PF4/UFH antibody detected by the ELISA. Third, some patients express a large amount of platelet associated PF4 and can thus develop clinically apparent HIT with levels of anti-PF4/UFH antibodies low enough to evade the screening ELISA test. A recent retrospective chart review identified cases of repeat HIT antibody testing following an initial negative result. While 12 % of these repeat tests returned positive, mainly among those patients whose initial ELISA was borderline, the only four who actually developed thrombotic complications were the same four patients whose pre-test “4 Ts” score had also increased in the interim, thus suggesting a true change in their clinical situation. In these patients, the positive ELISA merely confirmed the increased clinical suspicion raised by the climbing “4 Ts” score. This finding reinforces the notion that the occurrence of symptomatic HIT is best predicted through accurate assessment of the clinical situation; the ELISA test remains an adjunct and should be reserved for confirmation of the diagnosis in patients with a high pre-test probability.
A TATTOO PAINTS A PICTURE OF SARCOIDDavid A. Rand1; Julie Lin2; Elizabeth Zeeck3; Deborah Cook4. 1University of Vermont, Burlington, VT; 2University of Vermont, Burlington, VT; 3University of Vermont, Burlington, VT; 4University of Vermont, Burlington, VT. (Tracking ID #1939857)
LEARNING OBJECTIVE 1: Recognize that tattoo reactions can be a manifestation of systemic sarcoidosis
CASE: A 30 year old Caucasian male presented with a 10 day history of progressively worsening discomfort and irritation at multiple tattoo sites. Severe pain surrounding his leg tattoos limited his ability to ambulate and prompted a visit to the emergency department. All tattoos were placed professionally 10 years prior though one tattoo had been touched up with black, orange, and red pigment 4 months before presentation. The patient had a history of hyperlipidemia, hypothyroidism, as well as systemic sarcoidosis with associated hilar adenopathy and anterior uveitis, asymptomatic since remicade infusion therapy 2 years prior. On examination, all black tattoos were inflamed and raised with erythematous margins and superficial scaling. Areas with non-black pigmentation were completely spared. The result of a punch biopsy was notable for multinucleate giant cells consistent with granulomatous dermatitis. The patient was prescribed 60 mg of prednisone daily which was tapered over 4 weeks. His symptoms subsequently resolved completely and the appearance of the tattoos returned to baseline.
DISCUSSION: Sarcoidosis is a granulomatous disease of unknown etiology which involves the skin in up to one third of cases (1,2,3). Indeed, the word sarcoid originated from the Greek sarkodes, coined by the Norwegian Dermatologist Casear Boeck to describe “fleshy” skin findings resembling sarcoma (4). The presence of granulomatous reactions within tattoos has been reported since 1952 (5). In this case vignette, we report the case of a patient with known sarcoidosis presenting with granulomatous infiltration of multiple tattoos. While this patient had previously been diagnosed with systemic sarcoidosis, prior case reports have described the presence of non caseating granulomas within a tattoo as the initial presentation of systemic sarcoidosis (6,7,8). However, the presence of histologically identical granulomatous disease may also be associated with a foreign body reaction caused by a tattoo or scar, unrelated to sarcoidosis (9,10). Hence, identification of a non-caseating granuloma in the skin should be followed by a thorough workup for systemic sarcoidosis. In this case, the long latency period between placement of the tattoos and the granulomatous reaction likely suggests a sarcoidosis flare. However, the role of exposure to foreign bodies in sarcoidosis is still unknown and it is possible that the flare represents a delayed foreign body reaction. Also unclear is why only the black pigmented regions were affected (4). It is important for internists who care for patients with sarcoidosis to recognize its dermatologic manifestations in addition to the more common pulmonary and ocular presentations. This is especially relevant given the popularity of cosmetic tattooing. 1. Hanno R; Needelman A; Eiferman RA et al. Cutaneous sarcoidal granulomas and the development of systemic sarcoidosis. Arch Dermatol. 1981;117:203–207. 2. English JC; Patel PJ; Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725–743. 3. Samtsov AV. Cutaneous sarcoidosis. Int J Dermatol. 1992;31:385–391. 4. Iannuzzi MC; Rybicki BA; Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153–65. 5. Lubeck G; Epstein E. Complications of Tattooing. Calif Med. 1952; 2: 83–85 6. Post J; Hull P. Tatoo Reactions as a Sign of Sarcoidosis. CMAJ. 2012; 184 (4): 432–433 7. Antonavich D; Callen J. Development of Sarcoid in Cosmetic Tattoos. Arch Dermatol. 2005; 141: 869–872 8. Anolik R; Mandal R; Franks A. Sarcoid Tatoo Granuloma. Dermatology Online Journal. 2010; 16 (11): 19 9. Marcoval J; Mana J; Morena Abelardo; Gallego Isabel et al. Foreign Bodies in Granulomatous Cutaneous Lesions of Patients with Systemic Sarcoidosis. Arch Dermatol. 2001; 137: 427–430 10. Callen JP. The presence of foreign bodies does not exclude the diagnosis of sarcoidosis. Arch Dermatol. 2001;137:485–486
A TEMPERATE CLIMATE PATIENT PRESENTING WITH A TROPICAL DISEASE: A CASE OF BACTERIAL PYOMYOSITIS SECONDARY TO COMMUNITY ACQUIRED MRSAGrant Boschult; Jonathan S. Kurman; Kurt J. Pfeifer. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1927281)
LEARNING OBJECTIVE 1: Enhance clinical awareness of the increasing incidence of pyomyositis in temperate climates.
LEARNING OBJECTIVE 2: Consider the presence of pyomyositis in patients who present with localized musculoskeletal complaints in the setting of bacteremia.
CASE: A 28-year-old African American female with a past medical history of hypertension presented with 2 days of persistent, left-sided, “burning,” chest pain exacerbated by palpation, deep breathing, and lying supine. While in the emergency department the patient was found to be afebrile and tachycardic with a mild leukocytosis of 14,700/uL. A chest X-ray was performed, and no abnormalities were noted. Computed tomography (CT) of the chest with contrast was negative for pulmonary emboli or other pathology. The patient was subsequently discharged home with a presumed muscle strain, only to return to the emergency department 2 days later with complaints of worsening left-sided chest pain. The patient had a temperature of 100.1 F and a worsening leukocytosis. An electrocardiogram showed sinus tachycardia, and a chest x-ray was unremarkable. The patient was admitted for further evaluation and management. Two days after admission, blood cultures returned positive for methicillin-resistant Staphylococcus aureus (MRSA). The patient was subsequently started on intravenous vancomycin. Transthoracic and transesophageal echocardiograms were performed and showed no valvular or other abnormalities. An indium-tagged white blood cell scan showed an area of intense uptake in left mid-anterior hemithorax, consistent with the distribution of the chest pain. A repeat CT scan revealed an ill-defined mass-like inflammatory lesion in the left anterior chest wall extending into the intercostal fat, mediastinal fat, and pleural spaces, with some compression of the right ventricular outflow tract, as well as a moderate left-sided pleural effusion. A thoracentesis produced 250 mL of exudative and culture-negative fluid. Surgical drainage of the affected muscle was considered, but not performed, as a focal fluid collection or abscess was not identified. The patient was continued on IV vancomycin for a total 4 weeks and her symptoms gradually improved. A repeat chest CT was performed at the end of therapy, which showed resolution of the inflammatory mass and pleural effusion.
DISCUSSION: Pyomyositis is a purulent infection involving skeletal muscle associated with bacteremia and abscess formation. Classically seen in the tropics, this disease has been recognized with increasing frequency in temperate climates. Pyomyositis is often not an early diagnostic consideration due to its rarity in temperate climates and non-specific presenting signs and symptoms (fever, muscle pain and leukocytosis), often delaying initiation of appropriate therapy. If not recognized and treated in a timely manner, pyomyositis can progress to septicemia and septic shock. Predisposing factors include immunodeficiency, trauma, intravenous drug use and malnutrition. The most common associated pathogen is Staphylococcus aureus, responsible for approximately 95 % of tropical and 70 % of temperate cases. Treatment includes drainage of abscesses and empiric intravenous antibiotics, initially directed against MRSA and adjusted according to gram stain and culture results. It is generally recommended to continue IV antibiotics for 4 weeks and to repeat imaging at the end of therapy. This case illustrates the importance of considering the diagnosis of pyomyositis in patients who present with persistent fever, leukocytosis and focal muscle cramping and tenderness.
A TIGHT SQUEEZERebecca L. Hostetler1; Jeremy S. Markowitz2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2VA Pittsburgh Healthcare System, Pittsburgh, PA. (Tracking ID #1938174)
LEARNING OBJECTIVE 1: Recognize the clinical features of constrictive pericarditis and distinguish it from restrictive cardiomyopathy
LEARNING OBJECTIVE 2: Determine the best diagnostic workup for constrictive pericarditis
CASE: 46 year old man with a history of class III obesity and coronary artery disease status post coronary artery bypass graft 3 years prior transferred from an outside hospital with a 4 month history of increasing ascites, worsening dyspnea on exertion, jaundice, and a 50 lb weight gain. He had been intubated for increasing repiratory distress prior to arrival, after a large-volume paracentesis failed to sufficiently improve his respiratory status. His exam was notable for central venous pressure of 30, massive ascites, and 4+ lower extremity edema. His labs showed an acute liver injury in a cholestatic pattern and kidney injury of unknown duration. On arrival, the team initially attempted fluid removal with repeated large-volume paracentesis and IV diuretics; however, he developed refractory ascites, renal failure, and eventually shock requiring CVVHD and pressors. His liver failure continued to worsen, and peaked with a total bilirubin of 11.4 mg/dL, direct bilirubin 7.0 mg/dL, ALT 236 IU/L, AST 265 IU/L, and alkaline phosphatase 953 IU/L. Workup for the cause of his liver failure revealed negative testing for viral hepatitis, primary biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis. Right upper quadrant ultrasound disclosed no focal liver lesions, mild cirrhosis and patent vessels. Transjugular liver biopsy showed sinusoidal dilatation, moderate bridging fibrosis, and transhepatic gradient of 6 mmHg without significant portal hypertension. TTE showed normal systolic function with borderline pulmonary hypertension. Left and right heart catheterization were notable for four-chamber equalization of pressures, and CT chest revealed pericardial thickening with calcifications, confirming the diagnosis of constrictive pericarditis with hepatic congestion. Unfortunately, he was unable to be stabilized in order to perform a pericardectomy and passed away after being terminally extubated.
DISCUSSION: Our patient presented with constrictive pericarditis from cardiac surgery. The most common causes of constrictive pericarditis are viral/idiopathic, post-surgical, and post-radiation. Constrictive pericarditis complicates 0.2–0.3 % of cardiac surgeries. This case illustrates common challenges in diagnosing constrictive pericarditis, which include distinguishing congestive hepatopathy from primary liver disease, and distinguishing constriction from other causes of right heart failure, especially restrictive cardiomyopathy. Historical clues that aid in the diagnosis include prior cardiac surgery or chest radiation. Exam findings of constrictive pericarditis include signs of right heart failure (elevated JVP, ascites, pulsatile liver, peripheral edema.) Transthoracic echocardiography can exclude other more common causes of right heart failure (such as left heart disease and pulmonary hypertension) and sometimes shows characteristic findings of pericardial constriction such as ventricular interdependence. Pericardial thickening and calcifications on chest X-ray, chest CT, or cardiac MRI are also characteristic findings. Distinguishing constrictive pericarditis from restrictive cardiomyopathy usually requires simultaneous left and right heart catheterization to evalaute hemodynamics, cardiac CT/MRI to find the location of structural abnormalities, or both. Despite being a rare condition, there is a definitive treatment (pericardiectomy), increasing the importance of early recognition.
A TREMOR WITH GRAVE CONSEQUENCESAsad Jehangir; Bilal Shaikh; Ahmed Salman; Anthony Donato. Reading Health System, West Reading, PA. (Tracking ID #1927856)
LEARNING OBJECTIVE 1: Recognize Graves’ disease in patients with complaint of intention tremor.
CASE: A 34 -year-old-male presented to an urgent care center with a chief complaint of tremors for the last 3 months. Vitals revealed tachycardia with heart rate of 120, prompting them to refer him for emergency care. Exam showed mild diffuse enlargement of his thyroid gland to two times normal size without nodules and an associated thyroid bruit. Hyperreflexia was also noted, but opthalmoplegia and dermopathy were absent. A high-frequency, low amplitude tremor was present that worsened with intention. Labs revealed TSH of 0.01 uIU/mL (normal: 0.3–5.0 uIU/mL), free T4 of 5.59 ng/dl (normal: 0.58–1.64 ng/dl) and total T3 of 8.1 ng/mL (normal: 0.9–1.8 ng/mL). TSI and thyroid receptor antibody were positive, confirming Graves disease. He was started on methimazole and propranolol and referred for follow up with an endocrinologist. Patient has been maintained on methimazole and is awaiting definitive therapy at this time.
DISCUSSION: Graves’ disease is the cause of 60–80 % of cases of hyperthyroidism and usually presents with multiple symptoms including sweating, palpitations, tremors, weight loss, diarrhea and tachycardia as well as unique Graves’ disease findings of lid-retraction, proptosis and pre-tibial myxedema. However physicians should recognize it even when patients do not have overt symptoms of hyperthyroidism. This case demonstrates that patients can present with a solitary complaint of tremors as the presenting sign of hyperthyroidism. A new tremor is a symptom that can be a benign finding or it can serve as a harbinger for underlying systemic disease. The presence of a high-frequency, low-amplitude tremor should raise essential tremor, catecholamine excess (including alcohol withdrawal) and hyperthyroidism on a differential. The presence of weight loss or abnormal thyroid examination should prompt serum testing of thyroid function.
A TRICKY CLICKING: A CASE OF PULSATILE TINNITUSAlison R. Landrey. University of Vermont/Fletcher Allen Medical Center, Burlington, VT. (Tracking ID #1937486)
LEARNING OBJECTIVE 1: Recognize and evaluate for vascular etiologies of pulsatile tinnitus.
CASE: CC: left ear clicking HPI: A 79-year-old man presents with a constant “clicking” sound in his left ear progressing over 7 weeks. He states it is “like a ticking clock” and seems to be timed with his pulse. It is worse when supine and better when leaning his head back while sitting or standing. He also complains of episodic lightheadedness and nausea progressing over 4 weeks. The lightheadedness and nausea are worse with standing or sitting up from a supine position and better with lying down. He also endorses a mild intermittent non-throbbing frontal headache for 5–6 days. He denies ear pain, neck pain, eye pain, nasal congestion, sinus pressure or vision changes. He had been seen 1 month prior for the same complaint. He was noted at this visit to have been seen 6 weeks prior for ear fullness, which resolved with ear irrigation for cerumen impaction, but was associated with clicking in the left ear when opening his jaw. His ear canals this time were clear but he was thought to have a mild effusion behind the left tympanic membrane. Auscultation was not performed. He was prescribed a nasal corticosteroid for possible Eustachian tube dysfunction as a cause of the tinnitus. He stopped it after a week because he thought it was making the lightheadedness and nausea worse and did not seem to be helping the clicking. Past medical history: Prostate cancer, T2, gleason grade 9. Treated at age 75 with radiation and androgen deprivation therapy Osteoporosis Osteoarthritis Hyperlipidemia Current medications: Atorvastatin 10 mg daily Latanoprost eye drops Multivitamin daily Social history: He has never smoked. He currently drinks on 10 alcoholic drinks per week. He is a retired banker and lives with his wife. Family history None pertinent Physical Exam BP 160/75 | Pulse 68 | Temp (Src) 36.7 °C (98.1 °F) (Tympanic) Constitutional: He is oriented ×3. He appears well-developed and well-nourished. No distress. Head: Normocephalic and atraumatic. Right Ear: Tympanic membrane, external ear and ear canal normal. Left Ear: Tympanic membrane, external ear and ear canal normal. Nose: normal. Mouth/Throat: Uvula is midline, oropharynx is clear and moist and mucous membranes are normal. Eyes: EOMI, PERRLA, normal fundoscopic exam Neck: Normal range of motion. Neck supple. Cardiovascular: Normal rate and regular rhythm. 2/6 diastolic murmur 2nd intercostal space, right sternal border Radial pulses 2+ bilaterally Loud left carotid bruit Pulmonary/Chest: Effort normal and breath sounds normal Neurological: He is alert and oriented to person, place, and time. No cranial nerve deficit. Gait normal. Workup and Diagnosis: The patient was suspected of having a vascular etiology for his pulsatile tinnitus. A CT angiogram and an echocardiogram were ordered. He was also started on lisinopril for his elevated blood pressure. CT arteriography showed early venous opacification at the skull base to the left of midline about the left vertebral artery and epidural space, suspicious for an arteriovenous fistula. Echocardiogram showed a normal left ventricle and systolic function with mild aortic stenosis and moderate aortic regurgitation. A conventional angiogram confirmed a dural arteriovenous fistula originating in the left vertebral artery. The patient then underwent an uncomplicated coil embolization of the fistula. He had complete resolution of the clicking sound and dizziness.
DISCUSSION: Pulsatile tinnitus is the perception of a rhythmic noise timed with the pulse and is a relatively uncommon complaint in the primary care setting. It is most suggestive of a vascular etiology such as AV malformation, arterial stenosis, or compression of a blood vessel by a mass. Other etiologies include pseudotumor cerebri and Eustachian tube dysfunction. In our case, the diagnosis was missed on the first examination. The fact that the patient did have a prior visit for ear fullness with similar left ear clicking may have confounded the assessment, although the clicking was not pulsatile when associated with the ear fullness. It is important for the general internist to be aware of pulsatile tinnitus as a distinct presentation and to perform an appropriate exam and workup for vascular causes. This includes auscultation for bruits, which may have accelerated the diagnosis and treatment for our patient had it been done at the initial visit for his complaint.
A TWENTY-NINE-YEAR-OLD MAN WITH AN UNUSUAL CAUSE OF AN ABSCESSShivangi Vachhani; Anne Cioletti. George Washington University, Washington D.C., DC. (Tracking ID #1939152)
LEARNING OBJECTIVE 1: Discuss an unusual cause of an abscess, which is a botfly infection
LEARNING OBJECTIVE 2: Remind the readers that travel history is an important aspect of the history taking.
CASE: A 29 year old healthy male presented to the clinic with a two-day history of a left scalp mass. Two days prior to his initial presentation, he noticed three scabs on his left scalp with associated pruritis. These symptoms progressed to left temporal edema and purulent drainage from his scalp on the day prior to presentation. He denied any fevers, chills or any pain. His past medical and family history was negative, and he was not on any medications. He denied any tobacco or drug use and drank alcohol only socially. He did report recent travel to Belize 2 weeks prior to his presentation. His review of system was otherwise negative. Upon presentation, his vital signs were within normal limits, and he was afebrile. His physical exam showed a firm abscess with purulent drainage on the left scalp as well as a left temporal edema. He was started on sulfamethoxazole and trimethoprim to treat for suspected MRSA abscess. He noticed improvement of the left temporal edema and decrease in purulent drainage upon starting the antibiotics. Over the next few days, the patient started experiencing alopecia around the abscess as well as occasional parasthesia leading to increased pruritis. Despite finishing the course of his antibiotics, his abscess and drainage persisted, so he was re-started on another course of sulfamethoxazole and trimethoprim and instructed to use warm compresses over the area. After restarting the antibiotics and warm compresses, the patient’s wife tried to express purulent material when a larva was expressed instead. Analysis of this larva confirmed it was a larva of a bot fly. A total of three larvae were removed from his scalp. Upon the removal of the larvae, his symptoms improved, and he had complete resolution over the next few weeks.
DISCUSSION: This is a case of a young man with recent travel to Belize who presented with a two-day history of a scalp abscess and left temporal edema. He was appropriately started on sulfamethoxazole and trimethoprim to treat for community acquired MRSA with incomplete resolution of his symptoms; after a couple of weeks with attempts to drain the abscess, larvae of the human bot fly were extracted instead. The initial improvement of symptoms with antibiotics is believed to be due to a superimposed bacterial infection around the larvae, but without expression of the fly, symptoms would have persisted. The bot fly is a 12–18 mm in length bluish colored fly that resembles bumble-bee. The larva of this fly is known to infest the skin of mammals and live out the larval stage in the subcutaneous layer. The species of bot fly known to infect humans is called Dermatobia hominis. It is native to Central as well as South America. The adult fly lays its eggs on the abdomen of a mosquito where it hatches to form the first larval instar. When the mosquito bites the human, the larva penetrates the skin and burrows itself into the subcutaneous layers. As the larva burrows deeper, it feeds on the host's body and exudates. It uses spines on its body to anchor itself and breaths through posterior spiracles. The treatment is asphyxiation using either petroleum or a scotch tape which causes the larva to migrate out of its host. Although it is rarely fatal, the larva can live in subcutaneous layer for as long as 10 weeks and induces formation of a painful nodule. It can occur in any part of the body including eyes, ears, and nose. The exact prevalence of Botfly in United States is unknown; however given the increasing rates of travel to foreign countries, it is important to recognize the symptoms of this infection.
A UNIQUE CASE OF ACQUIRED PANHYPOPITUITARISM PRESENTING AS SYMPTOMATIC HYPONATREMIABrian Y. Park1; Daniel I. Kim1,2; Iqbal Munir1,2. 1Loma Linda University, Loma Linda, CA; 2Riverside County Regional Medical Center, Riverside, CA. (Tracking ID #1939505)
LEARNING OBJECTIVE 1: Hypopituitarism is a clinical condition with impaired synthesis of pituitary hormone(s) which has variable presentation and often difficult to diagnose. The clinical features of hypopituitarism depend on rapidity of onset of hormone deficiency and involvement of specific hormonal axis.
CASE: A 49-year-old female with a past medical history of hypertension and diabetes type II, presented with a one-month history of weakness, fatigue, and loss of appetite in our hospital. A detailed history revealed having no menstrual period since her last child birth in Mexico 20 years ago. Although her pregnancy was otherwise unremarkable, she had lactation failure after delivery. The patient was admitted to the hospital due to moderate hyponatremia (serum Na level 124 mEq/L). Her vitals were in the normal range; physical exam was normal except absence of axillary hair and very scant pubic hair. Clinically, she was euvolemic. Labs showed low T4 with inappropriately normal TSH. The patient was suspected to have pituitary failure and futher labs were ordered, which showed low insulin-like growth factor, low dehydroepiandrosterone, and normal prolactin level. She also had very low follicle-stimulating hormone and luteinizing hormone levels. Her basal cortisol was low with a normal ACTH level, and cosyntropin test showed a sub-optimal rise of cortisol following administration of cosyntropin. An MRI of the pituitary gland showed an empty sella. Patient was diagnosed with panhypopituitarism (when three or more hormonal axis are deficient). She was treated with levothyroxine and hydrocortisone replacement with resolution of hyponatremia and improvement of clinical condition.
DISCUSSION: This is a unique case of panhypopituitarism presenting with hyponatremia. Etiology of hyponatremia for this patient is likely both adrenal and thyroid hormone deficiency. History of lactation failure and amenorrhea following last child birth points toward Sheehan’s Syndrome. Sheehan syndrome occurs as a result of pituitary necrosis following severe postpartum hemorrhage. Empty sella in pituitary MRI, which is often a normal variant, may indicate a loss of pituitary tissue subsequent to Sheehan’s Syndrome. THis case is also unique having a delay of presentation of Sheehan’s Syndrome.
A WEAK, EXCITED, AND DRUNK HEARTMichael Zablow; Amir Latifi; Salman Haq. New York Methodist Hospital, Brooklyn, NY. (Tracking ID #1923584)
LEARNING OBJECTIVE 1: Recognize the etiology of cardiomyopathy and subsequent decompensations.
LEARNING OBJECTIVE 2: Recognize medication interactions, including those with diet and social habits
CASE: A 30 year old male with ADHD presented with 2 months of progressive shortness of breath and decreased exercise tolerance. He had generalized malaise, but denied fevers. His only medication was Adderall (Amphetamine/Dextroamphetamine), which he had been taking TID between 2006 and 2008, and again from 2010 to the present. While he denied tobacco and illicit drugs; he drank 1 bottle of wine 4–5 times weekly for 12 years. Family history was HTN in both parents. Physical exam was unremarkable. Chest X-ray had a small pleural effusion and cardiomegaly. Routine labs and cardiac enzymes were normal, ProBNP was 2,619 pg/ml. EKG showed sinus tachycardia, rate 125, left atrial enlargement, and left axis deviation. Echocardiogram found left ventricular ejection fraction to be 19 %. Cardiac MRI did not show infiltrative disease (i.e. amyloidosis, hemochromatosis, or sarcoidosis). Cardiac catherization was negative for CAD. Anti-dsDNA, ANA, HIV, Hepatitis C and Parvovirus IgM were negative. Parvovirus IgG was 6.6 (normal 0.0–0.89) and Coxsackie B3 titer was 1:8 (normal <1:8). He was discharged on an ACE-I, beta blocker, and loop diuretic. There is a black box warning for Adderall and structural heart damage. He agreed to discontinue Adderall and abstain from alcohol. He was outfitted with an external defibrillator and plans for a follow up echocardiogram in 3–6 months. Should there be no improvement in LVEF, he will need permanent defibrillator placement and cardiac transplant evaluation.
DISCUSSION: The low Coxsackie titer and negative Parvovirus IgM imply the infections are not acute. Coxsackie B3 and Parvovirus are known causes of myocarditis, which can progress to idiopathic dilated cardiomyopathy (IDCM) through mechanisms that are not well understood. IDCM is the second leading cause of heart transplant; Androletti found Enterovirus RNA (i.e. Coxsackie) in 37.5 % of explanted hearts with IDCM. Amphetamines increase cardiac work through indirect sympathetic activation via noradrenaline, dopamine and serotonin. Dilated cardiomyopathy is an infrequent complication of Adderall, occurring in <1 % of patients. By itself, alcohol is unlikely the primary cause of the cardiomyopathy; MCV and LFTs were normal. However, alcohol inhibits the breakdown of amphetamines, and furthermore, is a vasodilator. When combined, the two substances can place tremendous stress on the heart. It is by exclusion that we hypothesize the decompensated IDCM was caused by two mechanisms. Viral myocarditis caused the dilated cardiomyopathy, which was well compensated until cumulative damage from amphetamine and alcohol lead to a decompensated state. This case exemplifies the need for a meticulous history and medication reconciliation. Without recognizing the affect of Adderall and alcohol, cardiac damage and functional decline would have continued.
A WOLF IN SHEEP’S CLOTHING: HANSEN’S DISEASE MASQUERADING AS A VASCULITIC PROCESSSumit R. Naig2,1; Eunice Yu1; Susan Rhee3,1. 1Johns Hopkins Bayview Medical Center, Baltimore, MD; 2Johns Hopkins Bayview Medical Center, 21224, MD; 3Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1939034)
LEARNING OBJECTIVE 1: Recognize that steroid responsiveness does not confirm a primary vasculitic process and can delay diagnosis of an infectious process.
LEARNING OBJECTIVE 2: Recognize that Hansen’s disease can present with vasculitic complications
CASE: Mr. S is a 28 year old man who presented with severe pain from bilateral lower extremity ulcers. The lesions began 1 year after he moved to the United States from Costa Rica as painless, red plaques below the knees. Oral prednisone led to rapid resolution. Eight months later, the plaques reappeared and were again successfully treated with steroids. The lesions appeared with increasing frequency before progressing to ulcers. Mr. S reported subjective fevers and weight loss of 30 lbs. He had no other medical history. His medications were intermittent steroids and ibuprofen for pain control. He tried a 3 month course of methotrexate for the lesions without success. Family history was significant for ‘colitis’ in his mother although he denied such symptoms. Mr. S did not smoke, drink alcohol, or use illicit drugs. Physical exam was pertinent for a thin man in no acute distress, moon faces, and loss of lateral eyebrows and eyelashes. He had a normal neurologic exam except for decreased sensation in a median nerve distribution of the left hand. Below the knees, patient had multiple punched-out ulcers with wavy, violaceous borders that ranged from 4 to 12 cm in size. Bloodwork showed sedimentation rate of 47 mm/h and C-reactive protein of 9 mg/L. Mr. S had negative anti-nuclear antibody and anti-nuclear cytoplasmic antibody, making rheumatologic process unlikely. Hepatitis C and cryoglobulins were also negative. Multiple skin biopsies of the ulcers showed heavy acid-fast bacilli (AFB) positive staining, and a deep wedge biopsy showed heavy AFB+ bacilli within bubbly macrophages and nerves, as well as changes of small vessel vasculitis.
DISCUSSION: The morphology of the ulcers and a history of response to steroids suggested a vasculitic process. Unfortunately, skin biopsy was never pursued as an outpatient due to presumptive diagnosis of scleroderma vs. pyoderma gangrenosum and inconsistent follow-up, delaying diagnosis. The deep wedge biopsy that demonstrated AFB+ bacilli in nerves was critical to establish the diagnosis of Hansen’s disease. Hansen’s disease is a chronic granulomatous disease caused by Mycobacterium leprae or Mycobacterium lepromatosis that affects the skin and peripheral nerves. A variety of the diffuse lepromatous form is characterized by necrotic ulcerations of the skin of the lower extremities from reactive vasculitis, alopecia of the eyebrows and eyelashes, and is epidemiologically linked to Central America. Following diagnosis, steroids were restarted and the patient was referred to the National Hansen’s Disease Program for further treatment with dapsone, rifampin, and clofazimine.
A WOMAN AND HER ACUTELY UNSUSPECTING HEARTEugenia Tsai; Jenny Johnson; Darlene LeFrancois. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939371)
LEARNING OBJECTIVE 1: Recognize clinical manifestations of toxic shock syndrome
LEARNING OBJECTIVE 2: Diagnose endocarditis based on its risk factors and clinical presentation
CASE: A 23 year old woman with no significant medical history presented with 1 week of fever and rhinorrhea accompanied by diffuse myalgias. She had no history of congenital heart disease, rheumatic fever or intravenous drug use (IVDU). Her last menstrual period was 3 weeks prior to presentation and she denied any recent tampon use. Vital signs were notable for temperature 102○F, HR 130 bpm and BP 109/56 mmHg. She had injected conjunctiva, a diffuse macular rash and early necrosis of the right index finger. Cardiac exam revealed a 3/6 diastolic murmur at the right sternal border with radiation to the carotids. On hospital day 10, patient had desquamation of her palms. Blood work on presentation showed creatinine 1.6 mg/dL, AST 155 U/L and ALT 145 U/L. CBC revealed WBC 16.5 × 106/L, platelet count 34 × 109/L. Other notable labs included CRP 111 mg/dL, ESR 51 mm/h and CPK 596 U/L. A full infectious panel, including syphilis and HIV were negative. Multiple blood cultures grew methicillin-sensitive S. aureus. Transesophageal echocardiogram revealed a 0.6 cm round mobile vegetation on the aortic valve and moderate aortic valve regurgitation without any abscess formation; the remainder of the endocardium was unremarkable. The patient fulfilled diagnostic criteria for non-menstrual Staphylococcal toxic shock syndrome (TSS), complicated by infective endocarditis (IE). She was treated with a 6-week course of nafcillin and gentamicin. Three days after initiation of antibiotic therapy the patient was no longer bacteremic.
DISCUSSION: Toxic shock syndrome (TSS) is a toxin-mediated, potentially life-threatening condition that is typically associated with tampon use during menstruation. Pathogens include S. aureus, where TSS is caused by enterotoxin type B, and S. pyogenes. However one-half of reported TSS cases are non-menstrual. Diagnosis is made based on clinical features of fever, diffuse rash, hypotension, desquamation of the palms and soles and multiorgan involvement. Three of seven organ systems must be affected to meet criteria: GI (diarrhea or vomiting), muscular (myalgia or elevated CPK), mucous membrane (vaginal, oropharyngeal or conjunctival hyperemia), renal (elevated BUN or creatinine), hepatic (elevated transaminases or total bilirubin), hematologic (platelet <100 × 109/L) or CNS (altered consciousness). Endocarditis, or inflammation of the endocardium, is the result of aggregation of platelets, fibrin and inflammatory cells. IE by bacterial or fungal species involves direct adherence by more virulent species to the endocardium. Alternatively, microorganisms in the blood may attach to sites of nonbacterial thrombotic endocarditis (NBTE) and lead to infective endocarditis. In acute endocarditis rapid structural cardiac damage ensues, often leading to metastatic infection and fatal if left untreated whereas subacute endocarditis slowly damages the heart and rarely has hematologic seeding. Although many bacteria can cause endocarditis, only a few cause the majority of cases. S. aureus, streptococci and coagulase-negative staphylococci are the pathogens in a majority of acute bacterial endocarditis cases. IE more often occurs in those with underlying cardiac structural abnormalities including congenital or rheumatic heart disease. Patients with intracardiac devices may also be predisposed to endocarditis. Risk factors include IVDU, indwelling catheters, poor dental hygiene or HIV infection. As this case demonstrates, however, IE due to S. aureus can occur in patients with normal hearts and without risk factors. The most common presenting features of IE are fever and heart murmur, each clinically seen over 80 % of the time. Other features such as chills, myalgias, arthralgias and malaise, are also nonspecific and can suggest any number of diseases. Although seen in only 2–8 % of acute cases, clinical findings can include Osler nodes (tender subcutaneous nodules usually in the hands and feet), splinter hemorrhages (dark-red, linear lesions in the nail beds), Roth spots (retinal hemorrhages) and Janeway lesions (nontender rash on the palms and soles). Alarming sequelae include neurological complications such as stroke or encephalopathy. Diagnosis requires fulfilling 2 major, 1 major and 3 minor or 5 minor Duke criteria. This patient met the 2 major Duke criteria: persistently positive blood culture with a typical IE organism and a valvular mass on echocardiogram. Minor criteria include predisposition, fever, evidence of embolism, immunologic problems (e.g. Osler’s nodes), and a positive blood culture that does not meet major criteria. It is important for internists to maintain a high degree of suspicion for infective endocarditis, despite the lack of classic risk factors, as delay of treatment can lead to significant sequelae.
A YOUNG MAN WITH FEVER AND DIFFUSE MUSCLE PAINPriti Dangayach; Lee Lu; Vagish Hemmige. Baylor College of Medicine, Houston, TX. (Tracking ID #1926379)
LEARNING OBJECTIVE 1: Recognize the clinical features of tropical pyomyositis.
LEARNING OBJECTIVE 2: Diagnose and treat tropical pyomyositis promptly for better outcome.
CASE: A previously healthy 43-year-old construction worker presented with fever and muscle pain for 8 days. His initial symptoms included a high fever up to 1020 F with left hip pain radiating down his leg. Two days prior to presentation, he noticed left shoulder pain and right elbow pain with redness, swelling, and warmth. His pain was worsened by movement. He denied muscle trauma. His fever continued to spike daily to a maximum temperature of 105 0 F. He was monogamous, married, and denied any new sexual partners, penile discharge, or skin lesions. On examination, he was febrile to 102.9 ○F, tachycardic to heart rate in the 120 s, and normotensive. He had limited range of motion of his left shoulder, most pronounced with abduction, and of the left hip, mainly with flexion. There was left sided gluteal point tenderness. The right elbow was erythematous and warm without palpable effusion. There were no rashes, lesions, or open wounds. His WBC was 21.6 (91 % neutrophils) with ESR 71 mm/h and CRP 32.9 mg/L. The focal muscle tenderness on exam prompted further studies. CT imaging showed fluid collections in the left iliacus muscle (2.4 × 8 cm), left piriformis muscle (1.2 cm × 1.5 cm), and the subdeltoid bursa. The left iliacus abscess was drained, and cultures yielded Staphylococcus aureus. An attempt to drain the subdeltoid bursa was unsuccessful. Blood cultures grew methicillin susceptible Staphylococcus aureus. His transthoracic echo was negative for endocarditis. He was diagnosed with tropical pyomyositis and was initially started on intravenous vancomycin, which was changed to cefazolin when susceptibilities returned. He completed 6 weeks of therapy with resolution of all abscesses.
DISCUSSION: Isolated bacterial infection of the muscles has been named “tropical pyomyositis” due to its higher incidence in equatorial regions. In the tropics, most cases occur in young healthy males. In temperate regions, the associated risk factors are immunocompromised state, intravenous drug use, or significant medical comorbidities. The most common pathogen for tropical pyomyositis is Staphylococcus aureus, with increasing reports of methicillin resistant Staphylococcus aureus. Other described pathogens are streptococci, pneumococci, enteric gram negatives, and mycobacteria. Approximately 20–50 % of cases are associated with previous muscle trauma. The commonly affected muscles include quadriceps, glutei, pectoralis major, serratus anterior, biceps, iliopsoas, gastrocnemius, abdominal and spinal muscles.
A YOUNG WOMAN WITH CHEST PAIN AFTER A SORE THROAT AND FEVERRichard Wang. NewYork-Presbyterian Hospital Weill Cornell Medical Center, New York, NY. (Tracking ID #1936849)
LEARNING OBJECTIVE 1: Recognize the features of carditis in acute rheumatic fever
LEARNING OBJECTIVE 2: Recognize the diagnostic error of premature closure
CASE: A 33 year old woman with no significant medical history was admitted at this hospital with diffuse chest, abdominal, and back pain. Two weeks prior to presentation, the patient had had a sore throat with fever. These symptoms resolved after 1 week. Five days prior to presentation, the patient developed severe abdominal, chest, and back pain associated with fever, chills, and rigors. The pain was diffuse and often pleuritic. She took large doses of ibuprofen, up to 800 mg four times daily, with minimal improvement in symptoms. She was prescribed azithromycin at an urgent care center 1 day prior, but her symptoms persisted and she presented at the Emergency Department for further evaluation. On presentation, the patient was afebrile, tachycardic to 102 beats per minute, tachypneic to 26 breaths per minute, and normotensive. Her physical examination was otherwise normal. A complete blood count was remarkable for a leukocytosis of 23,400. Her serum creatinine was 5.89 mg/dL. The serum level of troponin I was 4.28 ng/mL. EKG showed normal sinus rhythm with no ST depressions or elevations. Urine toxicology screen was negative for all tested substances. Serum CRP was 10.95 mg/dL. ASO titer was elevated to 687 IU/mL (normal is <144 IU/mL). Throat culture was negative for Streptococcal species. Blood culture was positive for Streptococcus pyogenes. Accounting for her history of a sore throat and a positive streptolysin titer, the patient was diagnosed with acute rheumatic fever based on 1 major Jones criterion (carditis) and 2 minor Jones criteria (history of fever and elevated CRP). An echocardiogram was normal and showed no significant valvular disease. Her acute kidney injury was attributed to NSAID nephrotoxicity and resolved with intravenous fluids. The patient was initially treated with vancomycin, piperacillin-tazobactam, and penicillin VK, then subsequently narrowed to amoxicillin-clavulanate. Her pain was treated with ibuprofen and hydromorphone. She was discharged on the fifth day of her hospitalization with instructions to complete a 14-day course of amoxicillin-clavulanate. Two days after discharge, the patient returned to the Emergency Department with severe pleuritic back and chest pain. A chest X-ray was abnormal with a new opacification of the right lower lobe concerning for collapse. CT of the chest revealed an empyema of the right posterior thorax. The patient’s diagnosis was revised from acute rheumatic fever to streptococcal toxic shock syndrome from empyema. The patient subsequently underwent video-assisted thoracoscopic surgery for drainage and lung de-cortication. After a 14 day course of IV antibiotics, the patient made a full recovery.
DISCUSSION: The misdiagnosis in this case resulted in part from a misunderstanding and misapplication of the Jones criteria for the diagnosis of acute rheumatic fever. On physical examination and on echocardiographic imaging, the patient did not have any evidence of the valvular injury that is characteristic of carditis from acute rheumatic fever. In the absence of valvulitis, the patient was unlikely to have acute rheumatic fever. Moreover, it was incorrect to attribute the patient’s pain symptoms and elevated serum troponin to rheumatic carditis, and pre-mature closure prevented a search for alternative etiologies. In retrospect, the patient had low pre-test likelihood for acute rheumatic fever because initial attacks of acute rheumatic fever are rare in adults. Her history of sore throat 2 weeks prior to hospitalization was ultimately a red herring. A series of cognitive errors resulted in the failure to recognize and treat the correct diagnosis in this case, streptococcal toxic shock syndrome.
A-KNEE-MIA: BLOOD WHERE IT DOESN’T BELONGJonathan T. Cheah; Jason A. Korcak. Montefiore Medical Center, Bronx, NY. (Tracking ID #1940577)
LEARNING OBJECTIVE 1: Recognize hemarthrosis as a potential cause of acute monoarthritis.
LEARNING OBJECTIVE 2: Describe the etiology and risk factors, including systemic anticoagulation, for the development of hemarthrosis.
CASE: A 67-year-old woman presented with 3 days of right leg pain that began while walking and was exacerbated by movement. The patient denied any history of antecedent trauma. Past medical history was significant for bilateral hip replacement and atrial fibrillation on systemic anticoagulation with Warfarin. Temperature was 100.5 F and other vital signs were normal. There was swelling of the right lower extremity most prominent at the knee, as well as overlying ecchymosis. The knee and proximal lower extremity were warm and tender to palpation. Both active and passive movement of the knee were markedly reduced secondary to pain. Hemoglobin was 7.5 g/dL (the baseline was 10.0 g/dL), white blood cell count was 9.7 k/μL, INR was 6.4, and C-reactive protein was 223 mg/L. A radiograph of the right knee showed diffuse subcutaneous soft tissue edema and evidence of severe osteoarthritis. Knee aspiration revealed blood and blood clots, and cultures of the aspirate were without growth.
DISCUSSION: The complaint of joint pain is frequently encountered by the internist in both outpatient and inpatient settings. Although there is a broad differential, the most typical causes of acute monoarthritis include trauma, septic arthritis, and the crystal arthritides, gout and calcium pyrophosphate dihydrate deposition disease. Less frequent causes include hemarthrosis, erosive osteoarthritis, reactive arthritis, and tumors. Hemarthrosis most commonly affects the knee. Risk factors for the development of hemarthrosis include trauma and bleeding disorders. Less common associated conditions include septic arthritis, tumors such as synovial hemangiomas and pigmented villonodular synovitis, and impaired sensation and proprioception leading to abnormal loading and injury. In cases of trauma, hemarthrosis may occur secondary to damage of any component structures of the knee joint, but often arises from ligament or meniscal damage. Furthermore, underlying joint disease, such as osteoarthritis in this case, may be a contributing factor due to the development of abnormal anatomy and vasculature. Bleeding disorders that cause hemarthrosis are typically aquired or congenital deficiencies of specific coagulation factors, such as the hereditary hemophilias, rather than defects of the vessel wall, platelets, or fibrinolysis. Acquired deficiencies of coagulation factors leading to hemarthrosis are predominantly due to the effect of systemic anticoagulants. Hemarthrosis is a complication of Warfarin therapy in up to 1.5 % of patients. In comparison, the overall hospitalization rate for any Warfarin-related hemorrhage has been estimated at 3.8 % per person year. Hemarthrosis has also been documented with the use of the newer oral anticoagulants, including Rivaroxaban for the prophylaxis of venous thrombosis after knee and hip surgery. In conclusion, hemarthrosis should be considered in the differential diagnosis of acute monoarthritis, especially in individuals receiving systemic anticoagulation.
ABDOMINAL COMPARTMENT SYNDROME FROM MASSIVE PANCREATIC PSEUDOCYSTSJianhua A. Tau1,2; Jeffrey T. Bates1,2. 1Baylor College Of Medicine, Houston, TX; 2Michael E. DeBakey VA Medical Center, Houston, TX. (Tracking ID #1940161)
LEARNING OBJECTIVE 1: Diagnose the abdominal compartment syndrome (ACS) as a cause of end-organ failure in patients with acute pancreatitis.
LEARNING OBJECTIVE 2: Recognize the utility of bladder catheter transduction to diagnose ACS and that rapid decompression of increased abdominal pressure is the mainstay of therapy.
CASE: A 46-year-old male with a PMH of alcohol dependence was admitted to the intensive care unit with hypotension, acute abdominal pain and distention, and severe dyspnea requiring intubation. Physical examination revealed diffuse rales and a tense and tender abdomen. Laboratory studies were significant for a lipase >2000 U/L, and a CXR showed diffuse infiltrates. Abdominal CT revealed multiple fluid collections and large peripancreatic pseudocysts. He was diagnosed with severe pancreatitis and the acute respiratory distress syndrome (ARDS), and his hypotension was treated with rapid volume expansion. Initial renal function was intact, but by the fifth hospital day the renal function began to deteriorate; peak and plateau lung pressures were also increasing despite a protective ventilator strategy. Serial CT scans confirmed enlarging abdominal fluid collections. Abdominal compartment pressure (ACP) was measured every 6 h via bladder catheter transduction and was persistently greater than 25 mmHg. He was diagnosed with abdominal compartment syndrome (ACS), based on the combination of new organ dysfunction in the setting of an elevated ACP. Over the course of 63 days, he received six transcutaneous abdominal drains for decompression, which were effective in reducing his abdominal pressure below 20 mmHg. His renal function and inspiratory pressures improved within 48 h of each successful drainage; they ultimately returned to normal. The patient never required decompressive laparotomy.
DISCUSSION: Abdominal wall compliance initially reduces the degree to which an increasing abdominal girth can elevate the intra-abdominal pressure. However, when a critical abdominal girth is reached, abdominal wall compliance decreases abruptly. Further increases in abdominal girth beyond this critical level result in a rapid rise of intra-abdominal pressure and can result in abdominal compartment syndrome (>25 mmHg). ACS can cause ischemic compression of visceral organs, cardiovascular collapse from decreased venous return, and high peak and plateau lung pressures leading to barotrauma. ACS is often related to the need for and extent of volume resuscitation—creating a difficult balancing act in patients with severe pancreatitis, who require significant volume resuscitation. ACS may be underrecognized because it affects patients who are already critically ill and whose organ dysfunction may be incorrectly ascribed to progression of the primary illness—such as ARDS, sepsis, or pancreatitis itself. Since treatment can improve organ dysfunction, it is important that the diagnosis be recognized in critically ill patients with severe acute pancreatitis.
ABDOMINAL COMPARTMENT SYNDROME: A DEADLY CASCADEMandy S. Stull. Reading Health System, Ephrata, PA. (Tracking ID #1926050)
LEARNING OBJECTIVE 1: Abdominal Compartment Syndrome is a clinical entity resulting in organ dysfunction and multiorgan failure from elevated abdominal pressures. Abdominal compartment syndrome has a mortality that can range from 40 to 100 %.
LEARNING OBJECTIVE 2: Most patients who develop ACS have a tensely distended abdomen, significantly elevated intraabdominal pressures, progressive oliguria, hypotension, and increased ventilatory requirements.
CASE: 48 year male with diabetes, hypertension, and morbid obesity was admitted with tense scrotal and peripheral edema after stopping his furosemide 1 month prior. No evidence of heart failure on physical exam with normal chest radiography and BNP. No history of liver or kidney disease. His liver function tests, including albumin and INR were normal. No proteinuria on urinalysis with normal creatinine. On the second day of admission, the patient developed high pitched bowel sounds and a tense distended abdomen. CT scan of abdomen/pelvis showed not acute findings. Over the course of third hospital day; patient developed oliguric acute kidney injury; creatinine increased from 0.92 to 5.03. Patient then developed acute hypoxic hypercapneic respiratory failure which required BiPAP. He became progressively more hypotensive and ultimately required fluid resuscitation and vasopressors for blood pressure support. In setting of tense distended abdomen with oliguria, acute kidney injury, and hypotension, there was a concern for Abdominal Compartment Syndrome. The patient continued to decompensate requiring mechanical ventilation and multiple vasopressors. Foley catheter transduced pressures greater than 20 mmHg range. Bladder pressures were consistent with intra-abdominal hypertension; patient had evidence of multi-organ failure as well. Patient continued to decompensate. Repeat CT of abdomen/pelvis demonstrated pneumoperitoneum. Surgery revealed perforated right colon requiring right hemicolectomy. The abdomen was left open for surgical decompression with dressings to bridge the fascial edges. Septic shock persisted. Multiorgan failure ensued with further kidney injury and bowel infarction, shock liver, myocardial infarction and ultimately death.
DISCUSSION: Abdominal Compartment Syndrome is a clinical entity resulting in organ dysfunction and multiorgan failure from elevated abdominal pressures. Failure to recognize abdominal compartment syndrome can lead to a deadly cascade of events. Clinicians must have a high degree of suspicion for this diagnosis and a low threshold to obtain bladder pressures to identify high risk patients. This clinical entity is gaining increased recognition among the medical community as it has a high morbidity and mortality.
ABSENCE MAKES THE HEART GROW FONDERAimee E. Hiltbold; Catherine Jones. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926970)
LEARNING OBJECTIVE 1: Recognize the clinical presentation and the appropriate treatment of cardiac tamponade.
LEARNING OBJECTIVE 2: Define the pathophysiology of classic cardiac exam findings.
CASE: A 58-year-old man presents with 2 weeks of progressively worsening dyspnea and chest pain. He has experienced severely decreased functional capacity and is now unable to walk 5 ft without becoming dyspneic. His pain is described as substernal without radiation, and unrelated to physical exertion. He has smoked two packs per day for the past 30 years. He is tachycardic at 118 bpm and tachypneic to 22 breaths per minute. Blood pressure is 128/86 mmHg, but systolic blood pressure drops to 112 mmHg on inspiration. He appears uncomfortable, is sitting in the tripod position, and is unable to speak in full sentences. He has jugular venous distention to the angle of the mandible. Coarse breath sounds are auscultated bilaterally. He has distant heart sounds and the point of maximal impulse is difficult to locate. Chest radiograph reveals small bilateral pleural effusions, right interstitial and airspace disease, cardiac enlargement, and prominent right hilar lymphadenopathy, suggestive of malignancy. Electrocardiogram shows low voltage amplitude and electrical alternans. Bedside transthoracic echocardiogram revealed a large pericardial effusion. The patient was diagnosed with cardiac tamponade and an emergency pericardiocentesis was performed. Pathological evaluation of the fluid revealed hypercellular and atypical cells arranged in papillary groups. Immunohistochemistry was consistent with malignant papillary adenocarcinoma causing pericardial effusion and cardiac tamponade.
DISCUSSION: Chest pain is a common emergency encountered by internists. We often rely upon advanced tests and imaging for diagnosis. However, a thorough physical exam can focus the practitioner’s differential and expedite diagnosis. Physical exam findings of cardiac tamponade include hypotension, jugular venous distention, and muffled heart sounds—collectively known as Beck’s triad. A decrease in systolic blood pressure of greater than 10 mmHg with inspiration is known as pulsus paradoxus, and is highly suggestive of cardiac tamponade. Cardiac tamponade is caused by increased pressure on the heart, often from fluid accumulation within the pericardial space. Pericardial effusion may be secondary to infection, malignancy, ventricular rupture, trauma, or surgical procedures. Increased pressure limits diastolic filling, reduces cardiac output, and causes hypotension. The decreased forward flow of blood results in jugular venous distension. Auscultation reveals muffled heart sounds secondary to the accumulated pericardial fluid. Bedside transthoracic echocardiogram is useful in confirming fluid within the pericardial sac and can estimate the volume of effusion. EKG generally reveals diffuse low voltage complexes, with electrical alternans due to the pendular motion of the heart within the pericardial sac. Treatment of cardiac tamponade requires that the fluid surrounding the heart be evacuated via pericardiocentesis or a surgical pericardial window. When the tamponade is secondary to malignancy, treating the underlying malignancy is required. The internist should utilize physical exam findings, such as Beck’s triad and pulsus paradoxus, in addition to bedside TTE and EKG findings to promptly diagnose cardiac tamponade.
ACCELERATED CALCIFICATION OF A BIOPROSTHETIC VALVE IN END-STAGE RENAL DISEASEAllison J. Kwong; Douglas B. Jacobs; Matthew Spinelli; Paul D. Blanc. University of California, San Francisco, San Francisco, CA. (Tracking ID #1937187)
LEARNING OBJECTIVE 1: To recognize end-stage renal disease as a risk factor for early calcification of prosthetic valves, and review the relevant literature.
CASE: Our patient is a 61-year-old transgender male-to-female with HIV/AIDS and anuric end-stage renal disease (ESRD) on hemodialysis, who underwent bioprosthetic mitral valve replacement in 2008 for endocarditis of her native valve. She presented in early 2013 with symptoms of progressive heart failure, including orthopnea, weight gain, and exertional dyspnea. Other co-morbidities included type 2 diabetes mellitus, coronary artery disease with history of stents, smoking, and peripheral vascular disease requiring bilateral below-the-knee amputations. Her end-stage renal disease was attributed to HIV and diabetes, and she had been on hemodialysis since 1999, with a history of failed renal transplant in 2004. Physical exam revealed bibasilar crackles, 13 cm jugular venous distention, an audible S3, and a 3/6 holosystolic murmur at the left lower sternal border. Upon admission to the hospital, her calcium was 9.0, phosphorus was 3.6, and PTH was 420 (normal 12–65). Her calcium-phosphorus product had been intermittently elevated—to as high as 90—in the preceding year, despite prescribed phosphate binder therapy. The most recent CD4 count was 174, with an undetectable viral load on anti-retroviral therapy. Her initial EKG showed evidence of an old anteroseptal myocardial infarction and left axis deviation. An echocardiogram obtained during her admission showed new severe mitral valve stenosis, mild mitral regurgitation, no paravalvular leak, and peak and mean transvalvular gradients of 21 mmHg and 14 mmHg, respectively. The ejection fraction was estimated to be 50–55 %. Given her co-morbidities, she was deemed ineligible for either percutaneous valvuloplasty or repeat surgical mitral valve repair/replacement. She has since had frequent admissions for volume overload and is currently in hospice care.
DISCUSSION: Structural valve degeneration, which includes stenosis and/or regurgitation, is a known long-term complication of bioprosthetic heart valves. In the mitral position, bioprosthetic valves have an expected lifespan of at least 10–20 years, and 5-year durability rates approach 100 %. Accelerated calcification of bioprosthetic valves in patients with dialysis-dependent renal failure has been long-assumed, but described only in isolated case reports, and usually in the tricuspid and aortic positions. The mechanism of this rapid calcification is thought to be due to elevated calcium-phosphate product in the setting of end-stage renal disease and hyperparathyroidism. Though HIV and antiretroviral therapy could also be implicated in this case, these particular risk factors have yet to be associated with the accelerated calcification of non-native valves. Awareness of this potential early complication of bioprosthetic valves in patients with end-stage renal disease could lead to more timely diagnosis, management, and intervention. Strict control of hyperphosphatemia and hyperparathyroidism, as well as closer surveillance of valve function, is likely warranted among patients on hemodialysis with bioprosthetic valves. In this specific high-risk population, mechanical valves, which are less susceptible to calcification, may be a preferable option for those requiring valve replacement.
ACQUIRED ACRODERMATITIS ENTEROPATHICA: RECOGNIZING ZINC DEFICIENCY FOLLOWING GASTRIC BYPASS SURGERYGautam Mankaney; Thomas Radomski; Kevin Kraemer. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1939348)
LEARNING OBJECTIVE 1: Describe a classic presentation of zinc deficiency
LEARNING OBJECTIVE 2: Recognize the potential nutritional deficiencies following gastric bypass surgery
CASE: A 54 year-old Caucasian woman with a history of Crohn’s disease, Roux-en-Y gastric bypass surgery, and chronic kidney disease, presented with a progressive skin rash for several months. The patient noted a red rash with cracked and sloughing skin around her groin, buttocks, and upper extremities. The rash did not resolve with the use of topical corticosteroids or both topical and oral anti-fungal agents. She denied any fevers or new medications, but did have several weeks of associated diarrhea. She underwent a Roux-en-Y gastric bypass surgery about 8 years prior and endorsed poor eating habits and compliance with her vitamin supplements. The physical exam revealed a middle-aged appearing female in no distress. She was afebrile with stable vital signs. She had an erythematous, desquamating rash associated with excoriations and honey-colored crusting. The rash was predominant over her perioral, lumbosacral and inguinal regions. Her distal extremities also displayed palmar erythema and fissuring. The remainder of her exam was unremarkable A skin biopsy revealed non-specific histologic findings of parakeratosis, impetiginized regions, and chronic inflammation with dermal edema. A work-up for infections and autoimmune etiology was non-revealing. The patient was found to be nutritionally deficient with an albumin level of 1.4 g/dL. Further evaluation for micronutrient deficiencies revealed a markedly low plasma zinc level of 0.31 μg/ml (normal 0.55–1.50 μg/ml). She was diagnosed with acquired acrodermatitis enteropathica secondary to zinc deficiency and was started on zinc supplementation. A near-complete resolution of the rash was noted at follow-up 4 weeks later.
DISCUSSION: Bariatric surgery is one of the fastest growing surgical procedures in the United States. The Roux-en-Y gastric bypass surgery, the most commonly performed type of bariatric surgery, divides the stomach into two unequally sized pouches and connects the smaller pouch to the jejunum, effectively bypassing the duodenum and part of the proximal jejunum. Although intraoperative and early postoperative complications are rare and compare favorably with other frequently performed abdominal operations, late complications are becoming more visible. Micronutrient deficiencies are the most likely long-term complication and often present as clinical syndromes classic for the deficiency. Zinc is an essential cofactor for enzymes involved in keratinocyte maturation, among several other regulatory processes. Acquired acrodermatitis enteropathica, or zinc deficiency due to impaired metabolism, classically presents as a perioral, intertriginous, and acral dermatitis that may be associated with diarrhea, alopecia, and altered mental status. The dermatitis appears as erythematous patches of dry and scaly skin, an eczematous rash, or a vesiculopustular eruption. Several mechanisms contribute to the micronutrient deficiencies seen after bariatric surgery, including decreased oral consumption, impaired intestinal uptake, poor compliance with dietary supplementation, and pre-existing nutritional deficiencies seen in obesity. Zinc levels may be low pre and postoperatively; however, when symptomatic, oral repletion rapidly corrects symptoms, as in this patient. This case also illustrates the importance of recognizing nutritional deficiencies in patients who undergo bypass surgery. Other common deficiencies include vitamin B12, folate, iron, copper, calcium, and vitamin D. There are not any randomized-controlled trials that guide general practitioners on screening and supplementation; however, awareness of such deficiencies may lead primary care physicians to reinforce dietary compliance with their patients and more easily identify the signs and symptoms of micronutrient deficiencies when they occur.
ACRAL CD4 T CELL LYMPHOMA PRESENTING AS DUPYTUREN’S CONTRACTURERagisha Gopalakrishnan; Harris Naina. UT southwestern, Dallas, TX. (Tracking ID #1939624)
LEARNING OBJECTIVE 1: To recognize Acral CD4 T cell Lymphoma as a part of the differential diagnoses for Dupyuturen’s contracture.
CASE: A 90 year old Hispanic man with no medical history presented to his physician after developing redness and a knot like sensation in both of his hands for 1 year. On exam, there was erythema on the dorsum and palmar surfaces of both hands, but there was no evidence of lymphadenopathy, petechiae or ecchymosis. He denied any fevers, night sweats, pruritus, and weight loss. He was a former smoker, but denied any family history of malignancy. He was initially diagnosed with Dupuytren’s contracture and treated with topical steroids and clobetasone. However, this provided little symptomatic benefit, and a subsequent MRI of his left hand showed a small 8 mm lesion between the epidermal and subepidermal tissue. A biopsy showed a nodular proliferation of medium-sized to large, cytologically atypical and immunophenotypically aberrant T-lymphoid cells which were consistent with acral CD4 positive T-cell lymphoma. Subsequent PET imaging showed no evidence of systemic disease. He underwent surgical resection of the 8 mm nodule of his left hand. However, the disease continued to be spread to his right hand, and he developed gangrene of his thumb requiring amputation of his thumb. He underwent 35 cGy radiation to his right hand, but the disease recurred. He was treated with gemcitabine, with minimal response. His performance status declined rapidly and died on hospice care.
DISCUSSION: Acral CD4 T cell lymphomas (ACTL) are a rare form of cutaneous lymphomas. There are 15 cases of ACTL reported in literature, and all of these cases present in the lesions in the lower extremity, head or neck. Most patients diagnosed with ACTL have had an indolent clinical course with complete response rate greater than 80 % with local surgical therapy or radiation therapy. However, in 2 of the 15 cases of ACTL reported, systemic chemotherapy (vornistat or gemcitabine) was used when a patient could not qualify for local surgical or radiation therapy; this provided limited benefit, and both of these patients died. By presenting this case, we show for the first time that ACTL can present with lesions in the upper extremity. This suggests, that ACTLs can present as upper extremity lesions and should be considered as part of the differential of Dupuytren’s contracture. In addition, in this case, the disease recurred multiple times and was resistant to all three treatment regimens currently available for ACTL. Given the aggressive course and number of recurrences of this patient’s case, additional investigation is required to in additional treatment modalities when the existing treatment regimens fail.
ACRAL MELANOMA IN SITUKaren Y. Cheng1; Victoria T. Liu1; Pearl Yu2. 1UCSD, San Diego, CA; 2University of California, San Diego, La Jolla, CA. (Tracking ID #1925625)
LEARNING OBJECTIVE 1: Recognize the parameters for assessing pigmented cutaneous lesions that require further evaluation by a dermatologist
LEARNING OBJECTIVE 2: Describe the risk factors and management for melanoma in situ
CASE: A 59 year old white male with past medical history of prostate cancer, hypertension, and hyperlipidemia presented with a pigmented lesion that was changing in appearance on the plantar surface of his left first toe. The patient stated that there had been a pigmented lesion on the plantar surface of his left first toe for about 5 years. In the few weeks prior to presenting in clinic, he had noticed that several other pigmented lesions had appeared around the original lesion. There was no associated pain or pruritis. On exam, it was noted that he had 3 areas of black pigmentation measuring 5 × 5 mm, 6 × 4 mm, and a larger area consisting of a very dark 5 × 4 mm patch and a lighter 15 × 8 mm patch. He was referred to dermatology, where two 2 mm punch biopsies were taken from different parts of the larger area: one from the more distal dark black patch and another from the more proximal lighter black patch. Both of these biopsies showed proliferation of atypical pigmented melanocytes at the dermal-epidermal junction consistent with melanoma In situ. Additional biopsies were taken from the two other areas of pigmentation on the great toe after the dermatopathology demonstrated melanoma in situ and the patient is scheduled to discuss wide excision with possible plastic surgery repair with the dermatology surgeon.
DISCUSSION: The incidence of malignant melanoma in situ has been increasing and represents about 40 % of all melanomas diagnosed in the United States. Malignant melanoma in situ is a non-invasive precursor lesion which accumulates mutations to gain the ability to invade the underlying dermis and become invasive and metastatic melanoma. Risk factors for melanoma in situ include: family history of melanoma, greater number of severe sunburns, greater susceptibility to sunburns, and natural red or blond hair color. Melanoma is suspected based on the well-known ABCDE parameters: asymmetry, border irregularity, color variegation, diameter >6 mm, and evolution. Biopsy with histopathological findings of proliferating melanocytes that migrate into the epidermis and architectural asymmetry within the lesion are diagnostic of melanoma in situ. Standard treatment is excision with margins of 0.5 to 1 cm. Although acral skin is the most prevalent site of melanoma in non-white populations, this case represents an atypical anatomic site of presentation since white males typically have lesions on their trunk or back and the patient had no family history or other risk factors for melanoma in situ. However, the lesion did show asymmetry, irregular borders, color variegation, diameter greater than 6 mm, and recent change, demonstrating the necessity of having a high index of suspicion for melanoma when a lesion matches ABCDE criteria.
ACUTE AMIODARONE PULMONARY TOXICITY FOLLOWING LUNG RESECTIONOpeyemi Fadahunsi; Mandy S. Stull; Shobhit Gupta. Reading Health System, Reading, PA. (Tracking ID #1938472)
LEARNING OBJECTIVE 1: Recognize that amiodarone pulmonary toxicity (APT) can occur any time after commencement of amiodarone and it is a diagnosis of exclusion
LEARNING OBJECTIVE 2: Recognize the increased risk of acute APT following lung resection
CASE: An 80-year-old male with a 15-pack-year cigarette smoking history and coronary artery disease underwent a right upper lobectomy for lung adenocarcinoma (T2A N0 M0, Stage 1b). Preoperative transthoracic echocardiography (TTE) showed normal left ventricular function. Preoperative pulmonary function tests (PFTs) revealed a forced expiratory volume in 1 s (FEV1) of 2.19 L (71 % of predicted), forced vital capacity (FVC) of 2.86 L (71 % of predicted), FEV1/FVC ratio of 77 %, total lung capacity (TLC) of 4.45 L (66 % of predicted) and a diffusion capacity for carbon monoxide (DLCO) of 13.5 mL/mmHg/min (59 % of predicted). Postoperative (postop) course was complicated by subcutaneous emphysema which necessitated prolonged intubation. On postop day 4, he developed paroxysmal atrial fibrillation with rapid ventricular rate and was loaded with IV amiodarone for rhythm control at a rate of 0.5 mg/min which was then converted to 400 mg tid orally on postop day 8. He was transferred to a rehabilitation center on postop day 12 in a relatively stable condition. On postop day 15, patient presented to the hospital with severe dyspnea, dry cough and syncope. He denied chest pain, diaphoresis, nausea or fever. He had received a total dose of 12.5 g amiodarone in the preceding 12 days. There were no known environmental exposures. On physical examination, patient had diffuse dry crackles and no wheezes. Neck veins were not distended and there was no pedal edema. Arterial blood gas showed hypoxemia without CO2 retention. Cardiac enzymes were normal and there were no EKG changes. Laboratory studies showed a leukocytosis and elevated ESR. Chest CT scan revealed bilateral airspace opacities and mediastinal adenopathy. ACE level was normal and collagen vascular work up, including ANA, RF and ANCA, was negative. Blood culture did not grow any organisms. Postop PFTs revealed a severe restrictive disease: FEV1 of 1.24 L (41 % of predicted), FVC of 1.61 L (39 % of predicted), FEV1/FVC ratio of 81 %, TLC of 3.13 L (42 % of predicted) and DLCO of 6.5 mL/mmHg/min (24 % of predicted). TTE showed normal valvular and left ventricular function with elevated pulmonary artery (PA) pressure (80 mmHg). Cardiac catheterization which was done 7 months ago had shown normal PA pressure. Amiodarone was discontinued and he was started on prednisone due to suspicion for APT. He improved symptomatically and radiographically, however he was still requiring 3 L of intranasal oxygen. He was discharged home on oxygen and was placed on 1 month prednisone taper. On postop day 52 (4 days after completing steroid therapy), he again presented to the hospital with similar complaints of severe dyspnea with high oxygen requirements. Radiological findings were improved but not back to baseline. He underwent bronchoscopy which revealed normal bronchial mucosa. Bronchial washing cytology was negative for AFB or malignancy and there was no growth on culture. Microbiologic analysis of bronchial washing showed a neutrophilic leukocytosis. Clinically, he improved and he was discharged on a prolonged course of prednisone.
DISCUSSION: APT is the most severe adverse effect associated with the use of amiodarone. Pulmonary fibrosis following APT is irreversible, therefore anticipation and early detection of this potentially fatal side effect is important. Onset of APT has usually been observed after several months or years of amiodarone use. In the above case and a handful of other cases reported in literature, pulmonary toxicity can occur within a few days to weeks. The clinical findings in APT are non-specific and it remains a diagnosis of exclusion. The diagnosis of APT needs to be considered in high risk patients on amiodarone irrespective of dose, presenting with new or worsening respiratory symptoms or signs, new chest radiographic abnormalities or a decline in DLCO > 20 %. Risk factors in our case include old age, pre-existing lung disease, thoracic surgery, intubation and amiodarone dose ≥400 mg/day. In a subset of patients undergoing thoracic surgery who are intubated and require high levels of oxygen, it has been postulated that the risk of developing APT is further heightened due to increased susceptibility for lung damage. Studies on risk factors for APT development have not been conclusive, however, in patients with multiple risk factors, there needs to be a discussion on the risks and benefits of amiodarone treatment. Finally, management of APT requires discontinuation of amiodarone and commencement of steroids for greater than 6 months. As in the case presented, tapering steroids too early may lead to symptom recurrence.
ACUTE ANEMIA AFTER A URINARY TRACT INFECTION (UTI): A CASE OF HEMOLYTIC ANEMIA IN A NEWLY DIAGNOSED GLUCOSE-6-PHOSPHATE DEHYDROGENASE (G6PD) DEFICIENT PATIENTIrem Nasir. greenwich hospital, Greenwich, CT. (Tracking ID #1939299)
LEARNING OBJECTIVE 1: 1) Recognize a case of acute nonimmune hemolytic anemia in a patient with a new diagnosis of G6PD deficiency.
LEARNING OBJECTIVE 2: 2) Name drugs contraindicated in patients with G6PD deficiency.
CASE: A 69 year old Hispanic female who had a recent UTI, presented to us with shortness of breath, fatigue, and malaise ×6 days. She also had jaundice and dark urine ×1 day. She had just completed an 8 day course of nitrofurantoin and phenazopyridine (a urinary tract analgesic) the day prior. She denied fevers, cough, chest pain, nausea, vomiting, and diarrhea. There were no tarry/black stools. Her dysuria had resolved. There was no recent travel, sick contacts, or insect bites. There was no history of IVDA or risky sexual behavior. There was no known family history of any blood dyscrasias. On physical exam, patient was afebrile, icteric, heart regular rate, lungs clear, abdomen soft, nontender. Guaiac was negative. There were no rashes or petechiae. Her labs were notable for wbc22, hgb6.8 (decreased from a hgb 12 a few months prior), platelets 280, Cr 1, and a lactate of 1.5. Both her reticulocytes and LDH were significantly elevated at 12 % and 700, respectively. Total bilirubin was elevated at 4 with an indirect bilirubin of 3. AST, ALT, and INR were normal. Haptoglobin was low at <7. Peripheral blood smear had no schistocytes. Urinalysis showed high urobilinogen. CXR was neg. A diagnosis of acute hemolytic anemia due to nitrofurantoin and phenazopyridine was made and both drugs were immediately stopped. Aggressive supportive care was initiated and 1u pRBC was transfused. Her hgb improved to 7.7. On further testing, direct coombs test, ANA, Parvovirus IgM and PCR, Cold agglutinins, Mycoplasma IgM, EBV, and CMV titers were all negative. Hgb electrophoresis was negative. Her RBC G6PD activity level was low at 2.5 (4.6 to 13 reference range). A diagnosis of G6PD deficiency was made. Two weeks later, her hgb was 11 and both the reticulocytes and LDH were normal at 2 % and 196, respectively. Patient and family were advised to avoid all foods and drugs with known oxidative potential, such as nitrofurantoin and phenazopyridine, which can trigger an episode of nonimmune hemolytic anemia.
DISCUSSION: G6PD deficiency, an X linked disorder, is the most common enzymatic disorder of RBC, affecting 400 million people worldwide. A diagnosis of G6PD deficiency is made when there is decreased activity of this enzyme in RBC. False negative results can occur if the G6PD level is checked immediately following hemolysis, since the most severely deficient RBC have been removed and young reticulocytes have higher G6PD levels. In those cases, retesting a few months later is recommended. A female can be heterozygous or homozygous, resulting in half or all of her RBC vulnerable to hemolysis, respectively. G6PD deficient cells are incapable of coping with oxidant stress. G6PD protects RBC by replenishing reducing equivalents, NADPH and Glutathione reductase. Nitrofurantoin inhibits glutathione reductase and decreases generation of reduced glutathione. Phenazopyridine, which should only be prescribed for 2–3 days, is a well known oxidative drug. Other commonly used drugs like fluoroquinolones, sulfa drugs, and even NSAIDS and acetaminophen in high doses can cause hemolysis. Even black and red henna tattoo and hair dyes have been implicated. Clinicians must maintain a high index of suspicion for G6PD deficiency in any individual presenting with an episode of nonimmune hemolytic anemia, especially if temporally related to a culprit drug.
ACUTE CHOLANGITIS, SANS CHOLEAimee E. Hiltbold; Catherine Jones. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926993)
LEARNING OBJECTIVE 1: Apply the Tokyo guidelines to diagnose a cause of abdominal pain
LEARNING OBJECTIVE 2: Discuss treatment goals for acute cholangitis
CASE: A 61 year-old woman presented with 3 days of worsening abdominal pain, fever, and jaundice. Additionally, she reported dizziness with periodic confusion. Abdominal pain was located in the right upper quadrant with radiation to her right scapula. She noted dark urine and yellowing of her eyes. Pertinent past medical and surgical history was significant for a history of gallstones, prompting a cholecystectomy, and a Roux-en-Y gastric bypass procedure 10 months ago. She was febrile at 103 °F, tachycardic at 111 bpm, tachypneic at 22 bpm, with a blood pressure of 85/58 mmHg after receiving 3 l of normal saline. She was slightly confused and in moderate distress with severe 10/10 abdominal pain. She had scleral icterus and significant tenderness to palpation of the right upper quadrant with voluntary guarding. Laboratory findings included a leukocytosis of 20,000, 94 % neutrophils, bandemia, and prolongation of the PT to 12.3. Chemistry demonstrated BUN of 24 with a creatinine of 1.1. Liver panel evidenced an obstructive pattern with AST of 1030, ALT of 638, alkaline phosphatase of 1026, and total bilirubin of 5.8. Computed tomography revealed fluid in the gallbladder fossa with intra and extrahepatic biliary duct dilation. The patient met Reynolds’ pentad of acute cholangitis; however, secondary to her gastric bypass surgery she could not undergo ERCP. Interventional radiology performed percutaneous cholangiography with biliary drain placement, where she was noted to have a 1 cm stone in the distal common bile duct.
DISCUSSION: It is imperative for the general internist to quickly diagnose acute cholangitis to prevent significant morbidity and mortality. Cholangitis is a clinical syndrome characterized by fever, jaundice, and abdominal pain, known as Charcot’s triad. Confusion and hypotension may also occur in patients with suppurative cholangitis, producing Reynolds’ pentad. The Tokyo guidelines propose definitive diagnosis of acute cholangitis if the patient exhibits Charcot’s triad, or if there are two elements of Charcot’s triad plus abnormal liver tests, imaging revealing biliary dilation, and evidence of an inflammatory response—leukocytosis or elevated CRP. Infection occurs when bacteria from the gut translocate into an obstructed biliary tree or after introduction via instrumentation. Primary causes of biliary obstruction include gallstones, acalculous stasis, and malignancy. Bile duct stones usually form in the gallbladder, but can also form spontaneously in the bile duct after cholecystectomy. Treatment of acute cholangitis is aimed at treating associated sepsis, providing empiric antibiotics to cover enteric pathogens, and visualizing and draining biliary obstruction. This is typically done by emergent endoscopic sphincterotomy with stone extraction via ERCP. ERCP is not technically feasible in some patients, including those who have undergone a Roux-en-Y gastric bypass. In this instance, biliary drainage should be attempted via percutaneous transhepatic cholangiography with biliary drain placement or open surgical decompression. Acute cholangitis is associated with significant morbidity and mortality, and internists must be adept at providing prompt diagnosis and treatment.
ACUTE DIFFUSE MACULOPAPULAR RASH: MAYBE NOT SO “SWEET.”Derek A. Pae; David Linz. University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1942112)
LEARNING OBJECTIVE 1: Recall the differential diagnosis of acute febrile neutrophilic dermatosis
LEARNING OBJECTIVE 2: Diagnosis of Sweet’s syndrome
CASE: A 29 year old man presented to his doctor with 1 week of fevers and a painful rash. The patient first experienced a fever to 101 associated with shaking chills and drenching sweats, followed the next morning by a rash on his chest and abdomen. Over the following few days, the rash spread all over his body with painful blisters, draining milky-yellow fluid and the fevers did not abate. The patient finally sought medical attention because of the intense pain of the blisters and was subsequently admitted to the hospital. Past medical history was significant for Crohn’s disease diagnosed by colonoscopy 4 months prior. He worked as electrician, did not have any recent travel or sick contacts. His medications included azathioprine 200 XXX mg daily, which was initiated 4 months prior and 5 mg of prednisone daily, tapered from 40 mg daily over the past 2 months. Skin exam revealed multiple diffuse pustular lesions across neck, face, trunk and upper extremities sparing the palms and soles, multiple nodules on the lower extremities, and two painful erythematous nodules in groin and neck in various stages of healing. There were also two flaccid hemorrhagic bullae on the right shin. Labs revealed WBC of 21.5 and elevated ESR and CRP (99 mm/h; nl <23 and 22.5 mg/dL; nl <0.7 respectively). Blood and urine cultures were negative. CXR showed no evidence of pneumonia. Sigmoidoscopy showed severe inflammation with skip lesions and ulcers in the colon consistent with active Crohn’s colitis. Skin biopsies revealed neutrophilic dermatosis with mild vasculopathy consistent with abscess forming neutrophilic dermatosis/atypical Sweets syndrome. Patient did not respond to broad spectrum antibiotics, but showed marked improvement after the initiation of high dose steroids, with decreased pain, absence of fevers, and normal WBC.
DISCUSSION: Fever, leukocytosis, or skin rash are common chief complaints for physicians but the combination of all three can be a puzzling triad. This patient presented with acute febrile neutrophilic dermatosis, which should prompt a differential diagnosis that includes infection, malignancy, and auto-immune disease. Empiric antibiotics to cover a broad spectrum of organisms could be warranted while awaiting final pathology results. In acutely ill patients like ours with fever and leukocytosis who are taking immunosuppressants, pseudomonas and funal infection should be ruled out. Sweets syndrome is not uncommon, but the presence of abscess formation and hemorrhagic lesions in our case is exceedingly rare. The definitive way to diagnose this disease is through biopsy, as performed in this case. However, there are several underlying systemic diseases to consider, including malignancy, in a patient with such a syndrome. In this case, patient was already diagnosed with IBD, and the repeated sigmoidsocopy was consistent with Crohn’s flare. However, in another setting if such a patient presented with only the dermatological manifestation, investigation including sigmoidscopy may be warranted. Taking into account patient age, investigation for malignancy should be considered. There have been several but not many case studies regarding association between atypical sweet’s syndrome and myeloproliferative diseases, including leukemia. One final note is this patient was on azathioprine, which had been linked to sweet’s syndrome, and discussion regarding discontinuing this medication and watchful observation should be considered.
ACUTE ENCEPHALITIS IN AN AFEBRILE YOUNG ADULT PRESENTING WITH HEADACHES AND MYALGIASSharon Chow; Jennifer Way; Adrienne L. Clark. UCLA, Los Angeles, CA. (Tracking ID #1939510)
LEARNING OBJECTIVE 1: Describe an atypical presentation of acute encephalitis in a young adult
LEARNING OBJECTIVE 2: Discuss the broad differential and work up of meningoencephalitis in a patient with atypical presentation
CASE: RL was a 21 year old previously healthy male with a history of ADHD, impulsivity, and migraines who was initially admitted to the hospital for 3 days of headaches and diffuse myalgias. On presentation, the patient was afebrile with normal heart rate and physical exam, and all studies, including CBC, BMP, CK and blood cultures, were unremarkable. He was initially treated with supportive management, including intravenous fluids and analgesics, for suspected migraine and somatization disorder given no evidence of an organic component to his symptoms. However the patient’s mental status deteriorated on hospital day three following myoclonic-seizure activity and he became increasingly agitated and unable to follow commands with changes in his vitals including fever to a Tmax of 40.0C and tachycardia into the 160 s following a lumbar puncture (LP). He also developed severe muscle rigidity, opisthotonus, and upper motor neuron signs such as clonus and hyperreflexia on physical exam. MRI at that time showed subtle leptomeningeal enhancement and LP was significant for 104 RBC, 54 WBC (86 % Lymphocytes, 14 % monocytes), glucose 103, and protein 288. He was intubated and sedated for airway protection and started on broad spectrum anti-infective agents including ceftriaxone, vancomycin, and acyclovir for suspected meningitis. Given the severity of his acute decompensation, atypical physical exam findings, and elements in his history such as recent travel to Sweden and questionable immunization profile, a broad differential for both infectious and non-infectious causes was considered that included tetanus, rabies, and anti-NMDA receptor encephalopathies. Anti-infective therapy was broadened with doxycycline to cover atypical infection including rickettsial disease and tetanus toxoid was administered. Following negative viral and bacterial CSF cultures, the decision was made to initiate treatment for anti-NMDA receptor encephalitis with five doses of solumedrol and IVIG with further work up (including NMDA receptor and paraneoplastic serologies) pending. The patient showed marked improvement, and was extubated on hospital day eight with improved mental status and physical exam. Eventual CSF studies all returned negative with the exception of Mycoplama Pneumoniae and West Nile Virus IgG, both which resulted as positive. He was discharged home to complete a course of doxycycline for possible mycoplasma infection with close follow up in infectious disease clinic post discharge.
DISCUSSION: 1. Encephalitis can present with subtle neurologic symptoms including behavioral changes, agitation, and motor complaints such as paresis and myalgias without evidence of organic disease. High index of suspicion for CNS infection should be maintained for individuals with persistent symptoms. 2. Atypical causes of encephalitis including West Nile Virus and Mycoplasma Pneumoniae are difficult to diagnose based on laboratory data due to poor sensitivity and specificity of available studies. 3. Broad spectrum treatment for severe encephalitis should be initiated early as diagnostic results are often delayed. Furthermore, a confirmed etiology in most encephalitis cases is unable to be determined, thus illustrating the importance of prompt supportive management.
ACUTE HEPATITIS B INFECTION ASSOCIATED WITH RHABDOMYOLYSISMarissa D. Friedman. New York Presbyterian - Weill Cornell Medical Center, New York, NY. (Tracking ID #1911877)
LEARNING OBJECTIVE 1: Recognize instances when a patient with acute hepatitis B infection should receive treatment with anti-virals.
LEARNING OBJECTIVE 2: Discuss the potential for myopathy with the use of statins in patients with acute liver dysfunction.
CASE: In this case, a 66 year old female originally from Italy, with a history of coronary artery disease status post three vessel coronary artery bypass graft, was admitted to the hospital with 3 weeks of malaise, fever, nausea, jaundice, and diffuse abdominal pain. Her medications included simvastatin 80 mg daily. On physical exam, her sclera were icteric, skin with jaundice, and she had right upper quadrant abdominal tenderness to palpation. Labs were significant for a transaminitis with values of 877/724 (AST/ALT). A hepatitis panel was obtained which revealed, hepatitis B surface antigen positive, hepatitis B core antigen IgM positive, and Hepatitis A IgM negative, indicating an acute hepatitis B infection. On her second day of admission, she reported that she could not move her legs and her arms also felt week. Repeat exam revealed that strength was 3/5 in the lower extremities bilaterally and 4/5 in the upper extremities bilaterally. Creatine kinase (CK) level was found to be 5000. Over the next few days the CK continued to uptrend as did the transaminases, with peaks at 12,000, and 1300/1000 (AST/ALT) respectively. The patient also developed a rise in creatinine, thought to be secondary to rhabdomyolysis given presence of myoglobin in the urine. The patient remained bed bound, barely able to lift herself out of bed. Rheumatologic serologies were all negative, and the decision was made to begin anti-viral treatment with tenofovir and entecavir. A muscle biopsy was performed in attempt to rule out vasculitis, however the sample was too small, only revealing a small area of muscle necrosis. Overall, with anti-viral treatment, CK and transaminases started to downtrend. The patient slowly regained her strength and was discharged from the hospital.
DISCUSSION: This case presents a unique diagnostic dilemma as to the actual cause of the rhabdomyolysis and demonstrates instances when a patient with hepatitis B may benefit from treatment with anti-virals. Typical indications for treatment with anti-virals in acute hepatitis B include the presence of coagulopathy or encephalopathy. This patient had neither, however given the concurrent myopathy and an inability to fully rule out the hepatitis virus itself as potential cause, the decision was made to treat with anti-virals. Following initiation of tenofovir and entecavir, the patient did improve. Even so, the leading differential diagnosis for the cause of myopathy in this case was the patient’s use of statin while concomitantly developing acute viral hepatitis. In the current literature the link between statin use in the setting of acute viral hepatitis has never been studied and thus is not associated with any known increased risk of myopathy. There is evidence that patients with existing liver disease are at increased risk to develop myopathy, therefore it can inferred that an acute liver injury may invoke a similar mechanism leading to the same side effect. In considering this possibility, another interesting clinical practice question is raised as to whether or not patients on statins should receive a hepatitis B vaccination? Further research needs to be conducted to better elucidate the incidence of myopathy in patients on statins who develop acute viral hepatitis in order to answer this question.
ACUTE HEPATOTOXICITY: A COMPLICATION OF CHAPARRAL INGESTIONNicholas Tangchaivang. University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1925982)
LEARNING OBJECTIVE 1: Recognize an unusual cause of hepatotoxicity that would not be recognized if not searched for
CASE: A 65-year-old man with no significant past medical history presented to the Emergency Department with a 1 week history of fevers up to 103 F and chills. He endorsed myalgia, nausea, anorexia, night sweats, and fatigue. He denied abdominal pain, diarrhea, melena, weight loss, or recent travel. The patient denied using any medications including supplements and herbals. He had been seeing an acupuncturist regularly. Physical exam was notable for a temperature of 38.1C, blood pressure of 78/58, heart rate of 130, a jaundiced general appearance, scleral icterus, dry mucous membranes, and hepatomegaly. The patient was given IV fluids with improvement in blood pressure to 116/73 and heart rate to 113. Laboratory work-up revealed elevated liver tests with an AST of 178 U/L, ALT of 342 U/L, Total Bilirubin of 4.3 mg/dL, and Alk Phos of 257 U/L. CBC, Basic Metabolic Panel, and INR were within the normal range. An abdominal ultrasound revealed an enlarged liver with mild perihepatic ascites and marked gallbladder wall thickening with no evidence of cholecystitis. A CT Abdomen and Pelvis with Contrast confirmed these findings. There was no evidence of drainable fluid collections. IV fluid resuscitation was continued. Empiric antibiotics were not given due to a lack of an infectious source, normal WBC count, and hemodynamic stability following IV fluid resuscitation. Acute hepatitis workup was negative for Hepatitis A, Hepatitis B, Hepatitis C, Autoimmune Hepatitis, and acetaminophen toxicity. An abdominal ultrasound with Doppler was negative for vascular occlusion. Over the next 48 h, the patient had complete resolution of his symptoms without additional intervention. Bacterial cultures returned negative and the patient’s liver tests were downtrending. A call to the patient’s acupuncturist revealed that the patient had been taking Chaparral to promote liver health.
DISCUSSION: The actual prevalence of herbal product use and incidence of acute herbal hepatotoxicity are unknown. Based on available data, herbal products are implicated as a cause of hepatotoxicity in up to 10 % of drug induced liver injury and acute liver failure cases. Chaparral-induced hepatotoxicity typically manifests with symptoms that include fatigue, abdominal pain, dark urine, light stools, nausea, and diarrhea. Most patients have marked jaundice and elevated liver tests. Although most cases of hepatotoxicity resolve following cessation of Chaparral ingestion, some evolve onto cirrhosis or develop acute liver failure. Chaparral is made from the leaves of the creosote bush or greasewood. It has been used for its claimed antioxidant and anti-ageing properties as well as for treatment of various conditions such as cancer and AIDS. The mechanism of Chaparral-induced hepatotoxicity is not known but may be related to inhibition of lipoxygenase and cyclooxygenase pathways, cytochrome P450 inhibition, or the estrogen activity of chaparral metabolites. In this case, our patient presented with acute hepatotoxicity with marked hypotension. This may have led to acute liver failure had prompt IV fluid resuscitation not been employed. Awareness that the ingestion of alternative medicines can lead to severe hepatotoxicity is essential in cases of unclear liver disease. This case also reminds us that inquiring about the use of alternative medicines is an important aspect of taking a thorough medication history.
ACUTE LIVER FAILURE AS INITIAL MANIFESTATION OF DIFFUSE LARGE B CELL LYMPHOMAGargi Bajpayee; Matthew Kutner; Isabel Preeshagul; Alfred Burger; Lionel S. D’Souza; Franklin Kasmin. Beth Israel Medical Center of Mount Sinai, New York, NY. (Tracking ID #1940112)
LEARNING OBJECTIVE 1: Recognize Non-Hodgkin’s Lymphoma as a rare presentation of acute liver failure
LEARNING OBJECTIVE 2: Understand that prompt recognition and appropriate treatment of this disease is essential in preventing devastating outcomes
CASE: A 77-year-old man with remote history of prostate cancer (in remission) and former alcoholic presented to the emergency department for worsening jaundice and malaise for 1 month. The patient denied any recent travel, fevers, abdominal pain, diarrhea, or constipation and was current with his hepatitis vaccinations. The patient’s vitals were normal and physical exam was remarkable for diffuse jaundice, scleral icterus, and intermittent episodes of confusion. Laboratory work was significant for total bilirubin 17.3 mg/dL, direct bilirubin 14.5 mg/dL, AST 310 IU/L, ALT 232 IU/L, ALP 254 IU/L, albumin 2.6 g/dL, INR 1.9, LDH 2144 U/L, ferritin 663 ng/ml, ceruplasmin 54 mg/dl, acetaminophen level <10 ug/ml and absence of hepatitis A, B, C, D, EBV, CMV, VZV and HIV. ANA (anti-nuclear antibody), anti-LKMI (liver-kidney microsome) and ASMA (anti-smooth muscle antigen) were negative. Right upper quadrant ultrasound revealed diffusely infiltrated liver with normal portal and arterial blood flow. The patient was started on Rifaximin and Lactulose for worsening hepatic encephalopathy. Liver biopsy revealed large, heterogenous, neoplastic cells with vesicular chromatin and prominent nucleoli consistent with Diffuse Large B Cell Lymphoma. Shortly thereafter, the patient’s clinical and laboratory status deteriorated, requiring transfer to the MICU. Unfortunately, 2 days after induction chemotherapy with CHOP, the patient developed tumor-lysis syndrome and expired.
DISCUSSION: Acute Liver Failure (ALF) is a rare condition characterized by rapid deterioration of liver function resulting in the development of encephalopathy and coagulopathy in a patient without preexisting cirrhosis and an illness duration <26 weeks. Annual incidence of ALF in the US is estimated at approximately 2000 cases per year with an overall mortality rate of 80 %. Drug-induced (primarily acetaminophen), infectious, and autoimmune liver disease represent the majority of ALF cases. As was the case for our patient, Non-Hodgkin’s Lymphoma (NHL) is an extremely rare presentation of ALF, with less than 40 cases reported in the literature. Most diagnoses are confirmed by liver biopsy, however, are often made postmortem. In order to prevent devastating outcomes, it is essential to recognize that hepatic involvement from NHL is usually asymptomatic and should be suspected if liver enlargement and alterations in liver biochemistries, mainly ALP and GGT, are present. One should further suspect hepatic involvement if symptoms such as malaise, weight loss, and fever are present. Early diagnosis and initiation of appropriate chemotherapy are vital for prognosis; even with rapid introduction of therapeutic options, ALF secondary to NHL carries with it a mortality rate of greater than 90 %. In conclusion, this entity should be included in the differential diagnosis when evaluating a patient with rapidly progressive encephalopathy, coagulopathy and liver function derangement. Even when a common etiology seems likely (i.e. drug-induced or viral hepatitis), a thorough understanding of the wide differential diagnosis for acute liver failure, could result in early recognition and treatment of the disease thereby preventing adverse outcomes.
ACUTE MYOPERICARDITIS AFTER TETANUS, DIPTHERIA, AND PERTUSSIS VACCINATION IN A HEALTHY ADULTAdrienne L. Clark1; Laleh Boroujerdi-Rad2. 1University of California, Los Angeles, Los Angeles, CA; 2University of California, Irvine, Orange, CA. (Tracking ID #1919044)
LEARNING OBJECTIVE 1: Recognize that myopericarditis may rarely be observed after immunization
LEARNING OBJECTIVE 2: Weigh risks and benefits of invasive procedures such as cardiac angiography, particularly if alternatives are available
CASE: A previously healthy 28-year-old man presented with 1 day of sudden onset severe substernal chest pain, not associated with inspiration and improved by leaning forward. Three days prior he had received a single intramuscular tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine, and 2 days prior developed tactile fevers and myalgias. Vital signs and clinical exam were normal. He denied sick contacts, any history of vaccine reactions, or any cardiac risk factors apart from a 10-pack-year tobacco history. EKG showed diffuse upsloping ST segment elevations. Laboratory studies revealed WBC 13.3/mm^3, troponin 9.1 ng/mL, creatinine kinase 372 IU/L, and C-reactive protein 79.3 mg/L. Two-dimensional echocardiography showed normal left ventricle size and function and no effusion. His symptoms were thought consistent with pericarditis and he was started on high dose aspirin and colchicine. Overnight he was febrile to 38.1C, his troponin uptrended to 30.5 ng/mL, and his chest pain persisted. Cardiac catheterization showed normal coronary arteries. Several hours later he developed worsening chest pain and new, marked ST elevations in leads I, AVL, and V1-V6. Repeat angiography showed a newly dissected and occluded LAD, which was stented with restoration of TIMI 3 flow. He was discharged with an ejection fraction of 45 % on colchicine, clopidogrel, and aspirin. An infectious workup including Coxsackie B, echovirus, and adenovirus was ultimately negative, as were antinuclear antibody and rheumatoid factor. He re-presented several times over the next few months with atypical chest pain but normal cardiac enzymes and CRP. He underwent an exercise treadmill test-myoview and was able to exercise 10 min without EKG changes. Nuclear imaging showed a medium-to-large partially reversible perfusion defect in the apex and anteroseptal wall, but repeat catheterization showed a patent LAD stent and distal vasospasm. He was treated for vasospasm with isosorbide mononitrate and diltiazem.
DISCUSSION: Most U.S. cases of myopericarditis result from viral infection, although other pathogens, drugs, hypersensitivity, and autoimmune disorders are occasionally implicated. Cardiovascular complications due to vaccination are rare. Only two case reports of myopericarditis after Tdap vaccination exist, and of 20 million doses distributed from 2005 to 2007, three cases were reported in the U.S. postlicensure safety surveillance. While it is impossible to definitely exclude a viral etiology for this case, negative viral serologies and absence of symptoms prior to vaccination make it less likely. While early post-vaccination prodrome favors a hypersensitivity reaction, hypersensitivity myocarditis is usually a retrospective, circumstantial diagnosis. The diagnostic accuracy of endomyocardial biopsy remains poor and was not indicated. Coronary angiography may be performed if there is significant uncertainty as to whether the clinical picture reflects acute coronary syndrome versus myopericarditis. Cardiac MRI has been shown to be a highly sensitive (76 %) and specific (96 %) alternative for myocarditis detection and differentiation from infarction. However, it is not available in many resource-limited settings, including the county hospital to which this patient presented.
ACUTE NECROTIZING PANCREATITIS: ATYPICAL MANIFESTATION AND MANAGEMENTAtena Lodhi; Sanghee Hong. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1916249)
LEARNING OBJECTIVE 1: Identify presentations of severe acute pancreatitis without correlating high prognostic score.
LEARNING OBJECTIVE 2: Assess appropriate time and methods for nutritional support to minimize complications of acute pancreatitis.
CASE: A previously healthy 30-year-old male presented after a visit to outside hospital’s ED for a 3-day history of persistent abdominal pain and nausea. It was a constant, colicky pain located in the epigastrium and radiated to the back. At outside ED, he had elevated lipase (>3,000 U/L), leukocytosis (19,400 cells/mm3), and elevated serum glucose (141 mg/dL) but otherwise patient was afebrile and had unremarkable lab results. CT from outside ED showed findings of acute pancreatitis with peripancreatic free fluid. When patient presented to our ED, his lipase and glucose decreased but leukocytosis (23,500 cells/mm3) had worsened. His abdomen was non-distended but diffusely tender, predominately in the epigastric area. Social history was negative for extensive smoking or drinking history and extensive work up ruled out autoimmune, obstructive, malignant, hyperlipedemia-induced, or trauma-induced pancreatitis. Four days after admission, repeat CT was done when patient was tolerating a clear liquid diet and pain. It showed necrosis involving pancreatic head, neck, and proximal body. He was placed NPO and had two failed attempts of feeding through nasal-jejunal tube over 3 weeks. Four weeks after admission, patient had direct hyperbilirubinemia and subsequent CT showed an enlarging pseudocyst with dilated common bile duct, narrowing extrahepatic portal vein, and subhepatic inferior vena cava. Interventional gastroenterology was consulted for urgent drainage. Patient underwent endoscopic ultrasound guided cystogastrostomy with two double pigtail stents placement. The patient’s condition has improved markedly over next several days with resolution of signs of biliary obstruction.
DISCUSSION: Even with low prognostic score (<3 Ranson’s criteria and <8 APACHE II scale), acute pancreatitis may have high risk of developing complications. Although supportive medical management for all levels of pancreatitis shares a goal of maintaining adequate perfusion and prevention of infection, patients should be monitored closely for complications with CT severity index regarding extrapancreatic fluid collection and extent of pancreatic involvement. There is a controversy in management of sterile pancreatic necrosis. However, as complicating sepsis from necrosis accounts for more than 80 % of acute pancreatitis-related deaths, repeat imaging and frequent clinical exam, especially in the first 3 weeks to evaluate for endoscopic or surgical intervention was reasonable. Nutrition is another important component in management of patients with pancreatitis. Enteral feeding was shown to reduce mortality, infection, and hospital stay compared to parenteral feeding. About 20 % of pain relapse was reported with oral re-feeding and jejunal feeding was shown to reduce the risk. However, this case presented with worsening symptoms at jejunal feeding. It is likely from extent of enlarging pseudocyst already compressing on intra-abdominal cavities. This was a patient case with atypical presentation of severe acute pancreatitis and severe complications including necrosis and pseudocyst formation without spontaneous resolution. It is important to be familiar with this common condition with highly variable manifestation to ensure best clinical outcome.
ACUTE NEUROLOGICAL MANIFESTATIONS OF ATYPICAL TRAMADOL WITHDRAWALPranathi Sundaragiri1; Saraschandra Vallabhajosyula1; Sakshi Malhotra2,1. 1Alegent-Creighton University Medical Center, Omaha, NE; 2Vetrans Affairs Medical Center, Omaha, NE. (Tracking ID #1928252)
LEARNING OBJECTIVE 1: Recognizing lesser known contributors of altered mental status in substance abuse
LEARNING OBJECTIVE 2: Understanding addiction potential and neurological manifestations of tramadol withdrawal
CASE: Introduction: Tramadol is an analgesic medication that acts as a typical Mu-opioid receptor agonist with some non-analgesic activity mediated via serotonin and norepinephrine reuptake inhibition (SNRI) 1. With a low potency at Mu-receptors (1/10th affinity of Morphine) 2 it has been reported to have typical withdrawal symptoms on discontinuation due to its opioid-like action, despite being chemically unrelated to the opioids1-3. Atypical withdrawal symptoms predominantly involving the central nervous system (CNS), as presented in this case, have been infrequently reported in literature1. Case Report: A 71-year-old African-American female with past history of chronic kidney disease, osteoarthritis and hypertension presented with new onset altered mental status (AMS) and reduced verbal output of one-day duration. Review of systems was positive for diffuse myalgia, malaise and history of non-compliance with home medications since 1 week. Patient’s family reported that she took about 30 tramadol tablets the day prior for arthralgia. Neurological examination was significant for miosis (pupillary diameter 2 mm) and lower extremity proximal weakness with normal reflexes. Laboratory parameters were significant for mild leukocytosis and negative urine toxicology screen. She was empirically started on broad-spectrum antimicrobial therapy for suspicion of meningioencephalitis. Cerebro-spinal fluid (CSF) revealed mildly elevated protein and no infective etiology. Patient continued to be disoriented, with visual and auditory hallucinations. In addition, paranoia with delusions of persecution was noted. Magnetic resonance imaging was unremarkable for any acute pathology and antimicrobial therapy was de-escalated. Patient’s AMS gradually resolved with a short course of risperidal with subsequent normal mood and affect. The AMS was believed to be secondary to her acute tramadol ingestion with atypical withdrawal symptoms. Patient was cautioned against self-management of her medications and remained asymptomatic at six-month follow-up.
DISCUSSION: Tramadol has been popular with clinicians for analgesic use due to its non-scheduled nature, lack of ‘opiophobia’ and relative lack of side-effects4. It has, however, documented physical and psychological effects, with dose-dependent addiction potential and typical withdrawal symptoms similar to opiates1-4. It has been linked extensively to seizure disorder and general disorganization on EEG5,6. Atypical tramadol withdrawal noted in 1 of 8 cases of tramadol withdrawal, manifests as anxiety, panic attacks, delusions, confusion and paresthesia. Tramadol is hypothesized to exert its atypical features via the SNRI action, though this remains unproven. It does not have any age or gender predilection, but is however typically associated with a dose range of 50–1300 mg/day1. Acute high-dose tramadol use (as noted in our patient) or sudden decrease in tramadol use has been associated with atypical withdrawal3,7. There are no established guidelines on management. Various regimens proposed include methadone, low-dose benzodiazepines and reinitiating low-dose tramadol1,3,7. Gradual taper of tramadol has been recommended, but however further randomized controlled trials are required to establish standardized treatment protocols. References: 1. Senay EC, Adams EH, Geller A, Inciardi JA, Munoz A, Schnoll SH, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003 Apr 1;69(3):233–41. 2. Lanier RK, Lofwall MR, Mintzer MZ, Bigelow GE, Strain EC. Physical dependence potential of daily tramadol dosing in humans. Psychopharmacology (Berl). 2010 Sep;211(4):457–66. 3. Leo RJ, Narendran R, DeGuiseppe B. Methadone detoxification of tramadol dependence. J Subst Abuse Treat. 2000 Oct;19(3):297–9. 4. Ripamonti C, Fagnoni E, De Conno F. Withdrawal syndrome after delayed tramadol intake. Am J Psychiatry. 2004 Dec;161(12):2326–7. 5. Kahn LH, Alderfer RJ, Graham DJ. Seizures reported with tramadol. JAMA. 1997 Nov 26;278(20):1661 6. Riedel F, von Stockhausen HB. Severe cerebral depression after intoxication with tramadol in a 6-month-old infant. Eur J Clin Pharmacol. 1984;26(5):631–2. 7. Barsotti CE, Mycyk MB, Reyes J. Withdrawal syndrome from tramadol hydrochloride. Am J Emerg Med. 2003 Jan;21(1):87–8
ACUTE ONSET MUSCLE WEAKNESS AFTER EATING FIVE BOWLS OF FROSTED CEREALChristine N. Salvaggio; David I. Rotstein; Matthew T. Czaja; Sarang Kim. Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1931474)
LEARNING OBJECTIVE 1: Review the differential diagnosis and treatment of a patient presenting with acute muscle weakness and hypokalemia.
CASE: A 23-year-old man presents with acute onset appendicular muscle weakness after consuming five bowls of frosted cereal on the morning of admission. He had noted mild, progressive muscle weakness involving his lower and upper extremities for the past 6 weeks, as well as tremor, palpitations, diaphoresis, nausea, diarrhea and a 10-lb weight loss. The patient denies trauma, neck or back pain, numbness, bowel or bladder incontinence, dysphagia, or shortness of breath. He denies exposure to iodine or radiocontrast agents. He also denies family history of autoimmune diseases. On physical exam, his temperature is 97.4, blood pressure 134/52 mmHg, pulse 135, and respiratory rate 22 per minute. Cardiac exam reveals a tachycardic, irregularly irregular rhythm. Muscle strength is 3/5 in proximal muscle groups bilaterally, and 4/5 in the distal muscle groups bilaterally in both his upper and lower extremities. Deep tendon reflexes are 1+ and symmetric in the patella, achilles and brachioradialis. Exam is negative for lid lag, proptosis, thyromegaly, nodules, or thyroid bruit. The remainder of the exam is unremarkable. Laboratory investigation demonstrates a potassium level of 1.4 mEq/L. High sensitivity TSH is <0.01 mIU/L (normal range 0.35–5.50), and free T4 is 3.39 ng/dL (normal range 0.9–1.8 ). EKG reveals atrial flutter and a prolonged QT interval. Treatment was initiated with IV potassium and oral propranolol. Overnight, the patient’s weakness completely resolved. Thyroid ultrasound, TFTs and positive thyroid stimulating immunoglobulin confirmed the diagnosis of Thyrotoxic Hypokalemic Periodic Paralysis (HPP) in the setting of Graves’ disease.
DISCUSSION: Thyrotoxic HPP is a rare neuromuscular disorder related to a defect in muscle ion channels that occurs in association with hyperthyroidism. This case illustrates the importance of considering thyrotoxic HPP in a patient with acute paralysis and hypokalemia. The differential diagnosis of sudden tetraparesis includes Guillain-Barré syndrome, multiple sclerosis, myasthenia gravis and spinal cord trauma, ischemia, inflammation or tumor. Distinguishing characteristics of thyrotoxic HPP are thyrotoxicosis and hypokalemia. Thyrotoxic HPP predominantly occurs in Asian males in the third decade of life. Patients present with acute muscle weakness, commonly in the shoulders and hips. Deep tendon reflexes may be decreased, but ocular, bulbar, and respiratory muscles are usually spared. In these patients, elevated levels of thyroid hormone, exercise, alcohol consumption or high carbohydrate meals can increase the Na+/K+ pump activity on skeletal muscle cell membranes, driving potassium into cells and leading to a hypokalemia. Recognition of this syndrome is critical to the institution of appropriate therapy. Acute treatment involves potassium administration, which can hasten recovery and prevent life-threatening hypokalemic-related arrhythmias. While evidence-based guidelines do not exist, experts recommend KCl 10–20 mEq every 2 h. Potassium levels should be monitored during replacement, as rebound hyperkalemia has been seen in at least 40 % of patients. Non-selective β-blockers such as propranolol can diminish hyperadrenergic activity and the Na+/K+ ATPase dependent K+ cellular influx, which have been implicated in the pathogenesis of the disease. Additionally, patients with thyrotoxic HPP merit a thorough evaluation to determine the etiology of their hyperthyroidism. Only definitive treatment of thyrotoxicosis will prevent further occurrences of HPP. Our patient was diagnosed with Graves’ disease and treated with methimazole with plan for radioactive iodine ablation in the future.
ACUTE PANCREATITIS AS INITIAL PRESENTATION OF COCAINE-INDUCED VASCULITISAyorinde Ogunbameru; Mohammed Badr Jandali; Amer Issa; Waleed Quwatli; Timothy Woodlock; Wajid M. Choudhry. Unity Health System, Rochester, NY. (Tracking ID #1934655)
LEARNING OBJECTIVE 1: Recognize Acute Pancreatitis as an atypical and rare systemic manifestation of Cocaine-induced ANCA negative necrotizing immune glomerulonephritis
CASE: A 22 years old male with no past medical history, presented with a 2 day history of mid abdominal pain radiating to the chest with Shortness of breath. Patient was sent to the Emergency room for a Chest CT after routine lab test at Urgent care showed elevated D-Dimer. Patient denied any fever, chills, recent travel or history of thromboembolic disease. Patient was adopted and does not know his family history. BP was 139/74, HR 67/min, RR 18, O2 sat 98 % on room air. Clinical examination showed mild epigastric tenderness, otherwise unremarkable. Chest CT was negative for Pulmonary Embolism but showed some stranding at the tail of the pancreas suspicious for Acute Pancreatitis. Labs showed WBC 14.4/mm3, elevated Lipase (754), Cr(0.79), ESR(1), CRP(0.08), ALT(23), AST(71), ALP(139), GGTP(209). Patient was kept NPO, Intravenous normal saline and IV Dilaudid were commenced. Patient admitted to drinking ½ L of whiskey daily. Right Upper Quadrant Ultrasound did not show any evidence of gallstones but revealed fatty liver. Lipid panel and Triglycerides were normal. A urine toxicology screen was positive for cocaine and marijuana. Ethanol level was normal. On day #2/3 of admission, patient was noticed to have elevated Creatinine (3.71) with baseline (0.59) and thrombocytopenia (59) with baseline (159). SC Heparin was stopped. Patient subsequently became oliguric with a Urine output of (200 cm3 in 24 h) despite adequate fluid hydration (8 L). Renal Ultrasound did not show any hydronephrosis or stones. GI, Nephrology and Hematology were consulted. Follow up MRCP done showed heterogeneous pancreas suggesting inflammation. Patient was thought to have an atypical form of pancreatitis. IGG-4 test done to rule out auto-immune pancreatitis was negative. Patient’s labs showed thrombocytopenia, severe anemia, negative Platelet Factor-4, elevated direct bilirubin, low Haptoglobin, high LDH, elevated D-Dimer and positive FDPs. Schistocytes were seen on blood microscopy. Differentials of HUS/TTP or DIC were entertained but the definite diagnosis was still inconclusive. ADAMS-13 level was negative. Patient eventually became anuric and developed azotemia. A diagnosis of Acute Renal Failure with a likely vasculitic process was made. Urinalysis showed muddy brown casts, proteinuria and WBCs. FENA was 3.57. Work up for glomerulonephritis showed HIV, Hepatitis, ANCA, ANA, Anti-glomerular, Anti-cardiolipin, Scleroderma, Complement C3/C4 tests were negative. Hemodialysis was initiated. Kidney biopsy was done and revealed pauci-immune necrotizing glomerulonephritis with features of glomerular thrombotic microangiopathy. Patient was commenced on High dose IV Solumedrol and Rituximab. He was transfused with a total 9 units of Packed Red Blood Cells and he had 9 sessions of Plasmapheresis. Patient’s renal function and hematological indices improved and he was discharged in stable clinical condition.
DISCUSSION: My patient had an ANCA negative pauci-immune necrotizing glomerulonephritis (thought to be induced by cocaine) which initially presented as acute pancreatitis which is atypical and rare, making the diagnostic process challenging. Pauci-immune necrotizing glomerulonephritis is the most frequent cause of rapidly progressive glomerulonephritis and in 60 % of cases; it is associated with positive anti-neutrophil cytoplasmic antibodies (ANCA). It is either the renal manifestation of Wegener’s granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome, or a renal-limited vasculitis. Few case reports cite Wegener’s Granulomatosis affecting the gastrointestinal system with an initial presentation of pancreatitis which may be rapidly progressive and fatal. Vasculitic disease of the pancreas, even though rare, should be considered when other causes of pancreatitis have been excluded. References: 1. Mohammed Abu-Hilal et al., Acute Pancreatitis as First Presentation of Wegener’s Granulomatosis. Case Report, JOP. J Pancreas 2008; 9(3):300–304. 2. Saurabh Chawla et al., Acute Pancreatitis as a rare initial manifestation of Wegener’s Granulomatosis. A case based literature review, JOP. J Pancreas 2011 Mar 9; 12(2):167–169.
ACUTE RENAL FAILURE ASSOCIATED WITH MASSIVE HEMATURIA IN IGA NEPHROPATHYAsad Jehangir; Leena Jalota; Manoj Singla. Reading Health System, West Reading, PA. (Tracking ID #1928687)
LEARNING OBJECTIVE 1: Recognize IgA Nephropathy (IGAN) as a potential cause of acute kidney injury (AKI); either by crescentic IgA nephropathy or massive hematuria leading to tubular obstruction by red cell casts.
CASE: A 45 year old male with multiple co-morbidities recently discharged after being treated for stroke and urethral stricture with normal renal functions (BUN 25 mg/dl, creatinine 1.5 mg/dl) presented within few weeks with gross hematuria and decreased urine output. Initial labs revealed a creatinine of 10.96 mg/dl and a BUN of 76 mg/dl. Bladder scan showed no evidence of urinary retention. Additional work up including ANA, anti-streptolysin O, blood and urine cultures, anti IGM antibodies, urinary eosinophils were negative. Renal ultrasound showed normal sized kidneys. Renal artery duplex suggested less than 60 % stenosis of right renal artery Cystoscopy showed no evidence of obstruction. Subsequent renal biopsy showed ATN and IgA nephropathy. ACE inhibitor was discontinued and patient improved with initiation of temporary dialysis. Creatinine prior to discharge was 2 mg/dl.
DISCUSSION: IgA nephropathy is a relatively common but underdiagnosed disease as most cases have transient gross hematuria following upper respiratory infection. Others have persistent microhematuria and mild proteinuria associated with a benign course and uncommonly patients can have marked proteinuria. Rarely patients may present with AKI that requires dialysis, prolonged glucocorticoid and ACE inhibitor therapy. This report emphasizes the importance of recognizing that IgAN as a cause of AKI that may require dialysis. Furthermore, severe acute tubular necrosis may occur in IgAN and may be related to heavy glomerular bleeding.
ACUTE THORACIC CORD COMPRESSION DUE TO HIV-ASSOCIATED BURKITT’S LYMPHOMAKristen Lee; Ameeta Kalokhe; Schuyler D. Livingston. Emory University School of Medicine, Atlanta, GA. (Tracking ID #1939108)
LEARNING OBJECTIVE 1: Recognize the high risk of non-Hodgkin’s lymphoma in a patient with HIV/AIDS.
LEARNING OBJECTIVE 2: Describe potential serious causes of back pain in a patient with HIV/AIDS.
CASE: A 46 year-old African-American man with HIV, a CD4 count of 274/mcL and a viral load of 200 copies/mL, on combination antiretroviral therapy (cART), presented with 1 month of progressive mid-to-low back pain without fevers or night sweats. He had no neurological deficits and was discharged with a diagnosis of musculoskeletal back pain. One week later, he developed lower extremity weakness and numbness. Physical exam demonstrated decreased lower extremity strength, loss of sensation to light touch, proprioception, and pain below the umbilicus, patellar tendon hyperreflexia, bilateral ankle clonus, and decreased rectal sensation. Spine MRI showed extradural soft tissue masses at the T3-T4 and T10-T11 levels with neural foraminal and paraspinal spread with severe canal stenosis at the T3-T4 level suggestive of lymphoma. Intravenous dexamethasone was initiated, followed by emergent laminectomy and epidural mass resection. Pathological exam of the mass showed dense lymphocytic infiltrate. Flow cytometry revealed a monoclonal B-cell population, and FISH studies demonstrated expression of the c-myc oncogene with chromosomal translocation 8q24 consistent with Burkitt’s lymphoma (BL). Epstein-Barr virus (EBV) was detected in serum by PCR. CT of the chest, abdomen, and pelvis were negative for lymphadenopathy. Brain MRI showed no parenchymal lesions. Bone marrow biopsy was negative for malignant cells. PET scan showed increased FDG activity within the right trochanter. Systemic and intrathecal chemotherapy were initiated.
DISCUSSION: Non-Hodgkin’s lymphoma (NHL) is an AIDS defining malignancy that is 200–600 times more common in HIV-infected patients compared to the general population. High grade diffuse large B-cell or Burkitt-like lymphomas are more common in people living with HIV and are associated with EBV coinfection. The incidence of NHL has decreased in the cART era. A recent review of 61 cases of NHL in AIDS patients in France showed that the major risks for NHL included both longer and current exposures to a viral load above 500, and a CD4 below 200. Patients commonly present with “B” symptoms, and usual sites of involvement include bone marrow, lungs, abdomen, and CNS. Epidural spinal cord compression occurs in 0.1 to 6.5 % of NHL patients, either at the time of relapse or as the initial manifestation of NHL. Burkitt’s lymphoma (BL) is a highly aggressive, mature B-cell NHL. Endemic variant BL occurs in African children, usually presenting with a mass at the jaw or neck, and is associated with EBV infection. Sporadic BL usually presents with an abdominal mass. Immunodeficiency-related BL is seen in AIDS patients and often involves the lymph nodes, bone marrow, and CNS. Few cases of spinal involvement in adults with BL have been reported in the literature. BL is associated with unique cytogenetic translocations involving the c-myc oncogene. This case demonstrates the potential seriousness of back pain in patients with HIV/AIDS. The differential diagnosis includes cancers that metastasize to bone, compression fracture from osteoporosis, spinal epidural abscess, and NHL including BL. Clinicians should have a lower threshold for imaging HIV-infected patients with back pain when compared to the general population.
ACUTE URINARY RETENTION DUE TO SACRAL HERPES ZOSTERMaryam Mahmood; Anthony A. Donato. Reading Health System, Reading, PA. (Tracking ID #1900837)
LEARNING OBJECTIVE 1: Recognize uncommon causes of urinary retention
CASE: A 76-year-old woman with history of myasthenia gravis on chronic mycophenolate mofetil presented to the emergency department with a 2 day history of incomplete voiding, increasing urgency, and abdominal discomfort. Three days prior she had noted a painful unilateral vesicular rash over her right buttock diagnosed as zoster and treated with oral valacyclovir. On examination she was afebrile with stable vital signs. Abdominal examination revealed a tender bladder palpable at the level of the umbilicus, as well as was a unilateral erythematous, vesicular rash on the right buttock in the distribution of S1-S2 dermatomes. Polymerase chain reaction culture of an affected vesicle confirmed herpes zoster virus. Urinalysis was remarkable for pyuria and microscopic hematuria with negative urine culture. Renal ultrasound revealed no structural abnormalities. Postvoid bladder scanning confirmed significant unvoided urine. Foley catheterization was performed and 700 mL of urine was obtained. The patient was diagnosed with acute urinary retention secondary to zoster and discharged home with a Foley catheter with re-evaluation by Urology in 1 week.
DISCUSSION: Varicella zoster is a neurotropic virus that recurs in nearly a third of all adults, presenting as a painful unilateral vesicular rash that may result in post-herpetic pain syndromes. Less commonly the autonomic nervous system or viscera can be involved with associated morbidity. Herpes zoster associated voiding dysfunction is rare and typically occurs with lumbosacral involvement. The main clinical manifestations include cystitis, neuritis-associated retention and myelitis related overflow incontinence. Acute urinary retention associated with zoster is related to sacral reactivation causing Detrusor muscle atony. It is often accompanied by severe constipation and may persist for 2 to 6 weeks. It should be considered as a cause of acute urinary retention in patients with unilateral sacral dermatomal pain syndromes, with or without vesicular rash, as neurologic dysfunction can precede skin outbreaks.
ADDRESSING DRESSLER’S SYNDROMEEwa M. Rakowski. Montefiore Hospital, Bronx, NY. (Tracking ID #1937679)
LEARNING OBJECTIVE 1: Identify the etiologies of post myocardial infarction pericardial effusions
LEARNING OBJECTIVE 2: Recognize the diagnosis, pathophysiology and management of post myocardial infarction syndrome (Dressler’s syndrome)
CASE: A 71 year old man with history of uncontrolled diabetes and hypertension presented with 1 week of intermittent severe chest pain. Physical exam was unremarkable. Electrocardiogram revealed ST elevations in the inferior leads and concomitant Q waves. Cardiac catheterization revealed extensive three vessel disease including 100 % occluded right coronary artery with collateral vessels. Initial troponins were elevated. Overall presentation was consistent with delayed presentation of ST elevation myocardial infarction (STEMI) with multi-vessel disease not amenable to stenting. Echocardiogram showed normal ejection fraction, wall motion, right ventricular dilation and small pericardial effusion. Patient had a complicated medical course requiring intensive care. Two weeks later when acute issues were resolved work up for coronary artery bypass graft surgery was initiated. Repeat echocardiogram revealed a new large pericardial effusion with early tamponade physiology and an area of the ascending aorta concerning for hematoma. MRA chest confirmed pericardial effusion and revealed bilateral pleural effusions but excluded aneurysm and hematoma. CT surgery performed pericardial window with 300 cm3 of serosangious fluid drained. Pericardial fluid cytology was positive for extensive inflammation. In combination with clinical history and time course this was consistent with diagnosis of post myocardial infarction syndrome (PMIS). The patient was started on colchicine and recovered well.
DISCUSSION: With the advent of fibrinolytic therapy and cardiac catheterization the 30 day mortality of STEMI’s has decreased from 15 % to those medically managed to 3–5 % for those receiving optimal reperfusion therapy. Likewise there has been a significant decrease in post -myocardial infarction complications including pericardial complications such as early infarct-associated pericarditis and post myocardial infarction syndrome. Pericardial effusion is a common early complication of transmural myocardial infarction and is detected by echocardiography in one third of patients by day three post infarct. Half of these patients do not have a pericardial friction rub. These pericardial effusions are often irritative or due to hydropericardium or hemopericardium. Irritative effusions are usually small and result from increased vascular permeability. Hydropericardium should be considered in large Q wave infarcts that present with clinical heart failure. Hemopericardium can occur from spontaneous hemorrhage or secondary to thrombolytic and antithrombotic therapy or most fatally from myocardial wall rupture. The latter should be considered for any post myocardial infarct patient with persistent pericardial rub and drop in hematocrit. Finally, PMIS should be considered in patients who present with delayed pericardial effusion post acute or subacute infarct whether or not they have symptoms and especially if there are pleural effusions and infiltrates in absence of heart failure. PMIS, also known as Dressler’s syndrome occurs 1 week to several months post myocardial infarction. Clinically it presents with pericardial friction rub, malaise fever and leukocytosis. Half of patients will have a pericardial effusion which can be serous or hemorrhagic. Chest x-ray often shows pleural effusions and infiltrates. Historically PMIS had an incidence of up to 5 % post-STEMI and occurred more often in larger infarctions, specifically those anterior or inferior infarctions and in those with complicated hospital courses. With the advent of early re-perfusion therapy leading to decreased size of infarction this diagnosis has become less common. The pathogenesis behind PMIS is that myocardial necrosis releases cardiac antigens which stimulate antibody formation. An inflammatory response occurs from immune complex deposition in the pericardium, pleura and lungs. Therefore, a latent period of minimum 1 week is necessary for diagnosis and distinguishes PMIS from infarct-associated pericarditis which occurs immediately post-infarct. It is an important clinical distinction because PMIS is more likely to lead to larger effusions, life threatening tamponade, constrictive pericarditis and hemorrhage. With a diagnosis of PCIS the patient should be hospitalized and observed for cardiac tamponade. Non-steroidal anti-inflammatory drugs or colchicine are recommended however data is lacking. Given the increased propensity for bleeding, if anticoagulation therapy is strongly indicated the patient must be monitored closely. The presence of cardiac tamponade confers an increased 30 day mortality and requires urgent drainage. Symptoms of PCIS may recur but overall the prognosis is favorable.
ADULT ONSET STILL’S DISEASEKaren Y. Cheng1; Baran Ho2; Victoria T. Liu1; Helen Wang2; Pearl Yu2; Gregory Middleton3; Christina Le2. 1UCSD, San Diego, CA; 2University of California, San Diego, La Jolla, CA; 3University of California, San Diego, La Jolla, CA. (Tracking ID #1923776)
LEARNING OBJECTIVE 1: Recognize the clinical features of Adult Onset Still’s Disease
LEARNING OBJECTIVE 2: Diagnose Adult Onset Still’s disease
CASE: A 39 year-old woman presented with 2-months of throat discomfort and migratory joint pain of the hands, knees, and shoulders. Physical exam revealed a new onset holosystolic murmur and a mildly erythematous oropharynx. She had traveled to Hong Kong 8 months prior, but denied any unusual food exposures, arthropod bites, or sick contacts. One week later, the patient developed intermittent nocturnal fevers up to 39 °C and a transient urticarial rash over the trunk and extremities with dermatographism. Rheumatic fever was suspected due to the murmur and recent travel to Hong Kong during a known strep throat outbreak. Erythrocyte sedimentation rate (ESR) was elevated at 35 mm/h, but there was no evidence of infection on multiple blood cultures or serological examination for group A strep. The patient’s symptoms resolved and remitted over the next 2 months. During this period, comprehensive infectious and rheumatologic workup was pursued and all tests came back negative. However, CT imaging of the chest showed mid-axillary lymphadenopathy. The patient was admitted for further workup, with an emphasis on evaluation for occult malignancy and endocarditis. During this hospitalization, she developed a new nonpruritic, light-colored erythematous maculopapular rash, and experienced inflammatory polyarthritis with quotidian fevers. Echocardiogram showed no valvular vegetations. CT showed interval enlargement of axillary lymph nodes, prompting biopsy, which showed reactive follicular hyperplasia without evidence of lymphoma. A diagnosis of adult onset Still’s disease was made following the negative infectious and neoplastic workup and the patient was started on prednisone 40 mg daily with significant improvement.
DISCUSSION: Adult onset still’s disease (AOSD) is a rare condition that often presents as fever of unknown origin (FUO). Classic AOSD is characterized by high spiking fevers, arthralgias, and nonpruritic salmon colored rash. This case illustrates an atypical, indolent course of AOSD punctated by periods of improvement. Diagnosis is clinical and requires exclusion of infectious, neoplastic, and other rheumatologic disorders. A hallmark diagnostic feature of AOSD is a nonpruritic, maculopapular, salmon-colored rash. Atypical rashes have been described, but are rare. Diagnosis can be made using the Yamaguchi criteria, which has a 92.1 % specificity for AOSD if five criteria are satisfied. After admission, this patient satisfied three major criteria (fever, arthralgia, typical rash), as well as four minor criteria (sore throat, lymphadenopathy, liver dysfunction, and absence of rheumatoid factor and antinuclear antibody). A comprehensive workup was performed to rule out neoplastic and infectious etiologies of FUO.
ADULT ONSET UREA CYCLE DISORDER IN THE SETTING OF GASTRIC BYPASS SURGERYMichelle Kromas; Omar Mousa. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1939278)
LEARNING OBJECTIVE 1: Recognize a rare and potentially fatal complication of bariatric surgery
LEARNING OBJECTIVE 2: Diagnose and manage adult onset urea cycle disorders
CASE: We present a case of a 56-year-old male who developed altered mental status soon after Roux-en-y gastric bypass surgery (GBS). He presented initially to his PCP with intermittent neurological manifestations including confusion, tremors, inappropriate emotional responses, and ataxia. Multiple referrals left him with a diagnosis of Parkinson’s disease, for which he was prescribed Sinemet, with no improvement. He presented to our emergency department with symptom progression. Physical exam was significant for tremors, inability to concentrate, and memory impairment. He denied history of substance use or toxin exposure. Laboratory investigations including BMP, CBC, iron panel, hepatic function panel, carnitine level, zinc, manganese, Vitamin B12, Vitamin A, and Vitamin D levels which were unremarkable. Abdominal ultrasound and well as brain MRI were also non-revealing. Of significance was an ammonia level of 155mcg/dL. This finding spurred further workup significant for elevated urine orotic acid, consistent with a urea cycle disorder. Conservative management with low protein diet, lactulose and supportive care were initiated with improvement in the patient’s symptoms.
DISCUSSION: In the United States, 40 % of adults aged 20 years and over are obese prompting 200,000 bariatric surgeries annually. Hyperammonemia encephalopathy as a complication of gastric bypass surgery is very uncommon, especially when the etiology is adult onset urea cycle disorder. This rare non-specific neurologic presentation, in the absence of overt liver disease, presents a true diagnostic challenge. This may delay diagnosis and treatment, causing increased morbidity and mortality. Urea cycle disorders result from a deficiency in hepatic enzymes involved in the conversion of ammonia to urea thus impeding nitrogen disposal. Classically, these deficiencies become apparent in the neonatal period with failure to thrive and neurologic manifestations. However, a continuously growing body of literature has identified cases of disease manifesting in adulthood, likely secondary to a partial enzyme deficiency or a mutated enzyme that becomes apparent in the presence of an inciting stressor. Diagnostic tools include blood ammonia, plasma amino acids and urine organic acids as well as DNA or enzymatic testing. We indicate the importance of raising awareness among internists of this possible complication of gastric bypass surgery. Very few reports have described Post-GBS encephalopathy as a result of secondary nutrient deficiencies or unmasked urea cycle disorders. An early diagnosis may prevent associated complications by incorporating a simple and inexpensive intervention, dietary modification with protein restriction. Patient education about such potential complications can also reduce post-operative dissatisfaction. A high index of suspicion for unmasked urea cycle disorders post GBS can prevent the debilitating consequences of unrecognized and untreated disease and improve outcomes.
AGGRESSIVE ARTHRALGIA: A CASE OF GRANULOMATOSIS WITH POLYANGIITISClaiborne Childs. NYH-WCMC, New York, NY. (Tracking ID #1939157)
LEARNING OBJECTIVE 1: Describe an accelerated clinical presentation of an uncommon clinical condition and highlight its musculoskeletal manifestations.
LEARNING OBJECTIVE 2: Review the latest diagnostic criteria for Granulomatosis with Polyangiitis (GPA, formerly known as Wegener’s Granulomatosis)
CASE: A previously healthy 63-year-old woman presents to her PMD with a chief complaint of diffuse joint pain (knees, feet, shoulders) and swelling in her legs and ankles, with associated weight gain over the course of the proceeding week. Her PMD prescribes a short course of NSAID for presumed joint inflammation due to overuse. She returns to clinic 4 days later with no improvement in symptoms. Basic labs (CMP, CBC) as well as ESR, ANA, RF, ASO, and Lyme titers, all resulted as normal. Physical exam at the time revealed 1+ bilateral pitting edema in her lower extremities and pain with palpation of affected joints. (bilateral ankles, wrists, knees) No erythema or swelling was noted. Remainder of exam including, HEENT, cardiovascular, pulmonary, and abdominal exam were normal. The patient was instructed to continue oral NSAIDs and given a prescription for oral furosemide. Her lower extremity edema and arthralgia briefly improved. Three weeks following initial presentation, the patient develops worsening dyspnea, new cough, worsening lower extremity edema, and was noted by a family member to have decreased urinary frequency. The following day, she presents to the ED following an acute episode of cough and worsening dyspnea at rest. The patient was hypoxic to 80 % on room air. Labs in the ED were notable for: BUN (=128) and creatinine (=18.1, previous Cr = 0.75), anemia (Hgb = 6.7), and leukocytosis (WBC = 14). Chest radiograph showed diffuse alveolar opacities. While in the ED, the patient developed worsening hypoxia and hemoptysis. She was emergently intubated and transferred to the medical intensive care unit. Labs subsequently revealed elevated ESR (=129), CRP (=19) and a positive serum cANCA/PR3. A renal biopsy revealed Pauci-immune, severe diffuse crescentic/necrotizing glomerulonephritis with significant tubular dysfunction consistent with an ANCA positive vasculitis. The patient was given high dose steroids, cyclophosphamide and underwent plasmapheresis. She was extubated and clinically improved prior to discharge from the hospital. She remains on hemodialysis due to lack of recovery of renal function.
DISCUSSION: The clinical presentation of GPA includes: ENT manifestations (sinusitis, nasal crusting, bloody or purulent discharge) which present in 90 % of patients, lung involvement is present in 87 % of patients, signs of glomerulonephritis present in 77–85 % of patients and musculoskeletal symptoms present in 65–75 % of patients. Multiple diagnostic criteria exist for GPA: American College of Rheumatology (ACR, 1990) criteria include: (1) nasal/oral inflammation (oral ulcers, bloody discharge, etc.), (2) abnormal CXR (infiltrates, cavities, nodules), (3) UA abnormalities (hematuria, casts) and (4) biopsy proven granulomatosis. The presence of two or more criteria is 88 % sensitive and 92 % specific for GPA. Chapel Hill Consensus Conference Criteria (CHCC, 1994) includes: (1) granulomatous inflammation of the respiratory tract, (2) necrotizing vasculitis, and (3) positive c-ANCA with proteinase 3 (PR3) specificity. The more recent European Medicine Agency Algorithm (2007) includes: (1) abnormal chest radiograph (infiltrates, nodules, etc.), (2) upper airway/nasal or oral inflammation (bloody discharge, ulceration, etc.), (3) glomerulonephritis (hematuria or casts) and (4) positive c-ANCA. The more recent European Medicine Agency’s algorithm combines criteria of earlier ACR and CHCC criteria. Even though not in the diagnostic criteria, musculoskeletal symptoms are very common and may be the patient’s presenting symptom. GPA may uncommonly be rapid and progressive, therefore early diagnosis and treatment may be both life saving and organ sparing.
AIDS SUGAR RUSH: DIABETIC KETOACIDOSIS IN A NEWLY DIAGNOSED AIDS PATIENTFelix H. Lui1; Sara L. Swenson1; Diana Antoniucci2. 1California Pacific Medical Center, San Francisco, CA; 2California Pacific Medical Center, San Francisco, CA. (Tracking ID #1939735)
LEARNING OBJECTIVE 1: Review the differential diagnosis and work up of hyperglycemia in an AIDS patient
LEARNING OBJECTIVE 2: Highlight a rare treatment complication of AIDS/HIV
CASE: A 30 year-old Asian male recently diagnosed with AIDS and hepatitis C presents with generalized weakness for the past 2 weeks. Four weeks prior to admission, he was hospitalized for septic shock secondary to pneumocystis jirovecii pneumonia. He was discharged to a skilled nursing facility (SNF) to complete a 21-day course of IV pentamidine. In the hospital, his blood sugars were elevated (100 s), which were thought secondary to steroids received for his PJP infection. His steroids were stopped prior to SNF transfer. However, his blood sugars elevated to the 300 s during his SNF course and a hemoglobin A1C was 6.7 %. Approximately 2 weeks prior to admission, the patient noted a 10-pound weight loss, polyuria, polydipsia, and blurry vision. He denied fevers, chills, or recurrence of cough. Medications included prophylactic dapsone and HAART therapy with norvir, atazanavir, and epzicom, which had been started 2 months prior to his hospitalization. On exam, he was afebrile with dry mucous membranes. His blood glucose was 1584 mg/dl, with a bicarbonate of 22 mmol/L, anion gap of 23, pH of 7.28 and pCO2 of 46 mmHg. His urinalysis showed 3+ glucose and 1+ ketones, and a serum lipase was 512 U/L. A work-up for infection was unrevealing. A repeat hemoglobin A1C was 11.3 %. The patient was admitted to the ICU for aggressive hydration and insulin drip. Within 2 days, his blood glucose normalized, and subcutaneous insulin was started. We initially attributed his ketoacidosis and hyperglycemia to DKA from either new-onset type 1 diabetes mellitus (DM1) or diabetes secondary to HAART medications, so his HAART medications were held. However, his C-peptide level was low, and antibodies for GAD 65, IA2, and Insulin were negative. Given that his development of hyperglycemia coincided most closely with the initiation of pentamidine, we ultimately attributed his DKA and new-onset diabetes to pentamidine therapy. He was discharged with basal (glargine) and bolus (lispro) insulin, and restarted on his HAART therapy. At 6 month follow up, he had no recurrence of his ketoacidosis.
DISCUSSION: We report a case of pentamidine-induced diabetic ketoacidosis in an AIDS patient. Although we initially considered a diagnosis of autoimmune type 1 diabetes, his low C-peptide level and lack of autoantibodies did not support this. Given his lack of prior documented insulin resistance or type 2 diabetes, we turned to medication-related causes of hyperglycemia. Initially, the patient’s elevated blood glucose was thought to be secondary to steroids or HAART medications. Ritonavir and atazanavir have both been associated with the development of insulin resistance, hyperglycemia, and new-onset diabetes. However, his initiation of HAART therapy predated his hyperglycemia by 2 months. Moreover, he developed severe hyperglycemia only after starting pentamidine for PJP. Pancreatic dysfunction leading to hyperglycemia has been a rare side effect of pentamidine. Usually associated with hypoglycemia (6 %) and renal impairment (24 %), pentamidine has been linked less commonly to severe pancreatic toxicity and hyperglycemia, which would explain a low c-peptide level. Pentamidine, an aromatic diamidine, has been used in the treatment of PJP pneumonia in those allergic to sulfa medications and severe disease. Pentamidine may induce a direct cytolytic effect on pancreatic beta cells that initially leads to insulin release and hypoglycemia and, less commonly, eventual insulin deficiency and diabetes. Hyperglycemia during pentamidine therapy may be a predictor for the development of diabetes mellitus. This case emphasizes the potential for severe pancreatic toxicity leading to DKA in patients receiving IV pentamidine, especially in conjunction with other medications, such as protease inhibitors, that can affect glucose metabolism. As the AIDS population lives longer, we remain alert to the possibility that we may identify additional cases similar to this one.
ALL THAT GLITTERS ISN’T WISNNaomi Karlen; Melody Oncale. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925932)
LEARNING OBJECTIVE 1: Recognize the presentation and treatment of Warfarin induced skin necrosis in the acute inpatient setting.
LEARNING OBJECTIVE 2: Discover an algorithm to diagnose purpura.
CASE: A 61 year-old woman presented with chief complaint of 6 days of bilateral gluteal pain. The pain was described as burning, tingling, and associated with a feeling of puffiness. It progressively worsened until she felt the need to seek emergent care. She has a medical history of coronary artery disease and recently was hospitalized due to acute myocardial infarction. Physical exam revealed stellate pupuric skin lesions without necrosis over bilateral hips and sacrum. Each was tender to palpation and associated with involuntary guarding. There was no associated warmth, erythema, or swelling. Laboratory studies revealed no thrombocytopenia, PT 27.5, PTT of 38.4 and INR of 2.6. During her recent hospitalization for myocardial infarction, she experienced sudden onset of left foot numbness and pain. This was thought to be secondary to atherosclerotic plaque embolization. She was enrolled in a double-blinded warfarin study with an unknown dosage, which was started 21 days prior to presentation. Warfarin was immediately stopped and punch biopsy of the purpuric lesion was performed. The painful lesions improved without active treatment following cessation of warfarin. The biopsy revealed purpura without thrombi or vasculitis.
DISCUSSION: Skin lesions are one of the most common complaints an internist will encounter. When approaching new purpuric skin lesions of unclear etiology, having an algorithmic approach is helpful. Laboratory evaluation should include platelet count and a coagulation panel and a thorough history with medication reconciliation is imperative in assisting the differential. In a patient with normal platelets and prolonged PT/PTT, the differential includes coagulation factor deficiency, von Willebrand’s Disease, pharmacologic anticoagulation, and liver disease. The patient in this case was recently started on warfarin, and thus the initial differential should immediately include WISN. Although a rare complication, with 0.01–0.1 % prevalence, it can be life threatening if it goes unrecognized and untreated. WISN usually presents 3–6 days after starting warfarin therapy, but cases have been reported up to 3 years after starting therapy. WISN is more commonly associated with patients who are obese, middle-aged, female, and whose purpuric lesions appeared akin to early presentation of potentially necrotic lesions. Treatment is mainly supportive, with the goal to stop warfarin and reverse its effects with vitamin K and fresh frozen plasma. Consequences of lack of treatment include predisposition to sepsis and expansion of skin involvement. Despite not having biopsy-proven WISN, this patient experienced symptomatic relief and abatement of the lesions after withdrawal of the medication in addition to her laboratory studies being suggestive of WISN. In cases with an unclear diagnosis, the history may yield important clues. Internists must be thorough data gatherers and remember to consider medications as potential culprits. In the case of WISN, timely withdrawal of the offending agent may prevent the progression to life-threatening necrosis.
ALL THAT LOOKS LIKE “BRUGADA” IS NOT “BRUGADA” - CASE SERIES OF BRUGADA PHENOCOPY CAUSED BY HYPONATREMIASourabh Aggarwal; Vishal Gupta. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1940315)
LEARNING OBJECTIVE 1: To understand Brugada phenocopy
LEARNING OBJECTIVE 2: To understand patho-phhysiology of Brugada phenocopy associated with hyponatremia
CASE: Brugada syndrome (BS), a life-threatening channelopathy associated with reduced inward sodium current due to dysfunctional sodium channels, is characterized by ST-segment elevation with downsloping “coved type” (type 1) or “saddle back” (type 2) pattern in V1-V3 precordial chest leads. Brugada phenocopy, a term describing conditions inducing Brugada-like pattern of electrocardiogram (EKG) manifestations in patients without true BS, is an emerging condition. We describe a case series of Brugada phenocopy with hyponatremia. A 63 year old lady, with history of diabetes mellitus, hypertension and schizoaffective disorder, on haloperidol, presented to ER with confusion and altered mental status. She was drinking up to 12 l water and 4–5 beer cans every day. Physical examination, including vitals, was unremarkable except for confusion and disorganized thought process. Initial labs were significant for hyponatremia (Na 112 mEq/L). EKG showed prolonged QTc (547 ms) and “coved type” ST elevations in leads V1-V3. Cardiac markers were within normal limits. Electrophysiological studies and left heart catheterization were unremarkable. Her haloperidol was held and water restriction initiated. Her sodium level improved gradually with serial EKGs showing resolution of ST elevations and QTc interval returning to normal. A 54 year old male, with history of hypertension, presented to ER complaining of lethargy, vomiting, anorexia and decreased fluid intake for 7 days. He denied any cardiovascular symptoms. Physical examination was unremarkable except for signs of dehydration. Initial labs revealed significant hyponatremia (Na 106 mEq/L) with EKG showing prolonged QTc (526 ms) and a “saddle back” type ST elevation in leads V2-V3. Telemetry did not show any evidence of arrhythmia. He was fluid resuscitated with gradual return of sodium level towards normal, and serial EKGs showing resolution of EKG findings with improving sodium level.
DISCUSSION: Brugada phenocopy associated with hyponatremia has been very rarely described. There have been very few isolated case reports. This, to the best of our knowledge, is first case series of Brugada phenocopy with hyponatremia. Sodium channel blockers are used to unmask and/or induce EKG-manifestations of BS in susceptible patients. Electro-physiologically, hyponatremia works similarly by decreasing electrochemical gradient and causing decreased inward current, leading to Brugada phenocopy. We believe that reduced trans-membrane gradient was responsible for Brugada phenocopy in our patient which was reversible and resolved with improvement in sodium levels and potentially trans-membrane gradient. Prognostic implications of these changes are unknown, however both our patients are doing fine till date. Management of these patients is supportive with intensive observation. Clinicians should be aware of the association of Brugada phenocopy with hyponatremia and be vigilant for diagnosis of true BS in case EKG findings fail to resolve with supportive management.
AMIODARONE INDUCED THYROTOXICOSIS: A DELAYED EFFECTSuzanne J. Supplee; Shobhit Gupta; Shannon Schamel; Richard Alweis. Reading Health System, West Reading, PA. (Tracking ID #1939145)
LEARNING OBJECTIVE 1: Diagnose amiodarone induced thyrotoxicosis (AIT).
LEARNING OBJECTIVE 2: Recognize symptoms of amiodarone toxicity may manifest long after discontinuation of drug due to its long half life.
CASE: An 88-year-old male presented to clinic with a 1 month history of progressive dyspnea, lower extremity swelling, and weight loss. His past medical history included paroxysmal atrial fibrillation previously treated with amiodarone, which had been discontinued 7 months prior secondary to hepatotoxicity. Thyroid studies at the time of discontinuation were normal. Physical exam demonstrated weight loss, muscle wasting, intermittent tachycardia, and significant pedal edema. Laboratory studies revealed a suppressed TSH at 0.013 IU/ml, and an elevated free T4 at 3.4 ng/dl. A new goiter was noted on ultrasound and echocardiogram showed normal left ventricular function. Based on his constellation of symptoms and laboratory abnormalities, he was diagnosed with type 1, amiodarone induced thyrotoxicosis (AIT) and started on methimazole.
DISCUSSION: Amiodarone is a widely used anti-arrhythmic drug with a high iodine content that causes direct toxicity to the thyroid gland. Amiodarone induced thyrotoxicosis is associated with a three-fold increase in the rate of major adverse cardiovascular events. Three to five percent of patients treated with amiodarone in the US develop AIT 3 months to 4 years after starting therapy. Its long half-life of 100 days causes continued effect on thyroid hormone production even months after the drug is discontinued making the diagnosis a challenge. Clinical manifestations of AIT include development of arrhythmias, heart failure, weight loss, restlessness and low grade fever. Treatment is aimed at restoring a euthyroid state by using thionamide drugs, radioiodine, surgery, or steroids. This case highlights the importance of recognizing AIT, even in cases where amiodarone is not on an active medication list. It is critical, as AIT is associated with life threatening ventricular arrhythmias if not treated appropriately.
AMYLOIDOSIS PRESENTING ALONG WITH PERIPANCREATIC CASEATING GRANULOMATOUS LYMPHADENITISPaulina Alcalan; Valentine M. Ebuh; Michael Sheffield; Carlos Taboada. Dallas Methodist Hospital, Dallas, TX. (Tracking ID #1939187)
LEARNING OBJECTIVE 1: Recognize the clinical features of amyloidosis.
LEARNING OBJECTIVE 2: Diagnosis of Amyloidosis when other diagnoses do not fit.
CASE: A 44 y.o. HF with depression presented with 5 to 6 months of intermittent abdominal pain, nausea, vomiting, and diarrhea. She had recently been evaluated at another facility and had an exploratory laparotomy which revealed peripancreatic lymphadenopathy. Biopsy then revealed peripancreatic caseating granulomatous lymphadenitis. Patient presented to our facility with weakness and syncopal episodes. Review of symptoms was positive for weakness, 60 lb. weight loss over 3 months, dizziness, dyspnea, cough with clear phlegm, nausea, vomiting, abdominal pain, diarrhea and syncopal episodes. She denied smoking, alcohol and drug use. Her home medicines included meclizine and Celexa. On physical exam her blood pressure was 76/45, pulse 82, temperature 98.8, oxygen saturation was 97 % on room air. Exam was essentially unremarkable except for a macular rash on the sole of her right foot. Pertinent labs on admission revealed WBC 7.7 and hemoglobin 9.4. Basic metabolic panel, liver function tests and urinalysis were normal. Abdominal CT scan with contrast revealed small bilateral pleural effusions, patchy atelectasis, 5 mm right middle lobe pulmonary nodule, mild ascites, hepatomegaly, splenomegaly and nodular densities along the parietal peritoneum on the right posterolaterally. She was hospitalized with refractory abdominal pain and weakness. With biopsy report showing peripancreatic caseasting granulomatous lymphadenitis and pulmonary symptoms, there was originally a concern that patient had either a fungal or mycobacterial infection as the cause of her complaints. She was started on 4 drug therapy for presumed tuberculosis. Serologic tests including a Quantiferon gold test for TB, AFB smear and culture, HIV test, Urine histoplasma antigen, blastomyces antibody, brucella IgG and IgM, coccidioides antibody, and aspergillus antibody were all negative. Antinuclear antibody was normal and rapid plasma regain and treponema palladium were non-reactive. Lung biopsy and stomach/duodenum biopsies were done and revealed AL amyloidosis. Anti-mycobacterial therapy was discontinued and she was started on Velcade and dexamethasone.
DISCUSSION: Amyloidosis refers to extracellular tissue deposition of fibrils, which demonstrates characteristic apple-green birefringence when stained with Congo red and viewed under polarized light. In immunoglobulin light chain (AL) amyloidosis the fibrils are composed of fragments of monoclonal light chains. The incidence of AL amyloidosis is 6 to 10 cases per million, median age at diagnosis is 64 and it affects predominantly males. AL amyloidosis is a systemic disorder and can present with heart failure, nephrotic syndrome, peripheral neuropathy, and hepatomegaly. Presenting symptoms usually depend on the organs affected. Amyloidosis can involve virtually every organ in the body and should be considered in the differential diagnosis of obscure cases such as this one.
AN A (MASS) ING CASE OF LEUKOCYTOSISJessica R. Howard-Anderson; Edward Ha. University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1929441)
LEARNING OBJECTIVE 1: Distinguish and assess various causes of leukocytosis.
LEARNING OBJECTIVE 2: Recognize squamous cell carcinoma as a potential cause of extreme leukocytosis.
CASE: A 67-year-old female with a history of type 1 diabetes mellitus and a combined kidney and pancreas transplant 15 years ago (on immunosuppressive medications) presented to the hospital with 1 week of vomiting, diarrhea, fevers, and altered mental status. Further history revealed that she had a chronic wound in her right upper extremity that she had been debriding with scissors at home. On admission she had a temperature of 38.7 °C and was mildly tachycardic, but normotensive with a normal respiratory rate and oxygenation saturation. A complete physical exam was remarkable for an open ulceration in her right upper extremity that was approximately 6 cm long ×4 cm wide ×2 cm deep without any drainage or evidence of active infection. Her white blood cell (WBC) count was 27 × 103/uL with a neutrophilic predominance. A full infectious work up including cultures of cerebrospinal fluid, blood, urine, sputum and stool yielded a diagnosis of Clostridium difficile colitis. Cultures from her upper extremity wound initially grew coagulase negative staphylococcus, presumed to be a contaminant as there were no signs of infection on exam. A peripheral blood smear showed reactive granulocytosis. She was treated with oral vancomycin and intravenous metronidazole. Despite this treatment and an overall clinical improvement with normalization of her vital signs and resolution of her fevers, her leukocytosis continued to rapidly increase. Within 2 weeks her WBC count had increased to 78 × 103/uL. Concomitantly, her upper extremity wound had also rapidly grown in size. In 1 week it had progressed from an ulcer to a large exophytic mass, elevated approximately 3 cm above the skin. A biopsy of this mass revealed squamous cell carcinoma. A whole body PET-CT scan revealed no evidence of metastasis. A second culture of the mass 2 weeks after admission revealed vancomycin resistant enterococcus; treatment with daptomycin was initiated. Two days later there was still no significant change in her WBC count. At that time, approximately 16 days after admission, she was taken to the operating room for excision of the mass. Immediately after excision of the mass, her WBC count decreased from 69 × 103/uL to 36 × 103/uL, without other intervention. Over the next 6 days her WBC count continued to decrease to 8 × 103/uL and stayed in this range until discharge 1 week later.
DISCUSSION: This is an interesting case of extreme leukocytosis that persisted despite antibiotics. Leukemoid reactions are likely to be identified initially by general internists and so it is imperative to understand the common causes of extreme leukocytosis and initiate an appropriate diagnostic work-up. A complete WBC count and differential should be obtained along with a peripheral blood smear to identify the predominant cell type and any immature cells, blasts or atypical cells. Our patient had a neutrophilic leukocytosis, which is commonly associated with infections, states of stress (including emotional stimuli, exercise, pain, surgery or extreme temperatures), trauma, cigarette smoking, medications and reactions to non-hematologic malignancies. Myeloproliferative disorders such as polycythemia vera, chronic myelogenous leukemia, and chronic neutrophilic leukemia should be considered if there is no clear cause of neutrophilia. If myeloproliferative disorders are suspected, a specialist in hematology/oncology should be consulted to identify potential clonal cells and cytogenetic abnormalities. In this case our patient’s extreme and persistent elevation in WBC count despite appropriate antibiotics or inciting stressor suggested that her leukocytosis was most likely due to her squamous cell carcinoma. Her leukocytosis rapidly improved after surgical excision of the mass, further supporting this hypothesis. There have been other case reports in the literature documenting similar leukemoid reactions in patients with head and neck, lung, esophageal, gastric, bladder, gynecological, and cutaneous squamous cell carcinomas that improve with treatment of the malignancy. It has been hypothesized that this leukocytosis in squamous cell carcinomas is due to tumor production of granulocyte colony stimulating factor (G-CSF). Most reports of leukocytosis from squamous cell carcinoma have been described in cases of very aggressive tumors, frequently leading to death. Prompt diagnosis, staging and treatment for the malignancy is therefore essential.
AN ASYMPTOMATIC, PRO-ARRHYTHMIC INTRA-ATRIAL MASSAmara Hussain; Ilya Karagodin; Appesh Mohandas. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1934787)
LEARNING OBJECTIVE 1: To recognize the various types of extramedullary manifestations of acute myeloid leukemia.
LEARNING OBJECTIVE 2: To distinguish the pathophysiology and clinical presentation of cardiac myeloid sarcoma, a rare extramedullary manifestation of acute myeloid leukemia.
CASE: Extramedullary manifestations of acute myeloid leukemia (AML) are quite rare (<10 % of all cases). These extramedullary solid collections of leukemic cells, also referred to as myeloid sarcomas or chloromas, typically involve the skin, spine, orbits, digestive tract, and lymph nodes. Even more unusual is the presence of immature myeloid cells in the heart, also known as cardiac myeloid sarcoma (<1 % of cases). Cardiac myeloid sarcoma can occur as the initial presentation of AML, alongside marrow disease, or at the time of disease relapse. The small number of cases described in the literature have shown a marked predilection for the right atrium, and a striking male predominance. We present a case of an asymptomatic right intra-atrial mass in a 64-year-old male with a history of Monosomy 7 AML, allogeneic bone marrow transplant, graft-versus-host-disease, and chloroma of the right eye and tongue. At a routine visit to his oncologist, the patient was found to be in atrial flutter with 2:1 block at a rate of 146 bpm. A CT PE protocol highlighted a filling defect within the right atrium consistent with intra-atrial thrombus or mass. A cardiac MRI showed a large right atrial mass that extended from the superior vena cava to the inferior vena cava with several small adherent clots. To obtain tissue samples and facilitate a diagnosis, a right heart catheterization was performed with the aid of intracardiac ultrasound. Biopsy of the mass demonstrated cardiac muscle fibers with extensive fibrosis and an atypical infiltrate of small round blue cells consistent with myeloid sarcoma. Given the location of the chloroma, the patient was started on CLAG chemotherapy rather than adjuvant radiation therapy. Over the course of his hospitalization, the patient transitioned from a junctional escape rhythm with intermittent, non-sustained runs of ventricular tachycardia and atrial fibrillation to normal sinus rhythm. He was loaded with amiodarone and slowly tapered to a maintenance dose. Interestingly, the patient remained symptom-free throughout his entire treatment course. Follow-up cardiac MRI after CLAG chemotherapy demonstrated significant interval regression in the size of the mass (3 mm thick vs. 5.5 mm previously). There was also interval improvement of superior vena cava patency. The luminal diameter of the SVC was 4 mm prior to the initiation of chemotherapy, and 10 mm following the conclusion of chemotherapy.
DISCUSSION: The right atrial mass was the third extramedullary manifestation of this patient’s AML, whose marrow remained disease-free at presentation. The patient’s arrhythmias were likely caused by irritation of the SA node by the right atrial mass, causing sino-atrial exit block and intermittent failure of atrial depolarization. This fascinating case suggests that one or more episodes of myeloid sarcoma places an individual at higher risk for additional extramedullary manifestations in different anatomic locations.
AN ATYPICAL CAUSE OF ACUTE LOW BACK PAINRebecca Liu; Crystal Ritsema. Yale School of Medicine, New Haven, CT. (Tracking ID #1935200)
LEARNING OBJECTIVE 1: Recognize the atypical neurological manifestations of vitamin B12 deficiency
LEARNING OBJECTIVE 2: Diagnose and treat functional vitamin B12 deficiency in the setting of borderline low B12 levels
CASE: A 42 year-old female without significant past medical history presented with debilitating low back pain radiating down her legs, along with weakness, numbness and tingling of her upper extremities. Eleven months prior to this visit, she presented with acute low back pain radiating down her right leg and was diagnosed with sciatica. Ibuprofen, cyclobenzaprine, tramadol and prednisone were sequentially trialed but did not alleviate her symptoms. A lumbar spine MRI was unremarkable. She was lost to follow-up and re-presented with bilateral lower extremity pain and weakness in addition to weakness, numbness and tingling of her upper extremities. She also reported left facial droop, blurry vision and decline in memory and attention. Physical exam revealed a distressed woman, in pain and ambulating with a cane. Neurologic examination revealed normal cranial nerves, reflexes, strength and sensation in all extremities. MRI of the brain showed no evidence of demyelinating disease. Her hemoglobin, hematocrit, and mean corpuscular volume were 15.3 g/dL, 44.4 %, and 91 fL, respectively. Hemoglobin A1C was 5.1 %. TSH was 1.55 μU/mL. HIV and chronic viral hepatitis panel were negative. Antibodies to Borrelia burgdorferi were negative. Vitamin B12 level was 205 pg/mL, and on repeat was 189 pg/mL. Homocysteine (8.9 μmol/L) and methylmalonic acid (MMA) (0.24 μmol/L) were not elevated. On the basis of her clinical symptoms and these laboratory values, the diagnosis of functional vitamin B12 deficiency was made and parenteral B12 therapy was initiated. One month later, she reported dramatic improvement in the weakness, numbness and tingling in her arms as well as improvement in her lower back pain and weakness of left leg. Her B12 level at this visit had improved to 546 pg/mL. She was transitioned to daily oral B12 supplement, and on further follow-up continued to improve with complete resolution of her left leg and bilateral arm symptoms and only mild residual pain in her right leg.
DISCUSSION: The most common neurological manifestations of vitamin B12 deficiency are paresthesias, peripheral neuropathy, and subacute combined degeneration. This patient, with borderline-low vitamin B12 despite normal homocysteine and MMA, demonstrates atypical neurological manifestations of vitamin B12 deficiency that rapidly responded to B12 therapy. It is unusual for patients to exhibit B12 deficiency-associated symptoms with normal homocysteine and MMA. Savage et al. reported that only 1 out of 406 ‘clear-cut’ B12-deficient patients showed normal levels for both homocysteine and MMA. Nevertheless, there is evidence in the literature of patients with normal B12, homocysteine, and MMA levels who quickly respond to parenteral B12 with resolution of symptoms. In summary, this case details an atypical presentation of B12-deficiency associated polyneuropathy that proved highly responsive to B12 therapy. This case also highlights the importance for clinicians to develop comprehensive differential diagnoses prior to obtaining labs, and despite borderline normal lab results, to use overall clinical judgment to properly diagnose and treat patients with commonly encountered conditions in General Internal Medicine.
AN ATYPICAL ULCERATIVE COLITIS FLARE: TAKING A DEEPER LOOKAllison R. Bond2; Artur Viana1. 1Boston Medical Center, Boston, MA; 2Boston University School of Medicine, Boston, MA. (Tracking ID #1937106)
LEARNING OBJECTIVE 1: To recognize the signs and symptoms that may indicate an ulcerative colitis (UC) flare has been complicated by a secondary cause
LEARNING OBJECTIVE 2: To understand the risk of opportunistic infections that chronic immunosuppressive treatments can pose among patients with ulcerative colitis.
CASE: A 53-year-old man with ulcerative colitis presented with bloody diarrhea and abdominal pain. The patient had two prior ulcerative colitis flares in the 16 years since diagnosis, which were treated with a brief steroid course and did not require hospitalization or long-term immunosuppression. Five weeks prior to admission, the patient developed bloody diarrhea and intense abdominal pain, and was started on mesalamine without effect. He was subsequently admitted and received IV methylprednisolone and one dose of infliximab. His symptoms improved and he was discharged. However, when bloody bowel movements and abdominal pain recurred, he was readmitted. The patient had no fever or leukocytosis and was again placed on IV methylprednisolone, with oral and rectal mesalamine. He continued to have 10–15 bloody bowel movements a day, and a flexible sigmoidoscopy revealed transmural ulcerations with anal involvement deemed uncharacteristic of ulcerative colitis. Biopsy showed inflamed mucosa consistent with moderate ulcerative colitis, along with cytomegalovirus (CMV) in the mucosal cells. The patient was started on ganciclovir IV and continued on mesalamine; the dose of methylprednisolone was also reduced. Despite appropriate therapy, his symptoms progressed and a repeat sigmoidoscopy showed marginally improved deep ulcerations. He subsequently underwent a total colectomy with end ileostomy and a surgical specimen revealed nearly transmural ulcerations. He recovered from the colectomy without major issues and was discharged a week later.
DISCUSSION: This is a case of CMV colitis in the setting of acute immunosuppression and local mucosal inflammation. Gastrointestinal CMV can occur anywhere in the gastrointestinal tract, presenting as diarrhea, bloody stools, abdominal pain, fever, and weight loss. As these symptoms mimic ulcerative colitis, it is impossible to pinpoint when the patient developed CMV colitis. However, the infection likely exacerbated a pre-existing UC flare and prevented recovery. Immunodeficiency is the most common setting in which GI CMV is found, including patients with HIV/AIDS or immunosuppression (organ transplant, malignancy chemotherapy or steroid therapy). This case underscores the importance of considering CMV as a causative agent of diarrhea in systemically immunosuppressed patients. Once diagnosed, the patient’s CMV presented a treatment conundrum, as the immunosuppressants intended to alleviate the flare could possibly hinder the body’s ability to clear the CMV infection. It has been noted in previous studies that CMV, while commonly reactivated in patients with ulcerative colitis, may resolve without treatment. Furthermore, mortality rates among patients with concurrent UC and colonic CMV infection were formerly reported to be 33 %, with a need for surgical treatment in 80 % of patients. With the use of ganciclovir, however, a minority of patients have required surgery, and death from CMV superinfection is rare. Antiviral treatment was favored in this patient as his symptoms were thought to be due in large part to a CMV infection. Unfortunately, his symptoms worsened and he ultimately required intervention.
AN CASE OF SOLITARY OCULAR LANGHERHANS CELL HISTIOCYTOSIS PRESENTING AS PROPTOSISRagisha Gopalakrishnan; Harris Naina. University of Texas Southwestern Medical Center, Dallas, TX. (Tracking ID #1938796)
LEARNING OBJECTIVE 1: To recognize solitary orbital manifestations of langherhans cell histiocytosis (LCH) as part of the differential for unilateral proptosis and orbital tumors.
CASE: A 28-year-old Hispanic female with a history of hypothyroidism presented to her ophthalmologist after having unilateral blurry vision, proptosis, right upper eyelid swelling, and intermittent headaches for 1 year. She denied any fevers, chills, night sweats, changes in vision, denied using contacts. She did not smoke, and did not use recreational drugs, or smoke tobacco. On exam, she was noted to have significant proptosis in her right eye, but her exam showed was no evidence of conjunctival injection, focal neurologic deficits, skin lesions, or lymphadenopathy. Labs showed that her BMP was within normal limits, and TSH was 3.2 ( normal). Subsequent workup including a MR of the orbits performed showed an ill-defined superior right 4 mm anterior posteriorly ×10 mm transverse orbital mass with adjacent right frontal bone erosion. Biopsy of the mass showed a large infiltrate was strongly positive for CD1a and S100, which was diagnostic of Langerhans cell histocytosis (LCH). A PET scan, A MRI spine, and CT chest and CT abdomen and pelvis showed no evidence of systemic disease. Local radiation and or surgical excision have been previously used in the past to treat children who presented with solitary orbital manifestations of LCH. However, local surgery and/or local radiation could not be performed because the tissue obtained was too friable and thin. She was referred to malignant hematology clinic, and systemic therapy with cytarabine was recommended. However, the patient decided to undergo herbal treatment.
DISCUSSION: Langerhans cell histiocytosis (LCH) is a rare disease with clonal proliferation of dendritic histiocytes forming a pseudotumoral growth. Orbital manifestation of LCH is a rare form of LCH and are best studied in children. Local surgery and radiation therapy are used as first line therapies, and systemic chemotherapy is often used as an adjunctive therapy if local surgery or radiation therapy is not possible. There have been only 2 cases of solitary orbital manifestations of LCH documented in adults till date. Both patients survived with local surgery and radiation therapy. Hence, this case demonstrates that orbital LCH should be considered as part of the differential for proptosis and orbital tumors. It also underscores the need for further investigation into treatment protocols for solitary ocular manifestations of LCH in adults.
AN EMOTIONAL CASE OF A NEUROLOGIC DISEASEKatie Tipton; Kobina Wilmot. Emory, Decatur, GA. (Tracking ID #1940210)
LEARNING OBJECTIVE 1: Altered mental status can have an exhaustive differential which requires thorough work up to ensure correct diagnosis.
LEARNING OBJECTIVE 2: Psychologic derangements are present in at least half of all patients with multiple sclerosis.
CASE: A 25 year old female with no past medical history presented for evaluation of bizarre behavior. She was in her normal state of health until 5 months prior to presentation. At that time she developed significant paranoia, quit her stable job, had decreasing interaction with her family and fiancée, and developed full body tremors. Family also witnessed her walking the streets in the middle of the night, undressing in public and urinary incontinence. She was minimally interactive with staff, and physical exam was only positive for hyper-reflexia in lower extremities. During initial work up, she underwent lumbar puncture which showed mild pleiocytosis but glucose and protein levels were within normal limits. Infectious work up was negative, including HIV, HSV, CMV, VDRL, and blood, viral, and fungal cultures. Metabolic work up was grossly within normal limits except mildly suppressed vitamin D level of 16. Rheumatologic work up was negative, including ANA. Cat scan of her head was also within normal limits. During hospitalization her behavior remained altered including minimal interactions with all staff, inappropriate laughter, crying spells, and overall behavioral regression. Psychiatry was consulted, and she was started on Zyprexa with mild improvement in her symptoms. Prior to inpatient psychiatric hospitalization, an MRI brain was performed. This imaging revealed numerous (greater than twenty) white matter lesions of varying ages consistent with multiple sclerosis. Neurology was consulted but steroids were held in the setting of her acute psychosis.
DISCUSSION: Multiple sclerosis (MS) is an autoimmune inflammatory demyelinating disease of the central nervous system. This disease affects more women than men primarily between the ages of 23 and 30. Though symptoms vary greatly among all patients with MS, most patients have a primarily neurologic complaint such as vision, sensory, and/or gait changes at time of diagnosis. Though physical complaints are the most common, approximately half of all MS patients also have some emotional disturbance as well. The most common of these is depression, but patients also suffer from pathologic laughing and crying, euphoria, anxiety, and rarely psychosis. Our patient was a bit more unique as her entire presentation was psychological abnormalities. She experienced the pathological laughing and crying which is common with pseudobulbar palsy as well as anxiety and paranoia. Psychosis is more atypical with MS as it is considered to involve more gray matter rather than white matter. However, a subset of patients do experience psychosis particularly with frontal lobe and cognitive dysfunction. This case demonstrates the importance of a complete work up whenever a patient presents with altered mental status and behavioral changes. Since this patient was within the common age of presentation of a variety of psychiatric illnesses, her underlying demyelinating disease was almost misdiagnosed. Every patient with altered mental status should undergo a complete infectious, rheumatologic, metabolic, and neurologic work up to ensure potential underlying organic causes are found.
AN EXTREMELY RED EXTREMITYJulia Fleming; Darlene LeFrancois. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939692)
LEARNING OBJECTIVE 1: Identify the differential diagnosis for erythema in an extremity
LEARNING OBJECTIVE 2: Recognize the clinical presentation of pyomyositis
CASE: A 53 year-old man with uncontrolled diabetes mellitus type two on high dose steroids presented with redness that had progressed from his right hand to upper arm over the course of 3 days. He also noted pain and warmth of the arm. He reported no fevers or changes in strength or sensation in the hand. He noted no trauma or recent insect bites, and recalled no peripheral IVs in the arm despite having a recent hospitalization where he was diagnosed with hemophagocytic lymphohistiocytosis and initiated on steroids. Vitals were T 97.8 F, BP 153/65, HR 72, and RR 16. He was found to have erythema, warmth, tenderness, and accompanying 2+ pitting edema extending from the volar aspect of the right wrist to the mid-humerus. Induration and more severe tenderness but no overt fluctuance of the right forearm was appreciated. Passive wrist extension that stretched the flexor compartment of the forearm was particularly painful for the patient. Labs revealed a WBC 15.8 k/uL, and CPK 17 U/L. Blood cultures showed no growth. There was no deep venous thrombosis by ultrasound. Non-contrast CT of the forearm revealed extensive edema throughout the subcutaneous tissues and muscles with a discrete fluid collection that interdigitated the edematous flexor muscles. Several days of intravenous vancomycin, clindamycin, and ampicillin/sulbactam did not yield clinical improvement. He underwent surgical debridement of the forearm revealing purulent material infiltrating all fascial planes of the anterior compartment and fibrinous material covering the muscle surfaces, consistent with pyomyositis involving superficial and deep flexor muscle groups. Wound cultures grew methicillin-sensitive staphylococcus aureus.
DISCUSSION: Erythema of an extremity is a commonly encountered problem. It is often difficult to distinguish cellulitis from deep tissue infections but a systematic approach can assist in diagnosing less common sources of erythema. Starting from the skin and moving towards deeper structures allows for thorough identification of both infectious and non-infectious conditions, including: skin—cellulitis, skin abscesses, and contact dermatitis; fascia—necrotizing fasciitis; muscle—pyomyositis, diabetic myonecrosis, and necrotizing myositis; vasculature—deep venous thrombosis; joints—septic arthritis, and gout; and lastly bone—osteomyelitis. Particular exam findings that are concerning for pyomyositis include edema and increasing pain classically localized to a single muscle group but not infrequently involving multiple muscles whereas necrotizing fasciitis often presents with progressive fever and/or systemic toxicity, crepitus, and pain out of proportion to skin findings. Pyomyositis is an acute bacterial infection of the muscle due to hematogenous spread. Pyomyositis is commonly seen in tropical climates, but less commonly in temperate climates. Most cases in temperate climates are seen in patients with underlying immunodeficiency, such as HIV, diabetes or malignancy, as was the case with this patient. Staphylococcus aureus in the most common cause of infection, resulting in more than 75 % of cases seen in temperate climates. Bacteremia is seen in ~25 % of cases. Most common sites of involvement are the thigh, followed by the calf, buttock, upper extremity, and iliopsoas. Pyomyositis can be divided into three clinical stages. In the invasive stage (days 1–10), patients develop local, crampy muscle pain, swelling, and “woody” texture to the muscle. In the suppurative stage (weeks 2–3), patients are noted to have worsening fever, extreme muscle tenderness, and edema with presence of pus and often frank abscess in the muscle. Fluctuance is frequently not present. In the third stage, patients develop sepsis and systemic toxicity. Early diagnosis of pyomyositis may be difficult since findings are often nonspecific - pain and cramping of the muscle. A high index of clinical suspicion is necessary. Laboratory findings vary, although CPK is usually normal. Imaging studies - CT, MRI - are most helpful to make the diagnosis. MRI is more sensitive than CT for showing the full extent of tissue involvement. While early stage infections may be treated with antibiotics alone, later stage infections also require drainage.
AN EYE OPENING DIAGNOSISGurkaran Garcha; Neeti Reddy; Priti Dangayach; Himabindu Kadiyala. Baylor College of Medicine, Houston, TX. (Tracking ID #1939605)
LEARNING OBJECTIVE 1: Recognize malignant melanoma as a cause of ocular pathology via distant metastases
LEARNING OBJECTIVE 2: Review screening rationale and strategies for early detection of malignant melanoma by the General Internist
CASE: A 53 year old male presented to the Emergency Room with an inability to spontaneously open his right eyelid for 1 day. Three weeks prior to presentation, he noted drooping of his right eyelid which then progressed gradually to complete closure 1 day prior to presentation. He was able to open his eyelid fully with his hand. There was no loss of vision, diplopia, or headache. The degree of ptosis did not vary during the course of the day or with fatigue. No history of ocular surgery or trauma. Past medical history was significant for resection of a “skin cancer” from the first digit of his right foot 12 months prior to presentation, and the patient was lost to follow up afterwards due to loss of health insurance. The physical exam was significant for ptosis of the right eye leading to complete closure of the eye lid. Levator function was decreased but constant throughout the examination. Pupils were equal, round, and reactive to light. Extraocular movements were intact along with visual acuity and visual fields. A MRI of the orbits showed a 1.8 cm × 1.6 cm × 1.3 cm well defined intraconal mass in the superior aspect of the orbit, inseparable from the levator palpebrae and superior rectus muscles. A right orbitotomy revealed a grey colored irregular appearing mass, and pathology showed tumor cells positive for S100, Mart1 and HMB45, consistent with malignant melanoma. Further staging also revealed two small frontal lobe metastases which were surgically resected. Our patient is currently undergoing whole brain radiation therapy.
DISCUSSION: Melanoma of the skin is the most commonly fatal type of skin cancer. The American Cancer Society estimates 76000 new cases of invasive melanoma in 2013. Malignant melanoma can present with distant metastases leading to unusual presentations as in our patient. Patients with metastatic disease have a poor prognosis, with a 5-year survival rate of less than 20 %. Limited therapeutic options are available for these patients. Cytotoxic chemotherapy has not been shown to induce remission or prolong life. The therapeutic considerations include surgical metastasectomy, immunotherapy (IL 2 or ipilimumab), targeted inhibition of the MAP kinase pathway (dabrafenib), and radiation therapy to symptomatic sites of metastases. For the vast majority of patients, these approaches only prolong life by 1–6 months. Screening and early detection of melanoma by the primary care physician may offer a cost effective way to decrease melanoma mortality. Multiple studies report that clinicians are able to detect melanomas thinner than those self reported by patients. Although data from randomized controlled trials is lacking, large population based screening programs such as the SCREEN project have demonstrated up to a 50 % decrease in melanoma mortality. The American Cancer Society guidelines recommend routine skin examinations for early detection of melanoma, particularly in high risk individuals: atypical or high nevus counts (>25), ultraviolet exposures, and phenotypic traits (light skin, high density freckling, and green or blue eyes). The A, B, C, D, Es of melanoma recognition are a valuable tool for clinicians providing initial screening. Additionally, examination of the total skin surface can lead to a six fold increase in the likelihood of detecting a melanoma. Malignant melanoma may present with widely metastatic lesions leading to unusual presentations. Periodic screening for cutaneous melanoma may play a role in decreasing melanoma mortality.
AN HISTORICAL CLINICOPATHOLOGICAL ANALYSIS. HOW FLAVIUS JOSEPHUS, GUSTAV MOREAU, OSCAR WILDE, AND RICHARD STRAUSS OFFER INSIGHTS INTO THE MYSTERIOUS ILLNESS OF KING HERODCianna Leatherwood; Richard Panush. University of Southern California, Dept of Internal Medicine, Los Angeles, CA. (Tracking ID #1938067)
LEARNING OBJECTIVE 1: Recognition of Chronic Lead Intoxication as a possible diagnosis of the deleterious illness of King Herod the Great.
CASE: Herod the Great was “King of Jews”, appointed by the Roman Emperor and Senate to govern Judea; he lived from 73/74 BCE - 1 CE. He died from a mysterious illness that was depicted by Richard Strauss in his classic opera, Salome, considered by critics among the best of this genre. That opera was derived from a play of the same name by Oscar Wilde which was based on an 1876 painting, “Salome Dancing Before Herod”, by Gustav Moraeau. Josephus authored the definitive history of the Herodian epoch. We suggest a novel diagnosis of Herod’s illness and speculate about its historical impact. The operatic Herod was afflicted with an illness characterized by dementia, hallucinations, paranoia, alcoholism (from drinking the Emperor’s wine), violence, twitches, and sterility; different depictions showed him also with falls, chills, shaking, thirst, forgetfulness, and sleepiness. The historical Herod was described with severe abdominal pain, extremity swelling, and likely renal failure, in addition to his psychotic behavior.
DISCUSSION: We considered a differential diagnosis including vasculitis/systemic rheumatic disease, Behcet syndrome, sarcoidosis, thyroid disease, brain tumor, renal disease, amyloidosis, infections, malignancies, and paraneoplastic syndrome, among certain other possibilities, as unifying diagnoses. We suggest that he had chronic lead intoxication. He had compatible symptoms (encephalopathy and neuromuscular symptoms) and consumed excessive quantities of imperial wine, known to be highly contaminated with lead and likely associated with similar symptoms among Roman aristocracy. We are not aware that Wilde or Strauss had similar maladies and therefore do not believe their depiction of Herod to be based upon personal experiences. We therefore offer a novel diagnosis for the illness of the historic and operatic King Herod. Herod’s demented cruelties—an oppressive reign including the beheading of John The Baptist—exacerbated the political climate and may have contributed to the subsequent violent 7-year revolt culminating in the destruction of the second temple. How different might history have been if Herod the Great had been abstemious?
AN INTERESTING CASE OF CELLCEPT TOXICITYMona Hassan; Hiba Hadid; David Paje. henry ford health system, Detroit, MI. (Tracking ID #1938952)
LEARNING OBJECTIVE 1: To shed the light on one of the less common but devastating side affects of Mycophenolate mofetil, bowel necrosis.
CASE: We present a case of a 62 year old female with autoimmune hepatitis, on prednisone and Cellcept for 8 months, who presented with diarrhea for 1 month. The diarrhea was non-bloody in the form of 5 to 6 bowel movements per day. The patient also noted increasing fatigue and a 10 lb weight loss over a 6 month period. Stool work up, urine and blood cultures were all negative. There was no history of recent travel or exposure to sick contacts. Her symptoms began approximately 2 months after initiating it. The decision was made to hold Cellcept. A colonoscopy was performed and biopsies were obtained. Pathology revealed Bowel necrosis that was pathgnomonic of that found in Cellcept toxicity. Upon 2 week follow up the patient’s diarrhea had completely resolved.
DISCUSSION: Gastrointestinal injury can occur with short-term exposure to Cellcept. Cellcept induced gastrointestinal toxicity is thought to occur from injury to enterocytes and formation of immunotoxicologic reactions. Endoscopy reveals gross inflammatory changes in addition to mucosal injury. Our case emphasizes the importance of having a high index of suspicion in patients taking Cellcept presenting with diarrhea.
AN INTERESTING CASE OF CRYOFIBRINOGENEMIAAswini Kumar1; Aswanth Reddy2; Aditya Kalakonda1; Kiran Pokhrel1; Amit S. Dhamoon1. 1SUNY Upstate Medical University, Syracuse, NY; 2Saint Vincent Hospital, Worcester, MA. (Tracking ID #1933290)
LEARNING OBJECTIVE 1: Recognize cryofibrinogenemia in appropriate clinical settings.
LEARNING OBJECTIVE 2: Understand the importance of prompt diagnosis.
CASE: 25 year old male with H/O IV drug abuse presented to the emergency department with abdominal pain, diarrhea, arthralgia and purpuric lesions in the extremities. Labs showed leukocytosis and abdominal imaging revealed possible colitis. Treatment was initiated with IV antibiotics. Infective endocarditis was excluded by negative blood cultures and transesophageal echocardiogram. Vasculitis and rheumatological panel were unremarkable except for elevated ESR and low complements. Hepatitis B and C were negative and coagulation profile was normal. Subsequently he developed acute renal failure with hematuria and proteinuria. At that point, diagnosis was unclear and the patient was deteriorating. Skin biopsy of the lesions showed leukocytoclastic vasculitis with thrombosis of the dermis and renal biopsy revealed hypereosinophilic deposits suggestive of cryofibrinogenemia. There was significant improvement in renal parameters after treatment with corticosteroids.
DISCUSSION: Cryofibrinogenemia (CF), first described by Korst and Kratochvil in 1955 refers to the presence of plasma cryoproteins comprising fibrinogen, fibrin and fibrin split products. It can be primary, of unknown etiology or secondary to malignancy, autoimmune, infectious or thrombotic disorders. It is a potentially serious disease which commonly affects skin but can involve any organ causing thrombosis. There is paucity in medical literature about renal involvement of Cryofibrinogenemia (CF). CF is a disease often underrecognized in routine practice. High clinical suspicion is necessary and prompt diagnosis with assay is life saving. Clinicians should be aware of renal involvement in CF as it can be reversed with early treatment.
AN INTERESTING CASE OF FALSELY ELEVATED TSH LEVEL DUE TO HUMAN ANTI-MOUSE ANTIBODIES (HAMA) INTERFERENCE WITH THYROTROPIN ASSAYSamaneh Dowlatshahi; seyedAmirHossein AfsharImani; Erica Sinsheimer; Harvey Friedman. St Francis Hospital, Evanston, IL. (Tracking ID #1923838)
LEARNING OBJECTIVE 1: Heterophile antibodies that interfere with the TSH assay have been described in the past. Human antimouse antibody (HAMA), which is the most commonly encountered heterophile antibody, may be present in the serum of up to 10 % of patients. The incidence increases in people who have received or have been treated with radiolabeled mouse monoclonal antibodies.
LEARNING OBJECTIVE 2: It has been suggested that these heterophile antibodies are natural antibodies in normal people, although they could represent autoantibodies. We present a patient with falsely elevated TSH levels secondary to presence of HAMA.
CASE: A 45 year old male presents with an incidentally found abnormal thyroid panel which showed elevated TSH levels along with normal free T3 and free T4. Patient complaints of prolonged constipation. He was started on increasing doses of levothyroxine. At 6 weeks follow up TSH did not show any significant changes. TSH was repeated at another laboratory with the addition of mouse serum to the patient’s sample, and it was normalized.
DISCUSSION: A common and the first test to diagnose thyroid dysfunction is TSH measurement. HAMA is one of the multiple factors that can interfere with this test result and can result in costly diagnostic evaluation and unnecessary treatment. It is crucial to evaluate for the interfering factors prior to initiating unnecessary and potentially harmful clinical interventions. In this case we report the presence of HAMA as the interfering substance in the TSH assay.
AN INTERESTING CASE OF PITUITARY MACRO-ADENOMA PRESENTING AS SYMPTOMATIC INTERNAL CAROTID ARTERY COMPRESSIONSamaneh Dowlatshahi; seyedAmirHossein AfsharImani; Harvey Friedman. St. Francis Hospital, Evanston, IL. (Tracking ID #1923825)
LEARNING OBJECTIVE 1: Non-functioning pituitary macroadenoma are usually benign in origin, however mass effects may lead to serious clinical symptoms such as visual impairments, chronic headache, and pituitary insufficiency.
LEARNING OBJECTIVE 2: Obstruction of the internal carotid artery by a pituitary tumor is a rare occurrence, particularly in the absence of pituitary apoplexy. Pituitary macroadenomas can invade the cavernous sinus and rarely cause occlusion of the internal carotid artery (ICA). Most patients with symptomatic obstruction of the ICA by a pituitary tumor have been reported as a result of apoplexy. In this case report we present a patient with symptomatic carotid compression by a pituitary adenoma without evidence of apoplexy.
CASE: A 67 y.o. male patient presented with a right sided weakness, and 3 months history of progressive loss of vision on both eyes. Physical exam showed a bitemporal hemianopsia. The MRI revealed a 2.7 cm pituitary mass likely a macroadenoma, which was extending into the suprasellar cistern and was displacing the optic chiasm, and laterally the mass was pressing on cavernous portions of both internal carotid arteries. Also there was evidence of an acute stroke in the left pons. There was no radiologic evidence of apoplexy. Hormone studies at that time was consistent with panhypopituitarism, his prolactin level was initially 29 ng/ml (elevated but not at the extend of prolactinoma,) and a dilutional test showed even lower prolactin level of 21 ng/ml, so patient was diagnosed with a non-functioning macroadenoma. Surgical resection of the tumor and ICA decompression via the transsphenoidal route resulted in prevention of further symptoms. Histopathologic analysis confirmed a nonfunctioning pituitary adenoma without evidence of hemorrhage or intra-tumoral infarction. Patient was started on 20 mg prednisone twice daily which was reduced to 5 mg twice daily at 1 month follow up. TSH at 1 month follow up remained low and he was continued on 125 mcg levothyroxine daily.
DISCUSSION: There is a clinical impression that when tumors invade the cavernous sinus, compression of the internal carotid artery and cerebral ischemia is rare with pituitary adenomas and more common with other types of lesions but there are no actual data to support this impression. In this case report, we present a patient with symptomatic carotid compression by a pituitary adenoma without evidence of apoplexy.
AN INTERESTING CASE OF TRICHINELLOSISJason Sayanlar; John Meriwether. Georgetown University Hospital, Washington, DC. (Tracking ID #1942081)
LEARNING OBJECTIVE 1: To understand the clinical importance of Trichinellosis as a rare but serious cause of systemic infection.
LEARNING OBJECTIVE 2: To understand the clinical importance of Trichinellosis as a rare but serious cause of systemic infection.
CASE: A 38 year-old Caucasian male with no past medical history presented to the hospital with a one-day history of hematuria. Approximately 2 weeks prior, he reported consuming pork purchased from a local grocery chain. The next day he began experiencing fevers and diarrhea, which persisted for several days. As his diarrhea resolved, he noticed “puffiness” around his eyes, leg swelling, and general weakness. One week later, his diarrhea resumed, along with muscle pain in his arms, legs, and lower back. On the day of admission, he noticed bright red urine, which prompted him to present to the emergency department. Elevated transaminases gave concern for viral infection, including hepatitis and Ebstein-Barr, along with Legionella. However, significant serum eosinophilia was noted, suggesting a parasitic infection. His urinalysis indicated muscle injury (gross hematuria with few erythrocytes) and creatine phosphokinase (CPK) was markedly elevated- both suggesting a muscle-infiltrating disease. Markedly elevated IgE levels returned, and trichinellosis became the unifying diagnosis. An enzyme-linked immunosorbent assay (ELISA) was positive, and was later confirmed with western blot. Invasive diagnosis with muscle biopsy was not pursued. After initiating therapy with albendazole and prednisone, the patient’s abnormal lab values began to improve- eosinophilia peaked at 31 %, aspartate aminotransferase at 215, alanine aminotransferase at 370 and CPK at 3541. Within days, he noticed a significant improvement in peripheral edema and resolution of myalgia. He was discharged home on a two-week course of albendazole and a prednisone taper.
DISCUSSION: Trichinellosis is a rare parasitic infection caused by a nematode from the genus Trichinella. Ingestion of undercooked pork is the most common source of infection. However, wild boar, horse, walrus, moose, and bear have all been identified as potential sources. Infection is characterized by the enteral and the parenteral phases. Ingested larvae penetrate the host’s intestinal mucosa, traveling through vessels to ultimately reside in skeletal muscle fibers. Larval migration triggers an inflammatory response, releasing mediators such as histamine and bradykinin, which augment the permeability of host capillaries, resulting in widespread edema. Initial complaints may include gastrointestinal disturbances, fevers/chills, myalgias, or edema. Rarely, myocarditis and encephalitis are also seen. Diagnosis is made clinically, but clinicians should check a complete-blood-count, to assess for eosinophilia, and a metabolic panel with CPK, to assess for muscle damage. Anti-trichinella antibodies are detectable on ELISA after 3 weeks of infection, and are confirmed with western blot. Definitive diagnosis can be made with muscle biopsy (to look for larval infiltration), however, biopsy is reserved only for cases of uncertain diagnosis. Most cases are uncomplicated and self-limited. However, signs of systemic involvement such as hematuria, encephalopathy, pulmonary or cardiac inflammation should be treated with anti-helminthic therapy and corticosteroids.
AN INTERNIST’S WORST NIGHTMARE- MANAGING A RIVAROXABAN BLEEDNaveen Nannapaneni; Marwan Al-Hajeili. Wayne State University/Detroit Medical Center, Detroit, MI. (Tracking ID #1923321)
LEARNING OBJECTIVE 1: Manage an acute bleed while on rivaroxaban.
LEARNING OBJECTIVE 2: Recognize the utility of using prothrombin complex concentrate for reversal of rivaroxaban.
CASE: For decades the mainstay of outpatient anticoagulation has been warfarin, a problematic drug requiring close monitoring and which has several medication interactions. With the arrival of a new generation of oral anticoagulants, significant burdens on both the patient and the healthcare system have been alleviated. Nevertheless, shortfalls exist in regards to agents or protocols for reversal of these anticoagulants in the setting of an acute bleed, as exhibited in our case. A 39-year-old woman with a history of bilateral pulmonary emboli and schizoaffective disorder presented to the ER with a 2 week history of vaginal bleeding. She associates abdominal cramping and low back pain with the bleeding and endorses fatigue, dyspnea and lightheadedness. At her baseline she reports normal cyclical bleeding lasting less than 1 week. She reports being transitioned from warfarin to rivaroxaban 6 weeks ago. Physical exam revealed stable vitals, fresh blood and clots in the vaginal vault, and after they were cleared, bleeding from a closed external cervical os was identified. Her hemoglobin on presentation was 2 g/dL below her baseline. In the ER she was given intravenous fluids along with a dose of intravenous FEIBA (prothrombin complex concentrate, PCC) per ER protocol. Hematology was consulted and recommended transfusing packed red blood cells, decreasing the dose of, and ultimately holding, rivaroxaban and discontinuing the PCC due to concern of an increased risk of thrombosis. Additional attempts to stop the bleeding via intravenous conjugated estrogen and balloon tamponade recommended by gynecology were unsuccessful. After discussing the implication to her fertility, the patient was agreeable to a dilation and curettage with endometrial ablation which resulted in cessation of her bleeding. She was discharged on fondaparinux with hematology follow-up.
DISCUSSION: The acute management of a bleed while on rivaroxaban is a challenge for any physician. In our case, the patient was given PCC based on an ER algorithm derived from an individual study that suggests its efficacy for reversal. This protocol, however, was not continued after consultation with hematology as it was noted that the study was conducted in healthy subjects and followed thrombin and activated prothrombin times to gauge reversal, both of which are suboptimal methods of monitoring rivaroxaban. Moreover, the use of PCC is associated with an increased risk of further thrombosis, a significant concern given our patient’s history of unprovoked pulmonary emboli. At present there is no guideline regimen to induce reversal of rivaroxaban. As a result, supportive management including transfusions and compression or tamponade are performed, but cessation of bleeding ultimately requires metabolism and clearance of the drug. Our case reiterates the uncommon, and difficult, management of patients bleeding while on rivaroxaban.
AN OCULAR PLASMACYTOMA PRESENTING AS ASYMPTOMATIC, RED EYERagisha Gopalakrishnan; Harris Naina. UT southwestern, Dallas, TX. (Tracking ID #1939389)
LEARNING OBJECTIVE 1: To recognize that solitary ocular plasmacytomas can present as asymptomatic red eye.
LEARNING OBJECTIVE 2: To recognize that solitary ocular plasmacytoma behave clinically and biologically different from systemic multiple myeloma with ocular manifestations.
CASE: A 73-year-old gentleman with a medical history of hypertension was referred to an opthalmologist by his friend after his friend noticed that his right eye was turning red for 3 months. He denied any recent vision changes, fever, chills, weight loss, night sweats, dry mouth, or dry eyes. There was no family history of autoimmune disease, glaucoma, leukemia, or lymphoma. He did not smoke or wear glasses. On exam, a small nodularity was noted the lateral aspect of the patient’s right iris. There was mild erythema noted in the right eye, but there was no evidence of pallor, scleral icterus. Visual acuity was 20/20 on exam, and there was no evidence of the lymphadenopathy on exam. Slit lamp examination showed a nodularity on his right conjunctiva. Subsequent biopsy showed a dense subepithelial infiltrate composed of CD19+, CD20+ plasma cells expressing lambda light chains, consistent with ocular plasmacytoma. He was subsequently referred to malignant hematology clinic for further management. A serum protein electrophoresis (SPEP), serum free light chain assay, skeletal survey were done and showed no evidence of systemic manifestation of multiple myeloma. The patient underwent surgical resection, and has remained symptom free till date.
DISCUSSION: Primary ocular plasmacytomas represent less than 5 % of ocular neoplasms. In the literature thus far, most cases of ocular plasmacytomas have been in context of patients presenting with systemic manifestations of multiple myeloma. However, primary ocular plasmacytomas are a separate entity that behave clinically and biologically different from multiple myeloma. These tumors are often localized. They respond well to local radiation or surgery, and the complete response rate is greater than 80 %. Systemic chemotherapy is rarely required as their no evidence of systemic end organ damage such as hypercalcemia, renal failure, etc. On the other hand, in patients presenting with ocular manifestations of multiple myeloma, patient have evidence of systemic disease including disease involving disease. To distinguish these two entities, systemic evaluation including an SPEP, UPEP, serum free light chain assay, and histologic examination of bone marrow may be required. There have been 20 cases of ocular plasmacytomas reported in the literature, and most of these cases have been reported in the context of multiple myeloma. Till date, there are seven cases of solitary plasmacytomas. In all of these cases, patients report symptoms of vision loss, eye swelling, or blurry vision. On the other hand, our patient did not report such as symptoms. This suggests that primary ocular plasmacytoma should be considered as part of the differential of a chronic, asymptomatic red eye. In addition, this case also underscores that primary ocular plasmacytomas are a separate clinical entity, but close follow up is required to ensure that patients do not develop signs of systemic myeloma.
AN OPPORTUNE OBSTRUCTIONNicolas Cortes-Penfield1; Anna Kolpakchi1,2; Lee Lu1. 1Baylor College of Medicine, Houston, TX; 2Michael E Debakey VA Medical Center, Houston, TX. (Tracking ID #1938865)
LEARNING OBJECTIVE 1: Recognize gastrointestinal histoplasmosis as a serious cause of non-specific gastrointestinal symptoms in patients with AIDS
LEARNING OBJECTIVE 2: Recognize that gastrointestinal histoplasmosis may mimic other gastrointestinal disorders, including inflammatory bowel disease, on radiographic imaging.
CASE: A 40-year-old woman with AIDS and a CD4 count of 72 on HAART presented with several months of intermittent abdominal pain. She had had many visits to emergency room for this complaint. Abdominal CT 1 month prior to presentation showed small bowel dilatation without obstruction, which was not evaluated further. Three weeks prior, she was hospitalized at another facility with a partial small bowel obstruction (SBO), and small bowel thickening was observed on CT at that time. She was treated with steroids for presumed inflammatory bowel disease based on radiographic findings, but still had pain at discharge. She described the pain as severe, sharp, and cramping in the epigastric area. She denied nausea, vomiting, fever, chills, or change in bowel habits. On exam, her abdomen was distended and diffusely tender to palpation. An abdominal CT showed small bowel obstruction with numerous mesenteric lymph nodes. Due to the worsening of symptoms of SBO, she underwent exploratory laparotomy and was found to have extensive small bowel disease with multiple areas of obstruction and stricture. Pathology demonstrated granulomatous inflammation with budding yeasts characteristic of Histoplasma capsulatum, which also grew from surgical cultures. Treatment with liposomal Amphotericin B resulted in rapid improvement and resolution of her abdominal pain.
DISCUSSION: Disseminated histoplasmosis is common in patients with AIDS, and the gastrointestinal tract is involved in 70–90 % of cases, though isolated gastrointestinal histoplasmosis occurs in only 3–12 % of patients. Gastrointestinal histoplasmosis is not readily recognized because the symptoms are non-specific, the clinical presentations can mimic other AIDS-related enteropathies, and the radiographic appearance can be mistaken for other diseases such as colon cancer or inflammatory bowel disease. The most common presenting symptoms include abdominal pain, weight loss, fever, and diarrhea. Bowel obstruction, GI bleeding, and perforation are major complications. Tissue diagnosis is definitive. Treatment involves a 2-week induction phase with 3 mg/kg liposomal amphotericin B, followed by 12 months of oral itraconazole. Gastrointestinal histoplasmosis is a rare but treatable disease that should be included in the differential diagnosis in the immunocompromised patient with gastrointestinal complaints. Because antifungal therapy improves outcomes for >80 % of patients and early initiation of therapy decreases morbidity and mortality, it is important to be aware of different presentations of gastrointestinal histoplasmosis in order to treat this potentially life threatening infection in a timely manner.
AN UNCOMMON CAUSE OF ACUTE POST-OPERATIVE HYPOXIA: NEGATIVE PRESSURE PULMONARY EDEMASamantha L. Klebe; Kumar Vipul. Wellspan York Hospital, York, PA. (Tracking ID #1933859)
LEARNING OBJECTIVE 1: Recognize negative pressure pulmonary edema (NPPE) as an immediate post-operative complication of elective surgery.
LEARNING OBJECTIVE 2: Distinguish NPPE from other post-operative causes of hypoxia.
CASE: A 36 year-old African-American female with mild intermittent asthma was transferred with respiratory distress post-extubation from a scheduled knee arthroscopy under conscious sedation. On post-procedure withdrawal of laryngeal mask airway (LMA), her oxygen saturation was around 70 %. After a failed LMA re-insertion attempt, she tolerated rapid induction and intubation. Arterial blood gas confirmed hypoxemia with pO2 114 mmHg on FiO2 100 %. Chest x-ray (CXR) showed moderate pulmonary edema and proper endotracheal tube (ETT) placement. Electrocardiogram (ECG) confirmed sinus arrhythmia without acute changes. BNP was normal (20 pg/mL). Pink, frothy secretions were found in the ETT. On physical examination, there were coarse breath sounds with bilateral crackles. Pertinent negative findings included wheezing, rhonchi, cyanosis, murmurs, peripheral edema, or jugular venous distention. Vitals were stable, and the patient was supported on volume control mode of ventilation. Furosemide was administered with the goal of negative fluid balance. There was complete resolution of pulmonary edema on subsequent day’s CXR. The patient passed spontaneous breathing trial, and after confirmation of negative cuff-leak test, she was extubated successfully.
DISCUSSION: Recognition of NPPE is crucial as it is an uncommon but potentially life-threatening complication of elective surgery with reported mortality of 40 % (1). NPPE has two subtypes. Type 1 occurs acutely after inspiration against an upper airway obstruction including ETT or LMA, laryngospasm, or strangulation. Type 2 occurs after resolution of a chronic upper airway obstruction (1, 2). In type 1 NPPE, forced inspiration against an occluded airway causes negative intra-thoracic pressure, increased venous return, and increased left ventricular end-diastolic pressure leading to fluid extravasation from pulmonary capillaries into the alveolar spaces (2). Use of LMA is strongly associated with NPPE (1). NPPE usually affects young, healthy patients, as they can generate large negative intra-thoracic pressures (3). Clues from the anesthesiologist include difficult intubation or extubation, biting on tubing, or “bucking” the ventilator (3). Clinical presentation differentiates NPPE from other post-operative causes of hypoxia. Aspiration leads to chemical pneumonitis with abrupt dyspnea, tachycardia, fever, sputum, and infiltrates in selective tracheo-bronchial segments. Cardiogenic edema can be surmised by cardiac history, ECG or echocardiogram findings, or abnormal heart sounds (4). Acute bronchospasm presents with wheezing, small tidal volumes, prolonged expiration, and hypercapnia. Obstructive sleep apnea is exacerbated by narcotics, with prolonged and increased frequency of apneas or desaturation. With laryngeal edema, CXR is normal, and wheeze is absent. Finally, recovery from NPPE is faster compared to acute respiratory distress syndrome. Therapy is supportive with correction of hypoxemia and establishment of a safe airway. Diuretics may be used judiciously to decrease intravascular volume and hydrostatic pulmonary edema. It is important to recognize NPPE as a complication of elective surgery because treatment is highly effective, and misdiagnosis could lead to hazardous therapeutic choices.
AN UNCOMMON CAUSE OF VERTEBRAL OSTEOMYELITIS AND PARASPINAL ABSCESS LEADING TO QUADRIPARESIS IN A HEALTHY YOUNG MANAfaq Motiwala1; Jenny C. Lee2; Divyanshu Dubey3; Oanh K. Nguyen1. 1University of Texas Southwestern Medical Center, Dallas, TX; 2University of Texas Southwestern Medical Center, Dallas, TX; 3University of Texas Southwestern Medical Center, Dallas, TX. (Tracking ID #1938755)
LEARNING OBJECTIVE 1: Recognize coccidiodomycosis can present as disseminated disease in at-risk immunocompetent persons.
LEARNING OBJECTIVE 2: Recognize disseminated coccidiodomycosis as a potential cause of vertebral osteomyelitis and paraspinal abscess leading to quadriparesis in endemic areas.
CASE: A previously healthy 39 year old African American man presented to the emergency department with progressively worsening descending weakness of his bilateral upper and lower extremities. Three weeks prior to admission, he noted the onset of neck and shoulder pain, followed by hand clumsiness, decreased grip strength, increased stumbling and falls, and ultimate progression to an inability to lift his arms or walk. On the day of admission, he was bed-bound. Review of systems was notable for 15 lb weight loss over 4 months, night sweats, fatigue, and a ‘pustule’ over the sternum of 4 months’ duration, and negative for fever, cough, shortness of breath and altered mental status. He had no prior history of illness, did not take any medications and had no known sick contacts or high-risk health behaviors. Of note, he was a missionary in a small rural town on the northeast Mexican border and had also recently worked as an air conditioning repairman. Exam revealed a thin man in no apparent distress who was alert, oriented and appropriately responsive. Chest exam was notable for a 1 × 1 cm non-draining ulceration over the sternum; heart and lung exams were unremarkable. Neurologic exam was notable for 2/5 strength, decreased vibratory sensation, increased tone, and hyperreflexia in the bilateral upper and lower extremities; bilateral sustained ankle clonus; and decreased sensation to pinprick in the trunk (T4-L4 distribution). Cranial nerves 2–12 were intact and symmetric. Labs were notable for C-reactive protein of 2.9 mg/dL and erythrocyte sedimentation rate of 65 mm/h. Human immunodeficiency virus antibody was negative. Magnetic resonance imaging of the spine showed vertebral osteomyelitis and paraspinal abscesses at multiple spinal levels (C4-T1, T3-T4, L1-L2, S3-S4) with cord compression from C4-T1. Empiric broad-spectrum antibiotic coverage for methicillin-resistant Staphylococcus aureus, tuberculosis and brucellosis was initiated. Patient underwent cervical discectomy and incision and drainage to relieve cord compression. Surgical wound cultures, chest skin scraping and serum antibody tests were positive for Coccidioides spp. Dual antifungal therapy was initiated with amphotericin B for 6 weeks and fluconazole indefinitely.
DISCUSSION: Coccidioidomycosis is caused by inhalation of airborne spores of the fungus Coccidioides, endemic to the southwestern U.S. and parts of Central and South America. Approximately 60 % of individuals with primary coccidioidomycosis are asymptomatic. The remainder experience influenza-like symptoms, including cough, fever, arthralgias, myalgias, and fatigue. Progression from initial pulmonary infection to disseminated disease occurs in 5 % of symptomatic patients and 1 % of patients overall. Common sites of dissemination are skin and soft tissue, brain and spinal cord meninges, and bone. Risk factors for disseminated infection include cell-mediated immunodeficiency, pregnancy, male gender, and Filipino or African ancestry. Mainstays of therapy are oral azoles given for at least 6 months, or indefinitely in patients with immunosuppression or neuromeningeal involvement. Initial therapy with amphotericin B is recommended for disease that is rapidly progressive or involves a critical location (e.g., spinal column). Surgery is indicated with neurologic compromise, progression despite medical treatment, or refractory pain. In conclusion, disseminated coccidiodomycosis should be considered as a potential cause of vertebral osteomyelitis and paraspinal abscess in highly endemic areas, particularly among immunocompetent individuals with risk factors for disseminated illness.
AN UNCOMMON PRESENTATION OF A RARE PATHOGEN: CONSIDERING THE CAUSE OF PROLONGED HICCUPSSarah Nickoloff1,2; Anil Sharma1; Jesse Martin1. 1Medical College of Wisconsin, Milwaukee, WI; 2Zablocki VA Medical Center, Milwaukee, WI. (Tracking ID #1933243)
LEARNING OBJECTIVE 1: To recognize the differential diagnosis for prolonged hiccups.
LEARNING OBJECTIVE 2: To review the clinical manifestations and management of pulmonary actinomycosis.
CASE: A 67 year-old male with a 42 pack-year history of smoking presented to clinic with complaints of hiccups of 2 weeks duration and decreased appetite with nausea and vomiting over the past 4 days. He also had an 18-pound weight loss over the past 4 months. Past medical history was notable for a history of well-controlled hypertension and chronic low back pain. A chest X-ray demonstrated a 15.0 × 8.3 × 8.0 cm soft tissue mass density in the posteromedial left lower chest that was felt to be consistent with primary lung cancer. Labs were remarkable for leukocytosis of 20.9 K/μL, new anemia, thrombocytosis, hyponatremia, hypokalemia, hypochloremia, hypobicarbonatemia, elevated BUN, and elevated creatinine. He was admitted, where he was afebrile with a physical exam significant for poor dentition, decreased breath sounds and dullness to percussion at the left lung base. A CT scan revealed a left posterior basilar pleural effusion with pleural thickening, thereby shifting the most likely diagnosis from lung cancer to empyema. The patient was started on intravenous piperacillin-tazobactam and vancomycin after becoming febrile to 101.6 ° F. A chest tube was placed and set to suction. Pleural fluid analysis was significant for white blood cell count of 95,920 cells/μL (98 % neutrophils), pleural fluid to serum protein ratio of 0.3, pleural fluid to serum lactate dehydrogenase (LDH) ratio of 77, LDH greater than two-thirds the upper limit of normal, and pH of 7. The pleural fluid was determined to be exudative in nature with a pH of less than 7.2, therefore highly suggestive of an empyema. Pleural fluid Gram stain revealed branching, pleomorphic Gram positive rods, and culture grew Actinomyces turicensis. Antibiotic coverage was narrowed to oral amoxicillin/clavulanic acid. Over the course of his admission, the patient improved clinically with resolution of his symptoms. Leukocytosis resolved prior to discharge and regular chest X-rays during hospitalization demonstrated interval improvement in the empyema. Metabolic derangements improved with intravenous fluids and electrolyte replenishment.
DISCUSSION: Pulmonary actinomycosis is a rare, slowly progressing disease that can often present similarly to other infectious and inflammatory diseases, as well as mimic neoplastic processes. The responsible agent is the Actinomyces species, which enters the respiratory tract through aspiration of oral secretions. Risk factors include underlying pulmonary disease, alcoholism, and poor oral hygiene. Clinical manifestations are nonspecific and variable, though most common symptoms include cough, sputum production, hemoptysis, fever, chest pain, and weight loss. Radiologic manifestations can also vary and include consolidation, mediastinal and/or hilar lymphadenopathy, atelectasis, cavitation, or pleural effusion. Pulmonary actinomycosis is generally highly susceptible to penicillin; however, it typically requires a long course (6 to 12 months) of therapy. In addition to medical therapy, surgical or percutaneous drainage of abscesses or empyemas may be necessary, as was seen in this patient. This case underscores the importance of good oral hygiene and a high index of suspicion for this disease, particularly in patients with pulmonary symptoms and poor oral hygiene.
AN UNDERDIAGNOSED SYNDROME OF LOWER EXTREMITY PAIN AND WEAKNESS IN A PATIENT WITH DIABETES MELLITUSDaniele Massera; Darlene LeFrancois. Montefiore Medical Center, Bronx, NY. (Tracking ID #1936348)
LEARNING OBJECTIVE 1: Recognize the syndrome of diabetic lumbosacral radiculoplexus neuropathy as a cause of proximal muscle weakness and pain in patients with diabetes mellitus.
LEARNING OBJECTIVE 2: Manage diabetic lumbosacral radioculoplexus neuropathy with the use of steroids.
CASE: A 69 year-old man with a history of prior stroke and diabetes mellitus type 2 on insulin with a hemoglobin A1c level of 7.7 complicated by distal sensory neuropathy presented with 3 days of pain in his right thigh and inability to rise from a chair. He described the pain as constant at rest and worsening with standing and ambulation. He reported distal radiation of pain with a “shooting” quality and the sensation of leg swelling in the same distribution. Prior to the onset of his symptoms he could walk up to half a block with a cane, whereas now he was not able to stand without assistance. Motor exam did not reproduce pain but demonstrated moderately decreased strength of right hip flexors, quadriceps and hamstrings, and only mildly decreased strength of plantar flexion and extension. Tenderness to palpation of the right quadriceps without edema was noted. Reflexes were absent on both legs and sensation was decreased on both feet. Motor exam of the left leg was normal. The creatine kinase level was 154. Initial head CT showed prior infarction consistent with previous imaging, but no changes suggestive of recent ischemia. Nerve conduction studies showed bilaterally reduced amplitudes of sensory and motor action potentials in both lower extremities suggesting axonal damage without demyelinating changes. Needle EMG demonstrated spontaneous activity of the right quadriceps with preservation of distal motor nerve integrity correlating with the neurologic exam. Magnetic resonance imaging of the lumbar spine and hips did not show structural causes of radiculopathy. A high level of clinical suspicion combined with characteristic EMG changes in absence of structural lumbosacral disease confirmed the diagnosis of diabetic lumbosacral radiculoplexus neuropathy (DLRPN). The patient’s symptoms responded to a two-day course of methylprednisolone IV at a dose of 1000 mg/day. After treatment, his pain and weakness were markedly improved, and he was able to stand up and walk five steps without assistance.
DISCUSSION: Lower extremity pain and weakness are common presentations in primary care and hospital medicine settings. The differential diagnosis includes musculoskeletal, neurogenic and vascular etiologies, but also lesser known causes. In patients with diabetes mellitus, associated with a multitude of neuropathies and pain syndromes, the differential is especially broad. The most important features of our case that prompted further investigation are objective proximal muscle weakness and pain irrespective of rest or action. DLRPN was first reported in a 1955 paper by Garland as “diabetic amyotrophy”, and is prevalent in approximately 1 % of diabetics with a median age of 65 years. It was first described as unilateral syndrome of pain, weakness, wasting and areflexia with acute or subacute onset affecting buttock, thigh or the entire leg. It can progress distally or contralaterally, and is characterized by spontaneous recovery over months. Similarly to our patient, the syndrome can be, but is not necessarily associated with distal peripheral neuropathy. It usually affects diabetics with recent onset of disease and is unrelated to the degree of glycemic control. Weight loss and autonomic dysfunction are common features. Affected parts of the nervous system can include nerve roots, plexus or peripheral nerves. The etiology is largely unknown, but is thought to be due to ischemic injury of the affected axons by either microscopic vasculitis or metabolic derangements. Nerve conduction studies, electromyography and muscle biopsy are helpful diagnostic tools and typically reveal a multifocal process with primarily axonal degeneration. The natural course of this disease is characterized by debilitating pain and weakness for weeks to months causing considerable morbidity. Pain control with narcotic analgesics is often necessary in addition to non-steroidal anti-inflammatory agents. Several immunosuppressive therapies, e.g. steroids, intravenous immunoglobulin, cyclophosphamide and plasma exchange have been studied in small retrospective or non-randomized settings yielding conflicting results. One randomized double-blinded placebo-controlled trial of IV methylprednisolone in patients with DLRPN did not demonstrate a difference in improvement of the Neuropathy Impairment Score in the Lower Limbs (NIS-LL). However, improvement of pain and positive neuropathic symptoms was reported in the group receiving steroids. Our patient, who presented early in the course of the disease and was promptly diagnosed, responded to methylprednisolone with near eradication of pain and marked improvement of function.
AN UNEXPECTED CASE OF ACUTE HEPATITIS CSophie Cai1,2; Khendi T. White2; Brian Hoffman1,3. 1Harvard Medical School, Boston, MA; 2Brigham and Women’s Hospital, Boston, MA; 3VA Boston Healthcare System, Boston, MA. (Tracking ID #1940047)
LEARNING OBJECTIVE 1: Recognize challenges of acute Hepatitis C diagnosis and pursue appropriate work-up and treatment
LEARNING OBJECTIVE 2: Distinguish between hereditary hemochromatosis and secondary iron overload in patients with elevated iron studies
CASE: A 33-year-old otherwise healthy male veteran presented with 3 days of acute-onset scleral icterus, loose stools, and abnormal liver enzymes (AST 774, ALT 679, ALKPHOS 224, and T. Bili 7.8), with no other associated signs or symptoms by history or physical exam. He had been transferred from a four-month inpatient PTSD psychiatric hospitalization and denied history of alcohol abuse, IV drug use, blood transfusions, or needlestick injuries. He reported 2 years of no sexual activity. Family history was negative for liver or autoimmune conditions. Recent medication changes were notable for metformin initiation 10 days prior for an inappropriate diabetes diagnosis. Interestingly, he had been worked up 1 month prior for incidentally-found transient mild transaminitis (AST 75, ALT 80), at which time abdominal ultrasound had revealed fatty liver changes and viral hepatitis antibody panel had been negative. This transaminitis had been downtrending at time of last follow-up 3 weeks prior to his admission. Our initial leading diagnostic hypothesis was metformin-induced hepatotoxicity based on case reports of metformin-induced liver injury and diarrhea and our patient’s recent negative viral hepatitis workup. Four days after discontinuing metformin, however, his T. Bili and ALKPHOS began uptrending, later peaking at 12.7 and 244 respectively. To our surprise, comprehensive viral and autoimmune antibody workup returned positive for HCV antibody, confirmed by RNA viral load. Serum iron studies were also elevated (transferrin saturation 72 %, ferritin 1957); HFE genotype was H63D/wt (unassociated with hereditary hemochromatosis). Liver ultrasound again showed fatty liver changes.
DISCUSSION: Acute Hepatitis C rarely presents symptomatically (15 % of cases). Encouragingly, symptomatic presentation predicts up to 67 % likelihood of spontaneous viral clearance, allowing a three-month watchful waiting period before therapy consideration. For those who do not spontaneously clear the virus, HCV genotyping and assessment of HIV status are important for guiding therapy. Just-FDA-approved sofosbuvir and other interferon-free direct-acting antivirals offer new hope to patients with historically poorly-interferon-responsive HCV genotypes such as our patient’s HCV genotype 1b. In patients without known risk factors, diagnosis of acute Hepatitis C is often challenging. Proof of recent seroconversion, which allows definitive diagnosis, was possible in our case only due to the recent incidental transaminitis workup. Importantly, had we not ordered repeat hepatitis antibodies and relied on the previous month’s negative results, we would have missed this critical diagnosis. Also of note, our patient’s infection source remains uncertain—a not-uncommon problem in hepatitis patients. Thus, even in cases of low clinical suspicion, recent negative HCV antibody results should not preclude repeat evaluation. As HCV RNA and anti-HCV antibodies typically appear within 2 weeks and 6 months respectively of infection, healthcare-associated exposure in our long-hospitalized patient is one concerning possibility. In-depth repeat questioning also revealed possible history of a recently shared razor. Our patient’s markedly abnormal iron studies, which returned before we had confirmation of our patient’s acute Hepatitis C diagnosis, initially led us to suspect hereditary hemochromatosis. As hereditary hemochromatosis is known to be associated with HFE C282Y homozygosity (85–90 % of cases) and C282Y/H63D heterozygosity but not C282Y/wt heterozygosity, H63D homozygosity, or H63D/wt heterozygosity (our patient’s genotype), we later recognized that our patient’s underlying fatty liver disease was a possible cause of secondary hemochromatosis. In a recent retrospective review, Cherfane et al. report that failure to order and correctly interpret HFE genotyping among patients with elevated iron studies (transferrin saturation >45 % or increased ferritin) caused 38 % of patients with nonhereditary hemochromatosis genotypes to be inappropriately phlebotomized. Thorough workup and correct distinction between hereditary hemochromatosis and iron overload secondary to hematologic or chronic liver disease are critical to avoid such misdiagnosis. We look forward to following our patient’s progress in the coming months. Given limited existing literature on acute Hepatitis C, we in particular plan to track whether fatty liver changes on ultrasound and elevated serum iron studies can occur secondary to acute Hepatitis C, as such associations with chronic hepatitis have been previously reported.
AN UNEXPECTED CASE OF BIGEMINY AND NON-SUSTAINED VENTRICULAR TACHYCARDIACamille Clarke1,2; Danny McCormick1,2; Pieter Cohen1,2; Deepak Thatai1,2. 1Cambridge Health Alliance, Cambridge, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1939677)
LEARNING OBJECTIVE 1: Recognize ventricular arrhythmias as an atypical presentation of pericardial effusion and cardiac tamponade.
LEARNING OBJECTIVE 2: Appreciate the utility of echocardiogram in elucidating etiologies of non-sustained ventricular tachycardia
CASE: A 68 year old Latino male with coronary artery disease and coronary artery bypass graft surgery 8 years prior presented with symptoms of progressive exertional shortness of breath for the past 3 months with acute worsening in the preceding 3 days. He endorsed mild palpitations during these episodes but denied any accompanying chest pain, orthopnea, dizziness, syncope or abnormal constitutional symptoms. On arrival, he was noted to have persistent bigeminy with a 5 beat run of ventricular tachycardia. Vitals signs were within normal and electrocardiogram revealed sinus rhythm with persistent bigeminy but no ST-T segment changes. His basic metabolic panel was unremarkable, troponin negative and hematocrit 38. Chest x-ray showed minimal enlarged heart with no lung pathology. Physical exam revealed jugular venous distention to the angle of his mandible, lungs were clear and cardiac exam normal. On the night of admission patient had persistent bigeminy with significant couplets and a 40 beat run of ventricular tachycardia. He remained hemodynamically stable throughout. Echocardiogram was performed and showed inferoapical wall akinecity and two pockets of pericardial effusion behind the left atrium as well as a compressed right ventricle. He was transferred for cardiac catheterization, which revealed a patent cardiac graft but transudative pericardial fluid causing tamponade, which resolved after drainage.
DISCUSSION: Although ventricular arrhythmias have been reported as a presenting manifestation of metastatic or infectious cardiac arrhythmias it is an uncommon presenting symptom of transudative pericardial effusion. Cardiac tamponade, a life-threatening condition, is caused by a slow or rapid compression of the heart due to pericardial accumulation and intrapericardial pressure. Classic findings such as distant heart sounds, pulsus paradoxus, elevated jugular venous pressure are helpful in diagnosis and chest imaging revealing cardiomegaly or electrocardiographic changes can help direct clinicians towards this diagnosis. These signs and symptoms are not always present, however, and their absence could be misleading thus a high index of suspicion should be maintained in certain clinical contexts. Our patient had a history of pericarditis and a pocket of pericardial fluid that accumulated and compressed his right ventricle, leading to cardiac tamponade with resultant ventricular arrhythmias. It is very likely that, in addition to the effusion, the stiffness of his pericardium from prior disease contributed to this large relative compression. Though ischemia was an appropriate initial suspicion given his history of coronary artery bypass graft surgery and cardiac risk factors, timely echocardiogram was imperative. Subcostal four-chamber view revealed both the size and location of the effusion, which was causing significant chamber compression that resolved once the effusion was drained. In summary, for patients with history of pericarditis, the appearance of ventricular arrhythmias should raise the suspicion for cardiac tamponade. Cases may go undiagnosed because typical associated clinical findings are absent or unapparent thus timely identification through emergent echocardiography plays a key role in confirming the diagnosis.
AN UNLIKELY SUSPECT: GROUP B STREPTOCOCCUS ENDOCARDITIS AND ASSOCIATED COMPLICATIONSBrianna S. Siegel; Wan L. Lam. Beth Israel Medicine Center, Mount Sinai Health System, New York, NY. (Tracking ID #1925944)
LEARNING OBJECTIVE 1: Diagnose atypical presentations of infective endocarditis.
LEARNING OBJECTIVE 2: Recognize group B streptococcus as an invasive pathogen in nonpregnant adults.
CASE: An 80 year old man presented to his primary care physician with severe lower back pain for 2 months and was treated with epidural glucocorticoid injections. Several weeks later he went to the hospital with worsening back pain, accompanied by fever and chills. Pertinent history included rheumatic heart disease (RHD) and osteoarthritis. Physical examination revealed the patient was febrile 39C, tachycardic to 110 beats per minute, blood pressure 117/57 mmHg with a grade 3/6 systolic murmur at left sternal boarder. There was warmth over the lumbar spine accompanied by severe tenderness to palpation. MRI showed septic arthritis of the L4-L5 facet joints. Laboratory results included leukopenia 3.4 k/uL and an elevated C-reactive protein 27 mg/dL. Patient was admitted for septic arthritis, and was broadly covered with Vancomycin and Cefepime. All 4 blood cultures grew Streptococcus agalactiae, and antibiotics were narrowed to Penicillin G. Transthoracic echocardiogram was completed which revealed severe prolapse of the anterior mitral valve leaflet with a mitral valve mass. Soon after, the patient noted right hand weakness with numbness and gait instability. MRI revealed multiple punctate foci of ischemia within the cerebellar hemispheres, occipital lobes, and corona radiata compatible with septic emboli. The patient underwent transesophageal echocardiogram confirming a 1.8 × 1.7 cm mobile mitral valve vegetation. A mitral valve replacement was done using a bioprosthetic valve. Pathology of the vegetation revealed gram positive cocci, consistent with group B streptococcus (GBS). The patient was treated with Penicillin G for a total 8 of weeks.
DISCUSSION: GBS is an established pathogen in pregnant women and neonates, rarely causing infections in other populations (incidence of 4.4 per 100,000). Risk factors for GBS infections are age >60 years, diabetes, malignancy, alcoholism and human immunodeficiency virus. RHD is a risk factor for infective endocarditis, seen in 6 % of cases. This patient was at risk for GBS endocarditis because of his age and history of RHD. The case illustrates the invasive potential of GBS in non-pregnant adults who have risk factors for infection. The initial presentation suggested steroid injections were the etiology of the septic arthritis. However, positive blood cultures and a heart murmur uncovered endocarditis as the underlying cause. We believe the septic arthritis and embolic strokes were complications of GBS endocarditis. This case highlights both the potential virulence of GBS in the elderly with a history of RHD and the variability in clinical presentations of infective endocarditis.
AN UNRESPONSIVE PATIENT? IT MAY BE SERO-TONE-INVictoria Gutgarts1,2; Jonathan T. Cheah1,2; Athina Vassilakis1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1936837)
LEARNING OBJECTIVE 1: Recognize and diagnose serotonin toxicity in an unresponsive patient
LEARNING OBJECTIVE 2: Outline the initial management of serotonin toxicity
CASE: A 59-year old man with atrial fibrillation and prior stroke presented with a 2 day history of decreased interaction and responsiveness. At baseline, the patient was alert and oriented to time, place and person and was able to ambulate with assistance. Due to concerns for depression, Sertraline had been commenced 1 week prior to presentation with a subsequent episode of tachycardia to 120 bpm attributed to his atrial fibrillation. Initial vitals were significant for temperature 37.8 °C, blood pressure 173/118 mmHg and heart rate 95 bpm. Examination revealed a diaphoretic and unresponsive individual with no vocalization and localization to painful stimuli only. There was a resting tremor evident with increased tone, inducible ankle clonus and hyperreflexia bilaterally. White blood cell count was 7.9 K/UL, creatine phosphokinase 49U/L and basic metabolic panel unremarkable. Urine and serum toxicology were negative while blood and urine cultures were without growth. Imaging of the head (both CT and MRI) did not reveal any evidence of acute pathology. Sertraline was discontinued for possible serotonin toxicity with subsequent recovery to baseline level of functioning.
DISCUSSION: Admissions for acute changes in mental status are common. The initial differential is broad, encompassing infective, vascular, toxic and metabolic causes amongst others. The narrowing of this differential relies on obtaining a comprehensive collateral history, physical examination and initial investigations. Serotonin toxicity is characterized by a triad of changes in mental status, neuromuscular abnormalities and autonomic instability. History reveals the recent initiation, addition or change in dose of a serotonergic agent, generally within 24 h of presentation. Aids to the diagnosis of serotonin toxicity include the Hunter Toxicity Decision Criteria, reported to have a specificity of 97 %. Criteria include at least one therapeutic dose of a serotonergic agent within the past 5 weeks in addition to one of the following: spontaneous clonus, inducible clonus with agitation or diaphoresis, ocular clonus with agitation or diaphoresis, tremor with hyperreflexia, or hypertonia with temperature greater than 38 °C and ocular or inducible clonus. Furthermore, careful consideration should be given to other etiologies which can present in a similar fashion. For example, neuroleptic malignant syndrome may also manifest with the same triad of changes and an unresponsive individual. However, there will be prior use of dopamine antagonists and laboratory investigation often reveals elevated creatine phosphokinase, lactate dehydrogenase and transaminases. The spectrum of serotonin toxicity spans from mild to severe depending on the mechanism by which intrasynaptic serotonin is increased. The use of serotonin reuptake inhibitors may result in milder episodes, where patients present with a more indolent course. In contrast, in combination with monoamine oxidase inhibitors, moderately severe toxicity has been shown in 50 % of cases as the degradation of synaptic serotonin is additionally prevented. Severe toxicity can be seen with agents that cause the direct release of serotonin, such as Amphetamine. Regardless of severity, initial management comprises discontinuation of the serotonergic agent. Mental state changes such as agitation are often controlled with benzodiazepines, whereas physical restraints are not recommended as they can increase isometric muscle contractions resulting in lactic acidosis. Neuromuscular instability is addressed by halting excessive muscle activity through the use of benzodiazepines or non-depolarizing agents such as Vecuronium. Control of autonomic instability involves stabilization of pulse and blood pressure, with hyperthermia managed by external cooling and hydration, often requiring admission to the intensive care unit in severe cases. When initial management has failed, serotonin antagonists such as Cyproheptadine can be considered. In conclusion, the unresponsive patient can often prove a diagnostic challenge, but careful history taking and physical examination may help in providing clues towards the eventual diagnosis.
AN UNSOLVED MYSTERY CASE OF CENTRAL DIABETES INSIPIDUSRicardo Cruz; Jennifer Russo; Ryan Chippendale. Boston University School of Medicine/Boston Medical Center, Boston, MA. (Tracking ID #1935100)
LEARNING OBJECTIVE 1: Understand the differential diagnosis for central diabetes insipidus
LEARNING OBJECTIVE 2: Recognize the clinical features and diagnostic criteria of POEMS syndrome
CASE: A 26 year old male presented with complaints of dry mouth, polyuria, polydipsia, polyphagia, and a burning sensation in his lower extremities for 1 month. His physical exam was notable for a morbidly obese gentleman with decreased sensation of his lower extremities bilaterally. Labs demonstrated a markedly elevated serum sodium level (168), a low Antidiuretic Hormone (ADH) level (less than 0.1), and a serum and urine osmolality of 345 and 185 respectively, consistent with central Diabetes Insipidus (DI). Pituitary function testing was notable for low total testosterone and leutinizing hormone consistent with hypogonadotrophic hypogonadism. A brain MRI revealed a normal pituitary gland, hyperintensities within the cerebellum and corpus callosum, enlargement of the adenoids, and lymphadenopathy within the retropharyngeal and parotid nodes. Due to this an infiltrative cause of DI was suspected. Later that year, he developed acute respiratory failure secondary to diastolic heart failure, requiring placement of a tracheostomy and gastrostomy tube. At this time he was found to be anemic and have significant splenomegaly at 18 cm. Given the constellation of laboratory and physical findings, a unifying diagnosis of POEMS syndrome was considered. Further work-up resulted in T cell predominance on flow cytometry, a normal lactate dehydrogenase and haptoglobin level, and a monoclonal lamda gammopathy on serum and urine immunofixation. The vascular endothelial growth factor (VEGF) level was normal, and bone marrow was without evidence of plasma cell neoplasm, nonhodgkin lymphoma, or acute leukemia.
DISCUSSION: Central DI is a condition which there is lack of production of vasopressin by the pituitary. It is characterized by excessive urination and volume depletion leading to hypernatremia. Causes of acquired central DI include intracranial mass lesions, brain trauma, and infiltrative disorders including sarcoid or Langerhans Cell histiocytosis. POEMS syndrome is a rare paraneoplastic syndrome arising from an underlying plasma disorder. The acronym POEMS refers to some of the distinguishing features of the disorder including polyradiculneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes (hyperpigmentation, hypertrichosis, flushing). Other potential features include sclerotic bone lesions, Castlemans disease (lymph node hyperplasia), pleural effusion, edema, ascites, and thrombocytosis. The pathogenesis of this syndrome is not well understood but thought to be due to elevated VEGF production that enables angiogenesis. Diagnosing POEMS is based on a composite of clinical and laboratory features. The diagnosis is made when both mandatory major criteria (polyneuroradiculopathy and monoclonal plasma disorder) are met, along with 1 out of 3 other major criteria (Castleman’s disease, sclerotic bone lesions, and VEGF elevation), and 1 out of 6 other minor criteria are present (organomegaly, extravascular volume overload, endocrinopathy, skin changes, papilledema, thrombocytosis/polycythemia). Although suspicious for POEMS syndrome, after extensive work-up, this patient did not meet the major and minor criteria to solidify the diagnosis. Therefore, the primary etiology of this patient’s central DI remains an unsolved mystery.
AN UNUSUAL CASE OF ACUTE BACK PAINGaurav Rao1; Andrea Card2. 1Montefiore Medical Center of the Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center, Bronx, NY. (Tracking ID #1939550)
LEARNING OBJECTIVE 1: Identify the clinical features of serious back pain
LEARNING OBJECTIVE 2: Recognize the significance of hypercalcemia in the setting of concerning back pain
CASE: A 56-year old male with past medical history significant for a MVA trauma 15 years prior with subsequent right below knee amputation and right upper extremity paresis as well as mild mental retardation presented with a 3 week history of back pain. After presenting to his internist 2 weeks prior and an urgent care a week prior with less severe symptoms, the patient presented to the emergency department with excruciating lower back pain that persisted at rest, nocturnally, and was refractory to the acetaminophen, NSAIDs, muscle relaxants and hot packs he had been prescribed recently. The patient denied a history of similar symptoms, recent trauma, weight loss, or intravenous drug abuse. He had an electrocardiogram notable for sinus tachycardia at 116 beats per minute, distant heart sounds, severe thoracic vertebral tenderness, and no other neurological changes from baseline. Laboratory results were significant for a white blood cell count of 26.9 k/μL, corrected calcium of 15.6 mg/dl (12.3 mg/ml 2 weeks prior and 11.3 mg/dl 3 months prior at his internist’s office), ionized calcium of 6.3 mg/dl, and parathyroid hormone level of 18.9 pg/ml. Computed tomography of the abdomen revealed a hepatic and pancreatic mass, bilateral adrenal masses, lymphadenopathy and bony metastatic disease most prominent in the thoracic spine. A moderate size pericardial effusion was also visualized and confirmed with a transthoracic echocardiogram to be early cardiac tamponade and intrapericardial masses. Patient underwent a pericardial window the following morning and the pathology sent intraoperatively revealed adenocarcinoma of lung or hepatobiliary origin. The patient expired 2 weeks later on the floor secondary to pulseless electrical activity arrest unresponsive to resuscitation attempts.
DISCUSSION: Back pain is one of the most common presentations in the primary care setting, most commonly due to benign etiologies such as lumbar strain or sprain, degenerative disease or disc herniation. Most patients recover with minimal treatment, however proper evaluation is important to identify any serious underlying pathology especially if any key warning signs are present. Unremitting night pain or pain at rest, unexplained weight loss and failure to improve with conservative therapy should raise concern for insidious etiologies. Laboratory testing such as a cell blood count, inflammatory markers may be beneficial when infection, neoplasm, or an inflammatory condition is suspected. Alkaline phosphatase and calcium levels can identify conditions that affect bone metabolism, such as Paget’s disease or neoplasm, but are not needed in all patients with back pain. In our patient, the relentless, severe nature of the back pain were the warning signs and impetus for further work up. The subsequent hypercalcemia discovered was secondary to an increase in osteoclastic bone resorption in areas surrounding the metastatic malignant cells within the marrow space. This mechanism is responsible for 20 % of cancer related hypercalcemia with the rest predominantly PTHrP-induced. Cancers most commonly associated with direct metastasis to bone are cancers of breast, prostate, lung, lymphoma, thyroid, kidney and multiple myeloma. Hypercalcemia has been reported in 20–30 % of patients with cancer during the course of their disease and signifies a poor prognosis with approximately 50 % of such patients expiring within 30 days. Our patient had chronic gradual elevations of calcium for months explaining the lack of a clinical sequela suggestive of hypercalcemia such as neurological dysfunction or gastrointestinal symptoms, which is more common in acute elevations of calcium levels. Elevations above the body’s tightly controlled range of calcium should prompt early investigation and be treated to allow time to target the primary process responsible. This case underscores the diagnostic challenge of back pain, which is typically benign but internists should be vigilant of the clinical signs and laboratory findings which warrant concern for a more serious etiology.
AN UNUSUAL CASE OF HYPERAMMONEMIA - A CASE FOR CAUTIONRavneet Bajwa; Mayur Mody; Maryam Sattari. univeristy of Florida, Gainesville, FL. (Tracking ID #1940329)
LEARNING OBJECTIVE 1: Be familiar with hyperammonemia as an important idiosyncratic side effect of Valproic acid (VPA).
LEARNING OBJECTIVE 2: Recognize that VPA-induced hyperammonemia can occur even with normal VPA levels.
CASE: A 41-year-old male with a history of bipolar affective disorder presented with progressive altered mental status (AMS), lethargy, diffuse weakness, slurred speech and inability to perform simple activities of daily living which he had previously been able to do without difficulty. Vital signs were within normal limits. He was alert and oriented, but responded to questions slowly. Physical exam was otherwise normal. Labs revealed normal liver function tests. Ammonia level was 209 mcmol/L (reference range <60 mcmol/L). Head CT and chest x-ray were unremarkable. On review of patient’s medications, psychotropic medications included clonazepam, valproic acid (VPA), risperidone, venlafaxine, and Fluphenazine. Free VPA level was 5 mcg/mL (reference range 5–25 mcg/mL). Since he did not have any evidence of liver disease and inherited urea cycle disorders seemed less likely, his hyperammonemia was thought to be secondary to VPA. VPA was discontinued and lactulose was started. Ammonia level decreased to 84 mcmol/L and his mental status improved within 24 h. In 1 month follow-up, ammonia level was 43 mcmol/L. Lactulose was discontinued. Patient continues to remain asymptomatic and has normal ammonia levels to date off VPA and lactulose.
DISCUSSION: VPA has been associated with increased serum ammonia levels, even in the setting of normal renal and hepatic function. A possible mechanism for hyperammonemia includes VPA’s inhibition of carbamoyl phosphate synthase I (CPS I), an enzyme involved in the urea cycle. CPS I is ultimately responsible for converting ammonia to urea to allow excretion through the urine. With CPS I inhibition, plasma ammonia levels rise. VPA’s binding to carnitine and coenzyme A results in a reduction in fatty acid use for energy needs and dysregulation of the metabolism of nitrogenous waste, disrupting the urea cycle even further. Clinical presentation varies from asymptomatic hyperammonemia to symptoms resembling hepatic encephalopathy. Patients may present with AMS, somnolence, and asterixis, without other clinical stigmata of liver disease. Workup should include VPA levels (which may be supratherapeutic or therapeutic as in our case), as well as evaluation of liver structure and function to rule out concomitant liver disease. If symptomic, VPA may be stopped for a few days. Use of levocarnitine and high-flux hemodialysis has also been reported for treatment. Lactulose and non-absorbable antibiotics, such as rifaximin, reduce ammonia levels in acute treatment and can be used, in addition to dietary modifications (i.e. low protein diet), to prevent recurrences. While most cases of hyperammonemia with or without encephalopathy are due to liver disease, clinicians should be aware of unusual etiologies of hyperammonemia to prevent delay in diagnosis and treatment in patients without liver disease presenting with hyperammonemia. With the increasing indications and off-label uses of VPA, physicians should be aware of this potential complication of VPA and check ammonia levels in patients taking VPA who present with AMS.
AN UNUSUAL CASE OF PROLONGED FEVER OF UNKNOWN ORIGINDuminda Suraweera1; John Sy1; Elizabeth Akiyama2; Emil Heinze3. 1Olive View-UCLA Medical Center, Sylmar, CA; 2Olive View-UCLA Medical Center, Sylmar, CA; 3Olive View-UCLA Medical Center, Sylmar, CA. (Tracking ID #1939182)
LEARNING OBJECTIVE 1: Recognize the broad differential diagnosis in patients presenting with FUO including infectious, rheumatologic, and oncologic causes
LEARNING OBJECTIVE 2: Consider the implications of all the tests performed when considering a broad differential diagnosis to elicit the most likely etiology of the clinical presentation
CASE: The diagnostic workup for fever of unknown origin (FUO) remains challenging despite advances in medical technology and testing. Herein we present an unusual case of FUO with several confounding historical elements that detracted from the ultimate diagnosis of giant cell arteritis (GCA). A 50 year-old Guatemalan male with a history of sinusitis presented to our hospital approximately 4 months after the onset of daily fevers as well as upper and lower extremity myalgias. Approximately 5 months prior to his hospitalization, his travels included a hiking trip in Minnesota and a spelunking (caving) expedition in Kentucky. Three weeks after returning to Guatemala, he developed the aforementioned myalgias and fevers. Despite his myalgias resolving and an extensive infectious disease workup done in Guatemala (the patient received multiple antibiotics for treatment of Helicobacter pylori infection, a helminthic infection, prolonged sinusitis, and a typhoid infection), his fevers persisted. Due to his travel history, an infectious etiology was initially again pursued. Initial lab abnormalities included an elevated WBC to 14.2 and platelets to 744. ESR and CRP levels were elevated to 105 and 294, respectively. His infectious workup was negative including HIV, PPD, peripheral blood smear for malaria, and tests for brucella, Histoplasmosis, rickettsia, Strongyloides, Lyme disease, acute hepatitis, coccidioidomycosis, syphilis, and cryptococcus. A CT revealed rectal wall thickening and non-specific pulmonary nodules without evidence of malignancy. A flexible sigmoidoscopy and colonoscopy were unremarkable. Blood cultures revealed 1 out of 4 bottles positive for Streptococcus parasanguinis with sterile urine cultures. Repeat blood cultures remained negative and both TTE and TEE were unrevealing for vegetations. He was subsequently treated for his presumed Streptococcal bacteremia. During hospitalization, the patient developed vertical diplopia with decreased vision of the right eye. Ophthalmologic examination revealed boxcarring and a rheumatological workup was then pursued with specific concern for vasculitis. Further questioning revealed 3 episodes of blurry vision and diplopia in the previous 3 months that spontaneously resolved within 30 min. No abnormalities to the temporal artery were felt on examination and the patient never complained of headache. Myeloperoxidase (MPO) antibodies returned positive as well as rheumatoid factor and SS-B. SS-A, ANA, Anti-citrullinated peptide (anti-CCP) antibodies were also unremarkable. Although an MRI/MRA of his head did not show evidence of vasculitis, the presumed diagnosis of GCA versus ANCA associated vasculitis was given and he was initiated on pulse dose steroids followed by transition to oral steroids. A subsequent biopsy of his temporal artery was consistent with GCA and he was appropriately treated.
DISCUSSION: Low grade bacteremia without septicemia has been documented in otherwise healthy patients following oral manipulation. Since the patient had no symptoms of septicemia or infective endocarditis, an infectious etiology to his FUO was excluded despite having S. parasanguinis in one of four bottles. Given that subsequent blood cultures were negative, contamination was suspected. Workup for malignancy with imaging was also unremarkable, leaving a rheumatologic diagnosis as the most likely cause of his FUO. Previous studies on FUO have suggested that up to 22 % of FUO cases end up with rheumatologic diagnoses compared to only 16 % attributed to infectious causes. This patient’s FUO was ultimately associated with his diagnosis of GCA after meeting 3 of the 5 criteria for diagnosis (age > or = 50 years, ESR > 50 mm/h, and biopsy consistent with the diagnosis). GCA accounts for approximately 2 % of all cases of FUO, although rarely do patients not present with headache or visual symptoms. Despite his rheumatological work up revealing a positive SS-B and RF, the patient did not meet criteria for Sjogren’s syndrome or rheumatoid arthritis, two other known causes of FUO. This interesting case presenting with an otherwise unrelated travel history highlights the diagnostic dilemma when faced with multiple positive results and confounding factors. A detailed history to elicit specific details the patient might not associate with his present illness is appropriate in such cases. With the workup of FUO, the need for a systematic approach is also stressed. Elimination of each cause of FUO will usually lead to the correct diagnosis as in this case. Finally, all results should be considered in light of the clinical presentation as tests can be positive without clinical significance.
AN UNUSUAL CASE OF STATIN-INDUCED MYOPATHYLaura Nichols; Kurt J. Pfeifer; Chamindra Konersman. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1928602)
LEARNING OBJECTIVE 1: Recognize statin-associated necrotizing autoimmune myopathy (NAM) as a cause of prolonged muscle weakness and creatine kinase elevation after cessation of statin therapy
LEARNING OBJECTIVE 2: Diagnose statin-associated NAM utilizing clinical history and characteristic EMG and muscle biopsy findings
CASE: A 63-year-old woman presented with continued elevation of creatine kinase (CK) after discontinuation of statin therapy as well as waxing and waning proximal muscle weakness. She had been taking simvastatin for approximately 10 years but was transitioned to atorvastatin 1 year prior to onset of her proximal muscle weakness after undergoing repeat cardiac stenting. CK at that time was noted to be elevated to 10,829 U/L. Atorvastatin was discontinued, but CK levels continued to be elevated, ranging from 4000 U/L to over 10,000 U/L in the 2 years preceding her diagnosis. Serology was negative for myositis or connective tissue disease-associated antibodies. She had irritable myopathy on EMG, and necrotizing autoimmune myopathy was confirmed on muscle biopsy. The patient was diagnosed with statin-associated necrotizing autoimmune myopathy. She subsequently tested positive for an experimental anti-HMGCoA reductase antibody that is often present in patients with statin-associated NAM. The patient was treated with immunosuppressive therapy including high-dose steroids, methotrexate and intravenous immunoglobulin (IVIG) with significant improvement in her symptoms. She continues on these therapies currently due to the aggressive nature of her disease.
DISCUSSION: Self-limited statin myopathy has been described for several decades; whereas, statin-associated autoimmune necrotizing myopathy is an entity that has been described only in recent years. Though it is rare, statin-associated NAM is an important consideration in any patient who has prolonged symptoms of muscle weakness and elevated CK levels after discontinuation of statin therapy. In addition to consideration of alternative causes of muscle weakness, workup should include EMG and muscle biopsy. Signs of irritable myopathy on EMG and prominent necrosis with minimal inflammation on muscle biopsy are indicative of necrotizing autoimmune myopathy. In the future, anti-HMGCoA reductase antibody testing will likely be routinely available to aid in confirmation of the diagnosis. Given our patient’s ten-year history of simvastatin use and onset of symptoms only after initiation of atorvastatin therapy, there is reason to suspect relation to therapy with specific statins and possibly a dose-dependent toxicity. Though there are no controlled trials to aide in treatment selection, immunosuppressive therapy using high dose steroids is the mainstay of treatment. Methotrexate is commonly used as a steroid-sparing agent, and IVIG is utilized for particularly severe cases. Though response rates to standard therapies are generally good with most patients showing partial or complete response, approximately half of patients relapse after tapering immunosuppressive therapies. Given these challenges, continued research is necessary to better define statin-specific and dose-dependent risk as well as optimal treatment for this condition.
AN UNUSUAL CAUSE OF A “BROKEN HEART”Altaf Dawood. University of Nevada School of Medicine, Las Vegas, NV. (Tracking ID #1926357)
LEARNING OBJECTIVE 1: Pheochromocytomas are uncommon neuroendocrine tumors that typically present with paroxysmal headache, nausea, palpitations and hypertension. Rarely, Catecholamine secretion from pheochromocytoma induces a clinical syndrome mimicking acute coronary syndrome known as takotsubo cardiomyopathy or “broken heart syndrome”. “Reverse takotsubo” is an atypical variant of takotsubo’s cardiomyopathy causing left ventricular basal hypokinesis with apical hyperkinesia. We present a rare case of reverse Takotsubo syndrome with underlying pheochromocytoma.
CASE: A 53 year old Caucasian male with past history of hypertension and type II diabetes mellitus presented with anginal chest pain of 1 h duration. Electrocardiogram revealed diffuse T wave changes and troponin later came back elevated at 6.1, concerning for acute coronary syndrome. He was emergently started on antiplatelets and anticoagulants and underwent left heart catheterization. Angiographic evaluation revealed normal coronaries. Interestingly left ventriculogram revealed severe basal akinesis with apical hyperkinesia, consistent with “reverse Takotsubo” or stress induced cardiomyopathy. Transthoracic echocardiogram post procedure showed an ejection fraction of 35 % with features consistent with “reverse Takotsubo”. Patient was started on ACE Inhibitor and beta blocker for non-ischemic cardiomyopathy. During the admission patient was also noted to have elevated blood pressure reading of 170/105, but did not undergo any workup for secondary hypertension as an inpatient. Patient was subsequently discharged after optimization of therapy for cardiomyopathy. Several months later patient was re-admitted with markedly elevated blood pressure of 190/118 associated with dyspnea. Patient at this admission was worked up for secondary hypertension which revealed evidence of pheochromocytoma. He was found to have elevated plasma and urinary metanephrines and normetanephrines. CT abdomen done which was consistent with 11.8 × 11.6 × 11.2 cm left sided abdominal mass centered at the level of adrenal gland with solid and cystic component. After consultation with endocrinology and endocrine surgery, patient underwent left radical adrenalectomy. The tissue stained was positive for chromogranin, synaptophysin, S- 100 consistent with a diagnosis of pheochromocytoma. In the 2 months following tumor removal, Patient symptoms completely resolved and 6 months following tumor removal, 2D echo showed normal left ventricular systolic function.
DISCUSSION: Takotsubo cardiomyopathy is a unique form of transient non-ischemic cardiomyopathy. Reverse takotsubo cardiomyopathy is a rare variant with similar pathophysiological causes as classic takotsubo cardiomyopathy. Recognition and management of underlying cause is important in patients with takotsubo cardiomyopathy particularly with recurrent symptoms to improve morbidity and mortality.
AN UNUSUAL CAUSE OF CHRONIC COUGHDavid J. Epstein. UCLA, Los Angeles, CA. (Tracking ID #1927629)
LEARNING OBJECTIVE 1: Understand the diverse manifestations of sarcoidosis.
LEARNING OBJECTIVE 2: Know the diagnostic approach for suspected sarcoidosis, including how to rule out similarly-presenting disorders.
CASE: A 71-year-old woman with no significant past medical history presented with a cough, hoarse voice, and rhinorrhea. Her initial physical exam was unremarkable, and labs showed only mild anemia. After symptoms persistent with conservative management, a CT of the sinuses, neck, and chest was performed. Imaging showed no essentially no abnormalities of the sinuses or chest. However, CT of the neck showed a soft tissue density on the right side encasing the common carotid and internal carotid arteries and causing mass effect on the right oropharynx and hypopharynx with occlusion of the right internal jugular vein. PET-CT showed hypermetabolic activity of these masses concerning for lymphoma; in addition hypermetabolic lymph nodes were found diffusely in the mediastinum, hila, abdomen, and pelvis. A subsequent rigid laryngoscopy showed right vocal cord paralysis. An ultrasound-guided biopsy of the right neck soft tissue mass showed granulomatous inflammation, though was paucicellular. A subsequent excisional biopsy of the right neck lymph node showed nonnecrotizing granulomatous lymphadenitis. Gram stain, silver stain, and AFB stains showed no organisms. Bacterial, mycobacterial, and fungal cultures were sterile. Multiple other studies, including serologies for HIV, Brucella, Bartonella, syphilis, toxoplasmosis, coccidiodomycosis, histoplasmosis, and HTLV were non-reactive. Cryptococcal antigen and MTB interferon gamma release assay were negative. ACE level was elevated at 72. The patient was diagnosed with sarcoidosis. She was started on methotrexate and prednisone.
DISCUSSION: Sarcoidosis is a multi-system disease with an unknown etiology. Since it most commonly effects blacks between the ages of 10 and 40, clinicians may be less likely to recognize this condition in older non-black patients. Furthermore, since over 90 % of patients have lung involvement, patents with exclusively extra-pulmonary sarcoidosis may pose a diagnostic challenge. Almost every organ and organ system can be affected by the disease, including the skin, eyes, brain, musculoskeletal system, kidneys, and heart. The reticuloendothelial system can be involved, as in the patient above. Patients with sarcoidosis can have peripheral lymphadenopathy, hepatomegaly, and splenomegaly, with granulomatous involvement of these structures. Though most patients have an elevated ACE level, this finding has poor predictive value, therefore tissue diagnosis is almost always required. Histopathology demonstrates non-caseating granulomas. In combination with compatible clinical and radiographic findings, this finding on histopathology can confirm the diagnosis of sarcoidosis, but only when other disorders with similar presentations are ruled out. These include occupational lung diseases and hypersensitivity pneumonitides (in the case of lung involvement), tuberculosis, and histoplasmosis, among others. Therapy consists of oral glucocorticoids.
AN UNUSUAL CAUSE OF IRON DEFICENCY ANEMIA : A CASE OF PICA FOR ANTACIDS IN A PREGNANT WOMENVenu M. Ganipisetti1; Keeley M. Hack2; Mojtaba Akhtari2; Harvey Friedman1. 1Presence Saint Francis Hospital, Evanston, IL; 2University of nebraska, Omaha, NE. (Tracking ID #1934951)
LEARNING OBJECTIVE 1: Recognize the importance of monitoring the dosage of over-the-counter medications in all patients, particularly pregnant women.
LEARNING OBJECTIVE 2: Recognize the importance of educating pregnant women about pica and its potential complications.
CASE: Introduction: Pica is defined as an unusual craving and purposeful consumption of non-food substances for a period longer than 1 month. Even though, it is a commonly noticed phenomenon in pregnant women, it is frequently underestimated. Case: A 39-year-old, G6P5A0 Caucasian woman in her third trimester of pregnancy was referred to our medical center for evaluation of severe iron deficiency anemia (IDA). Her past medical history is unremarkable. At 34 weeks gestation, she presented to her local ER with severe nausea, vomiting and dehydration. She was found to have severe anemia despite reported compliance with her prescribed prenatal vitamins and supplemental iron. Her lab values were as follows: Hb 5.9 g/dL (normal range 12–16), MCV 73 fL (80–100), HCT 19.9 % (36–48), MCH 21.8 pg (26–34), MCHC 29.6 g/dL (30–37), RDW 19.2 % (11.5–15.5), Serum iron 97 ( 37–170), TIBC 613 ( 250–450), and Ferritin 4 ng/mL (8–250). She was transfused with 2 units of packed RBCs, set up for an outpatient IV iron infusion and referred to our hematology clinic. Upon evaluation and getting a detailed history and ruling out other possible causes of her IDA, it was found that she was taking calcium-carbonate antacid in unusual doses. During her pregnancy, she developed heartburn and began taking this medication as needed. She then developed craving for it and was taking approximately 15 tablets every day, which she continued for several months. She was instructed to stop taking the tablet, educated about pica and management of heartburn in pregnancy, and was treated with parenteral iron therapy.
DISCUSSION: The physiologic demands of iron are high during pregnancy and maintenance of iron homeostasis depends on intact absorptive and digestive processes of the gut. Any dietary factors interfering with iron absorption can have significant impact and can lead to iron deficiency anemia, which is associated with increased maternal and neonatal mortality during pregnancy. Calcium-containing antacids are generally considered to be safe during pregnancy, and are very routinely used. Several radioisotope labeling studies and single meal studies have suggested that calcium can be a major inhibitor of iron absorption. Also, due to its antacid property, it can alter the pH of the gut, further interfering with iron absorption. In our case, the patient was taking the antacids in excessive amounts after she developed craving for this medication. She did not mention this habit to her obstetrician and ER physician probably due to the possible embarrassment involved in discussing this unusual behavior. This unchecked behavior has lead to severe iron deficiency and would have been detrimental to both the mother and fetus, if it was unrecognized. Therefore, we stress the importance of obtaining a thorough and accurate medication history, including over-the-counter medications in all patients, particularly pregnant women. Pregnant women should be educated about pica and encouraged to discuss their dietary habits.
AN UNUSUAL PRESENTATION OFBURKHOLDERIA CEPACIAIN A HOSPITALIZED PATIENTDerar Albashaireh1; Marcus Zervos2. 1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Detroit, MI. (Tracking ID #1934402)
LEARNING OBJECTIVE 1:Burkholderia cepacia is an important pathogen implicated in nosocomial infection. Its diagnosis should prompt a thorough investigation to identify the source.
LEARNING OBJECTIVE 2: In intravenous drug abusers, Burkholderia cepacia is likely related to IV drug injection with contaminated materials.
CASE: A 19 year old male Caucasian patient, with past medical history significant of intravenous drug abuse (IVDU), presented with progressive productive cough, fatigue and fever of 2 weeks duration. On initial presentation, the patient was found to be hypotensive, tachycardic and febrile. He was admitted to the Intensive Care Unit for management of severe sepsis. A few hours later, his blood cultures were positive for methicillin resistant Staphylococcus aureus (MRSA). A two dimensional Echo confirmed the diagnosis of infective endocarditis involving the right tricuspid valve. The patient was started on Vancomycin for therapy of infective endocarditis. The patient clinically improved with serial repeated blood cultures which were negative. He was transferred to the general medical floor and the plan was to treat him for 6 weeks with IV antibiotics. However, he started to exhibit a drug seeking behavior in the hospital. After 2 weeks of IV antibiotics, he spiked a persistent fever. Blood cultures at that time were positive for Burkholderia cepacia. After further investigations, syringes and needles were found in the patient’s belongings by security personnel. Apparently, he was crushing his oral narcotics, diluting it with tap water and then injecting himself using non-sterile needles and syringes. He was treated with Piperacillin/Tazobactam, and his central line was removed. His fever resolved after 2 days. He was treated with IV antibiotics for 6 days that was switched to oral Bactrim after he decided to leave the hospital against medical advice.
DISCUSSION:Burkholderia cepacia is a gram negative bacilli that is widely distributed in the natural environment and has been isolated from water, soil, fruits and vegetables. It was discovered in 1949 by Walter Burkholder at Cornell University in rotting onions. B. cepacia is of particular concern for patients with cystic fibrosis (CF), in whom it can cause chronic endobronchial infection. It also is a well-known nosocomial pathogen among non-CF-patient populations. Numerous outbreaks of Burkholderia cepacia have been traced to contaminated products in a hospital setting, including tap, distilled, or deionized water; contaminated chlorhexidine; topical anesthetic agents; benzalkonium cholride; povidone-iodine solution; and quaternary ammonium solutions. Other outbreaks have been traced to mouthwash, albuterol nebulizer solution, infusion solutions, albumin infusion, blood gas analyzers and respiratory-therapy equipment. In our case, the contaminated syringes and needles were the most likely source of B. cepacia infection. Burkholderia cepacia infective endocarditis has been reported in injecting intravenous drug users. To our knowledge, it has never been reported in IVDU as a result of drug injection in the hospital. Surprisingly, it has been also reported in patients without predisposing factors. Burkholderia cepacia is an important pathogen implicated in nosocomial infection. Its diagnosis should prompt a thorough investigation to identify an environmental source and prevent further spread. In IVDU it should be suspected as likely related to IV drug injection with contaminated materials.
AN UNUSUAL PRESENTATION OF RESPIRATORY SYNCYTIAL VIRUSTricia G. charles -Cowan; Mahmoud Abdelghany; Christopher Begley. Conemaugh Health Systems, Johnstown, PA. (Tracking ID #1938623)
LEARNING OBJECTIVE 1: Human Respiratory Syncytial virus should be included in the differential diagnosis of acute respiratory failure in immunocompetent adults.
CASE: Respiratory Syncytial Virus (RSV) is a common and major respiratory pathogen that affects the lower respiratory tract in young children and infants. Adults at risk are the immunocompromised, institutionalized elderly patients with cardiopulmonary disease. It is estimated that RSV is responsible for 25 % of excess wintertime mortality, previously attributed solely to influenza. We report a case of a 42-year-old male with a past medical history of obstructive sleep apnea, morbid obesity and diabetes mellitus who presented to our hospital complaining of dyspnea, fever and cough for 1 week. Patient reported a maximum temperature at home of 40° Celsius with a nonproductive, persistent cough. He was recently diagnosed and treated for community acquired pneumonia with a course of ciprofloxacin. On admission the patient was found to be hypoxic with an oxygen saturation of 82 %, tachypnic with a respiratory rate of 24/ min and hypotensive with a blood pressure of 94/60 mmHg. Chest X-ray showed air space opacities in both mid to lower lung zones. Laboratory evaluation was significant for acute renal failure with a creatinine of 4.7 mg/dl, blood urea nitrogen 60 mg/dl, and bicarbonate of 15 meq/L. Blood cultures, respiratory culture and rapid influenza A and B were negative. The patient was admitted to the intensive care unit due to clinical deterioration with progressive hypoxia and tachypnea, which required mechanical ventilation. RSV was detected in the blood and sputum using ELISA technique. Treatment involved supportive care including ribavirin, bronchodilators, ventilator support and hemodialysis for acute renal failure. He later developed acute respiratory distress syndrome and died of end organ failure and complications associated with his illness.
DISCUSSION: Although RSV is common in children and immunocompromised adults, it is a rare cause of severe respiratory failure in adults. The CDC reports that people of any age can get RSV, but later infections are generally less severe. Elderly and adults with cardiopulmonary disease or the immunocompromised are at a higher risk of developing severe RSV. Transmission occurs primarily through close contact with contaminated fingers or fomites and self-inoculation. In addition, transmission via course aerosol produced by coughing or sneezing can occur. RSV typically starts 4 to 6 days after exposure and presents with respiratory tract involvement including cough, sore throat, wheezing, fever, rhinorrhea and decreased appetite. Diagnosis is made with history, immunofluorescence or ELISA of nasopharyngeal washes and aspirates. Treatment is supportive and involves hydration, suctioning of secretions, and anti-bronchospastic agents. RSV is usually self limiting in adults. In severe cases mechanical ventilation may be required. Currently there is no vaccination approved by the FDA for RSV and prevention involves proper sanitary techniques. RSV is typically under-diagnosed in adults. With the awareness of possible serious complications we should be more vigilant in diagnosis and aggressive in the treatment of the adult population.
ANAPHYLAXIS MIMICKING ISCHEMIC HEART DISEASE IN KOUNIS SYNDROMENaoki Takamatsu; Christine Kwan. Teine Keijinkai Hospital, Sapporo-shi, Japan. (Tracking ID #1929516)
LEARNING OBJECTIVE 1: Recognize that vasospasm causing typical acute coronary syndrome (ACS)-symptoms may occur during anaphylactic shock
LEARNING OBJECTIVE 2: Suggest a role of allergic insult behind the pathophysiology of cardiovascular (CV) disease
CASE: A 73 years old Asian woman comes with 1 h, worsening, dull, post-prandial epigastric pain. She is just discharged from the hospital 2 weeks ago for acute on chronic pancreatitis; she now describes a similar pain but denies all other review of systems. The patient’s medical history includes chronic pancreatitis, pancreas divisum, pancreatic calculus with endoscopic stenting, diabetes mellitus, and dyslipidemia; she takes glimepiride and atorvastatin. She has prior tobacco (88pack-years) and daily alcohol use (quit 8 years ago) but no recreational drugs. She is allergic to a cefoperazone/sulbactam which causes a rash and itchy throat. Family history is not significant. On exam, her vital signs include temperature 36C, heart rate (HR) 71, blood pressure (BP) 132/75, respirations 16, and O2 saturation 100 % room air. She appears calm and alert/oriented ×3. Abdominal exam shows a soft abdomen and epigastric tenderness with no rebound/guarding; otherwise, her exam shows no irregularities. Her labs show leukocytosis (12,900/μl), amylase 430 IU/L, and lipase 1300 IU/L, likely acute on chronic pancreatitis. Gabexate mesilate is given, which she has previously used without complications, but 8 min later, she complains of dyspnea, chest pain, and chest/extremities’ rash. Systolic BP drops to 40’s with bilateral wheezes; gabexate is withheld while epinephrine 0.1 mg IV is given. She becomes unresponsive 5 min later with diaphoresis, systolic BP 60’s, HR 120’s, and O2 saturation 80 % on 10 L reservoir mask. Another dose of epinephrine is given, and she regains consciousness 7 min later. Electrocardiogram reveals ST elevations in leads II, III, and aVF while echocardiogram shows a hypokinetic inferior wall, but coronary angiography has no abnormalities. While the anaphylactic shock has been managed with hydrocortisone, famotidine, and chlorpheniramine, nitroglycerin is given for coronary artery spasm. Recovery is uneventful with stenting for pancreatitis.
DISCUSSION: Kounis syndrome, first coincidentally described, is a manifestation of cardiac symptoms responding to an allergic stimulus. Any drug can trigger it although most are beta-lactams and contrast media. Meanwhile, anaphylaxis caused by the protease inhibitor gabexate rarely occurs, and no reports of Kounis syndrome induced by this drug has been found. The patient’s newly developed ACS-symptoms during anaphylactic shock suggest involvement of vasoactive mediators’ contractions of the coronary arteries. In this case, even with prior use, the culprit appears to be gabexate, and though few in number, reports suggest its careful monitoring >30 min after, especially repeat, use. Furthermore, evidence shows inflammatory cells’ infiltrating atheroma plaques even before actual plaque erosion occurs, not only as an acute inflammatory response during the coronary event. Perhaps an allergic reaction in the pathophysiology of CV disease exists as well. Highlighted is the translational impact of the linkage between physiological allergic responses to clinical cardiac involvement. Its significance not only lies in recognizing a rare complication of anaphylaxis but also gives insight into future implications for identifying patients at risk.
ANCA-ASSOCIATED VASCULITIS PRESENTING AS INTERSTITIAL LUNG DISEASEStephen A. McCullough; Nneka Ufere; Albert Yeh; Badri Modi; Kristian Olson. Massachusetts General Hospital, Boston, MA. (Tracking ID #1930631)
LEARNING OBJECTIVE 1: Diagnose ANCA-associated vasculitis (AAV) presenting as interstitial lung disease (ILD.)
LEARNING OBJECTIVE 2: Recognize the utility of rituximab for AAV.
CASE: Mrs. P is a 71-year-old woman with hypertension and hypothyroidism who presented with fatigue and dyspnea. Over the course of 1 month, she noted that her normal daily activities such as walking and grocery shopping became increasingly limited by fatigue and dyspnea. She presented to her PCP for evaluation and had laboratory studies that demonstrated normal general chemistries and CBC; elevated inflammatory markers with an ESR of 85 and a CRP of 134.3; and a UA notable for 2+ blood. A CT chest/abdomen/pelvis revealed diffuse basilar prominent subpleural ground-glass opacities and traction bronchiectasis consistent with ILD as well as a new 5 cm × 3 cm lobular para-aortic mass. There was a plan to further characterize her abdominal mass with an MRI, but she became severely dyspneic prior to this study and was admitted to our hospital. On admission she was hypoxemic to 80 % on room air, had increased work of breathing, and coarse bibasilar crackles. The remainder of her examination was unremarkable. Her admission laboratory studies were notable only for a positive ANA at 1:160; her general chemistries, CBC, anti-dsDNA, anti-Sm, anti-Jo-1, RF, anti-CCP, complement, SPEP, and UPEP were otherwise normal. A repeat CT chest confirmed an increase in subpleural ground glass opacities predominantly in the lower lung zones consistent with a Non-Specific Interstitial Pneumonia (NSIP)-type pattern. Shortly after her admission she was started on high dose prednisone and transferred to the Medical Intensive Care Unit for profound hypoxemia. Given her tenuous respiratory status, a bronchoscopy and open lung biopsy were deferred. Four days after her admission, she was found to be acutely confused with left sided weakness in the context of new paroxysmal atrial fibrillation (pAF.) She underwent an MRI which revealed an acute infarction in the posterior circulation, and TPA was administered with resolution of her neurologic deficits. Her MPO-ANCA then returned positive and she was started on cyclophosphamide, high dose prednisone, and she was anticoagulated with warfarin for pAF. She was intubated for progressive hypoxemia, though after completing 7 days of cyclophosphamide she was uneventfully extubated. Though she had improved, she continued to require between 4 and 6 L of supplemental oxygen at rest. As such, she was given rituximab as an adjuvant agent to reverse her pulmonary process. Four days after extubation, she developed a recurrence of pAF, worsening hypoxemia, and was found to have bilateral pulmonary emboli despite having a therapeutic INR. At this point, she was transitioned to low molecular weight heparin and her respiratory status slowly improved. Over the following week, her ANCA titer decreased to undetectable and she was ambulating without supplemental oxygen. Prior to discharge, she underwent a CT-guided biopsy to elucidate the etiology of her para-aortic mass, which revealed a lymph node infiltrated with a poorly differentiated carcinoma of Mullerian origin. She underwent three cycles of neoadjuvant paclitaxel and carboplatin therapy followed by total abdominal hysterectomy, bilateral salpingo-oopherectomy, retroperitoneal lymph node dissection, and omentectomy. Her final pathology revealed a microscopic high-grade serous adenocarcinoma in the left fallopian tube wall without evidence of metastatic disease. She has continued on adjuvant paclitaxel with plans to continue low molecular weight heparin until the end of her chemotherapy course and then potentially transition to warfarin therapy. Though she feels weak with chemotherapy, she remains improved, off oxygen, with only a borderline detectable ANCA and without evidence of malignancy.
DISCUSSION: This case highlights the need to consider AAV as a rare, reversible etiology of new pulmonary disease in a patient presenting with imaging findings concerning for ILD. In one retrospective analysis of 511 patients with AAV, 14 patients had a coexistent diagnosis of ILD, all of which had MPO-ANCA. Additionally, rituximab has come to the forefront in the management of patients with AAV. Rituximab has shown noninferiority to cyclophosphamide and steroids in inducing remission in AAV, and rituximab had no differences in maintaining the duration of remission or the frequency or severity of relapses from AAV. The combination of both rituximab and cyclophosphamide, as used in our patient, has yet to be studied.
ANCHOR ON NSAIDFrancis Lam; Laura K. Snydman. Tufts Medical Center, Boston, MA. (Tracking ID #1923051)
LEARNING OBJECTIVE 1: 1. Recognize the importance of checking HIV status regardless of patient risk factors. 2. Illustrate the value of a thorough differential diagnosis and appropriate work-up of someone with intra-renal AKI. 3. Recognize the significance of urinalysis and urine electrolyte studies in predicting the cause of nephropathy.
CASE: A 39-year-old obese black man with DM2 presented after routine labs from PCP’s office revealed a creatinine of 6.3 (0.9 1 year prior). A month ago, he used 1800 mg of ibuprofen daily for headache. For past 6 months, he reported polyuria but denied fever, chills, dysuria, hematuria, back or abdominal pain, URI symptoms, or sick-contacts. Patient appeared well. Blood pressure was 151/99 and HR was 98. He had no CVA tenderness or peripheral edema. Laboratory data showed Na 136, K 5.7, Cl 113, HCO3 14, BUN 43, creatinine 6.3, albumin 2.1, and Hgb 11.2. Urinalysis revealed SG 1.025, 3+ blood, 3+ protein, and 13 RBC without casts or eosinopils. Twenty-four hour urine collection revealed 18 g of protein. Ultrasound showed bilateral enlarged and diffusely hypoechoic kidneys suggestive of an infiltrative process. Other negative results included ANCAs, anti-GBM, RPR, SPEP/UPEP, viral hepatitis, and complement levels. HIV test returned positive, and biopsy revealed focal segmental glomerulosclerosis (collapsing variant) consistent with HIV nephropathy. A more detailed history regarding HIV risk factors was then obtained. He had many sexual partners in the past and had gonorrhea as a teenager. HIV was, therefore, most likely from unprotected intercourse in setting of multiple sexual partners.
DISCUSSION: This case demonstrates the importance of consideration of HIV nephropathy in patients with unexplained acute kidney injury. HIV nephropathy was first reported in 1984, and was highly associated with African American. Most had CD4 count above 200. It is characterized by proteinuria, and most had moderate to severe renal insufficiency by diagnosis. This case was a diagnostic challenge due to various risk factors that could explain his acute kidney injury. Because FSGS described a histologic diagnosis, clinical presentation and progression speed depended upon its etiology. Which diagnosis explains such a rapid and remarkable presentation of proteinuria? Focal segmental glomerulosclerosis (FSGS) from obesity, NSAID, or minimal change disease would not give such high proteinuria. Lack of casts in his urine made diabetic nephropathy unlikely. Other risk factors associated with FSGS included HIV, heroin usage, and vesiculoureteral reflux. In this case, biopsy confirmed the diagnosis. Our approach to the diagnosis demonstrates a high potential for confirmation bias; one could have easily anchored on the history NSAIDs usage and turned a blind eye to evidence not consistent with NSAID-induced nephropathy. This is a reminder to always confirm that the objective evidence fits the history.
ANCHORING HEURISTICS IN DIAGNOSISAnene Ukaigwe; Christain Espana-Schmidt. The Reading Health System, West Reading, PA. (Tracking ID #1939233)
LEARNING OBJECTIVE 1: Recognize anchoring heuristics and its effect on patient safety
CASE: A 90-year-old right-handed male came to the Emergency Department (ED) complaining of left upper extremity numbness and weakness lasting 15 min, 5 h ago at dinner. His past medical history included atrial fibrillation, CHADS2 score of four (for hypertension, age and previous stroke), hyperlipidemia, bilateral carotid stenosis and poor adherence to treatment recommendations. He had no other neurologic complaints. He had multiple ED visits in the preceding 6 months for dizziness and hypertensive urgency, refusing workup each times. BP on admission was 205/90 mmHg. The remaining vital signs and physical examination was unremarkable. CT brain did not reveal any acute changes. He received intravenous hydralazine in the ED for Hypertensive emergency. BP dropped to 130/70 mmHg and left upper extremity numbness returned. Symptoms again improved when BP increased to 175/100 mmHg. He was diagnosed with TIA; ABCD2 score of three and admitted. Twelve hours later, the symptoms returned. This time, his left hand was slightly cooler than the right on examination. Duplex scan revealed an occlusive clot in the brachial, radial and ulnar arteries. He underwent thrombo-embolectomy. Intraoperative findings showed fresh thrombus superimposed on an organized portion of clot suggestive of a cardio-embolic source. Post-operative course was uneventful. He was discharged home on anticoagulation.
DISCUSSION: Heuristics are the cognitive processes we develop for daily medical decision-making. They are “educated guesses” or “rules of thumb”. Heuristics hasten the decision-making process in time-constrained, performance-driven work environments. However, the danger lies in the potential risk for diagnostic and medical error. Medical errors have a huge impact on patient care and physician wellbeing. Of the various heuristics, our case illustrates anchoring heuristic. Anchoring heuristics, (premature closure) refers to reliance on initial diagnostic impression, despite information suggesting otherwise. This is exemplified in our patient, who was diagnosed as having a cerebrovascular accident and hypertensive emergency based on risk factors, hypertension and previous stroke, without extensive consideration of other peripheral vascular disease or embolic phenomena sharing the exact same risk factors. Although subsequent evaluation alerted the managing team to critical limb ischemia and averted loss of limb, the outcome could easily have been worse. Recent strides to improve patient safety have tackled errors with medical administration and reconciliation, healthcare-associated infections, and peri-operative complications. Unfortunately, diagnostic errors have received less attention, despite studies indicating that they are common and often due to cognitive shortcuts rather than knowledge deficits. Recognizing heuristics in daily practice and training is the first step to avoiding its disastrous consequences in patient care. Other ways to mitigate the effects of heuristics include simulation training to increase knowledge and experience, reflection-based strategies to improve clinical decision-making skills and provision of cognitive assistance through clinical decision support tools.
ANTERIOR MEDIASTINAL MASS-LUCKILY IS NOT CANCER!Rami Hazzi; Anil Kumar Reddy Anumandla; Gaurav Kistangari. Cleveland Clinic, Cleveland, OH. (Tracking ID #1936593)
LEARNING OBJECTIVE 1: Recognize that Silicone implant rupture can migrate.
LEARNING OBJECTIVE 2: Recognize that Silicone induced lymphadenopathy can be confused for malignancy.
CASE: A 56 year-old nonsmoking women with a history of rheumatoid arthritis, breast augmentation surgery followed by explant and silicone exchange due to implant rupture many years prior, presented with complaints of exertional dyspnea and palpitations for 1 month. Prior outpatient evaluation including echocardiography, exercise stress test and pulmonary function tests were unremarkable. During one of her outpatient visits she was found to be hypoxic and was sent to the emergency department (ED) for further evaluation. In ED, her vital signs and physical examination were unremarkable. Initial cardiac evaluation was negative for acute coronary syndrome. Computed tomography (CT) chest ruled out pulmonary embolism but revealed a 2.7 cm anterior mediastinal mass with mediastinal adenopathy along with a left supraclavicular adenopathy. The patient was known to have left supraclavicular adenopathy, for which she underwent FNA that was negative for malignancy, a month prior to admission. During the hospital course episodes of supraventricular tachycardia were seen on telemetry that were controlled with Metoprolol. No episode of hypoxia or exertional drop in oxygen saturation was noted during her hospital stay. CT guided core needle biopsy of the anterior mediastinal mass was inconclusive and revealed necrosis and debris. Subsequently, due to increased concern for malignancy, thoracic surgery was involved and complete excision of the mediastinal mass and supraclavicular lymph node was performed by video-assisted thoracoscopic surgery (VATS). Left upper lung wedge resection was also performed due to the adhesions between mediastinal area and lung. Review of the surgical specimens showed no malignancy but rather fibrosis and foreign body giant cell reaction to lipoid like material compatible with silicone. The lung biopsy revealed the same reaction predominantly within the alveolar capillaries and perivascular regions consistent with silicone emboli.
DISCUSSION: Silicone implants are widely used either for breast reconstruction surgery or for breast augmentation. Direct silicone injections into the breast tissue for augmentation were discontinued in the United States because of the widespread occurrence of adverse events, including the migration of silicone to distant sites. Implants were considered technically superior as the envelope and the scar capsule were designed to retain the gel and to prevent migration. However, Implant rupture can still occur and is often a late complication that can be either: intra capsular, extra capsular or migrated gel. Most ruptures have no obvious traumatic cause. The frequency of asymptomatic rupture is around 0.2-4 %. The silicone gel that migrates beyond the breast tissue incites an inflammatory reaction and silicone granuloma formation regulated by cell mediated immune reactivity and T cell stimulation. Silicone gel entering the lymphatics, either through overt implant rupture or slow leakage across the intact outer shell can result in regional migration to the draining lymph node basins. Migration may not be limited to the corresponding axillary lymph nodes and can spread to more distant sites such as internal mammary, inguinal nodes, and abdominal wall. Silicone leak can also spread in a retrograde direction once it reaches the jugular-subclavian venous confluence. The development of lymphadenopathy may raise concerns regarding new or recurrent malignancy. In addition, positron emission topography (PET) scanning may demonstrate positive FDG uptake in silicone-induced lymphadenopathy and further heighten the suspicion of malignant disease. Magnetic resonance imaging (MRI) is the imaging study of choice in diagnosing implant rupture. Individual plastic surgeons have recommended prophylactic removal of implants within 8 years of implantation to avoid the increased risk of rupture as the implants ages. Few have advised that in the absence of definitive studies, the source of silicone should be removed from patients with symptoms of systemic disease. Breast implant rupture should always be treated aggressively to prevent extra capsular spread, distant migration and inflammatory reactions. However it is not recommended to routinely screen women for implant leak without symptoms. Our case adds to a growing awareness of this phenomenon and emphasizes the need for continued vigilance for signs and symptoms of migration and to recognize silicone migration as a cause of lymphadenopathy in patients with breast implants, not to be confused with metastatic cancer or other malignancy or infectious disease.
ANTERIOR T WAVE INVERSION: HEART OR LUNG? LEFT OR RIGHT VENTRICLE?Naoki Misumida; Elisheva Levine. Beth Israel Medical Center, New York, NY. (Tracking ID #1925559)
LEARNING OBJECTIVE 1: Recognize anterior T wave inversion as a sign of right ventricular dysfunction in patients with pulmonary embolism.
LEARNING OBJECTIVE 2: Review the diagnostic and prognostic values of anterior T wave inversion in patients with pulmonary embolism.
CASE: A 62 year-old man with chronic hepatitis C presented with a three-day history of pleuritic chest pain and shortness of breath. The patient had no recent travel or immobilization. His blood pressure was 132/82 mmHg, pulse rate was 87/min, respiratory rate was 18/min, and oxygen saturation was 91 % on 2 L of oxygen via nasal cannula. Physical examination showed bilateral clear breath sounds without jugular venous distention or lower extremity edema and the cardiac exam was without any murmurs, rubs or gallops. EKG revealed sinus rhythm and T wave inversions in leads V1 to V4 with marked QT prolongation (QTc 606 ms). Laboratory results were significant for a D-dimer of 7.04 UG/ML and a troponin I of 0.117 ng/ml. Chest X-ray revealed an enlarged right pulmonary artery silhouette. These findings raised the suspicion of pulmonary embolism and empiric anticoagulation with enoxaparin was started pending further studies. Subsequent chest CT angiography showed bilateral extensive pulmonary emboli. The patient was successfully treated with enoxaparin, which was transitioned to warfarin. Echocardiography performed on the following day revealed right ventricular dilatation and right ventricular systolic dysfunction, whereas left ventricular size and systolic function were within normal limits. Coronary angiography was performed to exclude concomitant coronary lesions, and no obstructive lesions were found. The patient remained normotensive during his hospital stay and did not develop any ventricular arrhythmia. A repeat EKG obtained 1 month later showed normalized T-waves and a QTc of 424 ms.
DISCUSSION: Acute pulmonary embolism can produce several EKG abnormalities including right bundle branch block, S1Q3T3 pattern, and anterior T-wave inversion. These EKG changes are called right ventricular strain pattern and reflect the severity of pulmonary hypertension. One large observational study, which reviewed EKG’s of 354 patients with pulmonary embolism, found that anterior T wave inversion was seen in 32.2 % of the patients and S1Q3T3 pattern was seen in 8.5 % of the patients. T-wave inversion in V1-V4 had a positive likelihood ratio of 3.7. In addition to the diagnostic value, right ventricular strain pattern also carries a prognostic value; another study of 386 patients with pulmonary embolism revealed that right ventricular strain pattern was associated with an increased risk of all-cause mortality and clinical deterioration with a hazard ratio of 2.58. In this case, anterior T wave inversion was accompanied by a prominent QT prolongation. However, the prognostic value of this unique EKG change is unknown due to the limited number of case reports. In conclusion, early recognition of right ventricular strain pattern should alter the estimated pretest probability of pulmonary embolism and prompt more aggressive treatment before hemodynamic instability ensues.
ANTIBIOTICS NON-RESPONSIVE FOOT ULCER, RETURNED TRAVELLER FROM BOLIVIAHirokazu Ban; Stanley R. Yancovitz; Joseph Petrsoric. Beth Israel Medical Center, New York, NY. (Tracking ID #1927748)
LEARNING OBJECTIVE 1: Recognizing possible cutaneous leishmaniasis for returned travelers who present with soft tissue infection with ulcer who do not respond to antibiotics.
CASE: The patient was a 64-year-old man with no significant past medical history who presented to Emergency department with a progressively worsening right dorsal foot soft tissue infection with a painless ulcer formation over 6 weeks-old. He had recently visited Bolivia and joined river fishing trip where he was bitten by a sandfly about 4 months prior to admission. The patient started to notice an erythematous papule on his right dorsal foot about 6 weeks prior to admission which was gradually getting bigger in size and swollen and erythematous. And in the last 4 weeks, the lesion was spreading thin and started to have a painless ulcer formation with a raised rim. This prompted the patient to see a primary infectious disease doctor. He was treated with total 4 antibiotics courses with broad spectrum coverage (Doxycycline → Augmentin → Ciprofloxacin → Linezolid → Bactrim) and itraconazole for considered spider bite, tick related infection or fungal infection by a infectious disease specialist and a dermatologist without any improvement. Finally, patient was referred to another infectious specialist and advised to come to emergency department for tissue biopsy for possible nocardiosis, sporotrichosis or lymphocutaneous leishmaniasis. He did not have a fever, chills, weight loss, night sweat, appetite loss, chest pain, shortness of breath, nausea, vomiting, or diarrhea through the clinical course. On admission, a physical examination revealed normal vital signs and a significant 3–4 cm erythematous wound with a necrotic base and perilesional erythema with ulcer formation on right dorsal foot and sporotrichoid nodules ascending up the leg and lymphadenitis in the upper thigh. Admission lab findings were not significant. A vascular surgeon was called and did debridement and sent the sample to pathology and deep wound culture which came back positive for Leishmaniasis. Given complications with lympthangitis, patient started liposomal amphotericin B IV for 7 days and was discharged. The patient has been followed as an outpatient and we’ve observed sign of healing.
DISCUSSION: Cutaneous leishmaniasis is the 10th most common dermatologic diagnosis among returned travelers but still there is some difficulty making a correct diagnosis, sometimes even by specialists. In fact, his physicians were misled by long latent period and possible exposure to tick related infection. A definitive diagnosis is made by identifying amastigotes in tissue or promastigotes in culture, or by amplifying Leishmania-specific DNA or RNA in a PCR. Most cases of cutaneous leishmaniasis will be resolved by themselves without any specific treatment but in some specific situations, especially people who have a higher risk of developing mucosal leishmaniasis, systemic treatment is recommended. There are no licensed drugs for treatment of cutaneous leishmaniasis in the U.S. Intramuscular SbV treatment is the most common with a overall 76 % cure rate but which is not familiar drug among general practitioner. Even though there are no controlled studies, a recent small case series suggests liposomal amphotericin B can be used as a first choice drug which is commonly used among physicians. To prevent more serious complications from cutaneous leishmaniasis, it is important to make a correct diagnosis and appropriately treat those who have a risk of developing mucosal leishmaniasis.
APPROPRIATE RISK STRATIFICATION OF PATIENTS WITH ACUTE PULMONARY EMBOLISMZohair Ahmed; Nikhil R. Kalva. University of Illinois College of Medicine at Peoria, Peoria, IL. (Tracking ID #1939635)
LEARNING OBJECTIVE 1: Management in the setting of acute pulmonary embolism (PE) is dependent upon massive vs. sub-massive classification. For those patients that exhibit features from both of these classifications, there is no clear-cut algorithm to guide management. Clinical judgment, experience, and comfort level are crucial when there is no risk stratification tool. Here we report a case of successful thrombolysis in a patient with delayed cardiopulmonary arrest due to a saddle pulmonary embolism.
CASE: A 43 y.o. male with a past medical history significant for recently diagnosed unprovoked saddle PE presented with recurrent shortness of breath. He attested to compliance with Coumadin. He denied any chest pain, hemoptysis, fevers, chills, cough or flu-like symptoms. His initial vitals revealed a blood pressure was 130/85, heart rate of 86, respiratory rate of 16 and an oxygen saturation of 88 % on room air. He subsequently was placed on 3 L nasal cannula with improvement in his oxygen saturation to 95 %. His cardiac exam revealed normal heart sounds, no JVD, and lungs were clear to auscultation. His CBC, CMP, CXR, Troponin, and BNP were all within normal limits. His INR was in the therapeutic range at 2.3. Electrocardiogram revealed sinus tachycardia. CT angiogram of chest revealed stable saddle PE, with no increase in clot burden. The patient got up to use the bedside urinal, and complained of excruciating calf pain followed by severe shortness of breath. He was now placed on 15 l of oxygen delivered via non-rebreather facemask. He was tachycardic at 135 beats per minute with a BP of 110/80. He seemed very anxious and now had developed mild hemoptysis. Stat 2D TTE showed severe RV dilation and hypokinesis. Since BP was stable and the patient did not meet criteria for massive PE, the decision was made not to administer tPA at this time. Catheter directed tPA was also deferred for the aforementioned reasons. Four hours later a code blue was called for respiratory arrest. Pulseless electrical activity was noted on the bedside monitor. ACLS protocol was initiated and the patient was successfully intubated. A stat order for tPA was given. Approximately 24 min into the code, tPA arrived; and all 100 mg of it was given IV push. Shortly thereafter, return of spontaneous circulation was noted with evidence of a strong carotid pulse and rhythm consistent with sinus tachycardia. Maximum vasopressor support with Norepinephrine, Epinephrine and Vasopressin was initiated, and the patient was placed on therapeutic hypothermia for neuroprotection. Ten days later, the patient was transferred to a general floor with all neurological function intact, and was eventually discharged home in good condition.
DISCUSSION: This case illustrates the need for continued use of available risk stratification strategies in patients with acute pulmonary embolism. While systemic tPA remains a viable option in patients with pulmonary embolism with cardiopulmonary shock, its role in sub-massive forms remains controversial. While we eagerly await the results of the multicenter PEITHO study addressing this question, all patients should be assessed carefully upon presentation for indications and contraindications for thrombolytic therapy to potentially minimize immediate and long-term complications of acute pulmonary embolism.
ARIPIPRAZOLE INDUCED AGRANULOCYTOSIS: A RARE BUT IMPORTANT ASSOCIATIONGautam George1; Patrick R. Aquino2; Dalar Nazarian3; Susan Krikorian3. 1Mount Auburn Hospital- Harvard Medical School, Cambridge, MA; 2Mount Auburn Hospital- Harvard Medical School, Cambridge, MA; 3Massachusetts College of Pharmacy and Health Sciences, Boston, MA. (Tracking ID #1940055)
LEARNING OBJECTIVE 1: To identify a rare association between aripiprazole and agranulocytosis and understand the risk factors of drug-induced neutropenia.
CASE: A 57 year old woman with a past medical history of major depressive disorder and a documented history of topiramate induced neutropenia presented with complaints of a painful right thumb after a burn injury. She reported an attempt at incision and drainage that was made by another doctor 5 days ago, that yielded only blood. She was initiated on sulfamethoxazole/ trimethoprim at that point of time. Examination of her thumb revealed an area of erythema and tenderness, with an area of central induration. Her medications for depression included aripiprazole that was started a month prior to admission and fluoxetine. Upon admission her white blood cell 1290 cells/mcL and absolute neutrophil count was 0, consistent with agranulocytosis. Sulfamethoxazole/trimethoprim and aripiprazole were discontinued and she was initiated on daptomycin for a potential secondary skin infection to her burn injury. Filgrastim was also started because of profound neutropenia. She demonstrated immediate recovery of leukocyte count and the offending agents were discontinued.
DISCUSSION: Drug induced neutropenia is an idiosyncratic reaction that commonly occurs within 4 weeks of drug administration. Agranulocytosis is more commonly seen in patients above the age of 50, women and in those with a past history of neutropenia. Anti-epileptics, anti-thyroid drugs and certain antibiotics are common culprits. In our case the absence of pus prior to the initiation of trimethoprim/sulfamethoxazole made ariprazole the likely offending agent. Clozapine is an anti-psychotic drug that has a classical association with agranulocytosis, hence routine leukocyte count monitoring is advocated. Newer atypical antipsychotics such as aripiprazole are considered to be safer alternatives to clozapine and routine leukocyte count monitoring is not recommended. The exact pathophysiology of psychotropic-induced blood dyscrasias is unclear, but proposed mechanisms include a direct toxic effect to myeloid precursors, immune mediated destruction and peripheral destruction of neutrophils. As agranulocytosis can lead to life threatening infections, we recommend vigilance when initiating aripiprazole and other psychotropic drugs especially in the setting of pre-disposing factors.
ASCITES: AN UNCOMMON PRESENTATION OF LUPUSChristopher H. Blevins1; Clement J. Michet2. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN. (Tracking ID #1928897)
LEARNING OBJECTIVE 1: Recognize the Prevalence of Peritoneal Involvement in Lupus
CASE: An 84 year old man was transferred to our hospital for further evaluation and management of nausea, vomiting, diarrhea, a 40 lb weight loss and drenching night sweats. His illness narrative began 2 years ago with constipation but recently worsened to include the aforementioned symptomatology which prompted hospitalization. He had an extensive workup prior to arrival that included a PET-CT showing hypermetabolic mediastinal and axillary lymph nodes, a node biopsy that was negative for malignancy, an unrevealing bone marrow biopsy, an exhaustive infectious workup that was negative, an abdominal CT that showed mild to moderate ascites, esophagogastroduodenoscopy showing chronic duodenitis with biopsies that were negative for infiltrative disease and infection, and a colonoscopy that showed non-specific colitis. Before arrival, he also had an anti-nuclear antibody study that was positive. Upon our interview with the patient, his rheumatologic review of systems was positive for 2 years of sicca symptoms, photosensitive rash on his face, history of unprovoked deep vein thrombosis, pulmonary embolism, and morning joint pain and stiffness. On physical exam, he was ill appearing, receiving total parenteral nutrition, and his abdomen was distended and diffusely tender with signs of ascites. His labs revealed: white blood cell count of 1.9 × 109/L (3.5–10.5 × 109/L), ANA of 5.1 U (<1.0 U), anti-RNP of 1.0 U (<1.0 U), total complement of 12 U/mL (30–75 U/mL), C3 of 67 mg/dL (75–175 mg/dL), C4 of <3.0 mg/dL (14–40 mg/dL), IgG beta-2 glycoprotein of 35.8 U/mL (<10 U/mL) and IgA beta-2 glycoprotein of 14.6 U/mL (<10 U/mL). His ascites fluid showed a SAAG of 0.9 g/dL. He met diagnostic criteria for systemic lupus erythematous and was treated with Solu-Medrol 500 mg IV for 3 days before transitioning to oral prednisone with resolution of nausea, vomiting and night sweats. He was able to stop the previously started total parenteral nutrition feedings and return home.
DISCUSSION: Lupus peritonitis is a rare form of the serositis that is associated with systemic lupus erythematous (SLE). SLE is an autoimmune disorder that can affect any organ, with one of the hallmark clinical signs being serositis. Serositis refers to the inflammation of the serous lining of the lungs, heart, and abdomen. This usually presents as pericarditis, which is seen in 39 % of patients with SLE, and pleurisy or pleural effusions, seen in 30 % of patients. However, the GI tract can be involved in 40 % of patients with SLE. It is thought that most of the GI complaints surrounding SLE are a result of non-steroidal medications, corticosteroids, or cytotoxic medications used for SLE therapy with only a small proportion having abdominal pain as a direct consequence of the disease. It is thought that 8–11 % of patients with SLE present with ascites secondary to lupus. However, autopsy studies suggest that 60 to 70 % of patients with lupus have had an episode of peritonitis.
ASEPTIC MENINGITIS AFTER INTRATHECAL STEM CELL INFUSIONArthi Balu. UCSD Medical Center, San Diego, CA. (Tracking ID #1940354)
LEARNING OBJECTIVE 1: Review causes and treatment of aseptic meningitis.
LEARNING OBJECTIVE 2: Consider the safety and ethical consequences of experimental procedures.
CASE: A 27-year-old male with partial T6 paraplegia presented with 1 day of fever, headache, nausea, vomiting, and altered mental status. His history was remarkable for intrathecal infusion of fetal neuronal stem cells one-day prior. Per the patient, the cells were injected in the L4-L5 space at a clinic in Mexico. The therapy was undertaken in hopes of regenerating spinal tissue and reversing his paraplegia. On exam he was extremely sound and light sensitive, oriented only to self, and had worsening of his right lower extremity weakness. CT of the head was unremarkable and MRI of the lumbosacral spine was negative for epidural abscess. Analysis of the CSF revealed 170 RBC/mm3 and 6500 WBC/mm3 with 75 % neutrophils and 24 % macrophages. CSF chemistries were notable for glucose of 33, and protein of 900 mg/dL. Gram stain was negative. IV antibiotics and dexamethasone were initiated for bacterial meningitis. CSF cultures failed to grow any organisms, and testing for streptococcus pneumoniae antigen was negative. By hospital day 3 the patient had significant improvement—he was afebrile for 72 h, alert and oriented, and his peripheral WBC had fallen from 16 to 8. A repeat LP revealed WBC of 250, glucose of 49 and protein of 60 mg/dL. Gram stain and culture were again negative. The rapid improvement in the patient’s symptoms and CSF profile suggested a biochemical inflammatory meningitis due to the stem cell injection rather than true bacterial meningitis. The patients IV antibiotics and steroids were stopped. He continued to do well clinically and was discharged without further treatment.
DISCUSSION: Aseptic meningitis develops in the absence of pyogenic bacteria in the cerebrospinal fluid (CSF). The underlying cause may be viral, a drug reaction, or an auto-immune/inflammatory process. Though rare, aseptic inflammatory meningitis can occur after spinal injections. A CSF profile with elevated WBC and protein may not indicate bacterial meningitis in such cases. However, given the mortality of bacterial meningitis, initial management should include IV antibiotics and steroids. This treatment course can then be modified if gram stain and cultures are persistently negative. Of note, 3 days of antibiotics, though sufficient to sterilize the CSF, should have minimal effect on CSF cell counts and chemistries. Therefore, the rapid improvement of CSF abnormalities in this case along with negative cultures argued against a bacterial etiology. This distinction is important, as unlike bacterial meningitis, aseptic meningitis can often be managed with close clinical observation and pain medications alone. In drug-induced cases of aseptic meningitis, the offending agent should be withdrawn. Anti-virals may also be indicated if suspicion for HSV is high. Spinal stem cell injection has shown promise in regenerating spinal tissue in rat models, but has not been demonstrated to be safe or effective in humans. The immunogenicity of stem cells is under question, and there are no standards for the collection or administration of these cells. Despite the risks, these therapies are being marketed as curative by for-profit clinics. Such clinics overwhelmingly target the most vulnerable patients, who undertake great personal and financial risk in the hopes of a cure for their illness. As in this case, aseptic meningitis is one potential adverse effect of such experimental procedures.
ASYMPTOMATIC LARGE PITUITARY INCIDENTALOMA IN A PATIENT WITH SARCOIDOSISLeena Jalota; Ana Abaroa-Salvatierra; Richard Alweis. Reading Health System, Reading, PA. (Tracking ID #1934741)
LEARNING OBJECTIVE 1: Pituitory hormonal deficits should be addressed accordingly to identification of the cause as primary, secondary or tertiary.
LEARNING OBJECTIVE 2: Work up of pituitory incidentaloma includes MRI imaging, hormonal lab testing as well as visual field testing.
CASE: A 52 year old male with pulmonary sarcoidosis presented to his allergist for excessive tearing. CT scan of sinuses ordered for possible blocked nasolacrimal duct revealed abnormal expansion of the sella turcica. MRI suggested a homogeneously enhancing 4 cm soft tissue mass centered in the sella turcica extending into both the left and right cavernous sinuses as well as abutting the optic chiasm. TSH, free t4, t3, LH, FSH, testosterone, GH, IGF-1 and 24 h urine cortisol levels were normal with only abnormality a minimally elevated prolactin (24.4 ng/mL (2.64–13.13). Visual field testing was normal. Patient underwent trans-sphenoidal excision of the mass.
DISCUSSION: Pituitary incidentalomas are unsuspected pituitary lesions discovered on an imaging study performed for unrelated reasons, and are classified on the basis of size and hormonal activity. The most frequent deficit (30 %) is hypogonadotropic hypogonadism without hyperprolactinemia. The differential diagnosis of sellar incidentalomas is broad; in this case, given the pulmonary sarcoidosis, the initial concern was for neurosarcoidosis. However, almost all cases (91 %) of neurosarcoidosis were diagnosed with neurologic symptoms or clinical hormonal deficits, neither of which was present in our patient. Given the size of the tumor and the absence of visual field deficits, despite the displacement of the optic chiasm, this tumor likely had a slow growth pattern that usually corresponds to nonfunctioning macroadenomas. Surgical indications include resection of hormonally active tumors and those displacing the optic nerves on imaging studies or cause field deficits, but the future management would be directed based on pathology and immuno-cytochemical studies
ATRIAL FIBRILLATION CAUSED BY INDWELLING PERIPHERALLY INSERTED CENTRAL CATHETER (PICC)Anene Ukaigwe; Paras Karmacharya; Madan R. Aryal; Adetokunbo Oluwasanjo. The Reading Health System, West Reading, PA. (Tracking ID #1936732)
LEARNING OBJECTIVE 1: Identify indwelling Peripherally inserted Central Catheters (PICC) as a cause of new onset arrhythmias
LEARNING OBJECTIVE 2: Evaluate and successfully treat PICC associated arrhythmias
CASE: A 22-year-old female with no previous cardiac disease was admitted for treatment of meningitis. A right-sided PICC line was placed in arm for intravenous access and antibiotic administration. Chest radiographs had showed the PICC tip at the aorto-caval junction. A day later, she complained of palpitations. These started within an hour of PICC placement. Symptoms were worse with lying flat, arm movements and deep breaths. Electrocardiogram (EKG) showed atrial fibrillation (AF) with atrial and ventricular rate of 210/min and 78/min respectively. Previous EKGs at admission and dating back 6 months showed sinus rhythm. The PICC was thought to be the likely cause of AF given the positional variation of symptoms. The PICC withdrawn 1 cm from its prior location. Immediately after this, she returned to normal sinus rhythm. Placement at the distal third of the Superior Vena Cava ( SVC) was confirmed on chest radiograph. Thyroid function tests, complete blood count, electrolytes and echocardiogram were all within normal limits. She was asymptomatic and maintained sinus rhythm until discharge.
DISCUSSION: Peripherally Inserted Central Catheters (PICC) are commonplace in patients requiring long-term intravenous therapy in both inpatient and ambulatory settings but arrhythmias are an infrequent complication of indwelling PICC lines. While transient arrhythmias during PICC placement may occur, these resolve within minutes of insertion. Arrhythmias associated with indwelling PICC may be of atrial or ventricular origin and are caused by irritation of the myocardial wall by the tip of the PICC. Blind PICC placement at the bedside is a cost effective alternative to placement with direct radiologic guidance. However blindly inserted PICCs are less successful than those placed under direct vision (84 % v 100 %). Blindly placed PICCs are also more likely to migrate irritating the myocardium. Even uneventful and well placed PICCs, may still be complicated by arrhythmias due to PICC migration. Additionally, changes in body posture for example arm abduction, deep respiration and lying supine may vary the position of the PICC resulting in intermittent positional arrhythmias. Repositioning the PICC is often all that is needed for treatment of these arrhythmias; in our patient, the PICC was withdrawn from the aorto-caval junction into the distal third of the SVC for relief. More proximal PICCs that is proximal SVC increase the risk of PICC associated thrombosis while more distal placement may lead to cardiac complications including arrhythmias, cardiac perforation and tamponade. Cardioversion is rarely needed. About 0.9 % of the patients with central catheter associated arrhythmias eventually require cardioversion. In conclusion, the evaluation of new arrhythmias in patients with a PICC line should include assessment of the effect of postural changes on the PICC and the arrhythmias.
ATTENTION!! HENOCH-SCHöNLEIN PURPURA CAN OCCUR IN ADULTS WITH ACUTE ABDOMINAL PAIN AS AN INITIAL SYMPTOMKaname Uno1; Some Furukawa1; Masato Yoshihara1; Shinichi Mizuno2; Yoshinori Kobayashi3; Hiroshi Yamasita3; Mitsunori Iwase1. 1TOYOTA memorial hospital, Toyota, Aichi, Japan; 2TOYOTA memorial hospital, Toyota, Aichi, Japan; 3TOYOTA memorial hospital, Toyota, Aichi, Japan. (Tracking ID #1929572)
LEARNING OBJECTIVE 1: Note that abdominal pain can be the first symptom of Henoch-Schönlein purpura (HSP).
LEARNING OBJECTIVE 2: Recognize that the prognosis of the renal function is worse in adult HSP than in children.
CASE: A 67-year-old woman with a history of sigmoid colon cancer which was completely resected by laparoscopy 3 years before, complaining of acute abdominal pain. Five days before the admission, she developed acute abdominal pain, which was intermittent and sharp around epigastric area. Since her condition did not improve at all for 5 days, she was presented to our hospital. Vital signs were not remarkable but there was tenderness at the epigastric area and left lower area of the abdomen without rebound tenderness. Other physical examinations were not remarkable. On laboratory studies, WBC, CRP and D-dimer were elevated, 24300 /μL, 8.9 mg/dL, 14.8 μg/mL respectively. Abdominal CT image showed the thickening of the duodenum, which made her diagnosed with either acute gastroenteritis or ischemia enteritis in the duodenum and fluid therapy was initiated. Four days after the admission, in addition to abdominal pain, arthralgia of both wrists and left ankle occurred. At the same time, the purpura suddenly appeared in the legs and urine protein became positive. From these findings, HSP was suspected. The renal biopsy revealed mesangial IgA deposition and additional blood test found coagulation factor 13 decreased, which led to the final diagnosis of HSP. After the diagnosis, steroid pulse therapy was initiated for 3 days followed by oral corticosteroid therapy. Additionally, we conducted steroid pulse therapy for three times and continued oral corticosteroid therapy. At present, her creatinine is 1.34 mg/dL and urine protein is 1.37 g/day, which suggests an irreversible renal failure has already progressed.
DISCUSSION: HSP is the most common acute vasculitis in children, but relatively rare in adults. Patients with HSP present with purpuric rash, which is the most common initial symptom in both adults and children. On the other hand, some patients have only abdominal pain in early phase of HSP like this patient. In these cases, it is very difficult to differentiate the diagnosis of HSP. Some reported that the severe inflammation of duodenum is the first sign of HSP. Although the differential diagnosis for epigastric pain is broad, which include acute coronary syndrome, gastric and duodenum ulcer, acute pancreatitis, gastroenteritis and the first stage of appendicitis, other diagnosis such as HSP should be included, especially if there is an inflammation of duodenum. In general, patients with HSP who present with abdominal pain as the initial disease-related symptom have a significantly higher probability of developing nephrotic syndrome. The clinical presentation of HSP is severe in adult patients and the renal prognosis for HSP is poor compared with that of children. The percentage of patients with HSP nephritis that progress to renal failure or end stage renal disease has been reported to be around 16 % in adults. In our present case, the renal function may worsen in the future. In summery, there are some adult patients with HSP whose renal prognosis are worse than that of children. Clinician must keep in mind that abdominal pain can be the initial symptom of HSP, which can lead to renal failure in the end.
ATYPICAL CASE OF THROMBOCYTOPENIAClaire Campbell; Eugene Lee. California Pacific Medical Center, Pacifica, CA. (Tracking ID #1939648)
LEARNING OBJECTIVE 1: Recognize the clinical and laboratory manifestations of atypical Hemolytic Uremic Syndrome (HUS) as a cause of thrombocytopenia.
LEARNING OBJECTIVE 2: Review the management of atypical HUS, including the use of Ecluzimab, a terminal complement inhibitor.
CASE: A 39-year-old Asian female with no significant past medical history presented with 2 weeks of gingival bleeding and epistaxis. She also noted increased fatigue, frequent urination, and dark urine. She denied any fevers, chills, headaches, change in mental status or recent diarrheal illness. Her physical exam was significant for elevated systolic blood pressure of 170, gingival bleeding and petechiae over her bilateral lower extremities. There were no signs of hepatosplenomegaly or lymphadenopathy. Significant laboratory findings included platelets of 6,000, hemoglobin of 8, creatinine of 2.24, and BUN of 28. Peripheral smear did not reveal schistocytes. After platelet transfusion, her platelet count dropped. High dose intravenous steroids and a dose of intravenous immunoglobulin (IVIG) resulted in no change in her platelets. ADAMST13 activity was normal, C3 was low, C4 was normal, and LDH was elevated. Stool shiga toxin and CD 59 were negative. Bone marrow biopsy was negative. Given her renal failure, negative stool antigen, low C3, and lack of response to steroids and IVIG, atypical HUS was suspected. She received five cycles of plasmapheresis with modest improvement in her platelets and renal function. After receiving one dose of Ecluzimab, an inhibitor of the complement pathway, her platelet count improved to 76,000 and her creatinine dropped to 1.73. She was then scheduled for weekly Ecluzimab as an outpatient.
DISCUSSION: Hemolytic uremic syndrome should be suspected in patients presenting with thrombocytopenia, renal dysfunction and hemolytic anemia. Ten percent of HUS is not caused by shiga toxin or bacteria such as Streptococcous pneumoniae. Atypical HUS is caused by genetic abnormalities of complement regulation. In those patients without diarrheal illness, atypical HUS should remain high on the differential, but etiologies such as leukemia, paroxysmal nocturnal hemoglobinuria, HIV, ITP and TTP should be excluded. No gold standard test exists for atypical HUS, but given its high mortality rate, frequency of progression to end-stage renal disease, and limited treatment options, it must be considered. In this patient, atypical HUS was exemplified by low C3, normal C4, hemolytic anemia, thrombocytopenia, and renal failure. Her failure to respond to platelet transfusion and steroids are typical as well. Plasmapheresis may temporarily improve thrombocytopenia, hemolytic anemia, and renal failure, but recurrence occurs in up to 70 % of patients depending on the complement mutation. No randomized clinical trials exist, but use of plasmapheresis may decrease mortality from 50 to 25 %. Renal transplant is contraindicated given rejection rates as high as 90 %. Ecluzimab, an antibody that blocks terminal complement formation, has been shown in phase 2 trials to improve renal failure, decrease dialysis requirements, increase platelet counts, and improve quality of life. Ecluzimab is also hypothesized to reduce recurrence rates. Our patient had a drastic improvement in platelet count and renal function with a single dose, significantly more than with five cycles of plasmapheresis. Because it is a weekly to bi-weekly infusion, management can occur as an outpatient, as was the case with our patient. This case highlights how Ecluzimab holds great promise for the treatment of atypical HUS.
ATYPICAL PRESENTATION OF NEUROMYELITIS OPTICAZachary D. Horne; Paul Koffer; Benjamin Lloyd. The Reading Hospital, West Reading, PA. (Tracking ID #1939244)
LEARNING OBJECTIVE 1: Recognize the challenges in differentiating neuromyelitis optica (NMO) from multiple sclerosis (MS)
LEARNING OBJECTIVE 2: Recognize the importance of aggressive treatment in NMO
CASE: The patient is a 37 year old male with a history of cutaneous marginal zone B-cell lymphoma s/p XRT 3 years prior with a recently unremarkable PET scan who was sent to the ED for back pain, progressive parasthesias, bladder and bowel dysfunction, and abnormal spinal MRI findings. There was no precipitating illness or trauma. In the month prior to admission, the back pain gradually progressed. At the same time, he began to experience numbness and tingling of the right foot which became bilateral and gradually rose to the level of the waist. In the week prior to hospitalization, numbness extended to the umbilicus and groin with difficulty emptying his bladder and moving his bowels. He had no weakness until 5 days prior to presentation. He denied any visual changes or eye pains. CT of the head was negative. Thoracolumbar spine MRI showed an enhancing lesion at the level of T1-T4 and a non-enhancing lesion further inferiorly to the level of T11 as well as a T7 vertebral body lesion. Multiple vertebral spine marrow signal changes were also noted. B12/folate were normal. An LP done in the emergency department showed an increased protein level of 67 mg/dL (nl: 20–45 mg/dL). CSF studies were negative for IgG index, ACE, lyme, oligoclonal bands, or bacterial growth. A serum NMO antibody was ordered as a send out lab. At that time, the differential was felt to include recurrent lymphoma, transverse myelitis, spinal cord tumor, metastasis, neurosarcoidosis, Behcet syndrome, HIV, or less likely NMO or an MS variant. He was given a single dose of 10 mg IV decadron followed by 4 mg IV q6h for 48 h with a 60 mg prednisone taper over 6 days. With steroids his numbness/weakness improved dramatically. Two days later, he only had some numbness in the distal legs and perineum. Repeat MRI of the spine at that time showed moderate improvement of the thoracic cord with decreased enhancement and edema. He was discharge home with the prednisone taper. Following his discharge, the serum NMO antibody returned positive. He returned to the hospital 5 days later, the day following his last dose of prednisone, complaining of recurrent numbness up to mid-chest. He denied any eye pain or visual changes but was again constipated. He was given an infusion of rituximab 1 mg IV and started on solumedrol 500 mg BID for 5 days followed by prednisone 60 mg PO daily as maintenance. His symptoms improved significantly and he was discharged with appropriate follow up in place. He was scheduled for additional a rituximab infusion 2 weeks following discharge. Seven days following the second discharge, however, he returned to the hospital complaining of increasing weakness in both legs and parasthesias below T4. He had had mildly blurry vision while watching TV 3 days prior to returning, but denied current eye pain, visual loss, or diplopia. Repeat spinal MRI showed overall improvement of the originally abnormal thoracic and cervical signals without new or worsening lesions. He was transferred to an outside institution at that time for plasmapheresis and further management.
DISCUSSION: Because they are both demyelinating disorders, NMO and MS can be difficult to differentiate at initial presentation. Key differences between the two diseases include the prevalence of abnormal findings on brain MRI in MS, CSF neutrophilic pleocytosis with anti-myelin oligodendrocyte glycoprotein in NMO, higher levels of glial fibrillary acidic protein in NMO than MS, and the presence of anti-aquaporin 4 water channel IgG antibodies in NMO. Unvalidated diagnostic criteria for NMO have been proposed for the differentiation of NMO from MS, but not all cases fit these criteria, as there is a spectrum of NMO-like disorders, such as in our patient who presented without initial visual symptoms. A small minority of NMO cases can be monophasic, but the vast majority have a relapsing course which can present with optic neuropathy and myelopathy in any order or simultaneously. Most of the disability from NMO results from these relapses, unlike in MS where secondary progression is the culprit. Thought here are no randomized-controlled trials evaluating the efficacy of various treatment regimens for NMO, current treatment proposals include early and aggressive steroid immunosuppression with high-dose methylprednisone to be followed shortly thereafter by plasmapheresis. Maintenance immunosuppression should be utilized for up to 5 years because of the risk of relapse.
AUTOIMMUNE HEMOLYTIC ANEMIA WITH VTE: COMMON COMPLICATION OF A RARE DISEASESonikpreet Sonikpreet; Karthikeyan Venkatachalam; Jasleen Kaur; Alaeddin Maeza; Sarwan Kumar. Crittenton Hospital/Wayne state university, Rochester, MI. (Tracking ID #1938391)
LEARNING OBJECTIVE 1: Autoimmune hemolytic anemia (AIHA) is a rare disorder in which RBCs are prematurely decreased by either IgG or IgM auto-antibodies. VTE is a more serious, acute and often lethal complication of AIHA. There are many mechanisms described for the prothrombotic state in patients with AIHA; despite the thrombotic implications, risk of VTE is often overlooked.
CASE: We are presenting a case of 76 y/o female with AIHA associated with extensive proximal DVT. Seventy-six year old F with PMH of PUD & HTN was admitted with complaint of SOB on exertion since 1 month and near-fainting episode a week ago. On admission, her Hb was 3.8. Pertinent physical examination findings revealed conjunctival pallor but no evidence of bleeding, lymphadenopathy or Hepatosplenomegaly. Lab studies revealed elevated LDH, high retic count, Hct 11.8, MCV 128.4 and spherocytes on peripheral smear. Further investigations showed positive IgG Ab on coomb’s test. GI and MM work up was negative. Patient’s Hb started improving after blood transfusion and IV steroids. After 1 week, she presented with right leg swelling found to have DVT involving right common & proximal femoral veins; left common femoral & popliteal veins.
DISCUSSION: Although rare in incidence, AIHA is the most common cause of acquired hemolytic anemia. Several studies including a review of 47 patients with AIHA supporting the existence of a prothrombotic state in patients with AIHA revealed that PE was the most common cause of death. But the risk for PE is often neglected, leading to fatal consequences.
AUTOIMMUNE NECROTIC MYOPATHY AS A RARE SIDE EFFECT OF STATIN THERAPYColleen Pater; Alda Maria Gonzaga. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1937103)
LEARNING OBJECTIVE 1: Pursuit of an alternative unifying diagnoses when a disease course is not proceeding as expected in the outpatient setting
LEARNING OBJECTIVE 2: Recognition of autoimmune necrotic myopathy as a rare side effect of statin therapy
CASE: A then-70 year old Vietnamese female was noted on routine screening to have hyperlipidemia in July 2009. Her LDL did not significantly improve with lifestyle change, so she was started on monotherapy atorvastatin in October 2009. She tolerated the medication well for approximately 2 years, during which time her LDL cholesterol improved to goal. In February 2012, the patient presented for evaluation of falls and generalized weakness. She reported difficulty climbing stairs and lifting her arms and legs, as well as diffuse achiness. Physical exam was notable for bilateral, symmetric, proximal muscle weakness. Laboratory evaluation showed mild elevation of muscle enzymes with significant elevation in creatine phosphokinase (CPK) to 6300. Symptoms were felt consistent with statin-induced myopathy, and atorvastatin was stopped at that time; ezetimibe was started for hyperlipidemia. The patient reported clinical improvement in muscle weakness over the next month although CPK remained elevated at 5500, prompting a rheumatology referral. In March 2012, rheumatology evaluation noted a decreasing CPK, with a negative myositis panel, ANA, Sjogren antibodies (patient also complained of dry eyes), and serum protein electrophoresis. Electromyography was consistent with myopathic process and a left bicep muscle biopsy showed chronic and moderately active inflammatory myopathy. Differential diagnosis at the time included polymyositis/dermatomyositis, inclusion body myositis, and statin-induced myopathy. Interestingly, the myositis panel resulted in an S35 immunoprecipitation with bands suggesting the presence of an unidentified autoantibody. No immunosuppressive medications were started as CPK began downtrending and the patient slowly started improving, both subjectively and on physical exam. However, in August 2012, CPK rose again although the patient reported her strength was almost back to baseline. Ezetimibe was stopped. CPK remained elevated through March 2013 and the patient again presented with a slight decrease in muscle strength, both subjectively and on physical exam. She also was experiencing early symptoms of dysphagia. At this point, the patient was started on prednisone 1 mg/kg daily. MRI of bilateral thighs in May 2013 was normal and repeat electromyography again showed a diffuse chronic and active myopathic process. Muscle biopsy of left deltoid in May 2013 showed mild subacute, active necrotizing myopathy that seemed most likely autoimmune related; the clinical correlation was felt to be related to HMG-CoA autoantibody. After approximately 2 months of steroid therapy, the patient’s strength began to improve and a taper with weekly methotrexate therapy was started. Since then, the patient has continued to recover strength and her CPK has normalized, even with a decrease in steroids and methotrexate. She continues to focus on dietary modifications to lower her cholesterol.
DISCUSSION: Statin-induced myopathy is a well-known side effect of statin therapy and ranges in severity from asymptomatic elevations in muscle enzymes to life-threatening rhabdomyolysis. Most patients present within the first 6 months of therapy, with resolution of symptoms an average of 2 months after cessation of therapy. This patient’s initial presentation was consistent with statin-induced myopathy, but her symptoms did not improve with statin cessation. Further outpatient evaluation yielded a diagnosis of necrotizing myopathy. Recent case reports and small series indicate an immune-mediated necrotizing myopathy associated with statin use that persists after statin withdrawal. Symptoms can relapse with the addition of other lipid-lowering agents. Patients improved with immunosuppressive therapy and had frequent relapses when treatment was tapered, suggesting an immune-mediated etiology. Further investigation found a novel autoantibody at 200 and 100kd with a strong association to the immune-mediated necrotizing myopathy and very recently the autoantigen has been identified as HMG-CoA reductase, the pharmacologic target of statins. It is unknown at this time whether our patient’s S35 immunoprecipitate is this autoantigen, but certainly the remainder of her clinical presentation and course are consistent with autoimmune statin-associated necrotizing myopathy. Thus, the pursuit of a different unifying diagnosis when our patient’s disease did not progress as expected uncovered a rare complication of statin therapy and re-directed her medical therapy appropriately.
AVOIDING DIAGNOSTIC PITFALLS IN THE RECOGNITION OF DRESS SYNDROME: CONSIDER “SAYING YES TO THE DRESS!”Hili Rosen; Daniel I. Steinberg; Alfred Burger. Beth Israel Medical Center New York, New York, NY. (Tracking ID #1936000)
LEARNING OBJECTIVE 1: Recognize that lamotrigine is a cause of DRESS syndrome.
LEARNING OBJECTIVE 2: Recognize that DRESS syndrome and ACEI induced angioedema can look similar in presentation
CASE: A 70 year-old female with HTN, CAD on an ACE inhibitor (ACEI) and schizophrenia treated with lamotrigine for 2 months presented to the ER with facial puffiness of unclear duration. Angioedema due to her ACEI, accupril, was diagnosed. Accupril was stopped, and the patient was given one dose of dexamethasone, and discharged. Two days later, she returned to the ER with continued facial puffiness along with a full body rash and sore throat. On admission, vitals were T: 99.7, P: 102, RR: 18, BP: 97/62, O2: 96 %. Physical exam revealed diffuse macular rash with desquamation, lip fissures, and cervical lymphadenopathy. Labs from her initial ED visit were significant for AST = 585U/L, ALT = 655U/L, AlkP = 144U/L, TBili = 2.1 mg/dL, eosinophils 14 %. On current admission, labs were AST = 1272U/L, ALT = 1229U/L, AlkP = 156U/L, TBili = 2.3 mg/dL, eosinophils 12 %. The patient reported no abdominal symptoms, no history of liver disease, and no alcohol use. Hepatitis panel was negative for hepatitis A and C, and indicated previously cleared hepatitis B. Ultrasound of her abdomen showed no liver disease or obstruction. Drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) caused by lamotrigine was diagnosed. Upon review, it was felt her initial ER presentation was early signs and symptoms of DRESS rather than ACEI induced angioedema. During the patient’s hospitalization, her bilirubin peaked at 9.4 mg/dl (direct = 5.3 mg/dl) and INR at 2.4 within days of each other. On third day of admission, the patient was started on prednisone 50 mg. Her symptoms and labs normalized over the next 2 weeks and the patient was discharged.
DISCUSSION: Drug reaction with eosinophilia and systemic symptoms is a drug hypersensitivity reaction that commonly presents with a desquamative skin rash, peripheral blood eosinophilia, and involvement of other organs. Lamotrigine is one of the most common causes, and has been reported to cause DRESS in 1/1,000 to 1/10,000 exposures. Liver involvement is often mild, with transient transaminitis and elevated alkaline phosphatase levels. We present a case of DRESS that was initially missed, as it was felt to be ACEI induced angioedema instead. This case highlights the importance of medication reconciliation, including medication durations, and of conducting a thorough review of all potential medication side effects in patients presenting with angioedema-like symptoms. Also, more careful consideration of the initial LFT abnormalities could have allowed for broadening of the differential diagnosis, reducing clinicians’ bias towards ACEI induced angioedema, and recognition of the “illness script”—the pattern of history and physical findings—for DRESS. A separate clinical learning point is that case reports have found that DRESS patients with a high bilirubin and INR have increased mortality and increased need for liver transplantation. In our patient, this association did not hold true. Clinicians should be aware that patients with these lab abnormalities may still do well, as our patient did.
B IS FOR BACTERIA: FEVER, NIGHT SWEATS, AND UNINTENTIONAL WEIGHT LOSSVictoria Chia; Roxana Aminbakhsh; Xiangdong Xu; Ramin Motarjemi. UCSD, La Jolla, CA. (Tracking ID #1923851)
LEARNING OBJECTIVE 1: A subacute course of systemic symptoms requires a broad differential diagnosis. Though rare, Whipple’s disease is important for clinicians to keep in mind.
CASE: A 48-year-old Hispanic man presented with 2 weeks of spiking fevers, night sweats, and unintentional weight loss of 10 lb in 30 days. He denied diarrhea, abdominal pain, hematemesis, and melena. Of note, he endorsed 1 year of bilateral hip osteoarthritis. Physical exam revealed bilateral inguinal and left axillary lymphadenopathy. The patient was found to be anemic and leukopenic with hemoglobin of 9.0 and WBC of 2.7. Abdominal CT showed mesenteric and retroperitoneal lymphadenopathy. The patient was admitted for workup for neoplastic and infectious etiologies. Throughout hospitalization he continued to spike periodic fevers and was transfused for hemoglobin of 7.6 on hospital day 3. Nutrition was consulted due to weight loss and poor oral intake. Infectious workup ruled out HIV, CMV, EBV, hepatitis, and tuberculosis. Upper endoscopy showed Candida esophagitis which was treated with nystatin. The patient was discharged on day 5 with improved energy and appetite. Duodenal biopsy pathology revealed numerous PAS-positive, AFB-negative rod-shaped microorganisms engulfed by foamy histiocytes consistent with Whipple’s disease, confirmed by PCR assay on axillary lymph node biopsy. One month of daily intravenous ceftriaxone was initiated, achieving a dramatic clinical response within 2 weeks. This was followed by 1 year of oral antibiotic therapy.
DISCUSSION: First described by George Hoyt Whipple in 1907, Whipple’s disease is caused by the bacteria Trophyrema whipplei and has an estimated worldwide incidence of 12 new cases per year. [1] It is described as presenting in stages, with a prodrome of oligoarthralgia preceding diarrhea and malabsorption. [2], [3] It is diagnosed by histopathology showing PAS-positive, AFB-negative stain of infected tissues, and PCR assay of biopsy specimens. [4] Although the causative organism primarily infects the gastrointestinal tract, the disease can also have cardiac [5], [6] and neuropsychiatric [7], [8] manifestations. Based on his clinical presentation of “B” symptoms and lymphadenopathy, non-Hodgkins lymphoma and HIV were highest on the differential for our patient. This case illustrates the potential for Whipple’s disease to present with systemic symptoms consistent with hematologic malignancy or immune deficiency. We recommend that physicians be aware of the variable presentation of Whipple’s disease and to consider a prodrome of oligoarthritis in raising suspicion in a patient presenting with systemic symptoms. [1] Dutly and Altwegg. Whipple’s disease and “Tropheryma whippelii.” Clin Microbiol Rev 2001, 14(3):561 [2] Schwartzman. Whipple’s disease. Rheum Dis Clin N Am 2013, 39:313–231 [3] Jones et al. A stain in time. N Eng J of Med 2007, 356:68–74 [4] Zaidan et al. Whipple disease mimicking adult-onset Still’s disease and treated by anakinra: diagnosis using PCR. Scand J Rheumatol 2012, 41(4):321–323 [5] Algin et al. Tropheryma whipplei aortic valve endocarditis, cured without surgical treatment. BMC Research Notes 2012, 5:600 [6] Fenollar et al. Whipple’s disease. N Eng J of Med 2007, 356:55–66 [7] Uryu et al. Central nervous system relapse of Whipple’s disease. Intern Med 2012, 51: 2045–2050 [8] Amendolara et al. Whipple’s disease infection surgical treatment: presentation of a rare case and literature review. G Chir 2013, 34(4):117–121
BE CAREFUL WHAT YOU ASK FOR: SYSTEMIC LUPUS ERYTHEMATOSUS AND IMMUNOSUPPRESSIONMerrill H. Stewart. Tulane University School of Medicine, New Orleans, LA. (Tracking ID #1939986)
LEARNING OBJECTIVE 1: Identify common non-HIV populations at risk for Pneumocystis Pneumonia (PCP)
LEARNING OBJECTIVE 2: Know when to start PCP prophylaxis in patients on chronic immunosuppressive agents for rheumatologic disease.
CASE: A 43 year-old woman presented with 5 days of chest pain and subjective fever. The chest pain was noted to be sub-sternal, constant, and pleuritic. She also endorsed a cough productive of white sputum and shortness of breath. Her past medical history was remarkable for Systemic Lupus Erythematosus on chronic prednisone and hydroxychloroquine for 1 year, with a recent decrease in her prednisone dosage. She was tachypneic, hypoxic to 90 % O2 saturation on room air, with bilateral basilar crackles and decreased breath sounds at the left base. The JVP was not elevated, with a tachycardic regular rhythm on auscultation. No pulmonary embolus was seen on computed tomography. Chest X-Ray reveled diffuse bilateral pulmonary infiltrates with bilateral pleural effusions. A good left ventricular ejection fraction and small pericardial effusion were seen on an echocardiogram. White blood count was elevated at 13.9 thousand cells/μl, and sputum stain was positive for Pneumocystis jirovecii. She was treated with IV Trimethoprim-Sulfamethoxazole and high dose corticosteroids resulting in clinical improvement.
DISCUSSION: Despite its association with HIV, any immunocompromised population is at risk for PCP, particularly those on chronic glucocorticoid therapy like our patient, or with a hematologic malignancy. Other groups include those with rheumatologic diseases, solid organ and hematopoietic transplants, primary immunodeficiencies, and severe malnutrition. Among those on chronic glucocorticoid therapy, the highest risk of infection is seen when an additional immunosuppressive agent such as cyclophosphamide, rituximab, methotrexate, or hydroxychloroquine is used. Often PCP is seen in these populations when the glucocorticoid dosage is reduced. Guidelines for PCP prophylaxis in the non-HIV immunosuppressed population are primarily based on consensus. In general patients who receive greater than 20 mg daily of prednisone for 1 month AND have an additional cause of immunosuppression (malignancy, additional immunosuppressive drug) should be on prophylaxis. An exception being when prednisone is used with methotrexate for rheumatoid arthritis for which no prophylaxis is needed. Recommended therapy for prophylaxis in the non-HIV population is identical to the HIV population, with Trimethoprim-Sulfamethoxazole being first line treatment followed by atovaquone and dapsone. Trimethoprim-Sulfamethoxazole has been associated with an increased incidence of lupus flares, so atovaquone is often used as a first line agent in these patients. We see that our patient was on both prednisone and hydroxychloroquine for many months therefore she most likely would have benefited from some prophylaxis that could have prevented her infection and hospitalization.
BELL’S ISN’T RINGINGBrian Cruz; Paul Jacob. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926996)
LEARNING OBJECTIVE 1: Identify the common symptoms of lateral medullary infarction
LEARNING OBJECTIVE 2: Recognize stroke as a potential cause of peripheral facial nerve palsy.
CASE: A 61-year-old man presents with dysphagia after inability to swallow his morning medications. He also complains of weakness, headache, and vomiting. He has hypertension and a history of a stroke with minimal residual deficits. He is prescribed antihypertensives but frequently misses doses. He is in no acute distress. He has complete left-sided facial weakness but facial sensation is intact. It is difficult for him to swallow and his voice is hoarse. He has right-beating nystagmus on gaze to the left. Gait is not tested given concern for falls but he has full strength in all extremities. Blood pressure is 243/122 mmHg. The remainder of his physical exam and vital signs are normal. Computed tomography scan reveals an old area of encephalomalacia within the right frontal lobe and chronic small vessel disease, but no acute intracranial hemorrhage. Initial diagnosis is Bell’s palsy and hypertensive urgency. The following day he continues to have left facial paresis and nystagmus, and also has uvula deviation to the right on palatal raise. Magnetic resonance imaging of the brain reveals a focal ischemic lesion located at the pontomedullary junction extending along the left cerebellar peduncle, within the perfusion territory of the posterior inferior cerebellar artery (PICA). Other, less well-defined anomalies are seen in the left cerebellar hemisphere in the PICA distribution. The location is consistent with lateral medullary infarction.
DISCUSSION: Strokes are common and require immediate recognition. Stroke syndromes that lack characteristic features, however, can easily be missed. Also, there is considerable variability in the findings of certain stroke syndromes. Our patient was initially misdiagnosed with Bell’s palsy, which did not explain his nystagmus, difficulty swallowing, or “weakness”, which was determined to be disequilibrium. His symptoms were due to an occlusion in his posterior inferior cerebellar artery leading to lateral medullary infarction. The features of lateral medullary syndrome, also known as Wallenberg syndrome, are variable depending on the areas damaged, and typically only some of the features are present. Damage to vestibular nuclei leads to vertigo, nystagmus, and vomiting. Spinothalamic tract injuries cause loss of contralateral pain and temperature sensation, whereas descending sympathetic tract damage causes ipsilateral Horner syndrome. Damage to fibers of CN XI and X causes hoarseness, dysphagia, ipsilateral paralysis of palate, and decreased gag reflex. Cerebellar injury leads to ataxia and lateropulsion to the ipsilateral side. A PICA infarction causing facial nerve palsy is exceedingly rare, as the facial nerve nucleus in the pons typically receives its vascular supply from the anterior inferior cerebellar artery (3). However, there are variations in arterial anatomy and an occlusion of the PICA has been documented to cause peripheral facial nerve palsy (4). Given the importance of early treatment in improving outcomes for stroke patients, the internist must definitively rule out stroke whenever new neurological deficits are present before attributing the changes to another cause.
BEWARE THE KETTLEBELLMatthew A. Calzetta; Meredith B. Barnes. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926108)
LEARNING OBJECTIVE 1: Recognize potential serious complications that may follow common exercises
LEARNING OBJECTIVE 2: Learn risk factors and preventive measures to avoid such complications
CASE: A 44 year-old Caucasian woman presented with a one-day history of worsening low back pain and tenderness. The pain was aggravated by movement and minimally relieved by over-the-counter pain medications. One day prior to presentation, she had participated in her first hour-long kettlebell exercise class. She denied any incontinence, fevers or weight change. On exam, paraspinal muscle, but not vertebral, tenderness from the level of T9 to the sacrum was seen. Flexion, extension and rotation of the spine were severely limited by pain. Straight leg raise was negative bilaterally. There were no neurological deficits. Dorsalis pedis pulses were 2+. Laboratory studies revealed a total creatine kinase (CK) of 25,700, AST of 1160 and ALT of 406. Urinalysis showed moderate blood with no red blood cells on microscopy. Initial electrolytes were within normal limits. Plain spinal films showed no fractures. MRI spine ruled out compartment syndrome of the paravertebral musculature, but showed diffuse lower musculature inflammation. Aggressive intravenous fluid hydration with normal saline was started. The total CK continued to rise to a peak of 52,000 on day 3 before decreasing to 10,000 on the day of discharge at hospital day 6. The only electrolytes changes were mild asymptomatic hypokalemia and hypophosphatemia following fluid administration. Renal function remained normal.
DISCUSSION: Rhabdomyolysis is defined as the release of striated muscle contents into the circulation following traumatic or nontraumatic events. The contents of muscle cells consist of electrolytes, myoglobin and sarcoplasmic proteins, including creatine kinase, aldolase, lactate dehydrogenase, alanine aminotransferase and aspartate aminotranferase. Clinically, it is defined based on elevated serum creatine kinase (CK) levels of more than 1000 U/L. Rhabdomyolysis is classified into traumatic and non-traumatic causes. Crush syndrome is the typical traumatic cause. Nontraumatic causes include exertion-induced, including strenuous exercise, seizures, alcohol withdrawal syndrome, muscle hypoxia, genetic defects, infections, body-temperature changes, metabolic and electrolyte disorders, drug-induced, toxin-induced and idiopathic. Rhabdomyolysis clinically presents with limb weakness, myalgia, edema and dark urination. The major complications are acute kidney injury (AKI) secondary to myoglobinuria, with an incidence that ranges from 13 to 46 % of cases, and disseminated intravascular coagulation. This case demonstrates exercise-induced rhabdomyolysis without complication. Rhabdomyolysis has been demonstrated in military recruits, professional athletes and individuals participating in regular exercise. There are no reports of kettlebell-induced rhabdomyolysis in the literature. Risk factors that increase the likelihood of rhabdomyolysis from exertion include: eccentric contractions, in which tension is applied during muscle extension causing more muscle damage than observed with concentric contractions, hot weather with high relative humidity, competitive exercise, higher socioeconomic status, poor physical condition, restrictive clothing that impairs heat dissipation, certain medications and supplements, including diphenhydramine, SSRIs, caffeine and performance-enhancing supplements, and hypokalemia secondary to impaired potassium-induced vasodilation in muscle. This case highlights the need for individuals seeking to try new, intense exercises should see their primary care physicians for pre-performance evaluation and education.
BEYOND SKIN DEEP: AN ELUSIVE DIAGNOSISKathryn Sweeney. UNC Chapel Hill, Chapel Hill, NC. (Tracking ID #1939062)
LEARNING OBJECTIVE 1: Diagnose skin lesions when initial biopsies are unrevealing.
LEARNING OBJECTIVE 2: Recognize the clinical features of cutaneous lymphoma.
CASE: The patient is a 76-year-old man who presented to the Emergency Department with a lower extremity wound of 3 months duration that had become progressively larger with ulceration and foul-smelling drainage. He had seen his local primary care physician who referred him to Dermatology. Two punch biopsies were performed and non-diagnostic. He was treated with courses of Trimethoprim-Sulfamethoxazole and Dicloxacillin without improvement. His medical history was significant for tophaceous gout and CKD. The patient lived on a farm and gardened frequently. He was a widower and a lifelong non-smoker. Physical exam was notable for large, necrotic, ulcerative lesions (5 × 4 cm and 6 × 3 cm) on an erythematous base with eschar and foul-smelling drainage on the left lower leg. Admission labs were significant for an elevated creatinine (1.68) and mild pancytopenia (WBC 2.7, Hemoglobin 11.4, Platelets 103). Differential diagnosis on admission included infection (particularly fungal or atypical mycobacteria), vasculitis, pyoderma gangrenosum, and non-melanoma skin cancer. A punch biopsy showed suppurative and granulomatous dermatitis. Wound culture grew Pseudomonas aeruginosa. Because three punch biopsies failed to yield a diagnosis, an excisional biopsy was pursued. Pathology from the excisional biopsy revealed extensive cutaneous involvement by large atypical lymphocytes that were strongly and diffusely positive for CD20, CD10, CD45, and Bcl-6. The patient’s biopsy and clinical presentation led to a diagnosis of Primary Cutaneous Diffuse Large B-cell Lymphoma, Leg Type. Staging with bone marrow biopsy and PET/CT did not reveal evidence of extracutaneous disease. The patient is currently undergoing therapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone).
DISCUSSION: Primary cutaneous lymphomas are those lymphomas with skin manifestations but no evidence of extracutaneous disease. They can be further classified according to several histological, immunohistochemical and clinical features. Primary cutaneous lymphoma has an annual incidence of 1:100,000 and is the second most common site of extranodal Non-Hodgkin lymphoma (with the gastrointestinal tract being the most common). Twenty percent of primary cutaneous lymphomas are primary cutaneous B cell lymphoma, and 4 % can be further classified as primary cutaneous diffuse large B cell lymphoma, leg type. Patients with primary cutaneous diffuse large B cell lymphoma, leg-type often present with red nodules or tumors on the lower leg that grow rapidly. Diagnosis is generally performed by biopsy. As was seen in our patient, excisional biopsies are preferred to punch biopsies due to greater yield. Treatment usually consists of rituximab and anthracycline-based chemotherapy. Primary cutaneous diffuse large B cell lymphoma, leg-type tends to occur at an advanced age (median 77 years) with a relatively poor prognosis (5-year disease specific survival of 41 %). Compared to other cutaneous lymphomas, it has a greater tendency to relapse and disseminate to extracutaneous sites. It is essential to maintain a broad differential diagnosis when evaluating skin lesions. It is also important to employ more comprehensive diagnostic strategies when initial tests are unrevealing. For example, our patient had three non-diagnostic punch biopsies before an excisional biopsy revealed his diagnosis. When considering skin lesions that do not heal with usual measures, malignancy should always remain on the differential.
BIG PATIENT, BIG PROBLEM: GASTROINTESTINAL DYSMOTILITY IN A PATIENT WITH ACROMEGALYMeghan Gilroy; Emily Beck; Paul Aronowitz. UC Davis Medical Center, Sacramento, CA. (Tracking ID #1936092)
LEARNING OBJECTIVE 1: Recognize gastrointestinal manifestations of acromegaly.
CASE: A 57-year-old man presented to the emergency department with a chief complaint of enlarged tongue. Family members had noticed enlargement of his tongue and forehead over the past several months. He also complained of chronic constipation. On physical exam, the patient was found to have macroglossia, frontal bossing, and extremely large hands and feet. Serum IGF-1 was 771 ng/mL (reference range 81–225 ng/mL) and serum growth hormone following a two-hour glucose tolerance test was 7.75 ng/mL (reference range <2 ng/mL). The diagnosis of acromegaly was made. MRI of the brain revealed a pituitary prominence suggestive of microadenoma. The patient was scheduled for resection and octreotide therapy was initiated. Despite aggressive bowel regimen and cessation of opioid pain medications, constipation persisted. Barium swallow demonstrated esophageal dysmotility; small bowel follow through revealed delayed gastric emptying and prolonged small bowel transit.
DISCUSSION: Acromegaly is a rare clinical syndrome characterized by elevated serum levels of growth hormone (GH) and insulin-like growth factor-1 (IGF-1); incidence is 3 cases in 1 million per year. The syndrome is most commonly caused by primary GH excess with benign pituitary neoplasms accounting for over 90 % of cases. Less common etiologies include ectopic GH secretion, familial disorders of GH excess, and neoplastic overproduction of GH-releasing hormone. Common clinical manifestations of acromegaly include acral enlargement and hypertrophy of the tongue, frontal bone and jaw. Elevated GH has visceral effects as well, including enlargement of kidneys, liver and spleen, but does not generally affect organ function. Gastrointestinal manifestations include constipation and higher prevalence of cholelithiasis, colon polyps and colorectal cancer. Constipation is a result of impaired gastrointestinal motility. Large bowel and small bowel transit times have been shown to be prolonged in acromegaly, which predisposes patients to small bowel bacterial overgrowth. This is presumed to be caused by both the increased length of the intestine and excess GH and IGF-1. Treatment for acromegaly includes resection of the culprit adenoma if present and administration of a somatostatin analogue such as octreotide, which suppresses growth hormone secretion by negative feedback. Somatostatin analogues decrease gastrointestinal transit, which can exacerbate constipation. Acromegaly and octreotide therapy likely accounted for the gastrointestinal dysmotility discovered in our patient.
BIZARRE NEUROLOGICAL SYMPTOMS WITH THUNDERCLAP HEADACHE MAY STEM FROM REVERSIBLE VASOCONSTRICTIONSMasato Yoshihara1; Hidenori Oguchi1; Mitsunori Iwase1; Aya Ogura2; Yasuhiro Ito2; Yasuyuki Kishigami3. 1TOYOTA memorial hospital, Toyota, Aich, Japan; 2TOYOTA memorial hospital, Toyota, Ach, Japan; 3TOYOTA memorial hospital, Toyota, Aich, Japan. (Tracking ID #1929116)
LEARNING OBJECTIVE 1: Note that reversible cerebral vasoconstriction syndrome (RCVS) presents various symptoms and associated disorders.
LEARNING OBJECTIVE 2: Recognize that RCVS dose not always present reversible pathopysiological state.
CASE: The first case is a 55-year-old female with a history of migraine and taking some painkiller drugs occasionally. The day of admission, the patient suddenly felt thunderclap headache right after defecation. Since there were no significant physical signs including neurological deficits, emergency physicians chose to observe her carefully with administration of acetaminophens. Then, the pain was favorably controlled. Magnetic Resonance Image (MRI) performed on the fourth day after the onset showed cortical subarachnoid hemorrhage (cSAH) at the right parietal lobe. Cerebral angiography revealed vasoconstriction of the right anterior cerebral artery. Accordingly, the patient was diagnosed with RCVS associated with cSAH. Additionally the single photon emission computed tomography (SPECT) was performed, which detected decreased venous flow at the corresponding cSAH lesion. The patient was treated with a calcium channel blocker and the sequential magnetic resonance angiography (MRA) was performed, which showed improvement of the vasoconstriction. Although the patient favorably progressed, the decreased venous flow in SPECT unchanged even after the diagnosis of RCVS. The second case is a 36-year-old pregnant woman with no significant past obstetrical history. The patient began to feel headache at the beginning of labor. Right before and after the birth, two times of convulsion occurred and she was transferred to our hospital. On arrival, the patient was agitated, but there were no significant vital signs or physical signs. Computed tomography (CT) image showed hemorrhage of the left putamen and sedatives were administered. MRI performed on the same day did detect cerebral edema of the bilateral posterior lesions. On the third day, MRI showed the cerebral edema resolved and the patient was diagnosed with posterior reversible encephalopaty syndrome (PRES). The patient progressed favorably with intravenous magnesium sulfate and weaned from the sedatives on the fourth day. The initial MRA revealed no evidence of vasoconstriction, however, the MRA on the seventh day after the admission showed remarkable vasoconstrictions of the bilateral middle cerebral arteries and the basilar artery, which were consistent with RCVS. There were no symptoms including neurological deficits and the patient was discharged on the fourteenth day. Interestingly, the vasoconstriction in MRA had remained for 2 months after the diagnosis of RCVS.
DISCUSSION: RCVS is characterized by reversible multifocal narrowing of the cerebral arteries preceded by thunderclap headaches with or without associated neurologic deficits. Although this constriction generally resolves spontaneously within 3 months, RCVS develops a unique set of clinical imaging features such as subarachnoid hemorrhages, lobar hemorrhages and cerebral infarctions. Approximately 90 % of RCVS patients follow favorable clinical outcome. However, 10 % develop severe deficits, and some of them eventually die. Moreover, even among the patients with no clinical sequela, irreversible decreased venous flow on SPECT can be detected, which suggests potential loss of brain functions. The calcium channel blocker is considered to reduce headaches, but has no proven effects on hemorrhagic and ischemic complications. In summary, we experienced two female cases of RCVS, which presented different clinical manifestations and radiographic findings. Careful observation and appropriate prognostic evaluation are essential for any patient who present with thunderclap headache, which can be the initial symptom of RCVS or other fatal diseases such as subarachnoid hemorrhage.
BONE MARROW GRANULOMA: A DIAGNOSTIC CLUEGregory Madden; Pinar Oray-Schrom. Yale New Haven Hospital, New Haven, CT. (Tracking ID #1923773)
LEARNING OBJECTIVE 1: Discuss the differential diagnosis and investigative approach to a patient with bone marrow granulomas.
CASE: A 77 year old woman with history of hypertension, diabetes, uveitic glaucoma, and gout underwent a bone marrow biopsy for workup of incidental cytopenias and abnormal serum protein electrophoresis (M-protein 0.4 g/dL). The biopsy was diagnostic for monoclonal gammopathy of undetermined significance (5–10 % plasma cells) and demonstrated non-caseating granulomas. No pathogens were identified. She presented to the hospital several months later with shortness of breath. Vitals signs were within normal limits. Exam was notable for jugular venous distention, leg edema, and rales. Chest X-ray demonstrated pulmonary edema and calcified hilar nodules. Echocardiography measured her ejection fraction 30 % and she was diagnosed with new-onset congestive heart failure. Cardiac catheterization revealed diffuse, tri-vessel disease but no intervention was done. A suspicion for nonischemic cardiomyopathy prompted cardiac MRI, showing thick ventricles and areas of delayed enhancement consistent with cardiac sarcoid. The diagnosis of systemic sarcoidosis was further supported by evidence of hypercalcemia (11.3 mg/dL) and elevated ACE level (85 U/L). She responded well to medical therapy of her heart failure and remains independent at home. Her sarcoidosis was deemed quiescent and required no treatment.
DISCUSSION: Granulomas are collections of fused macrophages surrounded by a rim of activated T-cells formed in an attempt to contain bacteria, fungi, or other foreign material. Granulomas on bone marrow biopsies are rare and incidence is less than 3 %. According to one recent retrospective study of 57 cases of bone marrow granulomas, 33 % were identified as infectious, 21 % sarcoidosis, 9 % malignancy, 6 % drug or therapy-related, and 21 % unknown (Brackers de Hugo et al. 2013). Among bacteria, intracellular pathogens are most common: Mycobacteria (TB and non-tuberculous), Bartonella, Salmonella (typhoid fever), and Coxiella burnetii (Q fever, characteristic “doughnut” shaped granuloma). Invasive fungal infection should be suspected in immunocompromised individuals. HIV is independently associated with bone marrow granulomas in addition to other viral infections such as EBV, CMV, and HSV. Sarcoidosis is the single most common diagnosis related to bone marrow granulomas. Bone marrow granulomas are identified in 10 % of all sarcoid patients but may be present in over half of patients with sarcoidosis-related anemia or leukopenia. Among malignancies causing granulomas on marrow biopsy, lymphomas, leukemias, and myelomas have all been described. Finally, therapy-related bone marrow granulomas can be due to drugs (amiodarone, procainamide) or Bacillus Calmette-Guérin (BCG) in patients vaccinated against tuberculosis or treated for bladder cancer. Differential diagnosis of bone marrow granulomas should begin with appreciation for signs and symptoms of a systemic illness. Infection, sarcoidosis, malignancy, medications, BCG exposure, and sarcoidosis should be considered. Bone marrow samples containing granulomas should be stained with Grocott Methenamine Silver (fungi), Warthin-Starry (Bartonella), acid fast (mycobacteria), and Gram stains with appropriate cultures sent. PCR testing may also be useful. Although bone marrow granulomas can be an important diagnostic clue, no cause will be identified in up to one fifth of patients.
BORTEZOMIB-RELATED CARDIOMYOPATHYZachary D. Horne; Paul Koffer; Anthony A. Donato. The Reading Hospital, West Reading, PA. (Tracking ID #1938840)
LEARNING OBJECTIVE 1: Recognize the role of both anthracycline and non-anthracycline chemotherapies in new-onset cardiomyopathy
CASE: A 62 year-old male veteran with a history of multiple myeloma being treated for the last 6 months with weekly first-line bortezomib and dexamethasone who presented with subacutely progressing dyspnea and an acute decline in exercise tolerance over the 2 days prior to admission. Prior to the initiation of chemotherapy, baseline echocardiogram showed normal cardiac size and function with an ejection fraction (EF) of 65 %. He denied increased swelling of his legs, inability to lie flat, or paroxysmal nocturnal dyspnea. He was afebrile, tachypneic, and in normal sinus rhythm, with normal oxygen saturation breathing room air. On examination he was noted to have 10 cm of jugular venous distention as well as diffuse inspiratory wheezes. Brain naturietic peptide was elevated at 1692 pg/mL (nl: 0 = 100 pg/mL) and troponins were elevated at 0.86 ng/mL (nl: <0.06 ng/mL). He was also found to have acute on chronic renal insufficiency and thrombocytopenia. Cardiac ultrasound revealed dilated cardiomyopathy, with ejection fraction 43 %. He responded well to diuresis with intravenous loop diuretics and initiation of carvedilol, but could not tolerate angiotensin inhibitors due to angioedema. Due to his lack of chest pain, renal insufficiency, thrombocytopenia, and elevated LFTs, a cardiac catheterization was felt not to be indicated. His dyspnea improved to the point of being able to participate in short periods of physical therapy and he was discharged to cardiac rehabilitation. The patient ultimately passed away 3 months after discharge following an episode of gram-negative neutropenic sepsis.
DISCUSSION: As long-term survival of malignancies increases, the long-term side effects of chemotherapy are becoming more prevalent issues for physicians. The cardiotoxic effects of many chemotherapy agents are well known, and are most closely associated with anthracyclines, cyclophosphamide, and tyrosine-kinase inhibitors such as trastuzumab. Proteosome inhibitors such as Bortezomib are uncommon causes of cardiac decompensation and have been documented in only a few case reports. Recommendations from the 2010 European Society for Medical Oncology Guidelines provide that all patients undergoing chemotherapy treatment have a clinical evaluation for cardiovascular function and comorbidities, including a baseline echocardiogram, especially in patients being treated with anthracyclines, trastuzumab, or with cardiovascular risk factors (age >60, prior coronary artery disease, or prior mediastinal irradiation).
BRAIN ABSCESS: AN UNUSUAL COMPLICATION OF ODONTOGENIC INFECTIONRajesh Mourya1; Runa Shrestha2; Renuga Vivekanandan1. 1Creighton University Medical Center, Omaha, NE; 2SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1933122)
LEARNING OBJECTIVE 1: Brain abscess, commonly caused by gram positive cocci, is a localized, suppurative inflammation of the brain parenchyma. Common causes of brain abscess include local extension (from ear, para-nasal sinuses), direct trauma and hematogenous spread. Odontogenic infections are rarely associated with brain abscess.
CASE: A 77-year-old, African - American male, with past medical history of type 2 diabetes mellitus , essential hypertension, and benign prostatic hyperplasia, was brought to the emergency department with a 1 week history of fever, progressive headache, vomiting followed by confusion, lethargy and 1 episode of generalized tonic clonic seizure. On examination, he was febrile with temperature of 101.2° Fahrenheit, was lethargic and disoriented. Meningeal sings were negative. Computed tomography of the head was abnormal, therefore magnetic resonance imaging of the brain was done which revealed a 4.2 × 1.8 × 2 cm bilobed mass in the right inferior frontal lobe and right basal ganglia, suggestive of brain abscess. Maxillo-facial x-ray showed evidence of periodontal abscess. Complete blood count, basic metabolic panel, urine analysis, and chest x-ray were within the normal limit. The patient was empirically started on broad spectrum antibiotics including vancomycin, ceftriaxone and metronidazole. He underwent surgical drainage of the brain abscess and extraction of the infected teeth along with drainage of the periodontal abscess. Streptococcus viridans was isolated from the pus aspirates. Blood cultures were negative. Vancomycin was stopped and ceftriaxone and metronidazole were continued. After the drainage of the brain abscess and antibiotic therapy, we noticed marked improvement in his neurological status. The patient was discharged to a skilled nursing facility on intravenous ceftriaxone and metronidazole to complete 8 weeks therapy. Repeat computed tomography of the head after few months showed complete resolution of the abscess. Patient has been doing well without any residual neurological deficit.
DISCUSSION: Brain abscess as a complication of odontogenic infection is uncommon. There are few case reports documenting the association of brain abscess with odontogenic infection. Brain abscess is associated with high morbidity and mortality. Early detection and initiation of treatment, that include surgical drainage and prolong antibiotics therapy, is the key to the management of brain abscess. Maintaining good oral hygiene, and early recognition and treatment of odontogenic infections may decrease the risk of brain abscess.
BRAIN DRAIN: A CASE OF TRANSIENT HYDROCEPHALUS AND SEIZURE DUE TO NEUROCYSTICERCOSISHaley Kensing; Roger D. Smalligan; Miles Raizada; Mashrafi Ahmed. Texas Tech Univ Health Science Center, Amarillo, TX. (Tracking ID #1938850)
LEARNING OBJECTIVE 1: Diagnose neurocysticercosis.
LEARNING OBJECTIVE 2: Recognize neurocysticercosis causing transitory hydrocephalus.
CASE: A 34-year-old Hispanic male who immigrated from Mexico 15 years ago presented with status epilepticus. The patient has a history of seizures that began at the age of 10. The patient has had four episodes of status epilepticus: 27 years ago, 10 years ago, 3 years ago, current presentation. The patient reports that every episode has occurred at night when the patient was lying down. The episode lasts approximately 3 min and consists of severe headache, confusion, foaming from the mouth, and tongue biting. The patient had significant history of worm infestation in childhood. An initial Head CT showed hydrocephalus with dilated lateral & third ventricles and blunted sulci. Few punctate foci of calcification were present in left frontal lobe. Another Head CT 24 h apart showed complete resolution of the hydrocephalus. An MRI with contrast indicated a 1 cm complex cyst like mass in the 4th ventricle. The patient was started on phenytoin. No surgical intervention was recommended. Taenia solium antigen and antibody tests came back negative.
DISCUSSION: Internists see patients with seizures on almost a daily basis, and in this country seizures secondary to neurocysticercosis are not on the top of our differential. However, 50 million people worldwide have cysticercosis caused by ingestion of the egg stage of Taenia solium. Once the eggs hatch within the intestine, the oncospheres invade the bowel wall and disseminate hematogenously. There is involvement of the CNS 60–90 % of the time. The intraventricular involvement occurs in only 7–20 % of patients. Although the primary infection does not commonly occur in the United States, we still encounter neurocysticercosis in immigrants from Central and South America. Diagnosis of neurocysticercosis is generally made based off of clinical suspicion and imaging. Our patient was from Mexico and had a history of worm infestation. The two calcifications in the cerebral cortex and cystic lesion within the 4th ventricle confirmed our suspicion of neurocysticercosis. Although the serology testing was negative for both antigen and antibody to T. solium, this is most likely due to the fact that the primary infection was over 30 years ago and the cysts appeared calcified rather than active. The transitory obstructive hydrocephalus can most likely be explained by a migratory scolex within the fourth ventricle that at time migrated to obstruct the outflow of the cerebral aqueduct. Bruns’ syndrome describes this ball-valve mechanism that results from a migrating cyst during a change in head position. Our patient’s seizure episodes have always occurred at night or in the early morning when the patient was supine leading us to believe that scolex repositions itself during this time resulting in obstructive hydrocephalus and seizures. Treatment of neurocysticercosis includes destruction of the parasite and prevention of seizures. Albendazole is the antiparistic drug of choice and it is strongly recommended to use corticosteroids concurrently to prevent inflammation and further brain damage. The location of the intraventricular cyst within the fourth ventricle prevented it from being accessed by rigid endoscope. Therefore, open resection would be the only way to remove the cyst, which was considered inappropriate at this time as the risks outweighed the benefits. Treatment with albendazole and corticosteroid was also considered to try and shrink down the scolex, but other attempts in the literature have shown inconsistent efficacy and poor outcomes. Since the patient has only had four seizure episodes and this was the only confirmed case of transitory hydrocephalus, it was elected to begin phenytoin to increase the seizure threshold until such time when more rigorous therapy may be indicated.
BREAKING BAD: THE IMPORTANCE OF RECOGNIZING PHYSICIANS IMPAIRED BY SUBSTANCE ABUSE DISORDERSRebecca Glassman; Howard Libman; Erina Matsumoto. Beth Israel Deaconess Medical Center, Boston, MA. (Tracking ID #1925951)
LEARNING OBJECTIVE 1: Understand the epidemiology of substance abuse among physicians in the United States
LEARNING OBJECTIVE 2: Identify resources available for health care professionals with substance abuse disorders
CASE: A 54-year-old physician with a history of HIV infection and depression presented to the emergency room with altered mental status, after failing to arrive at his medical office. He was somnolent and minimally responsive, and laboratory studies were noteworthy for a toxicology screen positive for amphetamines. He was admitted to the intensive care unit for further management. Overnight, the patient was treated with lorazepam for agitation. When interviewed the following day, the patient communicated that he had used crystal methamphetamine the night prior. He was encouraged to seek help through the Massachusetts’ Physician Health Services, and expressed that he had been told to do so by several previous providers. He also reported a recent admission to a nearby psychiatric hospital for suicide attempt while under the influence of methamphetamine. Given evidence of repetitive abuse and failure to follow through with Physician Health Services, a report was sent to the Massachusetts State Medical Board.
DISCUSSION: The prevalence of substance abuse among health care providers is an estimated 6–8 %, similar to the general population but concerning given the level of responsibility placed in their hands. Studies have shown that large workloads and chronic work-related stress lead to early burnout among physicians. To counter-act the effect on mental health, physicians have been found to abuse drugs for performance enhancement (stimulants) and for self-treatment of pain, anxiety, and depression (opioids and benzodiazepines). In 1973, the American Medical Association published a report entitled “The Sick Physician,” which brought to light the prevalence of physician impairment secondary to substance abuse and prompted the creation of state and local programs. All 50 states now have impaired-physician programs sponsored by the state medical society aimed at providing physicians with rehabilitative services. In Massachusetts, this program is called Physician Health Service. It is independent of the state licensing boards and therefore free of punitive action unless the practitioner does not comply with treatment guidelines. For those who do not comply or have a severe enough disability to compromise their professional activities, state medical boards should be informed for both ethical and legal reasons. It is important to recognize the services available to physicians with substance abuse issues so that they can receive treatment early before endangering their patients.
BROADEN YOUR DIFFERENTIAL! LYME AS THE NEW “GREAT IMITATOR”Brin Freund; Abby Spencer. WPAHS, Pittsburgh, PA. (Tracking ID #1932217)
LEARNING OBJECTIVE 1: 1. To recall Lyme disease in patients with neurologic signs and symptoms.
LEARNING OBJECTIVE 2: 2. To outline the presentation of nervous system Lyme, neuroborreliosis. 3. To revisit the importance of thorough history taking and examination and re-evaluation of unsuccessful treatments.
CASE: A 64 year old male without significant medical history presented to the emergency department (ED) in June status post ground level fall with fever, testicular pain, headache, sore throat, malaise, cough, nausea, and abdominal pain. Neurological exam and labs were unremarkable. Discharge diagnosis was viral syndrome. He followed up with his primary care physician with cough and an annular truncal rash thought to be secondary to pertussis. Azithromycin and Robitussin AC were prescribed. He presented to the ED the following month with persistent testicular pain. He was evaluated by urology and prescribed Percocet for pain and antibiotics for epididymitis. Within a month he had three additional ED visits for persistent testicular and abdominal pain, constipation, bloating, weight loss, anorexia, and urinary retention. Repeat imaging demonstrated ileus versus constipation, possibly opiate induced. He decreased opiate intake during this time. Review of systems did not note presence or absence of neuropathy. Neurological exam was not documented. Colonoscopy showed possible ileus and impacted stool. Opiates were discontinued. Over a few weeks, his gastrointestinal symptoms persisted and he presented to another primary care physician. At this point, he also reported back and hip pain with leg weakness. He reiterated recurrent falls and was using a walker for balance. He reported terrible withdrawal symptoms from stopping the opiates and was overall miserable. Neurological exam elicited decreased reflexes and hip flexion strength with sensory deficits in the thigh and dorsal foot, right greater than left. Thoracolumbar MRI showed moderate spinal stenosis and disc disease. This prompted referral to neurosurgery who confirmed that findings did not support his symptoms and clinical exam. The neurology team was consulted and performed neurodiagnostics.. EMG demonstrated right-sided motor polyneuropathy in L2-L4. Extensive workup produced positive lyme serology in serum and CSF. He was admitted for LP and high dose Ceftriaxone was initiated. Near-complete resolution of gastrointestinal, testicular, and neurological symptoms was seen at 3 weeks. He walked into his hospital follow-up appointment with his primary care physician with full strength and no complaints.
DISCUSSION: Roughly 30,000 cases of Lyme disease are diagnosed in the U.S. yearly. Presenting signs and symptoms can be non-specific and involve nany organ systems. Although not commonly associated with Lyme, testicular involvement has been noted in the literature and discomfort is usually due to swelling and pain. About 10–20 % of Lyme cases involve the nervous system. Cranial and peripheral neuropathies and meningitis are well-known presentations in the U.S. Radiculopathy is more common in Europe as part of an infrequently encountered entity, Bannwarth syndrome. Sensory and motor symptoms are common. Autonomic involvement is less cited. Back and neuropathic pain are common, often overshadowing neurological deficits. As a result, workup is usually exhaustive before considering Lyme as the etiology of radiculopathy. Diagnosis of Lyme disease requires two-tiered antibody testing. CSF serology confirms central nervous system involvement. Imaging can delay diagnosis as it often demonstrates incidental and clinically insignificant findings but is one of the first tests ordered to workup radicular symptoms. Neuromuscular studies are necessary to pinpoint lesions and help guide further testing for etiology. Antibiotics are the standard treatment of Lyme. Oral medications are sufficient for early non-disseminated disease. However, when involving the central nervous system IV therapy is prescribed. Ceftriaxone is often the preferred agent in the US. This patient presented with multiple complaints all of which were at first attributed to opiate use. Given the multiple visits to the ED with persistent and worsening symptoms despite discontinuation of opiates, the diagnosis could have been re-considered and the patient re-evaluated more comprehensively. This case illustrates that plans of care should be re-assessed when symptoms persist despite initiating adequate treatment. By completing a thorough review of systems and physical examination while keeping a broad differential in mind, diagnoses may be missed less often.
BRUCELLOSIS IN A TRAVELER WITH FEVER AND KNEE PAINThuyet Ho. University of California, San Diego, San Diego, CA. (Tracking ID #1935253)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of brucellosis and the necessary evaluation to rule out complications.
LEARNING OBJECTIVE 2: Treat brucellosis in a patient who does not have access to home antibiotic infusion.
CASE: A 17 year old Kuwaiti man with no significant past medical history presented with 1 week of fever, diaphoresis, malaise, and left knee pain. The patient was visiting his brother-in-law in California for the past 3 weeks; he reported he was in his usual state of health until the onset of fevers and diaphoresis occurring 1 week prior. Then he woke up with acute left knee pain on the day of presentation. Physical exam showed significant sweating with mild swelling and severe tenderness to palpation of the left knee. Labs demonstrated mild transaminitis, thrombocytopenia, and coagulopathy. After an arthrocentesis and pan-culture were performed, intravenous Vancomycin was started empirically. A more thorough history revealed travels around the Saudi peninsula, exposure to birds, no recent sexual contact, and ingestion of unpasteurized camel milk several months prior to presentation. Repeat exam revealed a I/VI systolic murmur at the left lower sternal border and tenderness now localized to the pes anserine bursa. The bursa was aspirated and sent for culture. Patient remained intermittently febrile with minimally productive cough and generalized aches and pain. Thrombocytopenia and transaminitis continued to worsen. In the setting of camel milk ingestion, doxycycline was added given the suspicion for brucellosis. By the third day, blood cultures grew gram negative bacilli and pes anserine bursa eventually grew Brucella melitensis. Patient’s clinical symptoms improved when the antibiotics regimen was transitioned to oral doxycycline and intravenous gentamicin. Negative transthoracic echocardiography and MRIs of the spine and left leg ruled out endocarditis, spondylitis and osteomyelitis, respectively. Hepatitis serology, HIV, CMV serology, Cryptococcal antigen, malarial smear, and tuberculosis screen were negative as well. Ideally the patient would be sent home on doxycycline and intravenous gentamicin. However, due to his status as a visiting foreigner, he did not qualify for home infusion service. He was discharged on oral doxycycline and rifampin for at least 6 weeks with arrangement to follow up in infectious disease clinic in Kuwait.
DISCUSSION: Brucellosis is a zoonotic infection which can present in a broad clinical spectrum. It is transmitted to humans by contact with infected animal fluids or derived food products. This case illustrates the initial diagnosis and work up of fever in a traveler from the Middle East. When the risk factor of unpasteurized camel milk ingestion was identified in the setting of high grade fever and liver dysfunction, the focus was narrowed to brucellosis. It is important to recognize that Brucella may cause focal infection of any organ system. In this case, it was necessary to rule out endocarditis due to the murmur and positive blood culture, spondylitis due to back pain, and osteomyelitis due to bursa infection as these findings would change the course of treatment. Finally, it is important to know that treatment with oral doxycycline for 6 weeks and intramuscular streptomycin or intravenous gentamicin for 2 weeks is first-line therapy. However, if a patient does not have access to home infusion, then at least 6 weeks of oral rifampin can be substituted for the aminoglycoside. Relapse and treatment failure are not uncommon. Patients should be educated on avoiding risks for contracting Brucella and should follow up closely to monitor for relapse or treatment failure. In this case, it was important to have an Arabic interpreter by bedside to educate and engage the patient in treating this disease.
CALCIPHYLAXIS IN A PATIENT WITHOUT RENAL FAILUREAllison J. Kwong; Joseph Ebinger; Peter Hanna; Matthew Spinelli; Paul D. Blanc. University of California, San Francisco, San Francisco, CA. (Tracking ID #1937191)
LEARNING OBJECTIVE 1: To recognize, diagnose, and treat calciphylaxis in a patient with normal renal function.
CASE: Our patient is a 65-year-old Hispanic woman with a history of insulin-dependent diabetes mellitus, seronegative rheumatoid arthritis on methotrexate, and paroxysmal atrial fibrillation on warfarin, who presented to her primary care clinic with hyperpigmentation of her bilateral lower extremities, which progressed over the next 8 months to a symmetric livedoid rash. An outpatient skin biopsy of her right leg was performed but initially non-diagnostic. In the month following her biopsy, she began to describe intense pain at the biopsy site, where she had developed retiform purpura and associated ulceration. She was referred for admission to our medical center for expedited workup and symptom control. Slides from her prior skin biopsy were re-reviewed. Based on her clinical picture and histopathologic findings of intravascular and extravascular calcium deposition, a diagnosis of non-uremic calciphylaxis was made, most likely due to the use of warfarn. She had a normal creatinine, parathyroid hormone, vitamin D level, calcium, phosphorus, and calcium-phosphate product. Warfarin was withdrawn, and rivaroxaban was started in its place for primary stroke prevention given her history of atrial fibrillation. In consultation with our dermatology colleagues, we elected to treat her calciphylaxis with infusions of sodium thiosulfate 25 g three times weekly for 8 weeks. With this therapy, she experienced marked clinical improvement and resolution of the ulcer.
DISCUSSION: Calciphylaxis is most often associated with renal disease or abnormal parathyroid function, which cause derangements in calcium and phosphorus levels. These can lead to pathologic vascular calcification and microvascular occlusion, and thus the severe pain of cutaneous calciphylaxis and a high mortality due to sepsis. Non-uremic calciphylaxis exhibits these same histopathologic features of arteriolar calcification and microthrombi; however, the underlying pathophysiology has yet to be elucidated. It is an exceedingly rare, though increasingly recognized entity, associated in existing case series with female sex, white race, and obesity. Hypoalbuminemia, the use of warfarin or glucocorticoids, liver disease, and hypercoagulability have been identified as risk factors. Conventional therapies for calciphylaxis focus on the regulation of calcium and phosphorus levels with phosphate binders, cinacalcet, dialysis, and even parathyroidectomy, but these interventions are irrelevant in patients with normal renal function and electrolytes. Sodium thiosulfate—currently approved only for cyanide poisoning—is also thought to have some role in the chelation of calcium. It has recently emerged as an effective, off-label treatment option for calcific uremic arteriolopathy. Sodium thiosulfate has since been applied in non-uremic calciphylaxis with similar success, though the existing literature is still limited to observational data in fewer than 10 patients. The medication is generally well-tolerated, its main complications being nausea, vomiting, and an anion gap metabolic acidosis. Our patient developed self-limited episodes of atrial fibrillation related directly to her infusions; these were ultimately controlled with beta-blockade and a slower infusion rate. Alternate medications, such as bisphosphonates and cinacalcet, have also been proposed in the literature for the treatment of non-uremic calciphylaxis, but to date, sodium thiosulfate appears to be the most promising. In conclusion, we describe a case of warfarin-induced calciphylaxis, successfully treated with sodium thiosulfate, and aim to increase awareness of this rare diagnosis and its treatment in non-traditional patients.
CALCIPHYLAXIS OF EVILCatherine Trimbur1; Simon Hong2. 1Montefiore Medical Center, Bronx, NY; 2Montefiore Medical Center, Bronx, NY. (Tracking ID #1939009)
LEARNING OBJECTIVE 1: Recognize the clinical presentation and pathogenesis of calciphylaxis (calcific uremic arteriolopathy)
LEARNING OBJECTIVE 2: Understand the treatment and prognosis for patients with calciphylaxis
CASE: A 35 year-old woman with a history of diabetes and end-stage renal disease on hemodialysis presented with 4 days of nausea, vomiting, and bilateral flank pain. On admission, she was noted to have fever of 100.6 F, WBC of 16.4 and non-contiguous, hyperpigmented, indurated lesions on the left lower quadrant of her pannus, bilateral thighs, and right flank. The skin was exquisitely tender to light tough but not warm or erythematous. Labs revealed Ca of 7.9, Ph of 6.2 and PTH of 198. Patient was started on empiric antibiotics for cellulitis, without improvement. Biopsy of the site showed subcutaneous microvascular calcification and thrombosis. Diagnosis of caliphylaxis was made. The area biopsied did not heal in subsequent days, and she developed a black eschar. The patient was started on IV sodium thiosulfate with dialysis, a phosphate binder, calcimimetic and pain management. On discharge, she continued to have progression of lesions with areas of blackened skin necrosis.
DISCUSSION: Calciphylaxis, or calcific uremic arteriolopathy (CUA), is a rare disorder characterized by painful ischemic cutaneous necrosis on areas of skin with high adiposity. First described in 1898 by Bryant and White, then elaborated in animal models by Hans Selye in 1962, CUA has increased in incidence as a result of higher rates of end stage renal disease and raised awareness. The proposed mechanism of pathogenesis is mural calcification of arterioles of the dermo-hypodermic layers leading to intimal fibrosis of arterioles. The resultant arteriolar narrowing leads to decreased flow states, causing thrombus formation. Thrombi obstructing flow in the vasculature of the dermis is what ultimately leads to necrotic ulceration of the skin. Often associated with end stage renal disease, pathogenesis is thought to involved dysregulation of parathyroid, vitamin D, phosphate and calcium levels, as calcium-phosphate product (CPP) puts patients at increased risk for calcification. However, elevated CPP is neither sensitive nor specific and many patients with CUA have normal calcium and parathyroid levels, suggesting deeper levels of pathogenesis not yet elucidated. Patients with CUA generally present with exquisitely painful areas of skin necrosis, commonly on the abdomen, buttock and thigh, though can occur elsewhere. The initial decrease in blood flow as a result of intimal thickening leads to livedo reticularis and plaque-like subcutaneous nodules, which are usually signs of early disease. As blood flow continues to diminish and thrombi form, complete occlusion of vessels lead to ischemic ulceration, often leading to eschars that are highly susceptible to superinfection. This presentation often leads to delayed diagnosis of CUA, as it appears to be a skin infection. While diagnosis can be made via skin biopsy or clinically, biopsy is often avoided due to poor wound healing and risk of infection. Prognosis of CUA is extremely poor, with a progressively worsening clinical course. One year mortality rates approach 46 % and are higher if infection develops. Due to low incidence, there are no randomized controlled trials establishing treatment plan, but treatment is generally aimed at reducing CPP and PTH levels, wound care, including surgical debridement, and pain control.
CANDIDA TROPICALIS INFECTION IN A PATIENT WITH ESRDShenelle-Marie Wise; Kate Hust. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926150)
LEARNING OBJECTIVE 1: Recognize the clinical manifestations of and risk factors for candidemia, and initiate appropriate evaluation for disseminated disease.
LEARNING OBJECTIVE 2: Compare and contrast the prevalence, virulence and treatment of Candida tropicalis to Candida albicans and other non-albicans species
CASE: A 22-year-old man presented with 1 week of fevers, nausea and vomiting. He was febrile to 101° Fahrenheit but alert, oriented, and able to discuss his full medical history, which included end-stage renal disease with an indwelling hemodialysis catheter. Given his elevated white blood cell count, fevers, and tachycardia, he was admitted with sepsis. Over the following days his mental status gradually declined, and he was unable to respond to questions or follow commands. Blood cultures drawn on admission grew Candida tropicalis. Echocardiogram revealed vegetations on the aortic and tricuspid valves. MRI revealed multiple small lesions consistent with septic emboli in the frontal lobe, parietal lobe, and cerebellum.
DISCUSSION: Candidemia is an important cause of nosocomial bloodstream infections encountered by hospitalists. The clinical manifestations of candidemia vary from minimal fever to full-blown sepsis that is indistinguishable from severe bacterial infection. Invasive candidiasis is defined by hematogenous spread to multiple viscera (e.g., eye, kidney, heart valves, brain). The susceptibility to candida is increased in patients with indwelling catheters. Patients with end stage renal disease are further at risk for infection because of impairment in cell-mediated immunity and granulocyte function. Candidemia is diagnosed with fungal blood cultures, but additional studies should be considered to evaluate for disseminated disease. Due to risk for invasive infection, all patients with candidemia should undergo an ophthalmologic examination, even in the absence of ocular symptoms, to evaluate for endophthalmitis or chorioretinitis. Echocardiogram is recommended to evaluate for endocarditis. Central intravenous catheters should be removed in these patients as it leads to more rapid clearance of fungemia. Higher mortality has been documented when catheters remain in place despite treatment with an anti-fungal agent. Although C. albicans is the most common cause of candidemia, there has been increased isolation of non-albicans species of Candida in recent years. This has been due to the increasing numbers of immunocompromised patients, long-term use of in dwelling catheters, and the use of broad-spectrum antibiotics. In the US, the most prominent strains have been C. tropicalis, C. glabrata, C. parapsilosis, and C. krusei. Clinical and experimental observations have suggested that morbidity and mortality rates are higher for the non-albicans species of Candida compared to C. albicans. This is likely secondary to emerging anti-fungal resistance and increased infections in the immunocompromised patients. C. tropicalis has shown a moderate level of fluconazole resistance but is usually susceptible to amphotericin B and the echinocandins. The choice of anti-fungal therapy depends on relevant comorbidities, evidence of multi-organ involvement, history of recent azole exposure, and local prevalence of different Candida species. Fluconazole is the standard therapy for clinically stable therapy without risk factors for resistance. Therapy may be escalated to echinocandins in patients who are neutropenic and/or unstable and in those with risk factors for azole-resistance. For patients at risk for echinocandin resistance (eg, prior recent exposure to an echinocandin), or who develop candida endorcarditis, amphotericin B should be used until anti-fungal susceptibility testing results are available. Treatment duration is usually 2 weeks in patients without end organ involvement. In patients with candidal endophthalmitis, a 6-week duration is required, and with candidal endocarditis valve replacement is required along with 6 weeks of antibiotics.
CANNABINOID HYPEREMESIS SYNDROME - TRULY AN OXYMORON!Sathish kumar Krishnan; Hitu Khaira; Venu M. Ganipisetti. St. Francis Hospital, Evanston, IL. (Tracking ID #1926420)
LEARNING OBJECTIVE 1: Recognize cannabinoid hyperemesis syndrome (CHS) is characterized by episodic vomiting, abdominal pain and compulsive hot showering in chronic marijuana users.
LEARNING OBJECTIVE 2: Identify that the rarity of this condition can cause a diagnostic confusion leading to expensive and extensive investigations with a delay in treatment.
CASE: A 32 year old male presented to the emergency department (ED) with a three-day history of nausea, 10–15 episodes of vomiting a day and colicky abdominal pain. He denied eating anything out of the ordinary, sick contact or travelling recently. He denied any alcohol, tobacco or illicit drug use. Vitals were normal. On physical exam, his abdomen was soft and he had mild diffuse tenderness. There was no guarding or rigidity. Murphy’s sign was negative. Complete blood count, comprehensive metabolic panel, amylase and lipase were within normal limits. He was treated with intravenous fluids, morphine and anti-emetics. He had been hospitalized five times in the previous 2 years for similar symptoms. During this period, five CT scans and three ultrasound scans of the abdomen, and an esophagogastroduodenoscopy (EGD) were performed, all of which were normal. In one of those encounters, he had reported smoking marijuana. During this admission, he spent most of his day in the shower. When questioned, he reported symptomatic relief with hot showers. A urine toxicology screen was performed which was positive for cannabinoid. A diagnosis of cannabinoid hyperemesis syndrome was established. But, the patient left against medical advice. Two months later, the patient presented with same complaints and his urine toxicology showed cannabinoid. It was explained that marijuana was the cause of his symptoms and he was advised to abstain from smoking marijuana. On follow up in 5 months, he remained free of symptoms.
DISCUSSION: Marijuana is well known for its anti-emetic effect. Paradoxically, chronic use results in hyperemesis. The pathogenesis remains obscure. Patients are typically young adults with a long history of cannabis use. They present with recurrent episodes of nausea, vomiting, and dehydration. The exact incidence and prevalence are unknown. It is likely that this condition is under-recognized and under-diagnosed. Patients usually remain misdiagnosed for a considerable period. In one case series, the average number of ED visits was 7, prior to diagnosis. The lack of understanding and the delayed diagnosis can lead patients to self-medicate with the very substance that is causing the symptoms. As such, patient education is critical. The most intriguing component is the compulsive hot showering and is present in nearly all cases. When questioning a patient’s social history, it may be worthwhile to inquire about hot showering patterns, especially in those who deny their use of illicit drugs. It has been proposed that hot bathing may act by correcting the cannabis-induced disequilibrium of the thermoregulatory system in the hypothalamus. Hence, it is important to recognize CHS as it may be misdiagnosed as psychogenic vomiting or ‘drug seeking behavior’. It can prevent invasive and unnecessary workups, and lead to reduction in health care costs and morbidity.
CARBON MONOXIDE POISONING: A DIAGNOSIS NOT TO BE MISSED!Runa Shrestha1; Rajesh Mourya2; Brian A. Changlai1. 1SUNY Upstate Medical University, Syracuse, NY; 2Creighton University, Omaha, NE. (Tracking ID #1935530)
LEARNING OBJECTIVE 1: Carbon monoxide (CO), an odorless, colorless, tasteless gas, is formed by incomplete combustion of hydrocarbon from wood or fossil fuels. CO poisoning is the leading cause of poisoning deaths in the United States and often attributed to poor ventilation and malfunctioning machinery. The vague and variable manifestation with which it presents makes CO poisoning a diagnostic challenge.
CASE: A 61-year-old male, with history of hypertension, was brought to the emergency department by his co-workers when he was found to be unresponsive at work. He had been driving a forklift around a small enclosed warehouse for 3 h and developed a mild headache and dizziness before passing out. In the emergency department, he regained consciousness; however he complained of severe headache and unsteadiness. On examination, his vitals were stable but he was lethargic, ataxic and had facial flushing. Meningeal signs were absent. Diagnostic tests including complete blood count, basic metabolic panel, liver function test, ammonia level, coagulation panel and cardiac injury panel were within the normal limit. Electrocardiogram, chest x-ray and computed tomography of the head were normal. Carboxyhemoglobin level turned out to be 36 % (normal range is 0.2 to 6.5 %) and the patient was diagnosed with acute, severe CO poisoning, placed on 100 % oxygen via face mask and was immediately transferred to higher center for hyperbaric oxygen therapy (HBO). After 2 sessions of hyperbaric oxygen therapy, each of 90 min, there was complete resolution of the neurological symptoms. Repeat carboxyhemoglobin level after the hyperbaric oxygen therapy was 1.6 %. The patient was discharged home the next day without any neurological sequelae.
DISCUSSION: The manifestation of CO poisoning can be non-specific, ranging from mild headache to seizure, myocardial ischemia and coma, and may mimic any type of cardio-neurological disease. Due to the high affinity of carbon monoxide to hemoglobin, CO poisoning leads to severe impairment of tissue oxygenation resulting in end-organ damage and can be fatal if undetected or misdiagnosed. The diagnosis is suggested by a history of exposure to smoke or combustion products and a physical examination revealing insult to the nervous system. It is confirmed with an elevated carboxyhemoglobin level. Physicians should always consider hazardous environments as a possible etiology of a patient’s condition. Early detection and initiation of treatment with 100 % oxygen delivery and removal of the source improve morbidity and mortality. Patients exhibiting signs of severe poisoning (altered mentation, CO level more than 25 %, end organ damage) should be treated with HBO therapy. Public education and CO detectors are important prevention measures.
CARCINOID SYNDROME MASQUERADING AS AN ACUTE CORONARY SYNDROMEAjay Dharod; Peter R. Lichstein; Ramon Velez. Wake Forest Medical Center, Winston Salem, NC. (Tracking ID #1927139)
LEARNING OBJECTIVE 1: Identify clinical symptoms of carcinoid tumors recognizing that symptoms only occur with hepatic and pulmonary carcinoids.
LEARNING OBJECTIVE 2: Recognize cardiac involvement occurs in up to 50 % of patients with carcinoid syndrome.
CASE: Ms. R, a 48 year old non-smoking Caucasian female with hypertension, diabetes mellitus, hepatitis C, hyperlipidemia and anxiety, presented to the emergency room with 10/10, heavy, non-radiating, mid-sternal chest pressure that began while doing the dishes. She immediately took both alprazolam and Aspirin 325 mg without relief. She also complained of new-onset dyspnea, nausea without vomiting, dizziness, lightheadedness, diaphoresis, facial flushing, intermittent diarrhea, and rigors. A home blood pressure cuff revealed readings of 200 s/110 s. Her mother and sister both suffered from fatal myocardial infarctions and her brother underwent CABG. Her pain was initially 10/10 but improved with nitroglycerin in the ER. Vital signs revealed blood pressure 179/110 and pulse 130. On physical exam, Ms. R had facial flushing, wheezing throughout all lung fields and pitting edema at her ankles. EKG, high-sensitivity troponin-I and CXR were unremarkable aside from sinus tachycardia. Labs were notable for AST 129 and ALT 104. Morning cortisol, TSH, BNP, lipid profile, and HbA1c were normal. Renal artery duplex was unremarkable. CT PE ruled out pulmonary embolism but revealed an incompletely characterized enhancing mass in the liver. Abdominal MRI revealed a hypervascular mass centered within the caudate lobe concerning for hepatocellular carcinoma in the setting of background hepatomegaly and hepatic steatosis. Fine needle aspiration of the liver mass revealed a low-grade metastatic neuroendocrine tumor. 24 h-Urine 5HIAA (hydroxyindoleacetic acid) was 15.0 (Ref <6), Chromogranin A was 154 (Ref <15), 5-Hydroxytryptamine was 97 (Ref 26–265) and 24 h-Urine VMA (Vanillyl Mandelic Acid) was 2.0 (Ref <6). She was diagnosed with carcinoid syndrome. Octreotide scan did not locate a primary. The mass was deemed unresectable given close proximity to the inferior vena cava. She underwent chemoembolization complicated by bronchospasm, flushing, initial hypertension with subsequent hypotension and cardiomyopathy with EF 37 %, elevated right heart pressures and tricuspid regurgitation requiring intubation. After recovery, adenosine stress revealed no-inducible ischemia, EF 56 % and pliable tricuspid valve. She underwent second chemoembolization and, despite octreotide premedication, again required intubation. Post recovery, she underwent radiation of the carcinoid liver tumor. Ms. R suffered with continued diarrheal symptoms after her chemoembolization which improved with Somatostatin analogue treatment. She had no further episodes of chest pain.
DISCUSSION: Clinical symptoms (flushing, diarrhea, bronchoconstriction and telangiectasias) arise in patients with hepatic and pulmonary carcinoids secondary to secretion of vasoactive substances directly into the central venous system, bypassing hepatic metabolism (Moller JE, 2003; Fink, 2001). In Ms. R’s case, the presence of hepatic metastases allowed for her presentation with neuroendocrine crisis (flushing, bronchoconstriction, hypertension & hypotension). Chest pain has been reported in 1–19 % of patients and coronary artery spasm may occur during flushing episodes (Hage, 2003; Powell, 2011). Interestingly, chromogranin A concentration is an independent predictor of long-term mortality and heart failure hospitalizations in patients with acute coronary syndromes (Jansson, 2009). To our knowledge, there is no literature describing a direct relationship between carcinoid syndrome and acute coronary syndromes. Vasoactive substances cause cardiac valve leaflet fibrous endocardial plaques, classically on the tricuspid and pulmonary valves (Farb, 2000; Otto CM, 1999). Right-sided heart failure with worsening dyspnea, edema, ascites and cardiac cachexia occur with progressive disease (Moerman, 2012). Ms. R’s presentation of carcinoid crisis with bronchospasm, hypertension and hypotension twice in the setting of tumor ablation may relate to an acute exacerbation of underlying progressive right heart failure. Hypertensive carcinoid crisis is rare with few case-reports in the literature. Carcinoid hypertensive crisis typically occurs peri-operatively related to the stress of anesthesia and surgery by an unclear mechanism. Both hypertensive and hypotensive carcinoid crises can be managed with pre-, intra-, and post-operative Octreotide treatment (Yates, 2010; Warner, 1994). Overall prognosis is poor with mean survival of 1–2 years post diagnosis. Treatment is directed at medical therapy for right heart failure and treatment of hepatic metastasis with systemic chemotherapy, chemoembolization, radiofrequency ablation, and surgical resection if possible. Somatostatin analogues, serotonin antagonists, and alpha-adrenergic blockers provide partial symptomatic relief (Oberg, 2004; Strossberg, 2011; Strossberg, 2013).
CARDIAC TAMPONADE AS THE INITIAL PRESENTATION OF UNDIAGNOSED LUNG CANCERHirva Mamdani; Dipenkumar Modi; Theresa Vettese. Wayne State University, Detroit, MI. (Tracking ID #1939146)
LEARNING OBJECTIVE 1: To recognize cardiac tamponade as a possible initial presentation of underlying malignancy especially in high risk patients
LEARNING OBJECTIVE 2: To recognize the importance of good history and physical exam in the diagnosis of cardiac tamponade
CASE: A 59 years old African American man with extensive smoking history presented with complaints of exertional shortness of breath and dry cough of 1 month duration. He also had unintentional loss of about 10 lbs over 2 months prior to presentation. He did not have any fever, chills, night sweats, orthopnea, or PND. He also did not have any prior history of or exposure to tuberculosis or incarceration. On admission, he was found to be afebrile, but hypotensive (90/60), tachycardic (113), and tachypneic (respiratory rate 22/min). On physical exam, he was in mild distress, had jugular venous distension, muffled heart sounds, and diminished breath sounds on the left. EKG showed sinus tachycardia with low voltage QRS complexes. A bedside echo showed large pericardial effusion, diastolic collapse of right atrium and ventricle with paradoxical septal motion, and plethoric inferior vana cava. The patient was diagnosed with cardiac tamponade and was immediately taken for pericardiocentesis with removal of about 800 cm3 of hemorrhagic fluid. Lab studies were remarkable only for mild normocytic anemia. The patient showed significant hemodynamic and symptomatic improvement. Subsequently pericardial fluid cytology returned back positive for malignant cells concerning for adenocarcinoma. Subsequent CT thorax showed a left sided lung mass with left pleural effusion. Finally the patient was diagnosed with adenocarcinoma of lung with CT guided biopsy.
DISCUSSION: Malignant involvement of the pericardium is not an uncommon phenomenon, especially in patients with lung cancer, breast cancer, lymphomas, leukemias, and melanomas. It can manifest as pericardial effusion, cardiac tamponade, or constrictive pericarditis. Cardiac tamponade as the first clinical presentation of the underlying yet undiagnosed malignant process is uncommon. There have been a few case reports and small case series reporting lung cancer, breast cancer, adenocarcinoma of Fallopian tube, soft tissue sarcomas, primary cardiac sarcoma, metastatic hepatocellular carcinoma, and renal cell cancer presenting with cardiac tamponade secondary to malignant pericardial effusion. Having a high index of suspicion from history (including risk factors for malignancy) and physical exam as well as initial imaging studies are of utmost importance in timely diagnosis of the nature of the disease. Physical exam features of hypotension, tachycardia, pulsus alternans, pulsus paradoxus, distended neck veins, positive Kusmaul’s sign, and muffled heart sounds are important diagnostic clues. EKG is usually low voltage and may show electrical alternans. Echocardiography shows pericardial effusion along with diastolic collapse of the right sided heart chambers, increased respiratory variation in the peak mitral and tricuspid inflow velocities, and IVC dilatation. Initial therapeutic intervention with pericardiocentesis and/or pericardial window placement allows for rapid symptomatic relief. Fluid cytology is very useful in detecting the presence of the malignant cells and the nature of the underlying malignancy. However, its clinical utility is limited by its low sensitivity. Long term management is largely dependent on the extent and histologic features of the underlying malignant conditions. Different treatment options include systemic chemotherapy and/or radiotherapy in case of sensitive tumors such as lymphoma, leukemia, or breast cancer. Local sclerotherapy with intrapericardial instillation of various sclerosing agents such as tetracycline, bleomycin, or cisplatin can also be attempted. In some cases, pericardiectomy is necessary to prevent recurrent malignant pericardial effusion. In most of the cases, the condition is usually incurable and above modalities only offer palliation.
CASEATING GRANULOMAS, TB OR NOT TO TB?Bishr Alhafez; Arati K. Kelekar. Oakland University William Beaumont School of Medicine, Huntington Woods, MI. (Tracking ID #1939071)
LEARNING OBJECTIVE 1: To expand the possibilities in the differential diagnosis of caseating granulomas
CASE: A healthy 64 year old male with no significant past medical history presented with one episode of hemoptysis. He also complained of 3 weeks of left sided chest pain. He denied any history of fever, chills, night sweats, weight loss, dyspnea, palpitations, dizziness, or cough. The patient was not a smoker. He was a war veteran. Laboratory studies showed a mild neutrophilia. A chest X-ray revealed a large left upper lobe mass. A computerized tomography of the chest confirmed the presence of a 10 cm mass in the upper lobe of the left lung. Tissue analysis of a specimen obtained through transbronchial biopsy showed caseating granuloma with lamellated fibrous capsules and epithelioid histiocytes with central necrotic debris. No atypical or malignant cells were seen. This histology raised concern for tuberculosis. However, sputum culture for AFB, QuantiFERON testing and AFB staining of the biopsy tissue were all negative. A suspicious looking osseous lesion in the T6 vertebral body was biopsied. It revealed high-grade malignant spindle and epithelioid cell neoplasm. He was started on radiation therapy and received two cycles of chemotherapy with gemcitabine and docetaxel.
DISCUSSION: Primary lung sarcomas are rare and compromise less than 1 % of all primary lung tumors. They are associated with worse survival compared to other types of lung cancer. Epithelioid tumors are a rarer subtype of lung sarcomas. They are highly vascular and rapidly growing which predisposes them to tissue necrosis. This case raises the importance of considering lung sarcoma in the differential diagnosis of tuberculosis. It is prudent to suspect this diagnoses especially if the clinical presentation is not typical for tuberculosis.
CATASTROPHIC ANTIPHOSPHOLIPID SYNDROME IN A PATIENT WITH LUNG MALIGNANCYAakriti Gupta; Liam Zakko. Yale New Haven Hospital, New Haven, CT. (Tracking ID #1940029)
LEARNING OBJECTIVE 1: To learn about the clinical presentation of catastrophic anti-phospholipid antibody syndrome in the setting of malignancy
LEARNING OBJECTIVE 2: Review the importance of chart documentation, outpatient and inpatient physician communication, and chart review
CASE: Patient is a 67 year old lady with history of stage IIIA adenocarcinoma of the lung (diagnosed in 5/2013) who received 3 cycles carboplatin/paclitaxel and radiation treatment and extensive right lower extremity deep vein thrombosis (DVT) in 6/2013 that was anticoagulated with lovenox. As an outpatient, she was noted to have thrombocytopenia and her anticoagulation was held in 9/2013. Around the same time, she developed severe abdominal pain and significant diarrhea that lasted more than a week when she presented to the emergency department where she was febrile to 100.6 F with tachycardia. Exam was notable for subungual splinter hemorrhages, multiple erythematous macules and painful nodules in her palms and soles bilaterally. Laboratory tests revealed platelet count of 42000/cm3, mild transaminitis and hyperbilirubinemia. Chemistry panel was unremarkable (creatinine 1.0 mg/dl). Imaging of the abdomen showed mild ascending colitis as well as a non-specific heterogeneity in the liver. Infective endocarditis workup was unrevealing. We initiated antibiotics for infectious colitis. Her course over the ensuing week was complicated by worsening thrombocytopenia (11000/cm3), new infiltrate in right lung without fever or leukocytosis, new atrial fibrillation with ST depressions in V3-V6 leads and elevated cardiac enzymes. Finally, she developed acute kidney injury (creatinine 2.7 mg/dl) and oliguria with evidence of schistocytes on blood smear. At this time, chart review revealed that patient had been tested for antiphospholipid (aPL) panel in June as an outpatient that was markedly positive for anticardiolipin IgM, antiphosphatidylserine, beta-2-glycoprotein IgA, lupus anticoagulant and dilute viper venom test which were positive on repeat testing by us. Bone marrow biopsy revealed a large intravascular thrombus in the marrow. We diagnosed our patient with catastrophic antiphospholipid antibody syndrome (APS) thought to be triggered from discontinuation of anticoagulation and infectious colitis in the setting of lung malignancy with likely clot formation in the pulmonary vasculature, coronary arteries, liver, microvascular renal vessels, bone marrow, and microangiopathic hemolytic anemia. We treated her with anticoagulation, high dose steroids, plasmapheresis, IVIG, and rituximab with significant improvement in her organ function and her lab abnormalities including improvement in platelet count to 145000/cm3.
DISCUSSION: According to revised Sapporo criteria, definite APS is considered when there is presence of clinical evidence of vascular thrombosis/pregnancy morbidity (extensive DVT in our patient) AND serologic confirmation of aPL at least 12 weeks apart. Initially described in patients suffering from systemic lupus erythematosus, APS may occur in the setting of multiple autoimmune conditions and malignancies. Catastrophic APS is an accelerated form of this condition involving evidence of multiorgan involvement over a short period of time, laboratory confirmation of presence of aPL and histopathologic confirmation of small vessel occlusion, all of which were present in our patient. Manifestations commonly include thromboses in cerebral, pulmonary, cardiac, hepatic, or renal vasculature. Our patient was unique in having an intravascular thrombus in the bone marrow as well. Rapidly occuring and fulminant thrombotic complications seen in patients with malignancies should raise suspicion for catastrophic APS, and these patients may benefit from early and aggressive treatment of this often fatal syndrome. Treatment involves anticoagulation, plasmapheresis, pulse dose steroids and plasmapheresis, all of which our patient received. Finally, diagnosis and treatment of the patient was delayed since the initial diagnosis of APS was not documented in the chart. This case demonstrates the significance of thorough chart review and timely communication amongst the inpatient and outpatient providers.
CELLULITIS WITH AN ARRHYTHMIC TWISTAllison C. Heacock. The Ohio State University Wexner Medical Center, Columbus, OH. (Tracking ID #1939154)
LEARNING OBJECTIVE 1: Diagnose Brugada Pattern and Brugada Syndrome
LEARNING OBJECTIVE 2: Recognize provoking factors for Brugada Syndrome and indications for implantable cardioverter-defibrillator placement.
CASE: 43 yo male prisoner was admitted for left arm erythema, swelling and fever. He had received a prison tattoo 2 weeks prior to admission. Approximately, 10 days later he began to have swelling, erythema and decreased range of motion of his left elbow. He was treated with Bactrim but symptoms worsened and he developed a fever to 101° Fahrenheit. During review of symptoms the patient endorsed occasional substernal chest pressure occurring at rest with no associated symptoms. The pain was self-resolving. He denied any past medical history or surgical history. He was a former smoker. His cardiac family history was notable for coronary artery disease in his mother and maternal aunt and sudden cardiac death in a maternal uncle. He was taking no medications. On physical exam the patient was afebrile after receiving acetaminophen. He had left arm erythema and swelling of his elbow. The remainder of his exam was within normal limits including his cardiovascular exam. The patient was admitted and started on antibiotics. An electrocardiogram (ECG) was done due to his recurrent chest pain. This showed sinus tachycardia, incomplete right bundle branch block, “saddle back type” ST elevated in V2 with atypical ST elevation in lead V1 and V3. No t wave inversion. Troponins × 3 were normal. An ECG on hospital day two showed normal sinus rhythm with complete resolution of the RBBB and ST elevation. The patient was diagnosed with type 2 Brugada Syndrome, which was likely provoked by his fever. His ECG findings had resolved with defervescence of his fever. His chest pain was determined to be non-cardiac in origin and not secondary to his Brugada syndrome. The patient was discharged with anticipatory guidance including a list of medications and other Brugada Syndrome provoking factors to avoid.
DISCUSSION: Brugada syndrome is an autosomal dominant disorder characterized by typical ECG findings including right bundle branch block and ST elevation with increased risk for ventricular tachyarrhythmia and sudden cardiac death. Sudden cardiac arrest may be the initial presenting symptom in up to one third of patients. The typical ECG findings can also be found in asymptomatic patients without diagnostic clinical criteria and is defined as Brugada pattern. The typical ECG findings of type 1 Brugada pattern are “coved type” ST elevation with negative t waves in more than one right precordial lead (V1-V3). Type 2 is characterized by “saddle back type” ST elevation in more than one right precordial lead (V1-V3) with positive t waves. In order to diagnose a patient with Brugada syndrome as opposed to Brugada pattern they must have one of these typical ECG findings plus one of the following: History of documented ventricular tachycardia (VT) or ventricular fibrillation (VF), family history of sudden cardiac death at less than 45 years of age, family history of type 1 Brugada syndrome ECG changes, unexplained syncope, nocturnal agonal respiration or inducible VT during electrophysiology study. Our patient met criteria for Brugada syndrome due to his Type 2 Brugada ECG findings and family history of sudden cardiac death in his maternal uncle. There are several provoking factors of the Brugada ECG pattern. These include medications such as sodium channel blockers, beta blockers, tricyclic or tetracyclic antidepressants, lithium and local anesthetics. Other factors include vagal maneuvers, hypokalemia, hyperkalemia, hypercalcemia, alcohol and cocaine toxicity and fever. Data from a retrospective review by Amin et al. showed that fever was associated with Brugada ECG changes and was present in 4 out 22 patients with cardiac arrest. These findings may resolve with removal of provoking factors. This occurred in our patient when his ECG returned to normal after his fever defervescenced. The most important risk factor of sudden death in Brugada Syndrome is a history of ventricular tachyarrhythmia or syncope. The use of electrophysiology studies to induce VT/VF has not been shown to be predictive of risk and should not be used in risk stratification. The only treatment that has been shown to improve mortality from tachyarrhythmia is implantable cardioverter-defibrillator (ICD) and should be considered as first line therapy in all patients with Brugada syndrome and syncope, ventricular tachycardia or ventricular fibrillation. In conclusion, risk stratification of asymptomatic Brugada syndrome is ill defined but diagnosis should be made in order to provide patients with education on avoiding provoking factors and for ICD implantation on those patients with highest risk for sudden cardiac death.
CEREBRAL SALT WASTING SYNDROME OR SIADH: HYPONATREMIA IN A PATIENT WITH METASTATIC BRAIN LYMPHOMASeyedAmirhossein Afsharimani; Samaneh Dowlatshahi; Harvey Friedman. St. Francis Hospital, Evanston, IL. (Tracking ID #1926324)
LEARNING OBJECTIVE 1: Hyponatremia is common in the setting of central nervous system (CNS) disease which is usually attributed to SIADH. However, cerebral salt wasting (CSW) is another potential cause of hyponatremia, which is characterized by excessive natriuresis, hypernatremia and volume depletion with associated cerebral pathology.
LEARNING OBJECTIVE 2: Although clinical presentation of SIADH and CSW is similar, in CSWS, there is relative or overt hypovolemia whereas SIADH is associated with normal or hypervolemia. It is essential to differentiate these two disorders, in order to provide appropriate therapy.
CASE: A 59 year old female with history of diffuse large B cell lymphoma of breast on second cycle of R-CHOP chemotherapy, and recently diagnosed brain metastasis in right and left frontal parietal area, presents with increasing weakness. Her lips and tongue were dried because he had little oral intake of food and fluid for 15 days. Initial vital signs were significant for a BP: 76/53 mmHg, and a heart rate of 120/min. His serum sodium level was 131 mmol/l, potassium was 3.6 mmol/l, chloride was 98 mmol/l, urine sodium was 228 mmol/l, plasma osmolality was 273 mOsm/kg, urine osmolality was 540 mOsm/kg, and urine specific gravity was 1.014. The serum blood urea nitrogen level was 8 mg/dl, uric acid was 1.2 mg/dL, and creatinine was <0.20 mg/dL. Hormone levels from the laboratory test revealed normal antidiuretic hormone (ADH), renin, and, aldosterone level. Urine output showed 3.1 mL/kg/h. She was started on IV fluid replacement with normal salin which improved her BP to 85/65 mmHg. However, excessive urine output continued and increased up to 4 mL/kg/h. Although the urine sodium level and volume were not normalized, his serum sodium level increased to 133 mEq/L after sodium chloride infusion. Patient has been on dexamethasone high dose for 3 weeks before admission for excessive brain edema on recent imaging which resulted in a suppressed cortisol level. Patient was started on fludrocortisone 0.1 mg BID. Her sodium level improved to 136 mmol/l after 5 days of treatment and fludrocortisone was held. On the 5th day of treatment his urine sodium was 95 mmol/l.
DISCUSSION: CSW was once thought to be a misnomer, however recent studies have shown that it not onl exists, but also is not uncommon among patients with acute or chronic brain injuries. This condition can have significant negative consequences if not properly diagnosed and treated. It is important to differentiate CSW from SIADH. The key in diagnosis of CSW lies in volume status evaluation. The goel in treatment of CSW syndrome is to replace sodium and volume, and this can be achieved with combination of isotonic saline, hypertonic saline, and mineralocorticoids.
CERVICAL NECROTIZING FASCIITIS: CLINICAL MANIFESTATION AND MANAGEMENTShenelle-Marie Wise; Kate Hust. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926148)
LEARNING OBJECTIVE 1: Recognize the clinical manifestations of and risk factors for cervical necrotizing fasciitis.
LEARNING OBJECTIVE 2: Identify the differential diagnosis for necrotizing fasciitis and its appropriate diagnostic evaluation and treatment.
CASE: A 29-year-old woman presented with 1 week of fevers and pain along her left neck. A week prior to admission she complained of a sore throat and developed a small lump on her mandible, which increased in size, became erythematous, and painful. On presentation, her temperature was 102° Fahrenheit, and physical exam revealed erythema and tenderness extending from her left anterior neck to the 3rd intercostal space. CT scan revealed cellulitis and edema of the anterior left neck extending to left anterior chest wall with extensive periodontal disease and periapical abscess. Treatment was started with broad-spectrum antibiotics, but with worsening of the erythema and pain overnight, she was taken to the operating room for surgical exploration. Deep neck abscesses were drained and necrosis of both subcutaneous fat and muscle layers was debrided. Surgically obtained cultures grew Group A streptococcus. Her hospital course involved serial surgical debridements until her symptoms improved.
DISCUSSION: Necrotizing fasciitis is a rapidly progressing soft tissue infection that carries a significant mortality rate despite intensive treatment. More commonly seen in the abdomen, perineum, and lower extremities, the neck, owing to its rich vascular network, is a rare site for this condition. Given its rarity but high mortality, internists should consider this diagnosis in patients who present with neck pain and progressive and painful cellulitis. It is characterized by widespread destruction of the subcutaneous tissues and fascia, and gas formation in anatomic spaces. Overlying skin and muscles are spared initially but may undergo necrosis with disease progression. Cervical necrotizing fasciitis is most commonly caused by dental infections, especially from the mandibular molars. Less common causes are minor trauma leading to an opening in the skin, peritonsillar abscess, insect bites, and hypodermic needle infection. Conditions predisposing necrotizing infections include diabetes, drug use, obesity, immunosuppression, recent surgery, and traumatic wounds. Cervical necrotizing fasciitis has a reported mortality rate of 7 % to 20 %, depending on the extent of neck involvement. When the disease progresses into the thorax with descending necrotizing mediastinitis the mortality rate increases to 41 %. The affected area is usually erythematous, swollen, warm, and exquisitely tender. The process progresses rapidly over several days, with changes in skin color from red-purple to patches of blue-gray. In advanced infection, high fever and systemic toxicity are generally observed. This is in contrast to necrotizing cellulitis which may present with thin, dark wound drainage and gas formation in the skin but pain, swelling and systemic toxicity are not prominent features. Numerous case reports have documented pyodermagangrenosum misdiagnosed as necrotizing fasciitis. Pyoderma is an inflammatory dermatologic condition that presents with ulceration and tissue necrosis similar to infectious processes. It is often a diagnosis of exclusion and should be considered if there is no symptom improvement with antibiotics and cultures remain inconclusive. Additionally, pyoderma is often associated with pathergy, a phenomenon that may lead to worsening necrosis with surgical debridement. Laboratory findings are generally nonspecific. Abnormalities may include leukocytosis with a marked left shift, coagulopathy, and elevations in the serum creatine kinase, lactate, and creatinine. Soft tissue x-ray, CT scan and MRI are most helpful if gas is visualized in the tissue, but more often, imaging studies demonstrate soft tissue swelling. Surgical exploration is the only way to definitively establish the diagnosis, facilitate early debridement and allow specimens to be obtained for cultures. In addition to surgical debridement, mainstays in management are early airway protection and broad-spectrum antibiotics against group A streptococci, anaerobes, and methicillin-resistant Staphylococcus aureus. Acceptable regimens include administration of a carbapenem or beta-lactam/beta-lactamase inhibitor for activity against gram-positive, gram-negative, and anaerobic organisms. Clindamycin should be included for its effects against toxin-producing strains of streptococci and staphylococci, and an agent with activity against methicillin-resistant Staphylococcus aureussuch as vancomycin, daptomycin, or linezolid should be added. Antibiotic treatment should be tailored to Gram stain, culture, and sensitivity results when available.
CHANGE IN MENTAL STATUS AND RECURRENT HYPONATREMIA ATTRIBUTABLE TO BEER POTOMANIANaba R. Mainali; Ranjan Pathak; Madan R. Aryal; Richard Alweis. Reading Health System, West Reading, PA. (Tracking ID #1933869)
LEARNING OBJECTIVE 1: To be able to diagnose hyponatremia secondary to beer potomania.
LEARNING OBJECTIVE 2: To identify the indications of treatment with hypertonic saline in hyponatremia caused by beer potomania.
CASE: Introduction: Beer Potomania is a syndrome manifested by severe hyponatremia and mental status changes (agitation, confusion and seizures), seen in patients who consume excessive beer and have poor dietary intake. Early recognition is important as hyponatremia, if not symptomatic, corrects simply with normal diet and cessation of alcohol. Case Report: A 64-year-old chronic alcoholic woman presented with altered mental status, difficulty walking and confusion of 10 h duration. She progressively became more confused and agitated, and developed ambulatory dysfunction without loss of consciousness or witnessed seizure. She gave the history of drinking up to 20 cans of beer a day without significant food intake for 5 consecutive days. She had two similar episodes in the past requiring ICU admission, treated with 3 % hypertonic saline initially but was switched to normal saline due to too rapid correction. Physical exam revealed tachycardia, agitation and mild confusion with unstable gait. Laboratory tests revealed sodium 112 mEq/L, potassium 2.7 mEq/L, chloride 77 mEq/L, bicarbonate 15.9 mEq/L, blood alcohol level 0.27 % (by volume), ALT 59 U/L, AST 120 U/L, serum uric acid 3.6 mg/dL, plasma osmolality 241 mOsm/Kg, urine osmolality 99 mOsm/Kg, urine sodium 19 mEq/L and negative urine toxicology. Other hyponatremia like dehydration, SIADH were thus excluded. She was given normal saline and responded well.
DISCUSSION: Beer potomania is a disorder where dietary sodium and protein insufficiency lead to dilutional hyponatremia that is often seen in chronic alcohol abusers. The clinical picture and laboratory values are consistent with water intoxication (hyponatremia, hypochloremia and hypokalemia). The pathophysiology involves inability of kidneys to excrete sufficient amount of free water due to the loss of normal renal urea gradient. Aggressive correction of chronic hyponatremia with hypertonic saline should not be attempted unless there are complications like seizure due to high risk of central pontine myelinolysis.
CHEST PAIN IN A YOUNG WOMAN DUE TO IVC FILTER FRAGMENT IMBEDDED IN THE SEPTAL WALL OF THE RIGHT VENTRICLEYagna R. Bhattrai; Gabriel S. Lerman; Manzoor Rather; Eric Green; Martin O’Riordan. Mercy Catholic Medical Center, Upper Darby, PA. (Tracking ID #1927306)
LEARNING OBJECTIVE 1: Understand the risks of inferior vena cava (IVC) filter fracture and embolization.
LEARNING OBJECTIVE 2: Detect and prevent possible complications by appropriate screening and retrieving if no longer indicated.
CASE: Introduction: The fracture of an inferior vena cava filter (IVC) and its subsequent migration is a well-documented complication of the Brad Recovery IVC filter. While the lung constitutes the major destination of these fragments, migration to the ventricular chamber is a rare complication. Case: A 46-year-old woman with a history of COPD, depression, and prior IVC filter presented with non-radiating, left sided chest pain for several days, associated with occasional palpitations and exertional dyspnea. She was not on any regular medications. Physical exam was normal aside from chest pain and mild wheezes. A chest x-ray, EKG, and blood work (including cardiac biomarkers) were normal. A CT chest angiogram revealed a linear foreign body in the septal wall of the right ventricle and normal pulmonary arteries. An echocardiogram showed an echo dense linear structure protruding from RV septal wall into the RV cavity, without evidence of pericardial effusion. She underwent successful retrieval of the filter via interventional radiology. A visual inspection showed an IVC filter with missing tynes. She was symptomatically better after retrieval. We decided to leave the IVC fragment embedded in the RV septum because we felt the risk of removing a foreign body imbedded in the myocardium (probably for several years) outweighed the benefits.
DISCUSSION: The most common complications after IVC filter placement are recurrent PE, thrombosis of the IVC, and local access site complications. Filter fractures with embolization is relatively rare, with an estimated incidence of 1 to 2 % of cases. Two published studies have looked at a total of 83 patients with filter fractures. The incidence increased with longer filter dwell times and with certain types of filters. The majority of filter embolizations were in the lungs, and most are clinically “silent.” However, both right ventricular embolization complicated by cardiac tamponade have been reported. Although retrieval of the main filter body is typically successful, removal of the embolized fragments have had variable success. Patients with any retrievable filter should understand the risks associated with fracture and embolization. Evaluation for filter embolization should be considered in patients with a history of long term IVC filters who present with unexplained chest pain or shortness of breath.
CHEST PAIN MIMICKER: ACUTE GASTRIC VOLVULUSPraveena N. Iruku; Tareq Khader; Anna Maria Affan. St Vincent Charity Hospital, Cleveland, OH. (Tracking ID #1933868)
LEARNING OBJECTIVE 1: Diagnose the uncommon fatal causes of chest pain
LEARNING OBJECTIVE 2: Manage acute gastric volvolus
CASE: Case Presentation: This is a 66 year old female with past medical history of asthma and heart burn who presented to the emergency room with severe chest pain and left sided shoulder pain. Chest pain is described as sudden onset, left sided and epigastric in location, steady, and 10/10 in intensity, associated with some shortness of breath and nausea. She denied any abdominal pain, vomiting, diarrhea, loss of appetite or weight. She complained of some early satiety and bloating. She did not do any unusual weight lifting or activity. Her past history is significant for cholecystectomy and mesh repair for umbilical hernia. Social history is unremarkable. Physical examination demonstrated normal vital signs. Patient was alert, oriented and in moderate pain distress. Neck and shoulder exam were unremarkable. Chest auscultation revealed very prominent bowel sounds, otherwise normal air entry. Abdominal exam was unremarkable except for mild epigastric tenderness. Contrast Tomographic (CT) scan with a pulmonary embolism (PE) protocol revealed a large bilateral diaphragmatic hernia with possible obstruction and stomach rotated along its own long axis. There was no evidence of PE or myocardial ischemia. Multiple attempts to pass an nasogastric tube failed. Exploratory laparotomy showed major portion of the stomach, splenic flexure and transverse flexure of the colon in the chest. Fundoplication was performed to prevent recurrence.
DISCUSSION: Gastric volvulus is defined by abnormal rotation of the stomach of more than 180° there by creating a closed loop obstruction. It is mainly composed of three types, organoaxial, mesenteroaxial, and combined type. Organoaxial is the most common type of volvulus which means that the stomach rotates around its own long axis and is associated with large diaphragmatic hernia. Strangulation and necrosis commonly occur with organoaxial gastric volvulus and have been reported in 5–28 % of cases. The classic triad of gastric volvulus, described by Borchardt in 1904, consists of severe epigastric pain without vomiting, inability to pass a nasogastric tube and sometimes severe pain at the top of left shoulder which may be due to internal bleeding irritating the diaphragm upon respiration. Diagnosis is based on clinical suspicion, radiographic studies and endoscopy. Treatment is surgical and non operative mortality is very high. In conclusion, acute gastric volvulus is an important and timely diagnosis to make in any clinical setting given the increase in fatality with delay. It is an uncommon encounter and needs a high index of suspicion. We present a case of acute gastric volvulus and diaphragmatic hernia presenting with severe chest pain. The diaphragmatic hernia may be from diaphragm injury during her previous surgeries and it might have been complicated with adhesions leading to traction on the diaphragm and diaphragmatic hernia.
CHLORPROMAZINE-INDUCED HEPATITISAnita Mulye; Tara Lagu. Baystate Medical Center, Springfield, MA. (Tracking ID #1936726)
LEARNING OBJECTIVE 1: Diagnose drug-induced hepatitis with significant clinical signs and symptoms, imaging, and procedures (ie biopsy)
LEARNING OBJECTIVE 2: Recognize adverse effects of medications commonly prescribed
CASE: A 34yo woman with a history of bipolar disorder and attention-deficit hyperactivity disorder presented with a one-month history of nausea and vomiting of non-bloody non-bilious emesis, and anorexia. Three days prior to presentation, the patient developed severe right upper quadrant abdominal pain. On presentation to the emergency department, the patient was afebrile and other vital signs were stable, but she was noted to be severely jaundiced with scleral icterus and abdominal exam revealed right upper quadrant that was tender to palpation without rebound or involuntary guarding. HIDA scan indicated possible common bile duct dilation and abdominal ultrasound revealed a contracted gallbladder with possible non-shadowing stones. Computed tomography of the abdomen was unrevealing for acute processes and ERCP revealed no obstructive etiologies. Serum anti-mitochondrial antibody, anti-smooth muscle antibody was negative, and ceruloplasmin were all either negative or within normal limits, ruling out primary biliary cirrhosis, autoimmune hepatitis and Wilson’s disease, respectively. Anti-nuclear antibody was positive but with only a 1:400 titer. The patient subsequently underwent liver biopsy, which revealed significant cholestasis with marked eosinophilia, inflammation and bile duct edema. These findings were felt to be most consistent with drug-induced hepatitis. The team conducted a detailed review of the medications the patient had taken in the months prior to presentation, revealing metoclopramide 10 mg, clonazepam 0.1 mg three times daily, lithium 300 mg daily, methylphenidate 36 mg daily, chlorpromazine 25 mg three times daily (of which the patient was advised to take two at a time), ondansetron 4 mg every 8 h as needed. Her lithium dose had been increased a week prior to admission to the above dose with the intention to taper clonazepam. The patient also developed a diffuse pruritic urticarial type rash with eosinophilia several days after presentation.
DISCUSSION: Drug-induced hepatitis occurs in 1 out of every 1000 to 100,000 patients and is more common in women (1,2). The clinical manifestations of most drug-induced hepatitis resemble viral hepatitis with malaise, jaundice and transaminitis. However, different pharmacological entities have specific patterns of injury (i.e. hepatocellular, cholestasis, autoimmune, fibrosis, etc.). In cholestatic injury, there are four histological types: pure (canalicular, bland or noninflammatory), cholestatic, ductopenic, and sclerosing cholangitis (7). Symptoms typically develop within 1–6 weeks of initial ingestion of the medication and may continue evolving even after the agent is withdrawn (1,8). Some drugs have a strong allergic component, causing fever, rash, lymphadenopathy, and hepatic injury. Although chlorpromazine is typically associated with cholestasis, it is possible that a mild form of this “reactive metabolite syndrome” was the source of this patient’s pruritic rash as this developed several days after the patient began having other signs of hepatic injury (3,4). Chlorpromazine-induced hepatitis occurs in 0.2–2 % of patients (8), with 80–90 % of cases developing within the first 4 weeks (5). The mechanism by which chlorpromazine decreases canalicular function and bile flow has been hypothesized to be due to poor genetic sulfoxidation of free radicals and hydrocarbons making affected patients more susceptible to cholestasis (9). Light microscopy shows cholestasis and a predominance of mononuclear and eosinophilic cells, although hepatocellular injury and granuloma formation is possible as well (6). In the case of our patient, liver functions tests and bilirubin trended down with removal of the offending agent to near-normal levels approximately 42 days after initial presentation, and her abdominal pain gradually dissipated as well. The hypersensitivity or reactive metabolite syndrome improved with triamcinolone cream within 24 h of treatment. The etiology of her emesis and remains unclear, however her remaining symptoms are gradually resolving and thought to be due to chronic hepatitis from the inciting injury.
CHOLESTEROL AND CRAMPS: A PROBLEM OF PROLIFIC PRESCRIBING PATTERNSJeffrey K. Hom. University of California, San Francisco, San Francisco, CA. (Tracking ID #1939358)
LEARNING OBJECTIVE 1: Recognize the risk factors for muscle injury associated with HMG-CoA reductase inhibitors
CASE: A 54 year-old man with type 1 diabetes mellitus, hyperlipidemia, hypertension, and stage III chronic kidney disease presented to clinic with 2 days of “leg cramps”. The discomfort was “a sore ache” in both his calves that was worst at night. He denied a preceding viral prodrome, trauma, restless legs, dehydration, or distal parasthesias. He had taken gabapentin without relief. His other medications were amlodipine, atorvastatin, enalapril, insulin, and tramadol. His exam was notable for diffusely tender gastrocnemius muscles, without warmth, swelling, discoloration, or palpable cord. His distal extremities were well-perfused, with 2+ pedal pulses, and his sensation was intact to monofilament. He had full strength and ambulated without difficulty. Labs revealed an elevated creatine kinase (CK) (2605 U/L), creatinine (1.83 mg/dL, up from 1.65 mg/dL), and glucose (363 mg/dL). A urinalysis had been ordered but not obtained. Two weeks prior to presenting his atorvastatin had been increased from 20 mg to 40 mg nightly for persistently elevated LDL. Given the suspicion for statin-induced myositis, the patient’s atorvastatin was discontinued and aggressive hydration was recommended. Repeat labs 3 days later showed a CK of 459 U/L and a creatinine of 1.46 mg/dL. His cramps resolved over the following 2 weeks and his CK had returned to normal 1 month after his initial presentation.
DISCUSSION: One in four adults in the United States over age 45 is prescribed an HMG-CoA reductase inhibitor (“statin”), a number sure to increase under the new ACC/AHA guidelines. Muscle injury is known side effect of statins and should remain a concern in all patients taking them, regardless of the duration of treatment. The degree of injury ranges from myalgias to rhabdomyolysis, and patients may complain of cramps, aches, fatigue, or weakness. The mechanism by which muscle toxicity occurs is not well understood. While the incidence varies among statins due to differences in absorption and metabolism, higher doses are associated with greater risk. Other risk factors include hypothyroidism and renal and liver diseases. Additionally, because many statins are metabolized by cytochrome P450 3A4 (CYP3A4), concurrent use of medications that inhibit or compete for this enzyme, including amlodipine, increases susceptibility to developing myopathy. Myositis, as was suspected in this patient, is uncommon, occurring in 0.5–0.9 % of patients on statin monotherapy for hyperlipidemia. Resolution of symptoms and normalization of CK occur following withdrawal of the medication. For patients who develop muscle injury other than rhabdomyolysis, a trial of pravastatin or fluvastatin, two statins with less intrinsic muscle toxicity and not metabolized by CYP3A4, can be considered with close monitoring. While the occurrence of statin-induced myopathy is rare, the burden of disease from this adverse effect should not be overlooked when greater than 255 million prescriptions for cholesterol-lowering medications are written annually in the United States.
CHORDOMA: A RARE CAUSE OF PROGRESSIVE NEUROLOGIC SYMPTOMS AND HORNER’S SYNDROMEMarjan M. Hovaida. UCSD, San Diego, CA. (Tracking ID #1936961)
LEARNING OBJECTIVE 1: Recognize chordomas as rare bone tumors that commonly present as chronic, progressive neurologic symptoms refractory to routine management
LEARNING OBJECTIVE 2: Coordinate multidisciplinary care for complex patients
CASE: A 59 year old female with history of morbid obesity, diabetes mellitus complicated by CKDIII, hypertension and OSA presented to her primary internist with persistent left arm and neck pain and tingling for 9 months refractory to physical therapy that prevented her from typing at work. She also complained of dry eyes and progressive shortness of breath, previously attributed to worsening OSA with up-titration of her CPAP settings. Physical exam was notable for an obese Hispanic female with left neck fullness and left miosis and ptosis consistent with Horner’s syndrome. CT neck/thorax demonstrated a large, infiltrating pre-vertebral mass extending 20 cm from the lower clivus to the upper chest, displacing the trachea, posterior to the descending aorta and encasing the left subclavian, vertebral and common carotid artery. The patient was referred to ENT with laryngoscopy showing a patent but narrowed airway. Subsequent tracheostomy with exploration and biopsy identified metastatic adenocarcinoma on frozen section. However, formal pathology identified a classic type chordoma with cytokeratin and EMA positivity. Radiation Oncology recommended maximal resection with post-operative proton beam radiotherapy to residual disease and areas at risk for recurrence. Coordinated tumor de-bulking and spinal cord decompression was performed by Orthopedics, Neurosurgery and ENT, however tumor could only be partially removed due to high risk location. Repeat imaging demonstrated residual tumor within the spinal canal at the cervico-thoracic junction and mediastinum. She underwent 30 sessions of radiation, although repeat imaging showed increased tumor size and necrosis. Patient’s course was also complicated by multiple ED visits and hospitalizations for pain control, neurologic complaints and infection requiring close follow-up with her primary. After multiple discussions, patient and family requested focus on comfort-oriented treatment and was subsequently enrolled in hospice, although she was discharged after 6 months given her stable clinical status.
DISCUSSION: Chordomas are rare bone tumors characterized by slow growth, frequent local recurrence and rare systemic spread. They arise from embryonic remnants of the notochord and can be spheno-occipital (35 %), vertebral (15 %), or sacro-coccygeal (50 %). Approximately 7–10 % of chordomas are cervical and typically present in the 5th-6th decade without gender predilection. Nerve impingement, progressive pain and headaches are common symptoms. Radiographically, chordomas are usually solitary, lytic lesions ranging from 1 to 10 cm. In this case, the large size and considerable extension of the tumor were uncommon. Immunohistochemistry typically demonstrates positivity for EMA or cytokeratin. Initial treatment consists of wide, local excision, which is associated with longer survival and delayed recurrence, although as in this case, complete resection is often difficult secondary to involvement of vital structures and thus adjuvant radiation is employed. Limited literature reviews of molecular based therapy have also demonstrated symptomatic, and rarely, radiological response. Ultimately, chordomas are challenging to manage and often require a multi-disciplinary approach, demonstrating the importance of the primary provider in care coordination, advocacy and ongoing assessment of patient symptoms and goals of care through this complicated course.
CHRONIC PAIN CAUSED BY SCHWANNOMATOSISSheila Laleman; Christopher M. Wittich. Mayo Clinic, Rochester, MN. (Tracking ID #1936577)
LEARNING OBJECTIVE 1: Differentiate Schwannomatosis from Neurofibromatosis
LEARNING OBJECTIVE 2: Identify, manage, and treat Schwannomatosis
CASE: A 59-year-old Caucasian man presented for general medical exam with painful masses on his midback and right elbow. The midback mass was first discovered incidentally 4 years prior on CT to investigate for metastatic thyroid cancer. On serial CT scans, the mass had been stable. The mass was now painful with a constant, focal, and non-radiating area of “pin prick” pain near the medial scapular border at T6. There were no alleviating factors and the pain was more noticeable when he sat quietly. He first noted the enlarging right elbow mass about 2 years prior. He described a tingling, dysesthetic quality of the 4th and 5th digits of the right hand. His past medical history was significant for papillary thyroid cancer status post thyroidectomy with no evidence of recurrence and cavernous hemangiomas in the liver. No family history of tumors or neurofibromatosis. On examination, his hearing was normal. A soft tissue growth was palpated posteriorly at the level of T6. Deep palpation reproduced left medial scapular border tenderness. He had a mobile mass in the right proximal elbow just above the cubital tunnel. Palpation of the mass caused tingling sensations into his 4th and 5th digits. He had normal ulnar motor function in his extrinsic and intrinsic muscles of his hand. Thoracic MRI revealed a dumbbell shaped T2 hyperintense, T1 hypointense uniformly enhancing mass at the left T5-6 neural foramen measuring 1.6 × 2.3 × 0.9 cm. It contacted the left lateral margin of the dura without extending into the spinal canal, all consistent with a schwannoma. Right upper extremity MRI revealed a heterogeneous soft tissue mass that involved the right ulnar nerve. It was ovoid in shape with a well-defined margin measuring 4.5 × 2 × 1.9 cm, also consistent with a schwannoma. A head MRI was negative for vestibular nerve involvement. He underwent surgical resection of the right ulnar nerve tumor and pathology revealed a benign schwannoma. Gabapentin was recently initiated for long-term management of his pain.
DISCUSSION: We describe a case of multiple, peripheral schwannomas causing pain in a 59-year-old man. Schwannomatosis is a rare form of neurofibromatosis (NF) characterized by multiple schwannomas of cranial, spinal, and peripheral nerves. It is an uncommon disorder resulting in 0.58 cases per 1,000,000 yearly. In contrast to other forms of NF, patients with schwannomatosis do not develop vestibular tumors, deafness, or malignancies. Segmental schwannomatosis that affects only one body segment occurs in about one-third of patients. Schwannomatosis is a disease of adulthood (median age of diagnosis = 40 years). The main debility from schwannomatosis is chronic pain rather than neurological deficits. Pharmacologic management of schwannomatosis includes symptomatic pain relief with gabapentin, opioids, NSAIDs, tricyclic antidepressants, and SNRIs. Surgical management can include excision of the schwannoma. This case highlights that schwannomatosis 1) is a subset of NF, 2) does not have vestibular nerve involvement, 3) does not cause deafness or malignancies, and 4) can cause severe chronic pain.
CLINDAMYCIN CAUSES A MACULOPAPULAR RASH WITHOUT EOSINOPHILIA IN PRIMARY INFECTIOUS MONONUCLEOSISAlbert Do1,2; Donald Curran2,1. 1Yale-New Haven Hospital, New Haven, CT; 2West Haven Veterans Affair Hospital, West Haven, CT. (Tracking ID #1933467)
LEARNING OBJECTIVE 1: Recall diagnosis and treatment principles for infectious mononucleosis in a patient presenting with acute pharyngitis, and appreciate the possibility of clindamycin administration resulting in a non-infectious diffuse maculopapular rash, as well as other reported adverse dermatologic syndromes associated with clindamycin use
LEARNING OBJECTIVE 2: Recognize other antibiotics reported in the literature to be associated with non-infectious rash in infectious mononucleosis, including amoxicillin, azithromycin, and levofloxacin.
CASE: A 28 year-old male who had received all childhood vaccinations, presented to clinic with fevers to 101 °F, sore throat, and odynophagia for the past 4 days. His exam revealed severe left anterior cervical tenderness with lymphadenopathy. He exhibited pharyngeal erythema without exudates, but was without rash or hepatosplenomegaly. Due to concern for pharyngeal abscess suggested by his severe pain, he was given a 10-day course of clindamycin, though cultures eventually returned negative. On the final day of antibiotic therapy, he suddenly developed a diffuse, mildly-pruritic maculopapular rash without pustules, involving the head, palms, soles, and intertriginous regions including all flexural folds and axillae. No mucous membranes were involved. At this time, his white blood cell count was 8.1/μL with 49 % lymphocytosis (49 %) without peripheral eosinophilia (5 %). On consideration of infectious mononucleosis, his anti-heterophile antibody test was found to be positive, with elevated Epstein-Barr virus (EBV) antibody IgM titers elevated at 5.0 (upper limit of normal 1.1) and low IgG levels of <0.9. He was advised to discontinue antibiotics and closely monitor his rash. On follow-up 3 days later, he reported improvement in his symptoms.
DISCUSSION: Infectious mononucleosis (IM) is common, and manifests with lymphadenopathy, fevers, and pharyngitis (in 100 %, 98 %, and 85 % of patients, respectively). Clinically, pharyngitis in EBV and cytomegalovirus infections tend to be milder in severity. Diagnosis involves testing for the presence of anti-heterophile antibodies, with a sensitivity of 70 to 92 %, and a specificity of 96 to 100 %. The mainstay of IM management is supportive: anti-pyretics and analgesics, as well as limitation of contact sports due to splenomegaly, occurring in the first 3 weeks in 50 to 60 % of patients and with the associated risk of splenic rupture. Classically, patients with IM who receive ampicillin or amoxicillin develop a non-infectious maculopapular rash not thought to be a drug allergy. However, it has also been described with azithromycin, levofloxacin, piperacillin/tazobactam, and cephalexin. Clindamycin is a lincosamide antibiotic used in a variety of infections, including methicillin-resistant Staphylococcus aureus and anaerobic bacterial infections. A range of adverse dermatologic effects associated with clindamycin have been reported in the literature, including drug-induced hypersensitivity syndrome (DIHS), drug-related rash with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis. Unique to this case is the lack of eosinophilia or pustules, thus representing a clinical entity distinct from DRESS, DIHS, or acute generalized exanthematous pustulosis. In addition, this patient presents with a primary EBV infection, rather than a reactivation syndrome. Viral reactivation has been postulated to be the mechanism of action in clindamycin-associated rash. However, acute EBV infection in this patient suggests involvement of another mechanism, though the mechanism of this rash has not been elucidated to date.
CLUBBED WITH A REMINDER TO TEST FOR HIVMona Siddiqui1; Michael T. Melia2. 1Johns Hopkins University School of Medicine, Arlington, VA; 2Johns Hopkins University School of Medicine, Baltimore, MD. (Tracking ID #1939407)
LEARNING OBJECTIVE 1: Recognize the association between clubbing and HIV
LEARNING OBJECTIVE 2: Understand the differential diagnosis of clubbing
CASE: A previously healthy 34-year-old man was evaluated for 24 months of progressive digital clubbing. He denied fevers, night sweats, cardiopulmonary symptoms, travel, or unusual exposures. Physical examination demonstrated no pathologic lymphadenopathy, genital lesions or penile discharge. The patient had dramatic clubbing of all digits and erythematous nail beds.
DISCUSSION: The differential diagnosis for clubbing includes systemic diseases (including malignancy and inflammatory bowel disease) but CBC, CMP, ANA, RF, ESR and CRP were normal. Cardiopulmonary disease (including interstitial lung disease and cystic fibrosis,) was considered but echocardiography, pulmonary function testing, polysomnography and chest CT were unremarkable. Liver disease was on the differential but GGT and viral hepatitis serologies were normal. Infections (including TB and HIV) were considered and although PPD and RPR were nonreactive, HIV antibody test (with Western blot) returned positive. CD4+ lymphocyte count was 401/μL and viral load was 205,000 copies/mL. Among one convenience sample of 76 HIV-infected patients, 28 (36 %) had objectively confirmed clubbing, and HIV testing is recommended as part of a diagnostic algorithm. While HIV screening is now recommended for all patients aged 15–65 years, our case highlights the need for diagnostic testing based upon physical examination findings.
CNS LUPUS: A CHALLENGING DIAGNOSISAlexandra Perel-Winkler. St. Luke’s-Roosevelt, New York, NY. (Tracking ID #1937811)
LEARNING OBJECTIVE 1: To describe the challenges intrinsic to the diagnosis of CNS lupus.
LEARNING OBJECTIVE 2: To illustrate a clinical picture where an internist should have a high index of suspicion for CNS lupus.
CASE: A 46 year old African American female with a past medical history significant for positive lupus anticoagulant antibody (Ab), chronic leukopenia, and right sided anterior ischemic optic neuropathy, presented with a 2 day history of right sided weakness and slurred speech. The Emergency Department triaged the patient to the stroke team and a workup was initiated for suspected ischemic stroke. The patient’s history was significant only for the above. On examination, pertinent positive findings included right-sided upper extremity (RUE) and lower extremity (RLE) weakness of 4/5. No cranial nerve or left sided neurologic deficits noted on initial exam. Notable admission laboratory findings included leukopenia of 2.4, normal platelets and a prolonged partial thromboplastin time of 51.5 s, prolonged prothrombin time of 14.9 and an INR of 1.2. Non-contrast head CT showed a mild hypodensity in the left inferior internal capsule consistent with a recent infarct. Non-contrast MRI brain showed an inflammatory lesion of the left posterior limb internal capsule, cerebral peduncle, and left pons. Brain and neck MRA were unremarkable. On day three the neurologic exam progressively worsened until the patient was found to have a dense right-sided hemiparesis. MRI brain findings prompted workup for causes of demyelinating disease. MRI cervical and thoracic spine were negative for pathology. Lumbar puncture was performed with grossly normal results. On day six a basic rheumatologic panel was sent by the house-staff. Rheumatology was consulted based on the advice from a Neuro-Immunonologist who thought the imaging was less consistent with MS. Significant studies showed positive antinuclear Ab, positive double-stranded DNA, elevated B2-glycoprotein IgA, positive ribonuceoprotein Ab, positive smith Ab, positive anti-SSA Ab, with low complement 4. At this juncture a diagnosis of CNS Lupus was made through the integration of the clinical picture, the inflammatory findings on imaging and serology strongly positive for an Systemic Lupus Erythematous (SLE) flare. Subsequent to diagnosis, the patient has received a total of 10 days of pulse steroids, four cycles of plasmapheresis and two doses of monthly intravenous cyclophosphamide. On discharge from acute rehabilitation her RUE and RLE weakness was graded as 4/5.
DISCUSSION: Neuropsychiatric manifestations of SLE often occur early in the course of the disease, with recent research suggesting up to 39 % present within the first year of diagnosis. While CNS lupus is not a rare disease, it is not commonly confronted by the General Internist. The diagnostic challenge lies in the broad range of clinical presentations as well as non-specific imaging results that often preceed the diagnosis. CNS lupus can present with diffuse or focal neurologic findings, mimicking stroke, or as psychiatric in nature. Typically, neurologic manifestations of SLE are generalized, including confusion, lethargy, affective changes or coma, however, cranial nerve and focal CNS involvement does occur. Imaging can demonstrate a broad range of findings, including demyelination of white matter or ischemia, as well as radiographic signs suggestive of cerebritis or vasculitis. In this case, a middle-aged African American woman presented with neurologic findings and a known history for positive lupus anticoagulant. Her age, racial background and history of autoantibodies for lupus anticoagulant confer a higher risk of SLE, as such CNS lupus should have been considered when this patient presented with neurologic symptoms. It is essential to have a high index of suspicion for CNS Lupus in patients with known positive antibodies associated with SLE and neurologic symptoms in order to prevent a delay in treatment.
CNS TB WITH INITIALLY NEGATIVE AFBAlexis C. Haftka; Ashleigh Porter; Ravish Parekh. Henry Ford Hospital, Detroit, MI. (Tracking ID #1939078)
LEARNING OBJECTIVE 1: Assess an atypical presentation of CNS tuberculosis.
LEARNING OBJECTIVE 2: Diagnosis CNS tuberculosis without systemic findings.
CASE: An 82 year-old middle eastern male from Yemen with an extensive past medical history significant for a-fib, diabetes mellitus, cryptogenic cirrhosis, and prostate cancer was initially brought to the emergency room due to altered mental status and acute renal failure. CT scan and MRI revealed multiple ring enhancing lesions located in the left cerebellum and parietal lobe as well as in the right frontal lobe. The initial impression was infectious versus metastatic process as the patient had a recent history of prostate cancer, however, PSA levels were undetectable. The patient was placed on a prophylactic antibiotic regimen that included vancomycin, cefepime, and flagyl and initially had a marginal response with diminishing lesions, decreasing vasogenic edema, and improving mental status. Preliminary testing for infectious causes included an extensive workup including blood cultures, fungitell, PPD skin testing, chest xray and CT, bronchiolar lavage with culture, and Quantiferon TB gold which were all negative. Although the initial follow-up MRI showed a preliminary improvement in the size of the brain lesions, a subsequent MRI 1 month later showed profound worsening of the lesions with increasing vasogenic edema and new found mass effect impinging on the fourth ventricle. The patient’s course was further complicated by the development of generalized anasarca attributed to worsening renal versus liver function as well as poor nutritional status. The patient’s mental status and overall health continued to decline and additionally developed a-fib with RVR and respiratory distress. Furthermore, the patient was transferred to the intensive care unit with hypoxic respiratory failure due to increasing secretions and inability to protect his airway and was intubated for the remainder of his hospital stay. Therefore, brain biopsy was deferred until the patient stabilized 3 weeks later. The diagnosis of CNS tuberculosis was finally confirmed by drainage of the posterior brain abscesses revealing positive AFB cultures. The following day the patient had a bronchial lavage, which was also AFB positive. The patient was started on standard tuberculosis therapy but unfortunately expired after 8 days of antibiotic treatment due to worsening renal failure and electrolyte abnormalities inducing cardiac arrest.
DISCUSSION: Central nervous system tuberculosis is more frequently seen in endemic areas where there is a higher prevalence of tuberculosis. If seen in less prevalent areas, such as the United States, it is thought to be a post-primary result of systemic TB. CNS tuberculosis may present as a tuberculoma, meningitis, or spinal tuberculous arachnoiditis. Based on previous case reports the findings of CNS TB without systemic findings, such as pulmonary involvement, is very rare. Usually patient’s will present with seizure as a primary symptom, suggesting our patient had a very atypical presentation. He presented with altered mental status and new onset renal failure. The patient was also negative for AFB, Quantiferon Gold, and PPD. There appeared to be no evidence supporting the diagnosis of TB, especially in the CNS. This makes our case very unusual. For diagnosis purposes CT imaging of the head will show small rings with surrounding edema. As they mature they become larger by coalescing together and becoming lobulated. MRI is thought to be the best imaging study. Biopsy should only be done if the tuberculoma is located in a safe location where there is a decreased chance of causing any injury to the brain. There is mixed views, based on several studies, as to whether biopsy is the best approach to diagnosis. Treatment should always be started when there is a high clinical suspicion for TB for a better clinical outcome. First line therapy includes INH, Rifampin, Ethambutol, Streptomycin, and Pyrazinamide. For the first 2 months of therapy the patient should receive 4 agents (INH, Rifampin, Ethambutol and Streptomycin or Pyrazinamide). After this 2 month period, a patient should remain on therapy for additional 7–10 months of Rifampin or INH. Our patient was immediately started on the intense regimen of INH, Rifampin, Ethambutol, and Pyrazinamide, but unfortunately due to the late diagnosis of CNS TB, our patient was unable to benefit from treatment.
COARCTATION OF THE AORTA AND BICUSPID AORTIC VALVE IN A DISORDERED SCHIZOPHRENICCynthia Huang1; Priya Pillutla2. 1Harbor-UCLA Medical Center, Torrance, CA; 2Harbor-UCLA Medical Center, Torrance, CA. (Tracking ID #1922738)
LEARNING OBJECTIVE 1: To recognize the clinical features of coarctation of the aorta (CoA).
LEARNING OBJECTIVE 2: To manage CoA in the contemporary era.
CASE: The patient is a 45 year-old disordered schizophrenic diagnosed with CoA. Cardiac catheterization showed a bicuspid aortic valve (BAV) with moderate-to severe stenosis (calculated valve area of 1.2 cm2); an infraductal aortic coarctation with pressure gradient of 60 mmHg and a severely dilated aortic root of 5 cm. His care was complicated by his psychiatric illness and he was lost to follow-up but re-presented with heart failure. On physical exam, the patient had a 30 mmHg systolic pressure gradient between upper and lower extremities, delayed carotid upstrokes and a brachial to femoral pulse delay. Cardiovascular exam was notable for a diminished S2, an ejection sound and a harsh 4/6 mid-systolic murmur at the 2nd right ICS. He had a 1/4 holodiastolic murmur at the 2nd right ICS, and a continuous murmur over the posterior inter-scapular areas. His ECG showed LVH with repolarization abnormalities and CXR demonstrated the characteristic “3 sign” and rib notching consistent with rib erosion by dilated collateral vessels. The patient met current ACC/AHA guideline recommendations for intervention based both on the presence of a hemodynamically significant CoA and severe bicuspid AS. However, he lacked capacity to make medical decisions. After extensive discussions, his conservator opted against surgical intervention and to adopt DNR/DNI status.
DISCUSSION: CoA is a relatively common cardiac defect that affects about 7 % of the population with underlying CHD. It is frequently seen in patients with gonadal dysgenesis (e.g. Turner syndrome) and Noonan syndrome. It may also be associated with BAV, subvalvular aortic stenosis (SubAS), mitral valve abnormalities (e.g. parachute mitral valve), ventricular septal defects and cerebral artery aneurysms within the circle of Willis (up to 10 %). Adult patients with isolated CoA tend to remain asymptomatic. Symptoms, if present, tend to be of upper extremity hypertension such as headache, epistaxis, claudication or even intracranial hemorrhage. Mean survival in individuals managed conservatively, is 35 years of age with a 75 % mortality rate by 46 years of age. Sequelae include systemic hypertension, accelerated coronary artery disease (CAD), stroke, aortic dissection and heart failure. In the pre-surgical era, aortic dissection caused 19 % of the overall deaths in these patients (50 % in the setting of associated BAV). Currently, either surgical or percutaneous treatment is the standard of care in adults greater than 50 years of age. The surgical approach is via a left lateral thoracotomy and placement of an interposition graft, an end-to-end anastomosis or a subclavian flap. Transcatheter therapies such as percutaneous balloon angioplasty or stenting of the CoA are considered acceptable alternatives to surgery in the absence of contraindications. Balloon angioplasty alone however, is associated with a higher rate of re-CoA and aneurysm formation. In non-operable patients with CoA, medical management consists of beta-blockers, additional blood pressure control as needed, and endocarditis prophylaxis prior to dental procedures. Beta-blockers, by controlling both heart rate and blood pressure are advantageous in slowing the progression of aortic dilatation/dissection.
COEXISTING PRIMARY HYPERPARATHYROIDISM AND MULTIPLE MYELOMAYumiko Kinugawa; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1928987)
LEARNING OBJECTIVE 1: Recognize that elevated intact parathyroid hormone (PTH) does not exclude multiple myeloma in hypercalcemic patients
CASE: An 86 years old Asian woman with a history of chronic hypercalcemia presents with 2 months’ history of worsening upper back pain despite normal x-ray. She reports fatigue, paresthesias from her left buttock to posterior thigh, and numbness on bilateral plantar feet; she denies all other review of systems. Her pain is controlled with acetaminophen and non-steroidal anti-inflammatory drug. The patient’s past medical history includes hypercalcemia of unknown etiology ×6 years, spinal stenosis, peptic ulcer disease, hypertension, and constipation; she takes acetaminophen, tramadol/acetaminophen, loxoprofen, carvedilol, olmesartan, amlodipine, magnesium oxide, probiotic, and rabreprazole. She has no allergies, and her family history is unknown. She does not use tobacco, alcohol, or drugs. On exam, the patient’s vital signs are temperature = 36.6 °C, blood pressure = 138/78, heart rate = 100, O2 saturation = 100 % room air, and respiratory rate = 16. She is in no acute distress; oriented ×3. Significant findings include pain on palpation of 4th and 5th ribs bilaterally in the mid-axillary line, decreased bilateral patellar/Achilles tendon reflexes, and decreased pain/temperature sensation on her plantar feet. No back tenderness and negative straight-leg raising test; the rest of the exam shows no irregularities. Blood work reveals hemoglobin = 10.8 g/dL (baseline = 12), potassium = 4.9 mEq/L, calcium = 11.3 mEq/L, albumin = 4 mg/dL, creatinine = 2.3 mg/dL (baseline = 0.96), and intact PTH = 115 pg/mL (normal = 10–60). Bone scintigraphy reveals hot spots in T8-T9 and 3rd and 6th right ribs. Magnetic resonance imaging of the vertebrae indicates compression fractures on T8-T9. Bone densitometry shows T score = −1.6 at L1-L4 and −1.4 at femurs. Neck ultrasound and computed tomography reveal a thyroid mass suspicious of parathyroid adenoma. Although TcMIBI scintigraphy shows no abnormal uptake indicative of a parathyroid tumor, surgical intervention for probable parathyroid adenoma is recommended. Meanwhile, bilateral humerus and femur x-ray reveal no lytic lesions. Serum/urine protein electrophoresis show Bence-Jones protein; subsequent bone marrow biopsy confirms multiple myeloma with 34 % plasmacytosis. As she refuses surgery, she is thus started on chemotherapy.
DISCUSSION: Coexistence of primary hyperparathyroidism (pHPT) and multiple myeloma (MM) remains a rare clinical event. Whether the association is fortuitous or not continues to be a topic of discussion; however, a study by Arnulf et al. suggests that the prevalence of monoclonal gammopathies is higher in pHPT compared to controls. Initial manifestations of MM include anemia (73 %), bone pain (58 %), hypercalcemia (28 %), and elevated creatinine level >2 mg/dL (19 %), all of which can also be present in pHPT. No guidelines exist as to when coexisting MM should be suspected in pHPT cases, but several reports suggest that recurrent or treatment-resistant hypercalcemia (surgical or non-invasive) warrants MM work-up. Furthermore, considering that the median age of MM at diagnosis is 66 years and presuming that the prevalence of monoclonal gammopathies is higher in pHPT, screening for monoclonal gammopathies during initial assessment of hypercalcemia in elderly patients is recommended.
COMBINATION THERAPY IN A PATIENT WITH COMBINATION OF RHEUMATOID ARTHRITIS AND MULTIPLE SCLEROSISEricka Maximous1; Adegbenga Bankole2. 1Carilion Clinic-Virginia Tech Internal Medicine Residency, Roanoke, VA; 2Virginia Tech Carilion School of Medicine Department of Internal Medicine: Rheumatology, Roanoke, VA. (Tracking ID #1938800)
LEARNING OBJECTIVE 1: Recognize Different Modalities Available to Treat RA/MS
CASE: A 46 year old woman presented in April 2011 with bilateral hand and foot pain, swelling and morning stiffness lasting several hours daily. She had no rashes, ulceration, alopecia, sensory changes, muscle tenderness or weight changes. She has a history of multiple sclerosis (MS) not on treatment at the time of presentation. Physical exam reveals multiple Rheumatoid Arthritis (RA) deformities of bilateral hands with active synovitis including swelling of both metacarpophalangeal joints (MCP). She also had a left knee effusion and crepitations of the right knee. Pertinent labs during her workup include ANA Ab negative in July 2002, CCP Antibody, IgG 24.1 (Ref 0–5 U/ml) in April 2008, Rheumatoid Factor (Ref <30 IU/ML) <30 in April 2008, Sedimentation rate (Ref: 0–20 mm/HR) 24 in April 2011, C-reactive Protein (Ref: <1 mg/dl) 3.2 in July 2011, Sedimentation rate 8 in May 2013 and C-reactive Protein <0.4 in May 2013. Her hand X-rays showed diffuse osteopenia with soft tissue swelling. Large erosions and partial bony ankylosis were also seen. Her foot X-rays also were consistent with diffuse osteopenia and erosions. She was treated with Hydroxychloroquine and Methotrexate for RA. She remained active despite this, and as tumor necrosis factor (TNF) inhibitors are contraindicated in a patient with Multiple Sclerosis, she was started on Abatacept. On combination therapy, both her RA and her MS responded and both diseases have been in remission for over 12 months.
DISCUSSION: The occurrence and clustering of autoimmune disease in patients and families have been reported and well investigated (1). The most common autoimmune disease associated with RA is Sjrogen’s Syndrome (SS), though almost any disease can be associated with RA. We have known for many decades that tumor necrosis factor (TNF) may be either pathogenic or protective in different clinical situations. In RA this has proved to be of great therapeutic value. However, it is pivotal in the pathogenesis of inflammatory demyelinating disease of the central nervous system like MS. There have been multiple reports of anti-TNF induced and flares of MS (3). There have also been many reports not just of central nervous system neurological disease, but also peripheral disease (4). T cell directed therapies with CTLA4Ig (Abatacept) has been shown to be effective in both RA and MS, and were used successfully in out patient (6). In our patients we were able to maintain remission of both diseases with the use of combination therapy including Abatacept. She followed up with Neurology and had no MS activity or the need for other medications. References: 1. Multiple Sclerosis and Autoimmune Diseases, H. W. G. Baker, J. I. Balla, H. G. Burger, P. Ebeling, I. R. Mackay. Australian and New Zealand Journal of Medicine Volume 2, Issue 3, pages 256–260, August 1972. 2. The function of tumor necrosis factor and receptors in models of multi-organ inflammation, rheumatoid arthritis, multiple sclerosis and inflammatory bowel disease. George Kollias, Eleni Douni, George Kassiotis, Dimitris Kontoyiannis. Ann Rheum Dis 1999;58:I32-I39 doi:10.1136/ard.58.2008.i32. 3. Onset of multiple sclerosis associated with anti-TNF therapy, Nancy L. Sicotte, MD and Rhonda R. Voskuhl, MD. Neurology November 27, 2001 vol. 57 no. 10 1885–1888. 4. Inflammatory neurological disease in patients treated with tumor necrosis factor alpha inhibitors, Andrew J Solomon, Rebecca I Spain, Michael C Kruer, Dennis Bourdette. Mult Scler December 2011 vol. 17 no. 12 1472–1487. 5. Update on the use of abatacept for the treatment of rheumatoid arthritis, Esther F Vicente Rabaneda, Gabriel Herrero-Beaumont and Santos Castañeda. Expert Review of Clinical Immunology July 2013, Vol. 9, No. 7, Pages 599–621. 6. B-cell-targeted treatment for multiple sclerosis: mechanism of action and clinical data. Hawker, K. Current Opinion in Neurology. 2008, 21 (suppl 1):S19–S25.
COMMON MEDICATION, UNCOMMON COMPLICATIONSue-Wei Luu; Laura S. Lourdes; Umna Ashfaq. University of Florida, Gainesville, FL. (Tracking ID #1927964)
LEARNING OBJECTIVE 1: This case highlights the importance of checking the drug-drug interactions in patients on highly active retroviral therapy (HAART). Patient education regarding seeking early treatment for prolonged nonsexual erections is also critical when starting Trazodone.
LEARNING OBJECTIVE 2: Lastly we would like to educate all internists about the importance of early recognition and management, as well as the consequences of ischemic priapism.
CASE: A 33-year-old African American male with human immunodeficiency virus infection, migraine headaches, gastro-esophageal reflux disease and hypertension presented to the emergency department with new onset painful, persistent penile erection of 28 h in duration. His current medications at the time were norvasc, lisinopril, propanolol, sumatriptan, topiramate, pantoprazole, trazodone and emtricitabine-tenofovir, truvada, ritonavir combination of HAART. The patient had started taking trazodone 50 mg nightly as needed for insomnia for 9 months; last dose was 36 h prior to presentation. He had no history of priapism or penile trauma. He was evaluated by Urology and treated with therapeutic aspiration of 600 cm3 of blood from the corpus cavernosum and irrigation with complete resolution of symptoms. Within 8 h, the patient had recurrence of painful priapism without response to intracavernous injection of phenylephrine. An Al Ghorab distal penile shunt (involves excising a piece of the tunica albuginea from the tip of the corpus cavernosum) was then placed. The following day he again had recurrent priapism that was refractory to repeat treatment with aspiration, irrigation, and phenylephrine injection. A proximal Quackle’s penile shunt was then placed (creating a window between the corpus cavernosum and corpus spongiosum). He was also started on intracavernous pseudoephedrine and oral terbutaline with resolution of erection over 3 days, followed by gradual improvement in pain and swelling over the following 2 weeks. Upon follow-up, the patient reported lack of spontaneous erections suggesting persistent erectile dysfunction for which he was placed on Cialis as needed. Further evaluation revealed that the patient had sickle cell trait (hemoglobin electrophoresis: 62 % Hb A, 34 % Hb S).
DISCUSSION: Priapism is a medical emergency. It has an incidence of 0.73 cases per 100,000 men and ischemic priapism is the most common subtype. Without prompt treatment, ischemic priapism may lead to progressive fibrosis of the cavernosal tissues and erectile dysfunction. While priapism has been described in sickle cell trait, it is not a typical complication under normal circumstances. More significantly, the patient was taking ritonavir and trazodone concomitantly. Ritonavir is a protease inhibitor that inhibits CYP450 enzyme levels, causing greater than expected free levels of other concomitant medications like trazodone that is metabolized through the CYP450 pathway. Due to the temporal relationship of events, this patient’s new onset of ischemic priapism was attributed to the combination of ritonavir and trazodone. Trazodone has been known to cause priapism albeit rarely and usually associated with overdose; however, when combined with a CYP450 inhibitor, it is more likely to do so. Therefore, when starting a patient on trazodone, the internist should pay attention to any concomitant medications that may increase the levels of trazodone and educate the patient about seeking medical attention in case of prolonged erections. Early recognition and management is also vital as all the above interventions would have prevented the long term sequela of erectile dysfunction in this patient.
COMPLICATION OF REVERSIBLE POSTERIOR LEUKOENCEPHALOPATHY IN THE SETTING OF SUSPECTED HYPERTENSIVE EMERGENCY MANAGEMENTDavid Goldberg; Lauren C. Hogshire. Rutgers: Robert Wood Johnson Medical School, Piscataway, NJ. (Tracking ID #1901180)
LEARNING OBJECTIVE 1: Recognize Reversible Posterior Leukoencephalopathy Syndrome in the setting of hypertension accompanied by the characteristic findings on neuroimaging.
LEARNING OBJECTIVE 2: Manage Reversible Posterior Leukoencephalopathy Syndrome associated with hypertension appropriately.
CASE: A 48 year old African American woman with a past medical history of poorly controlled hypertension presented with a 3 week history of worsening vision, leg swelling, and intermittent right-sided but diffusely radiating headaches of moderate severity. Vital signs were significant for a blood pressure of 265/155 mmHg on initial evaluation. The physical exam revealed only bilateral nonpitting ankle edema. Electrocardiogram showed normal sinus rhythm and left ventricular hypertrophy. Initial lab work was significant for elevated creatinine. A head CT was not performed on initial assessment. Treatment for suspected hypertensive emergency was begun with an intravenous beta blocker and the patient was admitted. Upon evaluation the next morning, the patient was difficult to arouse with altered mental status. The neurological exam revealed dysarthria as well as focal left sided motor deficits. Blood pressure at this time was 190/100 mmHg. CT of the head showed white matter changes suspicious for RPLS which were confirmed on a subsequent MRI significant for diffuse subcortical lesions worse on the right. MRA was within normal limits. There was no evidence of focal hemorrhage or infarction. Intravenous management was begun with a beta blocker, calcium channel blocker, and vasodilator. By hospital day three, the patient’s blood pressure stabilized averaging 180/110 mmHg. She was then transitioned to an oral antihypertensive regimen and her neurological deficits steadily improved to baseline over the next few days. On hospital day six, she was discharged with a blood pressure of 160/90 mmHg. The patient remained well on last follow-up 10 weeks post-discharge.
DISCUSSION: Reversible Posterior Leukoencephalopathy Syndrome (RPLS) is a clinical syndrome of multiple etiologies defined by the characteristic diffuse subcortical white matter hyperdensities seen on CT and MRI. MRA is typically normal. RPLS is rarely encountered, making appropriate recognition and clinical management a challenge. Hypertensive RPLS is believed to develop insidiously as chronically increased intracranial pressure overcomes cerebral autoregulation. The result is endothelial dysfunction and disruption of the blood brain barrier with ensuing subcortical parenchymal edema. Symptoms include headaches, visual changes, mental status changes, and rarely focal neurologic deficits. The literature recommends management of hypertensive RPLS similarly to hypertensive emergency. Both are treated with aggressive reduction of the patient’s diastolic pressure to below 110 mmHg without exceeding a 25 % fall from the presenting mean arterial pressure. This case illustrates the sudden onset of severe focal neurologic deficits mimicking stroke in a patient being managed for symptomatic severe hypertension. We hypothesize that the patient had previously undiagnosed chronic RPLS at presentation. While prompt blood pressure control is recommended for the treatment of RPLS, in this case the patient’s underlying disorder left her unable to compensate for the rapid iatrogenic decrease in blood pressure, precipitating her acute decompensation.
CONCRETIO CORDIS: A CHALLENGING IMITATOR AND OFTEN DELAYED DIAGNOSISZakaria Almuwaqqat. saint francis hospital, Evanston, IL. (Tracking ID #1938684)
LEARNING OBJECTIVE 1: Importance of clinical evaluation and maintenance of high degree of suspicion in diagnosis of constrictive pericarditis.
LEARNING OBJECTIVE 2: Early diagnosis and referral for pericardectomy is essential for treating heart failure and preventing cardiac and liver complications.
CASE: We present a case of 76 year old male patient who was referred for Exercise stress test because of symptoms of dyspnea and dizziness on exertion together with abnormal liver function tests. Symptoms had been present for 6 weeks. Further questioning revealed symptoms of lower limb oedema and weight gain. He had lately become less active and not exercising, he had history of substance abuse 30 years ago, stopped smoking 30 years ago and denies excessive ETOH consumption. His Physical examination revealed a raised jugular venous pulse, Mild ascites, hepatomegaly and peripheral edema. Exercise Dobutamine stress Echo revealed Right ventricular hypertrophy with normal LV motion and systolic function, Complete transthoracic Echo was done revealing Normal LV size and contractility, Biatrial enlargement, exaggerated septal motion in early diastole, diminished LV filling during inspiration with dilated inferior vena cava and no respiratory variation, interestingly there was no demonstrable pericardial abnormality. Laboratory tests showed normal values for full blood count, BUN, electrolytes and Creatinine. His bilirubin level was 2.5, alanine Amino-transferase (ALT) 35 IU/l and alkaline phosphatase (ALP) 169 IU/l. An ECG showed sinus rhythm with non specific ST/T changes. An abdominal ultrasound was suggestive of hepatic vein dilatation. A CXR showed extensive pericardial calcification, Chest CT was confirming calcific constrictive pericarditis, patient had uneventful surgical partial pericardiectomy after which he had improvement in his dyspnea and peripheral edema.
DISCUSSION: Constrictive pericarditis is an uncommon condition, often of unknown etiology but can be caused by infections, inflammation of the pericardium, radiation therapy or occupational exposure, its initial presentation often mimics myocardial and non-cardiac diseases. This case illustrates one such presentation with Dyspnea and dizziness on exertion and abnormal Liver function test. Echocardiographic examination was consistent with combination of left and right sided heart failure. Early diagnosis and referral for pericardectomy is essential for treating heart failure and preventing cardiac and liver complications. Constrictive pericarditis was first described as “Concretio Cordis”, diagnosis can be difficult and often delayed, presenting usually with symptoms and signs of right heart failure. In this time constrictive pericarditis presented with symptoms of left sided heart failure due to diastolic dysfunction due to impaired Left ventricular filling. Other modes of presentation may mimics non cardiac disease such as ascites and pulsatile hepatomegaly (50 %) and less comonly as liver disease and hepatic coma. Evaluation of Jugular venous distention and wave form is essential to avoid missing the diagnosis. Etiology of constrictive pericarditis is diverse and range from idiopathic most commonly (attributed to previous pericardial injury) to post cardiac surgery, pericarditis, radiotherapy, medications, infectious and inflammatory diseases. Pericardial calcification on chest x ray varies depending on the etiology representing about half the cases of idiopathic pericarditis. Cardiac catheterization is the definitive investigation, revealing classical pressure waveforms confirming the pathophysiology of constriction, Echocardiography may help in diagnosis and chest imaging should be considered for visualization of pericardium although thickened pericardium isn’t essential for diagnosis. Surgical pericardiectomy remains the definitive treatment for symptoms relief and avoid complication especially liver dysfunction.
CONDITION THAT MAY MIMIC RHEUMATOID ARTHRITISEriko Kanehisa; Junwa Kunimatsu; Tatsuya Sato; Junko Maeda; Riri Watanabe; Atsuto Yoshizawa. National Center for Global Health and Medicine Hospital, Tokyo, Japan. (Tracking ID #1935376)
LEARNING OBJECTIVE 1: Recognize that clinicians should consider human T-cell lymphotropic virus type 1 (HTLV-1)-associated arthropathy (HAAP) when a patient from the endemic area of HTLV-1 presents with seronegative arthritis with an erosive joint, mimicking rheumatoid arthritis (RA).
LEARNING OBJECTIVE 2: Recognize that HAAP can occur prior to the onset of adult T-cell leukemia/lymphoma (ATLL).
CASE: A 56-year-old Japanese woman was presented with 8-year history of repeated symmetric polyarthralgia (shoulders, wrists, knees, and ankles). The symptom was occasionally associated with low-grade fever and fatigue, aggravated by over-exercise, and resolved spontaneously. Her past medical history contained miliary tuberculosis, hypertension, and dyslipidemia. She was born in Miyazaki Prefecture, which is one of an endemic area of HTLV-1 in Japan. Both her mother and sister were known HTLV-1 carriers. Physical examination revealed tender and swelling of left knee. Neither lymphadenopathy nor hepatosplenomegaly were noted. Laboratory studies showed normal complete blood count, liver function, serum creatinine kinase, serum calcium, and thyroid function. C-reactive protein and ESR were also normal. Anti-HBV, HCV, and HIV antibodies were all negative. Rheumatoid factor (RF) and anti-cyclic citrullinated peptide antibody (ACPA) were negative. Considering her birthplace, we decided to screen her HTLV-1 status to determine an etiology of the arthritis, and that showed positive by western blot analysis in the serum. MRI of the right wrist revealed active synovitis and bony erosions including proximal carpal bones. This pattern raised the possibility of RA, but we strongly suspected HAAP because of her HTLV-1 positivity. In this case, the synovial fluid could not be taken. However, we closely follow her in the outpatient clinic as a HAAP. To date, she is well without emerging an overt leukemia or lymphoma.
DISCUSSION: HAAP can take two forms: a leukemia-associated arthritis in patients with frank HTLV-1 leukemia and a RA-like syndrome in HTLV-1-positive patients who do not have leukemia. In the former syndrome, the joint tissue and synovial fluid contain infiltrating HTLV-1-positive malignant T-cells. In the latter syndrome, the histology of arthritis is very similar to that seen in classic RA, so to speak, “non-leukemic HAAP”. HAAP in the absence of leukemia is distinguished by negative RF and positive serologies for HTLV-1. In this case, her HTLV-1 serology was reported as positive. However, little clinical consideration was warranted for the diagnosis of ATLL. Most infected individuals do not experience any symptoms, and approximately only 2–6 % of individuals with HTLV-1 develop ATLL. Correct diagnosis of arthritis is often challenging. Few data have been published describing the HAAPs, and its clinical presentation and disease course can vary. Fortunately, our patient had a definite family history of HTLV-1 carriers, which promptly provided us useful information for differential diagnosis. Even in a high prevalence area, a lot of people may not know his or her own HTLV-1 status. Clinicians should consider HAAP when a patient from the endemic area of HTLV-1 manifested an erosive joint without positive diagnostic clues, such as major anti virus-specific antibodies, hormone levels, RF, and ACPA.
CONFUSION AND HYPOGLYCEMIA IN AN ELDERLY WOMENEunice Chuang. Mount Auburn Hospital, Cambridge, MA. (Tracking ID #1940061)
LEARNING OBJECTIVE 1: To recognize hypoglycemia as a cause of confusion.
LEARNING OBJECTIVE 2: To recognize hypoglycemia as a presentation of insulinoma, even in elder patients.
CASE: 88 year-old woman with a 44 year old diagnosis of a “touch of hypoglycemia” was admitted for an episode of confusion, dysarthria and right facial droop. Forty four years earlier after she was told she had a “touch of hypoglycemia”, she started diligently multiple daily small meals. In recent months, she noticed increasing episodes of weakness and nausea coinciding with capillary blood glucose of 40–60 mg/dL. These episodes were progressively more difficult to control with dietary regimen. During hospitalization, she was noted to have blood glucose (BG) levels below 45 mg/dL, in coincidence of which she was confused. Confusion resolved after she ate and blood glucose normalized confirming the Whipple’s triad. Laboratory tests obtained after 12 h fast while the patient was confused: BG 48 mg/dL (70–99 mg/dL) and inappropriately Detectable C-Peptide (1.41 ng/mL; >0.6), Insulin (6.9 mU/L; ≥3) and Proinsulin (61.4 pmol/L; <18.8). Normal Beta-hydroxybutyrate 0.12 mmol/L (<0.28 mmol/L) and 8 AM Cortisol 8.6 ug/dL (5.0–23.0 ug/dL). Sulfonylureas and Insulin Autoantibodies were negative. Abdominal ultrasound, CT and octreotide scan were consistent with 7 × 8 mm lesion distally in the body of the pancreas consistent with insulinoma. At 89 years of age, she underwent middle pancreatectomy without complications. Pathology confirmed benign unifocal insulinoma. Her symptoms resolved completely.
DISCUSSION: Insulinomas usually present with neuroglycopenic symptoms. The duration of symptoms is on average 1.5 years prior to diagnosis. There are sparse data of long standing functional insulinoma in the elderly. The purpose of this case is to report an unusual presentation of insulinoma in an elderly woman with symptomatic hypoglycemia for 44 years prior to the diagnosis. Her hypoglycemia was controlled by conservative dietary measures alone prior to diagnosis of insulinoma. This is an unusually benign, although symptomatic course of insulinoma over several years, still eventually resulting in life-threatening symptoms if not diagnosed and treated appropriately. Aging and recurrent severe hypoglycemic episodes impair the usual “protective” counterregulation responses to hypoglycemia and likely accounted for the emergence of uncontrollable symptoms in this elderly patient.
CONSERVATIVE MEDICAL TREATMENT ON NON-OCCLUSIVE MESENTERIC ISCHEMIA (NOMI) COMPLICATED WITH HEPATIC PORTAL VENOUS GAS (HPVG)Yuka Naito; Akiko Eiri; Hiroki Aihara; Masaki Tago; Jun Tokutomi; Motoshi Fujiwara; Motosuke Tomonaga; Tsuneaki Yoshioka; Masaki Hyakutake; Itaru Kyoraku; Shu-ichi Yamashita. Saga Medical School Hospital, Saga, Japan. (Tracking ID #1917116)
LEARNING OBJECTIVE 1: Indication of conservative treatment without surgical intervention on NOMI and HPVG.
CASE: An 81-year-old woman was admitted to our hospital because of severe abdominal pain and vomiting. She had been hospitalized in another psychiatric hospital for years because of her depression and dementia. She also had long history of severe constipation due to psychotic medications. Her bowel movement was controlled by daily prescription of laxatives until the day of admission when she started to have abdominal pain and vomiting after lunch. The abdominal CT scan without enhancement at the hospital showed massive gas in the portal vein and the lumen of small intestine, so she was transferred to our hospital. On examination, the temperature was 36.4C°, the blood pressure 117/60 mmHg, the pulse 92 beats per minute, the respiratory rate 20 per minute, and the oxygen saturation was 95 % while the patient was breathing ambient air. Although her abdomen was silent, tenderness was not severe without guarding. The abdominal CT scan with enhancement revealed a wide range of bowel ischemia and emphysema in intestinal wall with the enhancement of adipose tissue of mesentery in addition to portal venous gas. There was no thrombus in the mesenteric artery and vein. We diagnosed her illness as non-occlusive mesenteric ischemia (NOMI) and hepatic portal venous gas (HPVG). As her vital sign deteriorated into shock, so we considered surgery on her necrotic intestines. However, her previous psychiatric condition, older age and extensive range of intestinal ischemia made it difficult to indicate surgery that might have resulted in significant bowel resection. In addition, because of the absence of peritoneal irritability, improvement of shock only with infusion of crystalloid, the lack of marked increase of LDH and CK or severe acidosis, we chose the conservative medical treatment with fasting, intravenous fluid infusion and antibiotics. By the 14th hospital day, her condition gradually improved and intestinal ischemia and edema and HPVG disappeared on abdominal CT. Then, she started oral intake again without any problems. She was transferred to another local hospital for rehabilitation on the 22nd hospital day.
DISCUSSION: HPVG in the presence of NOMI is a life-threatening condition that usually requires surgical intervention when the marked ischemia of intestine is suspected on imaging studies such as abdominal CT. However, conservative management can be a choice when peritoneal signs are absent, enzyme leakages such as LDH and CK are low and severe acidosis is absent.
COPPER DEFICIENT MYELONEUROPATHY IN CELIAC DISEASESiddharth Sheth; Michael Elnicki. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1939687)
LEARNING OBJECTIVE 1: Recognize the relationship between copper deficiency and peripheral neuropathy
LEARNING OBJECTIVE 2: Evaluate copper levels in patients with celiac disease (CD) who present with myeloneuropathy
CASE: A 55-year-old Caucasian man with a history of hypothyroidism and celiac disease presented to our general internal medicine service with unintentional 30-lb weight loss and bilateral proximal leg weakness. Symptoms started insidiously and worsened over a five-month period. He had difficulty rising from a seated position and could not ambulate independently. Review of systems was negative for changes in appetite, abdominal pain, diarrhea, or skin rashes. Per chart review, the patient’s primary care physician had recently treated B12 deficiency with little improvement in symptoms. Further, celiac disease was diagnosed 5 years ago via endoscopy following workup for gastritis; however, the patient never initiated a gluten-free diet. Physical examination was notable for a thin male with stable vitals signs and clear mentation. There was diffuse muscle loss without focal atrophy. Lower extremity sensation and coordination were preserved, but vibratory sense and deep tendon reflexes were diminished. Gait was unsteady and wide-based. Laboratory findings revealed macrocytic anemia with leukopenia (hemoglobin 12.5 g/dL, white blood count 2.6 × 10^9/L, platelets 340 × 10^9/L and mean corpuscular volume 101.6 fL). Thyroid stimulating hormone, antinuclear antibody, lyme titers, zinc levels were normal. A full body computed tomography scan to assess for malignancy was negative. Additionally, a bone marrow biopsy evaluating for myelodysplastic syndrome showed slight hypocellularity with small lymphoid aggregates. Following neurology consultation, laboratory evaluation revealed markedly decreased serum copper (5 ug/dL, reference range 60–190 ug/dL) and ceruloplasmin (3.1 mg/dL, reference range 22–58 mg/dL) levels. The patient was treated with copper sulfate (1 mg IV weekly) and started on a gluten-free diet. His anemia and neuropathy improved significantly in 3 weeks. He also reported weight gain with strict dietary compliance supplemented by parenteral nutrition.
DISCUSSION: Peripheral neuropathy is a common office and hospital complaint. Diabetes, hypothyroidism, and B12 deficiency are typical causes; however, the differential is vast. In this case, our patient had a history of hypothyroidism and B12 deficiency, which were treated at presentation. He also had celiac disease, which was asymptomatic prior to the onset of weight loss. CD is an autoimmune enteropathy characterized by inflammation of small bowel mucosa. Commonly associated malabsorption deficiencies include low vitamin B12, folate, and calcium. Case reports have linked CD with copper deficiency. The exact location of copper absorption is unknown; however, the small intestine is reportedly involved. In our patient, worsening CD likely caused copper malabsorption, which manifested as the combination of anemia, neutropenia, and myeloneuropathy. More than three million Americans have CD, many of whom who are asymptomatic. As awareness increases, general medicine providers will likely diagnose and treat more patients with CD. Copper deficiency-associated neuropathy can be potentially irreversible; therefore, early detection of symptoms with appropriate treatment is paramount to prevent significant morbidity.
CRACK IS WHACK: CHARACTERISTIC FINDINGS IN LEVAMISOLE-INDUCED VASCULITISSalomon Puyana2; Anar Patel1; Harish Jasti1. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1934966)
LEARNING OBJECTIVE 1: Identify the clinical characteristics of levamisole-induced vasculitis
LEARNING OBJECTIVE 2: Recognize the diagnosis and management of this condition
CASE: A 57 year old female with a past medical history of rheumatoid arthritis presented with 2 days of a painful and progressive erythematous rash on her upper extremities, buttocks and knees. She was on infliximab, methotrexate and prednisone for control of her rheumatoid arthritis. She denied fevers, shortness of breath or chest pain. Social history was remarkable for tobacco use and prior incarceration. Physical exam revealed a slender, ill-appearing female. Vital signs were stable. Cardiac, pulmonary and abdominal exam were unremarkable. Skin exam was significant for erythematous and violaceous circular plaques on her elbows, buttocks, and bilateral knees as well as an eschar on the right middle finger. Laboratory studies were significant for an elevated CRP, low complement levels (C3, C4), and positive p-ANCA. Despite denial of illicit drug use, urine toxicology screen was positive for cocaine metabolites. Microscopic examination of a punch biopsy of a lesion from the mid-back revealed leukocytoclastic vasculitis and fibrinoid necrosis of the blood vessel wall with perivascular neutrophilic infiltrate. The combination of positive ANCA screen, recent cocaine use, and skin biopsy result was highly suggestive of the diagnosis of levamisole-induced vasculitis. The patient was continued on her previous dose of prednisone 20 mg daily and was counseled on abstinence from cocaine use.
DISCUSSION: Levamisole is a synthetic agent derived from imidazothiazole which was previously used as a veterinary antihelminthic and immunomodulator. In recent years, it has emerged as the prevalent adulterant of illicit cocaine in the US. A syndrome related to levamisole is becoming increasingly recognized as a serious and potentially life-threatening complication of cocaine use. Distinctive clinical characteristics suggestive of levamisole-adulterated cocaine use include neutropenia/leukopenia, cutaneous vasculopathy, and the generation of auto-antibodies. Most patients will have a positive urine toxicology screen for cocaine, and the presence of levamisole can be confirmed with gas chromatography-mass spectrometry. The predominant histopathology includes leukocytoclastic vasculitis and/or microvascular thrombosis making biopsy useful in narrowing the differential diagnosis. Commonly implicated auto-antibodies in this syndrome include ANCA, anti-phospholipid antibody, lupus anticoagulant, and anti-cardiolipin antibodies. The mainstay of treatment is abstinence from cocaine, not only for resolution of skin manifestations but also to prevent future recurrences. There is currently insufficient evidence to support the use of corticosteroids in treatment. Rarely, wound debridement and amputation is required to manage extensive skin and soft tissue necrosis. In addition to a high index of clinical suspicion and a detailed history, laboratory and histopathological findings can be helpful in making the diagnosis of levamisole-induced vasculitis.
CRACKING A RARE CASE OF ABDOMINAL PAINDevika Nair; Deepa Bhatnagar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924938)
LEARNING OBJECTIVE 1: Discover an example of congenital causes of abdominal pain
LEARNING OBJECTIVE 2: Recognize the appropriate imaging modalities used in diagnosing Nutcracker Syndrome
CASE: A 21-year-old woman presented with a one-year history of intermittent abdominal pain, nausea, and vomiting. She denied any triggering factors, drug use, sick contacts, weight loss, or blood in her stools. Vital signs on presentation were a temperature of 97 F, heart rate of 75 beats/min, respirations of 20/min, and a blood pressure of 143/90 mmHg. She had tenderness to deep palpation in the left lower quadrant as well as left costovertebral angle tenderness. Murphy’s sign was negative. Laboratory studies were only significant for microscopic hematuria and a negative urine pregnancy test. Her urine contained no white blood cells and was negative for leukocyte esterase. Her persistent costovertebral angle tenderness in the setting of a relatively normal urinalysis prompted a search for nephrolithiasis. A contrasted abdominal computed tomography (CT) revealed compression of her left renal vein by the left superior mesenteric artery. CT venography revealed a large pressure gradient between the left renal vein and inferior vena cava. It was thus determined that she was suffering from a rare condition known as Nutcracker syndrome. A stent was placed in her left renal vein, and her symptoms resolved completely.
DISCUSSION: Abdominal pain is a common complaint encountered by internists. A careful history and physical examination is essential, but cases like this one emphasize the importance of pursuing further testing when an initial evaluation is unrevealing. Nutcracker syndrome, or renal vein entrapment syndrome, occurs as the result of compression of the left renal vein as it passes between the abdominal aorta and the superior mesenteric artery. Though diagnostic criteria are not established, common manifestations include abdominal pain, nausea, hypertension, and microscopic hematuria. The phenomenon is commonly seen in adolescent females who present with pelvic pain and dyspareunia. Diagnosis is confirmed with an abdominal CT with IV contrast, but the gold standard test is venography. The left renal vein typically runs inferior to the superior mesenteric artery (SMA) and anterior to the abdominal aorta. Normally, the pressure gradient between the left renal vein and the inferior vena cava is less than 1 mmHg. A gradient of >2 cm on venography is highly suggestive of Nutcracker syndrome. This increased pressure results in the formation of collateral vessels. Communication between these vessels and neighboring renal calyces results in the hematuria that is characteristic of the syndrome. There are currently no specific guidelines for the treatment of Nutcracker syndrome. Patients may undergo observation alone, but those whose symptoms are severe receive renal vein transposition or renal vein stenting. With careful history taking and appropriate diagnostic studies, the morbidity associated with this rare condition can be significantly improved.
CRANIAL MASS IN A YOUNG MALE: TB OR NOT TBRadha S. Mehta; Gautam George; Indumathy Varadarajan. Mount Auburn Hospital, Cambridge, MA. (Tracking ID #1931849)
LEARNING OBJECTIVE 1: To diagnose a potentially curable disease by having a high index of suspicion in a patient with atypical manifestations involving several organ systems.
CASE: 25-year old male of Vietnamese descent presented with a lump on the left side of head, associated with fatigue, weight loss and night sweats. He has lived in the US all his life and has made short visits to Vietnam and the Dominican Republic. He endorsed prior smoking and a history of tuberculosis in his father. Physical examination was significant for sinus tachycardia and a nontender, nonerythematous, soft, left parietal mass. MRI Brain showed a heterogeneous mass in the diploic space of the left parietal bone that breached the cortex and was associated with epidural and subgaleal components. Chest CT revealed a pleural based mass invading left anterior ribs with accompanying bone destruction. IR-guided biopsy of the bone showed granulomatous inflammation and necrosis. PPD was strongly positive. Induced sputum and bronchoscopy specimen was positive for Mycobacterium tuberculosis by PCR and culture. Anti-tuberculosis therapy was initiated.
DISCUSSION: Tuberculosis is a chronic granulomatous infectious disease which can have bizarre manifestations. Disseminated form occurs when Mycobacterium tuberculosis bacilli spread from the primary site (usually lungs) to other organs by haematogenous or lymphatic route. Any organ system may be affected in this process of dissemination. Extremes of age and immunosuppression are the major risk factors for dissemination. In disseminated disease, usually the solid organs are affected in its micro nodular or miliary form, which manifests as diffuse enlargement of the organ or as multiple tiny lesions. The macro nodular variety is rare and it appears as a single hypo dense tumor-like lesion or as multiple hypo dense lesions with central enhancement in early lesions and as calcified lesions in advanced disease. Lytic lesions seen in skeletal tuberculosis may resemble other sinister pathology such as leukemia, neuroblastoma and Langerhan’s cell histiocytosis. In these clinical circumstances, a tissue biopsy for Tuberculosis PCR may prove to be of crucial diagnostic value. The tuberculin skin test can be a supportive diagnostic tool if positive, but a negative skin test does not exclude the diagnosis due to higher incidence of anergy in military TB. In general, the approach to antimicrobial therapy for treatment of miliary tuberculosis (TB) is the same as for pulmonary TB using the four drug regimen (Isoniazid, Rifampicin, Ethambutol and Pyrazinamide) for the first 2 months followed by two drug regimen for 4–7 months. The exact duration of treatment however is controversial.
CREUTZFELDT-JAKOB DISEASE (CJD) PRESENTING AS RAPIDLY PROGRESSIVE DEMENTIA IN A MIDDLE-AGED VEGETARIAN FEMALEMark Schwartz; Rory Shallis; Gabriela Ferreira. Rutgers Medical School, New Brunswick, NJ. (Tracking ID #1935680)
LEARNING OBJECTIVE 1: What is the differential diagnosis of rapidly progressive dementias?
LEARNING OBJECTIVE 2: What are initial diagnostic tests and when should a referral be made?
CASE: A 57 year-old female presented to the hospital with a 6 month history of rapid cognitive and functional decline, ataxia and urinary retention with associated recurrent urinary tract infections. One year prior to presentation, the patient experienced mood changes, fatigue, and 40 lb weight loss. A psychiatrist started anti-depressant therapy without improvement. A rheumatologist diagnosed the patient with Sjogren’s syndrome after labs showed elevated CRP, anti-RNP and anti-SSA, but prednisone did not improve symptoms. The patient became more ataxic, resulting in frequent falls and fractures requiring surgical repair. She eventually required assistance with all activities of daily living. Significant history included rheumatoid arthritis, B12 deficiency, bilateral knee replacements and carpal tunnel release. There was no history of organ transplantation, blood transfusion, or toxic exposure. The patient was a lifelong vegetarian. Family history was negative for neurodegenerative illnesses. On exam, the patient was alert with garbled speech and non-purposeful movements. There was no evidence of startle reflex or myoclonus. The patient had a labile affect with a short attention span. Neurologic exam revealed normal reflexes, muscle tone and strength. Labs including heavy metal screen and manganese were negative. MRI showed increased signal intensity in bilateral basal ganglia on FLAIR imaging; DWI was not performed. EEG showed bilateral posterior periodic 1.5–2Hz sharp waves during wakefulness that disappeared during sleep. CSF revealed elevated 14-3-3 protein. Diagnosis of sporadic CJD (sCJD) was made on the basis of clinical presentation, typical MRI FLAIR signals, elevated 14-3-3 and characteristic EEG findings. Patient’s family declined brain biopsy
DISCUSSION: Rapidly progressive dementias (RPD) are rare and most are caused by prion diseases which have no effective therapy. In a referral population of 825 cases of RPD (1), 54 % were prion diseases, 28 % were undetermined, and 18 % were nonprion related, and potentially treatable. Of nonprion conditions, 26 % were neurodegenerative, 15 % autoimmune, 11 % infectious, 11 % psychiatric, and 9 % other (vascular, toxic-metabolic, neoplasm related). Because of the rapidity of clinical deterioration and lack of therapies for prion diseases, clinicians must use a systematic approach to identify any potentially treatable causes. Initial diagnostic tests include labs for autoimmune, infectious or other metabolic illness, MRI brain with gadolinium to evaluate for neoplasm, demyelination, vasculopathy or neurodegenerative illness, and a psychiatric evaluation for pseudodementia in select patients. If these are unrevealing, the patient should see a neurologist for further evaluation including EEG, toxins including heavy metal poisoning, and a lumbar puncture including quantification of 14-3-3 protein to rule out CJD. This case illustrates the diagnostic challenges in CJD and RPD, which can present initially with nonspecific behavioral and constitutional symptoms. Diagnosis of CJD relies on clinical suspicion, imaging, EEG, elevated CSF biomarkers, and is confirmed by brain biopsy.
CRITICAL MASSMeghana Dhamdhere. St. Luke’s University Health Network, Bethlehem, PA. (Tracking ID #1901648)
LEARNING OBJECTIVE 1: Recognize cardiac metastasis as a cause in patients presenting with signs of cardiac failure with past history of tumors. Right ventricular (RV) metastases without either IVC or RA involvement are rare and diagnosis can be missed in view of more common causes like vegetations, thrombus or primary tumors of the heart.
CASE: A 71-year-old, with history of renal cell carcinoma (RCC-clear cell type with sarcomatous changes confined to the capsule), resected 2 years earlier, had been in his usual state of health until he presented with lower extremity edema, anasarca and shortness of breath. Two, biopsied, regional lymph nodes were negative. Echocardiogram revealed a large right atrial mass obstructing the tricuspid valve. He was also found to have a new pulmonary mass and pleural effusions suggestive of aggressive disease. CT scan of his abdomen and pelvis did not show obstruction of his IVC. He was admitted for acute kidney injury with severe hyperkalemia and severe bradycardia necessitating emergent CVVHD. His potassium improved on CVVHD, however while in the intensive care unit he developed mental status changes and worsening hypotension consistent with septic shock. He was started on empiric broad spectrum antibiotics and required vasopressor support. Given the patient’s history, metastatic tumor in the right atrium was the presumptive diagnosis. As surgical resection for cure was felt to unlikely and palliative surgical resection debulking is usually not indicated, the patient was made inpatient hospice according to his family wishes
DISCUSSION: The differential diagnoses of intracardiac masses include vegetation, thrombus and tumors. Most secondary tumors of the heart originate from leukemia, melanoma, lung cancer, breast cancer, and lymphoma. Cardiac metastases from RCC, which are extremely rare, usually occur in either of two circumstances. First, advanced RCC characteristically extends into the renal vein and the inferior vena cava in 5–15 % of patients, and into the right atrium in about 1 % of patients, thereby obstructing venous return to the heart. Second, there can be a primary tumor that metastasizes to the heart, which occurs in 10–20 % of patients who are dying of widespread, systemic RCC. Right ventricular metastases without either IVC or RA involvement are reported rarely.
CRYOGLOBULINEMIA ASSOCIATED WITH SECONDARY HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS (HLH)Shone Almeida; Soo I. Choi. Ronald Reagan Medical Center at UCLA, Los Angeles, CA. (Tracking ID #1924780)
LEARNING OBJECTIVE 1: Recognize the importance of identifying secondary causes of HLH
CASE: F.W. is a 43-year-old African American female who was transferred to UCLA with recurrent fevers, arthralgias, facial rash and abdominal pain. She was in otherwise good health until September 2012 when she began to experience persistent fevers, joint pain, and unexplained weight loss. She was admitted to three outside facilities over a 3 to 4 month period with no clear explanation for her symptoms. On evaluation at UCLA, she was noted to have markedly elevated ferritin at >20,000 ng/mL. Additional workup demonstrated anemia, thrombocytopenia, hypertriglyceridemia, and low NK cell activity with subsequent bone marrow biopsy revealing evidence of hemophagocytosis, confirming diagnosis of HLH. Evaluation for secondary cause of HLH revealed evidence of SLE (discoid lesions, pancytopenia with hemolytic anemia, multiple low-titer autoantibodies including + ANA, dsDNA, Sm/RNP, cardiolipin, and ribosomal-P protein antibodies, and hypocomplemetemia) as well as inflammatory myositis/myocarditis (CK >7000U/L and elevated troponin with decreased ejection fraction). She also had markedly positive cryocrit at 8 %. She was treated with a modified HLH-94 protocol consisting of pulse IV solumedrol followed by decadron taper and cyclosporine 200 mg twice daily. After a 2 month hospital course she was discharged in good condition.
DISCUSSION: Hemophagocytic Lymphohistiocytosis (HLH) is a rare syndrome resulting from pathologic activation of histiocytes and macrophages, leading to unchecked cytokine production and a persistent inflammatory state. HLH can occur as a primary process, familial disease, or secondary to malignancy, infection, and rheumatologic conditions. This report highlights a case of secondary HLH associated with underlying connective tissue disease with features of Systemic Lupus Erythematosus (SLE) and inflammatory myositis as well as cryoglobulinemia with good response to modified treatment regimen. The association with cryoglobulinemia is notable as there has been no report of HLH in setting of cryoglobulinemia in our review of current literature. Although a rare diagnosis, HLH is an important differential to consider in patients with recurrent fevers of unknown origin. Delay in diagnosis is often the biggest barrier to successful outcome, especially in a disease that carries greater than 50 % 5-year mortality. Additionally, identifying an underlying cause, infectious (i.e. EBV), malignancy, or as in this case, rheumatologic, has significant implications for treatment approach and prognosis.
CRYPTOCOCCAL MENINGOENCEPHALITIS: A CRUCIAL DIFFERENTIALSameer K. Avasarala1; Andrew Kure2; Anne Chen3. 1Henry Ford Hospital, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Henry Ford Health System, Detroit, MI. (Tracking ID #1923516)
LEARNING OBJECTIVE 1: Recognize the need to check cerebrospinal fluid (CSF) cryptococcal polysaccharide antigen and cryptococcal culture in any patient with abnormal CSF results.
CASE: A 48 year old homeless male with a past medical history significant for intravenous (IV) drug abuse and recent short term incarceration presented to the emergency room with a chief complaint of having the “worst headache of his life” for 5 days. His headache was associated with neck pain and photophobia. Review of systems was negative for fever, chills, nausea, and vomiting. On physical examination, he was afebrile and there were no signs of meningeal irritation or neurological deficits. He was alert and oriented to person, place, and time. His initial laboratory investigations did not show leukocytosis and his first set of blood cultures were negative. Computed tomography of his head did not show any evidence of an acute intracranial process. Initial CSF analysis revealed 236 leukocytes per microliter (17 % neutrophils and 76 % lymphocytes), glucose of 32 mg/dL, and protein of 117 mg/dL. Immediately after the CSF sample was acquired, the patient was started on intravenous (IV) acyclovir, vancomycin, and ceftriaxone as empiric therapy for both bacterial and viral meningitis. Gram stain, smear for acid fast bacilli, and India ink staining of the CSF were all negative. CSF cultures and fungal cultures were sent. After results demonstrated negative CSF herpes simplex virus polymerase chain reaction and no growth on CSF cultures after several days, all antimicrobials were discontinued. The patient was known to be human immunodeficiency virus (HIV) negative on previous testing, and repeat testing this admission was again negative. The patient clinically improved after 4 days of symptomatic therapy and was discharged with a primary diagnosis of aseptic meningitis. However, 10 days later his CSF fungal cultures identified Cryptococcus neoformans (C. neoformans) and the patient was called back for treatment. He stated that over the past few days, his headache had returned and was accompanied by nausea, vomiting, and a fever. When the patient was re-admitted his lumbar puncture had an opening pressure of 40 cm of water. He was treated with serial lumbar punctures, IV amphotericin B, and flucytosine. After 2 weeks, he was discharged on oral fluconazole as maintenance therapy with close outpatient follow up.
DISCUSSION: C. neoformans is a widespread saprophyte with a global distribution and is acknowledged as a common worldwide opportunistic pathogen. The two most common sites for infection with this encapsulated yeast are the lung and the central nervous system (CNS); although, this organism has been known to infect any organ. Pathogenesis is often related to inhalation of Cryptococcus from avian droppings or soil, with potential subsequent hematogenous spread. In the United States, C. neoformans is the predominant species with most cases reported as opportunistic infections. Cryptococcus causing meningoencephalitis most commonly affects those with an immunocompromised state: patients with Acquired Immune Deficiency Syndrome (AIDS), prolonged treatment with corticosteroids or other immunosuppressant therapy, organ transplantation, advanced malignancy, sarcoidosis and those who have been treated with other immunomodulating medications (i.e. monoclonal antibodies). Over the past few years there have been increasing reports of cryptococcal meningitis infecting patients with no known risk factors. It has been estimated that approximately 20 % of patients who have cryptococcosis without HIV infection have no apparent predisposing disease. An underlying cellular immune dysfunction is known to predispose to this infection and likely contributes to many of these cases. Although cryptococcal meningoencephalitis is an uncommon cause of meningitis, it can result in permanent cranial nerve damage and mortality. Several tests are used to help diagnose cryptococcal meningitis. India-ink preparation has an overall sensitivity of 50 %, and is over 80 % sensitive in those with AIDS. Between 93 and 99 % of patients have cryptococcal polysaccharide antigen in the CSF. In this particular case, our initial suspicion for cryptococcal meningoencephalitis was low due to the absence of risk factors, so CSF cryptococcal antigen was not checked. However, given the increasing number of cryptococcal meningitis cases identified in patients with no apparent risk factors, checking CSF cryptococcal antigen in any patient with abnormal CSF chemistries should be considered, especially given the potentially rapid progression toward permanent neurological damage and death.
CRYPTOGENIC LIVER ABSCESS IN A DIABETIC PATIENTDebjit Saha1; Sandeep Gupta2. 1Mount Sinai Medical Center, Miami Beach, FL; 2School of Medicine University of California, Irvine, CA. (Tracking ID #1939721)
LEARNING OBJECTIVE 1: Recognize the clinical clue of the pyogenic liver abscess in a diabetic patient with string test positive Klebsiella pneumoniae bacteremia.
LEARNING OBJECTIVE 2: Prompt initiation of antibiotic treatment and strict glycemic control are key interventions in preventing invasive syndromes and metastatic complications caused by hypermucoviscous Klebsiella pneumoniae strains with K1 and K2 serotypes.
CASE: A 53 year old Hispanic man with a history of type II diabetes mellitus presented with chills, fever, nausea, vomiting and abdominal pain over the past 36 h. He complained of epigastric, non-colicky, mild to moderate intensity abdominal pain associated with 5–6 episodes of non-bloody vomiting and shaking chills and high grade fever. Physical exam was significant for a temperature of 103 F, tachycardia (heart rate 134/min) and right upper quadrant abdominal tenderness on palpation without rigidity or rebound. Initial laboratory work-up showed mild leukocytosis (12,000), thrombocytopenia (133,000), hyperglycemia (363), anion-gap metabolic acidosis (anion gap of 20 and pH 7.20) with serum beta-hydroxybutyrate of 21. Liver function tests revealed an AST of 113, ALT of 126, Alk Phosp. of 202 and total bilirubin of 4.8. Abdominal ultrasound showed mild hepatomegaly with no evidence of cholelithiasis or acute cholecystitis. The patient was started with normal saline and insulin infusion. Intravenous levofloxacin and metronidazole was started after blood culture had been drawn. Following day, blood culture grew gram negative rods and patient went in to septic shock. He was shifted to ICU, antibiotics were changed to piperacillin-tazobactum. CT scan of the abdomen with contrast showed a 5 cm heterogeneous cystic/necrotic hepatic lesion in the posterior right hepatic lobe suggesting hepatic abscess. Blood culture grew highly mucoid K. pneumoniae with positive string test on day 3 of hospitalization. Antibiotic was changed to Ceftrixone and IR was consulted for percutaneous drainage. Following drainage, the patient became afebrile, LFT normalized and he was discharged after 4 weeks of intravenous antibiotics without any complications.
DISCUSSION: Our patient presented with diabetic ketoacidosis, precipitated by intra-abdominal infection. DM and specific virulent strains of K. pneumoniae were predisposing factors for the development of pyogenic liver abscess in this patient. Several studies have shown that these strains can infect the liver following translocation through intestinal epithelium. The invasive nature of these organisms can cause metastatic infective complications like bacteremia, meningitis, endopthalmitis and septic pulmonary emboli with empyema. Third generation cephalosporin with IR guided drainage is the standard of care.
CRYPTOGENIC ORGANIZING PNEUMONIA, A RARE AND OFTEN MISDIAGNOSED ENTITYSonia Rajput; Katherine Yu. UCLA-Olive View Medical Center, Sylmar, CA. (Tracking ID #1938213)
LEARNING OBJECTIVE 1: Recognize that cryptogenic organizing pneumonia is a part of the differential diagnosis when presumptive symptoms of pneumonia do not resolve despite antibiotic treatment
CASE: A 54 year-old male without significant PMH presented to the hospital with a 10-day history of dyspnea on exertion and orthopnea. He endorsed a productive cough with non-bloody sputum and night sweats, but denied fevers, myalgia/arthralgia, recent travel, sick contacts or homelessness. His respiratory symptoms failed to improve after a course of Azithromycin prescribed by his primary provider for empiric treatment of CAP vs. bronchiolitis. Upon evaluation, he was afebrile and tachycardic with an oxygen saturation of 90 % on room air. He had crackles bilaterally and no JVD or lower extremity edema. Laboratory analysis revealed hypoalbuminemia and a normal WBC and electrolyte count. Chest Xray showed diffuse patchy infiltrates in both lungs. High-resolution chest CT showed patchy ground glass opacities in a peribronchial distribution with findings suggestive of multifocal pneumonia. He was pan-cultured and started on ceftriaxone and azithromycin for presumed CAP. However, he continued to be tachypneic and O2 dependent despite antibiotic therapy. Coccidiomycosis, histoplasma, legionella, tuberculosis, cryptococcus, PCP and HIV were all subsequently negative, as were sputum and blood cultures. Transbronchial biopsy demonstrated “masson bodies” typically associated with cryptogenic organizing pneumonia. He was started on prednisone with marked improvement of his respiratory status and sent home days later.
DISCUSSION: Cryptogenic Organizing Pneumonia (COP) is a diffuse interstitial lung disease that affects the distal bronchioles and alveolar walls. It is a rare entity and accounts for roughly 6–7/100,000 admissions every year. COP usually presents in the fifth or sixth decade of life. Fifty percent of cases are idiopathic and the rest are associated with connective tissue diseases (e.g. rheumatoid arthritis), and a variety of drugs, including amiodarone. Symptoms such as cough, shortness of breath, and malaise are nonspecific and often get misdiagnosed initially as community acquired pneumonia (CAP). However a key clue is that symptoms usually last for 1–2 months and are refractory to antibiotic treatment. High resolution CT reveals patchy air-space consolidations, ground-glass opacities, and bronchial wall thickening with dilation. Biopsy typically reveals intraluminal plugs of inflammatory debris in alveolar spaces, called Masson bodies, as was seen in our patient. Treatment includes oral or parenteral corticosteroids for moderate or severe respiratory impairment, respectively. For patients who fail steroids, addition of cyclophosphamide is often indicated. Treatment usually lasts 4–8 weeks with improvement of chest imaging anywhere from several weeks up to 3 months. Internists should have a low threshold for COP when presumptive CAP symptoms do not resolve.
DAPTOMYCIN-INDUCED EOSINOPHILIC PNEUMONITISCamille Folkard; Raymond Munoz. Methodist Dallas Medical Center, Dallas, TX. (Tracking ID #1939567)
LEARNING OBJECTIVE 1: Recognize adverse drug reactions of daptomycin
LEARNING OBJECTIVE 2: Manage drug-induced acute lung injury
CASE: Eosinophilic pneumonitis is a relatively rare phenomenon that can be triggered by exposure to certain drugs or environmental agents. Daptomycin-induced eosinophilic pneumonitis typically presents within 2–4 weeks of therapy initiation as acute onset dyspnea, fever and new pulmonary infiltrates on imaging studies. Diagnosis is typically made by demonstrating eosinophilia in bronchoalveolar lavage fluid and a temporal relationship between drug exposure and symptom onset. Peripheral eosinophilia is not required for diagnosis and may be absent early in disease course. A 69 year-old woman with a past medical history of hypothyroidism, systolic CHF, anemia, hypertension, atrial fibrillation and coronary artery disease was admitted to MDMC with worsening shortness of breath and dyspnea on exertion. Several months prior, she had undergone left total knee arthroplasty and subsequently developed an infection of the prosthesis causing bacteremia. Revision was made with operative incision and drainage and exchange of the polyethylene liner by the orthopedic surgeon. Following this, she was found to have ongoing vancomycin-resistant enterococcus infection of the left knee prosthesis and started on IV daptomycin. While continuing treatment with IV daptomycin at a long-term acute care facility, she developed an episode of acute respiratory distress believed to be drug-induced and was switched from IV daptomycin to oral linezolid. Her respiratory symptoms improved and she was transitioned to Methodist Rehabilitation Hospital. This facility was unaware of the recent adverse drug reaction to daptomycin and after finding the patient pancytopenic secondary to linezolid therapy, started her back on IV daptomycin. Again, the patient developed acute respiratory distress with pulmonary edema and presented to MDMC as mentioned above. On admission, she was afebrile but with diffuse bilateral pulmonary infiltrates present on CXR. The patient was treated with removal of daptomycin (with the patient being already past the recommended antibiotic completion date), improved significantly in the following days and was discharged home.
DISCUSSION: This case demonstrates the value of a complete and thorough history. Daptomycin-induced eosinophilic pneumonitis, although rare, does occur and can present as acute lung injury with recurrences on re-exposure. Recognition is paramount. In this case, some classic presenting features of fever and peripheral eosinophilia were absent, which made the history that much more crucial in making the correct diagnosis. Demonstration of eosinophilia on bronchoalveolar lavage would have made a useful contribution, however the strong temporal association exhibited on two separate occasions and resolution of the symptoms upon removal of the offending agent were sufficient to confirm the diagnosis.
DEEPER THAN THE SKIN: DRESS SYNDROME AS A MEDICATION-RELATED COMPLICATION IN A HIV + PATIENTMeena Zareh1; Timothy Vossler1; Stephanie K. Zia1,2. 1Keck School of Medicine, Los Angeles, CA; 2Keck School of Medicine, Los Angeles, CA. (Tracking ID #1939849)
LEARNING OBJECTIVE 1: Recognize clinical features associated with DRESS syndrome
LEARNING OBJECTIVE 2: Recognize the importance and implications of assessing patients’ understanding of their medical conditions, medications, and side effects
CASE: A 50 year old African American male with HIV, Hepatitis C (HCV), chronic kidney disease, and hypertension presented with 1 week of a progressive, pruritic rash. Initially localized to the groin, the rash gradually spread to the bilateral upper and lower extremities and lips. The patient was in his usual state of health until 2 months prior to presentation, when he was enrolled in a HCV treatment trial using PEG-interferon, telaprevir, and ribavirin. Shortly thereafter, he experienced periods of shortness of breath and tachypnea, which he attributed to asthma. His HAART therapy consisted of abacavir, raltegravir, and lamivudine; however, the patient was unable to name his HAART regimen. Significantly, in the 5 month period prior to admission, the patient’s HAART therapy underwent several modifications, from monotherapy to multi-tablet regimens. On physical exam, the patient was febrile to 101.2°, tachycardic to 130, and tachypneic to 24. A morbilliform rash covered his upper and lower extremities and perineum. Inspection of the oral and anal mucosa and conjunctiva failed to reveal any lesions. Palpation of the inguinal and posterior auricular areas revealed firm, nontender lymphadenopathy. Significant laboratory data on admission included a leukocytosis of 11.0 K/cumm with 1.8 K/cumm eosinophils, a serum creatinine of 4.53 mg/dL, elevated from a baseline of 1.52, and bicarbonate concentration of 6 mEq/dL. In consultation with the allergy/immunology service, his primary doctors administered methylprednisolone at a dose of 0.6 mg/kg/day IV, with no clinically apparent response. After augmenting the dose to 1.5 mg/kg/day, the rash and eosinophilia receded over the next 2 weeks. Multiple recurrences complicated the patient’s hospital stay, as each attempt to wean the steroid dose resulted in a flare of symptoms. He developed multiple episodes of bacteremia and a gastrointestinal bleed, requiring four separate admissions to the MICU. The patient’s HIV viral load changed from undetectable to detectable, and his CD4 count began to decrease. Ultimately, he died of gram-negative sepsis.
DISCUSSION: Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is a severe reaction to medication first described in 1936. Historically associated with anti-convulsants such as carbamazepine, recently recognized culprit agents include many different medications, such as allopurinol and sulfasalazine. Signs of DRESS include morbilliform rash, fever, eosinophilia, lymphadenopathy, atypical lymphocytes, and end organ dysfunction. Proper management begins with prompt recognition and hospitalization, followed by removal of the offending drug, initiation of steroid therapy, and appropriate consultation. With an incidence between 1 in 1,000 to 1 in 10,000 drug exposures, DRESS requires a high index of suspicion to diagnose. As seen in this case, identifying the offending drug proves challenging in a patient with a complex medication history and limited health literacy about his condition and regimen. Health literacy, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” is integral to patients’ ability to adhere to treatment and achieve the best possible health outcomes. Approximately 36 % of US adults have basic or below basic health literacy skills. At-risk groups include African Americans and patients of lower socioeconomic backgrounds. Physicians can improve patients’ health literacy by utilizing strategies such as the teach-back method to assess patient understanding. Written materials such as pamphlets and medication lists can be given to patients to help promote patient empowerment and self-management of their conditions. As illustrated in our case, multiple medication changes, along with poor understanding by patients of their own care, can complicate the identification of the offending drug. If DRESS syndrome is suspected, prompt recognition and aggressive therapy should be initiated, with involvement of subspecialists. However, despite early identification and treatment, the mortality of DRESS is nearly 10 %.
DELIVERING THE DIAGNOSIS: ALCOHOLIC FOAMY CELL DEGENERATIONAbtin K. Farahmand2; Sabina Sandigursky1; Anthony A. Holmes1; Janina L. Morrison1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1936441)
LEARNING OBJECTIVE 1: Recognize an uncommon clinical presentation of alcoholic liver disease
LEARNING OBJECTIVE 2: Identify pathological characteristics of alcoholic foamy cell degeneration
CASE: A 58 year-old woman presented with intermittent epigastric pain, diarrhea and weight loss for 3 months. Her past medical history was significant for chronic alcohol abuse (1 pint of liquor daily for 20 years) with her last drink 30 days prior to admission. Her exam revealed normal vital signs, anicteric sclera, hepatomegaly, mild epigastric tenderness, and mild abdominal distention. Laboratory findings were notable for WBC 29.7 with 91 % granulocytes, INR 1.6, low albumin (2.2), total bilirubin 1.3, direct bilirubin 0.5, AST/ALT 79 and 8, respectively, alkaline phosphatase 408, and GGT 1352. Infectious work-up including hepatitis and HIV serologies, paracentesis, chest x-ray and urinalysis were unrevealing. Abdominal imaging (ultrasound with doppler and MRCP) revealed hepatomegaly without cirrhosis or vein thrombosis, mild ascites, and cholelithiasis without bile duct dilation. Her leukocytosis persisted, alkaline phosphatase remained elevated, and she underwent a liver biopsy. Liver biopsy revealed hepatocytes with both neutrophilic infiltrate and microvacuolar large-droplet steatosis, consistent with concurrent alcoholic hepatitis and alcoholic foamy degeneration.
DISCUSSION: Alcoholic hepatitis can present, as in this case, with epigastric pain, weight loss and diarrhea. The most common clinical manifestations also include jaundice, hepatomegaly and ascites. Laboratory abnormalities typically include increased serum bilirubin, elevated AST and ALT levels with AST/ALT ratio 2 or greater, elevated GGT, leukocytosis, and elevated INR. These laboratory abnormalities often resolve with cessation of alcohol use, though, more rarely, some abnormalities can persist for weeks to months after cessation, even in the absence of cirrhosis. As a result, the various manifestations of alcoholic liver disease must remain in the differential diagnosis when considering the presentation of patients with this constellation of history, symptoms, and laboratory findings. Alcoholic hepatitis is characterized by inflammation with neutrophilic infiltration of hepatocytes, usually corresponding to an elevated AST/ALT and leukocytosis. Alcoholic foamy degeneration (AFD) represents a separate pathological pathway, with neither inflammation nor fibrosis, but with significant degeneration of perivenular hepatocytes due to alcohol. AFD is characterized by transient elevation in AST/ALT but more prolonged elevation of alkaline phosphatase, without leukocytosis, mimicking obstructive biliary diseases. These two varied presentations of alcoholic liver damage are not often seen together. Importantly, alcoholic foamy degeneration is also thought to respond quickly to the cessation of alcohol use, though it is unknown whether persistence of the abnormal pathology portends a poor long-term prognosis for full recovery and resolution of symptoms.
DETERMINING THE SOURCE OF BLEEDING: A STRATEGIC DIAGNOSIS AND TREATMENT FOR OBSCURE GASTROINTESTINAL BLEEDING IN A YOUNG WOMANNagano Hiroyuki; Yukio Tsugihashi; Satoshi Okamori. Tenri yorozu Hospital, Tenri, Japan. (Tracking ID #1912637)
LEARNING OBJECTIVE 1: To recognize a small bowel tumor as a potential cause of obscure gastrointestinal bleeding in a young patient
LEARNING OBJECTIVE 2: To recognize fludeoxyglucose positron emission tomography (FDG-PET)/computed tomography (CT) as a significant tool for evaluating small bowel tumors
CASE: A 32-year-old Japanese woman presented with general fatigue and vomiting. She lost transient consciousness in the emergency room and was admitted to the Department of General Internal Medicine. Her blood pressure was 92/58 mmHg, regular pulse rate was 81 beats/min, respiratory rate was 20 breaths/min, and body temperature was 36.6 °C. Rectal examination revealed a melena. Furthermore, her hemoglobin was 9.1 g/dL, mean cell volume was 86 fl, iron level was 23 ug/dl, and ferritin level was 79 ng/ml. Her electrocardiogram was normal. Upper and lower endoscopies confirmed bleeding in the large intestine, the source of which could not be identified. Therefore, we suspected small bowel bleeding. Chest and pelvic radiographs incidentally revealed anterior mediastinal and pelvic masses. Contrast enhanced CT also revealed the masses, however the cause of bleeding remained unidentified. FDG-PET/CT revealed abnormal accumulations on the mediastinal and pelvic masses and a duodenal lesion. Small bowel endoscopy revealed an ulcerated lesion in the distal portion of the ligament of Treitz. This biopsy revealed atypical lymphocytes. CT-guided biopsy of the mediastinal mass also revealed atypical lymphocytes. The patient was then diagnosed with malignant lymphoma. Because of the risk of perforation associated with chemotherapy, we resected the duodenal lesion and pelvic mass. Histopathological examination of the resected specimen revealed diffuse large B-cell lymphoma. The patient was referred to the Department of Hematology, where she was treated by chemotherapy. The anterior mediastinal mass has now disappeared, and the patient is now in complete remission.
DISCUSSION: This case report illustrates that small bowel tumors such as lymphomas are a potential cause of obscure gastrointestinal bleeding in young patients and that FDG-PET/CT plays a significant role in the detection of these tumors. A previous study demonstrated that in patients below 40 years of age, as in this case, a small intestinal tumor is second most common cause (23 %) of obscure gastrointestinal bleeding. In this case, upper and lower endoscopies couldn’t identify the source of bleeding. Thus, we suspected a small bowel lesion including small intestinal tumor as the cause of obscure gastrointestinal bleeding. The young patient also had anterior mediastinal and pelvic masses along with obscure gastrointestinal bleeding. Therefore, we performed FDG-PET/CT in order to evaluate these masses and to survey the focus of obscure bleeding on small bowel. As a result, FDG-PET/CT revealed abnormal accumulations on the masses as well as the duodenal lesion that was not detected on contrast enhanced CT. Then, small bowel endoscopy revealed that a small bowel tumor with an ulcerated lesion was the cause of the bleeding. In conclusion, the strategic approach toward the determination of small intestinal bleeding and the masses using FDG-PET may help in the diagnosis and radical therapy.
DIAGNOSING MALIGNANT OTITIS EXTERNA - A LESSON TO IMPROVE PATIENT “HANDOFF”Anil Kumar Reddy Anumandla1; Gaurav Kistangari1; Avanti Reddy2. 1Clevaland Clinic, Cleveland, OH; 2Kasturba Medcial College, Mangalore, India. (Tracking ID #1939269)
LEARNING OBJECTIVE 1: Recognize the unusual presentation of malignant otitis externa
LEARNING OBJECTIVE 2: Recognize the importance of inadequate handoff during transfer of patient care
CASE: An 84 year old African American male presented to our hospital with nasopharyngeal mass and dysphagia. His past medical history was significant for hypertension, seizure disorder, chronic kidney disease and deep venous thrombosis. Prior to current admission, patient was twice admitted to a local hospital for poor oral intake and acute kidney injury. During that time he underwent CT head that revealed a right nasopharyngeal mass with osseous involvement of the right clivius. Biopsy of mass was considered with a presumed diagnosis of nasopharyngeal carcinoma and patient was referred to outpatient ENT physician at our tertiary care center. At the outpatient clinic, patient reported nausea, generalized weakness and inability to eat food. He was subsequently admitted for PEG tube placement as he also had a positive barium swallow study with increased risk of aspiration. Following PEG tube placement, patient’s hospital course was complicated by ileus, leucocytosis and low-grade fever. Empiric intravenous antibiotics were started for possible aspiration pneumonia. After 7 days of hospital course, the biopsy results of outside hospital were still not available and review of entire outside hospital records indicated no attempt at the biopsy; It was realized that a miscommunication during handoff made everyone assume that patient underwent biopsy at outside hospital. ENT physician was reconsulted and MRI head was done which revealed para-retropharyngeal abscess, contiguous extensive skull base osteomyelitis, and possible intracranial extension secondary to malignant otitis externa (MOE). Nasopharyngeal biopsy revealed purulence and frozen section was negative for malignancy. Post biopsy, patient was admitted to ICU as he became cyanotic and hypotensive, and was subsequently intubated for respiratory failure. Biopsy results confirmed MOE, and culture from purulent drainage grew Pseudomonas species and a rare yeast. Over the next 2 weeks tracheotomy was done to protect his airway. Treatment regimen was adjusted to micafungin and meropenem. Patient’s condition was discharge to longterm term acute care center in a stable condition.
DISCUSSION: The diagnosis of MOE should be considered in all immunocompromised patients, especially elderly diabetics, who have severe otalgia and symptoms of cranial nerve palsy. Decreased oral intake secondary to trismus may also be present. Iatrogenic factors such as aural irrigation may play a predisposing role. Pseudomonas among bacteria and aspergillus or mucor among fungi are common culprits. As the skull base is progressively involved, the adjacent exiting cranial nerves and their branches may be involved leading to cranial nerve deficits; sinus thrombosis, meningitis, and cerebral abscess may also complicate MOE and are late findings that portend a grave prognosis. Early nuclear and CT/MRI imaging, biopsy to rule out malignancy, and culture are essential for prompt diagnosis. Additionally, repeat biopsy and cultures are warranted to rule out an occult malignancy if the disease persists despite appropriate antibiotic therapy. Close follow-up is necessary due to it’s increased recurrence rates of 15 % to 20 % per year. Early recognition and early initiation of antibiotics are key to successful treatment. Ineffective patient handoffs, especially during transfer of care from other facilities, can lead to increased risk of preventable adverse events, prolonged hospitalization and reduced patient safety.
DIAGNOSING THROMBOTIC THROMBOCYTOPENIC PURPURA IN A PATIENT WITH SYSTEMIC LUPUS ERYTHEMATOSUSAlicia Stapleton1; Daniel Ling2; Daniel Kahn2. 1UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA. (Tracking ID #1939696)
LEARNING OBJECTIVE 1: Differentiate between thrombotic thrombocytopenic purpura (TTP) and lupus flare in a patient with systemic lupus erythematosus (SLE)
CASE: A 22 year old African American female with recently diagnosed systemic lupus erythematosus (SLE) presented to the emergency department complaining of worsening bilateral lower extremity edema and fatigue. She had been healthy until 2 weeks prior when she was admitted to the hospital with similar symptoms of fatigue and swelling and was found to have acute kidney injury with creatinine 2.1. Her ultimate diagnosis of SLE was solidified by a positive ANA at 1:1280 titer, elevated dsDNA, low C3 and C4, and a renal biopsy showing diffuse proliferative glomerulonephritis with crescents consistent with lupus nephritis. She was treated with rituximab, high dose steroids, and mycophenolate with improvement in renal function. Her labs at the current presentation were notable for a creatinine of 3.3, elevated from 1.9 at prior discharge. This was attributed to a worsening of her lupus nephritis although her C3, C4, and dsDNA had all improved since the last admission. She was treated again with methylprednisolone pulse and rituximab, and she was given leuprolide in preparation for outpatient dosing of cyclophosphamide. Her creatinine stabilized but did not improve. On the day of planned discharge, her platelets decreased from 233 to 131. A heparin platelet antibody test was sent to rule out heparin induced thrombocytopenia (HIT), and discharge was delayed for further monitoring. Over the next 48 h, her platelets continued to decrease to 47, and then her hemoglobin, which had been previously stable, decreased from 7.8 to 6.5. Despite these worsening abnormalities, she remained asymptomatic and her exam was significant only for isolated anasarca, with no fever, mental status changes, bleeding or bruising. Further work up of her anemia and thrombocytopenia revealed the following: LD 588, haptoglobin undetectable, reticulocyte count 1.06, total bilirubin 3.3, direct bilirubin 1.2, fibrinogen 297, INR 1.1, aPTT 27.4, and negative antiphospholipid antibodies. A peripheral blood smear showed 6 schistocytes per high power field. Given these findings consistent with microangiopathic hemolytic anemia (MAHA) in the setting of thrombocytopenia, she was diagnosed with thrombotic thrombocytopenic purpura (TTP). Hematology was consulted and performed 7 cycles of plasma exchange. Her platelets nadired at 15 before recovering, and her hemolytic anemia resolved with therapy. ADAMTS13 returned at 55 % activity, with normal being greater than 66 % by our lab standards. Her hospital course was complicated by worsening uremia leading to the initiation of hemodialysis.
DISCUSSION: TTP is a rare but dangerous entity that can be difficult to diagnose. This is particularly true in a patient with SLE, as the primary presenting signs of TTP can also be seen in a lupus flare. As our patient’s platelets decreased, TTP was low on our initial differential considering her stable hemoglobin, preserved mental status, and lack of fevers. She did have new impairment of her renal function but this was attributed to a flare of her recently diagnosed lupus nephritis. Our initial diagnostic step was to rule out HIT and to monitor. Worsening lupus flare causing immune-mediated platelet destruction was considered but thought unlikely given her ongoing immunosuppressive therapy. Only further work up revealed MAHA suggestive of TTP, prompting the urgent initiation of plasma exchange that was likely life-saving. Interestingly, her renal function did not improve despite her initial treatment for a lupus flare, suggesting that TTP was also contributing to her AKI, although no thrombotic microangiopathy was noted on her initial renal biopsy and repeat biopsy was not performed. Differentiating between TTP and lupus flare can be challenging as both can cause the pentad of hemolytic anemia, thrombocytopenia, kidney injury, fevers, and neurological symptoms, but is necessary given the divergent therapeutic pathways. TTP does not always present with this full pentad, especially in SLE patients, and can even be diagnosed with findings of only MAHA and thrombocytopenia if clinical suspicion is present. The finding of schistocytes on peripheral blood smear is more suggestive of TTP, whereas the immune-mediated hemolysis of lupus more characteristically produces spherocytes. Additionally, clinical deterioration despite aggressive immunosuppressive therapy for a lupus flare should prompt investigation for an alternative pathological process. This case demonstrates the often occult nature of TTP and the importance of a maintaining a high index of suspicion for this life-threatening syndrome.
DIAGNOSIS AND TREATMENT OF NON-TYPHI SALMONELLA INDUCED MYCOTIC ANEURYSMJung-Eun Ha. NYU School of Medicine, New York, NY. (Tracking ID #1928206)
LEARNING OBJECTIVE 1: Recognize the importance of a mycotic aneurysm in the differential diagnoses of non-specific abdominal complaints and fever
LEARNING OBJECTIVE 2: Discuss the distinct therapeutic approaches for a mycotic aneurysm and recognize the poor prognosis despite appropriate treatments
CASE: A 64-year-old man with hypertension and hyperlipidemia presented with a 10 day history of epigastric pain that radiated to his back, subjective fevers, and one episode of non-bloody non-bilious diarrhea. At first evaluation he was afebrile and hemodynamically Stable. A thoracic CT scan demonstrated a saccular lesion (please add the dimensions) with surrounding inflammation in the descending thoracic aorta. He then underwent an emergent thoracic endovascular aortic repair (TEVAR). Blood cultures grew pan-sensitive Salmonella enteritidis. Empiric antibiotic therapy with vancomycin and piperacillin/tazobactam were switched to ceftriaxone with a plan to treat for 6 weeks followed by chronic suppressive therapy in the setting of stent placement. A transesophageal echocardiogram ruled out endocarditis as the source of his aneurysm. On post-operative day 20, patient was readmitted with fever of 101.2 F, tachycardia, non-productive cough, and pleuritic chest pain radiating to left axilla. Vancomycin, piperacillin/tazobactam, and azithromycin were restarted. CT angiogram demonstrated air and debris surrounding the aortic graft concerning for the development of an abscess, of note no free air was described. Ceftriaxone was switched to ciprofloxacin. He developed a moderate-sized left pleural effusion, and thoracentesis cultures grew multidrug resistant Klebsiella pneumonia and yeast, for which polymixin B, tigecycline, and micafungin were started. An infected aortic graft was replaced by new homograft, and daptomycin was started after washout and debridement grew polymicrobes including vancomycin-resistant E. faecium, Candida glabrata, and Candida kruzei. Post-operative course was complicated by a finding of esophageal tear on CT and barium swallow that was communicating with the mediastinal and pleural space. While awaiting diversion vs. stent, patient became hypotensive to 50s systolic with 1–2 L bloody output in left pleural tube. Despite emergent TEVAR at the site of homograft tear, on day 36 from the initial presentation, patient was pronounced dead.
DISCUSSION: Mycotic aneurysm is a rare form aortic aneurysm with high rates of morbidity and mortality. It is more common in men older than 65 years of age, and those with risk factors for atherosclerosis. Presenting symptoms are non-specific and include abdominal symptoms, back pain, and fever; delayed diagnosis and treatment can lead to aortic rupture and increased mortality. Diagnosis is confirmed by positive blood cultures as well as intraoperative cultures. Non-typhi salmonella species are the most frequent pathogens, though they have a better prognosis than other micro-organisms. Several recent case reports have found that patients receiving emergent TEVAR had improved early morbidity and mortality and a comparable long term outcome when compared to patients receiving traditional open surgery. Most case reports used 6–8 weeks of third generation cephalosporin post-operatively given increased rates of ciprofloxacin-resistant salmonella. A systematic review showed that age 65 years or older, aneurysm rupture, and perioperative fever were predictors of persistent infection while preoperative antibiotics use for longer than 1 week and an adjunct intraoperative procedure were protective. The 12-month survival rate of those with sterile repeat blood cultures was 94 % while that of persistently infected group was 39 %. One case report of intraoperative, intra-aortic rifampin infusion noted a resolution of aneurysm sac at 4-month follow-up. Early diagnosis and TEVAR with adjunct procedure may improve prognosis of the rare but lethal mycotic aneurysm.
DIALYSIS DISEQUILIBRIUM SYNDROMEKhaled M. Abouelezz; Ahmed Abuzaid; Mohamed El khashab; Abhishek Matta. Creighton university medical center, Omaha, NE. (Tracking ID #1939703)
LEARNING OBJECTIVE 1: Recognize Dialysis Disequilibrium Syndrome as a cause of brain edema and death.
LEARNING OBJECTIVE 2: Recognize risk factors for Dialysis Disequilibrium syndrome.
CASE: A 59-years-old African American male with history significant for end stage renal disease status post bilateral transplant and insulin dependent diabetes mellitus admitted with altered mental status (GCS 7) hypothermia (94.4 F), hypotension, tachypnea, kussmaul’s breathing, severe dehydration and anuria. Blood tests showed elevated plasma glucose level (1000 g/dl), BUN 246 mg/dl, Creatinine 14.6 mg/dl with baseline 1.2 mg/dl, measured osmolality 437, calculated osmolality 438, and positive ketone in urine. Patient was diagnosed with diabetic ketoacidosis with acute kidney injury secondary to dehydration. Patient was intubated due to sever distress, given intravenous fluid with bicarbonate and insulin. Follow up blood work after 8 h showed BUN level 185 mg/dl. The decision was made to start the patient on hemodialysis. Patient had dialysis for 1 h. His BUN level after the dialysis was 124. Later the blood cultures disclosed gram negative rods bacteremia. Next day GCS dropped from 7 to 3. Patient was not breathing over the ventilator. CT of the head was done showed diffuse advanced global edema throughout the cerebral cortex with tonsillar herniation. Patient was given mannitol with no improvement. The patient deceased on the following day.
DISCUSSION: Our patient mostly developed dialysis disequilibrium syndrome which is a rare syndrome presented with neurologic manifestation mostly secondary to brain edema that affect dialysis patients, particularly when they are first started on hemodialysis. The pathogenesis is not clear but mostly secondary to reverse osmosis due to removing of urea or due to changing in the cerebral intracellular PH that can lead to cerebral edema. Risk factors include first dialysis treatment, markedly elevated blood urea concentration, chronic kidney disease, severe metabolic acidosis, older age, any condition that increases permeability of the blood brain barrier (such as sepsis, vasculitis, thrombotic thrombocytopenic purpura-hemolytic uremic syndrome or meningitis). Our patient had known kidney disease, sepsis. His BUN level dropped from 246 to 124 within 12 h after one dialysis session. He was intubated, that delayed recognition of his neurological status. Management of suspected DDS aims mainly to reduce the intracranial pressure of the patient. Standard maneuvers are to give mannitol or hypertonic saline to raise the blood osmolality and to hyperventilate the patient; however, these measures may be futile. The corner stone in the management is the prevention. The most important preventive measure is to limit the reduction in BUN per treatment so that there is a gradual reduction that is distributed over several days. Slow urea removal can be achieved by low blood flow rate of 150 to 250 mL/min with a small surface area dialyzer (0.9 to 1.2 m2), patients who have marked fluid overload can be treated with ultrafiltration. Patients with extremely elevated BUN or neurologic symptoms, dialysis should be initiated as an inpatient. Conclusion: Dialysis disequilibrium syndrome is a disease that can result from rapid drop in BUN in patient on dialysis especially during the first session, resulting in neurological manifestation range from nausea to herniation and death. The main cornerstone in the management is prevention by slow urea removal and early detection.
DIFFUSE CEREBRITIS IN ALCOHOL WITHDRAWAL AND MENINGITIS: NO ROOM FOR DIAGNOSTIC DELAYPoojita Shivamurthy; Sparsha Kukunoor. University of Connecticut Health Center, Farmington, CT. (Tracking ID #1933996)
LEARNING OBJECTIVE 1: Suspect meningitis early in patients with altered mental status in setting of alcohol withdrawal to prevent fatal complications.
LEARNING OBJECTIVE 2: Recognize infrequent complications of Pneumococcal meningitis including diffuse cerebritis and acute demyelinating encephalomyelitis (ADEM).
CASE: Fifty four year old male with alcohol abuse was brought to the hospital by friends for poor intake and not being himself for 2 days. His medical history was significant for heavy alcohol abuse. He drank a gallon of vodka and snorted heroin daily. He took no medications, lived alone and was unemployed. Limited review of systems was positive for headache, negative for fall, fever, cough and diarrhea. At arrival, he was afebrile, tachycardic to 120 beats per minute with blood pressure 160/90 mmHg and normal respiration. He was disheveled, agitated with an unsteady gait with poor oral hygiene. He had bilateral rhonchi on lung exam, normal intensity heart sounds, soft non tender abdomen without organomegaly. Neurological exam was non focal. Lab data showed hyponatremia (128 meq/L), hypochloremia (86 meq/L) with creatinine. His neutrophil count was 6400 per microL, Hemoglobin of 10 g/dl with platelet count of 282,000 per microL. Alcohol level was 33 mg/dl, urine positive for opiates and cannabis. Head CT was suggestive of mild nonobstructive hydrocephalus. Chest Xray showed patchy left lower lobe consolidation for which Vancomycin was given in the ER. He was diagnosed with alcohol withdrawal, received Ativan following which he got intubated for airway protection. In ICU, he was sedated with propofol. Blood cultures grew Streptococcal pneumonia which was thought to be secondary to pneumonia. To investigate quick deterioration in mental status, lumbar puncture was done in the ICU. CSF was turbid with WBC 1685 per microL, elevated protein at 625 mg/dl, and a strikingly low CSF glucose of 2 mg/dl growing streptococcal pneumoniae. He was immediately started on high dose of ceftriaxone, and dexamethasone but more than 15 h had elapsed prior to this. Transesophageal echocardiogram did not show vegetations. He remained hemodynamically stable. Following day, during sedation holiday, patient was unresponsive with GCS of 3, flaccid quadriplegia and absent deep tendon reflexes. Immediate head CT showed diffuse supratentorial white matter hypoattenuation and loss of gray-white differentiation in bilateral parietal lobes and cerebellum suggestive of extensive multifocal acute infarcts with superimposed cerebritis. There was a small suspicion ADEM based on intensity of demyelination. Hence, patient was given high dose prednisone (1 g daily for 5 days) while antibiotics were continued. Repeat MRA showed slight improvement in degree of restricted diffusion in the white matter but progression of cerebritis. Due to poor prognosis, family wished to focus on comfort. Patient expired 4 days after.
DISCUSSION: It is crucial to broaden our differential for altered mental status in alcohol withdrawal. Unrecognized sepsis or meningitis is detrimental. There was a delay in recognizing meningitis and hence in starting antibiotics and steroids (ideally within 4 h). This gives us opportunity to review literature on cerebritis and ADEM in meningitis. Cerebritis is a result of cerebral vascular involvement from infection or inflammation which causes altered mental status or focal deficits if infarcts occur. High clinical suspicion, contrast MRI are the diagnostic methods. Altered mental status in pneumococcal meningitis is an independent predictor of in-hospital mortality and neurological deficits1. It could be due to persistence of biologically active agents in killed bacteria which incite host inflammatory response. While early diagnosis of meningitis may prevent these complications, it is unknown if early diagnosis of cerebritis in timely treated meningitis has better prognosis. A case report with cerebritis from Klebsiella pneumonia in an alcoholic cites an animal study where alcoholic hosts were more susceptible due to lack of cytokine IL-7 response.2 Post infectious ADEM is a rare differential for cerebritis when there is intense demyelination.3 It occurs within few weeks of an infective process. T2-weighted images, FLAIR sequences, and contrast-enhanced MRI with gadolinium are preferred tests. High dose steroids is the treatment of choice. Time frame and no response to steroids goes against ADEM in our patient. References: 1. Pfister HW, Feiden W, Einhaupl KM. Spectrum of complications during bacterial meningitis in adults: Review of prospective clinical study. Arch Neurol.1993 Jun;50(6):575–81. 2. Majumdar M, Simes DC, Prabha RD. Cerebritis: An unusual complication of Klebsiella Pneumoniae. Indian J Crit Care Med.2009. Jan-Mar;13 (1):37–40. 3. Beleza P, Ribeiro M, Pereira J, Ferreira C, Jordão MJ, Almeida F. Probable acute disseminated encephalomyelitis due to Haemophilus influenzae meningitis. Dev Med Child Neurol. 2008 May;50(5):388–91.
DIFFUSE MESENTERIC VENOUS THROMBOSIS RESULTING IN BOWEL ISCHEMIA AND OBSTRUCTION WITH NORMAL LACTATE LEVELSYevgeniy Mikityanskiy; Gary Carpenter; Farah Daccueil; Evan Schloss; Nicholas Berbari; James Gardner. Winthrop University Hospital, Mineola, NY. (Tracking ID #1937639)
LEARNING OBJECTIVE 1: To reinforce the importance of a trusting physical exam findings, maintaining a broad differential diagnosis and constantly reevaluating the approach to treatment if the patient’s condition is not improving despite appropriate therapy.
LEARNING OBJECTIVE 2: To emphasize that sensitive laboratory studies may still be normal in atypical presentations of certain disease processes.
CASE: A 36 year-old male with no past medical or surgical history presented with 2 weeks of abdominal pain and constipation. He was initially evaluated at another emergency department with an abdominal CT scan and ultrasound, both of which were negative. The patient traveled to Florida where the pain worsened again and became accompanied by nausea and vomiting. On arrival to our hospital, the patient was hypertensive with an abdominal exam positive for hypoactive bowel sounds, voluntary guarding, diffuse tenderness to palpation, but no rebound or rigidity. Laboratory work up revealed leukocytosis, elevated INR, ESR and CRP, but normal liver related tests as well as a normal lactate level. Abdominal x-ray showed relative obstruction of emptying of all contrast from the stomach and duodenum. CT of the abdomen revealed duodenal wall thickening, marked wall thickening and edema of several jejunal loops in the left upper quadrant with associated mesenteric edema. The findings were consistent with enteritis. The patient was treated aggressively with intravenous fluids, broad spectrum antibiotics and pain control. However, his condition worsened daily with increasing leukocytosis, worsening abdominal pain despite high doses of opioids as well as profound tachycardia. Serum lactate measurements remained normal. The patient developed feculent vomiting, abdominal rigidity and rebound tenderness. A nasogastric tube was inserted for small bowel obstruction, which was confirmed byabdominal x-ray. The initial abdominal CT was reevaluated as showing extensive thrombus in the portal vein, superior mesenteric vein and splenic vein. Stat abdominal MR showed ischemia and necrosis involving proximal jejunal loops with presumed secondary thrombosis of several mesenteric veins. Emergent exploratory laparotomy with 60 cm jejunal resection revealed loops of jejunum with a sharp demarcation between necrotic and healthy bowel without any obvious anatomical etiology. Post-operatively, full dose low molecular weight heparin was initiated and the patient showed significant clinical improvement. Abdominal CT angiography showed patent mesenteric arterial system. Hypercoagulable workup revealed heterozygosity for factor V leiden gene mutation and prothrombin G20210A mutation suggesting that mesenteric venous thrombosis was, in fact, the primary event.
DISCUSSION: Mesenteric ischemia is typically arterial in etiology in patients with known risk factors. It is described as pain out of proportion to physical exam findings and elevated serum lactate is a rather sensitive marker used to aid in making the diagnosis. The pathophysiology of intestinal ischemia caused by venous thrombosis involves increased resistance in mesenteric venous blood flow causing profound bowel wall edema, fluid efflux into bowel lumen resulting in systemic hypotension, increase in blood viscosity leading to decreased arterial flow, submucosal hemorrhage and ultimately bowel infarction. This case of hereditary hypercoagulability induced mesenteric venous thrombosis with subsequent bowel ischemia and necrosis is unusual since most causes of bowel ischemia are indeed arterial in origin. Additionally, persistently normal lactate levels in the setting of severe bowel necrosis proved to be an uncommon as well as misleading phenomenon. This case also serves to reinforce the importance of trusting the physical exam, even if it does not perfectly correlate with pertinent laboratory and imaging findings, as well as maintaining a broad differential diagnosis if the patient’s condition is not improving despite seemingly appropriate medical treatment.
DIRE DIARRHEA: IPILIMUMAB INDUCED COLITIS AND ITS MANAGEMENTYouran Gao; Saumya Sharma; Rubina Boparai. Northshore-LIJ, Manhasset, NY. (Tracking ID #1899684)
LEARNING OBJECTIVE 1: Increase early detection of colitis in patients who present with diarrhea and abdominal while on ipilimumab for melanoma treatment.
LEARNING OBJECTIVE 2: Recognize the treatment options for ipilimumab induced colitis.
CASE: Case 1: A 49-year-old woman with metastatic melanoma developed abdominal pain 1 day after initial dose of ipilimumab at 3 mg/kg. After second dose she also developed small volume watery diarrhea occurring 3–4 times daily. She was started on oral prednisone 40 mg taper for 1 week. Within the week, patient’s diarrhea worsened to 5–6 per day, and she was admitted to the hospital. A colonoscopy was performed which showed pancolitis with diffuse erythema and edema. Methylprednisolone 60 mg IV q8 h was started and patient’s symptoms improved within 24 h. Patient was discharged home on oral prednisone 60 mg taper with complete resolution of symptoms within 1 week. Case 2: A 86-year-old man with metastatic melanoma presented with 3 day history of non-bloody diarrhea without abdominal pain. Two weeks prior, patient received second infusion of Ipilimumab at 3 mg/kg for the treatment of metastatic melanoma. CT scan of abdomen showed diffuse colonic wall thickening with pericolonic fat stranding suggesting pancolitis. Clostridium difficile testing was found to be negative and treatment with high dose IV steroids was started. Response to steroid use was suboptimal and patient continued to have diarrhea. Initiation of Infliximab as an alternate treatment was considered however not initiated due to patient’s poor cardiac function (EF 20 %). IV steroid treatment was continued and patient began to show improvement. He was discharged with slow oral prednisone taper with complete resolution of diarrhea within 2 weeks.
DISCUSSION: Ipilimumab, a monoclonal antibody to cytotoxic T-Lymphocyte antigen 4 (CTLA-4), is used for the treatment of metastatic melanoma. Inhibition of CTLA-4 results in activation of T cells which proliferate and infiltrate into tumors causing tumor cell death. However, this same mechanism also leads to increased immune activity against normal cells which is the underlying cause of side-effects associated with ipilimumab. The most commonly seen adverse event is colitis but skin, liver, and endocrine organs can also be affected. Steroids are usually used first but Infliximab can be used as second line. As in case 2, many patients may have contraindications to infliximab therapy. Both of these patients had colitis after 2 treatments of ipilimumab and both were successfully treated with high dose IV steroids. Case 1 had a faster and more sustained response to steroids mostly because of her age and lack of other comorbidities. In both instances, further treatment with ipilimumab was aborted because the risk of complications from recurrent colitis outweighed the benefits.
DISSEMINATED HISTOPLASMOSIS PRESENTING WITH PANCYTOPENIA IN AN AIDS PATIENTRibka Ayana1,2; Katherine C. Chretien1,2; Suzanne Sweidan1. 1George Washington University Hospital, Washington, DC, DC; 2 DC VA Medical Center, Washington, DC, DC. (Tracking ID #1939247)
LEARNING OBJECTIVE 1: Recognize clinical features of disseminated histoplasmosis
LEARNING OBJECTIVE 2: Adopt a cost-conscious approach to diagnosis of disseminated histoplasmosis
CASE: A 38 year-old man presented with 5 days history of fevers and shortness of breath. He also noted 30 lb weight loss, malaise, headache, gingival bleeding, and dark urine. He was diagnosed with HIV 10 years prior, but he was treatment naïve, followed by holistic doctors who treated him with various unknown herbal medications. The patient was chronically-ill appearing. He had scleral icterus and multiple, small, shallow, ulcers with a clean base. Lung exam revealed diminished breath sounds diffusely and crackles at the bases. Complete blood count revealed pancytopenia with white blood cell count of 1,850, hemoglobin of 5.4 g/dL, platelet count of 18,000 and a CD4 count of 0. His hepatic panel was notable for an albumin of 1.8, total bilirubin of 2.7, aspartate aminotransferase of 479, alanine aminotransferase of 104 and alkaline phosphatase of 141. Ferritin level was greater than 10,000 ng/mL. Lactate dehydrogenase was 7,108 with haptoglobin of less than 20 suggesting a hemolytic process. A thoracic CT scan revealed scattered tree bud opacity and bilateral pleural effusions, splenomegaly, and bulky necrotic left axillary lymphadenopathy. On admission, he was empirically started on moxifloxacin to cover for possible community-acquired pneumonia and sulfamethoxaxole/trimethoprim for possible pneumocystis pneumonia. Fluconazole was added for oral candidiasis. Further diagnostic studies were negative including hepatitis panel, serum RPR, stool AFB, quanteferon, serum cryptococcal antigen, and head CT scan. On the fourth day of hospitalization, he was transferred to the intensive care unit (ICU) with septic shock and disseminated intravascular coagulation. Clarithromycin, ethambutol and rifabutin were begun for empiric mycobacterium avium-intracellulare (MAI) infection treatment. The next day, a bone marrow biopsy was preformed and the aspirate smear as well as the core biopsy revealed histiocytes containing numerous intracellular yeast forms morphologically consistent with Histoplasma. Following the diagnosis of disseminated histoplasmosis, Ambisome was started at a dose of 5 mg/kg daily.
DISCUSSION: Although opportunistic infections are not seen as commonly in the post antiretroviral era, internists need to be adept at recognizing and diagnosing these infections as timely diagnosis and initiation of early, appropriate, therapy is critical for good patient outcome. It has been well-established that patients with AIDS have increased incidence of both AIDS defining and non-AIDS defining malignancies. Thus, when hematologic abnormalities are seen, concern for malignancy is warranted. Nonetheless, it is also important to consider infiltrative infectious processes when AIDS patients present with cytopenia. Disseminated histoplasmosis is an uncommon, potentially fatal, but treatable infection seen in immunocompromised patients such as those with advanced AIDS and CD4 lymphocyte count less than 100 cells/microL. While disseminated histoplasmosis is a well-recognized complication of AIDS, fortunately, it is fairly uncommon in the post antiretroviral era, which can lead to potential delayed or missed diagnosis. This patient presented with many of the clinical and laboratory features seen in disseminated histoplasmosis including fever, fatigue, night sweats, splenomegaly, cytopenia, elevated ferritin and liver enzymes. Failure to recognize the diagnosis in this patient led to unnecessary studies and delay in initiation of the appropriate therapy. In AIDS patients with disseminated disease, histoplasma antigen detection is the most sensitive and specific test. In this case, a urine histoplasma antigen test could have led to an earlier diagnosis and prevented complications as well as more costly, and more invasive studies.
DISSEMINATED MYCOBACTERIUM AVIUM COMPLEX INFECTION AS A CAUSE OF TREATABLE DEMENTIAHirotaka Kato; Matthew Harrington. Beth Israel Medical Center, New York, NY. (Tracking ID #1935439)
LEARNING OBJECTIVE 1: Recognize disseminated mycobacterium avium complex infection as an etiology of reversible dementia in AIDS patients.
LEARNING OBJECTIVE 2: Recognize the risk of early diagnostic closure in AIDS patients given concomitant infections can exist.
CASE: A 58 year-old male with recently diagnosed HIV presented with altered mental status in setting of 6 months progressive cognitive decline, visual hallucinations and paranoia. Patient reported subjective fevers, night sweats, weight loss, and diffuse pruritic nodular rash. On presentation, the patient was somnolent, afebrile. Neurologic exam revealed emotional lability, absent focal deficits or meningeal signs. The following laboratory tests were normal, including electrolytes, TSH, B12, folate, RPR/FTA-ABS, urinalysis, urine toxicology, and CSF studies. Toxoplasma, cryptococcus, and JC Virus serologies were also negative. HIV vial load was 1.2 million copies/mL, CD4 count was 2 cells/mL. MRI revealed diffuse white matter changes. Blood cultures detected Staphylococcus aureus (MSSA) in 1 of 4 initial cultures and 2 of 4 repeat cultures. The patient was treated with cefazolin for 6 weeks for presumed Infectious Endocarditis due to this persistent MSSA bacteremia. Opportunistic infection prophylaxis initiated with azithromycin and trimethoprim/sulfamethoxazole, however, antiretroviral therapy was deferred due to the risk of immune reconstitution syndrome. His mental status remained labile with aggressiveness, which was considered as HIV-associated dementia. Patient was discharged on day 10. The patient presented 2 weeks later with fever and rigors. Infectious workup was unrevealing. AFB blood cultures from the initial hospitalization detected mycobacterium avium complex. Within 1 week after clarithromycin, ethambutol and rifampicin were initiated, the patient defervesced and mental status resolved to baseline.
DISCUSSION: Symptoms of disseminated mycobacterium avium complex infection (MAI) are non-specific, including fever, diarrhea, and weight loss, which precede the onset of fever. Since it takes about 10 days to detect mycobacterium from blood culture, early diagnosis and treatment are challenging. To our knowledge, there exists no case report documenting disseminated MAI presenting as progressive cognitive impairment. Furthermore, concomitant bacteremia with disseminated MAI has not been described in the literature. This patient had fever, night sweats, which were consistent with symptoms of MAI, however, the presence of MSSA bacteremia misled to early diagnostic closure in the first hospitalization. We initially considered HIV-associated dementia as the cause of his early dementia and planned to initiate HAART later due to the concern of immune reconstitution syndrome, however, his significant cognitive improvement after the initiation of disseminated MAI treatment strongly suggests disseminated MAI as the cause of his progressive cognitive decline. Physicians should be aware of disseminated MAI as an etiology of neurocognitive decline or altered mental status in AIDS patients. Also, acid-fast bacilli culture must be considered for any patient with AIDS or unknown CD4 count presenting with non-specific symptoms, even without fever.
DISSEMINATED PYOGENIC INFECTION CAUSED BY STREPTOCOCCUS ANGINOSUS THROUGH HEMATOGENOUS SPREAD VIA INFECTIOUS ENDOCARDITISRie Ueno1; Ayumi Maeda2; Misako Nagasaka1; Wan L. Lam1; Dennis Karter1; David C. Perlman1. 1Beth Israel Medical Center, New York, New York, NY; 2Massachusetts General Hospital, Boston, MA. (Tracking ID #1934424)
LEARNING OBJECTIVE 1: Identify Streptococcus anginosus as one of the causes of infectious endocarditis
LEARNING OBJECTIVE 2: Recognize the importance of early detection of brain abscess during Streptococcus anginosus bacteremia
CASE: A 57 year-old female with a history of a perianal abscess presented with fevers and chills for 7 days. Two weeks prior the abscess had drained spontaneously. On admission, temperature 100.9 °F, BP 104/70, HR 112/min, and RR 15/min. Physical exam demonstrated mild right upper quadrant tenderness and a 1–2 mm well healed scar in 6 o’clock position of her anus. Labs showed WBC 15.7/mL with 88 % PMNs, ALP 202 U/mL, T bil 1.5 mg/dL, ALT 70 U/L, AST 145 U/L. Abdominal CT scan showed a 11.4 × 9 × 14 cm lobulated collection in the right hepatic lobe with satellite abscess measuring 2.4 × 2.2 × 1.8 cm in the left lobe. The patient received piperacillin/tazobactam 3.375 g IV q6 and underwent percutaneous drainage of the larger abscess. Cultures of the aspirate and 1 out of 2 sets of blood cultures grew Streptococcus anginosus. Antibiotics were changed to ceftriaxone 2 g q24 and metronidazole IV 0.5 g q8. Transthoracic echocardiogram was negative for vegetation and subsequent blood culture was negative. She was discharged on the same antibiotic regimen but presented 1 week later with memory deficits. Head CT and brain MRI showed more than 10 ring-enhancing brain lesions measuring 0.3–1.7 cm in the bilateral cerebral and cerebellar hemispheres, most prominently adjacent to the left ventricle with associated edema. Transesophageal echocardiogram (TEE) showed 0.7 cm vegetation on the aortic valve with a trace aortic regurgitation. Ceftriaxone was increased to 2 g q12. Repeat TEE 1 week later showed disappearance of the vegetation. Her symptoms improved and she was discharged with ceftriaxone IV 2 g q12. Head and Abdominal CT scans at 4 weeks of therapy showed interval resolution of the brain lesions and the liver abscesses.
DISCUSSION: The Streptococcus anginosus group (SAG), also known as the Streptococcus milleri group is a subgroup of viridans streptococci that consists of three distinct streptococcal species: S. anginosus, S. intermedius, and S. constellatus. Compared to other viridans streptococci, members of the SAG are more often associated with abscess formation, including liver and brain abscess through their cell surface adhesions and pyogenic extoxins but less often associated with infectious endocarditis. When endocarditis does occur, it is more common in patients with damaged or prosthetic heart valves than patients with normal native valves. A 2012 literature review identified 12 cases of disseminated pyogenic infection affecting multiple (2 or more) organs, caused by SAG, but none was accompanied with endocarditis. Our case describes a rare instance of liver and brain abscesses in the setting of infectious endocarditis by SAG. It is important to recognize SAG as one of the causes of native valve infectious endocarditis and to search for signs of dissemination to other organs. Brain abscess should be considered in any patient with SAG bacteremia who presents with cognitive deficits. Also our case suggests the importance of performing TEE to evaluate for endocarditis for patients with SAG bacteremia.
DISSEMINATED TOXOCARIASIS IN AN IMMUNOCOMPETENT HOSTParas Karmacharya1; Madan R. Aryal1; Ranjan Pathak1; Smith Giri4; Amrit Pokharel5; Pragya Shrestha2; Supriya Shrestha Tamrakar3; Richard Alweis1. 1Reading Health System, West Reading, PA; 2Nanjing Medical University, Nanjing, China; 3Guangxi Medical University, Guangxi, China; 4University of Tennessee Health Science Center, Tennesse, TN; 5Tribhuvan University Teaching Hospital, Kathmandu, Nepal. (Tracking ID #1935244)
LEARNING OBJECTIVE 1: Consider toxocariasis as a differential diagnosis in patients with persistent hypereosinophilia. Look for a history of exposure to dogs and cats in patients with multiple non-cavitating pulmonary and hepatic infiltrates and perform toxocara serology if present.
LEARNING OBJECTIVE 2: Treat promptly with albendazole or mebendazole with concomitant corticosteroid.
CASE: A 36 year-old-male presented with low grade fever, fatigue, and intermittent right upper quadrant abdominal pain for 1 week. Associated symptoms included nausea with 5 episodes of non-bilious vomiting and nonproductive cough. He lived in an apartment with 6 dogs and a kitten. On physical examination, he was afebrile with mild right upper quadrant tenderness. Labs included a white cell count 17,400/mm3 (eosinophils 18 %, absolute eosinophil count 3,220), and normal liver function tests. Serum immunoglobulin (Ig) E levels were 5564 U/ml; IgA, G and M as well as complement levels (CH50) were within normal limits. Flow cytometry did not reveal abnormal cell population. Additional tests, including antinuclear antibody, anti-neutrophil cytoplasmic antibody, stool examination for ova and parasites, serologies for HIV, hepatitis B and C, Aspergillus fumigatus, Trichinella spiralis, Histoplasma capsulatum, Toxoplasma gondii, Strongyloides stercoralis and quantiferon test were all negative. His serum toxocara Ig M antibody levels on ELISA was 3.19 (normal <1). Chest radiograph revealed bilateral scattered small ill-defined nodules bilaterally. Contrast enhanced CT scan of the chest and abdomen revealed ill-defined pulmonary nodules and multiple hypodense lesions in the liver. CT scan of the brain was unremarkable. Gram stain, acid fast stain and bacterial/fungal cultures of bronchial washings and endobronchial biopsy were negative. Urine and blood cultures were negative. He was treated with mebendazole 200 mg twice daily for 5 days for disseminated toxocariasis. Concomitant prednisone was started at 1 mg/kg/day and tapered over the next 2 months.
DISCUSSION: Toxocariasis is a human infiltrative larval infection caused by the dog ascarid, Toxocara canis and the cat ascarid, Toxocara cati1). While it is more common in the tropical regions of the world; it is estimated that human seroprevalence is 13.9 % in the United States (2) and that about 5 % of dogs and puppies in North America are infected (3). It commonly affects the pediatric and immunocompromised population; and rare in the immunocompetent. Most human infections are asymptomatic. Two of the well-recognized syndromes especially in children are visceral larva migrans and ocular larva migrans. Diagnosis is established on the basis of marked eosinophilia and presence of specific serum toxocara antibodies in the right clinical setting. Serum eosinophil levels may be used to assess therapeutic response. Mild forms of toxocariasis are self-limited and do not require anti-helminthic therapy; severe or persistent infections, such as in our case, can be treated with mebendazole and albendazole (4). Concomitant corticosteroids limit the inflammatory response. References: 1. Nicoletti A. Toxocariasis. Handb Clin Neurol. 2013;114:217–28. 2. Won KY, Kruszon-Moran D, Schantz PM, Jones JL. National seroprevalence and risk factors for Zoonotic Toxocara spp. infection. Am J Trop Med Hyg. 2008 Oct;79(4):552–7. 3. Mohamed AS, Moore GE, Glickman LT. Prevalence of intestinal nematode parasitism among pet dogs in the United States (2003–2006). J Am Vet Med Assoc. 2009 Mar 1;234(5):631–7. 4. Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev. 2003 Apr;16(2):265–72.
DO NOT LET THE MOMENTUM TAKE YOUReza Sedighi Manesh; Jeff Kohlwes; Jeffrey Dixson. UCSF, San Francisco, CA. (Tracking ID #1940211)
LEARNING OBJECTIVE 1: Apply Bayes’ theorem to improve diagnostic accuracy
LEARNING OBJECTIVE 2: Recognize diagnostic momentum to reduce diagnostic error
CASE: 67 y/o Japanese American who has been out of care for 15 years is brought to the emergency department by his brother with painless jaundice for 3 weeks. For 2–3 weeks prior to presentation, pt noted yellow eyes and skin, white stool, fatigue, and severe pruritis that was interfering with sleep. He denied abdominal pain, fevers, chills, diarrhea, nausea or vomiting but did note 15–20 lb unintentional weight loss over the last 1–2 months. He has had a good appetite without dysphagia or odynophagia, melena, or BRBPR. Past medical history was notable only for a remote stab wound in his LUQ from a disgruntled mistress for which he underwent laparotomy without bowel resection at another institution. He takes no medications and has no allergies. By social history he is a Vietnam vet, lives with his ex-wife and owns a video store. He previously drank 10–12 beers daily, but has cut back to 1–2 daily. He has a 50 pack year smoking history and used marijuana in the service, but otherwise denies any illicit drug use. Family history was negative for malignancy or liver disease. Exam was notable for normal vital signs, marked jaundice, a large surgical scar on his abdomen, and multiple excoriations over his abdomen consistent with his history of pruritis. He had no stigmata of chronic liver disease, no appreciable organomegaly, and no asterixis, but did have a possible fluid wave detected. Labs were notable for a predominantly direct hyperbilirubinemia with intact synthetic function. AFP and viral hepatitis serologies returned negative. CT abdomen pelvis with contrast showed marked intrahepatic and extrahepatic biliary dilation. An ampullary lesion could not be entirely excluded. EUS revealed a 2.3 × 2.8 cm mass in the uncinate process of the pancreas without vascular invasion, which was sampled by FNA. ERCP was performed and revealed a single, localized, 1 cm stenosis of the common bile duct that was successfully stented. FNA biopsy results returned “abundant benign pancreatic elements”. He was seen in general surgery pre-op clinic where all imaging, pathology, and laboratory results were thoroughly reviewed. A pylorus-preserving Whipple resection was performed. The surgical pathology report returned and showed duct-centered lymphoplasmacytic inflammation, ductilitis, fibrosis, and phlebitis with more than 100 IgG4 plasma cells per high power field, consistent with autoimmune pancreatitis type I, or IgG4-related sclerosing pancreatitis and cholangitis.
DISCUSSION: Diagnostic momentum is the conveyance of an initial working diagnosis from one team to another without adequate consideration of alternative possibilities. In this case the diagnostic momentum was initiated by the medicine service and subsequently accepted by the consulting services. The diagnosis of pancreatic adenocarcinoma, resulting in a potentially morbid procedure (i.e., pancreaticoduodenectomy), should have been seriously questioned with the benign pathology of EUS-guided biopsy. In medicine Bayes’ theorem, the act of refining the probability of a specific diagnosis with new information, can both improve diagnostic accuracy and reduce diagnostic errors due to diagnostic momentum. A method to determine how a single test or series of tests influences the posttest probability of a diagnosis, one can follow 4 steps introduced by Friedland et al. (REF 1). (1): Develop a differential diagnosis; (2): Determine the pre-test probability (i.e., in term of percentages from 0 to 100) of a particular diagnosis. The pretest probability is determined by personal experience and published data (i.e., use prevalence data for clinical symptoms and signs). (3) Convert diagnostic test information into likelihood ratios (LR) using sensitivity and specificity. If a test is positive, then the positive LR should be calculated. If the test is negative, then a negative LR should be calculated. (4) Using a nomogram or simple math to combine pretest probability and likelihood ratios to arrive at the final posttest probability of disease. In this case the tests completed to evaluate for pancreatic cancer (MRCP, CT-abd, EUS-guided biopsy, CA19-9) resulted in the posttest probability of pancreatic cancer decreasing from 50 to 11 %. If the clinicians had applied Bayes’ theorem, it is conceivable they would have paused and considered alternative diagnoses (e.g., type 1 autoimmune pancreatitis) prior to performing a pancreaticoduodenectomy.
DON’T BATHE IN THE CREEKUchechukwu Obih; Thomas Montgomery. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1926361)
LEARNING OBJECTIVE 1: Recognize the importance of obtaining a thorough social history
LEARNING OBJECTIVE 2: Identify one cause of water-borne illness
CASE: The patient is a 59 year old man who presents to the emergency department with complaints of chest pain, dyspnea, and chills. He also presents with a new swelling above his right eye. His past medical history is notable only for hypertension. His exam shows normal vital signs, an area of erythematous, fluctuant swelling above his right eye. Laboratory data is notable for an elevated white blood cell count of 17.6 g/dL and creatinine of 1.31 mg/dL. CT angiography of the chest reveals bibasilar consolidation, extensive bilateral hilar and mediastinal lymphadenopathy, and bilateral lung nodules. The patient leaves against medical advice only to return the next day with sepsis, with hypotension and tachypnea, and an elevated lactic acid of 5 mmol/L. He is placed on broad spectrum antibiotics but continues to decompensate. He develops multi-organ system failure affecting the kidneys, septic emboli to the liver, and septic emboli to the lungs, requiring ventilator support and pressors. Incision and drainage of his right eye abscess reveals Yersinia enterocolitica. Blood cultures also grow Yersinia enterocolitica. His antibiotics are switched to Ceftriaxone. Further exploration of the patient’s social history reveals that he lives downstream from a pig farm in rural North Carolina, nearby a creek in which he frequently bathed. He is treated with 3 weeks of Ceftriaxone 2 g daily. He requires tracheostomy for prolonged ventilatory requirements and hemodialysis is initiated secondary to renal failure.
DISCUSSION: Obtaining a thorough social history of environmental and dietary exposure to pigs is essential in the diagnosis of Yersinia enterocolitica given the nature of this bacterium. Yersinia enterocolitica, is a gram-negative coccobacilli frequently colonized in the oropharyngeal lymphoid tissues of pigs. It is transferred by consumption of undercooked pork and, on rare occasion, through untreated water. Incidence of Yersinia in North America is approximately 1000 cases per year, of which incidence is highest in children, often manifesting as a diarrheal illness. Infection occurs by bacterial attachment to gut epithelial walls or by the release of pore-forming toxins. A method of bacterial virulence also includes the release of proteins to avoid host cell mediated immune response. Very rarely does Yersinia cause septicemia, making this case exceptional. Yersinia growth can be overlooked given its colorless appearance on routine culture mediums. Diagnosis is obtained from lymphoid tissue, stool, or blood cultures. Treatment for septic patients includes ceftriaxone 2 g daily.
DON’T GO BREAKIN’ MY HEART: ACUTE STREPTOCOCCAL INFECTION CAUSING MYOPERICARDITISSara Jane Cromer; Priti Dangayach; Courtney N. Miller-Chism. Baylor College of Medicine, Houston, TX. (Tracking ID #1927210)
LEARNING OBJECTIVE 1: Diagnose acute streptococcal infection in the setting of a negative rapid strep test
LEARNING OBJECTIVE 2: Recognize that streptococcal infection can be complicated by myopericarditis which may mimic acute coronary syndrome (ACS)
CASE: A 20-year old African-American male with past medical history of hypertension and asthma presented with severe chest pain described as “the grim reaper sticking his scythe in my chest” in the setting of a several day history of sore throat, fever, chills, myalgias, and back pain. He denied a cough. His temperature was 100 °F, and he was hypertensive (160/93), tachycardic (120 beats/min), and tachypneic (24 breaths/min) with an O2 saturation of 99 % on room air. On exam, he was diaphoretic and had dry mucous membranes, tender anterior cervical lymphadenopathy, and erythema of the oropharynx. Initial labs were remarkable for white blood cell count of 24,600 cells/μL, with ESR of 77 mm/h and CRP of 30.2 mg/dL. His troponin on presentation was 0.487 ng/mL. Monospot, HIV, and rapid strep screening tests were all negative. Imaging included a normal chest X-ray. His initial EKG was normal. On hospital day #2, he again complained of severe chest pain, and a repeat EKG showed ST elevation in leads I, II, aVL, and V4-V6. His troponin peaked at 2.69 ng/mL, with total CK of 2,641 u/L and CKMB of 2.2 ng/mL. A transthoracic echocardiogram showed a normal ejection fraction and no wall motion abnormalities. A cardiac catheterization was performed, which revealed no obstructive culprit lesions. Treatment for myopericarditis was initiated with high-dose ibuprofen and the patient improved clinically, with resolution of chest pain and cardiac enzyme elevation, and normalization of his EKG. A throat culture returned β-hemolytic Group A Streptococcus on hospital day #4, and he was discharged in stable condition to complete a course of penicillin.
DISCUSSION: Group A Streptococcus is a common cause of bacterial pharyngitis. The Centor Score for predicting streptococcal pharyngitis based on clinical symptoms can aid in decision making. When the clinical suspicion is high for streptococcal infection, a throat culture (sensitivity 90–95 %) or PCR-based test should be performed as rapid antigen detection tests for streptococcal organisms have limited sensitivity (70–90 %, depending on technique). Throat culture is the gold standard for diagnosing acute streptococcal pharyngitis. Acute non-rheumatic streptococcal myocarditis has been reported to mimic ACS in young patients presenting with chest pain that have troponinemia and ST elevation. Descriptive studies have demonstrated that over 95 % of cases of myopericarditis in the setting of streptococcal pharyngitis or tonsillitis occur in young males (average age 28.6), and almost all present with chest pain, diffuse ST segment elevation, and elevated CK, CKMB, and troponin. Many of these patients (up to 67 % in one study) underwent cardiac catheterization despite their young age and very few risk factors. In the setting of an acute infection in a young patient, it is important to recognize myopericarditis in order to avoid unnecessary invasive testing. While ACS should always be on the differential diagnosis in a patient presenting with chest pain, it is important to recognize myopericarditis as a potential cause of chest pain in a young person with acute streptococcal infection.
DOWN IN THE DUMPS: SELECTIVE SEROTONIN REUPTAKE INHIBITORS AS A CAUSE OF DIARRHEATalia Kahn; Ryan Laponis. UCSF, San Francisco, CA. (Tracking ID #1936899)
LEARNING OBJECTIVE 1: Recognize selective serotonin reuptake inhibitors as a cause of chronic, non-inflammatory diarrhea
CASE: A 64 year-old man with a history of Crohn’s disease and severe major depression presented with 6 months of chronic, watery, non-bloody diarrhea. He described four to six watery bowel movements per day. He denied bloating, abdominal pain, fevers, chills, night sweats, weight loss, bowel movements at night, recent travel, camping, antibiotic use, or association with foods such as dairy or grains. Medications included adalimumab, aripiprazole, mirtazapine, and sertraline. His vitals as well as his abdominal, skin and rectal exams were unremarkable. A basic metabolic panel, TSH, liver function, and tissue transglutaminase were normal. Additionally, bacterial culture, clostridium difficile, and ova and parasite, including specific testing for cryptosporidium and cyclospora, exams were negative. Furthermore, elimination of lactose from his diet resulted in no improvement. Colonoscopy revealed minimal to quiescent colitis in the cecum and colon. Given this, a plan was made to check fecal fat and white blood cells, stool potassium and sodium, trial him on treatment for bacterial overgrowth, and possibly examine the small bowel by MR enterography. He returned, however, to clinic indicating that his psychiatrist had changed his sertraline to bedtime dosing, leading to resolution of his symptoms.
DISCUSSION: Our patient’s known diagnosis of Crohn’s disease and concomitant immunosuppression led to an extensive work-up of his chronic diarrhea and we overlooked a common cause of chronic, non-inflammatory diarrhea: medications. Over 700 drugs can cause diarrhea and this side effect can appear long after the initiation of the drug, leading to a delay in recognition. With respect to selective serotonin reuptake inhibitors (SSRIs), studies have shown that serotonin initiates peristaltic and secretory reflexes in the gut and potentiation of serotonergic signaling by inhibition of the serotonin reuptake transporter contributes to increased stool water and motility. Since SSRIs prolong the availability of physiologically released serotonin in both the central nervous system and gut, these medications can lead to the watery diarrhea described by this patient. Given that inflammatory bowel disease is often co-morbid with depression, SSRIs should not be overlooked in these patients as a cause of chronic, watery diarrhea even months after drug initiation.
DRESSED IN DISGUISEJeffrey M. Kroopnick1,2; Rosemarie Conigliaro1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1936772)
LEARNING OBJECTIVE 1: Recognize the clinical and laboratory presentation of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS Syndrome)
LEARNING OBJECTIVE 2: Identify factors that may play a role in the pathogenesis of DRESS
CASE: A 27-year old woman presents with one-day duration of rash and fever. She described the rash as red, pruritic, and burning. She also noted a flushing sensation and tingling throughout her body. Exam revealed fever of 102.5 °F; a non-vesicular erythematous rash with coalescing macules and papules on the face, neck, chest, abdomen, groin, and legs; a quarter-sized scar on her right lateral calf was also noted. She had facial swelling and cervical lymphadenopathy. Aspartate aminotransferase (AST) was 382 U/L and Alanine aminotransferase (ALT) 738 U/L; white blood cell count peaked at 26.7 k/uL with a maximum of 20 % eosinophilia and 12 % atypical lymphocytes. Skin biopsy revealed spongiotic and lichenoid dermatitis with eosinophils consistent with a drug eruption. Medication reconciliation disclosed that she had been receiving vancomycin infusions for two and a half weeks for a methicillin-resistant Staphylococcus aureus (MRSA) brain abscess and pulmonic valve vegetation diagnosed during a recent hospitalization. Her constellation of symptoms and laboratory findings were concerning for Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) with vancomycin as the likely culprit. Once this medication was discontinued, her rash improved, AST decreased to 60, ALT to 318, eosinophilia resolved (0 %), and atypical lymphocytes declined to 4 % post-discharge.
DISCUSSION: Rashes from medications are quite common; these may be benign, but sometimes more serious. DRESS has been estimated to occur in 1 in 1,000 to 1 in 10,000 drug exposures and carries a 10 % mortality rate, primarily from visceral organ involvement. It is typically characterized by a skin rash consisting of erythematous coalescing macules and papules without scale or vesicles, fever, eosinophilia or atypical lymphocytes, lymphadenopathy, and internal organ involvement, usually the liver and less frequently, kidneys, lungs, and central nervous system. The RegiSCAR (European registry of Severe Cutaneous Adverse Reaction) is a scoring system to analyze cases of DRESS as ‘no,’ ‘possible,’ ‘probable,’ or ‘definite’ by assessing for these characteristics, in addition to time of resolution and ruling out other causes, such as infection, viral hepatitis, and vascuilitic/rheumatologic etiologies. Our patient garnered 6 points, characterizing her as a ‘definite’ case. The most common offending agents in DRESS are anti-epileptic drugs such as phenytoin, carbamazepine, lamotrigine, and phenobarbital, and the xanthine oxidase inhibitor, allopurinol. While some antibiotics have been implicated in DRESS, there are only a few reported cases of vancomycin as the guilty agent. Interestingly, recent evidence suggests that viral replication, namely Human Herpes Virus (HHV)-6, and other herpes viruses may play a role in the pathogenesis of DRESS. It has been theorized that some of the inciting medications may elicit viral reactivation and a subsequent immune response. Unfortunately, there are no distinct clinical or laboratory entities to indicate when DRESS is life-threatening. Treatment typically consists of discontinuation of the implicated drug in addition to supportive care with topical steroids, emollients, anti-pyretics, adequate caloric intake, and correction of electrolyte and fluid abnormalities. In more extreme cases, systemic steroids may be necessary. DRESS is an important, and potentially fatal condition, that all physicians should recognize.
DUKE IT OUT: FINDING THE RIGHT DIAGNOSISFarah Kaiksow; Philip J. Putnam. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925935)
LEARNING OBJECTIVE 1: Diagnose bacterial endocarditis in the absence of echocardiographic evidence of endocardial involvement.
CASE: A 42-year-old man presented with a two-day history of right hand pain and swelling, which began the day prior while injecting heroin into his hand. He had been awoken from sleep that morning by a sharp, left-sided chest pain that worsened with deep inspiration and was associated with shortness of breath. Temperature was 104.4 °F, heart rate was 122 beats per minute, blood pressure was 169/109, respirations were 22 breaths per minute, and oxygen saturation was 84 % on room air. Past medical history was significant for opiate abuse, hypertension, Type 2 diabetes, and previous trauma to the right hand with residual orthopedic hardware. The patient’s hand was warm, swollen, and tender to palpation along the dorsum. Peripheral white blood cell count was significantly elevated and a plain radiograph of the hand showed soft tissue swelling with foreign bodies and no evidence of osteomyelitis. A chest x-ray was normal; CT PE protocol revealed multiple nodules in each lung, concerning for cavitation. A transthoracic echocardiogram was negative, but given the high suspicion for endocarditis, a transesophageal echocardiogram was performed, and was also negative. All three sets of blood cultures, drawn on admission, quickly resulted as gram-positive cocci in clusters, ultimately identified as Methicillin-Resistant Staphylococcus aureus. Despite the lack of visual evidence of endocardial involvement, the patient was diagnosed with acute bacterial endocarditis based on the Modified Duke Criteria.
DISCUSSION: Bacterial endocarditis is a life-threatening condition frequently treated by general internists. The estimated annual incidence is between three to nine cases per 100,000 people, with twice as many men as women effected. Patients classified as ‘high-risk’ include intravenous drug users and individuals with prosthetic valves or a prior history of valvular disease, and have a much higher infection rate. The diagnosis of bacterial endocarditis is made based on the Modified Duke Criteria, which have a greater than 80 % sensitivity, specificity, and negative predictive value. In 90 % of cases, vegetations are seen on transthoracic or transesophageal echocardiogram, which is one of the two major Duke Criteria. The other major criterion is bacteremia by an organism commonly known to cause endocarditis; if both major criteria are met the diagnosis of definitive bacterial endocarditis is made. In the other 10 % of cases, diagnosis must include at least three minor criteria, such as a predisposing condition, fever, vascular or immune phenomena, or positive blood cultures with an organism not commonly known to cause endocarditis. Definitive endocarditis can be diagnosed in a patient with one major and three minor criteria, or with no major but all five minor criteria. In this case, the patient met one major and three minor criteria: Staphylococcus aureus bacteremia, a predisposing condition (intravenous drug use), fever, and a vascular phenomenon (septic pulmonary emboli as seen on chest CT). With intravenous drug use on the rise, general internists should be familiar with the Modified Duke Criteria for diagnosing endocarditis, particularly when echocardiography does not correlate with clinical presentation.
DYNAMIC EARLY REPOLARIZATION PATTERN AND VENTRICULAR FIBRILLATION: CASE REPORT AND A BRIEF LITERATURE REVIEWVimalkumar Veerappan Kandasamy1; Satish Chandraprakasam2; Aryan Mooss2. 1Creighton University, Omaha, NE; 2Creighton University, Omaha, NE. (Tracking ID #1939222)
LEARNING OBJECTIVE 1: To recognize the dynamic nature and association of early repolarization (ER) pattern with idiopathic ventricular fibrillation.
LEARNING OBJECTIVE 2: To identify electrocardiographic characteristics that differentiate the benign ER pattern from the malignant variant.
CASE: A 43 year old Caucasian male was admitted following a witnessed out of hospital sudden cardiac arrest (SCA) without any preceding symptoms. Cardiopulmonary resuscitation was initiated within minutes of arrest. Initial presenting rhythm was ventricular fibrillation (VF) and 2 unsynchronized shocks successfully converted him to sinus rhythm. Upon return of spontaneous circulation, electrocardiogram (EKG) showed sinus tachycardia without signs of ischemia. Computed tomography of head showed no acute abnormalities. Since he was minimally responsive, he was intubated and hypothermia was initiated per hospital protocol. Cardiac examination was unremarkable. Troponin I peaked at 0.33 ng/ml 8 h after admission. Echocardiogram showed normal left ventricular systolic function without regional wall motion abnormalities. Upon re-warming, he had an excellent neurological outcome. Coronary angiogram (CAG) showed 99 % stenosis in the distal first diagonal artery and 75 % discrete stenosis in the proximal left anterior descending artery. He received drug eluting stent to both lesions given their hemodynamic significance by fractional flow reserve. Follow up EKGs showed 1 mm J-point elevation in the inferolateral leads with concave upwards ST segment elevation and notching at the end of QRS complex suggestive of early repolarization pattern. Cardiac magnetic resonance (CMR) demonstrated minor right ventricle (RV) wall motion abnormality but no evidence of fibro fatty infiltration of RV myocardium. It was inconclusive if the cardiac arrest was secondary to ischemia despite the presence of obstructive lesions noted in CAG. Absence of symptoms prior to SCA, lack of biomarker and echocardiographic/CMR evidence of myocardial infarction and/or structural abnormalities suggested the possibility of underlying electrical instability (ER pattern) initiating VF. After multi-disciplinary team discussion, an implantable cardioverter defibrillator (ICD) was placed for secondary prevention. He was doing well without any ICD therapy at 6 month follow up.
DISCUSSION: Early repolarization (ER) pattern consists of 2 EKG components: prominent J-point elevation ≥0.1 mV in adjacent leads with a slurred or notched QRS morphology and ST segment elevation. Prevalence of ER ranges from 5 to 13 %. Historically, ER pattern has been considered a marker of good health because it is more prevalent in athletes, younger persons, and at slower heart rates. On the contrary, its potential to cause serious ventricular arrhythmias was not recognized until recently. ER pattern when associated with symptomatic arrhythmias is known as ER syndrome. Haissaguerre et al. showed an increased prevalence of early repolarization among patients with a history of idiopathic ventricular fibrillation. Tikkanen et al. studied two populations of healthy adults and concluded that association between ER and increased risk of death from arrhythmia was found in persons with the horizontal ST segment pattern whereas risk for adults with rapidly up-sloping ST segment was similar to that of persons without ER. This association was also reported by Wu et al. in a large meta-analysis of 9 studies involving 141,095 subjects. However, there was no significant difference in risk of all cause or cardiac death in this study. The inferior or global distribution and higher J-point amplitude are known to be associated with increased arrhythmic risk both in general population and patients with idiopathic VF. In addition, horizontal ST segment elevation has also been identified as a high risk variable. In conclusion, early repolarization (ER) pattern is a common and benign electrocardiographic finding. As demonstrated in this case, ER pattern is dynamic and can vary in the same patient with change in body position, activity or over time. In select populations, the presence of certain subtypes of ER pattern may portend higher risk of death from arrhythmia. However no cause and effect relationship has been proven so far.
EARLY IMMUNE MODULATING THERAPY FOR PSEUDOTUMORAL ANOGENITAL HERPES IN HIV INFECTIONStacey Schott1; Veronique Nussenblatt1; Siham Mahgoub2; Khalil Ghanem1. 1Johns Hopkins University School of Medicine, Johns Hopkins Bayview Medical Center, Baltimore, MD; 2Whitman Walker Health, Washington, DC. (Tracking ID #1938713)
LEARNING OBJECTIVE 1: Recognize pseudotumoral forms of anogenital HSV2 in HIV infected individuals
LEARNING OBJECTIVE 2: Consider the use of early immune modulating therapy for anogenital HSV
CASE: A 41 year old man with HIV/AIDS since 2004, CD4 count of 35 cells/mm3 and undetectable viral load presented with a 2 month history of progressively ulcerated penile lesions despite multiple courses of valacyclovir. Two months after re-initiating HAART, a painless, small, round, fluid-filled pimple-like lesion spontaneously appeared on the dorsum of his penis, shortly followed by a similarly appearing second lesion on the ventral side. Analogous to two previous episodes of suspected HSV outbreak in the previous year that completely resolved with 2 weeks of standard valacyclovir treatment, the lesions were thought to be recurrent HSV and were again treated with valacyclovir 1000 mg twice daily for 14 days. While on valacyclovir, the lesions became ulcerated and the medication was increased to 1000 mg three times daily. Despite 1 month of treatment, the lesions continued to grow and ulcerate, becoming painful, sore and bloody. The patient denied fever, chills or other systemic symptoms. A trial of famciclovir and doxycycline for suspected superinfection was ineffective. Laboratory testing included: positive HSVI and II IgG serologies; negative RPR, FTA-Abs, Quantiferon, chlamydia and gonorrhea. Acyclovir (ACV) resistance was thought to be unlikely given the patient’s lack of prolonged valacyclovir exposure or history of suppressive valacyclovir, but viral culture verified acyclovir resistant, foscarnet sensitive HSV2. Biopsy of the ulcer was performed to rule out other etiologies including malignancy. While awaiting biopsy results, topical imiquimod 5 % cream was initiated three times per week for suspicion of pseudotumoral HSV2 and lesions dramatically healed after 1 month of use. Biopsy then confirmed HSV infection and demonstrated multinucleated cells with dense and predominately lymphocytic infiltrate.
DISCUSSION: HSV 2 is the primary agent of genital ulcerations and in HIV infected individuals herpetic lesions may be more extensive or last for longer periods. First line treatment for primary and recurrent genital ulcerations is acyclovir (or nucleoside analogues). However, atypical hypertrophic, ulcerative, or pseudotumoral forms of HSV exist and are usually suspected to contain drug resistant viral subtypes because they show poor response to acyclovir. It may be difficult to initially identify pseudotumoral forms as they appear to mimic epidermoid carcinoma, chancroid or lymphoma. The differential may also include HSV IRIS and atypical syphilis. A recent histopathologic, virologic and immunologic analysis elucidated that pseudotumoral lesions harbored ACV sensitive strains and ulcerative lesions harbored ACV resistant strains but patients with either of these types continued to fail anti-herpetic medications. The discovery of a predominance of polyclonal lymphoplasmocytic B cells in lesional infiltrates revealed a pseudolymphoma nature to the disease. Therefore, treatment with imiquimod, a toll- like receptor 7 agonist that boosts innate and adaptive antiviral immunity; or thalidomide, an anti-angiogenic, anti-proliferative immune modulator, may help overcome deficiencies in anti-herpetic immunity that persist in HAART treated patients to provide more consistent and lasting efficacy against the disease. In HIV infected individuals with suspected HSV2 refractory to antiherpetic drugs, early initiation of immune modulating therapy should be considered and may offer an effective, less toxic (than foscarnet) and more easily administered treatment choice for acyclovir resistant HSV infection.
EKG CHANGES IN A PATIENT WITH ACALCULOUS CHOLECYSTITIS: A RED HERRINGHarish Madala; Tessa Antalan; Sandeep Padala; Vamsi Korrapati; Kavitha Kesari; Susan J. Smith. Mclaren Regional Medical Center, Flint, MI. (Tracking ID #1922038)
LEARNING OBJECTIVE 1: Acute Cholecystitis can present with EKG changes suggestive of Myocardial Ischemia, usually as ST depression but very rarely ST elevation as well.
LEARNING OBJECTIVE 2: Importance of using clinical judgement when dealing with ambiguous clinical presentation to avoid anchoring bias.
CASE: A 53 year-old Caucasian male with a past medical history of diabetes, dyslipidemia, extensive smoking and family history of cardiac disease, presented with acute-onset midsternal pressure-like chest pain that had awakened him from sleep. There was also associated vague right upper quadrant abdominal pain and nausea. Physical examination was normal, except right upper quadrant abdominal tenderness. The white blood cell count was 13,600 per microliter. Initial EKG revealed diffuse ST segment elevation in leads I, II, III and V3-V6, along with peaked T waves in V3 and V4; two sets of troponins were negative. He was given intravenous nitroglycerin which provided moderate pain relief. An emergent cardiac catheterization was negative for focal obstructive coronary artery disease. Simultaneously he was started on intravenous antibiotics for suspected cholecystitis, which was confirmed by pericholecystic fluid seen on gallbladder ultrasound as well as by HIDA scan. The patient underwent laparoscopic cholecystectomy 2 days later, and was found to have acute on chronic gangrenous acalculous cholecystitis. Post-operatively, follow-up EKG’s revealed near normalization of the ST segment changes.
DISCUSSION: Acute cholecystitis is usually recognized by a triad of fever, leukocytosis and right upper quadrant pain. The two main types are calculous and acalculous cholecystitis. There have been multiple references to acute cholecystitis presenting with EKG changes such as T wave inversions or ST segment depressions, but there have only been a handful of instances where ST-segment elevation was present. The exact pathophysiology of the EKG changes in acute cholecystitis is unclear. Based on animal experiments, a possible relationship of gallbladder distension to increased heart rate, blood pressure and plasma renin levels has been postulated to cause transient changes in the coronary vasculature. In our literature review, we found 8 previous case reports of ST-segment elevation in patients with cholecystitis. Of these 8 cases, there was only one reference to acalculous cholecystitis while the rest were associated with gallstones. Our case reiterates the importance of exercising appropriate clinical judgment in the face of ambiguous findings. Having knowledge of this “red herring” in patients with cholecystitis could prevent unnecessary diagnostic testing and ensure timely administration of antibiotics as well as prompt surgery, if indicated.
ELECTROCARDIOGRAM CHANGES IN COMMON VARIABLE IMMUNODEFICIENCY RELATED ADRENAL INSUFFICIENCYNili Parekh1; Fagunkumar Modi2; Brijal P. Patel1; Ryland P. Byrd2,1; Thomas M. Roy2,1. 1ETSU, Johnson City, TN; 2ETSU, Johnson city, TN. (Tracking ID #1925143)
LEARNING OBJECTIVE 1: We present an adult patient with known history of common variable immune deficiency (CVID) who was identified to have adrenal insufficiency-associated QTc interval prolongation and t-wave inversion. Treatment with hydrocortisone resolved these endocrinopathy-associated myocardial electrical abnormalities.
LEARNING OBJECTIVE 2: Consideration of adrenal insufficiency early in hospitalization lead to prompt diagnosis and treatment which prevented catastrophic consequences of ventricular arrhythmia or death in this patient.
CASE: A 70 year-old male with atherosclerotic coronary artery disease and CVID was admitted for hypotension refractory to fluid challenges. He reported fatigue, loss of appetite and an unintentional weight loss of 40 lb of several months duration. His blood pressure was 82/42 mmHg. His hemoglobin was 11.9 g/dl and had an eosinophilia of 13.9 %. He was hyponatremic with normokalemia. The electrocardiogram (ECG) showed a QTc prolongation of 600 ms with nonspecific anterolateral T wave changes. Thorough history was taken and records were studied to rule out any prior use of glucocorticoids or other medications which could be the cause of adrenal insufficiency or QT interval prolongation before this hospitalization. Adrenal insufficiency was confirmed by low morning cortisol levels of 1.3 ug/dl which were drawn on morning after admission. Blood ACTH level was collected. Intravenous hydrocortisone was started immediately. Improvement in patient’s symptoms, blood pressure and EKG occurred with hydrocortisone supplementation. Serial ECGs showed gradual return to normal by the fifth day of treatment. He was later diagnosed with low serum ACTH and a partially empty sella on magnetic imaging studies.
DISCUSSION: We found one pediatric case report suggesting autoimmune lymphocytic hypophysitis in a patient with CVID. Panhypopituitarism begins with involvement of adrenocorticotrophic (ACTH) and growth hormone at earlier stages in CVID patients. In 1950s, ECG abnormalities in adrenal insufficiency were described. Studies of rat heart muscle show that glucocorticoid is essential for the calcium transport in sarcoplasmic reticulum and microsomal phosphorylase activity. There are other reportsin literature also suggesting adrenal insufficiency-related reversible cardiomyopathy and T wave changes but it is rare that such a finding is present in an adult patient with CVID.To our knowledge, this is the first case report of CVID, adrenal insufficiency and QTc abnormality in adult patient. Consideration of adrenal insufficiency early in hospitalization lead to prompt diagnosis and treatment which prevented catastrophic consequences of ventricular arrhythmia or death.
EMPTY SELLA SYNDROME PRESENTING AS EPISODIC HYPOGLYCEMIAEric R. Simon; Pinky Jha. Medical College of Wisconsin, Wauwatosa, WI. (Tracking ID #1938665)
LEARNING OBJECTIVE 1: Recognize empty sella syndrome as a cause of hypoglycemia
LEARNING OBJECTIVE 2: Diagnose and treat secondary adrenal insufficiency due to empty sella syndrome
CASE: A 38-year-old female with a past medical history of Crohn’s disease and hypothyroidism presented to the emergency room with dizziness after she skipped a meal due to nausea. On arrival, her finger stick blood glucose level was 41 mg/dL and it was corrected to 247 mg/dL with IV glucose. Over the past 18 months, she has had five previous known episodes of hypoglycemia that would always occur after she skipped a meal. She had no other associated symptoms. Her last Crohn’s flare, and oral steroid use, was in 2009. Her hypothyroidism was diagnosed 6 years ago and she was prescribed levothyroxine, however she only took it for 6 months before stopping. Her only home medication was acetaminophen as needed. Family history is positive for diabetes mellitus type 2 in her father. She does not smoke or drink. Physical exam was unremarkable. Laboratory findings included an elevated TSH of 9.38 uIU/mL, a low free T4 of 0.54 ng/dL, a normal hemoglobin A1C, a normal c-peptide level, and a normal pro-insulin level. During the hospital course, she continued to have multiple episodes of hypoglycemia that ranged between 40 and 60 mg/dL that would respond to oral glucose. Endocrinology was consulted and a cosyntropin (synthetic ACTH) stimulation test was performed, which showed low cortisol levels of 0.1 ug/dL, 0.2 ug/dL, and 0.3 ug/dL at 0, 30, and 60 min respectively. An ACTH level that was drawn 4 h after the cosyntropin stimulation test was <1.0 pg/mL. An MRI of the sella was then performed to evaluate for possible causes of secondary adrenal insufficiency and it showed a partially empty sella with a thin sliver of pituitary tissue at the floor of the sella. Subsequent additional laboratory work showed normal levels of FSH and LH along with an elevated prolactin and a low somatomedin C. She was started on hydrocortisone for her adrenal insufficiency and levothyroxine for her hypothyroidism. Her hypoglycemic episodes resolved after the initiation of steroid therapy.
DISCUSSION: Empty sella syndrome is a condition in which the sella turcica, which normally houses the pituitary gland, appears to be empty on imaging. This syndrome has been reported in 6–20 % of people, most commonly in multiparous women with obesity and hypertension. Empty sella syndrome can be asymptomatic or the patient may have various types of endocrine dysfunction. The most common endocrine abnormality is hyperprolactinemia and the most common hormone deficiency is growth hormone deficiency (measured by somatomedin C), both of which were seen in our patient. When the pituitary gland fails to produce ACTH, which normally stimulates the adrenal glands to produce cortisol, secondary adrenal insufficiency occurs. This can result in hypoglycemia because cortisol normally acts to increase blood sugar by increasing gluconeogenesis within the liver as well as blocking the uptake of glucose into cells throughout the body. Adrenal insufficiency can be diagnosed by the cosyntropin stimulation test, where an infusion of cosyntropin is given to the patient and plasma cortisol levels are measured over time. In primary adrenal insufficiency, cortisol levels will fail to increase in response to cosyntropin due to atrophy of the adrenal glands, and plasma ACTH levels will be high. In secondary adrenal insufficiency, cortisol levels will also fail to increase in response to cosyntropin because the adrenal glands are not used to being stimulated, but they will begin to respond and produce cortisol within 4–5 days. However in secondary adrenal insufficiency, plasma ACTH levels will be low, as was seen in our patient. Similarly, when the pituitary gland fails to produce TSH, secondary hypothyroidism occurs. The lab values for our patient, namely an elevated TSH and a low free T4, initially look like primary hypothyroidism. However with such a low free T4, one would expect the TSH to be even higher than it is, so there may be an element of secondary hypothyroidism as well. Treatment of empty sella syndrome is replacement of the deficient hormones, which included hydrocortisone and levothyroxine for our patient. Of note, with secondary adrenal insufficiency, the renin-aldosterone system is intact so mineralocorticoid treatment is not necessary.
EOSINOPHILIA IN THE CSF IN A PATIENT WITH ALTERED MENTAL STATUSVikas Khullar1; Lucas A. Burke1; James Wynne2,1; Peruvemba S. Sriram2,1. 1University of Florida -College of Medicine, Gainesville, FL; 2University of Florida -College of Medicine, Gainesville, FL. (Tracking ID #1938188)
LEARNING OBJECTIVE 1: Recognize the differential diagnosis of eosinophilia in the CSF.
LEARNING OBJECTIVE 2: Assess and understand the treatment options for patients with eosinophilic meningitis.
CASE: A 58 year-old-man with no past medical history presented to the emergency department complaining of headaches, blurred vision, nausea, vomiting and poor balance of 1 week duration. Physical exam was unremarkable except for mild imbalance. Laboratory workup was significant for leukocytosis of 15,000 cells/uL with 8 % eosinophils with normal blood chemistry and liver function tests. Urine toxicology screen was positive only for marijuana. Chest radiograph and urinalysis were unremarkable. Computed tomography of the head did not show any abnormalities and patient was admitted for further evaluation. The day after admission, patient’s neurological status deteriorated with acute onset confusion and agitation requiring sedative medication. Given acute decline, neurology was consulted and recommended lumbar puncture (LP); however, it was unsuccessful given patient’s severe agitation. Empiric treatment for infectious meningitis was initiated, including ampicillin, vancomycin, ceftriaxone and acyclovir. However, patient’s mental status continued to decline requiring intensive care unit admission and tracheal intubation. Patient subsequently underwent a LP and magnetic resonance imaging (MRI) for further evaluation. LP showed an opening pressure of 42 mmHg, clear cerebrospinal fluid (CSF) with 48 WBC #/cm2 with 14 % lymphocytes, 53 % eosinophils and 7 % basophils. CSF protein was 178 mg/dl [N = 15–45 mg/dl] and glucose of 58 mg/dl [N = 40–70 mg/dl]. CSF gram stain, india ink and cultures were negative. CSF VDRL, Cryptococcus Antigen, Coccidioides Antibody, HSV 1 and 2 DNA were also negative. Serum HIV antibody and antigen were both negative. MRI showed diffuse leptomeningeal enhancement most consistent with acute meningitis. Electroencephalogram was also ordered and was negative for seizure activity. Based on these investigations, a diagnosis of eosinophilic meningitis was established. Infectious diseases was consulted and recommended treatment with high dose steroids (1 mg/kg/day) for suspected parasitic meningitis and recommended no anti-helminthic medications due to concerns for causing increased inflammation. Hematology was also consulted to review CSF and concluded that the cells appeared mature in nature without blastoid features concerning for leukemia. With this intervention, patient’s mental status began to improve and he was successfully extubated. Once the patient returned to baseline mental status, he reported recently working in a wooded construction area about 2 weeks prior to presentation with sighting of multiple raccoons in the area. A presumptive diagnosis of parasitic meningitis likely secondary to Baylisascaris procyonis given possible raccoon exposure was made and patient was discharged on a slow taper of prednisone.
DISCUSSION: This case demonstrates an unusual cause of meningitis and highlights the importance of cell differential in the CSF for the diagnosis and identification of certain pathologies. Eosinophilic meningitis is defined as the presence of 10 or more eosinophils/uL or eosinophilia of at least 10 % of the total CSF leukocyte count. The presence of eosinophilia in the CSF is associated with a limited number of diseases, with invasion of the central nervous system by helminthic parasites (such as Angiostrongylus cantonensis, Gnathostoma spinigerum, Baylisascaris procyonis and other helminths) being the most common. Other infectious causes include other parasites such as neurocysticercosis, cerebral toxocariasis and fungal infections with most common being coccidioides immitis. The diagnosis of a specific organism is made based on history of possible exposure, the clinical presentation and CSF eosinophilia. Serologic testing for its diagnosis is only available in endemic areas. Non-infectious causes of eosinophilia in the CSF include malignancy (Hodgkin’s and Non-Hodgkin’s, eosinophilic leukemia), medications (such as NSAIDs, ciprofloxacin, IV vancomycin, IV gentamycin), and presence of ventriculoperitoneal shunts. Treatment of eosinophilic meningitis secondary to helminthic parasites is mainly supportive as anti-helminthics have not been shown to be effective and often worsen symptoms by increasing inflammation due to antigens released by the dying parasites. Repeated lumbar punctures and analgesics can provide relief in patients with persistent headaches due to increased intracranial pressure. Corticosteroids have been used and shown to reduce focal neurological deficits. Most patients with helminthic parasites invasion require no specific treatment and recover completely in 3 to 6 weeks.
EOSINOPHILIC GASTRITISPearl Yu1; Vivian Shing2. 1UCSD, La Jolla, CA; 2Canyon Crest Academy, San Diego, CA. (Tracking ID #1931860)
LEARNING OBJECTIVE 1: Recognize Eosinophilic Gastritis as a treatable disease that presents as nonspecific symptoms of dyspepsia, dysphagia and stomach bloating.
LEARNING OBJECTIVE 2: Understand the diagnosis and treatment of Eosinophilic Gastritis
CASE: A 62 yo female with history of osteopenia, factor 7 deficiency presents with stomach discomfort and indigestion after her colonoscopy procedure 3 months prior. She is not currently on medications nor dietary supplements except vit D. Patient describes symptoms of intermittent dysphagia, belching and stomach bloating. Her labs show normal CBC, comprehensive chemistry. Her Helicobacter pylori antibody and stool antigen test are both negative. An upper endoscopy is performed that shows a small healing gastric antrum ulcer otherwise negative. Random gastric biopsies show reactive gastropathy, erosions and an increased eosinophils greater than 30 HPF per HPF over 5 HPF. No evidence of Helicobacter pylori on routine stain. Esophageal and duodenal biopsies are all negative. Patient also has a RAST test which shows that she is mildly allergic to tomatoes, soy, peanuts and milk. Patient is put on proton pump inhibitors for 2 weeks without response and then is started on diet eliminations including seafood, soy, wheat, corn, egg, milk, peanut for 6 weeks trial. Patient reports life style of large amount of fish and soy consumption.
DISCUSSION: Eosinophilic Gastritis (EG) is a rare disease with limited case reports and there have been no prospective randomized therapeutic trials. The diagnosis is typically confirmed by endoscopic biopsies which reveal >20–25 eosinophils per HPF. Typical endoscopic findings include gastropathy with erythema and erosions. Lab findings may or may not show peripheral eosinophilia (20 % of the patients have normal absolute eosinophil count.). Treatment is empiric and based upon the severity of the clinical manifestations. Although food hypersensitivity plays an important role in EG pathogenesis, no food allergy test (skin, patch or allergen specific igE) has been shown to effectively identify the culprit. A prospective trial in adults with EG has demonstrated clinical remission with a 6 week course of dietary elimination. The six- food elimination diets employed in EG include soy, wheat, corn, egg, milk, peanut and seafood for 6 weeks. If the dietary changes are successful at reducing symptoms, foods can be added back slowly in a systematic fashion from the least allergenic to most allergenic. If dietary measures do not result in decrease symptoms and tissue eosinophilia, a trial of prednisone (20 to 40 mg/day) for 2 weeks followed by a rapid taper is the next treatment option. Other approaches include oral cromolyn, Ketotifen, montelukast. Untreated patients with EG may rarely remit spontaneously or progress to severe obstruction, malabsorption, malnutrition. Presentations and course is variable, and most may experience recurrence. Some patient may require long term maintenance therapy.
ERYTHEMA NODOSUM CAUSED BY CHLAMYDIAL INFECTIONYuki Otani; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1924164)
LEARNING OBJECTIVE 1: Recognize the importance of taking a sexual history even in patients with a nodular rash.
LEARNING OBJECTIVE 2: Assess the possibility of sexually transmitted diseases (STD) with erythema nodosum.
CASE: A 29 years old Asian woman presents with 2 days’ worsening rash on her bilateral lower legs; the lesions are round, red, raised, tender, non-itchy, and have no discharge. She also reports headache, dry cough, fever up to 39°, and chills despite non-steroidal anti-inflammatory drug use. She has no other constitutional, lung, abdominal, urinary, or musculoskeletal symptoms, in addition to no neck mass, new topical exposures, trauma, sick contacts, travel/hiking, or new pets; all other review of systems are negative. Her past medical history includes endometriosis and resected right ovarian chocolate cyst; she takes a gonadotropin-releasing hormone agonist (buserelin) and has no drug/food allergy. She does not use tobacco, alcohol, or recreational drugs. Her family history is not significant. Her physical exam shows temperature = 37.8C, heart rate = 92, blood pressure = 92/53, respiratory rate = 30, and O2 saturation = 99 % room air. She appears tired but alert/oriented ×3. Head/neck exam reveals bilateral posterior cervical lymphadenopathy, 1 on each side at 2–3 cm, which is mobile, rubbery, and tender on the right. Skin exam shows ~15 erythematous, tender, 0.5 cm nodules on her bilateral palms, anterior shins, and dorsum of her right foot. The rest of her exam shows no irregularities. Labs show no abnormalities in the CBC or chemistry, except for slightly elevated C-reactive protein. Rapid Strep Test is negative; throat cultures show only normal oral flora. Anti-nuclear antibody is elevated at 160× titer in a homogenous pattern, but anti-nuclear cytoplasmic antibody is negative. Transthoracic echocardiogram does not reveal any vegetations. Skin biopsy shows neutrophilic septal panniculitis without vasculitis consistent with erythema nodosum, but slit-lamp exam reveals no evidence of uveitis. On further questioning, she reports being sexually active with only her husband but no condom use even though she has had untreated chlamydia 2 years ago. Her husband also has had multiple sexual partners until last year. Her last menstrual period is yesterday. Chlamydia PCR is positive on throat swab and urine; gonorrhea, syphilis, and HIV are negative. She is thus treated with both minocycline and ceftriaxone; her erythema nodosum subsides within 10 days.
DISCUSSION: Erythema nodosum, the most frequent clinico-pathological variant of the panniculitides, has the highest incidence in 20–40 years old, like the above patient. The inflamed, tender, and nodular lesions, usually located on the bilateral anterior aspects of the legs, are associated with a wide variety of diseases although the two most common causes are streptococcal infection and medications; 60 %, however, is idiopathic. On the other hand, chlamydial infection is one of the most common STD’s, especially in those under 25 years. Because it usually remains asymptomatic, it can be unknowingly transmitted to sexual partners. Complications include pelvic inflammatory disease, ectopic pregnancy, and infertility. Erythema nodosum, however, is rarely caused by chlamydial infection; only 10 case reports have shown this association. Given its asymptomatic nature, however, one should still recognize that erythema nodosum may be caused by chlamydia and take the appropriate sexual history.
ERYTHRODERMA…THE OTHER DERMATOLOGICAL EMERGENCYMike Butterfield; Rachel Sandler; Kate Hust. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925918)
LEARNING OBJECTIVE 1: Generate a differential diagnosis for erythroderma and understand its life-threatening complications
LEARNING OBJECTIVE 2: Recognize the erythrodermic subtype of psoriasis and its management
CASE: A 61-year-old man presented with a rash beginning 5 months prior to arrival as well as chills and an unintentional 40-lb weight loss. The rash began on the extensor surfaces of both arms and subsequently encompassed his entire body, causing severe pruritus. An outside dermatologist diagnosed the patient with psoriasis. Courses of topical and oral steroids failed to change the patient’s symptoms, but etanercept achieved moderate relief. The patient ran out of etanercept 2 weeks prior to presentation, and his symptoms again flared. Physical examination was notable for cachexia, alopecia, and global erythroderma sparing only his face and genitals. He had 2+ non-pitting edema of the lower legs with lichenified skin changes, thickening of the palms and soles (keratoderma), and hypertrophic finger and toenails (onchyauxis). Non-tender supraclavicular, axillary, and inguinal lymphadenopathy was present. Initial laboratory workup revealed negative HIV serology and normocytic anemia. Lower-extremity ultrasound detected 3–4 cm inguinal lymph nodes bilaterally. Skin biopsy demonstrated psoriaform dermatitis, and flow cytometry of an excised right inguinal node later revealed an elevated CD4:CD8 ratio. T-cell receptor rearrangements were not present in the biopsy specimen or peripheral blood.
DISCUSSION: Erythroderma is a rare inflammatory skin condition defined by involvement of more than 90 % of body surface area. Patients display a “lobster-like” appearance with erythematous, warm, scaly skin that can be quite painful and pruritic. Generalized lymphadenopathy and skin lichenification may also be present. Erythroderma is a dermatologic emergency as widespread damage to the dermis compromises its role as an immunologic barrier, placing patients at risk for infection (particularly by staphylococcus, pseudomonas, and herpes) and sepsis. Heightened insensible losses may cause dehydration and electrolyte disturbances while cutaneous vasodilation may induce high-output heart failure. Erythroderma often represents the exacerbation of a pre-existing skin condition (eczema, psoriasis, contact dermatitis). Flares may be triggered by events such as stress or sudden cessation of medications. Alternatively, erythroderma may be a manifestation of underlying systemic disease such as lymphoma (including the Sézary Syndrome), paraneoplasic syndromes, lupus, graft-verses-host-disease, or hypereosinophilic syndrome. Though erythroderma only complicates 1–2 % of all cases of psoriasis, its presence must be promptly recognized. The onset of psoriasis in mid-to-late adulthood generally portends a milder natural history compared with those presenting at an earlier age; however, the proportion of erythrodermic cases appears to increase with age, approaching 5 % of new cases in those over 60. Rapid symptom control is often needed in the acute setting, but the evidence for treatment of erythrodermic psoriasis is limited. In addition to supportive measures such as topical steroids, moisturizers, and oatmeal baths, the National Psoriasis Foundation currently recommends cyclosporine or infliximab as first-line treatment, due to their quick onset of action.
ESRD + DIABETES = CRAZY LEGS?Sagar Y. Patel; Justin B. Miller; Thomas Montgomery. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1925056)
LEARNING OBJECTIVE 1: Discuss the diagnosis, prognosis, and treatment of diabetic uremic syndrome
LEARNING OBJECTIVE 2: Recognize the vast differential for hyperkinetic movements
CASE: A 60-year-old African American man with end-stage renal disease on hemodialysis complicated by anemia and secondary hyperparathyroidism, diabetes mellitus complicated by nephropathy, neuropathy, retinopathy, and previous episodes of hyperglycemia hyperosmolar state, hypertension, COPD, and chronic pancreatitis presented with 10 day history of lower leg jerking/uncontrollable movement that had worsened to point that he was unable to ambulate. He was hospitalized 2 weeks prior to his current admission for shortness of breath secondary to fluid overload from kidney disease and was noted to have some mild involuntary movements of his lower extremities at the time of discharge. Upon this current admission, the patient’s Gabapentin, Amlodipine, and Promethazine were held as these each had movement disorders listed as adverse side effects. He also underwent dialysis and received Cogentin but saw no improvement in symptoms. He denied taking any new medications, illicit drug use, trauma, new onset weakness, headache, or changes in vision or hearing. Physical exam revealed normal vital signs and choreiform movements of his bilateral lower extremities. Lower extremities otherwise had 5/5 strength, with toes downgoing bilaterally, and other reflexes untested due to involuntary movement. Exam of his upper extremities was normal. Other than a BUN of 29 mg/dL and creatinine of 5.62 mg/dL, chemistries and iron studies were within normal limits. Urine drug screen was negative. Creatine phosphokinase and erythrocyte sedimentation rate were elevated at 1480 IU/L and 68 mm/h, respectively. Rheumatologic labs (including ds-DNA, Chromatin, Jo-1, Centromere, RNP, Scleroderma, SSA, SSB, and Smith) were negative. A MRI of the brain revealed abnormal T2 signal change in bilateral basal ganglia (image included). Patient was ultimately started on Haldol and showed remarkable improvement in hyperkinetic movements.
DISCUSSION: The presentation of hyperkinetic movements comes with an extensive differential that includes Huntington’s disease, Wilson’s disease, restless legs syndrome, Sydenham’s chorea, tardive dyskinesia, drug-induced movement disorders, and psychogenic disorders, among others. Many of these causes are able to be rendered improbable based on history, physical exam, laboratory, and imaging studies. We considered many of these in our differential; however it was the history of end-stage renal disease and diabetes mellitus with previous hyperglycemia hyperosmolar states combined with classic MRI findings that directed us towards a diagnosis of diabetic uremic syndrome. Diabetic Uremic Syndrome was first reported by Wang, et al. of Taiwan in 1998. Since then, this syndrome has been characterized as acute hyperkinetic or hypokinetic extrapyramidal disorders associated with uniform neuroimaging findings of bilateral symmetrical basal ganglia changes in diabetic ESRD patients undergoing hemodialysis. The classic image findings in our patient are consistent with reports citing bilateral basal ganglia lesions ranging from focal putaminal and pallidal lesions to widespread involvement of the whole basal ganglia with perifocal edema. Prognosis is not clear but it appears in a number of cases patients had reversal of their acute neurologic impairments with lesions often disappearing during follow-up. The pathogenesis is unknown, with speculation that it may be related to uremic toxins, diabetic microangiopathy, metabolic acidosis, and hypoglycemia. Treatment seems to be primarily symptomatic with dialysis recommended if a toxic or metabolic mechanism is present. In our case, Haldol was relatively successful at suppressing involuntary movement. Most reported cases are from patients of Asian descent; however this case demonstrates that this syndrome is likely independent of genetic influences. It has also been discussed in the literature that this may not be a rare condition but rather underdiagnosed due to relative ambiguity. Better recognition of this syndrome can lead to better physician and patient education.
EVALUATION AND MANAGEMENT OF ACUTE INFERIOR MESENTERIC VEIN THROMBOSISSara-Megumi Naylor. UCLA Medical Center, Los Angeles, CA. (Tracking ID #1926398)
LEARNING OBJECTIVE 1: Mesenteric venous thrombosis (MVT) is a rare condition that can be due to inherited or acquired thrombophilia, local factors causing vessel wall injury from abdominal infections or surgery, or stasis. Patients can be asymptomatic or present with abdominal pain or signs of portal hypertension depending on the acuity of the thrombosis. With the increasing use of computed tomography (CT), the detection of MVT is increasing. Most sources recommend anticoagulation to prevent bowel infarction and recurrent thrombosis.
CASE: A 59 year-old Caucasian homeless man with history of alcohol abuse and cigarette smoking related COPD presented to the emergency department for progressive abdominal pain over 1 week. The abdominal pain was diffuse but most prominent in the left lower quadrant, severe, crampy and constant with no radiation. He reported associated fevers, chills, nausea, vomiting, and diarrhea. On exam he was well-nourished, in mild distress, afebrile, tachycardic and had mild abdominal tenderness in the left lower quadrant. Admission CT abdomen and pelvis with contrast showed extensive diverticulosis with significant sigmoid diverticulitis and colonic wall thickening with associated thrombus of the inferior mesenteric vein (IMV) extending into the splenic vein. The patient was initially admitted to the General Surgery service, however, with the plan for conservative management, was transferred to General Medicine. He was kept NPO, given IV fluids, and started on IV antibiotics. The patient refused therapeutic anticoagulation with heparin and received enoxaparin SQ while bridged to oral warfarin. We evaluated for a thrombophilic state which was negative except for mildly decreased protein C and antithrombin III activity levels which can be seen in infections. He improved and was discharged on a prolonged course of oral antibiotics and warfarin with the plan for a colonoscopy with eventual elective sigmoidectomy. The patient returned to the hospital 10 days later with recurrent abdominal pain and was found to have a large, multiloculated abscess and now air-filled IMV which was thought to be in direct connection with the diverticular abscess. He underwent surgical drainage of the abscess, sigmoid colectomy, with diverting colostomy. He was eventually discharged from the surgery service without prolonged anticoagulation. He was last seen in clinic 3 months after his surgery and was doing well. There has been no re-imaging of his abdomen.
DISCUSSION: In our patient, the IMV thrombus was likely provoked by his diverticulitis. We also suspect the IMV thrombosis caused relative ischemia and exacerbated the colonic inflammation. The case highlights the complexity of medical and surgical considerations and the importance of co-management of patients with MVT. In the era of widespread availability of CT scans and >90 % accuracy of CT scans to detect MVT, the diagnosis of MVT is no longer a challenge. However, the evaluation for the cause of the MVT and management remain complex. Literature suggests the inclusion of a coagulation profile, thrombophilia work-up, and in a more recent recommendation, a JAK2 sequence variation screen to evaluate acute MVT. Anticoagulation is the mainstay of therapy with supportive care given the most common cause of death of MVT is sepsis with multiorgan failure. The duration of anticoagulation depends on the cause of the MVT.
EXERCISING HICKAM’S DICTUM: A CASE OF SIMULTANEOUS PARASITIC, FUNGAL, BACTERIAL AND VIRAL INFECTIONSJohn Romond; Andrew Hoellein. University of Kentucky, Lexington, KY. (Tracking ID #1937736)
LEARNING OBJECTIVE 1: Demonstrate immunosuppression as a setting for multiple simultaneous infections
LEARNING OBJECTIVE 2: Describe the role of steroids in the conversion of Strongyloidiasis to hyperinfection syndrome
CASE: A 76 year-old man from eastern Kentucky presented with abdominal pain and intermittent melena for 1 month. He was recently diagnosed with lupus nephritis and started on mycophenolate and prednisone. On presentation, he was afebrile and in atrial fibrillation with a heart rate in the 120 s, his respiratory rate was elevated to 22 and he was normotensive. He was anemic with a hemoglobin of 7.9 but without leukocytosis. A CXR suggested bilateral lower lung airspace disease and follow up CT showed extensive areas of ground glass opacities. Shortly after admission he had coffee ground emesis and became more dyspneic. Upper and lower endoscopy revealed diffuse mucosal erythema and friability with contact bleeding. Following endoscopy his clinical condition worsened, and he became hypotensive and hypoxic. He was intubated and transferred to the ICU. Blood cultures returned positive for Enterococcus faecalis. Blood CMV DNA PCR was positive at 1100 copies/ml. Serum Cryptococcal antigen was positive with a titer of 1:64 and blood mycological evaluation returned positive for Cryptococcus. Biopsies taken from esophagus, stomach, duodenum and colon showed extensive Strongyloides stercoralis infection and bronchoalveolar lavage found both Strongyloides and Cryptococcus in the lungs. Despite aggressive therapy for each of these infections, our patient died.
DISCUSSION: Although William of Occam in the 14th century stated, “Plurality must not be posited without necessity,” the more recent quip of Dr. Hickam, “A patient may have as many diagnoses as he darn well pleases. “ proved the more applicable in this case. While the multiple diagnoses discovered in this patient were likely secondary to his immunosuppression, the role of steroids specifically in the development of overwhelming Strongyloidiasis has been well described. Investigation has shown that steroids diminish circulating eosinophils through decreased proliferation and accelerated apoptosis in addition to directly stimulating the Strongyloides to proliferate. Thus, as the worm burden rapidly increases the innate defense of the host is weakened and a massive infection of the gastrointestinal tract, blood stream, and lungs is termed “hyperinfection”. There are often secondary infections as bacteria may travel on the parasite or within the gut of the worm. Although wide variation exists in the literature due to small study populations, Strongyloides Hyperinfection alone has a mortality rate reported as high as 87 %.
EXTENSIVE AORTIC THROMBUS IN ULCERATIVE COLITIS: COMMON DISEASE WITH UNUSUAL COMPLICATIONSonikpreet Sonikpreet; Alaeddin Maeza; Jasleen Kaur; Sarwan Kumar. Crittenton Hospital/Wayne state university, Rochester, MI. (Tracking ID #1938323)
LEARNING OBJECTIVE 1: Thromboembolism is a serious but under-recognized complication of inflammatory bowel disease (IBD). Venous thrombosis is a well recognized but arterial thrombotic complications of IBD is extremely rare and poorly understood.
CASE: We describe a case of extensive arterial thrombus of descending aorta and its branches in association with severe Ulcerative Colitis (UC). A 54 y/o female with the history of chronic intermittent bloody diarrhea, presenting with worsening of symptoms for 3 months. Diagnosed proctitis on outpatient evaluation with no follow up, until the day she presented to the ER with severe bloody diarrhea and abdominal cramps. Associated with fever and weight loss of 30 lbs. Physical examination concluded mild diffuse abdominal tenderness. She was admitted and started on Ciprofloxacin and Flagyl. Stool studies were unremarkable except for positive leukocytes. Colonoscopy was performed suggesting nonspecific colitis with biopsy confirming UC. She was then started on IV steroids and Lialda. However, CT scan including angiography was done in ER, revealing multiple arterial thromboses in the abdominal aorta, distal superior mesenteric artery and the branches of proximal inferior mesenteric artery. Anticoagulation workup was negative. Heparin was started but the patient had massive bleeding episodes, necessitating discontinuation of heparin though APTT was within normal range. Eventually the patient recovered, following up with repeat CT angiography showing resolution of arterial thrombi.
DISCUSSION: Arterial thrombotic complications are rare in UC and need early recognition and appropriate management to prevent morbidity and mortality. Therapeutic management is difficult because of spontaneous hemorrhage, more clinical trials of therapy required to provide the appropriate options for treatment.
EXTENSIVE ARTERIAL AND VENOUS THROMBI AS A PRESENTATION OF HYPEREOSINOPHILIC SYNDROME WITH A UNIQUE COMPLICATION OF HEMOLYTIC ANEMIA AND POOR RESPONSE TO TREATMENTMatthew P. Deek; Mansi Shah; Lauren C. Hogshire. Rutgers- Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1899545)
LEARNING OBJECTIVE 1: Recognize the various clinical presentations of idiopathic hypereosinophilic syndromes
LEARNING OBJECTIVE 2: Identify unique complications of idiopathic hypereosinophilic syndromes.
CASE: A previously healthy 46 year old man, who recently emigrated from Dominican Republic with a diagnosis of bilateral lower extremity DVT on warfarin therapy, presented with progressively worsening bilateral lower extremity pain, cyanosis of his right foot, and 18 lb unintentional weight loss over 3 weeks. On exam, he was tachycardic with bilateral lower extremity edema, had dusky discoloration of the digits of his hands and feet with weak peripheral pulses. No rash, lymphadenopathy, respiratory wheezes, masses or organomegaly were present. Diagnostic tests revealed severe eosinophilia (WBC 30.4 × 103; eosinophils 20.7 × 103) and anemia (Hgb 9.6 g/dL). Vascular studies confirmed with CT showed extensive arterial thrombi of the right upper, left upper, and right lower extremity and venous thrombi of the IVC, right peroneal, right posterior tibial, right popliteal, right femoral, right external iliac, left popliteal, left femoral, left external iliac, and hepatic vein. An extensive investigation followed and ruled out infectious etiologies including parasites, HIV, and hepatitis. His hospital course was complicated by the development of hemolytic anemia for which he was treated with IVIG and required transfusions. Subsequent hematological work up including bone marrow biopsy revealed a monoclonal T-cell population, and he was diagnosed with hypereosinophilic syndrome with a clonal T-cell mediated lymphoproliferative disorder (CD3-/CD4-/FIP1L1-PDGFRA-). He was treated with a trial of high dose corticosteroids and adequate control of his eosinophilia was achieved. Due to his widespread arterial and venous thrombi, he was discharged on warfarin. Two weeks later, he returned with a gangrenous right foot and was found to have refractory hypereosinophilia (WBC, 21 × 103; eosinophils 5.3 × 103) with recurrent thrombosis, which required a transmetatarsal amputation.
DISCUSSION: Idiopathic hypereosinophilic syndrome (HES) is defined as persistent eosinophilia with end organ damage in the absence of a neoplastic process or reactive eosinophilia. Major organ damage can occur due to eosinophil infiltration, which may manifest as fibrosis, thrombosis with or without thromboembolism, cutaneous or mucosal involvement, edema, and neurologic deficits. Amongst idiopathic HES is a lymphocytic variant caused by an aberrant T cell lymphocyte population that overproduces the cytokine interleukin-5. Some patients with the lymphocytic variant HES may eventually develop T-cell lymphoma. This case represents a unique presentation of T-cell mediated HES with a lymphocytic variant for multiple reasons. Principally, the extent of eosinophil-mediated venous and arterial thrombi in this patient is greater than typically found in literature. Many patients with HES show some degree of hypercaoguability, but the precise cause of this is not known. One hypothesis is that the eosinophil-mediated protein release causes endothelial damage and activates the coagulation cascade, which may account for the persistence of thromboses and failure of anticoagulant therapy. Moreover, autoimmune hemolytic anemia is not a well documented clinical phenomena in the literature surrounding HES and the presence of complications such as this may be a marker for disease refractoriness and prognosis, and should be considered when determining treatment options.
EYES: A WINDOW TO THE HEARTRadha S. Mehta; Surbhi Rohatgi; Aliya Laeeq. Mount Auburn Hospital, Cambridge, MA. (Tracking ID #1931906)
LEARNING OBJECTIVE 1: To know the association of various organ systems involved in a patient presenting with one of the features of a rare syndrome.
LEARNING OBJECTIVE 2: To know the management including close follow up of a patient with a known rare mitochondrial encephalomyopathy.
CASE: 40-y/o gentleman with history of Kearns-Sayre syndrome presented at outside hospital with flu like symptoms where he was noted to have a heart rate in the 40s with complete heart block and was sent to our hospital for further management. He had symptoms of progressive fatigue and worsening shortness of breath waxing and waning over the last several weeks to months. He was a former smoker, used alcohol socially and had no family history of premature atherosclerosis. Physical examination was significant for pulse rate of 35 and eye exam showing ptosis and ophthalmoplegia. Rest of the exam was reassuring. His labs included BNP of 2000. INR of 1.3. WBC 6.8, hemoglobin 13.7, hematocrit 40.2, platelets 130. Sodium 143, potassium 4.3, chloride 106, CO2 25, glucose 87, BUN 6, creatinine 0.5, calcium 8.8, magnesium 2.7. Troponins <0.04, 0.11. TSH 1.78. CRP 33.5. albumin 3.2, total protein 5.7, T.bilirubin 1.7, D.bilirubin 0.7, AlkPhos 144, ALT 50, AST 79. HbA1c 6.5. PTH 59.1. Lyme antibody was negative. Echocardiogram showed a decreased EF of 20 %. He had received Isoproterenol at the outside hospital. We observed the patient overnight and he was hemodynamically stable. He got a single ventricular pacemaker with implantation of the ICD lead in case he needs ICD for his cardiomyopathy in the future. He was also started on B-Blocker and Lisinopril for his cardiomyopathy.
DISCUSSION: Kearns-Sayre syndrome (KSS) is a rare syndrome characterized by the triad of progressive external ophthalmoplegia, pigmentary retinopathy and cardiac conduction system disturbances; it is a mitochondrial encephalomyopathy which usually presents before the patient reaches the age of 20. Cardiac involvement has been shown to be the most important prognostic factor for life expectancy, and complete heart block is known to be the major cause of death in patients with KSS. Other cardiac manifestations reported are first or second degree of AV block, QT prolongation, torsades de pointes ventricular tachycardia, and rarely dilated cardiomyopathy. Intracardiac electrophysiological studies showed that the primary abnormalities are in the AV node-His-Purkinje system. In cardiac histopathological studies, fatty infiltration and fibrosis of the bundle branches and of the sinoatrial and atrioventricular nodes have been observed. The European Society of Cardiology guidelines for cardiac pacing, 2007 recommend pacemaker implantation with any degree of fascicular block in patients with neuromuscular diseases with class IIa indication, level of evidence C, or with second- or third-degree AV block with class I indication, level of evidence B.
FACIAL RASH AS A RARE INITIAL PRESENTATION OF PRIMARY CUTANEOUS CRYPTOCOCCOSISAmornpol Anuwatworn; Pramil Cheriyath. Pinnacle Health System - Harrisburg Hospital, Harrisburg, PA. (Tracking ID #1939763)
LEARNING OBJECTIVE 1: Recognize the clinical features of primary cutaneous Cryptococcosis
LEARNING OBJECTIVE 2: Investigate and manage primary cutaneous Cryptococcosis
CASE: A 26 year-old male with history of HIV and lymphoma presented with a 3 month history of facial rah associated with itching. He had been on antiretroviral medications since the age of 17 but stopped taking medicine 5 years ago. Two weeks prior to the admission, HAART regimen and bactrim were prescribed. He underwent skin biopsy by dermatologist and the histopathology showed cryptococcus. On examination, temperature was 38 centrigrade. There were umbilicated erythematous plaques and papules all over his face. There was no rash on all extremities or trunk. Laboratory results revealed white cell of 12 K/uL, hemoglobin of 8.2 G/DL, platelet count of 116 K/uL, CD4 count of 70 and HIV RNA of 9,908 copies/mL. Blood cultures grew Crytococcus neoformans. Chest x-ray was unremarkable. Amphotericin B was initiated however it was discontinued after he developed acute kidney injury. Intravenous fluconazole was administered. His symptoms improved and he was discharged with a 6 month course of oral fluconazole. He is currently following with his primary physician.
DISCUSSION: Primary cutaneous cryptococcosis (PCC) is an opportunistic infection in immunocompromised patients, and is characterized by cutaneous lesions, positive culture with no evidence of systemic manifestations. Skin lesions usually involve upper or lower extremities. We described a case of facial rash as an extremely rare initial presentation of PCC. PCC is caused by Cryptococcus neoformans or Cryptococcus gattii. Acneiform, palpules, plaques, tumoral mass, cellulitis, ulcerated and necrotic lesions are varied cutaneous forms. Umbilicated papules may be found in HIV patients as illustrated in this case. The main therapy includes systemic fluconazole or amphotericin. As PCC incidence is rare, the diagnosis may be delayed. PCC should be considered in the differential diagnosis of facial rash in immunocompromised patients. Skin biopsy and culture should be done.
FATAL ACUTE RESPIRATORY DISTRESS SYNDROME CAUSED BY DISSEMINATED NOCARDIOSIS: A CASE REPORTSatoshi Okamori; Nagano Hiroyuki; Yukio Tsugihashi; Hiroyuki Akebo. Tenri Hospital, Nara, Japan. (Tracking ID #1933943)
LEARNING OBJECTIVE 1: Recognize that suppression of cell-mediated immunity is a risk factor of Nocardia infection.
LEARNING OBJECTIVE 2: Recognize that disseminated nocardiosis has the potential to cause acute respiratory distress syndrome (ARDS) even under appropriate antibiotic therapy.
CASE: A 66-year-old Japanese woman was admitted to our hospital with wrist pain and fever. Approximately 5 months before admission, she developed hemophagocytic syndrome. She was treated with steroid pulse therapy and oral prednisolone and cyclosporine. One month before admission, she noted pain in her left wrist with progressive swelling. Three days before admission, she developed a fever which peaked at 38 °C. She was then admitted to our hospital. On examination, oxygen saturation was 92 % while breathing ambient air. On auscultation, coarse crackles were heard bilaterally. Subcutaneous nodules were palpable on the left wrist, left thigh and right inframammary region. Computed tomography (CT) revealed multiple nodules not only subcutaneously but also in the bilateral lungs and retroperitoneal space. Surgical biopsy of a subcutaneous nodule revealed an abscess with bloody pus, and bacteriological examination detected Nocardia farcinica. A diagnosis of disseminated nocardiosis was made and treatment with trimethoprim-sulfamethoxazole and imipenem-cilastatin was initiated. Shortly thereafter her respiratory status deteriorated with rigor and shivering. Chest X-ray and CT revealed bilateral consolidations, presenting acute respiratory distress syndrome (ARDS). The patient was intubated and treated with mechanical ventilation. Nocardia farcinica bacteremia was confirmed by blood culture. The patient responded poorly to antibiotic therapy and died of respiratory failure. Postmortem examination revealed multiple inflammatory regions with necrosis of the lung, kidney and perinephric tissue, confirming the diagnosis of disseminated nocardiosis. Diffuse alveolar damage, which is pathological feature of ARDS, was also observed.
DISCUSSION: Immunocompromise is a well-established risk factor for nocardiosis. Our patient had suppressed cell-mediated immunity due to oral prednisolone and cyclosporine, and was at a high risk of Nocardia infection. We informed the laboratory staff and they immediately conducted not only a standard gram stain but also a modified Kinyoun acid-fast stain, which provided the diagnosis of disseminated Nocardiosis and led to prompt antibiotic therapy. The incidence of nocardiosis has increased substantially in the past two decades, in association with an increase in the population of immunocompromised hosts. Nocardiosis should be considered in the diagnosis of fever and multiple nodules in immunocompromised patients, and this possibility should be communicated to laboratory staff. On admission, CT in our patient showed multiple nodular lesions. Even though antibiotic therapy was initiated, the CT findings changed to bilateral consolidation, with concurrent respiratory failure requiring mechanical ventilation. The patient was clinically diagnosed with ARDS, and post mortem examination of the lung pathologically confirmed diffuse alveolar damage. Nocardiosis can follow a rapidly progressive course in patients with severe immunosuppression. In particular, as Nocardia farcinica has a higher risk of dissemination and mortality and is more resistant to antimicrobial agents, distinguishing it from other Nocardia species is important.
FATAL CEREBRAL AIR EMBOLISM AS A COMPLICATION OF ESOPHAGOGASTRODUODENOSCOPYDavid E. Kim; Julie Yam; Tejaswini Joginpally; Woo J. Chang; Shilpa Kavuturu. Michigan State University, East Lansing, MI. (Tracking ID #1939483)
LEARNING OBJECTIVE 1: Recognize an uncommon but fatal complication of endoscopy
LEARNING OBJECTIVE 2: Manage suspected acute air embolism
CASE: An 88 year old female with a history of Alzheimer’s, hypertension, and a duodenal ulcer presented to the ED with 3 day history of generalized weakness, dizziness, and multiple falls. She used NSAIDs regularly for her arthritis. The patient was diagnosed with an upper GI bleed and symptomatic anemia with a hemoglobin of 4.7 g/dL. CT brain was unremarkable. After transfusion and stabilization she underwent an EGD under conscious sedation with propofol. Endoscopic findings included a grade B distal ulcerative espophagitis, an obstructive pyloric stenosis which was balloon dilated to 12 mm, and a 6 cm × 6 cm post bulbar duodenal ulcer with visible vessel and active bleeding with hemostasis achieved with clips and gold probe coagulation. Within minutes following the procedure, patient became hypotensive with blood pressure of 70/30 mmHg and tachycardic with pulse of 120 bpm and then became unresponsive with a GCS of 3. No arrhythmias were noted on telemetry. The patient was intubated for air way protection. Her hypotension shortly resolved after minimal IV fluids. Repeat CT brain showed multiple foci of air in the right frontal, temporal, and occipital regions with significant infarctions of the right cerebellum, left occipital lobe, and left parietal lobe. A transthoracic echocardiogram did not show evidence of an intracardiac shunt, air, wall motion abnormalities, or elevated pulmonary artery pressures. The left ventricular ejection fraction was 65 %. The patient was treated with 100 % oxygen therapy but the prognosis was poor. The patient was declared brain-dead and life support was withdrawn on hospital day 5. Post mortem autopsy did not show signs of a ruptured duodenal ulcer, GI AVM, GI fistulas, barotrauma, intracardiac air or shunt, or evidence of portocaval shunting.
DISCUSSION: Cerebral air embolism due to EGD is a rare but potentially fatal complication. To our knowledge there are only 10 other reported cases. There is increasing evidence that a certain volume and rate of air entry may overwhelm the filtration capacity of the pulmonary capillaries and allow the passage of venous air into the arterial circulation. In our patient we hypothesize that a combination of insufflated air and balloon dilation created an entry point and a large pressure gradient to introduce air into the visible duodenal vessel. This may have caused the transient hypotension via a temporary obstruction of the right ventricular outflow tract that was relieved when the venous air passed into the arterial circulation. The patient’s advanced age with dementia and sedation with Propofol were complicating factors for initial diagnosis and likely the clinical outcome. Cerebral air embolism can be indentified through CT scanning if done early. If venous air embolism is suspected, the patient should be placed head-down in a left lateral decubitus position to prevent the air bubble from obstructing the right ventricular outflow tract. Some authors have suggested that aspiration of air from the right ventricle through a central catheter may improve outcomes. The initial treatment is 100 % oxygen and hyperbaric oxygen (within 30 h) therapy to rapidly reduce the volume of air embolus.
FEVER OF UNKNOWN ORIGIN WITH TELANGIECTASIA AND INFLAMMATORY LESION OF ABDOMINAL SKIN AND RESPIRATORY FAILUREMotosuke Tomonaga1; Motoshi Fujiwara1; Masaki Tago1; Yuka Naito1; Jun Tokutomi1; Akiko Eiri1; Hiroki Aihara1; Tsuneaki Yoshioka1; Masaki Hyakutake1; Yuta Sakanishi2; Itaru Kyoraku1; Takashi Sugioka2; Shu-ichi Yamashita1. 1Saga Medical School, Saga, Japan; 2Saga Medical School, Saga, Japan. (Tracking ID #1902509)
LEARNING OBJECTIVE 1: Diagnose the cause of fever of unknown origin associated with teleangiectasia
CASE: A 75-year-old woman was admitted to our hospital because of redness and swelling of skin of lower abdomen and left thigh, dyspnea and fever. Two months before admission, pain developed in her lower abdomen, which also showed reddening of the skin. She visited another hospital and was diagnosed as cellulitis and was prescribed antibiotic, but her symptoms didn’t improve. Skin biopsy was performed, which showed only nonspecific inflammatory findings. In addition, dyspnea and high fever developed, so she was transferred to our university hospital. On examination, the temperature was 36.3 °C, the blood pressure 100/60 mmHg, the pulse 84 beats per minute, the respiratory rate 16 per minute, and the oxygen saturation was less than 90 % while the patient was breathing ambient air. Her skin of lower abdomen and left thigh was red, swelled, feverish and coarse with slight tenderness. The capillaries in the same area showed dilatation. The white blood cells were 3300/μl, and atypical lymphocytes were detected on microscopic image. LDH was 472 IU/l, soluble interloikin 2 receptor 1485 IU/l. The chest X-ray showed pleural effusion in both sides. Paracentesis was performed and pleural effusion was exudative without malignant cell. Her pleural effusion was intractable in spite of the treatments with chest drainage or diuretics. Gradually, the skin inflammation and telangiectasia extended to the upper abdomen, so we performed skin biopsy again showing invasion of large lymphoid cells to vessels that was considered as nonspecific findings. On the 21th hospital day, consciousness disturbance occurred. Laboratory data on the day showed serum sodium 113 mEq/l and blood glucose 45 mg/dl. Since we suspected the presence of adrenal failure, we started intravenous administration of hydrocortisone before the results of endocrinological examinations came back, which showed that she had panhypopitutitarism. Since we suspected her illness as intravascular lymphoma (IVL), we performed random skin biopsy, which made the diagnosis of diffuse large B-cell lymphoma (DLBL). At this time, she was in severe respiratory failure. She was intubated and put under ventilator treatment. Since her general condition was too bad to receive chemotherapy, we chose the treatment of best supportive care. She died 2 months after her hospitalization. We performed postmortem examination. The color of peritoneum was brown, and we suspected the invasion of lymphoma cells. On intracranial survey, there was adhesion of dura mater, and pituitary body was swollen, which suggest the intracranial invasion including pituitary body. Histopathological examination is currently in process, which we are going to show on our presentation.
DISCUSSION: Random biopsy of skin is essential when IVL is suspected, especially when a patient shows telangiectasia and inflammation of skin with diverse symptoms including fever of unknown origin.
FIBRINOLYSIS SECONDARY TO UROKINASE PRODUCTION BY TRANSITIONAL CELL CARCINOMAJorge Fuentes; Jesse Victor. University of Florida, Gainesville, FL. (Tracking ID #1939778)
LEARNING OBJECTIVE 1: Recognize the diagnostic, prognostic and therapeutic implications of urokinase production by transitional cell carcinoma.
LEARNING OBJECTIVE 2: Diagnose secondary fibrinolysis by thromboelastography analysis.
CASE: Seventy-three year old male with history of prostate cancer treated with androgen deprivation therapy, transitional cell bladder cancer with partial resection and deep venous thrombosis on coumadin presented to clinic for three-week duration of painless hematuria. CT of abdomen and pelvis revealed large bladder mass with mild to moderate hydronephrosis in the setting of creatinine of 1.0 and INR of 2.3. Patient was instructed to discontinue coumadin and return to clinic in 5 days for cystoscopy. Patient complied with coumadin discontinuation however returned in 3 weeks. During this visit cystoscopy revealed necrotic posterior bladder mass suspicious for transitional cell carcinoma. Labs revealed acute kidney injury with creatinine of 11.5 and INR of 8.3 despite discontinuation of coumadin. Renal ultrasound confirmed severe bilateral hydronephrosis. Intravenous hydration was initiated along with vitamin K and two units of fresh frozen plasma. Three-way foley was placed for continuous bladder irrigation. Interventional Radiology consulted for placement of bilateral nephrostomy tubes for obstructive nephropathy. Prior to nephrostomy tube placement, patient was afebrile and hemodynamically stable with moderate suprapubic tenderness and bright red blood with visible clots in foley bag. Labs consisted of creatinine of 12, corrected INR of 1.7 and decreased hemoglobin from 8.9 to 6.7 g/dL. Patient transfused two units of packed red blood cells with adequate response. He tolerated nephrostomy tube placement well with no requirement for blood products. Approximately 6 h post procedure, significant hypotension developed with decreased hemoglobin from 8.7 to 4 g/dL, lactic acid of 15 mmol/L, D-dimer 17.79 mg/L, fibrinogen <35 mg/dL, INR 3.7 and protime 36.1 s. Thromboelastography (TEG) analysis showed evidence of clot lysis with prolonged LY30 of 15 % (0-8 %), coagulation index of 3.1 (−3 to 3) and decreased MA of 40 mm (55–73) suggestive of secondary fibrinolysis. There was no evidence of microangiopathic hemolytic anemia given lack of thrombocytopenia and schistocytes on peripheral smear. Abdominal CT revealed developing retroperitoneal hemorrhage with new hematomas in left proximal thigh. Angiogram revealed no evidence of contrast extravasation in right/left renal and right/left iliac arteries. Patient was transferred to intensive care unit for management of hemorrhagic shock and transfused six units of packed red blood cells, four units of cryoprecipitate, four units of fresh frozen plasma with correction of coagulopathy. Renal function gradually improved over the course of hospitalization. Patient subsequently underwent successful urologic resection of bladder mass.
DISCUSSION: Urokinase is a serine protease produced by urothelium that promotes conversion of plasminogen to plasmin. It is used clinically as a thrombolytic agent in the treatment of massive deep venous thrombosis, pulmonary embolism and myocardial infarction. Effective thrombolysis with urokinase is evidenced by reduced fibrinogen, increased concentration of fibrinogen degradation products, shortened clot lysis time and prolonged PT and PTT. Urokinase plasminogen activator (uPA) has been implicated in tumor invasion and metastases as activated plasmin directly cleaves components of the basement membrane and extracellular matrix; permitting tumor cells to access lymph vessels and vasculature. Patients with transitional cell cancer have increased levels of plasma uPA compared to healthy controls. Moreover, patients with advanced stage transitional cell cancer and high uPA levels have poorer prognosis compared to similar staged tumors with low uPA levels; suggesting that uPA may serve as an independent prognostic marker. Hyperfibrinolysis in this patient was attributed to increased levels of urokinase in the setting transitional cell cancer. Hyperfibrinolysis is diagnosed on TEG analysis by LY30 >7.5 % or EPL >15 %. Coagulation index (CI) is used to distinguish primary and secondary fibrinolysis with values greater that 3.1 suggestive of secondary fibrinolysis. Therefore, LY30 of 15 % and CI of 3.1 in the setting of decreased fibrinogen, increased D-dimer and prolonged PT and PTT were suggestive of secondary fibrinolysis. Additionally, acute kidney injury from obstructive nephropathy may have exacerbated fibrinolysis by impaired renal clearance of urokinase. Antifibrinolytic drugs such as aminocaproic acid or tranexamic acid are used to treat fibrinolysis; however this was not administered as fibrinolysis resolved with improvement in renal function after nephrostomy tube placement. Further investigation of urokinase utilization by tumor cells is required as urokinase may serve as a marker for tumor recurrence or therapeutic target for prevention of metastasis.
FIRE IN THE BELLYJessica Pacifico; Sheira Schlair. Montefiore Medical Center, Bronx, NY. (Tracking ID #1937714)
LEARNING OBJECTIVE 1: Identify the differential diagnosis for recurrent abdominal pain and fever
LEARNING OBJECTIVE 2: Recognize the clinical manifestations of Familial Mediterranean Fever
CASE: A 37-year-old man presented with severe mid-abdominal pain and fever for 2 days. His temperature at home measured 102° Fahrenheit and he had associated rigors. He reported no nausea, vomiting, diarrhea, constipation, reflux symptoms, weight loss or rash. The abdomen was diffusely tender but not distended with no rebound or guarding; he had no rash and no lymphadenopathy. Liver tests, amylase and lipase were within normal limits and white blood cell count was not elevated. Computed tomography of his abdomen was unremarkable. For the past 3 years, he had similar episodes as often as once per week. At other times, up to 6 months would pass between episodes; they typically lasted 1–3 days with associated fevers ranging from 101 to 105° Fahrenheit. During some of the episodes, he would have thigh myalgias but no frank joint swelling, redness or warmth. Between episodes, the patient was asymptomatic. Prior studies included a colonoscopy, ultrasound of the abdomen and computed tomography of his abdomen that were all normal. The patient was born in Egypt and lived with his wife in New York City; he had smoked cigarettes infrequently in the past but quit many years ago, had minimal alcohol intake and noted no risk factors for human immunodeficiency disorder. The pain and fever resolved with no intervention the next day. Several months later, on a trip to visit his family in Egypt, he was diagnosed with Familial Mediterranean Fever through genetic testing and initiated on colchicine. Since that time, he has had no subsequent episodes of abdominal pain and fever.
DISCUSSION: A typical, basic evaluation of abdominal pain includes history, physical examination, labs including complete blood count, liver tests, amylase and lipase and imaging as needed. While the differential diagnosis for abdominal pain and fever is quite extensive, it narrows with several recurrences and repetitive non-revealing basic work ups. At that point, evaluation for infectious etiologies (e.g. typhoid fever, brucellosis, borreliosis, malaria, tuberculosis, HIV), rheumatologic etiologies (e.g. vasculitides, systemic lupus erythematous) and malignancy (e.g. lymphoma) should be undertaken. Additionally, the periodic fever syndromes should be considered. Amongst the periodic fever syndromes, abdominal pain is a common feature in Familial Mediterranean Fever (FMF), TNF-receptor 1 associated periodic syndrome, hyperimmunoglobulinemia D syndrome and Muckle-Wells syndrome. FMF is a genetic disease (most commonly autosomal recessive inheritance) that occurs mainly in people of Sephardic Jewish, North African, Arab, Turkish, Italian, Greek and Armenian descent. FMF is characterized by paroxysmal attacks of fever and serosal inflammation including peritonitis, pleuritis and synovitis, typically lasting 1–3 days and then resolving spontaneously. The most common manifestation of the disease is peritonitis presenting as abdominal pain. The presentation of the abdominal pain can range in severity from aching, generalized tenderness to guarding, rebound tenderness and rigidity that can mimic an acute surgical abdomen. Other acute manifestations include, but are not limited to, erysipelas-like dermatologic lesions, pericarditis, orchitis and aspetic meningitis. Laboratory abnormalities include elevations in the serum markers of systemic inflammation including leukocytosis, erythrocyte sedimentation rate and C-reactive protein, amongst others. The major long-term complication is secondary AA amyloidosis. Diagnosis can be made clinically via a detailed criteria set; the most commonly used has 4 major and 4 minor criteria, as well as 10 supportive criteria. FMF can also be diagnosed through genetic testing for mutations in the MEVF gene. MEVF encodes pyrin, a protein which plays a key role in the innate immune system and the inflammatory response. The exact mechanism triggering attacks is unknown at this point. A few founder mutations account for the majority of cases; it has been suggested that two of the most common mutations, V726A and M694V, originated in common ancestors from the Middle East that lived about 2500 years ago. The typical treatment of FMF is colchicine which both reduces the frequency of attacks and reduces the risk of secondary AA amyloidosis. Since a key feature of FMF is robust health between attacks, clinicians should guard against concluding the workup when a flare resolves. A high clinical suspicion for FMF should be maintained in a patient with recurrent abdominal pain and fever, especially when the patient belongs to a typical ethnic group. Expeditious diagnosis is paramount because the initiation of colchicine therapy markedly reduces the risk of renal failure secondary to AA amyloidosis, which remains the greatest source of mortality.
FROM A SORE THROAT TO A CEREBELLAR ABSCESS AND SEPTIC PULMONARY EMBOLI; AN ATYPICAL PRESENTATION OF A “FORGOTTEN DISEASE”Puneet Gill; Richard M. Butler. Virginia Tech Carilion, Roanoke, VA. (Tracking ID #1928647)
LEARNING OBJECTIVE 1: Recognize the potential for diagnostic error in the initial clinical presentation of Lemierre’s syndrome.
LEARNING OBJECTIVE 2: Recognize that Lemierre’s syndrome may present without the classic radiographic finding of thrombus in the internal jugular vein.
CASE: A 21-year-old female with a history of asthma presented to the emergency department for evaluation of left ear pain, sore throat and productive cough for the past 3 days. She was found to be febrile (T 102.7 F) and tachycardic, which resolved after receiving antipyretics. Rapid Strep screen was negative and patient was discharged home with presumed viral pharyngitis. She returned to the emergency department 5 days later with complaints of headache, neck pain and back pain. Family reported symptoms of confusion, drowsiness and slurred speech over the past 2 days. On exam patient was somnolent but arousable, ill appearing with dry mucous membranes and in mild respiratory distress. She had tender left-sided facial and neck swelling without erythema. A complete neurological exam was difficult due to altered level of consciousness, however no obvious focal deficits were noted. She was hypotensive, tachycardic, afebrile and saturating well on room air. Initial labs revealed leukocytosis, profound thrombocytopenia and elevated creatinine. CT head did not show any intracranial abnormality. CT chest showed multiple bilateral cavitary and non-cavitary parenchymal lesions increasing the index of suspicion for Lemierre’s syndrome with septic emboli to the lungs. Subsequent imaging of the neck revealed multiple small retropharyngeal abscesses and thrombophlebitis of left facial vein; the internal jugular veins appeared patent. Blood cultures returned positive for Fusobacterium necrophorum. Despite appropriate antibiotic coverage, her respiratory status declined. Repeat imaging of the brain and neck revealed a cerebellar mass and newly developed thrombus of the left internal jugular vein. The left internal jugular vein was ligated to prevent further septic emboli. The patient had a three-week hospital course, complicated by pleural empyema.
DISCUSSION: Lemierre’s syndrome was first coined in 1936, describing a condition that started as tonsillitis and progressed to suppurative thrombophlebitis of the internal jugular vein. It is usually caused by the gram negative anaerobe, Fusobacterium necrophorum. Diagnosis is supported by imaging studies showing thrombus in the internal jugular vein. This case of Lemierre’s initially lacked this classic radiographic finding, but instead showed thrombophlebitis of the facial vein. As antibiotics gained popularity, Lemierre’s syndrome became known as “the forgotten disease”. Fusobacterium necrophorum is generally sensitive to penicillin and amoxicillin. However, due to increasing concerns regarding overuse of antibiotics, physicians are encouraged to utilize conservative measures with symptomatic treatment for what is likely a viral illness. As antibiotic stewardship has become customary, there appears to be a resurgence of this syndrome in the literature. Unfortunately, the initial clinical presentation of Lemierre’s is vague and resembles viral pharyngitis. A high index of suspicion is needed when making this diagnosis, as it progresses rapidly and is associated with high mortality. It is important to recognize that there may be variations in the typical radiographic findings.
FULL COURT PRES: ALTERED MENTAL STATUS IN THE IMMUNE-COMPROMISEDCady (Blackey) Brown. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926243)
LEARNING OBJECTIVE 1: Review the work-up for altered mental status (AMS) in immune-compromised patients
LEARNING OBJECTIVE 2: Illustrate a less common cause of Posterior Reversal Encephalopathy Syndrome (PRES)
CASE: A 48 year-old woman with a history of diffuse large B-cell lymphoma, status-post allogenic stem cell transplant on cyclosporine, presented complaining of dysuria and fever. She was found to be neutropenic; she was admitted and treated with cefepime. Over the ensuing 24 h, she developed myoclonus and AMS. She was afebrile, mildly tachycardic and normotensive. ¬¬¬The physical exam revealed a woman with a Glasgow coma score of seven. She did not have abdominal distension or tenderness; her cardiac and lung exams were benign. She had myoclonus, but normal reflexes and intact cranial nerves. Her liver and renal function were normal. The blood cultures from admission showed no growth. Her cerebrospinal fluid studies (CSF) were normal. An EEG was consistent with encephalopathy. Both a non-contrast head CT and a brain MRI were normal. She remained unarousable over the following week. Bacterial cultures and viral studies of the CSF, including, herpes simplex virus, cytomegalovirus, arboviruses and west nile virus, were all negative. CSF toxoplasma and cryptococcus antigen tests were negative. A repeat MRI was done and showed edema in the bilateral occipital lobes consistent with PRES. Her immunosuppressive medication was changed from cyclosporine to sirolimus. One week later, her mental status began to improve and a repeat MRI showed less edema.
DISCUSSION: As transplant medicine increases in prevalence, more patients are immune-compromised. Thus, it is important to have an approach to AMS in this patient population. The differential diagnosis for AMS in immune-compromised patients is broad, but can be simplified into categories of infection, malignancy, metabolic, vascular and toxin/medication-induced. A thorough infectious workup, including lumbar puncture, blood cultures and serologic studies for possible pathogens must be initiated. Medications should be reviewed for possible culprits. Brain imaging and an EEG should be to done to evaluate for structural and or metabolic abnormalities. Among the less common causes for AMS in the immune-compromised, is PRES. This is a syndrome based on clinical and radiologic findings, with heterogeneous etiologies. Classic clinical manifestations include headache, AMS, visual disturbances and seizures. Symmetric white matter edema in the posterior cerebral hemispheres on MRI is the classic radiologic finding of PRES. Most commonly, uncontrolled hypertension is the underlying cause for PRES. However, immunosuppressive and immunomodulatory medications can also be the cause. Treatment involves removal of offending agent or control of offending cause (hypertension) in addition to supportive care. Recognizing PRES as a possible cause for AMS in the immune-compromised patient is particularly important because most patients recover fully if the underlying cause is reversed.
FULMINANT DISSEMINATED VARICELLA ZOSTER INFECTION IN AN IMMUNOCOMPETENT ADULTNeal Shah; Arthur Jeng. Olive View Medical Center, Sylmar, CA. (Tracking ID #1938866)
LEARNING OBJECTIVE 1: Varicella zoster virus (VZV) is a contagious childhood disease that affects both immunosuppressed and immunocompetent adults. While childhood vaccination efforts have significantly decreased those afflicted, a substantial adult population still exists who are at risk. VZV can have severe disease manifestations uncommonly seen in the current era, causing serious morbidity and mortality in the immunosuppressed.
CASE: A 44-year-old woman with no medical history presented to the ER with 3 days of non-radiating epigastric pain, shortness of breath, subjective fevers and rash that started on her trunk and spread to her arms, legs and face. She received a steroid injection 1-day prior at an outside clinic for her abdominal pain with no relief. She denied any travel, drug usage, new exposures, pets or other identifiable risk. She endorsed having “chickenpox” when young. On exam, she was febrile to 39.3 with mild tachycardia. She had bilateral conjunctival suffusion. Oral exam revealed extensive ulceration and stomatitis over her buccal mucosa, palate, and posterior oropharynx. On her skin, there were multiple erythematous maculo-papular lesions, some of which were vesicular and some of which were papular, throughout her face, back, chest, abdomen, legs, and arms including both palms. Abdominal exam revealed epigastric tenderness to palpation. Labs revealed a leukocytosis, hepatitis, and coagulopathy, consistent with disseminated intravascular coagulation (DIC). Serologies and PCR for HIV, syphilis, and typhus were negative. Viral cultures and HSV/VZV PCRs were sent from scrapings of the lesions. CT scan of the chest/abdomen/pelvis revealed extensive, bilateral nodular infiltrates and scattered ground glass opacities, along with fatty infiltration of the liver. She was empirically started on IV acyclovir and doxycycline, for concern of severe VZV or (murine) typhus. On day 2, the rash and oral/gingival lesions worsened. PCR for VZV returned positive, and she was switched to oral valacyclovir; all other antibiotics were stopped. Her VZV IgG was negative and IgM positive. Her coagulaopathy and hepatitis gradually improved. On day 4 the skin lesions began crusting over and she was discharged on day 5 with complete resolution on follow-up.
DISCUSSION: This case demonstrates the atypical severity of VZV in an immunocompetent adult. Although VZV is common in adults, it is usually reactivation (ie, shingles). Primary infections (ie, chicken pox) are less commonly seen in adults. Well-known adult complications of VZV include pneumonitis, can be life-threatening. However, conjunctivitis, severe hepatitis, and DIC are rarely seen and illustrate the wide spectrum of presentation. The steroid injection given in the outpatient clinic may have allowed this severe presentation of VZV. This case reminds clinicians of the severity that primary VZV can present with, even in an immunocompetent adult, underscoring the necessity of vaccination efforts.
FULMINANT MYOCARDITIS: THE ROLE OF VENTRICULAR ASSIST DEVICE AS A BRIDGE TO RECOVERYAmbreen Mohamed; Richard Soucier. University of Connecticut Health Center, Farmington, CT. (Tracking ID #1939220)
LEARNING OBJECTIVE 1: Recognize the clinical features of fulminant myocarditis
LEARNING OBJECTIVE 2: Discuss the role of mechanical circulatory support in fulminant myocarditis
CASE: This is a 52-year-old Japanese female with no significant past medical history who presents with complaints of fatigue and subjective fevers for 1 week. Patient had her sister recently visit from Japan as well as two daughters who were sick with upper respiratory tract infections. On the day of admission, patient developed chest comfort with increased pallor with weakness which concerned her family and was brought to the emergency room. On arrival, patient was noted to be febrile to 101.3, tachycardic in the 150’s and in significant respiratory distress. Physical exam revealed jugular venous distention, bibasilar crackles, and cool extremities. Patient became progressively became more lethargic and was placed on BiPAP of which she did not tolerate well and subsequently was intubated. Bedside echocardiogram showed an ejection fraction (EF) of 10 % to 20 %, trace pericardial effusion and a globally dyskinetic heart. With acute coronary syndrome (ACS) high on the differential, patient was started on a heparin drip and immediately taken to the cath lab only to find clean coronaries, normal right and left sided pressures, however a depressed cardiac index of 1.98. She continued to decompensate and was started on milirinone and lasix drips as well as an aortic balloon pump post cardiac cath. Patient was in cardiogenic shock, non ischemic in origin with the working diagnosis of fulminant myocarditis. She was transferred to an outside hospital where biventricular assist device (BiVAD) was placed so her heart could slowly recover. Patient’s course was unfortunately complicated by an ischemic stroke and she soon after was taken off life support and passed.
DISCUSSION: Fulminant myocarditis most often presents with cardiogenic shock. As seen in our patient, despite using maximal medical therapy, additonal mechanical ventilatory support may be needed. Ventricular assist devices offer a bridge to transplant or even recovery. Prognosis of acute viral myocarditis depends on several risk factors such as clinical presentation, ejection fraction and lower blood pressure levels on admission. Although fulminant myocarditis has been shown to have a higher in-hospital morality rate in comparison to those with acute nonfulminant myocaridits, early recognition of risk factors along with aggressive hemodynamic support has been shown to have an excellent long term prognosis.
FUNCTIONAL HYPOPARATHYROIDISM CAUSED BY HYPOMAGNESEMIAHaleigh James; Murali Duggirala. Mayo Clinic, Rochester, MN. (Tracking ID #1936960)
LEARNING OBJECTIVE 1: Diagnose and manage functional hypoparathyroidism as a result of hypomagnesemia
LEARNING OBJECTIVE 2: Recognize proton pump inhibitors as a potential cause of hypomagnesemia
CASE: A 68 year-old woman with CREST syndrome was brought to the emergency department after her husband witnessed her having a convulsive episode. She had no history of seizures. Physical exam revealed a mildly confused woman not oriented to time. She had no tongue lacerations or focal neurologic deficits. Initial ECG showed a prolonged QTc of 519 milliseconds. CT scan of the head was negative for any acute findings. Glucose was normal, but laboratory evaluation revealed several electrolyte abnormalities including a total calcium of 5.7 mg/dL (reference 8.9–10.1 mg/dL), magnesium of <0.5 mg/dL (reference 1.7–2.3 mg/dL), and potassium of 3.1 mmol/L (reference 3.6–5.2 mmol/L). Albumin was 3.5 g/dL (reference 3.5–5 g/dL) and parathyroid hormone (PTH) was 24 pg/mL (reference 15–65 pg/mL). Intravenous calcium gluconate, magnesium sulfate, and potassium chloride were administered prior to admission to the medical ICU. Upon admission, further questioning revealed that the patient had been experiencing episodic nausea and vomiting over the preceding several months and was recently diagnosed with gastroparesis. Past medical history was significant for gastroesophageal reflux disease, for which she was taking esomeprazole twice daily, and hypertension, but she was not taking any diuretics. With supplementation, the patient’s serum magnesium rose to 2.3 mg/dL (reference 1.7–2.3 mg/dL) and total calcium rose to 9.4 mg/dL (reference 8.9–10.1 mg/dL) by day 3 of hospitalization. PTH at that time was found to be elevated to 92 pg/mL (reference 15–65 pg/mL). The etiology of her hypomagnesemia was presumed to be a combination of her poor oral intake with frequent vomiting over the preceding few months, along with proton pump inhibitor use. She had no further seizures and was dismissed home on an oral calcium and magnesium supplementation regimen, as well as a lower dose of esomeprazole. She was instructed to follow up with her primary care physician for electrolyte monitoring and further investigation hypomagnesemia persisted.
DISCUSSION: This case illustrates functional hypoparathyroidism due to severe hypomagnesemia, resulting in marked hypocalcemia and seizure. Low serum magnesium causes hypocalcemia via inhibition of PTH release and bone resistance to PTH. Proton pump inhibitors (PPIs), as in this case, may cause hypomagnesemia via impaired active magnesium transport across transient receptor potential melastatin-6 and −7 (TRPM6/7) channels on intestinal epithelial cells. The risk is increased with concomitant vomiting, diarrhea, and diuretic use. Recognizing and treating hypomagnesemia is integral to correcting associated hypocalcemia because calcium supplementation alone does not reverse the functional hypoparathyroidism. When PPIs are the inciting factors of low magnesium, discontinuation of them leads to magnesium recovery.
GASTRIC ULCER PERFORATION: AN UNCOMMON CONSEQUENCE OF VOMITINGNeema Heivand; Sarah B. Fleisig; Hanna Freyle. Lenox Hill Hospital, New York, NY. (Tracking ID #1936233)
LEARNING OBJECTIVE 1: Clinically diagnose a perforated peptic ulcer
LEARNING OBJECTIVE 2: Recognize the clinical features of a perforated peptic ulcer
CASE: A 60-year-old female with a past medical history of Peptic Ulcer Disease (PUD) presented to the Emergency Department with a 3 day history of vomiting and diarrhea. She complained of 10–15 loose bowel movements per day and non-bloody, non-bilious emesis. Her presentation was prompted by inability to tolerate food or liquids without aggravating her symptoms. The patient did not complain of any abdominal pain or dyspepsia on presentation. She denied recent travel or ill contacts. PUD was diagnosed about 20 years ago and she currently was not on any antisecretory therapy. She did not take any medications and denied the use of non-steroidal anti-inflammatory drugs. The patient complained of worsening nausea, vomiting, and retching that was refractory to antiemetics overnight on hospital day one. On the morning of hospital day two, the patient complained of intense, abrupt-onset epigastric pain radiating to the back with associated right shoulder pain radiating down her right arm. Other than low-grade fever, vital signs were stable and within normal limits. On physical exam, the patient was in acute distress, writhing in pain. Abdominal exam revealed a soft, non-distended abdomen with bowel sounds present. However, the patient complained of intense tenderness to light palpation over the epigastric region and displayed guarding. Electrocardiogram was unremarkable with no change from prior studies and troponins were negative. Blood pressures taken in both arms were within 5 mmHg of each other and within normal limits. Lipase was mildly elevated at 419. Ultimately, a chest x-ray revealed free air below the right hemidiaphragm. An emergent surgical consultation was placed and the patient was sent to the operating room where a perforated gastric ulcer was revealed. Gastric tissue biopsy revealed H. Pylori infection.
DISCUSSION: Perforation is a life-threatening complication of Peptic Ulcer Disease. Although the pathophysiology of PUD is well known, aggravating factors that could result in perforation are not. The increase in intra-abdominal pressure and subsequent stomach contraction during vomiting may be a potential mechanism for perforation of an underlying gastric ulcer. This mechanism may be similar to that found in Boerhaave’s syndrome, where increased pressure results in rupture of the esophagus. The patient’s right shoulder pain could be explained by the right subphrenic presence of gastric contents. This case highlights the importance of early diagnosis of the acute abdomen and underscores the utility of the history and physical examination. Perforation should be kept on a clinicians list of differential diagnosis in a vomiting patient with history of PUD who complains of severe abdominal pain.
GIANT SPLENIC ARTERY ANEURYSM PRESENTING AS LOWER GI BLEEDINGChandra S. Dasari; Amareshwar Podugu; Steve Sanofsky. Canton Medical Education Foundation, Canton, OH. (Tracking ID #1926347)
LEARNING OBJECTIVE 1: We present a case in which a giant SAA, by causing venous obstruction in the intestinal circulation, led to extrahepatic venous hypertension causing GI bleeding, and was successfully treated with endovascular means using coil embolization.
LEARNING OBJECTIVE 2: Splenic artery aneurysms occur in slightly less than 1 % of the population. Rupture of a splenic artery aneurysm (SAA) carries a high mortality. Aneurysms generally are not treated unless they are larger than 2 cm, most treated aneurysms falling within the 2.5 to 3 cm range.
CASE: A 77 year male presented to the ER with a 3 week history of bloody stools and fatigue with a hematocrit of 16.5 which stabilized after receiving 4 units of blood. Neither upper GI endoscopy nor colonoscopy was able to localize the source of bleeding. A CT Angio of the abdomen demonstrated a heavily calcified 8.0 × 7.5 × 7.6 cm SAA. The patient continued to have ongoing episodes of slow GI bleeding while on the medical service. A bleeding scan was non-diagnostic. An arteriogram performed during an episode of bleeding also failed to locate the bleeding source, but did demonstrate the splenic artery aneurysm along with dilated veins felt to be part of the Superior Mesenteric venous system. Coil embolization of the giant splenic artery aneurysm, with occlusion of both inflow and outflow arteries, was performed in the Interventional OR Suite. The patient did not have any further episodes of GI bleeding and was discharged a few days later. A follow up CT angiogram the next day confirmed successful occlusion of the aneurysm. The patient has had no further bleeding episodes since.
DISCUSSION: SAA’s are the third most common abdominal aneurysm, following aortic and iliac aneurysms. They are usually discovered as an associated finding on an abdominal X-ray or CT scan, appearing as a spherical calcified mass in the right upper quadrant along the expected course of the splenic artery. The vast majority of SAA’s are asymptomatic. There is some controversy regarding when to prophylactically treat an asymptomatic aneurysm, although such considerations don’t occur until the aneurysm is more than 2 cm in diameter. There are a few groups of patients considered at higher risk for rupture, and these include women of childbearing age and those who are to undergo liver transplant. Treatment in these higher risk groups is considered for aneurysms 1.5 cm or greater. Treatment is indicated for symptomatic aneurysms. Aside from rupture of the aneurysm, which presents as abdominal pain and shock, and which carries a high mortality, symptoms can include abdominal pain in an otherwise stable patient, and rarely as GI bleeding due to erosion into surrounding organs such as the stomach, or as in our case, from venous compression causing portal hypertension. The most common etiology of SAA’s is atherosclerotic disease. Other etiologies include collagen vascular disease and portal hypertension. Pancreatitis can lead to false aneurysms of the splenic artery due to erosion of a pancreatic pseudocyst into the splenic artery. Although SAA’s have been treated with open surgery, the most common present day treatment for nonruptured aneurysms utilizes catheter based methods using either coil or glue embolization. Catheter based treatments have a low complication rate. Although treatment requires occlusion of the splenic artery at the site of the aneurysm, the spleen usually remains viable due to collateral flow from the short gastric arteries. Only on a rare occasion is a splenectomy required due to splenic infarction. There is a syndrome called PES (post embolization syndrome) which presents as fever, abdominal pain, pleural effusion, and rarely, pancreatitis. The syndrome probably involves partial infarction of the spleen and perhaps occasional embolic particles ending up in the pancreas. This syndrome can occur in up to 30 % of patients but is typically self limiting. Giant SAA’s causing extrahepatic portal venous obstruction has been reported but is very rare. We believe that the GI bleeding in our patient was due to elevated intestinal venous pressure caused by SMV compression by the 8 cm splenic artery aneurysm. Once the aneurysm was thrombosed as a result of coil embolization, the patient had no more bleeding episodes. He has remained symptom free for the 6 months that we have followed him since his treatment.
GIVE ME DOXYCYCLINE OR GIVE ME DEATHNaomi Karlen; Matthew N. Peters; Jared Roussel. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926161)
LEARNING OBJECTIVE 1: Recognize that serology for tick-borne illnesses can be negative during the first week and that PCR and close examination of peripheral blood smears should be performed in patients with high suspicion.
LEARNING OBJECTIVE 2: Identify doxycycline as a low cost, well tolerated treatment option to prevent potentially fatal infection with tick-borne illnesses.
CASE: A 62-year-old man presented with 5 days of fever. He described the fevers as intermittent and reported a maximum temperature of 103o F. He had a medical history of ischemic stroke and ongoing well-controlled hypertension. The patient recently completed a 30-day trip from Boston to New Orleans, during which he spent several days walking outside. However, he reported no insect bites. He denied recent sick contacts, cough, myalgia, and previous illicit drug use. On physical examination, all vital signs (including temperature) were within normal limits. Physical examination revealed no abnormalities; no rashes or breaks in the skin were noted. Initial laboratory values including CBC, CMP, PT and INR were within normal limits aside from a white blood cell count of 2.6 K/μL with 70 % segmented neutrophils, 10 % bands, and 12 % lymphocytes. Additional laboratory tests including blood/urine cultures, HIV, hepatitis panel, ehrlichia IgM/IgG, histoplasma antigen, HSV PCR, CMV PCR, ANA, and RPR were all negative. Despite the negative diagnostic testing, the patient was started on doxycycline due to a high suspicion for infection. Less than 48 h following admission, the patient acutely decompensated, went into hypocic respiratory failure, and was intubated. Further review of the admission peripheral blood smear revealed rare neutrophils with single basophilic intracytoplasmic inclusions highly suggestive of anaplasma morulas without intracytoplasmic monocyte inclusions. Doxycycline was continued. Within 48 h of intubation, the patient was extubated and reported feeling asymptomatic. He left the following day against medical advice. Anaplasma phagocytophilum was confirmed by polymerase chain reaction (PCR) more than a week after initially drawn.
DISCUSSION: Tick-borne diseases are an under-recognized cause of fever of unknown origin and accurate diagnosis requires documentation of a thorough and detailed history. It is critical to recognize that while antibody detection represents the gold standard of diagnosis, false negatives are frequently encountered during the initial (first week) of infection (polyvalent antibody sensitivity 82–100 %). PCR represents an alternative means of confirmatory test (sensitivity 67–90 %). However, the result is not readily available and thus cannot aid in immediate diagnosis. In patients with high-suspicion for tick-borne illness, further evidence for diagnosis can be provided by close re-examination of peripheral blood smears for the presence of morulae (stippled blue intracytoplasmic inclusions in neutrophils, present in 25–75 % reported cases in US, highest sensitivity during first week of infection). In patients highly suspected of carrying a tick-borne infection, doxycycline should be initiated early in the disease course. Doxycycline is not only a cheap and well-tolerated antibiotic, but also treats a variety of other tick-borne illnesses including Rickettsia and Borrelia spp.
GLIOMATOSIS CEREBRI AND THROMBOCYTOPENIA: A PREVIOUSLY UNKNOWN ASSOCIATIONSarah Nickoloff1,2; Appesh Mohandas1. 1Medical College of Wisconsin, Milwaukee, WI; 2Zablocki VA Medical Center, Milwaukee, WI. (Tracking ID #1935835)
LEARNING OBJECTIVE 1: Recognize that gliomatosis cerebri may be associated with idiopathic thrombocytopenic purpura that is resistant to therapy with intravenous immune globulin.
LEARNING OBJECTIVE 2: Recognize the implications of gliomatosis cerebri associated thrombocytopenia on choice of therapy.
CASE: A 68 year old male with a past medical history significant for myotonic muscular dystrophy, first degree AV block and subsequent pacemaker implantation, initially presented with dizziness. CT head revealed a large infiltrative mass involving the right temporal and parietal lobes, with extension into the white matter. Neurosurgery was consulted and MRI was requested, but could not be performed due to pacemaker implantation. The patient was medically stable at that time and was discharged home. Approximately 1 month later he was readmitted for altered mental status. Labs on readmission were significant for a platelet count of 4,000/uL. Thrombotic thrombocytopenic purpura and other secondary causes, such as disseminated intravascular coagulation, sepsis, HIV infection and bone marrow disorders, were ruled out. The etiology of his thrombocytopenia was determined to be idiopathic thrombocytopenic purpura (ITP), likely related to his brain tumor. Treatment with intravenous immune globulin (IVIG) was initiated, however it was not as effective as expected. Following IVIG therapy, platelet levels would temporarily recover to greater than 40,000/uL but would then fall to pre-treatment levels within 4 to 5 days. The patient received three IVIG infusions during his hospitalization, without lasting effect. Definitive therapy for this patient was dependent upon better characterization of the intracranial mass. MRI was performed under a specialized protocol for patients with implanted pacemakers, and results were consistent with gliomatosis cerebri. Radiation oncology and hematology oncology services determined that chemo- or radiation therapy would not be of therapeutic or palliative benefit. The patient’s mental status continued to decline, and he died on the inpatient hospice unit 18 days after admission.
DISCUSSION: Gliomatosis cerebri is a relatively rare clinical entity that is considered a high-grade glioma, and is associated with a very poor prognosis, typically measured in months. It often involves the majority of one brain hemisphere, but may affect both hemispheres, and diagnosis can be made with MRI. It is known that patients with central nervous system malignancies are at risk for developing bleeding disorders, however this is the first known case of a patient with concurrent ITP and gliomatosis cerebri. There is data to support treatment of gliomatosis cerebri with temozolomide and radiation, however high grade thrombocytopenia may occur in patients who receive temozolomide. Clinicians should be aware that gliomatosis cerebri may present with concurrent thrombocytopenia, which may impact treatment considerations.
GOOGLE IT: HYPERAMMONEMIA + ROUX-EN-YRohit Godbole1; Susan Stein2. 1Olive View - UCLA Medical Center, Sylmar, CA; 2Olive View - UCLA Medical Center, Sylmar, CA. (Tracking ID #1938826)
LEARNING OBJECTIVE 1: Diagnose L-carnitine deficiency in a patient with altered mental status by using the internet
CASE: A 58 year old morbidly obese woman was admitted for nausea, vomiting, abdominal pain, and poor oral intake of food. The patient had a history of Roux-en-Y bypass surgery 10 years prior to admission to treat her obesity (BMI of 83). She had been admitted multiple times in the past year for the same chief complaint with diagnoses of chronic relapsing pancreatitis and gastric dysmotility. BMI at this admission was 50. She complained of generalized weakness but otherwise appeared comfortable. After admission, she was awaiting placement of a jejunostomy tube for nutritional support. On hospital day 30, she suddenly became less responsive and the rapid response team was called. Her O2 saturation was 80 %, heart rate was 160 beats per minute, and finger stick glucose was 25 mg/dL. Fifty grams of glucose was administered by IV push and the patient became more responsive but did not return to baseline mental status. She aroused to voice but could not follow any commands. Neurological exam was non-focal other than diffuse muscular weakness. The patient was transferred to the ICU, started on empiric antibiotics for sepsis and heparin drip for a possible pulmonary embolus given a prior history of VTE. Basic chemistry, lactate, liver function tests, TSH, venous blood gases, blood and urine cultures were normal. An ammonia level was sent due to persistent altered mental status and was elevated at 119 μmol/L (ref 9–35 μmol/L). Over the next day, the patient remained altered and an encephalopathy due to metabolic derangement was suspected. Multi-vitamin and thiamine infusions were administered. Lactulose was started given the hyperammonemia but led to no discernible clinical improvement. At this point, work-up for altered mental status (AMS) had included ruling out infections, cerebrovascular events, myocardial infarction, endocrine abnormalities, and common metabolic and toxic insults. Once we had exhausted a number of options for diagnosis, we conducted an internet search using Google as our primary search engine. We entered the keywords “hyperammonemia + Roux-en-Y” into Google search, which revealed a case report with striking similarities to ours: a case of hyperammonemic encephalopathy that was caused by L-carnitine deficiency, as well as several reports of refractory hyperammonemia in Roux-en Y cases resulting in death. As a result of our search, we provided intravenous L-carnitine repletion and our patient’s mental status improved to baseline over the next several days. The total L-carnitine level prior to infusion was 15 μmol/L (ref 25–58 μmol/L) and free L-carnitine level was 6 μmol/L (ref 19–48 μmol/L) while 1 week post-infusion total L-carnitine level was 81 μmol/L and free was 70 μmol/L. The initial ammonia level of 119 μmol/L improved to 66 μmol/L after L-carinitine infusion.
DISCUSSION: After a search for common causes of AMS failed to reveal a specific etiology, we discovered a case report on the internet with similarities that led to the diagnosis. Both the case report patient and our patient had (1) a history of Roux-en-Y gastric bypass several years prior complicated by recurrent pancreatitis, (2) acute onset of altered mental status with diffuse muscular weakness, (3) low carnitine (total and free) level with hyperammonemia, (4) improvement in AMS with L-carnitine intravenous infusion, and (5) improvement in ammonia level with L-carnitine infusion. Primary L-carnitine deficiency is well recognized in pediatric literature however the disorder, primary or secondary, is not commonly described in general internal medicine literature. L-carnitine is involved in the transfer of fatty acids into mitochondria for beta oxidation and deficiency can lead to muscular weakness and encephalopathy as seen in this patient. Our case lends further evidence for secondary L-carinitine deficiency as a cause of hyperammonemic encephalopathy in a patient with prior Roux-en-Y bypass surgery complicated by chronic pancreatitis and poor nutritional status. It is noteworthy that the case report referenced was listed second on the list of search results, making it extraordinarily relevant. A simple Google search likely saved our patient’s life.
GROUP B STREPTOCOCCAL LEAD-ASSOCIATED ENDOCARDITIS IN A POORLY CONTROLLED DIABETICIlya Karagodin; Krutika Kuppalli; Marcie Berger. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1934824)
LEARNING OBJECTIVE 1: To manage and treat the risk factors that predispose patients to Group B Strep endocarditis.
LEARNING OBJECTIVE 2: To recognize the most common complications and sequelae of GBS endocarditis, as well as associated mortality rates.
CASE: Group B Strep (GBS) endocarditis, caused by the bacteria Streptococcus Agalactiae, is a rare infection traditionally thought to be a newborn disease. In recent years, the incidence of GBS endocarditis has been rising, particularly in the elderly and the immunocompromised. Populations at particular risk are patients suffering from diabetes, liver disease, alcoholism, cancer, COPD, urinary tract disease, chronic kidney disease, or HIV infection. The infection typically arises in native valves, and usually causes rapid clinical deterioration and valve destruction. Complications associated with GBS endocarditis include embolic phenomena, cardiac abscesses and fistulas, and heart failure. Mortality due to GBS endocarditis is high, with reported rates of 35–50 %. We report on a case of GBS endocarditis in a 55-year-old African-American male with a history of poorly controlled Type II Diabetes Mellitus, Stage 3 chronic kidney disease, coronary artery disease, ischemic cardiomyopathy (LVEF = 30–34 %), and NYHA Class II heart failure s/p single-chamber AICD placement for primary prevention 7 months prior to presentation. Ten days prior to presentation, the patient underwent surgical amputation of his right fifth toe due to gangrene and suspected osteomyelitis. The patient was subsequently admitted to the hospital for fever and abdominal pain, and found to have acute appendicitis. He underwent laparoscopic appendectomy, and following surgery, was found to have two positive blood cultures for Group B Strep. The patient was started on IV Ceftriaxone. Transesophageal echocardiogram showed a large, mobile cystic structure (2.4 × 1.1 cm) in the right ventricle that appeared to be attached to the right ventricular AICD lead. In addition, there was a small echodensity noted on the AICD wire as it crossed the tricuspid annulus, as well as mild tricuspid regurgitation. The differential included vegetation, abscess, or thrombus. At this point, IV Gentamicin was added to the patient’s regimen. CT chest showed three focal areas of consolidation in the upper lobes of the lungs consistent with septic emboli. Electrophysiology was consulted and proceeded to explant the AICD capsule and extract the AICD lead. Both the capsule and distal lead were sent for culture, and came back negative for GBS. The patient was sent home on IV Ceftriaxone (6-week course) and IV Gentamicin (2-week course) in improved and stable condition.
DISCUSSION: Our patient’s co-morbidities, particularly his poorly controlled diabetes (HbA1C = 10.3) and Stage 3 chronic kidney disease, placed him at high risk for GBS bacteremia. We postulate that the source of our patient’s infection was his diabetic foot ulcer, and that following his right toe amputation, the Streptococcus Agalactiae bacteria spread hematogenously, finding a nidus for infection on the right ventricular AICD lead, leading to GBS endocarditis of the tricuspid valve, and ultimately embolizing to the upper lobes of the patient’s lungs. To the best of our knowledge, this is the first reported case of GBS endocarditis in a patient with an AICD device.
HAND SANITIZER: THE NEW VODKA?Livia Hegerova; John Eaton. Mayo Clinic, Rochester, MN. (Tracking ID #1899672)
LEARNING OBJECTIVE 1: Use of hand sanitizer as an infection control strategy has become ubiquitous amongst health-care workers and the general public. Unfortunately, a new epidemic has emerged of cheap and easily accessible hand sanitizer ingestion, which contains greater than 60 % ethyl alcohol. This dangerous trend of toxic ingestion has recently been reported amongst teenagers in emergency rooms across the nation. Our institution treated multiple cases of hand sanitizer ingestion that required intensive level care and intubation.
CASE: Police brought a 50 year-old woman with past history significant for heavy alcohol use into emergency department after she was found inebriated lying in feces. Blood ETOH level in admission was 353 mg/dL, lactate 4.5 mmol/L, and she had a metabolic acidosis with anion gap of 15. CT head was performed which was negative for acute process. Upon awakening, she admitted to binging on wine prior to the episode. Her systolic blood pressure was in 90s after fluid resuscitation, thus she was transferred to ICU for concern of possible sepsis. Blood and urine cultures were negative, antibiotics were discontinued, and she was transferred back to the general floor service. A few hours after transfer to the medical floor, she was found to be unresponsive with incontinence of bowel and bladder. Her obtundation required intubation and transfer back to the ICU. CT head #2 again showed no acute process. Her spell was thought to be due to ETOH withdrawal seizure. She had no further episodes, was extubated and transferred out of intensive care. The next day, she was unresponsive and hypotensive once again. For the third time she was transported to the ICU and CT head #3 was negative. Interestingly, blood ETOH level was 369 mg/dL, which was curiously higher than her admission ETOH. It was noted that the bottle of instant hand sanitizer in the patient’s room was opened and empty lying near the bed.
DISCUSSION: Alcohol gel hand sanitizer in 70 % ethyl alcohol by volume and also contains isopropyl alcohol, hydroxyethyl urea, isopropyl myrisate, and propylene glycol. It widespread use has been shown to decrease infection rates in health-care settings. However, dispensers should be such that they do not allow removal and bedside ingestion by patients. Ingestion leads to a metabolic acidosis and lactate elevation consistent with acute ethyl alcohol and isopropyl alcohol ingestion. Physicians and public health officials may also consider warning parents of young people to watch for danger signs of over-the-counter cleanser ingestion.
HAPPENED IN MY SLE-EP—LUPUS MYELITISMike Butterfield; Sarah Tribune; Kate Hust. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925923)
LEARNING OBJECTIVE 1: Generate differential diagnosis for symmetric lower extremity weakness.
LEARNING OBJECTIVE 2: Recognize the clinical presentation of transverse myelitis as a classic, though rare, neurologic manifestation of systemic lupus erythematosus.
CASE: A 21-year-old man with a year-long history of rash presented with bilateral leg weakness, first noticed upon waking 3 weeks prior. Its severity was unchanged over time, and the patient was able to ambulate with difficulty. He noted an unintentional 30-lb weight loss over the preceding month. Medical history was otherwise notable for hypertension diagnosed 2 weeks earlier, with initiation of a combination anti-hypertensive medication. On examination, blood pressure was 157/89 mmHg and pulse 103 beats/min. Neurologic examination was significant for proximal leg weakness (3+/5), diffuse hyperreflexia (3+), bilateral upgoing plantar reflexes, and ataxia with heel-toe gait. He had a pink, rectangular patch on his posterior neck, faded patches on his dorsal forearms, and soft, non-tender pretibial nodules. Initial laboratory workup revealed mild pancytopenia and low reticulocyte count. Creatinine was 1.51 mg/dL, and urinalysis revealed hematuria with moderate proteinuria. ESR was 72 mm/h, CRP <0.50 mg/dL, and complement levels were low. T2 MRI of the cervical spine showed hyper-intensities at C1-2 and C5-6 levels. Anti-cardiolipin IgG, ANA and anti-dsDNA were positive, the latter two with high titers.
DISCUSSION: Internists commonly encounter weakness in clinical practice. Having a thorough approach is important to initiate appropriate management. The acute presentation of symmetric lower extremity weakness prompts a broad differential diagnosis, as pathology may be present anywhere from the spinal cord “on down”—the anterior horn, neuromuscular junction, peripheral nerves, or leg musculature. The presence of upper motor neuron signs should greatly assist in focusing the differential on spinal cord disorders. Transverse myelitis (TM), multiple sclerosis (MS), and space-occupying lesions are among the most concerning etiologies. If associated with autonomic symptoms (e.g. bowel or bladder incontinence), such findings should raise concern for cauda equine syndrome. Neuropsychiatric sequelae complicate over 60 % of cases of systemic lupus erythematosus (SLE), and are included among the diagnostic criteria for the disease. Transverse myelitis, an inflammatory disorder of the spinal cord, is a rare but classic manifestation of SLE (1–2 % of cases). Along with more common neurologic complications of lupus such as cerebrovascular disease and seizures, there is a strong association between TM and antiphospholipid antibodies, though their role remains controversial. The typical presentation of TM is an acute onset of motor and sensory deficits below the level of the lesion, sometimes associated with autonomic dysfunction. Though complete lesions occur, partial cord inflammation is more common; motor symptoms may exist in absence of sensory deficits or vice versa. MRI showing high-signal lesions with cord edema, typically on T2 imaging, is diagnostic. Intravenous corticosteroids are given to treat lupus-associated TM acutely, while plasmapheresis may be initiated in refractory cases. Prognosis is variable, with complete recovery occurring in approximately 50 % of patients, partial recovery in 30 %, and no improvement or clinical deterioration in the remaining 20 %.
HBV-ASSOCIATED CRYOGLOBULINEMIA WITH MEMBRANOPROLIFERATIVE GLOMERULONEPHRITISAkane Ryu; Christine Kwan; Yoshinosuke Shimamura; Koichi Hasegawa; Norihito Moniwa; Hideki Takizawa. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1937444)
LEARNING OBJECTIVE 1: Recognize that hepatitis B virus (HBV), not just hepatitis C virus (HCV), can also cause cryoglobulinemia
LEARNING OBJECTIVE 2: Treat mixed cryoglobulinemia (MC) in a multi-step approach based on its pathology
CASE: A 65-year-old Asian woman presents with proteinuria and elevated creatinine (Cr) on labs. She also has associated rash and edema on her bilateral legs ×5 years. She has no other symptoms. The patient’s past medical history includes latent HBV infection and hypertension for which she takes olmesartan, hydrochlorothiazide, and amlodipine. She does not use tobacco, alcohol, or recreational drugs. Her family history is insignificant. On physical exam, the patient’s vital signs include temperature = 37 °C, heart rate = 84, blood pressure = 158/84, respiratory rate = 16, and O2 saturation = 100 % room air. She appears in no acute distress; alert/oriented ×3. Jugular venous pressure = 5cmH2O. Bilateral lower extremities have pitting edema up to knees and multiple scattered 1 ~ 3 mm dark red, round purpura. The rest of the exam shows no irregularities. Abnormal laboratory results include hemoglobin 8.9 g/dL, albumin 2.9 g/dL, Cr 1.6 mg/dL (baseline 0.85 mg/dL), proteinuria (2.74 g/24 h), and hematuria (>100 red blood cells/high power field). Cryoglobulins and rheumatoid factor are positive with hypocomplementemia (C3 0.45 g/L-normal range 0.8–2.14 g/L and C4 0.06 g/L-normal range 0.13–0.6 g/L). Serum kappa:lambda ratio is 5 (normal range 0.26–1.65). HCV-RNA is negative while HBV surface/core/e- antibody are positive but negative HBV surface/e- antigen and viral load. Renal biopsy shows membranoproliferative glomerulonephritis (MG) with hyaline thrombus in the glomerulocapillary, consistent with cryoglobulinemic glomerulonephritis. Skin biopsy of the purpura reveals leukocytoclastic vasculitis. Bone marrow and inguinal lymph node biopsies show B-cell lymphocytic infiltration suggestive of lymphoproliferative disease. According to the results, a diagnosis of MC vasculitis with MG due to HBV infection causing B-cell proliferation is made, and treatment is initiated with methylprednisolone and rituximab. Meanwhile, her HBV load turns positive (<2.1 log copies/mL), and entecavir is started. Her purpura, edema, and proteinuria gradually improve (0.64 g/day), but her renal function does not completely return to baseline. HBV load becomes Undetectable 5 months later.
DISCUSSION: Cryoglobulinemia is a disease characterized by immunoglobulins that are soluble at 37 °C but precipitate in the cold, even in the microvasculature, and usually associated with inflammatory manifestations in the vessel walls. In type I cryoglobulinemia, a monoclonal immunoglobulin exists while in types II and III, called MC, a polyclonal immunoglobulin G (IgG) and an immunoglobulin M (IgM) with rheumatoid factor activity exist, the latter of which is either monoclonal in type II or polyclonal in type III. MC is often associated with HCV infection but less commonly with HBV. Few cases of cryoglobulinemia with HBV infection have been reported, so conventional treatment of HBV-associated cryoglobulinemia is not yet standardized. In this case, based on the pathology of HBV-associated MC, the patient receives multi-step treatment: antiviral therapy for suppressing HBV activation and stopping B-cell proliferation and steroid for controlling MC nephritis.
HEMATEMESIS: MORE THAN MEETS THE EYERobert Mocharla; Natalie Spaccarelli; Michael Janjigian; Douglas Bails. NYU School of Medicine, New York City, NY. (Tracking ID #1938941)
LEARNING OBJECTIVE 1: Recognize deviations from common clinical presentations that may indicate additional or alternate pathology.
LEARNING OBJECTIVE 2: Investigate abnormal diagnostic tests that are not explained by a working diagnosis.
CASE: A 22-year-old woman with no past medical history presented to the emergency department after an episode of hematemesis. One hour after drinking 2 alcoholic beverages, she began to retch and soon vomited non-bloody gastric contents. Minutes later, she vomited frank blood. She denied abdominal discomfort prior to or during the events. She denied using any medications, including non-steroidal anti-inflammatory agents. Her alcohol intake was limited to 1–2 drinks once monthly. She denied a family history of hematologic or gastrointestinal diseases. She reported an identical event 3 months prior that was not preceded by retching. Her initial physical examination was notable for a heart rate of 114 and pallor. The rest of the examination was normal. Laboratory testing revealed a pancytopenia (white blood cells 3,700, hemoglobin 8.6 g/dL, platelets 40,000), decreased total protein of 5.6 g/dL and albumin 3.0 g/dL (otherwise normal liver function tests), elevated INR of 1.49 and aPTT of 41.9 s. Emergent endoscopic evaluation revealed 2 columns of non-bleeding esophageal varices and diffuse petechial hemorrhage throughout the gastric mucosa. Abdominal ultrasound revealed a cirrhotic liver with normal biliary tree and no evidence of portal or splenic venous thrombosis. Additional examination and laboratory testing directed toward causes of cirrhosis revealed brownish rings in the corneal limbus (visible to the naked eye) and a low ceruloplasmin level of 5.9 mg/dL. Ophthalmologic slit-lamp examination confirmed the presence of Kayser-Fleischer rings and sunflower cataracts, establishing the new diagnosis of Wilson’s Disease (also known as Hepatolenticular Degeneration). The patient had no further episodes of hematemesis and was referred for copper chelation treatment.
DISCUSSION: Hematemesis is a common presentation encountered by clinicians. As this clinical entity can be the end result of a myriad of underlying pathology, possible diagnoses included in its differential diagnosis are many. In order to aid in a rapid and accurate diagnosis, clinicians are guided by the clinical context in which the event occurred, known medical history, and epidemiological characteristics. For our patient, experience with otherwise young and healthy individuals would usually dictate more benign causes of hematemesis (i.e. Mallory-Weiss tears, Peptic Ulcer Disease, Gastritis, etc.). However, her clinical presentation and history did not conform purely with what would be expected from these benign conditions. Particularly, she did not report repeated instances of dry retching or non-bloody emesis prior to hematemesis as would be expected with Mallory-Weiss tears. Additionally, she provided no symptoms to suggest a subacute or chronic gastrointestinal illness as may be expected with ulcerative disease or gastritis. Her history of a similar event (and with no preceding retching or non-bloody emesis) also was not easily explained if attributing her disease to a benign condition. Due to these clinical inconsistencies, we found it prudent to broaden our differential to include more chronic and serious pathology. With laboratory data showing pancytopenia and impaired synthetic liver function, we further suspected serious underlying pathology. Once it became evident that our patient exhibited cirrhosis at such a young age, we shifted our differential entirely and eventually arrived at the diagnosis of Wilson’s Disease. Wilson’s Disease, or Hepatolenticular Degeneration, is an exceedingly rare cause of cirrhosis and hematemesis. It is an autosomal recessive disease estimated to affect 30 per 1,000,000 individuals. It is characterized by impaired copper excretion and resultant deposition throughout the body, with a predilection for hepatic and neurologic structures. Patients generally present from age 20–40 with evidence of hepatic damage or dysfunction. Evidence of neuropsychiatric involvement usually manifests later in the course. Although investigation of hematemesis will rarely result in a new diagnosis of Wilson’s Disease, the points illustrated above are applicable to any clinical evaluation. Our patient’s history and laboratory data simply could not easily be grouped and explained by diagnoses normally expected among otherwise healthy patients of her age. A critical component of rapid and accurate diagnosis involves pattern recognition, but it is equally important to recognize deviations from these patterns and investigate them thoroughly. References: 1) Frydman M. Genetic aspects of Wilson’s Disease. J Gastroenterol Hepatol 1990;5:483–490.
HEMOLYTIC ANEMIA IN CHRONIC HEPATITIS C: ROLE OF RIBAVIRIN AND INTERFERONDipenkumar Modi; Hirva Mamdani; Diane L. Levine. Wayne State University, Detroit, MI. (Tracking ID #1939118)
LEARNING OBJECTIVE 1: To recognize ribavirin as one of the causes of anemia in patients receiving therapy for chronic hepatitis C
LEARNING OBJECTIVE 2: To recognize key aspects of managing anemia in patients on treatment for chronic hepatitis C
CASE: A 64 y/o African American woman with past medical history of chronic hepatitis C, and Iatrogenic hypothyroidism secondary to RAI ablation for Graves’ disease was admitted for severe anemia with hemoglobin of 4.8. Patient complained of significant fatigue, weakness and light headedness immediately after getting up from bed over couple of months prior to presentation. She was also feeling chest discomfort, worsening exertional dyspnea and palpitations over 3–4 weeks duration. Vitals showed no fever but marked tachycardia and hypotension. On physical examination, patient was profoundly pale. She had known Hepatitis C, Group 1a genotype, G1/S2 liver disease with fibrospect of 72. She had been on week 40 of Hepatitis C therapy with Ribavirin 1200 mg/day and Pegylated INF 180mcg/week with first 12 weeks of Telaprevir therapy. Laboratory findings showed severe anemia (hemoglobin 4.8 g/dl), normal MCV (90.2FL), normochromia (MCH 29.3 pg), leukopenia (WBC 1.7 K/CUMM), and thrombocytopenia (platelets 107 K/CUMM). Hemolytic work up showed elevated LDH (464Units/l) level, severely reduced haptogobin (<8 mg/dl), but disproportionately low reticulocyte count (1.7 %; 26,900/CUMM). She had negative coombs’ test, normal vitamin B12 and folic acid levels. Iron studies showed elevated Iron (259mcg/dl), ferritin (1750 ng/ml), Iron saturation (87 %) and normal Iron binding capacity (297mcg/dl). Baseline HCV PCR 14,630,419 IU/ml; <43 at 4 weeks, and undetectable at 8, 12, 24 & 36 weeks. Based on above laboratory findings and active Hepatitis C treatment history, diagnosis of anemia secondary to Ribavirin induced hemolysis and Inferferon induced bone marrow suppression was made.
DISCUSSION: Hepatitis C virus (HCV) infection is a major cause of chronic liver disease, leading to cirrhosis, end-stage liver disease, and hepatocellular carcinoma. Combination therapy with Ribavirin (RBV) and Interferon (IFN) is associated with higher rates of sustained virological, biochemical, and histological response compared to IFN monotherapy with improved response rates 42 to 46 % for patients with genotype 1 and 76 to 82 % for patients with genotypes 2 and 3. Hemolytic anemia is a major concern of treatment with Ribavirin. Anemia mainly results from increased RBC turnover with relative ATP deficiency and increased susceptibility to oxidative damage. Ribavirin is predominantly accumulated in Erythrocytes where it is principally phosphorylated by adenosine kinase into Ribavirin phosphates (monophosphate, diphosphate, and triphosphate). Ribavirin phosphates are unable to cross erythrocytes membrane. Overall the resultant effect would be an accumulation of Ribavirin and its active metabolites in erythrocytes which eliminate very slowly from Erythrocytes (half-life 40 days). After accumulation of Active triphosphate metabolites in erythrocytes, deficiency of adenosine triphosphate (ATP) in erythrocytes occurs. The low ATP level might indirectly affect the antioxidant defense mechanisms, by decreasing hexokinase-mediated production of glucose 6-phosphate. Genetic variants leading to ITPA deficiency protect against hemolytic anemia in HCV-infected patients receiving RBV. Interferon alfa contributes to hepatitis C treatment-induced anemia by directly inhibiting erythropoiesis by suppressing the proliferation of erythroid progenitor cells. Because bone marrow suppression caused by interferon prevents an adequate reticulocyte response, a compensatory reticulocytosis is often impaired in response to ribavirin induced hemolysis. The standard-of-care management of ribavirin induced anemia has been dose reduction to 600 mg/d when the hemoglobin level decreases to <10 g/dL. However, if the hemoglobin level remains <10 g/dL after RBV dosage reduction, the administration of EPO should be considered as well as reducing the dosage of pegy interferon to 1.0 mg/kg/week, especially if the reticulocyte counts are low. If RBV is permanently discontinued for management of anemia, then pegy interferon alfa and boceprevir must also be discontinued. Once the hemoglobin level is >10 g/dL, the dosage of RBV should be increased in 200 mg/d steps to a dosage less than the initial dosage of RBV. Once the hemoglobin level is >11 g/dL, the administration of EPO should be discontinued. It is important to recognize ribavirin as one of the causes of anemia in patients receiving therapy for chronic hepatitis C. Absence of brisk reticulocyte response should not preclude the diagnosis of ribavirin induced hemolysis because of co-administration of Interferon-alpha.
HEMOLYTIC ANEMIA IN PREGNANCYRagavi Elangovan. UCR SOM, Riverside, CA. (Tracking ID #1939855)
LEARNING OBJECTIVE 1: Identify high risk complications of paroxysmal nocturnal hemoglobinuria (PNH) and provide appropriate management.
LEARNING OBJECTIVE 2: Recognize clinical situations in which the benefits of eculizumab will outweigh the risks.
CASE: 23 year old female P0G1A0 at 23 weeks gestation presents to ER with headache, right lower extremity weakness and foot drop for 2 days. Platelet count upon presentation was 45. LDH, indirect bilirubin, and reticulocyte count were elevated. Coomb’s test was negative, and peripheral smear was also negative for schistocytes. Blood test for ADAMST13 protease activity was drawn upon admission. Presumptive diagnosis of thrombotic thrombocytopenic purpura (TTP) was made and patient was treated with plasmapheresis and steroids for 5 days. LDH declined but platelet count failed to improve. MRI of the brain revealed dural venous sinus thrombosis. Flow cytometry was done which revealed deficiency in CD 55/59 proteins and diagnosis of paroxysmal nocturnal hemoglobinuria (PNH) was made. ADAMST13 test returned as 95 % normal, therefore plasmapheresis and steroid treatment were discontinued. Patient was vaccinated against meningitis, and started on prophylactic penicillin, enoxaparin, and weekly eculizumab after extensive review of the Class C drug with colleagues and discussion with patient. Patient was followed by hematology and obstetrics for the rest of her pregnancy. She delivered a healthy baby at 38 weeks gestation via C-section. Patient will continue eculizumab and enoxaparin indefinitely.
DISCUSSION: PNH is a rare disease affecting 3000–6000 Americans with an incidence of 1.3 per million each year. Median age of onset is in thirties. PNH is a disorder characterized by an abnormality in PIG-A gene which leads to absence of complement regulatory proteins CD 55 and CD 59, with resulting increased sensitivity of red blood cells to hemolytic action of complement. Diagnosis is made with flow cytometry which reveals missing CD 55 and CD 59 proteins. PNH increases morbidity and mortality of the mother and fetus. Several complications may present in PNH including thrombocytopenia, smooth muscle dystonia, renal insufficiency, bone marrow failure, and thrombotic events. Thrombosis is the leading cause of death in PNH patients and this risk is increased in pregnancy. Anticoagulation with low molecular weight heparin (LMWH) is necessary if history of prior episode of thrombosis is present, if recurrent late fetal losses have occurred, or if PNH clone is >50 %. Treatment with eculizumab for patients with PNH has shown to decrease intravascular hemolysis and thrombotic events. Eculizumab is a monoclonal antibody that binds to C5 and inhibits terminal complement activation. It is made of IgG2 and IgG4 heavy chain sequence. Although IgG2 has minimal transmission, IgG does cross the placenta, and therefore eculizumab is a category C drug. There are no published studies on the use of eculizumab during pregnancy, so the decision to treat a pregnant patient with this drug must be made on a case by case basis. Smooth muscle dystonia, resulting from depletion of nitric oxide from the ongoing hemolysis, may prevent the progression of labor, and only 30 % of women deliver vaginally. However, administration of this drug will decrease smooth muscle dystonia, decrease the risks of premature delivery, and increase the likelihood of a vaginal delivery. Use of Eculizumab in the third trimester for patients with increased risk of thrombotic complications may be a good option. Pregnancy is not recommended for women with PNH given the high risk of adverse outcomes. Pregnant women with PNH should be followed closely by a hematologist as well as an obstetrician.
HEMORRHOIDS AS A CAUSE OF SEVERE TRANSFUSION DEPENDENT IRON DEFICIENCY ANEMIAVenu M. Ganipisetti; Pratyusha Bollimunta; Malav P. Parikh; Harsh V. Gupta; Harvey Friedman. Presence Saint Francis Hospital, Evanston, IL. (Tracking ID #1931908)
LEARNING OBJECTIVE 1: Recognize that Hemorrhoids are a common source of lower GI bleeding; however, hemorrhoids causing bleeding that leads to severe transfusion dependent iron deficiency anemia is quite rare.
LEARNING OBJECTIVE 2: Recognize that other causes for anemia should be thoroughly evaluated before considering treatment for hemorrhoids.
CASE: A 61-year-old Indian female presented to our hospital with a low hemoglobin of 2.1 g/dl. She had an episode of bright red bleeding per rectum about 15 days prior to presentation. She reported a chronic history of anemia for about 12 years requiring several blood transfusions in the past. She had a history of multiple self-limiting rectal bleeding episodes for which she sought medical attention and underwent multiple endoscopic studies. She had multiple colonoscopies, EGDs, and small bowel studies (including capsule endoscopy, push enteroscopy, and Merkel cell scan), which were all negative except for the presence of hemorrhoids. She was advised to undergo surgery for hemorrhoids, which she refused. She had taken ferrous sulfate tablets for a few years, but she stopped taking them as they made her constipated. Other tests including for celiac disease, gynecological disorders and coagulation tests were negative. She had four caesarian sections in the past that were all uneventful, and she denied any family history of bleeding disorders. Over the last few months, she had experienced severe fatigue, exertional chest pain, shortness of breath, and bilateral leg swelling and heaviness. On labs, she had microcytic anemia with a MCV of 57.9 fL and iron studies suggestive of severe iron deficiency anemia with a ferritin level of 3 ng/ml. Upon admission, she was given five units of PRBC transfusion with which her hemoglobin (Hb) improved to 10.5 g/dl. She again complained of an episode of a small amount of bright red bleeding in her stool, and a colonoscopy was performed. The colonoscopy showed Grade 2 hemorrhoids and was negative otherwise. She underwent a hemorrhoidectomy under anesthesia. She was discharged on ferrous sulfate tablets and was asked to continue taking them for at least 1 to 2 years without any interruption. No further bleeding episodes have been reported. The follow-up of hemoglobin at 1 month showed it has remained stable, and our plan is to follow up on hemoglobin monthly for atleast another 5 months.
DISCUSSION: Hemorrhoids are an extremely common source for rectal bleeding. Chronic hemorrhoidal bleeding can lead to iron deficiency anemia; however, massive amounts of bleeding leading to transfusion-dependent, iron deficiency anemia is quite rare. For example, a retrospective analysis done at two medical centers over a period of 15 years showed that the incidence of hemorrhoidal bleeding causing iron deficiency anemia was 0.5 patients per 100,000 population per year, and the mean Hb of the patients who were anemic before treatment in this study was 9.4 (+/− 0.97 SD). (1) It is imperative to exclude other causes before starting treatment for suspected hemorrhoidal bleeding. Only after thorough exclusion should the treatment of hemorrhoids begin. In our patient, a thorough evaluation over a period of at least 6 years did not show any other cause except for hemorrhoids. In these patients, transfusion independence and stable hemoglobin are expected after treatment. It is also important to follow up hemoglobin closely for a few months after treatment, and any further bleeding and/or drop in hemoglobin should be evaluated again. Reference: 1) Kluiber RM, Wolff BG. Evaluation of anemia caused by hemorrhoidal bleeding. Diseases of colon and rectum. 1994 Oct;37(10):1006–7.
HEPATIC SARCOIDOSIS PRESENTING AS CHYLOPERITONEUMBrett K. Sharpe; Atena Lodhi; Michael Schmalz; Kurt J. Pfeifer; Lawrence Ryan; Tessa Damm. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1926911)
LEARNING OBJECTIVE 1: Identify chyloperitoneum as both a presentation and complication of sarcoidosis.
LEARNING OBJECTIVE 2: Describe the diagnosis and management of hepatic sarcoidosis.
CASE: A 38-year-old female of mixed ethnicity with partial empty sella syndrome presented for unintentional weight loss, early satiety, constipation, and abdominal pain. Physical examination was significant only for diffuse abdominal tenderness. Labs were notable for elevated transaminases and alkaline phosphatase. Abdominal ultrasound detected ascites with a partially-occlusive portal venous mass. CT confirmed a soft tissue mass encasing the celiac and mesenteric arteries with extensive retroperitoneal adenopathy. Hepatology and Oncology were consulted for suspected lymphoma, but CT-guided biopsy of a celiac axis lymph node was negative for malignancy. Wedge resection liver biopsy revealed well-formed granulomatous infiltration, multinucleated giant cells, steatosis, and no significant fibrosis. Focal granulomas showed central necrosis without geographic necrosis, caseating necrosis, dysplasia, or malignancy. Stains for acid fast bacilli and fungal organisms were negative, as was workup for common variable immunodeficiency (CVID) and immunoglobulin G4 (IgG4) disease. Serum angiotensin converting enzyme (ACE) levels were normal. One month after initial presentation, the patient returned with profound ascites. Rheumatology was consulted. Paracentesis drained yellow-white opaque fluid with a serum ascites-albumin gradient >1.1, lymphocyte predominance, and no signs of infection. Visualization of the fluid prompted triglyceride analysis confirming chylous ascites. A presumptive diagnosis of hepatic sarcoidosis was made. No other organ systems were found to be symptomatically or radiographically involved to suggest widespread disease. The patient was started on medium chain triglycerides, furosemide, spironolactone, and high-dose prednisone. Liver enzymes, including alkaline phosphatase, normalized over 3 months. Despite aggressive treatment and improvement in biomarkers, serial large-volume paracentesis was required for symptom management.
DISCUSSION: To our knowledge, this is the first reported case of chyloperitoneum as a manifestation of previously undiagnosed sarcoidosis. Epidemiologic data suggests that clinically significant gastrointestinal involvement occurs in less than 0.9 % of all sarcoidosis cases, though subclinical hepatic granulomas are common. While chylothorax is a well documented complication of systemic sarcoidosis, there remains a relative paucity of literature describing chyloperitoneum attributable to this disease. Moreover, this has only been reported in chronic, severe disease. Even more infrequent are cases of isolated hepatic and peritoneal sarcoidosis leading to chylous ascites. Identification of noncaseating granulomas on biopsy remains essential to the diagnosis of sarcoidosis. All other etiologies, including infectious (notably mycobacterium), malignancy, drugs, CVID, and IgG4 related disease should be effectively ruled out prior to making the diagnosis of gastrointestinal sarcoidosis. Corticosteroids endure as a mainstay of treatment for symptomatic gastrointestinal sarcoidosis, with Methotrexate being reserved for those intolerant or unresponsive to steroids.
HEPATIC SUBCAPSULAR BILOMALarry J. McMann1; Sayf Al-tabaqchali1; McKenzie Thompson2; Azzat A. Ali1,2. 1Wayne State University School of Medicine, Rochester, MI; 2American University of the Caribbean School of Medicine, Cupecoy, Saint Martin (French part). (Tracking ID #1936978)
LEARNING OBJECTIVE 1: Recognize and diagnose biloma as a differential diagnosis of abdominal pain after laparoscopic cholecystectomy.
CASE: An 81-year-old male with a history of ischemic cardiomyopathy presented with epigastric pain and was admitted to our Internal Medicine service. He was found to have pancreatitis and had biliary sludge on abdominal ultrasound. He was scheduled for a laparoscopic cholecystectomy soon after resolution of his pancreatitis. The laparoscopic cholecystectomy was uneventful. He returned 7 days post-operatively with worsening right upper quadrant (RUQ) abdominal pain that radiated to his right shoulder. He had no other gastrointestinal or infectious symptoms. His comorbidities included chronic atrial fibrillation and ischemic cardiomyopathy with an implantable cardioverter-defibrillator (ICD). His medications included warfarin. He was afebrile. His physical exam was remarkable for exquisite RUQ tenderness but no guarding or rebound tenderness. Incision site was clean. His labs were notable for a direct bilirubin of 0.9 mg/dL, alkaline phosphatase of 230 u/L, International Normalization Ratio of 1.8 and leukocytosis of 20 thousand/mcL with a left shift. Computed Tomography (CT) of the Abdomen revealed a hepatic subcapsular fluid collection and was subsequently empirically started on ampicillin/sulbactam. Percutaneous drainage of the fluid collection under CT guidance, instantaneously drained 1.7 L with immediate pain relief. Fluid analysis revealed a bilirubin concentration of 20.6 mg/dL confirming the diagnosis of biloma. Fluid cultures had no growth. Attempts at localizing the leak were unsuccessful by endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) was contraindicated due to the presence of the ICD. The percutaneous drain output progressively declined over the course of 4 days indicating spontaneous resolution of the leak. A repeat CT scan showed complete resolution of the biloma. He was discharged home and seen in clinic a week later with no recurrence of symptoms.
DISCUSSION: Biloma is an extra biliary collection of bile. The incidence has become uncommon after the widespread acceptance, use as well as continued improvement in surgical technique in laparoscopy. Some studies suggest the incidence to be as low as 0.3 % to 0.6 %. Bile leakage usually originates from the cystic duct stump due to misplacement of the clips or injury of the common bile duct or accessory duct. Early CT or abdominal ultrasound to determine the extent of the bile leak can help. Standard cholangiographic techniques (ERCP & MRCP) usually cannot fill small bile ducts delineating the leak. Bile leakage may resolve by spontaneous sealing after percutaneous drainage. ERCP is therapeutic by allowing bile to run transpapillary rather than to allow extravasation at the site of the leak. Internists are commonly co-managing surgical complications. Biloma should remain on the broad differential diagnosis of abdominal pain after laparoscopic cholecystectomy. Reference #1: Pavlidis T, Atamatzidis K, Papaziogas B, Galanis I, Koutelidakis I, Papaziogas T. Biloma after laproscopic Cholecystectomy. Annals of Gastroenterology. 2002; 15(2), 178–180. Reference #2: Binmoeller KF, Katon RM, Shneidman R. Endoscopic management of postoperative biliary leaks: review of 77 cases and report of two cases with biloma formation. Am J Gastroenterol. 1991; 86(2):227–231.
HEPATITIS B VIRUS-ASSOCIATED CRYOGLOBULINEMIC NEPHRITISYoshinosuke Shimamura; Hideki Takizawa; Norihito Moniwa; Koichi Hasegawa. Teine Keijinkai Medical Center, Sapporo, Japan. (Tracking ID #1935339)
LEARNING OBJECTIVE 1: Highlights the benefit and efficacy of rituximab in association with antiviral therapy in small vessel vasculitis related to hepatitis B virus- associated cryoglobulinemia.
CASE: A 65-year-old Japanese female with histories of hypertension and chronic hepatitis B infection presents with a three-year of relapsing rash, and a three-month of proteinuria was admitted to hospital for further investigation. She has never smoked or used recreational drugs and only occasionally drinks beer. She has no family history of kidney diseases. On physical examination, blood pressure 158/84, pulse 84, and temperature 37.0° celcius. She had bilateral pitting edema of legs, extending up to her thighs. Raised purpuric lesions were noted on bilateral legs. The reminder of the physical examination, including neurologic examination was not significant. On her labs, significant values include blood urea nitrogen 35.8 mg/dL, and creatinine 1.6 mg/dL; decreased serum complement levels; and positive serum cryoglobulin. Urinalysis with microscopy reveals heme >100/high power field and dysmorphic red blood cells and urinary protein 2.7 g/day. A skin biopsy revealed leukocytoclastic vasculitis. Renal biopsy specimen included 28 glomeruli, one of which showed cellular crescents. Along with the findings of glomerular capillary endotheliosis, mild proliferation of mesangial cells and increase of mesangial matrix, diffuse segmental endocapillary hypercellularity with double contour, and intracapillary hyaline-like deposits were observed. Immunofluorescence staining demonstrated deposits of IgM and C3 in the glomerular basement region. Bone marrow biopsy revealed several lymphoplasmacytic aggregates, which were positive for CD20. Given her diagnosis of cryoglobulinemic vasculitis associated with HBV, she is given weekly rituximabx4 with subsequent oral prednisolone ×2 months with clinical improvement.
DISCUSSION: Mixed cryoglobulinimia (MC), type II and type III, refers to the presence of circulating cryoprecipitable immune complexes in the serum and manifests clinically by a classical triad of purpura, weakness, and arthralgias. In addition, it is associated with hepatitis C virus (HCV) infection and less common with hepatitis B virus infection (HBV). In recent study, efficacy of rituximab, a chimeric monoclonal antibody directed against CD20 antigen, is reported to treat patients that were refractory to conventional antiviral therapy in HCV-MC patients. However, both established treatments and efficacy of rituximab treatment for HBV-MC vasculitis are still unknown. We report here a case of HBV-MC vasculitis associated with lymphoproliferative disease, which was refractory to antiviral therapy but in which rituximab led to a decline in proteinuria and normalize renal function. In this case, we made two important clinical observations. First, rituximab significantly improves MC vasculitis and several clinical and immunologic parameters in patients with HBV-MC who had been resistant to standard immunosuppression therapies. Second, serum free light chain ratio would be a useful maker for response to rituximab therapy. To the best of our knowledge, the present case should be the first to demonstrate the usefulness of serum FLC ratio to monitor response to rituximab therapy in MC. Future controlled, randomized studies are needed to define the drug indications and the cost-efficacy profile in the different systemic features of the disease.
HEPATOCELLULAR CARCINOMA PRESENTING AS AN ACUTE INTRA-ABDOMINAL BLEED: A FATAL PRESENTATIONAbhishek Matta1,3; Abhilash Akinapelli1; Pavan Tandra2; Savio Reddymasu3; Liyan Xu4; Theresa Townley1; Jahnavi Koppala1. 1Creighton University Medical Center, Omaha, NE; 2University of nebraska Medical Center, Omaha, NE; 3Creighton University Medical Center, Omaha, NE; 4Creighton University Medical Center, OMAHA, NE. (Tracking ID #1939192)
LEARNING OBJECTIVE 1: Intra-abdominal hemorrhage should be suspected early in patients with a history of liver cirrhosis who present with acute abdomen and hemodynamic instability and/or drop in hemoglobin.
LEARNING OBJECTIVE 2: Ultrasound abdomen or Contrast enhanced CT of the abdomen can identify intraabdominal bleed as well as a hepatic mass and such patients may benefit from transcatheter arterial embolisation or an emergency surgical intervention.
CASE: A 64 y/o African-American gentleman presented to the emergency room with acute non-radiating lower chest and epigastric pain for 6 h. He had a history of hypertension, hyperlipidemia, type 2 diabetes mellitus and Heptitis C with cirrhosis. Blood pressure was 107/57 mmHg, heart rate 62/min, respiratory rate 18/min and temperature was 98.4oF at presentation. Physical examination revealed mild epigastric tenderness. Laboratory data revealed hemoglobin 11.4 g/dL, WBC 7 × 103/mcL, Platelets 74 × 103/mcL. Liver function tests were normal. Chest Xray was unremarkable. Three hours into the admission, the patient’s abdominal pain suddenly worsened. His systolic blood pressure was 70 mmHg and heart rate was 110/min. Patient was resuscitated with fluids and started on norepinephrine drip. Laboratory data revealed a drop in hemoglobin to 5.6 g/dL. Nasogastric tube revealed no blood. Packed red blood cells transfusion was immediately initiated. He suffered cardiac arrest and passed away on the way to the operating room despite aggressive resuscitation. Autopsy report revealed bleeding into the peritoneal cavity and a 3.5 × 3.0 × 2.5 cm ruptured, poorly circumscribed superficial tumor in the left lobe of the liver. Histopathology confirmed hepatocellular carcinoma (HCC) with well to moderately differentiated cells. The cause of death was determined to be massive hemoperitoneum secondary to ruptured HCC.
DISCUSSION: Hepatocellular Carcinoma (HCC) is the most common primary malignancy of the liver. Liver cancer in men is the fifth most frequently diagnosed cancer worldwide, and is the second leading cause of cancer-related death in the world. The spontaneous rupture of hepatocellular carcinoma occurs in 3–26 % of all HCC cases, is regarded as one of the most life-threatening conditions associated with HCC. The 30-day mortality ranges from 32 to 66.7 %. Various mechanisms have been proposed for spontaneous rupture of HCC including subcapsular localization, portal hypertension and regional increase of venous pressure due to obstruction of the venous outflow by direct tumor invasion, thrombocytopenia, coagulopathy due to altered prothrombin synthesis, trauma and central necrosis due to rapid tumor growth have been implicated in its Pathogenesis. HCC rupture with intra-abdominal bleed presents with acute epigastric or right upper quadrant pain, abdominal distension and signs of hemorrhagic shock. The diagnosis can be challenging in patients who present with rupture as the first manifestation of HCC and some cases may be misdiagnosed as acute appendicitis or perforated peptic ulcer. Laboratory data generally shows an acute drop in hemoglobin. Focussed abdominal sonography for trauma (FAST) can be performed in the emergency room and can aid in the rapid diagnosis of an intraabdominal bleed. CT abdomen can demonstrate the tumor and identify the high density intra-peritoneal free fluid suggestive of bleeding. Multiple options are available including transcatheter arterial embolization (TAE), surgery or a combination of TAE and staged hepatectomy. Surgical management includes hepatic segmentectomy with perihepatic packing, wedge resection with hepatic artery ligation and lobectomy. The consensus is that TAE followed by staged or delayed hepatectomy has the highest survival benefit and should be the procedure of choice. Patients who are poor candidates for surgery or TAE are managed conservatively.
HEPATOCELLULAR CARCINOMA SECONDARY TO METABOLIC SYNDROME: A MORBID ASSOCIATION FOR ALL PRACTITIONERS TO BE CONCERNED ABOUTDovid Moradi; Faraj Faour; Alfred Burger. Beth Israel Medical Center, New York, NY. (Tracking ID #1932163)
LEARNING OBJECTIVE 1: Review the prevalence of hepatocellular carcinoma in the United States
LEARNING OBJECTIVE 2: Discuss the association of hepatocellular carcinoma and metabolic syndrome and recognize an emerging health risk associated with metabolic syndrome
CASE: An 82 year old Greek born female, who had been out of contact with an MD for 15 years but previously diagnosed with hypertension, hyperlipidemia, and obesity (BMI > 30), was admitted after sustaining a slow fall to the ground. Physical exam was significant only for multiple ecchymosis on the right hip and elbows bilaterally. Labs showed a positive urinalysis, a T bili 3.3 mg/dL, alkphos 334 U/L, AST 138 U/L, ALT 102 U/L. A right upper quadrant ultrasound was ordered to evaluate the abnormal liver function tests and revealed multiple masses in the left hepatic lobe. A CT of the abdomen/pelvis confirmed masses extending from left to right hepatic lobes with portal vein occlusion. Testing was negative for hepatitis A, B, and C. INR was 1.1, alpha-Fetoprotein 48800 ng/mL, and CA19-9 77 U/mL. Liver biopsy showed carcinoma with clear cell features, favoring primary hepatocellular carcinoma (HCC) as the diagnosis. The patient was discharged to sub-acute rehab for her physical therapy and followed up as an outpatient with Oncology. It was determined she was not a candidate for chemotherapy due to ongoing poor functional performance; she was then referred to home hospice and passed away 7 weeks after diagnosis. Her initial fall was attributed to a sensitive E. Coli UTI treated with beta-lactam.
DISCUSSION: We present a case of HCC in a patient with non-alcoholic fatty liver disease (NAFLD) and the metabolic syndrome without other traditional high risk factors of HCC. Liver cancer is the fifth most common cancer in the United States and causes the third most cancer related deaths. Recently, Hepatology research has begun focusing on causes of HCC other than viral hepatitis and alcoholic cirrhosis. NAFLD is reported to be associated with up to 27 % of HCC cases in the United States. The prevalence of NAFLD is as high as 30 % in the general population and 90 % of those with morbid obesity (BMI > 40). NAFLD is the direct result of chronic liver damage due to metabolic syndrome. According to the CDC, the prevalence of metabolic syndrome was 34 % in the United States from 2003 to 2006, affecting up to 100 million people. Metabolic Syndrome increases the risk of developing NAFLD 4–11 times. NAFLD increases the risk of developing HCC by 2.8 %. As Internal Medicine practitioners who routinely manage the epidemic of obesity and the metabolic syndrome on a daily basis, we must recognize the emerging and relatively newly described risk factor for HCC. Although screening guidelines have not yet been implemented for this population future efforts should be considered in this high risk population.
HEROIN LIES THE PROBLEMSarah Moore; Catherine Firestein; Kate Hust. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924698)
LEARNING OBJECTIVE 1: Develop a focused differential diagnosis for shortness of breath in patients with recent intranasal heroin use.
LEARNING OBJECTIVE 2: Recognize the clinical presentation of pulmonary edema and understand the treatment of non-cardiogenic pulmonary edema.
CASE: A 49-year-old man with history of asthma presented with acute shortness of breath. He endorsed a daily, non-productive cough with recently increased frequency. The patient had a ten-year history of daily heroin use, and he had snorted a bag of heroin earlier that day. On exam, his temperature was 103° Fahrenheit, heart rate 117 beats per minute, and oxygen saturation 80 % while breathing room air. Pulmonary exam revealed diffuse wheezing with decreased breath sounds in the right lower lobe. Laboratory data was significant for normal brain natriuretic peptide, negative troponin, and white blood cell count of 22,000/μL. Chest radiograph and computed tomography showed right-sided alveolar infiltrates. Initial treatment was for community-acquired pneumonia and an asthma exacerbation. Bi-level non-invasive ventilation was started for respiratory support given his low oxygen saturation and pulmonary edema seen on chest imaging. Over the next 2 days, his symptoms improved, he was weaned from respiratory support, and there was complete radiographic resolution of the pulmonary edema.
DISCUSSION: Internists often encounter shortness of breath; when it is accompanied by fever, hypoxia and infiltrate on chest x-ray, infectious etiologies are generally at the top of the differential. In drug users who snort or smoke the substance, it is important to consider a wide differential. Heroin users are susceptible to aspiration pneumonia, acute lung injury, pneumonitis, and non-cardiogenic pulmonary edema. Cocaine users are at risk for pulmonary alveolar infiltrates, pneumothorax, hypersensitivity pneumonitis, bronchiolitis obliterans and diffuse alveolar damage or hemorrhage. Pulmonary edema generally presents with severe dyspnea, frothy sputum production, and hypoxia. Chest x-ray shows alveolar edema, generally with bilateral peri-hilar infiltrates but may be lobar or unilateral. Echocardiogram and pulmonary capillary wedge pressure help differentiate cardiogenic from non-cardiogenic causes. Most patients require only supportive care for resolution of the pulmonary edema, but they may be treated with intravenous diuretics, non-invasive positive pressure ventilation or intubation as needed. Non-invasive positive pressure ventilation can help prevent carbon dioxide retention and assist oxygenation. Nitrate therapy may be considered if there is associated hypertension and inhaled beta agonists if there is concern for bronchospasm. Non-cardiogenic pulmonary edema is frequently seen in fatal heroin overdoses, and maintaining clinical suspicion for heroin lung is important for close patient monitoring. The key to establishing this diagnosis is rapid improvement in symptoms and resolution of infiltrate on chest x-ray, usually within hours to a few days. Further investigation into management of heroin-induced pulmonary edema would help physicians better treat heroin overdose and hopefully prevent future deaths. It is important for internists to consider the pulmonary complications of illicit substances as drug use remains prevalent in the community.
HIDA SCAN AS AN IMPORTANT TOOL FOR DIAGNOSIS OF BILIARY DUCTAL OBSTRUCTION IN THE PRESENCE OF A NORMAL ULTRASOUNDKaiming Wu; Esther Hwang; Anthony A. Donato. Reading Hospital, West Reading, PA. (Tracking ID #1926870)
LEARNING OBJECTIVE 1: Describe the utility of various imaging modalities in the early diagnosis of choledocholithiasis
CASE: The patient is a 25 year old woman with no significant past medical history who presented with complaint of several episodes right upper quadrant abdominal pain over the prior 2 days which had resolved at the time of her admission. On exam, her abdomen was soft and non-tender with no fever or jaundice. She had no elevation in white blood cell count but was found to have elevated transaminases with AST 601 mg/dl (normal: 10–38 mg/dl) and ALT 602 mg/dl (normal:10–40 mg/dl) and elevated total bilirubin of 3.2 mg/dl (normal: 0.4–1.4 mg/dl) with a normal alkaline phosphatase of 107 units. A right upper quadrant ultrasound showed the presence of gallstones within the gallbladder without evidence of cholecystitis and with a non-distended common bile duct (5 mm). Following admission, a surgical consultant ordered a hepatobiliary iminodiacetic acid (HIDA) scan, which showed non-visualization of both the gallbladder and the common bile duct at 1, 2, and 4 h, indicating an obstruction in the common bile duct. She subsequently underwent an ERCP, which retrieved multiple stone fragments and pus from the common bile duct. On day 3, she underwent a laparoscopic cholecystectomy. She tolerated both procedures well and has been asymptomatic on follow-up after discharge.
DISCUSSION: Acute biliary ductal obstruction is potentially life-threatening when choledocholithiasis results in ascending cholangitis and is thus important for the internist to diagnose accurately. In patients with symptoms and laboratory findings suggestive of biliary ductal obstruction, the initial imaging study of choice is a right upper quadrant ultrasound, which can often be diagnostic. However, the sensitivity of ultrasound for detecting choledocholithiasis in the presence of non-dilated ducts is only 50 %. Many cases of early obstruction may be missed with ultrasound alone, since normal bile duct size may be age dependent, and retained stones are found in 9.6 % of ducts 0–4 mm in width. HIDA scan is most frequently used after an inconclusive right upper quadrant ultrasound for the diagnosis of acute cholecystitis. However, HIDA also presents a more sensitive and specific means of diagnosis of early common bile duct obstruction in the face of clinical and laboratory signs of obstruction but a normal right upper quadrant ultrasound.
HIDDEN IN PLAIN SIGHTDevika Nair; Deepa Bhatnagar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924986)
LEARNING OBJECTIVE 1: Understand the clinical presentation and management of a rectus sheath hematoma
LEARNING OBJECTIVE 2: Know when to suspect rectus sheath hematomas in a patient with a declining hematocrit
CASE: A 65-year-old woman was discovered to have a hemoglobin drop from 9.1 g/dL to 7.2 g/dL in 24 h while in the intensive care unit. She was being cared for after suffering a myocardial infarction. Her course was complicated by new-onset atrial fibrillation, resulting in a prolonged ICU stay. Her medications included prednisone for Graves-disease related opthalomopathy, clopidogrel, aspirin, and subcutaneous enoxaparin for deep venous thrombosis prophylaxis. Vital signs were as follows: temperature 98 F, heart rate 90 beats/min, blood pressure 132/90 mmHg, and respirations of 20/min with stable oxygen saturations. Exam revealed a palpable mass in the left lower quadrant that did not cross the midline as well as increased pain when the patient tensed her abdominal muscles. She had no visible areas of ecchymoses on her abdomen. Computed tomography of the abdomen and pelvis without contrast revealed heterogenous material in the patient’s pelvis consistent with blood products, as well as an inferior left abdominal rectus sheath hematoma. Using Doppler ultrasonography, it was determined that the source of the bleed was the patient’s inferior epigastric vein, which had been lacerated during a subcutaneous injection of enoxaparin. She was given transfusions of blood products, and external compression of the vessel was achieved using a bandage secured over her abdomen. Fortunately, her hemoglobin remained stable for the remainder of her hospital course.
DISCUSSION: Rectus sheath hematomas are an often-misdiagnosed cause of blood loss in the intensive care unit. The hematoma occurs when blood accumulates within the rectus abdominis sheath due to bleeding from lacerated inferior or superior epigastric vessels. Risk factors include subcutaneous injections, age, female sex, critical illness, previous paracentesis, and weakened connective tissue from chronic corticosteroid therapy. A study of 1257 patients admitted to the ICU at the Mayo Clinic in Jacksonville, FL revealed that 1.8 % had a previously misdiagnosed rectus sheath hematoma. Recent case reports suggest that with the increased use of anticoagulant therapy, these hematomas are becoming even more common. Fothergill’s sign and Carnett’s sign are physical exam findings useful in diagnosing rectus sheath hematomas. Fothergill’s sign is positive when the patient has a mass that does not cross the midline and remains palpable when the rectus muscles are tensed. Carnett’s sign occurs when a patient’s abdominal pain is worsened by contraction of the rectus muscles. Both of these maneuvers help differentiate rectus sheath hematomas from intraabdominal pathologies. Currently, no definitive treatment guidelines exist. Typically, the hematomas are self-limiting, as the bleeding tamponades itself. Strategies consist of using external compression, embolization of the bleeding vessel, or surgical evacuation. Surgery has the potential hazard of worsening the hematoma due to reversing the naturally-occurring intra-abdominal tamponade. Patients should be evaluated on a case-by-case basis, and physicians should take comorbidities into account before proceeding with treatment. This case illustrates the importance of including rectus sheath hematomas on the differential for abdominal pain in critically-ill patients.
HIDING THE CROWN: CROWNED DENS SYNDROME MIMICKING ASEPTIC MENINGITIS IN AN ELDERLY WOMANAkane Ryu; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1898238)
LEARNING OBJECTIVE 1: Recognize that another cause of neck pain, headache, and fever in the elderly can be from crowned dens syndrome (CDS)
LEARNING OBJECTIVE 2: Appreciate the usefulness of a cervical computed tomography (CT) scan in diagnosing CDS
CASE: An 86-year-old Asian woman with a significant past medical history of hypertension and osteoarthritis presented with 1 day’s history of acute-onset neck pain associated with headache. She described the posterior neck pain as constant throbbing, rated 10/10, non-radiating, not improved by anything, and worsened by movement. She reported a slightly higher temperature of 37.4 °C, but no other constitutional, neurologic, or rheumatologic symptoms. No sick contacts, visual changes, jaw claudication, or trauma. She did not have any medications, allergies, tobacco, alcohol, or recreational drug use; her family history was insignificant. On physical exam, the patient’s vital signs included temperature = 37.4 °C, heart rate = 85 bpm, blood pressure = 150/80, respiratory rate = 16, and O2 sat = 99 % room air. She appeared in no acute distress and alert/oriented ×3. Head and neck exam was significant for stiff neck, decreased active and passive range of motion (rotation, flexion, and extension), and tenderness to palpation over the cervical vertebrae. Neurological exam showed intact CN II-XII, intact sensation to touch and pain, motor strength 5/5 in all extremities, negative Kernig/Brudzinski signs, and 2+ reflexes. The rest of her exam showed no abnormalities. On labs, the patient’s complete blood count and chemistry panel showed no abnormalities except for slightly elevated white blood cell count (WBC = 10,770/μl) and elevation of C-reactive protein (CRP) (22 mg/dL). Cerebrospinal fluid (CSF) exam was within normal limits as was the cervical X-ray, head CT scan, and head magnetic resonance imaging. CDS was then suspected, so a cervical plain CT scan was done which revealed curvilinear calcifications of the transverse ligament of the atlas and crown-shaped calcium deposits surrounding the odontoid process. She was thus prescribed a nonsteroidal anti-inflammatory (naproxen 300 mg Qday) with relief of her symptoms within 1 week and normalized CRP.
DISCUSSION: Some typical causes of neck pain with possible fever and headache include meningitis, spondylitis, and polymyalgia rheumatica. While the above patient has acute onset of symptoms like in meningitis, she does not have altered mental status, and her CSF is normal. In addition, her time course is inconsistent with typical spondylitis and polymyalgia rheumatica. Crowned dens syndrome is characterized by acute neck pain in the elderly, especially women, and usually presents with radiodense deposits of hydroxyapatite or calcium pyrophosphate dihydrate in ligaments around the odontoid process, which create the appearance of a crown or halo surrounding the odontoid process on radiographic imaging. Evidence of inflammation, such as high CRP, is typical, as is a history of osteoarthritis. A short course of nonsteroidal anti-inflammatory medication usually completely alleviates symptoms. Given this woman’s presentation, therefore, in patients complaining of neck pain, headache, and fever, but with a low likelihood of meningitis or rheumatologic diseases, recognize that CDS can also present with a similar picture, and use a cervical CT scan for diagnosis.
HOLD ON STILL! THINK BEFORE ACTINGJae Yoon Park1; Louis Letendre2. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN. (Tracking ID #1936865)
LEARNING OBJECTIVE 1: Recognize the clinical features of adult onset Still’s disease
CASE: A 24-year-old woman with no significant medical history presented for evaluation of several weeks history of joint pains involving her wrists, ankles, and knees associated with daily fevers and evanescent rash. The symptoms began after an upper respiratory syndrome associated with sore throat, treated with empiric antibiotics. Initial conservative therapy with non-steroidal anti-inflammatory drugs had no benefit. With continued fevers and joint pain, she was admitted at outside institution and was found to have acute kidney injury, with biopsies suggestive of acute tubular necrosis. She was transferred to our institution for further care. On admission, physical exam demonstrated left axillary lymphadenopathy, an irregular erythematous patch on bilateral forearms, lacy reticular erythematous macules on abdomen, and no hepatosplenomegaly. Initial laboratory tests were remarkable for microcytic anemia, thrombocytopenia, mildly elevated transaminases [alkaline phosphatase 215 U/L (normal 37–98 U/L), aspartate and alanine aminotransferase 371 U/L and 561 U/L respectively (normal 7–45 U/L)], lactate dehydrogenase 1232 U/L (normal 122–222 U/L), C-reactive protein of 34 mg/L (normal <8 mg/dL), fibrinogen of 150 mg/dL (normal 200–430 mg/dL), triglyceride of 314 mg/dL (normal <150 mg/dL), and hyperferritinemia to 40,000 mcg/L (normal 11–307 mcg/L). Infectious work-up including blood cultures and serologic tests were unremarkable. Autoimmune panel was negative. Given concern for hemophagocytic lymphohistiocytosis, she underwent bone marrow biopsy which demonstrated a hypocellular marrow with histiocytic infiltrates and hemophagocytosis. To further evaluate the left axillary lymphadenopathy, subsequent PET scan demonstrated hypermetabolic left neck and left axillary lymphadenopathy with mild uptake in several other lymph nodes. Subsequent left axillary lymph node biopsy was negative for evidence of lymphoma. As evaluations for infectious, neoplastic, and autoimmune disorders were unremarkable, her constellation of symptoms in setting of laboratory and pathology findings were felt to reflect adult onset Still’s disease with a component of macrophage activation syndrome. She was initiated on glucocorticoids with improvements in her symptoms and was eventually started on methotrexate. At 6 month follow-up, her symptoms resolved with normalization of her blood counts, inflammatory markers and ferritin levels.
DISCUSSION: This demonstrates a rare case of adult onset Still’s disease. In the setting of non-specific signs and symptoms, the differential must remain broad before reaching a final diagnosis and initiation of treatment. Still’s disease is a rare multisystem inflammatory disorder characterized by daily fevers, evanescent rash, and arthritis. Yamaguchi criteria can be used after excluding infectious, neoplastic and autoimmune disorders. The initial treatment of choice in those with moderate or severe disease is glucocorticoids. Thus, in the appropriate clinical context of fevers, rash, and arthritis accompanied by supportive laboratory and clinical findings, Still’s disease should be in the differential diagnoses.
HOLES IN THE TRACKS OF MY HEART: NEW ATRIOVENTRICULAR BLOCK AND PERIVALVULAR ABSCESSMerrill H. Stewart. Tulane University School of Medicine, New Orleans, LA. (Tracking ID #1940172)
LEARNING OBJECTIVE 1: Know the differential for new atrioventricular heart block
LEARNING OBJECTIVE 2: Understand the significance of a perivalvular aortic abscesses
CASE: A 56 year-old man was post-operative day 2 from a toe amputation secondary to gangrene when he began to develop new bradycardia with a heart rate to 35 beats per minute. He reported no chest pain, no shortness of breath, no pre-syncope, and no new symptoms since his surgery. He initially presented 2 days prior with a fever, diagnosed with gangrene, and treated with intravenous clindamycin for the past 72 h in addition to the toe amputation. On exam he was found to be afebrile with a blood pressure of 101/55 mmHg. His heart rate was 47 beats per minute, irregular, without any murmur or rub. Electrocardiogram initially showed a new secondary degree (Mobitz I) atrioventricular block, and 1 h later a complete atrioventricular block. Troponin was 3.480 ng/mL, and left heart catheterization showed known prior diffuse disease with one discrete lesion eligible for percutaneous trans-luminal coronary angioplasty in the saphenous venous graft to his right coronary artery. Transesophageal Echocardiography revealed several aortic valve vegetations with an aortic valve abscess and likely perforation into the right atrium. He was treated with continuous antibiotics and his heart block improved to a first-degree atrioventricular block after 5 days. A final determination as to his surgical candidacy was pending at the time of this writing.
DISCUSSION: While almost half of atrioventicular heart block cases are simply age-related fibrosis of the conduction system, there are many other etiologies on the differential that the internal medicine physician must always consider. The second leading cause is ischemic, with 20 % of post-myocardial infarction patients developing a heart block. However any cause of cardiomyopathy or myocardial irritation/infiltration can also lead to a heart block. These include hypertrophic cardiomyopathy, rheumatic fever, lyme disease, sarcoidosis, amyloidosis, lupus, viral myocarditis, and bacterial endocarditis as we see in our patient. The etiology of our patient’s new heart block was either from direct abscess infiltration into the conduction system, or embolic vegetation into the coronary vasculature causing an ischemic event. Less common causes include familial heart block, hyperkalemia, thyroid dysfunction, neonatal lupus, hematologic malignancies, dematomyositis, Paget’s disease, and cardiac tumors. Perivalvular abscesses in bacterial endocarditis are relatively common, seen in approximately 30–40 % of cases. They are more often seen with prosthetic valves over native valves, and 20 % present with atrioventricular block versus 2 % in those without an abscess. Development of a new atrioventricular block with known endocarditis is 97 % specific for an abscess, and trans-esophageal echocardiography detects 80–90 % of all abscesses. Detection of perivavluar abscess is important in this population as 70 % end of requiring surgical intervention for persistent infection or heart failure versus 30 % in bacterial endocarditis without an abscess. Earlier detection can lead to sooner stratification and closer monitoring and is important to rule out when making the diagnosis of endocarditis.
HOW DEEP SHOULD YOUR FUNDOSCOPIC EXAM GO? A RARE CASE OF ENDOGENOUS ENDOPHTHALMITIS DUE TO KLEBSIELLA PNEUMONIAEGargi Bajpayee; Jonathan Martin; Isabel Preeshagul; Jason Filopei; David Chun; Jose A. Cortes. Beth Israel Medical Center of Mount Sinai, New York, NY. (Tracking ID #1939482)
LEARNING OBJECTIVE 1: Recognize the difference between exogenous and endogenous endophthalmitis as well as its associated predisposing risk factors.
LEARNING OBJECTIVE 2: Understand that endogenous endophthalmitis is a medical emergency that requires prompt diagnosis and immediate treatment in order to prevent devastating outcomes.
CASE: A 60-year-old Japanese man with DM type II presented to the emergency department for left eye blindness. One day prior, he experienced fevers, chills, and flashes of light in his left eye that rapidly progressed to complete eye blindness. He denied any additional symptoms. On physical exam, his right eye was without deficits, while his left eye had extensive erythema, lacrimation, and zero visual acuity. The remainder of his physical exam was normal. Initial laboratory testing was unremarkable, including normal CBC, BMP, and liver enzymes. Fundoscopic exam exhibited dense vitritis and slit-lamp exam showed extensive inflammation of the anterior chamber and vitreous humor. A CT with IV contrast of the orbit revealed uveoscleral inflammation consistent with left eye endophthalmitis. He was promptly given intravitreous antibiotics and steroids. With no history of ocular trauma or surgery, an endogenous infection was suspected, and a CT abdomen and pelvis revealed a 3.5 cm hepatic abscess. The patient was started on systemic antibiotics with Vancomycin, Cefepime, and Metronidazole to cover the most common intra-abdominal and intra-ocular pathogens. Percutaneous drainage of the abscess was performed and cultures revealed pan-sensitive K. Pneumoniae. In an attempt to restore visual function, the patient underwent left eye vitrectomy. Vitreous cultures also grew K. Pneumoniae, confirming the liver abscess as the primary source for the patient’s endophthalmitis. Following the surgery, the patient completed a 4 week course of intravenous ceftriaxone and oral steroids. After this therapy, the patient regained light perception in his eye.
DISCUSSION: The majority of endophthalmitis cases are acquired infections from exogenous sources secondary to ocular trauma or surgery. Endogenous endophthalmitis, however, is exceedingly rare. We performed a literature search and found a single center retrospective chart review spanning 10 years that identified 28 cases of endogenous endophthalmitis. In the United States, patients with endogenous endophthalmitis usually have primary endocarditis caused by S. pneumoniae or S. aureus. In contrast, in Asia, 60 % of endogenous cases occur from a liver abscess growing K. Pneumoniae, predominantly found in patients with DM type II. The standard therapy for endogenous endophthalmitis includes intravitreous and systemic antibiotics as well as vitrectomy. Although the effectiveness of vitrectomy is controversial, this aggressive procedure is utilized in most cases of severe vision loss. Fortunately for our patient, vitrectomy resulted in regaining light perception in the affected eye. Our case highlights the need to suspect and recognize the common causes of endogenous endophthalmitis. The cause of endogenous endophthalmitis is greatly dependent on whom you are treating. Given the large non-continental US population many internists may care for, it is important to understand that a sub-acute liver abscess is a prevalent source in Asian patients with DM type II. This information can help minimize the diagnostic work-up entailed in identifying a source resulting in lower cost and prompt therapy thus preventing the catastrophic sequela of blindness.
HOW MANY LICKS DOES IT TAKE? AN UNUSUAL CASE OF BACTEREMIAAndrew Ip; Abeer Memon; Robin Klein; Neil Winawer. Emory University, Atlanta, GA. (Tracking ID #1927795)
LEARNING OBJECTIVE 1: Recognize the presentation of Pasteurella multocida infections.
LEARNING OBJECTIVE 2: Appreciate the link between pet contact and Pasteurella infections.
CASE: A 53 year old African-American Male presents with bilateral leg pain. The patient reported pain and redness that had started around his knees and spread to his ankles bilaterally. The pain increased to the point where he was unable to ambulate. Past medical history was notable for stage 4 chronic kidney disease, diastolic heart failure and diabetes mellitus. He was recently admitted 10 days prior for generalized anasarca that resulted in bilateral ulcers of the anterior legs. This improved on discharge with local wound care and diuresis. Review of systems was unremarkable and he denied any recent travel, bug bites, or animal bites. Exam revealed tachycardia but no fever. Lower extremities were edematous with pitting to his thighs. His anterior calves were warm and tender with erythema. There was no evidence of joint swelling. Two healed ulcers were noted on both his legs anteriorly with mild overlying erythema but no discharge. Laboratory work revealed a WBC of 14.4 with 88 % neutrophils. The patient was treated for cellulitis with vancomycin. Blood cultures grew Pasteurella multocida. Antibiotic coverage was changed to ceftriaxone. On further questioning, our patient stated that despite not suffering any animal bites, he acknowledged that his two dogs did frequently lick his legs prior to the development of his pain. Repeat cultures were negative. The patient’s lower extremity pain was slow to resolve but imaging of lower extremities only revealed soft tissue swelling. Patient was discharged after 2 weeks of ceftriaxone.
DISCUSSION: Pasteurella Multocida is a gram negative coccobacilli commonly found in the oral cavity of healthy cats and dogs. It is best known for its association with cat and dog bites. Pasteurella infections most commonly present with skin or soft tissue involvement at the site of contact. Other clinical manifestations include upper respiratory infections, pneumonia, septic arthritis, osteomyelitis, and less commonly bacteremia. Complications due to inadequate treatment include tenosynovitis, osteomyelitis, and septic arthritis. There are multiple reported cases of infections following bites and scratches. Less common are reports of infection from contact through licking. Our patient had bilateral lower extremity cellulitis corresponding to areas where his dogs licked. In addition, the patient was found to be bacteremic with Pasteurella, which occurs in about 15 % of infections. Risk factors for this are multiple co-morbidities or underlying immune-compromise. In this case, our patient had both chronic kidney disease and diabetes mellitus. Pasteurella infections are very receptive to empiric therapy directed either towards a specific infection or in the setting of an animal bite. Second or third generation cephalosporin is recommended due to resistance of Pasteurella Multocida to first generation cephalosporins. Duration of therapy should be individualized, as treatment response may vary. This case highlights the importance of obtaining a complete social history including exposure to pet bites or saliva when presented with a case of cellulitis. Prompt recognition allows a clinician to effectively manage the complications of dog bites, or in our case, a dog lick.
HOW TO PREVENT MYOCARDIAL INFARCTION WITH VITAMIN SUPPLEMENTSNadia El Hangouche; Samian Sulaiman; Muhammad Akbar. Presence Saint Francis Hospital, Evanston, IL. (Tracking ID #1932360)
LEARNING OBJECTIVE 1: Coronary artery disease is affecting young population increasingly. Physician should always keep the possibility of acute coronary syndrom among the differential for young patient presenting with chest pain
LEARNING OBJECTIVE 2: In case of acute coronary syndrom occuring in a young patient, physician should consider screening for uncommon risk factors including vitamin B12 deficiency.
CASE: A 30 y old male presented to the emergency department for chest pain. He had a vague history of vitamin deficiency and active smoking for the past 5 years. Chest pain was described as mild squeezing in the left precordial area that started 4 days ago, it lasts couple of minutes, occures at rest, sometimes trigerred by eating or smoking, and resolves spontaneously after 3 to 5 min. Physical exam at presentation was unremakable and vitals were stable. On the ECG, there was T waves inversion and ST depression in apico lateral leads, that improved after resolution of the chest pain. Cardiac monitor showed multiple premature ventricular complexes. Troponin was borderline elevated : 0.14 at presentation up to 0.19 at 4 h (threshold of positivity : 0.08 ng/mL). A CT angiogram ruled out aortic dissection, pulmonary embolism or pneumothrax. Urine toxicology was negative. Patient was diagnosed with NSTEMI, recieved aspirin and was schedueled for a cath the day after. The angiogram revealed subtotal ostial LAD occulsion with a thrombus, possibly due to ulcerated plaque. Patient had a successful thrombectomy that left residual stenosis less than 40 %. Due to proximity of LAD stenosis to left main, patient was treated medically with integrillin, plavix, asprin and the plan was to obtain stress test in 4 weeks later to evaluate hemodynamic significance of this lesion and if needed consider high risk PCI or single vessel CABG. Patient was pain free. The work up revealed low vitamin B12 88 pg/mL (normal range 211–946 pg/mL), high homocystein level at 40 Umol/L (3.7–13.9 Umol/L), and positive antiphospholipid anbibody. Patient was started on coumadin and vitamin B12 supplements. On day 3 after the PCI, he had a severe typical chest pain. The ECG showed ST elevation with Pardee wave in anterior leads. Patient was taken to the cath lab stat and the angiogram revealed subtotal LAD occlusion that was treated with a Drug eluting stent. The recovery was uneventhfull.
DISCUSSION: Early onset CAD is increasing in frequency. Classical risk factors (age, sex, tabacco, hyperlipidemia, HTN, Diabetes) are well known, but physician need to keep in mind the possibility of advanced CAD in young population that is related to other less frequent risk factors, as in our patient. Our patient was 30 yo and yet he had a STEMI that is now considered related to his vitamin b12 deficiency and hyperhomocysteinemia. The initial workup was more directed toward PE or aortic dissection due to the low likelyhood of CAD in young patients. Later on, when he was diagnosed with ACS, his vitamin deficiency wasn’t worked up. It is only after the cath showed thombosis of the LAD that the connection with hyperhomocysteinemia and the ACS was made. The history of vitamin deficiency was initially “neglected” as his CBC was completely normal, with no neurological signs but retrospectively it appeared very relevant to the motif of presentation. He also had a positive antipholpholipid antibody, but this later is more known to cause venous thrombosis, and the connection with arterial thrombosis is less well established.
HYPERKALEMIA BY A MINOR LEAGUESoohwan Chun1; Manuela Calvo1,2. 1Montefiore medical center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1940101)
LEARNING OBJECTIVE 1: Recognize propranolol as a potential precipitator of hyperkalemia
LEARNING OBJECTIVE 2: Recognize role for an alternative non-selective beta-blocker, that is less associated with hyperkalemia
CASE: A 70 year-old woman presented with asymptomatic hyperkalemia. Her past medical history was significant for type 2 diabetes and liver cirrhosis, secondary to chronic hepatitis C. She reported taking the same dosage of furosemide and spironolactone for many years. There was no recent change in her diet or in the dosage of insulin. Her vital signs were within normal limits and her physical exam was unremarkable. The serum potassium was 6.4 meq/L and glucose was 360 mg/dL. Creatinine and hemoglobin were both at baseline, and creatine phosphokinase was 50 mcg/L. Venous pH was 7.29 [7.32–7.42]. Electrocardiogram was unremarkable. On further questioning, patient revealed that, several days ago, she started taking a new medication, propranolol, prescribed by her gastroenterologist for portal hypertension. The patient was treated with insulin and kayexalte; propranolol was discontinued. Hyperkalemia was corrected and did not recur.
DISCUSSION: Hyperkalemia is a common and probably one of the most worried electrolyte derangement, encountered by an internist. In most cases, the cause of hyperkalemia is readily identifiable (i.e., use of diuretics, or renal failure). However, in a less clear situation, it is important to approach systematically. One method is to think of causes that would lead to either increase in introduction, or decrease in removal of potassium to and from serum. Potassium is consumed from diet and stored mainly in cells. Two main ways of increasing introduction of potassium to serum are increase in consumption from diet and increase in movement of potassium out of the cells. Lysis of cells, such as in hemolysis or rhabdomyolysis, is one simple mechanism of introducing intracellular potassium to serum. Potassium ion shifts from cells to serum, in exchange for a hydrogen ion. Thus, acidemia is another way of pooling potassium from an intracellular source. Potassium is primarily removed by kidney, more specifically by principal cells in collecting tubules, mediated by renin-angiotensin-andosterone system. Problems with the hormone and the principal cells, or even a simple decrease in glomerular filtration will lead to reduction in removal of potassium. Beta-2-adrenergic receptors are present ubiquitously in many cells and their stimulation leads to uptake of potassium from serum. Thus, beta-2-receptor blockade, such as in use of a non-selective beta blocker, leads to small rise in serum potassium, that is often clinically insignificant. However, in presence of other factors that can contribute to rise in serum potassium, use of non-selective beta blocker can precipitate acute hyperkalemia, that can be potentially life-threatening. Both propranolol and nadolol, the two most commonly used non-selective beta-blockers in portal hypertension, have been associated with hyperkalemia. Use of non-selective beta blocker can precipitate hyperkalemia, especially when renal excretion of potassium is impaired, as in our patient with concurrent use of spironolactone, a potassium-sparing diuretic. A general approach is to remove the precipitating factors; however, in many cases, both the beta-blocker and the diuretic are equally important for treatment. Thus, it is necessary to look for a different non-selective beta-blocker, that is less associated with hyperkalemia. Carvedilol seems to be an example of such medication, because of its additional alpha-1 blockade. Inhibiting alpha-1 receptors not only produces smooth muscle relaxation, but also reduces potassium release from liver. Thus, carvedilol is a potential alternative in patients with hyperkalemia, induced by propranolol or nadolol.
HYPEROSMOLAR ANION GAP METABOLIC ACIDOSIS CAUSED BY MOUTHWASHDebjit Saha1; Seth Gottlieb2. 1Mount Sinai Medical Center, Miami Beach, FL; 2Mount Sinai Medical Center, Miami Beach, FL. (Tracking ID #1939579)
LEARNING OBJECTIVE 1: Identification of an osmolar gap associated with an anion gap is helpful in recognizing fatal intoxications with ethylene glycol or methanol ingestion. Consideration of other unusual etiologies is a crucial step to recognize and manage this deadly metabolic disorder effectively.
LEARNING OBJECTIVE 2: Due to the high ethanol content (21 %) and easy accessibility, mouthwashes can be abused by chronic alcoholics, especially those from a low socio-economic background. Though there are no specific antidotes available for the phenolic compounds in mouthwash (thymol, eucalyptol, and menthol), detailed clinical history, high index of suspicion and identification of the osmolar gap with an AG acidosis can be helpful in identifying this atypical presentation.
CASE: A 35-year old man with a history of alcohol abuse and pancreatitis presented with hematemesis and confusion. He had been binge drinking for a week and upon exhausting his alcohol stocks, he ingested “Listerine”. He complained of several episodes of bilious emesis and hematemesis with right upper quadrant pain and generalized abdominal discomfort. Physical exam was unremarkable except for dry mucous membranes and generalized abdominal tenderness. He had no focal neurological deficits. Initial lab work-up showed leukocytosis (21,000), thrombocytopenia (106,000), hyponatremia (122), hypokalemia (2.2), hypochloremia (56) with increased BUN (106) and creatinine (4.85). Arterial blood gas revealed pH of 7.59 and HCO3 of 40. Serum alcohol was 49 and urine was negative for toxic-screen and crystals. Lactic acid and beta-hydroxybutyrate were normal. Abdominal US and head CT were normal. He was admitted to the ICU where he received normal saline and pantoprazole infusion. Subsequently, hemodialysis was initiated for severe mixed acid base disorder with acute kidney injury. Serum ethylene glycol and methanol levels were drawn due to the high suspicion of toxicity and empiric Fomepizole was started, but the results came back negative. With supportive treatment and hemodialysis, the electrolyte imbalance corrected and his acidosis resolved.
DISCUSSION: The patient presented with an AG (26). Calculated ΔAG was 14 (26–12 = 14). The measured HCO3 (40) was more than the corrected HCO3 (24–14 = 10), which suggested a concomitant metabolic alkalosis with an AG acidosis. One usually develops hypochloremic metabolic alkalosis with intractable vomiting, but our patient’s disproportionate osmolar gap (30) and high AG could not be explained with his serum alcohol level and negative serum ethylene glycol/methanol screens respectively. The cause of this patient’s hyperosmolar AG metabolic acidosis was therefore attributed to the phenolic compounds (thymol, eucalyptol, and menthol) in “Listerine”.
HYPERTENSIVE EMERGENCY AS THE INITIAL PRESENTATION OF SYSTEMIC LUPUS ERYTHEMATOSUSCharles J. Lenz; Roger Yu. Mayo Clinic, Rochester, MN. (Tracking ID #1934759)
LEARNING OBJECTIVE 1: Diagnose systemic lupus erythematosus (SLE) in a patient presenting to the emergency department with hypertensive emergency in the absence of other classical symptoms of SLE.
CASE: A 25-year-old woman without significant past medical history presented to the emergency department complaining of a headache and fatigue that had been gradually worsening for a month. Over the 5 days prior to admission, the patient had also developed associated blurry vision and vomiting. The patient denied any other symptoms including rashes, arthralgias, oral ulcers, photosensitivity, or chest pain. She had not noticed any change in her urine. The patient was not on any medications at home. No family history of autoimmune diseases or renal disease. Initial assessment in the emergency department revealed a blood pressure of 226/128. Physical exam was otherwise unremarkable. There was no evidence of any neurologic deficits, rashes, or peripheral edema. The patient’s blood pressure was stabilized with hydralazine and nicardipine in the emergency department and she was admitted to the medical intensive care unit for further evaluation. Initial lab work revealed a creatinine of 1.6 mg/dL, hemoglobin of 8.9 g/dL, and an ANA > 12.0 (Normal <1.0). Urinalysis revealed 9.9 g of predicted 24 h protein, many dysmorphic RBCs, and fat in casts. Anti-ds-DNA antibodies, anti-RNP, and anti-Sm antibodies were elevated. Complement levels (C3 and C4) were low. The patient’s headache, blurry vision, and nausea improved after her blood pressure was controlled. However, the patient began to develop swelling of the lower extremities during the hospitalization. Salt restriction was instituted and the patient was started on Lasix to help with edema. The patient underwent renal biopsy which confirmed the diagnosis of class IV and V lupus nephritis. She was started on treatment with mycophenolate mofetil, prednisone, tacrolimus, and an aggressive anti-hypertensive regimen. The patient was discharged with close outpatient follow-up in stable condition.
DISCUSSION: Systemic lupus erythematosus is a rare disease that can present with many different clinical syndromes. The most commonly reported symptoms at initial presentation include arthritis, malar rash, fever, photosensitivity, serositis, and nephropathy. Hypertensive emergency is an uncommon and rarely reported presentation for SLE. It is important that clinicians are aware of this possible presentation as hypertensive emergency is a relatively common problem in the emergency room setting, and a broad differential needs to be maintained, especially in the setting of an abnormal urinalysis.
HYPERTENSIVE URGENCY, UNSTABLE ANGINA, AND ACUTE ANGLE CLOSURE GLAUCOMAMichael Dietz1,2; Hani Alkhatib1,2; Erika Osterholzer3,2; Joel Tsevat1,2. 1University of Cincinnati College of Medicine, Cincinnati, OH; 2VA Medical Center, Cincinnati, OH; 3University of Cincinnati College of Medicine, Cincinnati, OH. (Tracking ID #1939260)
LEARNING OBJECTIVE 1: Understand the importance of an in-depth review of systems including specific visual complaints when patients present with hypertensive urgency or emergency.
LEARNING OBJECTIVE 2: Recognize that internal medicine, emergency medicine, and family medicine practitioners are often the first clinicians to come in contact with patients with acute angle closure glaucoma, an ophthalmologic emergency.
CASE: A 67-year-old male with hypertension presented to the emergency room with left-sided, sharp, exertional chest pain radiating to his left scapula for 30 min. The pain had occurred once earlier that morning and intermittently for 2 weeks. His past medical history was notable for smoking and a prior ocular history of refractive error; he stated that his optometrist was monitoring him as a “glaucoma suspect” but the patient was asymptomatic and no treatment was planned. In the emergency room, his BP was 210/80 and his EKG showed ST depression in V4 and V5 and T-wave inversion in aVL and V2. Troponins were negative. He was admitted for acute coronary syndrome and treatment of hypertensive urgency. On the evening of his first hospital day, he noted blurry vision of his left eye without pain, redness, or diplopia. His pupillary exam that evening was reportedly normal with reactive, equal pupils. The following morning, the patient reported having had chest tightness when walking in the hallway and a return of blurry vision in his left eye. On exam, his BP was 183/81. His left eye was red; the pupils were reactive but not equal, with the left greater than the right. A head CT was negative. The patient was transferred to the ICU. Ophthalmology was consulted, and the patient was noted to have a normal right eye, and left eye with a fixed mid-dilated pupil (4 mm), conjunctival injection, a mildly hazy cornea, a very shallow anterior chamber, and an intraocular pressure of 60 mmHg (normal 10–21 mmHg). The patient was immediately treated with acetazolamide 500 mg orally and 3 rounds of timolol/dorzolamide and brimonidine eye drops, followed by indentation gonioscopy and additional parenteral and topical medication. His intraocular pressure returned to normal. The patient’s BP improved steadily with resolution of the intraocular pressure. The following morning, he underwent successful laser peripheral iridotomy. Though the patient initially denied eye pain, he later admitted to having eye pain prior to resolution of the elevated intraocular pressure, stating that he was anxious about being admitted and did not think about the pain until it was gone.
DISCUSSION: Visual complaints in the setting of hypertensive urgency should be investigated carefully, as many constitute ophthalmologic or neurologic emergencies, including, for example, retinal artery or vein occlusions, vitreous hemorrhage, acute hypertensive retinopathy, and TIAs or CVAs involving visual centers. Angle closure glaucoma is characterized by symptoms of blurry vision, eye redness, and severe eye pain. Patients frequently will also complain of headache and nausea or vomiting. Upon examination, the eye is red, with a mid-dilated, fixed pupil (approximately 5 mm and non-responsive to light), and the cornea may be hazy. Untreated acute angle closure glaucoma quickly leads to vision loss. Careful examination of the eyes and pupillary light response with a penlight should be performed in all patients, and confirmed if any uncertainties arise. Most antihypertensives are safe to use during an acute glaucoma attack, except for the vasodilator fenoldopam mesylate. This patient presented with hypertensive urgency, unstable angina, and acute angle closure glaucoma. A review of the literature revealed only one case report of acute glaucoma coinciding with hypertensive crisis, but the authors couldn’t prove cause and effect (1). While we can’t prove cause and effect either in this case, eye pain associated with acute angle closure glaucoma might have precipitated the hypertensive urgency, which in turn might have precipitated demand coronary ischemia and angina. 1. Razeghinejad MR, Heknat V, Mansouri K. Acute-angle closure glaucoma as the presenting sign of hypertensive crisis. Eye. 2010;24:1629–30.
HYPERTRIGLYCERIDEMIA-INDUCED ACUTE PANCREATITIS TREATED WITH PLASMAPHERESISMihaela C. Chelu; Mher Onanyan; Akshay Manohar; Tania Calzada; Daniel Goldsmith; Albert Empedrad. Capital Health Regional Medical Center, Trenton, NJ. (Tracking ID #1940166)
LEARNING OBJECTIVE 1: Demonstrate plasmapheresis as a definitive treatment for severe hypertriglyceridemia and pancreatitis.
CASE: The phlebotomist was alarmed when he drew milky white blood from the right antecubital of a 49 year-old African American obese man who presented to the emergency department complaining of severe upper abdominal pain for approximately 10 days. Laboratory findings showed: triglyceride 7313 mg/dL, total cholesterol 1153 mg/dL, lipase 2071 units/L, amylase 271 units/L, glucose 347 mg/dL, white blood cell count 17,200 cells/mm3. Computerized tomography of the abdomen revealed infiltration and haziness around the pancreatic head, body and uncinate process, confirming acute pancreatitis. On day 2, the patient’s condition was complicated by development of diabetic ketoacidosis (DKA) for which he was transferred to the Intensive Care Unit. Patient was started on insulin continuous infusion, which was continued for 3 days, then transitioned to subcutaneous insulin for 2 more days. This lowered of his TG level by 32 % to 5019 mg/dL. However, the patient still continued to have abdominal pain. Since he was at high risk of necrotizing pancreatitis, plasmapheresis was initiated on the general medical floor and the TG dropped dramatically by 78 % in a single session. Two additional plasmapheresis sessions were done lowering his TG level below 500 mg/dL. His symptoms resolving, the patient was discharged home on a low-fat diet on day 9, his TG 408 mg/dL and total cholesterol 118 mg/dL. He was prescribed Lantus 25 units subcutaneous daily, gemfibrozil 600 mg per mouth twice daily, and pravastatin 40 mg per mouth daily.
DISCUSSION: While intravenous insulin and gemfibrozil lower triglycerides, plasmapheresis is more effective in lowering levels quickly. Plasmapheresis is indicated in emergency situations when TG level is greater than 1000 mg/dL and should be continued until TG level have been lowered to less than 500 mg/dL. After the acute episode, rigorous pharmacological regimen and lifestyle modification are imperative, as is a discussion regarding screening of family members for lipid disorders.
HYPOGLYCEMIC HEMIPARESIS, THE STROKE MASQUERADERAlaa Elkhider; Naveen Nannapaneni; Joel Steinberg. Wayne State University/Detroit Medical Center, Detroit, MI. (Tracking ID #1923336)
LEARNING OBJECTIVE 1: Recognize hemiparesis as a potential manifestation of hypoglycemia.
LEARNING OBJECTIVE 2: Distinguish hypoglycemia from an acute cerebrovascular event in a patient presenting with hemiparesis.
CASE: The classic presentation of hypoglycemia involves adrenergic symptoms such as diaphoresis, palpitations and tremors. This however, overlooks the multitude of other signs and symptoms that hypoglycemia produces, which if missed, may lead to morbidity and even mortality. We present a case where just such an atypical symptom, hemiparesis, was initially believed to be the result of a stroke. A 63-year-old female smoker with diabetes and hypertension presented to the hospital with right-sided weakness starting acutely the morning of presentation. She reported having three similar previous episodes over the last month. She affirms compliance with her medications, which include glyburide, metformin, hydrochlorothiazide, triamterene and lisinopril, and describes anorexia with poor oral intake for several weeks. EMS evaluation identified a blood glucose of 42 mg/dL, in the absence of hypotension, which corrected with oral glucose, resulting in immediate resolution of her right hemiparesis. At ER arrival the patient had stable vital signs with an unremarkable physical exam including normal motor strength, sensation, reflexes, cranial nerves, and testing of higher cognitive functions. Laboratory investigations revealed abnormalities of blood glucose of 45 mg/dL, creatinine 5.1 mg/dL, BUN 38 mg/dL, albumin 1.8 g/dL and hemoglobin A1c 4.8 % with a normal lipid profile. The reported hemiparesis triggered the hospital’s stroke protocol initiating a neurology consultation in the ER. A non-contrast head CT, brain MRI/MRA, neck MRA and transthoracic echocardiography detected no acute abnormalities. After admission metformin and glyburide were discontinued given the suspicion of medication-induced hypoglycemia causing the recurring episodes of hemiparesis. The renal insufficiency resolved with intravenous fluid hydration. No further episodes of hemiparesis occurred during her hospitalization. Endocrinology consultants recommended against prescribing oral hypoglycemics on discharge given her previous episodes of hypoglycemia and euglycemia during hospitalization while off oral hypoglycemics.
DISCUSSION: Hemiparesis is a known, yet rare, presentation of hypoglycemia that can be mistakenly attributed to other etiologies. Our patient’s hypoglycemia was precipitated by impaired sulfonylurea clearance in the setting of acute renal insufficiency from poor oral intake and diuretic use. Prompt evaluation of serum glucose and obtaining diabetic history in patients presenting with focal neurologic deficits allow rapid identification of hypoglycemia as a potential cause. At present the pathophysiology of hypoglycemia induced focal neurologic deficit includes theories based on cerebral vasospasm, asymmetric cerebral blood flow, and selective neuronal vulnerability. Ultimately, should a patient present with acute hemiparesis in the context of significant risk factors for stroke, as in our patient, it would be presumptuous to simply attribute the deficit to hypoglycemia and disregard a cerebrovascular event. Rather, both hypoglycemia and other etiologies of stroke should be considered as they both carry risk of significant morbidity and mortality.
I’M NOT THE RASH YOU THINK I AM—A VASCULITIS WITH AN UNUSUAL CULPRITMinal A. Shah; Jeffrey T. Bates. Baylor College Of Medicine, Houston, TX. (Tracking ID #1939695)
LEARNING OBJECTIVE 1: Recognize that TNF-alpha inhibitors can paradoxically induce secondary autoimmune disorders such as vasculitis.
LEARNING OBJECTIVE 2: Distinguish vasculitis associated with Crohn’s Disease from vasculitis associated with TNF-alpha inhibitors.
CASE: A 52-year-old female with a history of well-controlled Crohn’s Disease and delusional parasitosis presented with a bilateral lower extremity rash. Over 5 years the rash would intermittently occur and spontaneously resolve. There were no other symptoms or signs, and she took no new medications. Her only medication was infliximab, which she would intermittently refuse because she thought she had a parasitic infection of the skin. Physical examination revealed multiple confluent erythematous papules, plaques and tender nodules ranging from 2 to 4 cm in diameter, extending bilaterally from her feet to her knees. Laboratory studies, including sedimentation rate, C-reactive protein, complement factors, and multiple autoantibodies were all negative. A punch biopsy showed acute inflammatory changes consistent with vasculitis. A careful review of her previous episodes revealed that her flares coincided with the administration of infliximab. Infliximab therapy was discontinued, and her rash resolved.
DISCUSSION: Inhibitors of tumor necrosis factor alpha (TNF-alpha) have revolutionized the management of inflammatory bowel disease. Despite their role as immunosuppressive agents, TNF-alpha inhibitors have been paradoxically implicated in secondary autoimmune disorders, including cutaneous and systemic vasculitidies. The incidence of vasculitis caused by TNF-alpha inhibitors is reported to be 0.2–3.9 % in the literature. In contrast to vasculitis associated with Crohn’s disease, vasculitis secondary to TNF-alpha inhibitors typically does not coincide with the worsening gastrointestinal inflammatory symptoms of abdominal pain, bloody stools or diarrhea. Furthermore, the rash is actually worsened by administration of the drug and is improved after cessation of therapy. The timing of the rash in relation to gastrointestinal symptoms, worsening of the rash after the culprit drug is administered, and biopsy findings suggestive of vasculitis are features diagnostic of vasculitis secondary to TNF-alpha inhibitors. Although the most common presentation is cutaneous vasculitis, it is also possible to have systemic involvement. The pathophysiology of systemic vasculitis is not well-known, although a type III hypersensitivity reaction is suspected. Treatment consists of switching to an alternative therapy for the primary autoimmune disorder. Interestingly, the formation of autoantibodies to TNF-alpha inhibitors is more likely to occur when maintenance doses of the medication are missed. Therefore, it is likely that our patients’ delusions of parasitosis and avoidance of her scheduled medication played a significant role in the development of her rash. Internal medicine physicians should be familiar with the full spectrum of skin manifestations in a patient with inflammatory bowel disease. When a patient presents with a vasculitic rash in the setting of well-controlled inflammatory bowel disease, vasculitis caused by a TNF-alpha inhibitor should be considered.
IDIOPATHIC PULMONARY FIBROSIS ASSOCIATED WITH ANCA VASCULITISHeena A. Birbal Jain; Saurabh K. Bansal. University of illinois college of Medicine at Peoria at Saint Francis Medical center., Peoria, IL. (Tracking ID #1917850)
LEARNING OBJECTIVE 1: Association of Idiopathic Pulmonary fibrosis with ANCA Vasculitis
CASE: A 73-year-old male of Indian descent presented with one-week history of fatigue, lethargy from outlying hospital. He was diagnosed with IPF 2 years ago. His creatinine on admission was 4.7 from baseline of 1.5. His renal failure was non-oliguric and electrolytes were stable. Urinalysis revealed active urinary sediment with RBC and RBC casts and random urine protein:creatinine ratio of 2.2 g. He was diagnosed with rapidly progressive glomerulonephritis (RPGN). Autoimmune workup including ANA, rheumatoid factor, anti-ro, anti-LA, anti GBM antibodies were negative except ANCA. C-ANCA resulted positive at 1:5620 and was specifically positive for anti PR-3 antibodies. Review of records from multiple hospitals revealed that he was never checked for ANCA antibodies before. He was diagnosed with ANCA related glomerulonephritis. Patient refused renal biopsy and was started on cyclophosphamide and prednisone. In the next few days he developed productive cough with blood streaks followed by respiratory failure and was placed on mechanical ventilation. Bronchoscopy was performed which showed extensive erythema in the bronchioles and return of RBC rich lavage. Cultures were negative and biopsy from the bronchus was negative for any acute pathology. His hypoxemia worsened and eventually succumbed to acute respiratory failure. Histology of lungs on autopsy showed extensive pulmonary fibrosis. Unfortunately, renal pathology was not done as a part of autopsy.
DISCUSSION: Idiopathic pulmonary fibrosis (IPF) is a rare disease with incidence of 20 in 100,000. IPF is a diagnosis of exclusion. Patients usually present with typical respiratory symptoms of dyspnea and cough, and most are not acutely sick at the time of presentation. Diagnosis is sought after pulmonary function test (PFT) reveal restrictive disease pattern and CT scan shows typical changes (bibasilar opacities with honey combing appearance). Autoimmune diseases such as Wegener’s, microscopic polyangiitis, lupus should be ruled out with appropriate labs. IPF is an uncommon disorder and is a diagnosis of exclusion. Based on literature review, most of such clinical presentations are associated with ANCA related disease. Also, in rare case reports it has been described that patients were diagnosed with IPF earlier and had ANCA antibody positive later. We believe that our patient had ANCA related vasculitis. It initially manifested as isolated lung involvement and was mistakenly labeled as IPF. Patient eventually developed a full-blown ANCA related vasculitis, which manifested as RPGN, alveolar hemorrhage and pulmonary capillaritis. The extreme levels of cANCA were indicative of high degree of inflammation. We recommend that all patients diagnosed with IPF should have ANCA antibodies checked at the time of diagnosis. This will help in better identifying patients with ANCA related pulmonary fibrosis, which is potentially treatable unlike the idiopathic form where no definite treatment is available.
IDIOPATHIC PULMONARY HEMOSIDEROSIS: AN ORPHAN DISEASENavneet Kaur; Pahul Singh. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1938947)
LEARNING OBJECTIVE 1: Early recognition of diffuse alveolar hemorrhage and its underlying cause to treat it in a prompt and timely manner.
CASE: A 62-year-old male presented to our institution with recurrent episodes of hemoptysis and exertional dyspnea for 1 month duration. He denied any chest pain, fever or hematochezia. Past medical history was significant for diabetes mellitus and 25 -pack -year smoking. Examination revealed normal vital signs and bibasilar crackles on lung exam. Laboratory values revealed hemoglobin of 7.3 g/dL, serum iron was 18 mg/dL, iron saturation was 5 %, MCV was 67.5. Chest radiograph showed bilateral lower lobe infiltrates. CT scan thorax showed multifocal ground glass opacities involving bilateral lower lobes consistent with alveolar airspace disease. 2-D echocardiogram was unremarkable. Bronchoalveolar lavage revealed intra-alveolar hemosiderin laden macrophages with no evidence of capillaritis, vasculitis or granulomas. After excluding all other sources of bleeding through extensive gastrointestinal workup and thorough immunologic profile, video-assisted thoracic lung biopsy was done which confirmed the diagnosis of IPH. Treatment was initiated with high dose of oral prednisone leading to marked improvement in the symptoms and the patient has been doing fine in last 6 months of follow-up.
DISCUSSION: Idiopathic Pulmonary Hemosiderosis (IPH) is a rare condition with unknown etiology with an incidence of 0.24–1.23 cases per million, causing recurrent episodes of diffuse alveolar hemorrhage that might lead to pulmonary fibrosis. IPH is characterized by abnormal accumulation of iron as hemosiderin in alveolar macrophages. Various etiological theories have been proposed of which auto-immune mechanism is most widely accepted theory. Clinical manifestations include hemoptysis, exertional dyspnea, iron deficiency anemia and parenchymal infiltrates on chest radiograph. CT thorax shows diffuse ground glass opacities and parenchymal infiltrates. Diagnosis of IPH is established upon eliminating all other secondary causes of alveolar hemorrhage and confirmation with lung biopsy which is gold standard diagnostic tool and reveals bland alveolar hemorrhage with absence of vasculitis or accumulation of immune complexes within lung parenchyma. Systemic corticosteroids are the cornerstone therapy in IPH. They decrease the episodes of alveolar hemorrhage during acute stage of disease and also control progression towards pulmonary fibrosis. To summarize, our case reiterates the importance of early recognition of diffuse alveolar hemorrhage which is a life threatening condition with prompt diagnosis of underlying syndrome to initiate therapy in a timely fashion.
IDIOPATHIC? SOUNDS LIKE A COP OUTMerrill H. Stewart; Deepa Bhatnagar. Tulane University School of Medicine, New Orleans, LA. (Tracking ID #1940000)
LEARNING OBJECTIVE 1: Understand cryptogenic and secondary organizing pneumonia
LEARNING OBJECTIVE 2: Identify the extra-articular manifestations of rheumatoid arthritis
CASE: A 63 year-old man presented with 3 weeks of worsening shortness of breath and generalized weakness. He also reported a dry cough and a history of heart failure. He was noted be afebrile, tachycardic, with an oxygen saturation of 100 %. He had no lower extremity edema. Proximal muscle groups were weaker than distal muscle groups in all extremities. Brain natriuretic Peptide was 50 pg/mL. Chest radiograph revealed no pulmonary edema and bilateral interstitial changes. Chest computed tomography revealed mediastinal lymph nodes and multi-focal “reverse halo,” or “atoll” signs. Serum rheumatoid factor was 860 IU/mL, cyclic citrullinated peptide antibody >300u/mL, creatinine kinase 853u/L, and aldolase 15u/L.
DISCUSSION: Cryptogenic Organizing Pneumonia (COP), formerly Brochiolitis Obliterans Organizing Pneumonia, can be grouped among the 5 idiopathic interstitial lung diseases. Fibroblasts proliferate in the alveolar ducts, moving from one adjacent alveolus to the next forming airway plugs. This preserves the existing lung architecture without any necrosis, while occurring in isolated focal patches throughout the lungs. When associated with an underlying disease or medicine it is termed a secondary organizing pneumonia, however the characteristics are the same as when it is cryptogenic. Implicated medications or conditions associated with organizing pneumonia include amiodarone, cocaine, connective tissue diseases, infectious pneumonias, diffuse alveolar hemorrhage, aspiration, and hypersensitivity pneumonitides. COP presents in 5th-6th decade of life with several weeks of cough, fever, dyspnea, malaise, and weight loss. The work up usually begins after failed antibiotic treatment for atypical pneumonias, and should include an investigation for any of the above associated conditions. Laboratory analysis should focus on ruling out infectious pneumonias and connective tissues disease. Chest Computed Tomography usually shows peripheral patchy focal air-space consolidation and ground glass opacities. Occasionally computed tomography also shows cavitary, crescentic, or ring shaped opacities. A “reverse halo” or “atoll” sign is an area of ground glass opacity surrounded by a dense crescentic ring, and is highly suggestive of organizing pneumonia. Ultimately tissue is required to make a diagnosis of Organizing Pneumonia, and often an open wedge resection is needed to obtain a sufficient sample. Only after all secondary causes have been ruled out and tissue shows consistent histopathology, can a diagnosis of Cryptogenic Organizing Pneumonia be made. Rheumatoid arthritis typically presents with joint involvement, however in 15–25 % of people it can have extra-articular manifestations, and occasionally these can precede joint involvement by years. They include rheumatoid nodules, interstitial lung disease, vascultitis, felty syndrome, sicca syndrome, amyloidosis, coronary artery disease, pericarditis, and peripheral neuropathy. It can also present with other connective tissue diseases in an Overlap Connective Tissue Syndrome. Our patient presents without any joint involvement, elevated cyclic citrullinated peptide titers, laboratory and clinical findings suggestive of polymyositis, and organizing pneumonia. The most consistent diagnosis would be an overlap connective tissue disease syndrome with secondary organizing pneumonia.
IGA NEPHROPATHY PRESENTING AS A RAPIDLY PROGRESSIVE GLOMERULONEPHRITIS IN AN ELDERLY WOMANMark H. Adelman; Eduardo Iturrate. NYU School of Medicine, New York, NY. (Tracking ID #1931286)
LEARNING OBJECTIVE 1: Recognize the clinical and pathologic features of IgA nephropathy that portend a poorer prognosis and thus require aggressive management
CASE: An 81-year-old woman presented to an outside provider with 3 months of post-prandial abdominal pain and bloating. Her symptoms were not relieved with a proton-pump inhibitor so she underwent upper endoscopy that was reportedly unremarkable. When seen in an outside hospital emergency department for acute worsening of her abdominal pain now associated with increased abdominal girth, the patient had an abdominal CT. This was notable for large volume ascites. The patient denied fevers, chills, cough, diarrhea, dysuria, hematuria and rash. She reported chronic, bilateral knee pain but no new joint pains. She was admitted to the outside hospital for workup of new onset ascites. After several days the patient signed out against medical advice and presented to our hospital for further management. Past medical history was significant for knee osteoarthritis, herpes zoster and bereavement disorder. Home medications were pantoprazole, diazepam and corticosteroid knee injections. There was no family history of autoimmune, renal or hepatic disease. The patient lives at home with her daughter, is independent in activities of daily living and denied tobacco, alcohol or illicit drug use. On physical exam at our hospital, vital signs were notable for a blood pressure of 172/102. She was in no acute distress. Abdomen was distended, firm and mildly tender to palpation diffusely. Legs were massively edematous. Labs were most notable for creatinine that rose from 1.3 mg/dL to 4.5 mg/dL over 12 days. Spot urine protein/creatinine was 9602 mg/g. Ascitic fluid was negative for SBP and malignant cells. ANA 1:640, ANCA negative. HIV, Hepatitis B/C all negative. Renal biopsy showed: proliferative, necrotizing glomerulonephritis, consistent with IgA nephropathy, severe, acute; tubular atrophy and interstitial fibrosis, mild; interstitial edema and inflammation, moderate. Prior to leaving the outside hospital, the patient had received 2 days of pulse-dose methylprednisolone after her renal biopsy results came back. She received a third dose of methylprednisolone at our hospital and cyclophosphamide on the recommendation of our nephrology consultant. We gave IV loop diuretics for her massive volume overload but the patient required initiation of hemodialysis via a tunneled catheter. Further doses of cyclophosphamide were held due to development of anemia and thrombocytopenia, as well as infectious complications including gram-negative sepsis. A long, tapering course of prednisone was continued. The patient has not required hemodialysis for approximately 3 months.
DISCUSSION: IgA nephropathy is believed to be the most common cause of primary glomerulonephritis worldwide. It occurs most commonly in the second and third decades of life and among males more often than females. The typical presentation is painless, macroscopic hematuria (40–50 % of patients), frequently temporally associated with an upper respiratory tract infection. Thirty to forty percent of patients present with microscopic hematuria with or without proteinuria. Much less commonly (<10 %), patients present with nephrotic syndrome or acute kidney injury associated with a rapidly progressive glomerulonephritis. Essential to the diagnosis of this condition is renal biopsy and the identification of glomerular IgA deposits on immunofluorescence microscopy. Several clinical features have been associated with a poor prognosis in studies of IgA nephropathy patients. These include sustained hypertension, persistent proteinuria >1 g/day, impaired renal function at time of diagnosis, and nephrotic syndrome. The Oxford classification is a histologic scoring system, validated in diverse cohorts, that incorporates findings on renal biopsy that are also associated with adverse outcomes independent of clinical features. The cornerstone of management in nearly all patients with IgA nephropathy is treatment of hypertension and/or proteinuria by ACE inhibition or angiotensin receptor blockade. Corticosteroids demonstrated some efficacy for preservation of renal function and improvement in proteinuria among patients with more significant proteinuria and normal baseline renal function in a randomized controlled trial. Immunosuppression with corticosteroids and cyclophosphamide is often used to manage rapidly progressive glomerulonephritis with cellular crescents seen on renal biopsy, based on observational data, but randomized controlled trial data is lacking. Our patient presented with a number of poor prognostic factors, mostly significantly the rapid progression of her condition, massive proteinuria and crescents on renal biopsy. Consequently, we aggressively managed the patient with steroids and a cytotoxic agent given the acuity and fulminant nature of her presentation.
IMMUNODEFICIENCY DIAGNOSED IN ADULTHOODJenny Koo1; Laura Y. Sue1; Pearl Yu2. 1UC San Diego School of Medicine, San Diego, CA; 2UC San Diego Medical Center, La Jolla, CA. (Tracking ID #1924024)
LEARNING OBJECTIVE 1: Recognize the clinical manifestations of IgA deficiency and its associated co-morbidities
LEARNING OBJECTIVE 2: Review the preventive and therapeutic options available for individuals with IgA deficiency
CASE: A 58 year old woman with allergic rhinitis, new onset asthma, gastroesophageal reflux disease, and history of Non-Hodgkins lymphoma [NHL] presented repeatedly in clinic for respiratory infections. Her symptoms included persistent sinus congestion, post nasal drip, productive cough, and wheezing. Fluticasone/salmeterol, montelukast, prednisone, nasal saline irrigation, and an as needed albuterol were prescribed to address the various refractory symptoms. Multiple courses of amoxicillin-clavulanate were ineffective. The patient did not have sensitivity to aspirin or a history of nasal polyps. She did not have a history of food allergies or autoimmune disease. She believed that her recurrent infections started after treatment for NHL 10 years prior. There was no tenderness to palpation over the frontal and temporal sinuses and the lungs were clear to auscultation bilaterally. Chest x-ray was negative and CT scan of the sinuses revealed bilateral inflammatory sinus disease in the maxillary, sphenoid, and ethmoid sinuses. Endoscopic sinus surgery improved sinus symptoms but the patient continued to have frequent respiratory infections. A subsequent serum immunoglobulin panel revealed severely low to absent levels of IgA (<5 mg/dL), with normal levels of IgG and IgM. The patient was therefore diagnosed with IgA deficiency. Testing for serum anti-transglutaminase antibodies, given the association between IgA deficiency and autoimmune processes, was negative. The patient was advised to discuss the new diagnosis, immunology testing of family members, prevention, and treatment options with an allergy/immunology specialist.
DISCUSSION: IgA deficiency is an isolated decrease in IgA with normal levels of IgG and IgM. It is the most common immunologic deficiency and is largely asymptomatic. When symptomatic, individuals have recurrent sinusitis and other respiratory tract infections, especially those due to encapsulated bacteria. GI infections are also common, including increased susceptibility to Giardia lamblia infection. The differential diagnosis includes emerging common variable immunodeficiency (or other immunodeficiencies) and drug-induced, mostly reversible IgA deficiency. Individuals with IgA deficiency are more likely to have food allergies, allergic rhinitis, and allergic asthma. Twenty percent will have concomitant autoimmune disease, such as rheumatoid arthritis, systemic lupus erythematosus, celiac disease, or inflammatory bowel disease. There is also the potential to develop anti-IgA antibodies and individuals with IgA deficiency may have anaphylactic reactions to blood transfusions. Patients should be vaccinated against Streptococcus pneumoniae and may consider testing for anti-IgA antibodies in case of possible future blood transfusions. Treatment is directed at any concomitant respiratory disorders (such as asthma) and infections as they arise. Prophylactic antibiotics and/or IVIG therapy can be considered.
IMMUNOSUPPRESSION: OPENING A CAN OF WORMS FOR HYPERINFECTION SYNDROME?Marc Cohen; Deborah Hemel. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939077)
LEARNING OBJECTIVE 1: Recognize the signs and symptoms of strongyloides infection.
LEARNING OBJECTIVE 2: Recognize risk factors for Hyperinfection syndrome.
CASE: A 58 year old female presented with a 2 year history of vomiting after nearly every meal. She also reported epigastric pain associated with vomiting and intermittent watery diarrhea for several years. The patient had undergone previous endoscopy showing gastric reflux disease and a hiatal hernia, but her symptoms did not improve with proton pump inhibitor therapy or lifestyle modifications. Relevant past medical history included longstanding rheumatoid arthritis treated with prednisone, hydroxychloroquine and methotrexate. Her social history was significant for intermittent trips to the Dominican Republic, from which she had emigrated many years prior. Admission labs were notable for white blood count of 12.4 k/uL with slight eosinophilia of 0.6 k/uL (normal range 0.0 to 0.3 k/uL), sodium 128 mEq/L, potassium 3.3 mEq/L, albumin 1.7 g/dL, and INR 1.5. On exam, she was a lethargic, ill-appearing female with vague abdominal tenderness, diffuse anasarca, and confluent bruising along the extremities. During the first week of her hospitalization her frequent vomiting persisted despite an aggressive anti-emetic regimen, her functional status continued to decline, and her albumin dropped to 1.2 g/dL. On hospital day 8 stool studies returned positive for strongyloides stercoralis, therefore she was started on Ivermectin. Her serum subsequently returned positive for strongyloides IgG. Her endoscopic biopsies revealed severe inflammation and strongyloides within the mucosal crypts of the stomach and duodenum, as well as marked villous flattening of the duodenum. The patient improved significantly on Ivermectin. She was discharged home on hospital day 16. She was seen in clinic 2 weeks after discharge at which time she reported resolution of her symptoms.
DISCUSSION: Strongyloides is a nematode that enters the body cutaneously, most classically when bare feet contact soil contaminated with infected human feces. The parasite lives primarily in tropical climates but is also found in parts of Appalachia. Many people with strongyloides are asymptomatic; those who develop symptoms generally have vague, transient pulmonary complaints or vague, chronic gastrointestinal complaints. Gastrointestinal symptoms include poor oral intake, epigastric pain, nausea, vomiting and diarrhea. As the nematodes proliferate in the gastrointestinal tract they can cause destruction of the villous architecture, thereby leading to malabsorption. The combination of anorexia, chronic vomiting and malabsorption can lead to life-threatening malnutrition, as was the case in our patient. A patient with a high burden of disease who is immunosuppressed is at risk of developing the dreaded Hyperinfection syndrome, which occurs when strongyloides travels beyond the gastrointestinal tract via the blood stream. Immunosuppressed patients are at elevated risk of this complication, although how elevated remains unclear. Once disseminated, strongyloides can affect many different organs, thereby leading to variable types of organ dysfunction. Additionally, once strongyloides interrupts the integrity of the bowel mucosa, patients become predisposed to sepsis due to enteric gram negative bacteria. If left untreated, the syndrome is fatal in up to 90 % of patients. Detection of strongyloides infection can be difficult given that stool samples have less than 50 % sensitivity. Serum ELISA testing appears to be much more effective, with reported sensitivities of greater than 80 %. However ELISA testing is costly and may not be widely available. Endoscopic biopsy is also a diagnostic option but should be undertaken only if the patient warrants an endoscopy as part of a gastrointestinal work up. Mild eosinophilia can be one clue to the diagnosis, however it is neither sensitive nor specific for strongyloides. Patients with chronic gastrointestinal complaints who have traveled to endemic regions should be tested for strongyloides as part of a parasitic work up. Physicians who care for patients who have spent extensive time endemic areas should consider screening for strongyloides prior to starting such patients on steroids or other immunosuppressive agents given the high fatality rate associated with Hyperinfection syndrome and the ease of treatment with Ivermectin.
INCESSANT PERICARDITIS IN A 31-YEAR OLD MALE FOLLOWING BIOPROSTHETIC AORTIC VALVE REPLACEMENTTheresa L. King; Jeffrey Beasley. University of Kansas, Kansas City, KS. (Tracking ID #1941415)
LEARNING OBJECTIVE 1: Recognize and treat incessant pericarditis, including early involvement by rheumatology for steroid-sparing treatment options.
CASE: A 31-year-old male with a benign medical history presented to an academic medical center with complaint of acute onset of extreme dyspnea with minimal exertion. An ECHO revealed moderate to severe aortic regurgitation and the presence of a bicuspid valve, which was thereunto unknown. He underwent aortic valve replacement (AVR) with a bovine tissue valve. His hospital course was uncomplicated. At 3 week follow-up, he was found to have a trivial pericardial effusion on ECHO, and was started on ibuprofen. Two weeks later he was admitted due to severe pleuritic, substernal and positional chest pain. He was found to have a moderate pericardial effusion on ECHO and CRP was elevated. A diagnosis of pericarditis/post-cardiac injury syndrome was made. He was started on indomethacin but relief was inadequate so steroids were started. He was discharged on indomethacin and a solumedrol dose pack. Ten days later the steroid taper was complete. Chest pain had resolved but he complained of mild dyspnea with exertion. Colchicine was added. Nine days later he developed severe pleuritic chest pain and was started on prednisone 60 mg qday which was tapered by 10 mg qday each week. Within days following completion of steroids, symptoms of pericarditis returned. During the year following surgery he underwent 4 slow steroid tapers with flares occurring within a month of cessation of steroids. Approximately 1 year following AVR he was again hospitalized with a severe flare. Steroids were initiated and rheumatology was consulted for consideration of starting a steroid-sparing agent. At follow-up with rheumatology, which was 14 months post AVR, azathioprine was started and the slow steroid taper was continued. Approximately 6 months after initiation of azithioprine, the patient was off steroids and continued to be symptom-free. Approximately 1 year after starting azithioprine, a slow taper was begun that was completed 1 year later. He remains symptom free.
DISCUSSION: The development of pericarditis following cardiac surgery is not an uncommon occurrence, with most cases involving men aged 20 to 50. Recurrent pericarditis refers to a syndrome in which acute pericarditis recurs after the agent inciting the original acute attack has disappeared or has ceased to be active. It involves considerable morbidity and can result in cardiac tamponade and constrictive pericarditis. Incessant pericarditis, as opposed to recurrent pericarditis, refers to cases with persistent symptom return within 6 weeks of previous resolution. Incessant pericarditis is extremely uncommon and very few case reports are available to guide treatment. Prolonged steroid use is associated with serious side effects, including an increased risk of infection, osteoporosis, psychosis, insomnia and glaucoma and should not be used long term. Additionally, steroids are a known risk factor for recurrence if used during the index case. Steroid-sparing immune suppressants should be considered, but carry an increased risk of infection, lymphoma and bone marrow suppression. The purpose of reporting this case is to increase awareness of this uncommon condition and to share management decisions and regimens, as no well-prescribed standard treatment exists for incessant pericarditis. Early involvement by rheumatology is encouraged for consideration of steroid-sparing agents.
INCIDENTAL HYPOXEMIASaroja Bangaru; Arash Harzand. Emory University, Atlanta, GA. (Tracking ID #1938711)
LEARNING OBJECTIVE 1: Recognize the subclinical presentation of hepatopulmonary syndrome
LEARNING OBJECTIVE 2: Anticipate and diagnose hepatopulmonary syndrome early and efficiently
CASE: A 60 year-old homeless man with cirrhosis 2/2 HCV presented to the ED with complaints of lower back pain. On triage, he was found to be hypoxic to low 80’s on room air. Further questioning revealed 4-month history of fatigue and occasional shortness of breath with exertion. He was otherwise asymptomatic with a normal CXR, so he was admitted for management. His cardiopulmonary exam was benign, and he had no stigmata of chronic liver disease. CMP revealed mild transaminitis but was otherwise normal. ABG revealed wide A-a gradient hypoxia that corrected with supplemental O2 to 96 %. Right to left intra-cardiac shunt was initially suspected as there was no evidence of diffusion impairment with normal lung parenchyma and desaturation on ambulating, and CT PE was negative. Surface echo with bubble study revealed late bubbles in the left atrium and left ventricle, suggesting a pulmonary AVM versus a PFO with intermittent shunt. It was decided that TEE should be performed to visualize atrial septum. A TEE with bubble study confirmed a small PFO without any significant right-to-left shunt or Eisenmenger’s physiology to explain his hypoxia. Pulmonary was consulted who agreed that the patient may indeed have pulmonary micro-AVMs that cannot be visualized with CT as they are capillary sized. The only therapeutic option was home supplemental O2 as the patient would likely not qualify for liver transplant due to untreated HCV. He was arranged with home O2 and discharged to a nursing facility as he was homeless. He was arranged with follow up at GI clinic for any additional recommendations given new diagnosis of hepatopulmonary syndrome and for consideration, if possible, of liver transplantation in the future.
DISCUSSION: Hepatopulmonary syndrome is characterized by arterial hypoxemia induced by pulmonary vascular dilation in the setting of liver disease. Estimates of its incidence are as high as 47 %, but it is frequently asymptomatic and under-recognized, making it a diagnostic challenge. This case increases awareness of HPS in hopes that it will be more readily recognized in cases of liver disease of varying severity. It demonstrates the need to anticipate a diagnosis of HPS because it is often subclinical and because it is associated with a worse prognosis. In reflecting on this case, the necessity of an extensive inpatient pulmonary work-up and trans-esophageal echocardiogram was debated. Integrating a patient’s clinical history with his presentation is necessary in order to make a diagnosis efficiently, without conducting an extensive and invasive work-up when it may not be necessary.
INDUSTRIAL LAUNDRY FACILITIES: NOT AS “CLEAN” AS WE EXPECTSean Townsend; Stephen Harder. University of Texas Southwestern Medical Center at Dallas, Dallas, TX. (Tracking ID #1939547)
LEARNING OBJECTIVE 1: Recognize the importance of occupational history in timely diagnosis and treatment of Legionnaires’ disease.
LEARNING OBJECTIVE 2: Appreciate the appropriate clinical indications for the Legionella urine antigen test.
CASE: A 44 year old African-American woman presented with 5 days of high fever, nausea and vomiting, diarrhea, and headache as well as 2 days of worsening productive cough and shortness of breath. She had no medical history prior to this illness. She denied any recent travel or sick contacts at home or work. She was an intermittent smoker, but denied alcohol use. She reported a long time occupation working in an industrial laundry facility handling freshly laundered items. On physical exam, the patient had a temperature of 102.9 F, blood pressure of 141/84, heart rate of 126, and respiratory rate of 28, with an oxygen saturation of 87 %. She was able to talk in full sentences despite breathing quickly. There were bibasilar rales, worse on the left, however no tactile fremitus or dullness to percussion. Laboratory studies revealed a white blood cell count of 12.6 × 103/μL with neutrophil predominance, alanine aminotransferase of 53 U/L, aspartate aminotransferase of 79 U/L, and an alkaline phosphatase of 159 U/L. Chest radiograph showed bilateral parenchymal consolidations. She was admitted with a preliminary diagnosis of community acquired pneumonia and sepsis, and treated with vancomycin, piperacillin/tazobactam, and azithromcyin. Given the patient’s known environmental exposure a Legionella urine antigen test was obtained which resulted positive, and she was changed to moxifloxacin monotherapy. A Legionella specific sputum culture grew Legionella pneumophila. Her clinical course then improved over 1 week with resolution of symptoms.
DISCUSSION: This case highlights an industrial laundry facility as an interesting source for exposure to Legionnaires’ disease. The Legionella urine antigen test has a sensitivity of 70–80 %, a specificity of >99 %, and remains positive for days to weeks after initial infection. Current IDSA/ATS guidelines recommend obtaining a Legionella urine antigen test in the evaluation of community acquired pneumonia in patients with recent travel, alcohol abuse, pleural effusion, failure of outpatient treatment, ICU admission, and nonresponding pneumonia, defined as clinical deterioration despite appropriate broad spectrum antibiotics. Patients should be carefully selected so as to reduce the number of false positive tests. This case is an example of a patient who did not meet accepted criteria, but in whom early recognition of pertinent occupational history leading to utilization of the Legionella urine antigen test by the general internist was essential in the timely diagnosis and treatment of Legionnaires’ disease. Strong clinical suspicion for Legionnaires’ disease based on occupational history should be considered as an addition to guidelines for the use of the Legionella urine antigen test.
INFECTIOUS GRANULOMATOUS DERMATITIS: A RARE PRESENTATION OF MYCOBACTERIUM TUBERCULOSISMary Ramirez; Jack Waller; Roger D. Smalligan. Texas Tech University Health Sciences Center, Amarillo, TX. (Tracking ID #1934995)
LEARNING OBJECTIVE 1: Recognize the clinical features of cutaneous tuberculosis
LEARNING OBJECTIVE 2: Recognize that cutaneous tuberculosis can persist for years and leave varioliform scars if not treated appropriately
CASE: A previously healthy 31-year-old Burmese male with no past medical history presented with lymphadenopathy, sore throat, nausea, abdominal pain, vomiting, and shortness of breath. A rapid strep test was positive and the patient was prescribed Amoxicillin. Seven days later he felt better but had a new swollen cervical lymph node and his axillary node was sore and swollen. Labs showed anemia and hypoproteinemia. A PPD was read as 50 mm. CT of the chest showed adenopathy of the left axilla, right hilum, and mediastinum. A sputum AFB culture was sent and he was started on directly observed therapy with daily isoniazid, rifampin, pyrazinamide, ethambutol, and vitamin B6. His culture later came back positive for Mycobacterium TB. Three weeks after starting treatment the patient presented with pruritic, vesiculopapular, crusted, and hyperpigmented skin lesions on the chest and extremities. The lesions were initially thought to be molluscum contagiosum but when they became more hemorrhagic 1 week later dermatology was consulted and a biopsy was performed to rule out tuberculosis miliaris disseminata and perforating folliculitis. Pathology showed vacuolar alteration along with lichenoid features with no evidence of molluscum and granulomatous dermatitis consistent with an infectious process.
DISCUSSION: Cutaneous lesions are a rare manifestation of Mycobacterium tuberculosis (MTB), occurring in only 1 to 2 % of infected patients. MTB is a slow growing acid-fast bacillus which is the predominant cause of cutaneous TB. Cutaneous TB has re-emerged in parts of the world where the incidence of HIV infection and multi-drug resistant TB is high. In the majority of cases, cutaneous TB is a manifestation of systemic involvement and can present in a variety of ways including as inflammatory papules, verrucous plaques, suppurative nodules, warty tumors, scarring reactions, or chronic ulcers among others. The different manifestations may vary due to the quantity of organisms in the lesions and predisposing factors of the host such as the patient’s age, immune competence status and previous TB sensitization. Four common forms of cutaneous TB include lupus vulgaris, tuberculosis verrucosa cutis, scrofuloderma, and papulonecrotic tuberculids. Papulonecrotic tuberculids consist of multiple symmetric papules, 1 to 5 mm in diameter with an umbilicated, necrotic center that commonly appear on the trunk and are often seen in adults with active tuberculosis disease elsewhere. This is precisely what was seen in our patient. Tissue biopsy often reveals a palisading granuloma and follicular necrosis. As with our patient, bacilli are usually absent in papulonecrotic tuberculoid lesions, and the PPD test is often strongly positive. Fever and constitutional symptoms often precede the appearance of skin lesions, and associated lymphadenitis is common. Although these lesions may spontaneously resolve over the course of several weeks, they often recur and if left untreated may persist for years, leaving varioliform scars. This case reminds internists of the cutaneous manifestations of TB that can appear even after treatment for TB has been started. It is important to initiate proper, directly observed therapy that encompasses an effective, standard anti-tuberculous regimen based on culture results to insure an adequate response to treatment and ultimately a cure for the patient.
INFECTIVE ENDOCARDITIS: AN UNUSUAL CULPRITNathaniel Ernstoff; Misako Nagasaka; Jonathan Katz; Charles M. Geller. Beth Israel Medical Center, New York, NY. (Tracking ID #1939094)
LEARNING OBJECTIVE 1: Recognizing Citrobacter koseri as a possible pathogen for endocarditis
LEARNING OBJECTIVE 2: Suspecting septic emboli in patients with visual disturbances
CASE: A 62 year old Haitian woman with past medical history significant for hypertension and end stage renal disease on hemodialysis presented with sudden onset of blurry vision in the right eye. Physical exam was significant only for decreased visual acuity and 3/6 diastolic murmur best heard at the apex. Initial labs were significant only for elevated BUN and creatinine. Initial workup for a transient ischemic attack was started and CT of the head did not show any acute changes. The loss of visual acuity did not resolve and given additional concern for multiple sclerosis, MRI brain was ordered. MRI showed multiple infarcts throughout the brain with the largest being in the left occipital lobe secondary to suspected embolic etiology. This lesion’s location was consistent with the patient’s symptoms though the rest of her neurologic exam was benign and no other embolic stigmata were observed. Transthoracic echocardiogram showed a thickened mitral leaflet with an opening size of 1.8 cm. Follow up with transesophageal echocardiogram showed a 1-cm mobile vegetation on the mitral valve. Blood cultures at this time returned positive for Citrobacter koseri in 2 sets of anaerobic and aerobic bottles and treatment was started with cefepime. The patient’s vision started to improve and the patient underwent emergent mitral valve replacement. Surgical findings included abnormal mitral valve with small friable vegetations on the posterior leaflet, a posterior annular abscess with frank pus and significant pericarditis throughout the pericardial sac.
DISCUSSION: Citrobacter koseri is an exceedingly rare cause of endocarditis. To our knowledge only 5 other cases have been reported. These 5 cases include a hemodialysis patient, two intravenous drug users, one pacemaker patient and a young immunocompetent adult. None of these cases reported additional findings of cardiac abscess and pericarditis. One separate case implicated Citrobacter koseri and Proteus mirabilis in a polymicrobial suppurative pericarditis leading to tamponade. Citrobacter is a gram negative bacillus and facultative anaerobe part of the Enterobacteriaceae family which is distinguished from other members of the Enterobacteriacaeae family for its ability to use citrate as a carbon source. Generally, Citrobacter koseri is known for causing infection in two distinct groups of patients. In neonates Citrobacter koseri can cause sepsis and meningitis leading to CNS abscesses and often death. These cases are sporadic and no clear infection source has been identified, though the natural habit of this bacteria is in water, food, soil, sewage and human excrement. The second group includes immunocompromised, elderly, and dehabilitated patients. Our patient does not fit either of these categories suggesting a third category exists that has not yet been defined. Further reports may help develop a clear source for this infection and elucidate this third group.
INFLUENZA A INFECTION IN A PATIENT WITH CONGESTIVE HEART FAILURE, A DYSPNEIC COMBINATIONKomal D’Souza; Robin Klein. Emory University School of Medicine, Atlanta, GA. (Tracking ID #1938669)
LEARNING OBJECTIVE 1: Identify common clinical manifestations of congestive heart failure and influenza infection.
LEARNING OBJECTIVE 2: Highlight the link between CHF decompensation and influenza infection.
CASE: A 58 year old male was admitted to an urban hospital with respiratory complaints in the month of December. He reported progressive dyspnea on exertion for the past month and a productive cough for 4 days prior to admission. He also noted orthopnea and pleuritic chest pain associated with coughing. He denied myalgias. His past medical history was significant for congestive heart failure (CHF) with a reduced left ventricular ejection fraction of 10–15 %. He reported compliance with an ace-inhibitor and beta-blocker, but did report limited understanding of dietary sodium and fluid restrictions. He also reported his grand-son who had visited with him recently was also ill with respiratory symptoms. On exam, the patient was afebrile, mildly tachypneic and hypoxic, requiring supplemental oxygen to maintain adequate peripheral oxygen saturations. He had crackles in his posterior lung fields and elevated jugular venous distention with a positive hepato-jugular reflex. His labs were significant for renal insufficiency and an elevated brain-natriuretic peptide. His chest x-ray showed cardiomegaly and a pulmonary edema pattern. The patient was treated for acutely decompensated congestive heart failure and the etiology of his decompensation was initially attributed to dietary non-compliance. The patient’s work of breathing was marginally improved with initial diuresis. On hospital day two, he became febrile with continued shortness of breath and cough. A respiratory virus panel nasal swab was collected and he was empirically started on an anti- influenza agent. His symptoms gradually improved and on the day of discharge, his respiratory virus panel resulted positive for the influenza A virus.
DISCUSSION: Acute decompensation of congestive heart failure (CHF) is one of the most common reasons for hospital admission in the United States. Most of the acute decompensations of this chronic disease can be attributed to progression of the underlying cardiomyopathy, dietary non-compliance, or inadequate medication regimens. Infections can also precipitate decompensation due to the pro-inflammatory response associated with infection. Influenza infection is also common, particularly in the winter months. Common manifestations include fevers, fatigue, myalgia, shortness of breath and cough. Patients with CHF are considered a high-risk group for severe influenza infections. Also, patients with CHF may be at a higher risk of hospitalization during the influenza season than during non-influenza seasons. Although patients with CHF who have been vaccinated against influenza may have a lower risk of hospitalization, these patients also may have difficulty mounting an immune response to newer antigens included in the annual influenza vaccine. Our patient presented with acute decompensated congestive heart failure triggered by influenza A infection. This case highlights the link between two common but potentially serious conditions: CHF decompensation and influenza. It is important to recognize the association between these conditions and to maintain a broad differential in considering the etiology of acute worsening of common chronic conditions. Furthermore, it is important to consider infectious etiologies for CHF decompensation so these infections can be managed appropriately to prevent further cardio-pulmonary distress.
INITIAL PRESENTATION OF MULTIPLE MYELOMA AS INTRAPARENCHYMAL BRAIN MASSIshan Malhotra; Abhinav Chandra; Yiwu Huang. Maimonides Medical Center, Brooklyn, NY. (Tracking ID #1935319)
LEARNING OBJECTIVE 1: A rare case of Intracranial periventricular Plasmacytoma who presented with headaches indicating the importance of Plasmacytomas in the differential diagnosis of intracranial/intraparenchymal tumors like meningioma .
LEARNING OBJECTIVE 2: It is critical to follow up patients frequently with a complete systematic work up to identify the transformation of Solitary Plasmacytoma into Multiple Myeloma.
CASE: 38 year old African female presented with complaints of severe headache which had started couple of weeks prior to presentation and was progressively becoming worse. Patient underwent a CT scan of the head which revealed a 3.2 × 3.3 × 3.7 cm lobulated hyperdense periventricular mass in the left temporoparietal area. MRI of the brain revealed a 3.1 × 2.6 × 3.6 cm lobulated mass in left lateral ventricle trigone. Patient underwent left craniotomy for tumor resection and the resected tumor was high grade malignant neoplasm with plasmablastic features and immunohistochemical stains revealed that the tumor cells were positive for CD138, CD30, MUM-1, Bcl-2, vimentin and lambda light chains and were negative for kappa light chains, CD3, CD20, PAX-5, CD79a, GFAP, cytokeratin, AE1/AE3, synaptophysin, chromogranin, EMA, S-100, Melan-A, CD45, CD56 and EBV (EBER-ISH). Ki-67 was about 80 %. Serum protein electrophoresis (SPEP) was sent that showed an M-spike of 3.3 g/dl that was IgG lambda. A bone marrow biopsy showed 100 % infiltration with plasma cells. Patient underwent a CT chest/abdomen/pelvis and a PET/CT scan which revealed multiple scattered subcutaneous masses throughout the body and an asymptomatic mass near spinal cord at C1. Patient was treated with VTD-PACE regimen (bortezomib, thalidomide, decadron, cisplatin, liposomal doxorubicin, cyclophosphamide, and etoposide) with excellent response to the treatment. She was referred for autologus stem cell transplant.
DISCUSSION: Malignancies of plasma cells comprise 1 % of malignant neoplasms which includes multiple myeloma, solitary plasmacytomas (including solitary bone plasmacytoma and extramedullary plasmacytomas) and immunoglobulin deposition syndromes. Cases with initial presentation of intracranial plasmacytomas are extremely rare. Central nervous system (CNS) involvement of multiple myeloma itself is not a common entity with the largest single center report of patients reported by Fassas et al. who published data of 18 cases over a course of 10 years. This is an extremely rare site for origination of brain tumors with differential diagnosis of brain tumors at this site being choroid plexus papilloma, ependymoma, subependymoma, subependymal giant cell astrocytoma, neurocytoma, meningioma, lymphoma and cerebral metastasis. Patients with CNS myeloma have poor prognosis with median survival being around 4–5 months. Our patient had excellent response with two cycles of VTD-PACE regimen with negative M-spike, normalization of IgG and decrease in size of subcutaneous nodules and C1 spinal lesion. She has survived for 5 months without autologus transplant and is currently on weekly cyclophosphamide, bortezomib and decadron.
INTERNAL CAROTID ARTERY DISSECTION - A CLASSIC PRESENTATIONOpeyemi Fadahunsi; Joelle Lauchner; Ana Abaroa-Salvatierra; Anthony Donato. Reading Health System, Reading, PA. (Tracking ID #1931485)
LEARNING OBJECTIVE 1: Recognize carotid artery dissection in patients presenting with a triad of unilateral headache or facial pain, neck pain and partial Horner syndrome.
CASE: We present an 18-year old female on oral contraceptive pills (OCPs) with a 2 month history of right-sided neck and periorbital pain. One week prior to admission she noticed new miosis and ptosis with no other neurological complaints and presented for evaluation. She specifically denied any trauma, rigorous activity, or personal or family history of connective tissue disease. Physical examination revealed unilateral ptosis and miosis, with no other abnormalities noted on examination. CT angiography of the neck demonstrated a 5 mm dissection of the right internal carotid artery. MRI of the brain was unremarkable. Echocardiography did not demonstrate any aortic root dilatation. This patient was admitted and placed on heparin with a warfarin bridge. She was discharged with instructions to complete 6 months of Coumadin therapy and to discontinue OCP use. At the 6 month evaluation, she continued to demonstrate findings of minimal right-sided ptosis and miosis with no other neurological findings. Repeat CT angiography of the neck and head revealed minimal residual irregularity of the distal cervical right internal carotid artery without significant stenosis. Coumadin was stopped and the patient was switched to Aspirin at this visit. A follow up appointment was scheduled in 1 year.
DISCUSSION: Although head, neck and facial pain are common complaints in the ambulatory setting, when presented with accompanying complaints of miosis and ptosis (partial Horner’s), one should have a high suspicion for carotid artery dissection. Early diagnosis may allow for consideration of anticoagulation or antiplatelet therapy with hopes of preventing a stroke event. Our case did not have any disabling deficit at the 6 month evaluation. This is consistent with findings in literature that showed excellent recovery in 70 to 85 % of cases of extracranial dissection.
INTESTINAL ASCARIASIS IN THE MODERN ERAParas Karmacharya1; Madan R. Aryal1; Pragya Shrestha2; Supriya Shrestha Tamrakar3; Ranjan Pathak1; Raju Khanal1; Satyajeet Roy4. 1Reading Health System, West Reading, PA; 2Nanjing Medical University, Nanjing, China; 3Guangxi Medical University, Guangxi, China; 4Cooper University, Camden, NJ. (Tracking ID #1935103)
LEARNING OBJECTIVE 1: Diagnose intestinal ascariasis which can present with non-specific symptoms and signs. Diagnosis requires high index of suspicion and can be usually made through a combination of blood counts showing marked leucocytosis with eosinophilia, stool studies and radiographic imaging.
LEARNING OBJECTIVE 2: Treat intestinal ascariasis with antihelminthic therapy which is usually effective except in few complicated cases where surgical interventions might be needed.
CASE: A 40-year-old woman presented with altered bowel movements, 10 lb weight loss and abdominal discomfort for 1 month. On examination, the patient was afebrile and had mild tenderness in the epigastric region. Prior to this, she had been on a week-long trip to Mexico. Patient’s complete metabolic profile, complete blood count, serum amylase and lipase, urine analysis and culture, and stool studies for white blood cells, ova, parasite, and culture were all either in the reference range or negative. An ultrasonography of the abdomen was normal. A computerized axial tomography (CT) scan of the abdomen with oral and intravenous radiocontrast material showed multiple tubular filling defects about 15 cm in length predominantly located in the jejunal lumen (Figure 1, 2 and 3), highly suggestive of intestinal parasites. She was treated with a one dose of oral albendazole 400 mg. After 1 week, her symptoms improved and she reported passage of 15–20 cm long cream colored cylindrical worms in her stool.
DISCUSSION: Most patients with intestinal ascariasis are asymptomatic, hence it can be undetected for years until they develop some symptoms (1,2). Diagnosis is usually made through a combination of blood counts showing marked leucocytosis with eosinophilia, stool studies and radiographic imaging. Complications can range from nutritional deficiency to obstruction of the bowel lumen, the bile or pancreatic duct, perforation, volvulus, intussusception, appendicitis, cholecystitis, biliary colic, cholangitis, hepatic abscess and pancreatitis depending on the site and severity of infestation (1,3). Antihelminthic therapy is usually sufficient except in few cases where surgical interventions might be needed (4). References: 1. Kanneganti K, Makker JS, Remy P. Ascaris lumbricoides: To Expect the Unexpected during a Routine Colonoscopy. Case Reports Med. 2013;2013:579464. 2. Suzuki A, Yabushita Y, Takahashi H, Inamori M, Nakao S, Suzuki K, et al. Gastrointestinal: Ascariasis. J Gastroenterol Hepatol. 2008;23(11):1770–1770. 3. Zheng P-P, Wang B-Y, Wang F, Ao R, Wang Y. Esophageal space-occupying lesion caused by Ascaris lumbricoides. World J Gastroenterol WJG. 2012 Apr 7;18(13):1552–4. 4. Tay K-V, Teo J-Y. Education and imaging. Gastrointestinal: Incidental findings of Ascaris Lumbricoides in patient presenting with ureteric colic. J. Gastroenterol. Hepatol. 2012 Jun;27(6):1127.
INTRACTABLE NAUSEA AND VOMITING IMPROVED THROUGH TARGETED SELECTION OF ANTIEMETIC MEDICATIONSRachel Havyer; Keith M. Swetz. Mayo Clinic, Rochester, MN. (Tracking ID #1938060)
LEARNING OBJECTIVE 1: List common pathways leading to nausea/vomiting.
LEARNING OBJECTIVE 2: Describe the various pathways associated with nausea/vomiting and appropriate pharmacologic targeting of receptors.
CASE: We present a case of nausea and vomiting (N&V) severe enough to require nutritional support, and discuss how appropriate evaluation and pharmacotherapy can lead to optimal outcome. An 84-year-old woman was transferred to our institution after a 21-day history of Intractable N&V associated with vertigo and inability to maintain hydration. Head MRI revealed a left cerebellar stroke. Ondansetron and prochlorperazine were given with no relief and haloperidol provided only modest improvement. The patient was initiated on parenteral nutrition due to lack of progress, and transfer to our institution was requested. Review of symptoms revealed that N&V dramatically worsened with head movement, suggesting a vestibular mechanism. Additionally, the symptoms started abruptly at the time of stroke diagnosis, suggesting a central source. Recommendations were made for anticholinergics (diphenhydramine) targeting the vestibular pathway, and dexamethasone targeting centrally. Haloperidol was continued in order to cover the dopaminergic receptors in the vomiting center. With these changes, the patient’s symptoms and quality of life improved significantly, allowing her to resume oral nutrition.
DISCUSSION: Nausea and vomiting is a common symptom that significantly affects quality of life, but all N&V is not the same. Patients with Intractable N&V require a detailed history and physical exam to investigate potential etiologies. Many pharmacologics exist for control of N&V, and some are often used routinely as part of hospital order sets. Medications prescribed for N&V without individual patient evaluation may result in lack of efficacy and results in resource overutilization (e.g. delayed hospital discharge, nutritional support). We promote a structured approach to N&V based on individual patient history and physical, and note that in cases of Intractable N&V, a careful review of etiologies and coverage of multiple neurotransmitters may be necessary to provide adequate symptom palliation.
IS CARDIAC CATHETERIZATION THE DEFINITIVE TREATMENT OF CARDIO EMBOLIC MYOCARDIAL INFARCTION FROM INFECTIVE ENDOCARDITIS?Leena Rahmat1; Vijay Gadiraju1; Shanmugam Uthamalingam2; Mathias Stoenescu2. 1Baystate Medical Center, Springfield, MA; 2Baystate Medical Center, Springfield, MA. (Tracking ID #1922897)
LEARNING OBJECTIVE 1: Myocardial infarction (MI) as a result of coronary artery septic embolization is a rare complication of infective endocarditis (IE), associated with a high mortality
LEARNING OBJECTIVE 2: Optimal therapeutic strategies remain controversial due to the risks from coronary intervention.
CASE: A 40-year-old male with a history of intravenous drug abuse (IVDA) presented with a three-day history of fever. His past medical history was significant for bacteremia, IE secondary IVDA requiring mechanical aortic valve replacement, hepatitis C, hypertension and hemorrhagic stroke. Physical examination was significant for a temperature of 102.2, sinus tachycardia, a systolic murmur and a normal neurological exam. He had a leukocytosis of 25000, and an echocardiogram revealed a 1.12 cm vegetation on the ventricular surface of the aortic valve. He was diagnosed with IE and was started on IV antibiotics. Blood cultures grew candida albicans and an antifungal was initiated. Cardiac surgeons deemed him a poor surgical candidate given his ongoing IVDA. During the hospitalization, he suffered an acute MI with ST-segment elevations in the infero-lateral leads on EKG and positive cardiac biomarkers (Troponin T 0.15, CK 688, and CK-MB 50.3). After weighing the risks and benefits, he underwent cardiac catheterization which demonstrated 100 % stenosis of the mid left anterior descending artery (LAD), consistent with embolic occlusion of the culprit vessel. The aspirated debris grew candida albicans. After the catheterization he suffered an embolic stroke with a frontal infarct resulting in expressive aphasia, comprehensive deficits, and behavioral issues. He improved during the hospital course and was discharged to rehabilitation.
DISCUSSION: IE is associated with a high in-patient mortality rate, ranging from 16 to 25 % and a high incidence of embolic events ranging from 13 to 49 %. Although septic embolization is a well delineated complication of bacterial IE, cardio embolic MI as a result of septic embolization from cardiac valve vegetation is rare, with an estimated incidence of 0.3–1 %. As rare as coronary artery emboli are, cardiac valves are the most common sources. Coronary angiography may establish the diagnosis of septic emboli in coronary arteries. There is a risk of dislodging a piece of vegetation into the systemic circulation if there is contact between the angiography catheter and the valve surface vegetation, which happened in our patient, resulting in a stroke. Fortunately our patient suffered a minor stoke and eventually improved but one would be at high risk of developing a major stroke and brain abscess from the dislodgement of the infected vegetation. The indication for percutaneous intervention mainly depends on the size of the infarct and degree of complications due to the MI. Surgical embolectomy using direct coronary incision has been described in literature as an alternative therapeutic option in unstable patients too. Cardioembolic MI is an uncommon and lethal complication of IE, associated with a high mortality. Its early recognition is vital in order to optimize management. The decision on coronary intervention should be made on a case by case basis considering the benefits vs. possible life-threatening complications.
IS THAT EFFUSION REALLY PARAPNEUMONIC? THE CHALLENGE OF AVOIDING CHEST TUBES IN HEPATIC HYDROTHORAX AND SPONTANEOUS BACTERIAL EMPYEMAHirotaka Kato; Dovid Moradi; Cameron S. Page. Beth Israel Medical Center, New York, NY. (Tracking ID #1935428)
LEARNING OBJECTIVE 1: Comprehend presentation, diagnosis and management of hepatic hydrothorax and spontaneous bacterial empyema.
LEARNING OBJECTIVE 2: Learn that chest tube is contraindicated for hepatic hydrothorax/SBEM and its complications and also understand the need for a low threshold of suspicion for hepatic hydrothorax in any cirrhotic patients with pleural effusion.
CASE: A 34 year-old male with hepatitis C and alcoholic liver cirrhosis presented with 1 day history of nausea, bilious vomiting and intermittent epigastric pain. The patient had elevated WBC but no fevers, SpO2 was 92 % on ambient air, and abdomen was tender to palpation in the right upper quadrant. Intra-abdominal processes were suspected, but abdominal ultrasound, HIDA scan, and paracentesis were all negative. Chest X ray revealed right pleural effusion and chest CT showed RLL infiltrate, so ceftriaxone and metronidazole were started for pneumonia with parapneumonic effusion. Thoracentesis showed an exudative fluid. Blood cultures detected Streptococcus pneumoniae but pleural fluid culture was negative. In the 48 h after thoracentesis, he developed aggressive re-accumulation of right pleural effusion and a chest tube was placed. Over the next 2 days nearly 4 L of pleural fluid was drained from the chest tube, and repeat samples showed a transudative fluid, consistent with hepatic hydrothorax. Chest tube was clamped to prevent further nutritional and albumin loss, and aggressive diuretic treatment was begun. His hospital course was complicated by worsening cirrhosis and variceal bleeding, which required blood transfusions and 3 days in the MICU. On hospital day 16 the patient accidentally pulled out his chest tube and a fistula formed between the pleural space and the chest wall. Due to active alcohol use, the patient was not a candidate for liver transplantation, and he was discharged to hospice for comfort care on day 22.
DISCUSSION: Hepatic hydrothorax and spontaneous bacterial empyema (SBEM) are rare complications of cirrhosis. They have been known to occur even in the absence of ascites. SBEM occurs in 15 % of hepatic hydrothorax patients. The diagnostic criteria include culture-positive or culture-negative pleural fluid, with PMN count greater than 500, or flank pus. At the time of chest tube placement this patient did not meet criteria for SBEM. Due to his poor prognosis and refusing tap, antibiotics were started before thoracentesis, however, which may have complicated the diagnosis. The presence of S. pneumoniae bacteremia in the setting of pleural effusion is supportive of the diagnosis of hepatic hydrothorax with SBEM. Chest tube placement is contraindicated in SBEM and hepatic hydrothorax. In this case, the clinical course included worsening cirrhosis and variceal bleeding, both of which are known complications of chest tube placement in hepatic hydrothorax. Chest tube placement might have accelerated the patient’s clinical course. Physicians should use caution when considering chest tubes in patients with cirrhosis. Even when imaging studies and pleural fluid suggest primary lung pathology, if the patient exhibits signs and symptoms of an intra-abdominal process then chest tube should be deferred until hepatic hydrothorax can be definitively ruled out.
ISOLATED VISCERAL KAPOSI’S SARCOMAKristin Bateman; Philip J. Putnam. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926112)
LEARNING OBJECTIVE 1: Recognize the incidence and presentation of visceral Kaposi’s sarcoma
LEARNING OBJECTIVE 2: Discuss the treatment course for visceral Kaposi’s sarcoma
CASE: A 26 year-old man presented with three-day progression of dyspnea on exertion. He experienced associated symptoms of odynophagia and dysphagia with an associated thirty-pound weight loss over 1 month. He has a history of untreated HIV diagnosed 5 years ago. He is not taking any medications. His exam revealed a pulse of 139 and fever of 101°, pale conjunctivae, cervical lymphadenopathy, white plaques in his oropharynx, and anal warts, with no gross blood on rectal exam nor skin lesions. A complete blood count revealed pancytopenia, and CD4 count of 3. Work-up of his microcytic anemia was consistent with iron deficiency and chronic inflammation. He was transfused two units of packed red blood cells. In the setting of oral thrush, iron deficiency anemia, and odynophagia with weight loss, the patient underwent esophagogastroduodenoscopy, which revealed esophageal candidiasis with esophagitis, and Kaposi’s Sarcoma of the stomach.
DISCUSSION: Kaposi’s Sarcoma (KS) is the most common cancer in HIV-infected individuals. Ninety percent of KS presents with cutaneous lesions, and about one-third of these individuals develop gastrointestinal metastases. KS also may metastasize to lymph nodes, lung, and liver. Overall, this angioproliferative disorder is an AIDS-defining illness, the spectrum of disease ranges from indolent skin manifestations to fulminant and extensive visceral involvement. Symptoms of gastrointestinal involvement are non-specific, and include chronic blood loss anemia, vomiting, diarrhea, and intestinal obstruction. Patients may also have asymptomatic visceral KS. The identification of visceral KS, particularly gastrointestinal, requires endoscopic biopsy. Endoscopic findings vary from patches to vascular submucosal nodules to bulky masses with ulcerations. Biopsy of patches in early disease tends to have low diagnostic yield, however, a negative biopsy result should not exclude KS. There is up to a 35 % false negative rate in gastrointestinal lesions, due to the variability of gross appearance of the lesions. Typically, disease limited to skin findings is treated with local therapy or electrochemotherapy. If there is visceral involvement, treatment includes antiretroviral therapy and systemic chemotherapy, the first-line treatment being liposomal anthracyclines. As visceral involvement portends a worse prognosis, early identification is crucial to start appropriate therapy. Patients with identified cutaneous lesions should be evaluated for visceral involvement as well. Overall, gastrointestinal KS is a difficult disease to identify, particularly when there are no associated cutaneous manifestations. The only independent risk factors identified in gastrointestinal KS are men-who-have-sex-with-men and CD4 cell count less than 100. With these risk factors and non-specific symptoms described earlier, primary care physicians should have a low threshold to refer for endoscopy to diagnose and treat this AIDS-associated malignancy.
IT IS MORE THAN A VOODOO. THE LIMBIC HEARTAhmed Abuzaid1; Hitham Al-Alshry1; Hamza Tantoush1; Allen Ameri1; Gale M. Etherton2,3. 1Creighton university, omaha, NE; 2UNMC, omaha, NE; 3VA Medical Center, omaha, NE. (Tracking ID #1934912)
LEARNING OBJECTIVE 1: The nervous system’s capacity to injure the heart has been described in a number of clinical reports. Excessive stimulation of the cortical limbic system is associated with hyperactivity of the catecholamine circuits. Cardiac involvement can be seen with excessive stimulation of the limbic system.
LEARNING OBJECTIVE 2: Hyperactivity of the catecholamine circuits can be precipitated by substance abuse, such as cannabis. Neurogenic cardiomyopathy is an uncommon presentation of cannabis can lead to misdiagnosis.
CASE: Our patient was a 60-year-old male with no significant past medical history. He was brought to the ED after persistent retrograde memory loss of 4 days duration. He denied any other complaints. He had a remote tobacco history, did not consume alcohol heavily but consumed cannabis 5 days prior to admission. He had no known drug allergy, no recent prescription drug intake and no significant family history. On examination, he was afebrile, blood pressure was 132/84 mmHg, and heart rate was 86/min. Physical examination was unremarkable except for impaired 3 min recall test. The results of routine biochemical tests were satisfactory. Serial cardiac biomarkers were mildly elevated. Urine screen was positive for cannabis only. An EKG showed NSR with deep T-wave inversions in anterior leads. TTE revealed severe anterior wall hypokinesia with estimated ejection fraction 30–35 %. A non-contrast head CT scan was unremarkable. Head MRI revealed patchy contrast enhancement in the left limbic region without mass effect or evidence of acute infarct, suggestive of limbic encephalitis. An electroencephalogram showed no evidence of seizure activity. Left heart catheterization showed non obstructive coronary disease and apical ballooning. Further evaluation of limbic encephalitis including viral serology and CSF analysis (chemistry, cell count, viral PCR panel, microbial cultures and cytology) were all unremarkable. A malignancy work up including whole body CT scan, para-neoplastic antibodies and a vasculitis panel were all negative. A diagnosis of neurogenic stunned myocardium as a manifestation of cannabis induced limbic encephalitis was established. Mini-Mental Status examination towards the end of the hospitalization was 26/30 with deficits in recalls and date abilities (unchanged since admission). Follow up showed significant resolution of his EKG, echocardiography and memory deficit with complete cannabis abstinence.
DISCUSSION: After excluding viral and autoimmune disorders, many patients with limbic encephalitis have CSF, EEG or MRI abnormalities, and rarely, myocardial compromise. Our patient’s cardiac abnormalities included EKG changes, mild elevation of cardiac biomarkers and transient LV dysfunction. Over activity of the sympathetic limb is the common phenomenon that associates the major cardiac pathologies seen in neurological insults. It is thus conceivable that overstimulation of catecholamine circuits in the limbic system due to cannabis ingestion could manifest as neurogenic heart disease. Providers should be aware of an uncommon presentation of cannabis ingestion.
IT’S NOT YET TIME TO HANG UP YOUR HATMarie Caldwell; Jonathan Kirsch. UNC Hospitals, Chapel Hill, NC. (Tracking ID #1895542)
LEARNING OBJECTIVE 1: Diagnose a long term complication of liver transplantation.
LEARNING OBJECTIVE 2: Recognize the anatomic complications of hepatic artery thrombosis.
CASE: A seventy year-old woman presented with 8 weeks of progressive abdominal pain. She underwent a liver transplant 12 years ago and had a previously uncomplicated course. Her abdomen was tender to palpation in the right upper and right lower quadrants without rebound or guarding. She had no scleral icterus or asterixis. Her transaminases (AST and ALT) were both over 2000 U/L, bilirubin was 1.4 mg/dL, INR was 1.2, and white blood cell count was 17 × 10^3/μL. Liver ultrasound revealed a hepatic abscess in the right lobe with poor visualization of the right hepatic artery. She was started on intravenous antibiotics and a percutaneous drain was placed into the abscess. Blood and abscess cultures grew Enterococcus faecalis. After abscess drainage a liver ultrasound was repeated and showed no hepatic arterial flow. A hepatic arteriogram confirmed a 100 % occlusion of the common hepatic artery, consistent with complete hepatic artery thrombosis (HAT). She was not a candidate for retransplantation due to her age and comorbidities. Despite the complete hepatic artery occlusion the patient’s transaminases and bilirubin trended down to normal. She continued to improve clinically and was discharged home with a drain in place and on antibiotics.
DISCUSSION: As more liver transplants are performed each year and transplanted livers are lasting longer, more hospitalists will be taking care of these patients. Short term complications include graft rejection and infections. Long term complications are not as well characterized in this patient population. HAT occurs in 1–10 % of liver transplant recipients, mostly in the first 30 days, and has a mortality of 73 %. Late HAT has a milder clinical course, likely due to the development of collateral circulation. Clinical presentation includes fever, elevated transaminases, and a biliary leak or hepatic abscess. Our patient had developed collaterals and improved after drainage of the abscess. HAT is diagnosed with Doppler ultrasound and can be confirmed with hepatic angiogram or MRI. Broad spectrum antibiotics are recommended as bacteremia is a common complication. Treatment includes drainage of abscess or fluid collection and broad spectrum antibiotics. Re-transplantation should be considered if the operative risk is acceptable. This case illustrates the unique and complex circulation of the liver, which is important to understand in patients with long lasting liver transplants. The portal vein supplies two thirds of the blood flow to the liver; the hepatic artery supplies the latter one third and supplies all of the blood to the biliary tract. HAT therefore tends to cause ischemia and rupture of the biliary tract. However, the liver parenchyma may be spared due to the unique circulation in the liver. Venous and arterial circulation mix within the hepatic sinusoids and the hepatocytes receive sufficient oxygen even without a functioning hepatic artery.
IT’S NOT ALL IN HER HEADNeetha Reddy; Manuela Calvo. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939333)
LEARNING OBJECTIVE 1: Recognize appropriate approach to hypereosinophilia
LEARNING OBJECTIVE 2: Recognize presentation, management and prognosis of hypereosinophilic syndrome
CASE: A 34 year-old woman presented with a 4 year history of intermittent severe abdominal pain associated with nausea and non-bloody diarrhea. She had no past medical history and took no medications. She had been hospitalized several times for abdominal pain in the past. No organic etiology had been found and psychiatric etiology had been considered. On exam abdomen was mildly tender to palpation in the lower quadrants. Initial eosinophil count was 2700 cells/mcl and peaked at 9500 cells/mcl. Infectious, atopic, and autoimmune workup was unrevealing. CT abdomen revealed diffuse thickening of the esophagus and portions of the small and large bowel. EGD and subsequent biopsy revealed marked eosinophils in the duodenal lamina propria. Bone marrow biopsy revealed marked eosinophilia as well. Bone marrow cytogenetics were normal. Echocardiogram and CT thorax were unremarkable. The patient was started on systemic steroids. Eosinophil count dropped to 0.1 cells/mcl and her symptoms improved.
DISCUSSION: Eosinophila is defined as >500 eosinophils/mcl of blood. Causes of eosinophilia include medications, infection, atopy and malignancy. Parasites that can cause eosinophila are strongyloides, toxocara, trichanella, schistosoma, hookworm, filariae, and entamoeba. In patients with pulmonary symptoms, allergic bronchopulmonary aspergillosis should be considered in those that have a history of asthma and coccidioidomycosis should be considered in those that have been in endemic areas. Rarely rheumatologic conditions and immunoglobulin deficiencies can lead to eosinophilia. Benign and malignant hematologic disorders (leukemia, lymphoma, mastocytosis, hypereosinophilic syndromes) can cause eosinophilia as well. These conditions can be evaluated for though thorough history, laboratory testing, and in the case of hematologic disorder, bone marrow biopsy. Hypereosinophilic syndrome is defined as >1500 eosinophils per microliter of blood with no other apparent etiology of eosinophilia (asthma, parasites etc.) accompanied by eosinophil mediated multiple end organ dysfunction. Hypereosinophilic syndrome can be further sub-classified into primary hypereosinophilic syndrome and overlap hypereosinophilic syndrome. In primary hypereosinophilic syndrome eosinophilic expansion is due to underlying hematologic malignancy. In overlap hypereosinophilic syndrome there is no underlying malignancy and only single organ involvement. Presentation of hypereosinophilic syndrome varies greatly depending on which organ systems are involved. 14‰ of patients with hypereosinophilic syndrome present with gastrointestinal symptoms such as abdominal pain, gastritis, enteritis, or colitis. Workup of suspected hypereosinophilic syndrome includes, first and foremost, ruling out other possible causes of hypereosinophila followed by bone marrow biopsy to assess for underlying malignancy. Patients should also have through laboratory and imaging workup to assess for end organ involvement. Once the diagnosis of hypereosinophilic syndrome is made patients are treated with prednisone (and imatinib in the case of primary hypereosinophilia). Prognosis is dependent upon degree of end organ damage, presence or lack of underlying malignancy, and degree of response to systemic steroids.
IT’S NOT ALWAYS A RELAPSE: SPORADIC CREUTZFELDT-JAKOB DISEASE IN A PATIENT WITH RELAPSING-REMITTING MULTIPLE SCLEROSISJulius Cesar G. Laban; Rex Wilford. Summa Health System, Akron, OH. (Tracking ID #1912662)
LEARNING OBJECTIVE 1: Recognize the clinical features of sporadic Creutzfeldt-Jakob disease in a patient with relapsing-remitting multiple sclerosis
CASE: A 47-year-old African-American female with 7-year history of relapsing-remitting multiple sclerosis (MS) was admitted for a 2-month history of rapidly worsening mental status, generalized weakness, gait abnormality, speech difficulty, and hallucinations. The patient denied any recent travel or family history of early-onset dementia. She was diagnosed with subacute MS relapse by her local neurologist 1 month prior to admission. Extensive neurologic, autoimmune, infectious, and metabolic work-up was done. Blood tests were unremarkable. Initial magnetic resonance imaging (MRI) of the brain showed moderate typical MS-appearing demyelination. The electroencephalogram exhibited diffuse slowing without periodic complexes. Cerebrospinal fluid (CSF) analysis revealed a mildly elevated protein (50 mg/dL), normal glucose without leukocytosis, and presence of oligoclonal bands. The CSF 14-3-3 protein test came back positive suggesting the diagnosis of sporadic Creutzfeldt-Jakob disease (CJD). This was further confirmed with repeat MRI of the brain (done 17 days after the previous one) that showed abnormal hyperintensities with diffusion restriction in bilateral caudate nuclei and putamen. The patient was discharged to a skilled nursing facility with progressive neurologic decline (exhibited myoclonus and akinetic mutism), and subsequently died 28 days after her initial presentation.
DISCUSSION: MS and CJD share a number of clinical, pathologic, and immunologic features that may be explained by the proposed “molecular mimicry” and autoimmunity that may exist between the two disease processes. These similarities may pose a diagnostic challenge to the clinician. Hence, it is not always a relapse, sporadic CJD should be considered in the differential diagnosis of a patient with established MS presenting with rapidly progressive dementia. To our knowledge, this is the first report of CJD in a patient with established MS in the United States.
K2, SPICE THE GUT DON’T LIKE: CANNABINOID HYPEREMESIS SYNDROME DUE TO THE SYNTHETIC CANNABINOID K2Anene Ukaigwe; Paras Karmacharya; Anthony Donato. The Reading Health System, West Reading, PA. (Tracking ID #1939115)
LEARNING OBJECTIVE 1: Diagnose Cannabinoid Hyperemesis Syndrome (CHS)
LEARNING OBJECTIVE 2: Recognize that Conventional Urine Drug Screen (UDS) is negative in cannabicyclohexanol (K2) users.
CASE: 38-year-old man with no significant past medical history presented with 1-week history of episodes of nausea and vomiting of clear fluids, associated with ill-defined epigastric pain. He has had previous episodes in the past 3 months. He reports that only hot showers relieve symptoms. Review of symptoms was not contributory. He admitted using cannabis for over 10 years, changing to K2 spice in the past year. On examination, vital signs were within normal limits. His abdomen was soft and non-tender. Bowel sounds were reduced. The remaining physical examination was unrevealing. He interrupted evaluation and care several times to take hot showers. Laboratory test showed sodium −123 mEq/L, BUN −160 mg/dl, Creatinine −4.78 mg/dl. Liver function test, amylase and lipase were normal. Abdominal x-rays did not reveal any bowel obstruction. Esophagogastroduodenoscopy was unremarkable. UDS was negative. Renal ultrasound and urinalysis was normal. Fractional excretion of sodium (FeNa) was 40 %. Given chronic cannabis use, cyclic vomiting, abdominal pain without other cause found on eveluation, CHS was diagnosed, complicated by pre-renal acute renal failure (ARF). He was treated with intravenous fluids and ondansetron. ARF resolved within 72 h. He was counseled on the need to quit all cannabinoids to prevent further episodes. He remained normal and abstinent at 2-month follow up.
DISCUSSION: Allen et al. recently described CHS in 2004. CHS is characterized by cyclical nausea and vomiting, abdominal pain and an unusual compulsion to take hot showers in the presence of chronic use of natural and now synthetic cannabinoid substances. Although antiemetic properties of cannabinoids drive the “medical marijuana” campaign, it is important to note that it may have paradoxical effects as in CHS. Due to relative novelty of CHS, it is often unrecognized by clinicians leading to huge health care costs in evaluating these patients with cyclical symptoms. It has been reported that it may take up to 9 years to arrive at a diagnosis. This delay may lead to patient and physician dissatisfaction. The treatment consists of supportive care. Intravenous fluids may be needed, as the vomiting may be severe enough to cause renal failure as in our patient. The only definitive treatment is complete cessation of the culprit cannabinoid, as evidenced by the fact that the symptoms resolve as drug levels wane. Cannabinocyclohexanol, is a synthetic cannabinoid, popularly known as K2 spice. It is increasingly used as a marijuana alternative among teenagers and young adult as it is readily available as herbal incense. Unlike marijuana, Cannabinoids are negative on UDS with K2 use, making it even more attractive to these patients. K2 is detected, only with gas chromatography mass spectrophotometry, which is not widely available. It is imperative for clinicians to recognize CHS, even with negative UDS, to provide cost effective care, help patients break the cycle of cannabinoid and CHS.
KNOWN ENEMY TO THE KIDNEY…ALSO A HEPATIC FOEGeorge Shelton1,2; Nivedita Lakhera3; Pradeep Yarra3; LeChauncy D. Woodard1,4. 1Michael E. DeBakey VA Medical Center, Houston, TX; 2Baylor College of Medicine, Houston, TX; 3Wake Forest Medical Center, Winston Salem, NC; 4Baylor College of Medicine, Houston, TX. (Tracking ID #1928538)
LEARNING OBJECTIVE 1: Recognize Ciprofloxacin as a Cause of Drug-Induced Liver Injury (DILI)
LEARNING OBJECTIVE 2: Differentiate DILI from Drug Rash with Eosinophilia and Systemic Symptoms (DRESS)
CASE: A 41 year-old African American male with past medical history significant for dilated cardiomyopathy (EF 30–35 %), diabetes, hypertension, hyperlipidemia, gout, obesity, and recent admission for acute renal failure and urinary tract infection presented to the emergency department 3 days after hospital discharge. He complained of pruritus, rash, nausea, and diarrhea. He was found to have acute renal failure and hepatic dysfunction. Labs at presentation included potassium 6.3, Cr 3.72, BUN 75, total bilirubin 2.9, Alkaline Phosphatase (AP) 351, AST 832, and ALT 959. Medications included spironolactone, allopurinol (last dose 4 weeks ago), lisinopril, ciprofloxacin, furosemide, and metolazone. On admission, urinalysis showed epithelial casts and proteinuria (Protein/Creatinine ratio of 0.46). FENa was consistent with pre-renal azotemia. Abdominal ultrasound revealed hepatosplenomegaly. Non-contrast CT revealed hepatic steatosis. The patient’s liver function tests peaked on hospital day 3 (Bilirubin 3.6, AP 493, AST 1059, ALT 1231). His INR was 2.04. Gastroenterology was consulted. Triglycerides, ceruloplasmin, and iron saturation were normal. Screening for viral (EBV, CMV, HIV, Hepatitis A- C) and autoimmune (anti-Smooth Muscle Ab and ANA) etiologies was negative. The patient was diagnosed with ciprofloxacin-induced- liver injury (CILI). Given his deteriorating hepatic failure, he was treated with N-Acetylcysteine and steroids with rapid improvement in hepatic (AP 97, AST 298, ALT 341, and INR 1.2) and renal (Cr 1.5) function at discharge.
DISCUSSION: CILI is a rare complication of a common medication. The mechanism of liver injury is thought to be a hypersensitivity response to fluoroquinolones. It occurs most commonly in adults over 30 years old, presenting with symptoms of liver injury within 1–10 days after drug exposure. Common symptoms include nausea, abdominal pain, jaundice, pruritus, fever, rash, and eosinophilia. In patients with immunologic symptoms such as fever, rash or eosinophilia, steroids may be effective. In patients with CILI, the R-ratio (percent increase in ALT above upper limit of normal (ULN)/percent increase in alkaline phosphatase above the ULN) is used to predict the pattern of liver injury. R-ratios of >5 suggest hepatocellular injury (5.83 for this patient), R-ratios <2 suggest cholestatic injury, and R-ratios of 2–5 suggest a mixed hepatocellular/cholestatic liver injury pattern. Fever is more common with cholestatic injury whereas rash is found in hepatocellular or cholestatic liver injury patterns. Mixed liver injury pattern confers the best prognosis and is not associated with rash. In one study, CILI carried a 15 % mortality rate--consistent with the 10 to 80 % mortality rate for DILI with acute liver failure. DRESS also primarily occurs in adults. It usually presents 2–6 weeks after exposure to agents such as anticonvulsants, allopurinol, sulfonamides, dapsone, minocycline, or vancomycin. Symptoms include fever, malaise, lymphadenopathy, and rash. Other signs and symptoms are related to liver (hepatomegaly and jaundice), renal (acute interstitial nephritis, proteinuria, and eosinophiluria), or pulmonary (cough, tachypnea, hypoxemia, pneumonitis, etc.) involvement. DRESS has an approximate 5 % mortality rate. This patient had features of DRESS and CILI. His hepatic and renal dysfunction could have represented DRESS with rash, AIN, and liver involvement vs. CILI with rash and renal hypersensitivity nephritis. The time course of his symptoms was consistent with both DRESS and CILI as he was exposed to allopurinol (DRESS) 4 weeks prior to presentation and exposed to ciprofloxacin (CILI) 4 days prior to presentation. However, this patient did not meet diagnostic criteria for DRESS. The European Registry of Severe Cutaneous Adverse Reactions (RegiSCAR) DRESS and Japanese consensus DIHS (Drug-induced hypersensitivity syndrome) diagnostic criteria both include a drug-related rash, fever, adenopathy, organ involvement, and hematologic abnormalities. This patient had a suspected drug-related rash and organ involvement; however, he had no adenopathy, fever, eosinophilia, or other hematologic abnormalities. Thus, he met 2 of the 3 required RegiSCAR criteria and only 2 of the required 5 Japanese Consensus DIHS Criteria. Given that he did not meet diagnostic criteria for DRESS and had an otherwise negative evaluation, his presentation was most consistent with CILI. He was treated with steroids given the presence of a rash indicating likely hypersensitivity. He was also given N-acetyl cysteine as this has been shown to improve transplant-free survival in some cases of DILI-related acute liver failure. His rapid response to these therapies further supported the diagnosis of hypersensitivity-mediated CILI.
LADY WINDERMERE’S RASHPaavani Komanduri. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1939180)
LEARNING OBJECTIVE 1: Describe the role of Mycobacterium Avium Intracellulare complex in creating cavitary lung lesion
LEARNING OBJECTIVE 2: Discuss the treatment of pulmonary MAI disease
CASE: Mrs. Z is a 53 year old with a history of anorexia nervosa and anemia who presented to her primary care doctor with a new onset of rash. The rash started 4 days prior to the visit as macular non-blanching lesions in her inner thighs that progressed to cover both lower extremities. Over the next 2 days they evolved and became purpuric lesions. She noted that for the last 1 month she had a non-productive cough and night sweats without fevers, dyspnea or orthopnea. She also noted mild arthralgia of her knees over the same span of time. Physical exam demonstrated a thin female in no distress. Her BMI was 14.9 and other vitals were within normal limits. Her cardiac, lung and abdominal exams were unremarkable. Her lower extremities were covered in a numerous 0.5 cm macules with interspersed palpable purpura. Her initial labs were remarkable for normal basic metabolic panel and ESR of 88 with hsCRP of 4.155. Chest X-ray showed an alveolar left lung infiltrate with a thin-walled right upper lobe cavitary lesion which was confirmed on chest CT. CT also showed bronchiectasis and small scattered nodules. She underwent induced sputum which eventually grew Mycobacerium Avium Intracelluare. Biopsy of her skin rash was consistent with a leukocytoclastic vasculitis due to the MAI. Further testing for a vasculitic cause of her purpura including ANA, ANCA, C3, C4, hepatitis B and C were all negative. Patient was started on azithromycin, ethambutol and rifampin which resulted in improved in her cough and resolution of her rash. However, after 6 months of therapy, she continued to have positive sputum cultures and moxifloxacin was added. Two months later, her disease worsened radiographically and she was started on inhaled amikacin which resulted in negative sputum culture.
DISCUSSION: Mycobacterium Avium Intracellulare is a ubiquitous bacteria composed of two species of bacteria. In the United States, pulmonary MAC can occur in up to 5.6 per 100,000, with 60 % of cases in females. It is traditionally found in AIDS and lymphoma patients with CD4 counts less than 50. MAC in non-immunosuppressed hosts is generally due to pre-existing pulmonary disease. Elderly thin women and anorexic women without predisposing pulmonary disease are thought to develop MAC due to deficient interferon-gamma pathways. Pulmonary disease in this population is historically referred to as Lady Windermere Syndrome. Patients most frequently present with chronic productive cough, but may not be diagnosed for months or years due to the relatively mild symptoms. Fever and hemoptysis are more common in patients that have culture positive sputum. Unlike patients with pulmonary tuberculosis, patients with pulmonary MAC are not infectious and close contacts and healthcare workers are not at risk of contracting the disease even if sputum cultures are positive. The mainstay of treatment is a triple drug regimen comprised of a macrolide, a rifamycin such as rifampin and ethambutol. In patients who fail this therapy, quinolones may be added, followed by either streptomycin or amikacin. Treatment typically lasts for 12 months. Unfortunately, patients with low BMI frequently cannot tolerate these regimens due to significant GI distress (nausea, diarrhea). Treatment is considered successful if radiographic regression and negative sputum cultures are achieved. Patients who fail chemotherapy and have sufficient lung reserve can undergo surgical resection. Successful treatment ranges from 20 to 90 % depending on the study. Pulmonary MAC is usually an indolent process with 50 % of non-immunosuppressed patients alive after 5 years. Poor prognosis is associated with fibrocavitary pulmonary disease, BMI less than 18.5 kg/m2, and anemia. Patients with these factors have high MAI related mortality and all-cause mortality.
LANGERHANS CELL HISTIOCYTOSIS OF LUNG AND BONEDipenkumar Modi; Hirva Mamdani; Diane L. Levine. Wayne State University, Detroit, MI. (Tracking ID #1936454)
LEARNING OBJECTIVE 1: To recognize Langerhans cell Histiocytosis as a rare cause of reticulonodular/cystic lung disease.
LEARNING OBJECTIVE 2: To recognize the wide spectrum of presentation of Langerhans cell Histiocytosis and various diagnostic modalities.
CASE: A 27 y/o African American woman with extensive smoking history was admitted for progressively worsening right sided pleuritic chest pain and dry cough over 2 weeks duration. She had decreased exercise capacity gradually worsening over past few months and on presentation, she was also remarkably dyspneic at rest. Review of systems was positive for fever, night sweats and 14 lb unintentional weight loss over 3 months. Chest x-ray on admission showed inferior scalloping at the posterior aspect of several ribs. CT thorax showed numerous cysts of different sizes and morphology within the upper and mid lung field and a 1.6 cm soft tissue mass within the right sixth rib. Pulmonary Function test showed moderate restrictive lung disease, with reduced total lung capacity, residual volume and DLCO. Thoracoscopic right lung wedge resection was performed which showed Multiple lymphohistiocytic infiltrates, consistent with Langerhans cell histiocytosis (LCH). Pleural biopsy showed fibroadipose tissue with focal chronic inflammation. Diagnosis of pulmonary LCH was made by immunohistochemistry studies which showed histiocytes positive for CD1a and S-100. They were negative for CD68 and AE1/AE3. Since patient was an active smoker, chemotherapy was not started and she was counseled about smoking cessation.
DISCUSSION: Langerhans cell histiocytosis (LCH) is a very rare clonal proliferative disorder characterized by uncontrolled proliferation of Langerhans cells (LC). LC represents the main antigen capturing, processing and presenting dendritic cells in the epithelial surfaces including skin, oral mucosa, and bronchial epithelium. The estimated incidence rate in adults is 1–2 adult cases per million populations with peak age at presentation being 30 years, whereas in pediatric populations, incidence rate is about 5 cases per million and usually affects children younger than 10 years. Various risk factors have been described in literature i.e. cigarette smoking, recurrent BRAF V600E mutation etc. Increased number of dendritic cells by altering normal physiologic turnover as well as non-clonal proliferation of Langerhans cells in cigarette smoking patients has been implicated as possible mechanisms for the development of pulmonary LCH. Resistance to apoptosis has also been proposed by up-regulating expression of anti-apoptotic proteins i.e. Bcl-2 or Bcl-xL by mature LCs. LCH has wide spectrum of presentation. General symptoms are fever, night sweats, loss of appetite, weight loss and asthenia. Pulmonary LCH presents with nonspecific symptoms i.e. nonproductive cough, chest pain and exertional dyspnea. Some patients also present with spontaneous pneumothorax or pulmonary hypertension. Eighty percent of LCH patients have bone involvement with main complaints being bone pain. It can present with various endocrine abnormalities among which Diabetes Insipidus is the most common manifestation, seen in up to 30–40 % of patients. Anterior Pituitary is involved in up to 20 %. In pulmonary LCH, bilateral symmetric reticulonodular infiltration is the most common finding on chest radiograph. Cystic changes may also be apparent within the infiltrates which typically has bilateral distribution with frequent sparing of costophrenic angles. The characteristic HRCT findings are nodules with/without cavitations, and different types of cysts (thin and thick walled) involving mainly upper and lower lung lobes with both peripheral and central lung field distribution. Obstructive, restrictive or mixed pattern are observed on pulmonary function tests. The reduced DLCO is the most commonly noticed abnormality in 70–90 % of patients. Histologically, LCH cells are characterized by their prominent cleaved nucleus with pale cytoplasm, and characteristically reactive for CD1a, langerin (CD207), S-100 protein, and CD11. The cells are also positive for vimentin, CD68, and HLA-DR. Smoking cessation is of utmost importance in patients with pulmonary LCH. Serial pulmonary function tests every 3 months in first year of diagnosis are performed to assess for progressive disease. Corticosteroid therapy should be initiated in patients with persistent pulmonary or constitutional symptoms, or evidence of progressive disease on serial PFTs. 2-CDA (cladribine), cyclophosphamide, and methotrexate may be considered in progressive pulmonary LCH despite steroid therapy.
LARGE PERICARDIAL EFFUSION ASSOCIATED WITH SEVERE PULMONARY HYPERTENSIONRavi Thimmisetty; Manogna Nookathota; Janardhana Gorthi; Ariel Modrykamien. Creighton University Medical Center, Omaha, NE. (Tracking ID #1926447)
LEARNING OBJECTIVE 1: Recognize the challenges in treating patients with large pericardial associated with severe pulmonary hypertension.
LEARNING OBJECTIVE 2: Stabilizes RV function in this group of patients Assess when NOT to drain
CASE: 60 year old female presented with worsening exertional dyspnea for 2–3 days. Past medical history includes: Group I Pulmonary Hypertension (PAH), Diabetes, Hypertension and Gastric antral ectasia. Vital signs were: temperature-97.4 F, B.P-130/80, heart rate-104, O2 sats 94 % on 2 l. Physical exam revealed jugular venous distension, tachycardia, distant heart sounds and bilateral pedal edema. Rest of the exam was unremarkable. Laboratory data was within normal limits. EKG showed sinus tachycardia with low voltage QRS complexes. Echocardiogram revealed a large pericardial effusion, right ventricular systolic pressure of 74 mmHg (35 mm from a prior study 6 months ago), left ventricular ejection fraction 60–65 %, moderately dilated right ventricle with reduced systolic function, flattened inerventricular septum consistent with RV pressure overload, diastolic left atrial compression, severely enlarged right atrium and no evidence of tamponade. She was diagnosed with worsening pulmonary hypertension associated with a large pericardial effusion. In view of high mortality in this setting, pericardiocentesis was not performed as the patient was hemodynamically stable. She was started on IV prostacyclins with significant improvement in symptoms and hemodynamic profile. Echocardiogram prior to discharge showed improved RV function compared to admission.
DISCUSSION: Right ventricular failure is the most common cause of death in patients with pulmonary hypertension, and RV function is the major determinant of morbidity and mortality in this patient population. Even though, pericardial effusion is an independent predictor of mortality in patients with pulmonary arterial hypertension, physiologically and hypothetically it stabilizes RV function. Pulmonary hypertension complicated by pericardial effusion carries a poor prognosis, and little data exists to support management options in this clinical scenario. Perhaps, the removal of large amounts of pericardial fluid from an over-distended right heart results in loss of RV muscle tone with interventricular septal bowing and decreased left heart filling pressures, causing death. Chronic pericardial effusions associated with severe PAH are best managed medically. If attempted, Pericardiocentesis should be done very slowly with a drain in-situ. Our patient was very symptomatic and there was no tamponade physiology described on the echocardiogram. However, the absence of tamponade physiology with severe PAH is misleading due to the lack of collapse of RA and/or RV secondary to elevated right sided filling pressures. IV Prostacyclin use can improve the clinical profile in patients with RV dysfunction in this situation. With early prostacyclin use, our patient improved both clinically and hemodynamically.
LARYNGEAL AMYLOIDOSISJenny Koo; Laura Y. Sue; Pearl Yu. UC San Diego, San Diego, CA. (Tracking ID #1922246)
LEARNING OBJECTIVE 1: Recognize the clinical manifestations of isolated amyloidosis versus systemic amyloidosis andhow to diagnose amyloidosis with histopathology.
LEARNING OBJECTIVE 2: Understand what organs can be affected in systemic amyloidosis and determine what work-up is required.
CASE: A 37 year-old female former singer presents with chronic, progressive hoarseness for 5 years. She had marked worsening of vocal quality over the prior 3 months with associated loss of vocal range, strain, and vocal fatigue. She denies reflux symptoms, dysphagia, or odynophagia and has no other systemic complaints. Flexible laryngoscopy revealed a stiffened right vocal with a yellow-orange lesion. A small lesion was also noted on the left anterior false vocal fold. Microdirect laryngoscopy was performed and biopsies were taken of the left false vocal fold lesion and the right true vocal fold lesion. Frozen sections revealed no evidence of neoplasm or malignancy. Biopsy specimens were positive with apple green birefringence on Congo Red stain, consistent with amyloidosis. Mass spectrometry revealed AL kappa type amyloid deposition. Additional work up was performed to rule out systemic amyloidosis. Her complete blood count, electrolyte panel, liver panel, thyroid panel, and urinalysis were normal. An electrocardiogram (EKG) revealed normal sinus rhythm and an echocardiogram was performed which showed no cardiac involvement. Patient had a normal 24-hour urine collection which suggested no renal involvement. Serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) were negative for multiple myeloma.
DISCUSSION: Amyloidosis is a process of extracellular deposition of fibrils formed by low molecular weight subunits. There is higher prevalence in males between the ages of 40 and 60. AL (fragments of immunoglobulin light chain) is the more common subtype in developed countries, while AA (fragments of acute phase reactants) is more common in developing countries. Amyloid deposition can occur in any organ, more commonly in the kidneys, heart, liver, spleen, and gastrointestinal tract. Localized forms of amyloidosis are less common, and typically affect abdominal organs and structures of the head and neck. Amyloidosis represents only 1 % of benign laryngeal masses, and is most commonly supraglottic. Diagnosis is made with Congo Red staining which reveals “apple green” birefringence. Treatment is excision by laryngeal microsurgery with the goal of maintaining the structural integrity of the true vocal folds if possible. Although it is rare for laryngeal amyloidosis to be associated with systemic amyloidosis, a number of reports have revealed laryngeal amyloidosis in the setting of multiple myeloma or extramedullary plasmacytoma. Patients with underlying malignancy as the source of amyloidosis are likely to have systemic involvement, and thus require additional evaluation including a complete blood cell count, liver function test, urine tests, EKG, echocardiogram, and SPEP/UPEP. This case represents a rare form of isolated amyloidosis in a patient that does not fit the demographics most commonly associated with this disease. A thorough evaluation was warranted in this patient to rule out any systemic disease given the profound morbidity of systemic disease.
LATE DIAGNOSIS OF CYSTIC FIBROSIS: A MISSED OPPORTUNITYBrianna S. Siegel; Peter Rattner; Patricia Walker. Beth Israel Medicine Center, Mount Sinai Health System, New York, NY. (Tracking ID #1938620)
LEARNING OBJECTIVE 1: Recognize the atypical presentations of cystic fibrosis
LEARNING OBJECTIVE 2: Diagnose non-classic cystic fibrosis in adults.
CASE: A 30-year-old man presented for further evaluation of chronic cough, worsening over the past 3 years. His cough was productive with thick yellow sputum, upwards of a cup per day. Pertinent history included chronic pancreatitis due to pancreatic duct strictures diagnosed at age 16. Patient had multiple pancreatic ductal dilatations and stent placements, eventually undergoing pancreaticojejunostomy Roux-en-Y procedure at age 26. Abdominal CT imaging at the time incidentally noted right lower lobe bronchiectasis. Patient started to develop a productive cough in the following year and was treated for multiple recurrent pneumonias with oral antibiotics. He was a current smoker with a 16-pack-year history, no drug or alcohol use, no pets and no recent travel. Physical exam was notable for crackles in the right lower lobe with digital clubbing bilaterally. Bronchoscopy revealed normal bronchial anatomy without endobronchial obstruction, and cultures grew only normal flora. The sweat chloride test was borderline at 47 mEq/L. Pulmonary function testing showed a mild combined obstructive and restrictive defect. Genetic testing revealed two mutations of the CFTR gene: D1152H/G542X.
DISCUSSION: Cystic fibrosis (CF) is the most common genetic disease affecting Caucasians. In adults, CF is diagnosed by evidence of disease in one or more organ systems with laboratory evidence of dysfunction in the cystic fibrosis transmembrane conductance regulator (CFTR) protein, or the identification of 2 disease causing mutations by DNA analysis. Our patient was found to have the D1152H mutation, which has significant variability in phenotype ranging from normal to CF. It is usually characterized by mild late onset pulmonary disease, pancreatic sufficiency and congenital bilateral absence of the vas deferens. Variability in sweat chloride levels is also common. Recognizing non-classic CF can be a significant challenge due to the wide phenotypic variance seen in these cases. In up to 10 % of cases of suspected CF, patients have been found to have mild disease or dysfunction of a single organ system along with borderline or negative sweat chloride tests. The problem is further compounded when rare or unidentified CFTR mutations are present and not routinely screened on commercial panels. There has been a rise in diagnosis of CF in adults. However, these diagnoses are frequently overlooked or delayed when physicians are unfamiliar with the expanded spectrum of CF manifestations. It is important for internists to recognize these atypical phenotypes. There is now a wide range in treatments available that can help improve quality of life, delay disease progression, reduce overall morbidity, and increase life expectancy. Patients like ours, with mutations associated with residual CFTR function, continue to represent the population of adult patients who present with atypical CF.
LATENT TUBERCULOSIS INFECTION CAUSING ERYTHEMA NODOSUMSrividya Bhadriraju1,2; Jeffrey T. Bates2,1. 1Baylor College of Medicine, Houston, TX; 2Michael E. DeBakey VA Medical Center, Houston, TX. (Tracking ID #1939724)
LEARNING OBJECTIVE 1: Recognize erythema nodosum as a manifestation of latent tuberculosis
LEARNING OBJECTIVE 2: Understand the diagnosis and treatment of tuberculosis-associated erythema nodosum
CASE: An 18-year-old Mexican female presented with a recurrent painful rash. Two years prior to presentation, the rash initially appeared as painful, raised, dark red and purple “bruises” over her shins, thighs and abdomen; it was associated with weight loss, low-grade fevers, malaise, anemia and alopecia. At that time, a clinical diagnosis of panniculitis with erythema nodosum (EN) was made, and she received intravenous corticosteroids with subsequent improvement. During the following year, she had recurrent episodes requiring repeated courses of oral prednisone for relief. Laboratory studies revealed elevated ESR and CRP, negative ANA, and a positive tuberculin PPD with induration to 9 mm; however, she never received treatment for latent mycobacterial infection at that time. At the current presentation, she complained of only the rash and denied any symptoms or signs of pulmonary tuberculosis. Physical examination revealed multiple 3 cm, painful, erythematous subcutaneous nodules on her bilateral upper thighs. Although a repeat PPD was negative, a QuantiFERON Gold test was positive. A punch biopsy of the lesion showed septal panniculitis with minimal lobular involvement. She was diagnosed with EN, and was treated with isoniazid (INH) for latent TB. She was later switched to INH, rifampin, pyrazinamide and ethambutol (four-drug RIPE therapy) after developing recurrent EN while on INH monotherapy. She clinically improved on this regimen and has had no further recurrence of EN.
DISCUSSION: Erythema nodosum is a delayed hypersensitivity reaction to antigens occurring secondary to streptococcal infection, autoimmune disease or fungal infections. A complete blood count, chest X-ray, anti-streptolysin O (ASO) titers, and TB skin testing are recommended to elucidate etiology. A biopsy is required only in atypical cases, and a deep excisional biopsy is preferred. It typically shows panniculitis with septal inflammation in the subcutaneous fat tissue, usually without associated vasculitis. A study from Turkey demonstrated that primary TB was the most common cause of EN, and most patients with primary TB presented with EN. Although men with EN were more likely to have active TB compared to women, women had an increased risk of developing EN from TB. Corticosteroids are discouraged for the treatment of TB-associated EN; a four-drug TB regimen is recommended for treatment. Latent TB-associated EN is rare, and the initial diagnosis can be challenging as repeated courses of steroids may result in a falsely negative PPD. Polymerase chain reaction (PCR) detection of TB in the tissue has high sensitivity and specificity, and should be considered in these cases.
LEFT ATRIAL MYXOMA: A ‘ZEBRA’ IN THE DIFFERENTIAL FOR ALTERED MENTAL STATUS & SEIZUREPrasanna Durairaj; Auras R. Atreya; Issra Jamal; Thomas Higgins. Baystate Medical Center/Tufts University School of Medicine, Springfield, MA. (Tracking ID #1940170)
LEARNING OBJECTIVE 1: Recognize that neurological manifestations can be the first presentation of atrial myxomas.
LEARNING OBJECTIVE 2: Identify high risk features of embolization on echocardiography.
CASE: A 41-year-old female with a past medical history of chronic migraines and recently diagnosed primary hyperparathyroidism presented to the emergency room with altered mental status associated with a fall and seizure-like activity. As per her family, she had been doing well earlier that day without any headaches, neck pain, fevers, nausea or vomiting. Soon after arrival in the ED, she was intubated for airway protection. It was noted that her pupils were unresponsive and dilated so she underwent an emergent CT scan of the head which did not reveal any bleed. She was admitted to the ICU where cerebrospinal fluid was obtained to evaluate for HSV meningo-encephalitis and empirical IV acyclovir and fosphenytoin load were administered. Further review of history revealed that she had 2 other episodes of syncope in the past few months that had been attributed to dehydration and orthostasis in the setting of a viral illness. The next day, brain MRI was obtained due to lack of neurological recovery and showed multiple acute to subacute infarcts involving the supratentorial and infratentorial brain parenchyma bilaterally, consistent with an embolic process. Physical examination did not reveal any cardiac murmurs. MRA/MRV obtained at the same time did not show venous thrombosis or arterial aneurysm/Dissection. A transthoracic echocardiogram (TTE) showed an atrial mass concerning for myxoma. Subsequently, a trans-esophageal echocardiogram (TEE) confirmed a large left atrial myxoma attached to the inter-atrial septum, with multiple highly mobile villous processes. She was scheduled for emergent cardiac surgery, which revealed the mass to be gelatinous and fibrous, requiring suction for complete removal. Histological examination confirmed myxomatous tissue. The patient, however, continued to have neurological deterioration, with increased ICP, midline shift on repeat head CT scan and no improvement despite a decompressive hemicraniectomy. Eventually, her family withdrew care to respect her advance directives.
DISCUSSION: Myxomas are generally thought to originate from multipotential mesenchymal cells of the endocardium and are the most common primary cardiac tumors. There is a female predominance in the presentation of myxomas and only a minority of cases is familial (Carney Syndrome). In 90 % of patients with left atrial myxoma, symptoms are either related to mitral valve obstruction, systemic embolization or constitutional symptoms. Neurological manifestations, particularly cerebral infarction, can be the presenting symptoms in nearly a third of the patients with left atrial myxomas while right atrial myxomas frequently cause heart failure and pulmonary embolization. A high degree of suspicion is needed to consider a diagnosis of myxoma. Many cases are detected incidentally during TTE for evaluation of other cardio-embolic etiologies such as thrombus. TEE has been proven to be superior to TTE in the diagnosis and characterization of myxomas. It is the mobility, not the size, of the myxoma which appears to be related to embolic potential. In our patient, the myxoma appeared to be large, villous, frond-like and friable, leading to devastating neurological complications which ultimately led to her death. Prompt cardiac resection of the tumor is associated with good outcomes since the mortality rate of 10–15 % in these patients is related to sudden death in the setting of coronary or cerebral infarction as well as complete obstruction of blood flow at mitral or tricuspid valves. In conclusion, this case highlights that the differential diagnosis needs to be expanded to include rare diagnoses or “zebras” on occasion, especially in young patients with severe atypical presentations.
LEFT ATRIAL SEPTAL POUCH THROMBUS: A COMMON PATHOLOGY IN AN UNCOMMON LOCATIONSourabh Aggarwal; Vishal Gupta. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1940266)
LEARNING OBJECTIVE 1: To understand emerging pathology of left atrial septal thrombus
CASE: Left atrial septal pouch (LASP) is a recently described anatomical entity that is formed by the caudal fusion of the area of overlap between septum primum and the septum secundum. The potential for thrombus formation inside this pouch remains debatable. We present an extremely rarely reported case of LASP thrombus. Seventy-five year old male, with a known history of coronary artery disease status post stent in right coronary artery and left circumflex artery, presented to us with complains of new onset chest pain which was non-exertional, non-radiating and not relieved by rest. On physical examination, he was tachycardic (110 beats/min) with irregularly irregular rate. No murmurs were heard. Rest of physical examination was unremarkable. 12-lead EKG showed irregular rhythm with no signs of ischemia, confirming the diagnosis of new-onset atrial fibrillation. Initial lab evaluation including troponin were unremarkable. His rate was controlled with Cardizem which alleviated his chest pain. He was taken into echocardiography lab for transesophageal echocardiography (TEE) and potential cardioversion. TEE was significant for moderately dilated left atrium and normal left ventricular systolic function. A thrombus was noted in the left atrium originating from septal pouch. No thrombus was noted in left atrial appendage and contrast study did not show any evidence of inter-atrial shunt. He was diagnosed with LASP thrombus and started on anticoagulation therapy.
DISCUSSION: Left atrial septal pouch thrombus is an extremely rarely described entity. LASP is a newly understood anatomical entity (described as recent as 2010) with prevalence significantly higher than patent foramen ovale (39 % vs 24 %). It is thought to represent an incomplete closure of the foramen ovale resulting in formation of a kangaroo pouch like blind recess with opening in left atrium. Due to its anatomical features, it serves as a potential site of stasis and thrombus formation. In nonvalvular atrial fibrillation, left atrial thrombi almost exclusively tend to arise in the left atrial appendage due to decreased velocity (<20–30 cm/s). In our case, due to partly preserved contractile function of the left atrial appendage, no thrombus occurred there. Very few case reports have demonstrated LASP as a site of origin of thrombus formation. The 2-D TEE is an established modality for the evaluation of intracardiac mass/thrombus. Further prospective studies are required to determine the impact of LASP as a potential cause of cardiac embolism and its optimum management. The present case report indicates that more attention is needed to diagnose this structure when TEE is performed in susceptible patients.
LEGIONELLA PNEUMONIA IN A PATIENT WITH ADVANCED LUNG CANCERValida Bajrovic; Christopher Sankey. Yale School of Medicine, New Haven, CT. (Tracking ID #1924440)
LEARNING OBJECTIVE 1: Recognize Legionella as an important etiologic factor in community acquired pneumonia, especially in the immunocompromised host.
LEARNING OBJECTIVE 2: Review epidemiological characteristics, diagnostic testing, and treatment options in Legionella pneumonia.
CASE: A 54 year-old Caucasian woman with stage IV non-small cell lung cancer (NSCLC), currently on erlotinib and dexamethasone, presented with a 2 day history of progressive dyspnea. Her family noted a dry cough and mild confusion 2 days prior to admission. She denied fevers, chills, sick contacts, hemoptysis or other associated symptoms. On admission the patient was tachycardic, hypoxemic (O2 saturation 85 % on room air, 93 % on 6 l of oxygen) and tachypneic. Her physical examination was remarkable for dyspnea at rest making it difficult for her to speak in full sentences. Rhonchorous breath sounds were appreciated bilaterally with bronchophony over the left lower lung field. Laboratory testing revealed hyponatremia (sodium of 129 mmol/L), leukopenia, thrombocytopenia, and an elevated lactic acid. A spiral CT of the chest demonstrated a new dense consolidation involving the left lower lobe and patchy ground glass opacities throughout both lung fields. The patient was admitted for close monitoring of her respiratory status and placed on broad spectrum antibiotics. Her legionella urine antigen returned positive, and moxifloxacin was added to her regimen. The patient’s respiratory status continued to worsen, requiring intubation and transfer to the medical intensive care unit. Given her immunocompromised state and continued hypoxemia, azithromycin was added to moxifloxacin to treat severe legionellosis. Her clinical status continued to decline over the next 48 h, and she passed away after being transitioned to comfort measures.
DISCUSSION: Legionella was first identified in 1976 during an outbreak at an American Legion Convention in Philadelphia. It has since been implicated in two clinical syndromes: pneumonia (both hospital and community-acquired) as well as Pontiac fever, a self-limited acute febrile illness. L. pneumophila is the most common species; it is a water-borne pathogen, and man-made reservoirs such as water distribution systems amplify the growth of the organism. The most common risk factors for Legionella pneumonia are cigarette smoking and chronic lung disease. Glucocorticoid administration and other forms of immunosuppression are also independent risk factors, as was the case in our patient. The diagnosis of Legionnaires’ disease can be made by both a urinary antigen test and Legionella culture of a respiratory specimen. The urinary antigen test is specific for only L. pneumophila serogroup 1; the majority of Legionnaires’ disease cases from the community are caused by this species and serogroup. The sensitivity is significantly higher in patients with severe compared with mild pneumonia (86 versus 38 %), while specificity is 97 to 100 %. Azithromycin or respiratory quinolones are effective for Legionella infection. In severely ill patients or those with extrapulmonary legionellosis, institution of prompt treatment is paramount and a combination antibiotic therapy of a quinolone plus azithromycin should be considered. Our case demonstrates the importance of recognizing the clinical presentation of legionella pneumonia in the immunocompromised host, as it carries a high mortality and requires timely administration of appropriate antibiotic therapy.
LEMIERRE’S SYNDROME CAUSED BYCLOSTRIDIUM CLOSTRIDIFORMEIgor Tkachyk; El-waleed Ali; Sonia Borra; Harish Patel. Kingsbrook Jewish Medical Center, Brooklyn, NY. (Tracking ID #1897113)
LEARNING OBJECTIVE 1: to present a case of Lemierre’s syndrome caused by Clostridium Clostridiforme
CASE: A 24 year old female with known sickle cell trait developed sore throat and low grade fever and was treated with azithromycin by her physician. Five days later her condition worsened and she was admitted with fever, malaise, dyspnea and vomiting. Temperature 38.8 °C (102 °F), blood pressure 124/72 mmHg, pulse 124/min, respirations 24/min. Her tonsils were red and swollen with mild exudate, neck was supple. Chest examination revealed decreased air entry and bilateral basilar crepitations. Abdomen was with mild diffuse tenderness, active bowel sounds. Laboratory results revealed: hemoglobin 12.4 g/dL, white cell count 23000/μL, platelets 50000/μL, blood urea nitrogen 26 mg/dL, creatinine 1.67 mg/dL. Chest X ray showed consolidation at both lung bases. Computed tomography confirmed extensive bilateral infiltrates and loculated pleural effusions, as well as a thrombus in the internal jugular vein. Blood cultures grew Gram negative anaerobic rods after 1 day, later identified as Clostridium Clostridiforme sensitive to cefotaxime, clindamycin and metronidazole. She tested negative for Hepatitis B and C as well as HIV. The patient became hypotensive, was hydrated with intravenous fluids, placed on mechanical ventilation and treated with antibiotics and vasopressors. Initially azithromycin, meropenem and vancomycin were given and later switched to metronidazole and piperacillin and tazobactam. Her condition improved and she was extubated and later underwent video assisted thoracotomy for treatment of the empyema. The patient recovered fully.
DISCUSSION: Lemierre’s syndrome is a serious infection usually caused by Fusobacterium necrophorum, but other microorganisms have been implicated: Klebsiella pneumoniae, Streptococcus intermedius, Staphylococcus aureus, Arcanobacterium haemolyticum. This is the first report of Lemierre’s syndrome associated with Clostridium Clostridiforme, which is one of the predominant anaerobes in the intestinal tract and infrequently cause infections such as intraabdominal abscesses and occasionally have been described as causative agent of deep neck infections. The three clinically important species: Clostridium bolteae, Clostridium Clostridiforme and Clostridium haltewayi are morphologically and microscopically indistinguishable from each other are involved in human infections, including bacteremia.
LEUKEMIA OR SARCOMA? ITS A DIAGNOSTIC DILEMMA!!Arushi Khurana; N. Gurukripa Kowlgi. University of connecticut, Farmington, CT. (Tracking ID #1925979)
LEARNING OBJECTIVE 1: To recognize various and unusual presentation of Acute Myeloid Leukemia and Myeloid Sarcoma
CASE: A 20 year old female with no previous history initially presented with symptoms of generalized weakness, fatigue, progressive dyspnea on exertion and was found to have profound anemia with hemoglobin level of 6 g/dl. After extensive workup for common causes like nutrient deficiencies, blood loss, infections, drugs, connective tissue or autoimmune disorders and bone marrow suppression her labs were suggestive of hemolysis. She was diagnosed with warm type autoimmune hemolytic anemia and given treatment with pulse dose steroids which remarkably improved her condition. She subsequently had 2 more similar admissions with relapsing hemolytic anemia on tapering steroids and hence was given IvIG and rituximab therapy with significant response. She developed sudden hypoxic respiratory failure requiring ventilatory support from unknown cause and eventually died of severe DIC within 1–2 days. Her unusual presentation and sudden death was finally revealed on autopsy which showed disseminated myeloid sarcoma with acute myelomonocytic features involving heart, lungs, liver, spleen, pancreas, adrenal glands and almost every major organ without any bone marrow involvement.
DISCUSSION: Myeloid sarcoma (MS) is a rare condition which consists of immature myeloid cells and occurs at an extramedullary site, most commonly bone, skin, or lymph node, although any part of the body may be affected. MS mostly consists of myeloblasts, with or without features of promyelocytic or neutrophilic maturation, which can totally or partially distort the tissue architecture. Most of the cases are found to have either myelomonocytic or monoblastic features. It may develop de novo or concurrently with acute myeloid leukemia (AML) or as first manifestation, precede it by months or years, or equally represent the initial manifestation of relapse in a previously treated AML in remission. Rarely has it been seen to be disseminated, present as autoimmune hemolytic anemia or manifest as DIC. AML in itself is a commonly seen neoplasm but presentations like these always prove to be diagnostic dilemma. Myeloid sarcoma represents a poor prognostic feature in patients with AML regardless of its spatial occurrence. It is highly unusual for myeloid sarcoma to be diffuse and present with DIC without evidence of AML in blood or bone marrow. We believe this presentation for myeloid sarcoma is first of its kind and cases like this require early multi-specialty consultations for appropriate work up.
LIFE THREATENING HYPOXIA DURING ELECTRICAL CARDIOVERSIONZakaria Almuwaqqat. saint francis hospital, Evanston, IL. (Tracking ID #1923592)
LEARNING OBJECTIVE 1: Reporting a potentially life threatening complication of trans-esophageal echocardiography and local anesthesia.
LEARNING OBJECTIVE 2: Importance of maintaining a high degree of suspicion and prompt recognition local anesthetics side-effects and providing appropriate treatment.
CASE: A 75 year old male patient in phase 2 cardiac rehab presents with increasing shortness of breath and recurrence of Afib after bi-Atrial maze procedure. PMHX includes CAD (coronary artery disease); HTN (hypertension); Paroxysmal atrial fibrillation; S/P angioplasty with stent; Aortic valvular stenosis; Hyperlipidemia; DM (diabetes mellitus); CKD (chronic kidney disease) stage 3, GFR 30–59 ml/min; and S/P aortic valve replacement. He is s/p AVR bioprosthetic valve, tricuspid annuloplasty, bi-atrial MAZE procedure with CABG (LIMA to LAD) 6 months ago. Medications: amlodipine, Zaroxyln, Lasix, lisinopril, glipizide, aspirin and carvideolol. Physical Examination: Vitals: BP; 145/90, HR; 105/, Temp; 98 °F, RR 18 min, SpO2; 98 % (before the procedure). General: alert, Ox3, not in distress Neck: JVP 13 cm H2O Lungs: bibasilar rales heart: irregular, S1 & S2 normal. faint systolic murmur Abdomen: liver edge smooth and nontender. Extremities: Bilateral Lower limb edema. Hospitalization Course: Patient was attached to non-invasive hemodynamic and electrophysiological monitoring equipment, TEE was done with local anesthesia and showed no LA thrombi. After achieving an appropriate level of sedation with propofol, a synchronized, biphasic 200 J shock was delivered and converted to NSR. The patient was hypoxic with O2 Saturations in the mid-80s while on a non-rebreather mask and non-sedated, for that he was given Lasix IV and flumazenil, afterward patient became cyanotic, less responsive, respirations slow, Methemoglobin level was obtained (45 %) and patient given methylene blue and placed on non invasive ventilation, his O2 saturation improved to 90s over an hour and patient recovered.
DISCUSSION: The patient developed an episode of benzocaine induced Methemaglobinemia which was used during preparation for TEE prior to electrical cardioversion. Methemoglobinemia can result in impaired oxygen delivery to tissues as well as a left shift of the oxygen-Hb dissociation curve, it’s a potentially life threatening emergency which can result in respiratory depression, altered consciousness, shock, seizures, and death. Mucosal benzocaine spray is used in most local anesthesia procedures I.e. endoscopy, bronchoscopy, awake intubation and TEE and has been associated with methemoglobinemia and its complications. Knowledge of this adverse medication reaction is essential for medical residents and house staff in ICU.
LIFE-THREATENING ARRHYTHMIA IN A HEALTHY YOUNG WOMAN WITH PECTUS EXCAVATUMNaoki Takamatsu; Christine Kwan. Teine Keijinkai Hospital, Sapporo-shi, Japan. (Tracking ID #1929494)
LEARNING OBJECTIVE 1: Recognize that pectus excavatum (PE) may cause life-threatening arrhythmias
LEARNING OBJECTIVE 2: Treat adult PE patients with surgery for reasons other than cosmetic purposes
CASE: A previously healthy, active 35 years old Japanese woman presents with 3 episodes of syncope in the last month. Her first episode occurs during a neck massage; she describes nausea and lightheadedness with urinary incontinence upon awakening. She denies paresthesias, seizures, and cardiovascular symptoms; all other review of systems is within normal limits. The patient does not have any past medical problems and does not take any medications or use tobacco, alcohol, or recreational drugs. Her father has PE, but no family history of sudden cardiac death (SCD). On exam, her vital signs include temperature 36.7C, heart rate 40, blood pressure 108/55, respiratory rate 14, and O2 saturation 99 % room air. Generally, she initially appears disoriented but quickly becomes alert/oriented ×3. Cardiac exam demonstrates a depressed sternum; otherwise, her exam shows no irregularities. Her labs show complete blood counts and chemistry within normal limits. Electrocardiogram shows pulse 35 with junctional rhythm. Meanwhile, during diagnostic workup, she goes into cardiac arrest with ventricular fibrillation (V-fib) but is successfully resuscitated. Even with the use of a pacemaker, however, she develops delayed pupillary light reflexes and extremity convulsions/rigidity, so she is placed on hypothermia protocol with subsequent recovery, albeit with slight retrograde amnesia. Diagnostic workup continues with chest computed tomography’s confirmation of a depressed sternum with pectus severity index (PSI) 6.8 (normal 2.5). Holter monitor records multiple ventricular dysrhythmias, 35 % being premature ventricular contractions with some R on T waves. Echocardiography, coronary angiography, electrophysiological study, and cardiac magnetic resonance imaging demonstrate no abnormality. The patient is treated with amiodarone and carvedilol and is discharged after getting an implantable cardioverter-defibrillator (ICD). Surgical repair is on hold due to having only one (PSI > 3.25) of five Nuss criterion.
DISCUSSION: PE, a congenital hereditary deformity of the chest, is often considered a benign condition although this anatomic alteration can result in compression of the heart, thereby decreasing exercise capacity and affecting right ventricular morphology and function. An association with supraventricular dysrhythmia has been well documented while only a few reports of ventricular dysrhythmia exist. The patient’s V-fib arrest occurs without any preceding cardiovascular symptoms or precipitating factors like exercise. In the absence of coronary heart disease and cardiomyopathy, the only suggestive cause remains to be her PE. Ventricular dysrhythmias associated with PE are a rare entity; however, since it remains to be the leading cause of SCD and because V-fib recurs in ~14 % of all V-fib resuscitations, ICDs are a necessity. Furthermore, surgical repair is often performed in children or in adults’ wanting cosmetic enhancement. The indications of repair in adults for medical purposes remain unclear due to lack of reports although the Nuss criteria is sometimes used. This case underscores the importance of PE in the recognition of its potentially life-threatening clinical presentation and gives insight into indications for surgical correction of PE in symptomatic adults.
LIFE-THREATENING HYPERSENSITIVITY REACTION TO ACE INHIBITOR USED IN SCLERODERMA RENAL CRISISSonja Gill. 1SUNY Upstate Medical University, Syracuse, NY; 2University of Toronto, Toronto, ON, Canada. (Tracking ID #1938979)
LEARNING OBJECTIVE 1: Identify and treat life threatening drug reactions
LEARNING OBJECTIVE 2: Recognize a rheumatologic emergency encountered in training and practice
CASE: A 68yo female presented to the emergency department after recently being discharged from the hospital for renal crisis in diffuse-type systemic sclerosis. She was discharged on an ACE-inhibitor, captopril, and came back 3 days later for fever, shortness of breath, pruritic rash and facial swelling. Her blood pressure was 215/90 mmHg and her skin diffusely swollen and tender with erythematous confluent patches covering 85 % of total body surface area. Creatinine was 5.8 mg/dL with white blood cell casts on microscopy, and she was diagnosed with acute hypersensitivity reaction secondary to captopril with recurrent renal crisis. Skin biopsy revealed partial necrosis of the epithelium with vacuolar change and spongiosis consistent with major erythema multiforme or Stevens-Johnson syndrome. Treatment with pulse dose steroids was initiated and captopril discontinued, noting the possibility that renal crisis may precipitously worsen. Over 2 days, the patient’s symptoms abated and the exfoliative rash was resolving, however, her renal function remained impaired with persistently elevated blood pressures. Preparations were made for hemodialysis. She was started on an inpatient antihypertensive regimen that included losartan, methyldopa and hydralazine. Over several days, her renal function improved, and blood pressure returned to baseline. Hemodialysis was avoided, and the patient was discharged home in hemodynamically stable condition with close rheumatology and nephrology follow-up. She was not started back on ACE inhibitor therapy and continues on ARB monotherapy without any significant adverse effects.
DISCUSSION: Renal crisis in systemic sclerosis is a life-threatening condition, and ACE inhibitors have thus far been the standard pharmacological treatment. In a patient with a serious adverse drug reaction to ACE inhibitor therapy, other modalities such as hemodialysis and renal transplant are usually considered to treat this condition. Prior to subjecting a patient to these lifelong interventions, however, we as internists may consider alternate management strategies to avoid this commitment. While employing the expertise of a rheumatologist and nephrologist, we may begin treatment with systemic steroids with strict blood pressure control. ARB monotherapy took the place of ACE inhibitors for the management of renal crisis in this case and thus, we may also ponder the hypothesis of whether ARB monotherapy may be of use in treating systemic sclerosis renal crisis, especially in those patients with adverse drug reactions to ACE inhibitors.
LISTERIA SEPSIS IN AN IMMUNOCOMPROMISED HOST WITH ADVANCED BREAST CANCERValida Bajrovic; Christopher Sankey. Yale School of Medicine, New Haven, CT. (Tracking ID #1924459)
LEARNING OBJECTIVE 1: Recognize listeria monocytogenes as an important bacterial pathogen in the immunocompromised host.
LEARNING OBJECTIVE 2: Review clinical characteristics and etiologic factors in listeria monocytogenes infection.
CASE: A 50 year-old Caucasian woman with history of stage IV breast cancer (ER/PR+, HER2/NEU -) with metastasis to liver and bone on hormonal chemotherapy presented with a 4 day history of fevers (104 °F), malaise, and anorexia. She denied dysuria, cough, or diarrhea; she had no indwelling central access. On admission, the patient was afebrile but tachycardic and hypotensive (blood pressure 86/58). Her physical examination was most notable for how well she appeared; she had an intact mental status, absence of meningismus, dry mucous membranes, pale conjunctivae and no localizing sign of infection. Laboratory testing revealed hyponatremia (serum Na 120 mmol/L), acute renal failure (creatinine 2.5 mg/dL), and a worsening of her chronic hypoproliferative anemia (hemoglobin 7.4 mg/dL, down from a baseline of 9 g/dL). She had a no leukocytosis and a normal lactic acid. Admission chest radiography showed no infiltrates and persistence of known bony metastases. The patient was admitted for hemodynamic monitoring as well as correction of her metabolic derangements. Over the first 24 h, she was aggressively volume-resuscitated with intravenous fluids and packed red blood cells. Her blood cultures were quickly positive for gram positive rods, which were initially presumed to be a contaminant and antibiotics were withheld. However, repeat cultures from the following day demonstrated the same organism, which was identified as listeria monocytogenes. Treatment with ampicillin was initiated, and she clinically improved. Her laboratory abnormalities resolved, antibiotics were switched to oral amoxicillin, and she was discharged home. Her subsequent recovery was uncomplicated.
DISCUSSION: Listeria monocytogenes is a pathogen implicated in infection of neonates, immunosuppressed patients, the elderly, and pregnant women. The great majority of listeria infections are sporadic, but outbreaks have been reported in association with unpasteurized milk, soft cheeses and delicatessen meat. Clinical syndromes associated with Listeria monocytogenes infection range from a self-limited gastroenteritis to invasive diseases including meningitis, meningoencephalitis, or bacteremia. Invasive infections most commonly occur in immunosuppressed patients, individuals at the extremes of age and pregnant women. Listeria sepsis occurs in patients of all ages. Adults with Listeria sepsis classically present with fever and chills but can be asymptomatic especially if immunocompromised, as was the case for our patient. Septic shock can develop and there may be seeding of the brain and/or meninges, leading to meningoencephalitis or cerebritis. The diagnosis of listeria bacteremia is best established by obtaining blood cultures. The antibiotic of choice for Listeria infection is ampicillin or penicillin G. Neither antibiotic achieves adequate bactericidal activity in the cerebrospinal fluid; thus, listeria central nervous system infections, endocarditis, and infections in neonates and immunocompromised patients are usually treated with combination therapy, with an aminoglycoside being added for synergy. Penicillin-allergic patients can be desensitized or treated with trimethoprim-sulfamethoxazole.
LITHIUM-INDUCED HYPERTHYROIDISM MIMICKING ACUTE CORONARY SYNDROMELucas A. Burke; Kiran Mogali; David E. Winchester; Margaret C. Lo. University of Florida, Gainesville, FL. (Tracking ID #1936553)
LEARNING OBJECTIVE 1: Diagnose and treat hyperthyroidism-induced coronary vasospasm in acute chest pain presentation.
LEARNING OBJECTIVE 2: Recognize the various thyroid dysfunctions that can result from lithium use, even at subtherapeutic levels.
CASE: A 50-year-old female with chronic obstructive pulmonary disease, tobacco use and bipolar disorder presented with acute, intense substernal chest pain and heart rate of 170 bpm. She had no previous cardiac history and no similar episodes in the past. She started taking lithium 2 months earlier for bipolar disorder. Her electrocardiogram showed inferior ST depression and an incomplete left bundle branch block (LBBB). Troponin T was elevated at 0.48 ng/mL. An emergent left heart catheterization revealed non-obstructive coronary artery disease and vasospasm of the left main and left anterior descending coronary arteries which resolved with intra-coronary nitroglycerine. She remained tachycardic and the electrocardiogram later showed multifocal atrial tachycardia. A subsequent thyroid-stimulating hormone level came back low (< 0.01 mIU/L) and free T4 elevated (3 ng/dl). Thyroid stimulating antibodies were negative however thyroid peroxidase (TPO) was positive. Thyroid ultrasound was unremarkable. Despite a sub-therapeutic lithium level (0.53 mmol/L), lithium-induced hyperthyroidism was suspected given its narrow therapeutic index. Lithium was discontinued and methimazole was started. After 2 days, she became asymptomatic and converted to normal sinus rhythm; she was discharged with cardiology and endocrinology follow-up.
DISCUSSION: The presentation of severe coronary artery spasm can be similar to acute coronary syndrome (ACS). Unlike ACS, coronary artery spasm is more easily reversible and can be prevented by treating underlying causes. Coronary artery spasm is part of variant angina and if left untreated, can lead to myocardial infarction by promoting coronary thrombus formation. Furthermore, coronary artery spasm can cause life-threatening arrhythmias including heart block (with right coronary artery spasm) or ventricular tachycardia (with left anterior descending coronary involvement). Coronary vasospasm has been reported in patients with overt hyperthyroidism. The management generally includes thionamides (methimazole or propylthiouracil) to treat the hyperthyroid state as well as long-acting nitrates or dihydropyridine calcium channel blockers to decrease spasm of the coronary arteries. Interestingly, lithium itself is also used to treat hyperthyroidism by blocking thyroid hormone release, although its use is certainly not first or second line. There is little in the medical literature regarding coronary vasospasm secondary to hyperthyroidism as evidenced by a review of 21 case reports describing this clinical scenario. Of these 21 cases, 14 were attributed to Graves’ disease (67 %), 2 to toxic multinodular goiter (10 %), 1 to amiodarone-induced hyperthyroidism (5 %) and the remaining cases did not provide the underlying etiology for the hyperthyroidism. This patient may have been in “Hashimototoxicosis” (initial hyperthyroid phase of Hashimoto’s disease) as evidenced by positive TPO antibodies and may eventually become hypothyroid due to underlying chronic autoimmune thyroiditis, with a predisposition for autoimmunity secondary to lithium. One study found that 20 % of lithium-treated affective disorder patients had elevated TPO antibodies vs. 7.5 % in non-lithium treated patients and 0 % in controls. Lithium has a narrow therapeutic index and can cause thyroid dysfunction (hypo or hyperthyroidism) even at sub-therapeutic levels. A particular case series showed a 3-fold increase of thyrotoxicosis in patients taking lithium. Lithium use has also been associated with a self-limited destructive thyrotoxicosis (lithium-associated thyroiditis). This particular type of hyperthyroidism falls under the category of subacute painless thyroiditis and typically resolves over the course of months to years with adequate treatment of the hyperthyroid state. In conclusion, this case highlights key points in the diagnostic evaluation of acute chest pain. First, non-ST elevation myocardial infarction or new LBBB do not establish a diagnosis of a type 1 myocardial infarction (secondary to acute plaque rupture) but could be secondary to acute coronary vasospasm (type 2 myocardial infarction; secondary to decreased oxygen delivery or increased oxygen demand). Second, hyperthyroidism must be considered with chest pain presentations, especially in patients with low Framingham risk score and isolated coronary artery vasospasm on heart catheterization. Finally, thyroid function should be evaluated in all patients who take lithium, given its narrow therapeutic index.
LITTLE KNOWN LYMPHOMA: SMALL LYMPHOCYTIC LYMPHOMA PRESENTING AS A PARANEOPLASTIC SYNDROME WITH ACUTE CNS DEMYELINATIONNicholas DeVito. Tufts Medical Center, Boston, MA. (Tracking ID #1925987)
LEARNING OBJECTIVE 1: 1. To recognize rare neurological paraneoplastic syndromes, appropriately identify their cause and the cancer of origin.
LEARNING OBJECTIVE 2: 2. To identify other paraneoplastic syndromes in hematologic malignancies and identify possible causes of these syndromes.
CASE: A 72-year-old woman with a past medical history of hyperlipidemia presented with progressive complete ophthalmoplegia, facial diplegia, slurred speech and right-sided ataxia for 6 weeks, preceded by transient monocular vision loss. She was worked up at an outside hospital with negative CT and MRI. She presented to our institution after several falls at home. Her vital signs were stable and she was alerted and oriented. She had shotty bilateral axillary lymphadenopathy. Her neurological exam was significant for complete ophthalmoparesis, left eye ptosis, dysarthria, severe finger-nose-finger dysmetria on the right, inability to sit up unsupported, and severe rubral head tremor. Laboratory values were unremarkable. Repeat MRI of the head revealed a well marginated, extensive T2/FLAIR signal abnormality extending from the midbrain to the pons posteriorly with subtle peripheral enhancement, suggestive of a demyelinating disease. CT of the chest, abdomen, and pelvis showed numerous enlarged lymph nodes. CSF revealed 10 white cells (82 % lymphocytic), >5 oligoclonal bands, normal protein/glucose, and elevated CSF IgG index and synthesis rate. This was suggestive of an antibody present in the CSF not present in the blood. Rheumatologic and infectious workup was negative. Axillary lymph node biopsy was consistent with small lymphocytic lymphoma (SLL). She was treated with high dose steroids, five sessions of plasmapheresis, and R-CHOP chemotherapy (Rituximab, Cyclophosphamide, Doxorubicin, Vincristine and Prednisone). Within days of starting treatment, her symptoms resolved. Post-treatment CSF studies and MRI were unremarkable 6 months later.
DISCUSSION: SLL is a mature B cell lymphoma characterized by accumulation of functionally incompetent monoclonal lymphocytes with the same morphologic and immunophenotypic features as chronic lymphocytic leukemia (CLL), but lacks peripheral blood lymphocytosis. Paraneoplastic and autoimmune complications occur in up to 25 % of all patients with CLL/SLL, The most common complications are autoimmune hemolytic anemia or immune thrombocytopenia, both of which were not present in this patient. CNS complications are rare except when there is direct invasion of leukemic cells. This represents the first known case of a demyelinating paraneoplastic syndrome due to SLL. This was a unique case of SLL presenting as paraneoplastic syndrome of brain stem demyelination as determined by imaging, CSF studies and symptoms. Brain stem demyelination is an autoimmune syndrome seen in small cell lung cancer, germ cell cancers or in viral infections. Malignancies can interfere with self-tolerance in the central immune system, resulting in aberrant antigen recognition and autoimmunity. Unfortunately we were unable to isolate a specific autoantibody in this case; however this highlights the fact that there is a plethora of research to be done in understanding the causes of paraneoplastic autoimmunity in CLL/SLL.
LOSING A BATTLE BUT NOT THE WAR: INSIGHTS INTO A VETERAN’S PREFERENCE FOR AGGRESSIVE MEASURES IN ADVANCED ILLNESSNeil Gupta1; John Thomas1,2. 1Yale University School of Medicine, New Haven, CT; 2Veterans Affairs (VA) Connecticut Healthcare System, West Haven, CT. (Tracking ID #1936952)
LEARNING OBJECTIVE 1: Appreciate the potential complexity surrounding goals of care discussions for patients with terminal illness.
LEARNING OBJECTIVE 2: Recognize that a decline in health status may prompt a change in goals of care for such patients.
CASE: A 96-year-old World War II veteran with prostate and bladder cancer with metastases to bone and brain presented to the hospital after an unwitnessed fall at home. Chart review revealed numerous cancer treatments over a span of several years, including a series of radiation treatments and transurethral resection of bladder tumor procedures. The patient’s son reported that his father had been living at home independently until a few weeks prior to admission, when his growing forgetfulness and loss of energy prompted the hiring of a home health aid. He had no focal neurologic deficits on exam. CT scan showed subarachnoid hematoma of the right frontal lobe. A chest x-ray showed a large right-sided pleural effusion, and CT of the abdomen and pelvis showed a new bladder wall mass, metastatic lesions in his lung, and bilateral hydronephrosis and hydroureter. Urinalysis was consistent with urinary tract infection. Due to intracranial hemorrhage, he was admitted to the intensive care unit for close monitoring. Goals of care discussions initially centered on the patient and family’s insistence upon aggressive measures, including full code status, despite the patient’s overall poor prognosis. The patient’s son confirmed that his father was always a “fighter,” and despite multiple prior hospitalizations, he was always able to return to living at home independently and without significant symptom burden, even in the face of metastatic cancer. Within hours of arrival to the hospital, a chest tube and bilateral nephrostomy tubes were placed. The patient tolerated these procedures well and was transferred out of the intensive care unit the next day. While on the medicine floor, he took a turn for the worse, developing delirium and a steady cognitive decline, eventually responding only to voice. In light of this, his family decided to focus on making him comfortable and enrolled him in an inpatient hospice program. He died the next day.
DISCUSSION: Within only a few days, the patient in this case had a dramatic shift in care preferences spanning opposite ends of the treatment spectrum. Such decision making would at first glance make little sense to a medical team fully cognizant of his overall prognosis. However, certain aspects of the patient and family’s perspective in initially insisting on aggressive treatment were compelling. The patient proudly identified as a veteran and maintained his “fighting” spirit in approaching chronic illness, not without prior successes, and his quality of life prior to this hospitalization was excellent. In his understanding, he was perhaps “winning the war,” but facing a new setback of unclear significance. From the perspective of the medical team, they had inherited a “losing battle” in terms of the seeming futility of aggressive treatment at such a late stage in the patient’s illness. Initial discussions about goals of care were awkward, as the team had just met the patient and family and were trying to gingerly reveal bleak prognostic information that perhaps had not been fully discussed previously. Ultimately, the patient’s poor prognosis declared itself fully, and with the aid of continued conversations between the medical team and family, a smooth transition to hospice care was made. This case illustrates the vital role of communication in providing compassionate, patient-centered care at the end of life. Preferences for patients with advanced illness have been shown to be highly dynamic, thus necessitating careful, ongoing discussions involving the patient and a family member who can serve as health care proxy when needed. It is unclear whether advance care planning in the outpatient setting for this patient would have altered his care trajectory while hospitalized, but in the least it may have more clearly established his values and better prepared both him and his family for in-the-moment decision making.
LOWER EXTREMITY EDEMA AND JVP ELEVATION: MORE THAN MEETS THE EYERyan Campbell-Massa1; Anna K. Donovan2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1940159)
LEARNING OBJECTIVE 1: Maintain a high index of suspicion for pericardial constriction in the appropriate clinical setting
LEARNING OBJECTIVE 2: Understand the diagnostic work-up and treatment options for chronic pericardial constriction
CASE: A 64 year old man with a history of hypertension and rheumatic fever as a child presented as a new patient to primary care with complaints of lower extremity edema. The lower extremity swelling was present for the preceding 10 years, managed on furosemide and metolazone. He denied exertional chest pain, dyspnea, orthopnea, or paroxysmal nocturnal dyspnea. He denied any history of heart failure or myocardial infarction. He had no history of radiation exposure, tuberculosis, acute pericarditis, or autoimmune disorders. He had a 15 pack year history of tobacco use, and quit 30 years prior to presentation. On physical examination, he was in no acute distress. His cardiac examination was remarkable for a II/VI systolic ejection murmur best appreciated at the right upper sternal border without radiation to the carotids, elevated jugular venous pressure (JVP) to 11 cm, and 1+ pitting edema to mid-shins bilaterally. No rubs or gallops were appreciated on auscultation. There was no pulsus paradoxus. Pulmonary examination demonstrated clear lung fields bilaterally without crackles. EKG demonstrated sinus bradycardia with a heart rate of 60 without ST segment or T wave changes. QRS voltage was within normal limits. On transthoracic echocardiogram (TTE), the pericardium was echobright consistent with possible pericardial thickening. TTE also demonstrated 10–12 % increase in mitral inflow velocity with expiration and 13 % increase in tricuspid inflow velocity with inspiration. The respiratory variation was not diagnostic of pericardial constriction, but the constellation of findings warranted further evaluation. Chest CT with contrast demonstrated focal thickening and calcification of the pericardium along the right heart border. Cardiac catheterization demonstrated equalization of right ventricular end-diastolic pressure (RVEDP) and left ventricular end-diastolic pressure (LVEDP), near-equalization of pulmonary arterial diastolic pressure and LVEDP, and an RVEDP that was greater than one-third of right ventricular systolic pressure. An early diastolic dip followed by a plateau (the “square root sign”) was also noted on hemodynamic tracing. Cardiothoracic surgery was consulted and recommended pericardiectomy. Given the patient’s lack of obvious risk factors, his constrictive pericarditis was presumably due to idiopathic or viral causes.
DISCUSSION: When seeing a new patient in clinic, it is essential to pause to consider the rationale for the prior management of a patient. Our patient was requiring two diuretics to appropriately manage his peripheral edema without a clear explanation of why. Given this patient’s unexplained elevated JVP and peripheral edema, especially in the absence of any history or electrocardiographic evidence of prior myocardial infarction, further workup was pursued. Heart failure is common in a primary care clinic, and its presentation can be similar to that of constrictive pericarditis. Patients with constrictive pericarditis often report a history of peripheral edema and decreased functional capacity. Physical examination commonly reveals elevated JVP but may also more rarely include pulsus paradoxus, Kussmaul’s sign, and a pericardial knock. Constrictive pericarditis is an uncommon entity. The etiology in a particular case is often not identified, and is most commonly attributed to idiopathic or viral causes. Other associated conditions include cardiac surgery, radiation exposure, infection of pericardium, and connective tissue disorders. Current guidelines recommend echocardiography for the initial evaluation of patients suspected to have pericardial constriction. Echocardiography may be diagnostic in some cases, especially with the use of Doppler assessment of hemodynamic changes in the respiratory cycle, which has been reported to have sensitivity and specificity of 85 % to 90 % in this setting. Imaging with CT scan and cardiac MRI can evaluate for pericardial thickening. Cardiac catheterization is a useful modality to definitively establish a diagnosis, and is typically performed prior to operative intervention. Hemodynamic findings frequently seen in constrictive pericarditis include increased right atrial pressure, elevated RVEDP to greater than one-third of RV systolic pressure, equalization of RVEDP and LVEDP, and an early diastolic dip followed by a plateau on hemodynamic tracing. Note that these findings were seen in our patient. Pericardiectomy is the definitive treatment for chronic constrictive pericarditis, but must be timed optimally. Early disease may not warrant surgical correction and can sometimes be temporized with diuretic therapy. Conversely, patients with late disease (NYHA Class IV) rarely benefit from surgery, which is associated with a 30–40 % mortality in that population.
LUNG HERNIATION POST CARDIO-PULMONARY RESUSCITATIONSourabh Aggarwal; Shrey Velani; Mark Loehrke. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1941459)
LEARNING OBJECTIVE 1: To understand rare complication of lung hernia post resuscitation
LEARNING OBJECTIVE 2: To know management of lung hernia
CASE: Chest compressions during cardiopulmonary resuscitation (CPR) can be traumatic to patients resulting in ribs/sternum fractures. Sternal fractures occur in 1 out of 5 and costal fracture in 1 out of 3 patients with resuscitation attempts. We report a rare complication of lung parenchymal herniation post-CPR. Fifty-six-year-old, previously healthy male, had Ventricular Fibrillation cardiac arrest and return of spontaneous circulation after 10 min of CPR. He was intubated and hemodynamically stabilized in the intensive care unit. Therapeutic hypothermia was initiated and rewarming done after 24 h. His neurological and cardio-respiratory status gradually improved over next 7 days. He was eventually extubated and placed on Bilevel positive air pressure (BiPAP). However, he started having respiratory distress with decelerating oxygen saturation. He had asymmetric chest wall movements with right side expanding more than left side. He was re-intubated and CT scan revealed displaced fracture from 3rd-6th ribs and herniated right-sided upper and middle lobe of lung tissue outside of the rib cage into pectoralis muscle. He was immediately taken to operating room where emergency repair of a large right lung hernia with a right pectoralis major muscle flap, open reduction and internal fixation of multiple right-sided rib fractures and drainage of the right pleural effusion was done followed by chest tube placement. He had an uneventful recovery, re-extubated and was transferred to floor.
DISCUSSION: Lung herniation post CPR has been very rarely described. A study of 705 post-CPR autopsies did not report even a single case of lung herniation. The rib fractures our patient received during CPR caused patient’s lung parenchyma to herniate which was complicated by initiation of BiPAP therapy. Most patients with lung herniation remain asymptomatic and a soft, reducible bulging mass may be noted in chest wall or neck fluctuating with the respiratory cycle, coughing or straining. Lung parenchymal hernias may appear as loculated subcutaneous air pockets on chest X-ray, however CT scan is the diagnostic modality of choice. Management is largely conservative in asymptomatic patients with careful monitoring of the respiratory function. Surgical intervention may be chosen in appropriate patients, especially those symptomatic with intractable pain, dyspnea, incarceration or ongoing effusion. Lung herniation should be considered as a differential in patients with a bulging mass in the anterior thorax, intractable pain at the site of potential fracture, ongoing dyspnea with no definite etiology, subcutaneous emphysema or pneumothorax after CPR.
LUNG HERNIATION—A UNIQUE CASE OF CHEST PAINChirag D. Patel; Van Holden. Rutgers—Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1938128)
LEARNING OBJECTIVE 1: Reviewing clinical and radiologic findings of lung herniation
LEARNING OBJECTIVE 2: Considering lung herniation as part of the differential diagnosis in a patient with atypical chest pain and associated risk factors.
CASE: A 57 year-old woman with a past medical history of morbid obesity, coronary artery disease status post coronary artery bypass surgery (CABG) with left internal mammary artery harvesting more than 5 years ago, hypertension, diabetes mellitus type II, and intermittent asthma presents with progressively worsening dyspnea over a month. It was associated with increased lower extremity edema, increased abdominal girth, paroxysmal noctural dyspnea, 3-pillow orthopnea, productive cough, and a “squeezing”, non-radiating, pleuritic chest pain. At baseline, she uses her nebulizer once a week and gets shortness of breath after walking up one flight of stairs. On admission, patient had dyspnea at rest despite using her nebulizers four times a day and medication compliance with furosemide and metoprolol. Her presentation was not characteristic of her asthma or anginal symptoms. The patient was hemodynamically stable except for 90 % oxygen saturation on 100 % non-rebreather. She was in respiratory distress with accessory muscle use; she had jugular venous distention, bilateral apical wheezing, decreased breath sounds at the bases, and bilateral lower extremity pitting edema. She was treated for presumed CHF exacerbation and started on BiPAP and intravenous furosemide. Her condition did not improve despite diuresis of more than four liters; thus, she was started on intravenous methylprednisolone for severe asthma exacerbation. The patient continued to have vigorous coughing spells despite antitussives. On hospital day five, she reported having sharp, pleuritic, left-sided chest pain radiating to the back after a violent coughing fit. She also had a focal bulge around the left parasternal area that was non-tender to palpation but had paradoxical movement with respirations. It was associated with a 30 mmHg systolic blood pressure difference in the arms. A CT angiography of the chest was obtained to evaluate for aortic dissection. It unexpectedly showed a diastasis between the 4th and 5th ribs where a 5.2 × 2.6 cm section of left upper lobe herniated. Adjacent to the defect was a metal clip from her cardiac surgery, suggestive of an intercostal muscle defect. Pulmonary and thoracic surgery recommended conservative management with observation in the acute setting because the patient’s pain was resolved gradually with local lidocaine and NSAIDS. She was discharged on oral furosemide and a prednisone taper with the plan for future surgical intervention. Our theory is that the patient’s previous cardiac surgery and parasternal clipping resulted in intercostal muscle weakness. Concurrently, her violent coughing spells causing increased abdominal pressure, and her periodic steroid use for asthma exacerbations prevented wound healing. All of these factors contributed to the patient’s lung herniation.
DISCUSSION: Lung herniation is an uncommon cause of chest pain with approximately 300 cases reported in the literature. The incidence may be even higher since many are asymptomatic. Herniation of the lung is usually classified as either congenital or acquired. Causes of acquired lung herniation include trauma, pathologic or spontaneous. Spontaneous herniations are a consequence of body habitus, COPD and hyperinflation; however, the majority of causes are a result of trauma or after surgery where the rib cage has been violated. Authors have reported intercostal lung hernias after numerous procedures interfering with the integrity of the thoracic wall (i.e. video-assisted thorascopic surgery, tube removal, minimally invasive direct coronary artery bypass grafting surgery, harvesting of internal mammary artery and thoracotomy). Specifically, harvesting left internal mammary artery for coronary bypass grafting along with the use of parasternal steel wires may interfere and damage the intercostal arteries leading to local ischemia. Consequently, thoracic wall integrity is compromised, increasing the risk of herniation, especially during vigorous coughing spells. Unique to our case is the fact that the lung herniation occurred years after her CABG. Most lung herniations due to surgical intervention described in the literature occurred weeks to months in the post-operative period. Numerous factors including body habitus, respiratory disease, and previous cardiac surgery contributed to her condition. This case illustrates the importance of understanding the clinical and radiologic findings of lung herniation also the risk factors associated with such an entity.
LYMPHADENOPATHY AND FEVERS AND TACHYCARDIA, OH MY!Chaitanya Madamanchi; Mukhtar Adem. University of North Carolina, Chapel Hill, NC. (Tracking ID #1923942)
LEARNING OBJECTIVE 1: To recognize clinical manifestations of Castleman’s disease
LEARNING OBJECTIVE 2: To recognize the importance of promptly initiating treatment
CASE: A 32 year-old woman with a history of asthma presented with 1 week of pleuritic chest pain. She also noted intermittent fevers, fatigue, and a dry cough. She denied weight loss, rash, or myalgias. She had a 15 pack-year smoking history and a family history of Systemic Lupus Erythematous. Physical exam was notable for tachycardia and decreased breath sounds at the lung bases bilaterally without wheezing or rhonchi. There were bilateral, nontender, palpable, one-centimeter lymph nodes in the inguinal region. Labwork revealed eosinophilia and ANA 1:160. Chest X-ray revealed bilateral ground glass opacities and pleural effusions. CT Chest/Abdomen/Pelvis revealed bulky mediastinal and cervical lymphadenopathy and anterior mediastinal soft tissue mass, in addition to small pericardial and pleural effusions, tree-in-bud opacities, and ascites. PET scan showed FDG (tracer) avid lymphadenopathy with a dominant conglomerate 6 × 4 cm anterior mediastinal nodal mass. Thoracentesis revealed exudative effusions. Bronchoscopy was unrevealing. Blood, urine, pleural fluid, and bronchial wash cultures were negative. Hospital course was complicated by daily fevers up to 102 F, tachycardia up to 150 s, and hypoxic respiratory failure requiring mechanical ventilation despite empiric treatment with broad-spectrum antibiotics. Biopsy of the anterior mediastinal lymph node revealed interfollicular and paracortical expansion of polyclonal plasma cells. Pathology was consistent with a plasma cell variant of Castleman’s Disease. Patient was started on solumedrol and tocilizumab, an IL-6 monoclonal antibody, with improvement in symptoms.
DISCUSSION: Castleman’s Disease, also known as angiofollicular lymph node hyperplasia, is a rare, lymphoproliferative disorder that can be found in nodal and extra nodal sites. It is encountered infrequently and thus is difficult to diagnose. The plasma cell variant is characterized by the presence of hyperplastic germinal centers in lymph nodes. These enlarged lymph nodes can cause local symptoms such as pain from tissue expansion, dyspnea, and cough from compression of trachea. This disease has been linked to excessive release of IL-6, which leads to excess lymphocyte proliferation. This immune response helps explain other manifestations including high fevers, weakness, and fatigue. It is important to recognize Castleman’s disease and obtain tissue diagnosis early, so that pharmacotherapy with glucocorticoids and IL-6 antibody can be initiated promptly. Failure to do so can result in death from fulminant infection, progressive disease with multi-organ failure, and conversion to lymphomas or uncontrolled HHV-8 infection.
LYMPHOMA TRAPPED IN BLOOD VESSELS: A RARE CASE OF INTRAVASCULAR B-CELL LYMPHOMAGagan Preet; Sreenivasa Chandana; Christine Dugan. WMU, Kalamazoo, MI. (Tracking ID #1936973)
LEARNING OBJECTIVE 1: To understand the pathology, clinical presentation, diagnosis and prognosis of intravascular B-cell lymphoma.
CASE: A 52-year-old Caucasian female presented with fatigue and diffuse abdominal pain for 4 weeks accompanied by 30-pound unintentional weight loss over 2 months duration. Her past medical, social and family history were non-contributory. On examination, she had hypotension (BP 70/50 mmHg), tachycardia (100 beats/min) and hypoxia (94 % oxygen saturation on 4 L/min oxygen). She was cachectic, had decreased breath sounds in lung bases and generalized abdominal tenderness. Initial labs revealed hemoglobin 11.6 mg/dL, WBC 5,000/mm3, platelets 15,000/μL, anion gap of 23 with lactic acidosis (9.1 mmol/L), LDH 2147 U/L, haptoglobin 98 mg/dl (normal 41–165 mg/dL) and ferritin 5127 ng/ml (Normal 13–300 ng/mL). She had worsening respiratory distress which required intubation. Fluid resuscitation was initiated, empiric broad spectrum antibiotics given and vasopressors started for hemodynamic support. CT scan of chest, abdomen and pelvis revealed bilateral pleural effusion, ascites and splenomegaly. An exhaustive work up including pan-culture, fungal serology, broncho-alveolar lavage, hepatitis panel, HIV, DIC panel, rheumatological workup (ANA, anti-dsDNA), transthoracic echocardiogram, colonoscopy, peripheral smear and flow cytometry were unremarkable. Despite all supportive measures, her clinical condition deteriorated fairly rapidly. She developed multi-organ failure and died within 7 days from the day of admission. Autopsy revealed extensive infiltration of small and medium sized vessels with large malignant lymphocytes. The lymph nodes were largely unremarkable. Immunohistochemistry was strongly positive for CD20, consistent with the diagnosis of intravascular B-cell lymphoma (IBCL).
DISCUSSION: IBCL is an extremely rare type of NHL characterized by selective clonal proliferation of lymphocytes, within the lumina of small blood vessels, particularly capillaries, without an extra-vascular tumor or nodal involvement. These lymphocytes lack CD29 and CD54 cell-surface proteins which are required for trans-vascular migration, hence malignant cells remain trapped in small-vessel lumina. Patients present with varied symptoms and are challenging to diagnose. Based on the presence of severe thrombocytopenia, anemia, elevated LDH, our patient did fit in to the category of IBCL associated with hemophagocytosis which is very rarely described in Caucasian population. Peripheral blood smears and flow cytometry can be normal as in our patient. Biopsy of the involved organ is the diagnostic test of choice with literature supporting random biopsy of even normal skin to confirm diagnose if no obvious lesions are present and suspicion is high. IBCL is a very aggressive tumor with grave prognosis and early diagnosis with intensive chemotherapy is crucial for better outcomes. Clinicians should be aware of this entity and should have high index of suspicion in appropriate patients.
MANAGEMENT OF HEPATITIS C VIRUS-INDUCED CRYOGLOBULINEMIC VASCULITIS IN THE PRESENCE OF COEXISTING DISEASES AFFECTED BY IMMUNOSUPPRESSANTSEsther Hwang; Madan R. Aryal; Kaiming Wu; Benjamin Lloyd. The Reading Hospital and Medical Center, West Reading, PA. (Tracking ID #1926781)
LEARNING OBJECTIVE 1: Recognize the challenges of treating hepatitis C-induced cryoglobulinemic vasculitis in the presence of coexisting diseases affected by immunosuppressants
CASE: A 57-year-old Hispanic male with past medical history of untreated hepatitis C, chronic pulmonary Mycobacterium Avium Complex (MAC) newly started on clarithromycin, incompletely treated latent tuberculosis (TB), and chronic bronchiectasis presented with a 3-month history of intermittent severe pain, discoloration, and swelling of his lower extremities. On physical examination, the patient had tender palpable purpura with brown copper deposits and punctate satellite lesions, significant pitting edema from ankles to knees, previously identified as leukocytoclastic vasculitis by skin biopsy. Positive lab results included serum cryoglobulins, rheumatoid factor, low C4, hepatitis C genotype 1 with viral load >23.5 million, and sputum culture growing Pseudomonas. ANA, ANCA, HIV, sputum acid-fast bacillus, and urinalysis were negative. CT chest revealed stable bronchiectasis. A multidisciplinary meeting was called with GI, ID, and pulmonary to discuss the impact of all possible treatments. The team decided to pursue symptom-based treatment with steroids, antihistamines, colchicine, diuretic, wound care, and conservative measures, such as leg elevation and fluid restriction. Over the next few days, the patient’s leg swelling improved. He was discharged on levofloxacin and the same inpatient regimen for cryoglobulinemic cutaneous vasculitis with steroid taper and wound care. The decision was made to start anti-virals after 6 months of clarithromycin therapy.
DISCUSSION: Creating this patient’s treatment plan was a balancing act requiring management of multiple diseases as well as many potential complications of different therapies. Immunosuppresant therapy for cryoglobulinemic vasculitis could worsen hepatitis C viremia, MAC, and bronchiectasis; interferon therapy for hepatitis could re-activate TB; latent TB could not be treated due to hepatic intolerance. Since there was no literature for this patient’s specific constellation of diseases and there were risks with every treatment option, decision-making was based on the principles of prioritizing treatment of diseases that cause definite harm while maximizing benefit and minimizing potential harm in the management of coexisting diseases.
MANAGEMENT OF METABOLIC ACIDOSIS IN PRE-EXISTING PROXIMAL RTAGuillermo E. Espinoza. NYPH-WCMC, New York, NY. (Tracking ID #1938719)
LEARNING OBJECTIVE 1: To understand the mechanisms underlying the electrolyte imbalances present in patients with proximal RTA.
LEARNING OBJECTIVE 2: To learn how an understanding of this pathophysiology impacts the treatment of critically ill patients with proximal RTA.
CASE: Patient is a 27 year old male with a past medical history significant for vertically transmitted HIV/AIDS, diffuse large B-cell lymphoma with intestinal involvement status post sigmoidectomy with end colostomy and proximal renal tubular acidosis secondary to tenofovir therapy. He presented to the hospital with complaints of increased ostomy output, decreased oral intake, generalized weakness and fatigue. He was noted to have C. diff positive ostomy output as well as a marked hyperchloremic hypokalemic metabolic acidosis with a bicarbonate less than 5, potassium of 2.2 and chloride of 122. At first, management and electrolyte repletion focused primarily on correcting a profound metabolic acidosis, for which the patient was briefly placed on a bicarbonate drip. Efforts were also made to correct the patient’s other concomitant electrolyte abnormalities, in particular his hypokalemia, which proved to be difficult to manage with replacement equating to 220 mEq of KCl daily. Repletion efforts eventually shifted to consolidation of supplementation in order to optimize his repletion regimen (e.g. KPO4 for phosphorus repletion and LR for volume repletion). Most notably, the patient’s potassium repletion changed from a KCl based regimen to a CH3CO2K based regimen. With this change the patient’s high potassium requirements decreased to 80 mEq of potassium daily as did his sodium bicarbonate requirements, though to a lesser extent, despite continued high ostomy output.
DISCUSSION: The treatment of acidemia in proximal RTA is complicated by the fact that alkali therapy can result in a HCO3 diuresis and increased urinary K+ losses. In order to avoid a refractory and persistent hypokalemia, efforts should be made to ensure a portion of the alkali replacement is in the form of a potassium salt such as potassium citrate or potassium acetate. This physiologic perturbation in patients with proximal renal tubular acidosis is illustrated by the fact that this patient’s potassium repletion requirements were markedly reduced once concomitant alkali therapy was added to his potassium repletion substrate, rather than addressing each of his electrolyte deficits individually.
MAY THURNER SYNDROMEManisha Bhide; Kandace Shepherd. University of Colorado Denver, Aurora, CO. (Tracking ID #1923475)
LEARNING OBJECTIVE 1: Discuss how a common anatomic variant can increase risk of left leg deep vein thrombosis.
LEARNING OBJECTIVE 2: Increase the awareness of this vital problem that causes morbidity in young adults and needs more aggressive management.
CASE: 53 years old, previously healthy, male presented to clinic for left leg pain, new unilateral varicose veins, purple discoloration, leg swelling and unable to bear weight. He denies any recent travel, trauma, illness, fever or chills. Past history significant for former smoker 15 pack years quit 10 year ago, hereditary spherocytosis, s/p splenectomy. Age appropriate cancer screening up to date, including normal colonoscopy. Exam revealed normal Ankle brachial index, but dusky, blue edematous leg with varicose veins. Systemic exam was normal. Ultrasound of the leg showed left common iliac vein occlusion, extending into Inferior Vena Cava (IVC), partial thrombus in external iliac and femoral veins. CT of abdomen pelvis noted- Extensive left lower extremity thrombus and thrombophlebitis. Non occlusive thrombus in the IVC beginning 6 cm below the right main renal vein with occlusive thrombus in the left common iliac left external and internal iliac, common femoral, femoral and deep femoral veins. CT chest confirmed moderate burden of pulmonary emboli to both lungs with small wedge lung infarction. Vascular surgery was contacted and TPA directed thrombolysis with left iliac vein stent was done. He was found positive for Factor V Leiden mutation. He was discharged on chronic anticoagulation. Course- 2 months later, he developed iliac vein stent thrombosis on INR 1.7 and needed re stenting Case 2–35 year female nonsmoker presented with extensive left leg DVT. CT abdomen diagnosed MTS. She underwent iliac vein stenting and 6 month anticoagulation. Her stent remains patent for >5 year
DISCUSSION: In 1851, Virchow noted increased incidence of left sided DVT (deep vein thrombosis). In 1957, May and Thurner noted hemodynamically significant compression of the left common iliac vein between the overlying right common iliac artery and the underlying vertebral body causing a venous spur. This was termed May-Thurner syndrome (MTS) or iliac vein compression syndrome. Venous spur develops due to collagen and elastin deposition and intimal fibrosis due to chronic arterial pulsations. Incidence of MTS is 20 % and accounts for 2–5 % of venous disorders in leg. It is more common in young women in 2nd-3rd decade. When accompanied by postpartum state, contraceptive use, immobility, hypercoagulable states it can precipitate a left leg DVT. Diagnosis is made based on clinical suspicion, venous ultrasound and CT or MR venography. Advanced techniques like intravascular ultrasound is sensitive in detecting the pathognomonic venous spur and helps to calibrate vessels before stenting. Long term anticoagulation alone may not prevent recurrence; hence more aggressive approach like intravascular stent placement is needed. Society of Vascular surgery 2012 guidelines do not recommend IVC filter placement, but do recommend catheter directed thrombolysis and mechanical thrombectomy to prevent post thrombotic syndrome. Usually anticoagulation is needed for at least 6 months post stenting. Longer duration of anticoagulation is recommended for pulmonary embolism. Literature review shows average post stent patency is about 70-80 % over 2 years. Thus it is important to know and identify this anatomic variant, since it affects management, prognosis and morbidity.
MELANOMA MASQUERADING AS HEMORRHOIDFumi Ito1; Hidenori Oguchi1; Mitsunori Iwase1; Masataka Shinoda2; Shinichi Mizuno1; Takahisa Suzuki2. 1Toyota Memorial Hospital, Toyota, Aichi, Japan; 2Toyota Memorial Hospital, Toyota, Aichi, Japan. (Tracking ID #1930588)
LEARNING OBJECTIVE 1: Recognize the possibility of malignancy even in patients with hemorrhoid.
LEARNING OBJECTIVE 2: Asses the need for pathological diagnosis in hemorrhoid.
CASE: A 63-year-old woman with a past medical history of internal hemorrhoid was admitted to our hospital for gradually developing edema of lower extremities. Her internal hemorrhoid had been followed by a practitioner who was specialized in anal diseases, and exsected three times during 4 months prior to admission. She denied dyspnea, orthopnea, fatigue, nausea, weight loss, headache, cough, any pain throughout her body. She had no history of medication, smoking or drinking alcohol. Vital signs showed the blood pressure of 103/60 mmHg, the pulse of 80 beats per minute, and the body temperature of 36.5 °C, the respiratory rate of 14 per minute, and the oxygen saturation of 96 % while breathing ambient air. Physical examination revealed slightly swollen abdomen without tenderness, and also severe edema in her lower bilateral extremities. Laboratory results including complete blood cell counts, basic metabolic panel were normal, but liver enzymes prominently elevated. Abdominal ultrasound showed ascites and multiple high-echoic lesions in the liver. Plain chest and abdominal CT scans revealed several small masses in the bilateral lungs and liver, and a tumor in the rectum. Colonofiberscopy revealed a melanotic tumor in anorectal region. Accordingly, malignant melanoma with metastasis was highly suspected. Biopsy was performed, and indicating positivity for malignant melanoma specific in Human melanoma black 45 (HMB45) immunostaining. The patient was diagnosed with malignant melanoma stage 4 and anorectal lesion was suspected of the primary site from imaging results. MRI and PET findings revealed multiple metastasis not only in both side lungs and liver, but also in iliac and femoral bones. At first, the standard chemotherapy with DAV (dacarbazine, nimustine hydrochloride and vincristine) was considered. However, the mono-therapy with dacarbazin was chosen, because her condition was seriously exacerbating with increasing ascites and emergence of dyspnea and appetite loss. After the mono-therapy with dacarbazin, her symptoms were substantially improved. Accordingly, DAV therapy was added once. Inspite of these chemotherapies, the patient passed away 2 months after admission.
DISCUSSION: Melanomas may stem from the mucosal epithelium lining in the respiratory, alimentary, and genitourinary tracts, all of which contain melanocytes, as well as from the skin. Anorectal mucosal melanoma accounts for approximately 0.05 % of all colorectal malignancies and only 1 % of all anal canal cancers. Importantly, mucosal melanomas generally carry a worse prognosis than those arising from cutaneous sites, with most patients developing recurrent and disseminated disease. The standard initial management for locoregionally confined mucosal melanoma is a complete wide local resection, which offers the best chance for long-term survival. Actually, some studies have shown early resection of primary mucosal lesions considerably improve the patient’s prognosis. The approach to the management of systemic metastases from a mucosal melanoma is based upon the treatment of metastatic cutaneous melanoma, and is limited. Anorectal mucosal melanoma is a very rare disease and likely to be missed at the time of exsection, though its prognosis is dismal especially in advanced metastases. Once we recognize that some hemorrhoid may be malignant tumor, we should asses the exsected hemorrhoid pathologically to prevent the tumor spread systemically. That will allow patients survive longer with more options for treatment including resection.
METRONIDAZOLE-INDUCED ENCEPHALOPATHYYuichiro Suzuki; Christine Kwan. Teine Keijinkai Medical Center, Sapporo, Japan. (Tracking ID #1932143)
LEARNING OBJECTIVE 1: Recognize that encephalopathy may be caused by the commonly used antibiotic, metronidazole
CASE: A 22 years old Japanese man presents with 12 days’ history of altered mental status while hospitalized. He is noted to have behavioral changes, disinhibition, dysarthria, and decreased response to external stimuli. At the time, he has no constitutional symptoms or other neurological changes. Of note, he has been hospitalized 2 weeks prior for fevers (39 °C), headache, left arm/leg weakness, and vomiting for which he has been diagnosed with Streptococcus constellatus right putamen brain abscess and prescribed ceftriaxone 2 g Q12H and metronidazole 500 mg Q6H in addition to stereotactic drainage. He has been clinically improving until now with new-onset encephalopathy not improved by sulpiride (anti-psychotic). Physical exam at this time shows vital signs of temperature:35.8C, blood pressure:108/59, heart rate:61, respiratory rate:10–15, and O2 saturation:92–98 % room air. Generally, he is awake but has depressed affect and psychomotor retardation. Neuro exam shows intact cranial nerves, motor strength 4/5 on his right extremities and 3/5 on his left, continued decreased sensation to light touch and position on his left extremities, 2+ reflexes bilaterally, (+) muscle rigidity, and unstable gait. Labs, including complete blood counts and chemistry, are within normal limits except for gamma-glutyl transpeptidase:184U/L, alkaline phosphatase:350U/L, aspartate aminotransferase:44U/L, alanine aminotransferase:73U/L, and creatine kinase:38U/L. Repeat head computed tomography (CT) 1 week after the first one shows no worsening of the abscess. Head magnetic resonance imaging (MRI), however, reveals high intensity areas in the retrosplenial region and bilateral cerebellar dentate nucleus. Given these imaging results consistent with metronidazole-induced encephalopathy, his metronidazole is switched to clindamycin with behavioral improvement the following day. Repeat MRI 1 week after shows a decrease of the high intensity signals with continued clinical improvement although still with some residual numbness, albeit improving, in his extremities.
DISCUSSION: Metronidazole is one of the mainstay drugs for the treatment of anaerobic infections, including brain abscesses, and Clostridium difficile diarrhea. Resistance remains rare, which is probably one of the reasons why this drug is commonly used worldwide. It can also reach high concentrations when taken orally, and its tissue penetration is excellent. Metronidazole can even effectively penetrate the blood brain barrier, hence why it is often used for brain abscesses. While the most common side effects of the drug is usually in the gastrointestinal tract, neurotoxicity can occur, usually when the dose exceeds the range of 21–135 g; the above patient has taken a total of 2000 mg/day × 41 days = 82 g. Metronidazole-induced encephalopathy, however, has only been reported in 21 case reports in 2011. Key radiologic findings on diffusion weighted MRI include bilateral, symmetric high intensity areas in the cerebellar dentate nuclei and corpus callosum, like the above patient. Most patients improve within 3–6 weeks after discontinuation of metronidazole, but some are left with irreversible severe neurologic disabilities. Given the possibility of encephalopathy, therefore, one should recognize the potential adverse effects of the commonly used antibiotic, metronidazole.
METRONIDAZOLE-INDUCED PSYCHOSIS: A CASE REPORT AND BRIEF REVIEW OF THE LITERATUREMargaret Park1; Christopher P. Redgate2; Estebes Hernandez1. 1UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA. (Tracking ID #1938516)
LEARNING OBJECTIVE 1: Recognize the neuropsychiatric side effect of metronidazole.
CASE: A 42 year old male with a history of end-stage renal disease, type 2 diabetes mellitus, and stroke presented with a 2 week history of acute episodes of altered mental status. The first episode occurred at the end of a hemodialysis session during a recent hospitalization for catheter- associated bacteremia and Clostridium difficile colitis. He became acutely agitated and repeatedly endorsed suicidal ideation. The episode lasted 20–30 min then resolved with the patient having no recollection of the event. Psychiatry attributed the episode to acute delirium in the setting of multiple medical issues. He was monitored for 24 h without a recurrent episode and discharged home. Upon discharge, he subsequently had multiple episodes similar to the first. Over the course of a week, the episodes increased in duration and frequency. Several emergency room visits failed to reveal a metabolic or organic cause. Subsequently, a persistent episode required inpatient admission for management of his symptoms and search for etiology. Initial testing for reversible causes of delirium were negative including blood cultures, thyroid function, liver function, blood chemistry, vitamin B1, and urinary drug toxin screen. A CT and MRI of the brain noted encephalomalacia in the right MCA territory consistent with prior stroke. Review of current medications revealed a long list of stable medications. The only medications over the past several weeks were antibiotics prescribed to treat bacteremia and colitis. He completed his course of ciprofloxacin on the day of admission and metronidazole was switched to oral vancomycin. He continued to have daily acute episodes of agitation and hallucinations requiring 24-hour supervision and intermittent use of restraints. Psychiatry again felt the episodes were more likely delirium versus a new underlying psychiatric condition. He was medically managed with risperdone twice daily and clinically improved over the course of 5–7 days. Patient was discharged with Psychiatry follow-up. Patient has been followed closely since discharge without recurrence of symptoms for greater than 6 months since hospitalization.
DISCUSSION: Previous cases of metronidazole-induced psychiatric side effects described in the literature often involved healthy, young patients. The low number of reported cases of psychiatric side effects, despite widespread use of metronidazole, may speak to the difficulty in confirming drug-related psychiatric adverse reactions in general but particularly in more medically complex patients in which this drug is often used. The exact mechanism of metronidazole neurotoxicity remains unknown. Metronidazole reaches near 100 % bioavailability, with a large volume of distribution and low serum protein binding. The drug undergoes extensive hepatic metabolism and rapidly and effectively crosses the blood brain barrier in concentrations that approximate serum levels, which could explain its potent albeit rare neurologic side effects. This drug reaction may have been confounded by his renal dysfunction despite appropriate dose reduction. That being said, after evaluation of the case reports collectively, a consistent dose or duration relationship with metronidazole and neuropsychiatric side effects has not been confirmed. Both direct and indirect neurotoxic effects have been hypothesized for metronidazole-induced neuropsychiatric side effects. Direct toxicity appears to occur through inhibition of neuronal protein synthesis and temporary axonal swelling or neuronal injury with subsequent death of Purkinje-fibers. The proposed indirect toxicity is thought to be due to oxidation of catecholamines to their corresponding semiquinone radicals when exposed to metronidazole or impaired thiamine utilization. This case highlights the importance of maintaining a broad and thorough differential when determining the cause of psychiatric symptoms. A detailed account of current medications with start and stop dates is a critical component in the assessment of new- onset psychiatric complaints and should be conducted upon presentation, particularly in the setting of polypharmacy and a medically complex patient. Delay in diagnosis can result not only in severe impairment, impacting the patient’s mental and physical well-being, but also in increased healthcare utilization as in this case.
MICROSCOPIC POLYANGIITISChristina M. Cruz; Darlene LeFrancois. Montefiore Medical Center, Bronx, NY. (Tracking ID #1940703)
LEARNING OBJECTIVE 1: Distinguish non-infectious from infectious causes of pulmonary consolidation
LEARNING OBJECTIVE 2: Recognize the clinical manifestations and diagnostic criteria of microscopic polyangiitis
CASE: Mr. M is a 70 year old man with prostate cancer treated with radiation therapy 3 years prior and a former smoker with significant emphysematous disease who presented with progressively decreasing exercise tolerance × 6 weeks. He initially presented 5 weeks previously with decreased exercise tolerance, cough, malaise, and subjective fever. He was treated for community acquired pneumonia, which was seen on CXR, and superimposed COPD exacerbation. Two weeks later, without interim improvement, he again presented with similar symptoms. Repeat CXR and CT thorax revealed multilobar consolidations. He was then treated for hospital acquired pneumonia. But 3 weeks thereafter, he again presented with progressively worsening dyspnea. His initial cough had persisted, productive of some white sputum, however fevers did not continue. He had also developed pleuritic pain significant weight loss and 1 week of painful paresthesias of his right foot. He did not note any lower extremity edema, palpitations, arthralgias, myalgias, rashes nor muscle weakness. On exam he had focal areas of decreased breath sounds but a normal heart exam. He had decreased sensation to light touch of right lateral and plantar foot, strength preserved. Initial laboratory studies were significant for a leukocytosis of 24,000 (increased from 12,000 5 weeks prior, 16,700 3 weeks ago and 18,800 1 week ago) with a neutrophilic predominance, no immature cells. Hemacrit was 29 % from a baseline of 40 % 6 weeks to this presentation. Stable creatinine with GFR >60 but urinalysis with 22 RBCs/hpf, 35 WBCs/hpf, 30 protein, no casts sent (microscopic hematuria on urinalysis apparent for months). ESR of 95 mm/h and AST 133, ALT 135 (previously normal). CXR demonstrated stable multifocal consolidations. During his hospital course he also developed rapidly progressive renal failure and labs significant for positive ANA titer at <1:40, Rheumatoid factor 770, positive ANCA (P3-at >8.0 U but negative MPO) normal hepatitis serologies, negative anti-GBM, normal C3 and C4. Renal biopsy results showed diffuse segmental glomerulonephritis, pauci-immune, consistent with ANCA-mediated renal disease. He was diagnosed microscopic polyangiitis and treated with high dose steroids and cyclophosphamide, along with plasmapharesis for rapidly progressive glomerulonephritis. Although he required hemodialysis, his renal function and other symptoms improved and did not require subsequent renal replacement therapy.
DISCUSSION: Microscopic polyangiitis (MPA) is a small vessel vasculitis. It is an ANCA positive vasculitis characterized by pauci-immune necrotizing small-vessel vasculitis without clinical or pathological evidence of necrotizing granulomatous inflammation. Clinical manifestations include constitutional symptoms, including fever and weight loss, as well as renal, pulmonary, gastrointestinal, skin and neurologic manifestations. Renal involvement is a primary feature and seen 80–100 % of reported cases. It is typically characterized as rapidly progressive glomerulonephritis. Pulmonary manifestations include hemoptysis and alveolar hemorrhage, infiltrates, pleural effusion, pulmonary edema, pleuritis, and interstitial fibrosis. It remains one of the most common causes of pulmonary-renal syndromes. Growing evidence indicates a role for ANCA in the pathogenesis of MPA, with over 80 % of patients having associated ANCA positive serologies, although they are not included in the diagnostic criteria. Diagnostic criteria, like the Chapel Hill Consensus Conference criteria, primarily define MPA based on pathologic findings. Treatment for MPA includes an induction phase with high dose steroids and usually cyclophosphamide, with maintenance prolonged maintenance therapy. Alternative regimens are being explored given the substantial toxicity of cyclophosphamide.
MOLLARET’S MESS: THE HEADACHE YOU JUST CAN’T SHAKECatherine Firestein; Cady (Blackey) Brown. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926145)
LEARNING OBJECTIVE 1: Explore the differential diagnosis for aseptic meningitis
LEARNING OBJECTIVE 2: Review definition, diagnosis, and treatment of Mollaret’s meningitis
CASE: A 40 year-old woman with a history of meningitis and migraines presented with complaints of a frontal headache with associated photophobia, nausea, vomiting, and neck stiffness. She denied altered mental status and endorsed subjective fever and chills. On exam, the patient was found to be afebrile and demonstrated mild photophobia and neck stiffness. Basic laboratory studies were only significant for white blood cell (WBC) count of 11400/microL. CT of the head was within normal limits. Cerebrospinal fluid (CSF) studies were as follows: protein 62 mg/dL, glucose 66 mg/dL, zero red blood cells, WBC 716 with 8 % polymorphonuclear cells, 74 % lymphocytes, 2 % monocytes, 1 % eosinophils, and 5 % basophils. As the lymphocytic predominance was more consistent with viral meningitis and the Gram stain and routine culture of the CSF fluid were negative, empiric antibiotics were discontinued. The patient continued to improve and was ultimately discharged from the hospital with no further treatment indicated. Four days later, the patient re-presented to the emergency room with similar complaints of headache, photophobia, nausea, vomiting, and neck pain. She remained afebrile with only mild photophobia and neck stiffness noted on physical exam. HSV-2 PCR from her prior CSF studies had returned positive and she was admitted for treatment of HSV meningitis. The infectious disease service was consulted and recommended treatment with acyclovir until her discharge date, at which time she was transitioned to oral antivirals and treated with valacyclovir for 7 days.
DISCUSSION: Based on clinical signs and symptoms, this case was concerning for aseptic meningitis. Aseptic meningitis is commonly encountered by the general internist; it is important to be familiar with an appropriate differential diagnosis. This includes infectious causes, such as viruses, parasites, spirochetes, fungi or mycobacteria, as well as non-infectious causes such as medications, Bechet’s disease, sarcoidosis and lupus. Mollaret’s meningitis, or recurrent aseptic meningitis, was named for the French physician who first wrote about cases of recurrent aseptic meningitis. Today, diagnosis of Mollaret’s meningitis is based on clinical findings and cerebrospinal fluid results. The disease is characterized by multiple episodes of meningitis, with symptom-free periods between episodes. Lymphocytosis is seen in the CSF and characteristic mononuclear (Mollaret) cells may be seen early on. For many decades, the etiology of this disease was unclear, though a viral etiology has long been suspected. Since the advent of polymerase chain reaction testing, Herpes simplex virus has been found to be the cause of the majority of cases of Mollaret’s meningitis. Treatment for this entity is still being debated. Case studies have shown benefit of antiviral medications in both treatment of acute illness and prevention of recurrence. However, acute episodes usually resolve spontaneously and many patients have long symptom-free intervals. Until more clear evidence exists, treatment decisions should be made individually for each patient, based on the severity and frequency of his or her symptoms.
MOTHER NATURE TO THE RESCUE? AN UNUSUAL RASHJane Andrews; A Domnica Fotino. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926245)
LEARNING OBJECTIVE 1: Recognize the treatment potential of omega-3 fatty acids for skin conditions
LEARNING OBJECTIVE 2: Understand the workup of urticaria
CASE: A 64-year-old woman presented with a two-day pruritic rash that began on her scalp and progressed diffusely. She had no past medical history of rashes, allergies, recent sick contacts, fevers, chills, new exposures, medications or foods. She noted worsening GERD symptoms and dysphagia in the days leading up to admission, to the point that she could not swallow, but denied other symptoms or triggers. She has a history of severe GERD, depression, celiac disease though compliant with a gluten-free diet, and multiple family members with Sjogren’s, systemic lupus erythematosus and rheumatoid arthritis. Home medications include Paxil 20 mg daily, ranitidine 150 mg po twice a day, and albuterol q6h prn for shortness of breath. Patient had all childhood vaccines including measles, mumps and rubella. Her vital signs were within normal limits. Her skin was dry and erythematous, with coalescing, papular patches throughout the abdomen, back, and extremities. No scaling or vesicles were present. The rash appeared uniform, with no predilection for sun-exposed areas or extensor surfaces. Genital and oral membranes were pink and without ulceration. No oral ulcerations or joint abnormalities noted. Lab work demonstrated comprehensive metabolic panel notable for elevated BUN and creatinine of 29 mg/dL and 2.54 mg/dL, which normalized over 48 h with intravenous fluids, and elevated total protein to albumin ratio (8.8 g/dL to 3.8 g/dL), elevated erythrocyte sedimentation of 58, elevated C-reactive protein of 1.31 mg/dL, positive anti-neutrophilic antibody (unknown titer), negative anti-neutrophil cytoplasmic antibody, and negative HIV-1/2 antibodies and normal complete blood count. Manual differential showed 52 % neutrophils, 42 % lymphocytes, 6 % monocytes, and 0 % eosinophils. The patient’s urticarial reaction appeared 4 days after starting Benadryl and prednisone, however the rash slowly reappeared after discharge when patient had stopped taking the Benadryl and prednisone. An outpatient physician suggested adding omega-3 fatty acids to her diet, and upon starting flax seed oil (a rich source of omega-3) the rash went away. She stopped taking the flaxseed oil months later and the rash reappeared. This cycle repeated itself two more times with the rash disappearing each time she restarted the flax seed oil.
DISCUSSION: Rashes frequently challenge general internists. When pattern recognition fails to identify the cause, lab work may be helpful. Elevated serum IgE levels can point towards atopic dermatitis, skin scrapings may point towards fungal infections or scabies, ESR, CRP and antibody testing can point towards autoimmune disease, and flow cytometry and immunophenotyping are useful if B or T cell lymphoma is on the differential. HIV testing (particularly PCR testing) is important, since exfoliative dermatitis is predictive of seroconversion and can point to HIV-associated infectious agents. Differential diagnosis of this patient’s urticarial rash included contact dermatitis, atopic dermatitis, shingles, dermatitis herpetiformis, bacterial or fungal infection, scabies and DRESS. However, the distribution and characteristics of the rash were not consistent with these diagnoses. The patient denied having started any new medications, making Drug-Reaction with Eosinophilia and Systemic Symptoms less likely. In this particular case, anti-inflammatories were used to treat a presumed inflammatory process. This case study demonstrates one patient’s experience with using flax seed to treat this condition. Flaxseed’s likely benefits derive from its anti-inflammatory effects. In fact, several dermatologic conditions can be treated with omega-3 fatty acid supplementation such as atopic dermatitis, atopic eczema, alopecia, psoriasis, dandruff, ichthyosis, follicular hyperkeratosis and photosensivity. The omega-3 fatty acids present in flax seed have been shown to inhibit cyclooxygenase, a precursor to arachadonic acid and to lower multiple inflammatory markers such as white blood cell count, C-reactive protein, and serum amyloid A. Physicians may rely on medications to offer symptomatic relief in urticaria, such as anti-histamines and steroids, however these may be accompanied by side effects such as drowsiness, skin changes and weight gain. Flaxseed oil offers a non-pharmacologic anti-inflammatory alternative.
MULTIPLE CHIEF COMPLAINTS: CAN THERE B1 UNIFYING DIAGNOSIS?Theresa Poulos1; Marisa Hernandez-Morgan2; Marcia Glass3. 1University of California, San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA; 3University of California, San Francisco, San Francisco, CA. (Tracking ID #1898051)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of high-output heart failure due to severe thiamine deficiency (wet beriberi).
LEARNING OBJECTIVE 2: Understand the pathophysiology of wet beriberi and identify individuals at highest risk of developing thiamine deficiency.
CASE: A 48 year-old woman presented with 5 days of abdominal pain and difficulty breathing, a week of hemoptysis, and painful swelling of her left lower extremity. Her history was notable for alcohol dependency with delirium tremens, COPD, and hepatitis C. She was afebrile and tender to palpation in the epigastric area, with erythema and induration of the left abdomen. She had two-plus pitting edema to the mid-thigh bilaterally; both lower extremities showed marked erythema and were warm and tender to touch. She had a tremor of the upper extremities bilaterally. Her toxicology screen was positive for alcohol, and lactate was elevated at 2.6 mmol/L. Lower extremity Doppler was negative for deep vein thrombosis. CT of the abdomen was only remarkable for diffuse subcutaneous edema. Transthoracic echocardiogram findings were consistent with a high cardiac output.
DISCUSSION: Fluid accumulation resulting in edema is a common presentation. Distinguishing between dependent and diffuse soft tissue edema can help to narrow the differential and result in more timely diagnosis and treatment. The underlying cause of this patient’s anasarca is high-output heart failure due to severe thiamine deficiency. Thiamine deficiency can manifest as a peripheral neuropathy (dry beriberi), or with predominantly cardiac symptoms (wet beriberi). Initially in wet beriberi, peripheral vasodilation results in a decreased SVR and increased venous return. Continued deficiency leads to impaired myocardial function because thiamine acts as a coenzyme in carbohydrate metabolism. Specifically, thiamine deficiency results in impaired utilization of lactate, which then accumulates in the blood causing elevated serum lactate, as was seen in this patient. While elevated blood lactate is nonspecific, it has been used in the diagnosis of beriberi. With continued vasodilation, the kidneys detect a relative volume loss and respond by conserving salt. Fluid is re-absorbed, leading to diffuse edema, consistent with this patient’s otherwise odd pattern of fluid retention. The body cannot produce thiamine, and is only able to store up to 30 mg in tissue. The half-life is 9 to 18 days, so individuals who lack thiamine in their diet will become deficient within a month. Thiamine deficiency is rare in developed countries because most foods are fortified, however the WHO has documented outbreaks of beriberi among refugees and in developing countries–particularly Thailand and in sub-Saharan African–where diets are based on thiamine-poor staples such as polished rice and cassava. This patient was deficient as a consequence of poor nutrition associated with her chronic alcoholism. Gastric bypass patients and individuals on “fad” diets are also at risk. Physicians need to consider thiamine deficiency when evaluating a patient with diffuse anasarca. The diagnosis is largely clinical, because blood thiamine levels may not accurately represent the amount in tissue. IV thiamine should be administered whenever deficiency is suspected.
MY HUSBAND ATE MOTH BALLS: METHEMOGLOBINEMIA AND HEMOLYTIC ANEMIA ASSOCIATED WITH NAPHTHALENE INGESTIONAmeera J. Ahmed. Baylor College of Medicine, Houston, TX. (Tracking ID #1939468)
LEARNING OBJECTIVE 1: − Recognize that elderly patients with dementia may be at increased risk of ingestion of common household items
LEARNING OBJECTIVE 2: − Identify that naphthalene moth balls may cause both hemolytic anemia and methemoglobinemia. Diagnose early signs of methemoglobinemia
CASE: Naphthalene based compounds were widely used as household deodorizers and repellents for moth larvae in the past. Their use has been phased out but not banned given the toxic side effects associated with accidental ingestion. There have been numerous cases of naphthalene toxicity in children reported in literature before the 1970’s but recent cases have been rare. Now naphthalene has been replaced with 1,4-dichlorobenzene which tends to be safer. A 74 year old African-American male with advanced vascular dementia was brought to the clinic with complaints of lethargy, confusion and dark colored urine. The patient’s wife reported that she had found the patient with mothballs in his hand 2 days prior to presentation and suspected that he had ingested them. On exam the patient was somnolent. Labs showed profound anemia, indirect hyperbilirubinemia and elevated reticulocyte count. On the second day of admission the patient’s oxygen saturation was found to be 70 % with no signs of respiratory distress. Co-oximetry of an arterial blood gas sample showed elevated methemoglobin levels (9.5 %). He was managed conservatively with IV hydration and packed red blood cell transfusions.
DISCUSSION: Naphthalene has been well known to cause oxidative stress to red blood cells and cause hemolysis. The degree of hemolysis is greater in people with glucose-6-phosphate dehydrogenase deficiency, which is important to consider in African American patients. The hemolysis tends to resolve once the offending agent is removed. Conservative management with transfusions is recommended. Methemoglobinemia occurs by the oxidation of ferrous (Fe2+) to ferric (Fe3+) hemoglobin. This causes the hemoglobin to become incapable of carrying oxygen and shifts the oxyhemoglobin curve to the left. If MethHb levels are >20 % treatment with intravenous methylene blue and/or oral ascorbic acid is recommended. The caveat to this being avoidance of intravenous methylene blue if glucose-6-phosphate dehydrogenase deficiency is suspected since methylene blue may cause oxidant stress leading to further hemolysis. Clinicians should have a high index of suspicion for ingestion in elderly patients with dementia presenting with confusion and lethargy. Although the use of naphthalene moth balls has decreased in recent years there are still cases of ingestions leading to hemolytic anemia and methemoglobinemia. It is important to suspect methemoglobinemia in patients with hypoxia detected on pulse oximetry with no signs of respiratory distress. Early recognition may be life saving for the patient.
MYCOTIC ANEURYSM RUPTURE ASSOCIATED WITH ENTEROCOCCAL ENDOCARDITISMelissa Lyle1; Christopher Aakre1; Jae Yoon Park1; Peter C. Spittell2. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN. (Tracking ID #1927596)
LEARNING OBJECTIVE 1: Using diagnostic criteria to recognize a mycotic aneurysm in patients with infective endocarditis
LEARNING OBJECTIVE 2: Understanding the importance of early detection of mycotic aneurysms
CASE: A 33-year-old male with history of intravenous drug abuse and chronic hepatitis C presented to an outside hospital with fatigue, anorexia, myalgias, and general malaise. Blood cultures indicated enterococcal bacteremia, and he was subsequently transferred to our institution. He had mitral valve enterococcal endocarditis 2 years prior, which resulted in severe mitral regurgitation. He underwent mitral valve annuloplasty with neochordae placement. He experienced an episode of MSSA endocarditis 1 year afterwards. On admission, physical examination was notable for a grade 2/6 apical systolic murmur and splinter hemorrhages on his fingernails. Transesophageal echocardiogram demonstrated severe mitral valve regurgitation with new masses on the P2 scallop and an estimated ejection fraction of 60–65 %. He was initiated on a 6 week course of IV Penicillin G and Gentamicin for treatment of enterococcal mitral valve endocarditis. Cardiovascular surgery recommended mitral valve replacement following completion of the antibiotics. On hospital day ten, he developed a progressive unilateral headache. At onset, he had no focal neurologic findings, but suddenly became unresponsive 20 min later. Examination revealed a fixed and dilated right pupil and no spontaneous movements. He was urgently intubated, and a head CT scan illustrated a large right intracerebral intraparenchymal hemorrhage measuring 6.4 × 6.9 × 5 cm with intraventricular extension into the frontal and posterior horns of the right lateral ventricle, and herniation with a 2 cm midline shift. Emergent neurosurgical evacuation was performed. After evacuation, he remained comatose with extensor posturing and showed no improvement over the next 3 weeks. He was subsequently dismissed to a long-term care facility.
DISCUSSION: Intracranial mycotic aneurysms are relatively rare, accounting for only 10 % of neurologic complications associated with infective endocarditis. Aneurysmal degeneration of an arterial wall can result from bacteremia or septic embolization. Septic emboli from infective endocarditis have a predilection for the distal branches of the middle cerebral artery. The emboli can lead to inflammatory changes of the adventitia and can destroy the intima, ultimately resulting in aneurysmal formation. Diagnostic criteria assist in determining if an intracranial mycotic aneurysm is definite, probable, or possible. Mandatory criteria include demonstration of intracranial aneurysm by neuroimaging, and supportive criteria include a recent history of a predisposing infection, particularly infective endocarditis, any angiographic features, or age less than 45 years. Early detection of mycotic aneurysms with either magnetic resonance angiography or computed tomography can prove vital in regards to early aggressive treatment with antibiotics and surgery to possibly prevent rupture. Clinicians must keep in mind mycotic aneurysm formation in patients with infective endocarditis, particularly in those who develop new neurologic symptoms.
NATURAL KILLER/T-CELL LYMPHOMA: A CANCER THAT HIDES IN PLAIN SIGHTNayiri Gharibian; Jeffrey Miller. University of California, Los Angeles Olive View Medical Center, Sylmar, CA. (Tracking ID #1934890)
LEARNING OBJECTIVE 1: Recognize the unique clinical features associated with natural killer/T-cell lymphoma
LEARNING OBJECTIVE 2: Diagnose natural killer/T-cell lymphoma in the setting of challenging pathologic and radiographic findings
CASE: A 33-year-old female without significant PMHx was evaluated in Ophthalmology clinic for 1 month history of “dacryocystitis with nasolacrimal duct obstruction of left eye” after a cooking injury. She was started on antibiotics and had an I&D 1 month later given no improvement. After failing conservative management, her antibiotics were broadened and she underwent a left dacryocystorhinostomy (DCR) with stent placement. She returned to the ED twice after DCR with persistent facial pain and swelling. Four months after initial presentation, she was referred to ENT clinic with complaints of a new ulcer on the roof of her mouth. Biopsies were obtained and sent for culture. Several days later, CT imaging showed a “hypodense rim-enhancing collection” of the anterior septum most consistent with an abscess. Meanwhile, biopsy pathology returned showing “extensively inflamed and partially necrotic tissue with bacterial colonization.” She was then referred to ID clinic and placed on different antibiotics. On-going documentation notes “an unusual infection in a patient with no medical history.” Eight months after initial presentation, new biopsies demonstrated atypical T-cells consistent with NKTCL. Repeat imaging showed “significant progression of facial lymphoma” with extension of the mass to the entire upper lip and left buccal space. Staging CT showed mild splenomegaly but was otherwise unremarkable. Chemo and radiation therapy were started. In the following months, the patient had multiple hospitalizations for issues related to her lymphoma and developed progressive pulmonary involvement by her NKTCL. Four months after diagnosis, she was admitted with sepsis. CT chest showed worsened adenopathy, parenchymal abnormalities and bilateral pleural effusions. Given such rapid progression of her disease and poor prognosis, she was placed on comfort care measures and died 4 days later.
DISCUSSION: Natural killer/T-cell lymphomas (NKTCL) are aggressive malignancies occurring worldwide, with a strong predilection for Asian and South American populations. They are usually extra-nodal with initial sites involving the naso/oropharynx. Compared with other lymphomas, NKTCL portends a much higher mortality rate. This case highlights the challenges in diagnosing NKTCL, and the vigilance needed when faced with an “unusual infection” of the naso/oropharynx. Physicians should specifically consider NKTCL when confronted with a mass or ulceration of the naso/oropharyngeal space. Retrospectively, this patient’s hard palate ulcer was characteristic of NKTCL invasion of the nasal cavity floor which was not recognized. On radiographic imaging, NKTCL can easily be mistaken for an infection or abscess. In addition, biopsies often only reveal necrotic tissue. The treating physician should alert the pathologist of the consideration of NKTCL and surgeons should take care to adequately sample soft tissue adjacent to necrotic tissue. If initial biopsy results are inconclusive but clinical suspicion remains high, repeat biopsies should be pursued. As demonstrated in this case, timely diagnosis of NKTCL is typically elusive though essential. There is no surgical cure. Standard therapies include chemotherapy and radiation, however, clinical outcomes for most patients remain poor. Complete respone to primary treatment is reported in about half of all patients. Studies estimate that 5-year overall survival for NKTCL is 42 %. Still, Stage I (limited) disease can be cured, but stage IV (more invasive) disease is much less likely to be cured.
NAUSEA, VOMITING AND DIARRHEA: COMMON SYMPTOMS WITH AN UNCOMMON ETIOLOGYArvind Kalyan Sundaram1,2; Julie Grimes1,2; Saira Samani1,2; Christopher Roy1,2. 1Mount Auburn Hospital, cambridge, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1939208)
LEARNING OBJECTIVE 1: To recognize the signs and symptoms of Ciguatera poisoning.
LEARNING OBJECTIVE 2: To emphasize the importance of detailed history taking to overcome the anchoring heuristics while treating patients.
CASE: A healthy 34-year-old female presented to the emergency department after two episodes of syncope in a week’s time. The patient had returned from Haiti a day before where a few days ago, she had developed nausea, vomiting, diarrhea along with generalized pruritus. At Haiti she was given intravenous fluids and anti-histamines. Upon arrival to the US, her symptoms persisted. She experienced two syncopal events, leading her to seek medical attention. While in the emergency department she developed excruciating right leg pain. On review of symptoms, she reported reversal of hot/cold sensation in her hands, as well as generalized weakness. She was asked whether she had any exotic fish while on her trip at Haiti, which she replied to positively for red snappers. The patient’s cardiovascular and neurological examination was within normal limits. However, she was positive for orthostatic hypotension. Her complete blood count, basic metabolic profile, and electrocardiogram were unremarkable. Beta-HCG was negative. The patient was admitted on a telemetry floor to watch for bradycardia. It was decided to withhold Mannitol administration. Neurology recommended Gabapentin for the patient’s right leg pain that was thought to be neuropathic, and Duloxetine for the increased generalized weakness experienced by the patient. Despite aggressive fluid resuscitation, she continued to have orthostatic hypotension. She was then started on Fludrocortisone, following which her symptoms improved. Ondansetron and Diphenhydramine were continued for nausea and pruritus respectively. She improved and was discharged after being counseled on avoiding fish, alcohol, caffeine and nuts for 6 months.
DISCUSSION: Ciguatera poisoning is a food borne disease commonly noticed in the tropical and subtropical regions, accounting for 20 % of the fish related food borne diseases in the US. Nausea, vomiting, diarrhea, tingling, numbness, temperature relate dyesthesias, orthostatic hypotension are some of the presentations of Ciguatera poisoning. There are no clinical tests to diagnose Ciguatera poisoning. Gastrointestinal symptoms usually resolve earlier while neurological symptoms take longer time. Treatment is largely symptomatic. Use of Mannitol is controversial. Some trials have advocated for its use within the first 48 h, while another randomized control trial showed no benefit with Mannitol versus Normal saline administration. The case illustrates the importance of obtaining a complete history and the danger of anchoring heuristics. Presenting with symptoms of gastrointestinal upset has a broad differential. However, obtaining a careful history provided a diagnosis that tied in the entire patient’s presenting features, and most importantly counseled on prevention, as recurrent symptoms could be worse than the initial illness. This would have otherwise been a lost opportunity.
NECROLYTIC ERYTHEMA ASSOCIATED WITH HEPATITIS CPriyanka Yaramada1; Shannon Miller2; Huy Au2,1. 1University of California, Riverside, Riverside, CA; 2Riverside County Regional Medical Center, Moreno Valley, CA. (Tracking ID #1923606)
LEARNING OBJECTIVE 1: A good clinical examination is necessary for evaluation of diseases. This case is to remind physicians to recognize a pathognomonic rash for the diagnosis of an indolent but common disease. In this case, a good skin examination led us to diagnose a dangerous but treatable systemic disease that has been progressing undiagnosed and untreated for several years.
LEARNING OBJECTIVE 2: Awareness of necrolytic acral erythema is important not only for accurate dermatologic diagnosis but also because of the potential for earlier diagnosis and treatment of hepatitis C infection. The appearance is similar to psoriasis or lichen planus and is often misdiagnosed as these alternate conditions.
CASE: A 42 y/o Hispanic female with a history of IV drug abuse and dermatitis since 2005 with recurrent episodes of cellulitis presented to the hospital with severe edema, erythema and pain of the right lower extremity for 3 days. She had been treated with topical steroids and steroid injections intermittently for her dermatitis since 2005. She denied Hepatitis C stating she was last tested in 2003. She was found to have cracked demarcated and pigmented skin lesions with extensive scaling on the dorsal aspect of both feet from the toes extending across the dorsum of the foot, advancing 4 cm up the anterior portion of the bilateral lower extremities. The lesions were also noted on the dorsal aspect of both hands from just below the nail beds to the wrist. There was fluid drainage from the lesions on her feet. A CT scan of the legs showed soft tissue inflammation. Labs revealed elevated INR (1.6), PTT (43), bilirubin (2.4) and low albumin (1.4). Abdominal CT was unremarkable. A hepatitis panel was positive for hepatitis C virus with the 1a genotype. A punch biopsy of one of the lesions showed mild hyperkeratosis, minimal acanthosis and slight psoriasiform hyperplasia with mild superficial dermal chronic inflammation with post-inflammatory hyperpigmentation. She was diagnosed with Necrolytic acral erythema (NAE). Her cellulitis improved with IV antibiotics (vancomycin and zosyn) and zinc supplementation. She was discharged to follow up with Dermatology and Hepatology.
DISCUSSION: Necrolytic acral erythema (NAE) is a rare condition, first described in 1996. It is a cutaneous manifestation of hepatitis C viral infection (considered an early cutaneous marker of hepatitis C) with onset typically between 35 and 55 years old. It is described as a well-defined, pruritic or burning, hyperkeratotic erythematous eruption that most often affects the acral surfaces. The pathogenesis of NAE is thought to be related to zinc dysregulation, which can occur as a result of hepatitis C induced metabolic alteration. Histopathologically, it closely resembles psoriasis. Treatment for NAE is to treat the underlying hepatitis C infection. Oral zinc replacement has also been successful in some cases.
NEISSERIA SICCA ENDOCARDITIS PRESENTING AS MULTIPLE EMBOLIC BRAIN INFARCTSJorge L. Salinas; Kobina Wilmot; Christine L. Kirlew; Mark Mulligan. Emory University School of Medicine, Atlanta, GA. (Tracking ID #1938692)
LEARNING OBJECTIVE 1: Learn about the typical presentation of Neisseria sicca endocarditis
LEARNING OBJECTIVE 2: Learn how to appropriately treat Neisseria sicca endocarditis
CASE: The patient was a 58 year-old man with a history of HIV infection (CD4 191/22 %; viral load <20 copies/cm3 on antiretroviral therapy), ischemic cardiomyopathy, and a myoxmatous mitral valve status post mitral valve replacement in 2006 who presented with a 14-day history of worsening encephalopathy. He had become progressively more aggressive, forgetful, and disoriented and was lethargic and somnolent on the day of admission. On presentation, the patient had a temperature of 37.8, was tachycardic, and had a blood pressure of 105/66. Physical exam revealed a Glasgow comma scale of 14 and a muffled valvular click and 3/6 systolic murmur heard best at the apex. He did not have splinter hemorrhages, conjunctival petechiae, Osler nodes, nor Janeway lesions. White blood cell count was 15,000 (85 % neutrophils) and INR 5.54. Of note, the patient was on coumadin due to presence of St. Jude’s mechanical mitral valve. A non-contrast computer tomography of the brain revealed a left frontal hemorrhage (Figure 1) as well as a right temporal and right cerebellar hemorrhage, scattered subarachnoid hemorrhages, and an intraventricular hemorrhage with rightward midline shift. The patient was admitted to the neurological intensive care unit (ICU). Anticoagulation was discontinued and fresh frozen plasma and prothrombin complex concentrate were administered to reverse prolonged INR. The initial gram stain from blood cultures indicated presence of gram positive cocci, but the organism was later determined to be a gram negative diplococcus that was identified as Neisseria sicca. Transesophageal echocardiography performed on day 3 of admission revealed mild mitral regurgitation and two small vegetations. CT surgery evaluated the patient and opted not to perform surgery due to preserved mitral valve functionality and concern for further intracranial hemorrhage in the setting of heparin administration during surgery. The patient was initially started on vancomycin, rifampin, gentamicin, and ceftriaxone. Blood cultures cleared within in 3 days. Antibiotic coverage was narrowed to ceftriaxone after final sensitivities (MIC 0.25) were determined. After a 9 day Neurological ICU stay and stability on multiple head computed tomography (CT) scans, his mental status had improved significantly. He was discharged to subacute rehab after 30 days of inpatient care and received ceftriaxone for a total of 12 weeks. Anticoagulation was held for the duration of antibiotic treatment due to risk of recurrent intracranial hemorrhage.
DISCUSSION: Neisseria sicca is a gram negative diplococcus (Figure 2) found commonly in the upper respiratory tract [1]. It is typically a commensal organism. To our knowledge, there only 21 reports of Neisseria sicca endocarditis in the existent literature. Immunosuppression and the presence of an artificial valve were two risk factors which predisposed our patient to infection with the organism [1–17]. Other risk factors include poor dentition and intravenous drug abuse [1–17] N. Sicca grows easily on blood culture. The organism is usually susceptible to beta-lactams [1, 2, 12, 15, 16] but obtaining sensitivities is highly recommended. In the literature, >90 % of cases present with embolic events [16], and the brain is involved in at least 65 % of cases. Due to the high rates of embolism early surgery may be an important consideration in patients with Neisseria sicca endocarditis. Current endocarditis guidelines recommend surgery in cases of prior embolism and large remaining vegetation [18]. However, it may be reasonable to argue for early surgery in patients with Neisseria sicca endocarditis even in the absence of prior embolism due to the high rates of embolism associated with the organism. In this case, the patient had already experienced embolic events but the remaining vegetations were small. The patient also had significant risk of bleed if heparin were administered during surgery. Surgery was, therefore, not performed. Conclusion Neisseria sicca is a rare cause of endocarditis which is highly prone to embolic events.
NEVER TRUST THE GOLD STANDARD: A DIFFICULT DIAGNOSIS OF IGA DOMINANT ACUTE POST-STAPHYLOCOCCAL GLOMERULONEPHRITISVikram Balakumar; Jodie Bryk. Univeristy of Pittsburgh, Pittsburgh, PA. (Tracking ID #1940173)
LEARNING OBJECTIVE 1: Integrate history, physical examination, laboratories and biopsies into the diagnosis of glomerulonephritis (GN) sub-types
LEARNING OBJECTIVE 2: Recognize IgA Dominant Acute Post-staphylococcal Glomerulonephritis (APSGN) as an emerging etiology of GN.
CASE: A 76 year old male with hypertension, diabetes mellitus II, and bilateral Charcot’s foot deformity presented with oliguria, cola-colored urine, and anasarca following completion of therapy for a non-healing methicillin-resistant staph aureus (MRSA) left toe ulcer status-post 2 months of amoxicillin, 1 week of trimethoprim-sulfamethoxazole and recovery course complicated by osteomyelitis for which he underwent left toe amputation and treatment with parenteral daptomycin. Upon admission, the patient was found to have BUN of 140 mg/dL and Cr of 5.2 mg/dL (baseline of 1.0 mg/dL 3 months prior to admission). An initial urinalysis revealed 3+ protein, positive urine eosinophils, gross hematuria, and urine protein/creatinine ratio of 12 mg/g. Urine microscopy was positive for dysmorphic red blood cells. His presentation was felt to be consistent with a diagnosis of glomerulonephritis (GN). The differential included ANCA-vasculitis associated GN, anti-GBM GN, and immune complex GN. ANCA and anti-GBM laboratories returned non-elevated. He was found to have decreased C3 with normal C4. Given the decreased C3 and history of MRSA infection, APSGN was felt to be the most likely etiology of GN. A renal biopsy was performed for definitive diagnosis and showed pauci-immune cellular crescents with no immune complex deposits on immunofluorescence. Hence, it was concluded that an ANCA-associated GN was the more likely diagnosis and APSGN less likely despite our clinical suspicions. During his hospital course, the patient developed worsening anasarca and renal failure, requiring the initiation of hemodialysis. Empiric initiation of plasmapheresis with cyclophosphamide was recommended for management of ANCA-associated GN. Although the biopsy results were considered the gold standard to diagnose GN, clinical suspicion for APSGN prompted a repeat biopsy. The repeat biopsy revealed proliferative glomerulonephritis with presence of IgA and C3 deposits consistent with a diagnosis of IgA dominant APSGN, as history and laboratories predicted. After the second biopsy, plasmapheresis and cyclophosphamide were not started. The patient showed marginal improvement in his renal function without medical intervention, but remained oliguric and ultimately was discharged on long-term intermittent hemodialysis.
DISCUSSION: Although renal biopsy is considered the gold standard in the diagnosis of etiology of GN, this case demonstrates the importance of the history and supplemental laboratories in interpretation of even supposedly definitive data. The importance of making a diagnosis based upon all available data in this case cannot be overemphasized, as the treatment would have been a cytotoxic medication and plasmapheresis, an intervention not without harm. Earliest cases of MRSA related ASPGN were reported in 1995 in Japan. Given the global increase in incidence of MRSA, it is likely that the incidence APSGN will increase as well. IgA dominant acute post-staphylococcal glomerulonephritis (APSGN) is more common amongst the elderly following staphylococcal skin infections developing up to 16 weeks after the initial infection. Overall, the prognosis of APSGN is poor; existing data suggest that an important predictor in renal recovery in ASPGN is the absence of chronic renal parenchymal changes. Although there have been no systematic evaluations of treatment options, there is currently no available evidence to support corticosteroids in addition to appropriate anti-staphylococcal therapy.
NEW ONSET HYPOGLYCEMIA IN A PATIENT WITH SEVERE DIARRHEA: EVALUATING THE CAUSESRebecca Koransky; Manuela Calvo. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939272)
LEARNING OBJECTIVE 1: Identify the most common causes of new onset hypoglycemia and prioritize an appropriate work up.
LEARNING OBJECTIVE 2: Identify some less common causes of hypoglycemia.
CASE: A 33 year-old man with AIDS presented with 1 week of watery diarrhea. Home medications included anti-retrovirals and Bactrim. The patient reported having 8–9 bowel movements a day, a 15 lb weight loss over 1 week and abdominal pain worsened by food. Vital signs were significant for hypotension and fever. On exam, abdomen was diffusely tender but non-distended, with no guarding or rebound tenderness. Laboratory data was significant for potassium of 2.4 meq/L, chloride of 116 meq/L, CO2 of 12 meq/L and glucose of 75 mg/dL. An infectious work-up of the diarrhea was done, and patient was found to have positive cryptosporidium Ag in his stool, for which he was treated with aggressive electrolyte replacement, anti-diarrheal agents and anti-retroviral therapy. On day 2 of hospitalization the patient reported that he was feeling dizzy and weak with palpitations and diaphoresis, glucose level was found to be 20 mg/dL. Patient was given D50 IV injections, but hypoglycemia did not significantly improve, and he was then started on a D10 drip at 125 cm3/h. Glucose levels did not tolerate any decrease in the rate of the drip and patient continued to be symptomatic from the low blood glucose. He had never had similar episodes of hypoglycemia in the past, and liver function was normal. Insulin, C peptide, and cortisol levels drawn with each hypoglycemic episode were unrevealing. ACTH stimulation test was performed, and results demonstrated appropriate adrenal response. Bactrim was held as potential cause of hypoglycemia and replaced with Atovoquone, with no improvement in hypoglycemic episodes. After 1 week of supportive treatment, diarrhea slowly began to improve and patient began to eat his meals. With this improvement in diarrhea, symptomatic episodes of hypoglycemia decreased, glucose levels remained stable and patient was weaned from D10 drip. On the day of discharge 3 weeks later, abdominal pain had resolved, patient was having only one to two bowel movements a day, and glucose levels were normal without any supplementation.
DISCUSSION: Severe infectious diarrhea is often seen in immunocompromised patients. As seen in this patient, severe diarrhea in the setting of malnourishment can lead to symptomatic hypoglycemia. Common causes of hypoglycemia include medications, sepsis, renal insufficiency, cortisol deficiency, and nonislet cell tumors. In this patient, differential diagnoses should also include bactrim-induced hypoglycemia and decreased production of endogenous glucose. The standard of care for hypoglycemia work up includes close review of medications and medical history and laboratory testing of glucose, insulin, C-peptide, beta-hydroxybutyrate, pro-insulin, sulfonylurea and meglitinide during hypoglycemic episode. ACTH stimulation test can be performed to rule out adrenal insufficiency. If endogenous insulin production is found from laboratory values, radiologic studies can be performed. Once these common causes of hypoglycemia have been ruled out, as they were in this patient, other less common causes of hypoglycemia should be considered. Bactrim has been shown to cause hypoglycemia, and was initially considered as a cause in our patient. Medication was stopped and replaced with Atovoquone but hypoglycemia did not resolve. In children, there have been studies of hypoglycemia during episodes of severe diarrhea, with failure of gluconeogenesis found to be most common cause of hypoglycemia. Other case reports have shown hypoglycemia in patients with severe diarrhea correlated with low glycogen stores. We believe this impaired gluconeogenesis in the setting of severe diarrhea and malnourishment to be the cause of the patient’s hypoglycemia. It is important for clinicians to recognize this process in patients with severe diarrhea in order to maintain good nutritional intake even with diarrhea and to prevent symptomatic and dangerous episodes of hypoglycemia.
NEWFOUND ASSOCIATION OF ERYTHEMA NODOSUM WITH RARE SCALP DISEASEKarl Kirschke; Robby Singh; Diane L. Levine. Wayne State University School of Medicine, Detroit, MI. (Tracking ID #1938659)
LEARNING OBJECTIVE 1: Recognize the clinical features of dissecting cellulitis of the scalp
LEARNING OBJECTIVE 2: Assess the current treatment modalities for dissecting cellulitis of the scalp
CASE: A 23-year-old male with a past medical history of dissecting cellulitis of the scalp (DCS) presented to the Emergency Department with a 1 month history of bilateral leg desquamation with hyperpigmentation and tenderness and chronic scalp lesions. The patient was diagnosed with DCS 1 year ago. He had a complicated course and was treated with multiple medications including doxycycline, clindamycin, TMP-sulfa, isotretinoin, intralesional corticosteroids and an incision and drainage; all with minor improvement. One month ago, the patient developed painful bruises on his legs and was diagnosed with erythema nodosum (EN). Shortly, thereafter he began to have well demarcated desquamation over his legs as well as increased tenderness. On admission, he was afebrile. Exam of the scalp revealed diffuse weeping lesions with crusting and moderate diffuse alopecia. Multiple 1–2 cm tender erythematous nodules were present over both shins with significant desquamation of the overlying skin. The remainder of the exam was normal. He was treated with vancomycin, fluconazole and terbinafine for suspected refractory cellulitis. Cultures were taken from his legs and scalp, which were negative. The leg biopsy showed spongiosis with features of cellulitis and abscess formation. Chest radiographs and urinalysis were negative. CRP and ESR were elevated. HIV, GC and RPR were all negative. ANA was positive with a titer of 1:320 and a speckled pattern. Anti-dsDNA antibody was negative. Over the course of the hospital stay, his pain improved, and the desquamation and hyperpigmentation began to resolve. However, the DCS showed little to no improvement during the course of his stay. He was discharged 1 week after admission with a diagnosis of dissecting cellulitis of the scalp with cellulitis NOS of the legs and given TMP-sulfa for 3 weeks and terbinafine for a total of 6 weeks. One week later, his leg swelling and desquamation had improved and his scalp showed mild improvement. Etiology of leg involvement was suspected to be autoimmune in nature though medication related EN could not be ruled out.
DISCUSSION: DCS is a rare chronic inflammatory disease affecting the hair follicles of the scalp. It begins with multiple painful nodules forming abscesses on the scalp and often progresses to disfiguring scarring alopecia. It most commonly affects African American males between 20 and 40 years of age. The etiology remains unknown but is thought to represent a follicular occlusion disorder. While many treatments have been attempted, few have yielded promising long-term results. There are no large trials for DCS but many treatments have been tried in small series. Rifampicin and isotretinoin have yielded positive results in treating DCS but are often found to be unsuccessful in severe disease. In these instances, adalimumab and IV infliximab have had success in decreasing discharge, inflammation and pain. Laser therapy has also been effective in the treatment of DCS leading to reduced reliance on systemic treatments. Surgical approaches including skin grafting have been successful in the most refractory cases of DCS. Koshelev et. al. recently reported the first case of DCS with associated pyoderma gangrenosum lesions but there have not been any DCS cases associated with EN. We believe this is the first report of dissecting cellulitis of the scalp with concurrent EN. However, we must also allow for the possibility that the multitude of antibiotics our patient received over the last 6 months, specifically sulfa antibiotics, may have caused EN. While a rare disease, DCS has a characteristic course which if recognized early can be treated more effectively using the alternative modalities discussed here.
NIFEDIPINE INDUCED GINGIVAL HYPERPLASIARoshni Naik; Alan Tso. Beth Israel Medical Center, New York, NY. (Tracking ID #1939130)
LEARNING OBJECTIVE 1: Recognize the risk of gingival hyperplasia with nifedipine use.
LEARNING OBJECTIVE 2: Review the management of nifedipine induced gingival growth.
CASE: A 68 year old male with history of hemorrhagic stroke and hypertension on nifedipine was seen for complaint of gum swelling for the past year. The patient started taking nifedipine at the time of his stroke 1 year prior. His medication list included nifedipine 60 mg daily, losartan 25 mg daily and aspirin 81 mg daily. Patient was not on any antiepileptic drugs. The patient saw the dentist over the past year with reports of poor oral hygiene. There was improvement in gum swelling after one dental hygiene cleaning visit. Oral cavity examination revealed gingival growth in between teeth in anterior maxilla teeth and anterior mandibular teeth with multiple posterior molar cavities. The patient was seeking alternative blood pressure medication as his symptoms started since his stroke. Nifedipine was stopped because of the known side effect of gingival hyperplasia. The patient was seen 11 days later and was reporting decreased symptoms of gum growth.
DISCUSSION: We present a case in which a patient developed gum swelling with nifedipine use. Gum hyperplasia can be very distressing as it can result in difficulties in mastication and speaking as well as troublesome breath odor. The mechanism of gingival hyperplasia is thought to be a result of metabolic byproducts from the medication or alterations in calcium metabolism. Initially there is an enlargement of interdental papillae of the gingiva that develop into a lobulated mass or nodule. The gingiva can extend over the teeth and crowns. Trials have shown that the prevalence of nifedipine induced gum hyperplasia ranges from 0.5 to 83 %. Gum overgrowth is generally seen within 1 to 9 months of starting nifedipine. Factors that increase risk of gum hyperplasia include young age, dosage of nifedipine, and poor oral hygiene. Younger patients are at higher risk because they have higher fibroblast metabolism and hormonal changes. Also, increasing dosages of nifedipine may result in increased risk of gum growth. Doses of 30 mg/day to 100 mg/day have been shown to result in gum growth. Patients with poor oral hygiene with high plaque index also are at greater risk of gum hypertrophy. Treatment generally consists of meticulous hygienic dental cleaning and plaque control. In addition, reduction of nifedipine dose or discontinuation of drug is advised. Regression can occur after 1 week of stopping the medication, and complete regression can happen within 15 days. Gingival growth may recur if nifedipine is resumed. Also, switching to another calcium channel blocker may not result in resolution of gum growth as gingival hyperplasia has been associated with other calcium channel blockers in both dihydropyridines (i.e. felodipine, nitrendipine, amlodipine) and nondihydropyridines (i.e. diltiazem and verapamil). In severe cases, gingival resection may be needed, but nifedipine must be stopped as gum growth generally recurs if nifedipine is resumed.
NITROUS OXIDE ABUSE LEADING TO HYPERHOMOCYSTEINEMIA AND PULMONARY EMBOLIEiran A. Warner1; Yamin Shwe2; Leonard Amoruso1; Erica Grabscheid1. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1939770)
LEARNING OBJECTIVE 1: Understanding The Complications Of Nitrous Oxide Abuse
LEARNING OBJECTIVE 2: Understanding The Complications of Vitamin B12 Deficiency
CASE: A 23 year old Caucasian man was admitted to the hospital with a 5 day history of progressively worsening parasthesias and numbness of the feet which spread to his legs, arms and hands. The patient admitted to nitrous oxide (whippets) abuse over the previous 6 months. PMH included migraines, anxiety, bipolar disorder and heroin abuse. There was no history of alcohol abuse, vegetarianism or pancreatic/small bowel/gastric disease. On physical exam neurological abnormalities included: proximal weakness in the lower limbs, diffuse hyporeflexia, bilateral impairment of vibration and positional sense at the toes, a wide-based stance and truncal ataxia. Labs: Vitamin B12 303 pg/mL (normal 211–911), folate 12.9 ng/mL (normal 4.1–22.0), homocysteine 83.7 μmol/L (normal 5–15), methylmalonic acid 6144 nmol/L (normal 87–318) and Hgb 11.4 g/dL (normal 13.5–17.5) with an MCV of 104.8 fL (normal 80–100). MRI of the c-spine showed T2 signal hyperintensity within the bilateral posterior columns, extending from the cervicomedullary junction to mid C5. The patient began treatment with Vitamin B12 1000 mcg IM daily. After 1 week of treatment, Vitamin B12 was changed to weekly dosing. Prophylactic sq heparin 5000 units three times daily was also started on the day of admission. Five days after admission pt developed fevers, shortness of breath and pleuritic chest pain. CT angiogram showed bilateral pulmonary emboli. No DVT’s noted on US. Pt was started on Lovenox 1 mg/kg q12 h with a bridge to warfarin. At time of discharge 2 weeks after admission, his neurological deficits were resolving.
DISCUSSION: Nitrous oxide (N20), because of its euphoric effects, is often a drug of abuse- especially among young adults. Nitrous oxide is generally administered as ‘whippets’, small canisters that contain a pressurized form of the gas (similar to whipped cream aerosol containers). One of N20’s harmful effects is its ability to cause Vitamin B12 (cobalamin) deficiency by oxidizing Cob (I) alamin to Cob (III) alamin. B12 deficiency can lead to ineffective erythropoiesis (and ultimately megaloblastic anemia) as well as demyelination of the brain and spinal cord. A consequence of Vitamin B12 deficiency is elevated homocysteine levels. Hyperhomocysteinemia causes an increased risk for thrombosis and atherogenesis. This risk likely explains why the patient, despite thrombo-embolic prophylaxis, developed bilateral pulmonary emboli. Nitrous oxide use leads to Vitamin B12 deficiency which begets hyperhomocysteinemia, a risk factor for thrombi. Due to the high prevalence of nitrous oxide abuse in young adults, it is important to screen for B12 deficiency in any individual presenting with unexplained neurologic abnormalities or thrombosis in this age group. To the best of our knowledge, there have been no other case reports of symptomatic pulmonary emboli in the context of Vitamin B12 deficiency secondary to nitrous oxide abuse.
NO BULGING DISKPatrick Quinlan; Ronald Herb. Reading Hospital, Wyomissing, PA. (Tracking ID #1933080)
LEARNING OBJECTIVE 1: Consider Neuralgic Amyotrophy in the differential of unilateral arm pain and weakness
LEARNING OBJECTIVE 2: Recognize the classic presentation and diagnostic workup for Neuralgic Amyotrophy
CASE: A 56yo M with a remote past medical history of radiculopathy secondary to a bulging disk at C6 presented as an outpatient for evaluation of numbness on the tips of the first and second digits and severe, “knife-like” neck pain. His pain was constant when lying down. He also noted numbness on the posterior aspect of the ipsilateral forearm. The patient stated that he had similar symptoms in the contralateral arm about 10 years prior when he was diagnosed with cervical radiculopathy. At that time, he was successfully treated with a course of oral prednisone and physical therapy. On exam, he was noted to have decreased range of motion of the left upper extremity with weakness with arm flexion, wrist extension and hand grip. Decreased sensation to light touch was also appreciated. The patient was referred to neurosurgery, and an MRI of the spine was performed which revealed no significant cord compression or bulging disk. Upon follow up, the patient had no improvement of his symptoms and had developed “obvious atrophy of the left bicep”. EMG was performed and was notable for findings consistent with Neuralgic Amyotrophy. With two - seven day courses of oral prednisone the patient had relief of his neck pain but only had minimal improvement of his neurologic symptoms. He did have pertussis 7 months earlier which may have been an autoimmune trigger leading the his Neuralgic Amyotrophy.
DISCUSSION: Neuralgic Amyotrophy, also called Parsonage-Turner syndrome, idiopathic brachial plexopathy, brachial plexus neuropathy, acute brachial radiculitis, and paralytic brachial neuritis is an inflammatory disorder of the brachial plexus classically presenting with pain, sensory abnormalities, and eventual paresis. The pathophysiology is assumed to be autoimmune in origin, but the precise mechanism is unknown. The differential diagnosis may include cervical radiculopathy, peripheral nervous system vasculitis, or pancoast tumor. Imaging studies may be warranted to rule out these other possible etiologies as was done in this case. It is also important to obtain accurate history to rule out any potential preceding brachial plexus trauma (accidents, surgery, radiation). When no cause is apparent, and the onset of symptoms is rapid and painful, Neuralgic Amyotrophy is the most likely diagnosis. EMG will confirm the diagnosis. Those patients treated with corticosteroids early in their disease course have earlier recovery from their paresis. In summary, recognize Neuralgic Amyotrophy as a possible cause of neck and arm pain followed by paresis and sensory deficits.
NO MONOPOLY ON MONO: A CURIOUS CASE OF A VIRAL SYNDROMEChelsea Bowman1; Marion Stanley1; Harry Lampiris2,1; Meg Pearson2,1. 1University of California, San Francisco, San Francisco, CA; 2Veterans Affair Medical Center, San Francisco, CA. (Tracking ID #1928138)
LEARNING OBJECTIVE 1: Assess for acute Ebstein Barr virus (EBV) infection with a negative heterophile antibody
LEARNING OBJECTIVE 2: Recognize diagnostic considerations in heterophile-negative mononucleosis syndromes
CASE: 32-year-old healthy man presents with 2 weeks of malaise and diffuse myalgias after returning from a bachelor party. He also noted low-grade fevers and mild diffuse arthralgias. He denied sore throat, nasal congestion, cough, abdominal pain, dysuria and penile discharge. He is monogamous with his wife. Exposure history was significant for ticks and fresh water swimming near his home in Northern California. He had no exposures to farm animals, household pets, international travel, or mushroom ingestion. His exam showed a clear oral pharynx, no lymphadenopathy or rash, and liver edge was palpable 3 cm below costal margin. Initial labs were significant for a mild transaminitis with AST of 43 U/L and ALT of 56 U/L. Other labs revealed prior hepatitis B infection, negative HIV antibody, and a negative monospot (heterophile antibody). One week after initial presentation, persistent symptoms and development of right upper quadrant pain resulted in repeat evaluation which was significant for a white blood cell count of 6 K/cmm with lymphocytosis (54 % lymphs), mild anemia and thrombocytopenia (hemoglobin of 12.5 g/dl, platelets of 124 K/cmm), and acute hepatitis without evidence of liver failure (AST of 255 U/L, ALT of 416 U/L, total bilirubin of 0.8 mg/dl, alkaline phosphatase of 54 U/L and INR of 1.2). Further work up included negative Hepatitis C RNA, Hepatitis B core antibody IgM, RPR, EBV viral capsid antigen IgM, and HIV PCR. Both EBV viral capsid antigen IgG and EBV nuclear antigen IgG were positive consistent with prior EBV infection. Abdominal ultrasound revealed mild hepatosplenomegaly (both liver and spleen measured 18 cm). Cytomegalovirus (CMV) antibody IgM and IgG returned positive at 2.1 and 3.95 respectively (Normal <0.9). The patient’s symptoms were treated with supportive care. Transaminases downtrended to AST of 89 U/L and ALT of 177 U/L, and symptoms resolved by week 6 of illness.
DISCUSSION: General internists commonly evaluate patients with infectious syndromes likely due to viral pathogens. Our patient’s constellation of symptoms and lab findings, including subacute fevers, malaise, fatigue, diffuse myalgias, lymphocytosis, transaminitis and splenomegaly, were strongly suggestive of infectious mononucleosis. EBV is the primary etiology of infectious mononucleosis with around 80 % of patients having a positive monospot. A negative monospot can occur in acute EBV within the first 2 weeks of symptom onset. As our suspicion for EBV remained high and the monospot was negative, additional testing with EBV specific antibodies was taken as the next diagnostic step. The presence of EBV nuclear antigen IgG within the first 4 weeks of symptom onset excludes acute EBV as a diagnostic consideration. CMV is the most common etiology of EBV-negative mononucleosis. Primary CMV infection presents as symptomatic in less than 10 % of immunocompetent patients. CMV is less likely than EBV to have features such as lymphadenopathy, splenomegaly and exudative tonsillopharyngitis but is more likely to present with significant transaminitis, typically affecting ALT more than AST. Secondary syphilis and acute toxoplasmosis are important bacterial and protozoal causes of acute mononucleosis-like illness, respectively. Patients presenting with symptoms compatible with a mononucleosis syndrome should have an evaluation for EBV with a monospot and, if negative, EBV-specific antibodies. If testing for EBV is unrevealing, CMV, secondary syphilis and acute HIV infection should be highly considered in the differential diagnosis.
NON-ALCOHOLIC BEER: A UNIQUE CASE OF ACUTE ALCOHOLIC HEPATITISAnkita Tandon1; Neal Fitzpatrick1; Karen Krok2. 1Penn State University Hershey Medical Center, Hershey, PA; 2Penn State University Hershey Medical Center, Hershey, PA. (Tracking ID #1934352)
LEARNING OBJECTIVE 1: Recognize that patients who are to abstain from alcohol should also abstain from non-alcoholic beer.
CASE: Acute alcoholic hepatitis (AAH) can develop in patients with chronic alcohol abuse or recent heavy intake. Patients who go untreated with severe acute alcoholic hepatitis (defined as Maddrey discriminant function (DF) >32) have mortality rates as high as 25–35 % within 1 month. Patients substitute non-alcoholic beer (NAB) for alcohol-containing beer, however, NAB is a misnomer as it also contains alcohol. Most brands contain 0.5–1 % alcohol by volume (ABV) compared to regular beer that contains approximately 4 % ABV. We describe a patient with severe AAH after drinking NAB. Sixty-nine-year-old woman presents with worsening abdominal pain and fullness, confusion and jaundice for the past week. She has a history of alcohol abuse but stopped drinking alcohol 3 years ago because she developed AAH. Since then she has been consuming 7–8 NABs per day and denies any other alcohol consumption (corroborated by her supportive family). Physical exam revealed icteric sclera, jaundiced skin and 3+ pitting edema. Labs revealed a creatinine of 4.1 mg/dL, ALT of 33u/L, AST of 107u/L, total bilirubin of 23.6 mg/dL, albumin of 2.6 g/dL, platelet count of 208 and INR of 1.8. CMV IgM, HSV IgM, hepatitis A, B, C serologies and EBV PCR were all negative. ASMA, ANA and AMA were also negative. Abdominal MRI without contrast did not show signs of liver cirrhosis, splenomegaly or varices, however, it did show ascites and a fatty liver. Within 4 days, her liver function worsened and she had a DF of 39. Given her anuric acute renal failure, she was started on pentoxifylline, prednisone and treated with octreotide, midodrine and albumin for hepatorenal syndrome. Ultimately she required a week of hemodialysis. Subsequently, her total bilirubin started trending down and eventually her kidney function improved as well. Two weeks later, the patient was back to her baseline at which point her creatinine was 0.8 mg/dL, INR was 1.3 and total bilirubin was 6.4 mg/dL. Given her MELD score of 39, she was evaluated for a liver transplant. She underwent extensive psychosocial evaluation of her alcohol consumption by a transplant psychiatrist, social worker, and transplant hepatologist. These specialists all agreed that she was honest about her consumption of only NAB. Ultimately no transplant was required as her liver function continued to improve.
DISCUSSION: The patient was drinking eight NABs everyday for 3 years. With 0.5–1 % ABV per NAB, her total alcohol consumption per day exceeded the amount consumed from one regular beer. The 2010 dietary guidelines for alcohol consumption recommend drinking no more than 1 drink per day for women. If not treated appropriately, AAH carries a high morbidity and mortality. AAH in association with low alcohol content beer has previously not been described in the literature. Patients with cirrhosis, on medications that should be avoided with alcohol, or with chronic liver disease are advised not to drink alcohol. These patients may gravitate towards NAB without realizing these drinks still contain alcohol. It is imperative to educate physicians and patients about the existence of alcohol in NAB. The amount of NAB that patients can consume remains unclear, and it is our recommendations that they avoid all NAB.
NON-ARTICULAR FELTY’S SYNDROME: AN UNCOMMON DIAGNOSISTarun Jain; Chetan Mittal; Bernard R. Rubin. Henry Ford Hospital, Detroit, MI. (Tracking ID #1936228)
LEARNING OBJECTIVE 1: Appropriately rule out alternate causes of neutropenia with splenomegaly.
LEARNING OBJECTIVE 2: Recognize an uncommon presentation of Felty’s syndrome
CASE: 73 year old caucasian female with past medical history of chronic kidney disease, essential hypertension, ischemic cardiomyopathy status post implantable cardioverter defibrillator and ventricular tachycardia on amiodarone. She was found to have leukopenia (1800 cells/μl) and neutropenia (700 cells/μl) on routine blood work which persisted despite discontinuation of amiodarone. Review of systems was negative for morning stiffness, joint pains, swelling, oral or anal ulcers, rash and family history of rheumatological diseases. Physical examination was unremarkable except for splenomegaly. There was no obvious synovitis or limited range of motion in any joint. Imaging confirmed splenomegaly (18 cm) but was otherwise unremarkable. She subsequently underwent bone marrow biopsy and multiple peripheral smears which were negative for alternate causes of neutropenia. Autoimmune work-up revealed negative direct antiglobin test, anti-nuclear antibody, C-3, C4, c-ANCA, p-ANCA and monoclonal protein evaluation. However, rheumatoid factor (RF) 180 IU/ml, cyclic citrullinated peptide (CCP) 35 IU/ml and erythrocyte sedimentation rate 65 mm/h were significantly elevated. X-ray of the hands revealed diffuse osteopenia but no joint erosions. Ultrasound of hands was performed Final diagnosis of Non-articular Felty’s Syndrome (FS) was proposed and she was started on daily prednisone 20 mg with subsequent improvement in leukocyte (4100 cells/μl) and neutrophil (1700/μl) count gradually. It is now planned to start her on Azathioprine.
DISCUSSION: FS is characterized by neutropenia and splenomegaly in patients with seropositive (RF+, anti-CCP+) rheumatoid arthritis (RA). As a result of neutropenia, affected patients are increasingly susceptible to certain infections like Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, herpes and fungi. Differential diagnoses in our case vignette include myeloproliferative syndromes, amyloidosis, systemic lupus erythematosus, large granular lymphocyte syndrome, tuberculosis, HIV infection, sarcoidosis and cirrhosis; all of which were ruled out by appropriate testing. The articular disease in FS is usually severe in terms of both erosions and deformity. In some affected individuals, FS may develop during a period when the symptoms and physical findings associated with RA have subsided or are not present. In such scenario, it may remain undiagnosed. Manifestations of FS without clinical but only with laboratory features of rheumatoid arthritis are extremely rare. We present a case of severe neutropenia and mild splenomegaly in a patient with high titers of RF and anti-CCP with no signs of synovitis. The current vignette highlights the importance of recognizing Non-articular FS without much delay to initiate appropriate management.
NON-KETOTIC HYPERGLYCEMIC CHOREAMahmoud Abdelghany; Andrea Fritz; Samuel Massoud. Conemaugh Memorial Medical Center, Temple University, Johnstown, PA. (Tracking ID #1923595)
LEARNING OBJECTIVE 1: Non-ketotic hyperglycemic chorea might be the first presentation of hyperglycemia, or it might be secondary to poorly controlled DM.
LEARNING OBJECTIVE 2: Non-ketotic hyperglycemic chorea is a benign disorder that could completely reversible if diagnosed early and treatment properly .
CASE: A 34-year-old white male presented to our hospital complaining of flailing-like movements of the right side of the body, polyuria, polydipsia and 20 lb weight loss in 1 month. He denied any other symptoms or history of drug abuse. The past history was significant for type II DM for which he was on insulin therapy but had not been taking it for a year because of financial problems. Laboratory investigations were only significant for fasting blood sugar of 230 mg/dl, with no anion gap, and glycated hemoglobin (HBA1c) of 13.6 %. CT scan of the head did not show any abnormalities. MRI of the brain showed high T2- weighted signal in the both putamina of the basal ganglia, with low T1-weighted signal in the left putamen. Physical exam showed mild hypotonia on the right side but no weakness. The patient was started on insulin and clonazepam. After 3 days; the patient’s abnormal movements markedly decreased. Two weeks later, the abnormal movements disappeared completely. The patient refused to have a repeat MRI of the brain after 6 months, but he continued to be completely asymptomatic.
DISCUSSION: NKH chorea is a rare disorder with unclear etiology. The prevalence in the Asian females increases the possibilities of genetic or environmental predisposing factors. Cerebral vascular insufficiency, petechial hemorrhage, hyperviscosity, depletion of both gamma-aminobutyric acid and acetylcholine secondary to metabolic changes have been suggested as possible mechanisms of the NKH chorea. Infection could be a trigger factor. NKH chorea might be the first presentation of hyperglycemia, or it might be secondary to poorly controlled DM. Rapid correction of hyperglycemia might cause NKH chorea. Typically in patients with NKH chorea, there is high T1- and low T2-weighted signal in the contralateral putamen and high density on CT of the brain. Absence of putamen abnormalities on the MRI or the CT of the brain was previously reported. Here, we report a case with high T2-weighted and low T1-weighted signals in the contralateral basal ganglion. A follow up brain MRI after 6 months usually shows disappearance of the initial findings. The prognosis of NKH chorea is good. It depends on early diagnosis and proper management of the blood glucose. Additionally, typical neuroleptic drugs and benzodiazepines are helpful in controlling choreic movements. DM should be highly suspected in older patients with newly diagnosed chorea.
NON-OCCLUSIVE MESENTERIC ISCHEMIA IN A PATIENT WITH NO CARDIOVASCULAR DISEASETakeomi Nakamura; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan. (Tracking ID #1934046)
LEARNING OBJECTIVE 1: Recognize that patients with no cardiovascular (CV) disease may still have non-occlusive mesenteric ischemia (NOMI)
LEARNING OBJECTIVE 2: Recognize that type 1 diabetes mellitus (DM-I) may be associated with NOMI
CASE: A 49 year-old Asian man presents with sudden onset, witnessed syncope and fall from a standing position. He loses consciousness for several seconds with spontaneous recovery and no residual confusion. Soon after, he has diaphoresis, fatigue, and watery diarrhea ×3. He reports eating oysters 24 h ago, but no other gastrointestinal/CV/neurological symptoms, pre-syncopal tunnel vision, or recent travel. Besides his DM-I, he has constipation and takes insulin, senna, and telmisartan. He smokes 1.5 packs/day and drinks 1 beer/day for 29 years but uses no recreational drugs. Family history is unremarkable. Physical examination shows temperature = 37.5C, pulse = 90, blood pressure = 50/38, respiratory rate = 20, and O2 saturation >95 % room air. He generally appears in no acute distress; alert/oriented ×3. CV, abdominal, and neurological exams demonstrate no abnormalities, as does the rest of the exam. Laboratory testing, including complete blood counts, chemistry, and arterial blood gas, is normal except for BUN = 37.4 mg/dL, creatinine = 2.72 mg/dL, glucose = 174 mg/dL, HbA1c = 7.6 %, creatine kinase = 210 IU/L, lactate = 34 mg/dL (3.3 − 14.9), pH = 7.23, HCO3 = 13 mmHg, pO2 = 78 mmHg, and PCO2 = 33 mmHg. Electrocardiogram reveals no abnormalities. Several hours later, he starts shivering with diffuse abdominal pain, so given a presumptive diagnosis of acute gastroenteritis, he is administrated IV fluids, scopolamine, and pentazocine with continuation of his symptoms in addition to development of hematochezia, decreased urine output, and abdomen’s becoming flat, hard, and diffusely tender with peritoneal signs and decreased bowel sounds. Non-contrasted computed tomography shows pneumonatosis cystoids intestinalis and gas in the portal vein consistent with mesenteric ischemia and colonic necrosis. He thus undergoes enteroanastomosis without any complications. After the operation, he clinically improves. Pathology confirms the above diagnosis of NOMI.
DISCUSSION: NOMI occurs when either the small/large intestine undergoes partial- or full-thickness necrosis in the absence of an overt organic vascular occlusion. It starts with non-specific symptoms of mild abdominal pain that gradually progresses although abdominal pain is absent in up to 25 % of patients. Abdominal exam may initially, therefore, be normal or reveal only mild abdominal distention or fecal occult blood. Typical risk factors for NOMI include medications, such as vasoconstrictors (digoxin, dopamine, or norepinephrine) and diuretics, dialysis, severe CV disease, dehydration, or cardiopulmonary bypass. In the above case, however, the patient has none of the above risk factors except for dehydration. Instead, he has a long history of DM-I, which may have contributed to some arteriosclerosis around the NOMI lesion. It and the diarrhea may also have contributed to his dehydration. One case report has shown acute inferior mesenteric arterial occlusive disease associated with diabetic ketoacidosis although no other cases have specifically reported an association between DM-I and NOMI. One should recognize, therefore, that NOMI may still occur in patients with DM-I and without known CV disease.
NON-UREMIC CALCIPHYLAXIS IN PATIENT WITH PROGRESSIVE ISCHEMIC ACRAL LESIONSGladys Rodriguez; Robert L. Fogerty. Yale School of Medicine, New Haven, CT. (Tracking ID #1940115)
LEARNING OBJECTIVE 1: Diagnosing non-uremic calciphylaxis in patients with acral lesions.
LEARNING OBJECTIVE 2: : Review management of non-uremic calciphylaxis.
CASE: A 47-year-old gentleman with a PMH of diabetes, hypertension, and chronic renal insufficiency presented to our hospital with progressive, ischemic acral lesions. He had an episode of acute kidney injury 2 months prior to presentation where he was noticed to have hypercalcemia to 14 with normal PTH. Around that time he had noted cracks in his fingers that subsequently progressed to blackened tissue. He was empirically started on prednisone and underwent a renal biopsy consistent with diabetic nephropathy. He was discharged on a prednisone taper and had stable lesions. Two months later he presented with progression of necrosis of his fingertips and wet gangrene on his right foot, He underwent ray resection of his second to fourth digits of the right foot and was restarted on steroids and empiric antibiotics, and transferred to our hospital. On physical exam he had multiple black necrotic lesions on his fingers and toes. On genital exam, he had a necrotic lesion on the glans of his penis with fibrinous material present around the corona. Labs showed WBC of 11, Hct 21,3, plt of 111, INR 2.3, BUN 43, Cr of 2.5. LFT’s showed elevated alkaline phosphatase of 143 and GGT of 210. LDH, Vit D, intact PTH, PTH-RP, ACE level, and alpha-1 antitrypsin levels were all normal. His haptoglobin was elevated at 341. SPEP and cryoglobulins were negative. He had a positive phospholipid neutralization test, and his dilute Russell viper venom test was elevated at 1.35. Urine CTX was positive at over 1000 suggesting high bone turnover. On imaging he had a CT abdomen that showed para-aortic adenopathy and splenomegaly. Chest CT was consistent with multiple unchanged pulmonary nodules bilaterally. Upper angiogram showed widespread vascular calcifications. Dermato-pathology showed right medial calf consistent with calciphylaxis. Left upper lobe bronchial alveolar lavage and FNA of lymph nodes were negative for malignant cells. Bone marrow aspirate was not indicative of leukemia or lymphoma. A mediastinoscopy with lymph node biopsy showed markedly hyalinized lymph nodes with bland necrosis, focal calcification, and scattered small non-caseating granulomas consistent with sarcoidosis. Surgically he underwent several bilateral digit amputations and right foot MTA for wet gangrene. He was started on sodium thiosulfate and trialed on bisphosphonates with a notable drop in both calcium and phosphate. Because of the response to therapy, sodium thiosulfate was discontinued and he was started on a steroid taper again with a plan to discontinue as outpatient.
DISCUSSION: This case is of interest to General Internists and Nephrologists due to the severe morbidity and high cost ramifications of this diagnosis. Calciphylaxis is a well-described entity in patients with end-stage kidney disease and renal transplant. Sodium thiosulfate has been used in patients with uremic calciphylaxis undergoing dialysis. However, non-uremic calciphylaxis (NUC) is well less characterized. Patients with NUC usually have a normal or low values of calcium, phosphate and PTH. NUC is associated with high mortality with no known specific effective treatment. Thus, calciphylaxis should be considered while evaluating skin lesions in patients even in the absence of end-stage kidney disease and renal transplantation.
NONTUBERCULOSIS MYCOBACTERIAL INFECTION IN AN IMMUNOCOMPETENT HOST WITH UNDERLYING LUNG DISEASEEmily H. Miller1; Geeta Laud2. 1Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center at Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1938672)
LEARNING OBJECTIVE 1: Recognize mycobacterium avium-intracellulare as an important pathogen in immunocompetent elderly men with chronic pulmonary disease
CASE: An 83 year-old former smoker with COPD on home oxygen, recently hospitalized and treated for community-acquired pneumonia presented with ongoing symptoms of dizziness, dyspnea and failure to thrive culminating in syncope. He revealed generalized weakness, subjective fevers, and an unintentional weight loss of 20 lb over 2 months with a cough productive of white sputum without hemoptysis. The patient was a cachectic elderly white male with clubbed digits, crackles and dullness to percussion in the left lower lung fields. A chest CT showed dense consolidation and nodular opacities of the left lower and upper lobes without appreciable improvement from his previous admission. The patient was suspected to have chronic aspiration pneumonia and was treated with antibiotics for both aspiration and nosocomial pneumonia, given his recent hospitalization. He improved with this treatment regimen, but further workup was pursued given the indolent nature of his symptoms. Sputum cultures were positive for rare acid-fast bacilli by fluorochrome stain as well as mycobacterium avium-intracellulare (MAI) by DNA probe. He tested negative for HIV. The patient was started on MAI therapy and was discharged home with close follow-up in the pulmonary clinic. Eventually, his sputum cultures grew MAI. He improved significantly on this treatment, reporting increased exercise tolerance and weight gain.
DISCUSSION: MAI is perhaps best known as an opportunistic infection in the immunocompromised host. However, nontuberculosis mycobacterial infections can present in immunocompetent patients, and should be considered in the differential diagnosis of indolent nonresolving pneumonia. The exact number of MAI infections in the United States is not known, because reporting of the disease is not mandatory. Current data suggests that the rate of nontuberculosis mycobacterial pulmonary infection is 47/100,000 in people over the age of 65 in the U.S., and is thought to be on the rise. It is thought that about 2/3 of sputum samples which test positive for mycobacterium contain nontuberculosis mycobacterium, while only 1/3 are M. tuberculosis, suggesting that MAI may be a more common infection than previously thought. Pulmonary MAI often presents in middle age or elderly immunocompetent white men who have pre-existing lung disease, such as COPD. Common symptoms include fever, weight loss, and fatigue and these patients are often treated for recurrent lung infections with little resolution of their symptoms. The underlying lung disease present in these patients can make diagnosis of MAI very challenging. CT findings such as lung nodules in a tree-and-bud pattern are suggestive of MAI in a patient with the previously described symptoms. The gold standard for diagnosis is sputum culture, but a DNA probe for MAI can also be useful in diagnosis as cultures take weeks to result. Indications for the treatment of MAI include clinical symptoms consistent with the disease, radiographic findings and isolation of MAI from multiple sputum samples. Treatment of MAI requires a lengthy multi-drug regimen, consisting of a macrolide (azithromycin or clarithromycin), rifampin and ethambutol taken three times a week. This regimen should be continued until sputum cultures are persistently negative for MAI for at least 1 year. Close follow-up during this treatment course is important to monitor for medication side effects and clinical improvement. This patient had a significant improvement in his symptoms and quality of life with MAI treatment, highlighting the importance of including atypical organisms in the differential diagnosis for male smokers with chronic or unresolving symptoms such as persistent cough or weight loss.
NORMOLIPEMIC XANTHOMAS; A RARE CUTANEOUS FINDING LEADING TO DIAGNOSIS OF MULTIPLE MYELOMADevin B. Malik; Sourabh Aggarwal. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1939102)
LEARNING OBJECTIVE 1: Recognize that the presence of xanthomas, especially when a patient is normolipemic, may represent an underlying systemic disease such as malignancy and may warrant further investigation.
CASE: We describe a 66 years old gentleman with a history of cutaneous lupus well controlled by topical steroid cream, who presented to primary care office for a new rash of 3 months duration. The patient denied any pruritus or pain from the rash. He denied any fever, sick contacts or recent travel. There was no personal or familial history of hyperlipidemia or xanthoma. Exam revealed flat, yellowish plaques in bilateral axillae as well as inguinal fold without any adeonpathy, xanthelsma palpebrarum, or tendon involvement. Laboratory investigation revealed total cholesterol of 172 mg/dL, triglycerides of 37 mg/dL, HDL of 70 mg/dL and LDL of 95 mg/dL. Complete blood count, complete metabolic profile including kidney function test, liver function test and thyroid profile were normal. Erythrocyte sedimentation rate was elevated at 63 mm/h. C reactive protein, complement level and cryoglobulins were unremarkable. A punch biospy of the skin lesion revealed mononuclear cell infiltrate with numerous foamy histiocytic cells consistent with xanthoma. Further testing with immunofixation demonstrated an IgG monoclonal protein with lambda light chains. Patient was referred to oncology where a bone marrow biopsy showed 20 % plasma cells with no signs of end organ damage present, therefore a diagnosis smouldering multiple myeloma was made.
DISCUSSION: DPNX is a very rare entity and presents as a yellowish maculo-papular lesion symmetrically found in flexural folds of skin. It is usually associated with hematological disorders, mainly leukemias and paraproteinemias and rarely can be first sign of an underlying malignancy. The novelty that surrounds the diagnosis is the absence of hyperlipidemia. It is postulated that there is an interaction between paraproteins and lipoproteins which are cleared by macrophages to form complexes and deposit in the skin. The monoclonal antibody interacts with LDL forming an abnormal Ig-LDL complex that is scavenged by macrophages and are deposited in skin, causing xanthomas. Macrophages are believed to have predilection for abnormal LDL complex as opposed to normal LDL allowing the latter to be degraded as per the usual metabolic pathway resulting in normal lipid profile in these patients. Therefore, in a patient with xanthomas and normal lipids, a serum protein electrophoresis should be done to exclude an underlying myeloma, with close monitoring for overt disease manifestations such as renal failure, and bone lesions. This case demonstrates the importance of investigating xanthomas in the absence of hyperlipidemia, as it can often be the first manifestation of hematological disease, therefore physicians should be aware this entity.
NOT ENOUGH OF A GOOD THINGDevika Nair; Deepa Bhatnagar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924913)
LEARNING OBJECTIVE 1: Recognize pericardial effusions as a complication of renal failure
LEARNING OBJECTIVE 2: Distinguish uremic pericarditis from dialysis-associated pericarditis
CASE: A 63-year-old woman with end-stage renal disease due to long-standing hypertension presented with dyspnea and pleuritic chest pain that had been present for weeks. She denied fevers, cough, recent surgeries or recent hospitalizations. Outside records indicated that many of her dialysis sessions had been terminated prematurely due to fatigue. Vital signs revealed a temperature of 98 F, pulse of 89 beats/min, blood pressure of 153/68, mm Hg and oxygen saturations of 94 % on 2 l nasal cannula. She had a pericardial friction rub, and pulmonary examination revealed no abnormalities. Laboratory studies were significant for a BUN of 30 mg/dL and a creatinine of 4 mg/dL. An electrocardiogram showed normal sinus rhythm, but an echocardiogram revealed a 2.4 cm pericardial effusion. The patient underwent daily hemodialysis sessions for 1 week without a change in her symptoms. It was thus determined that she was suffering from dialysis-associated pericarditis. After she received a pericardial window, her symptoms resolved.
DISCUSSION: Internists must be aware of cardiovascular complications seen in patients with end-stage renal disease. Two such complications are uremic pericarditis and dialysis-associated pericarditis. In both cases, the pathophysiology appears to be related to the accumulation of nitrogen residues and chemical irritants in the pericardial space. However, it is important to distinguish between the two, as management differs significantly. Uremic pericarditis occurs when the visceral and parietal membranes of the pericardium are inflamed. Such patients usually present with an acute rise in BUN, with values being greater than 60 mg/dL. Unlike the diffuse ST elevations seen in pericarditis from other causes, uremic pericarditis shows a normal ECG. This is because uremic pericarditis is a result of fibrin and uremic toxin deposition into the pericardium, rather than acute inflammation. There is less epicardial electric injury in uremic pericarditis, resulting in less noticeable ECG changes. Our patient was likely suffering from dialysis-associated pericarditis, which occurs over a more extended period of time. This should be suspected in end-stage renal patients who present with a BUN that is not significantly elevated despite multiple missed dialysis sessions. Unlike patients with uremic pericarditis, these patients often do not respond to extended hemodialysis sessions. The underlying pathophysiology is less understood, but the phenomenon may be due to increased fibrosis and adhesions of the pericardial fluid necessitating surgical intervention for adequate fluid removal. Any patient with renal failure who presents with a pericardial effusion should be monitored with serial echocardiograms to assess for resolution with dialysis. If the effusion does not resolve after 7 to 10 days of daily dialysis, current practice suggests the patient be treated for dialysis-associated pericarditis with pericardiotomy and window placement. Our case highlights this important, albeit less common, manifestation of pericardial disease in end-stage renal patients.
NOT EVERYTHING THAT LOOKS LIKE IS A CELLULITISSubodh Pandey; Subhas Sitaula; Swagatam Mookherjee; Bhaskara Madhira. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1939141)
LEARNING OBJECTIVE 1: Differentiate cellulitis from vasculitic rash
LEARNING OBJECTIVE 2: Recognize unusual presentation of adult onset Henoch-Schonlein purpura (HSP) and importance of immunofluorescence study
CASE: A 43 year-old man with no medical history, presented with a 2 month history of worsening bilateral lower extremity rash, ulcers and painful swelling. These symptoms started 2 week after taking celecoxib for suspected tendinitis. He had failed outpatient treatment with 1 week of Augmentin given by primary care and with Prednisone 60 mg with rapid taper given by a dermatologist. At the time of ER presentation, he had unbearable neuropathic pain with intense burning and pins and needle sensation and he received a dose of Vancomycin and Zosyn for suspected cellulitis and admitted to our service. On examination he was afebrile, with diffuse palpable purpuric rash on bilateral feet extending up to upper leg, some blisters with serosanguinous discharge and many ulcers with black eschar. Other review of system was completely normal including no eye, oral, lung, abdomen, renal or joint affliction. His lab work revealed normal renal and hepatic function, leukocytosis of 15,000 with normal differential and no signs of infectious source, presumably secondary to steroids. An extensive rheumatologic workup was completely normal and failed to reveal a possible etiology. A skin biopsy was done and immunofluorescence revealed granular deposition of IgA, C3 and fibrin around scattered small dermal vessels pathognomonic for HSP. Patient’s pain was adequately controlled and continued on Prednisone at 50 mg. No new skin lesions were noticed in his three-day of hospital stay and he was discharged with rheumatology follow up.
DISCUSSION: With the incidence of skin and soft tissue infection 24.6/1000 person-years, cellulitis is a common anchoring bias for an inflamed rash. The wide array of vasculitidies, with its systemic involvement and often-fatal course, should always be in the differential. More than 10 % of patients labeled as having cellulitis do not have it. Because the internists and the hospitalists usually take care of cellulitis, they should be able to differentiate other dermatologic conditions. HSP, also termed as IgA Vasculitis, is a primarily pediatric disease of small vessel with more than 90 % cases in less than 17 years age, with peak in 4–6 years of age. Although a variety of infectious and chemical triggers are recognized, the underlying cause of HSP remains unknown. At presentation in adults, clinical findings included palpable purpura (96 %), arthritis (61 %), and gastrointestinal symptoms (48 %) and renal insufficiency (30 %). In adults, renal involvement tends to be more severe in adults than in children as manifested by a higher frequency of nephrotic syndrome, hypertension, and an elevated serum creatinine. Biopsy commonly shows Leukocytoclastic vasculitis, but the immunofluorescence showing IgA deposition is pathognomonic. We present this case as an unusual presentation in adults without any systemic manifestation. Many a times, the classic purpuric lesions are marred by advanced ulcers and with significant edema and inflammation, commonly misdiagnosed and managed as cellulitis. Leukocytolastic vaculitis, also known as hypersensitivity vasculitis, is a term used for small vessel vasculitis and not a diagnosis in self. Other differential are cryoglobulinaemic, urticarial, ANCA-associated vasculitis, as well as vasculopathy and coagulopathy in SLE or in bacteremia/sepsis. Along with formalin specimen a second specimen in Michelle solution should also be sent to detect autoantibody deposition.
NOT JUST A SIMPLE PNEUMONIARachel Solomon; Jenny J. Lin. Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1935178)
LEARNING OBJECTIVE 1: Identify unusual causes of pneumonia in immunosuppressed patients
LEARNING OBJECTIVE 2: Recognize symptoms associated with Mycobacterium Avium Complex-related pneumonia
CASE: A 53 year-old woman with history of orthotopic liver transplant 20 years ago for chronic hepatitis B and hepatocellular carcinoma presented to her PCP with a two-week history of nasal congestion and cough. She was an active yoga instructor and had been doing well on minimal immunosuppression with sirolimus. She was afebrile and her clinical exam was normal so robitussin and a steroid nasal spray were prescribed for a likely viral URI. Two weeks later, she returned with persistent symptoms and fevers to 101 F. On exam, her lungs were clear and she was given Bactrim for presumed bacterial sinusitis. Two days later, the patient returned because she had persistent fevers. Even though her lungs remained clear, a chest x-ray was performed and revealed a left upper lobe infiltrate. She was started on a 14-day course of levofloxacin for presumed community-acquired pneumonia and her fevers and symptoms resolved. Six weeks later, however, the patient returned with recurrent cough and fatigue. She was afebrile, had a normal oxygen saturation, and her lungs remained clear. Repeat CXR showed a dense rounded opacity in the lingula concerning for possible abscess. A chest CT confirmed the lingular consolidation and showed left upper-lobe and right-sided bronchiectatic changes. She was referred to a pulmonologist and a week later, underwent bronchoscopy and thoracentesis for a new, left-sided pleural effusion. Cultures from the lingular biopsy and lavage grew Methicillin-sensitive Staphylococcus aureus. Pleural fluid studies suggested a hemorrhagic effusion. Clinically, the patient appeared well and remained afebrile. But a repeat chest CT revealed new left upper lobe lesions and worsening lingular consolidation with cavitation. The patient was hospitalized with concern for necrotizing Staphylococcal pneumonia. She received 3 days of intravenous ceftriaxone and in light of her clinical stability, was discharged home to complete 4 weeks of Bactrim. Post-discharge, tissue and fluid cultures from her bronchoscopy grew Mycobacterium Avium Complex (MAC).
DISCUSSION: Community-acquired pneumonia (CAP) is common and usually due to common pathogens such as Streptococcus pneumonia or Haemophilus influenzae. Atypical pathogens such Mycoplasma or Legionella can also cause CAP but often present more subacutely and sometimes with extrapulmonary symptoms (such as diarrhea or headache). In solid-organ transplant patients who are immunosuppressed, unusual or opportunistic infections must also be considered. Both Staphylococcus and MAC are less common culprits in the spectrum of pulmonary infections. Necrotizing Staphylococcus pneumonia typically affects older adults with underlying comorbidities. It is generally acute in onset and rapid in its progression to septic shock, ARDS, and frequently death despite treatment with appropriate antibiotics. Consistent with our patient’s presentation, pathologic MAC generally has a more indolent course with a variable symptom profile including chronic or recurring cough, sputum production, dyspnea, malaise, fatigue, chest pain, and hemoptysis. Notably, fever and weight loss may be absent. Although historically MAC-related illness was rare and generally isolated to middle-aged women (“Lady Windemeres”), those with underlying lung disease, and AIDS/HIV patients, non-tubercular mycobacterium has been implicated more frequently in the past two decades in pulmonary disease in both immunocompetent and immunocompromised hosts. While overall numbers remain low and data scarce, the incidence of mycobacterial disease in solid-organ transplant recipients appears to be increasing as well. Of the eight cases reported in liver transplant recipients, two were pulmonary specific and four were disseminated. Non-tubular mycobacterium pulmonary infections generally arise late in the post-transplant course. Radiography may show predominantly fibrocavitary disease or more nodular/bronchiectatic disease. As in our patient, the latter typically manifests as dense airspace disease localized to the mid- and lower- lung fields accompanied by multifocal bronchiectasis, clustered sub-centimeter nodules, and some cavitation. Our patient improved both clinically and radiographically on single-agent therapy. Her cavitary pneumonia was likely pathologic MAC revealed in the setting of an exacerbating MSSA superinfection. Her (albeit mild) immunosuppression may have protected her from the usual severe inflammatory response to an MSSA driven process. She has initiated treatment for MAC with rifabutin, moxifloxicin and azithromycin. As patients with solid-organ transplants are living longer and more likely to be followed by primary care physicians, clinicians should be aware of unusual presentations and causes of pneumonia, even among those who are minimally immunosuppressed.
NOT JUST ANOTHER DAY AT THE SPACamille M. Webb; Peter D. Bulova. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1937540)
LEARNING OBJECTIVE 1: Recognize that chronic schistosomiasis can remain relatively asymptomatic in the granulomatous form.
LEARNING OBJECTIVE 2: Identify previous travels as an important component of history taking.
CASE: A previously healthy 40-year-old female originally from Brazil presented to the Emergency Department complaining of 3 days of dark tarry stools and one episode of bloody diarrhea, associated with palpitations and lightheadedness. Review of systems was positive for a 14-pound unintentional weight loss over the past 4 months, and was negative for fever, abdominal pain, nausea or vomiting. Travel history was positive for yearly visits to Brazil, including a visit to a local hot springs spa 3 years prior. On presentation, temperature was 37.2, heart rate was 87 and blood pressure was 106/69. Physical exam showed a thin female in no acute distress and was positive only for conjunctival pallor. Rectal exam showed melanocytic heme positive stool. Laboratory studies revealed hemoglobin of 8.2, white blood cell count of 6.3, platelet count of 255, and albumin of 2.8. The patient was admitted to the medical floor where her hemoglobin continued to drop and she received two units of packed red blood cells and fluid resuscitation. An upper endoscopy showed gastritis without active bleeding. Colonoscopy showed small hemorrhoids with normal rectal and colonic mucosa, no evidence of blood. A biopsy from the terminal ileum revealed granulomas. The patient was discharged home, and the biopsy came back positive for Schistosoma organisms. She received praziquantel 40 mg/kg in two separate doses separated by 6 h with no recurrence of gastrointestinal bleed. Her hemoglobin at a follow up office visit was 13.6.
DISCUSSION: Schistosoma is a trematode worm responsible for Schistosomiasis (bhilariazis), a neglected tropical disease that affects more than 200 million people worldwide. It is endemic in more than 70 countries: throughout most of Africa, as well as Brazil, Venezuela, and the Caribbean, where it causes significant morbidity and mortality. S. japonicum and S. mansoni are responsible for most GI manifestations worldwide, while S. haematobium predominantly causes urinary manifestations. Schistosoma eggs are released from human urine or feces into fresh water. They then make their way in the form of mirasidia to snails, their intermediate hosts, mature and are released into fresh water, where they penetrate human skin and reside in mesenteric veins. Schistosomiasis is commonly obtained when swimming in fresh water in endemic areas, and in this case the disease was likely obtained during this patient’s visit to hot springs in Brazil. The disease can present in either its acute form (Katayama fever) or chronic form, as in this patient. Gastrointestinal and hepatic manifestations are common and include both upper and lower GI bleeding, polyposis, and microabscess formation, caused by host’s immune reaction to parasite eggs. Finding eggs in stool or urine is diagnostic but requires high suspicion for the disease, and treatment is 70 to 90 % effective with praziquantel, 20 mg/kg in two doses taken 6 h apart.
NOT JUST SKIN DEEP: PARANEOPLASTIC PEMPHIGUS DUE TO THYMOMAJosh H. Bukowski; Kaumakaokalani Shimatsu; Paul Aronowitz. University of California Davis, Sacramento, CA. (Tracking ID #1936741)
LEARNING OBJECTIVE 1: Understanding initial serologic evaluation of pemphigus
LEARNING OBJECTIVE 2: To learn about causes of paraneoplastic pemphigus
CASE: Pemphigus is a dermatological disorder characterized by acantholysis (loss of intrakeritinocyte adhesion), which leads to intraepithelial blisters in the skin and mucous membranes. Pemphigus is usually idiopathic, but in rare circumstances can be paraneoplastic in origin. When evaluating a patient with blistering skin lesions serologic studies can be useful in helping to narrow the differential diagnosis. Our case illustrates that despite the use of serologic markers, further work up should be pursued to rule out other rare etiologies such as neoplastic processes. A 49 year-old man with a history of diabetes mellitus, herpes simplex keratitis, and methamphetamine abuse presented from dermatology clinic with a two-month history of progressively worsening blistering rash that began on his fingers and hands, and spread to his torso, all extremities, face, oral mucosa, and groin. A skin biopsy was performed and he was begun on corticosteroids for what was believed to be pemphigus vulgaris. He was admitted to the hospital for concurrent management of his steroid-induced hyperglycemia and wound care. Biopsy results revealed intracellular epithelial deposition of IgG and C3 consistent with pemphigus. Though paraneoplastic pemphigus antibody serologies were obtained in an attempt to rule out paraneoplastic pemphigus, these studies came back negative. However, a chest radiograph revealed a retrosternal clear space that computed tomographic (CT) imaging of the chest found to be an anterior mediastinal mass. CT-guided biopsy of the mass revealed spindle cell thymoma. His skin lesions markedly improved with the addition of mycophenolate mofetil and clobetasol to his corticosteroid regimen. He was discharged with follow-up for surgical resection of the thymoma.
DISCUSSION: Pemphigus, is an organ-specific human autoimmune disease that is known to be associated with various tumors, autoimmunune disorders and some viral infections. The types of pemphigus are normally characterized by their clinical features and the identification of autoantibodies. These autoantibodies can be used to differentiate between paraneoplastic pemphigus and pemphigus vulgaris. Paraneoplastic pemphigus is characterized by antibodies against desmoplakins or desmosomal antigens in the setting of an identified neoplastic disorder. More than half of these neoplastic disorders are lymphoreticular in origin (thymoma, lymphoma, leukemia), with most remaining cases caused by Castelman disease, Kaposi sarcoma and other sarcomas. The pathophysiology of paraneoplastic pemphigus occurring with thymoma is not well understood but it is believed that damage induced by tumor growth within the thymus diminishes its ability to maintain self-tolerance and allows for development of autoimmune diseases such as pemphigus. This hypothesis is supported by case reports in which regression of bullous dermatoses occurred after resection of the thymoma. Our case illustrates that in the setting of pemphigus, serologic testing alone may not be adequate to rule out underlying malignancy as the etiology for bullous dermatoses and that further investigation looking for tumors commonly associated with pemphigus is warranted.
NOT YOUR TYPICAL “LUMPY JAW”: A CASE OF ACTINOMYCES OSTEONECROSIS OF THE MANDIBLEPrasanna Durairaj; Mihaela S. Stefan; Armando Paez. Baystate Medical Center/Tufts University School of Medicine, Springfield, MA. (Tracking ID #1940124)
LEARNING OBJECTIVE 1: Recognize the role of Actinomyces in osteonecrosis
LEARNING OBJECTIVE 2: Identify the histological features that distinguish Actinomyces related osteonecrosis from bisphosphonate related osteonecrosis (BRONJ) of the jaw
CASE: A 51 year old female consulted her primary care physician (PCP) for persistent 5 months left jaw pain, in the absence of preceding dental procedures. Past medical history includes: severe pulmonary hypertension on chronic oxygen supplementation, type II diabetes mellitus, and osteoporosis on weekly dose of Alendronate since 2007. The PCP diagnosed a dental infection; she was started on oral amoxicillin and also referred to the dentist. When seen by the dentist, she was noted to have trismus and facial swelling; hence, she was immediately referred to an oral maxillofacial surgeon for further assessment. The surgeon performed a sequestrectomy, where a fragment of necrotic bone was isolated from areas of healthy bone and sent for biopsy. Swab of the area was initially consistent with Streptococcus viridans and oral Clindamycin was prescribed. Four days later, she was admitted with fever and worsening jaw pain. She was noted to have SIRS criteria and appeared to be in moderate distress. Exam revealed left cervical lymphadenopathy, swelling with palpable lump of the mandible, and trismus. Oral exam did not show any exposed bone. Pathology report of the outpatient bone biopsy revealed extensive osteonecrosis with neutrophilic micro abscesses and bacteria with morphology suggestive of actinomyces. In the hospital, she was started on Penicillin 2 million units IV every 6 h and Alendronate was discontinued. The patient was not considered a surgical candidate for margin or segmental resection given poor vascularity of the region and her oxygen dependence. Penicillin dose was increased to 3 million units IV every 4 h for a 6 week course, to be followed by 6 months of oral antibiotics and possible debridement. Her symptoms improved in 48 h after antibiotics were adjusted and she was discharged home. At 2 week follow-up, she was tolerating the antibiotics well with almost total resolution of her jaw pain.
DISCUSSION: This case suggests that Actinomyces may have a role in the pathogenesis of BRONJ as the bacteria can instigate bone resorption by infecting living osteocytes. Bisphosphonates perpetuate mucosal breakdown by inhibiting keratinocyte life cycle and predispose the bone to entry of Actinomyces which form ‘sulfur granules’ (clumps formed during tissue invasion) at the site of the osteonecrotic bone. Previous reports suggest that 43/45 (93.5 %) patients with mandibular BRONJ were found to have direct association of Actinomyces colonies with bone. Although the estimated incidence of osteonecrosis of the jaw in those taking oral bisphosphonates is less than 1 case/100,000 person-years of exposure, long-term bisphosphonate use has to be periodically reevaluated to avoid this uncommon but serious complication. Additionally, once the presence of Actinomyces in recognized, prompt treatment of the infection is crucial for successful resolution of the symptoms.
ONCOGENIC OSTEOMALACIA: A CHALLENGING DIAGNOSISDietlind L. Wahner-Roedler. Mayo Clinic, Rochester, MN. (Tracking ID #1924460)
LEARNING OBJECTIVE 1: Recognize the clinical and laboratory features of oncogenic osteomalacia
LEARNING OBJECTIVE 2: Reinforce treatment plan for oncogenic osteomalacia
CASE: A 62 year old male patient presented to our institution in October of 2013 requesting a second opinion regarding the possible diagnosis of tumor induced osteomalacia. The patient was doing well until March 2012 when he developed upper back pain, which was treated with physical therapy. In October 2012 his back pain became progressively worse and he developed rib pain. He was seen by a local orthopedic surgeon where a whole body bone scan identified areas of increased uptake in the ribs raising concern of a possible underlying malignancy. However malignancy evaluation by laboratory testing was unremarkable. A repeat whole body bone scan in March 2013 showed some resolution of his previous lesions but new lesions specifically in the ribs which corresponded to rib fractures. There was further multilevel linear uptake in the vertebral column, most marked in the mid thoracic area, consistent with compression fractures. Increased uptake in the bilateral distal medial femoral condyles and the distal aspects of the tibia bilaterally was felt to be related to stress fractures. Irregular uptake in the upper left sacrum was interpreted as indicating a healing pelvic insufficiency fracture. Because of multiple bone fractures he had an extensive work up for malignancy including multiple myeloma. His serum protein electrophoresis was normal, alkaline phosphatase was markedly elevated ranging between 257 U/L in October 2012 to 400U/L in 2013. In the spring of 2013 he developed right hearing loss. His local ENT physician identified a growth in the right middle ear. A MRI of the head revealed a destructive enhancing lesion centered in the right jugular foramen with extension into the middle ear. He was further noted to have marked hypophosphatemia (phosphorus 1.8 mg/dl). He underwent a bone biopsy which showed significant osteomalacia. A biopsy of his right ear mass was consistent with a mesenchymal tumor. On presentation to our institution he had marked weakness and was in severe pain. He had difficulties rising from sitting to standing position, weakness with ambulation requiring the use of a cane for support. On physical examination there was no lymphadenopathy or organomegaly. ENT exam revealed some dried blood in the right ear canal and a middle ear mass inferiorly and posteriorly. Laboratory tests were remarkable for a markedly elevated alkaline phosphatase of 658U/L. Phosphate level was normal on Neutra-Phos. His outside bone scans were reviewed as were bone x-rays revealing multiple fractures due to his osteomalacia. Tissue from the right ear mass was obtained and stained for fibroblast growth factor 23 (FGF 23). Pathology was consistent with a non-calcifying phosphaturic mesenchymal tumor, positive for FGF23 expression by chromogenic in situ hybridization. Blood FGF-23 was elevated at 140 RU/ml (n < 100 RU/ml). At this point the diagnosis of “oncogenic osteomalacia caused by a phosphaturic mesenchymal tumor of the skull base (oncogenic osteomalacia)” was made. The diagnosis was discussed with the patient and an attempt to remove the underlying tumor was advised. The patient preferred to have this procedure done closer to home and returned to his LMD. During a follow-up conversation in December 2013 the patient stated that the tumor had been completely removed and his phosphorus levels were back to normal without replacement therapy.
DISCUSSION: Osteomalacia, a metabolic disorder of decreased mineralization of mature bone, has many causes including inborn errors of metabolism, insufficient levels of vitamin D or calcium, and even common disorders such as chronic kidney disease. Tumor-induced osteomalacia, also known as oncogenic osteomalacia, although relatively uncommon is an important cause of osteomalacia. This paraneoplastic syndrome, characterized by renal phosphate wasting due to increased urinary phosphate excretion caused by excessive synthesis and secretion of FGF23 by the tumor, is unique in that it can be cured by surgical resection of the tumor. Clinical characteristics include bone pain, pathologic fractures due to osteomalacia, and musculoskeletal weakness. Such vague symptoms often lead to a delayed diagnosis with subsequently delayed medical and surgical treatment as in the case presented. The diagnosis of a phosphaturic mesenchymal tumor (oncogenic osteomalacia) should be considered in any patient who presents with multiple bone fractures and hypophosphatemia. FGF 23 measurement helps to establish the diagnosis. Finding the tumor can be challenging, and may involve total body imaging (MRI); scintigraphy using octreotide or PET/CT. Phosphor supplementation should be continued until the causative tumor can be removed. Follow up FGF 23 measurements may serve as a biomarker of tumor burden and the efficacy of the therapeutic interventions.
ONE HEART, TWO HEART, RED HEART, GREEN HEART: A CAUSE TO CONSIDER IN A PATIENT WITH UNEXPLAINED HEART FAILUREDiego F. Alcivar Franco1,2; Kristy Deep1. 1University of Kentucky Medical Center, Lexington, KY; 2VAMC, Lexington, KY. (Tracking ID #1940126)
LEARNING OBJECTIVE 1: Recognize the clues that should lead a physician to consider cardiac amyloidosis as a cause of unexplained heart failure
LEARNING OBJECTIVE 2: Review the pathophysiology, diagnosis, and management of amyloid heart disease
CASE: A 68 year-old male presented with a 2 day history of progressive fatigue, palpitations, dyspnea on exertion, and two syncopal episodes. The syncopal episodes were preceded by lightheadedness, lasted only 1–2 min, and spontaneously resolved. The patient had recently received a diagnosis of heart failure with no known etiology. His medications included metoprolol, digoxin, aspirin, atorvastatin and furosemide. Vital signs showed a pulse of 53, blood pressure of 110/71 mmHg, and normal oxygen saturation. Physical examination revealed clear lung sounds, no murmur, and trace lower extremity edema. The serum creatinine was 1.42 mg/dL and N-terminal proB-Natiuretic peptide was 18,474. Chest radiography showed cardiomegaly. An electrocardiogram demonstrated an atrial rate of 180 with a 3:1 conduction block and a wide QRS. Echocardiogram showed an ejection fraction of 40 %, bi-atrial enlargement, concentric left ventricular hypertrophy with small ventricular cavity. His presentation and imaging were concerning for cardiac amyloidosis. Cardiac catheterization demonstrated non-obstructive coronary artery disease with elevated left and right-sided filling pressures and low cardiac output. Right ventricular endomyocardial biopsy was performed with Congo red stain positive for amyloid. Genetic testing showed wild-type transthyretin (TTR). The patient was treated with intravenous milrinone. Extensive evaluation for extra-cardiac amyloid deposition was negative. The patient underwent successful cardiac transplantation 3 months after presentation.
DISCUSSION: Cardiac amyloidosis is caused by accumulation of abnormally structured proteins which decrease mechanical compliance and disrupt cardiomyocytes. Three main types of primary amyloid protein can affect the heart: monoclonal light-chain amyloidosis (AL), mutated transthyretin in familial amyloidosis, and wild-type transthyretin. The wild-type TTR, often referred to as senile cardiac amyloidosis, typically presents as localized cardiac disease as in this patient. The severity can vary tremendously with many patients having only patchy amyloid deposits and little burden of disease. Cardiac symptoms are related to conduction abnormalities and restrictive physiology which can manifest as syncope, congestive heart failure, and less likely, pericardial disease. Clinicians should consider cardiac amyloidosis in a patient with unexplained heart failure and an echocardiogram with increased wall thickness and non-dilated left ventricular cavity who has no history of hypertension. Electrocardiographic evidence of heart block or conduction delays and low voltage are additional clues. Definitive diagnosis requires tissue biopsy. Loop diuretics and spironolactone are a mainstay of treatment to control symptoms of volume overload. Beta blockers and digoxin are often not tolerated due to exacerbation of conduction defects. ACE inhibitors are often not tolerated due to hypotension and calcium channel blockers are contraindicated due to their negative inotropic effect. Advanced heart disease may require transplantation. Investigational agents to stabilize the TTR molecule and prevent breakdown product accumulation are in active clinical trials.
ONE MAN’S TOE PAINMariam Majd; Ahmed Mohiuddin. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926238)
LEARNING OBJECTIVE 1: Identify the patients at risk for atypical presentations of endocarditis
LEARNING OBJECTIVE 2: Recognize the clinical manifestations of a rare gram positive cocci.
CASE: A 64 year-old man with end stage AIDS presented with 1 day of toe pain. He had a recent urinary tract infection 2 months prior that had been treated with trimethoprim/sulfamethoxazole. On exam, he had a low-grade fever and tachycardia. His left great toe was exquisitely tender with mild warmth and erythema over the toe. Cardiovascular exam revealed a grade 2/6 holosystolic murmur, heard loudest at the base of the heart. While undergoing MRI for further evaluation of the toe pain, the patient became hypotensive. His mental status quickly deteriorated. He developed septic shock and transferred to the ICU. Broad-spectrum antibiotics were begun. Within 24 h, gram stain of peripheral blood showed gram-positive cocci suggestive of streptococcus. His hemodynamic status worsened; despite attempts at resuscitation, he died of worsening sepsis. Autopsy and post-mortem blood cultures demonstrated Aerococcal mitral valve endocarditis and an infectious embolus to the toe. His prior urinary tract infection with Aeroccocus Urinae led to hematologic seeding of the mitral valve, an embolus to his toe, and fatal bacteremia.
DISCUSSION: Endocarditis is a problem commonly encountered by the internist. When the bacterial culprit is a rarely identified species, as in this case, the challenge of determining both the diagnosis and proper treatment is difficult. In infectious endocarditis, clinical manifestations are the result of both the direct effects of the nidus on the heart’s structure and function as well as end organ ischemia produced from embolic events. Patients do not always present with an array of typical physical exam findings; rather they may have only one or two signs of endocarditis. In addition, immunosuppression clouds the picture further with the variety of opportunistic infections to which they are susceptible. Aerococcus urinae is a rarely reported gram-positive coccus that can appear as pairs, tetrads, or clusters on gram stain. It is absent from the databases of many commercial identification systems and is frequently misidentified as a streptococcus, enterococcus, or staphylococcus, as was the case in our patient. Thus, the organism is thought to be drastically under-reported. Its sister species, A. Viridans, is a more common cause of endocarditis, but both organisms are known culprits. Patients at risk for this infection are elderly and institutionalized females, males with prostate disease, and the immunosuppresed. This organism should be considered in patients with these factors and those who are unresponsive to sulfonamide therapy like our patient. Aerococcus is susceptible to a variety of both β-lactam and non β-lactam antibiotics in vitro; despite this susceptibility, the prognosis is poor for elderly patients, especially those suffering from endocarditis. It is important for the physician to consider Aerococcus as a potential pathogen in both endocarditis and urinary infections. With the number of immunosuppresed and elderly patients on the rise, internists should be adept in identifying aeroccocal infection and its symptomatology.
ONE OF THESE THINGS IS NOT LIKE THE OTHERSkylar Souyoul; Edmond Fomunung; Michelle M. Guidry. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1927093)
LEARNING OBJECTIVE 1: Understand causes of cytopenia in rheumatoid arthritis
LEARNING OBJECTIVE 2: Recognize the adverse effects of methotrexate use
CASE: A 56-year-old woman presented with nausea, vomiting, weakness and fatigue. She was diagnosed with rheumatoid arthritis 6 years prior, and treated with methotrexate. On admission she had tachycardia, pancytopenia, acute kidney injury, elevated liver enzymes, and metabolic acidosis. Splenomegaly was not appreciated on exam. A methotrexate level was <0.02 uM/L. We diagnosed her with methotrexate toxicity and this medication was discontinued as we treated her with bicarbonate to correct the acidosis.
DISCUSSION: Rheumatoid arthritis (RA) is the most common form of chronic inflammatory arthritis. It is a systemic disease of unknown etiology that often results in joint damage and physical disability. Though joint symptoms predominate, RA frequently presents with extra-articular manifestations; hematologic abnormalities are common. Hematological involvement is most often manifested as a normochromic and normocytic anemia. Infrequently, neutropenia is encountered and raises several possibilities. Myelosuppression from methotrexate, Felty Syndrome, and T cell large granular lymphocyte leukemia (T-LGL) are possible diagnoses and share many features. Felty Syndrome is classically associated with the clinical triad of leukopenia, splenomegaly and deforming arthritis. It is seen in approximately 1 % of patients with RA, making it relatively rare. It tends to occur later in the disease process, as opposed to T-LGL which may occur early in the course of RA. T-LGL similarly presents with leukopenia and splenomegaly in the patient with RA, and is characterized by chronic indolent clonal growth of LGL cells. In our patient, the absence of splenomegaly, worsening renal insufficiency and presence of thrombocytopenia reflecting more global bone marrow involvement pointed away from these disorders towards methotrexate toxicity. Methotrexate is a folate antagonist recognized for its versatility in the treatment of a wide spectrum of disorders. It represents the first line among the disease-modifying anti-rheumatic drugs (DMARDs) in the treatment of RA. Myelosuppression and gastrointestinal toxicity are among the most common side effects of methotrexate toxicity. It is important to note that some of these adverse effects have been noted in patients taking therapeutic doses of methotrexate, as was our patient. In our patient, an exacerbating factor was the presence of renal insufficiency. Methotrexate is primarily excreted unchanged by the kidney and as such, should be used with caution in patients with renal impairment.
ONE TOUGH MUDDERThomas Cascino1; Kanako Mckee2; Jeff Kohlwes2. 1University of California, San Francisco, San Francisco, CA; 2San Francisco Veterans Administration Medical Center, San Francisco, CA. (Tracking ID #1939524)
LEARNING OBJECTIVE 1: Recognize primary coccidiodal infection after treatment failure for community acquired pneumonia.
LEARNING OBJECTIVE 2: Awareness of the anchoring heuristic.
CASE: A 31-year-old man presented with 1 day of left-sided pleuritic chest pain. Lungs were clear to auscultation without wheezes, rales, or rhonchi. On chest x-ray the patient had a left lower lung airspace consolidation, and he was given doxycycline for treatment of community-acquired pneumonia (CAP). The patient subsequently developed cough, fevers, and chills despite taking the doxycycline. He returned 1 week later and chest CT revealed a consolidation with a confluent focus in the lingula with scattered groundglass and centrilobular nodules, a small left pleural effusion, left hilar lymphadenopathy, and no pulmonary embolism. The patient was diagnosed with a non-resolving pneumonia and started on levofloxacin. He returned 4 days later with continued pleuritic chest pain, cough, malaise, and nightsweats. The patient declined hospital admission citing a personal obligation. He was given one dose of ertapenem with the plan to follow-up the next day. On follow-up, he had multiple painful nodules on the right shin consistent with erythema nodosum. Upon further questioning, he revealed that he had participated in a “Tough Mudder” endurance race near San Diego 1 week prior to symptom onset. He was admitted, started on fluconazole for presumed primary coccidiodal infection, and discharged after a brief hospital stay. Cocci antibody complement fixation was eventually positive with a titer of 1:4 and cocci ELISA was also positive, confirming the diagnosis. The patient was seen in follow-up 1 week after initiation of therapy with much improvement in symptoms.
DISCUSSION: Pleuritic chest pain, cough, and fevers are common problems encountered in outpatient medicine. The presence of an infiltrate on chest x-ray is the gold standard for diagnosis of pneumonia. The decision to treat with antibiotics as an outpatient is based on a multitude of factors including the history, physical exam, laboratory values, and psychosocial situation. It is important to be aware of the anchoring heuristic, the clinging to an original diagnosis despite evidence to the contrary, when treating common, nonspecific symptoms as an outpatient. One should consider alternative diagnoses when a patient fails to respond to treatment as expected. Primary coccidiodal infection is a common cause of CAP in endemic areas. There is a spectrum of presentations, many of which do not require treatment. In our patient, alternative diagnoses were pursued when the patient failed appropriate therapy for a bacterial pneumonia and developed errythema nodosum. Careful attention to the patient’s social, travel, and exposure history revealed clues about exposure to cocci during the outdoor race in an endemic area, which if elicited during a prior visit, may have led to an earlier diagnosis. The consideration of non-bacterial causes of pneumonia coupled with the compelling exposure history enabled a diagnosis of primary coccidiodal infection. The decision to treat was based on symptom severity (debilitating enough to keep patient out of work) and proximity to meeting two treatment criteria (>3 weeks of nightsweats and prominent hilar lymphadenopathy). Initiation of therapy with fluconazole resulted in improvement in the patient’s symptoms. Coccidiomycosis is a common cause of CAP in endemic areas. Physicians should be mindful of the anchoring heuristic and actively seek out alternative diagnoses when patients do not respond to empiric therapy for a presumed bacterial pneumonia.
OPENING PANDORA’S BOX: AN UNFORTUNATE CASE OF INFIDELITYSara Turbow2; Cameron Lambert1. 1Emory University, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA. (Tracking ID #1937404)
LEARNING OBJECTIVE 1: Illustrate the neurologic manifestations of syphilis
LEARNING OBJECTIVE 2: Review the challenges of diagnosing HIV and syphilis co-infection
CASE: A 38 year-old man presented to the hospital complaining of a one-month history of rash. The painful, intensely pruritic rash started on his torso and spread outward until it covered his whole body, including the palms and soles. Two weeks prior to presentation, the patient experienced several days of sore throat, cough, and fever. He also complained of night sweats, headache, fifteen-pound weight loss, pharyngitis and visual disturbances during this time period. The patient had a past medical history of childhood sinus cancer that was treated with surgery. His last HIV test was 6 months prior to admission and was negative. He is sexually active with men and recently left a 6-year relationship after his partner admitted to infidelity. On admission, he was afebrile and normotensive. His physical exam was significant for tonsillar erythema and diffuse and painful lymphadenopathy. An erythematous maculopapular rash extended from the scalp to the feet, including the palms and soles. It was tender to palpation with indistinct borders and was not present on the mucous membranes. Labs were notable for white blood cell count of 11.1 × 103/mm3, alkaline phosphatase 1165 U/L, ALT 110 U/L, AST 86 IU/L, and bilirubin 0.8 μmol/L. Lumbar puncture was performed which revealed 16 nucleated cells in tube 4 (56 % neutrophils) with a normal glucose and protein. RPR was positive with a titer of 1:64. Cerebrospinal fluid (CSF) VDRL was positive with a titer of 1:1. HIV antigen/antibody screening test as well as Western Blot were positive: HIV viral load was 1.2 million copies/mL and CD4 count was 593. Other CSF studies, including herpes simplex virus and cryptococcal antigen, were negative. The patient was treated with continuous IV penicillin G infusion. He was counseled regarding his new diagnosis of HIV and was started on antiretroviral therapy during this admission. His rash resolved and his neurologic symptoms improved.
DISCUSSION: This case illustrates the challenge of differentiating recent HIV infection from secondary syphilis, as well as the synergistic relationship they have during co-infection. Fifty to ninety percent of patients with HIV have symptoms at presentation. These are usually influenza- or mononucleosis-like syndromes, with fever, rash, myalgias, sore throat, and lymphadenopathy. Less than 20 % of patients present with encephalitis or meningitis (1). Even among those with neurologic signs or symptoms, it is not common for these findings to reflect a concomitant opportunistic central nervous system infection. Syphilis is increasing in incidence, especially in men who have sex with men (MSM). In 2006, 64 % of cases of primary and secondary syphilis reported nationwide were among MSM (2). Active syphilis increases the risk of HIV infection 2- to 5- fold (2). The classic manifestation of neurosyphilis is syphilitic meningomyelitis, characterized by slowly progressive lower extremity weakness and paresthesias. The most common form of neurosyphilis, however, is asymptomatic neurosyphilis; patients who are without neurologic symptoms but have evidence of syphilis infection in their CSF. A third presentation of secondary syphilis, syphilitic meningitis, occurs in 5 % of patients, usually within the first 12 months of infection and is associated with a variety of neurologic manifestations (3). The similarities between secondary syphilis and recent HIV infection can pose diagnostic challenges for clinicians. As mentioned above, HIV can cause many of the same symptoms as secondary syphilis such as rash, lymphadenopathy, and headache. Laboratory tests may also not be revealing, as both HIV and syphilis can cause changes in CSF studies and co-infection can lead to precipitous increases in viral load as well as rapid decreases in CD4 counts (3, 4). It is essential to understand the presentations of recent HIV infection and syphilis, whether isolated or during co-infection, to avoid missing either diagnosis. References 1. Douvuyiannis, M and Litman, N. “Acute Encephalopathy and multi-organ involvement with rhabdomyolysis during primary HIV infection.” Int J of Infect Dis (2009) 13, e299–e304. 2. Centers for Disease Control and Prevention http://www.cdc.gov/std/syphilis/STDFact-MSM-Syphilis.htm 3. Berger, J and Dean., D. “Neurosyphilis.” Handbook of Clinical Neurology, Vol. 121. Elsevier, 2014. 1461–1472. 4. Chang, C, et al. “Symptomatic and Asymptomatic Early Neurosyphilis in HIV-infected men who have sex with men: a retrospective case series from 2000 to 2007” Sex Health, 2011, 8, 207–213
OPHTHALMOPLEGIA AND HYPOPITUITARISM AS THE INITIAL MANIFESTATION OF METASTATIC SMALL CELL CANCERElliot Rhee; Rena Pollack. Montefiore Medical Center, Bronx, NY. (Tracking ID #1940180)
LEARNING OBJECTIVE 1: Recognize the clinical features of metastatic cancer to the pituitary
CASE: A 53 year-old man presented with 3 days of inability to open his right eye and diplopia. The patient denied any previous history of visual difficulties, but did mention a recent unintentional weight loss, back pain, and occasional headaches for the past few months. His only past medical history was a history of schizophrenia. Social history was significant for smoking one pack of cigarettes per day for the past 30 years. Vital signs were stable. Patient was found to be thin and cachectic with complete ptosis of the right eyelid. The right pupil was dilated, minimally reactive to light, and was fixed in the abducted position. The left eye was unaffected as well as all other cranial nerves remained intact. An admitting chest x-ray revealed collapse of the right middle lobe and hilar adenopathy. Initial CT of the head was unrevealing. Due to the continued persistence of ptosis and mydriasis on exam, an MRI was completed showing a 12 mm pituitary macroadenoma with deviation of the pituitary stalk to the right. Once this MRI result returned, a complete endocrine work-up was pursued due to concerns of endocrine axis dysfunction. Laboratory studies showed depressed levels of all hormones of the anterior pituitary as well as low levels of testosterone, cortisol, and free T4. A dedicated MRI with pituitary protocol showed a thickened infundibulum of 7 mm with heterogeneously enhancing soft tissue within the sella turcica. As a result of the findings on chest x-ray and MRI, a whole body CT scan was pursued as there was concern for diffuse metastatic disease. CT scan revealed a right lung mass with metastases to the liver, bilateral adrenals, ribs, thoracic and lumbar spines. Bronchoscopy was performed, and lung biopsy revealed small-cell neuroendocrine carcinoma.
DISCUSSION: Pituitary lesions are commonly encountered by general internists. It is estimated that about 20 % of the general population has a pituitary mass. Although pituitary adenomas are the most common type of sellar mass, and typically are benign, it is important to recognize that masses in this area can also be the result of diffuse metastatic disease as well as very rare instances of primary pituitary carcinoma. Approximately 5 % of patients with advanced malignancy are found to have pituitary metastases and are typically patients with lung or breast cancer. Furthermore, only 7 % of these patients with pituitary metastases become symptomatic during their lives. Once a pituitary adenoma is discovered, it should be fully evaluated for either hypersecretion or hyposecretion in addition to assessing for any symptoms. Patients may be asymptomatic or, if clinically significant, may have complaints of a non-specific headache, altered facial sensation, or vision changes such as diplopia or bitemporal hemianopsia. Panhypopituitarism and diabetes insipidus may also occur in patients with pituitary metastases due to destruction of the gland. It is critical to understand that pituitary lesions may be missed on routine CT scans, and that dedicated MRI of the pituitary is necessary when there is high clinical suspicion. Once a pituitary lesion is confirmed, it may not be easily distinguish on imaging alone. Some features, such as thickening of the infundibulum, invasion of the cavernous sinus, or invasion of the sella turcica, can be indicative of metastatic disease. Generally, treatment for pituitary metastases involves replacement of the deficient hormones as well as possible surgical resection. It is important for the clinician to recognize that pituitary masses have a wide array of clinical presentations and require full evaluation that may be sometimes missed with initial imaging. While pituitary metastases are rare and frequently asymptomatic, it is always important to consider metastatic disease in the differential diagnosis of a pituitary mass.
ORBITAL CELLULITIS WITH CAVERNOUS SINUS THROMBOSIS IN AN ELDERLY WOMAN: A CASE REPORTKathryn A. Jobbins; Jessie Leyse; Reham Shaaban. Baystate Medical Center, Springfield, MA. (Tracking ID #1928949)
LEARNING OBJECTIVE 1: Recognition of posterior orbital cellulitis complicated by cavernous sinus thrombosis in the elderly.
LEARNING OBJECTIVE 2: Treatment of posterior orbital cellulitis complicated by cavernous sinus thrombosis.
CASE: An 84-year-old woman with a past medical history of chronic sinusitis presented with an acute history of acute right eye pain, erythema, and decreased ability to move the right eye secondary to severe swelling that had gotten progressively worse over 3 days. Of note, she had been evaluated as an outpatient for worsening hearing loss for 1 month, and was treated for sinusitis with oral antibiotics 2 weeks prior to this event. On examination, she had decreased visual acuity on the right, pain with movement of the eye, and surrounding erythema, swelling and cellulitis of the right eye, forehead and cheek. The sinuses were tender to palpation throughout. A CT scan was performed in the emergency department demonstrated pre- and post-septal cellulitis of the right orbit with soft tissue swelling of the right cheek. There was also bony erosion of the inferomedial orbital wall and opacification of the frontal and maxillary sinuses with no intracranial extension. The patient was seen by ENT, ophthalmology, and infectious disease consultants who recommended starting nasal saline rinses, dexamethasone, ceftriaxone and vancomycin. She initially responded well to this treatment regimen, however, after 2 days continued to have difficulty with movement of the right eye consistent with a partial third and partial sixth cranial nerve palsy with ptosis. The patient then underwent a CT head angiogram and venogram study which showed a 6 mm filling defect in the right cavernous sinus likely representing a thrombus. At this point neurology and neurosurgery were consulted who recommended starting the patient on anticoagulation given the morbidity and mortality associated with the diagnosis. Of note, the patient never underwent any surgical intervention while admitted to the hospital and no formal tissue biopsy was obtained to determine the causative agent of her infective source. The patient continued to improve and was discharged to a rehabilitation facility after 8 days to complete her 8 week coarse of IV antibiotics and anticoagulation. At her follow up visit 2 months later, she had near complete resolution of all her orbital cellulitis but with persistent sinusitis symptoms and subsequent outpatient deep wound culture was positive for Serratia Marcescens.
DISCUSSION: Posterior orbital cellulitis complicated by cavernous sinus thrombosis is rarely seen in the elderly population. Cavernous sinus thrombosis carries the potential for significant morbidity and treatment is often not straight forward. The presented rare case of an 84-year-old female highlights the clinical features in order to recognize posterior orbital cellulitis complicated by cavernous sinus thrombosis and the treatment options with long-term antibiotic coverage as well as anticoagulation until symptoms have resolved.
ORGANIZING EOSINOPHILIC PNEUMONIA : AN ORPHAN DISEASENavneet Kaur; Pahul Singh. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1938989)
LEARNING OBJECTIVE 1: Importance of early and prompt diagnosis of eosinophilic pneumonia which is a rare parenchymal lung disease to initiate therapy in a timely fashion.
CASE: A 53-year-old female presented to our institution with fever, cough and exertional dyspnea for one week duration after hiking and exploring caves during her recent visit to Las Vegas 1 month ago. She denied hemoptysis, weight loss or joint aches. Past medical history was unremarkable. Examination revealed temperature of 101 F and bibasilar crackles on lung exam. Laboratory values were unremarkable. Chest radiograph showed bilateral lower lobe infiltrates. CT thorax revealed multifocal airspace disease within posterior aspect of bilateral lower lobes. 2-D echocardiogram was unremarkable. Peripheral blood smear and serology for Histoplasmosis, Coccidioides, Aspergillus, Cryptococcus and Blastomyces was unremarkable. Bronchoscopy was done and transbronchial biopsy showed organizing pneumonia with increased eosinophils with no evidence of malignancy on cytology, thus confirming the diagnosis of organizing eosinophilic pneumonia. Treatment was initiated with high dose of oral prednisone leading to marked improvement in the symptoms and the patient has been doing fine in last 2 months of follow-up.
DISCUSSION: Eosinophilic lung diseases are a group of diffuse parenchymal lung diseases characterized by infiltration of eosinophils of lung interstitium and alveolar spaces which may present as acute (<1 month) or chronic (>1 month) pneumonia. Exact etiology of eosinophilic pneumonia remains unknown. It has been suggested that it might be secondary to acute hypersensitivity reaction to an unidentified inhaled antigen. Clinical manifestations include febrile illness, non-productive cough, dyspnea and malaise. Laboratory values may reveal elevated erythrocyte sedimentation rate, increased Ace levels and peripheral eosinophilia. Chest radiograph and CT thorax reveals bilateral patchy ground glass or reticular opacities. Analysis of bronchoalveolar lavage fluid may reveal very high percentage (more than 25 %) of eosinophils. Lung Biopsy may reveal organizing diffuse alveolar damage with prominent eosinophilia. Diagnosis of eosinophilic pneumonia can be established without lung biopsy in immunocompetent patients with pertinent history and eosinophilia on bronchoalveolar lavage fluid in absence of any infection. Systemic corticosteroids are the cornerstone therapy in eosinophilic pneumonia that help in prevention and reversal of respiratory failure. To summarize, although rare, our case reiterates the importance of early and prompt diagnosis of eosinophilic pneumonia to initiate therapy in a timely fashion.
OUCH, HOT SPOTS! PANNICULITIS ASSOCIATED WITH PANCREATITISSteven Lilly1; Jake E. Turrentine2. 1Dallas VA Medical Center, Dallas, TX; 2University of Texas Southwestern, Dallas, TX. (Tracking ID #1938401)
LEARNING OBJECTIVE 1: Recognize that inflammatory skin lesions may rarely occur in the setting of pancreatitis which may mimic other systemic disorders.
LEARNING OBJECTIVE 2: Manage panniculitis in the setting of pancreatitis.
CASE: A 65 year-old male presented with diffuse abdominal pain, vomiting, jaundice, and “painful red spots” on both legs. These symptoms had been present for less than 1 week, but were worsening over the last 2 days, prompting his presentation. The rash was not pruritic, but was very painful when touched. Past medical history included diabetes mellitus type 2, hypertension, and psoriasis. His medications were metoprolol, insulin glargine, and etanercept. The patient denied smoking and alcohol use, and family history was noncontributory. On review of symptoms, he noted subjective fevers at home and loose stools, and stated that the current rash was unlike his previous psoriasis lesions. Physical exam demonstrated an obese man in mild distress, but vital signs were normal. Scleral icterus was present. His abdomen was severely tender to palpation, particularly in the midepigastric and RUQ areas, but there was no Murphy’s sign or masses noted. Cutaneous examination revealed several exquisitely tender erythematous subcutaneous nodules on the bilateral shins, medial feet, and ankles without overlying ulceration, necrosis, or drainage. The largest lesion was approximately 3 cm in diameter. Laboratory studies showed an elevated serum lipase of 1210 U/L. Liver function tests were elevated in an obstructive pattern: total bilirubin 2.9 mg/dl, alkaline phosphatase 510 U/L, ALT 166 U/L, and AST 147 U/L. Abdominal ultrasound and CT scan with contrast showed peripancreatic fat stranding, a dilated common bile duct of 1.2 cm, and two hyperdense structures in the distal CBD consistent with choledocholithiasis. Once the diagnosis of gallstone pancreatitis was made, the gastroenterology service performed an ERCP to remove the retained stones and placed a stent for biliary drainage. Regarding the patient’s painful skin lesions, the initial differential diagnosis of the medical team included soft tissue infection, erythema nodosum (EN), and vasculitis. Given the myriad potential inflammatory and infectious causes underlying these conditions, other supportive workup included a CXR; HBV, HCV, HIV, and fungal serologies; PPD; ASO titer; and blood cultures, all of which were negative. Dermatology was consulted and two 5 mm punch biopsies of the skin were obtained: one for tissue culture and one for routine histology. Tissue cultures were negative and pathology revealed a lobular panniculitis with a mixed inflammatory infiltrate, surrounding necrotic fat leaving “ghost-like” outlines, and calcification consistent with pancreatic panniculitis.
DISCUSSION: This patient presented with painful nodules on the lower extremities suggestive of an underlying systemic condition in addition to pancreatitis. Erythema nodosum (EN) was initially considered given the appearance and tenderness of the skin lesions, and can be caused by a wide variety of disorders including infections, autoimmune disorders, malignancy, and medications. Vasculitis was ruled out based on the clinical exam, laboratory workup, and skin biopsy. Our patient was on etanercept for psoriasis, a TNF-alpha inhibitor. Etanercept has not been linked to EN and, in fact is sometimes used as a treatment of refractory cases. Since it is an immunosuppressing agent, it is also important to rule out an underlying infectious etiology of skin nodules with tissue culture and appropriate ancillary workup. Based on the histopathology described above, the diagnosis in this case was an unusual form of panniculitis, generally defined as inflammation of the subcutaneous fat. “Pancreatic panniculitis” is a rare variant of panniculitis characterized by fat necrosis and ghost adipocytes thought to be caused by pancreatic enzymes which are released into blood circulation in the setting of pancreatic disease. Lesions typically involve the lower extremities, and can occur in the setting of acute or chronic pancreatitis with an estimated incidence of 0.3–3 %. They can also be associated with pancreatic carcinoma, especially if the lesions are ulcerated or found on other areas of the body. Occasionally, the skin lesions can precede abdominal symptoms associated with pancreatic disease, which can manifest up to months later. The primary therapeutic measure for pancreatic panniculitis is to treat the underlying pancreatic disorder. Importantly, if the lesions are extensive, ulcerating, or progress despite the resolution of pancreatitis; further work-up should be done to exclude other pancreatic pathology, particularly malignancy. In this case once the patient’s pancreatitis was clinically resolved, the panniculitis lesions improved significantly in the following weeks.
PAGET - SCHROETTER SYNDROME: A CASE TO REMEMBER!Muhammad O. Azam; Rudin Gjeka; David Aggen; Zain I. Kulairi; Sarwan Kumar. Wayne State University, Rochester, MI. (Tracking ID #1939542)
LEARNING OBJECTIVE 1: Recognize the pathogenesis of effort thrombosis is not the same as other venous thromboembolic disorders.
LEARNING OBJECTIVE 2: Managing with anticoagulation alone is inadequate and can lead to residual disability and complications including pulmonary embolism, post-thrombotic syndrome and recurrent thrombosis. An aggressive multi faceted treatment strategy consisting of catheter-directed thrombolysis, with possible early thoracic outlet decompression, is essential for best outcomes.
CASE: 34 year old female with no co-morbid conditions presented to the ED with complains of left upper limb swelling and heaviness that gradually developed over 1 week. She had pain, swelling and mild numbness which was exaggerated on minimal exertion. There was no history of any trauma. No associated shortness of breath, chest pain or any weight loss. She was married with 7 children. Patient was not on any oral contraceptive pills. There was no family history of malignancy or hypercoagulable condition. On examination at presentation, patient was hemodynamically stable, with left non-pitting upper limb swelling up to the elbow joint that was tender on palpation with intact peripheral pulses. Initial lab workup including CBC, PT, and PTT were all normal. A complete coagulation workup was also ordered. Anti-thrombin, factor V Leiden, lupus anticoagulant, protein C & S levels were all normal. A left upper extremity venous evaluation was performed using duplex imaging with color and spectral Doppler. The internal jugular vein was completely compressible with no evidence of thrombosis. However, the subclavian, axillary, brachial and basilic vein proximally was noncompressible and dilated with acute-appearing thrombus. Patient was started with heparin infusion and cardiology was consulted. A venogram study of the left sub-clavian, axillary and the brachial veins was performed showing compression of the sub-clavian vein with congenital web deformity and a small thrombus was found that did not required a thrombectomy. Patient was started with Warfarin; therapeutic INR of 2–3 was achieved and discharged home on Warfarin.
DISCUSSION: Spontaneous thrombosis of upper extremity veins presenting as swelling and pain was first postulated by Sir James Paget in 1875. Von Schroetter was first to relate this syndrome to thrombotic occlusion of axillary and sub-clavian veins in 1884. Spontaneous thrombosis of upper extremity veins is termed as, Paget-Schroetter Syndrome (PSS) or Axillosubclavian vein thrombosis (ASVT) or Effort Thrombosis. PSS is a disease of young active individuals. Seventy-five percent of the cases occur on the dominant upper extremity after a vigorous exercise. Significant evidence now supports the role of anatomical abnormalities involving the thoracic outlet that includes cervical rib, congenital bands, hypertrophy of scalenus tendons and abnormal insertion of the costoclavicular ligament in the pathogenesis of effort thrombosis. Color doppler ultrasonography is currently the preferred initial test in the evaluation of suspected UEDVT due to cost efficiency and easy availability. Contrast venography is the gold standard for the diagnosis of UEDVT, but is not a preferred modality due to invasive nature, and high cost. Magnetic resonance (MR) and computed tomographic (CT) venography are superior to ultrasonography with MR venography having sensitivity 100 %. However, its applicability is limited due to high cost. Complications include pulmonary embolism, post-thrombotic syndrome and recurrent thrombosis. Although, pulmonary embolism from PSS is known, but is much less as compared to patients with lower extremity DVT or catheter related upper extremity DVT. Our patient was predominantly left-handed. She is a housewife with 7 children the youngest child was 1 year old. Patient said that lately, she has been overusing her arm for holding her children and the fact that her swelling got worsened on increased usage of the left arm. Coagulation profile was negative. However, venogram showed a web deformity of the subclavian vein with a small thrombus. Venography was done on our patient with intention of possible therapeutic thrombectomy. Effort thrombosis has been managed conservatively with limb elevation and anticoagulation alone. However, studies have showed a high incidence of residual symptoms, disability and recurrent thrombosis with conservative management. Therefore, it is important for clinicians to approach this aggressively. Various treatment modalities have been proposed for thrombus evacuation and achieving vascular patency. These may include local catheter-directed or systemic fibrinolytic therapy along with anticoagulation and/or surgery like percutaneous and surgical venoplasty, venous bypass and stents. In our patient, no surgical intervention was considered due to the small size of the thrombus. She was eventually managed conservatively with anticoagulation.
PAINFUL PROGRESSIVE PROXIMAL PARESISEloho Ufomata; Harish Jasti. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1937752)
LEARNING OBJECTIVE 1: Evaluate a complaint of muscle weakness
LEARNING OBJECTIVE 2: Differentiate statin induced myopathy from HMG-CoA-antibody associated necrotizing myopathy
CASE: A 51 year old male with a history of hypertension, hypothyroidism and hyperlipidemia presented with weakness. Two months prior, he noticed persistent right shoulder pain, which was treated with an 8-day course of prednisone for a presumed shingles prodrome. He then developed weakness described as difficulty lifting both arms above his head, and lifting his legs while sitting, prompting presentation to the hospital. There, his labs were notable for a creatinine kinase of >4,000 and ANA of 1:80. His home medicine, red yeast rice, was discontinued due to possible causation, and he was discharged on prednisone 60 mg daily, with rheumatology follow up. During the next 4 weeks his condition worsened and he required assistance with ambulation and ADLs. He endorsed proximal muscle pain and dysphagia but denied fevers, chills, weight loss, rashes, chest pain, or SOB. He was re-admitted to the hospital for further work-up. Physical exam revealed a male in no acute distress, stable vital signs and unremarkable cardiovascular, respiratory, and integumentary exams. Neurological exam revealed normal cranial nerves, reflexes, cerebellar function, and sensation. Motor component was significant for 2/5 strength in the proximal muscles with intact strength in the distal muscles. Musculoskeletal exam revealed normal bulk and tender proximal muscles. Labs were notable for a normal CBC and BMP, with elevated transaminases, CK, LDH and aldolase. ANA and myositis panel (including anti-jo-1, anti-mi-2, and anti-SRP antibodies) were negative. EMG demonstrated a generalized myopathy with muscle inflammation/necrosis. Muscle biopsy revealed a necrotizing myopathy with membrane attack complex (MAC) deposition in the capillaries, and diffuse major histocompatibility complex (MHC) upregulation, suggestive of HMG-CoA-antibody associated necrotizing myopathy. He was treated with rituximab, methotrexate and physical therapy with improvement in his weakness and ability to perform ADLs
DISCUSSION: The complaint of weakness is nonspecific and can describe muscle weakness, fatigue, exercise intolerance or pain. A thorough history and physical is the key to diagnosis. With true muscle weakness, the neurological and musculoskeletal exams localize the lesion to a CNS, PNS, or myopathic origin. For adult myopathy, the etiology could be metabolic, immunologic, toxic, or infectious. Initial testing includes CMP, CK, aldolase and LDH. If abnormal, TSH, ANA, HIV and myositis panel are helpful in further work-up. EMG characterizes and localizes the abnormal area, which can then be biopsied to elucidate the etiology. Certain populations with myopathy require further investigation. Patients with dermatomyositis or polymyositis warrant age-appropriate malignancy screening and evaluation for interstitial lung disease due to the high prevalence and implications on mortality. Suspected statin myopathy, which progresses despite statin withdrawal, should prompt consideration of HMG-CoA-antibody mediated necrotizing myositis. Though rare, it is strongly associated with high CK levels, and biopsy shows limited inflammation and presence of MAC. The anti-HMGCR test is diagnostic, and treatment involves aggressive immunosuppresion. Weakness is a common complaint that can bode myopathic illness with significant consequences. A cost conscious evaluation can be performed by tailoring diagnostic tests to the illness script provided by the H&P, leading to a timely diagnosis and treatment.
PAINLESS AORTIC DISSECTIONJennifer Huang; Manuela Calvo. Montefiore Medical Center, Bronx, NY. (Tracking ID #1934199)
LEARNING OBJECTIVE 1: Identify atypical presentations of aortic dissection.
LEARNING OBJECTIVE 2: Recognize risk factors for aortic dissection.
CASE: A 70 year-old woman presented with 2 weeks of shortness of breath. She had a history of chronic obstructive pulmonary disease with a 110 pack-year smoking history. She also reported a productive cough, but denied chest pain or fevers. Her heart rate was 120 and her blood pressure was 110/70. She was afebrile and her oxygen saturation was 92 % on room air. She was able to speak in 5–6 word sentences only, and observed to have pursed lip breathing. She had a three out of six systolic murmur. Lungs were clear to auscultation without wheezes. There was no peripheral edema. Laboratory data was notable for a white blood count of 11 with 80 % neutrophilic predominance. Electrocardiogram was interpreted as sinus tachycardia without ST or T wave changes. Chest x-ray revealed hyperinflation without focal pulmonary consolidation. She was treated for a COPD exacerbation with inhaled bronchodilators, systemic steroids and antibiotics. Because she failed to respond to standard therapy for COPD, CT thorax with pulmonary embolism protocol was obtained to evaluate for PE versus other structural lung processes. The next morning, she was noted to be dyspneic and diaphoretic, but she again denied any chest pain. She was hypertensive with a blood pressure of 169/104 and continued to be tachycardic with a heart rate of 118. Her oxygen saturation was 94 % on room air and she remained afebrile. Her lungs were still clear to auscultation. No focal neurologic deficits were noted. CT chest revealed a new Stanford type A aortic dissection in a 7-cm ascending aortic aneurysm which severely compressed the SVC. The patient was evaluated by cardiothoracic surgery and transferred emergently to the operating room. She underwent ascending aortic dissection repair and was discharged to a rehabilitation facility.
DISCUSSION: Early recognition of aortic dissection, a life-threatening process, is important to the internist. It classically presents as acute onset of chest, back or abdominal pain, and is usually diagnosed in patients with hypertension or atherosclerosis. However painless dissection has been reported, and accounts for less than 10 % of all cases, often in older patients with diabetes, aortic aneurysm, or previous cardiovascular surgery, though our patient was not known to have any of these co-morbidities. These patients may present with syncope, symptoms suggestive of heart failure, or neurological deficits, and are more likely to have type A dissections that involve the ascending aorta. Other unusual presentations include myocardial infarction, aortic regurgitation, vocal cord paralysis, Horner syndrome, renal failure and limb ischemia. The typical diagnosis can usually be made in over 90 % of patients with at least one of the following: 1) classic acute chest, back, or abdominal pain; 2) mediastinal widening on chest x-ray; or 3) pulse or blood pressure variation. ECG is often normal or shows nonspecific ST and T wave changes. However imaging studies are often still needed for definite diagnosis, which can be made with CT, MRI, or transesophageal echocardiography. While patients with dissections limited to the descending aorta can be managed conservatively, those with type A aortic dissections are considered surgical emergencies. Due to the significant mortality and morbidity associated with late diagnosis, physicians must keep aortic dissection as a differential for any patient presenting with shortness of breath, even in the absence of classic symptoms like chest pain.
PAINLESS ENLARGING BREAST MASS, WHAT COULD IT BE?Dima Dandachi; Mashooque Dahar; Venu M. Ganipisetti. Presence Saint Francis Hospital, Evanston, IL. (Tracking ID #1933763)
LEARNING OBJECTIVE 1: Recognize the difference in presentation, prognosis and management between Primary breast lymphoma and Breast carcinoma.
LEARNING OBJECTIVE 2: Assess patients with Primary Breast Lymphoma for early Central Nervous system involvement.
CASE: A 59 years old Asian female patient, presented to the outpatient clinic after she noticed a right breast mass, rapidly increasing in size over the past 2 months. Patient denied any fever, chills, pain in her breast, weight loss. Past medical history is negative. Past surgical history is positive for tonsillectomy at the age of 12. She denied smoking, alcohol intake, or drug use. She does not taking any medications except multivitamins pill daily over the counter. She never had a colonscopy, pap smear done last year was normal and mammogram done 2 years back was negative for any lesion. Vital signs were normal. Complete physical exam was benign except for a circumscribed, firm, non tender, not fixed to chest wall right breast mass with no lymphadenopathy and skin changes over the breast. A Mammogram was done showing a rounded dense mass in the central portion of the right breast measuring 4 × 3.5 cm that was not seen in the previous mammogram done 2 years back. US breast done showed right heterogeneous breast mass highly suspicious for malignancy and a small lymph node in the right axillary region measuring 5 mm. US guided core needle biopsy of the right breast mass was performed. Patient was thought to have breast carcinoma. Two weeks later, patient presented to the hospital with back pain, inability to defecate and bilateral leg weakness. MRI showed spinal cord mass at level of L3 extending into the neural foramina bilaterally suspicious for malignancy. Patient was diagnosed with cauda equina syndrome, started on intravenous dexamethasone, received emergency radiation to lumbar spine. Pathology of the breast biopsy came out showing diffuse high grade large B-cell lymphoma as evidenced by positive and strong staining for CD-20. LDH level 1344 IU/L (normal 91–180). Diagnosis was made of primary Breast cell Lymphoma with spinal metastasis. Patient improved and got discharged home to be started on R-CHOP chemotherapy as outpatient and to continue on radiotherapy.
DISCUSSION: Primary Breast lymphoma (PBL) is used to describe malignant lymphoma detected in the breast in the absence of previous history of lymphoma and absence of widespread disease at the time of diagnosis, with or without regional lymph nodes involvement. It is a rare disease. It is only seen in 0.4–0.5 % of malignant breast tumors. It is usually misdiagnosed as breast cancer since it cannot be differentiated by clinical or radiographic findings. Breast lymphoma tends to be larger, grows rapidly, and is less likely to have skin erythema, peau d’orange and nipple involvement. Most of the lesions are oval shaped and circumscribed, no speculated margins or calcifications. To note that primary breast lymphoma was reported more among Chinese population similar to our patient. There are no clear guidelines regarding the best treatment modality. The use of combined chemotherapy and radiotherapy is considered to be more effective. Several studies showed that mastectomy did not affect the outcome in terms of survival or recurrence rates. Thus, it is not recommended. PBL has high incidence of central nervous system (CNS) involvement. Furthermore, CNS is the most common site of relapse. We are presenting a rare case of PBL misdiagnosed as breast carcinoma, complicated by early cauda equina syndrome.
PALPITATIONS AND METABOLIC DISTURBANCES IN A HEALTHY YOUNG MAN WITH CHRONIC HIGH-CAFFEINE ENERGY DRINK CONSUMPTIONAnkeet Bhatt1; Jonathan Salberg1,2; Mamta Shah1,2; Peruvamba Venkatesh2,1. 1University of Connecticut School of Medicine, Farmington, CT; 2Hartford Hospital, Hartford, CT. (Tracking ID #1927353)
LEARNING OBJECTIVE 1: Recognize energy drinks as a source of high concentration of caffeine and its potential adverse health risks including arrhythmia and metabolic disturbances.
LEARNING OBJECTIVE 2: Assess the impact of high caffeine energy drink consumption on serum and urine potassium contents.
CASE: HPI: 25-year-old male with a history of bipolar disorder, not on any medications, presents to the Emergency Department with 2 h history of acute onset of palpitations. Associated symptoms included 7/10, non-radiating, pressure like sub-sternal chest pain and three episodes of non-bloody, non-billious vomiting. He denied fever, chills, headache, loss of consciousness, shortness of breath or an infective prodrome. Of note, patient mentioned high intake of “Five Hour Energy” drink, usually 3–4 1.93 fl. oz. bottles each day. Last intake was 3 bottles prior to onset of symptoms. He drank 2.5 bottles of the drink the night before presentation. Patient has been using Five-Hour Energy shots for the past 3–4 months, with increasing intake over the past 1.5 months. Patient has never had the aforementioned symptoms before. He worked as a delivery truck driver and had a poor dietary habit, which included fast food infrequently. PMH: Bipolar disorder, Type II; history of UTI Allergies: Contrast dye, Depakote, Lithium SH: Occasional marijuana and alcohol use. Patient reports 3–4 beers/week. Married with 2 children. Avid athlete. PE: Vitals: On admission: temperature 98.5, BP 125/76, non-orthostatic, HR 120–130, RR 18, O2 sat 98 % on room air. General: He was awake, alert, oriented ×3. Physical exam within normal limits. Diagnostic Data: CBC/BMP on admission - WBC 11.4, hemoglobin 11.8, hematocrit 33.2, platelet count 226,000. Electrolytes (mEq/L): Sodium 140, potassium 2.4, chloride 101, bicarbonate 20,, BUN 12, creatinine 0.7 Lactate 5.4. Glucose 149 mg/dL. Anion Gap 19. Urine electrolytes (mEq/L): Sodium 73, Potassium 57, Chloride 41 Calculated osmolality: 293 mOsm/kg. Delta-delta Ratio >2. EKG: Heart rate of 118 beats per minute, sinus tachycardia, possible atrial tachycardia. ST depressions in leads V4 through V6. QTc is prolonged at 540 milliseconds. Echocardiogram: hyperdynamic LV ejection fraction of 70 %.
DISCUSSION: Energy drinks which contain a significant amount of caffeine have grown in popularity over the past decade, now compromising over $9 billion in sales with 6 billion drinks sold in the US in 2010. Five Hour Energy drinks contain a high dose (>1800 mg) “energy blend” contain taurine, glucoronic acid, caffeine, and other substances in small 1.93 fl. oz. container. These substances are mainly metabolized through the CYP 1A2 pathway and have the ability to cross the blood brain barrier. Toxicity with these substances can lead to seizures, agitation, psychosis, cardiac arrhythmia, and even death. Caffeine’s has multiple systemic effects on the body, including a competitive phophodiesterase inhibitor and adenosine receptor antagonist, inducing vasoconstriction and increased oxygen consumption. New studies in mice have shown that chronic caffeine consumptions can exacerbate renal failure, leading to the metabolic disturbances. This effect is particularly pronounced with concomitant metabolic syndrome. Research published in the NEJM showed 250 mg of caffeine increased plasma renin activity by 57 % 1 h after ingestion. While not previously described, such an increase in renin activity could account for renin-angiotensin-aldosterone axis activation and the phenomenon of hypokalemia with renal potassium wasting as seen in this patient. In addition, plasma norepinephrine and epinephrine concentrations increased 75 % and 207 % respectively with 250 mg caffeine dose, leading to significant sympathomimetic properties that could be responsible for a significant intracellular potassium shift, leading to witnessed profound hypokalemia even despite the patient’s elevated lactate level that likely suggests some cell lysis. Moreover, such physiology would account for the patient’s elevated delta-delta ratio, with a high AG acidosis secondary to elevated lactate and a concurrent metabolic alkalosis secondary to aldosterone activation. In summary, the clinical effects of high caffeine energy drink ingestion can have serious consequences that providers should be aware of in order to adequately counsel their patients on the safe use of these substances. The consequences can be quite pronounced, eliciting a significant sympathomimetic response that can affect cardiac conduction and the renin-angiotensin-aldosterone axis, leading to arrhythmia and metabolic disturbances. Caffeine’s intrinsic effect on cardiac conduction combined with profound hypokalemia associated with high caffeine consumption set the stage for dangerous arrhythmias. A ceiling of less than 500 mg of caffeine per day is generally considered a safe daily dose.
PANHYPOPITUITARISM, SARCOIDOSIS, AND AML: SIMULTANEOUS STORM OR COMPLEX CASCADE?Alice Williamson; Anne Weaver; Ramprasad Kandavar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926974)
LEARNING OBJECTIVE 1: Consider a broad, in-depth differential for fatigue.
LEARNING OBJECTIVE 2: Understand the wide range of symptoms associated with pituitary masses.
CASE: HPI A 66-year old man presented to the emergency department “feeling bad” for about 3 weeks. He endorsed fatigue, shortness of breath with exertion, feeling cold, anorexia, and intermittent fevers up to 101 ° F. His symptoms progressed until he could barely get out of bed. He also complained of worsened bilateral lower leg swelling over the past 3 months. His past medical history included hypertension and pancytopenia with bone marrow biopsy from 1 year prior to presentation consistent with iron-deficiency. His vitals signs at presentation included temperature of 99.2 F, heart rate of 89, blood pressure of 108/54, with respirations 18. He was in no acute distress, spoke slowly, and was fully oriented though his personality seemed blunted. Conjunctiva were pale and skin was flakey; spleen was moderately enlarged; and he had 2+ pitting, pedal edema. His exam was otherwise normal. He was pancytopenic with WBC 3.2, Hgb 8.7, MCV 85, PLT 121. His sodium was 128, ESR 82, total protein 8.2, and albumin 2.8. Chest x-ray revealed some interstitial fluid. Thyroid studies reveal central hypothyroidism (TSH 1.35, Free T4 0.41), and ACTH stimulation test resulted with baseline cortisol 1.06, 30-minute cortisol 4.53, and 60-minute cortisol 7.09. Pituitary pathology was suspected, and MRI brain revealed mild enlargement of the pituitary gland. Bone marrow biopsy revealed myelodysplastic syndrome with 1–2 % blasts. Follow Up Our patient was treated with hydrocortisone, levothyroxine, and testosterone, and was discharged home. Within 2 months, he developed a rash, which was biopsied and consistent with granulomatous dermatitis, possibly sarcoidosis. Still being worked up for the underlying cause of pituitary enlargement and due to concern for malignancy-associated pituitary disease, MRI was repeated as an outpatient in preparation for pituitary biopsy: enlargement had completely resolved 3 months after initial MRI. CT chest revealed mediastinal and hilar lymphadenopathy, and repeat bone marrow biopsy (performed 4 months after presentation) was consistent with acute myeloid leukemia with 40–50 % blasts.
DISCUSSION: Our patient initially presented with symptoms of pituitary insufficiency. Symptoms improved within the first few doses of hormone replacement. Sarcoidosis can infiltrate the pituitary, leading to symptoms of panhypopituitarism, the treatment of which is hydrocortisone. Our patient’s pituitary enlargement resolved with hydrocortisone and, in the meantime, he developed granulomatous dermatitis and was found to have hilar lymphadenopathy, both of which are consistent with sarcoidosis. While sarcoidosis is known to exist with malignancies, sarcodiodosis is not commonly associated with AML; when the two do coincide, the question remains: is the sarcoidosis actually a response to tumor antigen of AML, or does the impaired T-cell response of sarcoidosis predispose patients to AML? Further research and cotemporaneous cases need to be explored to help determine the pathways and interactions of this medical conundrum.
PARADOXICAL BREATHING: AN IMPORTANT PHYSICAL EXAM FINDING IN A PATIENT WITH METASTATIC MELANOMARiddhi Shah1; Ekta Kapoor2; Melissa Glenna1; Svetomir Markovic3. 1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Rochester, MN. (Tracking ID #1939293)
LEARNING OBJECTIVE 1: Recognize bilateral diaphragmatic paralysis due to drug-induced phrenic nerve palsy as an etiology of subacute dyspnea
LEARNING OBJECTIVE 2: Recognize the unique immunologic side effects of check point inhibitors, a novel class of antineoplastic agents
CASE: A 66-year-old male presented to his primary care physician with complaints of shortness of breath and fatigue for 1 week. He complained of significant dyspnea in the recumbent position, which markedly improved in upright position. He denied cough, fever, chest pain or similar prior complaints. His past medical history was significant for metastatic choroidal melanoma for which he was treated with 4 cycles of ipilimumab, an FDA approved cytotoxic T-lymphocyte associated antigen-4 (CTLA-4) inhibitor. A chest X-ray and echocardiogram of the heart were normal, and he was empirically initiated on oral antibiotics. He presented to our institution 2 days later with worsening symptoms. On examination, he appeared comfortable, and his vital signs were within the normal range. Pertinent findings included decreased breath sounds at the bases bilaterally and paradoxical breathing. A CT chest ruled out pulmonary embolism and acute pneumonitis. A sniff test to assess for diaphragmatic paralysis was normal. However, given that it may be normal in patients with bilateral diaphragmatic paralysis and our high index of suspicion based on physical examination, an electromyogram (EMG) was performed. This was suggestive of bilateral severe phrenic neuropathy. An ultrasound confirmed bilateral diaphragmatic paralysis. Examination of the vocal cords by direct laryngoscopy showed normal vocal cord function (thereby ruling out vagal nerve involvement). To assess for a mechanical cause for the bilateral phrenic nerve paralysis, an MRI of the cervical spine and brachial plexus was done. Both these studies were unremarkable. A serum paraneoplastic panel was normal. Given the lack of evidence for a direct infiltration of the phrenic nerves by melanoma, the absence of a serum antibody (based on a negative paraneoplastic panel), and the fact that ipilimumab has been associated with immunologic toxicities, a diagnosis of inflammatory amyotrophy secondary to ipilimumab was made (variant of Parsonage Turner syndrome). Since the patient’s respiratory condition deteriorated over the next 7 days, requiring non-invasive ventilation, he was started on high-dose corticosteroids. He had a dramatic improvement in his symptoms, and he was successfully weaned off the steroids over the next month. At his most recent follow-up 12 months later, he has unfortunately developed progressive melanoma requiring a change in his therapy. His respiratory status has remained stable with no shortness of breath.
DISCUSSION: Ipilimumab is the first immunomodulatory drug that received FDA approval for the treatment of metastatic melanoma by the FDA in 2011. It acts primarily by inhibiting CTLA-4, which in turn releases the inhibition of cytotoxic T-lymphocytes, and allows them to destroy the melanoma cells in vivo. Unfortunately, this reactivation of T-lymphocytes can have significant immunologic side effects. Indeed, in the original registration phase 3 trial that led to its approval, ipilimumab was associated with an immunologic side-effect in up to 60 % patients. The most common manifestations include skin rash, diarrhea, panhypopituitarism, and adrenal insufficiency. Other rare autoimmune conditions such as acquired hemophilia A, pure red cell aplasia, sarcoidosis and myasthenia gravis have also been reported. To the best of our knowledge, bilateral phrenic nerve paralysis has not been previously reported with ipilimumab. The vast majority of patients who experience severe toxicity as a result of ipilimumab are managed with high-dose corticosteroids for a short duration, followed by a rapid taper. This therapy is associated with high response rates. Interestingly, several reports suggest that patients who experience an immunologic event are more likely to have an anti-neoplastic effect, thereby suggesting that some degree of immune-mediated effects are desirable. Immune checkpoint inhibitors and other immunomodulatory drugs are making tremendous advances in the treatment of many cancers, and ipilimumab alone has been tested in 12 different malignancies. As internists, we need to be cognizant of its protean side effects. It is important to promptly recognize the manifestations of toxicities, including the rare ones such as bilateral diaphragmatic paralysis, for timely initiation of appropriate therapy. And finally, this case report underscores the importance of a thorough physical examination, since no investigations could have replaced the astute clinical observation of paradoxical breathing that clinched the diagnosis in our patient.
PARASITE CAUSING ACUTE ABDOMINAL PAINJessica C. Li; Sara L. Swenson. California Pacific Medical Center, San Francisco, CA. (Tracking ID #1939508)
LEARNING OBJECTIVE 1: Classical gastric anisakiasis manifests as acute abdominal pain 1–12 h after ingestion of raw fish and can also cause an allergic reaction. Treatment is removal of the parasite during endoscopy or symptomatic as the worm cannot survive within the human host for more than a few days.
LEARNING OBJECTIVE 2: A thorough history, including recent foods consumed, combined with prompt endoscopy is the key to suspecting a diagnosis of anisakiasis!
CASE: A 47 yo man with no significant past medical history presented to the emergency room with sudden-onset epigastric pain for the last 36 h. The pain was intermittent and 8/10 in severity at its worst, was dull and pressure-like with radiation to the lower abdomen and back, and was associated with decreased appetite. The pain was not associated with nausea, vomiting, diarrhea, constipation, hematochezia, hematemesis, or NSAID use. Notably, the patient reported eating mackerel at home the night before his symptoms developed. On physical examination, the patient was afebrile. Abdominal examination revealed normal bowel sounds and a non-distended, non-tender abdomen without hepatosplenomegaly. Labs were unremarkable. CT of the abdomen and pelvis revealed wall thickening of the mid and lower gastric body and antrum with mesenteric and retroperitoneal adenopathy most concerning for infiltrative gastric carcinoma with possible metastatic adenopathy. Subsequent upper endoscopy showed two non-bleeding gastric ulcers and a 2 cm anisakis worm exiting one of the ulcers. The worm was removed during the endoscopy as definitive treatment. The patient continued to experience some mild pain but was discharged in an improved condition.
DISCUSSION: This case illustrates a classic presentation of gastric anisakiasis. Anisakiasis includes all infections caused by members of the genus Anisakis. Most human infections are due to Anisakis simplex, a nematode most commonly found in salmon, herring, cod, and mackerel. Given its prevalence and increasing raw and undercooked fish consumption in the US, the incidence of anisakiasis should increase. If a third stage anisakis larva is ingested, it will attach to the stomach wall. The worm directly invades the stomach wall, causing pain, nausea and vomiting that occurs within 1–12 h after a meal. The burrowing worm can perforate the stomach wall or, as in our patient, cause an inflammatory reaction of the gastric wall. The worm can also cause an allergic reaction resulting in pruritis, rash, tingling of the oropharynx and anaphylactic shock. It can also reach the intestines causing diffuse abdominal pain, distention, ascites or even intestinal obstruction or perforation. Ileal involvement can mimic acute appendicitis. Laboratory testing can show an eosinophilia, which this patient did not have, especially in those with an allergic reaction. In the stomach, definitive treatment is removal of the worm. If the larvae makes it into the intestine, it usually passes through in a few days and treatment is symptomatic. However, a complication such as obstruction may require surgery. Albendazole has been used, but its effectiveness has not been studied in randomized trials. When taking a history for acute abdominal pain it is important to find out what the patient has eaten recently so as not to overlook the possibility of an intestinal nematode!
PARSONAGE-TURNER SYNDROME: AN UNUSUAL PRESENTATIONCharu Ramchandani; Waleed Quwatli; Khalid Abdel-Gadir. Unity Health System, Rochester, NY. (Tracking ID #1939501)
LEARNING OBJECTIVE 1: Identifying unusual presentation of Parsonage-turner syndrome involving phrenic nerve, leading to hemi-diaphragmatic paralysis.
CASE: 72 year old female came to the clinic few weeks after undergoing right total knee replacement with complains of shortness of breath on exertion, burning left neck and left upper arm pain interfering with her sleep. She denied any complaints of weight gain, palpitations, edema, chest pain, orthopnea or paroxysmal nocturnal dyspnea. Her past medical history was significant for rate controlled atrial fibrillation, hypertension and osteoarthritis. Her home medication consisted of Rivaroxaban for her atrial fibrillation and, Atenolol and Irbesartan for her high blood pressure. On examination her oxygen saturation at rest and exercise was normal, but on chest percussion there was dullness, decreased vocal fremitus and decreased breath sounds at the left lung base. On imaging, her Chest x-ray revealed atelectasis and elevated left hemi-diaphragm which on Sniff test concluded left hemi-diaphragm paralysis; computed tomography (CT) scan of the chest showed new moderate elevation of left hemi-diaphragm with atelectasis in the left lower lobe and the magnetic resonance imaging (MRI) of the cervical spine ruled out any nerve root compression. In 2009, patient had a similar history of pain, paresthesia and weakness of her left arm few weeks following her left knee replacement, for which she had an extensive work-up to find the cause. During that time, MRI was negative for any compressing or infiltrating lesion, but the nerve conduction study and electromyography concluded moderate left lower trunk brachial plexopathy strongly suggestive of acute brachial neuritis. Over years, her neuropathic pain was controlled with Gabapentin and left arm weakness improved with physical therapy.
DISCUSSION: Parsonage-turner syndrome also known as acute brachial neuritis or neuralgic amyotrophy is an idiopathic immune mediated neuritis with asymmetric involvement of brachial plexus. It is a rare condition most commonly reported as an idiopathic form triggered by surgery, viral infection, vaccination, trauma and strenuous exercise. A hereditary form of neuralgic amyotrophy has also been described in case reports which presents in a similar fashion with recurrent attacks preceding an inciting event. A typical case of Parsonage-turner syndrome presents with a dull aching/burning shoulder/arm pain within a few days to weeks after the inciting event and is followed by shoulder girdle and/or arm weakness. But very few cases have been reported in literature that involves a phrenic nerve, causing hemi-diaphragmatic paralysis leading to dyspnea. Important differential diagnosis to keep in mind is cervical radiculopathy which unlike brachial neuritis involves only one nerve root. Electromyogram and nerve conduction study are crucial to confirm the diagnosis but its findings should always be correlated with patient’s history and physical examination. Treatment is supportive with analgesic and physical therapy. But some studies have reported corticosteroid to be helpful during the acute phase, to expedite the recovery and reduce the pain. Intravenous immunoglobulin and plasma exchange are other therapies that have been reported with unknown results. In patients with persistent disabling diaphragmatic paralysis, laparoscopic plication of diaphragm is an option but data on its effectiveness is lacking. Patient’s recovery may take upto 3 years but in some cases, persistent residual deficits have been reported. In this case report brachial plexopathy and phrenic neuropathy following surgery and without any known etiology is strongly suggestive of Parsonage-Turner syndrome. We believe such presentation can be helpful to for internist/physician in recognizing this disorder in a timely fashion and thus avoid any unnecessary/expensive diagnostic and therapeutic interventions.
PECTUS EXCAVATUM: A RARE BUT POTENTIALLY REVERSIBLE CAUSE OF ATRIAL FIBRILLATIONMai Kaga; Leonard Amoruso; Peter Rattner. Beth Israel Medical Center, New York, NY. (Tracking ID #1895510)
LEARNING OBJECTIVE 1: Recognize important physical exam findings, such as pectus excavatum (PE), as a cause of atrial fibrillation (AF).
CASE: A 24 year old female, with no past medical history, presented to the emergency department (ED) complaining of palpitations, associated with dizziness, for 1 day. The patient was found to be in atrial fibrillation (AF) with rapid ventricular response at 158 beats per minute (bpm). The patient was medically cardioverted and sent home. The patient returned to the ED the next day because she “did not feel right.” Her electrocardiogram (ECG) showed normal sinus rhythm with a heart rate of 74 bpm, enlarged p waves, and anterior t-wave inversions. The patient was admitted to the cardiac care unit. Physical exam revealed a young, tall, thin woman with long limbs and deep voice. Pectus excavatum (PE) was noted on visual exam. Extremities were significant for long bones, and hyperlaxity, with positive Steinberg test and positive wrist sign. Cardiac exam revealed a loud p2, and a grade IV holosystolic murmur, heard best at the left heart border, with right ventricle heave. Transthoracic echocardiogram (TTE) revealed extrinsic compression of the right ventricular free wall. Cardiac MRI showed PE compressing the right ventricular free wall with narrowing of the right ventricular outflow tract. The patient was transferred to another institution to undergo a nuss procedure for surgical expansion of the chest wall.
DISCUSSION: The etiology of AF in this patient is most likely PE, causing mechanical impingement of the right ventricle, leading to dysfunction and right atrial enlargement. The clinical significance of PE depends on the severity, cardiopulmonary function, and cosmetic impact on the patient. The most common complaints among patients with PE are chest pain, poor endurance, and shortness of breath. Evaluation of PE is done with ECG, TTE, CT scan, and MRI. TTE evaluation can be difficult in patients with severe deformities. However, it is important to evaluate the degree of right ventricular compression in these patients to assess cardiopulmonary function. Surgical correction improves cosmetic appearance in most patients and cardiopulmonary functions in some patients. Generally accepted indications for surgery are severe deformity, cardiac compression and displacement, conduction abnormalities, restrictive abnormalities on pulmonary function testing and failed prior PE surgical correction. This case illustrates the importance of physical exam findings, such as PE, as a potentially reversible etiology of AF.
PELVIC ACTINOMYCOSIS MASQUERADING AS PYELONEPHRITIS AND NEPHROLITHIASISRobert P. McClung1; Sarah A. Holzman1; Jai Eun Lee1; Benjamin D. DeMoss2; Kimberly D. Manning1. 1Emory University School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA. (Tracking ID #1937946)
LEARNING OBJECTIVE 1: Recognize an uncommon pelvic infection associated with long-term use of an intrauterine device
LEARNING OBJECTIVE 2: Diagnose invasive actinomycosis using minimally invasive testing
CASE: A 59-year-old woman presented to the emergency department with subjective fevers, chills, flank pain, dysfunctional voiding symptoms and urine discoloration. Her past medical history was notable for asthma, an appendectomy and placement of an intact Lippe’s loop intrauterine device (IUD) 25 years ago. On physical exam, the patient was febrile to 38.8 °C with a heart rate of 124. She exhibited exquisite right-sided costovertebral angle tenderness and diffuse abdominal tenderness. Laboratory studies revealed leukocytosis (WBC 22.4 k with 90 % neutrophils), thrombocytosis of 495,000, and normocytic anemia (hemoglobin of 8.5 g/dL). Urinalysis was notable for 3+ leukocyte esterase, 3+ hemoglobin, numerous WBCs, and negative nitrites. CT scan of the abdomen and pelvis revealed right-sided hydroureteronephrosis without renal calculi and a 14.6 cm complex retroperitoneal mass extending from the proximal right ureter to the right adnexa. Broad-spectrum antibiotics were initiated, a nephrostomy tube was placed to relieve hydronephrosis, and the patient was admitted for management of presumed pyelonephritis and workup of her retroperitoneal mass. Differential diagnosis for her complex mass focused on neoplastic etiologies (ovarian malignancy or sarcoma) and infectious etiologies such as tubo-ovarian abscess. Her ovarian malignancy markers were unremarkable. Gonorrhea and chlamydia testing and blood and urine cultures were all negative. A Papanicolau smear and a bedside endometrial biopsy revealed innumerable infiltrating Actinomycetes. Ertapenem was selected to treat both Actinomyces species and a likely polymicrobial superinfection of the mass, both of which were later confirmed by endometrial culture. The patient improved markedly with appropriate antibiotic therapy, but open surgical management was eventually chosen based on the size of the mass and continued urinary obstruction.
DISCUSSION: Actinomycosis is a chronic granulomatous disease caused by anaerobic, gram-positive bacteria commensal to the oropharynx, gastrointestinal and genitourinary tract. In rare cases, this unusual organism produces invasive infection of the head and neck, thorax, or abdomen and pelvis. One common predisposing factor for abdominopelvic actinomycosis is appendicitis, especially with perforation and foreign body placement in the gastrointestinal or genitourinary tract. Pelvic actinomycosis is commonly associated with continuous IUD use of over 5 years. Approximately 7 % of IUD users have actinomyces species on cervical cytology, but only 2–4 % of these colonized IUD patients are estimated to develop invasive actinomycotic infections. Pelvic actinomycosis resembles a neoplasm on radiographic imaging and is commonly treated as such, frequently leading to surgical intervention. It is not until final surgical pathology results return that the true identity is uncovered. Early diagnosis requires a high index of clinical suspicion. Infections often resolve with antibiotics alone, though surgical debridement may still be required to manage abdominopelvic complications. This case demonstrates effective preoperative diagnosis of pelvic actinomycosis via endometrial biopsy in advance of exploratory surgery. This case also illustrates the importance of obtaining a complete sexual history. The patient’s longstanding IUD, which could have been overlooked, was the crucial link to her diagnosis and appropriate workup.
PERCUTANEOUS VACUUM THROMBECTOMY OF RIGHT HEART THROMBUSAhmed Al-Badri; Sean Wilson; Chad Kliger; Carlos E. Ruiz. Lenox Hill Hospital, New York, NY. (Tracking ID #1940316)
LEARNING OBJECTIVE 1: − Diagnose patients with large right heart thrombus when hemodynamically stable.
LEARNING OBJECTIVE 2: − Management of large right heart thrombus in surgically high risk patients using a novel technique.
CASE: The patient is a 71 year-old man with a past medical history of hypertension, anemia, chronic kidney disease and recent diagnosis of lung cancer with an 80 lb weight loss who presented to the emergency department complaining of dizziness associated with dyspnea on exertion and weakness for 36 h prior to presentation. Electrocardiogram showed sinus tachycardia and a new right bundle branch block. Computed tomography angiography (CTA) was performed revealing a large pulmonary embolus in the right main pulmonary artery extending into the right lower lobe arteries and the presence of an intracardiac filling defect. A transesophageal echocardiogram (TEE) revealed a large mobile mass, likely clot, in the right atrium (RA) extending from the superior vena cava with prolapse into the right ventricle (RV) during diastole. Given the patient’s medical comorbidities including the newly diagnosed lung cancer and poor nutritional status, the patient was deemed too high risk for surgical embolectomy. Thrombolytic therapy was considered to be high risk as well because of the potential for thrombus fragmentation and distal embolization. Therefore, percutaneous retrieval of the clot via vacuum thrombectomy with the AngioVac ® suction cannula (Vortex Medical, Norwell, MA) was attempted and complete en bloc removal of the right atrial thrombus was achieved without complication.
DISCUSSION: Right sided heart thrombi can develop directly within the right heart chambers or from embolization of peripheral venous clots that accidentally lodge in right heart structures on their way to lungs. Type A thrombi with a worm-like shape are extremely mobile, frequently move back and forth through the tricuspid orifice, and may cause cardiovascular collapse when entrapment occurs. They are relatively rare and can be seen in 4–18 % of patients presenting with acute pulmonary embolism. Patients with type A thrombi have a very poor prognosis with high early mortality rates of 44 % with severe and often fatal pulmonary embolisms. Whereas Type B thrombi attach to the atrial or ventricular wall indicating that they are probably of local origin. Mobile right heart thrombi causing acute pulmonary embolism require urgent aggressive therapy, but current management strategy remains controversial. Thrombolytic therapy can be successfully used for some patients but carries a 22 % risk of major hemorrhage. In addition, thrombolytic therapy should be used with caution with large mobile thrombi, as the risk of fragmentation and embolization is high. Surgical removal of the clot is another option, but multiple medical comorbidities may prohibit the operative management. Vacuum thrombectomy using the AngioVac® suction cannula (Vortex Medical, Norwell, MA) is an attractive modality allowing complete en bloc removal of the right atrial thrombus potentially avoiding a complex, high risk surgical procedure.
PERSISTENT HYPOGLYCEMIA: THE PANCREAS REVEALS ITSELFRekha Thammana. Emory University, Atlanta, GA. (Tracking ID #1937841)
LEARNING OBJECTIVE 1: Recognize chronic pancreatitis as a cause of both hyperglycemia and hypoglycemia.
LEARNING OBJECTIVE 2: Choose diabetic regimens that minimize hypoglycemia in patients with chronic pancreatitis.
CASE: A 58 year old African-American man presents to an urban safety-net hospital after he was found obtunded at the entrance of a local church. He is a known diabetic whose last medication of record was metformin. On admission, his blood glucose was 10 mg/dL. On computed tomography of the abdomen, multiple calcifications were seen at the pancreatic head. He was admitted to the intensive care unit and placed on an intravenous dextrose solution. His mental status improved after 48 h of intravenous dextrose. At the time of his initial presentation, his insulin level was 8.05 mcu/mL. His C-peptide level was less than 0.10 ng/mL, and his oral hypoglycemic screen was negative. He later revealed a history of alcohol abuse and chronic pancreatitis. He was actually taking premixed insulin 70/30 for management of his diabetes. His persistent hypoglycemia was due to excess exogenous insulin administration in the setting of a blunted hypoglycemic response due to chronic pancreatitis.
DISCUSSION: Chronic pancreatitis is an under-recognized etiology of diabetes. Alcohol abuse accounts for 70–90 % of cases of chronic pancreatitis, with most remaining cases due to genetic causes like cystic fibrosis. Alcoholic chronic pancreatitis has a median age of onset of 44, and it is associated with reduced pancreatic endocrine and exocrine function. Up to 80 % of patients with alcoholic chronic pancreatitis will develop diabetes within 10 years of chronic pancreatitis diagnosis. Endocrine dysfunction will involve deficiencies in both insulin and glucagon production. Normal pancreatic function dictates a decrease in insulin excretion at a serum glucose of 80–85 mg/dL. In our patient’s case, insulin levels remained relatively high because of exogenous administration. His intrinsic insulin production was non-existent, as evidenced by his low C-peptide level. Glucagon is normally triggered at a glucose of 60–75 mg/dL. While glucagon levels were not investigated, we suspect that our patient’s glucagon response to hypoglycemia was blunted or absent due to his history of chronic pancreatitis. While he should have had a preserved stress response to hypoglycemia with the release of epinephrine, it was not enough to counteract hypoglycemia without intravenous dextrose. Chronic undernourishment from homelessness and alcohol abuse may have played a role in decreasing glycogen stores, thus also preventing a robust response to hypoglycemia. Given the likelihood of an underreported substance abuse history, clinicians should explore the possibility chronic pancreatitis when first diagnosing patients with diabetes. Their management strategy should differ in patients with chronic pancreatitis given the significant risk of hypoglycemia. Clinicians should manage this population in a similar way to type I diabetics, mostly avoiding oral hypoglycemics. Ideally, these patients can be managed with basal-bolus insulin, as this is the most physiologic regimen. Premixed insulin, which our patient was taking, carries a higher risk of hypoglycemia and should also be avoided. Most importantly, more liberal glycemic control is acceptable in a population with secondary diabetes as the risks of hypoglycemia are so high. While hypoglycemic events are not uncommon in diabetic patients, not all hypoglycemia is created equal. It is important to view patients in the context of their full medical, social and family history. This case highlights the importance of understanding the complexity of a patient’s disease process and customizing their care appropriately.
PHEO-FI-FO-FUM !Lawrence Purpura; Seema Qayum. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1927104)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of a pheochromocytoma/extra-adrenal paraganglioma
LEARNING OBJECTIVE 2: Learn the most sensitive/specific biochemical testing for diagnosing a pheochromocytoma/extra-adrenal paraganglioma
CASE: A 36 year-old woman presented in hypertensive emergency with a blood pressure of 244/143, accompanied with bitemporal, 9/10 throbbing headache. She reported having similar headaches periodically for the past 4 months, associated with increased anxiety and elevations in her baseline systolic blood pressure, despite taking her home anti-hypertensives. She had mild right upper quadrant tenderness to deep palpation, but neurological, pulmonary, and cardiac exams were normal. Labs were within normal limits. The patient had a history of a right 4 × 2 × 5 cm retrocaval mass on computed tomography and had initially presented to the hospital that day for endoscopic ultrasound guided biopsy. A secondary hypertension work-up revealed normetanephrines of 2165 pg/mL (normal: 0–145) and metanepherines of 21 (normal: 0–62). An outpatient 123-I-metaiodobenzylguanidine scan revealed abnormal uptake in the area of the retrocaval mass with no other sites of uptake. She was pretreated with doxazosin for 2 weeks then underwent open laparotomy for the removal of the mass. Pathology confirmed diagnosis of extra-adrenal paraganglioma, and repeat plasma-free and fractionated metanephrines and blood pressure 2 months later were normal.
DISCUSSION: Pheochromocytomas are neuroendocrine tumors comprised of chromaffin cells and found mainly in the adrenal medulla, however 10–20 % are extra-adrenal and known as “extra-adrenal paragangliomas.” Both have the ability to secrete catecholamines and produce symptoms, most commonly hypertension, tachycardia, pallor, headache, panic or anxiety attacks; The triad of headache, palpitations and diaphoresis carries a high sensitivity for pheochromocytoma. Classical symptoms, uncontrolled hypertension, an adrenal incidentaloma, or a family history of pheochromocytoma warrant catecholamine biochemical testing, with plasma-free metanephrines being the most specific and sensitive test. If biochemical tests are unequivocal, imaging can be performed with T2-weighted magnetic resonance imaging being the choice modality. If high risk of malignancy, a 123-I-metaiodobenzylguanidine scan is performed to look for metastases. Surgical removal is the standard of care for most pheochromocytomas, and to prevent catecholamine-induced complications during surgery, the patient is pretreated with alpha-adrenoreceptor blockade for 10 to 14 days. Phenoxybenzamine is the drug of choice due to its noncompetitive alpha-blockade, however prazosin and doxazosin may also be used. A beta-adrenoreceptor blocker is added to competitive alpha-blocker after several days; care must be taken to avoid the loss of beta-adrenergic induced vasodilation before alpha-blockade, as unopposed alpha-vasoconstriction can lead to hypertensive emergency. The patient requires at least 1 day of intensive care observation post-resection to monitor for hypotension and hypoglycemia. Non-hereditary, unilateral cases carry good prognosis, but persistent hypertension is common.
PHOSPHATE NEPHROPATHY DUE TO COLONIC IRRIGATION THERAPYVijan Joshi; Naoka Murakami; Wan L. Lam. Beth Israel Medical Center, New York, New York, NY. (Tracking ID #1937123)
LEARNING OBJECTIVE 1: Distinguish phosphate nephropathy from other forms of acute kidney injury.
LEARNING OBJECTIVE 2: Recognize that colonic irrigation treatments used in alternative medicine pose a potential risk for phosphate nephropathy.
CASE: A 52-year-old male with a past medical history of HIV on HAART (CD4 470, viral load undetectable), presented with nausea and vomiting for 3 days, and anuria for 1 day. Vital signs on admission were all within normal limits. Physical exam was significant for oral thrush and mild tenderness to palpation in the lower quadrants of the abdomen. Labs were significant for acutely elevated BUN (75 mg/dl), creatinine (11.91 mg/dl, baseline 1.14 mg/dl 3 months prior to presentation), K 5.5 mEq/L, Ca 7.9 mg/dL, Phos 11.1 mg/dL and an anion gap metabolic acidosis (pH 7.24, CO2 33 mmHg, HCO3 17 mg/dL). Urinalysis was positive for blood and protein, but negative for WBCs and casts. Hemodialysis was initiated for symptomatic uremia on the third day of hospitalization. Additional history revealed that the patient had begun receiving colonic irrigation treatments 3 months prior to admission, and had thus far received three enema treatments. It was suspected that his acute renal failure could be due to high phosphate containing enemas. A kidney biopsy was performed, which demonstrated marked diffuse deposition of calcium phosphate in the tubules consistent with phosphate nephropathy, with concomitant tubular atrophy and interstitial fibrosis. The patient’s symptoms improved after initiation of hemodialysis, and he was instructed to discontinue his colonic treatments upon discharge.
DISCUSSION: This case illustrates a potential complication of colonic irrigation therapy. Phosphate nephropathy is used to describe acute renal failure with characteristic histologic findings on renal biopsy of widespread calcium phosphate deposition in the renal tubules. Typically, this nephrocalcinosis is associated with hypercalcemia, but in acute phosphate nephropathy, the precipitant is a large phosphate load delivered to the distal nephron. While the mechanism by which this causes acute renal failure is unknown, it is hypothesized that an increased intratubular phosphate concentration results in the precipitation of calcium phosphate salts, causing luminal obstruction and inflammation. Our patient’s laboratory results were consistent with hyperphosphatemia and normocalcemia, and there was no other clear precipitant of these abnormalities based on his history and medications. While the adverse effects of phosphate-containing enemas including renal failure are well documented, our case is unique in that it highlights a disturbing consequence of a form of alternative medical therapy that has been receiving increasingly more popular media attention. The FDA currently does not regulate the use of colon-cleansing regimens, and alternative medicine practitioners are not required to verify the contents of their enema products. In 2006, the FDA issued a warning regarding the potential for kidney injury in patients taking oral sodium phosphate bowel cleanses, and the FDA required that a boxed warning be added to two oral sodium phosphate containing medications in 2008. While most of the literature surrounding phosphate nephropathy involves phosphate-containing bowel purgatives used for the purposes of colonoscopy preparation or constipation relief, there is little literature published on the adverse effects of colonic irrigation when used as a form of alternative medicine. Physicians should be aware of the side effects that colonic irrigation therapy can carry for their patients, and should consider the possible risks associated with any alternative medical therapy.
PHYTOBEZOAR IN THE SETTING OF DIABETIC GASTROPARESISJenny Koo; Laura Y. Sue; Pearl Yu. UC San Diego, San Diego, CA. (Tracking ID #1922249)
LEARNING OBJECTIVE 1: Recognize the signs and symptoms of small bowel obstruction, and know the risk factors for developing a phytobezoar.
LEARNING OBJECTIVE 2: Understand the long term management after diagnosis of a phytobezoar
CASE: A 76 year old female with history of diabetes mellitus type 2 and no prior abdominal surgery presents to the emergency department with 2 days of left upper quadrant pain, nausea, and vomiting. She was diagnosed with diabetic gastroparesis and discharged home with metoclopramide. The patient returned the next day with worsening abdominal pain with vomiting and inability to tolerate oral intake. Computer tomography (CT) scan of the abdomen revealed small bowel obstruction. A nasogastric tube was placed, and patient was admitted. She was found to have a focal cut off point in the distal ileum and would require surgery to correct this. Exploratory laparotomy with enterotomy was performed. The jejunum was significantly dilated and hyperemic, a rock-hard intraluminal mass was found at the mid to distal jejunum a transition point. The mass was mobile and not consistent with a bowel wall tumor. The mass was described intraoperatively as “greenish, irregularly shaped bezoar consistent with a phytobezoar.” Post-operatively, the patient resumed normal bowel function within 10 days, tolerated oral intake of a regular diet and fluids. Patient was advised to minimize insoluble fiber intake and increase fluid intake.
DISCUSSION: Phytobezoars are formed from high indigestible fiber. Some common predisposing factors to formation of phytobezoars include excessive fiber intake, decreased gastric motility (ie. diabetic gastroparesis, hypothyroidism), adhesions secondary to abdominal surgery, and inadequate mastication. Phytobezoars account for as much as 2–5 % of mechanical small bowel obstructions; however, clinical presentation of a phytobezoar with a surgical abdomen is rare (only 1.1 %). Patients may present with nausea, vomiting, and abdominal pain. The most common locations for phytobezoar obstruction are in the stomach (due to inability to pass the pyloric sphincter) or at the terminal ileum. Diagnosis is made with computer tomography (CT) scanning, which would show mottled gas pattern and a dilated small bowel proximal to block. A well-defined mass with mottled appearance associated with an encapsulating wall is suggestive of a phytobezoar. Treatment may include gastric lavage, endoscopic removal, or in this case, surgical removal. Long term management includes reducing intake of insoluble fibers, and reducing risk factors for gastroparesis. This case illustrates an uncommon cause of mechanical small bowel obstruction. The patient’s history of diabetes mellitus predisposes her to gastroparesis, which in turn increases her risk of forming a phytobezoar obstruction.
PITFALL OF OMEPRAZOLE: COMMONLY PRESCRIBED IN THE WORLDSyo Tano1; Koichiro Kimura1; Masato Yoshihara1; Munehisa Atsumi1; Shinichi Mizuno2; Mitsunori Iwase1. 1TOYOTA memorial hospital, Toyota, Aichi, Japan; 2TOYOTA memorial hospital, Toyota, Aichi, Japan. (Tracking ID #1929571)
LEARNING OBJECTIVE 1: Recognize that the treatment approach to syndrome inappropriate secretion of ADH (SIADH).
LEARNING OBJECTIVE 2: Describe the signs and symptoms of hyponatremia associated with Omeprazole.
CASE: A 61 year-old man with no remarkable past medical history complained palpitation and hand tremor. The patient had abdominal pain and loss of appetite 1 week before and proton pump inhibitor (PPI), Omeprazole was prescribed the day before admission. Four hours after he took the medicine, palpitation, trembling, nausea and continuous dizziness occurred gradually. Since the symptoms were not improved even on the next day, he came to our hospital. Vital signs and physical examinations were normal except for tremor of his right hand. He was restless, but his consciousness was alert. There were no remarkable neurological findings. Laboratory studies showed serum sodium decreased at 114 mEq/L, high CK and low serum osmolality. Urine osmolality was high and urine sodium was also high. Other studies including complete blood cell count, serum chemistry, and endocrine tests: thyroid pituitary, adrenal functions were normal, but secretion of ADH was elevated at 6.5 pg/mL. There were no abnormal findings on the chest X-ray and the head, chest and abdominal CT images. Thus, he was diagnosed as SIADH of unknown etiology. Initial treatment was fluid restriction, 3 % saline and discontinuation of Omeprazole. Since the sodium level elevation was faster than expected with 3 % saline, it was necessary to use sodium free infusion. At the same time, his urine osmolality was decreased from 493 mOsm/kg H2O to 62 mOsm/kg H2O. After 2 days of fluid treatment, the serum sodium level returned to normal range and he was discharged free of any symptoms.
DISCUSSION: SIADH is thought to be caused by variable etiologies such as CNS disorder, tumor, surgery, infection and medicine. The treatment includes combination of water restriction and intravenous saline, while the treatment of underlying diseases or problems are needed. It is important to avoid overly rapid correction of serum sodium level because it is known as the risk of central pontine myelinolysis (CPM). In the presented case, the cause of SIADH was thought to be Omeprazole because of his medical history and clinical course after the admission. Although many papers which suggest the usefulness of PPI such as Omeprazole, there are not many papers reporting about its side effects. A few reports described the appearance of hyponatremia and rhabdomyolysis associated with Omeprazole. Although the mechanism is uncertain, it is suggested that Omeprazole make sodium excrete in urine or increasing secretion of ADH. Shiba, et al. presented a case of hyponatremia caused by Omeprazole. In his case, the serum sodium level was not corrected despite extensive supplementation of sodium before discontinuation of Omeprazole. In our case, since the sodium level elevation was faster than expected, it was needed to use sodium free infusion to avoid CPM. The reason of the rapid improvement of the SIADH was thought to be discontinuation of Omeprazole. In summery, although the frequency is relatively low, PPI like Omeprazole, which is commonly prescribed all over the world, has critical side effects such as hyponatremia and rhabdomyolysis. Therefore it is necessary to recognize the importance of medical history and consider SIADH as a differential diagnosis in patient with nonspecific symptoms prescribed with Omeprazole.
PLEURAL EFFUSION AND DYSPNEA FROM AN UNLIKELY SOURCELaura Nichols; Kurt J. Pfeifer; Apoorv Broor. Medical College of Wisconsin, Wauwatosa, WI. (Tracking ID #1928599)
LEARNING OBJECTIVE 1: Describe a case of intrahepatic cholangiocarcinoma with an unusual presentation of dyspnea and pleural effusion
LEARNING OBJECTIVE 2: Diagnose cholangiocarcinoma using histologic stains to differentiate from metastatic malignancies such as colon or lung
CASE: A 57-year-old man with a history of diabetes mellitus and cirrhosis secondary to alcohol abuse presented with 10 days of pleuritic chest pain and dyspnea. Admission examination revealed tachycardia, oxygen saturation of 91 % on room air and dullness to percussion with decreased breath sounds over the left lung. White blood cell count was elevated to 63,800/mm3 with 80 % neutrophils. Liver enzyme testing revealed elevated alkaline phosphatase of 340 U/L. Chest CT revealed a very large, loculated left pleural effusion with periaortic and retrocural adenopathy. Pleural fluid analysis was consistent with an exudative process (LDH 1493 U/L and total protein 4.2 g/dL). Multiple samples were negative for malignant cells. CT scan of the abdomen was performed to investigate the patient’s lymphadenopathy and demonstrated a 4.5 × 4.0 cm hepatic lesion with periaortic, retrocrural, and aortocaval lymphadenopathy. Extreme leukocytosis with peak WBC count of 106,000/mm3 was thought to be reactive, and peripheral smear and flow cytometry confirmed only 15 % monoclonal CD20-positive B cells compatible with a B cell lymphocytosis. Biopsy of the liver mass was performed and interpreted as adenocarcinoma with features favoring biliary origin (cholangiocarcinoma). Negative results for napsin A and TTF-1 made metastatic lung adenocarcinoma unlikely. Positive high-molecular-weight cytokeratin, in addition to positive results for CK 17 and HBME favored a biliary origin. Given the extent of his disease, the patient elected not to undergo treatment and was discharged to hospice.
DISCUSSION: Cholangiocarcinoma is an uncommon malignancy, accounting for only 3 % of gastrointestinal neoplasia. Of these, only 10 % involve the intrahepatic biliary system. Intrahepatic cholangiocarcinoma generally presents with dull right upper quadrant pain, weight loss, and elevated alkaline phosphatase levels or is incidentally discovered on imaging. Though our patient had multiple risk factors for cholangiocarcinoma (cirrhosis secondary to alcohol abuse and diabetes), his was an atypical presentation with pulmonary metastasis and pleural effusion. Though 10–20 % of patients have peritoneal involvement at presentation, distant metastasis is uncommon and spread generally occurs through direct extension. Furthermore, our patient had significant leukocytosis consistent with leukemoid reaction. Though this has been described in previous case reports of GM-CSF-producing cholangiocarcinoma, it is an exceedingly rare entity. Cholangiocarcinoma can be difficult to differentiate from other adenocarcinomas such as those originating from the colon or lung. However, as in this case, special stains can be performed to more definitively diagnose this malignancy.
PNEUMONITIS, EOSINOPHILIA AND INFERTILITYEunice Chuang; Leila Ganjehe. Mount Auburn Hospital, Cambridge, MA. (Tracking ID #1939989)
LEARNING OBJECTIVE 1: To recognize In Vitro Fertilization as a possible cause of eosinophlic pneumonia.
CASE: 39 year old Filipino women presented to the ED with shortness of breath, dry cough and lightheadedness for 4 days. She is usually very active and noted mild orthopnea and dyspnea while running. Denied chest pain, edema, and fever. Patient is undergoing fourth cycle of in vitro fertilization. She had used Lupron, esterase and vaginal progesterone. This cycle was different in that the progesterone has been administered in a sesame oil vehicle, injected intramuscularly. This started about 3 weeks prior. She has no other significant past medical history or medication. Denied tobacco or alcohol. In the ED, afebrile, BP 108/66, HR 111, RR 30, sO2 86 % RA. In mild respiratory respiratory distress, lungs with few soft crackles and decreased breath sounds in the basis, cardiovascular exam unremarkable except minimal elevated jugular venous pressure of 6–7 cm of water with no hepatojugular reflux. Carotids are 2+ and equal without bruit. Extremity with no edema. WBC 14.52 k/CMM with 14 % Eosinophil, Eos Count 290/cmm, hemoglobin 14.1 g/dL, hematocrit 39.8 %, platelet count 321 K/cmm, first troponin 0.15 ng/mL. Chest Xray showed diffuse interstitial infiltrates as well as small bilateral pleural effusion. Patient was admitted with diagnosis of eosinophilic pneumonitis. She was started on methyprednisolone 1 g daily for 2 days and changed to prednisone as she was improving. Echocardiogram showed EF 45–50 % with global hypokinesis with no valvular disease. A drug-induced eosinophilic pneumonia was suspected. The OBGYN recommended stop the i.m. form of progesterone also because of failure of the IVF (decrease in Hcg). Patient was discharged on prednisone. On 2 weeks follow up, patient was asymptomatic, repeat CXR was improved. She was tapered off the steroids over 30 days with no recurrence of the symptoms.
DISCUSSION: Eosinophilic pneumonia is a syndrome characterized by nonspecific pulmonary symptoms varying from mild to severe, life-threatening, respiratory failure. The diagnosis is usually suggested by peripheral alveolar opacities at the chest X-ray, with alveolar and usually peripheral blood eosinophilia. Acute eosinophilic pneumonia may be idiopathic or be related to various causes such as parasitic infections and drug-induced, such as amiodarone, methotrexate, NSAIDs. The addition of GnRH agonists to the IVF treatments has been used for the Luteal phase supplementation and it has mainly consisted of progesterone or hCG. Progesterone can be administered orally, i.m., or vaginally. We report a case of acute eosinophilic pneumonia induced by i.m. administration of progesterone used as luteal phase support after IVF. Symptoms improved as the i.m. form was discontinued and corticosteroids started. Sesame oil (used as excipient) and benzyl alcohol (used as preservative) could both be incriminated in the development of the type IV delayed hypersensitivity reaction. Although such reactions are exceedingly rare, specialists providing care to patients using these products should beaware of potential adverse reactions and their subsequent management.
POLYCYSTIC OVARY SYNDROME IN ASIAN-AMERICAN ADOLESCENT WOMENVictoria T. Liu; Karen Y. Cheng; Pearl Yu. University of California, San Diego, La Jolla, CA. (Tracking ID #1939487)
LEARNING OBJECTIVE 1: Recognize clinical features of polycystic ovary syndrome in Asian-American, adolescent women.
LEARNING OBJECTIVE 2: Evaluate polycystic ovary syndrome in adolescent women.
CASE: An 18 year old Chinese-American girl with unremarkable medical history presented for oligomenorrhea since menarche at age 12. Previously, menses had been 3–4 times yearly, but recently decreased to once yearly. Patient complained of weight gain, and slight hair growth between breasts and legs. She denied fatigue, cold intolerance, and acne. Family history was remarkable for breast cancer in mother. Physical exam revealed deepening of voice; no thyromegaly, acanthosis nigricans, acne or hirsutism. Initial testing revealed borderline free testosterone (16 ng/dL, female reference 1.2–9.9 ng/dL), total testosterone (71 ng/dL, female reference 9–55 ng/dL), dehydroepiandrosterone (DHEA) (7.78 ng/mL, female reference 1.33–7.78 ng/mL), and luteinizing hormone: follicle stimulating hormone ratio of 2. Also notable were decreased sex hormone binding globulin (18), mildly elevated hemoglobin A1C (HgbA1C) of 6.2 %. Thyroid stimulating hormone, and anti-thyroperoxidase antibody were within normal limits. Pelvic transabdominal ultrasound showed no cystic ovaries. Patient was diagnosed with probable polycystic ovary syndrome (PCOS). Due to family history of breast cancer, we recommended progestin-only therapy to regulate menstrual cycles, induce withdrawal bleeding, and reduce the risk of endometrial hyperplasia. We also encouraged lifestyle modification for elevated HgbA1C suggesting insulin resistance, and referred patient to endocrinology for further evaluation.
DISCUSSION: Currently, 3 major sets of diagnostic criteria exist for PCOS. The National Institutes of Health (NIH) criteria require 1) oligomenorrhea or amenorrhea, and 2) either clinical or biochemical hyperandrogenism. The Rotterdam criteria require 2 of the 3 following: the 2 NIH criteria, and polycystic ovaries by ultrasound. The Androgen Excess and PCOS Society criteria are similar, but require hyperandrogenism to be present. Diagnosis of PCOS remains difficult because there is no full consensus on diagnostic criteria. The most common clinical features of PCOS in adolescent women are hirsutism, menstrual irregularities, obesity, acanthosis nigricans and persistent acne. PCOS hirsutism typically grows in a male pattern. However, Asian-American women are less likely to show overt hirsutism, so index of suspicion must be high. Approximately two-thirds of PCOS patients have anovulatory symptoms, ranging from amenorrhea to dysfunctional uterine bleeding. However, diagnosis in adolescents is complicated by the fact that even in the general adolescent population, approximately half of menstrual cycles are anovulatory in the first 2 years after menarche. Polycystic ovaries are less frequently found on ultrasound in adolescent compared to adult PCOS patients (69 vs. 87 %), and polycystic ovaries can be a transient finding in adolescents. Approximately 50 % of PCOS patients are obese. Lastly, 50–75 % of PCOS patients have insulin resistance. In evaluating probable PCOS, androgen excess should first be confirmed by laboratory testing. Notably, the standard testosterone assay may not be accurate in women, so confirmation by mass spectrometry is recommended. Subsequently, other causes of hyperandrogenism should be excluded by endocrine testing (eg. congenital adrenal hyperplasia, Cushing syndrome) and ultrasound (eg. ovarian tumor, adrenal tumor).
POORLY CONTROLLED CHRONIC MYELOGENOUS LEUKEMIA AND AN UNEXPECTED LEGAL GUARDIANCharles J. Lenz; Roger Yu. Mayo Clinic, Rochester, MN. (Tracking ID #1939575)
LEARNING OBJECTIVE 1: Recognize the importance of identifying patients with court appointed legal guardians in the health care setting.
LEARNING OBJECTIVE 2: Recognize the role of a court appointed legal guardian in the decision making process for a legally incompetent patient who appears to possess capacity to make medical decisions.
CASE: A 34-year-old gentleman with a past medical history significant for substance abuse, chronic pain, and chronic myelogenous leukemia (CML) in the chronic phase was admitted to the hospital for worsening pain in the bilateral hips, knees, and clavicles. On admission, the patient was started on IV hydromorphone which controlled the pain quite well. The patient had a reported history of medication non-compliance and admitted to being on a self-reduced dose of ponatinib. Physical exam was unremarkable. There were no apparent abnormalities in mental status. CBC revealed blood counts consistent with well-controlled CML. Out of concern for medication non-compliance and undertreated CML a peripheral smear and peripheral blood PCR for BCR-ABL were performed. The peripheral smear and manual differential were negative for blasts. The PCR for BCR/ABL p210 mRNA transcripts revealed 81.8 % bcr/abl (p210):abl on the international scale. On this scale, 0.1 % is considered a major molecular response and indicates good control. This patient’s results were indicative of very poorly controlled CML and likely medication non-compliance. This was very concerning to the medical team, and the patient was educated about the importance of taking his medications as prescribed. At this point, the patient was transitioned from IV hydromorphone to oxycodone with continued control of his pain. Social work was involved to discuss outpatient options which could potentially increase medication compliance. It was through the assistance of social work that at this point it came to the medical team’s attention that the patient had a court appointed legal guardian and conservator. The document appointing this patient’s guardian had been on file within the hospital system at the time of admission and supplied the guardian with the power to make all medical decisions for the patient. The medical guardian had the sole power to provide consent for treatment. The patient had been appointed a guardian due to lacking sufficient understanding or capacity to make or communicate responsible decisions concerning needs for medical care, nutrition, clothing, shelter, and safety in the setting of ongoing substance abuse. The medical team reached out to the patient’s guardian who expressed concern that the patient was not taking his necessary medications at home and continuing to abuse substances. The guardian also requested that the patient be transitioned to a less potent narcotic pain reliever given his history of substance abuse. The patient was informed of this discussion and the plan to transition from oxycodone to tramadol. The patient became irate and wished to leave the hospital against medical advice (AMA). The medical team felt this would not be in his best interest unless all outpatient options to increase medication compliance were exhausted. The patient’s guardian agreed that the patient should remain in the hospital. The patient did not meet criteria to be placed on a 72-hour-hold. However, given his guardian’s wishes, security was notified that the patient would need to be held in the hospital if he attempted to leave. After a long discussion, the patient agreed to stay without the need to physically detain him. Eventually he was discharged to a location agreed upon by both the patient and his guardian with tramadol for pain control.
DISCUSSION: This case illustrates a couple of important legal and ethical points. First, it illustrates the importance of a systematic approach to clearly identify patients with legally appointed decision makers in the healthcare setting. This ensures that the appropriate person be consulted for important decisions regarding both treatment and consent. Secondly, this case illustrates the ethical responsibility of the medical team to hold an incompetent person in the hospital if the medical decision maker agrees that the patient should stay. This responsibility persists even when legally incompetent patients exhibit apparent capacity to make a decision, and when the patient does not meet criteria to be placed on a 72-hour-hold.
POSITIVE SPUTUM AFB STAINING: IS IT ALWAYS TUBERCULOSIS?Dipenkumar Modi; Hirva Mamdani; Theresa Vettese. Wayne State University, Detroit, MI. (Tracking ID #1939101)
LEARNING OBJECTIVE 1: To recognize nontuberculous mycobacteria as an important cause of AFB positive sputum
LEARNING OBJECTIVE 2: To recognize the importance of PCR in final identification of mycobacterial species in AFB stain positive sputum
CASE: A 64 year old Caucasian man presented with left sided pressure like chest pain after using cocaine. He had similar self-limited episodes of chest pain in the past. On review of systems, he reported having fever, night sweats, and unintentional loss of about 10 lbs over 6 weeks along with cough productive of yellowish sputum for 1 week. Chest X-ray showed left upper lobe nodular opacities with ill-defined/speculated borders. Review of past history revealed that he had been having chronic left upper lobe cavitation for 4–5 years which had never been worked up in the past. He also had a positive PPD while in prison about 15 years ago with suboptimal treatment for latent tuberculosis for 3 months. CT Thorax showed 3.6 × 2.2 × 2.7 cm size cavities in left upper lobe with hyper-densities within the lumen. Based upon above presentation, tuberculosis was the most likely possibility. Patient was kept under isolation and three sputum samples were sent for AFB stain and culture, out of which two samples came back positive for AFB. Subsequent mycobacterial PCR testing revealed it to be nontuberculous mycobacteria. Because of presence of hyper-densities within the cavity, aspergillus infection was also one of the possibilities, which was ruled out with low serum aspergillus antigen level. Finally diagnosis of Mycobacterium Kansasii lung infection was made based upon sputum PCR testing.
DISCUSSION: AFB smear- positive sputum, especially in the presence of a cavitary lung lesion is generally considered to be Mycobacterium tuberculosis unless proven otherwise. However, this test is not specific for tuberculous mycobacteria. Non-tuberculous mycobacteria (NTM) related lung disease can also have similar presentation with AFB positive sputum which poses a significant diagnostic challenge. Mycobacterium kansasii has traditionally been considered the most virulent of the NTM. It is the second most common NTM after Mycobacterium avium complex. It does not require contact tracing as it is not transmitted by person-to-person contact. M. kansasii infection most commonly manifests as a chronic pulmonary disease mimicking classic tuberculosis. Less commonly, the organism causes extra-pulmonary disease, such as scrofula-like lymphadenitis, sporotrichosis-like cutaneous infection, osteomyelitis, and tenosynovitis. Risk factors for M.kansasii lung infection include smoking, alcoholism, prior tuberculosis, and HIV infection. Its clinical and radiographic presentation is indistinguishable from MTB, including low grade fever, productive cough, and weight loss with radiologic evidence of cavitary lesion mostly involving upper lobes. Because of this, it is very important to consider the possibility of NTM in such patients and mycobacterial PCR is helpful in making the diagnosis. Treatment mainly includes daily isoniazid (300 mg/day), rifampin (600 mg/day), and ethambutol (15 mg/kg/day) until culture negative on therapy for 1 year.
POST-PRISON BLUES: UTILIZING A PRIMARY CARE STUDENT-FACULTY COLLABORATIVE CLINIC TO CONCURRENTLY TREAT HEROIN ADDICTION, PTSD AND HEPATITIS CKimberly Sue1; Harper Hubbeling1; Christine Kuo1; Katy Brubaker1; Luyi Xu1; Carina Fernandez-Golarz1; Marya J. Cohen1; Alex Keuroghlian2. 1Harvard Medical School/MGH-Chelsea, Chelsea, MA; 2Massachusetts General Hospital, Boston, MA. (Tracking ID #1930384)
LEARNING OBJECTIVE 1: (1) Recognize that patients leaving prison are at high-risk for chronic and infectious diseases, psychiatric illness, substance use disorders and violent victimization
LEARNING OBJECTIVE 2: (2) Recognize, manage and coordinate care for some common multidisciplinary clinical problems for patients leaving prison and identify common psychosocial stressors for patients recently released from prison within our co-located primary care and psychiatric clinic
CASE: HPI: Mr. M is a 54-year-old man with a history of mood disorders, heroin addiction, Hepatitis C and over 25 total years in prison presenting to establish primary care, psychiatric care and suboxone maintenance treatment. Our clinic is uniquely oriented towards serving post-incarcerated patients with co-located medical and psychiatric services provided by medical students working with staff faculty supervision. PMH: Significant for cocaine and heroin dependence. He relapsed on heroin 6 months after release from prison in the context of depression and posttraumatic stress disorder (PTSD). Experiences nightmares and flashbacks. Two suicide attempts in prison and four lifetime overdoses. Hepatitis C diagnosed while incarcerated in 2003, treatment naive. Social History: Grew up in single-parent Italian household, survived childhood sexual abuse. He has spent a total of 27 years in prison mostly related to crimes to support drug use. He is currently unemployed. Sexually active with girlfriend. Twenty pack-year smoking history. Physical Exam: General: Tall man, overweight, many tattoos, well-groomed, track marks on R hand, anxious affect Abd: Soft, nontender, no masses, no hepatosplenomegaly. No evidence of stigmata of chronic liver disease Diagnostic Studies: Urine Tox: Positive for opiates, cocaine, buprenorphine LFTS: AST 92, ALT 112 Hep Serologies: HBVsAb Positive, HBVsAg Negative, HCG\VAb Positive, Genotype 1A, VL 7,910,000, HIV Negative
DISCUSSION: Mr. M is a 54-year-old man seeking to establish primary care and treatment for heroin addiction, depression and PTSD. His case is further complicated by hepatitis C infection and history of lengthy incarceration. In our co-located clinic, we provided Mr. M with weekly CBT for PTSD, prazosin for nightmares, doxepin for depressed mood and insomnia, and 12 mg daily suboxone for heroin addiction. We also manage his Hepatitis C and future treatment given elevated risks for depression or suicidality. Our student-faculty clinic provides streamlined treatment for this patient’s medical and psychiatric illnesses as well as addressing social factors such as unemployment. The patient benefits from active communication and collaboration between teams about his treatment as well as the clinic’s efforts to create a positive environment and a consistent relationship with the patient. Such patients often are unable to keep their appointments for many reasons including experiencing medical mistreatment in prison, a general mistrust of healthcare systems, feeling stigmatized or judged, lack of transportation or even lacking basics like clothing or a cellphone. Individuals emerging from the prison system are both sicker and at greater risk of death than the general population; for the first 2 weeks post-release patients face an alarmingly acute mortality risk: 3–8 fold above the general population (Binswanger et al. 2007). Perhaps the most confounding aspect of taking care of these patients is the complex interrelationship between chronic conditions and treatments: for example, PEG-IFN/RBV treatment for Hepatitis C potentially exacerbating mental illness (Maru et al. 2010). Inmates use street drugs to self-medicate for untreated psychiatric illness and psychiatric issues characterized as “post-incarceration syndrome” limit help-seeking behavior and willingness to trust service providers (Rich et al. 2001). Consistent with these findings, Mr. M faces increased risks of morbidity and mortality upon release from prison. Such patients have pressing social situations such as homelessness and ongoing drug use that must be addressed simultaneously or even prior to addressing medical and psychiatric needs. In our clinic, we assisted the patient with Social Security disability and transportation needs. The structure of our student-faculty clinic, with special attention to patients with histories of incarceration, is an exemplar model for addressing health disparities and providing excellent clinical care for this vulnerable population. References: Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. Maru DS, Bruce RD, Basu S, Altice FL. Clinical outcomes of hepatitis C treatment in a prison setting: feasibility and effectiveness for challenging treatment populations. Clin Infect Dis. 2008;47(7):952–961. Rich JD, Holmes L, Salas C, et al. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. J Urban Health. 2001;78(2):279–289.
POST-TRANSFUSION PURPURA: A DIFFICULT DIAGNOSISGaurav Goyal; Peter Silberstein. Creighton university medical center, Omaha, NE. (Tracking ID #1927374)
LEARNING OBJECTIVE 1: Recognize the entity of post transfusion purpura in the appropriate clinical setting.
LEARNING OBJECTIVE 2: Distinguish between PTP and other causes of thrombocytopenia like ITP and drug induced Thrombocytopenia.
CASE: HPI: 78 y/o Caucasian female presented to the ER after she developed sudden onset bleeding from the oral mucosa and bloody stools. She was recently discharged from the hospital 9 days ago when she was admitted due to trauma causing subdural hematomas and received 1 unit of platelet transfusion at that time. Her platelet level on discharge was 190,000/microL. She had an uneventful course after that until she developed spontaneous bleeding. Past medical history was significant only for anemia of chronic kidney disease and gout. Initial Laboratory studies: Platelet count on admission was found to be 4000. Other laboratory studies showed LDH 343, INR 1.0, PTT 23, Absolute reticulocyte count 129.8, HgB 7.3, Fibrin Degradation products 10–40, Haptoglobin 58, Total bilirubin 0.7, creatinine 2.3, AST 22, ALT 13. Peripheral smear showed no evidence of schistocytes. Hospital course: The patient was already started on Dexamethasone 40 mg daily on the suspicion of immune thrombocytopenia. The platelet count dropped further to 2000 the next day. PTP was then suspected and the patient was started on high dose IVIG at 1 g/kg/day for 2 days along with the continuation of the Dexamethasone for a total of 4 days. Platelet count went up to 14,000 and 35,000 on days 2 and 3 respectively and the bleeding stopped spontaneously with that, thus pointing towards PTP. Patient was tested for antibodies to platelet antigen PlA1, now known as Human platelet antigen 1a (HPA-1a) and she tested positive for the same, thus confirming our suspicion of PTP. Patient was later seen as an outpatient follow up and her platelet count was 148,000 after 2 weeks and she did not have any further episodes of bleeding. For further confirmation, we performed platelet genotyping which showed that the patient was homozygous for the rare allele b/b (most common one being a/a which is present in 98 % of the population).
DISCUSSION: Post-Transfusion purpura is a rare transfusion reaction that can occur after transfusion of any platelet-containing product (red cells, platelets, or granulocyte concentrates). Female to male ratio in the total of about 250 reported cases is 26:1. Ninety-eight to ninety-nine percent of Caucasian women are PlA1/HPA-1a positive, as are their spouses. PTP might be thought of as a delayed transfusion reaction involving platelets. Patients with PTP can present with severe thrombocytopenia that develops 5 to 10 days following transfusion. PTP can be confused with drug- induced or immune thrombocytopenia, since the blood and bone marrow smears are consistent with immune platelet destruction in all these disorders. Since drug induced thrombocytopenia and de novo ITP appearing in someone who has recently been transfused is relatively rare, the appropriate hiatus time until the appearance of thrombocytopenia, and its severity, must alert the physician to the correct diagnosis. Nonetheless, the diagnosis of PTP is confirmed by identification of alloantibodies to HPA-1a/PlA1 and the absence of the platelet antigen HPA-1a, both of which conditions were satisfied in the above case. The management of PTP includes high dose IVIG (400 to 500 mg/kg per day, usually for 5 days or 1 g/kg per day for 2 days) and it usually takes about 4 days for the platelet count to increase up to the level of 100,000/microL. The clinical course of PTP may be severe with a mortality rate of 10-20 %. It emphasizes the importance of being alert to the possibility of PTP in appropriate clinical setting, along with being aware of the possible pitfalls in the diagnosis of this under-diagnosed condition. References: Post-transfusion purpura: A challenging diagnosis. Mordechai Shtalrid MD, Lev Schvidel MD, ElJakim Vorst, Eran E. Weinmann MD, Alain Berrebi MD and Erica Sigler MD. IMAJ 2006;8;672–674 Becker T, Panzer S, Maas D, et al. High-dose intravenous immunoglobulin for post-transfusion purpura. Br J Haematol 1985; 61:149. Berney SI, Metcalfe P, Wathen NC, Waters AH. Post-transfusion purpura responding to high dose intravenous IgG: further observations on pathogenesis. Br J Haematol 1985; 61:627. Legler TJ, Köhler M, Mayr WR, et al. Genotyping of the human platelet antigen systems 1 through 5 by multiplex polymerase chain reaction and ligation-based typing. Transfusion 1996; 36:426.
POTENTIALLY DELAYED DIAGNOSIS IN AN OBESE ASTHMATIC PATIENTJenny Koo1; Laura Y. Sue1; Pearl Yu2. 1UC San Diego School of Medicine, San Diego, CA; 2UC San Diego Medical Center, La Jolla, CA. (Tracking ID #1924018)
LEARNING OBJECTIVE 1: Evaluate acute or worsening dyspnea in a patient with asthma
LEARNING OBJECTIVE 2: Describe the differential diagnosis for a mass in the anterior mediastinum
CASE: A 52 year old woman with asthma, morbid obesity, gastroesophageal reflux disease [GERD], and untreated obstructive sleep apnea [OSA] presented with 2 weeks of non-bloody productive cough, worsening dyspnea, and “rattling” in the chest. In the preceding 6 months, the patient had had three upper respiratory infections [URIs]. The infections had caused worsening of asthma symptoms, including increased chest tightness and recently, orthopnea. Symptoms did not respond to oral corticosteroids, including a prolonged gradual taper. The patient also reported 3 months of intermittent dysphagia with solid foods and recent onset of night sweats. There was no dysphagia with liquids, fever, chills, or weight loss. The lungs were clear to auscultation bilaterally and peak flow was approximately 80–90 % of predicted. The patient was thought to be having another asthma exacerbation. She was advised to use her short-acting beta-agonist inhaler as needed and to monitor peak flow values. Because of the chronicity of symptoms, a chest x-ray was ordered. It showed marked widening of the mediastinum. Follow-up CT chest revealed a large infiltrative anterior mediastinal mass that compressed the left mainstem bronchus, left brachiocephalic vein, and possibly the aorta and main pulmonary artery. Core needle biopsy of the mediastinal mass revealed aggressive B cell lymphoma. Subsequent imaging and biopsies did not show involvement beyond the mediastinum. The patient was started on a multi-cycle regimen of methotrexate and R-EPOCH chemotherapy for her Stage I-EB lymphoma.
DISCUSSION: The anterior mediastinum includes the thymus, extra-pericardial aorta and its branches, great veins, and lymphatic tissue. Therefore, the differential for an anterior mediastinal mass includes thymoma, germ cell tumor, mediastinal cyst, or lymphoma. It can also rarely include extension of thyroid or parathyroid tissue. The patient with an anterior mediastinal mass can be asymptomatic or can present with chest pain, cough, or compressive symptoms of dyspnea and dysphagia, as this patient did. Given the history of moderate persistent asthma, the patient’s symptoms were initially attributed to an asthma exacerbation in the context of repeated URIs and increased workplace stress. She was appropriately advised to continue corticosteroid/long-acting beta-agonist therapy for her asthma and to manage co-morbidities, including GERD and OSA. It is possible that the patient’s morbid obesity and perimenopausal state also contributed to a delayed diagnosis, as she had night sweats but no other constitutional symptoms such as weight loss. Furthermore, the patient’s morbid obesity may have been a risk factor for lymphoma development. Possible mechanisms for the elevated risk include increased levels of circulating adipocytokines in obesity and the development of insulin resistance with insulin-like growth factor-I production, which promotes cell proliferation. This case illustrates the importance of chest imaging in cases of prolonged, unresponsive acute exacerbations of chronic asthma, especially in patients with previously well-controlled asthma.
PRE-ECLAMPSIA AND HELLP SYNDROME AS AN INITIAL PRESENTATION OF PRIMARY ANTI-PHOSPHOLIPID SYNDROMEAmy Loden. Washington University, Saint Louis, MO. (Tracking ID #1936036)
LEARNING OBJECTIVE 1: Recognize the internists role in the treatment of medical complications arising during pregnancy
LEARNING OBJECTIVE 2: Diagnose and confidently treat ante-partum complications and manage post-partum health of women based on obstetric diagnoses
CASE: A 28 year old G1P0101 was referred by her obstetrician to an internist for persistent hypertension following preterm delivery at 29 and 6/7 weeks secondary to pre-eclampsia and HELLP Syndrome (hemolysis, elevated liver transaminases and low platelets). She had no prior medical or surgical history, and no known allergies. She was taking amlodipine 5 mg daily and hydrochlorthiazide 25 mg daily which were started by her obstetrician when hypertension failed to resolve immediately post-partum. She had no toxic habits. Her father has hypertension. She had normal vital signs with a blood pressure of 125/75 and fundoscopic, cardiovascular, neurologic, musculoskeletal and dermatologic examinations were unremarkable. She was advised to stop anti-hypertensive therapy and subsequent ambulatory blood pressure monitoring was normal. Initial studies were notable for positive ANA with a titer of 1:80. Subsequent evaluation showed no anti-dsDNA antibodies, normal ENA panel and 24 h urine, but was notable for positive anti-β2 glycoprotein IgG antibody at 17.8 units/mL (normal level is <10 units/mL). Repeat testing 12 weeks later again revealed IgG antibodies against the β2 glycoprotein at 22.4 units/mL. Anti-cardiolipin and anti-lupus anticoagulant antibodies were never positive. She was diagnosed with primary antiphospholipid syndrome. Treatment was initiated with daily aspirin. She was advised of her increased future risk for hypertension and both cardiovascular and cerebrovascular disease given her history of pre-eclampsia and will follow-up annually with her internist. The patient’s obstetrician and internist agreed with the pre-conception treatment plan and to initiate heparin upon discovery of pregnancy.
DISCUSSION: Patients with a history of pre-eclampsia should be followed post-partum for monitoring and preventative care for cardiovascular and cerebrovascular disease.[1,5] Internists should be aware that women meeting certain obstetric criteria (more than three miscarriages prior to 10 weeks gestation, fetal death after 10 weeks gestation, or preterm delivery from eclampsia or pre-eclampsia) need immunologic evaluation for APS.[2,3] If anti-cardiolipin, anti-β2 Glycoprotein, or anti-lupus anticoagulant antibodies are detected, a repeat assessment should be performed no sooner than 12 weeks. [2,3] Patients with APS should take daily low dose aspirin and should not use contraceptives or hormone replacement therapy containing estrogen. [2,4] Upon discovery of pregnancy, internists should be comfortable maintaining a low dose aspirin regimen and initiating heparin for patients with APS.[2,4] Because these patients have a high risk of early miscarriage, failure to follow these guidelines, even to wait until the patient’s first obstetric visit (commonly between 8 and 10 weeks), significantly increases the chance of pregnancy loss.[2,4] Multi-specialty collaboration is essential for early diagnosis for women at risk for ante- and post-partum medical complications. Internists do not frequently consider obstetric complications as they may relate to a patient’s current or future medical problems and obstetricians may not adequately stress to patients the future risks indicated by ante-partum medical complications. As illustrated by this case, the referral by the patient’s obstetrician for persistent post-partum hypertension was appropriate for multiple reasons. First, ensuring that the obstetric diagnoses of preterm delivery secondary to pre-eclampsia and HELLP Syndrome are communicated to the patient’s internist inform aggressive monitoring and preventative care for cardiovascular and cerebrovascular disease in the post-partum setting and allow for new diagnoses to be discovered. Second, the treatment protocol for APS to be instituted upon discovery of pregnancy will reduce the risk of early pregnancy loss regardless of whether the patient’s obstetrician or internist discover the pregnancy. Finally, the communication between the patient’s obstetrician and internist revealed the patient’s need for preconception counseling for future pregnancies based on a new diagnosis. 1. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Brown MC, et al. Eur J Epidemiol. Jan 2013. 2. Antiphospohlipid syndrome in obstetrics. Danza A, et al. Best Pract Res Clin Obstet Gynaecol. 2012 Feb. 3. Practice Bulletin No. 132: Antiphospholipid syndrome. Committee on Practice Bulletins—Obstetrics, American College of Obstetricians and Gynecologists. Obstet Gynecol. Dec 2012. 4. Obstetric antiphospholipid syndrome. Galarza-Maldonado C, et al. Autoimmun Rev. Feb 2012. 5. Etiology and management of postpartum hypertension-preeclampsia. Sibai BM. Am J Obstet Gynecol. June 2012.
PREMATURE CLOSURE AND DELAYED DIAGNOSIS: A CASE OF ABOMINAL PAINJason Dukes2; Lee S. Shearer1. 1Weill Cornell Medical College, New York, NY; 2Weill Cornell - New York Presbyterian Hospital, New York, NY. (Tracking ID #1937942)
LEARNING OBJECTIVE 1: To recognize clincal features of abdominal pain that should prompt further evaluation.
LEARNING OBJECTIVE 2: To recognize the risk of cognitive biases such as premature closure of inquiry.
CASE: Initial Presentation and Diagnosis: −A 70 year-old woman with PMH HTN presented to the ED with RUQ/epigastric pain radiating to the back. -She had poor appetite, but normal bowel movements, no nausea, vomiting, diarrhea, fever, chills, CP, SOB. Pain was not associated with food. -On exam, the patient was afebrile with normal vital signs, and RUQ/epigastric ttp without rebound or guarding. -Labs, including CBC, BMP, LFTs, amylase, lipase, were within normal limits. -Patient was treated with nexium, famotidine, Maalox, and viscous lidocaine with little relief. -A RUQ U/S and AXR were obtained which demonstrated multicystic structure posterior to the pancreas. -CT A/P (Figure 1) demonstrated a multiloculated cystic mass of the body/tail pancreas measuring 9.0 × 10.6 cm. -EUS/FNA was performed. The pancreatic cystic fluid demonstrated acellular proteinaceous material negative for malignant cells. She was diagnosed with a benign pancreatic cyst as the cause of her pain. -Given the patient’s persistent abdominal pain, there was a plan for surgical intervention, but patient declined. Instead, she was managed medically as an outpatient with vicodin and tramadol. Interval History: -Over the course of a year, the patient was noted to have a significant decline in function with increasing pain not relieved in any position, decreased PO intake, and constipation. -Repeat CT A/P (Figure 2) showed an interval increase in size of a multiseptated pancreatic tail cystic lesion with internal areas of calcification, again probably representing a benign neoplasm. Additionally, new lytic changes involving the T11, T12 and L1 vertebral bodies with associated peripherally enhancing right paravertebral fluid collection involving the right psoas muscle and right erector spinae muscle with possible epidural extension. -An MRI (Figure 3) identified lesions involving the vertebral bodies and posterior elements of T11, T12 and L1 with pathologic compression fractures of T11 and T12. There was also epidural extension and retropulsion of the pathologic fracture of the T11 vertebral body resulting in marked canal stenosis with cord compression and intramedullary edema and a discrete lytic lesion in the T9 lamina/spinous process. -The patient was emergently taken to neurosurgery for decompression with T9-L2 fusion. Revisiting the Diagnosis: -The patient’s presentation and radiographic findings were puzzling and it was difficult to pinpoint a unifying diagnosis to reconcile all of her symptoms. The differential diagnosis revolved around infectious and malignant etiologies. -Arguments for tuberculosis were location (lower thoracic and lumbar vertebrae), involvement of disc space and paravertebral fluid collection in the psoas muscle. However, there was no significant anterior subligamentous spread or anterior vertebral body destruction which is more typical of tuberculosis. -A malignant etiology such as multiple myeloma or lymphoma was also considered. However, when comparing prior imaging studies, there appeared to be contraction of the T9 spinous process lesion, suggesting a more indolent process that healed in one area but progressed in another, which is not consistent with malignancy. -Ultimately, pathology identified diffuse large B cell lymphoma and the patient is currently undergoing RCHOP treatment.
DISCUSSION: 1) The patient’s abdominal pain was persistent, poorly controlled, and associated with a progressive decline in function. Her age (>50), gender, duration of pain >1 month, and pain that was not relieved by lying down were additional concerning clinical features that prompted further evaluation. 2) In clinical decision making, it is important to acknowledge cognitive biases such as premature closure that may impact patient care. Premature closure of inquiry, or search satisfaction, occurs when development and evaluation of a broad differential diagnosis is terminated once one diagnosis seems to explain the symptoms. Alternative diagnoses are not further pursued. In this case, premature closure may have occurred when the patient’s abdominal and back pain were attributed to the enlarging pancreatic cyst. Avoiding such cognitive pitfalls may have identified this lymphoma at an earlier stage.
PRIMARY COLORECTAL LYMPHOMA PRESENTING WITH PRESYNCOPE: SOMETIMES HOOFBEATS DO COME FROM ZEBRASLauren E. Radziejewski; Nina M. Schwenk; Christopher M. Wittich. Mayo Clinic, Rochester, MN. (Tracking ID #1934858)
LEARNING OBJECTIVE 1: Recognize unusual and serious causes of presyncope.
LEARNING OBJECTIVE 2: Diagnose primary colorectal lymphoma presenting as a presyncopal event.
CASE: A 70-year-old retired nurse presented to the outpatient clinic after a presyncopal event. It occurred upon rising from a chair after consuming one alcoholic beverage. During the week following the event, she continued to experience transient lightheadedness and bilateral pulsatile tinnitus. Her past medical history was significant for hypothyroidism, osteopenia, melanoma in situ status post wide local resection, hiatal hernia, and diverticulosis. Her age-appropriate cancer screening was up-to-date. Her last colonoscopy, 7 years prior, was technically difficult due to sigmoid stricturing. At presentation, her blood pressure was 143/61 mmHg, pulse 82 beats per minute, and oxygen saturation 96 %. She appeared well, was alert, and neurologically intact. Skin turgor was normal and mucous membranes were pink. Examination of the heart, lungs and abdomen were normal. She recently noticed occasional red blood spotting on toilet paper after wiping, which she attributed to bleeding hemorrhoids. Laboratory studies revealed normocytic anemia, with a hemoglobin 8.3 g/dL and MCV 87.5 fL. An upper endoscopy demonstrated a single, non-bleeding Cameron erosion and non-obstructing Schatzki ring. An initial colonoscopy was aborted due to difficulty advancing beyond the known stricture. A fecal hemoglobin study was obtained and was found to be positive despite absence of active bleeding in the esophagus. Repeat colonoscopy, under anesthesia, was therefore performed. This revealed an ulcerated, non-obstructing mass in the proximal ascending colon measuring 5 cm in length. Histologic examination demonstrated diffuse large B-cell lymphoma. Subsequent PET confirmed the avid circumferential mass in the ascending colon with adjacent conglomerate FDG avid lymphadenopathy. Bone marrow biopsy revealed no atypia. She was initiated on R-CHOP therapy, and has received 3 cycles to date with excellent initial response to therapy.
DISCUSSION: Dizziness accounts for more than 2 million emergency department visits in the United States annually. Potentially morbid causes of syncope include myocardial infarction, cardiac dysrhythmia, pulmonary embolism, stroke, and hemorrhage. Less serious causes include anxiety, vestibular dysfunction, POTS and venous insufficiency. Primary colorectal lymphoma is a very rare occurrence, responsible for only 0.1–0.5 % of all colorectal malignancy. Of these, most tumors occur within the cecum, perhaps due to a high percentage of lymphatic tissue. Diffuse large B-cell lymphomas represent the most common histological subtype. Typical presenting symptoms include abdominal pain, unintended weight loss, and changes in bowel habits. Risk factors include male gender, history of inflammatory bowel disease, and immunodeficiency. Treatment modalities include surgical resection, radiation, and chemotherapy. Prognosis varies with treatment. CHOP therapy has been the mainstay with long term survival averaging 40–55 %, while the addition of Rituximab appears to improve prognosis by 10–15 %. We describe a case of presyncope in a previously healthy 70-year-old woman. Evaluation ultimately revealed a rare colonic malignancy for which the patient demonstrated atypical symptoms and possessed no risk factors. This case highlights the importance of avoiding premature case closure during the initial evaluation of dizziness and near syncope, particularly in a previous healthy individual.
PRIMARY DUODENAL PLASMACYTOMA AS AN UNCOMMON CAUSE OF GASTROINTESTINAL BLEEDINGDevalkumar Rajyaguru. University of Pittsburgh Medical Center-Mercy, Pittsburgh, PA. (Tracking ID #1928737)
LEARNING OBJECTIVE 1: Recognize this rare entity as a cause of gastrointestinal tumors
LEARNING OBJECTIVE 2: Manage primary gastrointestinal plasmacytoma
CASE: A 70-year-old Caucasian male presented with 4 week history of exertional shortness of breath and fatigue. His past medical history was notable for coronary artery disease, atrial fibrillation, hypertension and type 2 diabetes mellitus. Patient was taking Coumadin for his atrial fibrillation. Physical examination showed conjunctival pallor, but was otherwise unremarkable. He was also noted to have positive hem occult stools. Abnormal laboratory values on admission included a hemoglobin level of 6.8 g/dL and an international normalized ratio (INR) of 3.3. Patient was transfused 2 units of packed red blood cells and upper gastrointestinal endoscopy was performed, which showed a large malignant looking fungating, infiltrative, ulcerated mass with bleeding areas in the second part of duodenum. Biopsies were taken with a cold forceps for histology. In addition, biopsy with jumbo forceps was also performed and more than 15 pieces were sent to pathology for further evaluation. The histology demonstrated multiple portions of duodenal mucosa with masses of apparent plasma cells, which stained positive for lambda light chains. Neoplastic cells were reactive for plasma cell marker CD138, finding consistent with plasma cell neoplasia. The negativity for the B-cell marker CD20 excluded the possibility of marginal zone B-cell lymphoma of mucosa. Serum electrophoresis and immunofixation did not show any monoclonal immunoglobulins. Urine immunofixation identified a monoclonal protein as a free monoclonal labda type, a finding identified in approximately 25 % of plasmacytoma cases. The serum light chain assay yielded kappa of 18.3 mg/L and lambda as 783 mg/L, with a Kappa/Lambda ratio of 0.02. Skeletal survey did not show any evidence of a lytic or blastic osseous lesion. Positron emission tomography (PET)/CT scan was performed which showed 6.4 × 5.6 × 10 cm mass at the region of second portion of duodenum with mild fluorodeoxyglucose (FDG) uptake with standardized uptake value (SUV) of 2.4. Subsequent bone marrow biopsy showed mildly hypercellular bone marrow with normal trilineage hematopoiesis with less than 5 % plasma cells. Together, these findings confirmed a final diagnosis of a primary extramedullary plasmacytoma of the duodenum.
DISCUSSION: Plasmacytomas are localized collections of neoplastic monoclonal plasma cells that form masses in bone or other organs. It accounts for approximately 3 % of plasma cell malignancy. Plasmacytomas can be either primary, without signs of bone marrow involvement such as solitary plasmacytoma of bone or solitary extramedullary plasmacytoma, or may occur in association with multiple myeloma representing extraskeletal spread of the disease. Primary extramedullary plasmacytoma is a rare form of the disease with 7 % only manifesting in the gastrointestinal tract. The presenting symptoms of gastrointestinal plasmacytomas may present with anorexia, weight loss, nausea, abdominal pain, vomiting, occult blood loss and rarely with overt gastrointestinal bleeding. Endoscopically, plasmacytoma may appear as discrete ulcers, ulcerated mass, thickened gastric folds, multiple polyps, small plaques or diffuse infiltrative lesions. Thus, as the endoscopic appearance of plasmacytomas varies significantly and may be similar to other more common conditions such as poorly differentiated or metastatic neoplasms, lymphoma and gastrointestinal amyloidosis. Thus, pathological and immunohistochemical examination of endoscopic biopsies is crucial for making an accurate diagnosis. In a patient with solitary plasmacytoma, multiple myeloma has to be ruled out because this requires systemic treatment. No general consensus guidelines for treatment currently exist. However, based on the well-known radiation sensitivity of plasma cell tumors, radiotherapy is accepted as a standard therapy. Surgery for extramedullary plasmacytomas can also offer cure and may be the preferred treatment for some patients. If complete resection is not feasible, then combined radiation or chemotherapy is recommended, especially for large or poorly differentiated tumors. To date, there are no long term follow-up studies of gastrointestinal plasmacytomas. The course of extramedullary plasmacytoma is generally favorable with a 70 % disease-free survival at 10 years. The rate of progression of extramedullary plasmacytoma to multiple myeloma ranges from 11 to 30 %, at 10 year. After any successful initial treatment, progression of solitary plasmacytomas to multiple myeloma is possible and long term follow up is necessary. This case illustrates the importance of awareness of this rare entity when considering evaluation of gastrointestinal tumors. A diagnosis of primary gastrointestinal plasmacytoma entails detailed work-up for multiple myeloma and a strict oncologic surveillance.
PRIMARY HYPERPARATHYROIDISM IN PREGNANCY PRESENTING AS ACUTE PANCREATITIS IN SECOND TRIMESTERNick Youssefi; Christopher Russo. University of California, San Francisco Fresno, Fresno, CA. (Tracking ID #1934186)
LEARNING OBJECTIVE 1: The purpose of this clinical vignette is to aid physicians recognize how to diagnose and manage concurrent hyperparathyroidism and acute pancreatitis, especially in the pregnant population.
CASE: A 28 year old, gravida 1 para 0 female presents to the emergency room with 1 day history of abdominal pain, epigastric, radiating to her back. Associated nausea, vomiting, decreased appetite. Patient never had these symptoms before. No history of alcohol consumption and patient was only taking prenatal vitamins. Patient had received in vitro fertilization prior to this pregnancy and her gestational age was 17 weeks. Physical examination reveals patient is alert and abdominal exam reveals epigastric tenderness with minimal rebound tenderness and guarding. Laboratory studies reveals elevated serum Lipase 3356 U/L (12–53), serum Amylase 2967 U/L (20–130), serum WBC 24,000 k/UL (4–11), serum Calcium 13.5 mg/dL (8.5–10.5), serum Parathyroid hormone 177 pg/mL (14–72), and low serum Phosphorus 1.5 mg/dL (2.7–4.5). Ultrasound abdomen reveals enlarged pancreas measuring 5.5 cm in thickness. Ultrasound of the neck reveals a 2.1 cm lesion in the inferior segment of the right lobe posterior to the thyroid gland. A diagnosis of hyperparathyroidism-induced acute pancreatitis is made based on clinical, laboratory, and radiological evidence. Endocrinology is consulted and started Calcitonin 200 units twice daily, fluid resuscitation, and Lasix 20 mg every 8 h. Surgery is consulted and parathyroidectomy is performed and histopathology is consistent with parathyroid adenoma. Patient tolerates procedure well and is discharged home with calcium supplementation. The patients serum calcium and PTH levels normalizes 2 days post-operative with serum WBC and lipase levels gradually normalizing 1 month later. Patient is currently 30 weeks gestation with no symptoms and is expecting twins.
DISCUSSION: Acute pancreatitis and hyperparathyroidism in pregnancy is very rare. After a thorough review of the literature, there were only 2 published papers describing 14 total patients who were diagnosed with hyperparathyroidism induced acute pancreatitis in pregnancy. The incidence of acute pancreatitis in patients with hyperparathyroidism is reported to be only 1.5 %. During pregnancy, active ionized calcium decreases, which causes a resulting increase in secretion of the parathyroid hormone. Furthermore, the existence of parathyroid hormone increases the risk of pancreatitis. Acute pancreatitis should be in the differential diagnosis of unexplained nausea, vomiting, abdominal pain during pregnancy and hypercalcemia should prompt evaluation for concurrent hyperparathyroidism.
PRIMITIVE NEUROECTODERMAL TUMOR OF THE SPINE 25 YEARS AFTER PINEOCYTOMA RESECTIONAvan Armaghani1; Benji Zusman1; Danny Estupinan2; Jesse Kresak3; Meredith Wicklund2; Peter W. Stacpoole1. 1University of Florida, Gainesville, FL; 2University of Florida, Gainesville, FL; 3University of Florida, Gainesville, FL. (Tracking ID #1936947)
LEARNING OBJECTIVE 1: Recognize that although pineocytoma is a benign tumor of the pineal gland, it is part of a spectrum of diseases and can undergo malignant transformation to pineoblastoma or primitive neuroectodermal tumor.
LEARNING OBJECTIVE 2: Recognize that patients with a history of pineocytoma who have signs, symptoms and imaging that are suggestive of normal pressure hydrocephalus (NPH), should have a contrasted MRI of the spinal cord to rule out possible primitive neuroectodermal tumor of the spine.
CASE: A 72 year-old male with past medical history significant for resection of a pineocytoma 25 years ago, type II diabetes mellitus, hypertension, hyperlipidemia and obstructive sleep apena, presented with a four-month history of progressive worsening gait disturbance, frequent falls, urinary and fecal incontinence and cognitive decline. Approximately 1 year ago, the patient began experiencing progressively worsening back pain, which was refractory to physical therapy, NSAIDs and cortisone injections. An MRI of the spine was performed at that time and suggested arthritic changes with worsening spinal stenosis. The patient subsequently underwent an L3-L4 spinal fusion, but his symptoms did not improve post-operatively. Over a four-month period following the surgery, the patient became increasingly weak, developed gait impairment, experienced frequent falls, urinary and fecal incontinence and short-term memory deficits. Given the patients progressive cognitive decline, he was hospitalized for further workup. A head CT showed ventriculomegaly without apparent obstruction or pineal tumor recurrence. A diagnosis of NPH was initially proposed, but two high volume lumbar punctures provided no relief of his symptoms. CSF studies showed markedly elevated protein (242 mg/dl) with pleocytosis out of proportion to the red blood cells (RBC: 30,000 mm3; WBC 60 mm3, poly 58 % lymph 42 %). Gram stain and bacterial culture were negative. A CSF flow study showed communicating flow without compressive lesions. White blood cell count was 17 thou/mm3, and urine culture grew >100,000 col/ml enteroccous faecalis. The patient was discharged home with antibiotics with plan to follow-up in 1 month. The patient’s clinical status continued to worsen and he was re-admitted approximately 1 week later. Physical exam was notable for severe bradyphrenia and bradykinesia, frontal release signs, Parinaud’s syndrome, and diffuse hyper-reflexia. A repeat lumbar puncture was performed and CSF studies revealed xanthochromia, elevated protein 284 mg/dl, RBC 10,150 mm3. Cytology returned no malignant cells. Bacterial, fungal, AFB culture, cryptococcal antigen, CMV PCR, and VDRL were all negative. Contrast MRI of the cervical, thoracic and lumbar spine showed innumerable enhancing nodules along the surface of the spinal cord in all regions. Notably in the lumbar region, the largest nodule measured 8 × 10 mm and displaced the cauda equina nerve roots to the right. CT chest, abdomen and pelvis did not identify a primary source of malignancy. An L2 laminectomy with intradural tumor resection was performed. Pathology results showed malignant small blue cell tumor, with neuroendocrine features consistent with primitive neuroectodermal tumor (PNET). The patient’s clinical status continued to decline. He was discharged to hospice before passing away 1 week later.
DISCUSSION: PNETs are a group of rare, highly aggressive tumors composed of undifferentiated ‘small round blue cells’ that resemble the embryonic neural tube. These tumors can be present both peripherally and centrally. Within the CNS, they are most common in the cerebellum but can also present in the spinal cord. Only about 1 % of all PNETs are found in the spinal cord and can be seen intramedullary, intradural-extramedullary and extradurally. Spinal PNETs often present with neurologic signs and symptoms referable to a spinal or root level. Our patient presented with progressive neurological dysfunction initially concerning for NPH. However, CSF pleocytosis and elevated protein in the absence of identifiable cerebral origin was concerning for a spinal CSF blockage. Contrasted imaging studies of the spinal cord revealed enhancing nodules, with biopsy confirming PNET. Given the patients history of resected pineocytoma, this presentation may represent late recurrence with transformation to a PNET, or a primary spinal PNET. Although pineocytoma is a benign disease, it is part of a spectrum of diseases and has been shown to undergo malignant transformation to a pineoblastoma or PNET. Therefore, it is important to recognize that patients with history of pineocytoma who present with signs, symptoms and imaging that are suggestive of NPH may have recurrence of the tumor. Prognosis for PNET remains poor with 5-year survival less than 10 % in adults over the age of 45. Treatments including radical resection, and radiation/chemotherapy have not been proven to be effective in prolonging survival in patients with this devastating disease.
PROBABLE LABETALOL-INDUCED ANGIOEDEMA: A CASE REPORTAkihiro Kobayashi1,2; Samuel Acquah2. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1927532)
LEARNING OBJECTIVE 1: Consider labetalol as a potential cause of angioedema
CASE: 79 year-old-woman presented to the hospital for hypertensive urgency. She had a history of chronic hypertension for which she was on Amlodipine 10 mg daily and Chlorthalidone 50 mg daily. No personal or family history of angioedema. Initial blood pressure was 234/117 mmHg and she received oral Amlodipine 5 mg, Losartan 50 mg and Metoprolol 50 mg on admission for better blood pressure control. After admission the patient remained hypertensive and intravenous Labetalol 20 mg was given. Three hours after administration of Labetalol, patient developed angioedema manifested by lip and tongue swelling requiring endotracheal intubation. Laboratory studies showed normal C4 and C1 inhibitor function. Losartan and Metoprolol were discontinued and Labetalol and Amlodipine were continued to treat blood pressure. Her symptoms resolved in 3 days with intubation and supportive treatment after which she tolerated extubation. Four days after resolution of swelling she developed a second episode of angioedema requiring a second intubation. Amlodipine was discontinued. Labetalol was however continued and titrated up to 800 mg every 8 h for blood pressure control. This second reaction resolved after 5 days of intubation and supportive treatment and patient was again extubated. However, the patient developed third episode of angioedema 4 days later which was more severe compared with the previous 2 episodes. This third episode required a longer intubation (8 days). Labetalol was the only medication which had been used consistently all three times and the severe reaction was thought to be due to increased doses of Labetalol. Application of the Naranjo adverse drug reaction probability scale determined a probable link between Labetalol and Angioedema.
DISCUSSION: Labetalol is a beta-blocker with alpha-blocking activity. It is widely used for the treatment of essential hypertension, hypertensive urgency/emergency. Its beta-blocking activity decrease heart rate and cardiac output and alpha-blocking activity produce vasodilation, which is thought to be a mechanism of peripheral pitting edema. Although the exact mechanism of angioedema due to BBs is not well understood, a previous case report has proposed a theory by which BBs increase histamine release by decreasing intracellular cyclic adenosine monophosphate leading to angioedema. We carefully reviewed all medications that the patient received during the 3 episodes of angioedema. Labetalol was the only medication which had been used consistently all three times. The application of the Naranjo adverse drug reaction probability scale determined a probable link between labetalol and angioedema. We also found that each subsequent episode of angioedema was worse than the previous, which can be correlated with the increased doses of labetalol. Although ACEs-induced angioedema is not thought to be associated with dose, our clinical observation found a link between her symptoms and the dosage of labetalol, which may suggest non-allergic etiology of labetalol-induced angioedema. We believe this is the first case report to link Labetalol to angioedema. Since Labetalol is widely used to treat various cardiovascular conditions, clinicians should aware of the possibility of Labetalol as a cause of angioedema.
PROFOUND PANCYTOPENIA AND HEPATITIS: HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS (HLH) OR HEPATITIS-ASSOCIATED APLASTIC ANEMIA?Amy Clouse; Nancy Feldman. Olive View - UCLA Medical Center, Sylmar, CA. (Tracking ID #1937072)
LEARNING OBJECTIVE 1: Distinguish HLH from hepatitis-assosciated aplastic anemia using diagnostic criteria.
LEARNING OBJECTIVE 2: Differentiate findings on bone marrow biopsies in HLH versus aplastic anemia.
CASE: Mrs. R is a 36 year old woman with no significant past medical history, who presented with 2 weeks of fatigue, dizziness, abdominal pain, joint pain and epistaxis. On admission, she was profoundly pancytopenic with an ANC < 100, platelet count 12 k, hemoglobin 7.9, transaminitis (AST/ALT 400/500’s), alkaline phosphatase of 130–150’s, and elevated total bilirubin (5, increased to 19). She denied any prior drug or toxin exposure, and autoimmune workup was negative. She did endorse URI symptoms several weeks prior to admission. A broad infectious workup for hepatitis was unrevealing other than mild EBV and CMV viremia, with PCR’s of 5000 and 400, respectively. She had evidence of prior infection with parvovirus. The acute hepatitis panel was negative. On imaging, she had hepatomegaly, but no splenomegaly. Liver biopsy showed possible “feathery necrosis”, but did not show hemophagocytosis. She had three bone marrow biopsies, which showed hypocellularity with <5 % cellularity without evidence of hemophagocytosis, consistent with aplastic anemia. HLH characteristically has a normocellular bone marrow and splenomegaly. Despite these studies, she met 5 of the 8 proposed criteria for HLH: 1) elevated soluble IL-2; 2) elevated triglycerides (400’s); 3) pancytopenia; 4) hepatitis with significant jaundice and; 5) daily fevers >38.5. She also had a progressively elevating ferritin (1770 at admission to >8000). As she met criteria for both HLH and hepatitis-associated aplastic anemia, she was treated for both. Following treatment for EBV with IVIG and valcyclovir, she was given solumederol, cyclosporine, and ATG, all without improvement. Ultimately, the patient expired from complications of prolonged pancytopenia after more than 2 months of hospitalization.
DISCUSSION: Hemophagocytic lymphohistiocytosis (HLH) and aplastic anemia are two separate diseases processes. In this case where the patient fits the diagnostic criteria for both, a therapeutic challenge arises in the absence of a clear diagnosis. This prompts a review of how to distinguish aplastic anemia from HLH. Both are characterized by immune dysregulation, and can be associated with hepatitis and jaundice. Both can be precipitated by viral infections and autoimmune syndromes. Bone marrow biopsies may be helpful in distinguishing the two diseases, but the absence of hemophagocytosis in the bone marrow does not preclude HLH. The critical juncture in this case was the cellularity of the bone marrow. In almost all cases of HLH, the bone marrow cellularity in HLH is normal to slightly decreased, while by definition it is profoundly hypocellular in aplastic anemia. There are case reports of untreated HLH evolving to aplastic anemia, which may explain why Mrs. R fit criteria for both. Her prognosis was poor with either diagnosis. The treatment of both disorders involves immunosuppression, to which unfortunately this patient did not respond.
PSEUDORENAL FAILURE CAUSED BY SPONTANEOUS RUPTURE OF THE URINARY BLADDERNaokatsu Ando1; Naoya Taki1; Ayako Kumabe1; Yoshioki Nishimura1; Michiko Kudo1; Tsuneaki Kenzaka1; Gurpreet Dhaliwal2; Masami Matsumura1. 1Jichi Medical University, Shimotsuke, Japan; 2University of California, San Francisco, and San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1935039)
LEARNING OBJECTIVE 1: Diagnose azotemia associated with massive ascites.
LEARNING OBJECTIVE 2: Recognize rupture of the urinary bladder as a rare cause of azotemia.
CASE: A 63-year-old man presented with a 2 month history of abdominal distension. Two months before admission, the patient noticed dysuria which improved spontaneously within several days. Shortly thereafter abdominal distension developed and progressed over the next 2 months. At an outpatient visit 4 days before admission, he had gained 2.4 kg of body weight and the serum creatinine was 0.8 mg/dL. Three days before admission, dysuria recurred. He had had a 30 year history of diabetes mellitus, 1 year history of dyslipidemia, and 7 year history of transitional cell carcinoma of the bladder treated by nine episodes of transurethral resection of bladder tumor (TUR-BT). The latest TUR-BT was performed 6 months before this admission. He was receiving 200 mg per day of bezafibrate and 26 units per day of short acting insulin. There was no history of trauma, fever, abdominal pain, myalgias, hematuria, dyspnea, or edema. On examination, his abdomen was profoundly distended but non-tender. There were no signs of end stage liver disease. Laboratory findings included a serum albumin 5.0 g/dL, urea nitrogen 87 mg/dL, creatinine 6.1 mg/dL, and potassium 5.5 mmol/L. Urinalysis revealed 3+ proteinuria and 1+ occult blood with white cells 30–49 per high-power field and no red cell casts. Urine biochemistry showed urea 612 mg/dL, creatinine 110 mg/dL, potassium 25 mmol/L, and protein 1.5 g per gram of creatinine. Fractional excretion of sodium was 3.2 %. Urine culture was not obtained. Computed tomography (CT) scan showed massive ascites without hydronephrosis, cirrhosis, or masses. Clear yellow-colored peritoneal fluid obtained by abdominal paracentesis revealed albumin 0.3 g/dL, urea 134 mg/dL, creatinine 21.4 mg/dl, and potassium 7.6 mmol/L. Serum-ascites albumin gradient was 4.7 g/dL. The peritoneal fluid white blood cell count was 170/μL with 92 % macrophages, 4.5 % neutrophils, and 3.5 % methothelial cells. Cytology showed no atypical cells. Within 17 h of urinary catheter placement, 4,800 mL of urine was excreted and abdominal distension improved dramatically. Urine cytology showed mesothelial cells which were consistent with those in peritoneal fluid. On hospital day 3, serum creatinine normalized to 0.8 mg/dL. Retrospective evaluation of the CT scan from admission showed partial wall thinning in the apex of the urinary bladder which was consistent with the lesion of the latest TUR-BT. We diagnosed pseudorenal failure caused by spontaneous rupture of the bladder. On hospital day 8, cystography revealed no perforation of the bladder. The patient was discharged from the hospital with an indwelling transurethral catheter.
DISCUSSION: This patient had a pseudorenal failure serum biochemical profile caused by leakage of urine into the peritoneal cavity, where urea, creatinine, and electrolytes equilibrated across the peritoneum with the blood. Spontaneous rupture of the bladder due to wall fragility induced by multiple TUR-BT procedures was suspected. Pseudorenal failure occurs when azotemia results from reabsorption of urine solutes though peritoneum after intraperitoneal bladder rupture rather than through a reduction in the glomerular filtration rate. Physicians should consider urinary ascites when ascites without a known cause of portal hypertension is accompanied by blood tests that suggest acute kidney injury.
PULMONARY ARTERIAL HYPERTENSION AND HUMAN IMMUNODEFICIENCY VIRUS INFECTIONAvan Armaghani1; Ashkan Karimi1; Talha Nazir3; Hassan Alnuaimat2; Richard Conti3. 1University of Florida, Gainesville, FL; 2University of Florida, Gainesville, FL; 3University of Florida, Gainesville, FL. (Tracking ID #1934516)
LEARNING OBJECTIVE 1: Recognize that pulmonary arterial hypertension (PAH) is a rare complication of HIV infection, and testing for HIV should be included in the work-up of patients with newly diagnosed PAH.
CASE: A 49-year-old male presented from an outside hospital with several months history of progressive shortness of breath. A right heart catheterization performed at the outside hospital recorded right atrial pressure of 32 mmHg, right ventricular pressure of 93/32, pulmonary artery pressure of 103/55, and pulmonary capillary wedge pressure of 19 mmHg. The patient was transferred to our hospital for further workup and management of PAH. A trans-thoracic echocardiogram revealed normal left ventricular function but a severely dilated right ventricle, severe right ventricular systolic dysfunction, and severely elevated right ventricular systolic pressure of 106 ± 5 mmHg. CT scan of the chest showed normal lung parenchyma. V/Q scan did not show evidence of pulmonary embolization and ruled out chronic thromboembolic cause of PAH. The patient did not have any clinical manifestations to suggest connective tissue disorders and serologic work-ups including ANA, rheumatoid factor, c-ANCA, p-ANCA, anti-SCL-70, anti-Sm, anti-Sm-RNP, anti-SSA, and anti-SSB antibodies were negative. The antigen/antibody combo test for HIV returned positive and was confirmed by western blot. HIV virus titer was measured in blood by PCR at 76,000 copies/ml and CD4 count was 131 cells/mm3. The patient reported high-risk heterosexual behavior several years ago, and he received blood transfusion after colorectal surgery for diverticulitis in 2009 both posing as possible risk factors for acquiring HIV infection. However, the patient denied any sign/symptoms to suggest neglected HIV diagnosis prior to the current presentation. The patient was ultimately diagnosed with group 1 pulmonary hypertension (WHO classification) secondary to HIV infection. He was started on furosemide, tadalafil, and ambrisentan for treatment of PAH and was referred to the local health department to initiate HAART therapy for HIV infection.
DISCUSSION: This case report will familiarize internists with the work-up for pulmonary arterial hypertension (PAH), which includes testing for HIV. PAH is a rare complication of HIV infection, the first case was reported in 1987. HIV has been shown to cause plexogenic pulmonary arteriopathy, medial hypertrophy, intimal fibrosis, pulmonary veno-occlusive disease, and in situ thrombosis, which all lead to PAH. Typically, PAH in the context of HIV infection occurs late in the disease process in patients who already have other stigmata of HIV or AIDS. However, in this case HIV infection was discovered as part of the initial work-up for PAH in an otherwise healthy patient.
PULMONARY EMBOLISM: AN UNUSUAL CONSEQUENCE OF AMEBIC LIVER ABSCESSESMitchell Luu; Ryan Laponis. University of California, San Francisco, San Francisco, CA. (Tracking ID #1937130)
LEARNING OBJECTIVE 1: Develop a differential diagnosis and initial work-up for liver abscesses
LEARNING OBJECTIVE 2: Diagnose and treat extra-intestinal amebic infections
CASE: A 53 year-old homeless man presented with 6 months of progressive right upper quadrant discomfort, malaise and intermittent fevers. Significant exam findings included a palpable liver edge 10 cm below the costal margin, and a grade 3/6 systolic murmur best heard at the left lower sternal border. Transthoracic echocardiography showed a 3 cm irregular mobile mass extending from the right atrium into the right ventricle, consistently with thrombus. CT abdomen revealed a 17 cm complicated cystic lesion in the liver. The patient later developed hypoxia and severe respiratory distress, and a CT angiography of the chest demonstrated a large subsegmental pulmonary embolus. The patient underwent interventional radiology-guided drainage of the hepatic lesion, with removal of 2 liters of “anchovy-paste” purulence. Repeat CT abdomen revealed persistent hepatic abscesses, with thrombus extending from the right hepatic vein into the inferior cava and right atrium. Lab tests revealed leukocytosis without eosinophilia and an elevated ESR. Liver function tests, including synthetic function were normal. Blood bacterial, fungal and mycobacterial cultures were negative. Stool culture and ova-parasite studies were negative. Bacterial and fungal cultures of the liver abscess were negative. Liver cytology was negative for malignancy and amoeba. HIV and viral hepatitis serologies were negative. Amebiasis IgG levels returned back elevated. The patient was diagnosed with an amebic liver abscess complicated by an intracardiac thrombus and subsequent pulmonary embolus. He was treated with anticoagulation and 10 days of metronidazole.
DISCUSSION: Liver abscesses are very rare and are generally classified by three etiologies: 1) pyogenic, 2) amebic, and 3) fungal. Bacterial infections are the most common (80 %) and are often due to multiple organisms, predominantly E. Coli and K. Pneumoniae. Amebic liver abscesses occur in 10 % of cases and are most often due to E. Histolytica. Fungal abscesses are primarily from C. Albicans. Initial evaluation includes complete blood count, liver function tests, blood cultures, serology for E. Histolytica and imaging with ultrasound, CT or MRI. After initial evaluation, percutaneous needle aspiration should be performed for microbiologic and pathologic evaluation. Entamoeba histolytica is a single-cell parasite with high prevalence in developing countries. In the United States, amebiasis is commonly seen in travelers to endemic regions, immigrants from countries with poor sanitation, institutionalized persons, and men who have sex with men. Most infected individuals are asymptomatic, but common symptoms include diarrhea, weight loss and fevers. Amebic liver abscesses are the most common extra-intestinal amebic infection. Diagnosis of amebic liver abscesses requires: 1) space-occupying liver lesion and 2) positive serology. Ultrasound and CT are sensitive for identifying the space-occupying lesion. Serology is highly sensitive (>94 %) and specific (>95 %) for infection, but may be falsely negative in the first 7 days of infection. Complications include abscess rupture, peritonitis and hepatic vein/IVC thrombosis (as was seen in this patient). Treatment involves a 7–10 day course of oral metronidazole and has a cure rate >90 %. Although not required for treatment, aspiration or surgery should be considered for cysts with imminent rupture, clinical deterioration, or lack of response to therapy.
PULMONARY HYPERTENSION AS A PRESENTING FEATURE OF METASTATIC GASTRIC CANCERDaniel Ling1; Rajan Saggar2. 1UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA. (Tracking ID #1925543)
LEARNING OBJECTIVE 1: Recognize pulmonary tumor thrombotic microangiopathy as a rare cause of pulmonary hypertension complicating metastatic adenocarcinoma
LEARNING OBJECTIVE 2: Evaluate a new diagnosis of pulmonary hypertension
CASE: A 58 year old Korean female with remote history of pulmonary tuberculosis presented to her primary care physician with 1 month of progressive dyspnea on exertion, palpitations, and dysphagia. Physical examination was remarkable for decreased breath sounds at the right base but no rales, peripheral edema, or jugular venous distention. Chest x-ray demonstrated a right-sided pleural effusion. Pleural fluid studies from thoracentesis revealed an exudative effusion, but microbiology and cytology were negative. Upper endoscopy was performed to evaluate the patient’s dysphagia and was unremarkable; she was started on omeprazole for presumed gastroesophageal reflux. CT angiogram of the chest was negative for pulmonary embolism, but did reveal bronchiectasis, dilated pulmonary arteries, and spiculated lung nodule. Echocardiogram showed preserved left ventricle systolic function; however, the estimated pulmonary artery pressure was elevated (50 mmHg). The patient’s pleural effusion continued to reaccumulate requiring recurrent thoracentesis, and she was subsequently admitted to the hospital for worsening dyspnea and hypoxia. Repeat echocardiogram showed worsening of estimated pulmonary artery pressure (88 mmHg). Right heart catheterization confirmed the severity of her pulmonary hypertension and also demonstrated normal pulmonary capillary wedge pressure and cardiac output. The patient had no history of relevant exposures or family history of pulmonary hypertension (PH). Further evaluation included HIV testing, V/Q scan, liver function tests, and ANA, Scl-70, SSA/SSB, RF, and RNP/SM antibodies, which all returned negative. Pulmonary function tests showed mixed severe obstructive and restrictive disease, which in combination with her prior CT results raised the question of PH due to lung disease. However, these findings were not thought to adequately explain the degree of PH, suggesting that an idiopathic component was also present. A pleural drainage catheter was placed and she was started on sildenafil with improvement in symptoms prior to discharge. One month later she was readmitted with worsening dyspnea on exertion and fatigue as well as back pain. Labs were notable for hemoglobin of 5.3. CT angiogram of the chest was again negative for pulmonary embolism but did show new sclerotic and lytic lesions of the spine. Upper endoscopy revealed a 6 cm irregularly shaped gastric ulcer; biopsy returned with signet ring gastric adenocarcinoma. The unusual aspects of her presentation now appeared consistent with a diagnosis of pulmonary tumor thrombotic microangiopathy secondary to metastatic gastric cancer. Despite numerous attempts at hemostasis including repeat endoscopy and gastric artery embolization, she continued to have severe bleeding episodes and eventually transitioned to comfort care.
DISCUSSION: This patient presented initially with dyspnea on exertion which appeared to be multifactorial due to recurrent pleural effusion, pulmonary hypertension without right heart failure, and mixed obstructive and restrictive lung disease, but a unifying cause of these findings remained unclear. Assessment included a right heart catheterization to confirm the diagnosis of precapillary PH and exclude left heart failure as the underlying etiology. An appropriate workup for PH was performed including evaluation for connective tissue, pulmonary, liver, and chronic thromboembolic diseases. While PH related to lung disease and idiopathic PH were considerations for this patient, several factors supported an alternative explanation. Severe PH with mean pulmonary artery pressure greater than 35 mmHg is reported in only 1–5 % of patients with obstructive lung disease. Furthermore, pleural effusions are typically only seen in PH with concurrent right heart failure. Generally, a diagnosis of idiopathic PH should remain open to reconsideration as new developments arise in the clinical course. This patient’s aggressive metastatic gastric adenocarcinoma eventually declared itself, providing a unifying explanation of her overall presentation. Pulmonary tumor thrombotic microangiopathy is a rare entity that is typically associated with mucin-secreting adenocarcinomas, and most commonly gastric cancer. Tumor emboli to the lungs cause occlusion of small arteries with intimal proliferation and activation of the coagulation cascade, leading to pulmonary hypertension and eventually cor pulmonale. Clinically, patients can have a subacute to fulminant progression of dyspnea and hypoxia. CT angiogram and V/Q scan are insensitive tests but may show small subsegmental filling defects. Definitive diagnosis requires pathological examination. Therapy primarily involves treatment of the underlying malignancy, although case reports have also described the use of anticoagulation or steroids.
PYOGENIC HEPATIC ABSCESS SECONDARY TO STREPTOCOCCUS ANGINOSUS: A RARE COMPLICATION OF SIGMOID DIVERTICULITISAdrienne L. Clark1; Francis E. Dailey2; Jeffrey R. Lewis3. 1University of California, Los Angeles, Los Angeles, CA; 2Saint Louis University, Saint Louis, MO; 3University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1918791)
LEARNING OBJECTIVE 1: Recognize that sigmoid diverticulitis may lead to hepatic abscess
CASE: A 59-year-old female presented with 1 week of progressive nausea, abdominal pain, and tactile fevers. She had a history of diverticulosis on colonoscopy 2 years prior, and 2 episodes of presumed diverticulitis 6 months and 1 month prior which had self-resolved after 2–3 days. She was tachycardic with involuntary guarding on palpation of the epigastrium and left lower quadrants. Laboratory studies revealed WBC 19.5/mm^3, 86 % neutrophils, and newly elevated liver enzymes (AST/ALT 117/237, alkaline phosphatase 154, GGT 103 U/L). CT abdomen/pelvis with contrast revealed diverticulosis with diverticulitis in the proximal third of the sigmoid colon without evidence of abscess and a multiseptated rim-enhancing lesion in hepatic segments 7 and 8 measuring 8.7 × 10.4 × 8.8 cm, consistent with abscess contiguous with the middle hepatic vein. She was started on piperacillin/tazobactam. She underwent percutaneous CT-guided abscess drainage with placement of an indwelling pigtail catheter on hospital day 2. Abscess fluid grew pan-sensitive Streptococcus anginosus. She was transitioned to ertapenem, although blood cultures from time of admission and anaerobic cultures were ultimately negative. Drain output slowed, her leukocytosis persisted, and repeat imaging on HD#6 showed a stable abscess. She underwent drain replacement on HD#7 and subsequent operative hepatotomy on HD#11, with two JP drains left in place post-operatively. While repeat imaging showed persistent abscess, she clinically improved, and was discharged home ambulatory and on an oral pain regimen to complete 6 weeks of IV ertapenem. After a relatively symptom free interval, she developed several months of intermittent diarrhea and left lower quadrant pain. Given her history of likely recurrent sigmoid diverticulitis, she underwent semi-elective sigmoid colectomy 15 months later.
DISCUSSION: Sigmoid diverticulitis may rarely lead to cases of hepatic abscess with or without coexistent pylephlebitis. Liver abscess is most frequently associated with biliary tract disorders such as stones, obstructive malignancy, strictures, and congenital conditions. It may also be caused by hematogenous dissemination of organisms in association with systemic bacteremia or transient local portal circulation bacteremia, leading to liver abscess directly or via localized septic thrombophlebitis. Patients with liver abscess typically present with nonspecific constitutional symptoms and diffuse abdominal pain/tenderness. Early and accurate diagnosis relies on prompt identification and localization with ultrasound or CT imaging. Treatment focuses on both timely administration of broad-spectrum antibiotics and percutaneous or surgical drainage. The S. anginosus which grew from this patient’s cultures is a member of the “Streptococcus milleri Group” (SMG) of bacteria now actually classified into three distinct species, S. intermedius, S. constellatus, and S. anginosus. The first case of SMG hepatic abscess was reported in 1975. Since then these have been identified as one of the important pathogens of liver abscess, although a sigmoid diverticular source is rarely reported. SMG are considered part of the normal flora of the gastrointestinal tract but with known potential to cause abscesses and systemic infections. If isolated from culture with no clinically apparent abscess, this should prompt further radiographic evaluation.
PYOGENIC LIVER ABSCESSSaranya Sasidharan; Jessica Hurst. Boston Medical Center, Boston, MA. (Tracking ID #1939048)
LEARNING OBJECTIVE 1: While pyogenic liver abscesses are most often the result of biliary tract disease and comparatively less frequent, failure to consider an intrahepatic infection early when confronted with a mixed hepatocellular/cholestatic pattern can delay treatment and worsen prognosis.
LEARNING OBJECTIVE 2: There may be a role for colonoscopy in the workup of liver abscess of unknown origin.
CASE: A 62 year old man presented with 1 week of fatigue, anorexia, myalgias, and chills. He reported dark urine and yellowing of his eyes and skin. He admitted to taking naproxen, as well as cold medicine with acetaminophen several days prior. He denied fevers and abdominal pain. He reported consuming up to 12 beers per day. Past medical history included arthritis, and PTSD. He was afebrile, normotensive, but tachycardic to 110. He had scleral icterus and jaundice without spider angiomas or palmar erythema. His abdomen was obese, nontender without hepatomegaly. He was oriented without asterixis. Labs were notable for creatinine 2.4, WBC 14, AST 569, ALT 430, alkaline phosphatase 486, total bilirubin 12.5, direct bilirubin 10.0, INR 1.3 (previously <1), acetaminophen level 6. Ultrasound showed diffuse steatosis and gallbladder sludge, but no ductal dilatation or portal vein thrombus. A 4.1 cm ill-defined area of fatty sparing in the right lobe and 2.8 cm area in the left were also noted. The initial diagnosis was presumed alcoholic hepatitis, with a component of acetaminophen related injury, without evidence of acute liver failure. His renal function improved with fluids. However, his leukocytosis worsened to 21, INR elevation persisted, and although most of his LFTs improved his bilirubin lagged. He developed low grade fevers; ceftriaxone and metronidazole were started. CT showed two liver lesions (up to 5.4 × 5.6 cm) concerning for abscesses, with gallbladder distention and pericholecystic fat stranding concerning for perforation. Serial CT-guided drainage of the liver abscesses revealed methicillin-susceptible staph aureus. Transthoracic echocardiogram, chest xray, and blood cultures were normal. Antibiotics were switched to nafcillin and the patient improved.
DISCUSSION: There has been a rise in the incidence of pyogenic liver abscess (PLA), now reported to be 3.6 per 100,000. The mortality rate of PLA has remained stable at 5.6 %; poor prognostic indicators include acute respiratory failure, gas forming liver abscess, or anaerobic infections. Mechanisms of hepatic seeding are often the result of biliary disorders (producing polymicrobial infections) and less often due to bacteremia or systemic infection (producing monomicrobial infections, often due to staph or strep). In 7.4 % of patients initially diagnosed with cryptogenic abscess, colonoscopy reveals mucosal abnormalities ranging from high grade dysplasia to adenocarcinoma. This case was unusual for several reasons. First, diagnosis was delayed due to the presence of alcohol and acetaminophen use. The patient’s lack of abdominal pain and initially fever obscured the true diagnosis, although the mixed pattern of LFT abnormalities, worsening leukocyctosis, and development of fevers were clues that this case was not classic for alcoholic hepatitis. Second, a single microorganism, staph aureus, was identified, but there was no evidence of hematogenous spread and a primary source of infection was never identified.
QUADRIPLEGIA IN A PATIENT WITH WEST NILE ENCEPHALITISRathan Reddy1; Kenneth C. Raney1; Gregg Shalan2. 1Methodist Dallas Medical Center, Dallas, TX; 2Methodist Dallas Medical Center, Dallas, TX. (Tracking ID #1939045)
LEARNING OBJECTIVE 1: Diagnose a viral illness in its acute stage
LEARNING OBJECTIVE 2: Recognize an atypical presentation of West Nile encephalitis
CASE: West Nile virus can cause neurologic disease in the form of meningitis and encephalitis. It is important to consider in patients who present with acute febrile illness in the presence of altered mental status, especially during mosquito season in summer and early fall. A common manifestation of neuroinvasive West Nile disease is a poliomyelitis-like asymmetric flaccid paralysis. It is quite rare for the disease to result in quadriplegia. A 65 year old Caucasian male with a past medical history of diabetes, hypertension, osteoarthritis and hyperlipidemia presented to our hospital with acute onset fever, emesis and altered mental status. The patient’s wife reported he was sent home from work earlier that day due to nausea and vomiting. Given the patient’s acute decline in mental status, a lumbar puncture was performed immediately upon admission. CSF analysis was unremarkable, demonstrating a WBC count of 1/mm3, elevated glucose of 108 mg/dl and a normal protein of 51 mg/dl. The patient’s CSF studies were negative for VDRL, cryptococcal neoformans, and HSV. Originally, the patient’s West Nile antibodies were negative, however, CSF analysis with West Nile PCR tested positive. Over the course of the next week, the patient’s initial symptoms began to resolve, including a return to baseline mental status. The day after clinical improvement, the patient once again spiked a fever and the following morning, he became somnolent and was unable to answer questions or follow commands. Again, because of his rapid clinical decline, lumbar puncture was repeated. Cytology of the CSF showed a WBC count of 185/mm3 and repeat titers for West Nile IgG and IgM returned elevated. The patient continued deteriorating rapidly, soon requiring intubation and mechanical ventilation. He became flaccid in all four extremities. A neuromuscular study performed by the neurocritical care specialist showed absent reflexes and complete paralysis of all four extremities. A short trial of IVIG was attempted, however, provided no benefit. He remained intubated for 14 days before the family decided to withdraw care in honor of the patient’s wishes.
DISCUSSION: Due to the severity of our patient’s disease and unique and rapid onset of quadriplegia, little could be done to prevent mortality. This case illustrates how awareness of atypical presentations of common diseases is important for timely diagnosis and implementation of appropriate therapy.
RAPIDLY PROGRESSIVE AND CATASTROPHIC OUTCOME OF ATHEROSCLEROTIC DISEASEMichelle M. El-Hosni; Dipenkumar Modi; Diane L. Levine. Wayne State University School of Medicine, Detroit, MI. (Tracking ID #1939394)
LEARNING OBJECTIVE 1: Diagnose peripheral artery disease and recognize features of critical limb ischemia
LEARNING OBJECTIVE 2: Recognize racial disparity in the diagnosis and progression of peripheral artery disease
CASE: A 75-year-old African American woman with a past medical history of untreated hypertension and depression was admitted for progressive worsening dry gangrene of the left foot over 3 months duration. She noticed 40–50 lb weight loss over the last 6 months and reduced exercise capacity. The patient was found to be afebrile, hypertensive, and tachycardic. Physical examination revealed bilateral prominent carotid bruits, undetectable bilateral femoral and lower extremity pulses, and left pedal edema with necrotic skin lesions over the first three digits. Laboratory results revealed elevated troponins (0.772) without ST-T wave changes, LDL (154) and HBA1C (7.6) Arterial Duplex was obtained which showed monophasic blood flow in common femoral arteries but absent blood flow in femoral veins, popliteal, posterior tibial, anterior tibial and peroneal veins bilaterally consistent with critical limb ischemia. CT Angiogram of the abdomen showed severe atherosclerotic disease involving the abdominal aorta with eventual complete occlusion of the distal abdominal aorta beyond the origins of the renal arteries, and opacification through the bilateral iliac arteries, superficial femoral and popliteal arteries. TTE showed small left ventricular cavity with near cavity obliteration, moderate LVH and hyperdynamic left ventricular systolic function with impaired relaxation pattern. Patient was managed for NSTEMI with IV heparin. Surgical intervention was deferred because of recent ACS. The patient was readmitted 1 week later with worsening dry gangrene of the left foot. On hospital day 2, she developed new-onset atrial fibrillation with rapid ventricular response. On EKG, STEMI was noticed with rapid up-trending troponins up to 13.6. Repeat TTE revealed new appearance of severe hypokinesia of basal to mid inferior and infero-lateral segments. Cardiac catheterization revealed 95 % stenosis of the proximal LAD and total occlusion of both the proximal LCX and distal RCA. Two bare metal stents were placed in the proximal and mid LAD. Head CT without contrast was obtained because of declining mental status, which revealed left maxillary sinusitis, possible subacute infarction involving inferior right precentral gyrus, chronic microvascular disease, and intracranial calcific atherosclerosis. Her clinical condition progressively worsened with continuous rise in troponins leading to cardiac arrest. Despite aggressive effort, the patient expired.
DISCUSSION: Peripheral artery disease (PAD) is a common circulatory problem in which narrowed arteries reduce blood flow to limbs. According to the ACC/AHA practice guidelines, risk factors for atherosclerosis, such as cigarette smoking, diabetes, dyslipidemia, and hypertension increase the likelihood of developing lower extremity PAD. Lower extremity critical limb ischemia (CLI) occurs in 1–2 % of patients above 50 years of age with PAD. CLI outcomes at 1 year are: 50 % alive with both limbs, 25 % amputation, and 25 % cardiovascular mortality. In all patients with PAD, antiplatelet therapy is recommended to reduce cardiovascular risk. Primary amputation is more frequently performed on patients with PAD who are nonwhite, low-income, and uninsured. Specifically, African American patients undergo amputation at 2–4 times the rate of white patients. The advanced ischemia observed in this population suggests a delayed diagnosis of PAD, likely due to a lack of primary care. Better education of the symptoms and consequences of PAD to the general population and providers may reduce the rate of amputation, especially among the economically disadvantaged. This patient’s chronic, untreated HTN likely predisposed her to the development of atherosclerosis and aorticoiliac occlusive disease (PAD), confirmed by Arterial Duplex and CT Angiography. Early blood pressure control could have stunted this fatal progression. If untreated, PAD results in critical limb ischemia, as evidenced by worsening lower extremity pain, non-healing wound/ulcer, and skin discoloration/gangrene. Per guidelines, antiplatelet therapy was initiated to reduce the risk of MI, stroke, and vascular death. Anti-hypertensives, statins, and blood glucose control were used for risk factor reduction. IV antibiotics were indicated until cellulitis and risk of infection could be ruled out. Patient was ineligible for surgical revascularization due to co-morbid cardiac abnormalities. Amputation of gangrenous tissue was deferred as it would lead to chronic non healing ulcer due to significantly diminished circulation and risk of infection. The patient’s rapid demise may have been prevented by early, aggressive treatment and risk reduction.
RAPIDLY PROGRESSIVE INTRACRANIAL GIANT CELL ARTERITIS; A RARE AND CATASTROPHIC PHENOMENONDevin B. Malik; Sourabh Aggarwal. Western Michigan University School of Medicine, Kalamazoo, MI. (Tracking ID #1939169)
LEARNING OBJECTIVE 1: Recognize that Giant Cell Arteritis (GCA) may present with stroke like symptoms, and could represent intracranial GCA which is exceedingly rare, as stroke in GCA is usually due to extracranial stenosis of carotid and/or vertebral arteries.
CASE: A 79 year old lady presented to us complaining of frontal headaches and odynophagia. Physical examination was unremarkable. Labs revealed an elevated erythrocyte sedimentation rate (ESR) of 82 mm/h. Computer tomography angiogram (CTA) done to evaluate headaches was unremarkable. The patient was referred to a rheumatologist for further evaluation with labs revealing ESR of 115 mm/h. ANA and ANCA tests were negative but a temporal artery biopsy was diagnostic for GCA. Prednisone 60 mg daily was started with gradual improvement of symptoms. Prednisone was slowly tapered over 3 months to 30 mg daily when patient developed right-sided weakness, dysarthria and word finding deficits. CTA of head showed infarcts in left frontal deep matter and cerebral white matter. New multifocal stenosis including stenosis of bilateral cavernous and paraclinoid internal carotids arteries, proximal portions of left anterior cerebral, middle cerebral and left posterior communicating artery and distal cervical left vertebral artery were found compared to previous CTA. These were consistent with intracranial vasculitis. Aspirin 81 mg was started. Lumbar puncture and echocardiogram were unremarkable for any other etiology. She was started on high dose steroids and cyclophosphamide, however the patient opted for hospice.
DISCUSSION: Intracranial vasculitis leading to CVA in a patient with biopsy proven GCA has been reported extremely rarely. GCA almost exclusively affects the extracranial vessels sparing the intracranial vessels It is postulated that the pathologic inflammation of GCA targets the arterial elastic tissue of extracranial vessels and the intracranial vessels are spared as they have little or no elastic tissue in their media and adventitia layers. Our patient developed intracranial vasculitis while on steroids which to the best of our knowledge has never been reported previously. This case of intracranial vasculitis highlights an extremely rare cause of CVA and to our knowledge is the first report of GCA associated intracranial vasculitis developing while on corticosteroid therapy.
RARE CAUSE OF A “BROKEN HEART” IN RHEUMATOID ARTHRITISJennifer Zora; Aluoch Aloice; Robin Klein. Emory, Atlanta, GA. (Tracking ID #1940118)
LEARNING OBJECTIVE 1: Recognize the pathophysiology of hyperviscosity syndrome.
LEARNING OBJECTIVE 2: Review the clinical manifestation of hyperviscosity syndrome.
CASE: A 45 year old female presents with progressive shortness of breath and lightheadedness. Past medical history was notable for Rheumatoid Arthritis treated with weekly abatacept. Physical exam demonstrated jugular venous distension but not synovitis, joint effusion, or rash. Laboratories revealed a positive anti-cittrulinated protein antibody and rheumatoid factor, negative double-stranded Deoxyribonucleic acid (DNA), platelet count of 128,000 per microliter, an international normalized ratio of 1.5, total protein of greater than 12 g per deciliter (gm/dL) and albumin of 2.4 g/dL. She underwent right heart catheterization which revealed a cardiac index of 1.39 L/min, pulmonary artery pressure of 45/27 mm Hg (mm Hg) and severe RV dysfunction with a mixed venous oxygen (MVO2) saturation of 22 % and pulmonary capillary wedge pressure of 7 mm of Hg. She was started on dobutamine and epoprostenol sodium therapies with for decompensated right heart failure. Ventilation perfusion scan was obtained and demonstrated multiple mismatched defects in the right lung characteristic for acute pulmonary embolism. Heparin therapy was started and was complicated by persistent, severe epistaxis. Repeated clotting of her blood specimen tubes for lab draws was also noted. Her simultaneous increased bleeding and clotting was perplexing. Her viscosity was found to be very high at 8.4 (normal range 1.4–1.8 units), and serum protein electrophoresis revealed polyclonal gammopathy. Notably, Von Willebrand factor function and quantity and factor VIII levels were within normal range. She was diagnosed with hyperviscosity syndrome. She underwent plasmapheresis twice, and her viscosity normalized. Following this, CT chest did not demonstrate evidence of true pulmonary embolism, and heparin was stopped. She was ultimately discharged on a decreased dose of epoprostenol sodium with normalization of her MVO2.
DISCUSSION: Hyperviscosity syndrome is a rare, potentially reversible complication of rheumatoid arthritis caused by polyclonal gammopathy. Monoclonal gammopathies such as multiple Waldenström macroglobulinemia causes 85 % of cases of hyperviscosity in contrast to polyclonal gammopathy. The primary mechanisms postulated for hyperviscosity in rheumatologic disease include binding of rheumatoid factor immunoglobulin M (IgM) and or immunoglobulin G (IgG). Hyperviscosity syndrome leads to both abnormal clotting and bleeding tendencies. The exact mechanism for the bleeding caused by this process is not understood but could involve platelet dysfunction and/or clotting factor destruction. Likely, slow movement of the viscous blood of blood in the pulmonary vascular system led to this patient’s (incorrectly) suspected pulmonary embolism and her severe pulmonary hypertension. Initial therapy with plasmapheresis was largely effective therapy for our patient. Long-term immunosuppression will be attempted with in an effort to potentially reverse her pulmonary hypertension/right heart failure and free her from her reliance on chronic epoprostenol sodium therapy. Thus, this case demonstrates that it remains important to maintain a broad differential for cardiopulmonary complaints in our patients with rheumatologic disease. In this case, right heart failure was caused by a rare complication of rheumatoid arthritis, hyperviscosity syndrome. History, physical and careful analysis of abnormal laboratory values remain paramount in these complex patients.
RARE CAUSE OF THROMBOCYTOPENIASparsha Kukunoor. University of Connecticut, hartford, CT. (Tracking ID #1940274)
LEARNING OBJECTIVE 1: Identify the relationship between thrombocytopenia and transfusion
LEARNING OBJECTIVE 2: Recognize the differential diagnosis of acute thrombocytopenia in a critical care setting
CASE: 26 year old man with end stage renal disease, hypertension, anemia due to chronic kidney disease, diabetes who was admitted to the ICU for hypoxic encephalopathy was diagnosed to have worsening anemia after 3 weeks of ICU stay, he then received one unit of packed red blood cell transfusion. Five days later he was found to have acute drop in platelet count from 389,000/UL to less than 5.000/UL the next day. Only symptom being epistaxis. Peripheral smear did not show platelet clumping or schistocytes. There was evidence of toxic granulation, decreased lymphocytes and no platelets were visible. Bone marrow suppression was unlikely due to the acute drop. ADAMTS 13, Direct Coombs test, triglyceride, ferritin, HPF4, vitamin B12 and folate and tick borne antibody screen was negative. A immune related event was suspected at this point due to the acuteness. Platelets were transfused with no improvement in post transfusion platelet counts. Post transfusion purpura was considered and human platelet antigen genotyping and antibody testing was sent out. Methylprednisolone 40 mg IV every 6 h was started along with IVIG treatment. There was no improvement in his thrombocytopenia. After 2 days plasmapheresis was started on a daily basis, this showed a gradual improvement in his platelet counts to 70,000/UL in 3 days time. His tests confirmed anti-HPA-1a antibody. He was later transferred on to hospice care due to his encephalopathy and other comorbidities and finally died.
DISCUSSION: Post Transfusion purpura is a form of severe thrombocytopenia occuring after transfusion of blood products. It is usually seen in individuals with HPA negative platelets, most often seen in multiparous women who have been immunized with HPA positive pregnancy. It can also be seen in men 5–10 days after transfusion with a sudden decrease in platelet count. It is seen in the form of an ananmestic response with the formation of HPA antibodies which react with the individuals own platelets which are HPA negative. The mechanism of this still remains unclear, a number of subtypes of HPA have been reported in the past. Our patient had no history of transfusion in the past or any history of thrombocytopenia. Diagnosis is based on the identification of the antibody in the serum of a patient who lacks the corresponding antigen, anti-HPA-1a being the most common, these tests may take days to weeks. Therapy should not be delayed. Platelet transfusion is generally not helpful in the management of this condition as the platelet count drops further even with platelet transfusions. The treatment of Post Transfusion Purpura is steroids, IVIG, exchange transfusion and sometimes plasma pheresis. Our patient was refractory to steroids and IVIG, and responded well to the plasmapheresis.
RARE PRESENTATION OF GASTROINTESTINAL TUBERCULOSISFadi Niyazi. Henry Ford Hospital, Detroit, MI. (Tracking ID #1927265)
LEARNING OBJECTIVE 1: In the United States, tuberculosis is relatively rare, and primarily manifests as pulmonary disease. This case describes a rare presentation of extra-pulmonary tuberculosis.
CASE: A 42 year old previously healthy male, who moved to United States from India in 2001, presented 6 weeks after an open repair of incarcerated right inguinal hernia with a 3 week history of difficulty passing urine and abdominal fullness associated with decreased appetite. He was initially evaluated by a urologist for urinary symptoms and started on Tamsulosin, and he tried over the counter medications for his gastrointestinal symptoms with no relief. With continued symptoms and increased abdominal discomfort he presented to the emergency department. The patient admitted to having a positive PPD test when he first moved from India, but did not complete a full course of medical treatment. He denied hematemesis, weight loss, night sweats, chills, nausea, vomiting, melena or hematochezia. Exam revealed a soft but mildly tender abdomen, positive fluid wave, no hepatosplenomegaly, normal bowel sounds, and no palpable pelvic lymph nodes. CT abdomen and pelvis revealed multiple intra-abdominal hypodense lesions that may represent low attenuation lymph nodes, with ascites. Differential diagnosis included broadly infectious etiologies versus neoplasia. Labs showed PSA of 1.01 ng/mL, and colonoscopy was entirely normal. Diagnostic laparoscopy with lymph node and peritoneal biopsy was performed, with intra-operative findings including multiple milliary peritoneal implants, inflamed peritoneum, and clear greenish ascites, with 3 l subsequently drained. Peritoneal fluid analysis showed cell count of 1385 WBC/uL with predominant lymphocytes and monocytes, glucose of 89 mg/dL, protein of 5.7 g/dL, albumin of 3.4 g/dL, and was negative for malignant cells by flow cytometry. Intra-operative frozen sections examined under microscope revealed organizing necrotizing and non-necrotizing granulomatous inflammation, consistent with gastrointestinal tuberculosis, with no evidence of neoplasm. Patient was started on isoniazid, pyridoxine, rifampin, pyrazinamide and ethambutol with clinical improvement noticed in an outpatient visit few weeks later.
DISCUSSION: Gastrointestinal tuberculosis is defined as infection of the peritoneum, hollow or solid abdominal organs, or abdominal lymphatics with Mycobacterium tuberculosis. Gastrointestinal tuberculosis is rare in the United States, but represents the sixth most common extra-pulmonary location worldwide. Patients usually present with non-specific gastrointestinal symptoms, and the diagnosis is often delayed and is made through a combination of radiologic, endoscopic, microbiologic, histologic, and molecular techniques. Surgery is occasionally required for diagnosis. Antimicrobial treatment is the same as for pulmonary tuberculosis.
RECOGNIZE THE IMPORTANCE OF PRE-EMBOLECTOMY CT PULMONARY ANGIOGRAPHY IN SUSPECTED MASSIVE PULMONARY EMBOLISMAkihiro Kobayashi1,2; Pierre Kory2. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1938452)
LEARNING OBJECTIVE 1: Recognize the importance of pre-embolectomy CT pulmonary angiography in suspected massive pulmonary embolism.
CASE: A 68 year-old man was admitted for evaluation and treatment of obstructive uropathy due to benign prostatic hyperplasia. On his second day of hospitalization, he suddenly developed shortness of breath. Vital signs revealed blood pressure 80/60 mmHg, heart rate 110/min, respiratory rate 30/min, and 90 % saturation while receiving supplemental oxygen via face mask at 10 L/min. His chest was clear to auscultation and a chest radiograph was unremarkable. Pulmonary embolism (PE) was suspected, however, CT pulmonary angiography (CT-PA) could not be performed due to the development of severe hypotension requiring norepinephrine followed by respiratory failure requiring tracheal intubation. Immediate transfer to the medical intensive care unit (MICU) was performed. In the MICU, a bedside transthoracic echocardiogram (TTE) revealed a severely dilated right ventricle (RV) with reduced function. Bedside compression venous ultrasonography revealed a thrombus in the left common femoral vein. Despite initiation of intravenous heparin for presumed massive PE, the patient remained hypotensive requiring escalating doses of norepinephrine. Due to hemodynamic instability, transport for confirmatory CT-PA was deferred and empiric intravenous tissue-plasminogen activator (t-PA) was initiated based on the high clinical pretest probability of massive PE. Despite t-PA, his hypotension persisted and surgical consultation for thrombectomy was sought. Due to worsening hemodynamics the patient was rushed to the operating room for surgical thrombectomy. A pre-operative transesophageal echocardiogram did not reveal central pulmonary emboli. Main and right pulmonary artery dissection with catheter exploration was performed but no thrombotic material was obtained. An inferior vena cava filter was placed. Heparin was continued, and his hypotension and respiratory failure resolved over days. A CT-PA on post-operative day 2 revealed bilateral segmental and subsegmental pulmonary emboli.
DISCUSSION: Emergent surgical embolectomy in massive PE is indicated when thrombolytic therapy is contraindicated or has failed and should be considered when hemodynamic instability is likely to cause death before thrombolysis can take effect. Current guidelines have stated that thrombolysis and thrombectomy are justified without a definitive diagnosis of PE in patients with suspected massive PE and RV dysfunction on TTE. Although thrombectomy may be justified without a CT-PA, existing literature suggests that extraction of emboli is limited to the level of segmental pulmonary arteries. This patient required escalating doses of vasopressor despite treatment with both intravenous heparin and t-PA. An emergent surgical embolectomy was performed without a pre-operative CT-PA to establish both the presence and location of thrombi and, as a result, no embolic material could be obtained. The presumed failure of surgical embolectomy was due to the majority of emboli residing in the subsegmental pulmonary arteries at the time of operation. This outcome suggests that, although patients with suspected massive PE are at high risk of death, the importance of avoiding unnecessary and highly invasive procedures such as thrombectomy may outweigh the risks of delay and transport incurred by CT-PA. Thus, CT-PA should be more strongly consided before surgical embolectomy in suspected massive PE.
RECURRENT ACUTE CORONARY SYNDROME DURING EXACERBATIONS OF IMMUNE THROMBOCYTOPENIC PURPURA: THE ROLE OF PLATELET MICROPARTICLESDavid E. Kim1; Kenneth A. Schwartz2. 1Michigan State University, East Lansing, MI; 2Michigan State University Breslin Cancer Center, Lansing, MI. (Tracking ID #1938718)
LEARNING OBJECTIVE 1: Recognize that ITP can present as a pro thrombotic state possibly via the generation of platelet microparticles
LEARNING OBJECTIVE 2: Manage acute thrombosis in setting of ITP
CASE: 67 year old male with history of chronic episodic ITP with normal platelet counts between episodes of acute thrombocytopenia, was admitted to the hospital for lower extremity petechiae and blood filled blisters of the oral mucosa with a platelet count of 1 K/uL. His past medical history was significant for splenectomy due to sarcoidosis, pre-existing coronary artery disease, and hypertension. The patient was treated with high dose steroids and IVIG. During the infusion he suddenly developed 10/10 substernal chest pain with difficulty breathing and diaphoresis. Subsequent EKG showed ST depression in anterolateral leads and blood work was significant for elevated troponin of 4.75 ng/mL. Due to his persistently low platelets, the patient did not undergo cardiac cath during his hospitalization. He was continued on high dose steroids and was discharged home after his troponins started to down trend and his platelets stabilized. Further review of his medical records showed that this was the second NSTEMI in the setting of an exacerbation of acute on chronic ITP. His first episode was 5 years ago when he was admitted for an NSTEMI, again in the setting of an ITP exacerbation with a platelet count of 39 K/uL. Cardiac cath at the time showed a chronic occlusion of his RCA with extensive collaterals. PCI of the RCA was attempted but was unsuccessful. Patient had been on 81 mg of aspirin since. A hypercoagulable work up at the time consisting of anticardiolipin antibodies, antithrombin III, prothrombin gene mutation, lupus inhibitor, and protein C and S deficiencies were unremarkable. Serial outpatient platelet counts confirmed his baseline platelets were 200–300 K/uL during the interval (2008 and 2013) between his cardiac events.
DISCUSSION: We hypothesize that in the setting of pre-existing coronary artery disease, acute coronary syndrome may be precipitated via rapid precipitous antibody mediated decreases in platelet count as occurred in our patient and that platelet microparticles generated during the rapid destruction of platelets may help mediate the prothrombotic state. Microparticles are submicron vesicles shed from various cell types that play a role in coagulation, vascular injury, cell signaling, vascular injury, and homeostasis. Platelet microparticles in particular was first described in 1967 by a British Physician, Peter Wolfe who discovered that these particles had pro-coagulant properties. Since then platelet microparticles have been implicated in both arterial and venous thrombotic disease. Our case demonstrates this hypothesis to dramatic effect as our patient’s precipitous drop in platelet count has a clear temporal relation to his two episodes of acute coronary syndrome. Management of thrombosis during an exacerbation of ITP is not currently addressed by guidelines. The consensus agreement is that anticoagulation is acceptable at platelet counts 40–50 K/uL and that the underlying ITP should be aggressively treated.
RECURRENT BENIGN LYMPHOCYTIC MENINGITIS (RBLM) IN A PREGNANT WOMANDelia Lee; Kurt J. Pfeifer; Mark A. Beilke. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1895597)
LEARNING OBJECTIVE 1: Diagnose recurrent benign lymphocytic meningitis (RBLM), also known as Mollaret’s meningitis
LEARNING OBJECTIVE 2: Tailor treatment of RBLM in pregnant patients
CASE: A 40-year-old African-American woman who was 11-weeks pregnant presented with a 3-day history of throbbing headache associated with photophobia, phonophobia, nausea, vomiting, and nuchal rigidity. She was healthy except for having a history of two episodes of viral meningitis 6 and 17 years prior. She denied association between pregnancy and prior episodes of viral meningitis. Physical exam revealed an alert but mildly distressed woman with tenderness at the temples, mild cervical adenopathy, reproducible nuchal rigidity and positive Kernig’s sign but without focal neurological deficits. Complete blood count was normal, and basic metabolic panel was only notable for hypokalemia. Blood cultures were drawn on admission but showed no growth. Cerebrospinal fluid (CSF) studies showed high protein, normal glucose, reactive pleocytosis, and herpes simplex virus (HSV) NAAT positive for HSV-2. Pelvic ultrasound confirmed a single, live intrauterine pregnancy with estimated 11 week gestational age. She completed a 5-day course of intravenous acyclovir and was discharged from the hospital with plans to complete a two-week course of therapeutic-dose of valacyclovir, followed by suppressive valacyclovir at least through the pregnancy. Two days after hospital discharge, her symptoms completely resolved. She completed 5 days of therapeutic valacyclovir but stopped prematurely due to disliking the large pill size. After further discussion, she was agreeable to the suppressive valacyclovir with smaller pills, and subsequently she has had no other documented recurrences.
DISCUSSION: RBLM is postulated to be caused by a reactivation of HSV-2 that may not be concurrent with mucocutaneous manifestations. Incidence is 1–2/100,000, occurring more often in women. Initial treatment is typically intravenous acyclovir, but there are no guidelines regarding treatment and suppression of RBLM, particularly in pregnant women. However, valacyclovir can reduce the number of genital HSV outbreaks during pregnancy. A recent randomized controlled trial demonstrated that with suppression therapy there was no prevention of recurrence. Additionally, there was a possible rebound of recurrence after completion of suppression though a decrease of mucocutaneous outbreaks. However, this study had several exclusion criteria, including pregnancy. In conclusion, we assert that the potential to prevent herpes transmission to the fetus justifies prescribing suppressive therapy for a pregnant woman with RBLM despite the paucity of supportive study data.
RECURRENT BENIGN LYMPHOCYTIC MENINGITIS (RBLM) IN A PREGNANT WOMANDelia Lee; Kurt J. Pfeifer; Mark A. Beilke. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1895597)
LEARNING OBJECTIVE 1: Diagnose recurrent benign lymphocytic meningitis (RBLM), also known as Mollaret’s meningitis
LEARNING OBJECTIVE 2: Tailor treatment of RBLM in pregnant patients
CASE: A 40-year-old African-American woman who was 11-weeks pregnant presented with a 3-day history of throbbing headache associated with photophobia, phonophobia, nausea, vomiting, and nuchal rigidity. She was healthy except for having a history of two episodes of viral meningitis 6 and 17 years prior. She denied association between pregnancy and prior episodes of viral meningitis. Physical exam revealed an alert but mildly distressed woman with tenderness at the temples, mild cervical adenopathy, reproducible nuchal rigidity and positive Kernig’s sign but without focal neurological deficits. Complete blood count was normal, and basic metabolic panel was only notable for hypokalemia. Blood cultures were drawn on admission but showed no growth. Cerebrospinal fluid (CSF) studies showed high protein, normal glucose, reactive pleocytosis, and herpes simplex virus (HSV) NAAT positive for HSV-2. Pelvic ultrasound confirmed a single, live intrauterine pregnancy with estimated 11 week gestational age. She completed a 5-day course of intravenous acyclovir and was discharged from the hospital with plans to complete a two-week course of therapeutic-dose of valacyclovir, followed by suppressive valacyclovir at least through the pregnancy. Two days after hospital discharge, her symptoms completely resolved. She completed 5 days of therapeutic valacyclovir but stopped prematurely due to disliking the large pill size. After further discussion, she was agreeable to the suppressive valacyclovir with smaller pills, and subsequently she has had no other documented recurrences.
DISCUSSION: RBLM is postulated to be caused by a reactivation of HSV-2 that may not be concurrent with mucocutaneous manifestations. Incidence is 1–2/100,000, occurring more often in women. Initial treatment is typically intravenous acyclovir, but there are no guidelines regarding treatment and suppression of RBLM, particularly in pregnant women. However, valacyclovir can reduce the number of genital HSV outbreaks during pregnancy. A recent randomized controlled trial demonstrated that with suppression therapy there was no prevention of recurrence. Additionally, there was a possible rebound of recurrence after completion of suppression though a decrease of mucocutaneous outbreaks. However, this study had several exclusion criteria, including pregnancy. In conclusion, we assert that the potential to prevent herpes transmission to the fetus justifies prescribing suppressive therapy for a pregnant woman with RBLM despite the paucity of supportive study data.
RECURRENT CASE OF ASEPTIC MENINGITIS FROM IBUPROFENParas Karmacharya1; Naba R. Mainali1; Madan R. Aryal1; Ranjan Pathak1; Raju Khanal1; Supriya Shrestha Tamrakar3; Pragya Shrestha2; Benjamin Lloyd1. 1Reading Health System, West Reading, PA; 2Nanjing Medical University, Nanjing, China; 3Guangxi Medical University, Guangxi, China. (Tracking ID #1935167)
LEARNING OBJECTIVE 1: Recognize that the clinical course as well as CSF findings of NSAIDs induced aseptic meningitis may be similar to that of acute bacterial meningitis. It should be considered in the differential diagnosis of patients with underlying autoimmune connective tissue disorders and recurrent aseptic meningitis.
LEARNING OBJECTIVE 2: It may be appropriate to screen for autoimmune diseases in healthy subjects developing NSAIDs induced aseptic meningitis. Patients developing this should avoid all types of NSAIDs as these have been described with many NSAIDs and a recurrence can be more severe.
CASE: A 28-year-old female with a history of mixed connective tissue disease on low dose prednisone and Ibuprofen presented with high grade fever, frontal headache, nausea and generalized bodyaches for 1 day. She had been taking ibuprofen 600 mg two to three times a day for the past 2 days for her arthralgia. Physical examination revealed an alert lady with a temperature of 103 °F and hypotension. Neck flexion was slightly limited because of pain. Kernig’s and Brudzinzki’s signs were absent and no focal neurological deficits were elicited on exam. She was started on broad-spectrum antibiotic coverage with cefepime, vancomycin and acyclovir for possible infectious meningitis. Cerebrospinal fluid analysis showed neutrophilic pleocytosis with negative bacterial, viral and fungal cultures. The antibiotics were subsequently discontinued after 3 days. She did not receive any NSAIDs during her hospital course. Her symptoms completely resolved with no neurological sequelae. She was advised not to take NSAIDs and hasn’t had a second recurrence as of now.
DISCUSSION: NSAID induced aseptic meningitis is extremely rare, however, the widespread use of ibuprofen, as well as other NSAIDs, particularly for rheumatological diseases makes it an increasing possibility (1). Ibuprofen is the most frequently implicated culprit (2,3). The clinical course as well as CSF findings may be similar to that of acute bacterial meningitis, so it should be considered in the differential, mainly in patients with underlying autoimmune connective tissue disorders and in patients with recurrent meningitis. In fact, NSAID induced meningitis must be considered in any case of recurrent aseptic meningitis, and it may be appropriate to screen for autoimmune diseases in healthy subjects developing this. References: 1. Lee RZ, Hardiman O, O’Connell PG. Ibuprofen-induced aseptic meningoencephalitis. Rheumatol Oxf Engl. 2002 Mar;41(3):353–5. 2. Jolles S, Sewell WA, Leighton C. Drug-induced aseptic meningitis: diagnosis and management. Drug Saf Int J Med Toxicol Drug Exp. 2000 Mar;22(3):215–26. 3. Moris G, Garcia-Monco JC. The challenge of drug-induced aseptic meningitis. Arch Intern Med. 1999 Jun 14;159(11):1185–94.
RECURRENT CONGESTIVE HEART FAILURE, WHEN IT IS NOT ALL ABOUT THE HEARTAmornpol Anuwatworn; Imelda A. Cirilo; Viswanathan Iyer; Pramil Cheriyath. Pinnacle Health System - Harrisburg Hospital, Harrisburg, PA. (Tracking ID #1939708)
LEARNING OBJECTIVE 1: Recognize the clinical manifestations of severe pulmonary hypertension caused by high output heart failure due to large atriovenous fistula
LEARNING OBJECTIVE 2: Investigate and manage severe pulmonary hypertension caused by high output heart failure due to large atriovenous fistula
CASE: A 71 year-old man with a history of ESRD requiring transplantations in 1998, 2008, non occlusive CAD, hypertension, OSA and COPD presented with 1 year history of progressive exertional dyspnea and recurrent symptoms of congestive heart failure. Brachial cephalic atriovenous (AV) fistula was implanted in 2007 but it was unused after the successful second transplantation. Examination showed a markedly enlarged right upper extremity AV fistula with thrill and flow murmur. Chest x-ray revealed congestion. Pulmonary function test showed a mild obstructive pattern. Echocardiogram showed normal left ventricular size and function, flattened septum, no aortic stenosis. Right ventricular size was moderately dilated and right ventricular systolic function was moderately reduced. There were moderate tricuspid regurgitation and biatrial enlargement. Pulmonary arterial systolic pressure (PASP) was measured at 71 mmHg. He underwent right heart catheterization and AV fistula was temporary occluded with the use of a blood pressure cuff. The results included PA pressure 64/34 with a mean of 44, PCWP of 24 mmHg. Thermodilution prior to occlusion was 6.7 l/min. Post-occlusion, thermodilution gave a cardiac output of 5.4 l/min. There was reduction in cardiac output with occlusion of the AV fistula, roughly 1.3 l/min. He was diagnosed with severe pulmonary hypertension caused by high output heart failure due to unused large AV fistula. He underwent AV fistula ligation. Repeated echocardiogram at the end of 2 weeks, PASP has already dropped to 50 mmHg and he clinically improved.
DISCUSSION: Etiology of pulmonary hypertension is diverse. We report a rare case of pulmonary hypertension caused by high output heart failure due to AV fistula. As illustrated in this case, the patient had severe pulmonary hypertension with no left-sided valvular heart disease or septal defects. Even though he had COPD, the mild severity of COPD was unlikely a cause of his severe pulmonary hypertension. The right cardiac catheterization revealed high output heart failure. The improvement of his symptoms and PASP after AV fistula ligation confirmed that large AV fistula resulted in high output heart failure leading to severe pulmonary hypertension. In patients with pulmonary hypertension who have ESRD and AV fistula, high output heart failure due to enlarged AV fistula may be a culprit.
RECURRENT PLEURAL EFFUSION AS THE PRESENTING MANIFESTATION OF MULTIPLE MYELOMALawrence Giove; Nikhil Kapila; Andrew Hamarich. University of Connecticut, Farmington, CT. (Tracking ID #1937498)
LEARNING OBJECTIVE 1: Recognize that pleural effusion is a rare initial manifestation of multiple myeloma.
CASE: A 70-year-old man presenting to the hospital with recurrent bilateral pleural effusion of unclear etiology. Previously, pleural fluid studies revealed a transudate effusion with negative cytology for malignancy or infection. Upon presentation, he complained of chronic cough and worsening dyspnea. He denied previous cardiac or pulmonary disease, trauma, cancer, or exposures. His social history was significant for 35 pack years of tobacco use, having quit 15 years prior. Physical exam revealed an elderly man, in mild respiratory distress. He was noted to have limited chest excursion with decreased breath sounds at the lung bases. The remainder of his exam was unremarkable. White blood count was 8300 cells/mm3, hemoglobin was 11.9 g/dL, serum creatinine was 3.0 mg/dL and serum calcium was 8.4 mg/dL. A chest x-ray revealed mild cardiomegaly, prominent vascular markings, and bilateral pleural effusions. Echocardiogram showed left ventricular ejection fraction of 65 % without evidence of pulmonary hypertension. Subsequently, the patient underwent a video assisted thoracoscopy, right basilar lung biopsy, pleural biopsy, and talc pleurodesis. Initial pleural studies revealed an exudative effusion with a white blood cell count of 350 cells/mm3, 95 % mononuclear cells, lactate dehydrogenase was 229 IU/L, fluid protein was 2900 mg/dL, and pH 7.5. The fluid and pleural biopsy were negative for infection, plasma cells or other tumor cells. Pathology of the lung biopsy revealed characteristic apple green birefringence compatible with amyloid deposition. The patients serum protein electrophoresis was without the presence of an M protein, however, his urine immunofixation was significant for the presence of lambda free light chains. A bone marrow biopsy revealed 20 % plasma cells, which exhibited lambda light chain monotypia. His hospital course was complicated by an episode of ventricular tachycardia, which was treated with intravenous lidocaine. Cardiac MRI was performed and findings were consistent with amyloid deposition in the myocardium. The patient met the diagnostic criteria for multiple myeloma with >10 % plasma cells on bone marrow biopsy and monoclonal protein in the urine. The etiology of his recurrent pleural effusions was secondary to amyloid deposition in the setting of a light chain restricted plasma cell dyscrasia. He was started on bortezomib, cyclophosphamide, and decadron in the outpatient setting and currently is in remission.
DISCUSSION: Multiple myeloma accounts for 1 % of all cancers and 10 % of all hematologic malignancies. It is primarily a disease of the bone marrow, but can involve other organ-systems. Thoracic manifestations include plasmocytomas, mediastinal lymphadenopathy, bony lesions and pleural effusions. Pleural effusion in myeloma can occur due to several mechanisms. These mechanisms include the involvement of the pleural space from adjacent skeletal or parenchymal tumors, lymphatic obstruction, nephrotic syndrome, chronic renal failure, restrictive cardiomyopathy, and pulmonary amyloidosis. Direct myeloma involvement of the pleural space is extremely rare occurring in less than 1 % of cases. Persistent pleural effusions develop in 1 to 2 % of patients with systemic amyloidosis and appear to be caused by pleural infiltration with amyloid deposits. In myeloma, these amyloid deposits are a result of deposition of protein from immunoglobulin light chain fragments. Light chain myeloma can be missed on serum electrophoresis and urine electrophoresis should always be done. Pulmonary amyloidosis can be diagnosed by bronchoscopic lung biopsy. Pleural involvement can be diagnosed by presence of plasma cells in pleural fluid or a pleural biopsy. Persistent pleural effusions due to amyloidosis or myelomatous involvement of the pleural space are associated with a poor prognosis and limited response to treatment.
RECURRENT PLEURAL EFFUSION IN A PATIENT WITH NEPHROLITHIASIS: A CASE FOR CAUTIONAderonke Salau-Okeleji; Michael Riverso; Maryam Sattari. University of Florida, Gainesville, FL. (Tracking ID #1933671)
LEARNING OBJECTIVE 1: Recognize urinothorax as a rare cause of pleural effusion, especially in patients with recent urinary tract manipulation
LEARNING OBJECTIVE 2: Become familiar with clinical presentation of urinothorax
CASE: A 70-year-old male with a history of hypertension and nephrolithiasis presented with weakness, productive cough, and decrease in oral intake and urine output. The patient had recently undergone percutaneous nephrolithotomy for bilateral staghorn calculi and hydronephrosis, shortly after which he had developed an asymptomatic right-sided pleural effusion. He was initially treated empirically with Augmentin for “parapneumonic effusion.” However, he had presented again with shortness of breath and cough and undergone repeat thoracentesis with removal of 1.7 L and 2.7 L of “exudative” pleural fluid. On presentation, the patient was tachypneic, hypoxemic, and had decreased right-sided breath sounds. The most significant lab abnormality was a serum creatinine of 3.9 mg/dL. Chest x-ray confirmed recurrence of right-sided pleural effusion. Thoracentesis removed 1.5 L of pleural fluid. Since the effusion was recurrent and had appeared in the setting of recent urological manipulation, pleural fluid creatinine was checked in addition to conventional studies. Fluid-to-serum creatinine ratio greater than 1 confirmed the diagnosis of urinothorax. Acute kidney injury was thought to be obstructive in nature and improved with Foley catheter placement. To prevent recurrence of effusion, the patient underwent talc pleurodesis with chest tube placement, followed by repeated doxycycline pleurodesis. Chest tube was eventually removed successfully.
DISCUSSION: Urinothorax, a rare form of pleural effusion, results from accumulation of urine in the pleural space. Reported etiologies include obstructive uropathy, blunt and iatrogenic trauma, urinary tract malignancy, and renal transplantation. The appearance and odor of the pleural fluid is often consistent with urine. The fluid usually fulfills Light’s criteria for a transudate with low glucose and pH. However, elevated LDH levels may lead to misclassification as an exudative effusion, as demonstrated by our case. Furthermore, the biochemical characteristics of the pleural fluid may become modified depending on duration of its presence in the pleural space or after repeat thoracentesis. The pleural fluid-to-serum creatinine ratio >1.0 might be the most reliable marker for this condition. Various techniques, including Mercaptoacetyltriglycine (MAG3) renogram, may aid in establishing the diagnosis of urinothorax by demonstrating leakage of the tracer from the urinary tract into the pleural space. While urinothorax may resolve with relief of urinary obstruction, iatrogenic/traumatic cases associated with a direct tract to the pleura may persist or recur, as in our case. As urological procedures become more common, urinothorax will likely increase in incidence. As our case demonstrates, urinothorax can often go undiagnosed. Timely diagnosis requires a high index of clinical suspicion and should be considered whenever a pleural effusion occurs in the setting of urinary tract obstruction or recent urological intervention. The creatinine level of pleural fluid, a biochemical parameter not routinely measured, should be determined. Furthermore, earlier thoracentesis is more likely to reveal the characteristic parameters of urinothorax.
RECURRENT PNEUMONIA OR PULMONARY ALVEOLAR PROTEINOSIS: A CONCEALED DIAGNOSISFayruz Araji1; Omar Mousa2; Daniela Moran3. 1Universidad Francisco Marroquin, Guatemala, Guatemala; 2SUNY Upstate Medical University, Syracuse, NY; 3Lung and Asthma Clinic, Houston, TX. (Tracking ID #1934266)
LEARNING OBJECTIVE 1: Diagnose Pulmonary Alveolar Proteinosis when the presentation is challenging with different mimickers of the disease.
LEARNING OBJECTIVE 2: Recognize that outcomes are worrisome for disease progression with high rates of recurrence and mortality.
CASE: We hereby present a case of a 49-year old Middle Eastern male patient who presented with worsening exertional dyspnea and productive cough with thick secretions for 3 months. In the preceding 6 months, he was evaluated multiple times for abnormal chest X-rays and clubbing and he was treated for recurrent pneumonia with oral antibiotics and glucocorticoids. He noticed weight loss of 20 lb but denied other symptoms. He had a history of recurrent sinusitis with no lung disease or a family history of similar illnesses. He worked as an aircraft maintenance technician and reported exposure to fiberglass and metal dust. He had a 25 pack-year smoking history with no recent travel. Physical examination revealed tachycardia (110 bpm) and hypoxemia (O2 saturation 92 % on 6 L O2). He had clubbing, bilateral diffuse crackles and the exam was otherwise unremarkable. He had bilateral interstitial alveolar infiltrates on the chest X-ray and the CT scan showed diffuse ground glass opacities bilaterally. Bronchoscopy was unremarkable and a single bronchoalveolar lavage culture was positive for nontuberculous mycobacterium. His symptoms worsened despite inpatient care and close monitoring. He required a video-assisted thoracoscopic surgery and anatomic pathology showed filling of the alveolar spaces with eosinophilic acellular finely granular material that stained positive with PAS, consistent with Pulmonary Alveolar Proteinosis. He received high volume bilateral lung lavage, oxygen therapy, GM-CSF 250 mcg SQ daily and anti-mycobacterial treatment with rifampin and ethambutol. The hospital course was complicated by non-sustained ventricular tachycardia. He improved slowly after a prolonged hospital stay.
DISCUSSION: Pulmonary alveolar proteinosis (PAP) is a very rare disease of the lungs with an estimated annual incidence and prevalence as high as 0.49 and 6.2 cases per million, respectively. The natural history of PAP has been studied over the past 6 decades through less than 1000-reported cases. The diagnosis is easily missed and delayed due to the mimickers of its various presentations, including disorders with similar radiographic manifestations. With only 8 % of patients experiencing clinically significant spontaneous improvement, delay in the management increases the mortality risk. Healthcare providers should have a high index of suspicion for PAP in patients with recurrent pneumonia. Raising awareness about the stepwise plan of treatment with whole lung lavage, inhaled GM-CSF then rituximab improves the clinical outcomes and the pulmonary function. Early intervention with such therapeutic modalities remains the standard of care until further immunologic mechanisms are discovered.
RECURRENT RASH WITH FEVERSadie Trammell Velasquez. 1University of TX Health Science Center at San Antonio, San Antonio, TX; 2South Texas Veterans Healthcare System, San Antonio, TX. (Tracking ID #1936647)
LEARNING OBJECTIVE 1: Identify the differential diagnosis of fever and rash in an adult.
LEARNING OBJECTIVE 2: Recognize the clinical presentation of Adult-Onset Still’s Disease and understand the treatment and clinical course of Adult-Onset Still’s Disease.
CASE: A 20 year-old woman presented with 3 days of fever, rash and arthralgias. Arthralgias were of elbows, ankles and back. She describes her rash as non-painful and non-pruritic that has progressed to cover her arms, palms and legs. She has also had associated myalgias and a sore throat. Her temperature was 39.4οC; heart rate 145 bpm; blood pressure 127/76 mmHg. She was tachycardic with regular rhythm. Skin exam revealed erythematous, somewhat blanching thin plaques with slight edema scattered on her bilateral arms, bilateral and medial aspects of legs, lateral thighs/hips and lower chin/neck and spared her torso; bilateral palms had macular lesions, slightly raised papules (PICTURE). The remainder of her exam was normal. Her WBC was 8 with 31 % bands; hemoglobin was 13 and platelet count of 253,000. Her liver function tests were normal. Her LDH was elevated at 550 IU/L and ferritin elevated to 1411 ng/mL. Her RPR was negative in addition to ANA, HIV antibody, HIV PCR, respiratory viral PCR, monospot heterophile antibody, CMV and throat culture. Her complements were normal. The patient was admitted and started on high dose ibuprofen with continued fevers yet resolution of her rash. On hospital day four she was initiated on prednisone 20 mg daily with resolution of her fevers. She followed up with Rheumatology 3 weeks after discharge.
DISCUSSION: Fever and rash are common findings that the general internist (hospitalist) encounters. A stepwise approach to determining the etiology of this constellation of symptoms should be taken and careful attention should be taken to assure that a treatable cause is not overlooked. The differential diagnosis with erythematous, slightly edematous rash with fever includes reactive, viral exanthema, autoimmune/connective tissue disease, Adult Onset Still’s disease (ASD). Viral etiologies are to be considered given her sore throat, arthralgias and other nonspecific complaints. In our patient with fever and rash, the associated arthralgias clued the diagnosis of ASD. Currently there is no specific test or combination of tests that can be used to establish the diagnosis of ASD. The Yamaguchi criteria have the highest sensitivity in patients with a definite diagnosis of ASD. This criteria requires five features for diagnosis, two being the major criteria. ASD has been associated with markedly elevated serum ferritin concentrations in as much as seventy percent of patients.
RECURRENT VS. LINGERING LEGIONELLA? A CASE HIGHLIGHTS RISK FACTORS, DIAGNOSTIC CHALLENGES AND KNOWLEDGE GAPS IN THE AFTERMATH OF HURRICANE SANDYMadeline R. Sterling. New York Presbyterian - Weill Cornell, New York, NY. (Tracking ID #1927313)
LEARNING OBJECTIVE 1: Review clinical features of Legionella Pneumonia and understand how a clinical test (Urine Antigen) is applied and interpreted.
LEARNING OBJECTIVE 2: Demonstrate how the incidence of Legionnaire’s disease is affected by environmental exposures and patient characteristics.
CASE: A 73 year-old man with CLL (stage 3, on immunosuppression) and hospitalization 1 year prior for Legionella pneumonia, presents from home to our hospital with 3 days of intermittent fevers and 1 week of blood-tinged sputum. He reports a maximum oral temperature of 103 F, associated with a productive cough. He notes dyspnea and hemoptysis of blood-tinged sputum for the last week. He denies night sweats, weight loss, lymphadenopathy, rhinorrhea, headache, neck stiffness and chest pain. He is retired and is able to walk 20 city blocks without dyspnea at baseline. He denies recent travel or Tuberculosis exposure. The patient’s apartment was victim to flooding from Hurricane Sandy; his apartment sustained extensive water damage. He did not relocate due to finances. He has not been to a primary care provider since his last hospitalization. On presentation he was afebrile and breathing comfortably (O2sat 98 %) on 2 L NC. He was alert and oriented, speaking in full sentences, without blood in his oropharynx. His lung exam was notable for decreased breath sounds on the right, without dullness to percussion. CT was remarkable for diffuse bilateral groundglass opacities, right greater than left, suspicious for diffuse alveolar hemorrhage. Blood cultures, PCR for atypical pneumonias and fungal cultures were negative. Urine Legionella antigen was positive and he was treated with Levaquin for 7 days. The patient was hemodynamically stable and improving; a diagnostic bronchoscopy was deferred.
DISCUSSION: Legionella, which was first discovered in a 1976 Philadelphia outbreak linked to water supply and air conditioning units, is a common cause of community-acquired and nosocomial Pneumonias. When the clinical situation appropriate, a urine antigen test is used to detect L. pneumophila. The test, which is relatively cheap and rapid, has a sensitivity of 70 % and specificity of 99 %. Although easy to diagnose, clearance is difficult to pinpoint, particularly in immunocompromised hosts such as this patient. Following treatment, it is not recommended to check urine antigen in the outpatient setting, since false positive tests are likely in the short term. In fact, immunocompromised patients can shed the antigen upwards of 300 days post-treatment. Not only is this patient at risk due to his lymphoma treatment(s), but he remained in his flood-zone apartment during (and after) the largest Atlantic hurricane on record, Sandy. Although Legionella has an incubation of 2 to14 days after exposure, several hard-hit regions took several months to be restored and cleaned. It is unclear how flooding and stagnant water affected his clinical state and susceptibility for this bacterium. Further research ought to examine the association between hurricane-affected areas and disease incidence. If Legionella incidence is higher in flood zones, then patients with clinical risk factors or prior infections ought to be screened more vigilantly and counseled regarding early evacuation by their primary care providers.
RED, HOT, SWOLLEN, AND TENDER: A CASE OF CELLULITIS?Aderonke Salau-Okeleji2,1; Margaret C. Lo2,1. 1Univeristy of Florida, Gainesville, FL; 2University of Florida, Gainesville, FL. (Tracking ID #1939038)
LEARNING OBJECTIVE 1: Distinguish between the clinical, diagnostic, and therapeutic features of refractory cellulitis vs. drug-induced myositis
LEARNING OBJECTIVE 2: Recognize the adverse health effects of popular energy drinks, the associated risk factors in the development of these adverse effects, and the need for screening for abuse of energy drinks.
CASE: A 30 year-old healthy, athletic Caucasian male was admitted by his PCP for refractory cellulitis after he failed to respond to a 7-day course of oral doxycycline for worsening right arm swelling with pain and redness. He denied any trauma or associated fevers, chills, right arm paresthesia or weakness. Vital signs on admission were all normal including temperature. Physical exam revealed a severely erythematous right upper extremity with increased warmth, dependent +2 pitting edema and taut skin extending from proximal biceps to distal elbow. Rest of the cardiopulmonary, skin, musculoskeletal and neurologic exam was unremarkable. Admission laboratory values including BMP, CBC, CRP, ESR, and blood cultures were all normal. Upon hospitalization, the patient was started empirically on IV Vancomycin for presumed refractory cellulitis that had failed out patient management. However, when he failed to improve on hospital day 2, investigation for noninfectious causes was initiated in light of no other objective evidence of systemic infections. Right upper extremity Doppler ultrasound was negative for DVT. Further studies including CPK level came back severely elevated at 11640 U/L with corresponding elevated aldolase value of 30.8 U/L. Urine myoglobin and anti-Jo 1 antibody titers were negative; ESR/CRP levels remained normal. Subsequent MRI of the right arm showed nonspecific myositis and swelling of the biceps, brachialis, and pronator teres. Further history from the patient revealed that 1 week prior to presentation he and his friends had vacationed at South Beach for Spring Break week where he had “gone clubbing all night, every night” and had gone weight-lifting during the day. To stay awake, he would drink 3–4 cans/day of Red Bull and 2–3 shots/day of 5-hour Energy. With this history, antibiotics were discontinued and supportive measures including IV fluids, arm elevation, and ice were started. His right arm symptoms resolved and his CPK level normalized 2-weeks later at his PCP follow-up visit.
DISCUSSION: Energy drinks such as Red Bull, Monster, and 5-hour Energy have become quite the craze in young adult culture with self-report surveys of consumption in 30–50 % of adolescents and young adults. Touted for positive effects on physical and mental endurance, growing evidence in the literature has now surfaced that energy drinks are not as harmless as advertised. Multiple studies have revealed adverse health effects such as obesity, seizures, cardiac anomalies (hypertensive urgency, tachyarrhythmias), strokes, rhabdomyolysis, mood disorders (mania, anxiety attacks), and even death. Our case adds to the literature by highlighting the potential for energy drinks to cause myositis. Such clinical presentations can become a diagnostic challenge by mimicking cellulitis. However, unlike cellulitis, clinicians must recognize that drug-induced myositis exhibits no systemic signs of infection (i.e. fevers, leukocytosis, elevated ESR/CRP), often fail to respond to antibiotics, and produces severe CPK and aldolase elevation. Risk factors for incurring the detrimental effects of energy drinks include mixture with alcohol and dehydration. Sleep deprivation and extreme exercise workouts can also be included as risk factors, as revealed in our case. Since there are no current diagnostic guidelines for energy drink abuse, a detailed and targeted social history for energy drink ingestion, either alone or with alcohol, is instrumental in the prompt recognition and management of their adverse effects. Screening by clinicians is particularly important for athletes, young adults with high-risk behaviors, certain health conditions (i.e. seizures, diabetes, obesity, hypertension, cardiac anomalies), and those with unexplained myalgias/myositis, behavioral/mood changes, anorexia, or sleep problems.
REDISCOVERING AN ANCIENT DIAGNOSISStephanie Behringer; Gianni Carrozzi. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939336)
LEARNING OBJECTIVE 1: Recognize visceral manifestations of tertiary syphilis in a patient with hepatic lesions
CASE: A 32 year-old man with HIV (normal CD4 count, on HAART), high risk sexual behavior and polysubstance abuse presented with 4 weeks of vague abdominal pain. The pain was diffuse and dull in nature, intermittent and would last several days before resolving on its own. He denied fevers, chills or weight loss and was well appearing. Infectious workup was notable for a positive serum RPR test with a titer of 1:256, but was otherwise negative. His primary care doctor and the New York State Department of Health confirmed that he had been diagnosed with syphilis in the past. However, it was unclear whether he had been successfully treated, and he continued to engage in high-risk sexual behavior, exposing himself repeatedly to reinfections and had poor medical follow up. A CT scan of the abdomen revealed scattered ill-defined hypodense lesions within the liver.
DISCUSSION: Syphilis is caused by the spirochete Treponema pallidum and is virtually always sexually transmitted. About 6 % of patients with HIV infection have serologic evidence of syphilis. If left untreated, 25–40 % of patients will develop late phase syphilis, also known as tertiary syphilis. Tertiary syphilis can manifest itself anytime from 1 to 30 years after primary infection and has become a forgotten diagnosis in parts of the world where screening and antibiotic treatment have made advanced stages of this disease a rare finding. In the past, however, tertiary syphilis used to be a common diagnosis leading to visceral involvement with space occupying lesions known as syphilitic gummata (or syphilomata). These lesions are granulomas that contain a central necrosis and are surrounded by inflammatory tissue that can mimic metastatic disease or sarcoidosis. In some cases, they are found in the liver, but can develop in any organ. In cases of hepatic involvement, patients can present with abdominal discomfort, mild hepatitis, jaundice and fatigue. Depending on size and location, syphilitic gummata can cause portal hypertension, variceal bleeding, hepatic vein thrombosis, ascites and liver failure. They are not malignant in nature, but can lead to biliary obstruction. Antibiotic treatment usually results in complete resolution of the lesions. The diagnosis of tertiary syphilis with visceral involvement is confirmed by high serologic markers (serum RPR titer >1:32) and by response to treatment with penicillin. Biopsies of gummata may be indistinguishable from other granulomatous diseases unless spirochetes are visualized within the tissue samples. Treatment of tertiary syphilis requires a prolonged antibiotic course with penicillin as spirochetes are slowly growing bacteria. Therapeutic levels are achieved with long-acting depot penicillin preparations. The current guidelines recommend Benzathine penicillin G 2.4 million units IM once a week for a total of 3 weeks.
REDUCING POLYPHARMACY IN THE ELDERLY-ROUND AND ROUND WE GOCeleste Newby; Alegra Venditto. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924994)
LEARNING OBJECTIVE 1: Discuss the challenge of managing polypharmacy in the elderly.
LEARNING OBJECTIVE 2: Highlight physician barriers to reducing polypharmacy in the elderly and the need for greater evidence-based strategies to reduce polypharmacy
CASE: A 69-year-old man with multiple medical problems presented to his primary care physician (PCP) for medication review after expressing confusion about his regimen. He also sees four subspecialty physicians who manage his chronic diseases. Review of his medication list via the electronic medical record revealed twenty total medications; all five of his physicians had prescribed medications. As requested, the patient presented to clinic with his home medications in two large duffel bags containing a total of 45 medication bottles. In addition to his currently prescribed regimen, the patient had two expired antibiotics, three duplicate medications, and medications for blood pressure and muscle pain that had been previously discontinued. After review, 25 medication bottles were given to pharmacy for destruction. A complete medication list, including essential and as-needed medications, was reviewed with patient. The electronic medical record was reconciled accordingly, with all extraneous medications eliminated. The patient returned to primary care clinic 1 month later after seeing several specialists. Four new medications had been added to his list. Again, the medication list was reviewed and edited with the patient as it had been the month prior.
DISCUSSION: Polypharmacy is a well-known topic to most internists, and an important consideration in caring for any elderly patient. One in six hospital admissions (one in three for age >75) for older adults can be attributed to an adverse drug effect. Older patients often have multiple chronic diseases, and long medication lists consisting of both essential and as-needed prescriptions. The clinical picture is complicated further by multiple prescribers. Medication lists can easily grow or change when patients have new complaints or are involved in care transitions. Even with electronic medical records, keeping medication lists current and appropriate can be a daunting task. The PCP often feels a responsibility to reduce polypharmacy, as he or she is the main coordinator of a patient’s care. While studies have reported that the number of prescribing physicians is an independent risk factor for adverse drug reactions in the elderly, physicians report awkwardness and reluctance to discontinue a medication prescribed by another physician. Additional barriers include difficulty in convincing patients to discontinue long-term medications, and problems distinguishing between new complaints and medication side effects. While there is great interest in improving appropriate medication use in the elderly, how to best accomplish this goal is still unclear. A recent Cochrane review found that while the Beers criteria and Medication Appropriateness Index (MAI) appeared beneficial in reducing medication-related problems and inappropriate prescribing, it was not clear that these interventions translated into clinically significant improvements. More evidence-based strategies are needed to implement meaningful change in the area of polypharmacy to improve safety for older patients.
REFRACTORY HYPOGLYCEMIA IN A TYPE 1 DIABETIC PATIENT - CLUE TO ADDISON’S DISEASE AND AUTOIMMUNE POLYENDOCRINE SYNDROME TYPE 2Anene Ukaigwe; Adetokunbo Oluwasanjo. The Reading Health System, West Reading, PA. (Tracking ID #1936686)
LEARNING OBJECTIVE 1: Recognize features of Autoimmune Polyendocrine Syndrome type 2 (APS-2).
LEARNING OBJECTIVE 2: Manage and appropriately screen APS-2 patients.
CASE: A 47-year-old Caucasian female presented for the third time to the emergency room with hypoglycemia and hypotension. For 3 months, she had recurrent hypotension, hypoglycemia, fatigue, orthostatic dizziness, weight loss and vomiting. She had a 16-year history of T1DM. Glycemic control was stable for 6 years on same dose of insulin. She had hypothyroidism for 5 years, also stable on levothyroxine. She denied recent travel, lifestyle or medication changes. Insulin dose was adjusted several times but hypoglycemic episodes persisted, occurring 2–3 times weekly. For her symptoms, she had seen a Cardiologist, Neurologist, Otorhinolaryngologist, Primary Care and Emergency Physicians. Work up thus far excluded Multiple Sclerosis, cobalamin deficiency, myasthenia gravis, hemochromatosis, vestibular, cardiac and rheumatologic disease. On examination she was alert and oriented, hypotensive; Blood Pressure = 87/53 mmHg and tachycardic; Heart rate = 124/min. Her skin was diffusely tan. The remaining exam was unrevealing. Labs showed Complete Blood Count, renal, liver and thyroid function tests were within normal range. Blood glucose was 70 mg/dl. Adrenal insufficiency was suspected based on hypoglycemia, hypotension, tachycardia and tan skin. This was confirmed with serum cortisol = 0.8mcg/ml (normal 8.7–22.4mcg/dl) and ACTH = 298 pg/ml (normal 10–60 pg/ml). After intravenous hydrocortisone and fluids, symptoms resolved. Given hypothyroidism, adrenal insufficiency and T1DM further antibody tests confirmed APS-2.
DISCUSSION: APS-2 is an autosomal dominant disease affecting HLA genes. APS-2 is characterized by Addison’s disease, autoimmune thyroid disease and type I diabetes mellitus. Other associated disorders include Pernicious anemia, celiac disease, Hepatitis, Hypogonadism, Hypophysitis, vitiligo. Unlike APS-2, APS-1 affects only children. APS-2 occurs more in females and is often diagnosed between ages 30s to 40s. Although APS-2 is uncommon (1.4–4.5 per 100,000), its prevalence increases when subclinical cases are included (150 per 100,000) implying it is not as rare as believed. The clinical presentation depends on specific APS-2 component disorders and involved organs. However, conventional treatment for each component disorder is often sufficient. Specialist care is required only as needed. The importance of APS-2 is illustrated in our patient. More than one APS-2 disorder should raise vigilance for associated disorders given that clinical features of these disorders are nonspecific. In addition, the interval between development of one disorder and the next can be as long as 20 years, making screening necessary for early initiation of disease-specific management. Experts recommend that patients with two APS-2 disorders should be screened every 1–2 years until 50 years old. In addition to detailed history and physical examination, screening includes autoantibody testing for T1DM, thyroid disease, Addison’s disease, Celiac disease and autoimmune hepatitis. Vitamin B12, sex hormone and blood glucose levels including liver and thyroid function tests are also useful.
RELATED CEREBRAL HEMORRHAGE WITH AN INFECTED ABDOMINAL AORTIC ANEURYSM AND VERTEBRAL OSTEOMYELITIS?Suzue Hirano-Kuwata; Yumiko Kanzaki; Hirokazu Mizohata; Keishi Kuriyama; Kentaro Isoda; Kenichiro Hata; Yukimasa Ooi; Akira Ukimura. Osaka Medical College Hospital, Takatsuki, Osaka, Japan. (Tracking ID #1934970)
LEARNING OBJECTIVE 1: Manage the complications of bacteremia.
LEARNING OBJECTIVE 2: Recognize the causes of intracranial hemorrhage.
CASE: A 73-year-old man with hypertension, coronary artery disease, and peripheral artery disease presented with severe lumbago and fever. Despite several different types of intravenous antibiotic treatments at another hospital, his symptoms remained over 2 weeks. He was transferred to our institution for further treatments. On admission, his body temperature was 38.0, his heart rate was 74 beats/min, and respiratory rate was 18 breaths/min. Laboratory studies showed a WBC count of 10160/μL (79 % neutrophils, 13 % lymphocytes), and a CRP concentration of 155 mg/L. He was diagnosed as vertebral osteomyelitis (disk-space infection) based on a hyperintense lesion of the spine on MRI. Streptococcus sanguinis was detected in one of three blood cultures. The transthoracic echocardiogram revealed no valvular vegetation, no other evidence of infective endocarditis, nor any regurgitant murmur was heard. His symptoms gradually improved with antibiotic therapy, but a CT scan showed a newly developed abdominal aortic aneurysm with periaortic soft tissue infiltration. The diameter of the abdominal aorta was 35 mm; it had been 20 mm on admission and we recognized it as an infectious aortic aneurysm. The aneurysm was adjacent to the vertebral osteomyelitis and despite sustained antibiotic treatment, the aneurysm enlarged. Eventually he had a graft implantation operation and was discharged 22 days after surgery. Two months after the aortic operation, he presented with left hemiplegia. A CT scan of the head showed a right putamenal hemorrhage, and he had an open craniotomy and an evacuation of the hematoma. He survived but was left with significant disability.
DISCUSSION: We describe a case of vertebral osteomyelitis, an infected abdominal aneurysm, and cerebral hemorrhage, which occurred in a short period of time. One possible cause of all three phenomena is hematogenous spread of infection. Vertebral osteomyelitis most often results from hematogenous seeding. Infected aortic aneurysms are also related to hematogenous spread of infection. Co-existence of an infected aneurysm and vertebral osteomyelitis is occasionally reported, and is thought to be caused by contiguous involvement of the vessel wall from adjacent pyogenic vertebra. Our patient presented with cerebral hemorrhage only 4 months after the initial symptoms. The most common cause of cerebral hemorrhage is hypertension, but intracranial infectious aneurysm is one of the causes. A minimum of 4 to 6 weeks of antimicrobial therapy is recommended for intracranial infectious aneurysm, but there remains a high risk for rupture even during appropriate medical treatment. It may be beneficial to perform cerebrovascular imaging on patients with a suspected infectious aneurysm. We are not sure whether this cerebral hemorrhage is relevant to an infected cerebral aneurysm, without previous examinations of cerebral arteries. This case involved vertebral osteomyelitis with an adjacent infected aneurysm and subsequent cerebral hemorrhage. Hematogenous spread of infection can explain the sequence of phenomena, though it is not proven. This case provides us an opportunity to consider further therapeutic plans that might lead to a better prognosis.
RESISTANT HYPOGLYCEMIA FROM GLYBURIDE-CIPROFLOXACIN INTERACTIONSuzanne J. Supplee; Anthony A. Donato. Reading Health System, West Reading, PA. (Tracking ID #1939107)
LEARNING OBJECTIVE 1: Recognize a drug interaction between glyburide and ciprofloxacin may lead to potentially fatal hypoglycemia.
CASE: A 50 year-old male with a history of diabetes mellitus type 2 on long-term combination glyburide/metformin therapy who was recently treated with a 14 day course of ciprofloxacin for venous stasis ulcers presented to the ED after his sister noticed he was disoriented, mumbling, diaphoretic and unarousable, but exam was otherwise non-focal. EMS recorded a finger stick blood glucose at 33 mg/dl. The patient was given one ampule of D50 en route. Upon arrival to the ED, the patient required another 3 ampules of D50 to get serum glucose over 100 mg/dl. A 5 % dextrose in half normal saline solution at 150 ml/h was required to stabilize his blood sugars over the next 24 h. The patient denied any recent change in medications except for the ciprofloxacin course completed 10 days prior, and in fact had not taken the oral hypoglycemic in the 24 h leading up to admission. He denied medication misuse, exogenous insulin or alcohol use. He denied any previous episodes of hypoglycemia. Laboratory values included a normal TSH and WBC count. Abdominal CT was negative for pancreatic mass. Abnormal laboratory values at the time of hypoglycemia included a C-peptide of 8.1 ng/ml (normal: 1.1–4.4 ng/ml) and free Insulin of 59 μ IU/ml (normal: 1.4–14 μ IU/ml).
DISCUSSION: Hypoglycemia is a common medical complication in patients receiving pharmacotherapy for diabetes that may result in permanent neurologic deficits and even death if unrecognized. With over 285 million people diagnosed with diabetes worldwide, many require oral hypoglycemic agents for disease management. A possible interaction between glyburide and ciprofloxacin has been reported, resulting in reduced drug clearance and a prolonged hypoglycemic effect of glyburide. Recognition of potential drug side effects is critical in the management of complex medical patients. Ciprofloxacin causing hypoglycemia in patients taking glyburide may be under-reported as the mechanism of action is poorly understood, therefore a causal relationship overlooked. A thorough medication history in hypoglycemia is essential to uncover potential adverse drug interactions. In patients on sulfonylurea therapy presenting with hypoglycemia of unknown etiology, ciprofloxacin should be considered as a potential cause and prescribed cautiously in patients currently on glyburide therapy.
RETIFORM PURPURA AS A CLUE TO DIAGNOSISSarah Apgar. Yale-New Haven Hospital, New Haven, CT. (Tracking ID #1938728)
LEARNING OBJECTIVE 1: Recognize the clinical features of retiform purpura
LEARNING OBJECTIVE 2: Understand the differential diagnosis of retiform pupura
CASE: A 50 year-old asplenic man with a history of hypertension presented with 4 days of nausea, vomiting and diarrhea and 1 day of lower extremity burning pain and numbness. Two days prior to admission he noted red spots on his upper thighs which became larger blotches on his feet and ankles followed by bluish discoloration of his third toe. Upon admission, he was afebrile, tachycardic at 125 with a blood pressure of 123/82. Physical examination demonstrated an ill man with a non-blanching purple mottled rash on the legs and feet without neurologic deficit. Blood work revealed a creatinine of 4.8 mg/dl, white blood cell count of 40 with 36 % bands, platelet count of 67, normal coagulation studies and lactic acid of 3.3. He was admitted to the intensive care unit and started on broad spectrum antibiotics and intravenous fluids. Further investigation revealed a D-dimer of >10,000, fibrinogen of 959, negative anti-cardiolipin antibodies and ANA < 1:40. A skin biopsy was compatible with disseminated intravascular coagulation and purpura fulminans without evidence of vasculitis. Extensive infectious evaluation did not reveal a specific pathogen as the etiology of his sepsis. The patient subsequently required a transmetatarsal amputation of the left foot, as well as amputation of his third and fifth toes on the right for treatment of gangrene.
DISCUSSION: Purpura is defined as visible hemorrhage into the skin or mucous membranes. It can be classified by size, palpability of the lesions and presence of the livedoid pattern. Retiform purpura results from occlusion in the vessels that cause the livedo reticularis pattern. What is observed clinically is hemorrhage into the skin around occluded dermal vessels resulting in a “puzzle-piece” morphology. Two major causes include vasculitis and microvascular occlusion syndromes which manifest as inflammatory or non-inflammatory retiform purpura respectively. The major distinguishing factor between the two is palpability of the lesion; however, there is significant overlap clinically and often a biopsy is required for diagnosis. Microvascular occlusion syndromes can be caused by thrombotic, embolic or infectious phenomena. Some common etiologies include anti-phospholipid antibody syndrome, calciphylaxis, warfarin necrosis, cholesterol emboli and disseminated intravascular coagulation (DIC). DIC results from massive activation of the clotting cascade and manifests clinically with either bleeding or thrombosis. Purpura fulminans is a severe form of DIC which results in extensive areas of skin necrosis usually over the extremities and buttocks. It is most frequently found in the setting of sepsis, specifically with encapsulated organisms, placing asplenic patients at high risk. Typical laboratory findings in DIC include elevated D-dimer, prolonged clotting times, thrombocytopenia and low fibrinogen; however, the balance between thrombin generation, clotting factor depletion and thrombolysis can lead to variable results. In this case, the diagnosis of DIC was originally questioned given the elevated fibrinogen level, resulting in a delay in starting anticoagulation. Subsequent recognition of the clinical exam finding of purpura fulminans led to initiation of treatment with later pathologic confirmation on skin biopsy. This case highlights the importance of recognizing the clinical exam finding of retiform purpura as this will guide the differential diagnosis of a patient with sepsis and a rash.
RETROPERITONEAL FIBROSIS AND PERIAORTITIS, IS THIS AN IGG4-RELATED DISEASE?Laila Shiekh Sroujieh1; Alexis C. Haftka1; Iyer Gayathri2. 1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Detroit, MI. (Tracking ID #1935038)
LEARNING OBJECTIVE 1: Identify IgG4 related systemic disease as a disease of multiorgan involvement that’s been newly recognized
LEARNING OBJECTIVE 2: Identify retroperitoneal fibrosis extending to iliac vessels as a cause of compression and venous stasis followed by DVT/PE
CASE: A 50 year old male patient with past history of hypertension, CKD and chronic lymphedema presented to the ED complaining of shortness of breath, chest pain, fever and cough. In the ED he was febrile, tachypnic and tachycardic. His labs revealed a white cell count of 14.7. Physical examination was unremarkable except for chronic edema in bilateral lower extremities. CXR revealed airspace disease that was questionable for pneumonia. He was started on antibiotics and was admitted as a case of CAP. In addition to his respiratory symptoms, he was complaining of severe abdominal pain. Abdomen CT scan was obtained and revealed a large pericardial effusion, retroperitoneal fibrosis and left hydroureter. A 2D echo was then obtained and revealed concern for cardiac tamponade in addition to aortic root and ascending aortic dilation. Pericardiocentesis was then performed with removal of 410 ml of serosanguinous fluid, with eventual drainage of an additional 160 ml by pericardial drain post procedure. Chest CT scan was obtained to evaluate the aorta and it confirmed aortic root and ascending aorta dilatation. Chest CT scan also revealed multiple bilateral segmental and subsegmental pulmonary emboli. Heparin drip was started. Bilateral lower extremity dopplers were obtained and were positive for an acute left peroneal DVT. Outside records were obtained showing presence of retroperitoneal fibrosis and history of aortic dissection and aneurysm back in 2010. In light of all these findings diagnosis of IgG4 related disease was a concern. Rheumatology was consulted and they thought that with the retroperitoneal fibrosis and history of aortic dissection and aneurysm back in 2010, IgG4 disease is the likely etiology of extensive fibrosis with peri-/aortic involvement. A biopsy of the retroperitoneal fibrosis was done and was sent for special staining for IgG4. Results of the biopsy are still pending. Patient was started on high dose steroids (1 mg/kg) and was discharged home with a plan to follow up with rheumatology for steroid tapering and repeat CT scan as outpatient pending biopsy results.
DISCUSSION: IgG4 related disease is a newly recognized multisystem disease. It has been described in every organ system: the biliary tree, salivary glands, periorbital tissues, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate, thyroid, pericardium, and skin. Many medical conditions that have long been viewed as conditions confined to single organs are now acknowledged to fall within the Spectrum of IgG4-Related Disease. For example Mikulicz’s syndrome (affecting the salivary and lacrimal glands), Küttner’s tumor (affecting the submandibular glands), Riedel’s thyroiditis, Retroperitoneal fibrosis (Ormond’s disease) Periaortitis and periarteritis to name a few. These different conditions were previously thought to be unrelated. The pathogenesis of IgG4-related disease (IgG4-RD) is poorly understood. Diagnosis of IgG4-related disease is defined by both elevated serum IgG4 (>1.35 g/l) and histopathological features, including storiform fibrosis, obliterative phlebitis, and lymphocyte and IgG4+ plasma cell infiltration (IgG4+ plasma cells/IgG+ plasma cells ratio >50 % on a highly magnified slide); tissue eosinophilia may also be present. Glucocorticoids are typically the first line of therapy. They appear to be effective in the majority of patients but disease flares are common. Azathioprine, mycophenolate mofetil, and methotrexate are used frequently as glucocorticoid-sparing agents or remission-maintenance drugs after glucocorticoid induced remissions. For patients with recurrent or refractory disease, B-cell depletion with rituximab appears to be a useful approach. Additionally, there have been case reports and studies about the development of lower extremity DVTs leading to PEs in patients with retroperitoneal fibrosis due to involvement of iliac vessels and in those cases treatment was steroids in addition to anticoagulation.
RETROPERITONEAL HEMORRHAGE ARISING FROM A RENAL MASS: A CASE REPORTJean Canham. University of North Dakota School of Medicine and Health Sciences, Bismarck, ND. (Tracking ID #1924635)
LEARNING OBJECTIVE 1: Recognize the possibility of spontaneous hemorrhage as a complication of anticoagulation in the setting of renal cell carcinoma.
CASE: A 91 year old female with a past medical history significant for stasis dermatitis, lower extremity edema, and a known left renal mass presented to the emergency department with complaints of a swollen and painful right leg of 1 day’s duration. The renal mass had been previously detected on a CT scan, but the patient and her family had declined any work-up or treatment for it because of her advanced age. Physical exam revealed 3+ edema and redness to the mid-thigh of the right lower extremity. Initial labs included a CBC demonstrating WBC of 11.6 and a microcytic anemia with a hemoglobin of 10.5. Doppler ultrasound of the right lower extremity revealed a large occlusive thrombus extending from the common femoral to the popliteal vein. She was admitted and started on therapeutic heparin and warfarin. The patient initially improved on anticoagulation therapy, but 36 h after starting heparin she began to experience left flank pain. A drop in her hemoglobin was noted. An abdominal CT was performed which revealed internal hemorrhage of the left renal mass, which appeared to represent likely renal cell carcinoma. A large amount of blood and hematoma were seen in the left retroperitoneum. An extensive tumor thrombus extending from left renal vein to the inferior vena cava was also seen. Heparin was immediately stopped and vitamin K was administered. Despite these measures, her hemoglobin continued to drop and she became hypotensive. Resuscitative efforts were initiated, but her hemodynamics failed to improve and the patient expired.
DISCUSSION: Renal cell carcinoma is known to be highly vascular, posing bleeding complications in surgical settings. However, little is known about the risk of spontaneous hemorrhage in RCC when anticoagulation therapy is initiated. Anticoagulation brings with it the inherent risk of bleeding, but this case forces us to ask if patients with renal cell carcinoma are particularly vulnerable to catastrophic spontaneous hemorrhage when anticoagulated.
REVENGE OF VIRCHOW’S TRIAD: MAY-THURNER SYNDROMEMegan Sisk; Paula Wichienkuer; Mark Gibson. PPMC, Portland, OR. (Tracking ID #1896509)
LEARNING OBJECTIVE 1: May-Thurner syndrome should be considered in cases of DVT in young patients, unprovoked clot, or extensive proximal clot burden.
LEARNING OBJECTIVE 2: Definitive treatment should be pursued if the patient is symptomatic from complications related to May-Thurner.
CASE: A 59 year old man presented to the ED with acute onset of left lower extremity swelling. His leg was normal at 6 am and by noon he had significant swelling, pain, and was unable to ambulate. On physical exam he had 3+ edema to the thigh, cyanosis, and the dorsal pedis pulse could be found using Doppler only. Ultrasound showed extensive occlusive clot burden extending from the left common femoral, profunda femoris, and proximal femoral veins. Due to concern for limb ischemia, he was taken for catheter directed thrombolysis. CT imaging for preparation of vascular access showed occlusive clot and compression of the left common iliac vein consistent with May-Thurner Syndrome. After 24 h of thrombolysis, the catheter was removed and angioplasty with stent placement of the left common iliac vein was performed. By day 4, the patient was discharged with complete resolution of his symptoms.
DISCUSSION: In 1851, Virchow first proposed the idea that a LLE clot could be caused by this compression of the vein by the artery. In 1957, May and Thurner confirmed this idea and the principles of Virchow’s Triad through autopsy studies where they noted effects of endothelial damage and turbulent flow. May-Thurner Syndrome leads to DVT of the left lower extremity due to the narrowed turbulent flow caused by the compression and repetitive trauma on the left common iliac vein. The vein traverses between the right common iliac artery where it can be compressed against the spine at L5. Additionally, the constant pulsatile force leads to fibrosis of the vein wall. May-Thurner Syndrome is being identified more often due to an increase in catheter directed endovascular treatments. While findings are often found incidentally during CT or ultrasound, venogram remains the gold standard. Treatment typically involves angioplasty with stent placement to support the vein from further compression. The exact length of anticoagulation and recommendations regarding prophylactic stenting remain controversial. This case demonstrates the importance of evaluation for additional causes in an unprovoked DVT. May-Thurner syndrome should be considered in cases of DVT in young patients, unprovoked clot, or extensive proximal clot burden. Definitive treatment should be pursued if the patient is symptomatic from complications related to May-Thurner.
REVERSIBLE ENCEPHALOPATHY IN AN ELDERLY PATIENT WITH END-STAGE RENAL DISEASENaoki Misumida; Krupa Majmundar. Beth Israel Medical Center, New York, NY. (Tracking ID #1925564)
LEARNING OBJECTIVE 1: Recognize cefepime-induced encephalopathy as a cause of altered mental status in patients with chronic kidney disease.
LEARNING OBJECTIVE 2: Review the typical clinical course of cefepime-induced encephalopathy.
CASE: A 93 year-old female with a history of end-stage renal disease on hemodialysis presented from nursing home with a five-day history of shortness of breath and dry cough. Her blood pressure was 131/66 mmHg, heart rate was 65/min and SpO2 was 92 % on room air. She was afebrile. Her cognitive function was unchanged from her baseline and neurological examination was unremarkable. She had coarse crackles on right lung base. Laboratory data did not show leukocytosis. Chest X-ray showed right lower lobe infiltration. She was admitted for suspected healthcare-associated pneumonia and fluid overload, and treated with cefepime (2 g/day), vancomycin (500 mg, once) and azithromycin (500 mg/day). Hemodialysis was performed on the following day and her dry weight was lowered. After hemodialysis, her respiratory condition improved and the infiltration on chest X-ray resolved. All of the antibiotics were discontinued based on her clinical improvement on the second day. On the third day, she became confused with temporo-spacial disorientation and expressive dysphasia. Extensive work-up including laboratory tests, head CT scan and brain MRI did not reveal the cause of acute mental status change. Metabolic encephalopathy and central nervous system infection were considered and excluded. She started to improve gradually on the fifth day and returned to her baseline level of mental status on the sixth day. Because of the temporal association of the symptom onset and drug administration, as well as complete improvement after drug discontinuation, a final diagnosis of cefepime-induced encephalopathy was made. Patient was discharged without any sequelae.
DISCUSSION: Cefepime is a fourth-generation cephalosporin used to treat severe infection, which is mainly excreted by the kidney. Cefepime-induced encephalopathy has been sporadically reported worldwide over the last decade. The neurotoxic side effects are likely secondary to suppression of inhibitory neurotransmission mediated through gamma-aminobutyric acid-A receptor. A review of 42 cases of cefepime-induced encephalopathy most commonly observed confusion with temporo-spatial disorientation (96 %), myoclonus (33 %) and seizures (13 %) in affected patients. Almost all affected patients have had renal failure and the dose of cefepime was relatively higher for the level of renal failure. In our case, the dosage of cefepime should have been adjusted more precisely according to the creatinine clearance even though it was stopped on the second day. The latency varied between 1 to 10 days. Symptoms usually regress within 2 to 7 days after stopping cefepime. In conclusion, physicians need to be aware of this potential adverse effect although it is uncommon. To avoid this complication, dose adjustment should be undertaken in patients with chronic kidney disease.
REVERSIBLE MYELONEUROPATHY IN A YOUNG WOMANXimena A. Levander1; Traci A. Takahashi3,1; Maxwell Ma2. 1University of Washington, Seattle, WA; 2University of Washington, Seattle, WA; 3VA Puget Sound Healthcare System, Seattle, WA. (Tracking ID #1928649)
LEARNING OBJECTIVE 1: Diagnose B12 deficiency and distinguish it from other etiologies of myeloneuropathy.
LEARNING OBJECTIVE 2: Recognize nitric oxide abuse as a potential cause of B12 deficiency.
CASE: A 35-year-old woman presented to clinic with 1 week of bilateral upper and lower extremity numbness. The paraesthesias occurred suddenly and felt like her extremities “fell asleep but never woke up.” She also reported difficulty ambulating, requiring a cane to walk even short distances. Symptoms had neither improved nor worsened since onset. Review of systems was notably negative for vision changes, headaches, new neck or back pain, and urinary or bowel incontinence. She denied any recent infections, sick contacts, travel, injury or immunizations. Medical history was significant for PTSD, depression, chronic pain, and cervical and lumbar surgeries. Her medications included morphine, etodolac, citalopram, lorazepam and a multi-vitamin. Family history was unremarkable. She had a 20-pack-year smoking history but denied any alcohol or illicit drug use. On physical exam she had normal vital signs except for a BMI of 30. Her neurological exam was notable for decreased pinprick sensation in a stocking and glove distribution bilaterally and hyper-reflexia in the lower extremities. Her gait exam demonstrated spasticity and sensory ataxia such that she was unable to ambulate unassisted. The neurology service admitted her and initial laboratory results were notable for normal electrolytes and a slight normocytic anemia. She had normal TSH and copper levels. Her RPR, treponemal antibody and ANA panel were negative. Her B12 level was 253 pg/mL (normal >211 pg/mL). Both her methylmalonic acid and homocysteine were elevated. MRI brain was unremarkable. MRI C and T spine demonstrated non-contiguous bilateral dorsal column lesions with high T2 signal that was non-enhancing with contrast. On further questioning, she revealed almost daily use of inhaled nitrous oxide for the past few weeks. She was started on cobalamin 1,000 mcg IM daily for 6 doses then switched to 1,000 mcg PO daily for 2 months. She was discharged to rehab and advised to stop using nitrous oxide. Within 1 month her ataxia resolved and she only had minor residual sensory deficits. In 2 months her B12 level was 1,092 pg/ml.
DISCUSSION: Nitrous oxide is an inhaled anesthetic used in minor medical and dental procedures. Its recreational use started shortly after its discovery in the eighteenth century, when English chemist Humphry Davy demonstrated its psychogenic effects. Today, nitrous oxide continues to be an inhaled drug of abuse, obtained from medical settings or from whipped cream cartridges, commonly referred to as whippets. The toxicity of nitrous oxide is thought to be caused by irreversible binding of the cobalt ion in cobalamin, rendering it unable to function as a coenzyme with methionine synthase. The enzymatic reactions catalyzed by methionine synthase are critical for DNA synthesis and for regeneration of carbon donor groups. Primary care providers need to be aware of the medical complications of nitrous oxide abuse since patients may present to clinic with its sequelae and may not readily volunteer information regarding abuse on social history screening. The differential diagnosis for our patient’s initial presentation was extensive and most worrisome for anatomic injury given her spinal surgical history but also included autoimmune conditions, malignancies, nutritional deficiencies and infections. Her MRI findings were consistent with many conditions on this differential and a lumbar puncture with cerebrospinal fluid analysis was the next step in evaluation. However, the patient later revealed her substance abuse history deeming this diagnostic procedure unnecessary. A high degree of suspicion was required given she denied any substance abuse both in clinic and to the initial inpatient team. Case reports of nitrous oxide toxicity have been described in toxicology, neurology, emergency medicine and anesthesiology texts and highlight patients presenting with myeloneuropathy and/or megaloblastic anemia. Most patients reported prolonged nitrous oxide abuse and had true B12 deficiency, unlike our patient who had a borderline low normal B12 level. Because of this lab value and her well-nourished appearance, the inpatient team tested her methylmalonic acid and homocysteine levels, which came back elevated. Given her presenting symptoms, MRI findings and the lab results, as well as her response to high dose B12 repletion, nitrous oxide had caused an effective B12 deficiency. Fortunately, symptoms of nitrous oxide abuse related cobalamin deficiency often resolve upon stopping nitrous oxide use and aggressively repleting B12.
REVERSIBLE POSTERIOR LEUKOENCEPHALOPATHY SYNDROME: MRI SAYS IT ALLCharu Ramchandani; Waleed Quwatli; Chris Burke. Unity Health System, Rochester, NY. (Tracking ID #1939239)
LEARNING OBJECTIVE 1: Recognizing the clinical and radiologic findings in reversible posterior leukoencephalopathy syndrome for the timely initiation of treatment.
CASE: A 28 year old African American female presented to the hospital with a constant headache in the frontal region, 9/10 in severity not responding to over the counter pain medications. The pain was associated with fever, nausea, right sided neck pain, blurred vision and photophobia. She was seen by her primary care doctor a week ago who prescribed her amoxicillin for sore throat. Her past medical history was significant for viral meningitis in 2006 and atopic eczema. There was no significant family history. She denied any recent sick contacts or travel outside the country. On physical examination, vital signs were stable, oral examination revealed mild pharyngeal erythema, and pain on flexion of the neck. There was no associated photophobia, vesicular rash or any focal neurologic deficits. Laboratory values were remarkable for white blood cell count 17000/cu mm; Cerebro-spinal fluid (CSF) showed - 8/cu mm of red blood cell, 15/cu mm WBC with 26 % segmented cells and no organisms on gram stain. CSF protein and glucose were 17.5 and 54.5 mg/dl respectively. Head Computed tomography (CT) scan with contrast was normal. Patient was seen by the infectious disease concerning for meningitis for which she was started on Vancomycin, Ceftriaxone and Acyclovir with a pending CSF culture and polymerase chain reaction (PCR) for Herpes simplex virus (HSV) 1 and 2. Three days after the admission, patient continued to have persistent headache, nausea, vomiting and her antibiotics were stopped because PCR for HSV and CSF culture came back to be negative. On the 7th day, she experienced two episodes of generalized tonic clonic seizure along with hypertensive urgency/persistently elevated blood pressure readings. Immediately, she was started on Keppra for seizures and Nicardipine drip for her blood pressure control and was taken for a repeat CT scan. Repeat CT head showed decreased attenuation within the right parieto-ocipital region which was suspicious for an acute infarct. Magnetic resonance imaging (MRI) showed numerous areas of patchy ill-defined high T2 and flair signal in bilateral supra- and infra-tentorial white matter with effacement of overlying sulci and fissures suggestive of reversible posterior leukoencephalopathy. Over the next few days, Nicardipine was stopped and she was started on oral Labetalol. After controlling for her high blood pressure, her headache and blurry vision resolved, and she was discharged home on a regimen of oral Labetalol. A repeat MRI month after the discharge showed resolution of the high T2 flair signal in bilateral supra- and infra-tentorial white matter along with continued improvement in her symptoms.
DISCUSSION: Reversible posterior leukoencephalopathy syndrome (RPLS) is a clinic-radio-neurologic entity presenting as headache, visual symptoms, seizure with accompanying symmetrical white matter edema in posterior cerebral hemispheres on MRI brain. Hypertensive encephalopathy, eclampsia and use of cytotoxic or immunosuppressant drugs are the most common causes of RPLS. Etiology remains unclear, but some of the proposed mechanisms which could lead to RPLS are: (1) failure of auto-regulation of cerebral blood flow in severe hypertension leading to cerebral hyperperfusion and breakdown of blood brain barrier; (2) damage of vascular endothelium with cytotoxic agents leading to disruption of blood brain barrier and vasogenic edema. Primary involvement of the parieto-occipital region is not well understood. MRI is the best diagnostic modality to support the diagnoses of RPLS. Treatment consists of rapid lowering of blood pressure and discontinuation of any offending agent as mentioned earlier. In this case report, the patient was neither pregnant nor on any immunosuppressive drugs and the most likely underlying etiology/triggering event could be the rapid elevation of blood pressure on an unrecognized essential hypertension. Improvement of her symptoms with control of hypertension and resolution of MRI findings further supports the diagnosis of RPLS. RPLS can be easily confused with a stroke/stroke mimic based on CT scan findings and MRI should be obtained to help differentiate the diagnoses. Differentiating RPLS from stroke is very important for early management strategies in both the conditions. RPLS is a reversible condition if recognized early and treated promptly. It is essential for the internists to recognize this entity early to avoid long term complications in patients presenting in a similar fashion.
RIBBON-SHAPED STOOL IS NOT ALWAYS CANCERMaryam Sattari; Ravneet Bajwa; Robert S. Egerman. univeristy of Florida, Gainesville, FL. (Tracking ID #1935612)
LEARNING OBJECTIVE 1: Recognize signs and symptoms of retroperitoneal fibrosis
LEARNING OBJECTIVE 2: Become familiar with diagnosis, management, and treatment options for retroperitoneal fibrosis
CASE: A 47-year-old male presented with 2 months of abdominal pain, constipation, fatigue, and 20-lbs. weight loss. He described “something pushing” on his colon and the urge to defecate. He had also noted a change in his stool caliber and described straining 4–6 times daily and difficulty passing “ribbon shaped” stools. Past medical history was remarkable for migraine headaches and use of ergot-based medications 10 years prior to presentation. Physical exam, including vital signs, was normal. Labs, including CBC and renal function, were also normal. Abdominal and pelvic CT scan showed periaortic soft tissue thickening surrounding the infrarenal abdominal aorta and proximal common iliac arteries, suggestive of retroperitoneal fibrosis (RF). Peripheral blood flow cytometry did not show atypical findings. Colonoscopy and EGD were normal. Patient was started on high dose steroids (1 mg/kg), reported complete symptom resolution within days, and had marked radiographic improvement in the extent of disease. After a month, daily prednisone dose was decreased to 10 mg. After remaining symptom-free and having stable imaging for 8 months, patient presented to an outside facility with recurrent symptoms, including “flat stools.” Outside CT reported aortitis. Addition of cellcept has resulted in improvement of his symptoms to date.
DISCUSSION: RF encompasses a range of diseases characterized by presence of fibro-inflammatory tissue in the retroperitoneum. Presenting signs and symptoms are non-specific and include fever, pain in abdomen/flank/back, anorexia, weight loss, renal failure, hypertension, and deep venous thrombosis. While the majority of RF cases are idiopathic, others are associated with recognized etiologies, such as malignancy, certain infections, drugs (e.g. ergotomines, hydralazine and beta blockers), abdominal aortic aneurysm, radiation therapy, surgery, or trauma. It has also been suggested that RF is mediated by the immune system. In fact, idiopathic RF may be part of a systemic fibrosing disease, such as immunoglobulin G4 (IgG4)-related disease. We believe our patient’s RF is either IgG-related or associated with his previous use of Ergot compounds. Laboratory findings are also nonspecific and consist of anemia and elevated erythrocyte sedimentation rate and serum creatinine. CT and MRI are the best diagnostic modalities for RF. As illustrated by our case, classical radiographic findings include a confluent mass surrounding the infrarenal aorta and other retroperitoneal structures. Biopsy is not necessary for the diagnosis, but is appropriate if malignancy or infection is suspected, location of fibrosis is atypical, or there is inadequate response to initial treatment. Careful history and physical exam would reveal causes of secondary RF, such as malignancy or drugs. Suspected drugs should be discontinued. If appropriate, patients should undergo age-appropriate malignancy screening. Surgical treatment might be required for obstructive complications. Successful nonsurgical management of idiopathic RF with various immunosuppressive agents (e.g. corticosteroids, azathioprine) and hormonal medications (e.g. tamoxifen) have been reported. This case highlights the importance of maintaining a high index of suspicion for RF, even in patients without classical urinary symptoms. Prompt diagnosis and treatment not only provide symptom-relief, but can also preserve renal function, prevent other organ involvement, and reduce need for surgical intervention.
RIZATRIPTAN INDUCED RENAL INFARCT IN A MIDDLE AGED MALE WITH MIGRAINESSaurabh K. Bansal; Emani Vamsi. University of Illinois College of Medicine at Peoria, Peoria, IL. (Tracking ID #1938756)
LEARNING OBJECTIVE 1: With this case we would like to emphasize to practicing physicians to be able to recognize renal infarction as one of the potential side effects of the Rizatriptan.
LEARNING OBJECTIVE 2: With this case we would like to emphasize to practicing physicians about the vaso-occlusive and ischemic side effects of Triptan class of medications.
CASE: 44 year old male presented with 1 week history of nausea, vomiting and vague diffuse abdominal pain. He denied fever, chills, dyspnea, diarrhea and abnormal weight gain/loss. He had history of migraines and was on Topamax for preventive therapy and Rizatriptan for as needed therapy for recurrent headaches. He took approximately two tablets of rizatriptan per week for last few weeks. He denied any personal or family history of autoimmune disorder or clotting disorders. Reported smoking marijuana rarely but no cocaine. On visual appearance he appeared dehydrated. Vital signs were normal, pulse rate 92 beats/min and blood pressure of 115/72 mm of Hg. Abdomen was soft with reproducible tenderness in the left CVA region. No murmur was heard during the cardiovascular examination. CT scan with contrast of abdomen showed hyperechoic wedge shaped shadow on the upper pole of the left kidney. This was highly suggestive of a renal infarct. Hemoglobin, creatinine, electrolytes, liver function tests and urinalysis were all within normal limits. Urine drug screen was only positive for cannabinoids. ESR, CRP elevated at 33 and 6.79 respectively. Prothrombin time and PTT minimally elevated at 16.9 s and 41 s respectively. ANA, RF and ANCA, Factor V leiden, lupus anticoagulant and homocysteine tests were all negative. Protein C&S levels were slightly lower than normal levels. EKG showed sinus rhythm and 2D Echocardiogram did not show any LV thrombus. Renal Doppler ultrasound did not show any renal artery stenosis. He was managed conservatively and improved slowly in the next few days. No further complications were noted. Repeat urinalysis and creatinine were normal.
DISCUSSION: Rizatriptan/maxalt is fairly safe medication in terms of side effects. Myocardial infarction, stroke, GI ischemia or splenic infarction had been mentioned on the prescriber’s sheet. Renal infarction is not mentioned anywhere in the list of side effects. Renal Infarction is a rare disorder. Most common causes of renal infarction are - Thromboemboli or in-situ thrombosis. Patients with embolic phenomenon have atrial fibrillation, cardiac thrombus, endocarditis or aortic atheroma. Patients with non-embolic occlusion have renal artery dissection, fibromuscular dysplasia or hypercoagulable state. In our patient, hypercoagulable workup was negative by lab testing and negative renal duplex study ruled out renal artery stenosis or dissection. EKG and in hospital cardiac monitoring for 72 h showed normal sinus rhythm. Transthoracic Echocardiogram was negative for any cardiac thrombus or vegetations. We believe in this healthy adult middle aged male, renal infarct was a result of prior Rizatriptan use. Rizatriptan had been previously associated with coronary ischemia, gastrointestinal ischemia and splenic infarcts due to peripheral vasoconstrictive properties. So this is completely plausible to have vasoconstriction elsewhere resulting in ischemia, such as what happened, presumably, in a segmental branch of left renal artery in our patient. Renal infarct due to Rizatriptan had only been reported once before (see reference 1), describing two such cases1. Our patient was discharged home with advice not to use Rizatriptan again. No anticoagulation was started since we did not find any evidence of hypercoagulability or clotting disorder or this as an acute embolic/thrombotic event. References: 1) Renal infarction during the use of rizatriptan and zolmitriptan: two case reports. Fulton JA, Kahn J, Nelson LS, Hoffman RS. Clin Toxicol (Phila). 2006;44(2):177–80.
ROUX EN Y AM I SO TIRED?Rachel Sandler; Catherine Jones. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926241)
LEARNING OBJECTIVE 1: Identify gastric bypass surgery as a risk factor for iron deficiency anemia
LEARNING OBJECTIVE 2: Recognize the nutritional deficiencies associated with gastric bypass surgery
CASE: A 43-year-old African American woman presents with complaints of fatigue and shortness of breath worsening over the past year. She also noted associated chest pressure when having long conversations and with exertion. Past medical history was notable for recurrent episodes of anemia requiring transfusion along with laparoscopic gastric bypass surgery that was converted to an open procedure over 10 years ago. Her only medication was a multivitamin. On physical exam, vital signs were normal. She had anterior rim pallor and prolonged capillary refill. She had a 2/6 systolic flow murmur and lungs were clear to auscultation. Complete blood counts showed hemoglobin of 4.4 g/dL and a mean corpuscular volume of 52.7 fl. Peripheral blood smear showed microcytes and polychromasia. Ferritin was 1.9 ng/mL. Hemoglobin electrophoresis showed no evidence of hemoglobinopathy. On chart review, 3 years ago iron studies revealed iron of 9 μg/dL, iron saturation 9 %, and total iron binding capacity 419 μg/dL. Transferrin was 322 mg/dL.. Ferritin at that time was 2.9 ng/mL. During her hospital course, she was transfused 2 units of packed red blood cells with appropriate rise in her hemoglobin and significant improvement in her symptoms. She was initiated on a trial of oral iron therapy prior to discharge.
DISCUSSION: While gastric bypass surgery has become a common and effective approach to treating obesity, this surgery, particularly Roux-en-Y, is not without its long-term complications, including iron deficiency anemia. The Roux-en-Y gastric bypass works by both restricting the size of the stomach through the creation of a remnant pouch and malabsorption by shortening the small intestine. Positive effects of this procedure include significant weight loss, reduction in cholesterol and triglyceride levels, and reversal of type 2 diabetes. However, as in this patient, 6–50 % of patients develop clinically significant iron deficiency anemia after Roux-en-Y surgery secondary to disruption of iron absorption in the duodenum and proximal jejunum, which are bypassed in the procedure. As gastric bypass procedures have become a more common method for treating obesity, a growing body of evidence has shown that nutritional deficiencies are common after surgery. Iron and vitamin B12 are particularly common micronutrient deficiencies, along with the fat-soluble vitamins (A, D, E, and K) and thiamine (vitamin B1). In addition to factors directly influencing iron absorption, chronic inflammation due to obesity and changes in iron hemostasis related to decreased hepcidin can also play a concomitant role in anemia in bariatric surgery patients. In some cases, oral iron supplementation is sufficient to replete iron stores, especially at higher doses, and with reducing agents like Vitamin C. Some cases do require IV iron for resolution. Recognition of iron deficiency in the setting of bariatric surgery is essential to recognize as a complication of this common obesity treatment.
RUPTURE OF SINUS OF VALSALVA ANEURYSM: A RARE BUT IMPORTANT CAUSE OF HYPOTENSION AND RENAL FAILUREAhmed Salman; Patrick Quinlan; Anthony Donato. Reading Health System, West Reading, PA. (Tracking ID #1934613)
LEARNING OBJECTIVE 1: In patients presenting with acute hemodynamic instability and new cardiac murmurs, cardiac etiology should be suspected .
LEARNING OBJECTIVE 2: A bedside transthoracic echocardiogram is an effective approach to rule out rupture of sinus of valsalva aneurysm .
CASE: Aneurysms of Sinus of Valsalvas (ASVs) are rare cardiac anomalies found at autopsy studies in 0.09 % of the population, as the result of congenital malformations, connective tissue disease (e.g. Ehler-Danlos, Marfan’s), infections or thoracic trauma. While typically asymptomatic, rupture of the aneurysm will result in profound hypotension and renal failure. Fifty-seven year old man presented to emergency department with a 5 day history of non-radiating mild precordial chest pain associated with nausea, vomiting and decreased urine output. On examination he was afebrile with a blood pressure of 70/40 and a pulse rate of 95 beats per minute. Despite receiving 4 l of IV normal saline, his blood pressure continued to range between 80 and 100 systolic. Initial workup revealed elevated BUN and creatinine concentrations (190 mg/dl (Normal 5–26 mg/dl) and 17.6 mg/dl (Normal 0.5–1.5 mg/dl) respectively). On physical exam the patient was noted to have a continuous 3/6 murmur on left sternal border with a friction rub. Given the refractory hypotension and new murmur, a transthoracic echocardiogram was urgently performed, which revealed a ruptured 1.4 cm aneurysm of the sinus of valsalva. Cardiothoracic surgery was consulted, who took the patient urgently to open repair. The patient required 10 days of hemodialysis support post-operatively but recovered kidney function (Creatinine 1.65 mg/dl) by time of discharge.
DISCUSSION: Rupture of Sinus of Valsalva should be suspected in patients presenting with acute hemodynamic instability and new cardiac murmurs. Prompt diagnosis of this rare condition is required for appropriate surgical management.
SCLEROSING MESENTERITIS - A RARE DIAGNOSIS THAT MAY PRESENT AS ACUTE ON CHRONIC ABDOMINAL PAINAnil Kumar Reddy Anumandla; Gaurav Kistangari; Omair Javed. Clevaland Clinic, Cleveland, OH. (Tracking ID #1939221)
LEARNING OBJECTIVE 1: Learning the differential diagnosis and treatment of Sclerosing Mesenteritis
CASE: A 66 year old man presented with complaints of worsening epigastric abdominal pain for 4 days and inability to tolerate oral intake due to severe pain. He reported similar but milder post-prandial epigastric discomfort with associated 15 lb weight loss over the past year. His past history was significant for lung cancer (treated 10 years ago) and autoimmune hemolytic anemia. At presentation his vitals signs were stable. Physical examination was benign aside from severe tenderness in epigastric region. Admission labs including CBC and BMP were normal except for mild leukocytosis. Lactate was normal. Computed tomography (CT) abdomen revealed a 10 cm non-heterogeneous fatty mass extending from the root of the mesentery suggestive of SM. There was no evidence of bowel obstruction so he was treated with medical management—a trial of immunosuppressive therapy with high dose prednisone 40 mg daily and colchicine 0.6 mg BID. His pain responded dramatically over the next 2 days after which he tolerated a regular diet without any discomfort. The need for biopsy was discussed extensively but given the significant improvement with medical therapy, it was felt that percutaneous biopsy might not be useful, as it would not change management. As such, the patient was discharged on prednisone and colchicine, with the option of doing laparoscopy for definitive diagnosis in the future if he fails to respond to medical treatment. Given the association of SM with malignancy and the patient’s history of lung cancer, Chest CT was done which showed no evidence of recurrence of his malignancy.
DISCUSSION: Sclerosing mesenteritis (SM) is a rare idiopathic inflammatory and fibrotic condition affecting the mesentery. The treatment of SM is tailored according to the severity of the presentation. For patients who do not have significant symptoms, a conservative approach can be followed, as the disease course is often self-limited. For symptomatic patients without obstructive symptoms, a trial of medical therapy with immunosuppressants is recommended, as illustrated in this case. If the patient has bowel obstruction or is refractory to medical therapy, then surgery is an option. SM is associated with a number of other conditions including malignancies, autoimmune disorders, or abdominal surgery/trauma. As such, a thorough diagnostic evaluation should be performed to rule out any other underlying pathology. In this case, the patient’s history of lung cancer prompted a CT chest to ensure no recurrence of his cancer.
SEEING THINGS - AN UNUSUAL CAUSE OF VISUAL HALLUCINATIONSPayel J. Roy1; Anand Kartha2. 1Boston University Medical Center, Boston, MA; 2VA Boston Healthcare System, West Roxbury, MA. (Tracking ID #1938747)
LEARNING OBJECTIVE 1: Assess the differential diagnosis of visual hallucinations
CASE: Mr. L presented with a chief complaint of “I was hallucinating this morning.” He is a 64 year-old man with a history of cerebrovascular accident without residual deficit, coronary artery disease, hypertension, diabetes mellitus, and pulmonary embolism status post warfarin treatment. On admission, Mr. L noted increasing confusion, memory loss, and sudden onset of visual hallucinations (VH), including speaking to a nonexistent woman and wrestling a nonexistent man. Mr. L was aware of the hallucinations throughout the event and expressed concern about them. His family history was significant for Alzheimer’s dementia in his mother. Physical exam revealed left abducens nerve palsy, right pronator drift, and slowed rapid-alternating movements. Mr. L was alert and pleasant, oriented only to name and place, had naming, abstraction, and perseverating difficulties, and 0/3 object recall at 5 min. Labs revealed a creatinine of 4.8 (baseline 1.1) and normal urinalysis. The rest of his labs, including CBC, CMP, urine toxicology, and hypercoagulable work-up, were normal. Electroencephalography was normal. MRI brain without contrast showed a subacute left hippocampal infarct.
DISCUSSION: The differential diagnosis of Mr. L’s hallucinations included toxic-metabolic syndrome, possibly from acute kidney injury; seizures, given his confusion; dementia, given his family history; ophthalmologic causes, including macular degeneration, though usually only seen in patients with complete visual loss (Charles Bonnet syndrome); psychotic disorder, given the threatening nature of hallucinations; and peduncular hallucinosis, or VH arising from infarction of the midbrain. Mr. L’s acute kidney injury resolved with fluids but his hallucinations persisted and his electroencephalogram was normal, making toxic-metabolic syndrome and seizures less likely. Optometry evaluated patient; he had no visual deficits and his left abducens nerve palsy was deemed related to his diabetes mellitus. Patient had no prior history of psychiatric illness and the acute onset of symptoms makes psychotic disorder and dementia less likely. Infarction of the midbrain was ruled out by MRI, thus making hippocampal infarction the most likely cause. The hippocampus is supplied by the posterior cerebral artery and its branches. Hippocampal infarction can cause memory loss and confusion. Auditory hallucinations have been seen from a lesion restricted to the hippocampus, however VH from hippocampal infarction have not been expressly seen in the literature. Instead, patients with positive spontaneous visual phenomena, including VH, have been found to have associated hippocampal lesions in the setting of agitated delirium and hemianopia. The above presentation, work-up, and subsequent Neurology consultation affirmed hippocampal infarction as the cause of Mr. L’s VH. Visual hallucinations are not an uncommon presentation in general practice and can be a marker of serious medical illness. Internists should be able to assess for medical, neurologic, and psychiatric causes of these hallucinations. Key features leading to diagnosis in our patient included a thorough history of symptom acuity, risk factors for organic causes, a thorough neurologic exam, a broad differential diagnosis, and appropriate consultation and MR imaging use.
SEIZING THE DAYRachel Sandler. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925914)
LEARNING OBJECTIVE 1: Identify key risk factors for intimate partner violence during history taking and physical examination
LEARNING OBJECTIVE 2: Recognize the importance of screening for intimate partner violence in patients at risk
CASE: A 55 year-old woman was admitted for new-onset seizures. She was noted to have nausea, vomiting, and blurry vision associated with a posterior occipital headache. She had an initial witnessed tonic-clonic seizure followed by multiple subsequent seizures while accompanied by EMS. She was also noted to have severe thoracic back pain. She had a history of multiple rib fractures. She did not smoke, but admitted to drinking 1 to 2 beers daily 6 times weekly. Physical exam was notable for elevated blood pressure at 165/89. She was also found to have diffuse ecchymoses on her arms and legs along with spinal tenderness along the thoracic spine. She had no focal neurologic deficits. Her laboratory studies revealed AST elevation 59 units/L with AST/ALT ratio of approximately 2:1. MRI brain showed no evidence of hemorrhage. MRI of the thoracic spine showed moderate compression fracture of T9 consistent with post-traumatic origin. During her hospital course, the patient’s seizures were treated with levetiracetam. She also underwent kyphoplasty of her compression fracture with improvement in her pain post-operatively. Prior to discharge, patient revealed that she had a long history of suffering from intimate partner violence including being hit and beaten by her husband for the past 30 years.
DISCUSSION: Intimate partner violence includes threatened, attempted, or completed physical or sexual violence or emotional abuse by former or current intimate partners whether a spouse, ex-spouse, or dating partner. Such violence is experienced by 35.6 % of women and 28.5 % of men in the United States in their lifetime. Recognizing patients at risk is crucial to help prevent the morbidity and mortality associated with this condition. A variety of health conditions and risk behaviors have been associated with intimate partner violence including stroke, heart disease, arthritis, HIV risk factors, current smoking and heavy drinking. Conditions like irritable bowel syndrome, frequent headaches, chronic pain, depression, anxiety, and insomnia have all been found as consequences of intimate partner violence. Patients may also show physical evidence of trauma not consistent with the history provided. In this case, the patient had multiple risk factors including frequent alcohol use both by history and laboratory studies and history of multiple rib fractures as well as evidence of a traumatic spine fracture. In January 2013, the United States Preventive Services Task Force released a grade B recommendation for screening women of childbearing age for domestic violence. Multiple screening tools including the HITS (Hurt, Insult, Threaten, Scream), HARK (Humiliation, Afraid, Rape, Kick), and STaT (Slapped, Threatened, and Throw) have been validated with high sensitivity and specificity for identifying patients at risk for intimate partner violence. Using these simple tools can help open up a larger conversation for patients about an incredibly personal topic. Opening up the conversation with patients will allow physicians and patients to recognize situations of abuse and move towards greater action towards prevention and providing treatment for victims of intimate partner violence.
SEROTONERGIC REACTION MANIFESTING AS DELAYED TOXICITY: RESPONSE TO CYPROHEPTADINE THERAPYSaraschandra Vallabhajosyula1; Pranathi Sundaragiri1; Ariel M. Modrykamien1,2. 1Alegent-Creighton University Medical Center, Omaha, NE; 2Alegent-Creighton University Medical Center, Omaha, NE. (Tracking ID #1939506)
LEARNING OBJECTIVE 1: Understanding the clinical presentation and management of serotonin syndrome, highlighting the role for cyproheptadine therapy
LEARNING OBJECTIVE 2: Identifying delayed manifestation of serotonin toxicity manifesting 3 months after medication alteration
CASE: Introduction: Serotonin (5-HT) neurons participate in sleep-wakefulness cycles, mood, food and sexual behaviors, and thermoregulation via the central brainstem midline raphe nuclei and on vascular tone and gastrointestinal motility in the periphery1,2. Serotonin syndrome (SS) is a clinical triad of mental status changes, autonomic hyperactivity and neuromuscular abnormalities mediated via 5HT2A receptors1-3. First reported in 1980s, there were 26,733 cases and 93 deaths in 20022,3. Case Report: A 53-year-old Caucasian female with past history of diabetes, hypertension, osteoarthritis and depression presented with worsening dyspnea, tremors and loss of balance of one-day duration. Three months prior, the patient developed tremors after increase in sertraline dosage. Review of systems was positive for urinary retention, forgetfulness and cough. Home medications included promethazine, diphenhydramine, citalopram, bupropion, hydrocodone, morphine, metformin and sertraline. Vital signs at presentation—temperature 102.7 °F, heart-rate 103/min, blood pressure 212/183 mmHg, respiratory rate 20/min & oxygen saturation 80 % on ambient air. Examination demonstrated dry mucous membranes, rigid abdominal wall, tachycardia, confusion, disorientation and resting myoclonus. Laboratory studies revealed mild leukocytosis, hyponatremia and acute kidney injury (AKI) with creatinine 4.0 mg/dL (baseline 0.9 mg/dL). A mixed respiratory/metabolic acidosis (pH 7.27), with elevated serum lactate (2.4 mmol/L) and creatinine phosphokinase (CPK) (921 U/L), was noted. Thyroid and liver function testing was normal and imaging studies for chest, abdomen and retroperitoneal regions were unremarkable. Home medications of sertraline, promethazine, metformin and diphenhydramine were held. Patient did not respond to empirical physostigmine therapy for suspected central anticholinergic syndrome. Supportive measures including intravenous hydration, positive pressure airway support, bronchodilator and diazepam therapy were initiated. Patient’s labile blood pressure ranging 94 to 224 mmHg was controlled with esmolol as needed. In view of insignificant improvement, cyproheptadine therapy was initiated—loading 12 mg, then 2 mg for 8 doses (total 28 mg). Patient’s confusion, myoclonus and dyskinesia resolved with return of baseline renal function confirming a diagnosis of SS. She was transitioned to lower doses of citalopram and bupropion, with no recurrence of symptoms at six-month follow-up.
DISCUSSION: SS is a dose-dependent continuum of clinical manifestations noted in all age groups 1–4, with onset usually immediate with ranges of 4–6 h after initial use, overdose or change in dosing with occasional reports of delayed onset (12 h) in slow release preparations2,3. Since it is a clinical diagnosis, multiple criteria in the past have been used, which were not very specific1,3,4. Currently, Hunter Serotonin Toxicity Criteria (sensitivity 84 %, specificity 97 %), which quotes clonus (spontaneous, ocular and inducible), agitation, diaphoresis, tremor and hyperreflexia as accurate predictors, is applied2,4. Occasionally, hyperreflexia and clonus are absent, which can be explained by the extreme state of muscle rigidity3,4. Bowel sounds, skin discoloration and rapidity of onset help distinguish from alternate diagnoses2. Non-specific laboratory findings include leukocytosis, high CPK and low bicarbonate with no correlation to serum serotonin levels. Management entails discontinuation of serotonergic agent and supportive therapy for prevention of respiratory failure, AKI and agitation with intravenous hydration, anxiolytics, chemical paralysis and mechanical ventilation 1–4. Direct-acting sympathomimetic agents and short acting anti-hypertensives are used to treat extremes of blood pressures2. Cyproheptadine, a histamine-1 receptor antagonist with non-specific action at 5HT1A and 5HT2A receptors, in a dose of 12–32 mg in a 24-hour period, has shown good response in management of SS. Other agents used include chlorpromazine, olanzapine, propranolol, bromocriptine and dantrolene, but are currently not recommended. However, further clinical trials are required to validate the use of cyproheptadine in SS2,3. References: 1. Birmes P et al. Serotonin syndrome: a brief review. CMAJ. 2003 May 27;168(11):1439–42. 2. Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005 Mar 17;352(11):1112–20. 3. Isbister GK, Buckley NA. The pathophysiology of serotonin toxicity in animals and humans: implications for diagnosis and treatment. Clin Neuropharmacol. 2005 Sep-Oct;28(5):205–14. 4. Dunkley EJ et al. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003 Sep;96(9):635–42.
SEVERE HYPERBILIRUBINEMIA IN A HEALTHY 18-YEAR-OLD MALEDennis D. Wang1,2; Chris Chu1,2; David McCants1,2. 1Baylor College of Medicine, Houston, TX; 2Ben Taub General Hospital, Houston, TX. (Tracking ID #1935177)
LEARNING OBJECTIVE 1: Hyperbilirubinemia is a common symptom in newborns and mid-age patients with liver or biliary diseases, but is relatively uncommon in healthy 18-year-olds. It is important to take a complete and thorough family history in teenage patients who presents with acute onset jaundice because hereditary spherocytosis often precipitates bilirubin stones, and the patient may be easily be misdiagnosed with obstructive biliary disease instead. Obtaining a blood smears can also be helpful in making the diagnosis.
LEARNING OBJECTIVE 2: In patients with a functioning liver presenting with hyperbilirubinemia secondary to hemolytic anemia, the hyperbilirubinemia can be predominantly direct rather than indirect. As in this case, the patient initially presented with a total bilirubin of 50.8 mg/dL and direct bilirubin of 38.5 mg/dL, but RUQ ultrasound and CT abdomen did not reveal any signs of biliary obstruction. Therefore, it is important to also work up any patient with direct-bilirubin predominant hyperbilirubinemia for causes that increases bilirubin production.
CASE: An 18-year-old otherwise healthy Hispanic male presents with a 2-week history of RUQ and right flank pain and nausea, which were exacerbated by eating solid food. On the day before admission, he began noticing that his skin and the sclera of his eyes turning bright yellow, which prompted him to come into the emergency room. Over the same time frame, he also noticed that his urine had become darker than usual. The patient denies fevers, chills, diarrhea, constipation, hematochezia, melena, dysuria, unintentional weight loss, drug or heavy alcohol use, recent travels, or any sick contacts. He has no known history of biliary or liver disease. At the emergency room, the patient was found to have a total bilirubin level of 50.8 mg/dL (Ref: 0.2–1.0), direct bilirubin level of 38.5 (Ref: <0.2) mg/dL, and reticulocyte count of 12.1 %. Alkaline phosphatase was only mildly elevated and the patient was not anemic. Coobs tests, hemoglobin electrophoresis, and direct RBC antibody tests were all negative. Upon further inquisition of his family history, the patient’s mother reveals that herself and her brothers had a history of jaundice when they were young, and she had her spleen removed at the age of 19 due to an unknown illness. CT abdomen and pelvis and abdominal ultrasound showed only mild hepatosplenomegaly, fatty liver, and cholelithiasis without cholecystitis or any signs of biliary obstruction. We obtained a peripheral blood smear, which showed predominantly spherocytes (70 to 80 %) and a diagnosis of hereditary spherocytosis was made.
DISCUSSION: Hereditary spheroctosis is a relatively common genetic disease affecting 1 in every 5000 people of northern European origin. The most common mutation is autosomal dominant and in the ankyrin gene, which results in RBC membrane instability and loss during exposure to shear force. Common clinical presentations include anemia, splenomegaly, cholelithiasis, and jaundice at an early age. However, as in this case, affected patients may remain asymptomatic until adulthood. In addition to hyperbilirubinemia, laboratory findings may include decreased Hgb with an elevated reticulocyte count, elevated MCHC, RDW, pseudohyperkalemia, and the characteristic spherocytes on peripheral blood smear. The osmotic RBC fragility test only has a sensitivity of about 70 %. Management is primarily focused on providing symptomatic relieve, including surgical splenectomy and cholecystectomy. This case highlights the importance of obtaining a complete and thorough family history and considering the workup of pre-hepatic pathology in young and healthy patients presenting with direct-bilirubin predominant hyperbilirubinemia.
SEVERE HYPONATREMIA IN A PATIENT WITH ESRD CORRECTED BY HYPERTONIC INFUSION WHILE REMOVING ISOTONIC VOLUME FOLLOWED BY HEMODIALYSISAlexander Pine1,2; Megan S. Lemay1,2; Antony J. Cusano1,2. 1Yale University School of Medicine, New Haven, CT; 2Waterbury Hospital, Waterbury, CT. (Tracking ID #1925990)
LEARNING OBJECTIVE 1: Recognize challenges and options for safe sodium correction in patients with ESRD requiring hemodialysis.
LEARNING OBJECTIVE 2: Correct severe hyponatremia in a patient with ESRD by infusing hypertonic saline while removing isotonic fluid followed by hemodialysis.
CASE: A 56-year old woman with history of schizophrenia treated with clozapine, ESRD of unclear etiology on HD presented with confusion, vomiting, diarrhea, and sodium of 112 mEq/L. Three days prior sodium was 134 mEq/L. Vital signs were unremarkable. She had moderate jugular vein distention of approximately 9–10 cm of water, positive hepatojugular reflux. Breath sounds were distant, inspiratory crackles and expiratory wheezes were heard bilaterally. She had significant edema up to mid-calves in both lower extremities. Potassium was 4.0, chloride 74, bicarbonate 24, serum creatinine 5.71 mg/dL, BUN 28 mg/dL. Plasma osmolality was 240 mOsm/kg. She was not anuric; specific gravity was 1.005. Urine osmolality was 154 mOsm/kg and urine sodium 67 mmol/L. We thought that rapid hyponatremia was the side-effect of clozapine causing psychogenic polydipsia. She was fluid-restricted. Initially, the patient underwent 3 L of isotonic fluid removal by ultrafiltration followed by an infusion of 3 % saline. This two-step procedure brought sodium from 112 to 118 mEq/L. Subsequently, adjustments with hypertonic saline and water raised sodium to 124 mEq/L after the period of 48 h. Next, using the dialysate with high sodium concentration of 140 mEq/L, we initiated HD and raised sodium to 130 mEq/L in 3 h. Immediately after HD, water was given to taper sodium to 127 mEq/L. The second HD increased sodium to 132 mEq/L.
DISCUSSION: The patient with ESRD, low ejection fraction of less than 20 % was admitted with severely depressed serum sodium that was thought to be a side-effect of clozapine causing primary polydipsia. The management of hyponatremia in patients with ESRD presents a challenge. This is because the transfer of sodium during hemodialysis can exceed established safe correction rates owing to significant serum-to-dialysate sodium differential. Sodium correction should not exceed the rate of 10 mEq/L/24 h to avoid central pontine myelinolysis, a process in which sudden augmentation in extracellular osmolality by rapid increase of sodium concentration leads to intra-to-extracellular water shift that may cause irreversible damage of CNS neurons. Considering the significant differential between serum sodium and that of dialysate concentrations (112 vs of 140 mEq/L, the lowest available to us), we delayed hemodialysis out of concern that it would correct too rapidly. To avoid rapid correction of sodium in a patient with severe hyponatremia we brought serum sodium closer to that of available dialysate by infusing hypertonic saline while removing isotonic volume. This was done to effectively increase the total body sodium without causing further volume expansion in this patient who exhibited signs of fluid overload. Wendland et al. (2012) described a method to mitigate sodium transfer and thus maintain safe serum sodium correction rate, in which hemodialysis was performed at a slower transfer rates (2 mEq/L/h) while using the dialysate with reduced sodium concentration (130 mEq/L vs 140 mEq/L available to us). Of course, this method prolongs the hemodialysis time. Furthermore, we were concerned with volume status that was consistent with fluid overload. While in euvolemic patients infusion of free water during hemodialysis could be used to achieve safe serum sodium transfer rates, we could not use this approach as our patient was showing signs of fluid excess. Therefore, we used a two-step approach in which we first safely raised serum sodium without expanding the volume, and then followed by safe sodium transfer during hemodialysis. With this case, we describe challenges of the safe rate for sodium correction in patients with hyponatremia in the settings of ESRD, and how to avoid over-correction. Reference: Wendland, et. al. Seminars in Dialysis. 25:1, pp. 82–85, 2012.
SEVERE HYPONATREMIA IN BEER POTOMANIA: A CASE FOR CAUTIONKristopher P. Kline1; Jorge Fuentes1; Amir Kazory1,2. 1University of Florida, Gainesville, FL; 2University of Florida, Gainesville, FL. (Tracking ID #1926328)
LEARNING OBJECTIVE 1: Manage severe hyponatremia with careful selection of fluids, monitoring and adjustments.
LEARNING OBJECTIVE 2: Recognize the clinical features for rapid overcorrection of hyponatremia.
CASE: Hyponatremia, defined as a serum sodium level less than 135 mEq/L, is a potentially fatal electrolyte abnormality. Patients with acute severe hyponatremia can present with headache, nausea, vomiting, confusion, disorientation, and lethargy. The syndrome “beer potomania” is used to describe a patient who presents with hyponatremia in conjunction with low daily solute intake and excessive beer drinking. A 63-year-old woman with a past medical history of hypertension, ethanol abuse, and depression presented with a two-day history of worsening confusion and lethargy. Vital signs were within normal range except for a respiratory rate of 24/min. She was diaphoretic, somnolent, oriented only to self, and opened eyes to verbal stimuli and sternal rub. Laboratory studies revealed severe hyponatremia with a serum sodium of 101 meq/L, low serum osmolality of 215 mOsm/kg, urine osmolality of 137 mOsm/kg, and a low urine sodium of 4 meq/L. Based on her history, clinical presentation, and laboratory values a diagnosis of hyponatremia secondary to beer potomania was made. She was initially treated with 3 % hypertonic saline followed by isotonic solutions the rate of which was carefully adjusted according to the rate of serum sodium correction. However, she developed a significant increase in urine output followed by a sudden increase in serum sodium level (124 mmol/L at 24 h) which was successfully managed by administration of hypotonic solutions. Her neurologic symptoms slowly resolved during admission without further complications.
DISCUSSION: Beer potomania represents a normovolemic variant of hyponatremia with appropriate suppression of ADH and urinary dilution. This typically ensues after daily consumption of greater than 5-liters of fluid (approximately 14 cans of beer) given a maximal urinary dilution of 50 mOsm/L with 250 mOsm of obligatory solute loss per day. The disease entity is particularly difficult to manage as the patients are at serious risk of rapid correction of hyponatremia and its neurological sequelae. The appropriately low ADH levels limit free-water absorption in the kidney and explain why these patients could develop brisk diuresis when solute (e.g. IV saline solution) or a high-protein diet is started. In patients with severe symptoms, rapid correction of serum sodium by 4–6 mmol/L with hypertonic saline in the first 6 h is indicated. Slower rate of correction with less than 10 mmol/L in the first 24 h and less than 18 mmol/L in the first 48 h should be enforced to prevent potentially permanent neurologic complications. This case demonstrates the importance of the diagnosis of beer potomania and highlights treatment goals as well as the susceptibility of these patients to present with overcorrection of serum sodium levels despite careful selection of fluids and adjustment of their rate of administration.
SEVERE HYPONATREMIA: IS YOUR PATIENT ALCOHOLIC?Dipenkumar Modi; Hirva Mamdani; Theresa Vettese. Wayne State University, Detroit, MI. (Tracking ID #1939047)
LEARNING OBJECTIVE 1: To recognize Beer Potomania as an uncommon but important cause of hyponatermia in Alcoholics
LEARNING OBJECTIVE 2: To recognize the role of serum and urine osmolality in diagnosing Beer Potomania To recognize key principles of managing Hyponatremia
CASE: A 55 years old African American man with significant past medical history of chronic alcoholism was admitted for confusion and seizures. The patient also had generalized weakness for 5–7 days duration prior to admission. He was drinking 40 oz beer daily for more than 35 years. He had been drinking more beer (around 64 oz) for many weeks prior to admission because of stressful condition in family. His oral intake had been very irregular, reduced and even missed because of heavy drinking. On physical exam, patient was afebrile and normotensive. He appeared confused, severely cachectic and malnourished. Patient had no focal neurologic deficits, jugular venous distension, lower extremity edema, or stigmata of chronic liver disease. Clinically patient did not seem like dehydrated and was not on any diuretic or antipsychotic medication. Laboratory studies revealed severe hyponatremia (96mMol/L). Patient had low serum osmolality (213 mOsm/kg), low Urine Na+ (11mMol/L), and low urine osmolality (121 mOsm/kg). Further studies showed severe hypokalemia (3.2mMol/l), hypochloremia (60mMol/L), hypocalcemia (7.3 mg/dl) and hypophosphatemia (1.6 mg/dl), undetectable BUN (<1 mg/dl) and creatinine (<0.1 mg/dl), as well as hypomagnesemia (1.3 mg/dl). Liver function tests, TSH, and serum cortisol levels were unremarkable. Chest x-ray did not show any lung lesion. CT head revealed mild generalized brain atrophy. Finally diagnosis of beer potomania was made based on hyponatremia with relative low serum osmolality and low urine osmolality.
DISCUSSION: Beer Potomania is an uncommon cause of hyponatremia in alcoholic patients. It is a condition characterized by severe hyponatremia without any obvious cause, low serum and urine osmolality, clinical findings consistent with protein malnutrition and consumption of large amount of alcohol. Hyponatremia has been observed in 17 % of chronic alcoholics in the study by Liamis et al. Hypokalemia, mild neurological symptoms (confusion), low BUN, brisk diuresis in response to solute intake and low urine sodium level have also been frequently noticed. Hyponatremia is mainly caused by very high water intake that exceeds excretory capacity. Patients with beer potomania have a history of significant beer drinking in conjunction with poor diet. The net result is very low osmole intake because beer has very little sodium and no protein but has some calories that prevent endogenous protein breakdown. Because obligatory solute loss in a day is approx. 250 mOsm in these patients, with a urinary dilution capability of 50 mOsm/L, water intake greater than 5 l results in hyponatremia. Moreover, ADH levels are frequently suppressed because negative suppression of osmo-receptors from hypotonic serum secondary to excessive beer intake. Patient with beer potomania are at increased of developing Osmotic Demyelination Syndrome because of degree and chronicity of hyponatremia. The goal Sodium increment should be below 10 mEq/L in first 24 h and less than 18 mEq/L in the first 48 h. If the patient has neurological symptoms, correction of sodium level by 1–2 mEq/h in the first 2–3 h is acceptable. If the sodium increment occurs at a rate that exceeds goal, D5W infusion should be started to match urine output. Desmopressin may be considered if diuresis occurs at an excessive rate that the infused D5W is unable to match.
SEVERE MALARIA CAUSING PROFOUND HEMOGLOBINURIA AND ACUTE KIDNEY INJURYJames F. Dylewski1; Jennifer Axelband2; Thong Le3. 1St. Luke’s University Hospital, Bethlehem, PA; 2St. Luke’s University Hospital, Behtlehem, PA; 3St. Luke’s University Hospital, Bethlehem, PA. (Tracking ID #1915761)
LEARNING OBJECTIVE 1: Recognize the clinical features of Blackwater fever
LEARNING OBJECTIVE 2: Assess the role of artesunate in treatment of malaria
CASE: A 40 year-old, otherwise healthy, African American male presented with episodic fever for 2 weeks. A thorough history yielded that he had visited Nigeria 1 month ago. Prior to his trip, he had obtained atovaquone/proguanil for malaria prophylaxis, but was noncompliant. Upon his return, he was diagnosed with malaria and was treated with doxycycline and hydroxychloroquine. He reported compliance with the medications, but continued to have fevers. Three days elapsed before the patient returned for evaluation. He was subsequently found to be hypotensive, necessitating transfer to our ICU for treatment of septic shock from severe malaria. The patient received aggressive volume resuscitation and vasopressor hemodynamic support. Preliminary laboratory studies showed a creatinine (Cr) of 1.35 mg/dL and hemoglobin (Hgb) 14.0 g/dL. Urinalysis demonstrated small dipstick positive blood without RBC on microscopy. A malaria smear identified the species as Plasmodium falciparum with 24.7 % parasitemia. The patient was given atovaquone/proguanil and the CDC was contacted. Given the severity of his condition, artesunate was obtained from the CDC and administered in conjunction with atovaquone/proquanil. Several hours after receiving the artesunate, the patient became febrile, tachypneic, tachycardic, and encephalopathic necessitating intubation. The patient’s urine was noted to change color from clear yellow to opaque, dark red. Blood chemistries 24 h into treatment revealed a Cr of 2.32 mg/dL, Hgb 10.9 g/dL and parasitemia 0.2 %. The patient completed his course of artesunate and atovaquone/proguanil with marked improvement. By day 3, vasopressors were titrated off and he was extubated. By day 7, the patient’s Cr improved to 1.30 mg/dL and urine color was dark yellow with moderate dipstick positive blood with only 2–4 RBCs/hpf. The patient was deemed clinically stable and discharged with close outpatient follow up.
DISCUSSION: Malaria is one of the most common infections globally with 300–500 million annual cases worldwide. However, in the US there are less than 2000 cases/year with only about 10 % being considered severe. Fever, rapid developing anemia, acute kidney injury and hemoglobinuria associated with malaria is Blackwater Fever. With prophylaxis, early detection and malaria’s domestic eradication in 1951, Blackwater Fever essentially disappeared in the US. It is felt this complication arises from massive hemolysis associated with treating malaria. Though rare, it can progress to renal failure and is associated with higher morbidity and morality. Artesunate is an intravenous antimalarial agent that is part of a class of drugs referred to as artemisinins. Artemisinins are believed to work by inhibiting DNA replication and transcription in Plasmodium species. Though considered a first-line therapy in most malaria endemic countries, in the US, artesunate is an orphan therapy for severe P. falciparum and can only be obtained from the CDC. Currently, the indications for obtaining artesunate are: severe malaria disease, high level of parasitemia, inability to take oral medication, lack of timely access to intravenous quinidine, quinidine intolerance or contraindications, or failure of quinidine therapy.
SEVERE REFRACTORY HYPERCALCEMIA IN A RARE CASE OF B-CELL PROLYMPHOCYTIC LEUKEMIAKah Poh Loh1; Saurabh Dahiya2; Karan Singh1; Leslie Howard2; Maura J. Brennan3. 1Baystate Medical Center/Tufts University, Springfield, MA; 2Baystate Medical Center/Tufts University, Springfield, MA; 3Baystate Medical Center/Tufts University, Springfield, MA. (Tracking ID #1942036)
LEARNING OBJECTIVE 1: Recognize the clinical presentations of prolymphocytic leukemia (PLL)
LEARNING OBJECTIVE 2: Evaluate PLL using a systematic approach
CASE: An octogenarian presented with 2 weeks of progressive weakness, subjective fever and left upper quadrant pain. He had no history of any hematologic disorder but physical examination revealed massive splenomegaly with no hepatomegaly. He had a marked lymphocytosis with immature cells and smudge cells on the peripheral smear. A CT abdomen and pelvis verified splenomegaly and bulky lymphadenopathy. An EBV test was positive; flow cytometry revealed CD5-, CD19+ and CD20+, monotypic, kappa-restricted cells consistent with a monoclonal B-cell malignancy. He was diagnosed with a B-cell prolymphocytic leukemia/lymphoma. Shortly thereafter he became weak and delirious with worsening leukocytosis, hypercalcemia (17.3) and hyperuricemia (12.4) secondary to his leukemia. He was aggressively hydrated and given furosemide, dexamethasone, calcitonin and zoledronic acid with minimal improvement in his calcium level. Comfort measures were instituted and he died shortly thereafter.
DISCUSSION: This case is special in that the authors report the first case of refractory hypercalcemia due to B-PLL in an elder. B cell prolymphocytic leukemia (PLL) is rare; it is characterized by marked leukocytosis and splenomegaly and comprises less than 1 % of B cell leukemias. It was first described in the 1970s. Older men are at higher risk and progression can be very rapid. The disease usually becomes clinically apparent within 1–2 years; the majority of patients present with B-symptoms and splenomegaly. Diagnosing PLL relies on identification of promyelocytes in the peripheral blood. Therapy is only indicated for patients with symptomatic and progressive disease. Rituximab, fludarabine and anthracycline monotherapy (or combination therapy) are used to treat PLL but the prognosis is worse than CLL; the median survival is 65 months. Our patient’s B-PLL was complicated by hypercalcemia which was unresponsive to all treatment. This precluded any attempt at chemotherapy. To our knowledge this is the first reported case of B-PLL presenting with severe refractory hypercalcemia.
SEVERE RHABDOMYOLYSIS FROM INFLUENZA A PH1N1 (2009) VIRUS INFECTION: SUSPECT EARLY AND TREAT AGGRESSIVELYEmily R. Haggerty; Amit Sharma; Viren Kaul; Omar Mousa; Phillip Aleksiejuk; Karthikeyan Sitaraman. SUNY Upstate Medical University, Syracuse, NY. (Tracking ID #1939022)
LEARNING OBJECTIVE 1: Diagnose rhabdomyolysis in influenza infection despite the absence of previously reported clinical risk factors of influenza severity for effective management.
LEARNING OBJECTIVE 2: Recognize that high creatine kinase (CK) levels with early initiation of renal replacement therapy (RRT) positively impacts clinical outcomes and length of hospital stay.
CASE: A previously healthy 31yo African American male presented with low back pain radiating to the lower extremities for 1 week and fever for 1 day. Additional history included recent upper respiratory tract infection associated with diffuse body aches 1 week prior to admission. Our high clinical suspicion for influenza was later confirmed by respiratory panel positive for influenza A pH1N1 (2009) infection. By this time, the patient’s renal function had deteriorated from a creatinine of 2.2 mg/dL to 7.2 mg/dL with severe transaminitis. Initial CK levels were normal but riding on the clinical suspicion of rhabdomyolysis, serial CK levels were ordered. The subsequent level was 615840 U/L (peak 677560 U/L). Interestingly, serum electrolytes were normal except for hyperphosphatemia and, despite severe myoglobinuria, the patient’s urine output remained normal. We excluded other vascular, toxic and metabolic causes for rhabdomyolysis leading to a diagnosis of severe influenza induced rhabdomyolysis. The hospital course was eventually complicated by resistant hyperkalemia and normal anion gap metabolic acidosis. Ultimately, the patient required RRT. CK levels improved, renal function stabilized and the patient continued to respond well to anti-virals and supportive management. There was no indication for intensive care support at any point during the hospital course.
DISCUSSION: The incidence of influenza-induced rhabdomyolysis has been poorly reported in the literature. In addition, internists rarely encounter such a serious complication. Our case highlights the heterogeneity of the presentation of influenza rhabdomyolysis, with absence of the traditional risk factors for severe influenza complications including extremes of age, multiple medical comorbidities, immunosuppression, pregnancy, morbid obesity and residence in a chronic care facility. Recent data refutes a correlation between these risk factors for severe influenza and actual outcomes. Furthermore, published case reports of influenza-induced rhabdomyolysis with acute renal failure are primarily in young, healthy individuals, supporting our observation. Maintaining a high level of suspicion for influenza rhabdomyolysis in addition to aggressive monitoring at any age or health status is essential for preventing poor outcomes. More specifically, CK has been proposed as a biomarker of H1N1 infection severity. Correlation between elevated CK and morbidity has been observed with twofold increase in RRT requirement in patients with CK ≥500 UI/L. Since RRT decreases CK levels while simultaneously improving symptomatology, we highly support the initiation of early RRT in patients with elevated CK in order to decrease morbidity and length of hospital stay. Future research is required to quantify appropriate CK levels for the initiation of RRT, regardless of other indications.
SEVERE SIRS FOLLOWING 23-VALENT PNEUMOCOCCAL VACCINATION IN A PATIENT WITH BEHçET’S DISEASEVijay Kotecha2; Kevin D. Hauck1; Matthew Shaines1. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicne, Bronx, NY. (Tracking ID #1939218)
LEARNING OBJECTIVE 1: -Understand common reactions to the 23-valent pneumococcal vaccine
LEARNING OBJECTIVE 2: -Recognize the role of streptococcal antigens in Behcet’s disease
CASE: A 41 year-old man with a history of Behcet’s disease treated with azathioprine presented with 1 day of fevers, rigors and severe right arm and shoulder pain. His symptoms started 12 h after receiving the 23-valent pneumococcal vaccine in his right deltoid. Vital signs on admission were notable for temperature of 104.8° Fahrenheit and heart rate of 120. There was full range of motion at the shoulders. There was a 12 cm poorly demarcated area of erythema, warmth, fullness, and exquisite tenderness to palpation over the right deltoid. Labs were notable for C-reactive protein of 24 mg/dL and white blood cell count of 20,000. Blood cultures showed no growth. A sonogram of the right deltoid was unremarkable. He was treated supportively with intravenous fluids and acetaminophen. By hospital day two, his arm pain and fevers had resolved, and he was discharged home without further incident.
DISCUSSION: Behçet’s disease is a rheumatological condition found most commonly in those of Turkish or Middle Eastern descent. Behçet’s may cause vasculitis of vessels of all sizes, and classically manifests as recurrent oral, genital and skin ulcerations. It may also involve the brain, heart, kidneys, lungs, joints and eyes and can progress to blindness, severe gastrointestinal bleeding, and permanent neurological deficits. Treatment depends on the extent of disease progression, but generally requires immunosuppression with glucocorticoids followed by azathioprine, infliximab or cyclosporine. The Centers for Disease Control and Prevention recommend administration of the 23-valent pneumococcal vaccine to immunocompromised adults, including those patients taking immunomodulating agents. About 50 % of adults will experience mild reactions to this vaccine, usually a local inflammatory response at the site of injection. Systemic reactions, including fevers and arthralgias, occur in less than 1 % of recipients. Severe reactions, such as seen in this patient, are exceedingly rare. To our knowledge, this is the fifth reported case of a severe systemic inflammatory response after administration of the 23-valent pneumococcal vaccine in a patient with Behçet’s disease. Prior cases occurred similarly, with rapid onset of fevers to greater than 104, severe pain at the injection site, rigors and C-reactive protein levels of 16 to 40 mg/dL. As in our patient, symptoms mostly resolved by 48 h with supportive care. The origins of Behçet’s disease are incompletely understood, but are known to include genetic factors, such as HLA-B51, and alterations in innate and cellular immunity in response to environmental antigens. Of particular interest are streptococcal species. When compared to controls, Behçet’s patients have significantly higher titers against certain species of streptococcus. Exposure to these antigens, such as from skin testing, causes upregulation of the pro-inflammatory cytokines IL-6 and TNF-alpha which in turn can lead to hypersensitivity reactions and exacerbations of Behçet’s. Hypersensitivity reactions to streptococcal antigens are frequent enough that is part of the Japanese diagnostic criteria for Behçet’s. A reaction to one of the streptococcal antigens in the 23-valent pneumococcal vaccine would explain our patient’s severe SIRS response.
SHIGELLOSIS AS A SEXUALLY TRANSMITTED DISEASE IN A HIV INFECTED MALEMatthew McCarra. University of California San Diego, San Diego, CA. (Tracking ID #1939768)
LEARNING OBJECTIVE 1: Recognize Shigella as a sexually transmitted infection in the men who have sex with men population
LEARNING OBJECTIVE 2: Recognize the limitations of stool cultures in diagnosis of Shigella dysentery
CASE: A 36 year-old man with a history of AIDS, off HAART due to non-compliance (CD4: 55 and viral load 120,000), presented to our emergency department for diarrhea and crampy abdominal pain. He endorsed two months of more than 20 loose, watery stools daily without blood or mucus and he had been admitted on two previous occasions for these complaints. He denied fevers, chills, nausea, or vomiting but endorsed recent 10 lb weight loss. Prior workup included multiple stool studies that showed blood and moderate white blood cells however negative for infectious source on stool culture negative tests for Cyclospora, Clostridium difficile, and Giardia which were negative. A colonoscopy showed severe colitis with erythema, friability, and adherent white exudate, without discrete ulceration. Biopsy of the colon was performed that demonstrated acute colitis with erosions and pseudomembranous exudate. A single cell stained positive for CMV. During that admission HAART—darunavir and abacavir/lamivudine—and gancyclovir (5 mg/kg) for presumptive CMV colitis was initiated with notable improvement in his symptoms. On discharge he was transitioned to oral valgancyclovir (900 mg BID). He did well at home for 3 weeks before recurrence of symptoms when he represented at time of the presentation of discussion. He was sexually active with men with a new sexual partner a month prior to onset of the symptoms. He denied any travel outside of the country but had recently traveled to Philadelphia. His medications included darunavir abacavir/lamivudine, valgancyclovir, azithromycin, trimethoprim/sulfamethoxazole, fluconazole, and promethazine. He was admitted for additional workup of severe diarrhea and pain control. At time of admission stool cultures were repeated, blood cultures were obtained, and he was transitioned back to IV gancyclovir with concern of malabsorption given severe duodenitis/colitis observed on prior imaging. Vital signs were normal and physical exam was remarkable for a cachectic male, temporal wasting, hyperactive bowel sounds with severe abdominal tenderness to palpation diffusely. There was no rebound tenderness, rigidity, or involuntary guarding. Admission labs were remarkable for K 2.8 mmol/L, creatinine to 2.11 mg/dL from baseline of 0.8 mg/dL. Initially his symptoms failed to improve and his pain persisted requiring large doses of IV hydromorphone. On hospital day 6, four of four admission blood cultures came back positive for Shigella flexneri resistant to amikacin, ampicillin, cefuroxime, gentamicin, and trimethoprim/sulfamethoxazole. He was started on IV ceftriaxone 1 g daily with notable improvement and completed a 2 week course at a skilled nursing facility.
DISCUSSION: Shigella is a common cause of bacterial associated diarrhea with more than 400,000 cases estimated in the United States every year. Clinical manifestations typically include diarrhea, abdominal pain, hematochezia, and fever. Shigella is the third leading cause of bacterial diarrhea in the United States. HIV positive individuals are at increased risk of shigellosis, with highest risk among men who have sex with men (MSM). Shigella was first recognized as a sexually transmitted disease in the MSM population in the 1970s with direct oral-anal contact as the primary risk factor. As in our patient, increasing antimicrobial resistance rates, >90 % in one study, have been found particularly to doxycycline, tetracycycline, aminoglycosides, cephalosporins, and trimethoprim/sulfamethoxazole. Stool culture is considered the gold standard for diagnosis however remained negative in the presented patient despite multiple cultures. One study demonstrated rates of isolation to be 11–12 % which poses a significant barrier to diagnosis of the disease and subsequent treatment. The present case highlights the need for heightened physician awareness of Shigella as an STD in individuals partaking in oral-anal sexual practices. Furthermore, if suspicion for Shigellosis is high, repeated stool testing may be necessary given poor rates of isolation.
SHOSHIN BERIBERI MASQUERADING AS SEPTIC SHOCKGautam George1; Fabian Reimold1; Carey C. Thomson2. 1Mount Auburn Hospital- Harvard Medical School, Cambridge, MA; 2Mount Auburn Hospital- Harvard Medical School, Cambridge, MA. (Tracking ID #1939956)
LEARNING OBJECTIVE 1: To recognize shoshin beriberi which is a fulminant form of thiamine deficiency and its manifestations in a critical care setting
LEARNING OBJECTIVE 2: To understand the pathophysiology of thiamine deficiency causing lactic acidosis and cardiovascular instability
CASE: A 65 year old woman with a history significant for incarcerated ventral hernia repair complicated by enterocutaneous fistulae managed conservatively with bowel rest and total parenteral nutrition for 2 months, presented with lethargy, abdominal pain and changes in mental status. Initial findings were significant for profound hypotension, tachycardia, hypoxia and lactic acidosis. She was admitted to the intensive care unit for management of presumed septic shock. Repeated physical examinations, radiologic and laboratory examinations did not yield a source of infection. Broad spectrum antibiotics, aggressive fluid resuscitation, and vasopressors were initiated. Significantly elevated lactate levels persisted despite resuscitation and stabilization. Due to persistent mental status changes, magnetic resonance imaging of the brain was performed which revealed an abnormal signal in the thalami and dorsal midbrain. A presumed diagnosis of Wernicke’s encephalopathy from thiamine deficiency was made and intravenous thiamine was started. Subsequently, her hemodynamics improved and lactic acidosis resolved with concurrent improvement in her mental status.
DISCUSSION: In our case, we report a patient who had been on total parenteral nutrition without adequate thiamine replacement for a prolonged duration that resulted in severe thiamine deficiency. Thiamine deficiency, which is commonly seen in alcoholics, can also be present in critically ill patients. Manifestations of this nutritional disorder can be varied and can range from polyneuropathy, cardiovascular disease, neurological changes as seen in Wernicke-Kosarkoff syndrome and severe lactic acidosis. Fulminant cardiovascular manifestations of thiamine deficiency include hypotension, tachycardia and lactic acidosis and is referred to as Shoshin beriberi. Thiamine is an essential co-factor in important de-carboxylation reactions in the Krebs cycle and decrease in its activity can lead to decrease in pyruvate formation and buildup of lactate that leads to mitochondrial dysfunction. It is important that this disorder be considered in critically ill patients with potential predisposing risk factors, as early diagnosis and treatment can result in preventing hemodynamic compromise and life threatening acidosis.
SICK SINUS SYNDROME TREATED WITH AN ANTIBIOTICAhmet A. Oktay; Harvey Friedman. Presence St. Francis Hospital, Evanston, IL. (Tracking ID #1935012)
LEARNING OBJECTIVE 1: Increasing the awareness about an atypical presentation of Lyme carditis.
LEARNING OBJECTIVE 2: Recognizing the importance of timely diagnosis and appropriate management of Lyme carditis.
CASE: A 59 y/o male patient presented to the emergency department because of dizzy spells and near-syncope experienced multiple times a day for the past 3 weeks. His symptoms were brief (<30 s) and paroxysmal with no association with any certain activity. He did not have any chest pain, shortness of breath, palpitations or fainting spells and denied any similar complaints in the past. He had a past medical history of hypertension for which he was taking Lisinopril 5 mg daily. He was also on supplemental fish oil, coenzyme Q and flax seed. He had no known allergies and his family history was non-contributory. He lived with his family in Chicago, drank ~1 bottle of wine every week and had no history of cigarette smoking or substance abuse. He reported going on a hiking trip in Upstate New York in September, which was a month ago. Right after returning from this trip, he developed erythematous rash on both arms, which lasted for a couple days and was accompanied by generalized fatigue, subjective fever and arthralgia in multiple joints. On examination, the temperature was 36.9 °C, the blood pressure 156/87 mmHg and the heart rate 64 bpm. His physical exam was normal except irregular heart rhythm. His ECG showed sinus bradycardia (ventricular rate: 56 bpm) with first-degree atrioventricular (AV) block and a sinus pause (3 s) with junctional escape beat. Initial laboratory workup including CBC, electrolytes, TSH and troponin (×3) were all within normal limits. After admission to the hospital, he continued to experience paroxysmal lightheadedness episodes frequently and these were accompanied by sinus pauses (3 to 7 s) on telemetry. Transcutaneous pacing pads were placed but he did not require any external pacing. Echocardiography was done which did not show any structural or functional cardiac abnormalities except mild mitral and aortic regurgitation. Although there was no recollection of tick-bite, history of skin rash, constitutional symptoms and arthralgia following a hiking trip, presence of first degree AV block and absence of any signs of structural and ischemic heart disease led us to the diagnosis of Lyme carditis as the cause of symptomatic sick sinus syndrome in our patient. He was started on IV ceftriaxone. The diagnosis of Lyme disease was later confirmed by serologic testing; ELISA was positive for IgG antibody and Western Blot positive for IgM and IgG antibodies. The patient showed slow but progressive improvement throughout his 14-day hospital stay. Sinus pauses became shorter and less frequent and the symptoms resolved. However, first degree AV block persisted. He was discharged home on oral doxycycline.
DISCUSSION: Lyme disease is a tick-borne systemic disease caused by the spirochete Borrelia burgdorferi. Cardiac involvement is seen in 4 to 10 % of patients with Lyme disease. The cardinal manifestation of Lyme carditis is self-limited conduction system disease, most commonly involving AV node. Additionally, endocarditis, myocarditis, pericarditis or tachyarrhytmias have been reported. The unique aspect of our case is the clear association between Lyme carditis and symptomatic sick sinus syndrome with sinus pause, in addition to AV node dysfunction. Lyme carditis is well known to cause AV node dysfunction. But there have been only a few case reports describing sick sinus syndrome induced by Lyme disease. Treatment options for Lyme carditis have not been validated with randomized controlled trials. However, if clinical suspicion is high as was in our case, antibiotic therapy should be initiated without waiting for lab confirmation. We think that; being aware of atypical presentations of Lyme carditis can help physicians with timely diagnosis of this treatable disease and save patients unnecessary invasive diagnostic and therapeutic procedures.
SICK TO YOUR STOMACH: IATROGENIC BOWEL ANGIOEDEMAChristopher Velez; Eric Stevens; Robert L. Goodman. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939114)
LEARNING OBJECTIVE 1: Review the epidemiology of angioedema.
LEARNING OBJECTIVE 2: Recognize angiotensin-converting enzyme inhibitor (ACE) inhibitor-mediated bowel angioedema as a cause of gastrointestinal distress
CASE: A 52-year-old African American man with a history of ischemic cardiomyopathy in the setting of hypertension, hyperlipidemia, type 2 diabetes mellitus, and active tobacco abuse presented with 2 weeks of abdominal discomfort and diarrhea along with several hours of oropharyngeal edema. The patient stated he usually had one or two well-formed bowel movements every day; recently, he had six loose-to-watery bowel movements daily. His diarrhea was non-mucoid, non-bloody, and there were no constitutional symptoms. He had no travel history, sick contacts, dietary changes, or antibiotic use. When the patient additionally developed acute tongue swelling, he presented to the emergency department. His medications included aspirin, metoprolol, lisinopril, furosemide, spironolactone, and atorvastatin; there were no recent changes. His physical exam was remarkable for tachycardia, dry mucous membranes, and an asymmetric swelling of the tongue without any localized erythema or urticaria. Although there was no respiratory stridor, diffuse abdominal discomfort was present. Laboratory studies revealed a leukocytosis of 12.1 k/μL, normal liver tests, and unremarkable serum amylase and lipase levels. With discontinuation of lisinopril for 48 h and subsequent administration of prednisone and diphenhydramine, the patient’s tongue swelling and gastrointestinal distress completely resolved.
DISCUSSION: Angioedema is a clinical phenomenon defined both by its acuity and discrete anatomic localization. Once hereditary angioedema is no longer being considered, only 20–40 % of evaluations are diagnostic. The association between angiotensin-converting enzyme (ACE) inhibitors and angioedema is classic, but it occurs in less than 1 % of patients taking these agents; angiotensin receptor blockers, calcium channel blockers, nonsteroidal anti-inflammatory drugs, antibiotics, and opiates also have been implicated. Yet, there has been an estimated 67 % increase in ACE inhibitor-mediated angioedema over the course of 2005 through 2009 correlating with a three-fold increase in the use of these agents. Risk factors for ACE inhibitor-mediated angioedema, as in the case of this patient, include African ancestry and a history of smoking; other reported risk factors are elderly age, and female gender. Even though the majority of patients report symptoms involving the lips and/or the tongue, angioedema can impact diverse sites including the bowel. Manifestations of visceral angioedema are typically underappreciated and likely underreported, making it difficult to determine the true incidence. Additionally, abdominal symptoms are typically non-specific such as pain, nausea, vomiting, and diarrhea. While visceral involvement may be detected radiographically, the strongest proof of the correct diagnosis of iatrogenic bowel angioedema remains a symptom-free clinical course after discontinuation of the offending agent. This patient experienced simultaneous resolution of gastrointestinal distress and oropharyngeal swelling with no further recurrence noted during subsequent visits to our institution after lisinopril had been stopped. This case illustrates not only the greater consideration that that should be given to ACE inhibitor-mediated angioedema given the increasing use of these agents, but also the importance of diagnosing iatrogenic angioedema beyond the oropharynx which may yield more rapid symptomatic relief without the need for expensive and invasive testing.
SICKLE CELL INTRAHEPATIC CHOLESTASIS: REVERSAL OF HEPATIC FAILURE WITH AGGRESIVE EXCHANGE TRANSFUSION IN A REFRACTORY CASEMusa A. Sharkawi; Noormuhammad Abbasakoor; Amy Tien; Robert R. Faust; Atoussa Goldar-Najafi. Lahey Hospital & Medical Center, Burlington, MA. (Tracking ID #1919578)
LEARNING OBJECTIVE 1: Recognize the causes of liver dysfunction in a sickle cell anemia patient
LEARNING OBJECTIVE 2: Manage patients with sickle cell intrahepatic cholestasis
CASE: A 22 year old Jamaican male with sickle cell disease (HbSS), presented with crampy abdominal pain, scleral icterus, epistaxis, tender hepatomegaly and found to have labs significant for a total bilirubin of >60 mg/dL, direct bilirubin of 43.5 mg/dL, White Blood Cell Count of 19,000, haemoglobin S (HbS) level of 26.7 % and International Normalized Ratio (INR) of 8. He was transferred to us from an outside hospital for further management of liver failure 7 days after a cycle of exchange transfusion was unsuccessful in reversing his hemorrhagic diathesis. He was treated with aggressive supportive therapy which constituted high flow oxygen, intravenous fluid hydration and daily folic acid supplementation. His coagulopathy required multiple fresh frozen plasma (FFP) transfusions and vitamin K supplementation. His symptoms were unremitting, hence a transjugular liver biopsy was performed to discern the underlying pathology. This was very remarkable for hepatic parenchyma with marked sinusoidal dilatation containing densely packed aggregates of “crescent shaped” red blood cells and hepatocanalicular cholestasis [Figures 1–2]. A further cycle of exchange transfusion was then performed with a lower HbS level goal of <10 %. His HbS level post-exchange transfusion was 8.6 % after which the coagulopathy and liver function gradually improved and the patient was discharged home on day 11 of hospitalization.
DISCUSSION: Sickle cell disease is a relatively common condition in populations of African descent that presents with numerous manifestations of varying severities. Common manifestations of hepatobiliary disease in sickle cell anemia include cholelithiasis, viral infection, iatrogenic hemochromatosis, vascular occlusions, hepatic sequestration and acute sickle hepatic crisis all under the umbrella term of “Sickle Cell Hepatopathy” [1]. Sickle cell intrahepatic cholestasis represents a potentially lethal and exceedingly rare variant of sickle hepatic crisis with only 18 cases described in the literature thus far. The underlying pathology is thought to be extensive sickling within the hepatic sinusoids leading to widespread ischemic damage [2]. Patients typically present with intense jaundice, tender hepatomegaly, coagulopathy and extreme hyperbilirubinemia which can progress to hepatic encephalopathy and florid renal failure. Current literature advocates early exchange transfusion as the treatment of choice with a HbS goal of less than 20–30 % [3–4]. In our experience, expeditious recognition and aggressive intervention with exchange transfusion HbS goal of <10 % and intensive supportive care can result in a favorable outcome in refractory cases. References: 1- Banerjee, S., Owen, C. and Chopra, S., Sickle cell hepatopathy: Hepatolog 2001; 33: 1021–1028 2- Shao SH, Orringer EP, Sickle cell intrahepatic cholestasis: approach to a difficult problem: Am J Gastroenterol. Nov 1995;90(11):2048–50 3- O’Callaghan, S G O’Brien, M Ninkovic, G P Butcher, C S Foster, J R F Walters, I A G Roberts, Chronic intrahepatic cholestasis in sickle cell disease requiring exchange transfusion: Gut 1995; 37: 144–147 4- Karina Irizarry, Hans Christof Rossbach, Joseph R. A. Ignacio, Michele P. Winesett, Greg C. Kaiser, Mudra Kumar et al., Sickle cell intrahepatic cholestasis with cholelithiasis: Pediatric Hematology and Oncology, 2006; 23:95–102
SINUSITIS CAUSING LEFT SIDED HEMIPARESISNeal George. Conemaugh Memorial Medical Center, Johnstown, PA. (Tracking ID #1943143)
LEARNING OBJECTIVE 1: How to differentiate possible etiologies to the pathogenesis of brain abscesses.
LEARNING OBJECTIVE 2: How to approach adult patients with brain abscess.
CASE: 65 year old Caucasian female with a history of insulin dependent diabetes mellitus, hypertension, and hypothyroidism presented to the emergency department via private car with complaints of a 3 day history of leaning towards the left side with progressive left sided weakness. No preceding fever or trauma. The patient presented with stable vital signs and with a Glasgow coma scale of 15. No dysarthria was present. Physical exam was remarkable for a 0-1/5 motor strength in the left upper and lower extremity with intact sensation throughout. Admission WBC was 7.3 thousands/cumm with a differential significant for 68 % neutrophils. The remainder of the admission laboratory studies were unremarkable. CT head revealed a 2.2 cm mass in the right cerebral hemisphere with moderate adjacent vasogenic edema without midline shift or hydrocephalus and no acute intracranial hemorrhage was noted. MRI of the brain revealed a peripherially enhancing mass measuring 2.4 × 1.8 × 2.3 cm located in the high right cerebral hemisphere with surrounding vasogenic edema. There was also membranous thickening and/or soft tissue density posterior-inferior aspect of the left maxillary sinus. The patient was evaluated by neurosurgery who performed a image guided craniotomy with excision of deep frontoparietal mass on the fourth day of admission. Surgical pathology of the frozen secton revealed acute necro-inflammatory debris with some atypical cell clusters. Culture of the brain tissue resulted in pansensitive growth of S. intermedius and S. constellatus on day number seven. Blood and urine cultures remained negative. Tranesophageal echocardiogram revealed a patent foramen ovale by and Atrial septal aneurysm by color flow doppler. The patient was treated with Decadron 8 mg IV every 6 h and Ceftazidime 1 g every 8 h. Subsequent imaging with dedicated CT of the sinuses revealed ethmoid and maxillary mucosal thickening consistent with sinusitis which was thought to be the possible etiology as previous reports corroborate cerebral abscess formation via intracranial extension from sinogenic sources.
DISCUSSION: Brain abscesses remain a consideration despite improvements in detection and treatment of sinusitis. Three mechanisms have been eluded to as etiologies for seeding brain abscesses. (1) Direct extension: infections stemming from the sinuses, teeth, middle ear, or mastoid may gain access to the venous drainage of the brain via valveless emissary veins that drain these regions. (2) Hematogenous dissemination from distant infection sites often results in multiple brain abscesses. (3) Following penetrating head injury or neurosurgery. However, up to 30 % of abscesses are crytogenic and have no clear source. Upon review of the current literature, there is a single case report of a patent foramen ovale and atrial septal aneurysm presenting with Streptococcus constellatus brain abscess. Jan et al. describes a case of 47 year old white male with patent foramen ovale with oral flora causing a S. intermedius brain abscess. However the patient reported here had a single solitary cerebral abscess and negative blood cultures making hematogenous spread an unlikely etiology. S. Intermedius infection tended to be associated with hematogenous spread or were deepseated, whereas those do to S. constellatus were more often superficial. S. constellatus had more of a predilection to cause odontogenic and intra-abdominal disease. This patient’s brain abscess was likely due to maxillary and ethmoid sinusitis via direct extension to the brain via venous drainage. Previous studies have shown that there is a greater predilection for S. intermedius and S. constellatus to generate cerebral abscesses. Brain abscesses larger than 2.5 cm, stereotactic aspiration or open brain biopsy with evacuation should be strongly considered for microbiological diagnosis which is helpful as given the wide range of possible pathogens and the prolonged course of IV antibiotics. One approach has been to treat neurologically stable patients with early infections with IV antibiotics alone. Aspiration can be attempted when the infection appears more encapsulated and liquefied, to maximize the yield of an aspiration procedure. Large abscesses (>2.5 cm) should generally be aspirated or excised. There is unfortunately no studies evaluating empiric therapy for cerebral abscess which may be appropriate given the number of different pathogens but those associated with paranasal sinusitis, otitis, or mastoiditis can be empirically treated with third-generation cephalosporins (ceftriaxone, ceftizoxime) combined with IV metronidazole.
SJOGREN’S SYNDROME-ASSOCIATED NEUROPATHY AND CIRRHOSISLillian Chen; Phillip S. Ge; Digish D. Shah. University of California- Los Angeles Medical Center, Los Angeles, CA. (Tracking ID #1940157)
LEARNING OBJECTIVE 1: Recognize that in the majority of patients with Sjogren’s syndrome-associated neuropathy, the neurologic manifestations precede the sicca symptoms.
LEARNING OBJECTIVE 2: Recognize that Sjogren’s syndrome can rarely cause cirrhosis.
CASE: A 56 y.o. female with history of hypothyroidism, anemia, and thrombocytopenia presented with a 1 year history of unilateral left-sided numbness that gradually progressed to left-sided weakness and numbness of the right foot. She denied any history of heavy alcohol or drug use. Neurological examination showed 3/5 strength in the proximal left lower extremity, 4/5 strength in the distal left lower extremity, 4/5 strength in the left upper extremity, 5/5 strength in the right upper and right lower extremities, absent sensation in the left upper and bilateral lower extremities, and areflexia of the three affected extremities. The remainder of her physical examination was unremarkable. Labs were notable for white blood cell count 2.9 × 103/μL, hemoglobin 9.6 g/dL, platelets 41 × 103/μL, alkaline phosphatase 230U/L, AST 38U/L, ALT 24U/L, total bilirubin 0.6 mg/dL, albumin 3.0 g/dL, INR 1.2. TSH was 7.8μIU/mL with normal fT4. MRI head/neck revealed multiple parotid cysts. Abdominal ultrasound revealed cirrhosis. On hospital day two, she had massive hematemesis and EGD showed bleeding esophageal varices that were banded. Subsequent laboratories showed ANA >1:1280, positive anti-SSA, and low C3 and C4; other rheumatologic workup including cryoglobulins was negative. HIV, HTLV-1, viral hepatitis panel, anti-mitochondrial and anti-smooth muscle antibodies were negative. Liver biopsy showed macrovesicular steatosis and bridging fibrosis compatible with lupus-related liver disease. CSF studies were normal. EMG/NCS showed sensorimotor polyneuropathy with predominantly axonal features. Sural nerve biopsy showed axonal degeneration and myelinated fiber loss. She was thus diagnosed with mononeuritis multiplex. Schirmer test was positive. Parotid gland biopsy was ultimately non-diagnostic; however she met criteria for Sjogren’s syndrome, as she also endorsed dry eyes and mouth starting 1 month prior to admission. She was started on pulse steroids with some improvement in strength and was transitioned to prednisone and ultimately started on rituximab.
DISCUSSION: Neurologic involvement occurs in about 20 % of patients with primary Sjogren’s syndrome. The presentation can be diverse, with sensory ataxic neuropathy and painful sensory neuropathy being the most common. However, mononeuritis multiplex and other neuropathies can also be seen. Even though dry eyes and mouth are the most common symptoms in patients with Sjogren’s syndrome, patients can have debilitating neuropathy as the initial presentation. A majority of patients develop neuropathy prior to the formal diagnosis of Sjogren’s syndrome. Sjogren’s syndrome should thus be considered in the evaluation of peripheral neuropathy despite the absence of classic sicca symptoms. Approximately 40 % of patients with primary Sjogren’s syndrome may have abnormal liver chemistries; however they are usually asymptomatic or have subclinical disease. The most common diagnoses, when found, are primary biliary cirrhosis, autoimmune hepatitis, and hepatitis C infection. Primary Sjogren’s syndrome-associated cirrhosis is considered very rare, however once detected it should be treated similarly to cirrhosis from other etiologies.
SKIN NODULES IN A PATIENT WITH RHEUMATOID ARTHRITIS… COMMON OR DEADLY?Crystal Hlaing; Ryan E. Jones; Tara Norris. Methodist Dallas Medical Center, Dallas, TX. (Tracking ID #1940175)
LEARNING OBJECTIVE 1: Review common dermatologic manifestations of rheumatoid arthritis.
LEARNING OBJECTIVE 2: Be able to differentiate similar-appearing dermatologic conditions associated with rheumatoid arthritis.
CASE: A very pleasant 80-year-old Caucasian woman with a past medical history of RA and hypertension presented to the emergency department (ED). She stated that a rash had started on her left thigh 1 month prior to this ED visit. It had progressed to involve the right thigh and right upper arm, as well as distal interphalangeal joints and finger tips of both hands. The patient was given a 4-week course of amoxicillin-clavulanate for presumed cellulitis approximately 2 weeks prior to admission. She did not have any improvement with this treatment, however, and in fact experienced progression while on the antibiotic. The patient complained of pain and discomfort in the affected areas, but denied any fever or chills. She had been on methotrexate (MTX) and prednisone prescribed by her rheumatologist for several years. She was also taking a calcium supplement and valsartan/hydrochlorothiazide. She denied any exposure to gadolinium or having an MRI in the past. She reported allergy to sulfa medications. She denied any toxic habits, poor living conditions, or family history of skin disorders, On exam, the patient was afebrile and nontoxic appearing. She had marked erythema and patchy induration of her bilateral inner thighs, with a 1 cm × 1 cm area of skin necrosis over her left inner thigh. The skin on the extensor aspect of her right upper arm was erythematous and swollen and had an extensive area of induration. Both the patient’s palms and the fingertips of her right hand were also affected. There was a 0.5 cm × 0.5 cm subcutaneous nodule at the tip of her right second digit. All affected areas were tender but lacked significant warmth to the touch. The patient’s laboratory studies were notable only for mild anemia (hemoglobin of 10.0), corrected calcium of 10.3 (normal: 8.4–10.2), and phosphorous of 2.6. She had no leukocytosis, and renal function and blood sugar were normal. As patient did not have signs such as fever or leukocytosis, infectious processes were thought to be less likely. Differentials most highly considered were: rheumatoid nodulosis, calciphylaxis, and vasculitis. Dermatology was consulted. Skin biopsies from right upper arm and left medial thigh lesions were performed. The patient was discharged home prior in stable condition, instructed to follow up with her rheumatologist in a few weeks. She was told to not to take her calcium supplement, prednisone, or MTX for the time being. Pathology report states that granulomatous inflammation throughout the dermis and panniculus was seen. Pathologist’s comment stated that this was most likely granulomatous vasculitis associated with RA. The patient’s rheumatologist concluded that the patient’s areas of induration were likely due to underlying vascultiis, and the nodular lesions most likely represented methoxtrexate-induced accelerated nodulosis (MIAN). The patient’s methotrexate was held, and upon 1-month follow-up, she reported complete resolution of all skin lesions (with the exception of a small scar in the left medial thigh where the most advanced lesion had been).
DISCUSSION: Our patient’s lesions were ultimately felt to be methotrexate-induced accelerated nodulosis (MIAN) along with rheumatoid vasculitis. This case highlights the differential diagnosis of erythematous and nodular skin lesions in a patient with rheumatoid arthritis. The first thing to rule out was calciphylaxis, due to its high potential for mortality. Calciphylaxis has occurred in patients on immunosuppressant medications and those with vasculitis, such as our patient, but it is much more commonly seen in patients with end-stage renal disease. Furthermore, our patient’s calcium phosphate product (CPP) was not greater than 70, which is usually seen with calciphylaxis. Furthermore, the patient’s upper extremities were involved, which is rare in calciphylaxis. Finally, the skin biopsy failed to show intravascular calcium deposition in the dermal media, thus ruling out this deadly condition. MTX is postulated to accelerate rheumatoid nodule formation (hence the term MIAN) by stimulation of adenosine A1 receptors, which leads to increased giant cell formation. Differentiating between usual rheumatoid nodules and MIAN is important, as management differs for these two conditions. The histopathology of the two cannot be easily differentiated. Some factors that point towards MIAN are: nearly all patients with MIAN are seropositive for RF, and 25 % have a concurrent vasculitis. Furthermore, lesions on atypical sites such as finger tendons, smaller (less than 5 mm) lesions, rapid development of lesions, and absence of extra-articular involvement point towards MIAN, with most patients having been on methotrexate for at least 3 months.
SKIN RASH, IS IT AN INFECTION?Mahmoud Abdelghany; Samuel Massoud. Conemaugh Memorial Medical Center, Johnstown, PA. (Tracking ID #1922858)
LEARNING OBJECTIVE 1: − Eruptive xanthoma is a cutaneous disease results from hypertriglyceridemia and poorly controlled diabetes.
LEARNING OBJECTIVE 2: − Early recognition of eruptive xanthoma is crucial to avoid more serious sequelae including acute pancreatitis and ophthalmic complications.
CASE: A 50 -year-old obese man with a past history of hypertension, hyperlipidemia and recently diagnosed diabetes presented complaining of skin rash for 1 week. He denied any history of fever, chills, myalgia, abdominal pain, visual changes, history of new drug use or contact with anyone with similar symptoms. His medications included lisinopril, simvastatin, niacin, metformin. On physical examination, the lesions were small reddish yellow non-pruritic tender papules covering the extensor surfaces of knees, forearms, the abdomen and the back. Laboratory evaluation showed total cholesterol level 1045 mg/dl, triglyceride level 7855 mg/dl, TSH 0.52 uIU/ML, fasting blood glucose 441 mg/dl and HBA1c 12.6 %. Three months before the laboratory evaluation showed total cholesterol 163 mg/dl, triglyceride level 614 mg/dl, fasting blood glucose 158 mg/dl and HBA1c 7.5 % and the patient was first diagnosed with diabetes mellitus. Histologic analysis of a lesion-biopsy specimen showed foamy macrophages and loose lipids, which confirmed the suspicion of eruptive xanthomas. Immediately after the diagnosis, the patient was started on a strict glycemic and lipid control. Metformin and statin doses were increased and insulin was added. Three weeks later there was marked improvement of the skin lesions.
DISCUSSION: Eruptive xanthoma is a cutaneous disease that most commonly arise over the extensor surfaces of the extremities, buttocks and shoulders. High levels of serum triglycerides and uncontrolled diabetes mellitus could be the cause. Hypothyroidism, end-stage renal disease and nephrotic syndrome can cause secondary hypertriglyceridemia. This condition may be associated with ophthalmologic deposition of cholesterol, such as lipemia retinalis (salmon-colored retina with creamy white retinal vessels), abdominal pain, and hepatosplenomegaly. Treatment involves dietary restrictions, exercise and medical management. Insulin, statin and gemfibrozil may be necessary for rapid control of the diabetes and hyperlipidemia. Early recognition and proper control of hypertriglyceridemia can prevent more serious complications as acute pancreatitis.
SPINE MRI AS WORK UP FOR SORE THROAT: A CASE OF MISSED PHARYNGITIS LEADING TO THE DIAGNOSIS OF ACUTE RHEUMATIC CARDITISLauren Mehner1; Melissa Reidy1; Luke Peters1; Daniel Chan2; Maria G. Frank3. 1University of Colorado, Aurora, CO; 2University of South Dakota, Sioux Falls, SD; 3Denver Health Hospital Authority, Denver, CO. (Tracking ID #1922217)
LEARNING OBJECTIVE 1: To raise awareness over the low but definite incidence of acute rheumatic fever (ARF)
LEARNING OBJECTIVE 2: To describe a case of ARF presenting with carditis and polyarthralgias
CASE: Thirty-five year-old female with no significant medical history presented to the ED complaining of 1 week of odynophagia, malaise, polyarthralgias, fever, back pain and headaches. Because she received epidural anesthesia for a vaginal delivery 1.5 months prior, she was evaluated with a spine MRI, which was unremarkable, and was discharged home with symptomatic treatment for back pain. She returned to the hospital 2.5 weeks later complaining of persistent polyarthralgias with additional large joint involvement, malaise, and subjective fever and was admitted to the medicine wards for further work-up. Her exam was significant for a new systolic murmur, best heard in the mitral area, and polyarthritis without synovitis. Her laboratory tests revealed ASO of 491 with ESR above 80 and CRP of 73.90. Bilateral hand X-rays were normal. A Trans-Thoracic Echocardiogram (TTE) showed severe Mitral Regurgitation and moderate Aortic Regurgitation. Because she met 2 major and 2 minor Jones criteria plus the evidence of a preceding Group A beta-hemolytic Streptococcus infection (GABHS), she was diagnosed with ARF. She was started on Penicillin G with a plan to receive monthly doses for a total of 10 years, as well as biannual TTE.
DISCUSSION: Acute rheumatic fever (ARF) has not been a reportable disease in the US since 1977 and ever since its diagnosis has been anecdotal. The advent of antibiotics, early diagnosis and treatment with rapid strep tests and cultures, as well as the described changes in streptococcal M proteins have led to a near disappearance of this malady in the developing world. ARF is a preventable disease; in fact, several studies on the treatment of GABHS pharyngitis to prevent ARF concluded that there would be a reduction in ARF cases by as much as 60 % if pharyngitis was appropriately treated, especially in endemic areas. While ARF remains high on the differential among immigrant populations and when practicing in endemic countries, this case serves as a reminder to remain vigilant in the U.S. as well. Common reasons for missed diagnosis and treatment failure among providers include absence of clinically significant preceding pharyngitis, anchoring biases, and failure to include ARF in the differential due to the extremely low disease incidence in the U.S. Additionally, patient factors such as failure to seek care for pharyngitis and poor antibiotic compliance contribute to the persistence of ARF. Because of the high risk of recurrence upon re-exposure to GABHS, it is essential that providers correctly diagnose ARF and begin patients on secondary prophylaxis. Our case demonstrates the need to raise awareness in the medical community around this infrequent condition as well as the need to be cognizant of our personal clinical biases.
SPONTANEOUS RENAL SUBCAPSULAR HEMORRHAGE AS A POSSIBLE COMPLICATION OF EXTERNAL RADIOTHERAPYTarun Jain; Suraj Raheja. Henry Ford Hospital, Detroit, MI. (Tracking ID #1939661)
LEARNING OBJECTIVE 1: Recognize the common and uncommon causes of spontaneous renal subcapsular hemorrhage.
CASE: Spontaneous subcapsular renal hemorrhage is a severe condition that leads to the abrupt removal of a kidney in two-thirds of cases. The primary causes described in the literature include renal tumors, vascular disease, and infections. We present a rare case of spontaneous subcapsular renal hemorrhage in the absence of these common causes, and as an apparent complication of radiation therapy used for the treatment of prostate cancer. We present an 84 year old male with past medical history of prostate cancer T2bN0M0 treated definitively with hormones and external radiation therapy 10 years ago. He presents with a 2 day history of sudden onset left sided lower abdominal pain. The patient denied hematuria, dysuria, lower urinary tract symptoms, hematuria, history of nephrolithiasis or history of UTIs. As part of his workup, abdominal computed tomography (CT) was performed, which demonstrated left hydroureteronephrosis with obstruction at the left ureteropelvic junction. The left kidney was also noted to have very thin parenchyma. Urology was consulted and noted that the obstruction may be a result of his previous radiation therapy, but because his PSA was stable there was no immediate urologic surgical intervention. He was discharged with analgesics and arranged for outpatient Urology follow-up. The patient, however, returned 1 week after this initial presentation, with complaints of persistent pain not alleviated by analgesics. Review of systems on this second presentation was negative for fever, nausea, vomiting, dysuria, frequency, urgency or hematuria. On physical exam, there was suprapubic fullness along with left lower quadrant and suprapubic tenderness. The patient’s creatinine was elevated to 3.5 mg/dl from a baseline of 1.5 mg/dl, but he had no elevation in his leukocyte count and his hemoglobin was not significantly decreased from his previous presentation. Repeat abdomen-pelvis CT scanning now demonstrated a new spontaneous hemorrhage in the subcapsular space of the left kidney, extending into the dilated intra-renal collecting system, along with worsening hydrouretonephrosis. Urology initially debated between ureteral stent with nephrostomy versus nephrectomy, but it was ultimately decided to manage the patient conservatively.
DISCUSSION: A meta-analysis of subcapsular and perirenal hemorrhages reported tumors as the etiology in over 61 % of cases. Vascular diseases, including polyarteritis nodosa, aneurysms and arterio-venous malformations, were a collective 17 % of cases. Infectious etiologies of abscess and pyelonephritis totaled 2.4 % of cases. No cause was identified or reported in approximately 7 % of cases, with the remaining 13 % being attributed to miscellaneous causes. These included uncontrolled hypertension, cyst rupture, nephrosclerosis and pre-eclampsia. Except for the exposure to radiation therapy, no particular cause for spontaneous hemorrhage could be identified in this patient. Physicians routinely encounter renal tumors, vascular diseases and infections of the renal system. Related to these common findings, this case renews the awareness of sub-capsular or peri-renal hemorrhage, and the need to assess these patients knowing the frequency of abrupt nephrectomy as a treatment outcome. In addition, physicians should be able to integrate the less commonly encountered causes that have been highlighted. Our case suggests radiation therapy as an additional risk factor for this hemorrhagic event.
SPONTANEOUS TUMOR LYSIS SYNDROME DUE TO NEUROENDOCRINE TUMORWaleed Quwatli; Charu Ramchandani; Mahesh Krishnamurthy. Unity health system, Rochester, NY. (Tracking ID #1939411)
LEARNING OBJECTIVE 1: Spontaneous tumor lysis syndrome (TLS) due to no-hematologic malignancy is rare but it is very crucial to be recognized and treated promptly.
CASE: A 60 year old male who was referred to the emergency room by a gastroenterologist for progressive abdominal pain and rapidly growing hepatomegaly for 1 month associated with worsening liver and renal functions. Review of system was positive for nausea, vomiting, diarrhea, anorexia, weight loss, weakness, jaundice, shortness of breath and oliguria. His past medical history was significant for Ankylosing spondylitis treated with Adalimumab and Methotraxate both of which were discontinued few months prior to presentation due to transaminitis and elevated creatinine. On physical examination he was hypotensive, tachypneic, tachycardic, mild icteric jaundice, flushed face. Lung exam showed bibasilar crackles with mild diffuse wheezing, heart was with normal sounds, abdomen exam showed massive hepatomegaly without stigmata of chronic liver disease. His lab tests showed BUN 66 mg/dl, Creatinine 4.8 mg/dl (baseline 1.4 mg/dl), potassium 4.9 mEq/L, phosphorus 5.3 mg/dl, uric acid 26.1 mg/dl, ALT 63 u/l, AST 284 u/l, total bilirubin 2.7 mg/dl, direct bilirubin 2.2 mg/dl, LDH 1292 u/l. Computed Tomography of the abdomen without contrast showed heterogeneous hepatomegaly with irregular contour. Based on the laboratory tests and the rapidly growing hepatomegaly there was a high suspicion of spontaneous tumor lysis syndrome. The patient developed non sustained ventricular tachycardia for that he was transferred to the ICU where dialysis was initiated, Rasburicase was given intravenously. Magnetic resonance imaging of the abdomen showed innumerable lesions throughout the liver. Biopsy showed well differentiated neuroendocrine tumor. Repeated Uric acid level was <1 mg/dl. The patient refused chemotherapy and further work up to identify the primary origin. He deteriorated rapidly, developed multi-organ failure and passed away.
DISCUSSION: Tumor lysis syndrome (TLS) is an oncologic emergency that is caused by massive tumor cell lysis and release of large amounts of potassium, phosphate, and uric acid into the systemic circulation leading to hyperuricemia, hyperkalemia, hyperphosphatemia, and secondary hypocalcemia. This can lead to significant morbidity, putting patients at risk of severe clinical consequences that include acute kidney injury, cardiac arrhythmias, pulmonary edema, fluid overload, seizures, and even death. Laboratory TLS is defined as any two or more of the following metabolic abnormalities and presents within 3 days before or 7 days after instituting chemotherapy: hyperuricemia, hyperkalemia, hyperphosphatemia, and hypocalcemia. Clinical TLS is defined as laboratory TLS plus one or more of the following that was not directly or probably attributable to a therapeutic agent: increased serum creatinine concentration (≥1.5 times the upper normal limit), cardiac arrhythmia/sudden death, or a seizure. TLS is associated most commonly with initiation of aggressive chemotherapy for hematologic malignancies like non-Hodgkin lymphomas and acute lymphoblastic leukemia. Spontaneous TLS is not commonly seen and just few cases of spontaneous TLS due to neuroendocrine tumor (NET) have been reported in literature. Spontaneous acute renal failure associated with marked hyperuricemia prior to the initiation of therapy has been described in lymphomas and acute leukemias. It usually occurs in patients with bulky, rapidly proliferating, treatment-responsive tumors. Interestingly, spontaneous TLS is associated with hyperuricemia but frequently without hyperphosphatemia because the high serum uric acid levels are related to rapid nucleoprotein turnover and the tumor is able to reutilize released phosphorus for resynthesis of new tumor cells. Effective management involves the combination of treating specific electrolyte abnormalities, and/or acute renal failure, and the use of allopurinol, a xanthine oxidase inhibitor administered to reduce the conversion of nucleic acid byproducts to uric acid in order to prevent urate nephropathy and subsequent oliguric renal failure. Rasburicase is a recombinant urate oxidase responsible for the oxidation of uric acid to allantoin which is more soluble in urine than uric acid and because of its rapid onset of action, it is indicated when uric acid levels cannot be lowered sufficiently by standard approaches. A loop diuretic and intravenous fluids is frequently needed, and hemodialysis may be indicated if the patient developed severe oliguria/anuria, persistent hyperkalemia, or hyperphosphatemia induced symptomatic hypocalcaemia. Spontaneous TLS due to NET is extremely rare, and spontaneous TLS by itself is an oncologic emergency which should be included in the differential diagnosis of patients with rapidly growing tumors who present with acute kidney injury even if they did not receive chemotherapy.
STAPHYLOCOCCUS LUGDUNENSIS: THE GREAT CONS ARTISTJulie M. Collins; Chad S. Miller. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926986)
LEARNING OBJECTIVE 1: Demonstrate the pathogenicity of coagulase-negative staphylococcus.
LEARNING OBJECTIVE 2: Review the clinical presentation of infective endocarditis.
CASE: A 49-year-old woman with HIV (CD4 count 101 cells/uL) and end stage renal disease presented with 9 days of progressive shortness of breath after a revision of her arteriovenous (AV) fistula for dialysis. She also noted generalized fatigue, subjective fever, four-pillow orthopnea and new-onset paroxysmal nocturnal dyspnea. Her temperature was 99.2 ° F, blood pressure 132/74, respirations 16, and saturation 99 % on room air. She had a 3/6 systolic ejection murmur noted at previous admissions as well as a new regurgitant murmur loudest in the mitral position, jugular venous distention, and 1+ lower extremity pitting edema. There was no erythema surrounding her right upper extremity AV fistula. WBC count was 14.2 × 10e3/uL with left shift. On day 2, she developed a fever to 101.6 ° F. Blood cultures from two sites grew coagulase-negative staphylococcus and repeat cultures were drawn. Blood cultures remained persistently positive for Staphylococcus lugdunensis for 8 days. A transthoracic echocardiogram (TTE) with bubble study showed an ejection fraction of 55–60 %, no shunt, and a vegetation on the atrial aspect of the anterior mitral leaflet. She was treated with nafcillin while inpatient and then transitioned to 6 weeks of cefazolin with dialysis.
DISCUSSION: Internists commonly encounter heart murmurs, and their etiology can be either benign or pathogenic. A high degree of suspicion for infective endocarditis (IE) with a new or changed heart murmur is imperative because endocarditis can rapidly cause irreversible damage to the heart. IE in chronic hemodialysis patients is significantly more common and causes greater morbidity and mortality than in the general population, being second only to cardiovascular disease as the leading cause of death in this group. Staphylococcus lugdunensis is a coagulase-negative staphylococcus (CONS) that like other CONS infections can range from a harmless skin flora to a life-threatening pathogen. S. lugdunensis affects native valves with greater frequency than prosthetic valves, unlike other CONS. IE due to this organism is characterized by a high mortality and rapid tissue destruction. Often, hospital laboratories will report non-aureus isolates only as CONS, but speciation of the organism can assume great importance in defining therapeutic approach. For example, the clinical outcome in the treatment of S. lugdunensis is much more favorable with valvular replacement than with antibiotics alone. Despite their frequency as contaminants, CONS have become important nosocomial pathogens, accounting for 9 % of all nosocomial infections. CONS are also the third most common cause of blood stream infections. The incidence of CONS bacteremia in patients with foreign bodies such as a port is increased compared to the general population due to their strong adherence to polymer surfaces and biofilm formation. It is important to assess the clinical picture when faced with CONS-positive blood cultures because these organisms are not always contaminants, and can cause significant morbidity and mortality when not treated appropriately.
STEAK IT’S WHAT’S FOR DINNERElizabeth Bowles; Molly Doose. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924659)
LEARNING OBJECTIVE 1: Consider acquired bronchoesophageal fistula in acquired immunodeficiency syndrome patients presenting with aspiration pneumonia in an atypical location.
LEARNING OBJECTIVE 2: Recognize populations at risk for acquired bronchoesophageal fistula and the importance of timely intervention.
CASE: A 50 year-old man with acquired immunodeficiency syndrome presented with 2 months of worsening cough, shortness of breath, and fever. He described a forceful cough associated with solid food or liquid intake and subsequent emesis, with a fifty-pound weight loss over the preceding 4 months. Upon examination, the patient was noted to be cachectic, with tachypnea and hypoxemia that responded well to oxygen supplementation via nasal cannula. No abnormal breath sounds were auscultated. Chest radiograph had no acute findings; however cough after oral intake prompted a modified barium swallow and chest computed tomography to evaluate further for aspiration. Modified barium swallow revealed no frank aspiration. Computed tomography revealed a left lower lobe consolidation with bronchiectasis, cavitation, air fluid levels, and punctate calcifications. Failure of response to typical therapy prompted bronchoscopy, which revealed vegetable matter with skeletal muscle fibers on biopsy of the consolidation. On esophagogram, contrast extravasation into the medial left lower lobe was consistent with a fistula. Esophagogastroduodenoscopy confirmed a 3 cm long false lumen in the esophagus, about 34 cm from the entry site, with esophageal mucosa on one side and bronchial tissue on the other. At the distal aspect of the lumen, there was a small opening, representing a discrete fistulous tract entering the lung.
DISCUSSION: In patients with known acquired immunodeficiency syndrome presenting with respiratory distress, infectious etiology including pneumocystis pneumonia, tuberculosis, viral, or bacterial pneumonia should be considered, with empiric therapy initiated quickly. When a patient’s symptoms persist despite appropriate therapy, further workup must be considered. Though rare, bronchoesophageal fistulas have been reported in acquired immunodeficiency syndrome patients, presenting with progressive dysphagia, weight loss and episodes of cough on intake of food. Imaging findings consistent with aspiration pneumonia should prompt continued workup for a fistula. Diagnosis can be made by barium esophagogram, with location and size of the fistula determined by bronchoscopy or esophagogastroduodenoscopy. Other patient populations at risk for acquired esophago-airway fistulas include patients who have undergone tracheal intubation, ingested corrosives, sustained chest trauma or iatrogenic injury, suffered granulomatous mediastinal infections, had prior surgery on the esophagus or tracheobronchial tree, or those with indwelling stents. In patients presenting with an esophago-airway fistula without one of the above risk factors, malignancy, especially esophageal carcinoma, must be considered. Therapies for an esophago-airway fistula include esophageal stenting, esophageal exclusion, esophageal bypass, and fistula resection and repair. Insertion of a coated self-expandable metal stent is the treatment of choice for an individual with malignant esophago-airway fistula. Without treatment, the median survival time may be 1 to 6 weeks, with aspiration pneumonia as the usual cause of death.
STEMI, ELEVATED PTT AND ANEMIA: A LIFE THREATENING SYNDROMEZakaria Almuwaqqat. saint francis hospital, Evanston, IL. (Tracking ID #1939026)
LEARNING OBJECTIVE 1: − Early diagnosis of antiphospholipid syndrome in a previously healthy young patient presenting with chest pain and elevated PTT.
LEARNING OBJECTIVE 2: − Importance of early anticoagulation therapy to prevent recurrent myocardial and cerebral infarction as well as failure of coronary intervention. - recognition of one of the cardiac manifestations of antiphospholipid syndrome.
CASE: 30 year old African American male patient presented to the emergency department with intermittent chest pain for 4 days associated with diaphoresis, arm numbness and tingling, palpitations. Patients reported that he would eat, smoke a cigarette, then get these symptoms; resolved within 4–5 min. patient described chest pain as “grabbing” pain, 10/10 retrosternal radiating to the arm. Episodes were becoming more frequent. Took 500 mg of tylenol twice without relief. Past medical history is significant for vitamin B12 deficiency. Patient admitted to smoking history of 1 ppd for the past 10 years. Patient had no recent travel. Denies any personal or family history of blood clots, DVT, cardiac disease, stroke or DM. Patient has history of pernicious anemia, has not been getting his B12 Injection. Family history was negative for coronary artery disease, thrombophilia and hyperlipidemia His physical examination: Alert, oriented ×3, not in distress, neck no jugular venous distention, chest clear no rales, heart regular sate and rhythm, no murmur or gallops, abdomen soft, non-tendern and non distended, extremities warm and without edema. EKG revealed Normal sinus rhythm with anterolateral ST segment depression, labs showed elevated troponin, Hemoglobin 14.1, MCV 93, WBC 4.5, Plt 260, Cr 0.76, BUN 8, INR 1.1, PTT 200. Patient had chest CT to rule out aortic dissection revealing possible stenosis of LAD coronary artery, patient subsequently underwent cardiac angiogram which showed subtotal ostial LAD stenosis with thrombus possibly due to ulcerated plaque had successful thrombectomy with aspiration catheter and residual lesion less than 40 %, patient due to proximity of LAD stenosis to left main patient was referred for medical treatment and repeat of stress test in 4 weeks to evaluate hemodynamic significance of the lesion and if needed consider high risk PCI or single vessel CABG Patient was admitted to intensive care unit and chest pain resolved completely, however in the second day he started to complain from recurrent severe chest pain, EKG showed new ST elevation in anterolateral leads, emergency cardiac angiogram with drug letting stent inserted in proximal LAD.
DISCUSSION: Patient had work up for premature coronary artery disease and hypercoagulable state, his PTT was 200, lupus anticoagulant work up was positive for lupus antibodies, his intrinsic factor blocking antibody was also positive, ANA was negative and complement levels were normal, his vitamin B12 level was low and homocysteine was elevated, patient was diagnosed with antiphospholipid syndrome and started on therapeutic dose low molecular weight heparin and warfarin subsequently. Antiphospholipid syndrome is an autoimmune disease characterized by venous and/or arterial thrombosis and/or recurrent fetal loss and the presence of antiphospholid antibodies. The case illustrates one of the cardiac manifestations of antiphospholipid syndrome, its an important and potentially treatable cause of myocardial and cerebral infraction, its also a recognized cause of sudden death and failure of coronary intervention during myocardial infraction treatment, other manifestations includes ventricular thrombosis, pulmonary embolism, arterial thrombosis, pregnancy losses, recurrent coronary events and valvular heart disease which is based on the presence of thickening or vegetation of the valves (mainly mitral and aortic) as described by Libman and Sacks for patients with systemic lupus erythematosus (SLE).
STERILE PYURIA - A CLASSIC TALE WITH A MODERN TWISTCeleste Newby; Krystle Barhaghi; Marlowe Maylin. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925002)
LEARNING OBJECTIVE 1: Identify the clinical presentation and methods for detection of genitourinary tuberculosis
LEARNING OBJECTIVE 2: Discuss the differential diagnosis for sterile pyuria in modern medicine
CASE: A 51 year-old man with no past medical history presented with subjective fevers and weight loss for 1 month; review of systems was otherwise negative. A palpable supraclavicular lymph node was the only abnormal finding on physical exam. The patient’s chest radiograph was normal. Urinalysis on admission was negative for nitrites and bacteria, but positive for leukocyte esterase. The patient was intermittently febrile to >39° Celsius during admission, but multiple blood and urine cultures were negative. The patient complained of dysuria on day 3. A repeat urinalysis showed large leukocyte esterase, but urine cultures remained negative. CT scans were notable for diffuse abdominal lymphadenopathy and wedge-shaped deformities of both kidneys. The patient underwent excisional lymph node biopsy secondary to concern for lymphoma. The tissue was Fite stain positive for mycobacterial species. On further discussion, the patient admitted being diagnosed with HIV 20 years ago, but never sought medication attention. Acid-fast bacilli (AFB) cultures from the urine were positive for mycobacterium tuberculosis several weeks later.
DISCUSSION: In the past, sterile pyuria suggested the presence of genitourinary tuberculosis (GU-TB). GU-TB is seen in approximately 30 % of extra-pulmonary tuberculosis cases and is usually the result of dissemination from pulmonary disease. Patients with GU-TB rarely exhibit lung disease or respiratory symptoms. Extra-pulmonary TB has a higher prevalence in the setting of immunosuppression such as in HIV or organ transplant recipients. GU-TB is difficult to recognize, as bacterial urine culture media are less favorable for mycobacterial growth and may not provide a high yield. AFB urine culture has a 37 %–79 % sensitivity and is the gold standard in diagnosis of GU-TB. Multiple urine samples can increase sensitivity, and some suggest early morning samples are best. AFB cultures, however, can take up to 8 weeks to result. Newer PCR techniques have variable sensitivity (25–93 %) with high specificity (95–100 %) but currently are not widely available. While symptoms of a urinary tract infection coupled with pyuria and negative bacterial growth can suggest GU-TB in the appropriate clinical setting, it is important for internists to note that sterile pyuria has a larger differential diagnosis. In an era of widespread antibiotic use, the most likely result of sterile pyuria is recent or incomplete antibiotic use rather than tuberculosis. Negative urine cultures can also been seen with atypical infections such as Chlamydia and Ureaplasma species, and can also can be seen in autoimmune disease, prostatitis, nephrolithiasis, and malignancy. In most cases of sterile pyuria, a thorough review of medication and sexual history can provide the diagnosis.
STEROIDS AND WORMS: DIAGNOSING A RARE CAUSE OF ABDOMINAL PAIN IN ADVANCED AIDSNihal Patel; Olga Aroniadis; Sheira Schlair. Albert Einstein College of Medicine - Montefiore Medical Center, Bronx, NY. (Tracking ID #1934583)
LEARNING OBJECTIVE 1: Identify the use of corticosteroids as a risk factor for developing Strongyloides stercoralis (SS) hyperinfection syndrome
LEARNING OBJECTIVE 2: Recognize the rare presentation of SS hyperinfection syndrome in advanced AIDS patients
CASE: A 44 year-old Puerto Rican man with long-standing poorly controlled HIV/AIDS (CD4 = 34 cells/mm3), a history of Pneumocystis jirovecii pneumonia (PCP) and moderate persistent asthma presented to the hospital with 2 weeks of progressively worsening exertional dyspnea and a productive cough. Recurrent PCP was suspected due to marked hypoxemia, and he was started on empiric trimethoprim-sulfamethoxazole (TMP/SMX) and corticosteroids. Several hours later he developed a high-grade fever (>104.00 F), increased dyspnea, wheezing, sharp constant epigastric pain, loose stools, nausea and a serpiginous rash on his proximal thighs and buttocks. Initially, a drug reaction to the administered TMP/SMX was presumed, however his abdominal complaints remained unexplained. Blood work revealed a white blood cell count of 3400/μl with eosinophilia (37 %). An abdominal CT scan did not indicate any acute pathology and stool studies for ova and parasites were negative. On further questioning, the patient reported chronic abdominal pain and several episodes of acutely worsened pain associated with dyspnea, loose stools and anorexia with each episode occurring after corticosteroid administration. SS hyperinfection was suspected in light of this history and serum testing for SS IgG was performed, which was positive. The patient was treated with a course of ivermectin for 2 weeks and his symptoms resolved, confirming SS hyperinfection syndrome.
DISCUSSION: Immunocompetent patients infected with SS are often asymptomatic. Some patients may have vague waxing and waning gastrointestinal, cutaneous or pulmonary symptoms; and blood tests in chronically infected patients commonly indicate eosinophilia. Diagnosis can be achieved via stool microscopy for ova and parasites although this test has a low sensitivity due to intermittent larval excretion in stool. ELISA testing to detect IgG is considered superior with a high sensitivity (83–89 %) and specificity (97 %) based on commercial assays. SS hyperinfection syndrome occurs when chronically infected patients with SS become immunosuppressed, resulting in an uncontrolled over-proliferation of larvae within organs involved in autoinfection such as the lungs and GI tract. The use of corticosteroids, which results in the impairment of cell mediated immunity, is the strongest risk factor for developing this syndrome. Classic manifestations of the hyperinfection syndrome include fever, nausea, vomiting, diarrhea, anorexia, abdominal pain, dyspnea, wheezing and/or cough, as in this patient’s case. Chest radiographs can indicate pulmonary infiltrates; and following hyperinfection, gram negative septicemia secondary to the translocation of gut flora may also occur. Surprisingly, this syndrome in severely immunocompromised patients with advanced HIV/AIDS is rare, with few cases reported to date. It might be expected that HIV/AIDS patients who are lacking cell mediated immunity are predisposed to SS hyperinfection. This is not the case however, since HIV-infected patients typically have a loss of Th1 immune activity but preserved Th2 activity. These changes, particularly the preservation of Th2 activity, have been proposed to play a role in preventing hyperinfection and the dissemination of SS. Treatment with steroids nonetheless can trigger an SS hyperinfection syndrome. This case highlights the vigilance required when contemplating corticosteroid administration in HIV positive patients with depressed CD4 counts, especially when SS may be suspected.
STEVEN JOHNSON SYNDROMEAhmed Abuzaid; Khaled M. Abouelezz; Mohamed El khashab. Creighton university medical center, Omaha, NE. (Tracking ID #1940193)
LEARNING OBJECTIVE 1: Recognize causes of Steven Johnson Syndrome.
LEARNING OBJECTIVE 2: Recognize proper management of Steven Johnson Syndrome
CASE: A 74-year-male with past medical history of hypertension and gout that was started on allopurinol 2 months before admission. He presented with fatigue, progressive generalized skin lesions which started suddenly 2 weeks before the admission, all over his body, involving his hands and feet, associated with odynophagia and eye redness. On examination, Blood pressure 152/75, temperature 99.0, respiratory rate 19, heart rate 70. Skin showed red macules, papules and patches all over his body. Also he had multiple superficial ulcers involving his face, chest and arms with postive nikolisky sign. Eye examination showed bilateral conjuncitval erythema. Blood test showed bicarbonate 21 mmol/l, creatinine 1.6 mg/dl, BUN 31 mg/dl, glucose 189, WBC 6.1 K/μL. Patient was admitted for close observation, allopurinol was stopped. He was given IV fluid, feeding tube was placed because of sever odynophagia and punch biopsy was done. Punch biopsy showed interface bullous dermatitis with necrotic keratinocytes, consistent with early phases of Steven Johnson syndrome. Patient developed more ulceration in his face, chest and arm, almost 15 % of his body surface area and multiple bullae. Blood culture showed gram negative rods. Patient was started on IV antibiotics and transferred to burn unit for further management.
DISCUSSION: Our patient developed steven Johnson syndrome mostly secondary to allopurinol. This is a rare and severe disease that affects skin and mucous membrane with necrosis and sloughing of the epidermis in a reaction to medication or infection. Most common medications are allopurinol, sulfonamides, carbamazibine and phenoparbital. It presented usually with fever and influenza-like symptoms then maculpapular lesions which progress to vesicular and bullous skin lesions followed by sloughing. The most important step in the management is discontinuing the offending medicine and supportive treatment. Close observation is needed to avoid serious complication like dehydration and sepsis, usually symptoms resolves within 4–6 weeks. No definite data about using steroids or IVIG as supportive therapy. Prognosis of the disease is determined usually by using the SCORTEN score, which calculated according to the patient age, history of malignancy, tachycardia, percentage of detached skin and levels of HCO3, glucose and urea level. Patient with high score should be treated at specialized unit. Our patient was transferred to a burn unit after his lesions get worse and the detached area of skin was more that 15 % of body surface area. Patient should wear a bracelet to identify the offending medicine. Conclusion: Steven Johnson syndrome is a serious mucocutaneous disease results from a reaction to medicine or disease. It can be life threatening condition. The corner stone in management is discontinuing the offending medicine and supportive treatment in a specialized unit if sever. .
STEVEN JOHNSON SYNDROME FROM ERTAPENEM: A UNIQUE CASE REPORTKarthik Ragunathan1; David Slagle2. 1OSF St. Francis medical center, peoria, IL; 2OSF St. Francis medical center, peoria, IL. (Tracking ID #1923710)
LEARNING OBJECTIVE 1: Recognize the need to avoid all beta lactam containing antibiotics in a patient with previous Steven Johnson Syndrome (SJS) to any beta lactam antibiotic
CASE: 75 year old asian male with past history of IgG Kappa multiple myeloma, thrombocytopenia, stroke, chronic kidney disease presented to the ED with complaints of non-traumatic fall. He also had history of fever, chills, foul smelling urine and confusion for 1 day. Review of systems was significant for chronic weakness and reduced appetite. Examination showed diffuse petechial rash in face, legs Initial labs showed WBC of 2.5 with absolute neutrophil count of 440, Hb of 7.3, platelets of 30. CMP showed creatinine of 3.79 (baseline 1.8). Urine analysis showed 50–200 WBC, esterase 2+, nitrite and bacteria positive. Initial procalcitonin was 46.55 which increased to 107.42 in 3 days. Chest Xray did not show any opacity. Nasal MRSA screen was positive and HIV ELISA was negative. Initial concern was for neutropenic fever from urinary tract infection in an immunocompromised patient. He has had previous SJS reaction to ampicillin and was also allergic to penicillin causing hives. He was given one dose of Ertapenem and Vancomycin. He developed a new skin rash the following day and was diffusely erythematous throughout the body. Both the antibiotics were stopped due to concern for SJS and gentamycin was started. Initial urine culture was positive for E. Coli resistant to cefoxitin and levofloxacin but subsequent urine cultures were negative. Clinical course was complicated because of obtundation, decerebrate posture requiring intubation and ventilator support. CT, MRI of brain was negative. His clinical status did not improve with continuing fevers, skin rash desquamating to purplish patches in few regions of body, facial swelling and he eventually deceased after comfort care was chosen by his power of attorney.
DISCUSSION: To our best of knowledge, this is the first reported case of SJS secondary to Ertapenem exposure. Previous studies have reported mixed results for allergic reactions from cross reactivity between penicillin and carbapenem class of drugs [2–4]. Two studies showed incidence of patients with a reported or documented penicillin allergy experiencing an allergic-type reaction to a carbapenem was 11 % [2] and 9.2 % [3] although it does not quantify the exact types of allergic reaction. Other study reported that it is safe to use meropenem in patients with history of allergic reactions to penicillin [4]. One previous case report reported toxic epidermal necrolysis (TEN) to meropenem in a patient with documented TEN to cefotaxime [5]. SJS occurs in 1–2 cases per million person years [1]. Common drugs causing SJS include allopurinol, antibiotics (Suflonamides, penicillins and cephalosporins), carbamazepine, lamotrigine. Risk factors for SJS are HIV, immunologic diseases (multiple myeloma in my patient), viral infections. Typical presentation is a prodrome of fever followed by erythroderma, facial edema, mucosal erosions and bleeding. Although skin biopsy can be used to confirm the condition, clinical diagnosis in the setting of trigger factor is mostly used for diagnosis. Differential diagnoses include erythema multiforme, erythroderma, toxic shock syndrome, staphylococcal scalded skin syndrome. Definitive treatment is to stop the offending drug and give supportive wound care, fluid replacement, and sterile environment along with therapies such as systemic corticosteroids, intravenous immunoglobulin and cyclosporine. Overall mortality is 10 % with sepsis, acute respiratory distress syndrome and multi-organ failure as the most common etiologies. The main objective of our clinical observation is to emphasize the need to avoid all beta lactam containing antibiotics in a patient with documented severe hypersensitivity reactions such as SJS, TEN to any beta lactam antibiotic. We also emphasize the need for proper documentation of allergic reactions to drugs to avoid errors by documenting pseudo-allergies. Reference 1. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis : Expert Rev Clin Immunol. 2011 Nov;7(6):803–13; quiz 814–5. doi: 10.1586/eci.11.66 2. Sodhi M, Axtell SS, Callahan J, Shekar R. Is it safe to use carbapenems in patients with a history of allergy to penicillin? J Antimicrob Chemother 2004; 54:1155. 3. Prescott WA Jr, DePestel DD, Ellis JJ, Regal RE. Incidence of carbapenem-associated allergic-type reactions among patients with versus patients without a reported penicillin allergy. Clin Infect Dis 2004; 38:1102 4. Cunha BA, Hamid NS, Krol V, Eisenstein L. Safety of meropenem in patients reporting penicillin allergy: lack of allergic cross reactions. J Chemother 2008; 20:233. 5. Paquet P, Jacob E, Damas P, Piérard GE. Recurrent fatal drug-induced toxic epidermal necrolysis (Lyell’s syndrome) after putative beta-lactam cross-reactivity: Case report and scrutiny of antibiotic imputability. Crit Care Med. 2002 Nov;30(11):2580–3
STEVENS - JOHNSON SYNDROME: AN UNUSUAL ADVERSE REACTION TO AZITHROMYCINRuna Shrestha1; Rajesh Mourya2; Ramsay Farah1. 1SUNY Upstate Medical University, Syracuse, NY; 2Creighton University, Omaha, NE. (Tracking ID #1932843)
LEARNING OBJECTIVE 1: Stevens - Johnson syndrome (SJS) is a rare, life threatening, idiosyncratic reaction characterized by fever and mucocutaneous lesions causing epidermal necrosis and sloughing. Medications and infections are the two most common causes of SJS. Here we present an interesting case in which SJS was seen as an unusual adverse reaction to a commonly used antibiotic.
CASE: A 19-year-old, healthy, African-American male, presented to the emergency department with a 3 day history of fever, chills, fatigue followed by painful mucocutaneous blisters that initially started in his oral cavity but rapidly progressed to involve the whole body. Two days prior to the onset of these symptoms, he was started on azithromycin by his primary care doctor for treatment of upper respiratory tract infection. He was allergic to penicillin which caused facial swelling, and he had never been on macrolide antibiotic before. On examination, he was febrile with temperature of 39.5° Celsius, and had sinus tachycardia with heart rate of 110/min. Skin examination revealed multiple, tender vesico-bullous lesions, with surrounding erythema, all over the body including palms and soles. He also had erythema, blistering with sloughing of the oral mucosa and edema with injection of the conjunctiva. The patient was empirically started on acyclovir for disseminated Herpes infection; however it was stopped after all the infectious work up including Herpes, Mycoplasma, and HIV, were negative. Autoimmune work up was also negative. Skin biopsy done on the second day of admission showed interface dermatitis with vacuolar alteration and subepidermal bulla formation with epidermal necrosis, features consistent with Stevens-Johnson syndrome. Immunofluorescence study was negative. Therefore, a diagnosis of azithromycin induced Stevens- Johnson syndrome was made and the patient was transferred to Burn service for extensive care. He improved after supportive treatment with special attention to wound care, ocular care, pain control, fluid and electrolyte balance.
DISCUSSION: Azithromycin, a semisynthetic macrolide, is one of the most commonly prescribed antibiotics in the United States. It is usually well tolerated; however serious side effects like Stevens-Johnson syndrome may rarely occur. There are rare case reports documenting the association of SJS with azithromycin, mostly in children. SJS is a medical emergency which can be fatal if untreated. Early recognition and initiation of supportive therapy is the key to the management of SJS. Physicians should be aware of the unusual association of azithromycin with SJS and thus, limit unnecessary use of this antibiotic.
STONES EVERYWHERE!Sathish kumar Krishnan; Hitu Khaira; Malav P. Parikh. St. Francis Hospital, Evanston, IL. (Tracking ID #1924585)
LEARNING OBJECTIVE 1: − Recognize that pulmonary alveolar microlithiasis (PAM) is a rare parenchymal lung disease often diagnosed incidentally during pulmonary radiography for other reasons.
LEARNING OBJECTIVE 2: − Identify that extra-pulmonary calcifications can be the initial manifestation of PAM.
CASE: A 44 year old gentleman presented for right sided flank pain for 6 days. He denied any constitutional symptoms, nausea, vomiting, diarrhea or dysuria. His past medical history included asthma and infertility. He was on albuterol inhaler as needed. He had 26 pack years of smoking history. His vitals were stable and physical exam was significant for mild tenderness in the right lower quadrant. A CT of the abdomen showed multiple renal stones bilaterally and a 7 mm stone in right ureter just above the ureterovesical junction. He was treated with analgesics and IV fluids. He developed shortness of breath on day 2 of hospitalization. His physical exam revealed diffuse bilateral wheezing and coarse crackles. A chest X-ray revealed bilateral diffuse micro nodular opacities. A CT of the chest showed bilateral diffuse calcified micronodules, interlobular septal thickening, pleural calcification and sub pleural cysts. PFT showed moderate restrictive pattern. He was treated symptomatically with oxygen and bronchodilators, and his shortness of breath improved. Biopsy of the lung showed concentrically arranged laminated calcified bodies and PAS positive psammoma bodies like microliths consistent with PAM. Considering his infertility and the diagnosis of PAM, an ultrasound of the scrotum was done, which revealed decreased left testicular volume and multiple calcified microliths in both the testes and epididymis
DISCUSSION: Pulmonary alveolar microlithiasis is a rare chronic lung disease characterized by deposition of calcium phosphate microliths in the alveoli. The etiology is not clearly evident. It is considered to be due to mutations in the gene encoding a sodium phosphate co-transporter. It is usually diagnosed in the third or fourth decades of life. About one half of the patients exhibit no clinical symptoms and are diagnosed incidentally by pulmonary imaging. Patients who are symptomatic, usually have shortness of breath, non-productive cough and chest pain. Chest X-ray usually demonstrates diffuse bilateral micro-nodular calcifications, predominant in the middle and lower zones. It is described as ‘sand storm appearance’. HRCT depicts widespread micro-calcifications and ground glass opacities, which may appear like the ‘crazy paving’ pattern of alveolar proteinosis. Extra-pulmonary involvement is rare and is characterized by calcifications in various tissues including liver, kidney, pancreas, intestines, testes, ovaries and heart valves. Our patient had nephrolithiasis and calcific depositions in testes and epididymis causing atrophy of the testis and obstructive azoospermia. There is no effective treatment for PAM, with the exception of lung transplantation. The clinical course of the disease is highly variable and the long term survival is unknown. An increased awareness and a better knowledge of the epidemiological characteristics of the disease could help to diagnose a larger number of cases and to gain insight into its etiology and pathogenesis.
STREPTOCOCCUS AGALACTIAE INFECTIVE ENDOCARDITIS OF A NATIVE MITRAL VALVEMahmoud Abdelghany; Louis Schenfeld. Conemaugh Memorial Medical Center, Temple University, Johnstown, PA. (Tracking ID #1923601)
LEARNING OBJECTIVE 1: Streptococcus agalactiae endocarditis is a virulent invasive infection that can lead to serious complications and death.
LEARNING OBJECTIVE 2: Both medical and surgical treatments are usually necessary for Streptococcus agalactiae endocarditis, Successful medical treatment alone, as in our case, has been reported.
CASE: An 86-year-old female presented complaining of chills, excessive sweating and feeling sick for 2 days. Her past medical history was significant for degenerative mitral valve disease with mitral regurgitation and endometrial cancer for which she had abdominal surgical removal followed by radiation therapy. Postoperative course was complicated with multiple intra-abdominal abscesses, intestinal obstruction and radiation enteritis treated surgically 4 months before that presentation. On admission, her vital signs were stable except for fever with a temperature of 39.1 °C (102.4 °F). Auscultation revealed systolic murmur over the cardiac apex. Two blood cultures were positive for Streptococcus agalactiae (S. agalactiae), also referred as group B streptococcus (GBS). The patient was started on intravenous penicillin G. Transthoracic echocardiography showed mobile vegetation measured 2.15 cm in size, and increased severity of mitral regurgitation compared to an echocardiography done 4 months earlier. CT scan of the head did not show any acute intracranial abnormalities. Combined antibiotic therapy and mitral valve replacement were recommended but the patient refused and requested medical treatment only. She completed four-week course of penicillin uneventfully and without complication. After 9 months, she continued to be asymptomatic with no limitations.
DISCUSSION: S. agalactiae is a rare cause of endocarditis in adults. It is clear that group B streptococcus endocarditis is much more virulent disease than endocarditis due to other streptococci and as virulent as Staphylococcus aureus. Immunocompromised patients are at a higher risk of GBS endocarditis. Transesophageal echocardiography is more sensitive and preferred over the transthoracic echocardiography when transthoracic imaging windows are limited. GBS infective endocarditis may be complicated by major emboli commonly to the brain causing meningitis, brain abscess or encephalopathy. Some genotyping studies had shown that isolates belonging to one particular genotype cluster, sequence type 17 (ST17), are associated with more invasive behavior. Early medical and surgical treatments have been recommended. However, other literatures described cases of GBS endocarditis with favorable outcomes after conservative medical treatment with antibiotics only. Penicillins are the drugs of first choice for the treatment of GBS infections. The benefit of addition of aminoglycosides is still controversial. Although the synergistic effect is confirmed, other literatures could not confirm the superiority of this combination versus penicillin alone. It is clear that GBS endocarditis is a virulent invasive infection. Early antibiotic therapy with or without surgical treatment is crucial to avoid fatal complications.
STROKE AS THE INITIAL MANIFESTATION OF NEPHROTIC SYNDROMEMary Anne S. Chacko; Javad Vaziri; Michael Sheffield. Methodist Dallas Medical Center, Dallas, TX. (Tracking ID #1936999)
LEARNING OBJECTIVE 1: Identify presenting symptoms for patients with nephrotic syndrome
CASE: The patient is a 46 year old male with a past medical history significant for hyperlipidemia and hypertension but had no history of renal issues or stroke. He was discovered with left sided weakness and aphasia on the day of admission about 14 h after he was last seen. Home medications included metoprolol and simvastatin. He smoked a pack per day. Family history was significant for hypertension and diabetes. Review of systems was significant for numbness and weakness on his left side. Vital signs on presentation were normal except for BP of 173/84. He could say one or two words. He attended on the right side of his body but neglected his left side. Face was symmetric and without droop. Neck was supple and without bruits. He had no movement in the left upper extremity and decreased movement in the left lower extremity. Toes were upgoing on his left foot. Neurological exam was intact on the right side. Periorbital edema and lower extremity swelling were absent. Significant labs included WBC 17.8, Hemoglobin 15.2, Platelet count 150,000, PT 13, INR 1.0, Creatinine 1.13, Glucose 128, Troponin <0.012, BNP 282 and Albumin 2.4. Lipid panel was abnormal. Urinalysis showed >300 protein and moderate blood, He excreted 24 g of protein in 24 h. UPEP and SPEP did not show a monoclonal component. Rheumatoid factor was elevated and C3 complement was decreased. CT of the brain indicated an infarct in the right middle cerebral artery distribution with cerebral edema. CT angiogram of head and neck showed occlusion of the M1 segment of the right MCA but no other intracranial stenoses or occlusions. Transesophageal echocardiogram indicated normal left ventricular systolic function and an ejection fraction of 60–65 % with no evidence of thrombus or shunting. Renal ultrasound showed normal arterial and venous blood flow to kidneys and no hydronephrosis. Kidney biopsy showed membranous glomerulonephropathy with secondary focal segmental glomerulosclerosis and mild-moderate arteriosclerosis. The patient did not have significant vascular disease. There was no cardiac evidence of emboli or a shunt. He was anticoagulated with heparin and warfarin and was eventually discharged on aspirin and warfarin with a goal INR of 2.5. He was treated with methylprednisolone and cyclophosphamide for membranous glomerulonephropathy, He was densely hemiplegic at the time of discharge. His neglect had improved, he had better behavior control and was more cognitively aware.
DISCUSSION: Since the first reported association of renal vein thrombosis with nephrotic syndrome in 1837, thrombosis is known to be one of the main complications of nephrotic syndrome. Patients with nephrotic syndrome may have a hypercoagulable state due to several reasons. These include the loss of clotting inhibitors (antithrombin III, Protein C and Protein S) via urinary loss, increased platelet aggregation, decreased fibrinolytic activity, increased concentration of pro-coagulatory factors, hemoconcentration due to hypoalbuminemia and diuretic use and corticosteroid treatment that could increase the concentration of clotting factors and decrease fibrinolytic activity. The hypercoagulability of patients with nephrotic syndrome could be an important trigger for both arterial and venous thromboses. Arterial thromboses are less frequent than venous thromboses and occur most commonly in the femoral arteries. Here we report the case of a patient with ischemic stroke in the distribution of the right middle cerebral artery as the first manifestation of nephrotic syndrome. Thus stroke can be an early manifestation of nephrotic syndrome and should be considered as a possible complication of the syndrome when common causes of ischemic stroke have been excluded. This patient highlights the need for a methodical approach to the patient with a new stroke.
SUBMANDIBULAR MASS WITH GENERALIZED LYMPHADENOPATHY DUE TO IGG4 RELATED DISEASESangmee Bae; Soo I. Choi. UCLA, Los angeles, CA. (Tracking ID #1933895)
LEARNING OBJECTIVE 1: Recognize IgG4 Related Disease in a patient with a nonspecific mass or organ enlargement with associated or generalized lymphadenopathy
LEARNING OBJECTIVE 2: Diagnose IgG4 Related disease with characteristic histopathologic findings and IgG4 specific staining
CASE: A 68 year old Korean female with a history of chronic hepatitis B and Hashimoto’s thyroiditis presented with bilateral painless firm submandibular masses. She had noticed bilateral neck masses that would alternately appear and resolve over the past few years, and intermittent chills and night sweats without weight loss. CT imaging showed enlarged salivary and lacrimal glands as well as generalized adenopathy of the neck, thorax, abdomen, and pelvis. Further history elucidated mild dry mouth and dry eyes, and exam also demonstrated evidence of lacrimal gland swelling. Laboratory testing was notable for positive ANA at 1:320 titer and elevated ESR at greater than 100 mm/h. Other serologies, including dsDNA, Sm/RNP, SSA/SSB, were negative, and LDH was normal. Fine needle aspiration of the submandibular gland revealed a scant mixed population of lymphoid cells, but was nondiagnostic. Subsequent excisional biopsy demonstrated no malignant cells, but the submandibular gland was marked by dense nodular fibrosis which appeared focally storiform. Further staining showed markedly increased IgG4 positive plasma cells, highly suggestive of IgG4-related sclerosing sialadenitis. Her serum IgG4 levels were also found to be markedly elevated at 1037 mg/dL (normal 8–140 mg/dL) consistent with this diagnosis. She was treated with prednisone leading to prompt resolution of submandibular and lacrimal gland swelling as well as improvement of lymphadenopathy.
DISCUSSION: IgG4 related disease (IgG4 RD) is an increasingly recognized clinical entity, characterized by lymphoplasmacytic infiltrate that stains positively for IgG4-bearing plasma cells in affected organs. Common presentations include a mass or enlargement of the affected organ with associated lymphadenopathy. Historically, it has been described in the head and neck glands (previously called Mikulicz’s disease) and pancreas (type 1 autoimmune pancreatitis), but recently clinicians are recognizing that it can involve nearly any organ system, including the orbits, aorta, bile ducts, kidney and lungs. Lymphadenopathy is a common finding in patients, often discovered by generalists who serve as initial providers. Especially when encountered with a tumerous mass or localized swelling in the head and neck, the differential workup should be inititiated by the generalist, and include studies for viral or mycobacterial infection, autoimmune disease such as Sjogren’s syndrome, granulomatous disease such as sarcoidosis, and malignancies such as lymphoma or squamous cell carcinoma. IgG4 RD is an important additional differential to consider in these patients which will have significant implications on treatment and prognosis. It is also important to note that greater than 50 % of cases can present with multiple organ involvement and generalized lymphadenopathy. Diagnosis of IgG4 RD requires immunohistochemical staining specific for IgG4, which is typically not routinely performed. Distinctive histopathological patterns include prominent infiltration of lymphocytes and plasma cells with storiform or swirling fibrosis as well as obliterative phlebitis. Mild peripheral eosinophilia and elevated serum IgG4 levels may also provide additional evidence to support the diagnosis of IgG4 RD. While lymphoproliferative malignancies are treated with systemic chemotherapy, IgG4 RD is treated with systemic glucocorticoids as a first line agent, and additional immunosuppressive therapy such as azathioprine, mycophenoate mofetil, and rituximab may be used in recurrent or refractory cases. Distinctive histopathological patterns include prominent infiltration of lymphocytes and plasma cells with storiform or swirling fibrosis as well as obliterative phlebitis. Mild peripheral eosinophilia and elevated serum IgG4 levels may also provide additional evidence to support the diagnosis of IgG4 RD.
SURVIVING PAINLESS JAUNDICE-A TEST FOR PATIENT AND PHYSICIANAbdul Haseeb; Jeannine Engel. University of Utah School of Medicine, Salt Lake City, UT. (Tracking ID #1939659)
LEARNING OBJECTIVE 1: Diagnose drug induced liver injury.
LEARNING OBJECTIVE 2: Recognize when to manage markedly elevated bilirubin levels with watchful waiting and no invasive testing.
CASE: A 92-year-old male with a history of ischemic cardiomyopathy and atrial fibrillation on chronic Coumadin therapy, presented to the acute-care-clinic with complaints of painless jaundice, pruritus, dark urine, and decreased appetite. The patient denied any history of hepatitis or alcohol use. Laboratory findings were significant for elevated total bilirubin 17.5 mg/dl, direct bilirubin 10.8 mg/dl, INR 4.8, alkaline phosphatase 1023 U/L, AST 230 U/L, and ALT 227 U/L. CT scan of the abdomen showed no abnormalities of the liver, pancreas or biliary tree. Initial assessment included a full review of his medication history. Two weeks prior to his current presentation, he later recalled completing a seven-day course of amoxicillin/clavulanate for a diagnosis of acute sinusitis. This was thought to be the culprit for his drug induced liver injury. Given the elevated INR, the patient’s Coumadin was stopped and his INR returned to therapeutic range within 4 days. The patient was treated symptomatically for his pruritus and started on Ursodiol when his bilirubin level surpassed 30 mg/dL. The patient’s liver enzymes and total bilirubin peaked 1 week after the initial presentation and then started to gradually downtrend. Although he felt better within 4 weeks, it took nearly 4 months for his laboratory values to normalize. No invasive procedures or additional imaging were performed, and no specialty consultations (save a phone call) were obtained.
DISCUSSION: The differential diagnosis of jaundice is large. To narrow the list, the pattern of hepatocellular, cholestatic, or isolated hyperbilirubinemia can be discerned from the liver function test (LFT) pattern. Once neoplasms and dilated bile ducts have been excluded with imaging, and the usual infectious and toxic exposures and alcohol disqualified by history, and inherited disorder made unlikely by the patient’s age, suddenly the possible diagnoses are fairly small. What seemed to be a death sentence on presentation for our patient, was rapidly becoming good news. Drug induced liver injury (DILI) has an incidence of 13.9 + 2.4 cases/100,000 and is estimated to affect 44,000 individuals annually in the United States. Despite the low incidence, 10 % of the patients with drug-induced jaundice will die. Most cases of DILI are due to either a dose dependent acetaminophen-type reaction or an idiosyncratic reaction. The data from prospective registries, such as the Drug Induced Liver Injury Network, indicates amoxicillin/clavulanate as a major culprit of idiosyncratic reactions. DILI can be classified based on the pattern of the liver injury: hepatocellular, cholestatic, or mixed. DILI remains a diagnostic challenge. Diagnosis of DILI is usually made through the process of causality assessment, which interestingly is similar to any criminal investigation. A few steps include: “Was the drug in the right place at the right time?”, “Does this drug have a prior record?”, “Are the characteristics of liver injury consistent with the implicated drug?”, “Are there other more reasonable explanations for the liver injury?”. Depending on the case scenario and the comorbidities, testing for Hepatitis A, B, C and sometimes E, iron/copper overload, alpha-1-antitrypsin deficiency, Celiac disease, alcohol abuse, and ultrasound of the liver are to be undertaken before diagnosing DILI. Amoxicillin/clavulanate is known to cause cholestatic or mixed liver injury with jaundice approximately 2 to 3 weeks after the medication has been stopped, as seen in our case described above. Hence, prior medication history is key in making the diagnosis. Improvement of the liver function tests is slower with drugs that induce a cholestatic injury compared to hepatocellular injury. Hepatic necrosis is uncommon in cholestatic injury, thereby having a lower mortality when compared to the other patterns. The rates of hepatic necrosis are 3 % in amoxicillin/clavulanate, compared to 65 % with isoniazid related hepatocellular injury. Elderly patients, like in our case, are prone to cholestatic/mixed pictures of DILI. Several strategies can be used to prevent DILI, which include patient/physician education, liver function test screening, and active legislation to restrict the potentially toxic drugs. Clinicians can utilize the National Library of Medicine “LiverTox” database, which uses prospective registries as an excellent point of care resource to identify potential drug culprits. When presented with patients such as our elderly gentleman, with impressively high lab values which continue to increase, the fallback is often to consult or proceed with invasive testing. Sometimes the best medicine is to do nothing.
SWEET PEE: AN UNCOMMON CAUSE OF GLYCOSURIAJames M. Kuo1,2; Carmen M. Ramis1. 1Weill Cornell Medical College, New York, NY; 2New York Presbyterian Hospital, New York, NY. (Tracking ID #1933883)
LEARNING OBJECTIVE 1: Distinguish between the different causes of glycosuria
LEARNING OBJECTIVE 2: Treat diabetes using medications that work via glycosuria
CASE: 28 yo male presented for an initial visit for STI screening and right sided back pain worse with movement. No hematuria, dysuria, or foamy urine. Past medical history remarkable for right sided nephrolithiasis 1 year ago. No medications or allergies. Family history notable for type 2 diabetes in aunt and grandmother and hypertension in mother and aunt. Social history of binge drinking on weekends, smoking 2–3 cigarettes/day, and describes himself as Hispanic. On exam, T 37C, HR 80, BP 120/80, RR 16, BMI 33.3. HEENT: NC/AT, PERRL, EOMI; Neck: no acanthosis; CV - rrr, no m/r/g; Lungs - ctab; Abd - obese, +bs, soft, nt/nd; MSK - no deformity, pain reproducible with movement, no flank tenderness. Labwork notable for dipstick UA - >2000 glucose, pH 5.0, no blood or protein. Formal UA confirmed >1000 glucose, pH 6.0, and no blood or protein. Pt had non fasting labs of Na 138 K 3.8 Cl 100 HCO3 24 BUN 17 Cr 0.77 Gluc 140 Ca 9.2. His A1c was 5.7 %. Repeat UA demonstrated >250 glucose, pH 6.0. STI screening was negative. The patient’s back pain improved with acetaminophen.
DISCUSSION: The most common cause of glycosuria is diabetes mellitus where sodium-glucose co-transporters (SGLT2) in the proximal convoluted tubule, which reabsorb 90 % of filtered glucose, become saturated and glycosuria usually commences once blood glucose levels are >185 mg/dl. It is unlikely in this patient given his A1c of 5.7 %. Fanconi syndrome causes global proximal convoluted tubule dysfunction and can also lead to glycosuria. Causes include genetic abnormalities, heavy metal poisoning, medications, and amyloid. Patients typically have bicarbonate wasting, urine pH > 7.5, and electrolyte abnormalities, none of which were present in this patient. Patients with nephrotic syndrome may have glycosuria but this patient did not have protein in his urine and lacked symptoms. Finally, familial renal glycosuria causes glycosuria via a defect in the SGLT2 transporter. It is very rare with a prevalence estimated to be 0.29 %. It is the most likely diagnosis in this patient as he repeatedly has large glycosuria in the absence of hyperglycemia or other renal dysfunction. The diagnosis can be confirmed via genetic testing, but it has a benign outlook so further testing is generally not indicated. Case reports indicate that some patients may have an increased risk of UTIs but otherwise no long term adverse effects. Further outcomes can be extrapolated from SGLT2 inhibitor drugs, such as canagliflozin, which are now being used to treat diabetes. Benefits include an A1c reduction ~0.5–0.7 %, weight loss via glycosuria ~1.8 kg, modest blood pressure reduction ~4.5 mmHg, and rare hypoglycemia. However, patients have an increased risk of genitourinary infections and the long-term cardiovascular and renal safety profiles are still unknown. This patient’s glycosuria likely protected him from becoming diabetic despite multiple risk factors, including obesity, Hispanic ethnicity, and family history.
SWOLLEN FEET AND PALPITATIONS AFTER DRAINING A PNEUMOCOCCAL EMPYEMAAnkita Tandon; Cynthia H. Chuang; Jed Gonzalo; Eileen Hennrikus. Penn State University Hershey Medical Center, Hershey, PA. (Tracking ID #1934365)
LEARNING OBJECTIVE 1: Recognize that large volume thoracentesis can result in systemic effects of hypoproteinemia.
CASE: Empyema is a life threatening complication of pneumococcal pneumonia requiring tube thoracostomy to drain the exudate. Common complications of chest tube placement include pneumothorax, tension pneumothorax, infection and organ perforation. The lesser recognized complication of systemic hypoproteinemia with resulting fluid shifts can result in significant complications. Fifty-three-year-old woman with no medical history presented with fatigue, low-grade fevers, dyspnea and left-sided pleuritic chest pain. Physical exam revealed no breath sounds in the left lung, labs were significant for leukocytosis, hyponatremia, and a slightly low albumin level at 3.2 g/dL. Chest CT showed numerous large loculated left-sided fluid collections. Three simultaneous chest tubes were placed and streptokinase was administered, resulting in the drainage of 3 l of purulent fluid over the next 3 days. By day four, her leukocytosis, fever, dyspnea and chest pain had improved, but she developed new 2+ lower extremity edema and palpitations. Physical exam revealed a pericardial rub. Subsequent work-up revealed a markedly low pre-albumin level (10 mg/dL), an electrocardiogram showed atrial flutter with rate of 170 beats per minute, and echocardiogram revealed a moderate pericardial effusion without tamponade physiology. Presumed diagnosis was pericardial effusion and peripheral edema as a complication of protein loss associated with large volume thoracentesis. With protein supplements and diuretics, the effusion and lower extremity edema improved. After a week, the chest tubes were removed. She was discharged on anticoagulation and a beta- blocker for heart rate control. She was cardioverted a month later. At subsequent follow-up appointments, she has clinically improved and repeat chest x-rays are clear.
DISCUSSION: We report a case of lower extremity edema and pericardial effusion resulting from protein loss and decreased oncotic pressure upon removal of 3 l of purulent fluid from the pleural space. Although, she was also hypoalbuminemic to begin with, so a part of these fluid shifts was from the disease process itself. While total protein loss is known to occur after tube thoracostomy, systemic manifestations resulting from decreased oncotic pressure is a less reported complication. Therefore, it is unclear if there are patients at particularly high risk who may benefit from a high protein diet prior to large volume empyema-related thoracostomy. It is also unclear whether such patients need to be preemptively placed on cardiac monitors despite no cardiac history due to risk of developing arrhythmias with pericardial effusions. Either way, one must be vigilant of subsequent systemic side effects of a seemingly localized pulmonary process that was treated and improving.
SYMPTOMATIC HYPOCALCEMIA, VITAMIN D DEFICIENCY AND ANEMIAEunice Chuang. Mount Auburn Hospital, Cambridge, MA. (Tracking ID #1940011)
LEARNING OBJECTIVE 1: To recognize that hypocacelmia, vitamin d deficiency and anemia are presenting symptoms of celiac disease.
CASE: A 22-year-old female without past medical history presented with numbness and tingling in the extremities as well as cramps in her hands and calves for the past few weeks. She also noted that she has a history of fatigue for many years. Denies weight loss. Has had intermittent nonbloody diarrhea for many months. Physical exam showed stable vitals and remarkable for palor. Lab showed hemoglobin of 5.8 g/dl, MCV of 61.7, MCH 16.2 and calcium of 5.8 mg/dl, albumin of 3.2 mg/dl, PTH was elevated at 296 and vitamin D was low at 5 ng/ml. Iron studies showed undetectable iron and ferritin of 4. She was started on IV calcium supplementation with good response. Endocrinology and GI were consulted. Celiac studies were sent with positive endomysial antibody and gliadin IGA. Patient was discharged with instructions of gluten free diet and on calcium and calcitriol supplemtation and close follow up with primary care physician.
DISCUSSION: Celiac disease is an immune-mediated inflammatory disorder of the small intestines induced by the prolamins of certain cereals causing loss of villous height, crypt hypertrophy leading to malabsorption. It is one of the most common lifelong disorders in Europe and the USA. In adults, presentation of celiac disease varies from asymptomatic to severely symptomatic, depending on the severity and the extent of mucosal involvement. Gastrointestinal symptoms are more common and include other conditions such as diarrhoea, weight loss, malaise, lethargy and abdominal pain. It is important to recognize vitamin D deficiency and hypocalcemia as presenting symptom of celiac disease. Hypocalcaemia is thought to occur due to the negative calcium balance, due to loss of villous surface area, with unabsorbed calcium binding to excess fatty acids in the intestinal lumen as a result of fat malabsorption. There is impairment of active intestinal calcium transport mechanisms because of depletion of calbindin from enterocytes. Decreased vitamin D also contributes to decreased calcium absorption. Hypocalcaemia stimulates PTH to correct for low calcium level. Secondary hyperparathyroidism occurs due to vitamin D and calcium malabsorption. It is important to recognize that hypocalcemia, vitamin D deficiency, elevated PTH in a patient with anemia can be signs of malabsorption, which can lead to diagnosis of celiac disease.
SYNCOPE DUE TO COLD WEATHERSparsha Kukunoor; Poojita Shivamurthy. University of Connecticut, hartford, CT. (Tracking ID #1939777)
LEARNING OBJECTIVE 1: Identify the association between acute hemolytic anemia and syncope.
LEARNING OBJECTIVE 2: Recognize the importance of finding cold agglutinins on peripheral smear.
CASE: 81 year old female presented to the emergency room after witnessed syncope while working outside in the cold doing volunteer work for her church. Her syncopal event was not preceded by aura, fatigue and lasted a few seconds. On coming to the emergency room she was short of breath and fatigued. Further questioning revealed a similar episode 2 years ago, during which time she was diagnosed with cold agglutinin disease with titers of 1: 512. Laboratory investigations revealed hemoglobin of 6.9 g/dl from a baseline of 10.0 g/dl. Peripheral smear was found to have cold agglutinins. This was confirmed with direct anti-globulin test which showed positive poly-specific test and mono-specific test positive for complement protein C3d/C3b and negative for IgG. She was admitted and was given warmed packed red blood cells. Other laboratory data revealed monoclonal gammopathy, IgM kappa type with M component of 0.67. Bone marrow biopsy and CT of abdomen and pelvis showed no evidence of lymphoproliferative disease. She dramatically improved the next day and did not require any further transfusions.
DISCUSSION: Cold agglutinins (CA) are antibodies that agglutinate erythrocytes at an optimum temperature of 0-4C. CA may be found in the serum of normal individual in the polyclonal form however in Cold Agglutinin Disease (CAD) they are monoclonal and in high titers (1). Usually effects female population in the 7th decade. CAD has an incidence of one in one million per year. A single institutional experience showed that in patients with 43,000 patients having a monoclonal gammopathy, less than 1 % had cold-reactive autoantibodies (2). The autoantibodies can be primary as in our case or secondary due to autoimmune disease, malignancy or infections. Clinical features include anemia, cold induced symptoms like acrocyanosis, Raynaud disease, livedo reticularis and sometimes cutaneous necrosis. Diagnosis is made by positive Coombs test to anti - C3, CA titers and thermal activity. Work up including a bone marrow aspiration should be done for secondary causes. Non-pharmacological management like avoidance of cold is the cornerstone of therapy. Studies as lacking and thermal amplitude of the CA antibody in many patients is such that physiologic peripheral cooling results in antibody binding sufficient to cause anemia. Pharmacological therapy has been unsuccessful until recently. Half of the patients respond to rituximab monotherapy. Fludarabine-rituximab combination therapy is very effective, resulting in 75 % response rate, Complete remissions in about 20 %, Toxicity is a concern, and benefits should be carefully weighed against risks (1).
SYSTEMIC LUPUS ERYTHEMATOUS MIMICKING SEPSISMing Zhao1; Charu Ramchandani1; Peter M. Deane2; Carlos D. Palacio1. 1Unity Health System, Rochester, NY; 2Allergy-Asthma-Immunology of Rochester, PC, Rochester, NY. (Tracking ID #1939134)
LEARNING OBJECTIVE 1: Recognize neuropsychiatric symptoms in systemic lupus erythematous (SLE).
LEARNING OBJECTIVE 2: Distinguishing SLE flare from sepsis.
CASE: Patient is a 38 year old female who was admitted to hospital due to worsening weakness, fatigue, shortness of breath and constant headache. Her past medical history was significant for systemic lupus erythematous (SLE) diagnosed 20 years ago. Patient stopped treatment for SLE 3 years ago. At the time of her admission, she was found to have systemic inflammatory response syndrome (SIRS), with WBC 14500, respiratory rate 36/min and heart rate 120/min. On examination patient was somnolent, breath sounds were decreased at the left lung base with scattered rhonchi and fine rales. Her labs were remarkable for white blood cell count (WBC) 14500, Hemoglobin 10 g/dl and serum creatinine 1.52 mg/dl. Shortly after admission, patient spiked high fever of 40° celsius along with worsening severe headache, increased confusion, irritability, memory impairment and lethargy. Given her severe headache, fever and SIRS, there was concern for sepsis secondary to meningitis/encephalitis. CT head and MRI/MRV did not show any abnormality. Cerebrospinal fluid (CSF) showed normal WBC, glucose and protein level with gram stain negative for organisms. She was empirically treated with Vancomycin, Ceftriaxone, Ampicillin and Acyclovir. However, given her history of SLE, there was also concern for SLE flare which could have led to her symptoms. Urine analysis was remarkable for 3+ proteinuria and numerous red cells. Chest x-ray showed cardiomegaly and small bilateral pleural effusions. Echocardiogram showed biatrial enlargement, right ventricular dilatation, severe tricuspid regurgitation, moderate mitral regurgitation, and 55 % left ventricular ejection fraction. We checked her serum C3 and C4 complement level, which were very low. We also checked her serum C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and ds-DNA, which all came back highly elevated. Rheumatology was consulted, following which she was started on intravenous cyclophosphamide and methylprednisone. Antibiotics were stopped. Eventually her fever and headache resolved and her mental status improved markedly. Over the course of her stay her ESR came back to normal and CRP improved. Her renal biopsy showed stage 4 lupus nephritis.
DISCUSSION: Neurologic and psychiatric symptoms are commonly seen in patients with SLE, either prior to the diagnosis or during the course of their illness. Neuropsychiatric systemic lupus erythematosus (NPSLE) is associated with a worse prognosis and more cumulative damage and represent an important cause of morbidity and mortality in SLE. Unfortunately, there are no diagnostic tests that can establish a specific diagnosis of NPSLE, and thus, the approach to patients with neuropsychiatric symptoms require establishment of the diagnosis of SLE and distinguish from other causes of nervous system abnormalities, such as medication effects, metabolic abnormalities and infection. It is always important to suspect infection in patients with SLE and central nervous system manifestations. Immune response in SLE is impaired due to defect in different components of humoral and cell mediated immune process, making patients prone to infection. Immunosuppressive action of the standard therapeutic regimen also increases the susceptibility to infection. However, sometimes, clinical manifestations of SLE can be indistinguishable from infection. Patients with highly active SLE may present with a picture mimicking infection or even sepsis. With severe inflammation and disease activity, such patient may present with high fever, tachycardia, hypercapnea and high WBC, just like our patient. In such circumstance, patients may benefit from immunosuppressive treatment such as corticosteroids, rather than antibiotics. Certain medications, such as Acyclovir, may even give patient a higher risk of worsening renal function and should be avoided as possible as we can. A typical workup for such circumstance may include a detailed history and physical exam to look for any clues of infection, serologic and imaging studies to look for the severity and activity of the disease as well as the possibility of underlying infection. A high ds-DNA titer may indicate highly active SLE rather than infection. Also complement levels are low in SLE flare versus high in infection. Other biological markers reported in several studies to identify infection in SLE patients are CRP, sedimentation rate, ferritin, procalcitonin, and delta neutrophil index. In conclusion, neuropsychiatric symptoms are commonly seen in patients with active SLE and should be distinguished from infection such as meningitis/encephalitis. Highly active SLE may also present with a picture mimicking infection or even sepsis. The diagnoses and treatment should always be based on a comprehensive evaluation.
TAKOTSUBO CARDIOMYOPATHY WITHOUT AN ACUTE STRESS TRIGGERRanjan Pathak; Paras Karmacharya; Leena Jalota; Benjamin Lloyd. Reading Health System, West Reading, PA. (Tracking ID #1938289)
LEARNING OBJECTIVE 1: Clinicians should consider Takotsubo cardiomyopathy in the differential diagnosis of patients presenting with chest pain, even without a history of recent stress.
CASE: A 92 year old female with no significant cardiac history presented to the emergency room complaining of non-radiating pressure-like chest discomfort of 2 h, dyspnea, nausea and vomiting. She denied any history of recent stress. Her Serial EKGs revealed dynamic changes with inferior, anterolateral ischemic changes with ST elevation and T inversion. A diagnosis of inferior wall STEMI and acute congestive heart failure was made. Given her age, a decision was made to manage her conservatively. However, she continued to have chest discomfort with rising Troponin (peak 14.09), CK-MB levels and was ultimately taken for cardiac catheterization on the third day. Coronary angiography showed non-obstructive coronary artery disease. Left ventriculography revealed hyperdynamic basal segment with a normal apex. The mid segment was severely hypokinetic to akinetic consistent with atypical TC. She was medically managed with aspirin, statin, beta blocker, and ACEI with significant improvement in symptoms.
DISCUSSION: Takotsubo cardiomyopathy (TC) is an acute segmental myocardial dysfunction of the left ventricle without significant lesion of the coronary artery. It presents with chest pain, electrocardiographic changes and elevated troponins frequently masquerading as acute coronary syndrome. Of the four variants, the most common type consists of apical ballooning and with hyperkinetic or normal basal region. TC is usually associated with acute or chronic emotional or physical stress. While the role of chronic stress in TC is unknown, stress as trigger may be absent in 15 % of cases. The mid ventricular variant is seen in about 17 % of the cases. The absence of the common apical left ventricular abnormality and lack of preceding stressor makes our case atypical. Clinicians should be aware of this unique syndrome, its variants and consider this in the differential diagnosis of patients presenting with chest pain, especially in post-menopausal women even without a history of recent stress.
TB OR NOT TB: TUBERCULOUS ENTERITIS PRESENTING AS APPENDICITISJaimin Amin; Arthur Jeng; Stanley K. Dea. Olive View-UCLA Medical Center, Sylmar, CA. (Tracking ID #1939731)
LEARNING OBJECTIVE 1: Recognize the clinical presentation of tuberculous enteritis and discuss the appropriate diagnostic and therapeutic management
LEARNING OBJECTIVE 2: Differentiate between M. tuberculosis and M. bovis
CASE: A 56 year-old Mexican man presented with 2 days of severe abdominal pain accompanied by fevers, weight loss, and non-bilious emesis. On examination, he was febrile and tachycardic with rebound tenderness of the epigastrium and periumbilical abdomen. Laboratory studies were significant for WBC 7.1 with 80 % neutrophil predominance, hemoglobin 8.4 with MCV 79, BUN 31 and Cr 1.1 and isolated alkaline phosphatemia 303. An abdominal CT scan demonstrated two large complicated cystic lesions with lymphadenopathy. The first lesion measured 5 × 5 cm and was located in the right lower quadrant adjacent to the third portion of the duodenum with a dilated appendix concerning for perforated appendicitis. The second lesion measured 3 × 3 cm and was found within the body of the pancreas suggestive of pancreatic malignancy. Surgery was consulted for exploration and appendectomy but deferred. Endoscopic guided biopsy of the pancreatic cyst was unremarkable. CT guided drainage of the right abdominal cyst revealed acid-fast bacilli, which grew M. tuberculosis complex, identified as M. bovis. Initiation of rifampin, isoniazid, and ethambutol resulted in resolution of symptoms and normalization of imaging.
DISCUSSION: This case emphasizes a lesser common clinical presentation of tuberculosis, that involving the GI tract. Although the initial evaluation was suggestive of appendicitis and/or pancreatic malignancy, further evaluation by CT guided drainage led to the demonstration of acid fast bacilli and the diagnosis of tuberculous enteritis from M. bovis. M. tuberculosis and M. bovis are related to the extent that it is not possible to distinguish these two mycobacteria by genetic amplification means (eg. PCR). However, they are distinguishable by biochemical means. They can both tuberculosis in humans, although their epidemiological reservoirs are different. M bovis is known to cause tuberculosis in cattle and may have evolved into M. tuberculosis. However, humans can be infected with this zoonotic pathogen by consuming unpasteurized dairy products from afflicted cattle. Because of the oral route of entry, M. bovis most commonly presents within the GI tract. Due to their ability to survive in mononuclear leukocytes and the density of lymphoid tissue within Peyer’s patches. M. bovis enteritis frequently mimics appendicitis or colon cancer, which are commonly the initial diagnoses. Suspicion for M. bovis, rather than M. tuberculosis, should arise when the isolate is resistant to pyrazinamide (PZA), given its universal genotypic resistance to this anti-mycobacterial drug. Treatment involves 6–9 months of standard anti-tuberculous medication, with the exception of PZA.
TENSION PNEUMOTHORAX IN OUT-PATIENT CLINICManisha Bhide. University of Colorado Denver, Aurora, CO. (Tracking ID #1923481)
LEARNING OBJECTIVE 1: To recognize that certain causes of dyspnea need urgent triage. Relatively stable outward appearance may be deceptive in cases of chest pressure and dyspnea
CASE: 39 year old male teacher, nonsmoker came to out-patient medical clinic with 7 days of worsening dyspnea, moderately severe chest pressure, dry cough and pleuritic chest pain. Past medical history was significant for hypertension, seasonal allergies and mild intermittent asthma. Family history was noncontributory. Exam revealed afebrile patient with heart rate of 96/min, BP 130/86 and respiratory rate of 18/min with increased work of breathing. Breath sounds were decreased on Rt side. Rt sided hyper resonance was present on percussion. EKG showed normal sinus rhythm with Rt axis deviation. Chest X-ray showed large right tension pneumothorax. Urgent Chest tube with water seal device and suction placement was done. Pneumothorax resolved over 4 days. CT Chest did not show any blebs or lung abnormality.
DISCUSSION: Differential diagnosis of dyspnea and pleuritic pain in a young male includes pulmonary embolism, pleurisy, autoimmune diseases and pericarditis. Chest pain with dyspnea and respiratory abnormalities should stimulate us to put pulmonary pathology higher on the list of differential diagnosis. Hyper resonance on percussion can indicate COPD, but in a young male, nonsmoker it could be due to pneumothorax. Presence of air in the pleural space, with no obvious underlying lung pathology or HIV or trauma, is termed as spontaneous pneumothorax. The incidence ranges from 7.4 to 18/100,000 per year among men. The incidence is lower in women at 1.2/100,000. Smoking, connective tissue disease and family history are thought to increase the risk by sub-pleural bullae formation and degradation of elastic tissue. The American College of Chest Physicians has established guidelines for management of spontaneous pneumothorax. For large pneumothorax, hospitalization and placement of chest tube with water seal device, with or without suction is recommended. Procedures to prevent recurrence, like pleurodesis are usually reserved only for second occurrence or for professionals like pilots and divers. Routine Chest CT is not recommended to find cause for first time pneumothorax, but CT may be done for management of secondary or complex pneumothorax. Shift of mediastinum along with unstable vitals like tachycardia, hypotension are indicative of tension pneumothorax. This case is important to remember because outwardly stable patients can conceal a tension pneumothorax which can lead to compression of the mediastinum and can have rapid clinical deterioration and death if unrecognized.
TERTIARY LGV DIAGNOSIS AFTER FISTULOTOMY: UNDER-SCREENED, UNDER-DIAGNOSED, AND UNDER-TREATEDRobert Spencer; David M. Levine; Richard E. Greene; Andrew A. Chang. New York University Medical Center, New York, NY. (Tracking ID #1939016)
LEARNING OBJECTIVE 1: Formulate a differential diagnosis for rectal pain in MSM
LEARNING OBJECTIVE 2: Recognize and diagnose lymphogranuloma venereum
CASE: A 27 year-old gay man presented to the ED with 2 weeks of much-worsened 7/10 rectal pain with bloody purulent discharge, fevers, chills, tenesmus, and a week of a rapidly enlarging tender L-sided inguinal mass. Five years prior to presentation he was the victim of a sexual assault involving forced receptive rectal penetration by the assailant’s penis and a sharp object causing a rectal abscess requiring incision and drainage (I&D) and infection with HIV. Until last year, he noted only mild rectal tenderness without drainage. At that time (CD4 800 [40 %], VL <20, on ART × 4 months), he noted progressive pain with purulent discharge from the previous incision site, prompting a second I&D that failed to entirely heal despite various PO antibiotic regimens over months. On exam, a 1 cm-long 9-o’clock perianal skin break without tenderness, fluctuance, or erythema, and a tender 5 × 2 cm mobile L-inguinal mass were noted. Blood work and urinalysis were within normal limits including urine cultures, urine gonococcal/chlamydial NAAT, blood cultures, RPR, and quantiferon gold. A CT scan demonstrated rectal wall thickening with surrounding infiltrative change and left inguinal lymphadenopathy without abscess. We clinically diagnosed lymphogranuloma venereum (LGV) and initiated treatment with doxycycline. Endoscopic ultrasound and fistulogram revealed an anal fistula, which was excised. Subsequent novel PCR analysis of the formalin-fixed paraffin embedded fistula specimen confirmed Chlamydia trachomatis serovar L2, while the NAAT rectal swab also confirmed Chlamydia. The patient’s inguinal lymphadenopathy and rectal pain subsided entirely following a 21-day course of doxycycline.
DISCUSSION: Taking an in depth history and formulating a broad differential for rectal pain in MSM are essential. We considered the differential for proctitis: infectious (C. trachomatis, N. gonorrhoeae, HSV, syphilis, intramuscular abscess, LGV), anatomic (trauma, hemorrhoids, cryptitis, anal fissure, rectocele), ischemic, malignant, and proctalgia fugax. We also considered the causes of inguinal adenopathy: chancroid, herpes, syphilis, LGV, lymphoma, tuberculosis, abscess, and bubonic plague. LGV was rarely reported in industrialized countries prior to 2003, when the first of many reports circulated in what has now been termed a “silent endemic disease” of MSM. LGV is a sexually transmitted infection caused by serovars L1-L3 of C. trachomatis, due to their tropism for lymphatic tissue. Risk factors include co-infection with HIV and/or hepatitis C, along with high-risk sexual behavior. Primary LGV presents with a frequently unnoticed painless genital papule or mucosal inflammation at the site of inoculation that may ulcerate and heal spontaneously. Secondary LGV presents 2 to 6 weeks later with involvement of lymph nodes that drain the area of the primary lesion. This may go unnoticed when primary infection occurs in the rectum, as the deep iliac nodes are often less symptomatic. Tertiary LGV involves chronic granulomatous change and lymphatic obstruction leading to fistula and stricture formation. In the US, LGV largely remains a clinical diagnosis, as no commercial PCR assays are available for serovars L1-L3. This often leads to delayed diagnosis and treatment, as in the case of our patient. Providers must be aware of LGV’s resurgence and consider rectal screening in MSM.
THE ANTIBIOTIC THAT CAUSED THE ITCH: INTRACTABLE PRURITIS AND JAUNDICE AFTER TREATMENT FOR SINUSITISJack Badawy; Ashley Garcia-Everett; Kanapa Kornsawad. University of Texas Health Science Center, San Antonio, TX. (Tracking ID #1938988)
LEARNING OBJECTIVE 1: Recognize medication adverse reaction as an important cause of liver failure
LEARNING OBJECTIVE 2: Emphasize a thorough history as a key diagnostic tool in medicine
CASE: A 71-year-old man with no significant past medical history presented with 1 week of intractable pruritus, jaundice, and anorexia. He initially noticed darkening of his urine which progressed to painless jaundice over the next few days. He denied a history of alcohol use. Home medications included aspirin, fish oil and a multivitamin. He had recently completed a 3 week course of amoxicillin-clavulanate for chronic sinusitis. He had no familial history of liver disease. On physical examination he was afebrile, jaundiced with scleral icterus, had multiple excoriations to his limbs and no hepatosplenomegaly. Initial laboratory results demonstrated aspartate and alanine aminotransferases of 171/380 IU/L, alkaline phosphatase of 260 IU/L, T.bilirubin of 5.2 mg/dL and INR of 1.3. Serological evaluation for viral hepatitis and autoimmune hepatitis were negative. A liver ultrasound was normal. He had a normal MRCP and eventually an EUS and ERCP with sphincterotomy and stent placement. Bile duct biopsy and brushing were normal. Liver biopsy showed extensive intrahepatic cholestasis with bile plugs suggestive of large bile duct obstruction which in the given clinical setting were consistent with drug toxicity related to amoxicillin-clavulanate therapy. His pruritis was refractory to multiple therapies including ursodeoxycolic acid, cholestyramine, rifampin and prednisone. His hyperbilirubinemia (peak total bilirubin of 20 mg/dL), coagulopathy and transaminitis began to improve with supportive measures prior to discharge.
DISCUSSION: Idiosyncratic drug induced liver injury is responsible for 11.1 % of all cases of acute liver failure, with antimicrobials being the most common causative group. Of antimicrobials, amoxicillin-clavulanate has the highest incidence of drug-induced hepatotoxicity accounting for 13–23 % of cases. Males are most commonly affected with a mean age of 60; longer duration of treatment (>2 weeks) is also associated with higher risk. Hepatotoxicity is clearly linked to the clavulanic acid moiety, with a 5- to 9-fold increase for the combination versus amoxicillin alone, giving an estimated incidence rate of 9.91 cases of jaundice per 100,000 prescriptions of amoxicillin-clavulanate. The cause is often elusive because the symptoms typically arise after completion of the antibiotic regimen (average delay of 17 days) and therefore a thorough inquiry into drug history is key. Treatment includes withdrawal of the offending agent and symptom management with ursodeoxycolic acid (which may improve the cholestasis) and cholestyramine. Despite this some patients may progress to fulminant hepatic failure resulting in transplantation or death. Amoxicillin-clavulanate is a one of the most widely prescribed antibiotics worldwide. Reports of adverse reaction with cholestasis, abnormal liver function test were less than 1 %, however, while rare, the morbidity and mortality associated with drug induced hepatoxicity is significant. This case emphasizes the importance of the judicious use of antibiotics.
THE CASE OF MS. A. EARLY SUPPORT FOR A GRASS-ROOTS, TEAM-BASED APPROACH TO AMBULATORY CARE IN A RESIDENT CLINICNora Segar; Manik Chhabra; Janet J. Ho; Megan S. Lemay; Faye Farber; Sarita Soares; Julie R. Rosenbaum; Stephen Holt; Tracy Rabin. Yale University, New Haven, CT. (Tracking ID #1939139)
LEARNING OBJECTIVE 1: Identify the challenges of caring for complex patients in a traditional model of ambulatory resident education.
LEARNING OBJECTIVE 2: Describe the implementation and potential benefits of a resident-organized, team-based outpatient care model.
CASE: Ms. A is a 52-year-old, unemployed, high-school-educated, Puerto Rican mother of three, and the primary care giver for her grandson and frequently hospitalized mother. She has uncontrolled diabetes with average hemoglobin A1C of 11, hyperlipidemia, asthma, tobacco dependence, hidradenitis suppurativa with recurrent groin abscesses, uncontrolled depression with history of a prior suicide attempt, and chronic pain secondary to spinal stenosis and adhesive capsulitis, managed with opioids. Of note, she has previously violated the clinic’s controlled substance agreement by taking non-prescribed opiates for worsening pain. Lead author NS has followed Ms. A at our resident continuity clinic since starting training 2 ½ years ago. During this time she has seen Ms. A 20 times and spoken with her over the phone on a weekly basis. In our established care model, NS cares for her with the support of a faculty preceptor. When NS is unavailable, other residents not familiar with Ms. A provide interim care. Our clinic does not currently employ social work staff, full-time mid-level providers, or a dedicated behavioral health team integral to the successful multidisciplinary care of patients like Ms. A. These resource limitations, in combination with complex resident schedules that often prioritize inpatient rotations, result in a fragmented clinical experience. For example, in addition to three hospitalizations and six emergency department visits, Ms. A has been seen 15 times by 11 distinct clinic providers other than NS in the past 2 ½ years. One model for effective outpatient care and improved training environment is the Patient Centered Medical Home (PCMH), a team-based, multidisciplinary approach to primary care for complex patients. At our clinic, a core group of interested residents have organized a pilot PCMH model called the Chase Ambulatory ICU (ChICU) designed to coordinate care for a subset of our highest risk patients and to improve resident satisfaction with the clinic experience. Enrolling Ms. A in the ChICU meant: 1) Establishment of mutual provider-patient goals, which, in her case, included compliance with the clinic’s controlled substance agreement, smoking cessation, and improved diabetes control; 2) Direct access to residents familiar with the patient through a direct-to-provider pager system; 3) Structured monthly team sign-out of patient updates and goals with a core group of known covering resident providers; 4) Completion of a home visit assessment. Two weeks post enrollment, while NS was away on a six-week international health elective, Ms. A was hospitalized for an asthma exacerbation under the care of a medicine resident who had received sign-out, supervised by the faculty preceptor. The same resident then saw her in post-hospital follow up. She has since met the goal of tighter diabetes control with improvement in her AIC from 11 to 8 through frequent structured visits to residents who are familiar with her care. She has been compliant with the controlled substance agreement as evidenced by multiple appropriate urine toxicology screens. Additionally, the home visit helped the care team to appreciate her bio-psycho-social complexity as well as to identify further barriers to accomplishing our mutual goals.
DISCUSSION: Patients with low health literacy, complex medical disease and low socioeconomic status may have difficulty navigating a fragmented and complex primary care system. Residency training models focused on inpatient training at the expense of outpatient continuity of care further complicate this fragmentation. Ambulatory ICU models designed to improve continuity of care may improve patient health outcomes for the under-served, medically complex patients served by residency clinics. Although these models traditionally rely heavily on incorporation of non-physician health care providers, we feel the above clinical vignette demonstrates the potential benefits of a structured, resident-driven intervention to improve the quality and continuity of care we provide for patients like Ms. A. Key teaching points: 1) Team-based care can improve outcomes for the complex patients cared for in residency clinics 2) Grassroots, resident-organized teams have the potential to improve outcomes even in the absence of interdisciplinary support and full-time clinic staff.
THE DEVIL IS IN THE (BLOOD SMEAR) DETAILSNaveen Nannapaneni; Adeeb Bulkhi; Marwan Al-Hajeili; Carter Bishop. Wayne State University/Detroit Medical Center, Detroit, MI. (Tracking ID #1923332)
LEARNING OBJECTIVE 1: Recognize the utility of a peripheral smear.
LEARNING OBJECTIVE 2: Diagnose thrombotic thrombocytopenic purpura.
CASE: Thrombotic thrombocytopenic purpura (TTP), characterized by low levels of ADAMTS13, abnormal platelet and endothelial activation, microvascular fibrin deposition, and hemolysis, is a disease that carries a high mortality rate. The early recognition of, and emergent plasmapharesis for, TTP results in favorable outcomes. Delay in making the diagnosis can lead to unnecessary investigations, incorrect therapies, prolonged hospitalization and even mortality. A 53 year-old woman with lupus was brought to the ER with progressive confusion, generalized pain, weakness and fatigue going on for 3 days. She was unable to provide further history due to her confusion. On exam her vitals were stable and aside from being confused, had no other abnormality. CBC showed an anemia, 11.2 g/dL, and severe thrombocytopenia 11/μL. She had evidence of hemolysis with an elevated LDH 816 U/L and low haptoblogin 10 mg/dL. After being admitted she was transfused with platelets pending a hematology consultation. Hematology suspected a broad differential including immune thrombocytopenia (ITP), plaquenil-induced and hydrochlorothiazide-induced thrombocytopenia and recommended starting corticosteroids while holding the implicated medications. The patient continued to deteriorate without improvement in her platelet count despite receiving platelet transfusions and incurred further mental status decline. Neurology was consulted and suspecting a stroke, performed a CT followed by MRI/MRA of the head, which were all negative for an acute process. Additional evaluation by EEG revealed no epileptiform activity. A second opinion by another hematologist was requested, and after review of the peripheral smear revealed schistocytes, a diagnosis of TTP was made. Immediate daily plasmapharesis was performed and platelet transfusions were discontinued resulting in progressive clinical improvement. Further workup showed a decreased ADAMTS13 activity level, 35 %. She was discharged after plasma exchanges resulted in a return to her baseline mentation and stabilization of hemoglobin and platelet count.
DISCUSSION: The classic presentation of TTP involves the pentad of fever, hemolytic anemia, thrombocytopenia, acute renal failure and neurologic changes. While all five findings are not necessary for diagnosis, whenever a patient presents with microangiopathic hemolytic anemia and thrombocytopenia, the diagnosis of TTP must be entertained. When included, interventions such as platelet transfusions, and corticosteroids alone, would not be considered as they cause further harm by additional platelet activation and confer no benefit, respectively. Review of a blood smear should be performed as the presence of numerous schistocytes provides rapid, inexpensive, and reliable evidence of TTP. Once diagnosed, the patient should undergo plasmapharesis. As in this case, if the individual problems in TTP are not assessed in a greater constellation there can be inappropriate investigations and therapies which can lead to an unfavorable outcome.
THE DILEMMA OF MANAGEMENT OF CARDIAC TAMPONADE IN THE PRESENCE OF SEVERE PULMONARY HYPERTENSION: OUR EXPERIENCEVimalkumar Veerappan Kandasamy; Ajaykumar Kaja; Tammy O. Wichman. Creighton University, Omaha, NE. (Tracking ID #1939129)
LEARNING OBJECTIVE 1: To recognize pericardial effusion as a common cause of worsening respiratory status in a patient with pulmonary hypertension.
LEARNING OBJECTIVE 2: To understand the complications of pericardiocentesis in patients with severe pulmonary hypertension presenting with cardiac tamponade.
CASE: A 33 year old Caucasian female with past medical history of pulmonary hypertension (PH) WHO group 1, functional class 3 at baseline, was admitted with complaints of worsening shortness of breath (SOB) and cough for the last 2 weeks. She had SOB at rest with increased oxygen requirements at the time of admission. She was on treprostinil continuous infusion, tadalafil, ambrisentan, digoxin and warfarin for PH. Jugular venous distention and positive Kussmaul sign were noted on examination. The patient went into hypoxic respiratory failure and subsequently intubated. Echocardiogram showed a large pericardial effusion with tamponade physiology with left atrial and ventricular collapse. The right ventricle (RV) was severely dilated and systolic function was severely reduced with RV systolic pressure of 161 mmHg. Pericardiocentesis was performed through a subcostal approach and 40 ml of hemorrhagic fluid aspirated. Pigtail catheter was left in the pericardial cavity and 50–100 ml of pericardial fluid was drained every 4 h. Patient also was started on antibiotics and vasopressors. A total of 2300 cm3 of fluid was aspirated from pericardial cavity with slow intermittent drainage over the next few days. Her clinical condition slowly improved over the week and vasopressors were weaned off. She was slowly diuresed and subsequently extubated and oxygen requirements came down. Although patient improved, her baseline oxygen requirement was higher than pre-admission levels and she was discharged with 2 L oxygen at rest and 4 L oxygen with activity and at night. She was referred to transplant center for lung transplantation.
DISCUSSION: Pulmonary arterial hypertension (PAH) in its advanced stages is complicated by right heart failure (RHF) and pericardial effusion. The optimal treatment of large or hemodynamically significant pericardial effusions in this group is not defined. The prevalence of pericardial effusion can be as high as 54 % and it is one of the predictors for mortality. It is hypothesized that a high PA pressure reduces lymphatic and venous return to a pressure-overloaded RA, leading to the pericardial effusion and eventual tamponade. The full picture of RV failure with low cardiac output and elevated RV filling pressures is typically seen in PH groups 1 and 4. When patients present with worsening RHF, echocardiogram to evaluate for pericardial effusion is an essential component of management. Multiple case reports have been published with various treatment strategies. In a case series of 6 patients by Hemnes et all, both pericardiocentesis and pericardial window placement were associated with significant postprocedural mortality. It was postulated that after removal of pericardial fluid, the already pressure- and volume-overloaded RV can enlarge further, resulting in further septal bowing and subsequently diminishing the LV size leading to worsening left heart filling, left HF, hypotension, and death. Our case report emphasizes the fact that removal of pericardial fluid in small quantities over longer period with adequate hemodynamic support could be a good treatment option for these patients, as it provides time for the right ventricle to adapt to the changing hemodynamics. More experience is needed before concluding this as a standard of care.
THE ELUSIVE DIAGNOSIS OF PULMONARY EMBOLISM; A CASE REPORTMai Kaga; Leonard Amoruso; Peter Rattner. Beth Israel Medical Center, New York, NY. (Tracking ID #1897760)
LEARNING OBJECTIVE 1: Recognize the limitations of using a single imaging modality for diagnosis of pulmonary embolism
LEARNING OBJECTIVE 2: Diagnose pulmonary embolism using imaging modalities in addition to laboratory values and clinical decision making tools
CASE: 35 year old male with history of heroin abuse presented with altered mental status after a witnessed heroin overdose. In the emergency department (ED), after receiving intravenous naloxone, the patient’s mental status improved. The patient disclosed that in the days prior to admission, he had a cough productive of yellow sputum. He had also been experiencing non-radiating chest pain occurring at rest, described as pins and needles for 1 day. He denied fevers, chills, shortness of breath, dysuria, and muscle aches. The patient’s initial vitals were remarkable for mild tachycardia to 105; otherwise, he was afebrile and normotensive. Heart sounds were normal with no murmurs, lungs were clear, and there was no evidence of lower extremity edema or JVD. Initial laboratory values were remarkable for elevated creatinine to 2.31, elevated AST/ALT to 585/678 respectively, as well as an elevated troponin of 2.1 with CK/CKMB elevated to 7857/49.3. Initial EKG showed TWI in leads V2-V4 with no old EKG available for comparison. Initial CXR was consistent with a multifocal pneumonia. Bedside TTE, done in the ED, showed left ventricular dysfunction with preserved ejection fraction (EF), as well as right ventricular dilation with possible strain. Concern for a PE led to a ventilation/perfusion (V/Q) scan, the result of which was low to very-low probability for PE. The patient was started on treatment for community acquired pneumonia as well as aspirin, statin and heparin drip for possible NSTEMI. The patient was admitted to telemetry for monitoring. While on the telemetry unit, the patient’s troponin continued to rise, peaking at 9.8. The patient was subsequently transferred to the cardiac care unit. An official TTE was performed which showed normal left ventricular size and function with an EF of 65 %. However, there was right ventricular hypokinesis and dilation. The patient underwent a left heart catheterization, which showed no evidence of obstructive disease. During the course of stay, the patient’s creatinine improved and a CT Angiogram of the chest was performed, which showed a large segmental pulmonary embolism. The patient was continued on a heparin drip while being bridged to warfarin. He completed his course of antibiotics for community acquired pneumonia and was discharged on warfarin to be followed as an outpatient.
DISCUSSION: The current gold standard for diagnosis of PE remains pulmonary angiography. In more recent years, studies, including PIOPED I/II, have shown both CT angiography as well as V/Q scan in combination with the use of clinic decision making tools, such as modified Well’s criteria, as both sensitive and specific. IThe initial modified Well’s score of this patient, 1.5, put the patient into a low risk category. The V/Q scan was very low probability for PE. When using the information put forth by the PIOPED and PIOPED II study, this patient still had a 4 % chance of having a PE, despite the negative V/Q scan results. It is critically important to not abandon the diagnosis of PE, despite having a near normal V/Q scan, in the setting of additional clinical information which may indicate the need for further imaging to diagnose PE.
THE FAçADE OF FAMILIARITY—A MISSED CASE OF MYXEDEMA COMALaura Harrison; Leena Rahmat. Baystate Medical Center, Springfield, MA. (Tracking ID #1939256)
LEARNING OBJECTIVE 1: Diagnose myxedema coma, and recognize it as a medical emergency.
LEARNING OBJECTIVE 2: Recognize difficulties created by experiential thinking when diagnosing a rare condition in the geriatric patient.
CASE: An 87 year-old male with a past medical history of advanced dementia, coronary artery disease, and hypertension was admitted from a long-term care (LTC) facility with unresponsiveness in the setting of subacute on chronic cognitive decline. On arrival to the hospital he was hypothermic with a temperature of 96.2 °F and bradycardic with a heart rate of 22. Physical examination was remarkable for lethargy, dry mucus membranes, and Glasgow coma scale (GCS) of 7. Labs were remarkable for serum sodium of 166 and serum creatinine of 3.5. Despite hydration and objective improvements in serum sodium level and renal function, clinically he remained unchanged. A thyroid stimulating hormone (TSH) level was checked on hospital day number 7, which returned at 219. The previous TSH level was normal. Intravenous thyroxine was started and the patient’s GCS increased from nine to 12. He was discharged to the LTC facility. Because of significant improvement in cognitive function, comfort goals were instituted and the patient expired 19 days after discharge.
DISCUSSION: Myxedema coma as a diagnosis makes this case unique. As a rare medical emergency, this case provides beneficial teaching points. Such uniqueness creates an environment where experiential thinking perpetuates a poor clinical outcome. This geriatric patient’s multiple, and common, co-morbidities further illustrate the downfalls of experiential thinking when clinicians face unique diagnoses in a façade of familiarity.
THE FEBRILE TRAVELER TO INDIA: A CASE OF TYPHOID FEVERLucinda B. Leung. UCLA Medical Center, Los Angeles, CA. (Tracking ID #1900811)
LEARNING OBJECTIVE 1: Recognize immigrants returning home to visit friends & relatives (VFRs) as a population vulnerable to typhoid fever and target them for immunization.
LEARNING OBJECTIVE 2: Manage typhoid fever when antibiotic-resistant strains of salmonella typhi are involved.
CASE: 41-year-old healthy male presents with fever and malaise, following travel to India one-month prior. The patient emigrated from India as a child, frequently visiting without routine vaccinations. One week after returning, he developed subjective fever, malaise, fatigue and non-bloody diarrhea. He denied abdominal pain, upper respiratory symptoms, cough, headache, palpitations, rash, and sick contacts. His diarrhea had improved but he continued to feel weak and febrile. On admission, he was febrile (Tm 40s), tachycardic (max HR 100 s), normotensive, and hypovolemic on exam. Labs showed mild leukocytosis, hyponatremia and transaminitis. Viral serologies, urine cultures, stool cultures, ova and parasite, hepatitis panel, malaria prep, dengue antibody, HIV, MTB quantiferon gold were negative. Blood cultures grew Salmonella typhii, resistant to cipro. His antibiotic was narrowed to ceftriaxone for a total 2-week course. Three weeks after antibiotic completion, his fevers returned and his blood cultures again grew Salmonella. Liver ultrasound did not reveal any abscess. Echocardiogram did not reveal any valvular vegetation. Tagged WBC scan did not reveal a metastatic source of relapse. He was treated with another 4-weeks of ceftriaxone, then transitioned to 2-additional weeks of azithromycin. He remains afebrile and well to date.
DISCUSSION: Typhoid fever should be suspected in a febrile returning traveler, along with malaria, rickettsial diseases, hepatitis, leptospirosis and dengue. There are 200 to 300 cases of S. typhi annually in the United States. However, most cases occur in endemic regions, where there is overcrowding and poor sanitation (e.g., India, Southeast Asia). Typhoid fever is acquired by direct or indirect fecal-oral spread. Since they have less control over their diet, travelers who visit friends and relatives are at increased risk for enteric fever. Typhoid fever is caused by S.typhi, following an incubation period of 5 to 21 days. The serotype S. paratyphi also causes enteric fever. Humans are the only reservoir for Salmonella. Patients present with sustained fever, anorexia, malaise, and vague abdominal discomfort. Diarrhea often appears early in the course and resolves before fever. Physical exam may reveal pulse-temperature dissociation, hepatosplenomegaly or rose spots. Complications include intestinal perforation, encephalopathy, relapse after clinical cure, and asymptomatic chronic carriage. Laboratory findings are nonspecific, such leukocytosis, anemia or transaminitis. S. typhi may be isolated in blood, stool, urine, bone marrow and duodenal aspirate cultures. Typhoid fever occurs in unimmunized travelers and 30 % of immunized travelers. Multidrug-resistant Salmonella strains are usually found in travelers to the Indian subcontinent. Due to increasing resistance, there has been a shift away from chloramphenicol, ampicillin, and trimethoprim-sulfamethoxazole. For susceptible strains, fluoroquinolones appear to be most effective and used empirically most often. Ceftriaxone (and oral cefixime) and azithromycin are also used for empiric therapy.
THE GREAT MASQUERADER, A BYGONE ACQUAINTANCE OR A PRESENT-DAY FOE?Maria Fan. University of California, San Francisco, San Francisco, CA. (Tracking ID #1937836)
LEARNING OBJECTIVE 1: Perform evidence-based lab and imaging assessment of cognitive impairment and dementia
LEARNING OBJECTIVE 2: Interpret RPR titers to guide clinical suspicion for neurosyphilis
CASE: An 82 year-old African American woman with a history of HTN, hypothyroidism, smoking, and chronic daily alcohol use was seen in clinic for follow-up of cognitive impairment, including difficulty recalling prior clinic conversations with her physician. The patient reported some general “forgetfulness” but declined to provide specifics. She also reported that her father had had syphilis so that she was treated for syphilis at age 9 with penicillin. Her examination was notable for Montreal Cognitive Assessment (MoCA) scores of 17/30 and 16/30 on two separate occasions with a PHQ-9 score of 3/27 suggesting minimal depressive symptoms. The remainder of her physical exam was unremarkable, without any focal neurologic deficits, rigidity, tremor, or gait abnormalities. Laboratory testing revealed normal TSH, B12, and thiamine levels. HIV was negative. RPR testing returned reactive with a titer of reactive undiluted, confirmed with reactive treponemal antibody. After discussion with Infectious Disease, a plan was made to treat the patient for late latent syphilis, with no plan for lumbar puncture to examine for neurosyphilis given the rarity of neurosyphilis in the era of antibiotics, low serum RPR titer, and patient preference.
DISCUSSION: The estimated prevalence of dementia in the United States is 6.5 % for those aged 60 years or greater, with Alzheimer disease representing 60–80 % of cases and vascular dementia 10–20 %. The American Academy of Neurology (AAN) has published guidelines for the laboratory and imaging evaluation of cognitive impairment and dementia, but what is done in clinical practice remains variable. The current AAN recommendation includes screening for B12 deficiency, hypothyroidism, and structural neuroimaging with either non-contrast CT or MRI. This is in contrast to the prior AAN 1994 practice guidelines that recommended examination of CBC, electrolytes, glucose, BUN/creatinine, folate, B12, thyroid function, and syphilis serology. In 2011, there were 18,576 cases of late and late latent syphilis in the United States (case rate of 6 per 100,000), with Los Angeles County, CA, and Cook County, IL, accounting for the most cases. Given the decline of neurosyphilis cases in the antibiotic era, the AAN now recommends not screening for syphilis unless the patient has a specific risk factor, evidence of prior syphilitic infection, or resides in a high prevalence area. Importantly, studies have found that a serum RPR titer of ≥1:32 highly predicts presence of neurosyphilis, defined as a positive CSF VDRL or CSF pleocytosis, regardless of HIV status or prior syphilis treatment history. A serum RPR titer of ≥1:32 has been suggested as a threshold to consider lumbar puncture to examine for neurosyphilis. In summary, this case reviews the laboratory and imaging evaluation of cognitive impairment and dementia in addition to illustrating the complexity of syphilis serology in considering neurosyphilis.
THE INCREDIBLE FUSS OVER ATYPICAL HUSAnita Bhagavath; David Chun; Jason Filopei; Gina Elhammady; Andrew Bohmart. Beth Israel Medical Center, New York, NY. (Tracking ID #1928693)
LEARNING OBJECTIVE 1: Recognize the clinical features of atypical hemolytic uremic syndrome.
LEARNING OBJECTIVE 2: Recognize the differences between typical HUS and atypical HUS.
CASE: 60yo F with PMHx of Hepatitis C presented with shortness of breath for 2 days, associated with chest tightness and lightheadedness. Further questioning revealed she had 2 days of bloody stools, hematuria, and minor nose bleeds. Physical examination was remarkable for dried blood in the nares, pale conjunctiva, and a flow murmur. Rectal exam showed brown stool. Admission labs revealed acute on chronic kidney disease, new normocytic anemia, and mild thrombocytopenia (Creat 4.75 g/dL, baseline 1.55, Hgb 7.8 g/dL, baseline 11.9, Plt count 130 K/uL, baseline 237, all 1 month prior). Stool sample was occult positive. Urinalysis was yellow, with large blood (>182 RBCs). Anemia work up showed schistocytes on peripheral smear, lactate dehydrogenase (LDH) 999, haptoglobin 16, and normal bilirubins. C3 was elevated (250 mg/dL) and C4 was low (3 mg/dL). The patient underwent emergent plasmapheresis and hemodialysis, with marked improvement in clinical status and laboratory abnormalities (Hgb 10.8, LDH 498, Plt 206, Creat 2.98). Stool cultures were negative and ADAMTS13 activity was normal, ruling out toxin-mediated hemolytic uremic syndrome and thrombotic thrombocytopenic purpura, respectively. Renal biopsy findings were consistent with HUS and a final diagnosis of atypical HUS (aHUS) was made. She was discharged with a plan to continue hemodialysis and begin outpatient ecluzimab therapy.
DISCUSSION: HUS is characterized by the triad of hemolytic anemia, severe thrombocytopenia, and renal impairment. Commonly this is secondary to Shiga toxin-producing enteric infections and presents as bloody diarrhea. In contrast, aHUS is both toxin and diarrhea negative, and is secondary to dysregulation of the alternate complement pathway. Our case of aHUS was unique because it presented with bloody diarrhea, only mild thrombocytopenia, and elevated rather than decreased C3 levels. These atypical presentations can result in delayed diagnosis and worsened outcomes. Plasmapheresis is the first-line therapy for aHUS and early initiation leads to better outcomes. Response is monitored by normalization of platelets, hemoglobin and LDH. Recently, a better understanding of the pathophysiology behind aHUS has led to the emergence of ecluzimab, a humanized anti-C5 monoclonal antibody. This drug inhibits the critical steps in the alternative complement pathway and is currently being evaluated in clinical trials. This new treatment option is changing the therapeutic approach to aHUS, One should recognize that aHUS can present with or without bloody diarrhea and the hallmark laboratory data may not always follow the classic pattern. This is important as early intervention with plasmapheresis and more cutting edge therapy such as ecluzimab may be critical to improved outcomes.
THE INDELIBLE DIRECTIVE: A CASE SERIES REPORT OF PATIENTS WITH DNR TATTOOSYevgeniy Mikityanskiy; Sagar Patil; Paul Leis; Jonah Feldman. Winthrop University Hospital, Mineola, NY. (Tracking ID #1937593)
LEARNING OBJECTIVE 1: To help guide treatment decisions for patients with DNR tattoos who may not be able to communicate their wishes.
CASE: Tattooing as a form of artistic expression remains as popular as ever, and some people are now choosing their ink based upon their attitudes towards health care. A 69-year-old widowed man with “Do Not Resuscitate” tattooed on his left forearm and past medical history of lung cancer presented to our emergency room with shortness of breath and fever. He was found to be in acute respiratory failure from pneumonia. Though he had difficulty speaking, he was able to communicate that he wished full resuscitation efforts to be made, including intubation, if needed. Mechanical ventilation as well as appropriate treatment was initiated, which led to a complete recovery. He explained that the tattoo represented his frustration with the health care system after losing his wife to cancer several years prior, but his attitude about health care changed after establishing a rewarding doctor-patient relationship with a new primary care physician. He was healthy when the tattoo was inked, and he never intended for it to be taken as an advance directive.
DISCUSSION: To help guide treatment decisions for future patients who may not be able to communicate their wishes, we searched Pubmed and Google scholar for articles containing the phrase “do not resuscitate” and the word “tattoo.” Review of these articles revealed four previously published case reports, which formed a series of five cases when added to our own. Based on these reports, we identified three reasons why a DNR tattoo should not be actionable in clinical practice. 1) A tattoo inked years ago may not be an accurate reflection of a patient’s current wishes. 2) DNR tattoos are ambiguous and are often intended to make a public statement unrelated to decisions about resuscitation. 3) DNR tattoos are not legally binding. While the third reason reflects a technical concern, the first two give insight into the true feelings of patients who get this type of tattoo. In our case series, patients with tattoos had a change in preference regarding resuscitation status in 2/5 cases. The meaning behind the tattoo did not coincide with specific decisions about resuscitation in 3/5 cases. In total, we found that tattoos did not accurately reflect patient resuscitation preferences in 4/5 cases. From this first known case series of patients with DNR tattoos, we conclude that clinicians should strongly consider resuscitating patients unless they have appropriate documentation. Tattoos, however, should be used as a starting point for conversations regarding preferences for care. In our case, this discussion led to a narrative that enriched the relationship between the patient and his healthcare providers.
THE MYSTERIOUS GREEN URINE!Venu M. Ganipisetti; Pratyusha Bollimunta; Sathish kumar Krishnan; Malav P. Parikh; Harvey Friedman. presence saint francis, Evanston, IL. (Tracking ID #1923585)
LEARNING OBJECTIVE 1: 1) Recognize that Propofol administration can be associated with green urine in patients.
LEARNING OBJECTIVE 2: 2) Recognize that this finding is benign and does not cause harm to the patient. Discontinuing the medication will normalize the urine color in few hours and will establish the diagnosis.
CASE: A 44-year-old African-American male with no known past medical history, presented to our Emergency department with blunt head trauma resulting in intracranial hemorrhage. Upon arrival, he was agitated, minimally responding to verbal stimuli, and was intubated emergently in the ER and later transferred to the ICU for close observation. He was started on a Propofol and Fentanyl infusions for sedation and analgesia. Sedation vacation was tried each day during the hospital course, however the patient became agitated, restless, and hypertensive upon weaning. He continued to require propofol and fentanyl at high doses. On day 10 of admission, we observed that his urine in the foley bag was green. At that time, his labs were normal except for elevated alkaline phosphatase 177 and serum albumin 2.9. His medications at this time were Lisinopril, Amlodipine, Unasyn (for facial injuries), and Dilantin. Cultures were negative for bacterial growth. Ultimately, Propofol was stopped and patient was switched to an Ativan drip. We monitored the urine color, which changed back to yellow within 6 h. No further work up was done.
DISCUSSION: Propofol is a commonly used sedative in critical care settings. Green urine color with propofol is a benign and rarely reported finding. To date, only 13 cases are reported in the literature. It has been proposed that green color occurs due to the presence of metabolites in urine. Propofol is metabolized in the liver by glucoronide conjugation and excreted in urine predominantly as the 1-glucuronide, 4-glucuronide, and 4-sulfate conjugates of 2,6-diisopropyl-1, 4 quinol which imparts green color to urine. Urine alkalinization increases the formation of these metabolites. A second proposed potential mechanism is entero-hepatic circulation failure due gallbladder hypomotility and extra-hepatic glucuronidation in the kidneys, which might be the cause of green urine in our patient. Other common causes for green urine include pseudomonas infection (Pyocyanin pigment), hartnup disease, indicanuria, ingestion of triamterene, amitriptyline, indomethacin, methocarbamol, promethazine, cimetidine, food coloring, listerine mouthwash, clorets mints, indigo dyes, and methylene blue. All these were excluded in our patient. The temporal relationship of normalization of urine color upon discontinuing propofol indicates it is the most likely cause of this finding. Presence of propofol metabolites in urine is benign and does not affect kidney function or cause harm to the patient. Although this finding is benign, it may cause unnecessary apprehension in Physicians and family members. Notably, in an informal survey of over 30 Anesthesiologists, only one was aware that propofol could cause green urine. This case illustrates that an awareness of this benign finding is important and may prevent unnecessary testing. We were able to avoid all unnecessary further workup in this patient while providing reassurance to the patient’s family members.
THE OUTPATIENT MANAGEMENT OF KETOSIS-PRONE DIABETES AT BELLEVUE HOSPITALArnab K. Ghosh; Jamie Osman; Natalie K. Levy. NYU, New York, NY. (Tracking ID #1920760)
LEARNING OBJECTIVE 1: 1) Recognize the epidemiology and classification of Flatbush/Ketosis-Prone Diabetes Mellitus and its common presentation as diabetic ketoacidosis.
LEARNING OBJECTIVE 2: 2) Recognize the need to carefully monitor glucose levels in ketosis-prone diabetic patients, who are at risk for hypoglycemia to prevent hypoglycemia.
CASE: A 53YO Mexican previously well male was admitted with a week-long history of polyuria, polydipsia, dry mouth, and a 30 lb weight loss over the past 2 weeks. He denied any personal or family history of diabetes mellitus. On examination he was clinically dehydrated. His labs were significant for K 5.5 mmol/L, HCO3 21 mmol/L, chloride 88 mmol/L glucose 1190 mg/dL, anion gap of 22, urinalysis showing ketones and glucose. Venous blood gas pH was 7.284. The patient was diagnosed with diabetic ketoacidosis and treated with intravenous fluids, potassium supplementation and insulin therapy. His symptoms resolved without incident. No precipitating factor was found. He was discharged home on glargine 10 units at night and metformin 1000 mg twice a day. The patient was seen in clinic. His glutamic acid decarboxylase (GAD) antibody and islet cell antibody were negative, fasting C-peptide was 2.23 ng/mL (N: 0.8–3.1 ng/mL) and HbA1c 15.8 %. He was only taking 6 units of glargine for unclear reasons. Based on his home blood glucose readings, his glargine dose was increased to 20 units nightly over these first two visits. For 2 subsequent visits over the next 5 weeks this insulin dose, plus metformin, led to controlled fasting blood glucose. The patient was lost to follow up for the next 2 months. When he returned to clinic 4 months after his initial discharge, he had ceased taking his insulin and metformin, owing to symptoms of hypoglycemia. Repeat HbA1c was 7.1 %. Because his fingerstick glucose remained elevated, the patient was restarted on metformin.
DISCUSSION: This case represents a case of a patient with Ketosis-Prone Diabetes (KPD) initially presenting with DKA. In the literature, KPD has been noted in the Hispanic and African-American populations, the diagnosis occurring in the fourth or fifth decade of life. Most patients diagnosed with KPD tend to be obese, and 80 % have a family history of type 2 diabetes mellitus. To place a KPD patient into the AB classification system, they need to be tested for both autoantibodies and beta cell reserve. Our patient was GAD and Islet Ab negative. His fasting C-Peptide level was normal, placing him in the A-B+ category, the most common category for new diabetics presenting in DKA. Patients with a new diagnosis of DM in DKA have a varied post discharge course. Some will need lifelong insulin. Others will have recovery of beta cell function and be able to come off of their insulin. A classification of A-B+ is associated with the highest likelihood of achieving insulin independence. Smiley et al. recommend KPD patients be followed every 2 weeks for the first 2 months for insulin adjustment. If found to have fasting blood glucose values of <130 for 2 weeks (or if there is any hypoglycemia) then tapering should occur, decreasing the dose by 25 % at each visit. In our patient’s case, his fasting glucose values <130 at weeks 4, 5, and 7 should have prompted a tapering of his glargine. When he returned ~4 months after hospital discharge, he had tapered his insulin off himself.
THE PERFECT LIPODYSTROPHY STORMVictoria Gutgarts1,2; Ewa M. Rakowski1,2; Bettina Fries1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1938598)
LEARNING OBJECTIVE 1: Define and identify the causes of acquired lipodystrophy.
LEARNING OBJECTIVE 2: Discuss the complications and management of lipodystrophy.
CASE: A 45 year-old woman with uncontrolled diabetes, hypertriglyceridemia, and human immunodeficiency virus (HIV) on antiretroviral medication presented with 1 day of worsening epigastric abdominal pain. The patient described the pain as constant, severe and radiating throughout the abdomen, with associated nausea and vomiting. Vital signs were notable for a temperature of 101 F. Abdomen was mildly distended with guarding and epigastric tenderness. Murphy’s sign was negative. Eruptive xanthomas were present at the elbows bilaterally as well as loss of subcutaneous fat over the arms, legs, and buttocks. Initial laboratory values were significant for a hemoglobin A1c of 12, lipase of 11,794, amylase of 1,857, and fasting triglycerides of 8,046. Patient was managed for acute pancreatitis secondary to hypertriglyceridemia. She was started on intravenous fluids and insulin. An apolipoprotein B level of 265 (normal 49–103) supported an underlying familial combined hyperlipidemia. Additionally, the patient was diagnosed with acquired HIV associated lipodystrophy.
DISCUSSION: The term lipodystrophy was derived from the Greek language, and has the literal translation of fat ill nourishment. This term is often used to describe a collective group of disorders characterized by degeneration of complete or partial adipose tissue. The two main types of lipodystrophy are congenital and acquired. The congenital type is autosomal recessive, and results from mutations in genes that interfere with lipid synthesis and differentiation. Acquired lipodystrophies are hypothesized to result from infections, medications, and autoimmune disorders. HIV is a common infection that can cause acquired lipodystrophy. In specific, it is the treatment with protease inhibitors that may impair differentiation of adipocytes and lead to apoptosis of peripheral adipose tissue. The mechanism for this is suggested by a homology in the catalytic site of HIV protease to proteins involved in lipid metabolism. Circulating lipids are then free to deposit in central tissues such as the abdomen and breasts. Other types of acquired lipodystrophies are named based on the amount of affected peripheral tissue. As an example, acquired generalized lipodystrophy, or Lawrence Syndrome, involves a generalized loss of fat, whereas, acquired partial lipodystrophy, or Barraquer-Simons syndrome, spares the abdomen and lower extremities. A localized lipodystrophy can also occur, often from subcutaneous injection of drugs such as insulin. The diagnosis of lipodystrophy is essential to prevent the many complications that can occur. The destruction of adipose tissue results in a decreased production of the leptin hormone, which normally acts at the hypothalamus to inhibit appetite. Loss of this hormone results in hunger and increased caloric intake. Increased calories have few adipocytes to deposit in, resulting in ectopic lipid deposition and muscle hypertrophy and hepatic steatosis. Elevated triglycerides in specific, can lead to acute pancreatitis. Patients with conditions like familial hyperlipidemias are at a higher risk, given the increased triglycerides at baseline. A lipid profile can be checked in suspected cases, followed by apolipoprotein levels. Excess lipids can lead to other complications like insulin resistance and eventually diabetes. Insulin resistance can also affect the reproductive system, leading to polycystic ovarian syndrome and issues with infertility. Management of lipodystrophy begins with lowering the primary lipid abnormality. Statins and fenofibrates are often used to lower elevated LDL and triglycerides, respectively. Thiazolidinedione and metformin are two additional agents which act to improve target cell’s response to insulin and reduce fat atrophy. Switching to different protease inhibitors has also been suggested in patients with HIV lipodystrophy. Studies have also shown that leptin replacement therapy with analogs like metreleptin has reduced hyperglycemia, hypertriglyceridemia, and decreased liver size. Along with pharmacological management, preventative therapies like diet and exercise can help reduce complications even in the setting of underlying lipid disorders and acquired diseases. Managing patients with lipodystrophy can be challenging, especially when patients have underlying conditions like diabetes, familial hyperlipidemia, and HIV. It is therefore essential to diagnose lipodystrophy early and utilize a multi-modal approach to treatment to prevent future complications of the disease.
THE PERFECT STORM: A FEBRILE ANAPHYLACTOID REACTIONJason P. Williams1; William Reid1; Raffi Tachdjian2. 1Ucla, Marina del Rey, CA; 2Ucla, Los Angeles, CA. (Tracking ID #1927138)
LEARNING OBJECTIVE 1: Distinguish anaphylactoid reactions from IgE mediated anaphylaxis.
LEARNING OBJECTIVE 2: Recognize a novel association of mast cell degranulation and fever in the setting of granulocyte colony stimulating factor
CASE: A 30 year old female with BRCA-1 and triple negative bilateral breast cancer presented with a fever and rash. She previously had a bilateral mastectomy, radiation, and recently completed her third cycle of docetaxel and cyclophosphamide 9 days prior to admission. Eight days prior, she received pegylated granulocyte colony stimulating factor (G-CSF). Cephalexin was prescribed over the phone for bilateral arm swelling that turned out to be lymphedema. She tolerated her first dose, but woke 4 h after the second dose of cephalexin with a diffuse pruritic rash. In the ER, her temperature was 38.0, heart rate 132 and blood pressure 86/47. Her extremities and torso exhibited erythematous, well circumscribed, raised plaques with central pallor consistent with urticaria (image available for presentation). There was no stridor or wheezing. Four hours later she developed angioedema of her lips, sparing her tongue. These symptoms quickly resolved with IM epinephrine, IV fluids, diphenhydramine, and methylprednisolone. She had a recurrence of her angioedema on hospital day 2 that again improved with IM epinephrine. Prior to corticosteroids, the WBC was 30,000 with 92 % neutrophils. Without any significant course of antimicrobials, the WBC normalized by hospital day 3. The patient spiked nightly fevers that were associated with flares of urticaria until hospital day 4. Penicillin skin testing done at the bedside was negative. An infectious work up was negative including repeated blood and urine cultures, stool C. Difficile PCR, serum CMV PCR, monospot, and nasal respiratory viral PCR. CT of the chest, abdomen and pelvis was unrevealing other than pericholecystic fluid with a normal HIDA scan. Ultrasound of the four extremities was negative for DVT. The patient was discharged on hospital day 5. She has since completed several more cycles of chemotherapy without further complications.
DISCUSSION: The differential for a rash and fever is broad. Infectious etiologies are possible, though her extensive work up was negative. Her tumor burden, if any, is too minimal to account for such profound symptoms. Reintroduction of her chemo has been uneventful. The antecedent antibiotic prompts consideration of a drug reaction. Drug Reaction and Eosinophilia with Systemic Symptoms (DRESS), Serum Sickness, and Stevens-Johnson can present with fever and rash, but none develop this rapidly nor do they account for her angioedema. The patient’s urticaria, angioedema and hypotension meet criteria for anaphylaxis and she responded appropriately to treatment. Anaphylaxis is an immediate hypersensitivity reaction, so the 10 h delay in symptom onset argues against an IgE mediated process. Anaphylactoid reactions are pseudoallergies that are clinically identical to anaphylaxis except anaphylactoid reactions can have a delayed presentation following drug exposure. This pseudoallergy results from direct stimulation of mast cells without cross linking to IgE. This explains why penicillin skin testing is negative in anaphylactoid reactions and positive in anaphylaxis. In the acute setting, anaphylaxis and anaphylactoid reactions are treated identically. Unlike IgE mediated reactions, pseudoallergies do not always preclude reexposure to the offending drug. One cases series found that if a reaction to a cephalosporin occurred greater than 1 h after exposure and the patient had negative skin testing, they completely tolerated reexposure to the drug. Neither anaphylactic nor anaphylactoid reactions result in fever or neutrophilia. However, the recurrent fever and simultaneous flares of urticaria suggest that they were linked. She did receive G-CSF which is associated with fever, neutrophilia, and a heightened neutrophil functionality. In vitro, these G-CSF primed neutrophils have been shown to release significant quantities of IL-6 when exposed to TNF-alpha. Mast cells are a significant source of TNF-alpha. Together, TNF-alpha and IL-6 produce fever. This novel clinical combination of mast cell degranulation stimulating G-CSF primed neutrophils appears to be the perfect cytokine storm for an anaphylactoid induced fever. Further study into the exact mechanism and biomarkers are warranted.
THE SHOUT OF A MURMUR: A DRAMATIC PRESENTATION OF MITRAL REGURGITATIONMara E. Murray Horwitz; Jennifer Siegel. Boston Medical Center, Boston, MA. (Tracking ID #1939427)
LEARNING OBJECTIVE 1: Review the sequelae of severe untreated mitral regurgitation (MR), including right heart failure, pulmonary hypertension, and atrial fibrillation;
LEARNING OBJECTIVE 2: Appreciate key physical exam findings associated with MR, and understand how the diagnosis of MR is made.
CASE: A 67 year old woman presented with altered mental status and leg pain. She was unable to provide further history. Past medical history was inferred from medications in her purse as significant for congestive heart failure (pill bottles of Furosemide 80 mg twice daily, Metoprolol 25 mg twice daily, and Lisinopril 5 mg daily), and atrial fibrillation (pill bottle of Pradaxa 150 mg daily). In the ED, her temperature was 96.9, blood pressure was 121/85, pulse was 120, respiratory rate was 18, and oxygen saturation was 100 % on room air. Exam was notable for somnolence, irregularly irregular cardiac rhythm, IV/VI holosystolic murmur heard throughout the precordium and posterior chest, and 3+ pitting edema to the sacrum. Laboratory studies were notable for a white blood cell count of 8.3, BUN of 41, creatinine of 2.01, alkaline phosphatase of 200, mild transaminitis, troponin of 0.039, BNP of 1632, and lactate of 2.3. Her EKG confirmed atrial fibrillation. A CT scan of her head was unremarkable. Chest x-ray showed pulmonary vascular congestion. She was admitted to the Medicine service for acute and chronic heart failure of unknown etiology. Upon arrival to the inpatient floor, a diagnostic trans-thoracic echocardiogram was performed. It revealed redundant mitral leaflets with severe mitral regurgitation (MR) causing pulmonary vein flow reversal, severe tricuspid regurgitation, inferior vena cava dilation, and hepatic vein flow reversal. She had a left ventricular ejection fraction of 50–55 %, mild right ventricular enlargement, and severe bilateral atrial enlargement. Her hospital course consisted of a 40-pound diuresis, with subsequent normalization of her renal and liver function tests and improvement in her mental status. She was considered for mitral valve repair or replacement, but unfortunately declined pre-surgical evaluation and left against medical advice.
DISCUSSION: This patient’s presentation illustrates the sequelae of severe mitral regurgitation (MR), while her hospital course reminds us of the classic physical exam findings and diagnostic studies for this condition. As seen here, severe MR can cause congestive heart failure by way of pulmonary hypertension, tricuspid regurgitation, and right heart failure. Resultant venous congestion can cause multi-organ damage, such as the altered mental status, acute kidney injury, and hepatic congestion seen in this patient. Long-standing MR with atrial enlargement may precipitate atrial fibrillation, which in retrospect was the first diagnostic clue toward her diagnosis. Several classic physical exam findings of MR were found in this patient. First, a holosystolic ejection murmur radiating to the apex, axilla, or back is almost always present. A wide split S2 and an S3 gallop may also be heard. When MR leads to right heart failure, as illustrated in this case, the systemic signs of congestive heart failure (dyspnea, lower extremity edema, encephalopathy, and congestive hepatopathy) will ensue. Echocardiogram makes the diagnosis of MR, in which severity is based on valve width, area, regurgitant volume, and presence of flow reversal. Of note, there is little correlation between the loudness of the murmur and MR severity, although grade I-II murmurs are rarely severe. The chambers of the heart are also affected. Left ventricular enlargement is common with severe MR, while left atrial enlargement is common with chronic MR. In this patient, severe MR was diagnosed by flow reversal. Left ventricular and atrial enlargement seen on her echocardiogram suggested that her MR had been both severe and chronic, respectively. This woman paints a dramatic portrait of severe, chronic, and untreated MR. The diagnosis was suggested in every element of her past medical history, physical exam, and laboratory studies, and was ultimately confirmed by echocardiogram.
THE SIMPLEST ANSWER IS THE BEST ANSWERErica Altschul; Allison Selby. Lenox Hill Hospital, New York, NY. (Tracking ID #1933727)
LEARNING OBJECTIVE 1: Formulate differential diagnosis of bradycardia
LEARNING OBJECTIVE 2: Recognize the importance of medication side effects in the differential diagnosis of bradycardia
CASE: This 68 year old man with a history of hypertension, ESRD on hemodialysis, and glaucoma was referred to Lenox Hill Hospital in New York, NY by his dialysis center for asymptomatic bradycardia (around 30 bpm) for 1 h. His home medications included amlodipine, carvedilol, allopurinol, omeprazole, ASA, dorzolamide/timolol eye drops, brimonidine tartrate eye drops, and travoprost eye drops. The patient’s past surgical, family, and social histories were not significant. Review of systems was notable for chronic and unchanged dyspnea on exertion as well as exertional chest pain. In the ED, his heart rate was 32 bpm, blood pressure 105/60, respiratory rate 18, and saturation of 98 % on room air. Physical exam was remarkable for bradycardia, 2+ pitting edema bilaterally, and a left arm AV fistula. An EKG demonstrated a junctional rhythm at 35 bpm. An echocardiogram demonstrated mild left ventricular hypertrophy with an EF of 50–55 %. The patient was admitted to telemetry for monitoring. His home medications were continued except amlodipine and carvedilol secondary to hypotension and bradycardia, respectively. Due to persistent bradycardia, permanent pacemaker placement was considered but not done due to right subclavian vein occlusion and his AV fistula precluded left subclavian access. The patient was considered a poor surgical candidate for an epicardial pacemaker given his comorbidities. The patient’s timolol/dorzolamide eye drops were discontinued with the belief they could have been causing his bradycardia, after which his heart rate improved to greater than 60 bpm. The patient was discharged on alternative glaucoma therapy as recommended by ophthalmology (Dimonidine and Dorzolamide).
DISCUSSION: Bradycardia is defined as a heart rate less than 60 beats per minute. When a patient presents with bradycardia, it is important to consider the possible causes; including, cardiac disease including sick sinus syndrome, high degree AV block, endocarditis, and myocardial infarction; electrolyte imbalances; hypothermia; and hypoglycemia. Medication side effects are often overlooked, with common culprits including centrally acting alpha-2 agonists, cholinesterase inhibitors, calcium antagonists, digitalis, and beta-blockers. Studies have shown that ophthalmic Timolol is similar to intravenous Timolol having comparable systemic bioavailability, plasma kinetics, and cardiopulmonary effects, mainly bradycardia. This effect on the heart rate is even more noticeable during exercise. The impact on blood pressure is considered less significant, likely because of the compensatory increase in systemic vascular resistance due to the lowered heart rate. Bradycardia due to Timolol has been documented in many case studies and is associated with syncope, especially in the older population and patients with pre-existing cardiovascular morbidity. It is important to look closely at medications as they can be a reversible cause to a patient’s chief complaint
THE TRIPLE GI THREAT OF CMV: A CASE OF CMV ESOPHAGITIS, HEPATITIS AND PANCREATITIS IN NEWLY DIAGNOSED HIVKendrick B. Gwynn1; Ameeta Kalokhe2; Robin Klein1. 1Emory University School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA. (Tracking ID #1938187)
LEARNING OBJECTIVE 1: Recognize the less common gastrointestinal manifestations of cytomegalovirus disease in HIV-positive patients
CASE: 41 year old male to female transgender with no significant past medical history presents with 4 weeks of odynophagia exacerbated with food and acidic liquids. She denied use of alcohol and illicit substances, but noted taking NSAIDs to relieve the pain. Review of systems was notable for anorexia, weight loss and night sweats. Exam revealed two palpable anterior cervical lymph nodes. No oral lesions or thrush was noted and abdominal exam was benign. Labs were notable for AST 786 U/L, ALT 218 U/L, Alkaline phosphatase 492 U/L, total bilirubin 4.1 mg/dL with direct component 2.9 mg/dL. Abdominal ultrasound showed no gallstones and patent hepatic veins. Acetaminophen level was negative. HIV ELISA and Western Blot were positive. CD4 was 22/mcL and viral load log 6.08 copies/mL. Endoscopy showed chronic active esophagitis, a 5 cm proximal ulcer and chronic inactive gastritis. Biopsies of the ulcer were taken, but while awaiting pathology results, the patient developed severe epigastric abdominal pain. CT scan showed pancreatitis but no gallstones. Lipase, AST, and ALT were 1750 U/L, 1800 U/L and 360 U/L, respectively. MRCP showed no pancreatic masses or evidence of obstruction. Triglyceride level was mildly elevated at 247 mg/dL. Further infectious workup was unrevealing including blood cultures, AFB blood cultures, tuberculin skin test, histoplasma antigen, Bartonella henslae antibody, Mycoplasma antibody, cryptococcal antigen, and viral hepatitis serologies. Eight days into the hospital course, pathology results of the esophageal biopsy returned, demonstrating an absence of cytopathologic changes typically seen with viral esophagitis, but immunohistochemical staining revealed CMV. CMV IgG was positive, IgM was negative and CMV-PCR was 1438 copies/mL. Dilated fundoscopic exam was without evidence of CMV retinitis. Induction therapy with IV ganciclovir renally dosed followed by oral valganciclovir 900 mg twice daily was initiated. Abdominal pain resolved 5 days into induction therapy and liver enzymes normalized. The patient was discharged to complete 21 days of induction therapy, followed by valganciclovir secondary prophylaxis, and was linked to comprehensive outpatient HIV care.
DISCUSSION: Cytomegalovirus infection can cause a variety of infections in immune compromised patients including retinitis, encephalitis, and esophagitis. A retrospective study found that a third of patients co-infected with CMV and AIDS manifested gastrointestinal disease. Nearly half of patients with gastrointestinal disease have esophagitis and 10 % have pancreas or liver involvement. Degree of CMV viremia by PCR does not necessarily indicate the presence of end-organ damage and cannot be solely used to diagnose end-organ disease. Esophagitis can also be due to other infections including HSV, HIV-associated aphthous ulcer, Candida, or tuberculosis but were all negative in this case. CMV remains the most common viral cause of esophagitis in immunocompromised patients. Literature review found seven cases of pathologically evident CMV pancreatitis, three of those presenting with clinical pancreatitis and one of which was associated with HIV, the others in post renal transplant patients. Pancreatic involvement by CMV has been reported in autopsies even without clinically observed pancreatitis. CMV has also been implicated as a cause of acute granulomatous hepatitis. Studies have shown higher rates of CMV in perinatally HIV infected children presenting with hepatitis. CMV hepatitis has been reported in the setting of acute HIV infection. Our case represents a rare presentation of CMV infection manifesting as concomitant esophagitis, pancreatitis and hepatitis in a newly diagnosed HIV infected patient. Physicians should be aware of the less common gastrointestinal manifestations of CMV infection in HIV-infected patients.
THE UNUSUAL SUSPECT: PARANEOPLASTIC MONONEURITIS MULTIPLEXJane J. Lee1; Gaetan Sgro2. 1University of Pittsburgh Medical Center, Pittsburgh, PA; 2VA Pittsburgh Healthcare System, Pittsburgh, PA. (Tracking ID #1936766)
LEARNING OBJECTIVE 1: Include paraneoplastic syndrome in the differential diagnosis of mononeuritis multiplex.
LEARNING OBJECTIVE 2: Recognize that mononeuritis multiplex can precede any other manifestation of a primary malignancy.
CASE: A 44 year old Caucasian man presents with acute lower back pain for 2 days. He has a history of a recent left orchitis and epididymitis treated with antibiotics, and multiple cranial nerve palsies and mononeuritis multiplex of unknown etiology that had persisted for 3 years. His previous symptoms had included left sixth and third cranial nerve palsies and unilateral, intermittent limb pain. He had previously undergone an extensive work up for rheumatologic, metabolic, toxic, and neoplastic etiologies, which was negative. Cerebrospinal fluid analyses were normal. Electromyography showed a right ulnar nerve focal neuropathy. A sural nerve and muscle biopsy showed mild axonal degeneration and chronic neurogenic changes, respectively. Numerous MRI and CT scans of his head and spine were unremarkable. A whole body gallium 67 imaging study was negative. Anti-hu antibody was negative. His neurologic symptoms were treated with intermittent steroids. On presentation, his exam was notable for anisocoria (left pupil larger than the right) with impaired adduction of the left eye, decreased light touch sensation on both sides of the forehead, and 3/5 strength in right hip flexion and ankle dorsiflexion. He had a palpable, non-tender left testicular nodule. Labs were only notable for new thrombocytopenia, with a platelet count of 37,000. A spine MRI with contrast showed new enhancement of the conus medullaris that was concerning for leptomeningeal involvement of a malignancy. A brain MRI now demonstrated a new left cavernous sinus mass. He underwent a bone marrow biopsy, which revealed a diffuse large B-cell lymphoma. He also underwent a left orchiectomy, and pathology showed a primary testicular lymphoma. PET/CT scan showed scattered lymph nodes as well as lesions in the spleen, thyroid, adrenal gland, and skeleton that were hypermetabolic and consistent with metastatic disease. The final diagnosis was primary testicular lymphoma, diffuse large B-cell type, with CNS and bone marrow involvement, and paraneoplastic mononeuritis multiplex. His neurologic symptoms improved dramatically after initiation of chemotherapy.
DISCUSSION: Involvement of the peripheral nervous system occurs in 5 % of lymphoma cases, mostly in non-Hodgkin lymphomas. Neuropathy in lymphomas is either a result of neurolymphomatosis (i.e. direct invasion of lymphoma cells into the peripheral nervous system, which is diagnosed pathologically or by positive signals on PET imaging) or a paraneoplastic syndrome, which is much less common. This case illustrates mononeuritis multiplex as the initial presentation of lymphoma, preceding the lymphoma diagnosis by several years. Malignancy was included in the differential during his prior work up, but was never proven until this presentation. Ultimately, his mononeuritis multiplex was attributed to a paraneoplastic disorder based on nerve biopsies and PET scans that failed to show direct lymphoma involvement of the peripheral nerves, as well as the fact that his symptoms resolved after chemotherapy. References 1. Hughes RA, Britton T, and Richards M. Effects of lymphoma on the peripheral nervous system. J R Soc Med. 1994 September; 87(9): 526–530. 2. Tomita M, et al. Clinicopathological features of neuropathy associated with Lymphoma. Brain 2013: 136; 2563–2578
THE UPSURGE OF EOSINOPHILSParas Karmacharya1; Madan R. Aryal1; Carol Kalathas1; Michael Goonewardene1; Ranjan Pathak1; Pragya Shrestha2; Supriya Shrestha Tamrakar3; Anthony Donato1. 1Reading Health System, West Reading, PA; 2Nanjing Medical University, Nanjing, China; 3Guangxi Medical University, Guangxi, China. (Tracking ID #1935129)
LEARNING OBJECTIVE 1: Recognize Hypereosinophilic Syndrome (HES) as an important but uncommon cause of extreme elevation of eosinophil counts, that can result in significant end-organ damage if not treated.
LEARNING OBJECTIVE 2: Recognize glucocorticoid as the first line treatment to reduce the number of tissue eosinophils.
CASE: A 69-year-old female presented with low grade fever, dyspnea on exertion, fatigue and confusion for 1 week. She denied history of rash, recent travel or asthma in the past. On exam, the patient appeared confused but without focal neurological deficits. She had a high white cell count of 25.7c/mm3 with 59 % eosinophils and absolute eosinophil count of 15,000c/mm3. Electrocardiogram showed some t-wave inversions on anterolateral leads, along with troponin level - 15 ng/ml, BNP - 1028 pg/ml. Patient had a creatinine of 2.49 mg/dl (baseline: 0.96 mg/dl, 2 months prior) with urinalysis showing many eosinophils. An extensive workup was performed to rule out secondary causes of eosinophilia, including stool studies for ova and parasites and serology for helminthic infections, autoimmune vasculitis, and collagen vascular disease, which all proved negative. Bone marrow aspiration and biopsy revealed marked eosinophilia (40 %), without any evidence of leukemia or lymphoma. Fluorescence in situ hybridization (FISH) analysis for genetic mutations of FIP1L1-PDGFRA and BCR/Abl were negative. Treatment with oral prednisone led to dramatic lowering of white cell counts and eosinophils with resolution of all symptoms. Her prednisone was slowly tapered from 60 mg to 5 mg over 3 months with her symptoms returning to baseline and normalization of lab parameters.
DISCUSSION: The diagnosis of idiopathic HES must exclude other causes of eosinophilia such as hematological diseases (especially eosinophilic leukemia) and reactive eosinophilia due to parasitic infections, allergic diseases, drug reactions, autoimmune disease, neoplasm, and vasculitis as these disorders require specific interventions directed at the underlying cause rather than the eosinophilia itself. Therapy is aimed to reduce the number of eosinophils in tissue, and glucocorticoids are first-line. Cytotoxic agents, interferon-α and monoclonal antibodies are considered in refractory cases. A subgroup of patients with FIP1L1-PDGFRA mutation has a favorable response to imatinib mesylate (1). Our patient’s multisystem presentation required consideration of a broad differential as well as ruling out infectious etiologies prior to therapy. Special attention to the organ systems involved (CNS, lungs, heart and kidneys), striking peripheral eosinophilia, bone marrow biopsy findings and ruling out other possible causes led the clinicians to a diagnosis of acquired hypereosinophilic syndrome (HES), which would not be a part of routine differential diagnosis. References: 1. Valent P, Klion AD, Horny H-P, Roufosse F, Gotlib J, Weller PF, et al. Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol. 2012 Sep;130(3):607–612.e9.
THE WILY WOLF: PERSISTENT FEVERS, TRANSAMINITIS, AND PANCYTOPENIA SECONDARY TO SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) IN PREVIOUSLY HEALTHY MALESyed Ali2,1; Katerina Kovalenko2; Weija Wang2; Laura K. Snydman2. 1Tuft University Medical School, Medford, MA; 2Tufts Medical Center, Boston, MA. (Tracking ID #1925626)
LEARNING OBJECTIVE 1: 1. Understand that SLE may present initially with normal or only mildly abnormal serologic findings but may change with disease course, and negative biomarkers should be interpreted in the context of the clinical picture.
LEARNING OBJECTIVE 2: 2. Importance of having a broad differential and a type II clinical reasoning approach for patients with non-specific systemic symptoms.
CASE: A 28-year-old Cape Verdean man with no past medical history presented to an outside hospital with 1.5 months of proximal muscle weakness, myalgias, fevers, palmar rash, fatigue and 15 lb weight loss. He was found to have transaminitis and pancytopenia. An extensive infectious disease, rheumatologic and hematology/oncology workup, which included palmar biopsy and bone marrow biopsy, did not yield a diagnosis and he was discharged after 3 weeks. Two weeks later, he was admitted to our hospital with these same complaints in addition to low back pain. Exam was significant for 3/5 proximal muscle strength (quadriceps, biceps, triceps), left inguinal lymphadenopathy and palmar rash. Laboratory data revealed transaminitis (AST 600 s, ALT 200 s), severe pancytopenia (WBC 0.9, HgB 7.3, HCT 21.1, plt 76), CPK > 1200, and elevated serum ACE 111. Imaging revealed a splenic infarct and myositis. Biopsy of paraspinal muscle, left inguinal lymph node and bone marrow was unrevealing. Infectious disease workup, including hepatitis, HIV, HTLV, malaria, CMV, EBV, RPR, tick-borne illnesses, parvovirus, toxoplasmosis, legionella, cryptococcus, enterovirus, coxsackie, and histoplasmosis was negative. All rheumatologic tests were unremarkable except for a slightly elevated ANA 1:160 in the setting of negative ds-DNA and anti-Smith antibody. PPD was negative, and Quantiferon Gold was indeterminate × 2, however these results were felt to be inconclusive due to the patient’s profound pancytopenia. The patient was treated with Cefepime for neutropenic fever but continued to spike temperatures >39 °C. After 2.5 weeks, our differential diagnosis included military tuberculosis (his son was being treated for latent TB), an unclear autoimmune process, sarcoidosis, and hemophagocytosis. Anti-TB treatment with moxifloxacin, ethambutol, and rifampin was started but didn’t show improvement after 4 days. Then the anti-TB medications were stopped and IV Solumedrol was started to treat a possible autoimmune process. Once steroids were started his blood counts improved and he began to feel well enough for discharge to inpatient rehab. At his follow up appointment in Rheumatology a month later, his ANA was 1:320 and his repeat ds-DNA was positive. Despite feeling 85 % of his normal self, his protein/creatinine ratio was uptrending, raising concern for developing lupus nephritis.
DISCUSSION: This case demonstrates the protean manifestations of SLE in a young, otherwise healthy male. SLE is a chronic inflammatory disease of unknown etiology that typically presents with a constellation of constitutional, hematologic and serologic findings and can affect almost any organ. Almost all patients experience fatigue, fever and arthralgias. A significant portion also have hematologic findings, including anemia, leukopenia, thrombocytopenia, and pancytopenia. A formal diagnosis of SLE requires the presence of 4 out of 11 criteria: malar rash, discoid rash, photosensitivity, oral ulcers, arthritis, serositis; renal, neurologic and hematologic disorders; and elevated ANA and one other serologic marker (anti-dsDNA, anti-Sm, APLA). Our patient has 3 criteria: pancytopenia, elevated dsDNA, and elevated ANA. His developing lupus nephritis would make it 4 criteria and a definite diagnosis. Approximately half of patients who present with a positive ANA and fewer than 4 criteria eventually accumulate enough criteria for a diagnosis of lupus. It is interesting to note that although dsDNA only has a 75 % sensitivity for SLE, it is a risk factor for developing lupus nephritis. Other risk factors include being young, male, black, and having positive anti-Smith and lupus anticoagulant. Serologies may be equivocal and can fluctuate throughout the disease course, so it is important to interpret them in the context of the clinical picture, and to recheck them if clinical suspicion of SLE remains high. SLE can be difficult to diagnose due to its variable presentation. It’s important to remember that although 84 % of patients with SLE are female, there are 25,000 males with this disease in the US, so keep it on the differential for patients presenting with systemic, nonspecific symptoms. Next, SLE is resistant to type 1 reasoning due to its unpredictable pattern. It is therefore important to apply type II clinical reasoning and to systematically develop a differential. Finally, cases like this require the collaboration of multiple teams who need to practice good communication and documentation. The coordination of care falls to the primary team to ensure sound (and safe) clinical decision making based on synthesized data and opinions.
THE WRONG SIDE OF THE TRACKSUchechukwu Obih; Beth Susi; Thomas Montgomery. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1926364)
LEARNING OBJECTIVE 1: Discuss the importance of obtaining thorough social history.
LEARNING OBJECTIVE 2: Identify a noninfectious cause of thrombotic thrombocytopenic purpura (TTP)
CASE: A 21 year old man presented with weakness and lethargy of 1 week’s duration. He complained of nausea, vomiting, diffuse abdominal achiness, chills, and headaches. His past medical history was notable for chronic back pain secondary to a horsing accident as a child. Exam showed a heart rate of 100, diffuse abdominal tenderness, and splenomegaly. His sclera, face, chest, back, and arms were jaundiced, with petechiae on his upper back, and a large tattoo on his left forearm and upper back. No focal neurologic deficits were present. Laboratory was notable for white blood cell count of 7.4 g/dL with 20 % bandemia, hemoglobin of 5.5 g/dL, MCV 114, platelets of 13 K/uL. Other pertinent labs included potassium of 2.8 mmol/L, creatinine of 1.59 mg/dL, albumin 2.6 g/dL, total protein 5.1 g/dL, total bilirubin 4.0 mg/dL, alkaline phosphatase of 54 IU/L, ALT 241 IU/L, AST 137 IU/L, and CPK 78 IU/L. Lactate dehydrogenase was elevated at 1,627, haptoglobin was low at 2 and peripheral smear showed 1+ schistocytes. Urine drug screen was negative for Tylenol, salicylates, ethanol, barbituates, marijuana, or opioids. Hepatits C was positive with viral load of 51,000 copies. HIV was negative. He was admitted to the intensive care unit to begin plasma exchange and steroids for concern of thrombotic thrombocytopenic purpura (TTP). His thrombocytopenia and anemia had slow resolution and plateaued by cycle ten of exchange. As his jaundice and petechiae improved, track marks were noted in the left antecubital fossa. The patient revealed that his brother presented to another hospital with similar symptoms and was also diagnosed with TTP. He admitted to injecting extended-release oxymorphone with his brother 1 week prior to the start of his symptoms. Plasma exchange and steroids were discontinued with improvement in anemia and thrombocytopenia.
DISCUSSION: Obtaining a thorough social history, including exposure to medications and illicit drugs is important in diagnosing thrombotic thrombocytopenic purpura (TTP). TTP is defined by the pentad of microangiopathic hemolytic anemia determined by the presence of schistocytes, elevated LDH and low haptoglobin, thrombocytopenia, fever, neurologic symptoms, and renal dysfunction. Etiology has been associated with ADAMSTS-13 activity deficiency and with Shiga-like toxin from diarrheal illness caused by enterohemorrhagic Escherichia coli O157:H7. A number of medications, such as cisplatin, bleomycin, and mitomycin have been implicated in the development of TTP in some patients. TTP induced by intravenous injection of extended release oxymorphone is a rare cause, of which there have been a few reported cases to the Centers for Disease Control. Treatment for drug induced TTP has not been established. While plasma exchange has become the mainstay of treatment for TTP secondary to ADAMTS13 deficiency or E. coli, evidence of use in drug induced TTP is not robust and is anectodal. Supportive care is often the treatment of choice.
THERE’S AN UNCOMMON FUNGUS AMONG USPrathyusha Savjani. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926142)
LEARNING OBJECTIVE 1: Understand the importance of obtaining tissue diagnosis in patients with cerebral infections while on immunosuppressive agents to accurately identify the disease.
LEARNING OBJECTIVE 2: Recognize how the differential diagnosis for infection changes based on the immunosuppressive agent being used
CASE: A 62 year-old African American man with a history of cadaveric kidney transplant presented with sudden onset of right arm weakness. MRI of the brain was obtained due to concern for stroke. On imaging, it was discovered that he had multiple peripherally enhancing lesions scattered throughout the cerebral parenchyma. The differential for such findings included metastatic disease, primary malignancy, infectious etiologies, and demyelinating processes. Cerebrospinal fluid analysis was normal as was serum testing for infectious etiologies of cerebral abscesses. He then underwent craniotomy with biopsy with preliminary fungal cultures showing light mold. Pathologic evaluation of the brain sample demonstrated acute granulomatous cerebritis containing pigmented hyphal forms consistent with dematiaceous fungi. Final fungal culture results yielded Fonsecaea pedrosoi. Investigation to identify a primary source of entrance for this organism included thorough investigation of the skin and sinuses. The only skin lesion noted was a chronic non-healing ulcer on his back that was previously biopsied and determined to be radiation dermatitis as a result of fluoroscopic procedures. Dermatology was consulted and did not believe that this skin finding was consistent with a fungal infection. The sinuses were patent with no thickening of any mucosal tissue on both CT and MRI of the head and thus sinus disease was ruled out. Treatment options were discussed including Amphotericin B, Itraconazole, Voriconazole, as well as surgical debridement of the abscesses. The patient chose not to undergo any further invasive procedures, and treatment was initiated with Amphotericin B and Voriconazole and the transitioned to Itraconazole at discharge. He was followed-up in the outpatient setting by the infectious disease team with a repeat MRI of the brain several weeks after treatment. It showed stable lesions that had neither grown nor shrunk in size. The patient’s symptoms remained stable with no improvement but also with no deterioration of neurologic deficits.
DISCUSSION: Chromoblastomycosis of the central nervous system by F.pedrosoi is a very rare disease throughout the world and even more rare in the United States. This fungal organism is generally found in rotten wood and soil in humid regions. Most reported incidences of this infection involve skin and subcutaneous infection from direct inoculation, which can occur in both immunocompetent and immunocompromised hosts. Most of the previous cases come from Asia, South America and Africa where the environment is friendlier to this organism. Cases of brain abscesses with this organism have been reported in patients with an altered immune system and most had a primary cutaneous site of inoculation. The mechanism by which this organism reaches the central nervous system is not known. This patient was on Tacrolimus, which by inhibiting T-cell activation, likely predisposed this patient to developing this fungal infection. One should build a differential diagnosis based not only on imaging, previous cases, and patient’s exposures, but also on the immunologic effects of the immunosuppressant being used. T cells are the cornerstones of immunologic response to fungal infections, and suppression of T cell function by medications such as Tacrolimus may predispose to fungal infections consisting of very rare organisms.
THESE DEVICES CAN BREAK SKIN!!!Samian Sulaiman; Muhammed Sherid; Salih Samo; Shahriar Dadkhah; Nadia El Hangouche; Muhammad Shahreyar; Addis Asfaw; Ahmet A. Oktay; Ana Inashvili; Husein Husein; Preethi Subramanian. St. Francis Hospital. Evanston, evanston, IL. (Tracking ID #1938782)
LEARNING OBJECTIVE 1: Despite improvements in the design and implantation techniques of permanent pacemakers, infection and skin erosion of the pacemaker pocket remain a serious problem. Continuous or recurrent pain at the pocket site should raise suspicion of infection. It is crucial to identify early signs of pocket infection before these devices breaks skin. Regular pacemaker check-up helps avoid late complications of pacemakers
CASE: − A 77 y/o Male who presented with redness and discomfort over his pacemaker pocket in the left upper chest. The pacemaker was implanted 2 years ago. The current complaint started 4 weeks ago. Despite outpatient oral antibiotics, his erythema progressively worsened and developed into a superficial ulcer with draining pus. Patient was admitted to our hospital to receive IV antibiotics. - On physical exam, Tenderness and erythema were noticed at pacemaker site with a superficial small ulcer. Patient was afebrile and rest of vital signs were normal except for irregular heart beats. - His past medical history was significant for atrial fibrillation, Diabetes mellitus, hypothyroidism and Hyperlipidemia. His medications included Coumadin, levothyroxine, atorvastatin, Cardizem, metoprolol and metformin - Patient was started on IV vancomycin and Zosyn. Blood and wound cultures were neg. Transthoracic Echocardiography did not show any vegetation. CT chest (see Figure 3) showed Skin and soft tissue thickening superficial to the pacemaker device but no abscess was present. His erythema and drainage resolved and he was discharged home on oral augmentin on sixth day of admission. Ten days after discharge, he presented again with a skin break at pacemaker’s pocket. Patient reported episodes of local irritation to which he responded by rubbing his skin. On physical exam, part of pacemaker hardware was exposed (see Fig 1). Cardiothoracic surgeon replaced the pacemaker and extracted intra-cardiac leads. Pacemaker lead tip culture grew Staph Epidermis susceptible to multiple antibiotics including vancomycin. Patient received extended course of antibiotics for 4 weeks.
DISCUSSION: The overall incidence of pacemaker-related infections is 1.9 per 1000 device-years. Several factors are associated with an increased risk of Permanent pacemaker infections, including diabetes mellitus, malignancy, operator inexperience, advanced age, corticosteroid use, anticoagulation, recent device manipulation, chronic renal failure, and bacteremia from a distant focus of infection. Early post-implantation infections are most commonly caused by Staphylococcus aureus and late infections most commonly by Staphylococcus Epidermis. There is a general consensus that once there is deep pacemaker pocket or lead infection, removal of the whole pacemaker system followed by an extended course of appropriate antibiotics results in the best prospect for long term eardiaction of infection. If pacemaker erodes the overlying skin, it is considered contaminated and current opinion favors replacement of the generator and leads. The mortality of persistent infection when infected leads are not removed can be as high as 66 %.
THIS IS MORE THAN A SIMPLE AKI!Hani Snounou. Saint Francis Hospital, Evanston, IL. (Tracking ID #1934404)
LEARNING OBJECTIVE 1: To recognize the reciprocal relationship between the uric acid level and acute kidney injury.
CASE: A 62 year old male presented with melenic stool, generalized weakness, low Urine output for 1 week duration. He is a reformed alcoholic with underlying cirrhosis but he admits returning to drink 2 weeks before the admission due to social stress. Otherwise he has a past medical history of Diabetes mellitus, Hypertension, diastolic CHF and COPD. Home medications were metformin, glimepiride, lisinopril, Lasix, advair and albuterol PRN. Physical examination at the time of admission was remarkable for obesity with BMI of 44, jaundice and mild tenderness in the right upper quadrant and epigastric area, the rectal exam with melenic stool. His initial labs showed creatinine of 7.2 mg/dL (with a historical creatinine of 0.9 1 year ago), BUN of 98 mg/dL, NA of 130 mmol/L, chloride of 84 mmol/L, hemoglobin of 12.1 g/dL, PLT of 129 K/mL, normal INR/PT, AST of 311 IU/L, ALT of 194 IU/L, total bilirubin of 4.9 mg/dl with direct bilirubin of 3 mg/dL, alkaline phosphatase of 163 IU/L. Hospital Course: The initial AKI workup showed a CK of 424 IU/L, Uric acid of 23.2 mg/dL, FENA of 1.24 %, urine PH of 5 with +30 protein without casts seen; CT abdomen without contrast showed fatty liver, normal kidneys texture without hydronephrosis or ascites. The patient underwent EGD and colonoscopy and no active bleeding was found. He was placed on half saline with 75 Meq of sodium bicarbonate at 100 cm3/h and was given one dose of rasburicase 5 Mg. His creatinine and the Urine output improved during the admission as well as the uric acid level as following: Creatinine trend: 7.2----->6.6------>5----->4.0 Uric acid trend: 23.2---->22---->20----->16 He was discharged and asked to follow up with his PCP when he had a repeat blood workup after 2 weeks showing normalization of the creatinine to 0.9 mg/dL and a uric acid of 7.8 mg/dL.
DISCUSSION: Acute uric acid nephropathy or UAN is a well known syndrome most frequently encountered in the course of rapid cell turnover such as leukemias and lymphomas, and the added acceleration of cell lysis that occurs with chemotherapy and radiation. But this pathology can be seen even with no malignancy history as in our case. The uric acid elevation can be the reason or the consequence of the AKI but a level above 12 is rarely to be due to the AKI by itself. High tubular fluid flow diuresis achieved by hydration is the primary mechanism of both protection and treating acute uric acid nephropathy. Urine alkalinization is controversial since it may sometimes accelerate phosphate precipitation in the kidneys and thereby worsen the renal failure, but this technique still commonly used. Using rasburicase helps to bring the uric acid level faster and can be considered as treatment option and a good outcome can be seen even with a single dose as in our case. Finally hemodialysis therapy may be required both to correct azotemia and to reduce the body burden of uric acid.
THROW ME A BONE: A CASE OF LANGERHANS CELL HISTIOCYTOSIS PRESENTING AS RIB PAIN IN A 35-YEAR-OLD WOMANJulia P. Brockway1; Elena Katz2; Sudha Dubey1. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1936915)
LEARNING OBJECTIVE 1: Recognize Langerhans cell histiocytosis as an uncommon etiology of bone pain and lytic bone lesions in adults.
LEARNING OBJECTIVE 2: Learn how to diagnose Langerhans cell histiocytosis and assess for multi-organ involvement.
CASE: A 35-year-old African American woman presented with intermittent right breast pain for 2 months. Three months prior she had presented to an outside clinic with a right breast lump. Ultrasound of the breast at that time showed two breast masses and a suspicious enhancement at the right fifth rib. The breast masses proved to be fibroadenomas on core biopsy. She was then referred for CT scan of the chest, after which she transferred her care to our institution. She now had right breast pain and a throbbing rib pain inferior to the breast. She also noted an unintentional 7 lb weight loss over 2 months. She denied fevers, night sweats, shortness of breath, or cough. Her right breast was tender to palpation in the lower inner quadrant and had a palpable, non-tender mass at 10 o’clock. There was no cervical, supraclavicular, or axillary lymphadenopathy. Lung exam was unremarkable. CBC showed mild neutropenia with an ANC of 1400/uL, hemoglobin of 12.5 g/dL, and platelets of 180 K/uL. Liver and renal function tests were normal, and calcium level was 8.7 mg/dL. Serum and urine protein electrophoresis showed no abnormal bands. CT scan of the chest revealed lytic lesions in the fifth and sixth ribs with an associated expansile soft tissue mass at the fifth rib. Biopsy of the rib mass was performed and pathology revealed eosinophilic granuloma, with no tumor seen. Immunohistochemistry stained positive for CD1a, S100, and CD207, consistent with a diagnosis of Langerhans cell histiocytosis (LCH). PET CT scan showed additional suspicious foci at the left hip and left maxilla, and interval development of numerous thin-walled cysts in the mid- to upper- lungs suggestive of pulmonary eosinophilic granulomatous disease. Bone marrow biopsy showed normocellular marrow. The patient was diagnosed with multi-system LCH without “risk organ” involvement. She was referred to hematology/oncology to explore treatment options, and her care was ultimately transferred to an outside cancer center to participate in a clinical trial.
DISCUSSION: LCH is an uncommon cause of lytic bone lesions in adults. The estimated incidence is one to two cases per million adults; however, the true incidence is not known, and LCH is thought to be under diagnosed. The differential diagnosis for lytic skeletal lesions, depending on a patient’s age, includes primary bone or soft tissue tumor, multiple myeloma, and metastatic disease. Definitive diagnosis can therefore only be made by biopsy of a suspicious lesion. LCH is a disorder of histiocytes that originates from the myeloid dendritic cell, a precursor of the Langerhans cells found in skin and mucosa. Pathophysiology is ambiguous, though evidence suggests a neoplastic process, a reactive process, or a combination of both. Histiocytes infiltrate various organs, including bones, skin, lymph nodes, the liver, the spleen, the lungs, and the central nervous system. While the most common presentation is pain due to lytic bone lesions, patients may also present with dyspnea due to lung involvement, rash, gingival hypertrophy, weight loss, fever, lymphadenopathy, splenomegaly, or polydipsia, polyuria, ataxia, or memory problems due to CNS involvement. About half of all patients diagnosed with LCH present without systemic symptoms and with involvement of only one organ, such as the lungs in primary pulmonary LCH. The rest are considered to have multi-system LCH, involving two or more organ systems with or without involvement of the “risk organs” (bone marrow, spleen, and liver) which portend a worse prognosis. Classification of a patient’s disease is critical, as it determines the specific type of treatment needed. All patients should be evaluated after initial diagnosis with a thorough physical exam, CBC, renal and liver function studies, skeletal survey, chest x-ray, and PET CT scan. Patients with multi-organ involvement or cytopenias must undergo bone marrow biopsy. Treatment of LCH depends on patient age and whether it is single or multi-system disease with or without “risk organ” involvement. For adults with single site disease, management ranges from watchful waiting to local methods such as curettage, topical steroids, or radiation therapy. For patients with multisystem disease, data is limited, and patients are encouraged to participate in clinical trials. The mainstay of treatment is chemotherapy. Prospective trials have shown that the majority of these patients respond to initial treatment; however, patients must be closely followed for disease recurrence after completing therapy. Further research is needed in order to better understand LCH, its pathophysiology, and its treatment. It is important for clinicians to be aware of this rare but potentially treatable disease and the various ways that it can present.
THYROID-INDUCED ATRIAL FIBRILLATIONFarah Kaiksow; Philip J. Putnam. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925927)
LEARNING OBJECTIVE 1: Diagnose thyroid disease as a cause of new-onset atrial fibrillation.
LEARNING OBJECTIVE 2: Recognize that thyroid disease workup can be limited by amiodarone administration.
CASE: A 65-year-old man presented with sudden-onset shortness of breath for 1 day. He was at home watching television when the dyspnea started. After a few minutes he began to have blurry vision and lightheadedness. The patient denied any associated chest pain or tightness. Past medical history was significant for hypertension and Type 2 diabetes, both well controlled. Review of systems was positive for dyspnea on exertion over the preceding 2 weeks that was associated with symptoms of a mild upper respiratory tract infection including rhinorrhea and cough. The patient’s heart rate was 136 and electrocardiogram revealed atrial fibrillation with rapid ventricular response. Vital signs were otherwise within normal limits. The patient had mild crackles at both lung bases and an otherwise normal exam. A diagnosis of mild heart failure secondary to new arrhythmia was made and amiodarone was started to control the heart rate and rhythm. Upon further workup, blood tests revealed an undetectable thyroid stimulating hormone level and an elevated free T4. The patient had previously been euthyroid. The diagnosis was then amended to include hyperthyroid as the underlying cause of the atrial fibrillation. While viral thyroiditis was thought to be the most likely source of the hyperthyroid disease, further workup with radioactive iodine uptake scan was not able to be performed because of the initial administration of amiodarone.
DISCUSSION: Atrial fibrillation is the most common arrhythmia diagnosed in the United States and thus a condition in which general internists should be well versed. Approximately 1 % of cases of this arrhythmia can be linked to hyperthyroidism, and about 1.7 % of patients with new hyperthyroid disease have simultaneous atrial fibrillation. Although hyperthyroid is much more common in women than in men, hyperthyroid-induced atrial fibrillation is more than twice as common in men than women. When a patient presents with new-onset atrial fibrillation, the minimum workup that should be performed includes a 12-lead electrocardiogram, chest x-ray, transthoracic echocardiogram, and thyroid functions tests. The goal of this workup is to rule out treatable causes of atrial fibrillation, such as hypertension, heart failure, myocardial ischemia, pulmonary disease, and thyrotoxicosis. In hemodynamically stable patients, there is no need to urgently control the abnormal rhythm. First line therapy is rate control with beta-blockers or calcium channel blockers. In cases where hypotension or heart failure is a significant concern, amiodarone is a reasonable alternative. However, if there is any concern for possible thyroid disease as the etiology of the arrhythmia, amiodarone should be avoided as it can both exacerbate thyroid disease and invalidate results of a radioactive iodine uptake scan. In this case, given the patient’s stable vital signs, absent history or exam findings of significant heart failure, and recent upper respiratory infection symptoms, it would have been reasonable to postpone amiodarone administration until further lab results were available.
THYROTOXIC HYPOKALEMIC PERIODIC PARALYSISSaifullah Nasir1,2; Jeffrey T. Bates2,1. 1Baylor College of Medicine, Houston, TX; 2Houston VAMC, Houston, TX. (Tracking ID #1939642)
LEARNING OBJECTIVE 1: Recognize Thyrotoxic Hypokalemic Periodic Paralysis (THPP) as a potential cause of weakness or paralysis.
LEARNING OBJECTIVE 2: Manage the hypokalemia and hyperthyroidism of Thyrotoxic Hypokalemic Periodic Paralysis (THPP).
CASE: A 36-year-old Vietnamese female without prior medical history presented with acute onset of several hours of bilateral lower extremity weakness. Over the previous 3 months, she had noticed a 10–15 lb unintentional weight loss, an intermittent throat pain which resolved with pain medications, and an occasional tremor of her hands. There was no trauma, recent illness, vision problems, or dizziness. Physical examination revealed tachycardia to 110, non-tender thyromegaly with a right thyroid lobe larger than the left, and an enlarged isthmus. There were no palpable thyroid nodules, no lymphadenopathy, and no thyroid bruit. There was no lid lag and no periorbital edema or chemosis. The patient’s lower extremity weakness was localized to her proximal thighs, but she was able to stand with some support. Laboratory data showed a potassium of 2.3 mmol/L, TSH of <0.01 U/mL, free thyroxine level of 4.08 ng/dL, and a free T3 of 18.25 pg/mL. An ultrasound of the neck revealed a diffusely enlarged thyroid gland with increased vascularity and no discrete nodules. Her potassium was repleted and her weakness immediately resolved. She was diagnosed with hyperthyroidism and started on both propranolol and methimazole.
DISCUSSION: Thyrotoxic hypokalemic periodic paralysis (THPP) occurs in up to 1.9 % of Asian males with hyperthyroidism. It can also occur less frequently in females as well as patients of other ethnicities. In cases of periodic paralysis weakness resolves completely with correction of hypokalemia. A hyperadrenergic state from hyperthyroidism leads to an increase in insulin secretion, which then leads to an intracellular shift in potassium. Serious complications include respiratory failure from weakness of the diaphragm and arrhythmias from hypokalemia. Clinicians should recognize THPP as a possible cause of paralysis or muscle weakness. Prompt treatment of hypokalemia and hyperthyroidism is necessary for resolution of paralysis and to prevent future attacks. However, clinicians should also be careful not to overcorrect hypokalemia, as the total body potassium in these patients is not low.
THYROTOXIC HYPOKALEMIC PERIODIC PARALYSIS IN A HISPANIC PATIENT: A RARE PRESENTATION OF GRAVES’ DISEASEAbhishek Matta; James Fulton; Jahnavi Koppala; Ahmed Abuzaid; Khaled M. Abouelezz; Arun Nagabandi. Creighton University Medical Center, Omaha, NE. (Tracking ID #1939520)
LEARNING OBJECTIVE 1: Thyrotoxic hypokalemic periodic paralysis should be considered in the differential diagnosis of patients presenting with acute paraplegia or periodic paralysis and the initial work up should include TSH and potassium level
LEARNING OBJECTIVE 2: Potassium replacement and propranolol will lead to rapid recovery from paralysis
CASE: A 26 y/o Hispanic gentleman presented to the emergency room with sudden onset weakness of lower extremities. He denied having such episodes in the past. He denied any weight loss, heat intolerance, anxiety, palpitations, tremors or increased perspiration. He denied any family history of periodic paralysis. His vitals were stable. Neurological examination revealed a power of 1/5 in the low extremities and 3/5 in the upper extremities. Sensations to fine and crude touch were intact. Deep tendon reflexes were diminished. Labs revealed a serum potassium of 1.8 meq/L and TSH of 0.02 mIU/L. EKG revealed prominent U waves. He was started on IV potassium supplementation and he recovered his muscle strength within 6 h. Further investigations revealed a T4 level of 2.32 ng/dl, T3 8.9 ng/dl, TSH receptor antibody 5.78 IU/L, Thyroid stimulating Ig 156. RadioIodine uptake scan of the thyroid showed increased homogenous uptake suggesting Grave’s disease. Patient was started on propranolol and methimazole.
DISCUSSION: Thyrotoxic periodic paralysis (TPP) is more common in Asians compared to Hispanics, Caucasians or African-Americans. The incidence on TPP in thyrotoxic patients in North America was found to be 0.1–0.2 %. TPP occurs predominantly in men. TPP has been reported with Grave’s disease, toxic nodular goiter, iodine-induced thyrotoxicosis, excessive thyroxine use, solitary toxic thyroid adenoma, lymphocytic thyroiditis and thyrotropin-secreting pituitary adenomas The usual age at presentation is 20–40 years. Thyroxine directly stimulates the Na+K+ATPase pump directly leading to increased transport of potassium into the cells and subsequent hyperpolarization of the cell membrane leading to paralysis. Hyperthyroidism can also lead increased epinephrine release from the adrenal gland which can stimulate the Beta-2 receptors on skeletal muscles and increase K+ uptake into the myocytes. TPP only affects the skeletal muscles. The episodes of paralysis are usually periodic and typically start in the proximal muscles of the lower limbs. The triggering factors include exercise, trauma, high carbohydrate diet, emotional stress or cold exposure. Sensory system and mental status are unaffected. Acute management of TPP involves potassium supplementation. Definitive control of hyperthyroidism completely abolishes the attacks of TPP and includes antithyroid medications, surgical thyroidectomy and radioiodine therapy.
TICK-TALK, TICK-TALK: WHEN A FEVER, HEADACHE AND STIFF NECK ISN’T MENINGITISAkshay Manohar; Andrei Yankovich; Sergey Gerasim; Daniel Goldsmith. Capital Health Regional Medical Center, Trenton, NJ. (Tracking ID #1939366)
LEARNING OBJECTIVE 1: Recognize that babesiosis can present in a myriad of symptoms that mimic other illnesses.
LEARNING OBJECTIVE 2: Suspect babesiosis in patients travelling to or living in endemic regions
CASE: A 49-year-old Hispanic male had 2 weeks of non-radiating occipital headache, fevers and chills in early August. The headache progressed and he developed neck stiffness on moving his head side to side, but not up and down. He denied rash, insect-bite, neurological, respiratory, cardiac or abdominal symptoms. He had a past history of dyslipidemia for which he took a statin. He denied any sick contacts. He worked as a road paver and travelled often from central New Jersey where he lived to Pennsylvania, Maryland, Virginia and Washington, DC for work. He denied recent foreign travel or ever entering wooded areas. His physical exam was positive for fever, and neck-stiffness when moving his head side to side. Initial outpatient testing showed a normal basic metabolic panel, mildly elevated bilirubin (1.5 mg/dL) and alkaline phosphatase (178 U/L). Complete blood count showed normal leukocyte count of 7,000 cells/mm3 with 32 % segmented neutrophils, 19 % bands and thrombocytopenia of 55,000 platelets/mm3. He was referred to the ED and underwent lumbar puncture with normal results. Computerized tomography of the abdomen showed multiple hypoattentuations in an enlarged spleen suggestive of infarctions or metastases. A “Malaria” smear was ordered showing ringed trophozoites with light blue cytoplasm and red chromatic dots, confirming babesiosis. The patient was started on Atovaquone, Azithromycin and empirically treated for Lyme disease with Doxycycline. Subsequent testing confirmed positive results for Lyme Disease.
DISCUSSION: Clinical features of Babesia microti infection vary from asymptomatic to severe viral-like symptoms of fever, myalgia, headache, neck stiffness and photophobia. Evidence of hemolytic anemia and thrombocytopenia is common. Severe manifestations such as splenic infarction and rupture, acute respiratory distress syndrome, congestive heart failure, renal failure and disseminated intravascular coagulation can occur. Patients usually present in endemic regions ranging from Massachusetts to Central New Jersey during the summer months. Given the wide variety of symptoms, patients may present to out-patient clinics or emergency rooms with a wide spectrum of complaints mimicking other illnesses. Diagnosis is confirmed on Giemsa-stained thin blood smears showing ringed trophozoites (Babesia microti) that strongly resemble Plasmodium falciparum. Requiring a skilled technician, parasites may be missed especially when parasitemia is low. Polymerase chain reaction may be used if smears are negative but the diagnosis is suspected. As endemic regions overlap, co-infection by Babesia, Borrelia and Anaplasma occurs commonly.
TICKLE MY NOSE BUT DON’T BREAK MY HEARTPavan Kapadia1,2; Sean M. Lockwood2,1. 1University of Kentucky Medical Center, Lexington, KY; 2VAMC, Lexington, KY. (Tracking ID #1940110)
LEARNING OBJECTIVE 1: Identify nasal packing and intranasal vasoconstrictors as potential causes of Takotsubo cardiomyopathy
LEARNING OBJECTIVE 2: Explore the mechanism of intranasal vasoconstrictors in Takotsubo cardiomyopathy
CASE: A 74-year-old Caucasian female with a medical history of coronary artery disease, hypertension, COPD and diastolic heart failure presented with acute and profound non-traumatic epistaxis requiring intranasal phenylepherine in addition to nasal packing with PVA Expandacell foam (Rhino Rocket) and transfusion of a unit of packed red blood cells. The patient was otherwise asymptomatic but after nasal packing she developed substernal, pressure-type chest pain with only partial resolution of symptoms after 3 sublingual nitroglycerin tablets. Vital signs: Temp 99 °F, BP 134/88, HR 111, RR 34, O2 Sat 90 % on 2 L. Physical examination was notable for nasal packing and tachycardia on cardiovascular exam. Routine labs were within normal limits however initial troponin I was 0.16 ng/mL, with maximal elevation to 3.33 ng/mL. Electrocardiogram showed sinus tachycardia with new S-T segment elevation in V2-V4. Left heart catheterization showed non-obstructive coronary artery disease however left ventriculography showed a reduced ejection fraction of 25 % with mid-ventricle band akinesis with preserved apical and basal contraction, all consistent with Takotsubo cardiomyopathy. The patient was started on metoprolol and lisinopril prior to discharge and demonstrated return to baseline systolic function at 4 months on transthoracic echocardiogram.
DISCUSSION: Takotsubo cardiomyopathy (TCM), also known as stress cardiomyopathy, is a reversible condition often presenting with anginal chest pain or dyspnea that was first described in Japan for the octopus-like movement exhibited by the left ventricle during systole in heart failure frequently triggered by stressful events. Based on the Mayo Clinic diagnostic criteria, there are 4 major conditions that must be met: 1) transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments; 2) absence of obstructive coronary disease; 3) new electrocardiographic abnormalities or cardiac biomarker elevation; 4) absence of other identifiable causes, including pheochromocytoma or myocarditis. Post-surgical and post-traumatic nasal packing with intranasal application of vasoconstrictors such as epinephrine or oxymetazoline have been reported in several cases as inciting events for TCM. We present a case of TCM after intranasal phenylephrine administration. Given that phenylephrine causes vasoconstriction in much the same manner as the others and remains a core component of epistaxis treatment in most emergency departments, this highlights the importance of judicious use of vasoconstrictors as a whole in at risk populations. One mechanism hypothesized for the syndrome is an increased sympathetic stimulation and a sudden surge of catecholamines incited by stressful events causing acute vasospasms or exacerbating pre-existing conditions such as microvascular dysfunction and left ventricular outflow tract obstruction and essentially stunning the myocardium. It is hypothesized that intravenous administration and similarly the intranasal application of vasoconstrictors such as phenylephrine can cause a similar manner of catecholamine surge and can thus trigger a TCM.
TIME IS OF THE ESSENCE: A PATIENT PRESENTING WITH ALTERED MENTAL STATUS AND A RISING CREATINE KINASEMegan E. Rau. Wake Forest University, Winston-Salem, NC. (Tracking ID #1940107)
LEARNING OBJECTIVE 1: Recognize the less common early signs and symptoms of acute aortic dissections to promote early detection and intervention.
LEARNING OBJECTIVE 2: Reinforce that CT and TTE are the most commonly used imaging modalities in the acute setting to diagnose an aortic dissection.
CASE: A 47-year-old man was driving to a lunch meeting when he experienced shortness of breath, dull chest pain, left arm pain, the inability to speak, and left sided paralysis. Upon arrival to the outside hospital emergency department (ED) the patient’s shortness of breath, chest pain, aphasia, and left sided weakness had resolved. A CT head image was performed followed by an MRI brain scan; both negative for intracranial abnormalities. Labs included a urine drug screen, CBC, CMP, blood alcohol, troponin, urine analysis, creatine kinase (CK) and ammonia level. Noted abnormalities included hyponatremia and slightly elevated CK. While in the ED he developed intense bilateral leg pain and became extremely agitated. He was given 1 mg Dilaudid, 4 mg Ativan, and finally 10 mg of Haldol. Due to continued altered mental status the patient was transferred to Wake Forest Baptist Medical Center (WFBMC) for further evaluation. At the WFBMC ED, the patient continued to be altered and the only abnormal vital sign was a temperature of 101.2° Fahrenheit. A lumbar puncture was performed and unremarkable. Repeat labs revealed WBC 13.1, Na 127 mmol/L, troponin WNL, lactic acid WNL, CK 8,861 U/L, TSH within normal limits (WNL), and HIV negative. Electrocardiogram was unremarkable and chest x-ray showed prominent interstitium with indistinctness of interstitial markings. He was then admitted for further monitoring. At admission his only complaint was a dull, non-radiating pain in the arch of his left foot. History was relevant for a brother who had a heart attack at age 48. Physical exam was notable for dilated, sluggish pupils, and slow speech. His CK was trended and continued to rise over night from 9,737 U/L to 10,593 U/L to 14,536 U/L by mid morning. A transthoracic echocardiogram (TTE) with bubble study was performed to evaluate for a cardiac shunt. No shunt was found but the image revealed a Type A aortic dissection with an intimal flap visualized in the ascending aorta. The flap originated a few millimeters beyond the sinotubular junction and the distal point was unable to be visualized. He also had a moderate sized loculated anterior pericardial effusion. Cardiothoracic surgery was immediately consulted and he was taken for emergency repair. Unfortunately during transport the patient developed chest pain, bradycardia, and pulse-less electric activity requiring initiation of cardio-pulmonary resuscitation. The patient was intubated and surgery was immediately performed. The dissection was repaired and after recovery from his surgery, the patient was discharged home 18 days after admission.
DISCUSSION: Aortic aneurysms are the 13th leading cause of death in the United States with 15,000 people dying each year after rupture. This is due to most aortic aneurysms going undetected until rupture. Once the aneurysm ruptures the mortality rates are as high as 90 %. It is crucial that providers be cognizant of the deadly potentially and need for early, rapid detection of aortic aneurysms. Chest pain is the most common symptom but acute aortic dissection may mimic the signs and symptoms of other acute diseases including abdominal pain, acute mental status changes, and rhabdomyolysis. An elevated CK in a patient with chest pain, even if transient, qualifies acute aortic dissection to be placed on the differential and further evalution to take place. The most common imaging modality world wide for the diagnosis of acute aortic dissection is the spiral CT and a less invasive option is the echocardiogram. Once an aneurysm is diagnosed intervention can be performed. It is paramount that providers have knowledge of aortic disease including symptoms beyond the most common of severe chest pain to prompt early diagnosis. By physician awareness of the less common presentation of aortic disease the time to diagnosis can continue to improve and continue to save lives. In the case of the patient presented, he had a history of intermittent chest pain, altered mental status and elevated CK. Imaging was delayed over 18 h and a TTE was initially ordered to evalute for a possible shunt, not an acute dissection. This patient was lucky imaging was ordered and when his aneurysm ruptured an operating room was only a few feet away.
TO THE RETROPERITONEUM AND BACK: AN INTERNIST’S TALEPatrick Snyder; Karin Warltier. NYU, New York, NY. (Tracking ID #1927562)
LEARNING OBJECTIVE 1: Recognize the clinical presentation and etiologies of retroperitoneal fibrosis
LEARNING OBJECTIVE 2: Treat retroperitoneal fibrosis
CASE: The patient is a 64 year old Greek man with a past medical history of migraine headaches who presented with abdominal pain. He had been in good health until 2 months prior to admission when he began experiencing sharp epigastric pain that radiated to his lower abdomen, groin and flanks. The pain was associated with fatigue, a 20 lb weight loss, daily sweats and subjective fevers. Examination revealed a frail appearing man with normal vital signs and epigastric tenderness. Laboratory studies included an ESR of 94 mm/h and CRP of 64 mg/L. A contrast enhancing CT scan of the abdomen and pelvis showed an aneurysmal aorta measuring 2.8 × 2.9 cm with atherosclerotic calcification and irregularity of the wall associated with enhancing near-circumferential periaortic soft tissue thickening beginning just below the renal arteries and extending to the aortoiliac bifurcation. The enhancing area measured up to 15 mm in thickness and encased the aorta with sparing of the posterior side. There was no ureteral involvement. Medication reconciliation was negative for retroperitoneal fibrosis (RPF) associated medications. Markers for syphilis, hepatitis B, hepatitis C, ANA and ANCA were all negative. PSA was 5.7. Serum IgG4 was mildly elevated, and Quantiferon Gold screen was positive. Systemic steroid therapy was initiated, which improved his abdominal pain significantly. CT guided biopsy was performed and revealed dense collagenous fibrosis with heterogeneous lymphoplasmacytic infiltration without increase in IgG4 expressing plasma cells. Flow cytometry was without immunophenotypic evidence of lymphoma. The diagnosis of idiopathic RPF was confirmed.
DISCUSSION: Retroperitoneal fibrosis, originally known as Ormond’s disease, is characterized by the presence of mixed fibrous and inflammatory tissue surrounding the aorta. It is a rare disorder most commonly affecting middle-aged to elderly men [1]. Back and flank pain are the most common presenting symptoms, occurring in over 90 % of patients [1]. B symptoms, including fatigue, anorexia and weight loss can be seen in 50–60 % of cases [2]. Other retroperitoneal organs, including renal arteries, the inferior vena cava, iliac veins and ureters, are also prone to entanglement. Compromise of the renal arteries can cause hypertension. Blockage of the inferior vena cava or iliac veins may lead to peripheral edema. Obliteration of the ureters can be associated with urinary frequency, urgency, oliguria and elevated serum creatinine. Indeed, one study indicated 33 % of cases of RPF present with new-onset hypertension, 23 % with peripheral edema and 67 % with obstructive uropathy [2]. Diagnosis can be made on the basis of abdominal imaging, either sonography or CT. Though presumptive diagnosis can be made solely on the pathognomonic finding of a homogenous periaortic plaque encasing the abdominal aorta on imaging, biopsy is often pursued for confirmation. A histologic pattern of fibroblast proliferation, sclerosis and infiltration of mononuclear cells is characteristic [3]. RPF can occur as a primary idiopathic or secondary condition. A secondary cause of RPF can be identified in nearly 30 % of patients [4]. Common culprits include medications (ergot alkaloids, dopamine agonists and beta blockers), malignancy (lymphoma, carcinoid tumor, breast, prostate and bladder carcinoma), infection (tuberculosis, histoplasmosis and actinomycosis) and history of prior abdominal or pelvic radiation or surgery (lymphadenectomy, colectomy or aneurysmectomy). Multiple theories have been proposed regarding the pathogenesis of primary RPF, but two predominate. The first suggests that it is a localized inflammatory response to oxidized low-density lipoproteins (LDL) from atherosclerotic plaques in the abdominal aorta that have breached its medial layer [3]. The other theory argues RPF is a sequela of a broader systemic autoimmune process. In more recent years, investigation has been done linking idiopathic RPF to the spectrum of IgG4 related disease. In general, therapy is aimed at limiting progression and promoting regression of fibrosis and preventing recurrence of disease. If the RPF is secondary to another cause, treatment is directed at the root problem. While no gold standard based on randomized control trials exists for treatment of primary RPF, steroids are generally first line therapy. Prednisone is routinely dosed at 1 mg/kg daily for the first month then tapered by various protocols for a net length of therapy between 6 months and 2 years [5]. Mycophenylate mofetil, methotrexate and tamoxifen are alternatives if steroids are contraindicated. If obstructive uropathy is present, ureteral stenting, percutaneous nephrostomy or surgery may complement medical management. Progression or regression of disease can be monitored by pain assessment, repeat imaging and trending of ESR and CRP.
TO TREAT OR NOT TO TREAT: AN ASYMPTOMATIC LADY WINDERMERE SYNDROMEKevin A. Johnson; Maryam Sattari. University of Florida, Gainesville, FL. (Tracking ID #1935022)
LEARNING OBJECTIVE 1: Recognize clinical and radiographic characteristics of Lady Windermere Syndrome
LEARNING OBJECTIVE 2: Be familiar with important considerations in diagnosis and treatment of Lady Windermere Syndrome
CASE: A 69-year-old female with history of hypertension and diabetes presented with 4 weeks of night sweats, cough productive of clear sputum, and weight loss. She had recently retired from working in an assisted living facility and denied smoking, fever, chills, history of connective tissue or lung disease, sick contacts, or recent travel. Physical examination revealed a thin woman in no apparent distress. Laboratory testing did not reveal significant abnormalities. Computed tomography of chest, abdomen, and pelvis demonstrated small foci of consolidation with air bronchograms in the right middle lobe and lingula, radiological findings consistent with Lady Windermere Syndrome. Bronchoscopy did not reveal any endobronchial lesions. Culture of bronchoalveolar lavage fluid yielded Haemophilus influenzae (H. flu), but was negative for acid-fast bacilli and fungus. She was treated with 2 weeks of Amoxicillin and reported complete resolution of symptoms within 5 days of initiating antibiotics.
DISCUSSION: The term “Lady Windermere syndrome” describes Mycobacterium avium Complex (MAC) infection in right middle lobe or lingula in elderly, often thin, immunocompetent women without significant smoking history or underlying pulmonary disease. The syndrome is named after a Victorian character in Oscar Wilde’s play Lady Windermere’s Fan. Voluntary suppression of cough and expectoration in these fastidious women is hypothesized to cause reduced clearance of secretions, thus resulting in a chronic nidus for inflammation and predisposing to infection. Typical radiological findings include cylindrical bronchiectasis and reticulonodular infiltrates involving the right middle lobe or lingula. The disease may have an insidious onset and symptoms, including fever, weight loss, malaise, cough and hemoptysis, may be present for months or years before the diagnosis is made. Early cases may be asymptomatic and only discovered incidentally. Diagnosis can be made by polymerase chain reaction, but identification of the organism from the sputum is difficult. H. Flu typically, on the other hand, usually causes community acquired pneumonia with more acute onset of symptoms, including fever and productive cough. This diagnosis was unexpected in our patient who presented with symptoms and radiographic findings suggestive of an indolent infection. Given the rapid resolution of her symptoms on amoxicillin, we suspect that H. flu was the organism responsible for her presenting symptoms. However, we cannot rule out an underlying asymptomatic MAC infection, responsible for her radiographic abnormalities. MAC must be considered in elderly women with unexplained respiratory symptoms and a tree-in-bud appearance on CT. Our case also demonstrates the importance of bronchoscopy and obtaining cultures when dealing with possibly MAC infections. In fact, making a diagnosis of MAC disease does not mandate therapy, which is a decision based on weighing the risks and benefits of anti-mycobacterial drugs with potentially severe toxicities in these often frail patients. Given the emerging resistance of MAC, treatment should only be initiated once cultures are available and sensitivities can be ascertained.
TOCILIZUMAB-ASSOCIATED “MIGRAINE”Maria Shtessel; Muhammad S. Shahid; Chaya Abelow. Montefiore Medical Center, Bronx, NY. (Tracking ID #1937861)
LEARNING OBJECTIVE 1: Diagnosis and management of cryptococcal meningitis in a non-HIV immunocompromised host.
LEARNING OBJECTIVE 2: Recognize the risks associated with interleukin-6 receptor inhibitors.
CASE: A 40 year-old female with a history of migraines and rheumatoid arthritis (RA) presented with 2 weeks of worsening frontal headache associated with nausea and vomiting. She reported that this headache was worse than her usual migraine headaches. Her history was significant for the use of tocilizumab and prednisone for treatment of RA. She was afebrile and her neurological exam was within normal limits. A CT of the head (CTH) was unremarkable. The patient was initially started on treatment for a presumed migraine. On day two of hospitalization she developed symptoms of photophobia, phonophobia and blurred vision. A lumbar puncture was performed, which revealed an opening pressure of 16 cmH20 [normal range 9–18], colorless CSF, WBC 93 [0–5 WBC/mm3], neutrophils 58 %, lymphocytes 42 %, glucose 21 mg/dL [50–75], total protein 195 mg/dl [10–40] and cryptococcal titer of 1:65000. Blood and CSF cultures grew C. neoformans. The patient was started on amphotericin B with flucytosine as induction therapy for cryptococcal meningitis. Two weeks into her admission, the patient had an episode of loss of consciousness while being transferred to a commode. A repeat CTH revealed enlargement of the lateral and third ventricles, consistent with a communicating hydrocephalus, as well as new left lentiform nucleus hypodensities suggestive of cryptococcomas. A lumbar drain was placed for treatment of communicating hydrocephalus. Repeat CSF analysis demonstrated non-sterile CSF with a cryptococcal titer of 1:1000. After completion of induction therapy, the patient was started on fluconazole 800 mg daily for consolidation therapy for a total of 8 weeks. She was discharged on fluconazole 200 mg daily for maintenance therapy for 6–12 months.
DISCUSSION: Headache is a common complaint encountered by the internist. Unrelenting headache, nausea, vomiting, photophobia/phonophobia are common symptoms of meningitis. The differential diagnosis of meningitis in an immunocompromised host includes the same bacterial and viral pathogens as would be suspected in an immunocompetent patient, however, physicians must also be aware of rarer pathogens. These include mycobacterium tuberculosis, fungal organisms such as cryptococcus, sporothrix, histoplasma, and parasitic infections such as toxoplasma, cysticercosis, and schistosoma, among others. Cryptococcal meningitis tends to have a more indolent course with headache being a common initial symptom, as in this patient. The increasing use of IL- 6 inhibitors in combination with traditional disease-modifying antirheumatic drugs (DMARDS) for recalcitrant RA requires internists to have a high index of suspicion for unusual pathogens. Tocilizumab is a humanized monoclonal antibody against the interleukin 6 receptor utilized mainly in the treatment of rheumatoid arthritis and juvenile idiopathic arthritis. While reactivation tuberculosis is a well known complication with the use of DMARDS, cryptococcosis and cryptococcal meningitis are less common side effects of such immunosuppressive therapy. Approximately 20 % of the total cases of cryptococcal meningitis occur in individuals who do not have HIV. In hospital mortality ranges from 10 to 12 % for all patients with cryptococcal meningitis. Laboratory diagnosis can classically be made with India ink staining of CSF, but the yield of this test is lower in non-HIV patients. CSF cultures tend to be positive in 90 % of non-HIV patients. CSF cryptococcal antigen is very sensitive and specific for Cryptococcus, but serial measurements of cryptococcal antigen cannot be used to monitor therapy adequately. Response to treatment needs to be accessed via repeat lumbar puncture 2 weeks after induction therapy. Standard treatment includes high dose amphotericin B and flucytosine for the induction phase followed by fluconazole for the consolidation phase of treatment. Management of intracranial pressure is also critical for a better prognosis in cryptococcal meningitis. Patients with severe symptoms and opening pressure greater than 25 mmHg should have their pressure reduced by 50 % or below 20 mmHg. Repeat lumbar punctures, a temporary lumbar drain, or a ventriculoperitoneal shunt may be necessary.
TOO BLUE NOT TO BE TRUE: A NIGHT FLOAT’S DIAGNOSTIC DILEMMAMinal A. Shah; Anita Sahu; Jeffrey T. Bates. Baylor College Of Medicine, Houston, TX. (Tracking ID #1939668)
LEARNING OBJECTIVE 1: Understand saturation gap and how it aids in the diagnosis of methemoglobinemia.
LEARNING OBJECTIVE 2: Identify lidocaine as a medication that commonly causes methemoglobinemia in the inpatient medicine setting
CASE: A 61-year-old female with no past medical history was admitted for surgical resection of a benign pelvic mass. Her post-operative course was complicated by a small bowel obstruction requiring placement of a nasogastric tube for decompression. She complained of a sore throat, so topical benzocaine was administered prior to insertion. Six hours later, her oxygen saturation was measured at 77 %. She reported no shortness of breath or discomfort. The pulse oximeter was repositioned several times with no change in the oxygen saturation. Physical examination was remarkable for tachycardia, cool extremities, and mild cyanosis of the lips, hands, and feet. Lung fields were clear, and she remained alert and oriented. Her saturation did not improve with 100 % oxygen. An arterial blood gas was drawn and was noted to be dark brown in color. The results were pH 7.45, pCO2 of 37, paO2 of 355, and a calculated oxygen saturation of 100 %. Given the cyanosis, abnormal coloration of arterial blood, and saturation gap, methemoglobinemia was suspected. The methemoglobin level returned at 57.7 %. Intravenous methylene blue (1 mg/kg) was slowly infused, and the cyanosis resolved within minutes. Her oxygen saturation improved to 93 %, and the methemoglobin level 1 h after administration was less than 5 %. Chart review revealed the only oxidizing agent she had received was the topical benzocaine spray.
DISCUSSION: Patients with methemoglobinemia may have tissue hypoxia with no symptoms. Additionally, subtle signs of tissue hypoxia such as mild cyanosis can be missed if the physician focuses solely on the chest examination. In most clinical scenarios a normal blood gas is reassuring; however, it is important to remember that a blood gas does not evaluate for all causes of tissue hypoxia. The oxygen saturation reported with an arterial blood gas is calculated assuming a normal hemoglobin. A greater than 5 % difference in the oxygen saturation measured by pulse oximetry and the calculated oxygen saturation indicates a saturation gap. This finding should prompt evaluation for abnormal hemoglobin variants. Furthermore, although methemoglobinemia is regarded as a diagnosis typically encountered in the emergency department, studies indicate it is most often diagnosed by internal medicine physicians. General internists should be able to recognize the medications that induce methemoglobinemia and minimize their use, given the rare but life-threatening complication of methemoglobinemia.
TOO MUCH OF “A” GOOD THINGMitra Barahimi1; Lauren Beste1,2. 1University of Washington, Seattle, WA; 2VA Puget Sound Healthcare System, Seattle, WA. (Tracking ID #1930680)
LEARNING OBJECTIVE 1: Recognize key clinical and diagnostic features of non-cirrhotic portal hypertension
LEARNING OBJECTIVE 2: Summarize the differential diagnosis and workup of non-cirrhotic portal hypertension
CASE: A 54-year-old man with a history of obsessive compulsive personality disorder presented to the hospital with abdominal pain and peripheral edema. He had no known medical history, other than obsessive compulsive personality disorder, and had avoided medical care for over 20 years. He denied foreign travel or family history of liver disease. He reported consuming probiotics and vitamin A supplements. Physical exam demonstrated cachexia, large ascites, and lower extremity edema. Labs were notable for mild transaminitis, normal liver synthetic function, no proteinuria or other signs of renal disease, and negative HIV. Liver ultrasound showed no evidence of cirrhosis, masses, or hepatic vascular occlusion. The patient was discharged on diuretics with outpatient Hepatology followup. Complete workup for causes of liver disease was negative and a TTE was unremarkable. Transjugular liver biopsy was significant for elevated portal venous wedge pressures, confirming portal hypertension. Hepatic histopathology showed no diagnostic alterations. He was diagnosed with non-cirrhotic portal hypertension, a rare condition associated with only a handful of etiologies including schistosomiasis, HIV, and hypervitaminosis A. Additional histopathologic evaluation revealed rare hypertrophic hepatic stellate cells, suggesting vitamin A-induced hepatotoxicity. After further questioning, the patient reported consuming up to 1,000,000 IU of vitamin A per day, well above the RDA of 900 IU/day. He endorsed extrahepatic signs of vitamin A toxicity including nail fracturing, anorexia, xerosis of his lower extremities, and hair thinning in his pubic region. He was subsequently referred to Nutrition and Mental Health for further counseling regarding his dietary habits.
DISCUSSION: Vitamin A hepatotoxicity has been reported at doses exceeding 50,000 IU/day. This case illustrates that hypervitaminosis A should be suspected in HIV-negative individuals with non-cirrhotic portal hypertension. The mechanism of vitamin A-induced portal hypertension is poorly understood but is believed to result from hypertrophy of hepatic stellate cells as they absorb the vitamin. With regard to prognosis, several case reports describe spontaneous resolution of vitamin A-induced portal hypertension, as well as several examples of progression to death or liver transplantation. At present, there is no treatment to accelerate vitamin A excretion. The patient’s prognosis remains guarded, though absence of liver fibrosis on biopsy suggests the potential for recovery.
TOO MUCH OF A GOOD THING: THE OVERDIAGNOSIS AND TREATMENT OF A GERMAN TOURISTJonathan L. Robbins; Gregory M. Bump; Harish Jasti. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1925980)
LEARNING OBJECTIVE 1: Identify the risks of diagnostic testing in patients with a low pretest probability of serious disease.
LEARNING OBJECTIVE 2: Describe the danger of healthcare overuse to individual patients and to the healthcare system.
CASE: An 18 year-old German man on vacation in the United States presented to the emergency department with a one-month history of coughing spells that occurred at night while lying supine, lasted for a minute, and resolved when he sat upright. He denied fevers, chills, weight loss, sputum production, hemoptysis, dyspnea, or chest pain. His past medical history was significant for pneumonia in early childhood that required inpatient hospitalization. He was a high school student with no TB risk factors, alcohol or drug use. Physical examination revealed a well-appearing, physically fit man with normal vital signs. The physical exam was entirely normal. Routine laboratory testing was normal. An HIV test was negative. A chest x-ray (CXR) was read as a large loculated right hydropneumothorax worrisome for empyema. A CT scan of the chest demonstrated a large intraparenchymal fluid and gas collection. A CT-guided pigtail catheter was placed. Fluid from the lesion contained many WBCs, but there were no bacteria on gram stain. Acid fast bacilli and bacterial culture were negative. Rare aspergillus fumigatus were subsequently cultured and the patient was started on voriconazole. Upon further review, given the patient’s clinical stability and absence of symptoms throughout the hospitalization, antifungal therapy was discontinued. The pigtail catheter was removed. The patient was discharged with the diagnosis of non-infectious pneumatocele resulting from disruption of the lung architecture from childhood pneumonia. The aspergillus was thought to be a secondary colonizer of the pneumatocele. The patient returned to Germany without incident.
DISCUSSION: The decision to perform a CXR in this patient, who presented with a cough and normal laboratory findings and exam, resulted in an extensive inpatient work-up, including six chest X-rays, two chest CTs, and placement of a pigtail catheter. Diagnostic testing in patients with a low pre-test probability of serious disease has been shown in a recent meta-analysis to have no effect on symptom status, nor on reducing patients’ illness worry or anxiety if the diagnostic tests are negative. Furthermore, when the prevalence of a serious condition is between 0.5 and 3.0 %, a diagnostic test with both 90 % sensitivity and 90 % specificity would produce 4 to 19 false-positive results for every true-positive, which leads to invasive and expensive further testing. With respect to the case, one study found that 19 % of all patients with acute cough who underwent a CXR had an incidental finding, only 3 % of which were clinically relevant. Healthcare overuse is defined as a health care service that is provided under circumstances in which its potential for harm exceeds the possible benefit. The Institute of Medicine has found that healthcare overuse results in least 210 billion dollars of unnecessary expenditure per annum. Almost half (42 %) of US primary care physicians believe their own patients receive too much medical care. Incidental findings discovered on imaging are common and frequently result in healthcare overuse. It is essential that providers act judiciously in the choice to use diagnostic tests in patients who are unlikely to have serious disease, as in this case of an 18 year-old man with cough.
TOXIC LEUKOENCEPHALOPATHY FROM HEROIN OVERDOSE - ATYPICAL PRESENTATION AND RECOVERY WITH RESIDUAL AUTONOMIC DYSFUNCTION AND SPASTICITYTaraka Vijay Gadiraju1; Dilpreet K. Singh1; Santhi Gokaraju2; Mary Jo Farmer3. 1Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 2Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 3Baystate Medical Center/Tufts University School of Medicine, Springfield, MA. (Tracking ID #1939347)
LEARNING OBJECTIVE 1: Identify the atypical presentation and recovery of Toxic leukoencephalopathy from heroin overdose (Chasing the Dragon), with residual autonomic dysfunction and spasticity.
LEARNING OBJECTIVE 2: Recognize that initial intensive care management followed by supportive care with multidisciplinary approach from occupational therapy, speech therapy, physical therapy and later appropriate rehabilitation can bring dramatic results in few weeks despite high mortality in these patients.
CASE: A 24 year-old-male patient with history of anxiety, depression, OCD, IVDU and drug abuse was brought to the hospital after he was found unresponsive and covered with vomit around his mouth. Patient was seen by his mother 10 h prior to this event and was in his usual state of health. On presentation, he was unresponsive with a GCS of 4, hypotensive with agonal respirations and no response to naloxone. He was intubated, fluid resuscitated and was started on Norepinephrine drip prior to being transferred to ICU. Vancomycin and piperacillin-tazobactam were also started for possible aspiration pneumonia and sepsis. His home medications were fluoxetine and alprazolam. Four weeks prior to this episode, had was admitted to an outside hospital for drug overdose where his girlfriend died on scene but the patient was fortunate enough to be discharge 3 days later to drug rehab program. Exam was benign except for neurologic exam significant for spasticity and GCS of 4. Laboratory work significant for leukocytosis, renal failure, hyperkalemia, rhabdomyolysis, elevated LFTs, lactic acidosis with an osmolar gap of 10. Utox positive for heroin, cocaine, benzodiazepines, and cannabinoids. EEG showed diffuse alpha and excessive beta activity; revealed no active seizure activity, but was consistent with postictal activity/global hypoxia/possible cerebral dysfunction. EKG revealed sinus tachycardia with peaked T waves. CT brain was negative for acute pathology. Chest x-ray was negative for pneumonia. The patient was weaned off the pressor support, remained afebrile with resolution of leukocytosis and the antibiotics were discontinued after 2 days. Patient had many episodes of whole body tremors, posturing, diaphoresis, sinus tachycardia, tachypnea lasting a few minutes but his mental status has not much changed in the first 48 h. These episodes responded to fentanyl and later needed Propofol drip. Twenty-four hour video EEG was negative for seizure activity during the episodes and were thought to be from opioid toxicity/withdrawal. MRI later on showed findings suggestive of diffuse leukoencephalopathy and he was diagnosed with acute toxic leukoencephalopathy secondary to heroin inhalation. He was supportively managed with a hope that it improves over weeks to months.
DISCUSSION: Leukoencephalopathy due to heroine abuse was recognized for over 30 years but the etiology and pathophysiologic factors are still poorly understood. It may result from the inhalation, intravenous injection, or ingestion of substance abuse drugs. The mortality ranges from 23 to 48 %, however, such occurrences are rare, sporadic, and not well studied. Leukoencephalopathy caused by inhalation of heroin, also known as “chasing the dragon” syndrome is one of the most studied of these rare occurrences and the clinical syndrome was describe to progress in 3 stages over A course of weeks on most occasions. However, our patient had a dramatic presentation with sepsis like picture on presentation associated symptoms of all stages. He was extubated 2 weeks later and was able to follow commands but continued to have residual autonomic dysfunction which is also unique to our patient and to our knowledge not described in earlier cases. He also continued to have symptoms like fever, rigidity/spasticity, with increased CPK on presentation similar to neuroleptic syndrome but all his symptoms resolved except for spasticity being treated with baclofen. Our patient is still in the hospital 6 weeks later awaiting for placement and we were able to observe his graded improvement over time with supportive care from occupational therapy, speech therapy, physical therapy and now planning on discharge to rehabilitation. Coenzyme Q and vitamin supplements, typically vitamin C and vitamin E, and other antioxidant therapies have been suggested to treat heroin-induced leukoencephalopathy patients. However, there is no strong evidence to support these choices and our patient improved with supportive care in addition to baclofen for the spasticity and amantadine for cognitive impairment. The wide array of causes and unclear understanding for the pathophysiology, with no known cure or treatment makes this an interesting disease and our case stands out with unique presentation of toxic leukoencephalopathy with the typical stages of improvement and residual deficits.
TRANSFUSION MIMICKING ARDSRavi Thimmisetty; Manogna Nookathota; Ariel Modrykamien. Creighton University Medical Center, Omaha, NE. (Tracking ID #1926462)
LEARNING OBJECTIVE 1: ● To know the types of transfusion reactions. ● TRALI is a rare, clear and present danger to the lungs
CASE: A 59 year old woman came to clinic for elective bronchoscopy for a 2 cm right upper lobe mass. Work up showed hemoglobin 3.4 g and she was admitted. ROS was negative except for some mild exertional dyspnea. PMH included moderate COPD, hypertension, hyperthyroidism, SVT s/p ablation and vitamin D deficiency. Home medications were Spiriva, Ventolin HFA, Norvasc, Synthroid, Lunesta, Cingualar, Zyrtec, Mimvey. She smoked a pack per day, denied alcohol and worked in a public school. Vitals were normal. Physical exam was unremarkable except for Hepatosplenomegaly. Imaging showed normal chest x-ray. CT scan showed central, lobular, paraseptal emphysematous changes; 2 cm speculated soft tissue density in right upper lobe. Rest of labs were unremarkable except anemia (Hb 3.4) and thrombocytopenia (21). She received 1 unit of PRBC, 2 units of platelets. During second unit of PRBC she developed fever, dyspnea, tachypnea, tachycardia and hypertension. We immediately stopped blood products and intubated her. Stat CXR showed bilateral airspace and interstitial opacities - given rapid appearance of findings; may represent changes related to fluid overload/pulmonary edema. Echo was normal. Repeat CBC showed Hb 5.5, platelets 111. One more unit of PRBC was given without any complications. Patient improved with positive pressure ventilation and was finally extubated on 2nd day. She was eventually discharged on room air.
DISCUSSION: TRALI (Transfusion Related Acute Lung Injury) occurs at a rate of approximately 0.04 to 0.1 % of transfused patients or in approximately 1 in 5000 transfused blood components. Most of the cases are under reported. Within the last 5 years TRALI reactions have been recognized as the leading cause of transfusion-related fatalities in the United States, surpassing hemolytic and septic transfusion reactions. Mortality rates associated with TRALI/possible TRALI have been reported to be as high as 41 to 67 %. TRALI is a clinical diagnosis. Acute onset of hypoxemia during or within 6 h of transfusion, bilateral infiltrates on CXR, no previous Acute Lung Injury, no evidence of circulatory overload points towards a diagnosis of TRALI. Though TRALI has been associated with virtually all blood products, high-plasma-volume components such as plasma, apheresis platelet concentrates, and whole blood have been consistently shown to carry the greatest risk per component or per transfusion episode. To reduce serious transfusion reactions, inappropriate transfusions must be minimized and the decision to transfuse blood products should be taken with care. It is one life-threatening condition which when diagnosed at bedside promptly, can have the potential to save the patient’s life. With prompt recognition and supportive measures, we can reduce mortality and also prevent further episodes of TRALI from that donor blood.
TRICKED BY PERSISTENT ST ELEVATIONSNaomi Karlen; George Bensabat; Philip J. Putnam. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1925938)
LEARNING OBJECTIVE 1: Identify potential causes of ST segment elevation on ECG.
LEARNING OBJECTIVE 2: Identify non-invasive or minimally invasive diagnostic tests that can be utilized in the diagnosis in hypertrophic cardiomyopathy.
CASE: A 55 year-old woman presented with altered mental status. The patient’s family stated that she had become intoxicated and was involved in a verbal altercation with her daughter before complaining of chest pain and becoming obtunded. They reported a past medical history of hypertension, coronary artery disease, and previous AICD implantation. Vital signs revealed blood pressure 74–139/42–87 mmHg and heart rate 52–76 beats/min. Physical examination was notable only for inability to follow commands. Initial lab work revealed troponin I 0.02 ng/ml, NT-proBNP 1923 pg/ml, and blood alcohol level 91 mg/dl. ECG revealed ST elevation in the anterior leads with reciprocal inferolateral ST segment depression. Emergency cardiac catheterization demonstrated patent coronary arteries. Subsequent left ventriculography showed a premature ventricular contraction, after which a paradoxical decrease in pulse pressure was observed. This is consistent with the Brockenbrough-Braunwald-Morrow sign, diagnostic of hypertrophic cardiomyopathy (HCM). Following cardiac catheterization, additional medical records were obtained which demonstrated persistent ST segment elevation on previous ECGs.
DISCUSSION: While the differential diagnosis of an ECG demonstrating ST segment elevation is broad, clinicians must quickly initially identify or rule out acute myocardial infarction. Other diagnoses include HCM, acute pericarditis, bundle branch blocks, and left ventricular hypertrophy. Persistent ST elevations have been observed in patients with HCM. Occurring in one out of 500 people, HCM is a relatively prevalent disease that remains under-diagnosed and continues to be the most common cause of cardiac-related sudden death in people under the age of 30. The presenting symptoms can mimic myocardial infarction with chest pain, palpitations and syncope. Early identification of HCM patients is imperative so that appropriate treatment can be implemented. The mechanism of persistent ST elevation in these patients is unclear, but subepicardial fibrosis may play a role. Prior to invasive testing, a thorough family history for sudden cardiac death is the easiest initial screen for HCM. Diagnosis can be made non-invasively with echocardiogram or cardiac MRI. Imaging demonstrates increased thickness of the left ventricular wall and obstruction of the left ventricular outflow. Finally, cardiac catherization can additionally show the Brockenbrough-Braunwald-Morrow sign, as in our patient. When confronted with ST-elevation on EKG, physicians must quickly diagnose and treat the underlying disorder to prevent life-threatening events. Although most physicians would appropriately focus on myocardial infarction as the most likely cause, it is prudent to maintain a reasonable differential diagnosis and pursue alternative studies when an acute coronary syndrome is ruled out.
TROUBLES WITH TRABECULATIONSBrian Cruz; Charles E. Murphy. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926965)
LEARNING OBJECTIVE 1: Identify the features of isolated left ventricular noncompaction (LVNC)
LEARNING OBJECTIVE 2: Review the management of LVNC cardiomyopathy
CASE: A 28-year-old woman presents with palpitations. Her palpitations are long-standing for the past 15 years, occurring at least three times per week and lasting for a few minutes. They are associated with chest pressure, diaphoresis, dyspnea, and often lead to presyncope. She denies dyspnea on exertion or orthopnea. She was diagnosed in the past with supraventricular tachycardia and underwent an unsuccessful catheter ablation. She takes propranolol for palpitations and naproxen as needed for migraines. She denies use of tobacco, alcohol, and illicit drugs. There is no family history of palpitations or heart problems and her four children have no medical conditions. Vital signs, physical exam, and laboratory studies are all within normal limits. Electrocardiogram reveals normal sinus rhythm with ST depression and T wave inversions with biphasic T waves in an inferolateral distribution. Transthoracic echocardiogram with echocontrast reveals a normal left ventricular ejection fraction and left ventricular noncompaction, which is confirmed by a computed tomography scan of the heart.
DISCUSSION: Congenital cardiac abnormalities are commonly detected during childhood, but the internist may be the first to diagnose rare abnormalities that are asymptomatic until adulthood. Isolated left ventricular noncompaction is a primary genetic cardiomyopathy that results from the failure of resorption and remodeling of endomyocardial trabeculations during fetal cardiac development (1). Patients frequently remain asymptomatic until adulthood, and present with nonspecific symptoms that include dyspnea, palpitations, chest pain, and atrial fibrillation (2,3). Some patients present with heart failure or embolic events (4). The electrocardiogram is usually abnormal, but there are no characteristic changes; common abnormalities include bundle branch block, fascicular block, atrial fibrillation, and ventricular tachycardia. Diagnosis is usually made by echocardiogram, and although there is no gold standard, proposed echocardiographic criteria generally require prominent trabeculations with intertrabecular Doppler flow. One set of criteria requires a ratio of noncompacted to compacted myocardium greater than two (5). Once diagnosis has been made, it is recommended that first-degree relatives also undergo echocardiographic evaluation. Prognosis depends on the severity of disease at the time of presentation: those who present with severe heart failure or cardiac complications are at the highest risk for future cardiovascular death or heart transplantation. Other common complications include ventricular arrythmias requiring implantable cardioverter-defibrillator (ICD) placement, progression of heart failure, and thromboembolic events. However, asymptomatic patients diagnosed incidentally or via screening appear to develop fewer complications and have an overall good prognosis (5). Controversial points include whether use of anticoagulation and placement of an ICD for primary prevention should follow standard cardiac guidelines or a more lenient criteria in those with LVNC.
TUBULOINTERSTITIAL NEPHRITIS AND UVEITIS (TINU) SYNDROME IN AN ELDERLY ADULTXu Wu1; Samer Nasser2,1. 1Conemaugh Memorial Medical Center, Johnstown, PA; 2Kidney Center, Johnstown, PA. (Tracking ID #1934322)
LEARNING OBJECTIVE 1: Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare autoimmune disorder that mainly affects young women and adolescents with a median age of 15 years. No identifiable risk factors have been found in most of cases although prior infection or the use of antibiotics and nonsteroidal anti-inflammatory drugs have been implicated in some instances. First described in 1975, most cases have since been documented in ophthalmology and pediatric medical literature and very rarely has it been reported in the older population.
CASE: We report a 60-year-old female patient who was referred to the Renal Clinic by her primary care physician for elevated serum creatinine together with uncontrolled hypertension. She had fever and fatigue with red and painful eyes. However, she did not have any recent history of infection or newly prescribed analgesic medications. The patient’s initial blood work revealed a Creatinine of 2.3 (baseline of 1.0) and subnephrotic range proteinuria and hematuria. The work up of the proteinuria and hematuria revealed normal complement levels, negative antinuclear antibody, myeloperoxidase, proteinase-3, hepatitis panel, and glomerular basement membrane antibodies. Ophthalmology referral for eye pain revealed uveitits for which she was treated with systemic and topical steroids for her eye symptoms. A kidney biopsy was done and showed an interstitial inflammatory process associated with tubulitis, which was consistent with active tubulointerstitial nephritis. Given the kidney biopsy results and the uveitis, she was diagnosed with TINU syndrome. This patient was treated with prednisone 1 mg/kg daily for 3 months followed by a tapering dose. Her renal function recovered without recurrence and she followed up with her ophthalmologist regarding the uveitis.
DISCUSSION: This case illustrates one of the few older patients who developed TINU syndrome, and whose kidney function successfully recovered after a course of steroid treatment. Noticeably, we did rule out certain autoimmune diseases relatively commonly seen before the diagnosis of TINU syndrome owing to some overlapping manifestations. Thus, this case delineates the importance of extensive system review in renal disease as well as the importance of appropriate referral and collaboration between specialties to obtain the correct diagnosis that dictates the appropriate management.
TUBULOINTERSTITIAL NEPHRITIS AND UVEITIS SYNDROME COMPLICATED BY IGA NEPHRITISTakahiro Tsushima; Christine Kwan. Teine Keijinkai Hospital, Sapporo, Japan, Sapporo, Japan. (Tracking ID #1930167)
LEARNING OBJECTIVE 1: Recognize that tubulointerstitial nephritis and uveitis syndrome (TINU) with IgA nephritis (IgAN) can occur in the presence of Graves disease
CASE: A 64 years old Japanese woman presents with sore throat and hematuria ×3 days. She describes urinating several tablespoons of blood/time, but no dysuria, frequency, or urgency. She reports elevated temperature (37.5C), chills, and fatigue. All other review of systems shows no abnormalities. Besides Graves disease, she has hypertension and chronic kidney disease stage III and takes propylthiouracil, amlodipine, and candesartan; she has no allergies. She has never smoked or used recreational drugs and only occasionally drinks beer. She has no family history of kidney diseases. On physical examination, her vital signs show temperature37.1C, heart rate 94, blood pressure 115/80, respiratory rate 12, and O2 saturation 98 % room air. On head and neck exam, her oropharynx is erythematous with swollen tonsils and pus; she has multiple tender, mobile, 5 mm bilateral cervical lymphadenopathy. Her thyroid, chest, and abdominal exams show no abnormalities, as does the rest of her exam. On her labs, significant values include white blood cell 23,310/μL, blood urea nitrogen (BUN) 15.4 mg/dL, and creatinine (Cr) 1.4 mg/dL (baseline); thyroid function panel is within normal limits. Rapid Strep Testing is positive with Streptcococcus pyogenes on throat culture for which she is given ceftriaxone. Urinalysis with microscopy reveals heme >100/high power field and dysmorphic red blood cells but no proteinuria. Two weeks later, though, she develops bilateral ciliary injection and photophobia; slit lamp exam reveals anterior chamber uveitis. Labs show BUN 26 mg/dL and Cr 2 mg/dL; anti nuclear antibody is 1:320 and IgA 497 mg/dL (normal 90–400 mg/dL). Urinalysis reveals protein 3200 mg/day and β2-MG 1347/μL (normal 0–250/μL). Kidney biopsy shows 1 cellular crescent, increased mesangial cell proliferation, and deposition of IgA and C3 in the glomeruli, consistent with IgAN. The interstitium, however, shows edematous changes and infiltration of granular leukocytes. Given her diagnosis of TINU syndrome complicated by IgAN, she is given methylprednisolone ×3 days with subsequent oral prednisolone ×2 months with clinical improvement.
DISCUSSION: TINU syndrome, with onset usually in women <20 years old, is associated with systemic symptoms of mild fever, weight loss, and fatigue. Renal manifestations include sterile pyuria, hematuria, proteinuria (<3 g protein/24 h), and acute renal failure. Typical biopsy findings include interstitial edema and infiltration by inflammatory cells, as the above patient. IgAN, however, is defined as glomerular nephritis resulting from IgA and C3 deposition around mesangial areas. It can present with mild fever, fatigue, mild proteinuria (300–1000 mg/day), hematuria, and upper respiratory infection symptoms. Rarer associations include dermatitis herpetiformis, seronegative arthritis, and inflammatory bowel disease. Only several case reports, however, have shown TINU complicated by IgAN; even still, most of them occur in the presence of the autoimmune diseases, spondyloarthritis and primary biliary cirrhosis. No reports have yet shown a relationship between Graves disease, such as the above patient, with TINU+IgAN. Given this possible association, even in those who are clinically euthyroid, one should recognize the possible renal complications of Graves disease.
TUMOR-INDUCED OSTEOMALACIA CAUSED BY A FGF-23 PRODUCING MESENCHYMAL TUMORSophia Hu1; Sara Lubitz2. 1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ. (Tracking ID #1930552)
LEARNING OBJECTIVE 1: To recognize tumor-induced osteomalacia (TIO) as a rare and reversible form of osteomalacia and hypophosphatemia caused by a fibroblast growth factor 23 (FGF-23) producing mesenchymal tumor.
CASE: A 52 year-old female was in good health until after her first pregnancy in 1986, when she developed muscle cramps with exercise. Over a few years, these cramps became debilitating myalgias, and she developed a waddling gait. Initial labs showed serum phosphate 1.2 mg/dL, calcium 8.4 mg/dL, urine phosphate 1506 g/24 h (normal 400–1300), 25-hydroxyvitamin D 37 pg/mL, 1,25-dihydroxyvitamin D 60 pg/mL (normal 15–75), and mid-molecule PTH 379 pg/mL (normal 50–330). No glycosuria nor aminoaciduria were noted. Neutra-Phos 4 g daily and calcitriol were initiated. Transiliac crest bone biopsy findings were consistent with severe osteomalacia, at which time she was diagnosed with vitamin D-resistant hypophosphatemic osteomalacia. She continued to have symptoms of bone pain, myalgias, fatigue and depression, with elevated creatinine to 2.8 mg/dL. She also remained hypophosphatemic to 1.6 mg/dL despite daily phosphate and calcitriol replacement. About 20 years after initial presentation, she noted a mass on her right forearm. A PET scan of the mass showed hypermetabolic activity at that site. In November 2009, she underwent resection of the mass with pathology showing phosphaturic mesenchymal tumor 4.5 × 3.5 × 2 cm, mixed connective tissue variant. Subsequently, her phosphate levels gradually increased to 3.2 mg/dL, creatinine improved to 1.5 mg/dL, and urine phosphate normalized to 948 mg/24 h. FGF-23 was measured to be 157 RU/mL (normal <180), however there were no preoperative values for comparison. In March 2011, she was titrated off all phosphate supplements and phosphate levels have remained normal.
DISCUSSION: TIO is a rare acquired disorder characterized by osteomalacia and severe hypophosphatemia. In this recently described disease, mesenchymal tumors produce FGF-23, a phosphaturic hormone which inhibits renal phosphate reabsorption and reduces renal 1,25-dihydroxyvitamin D production, resulting in hypophosphatemia, phosphaturia and eventual osteomalacia. The pathways involved and clinical presentations are similar to the inherited forms of vitamin D resistant rickets, which include X-linked hypophosphatemic rickets (XLH) and autosomal dominant hypophosphatemic rickets (ADHR). In all of these conditions, phosphate and calcitriol replacement are the cornerstone of treatment. However, unlike XLH and ADHR, TIO is acquired and can potentially be reversed once the FGF-23 producing tumor is localized and resected. In our case of TIO, the patient’s hypophosphatemia and osteomalacia completely resolved with tumor resection. Interestingly, 20 years had elapsed between the initial presentation and the discovery of this rare FGF-23 producing mesenchymal tumor.
TWO IS BETTER THAN ONE: PRESENTING WITH TWO PRIMARY MALIGNANCIESAdam Schwartz. NYP/Cornell, New York, NY. (Tracking ID #1926346)
LEARNING OBJECTIVE 1: Recognize unusual but treatable presentations of malignancy
LEARNING OBJECTIVE 2: Correlate anatomy and oncology
CASE: Patient is a 68 year-old woman with a significant tobacco history who initially presented to an outside hospital in December of 2012 with bronchitis. During that hospital stay she was found to be anemic. At New York-Presbyterian Hospital, patient underwent a colonoscopy which demonstrated invasive adenocarcinoma in the ascending colon. Subsequent PET CT revealed two lung nodules in the right upper lobe but with sparing of the liver. The lack of liver involvement suggested that the liver nodules may represent a distinct malignancy, indicating that both the colon and lung malignancies would be amenable to separate interventions and possibly carry a superior prognosis compared to that of metastatic colon cancer. Fine needle aspiration biopsy of one of the lung nodules was performed, which revealed squamous cell carcinoma. Patient underwent complex right hemicolectomy and subsequently received radiation therapy for her lung cancer. Patient remains alive at this time and still receives her care at New York-Presbyterian.
DISCUSSION: Though seemingly counterintuitive, this patient’s prognosis was improved when the pulmonary nodule seen on PET CT was found to be a second primary malignancy. Had the nodule represented widely metastatic colon cancer, her options for surgical cure would have been greatly diminished. Instead, she was found to have two intervenable malignancies. The decision to biopsy the lung—rather than to attribute the nodule to metastatic colon cancer—was driven by the absence of metastatic lesions in the liver. Because blood flow from the colon passes through the liver on the way back to the heart, it would be highly unusual to have colon cancer metastasize to the lungs without also seeding the liver.
UH OH, THAT’S HIGHRyan Brown. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1924906)
LEARNING OBJECTIVE 1: Review indications for high-dose versus low-dose methotrexate treatments.
LEARNING OBJECTIVE 2: Recognize signs, symptoms and treatment of methotrexate toxicity.
CASE: A 66 year old woman was admitted to the hospital for methotrexate chemotherapy. She had a history of diffuse large B cell lymphoma previously treated with four cycles of R-CHOP therapy along with two cycles of methotrexate and leucovorin. A third cycle of methotrexate treatment was initiated in the hospital. After a few days the patient developed clinical toxicity characterized by altered mentation, increased creatinine from 0.9 to 4.3, increased AST and ALT and pancytopenia with a low reticulocyte count. Twenty-fours post-transfusion, her serum methotrexate level was elevated at 46. The methotrexate level remained elevated at 48 h and 72 h, with levels of 15 and 6, respectively. On the fifth day of hospitalization, the rescue drug Glucarpidase was given. A second dose was given on hospital day eight. Subsequently, the creatinine, AST, ALT, pancytopenia and altered mental status all began to improve. By discharge on hospital day 32, all evidence of methotrexate toxicity had resolved.
DISCUSSION: Methotrexate is a folate antagonist that has anti-proliferative, anti-inflammatory and immunomodulating effects; it is used for multiple causes. At higher dose levels (>500 mg), it is used mainly to treat hematologic malignancies. However, it is also used in the treatments of breast, gastrointestinal and head and neck cancers. At lower doses (weekly doses of 7.5 to 25 mg), it is commonly used for treatment of rheumatoid arthritis, psoriasis, systemic lupus erythematous, crohn’s, ectopic pregnancy, multiple sclerosis and many others. In this case, methotrexate in conjunction with the folic acid analog leucovorin, had been used twice previously for treatment of diffuse large B cell lymphoma. On the third round of this treatment, the patient developed toxic effects. Common side effects of high dose methotrexate are nephrotoxicity and hepatoxicty. When giving methotrexate at these levels, aggressive pre- and post-administration treatment with intravenous fluids, urinary alkanization and leucovorin should be performed. If the patient develops nephrotoxicity, plasma methotrexate levels will remain elevated. At this point, an anti-methotrexate agent is necessary. Other side effects of high dose methotrexate are encephalopathy, stomatitis, and drug rash. Hematologic adverse effects are more common with low dose methotrexate, although the patient in this case developed bone marrow suppression with high-dose therapy. With long-term low dose oral therapy, hypersentivity pneumonitis can also occur. Treatment for methotrexate toxicity is Glucarpidase. It is a recombinant bacterial enzyme that converts methotrexate to inactive metabolites. It is needed when renal clearance of methotrexate has been compromised resulting in elevated plasma levels causing systemic effects. If the methotrexate level is still greater than 10 at 48 h, then glucarpidase should be given. It will decrease the level by 98 % in 30 min. It is rare but a second dose may be needed, as in this case.
UNCOMMON CAUSE OF COMMON PROBLEM: TESTICULAR TUMOR LEADING TO GI HEMORRHAGENaba R. Mainali; Madan R. Aryal; Anthony Donato. Reading Health System, West Reading, PA. (Tracking ID #1934053)
LEARNING OBJECTIVE 1: To be able to identify a rare cause of GI bleeding secondary to testicular tumor metastasis in an appropriate setting.
LEARNING OBJECTIVE 2: To describe the diagnosis and management of the metastatic disease of testicular germ cell tumor.
CASE: Introduction: Testicular tumors are the most common solid tumors in young adult males, usually presenting with painless solid testicular mass. Germ cell tumors, the most common pathology, have high propensity of distant metastasis. Common sites of metastasis of testicular carcinoma include brain, lungs and liver. Hemorrhagic metastasis to stomach is a rare entity and represents bad prognostic sign. Case Report: A 24 year old male with recent diagnosis of mixed germ cell testicular tumor metastatic to lungs was admitted to the hospital for the evaluation of fatigue and black stool per rectum. He had been treated with orchiectomy and started on chemotherapy with BEP (Bleomycin, Etoposide and Cisplatin). Review of systems was otherwise negative. On physical exam, his blood pressure was 98/64 mmHg. He had pallor on the conjunctiva, but examination was otherwise non-focal. Laboratory studies revealed hemoglobin 7.8 g/dl, hematocrit 24.2 %, platelets 372,000/cmm3 and hemoccult testing was positive. Beta Human Chorionic Gonadotropin was 52332 MIU/ML (normal 0–5 MIU/ML) and Alpha Feto Protein was 27.6 ng/ml (normal: 0.0–14.9 ng/ml). He was given packed red blood cell transfusions, and an urgent Esophagogastroduodenoscopy revealed a single gastric ulcer along the anterior body of the stomach. The ulcer was biopsied, and showed a mixed germ cell testicular tumor metastatic to the stomach. Chemotherapy with BEP was continued and his hemoglobin became 11.1 g/dl. After the second cycle of chemotherapy, his beta HCG became 100 MIU/ML and AFP dropped to 2.6 ng/ml.
DISCUSSION: The accurate diagnosis of gastrointestinal bleeding secondary to testicular carcinoma metastasis requires high index of suspicion with esophagogastroduodenoscopy and biopsy of the lesion. With the introduction of cisplatin based chemotherapy, metastatic tumor represents highly curable malignant disease. The combination of bleomycin, etoposide and cisplatin (BEP) given at 3-week interval still remains the treatment of choice for the metastatic disease of testicular germ cell tumor.
UNCOMMON PRESENTATION OF DIGOXIN TOXICITY IN SETTING OF ACUTE ON CHRONIC KIDNEY DISEASE AND AGGRESSIVE DIURETIC USE REQUIRING URGENT TREATMENTHirokazu Ban; Maurice Rachko; Madeeha Saeed. Beth Israel Medical Center, New York, NY. (Tracking ID #1922264)
LEARNING OBJECTIVE 1: Recognizing that digoxin toxicity can cause life-threatening arrhythmia, like ventricular tachycardia which may requires urgent Dig-binding treatment.
LEARNING OBJECTIVE 2: Recognizing that diuretics use can lead to digoxin toxicity.
CASE: We present a case of an 85 year-old man with past medical history of dilated non-ischemic cardiomyopathy (ejection fraction of 15 %), non-sustained ventricular tachycardia (NSVT) with automatic implantable cardioverter defibrillator (AICD), atrial fibrillation on coumadin, stage IV chronic kidney disease. Patient was recently discharged from another hospital after being treated for a non-ST elevation myocardial infarction (NSTEMI) where he was started acutely on digoxin and his furosemide dose was increased from 40 mg po twice a day to 80 mg po twice a day and metolazone 2.5 mg po daily was added to treat his heart failure. The patient’s chief complaint was only decreased appetite. He presented to an outpatient clinic with alarming AICD and was found to have had multiple episodes of defibrillator shocks for sustained ventricular tachycardia that did not respond to antitachycardia pacing. The patient was admitted to the coronary care unit. His vital signs were all within normal limits and his physical exam was significant for irregularly irregular heart sound with III/VI holo-systolic murmur at right sternal border. Initial lab results were significant for creatinine of 3.36 mg/dl (baseline 2.6 mg/dl), serum digoxin level of 2.2 ng/ml (goal 0.5–0.9 ng/ml), potassium of 4.0 meq/L, magnesium of 2.4 mg/dl, and troponin I of 0.157 ng/ml. Chest x-ray revealed cardiomegaly with small right pleural effusion and his ECG showed polymorphic NSVT. Digoxin toxicity was suspected and the patient received 4 vials of digoxin-specific Fab fragments. The polymorphic NSVT resolved after the dose of digoxin-specific Fab fragments. Due to his acute kidney injury, enalapril, furosemide, metolazone were held. On hospital day 2, patient remained free of any further NSVT episodes and was transferred to a telemetry floor for continuous monitoring. His creatinine improved to 2.19 mg/dl near baseline and the patient was discharged with cardiology follow up on hospital day 4.
DISCUSSION: Digoxin is commonly used to treat atrial fibrillation and congestive heart failure. Its well known cardiac side effects include increased automaticity and decreased AV node conduction such as atrial tachycardia with complete AV block and bidirectional ventricular tachycardia which has been related to higher mortality. Often digoxin toxicity occurs in the setting of aggressive diuresis, as in our patient. Due to the narrow therapeutic range of digoxin and the significant overlap between therapeutic and toxic ranges, even slight elevations of digoxin levels can cause acute digoxin toxicity. This is especially problematic among patients with advanced heart disease, underlying atrial fibrillation (suggestive of diseased myocardium at risk), and renal failure. These risks are potentiated by use of increasing diuretic dosages without adequate monitoring. Given these adverse effects, the use and dosage of digoxin routinely have declined in general cardiology practices. Digoxin toxicity is now seen infrequently and acute hospitalizations have declined, however, it must remain on the differential as the potential culprit when patients with above-mentioned diseases on digoxin present with cardiac arrhythmias. Recognizing digoxin toxicity is paramount in treating it adequately. In this case, the patient was urgently treated with digoxin-specific Fab fragments and withholding nephrotoxic agents with good results.
UNCOMMON SEPSIS FOLLOWING PANCREATIC SURGERYArvind Kalyan Sundaram1,2; Carey C. Thomson1,2. 1Mount Auburn Hospital, Cambridge, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1939655)
LEARNING OBJECTIVE 1: To recognize Aeromonas Hydrophilia infection as a rare cause of sepsis with respiratory failure
CASE: 69 Year old male was admitted to the Intensive Care Unit (ICU) after developing fever and hypotension following an elective pancreatectomy for a pancreatic adenocarcinoma. Prior to the admission patient was evaluated for painless jaundice. On hospital day two, he developed several episodes of fever to 102 F and hypotension requiring vasopressors. After obtaining blood, urine, sputum and abdominal drainage culture, he was treated with broad spectrum antibiotics including Vancomycin, Levofloxacin and Metronidazole. Despite this coverage, he continued to have fevers and remained hypotensive, ultimately requiring large volume fluid resuscitation and multiple vasopressors to maintain a blood pressure, and mechanical ventilation for respiratory support. His past medical illness is significant for Hypertension and Gastroesophageal reflux disease. He was Aremenian born and lived there as an adult, and had a prior history of heavy alcohol use. Examination did not reveal any sources of infection. Labs were significant for white blood cell count of 21,000 cells/mm3 with a band of 11 %, Hematocrit of 37 %, Platelet of 70,000/mm3, Elevated Alanine transaminase and Aspartate transaminase of 55 IU and 58 IU respectively, Amylase of 805 units/l and lipase of 1300 units/l. Serum chemistry and coagulation profiles were within normal limits. Chest radiograph showed mild congestion and large bilateral pleural effusions, Computed Tomography scan of abdomen and pelvis revealed a stable sub-capsular hematoma and was otherwise unremarkable. Jackson Pratt (JP) abdominal drain and sputum cultures grew gram negative bacilli which were later speciated as Aeromonas Hydrophilia. The JP drain also grew Sphingomonas Paucimobilus. The blood cultures and urine culture were negative. Patient gradually improved and was later extubated. He completed a total of 14 day course of Levofloxacin and was discharged to acute rehabilitation center for recovery.
DISCUSSION: Aeromonas infections in humans are rare and are more commonly seen in immune-compromised host including cirrhosis and malignancy. Among the 14 different Aeromonas spp., A. Hydrophilia, A. caviae and A. sobria account 80–90 % of the human isolates. These three species are commonly involved in aeromonas infections causing cellulitis, septicemia, meningitis, myositis, peritonitis, gastroenteritis, respiratory tract infections, hemolytic uremic syndrome and hepatobiliary disease. Aeromonads are gram negative, non- spore forming, facultative anaerobic bacilli that produces beta- lactamase and are extensively distributed in the environment through soil, water and are present in contaminated meat including chicken and ground beef. The bacteria can be acquired through wound contaminated with soil and water containing Aeromonad spp., consumption of contaminated water or meat or through medicinal leech therapy. The most common portal of entry of A. Hydrophilia causing bacteremia or sepsis in patient is through the gastrointestinal tract and skin lesions. Though the incidence is low, mortality rate of Aeromonas bacteremia or septicemia is around 70 %. Studies have shown that Aeromonas bacteremia have high acute mortality and should always be considered as one of the pathogens that can cause sepsis in patient with cirrhosis or neoplasm. Penicillin and first generation Cephalosporin are inherently resistant to Aeromonas species and the most effective antimicrobial includes Fluroquinolones, Carbipenems and third generation Cephalosporin.
UNHAPPY FEET: VORICONAZOLE ASSOCIATED TOXIC PERIPHERAL NEUROPATHYJayanth Adusumalli; Abhishek Singla; Avyakta Kallam; Edward Horowitz. Creighton University Medical Center, Omaha, NE. (Tracking ID #1900481)
LEARNING OBJECTIVE 1: To recognise that chronic Triazole therapy can be the primary cause of peripheral neuropathy.
LEARNING OBJECTIVE 2: To discuss management of this potentially irreversible complication.
CASE: A 53 year old male was diagnosed with rare invasive Aspergillus infection of the heart. He underwent mass resection of the right ventricle along with tricuspid valve replacement and was started on long-term voriconazole therapy. His past medical history included allergic bronchopulmonary aspergillosis, IgA deficiency and hypertension. Approximately 1 year after starting voriconazole, he complained of progressively increasing numbness, tingling and weakness of both his feet to the point where he found it difficult to walk. Neurological examination: Motor exam revealed power of 5/5 in all muscle groups along with 2+ deep tendon reflexes. Sensory exam revealed diminished fine touch and vibration sense in the feet, the left side being more involved than the right, along with loss of proprioception in the first and second toe on the left side. Laboratory tests revealed that the patient’s Hemogram, electrolytes, Vit. B 12 level, TSH, MMA, SPAP were all within normal limits. Voriconazole serum levels throughout therapy were all within the therapeutic range. Voriconazole was discontinued in favor of posaconazole. This resulted in marked improvement of symptoms over 2 months. On the basis of the temporal relationship of PN to the initiation of voriconazole therapy and subsequent improvement on cessation in the absence of other etiologies, a diagnosis of voriconazole induced PN was made.
DISCUSSION: Triazole antifungals have been known to potentiate PN caused by other agents such as vincristine, but are now being recognized as primary causes of peripheral neuropathy, with both short term and long term use. Symptoms may be sensory, motor or both. The mechanism is still under debate. One recent study claimed incidence of PN with chronic triazole therapy without any other contributing factors to be as high as 10 %, itraconazole being the most frequent culprit. It is important for physicians to be aware that chronic triazole therapy can be the primary cause of PN as it is rare, potentially irreversible and can manifest even with therapeutic serum levels as in our patient. Management includes complete neurological exam at initiation of therapy and subsequent follow up to catch it early, switching the anti-fungal agent preferably to a non-triazole if neuropathy manifests.
UNPREDICTABLE NATURE OF TOLVAPTAN IN THE TREATMENT OF HYPERVOLEMIC HYPONATREMIAIshan Malhotra; Kalyan Janga; Sheldon Greenberg; Shilpa Gopinath. Maimonides Medical Center, Brooklyn, NY. (Tracking ID #1937102)
LEARNING OBJECTIVE 1: Severe chronic hyponatremia must be managed with extreme care especially in patients with chronic debilitating illness. Rapid re-induction of hyponatremia immediately after the diagnosis of Osmotic Demyelinating Syndrome (ODS), within 24–36 h, can reverse the symptoms of ODS and is the treatment of choice.
LEARNING OBJECTIVE 2: Tolvaptan should be only dosed after checking Serum sodium levels .
CASE: A 51 year old male who presented with congestive heart failure exacerbation on admission had a serum sodium of 122 mmol/lt. Patient was fluid restricted and aggressive diuresis was done and as there was no rise in serum sodium levels, Tolvaptan 15 mg was started on hospital day 6. Patient showed improvement after receiving the first dose of Tolvaptan and on hospital day 7 his serum sodium was 126 mmol/L. On day 8 he had a rapid increase in his serum sodium level from 126 mmol/lt to 142 mmol/l after he received the second dose of Tolvaptan. His serum sodium levels further increased from 159 mmol/L to 167 mmol/L on day 8. At this point, tolvaptan was stopped. The patient developed signs of osmotic demyelination syndrome which failed to resolve after rapid correction with hypotonic fluids and desmopressin and was transferred to the medical intensive care unit for further management of hypernatremia.
DISCUSSION: Rapid correction of hyponatremia with tolvaptan can cause osmotic demyelination syndrome (ODS). In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable. Slow correction of serum Na (less than 12 mmol/L/day) is recommended to prevent the emergence of this syndrome (1). There is no standard therapy once ODS sets in. Fluid should not be restricted in patients with hyponatremia who are started on Tolvaptan and serum sodium concentration should be monitored every 6–8 h in order to avoid rapid correction of sodium levels (2) along with frequent urine output monitoring. Rapid re- induction of hyponatremia with hypotonic fluids like 5 % dextrose water and half normal saline along with desmopressin has been shown to improve mortality and even reverse the signs and symptoms of ODS and is currently the favored strategy to treat patients with ODS due to hypernatremia. The present case tells us that severe chronic hyponatremia must be managed with extreme care especially in patients with chronic debilitating illness due to the unpredictable nature of tolvaptan to raise serum sodium levels. In most hospital settings, warfarin dosing happens after checking daily prothrombin time. Similarly tolvaptan should be administered after checking serum sodium levels for that day and it should not be started as a standing order while initiating treatment. References 1. Rockville, MD: Otsuka America Pharmaceutical, Inc.; May, 2009. Samsca (tolvaptan), package insert. 2. Schrier RW, Sharma S, Shchekochikhin D Nat Rev Nephrol. 2013 Jan; 9(1):37–50.
UNUSUAL EARLY MALIGNANT TRANSFORMATION IN PANCYTOPENIA: CASE REPORT AND DISCUSSIONDinuli H. Delpachitra; Cherian Verghese. University of Toledo, Health Sciences, Toledo, OH. (Tracking ID #1930082)
LEARNING OBJECTIVE 1: Recognize early transformation of hypoplastic bone marrow to acute myeloid leukemia.
CASE: A 74 year old woman with a past medical history of hypertension, osteoarthritis and anxiety disorder presented with fatigue and generalized weakness lasting a few weeks. On physical examination she was thin but in no acute distress. Her initial blood work showed pancytopenia with a hemoglobin of 6.1 g/dL, white blood cell count of 1.5 × 103/mm3, platelet count of 16,000/mm3. In comparison, a previous complete blood count revealed a hemoglobin of 12.4 g/dL, white blood cell count of 3.7 × 103/mm3, and a platelet count of 133,000/mm3. At the time of presentation, her medications included atenolol, lorazepam, and multiple daily vitamins. Her history was negative for any recent infections or new medications. Peripheral blood smear did not reveal any blasts. Bone marrow biopsy was consistent with an aplastic marrow with rare ringed sideroblasts. Myeloid blasts were <5 %. The paroxysmal nocturnal hemaglobinuria panel by flow-cytometry was negative. Cytogenic studies demonstrated deletion of 17q. Molecular studies however, were negative for FLT3 gene mutation. A repeat complete blood count after 2 weeks demonstrated persistent pancytopenia but with 23 % percent blasts in the peripheral blood. Bone marrow biopsy was repeated to address the concern of leukemic transformation and it showed 32 % blasts. Immunophenotype analysis showed an abnormal myeloblast population expressing CD13, CD34, HLA-DR and CD11b. The cells lacked expression of CD33, CD9, CD71, and CD117. These findings were consistent with acute myeloid leukemia transformation.
DISCUSSION: The risk of transformation to Acute Myeloid Leukemia (AML) is generally considered to be less likely with hypoplastic MDS. Several clinical, morphological and chromosomal factors have been studied to develop a system of predicting leukemic transformation in MDS patients. The Revised International Prognostic Scoring System (IPSS-R) was published in 2012 as a valid tool to predict survival and risk of transformation to AML. However, its validity in predicting transformation in a hypoplastic marrow is unclear. Several causes of leukemia in a pancytopenic marrow exist and include hairy cell leukemia, hypoplastic MDS, myelofibrosis and paroxysmal nocturnal hemaglobinuria. Non-malignant causes of pancytopenia are well known and include medications, radiation, Systemic Lupus Erythematosus and infections such as Malaria and MiliaryTB. Our patient had Acute Myeloid Leukemic transformation within weeks of her diagnosis. Such rapid evolution is not predicted by the available IPSS-R risk stratification. Since our patient presented with an abnormal myeloblast population expressing CD13, CD34, HLA-DR and CD11b, we can postulate that the appearance of mutations like 17q deletion may be predicative of aggressive behavior in a hypoplastic marrow. Cytogenetic abnormalities are considered unlikely with benign causes of pancytopenia. Early recognition of this transformation is crucial as selected patients may benefit from enrollment in clinical trials.
UNUSUAL HEADACHE - UNUSUAL CAUSE: DURAL SINUS THROMBOSIS DUE TO MTHFR DEFICIENCYShah Habib; Mashrafi Ahmed. Texas Tech Univ Health Science Center, Amarillo, TX. (Tracking ID #1938999)
LEARNING OBJECTIVE 1: Recognize dural venous sinus thrombosis as an unusual but life threatening cause of headache
LEARNING OBJECTIVE 2: Methylenetetrahydrofolate reductase (MTHFR) is a rare prothrombotic state associated with dural sinus thrombosis
CASE: A 29 year old young Caucasian female presented with persistent, sharp and stabbing headache over the front and back of her head for 6 weeks. It started suddenly, and was excruciating in intensity. She had no history of oral contraceptive pill use, but had history of migraine headache which was different from this episode. She had few episodes of nausea and vomiting with some tingling sensation at the distal upper limbs, and mild paresis of the right 6th cranial nerve on presentation. On opthalmoscopic examination she had mild blurring of the temporal side of the optic disc with intact venous pulsation. MRI brain revealed thrombosis of the sagittal sinus extending into the right transverse sinus. Initial workup for prothrombotic defects, infection, malignancy and pregnancy were negative. Further extensive workup revealed MTHFR deficiency and high homocysteine level. The patient was treated with enoxaparin bridged with warfarin.
DISCUSSION: Dural sinus thrombosis is uncommon, with an overall incidence of <1 per 100,000 cases annually. The disorder is more common in neonates and children than in adults, and among young adults more common in women than men. The mean age of onset is 39 years. The major risk factors for dural sinus thrombosis in adults are prothrombotic conditions, oral contraceptives, pregnancy and the puerperium, malignancy, infection, head injury, and mechanical precipitants. The clinical presentation of dural sinus thrombosis is highly variable. The onset can be acute, sub-acute, or chronic. Headache (of gradual, acute, or thunderclap onset) is the most frequent symptom, occurring in almost 90 % of patients, and may occur as a part of an isolated intracranial hypertension syndrome, with or without vomiting, papilledema, and visual problems. Head CT scan is normal in up to 30 % of dural sinus thrombosis cases, and most of the findings are nonspecific. Brain MRI in combination with MR venography is the most sensitive examination technique for demonstrating the thrombus and the occluded dural sinus or vein. Although a 2010 meta-analysis by Gouveia Lo, et al. did not show MTHFR deficiency as a risk factor for dural venous thrombosis, but in our case, it was the inciting factor. Treatment for dural sinus thrombosis is anticoagulation with low molecular weight heparin bridged with warfarin, Warfarin should be continued 6–12 months.
UNUSUAL PRESENTATION OF MAC INFECTIONTatyana Taranukha; Eric R. Simon; Pinky Jha. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1930392)
LEARNING OBJECTIVE 1: Recognize atypical presentation of MAC infection in an immunocompromised patient.
LEARNING OBJECTIVE 2: Review management of disseminated MAC.
CASE: 28 year old female with history of AIDS (previously on HAART) and pancytopenia presented as a direct admission for evaluation of elevated liver transaminases. Laboratory findings were significant for AST elevation of 964, ALT of 220, Alkaline phosphatase of 871, CD4 count of 8, WBC count of .5 and platelets of 87. On presentation, patient appeared comfortable and was not complaining of any symptoms. Physical exam and review of systems were unremarkable. Initially, all hepatotoxic drugs were discontinued and Infectious Diseases and Hematology were consulted for further treatment recommendations. Over the course of hospitalization, patient underwent an extensive microbiology work up as well as imaging of the abdomen, the hepatobiliary tree and biopsies of the bone marrow and liver. Results were significant for a positive AFB blood culture. Bone marrow biopsy showed non-necrotizing granulomatous inflammation with acid fast positive organisms and liver biopsy revealed granulomatous hepatitis with acid fast bacilli. Based on biopsy results and positive blood culture, disseminated MAC (DMAC) with multiorgan involvement was thought to be responsible for the pancytopenia as well as the hepatocellular liver injury. Azithromycin, Rifabutin, and Amikacin were chosen as triple therapy for DMAC as the patient had advanced AIDS with a low CD4 count. WBC count increased with Neupogen administration. During hospitalization patient continued to remain asymptomatic, however, her liver function tests significantly improved after the initiation of antibiotics.
DISCUSSION: Here, we present a patient with disseminated MAC causing granulomatous hepatitis and bone marrow suppression who has remained asymptomatic throughout her illness. DMAC is a life threatening infection caused by either M. avium or M. intracellulare that carries up to a three-fold risk of death in patients with AIDS. MAC infections typically affect the respiratory or GI tract and symptoms include fevers, night sweats, abdominal pain, diarrhea and weight loss. The infection is acquired through inhalation or ingestion of organisms from soil or water and can subsequently spread through the lymphatics in an immunocompromised host. DMAC typically occurs after the CD4 count drops below 50 cells/mm3 and in patients with CD4 counts of less than 10 cells/mm3, the yearly incidence rate has been reported to be as high as 39 %. First line agents for treatment are Clarithromycin and Azithromycin followed by Ethambutol and Rifabutin. IDSA guidelines suggest that at least two drugs should be initiated for the treatment of DMAC due to concern for development of resistance. In our patient, however, we elected to use a three drug therapy of Azithromycin, Rifabutin, and Amikacin due to the patient’s severe immunocompromised state. Ethambutol was avoided due to patient’s history of optic neuritis. Therapy will be continued for at least a year and until the CD4 count remains above 100 cells/mm3 for at least 6 months.
UNUSUAL SUSPECTS: RENAL SIDE EFFECTS OF PENICILLINSCady (Blackey) Brown; Deepa Bhatnagar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926138)
LEARNING OBJECTIVE 1: Illustrate a rare cause of hypokalemia
LEARNING OBJECTIVE 2: Review the various causes of nephrotoxic effects of antibiotics
CASE: A 46 year-old man with a history of hepatitis C cirrhosis and osteomyelitis of the humerus was sent from infectious disease clinic to the emergency department because of fatigue and weakness. He denied any dizziness, fever or chills. He denied hematemesis, hematochezia and melena. He denied any recent diarrhea and reported having normal oral intake. Two weeks prior he had been initiated on a regimen of nafcillin and rifampin for osteomyelitis. The physical exam revealed stable vital signs and a thin man with scleral icterus in no acute distress. The cardiovascular and lung exams were normal. The abdominal exam revealed mild ascites. The neurologic exam was normal, including normal gait and absence of asterixis. Laboratory results revealed a potassium level of 1.9 and magnesium of 1.8. All other electrolytes were normal and liver enzymes were at baseline. The electrocardiogram revealed flattened T waves. He required aggressive potassium repletion over the ensuing 48 h. However, discontinuation of nafcillin led to normalization of potassium. Supplementation of potassium was then stopped and the potassium level remained normal with symptomatic improvement.
DISCUSSION: Antibiotics are among the most frequently prescribed medications. However, their use is often limited by potential renal toxicity. Internists must make decisions regarding antibiotic therapy by weighing the potential side effects of a medication and the co-morbidities of the patient. A number of antibiotics are known to have renal side effects, particularly decreased glomerular filtration rate (GFR). Vancomycin, cephalosporins, amphotericin, aminoglycosides and bactrim all have the well-known risk of causing acute renal failure. Penicillins, on the other hand, are often a safe choice when considering renal side effects. However, penicillins can affect electrolyte, fluid and acid/base status through renal mechanisms even though they do not affect GFR. In particular, penicillins have been shown to cause hypokalemia. Within the principal cells of the collecting duct, penicillin acts as a non-reabsorbable anion. This causes a luminal negative charge in the setting of increased aldosterone-driven sodium reabsorption. This negative charge stimulates potassium secretion and can cause severe hypokalemia, as was seen in this case. Since antibiotics are so commonly prescribed, it is important for internists to be familiar with the spectrum of renal side effects of these medications, not just their impact on GFR. This familiarity allows the cause of electrolyte, acid-base or fluid derangements to be identified and treated prior to the onset of significant morbidity.
URACEMIC SICK!Michael Jesinger; Diego F. Alcivar Franco; Andrew Hoellein. University of Kentucky, Lexington, KY. (Tracking ID #1938763)
LEARNING OBJECTIVE 1: Describe the presentation, clinical evolution, diagnosis and management of Tumor Lysis Syndrome.
LEARNING OBJECTIVE 2: Outline the approach to hyperuricemia, highlighting the importance of malignancy work up.
CASE: A 65 year-old man with a history of Chronic Kidney Disease Stage III and renal cell carcinoma status post left-sided nephrectomy 6 months ago, was admitted with altered mental status. He was found to have acute kidney failure with a creatinine of 5.5 mg/dL, hypercalcemia of 12 mg/dL, metabolic acidosis, and hyperkalemia. Despite volume resuscitation and naltrexone, his altered mental status persisted. Further evaluation found uric acid 18 mg/dL and phosphate 5.3 mg/dL. Our patient now met Cairo-Bishop criteria and was given rasburicase for hyperuricemia. However, suspicion for tumor lysis at this point was low given that the patient did not receive chemotherapy within the last month and extensive evaluation with peripheral smear, esophagoduodenoscopy, colonoscopy, CT of chest, abdomen, and pelvis, and whole body bone scan were without overt signs of tumor burden. Abdominal ultrasound showed irregular hepatic parenchyma concerning for cirrhosis. A transjugular liver biopsy was performed and revealed metastatic renal cell carcinoma which was likely the source of this tumor lysis syndrome. Despite improvement of uric acid to 4 mg/dL, his mental status continued to worsen and after discussion with family members, our patient was transferred to Hospice for comfort care.
DISCUSSION: Tumor lysis syndrome (TLS) is a catabolic disorder in the setting of malignancy with a high proliferative rate, large tumor burden, high sensitivity to treatment, chemotherapy, cytolytic antibody therapy, radiation therapy, or sometimes glucocorticoid therapy can result in the rapid lysis of tumor cells and is considered an oncologic emergency. It is most commonly observed in poorly differentiated lymphomas and leukemia especially in patients undergoing chemotherapy. However, TLS has been rarely described after treatment of nonhematologic solid tumors and in patients not undergoing cytotoxic therapy. Our review of the literature found no reports of renal cell carcinoma-induced TLS. Clinicians should have a high suspicion for tumor lysis syndrome in any patient with a history of malignancy and especially in those with renal compromise. The mainstay of treatment is prevention. Early recognition of TLS is crucial as its sequelae of electrolyte imbalances can result in potentially fatal cardiac arrhythmias or renal failure. The Cairo-Bishop score is based on laboratory changes of hyperuricemia, hyperphosphatemia, hyperkalemia and hypocalcemia and clinical changes of worsening renal function, seizures or changes in mental status and cardiac arrhythmias. Two laboratory and one clinical change is diagnostic. Patients at risk for tumor lysis should be treated prophylactically with allopurinol. In TLS, aggressive hydration and rasburicase often result in rapid improvement of renal function and resolution of symptoms. Allopurinol prevents uric acid from forming while rasburicase functions as a synthetic uric oxidase promoting degradation of uric acid.
URINOTHORAX AS A RARE CAUSE OF DYSPNEASrividya Bhadriraju1,2; Jeffrey T. Bates2,1. 1Baylor College of Medicine, Houston, TX; 2Michael E. DeBakey VA Medical Center, Houston, TX. (Tracking ID #1939593)
LEARNING OBJECTIVE 1: Recognize urinothorax as a rare cause of severe dyspnea in patients who have undergone recent urologic instrumentation
LEARNING OBJECTIVE 2: Understand the pathophysiology and diagnostic challenges of a urinothorax
CASE: A 62-year-old female with a history of aortic valve replacement on warfarin presented with increased urinary frequency and hematuria; an abdominal CT scan showed a right renal calculus. She was admitted and underwent a right percutaneous nephrolithotomy with placement of a percutaneous nephrostomy tube. On post-operative day eight, she complained of worsening dyspnea at rest associated with non-radiating substernal chest pain, mild nonproductive cough, orthopnea, and mild nausea. Physical examination revealed hypoxia to 82 % on room air, tachypnea, decreased breath sounds in the right lower lung field, and bloody output from the nephrostomy tube. The nephrostomy tube was removed, and a chest x-ray showed a large right pleural effusion. The patient underwent a right thoracentesis with removal of 1.1 l of malodorous, bloody fluid. Pleural fluid analysis demonstrated a urine-like odor, low protein, an elevated LDH, and an elevated pleural fluid-to-serum creatinine ratio of greater than 1.0. She was diagnosed with urinothorax, and clinically improved after the thoracentesis.
DISCUSSION: Urinothorax results from an accumulation of urine in the pleural space. Initially, leakage of urine into the retroperitoneal space forms a urinoma; urine then moves directly into the pleural cavity due to either an anatomic diaphragmatic defect or via lymphatic drainage into the mediastinum. Although urinothorax commonly occurs ipsilateral to the obstructed kidney, it is rare in unilateral obstruction if the contralateral kidney function is normal. Pleural fluid analysis typically reveals an elevated pleural fluid-to-serum creatinine ratio (much greater than one), a low glucose, a low pH, and a transudative effusion. However, effusions are often misclassified as exudative due to the high LDH. A urinothorax is the only cause of a transudative pleural effusion with a low pH. Renal scintigraphy will demonstrate leakage of tracer from the urinary tract into the pleural space. Once the renal obstruction is relieved, the urinothorax typically resolves. Although obstructive renal disease is common, urinothorax is less frequently recognized. The diagnosis should be considered in patients with a pleural effusion in the setting of obstructive uropathy, trauma from urologic procedures (such as attempted percutaneous nephrostomy, kidney biopsy, or lithotripsy), urinary tract malignancy, or a renal transplant. Severe dyspnea, although present in this case, is uncommon and has been reported only a few times in the literature.
VENOUS AND ARTERIAL HYPERCOAGULABILITY AS PRESENTING MANIFESTATIONS OF PANCREATIC ADENOCARCINOMASudeep D. Thapa; Mohammed W. Imam; Lucero C. Chueca Villa. Henry Ford Hospital, Detroit, MI. (Tracking ID #1926773)
LEARNING OBJECTIVE 1: Recognize that pancreatic cancer related hypercoagulability can present as stroke, deep venous thrombosis and pulmonary embolism
LEARNING OBJECTIVE 2: Recognize that patients with new onset resistant diabetes mellitus may have pancreatic malignancy
CASE: A 58 years old African American male with history of smoking for 30 pack years, hypertension, STEMI, uncontrolled new onset diabetes mellitus, presented with transient speech and gait abnormality to the Emergency Department. He presented with history of slurring of speech and inability to ‘think of the right words’ while talking on the phone. He had no difficulty understanding what was being said to him. On presenting to the ED, new onset flattening of the left nasolabial fold was noted. Patient also reported right calf tenderness and mild swelling for 3 days. He also complained of a brief episode of chest discomfort which resolved spontaneously. He denied fever, headache, palpitations and weakness in his limbs. Of note, he also had a history of new onset uncontrolled Diabetes mellitus diagnosed 1 year prior and 30 lb weight loss in 3 months. He had consistently elevated Hba1c despite treatment. On investigations, mild elevation of troponin which peaked at 0.12 mcg/L was noted, there were no new ECG changes. CT scan of the head did not show any acute abnormalities. CT scan of the abdomen showed hypodense mass within the body tail junction of the pancreas measuring 4.8 × 3 cm and multiple masses were noted throughout the liver. Diffusion weighted MRI of the brain was done which showed an area of acute infarction involving the left frontal gyrus, punctate focus of acute infarction in the left centrum semiovale and punctate focus of acute early infarction in the right centrum semiovale. CT scan of the chest showed multiple small bilateral emboli and small left common femoral deep venous thrombosis. 2 D echocardiogram showed hypokinesis consistent with the patient’s history of myocardial infarction. No intra-cardiac thrombus or vegetation was noted. A liver biopsy of the metastatic mass was done and histopathology confirmed pancreatic adenocarcinoma, strongly positive for CK7 and CK19 on immunostaining.
DISCUSSION: Malignancy is a hypercoagulable state and pancreatic adenocarcinoma in particular is asscociated with intravascular thrombosis. Reports of patients presenting with stroke as the initial manifestation of cancer have been published and bi-hemispheric disseminated multiple ischemic lesions are particularly suggestive of an underlying malignancy. Deep venous thrombosis is a well-known manifestation of cancer and precedes the diagnosis of malignancy in more than 7 % of the cases. Malignancies in general and adenocarcinomas in particular are associated with increased thrombogenecity both in the venous and arterial blood vessels. Both pancreatic neuroendocrine tumors and pancreatic adenocarcinoma are related to new onset treatment resistant diabetes mellitus. Cancer induced tissue damage leads to diabetes due to islet cells and beta cell destruction. Furthermore, patients with diabetes have been shown to have increased risk of pancreatic cancer. Therefore, diabetes can be both a potential cause and effect of pancreatic cancer. In summary, pancreatic cancer should be considered in patients presenting with new onset treatment resistant diabetes and also in patients presenting with thrombosis of the venous and arterial blood vessels.
VENTRICULAR FIBRILLATION ARREST IN A PATIENT WITH PRINZMETAL’S ANGINAVenkatesh Alapati; Francis Golier; Maria Sobolev. Montefiore Medical Center, Bronx, NY. (Tracking ID #1937220)
LEARNING OBJECTIVE 1: Identify ventricular fibrillation arrest and treat it appropriately
LEARNING OBJECTIVE 2: Recognize Prinzmetal’s angina as a rare cause of ventricular fibrillation
CASE: A 57 year-old woman presented with sudden onset, severe substernal chest pain lasting 20 min. She was hypertensive (190/102 mmHg) with an otherwise unremarkable cardiac exam. Laboratory testing revealed elevation in troponin (0.3 ng/mL). Electrocardiogram demonstrated ST segment elevations in the inferior leads. During initial evaluation, the patient had a ventricular fibrillation arrest and immediately received chest compressions with one electrical defibrillation before return of sinus rhythm. She underwent emergent cardiac catheterization revealing normal coronary arteries without thrombus or occlusion. She was admitted to the Coronary Care Unit for further management. A diagnosis of Prinzmetal’s angina was made based on the presenting ST segment elevations in the setting of angiographically normal coronary arteries. Calcium channel blockers were initiated to prevent subsequent coronary spasm. She had no further episodes of chest pain and was discharged home.
DISCUSSION: Ventricular fibrillation is the most frequent mechanism of sudden cardiac death. It is electrically characterized by rapid, irregular waveform with variable amplitude, which can ultimately evolve into asystole. Adult Cardiac Life Support (ACLS) protocols should immediately be initiated once ventricular fibrillation is recognized. If return of spontaneous circulation is achieved, the underlying cause of ventricular fibrillation should be investigated. Myocardial infarction and electrolyte imbalances are the most common causes of ventricular fibrillation. Coronary vasospasm, or Prinzmetal’s angina, is a rare cause of myocardial infarction and ventricular arrhythmias. Prinzmetal’s angina is typically characterized by cyclical, non-exertional, chest pain with associated ST-segment elevation on electrocardiogram. Episodes are triggered by coronary vasospasm. The prevalence of the disease is not well known. In the United States, 4 % of patients who undergo coronary angiography show evidence of focal spasm. While ST-segment elevations in the absence of coronary occlusion is suggestive of Prinzmetal’s angina, provocative tests with potent vasoconstrictors (ergonavine or acetycholine) can be used during angiography to make a definitive diagnosis. Calcium channel blockers and long-acting nitrates are effective chronic therapies for coronary vasospasm. Myocardial infarction and life-threatening arrhythmias occur in approximately 25 % of untreated patients with Prinzmetal’s angina. Patients who experience an arrhythmic complication, especially ventricular fibrillation and sudden cardiac arrest, have a poor prognosis. Further investigation is warranted to determine if these patients will benefit from Automatic Implantable Cardioverter Defibrillators (AICD) or life vests as secondary prevention. Recognition and treatment of ventricular arrhythmias can save lives. Early recognition of Prinzmetal’s angina allows for appropriate treatment and prevention of potentially fatal complications.
VISUAL LOSS AT THE HEART OF THE MATTERLaura Hart; Harish Jasti. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1925881)
LEARNING OBJECTIVE 1: Recognize the presentation of a transient ischemic attack (TIA).
LEARNING OBJECTIVE 2: Utilize the American Heart Association (AHA) guidelines to perform a cost-conscious evaluation of a TIA.
CASE: A 58 yo female with a history of hypertension, type 2 diabetes, and obstructive sleep apnea presented after five episodes of transient right-sided visual field loss that occurred over the course of 2 days. During the episodes, she also noted associated zig-zag lines in her remaining visual fields, but felt that the visual loss respected the vertical (i.e. that her left visual field was preserved in both eyes). There was no associated numbness, tingling, vertigo, light-headedness, double vision, headache, or dysphagia. Review of systems was notable for dyspnea on exertion further than two blocks. She had no chest pain with or without exertion. She presented to an ophthalmologist on day 1 of symptoms and was diagnosed with an ocular migraine. When she continued to have episodes, she presented to a local ED for further evaluation. Head CT was negative for evidence of ischemia or hemorrhage. The patient was transferred to our institution for further evaluation. On arrival, the patient had a normal neurologic exam with no current visual field defects, which raised concern for TIA as the etiology of symptoms. A diagnostic angiogram demonstrated a 4.5 mm aneurysm located near the cerebellar artery and basilar artery junction but no vessel occlusion to suggest atherosclerotic disease as the etiology of symptoms. Subsequent echocardiogram noted a large, mobile left ventricular thrombus in an akinetic left ventricle. Based on these results, the patient’s visual symptoms were felt to be due to embolic events from the thrombus, which likely developed after a remote MI caused left ventricular infarction. Cardiac MRI showed viable myocardium, and the patient underwent cardiac catheterization and stent placement, after which she was placed on warfarin for treatment of the LV thrombus.
DISCUSSION: TIAs are defined by the AHA as brief episodes of neurological dysfunction resulting from focal cerebral ischemia and not associated with permanent cerebral infarction. TIAs are common, with approximately 200,000 to 500,000 occurring each year and an estimated incidence rate of 0.37 to 1.1 per 1000 per year. Due to the high risk of stroke after a TIA, a thorough work-up should be done to determine the etiology and treat accordingly. The AHA has developed guidelines for evaluation of patients after a TIA. Class I recommendations include head imaging, which is done both for diagnosis of TIA versus stroke, and for its prognostic value. MRI is preferred due to its higher yield. While only 13 % of CTs done after a TIA show clinically relevant ischemia, 46–81 % of MRIs show clinically relevant ischemia. Additionally, the prognostic ability of MRI is better characterized, with changes on diffusion-weighted imaging (DWI) on MRI correlating with an increased risk of stroke. In one study, the risk of stroke within 90 days of TIA was 10.8 % in patients with changes on DWI versus 4.3 % in patients without such changes. Additionally, patients should have non-invasive head and neck vessel imaging, via CT angiogram or MR angiogram performed concurrently with head imaging or as a separate study with carotid dopplers. This imaging is done to determine those patients who are most likely to benefit from carotid endarterectomy or other vessel intervention to prevent stroke. If non-invasive imaging is unclear, a cerebral angiogram should be completed, as this is the gold standard for evaluation of cerebral vasculature. Echocardiogram is a Class II recommendation in the evaluation of a TIA, as the yield is low (approximately 3 %) in the absence of history. However, an echo can be of diagnostic value when the initial evaluation has not revealed a definitive etiology, with yields improving to 61 % for a TEE. Additional Class II recommendations include EKG on presentation, and CBC, CMP, coagulation studies, and fasting lipids to be done as soon as possible to ensure that all other stroke risk factors are evaluated and treated accordingly. In summary, TIAs are common and can present with focal neurologic changes. While no evidence of infarction is noted in patients with a TIA, they are at an increased risk for stroke in the future, and therefore require a thorough work-up for the etiology and for risk stratification and management. Thoughtful utilization of the AHA guidelines allows for complete and cost-conscious care for patients who have suffered a TIA. Source: Definition and Evaluation of Transient Ischemic Attack. Stroke. 2009; 40: 2276–2293
WE SEE WITH OUR EYES, BUT WE SEE WITH OUR BRAINS AS WELL - PHANTOMS IN THE BRAIN: CHARLES BONNET HALLUCINATIONSKaran Singh; Vijairam Selvaraj. Baystate Medical Center, Springfield, MA. (Tracking ID #1926071)
LEARNING OBJECTIVE 1: Charles Bonnet syndrome (CBS) was first described in 1760 when he noticed his grandfather, who was blinded by cataracts, describing birds and buildings that Bonnet could not see. The prevalence of complex visual hallucinations in patients with visual impairment is estimated to be 11–15 %. They are usually transient and are often noted to occur among the educated. We describe the case of a visually impaired and psychologically intact male who reported having visual hallucinations to illustrate the importance of considering alternate explanations apart from psychological or drug induced causes when faced with these complaints.
CASE: 70 year old male with no significant medical history except for glaucoma who was functioning independently at baseline was brought in to the hospital by family as patient reported seeing “diminutive ninjas” inside his house. He was awake, alert and oriented and was able to carry a normal conversation. The patient was initially reluctant to describe his symptoms although sympathetic questioning revealed well organized and brilliantly clear, complex visual hallucinations, that were sharper than his usual vision. Prior occurrence of these symptoms had led him to realize they were not real although was frustrated by them. He was noted to have paranoid delusions that his wife may be involved with his hallucinations. MOCA testing revealed score of 21. Lab studies were normal. Eye exam revealed severe visual impairment secondary to the glaucoma. MRI of his brain revealed right occipital encephalomalacia that was related to an old infarct. Psychiatry was consulted and a diagnosis of Charles Bonnet syndrome was made although it was noted that this fixed delusion is fairly atypical.
DISCUSSION: The prevalence of CBS is grossly underestimated to be between 1.84 and 3.5 % in the geriatric population. Even though patients may not voluntarily disclose visual hallucinations, they tend to respond to leading questions about the same. The proposed hypothesis is that in visually impaired individuals, the visual cortex compensates with abnormally increased activity and conjures up hallucinations from random firing of nerve cells. Although it is a diagnosis of exclusion, the syndrome is often under-diagnosed in clinical practice due to patients’ reluctance to admit to hallucinations for fear of being labeled mentally unstable in addition to physicians’ lack of awareness of the diagnosis. Physicians need to screen older adults with visual impairment for this syndrome and also be able to provide high quality education as reassurance and explanation can have a powerful therapeutic effect. Improving the visual function and addressing social isolation are also helpful in improving quality of life.
WEIGHT LOSS AND IDIOPATHIC VENTRICULAR TACHYCARDIA: A “GRAVE” SITUATIONClaire Larson; Ryan Laponis. UCSF, San Francisco, CA. (Tracking ID #1920287)
LEARNING OBJECTIVE 1: Review the common causes of ventricular tachycardia
LEARNING OBJECTIVE 2: Recognize hyperthyroidism as a rare but important cause of “idiopathic” ventricular tachycardia
CASE: A 53 year old man with a history of hypertension and obesity presented with a 3 week history of fatigue and dyspnea on exertion. He reported a week-long flu like illness prior to symptom onset, and since then had decreased exercise tolerance, shortness of breath, palpitations and diaphoresis. He denied chest pain. Review of systems was positive for an 80 lb weight loss over the past 8 months. He reported a family history of hypertension, myocardial infarction, stroke, thyroid disease, and no sudden cardiac death. Exam was remarkable for a heart rate of 92. Chemistries, complete blood count, and chest x-ray were unremarkable. He underwent a stress echocardiogram which showed 1 mm upsloping ST changes in V5/V6, an apical wall motion abnormality, and multiple episodes of monomorphic non-sustained ventricular tachycardia (NSVT). He underwent coronary angiography, which showed no angiographically significant disease. He was discharged on metoprolol and verapamil, with a diagnosis of idiopathic VT. At a Cardiology appointment 10 days later, labs from his initial visit revealed an undetectable TSH and elevated free T4. He was referred urgently to Endocrinology, and at his visit there was noted to have lid lag, proptosis, thyromegaly and tremors. Laboratory evaluation and ultrasound confirmed a diagnosis of Graves’ Disease. He was started on methimazole and continued on the beta blocker. Over the next 2 months, his symptoms of palpitations and dyspnea on exertion resolved. Ziopatch monitoring showed no recurrent ventricular arrhythmia, a repeat stress test revealed no arrhythmias, and he had gained 20 lb.
DISCUSSION: Most NSVT is due to either structural heart disease (most commonly due to coronary artery disease or a cardiomyopathy), or abnormal cardiac ion channels/structural proteins. Ten percent of cases are idiopathic. For patients with idiopathic monomorphic VT, the ECG between episodes, stress test, and coronary angiography should be normal. The most common form of idiopathic VT, Right Ventricular Outflow Tract VT, accounts for 70 % of all cases, and is caused by catecholamine-mediated delayed afterdepolarizations, triggered by exercise or stress. Cardiovascular symptoms in hyperthyroid states are common. T3 is transported into the cardiac myocyte, and produces findings similar to those of beta adrenergic stimulation. Clinical findings may include increased: heart rate, pulmonary artery pressure, cardiac output, ejection fracture, and myocardial oxygen consumption; and decreased: SVR and diastolic blood pressure. Sinus tachycardia is the most common rhythm abnormality in hyperthyroidism, while arrhythmias are primarily supraventricular, with atrial fibrillation occurring in 5 to 15 % of patients. Ventricular arrhythmias due to hyperthyroidism are extremely rare, particularly in the absence of underlying cardiac disease. Review of the literature reveals at least seven cases of thyrotoxicosis induced VT, with three cases in the setting of underlying CAD. In all of the patients, the ventricular arrhythmias resolved with a euthyroid state. This case highlights the initial work-up and management of ventricular tachycardia, and underscores the many cardiovascular effects of Graves’ disease, including the rare side effect of ventricular arrhythmia.
WEIL HE WAS RENOVATINGPoppy Markwell; Rachel Sandler; Patricia Harlan; Jeff Percak. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926980)
LEARNING OBJECTIVE 1: Demonstrate the risk of leptospirosis during demolition work
LEARNING OBJECTIVE 2: Recognize the clinical presentation, diagnosis and treatment of leptospirosis
CASE: A 61-year-old man with no past medical history presented with 4 days of bilateral lower extremity muscle pain and subjective fevers. He also reported decreased urine output. Over the preceding weeks, he reported doing strenuous work, including demolition and renovation of a blighted New Orleans apartment. He denied recent illness, sick contacts, animal contact, or travel in the last 6 months. On physical exam, patient was febrile and leg muscles were tender to palpation bilaterally. Initial tests suggested rhabdomyolysis with CK >8000 and creatinine elevated at 4.9. Thrombocytopenia and mild transaminitis were noted. Profound hyperbilirubinemia developed during his hospital course. Renal failure ultimately required dialysis. Broad-spectrum antibiotics were given initially and changed to ceftriaxone when leptospirosis was considered. The patient fully recovered renal and liver function prior to discharge. Serologic testing ultimately confirmed leptospirosis.
DISCUSSION: Leptospirosis is a globally encountered zoonotic infection caused by the spirochete Leptospira interrogans, commonly through exposure to mucous membranes, conjunctiva, or breaks in the skin with infected animal urine. While common in tropical areas, the disease is re-emerging in the developed world. The occupational risk of veterinarians, miners, sewer workers and others who may contact animal urine has long been established. Demolition has been suggested as a risk factor, presumably due to exposure to materials contaminated with rodent urine. The disease classically presents as a biphasic illness: an acute phase with leptosires in the blood for about a week and an immune phase with antibody and inflammatory response. Symptoms range from self-limiting febrile illness to acute kidney injury to classic Weil’s disease with jaundice, renal failure, and hemorrhage. The mortality of Weil’s Disease is 10 %. Pulmonary complications and mild rhabdomyolysis are also common features. The gold standard to diagnose leptospirosis is the microscopic agglutination test. Serologic testing, including rapid tests, is also useful as culture of Leptospira is difficult. Penicillin, doxycycline, and cephalosporins are all used to treat leptospirosis. However, the benefit of antibiotics in acute leptospirosis infection is debated. Corticosteroids have been used to limit the damage from host immune response. Supportive care is the mainstay of treatment of severe cases. This case reminds the internist that leptospirosis can be a disease of the tropics but should be considered in cases of febrile illness in persons who have risks of exposure as may be encountered during demolition and renovation.
WHAT IS POTENTIALLY CONCEALED IN UNCONSCIOUS PATIENT WITHOUT DEFINITE ORIGINKanoko Fukaya; Chiaki Murase; Munehisa Atsumi; Mitsunori Iwase. TOYOTA Memorial Hospital, Toyota, Japan. (Tracking ID #1928587)
LEARNING OBJECTIVE 1: Recognize that severe sepsis can be an important cause of unconsciousness.
LEARNING OBJECTIVE 2: Remind Group A streptococcus as responsible bacteria in the rapidly progressive cellulitis.
CASE: An 87-year-old woman came to our emergency department with a history of unconsciousness. Three hours before admission, her family found her unconscious at home. She became conscious rapidly when her family called. She had no prodromal symptoms such as chest pain, headache, cold sweats, and nausea. She had atrial fibrillation without treatment and chronic heart failure on medication. She had noticed pitting edema in both legs for recent several years, but she had neither tenderness nor laterality. She also had a past history of cerebral infarction with no sequelae about a decade ago, and gastric ulcer 7 years ago. Her current medications included aspirin, azosemide, and omeprazole. On examination in the emergency department, she was alert and oriented. The body temperature was 37.2 °C, the blood pressure of 80/56 mmHg, the pulse of 51 beats per minute with irregularity, the respiratory rate of 16 breaths per minute, and the oxygen saturation 98 % while breathing ambient air. The conjunctivas were neither anemic nor icteric. The respiratory sound was clear in both lungs, and no murmur was detected. The abdomen was soft and flat without any tenderness. Neurological findings were unremarkable. EKG showed atrial fibrillation without ST-segment deviations. Though the serum troponin-I level was minimally elevated (0.28 ng/mL) at first, no additional change was detected with follow exam after 4 h. No fresh infarcted regions were found in the plain CT scan and MRI of the brain. The cause of unconsciousness wasn’t revealed. We examined her again from head to toe, removing her socks. Then, we found redness, swelling, tenderness, and warmth in her left lower extremity, especially foot. There was no trauma but tinea lesions were seen at her toe. The laboratory data revealed that white-cell-count increased 20,300/μL, C-reactive protein 1.7 mg/dL, and D-dimer 11.7 μg/mL. Hemoglobin and Electrolytes, AST, CK and lactic acid were in normal range. Adding the enhanced CT image, both deep vein thrombosis and pulmonary embolism was denied. Then, cefazolin was started for the treatment of cellulitis. After admission, her blood pressure decreased to 75/48 mmHg and the pulse was 76 beats per minute. Furthermore, the redness area of the left leg lesion rapidly progressed from the foot to the knee in several hours. She didn’t have the episode such as water exposure or cat bite. We decided to add vancomycin and clindamycin. On the following day, Group A beta-hemolytic streptococcus was determined from the two sets of blood cultures on admission, then we changed the antibiotics to ampicillin and clindamycin. The treatment of antibiotics lasted for 2 weeks, and cellulitis was improved without progression to necrotizing fasciitis. Fortunately, she could go home on foot on day 20.
DISCUSSION: The chief complaint of this case was unconsciousness and its major differential diagnoses include cardiac diseases, hemorrhage, pulmonary embolism, and neurologic disorders. As for this case, these common underlying diseases were ruled out for the first step in the emergency department. It is said that when we see patients under the unexplainable conditions like consciousness disturbance, hypotension or something like that, we must not miss the signs of early sepsis. Finally we found cellulitis on her left leg by scrutinized physical examinations from head to toe. We did learn that the unconsciousness of unknown origin may be due to early sepsis. Additionally, as for the cellulitis of this case, not only did her skin findings get worse rapidly, but she became also hypotensive. Rapidly progressive erythema with signs of systemic toxicity should be considered of severe infection caused by group A beta-hemolytic streptococcus. Group A streptococcus (GAS), also called “flesh-eating bacteria”, causes a wide range of infections and severe complications. Importantly, it may induce severe invasive infections such as necrotizing fasciitis and streptococcal toxic shock syndrome. One study shows that the overall case fatality rate of GAS infection was 11 % but that was much higher in patients with toxic shock syndrome (55 %) and necrotizing fasciitis (58 %). Additionally, amputation was performed in 22 % patients with necrotizing fasciitis. In this valuable case, proper antibiotic therapy was performed and finally we could save the patient’s life and her left leg. Therefore, we should start antibiotics promptly under critical condition such as “flesh-eating bacteria”.
WHAT IS THIS RASH OVER THE JOINTS?Ryan Morton1,2; Muhammad Usman2; Lucero C. Chueca Villa2,1. 1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Hospital, Detroit, MI. (Tracking ID #1937537)
LEARNING OBJECTIVE 1: Recognize the clinical characteristics of Löfgren’s syndrome
LEARNING OBJECTIVE 2: Expand the differential diagnosis of skin rash and arthralgias
CASE: This is a 31 year old Maltese male with a past medical history of type 2 diabetes mellitus presenting to his PCP with a 1 week history of left wrist swelling and erythema after a hunting trip in northern Michigan in November. He was prescribed Bactrim for potential cellulitis. Five days later he returned with worsening symptoms. More joints were involved as both elbows, ankles, and his left knee were also swollen with a blanching, erythematous cutaneous rash distributed only over the joints. He reported subjective fevers throughout the course of the disease but had no recorded temperature. Lyme titers were drawn, arthrocentesis was performed in the left ankle, and doxycycline was prescribed with follow up in 4 days for potential Lyme disease. At follow up, he was tachycardic and had a leukocytosis of 18,000 cells/mL so he was admitted to Henry Ford Hospital. He denied any target shaped lesions, sore throat, bug bites, sexual contact, history of STD’s, contact with carcasses, family history of autoimmune disease, chest pain, shortness of breath, abdominal pain, dysuria, or diarrhea. A salmon colored macular rash on his chest was also observed on admission, which had been unnoticed by the patient. Lab tests showed slight elevations in AST and ALT and a marked drop in albumin of 2.2 g/dL. He had a slight microcytic anemia with low serum iron and significantly elevated ferritin at 900 ng/mL. Blood and synovial cultures were negative for growth and Lyme titers were negative. Other infectious etiologies were ruled out as HIV, hepatitis B, hepatitis C, and syphilis showed negative results. Parvovirus was positive for IgG but negative for IgM. An ANA was slightly positive with titer levels of 1:160 and a speckled pattern of immunofluorescence but double stranded DNA tests were negative. Other autoimmune etiological tests were negative including RF, ENA, ANCA, and celiac panel tests. A chest x-ray was performed that showed right sided hilar adenopathy suspicious for sarcoidosis, confirmed by a CT scan of the chest. Elevated ACE levels of 64 U/L, lysozyme levels of 23 ug/mL, and a biopsy showing septal panniculitis consistent with erythema nodosum confirmed the diagnosis of Löfgren’s syndrome. The patient was diagnosed with sarcoidosis, discharged, and is currently on a treatment regimen of prednisone and methotrexate with significant improvement of his symptoms.
DISCUSSION: Löfgren’s syndrome is an acute type of sarcoidosis that is defined by the triad of migratory arthralgias, bilateral hilar lymphadenopathy, and erythema nodosum. It is most frequently found in women, and is more common in Scandinavian and Irish populations. Erythema nodosum presents as erythematous tender nodules. Lesions can appear on any extremity or on the trunk, but are typically present on the pretibial surfaces of both legs. These are deep, evolving lesions which usually are difficult to visualize initially. Lesions progress to red or violet cutaneous lesions and spontaneously resolve over 2 to 8 weeks. Non specific symptoms such as fever, malaise and polyarthralgias frequently accompany erythema nodosum. The etiology is unknown but a Type IV delayed hypersensitivity reaction is the most likely pathogenesis suspected at this time. As other symptoms in addition to erythema nodosum spontaneously remit as well, the prognosis associated with Löfgren’s syndrome is quite good. Males presenting with sarcoidosis generally do not have erythema nodosum, rather they typically present with bilateral ankle arthritis. Our patient was atypical in a number of ways, in that no nodules were palpated, his lesions were non-tender and only distributed over the joints, and his sex and ethnicity make sarcoidosis less likely. This atypical presentation of sarcoidosis and erythema nodosum should be considered in the differential diagnosis of any patient presenting with polyarthralgias or unexplained erythematous cutaneous lesions. This would avoid the unnecessary testing seen in our patient, facilitating appropriate diagnosis and prompt treatment.
WHEN DOCTORS THINK THEY KNOWDima Dandachi; Venu Pararath Gopalakrishnan. Saint Francis Hospital, Evanston, IL. (Tracking ID #1925291)
LEARNING OBJECTIVE 1: Suspect Septic Pulmonary Emboli in a patient with multiple bilateral peripheral pulmonary nodules and fever with or without obvious predisposing factors.
LEARNING OBJECTIVE 2: Treat Septic Pulmonary Emboli early with prompt antimicrobial therapy to achieve a successful outcome.
CASE: A 54 years old, previously healthy male patient, presented to our hospital with acute onset left sided severe chest pain that progressed in intensity over 1 week The pain was sharp in character, worsened with inspiration, and not relieved with 10 tablets of ibuprofen a day. He complained of mild dry cough and occasional chills but didn’t have any documented fever, sputum, hemoptysis or shortness of breath. Review of system was positive for bright blood per rectum occasional for the last year that was attributed to hemorrhoids. Denied any unintentional weight loss, nausea or vomiting. He had a root canal procedure done 3 weeks ago. His is a smoker 30 pack year, drinks alcohol occasionally, denied any IV drug abuse, works as a cab driver. In the Emergency Department patient was in severe distress because of pain. Patient was afebrile and hemodynamically stable male with Clinical examination revealed normal heart and respiratory findings. Abdominal exam was positive for mild epigastric tenderness, fecal occult blood test was positive. Hemogram revealed WBC of 12.8 k/mm cu, hemoglobin 11.9 g/dL and MCV 89 fl. CT Chest with contrast done was negative for pulmonary embolism, but showed multiple bilateral pulmonary nodules suspicious for malignancy. Left upper lobe showed subpleural 2.4 × 1.5 cm rounded opacity, emphysematous changes, left hilar lymphadenopathy and moderate size left sided effusion. CT abdomen and pelvis showed folds in the stomach are thickened, otherwise unremarkable. The patient was informed about the most likely possibility of a gastrointestinal malignancy with lung metastasis or primary lung malignancy. Next day, EGD done was negative. Colonoscopy showed non-bleeding internal hemorrhoids, the rest of the exam was normal. He underwent percutaneous CT guided lung biopsy. Pathology report surprisingly showed distended alveoli filled with polymorphonuclear leukocytes mixed with fibrin, no evidence of malignancy, findings consistent with septic emboli. Special stains for organisms were negative. Blood cultures were negative, Trans-esophageal echocardiograph was normal. Mandibular film done was negative for dental abscess. HIV serology, Quantiferon gold, Beta-d glucan, Aspergillus, mycobacterial culture of sputum and pleural fluid were negative. During hospital stay patient developed fever when antipyretics were stopped and his WBC count increased. Left sided thoracocentesis was done and pleural fluid analysis revealed exudative fluid by light’s criteria. Both gram stain and culture of pleural fluid were negative. Patient started empirically on Ceftriaxone and Vancomycin. Patient improved significantly. Antibiotics were continued for 14 days. He was discharged home in a stable condition.
DISCUSSION: Septic pulmonary emboli (SPE) is a serious and uncommon condition that poses a diagnostic challenge. Patients with septic pulmonary emboli who are diagnosed early and treated with broad-spectrum antibiotics have a better prognosis than patients with a delayed diagnosis. Establishing the diagnosis of septic pulmonary emboli is not always straightforward, as the radiographic findings may be non-specific. Blood cultures may be negative initially and there may not be a detectable heart murmur. Septic pulmonary emboli travel to the lungs from numerous sources, including infected heart valves, peripheral sites of septic thrombophlebitis, and infected indwelling venous catheters. Other patients at risk are those with odontogenic infections. In patients with a history of intravenous drug use, the most common source of septic pulmonary emboli is an infected tricuspid valve. An echocardiogram can be obtained to evaluate for the presence of tricuspid valve vegetations. However, echocardiography may be limited technically and very small vegetations (less than 3 to 4 mm) may not be detected. Usual presenting symptoms are often non specific. Similarly, chest radiography is not helpful to establish a diagnosis. CT is more useful, usually shows multiple nodular opacities peripherally located. SPE can be suspected by the presence of potential source of underlying infection, febrile illness and multiple pulmonary nodules. Most common pathogen involved is Staph Aureus. We report a case of septic pulmonary emboli that was misdiagnosed as malignancy. SPE can be fatal therefore early diagnosis and appropriate antibiotic therapy are important for the control of the infection.
WHEN EYES DROOP AND THINGS GET BLURRY - THINK BOTULISMRobert H. Cooper1; Roger D. Smalligan2; Casie Stoughton4; J. M. Richardson4; Deree Duke4; Aimee L. Geissler3; Agam K. Rao3; Sarah D. Bennett3; Reid Harvey3; Sara Syeda1; Beverly Nixon-Lewis1. 1Texas Tech University HSC, Amarillo, TX; 2Texas Tech University HSC, Amarillo, TX; 3Centers for Disease Control and Prevention, Atlanta, GA; 4Potter-Randall Bi-County, Amarillo, TX. (Tracking ID #1934880)
LEARNING OBJECTIVE 1: Recognize presenting symptoms of botulism to treat the patient and stop an outbreak.
LEARNING OBJECTIVE 2: Differentiate botulism from other neuromuscular disorders.
CASE: A previously healthy 32-year-old Iraqi man presented with blurry vision and difficulty speaking for 3 days. He denied fever, chills, headache, neck stiffness, nausea, vomiting, diarrhea, constipation, chest pain and shortness of breath. He had no recent travel, denied smoking, alcohol and drug use. There was no FH of neurologic disorders. On physical exam he was alert, oriented and had normal vital signs. Heart, lung and abdominal exams were normal. Neuro exam showed ptosis, disconjugate gaze and reactive pupils. He had dysarthria, bilateral facial droop and neck weakness, and no gag reflex. No other deficits in strength were observed and DTR’s were normal. Initial testing included CBC, CMP, UDS, LP and MRI of the head and neck, all of which were negative or nonspecific. A Tensilon test was negative and additional tests for heavy metals, acetylcholine receptor antibodies and polio were negative. The patient identified two ill contacts who presented with similar signs and symptoms within the previous month, both were diagnosed with atypical myasthenia gravis due to a slightly positive Tensilon test and neither responded to pyridostigmine. One of these contacts had been discharged a few weeks earlier and the other was admitted days earlier and required mechanical ventilation. This similar presentation of three friends within 1 month raised the suspicion of botulism. The local health department and the CDC were notified immediately. After careful review of the case histories, signs and symptoms, botulinum antitoxin was released and administered within 8 h to the two patients who had ongoing progression of symptoms. The apartment shared by all three case patients was searched and potentially contaminated foods which were tested. A fourth case (acquaintance of the 3) was identified at a separate hospital. After many hours of interviews, a common food source was found that the four case patients had eaten at two different apartments on at least three separate occasions. The shared food product was a common Middle Eastern dish known as turshi and was prepared by the case patient with the earliest symptom onset. The turshi was made with fresh vegetables that were fermented at room temperature for weeks. No turshi was available for definitive testing; however, fermented vegetables are known to be associated with botulism outbreaks. Serum and stool samples from the case patients were negative for botulism by mouse bioassay. EMG/NCV testing was conducted on two of the case patients and results were inconclusive. In addition to the botulinum antitoxin administered, supportive care was provided to each patient, three of whom showed slow but consistent improvement and were discharged home. All were given education on proper food preparation techniques. The intubated patient required tracheostomy and longer term mechanical ventilation, but continues to improve slowly.
DISCUSSION: Although on average around 17 cases of adult botulism, caused by toxin production of Clostridium botulinum, are confirmed annually in the USA, myasthenia gravis and Miller-Fisher variant of Guillain-Barre syndrome can have similar presentations to botulism leading to botulism cases being misdiagnosed. Much of the confusion is due to the rarity and the varied way in which botulism can present, including combinations of ptosis, diplopia, slurred speech, dysphagia, dysarthria, muscle weakness and respiratory depression. Classically, it presents with descending paralysis with cranial nerve deficits. Work-up can be misleading as well since false-positive Tensilon tests can occur as in 2 of our cases. EMG/NCV studies are difficult to interpret unless the operator has experience with botulism. Although honey is often associated with botulism, it is only relevant in infant botulism cases. Home canned foods are the most common source of foodborne botulism, while black tar heroin is the most common cause of wound botulism. If botulism is diagnosed promptly, antitoxin can be administered to neutralize circulating toxin, halt symptom progression and shorten disease course; however, existing nerve damage is not reversed. Supportive care is required for days to months to allow for nerve regeneration. CDC has an on-call botulism team available 24/7 to discuss suspected cases and release antitoxin immediately when a single case or outbreak occurs. In conclusion, it is imperative for physicians to include botulism in the differential diagnosis of patients with ptosis, ocular and bulbar symptoms, facial paralysis and dysphagia in addition to descending flaccid paralysis as prompt administration of antitoxin can significantly improve outcomes. Early involvement of the health department and CDC is also needed to identify the food source in the event of a botulism outbreak and thus prevent additional cases of intoxication.
WHEN OCCAM’S RAZOR FAILS: LINEZOLID INDUCED LACTIC ACIDOSIS IN A PATIENT WITH SEVERE AORTIC ATHEROSCLEROTIC DISEASEKaran Singh; Sunitha Alluri. Baystate Medical Center, Springfield, MA. (Tracking ID #1926067)
LEARNING OBJECTIVE 1: Linezolid induced lactic acidosis was first reported in 2003, and till date there are only few case reports about the same. Linezolid is often used for prolonged duration and thus it is important to keep this side effect in mind.
CASE: 65 yo M with a complicated PMH which included uncontrolled Diabetes, with numerous prior complicated diabetic infections on Linezolid since the past 6 weeks. He had severe PVD, CKD, CAD s/p CABG along with severe diabetic gastroparesis. He presented with vague complaints of nausea, vomiting and lethargy for 3 days. He clearly denied any abdominal pain. He denied any constipation or diarrhea. He resided in a nursing home and review of their records did not reveal any episodes of hypotension. He was in NSR and his abdomen was soft and non-tender. He had a wound vacuum on, and the wound itself was healthy. His labs revealed a lactate of 6, with an AG of 20 and bicarbonate of 21. He was also pancytopenic and his platelet and WBC counts were normal 2 months back. A CAT scan was done of the abdomen which did not reveal any evidence of colitis. Considering his overall picture, it was thought to be type B Lactic acidosis secondary to Linezolid. On review of his records, there were no new medications except Linezolid. Patient’s lactic acidosis and thrombocytopenia both resolved within 5 days of stopping Linezolid
DISCUSSION: There are limited choices for oral antibiotic therapy in disease caused by resistant gram positive organisms. This is what has made Linezolid an attractive option when IV access is not feasible or when the duration of treatment is long. Linezolid is currently FDA approved for the treatment of Vancomycin resistant Enterococcus, nosocomial pneumonia caused by Staphylococcus and Streptococcus, complicated skin and skin structure infections and community acquired pneumonias. The mechanism by which this drug causes lactic acidosis has not completely been elucidated. Mitochondrial toxicity has been proposed as a causative mechanism. There have also been mortalities reported due to this adverse effect. There is no proven therapy to treat Linezolid induced Lactic Acidosis. In addition to cessation of the drug, thiamine has been used in treatment (potential benefits without harm). A review of the literature reveals that the majority of episodes occurred in older patients and those getting prolonged therapy, and resolution of lactate levels varied from 2 days to 2 weeks. This case and others described in the literature demonstrate importance of continuous monitoring of medication related adverse effects and those factors which might predict which patients are at higher risk
WHEN SEIZURES CAUSE DROWNING - WITHOUT THE WATERAlice Williamson; Eric Kasprowicz; Ramprasad Kandavar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926987)
LEARNING OBJECTIVE 1: Identify common and uncommon causes of seizure
LEARNING OBJECTIVE 2: Understand the importance of seizure management
CASE: A 31 year old woman presented to the emergency department after having a grand-mal seizure at work. The seizure resolved prior to EMS arrival. In the emergency department, she had another grand-mal seizure that resolved with lorazepam. She also developed shortness of breath and was found to be hypoxic requiring supplemental oxygen via nasal cannula. She was admitted to medicine for further support and work-up. Of note, she had a known seizure disorder but had been unable to fill her one of prescriptions. Also, our patient had suffered from past episodes of pulmonary edema requiring intubation during episodes of seizures. On exam (when patient was no longer post-ictal), vitals were normal except respirations were 22 with oxygen saturation 85 %. She was alert and oriented, able to speak in full sentences though with a little bit of respiratory distress. She had faint bibasilar crackles on lung exam. CBC and metabolic panel were normal. Valproic acid level was less than 3. Chest x-ray revealed a cardiomediastinal silhouette that was enlarged with continued findings of volume overload including interstitial and alveolar edema, central venous congestion and mild bilateral pleural effusions (consistent with previous chest x-rays taken after she had seized).
DISCUSSION: While uncommon, we diagnosed our patient with neurogenic pulmonary edema (NPE). NPE is defined as clinical syndrome characterized by the acute onset of pulmonary edema following a significant central nervous system insult (1). Upon close review of her medical record and prior imaging, we discovered that our patient had been admitted on three separate occasions due to seizures associated with hypoxia and pulmonary edema, all of which required ICU admission and at least one requiring intubation. Previously, she had been diagnosed with aspiration pneumonitis associated with her seizure activity. While such a diagnosis is plausible, the recurrence of these episodes led our team to establish the diagnosis of neurogenic pulmonary edema. During this admission, she was treated with intravenous furosemide and supplemental oxygen via nasal cannula. This diagnosis of NPE further underscores the importance of controlling our patient’s seizure disorder.
WHEN SHOULD WE CONSIDER SYSTEMIC LUPUS ERYTHREMATOSUS IN PATIENT PRESENTS WITH GUILLAIN-BARRE SYNDROMEHamza H. Tantoush; Ahmed Abuzaid; Haitham Al Ashry. Creighton University Medical Center, Omaha, NE. (Tracking ID #1917176)
LEARNING OBJECTIVE 1: Lupus should be considered in patients with Guillain-Barré syndrome who do not respond to intravenous gamma globulins
CASE: A 59 years old female presented with progressive muscle weakness of arms and legs proximal more than distal, together with parasthesia in both hands and feet for one-month duration. Her medical history was remarkable for depression, hypertension, and GERD. Physical examination on admission revealed a blood pressure of 156/86-mmHg and Neurological examination showed absent deep tendon reflexes, and severe symmetrical muscle weakness lower and upper limbs proximal more than distal. Cranial nerves are all normal. Sensory examination showed diminished sensation to light touch pain, vibration and sense of position. The sensory perception was more impaired distally compared to proximally and on the trunk. Patient did not show any urinary bladder or anal sphincters problems. Laboratory revealed an increased esr, crp, normal creatinine, low serum albumin normal LDH, low Platelets, low leucocyte count Folic acid and B12 all normal. Serum and urine protein electrophoresis were negative; The cerebrospinal fluid revealed protein cellular dissociation; urine analysis revealed high urine protein of spot protein creatinine ratio increased. Brain and neck magnetic resonance imaging did not show any pathologic lesions suggesting her weakness. The electromyogram and nerve conduction velocity also indicated sensorimotor demyelinating polyneuropathy. Treatment was started with oral prednisone and intravenous immunoglobulin G for 3 days. No improvement in her muscle weakness. Because of significant proteinuria, additional investigations were performed, including autoimmune serology. These revealed a positive antinuclear antibody ANA test, anti dsDNA, negatives both C/P ANCA, and decreased C3 and slightly decrease C4 values which raised the suspicion of SLE diagnosis. A percutaneous kidney biopsy was performed, which showed membranous lupus nephritis Class V. Because of this severe form of lupus nephritis the patient was treated from day 8 with Mycophenolate along with the high doses oral prednisone. This treatment regimen was tolerated rather well.
DISCUSSION: The prevalence of SLE in patients with Guillain-Barré syndrome has been reported to be between 0.6 and 1.7 %. Diagnosis of Guillain-Barré syndrome is confirmed if the CSF, and clinical neurophysiology studies show typical abnormalities Acute inflammatory demyelinating polyneuropathy, is the most common form of Guillain-Barré syndrome in the most parts of world. Because of the combination of Guillain-Barré syndrome and lupus nephritis, it is difficult to formulate an optimal therapeutic regimen. The treatment strategy is important in early phase of acute neuropathies with pulse steroid and plasma exchange. The association of Guillain-Barré syndrome with lupus seems to have implications for both treatment and prognosis. Prednisone and immunosuppressive therapy cyclophosphamide or mycophenolate should be considered in patients with, Guillain-Barré syndrome as a feature of lupus nephritis.
WHEN SIZE BEGINS TO MATTER: ISONIAZID-INDUCED GYNECOMASTIA IN A PATIENT WITH LATENT TUBERCULOSISJoanna Marie B. Aquino-Laban1; Aimee L. Mandapat2. 1Summa Health System, Akron, OH; 2Summa Health System, Akron, OH. (Tracking ID #1912687)
LEARNING OBJECTIVE 1: Recognize the clinical features of isoniazid-induced gynecomastia in a patient with latent tuberculosis
CASE: A 65-year-old asymptomatic African-American male presented with a positive tuberculosis (TB) skin test (~22 mm) found during routine testing for hospital volunteers. He is a retired chemist and denied any recent travel, but reported possible TB exposure during his previous volunteer job in a hospital. Chest x-ray was negative. The patient was diagnosed with latent TB infection, and was started on a 9-month regimen of daily isoniazid and pyridoxine. About 7.5 months after initiation of therapy, the patient noted bilateral breast swelling and tenderness. He denied headache, blurred vision, nipple discharge, or changes in secondary sexual characteristics. Blood work showed mild elevation of estradiol, follicle stimulating hormone, and prolactin. Mammogram confirmed the presence of gynecomastia. Given the temporal association of the anti-TB drug to the occurrence of breast swelling, isoniazid was immediately discontinued. One month after withdrawal of the drug, the patient reported partial resolution of his symptoms. He continues to feel better as of this writing.
DISCUSSION: Gynecomastia is a rare but recognized side effect of isoniazid therapy with at least 14 cases reported worldwide. Proposed mechanisms include altered vitamin B6 breakdown leading to defective hepatic estrogen-androgen metabolism, increase in gonadal function after weight gain (“refeeding gynecomastia”), and inhibition of cytochrome P450 system that may impair estrogen metabolism in the liver. Better understanding of this drug association can lead to prompt recognition and appropriate management. To our knowledge, this is the first case report of this rare side effect of isoniazid in the United States, and first in latent tuberculosis worldwide.
WHEN THE MCV IS THE MVP!Alice Williamson; Arti Allam; Ramprasad Kandavar. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1926978)
LEARNING OBJECTIVE 1: Understanding the importance of the entire CBC
LEARNING OBJECTIVE 2: Comprehending the work-up for abnormal CBC values
CASE: A 24-year old woman with sickle cell disease presented to the emergency department complaining of bilateral lower extremity pain as well as back pain and stomach pain. She stated that the pain was consistent with her sickle cell type pain began 2 days prior to presentation. Her vitals included a temperature of 37.1, pulse of 78, blood pressure of 120/80, respiratory rate of 16, and O2 saturation of 100 % on 2 L nasal cannula. She was in mild distress, complaining of diffuse pain, but alert and oriented. She had mild scleral icterus and a 2/6 systolic murmur. Her lungs were clear to auscultation bilaterally, and her abdomen was soft with diffuse right upper quadrant and epigastric tenderness to palpation. Bowel sounds were present, and her extremities were warm with no rashes or edema. Laboratory values included WBC 10.5, Hgb 7.9, PLT 477, MCV 109.1, RDW 15.7, Na 139, K 3.8, Cl 105, Bicarb 22, BUN 4, Cre 0.4, Ca 8.9, Folate level 18.4, and B12 level 163. Further Work-Up revealed an Anti-Intrinsic Factor Antibody Negative (normal), Anti-Parietal Cell Antibody 38.6 (high), and Methylmalonic Acid (MMA) 129 (within normal range based on healthy blood bank donors).
DISCUSSION: Pernicious anemia is not commonly associated with sickle cell anemia; however, B12 deficiency may be under diagnosed in black patients (1, 2). As of 2010, only four cases of these disease coexisting were documented (3). In a patient with chronic pain issues due to sickle cell disease, vitamin B12 deficiency could easily be overlooked as a contributor to a patient’s pain. This case is peculiar in that her B12 was low and she had Anti-Parietal Cell Antibodies present but her MMA was within normal range—a range defined as normal based on the values of healthy blood bank donors. This may be associated with the proposed changes in metabolic pathways in patients who have cobalamin deficiency (4). Another possible explanation is a low serum transcobalamin, though this was not assessed in our patient nor would that explain the antibodies to parietal cells (3). Regardless of these contradictions and based on the risk-vs-benefit of starting Vitamin B12 replacement, we treated this patient for B12 deficiency. This case reminds clinicians to scrutinize every CBC and to question abnormalities. In this case, a patient with HbSS should have a low MCV, not a high MCV.
WHEN THE PAST CLOUDS THE PRESENT: A UNIQUE CAUSE OF ACUTE ON CHRONIC BACK PAINCraig Mescher; Asher Tulsky. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1938733)
LEARNING OBJECTIVE 1: Appreciate that bias exists in the care of patients who present with low back pain.
LEARNING OBJECTIVE 2: Recognize the importance of identifying red flags in acute back pain and their impact on pretest probability for serious disease particularly in patients on chronic opiates.
CASE: A 49 year old female with a history of fibromyalgia with chronic back pain on opiate medication and left breast atypical ductal hyperplasia initially presented to the ED with new onset right lower back pain radiating to her right groin and thigh not controlled by her usual pain regimen. A lumbar spine x-ray was negative for bony lesions and she was discharged home with pain medications. Six days later she returned to the ED now with low back pain radiating down both legs. A CBC showed WBC 17.6, hemoglobin 9.6 and platelets 42 K, normal one-year prior. She was treated with methylprednisolone, cyclobenzaprine, and Percocet for presumed sciatica and told to follow up with her PCP regarding her CBC. Two days later she again presented to the ED as her back pain was not controlled, she was admitted for further work up. A CBC now revealed a WBC 18.5 with a differential of 23.1 % neutrophils, 6.5 % lymphocytes, 38.9 % blasts, 13 % myelocytes, 10.2 % metamyelocytes, hemoglobin 8.3 and platelets 23 K. She was to be transferred to the cancer institute for further care when shortly before transfer she developed severe back pain with numbness of her feet and the inability to move her legs. Neurological exam now showed markedly diminished strength of both proximal and distal lower extremity muscle groups in addition to loss of deep tendon reflexes and rectal tone. MRI of her lumbar spine demonstrated a 5.2 × 1.4 cm mass within the dorsal epidural space from L2-L4 with extension into bilateral L3 neural foramina. She underwent emergent neurosurgical resection of the mass, which on pathology was diagnosed as a myeloid sarcoma. Peripheral cytogenetics were positive for acute myelogenous leukemia with a 8;21 translocation. She received induction chemotherapy with idarubicin plus cytarabine followed by spinal radiation and HIDAC consolidation therapy.
DISCUSSION: Low back pain is a common presenting complaint among patients with a reported one-year prevalence as high as 73 %. It is often of a benign etiology and treated conservatively. Prejudices exist that affect the management of low back pain. African American race, low socioeconomic status, and patients with any history of substance abuse receive more conservative measures. Imaging studies are pursued early in patients with red flag symptoms that suggest a serious spinal cause. These include weight loss, history of cancer, age over 50, urinary retention, fever, saddle anesthesia, intravenous drug use, and progressive neurological symptoms. When red flag symptoms are absent, a serious spinal cause is almost always ruled out, but in as many as 80 % of people one red flag sign is present while the prevalence of serious cause is 0.9 % suggesting higher sensitivity than specificity. Additionally, failure of conservative measures adds to the sensitivity of detecting a malignant process. Cauda Equina syndrome is as such a rare but serious entity and clinical judgment is prudent. Myeloid sarcomas, or chloromas, are tumor masses composed of immature myeloid cells found outside of the bone marrow. These are rare presentations of hematologic malignancies that can occur with or independent of a bone marrow process. Although there is no ideal treatment, the primary treatment method is chemotherapy and radiation of the underlying malignant process. Surgical removal of the sarcoma is not needed unless required emergently. Cytogenetically, the 8;21 translocation had been repeatedly associated with myeloid sarcomas.
WHEN THINGS DON’T FIT … THINK ACROMEGALY. A CASE SERIESPatrick Quinlan; Mrunalini Deshmukh; Arti Patel. Reading Hospital, Wyomissing, PA. (Tracking ID #1934133)
LEARNING OBJECTIVE 1: Recognize the various presentations of Acromegaly in different settings.
CASE: A 59 year old male with a PMH of resistant HTN, OSA, and DM II presented to Rheumatology for evaluation of persistent right hip pain for 1 year, in addition to the increasing size of his hands, feet, and head circumference. Rings and shoes that he had worn previously no longer fit. Considering the patient’s advanced degenerative arthritis, deep voice, enlarged tongue, enlarged mandible and general physical habitus, the diagnosis of Acromegaly was suspected. The patient was found to have elevated IGF (629 ng/ml) and an MRI of the brain revealed an 11 mm mass. The patient was referred to neurosurgery for transphenoidal Resection. A 34 year old female with a PMH of PCOS, depression, and OA presented to her general internist with the chief complaint of a change in her physical appearance in comparison to her twin sister. She was found to have an elevated growth hormone level of 5.01 ng/ml. She was subsequently referred to endocrinology; at the time of presentation she also had galactorrea. Her prolactin level was 32.7 ng/ml. She was also noted to have an 11 mm mass on MRI of the brain. A 34 year old, Hispanic female with a PMH of carpel tunnel syndrome, presented to the emergency room complaining of a severe headache for 1 day. She had intermittent mild headaches in the past. CT scan of the brain was done which revealed a sellar-based invasive mass. MRI of the brain confirmed an infiltrating mass lesion of the sella tursica which measured 37 × 28 mm with partial encasement of the cavernous carotid arteries bilaterally. The patient had noticed a change in her facial features over the last 5 years with enlargement of her nose, lips and tongue. Ring and shoe sizes were increased. She was found to have an elevated growth hormone level of 2103 mg/dL and a fasting insulin-like growth factor of 1022 mg/dl.
DISCUSSION: Acromegaly is a condition that results when the anterior pituitary gland produces excess growth hormone (GH) after epiphyseal plate closure at puberty. Classic features include frontal bossing, increased teeth spacing, arthritis, and enlargement of the tongue, lips, nose, hands and feet. It takes several years to manifest these classic features. The first patient in this series exhibited these typical features. The second patient in the series had galactorrea and a change in facial and physical appearance in comparison to her twin sister as presenting features. This is not surprising as 20–30 % of patients with GH secreting pituitary adenomas also co-secrete prolactin. Although the classic feature of a sellar mass is bitemporal hemianopia, severe headache can be a presenting feature of a pituitary mass and Acromegaly. All three patients were asked to bring their old pictures to see the change over the years. In all three patients diagnosis was confirmed by glucose suppression test.
WHERE ARE THE BLISTERS? A CASE OF BULLOUS PEMPHIGOID WITHOUT BULLAEVictoria T. Liu; Karen Y. Cheng; Pearl Yu. University of California, San Diego, La Jolla, CA. (Tracking ID #1940162)
LEARNING OBJECTIVE 1: Recognize drug-induced, urticarial bullous pemphigoid when bullae are not present.
LEARNING OBJECTIVE 2: Diagnose bullous pemphigoid when direct immunofluorescence and serologies are negative.
CASE: An 80-year-old male presented with a 2 week history of rash, distributed mainly on the abdomen and flanks. The rash is associated with pruritus, but no pain or burning. He denied recent changes to medications, topical exposures, hospitalizations, antibiotic use, and increased sun exposure. Medical history was significant for hypertension on lisinopril, and chronic obstructive pulmonary disease (COPD) on low dose prednisone (6 mg daily). Physical exam revealed non-scaly urticarial pink plaques confined to the abdomen and flanks. A punch biopsy showed superficial perivascular inflammation with prominent eosinophils. A second biopsy was obtained for direct immunofluorescence (DIF), which was negative. In the meantime, the patient improved symptomatically with topical clobetasol. Patient’s serum was sent for indirect immunofluorescence (IIF), and enzyme-linked immunosorbent assay (ELISA) for antibodies against bullous pemphigoid (BP) antigen 180 and 230. IIF showed positive IgG staining on monkey esophagus substrate at 1:5120 (high) and on human substrate 1:640 (high). Salt split skin assay showed staining on the epidermal roof, consistent with BP. The serum was negative for BP180, BP230 and IgA. Lisinopril was discontinued and replaced with losartan. One month later, patient reported great improvement with resolution of pruritus, and physical exam showed resolving plaques.
DISCUSSION: When assessing rashes in the elderly, BP should be included in the differential. The median age at presentation for BP is 80 years, the same age as our patient. The most commonly involved sites are the trunk, extremity flexures, axillae, and inguinal folds, but up to 30 % of cases remain localized to one area. Though of course the classic presentation of BP is tense bullae, other variants include urticarial, eczematous, vesicular, verruciform, and even pruritus without any visible lesions. If there is urticaria, it can be during the prodromal phase preceding the development of bullae, or an urticaria-only variant of BP, as was the case with our patient. Urticarial BP can be distinguished from true urticaria because the lesions of BP are not transient. Classically, BP is considered an intrinsic autoimmune disorder, but exposure to drugs or infections can also precipitate it, likely due to cross-reactivity of antibodies with the basement membrane. Our patient appeared to have a drug-induced variant of BP, given that his rash resolved with the discontinuation of lisinopril. The absence of elevated ELISA for the most common antigens for BP (BP180 and BP230) can support the diagnosis of drug-induced BP, but it is also possible that our patient had a less common protein target (eg. BP200). Interestingly, our patient’s clinical presentation and lab results could both have been muted by chronic prednisone for his COPD. Another important lesson from this case is that BP can be diagnosed even in the absence of positive DIF or serological findings. In a patient with suspected BP, the standard approach is to begin with a punch biopsy of the lesion for H&E staining and of the perilesion for DIF. Though DIF is the reference standard, diagnosis can be made with serum specimens for IIF and ELISA to detect circulating basement membrane antibodies. This case illustrates a non-classical variant of BP that can obscure the diagnosis.
WITH A SPONGY HEARTCindy Wang; Matthew Shaines; Daniel Spevack. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939728)
LEARNING OBJECTIVE 1: To learn the classification of cardiomyopathies
LEARNING OBJECTIVE 2: To recognize, diagnose, and treat non-compaction cardiomyopathy
CASE: 65-year old male with no significant PMH complained of shortness of breath for 2–3 days. In the same time his exercise tolerance had acutely decreased to a few steps. His father had a myocardial infarction at age 58. On exam, there was a 3/6 systolic murmur, crackles bilaterally at the bases, and 1+ pitting edema bilaterally. Lab results showed troponin peaking at 0.03 ng/mL and a pro-BNP 3653 pg/mL. Electrocardiogram showed atrial flutter and left ventricular hypertrophy. Echocardiogram revealed severe diffuse hypokinesis and an ejection fraction of 30 %. Cardiac catheterization demonstrated normal coronary arteries. MRI showed extensive spongy trabeculation in the LV apex consistent with non-compaction cardiomyopathy. Extensive delayed enhancement (indicating scarring) of the mid-myocardial layer was present in the septum, apex, and lateral walls. The patient was started on medical management and an ICD was implanted.
DISCUSSION: Cardiomyopathies (CMs) can be classified into two groups—primary and secondary. Primary CMs are limited to the heart, while secondary CMs are cardiac manifestations caused by other systemic diseases. The secondary or “extrinsic” CMs are due to metabolic, endocrine, neuromuscular, inflammatory, or nutritional causes. Ischemic CM is used to identify coronary artery disease as the etiology of heart failure, and is the most common cause of heart failure in developed countries. The primary CMs are fewer in number and are separated into three types—genetic, mixed, and acquired. Acquired CMs include inflammatory (myocarditis), stress-provoked (tako-tsubo), tachycardia-induced, and peripartum. Mixed CMs include dilated and restrictive, which are combinations of genetic and nongenetic. Genetic CMs include hypertrophic, glycogen storage disease, conduction defects, mitochondrial, ion channels disorders (Brugada), and left ventricular non-compaction. Non-compaction cardiomyopathy (NCCM) is a congenital disease of the heart muscle caused by a disruption in the process of myocardial compaction during embryogenesis. The resulting myocardium becomes “spongy” in appearance, with trabecular myocardial fibers forming sinusoidal recesses that communicate with the left ventricular cavity. It is both sporadic and familial, with at least nine specific gene mutations identified. Some examples of reported mutations are troponin T/I, tropomyosin, myosin heavy chain, and myosin binding protein. It manifests clinically as congestive heart failure, arrhythmia, and arterial thromboembolic events. The prevalence is uncertain but has been found in 0.014–0.26 % of all adults referred to echocardiography. The average age of diagnosis is typically in the 40s, but has been diagnosed as early as 11 months and as late as 94. The differential includes other CMs (dilated, restrictive, hypertrophic), myocarditis, pericarditis, aberrant chordae tendineae, left ventricular thrombi, and intramyocardial hematomas/abscesses. Echocardiography is the test of choice for diagnosis, but cardiac MRI is also utilized. Treatment involves heart failure and arrhythmia management, following the same guidelines as other patients. Long-term anticoagulation has been proposed due to the higher incidence of embolic events, but there are no concrete guidelines. Patients should be screened for other musculoskeletal disease. Due to its hereditary nature, first-degree relatives should consider echocardiographic screening or genetic testing.
WOMAN, INTERRUPTED: AN UNUSUAL CAUSE OF PSYCHOSISSara Attalla; Deborah Hemel. Montefiore Medical Center, Bronx, NY. (Tracking ID #1939021)
LEARNING OBJECTIVE 1: Recognize hallmark neuropsychiatric symptoms of anti-NMDA receptor encephalitis
LEARNING OBJECTIVE 2: Initiate treatment as early as possible to optimize chances for recovery
CASE: A 31 year-old female with no past medical or psychiatric history presented with acute behavior changes. According to her family, the patient was in her fully functional state of health until 1 week prior when they noted changes in mood; she cried frequently, appeared anxious, and had difficulty sleeping, all of which were uncharacteristic. On the day of admission she was disoriented, paranoid and aggressive, prompting her family members to call EMS. Vital signs were within normal limits. CT head was unremarkable. Lumbar puncture (LP) revealed 25 white blood cells with 96 % lymphocytes. On initial exam she was alert and oriented but had poor recollection of recent events. Shortly afterwards the patient began screaming uncontrollably and attempted to leave the hospital. She became combative, and appeared to be responding to internal stimuli. She required several rounds of Haldol and Ativan for sedation. Over the next several days, she experienced numerous similar episodes requiring remarkable physical and chemical restraint. An extensive infectious work up was negative, and a brain MRI showed no gross abnormalities. EEG demonstrated cerebral dysfunction in the L temporal and R parasaggital regions. On hospital day 7, a CT scan of the patient’s abdomen and pelvis was performed as there was growing concern for a paraneoplastic process. Imaging revealed a large mass encompassing both ovaries. She was taken to the OR on hospital day 9 for bilateral salpingo-oopherectomy. Pathologic examination revealed a low-grade immature ovarian teratoma. She was subsequently started on high dose steroids and plasmapheresis. She experienced minimal neurologic improvement and so IVIG was initiated. Shortly after her last treatment, she began to show recovery in communication and comprehension. Her mental status improved, and she was discharged home on hospital day 44. CSF later returned positive for anti-NMDA receptor antibodies, confirming the diagnosis. Upon outpatient follow-up 10 weeks after presentation, neurologic function was noted to be nearing her baseline, although she had no recollection of her hospitalization or the events leading up to it.
DISCUSSION: Paraneoplasic limbic encephalitis is a challenging illness to diagnose and treat. A form of this that has been gaining increasing attention is anti-N-methyl-D-aspartate (NMDA) receptor encephalitis, which was identified in 2007. Manifestations of this illness include dramatic psychotic symptoms, altered consciousness, seizure-like activity, catatonia, dyskinesias, and autonomic disturbances. It is believed to be an autoimmune mediated disorder that results in excitotoxicity of the NMDA receptors found mainly in the limbic system. Anti-NMDA receptor encephalitis is prevalent in young women and is often associated with benign tumors, the most notable being ovarian teratomas. Common workup may reveal lymphocytic pleocytosis in CSF and abnormal frontotemporal activity on EEG. Definitive diagnosis is established by the presence of antibodies in CSF. First line treatment includes removal of tumor, if there is one, and combinations of plasmapheresis, steroids and IVIG. Studies have shown that prognosis is improved when the disease is identified and treated promptly. However, there is typically a significant delay in diagnosing anti-NMDA receptor encephalitis as patients are often misdiagnosed with a primary psychiatric illness. It is therefore important to think of this illness once common etiologies of encephalitis have been excluded.
WORKING OUT WITH MINIMAL CHANGEDerek Worley. Lenox Hill Hospital, New York, NY. (Tracking ID #1938580)
LEARNING OBJECTIVE 1: 1.) Recognize the need for detailed histories
LEARNING OBJECTIVE 2: 2.) Generate awareness of supplement use in the general population
CASE: A 33 year old previously healthy male presents with 3 days of bilateral lower extremity edema. The patient also endorsed oliguria and urgency during the previous week. Associated symptoms included lethargy, decreased appetite, and weight gain. He denied any family history of renal disease. The patient stated that he lifts weights most days of the week. His diet consists of low sodium, high protein intake, complex carbohydrates, and no vegetables. The patient also endorsed starting a dietary supplement called Tribulus approximately 1 month prior. He denied any other medication or supplement use. On his vitals were stable and his exam was significant for generalized anasarca with +1 pitting edema of the lower extremities to the tibial plateau. The serum creatinine was 1.89 mg/dL and a urinalysis showed >300 mg/dL of protein and moderate urine blood. Based on the findings the patient was diagnosed with a nephrotic syndrome. For further investigation the patient received a percutaneous renal biopsy, which revealed diffuse foot process effacement, supporting a diagnosis of minimal change disease.
DISCUSSION: Minimal change disease (MCD) is a major cause of nephrotic syndrome in children and adults. Lesions of the podocyte or glomerular epithelial cell define this disease. Most cases of MCD are idiopathic. However it can be associated with drugs, neoplasms, infections, and other glomerular diseases. Here we present a patient with suspected tribulus terrestris induced minimal change disease. Tribulus is a derivative of a weed found in warm climates, hypothesized to increase natural testosterone levels. Tribulus terrestris is taken by many because of the desire to enhance athletic performance. There is limited data as to whether or not this supplement increases the body’s own ability to produce testosterone. However animal research has proved this substance to be nephrotoxic. There are case reports suggesting that tribulus can be nephrotoxic in humans as well, however the he exact mechanism of the nephrotoxicity of Tribulus remains unknown. We recommend that clinicians screen their patients for use of dietary supplements as some clearly can have harmful side effects.
CLINICAL PRACTICE INNOVATIONS (CPI) “SWEETBEATS” DIABETES CLINIC: YOUR ONE STOP SHOPReena Agarwal2; Marta Rico2; Carol N. Lau1; Joanna White1. 1Montefiore Medical Center, Bronx, NY; 2Montefiore Medical Center, Bronx, NY. (Tracking ID #1939147)
STATEMENT OF PROBLEM OR QUESTION: It is unclear what is the best format to deliver diabetes care to a population with a high prevalence of uncontrolled diabetes.
OBJECTIVES OF PROGRAM/INTERVENTION: 1. To develop a multi-disciplinary “one-stop shopping” approach to diabetes care in order to make a diabetes management visit more convenient for the patient. 2. To integrate residents into this multi-disciplinary setting. 3. To improve the overall diabetes care of our patients
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT: The Bronx has a 12.1 % prevalence of diabetes mellitus, as compared to 8.3 % in the United States. Within our practice the prevalence is 18.2 %, of which 20 % are uncontrolled (have HgbA1c’s above 9 %). Our practice is a teaching site for internal medicine residents within a large academic medical center. It is a Federally Qualified Health Center and therefore a referral center for patients who are uninsured or unable to find a provider. Our population includes those with complex medical and psychiatric problems, significant psychosocial needs and low health literacy. We have a large proportion of patients with uncontrolled diabetes, and a continual influx of new patients who have not addressed their diabetes or are recently diagnosed. Our office offers multiple services for these patients including a health educator, dietician, social worker and pharmacist. However, seeing each of these providers quickly increases the burden of visits on our patients and can lead to a high no-show rate. We developed a weekly “Sweetbeats” diabetes clinic which incorporates a multi-disciplinary team in one clinical session. Patients are referred by providers either at an office visit or when a high HgbA1c is found by laboratory testing. As each patient checks in for their visit, the team huddles and assigns each patient 2–3 providers based on a review of their needs. The residents are integral to the huddle, and each patient sees one medical resident for medication management. We use the “one-stop” shopping approach even for the patient’s room assignment: the patient stays in one room and the providers rotate between patients.
MEASURES OF SUCCESS: The evaluation of Sweetbeats diabetes clinic is folded into our Primary Care Medical Home quality indicator monitoring. We monitor the quarterly HgbA1c, and annual LDL and urine microalbumin. We are in the process of improving our ability to track annual podiatry and ophthalmology visits as well.
FINDINGS TO DATE: We are reporting data for the year of 2012. During this time we were referred a total of 151 patients. Our no-show rates range from 30 to 70 % per session with no clear trend over the calendar year. The average Hgba1c prior to their Sweetbeats DM clinic visit was 10.14 %, this improved to 8.99 %. In addition, the average LDL decreased from 106 to 99.9. However, the number of patients who had a urine microalbumin checked decreased from 110 to 72.
KEY LESSONS FOR DISSEMINATION: In an office with multiple resources we were able to develop a multi-disciplinary clinical session for patients with uncontrolled diabetes. This is more convenient for the patient by limiting the number of visits required. For those patients who do come, we have found improved diabetes control. A major barrier is our continued high no-show rate. We are in the process of eliciting some of the reasons behind this poor patient turnout.
A COMPREHENSIVE CLINIC-BASED STRATEGY TO PROMOTE SAFE OPIOID PRESCRIBING FOR CHRONIC NON-CANCER PAIN IN THE PRIMARY CARE SETTINGJocelyn James; Jared W. Klein; Lisa Chew; Joseph Merrill; Sara L. Jackson. University of Washington, Seattle, WA. (Tracking ID #1939027)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Use of opioids for chronic non-cancer pain, particularly at high doses, carries significant risk without consistently improving function or quality of life; providers, including trainees, find opioid prescribing a particularly challenging aspect of primary care.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Develop and implement opioid prescribing policies and monitoring plans for patients on chronic opioids; 2. Train providers in the delivery of safe and effective chronic pain treatment; 3. Educate patients regarding the risks of opioids and non-opioid strategies for chronic pain management;
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Harborview Medical Center (HMC) in Seattle, WA, is an urban safety-net teaching hospital with a mission to serve medically and socially vulnerable populations. HMC’s Adult Medicine Clinic (AMC) has over 60 resident and attending providers and more than 5000 patients, including 27 % with Medicaid and 24 % uninsured. Coexisting medical, psychiatric and addiction disorders are common. As escalating opioid-related deaths in WA State highlighted the need for improved opioid prescribing practices, AMC implemented a clinic-wide strategy to promote safer prescribing of opioids for chronic pain. In 2010, a multidisciplinary committee of primary care providers (PCPs), pharmacists, nurses, a psychiatrist, a social worker, and an addiction medicine specialist developed opioid prescribing policies and protocols. Guidelines address depression and substance abuse screening, drug selection, dose titration, urine toxicology testing, review of the WA State Prescription Monitoring Program (PMP) database, and agreement violations. A ceiling dose of 120 mg morphine equivalents per day (MED) is recommended and providers are encouraged to taper patients on higher doses. Clinic pharmacists create monitoring plans for patients and maintain a registry to track prescribing practices. The opioid review committee meets monthly to review protocols and discuss cases of patients on high doses or with challenging needs, providing recommendations to PCPs. Provider education is an ongoing component of AMC’s opioid strategy. Training incorporates best practices in opioid prescribing, non-opioid pharmacotherapy and non-medication treatments such as Cognitive Behavioral Therapy and motivational interviewing skills. Finally, a patient care controlled substances agreement is used to educate patients about the risks of chronic opioid therapy and set behavioral expectations.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We recorded the number of educational sessions and cases reviewed by the multidisciplinary committee. Clinic registry data allowed us to quantify patients on chronic opioids and those on extremely high (>1000 mg MED) or high (>120 mg MED) doses before and after implementation of the strategy.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): From 2010 to 2013, three or more training sessions on chronic pain management were held each year for residents. The multidisciplinary committee provided recommendations on 99 cases, an average of 2.4 per month. The number of patients receiving opioids for chronic pain fell 39 % from 591 to 358; the percentage on extremely high doses fell from 10 % (n = 60) to 2 % (n = 7), and the percentage on high doses fell from 35 % (n = 197) to 19 % (n = 69).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): We created a clinic-wide strategy to promote safer chronic opioid prescribing in a large academic safety-net primary care clinic. Through increased education, communication, and decision support around pain management, we reduced the total number of patients on chronic opioids and the number of patients on high-dose opioids.
A METHODOLOGY USING INTERNET BASED RESOURCES AND WEBSITES TO IDENTIFY COMMUNITY RESOURCES AND SOCIOECONOMIC FACTORS OF PATIENTS ATTRIBUTED TO A GENERAL INTERNAL MEDICINE PRACTICE LIVING WITHIN A SPECIFIC METRO ZIP CODEScott Joy1,2; Jordan T. Wehe2; Gavriel Roda2; Edward A. Soto2; Cara Campbell2; Aaron B. Galbraith2. 1The Colorado Health Foundation, Denver, CO; 2University of Colorado-Denver, Denver, CO. (Tracking ID #1936054)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Providing referrals to community resources is a required element for PCMH certification, but community resources are widely dispersed within a given geographical region covered by a general internal medicine practice, and resources that catalog and illustrate these community services are not readily availble to patients and general internal medicine practices.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Identify within the metro Denver area the most common zip code address of patients who are attributed to a particular primary care practice. 2. Explore internet based resources/websites that are available to identify physical community resources (recreational centers, churches, schools and parks) and their location within this zip code. 3. Develop a map of these community resources that can be used by the practice and given to patients who live within the particular zip code.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): A query of existing billing data was performed to identify the most common address zip code of patients receiving care within a general internal medicine practice. It was determined that the metro Denver zip code 80205 was the most common address zip code for patients within the practice. A team of 4 undergraduate students in the BA/BS-MD program at the University of Colorado Denver was tasked with searching for internet based resources/websites that would provide detailed data on community resources available in this particular zip code. A comprehensive internet search located the following website (www.city-data.com/zips/80205.html) that allowed for detailed evaluation of physical community resources (churches, recreational centers, schools and parks) within zip code 80205. The website www.maps.google.com was used as an additional resource. The Colorado specific website www.piton.org was identified as a tool to identify relevant demographic information within each neighborhood in the specific zip code, including total population, average household income, % persons in poverty, and crime rate per 1,000 persons.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Determine the total number and addresses of physical community resources (churches, schools, recreational centers, parks) available within the targeted zip code. Create a map of the targeted zip code that includes locations of the physical community resources within the targeted zip code. Identify key socioeconomic factors for people living in each of the neighborhoods within the target zip code.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Our team’s analysis found that zip code 80205 has the following physical community resources: 9 Churches 9 Parks 3 Recreational Centers 1 Denver Police Community Resource Center 18 Schools Locations of the churches, parks, recreational centers and schools were placed on an electronic map of zip code 80205 found on the city-data.com website for reference. This document can be printed and given to patients to educate them on community resources available in their neighborhood. Zip code 80205 was found to have 5 distinct neighborhoods with the following socioeconomic demographics. Range of total population in each neighborhood: 3,106 to 12,710, average 5,927 Range of average household income: $35,519 to $44,847, average $40,313 (Metro Denver average is $55,129) Range of % of persons in poverty: 14.29 % to 31.5 %, average 26.1 % (Metro Denver average is 14.3 %) Range of crime rate/1,000 persons: 53.77 to 125.02, average 71.53 (Metro Denver average is 60.19)
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The existing internet based websites www.city-data.com and www.maps.google.com can be used by any general internal medicine practice within the United States to identify physical community resources for their patients. A map of resources within the zip code can be created from this data and provided to the practice and to the patients living within the zip code to allow all to understand the community resources available. A general internal medicine practice can also use demographic and socioeconomic factors to target clinical and social resources more effectively. Next steps will be to use the detail provided in this search to reach out and collaborate with community leaders to determine best ways to meet the needs of shared citizens living in these neighborhoods to maximize health outcomes.
A NURSE VISIT PROTOCOL COMBINED WITH POPULATION MANAGEMENT REPORTS IMPROVES QUALITY METRICS IN HYPERTENSIONJason Higdon; Monica Agrawal; Jennifer Zreloff. Emory University School of Medicine, Atlanta, GA. (Tracking ID #1937459)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): As the focus of healthcare shifts towards providing high quality care for chronic medical conditions, we must develop novel ways to provide better care, meet quality metrics, and manage ever-increasing demands in primary care.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): In a university-based and NCQA recognized Patient-Centered Medical Home (PCMH), we sought to improve the percentage of patients with hypertension who achieved a goal blood pressure of less than 140/90.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Our PCMH pilot practice consists mostly of patients on an employer-sponsored health plan. Using a team-based approach we focused on staff education and empowerment, population management reports, and documentation in our electronic medical record to deliver protocol-driven care to our patients with hypertension. 1. An in-service was done with the entire team including all providers, nurses, and medical assistants to reinforce proper measurement of blood pressure including timing, position, and cuff size. Competencies were observed and scored by the team physicians to ensure buy-in and comfort with a nurse visit protocol. 2. A nurse visit protocol was written for hypertension follow-up visits. This included a standard nursing note for our electronic medical record which includes the patient’s medication list, an assessment of medication compliance/side effects, current and most recent blood pressure readings, and follow-up of most recent self-management goals. The protocol includes parameters to identify potentially dangerous vital signs. For patients whose blood pressure is not at goal, the nurse automatically makes a 1 month follow-up visit for reassessment. In our patient population this type of nursing visit is offered at no cost to the patient. 3. We developed a monthly hypertension population management report that lists all patients with a diagnosis of hypertension whose last blood pressure anywhere in our system (excluding inpatient and ER visits) was above 140/90. It delineates if their most recent blood pressure reading in our clinic was at goal or not and notes if they have an upcoming appointment. We use this to generate health reminder letters to our patients which are largely delivered through our patient portal.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Each month, we track the percentage of all patients in our clinic who have hypertension whose last reading was <140/90.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Our baseline percentage of patients at goal was approximately 64 % which was on par with institutional and national benchmarks. Our peak level of patients at goal was 76 % in October 2013 with the largest improvement coming after the implementation of the standardized nurse visit follow-up for patients who were not previously at goal. Through the end of 2013 we were at 72 % of patients at goal.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1. Using standardized, protocol-driven care provides the foundation for team-based care 2. When physicians actively empower and educate team members to provide care beyond their typical roles, more buy-in occurs which leads to improved monitoring and quality of care 3. Access to accurate data is crucial in implementing population based-care for chronic medical conditions
A PANEL MANAGEMENT APPROACH TO SHARED DECISION MAKING FOR COLORECTAL CANCER SCREENINGKathleen Fairfield1,2; Christine Peura2; Elizabeth Herrle1; Lauren Daniels1; Mary McDonough3; Donald Medd1; Deborah Pyle1; Mark Bouchard3. 1Maine Medical Center, Portland, ME; 2Maine Medical Center, Portland, ME; 3Maine Medical Center, Portland, ME. (Tracking ID #1935561)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Use of decision aids (DAs) in shared decision making (SDM) increases patient knowledge, resulst in greater patient comfort with decisions and improves patient participation in decision making. However, using DA in primary care practice can be cumbersome due to practical limitations on providers recommending and disseminating DAs, the need to arrange appropriate follow up discussions with patients, and ensuring the ability to act on patient decisions in a timely manner.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): (1) To demonstrate the feasibility of a panel management approach to SDM for colorectal cancer screening (CRC) using DAs in primary care with follow up telephone decision support and the ability to order a screening test if chosen by the patient at the time of the decision support conversation. (2) To determine the effectiveness of this approach in varied practice settings.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We identified English-speaking adults between the ages of 50–75 from three primary care practices (all with resident learners) who were not current on CRC screening according to a review of their medical records, which included a transition to Epic during the record review for all three practices. Primary providers then excluded patients who had active serious medical conditions or for whom screening was otherwise inappropriate at the current time. Patients received a CRC DA through the mail that included a booklet, DVD, and a signed letter from their primary care provider. Patients were called 2 weeks after mailing of DA by a member of the medical team (RN or MA) for follow up decision support.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Chart reviews were completed 6 months after the mailing to determine (1) if the patient had been reached for decision support, (2) had completed CRC screening, or (3) reported using the DA and making a decision not to be screened.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 1,484 DAs were mailed to patients but 258 (17.4 %) patients were found to have been previously screened, medically unfit, transferred, or did not speak English before follow up support, and those patients were excluded from the remainder of the study, leaving an N of 1,226. 663 (54.1 %) were reached for follow up support and 148 (28.7 %) were further excluded from the study, leaving an N of 1,078. Of the remaining 515 patients reached for follow up support, 226 (43.9 %) patients stated they reviewed the DVD/booklet: 77 (34.1 %) declined screening, 41 (18.0 %) were interested in a FIT test, 79 (35.0 %) were interested in a colonoscopy, and 28 (12.4 %) did not make a decision. Two hundred four patients did not review the DVD/booklet: 93 (45.6 %) declined, 21 (10.3 %) were interested in a FIT test, 33 (16.2 %) were interested in a colonoscopy, and 57 (28.0 %) did not make a decision. Further chart review and office visits found two additional patients that had already been screened, leaving a final N of 1,076. Six months has elapsed for 940 patients. Of these, 143 (15.2 %) have completed a screening: 51 (5.4 %) chose a FIT test and 93 (9.9 %) chose a colonoscopy. The 111 (77.6 %) patients that were reached for follow up support were more likely to complete a screening compared to the 32 (22.4 %) who were not reached (32) (p < 0.001).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The panel management approach to SDM is feasible and required little time on the part of the PCP, but did require a significant amount of time for other office personnel including time for decision support, which increased effectiveness. To sustain this model, EMRs need to be populated with information on prior screenings, and to systematically identify unscreened patients as they turn 50 or join a practice. This approach, including the help of other team members, provides an opportunity for SDM outside the office visit and could fit well in a patient centered medical home model. The overall effect of this SDM process on increasing screening rates was small in this study, but decision support increased effectiveness.
A PATIENT CENTERED PAIN MANAGEMENT PROTOCOL: A BIO-PSYCHO-SOCIAL APPROACH TO THE MANAGEMENT OF CHRONIC PAINKatherine Kueny; Tara Turner; Susan Burbach. University of Nebraska Medical Center, Omaha, NE. (Tracking ID #1935632)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Although chronic pain is one of the most common complaints seen by general internists, it is also one of the most multifaceted and complex conditions to effectively manage in a primary care setting, lending itself well to utilize a patient-centered, bio-psycho-social approach to pain management.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To provide quality and safe chronic pain management by implementing a patient-centered, bio-psycho-social approach to pain management in a resident-run outpatient clinic. 2. To improve the communication and documentation of pain contracts between the ER and outpatient clinic setting. 3. To provide comprehensive resources and education on various strategies for managing chronic pain for all patients seeking treatment for chronic pain.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): A bio-psycho-social pain protocol was implemented in a resident-run general internal medicine outpatient clinic, and incorporated as part of our patient centered medical home model. The protocol was developed to standardize clinic management of chronic pain, improve patient education of pain management, standardize the use and management of pain contracts, establish methods of communicating a patient’s pain management plan with other departments in the organization, and to incorporate behavioral management of chronic pain as part of the standard treatment plan. The development of the model included perspectives from physicians, nurses, and behavioral medicine clinicians, as an effort to incorporate an inter-professional approach to pain management. As part of the new protocol, every patient who is on a pain contract is required to attend a chronic pain class, taught by behavioral medicine clinicians. Changes have also been made in the EMR to better document the status of pain contracts, so that other departments are aware of this information. In addition, narcotic prescriptions were changed to be written every 28 days, so that refills always landed on the same clinic day with the same attending physician. Every patient with a diagnosis of chronic pain now receives a pain management folder, which includes additional resources and education on pain management.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We plan to evaluate multiple layers of the new chronic pain protocol ranging from patient satisfaction, adherence to pain contracts, self-management behaviors, depressive screening scores, and frequency of ER visits. We plan to use qualitative metrics to gather patient perceptions and satisfaction tied to the new protocol and chronic pain education class. Utilizing data on our clinic’s standard PhQ-2 and PhQ-9 depression screenings, we will assess the impact a comprehensive, bio-psycho-social approach has on depression symptoms. We have worked with the university emergency room to develop a plan for researching the impact of the protocol changes on frequency of emergency visits. We also plan to use quantitative measures to assess a change in patient’s self-management behaviors following the education class. We anticipate an increase in adherence to pain contracts due to incorporating the patient more in the pain management plan from the beginning of treatment.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The new protocol has been in place for 1 year now. In response to the documentation changes related to the protocol, continuity and consistency of pain management treatment plans have improved particularly between the ER and our particular outpatient clinic. This has reduced the frequency of miscommunication and improved consistency of treatment plans between the inpatient and outpatient setting. The integration of behavioral medicine as part of the standard pain management protocol has increased our ability to treat co-morbid psychosocial conditions that have been reported to exacerbate chronic pain. Also, physicians have reported less frustration with narcotic refills, since moving to 28 day refills ensuring that the same physician is responsible for refills.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Treating chronic pain from a bio-psycho-social framework has reduced frustration and miscommunication among providers. Patients benefit from a focus on written and verbal education regarding pain management. Incorporating and assessing biological, psychological, and social factors from the start of treatment assists the physician and patient in developing a more comprehensive and effective management plan. Standardizing the clinic’s protocol on pain management has improved the consistency of education and resources that patients are exposed to. It is yet to be determined the long-term impact this new protocol has on narcotic use and patient/provider satisfaction. We are also revising the program to better monitor attendance of the chronic pain education class and adherence to pain contracts.
A RANDOMIZED CONTROLLED TRIAL OF A DAILY “I.R.A” MEDICAL HUDDLERahul Vanjani1; Nancy Chang1; Maria Arkipoff1; Steven Shea1,2; Jessica R. Singer1. 1New York Presbyterian Hospital - Columbia University Medical Center, New York, NY; 2Mailman School of Public Health - Columbia University, New York, NY. (Tracking ID #1936985)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Providers and staff at academic clinics often work in silos rather than as integrated members of a medical team, and this may result in low job satisfaction, poor work environment and feelings of burn out, ultimately resulting in inefficient care delivery.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To implement a daily medical huddle including all members of the patient care team with the following objectives: 1. Create a structured system for communication about clinic logistical and patient care 2. Foster social cohesion—a sense of team—between team members 3. Improve work satisfaction and decrease burnout among team members
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We conducted a randomized controlled trial to pilot a daily medical huddle from August to November 2013 in an urban, academic, joint faculty and resident outpatient primary care practice that provides 75–80,000 visits/year. The clinic has four structurally similar modules, each with relatively consistent teams of staff and providers. Two of the four modules in our clinic were randomized to the huddle intervention. The huddle was based on a customized framework we designed entitled I.R.A. (introduction, reflection, anticipation). Clinical duties were suspended each morning at 9:00 am to allow all team members (attending physicians, residents, medical assistants (MAs), registered nurses (RNs), front desk staff) in the intervention modules to congregate in a circle in order to engage in a process of organized introduction by name and role, reflection on what went well the day prior and what did not, and anticipation of upcoming logistical problems or patient issues. The huddles were led by the medical assistant in order to empower a non-clinical member of the team. Huddles generally lasted 5 min and team members were encouraged to stand rather than sit as a way of promoting efficiency and remaining cognizant of time.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): An 8-item modified version of the Staff Experience Survey from the University of Chicago and the Commonwealth Fund was used to measure job satisfaction, burnout, problem-solving, efficiency, communication and work environment characteristics on a 5 point Likert scale. The survey was administered to a convenience sample of staff and providers at baseline and upon completion of the 4 month intervention period. For each survey respondent, a change score was calculated for each of the items (score after intervention - score prior to intervention). For bivariate analysis, t-tests were performed to assess differences in item scores between groups. Linear regression with interaction terms was used to test for differential response to the intervention by providers and staff members.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We surveyed 48 people in our clinic and received responses from 41 individuals (response rate 85 %); 45 % were providers and 55 % were RN/MA/front desk staff. About 2/3 of the respondents were from the intervention modules. Prior to the intervention, the responses from control and intervention modules did not differ on any of the items. However, physicians were more likely to report lower feelings of job burnout (2.2 ± 0.6 vs 3.0 ± 1.1, p < 0.01) and higher job satisfaction (4.1 ± 0.9 vs 3.4 ± 0.9, p < 0.01) compared with non physicians staff members. Physicians were also more likely to report that their module functioned as a team (3.3 ± 0.9 vs 2.7 ± 0.9, p = 0.05) and feel like the work they perform is appropriate for their level of training (3.9 ± 0.7 vs 3.3 ± 1.0, p = 0.03). After the intervention, there were no significant differences between control and intervention modules in any of the items. We found that providers and staff responded differently to the intervention. Providers in the intervention modules perceived an improvement in teamwork (p-interaction = 0.02) and problem solving (p-interaction < 0.01) compared with staff; there were no differential responses in the other items.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Our pilot RCT demonstrated that a structured daily huddle can improve teamwork and problem solving from the perspective of the physician providers, but similar improvements were not noted by other staff members. As many clinics have already or will soon implement huddles as part of the patient centered medical home, it is important to recognize that huddles may have unintended consequences and effect groups differently. We did not see improvement in job satisfaction, burnout, efficiency, communication and work environment characteristics which may be attributed to small sample size, non-blinded design, short intervention period, or occasional cross-over of staff between intervention and control modules. We also note that our choice of downstream benefits to assess in the survey may not have included some relevant processes such as improved patient care and culture of safety. Based on overwhelmingly positive anecdotal feedback from staff and providers, the huddle has been adopted by all modules in our clinic. Next steps will include sharing our findings with the teams and seeking suggestions for how to improve the huddles.
A RESIDENT-LED INTERVENTION TO IMPROVE TEAM-BASED CARE IN AN INTERNAL MEDICINE CONTINUITY CLINICStephanie Nothelle; Eunice Yu; Laura Hanyok. Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1937682)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Internal medicine trainees need to master the skills of delivering high-quality care for complex patients in an outpatient, team-based patient-centered medical home; however, many trainees still practice in clinics that have not adopted this care model.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To design a low-cost, low-time intensity intervention to promote team-based care in the house staff outpatient practice 2. To improve understanding of roles and value of team members among residents
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Two interventions were instituted, pre-clinic huddles and monthly multidisciplinary meetings. The interventions took place in the General Internal Medicine practice at Johns Hopkins Bayview Medical Center, an academic medical center, where 45 residents in both primary care and categorical internal medicine tracks are primary care providers. In this practice, resident and attending physicians are assigned to one of three clinical “pods” where a consistent team of medical assistants (MAs) and medical office assistants (MOAs) works. Pre-clinic huddles took place in the 15 min prior to the first scheduled clinic appointment in each of these pods and included the house staff providers, MAs, and MOAs as well as an attending physician. The huddle started with a non-medical “question of the day” that also served as a team building exercise. The MAs reviewed issues that could contribute to workflow limitations that day, such as staffing shortages or vaccine availability. Then, each resident briefly reviewed their list of patients with the team, with a focus on making staff aware of workflow issues such as need for an interpreter or for procedure setup. Multidisciplinary meetings took place once a month and were focused on Medicare and Medicaid patients identified as high-risk for health care utilization by the Johns Hopkins Community Health Partnership (JCHiP), a separate program. The team was comprised of a nurse case manager, a community health worker, a behavioral health coach, resident physicians, and an attending physician. The nurse case manager led these meetings by reviewing each active or newly enrolled patient who had a house staff provider and inviting the team to comment on active problems. Each team member shared information on the patient and a problem-solving discussion was initiated. At the conclusion of discussion, the plan of care was updated appropriately in the EMR.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Pre-clinic huddles are being evaluated by an anonymous survey administered to residents and medical office staff prior to initiation of huddles and then 6 months later. The survey uses a Likert scale to measure how frequently house staff discuss patient and workflow issues with MAs and MOAs prior to a clinic session, the perception of working in teams in clinic and whether or not the huddle is enjoyable. The survey also asks for open responses regarding usefulness and areas for improvement. The multidisciplinary meeting is being evaluated 6 months after implementation using quantitative and qualitative survey questions. Using Likert scale-based responses, the survey assesses perception of the impact of the meetings on patient care, house staff understanding of the roles of each team member including themselves, and understanding of the value of multi-disciplinary care as a result of the meetings. Open response questions again assess usefulness and areas for improvement.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Thirty-one of the 45 eligible house staff completed the pre-intervention survey. Seventy-three percent reported that they touched base with MAs and MOAs prior to clinic sessions less than half of the time, and 22 % never did. On a scale of 1–4 [with 1 meaning not at all and 4 meaning a great deal], house staff responded on average 3.6 that they feel that they work in teams with MAs and MOAs, while MAs and MOAs responded on average 2.7. Six months after the intervention, medical office staff view the huddles favorably and feel more strongly that they are working in a team with house staff, rating of 3.17 out of 4. Results of the post-intervention resident surveys on huddles and multidisciplinary meetings will be available in February 2014.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1. Prior to the establishment of dedicated time for collaboration such as a huddle, most house staff in our practice did not discuss patient care regularly with other team members such as MAs and MOAs. 2. Small, low cost interventions such as pre-clinic huddles that bring together providers and office staff regularly can improve team based care. 3. Non-physician team members may perceive teamwork differently than physician team members.
A SYSTEM FOR TRANSITIONAL CARE MANAGEMENT IN THE PATIENT CENTERED MEDICAL HOMECarol R. Fleischman. University of Pennsylvania, Radnor, PA. (Tracking ID #1940768)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The patient centered medical home is considered a key factor in preventing readmissions, yet our hospitalized patients may be falling through the cracks; if we leave our follow up plans to individual practice, and do not have a system, our patients may be at risk for readmission due to not getting timely or medically relevant follow up care
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Centralize our admission notification and increase our awareness of when patients are admitted to any hospital in our region Accomplish telephone follow up with the patient promptly upon discharge, performing the key functions of medication reconciliation, and assessing any unmet needs. Ensure prompt follow up appointment with the patient’s primary care internist or relevant subspecialist.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Penn Medicine at Radnor is an eight-physician general internal medicine practice located in a suburb of Philadelphia, part of the Clinical Practices of the University of Pennsylvania. Patients from Penn Medicine at Radnor can be admitted to a number of University of Pennsylvania Health System hospitals as well as other hospitals in our region which are not affiliated with our health system. Our health system sends an electronic discharge notification to the primary care physician. The outlying hospitals all have disparate means of notifying the patient’s primary physician of a hospital stay. Notification of admissions and discharges was sporadic and unreliable. Furthermore, each physician dealt with admission notifications differently, and full schedules sometimes made it difficult to schedule follow up visits after hospitalization. Our goal was to devise a centralized system to track our admissions and collect relevant data about them at the practice level. All admission and discharge notifications, whether emails, faxes, or phone calls, were routed to one person as well as continuing to be routed to the patient’s primary physician. All admissions were then logged onto monthly spreadsheets which were placed on an external drive that was accessible yet secure for data analysis. We hired a care management RN, who makes follow up calls to patients after discharge and completes a Care Management form in our electronic medical record (Epic). We now also track the calls and patient’s follow-up visit date on the admissions spreadsheet.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): This system measurably improved our timely awareness of admissions and discharges. Between September 2011, when we fully implemented this program, and now, there was a steady increase in the number of admissions we captured per month. In recent months, we are tracking a stable average of about 100 admissions per month. We also achieved a marked improvement in scheduling 7–14 day follow up visits. Patient satisfaction survey. We created and distributed a survey to assess patient perception of whether the follow up calls assisted them with medication concerns, efficacy in self-management, follow up care, and overall sense of continuity and security regarding their care. The data collection for this survey is currently underway.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Between September 2011 and September 2013 the percentage of patients receiving a follow up within 7 to 14 days of discharge increased from 27 to 60 %. In 2011, 20 % of discharged patients did not receive a follow up visit. In 2013, less than 1 % did not receive a follow up visit.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Transitional care management cannot be left to chance. We designed a simple yet reliable system for tracking admissions and discharges, identifying problems after discharge, and scheduling follow up care. We leveraged existing resources within our health system (Events of Interest, Care Connectors) and reached out to hospitals that are not part of our system. Having a point person or small team responsible for connecting discharged patients to their follow up care is a much better system than relying on each physician’s diverse practice in receiving faxes/records regarding discharges and getting patients in. A care management nurse, using a templated phone encounter form, can quickly and efficiently uncover lapses/needs and assess patient status. Efficient and timely follow up also requires dedicated session time for hospital follow ups. Much effort is being expended on the hospital side of the readmission equation. However, outreach from the outpatient setting—the patient’s medical home—may be just as important in ensuring continuity and preventing readmissions.
A UNIQUE MODEL FOR MULTIDISCIPLINARY BEDSIDE ROUNDS IN AN ACADEMIC TEACHING HOSPITALEric A. Young1,2; Jaime Paulk1; James M. Beck1,2; Mel Anderson1,2; McKenna Burck1; Stephen Szapor1; Adam Roberts1; Chad Stickrath1,2. 1Denver VA Medical Center, Denver, CO; 2University of Colorado School of Medicine, Aurora, CO. (Tracking ID #1939319)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Valuable models for improving interprofessional communication through multidisciplinary bedside rounds (MBR) have been described in the literature; however, these models often depend upon geographic localization of patients and providers.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Our goal was to create a sustainable model for MBR on a medical unit in an academic teaching center without geographic patient or provider localization.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Our hospital is an academic, tertiary care teaching center with five housestaff teams caring for patients on three medical wards and in an open ICU. As part of a Rapid Performance Improvement Workshop (RPIW) aimed at improving patient flow, we developed a strategic plan for implementing MBR on a pilot 27-bed medical unit. Key components of the intervention included: 1. Shifting of the morning medication administration time from 9 am to 7 am, allowing nurses to join the resident teams on bedside attending rounds 2. Creation of a Provider Sign-In Sheet posted at the charge nurse desk with contact information for both nurses and physicians caring for each patient 3. Development of a protocol for housestaff teams to use the Provider Sign-In Sheet and Cisco© phones to quickly identify and contact each patient’s nurse prior to starting bedside presentations 4. Creation of a system for auditing day-to-day completion of multidisciplinary rounding using nursing self-report 5. Implementation of bimonthly displays of each housestaff teams’ frequency of multidisciplinary rounding, coupled with rewards for performance
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The intervention was evaluated using two methodologies: 1. Quantitative improvement in the frequency of physician-to-nurse communication during teaching rounds was assessed using daily nursing self-reports. 2. Qualitative evaluation using a 28-question survey adapted from available instruments and refined through cognitive interviewing. Constructs included overall satisfaction and perceived impact on teamwork culture, interprofessional communication, nurse job satisfaction, provider workload and impact on future practice. The survey was administered anonymously to nurses, medical students, residents and attending physicians who had participated in MBR in the preceding 5 months. Results were analyzed using descriptive statistics and differences between provider groups were assessed using Fisher’s Exact Test.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Our MBR initiative has been successfully employed for 5 months. During that time we have gathered daily nurse self-reports for 759 patient encounters, out of which multidisciplinary rounding occurred in 669 (success rate 88 %). Previous observational work from our hospital demonstrated that physician-to-nurse communication on rounds occurred only 5 % of the time; thus, we have achieved an 83 % improvement in interdisciplinary communication during medical teaching rounds. Ninety-five out of 142 providers completed the qualitative survey (67 %). In general, satisfaction was high, with similar percentages of nurses and physicians agreeing that the initiative should be expanded to other wards (100 % and 97 % respectively, p = 1.0). Eighty-five percent of resident physicians agreed that MBR should be incorporated at other hospitals in which they train. Physicians and nurses agreed that mutual understanding of care plan changes increased since the initiative began (nurses 93 % and physicians 94 %, p = 1.0). The perception of improved collaboration was similar, with 94 % of nurses and 93 % of physicians agreeing that they worked more often as a well-coordinated team (p = 0.68). Nursing job satisfaction improved, with 65 % reporting increased job satisfaction since the onset of the MBR initiative. MBR did not appear to significantly impede provider workflow as 87 % of nurses reported MBR was an efficient use of their time. Similarly, 85 % of physicians indicated that MBR only prolonged rounds by 10 min or less. Finally, MBR did not appear to hinder the educational value of teaching rounds, with 40 % of residents reporting that MBR increased the educational value of rounds and the other 60 % reporting no effect.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1) Multidisciplinary rounding is feasible in an academic institution without geographic patient and provider localization 2) Key lessons we have learned: a. The process for communication must be streamlined b. The system should strive to be workload-neutral c. Sustainability requires some means of auditing and providing performance feedback
ACTIVE REFERRAL MANAGEMENT - A SPECIALIST/PCP COLLABORATION TO ADDRESS ACCESS, VALUE, AND EXPERIENCESandhya K. Rao1; Ryan Thompson1; Creagh Milford1; Nancy Wei3; Calvin A. Richardson2; Sara Hoffman2; Timothy Ferris1. 1Massachusetts General Hospital, Boston, MA; 2Massachusetts General Physicians Organization, Boston, MA; 3Massachusetts General Hospital, Boston, MA. (Tracking ID #1939604)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Can a specialist-based referral review program reduce avoidable specialist visits by replacing the office based consultation with non-visit based alternatives for physician to physician consultation?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Develop a mechanism for referring clinicians to access specialist expertise through alternatives to face to face patient encounters 2. Reduce wait days and total visits per patient 3. Improve patient and provider experience
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): There are two related components to our intervention: 1. Active Referral Management: Specialty identifies referral reasons for which a face to face visit may be avoidable. Using our electronic referral management platform, the specialist reviews all incoming referrals in those areas weekly. When appropriate, the specialist emails the referring physician directly with recommendations, either to replace the visit, or to suggest additional tests or therapies to initiate prior to the specialist visit. Patients identified as urgent are triaged appropriately. Specialists are paid a quarterly stipend based on projected volume of incoming referrals 2. Curbside Consults: In two of our participating specialties, clinicians will have the option to submit a request for a “MD to MD” consult. Both take place in the ambulatory primary care and specialty practices of an urban academic medical center which is part of an integrated delivery system and uses both an electronic medical record and referral management system.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Key Process Measures 1.% of total incoming referrals reviewed: Aim is approximately 50 % to ensure broad impact. However, selecting appropriate referral reasons for review drives overall efficiency of the program, so some specialties will be lower. 2.% of referrals alternatively managed: Core performance measure of program; reflects both effectiveness of our case selection as well as utility of program. 3.% of referrals with pre-consultation tests/treatment recommended to referring MD: Secondary process measure which may drive reduction in scheduled follow up visits to specialist, improved patient/provider satisfaction, and both clinical and patient-reported outcomes 4.% of referrals with visit scheduled urgently: Measure of collateral benefit in which referrals not initially flagged for urgent scheduling are triaged by specialist Outcome Measures 5. Wait days—expect to reduce as visits are deferred 6. Referral rate—expect to reduce as PCPs are educated 7. Total visits per unique patient- expect to reduce with reduced follow up visits 8. Lab/Imaging utilization per referral—expect to reduce with PCP education 9. Patient/patient satisfaction—expect to improve with improved timeliness Balance Measures 10. Cost per visit avoided 11. Time per visit avoided
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Diabetes: approximately 6 months Percentage of referrals reviewed - 100 % Number of referrals reviewed - 359 % alternatively managed - 13 % % with previsit planning - 30 % Outpatient capacity gain - 60 h over 6.5 months Specialist time per visit avoided - 1 h Thyroid: approximately 5.5 months Percentage of referrals reviewed - approximately 10 % Number of referrals reviewed - 40 % alternatively managed - 55 % % with previsit planning - 0 % Outpatient capacity gain - 11 h in 5.5 months Specialist time per visit avoided - 30 min General Endocrinology: 1 month Percentage of referrals reviewed - 50 % Number of referrals reviewed 93 % alternatively managed - 18 % % with previsit planning -pending Outpatient capacity gain - 17 h Specialist time per visit avoided - 1 h Total of 85 visits avoided, approximately 75 h of clinical time invested. Cost at the time of writing is approximately $115 per visit avoided.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Through our three pilots thus far, we have learned that together, PCPs and specialists are able to manage a significant portion of referrals through non visit based activities. Specific lessons include: 1. Process mapping is key: Without developing a detailed, interdisciplinary understanding of the existing referral process, overlaying this new process will be disruptive and of limited value. 2. Use the PDSA model during all stages of implementation: With the high potential for dropped balls, unscheduled appointments, and confusion for patients/providers, weekly interdisciplinary huddles during which key process indicators and cases are reviewed are critical. 3. Well defined clinical scope, focusing on questions most appropriate for non-visit based consultation is critical to achieving efficiency, but may limit overall impact. 4. A quarterly stipend based payment for 1–2 clinicians per specialty, as opposed to a fee-for -service model, encourages an efficient, “programmatic” orientation. 5. Our progress to date has required approximately 75 h of specialist time to avoid 85 visits. Over time, we hope to improve the precision with which we define the scope of referrals reviewed to optimize our use of specialist time.
ADDRESSING FREQUENT UTILIZATION OF THE EMERGENCY DEPARTMENTParas Mehta; Animita Saha; Ethan Sherrard; Tamara D. Burdon; Joseph Brancatto. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1941752)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Frequent ED utilizers’ (FUEDs) multiple physical and behavioral health needs are not adequately addressed in the ED resulting in the overutilization of high-cost, low-value services.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Reduce number and frequency of emergency department visits. 2. Educate patients about services provided within Medical Home and link to services as needed. 3. Utilize integrative care team to reduce costs of patient care.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): This pilot was conducted in a hospital-based inner city clinic where majority of patient population is uninsured or underinsured. The entire program started with formation of an interdisciplinary team comprised of the clinic Directors, acupuncturist, behavioral health counselor, social worker, patient navigator, care managers and program coordinator. We used the hospital system’s billing system to identify FUEDs to invite to the Drop-in Self-Management Group. The targeted population has been able to access the clinic, as evidenced by at least one visit in the past 2 years. The main innovative and novel intervention is a once a week, Drop-In Self-Management Group (DISMG) held in the clinic location. Patients who attend were provided with a light snack and transportation help The purpose of the DISMG are: 1. Intensive care management with very low Care Coordinator to patient ratios. 2. Behavioral health services on-site using co-located therapists, and linkage to a behavioral health provider as needed. 3. Linkage to a PCP in the office 4. Education about how to appropriately navigate the healthcare system 5. Referrals to community resources based on need 6. Acupuncture is offered to interested patients to help address the biopsychosocial continuum in patients with high levels of anxiety or chronic pain. 7. Self-management support is enabled by motivational interviewing. Participants are given a toolkit containing disease-specific educational resources and Templates. A patient coordinator will make regular contact with the targeted patients using their preferred method of communication. When a patient does visit the ED, the hospital’s Social Workers will re-educate the patient and will close the communication loop with the Clinical Care Coordinator to follow up with the patient the next day. Following a hospitalization, a transitional care visit may occur telephonically, in the clinic, and/or in the patient’s home, depending on the patient’s need.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The most important indicator of success is how well the participating FUEDs are linked with available resources. Several factors that contribute to success are successful linkage to a PCP and behavioral health counselor (if necessary). An increase in use of these low-cost services indicates improved patient understanding of how to properly utilize healthcare services. We are also examining the effect of the program on the patients’ perception of how well they can manage their health effectively; self-efficacy plays a tremendous role in an individual’s overall health status. The effectiveness of the program is ultimately gauged by the reduction of ED visits and associated costs. The greater the reduction in costs, the greater the success of the program.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): All patients identified as being a FUED eligible for our program were successfully linked with a PCP. We realized a 37 % reduction in ED use, with annual number of visits dropping from 13.4 to 8.4. This equates to a 1.94 million dollar estimated reduction in annual charges for the 16 patients who have attended at least one group. The availability of drop-in medical appointments after group averted at least two visits to the emergency department. Eighty-eight percent of the patients received social work services, while 25 % see the integrated behavioral health counselor weekly. All uninsured patients were linked with the sliding scale department and were eligible for reduced-cost care or government-subsidized insurance, impacting the uncompensated care provided by the clinic. All group participants have a behavioral health diagnosis and multiple comorbidities. A supportive group environment is essential for maximum patient benefit. Most group participants have chronic pain. Incorporating acupuncture proved to be effective in reducing pain by average of 30 %.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The process should start with team building with members who play key role in transitioning patients from ED to their medical home. Key points to remember after the initial phase are: 1. Motivational Interviewing to promote patient engagement and self-management, group facilitator nees to be trained in this technique 2. Intensive care management and social work involvement for educating patients about available services within clinic or community 3. Addressing Behavioral Health issues 4. One specific group model will not fit every practice, need to tailor to population or practice
ADOPTION AND UTILIZATION OF E-CONSULTS IN A VETERANS AFFAIRS HEALTHCARE SYSTEMVarsha Vimalananda1; Gouri Gupte3; Justice Clark2; Jay D. Orlander2; Steven R. Simon2. 1Center for Health Organization and Implementation Research (CHOIR), Bedford, MA; 2VA Boston Healthcare System, Boston, MA; 3Boston University School of Public Health, Boston, MA. (Tracking ID #1926077)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Patient-centered medical homes (PCMHs) should improve patient access to healthcare; however, access to specialists may be limited by long distances and wait times, and PCPs often lack ready access to specialty expertise.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To improve access to specialty care for ambulatory patients and PCPs through electronic consultations (e-consults).
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Setting: VA Boston Healthcare System (VABHS) provides primary care through PCMHs to 32,000 Veterans at 3 hospitals and 8 community-based clinics. It is the main referral center for the New England VA Network. Implementation: E-consult implementation for VABHS medical specialties began in 1/2011. Discussions with primary care leadership and emails to PCPs described the availability and purpose of e-consults. By early 2013, e-consults had expanded to include most clinical services, including mental health and pharmacy. Any VABHS provider can request e-consults. Providers at some other New England VA facilities also have limited access to VABHS e-consults. Process: E-consult requests generated in the electronic health record are routed to the consulting service. Within 3 working days, specialists are expected to initiate a dialogue with the requesting provider or convert the e-consult to a traditional patient appointment.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We examined trends in adoption and utilization of e-consults at VABHS quantitatively and qualitatively. We identified the most common requesters, recipients, requester-recipient service dyads, and requesting provider types. We measured the median time to completion. We then examined the full text of e-consult requests and responses from primary care and between the commonest requester-recipient dyads to better understand e-consult utilization. We are now conducting semi-structured interviews with key stakeholders (leadership, administrators, clinicians).
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Within VABHS, we found: − Top requesting Departments: Medicine (59 %), Surgery (35 %), and Other (6 %) - Top requesting Sections within Medicine: Primary Care (76 %), Pulmonary (4 %), Cardiology (3 %). - Top requesting Sections within Surgery: Orthopedics (41 %), General Surgery (15 %), Optometry (11 %) - Top recipients: Cardiology (11 %), Orthopedics (11 %), Sleep (11 %), Hematology (10 %), and Pulmonary (5 %). - Top requester-recipient dyads: Orthopedics-Orthopedics (65 %), Optometry-Ophthalmology (18 %), Ophthalmology-Optometry (6 %) - 591 intra-specialty e-consults; 85 % within Orthopedics. - Requesting provider types: NPs (34 %), MD attendings (24 %), MD residents/fellows (10 %). - Median time to completion across specialties: 2.2 working days (IQR 0.9–9.6). On review of e-consult full text and in initial interviews with key stakeholders, we found both expected and unexpected uses of the technology. The majority of e-consults requests are clinical. Expected clinical uses include requests for data interpretation and advice on workup and treatment. Unexpected clinical uses vary. For example, we noted questions about workup prior to a scheduled specialty visit, and e-consults to Infectious Disease from a long-term care unit (inpatient) as a means to address non-urgent issues. Orthopedics places most of the intra-service e-consults as a means to document a detailed pre-operative chart review. There are multiple examples of administrative uses of e-consults, all of which represent unexpected use. For example, Pulmonary receives e-consults as a mechanism for granting access to low-dose lung cancer screening CTs, currently a limited resource for which Pulmonary is the gatekeeper. In Optometry, e-consults are commonly used for appointment scheduling.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): E-consults are frequent at VABHS. Nearly one-third originate from clinicians outside VABHS, representing robust use of the e-consult mechanism to improve specialty access for patients at locations with more limited specialty services. Within VABHS, as intended, Primary Care is the most frequent Section utilizing e-consults. Response time is generally satisfactory but widely variable. Access to specialty clinical input is a common use of e-consults. Surprisingly, we find many examples of the e-consult mechanism being utilized for other clinical and administrative uses. These represent unexpected ways that e-consults are used to achieve electronic communication and documentation within and between specialties. While these applications may meet the needs of the institution, providers and patients, they do not fulfill the original intention of e-consults. Therefore, measuring the volume of e-consult use alone may provide misleading and insufficient information in the assessment of improved patient and PCP access to specialty care. Further investigation is needed to better understand the processes leading to wide variation in response time; the rationale for unexpected uses of the e-consult mechanism; and what features of the e-consult program represent valid measures of quality care.
AN INTERDISCIPLINARY INTERVENTION TO REDUCE THE RISK OF ADVERSE EVENTS IN HOSPITALIZED PATIENTS WITH NUT ALLERGYChristina Lee1; Barry Schlossberg2; Sally Wong2; Daniel I. Steinberg1. 1Beth Israel Medical Center, New York, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1933394)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): A sentinel event of anaphylaxis in a staff member revealed that food items on the hospital menu were improperly labeled as to whether they contained nuts, prompting concern that patients with nut allergy were at risk for adverse events.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Ensure that no nut-allergic patient suffers an allergic reaction to improperly labeled hospital food. 2. Explore the process of how information about patient food allergy is documented in the medical record.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): A medical resident ate a turkey salad prepared by the hospital food service and developed immediate abdominal pain and urticaria. The resident had a history of anaphylaxis to nuts, and went to the ED where anaphylaxis was diagnosed and treated. The turkey salad was found to contain walnuts but was not labeled as such. The resident was concerned that other food items may not be properly labeled and that patients with nut allergy could be at risk for anaphylaxis. The prevalence of nut and/or peanut allergy in the general population is reported as up to 1.4 %. Tree nuts (of which walnuts are a sub-type) are one of eight foods that account for 90 % of all food-allergy reactions (http://www.cdc.gov/healthyyouth/foodallergies/). The resident and medicine residency program director contacted the directors of food services and of nutrition. Review of the hospital menu found that three items containing nuts were not properly labeled. An additional patient safety issue was identified. Our institution’s food service uses software (CBORD Nutrition Service Suite) to select foods compatible with a patient’s allergies. We discovered there is a delay in patient allergies being entered into CBORD. This system does not automatically receive allergy information from the computerized physician order entry software (GE Centricity Enterprise) that providers use to record patient food allergies upon admission. Manual information transfer between these systems is required, resulting in a window of up to 12 h in which patients could be served foods they are allergic to. Two solutions were considered-- consistent labeling of all foods containing nuts, or removal of nuts from all food served in the hospital. The latter was chosen as it was more reliable, simpler and did not result in any loss of nutritional value.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1. Ability to remove all nuts from food items on the hospital menu. 2. Closing the communication gap between our computerized physician order entry (CPOE) and our food services database.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 1. Within days of our interdisciplinary intervention and a review of the menu, nuts were removed from all hospital food items. 2. To date there have been no further reported events of nut allergy to food prepared in the hospital kitchen. 3. An ongoing goal is to correct the delay in information transfer between our CPOE and our food services database.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): We present this case to point out that it cannot be assumed that all hospital food menu items are clearly labeled as to whether they contain nuts or other food allergens. In addition, providers should be aware that a delay in communication regarding patient food allergies may exist between their institution’s CPOE system and the food services database used to generate patient meals. Such a delay could jeopardize patient safety. In this case, we identified a risk of nut allergy, however the same question we asked and process we followed could be applied to other food allergens (for example gluten, eggs or dairy). Different food allergens may require different solutions. In the case of nuts, complete removal from the menu was feasible. For eggs and gluten, proper labeling may be a more practical approach. We found that engaging an interdisciplinary team consisting of a resident, a program director, and food services and nutrition staff was easy and effective. Automatic and more immediate communication of patients’ food allergies to a hospital’s food service should be the goal. Efforts continue at our institution to solve this issue.
ARE YOU EX-FOLEY-ATING? A HOSPITAL-WIDE INTERVENTION TO DECREASE URINARY CATHETER USE, INCLUDING NURSE-DIRECTED POSITIVE-REINFORCEMENT STRATEGIESJennifer Meddings2; Cynthia Budelmann1; Heidi Reichert2. 1Greenville Health System-Laurens County Memorial Hospital, Clinton, SC; 2University of Michigan, Ann Arbor, MI. (Tracking ID #1939856)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Encouraging nurses to remove unnecessary urinary catheters quickly is challenging and important because nurses often are required to perform more bedside tasks regarding incontinence after catheters are removed.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To reduce unnecessary Foley catheter use and catheter-associated urinary tract infection rates, with a focus on education and positive-reinforcement strategies for nurses.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): In a 90-bed acute care community hospital with 8 critical care unit beds, several interventions were implemented in 2012 including: 1) February hospital policy regarding urinary catheter use requiring catheters to be ordered by physicians only for approved indications, daily assessment of necessity, standard expectations for bedside care regarding placement and maintenance, and encouragement for nurses to remind physicans to remove unnecessary catheters; 2) March 2012 entry into the ‘On-the-CUSP: STOP CAUTI’ program from the Agency for Healthcare Research and Quality (http://www.onthecuspstophai.org/on-the-cuspstop-cauti/) involving educational toolkits and data collection resources to reduce CAUTIs, with feedback of Foley catheter utilization rates to nurse leaders and units; 3) April 2012 purchase and training for bladder scanner; 4) July 2012 initiation of the “Are you ex-Foley-ating” campaign by the infection preventionist to encourage nurse removal of catheters including entertaining nurse-humor posters, daily rounding by the infection preventionist with nurses (for positive reinforcement and just-in-time education), monthly feedback and by rewarding each catheter removal with a small wrapped gift with an appreciation note (exfoliating cream for the first catheter removal, and candy for additional catheter removals).
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Before-and-after hospital-wide and critical care unit rates of Foley catheter utilization (i.e., ratio of Foley catheter days to patient days) and catheter-associated urinary tract events were monitored on monthly basis, with monthly feedback provided to each unit.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Hospital-wide urinary catheter use ratios in 2011–2013 varied between 0.17 and 0.30, before and after interventions, with no sustainable reduction from an average of 0.2. CAUTI events also did not decrease, yet the CAUTI definition (as defined for National Healthcare Safety Network surveillance reporting) also changed over time. Critical care unit measures of urinary catheter use and CAUTI events varied widely, not unexpectedly given only 8 beds. Unfortunately, despite multiple interventions including an enthusiastic response for the “ex-Foley-ating” nurse-directed interventions, no sustained reduction in urinary catheter use was demonstrated.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): In this small community hospital, despite multiple interventions, including standard strategies (education, policies, feedback) and nurse-directed positive-reinforcement strategies, urinary catheter use did not decrease. Given nurse enthusiasm for the “ex-Foley-ating” campaign, it is possible that specific nurse empowerment to remove unnecessary catheters by protocol (without requiring individual physician orders) may have further reduced catheter use; yet, despite requests by infection control since February 2012, this hospital’s nurses are not empowered to remove catheters.
BRIDGING THE CHASM-ADVANCED ILLNESS MANAGEMENT: HIGHER QUALITY, LOWER COSTSandy Balwan; Ramiro Jervis; Joseph Conigliaro; Kristofer L. Smith. North Shore LIJ Health System, Manhasset, NY. (Tracking ID #1936650)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Can delivering in-home care, to elderly patients with multiple chronic illnesses and functional impairment, focused on prompt response to changes in clinical condition and high quality transitions, result in lower total cost of care?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) Leverage information technology including real time notification to Improve care coordination between hospital, physician group, and home/community services. 2) Create an on-demand program to respond to patient’s changes in clinical status through same day urgent visits, 24/7 telephonic triage and off-hours community paramedicine. 3) Improve patient specific metrics (hospital length of stay, number of hospital encounters, readmissions, patient satisfaction, percent of death at home).
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The North Shore LIJ Health System Advanced Illness Management (AIM) House Calls Program is a multidisciplinary team of physicians, nurse practitioners and social workers with central support personnel including a nurse intake manager, practice manager, biller, data analyst, project manager, administrative assistant, medical coordinators, medical director, and director of quality and case management. Program eligible patients require two or more chronic conditions, a recent hospitalization or unmet symptom need, and meet Medicare definition of home boundedness. Patients must also be willing to allow AIM providers to serve as their primary care provider. Patient Characteristics: Mean age was 85 years, 72.2 % female and 27.6 % male. Most needed assistance with 5–6 ADL’s (65 %). The most common diagnosis were diabetes, protein-calorie malnutrition, decubitus ulcer of the skin, congestive heart failure, cardiac arrhythmias, COPD, renal failure, stroke, vascular disease, and Parkinson’s and Huntington’s disease.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Quantitative measures to evaluate the program include hospital admission rate, 30 day readmission rate, hospital length of stay (LOS), percent of in-home post discharge medicine reconciliations performed within 48 h, percent of patients with advanced care planning and percent of patients who die at home. Qualitative metrics included American Academy of Home Physicians surveys of patient satisfaction, likelihood to recommend the program, and whether the program met patient needs.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Among the enrollees in the program, the percentage of patients who had a post-admission contact within 48 h rose from 45 % in quarter 3 of 2012, to 85 % in quarter 3 of 2013. The acuity of patients entering the program, increased over time with the average HCC diagnosis risk score increasing by 46 % by quarter 3, 2013. Mean hospital LOS decreased from Q4 in 2012 (8.61 days) to Q3 in 2013 (7.28 days). Compared to the year prior to enrollment, patient experienced a 37 % decrease in hospital admissions. Hospital 30 day readmission rate was 17 % for patients discharged to rehabilitation facilities and 12 % for patients discharged to home. Post discharge in-home medication reconciliation was performed within 48 h of discharge for 94 % of patients in quarter 3, 2013 compared to 63 % in quarter 2, 2012. Of the total patients enrolled in the program, 95 % had an advanced care plan in place. In 2013 65 % of patients were able to die at home. Patient satisfaction: When asked about likelihood to recommend the program, 84 % responded “definitely yes” in September 2013 compared to 77 % in October 2012. Seventy one percent responded “definitely yes” when asked if they were seen by the team within 36 h for urgent medical problems in 2013, compared with 63 % in 2012. When asked about receiving answers to medical questions the same day, 65 % responded “definitely yes” in 2013 compared with 45 % in 2012. Sixty five percent responded that the program reduced their trips to the ED in 2013 compared with 56 % in 2012. Eighty percent of patients felt that the program improved their quality of life in 2013 compared with 71 % in 2012.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Implementation of a high quality advanced illness management program can decrease admission rates, hospital length of stay and increase patient satisfaction despite an increase in overall patient acuity. AIM programs can provide person-centric planning to balance curative and comfort care as disease progresses. Such programs must include an interdisciplinary team, and provide coordination of care between hospitals, physicians, home, and community services. However, the needs of the community can quickly outpace program resources. Our wait list is currently over 100 with a 3–4 month wait for non-acute referrals. Programs must also ensure buy in from senior leadership, finance and quality departments, and must leverage informatics to achieve high reliability. The employment of community paramedicine to assist with patient evaluation and triage during off hours is also critical to program success.
BRIEF CLINICIAN SURVEY CAN PRODUCE REMEDIABLE FACTORS TO REDUCE CLINICIAN BURNOUTSara Poplau3; Scott Shimotsu2; Mark Linzer1. 1Hennepin County Medical Center, Minneapolis, MN; 2Hennepin County Medical Center, Minneapolis, MN; 3Hennepin County Medical Center, Minneapolis, MN. (Tracking ID #1926205)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Clinician stress and burnout rates are high and rising across the country.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Many contributors to these conditions have been studied. We piloted a brief survey to determine areas for work life improvement within medical departments at an upper Midwestern safety net hospital.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The survey was administered by a new Provider Wellness Committee charged with improving clinician wellness throughout the institution. We developed a brief questionnaire that was distributed electronically via Survey Monkey to clinicians. The instrument was adapted from prior worklife measures from the MEMO study (Minimizing Error Maximizing Outcome). It is comprised of 10 quantitative questions concerning stress, burnout and their predictors, and one open ended question about stress. The survey was sent to all 540 inpatient and outpatient clinicians in the hospital system, including dentists, psychologists, physicians and advanced practice providers (NPs and PAs).
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The survey queried job satisfaction, stress, burnout, workload; time for documentation, work environment (chaotic, busy, calm), values alignment with leadership, teamwork, time spent at home using the electronic medical record (EMR), and EMR proficiency. The analysis included simple counts and frequencies of outcomes by department. We used adjusted logistic regression to evaluate factors that predicted burnout, and performed latent class analyses to determine characteristics of satisfied and dissatisfied clinicians. We hypothesized that burnout rates would vary among departments, along with the predictors.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Of the 540 providers, 352 (65 %) clicked on the survey and 314 (58 %) completed it. Of the 314 providers who completed the survey, 166 (53 %) filled in the open ended question about stressors, some typing pages of commentary. Of the respondents, 59 % were female, 85 % were white, and 19 % were part-time. Fifty-four percent were physicians, and 34 % were APPs. Burnout rates ranged from 0 to 50 %. In general, most providers were satisfied with their jobs (82 %), although 60 % noted a high degree of stress. Approximately 45 % noted poor or marginal control of their workloads, 51 % had insufficient time for documentation, and 44 % spent excessive time at home using the EMR. Adjusted regression analyses showed that burnout was predicted by stress (Odds Ratio (OR) 13.8, 95 % CIs 5.3, 35.7), lack of control (OR 5.5, CIs 2.6, 11.3), values alignment (OR 0.28, CIs 0.13, 0.63) and lack of EMR proficiency (OR 3.1, CIs 1.1, 8.8). Satisfied clinicians demonstrated low burnout, high values alignment, excellent teamwork, and high EMR proficiency. These findings were presented to a 4 h Provider Wellness Committee retreat with department Wellness Champions to determine tailored interventions for wellness and lower burnout. Intervention focal areas included communication, team building, promoting work control, and minimizing EMR stress. For example, a seminar may be convened to improve providers’ abilities to navigate through the EMR with “short cut” keystrokes or toggling.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): This pilot process shows it is possible to use a brief survey tool to inform an institution and address work life challenges and high burnout rates. Wellness-oriented interventions should focus on lack of control, values alignment, EMR proficiency and teamwork. The impact from wellness interventions on important outcomes such as clinician turnover and quality of care remains to be determined.
CAN E-CIGARETTE HELP PATIENTS TO REDUCE OR STOP SMOKING IN PRIMARY CARE PRACTICE?Jean-Paul Humair; Rodrigo Tango. University Hospitals of Geneva, Geneva, Switzerland. (Tracking ID #1938888)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The evidence about the acceptability and effectiveness of the electronic cigarette (E-cigarette) to reduce or stop tobacco use in primary medical care is very limited but plausible.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): This exploratory study assessed whether the E-cigarette was acceptable for patients, helpful for a short-term reduction or cessation in tobacco smoking and defined the profile of regular E-cigarette users.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Since mid-2013, E-cigarette was offered as a new aid to smokers who attended an outpatient clinic of an urban university hospital in Switzerland. All smokers received the usual motivational and behavioral counseling. Those who wished to reduce tobacco use or failed to stop smoking with usual cessation therapy (nicotine replacement, varenicline, bupropion) were offered to use E-cigarette with nicotine.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Acceptability will be evaluated with the proportion of patients using the E-cigarette daily for several months. The effectiveness will be assessed by proportions of E-cigarette users who either reduced their tobacco consumption by at least 30 % or quit smoking completely at the end of follow-up and at 1 year. Effects of E-cigarette on withdrawal and mental symptoms, changes in expired CO measurements, patient satisfaction and adverse events must also be measured.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Seventeen patients chose to use the E-cigarette. They were heavy and dependent smokers consuming a daily average of 23 cigarettes and smoking their first cigarette 16 min after waking up. A somatic tobacco-related illness (65 %) and a mental disorder (82 %) were very common in this sample. All patients but one used the E-cigarette daily either to reduce their tobacco use (59 %) or to quit smoking (41 %). Most patients (88 %) changed their behavior positively with either tobacco reduction or cessation during an average follow-up of 3 months. Half of patients (47 %) decreased their mean cigarette consumption by 57 %; the reduction was lower than 30 % for a single patient using E-cigarette without nicotine. A similar proportion (41 %) reported to have achieved tobacco abstinence. Pharmaceutical nicotine replacement or varenicline were used at some stage by 59 % of patients in association with the E-cigarette. Patients reported no significant side effects but were often unclear about their nicotine intake and levels of nicotine in E-liquid cartridges.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): E-cigarette with nicotine is well accepted and used daily by most patients willing to reduce consumption or to quit smoking after failed attempts. Short-term results in this very small sample suggest that E-cigarette might be effective to help smokers attending in primary care to reduce or stop tobacco use. Clinicians may start offering to some smokers the E-cigarette, which enlarges the choice of smoking cessation aids. As stronger evidence is needed, clinical trials with larger samples should test the effectiveness of E-cigarette to change smoking behavior and maintain it in the long-term among patients in primary care practice.
CAN PHYSICIAN REVIEW OF READMISSIONS IMPACT PROVIDER PERCEPTIONS AND REDUCE READMISSION RATES?Edmund A. Liles1; Carlton R. Moore1; Beth Ann Brubaker1; Jonathan Kirsch1; Paul Ossman1; Monica Reynolds1; Jacob Stein2; John M. French1. 1University of North Carolina School of Medicine, Chapel Hill, NC; 2University of North Carolina School of Public Health, Chapel Hill, NC. (Tracking ID #1938216)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): If hospitalist physicians perform chart reviews and root-cause analyses on their readmitted patients, will it change their perceptions of the causes and preventability of readmissions, and reduce overall readmission rates?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Hospitalist physicians conduct chart reviews and root-cause analyses on all of their patients readmitted within 30-days of hospital discharge 2. Assess impact on hospitalist physician perception of cause and preventability of readmissions 3. Assess impact on 30-day all-cause readmission rate
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We present a before-after (uncontrolled) trial evaluating timely feedback of readmissions to hospitalist physicians. As a part of routine patient tracking, the quality improvement department of UNC Hospitals creates a daily list of patients who are currently registered as receiving care within UNC Hospitals (inpatient, observation, procedure or emergency department). For this study, that list is filtered to include only those patients who were an inpatient within the last 30 days and cared for by a faculty member from the Hospital Medicine Program. Patients are removed from the list if they have planned readmissions (UNC Psychiatry or Rehabilitation on the same day, or return to the North Carolina Cancer Hospital for planned chemotherapy). The hospitalist physician for the index admission is notified on the day of a readmission. The hospitalist physician is responsible for performing a chart review and root-cause analysis on the readmission. The chart review and root-cause analysis is a structured tool adapted from the Institute for Healthcare Improvement STAAR Initiative.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The primary measure of success is a reduction in the 30-day readmission rate. We also assessed physician perceptions regarding the causes of readmissions and estimates of preventability, both before and after the intervention. Since a reduction in readmissions may be a result of physicians keeping patients in the hospital longer, we also collected data on length of stay during the study period. The notifications and chart reviews began July 1, 2013 and are ongoing. Descriptive statistics are presented. Continuous variables are analyzed via t-test for means and chi-squared for proportions. A Shewhart P chart is used to describe 30 day readmission rates over the course of the study.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 30 day all cause readmission data is currently available through the end of October 2013. For the 18 months prior to the intervention our 30 day all cause readmission rate was 12 %, since starting our intervention the rate has decreased to 10 % (chi-squared, p = .18). The Shewhart P chart for 30-day readmissions shows a possible trend toward reduced readmissions since the start of the intervention in month 19. Average length of stay increased from 4.73 days over the prior 18 months to 5.01 for the 4 months since the intervention (t-test, p = 0.1). At baseline the top three contributors to readmissions were felt to be patient understanding, medication non adherence, and substance abuse/addiction. After 6 months of the intervention, the top three contributors were felt to be substance abuse/addiction, medication non adherence and lack of primary care. Based on the STAAR tool chart review, the index hospitalization and readmission had the same diagnosis in 50 % of cases. Thirty percent of the readmissions were labelled preventable. The two most common categories contributing to readmission were problems with adequate follow up and medication errors or complexity.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Our intervention of readmission notification and chart review has resulted in a downward trend in readmission rates without significant changes in length of stay. The initial results are promising and our data collection and analysis is ongoing. Physicians continue to feel the majority of readmissions are not preventable. Chart review and physician perception indicate follow up and medication adherence are major concerns. Our faculty group continues to discuss our readmission rates during monthly faculty meetings and we have formed a complex care committee to develop individualized care plans for our highest needs patients.
DEVELOPING A GERIATRICS CONSULT CLINIC IN THE SAFETY NETAnna H. Chodos1; Christine Ritchie1,2; Janet Myers2; Hali Hammer3; Edgar Pierluissi1. 1UCSF, San Francisco, CA; 2UCSF, San Francisco, CA; 3UCSF, San Francisco, CA. (Tracking ID #1938100)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The health care safety net provides primary care to medically and socially complex older adults, but there are rarely geriatrics specialists available in this setting.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): A. Create an outpatient geriatrics consult service in the San Francisco Department of Public Health’s (SFDPH) safety net healthcare system using eReferral, an existing electronic health care record (EHR) referral mechanism. EReferral allows for iterative conversation between primary care providers (PCPs) and specialists, and allows efficient communication of recommendations and scheduling. B. Measure the proportion of geriatrics referrals that were managed through: 1) electronic advice (e-advice), or 2) e-advice and co-management (eg. direct social work referral, call patients or caregivers) without seeing the patient, or 3) comprehensive geriatrics assessment (CGA) of the patient in an outpatient setting. C. Measure consult’s impact on PCP satisfaction and PCP’s feelings of self-efficacy in geriatrics.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): In October 2012, we began a geriatrics outpatient consult service for 2 SFDPH primary care clinics, for patients age 65 or older. We accept consults via eReferral, and the staff of 1 geriatrics fellow and 1 attending meet twice weekly to review consult questions and accompanying patient records, and triage to 1, 2, or 3 as listed above. We have a once monthly half-day clinic for CGA and do home visits as needed.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We measured the number of consults received, time spent for consults, and nature of referral questions. We used surveys to assess providers’ satisfaction and self-efficacy with geriatric conditions after the consult.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Over 54 weeks, PCPs referred 100 patients to the geriatrics consult service and 2 geriatrics providers each spent an average of 77 min (median 60 min) weekly reviewing and responding to them. Of the 100 patients referred, 20 were managed with e-advice only, 17 were managed with e-advice and time-limited co-management, and 63 were seen in the clinic. Most consults (68 %) listed >1 reason for referral and 21 % asked for CGA or management of medical complexity. Common consult questions were cognitive impairment (60 %), social issues (27 %), medication review (26 %), and falls (19 %). For the 63 patients seen (in 13 clinic sessions and 11 home visits), each visit took an average of 2.1 h per patient. Provider surveys (response rate 65.9 %) showed 94.9 % would use it again, 78.3 % strongly agreed that their question was addressed to a satisfactory level, and 97.3 % felt their geriatrics knowledge improved.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): A Geriatrics consult clinic can provide effective support to PCPs in the safety net setting without seeing every patient. The most frequent reasons for referral were cognitive impairment, medical complexity and social issues. Providers felt the service was useful, including for patients seen with e-advice only. The next steps are to examine: 1) the nature of consult questions dealt with via e-advice vs. CGA, 2) the interventions of the geriatrics consult clinic, 3) patient outcomes before and after geriatrics consult, eg. number of inappropriate medications as determined by Beers criteria; health care utilization; documentation of advance care planning, and 4) identify ways to improve specialists’ time-efficiency, particularly with CGAs.
DEVELOPMENT AND IMPLEMENTATION OF AN ELECTRONIC REGISTRY TO SUPPORT ADHERENCE TO OPIOID PRESCRIPTION GUIDELINES AMONG ADULT PRIMARY CARE PROVIDERSChristopher W. Shanahan1; Donna Beers1; Vinay Hoolloomann3; Karen E. Lasser1; Jane M. Liebschutz1,2. 1Boston University School of Medicine, Boston, MA; 2Boston University School of Public Health, Boston, MA; 3VINK Software Technologies Inc., Acton, MA. (Tracking ID #1937571)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): To design, develop and implement an electronic registry for use in primary care by a nurse case manager to improve care of patients being treated with opioid medications for chronic pain.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Develop, implement, and test an electronic registry of patients with chronic non-cancer pain being treated with long-term opioid medications for use by a dedicated Nurse Case Manager (NCM), with a goal of maximizing efficiency and safety while minimizing risk of addiction and diversion. 2. Ensure that the electronic registry is intuitive, user-friendly, and closely supports the NCM’s actual workflow. 3. Develop, implement, and test tailored reports for use by the NCM, the project investigators, and specific primary care providers for use within an academic detailing session to improve provider performance and adherence to chronic pain management and opioid prescribing care guidelines (American Pain Society - American Academy of Pain Medicine).
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The electronic registry was developed to support evidence-based case management within a cluster randomized control trial comparing adherence to guideline based care of patients treated for chronic pain with opioids in primary care based practices (internal medicine and family medicine) in an urban safety net hospital and three community health centers in Boston. Primary care physicians (PCP) will be randomized to one of two conditions: intervention (nurse care management, registry, electronic decision support tools, and academic detailing) or control condition (electronic decision support tools only). Chronic pain patients (560) and PCPs (56), both control and intervention, will be followed for 12 months after study enrollment to assess the primary outcomes of rates of PCP adherence to chronic opioid therapy guidelines and opioid misuse among patients. The intervention group will receive intensive practice support from the NCM, who has access to the electronic health record and a state-of the art electronic registry tool designed and built by the study’s technology team. The registry provides a dynamic, filterable work list which is clickable and linked web-based forms to facilitate various clinical encounters including: medication refills, risk assessment, clinical assessment, and treatment plan creation, along with flexible reporting which provides both practice and provider specific monitoring for care management and academic detailing.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The following specific aims will serve as measures of this study’s success: 1) Evaluate the relative effectiveness of the intervention compared to the control condition on rates of PCP adherence to chronic opioid therapy guidelines. 2) Evaluate the relative effectiveness of the intervention compared to the control condition on rates of clinically significant reduction in opioid misuse by patients. 3) Develop a road-map for widespread dissemination of the implementation strategy, through qualitative assessments and a cost analysis.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 1. Development of a computer application to support actual clinical workflow for programmatic interventions that is simultaneously being developed in terms of staffing and workflow is feasible but complicated. 2. Design and development of efficient workflow enhancing technology is labor intensive and requires rapid design and development cycles. 3. Theoretic design work is critical but only provides the starting point for the full understanding of the workflow of a new clinical process. Flexibility and iterative open dialogue combined with sufficient time to develop, test, and revise is critical. 4. Screen shots of developed key components of the functional registry, an integrated workflow/application diagram will be presented.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Development of an advanced, automated case-management registry, must be grounded in actual clinical practices and processes. Success of the development process is critically dependent on a trusting and bidirectional partnership between clinical users and application developers based on mutual respect and a shared goal of creating the most clinically effective application possible.
DIABETIC GROUP VISITS: A “REAL WORLD” PILOT PROGRAMMarshall Fleurant1; Megan Bergstrom3,1; Bonnie Burke4; Gertha Dabady1; Karen Chalmers2; James Rosenzweig2; Karen E. Lasser1. 1Boston University School of Medicine, Boston, MA; 2Boston University School of Medicine, Boston, MA; 3Boston Medical Center, Boston, MA; 4Boston Medical Center, Boston, MA. (Tracking ID #1934535)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Can we utilize a series of diabetic group visits to improve self efficacy for patents with diabetes, maintain patients’ access, complete diabetic processes of care and achieve improved hemoglobin AIC (HbA1c) control?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1.) Evaluate the feasibility of the diabetic group visit series as a mechanism to treat patients with diabetes within a large urban safety-net patient centered medical home 2.) Evaluate patient health beliefs before and after group visits 3.) Maintain or improve HbA1c levels over the course of the group visit series
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): This program consists of four group visits and a set curriculum occurring over 3 months. Every 3 weeks patients meet, these visits are designed to increase patient self-efficacy and improve HbA1c levels. The curriculum encompassed the pathophysiology of diabetes, medication use and safety, diabetic nutrition and weight loss, and helpful resources to help treat your diabetes. Each visit is 2 h long and facilitated by a multidisciplinary team. The visit begins with a lecture followed by an interactive session led by a nurse practitioner to reinforce lessons learned and allow patients to share experiences. During interactive sessions, patients leave the group for individual medical consultations with a provider. A pharmacist or nutritionist may lead interactive sessions during the second hour. Our experience includes both a spring and fall series with eight group visits in total.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We measured patients’ attendance, HbA1c levels before and after the series, and measured health care utilization including outpatient and emergency department visits as well as hospitalizations. We also collected data on process measures such as testing for HbA1c, urine microalbumin, and low-density lipoproteins (LDL). We assessed patient health beliefs using a previously validated “Diabetes Related Health Beliefs” survey.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We invited two primary care providers (PCP’s) patients (n = 167) who were identified as diabetics by the electronic medical record problem list. In total 20 patients participated. Approximately 13 patients attended the four visit spring series and 8 attended the four visit fall series. One patient attended both series. We measured HbA1c 6 months after the completion of the spring series; 10 of 13 patients experienced declines in HgA1c from baseline. The average decrease in HbA1c was 0.52 % (Standard Deviation, 1.75 %). In the year prior to group visits, only 10 of the 20 participants saw the same PCP continuously (defined as at least 50 % of all PCP visits were with the same provider). However during the group visits 16 of the 20 participants saw the same PCP continuously and 10 of 20 patients went to group visits solely for their primary care needs. Group visits appeared most effective in capturing process measures for patients that were infrequent utilizers of care. Exactly 82 process measures were completed in the 6 months before and after the first group visit. Approximately 20 % of all labs were processed during the group visits. Among patients whom attended 10 or less total outpatient visits in the year, 40 % of process measures were processed during group visits vs only 5 % for patients who attended greater than 10 total outpatient visits per year. Group visits seem to affect participants perceptions on the role of medication in the care of diabetes but not the role of diet. Prior to the group visit series, 43 % who completed the survey (n = 7) were confused by all the medications given to them by their doctor, after the group visit series 17 % (n = 6) endorsed this belief. However approximately 57 % agreed that medications would control diabetes before the group visit series vs 33 % after the group visit series. Patient’s beliefs regarding the role of diet in the control of diabetes did not change. For example over 70 % of patents before and after the group visit series believed that diet could help control complications related to diabetes or that they should continue to follow their diabetic diet even if they did not feel better. Approximately 50 % of patients before and after the group visit series felt that their diabetes was well controlled.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Among a selected group of patients who participate, group visits can improve continuity within primary care and improve HbA1c. Group visits may also play a role in meeting recommended process measures for a selected subset of patients. Strongly held beliefs prior to group visits may be difficult to alter, patient’s self perception on medications or diet are important factors to consider when designing a program.
DIABETIC RETINOPATHY IS COMMON AMONG PATIENTS SEEKING CARE FOR DIABETES IN A COMMUNITY HEALTH CLINICCarolyn F. Pedley1; Claudia L. Campos1; Emily W. Gower3; Daniel Nelson2; David Friedman4; Ramon Velez1. 1Wake Forest School of Medicine, Winston-Salem, NC; 2Wake Forest School of Medicine, Winston-Salem, NC; 3Wake Forest School of Medicine, Winston-Salem, NC; 4Johns Hopkins School of Medicine, Baltimore, MD. (Tracking ID #1939136)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): What is the incidence of diabetic retinopathy identified by high resolution retinal photography in a community health clinic?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To screen diabetic patients in a community-based adult medicine clinic using a high resolution non-mydriatic retinal camera. To evaluate retinal images for diabetic retinopathy and other ocular pathology To calculate the incidence of diabetic retinopathy in this underserved population
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The Downtown Health Plaza is a safety net university-affiliated outpatient clinic that provides health care for approximately 1,700 adults with diabetes. The majority of patients are uninsured or are covered by Medicaid. The clinic serves as a training site for medical residents supervised by eight faculty physicians. The retinal camera, computer, software and study protocol were provided by a research grant awarded to the Johns Hopkins research group with funds from the Centers for Disease Control. Retinal photographs were read at the Wills Eye Center in Philadelphia, PA and participants were referred to the Wake Forest Eye Center or their preferred ophthalmologists for further management as needed
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The success of the program was measured by the number of diabetics screened and the photographs having sufficient quality to identify retinal pathology. Follow up appointments with Ophthalmology for those with significant retinopathy also were tracked.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 180 participants were screened over a 6 month period. Participants’ ages ranged from 19 to 91 and 67 % (n = 120) were female. We were unable to obtain photographs for 1 individual due to difficulty positioning her in front of the camera. An additional 13 % of photographs could not be read due to poor image quality or inability to view the retina because of corneal or lens opacity. Among the remaining 156 participants, 29 %(n = 46) had abnormal retinal findings requiring referral to an ophthalmologist, with 17 requiring urgent follow up due to severe diabetic retinopathy. Only 26 % reported seeing an eye doctor in the last year and less than 50 % had seen an eye doctor in the last 2 years.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): A significant number of screened participants had retinopathy requiring further management by ophthalmology. Given the low rate of eye care utilization in this population and the success of this program in screening participants, the use of camera screening for diabetic retinopathy in primary care should be considered on a broad scale. Such programs would increase diabetic retinopathy awareness in these populations. Challenges: There is considerable expense in purchasing the camera, software, reading, data tracking and personnel in implementing a screening program utilizing retinal photography. The tracking of participants involves sharing information across several settings including the clinic, the reading center, patients, providers, and the ophthalmology group.
EMBRACING THE HUDDLE IN A RESIDENT TEACHING CLINICEdward Ewen; Sarah Schenck; John Donnelly. Christiana Care Health System, Newark, DE. (Tracking ID #1938872)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Despite ongoing efforts to improve the consistency and quality of care delivered in our resident teaching clinic our performance had stalled after modest improvement in several measures, in part due to unrecognized or missed opportunities to affect care during the course of scheduled patient visits.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): A pre-session huddle each day to: 1) Identify opportunities for improvement immediately prior to the patient visit 2) Improve the overall consistency and quality of care delivery 3) Optimize Systems Based Practice in the setting of a Patient Centered Medical Home by more fully integrating the medical assistants into the resident-patient office workflow
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): A Huddle is an informal meeting between a provider and medical assistant to discuss, anticipate and prepare for the needs of the patients in an upcoming clinical session. In order to successfully role out the patient care Huddle, we started with physician and staff education. A presentation was given to all of the providers as part of the Preclinical Pearls teaching curriculum. The staff was also given education about the importance of the Huddle. To standardize the information that was shared during the Huddle, a form specifically designed for this purpose was completed by the residents and discussed with the Medical Assistant before the morning session. To ensure the completion of the Huddle, a 15 min block of time was incorporated into the schedule every morning. Faculty preceptors were assigned the responsibility of making certain the Huddle was completed each day. The Huddle was initiated in July 2011.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Since the Huddle emphasized preventative health care and chronic disease management, we focused on two aspects of care that could be directly impacted and facilitated by a pre-visit huddle; annual foot exams in diabetic patients and pneumonia vaccination in patients 65 years and older. To measure the success of our intervention we surveyed the residents on their impressions of the Huddle immediately prior to and 1 year after initiating the Huddle. We also analyzed pre and post intervention completion of annual diabetic foot exams and pneumonia immunization using a simple 2-rate chi-square test and a segmented Poisson regression to compare rates and trends 3 years prior to and 2 years following the intervention.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The Huddle was well-received by residents who indicated improvement in both communication with staff and efficiency in care delivery in 4 of 5 items surveyed. For 2 years prior to the intervention residents were receiving regular feedback on their diabetic foot exam performance, however, pneumonia vaccination reporting was started 1 year after Huddle initiation. The rate of annual foot exams increased from 42.5 % before to 63.8 % after intervention (p < 0.001) with a significant increase in the rate of improvement from 0.28 to 0.63 % per month (p = 0.001). Pneumonia vaccination rates initially fell in the first year following the Huddle from 60.1 to 58.3 % (p = 0.5), however, once performance feedback was provided to the residents the rate climbed from 58.3 to 70.4 % (p < 0.001) and was accompanied by a significant increase in the rate of change from 0.01 to 0.5 % per month (p < 0.001).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The Huddle, when combined with provider-specific performance feedback, can lead to significant improvements in the quality and consistency of care delivered in a resident teaching clinic. In our experience, a planned roll-out with education for both physicians and staff was needed before starting the Huddle process. The development of a Huddle checklist/form provided greater process uniformity and efficiency. In addition, protected time in the schedule for the Huddle to take place was essential for successful integration into the office workflow.
ENHANCING APPROPRIATE USE OF CARDIAC TELEMETRY TO IMPROVE CARE AND REDUCE WASTEDaniel Henderson; Christopher Kelly; Deepa Kumaraiah. Columbia University Medical Center, New York, NY. (Tracking ID #1934836)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Is a quality improvement effort to limit overuse of continuous electrocardiographic monitoring in general medical inpatients associated with improved rates of appropriate use?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): I. To define clinical guidelines for the use of cardiac telemetry for general medical ward patients, a population for whom no such guidelines exist, in a large, urban, academic medical center. II. To redesign the process of ordering cardiac telemetry around such guidelines, with oversight of extended use of telemetry, in order to curtail overuse. III. To evaluate the redesigned ordering process for effects on use and overuse of cardiac telemetry.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): In 2013, our hospital, a 710-bed academic general hospital member of a 1600-bed academic medical center, faced unprecedented demands in the wake of a recent natural disaster and temporary closure of several major hospitals. In this context, our institution identified continuous cardiac telemetry as a source of delayed care and waste of resources. We redesigned the process of telemetry ordering to promote appropriate use and minimize resource constraints. Cardiac telemetry, once found only in coronary care units (CCUs), is now widespread in nearly all units of most hospitals, despite limited or absent clinical evidence for its utility beyond a limited set of cardiac conditions. A handful of studies have loosely linked telemetry with bottlenecks to patient flow, particularly emergency department (ED) waiting, and with adverse clinical outcomes as a result. In fall 2013, we redesigned our telemetry ordering process to curtail inappropriate use and relieve system pressures due to overuse. Through a systematic literature review, we identified a limited evidence base for telemetry use, especially in patients without major cardiac problems, where guidelines are sparse. We developed a list of conditions for which telemetry was clearly or probably indicated, with thresholds for discontinuation. We also created a set of conditions where telemetry was commonly ordered, but clearly not indicated. This information was disseminated and incorporated into order-entry functions of the electronic health record system for timely availability at the point of care. This presentation details our evaluation of telemetry orders in one-month periods before and after implementation to assess the appropriateness of orders, within the ongoing evaluation of the project’s effectiveness in curtailing telemetry overuse and its sequelae.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We measured the proportion of appropriate orders, per the new guidelines. Appropriate orders had one clear indications, and inappropriate orders, clearly non-indicated ones, as assessed by order free text data and focused chart review. Benefit of the doubt was assumed, and cases where a determination could not be made were counted as indeterminate. The goal was a 33 % or greater reduction in inappropriate use between study periods.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We will present our institutional guidelines for telemetry in general medicine ward patients, as well as the analysis of the improvement project. Initial evaluation of 100 randomly-selected patient telemetry orders from both study periods revealed 46 % inappropriate orders in the pre-intervention period, and 32 % in the post-intervention period, a 30.4 % reduction, and a statistically significant effect at the 5 % level by the chi-squared test. Indeterminate orders made up 12–18 % percent of reviewed entries. These initial results show a significant effect, just below the specified goal of the measure. To ensure 80 % power for a 20 % effect, further analysis of 500 patients will be presented in the final results, along with stratified analyses to assess for confounding due to differential ordering practices by provider and service types.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Telemetry is frequently overused, and this overuse is responsive to a simple intervention to improve practice. Guidelines for the appropriate use of telemetry can be developed to guide its use where a dearth of evidence exists, significantly improving appropriateness. Clinicians respond to informational interventions at the point of care.
FACTORS CONTRIBUTING TO READMISSIONS FOR PATIENTS WITH ISCHEMIC HEART DISEASEVishal Patel; William S. Weintraub; Roger Kerzner; Edmondo Robinson; Tabassum Salam; Daniel J. Elliott. Christiana Care Health System, Newark, DE. (Tracking ID #1934521)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Despite intense scrutiny on the need to reduce readmissions, surprisingly little is known about the factors which lead to readmissions. Understanding these factors could help more appropriately target interventions to improve care transitions.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): We performed a thorough case review of all patients with ischemic heart disease readmitted within 30 days of discharge from percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). We sought to identify factors leading to readmission, determine preventability, and implement real time interventions to circumvent these readmissions.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Structured case review of all adult inpatients at a single tertiary care institution discharged from May 2013 to date with an index visit that included ischemic heart disease with revascularization who were readmitted within 30 days of discharge. All patients were enrolled in an integrative and innovative care management program prior to index discharge and consented for this review. Case review involved chart audits, interviews with re-admitting physicians, patients, and overall case adjudication by a physician team using a standard tool.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Demographic information and patient characteristics were collected to determine its relation to preventability. Data on preventability, location where efforts to prevent revisit could have been targeted factors for readmission, and role for care management to further engage the patient were also collected.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Forty-five patients had an unplanned 30 day readmission. Forty-seven percent (21) of the readmissions were assessed as potentially preventable; 11 % were very likely to be preventable and 36 % were likely to be preventable. Of the preventable readmissions, 48 % (10) could have been prevented prior to index discharge and 33 % (7) could have been prevented at home or nursing home. There was role for case management to further influence patient’s care in 95 % of the preventable cases. During discharge process, patients were, on average, started on 7 new medications from admission and issues related to medication reconciliation were seen in 15 % of the cases. The major factor during discharge process was not having a follow up appointment scheduled within 2 weeks of discharge (40 %). Major issues for home and outpatient care included inadequate services provided by home health services or nursing home (25 %), difficulty to manage symptoms at home (22 %), and poor communication with patients (28 %). In terms of hospital readmission, 70 % of all patients were readmitted for cardiac causes.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): This study has identified key factors for readmission and has shown that case management has a crucial role in preventing these events. Issues around communication and fostering partnership can help improve care transitions. Implementation of a multi-disciplinary group will help to customize targeted interventions with emphasis on the discharge process from index visit and management of post-acute care cardiac symptoms at home.
FEASIBILITY OF DIABETIC RETINOPATHY SCREENING USING A NON MYDRIATIC CAMERA IN A COMMUNITY HEALTH CLINICClaudia L. Campos1; Carolyn F. Pedley1; David Friedman2; Emily W. Gower4,3; Daniel Nelson3; James L. Wofford1; Ramon Velez1. 1Wake Forest University, WInston-Salem, NC; 2Wilmer Eye Institute-Johns Hopkins School of Medicine, Baltimore, MD; 3Wake Forest University, Winston - Salem, NC; 4Wake Forest University, Winston Salem, NC. (Tracking ID #1938696)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Is routine screening of diabetic retinopathy with a non mydriatic camera feasible in the primary care setting?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): − To perform routine retinopathy screening using a high resolution retinal imaging camera on all diabetic patients that present for regular clinic visits in the Adult Medicine Clinic - To train clinic personnel to operate a non mydriatic camera and upload photographs for remote grading - To determine patients’ self-report experiences with the screening process and elicit patients’ input for improving the screening process
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Located in Winston-Salem, North Carolina, USA, the Downtown Health Plaza Adult Medicine Clinic is affiliated with Wake Forest Medical Center, involves resident training and serves as a safety net for the community. It typically logs more than 25,000 adult clinic visits each year and serves a large number of Medicaid and uninsured patients. Three physician assistants, eight faculty and 40 resident physicians have clinic sessions 1–3 times a week with the support of 9 nursing staff (2 CMAs, 6 LPNs and 3 RNs). Diabetic participants were offered retinal photography as they came to clinic for regular appointments. Photographs were performed at the time of the appointment and a small number (34/180) were given appointments for photographs at a later date -Personnel training: Designated nursing staff received training to operate the camera and upload pictures on the computer system; 3 LPNs completed an -in person- four hour training course. A research assistant was also trained to take photographs when the nurses were unavailable or too busy. -Patient recruitment and intervention: during patient rooming, nurses recommended retinopathy screening to all diabetics presenting for a clinic visit. Immediately after the clinic visit (or before when the providers were running behind), the patients were consented and fundus photography was performed in a private darkened room. At the beginning of the program, we attempted scheduling of participants to return for photographs at a separate time point. Midway through the program nursing personnel changes made it difficult for the nurses to have the time to consent the patients, enter data into the computer and to take the photographs. After that point, a designated research assistant performed most of these activities. The nurses continued to control patient flow. - Uploading of Images: nurses and coordinator uploaded the images to the Wills Eye Telemedicine Center. Prior to upload they were able to review images and share them with the clinicians. - Post review follow up, referral, and patient satisfaction survey: Participants were contacted by phone with their results and referred for appropriate follow up care. A copy of the findings was also sent to their primary care provider. A post- screening questionnaire was conducted 2–3 months after screening.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Number of participants screened on a weekly basis
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Prior to designating a full-time research assistant to helping, 1–2 participants were screened per day for 2 days each week. After employing the research assistant, screenings were performed nearly every day, and the number screened per day more than doubled, averaging 4 per day, 5 days per week. On busy clinic days, 8–10 participants were screened when the research assistant was present. 61/180(34 %) retinal screenings were scheduled for a later appointment date. Of 61 scheduled visits, participants only kept 34 (55 %).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): A program of screening retinal photography can be implemented in a busy clinic practice. With limited clinical resources and the time required to perform and track the photographs, there must be dedicated personnel to perform these duties. Timing of the test during clinic visits is a more effective system to serve our low income patients. Nurses were a vital component in recruiting patients and maintaining the flow of participants.
GETTING HIP TO VITAMIN D: A HOSPITALIST PROJECT FOR IMPROVING THE ASSESSMENT AND TREATMENT OF VITAMIN D DEFICIENCY IN ELDERLY PATEINTS WITH HIP FRACTUREJohn Stephens1; Christine Williams1; Eric Edwards1; Darren A. DeWalt2; Paul Ossman1; Edmund A. Liles1. 1UNC Hospitals, Chapel Hill, NC; 2UNC Hospitals, Chapel Hill, NC. (Tracking ID #1927582)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Our hospitalist group, which co-manages all patients with hip fracture at our institution, had no standardized approach for the assessment and treatment of vitamin D deficiency in patients with fragility fractures, despite Endocrine Society recommendation for screening this population and prior studies demonstrating high prevalence of deficiency.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To standardize and improve our group practice for the assessment and treatment of vitamin D deficiency in elderly patients with hip fracture. To measure the prevalence of vitamin D deficiency in elderly patients with low trauma hip fracture at our institution.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We reviewed medical evidence, including major practice guidelines, for screening for vitamin D deficiency in elderly patients with low-trauma hip fracture and assessed our group’s adherence to best practice. Review of all hip fracture patients cared for by our group from June 2010 through October 2012 revealed that only 38 % had been assessed for vitamin D deficiency. Of those patients who had a level checked, 61 % were found to be vitamin D deficient using a cutoff of <30 ng/mL. Of those deficient, only 39 % were treated with the appropriate dose of vitamin D. Our conclusion was that group performance on this issue was varied and substandard. In October 2012, we created an intervention to address these findings. We presented a review of evidence and data from our practice to the hospitalist group. Concurrently, we altered the hip fracture order set in the hospital computerized physician order entry system to include prechecked boxes for measurement of vitamin D level at admission and empiric supplementation with 1000 international units of vitamin D.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We studied implementation of the new order set by searching the hospital database for patients with ICD-9 codes for femoral neck fracture linked with discharge physicians in our group. Outcome measures included the percentage of patients screened for vitamin D deficiency and percentage of deficient patients discharged on the correct dose of vitamin D, both before and after intervention. We also described the prevalence of vitamin D deficiency in this population.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Following our intervention, 95 % of hip fracture patients were checked for vitamin D deficiency, compared with 38 % before intervention. The proportion of patients with vitamin D deficiency who were discharged on the correct dose of vitamin D also improved, rising from 39 % before to 67 % after intervention. The prevalence of vitamin D deficiency was 49.5 %.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The prevalence of vitamin D deficiency in elderly hip fracture patients at our institution is high. Our hospitalist group practice performance in screening for vitamin D deficiency in this population was varied and not in adherence with current practice guidelines. With a review of best evidence and alteration of the hip fracture computerized physician order entry order set, we successfully standardized group practice and improved adherence to practice guidelines.
IMPLEMENTATION OF A RESIDENT HOSPITAL DISCHARGE CLINIC AT AN URBAN ACADEMIC MEDICAL CENTERMaria Hamm de Miguel; Amanda Ramsdell; Steven Shea; Nancy Chang; Luis M. Ducasse. Columbia University, New York, NY. (Tracking ID #1938847)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Hospital discharge is a vulnerable time for patients, prone to adverse events which may be mitigated by rapid follow up (<2 weeks) in a patient centered medical home setting within the same institution.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To provide timely follow-up to medicine patients within a resident PCMH in order to reduce ER visits and hospital readmissions 2. To improve the quality of the discharge process through continuity and communication between inpatient and outpatient 3. To educate residents on the importance of transitions of care
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Patients discharged from medicine teams at New York Presbyterian Hospital - Columbia University Medical Center, with participating Medicaid/Medicare plans or uninsured are given rapid follow up with a designated PGY2 (<2 weeks) in the resident continuity clinic on campus. The community served is diverse but primarily Hispanic, of low socioeconomic background, and with multiple co-morbidities, At the appointment, patients are assessed clinically and functionally, medication reconciliation is completed, new labs and tests are planned as needed, and continuity appointments are made or confirmed.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1. 30-day ER visits and hospital readmission rate [Data pending] 2. Quality metrics on the discharge process and post-discharge period: a. Quality of the discharge summary b. Medication reconciliation c. Interim events d. Interventions required at discharge clinic appointment e. Hospitalist vs. resident team comparison 3. Resident survey of educational benefit [Data pending]
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 423 patients were scheduled from 6/17/13 to 11/4/13, and 228 patients came. The high no show rate (46 %) is a critical finding that requires further investigation. Quality metrics are available for 147 patients, a 64 % completion rate. Discharge summaries were submitted for 90 % of patients. Ninety-three percent included relevant hospital events, 86 % an updated discharge medication list, 61 % PMD follow-up, and 66 % pending labs/test when required. At the visit, 27 % had incorrect medications, 16 % had difficulty obtaining new medications, 26 % were not taking medication as prescribed, and 12 % had new side effects. Patients reported new or persistent symptoms 42 % of the time. Only1-6 % of patients had adverse events including falls, ER visits, or new limitations in mobility or functional status. Medications were adjusted in 41 %, lab follow-up in 31 %, social work referral in 12 %, and referral to the ED in 2.8 %. Forty-three percent required new primary care appointments, and 26 % required specialist. Comparing quality metrics for resident and hospitalist teams using a chi-squared analysis (power >80 % for alpha = 0.05) the majority of variables did not show a significant difference. Residents were more likely to complete discharge summaries (OR = 4.5, 95 % CI 1.5–13.8, p = 0.05) but were more likely to require a PMD or specialist visit to be made (PMD: OR 0.5, CI 0.2–0.98, p = 0.04, specialist: OR 0.4, CI 0.2–0.8, p = 0.02).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The implementation of a discharge clinic has highlighted how vulnerable the post-discharge time is, and identified multiple areas for process improvement. The rate of interim adverse events is low (1–6 %), but the potential for new events is high, due to persistent conditions, need for lab follow up, medication errors, and lack of adequate follow up planning. We found few differences between resident and hospitalist team patients. The challenges are a high no-show rate, a moderate completion rate of quality metrics, inadequate quality of discharge summaries, and inadequate continuity planning. These deficiencies indicate areas for further investigation and improvement.
IMPLEMENTATION OF A SCREENING PROGRAM TO ADDRESS UNHEALTHY ALCOHOL USE IN AN ACADEMIC GENERAL INTERNAL MEDICINE CLINICEmily K. Sturkie; Daniel E. Jonas; Carol Golin; Catherine Grodensky; Jennifer Kinley; Shana Ratner; Thomas M. Miller. University of North Carolina, Chapel Hill, NC. (Tracking ID #1936705)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Unhealthy alcohol use is common, but usually goes undetected and unaddressed in primary care
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To uniformly screen all patients in clinic for unhealthy alcohol use 2. To identify patients who would benefit from a primary care based harm reduction intervention 3. To use motivational interviewing techniques to counsel patients with unhealthy drinking and to provide appropriate referral resources for patients with alcohol use disorders
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The University of North Carolina Internal Medicine Clinic is an academic practice serving approximately 12,000 patients. The clinic uses a visit planner to prompt clerks, nurses, and doctors to perform disease management and health maintenance interventions. Utilizing this planner, we introduced a program to screen and counsel patients for unhealthy drinking. We developed educational materials and conducted a half-day workshop in motivational interviewing and intervention protocol for teaching faculty. We produced a guide to lead providers through a motivational interviewing-based intervention for risky drinkers and a separate, parallel pamphlet for patients that included educational materials and a log to track consumption. To train housestaff, we developed curricula for two pre-clinic conferences. To screen patients, nurses are annually prompted to ask patients if they drink alcohol. Those responding affirmatively answer a second question about the number of times in a year they drink > four drinks (> five for men under 65). Nurses ask those with positive responses to complete the AUDIT to identify patients with alcohol use disorders. Physicians score the AUDIT and start a two visit intervention for patients without alcohol dependence. In the first visit, physicians address unhealthy drinking, explore patients’ interests in changing their behavior, and encourage patients to keep a log of alcohol consumed. At the second visit, physicians review the log with the patient and assist with setting goals to reduce unhealthy drinking. Patients with alcohol use disorders are referred for more intensive treatment.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Number of patients screened, proportion of eligible patients who are appropriately offered counseling or referred, and how faculty perceives the usefulness of the guides.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): In the first 3 months of the program, we screened 1,695 patients. Of those patients, 5 % (n = 87) screened positive and completed the AUDIT. We performed chart reviews of 74 patients who screened positive. In the clinic note, physicians mentioned alcohol use in 54 % (n = 40) and documented counseling in 38 % (n = 28). Three of the 74 patients screened positive for alcohol use disorders, but none of these patients were referred to alcohol use treatment programs. A provider survey was distributed after implementation of the prompt. Of the 11 providers who responded, 80 % (n = 9) felt that the guides were helpful.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): We have been successful at implementing alcohol screening in our practice to identify patient with unhealthy alcohol use. We developed resources to guide physicians through screening and motivational counseling. Our next step is to improve the consistency with which we counsel, refer patients with alcohol use disorders, and document our interventions.
IMPROVING ATTENDANCE TO PRIMARY CARE APPOINTMENTS: RANDOMIZED CONTROL TRIAL OF TEXT MESSAGING TO PATIENTS AT A COMMUNITY HEALTH CENTERSanja Percac-Lima1,2; Patrick R. Cronin3; Anjali Thakkar4; Adrian Zai2,3. 1Massachusetts General Hospital, Chelsea, MA; 2Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Boston, MA; 4Harvard Medical School, Boston, MA. (Tracking ID #1939188)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Poor adherence to medical appointments not only negatively impacts the quality of care, but also reduces access to care for other patients. In 2012, the Massachusetts General Hospital Chelsea HealthCare Center (MGH Chelsea) adult medicine practice had the highest no-show rate in our hospital’s primary care network. A previous pilot study revealed that forgetfulness and miscommunication were the most common patients’ reasons to no-show to their appointments.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Implement text messaging to patients at a community health center and using a randomized control trial (RCT) evaluate its effect on appointment attendance
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): MGH Chelsea is a community health center serving predominantly Latino, non-English speaking and low-income patients. Adult patients seen at the practice were eligible for the study and randomly assigned into two arms: 1. Control: receive usual care—a reminder phone call 2 days prior to their appointment 2. Intervention: receive usual care and text message reminder 7-days and 1-day prior to the appointment We designed an informatics tool to automatically: (1) provide Patient Services Coordinators with electronic rosters of patients who are due for a call reminder, and (2) send text message reminders to patients prior to their appointments.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The primary outcome was the no-show rate in the control and intervention groups. The secondary outcomes included: the no-show rate by age, race, gender, language and insurance, by text message outcomes in the study arms, cancelled/rescheduled appointments and return-on-investment.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The RCT started on August 1st, 2013 after 2 weeks of testing phase and randomization. In the intervention there were 3550 unique patients and, 716 (20.2 %) of patients consented to receive text messages, 93 (2.6 %) opted out and 2,061 (58.1 %) did not respond, and 680 (19.2 %) did not have a cell phone number. The no-show rate was slightly lower in the intervention than control (1101/6093 = 18.1 % vs 339/1395 = 19.6 %, p = 0.24). However, in the intervention, the subgroup of appointments where patients consented to receive text messages had significantly lower no-show rate 13.3 % vs. 19.2 % (p < 0.0001) than those who did not consent.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Improving attendance to primary care appointments in underserved populations is challenging. Although the text message intervention lowered the no-show rate, a significant number of patients do not respond to the addition of a text message reminder. Patients who consent to text messages have significantly better attendance with primary care appointments. Exploring the reasons why patients do not respond to receive messages and improving consent process to text messaging could improve the impact of the intervention.
IMPROVING COLORECTAL CANCER SCREENING UTILIZING LEAN SIX SIGMA METHODOLOGY IN AN ACADEMIC GENERAL INTERNAL MEDICINE CLINICShana Ratner1; Brooke B. McGuirt1; Kathryn A. Brennan1; Jonathan Thornhill2; Summer Hogan2; Kim Young-Wright3; Shaun McDonald3; Thomas M. Miller1; Michael Pignone1,4. 1University of North Carolina at Chapel Hill, Chapel Hill, NC; 2University of North Carolina-Chapel Hill, Chapel Hill, NC; 3University of North Carolina-Chapel Hill, Chapel Hill, NC; 4University of North Carolina- Chapel Hill, Chapel Hill, NC. (Tracking ID #1928120)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Colorectal cancer (CRC) screening rates were sub-optimal in the University of North Carolina Internal Medicine Clinic (UNC IMC) with many potential root causes.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) Use Lean Six Sigma methodology to identify root causes of the sub-optimal screening rate 2) Pilot and test methods of outreach for unscreened patients 3) Improve the CRC screening rate in the Internal Medicine Clinic
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The UNC IMC is an academic general internal medicine clinic with approximately 12,000 patients. We formed a multidisciplinary team to improve CRC screening, using Lean Six Sigma methodology. The team interviewed patients, physicians, clinic staff, and GI procedures staff to map the processes for stool cards and colonoscopy and identify barriers to screening. Root cause analysis identified 68 root causes of sub-optimal screening rates. Using multi-voting and an impact-effort grid, we chose 5 for rapid cycle improvement. We identified the exclusive use of a “visit-based approach” without supplementation from a population-based approach and poor documentation of outside studies as key root causes that we could test with chart reviews and outreach letters. We tested two approaches to overcoming these root causes: 1) sending outreach letters to patients who turn 50 and may not have scheduled visits (signed by the medical director); 2) having providers review their panels of unscreened patients to update documentation of outside studies and offer screening via personalized letters. We scheduled 17 residents and 3 attendings to complete panel reviews in phase 1 of the project.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): CRC screening rate in active clinic patients ages 50–75.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Non-personalized letters sent to patients at age 50 had minimal success: 2 % (1/48) of those receiving letters completed screening with 3 month follow up. Physicians who performed panel reviews in phase 1 (n = 20) had an average of 57 patients on attending lists and 16 patients on resident lists. Phase 1 physicians sent a total of 313 letters. The screening rate improved by a mean absolute increase of 5.0 % (range: −8.7 % to +18 %) in physicians who completed chart reviews and letters in phase 1 versus those who are scheduled to complete them in phase 2 (mean absolute increase 0.4 %). From January to December 2013, the overall clinic CRC Screening rate improved from 62.8 % (4609/7337) to 66.0 % (4943/7489), p < 0.0005, with an increase in the screening rate every month since the project began.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Centralized, non-personalized outreach letters to patients at age 50 had low efficacy. Individual physician chart reviews and personalized letters coming from the PCP improved screening more effectively.
IMPROVING TRANSITION OF CARE FOR PATIENTS WITH HIGH RISK FOR READMISSIONRaghid Zeitouni; Animita Saha; Katherine E. Gettys; Kelly Avey; Tamara D. Burdon. Carolinas Medical Center, Charlotte, NC. (Tracking ID #1937631)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): A 2009 analysis of Medicare patients showed that 50 % of patients readmitted within 30 days had not seen their physician since their last discharge, poor transition not only increase healthcare cost but also has a detrimental effect on patient and their family’s wellbeing.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Identifying patients with high risk for readmission at the time of hospital admission 2. Checking in with patients 2 days post discharge by a pharmacist/social worker and establishing an appointment within 5–7 days of discharge with their PCP’s office 3. Validating if this process reduces readmission.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): This pilot study was conducted in an Internal Medicine residency clinic where majority of patient population is uninsured or underinsured, has high disease burden and tremendously low overall and health literacy. The entire program started with formation of a team which involved Faculty physicians, Internal Medicine residents, nurses, pharmacist, social worker, case managers and quality improvement (QI) coaches. This started initially as part of an AHRQ funded ImPact grant where our clinic participated but then we continued with it even after the grant ended. Inpatient staff team used IHI risk stratification tool to determine post discharge follow up in clinic where several slots were available to accommodate these patients. When a follow up appointment was made at the time of discharge, the scheduler sent a notification to the care provider-MD, pharmacist and social worker. This triggered a phone call by the pharmacist who according to a checklist designed by IHI (STARR) did medication reconciliation, identified social and financial barriers limiting access to medications, food or appointment and importantly reminded the patient or family about the appointment. Presence of social or financial barriers triggered a phone call by a social worker or case manager. All communications were recorded in EMR and were available to MD’s. While in the Medical home they spend time with the pharmacist, care coordinator, social worker and primary care provider. This special emphasis on medication reconciliation, barriers to care, access issues and teach back all helps the MD formulate a more comprehensive plan of care.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The most important success was bringing the team together; there was representation from every component of the clinic team who took the role of champions. The other important measure of success was collaborating with our pharmacist team who played a tremendously important role if not the most important role and realization that lack of understanding about changes in medication regimen is almost 100 % ubiquitous and perhaps one of the factors that can be impacted the most. Educating and training faculty and residents and staff in the QI process and developing an QI mindset is an important achievement of this entire process. Improved access increased the comfort level and satisfaction of inpatient care team in making smooth transition for the patients. Quantitatively, we have definitely seen that we touched significant number of high risk patients and the 2 day post discharge phone call made a tremendous impact in getting these patients to their appointmant. This entire process resulted in reduction of readmission.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): During the pilot 72 patients were identified by inpatient team as high risk got an appointment within 5–7 days post discharge. We could reach 66 % of patients by phone, of which 74 % made it to the appointment. Among the group of patients that could not be reached by phone, only 12.5 % showed up for the appointment. This finding is statistically significant and shows the importance of 2 days post discharge phone call. All patients who were identified by inpatient team as high risk got an appointment within 5–7 days post discharge. We could reach 66 % of patients by phone, of which 74 % of patients made it to the appointment. Among the group of patients that could not be reached by phone, only 12.5 % showed up for the appointment. Among patients who made hospital follow up appointment, 27 % of patients got readmitted within 30 days, on the other hand 45 % of patients who did not make it to the appointment 45 % got readmitted within 30 days. These findings are statistically significant as well.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The process should start with team building with members who play key role in transitioning patients from inpatient to their medical home. Key points to remember after the initial phase are: 1. Timely Access to Care 2. Post discharge visit Planning: this needs to start before patient leaves hospital 3. Two days post discharge phone call by pharmacist and SW/care managers
INNOVATION IN SHARED MEDICAL APPOINTMENTS (SMAS) FOR DIABETES MANAGEMENT: ENGAGING RESIDENTS IN INTERDISCIPLINARY LEADERSHIP AND SELF-DIRECTED CURRICULUM DEVELOPMENTChristina B. Pham; Jennifer Huang; Dylan Bothamley; Patrick T. Lee; Yamini Saravanan. Harvard Medical School/Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1936691)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The shared medical appointment (SMA) is a model of care with potential to significantly improve patient experience and outcomes for patients with chronic disease. Currently, few US internal medicine residency programs provide formal training in leading SMAs. The SMA format should be integrated into residency training because it provides internal medicine trainees an opportunity to develop: 1. leadership skills to direct an interdisciplinary team 2. experience in applying quality improvement theories 3. skills that engage and educate patients in non-traditional formats
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Understand the evidence behind the SMA model and why it works for diabetes management. 2. Explore how the SMA is an effective tool for the development of resident skills in all six Accreditation Council for Graduate Medical Education’s (ACGME) core competencies: patient care, medical knowledge, practice-based learning and improvement, systems-based practice, professionalism, and interpersonal skills and communication. 3. Engage, teach, and mentor residents to lead SMAs.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We developed and implemented a new structure for internal medicine resident-led SMAs for diabetic patients at the Cambridge Hospital Primary Care Center - one of the teaching clinics at the Cambridge Health Alliance - an urban safety net, Harvard Medical School-affiliated community hospital. Training residents in leading SMAs has (1) increased resident case volume and allowed for care of diabetic patients in traditional and non-traditional formats, (2) provided opportunity for leadership of interdisciplinary care teams, and (3) allowed residents a practicum to apply quality improvement principles in daily practice. We designed an SMA process where third year residents lead the planning, execution, and de-brief of an interdisciplinary team every 6 weeks. The team consists of a medical assistant, dietician/diabetes educator, pharmacist, medical student/junior resident, senior resident, and teaching attending. During the SMA, the senior resident examines patients, engages them in active management of their diabetes, and teaches a patient-directed educational curriculum. Most importantly, however, the resident fosters an environment of peer mentorship, which patients repeatedly cite as the overarching value that keeps attendance high. At the end of the session, the resident runs a de-brief and enters ideas for process improvements into a change log that feeds into future plan-do-study-act (PDSA) cycles. The implication for this innovation is that our process can easily be replicated at other internal medicine residencies, to not only produce a cadre of physicians with evidence-based training and experience with SMAs, but most importantly, to offer more patients an effective way to manage their diabetes.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): − Patient exit surveys - Qualitative one-on-one patient interviews - Provider exit surveys - Patient attendance and attrition data - Clinical diabetes metrics
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): − Improved patient satisfaction with self-management of their diabetes based on formal exit interviews - Marked enthusiasm and positive feedback on evaluations from patients, who are requesting more frequent sessions - Resident’s active leadership of an interdisciplinary team surrounding diabetes management - Structured resident training in the mechanics of SMA implementation - Development of resident skill set in leading SMAs and designing curriculum based on patient needs and quality improvement metrics - Based on formal evaluations, marked enthusiasm and positive feedback from residents, who are requesting to lead more sessions than originally planned
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): The SMA is an effective format for care of diabetic patients. There is increased patient empowerment and satisfaction with self management of their disease. The SMA is an effective tool for the development of resident skills in the ACGME core competencies. FEASIBILITY OF MAINTAINING PROGRAM AND TRANSFER TO OTHER PROGRAMS: We have shown that this program can be run and maintained by a staff of one to two medical assistants, one medical student or junior resident, one diabetic educator, one resident physician, and one attending preceptor. We run our 120 min groups (60 min for all labs, exams, community time; 60 min for formally led group time) on a 6-week cycle, which is proving sustainable for both providers and patients. Importantly, this structure was scalable to a financial break-even point at approximately 12 patients per SMA session. With the commitment of program leadership and the allocation of appropriate staffing for the project, this structure can be implemented by internal medicine programs with large diabetic populations.
INTEGRATING BEHAVIORAL HEALTH SERVICES AND PRIMARY CARE AT AN URBAN, SAFETY-NET TEACHING HOSPITAL: A PILOT PROGRAMChristine A. Pace1; Joanna Buczek2; Alissa Cruz1; Lee Ellenberg1; Foote Jonathan2; Ellen W. Ginman1; Cindy M. Gordon2; Hannah M. Marks1; Robert Sokolove1,2; Jeffrey H. Samet1; Charlotte Wu1. 1Boston University School of Medicine, Boston, MA; 2Boston University School of Medicine, Boston, MA. (Tracking ID #1923614)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Although behavioral health conditions are known to affect the overall health of primary care patients, barriers to effective behavioral health care at Boston Medical Center’s Adult Primary Care Clinic (including the lack of systematic behavioral health screening and the delivery of most behavioral health services in another department) have led to missed opportunities for early identification of these conditions as well as gaps in patient access and coordination of care.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To improve early identification of depression and unhealthy substance use; improve access to psychotherapy and substance use counseling; and improve the quality of on-site care for depression and unhealthy substance use through primary care provider trainings and collaborative care protocols.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Boston Medical Center’s Adult Primary Care Clinic is a 36,000-patient practice at an urban, safety-net, academic teaching hospital. This pilot program of integrated behavioral health services is located in one of the clinic’s ’s six teams, with the goal of spreading an optimized program across all teams. The pilot involves the following new elements: 1) Standardized, annual screening for depression and unhealthy substance use, initiated by front desk staff and medical assistants; 2) Short-course psychotherapy and substance use counseling by an on-site, full-time licensed clinical social worker (LICSW), with facilitated referrals to specialty behavioral health for patients requiring long-term treatment; 3) A community resource expert who connects patients with resources such as food stamps or transportation; 4) Depression care management, modeled after IMPACT, in which the LICSW collaborates with providers to assess, educate and counsel patients with depression and adjust treatment as needed; 5) Staff and provider training on the rationale for behavioral health screening, the screening and referral workflows, and, for providers, brief interventions for unhealthy substance use and evidence-based depression treatment in primary care.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Metrics include: 1) Proportion of patients who receive annual screening for depression and unhealthy substance use; 2) Of patients referred to the LICSW: a) proportion given an appointment within 14 days; b) proportion who attended their appointment; 3) Proportion of patients with a diagnosis of depression who have a recorded PHQ9 score in their medical record; 4) Provider satisfaction with behavioral health services, measured by pre- and post-intervention surveys.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): A 26 question pre-intervention survey was completed by eight attending providers and five residents (n = 13). PHQ9 and referral data were obtained from hospital databases. Early pilot metrics will be available in April. Baseline findings include: 1) Approximately half of providers reported annual screening for depression with the majority of patients. All providers reported annual screening for unhealthy substance use with the majority of patients, but few reported consistently doing brief interventions. Providers reported a low level of staff assistance with screening. 2) With 10 being the highest score, the average satisfaction with available behavioral health services was 4.4. Although providers rated the importance of communication with behavioral health specialists as 8.4, the average rating for communication with these specialists was 3.6. 3) In a review of referral data over two week-long periods of the 2012–13 academic year, 100 % of adult primary care patients referred to the specialty Behavioral Health clinic were given appointments for a group clinic orientation, but only 25 % percent attended a clinical intake visit within 6 months. 4) Of patients with depression in their problem list, only 2.5 % had a recorded PHQ9 score in their record prior to the pilot.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Our novel pilot program of behavioral health integration in a safety net, academic hospital primary care setting has yielded several lessons: 1) Customizing screening workflows to our clinic and electronic record was challenging, requiring months of pre-testing with staff and problem-solving with the multi-disciplinary team. Such efforts, however, heightened staff engagement and helped us anticipate problems prior to implementation. 2) Despite the pilot’s small scale, each step has benefited from extensive collaboration between Behavioral Health and Primary Care. To ensure that participating providers and administrators have sufficient time for the project, such collaboration has required buy-in from departmental leadership, with a plan for sustainability and dissemination. 3) Even with high levels of institutional support and interdisciplinary collaboration, it is challenging to support non-billable efforts from providers such as psychiatrists when fee-for-service payment still dominates. Creativity is required to adapt evidence-based models such as IMPACT in an era of mixed payment models.
INTEGRATING CARE FOR HEPATITIS C VIRUS INFECTION WITH OFFICE-BASED THERAPY FOR OPIOID DEPENDENCEChristine A. Pace1,2; Judith I. Tsui1,2; Claudia Nader3; Lexie P. Bergeron2; Colleen T. LaBelle2; Jeffrey H. Samet1,2. 1Boston University School of Medicine, Boston, MA; 2Boston Medical Center, Boston, MA; 3St. Elizabeth’s Medical Center, Brighton, MA. (Tracking ID #1942516)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Individuals receiving opioid agonist treatment (OAT) are an accessible population with very high HCV prevalence, yet a minority of them receive appropriate HCV care, including treatment.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) To provide on-site HCV care (including counseling, education, and appropriate testing) for treated opioid dependent patients in general internal medicine clinics. 2) To increase the number of opioid dependent patients who receive pharmacotherapy for HCV.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The HCV-OBOT Program grew out of a desire to provide integrated HCV and substance use treatment in a population with a high prevalence of HCV. The Office-based Opioid Treatment (OBOT) Program based in the General Internal Medicine (GIM) clinic at Boston Medical Center has been in existence since September of 2003. It is a collaborative care model in Primary Care between nurse care managers and physician generalists to provide treatment (primarily buprenorphine/naloxone) for opioid dependent patients. It cares for over 400 patients, approximately half of whom are infected with HCV. The goal of the program is to reduce barriers to appropriate HCV care including treatment by providing on-site care for HCV. The program building on existing OBOT resources, including 3 full-time nurse care managers, was initiated by two physicians with HCV treatment experience, one an infectious disease specialist and the other a general internist/addiction specialist.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1) Number/percent of OBOT patient who receive appropriate confirmatory testing (HCV viral load). 2) Number/percent of OBOT patients who undergo HCV evaluation. 3) Number/percent of OBOT patients who are treated for HCV.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The HCV-OBOT Clinical Pathway was established in spring of 2010. In 2011, there were 424 patients enrolled in the OBOT program. Ninety-seven percent were screened for HCV on intake, and of those screened, 227/55 % were antibody positive, a slightly lower prevalence than that observed in methadone clinics. Among seropositive patients, 209/92 %, had an HCV viral load test completed, and of those, 157/75 % were positive demonstrating chronic infection. Nearly one-half of those (70/45 %) agreed to see an HCV medical provider and received an appointment, but only 42/60 % kept their appointment. Most medical visits centered on education, counseling, and work-up towards treatment. Ten patients have been treated, representing 6 % of the eligible sample, and eight patients have been cured of HCV.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): We found that it was feasible to implement a pathway for providing on-site HCV care in a large office-based opioid treatment (OBOT) program. Patients were receptive to receiving HCV care in conjunction with treatment for their opioid addiction. Although the no-show rate for appointments was high, the clinic provided an opportunity for a small number of patients to be cured of their infection. Challenges to be addressed in the future include overcoming misconceptions at the patient and provider level regarding HCV treatment, and navigating rapidly changing treatment options.
INTENSIVE PRIMARY CARE FOR HIGH READMISSION RISK ADULTSColleen Lynch; Ania Wajnberg; Mathew Jacob; Maria Basso Lipani; Susan Bernstein; Claudia Colgan; Jill Kalman; Alex Federman. Mount Sinai School Of Medicine, New York, NY. (Tracking ID #1933012)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Does intensive, team-based primary care consisting of low patient:provider ratios, open access, and social work services improve outcomes for high risk adults?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To examine the impact of intensive primary care on hospital stays, emergency department (ED) visits, and outpatient quality measures in a population of adults with high risk of readmission.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Mount Sinai Medical Center created the current Internal Medicine Associates- Preventable Admissions Care Team (IMA/PACT) primary care clinic in the fall of 2012. Patients are referred from PACT, an inpatient social work- led transition program begun in 2010 that has been shown to reduce hospital utilization. Core to the model is connection to a medical home; patients that do not have a primary care provider are referred to IMA/PACT. Patients are also referred by physicians within the Sinai system if they have similar high-risk criteria as the PACT program, including >2 ED visits or hospital admissions in the past 6 months, ≥3 chronic illnesses, and psychosocial complexity. Psychosocial complexity is subjectively determined based on markers including low income, low health literacy, psychiatric diagnoses, housing instability, and substance abuse. IMA/PACT is housed within the IMA clinic, an urban academic training practice. Care is delivered by teams consisting of 1 physician (MD), 1 nurse practitioner (NP), and 1 social worker (SW). Two teams are currently active and each team manages a panel of 200 patients. MD and NP roles are similar in terms of patient care, but MD team members provide NP oversight and clinical support. Providers become familiar with the entire team’s patients, and patients can see either panel provider for urgent visits. Open access is achieved by reserving one third of provider’s daily slots for urgent visits. Patients see their SW at every scheduled MD/NP visit, allowing for rapid evaluation of psychosocial issues and ongoing supportive care for mental health and chronic illness management. New visits are 1 h, and follow up or urgent visits are 30 min in duration for all (MD/NP/SW) visits. Team meetings are held weekly and the clinic is physically within one hallway, allowing for real-time communication around active patient issues. The high level of collaboration between MD/NPs and SW results in a holistic approach to patient care.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We are comparing 6- and 12-month all-cause ED visits and hospitalizations before and after IMA/PACT enrollment with a concurrent control group of patients not enrolled in the program but matched by clinical risk and healthcare utilization characteristics. We will also assess the program’s impact on intermediate outcomes like blood pressure control and HgbA1c values, and on process measures like receipt of vaccinations and diabetic retinopathy screening.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): From September 2012 to October 2013, 171 new patients were enrolled in the program, 77 % from the PACT program. The average age is 63 years, 63 % are female, 70 % have Medicare, 45 % have Medicaid, and 18 % are dually eligible. The average number of chronic medical conditions is 7; diabetes, hypertension, and asthma/COPD are the most common. Preliminary data show a 27 % reduction in hospital stays and a 44 % reduction in ED visits in the 6 months after program enrollment.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Patients at the highest risk for ED visits and hospital stays may benefit from intensive, multidisciplinary team-based primary care.
INTERPROFESSIONAL TRAINEE DEVELOPMENT OF AN AFTER VISIT SUMMARY IN A COMMUNITY-BASED OUTPATIENT CLINIC TO IMPROVE PATIENT SATISFACTIONChelsea Bowman1; Eugene Fan1; Joseph A. Hippensteel1; Anna Strewler2; Jonathan Van Nuys2,1; Daniel Wheeler1; Shalini Patel2,1; Meg Pearson2,1. 1University of California, San Francisco, San Francisco, CA; 2Veterans Affair Medical Center, San Francisco, CA. (Tracking ID #1928178)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): An after-visit summary (AVS) improves patient satisfaction in regards to patient-provider relationships and communication. However, our community-based outpatient clinic (CBOC) had no standardized mechanism to provide patients with an AVS.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) Develop an AVS incorporating contributions from patients, staff and providers 2) Increase percentage of patients who receive an AVS 3) Increase overall patient satisfaction with understanding of their treatment plan
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): An interprofessional team consisting of internal medicine residents and nurse practitioner (NP) trainees led by clinic attendings formed to improve written communication at our CBOC. First, we surveyed patients, staff and providers to assess the perceived need for an AVS and to identify key content areas to include in the summary. The survey data was used to create a prototype AVS, which was distributed to all clinic staff for feedback and revision. We piloted this revised AVS with select providers to determine ease of use prior to dissemination. The AVS was distributed to all providers who maintained a primary care panel in the clinic including 5 internal medicine attendings, 12 internal medicine residents and 1 NP student. We collected patient survey data to establish current baseline practices of providing written communication and patient satisfaction scores on communication. These surveys were continued after AVS distribution to evaluate the effect of the intervention.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The primary outcome was defined as the percentage of patients who received written communication after their clinic visit; our goal is to increase this percentage from 73 to 90 %. Our second goal is to increase the percentage of patients that “strongly agree” they understand their treatment plan and increase patient overall satisfaction with the understanding of their treatment plan. Outcomes will be based on the patient survey data collected both pre- and post-AVS implementation.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Key content areas identified by both providers and patients considered beneficial for an AVS included: medication changes, when to get laboratory or radiology tests, pending referrals and next appointments. While 81 % of providers reported they used written communication at clinic visits, only 73 % of patients reported they received written communication prior to AVS implementation. An overwhelming percentage of providers preferred a written AVS compared to a computer based AVS, 82 % vs. 18 % respectively. A preliminary pilot of the AVS showed an increase in patient reported receipt of written communication from 73 to 83 %. In addition, the percentage of patients who “strongly agreed” they understood their treatment plan increased from 56 to 67 %. Similarly, patients overall satisfaction with their understanding of the treatment plan increased from 81 % (62 % strongly agree and 19 % agree) to 89 % (33 % strongly agree and 56 % agree). AVS dissemination and data collection are ongoing.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Incorporating patient, staff and provider preferences in the development of an AVS in a CBOC can improve written communication between providers and patients and improve patient satisfaction with their understanding of the treatment plan. Incorporating clinic staff in the development of an AVS contributed to the adoption and sustainability of our project. The AVS has become a patient education tool used widely by clinic staff, including mental health providers and nurses, to help enhance communication. An AVS must be appropriately targeted and efficient to ensure provider participation.
INTRODUCTION OF A COPD TEMPLATE IN AN INTERNAL MEDICINE RESIDENT CLINIC TO IMPROVE DISEASE MEASURE RECORDINGJonathan N. Byrd. Washington University in Saint Louis School of Medicine, Saint Louis, MO. (Tracking ID #1927252)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): COPD is an extremely common condition with high and continually increasing morbidity; however, failure to establish an accurate diagnosis or to document functional status, risk factors, or immunization status can lead to inappropriate management plans as well as inefficient use of physician clinic time.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Improve accurate diagnosis of COPD and condition severity 2. Improve reporting and verification of influenza and pneumonia immunization 3. Improve reporting of smoking status 4. Lead to improved allocation of clinic time and guide management decisions
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The ABIM’s Chronic Obstructive Pulmonary Disease Practice Improvement Modules™ and the 2013 Global Initiative for Chronic Obstructive Lung Disease guidelines were used to identify several measures to incorporate into an EMR template to be used in the internal medicine outpatient resident clinic at Washington University in St. Louis. These measures included FEV1/FVC percent, FEV 1 %, GOLD stage, mMRC functional status grade, oxygen necessity, arterial blood gas metrics PCO2 and PaO2, history of intubation, smoking status, and pneumonia and influenza vaccination status. Interns in the residency program were used as study subjects. Planned intervention included a 15 min presentation to all interns reviewing COPD pathophysiology, diagnostic criteria per the GOLD guidelines, management approaches based on functional status and lung spirometry, and instruction on use of the COPD template in the EMR. Posters advertising the COPD template with instructions were posted throughout the resident clinic. The interns’ patient panels were assessed 3 weeks prior to intervention for number of COPD patients, documentation of COPD diagnosis, PFTs, smoking status, and influenza and pneumonia vaccination status. The interns were assessed for 6 weeks after the intervention for the use of the COPD template and documentation of above variables.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Rate of the COPD template use in the resident clinic as well as the rate of recording pulmonary function, smoking status, influenza and pneumonia vaccination status with and without use of the COPD template.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 33 COPD patients were evaluated before intervention vs. 48 COPD patients to date (4 weeks post intervention). Template usage rate was 12.5 % (6/48). Reporting rate before intervention was 90.9 %(30/33) for smoking status, 66.7 % (22/33) for influenza vaccination, 72.7 % (24/33) for pneumonia vaccination, and 60.6 % (20/33) for PFTs. Rate after intervention among non template users was 85.4 %(41/48) for smoking status, 68.5 % (33/48) for influenza vaccination, 68.5 (33/48) for pneumonia vaccination, and 52.1 % (25/48) for PFTs. Among template users reporting rate for these variables were universally 100 % (6/6). Notably 12.3 % (10/81) of assessed patients were not documented as having COPD despite adequate diagnostic information.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Based on preliminary data, structured tools in clinical documentation of COPD do improve incidence of recording among internal medicine residents when used; however, incorporation rate of COPD template in clinic notes was far less than expected. Additional strategies such as weekly email reminders or clinic attending instruction to encourage template use may aid in further achievement of above objectives. This tool can be used to focus clinic time on deficits including readiness for smoking cessation or need for immunizations.
LESSONS LEARNED IN IDENTIFYING PATIENT SELF MANAGEMENT GOALS AND PLANS AND ADDING GROCERY STORE BASED NUTRITIONAL SERVICES TO THE MEDICAL NEIGHBORHOOD OF A GENERAL INTERNAL MEDICINE PRACTICEScott Joy1,3; Jennifer Cullingford2; Jeannie Schwendtner2; Oswaldo Hernandez4; Gerardo Caldera Rosales4. 1The Colorado Health Foundation, Denver, CO; 2King Soopers, Denver, CO; 3University of Colorado, Denver, CO; 4High Street Primary Care Center, Denver, CO. (Tracking ID #1935130)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Criteria for certification as a PCMH specify that patients must be asked about their self management goals and plans, which often include eating a healthier diet, but follow-up for nutritional services can be variable and may not be covered by insurance plans.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Develop a self management goal/plan sheet to give to patients to understand the patient’s most important goal to improve their health. Identify patients in a general internal medicine practice who choose a goal of eating a healthy diet. Identify a retail grocery store chain that offers nutritional services in metro Denver, CO, and explore opportunities for partnership between the general internal medicine practice and nutritional services led by registered dieticians that are offered at the grocery store.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): A must-pass element of PCMH is that the practice develops and documents self-management plans and goals in collaboration with patients and families, provides educational resources or refers patients/families to educational resources to assist in self-management. Our academic GIM practice developed a one page, self management plan/goal form which includes the following: Graphics that represent various health goals that a patient can choose by circling the relevant graphic. Sections asking for the patient to document a written plan on how they will reach that goal. A Likert scale of 0 to 10 that the patient uses to report their confidence at changing their behavior. All patients who arrive for a clinic visit related to diabetes management are given this form by a medical assistant during the rooming process and are asked to complete the form. The provider reviews the form with the patient, the patient and provider sign the form, the document is scanned into the electronic medical record, and the patient is given the paper copy of the form to take with them post-visit. A local grocery store chain (King Soopers) offers free nutritional services to customers, including individual consultations, meal planning assistance and grocery store tours. The closest King Soopers store is 1.7 miles from the clinic practice site. These services are unique compared to nutritional services offered within the hospital, as the majority of the education is done in the store aisles where consumers can review and discuss the nutritional value of the foods and products they frequently purchase. Nutrition education conducted in the store teaches patients to become more comfortable with label reading and choosing the nutritious while staying within their budget. Clinic leadership met with health/wellness leadership from King Soopers to develop a referral process for patients to connect with this free nutritional service. Patients who circle the goal of eating a healthy diet are verbally informed of the King Soopers option for nutrition counseling. If a patient expresses interest in attending, a secure e-mail is sent to the King Soopers dieticians. Patients are also given a folder after the visit that includes the NDEP booklet Living with Diabetes, information regarding King Soopers Nutritional Calendar of Events, seasonal healthy nutrition/meal planning, and NuVal information. The King Sooopers dietitians contact the patient by phone to schedule an appointment.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): What percentages of patients with diabetes were given the self management plan/goals form during their visit? What percentages of patients were open to receiving nutritional counseling from a retail grocery store team of dietitians?
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Self management forms were given to 33 %, 50 %, and 100 % of patients with diabetes who had an appointment in the general internal medicine practice over the initial 3 weeks of the pilot program. To date, 10 referrals (80 % female, average age 50.3y) have been sent to the King Soopers dietitian team. All patients were contacted by telephone by King Soopers dietitians (80 % in person, 20 % unavailable, voice mail message left). Of the patients contacted in person, 3 patients (37.5 %) have had a consult scheduled (1 patient arrived, 1 patient no-show, 1 patient future appointment scheduled), 3 patients (37.5 %) requested a future phone call to schedule, 2 patients (25 %) refused an appointment.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): A process can be developed to create a patient self management goal/plan form that meets PCMH criteria. Workflows can be developed that allow a GIM practice to provide this goal form to patients, and patients can complete the form during their office visit. A general internal medicine practice can collaborate with a retail grocery store chain to engage patients in nutritional counseling and access free services to promote healthier behaviors and choices. Clinical outcomes regarding this initiative, such as improvement in body weight, cholesterol and BP values remain to be determined.
MULTI-DISCIPLINARY HUDDLES TO IMPROVE CARE AND REDUCE COSTS FOR HIGH COST PATIENTS IN A SHARED-SAVINGS PROGRAMGary Fischer1; Jennifer Hall3; Pamela Dittoe2; Joanne Riley1. 1University of Pittsburgh, Pittsburgh, PA; 2UPMC, Pittsburgh, PA; 3UPMC Health Plan, Pittsburgh, PA. (Tracking ID #1935538)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Patients with the highest medical costs often have psychosocial and socioeconomic barriers in addition to their medical conditions, resulting in fragmented care, polypharmacy, multiple specialists, and avoidable emergency department visits and hospitalizations.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Identify reasons for fragmented care and frequent emergency department visits and hospitalizations among high-risk, high-cost patients and develop individual, patient-centered interventions. 2. Improve the quality of care in high-risk, high-cost patients, as measured by decreasing avoidable emergency department visits and hospitalizations and decreasing fragmentation (i.e. fewer subspecialty visits). 3. Decreased the cost of care in high-risk, high-cost patients.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): University of Pittsburgh General Internal Medicine (UPP-GIM), a large, academic general internal medicine practice, with XX faculty physicians, XX residents, and XX patients entered into a shared-savings agreement with the UPMC Health Plan (HP), including its commercial, Medicare, and Medical Assistance products. The HP provides monthly data on our highest cost patients and has embedded a practice-based case manager (PBCM) into the clinic, who has access to insurance claims of all HP patients. A quality improvement team consisting of the practice medical director, division administrator, clinic nurse manager, and PBCM implemented a system of scheduled, multi-disciplinary team meetings (huddles) for each patient, with the aim of developing an individualized comprehensive care plan for the patient if needed. Huddles included the PCP, the nurses and secretary assigned to that PCP’s patients, social work, pharmacy, and the PBCM. The meetings were scheduled to ensure PCP availability, and included the resident and preceptor for resident patients. Prior to the meeting, the PBCM obtained claims information about the patient and attempted to contact the patient to determine housing situation, home supports, ability with ADLs and IADS, barriers to care including transportation or financial barriers, use of home medical equipment, and perception that care is coordinated. Anticipated interventions resulting from the huddles included increased PCP visits, consolidation or decrease in subspecialists, referral to mobile social work and behavioral health services provided by HP, assistance with transportation, and education of patient in self-management and appropriate venues to seek care,
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1. Decreased unplanned care as measured by visits to emergency department, urgent care centers, and unplanned hospitalizations. 2. Decreased overall costs of care for the patients enrolled in the program (i.e. claims paid by the HP in a specified time period before and after the huddle). 3. Increase in the number of patients who state that their care is “coordinated.”
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): There have been huddles on 8 patients so far. In 6 cases, needs were identified, including medication reconciliation, in-home assistance (including nursing, PT, OT, and speech), coordination of appointments, behavioral health and substance abuse treatment, financial assistance, dental care, transportation assistance, and housing issues. Interventions included monthly visits by mobile team for medication assistance and appointment coordination, medication review with patient by pharmacist, provision of dental discount cards, mobile social work and behavioral health teams, and increased PCP involvement during hospitalizations. Although follow-up so far as been only a few months, a decrease in unplanned utilitzation has been observed. By April, there will be quantitative data available on a greater number of patients.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1. Close collaboration between payors and providers can facilitate improved care of high-risk, high-cost patients. 2. Multidisciplinary huddles, involving the patient’s PCP and preceeded by careful case review and discussion with patients, can identify potential solutions to patient needs and barriers to care, and may improve care, decrease unnecessary utilization, and decrease costs.
ON-SITE COACHING TO BUILD AN ENGAGED, SKILLED WORKFORCE FOR COLLABORATIVE CARE IN AN INNER CITY PUBLIC HOSPITAL SYSTEMDamara N. Gutnick1,2; Maura Porricolo4,3. 1NYU School of Medicine, New York, NY; 2New York City Health and Hospitals Corporation, New York, NY; 3North Central Bronx Hospital, Bronx, NY; 4Jacobi Medical Center, Bronx, NY. (Tracking ID #1935127)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): While workshops expose learners to theory and skills, implementation of skills such as Motivational Interviewing (MI), Brief Action Planning (BAP) and other self-management support (SMS) strategies requires individual and team-based coaching.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To develop provider competencies in communications skills including MI, patient-centered goal setting using BAP, adherence counseling and other SMS strategies. 2. To improve provider self-efficacy and efficiency in delivering these skills in clinical practice through coaching and feedback.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The NYC Health and Hospitals Corporation (HHC) is a large public healthcare system with 11 hospitals and 6 Diagnostic & Treatment Centers. It serves a diverse inner city population of approximately 1.3 million annually. With NYS Medical Home Demonstration funding, HHC is implementing the TEAMcare model of collaborative care (Katon W et al. N Eng J Med 2010.) Care Managers (CMs), with supervision of a psychiatrist and internist team, work closely with patients with comorbid chronic illnesses including depression. The goal is to coordinate care, provide SMS, and facilitate patient-centered goal setting and patient engagement. Rapid delivery system redesign demands practice-based support. We describe an innovative coaching program designed to develop care teams that consistently utilize Motivational Interviewing (MI), Brief Action Planning (BAP) and other self-management support (SMS) strategies with their patients to improve health outcomes and staff satisfaction. Two HHC network coaches provide biweekly hands-on and telephonic support to care teams at 15 HHC ambulatory practices. Coaches use direct observation, and role-play, with individuals and groups, to identify gaps and inefficiencies in the care of patients with complex situations. Short (5–7 min) live coaching mini-sessions during routine clinical care, target topics such as adherence counseling and effective ways to give information and advice. Nurses quickly learn to recognize the emergence of commitment language (“change talk”) as a queue to begin patient-centered action planning, start using reflections, affirmations and summaries to evoke change talk, and effectively integrate SMS into clinical practice to increase patients’ self-efficacy and engagement. The following two coaching examples provide further understanding. A CM identified time management as a personal challenge. Overwhelmed by the number and breath of patient complaints, she questioned her ability to complete a visit within the allotted time. Using role-play, the coach identified inefficiencies in the way she elicited patient concerns and then introduced skills for upfront agenda setting through “surveying,” and a method for giving information and advice using “ask-tell-ask” to structure the visit. Role-play allowed the learner to practice these skills and build confidence prior to real-practice application. Another CM described frustration related to a depressed patient who was unfocused and “cried during the entire visit.” Coaching included effective use of silence, “naming the emotion,” reflective listening, and affirmations. The CM practiced via role play, while the coach provided instant feedback. This process resulted in the CM preparing specific affirmations of her patient’s inner strengths to use during the next visit. Even brief targeted coaching interventions of 5–7 min delivered by the coach during a busy HTN treat-to -target clinical session, were perceived as helpful by nurses who had previously attended an introduction to MI session but admitted they had not applied any of the skills into practice.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1. Increasing self-efficacy of CM’s in applying new skills into clinical practice. 2. Shortening the time and ease of TEAMcare implementation via skill-building.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Generating staff “buy-in” for any initiative is challenging in today’s healthcare environment. Despite attending an introductory MI workshop, nurses were unable to apply the skills to clinical practice. Coaching expedited skill building and increased CM self-efficacy and engagement, which created enthusiasm for successful program implementation. CMs perceived the use of MI, BAP and SMS strategies as not only effective, but also efficient. For example, one nurse reported that she was surprised at her patients’ baseline knowledge of HTN self-management and that the “Ask-Tell-Ask” technique “saved time,” by permitting her to target patient specific knowledge gaps as opposed to providing a standard health education message to all.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): On-site coaching is a pragmatic way to develop communication competencies of healthcare providers and accelerates implementation of innovative practice models by increasing self-efficacy of adult learners (CMs). It also facilitates PCMH transformation by building a more empowered and engaged workforce.
PRIMARY CARE PROVIDER FEEDBACK FOR IMPROVING CLINICAL PROGRESS REPORTS ON WEIGHT MAINTENANCEMichael Eng; Kathleen M. McTigue; Laurey R. Simkin-Silverman; Kimberly A. Huber; Lacey Funair; Molly B. Conroy. University of Pittsburgh, Pittsburgh, PA. (Tracking ID #1925673)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Clinical progress reports for referring primary care providers (PCP) are an essential component of delivering a behavioral lifestyle program in coordination with primary care; the content, format, and delivery method of reports that best suits PCPs is unknown.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): −Design a simple but informative clinical progress report to provide referring PCPs real-time updates about their patients’ participation in a weight maintenance behavioral lifestyle program -Obtain feedback from PCPs about how report could be improved to better suit their needs -Describe feedback from PCPs used to improve clinical reports
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The clinical progress reports were developed as part of the Maintaining Activity and Nutrition through Technology-Assisted Innovation in Primary Care (MAINTAIN-PC) study. The goal of MAINTAIN-PC is to evaluate the use of Health Information Technology (HIT)-delivered tools and health professional support to help primary care patients successfully maintain weight loss. Specifically, we have developed a flowsheet for weight, diet and physical activity data and standardized patient surveys; both tools are used to deliver a coaching protocol through the patient portal of the electronic health record (EHR). We are recruiting primary care patients and their providers from a group of outpatient clinics affiliated with University of Pittsburgh Medical Center (UPMC); a PCP referral is required for study participation. PCPs of patients randomized to the coaching arm of the study will receive clinical reports delivered via the EHR 24–48 h prior to routine clinic appointments. PCPs of patients randomized to the tracking (control) arm of the study will receive paper clinical reports delivered on an annual basis, and not necessarily in coordination with patient care.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Prior to start of recruitment and randomization, we asked PCPs for feedback on a draft of the clinical progress report we had designed for MAINTAIN-PC. The report was a one-page, brief summary of patient progress to date, interpretation of patient data (e.g., current patient strengths and challenges), and recommendations, including tips for PCP counseling. At the bottom of the report was a graph of patient weight since starting MAINTAIN-PC. Data for the progress report will be obtained from the patient-entered flowsheets and from subjective comments provided by coaching staff. We asked PCPs to comment on the content, format and delivery method of the report draft. We used both a written survey as well as structured interviews to gather PCP feedback; we gathered feedback until we reached thematic saturation. We plan to ask the referring PCPs for additional feedback on the reports and other aspects of the MAINTAIN-PC at 1 year and 3 years after beginning the program.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We received feedback on the draft report from 17 PCPs. Responding PCPs included those in large, academic practices as well as those in smaller, private practices. The content that they rated the highest was the weight graph and the tips for PCP counseling. The brief format was favorably rated, but they requested more bulleted information and fewer paragraphs of text. There was a wide range of responses for preferred method of delivery within EHR: patient encounter (n = 4), referral letter (n = 4), staff message (n = 3), and phone message (n = 3), and other (n = 1) were all selected as preferred means of delivery. While formatting constraints will not allow a weight graph to be embedded directly in the report delivered via the EHR, PCPs will be able to link to graphical data.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): PCPs replied favorably about clear visualization of patient data (e.g., graphs, bulleted text) on the draft report. There was no consensus about how the report should be delivered in the EHR. With the PCP feedback, a revised progress report was created and will be implemented in the coming months.
PRIMARY CARE-BASED COMPLEX CARE MANAGEMENT FOR LOW-INCOME PATIENTS WITH MULTIMORBIDITYJulia Finch1; Fern Ebeling1; Lindsay Evans1; Lisa Tang1; Alice Y. Mao2; Rachel Willard-Grace2,1; Louise Aronson2,1; Leslie Dubbin2,1; Anneliese Johnson2,1; Reena Gupta2,1; Claire Horton2,1; Elizabeth Davis2,1. 1San Francisco General Hospital, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1940154)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): A small number of complex patients account for a disproportionately large number of our clinic’s total hospital admissions.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) Reduce hospitalizations and ED visits. 2) Improve patient satisfaction and functional status, and 3) Improve provider satisfaction
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The Care Management Program is embedded in San Francisco General Hospital’s General Medicine Clinic, an outpatient primary care clinic. We enroll high-risk, high-utilizing patients who receive their primary care at the General Medicine Clinic. Our nurse-led interdisciplinary team conducts an initial assessment in the patient’s home in order to identify the patient’s individual concerns, barriers and goals for his/her health. After creating a patient-centered care plan, a health coach works with patients, primarily through a direct phone line, to achieve goals and provide health education. The nurse works closely with the patient’s primary care provider to manage complex medical issues and address any urgent medical concerns. Additionally, when a patient is admitted, the Care Management Team communicates with the inpatient team and primary care provider to coordinate patient discharge, thereafter providing focused support for the following 2 weeks to help prevent re-admission. The team aims to improve patient self-management through a focus on medication adherence, teaching about “red flags” to allow for early intervention, and appropriate use of services. As patients stabilize and improve, they are moved to less intensive levels of care and eventually graduated from the program.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We use a Microsoft Access database to track our care management activity and our patients’ utilization data, including the number of admissions, length of inpatient stays, and number of Emergency Department (ED) visits. We also assess patient and provider satisfaction using surveys and input from a patient advisory board.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We collected utilization data from 65 patients for the year prior to enrollment in the program and the time since enrollment. After annualizing the data, we found a 41.6 % decrease in number of hospital admissions and a 9.2 % decrease in ED visits. Looking at the 45 patients enrolled in our program for at least 1 year, we see a 40.2 % decrease in hospital admissions and a 15.3 % decrease in ED visits. Qualitative interviews with 13 patients currently enrolled in the Care Management Program revealed that most patients feel much more motivated to participate in healthier behaviors and feel that their self-management skills have improved as a result of enrollment in the program. Provider surveys showed satisfaction across multiple domains: communication with patients and family members, coordination of care, monitoring chronic conditions, referrals to community resources, and efficiency of office visits.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Nurse-led interdisciplinary teams that provide focused care and support for high risk patients can decrease the number of expensive hospital admissions and ED visits. Trusting relationships with care team members can motivate patients to change behaviors and improve self-management. Embedding the program in a primary care clinic enhances rather than detracts from the patient’s relationship with their primary care provider and helps avoid duplication of services. This type of program has the potential to improve patient care and satisfaction while also reducing costs for hospitals and insurance providers.
PROJECT RED: QUALITY IMPROVEMENT (QI) WITH EXPLORATORY AND PRESCRIPTIVE BENEFITSGeorge Shelton1; Aanand D. Naik1,2; Barbara Trautner1,2. 1Michael E. DeBakey VA Medical Center, Houston, TX; 2Baylor College of Medicine, Houston, TX. (Tracking ID #1934126)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Our facility’s all-cause readmissions do not meet the quality benchmark set by our VA Integrated Services Network (VISN 16).
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Determine if Project Re-Engineered Discharge (RED) reduces readmissions to our hospital compared to the prior 18 months Improve inpatient discharge process flow and coordination
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Our hospital readmission rates have averaged 14–15 % over the past quarter, while the benchmark for excellence is below 13.1 %. Project Re-Engineered Discharge (RED) is an 11-Element intervention, supported by the Agency for Health Research and Quality (AHRQ), which has been an effective means of decreasing readmissions in some settings. In a non-VA teaching hospital, RED demonstrated 30 % reductions in 30-day readmissions and/or emergency room visits. Our proposal adapts Project RED into the VA health care system. Each element addresses specific components of discharge planning and incorporates systems improvements within existing inpatient workflows and routines. (see below for RED element descriptions and measures).
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We will conduct a pre-post comparison of our readmission and emergency department use rates comparing FY2015 to FY2014. We will then compare our readmission rates to other VA medical centers (VAMCs) nationally and within our VISN--seeking a 25 % greater rate of improvement vs. similar sites (i.e., differences in differences, quasi-experimental design). Additionally, each element will demonstrate clinical improvements via process measure milestones specific to their element’s work (below). Process Measures by Element (as measured by manual chart review and/or computer audit): 1) Patient Education - Number of standardized patient education encounters delivered during hospitalization 2) Follow-Up Appointments -Percentage of patients with scheduled follow-up appointments prior to discharge 3) Follow-Up Tests & Studies - Number of labs/tests completed prior to hospital follow-up 4) Organizing Post-Discharge Care -Number of documented interdisciplinary team meetings within 48 h of admission 5) Medication Reconciliation - Percentage of patients with appropriate beta-blocker documentation 6) Guidelines Fidelity-Number of Case Manager Checkpoints completed within 48 h of patient admission 7) Action Plan for Problems -Number of patients receiving instructions on who to call should problems arise 8) Discharge Summary - Number of discharge summaries sent to PCP with complete discharge instructions 9) TeachBack Confirmation -Documented use of TeachBack at discharge 10) After Hospital Care Plan - Number of patients receiving a patient-centered After Hospital Care Plan 11) Post-Discharge Phone Call -Number of Patient-Aligned Care Team (PACT) phone calls completed within 48 h of discharge
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): In Project RED’s pilot phase, all-cause readmission rates decreased to 11.1 % and 12.4 % in successive months, the lowest in 18 months. It is unclear if these changes are due to early Project RED efforts or are sustainable; however, we will evaluate this going forward. Project RED process measures (above) show gradual improvements. In our pilot phase, the scheduling of follow up appointments before discharge increased by 11 % to 57 %. Further, appropriate beta-blocker documentation has increased by 8 % to 83.8 % and patient discharge instruction documentation increased by 9 % to 84 %.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Project RED has dual benefits of methodically uncovering system design issues in the discharge process while providing a framework to resolve them. Emphasis on evidence-based solutions has been a tool to strategically loosen staff fixations on the familiar but unsuccessful methods of delivering care. Project RED at our VAMC also capitalizes on mandatory hospital-wide lean management training which refocuses staff efforts away from individual performance and towards the systems and structures individuals perform within. Project RED facilitated breaking down clinical silos and streamlining discordant work. The silos impeded effective system redesign as some hospital staff were unaware of complimentary, duplicating, or sometimes contradictory efforts. By strategically ensuring that each element team had voices from QI, medical care, and operative care, we funneled projects from the larger hospital into Project RED. Project RED leaders also attend monthly systems redesign meetings that cut across clinical divisions and help establish a shared understanding between Project RED and other VA QI work. Lastly, coordination between and within element teams was challenging, yet vital. Aspects of one element’s work overlapped with or hinged upon the work of other element teams. Individuals also had varying levels of understanding of and motivation for adopting lean management principles. Thus, we appointed facilitators who attend all element team meetings to: 1) review lean management and systems redesign principles, 2) inform of synergistic work, and 3) facilitate progress forward.
QUALITY INITIATIVE TO INCREASE PROVIDER USE OF URINE DRUG TESTING FOR CHRONIC PAINDavid S. Levitt1,2; Nicholas Meo1,2; Christopher P. Chen1,2; Christopher M. Murphy1,2; Christopher Vanderwarker2,1; Joyce E. Wipf2,1; Catherine P. Kaminetzky2,1. 1University of Washington, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA. (Tracking ID #1935800)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Prescription opiate misuse and abuse has become a patient safety crisis in the United States with unintentional overdoses and deaths rising dramatically in recent years.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Our overall goal was to promote safe and responsible use of opiates in chronic non malignant pain amongst providers in our local primary care clinic, where 8 % of patients on are a narcotic pain contract (NPC). Urine drug testing (UDT) is recognized as essential practice to safe opiate prescribing. In November 2012 only 27.9 % of patients in our clinic on a NPC had UDT in the last year. Our primary objective was to increase the rate of UDT completed annually by providers, so that no provider had a rate less than 60 %.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): This quality improvement project was completed in 3 phases. In the planning phase, a retrospective chart review was performed examining all patients on NPCs as of November 1, 2012. Data collected included the date of last clinic visit, provider, opiate medication, dose, quantity, and last fill date. Inclusion criteria included primary care patient on a narcotic pain contract. Exclusion criteria included cancer diagnosis or current fentanyl prescription. The intervention phase began by holding an educational session with providers. State and national safety data with current clinic baseline measures were presented. As a group, a goal UDT target rate was identified. Panel information was provided to providers, including patient name; last UDT; and narcotic drug name, dose, and quantity of last fill. Providers were shown benchmarked summary statistics and encouraged to audit a small selection of charts from their panel. Finally, the electronic medical record template for the NPC note was modified to include a lab order hyperlink to facilitate ordering of the UDT. The post intervention phase assessed the number of patients on NPC, morphine equivalent dosing and the provider UDT rate. A regularly populated report was generated for sustainable improvement and panel management purposes.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Percent of urinary drug screens completed in patients on Narcotic Pain Contract in the last year.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The incidence of patients on a NPC with UDT rose from 27.9 to 59.4 %. Providers meeting the goal of a 60 % screening rate rose from 19 to 64 %. An unexpected finding was that 50 % of providers had a decrease in the number of patients in their panel on a NPC in the post intervention assessment. The number of patients on a NPC serves as a surrogate measure of patients on chronic opiates because our pharmacy will not process chronic opiate prescriptions without a NPC.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): UDT in patients receiving chronic opioid therapy is central to safe opiate prescribing and was identified as an area for improvement in our clinic. We dramatically increased the percentage of patients with UDT by providing benchmarked data to providers and embedding UDT ordering into the narcotic pain contract workflow. Our intervention also had the unexpected effect of decreasing the absolute number of patients receiving opiates in clinic.
REAL-TIME PATIENT SURVEY DATA DURING REAL-TIME CLINICS: IMPLEMENTING TECHNOLOGY-ENHANCED RAPID-CYCLE QUALITY IMPROVEMENTJames L. Wofford; Claudia L. Campos; Sheila R. Stevens; Robert E. Jones. Wake Forest University, Winston-Salem, NC. (Tracking ID #1934790)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Surveying patients is increasingly important for evaluating and improving healthcare delivery, but practical survey strategies during routine care activities have been challenging.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To assess the feasibility of using an integrated data management tool for conducting patient surveys during routine office care activities at a community health center primary care clinic
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We studied the feasibility of implementing a commercially available integrated data management tool (web-based survey creation, deployment on tablet computers, cloud-based management of survey data, and real-time web-based accumulation and display of survey results) in conducting patient surveys. Over a 1 month period, we conducted four patient surveys, each consisting of three questions focused on a specific patient care domain (dental care, waiting room experience, care access/continuity, and internet connectivity). Surveys were conducted among patients attending a clinic appointment on 1–2 designated survey days each week. Clinic personnel (nurses and secretaries) offered and proctored the tablet computer survey.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Number of patients provided the survey Percent of patients completing survey Time to complete the survey and individual questions
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Of the 727 patients who attended office visits during the clinic days when a survey was being offered, 316 patients (43.4 %) attempted the survey, and 293 (40.3 %) ultimately successfully completed the survey. For the four 3-question surveys, the average time per survey was overall 40.4 s, with a range of 5.4 to 20.3 s for individual questions. Yes/No questions took less time than multiple choice questions (average 9.6 s versus 14.0). Average response time showed no clear pattern by order of questions or by proctor strategy, but monotonically increased with number of words in the question (<20 words, 21–30 words, >30 words) - 8.0,11.8, 16.8, seconds, respectively.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): This technology-enabled data management system was successful in capturing patient opinions, accelerated turnaround of survey data, and had minimal impact on a busy primary care clinic. This new model of data collection and management is feasible and sustainable in a busy office setting, supports and engages clinicians in the quality improvement process, and harmonizes with the vision of a learning healthcare system.
REDESIGNING A RESIDENT CONTINUITY CLINIC TO PROVIDE EFFECTIVE POPULATION HEALTH MANAGEMENTAlex H. Cho1; Mark Dakkak1; Adia K. Ross1; Wei Duan-Porter1,3; Lynn Bowlby1; Daniella A. Zipkin1; Lawrence Greenblatt1; Natasha T. Cunningham1,2; Jessica Simo4; Gina Green4; Holly Causey4; Benjamin Smith4; Chris Samples4; David Zaas1; Aimee K. Zaas1; Eugene Z. Oddone1,3. 1Duke University School of Medicine, Durham, NC; 2Duke University School of Medicine, Durham, NC; 3Durham VA Medical Center, Durham, NC; 4Duke University Health System, Durham, NC. (Tracking ID #1936906)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): How does an adult medicine safety net clinic predominantly staffed by residents reinvent itself to provide more effective population health management?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Reduce excessive care utilization by patients with co-morbid mental health and substance abuse disorders. 2. Improve post-hospitalization follow-up for clinic patients. 3. Improve continuity and quality of patient care and resident education, simultaneously.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Over a 2 year period, the Duke Outpatient Clinic (DOC), a resident clinic caring for underserved and uninsured patients, undertook an effort to restructure its services to better serve its population and address avoidable utilization of ED and inpatient care. An overarching Six Sigma DMAIC framework (define; measure; analyze; implement; control) was used. Improvement of resident education was also an important goal. Three major interventions were proposed, and financial modeling done to make a case for the initial investment required; these were launched in July 2013: Clinic-based mental health-primary care coordinated care model To address the needs of DOC patients with co-morbid mental health conditions and high rates of ED and inpatient utilization, the HomeBASE program was created. This complex medical management intervention is supported by a care team consisting of two care managers, social worker, a mental health-trained advanced practice provider (MH-APP), and a dually trained medicine-psychiatry attending (MPA). Patients in the program are stratified into four levels of care management that vary by intensity. Detailed care plans created and entered into their records to guide other providers. All patients in the program also receive enhanced same-day clinic access to the MH-APP. The MPA supervises resident providers and provides onsite consultation. Managing post-discharge transitions of care Discharge from the hospital is a vulnerable time for patients in bridging care and maintaining accurate medical records and medication lists. To improve their transition to primary care, a team consisting of DOC front desk staff and pharmacists was formed to contact patients and perform medication reconciliation in advance of a structured post-discharge clinic visit. Clinc-based resident ‘firms’ Continuity had been a major challenge, not just between resident providers and their patients, but also between residents and their attendings. Acting on a resident proposal, a clinic-based ‘firm’ structure was adopted, in which residents are organized into teams with a lead attending, secondary attendings, a lead RN, and two certified medical assistants. These ‘firms’ are also now the basis for population management and quality improvement efforts.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): A ‘dashboard’ of metrics, updated quarterly, was created to monitor key components of the DOC redesign; including resident-attending and resident-patient continuity, post-discharge phone contacts and follow-up appointments, and the relatively hard outcomes of utilization (i.e., ED visits and hospitalizations) and direct costs for these services.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Findings 3 months after the start of implementation are promising. Ninety-four percent of resident clinic sessions were scheduled with assigned attendings and 42 % of patient visits were with resident PCPs. Every DOC patient who could be contacted was within 2 business days of hospital discharge, and the percent of patients with follow-up appointments within 14 days of discharge increased from 59 to 84 %. The coordinated care program has enrolled 38 patients; their ED visits and hospitalizations have decreased, driving a reduction in both numbers for the clinic overall. Direct costs for the inpatient care of DOC patients are $300,000 lower compared with the same period a year ago.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Many academic resident-based primary care clinics care for socially and medically complex populations. Optimal patient care and resident education need not be mutually exclusive ideals. The DOC redesign for improved population health management and resident education was based on the Six Sigma DMAIC approach (Define, Measure, Analyze, Implement, Control). Interventions were designed over the course of a two-year iterative process that sought from stakeholder groups, conducted some pivotal pilots, and reviewed the internal and external landscape. Continuous monitoring of a ‘dashboard’ of metrics will guide further refinements, improvements, and expansions of these interventions at the DOC going forward. The clarity of goals and focus in execution facilitated by the use of the DMAIC framework have been critical to its success. In addition, leaders of resident clinics may not be accustomed to making more than broad economic arguments for investment in changes they are advocating; we found that making a specific financial case was critical to understanding what would be sustainable long-term, and earning the support of health system leadership.
REDUCING NON-URGENT EMERGENCY ROOM VISITS DURING PRIMARY CARE BUSINESS HOURS: A COLLABORATIVE APPROACHAlexandra Norcott1,2; Esterina Anderson1,2; Sarah Dann1,2; Anne Hyson1,2; Cali Luco1,2; Emily M. Meyer1,2; Susan A. Zapatka1,2; Rebecca Brienza1,2. 1U.S. Department of Veterans Affairs, West Haven, CT; 2Yale School of Medicine, New Haven, CT. (Tracking ID #1938708)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Emergency room (ER) overutilization for non-life-threatening issues has been closely associated with overcrowding, loss of continuity, and patient dissatisfaction. In an effort to address these challenges, the West Haven Veterans Affairs Medical Center (WHVA) Center of Excellence in Primary Care Education (COEPCE) initiated a quality improvement (QI) project designed to decrease ER utilization for non-life-threatening issues during primary care’s (PC) regular business hours. This work is being undertaken at the WHVA through the Primary Care-ER committee and in collaboration with five other COEPCE sites across the country. The WHVA COEPCE has a strong QI curriculum and was able to combine the work of these groups with trainee clinical experience to achieve an interprofessional perspective.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): This QI initiative primarily aimed to decrease ER utilization during office hours and also aimed to promote interprofessional team learning and application of QI methods, and develop best practices for application at other clinical sites.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): This COEPCE is one of several patient aligned care teams (PACTs) at the WHVA. The WHVA COEPCE consists of three interprofessional teams, which include medical doctor (MD) and advanced practice registered nurse (APRN) faculty, registered nurses (RNs), licensed practical nurses (LPNs), MD residents, APRN fellows, undergraduate clinical students, pharmacists, and health psychologists. The COEPCE provides longitudinal care for 9 % of the Veterans seen across the VA Connecticut Healthcare System, who have access to the WHVA ER. In January 2013, COEPCE began collaborating with the PC-ER committee, which includes representatives from all PC clinics as well as the COEPCE in order to optimize PC and ER resources in conjunction with ongoing QI learning with COEPCE trainees. COEPCE held small group, ER specific, problem-based learning sessions designed to teach QI methodology, with subsequent Plan-Do-Study-Act cycle initiation (PDSA). In conjunction with the committee findings and the aid of the ER staff, the COEPCE initiated a series of interventions aimed to increase visibility and accessibility of PC resources available to Veterans. Such interventions included letter campaigns, informative posters/signage, referral to PC appointments directly from ER triage, and increasing the number of PC urgent visit (UV) appointment slots available starting in July 2013.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): At baseline, low-acuity (as defined by Emergency Severity Index scores of 4 or 5) needs constituted 12.9 % of WHVA ER visits during PC business hours. We calculated the number of non-urgent ER visits during PC business hours over total number of ER visits. These values were further organized according to where the Veteran was assigned: the COEPCE or Firm A, which implemented similar interventions but did not increase UV appointments. We also measured provider availability as assessed by number of UVs.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): A total of 13,533 non-urgent ER visits occurred between January 1, 2012 and December 31, 2012 with 1754 (12.9 %) occurring during PC business hours. A total of 12,817 non-urgent ER visits occurred between January 1, 2013, and December 31, 2013 with 1080 (8.4 %) occurring during business hours. Overall, this was a 26 % reduction in all ER visits during business hours with a 47 % reduction in the COEPCE (368 to 194) and 44 % reduction in Firm A (779 to 438). COEPCE UV’s increased 41 % from an average of 15.8 visits/week prior to July 2013 to 36.2 visits/week. The average percent reduction for non-urgent ER visits during PC business hours from July 2013 to November 2013 was 48.4 % for Firm A and 59.4 % for our COEPCE.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): In an effort to quickly optimize resource allocation many interventions/changes were implemented in a brief timeframe. This approach, although practical, confounds our interpretation of which intervention was most influential. It does appear, however, that the increase in UV appointments is particularly influential as the relative reduction in ER utilization for the COEPCE was 3 % higher when compared to Firm A. We recognize that ER utilization is, in itself, multifactorial and addressing non-urgent ER utilization will require multiple distinct interventions. Going forward we will endeavor to more methodically compare interventions across different PC teams. This was the first interdisciplinary, interdepartmental, and multi-site QI project that our COEPCE participated in. It has helped us to learn about one another’s challenges and make reasonable changes that would not adversely affect other departments. Our PACTs are more apt to work collaboratively together as a result of this endeavor and will inform future QI work at the WHVA COEPCE.
SAFE MED RECONCILIATION (SATISFY PATIENTS USING A MEDICAL RESIDENT EDUCATIONAL INTERVENTION TO IMPROVE OUTCOMES)Jessica Logan1,2; Cherinne Arundel1,3; Rebecca Swenson4; Ribka Ayana1,2. 1 DC VA Medical Center, Washington, DC; 2George Washington University, Washington, DC; 3Georgetown University, Washington, DC; 4Dartmouth College, Lebanon, NH. (Tracking ID #1937806)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Does a targeted intervention aimed at improving the medication reconciliation process with internal medicine residents reduce medication errors?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): −Improve the accuracy of discharge medication lists -Improve residents’ ability to perform accurate medication reconciliation
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Medication errors are an important preventable cause of adverse events. Improvement of the medication reconciliation process has been identified as a national patient safety goal by The Joint Commission (TJC).(3) A review of our patient population revealed that many patients had more than 8 medications and roughly 37 % of discharges had medication omissions, 16 % had duplicate medications, and in 75 % of cases there was a discrepancy between the discharge medication list provided to the patient and the discharge summary. An additional review of a 114 medical records revealed that 42 % of admitted patients had problem medications such as insulin, narcotics, and anticoagulants which have been associated with an increased risk of readmission. (7,8,9) Our internal data from the DCVAMC, complimented by a literature review, highlights that inaccurate medication reconciliation can lead to ineffective hospital discharges and transitions of care. While the significance of medication reconciliation is well-described, it remains error-prone and rarely formally taught to trainees. Our target populations are Internal Medicine residents and medical students rotating at the DCVAMC (18 interns/residents monthly and 16–20 students for a total of about 440 learners per academic year) and approximately 2400 patients admitted to the medicine ward annually. The purpose of this Clinical Practice Innovation is to determine if a real-time, educational intervention with residents on medication reconciliation impacts the accuracy of discharges. The SAFE MED RECONCILIATION project was a two part learning session held during morning report with residents and medical students. In the sessions, the importance of medication safety was highlighted and how to perform proper medication reconciliation was reviewed. This was complimented by a discussion of relevant quality improvement concepts. Resident performance was assessed at the start and end of the month using an evaluation rubric. The overall impact of the study was evaluated by pre intervention and post intervention chart reviews.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Accuracy of medication list was measured by chart review before and after the intervention. A random sample of 150 discharge summaries and discharge instructions were analyzed pre-intervention and post-intervention to assess the global impact of the intervention over time. A rubric with explicit instructions to assess accuracy was used by two hospitalists and determined by consensus. Data was analyzed by each individual item on the rubric as well as analyzed by summative score. The following variables were assessed: extraneous medications, duplicate medications, medication omissions, discrepancies with discharge summary, if medications were sorted by disease, if pharmacy medication reconciliation was done and number of medications. The number of admissions was also collected.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Chart review revealed our population to be vulnerable to medications errors with 57 % of patients having more than eight medications on discharge and 17 % having more than 15 medications on discharge. Preliminary data of the 150 discharge instruction revealed that in the pre intervention group there were 14.67 % extraneous medications compared with 6.67 % in the intervention group. Pre intervention there were 30.67 % medical records with a discrepancy between the discharge medication instructions and the discharge summary compared with 12 % in the intervention group. Medication omissions occurred in 17.33 % of discharges pre intervention compared with 14.67 % post intervention. Before the educational intervention, 28 % of discharge medications were sorted by disease compared with 65 % after. There was little improvement in the number of duplicate medications (18.67 % vs 17.33 %) or rates of pharmacy reconciliation (89.33 % vs 90.67 %).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Medication Reconciliation is a complex process with many opportunities for intervention. A real time educational intervention with residents is time consuming and difficult to keep relevant for repeat learners. In our institution, we have residents from various programs, which makes timing of the intervention difficult. Our project suggests that the accuracy of discharge medication reconciliation can be improved, but it remains difficult to assess patient related outcomes such as satisfaction and medication safety. In addition, there are multiple systems issues that contribute to medication errors. These issues must be analyzed and addressed to truly impact change.
STAAR: IMPROVING THE RELIABILITY OF CARE COORDINATION AND REDUCING HOSPITAL READMISSIONS IN AN ACADEMIC MEDICAL CENTERJocelyn A. Carter A. Carter; Gwen Crevensten. Massachusetts General Hospital, Boston, MA. (Tracking ID #1934428)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Can innovations in healthcare delivery on a medical ward effectively reduce avoidable readmissions by improving care coordination for patients at risk for readmission?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) To reduce readmissions on the Ellison 16 medical ward (36-bed unit) to 10 % 2) To improve care coordination at discharge for patients at risk for readmission
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Initial measurement of Ellison 16 medical ward (a 36-bed general medicine unit) 30-day hospital readmission rates were less than ideal (18.3 %) prior to the interventions. The goal for readmission rate reduction to 10 % was set by an MGH Hospital-wide initiative. Staff education on readmissions (local and national landscape), survey of ward staff (physicians, nurses and unit managers) as well as on-site observations of discharge processes were completed prior to initiating the interventions. All patients admitted to the Ellison 16 medical ward were evaluated for inclusion from 07/2009–7/2013. If high risk criteria were met, patients were enrolled and received interventions which included care coordination with a inpatient discharge nurse (who provided education to patients/care givers, coached patients on their discharge care plan and served as a centralized navigator for the care team) and a discharge pharmacist (who facilitated medication reconciliation, counseled patients/caregivers on medication usage, and conducted post-discharge calls to patients). General interventions also occurred during this time period and included reorganization of daily resident team rounding and discharge reconciliation processes.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1) All cause 30-day readmission rates using statistical process control analysis 2) Patient survey data tracking inpatient satisfaction and discharge experience satisfaction
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): 1) Overall, readmission rates on Ellison 16 decreased from 18 % (avr) before the interventions to 14.79 % (avr) after the interventions were implemented (p < 0.05). 2) During the study period, the discharge nurse intervention decreased readmissions to 15.9 % amongst high risk patients (p = 0.59). 3) During the study period, the discharge pharmacist intervention decreased readmissions to 12.9 % amongst high risk patients (p = 0.55). 4) During the study period, post-discharge pharmacy calls demonstrated that 52 % of patients deviated from medication instructions after leaving the hospital. 5) During the study period, inpatient/discharge experience satisfaction did not change during the study. 6) Readmission rates for patients on Ellison 16 that did not receive the designated nursing or pharmacy interventions decreased to 15.8 (p = 0.61) and 16.2 (0.31) respectively.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1) Reducing hospital readmissions on a general medicine unit is a complex process and requires input from physicians, nurses, case managers, patients and unit leaders. 2) Careful study of the processes of care and perspectives of key stakeholders is important in developing inpatient/discharge interventions. 3) While single interventions may not demonstrate statistically significant change in readmission rates, involvement of key stakeholders and awareness of readmissions as an organizational priority may effectively impact avoidable readmissions. 4) Patient satisfaction scores may not be impacted by care coordination improvements or reductions in readmission rates. 5) Additional studies are needed to validate inpatient/discharge nursing and pharmacy interventions in a setting of cultural change related to educating staff on readmissions.
STANDARDIZING THE DISCHARGE PROCESS WITH AN ELECTRONIC MEDICAL RECORD-BASED CHECKLIST - A RESIDENT-LED QUALITY IMPROVEMENT INITIATIVEChapy Venkatesan; Nancy Maaty; Kimberly Lui; Shirley Kalwaney; Alita Mishra; Jillian K. Price; Yun Fang. Inova Fairfax Hospital, Falls Church, VA. (Tracking ID #1936879)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Prevention of avoidable readmissions and improvement of patient throughput are high priority initiatives, yet there is no standard discharge process for residents to follow.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Improve readmission rate and patient throughput for patients cared for by a teaching service. 2. Empower residents to lead quality improvement (QI) initiatives.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Our QI team is located at a large community-based teaching hospital and consists of a 12 person transitional residency, two chief residents, and three hospitalist faculty physicians. All team members completed the IHI Open School QI modules. During the first team meeting, readmission prevention, improvement in hospital throughput, and the teach back technique were reviewed. The residents subsequently designed a best practice discharge process with a checklist in the electronic medical record. The intervention, enumerated in the checklist, consisted of 1) determining risk of readmission, using the Society of Hospital Medicine “The 8P’s Risk Assessment Tool”, 2) advanced notification and engagement of patients, families, and team members regarding discharge, 3) reminders to arrange early outpatient follow up appointments, 4) prompts to educate patients about their diagnosis and medications, and 5) in person resident-to-patient medication and diagnosis education using teach back. Residents were encouraged to perform the intervention for patients who were at high risk for readmission. When the intervention was completed, a final progress note with the checklist was generated and sent to the chief residents for record keeping. The QI team performed successive PDSA cycles with the goal of increasing the number of patients exposed to the intervention. The primary solution was to capitalize on the inherent competitive spirit of many of the interns by publicly displaying performance at morning report. “High performing” residents were able to advise their colleagues on how to perform this intervention more efficiently. Patients cared for by the teaching service who were not exposed to the intervention during the same time period, served as a comparison group. Future PDSA cycles will focus on refining specific components of the intervention until readmission and throughput goals are met.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): The QI team is tallying the number of interventions completed per week. Hospital administrative data is being utilized to determine 30 day readmission rates and will eventually be used to adjust outcome rates for differences in diagnosis, severity of illness, and other risk factors for readmission. Bed management data is being utilized to determine timing of discharge order and discharge time. Resident experience with the QI process and patient satisfaction with the intervention will be measured using survey instruments and focus groups. Direct observation using the University of Iowa “Teach-back Observation Tool” will be used to measure usage of the teach back technique and time spent during patient education. Finally, adherence to follow up and patient disease and medication knowledge will be assessed using patient questionnaires.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): A total of 254 patients were exposed to the intervention between September 2013 and December 2013. After resident performance was publicly displayed, the number of interventions per week increased from 7 per week to 19 per week. During October 2013, intervention data was available for 102 patients. This group of patients was at high risk of readmission. Forty-six patients (45 %) were aged 65 years or older, and 73 patients (72 %) were Medicare, Medicaid, or self-pay patients. Sepsis, pneumonia, heart failure, or GI hemorrhage was the primary discharge diagnosis in 78.4 % of patients. Thirty-two percent of patients reported a hospitalization within the prior 6 months, and 13 % were hospitalized in our own health system within the previous month. Nearly 20 % of patients were taking at least two high risk medications, and 65 % of patients met criteria for poly-pharmacy. The median case mix index (CMI) was 1.48. The comparison group, consisting of 331 patients, had a similar profile to the intervention group in terms of age, payor, and diagnosis. However, the median CMI was 14 % lower than in the intervention group. The 30 day readmission rate, within our five hospital health system, in the intervention group was 12.6 % versus a 15.4 % rate in the comparison group. The average time between discharge order and discharge time was 163 min in the intervention group versus 267 min in the comparison group.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Empowering residents to lead a QI initiative can be effective in improving use of an intervention. Pilot data suggests that following a standard discharge process, with a checklist embedded in an electronic medical record, can result in improvements in 30 day readmission rates and patient throughput.
SUCCESSFUL IMPLEMENTATION OF A LARGE SCALE HEPATITIS C SCREENING PROGRAM AMONG BABY BOOMERS IN AN URBAN PRIMARY CARE CENTERLesley Miller1; Shelly-Ann Fluker1; Kristina L. Lundberg1; Francois Rollin1; Brandi Park1; Kristi Quairoli3; Anne Spaulding2. 1Emory University, Atlanta, GA; 2Emory University, Atlanta, GA; 3Grady Health System, Atlanta, GA. (Tracking ID #1937462)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The CDC and USPSTF now recommend one-time hepatitis C virus (HCV) testing for all baby boomers, however implementation of this large-scale screening in primary care practices, as well as linking newly positive patients to care, remain challenges that require innovative approaches.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): The objectives of this CDC-funded demonstration project were to 1) Train internal medicine residents to implement birth cohort HCV antibody testing in their continuity clinics that serve an urban, medically underserved population. 2) Using residents as screeners, test 2,000 patients for HCV antibody over a one-year period, increasing the number of persons aware of their previously undiagnosed HCV infection. 3) Link HCV positive patients to onsite counseling, preventive services, care and treatment at the primary care-based, generalist-run Grady Liver Clinic or with their primary care providers.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): The program was implemented in the Primary Care Center (PCC) at Grady Memorial Hospital (Atlanta, GA), an urban teaching hospital serving a primarily African American, medically underserved population. The PCC has 58,000 patient visits annually. The first phase of the program was an educational intervention for all 147 internal medicine residents with continuity practices in Grady’s PCC. Project faculty sent an email to residents describing the project structure and goals, and included teaching pearls supporting hepatitis C screening. Faculty followed up with one-on-one educational interventions for all residents during which a hepatitis C screening reminder was added to the electronic medical record template. Residents then proceeded with hepatitis C screening among patients in the 1945–1965 birth cohort during continuity visits. The project coordinator abstracted charts for results of HCV antibody testing, contacted all HCV antibody positive patients, and linked positive patients to an educational session followed by a physician visit at the Grady Liver Clinic. Patients with positive HCV antibody tests were sent for confirmatory HCV RNA testing.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We evaluated the success of each of the 3 program objectives by measuring 1) the number of residents reached with the educational intervention, 2) the number of patients who received HCV antibody testing and 3) the number of HCV antibody positive patients who attended a linkage to care visit. Data were collected over a 1 year period on the total number of HCV antibody tests ordered and drawn, the number of patients testing positive for HCV antibody, HCV RNA and presenting for a linkage visit.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): At the end of the first project year, 147 residents (100 %) had received the educational intervention and had screened 2,439 PCC patients for HCV antibody, well over the 2,000 tests predicted. Of the 2,439 screened, 190 (7.8 %) tested positive for HCV antibody. Of the antibody positive patients, 149 (78 %) were tested for HCV RNA. Of these 149 with HCV RNA results, 104 (70 %) were RNA positive, confirming chronic HCV infection. Of the 104 with confirmed HCV infection, 96 % followed up with an internist, either with their PCP or at the Grady Liver Clinic.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Large scale implementation of new hepatitis C screening guidelines was feasible in a resident primary care practice and yielded an unexpectedly high prevalence of HCV infection that was previously undiagnosed. We achieved very high rates of linkage to care for HCV antibody positive patients, and all linkage was to general internists, whether in our primary-care based Liver Clinic or with primary care providers. It is likely that testing in similar populations would yield an equally high prevalence of undiagnosed hepatitis C, a compelling reason to screen. Our model suggests that generalists can become adept at initial, and if interested, in-depth hepatitis C care to manage patients identified through screening.
THE AFFORDABLE CARE ACT: HELPING PATIENTS SIGN UP FOR HEALTH COVERAGE THROUGH THE MARKETPLACESita Bushan1; Robin H. Roche2,1; Shana Ratner1. 1University of North Carolina- Chapel Hill, Chapel Hill, NC; 2AccessCare, Morrisville, NC. (Tracking ID #1938430)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Nearly 2000 uninsured patients in our clinic needed assistance with and education about the Affordable Care Act (ACA).
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To assess patient interest in assistance with signing up for the Affordable Care Act To educate both patients and providers about the Affordable Care Act To pilot a Saturday Sign Up Day to assist patients with signing up outside of regular clinic hours
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): UNC Internal Medicine Clinic (IMC) is an academic general internal medicine practice in North Carolina, a state which did not expand Medicaid. About 20 % of our patients are currently uninsured. Patient surveys were given to uninsured patients at clinic to assess the demand for assistance with signing up for the Marketplace. We developed educational materials in both English and Spanish for our patient population, including lists of local community resources, and provided education to staff through presentations and emails. A front desk-prompt was developed to direct uninsured patients to our financial counselor. Three clinic members trained to become Certified Application Counselors (CACs). We collaborated with UNC School of Medicine and Legal Aid to recruit CACs and Navigators to pilot a Saturday Sign Up Day where patients could meet with a CAC to enroll in marketplace, explore their options, and sign up for health insurance. After determining patient satisfaction with the Saturday Sign Up Day, we are planning a larger scale enrollment event in January.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Patient surveys were collected to assess demand for assistance. Data collected from the pilot Saturday Sign Up Day included number of appointments and walk-ins, number of no-shows for appointments, number of applications filled out, other social needs to address, and barriers to obtaining health insurance.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Twelve surveys of uninsured patients were collected, and 11 of these patients had not completed the application for the Health Insurance Marketplace. Most patients expressed interest in receiving help at the clinic. The Saturday Sign Up Day pilot offered 15 appointments, 100 % of which were scheduled. Fourteen patients completed appointments (9 scheduled, 5 walk-ins). Half completed an application (7/14). The most common barrier to obtaining health insurance was income level that caused patients to fall in the coverage gap between Medicaid and Qualified Health Plans. Staff also assisted patients in obtaining Medicare Part D coverage, applying for Medicaid, and obtaining information about food stamps. Education of staff members about the ACA resulted in 15 referrals to the Saturday Sign Up Day. A larger scale event is being planned in January for 120 patients, utilizing lessons learned from the pilot sign up day. Booths from local social service groups will be available to assist patients with other social needs.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Assistance with the ACA application in the clinic setting encourages patients to apply. Events like the Saturday Sign Up Day represent one method of providing assistance to patients that bypasses space and time constraints of the regular clinic day. Assisting patients with the ACA offers opportunities to help with other social services such as medication coverage, Medicaid, and food stamps.
THE CARE PROJECT: A MULTI-DISCIPLINARY APPROACH TO IMPROVE THE CARE OF HOSPITAL SUPER-UTILIZERSSaraswati R. Iobst1; Kelly Berchou1; Kristin Muzina2; Caroline Hoppenheim2; Riya George1; Celine Goetz1; Katie Salib2; Yvette Rolon-Fink2; Carol DeJesus2. 1New York Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 2New York Presbyterian Hospital/Weill Cornell Medical Center, New York City, NY. (Tracking ID #1934712)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Hospital super-utilizers often receive inadequate care despite exorbitant costs incurred to the medical system; a multidisciplinary team that focuses on an individualized approach to care has been demonstrated in the literature to improve care and reduce costs in this patient population.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): Our primary aim is to decrease annual inpatient admissions among hospital super-utilizers by an average of 30 % over a 12-month period. We also aim to perform in-depth assessments of each enrolled patient to identify barriers to care and unmet needs contributing to frequent hospitalizations; and based on this assessment, to develop individualized intervention plans that can be qualitatively measured for success. For example, if we identify lack of stable housing as a barrier, then obtaining stable housing would be a measure of success.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Our program, entitled the CARE Project, focuses solely on hospital super-utilizers and is the first of its kind at Weill Cornell Medical Center. We have created a multi-disciplinary care team comprised of representatives from hospital medicine, social work, primary care, and emergency medicine. We are using a community-based model, meaning we follow patients in both the inpatient and outpatient setting. We have defined a hospital super-utilizer as a patient with five or more inpatient admissions to the Medicine service within a 12-month period. We plan to enroll a total of 10 patients over a 12-month pilot period. After initial engagement with a patient, we perform an in-depth needs assessment to identify barriers to care and unmet needs contributing to frequent hospital admissions. Based on our findings, we create an individualized care plan in collaboration with the patient, caregivers, and providers. Many of our interventions are directed towards unmet psychosocial needs as well as facilitating care coordination and communication between providers as well as between providers and patients.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): We will compare the following variables from the 12 months prior to project enrollment to the 12 months after enrollment for each patient: number of admissions to the general medicine service; number of 30-day readmissions; average length of stay (LOS) per admission; number of ED visits; and cost data (hospital charges vs. actual reimbursement). We will also qualitatively assess the outcome of each patient’s individualized intervention plan.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): We have thus far enrolled 4 patients; enrollment is ongoing. Below are brief descriptions of our first 2 cases: Patient 1: 67 year-old man with congestive heart failure (CHF) who has been admitted to our hospital ten times over the past year for CHF exacerbations. He had not been to his PMD or cardiologist for almost 2 years. After 1 month of intensive engagement, he revealed that he was undomiciled. In addition, he was developing blindness from severe cataracts. Our initial intervention plan included re-establishing care with a primary care physician. He also underwent successful cataract surgery, which required obtaining temporary housing and significant care coordination. The most critical remaining goal of our intervention plan is to obtain permanent housing. Patient 2: 34 year-old man with sickle cell anemia complicated by severe iron overload and Mediport colonization leading to recurrent bacteremia and frequent admissions for sickle cell pain crises. He has had seven hospitalizations over the last 12 months, averaging 33 days each. As he is frequently hospitalized, we have become his support network in the hospital, visiting with him frequently. We have successfully coordinated care with his inpatient providers and have succeeded in having his Mediport removed. We have also arranged an appointment with a multi-disciplinary sickle cell anemia clinic that has access to outpatient infusion capabilities and active pain medication management. We also have obtained insurance approval for outpatient chelation therapy.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): 1. As the current healthcare system is fragmented and often ineffectual in caring for super-utilizers, a commitment to innovation and clinical re-design is crucial to any program that aims to improve care in this patient population. 2. Engage stakeholders early and continuously. Stakeholders need to be from both the outpatient and inpatient settings, as well as multi-disciplinary. 3. As these patients often have significant psychiatric co-morbidities, partnering with a psychiatrist is crucial. 4. We have found assisting these patients to be a very time intensive process. They require ongoing psychosocial support and help navigating a complex, fragmented system. Much of our initial work is spent engaging patients and relationship building. 5. Hospital super-utilizers represent a diverse group in terms of diagnoses and underlying problems leading to over-utilization of hospital resources, which is why a highly individualized approach is critical.
THE MAGIC DESK PROJECT: REDESIGNING THE DESK IN THE CLINIC EXAM ROOMIra Helenius1; Daniel Becker1,2; Sarai C. Martinez-Suazo1; Reuben M. Rainey2; Roger C. Sherry2; Theo Van Groll2; Natalie May1. 1University of Virginia School of Medicine, Charlottesville, VA; 2UVA School of Architecture, Charlottesville, VA. (Tracking ID #1928402)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): In the presence of the electronic medical record [EMR], do desk shape and computer/printer position influence clinician-patient interactions and clinic visit satisfaction?
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1) reduce the temptation to stare at the EMR while talking and listening to the patient; 2) collaborate with architects, furniture designers, and craftsmen to redesign the clinic desk, improve access to the computer screen, and reorganize the space around the desk; 3) to determine if these changes affected the patient-clinician interaction during a regular office visit .
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): With a health and design grant from the School of Architecture and an internal grant from the Division of General Medicine, we conceived, designed, built, and installed the “magic desk” in an exam room at an internal medicine clinic. This desk is a curved wooden platform that is anchored to the wall, appears to float in place, and makes it easier for the patient to share the computer screen with the doctor or nurse. It has a built in swivel for moving the screen in or out of view, per HIPPA restrictions. For images see: http://uvadesignhealh.org/docs/news/fellow-project-eye-contact-in-exam-rooms.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): In order to determine the effect of the desk on the clinical encounter we designed a survey for patients and one for doctors. Patients were randomly assigned to be seen by their regular physician or nurse practitioner in either the redesigned room or in the standard room. The standard desk was a sheet metal desk with square corners and stationary computer screen. After the visit the research assistant asked patients if they felt the EMR was good for their health care, whether their doctors looked at them more than the computer, seemed interested in listening to them, shared EMR information with them, and spent enough time with them. Doctors were surveyed at the end of each session and asked if being in the redesigned room made it easier to listen to patients, maintain eye contact, and finish the note during the visit. We also asked if the doctors preferred one room to the other.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): The study was conducted in the summer of 2013. There were 43 study room patients, 36 standard room patients, 11 attending physicians, 1 nurse practitioner. One patient refused to complete the after visit survey. All patients were at clinic for routine follow-up visits. There were no significant differences in the demographics of the two groups of patients: each group had slightly more women than men, slightly more white than non-white patients, and approximately half the patients were older than 50 years. The length of the doctor patient relationship was also similar in the groups: approximately 25 % knew the doctor longer than 5 years. Comparison of the patient survey results from the patients seen in the redesigned room versus those seen in the standard room showed no significant differences. Almost without exception patients felt the EMR was good for their health care. Regardless of the room, almost all patients felt their doctors looked at them more than the computer, spent enough time with them, and were interested in their stories. In general, these patients were highly satisfied with their doctors and their care. Results of the doctor survey showed that in 75 % of the sessions, the doctors preferred the redesigned room to the standard room. Eighty percent of the time they felt that the redesigned room made eye contact easier. The redesigned room did not make it easier to listen; nor did it improve efficiency. As pretty as the desk is, moving the printer out of the way also made a lasting positive impression on the doctors working in that room.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): This collaboration helped us rethink and reimagine the space and information we share with our patients. Although the magic desk and the design changes that came with it did not make a measurable difference in doctor-patient interactions or patient satisfaction, the doctors preferred it and noted that it reminded them to share the EMR and then made it easier to do so. Perhaps the patients were already so pleased with their doctor that re-designing access to health information did not have an easily measurable impact.
THE PROJECT RED CHIP (REDUCING DISPARITIES AND CONTROLLING HYPERTENSION IN PRIMARY CARE) CARE MANAGEMENT INTERVENTION: AN EVALUATION OF ITS EFFECTIVENESS & IMPLEMENTATIONTanvir Hussain1,2; Whitney K. Franz2,4; Emily L. Brown2,4; Kara Taylor2,4; Mekam T. Okoye2; Arlene Dalcin2; Kathryn A. Carson3; Katherine Dietz2; Jennifer Halbert2; Romsai T. Boonyasai1,2; Jill A. Marsteller2,3; Lisa A. Cooper1,2. 1Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Center to Eliminate Cardiovascular Health Disparities, Baltimore, MD; 3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 4Johns Hopkins HealthCare LLC, Baltimore, MD. (Tracking ID #1939834)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): Proliferation of care management (CM) programs for chronic disease care, despite mixed effects, urges deliberate evaluation of the implementation components that predict success.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. To evaluate the effectiveness of CM in improving blood pressure (BP) and reducing hypertension (HTN) disparities in primary care. 2. To describe implementation of a CM intervention and inform the design of future programs
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Developed using a community-based participatory approach, our CM program invites HTN patients ≥18 years with uncontrolled BP (≥140/90) within the last 6 months to participate in 2 h of in-person CM—first session 1 h, followed by two half-hour sessions, over 3 months. Registered Dietitians (RDs) and Doctors of Pharmacy (PharmDs) trained in motivational interviewing educate patients about HTN and encourage adherence to medications, DASH diet, physical activity, and self-monitoring behaviors; patients with BP ≥160/100 preferentially see PharmDs to focus on medication adherence. The intervention is being implemented across six clinic sites in Baltimore, three of which care for underserved populations. Now completed at clinic 1 (inner city, underserved site), the intervention is underway at clinics 2 and 3.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): 1. BP improvement 2. Adoption rates (% enrolled, % completing intervention) 3. Patient satisfaction
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Adoption: Of 897 eligible at clinic 1, we contacted 509 (57 %) patients. Of the 319 scheduled, 175 (55 %) completed session 1 and 65 (20 %) completed all three sessions. Fidelity: Mean BP of patients (n = 155) starting with RDs was lower than expected, 135/80; however, patients continued the program given the variable nature of BP. For those (n = 20) starting with PharmDs, mean BP was 153/90. Average total contact time was 149 mins. (Data for clinics 2 and 3 will be available in Spring 2014.) Patient Acceptability: Among patients completing all three sessions across the three clinics to date (n = 100), 35 (65 %) patients responded to the post-intervention patient experience survey. Sixty-three (97 %) respondents reported ideal session length is at least 30 mins. Forty-one (63 %) wanted more sessions. Thirty-three (56 %) would have found the addition of phone sessions helpful; email, text messages, and online support were viewed less favorably. Two-thirds responded that education on taking medications, following a DASH diet, reading food labels, and exercise were each very helpful in controlling BP; half reported that weight loss and BP self-monitoring education were very helpful. Effectiveness: BP control data are pending. Among our survey respondents, mean reduction in individual systolic BP and diastolic BP was 5.4 mmHg (SD = 16.9) and 4.5 mmHg (SD = 9.7), respectively, between sessions 1 and 3. BP improvement was associated with trust in care managers, medication adherence, developing a BP treatment plan the patient could carry out in daily life, and patient confidence to actually do the things needed to take care of one’s BP.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Integrating CM programs into clinical settings is challenging. Seeking provider and staff input during the design phase, encouraging CM telephone outreach to and physician referral of eligible patients, and allowing local adaptation of the intervention can enhance adoption. Patients are highly satisfied with care managers and value disease education and behavior change support. Preliminary results suggest developing a realistic patient treatment plan and increasing self-efficacy through CM will help improve BP.
TRANSFORMING CARE TRANSITIONS: IMPLEMENTING PROJECT RED AT A VETERANS AFFAIRS MEDICAL CENTERMelissa Bachhuber2,1; Jeanette Broering3,1; Christine Welles4; Margaret Wallhagen3. 1San Francisco VA Medical Center, San Francisco, CA; 2University of California San Francisco, San Francisco, CA; 3University of California San Francisco, San Francisco, CA; 4University of Colorado, Denver, CO. (Tracking ID #1937156)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): The San Francisco Veterans Affairs Medical Center data demonstrate that Veterans over age 65 have 16.8 % and 28.6 % 30 and 90 day all-cause readmission rates, respectively. Comprehensive strategies to reduce readmissions are needed.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): To implement the evidenced-based transitional care model, Re-engineered Discharge (Project RED) on the inpatient medicine service for high risk Veterans in order to reduce 30 and 90 day all-cause hospital readmissions.
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): Five Project RED nurse care coordinators were assigned to each inpatient medicine team at a Veterans Affairs Medical Center. Care coordinators followed medicine inpatients based on high risk criteria including: Age >65, >10 medications, homeless status, substance abuse or mental health comorbidity, living alone, no assigned PCP, prior hospitalization within past 90 days, >3 ER visits in 6 months, and admission diagnoses including CHF, pneumonia, or ischemic heart disease. Care coordinators provided comprehensive discharge planning, care coordination, and after hospital care plans to high risk patients. Providers including pharmacists, physicians, social workers, clerical staff, and outpatient primary care teams had designated roles in completing components of RED such as medication reconciliation, handoff communication, telephone follow up, and appointment scheduling.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Primary outcome measures include 30 and 90 day all cause readmissions for patients receiving the Project RED intervention. Seven process measures of transitional care will be analyzed by chart review including medication reconciliation, electronic handoff note to primary care team, post-discharge phone call within 48 h, discharge summary completed within 48 h, follow up appointment within 14 days scheduled and attended, and after hospital care plan provided to patient. Length of stay will be followed as a balance measure.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): A total of 726 Veterans from the inpatient medicine service received the Project RED intervention from December 2012 to July 2013. Two hundred and thirty three (32 %) electronic medical records were randomly selected for review. Seven were excluded due to death during hospitalization or leaving against medical advice. Veterans acted as their own control for history of hospitalization prior to receiving the intervention. Veterans were on average 69 years-old (±12); 97 % male; 37 % with mental health comorbid condition; and 22 % with poly substance abuse. Forty three percent of Veterans had been previously hospitalized within 30 days of participating in the Project RED intervention. Post-intervention 30 day and 90 day readmissions were 20 % and 31 % respectively. Average length of stay was higher among PR recipients (8.7 versus 5.4 days) when compared to all Veterans admitted from December 2012 to July 2013. Process measures (target goal versus actual achieved) were: Medication reconciliation (100 % vs. 90 %); electronic handoff note to primary care team (80 % vs. 72 %); Veteran reached by phone call follow-up within 48-hours (95 % vs. 81 %); discharge summary completed within 48-hours (80 % vs. 83 %); 14-day follow-up appointment scheduled (90 % vs. 69 %); 14-day follow-up appointment attended (80 % vs. 55 %); after hospital care plan in place (80 % vs. 51 %).
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Early data suggests RED implementation at a Veterans Affairs Medical Center may be successful in reducing 30 and 90-day readmissions among high risk Veterans. Role clarity for providers involved in each component of the intervention (physicians, pharmacists, nurse care coordinators, social workers), coordination of follow-up care, and timely creation of the after hospital care plan are important considerations for successful implementation. The electronic medical record was instrumental to communication of the electronic handoff and discharge summary to the primary care team. Given the complexity of the intervention, multidisciplinary leadership support within the organization is needed for implementation.
WHY DO OUR PATIENTS REALLY GET READMITTED? COMPARING THE DISCHARGING PHYSICIAN AND PATIENT’S PERCEIVED REASONS FOR HOSPITAL READMISSIONMonica Reynolds; John M. French; Jonathan Kirsch; Beth Ann Brubaker; Edmund A. Liles. University of North Carolina, Chapel Hill, NC. (Tracking ID #1939323)
STATEMENT OF PROBLEM OR QUESTION (ONE SENTENCE): If discharging physicians are not informed of their patients being readmitted, it can be difficult to know the reasons and learn from our patients experience.
OBJECTIVES OF PROGRAM/INTERVENTION (NO MORE THAN THREE OBJECTIVES): 1. Assess impact of real time feedback from both patient and attending physicians on readmission preventability and causes 2. Compare perceptions of the reason for a readmission between discharging physician and the readmitted patient
DESCRIPTION OF PROGRAM/INTERVENTION, INCLUDING ORGANIZATIONAL CONTEXT (E.G. INPATIENT VS. OUTPATIENT, PRACTICE OR COMMUNITY CHARACTERISTICS): We present an observational study in a large academic medical center assessing the opinions of patients and physicians on whether hospital readmissions are preventable. While many studies on readmissions prevention focus on close follow-up appointments, post-discharge phone calls and bundled programs, there is a paucity of literature utilizing real-time patient and physician feedback for insight. In 2012, the Centers for Medicare and Medicaid Services defined readmission criteria and measures under the Hospital Readmissions Reduction Program (HRRP). It is often difficult for a physician to know if a patient gets readmitted within 30 days and feedback from these patients is generally difficult to obtain, though we believe that we can learn from these patients and possibly reduce future readmissions. We established a real-time system for alerting the discharging physician of a readmission so we could learn from our patients. Discharging physicians were provided real-time feedback of readmissions through daily emails with patient’s medical record number. They were then responsible for performing a chart review adapted from the Institute for Healthcare Improvement STAAR Initiative. Physicians were asked to comment on social conditions or mental illness that could have contributed to the readmission and to discuss what should be done to prevent future readmissions. Patients were in turn interviewed during their readmission and asked questions regarding prior discharge instructions, medication compliance, follow-up appointments/phone calls and overall support once outside the hospital. They were also asked to comment on whether they believed this readmission was preventable and ways to prevent a future admission.
MEASURES OF SUCCESS (DISCUSS QUALITATIVE AND/OR QUANTITATIVE METRICS WHICH WILL BE USED TO EVALUATE PROGRAM/INTERVENTION): Prior to these notifications and chart reviews and again after 6 months, physicians were surveyed on their perception of readmissions in general and their preventability. Outcomes of interest were 30 day readmission rates, physician and patient perspectives and estimates of preventability. The notifications and chart reviews began July 1, 2013 and are ongoing.
FINDINGS TO DATE (IT IS NOT SUFFICIENT TO STATE “FINDINGS WILL BE DISCUSSEDâ€□): Of 15 patients interviewed, 13 of 15 stated they were able to take their discharge medications as prescribed. However, the two remaining felt that the one intervention to prevent their readmission was directly related medication compliance. Thirteen of 15 did not find discharge instructions confusing of hard to interpret. Thirteen of 15 felt that they had proper support once leaving the hospital with the majority citing family members as their primary support. Only 5 of 15 were able to follow-up with a primary care physician. However, 10 of 15 did receive follow-up phone calls from either and hospital RN or MD. Overall, 13 of 15 patients interviewed felt the readmission was not preventable. As a whole, most patients believed they were prematurely discharged before their medical condition was fully treated or diagnosed. This was related to pain management in 4 of 15 patients and an unclear diagnosis at discharge in 3 of 15 patients. Based on initial attending physician survey, 13 % of attending physicians felt less than 10 % of readmissions were preventable but this increased to 30 % after 6 months of timely notification and chart reviews. At baseline, the top three contributors to readmissions were felt to be patient understanding, medication non-adherence, and substance abuse/addiction. After 6 months of the intervention, the top three contributors were felt to be substance abuse/addiction, medication non-adherence and lack of primary care.
KEY LESSONS FOR DISSEMINATION (WHAT CAN OTHERS TAKE AWAY FOR IMPLEMENTATION TO THEIR PRACTICE OR COMMUNITY?): Surveying physicians and interviewing readmitted patients in real-time may allow for expedited root cause analysis of the readmission and eventually lead to a reduction in all cause readmission rates. Overall, 87 % of patients felt their readmission was unavoidable. Physician chart review indicated that medication adherence was a major concern but in contrast 87 % of patients stated they did not have trouble taking their medications. Close follow-up was also a concern for physicians and indeed only 33 % of patients endorsed visiting a primary care physician. To prevent readmissions, patients believed they should be included in discussions regarding discharge readiness and final discharge diagnosis.
INNOVATIONS IN MEDICAL EDUCATION (IME) “MS. B CHANGES DOCTORS”: USING A COMIC AND PATIENT TRANSITION PACKET TO ENGINEER PATIENT-ORIENTED CLINIC HANDOFFS (EPOCH) IN A RESIDENT CONTINUITY CLINICAmber Pincavage1; Wei Wei Lee1; Laura Ruth Venable1; Megan Prochaska1; Daina Staisiunas1; Kimberly J. Beiting2; M. K. Czerwiec3; Vineet Arora1. 1University of Chicago, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3Northwestern University, Chicago, IL. (Tracking ID #1940083)
NEEDS AND OBJECTIVES: While patients are especially vulnerable as they transition during the year-end clinic handoff, patient input to improve the resident clinic handoff process has been lacking. The aim of this study was to implement and assess the impact of a patient-centered transition packet and clinic handoff comic on patient-centered handoff outcomes.
SETTING AND PARTICIPANTS: This study took place at one urban academic internal medicine residency continuity clinic at the University of Chicago. High-risk clinic handoff patients were identified by departing residents and asked to participate in interviews.
DESCRIPTION: To create a patient-centered process, we interviewed over 100 patients shortly after their transition for suggestions in 2011. Using this input, 2 months before the 2012 handoff, patients were sent a “transition packet” with a goodbye letter form the departing resident, a welcome letter from the new resident with their picture and personal information (i.e. hobbies), a certificate of teaching recognition, and a visit preparation tool to improve communication with the new PCP. In 2013, a patient comic was created to boost recall of the packet, draw attention to the packet and educate patients about the clinic handoff called, “Ms. B Changes Doctors.” In 2012 and 2013 (post-packet), patients were interviewed by phone on the impact of the packet on: awareness of the transition, ability to correctly identify the primary care physician (PCP) after the handoff, and satisfaction with the handoff. Patient outcomes (number of patients missing their first visit with their new PCP) were determined by performing chart review. Likert scale questions and outcomes were summarized descriptively and compared using chi square tests and trend analysis for proportions where appropriate. The 2011 cohort of patients (who did not receive the packet) served as a control group.
EVALUATION: Interviews were conducted with 103 patients in 2011, 113 in 2012 and 107 in 2013. The majority of patients after the packet were aware of the clinic handoff (99 %, 103/113 in 2012 vs. 99 %, 106/107 in 2013). Half (44 % 50/113) of the patients interviewed in 2012 recalled receiving any part of the transition packet, however, this increased with the patient comic in 2013 (64 %, 69/107, p < 0.001). The number of patients able to correctly identify their PCP increased after the comic was added (77 % 87/113 in 2012 vs. 98 % 105/107 in 2013 p = 0.002). Out of the patients who recalled the transition packet, the majority of them agreed (70 %, 19/27 in 2012 and 65 %, 45/69 in 2013) the information helped them build a relationship with their new physician and the packet helped them prepare for their first visit with their new physician (70 %, 18/26 in 2012 and 67 %, 46/69 in 2013). Of those who recalled the comic during the interview, 87 % (26/30) thought the comic was helpful and 60 % (18/30) agreed the comic helped prepare them for the transition. Lastly, there was a decrease in the percentage of the number of patients who missed the first visit with their new physician from pre-packet to post-packet (43 %, 139/323 in 2011 vs. 31 %, 82/264 in 2012 and 26 % 70/273 in 2013, p < 0.001). When asked about the welcome letter she received one patient commented, “It was nice because it gives the patient the chance to see and know something about the new doctor they’re going to be meeting.” Another patient reported it “made her look forward to her first appointment.” Another patient when asked about the certificate of recognition stated, “it was cute and acknowledged me and made me feel appreciated.” Another patient reported, “it’s on my wall!” When asked about the comic, one patient responded, “it was cute and it stood out: it’s what made me call in and make an appointment.” Another patient thought it was “funny and informative.” One patient thought the visit tool was “informative and helped me ask certain questions”, while another thought it was a “great opportunity for the new PCP to learn about me right away.”
DISCUSSION/REFLECTION/LESSONS LEARNED: A patient-centered clinic handoff was helpful to patients and may have encouraged patients to return for care after the handoff. The comic may have increased transition packet recall while both the comic and the packet was effective and helpful to patients.
A DECADE OF CHANGE IN ATTITUDES TOWARD THE HOMELESS AMONG PRIMARY CARE INTERNAL MEDICINE RESIDENTSFrances Norlock; Laura Sadowski; Meghan Kapolnek. Stroger Hospital of Cook County, Chicago, IL. (Tracking ID #1939203)
NEEDS AND OBJECTIVES: The prevalence of homelessness is increasing. Few resident programs offer formal training in how to provide care for the homeless. Educators implemented a homeless medicine rotation to decrease residents’ stigma associated with homelessness and improve the clinical care resident physicians provide to homeless patients. Investigators wanted to assess the difference in attitudes toward homelessness between primary care internal medicine (PCIM) residents over the past decade (2002 and 2012). It was hypothesized that the 2012 cohort would have less prejudice towards the homeless prior to the rotation and less of a change in stigma score. This was supported by the passing of the Affordable Care Act (ACA) in 2010 and increased funding for programs that support underserved populations; the recent financial crisis of 2008 which may be viewed by residents as an external cause of homelessness; and the impact of social media since 2003 and potential positive informational effect it could have had on the 2012 residents.
SETTING AND PARTICIPANTS: PCIM residents participated in a 2 week homeless medicine rotation based at an urban, public hospital focused on collaborating with partners in the community. Residents participated in group seminars on campus and engaged in tours and clinical experiences in the community, including working with patients in shelters, clinics and residential housing programs.
DESCRIPTION: Curriculum consisted of small group seminars on epidemiology, chronic disease management and lifestyle issues affecting health outcomes in the homeless. Learners worked in community-based clinics that served the homeless and were assigned evening shifts to care for those in shelters with medical issues as well as facilities where women and children resided. Residents’ attitudes were assessed pre- and post-rotation using an 11 item Attitudes Toward Homelessness Inventory (ATHI) consisting of 4 subscales which attribute homelessness to societal cause; personal cause; having a willingness to affiliate with the homeless; and belief that homelessness is a solvable problem. A higher summation score of the 4 subscales equates to improved attitudes and lower stigma of homelessness. A meaningful difference score of 5.5 was set a priori.
EVALUATION: The 2012 cohort (n = 12) had a pre-rotation mean summation score of 42.0 compared to 45.4 in the original cohort (n = 18) indicating less stigma a decade ago prior to the onset of the rotation (although the mean difference of 3.4 was not meaningful). Post-rotation the mean summation score was 46.8 in 2012 compared to 51.7 a decade earlier with an improvement in mean change score of 5.0 and 6.3, respectively. The 2012 cohort’s total sum mean change score of 5.0 was in the positive direction and was close to the meaningful change criteria of 5.5. The greatest increases in mean change scores for 2012 were for societal cause (1.67) and affiliation (1.67); a decade earlier the greatest mean change score was 3.0 for the societal cause subscale.
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents had lower stigma towards the homeless at the onset of the rotation in 2002 compared to current residents as well as a greater improvement in attitude and lower stigma toward the homeless. These findings may be due to an unknown variation in the demographic composition between resident cohorts as well as possible variation in the educational didactic and clinical experiences a decade later.
A MEDICAL SPANISH ELECTIVE WITH A SPECIAL EMPHASIS ON LINGUISTIC HUMILITYCristina M. Gonzalez1; Yovana Q. Coupey2; Maria A. Marzan2; A. Hal Strelnick2. 1Albert Einstein College of Medicine/Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine/Montefiore Medical Center, Bronx, NY. (Tracking ID #1938843)
NEEDS AND OBJECTIVES: More than 10 % of the US population has limited English proficiency (LEP). Medical students will be caring for these patients, yet there are few medical language programs described in the literature. Our objective is to describe a medical Spanish elective highlighting enhancements made and lessons learned.
SETTING AND PARTICIPANTS: First and second year students at Albert Einstein College of Medicine in Bronx, NY.
DESCRIPTION: This lunch-time elective meets 16 times for 1.5 h a session in the first semester and 12 sessions in the second. Its goal is to increase students’ ability to communicate in Spanish in a clinical setting by focusing on conducting a medical interview in a linguistically effective and culturally appropriate manner. Students are placed in one of six levels according to an oral assessment directed by an instructor in conversational Spanish. The instruction for each level is tailored to those learners. Recently three enhancements occurred. Students practice interviewing community volunteers (real patients). We have hired professional Spanish language instructors trained in medical terminology and patient-centered history taking. There is also a strong emphasis on linguistic humility. Students interview real patients and practice linguistic humility by learning how to recognize their own limitations and bring in and work effectively with an interpreter (first four levels) or develop strategies to seek clarification from their patients (advanced two levels). Students are assessed via a final interview, written exam, homework assignments, and attendance. Grading rubrics developed by the instructors for the final interview focus on accuracy, coherence, creativity, and vocabulary. During the final interview, students interview a standardized patient (SP) with an interpreter (if needed). The Spanish instructor, SP, and interpreter (if needed) each assess the student’s performance. Students must attend at least 80 % of the sessions in order to sit for the exam and pass the course.
EVALUATION: In the first cohort, 84 first-year students registered with 75 % attending 80 % or more classes, 100 % of whom passed the course (score range 92–96 %). A total of 29 s-year students returned for the second semester, with 19 attending 80 % or more of the classes, 100 % of whom passed the course (score range 89–100 %). The second cohort of students had 97 first-year students register for the course, with 74 attending 80 % or more classes, 100 % of whom passed the course (score range 88–97 %). Second semester grading is underway. Students rated the areas of instruction that were most useful. The most frequently cited strengths were the interviews with real patients, as opposed to SP, and their instructors. The most cited change would be to include more instruction in grammar earlier in the course.
DISCUSSION/REFLECTION/LESSONS LEARNED: The three enhancements to the course positively impacted the students’ experience. Students early in their medical school experience are excited to speak to real patients. This may be a way for programs to attract participants. Our experience also lends support to making the investment in professional language instructors trained in medical interviewing. Finally, an emphasis on linguistic humility is important, as there have been reports of decreased interpreter use after a brief period of Spanish language instruction, when an interpreter was actually needed. The use of professional interpreters or bilingual providers improves the quality of care for patients with LEP thereby reducing disparities.
A MODEL SEMINAR FOR PRECLINICAL HEALTHCARE SAFETY AND QUALITY INSTRUCTIONJohn R. Joseph; Huixia Wei; Vahid Pasovic; Caitlin Biedron; Amy Li; Diane L. Levine. Wayne State University School of Medicine, Detroit, MI. (Tracking ID #1939503)
NEEDS AND OBJECTIVES: The importance of incorporating patient safety and quality improvement topics in undergraduate medical education is evidenced by the American Association of Medical Colleges (AAMC) recommendation to integrate these concepts as early as the first year of medical school. Efforts are presently underway to recognize important attributes students should possess at graduation from medical school called “Core Entrustable Professional Activities for Entering Residency” (CEPAER). Among these activities is the ability to identify system failures and contribute to a culture of safety and improvement. The Wayne State University School of Medicine student chapter of the Institute for Healthcare Improvement (IHI), with support from school administration, set to increase exposure to these topics for preclinical students by hosting a voluntary patient safety seminar.
SETTING AND PARTICIPANTS: The seminar was held in school facilities on a Saturday morning. It was offered as one option to fulfill a requirement for a Saturday seminar through the school’s Co-curricular Program for which students commit to 75 h of community service and 75 h attendance at educational lectures which may be used for credit for 1 month rotation during student’s fourth year. The seminar was open to the entire student body and advertised through school-wide emails and poster displays.
DESCRIPTION: The seminar began with an introduction to basic safety and quality principles. Next, students split into six groups and rotated through three different breakout activities lasting roughly 30 min each. These included a discussion on human factors engineering, a case study in infection control, and an interactive activity highlighting teamwork and communication. Each session was facilitated by a volunteer faculty whose clinical practice includes formal safety or quality responsibilities (i.e. Assistant Chief of Quality and Safety). The small group sizes of roughly 17 students and interactive design of activities/discussions fostered good discussion and provided an intimate setting for questions and comments. The seminar ended with a summary of the current state and future directions of healthcare safety and quality delivered by a former chief quality and safety officer of a local medical center.
EVALUATION: A total of 104 students and 6 faculty facilitators participated in the seminar. The seminar lasted 2.5 h in total. Identical surveys were distributed before and after the event for purposes of evaluating changes in knowledge and attitudes towards safety and quality. The initial survey was completed by 86 students (83 % response rate) and the post-seminar survey by 79 students (76 %). The responses were aggregated and analyzed. Five multiple-choice questions evaluated knowledge related to safety and medical errors. Student’s knowledge increased on all questions. The remaining 15 questions evaluated knowledge as well as attitudes towards safety and quality using a 5-point Likert scale (1 = Strongly Disagree to 5 = Strongly Agree). Students showed improvement in 13 of 15 questions as evidenced by movement of the mean towards the desired response. The seminar was very well received with all respondents indicating the seminar was good to excellent.
DISCUSSION/REFLECTION/LESSONS LEARNED: A voluntary seminar is an effective way to introduce medical students to key concepts in patient safety, quality and quality improvement techniques. The event was well received by preclinical students and survey data revealed an increase in knowledge and improvement in attitudes towards safety and quality immediately following the event. The majority of students indicated that they would like to see similar content added to the formal medical curriculum. The incorporation of smaller breakout sessions led to challenges in logistics and planning, including finding additional qualified faculty volunteers. The smaller groups and interactive activities were very well received by students and facilitators, however, and the authors recommend this strategy over traditional lecture-based learning. This proved especially true for topics such as the different types of error (i.e. near miss versus no harm incident) that can be difficult to grasp for preclinical students. Next steps include improving the event based on targeted feedback and incorporation into the formal medical school curriculum.
A NEW APPROACH TO OUTPATIENT GERIATRICS TRAINING: AN INTERPROFESSIONAL POLYPHARMACY INTERVENTION USING THE SHARED MEDICAL APPOINTMENT MODELJohn Thomas1,2; Anne Hyson1,2; Marcia C. Mecca1,2; Kristina Niehoff2; Susan A. Zapatka2; Susan T. Langerman2; Leila Islam2; Rebecca Brienza1,2. 1Yale University School of Medicine, New Haven, CT; 2Veterans Affairs (VA) Connecticut Healthcare System, West Haven, CT. (Tracking ID #1934252)
NEEDS AND OBJECTIVES: Despite the growing number of elderly patients seen in primary care practices across the United States, dedicated outpatient geriatrics training for Internal Medicine (IM) residents and other health professionals remains limited. Our main objective was to pilot a team-based geriatrics intervention for patients with polypharmacy as an innovative approach to geriatrics education for IM residents and other health professional trainees. Our secondary objective was to evaluate the potential of this intervention to facilitate trainee education in outpatient geriatrics.
SETTING AND PARTICIPANTS: In an interprofessional outpatient team-training program at a VA hospital, we involved IM residents, nurse practitioner (NP) fellows, health psychology residents, and pharmacy residents (hereafter referred to as trainees) in the intervention.
DESCRIPTION: The intervention consisted of a shared medical appointment (SMA) and individual provider visit. The patients were ≥80 years old, with ≥10 medications, and were referred by their provider to participate. The SMA was co-facilitated by the trainees and consisted of interactive discussions about patients’ experiences with medications. The individual visit, which was also conducted by the trainees, included standard geriatric assessments (St. Louis University Mental Status Exam, activities of daily living, and orthostatics), medication reconciliation, shared decision making regarding medication changes, and a detailed follow-up plan. Discussions were aided by the Beers criteria and a compilation of organizational disease-based guidelines. Afterward, we administered an anonymous online survey to the trainees to assess their experiences with the program.
EVALUATION: After the pilot, we administered an anonymous online survey to the trainees to assess their experiences with the program. Of the 4 IM residents, 2 NP fellows, and 1 pharmacy resident who participated in both the SMA and provider visit, all but 1 completed the survey (86 % response rate). All respondents agreed or strongly agreed that the program “has the potential to substantially improve my ability to safely decrease inappropriate prescribing for older patients.” All respondents agreed or strongly agreed that the following aspects of the program, among others, were valuable for their education and development as clinicians: “geriatric assessments,” “shared medical appointment,” “working with an interprofessional team,” and “shared decision making process.” For this same question group, one respondent was neutral about “safe follow-up planning and execution.” The free text comments were generally positive, but 4 respondents expressed the need for improved communication with the primary provider before and/or after the intervention.
DISCUSSION/REFLECTION/LESSONS LEARNED: We successfully piloted a team-based, outpatient geriatrics intervention for patients with polypharmacy. The participating trainees agreed that numerous aspects of the program were valuable for their education and development as clinicians. Future work will include enhancing communication with primary providers regarding clinical findings and medication changes, and introducing interprofessional trainee seminars focused on topics related to polypharmacy.
A NOVEL AMBULATORY CARE CURRICULUM: TEACHING THE SKILLS OF INFORMATION MANAGEMENT AND LIFE-LONG LEARNINGMargaret Horlick1,2; Jennifer Rockfeld2; Mary Fishman2; Patrick M. Cocks2; Barbara Porter2. 1NY Harbor VA Healthcare Center, New York, NY; 2NYU School of Medicine, New York, NY. (Tracking ID #1940151)
NEEDS AND OBJECTIVES: How do we teach the skills required for lifelong learning? Curriculum objectives: 1. Residents will demonstrate the skills needed to maintain their medical knowledge over the course of their career. 2. Residents will demonstrate the ability to teach their peers and lead a small group discussion. 3. Residents will practice self-reflection in regards to their medical knowledge, patient care, and teaching skills.
SETTING AND PARTICIPANTS: This curriculum was given to PGY-2 s and PGY-3 s during their 2 ambulatory care blocks each year. There were a total of 84 residents who participated in the curriculum.
DESCRIPTION: In this era of multiple information sources and changing practices, it is essential that residents develop facility with the skills required to keep up with the literature, answer a patient-centered clinical question, critically appraise articles, teach their peers, and integrate feedback and new information into their own practice improvement. To address these essential skills and to evaluate residents in the appropriate reporting milestones, we developed an ambulatory care curriculum in lifelong learning. Through several different exercises, residents learn to quickly and critically browse abstracts from the current literature, to ask patient centered clinical questions and find practical, evidence-based answers, identify their own knowledge gaps and to make short presentations to their peers on a current development in outpatient medicine. Each resident led conference includes the collection of written peer feedback, which the resident uses in guided self-reflection to develop an improvement plan for future presentations.
EVALUATION: Individual conferences are well received and we have observed improvement in the targeted skills as senior residents have taken the course for the second and third time. The quantitative evaluation of the conferences ranges from averages for each conference of 4.36 to 4.6 on a 5-point Likert scale. Qualitative comments include the following: “Good to learn how to critically appraise lit[erature]”, “Good way to practice presentation” “Good for life-long learning skills” “Nice to see how attendings look up a clinical question” “Really good, liked using interesting clinic cases we’ve just seen” “Great to see different approaches to searching questions” “Very useful, made me enthusiastic about reading up on my patients.” “Was a good exercise how to formulate and search for clinical questions.”
DISCUSSION/REFLECTION/LESSONS LEARNED: Over the past year and a half we have learned that a key to teaching lifelong learning skills is for residents to use these skills as they learn topics that are relevant to their current clinical practice. As examples, honing teaching skills is coupled with delivering essential outpatient content and critical appraisal skills is coupled with reviewing recently published abstracts. Our curriculum fuels clinical curiosity as we develop as physicians and teachers. Over the course of the last 18 months, we have observed the residents providing more specific and constructive feedback to their peers suggesting that regular opportunities to give structured feedback improves the content and usefulness of that feedback. We have found that residents are more likely to incorporate the feedback from their peers in their self-evaluations than feedback given only by faculty.
A NOVEL APPROACH TO INTERPROFESSIONAL EDUCATION (IPE) FOR RESIDENTS ON AN INPATIENT MEDICAL SERVICEMatthew F. Griffith1; Darcy Donaldson3; Eric A. Young2,1; Robert Burke2,1. 1University of Colorado, Aurora, CO; 2Denver Veterans Affairs Hospital, Denver, CO; 3Denver Veterans Affairs Hospital, Denver, CO. (Tracking ID #1929844)
NEEDS AND OBJECTIVES: Poor interprofessional communication is the leading cause of medical errors. The quality of communication and collaboration between members of interprofessional teams is associated with patient morbidity. However, few residency programs integrate interprofessional communication training into their inpatient curriculum. Published examples of interprofessional education (IPE) training have focused on pre-clinical medical students, CRM training of operating room staff or resource-heavy TeamSTEPPS events that last multiple hours to multiple days. Few have targeted Internal Medicine residents. Additionally these models tend to focus on communication during the care of a patient in crisis, through high fidelity simulation, rather than the interprofessional communication skills needed to avoid these crises. Our objective was to design an intervention to improve interprofessional collaboration and communication at the primary training site of medical residents, the inpatient medicine ward, that achieved similar outcomes to existing models and required fewer resources.
SETTING AND PARTICIPANTS: The Denver VA is a 167 bed tertiary care facility. Inpatient housestaff belong to the University of Colorado Internal Medicine resident training program. The residents in the University of Colorado training program rotate through inpatient rotations at four hospitals in the Denver metro area in four-week blocks. The VA was chosen as the site for this teamwork training based on feedback from residents that indicated their communication with nursing was the least successful at this site compared to the others. Nurses in their first year of employment at the VA participate in an on-the-job training program with protected time to participate in quality improvement and patient safety activities. Nurses from this cohort participated in this training during protected education time that coincided with the regularly scheduled resident lunch conference at the Denver VA Hospital. Medical students attending the University of Colorado School of Medicine, as part of their Internal Medicine clerkship at the VA, also took part in the conference.
DESCRIPTION: Prior to the conference, a Chief Resident in Quality and Patient Safety and members of nursing education and leadership arranged a one-shift structured shadowing experience for a medicine resident and an RN. This experience allowed both practitioners to observe the daily workflow of the other profession and report back observations regarding barriers to communication and teamwork elucidated by their new perspective. The conference consisted of an introductory discussion of common communication errors between professions, a problem-based learning activity requiring multidisciplinary teamwork, a discussion led by the providers who participated in the shadowing focusing on lessons learned during their experience, and a debriefing focused on specific behaviors both professions could adopt to improve collaboration between professions.
EVALUATION: A 5-question survey was distributed to participants before and after the conference, using a 10-point Likert scale (10 = highest) to rate agreement with prompts assessing changes in attitude, understanding of topics presented, and utility of the conference. Although 61 % of participants reported prior training in interprofessional communication, they reported significant increases in their comfort communicating with providers of other professions (before training 7.5, after training 8.0 p < 0.01), their ability to identify common causes of communication error (6.9, 7.8 p < 0.03), their ability to describe what a practitioner of the other profession does in the hospital (5.2, 7.2 p < 0.01) and their ability to involve practitioners of other professions in efforts to improve communication (7.1, 8.1 p < 0.01). Practitioners of both professions felt that this conference improved their understanding of interdisciplinary communication and 91 % of participants would highly recommend (score of 8 or higher) this training for their colleagues. We will evaluate resident assessment of nursing at the end of the year to see if this conference, when repeated with different cohorts of residents, improves assessments of VA nursing performance and communication.
DISCUSSION/REFLECTION/LESSONS LEARNED: Few residency programs integrate IPE into their resident curriculum and fewer still integrate it into the inpatient ward experience where excellent communication between providers is crucial. We have described a novel, one-hour multidisciplinary session requiring few resources that improved providers’ self-identified ability to identify and address communication issues between professions and was highly regarded by participants. We anticipate that by repeating this conference regularly we will improve resident and nursing communication at our hospital, enhancing patient safety.
A NOVEL EVALUATION SYSTEM USING DIRECT OBSERVATION AND FORMATIVE FEEDBACKJeremy Smith; David Feldstein; Christie Seibert; Bennett Vogelman. University of Wisconsin, Madison, WI. (Tracking ID #1897528)
NEEDS AND OBJECTIVES: Direct observation of trainees has been shown to increase frequency of feedback, identify clinical deficiencies otherwise unrecognized, increase learner confidence, and improve learners’ clinical skills. At our institution, however, direct observation of clinical skills was not being performed regularly. We also recognized that within the ambulatory block rotation, the single end-of-rotation summative evaluation being used by each faculty evaluator was inadequate and potentially lacking in validity, because each resident might interact with multiple different faculty during the rotation. Therefore, we designed a novel evaluation system and implemented it into residents’ ambulatory block rotation to address these needs. Our objectives were to: 1. Increase the amount of direct observation of residents. 2. Improve faculty’s attitudes towards direct observation. 3. Increase residents’ feedback and improve the quality of residents’ evaluations by moving from a single summative evaluation to multiple formative evaluations throughout the rotation. 4. Begin to develop an institutional culture wherein direct observation is seen by faculty and learners to be an integral part of the training process.
SETTING AND PARTICIPANTS: Twenty-nine residents per year rotate through a university-based ambulatory block rotation. Residents spend 1–3 months seeing outpatients 5 days per week, primarily in a general internal medicine clinic. Fourteen different faculty supervise residents on this rotation.
DESCRIPTION: Each resident was required to obtain 9 observations over the course of the ambulatory block, comprised of 3 observations from each of 3 clinical domains: history-taking, physical exam, and counseling/decision-making. We developed single-page, literature-based evaluation tools for each clinical domain, which were given to residents at the start of the rotation. They were instructed to work with their faculty member to select appropriate patients for observation. Residents gave the relevant form to the faculty member prior to the encounter, and faculty completed the form while observing the resident. After the encounter, the faculty provided the resident with feedback, and the completed form. The forms were collected at the end of the rotation. These 9 formative evaluations took the place of a single summative end-of-rotation evaluation.
EVALUATION: A total of 256 patient encounters were directly observed over 12 months. Twenty-six of 29 residents (90 %) completed all 9 observations. End of rotation questionnaires were completed by all participating residents; faculty evaluators were surveyed 6 months after program implementation. Residents found the new system valuable, with 85 % reporting they had permanently changed aspects of their history-taking, physical exam, or counseling based on the feedback received. Forty-two percent of residents reported having previously been directly observed a total of 3 times or less throughout his/her residency; 100 % of residents were directly observed at least 7 times over the course of the rotation. Faculty reported that the program increased their use of direct observation. Forty-two percent of the faculty reported conducting direct observation at least 6 times per year prior to the program, and 75 % reported conducting at least 6 observations in the 6 months since the program started (p = 0.01 for change in number of observations). Faculty attitudes toward direct observation also improved. Sixty-seven percent of faculty felt this new system made it more likely or much more likely that they would conduct direct observation in the future. Faculty rated on a 1–5 scale how burdensome they thought the observations were going to be, and how burdensome they actually found them to be; there was a significant (p = 0.015) improvement in faculty perceptions of the burden of direct observation. When asked to rate how useful they found the direct observations in terms of their ability to evaluate and provide feedback, on a 1–5 scale (5 = extremely useful), 92 % rated 4 or 5. 83 % of faculty preferred the new system to the prior evaluation system which used a single summative evaluation.
DISCUSSION/REFLECTION/LESSONS LEARNED: The new evaluation system was successful in increasing direct observation of residents, and improving faculty attitudes toward direct observation. Some residents and faculty suggested that the observations should be more learner-centered and flexible, allowing the number of observations in each clinical domain to be modified based on the learner’s self-assessed needs. Some residents noted the significant effort required to collect the 9 observations, though we believe putting the onus on the residents to obtain the observations was key to accomplishing them. Future efforts will focus on measuring whether this system leads to increases in direct observation conducted by participating faculty in other venues, and modifying the system so that the observations are conducted based on learner self-identification of areas needing improvement.
A PATIENT-CENTERED MEDICAL HOME (PCMH) RESIDENT ROTATION: TEACHING INTERNAL MEDICINE RESIDENTS THE PRINCIPLES OF PCMH THROUGH COMMUNITY-BASED PRIMARY CAREJanina L. Morrison1,2; Jonathan Swartz3,4; Donald Raum1,2; Rosemarie Conigliaro2,1. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY; 3Montefiore Medical Center, Bronx, NY; 4Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1938757)
NEEDS AND OBJECTIVES: Montefiore Medical Center (MMC) encompasses 22 primary care clinics, including six teaching sites. Since 2008, MMC has invested in transforming each clinic into a Patient-Centered Medical Home (PCMH), starting with the non-teaching community sites followed by the teaching sites. Resident participation in PCMH initiatives, coupled with structured educational activities, can better prepare residents for independent clinical practice and ensure that practice improvements reflect their needs. Recognizing this, medical directors and medical educators at MMC collaborated to create a PCMH rotation for residents with the following goals: (1) to introduce residents to the principles of the PCMH and, (2) to provide residents with an ambulatory experience in a community PCMH practice.
SETTING AND PARTICIPANTS: All third-year categorical internal medicine residents complete the 4-week PCMH rotation. Each resident is supervised at a community site by a primary care provider. These community providers complete several faculty development sessions on academic precepting to prepare for this rotation. The residents also attend their continuity clinic weekly and participate in didactic sessions facilitated by a PCMH faculty mentor trained in quality improvement.
DESCRIPTION: During the rotation, residents see patients at the community site and observe patient-care sessions with PCMH team members including the chronic care nurse, pharmacist, and diabetes educator. Residents participate in PCMH planning meetings at the community sites and their continuity sites. Facilitated by the didactic sessions, residents complete panel management activities for their continuity patients recently discharged from the hospital. Residents also discuss their patient outcomes data, including patient satisfaction. Residents complete an online curriculum of PCMH lectures on Patient Access, Quality Improvement, The Patient Experience, Health Insurance and Payment Methods, and Behavior Change.
EVALUATION: Residents complete evaluations of the rotation and a retrospective pre-post survey to evaluate changes in knowledge, attitudes, and behaviors. Each monthly cohort has two sessions in which we collect qualitative feedback. As of January 2014, 19 residents have completed the rotation. In the evaluations received thus far (N = 9), 100 % of residents reported the rotation was more than adequate or outstanding in meetings its educational objectives. The retrospective pre-post-survey (N = 9, data collection ongoing) has demonstrated improved ability to identify PCMH resources (33 % pre, 77 % post), use PCMH resources (33 % pre, 88 % post), and use patient data for quality improvement (55 % pre, 77 % post). Qualitative feedback has been strongly positive regarding the benefits of exposure to efficiency in primary care, identification of optimal continuity of care, and the potential for teamwork in increased physician satisfaction.
DISCUSSION/REFLECTION/LESSONS LEARNED: The unique combination of exposure to community medicine and participation in PCMH initiatives has provided a rich learning experience for our residents. Next steps include expansion of the curriculum to first year residents, extending resident participation in PCMH planning efforts, and analysis of resident utilization data before and after participation. Going forward, we expect to see our residents as quality improvement champions, both within our institution and in their future endeavors as physicians.
A PORTABLE FACULTY PEER OBSERVATION AND FEEDBACK PROGRAM TO BUILD AMBULATORY TEACHING SKILL CAPACITYAthina Vassilakis1,2; Sheira Schlair1,2. 1Montefiore Medical Center, Bronx, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1939337)
NEEDS AND OBJECTIVES: With increasingly complex healthcare delivery systems and limited trainee ambulatory care hours, clinician educators have increasing demands that may challenge their teaching effectiveness. Peer mentoring can be an effective way to provide ongoing faculty development. It has been linked to greater work satisfaction and improved work relationships. This study aims to use a faculty-generated list of ambulatory teaching skills to guide a peer observation and feedback (POF) exercise for teaching improvement in the ambulatory setting. Our objectives are that following the intervention, participating faculty will be able to goal-set to improve teaching skills and identify teaching strengths and weaknesses in order to deliver effective feedback on teaching skills.
SETTING AND PARTICIPANTS: The intervention is taking place in an urban ambulatory academic general medicine clinic at Montefiore Medical Center in Bronx, NY, between January 2014 and June 2014. All faculty have been invited to participate with no exclusion criteria.
DESCRIPTION: Faculty participation is voluntary. During a routine clinic faculty meeting, faculty brainstormed the skills they believed to constitute effective ambulatory teaching. These skills were then used to generate a “peer observation and feedback instrument” (POF-I), which is being used to facilitate the POF exercise. Faculty complete a pre and post intervention survey about their expectations, knowledge, and attitudes regarding teaching skills and POF. Participants will arrange for POF on a monthly basis for 6 months, and will complete a POF-I for each encounter (one form for observing faculty, one form for observed faculty). They will observe and give feedback once monthly during their administrative time. They are also observed monthly and given immediate feedback during their regularly scheduled precepting sessions.
EVALUATION: Outcomes studied (via encounter-based POF-Is and surveys) will include faculty’s self and peer assessed ability to (1) set goals to improve teaching skills, (2) identify strengths and weaknesses of teaching encounters, and (3) deliver effective feedback on teaching skills. Programmatic evaluation will be ongoing. Data collection will be complete by Spring 2014. Analysis will include calculation of mean number of goals set, teaching skills, and teaching domains (chosen for individual teaching improvement), and feedback skill evaluation scores. Paired t-tests will be used to examine associations between outcomes. Initial process evaluation data showed that during group brainstorming, faculty was engaged in the activity, and was spontaneously able to list skills in six of the seven “Stanford Faculty Development Center” educational categories. Thus far, eight faculty members have opted to participate in the POF process. Despite some initial reservations, their contribution to the development of the POF-I seems to have promoted their interest in the POF exercise.
DISCUSSION/REFLECTION/LESSONS LEARNED: The extensive list of teaching skills developed during brainstorming demonstrates the collective knowledge that can be cultivated through collaborative work and peer mentoring. The observation that faculty’s initial resistance to peer evaluation lessened with engagement in the peer feedback process highlights existing barriers to enacting sustainable peer feedback programs. It also suggests that learner buy-in is essential during assessment method development and ground rule setting for faculty to be willing to share vulnerability in peer assessment.
A STRUCTURED INITIATIVE THAT ENHANCES RESIDENT AND FACULTY RESEARCH PRODUCTIVITY IN A COMMUNITY HOSPITAL SETTINGMarianne Smith; Anita Szerszen; Suzanne El-Sayegh; Ursula Viola; Kathleen Ahern; Morton Kleiner; Neville Mobarakai; Terenig Terjanian; Mario R. Castellanos. Staten Island University Hospital, Staten Island, NY. (Tracking ID #1929408)
NEEDS AND OBJECTIVES: As a community-based hospital, our resources to produce research for our faculty and residents are extremely limited in comparison to large academic medical centers with strong infrastructures. Research productivity is essential for community-based hospitals that support physician training programs. Research activity is needed to fulfill ACGME scholarly requirements for both residents and faculty. Increasing faculty clinical responsibilities limit dedicated time for research. Key components of a successful program include a director, clear goals, a curriculum in research, dedicated time, a presentation forum and faculty mentors. While some of these elements were already in place in our department, much of the research was fragmented and there was no central forum to review and critique individual resident research progress. We proposed that research proficiency could be established by developing a complementary research initiative that re-organized resources already in place and centralized the entire research process, focusing on engaging residents and faculty in original research. With limited funding, we developed an infrastructure to enhance scholarly activity. Our objectives of the program were to: 1. identify key personnel in the department to lead this initiative, 2. create a research curriculum to build a culture of scholarship for lifelong professional development, 3. develop and centralize a system to monitor research goals, activity and progress. We were able to significantly advance our department’s research productivity with our multifaceted approach.
SETTING AND PARTICIPANTS: Staten Island University Hospital is a 700 bed community based hospital in an outer borough of New York City. Our Internal Medicine Residency Program has 107 residents, 90 being categorical. Every PGY3 is required to present a research project at the annual Resident Research Competition prior to graduation. For our initiative, at the beginning of the academic year all PGY 3 residents were assigned, and met with, research mentors, who are faculty of the Department of Medicine Research Committee. Our hypothesis was that with proper guidance, we could increase the number of original projects versus case reports for the competition. Since all projects are required to have a faculty principal investigator (PI), more of our faculty would be involved in projects. The Clinical Research Manager provided education and support. Members of the research committee reviewed progress.
DESCRIPTION: In the 2012–13 academic year, we focused attention to develop a new strategy for resident research education. This included bi-weekly departmental research committee meetings to review and develop policies, resolve critical issues and monitor productivity. All PGY3 residents met with their assigned research mentors. A mentoring assessment was performed to evaluate resident projects to ultimately be presented at the annual Resident Research Competition. Follow up meetings were mandatory. The mentors assisted residents to develop projects and linked them with faculty Principal Investigators. The Departmental Research Manager focused efforts on research education, assisting with protocols and developing a research intranet site.
EVALUATION: Formative evaluation to date suggests that the residents feel that the top three most helpful resources are: research mentor meetings, PI guidance and research education/lectures. Many residents also commented that they would like the mentor meetings to start in their PGY1 year. There is an ongoing systematic evaluation in progress. Original resident research increased from 28.75 % in 2012 to 50 % in 2013. ACGME survey results showed a 19 % increase in satisfaction with scholarly activity from 2012 to 2013.
DISCUSSION/REFLECTION/LESSONS LEARNED: Conducting research for clinical investigators is a challenge, yet essential for introducing innovative therapies and advancing patient care. The restructuring of our research program has accomplished increased support and guidance for the residents though the mentors, the Clinical Research Manager and varied educational resources. We have increased resident satisfaction, increased original research, and created a more user friendly method for resources and submission of protocols. There is also now a more centralized venue for discussion and feedback by the committee, as well as, organized tracking of individual progress. Assessment of faculty publication productivity is in progress and will be examined as part of summative evaluation. At present, program evaluation indicates that outcomes are being met and the multifaceted processes in place are effective. These efforts should eventually support our faculty to obtain publications and pilot data. This initiative was carried out without significant increases in our research budget. We believe that our initiative is reproducible in other programs.
ACCELERATING AMBULATORY APLOMB: A NOVEL IMMERSION BLOCK CURRICULUM FOR INTRODUCING INTERNAL MEDICINE R1S TO CONTINUITY CLINICJared W. Klein1,2; Ginger A. Evans1,3; Anna Golob1,3; Caroline Rhoads1,2. 1University of Washington, Seattle, WA; 2Harborview Medical Center, Seattle, WA; 3VA Puget Sound Health Care System, Seattle, WA. (Tracking ID #1935733)
NEEDS AND OBJECTIVES: Interns in our program historically reported a long interval between beginning continuity clinic and developing confidence and competence with basic clinic processes and disease management. We believe this was driven by their low-level, intermittent exposure to clinic. Therefore, we created an intern ambulatory immersion block with the following objectives: (1) improve intern comfort in continuity clinic by familiarizing them with clinic processes and support staff and (2) develop ambulatory skills including information management, communication, and disease-specific knowledge.
SETTING AND PARTICIPANTS: All interns in our large, multi-site, university-affiliated internal medicine residency program participate in a four-week ambulatory immersion block without inpatient responsibilities during one of the first 3 months of intern year.
DESCRIPTION: The immersion block is comprised of direct ambulatory patient care and a didactic curriculum. Interns spend three to five half-days per week seeing patients in continuity clinic, building a panel and learning to work with their interdisciplinary care team. The didactic curriculum, delivered during three to five half-day sessions per week, includes seminars on: (1) Disease management: core primary care conditions taught by an interdisciplinary team of physicians, pharmacists, dieticians and physical therapists; (2) Practice management: developing systems of care including charting, tracking patients and between-visit care; (3) Communication skills: agenda-setting, shared decision-making, medication counseling, and communicating test results; (4) Select physical exam skills: joint exams, cardiac exam, etc.; and (5) Evidence-based practice: formulating clinical questions, finding current evidence and effectively utilizing information resources.
EVALUATION: Interns who participated in immersion blocks during the 2013–2014 academic year (n = 54) completed pre- and post-block surveys to assess the utility of the immersion curriculum. Substantially all of the interns reported exposure to primary care during medical school, with most reporting a four-week experience. In a free response question asking interns to describe their emotional state before clinic, trainees reported feeling excited but also anxious and overwhelmed. After completing the rotation, interns reported increased confidence in a wide spectrum of skills, as measured by the amount of attending supervision they felt was necessary (complete, partial, minimal or none). For example, at the beginning of the immersion block, 35.8 % of interns felt they needed complete supervision when diagnosing common musculoskeletal complaints, but only 5.6 % of interns felt they needed that same level of supervision at the conclusion of the rotation. Similarly, there was a 44.2 % increase in the number of interns reporting they could independently negotiate a mutually agreeable agenda for a clinic visit. All respondents felt the skills learned during the immersion block would be relevant to their future careers.
DISCUSSION/REFLECTION/LESSONS LEARNED: Adoption of a curriculum to familiarize internal medicine interns with continuity clinic at the beginning of their training increases early confidence with important primary care skills. Our data suggest this curriculum may set the stage for a more fulfilling experience with primary care throughout residency.
ADAPTING TO A MILLENNIAL LEARNING ENVIRONMENT: AN INTERNAL MEDICINE RESIDENCY CURRICULAR IMPROVEMENT PROJECTSuzanne Brandenburg1; Cynthia Brandenburg2; Mel Anderson1,3. 1University of Colorado, Aurora, CO; 2Champlain College, Burlington, VT; 3Denver VA Medical Center, Denver, CO. (Tracking ID #1939274)
NEEDS AND OBJECTIVES: Because both the learning styles of today’s residents and the practice of medicine itself are changing, the effectiveness of traditional lecture-based content delivery is rapidly diminishing. The current project reflects ongoing efforts to innovate and transform didactic sessions in response to the unique needs and characteristics of “millennial” learners in order to better prepare them for the realities of medical practice in the digital age.
SETTING AND PARTICIPANTS: At the University of Colorado’s Internal Medicine Residency Program, curricular transformation of weekly academic half day sessions, delivered by faculty for 2nd and 3rd year residents, will occur over a 3-year period.
DESCRIPTION: The 3-year strategy for curricular transformation includes: 1) Assess needs through faculty and resident surveys. 2) Reduce the amount of specific content covered in sessions; promote critical thinking through interactive activities and capitalize on available technology to enhance information literacy when accessing digital information. 3) Garner faculty interest and provide faculty support and professional development for transforming pedagogy. 4) Involve the learners (specifically residents in the “clinician-educator” pathway) in curriculum redesign. 5) Pilot transformed sessions. 6) Solicit resident feedback. 7) Modify transformed sessions as needed. 8) Implement fully transformed curriculum.
EVALUATION: The effectiveness of curricular change will be assessed using a variety of measures, including post-session feedback via immediate online surveys, average ABIM Certification exam scores, annual faculty and resident satisfaction surveys, and periodic surveys of program graduates.
DISCUSSION/REFLECTION/LESSONS LEARNED: Initial survey results indicate that while both residents and faculty see room for improvement in educational sessions and residents are generally less satisfied with the current curriculum than faculty. For example, when asked to respond on a 4-point Likert scale to the statement “the sessions are a valuable part of resident training” (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree), the average was 2.81 for residents compared to 3.23 for faculty. When asked to respond to “the sessions are important to help residents become confident independent practicing physicians,” the resident average was 2.65 versus 3.03 for faculty. Resident feedback regarding piloted transformed sessions has been positive; preliminary post-session feedback from the first transformed cardiology session indicated 100 % of residents found the session’s objectives to be both meaningful and successfully met. However, since we are only in the first year of our curriculum transformation, more time will be needed before any substantive conclusions can be drawn. Challenges include engaging the large group of faculty who traditionally lecture to residents based on their fields of expertise but have no specific protected time to either learn new teaching approaches or adapt their materials. Furthermore, we recognize the need for a nuanced evaluative tool to measure complex critical thinking and decision-making skills; we hope to develop a modified version of Script Concordance to serve this need. Additional strategies we are considering for the next phase of the project include improvement of independent and online learning materials, facilitated resident and faculty focus groups, and establishment of a Faculty Learning Community.
ADVENTURES IN PILOTING AN INTERPROFESSIONAL OBESITY CURRICULUMTamasyn Nelson; Melanie Jay; Shonna Yin; Allison Squires; Charity Hung; Lisa Altshuler. New York University Medical Center, New York, NY. (Tracking ID #1936644)
NEEDS AND OBJECTIVES: Treating obesity is a complex task and barriers to effective counseling include lack of adequate time during clinical encounters and insufficient provider training. Further, providers become frustrated when they perceive that obese patients are not motivated to change their lifestyles. Implementation of obesity curricula within graduate health professions education programs to address these barriers is important. Use of a curriculum that incorporates an interprofessional approach may foster and facilitate collaborative efforts among health professionals; a multi-disciplinary approach to the treatment of obesity is considered to be especially effective. We sought to design an interprofessional curriculum in obesity counseling that could be individualized based on learner needs and would be appropriate for use across the lifespan and which focused on acquisition of skills related to two domains: 1) motivational interviewing (MI) and 2) health literacy.
SETTING AND PARTICIPANTS: The curriculum was piloted in the Department of Pediatrics in an urban academic hospital with three residents and two nurse practitioner students. It is scheduled to be piloted with Ob/GYN and internal medicine residents.
DESCRIPTION: The curriculum included 3 one-hour interactive sessions followed by an evaluative OSCE. Materials for the sessions were compiled by adapting existing curricula that had been developed separately for pediatrics and internal medicine residents. To this curriculum we included additional items based on a needs assessment obtained from the program director and trainees. The first session included discussion about perceived barriers to obesity treatment and a review of health literacy principles and obesity counseling as well as a brief introduction to MI. The second session focused on challenges in the assessment of the literacy levels of patients and an introduction to specific MI skills, such as change talk and goal setting. The third session was reserved for role playing using the skills learned in the first two sessions. Each session concluded with plans for skills practice within the clinical setting.
EVALUATION: We evaluated the curriculum with a 10-minute OSCE station counseling a resistant adolescent on weight reduction. Participants were assessed on use of counseling techniques, including MI skills. Following the OSCE, qualitative feedback was obtained from the trainees via a written survey and audio-taped debriefing session.
DISCUSSION/REFLECTION/LESSONS LEARNED: Learners had strong feelings of frustration and resignation about their experiences with obesity counseling and were initially resistant to using MI. To address this, we strove to create an environment where learners could be honest about their perceptions and attitudes. Feedback from participants indicated that there was increasing acceptance of MI over the sessions. Learners highly valued the opportunity to learn in an interprofessional setting, identifying areas of similarity and difference in approach to obesity counseling.
ADVOCATING FOR ADVOCACY TRAINING IN MEDICAL SCHOOL: TOO LITTLE TOO LATE?Valerie G. Press; Cassandra D. Fritz; Monica Vela. University of Chicago, Chicago, IL. (Tracking ID #1934127)
NEEDS AND OBJECTIVES: The question of whether physician advocacy should be a mandatory component of medical school training is not new, though to date, data are limited on the impact of such mandatory curricula. The objectives were to: 1) explore students’ understanding of advocacy in medicine; 2) provide a structure for students to explore advocacy and their commitment to advocacy; and 3) help first year medical students begin to define themselves as advocates within the profession of medicine.
SETTING AND PARTICIPANTS: This was a prospective qualitative study that followed 88 first year medical students in the Fall 2013 Health Care Disparities (HCD): Advocacy and Equity course as they learned about topics on health and health care disparities, heard from experts across multi-disciplinary fields about advocacy in medicine, and participated in experiential learning through group community projects and a field trip to our county hospital. Our IRB exempted this study.
DESCRIPTION: HCD is a first year course with mandatory attendance. We thought that this course provided an ideal opportunity for new medical students to learn about and explore advocacy in a formal and guided manner. Therefore, the 2013 HCD course was modified to include advocacy-specific learning: lecturers provided their view and experience with advocacy, written assignments focused on guided essays that encouraged self-reflection, and advocacy-specific lectures and large group discussions were introduced. To explore students’ understanding of advocacy in medicine prior to matriculation, students were surveyed on their pre-course experience, knowledge and beliefs about advocacy related topics. To provide a structure for students to explore advocacy and their commitment to advocacy the students participated in lectures, small group projects, in-class discussions, and a field trip to Cook County Hospital. To help first year medical students begin to define themselves as advocates within the profession of medicine, students completed several mid-course self-reflective essays gauging their reactions to, and understanding of, the topics being presented. To explore students’ understanding of advocacy in medicine after completing the course, the students completed a follow-up survey. Short essays were independently coded by three investigators; short-answer statements were answered on a five-point likert scale.
EVALUATION: The pre-course survey showed that the vast majority of students (93 %) had prior experience working with underserved populations, and 77 % spent greater than 15 h on this activity. About half (53 %) said that they or someone they knew had faced a health or health care disparity. After taking the course, students noted that their definition of advocacy broadened to incorporate multiple modalities. Prior to taking the course, 73 % of students agreed/strongly agreed, 24 % were neutral, and 3 % disagreed/strongly disagreed with the statement: “I consider myself an advocate;” after the course those in agreement increased to 86 %, those who were neutral deceased to 10 %, and those who disagreed remained at 3 % (p = 0.006). There were not significant differences between pre/post-course sentiments about whether access to basic health care is a fundamental human right (p = 0.3) or whether all medical students should become involved in community health efforts (p = 0.1).
DISCUSSION/REFLECTION/LESSONS LEARNED: Our course provided an ideal format of guided learning in which to explore medical students’ understanding of, and commitment to, advocacy in medicine through experiential learning activities and self-reflective assignments. We found that several students began to define themselves as advocates specifically within the field of medicine. However, we did not find that their beliefs about access to health care or participating in community efforts changed after taking the course. Therefore, beliefs underlying the core elements of advocacy are likely formed prior to matriculation, while self-identification as “an advocate” may be more malleable. Our study has limitations. This course took place at a single institution without a comparator group. Therefore we cannot comment on whether our results are generalizable or would differ if the course activities were not mandatory. With the nation’s growing attention and dedication to addressing and eliminating health and health care disparities, physicians will need to understand that our profession extends beyond the clinical encounter into the socio-cultural context. However, based on our results, beliefs on advocacy are likely formed prior to medical school matriculation, hence medical school curriculum, mandatory or otherwise, may be too little too late. Therefore, if an additional goal of medical schools is to promote a field of physicians dedicated to advocacy, admissions committees should recognize the limitations of post-matriculation education, and may consider evaluating for evidence of existing motivation for advocacy efforts during the application process through applicant responses in essays or interviews.
AN INTERACTIVE ONLINE MODULE TO ADDRESS LGBT HEALTH DISPARITIESPhilipp Hannan1; Rita Lee2. 1CU SOM, Aurora, CO; 2University of Colorado, Denver, CO. (Tracking ID #1926376)
NEEDS AND OBJECTIVES: Within the health care system, lesbian, gay, bisexual, and transgender (LGBT) persons face inequity that contributes to health disparities. A 2011 survey found 21 % of LGB individuals had been refused services by health care providers due to their sexual orientation, a rate that increased to 53 % among transgender respondents. Sixty-five percent of LGB and 85 % of transgender respondents felt there were insufficient adequately trained health care professionals to address their LGBT-specific needs. Only 61 % of respondents were “out” to their providers; of those that were not “out,” 41 % feared their provider was not supportive of LGBT people. The key features that would make their provider LGBT-friendly were provider comfort with their sexual orientation or gender identity, LGBT-inclusive forms, and specific knowledge around LGBT health issues. A 2013 survey of Colorado physicians showed 82 % were “totally comfortable” with LGB patients and 51 % were “totally comfortable” with transgender patients if they self-disclosed their sexual orientation or gender identity. However, only 47 % reported being “totally comfortable” asking patients about sexual orientation or gender identity. Most indicated a desire to make their practice more LGBT-friendly. Thus, a conundrum exists. Most providers perceive themselves to be LGBT-friendly and are comfortable if LGBT patients self-disclose their sexual orientation or gender identity, but they don’t ask. LGBT individuals want friendly providers, but don’t tell due to fear of discrimination. We can begin to address these issues by improving provider comfort with asking about sexual orientation and gender identity, increasing their knowledge around LGBT health issues, and providing tools to create an LGBT-friendly practice. Therefore, we developed an online educational module with the following learning objectives: 1. To describe the health disparities LGBT individuals face 2. To describe the specific healthcare needs of LGBT individuals 3. To list the steps a practice or healthcare provider can take to create a welcoming and safe environment for LGBT individuals
SETTING AND PARTICIPANTS: A one-hour long, interactive, online module that is available to all health care providers with internet access.
DESCRIPTION: Using Adobe Captivate, we developed an online module that addresses LGBT demographics and each of the learning objectives listed above. Based on adult learning theory, the module includes: availability to interested learners at their convenience (timely); pre- and post-tests to document knowledge gains (goal-oriented), embedded videos showcasing LGBT experiences (relevant), links to online resources for additional learning (self-directed), and simple, explicit instructions on creating a more welcoming environment for their LGBT patients (practical). Much of the module is interactive to enhance learner engagement. The module is approved for 1 h of continuing medical education credit.
EVALUATION: This is a new module and no evaluation data is available at this time. There is an optional evaluation survey embedded in the module. The module is also being monitored via Google Analytics to track number and location of learners.
DISCUSSION/REFLECTION/LESSONS LEARNED: Our hope is that creating an hour-long, clinically-relevant, practical, interactive, online module will increase provider engagement with the material. Ultimately, our goal is to increase the number of health care providers that have the knowledge, attitude, and skills to provide culturally responsive, clinically appropriate care for LGBT patients. Our dissemination strategy will require a multifaceted approach to reach a broad audience.
ONLINE RESOURCE URL (OPTIONAL): somed.ucdenver.edu/cme/lgbtcme.html
AN INTERDISCIPLINARY COLLABORATION SERVING AS THE BASIS FOR INTERDEPARTMENTAL GLOBAL HEALTH EDUCATIONMinesh Shah1; Huang Amy2; Clemence Sullivan1; Lillian Francia1; Andrew Dykens1. 1University of Illinois-Chicago, Chicago, IL; 2University of California San Diego, San Diego, CA. (Tracking ID #1934748)
NEEDS AND OBJECTIVES: As interest in global health grows, many residency programs have developed global health tracks or rotations for trainees. At the University of Illinois at Chicago (UIC), collaborative global health tracks have been developed for residents in the departments of family medicine, internal medicine, and internal medicine-pediatrics. The tracks focus on an interdisciplinary collaboration to establish community-based participatory research at the local level in a low-income country, through which residents learn first-hand how to conduct responsible, sustainable, and community-based projects. The international experiences are supported by an interdepartmental longitudinal 3-year curriculum that includes topics in community and public health, tropical medicine, health disparities, and the social determinants of health.
SETTING AND PARTICIPANTS: The global health tracks at UIC work through a partnership between a low-or-middle-income country (LMIC) community, Peace Corps, and an academic medical center. The partnership facilitates local level primary health care access with community-participatory primary health care services quality improvement as the aim. Our current project brings together the community of Guaymate, Dominican Republic; Peace Corps Dominican Republic; and UIC. Residents from the three aforementioned departments are engaged in ongoing planning and participate in faculty-led biannual site visits to advance partnership strengthening, assessment, development, implementation, evaluation, and dissemination through an iterative cycle.
DESCRIPTION: In the summer of 2012, we identified Guaymate, Dominican Republic as an ideal community partner. With a Peace Corps volunteer (PCV) as a liaison, we integrated into the healthcare community. Through focus group discussions and an onsite needs assessment, we identified several areas of need, and are currently coordinating the implementation of a broad health services quality improvement project in the Guaymate Municipal Hospital. The resident role is to assist with planning, facilitate local meetings, conducting data collection interviews, and assist faculty with bidirectional Continuing Medical Education seminars with local physicians. In Chicago, residents have monthly project meetings, during which they divide up tasks that include: contributing to writing and submission of the IRB protocol, curriculum development for the Guaymate QI project, logistics planning of site visits, and communication efforts with onsite partners.
EVALUATION: Evaluation tools have been created for the collaborative partnership and the global health tracks. Survey instruments assess partnership participation and satisfaction, and community-defined outcomes. Residents are also evaluated on knowledge, skills and attitudes related to global health topics.
DISCUSSION/REFLECTION/LESSONS LEARNED: The goal of this partnership approach is to offer responsible global health education through LMIC community engagement that fosters the sustainable strengthening of local health services. Our approach de-emphasizes global health education through intermittent clinical service provided by US personnel and cultivates skills of community engagement, health systems strengthening, and health services implementation research. The interdisciplinary effort allows residents to build relationships with non-medical professionals, while the interdepartmental aspect broadens residents’ viewpoints. Each piece of this collaboration complements another. The model is designed for replication in other international communities and academic medical centers.
ONLINE RESOURCE URL (OPTIONAL): Departme of Family Medicine Global Community Health Track: https://sites.google.com/a/uic.edu/uic-dfm-global-community-health2/ Department of Med-Peds Global Community Health Track: http://chicago.medicine.uic.edu/departments___programs/programs/residencies/combined_medicine_pediatrics_/global_community_health_track/
AN INTERPROFESSIONAL CARE TRANSITIONS CURRICULUM FOR AMBULATORY INTERNAL MEDICINE RESIDENTS AND NURSE PRACTITIONER STUDENTSMelissa Bachhuber2,1; Shalini Patel2,1; Candace Kim3; Bridget O’Brien2,1; Rebecca L. Shunk2,1. 1San Francisco VA Medical Center, San Francisco, CA; 2University of California San Francisco, San Francisco, CA; 3San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1939309)
NEEDS AND OBJECTIVES: Primary care providers play an essential role in care transitions of patients across the continuum of care, yet little formal training in care transitions occurs in the ambulatory care setting. We developed an interprofessional care transitions curriculum aimed to enhance trainees’ understanding of care transitions from perspectives of patients, multidisciplinary providers, and systems of care. The specific program objectives included: 1) Define the role of the primary care team in preventing hospital readmissions and the importance of an interprofessional approach to patient care to reduce readmissions; 2) Identify barriers to effective care transitions and describe transitional care models and local programs, 3) Recognize characteristics of patients appropriate for transitional care programs.
SETTING AND PARTICIPANTS: At the San Francisco VA Primary Care Clinics, internal medicine resident trainees are paired with nurse practitioner (NP) students in practice teams and care for a shared panel of patients. Residents and NP students attend curricular sessions together in a collaborative learning environment.
DESCRIPTION: The interprofessional care transitions curriculum was delivered in eight sessions to internal medicine residents (n = 20) and NP students (n = 14) over 2 months per academic year. The curriculum overview session discussed national and local care transitions data, such as hospital readmissions and emphasized four transitional care models. Key components of care transitions including functional assessment, palliative care, hospice, social services, living environments, and care coordination were emphasized in case-based sessions with an interprofessional faculty expert. Trainees applied transitional care concepts in a session reviewing a preventable readmission case focused on congestive heart failure management. Trainees conducted a home visit on a patient from their own primary care panel. Nine faculty members from geriatrics, occupational therapy, physical therapy, social work, nursing, and pharmacy participated as content experts for components of the curriculum. The content of each session was developed through collaborative efforts of primary care faculty with an interprofessional faculty expert lead.
EVALUATION: A total of 34 trainees participated in the care transitions curriculum over two academic years. Trainees evaluated the curricular sessions on a 5 point Likert scale and provided written feedback. Overall, trainees rated the curricular sessions as a mean 4.6 in overall quality of the learning session and 4.4 in likelihood for changes in clinical practice as a result of the sessions. Qualitative comments from trainees highlighted aspects of the sessions they found most valuable, including: insight into key components of successful care transitions and enhanced understanding of the role of the primary care team in transitional care.
DISCUSSION/REFLECTION/LESSONS LEARNED: The implementation of an interprofessional care transitions curriculum is feasible in an ambulatory care setting. Our care transitions curriculum enhanced trainees’ understanding of barriers to effective care transitions, transitional care programs, and increased awareness of the primary care team role in preventing hospital readmissions. Bringing together interprofessional faculty to emphasize key components of care transitions provided trainees with a better understanding of interprofessional team member roles during care transitions and was important to the success of the curriculum. Primary care faculty worked closely with interprofessional faculty content experts, particularly if they were less experienced with a case-based approach to education and with teaching primary care trainees.
ASSESSING AND IMPROVING PATIENT CARE SKILLS THROUGH A BOOTCAMP FOR NEW RESIDENTSLuke Cunningham; Chirayu Shah; Nainesh Shah; Prathit Kulkarni; Kaushal Patel; Steffanie Campbell; Anoop Agrawal; Richard J. Hamill. Baylor College of Medicine, Houston, TX. (Tracking ID #1937842)
NEEDS AND OBJECTIVES: As new residents start their Internal Medicine training in July, many studies have raised concerns about patient safety associated with inexperienced residents, also termed the “July effect.” Based on surveys conducted at our Internal Medicine residency program, there is considerable variation in the patient care experiences and skills of incoming interns starting residency training with only 53 % of incoming interns receiving a course for transition to intern year. Reviews of recent intern experiences revealed insecurities in communication, cross-cover, and procedural responsibilities. Studies evaluating this relationship between clinical knowledge and experience have generally concluded that the decline in knowledge is accompanied by a decrease in quality of care.
SETTING AND PARTICIPANTS: During Internal Medicine resident orientation at Baylor College of Medicine in June 2013, 68 interns participated in a full day training bootcamp divided into three sessions: Procedural training, 8 Cross-cover case simulations, and Teaching Sessions. The teaching sessions were entitled Art of Handoffs, Art of Floating, Art of Patient Presentations, and Art of Efficient Note Writing. All sessions were completed within the medical classrooms and within simulated patient rooms.
DESCRIPTION: The procedural training included hands-on practice with basic ultrasound techniques, central line placement, and managing a code blue situation. Faculty led small groups of interns (4–6) through central line placement and mock code situations with each intern having the opportunity to place a line independently. Cross-cover simulations were done one-on-one with common overnight patient issues: chest pain, shortness of breath, altered mental status, hypotension/sepsis, atrial fibrillation with rapid ventricular rate, acute GI bleeding, acute stroke, and headache. Each session was limited to a duration of 15 min with 3 min reserved for individual feedback.
EVALUATION: All residents were sent a pre-intervention and post-intervention survey about their self-reported comfort level with communication skills, procedural skills, and cross-cover scenarios. There was significant improvement in comfort level for each cross cover scenario: chest pain 3.0 to 4.0, shortness of breath 2.8 to 4.0, altered mental status 2.6 to 3.6, hypotension/sepsis 2.7 to 3.6, atrial fibrillation 2.6 to 3.6, acute GI bleeding 2.4 to 3.7, acute stroke 2.3 to 3.7, and headache 3.1 to 3.8 [n = 67, response rate 98.5 %, Likert scale 1 = very uncomfortable, 5 = very comfortable]. Resident self-reported comfort level with the following procedures also increased: central line placement 1.6 to 2.9, code blue scenario 2.0 to 3.3, and using an ultrasound 2.8 to 3.6 [Likert scale 1 = very uncomfortable, 5 = very comfortable]. Seventy-seven percent strongly agreed and an additional 17 % agreed that Bootcamp should be continued for future orientation sessions.
DISCUSSION/REFLECTION/LESSONS LEARNED: The full day training workshop prior to starting residency significantly improves intern comfort with patient care management skills and likely patient care. The workshop also helps the residency program to implement milestone-based assessments and track further progression during intern year. Future directions include improving observed assessment of handoff skills and assessing impact on patient safety.
ASSESSING THE IMPACT OF A RESIDENT TOOL CREATED BY SENIOR MEDICAL STUDENTS PURSUING CAREERS IN INTERNAL MEDICINERonald Omino; Elizabeth Grier; Katherine L. Fontichiaro; Diane L. Levine. Wayne State Univ SOM, Detroit, MI. (Tracking ID #1939492)
NEEDS AND OBJECTIVES: At the beginning of a clerkship, there is often a great deal of confusion regarding what is expected of both the residents and the students. Generally, the students will receive some sort of course syllabus with a list of goals and objectives for the clerkship that helps to provide some guidance. However, the expectations of the residents are not usually as clearly described. The LCME ED-24 describes, “Residents and other instructors who do not hold faculty ranks (e.g., graduate students and postdoctoral fellows) receive a copy of the course or clerkship/clerkship rotation objectives and clear guidance from the course or clerkship/clerkship rotation director about their roles in teaching and assessing medical students.” In order to address this expectation, we have created an “Orientation to My Team” document and a “Teaching Manual for Resident Physicians”. Our goal is to provide more structured guidance for internal medicine residents who teach medical students on the wards. Once the tools have been distributed residents will be given time to personalize their orientation document. We will then assess the impact of these tools on the quality of the team orientation and resident teaching quality and effectiveness during the Internal Medicine Clerkship.
SETTING AND PARTICIPANTS: Wayne State University Internal medicine residents at the Detroit Medical Center, a large academic healthcare system in Detroit, MI, as well as, third-year medical students at Wayne State University School of Medicine who are on the Internal Medicine Clerkship.
DESCRIPTION: A committee was created consisting of fourth-year medical students at Wayne State University School of Medicine who plan to pursue residency in internal medicine. This committee created a list of specific instructions for residents to use when initially orienting the new medical students to their ward teams. The committee also put together a list of tips on how to help the students learn as much as possible during the clerkship and how to get the most value out of their clinical experience. These recommendations were based on the personal experiences of the fourth-year students during their clerkships, and included topics that they had found helpful or that they had wished were discussed with them during their internal medicine clerkships. In order to effectively implement the use of these tools, at the beginning of each new clerkship rotation residents will be given the lists and instructed to read and go over them with the medical students on their team. Signatures from both the medical students and the residents will be collected to make sure the form was discussed in its entirety.
EVALUATION: A survey at the end of the students’ internal medicine clerkship will be used to assess the impact that the resident orientation had on their ward experience. Students will score their team orientation and the contributions of the interns and residents to their education on the wards. These surveys will be compared to identical surveys that were completed by medical students before the creation and use of the resident orientation tool.
DISCUSSION/REFLECTION/LESSONS LEARNED: Results are currently pending. The goal is that with written guidance provided to the residents that outlines their expectations, they will better understand how to help their students get acclimated to the clinical setting and gain as much educational value as possible out of the Internal Medicine Clerkship. The specific tools used in this project will be available for use.
ONLINE RESOURCE URL (OPTIONAL):https://drive.google.com/file/d/0B9GC533GPAp_TjUtREkzUjVTVWs/edit?usp=sharing
BLENDING RESEARCH AND RESIDENCY: THE CLINICAL SCIENTIST AND INTERNATIONAL SCHOLARS TRACKSPeter D. Bulova; Kathleen M. McTigue. UPMC, Pittsburgh, PA. (Tracking ID #1934592)
NEEDS AND OBJECTIVES: To recruit an elite and diverse group of medical graduates who have a clear ambition to pursue careers in academic medicine, both from US and international medical schools To train future clinician-investigators to serve as key contacts and bridges for international collaboration in medical clinical research and medical education. To develop future leaders in research and academic medicine To develop programs to help residents gain research skills and experience in the context of internal medicine residency training.
SETTING AND PARTICIPANTS: Over the past decade, we have recruited US and International medical graduates for two research-tailored tracks (Clinical Scientist Track and International Scholars Track) within our categorical residency program. Selection is based on evidence of excellence in clinical care and interest in a career involving research. At the end of the 3-year residency, graduates are eligible to sit for the American Board of Internal Medicine (ABIM) Certification Examination. Clinical training in the research-tailored tracks is similar to that of the categorical training program and conforms to requirements of the Residency Review Committee and the ABIM. Time is protected for didactic research training and mentored research experiences designed to produce first-authored manuscripts.
DESCRIPTION: Residents participate fully in our traditional 3 year residency. They devote 2 elective months to formal clinical research training using an established curriculum, and one or more research projects. Residents have assigned clinical and general research mentors. In addition, each resident chooses a research mentor (or mentoring team) for their mentored research project, specific to his/her field of study. Mentored research occurs throughout the residency. All participate in a monthly seminar series to discuss research issues and gain research presentation skills.
EVALUATION: These residents have performed extremely well in our residency. All have successfully completed the residency, were eligible to sit for, and passed the boards. The number of publications of our program participants far exceeds that of our categorical residents, while they have still performed well clinically. For example, in 2011–2012 the international scholar residents averaged 2 publications in peer reviewed journals per resident (32 by 16 residents), compared with an average of 0.5 per categorical resident. The mentored research component of these tracks has served as model for integrating research more broadly into our clinical program. Among 14 graduates who responded to post education surveys, all took positions in a school of medicine; 54 % as fellows, 23 % as residents, and 23 % as clinical educators. Program graduates (n = 14) assessed the program on a 7-point Likert scale, quite strongly agreeing that they were satisfied with the overall quality of the coursework [mean 6.0 (SD 1)], that the program expanded their research skills [5.9 (SD 1.0)], increased their interest in multi-disciplinary research [5.2 (SD 1.5)], and contributed positively to their overall training [5.92 (SD 1.0)].
DISCUSSION/REFLECTION/LESSONS LEARNED: The programs have added diversity and an avenue for research to the program without compromising the clinical mission. Residents have found the integration within the general categorical program to be its most important component. Recruitment of talented scholars from around the world to a specific curriculum has created a successful model of academic training for international medical graduates seeking research careers in subspecialties of internal medicine. The International Scholars and Clinician Scientists have served as models for integrating research and scholarly projects into our categorical clinical program.
ONLINE RESOURCE URL (OPTIONAL):http://www.residency.dom.pitt.edu/Program_Overview/tracks/isp.htmlhttp://www.residency.dom.pitt.edu/Program_Overview/tracks/cstp.html
BUILDING THE DIVERSITY BRIDGE ABROAD: THE STRATEGY TO IMPLEMENT PRE-GRADUATE CULTURAL COMPETENCY MEDICAL EDUCATION IN LAUSANNE, SWITZERLANDAlejandra Casillas1,2; Sophie Paroz3; Elody Dory1; Francis Vu1; Patrick Bodenmann1. 1Lausanne University Hospital, Lausanne, Switzerland; 2Hopitaux Universitaires de Geneve, Genève, Switzerland; 3Lausanne University Hospital, Lausanne, Switzerland. (Tracking ID #1934518)
NEEDS AND OBJECTIVES: Although the United States has been central in bringing cultural competency (CC) into the discussion of high-quality care, health systems all over the world are faced with the effects of global immigration and the widening disparities gap between socioeconomic classes. Lausanne University Hospital is one of five Swiss academic medical centers chosen to develop programs addressing CC. Here we focus on our CC medical student training as a model for other international settings looking to build CC curricula based on best practices, but tailored to their local context.
SETTING AND PARTICIPANTS: At Lausanne University Hospital, diversity is part of clinical practice. Just over a third of the patient population is non-Swiss, and include undocumented and recently arrived refugees. The center serves other high-risk and vulnerable populations. The strategies presented here focus on medical students at the Lausanne center. Given the midpoint of medical studies and the beginning of clinical activity, we specifically concentrate on student evaluations (n = 80) of the three CC training modules at the 3rd year level (of six) for 2012–2013.
DESCRIPTION: Tailored to our European context, this curriculum is influenced by programs developed by experts at the Massachusetts General Hospital and Harvard Medical School. A CC-focused session is delivered to students at various points each year. Primary topics are social determinants of health, cultural groups in the local community, stereotypes, and unintended biases. Early sessions begin with medical anthropology material which raise consciousness of the learner’s own potential biases. By the 3rd year, education evolves to a more case-based medical training- focusing on the social determinants of health through clinical vignettes linked to disparities (mental health, HIV). The three sessions are: Health and Migration, Communication/Trialogue (working with an interpreter), and LGBT health disparities. In the 4th and 5th years, students may enroll in a 12-week health disparities elective and community immersion experience, respectively. In the 6th year, these students rotate in the ambulatory clinic for a month and develop a health disparities project (thus exposing them to our primary care residency for potential recruitment).
EVALUATION: We present an evaluation of a portion of this curriculum for the 3rd year students. In November 2013, students submitted evaluations for the three CC half-day seminars specific to their year (n = 80); classes incorporated the presence of a patient, group interviewing guided by the instructor, videos of simulated case encounters, and case discussions. Sessions were conducted in groups of 20–30 students with an overall mean satisfaction score of 4.1/5 (highest-5). “General interest” and “acquired knowledge” were highest for the Health and Migration session (4.5 and 4.1, respectively).
DISCUSSION/REFLECTION/LESSONS LEARNED: We describe one of the few medical student CC curricula in Europe. We present the theoretical framework and pedagogical models that have been most applicable to our endeavor since its inception in 2005, educational content, developmental approach, and assessment by 3rd year medical students in clinical rotations. In summary, we provide a “roadmap” for international health-education systems developing CC student training, in the context of their local setting.
CARING FOR REFUGEES AND ASYLUM SEEKERS: PRIMARY CARE AND FORENSIC DOCUMENTATION IN REFUGEE HEALTH AS PART OF AN INTERNAL MEDICINE RESIDENCY CURRICULUMJessica Hurst; Matthew T. Corey. Boston University, Boston, MA. (Tracking ID #1936655)
NEEDS AND OBJECTIVES: 1. Increase resident knowledge about refugee medical needs and legal, social, and educational resources in greater Boston. 2. Provide residents with hands-on experience in forensic medical examinations for asylum-seekers. 3. Provide continuity of primary care for refugee patients.
SETTING AND PARTICIPANTS: Setting: A clinic dedicated to the primary care and forensic medicine needs of Boston refugees. Preceptors are attending physicians from the division of general internal medicine at Boston Medical Center, New England’s largest safety-net hospital. Participants: Interested categorical and primary care internal medicine residents.
DESCRIPTION: The innovation has two components. 1. Forensic Medical Evaluation Elective: This elective has been available to primary care residents for approximately 12 years. It consists of one afternoon per week of supervised visits with patients who are applying for asylum. Residents assist in reviewing cases and conducting a forensic medical exam to document evidence of prior ill-treatment based on the Istanbul Protocol. 2. Refugee Primary Care: This was started as a pilot with one resident in January 2013 and expanded to any interested residents in July 2013. As part of their ambulatory week, residents may choose a second continuity clinic in refugee primary care, supervised by faculty with expertise in refugee health and forensic evaluation.
EVALUATION: 1. Forensic Medical Evaluation Elective: Between one and three primary care residents have participated annually. Several program graduates have gone on to conduct forensic medical exams in their primary care practices. 2. Refugee Primary Care: Five residents have chosen to participate. Throughout 2013, there have been a total of 36 visits with 28 unique patients from 9 different countries. 3. Plans to measure quality and results: Monitor patient health metrics and outcomes, design tools to evaluate resident experience and pre- and post-rotation knowledge in refugee health.
DISCUSSION/REFLECTION/LESSONS LEARNED: Current strengths: 1. Training residents in the discipline of global health at their home institution. 2. Disseminating current best-practices in refugee health; participating residents share their knowledge of refugee health screening and available resources with others in the residency program. 3. Supporting Boston Medical Center’s longstanding mission to provide care for the underserved. 4. Utilizing BMC’s rich supply of phone and in-person interpreter services, covering 203 languages. 5. Expanding residents’ landscape of potential careers in general internal medicine. Areas for improvement: 1. Developing a formal, written curriculum, both for participating residents and as a published model for other institutions. 2. Expanding the program to include residents from other specialties, in order to provide unified, multidisciplinary care for refugees with complex care needs. Sustainability and dissemination to other institutions: 1. Maintaining the existing program at Boston University will require recruiting new faculty members and encouraging upper-level trainees to take on teaching roles. 2. Financially, the primary care program is self-supported based on billing Mass Health (Massachusetts’ Medicaid program) for services. This may be problematic in states with less robust health insurance options for refugees. Forensic medical evaluation is not covered by any insurance plan and must be supported through highly competitive grant funding. 3. Adoption of a refugee clinic model at other institutions depends on dedication of clinic space, ancillary staff, faculty time, and resident ambulatory elective time.
CARING FOR THE HOMELESS AND UNDERSERVED: AN ONLINE, SYSTEMS-BASED, INTERPROFESSIONAL CURRICULUMDavoren Chick1,3; April Bigelow2; F. Jacob Seagull3; Heather Rye5; Pamela Davis1,4; Brent C. Williams1. 1University of Michigan, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI; 3University of Michigan, Ann Arbor, MI; 4University of Michigan, Ann Arbor, MI; 5University of Michigan Health System, Ann Arbor, MI. (Tracking ID #1938597)
NEEDS AND OBJECTIVES: Many medical residents lack formal training regarding social determinants of health, public healthcare systems, or special interprofessional care needs of the medically underserved. Internal medicine curricular milestones include an expectation that residents reflect awareness of socioeconomic barriers impacting patient care, but a national curriculum has not been formalized. Locally, University of Michigan internal medicine residents scored an average of 44 % on a baseline needs assessment quiz in these content areas. Residents who rotated through underserved clinical venues with a traditional informal curriculum showed no significant improvement in knowledge. To address identified needs, we developed a sharable online curriculum regarding public healthcare systems and bio-psychosocial care for the underserved. We stressed interdisciplinary education and innovative adult learning methods by forming an interprofessional curriculum design team and incorporating a novel, game-based learning tool.
SETTING AND PARTICIPANTS: With support from a Graduate Medical Education Innovation grant from the University of Michigan Medical School, we formed a curriculum design team comprising the fields of nursing, social work, internal medicine, pediatrics, medical education, communications, and graphic design. The final curriculum was posted to a freely accessible website. Current participants include over 250 registered learners from numerous medical and nursing institutions across the United States.
DESCRIPTION: Through iterative refinement, the curriculum design team identified two relevant curricular domains supporting care of at-risk populations. Each of the two domains was divided into knowledge content modules: Domain 1. Public Healthcare Systems includes modules on epidemiology of the homeless and medically uninsured, public health insurance systems, and public healthcare delivery systems; Domain 2. Bio-Psychosocial Model of Care includes modules on biomedical needs of the homeless, social determinants of health, the bio-psychosocial model of health, and interprofessional team care. We produced case-based learning modules for each of these content areas and packaged the curriculum in a professionally designed web site: “Caring with Compassion”. The website includes an individualized learner dashboard, case-based didactic modules, extension resources, a trifold case formulation pocket guide, and a milestone-based assessment tool. The core knowledge curriculum is supplemented with a case-based online game that integrates core content into an enjoyable, low-risk learning experience.
EVALUATION: Nationally, hundreds of residents have enrolled in this curriculum. Additionally, the curriculum is in use by nurse practitioner and medical students, and is now a core resource for University of Michigan Medical School and School of Nursing courses regarding care of underserved populations. Faculty across multiple institutions report assigning the website for independent learner review and using the resources during small group discussions. Qualitative feedback has been highly positive, with residency program directors stating that the curriculum addresses significant gaps in the traditional graduate medical curriculum. Preliminary quantitative outcome data demonstrates highly significant improvement in multiple choice examination scores following exposure to the modules and game for all assessed content areas [n, pre-test, post-test, T test p value]: epidemiology of populations in need (42, 49 %, 81 %, p < 0.0001); health care delivery systems knowledge (19, 53 %, 67 %, p < 0.002); homelessness and disease (20, 59 %, 82 %, p < 0.0001); public health insurance (30, 52 %, 80 %, p < 0.0001); team care (14, 45 %, 64 %, p < 0.001); social determinants (29, 51 %, 56 %, p = 0.022).
DISCUSSION/REFLECTION/LESSONS LEARNED: This freely shared online curriculum addresses identified national and local gaps in socioeconomic and sociobehavioral knowledge for medical learners. Curricular components can be used individually or as a comprehensive curriculum. Medical educators and learners have expressed appreciation both for the cohesiveness of the compiled curriculum and for the flexibility of implementation options provided by the online modular format. Further plans include expansion of faculty development tools, expansion of the learning game through addition of a second game case scenario, and continual revisions based on curricular feedback. Challenges moving forward include securing time and resources to update content, maintain the website, and measure and monitor learner outcomes. High quality, freely accessible, interprofessional online curricula are highly appreciated resources for academic medical and nursing institutions. Shared online curricula are an important and valued direction for the future of a national medical curriculum and for academic recognition of medical education scholarship.
ONLINE RESOURCE URL (OPTIONAL):http://caringwithcompassion.org
CHAPLAINS ON THE MEDICAL TEAM: AN INTERPROFESSIONAL PARTNERSHIP IN PATIENT CAREPatrick Hemming; Paula Teague; Ty Crowe; Rachel Levine. Johns Hopkins University, Baltimore, MD. (Tracking ID #1931022)
NEEDS AND OBJECTIVES: Many patients identify spirituality as important to their coping and medical decision making, but physicians generally have little training in spiritual assessment. Increased collaboration between physicians and hospital chaplains may encourage greater attention to patients’ values. With this goal, we developed a shared educational experience for internal medicine ward teams and chaplain trainees in clinical pastoral education (CPE). The overall objectives are to: 1. Increase medical residents’ confidence in talking to patients about spiritual needs 2. Increase medical residents’ awareness of chaplains’ roles 3. Increase collaboration between residents and chaplains in patient care
SETTING AND PARTICIPANTS: Beginning in 2011, we paired CPE trainees with one of the Internal Medicine resident inpatient teams at JHBMC. These CPE trainees are Masters-level theology students pursuing a clinical inpatient experience prior to becoming chaplains. Each CPE trainee spends 1 or 2 days per week over a 3–4 week rotation with the medical team: attending, senior resident, two interns, two medical students. From 2011 until September 2013, eight CPE trainees had participated.
DESCRIPTION: The curriculum includes three phases: orienting, rounding, and partnering. Orienting: medical interns have an hour-long introduction to a spiritual assessment tool and chaplains’ roles. CPE trainees’ orientation includes an introduction to the medical team structure, and guidance about contributing appropriately to rounds. Rounding: the CPE trainee accompanies the team at bedside for at least 3 days over the rotation, and contributes to the discussion and plan. Partnering: CPE trainees and medical residents collaborate informally outside of rounds to care for patients identified as having need of a chaplain.
EVALUATION: Between October 2011 and May 2013, a pilot was conducted to evaluate the feasibility and appropriateness of the curriculum. We conducted focus groups with participating attending physicians (one group of 10), CPE trainees (one group of 3, one group of 4) and medical residents (one group of 4). Transcripts of the focus groups were recorded and analyzed by two researchers to develop a coding template that was applied to the transcript to develop themes. Regarding the educational experience, several themes emerged: 1. Physicians reported greater confidence addressing patients’ spirituality from observing CPE trainees’ communication techniques (listening, observing, and using appropriate language). 2. Physicians saw CPE trainees as a liaison between the team and patient, and valued the emotional support CPE trainees provided to the team. 3. Keys to a successful collaboration include: (a) introduce team members by role (b) set clear expectations for team members (c) provide opportunities for feedback. The observations from theme 3 prompted specific changes in our curriculum. In a separate survey of medical residents (response rate 34/57 = 57 %), 83 % (vs. 17 % neutral) agreed that the rotation with CPE interns was beneficial to their learning by comparison with other rotations.
DISCUSSION/REFLECTION/LESSONS LEARNED: Involving physicians and chaplains in an interprofessional curriculum is an innovative approach to medical education and offers an effective strategy to simultaneously improve teaching in both professions and enhance patient care.
CLOSING THE FEEDBACK LOOP -EVALUATING AN INNOVATIVE SYSTEM TO PROVIDE FEEDBACK TO FACULTY ABOUT THEIR STUDENT ASSESSMENTSNeil Mehta1; Alan L. Hull2; Amy S. Nowacki3. 1Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH; 2Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH. (Tracking ID #1933607)
NEEDS AND OBJECTIVES: Students need ongoing formative feedback that identifies specific strengths and areas for improvement, to compare this feedback to established goals and expectations, and to develop plans to improve targeted areas to become self-regulated learners. We have developed a web-based Clinical Assessment System (CAS) that allows all preceptors to provide timely formative feedback based on observed clinical encounters. While finding the time to provide formative feedback is a challenge, a bigger challenge is that clinical preceptors are more familiar with providing summative end-of-rotation feedback and may be unaware of the type of feedback that is most useful to help students identify learning needs, seek new knowledge or skills, and improve performance and understanding. To address this issue, we enhanced CAS to allow students to assess the usefulness of the formative feedback they receive from the clinical preceptors. The objectives of this project are to determine if these assessments can: 1. Reliably and validly identify preceptors for faculty development or for recognition; 2. Be aggregated to identify disciplines or clinical training sites for faculty development.
SETTING AND PARTICIPANTS: The study included 48 students from 1 of 3 tracks of a medical school during their core clinical rotations based at 3 medical centers. The track uses a competency-based portfolio system for assessment. This system requires students to write a reflective essay on 9 different competencies citing their formative assessments as evidence of meeting standards in each competency.
DESCRIPTION: The students log all their educationally significant patient encounters in CAS using any internet enabled device. The preceptors provide competency-based narrative formative feedback (both strengths and areas for improvement) for each of these encounters. When viewing this formative feedback online, students can rate the usefulness of the feedback using a 5-point Likert item of agree-disagree to the statement “This form identifies specific behaviors/skills that I did well and/or I can improve upon”. The student rating is presently not shared with preceptors.
EVALUATION: Students rated the usefulness of 1,181 (59 %) forms out of 2,001 formative assessments completed by faculty between July–December, 2013 as follows: 56 % Strongly Agree (SA); 33 % Agree (A); 7 % Neutral (N); 2 % Disagree (D); and 1 % Strongly Disagree (SD). Forty-two forms were rated D or SD. Twenty-four of these 42 forms had non-specific comments (e.g. “good history”) rather than specific feedback about observed interactions while 11 had no competency specific comments. Only 4 of these forms were blank. Twenty-four of these forms were from 3 students. Other observations of these 42 forms included faculty copying and pasting the identified criteria into the feedback boxes and faculty who entered a number (e.g. 9/10) instead of comments in the feedback box. Each form rating was dichotomized as Useful (SA/A) versus Not Useful (N/D/SD). When restricted only to disciplines with at least 50 assessed forms, the usefulness of the forms differed according to discipline (73 % surgery, 83 % aging, 88 % pediatrics, 89 % OB/GYN, 91 % internal medicine, 91 % family medicine; Chi-square test p = 0.001). The usefulness of the forms also differed according to clinical site (82 % vs. 87 % vs. 90 %; Chi-square test p = 0.05). Faculty level statistics were computed for the disciplines with the largest number (internal medicine, n = 134) and the most diversely rated (surgery, n = 32) faculty. The majority of these faculty (81 %) had 3 or fewer forms rated by students. Points were assigned to each student’s assessment of the usefulness of each form they rated: SD = 0, D = 2, N = 5, A = 8, SA = 10; the average for each faculty being the feedback score. The median feedback score was 9.3, Q1 = 8 and Q3 = 10. Nineteen faculty (11 %) had average scores below 6 and were identified as providing student-reported non-useful feedback.
DISCUSSION/REFLECTION/LESSONS LEARNED: Formative assessments are critical to help students develop into self-regulated learners by letting them close the gap between goals and performance. Providing useful feedback to students is a faculty skill that can be improved. We describe a system for students to assess the usefulness of feedback they receive. Our analysis suggests that these data can be used to identify faculty who could benefit from faculty development on providing feedback and recognize faculty who consistently provide useful feedback. The next step is to validate the results with a different cohort of students doing their clinical rotations at the same sites, in the same disciplines with the same group of faculty. We also plan to compare student and expert assessments of usefulness from a randomly selected group of assessments and study the utility of using student assessments of usefulness as an outcome marker for faculty development. If borne out by these studies, this model can be replicated on other assessment systems and help both students and faculty in academic programs.
COLLABORATING WITH COMMUNITY ORGANIZATIONS AND NON-MEDICAL PERSONNEL TO IMPROVE RESIDENTS’ MEDICAL SPANISH SKILLS INCLUDING COGNITIVE RETENTION AT 6 MONTHSFrances Norlock; Laura Sadowski; Jennifer Feld. Stroger Hospital of Cook County, Chicago, IL. (Tracking ID #1934926)
NEEDS AND OBJECTIVES: Cultural and language barriers have been documented as risk factors for disease, mortality, morbidity, access to health care and receipt of health care services. Spanish is the native language among 25 % of patients cared for by trainees at our institution and educators felt it was important to familiarize residents with this specific language. The objective of this medical education innovation was to improve healthcare providers’ medical Spanish skills so that they could better communicate with Latino patients. Unique to the educational innovation compared to previous language curriculums was the assessment of language retention 6 months after completion of the rotation.
SETTING AND PARTICIPANTS: Fifteen internal medicine residents and 1 genetic counselor completed a dedicated medical Spanish rotation at an urban, public hospital. Language skills were taught through daily didactic language instruction; role-playing with professional patients; homestays with Latino families to practice conversational skills; shadowing physician visits in clinics serving the Latino population to improve listening skills; as well as completing an intensive computer-based Spanish language CD and a computer-based medical Spanish CD.
DESCRIPTION: Over the past 3 years 16 trainees spent 4 weeks in an intensive Spanish language course taught by an experienced Spanish language instructor. Didactic sessions were held each morning for 3 h before residents went to a variety of experiences to reinforce the language skills learned in the morning sessions. Role-playing sessions were moderated by the language instructor and were held between trainees and professional patients to improve listening and speaking skills. Each trainee participated in 5 home stays with Latino families in their homes to practice Spanish conversational skills. Trainees shadowed physicians twice during ambulatory patient visits in clinics serving the Latino population to improve listening skills. Lastly, trainees completed the computer-based Spanish language CDs in one assigned afternoon. Language acquisition (writing, listening, and reading) and cognitive retention of medical Spanish were measured at the beginning and end of the 4 week rotation and 6 months after completion of the program.
EVALUATION: After 4 weeks educators found a 48 %, 26 % and 57 % mean change improvement prior to the start of the rotation in written, listening, and reading skills, respectively. Among trainees there were sustained improvements 6 months later with a mean change in improvement prior to the start of the rotation of 39 %, 12 % and 50 % in written, listening, and reading skills, respectively.
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents were able to make improvements in medical Spanish writing, listening and reading skills with a 28-day language instruction course both at the end of the rotation and 6 months after completion of the rotation. This is the first time educators have shown a sustainable improvement over a 6 month follow-up period. The number of role-playing sessions with professional patients was increased based on feedback from the initial group of trainees. In the future, a speaking assessment will be included using a professional patient and evaluator as the Program Director felt this was an important component to evaluating future rotations.
COMMON DOLLARS, COMMON SENSE: HARMONIZING A HIGH VALUE CARE CURRICULUM ACROSS AMBULATORY AND INPATIENT SETTINGS IN AN ACADEMIC MEDICAL SYSTEMReshma Gupta; Jacob Berman; Andrew Dervan; Anshu Abhat; Leah Marcotte. University of Seattle, Washington, Seattle, WA. (Tracking ID #1933710)
NEEDS AND OBJECTIVES: The Institute of Medicine estimates that as much as one-third of healthcare spending is waste. Although physicians play a central role in allocating healthcare resources, a recent cross-sectional study of physicians in JAMA showed that only 36 % of physicians see themselves as having a major responsibility to help reduce healthcare costs. In this context, training the rising generation of clinicians to deploy healthcare resources wisely has become essential. How do we empower residents to make high value, cost-conscious decisions at the point of care in an increasingly complex healthcare system? Objectives: - Enhance provider understanding of payment systems to illuminate the financial impact of clinical decisions on patients and the healthcare system - Shift paradigms from an inpatient vs outpatient dichotomy to a comprehensive view of cost and quality that spans time, disease and care settings - Motivate trainees to recognize the importance of physicians in providing resource-conscious healthcare
SETTING AND PARTICIPANTS: Across ambulatory and inpatient settings in a large, three hospital academic system including the University of Washington, Harborview, and Veterans Medical Center in Seattle for all internal medicine residents.
DESCRIPTION: We developed a curriculum focused on health systems and high value, cost-conscious care. Our curriculum includes 15 large group lectures providing a framework and vocabulary for health systems, ten small group workshops on delivering cost-conscious care, including six drawn from the Alliance for Academic Internal Medicine High-Value Care curriculum, and multiple initiatives throughout our program to make cost data more accessible to providers at the point of care. The large lectures cover topics including health systems structure, payment and financing, quality improvement, new health delivery models, and advocacy. The small group workshops are delivered through 30 min clinic conferences and 45 min inpatient morning reports in a coordinated effort across our three hospitals. We use hospital-specific data when possible and challenge participants to consider the most appropriate care setting for a given patient and problem.
EVALUATION: We conducted qualitative interviews of 15 medicine residents, probing their experiences in delivering coordinated, efficient care across ambulatory and inpatient settings. The themes extracted from these data include trainees’ limited health systems fluency and observed difficulties in coordinating care to avoid system redundancies and frequent ED visits. Motivated partly by these data, we implemented this curriculum within the first three rotational blocks of our academic year. We will use survey data and semi-structured qualitative interviews to evaluate the impact of this curriculum on resident cost-consciousness, health systems knowledge, and ordering habits.
DISCUSSION/REFLECTION/LESSONS LEARNED: Implementing a broad-based health systems/high-value care curriculum across a large academic medical system is feasible. Key to this effort has been giving residents the background (though larger lectures) and tools (through workshops) to use actual local cost and outcome data to provide high value care. It was essential to identify key champions across ambulatory and inpatient settings to achieve this. Structuring the curriculum to span various didactic venues has enriched the learning experience and improved educational continuity by comprehensively exposing trainees to multiple models and cultures of care delivery.
COMMUNITY HEALTH IMMERSON CURRICULUM FOR PRIMARY CARE RESIDENTSRobin E. Canada. 1University of Pennsylvania, Philadelphia, PA; 2Department of Public Health, Philadelphia, PA. (Tracking ID #1927792)
NEEDS AND OBJECTIVES: The University of Pennsylvania Primary Care Residency Program attracts residents who desire to care for the underserved, and our hospitals and clinics serve economically disadvantaged populations from West and Southwest Philadelphia. However there was little curriculum time or clinical experiences specifically addressing the needs of either patients or trainees. Thus, we developed our Community Health Immersion Curriculum, which was initiated in September 2013. The objectives were to: 1. Train physicians to understand the social determinants of health in order to better care for patients and prevent burnout. 2. Provide experience working in community sites to: a. Improve the practice of medicine with vulnerable populations though understanding the patient’s life context, the resources available, and barriers to care b. Improve discharge practices for vulnerable populations c. Provide experience for career planning
SETTING AND PARTICIPANTS: This Community Health Immersion is mandatory for the Primary Care residents in their junior year; (n = 6–8 annually) Residents rotate at one of the safety-net health clinics in West Philadelphia (Health Center #4), an HIV primary care site (The Jonathan Lax Center), and a student-run free clinic (United Community Clinic) during 1 month.
DESCRIPTION: Residents participate in a longitudinal didactic series on the social determinants of health throughout their Junior and Senior years. Presenters are researchers and practitioners working in academics, public health, and the community. Topics include: Community Health Centers, Social Determinants of Health, Gun Violence and Structural Causes of Disease, Racial Disparities in Cancer Screening, Research in Health Disparities, Homelessness, Immigrant Health, Mental Health Disparities and services in Philadelphia, Health Literacy, Tobacco Cessation and Obesity efforts. Additionally, trainees spend a month in the community practicing, tour community non-profits that address social determinants of health, and attend meetings on transitions of care. We plan to partner with a community-based organization to offer health topics and screening.
EVALUATION: Residents write a reflection of the month, meet with the course coordinator, and complete a standardized online evaluation. We aim to perform interviews of the residents completing the curriculum, and compare those to controls.
DISCUSSION/REFLECTION/LESSONS LEARNED: Two residents have rotated through our community health month. Their feedback was overwhelming positive. Resident 1: “Understanding where your patients are coming from is an important way to prevent burnout in trainees and one of the best ways to do this is show examples of community medicine at work so that the triumphs and challenges of patients can empower the trainee to care for patients competently and compassionately.” “I am such a better inpatient doctor, understanding how my patients access care after discharge.” Resident 2: “Ms. H’s social situation - her lack of insurance, lack of support, and lack of disposable income - were not taken into account when she was discharged.” “The rotation has made me rethink my career in academic oncology.” Notably, a senior resident, who did not get the experience, commented that she “wished we had done this earlier—it might have changed my career.” From this intervention we have learned that our residents are hungry for the opportunity to learn more about their patients through education and practice in community settings. We hope that this intervention will create doctors that better understand and serve their community.
CONTINUITY CLINIC IMMERSION FOR INTERNAL MEDICINE INTERNS: IMPROVING EFFICACY IN AMBULATORY CARE EARLY IN RESIDENCY TRAININGSoraya Azari1; Emily E. Hurstak1,2; Katherine Julian1; Maya H. Dulay2,1; Shalini Patel2,1. 1UCSF, San Francisco, CA; 2San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1933684)
NEEDS AND OBJECTIVES: Internal medicine residents spend approximately two-thirds of their training in the inpatient setting. With new duty hour changes and requirements, many training programs find it increasingly difficult to teach internal medicine interns how to provide effective primary care. Barriers include limited time spent in continuity clinic, patient complexity, and complex systems of care in resident continuity clinic settings. Our objective in designing this curriculum is to improve intern ambulatory medical knowledge, clinic systems of care knowledge and skills, and to enhance satisfaction with the continuity clinic experience.
SETTING AND PARTICIPANTS: All internal medicine interns at UCSF residency program were scheduled to take part in a one-month intensive ambulatory curriculum from June 2013 through January 2014 during the first 6 months of internship. Interns participated in the curriculum grouped by their clinic site: a university-based clinic, a Veteran Administration-based clinic and a county hospital-based clinic. Core clinic faculty, allied healthcare providers, and the ambulatory chief resident delivered the curriculum.
DESCRIPTION: Core ambulatory faculty from each clinic site met and agreed upon the immersion curriculum topics to be covered. This month-long intern immersion curriculum involved: 1. Increased continuity clinic sessions; 2. Ambulatory core didactics to increase medical knowledge on common primary care complaints and diseases; 3. Targeted curriculum aimed at enhancing effective team-based care through shadowing interdisciplinary team members and receiving interactive didactics from allied healthcare providers (ex: physical therapy, mental health providers, and social work); 4. Interactive didactics focused on navigating clinic systems including charting effectively in an electronic medical record, telephone and electronic communication with patients, and panel management; 5. Reflective sessions to allow interns to discuss challenges and accomplishments encountered in developing their ambulatory care skills; and 6. Dedicated time and opportunities to develop relationships with outpatient mentors.
EVALUATION: We delivered this educational innovation customized for each of our continuity clinical sites to 58 interns over 6 months. All internal medicine interns were surveyed every month from July 2013 through February 2014 regarding their perceived efficacy in their continuity clinic using an anonymous (coded by clinic site) paper-based survey tool. Comparisons will be made between responses from interns who have completed immersion curriculum to those who had not yet received the immersion curriculum in order to assess program effectiveness in improving medical knowledge, efficacy, and competence in continuity clinic settings. Independent evaluations of immersion didactic speakers were also obtained at all three clinic sites in order to guide future sessions and curriculum development. Qualitative data were also collected at the three sites. Examples of resident comments included: “The best part was having closely spaced clinic sessions which allowed me to get to know the clinic system” and “I also benefitted from shadowing a senior resident and learning their work flow.” “I found it helpful to discuss the approach to a patient with chronic pain…. and appreciated learning about evaluating a u-tox result”. Preliminary survey data reveal improved self-reported clinical efficacy, familiarity with staff and systems, and medical knowledge in continuity clinic settings. Interns valued shadowing opportunities, which fostered getting to know clinic staff, faculty, and resident mentors on a personal and professional level. The highest rated didactics were practical, concise, case-based sessions. Negative feedback included not receiving curriculum early enough in the academic year and too many sequential didactic sessions in a day. Responses were similar for primary care track and categorical interns.
DISCUSSION/REFLECTION/LESSONS LEARNED: Essential aspects of this program include scheduling immersion months as early in the academic year as possible, identifying clear learning objectives and checklists for shadowing activities, and involving ancillary team members and associated health professionals with formal and informal teaching responsibilities. Having a large number of learners immersed in clinic simultaneously can be a burden on staff and clinic resources, but developing best practice guidelines will aid core faculty to design and deliver effective immersion curriculum in the future. The success of this educational innovation has prompted discussion on the design and implementation of an advanced clinic immersion month for 2nd year residents to cover higher-level topics. Addressing the primary care workforce shortage requires creative curricular development to engage residents and improve clinic satisfaction so that they may envision rewarding careers as primary care providers.
ONLINE RESOURCE URL (OPTIONAL): NA
COOK HEALTHY EAT FRESH (CHEF): A PILOT STUDY OF AN INTERDISCIPLINARY SEMINAR TO AUGMENT MEDICAL STUDENT TRAINING IN NUTRITION AND CULINARY SKILLSRob Caldwell1,2; David M. Levine1; Scott Vasher3; Jared Beller3; Lisa Sasson4; Melissa Lumish3. 1New York University School of Medicine, New York, NY; 2New York City Health & Hospitals Corporation, New York, NY; 3New York University School of Medicine, New York, NY; 4New York University, New York, NY. (Tracking ID #1895433)
NEEDS AND OBJECTIVES: Health care providers are regularly expected to educate their patients in nutrition and weight management, yet formal medical student training is deficient in these areas. In response, our interdisciplinary team enhanced, implemented, and assessed a medical student seminar on healthy eating and cooking to focus on nutrition knowledge, food selection and preparation, and health promotion. This pilot also sought to assess the course’s impact on participants’ eating behaviors and perspectives surrounding nutrition and cooking as well as inspire them to share their practices with their patients.
SETTING AND PARTICIPANTS: 25 volunteer medical students at New York University (NYU) School of Medicine (SOM) participated in CHEF: Cook Healthy Eat Fresh. CHEF is an interdisciplinary para-curricular seminar led by faculty and student/resident volunteers from NYU’s SOM and Department of Nutrition, Food Studies, and Public Health.
DESCRIPTION: With new objectives-based teaching strategies, CHEF created a hands-on environment where medical students learned basic culinary techniques while gaining an understanding of nutrition fundamentals and patient counseling. Students engaged in four 3-hour cooking sessions in a teaching kitchen and four 50-minute didactic sessions in a classroom. Cooking session themes included the Mediterranean and DASH diets, which were linked to classroom topics including the sociocultural aspects of nutrition, barriers to dietary change, and making informed food decisions.
EVALUATION: Eleven students enrolled and completed evaluations, examined through intention to treat analysis where possible. Nutrition promotion was assessed through the validated Nutrition in Patient Care Survey. Students significantly improved on 3 out of 5 scales (p < 0.05). Participants’ dietary practices were measured pre/post through the validated Automated Self-Administered 24 h Diet Recall (ASA24). Participants’ intake of total calories decreased by 99.9 kcal (p = 0.45). When the ASA24 scores were converted to the Healthy Eating Index (HEI) 2010, mean population scores increased from 70.66 to 73.89. Due to the complex HEI calculation, this portion of the analysis was performed among survey completers only. Food selection and preparation were evaluated through both a pre/post self-efficacy questionnaire and kitchen skills observation rubric. Self-efficacy improved in skill areas including roasting, simmering, sautéing, and stir frying (p < 0.05). Students’ perception of their ability to prepare meals adhering to the DASH and Mediterranean diets, as well as time-efficient and budget-appropriate meals also improved (p < 0.05). Post-course, students on average felt they could incorporate healthy cooking and eating in their lives “with little difficulty,” a significant improvement. Pre/post observation rubrics of kitchen skills did not demonstrate significant changes. Nutrition knowledge was assessed with exit surveys after each didactic session, which demonstrated >80 % mean mastery of content objectives.
DISCUSSION/REFLECTION/LESSONS LEARNED: CHEF demonstrated a trend toward improvement in participant behaviors and perspectives. We look forward to enrolling more students in subsequent semesters to fully evaluate the effects of CHEF. Here we describe an innovative seminar for the training of future physicians such that they eat and cook more healthfully and are more comfortable discussing healthful dietary behaviors, cooking skills, and weight management with their patients.
CREATING A REPORT CARD TO MEASURE AND REPORT INTERNAL MEDICINE RESIDENT COMPETENCIES IN THE USE OF THE ELECTRONIC HEALTH RECORDScott Joy1,2; Brian Dwinnell1,2. 1The Colorado Health Foundation, Denver, CO; 2University of Colorado, Denver, CO. (Tracking ID #1935156)
NEEDS AND OBJECTIVES: Effective and efficient use of electronic health records (EHR) is a skill that internal medicine residents need to develop early in their careers. There is no agreed upon standard upon which to evaluate a resident’s skill regarding proper documentation within the EHR. We sought to develop a scorecard of relevant EHR documentation skills to provide feedback to residents on their performance regarding documentation of key data within the EHR.
SETTING AND PARTICIPANTS: 18 primary care track internal medicine residents (6 interns, 6 junior residents, 6 senior residents) at the University of Colorado who have their continuity clinic at High Street Primary Care Center at Presbyterian/St. Luke’s Medical Center in Denver, Colorado.
DESCRIPTION: A checklist was developed that evaluated 11 key factors relevant to effective documentation in a general internal medicine practice, which included: 1. Meaningful Use (4 criteria, updated problem list, medication reconciliation performed, allergies verified, documentation of smoking cessation counseling provided). 2. Evaluation and Management Coding (5 criteria, documentation of new/established patient, complexity of diagnosis, amount of data reviewed, E/M and teaching code entered in billing section) 3. PCMH Requirements (2 criteria, goals for clinically important conditions documented, follow-up plan documented (f/u with whom, why and when). These criteria were reviewed with each resident, and a summary sheet of the criteria were posted in obvious areas in the resident work area. At the end of a 6 month evaluation period, faculty retrospectively reviewed 3 resident notes from the evaluation period, including at least one progress note that was relevant to one of the practice’s PCMH Clinically Important Conditions (diabetes, coronary artery disease, or depression). If the resident adequately documented the key factor in the note or if that factor was not applicable in that particular encounter, the resident received a point. If the key factor was not documented, the resident received 0 points. The sum of the points the resident obtained in each key factor was determined, and the percentage of resident key factor points/total key factor points was calculated.
EVALUATION: The range of resident scores regarding competencies in documenting within the EHR was 69 % to 100 %. The average score for the entire group was 84 %. The average score for the group of Interns was 92 %, range 80 % to 100 %, 67 % scored above average. The average score for the group of junior residents was 83 %, range 76 % to 93 %, 33 % scored above average. The average score for the group of senior residents was 77 %, range 69 to 90 %, 33 % scored above average.
DISCUSSION/REFLECTION/LESSONS LEARNED: A report card that evaluates resident competencies at meeting critical documentation goals in an EHR can be developed. Interns who had no previous interaction with old methods of documentation within the practice had the highest percentages of compliance with EHR task completion. Ongoing training and feedback regarding appropriate documentation skills using EHR for residents is paramount to optimizing the potential of the EHR.
CULTURAL COMPETENCE EDUCATION IN A SIMULATED CLINICAL ENVIRONMENT : A PILOT EXPERIENCESophie Paroz1; Raphaël Bonvin2; Alejandra Casillas3; Sara Vadot2; Francine Viret2; Amaury Daele4; Patrick Bodenmann3. 1Lausanne University Hospital, Lausanne, Switzerland; 2University of Lausanne, Lausanne, Switzerland; 3University of Lausanne, Lausanne, Switzerland; 4University of Lausanne, Lausanne, Switzerland. (Tracking ID #1926053)
NEEDS AND OBJECTIVES: Patients accumulate socio-cultural factors that interact with their care. In addition, contemporary european health services are confronted with a growing diversity according to language, country of origin, education, and/or religious beliefs. At the Department of Ambulatory Care and Community Medicine in Lausanne University Hospital, Switzerland, half of the patients are immigrant. The first attempts to manage diversity emerged 15 years ago, and included the development of a cultural competence (CC) curriculum for frontline medical doctors. In 2010, a survey showed that their self-perceptions of CC skillfulness was low and that their CC needed strengthening. New education strategies have therefore been implemented. Our main objective was to improve the clinical impact of CC education efforts. The secondary objective was to increase the perceived relevance of CC care, among providers.
SETTING AND PARTICIPANTS: The Department of Ambulatory Care and Community Medicine is an academic center comprised of 100 physicians. During residency training, a mandatory 4 h CC education module is in place, based on traditional and moderately interactive teaching media (clinical encounter videos, powerpoint, case vignettes). The first session focuses on adressing language and literacy issues, the second session on social context, and the third on beliefs and stereotypes. The fourth and final session emphasizes learned/prior principles through clinical cases. Prior to these efforts, only oral or written patient cases had been used. The target populations are general medicine residents and chief residents. The trainer is an attending physician.
DESCRIPTION: A pilot experience was supported by an education-innovation grant from Lausanne University and took place in September 2013. It focused on the 90 min fourth session of the module and was developed in accordance with a patient-based approach in a simulated interactive and supervised clinical environment. Two clinical scenarios were created based on an « upstream evaluation » of learners’ needs. The first case involves a young Moroccan student with an undiagnosed gonococcal throat infection. Prejudice, sexual risk behaviour and sexual orientation were addressed in this vignette. The second case is about a 40 year old Albanian woman presenting with somatoform disorders. Treatment adherence, social integration and gender were touched upon in this segment. The following specific skills were integrated in the scenarios : to determine the socio-cultural factors affecting medical care; to identify a patient’s understanding of his/her illness; to show the learner how to « teach-back »; to negociate a treatment plan. Two simulated patients were trained for the role plays. A duration of 45 min was alloted to each case, this included group debriefing and a post-debriefing role play. Development of the session was supervised by a collaborative, interdisciplinary team of medical doctors, CC care specialists and educationists. Eleven physicians participated, five of them volunteered for the role play, and the rest were active observers.
EVALUATION: The experience was initially evaluated by an ad hoc form distributed directly after the session. Nine out of ten learners (n = 10, 1 missing) rated their satisfaction as « very satisfied ». Eight out of ten considered that simulated patients helped them improve their CC and that the class increased their comprehension of CC. One month later, a focus group reunited six of the learners to complete these results. Clinical cases and simulated patients were considered « realistic » and the increased opportunities for interaction in the class were highly appreciated. The application of CC through a simulated environment was considered advantages in increasing self-reflection and improving individual provider practice. Specific and planned improvements include 1) more time dedicated to the group debriefing, and 2) adding a discussion about the potential consequences of the generalisation of population groups related to CC learning cases.
DISCUSSION/REFLECTION/LESSONS LEARNED: The use of simulated patients has long been used in medical education. However, to our knowledge, this project is one of the few uses of simulated patients in a CC curriculum. Getting past a traditional CC curriculum and offering an educational setting that insists on interactivity, self reflection and real clinical practice is a relevant way to match the triad at the heart of CC « knowledge, attitude and skills ». As globalisation makes CC essential for medical practice, other settings are encouraged to take advantage of this international example : using innovative teaching medium adapted to the local contextual issues about diversity.
DESIGNING AND PILOTING A CURRICULUM IN CLINICAL EMPATHY FOR INTERNAL MEDICINE RESIDENTS, IN ORDER TO IMPROVE CLINICAL SKILLS IN CROSS-CULTURAL PATIENT CARENathan Bertelsen1,2; Michelle DallaPiazza1; Louis H. Miller1; Antoinette Schoenthaler2,1. 1NYU School of Medicine, New York, NY; 2NYU School of Medicine, New York, NY. (Tracking ID #1937125)
NEEDS AND OBJECTIVES: Competency in cross-cultural sensitivity, awareness and communication is considered an essential skill for physicians. Clinical empathy is increasingly recognized as a skill linked to improved patient satisfaction, adherence, continuity, and trust in health care providers and systems. Accreditation Council for Graduate Medical Education (ACGME) internal medicine milestones include the expectation that all graduating residents demonstrate competency in cross-cultural care. The current project hypothesized that clinical empathy is a measure that can demonstrate this competency. To that end, a pilot curriculum was developed, in order to define, teach and assess clinical empathy for residents in internal medicine.
SETTING AND PARTICIPANTS: NYU School of Medicine offers a large ACGME residency training program in internal medicine in a diverse setting of New York City. Faculty with expertise in working with multicultural patient populations in various ways, as well as GME program leadership, were identified to develop content for this curriculum. These patient populations included immigrants who experienced psychological and physical trauma, persons living with HIV, and community groups dedicated to reducing health disparities. Over 90 current second- and third-year internal medicine residents participated in groups of 10–15 residents, over 7 monthly ambulatory care clinical rotations at Bellevue Hospital, a municipal hospital and teaching site for NYU.
DESCRIPTION: After reviewing clinical empathy literature and drawing on similar exercises used in other venues, teaching exercises were piloted in a one-hour session to each successive group of residents. Background on clinical empathy theory, self-awareness exercises, and videos were used. Clinical cases to illustrate empathetic challenges were discussed, which included adherence, informed consent, health literacy and numeracy, trust and continuity, language and interpreters, traditional health beliefs, and the concept of the healing environment.
EVALUATION: Throughout each session, residents were encouraged to explore their own cultural identities, engage actively in discussion of clinical empathy, and to share personal experiences of clinical empathetic challenges with their peers. Participating faculty used the new ACGME milestone #18, measuring whether each resident “responds to each patient’s unique cultural needs,” as a general guide for discussion. Resident feedback was reviewed after each exercise and adapted to each successive session, with the ultimate goal of a modular curriculum that can be adapted to multiple venues.
DISCUSSION/REFLECTION/LESSONS LEARNED: Clinical empathy offers a promising clinical measure in which to demonstrate effective cross-cultural patient care. Initial feedback from the residents indicated that they had difficulty understanding the relevance of clinical empathy to patient care through theoretical discussions on culture and empathy. However, the combination of self-awareness exercises and case-based examples which illustrated clinical empathy translating into better outcomes was more successful. One hour in a classroom was a major challenge to engage residents, while having more time and incorporating standardized patients would have likely improved outcomes. A major limitation was the need for an objective structured clinical examination in which to demonstrate improved skills in clinical empathy among residents. To this end, a focus group of faculty in general internal medicine at NYU has been identified to review and standardize these findings into a modular curriculum, which can be shared among multiple instructors within the ACGME milestone context, in order to define, teach and assess clinical empathy for training residents in cross-cultural patient care.
DEVELOPING AN ENTRUSTABLE PROFESSIONAL ACTIVITY (EPA) FOR RESIDENT-LED SHARED MEDICAL APPOINTMENTS (SMAS)Yamini Saravanan; Rebecca Toutant; Richard Pels; Patrick T. Lee. Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1939296)
NEEDS AND OBJECTIVES: As academic, primary care clinics transform into Patient-centered Medical Homes (PCMH), how can Internal Medicine residency programs develop Entrustable Professional Activities (EPAs) to help faculty understand and evaluate newer PCMH skills? Entrustable Professional Activities (EPAs) capture clinical practice in an integrated manner, reflecting the multiple medical competencies that are involved in any one clinical activity (1,2,3). “Entrustment” specifies the competencies required for the resident to practice with progressive independence (1). As clinical practices transform to PCMHs, teaching faculty in these practices are unfamiliar with the principles of PCMH transformation and feel unprepared to teach trainees (2). We present our initial experience collaborating with residents to develop an EPA for a resident-led Shared Medical Appointment (SMA), an important strategy in PCMH deployment (3). The objectives are to: 1. Demonstrate a process by which our site collaborated with third year residents to identify an EPA for a resident-led SMA for diabetic patients. 2. Identify a set of preliminary clinical behaviors that characterize the EPA for resident-led SMAs.
SETTING AND PARTICIPANTS: The Primary Care Center (PCC) is a teaching, adult medicine clinic for nine internal medicine residents at the Cambridge Health Alliance, a safety-net community health system affiliated with Harvard School of Medicine. The PCC started resident led SMAs for diabetic patients in September of 2013. Every 6 weeks, third-year Internal Medicine residents co-lead an SMA.
DESCRIPTION: We conducted a series of three focus groups on residents to identify learning needs and to invite resident co-leadership in the SMA initiative. A series of skill building seminars, entitled “learning dinners,” were developed and hosted every 2–3 months. These learning dinners were co-led by a physician and a dietitian, with experience in group facilitation. An iterative reflection and narrative process facilitated ongoing learning and improvement. One week before each SMA, the third year resident and dietitian met to identify themes for discussion and to plan methods of facilitation. This plan was recorded in an e-group site, Evernote®, allowing colleagues and preceptors to provide constructive feedback. After each SMA, the resident posted “learning narratives” on Evernote. These included both Likert scale and open ended items to facilitate personal reflection. The physician and dietitian faculty provided additional feedback via e-mail after reading the learning narrative and observing the group. The feedback centered around specific behaviors to effectively mange the huddle or group that the resident did or did not demonstrate.
EVALUATION: We will qualitatively analyze the learning narratives, and feedback messages to identify common behaviors that made the group successful. These behaviors will in turn inform writing an EPA for a resident-led SMA. We will share the developed EPA with residents and SMA experts for further validation. We will present summarizes description of this EPA, mapped to specific behavioral expectations for the resident, and relevant competencies and PCMH principles.
DISCUSSION/REFLECTION/LESSONS LEARNED: This educational innovation outlines a process that can be used by other educational programs to develop EPAs for PCMH activities or for other novel clinical compentencies in which faculty may have little or no experience. Further study needs to be done on whether these EPAs or the EPA paradigm more generally prove valuable for faculty and residents. Developing an EPA for any activity in which medical faculty are unprepared to teach and supervise will help (1) identify learning needs for residents and faculty (2) develop cross-disciplinary mentorship for residents, and (3) provide more concrete criteria for faculty to evaluate residents. The process presented is reproducible and relevant to other clinical programs.
DEVELOPING AND IMPLEMENTING AN INTERN TEACHING CURRICULUMAnna K. Donovan; David Linz; Carla Spagnoletti. University of Pittsburgh School of Medicine, Pittsburgh, PA. (Tracking ID #1934963)
NEEDS AND OBJECTIVES: Teaching skills are critical for physicians, as evidenced by their inclusion in the Practice-Based Learning and Improvement ACGME Competency. These skills are honed slowly over many years, and can be thought of as taking place on a developmental continuum. Residency is the first venue where most physicians have an opportunity to formally teach. Yet, few published interventions describe teaching interns how to teach. A survey of our Internal Medicine interns and medical students in 2012 revealed that interns value teaching and significantly impact medical students’ learning on the wards; yet, the interns felt largely unprepared to teach. Given the findings of this needs assessment survey (Linz and Spagnoletti, JGIM Supplement of SGIM Annual Meeting Abstracts, July 2013), we developed a curriculum to prepare interns for medical student teaching on the wards. Our clinician-educator faculty met several times to determine the teaching skills most essential for interns and concluded that the curriculum should focus on: role modeling, selecting and optimizing teachable moments, thinking out loud, and coaching.
SETTING AND PARTICIPANTS: Sixty-one of our 85 IM, Medicine-Pediatrics, Preliminary Medicine, and Transitional Year interns attended a three-and-a-half hour workshop. By having this workshop in September, it was hoped that most interns would have had an opportunity to teach medical students and identify some challenges in doing so. Coverage of clinical responsibilities was arranged so that all interns except those on nights or vacation could attend. Nine clinician-educator faculty facilitated the small group portion of the workshop.
DESCRIPTION: After completing a pre-curricular survey, interns attended a 75 min, large group session that included: an introduction from the Residency Program Director on the importance of the intern’s role in teaching medical students; a discussion from the Clerkship Director on the “Care and Feeding of Medical Students”; an introduction to teaching skills important to interns; and a discussion and demonstration of the key steps of role modeling. The remaining 2 h of the workshop were spent in small groups consisting of four to seven interns and one facilitator. The small group format for “teachable moments” and “thinking out loud” included a question and answer session about use of each of these skills, a brief didactic about how to use the skills, an example case script demonstrating each skill, and an opportunity for group members to practice each skill in an observed role play. After the teachable moments and think out loud sections, facilitators briefly discussed the role of interns as coaches who provide informal, regular, timely feedback. Then, the group brainstormed ways to give effective feedback. Finally, facilitators helped interns to set two teaching goals for the year using the SMART (Specific, Measurable, Attainable, Relevant, Timely) Goals framework. Faculty mentors will follow-up on these goals with the interns at a teaching workshop planned for spring and at their end of the year advising session.
EVALUATION: The pre-curricular survey assessed teaching knowledge, frequency of various teaching activities, and self-reported quality of teaching activities. Eighty-three percent of interns surveyed felt that interns play an important role in the education of medical students, and 89 % felt enthusiastic about teaching. However, 60 % of interns lacked confidence in their teaching ability, 68 % were unsure about teaching expectations, and 69 % did not feel well prepared to teach. Interns will complete the same survey at the end of the intern year to compare changes in teaching knowledge, frequency, and quality. Additionally, this year’s interns will be compared to last year’s intern class, which completed the same survey but did not receive the curriculum. Additionally, medical student clerkship evaluations of interns include a component about teaching quality which will be compared before and after the curriculum. Finally, intern attendees completed learner satisfaction questions and comments. Overall, interns rated both the large and small group activities highly. Greater than 95 % of interns felt that the large and small group activities around teachable moments, thinking out loud, and coaching were either moderately or very useful, while 87 % of interns felt the role modeling section was moderately or very useful. Additionally, 83 % felt that the workshop “highly” or “very highly” affected the way they think of themselves as medical student teachers, and 85 % felt that the curriculum would change their behavior.
DISCUSSION/REFLECTION/LESSONS LEARNED: With programmatic support including faculty and intern time, an intern teaching retreat is both feasible and well-received. We intend to use the content of this workshop to inform the development of a longitudinal residents-as-teachers curriculum involving two additional interactive workshops, which are slated for the end of the intern year and the middle of the second year of residency.
DEVELOPING QUALITY-CONSCIOUS PHYSICIANS: THE VALUE OF A RESIDENT-LED QUALITY IMPROVEMENT INITIATIVEAlexandra Perel-Winkler; Amit K. Hiteshi; Deepti Zalavadia; Tamara Goldberg. St. Luke’s-Roosevelt, New york, NY. (Tracking ID #1937960)
NEEDS AND OBJECTIVES: Implementing quality improvement (QI) initiatives in the outpatient setting is vital for training physicians, particularly within the context of a performance-based health care system. Yet few curricula have effectively utilized residents as project leaders. One major barrier has been the constraint of a rotating-provider schedule. Objectives: 1. To illustrate that empowering residents as leaders in the design and implementation of quality improvement work is a valuable educational experience. 2. To demonstrate that our resident-led, practice-based quality improvement initiative is feasible amidst a rotating-provider schedule.
SETTING AND PARTICIPANTS: One hundred thirty-eight Internal Medicine residents are divided into quartiles which rotate through a two-week primary care block every 6 weeks. Residents are assigned to one of three urban community outpatient clinics for their continuity practice. At each center, a faculty site director oversees the projects and clinical care team members participate in implementation. Two residents per quartile at each site are designated ‘QI leaders’ and are responsible for driving the action phase of the curriculum.
DESCRIPTION: Foundation phase: Prior to project implementation, residents participated in faculty-led didactic sessions focused on general principles of quality improvement, and more specifically, the PDSA (Plan-Do-Study-Act) model. Action phase: During week one of the primary care block, residents implement site-specific PDSA projects addressing a core quality indicator. During week two, results are analyzed in small group learning sessions, and new PDSA projects are generated for the upcoming block. While all residents participate, the QI leaders are responsible for PDSA selection, coordination with residents and staff, data collection and analysis, and project ‘hand-offs’ to the upcoming block leaders. In order to better understand project feasibility and the educational value of this leadership role, we developed a survey tool addressed to all QI leaders.
EVALUATION: Using a self-designed questionnaire, we surveyed fellow QI leaders after the completion of the first action phase of the project to assess: attitudes, project feasibility, QI knowledge, and communication. The overall response rate was 18 out of 21 resident leaders (86 %). Favorable attitudes towards QI projects increased from 22 % pre-initiative to 72 % post-initiative. This pilot was considered feasible to lead (83 %) and execute (89 %). Leaders noted improved self-knowledge of design (83 %) and implementation (83 %) of PDSA’s after partaking in the curriculum. Sixty-five percent felt inter-block communication between residents was improved, while half felt the project increased intra-block communication.
DISCUSSION/REFLECTION/LESSONS LEARNED: Within the context of a rotating-provider schedule, our resident-led quality improvement initiative appears feasible and educationally valuable. Our results strongly suggest that integrating this leadership model into a trainee curriculum can improve attitudes toward QI work, increase knowledge of practice improvement, and augment resident QI exposure without oversaturating their schedules. Of note, while this continuous PDSA cycle format provides a simple structure and appears to improve inter-block communication among residents, intra-block communication barriers should be explored further. In sum, as more Internal Medicine programs adopt a 6 week inpatient-2 week outpatient schedule, our rapid-cycle PDSA curriculum highlights a viable way to enhance resident training and create quality-conscious physician leaders.
DEVELOPMENT OF A BEDSIDE TEACHING SERVICE TO ENHANCE PHYSICAL EXAMINATION AND CLINICAL REASONING SKILLSLisa Altshuler; Danise Schiliro; Douglas Bails; Patrick M. Cocks; Ellen Cogen; Jesenia Fernandez; Margaret Horlick; Michael Janjigian; Louis H. Miller; Valerie Perel; Sondra Zabar. NYU School of Medicine, New York, NY. (Tracking ID #1938440)
NEEDS AND OBJECTIVES: Deficiencies in physical examination skills among medical students, residents and even faculty have been documented for decades. Residents also are spending less time in educational activities and in direct patient care. Recent studies have suggested that with the new work hour rules, interns spent only 12 % of their time in direct patient care. With decreases in length of inpatient stays, patients are being discharged with more complex follow-up needs, highlighting the need for effective communication with outpatient providers. Bedside teaching offers the opportunity to develop and strengthen clinical skills, including physical diagnosis, clinical reasoning and communication skills. Additionally, the importance of clear, targeted verbal and written communication of care plans and clinical needs is essential to patient safety and good clinical care. We designed a focused 2 week rotation addressing these educational needs.
SETTING AND PARTICIPANTS: We designed an inpatient rotation at Bellevue Hospital Center, a public hospital. First and second year Internal Medicine residents at New York University School of Medicine were participants, with two first year and one second year resident per 2-week rotation. To date, 45 residents have completed the rotation.
DESCRIPTION: Based on focus groups, surveys, in-depth interviews of faculty and residents, and literature reviews, a 2-week inpatient rotation was designed and implemented to 1) to improve physical diagnosis, clinical reasoning and written and oral communication abilities in residents, 2) strengthen attending faculty’s comfort with teaching these skills. The rotation utilizes two 90-minute daily bedside teaching, and targeted physical examination and clinical reasoning sessions daily, at least one delivered by “master clinicians” and supported by attending faculty. Daily direct observation and detailed feedback of resident performance in these domains supports learning.
EVALUATION: An evaluation model was developed linking resident skill on performance-based measures of clinical reasoning and communication to quality of care outcomes. Resident measures including physical examination skill (adapted mini CEX) and retrospective pre-post measure of perceived skill, and quality of discharge summaries, are being tracked post-intervention to assess maintenance of effects. Patient level outcomes include length of stay, readmissions, patient satisfaction and disease-specific measures. Impact of master clinician teaching on attending faculty is being assessed as a faculty development effort, thus broadening the curriculum’s reach.
DISCUSSION/REFLECTION/LESSONS LEARNED: Initial results suggest the curriculum is well received by learners and faculty. The opportunity for deliberate modeling of physical examination skills and connection of examination results to clinical reasoning pathways by master clinicians provides unique training that is unavailable in other settings. This model for assessing the curriculum outcome can contribute to efforts to link curriculum, clinical care and health outcomes in general.
DEVELOPMENT OF A NOVEL PRE-CLINICAL MEDICAL SPANISH PROGRAM AT ONE UNITED STATES MEDICAL SCHOOLDanielle Dougherty1; Louisa Holaday1; Jonathan Waldmann1; Zahra Dawson1; Joel Purkiss1; Angad Singh2; Lauren Rodriguez4; Nathan Stern3; Stephanie Eldred1; Ali Dulchavsky1; Sarah Bell1; Tomas Huerta1; Elizabeth Feenstra1; Nita Valikodath1; Rajesh Mangrulkar1. 1University of Michigan, Ann Arbor, MI; 2University of Washington, Seattle, WA; 3University of California - San Francisco, San Francisco, CA; 4Henry Ford Hospital, Detroit, MI. (Tracking ID #1940164)
NEEDS AND OBJECTIVES: The Latino population in the United States faces many cultural and linguistic barriers to health care, contributing to poorer health outcomes when compared to their non-Latino counterparts. Research has shown that language barriers between patients and their providers adversely impact the quality of care the patients receive and result in longer hospital stays, more medical errors, and lower patient satisfaction. Latinos are the largest ethnic minority in the US, comprising 16 % of the population, and 30 % by the year 2050. There is not expected to be a proportionate increase in Spanish-speaking physicians, which suggests an alarming rise in language-related health care disparities. Even now, in California, there are 318 physicians per 100,000 English-proficient patients while there are only 38 Spanish-speaking physicians per 100,000 LEP Latinos.4,5. Thirty-three percent of Spanish-speaking persons in the United States report speaking English less than “very well,”3 and thus the need for Spanish-speaking, culturally competent physicians is apparent and increasing. A 2005 systematic review found that cultural competence training improves knowledge, attitude, and skills of health professionals and impacts patient satisfaction.
SETTING AND PARTICIPANTS: The University of Michigan Medical School (UMMS) Medical students in their pre-clinical years are taught by a professional Spanish instructor in a small classroom twice a week. The faculty advisor, a native Spanish-speaker dedicated to the program, also attends the class to provide valuable clinical insight, answer questions, and provide feedback.
DESCRIPTION: The pilot year was 2010–2011, and after 3 years of further development, overseen by the Medicine in Spanish Student Curriculum Committee (MSCC) and through feedback and guidance from the Office of Medical Student Education (OMSE) and the Curriculum Planning Committee (CPC), the course has been finalized as a for-credit pre-clinical elective for 2013–2014, the first at UMMS. There are two cohorts of 14 students, who receive 2.5 h of class/week for 15 weeks total. The curriculum was designed to mirror the M1 course schedule, using organ-based systems with cultural-competency education interspersed throughout. Students receive a coursepack at the beginning of the course, and additional resources and assignment information is available on a CTools website (a University of Michigan web-based environment used by instructors, researchers and students). Class weeks are as follows: Review (including anatomy and grammar) and general history and physical questions Cardiology Pulmonology Endocrine and Renal Neurology Psychiatry Folk Illness and Household Remedies Musculoskeletal Oncology Gastrointestinal Reproductive and Genitourinary Informal simulated patient interview Practice weeks with trained Spanish-speaking community members. Students are required to shadow a Spanish-speaking interpreter in the hospital for one half-day to give students the opportunity to witness a physician encounter in Spanish and also to gain experience in using an interpreter, a skill that will certainly be needed in the future for other non-English patient encounters. Overseen by the Faculty Advisor, students develop an educational session for Spanish-speaking community members
EVALUATION: Students are evaluated using three quizzes, one final exam, and a final Standardized Patient Interview in Spanish using SPIs trained through the rigorous University of Michigan program. These interviews are graded using a rubric that was developed with the assistance of the Standardized Patient Program at UMMS. Students provide feedback on the class each week using the same forms that are utilized for feedback on all pre-clinical classes at UMMSm and two student focus groups are held.
DISCUSSION/REFLECTION/LESSONS LEARNED: In 2010, a pilot course for Medicine in Spanish was initiated at UMMS to help in graduating physicians who are able to provide excellent care in Spanish. It became a formal, for-credit, UMMS-endorsed elective at the end of its third year after many years of development and collaboration between students, faculty, and the administration. Over the course of the first 3 years, many changes were implemented, including redeveloping the curriculum, appointing a faculty advisor, hiring a new instructor, adapting the schedule, developing novel assessments, integrating with existing technology at UMMS, implementing a structured community service project, and ensuring adequate feedback on the course from the students. We are now working on developing and improving additional components of a longitudinal Medicine in Spanish program at UMMS, including the creation of a faculty-led case discussion group for fluent and native speakers in 2012–2013, dedicated space for students in Spanish-speaking clinics in their clinical year, and further development of a Beginner’s course, which is currently taught by student volunteers. We are also constantly improving the course’s approach to cultural competency.
EDUCATING FOR CHANGE: MEDICAL STUDENTS DEVELOP ORGANIZATIONAL LEADERSHIP SKILLS THROUGH STUDENT-DRIVEN COMMUNITY-BASED FIELD PROJECTSBrent C. Williams1; Senait Fisseha2; Joy Williams3; Patricia Mullan4. 1University of Michigan, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI; 3University of Michigan, Ann Arbor, MI; 4University of Michigan, Ann Arbor, MI. (Tracking ID #1929187)
NEEDS AND OBJECTIVES: Leadership training in medical education is now widely recommended, though consensus is lacking on the appropriate scope and best methods for leadership curricula. A central goal of our newly created Global Health and Disparities (GHD) co-curriculum is to “prepare medical students to be agents of sustainable change to reduce domestic and global health disparities”. Therefore we developed an experiential leadership curriculum focusing on working with and developing organizations to promote change to address health disparities. Learner objectives are to: a) identify personal characteristics related to effectiveness as an organizational leader, and b) build, critique, and refine a collaborative project to address health disparities using frameworks and processes of demonstrated effectiveness in team and organizational development, and c) develop a personal learning plan for becoming a more effective leader.
SETTING AND PARTICIPANTS: 34 s year medical students enrolled in the GHD co-curriculum at the University of Michigan during 2013–14, and 9 community-based organizations in a 60-mile radius of the medical campus. All GHD activities are in addition to the formal medical school curriculum.
DESCRIPTION: The GHD co-curriculum consisted of three main components: ● Field projects with community-based organizations (CBOs). Groups of 3–5 students contacted selected CBOs to design and implement a new project or program over 7 months, of immediate value to the CBO and/or its constituents. CBOs were coached to co-design the intervention with the students. A total of 9 CBOs were recruited to participate, and included community health centers, a rural psychiatry outreach program, free clinics, school-based clinics, and the UM Community Outreach Program. ● Four two-hour seminars. Instructional methods included discussions with organizational leaders in health disparities, student-led case studies, and field team discussions and presentations applying key concepts. Conceptual frameworks for team and organizational leadership are based on: a) stakeholder analysis (including collaborators, customers, suppliers, and external stakeholders), b) the GRPI (Goals - achieving consensus on clear, achievable goals; Roles - distribution of authority, responsibilities, and tasks; Processes - decision-making, scheduling, communication; and Interactions - managing interpersonal relations) model of team development, and c) Community Based Participatory Research (CBPR), with its focus on joint decision-making, power-sharing, and mutual accountability across academic-community partnerships ● Final presentations to CBOs and GHD. Student teams present a ‘deliverable’ to the CBO and, in a separate session, a description of the project and lessons learned to GHD students and faculty.
EVALUATION: Program evaluation will include: ● Pre- and post-intervention surveys of students’ self-rated leadership skills using the validated Empowerment Leadership Questionnaire. ● CBO leadership interim and final online surveys and phone interviews measuring program processes and outcomes, effects on the CBOs, and ratings of individual and groups of students. ● Review of students’ interim written assignments for inclusion of key concepts. ● Final project write-up evaluation of project completion rates, inclusion of key concepts in project descriptions, reflections that include practical applications of lessons learned.
DISCUSSION/REFLECTION/LESSONS LEARNED: The scope and methods of current leadership curricula vary widely among medical schools; many curricula focus on team function in medical practice, and are classroom or short-exercise based. In contrast, our curriculum is intended to focus on organizational leadership to foster change. Guiding principles are that: a) leadership is learned mainly by doing with structured reflection and feedback rather than learning without an authentic context, b) learning about change agency requires that students engage in risk-taking by developing and testing new ideas rather than observe existing organizational operations, and c) building genuine collaborations across differing cultures and organizations that includes structural and process-based attention to accountability and shared decision-making is essential to leadership skills development. Challenges include: a) keeping students’ time burden manageable while engaging them with (at times distant) CBOs, and b) creating and maintaining opportunities for new projects each year among a diverse network of voluntary CBOs, and c) securing faculty time to implement and evaluate the leadership curriculum.
EVALUATING COMPATIBILITY MATCHING IN A COMBINED INTERNAL MEDICINE AND PEDIATRICS RESIDENCY MENTORING PROGRAMDaniel McFarlane1,2; Curt Walker1. 1The Ohio State University Wexner Medical Center, Columbus, OH; 2Nationwide Children, Columbus, OH. (Tracking ID #1936648)
NEEDS AND OBJECTIVES: Medical residency training is a challenging period when residents make important decisions that steer the direction of their careers. It can be difficult to determine which experiences serve as validation of career goals and which experiences aid in personal growth. Mentoring relationships have often served the function of providing personalized guidance and support to individuals in these learning contexts. Although studies on formal mentoring relationships have encompassed numerous professional contexts, few have examined components of compatibility between medical trainees and professionals and their effect on the success of the mentoring relationship. This is the aim of our study.
SETTING AND PARTICIPANTS: The current initiative aimed to develop a multidimensional matching process using components of compatibility based on demographics and personal preferences to pair combined internal medicine and pediatrics (Med-Peds) residents with similarly trained attending physicians. We assessed relationship outcomes associated with the matching process to determine the role of compatibility in realizing mentoring benefits.
DESCRIPTION: Outcomes of a structured mentor program that paired one Med-Peds resident (nResident = 19) with one attending physician (nMentor = 19) were compared to those of a class based mentor program (1 mentor paired with 8–10 residents; nClass = 17). Enrolled residents and volunteer mentors were given a survey that assessed demographics, personal interests, values, and professional goals. All mentors were Med-Peds trained despite representing different professional specialties. We derived compatibility scores from a combination of weighted survey responses and randomly assigned trainees to either a matched or unmatched group to test the role of compatibility in mentoring outcomes. The matched group (nMatched = 10) paired residents with the corresponding mentor who received the highest compatibility score. The unmatched group (nUnmatched = 9) randomly paired residents with the remaining mentors regardless of compatibility score. Mentors and residents were kept blind of their assignments and the purpose and expectations of the program were explained to all participants.
EVALUATION: We administered a program evaluation survey after 1 year to assess differences in relationship outcomes. Results of a series of z-tests for proportions showed supportive, yet non-significant trends in resident outcomes for matched mentor pairs compared to class based and unmatched pairs. Data were not sufficient to assess differences in mentor outcomes.
DISCUSSION/REFLECTION/LESSONS LEARNED: Matching residents with mentors provides a foundation of compatibility that can facilitate stronger more fulfilling mentoring relationships versus random assignment. Compatibility based on professional goals was most sought after, followed by personal interests. We continue to enroll new residents and mentors (nResident = 29) to further investigate the role of compatibility in mentoring outcomes. Personality typing was also considered as a foundation for compatibility and we intend to study if matching based on personality type would provide stronger outcomes. Based on our data, full benefits of a mentoring relationship were not realized in either group. Therefore, future steps include targeted education to develop mentoring skill sets as well as to ensure that mentees are receptive to mentor guidance.
EVALUATION OF THE MAINTENANCE OF COMPETENCY PROGRAM: PILOT YEAR 1Nancy Stewart; Nicole M. Twu; Frank Zadravecz; Meredith Borak; Dana P. Edelson. The University of Chicago, Chicago, IL. (Tracking ID #1940145)
NEEDS AND OBJECTIVES: Approximately 200,000 patients experience a cardiac arrest in United States hospitals each year, with a mortality rate of over 80 %. Cardiopulmonary resuscitation (CPR) is the mainstay of therapy for these patients but CPR is a complex psychomotor skill that is difficult to perform well. The standard of care for training and certification in this lifesaving skill is biannual, instructor led courses. Yet, prior research suggests that the skills developed in training decay well before the end of the two-year certification period, with the most rapid skill decay occurring within the first 6 months. We sought to test the feasibility of a program of self-service, quarterly training in Basic Life Support (BLS), as an alternative to in-person biannual bolus training.
SETTING AND PARTICIPANTS: All nurses and nursing assistants caring for adult patients at the University of Chicago were eligible to participate. The study was jointly supported by the American Heart Association (Dallas, TX) and Laerdal Medical (Stavanger, Norway) and was approved by the University of Chicago Internal Review Board. Participation was voluntary, with written consent, but subjects were offered a $5 gift card upon completion of the 1st and 4th quarters.
DESCRIPTION: The University of Chicago served as a pilot site for the Resuscitation Quality Improvement (RQI) program developed jointly by the American Heart Association and Laerdal. The program involved the use of specially designed self-service CPR mannequins sitting on top of mobile carts connected to laptop computers. These carts were placed in close proximity to clinical areas to enable participants to interact with the system during breaks as each quarterly module was designed to require less than 10 min to complete. Modules alternated between psychomotor skills stations, requiring participants to perform chest compressions and or assisted ventilation, and cognitive modules. Participants received reminder emails when they were due to complete a new module. If more than 6 months lapsed between modules the subjects were deemed to have dropped out. These subjects were then surveyed to assess barriers to participation.
EVALUATION: Following the open enrollment period, 123 participants were consented. Sixty- three (51 %) of participants completed Q1, 41 (33 %) of participants completed Q2, 50 (41 %) of participants completed Q3 and Q4. Of the 123 study participants, 44 completed the post-drop out anonymous survey, and of those, only six respondents stated they completed at least one module. Forty-one (93 %) of respondents primarily works day shifts. Thirty-six (82 %) respondents thought the MOC would be more convenient. Twenty-three (52 %) respondents thought the MOC would help maintain their skills. Survey results determined major barriers to completion included a lack of time to leave clinical responsibilities 36 (82 %), difficulty actively compressing the manikin 18 (41 %), and a lack of administrator support including reminder e-mails/notifications 17 (39 %).
DISCUSSION/REFLECTION/LESSONS LEARNED: This pilot program demonstrated the difficulties encountered in implementing a self -service training model during clinical work. Avoiding a full day course every 2 years may not be sufficient incentive for clinical care providers to switch to a new training modality. Successful implementation of such a program may require a mandate and/or additional incentives. Also, combining instructors with the carts to actively encourage participants to interact with the system could potentially maximize participation. Finally, alternative ways to engage nursing staff in the program will need to be evaluated, such as integrating the MOC during other nursing requirements.
FLIPPING THE CLASSROOM INTO THE HOSPITAL: INTERACTIVE CONTENT TO INTEGRATE BASIC SCIENCE INTO THE CLERKSHIPCharles D. Magee; Lynn Byars. Uniformed Services University, Bethesda, MD. (Tracking ID #1939408)
NEEDS AND OBJECTIVES: Our university has undertaken curricular reform, aiming to integrate clinical and basic sciences into an 18-month pre-clerkship, 12-month clerkship, and 18-month post-clerkship model. The pre-clerkship curriculum consists of a modular, systems-based introduction to basic and clinical science. The new pre-clerkship timeframe was truncated to 18 months, resulting in a substantial reduction in contact time with the basic science faculty. The clerkship curriculum consists primarily of traditional inpatient and outpatient clinical experiences. Basic sciences were identified as threads to be integrated across the entire curriculum. Prior to curriculum reform, basic science concepts were minimally integrated into our internal medicine clerkship. We aim to develop an effective method for integrating basic science concepts into the clerkship setting while harnessing the expertise of our basic science faculty to improve clinical performance measures. Objective: To deliver interactive, self-paced, instructional material to solidify key basic science concepts immediately preceding integrated clinical teaching activities via: - Collaboration with basic science faculty to develop expanded educational roles into the clerkship setting; and - Development of educational activities that align clinical and basic science knowledge in internal medicine clerkship educational objective.
SETTING AND PARTICIPANTS: Our university is a US allopathic medical school with clerkship students rotating in hospitals across the United States. This innovation is designed for clerkship students rotating on both ambulatory and inpatient internal medicine.
DESCRIPTION: The internal medicine clerkship implemented weekly interactive group sessions (IGS), which are case-based discussions of internal medicine topics led by a clinician-educator. The learning objectives for each IGS session include approximately 20 % basic science material. An identified challenge to successful IGSs is that the physicians who deliver all didactic material are typically less facile at basic science instruction. Additionally, our students complete clerkships at sites across America, making direct contact time with basic science professors impossible to realize in all clerkships. Collaborating with basic science faculty, basic science objectives are being converted into web-based didactic sessions to precede the IGS topic. Each session has 10–15 min of online material featuring narrative and interactive slides, embedded video and animation, and formative quiz questions to allow assessment of content mastery.
EVALUATION: For the innovation pilot, we are tracking timing of module completion prior to each IGS, time spent on the module, number of times accessed, and answers from pre-, post-, and embedded quiz questions. Surveys of students and faculty will assess satisfaction and perceived value with this innovation. Qualitative comments will be analyzed for themes that can direct the development of future content.
DISCUSSION/REFLECTION/LESSONS LEARNED: “Flipping the classroom” is an educational technique to allow student mastery of required knowledge prior to participation in expert-led synthetic activities. This offers a solution for meaningful integration of basic science content into the clerkship. This innovation allows basic science faculty to reach learners outside the classroom. Our basic and clinical scientists have welcomed this innovation. Our innovation aims to foster integration by delivering basic science expertise to the clerkship environment for transfer and synthesis of basic science knowledge to patient care.
GERIWARD FALLS: AN INTERPROFESSIONAL TEAM-BASED CURRICULUM ON FALLS PREVENTION AND SYSTEMS-BASED CARE FOR THE HOSPITALIZED OLDER ADULTStephanie Rennke1; Claire Larson1; Julie Vavuris3; Vicki Jue2; Josette Rivera1; Betty Smoot4. 1UCSF, San Francisco, CA; 2UCSF, San Francisco, CA; 3UCSF, San Francisco, CA; 4UCSF, San Francisco, CA. (Tracking ID #1939775)
NEEDS AND OBJECTIVES: Interprofessional collaboration is key for both student education in geriatrics and in the care of older adults, but is often underemphasized in medical education. Falls are a source of significant morbidity and mortality in the geriatric population. GeriWard Falls is an interprofessional team-based curriculum for health professions students to conduct a comprehensive falls risk evaluation at the bedside. The objectives included: 1) identify epidemiology and risk factors for falls; 2) work as a team to perform a focused inpatient falls risk assessment; and 3) propose a systems-based intervention to prevent falls.
SETTING AND PARTICIPANTS: The curriculum was piloted at a large academic medical center with patients over 65 years admitted to the medicine or cardiology service. Health professions students on clinical rotations in the hospital participating in the pilot included third-year medical, fourth-year pharmacy, third-year physical therapy, and graduate level nursing students.
DESCRIPTION: Interprofessional teams of 4–5 students met for a 2 h exercise which consisted of three parts: 1) a 90-minute bedside clinical exercise and completion of a bedside falls assessment, interviews with patient, caregivers and staff, physical examination and medication review; 2) development of a falls care plan and direct written communication with the patient and the primary inpatient medical team regarding prevention strategies and 3) propose systems-based interventions to reduce fall risk. Following the clinical exercise the students discussed their recommendations with a nursing, pharmacy or medicine faculty facilitator, and then contacted the primary medical team with their recommendations. The facilitators scored the student teams using a rubric on their falls assessment worksheet, system-based interventions proposal, and oral presentation.
EVALUATION: Twenty-three students participated in a pilot session in October 2013. Using a 5-point Likert scale, over 90 % of students agreed or strongly agreed that they learned skills applicable to future practice. Faculty rated the student presentations highly, citing the students’ ability to effectively collaborate, identify risk factors for falls, and propose systems-based interventions. The primary medical teams found the recommendations useful, and planned to implement at least one of the recommendations detailed in the student team’s falls care plan. On the post session survey completed by students, the score range for each component was 4–5 (“very good” to “excellent”) including: usefulness of the activity, overall quality of the session and likelihood that students will make changes in clinical activities.
DISCUSSION/REFLECTION/LESSONS LEARNED: GeriWard Falls is an innovative curriculum that emphasizes interprofessional collaboration during a clinical encounter with a hospitalized older adult. The activity was engaging for students, and helped them achieve competency with fall risk assessment. Communication of the students’ assessment to the primary medical team was not only useful to the primary team, but also helped students understand how systems can affect patient care.
GIVING EARLY MEDICAL STUDENTS A “HOME”: STUDENTS CAN MEANINGFULLY CONTRIBUTE TO CARE ON A YEAR-LONG CONTINUITY ROTATION IN A PCMHJennifer Mackinnon; Martin Muntz; Julie L. Mitchell. Medical College of Wisconsin, Milwaukee, WI. (Tracking ID #1940081)
NEEDS AND OBJECTIVES: To integrate early students into the Patient Centered Medical Home (PCMH). To develop a robust list of level-appropriate clinical tasks for early students that concurrently contribute to high quality patient care and advance learner knowledge and skills.
SETTING AND PARTICIPANTS: Our institution pairs a student with a preceptor in a year-long continuity course spanning the second half of the first year and the first half of the second year. Recruiting preceptors is a challenge that can be turned into an opportunity once appropriate clinical tasks are identified to advance the goals of the medical home and student education. To identify these tasks, the authors conducted local and regional workshops consisting of community and academic preceptors in internal medicine, pediatrics and family medicine. Sharing personal experiences, attendees added to the task list after considering principles of a medical home and evidence-based examples of how students can contribute. Sixty-seven physicians (including a fraction of residents) participated in the workshops. After removing duplicates and combining related ideas, 37 tasks were categorized within the PCMH standards. Examples include items related to specific history-taking and exam (such as standardized templates and blood pressure retakes), between-visit care (such as sharing results and ensure instructions were followed), connections to community agencies and strategies during transitions.
DESCRIPTION: Inspired by our list of clinically and educationally meaningful tasks for early students, we prepared students assigned to PCMH preceptors to contribute to care in a pilot program. Ten early students were provided an introduction to the PCMH and tools within our EHR, protocols to manage a diabetes registry, and a review of key preventive health guidelines. They were also given instructions on chronic condition management, including a pre-visit planning checklist. Students then worked within their preceptor-led clinic team in the continuity course. Preceptors were given independence in selecting specific clinical tasks they expected their students to master.
EVALUATION: We developed a robust list of tasks relevant to the early student that also allows students to contribute to care, setting up early students as valuable team members for preceptors in a PCMH. This value-added task list, which was generated with the help of both junior and more experienced physicians representing each of the primary care specialties, provides a “menu” of options to individualize teaching and add value for different teachers, learners, and patient populations. To our knowledge, this is the first list of PCMH-related tasks for early students.
DISCUSSION/REFLECTION/LESSONS LEARNED: Despite creating a list supported by a consensus of preceptors, we found individual preceptors widely varied in their expectations of students, based on their personal practice priorities and their own experience with items on the task list. Some preceptors voiced disagreement with students performing tasks that could be performed by other team members, and some preceptors were not proficient enough with the EHR tools and registry protocols to model use to students. Institutional educational leaders will use the task list and preceptor and student reactions to it to tailor preceptor preparatory materials and recruiting strategies. Further work will include the feedback of medical students currently enrolled and those recently graduated from this new program.
ONLINE RESOURCE URL (OPTIONAL): Link to Medical College of Wisconsin Faculty Development toolbox.
GOALS OF CARE AMBULATORY RESIDENT EDUCATION (GOCARE), A PILOT CURRICULUMMarianne Camargo1,3; Jacqueline K. Yuen2; Stephen Berns2; Diane E. Meier2. 1Rutgers, New Jersey Medical School, Newark, NJ; 2Mount Sinai Hospital, New York, NY; 3Mount Sinai Hospital, New York, NY. (Tracking ID #1900318)
NEEDS AND OBJECTIVES: Goals of care discussions frequently occur in the hospital setting, often after patients have lost decision making capacity, leaving health care providers and surrogates to make difficult treatment decisions with limited understanding of patients’ treatment preferences. This follows from missed opportunities to have advanced care planning (ACP) discussions with patients and their families in the outpatient setting. To address this gap, we piloted a curriculum to: 1. Enhance residents’ understanding of the importance of ACP in the ambulatory care setting. 2. Improve residents’ communication skills during outpatient ACP discussions. 3. Facilitate documentation of ACP discussions using the electronic medical record (EMR).
SETTING AND PARTICIPANTS: Second year Internal Medicine (IM) residents (N = 42) participated in the GOCARE curriculum as part of their 4-week ambulatory block from January to June 2013 at an urban, academic ambulatory care practice.
DESCRIPTION: The GOCARE curriculum content was guided by a focus group of IM residents on their communication training needs, a literature review of ACP communication strategies, and instruction from content experts. The instructional method was modeled after a workshop associated with improved communication skills for oncology fellows. It included didactics, a demonstration role-play by faculty, and a communication lab using trained simulated patients and family members for skills practice. The curriculum was delivered through weekly small group sessions of 6–9 residents led by 2 faculty members. In addition, residents completed at least one outpatient visit focusing on ACP discussions with 1–2 patients from their continuity panel who had chronic disease and a high likelihood of hospitalization. The (EMR) was re-configured to facilitate documentation and accessibility of ACP discussions.
EVALUATION: We used paired pre/post surveys to assess residents’ self-rated preparedness for communication challenges during outpatient ACP discussions before and after GOCARE. The survey used a descriptive 7-point Likert-type scale to rate the level of resident preparedness to perform the following: discuss health care proxy designation, deliver bad news, engage in ACP discussions, discuss treatment options with seriously ill patients and/or their families, elicit goals of care, discuss prognosis, and discuss hospice care. After GOCARE, the mean rank for all seven items increased 1–3 points on the scale, and this change was statistically significant (p < 0.001) for all comparisons. In addition, we compared residents’ willingness to initiate specific ACP discussion topics with patients and their families in the ambulatory setting. After GOCARE, more residents were willing to initiate conversations regarding goals of care (61 % vs. 93 %, p = 0.002), treatment options, including comfort care (54 % vs 90 %, p < 0.001), preferences on life-sustaining treatments (68 % vs. 93 %, p < 0.001), and resuscitation preferences (63 % vs. 93 %, p = 0.006). Furthermore, 95 % of residents had documented ACP conversations in the EMR for at least one patient during the course of the curriculum.
DISCUSSION/REFLECTION/LESSONS LEARNED: This pilot curriculum was created to improve residents’ understanding, attitudes and communication skills during outpatient ACP discussions. We found that residents’ self-efficacy with ACP discussion significantly improved after GOCARE. However, we did not use an objective method to rate change in communication skills. In the future, we plan to utilize pre-post curriculum OSCEs with standardized patients to objectively assess change in residents’ communication skills.
HANDOFF TRAINING FOR MEDICAL STUDENTS: EFFECTIVENESS AND SUSTAINABILITY OF KNOWLEDGEChristopher J. Smith; Grant Peterson; Gary L. Beck. UNMC, Omaha, NE. (Tracking ID #1938318)
NEEDS AND OBJECTIVES: The transfer of patient care between healthcare providers is a vulnerable time for patient safety. Incomplete handoffs can lead to adverse outcomes, yet few medical schools provide formal instruction on handoffs. The limited research evaluating handoff curricula for medical students has not examined the sustainability of acquired skills. To address these issues we developed a workshop to instruct senior medical students on handoff communication and examined its impact on participants’ immediate and extended attitudes and knowledge. The objectives for workshop participants were to: 1. Understand how poor communication during transitions of care impacts patient safety. 2. Identify key elements of effective handoff communication. 3. Demonstrate a standardized strategy for written and verbal handoff communication.
SETTING AND PARTICIPANTS: The intervention took place at a large, state-funded university in February and April 2013. An elective workshop in handoff communication was offered as part of residency preparatory program for senior medical students. Up to 12 students could participant in each session.
DESCRIPTION: During the 4-hour workshop, best-practices for handoff and discharge summary communication were reviewed. Following a brief didactic session, participants applied their skills to clinical scenarios in interactive small groups. Large group discussions were utilized to reflect upon the exercises and generate discussion.
EVALUATION: Participants’ attitudes and knowledge were tested pre- and post-intervention. A follow-up test was sent to participants and a control group in June 2013 to evaluate retention. Those completing the follow-up test received a $10 gift card. Attitude-based questions were rated on a 5-point Likert scale. Knowledge was tested with multiple choice questions and open-ended responses to clinical vignettes. Vignettes were scored on a 10-point scale by two blinded faculty members, with disagreements settled by consensus. Materials were tested for clarity prior to distribution. Twenty-four students participated in the seminar. All participants took the pre- and post-tests, and there was significant improvement in 12 of 13 attitude-based questions, 4 of 9 knowledge-based multiple-choice questions, and clinical vignette scores. Sixteen seminar participants and 21 control-group students took the follow-up test. Eleven participants completed vignette questions for all three tests. There was significant improvement between pre- and post-tests (6.34 vs. 8.55, p < 0.001), but this improvement decreased in follow-up (7.45). Only the April cohort maintained a significant improvement through follow-up testing (W = 0.831, p = .003). There was no difference in follow-up vignette scores between seminar participants and the control group.
DISCUSSION/REFLECTION/LESSONS LEARNED: Students’ attitudes and knowledge improved immediately following handoff training, but gains in knowledge declined in the following months. This is likely because students did not have the opportunity to routinely apply these skills in a clinical context. These findings support that, while handoff training is effective in improving attitudes and knowledge, it should coincide with assumption of clinical responsibilities.
HEALTH LITERACY IN TRANSITIONS OF CARE: AN INNOVATIVE OBJECTIVE STRUCTURED CLINICAL EXAMINATION FOR FOURTH YEAR MEDICAL STUDENTSReena Karani1; Kimberly Bloom-Feshbach1; Dana Casey1; Lucy Schulson1; Jonathan Giftos2; Peter Gliatto1. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Albert Einstein College of Medicine, Bronx, NY. (Tracking ID #1937013)
NEEDS AND OBJECTIVES: Only 12 % of Americans are considered to have proficient health literacy. Low levels of health literacy have been associated with multiple adverse outcomes. Recent evidence also indicates that low health literacy is a risk factor for hospital readmission. As part of a health literacy curriculum at the Icahn School of Medicine at Mount Sinai, we designed and implemented an innovative Objective Structured Clinical Examination (OSCE) to assess fourth year medical students’ ability to appropriately screen, counsel, and provide discharge instructions to patients of limited health literacy. Other institutions have implemented health literacy standardized patient encounters. Our OSCE is unique in that it a) focuses on the hospital discharge process, b) assesses fourth year medical students as part of an internship preparatory clerkship and c) specifically evaluates the efficacy of an evidence-based health literacy workshop.
SETTING AND PARTICIPANTS: Between January and April 2014, all fourth year students (n = 140) will undergo the Health Literacy in Transitions of Care OSCE with trained standardized patients (SP).
DESCRIPTION: In the OSCE, the fourth year student will prepare a patient for a safe hospital discharge. As part of this process, the student must screen the patient for low health literacy and educate the patient about diagnosis (pulmonary embolus), management (oral anticoagulation), and outpatient follow-up (INR monitoring). The student will also be required to write discharge instructions appropriate for patients of low health literacy. In order to allow for future research on the relationship between student participation in an evidence-based health literacy workshop and performance on the OSCE, 40 % of the class will serve as a control, receiving the workshop following administration of the OSCE.
EVALUATION: To assess a student’s ability to communicate with patients of low health literacy, the trained SP will complete a checklist. The checklist includes student performance on the following items: health literacy screening, use of plain language, delivery of a focused message, and teach-back, among other evidence-based communication techniques. The Flesch-Kincaid readability tool will be utilized to assess the reading level of the student’s written discharge instructions. The encounter will also be video recorded to assess inter-rater reliability between trained scorers. For feedback, each student will view his or her graded checklist and discharge instructions. After data collection is complete, we will assess the relationship between workshop participation and performance on the OSCE.
DISCUSSION/REFLECTION/LESSONS LEARNED: Transitions of care are a particularly vulnerable time for all patients. The Health Literacy in Transitions of Care OSCE is an innovative tool to train future interns to identify and better communicate with patients of all health literacy levels during the hospital discharge process. Curricula such as ours may ultimately make this time safer and improve health outcomes. *KBF, DC, and LS contributed equally and should be considered co-first authors
HOME VISITS FOR MEDICALLY COMPLEX PATIENTS IN A TERTIARY ACADEMIC MEDICINE CLINIC AS A TOOL FOR RESIDENT EDUCATION AND READMISSION PREVENTIONDuncan Vincent; Paul Chelminski. University of North Carolina Hospitals, Chapel HIll, NC. (Tracking ID #1897469)
NEEDS AND OBJECTIVES: Home visits are a much-valued but under-utilized way to provide care. Historically, providers have offered these in urban settings for logistical ease. We developed a multi-modal educational and clinical initiative with three principle aims: provide structured care outside of a standard clinic visit; provide rapid post-hospitalization follow-up for a subset of patients to decrease readmissions; and integrate resident physicians into this process as practitioners and learners.
SETTING AND PARTICIPANTS: The Charles Sanders Clinical Scholars Grant was created to promote personalized and humanistic medical care at the University of North Carolina at Chapel Hill as part of the educational mission. The first recipient of the award (an attending clinician educator) developed a home visit program that integrated resident physicians. Residents on ambulatory blocks accompanied the attending on home visits. The population consisted of established patients in the UNC Internal Medicine Clinic, which is a blended faculty and resident practice. Shortly after its inception, the program expanded to make the resident the lead physician in an initiative to decrease readmissions of recently discharged, high risk patients.
DESCRIPTION: Home visits were arranged by a multidisciplinary team including a social worker. They were conducted by the attending physician and usually one resident physician (sometimes a pharmacy resident). Residents were the lead physician for hospital follow-up visits. Medication reconciliation occurred at each visit with direct inspection of the patient’s pill bottles. Patients received counseling about medication adjustment, new prescriptions, laboratory, or imaging studies. Almost all visits were billed. After the visit, residents wrote a brief reflection of the experience. A master map was created of all the home visit locations.
EVALUATION: To date, there have been 62 unique home visits and 16 subsequent follow-up visits. Mean age of patients was 70 years (range 29–95 years). Fifty-two percent were male. Mean and median distances traveled round trip were 20 and 13 miles respectively that spanned six counties (range 0–95 miles). Average length of the visit was 30 min (range 10–75 min). Seventy-six percent of patients were insured with Medicare, 16 % with private insurance, 2 % with Medicaid, and 6.5 % were uninsured. Seventy-seven percent of patients were Caucasian and 21 % were African American. The patients were medically complex: 56 % had hypertension, 22 % had congestive heart failure, 29 % had coronary artery disease, 13 % had atrial fibrillation, 17 % had COPD, 16 % had diabetes, and 13 % had depression. Only ten visits (16 %) were conducted outside of usual clinic hours. Twenty-four visits (39 %) were urgent care visits for acute complaints. Ten percent of home visits were conducted for palliative care and hospice monitoring. An internal medicine resident was present for 75 % of the visits. There was a new prescription at 30 % of all visits. Forty-three percent were hospital follow-up visits occurring within 14 days of discharge. Seven percent of these patients were readmitted to the hospital within 30 days of discharge. By comparison, our general medicine clinic population has a 19 % re-admission rate within 30 days. A gift was offered at 17 % of visits. In 20 % of the households, the television was on in the examining space. A sampling of learner reflections after the visits revealed an enhanced appreciation for the social and environmental dimensions of care.
DISCUSSION/REFLECTION/LESSONS LEARNED: Home visits span a broad spectrum of patient encounters, from acute to chronic to palliative care. Interestingly, the median visit duration was not extended when compared to a standard clinic visit. We have demonstrated the feasibility of home visits in a non-urban teaching medical center. They circumvent barriers to prompt, patient-centered care that prevail in the traditional clinic visit. They can potentially prevent hospital readmissions and decrease resource utilization. Integrating learners into home visits promotes humanism in medicine. Resident-composed reflections emphasize the reciprocal nature of care between patients and providers in this non-time-pressured and non-regimented setting.
HOW PATIENT-CENTERED ARE YOU? THE IMPLEMENTATION AND ASSESSMENT OF A TRAIN-THE-TRAINER SHARED DECISION MAKING CURRICULUM FOR HOSPITAL BEDSIDE ROUNDSStephanie Rennke1; Bradley Monash1,5; Rebecca Blankenburg2; Debbie Sakai2; Stephanie M. Harman3; Adeena Khan1; Clarence H. Braddock4; Patrick Yuan1; Jason Satterfield1. 1UCSF, San Francisco, CA; 2Stanford University, Stanford, CA; 3Stanford University, Stanford, CA; 4UCLA, Los Angeles, CA; 5UCSF, San Francisco, CA. (Tracking ID #1939726)
NEEDS AND OBJECTIVES: Patient-centered medical care remains a primary goal of all health care providers and medical centers. Institutions are under increasing pressure to improve patient-centered outcomes, including patient satisfaction, and patients are taking a more active role in their own healthcare. Although the majority of providers believe they practice patient-centered care, patients frequently do not understand their condition or care plan, and their psychosocial characteristics are not considered. One of the primary means for improving the patient-centeredness of the care we provide is through patient engagement and shared decision-making (SDM). The objective of the curriculum is to improve patient engagement and SDM using a multi-modal strategy including train-the-trainer workshops, an educational campaign and expert observations with a real time feedback and audit system.
SETTING AND PARTICIPANTS: The curriculum is being piloted in 2013–2014 over a 6 month period at two large academic medical centers with internal medicine hospitalists, pediatric hospitalists and internal medicine and pediatric chief residents and residents.
DESCRIPTION: We developed a patient engagement and SDM curriculum as a multimodal strategy with three parts: 1) a series of train-the-trainer workshops for residents, chief residents and hospitalist faculty, with interactive exercises and videotaped role plays on SDM using the ASK-INFORM-ASK model; 2) an educational “campaign” and roll out including pocket cards, announcements, posters, reminders; and 3) expert faculty observations with real-time assessment with audit and feedback to the inpatient teams. A validated instrument, the Rochester Participatory Decision Making Scale (RPAD), is being used as a pedagogical tool and as a means to assess physician engagement in SDM. Program evaluation will include retrospective pre-post workshop questionnaires, RPAD ratings, and pre-post patient surveys.
EVALUATION: To date, a total of 20 medicine residents, fellows, and hospitalists have participated in the workshops. All participants showed improved confidence in using SDM tools, with a mean increase of 0.456 on a 4-point Likert scale. Participants rated their knowledge and self-efficacy in SDM higher after participating in the curriculum in all categories. The largest impact was on participants’ confidence with inviting patient and family participation in SDM (mean increase of 0.850), followed by confidence with asking about patient/family agreement with the decision and examining the patient’s or family’s concerns and problems with follow through (mean increase 0.800 and 0.700 respectively). Residents and hospitalist faculty agreed or strongly agreed that they learned skills applicable to future practice. There will be eight additional workshops in 2014, which will train approximately 40 residents and 40 hospitalists prior to the campaign launch and expert observations.
DISCUSSION/REFLECTION/LESSONS LEARNED: This train-the-trainer curriculum, including an educational “campaign” and use of a validated instrument to evaluate SDM at the bedside, is a novel approach to medical education and faculty development and improves learner self-efficacy. Participants were recruited to disseminate SDM and to actively engage other trainees and faculty by role modeling best practices and teaching SDM to the inpatient teams.
IDENTIFYING COMMUNICATION NEEDS FOR PALLIATIVE CARE PATIENTS TO DEVELOP A NARRATIVE BASED EDUCATIONAL TOOLLindsey N. Clark1; Henry Mortimer2; Ruth Evans3; Sarah H. Parker1; William S. Krimsky3. 1MedStar Institute for Innovation, Washington, DC, DC; 2Mortimer Communications Inc., Baltimore, MD, MD; 3MedStar Franklin Square Hospital, Baltimore, MD. (Tracking ID #1940054)
NEEDS AND OBJECTIVES: Communication between patient and physicians is repeatedly recognized as a key component for providing safe, high quality care to patients, particularly those dealing with chronic illness or requiring palliative treatment. However, only a small percentage of residents/physicians report having communication training. Further, didactic formats such as lectures, or simply shadowing another physician, may not be the most effective method to teach residents adequate communication techniques. Research suggests that medical learners need to be engaged in real patient experiences combined with reflective exercises to optimize communication skills. Combining these two elements into an education tool can lead to a change in behavior for better patient communication. This presentation will center on ongoing work to develop a narrative based education tool that combines actual patient chronicles spanning the arch of disease, from diagnosis through death, in conjunction with reflective exercises to enhance and teach communication skills to residents. This work is innovative as it utilizes actual and longitudinal patient narratives recorded in the healthcare setting, the micro-system where these issues occur. Thus, it can serve as a platform for developing education tools on communication with patients.
SETTING AND PARTICIPANTS: Participants included 26 patients and/or their care-providers with chronic and/or life-altering illnesses receiving treatment at a large urban medical center in Baltimore, MD.
DESCRIPTION: From 2009 through the present, semi-structured interviews were conducted with patients and, whenever possible, with their care-providers, families, etc. The interviews were conducted by a specialist who was treating the patients at the time of the interviews. The interviews were conducted in the office setting, outside of the patient’s treatment session. All interviews were videotaped and transcribed. Patients and their care-providers were asked to reflect on their experiences regarding their initial diagnosis, treatment options, and the manner in which physicians relayed information about their health condition. Patients were asked six main questions and also given the opportunity to describe other experiences that were meaningful to them during their care process. To determine specific communication areas that are critical for communication, qualitative analysis using a grounded theory approach will be conducted on the video transcripts. Two researchers will independently code 5 of the interviews. Coding results will be compared and discussed, resulting in a final coding scheme that will be used for all interviews to identify emerging themes.
EVALUATION: This project presents a patient centered curriculum for communication during critical aspects of patient care. For the work presented here, the evaluation will be the final coding scheme, which will then be refined based on iterative review by patients and clinicians.
DISCUSSION/REFLECTION/LESSONS LEARNED: In the next phase of the project, these emerging themes will be used to develop the content of an educational tool that combines patient and care-provider narratives with reflective exercises in order to enhance resident communication skills. The final phase of the project will include testing the tool for effectiveness. Utilizing patient and care provider experience as the foundation for curriculum development is a unique method for education in healthcare. With patient experience becoming rapidly more important for reimbursement, utilizing a patient centric approach to education specifically around communication is critical.
IMPACT OF A HOSPITAL MEDICINE ROTATION DURING INTERNAL MEDICINE RESIDENCYLuke Cunningham; Chirayu Shah; Erica Hubenthal; Doris Lin; Steffanie Campbell; Jeffrey T. Bates. Baylor College of Medicine, Houston, TX. (Tracking ID #1937882)
NEEDS AND OBJECTIVES: With the implementation of the ACGME duty hour restrictions for PGY1 residents in Internal Medicine, their exposure to inpatient medicine has declined. They are increasingly assuming care of patients admitted by other physicians rather than evaluating and developing management plans for new patients. Glasheen, et al. have also noted deficiencies in current Internal Medicine training for the growing role of hospitalists as they extend beyond traditional direct patient care. Non-clinical training needs include health-care economics, patient safety/quality improvement, continuums of care, leadership, and communication. Our objective was to create a new required PGY2 Internal Medicine rotation with a curriculum focused on skills needed for a physician primarily practicing inpatient medicine. The rotation would also provide increased inpatient experience with initial workup, assessment, management, and transitioning care of admitted patients. Program evaluation was done through pre- and post-rotation surveys. In addition, we also evaluated the curriculum delivery method.
SETTING AND PARTICIPANTS: The Resident Inpatient Training Experience (RITE) rotation is a one-month rotation at Baylor College of Medicine required for all PGY2 categorial Internal Medicine residents. Two PGY2 residents are assigned to each of the two hospital settings—Michael E. DeBakey VA Hospital and Ben Taub General Hospital. Over the course of an academic year, all 44 categorical PGY2 residents will rotation for at least 1 month on this rotation.
DESCRIPTION: An experienced hospitalist serves as the attending physician and works one-on-one with the residents without any students or interns. The RITE team admits an average of 16–18 patients from 7 am to 5 pm 4 days each week. There are no overnight responsibilities. The residents attend one or two half-day continuity clinics each month to fulfill the requirements. The curriculum is provided to each resident in a workbook format divided into three modules: Basic Principles in Patient Safety and Quality Improvement, Advanced Quality Improvement and Cost Conscious Care, and Billing/Coding. Using principles from the flipped classroom model, the residents are expected to independently read the workbook and complete basic exercises. Each Monday morning, hospitalist faculty lead a facilitated exercise on applying the principles of the weekly module. Residents are asked to answer a pre-rotation and post-rotation survey.
EVALUATION: The pre-rotation survey (n = 20, response rate 87 %) showed that residents identified deficits in their training in hospital reimbursement (85 %), hospital metrics (80 %), physician billing/coding (75 %), quality improvement (35 %), and patient safety (25 %). The post-rotation survey (n = 16, response rate 84 %) showed 81.25 % strongly agreed and 18.75 % agreed that the rotation was important for training and education. The same number responded that the rotation would help their skills in leading a traditional ward team supervising interns and students. The residents’ self-assessment of knowledge in the following categories increased: discharge planning/transitions of care (3.55 to 3.94), patient safety (3.6 to 3.86), quality improvement (3.45 to 3.56), cost conscious care (2.95 to 3.56), hospital reimbursement (2.5 to 2.94), physician billing/coding (2.2 to 2.88) [Likert scale 1 = very poor to 5 = excellent]. The interest to pursue a career in hospital medicine increased for 56.25 % of the residents on the RITE rotation. 62.5 % of residents preferred the independent workbook for curriculum delivery.
DISCUSSION/REFLECTION/LESSONS LEARNED: With a reduction in inpatient experience during intern year due to the ACGME duty hour restrictions, the addition of a required PGY2 hospitalist rotation during Internal Medicine residency helps to increase knowledge of many training needs identified for future hospitalists. The residents viewed the RITE rotation as important for their training and increased their confidence in leading a ward service. The rotation also led to more residents interested in pursuing hospital medicine as a career. Residency programs should consider alternative methods for curriculum delivery outside of the traditional didactics and Powerpoint slides. From this study, residents preferred using a workbook followed by a facilitated exercise.
IMPACT OF A TARGETED IPE CURRICULUM ON MEDICAL STUDENTS’ PERFORMANCE; AN IPC OSCE CASEJennifer Adams1; Maja Djukic2; Marc Triola1; Sondra Zabar1; Adina Kalet1; Linda Tewksbury1; Jennifer Ogilvie1; Sabrina W. Lee1; Colleen Gillespie1. 1NYU School of Medicine, New York, NY; 2NYU School of Nursing, New York, NY. (Tracking ID #1938507)
NEEDS AND OBJECTIVES: Interprofessional collaboration (IPC) is increasingly recognized as fundamental to patient-centered medical care. Interprofessional education (IPE) has been associated with improved collaboration in practice and patient outcomes. Still, many medical schools have limited training in IPE. The NYUSOM and NYUCN, with support from the Josiah Macy Jr. Foundation, developed and implemented a comprehensive IPE curriculum for its students. The impact of this curriculum was evaluated by comparing performance in an IPC-focused OSCE (Objective Structured Clinical Examination) case between two medical school cohorts, the first naïve to the curriculum and the second who had completed the curriculum.
SETTING AND PARTICIPANTS: An IPE case was implemented as part of the end-of-third-year comprehensive clinical skills OSCE. The case prompted students to create an interprofessional care plan with a nurse for the patient they saw in a previous case, a 15-minute interview with a patient who came into urgent care with chief complaint of shortness of breath.
DESCRIPTION: Students were expected to use the SBAR (situation, background, assessment and recommendation) technique to communicate with the Standardized Nurse (SN) and to use CUS communication tool (I’m concerned; I’m uncomfortable; This is a matter of patient safety) if the nurse relayed any incorrect information. The SN was trained to make a specific mistake. A behaviorally anchored checklist was developed to assess IPC, including 4 items to assess use of SBAR, 1 item focused on using CUS to respond to the SN’s information error, and 3 items focusing on core dimensions of collaborative practice (introducing professional role, collaborating in identifying next steps and implementing an interprofessional team care plan). Each of these used a 3-point response scale of “not done”, “partly done”, and “well done” and a composite score of % items rated by the SN as “well done” was calculated for each of the 3 IPC domains. Chi-square and t-tests were used to assess the significance of differences between frequencies and mean scores.
EVALUATION: 165 curriculum-naive third year medical students completed the case and 123 post-curriculum third years completed the case the following year. The overall OSCE scores did not differ significantly between cohorts. The overall IPC score did not differ significantly between cohorts (pre = 21 % vs post = 15 %; p = .32). In both cohorts, less than a third (28 % pre and 25 % post) of students collaborated with the nurse in developing a plan of action (p = .59). Significant differences (p < .05) were noted in the use of SBAR and CUS communication tools. Overall, mean SBAR and CUS scores for students completing the curriculum were significantly greater than students who did not (p < .05). Also, 72 % of pre-curricular students compared to 94 % of the post-curricular students used SBAR to present a patient-centered situational assessment (p < .05). Only half of the pre-curricular students used SBAR to comprehensively present the patient’s background, while 81 % of the post-curricular students employed this tool (p < .05) and 41 % of the pre-curricular versus 53 % of the post-curricular students used SBAR to provide their assessment of the situation (p < .05). Only 27 % of the pre-curricular students used CUS in a skillful and respectful way in response to the nurse’s error, while 40 % of the post-curricular students used this tool effectively (p < .05).
DISCUSSION/REFLECTION/LESSONS LEARNED: A targeted IPE curriculum effectively taught focused IPC skills (SBAR and CUS), but did not affect the overall ability for students to collaborate with a nurse and develop an IPC plan. This study illustrates that core skills can be taught and employed in a clinical setting and validates continued emphasis and dedicated curricular for IPC skills. However, full collaborative practice might require more experience in creating IPC care plans as well as continued exposure and education in this arena.
IMPLEMENTING A NOVEL MEDICAL STUDENT HEALTHCARE FOR THE HOMELESS CURRICULUMAndrew Coyle; Lauren Peccoralo. Icahn School of Medicine at Mount Sinai, New York, NY. (Tracking ID #1936375)
NEEDS AND OBJECTIVES: On any given night more than 50,000 individuals in New York City reside in shelters, an increase of nearly 70 % over the last 10 years. As nearly half of homeless individuals do not have health insurance, many do not receive regular medical care or receive care solely through shelter-based medical initiatives. Complex psychosocial circumstances affect health at all levels, limiting access and interrupting continuity, and often results in poor overall health. The expansion of Medicaid through the Affordable Care Act should improve homeless individuals’ access to the broader healthcare system, resulting in increased exposure for trainees. However, medical students at the Icahn School of Medicine at Mount Sinai (ISMMS) have no formalized training in or exposure to issues in homeless health. The objectives of this curriculum are to explore the social and psychological implications of homelessness on health, to discuss available resources for homeless persons and how to facilitate access, and to educate trainees on appropriate treatment strategies for high-prevalence conditions. Finally, the curriculum will enhance and standardize the clinical experience through case-based learning.
SETTING AND PARTICIPANTS: Third year medical students at ISMMS spend 1 month on an ambulatory clerkship. All students participate in the didactic portion of the curriculum while 25 % of students rotate through clinical sites in city homeless shelters that provide both routine and urgent care. The shelter clinics have private examination rooms and are staffed with a social worker, registered nurse, and attending physician.
DESCRIPTION: The central component of the curriculum is a didactic session given to all students. The objective of the first half of the session is to review the characteristics/demographics of the homeless population, implications of homelessness on health, available resources for homeless persons, and the reasons for the significant rise in homelessness. The objective of the second half is to discuss population-specific screening and treatment strategies for common conditions in the homeless population (including diabetes/hypertension, HIV, Hepatitis C, and TB) via interactive cases. Students work through short cases as a group and discuss challenges of caring for homeless persons, such as selecting low-cost medications, optimizing medication adherence in patients with complex social issues, and arranging preventive care. This session has been piloted with approximately 50 medical students this academic year. In addition to the didactic sessions, the curriculum will enhance and standardize the clinical experience for those students who rotate through the shelter clinics. Working with clinic preceptors, a list of frequently encountered conditions and clinical scenarios will be generated to create a database of case-based handouts. In conjunction with patient encounters, these will facilitate more robust preceptor-student discussion about medicine in the shelter setting. For example, a handout on breast cancer screening might include current USPSTF and ACS recommendations and data on national and homeless-specific screening rates. This handout could then be used by the preceptor, in the setting of seeing a patient due for mammography, to discuss challenges of completing preventive care in the homeless population.
EVALUATION: Students will complete a pre- and post-curriculum survey. The pre-test (needs assessment) will gauge baseline levels of knowledge, as well as prior experiences and comfort level with the homeless population. Students will also take the Attitudes Toward Homelessness Inventory (ATHI), a validated tool. After the curriculum, students will take a post-test and retake the ATHI to assess for knowledge or attitudinal changes.
DISCUSSION/REFLECTION/LESSONS LEARNED: Homeless individuals represent a growing and complex population in health care, and it is important that practitioners be well-versed with the challenges to providing high-quality care. Significant variability in student knowledge has been noted in current teaching sessions where students have voiced numerous common misconceptions about the homeless population (for example, that the street homeless are representative of the overall population, when in fact they represent less than 10 % of the overall population). This demonstrates that significant educational work is needed. Early formative feedback from students about the didactic pilot has been positive and has highlighted the unique nature of the curriculum. This curriculum gives students a base of knowledge about homeless healthcare through didactics and case-based discussion, and, in conjunction with direct patient encounters for those who rotate at the clinical sites, will provide necessary exposure to the unique social and medical characteristics of the homeless population.
IMPLEMENTING CHANGE IN CLINICAL PRACTICE CULTURE: PAIN AND OPIOID MANAGEMENT BOOTCAMPS FOR VA CLINICIANSKaren H. Seal2,1; Emily Sachs1; Tracy Lin1; Gary Tarasovsky1; Daniel Bertenthal1; Christopher J. Koenig2,1. 1SFVAMC, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1931958)
NEEDS AND OBJECTIVES: Primary care providers (PCPs) prescribe opioids for chronic non-cancer pain, despite a lack of evidence for their use. In turn, some patients, particularly those with comorbid mental health conditions, use opioids in excess to self-medicate psychosocial distress, sometimes with lethal consequences. Current clinical practice guidelines (CPGs) emphasize the biopsychosocial model of chronic pain self-management, yet CPGs are rarely used, and PCPs are not comfortable counseling patients about safer opioid use and non-opioid, non-pharmacological strategies for pain self-management. This interactive training aimed to educate providers about: (1) safer opioid prescribing and pain self-management, and (2) how to communicate more effectively with challenging chronic pain patients.
SETTING AND PARTICIPANTS: For this implementation project, we partnered with leadership at the San Francisco VA Medical Center (SFVAMC) to develop a 90-minute “Pain and Opioid Management Bootcamp” with an accompanying formative evaluation. Three opioid bootcamp trainings have taken place, two of which were broadcast by V-TEL (video telehealth) to 6 affiliated VA CBOCs throughout Northern California. To date, 140 clinical staff members have participated in the bootcamp and 125 (89 %) have completed pre- and post-training evaluations.
DESCRIPTION: In this interactive training, learners “assist” a PCP in a dramatized clinical scenario to make several clinical decisions about pain management. Using lessons from the training, learners manage a new complex chronic pain patient with comorbid mental health problems, including a history of heavy drinking, who is inappropriately prescribed benzodiazepines for posttraumatic stress disorder. In this scenario, the patient requests the same high-dose opioid regimen he received from a previous provider. The training reviews data on the questionable benefits and known harms of chronic opioid therapy including overdose, endocrine disruption, sleep disturbance, etc.… Throughout the training, the PCP models the use of Universal Precautions for opioid prescribing including: (1) Assessment of pain and risk for opioid misuse (using standard screens); (2) Consideration of non-opioid and non-pharmacological adjuncts and alternatives; (3) Shared decision-making in developing an Opioid Pain Care Agreement; and (4) Monitoring and re-adjustment (if the opioid trial fails, e.g., necessitating taper). The PCP models the use of the “VEMA” (validation, education, motivation, and activation) communication framework to implement Universal Precautions while maintaining a therapeutic relationship to reduce patient harms.
EVALUATION: Mixed methods were used to evaluate the training. T-tests were used to evaluate changes before and after the training using scaled and multiple choice items, and qualitative methods were used to describe open-ended feedback. To date, there have been significant improvements in knowledge and perceived comfort regarding safe opioid prescribing and chronic pain management (all p-values < 0.001). Learners were confident that they would apply lessons learned to their clinical practices (scale of 0 to 4, mean score = 3.34, SE = 0.07).
DISCUSSION/REFLECTION/LESSONS LEARNED: With stakeholder support, brief trainings can be implemented in clinical practice groups to successfully educate clinicians about safer opioid prescribing, which can begin to shift the practice culture toward a biopsychosocial model for chronic pain self-management. This training has been archived as a training DVD and is being adapted as a web-based training for dissemination. Future evaluations will investigate changes in clinical practice behavior.
IMPROVING APPROPRIATE PPI THERAPY INITIATION AND POST-DISCHARGE PRESCRIPTIONS; HOUSE STAFF EDUCATION PROJECT AND COST-SAVING ANALYSIS AMONG VA MEDICINE INPATIENTSTalia S. Gracer1; Victor Moles2,1; Cherinne Arundel2. 1Medstar Georgetown University Hospital, Washington, DC; 2Washington, D.C. Veterans Affairs Medical Center, Washington, DC. (Tracking ID #1934729)
NEEDS AND OBJECTIVES: Proton pump inhibitors (PPIs) were first marketed in the late 1980s, and since that time PPI use has skyrocketed, now ranking second in pharmaceutical expenditure worldwide, estimated at $11 billion annually in the US alone. This substantial cost prompted evidence-based strategies for PPI use, including the American Society of Health-System Pharmacologists (ASHP) Therapeutic Guidelines on Stress Ulcer Prophylaxis (SUP). These indications for SUP are limited to ICU patients, yet inappropriate prescribing of PPIs for the purpose of SUP in low-risk patients is a national problem that is costly and potentially harmful to patients. Prior literature proved significant improvements in appropriate PPI prescribing after one-time educational interventions by pharmacists and physicians. The culture of inappropriate PPI prescribing is evident in our institution. We feel it can be changed through education of Medicine trainees, as they are very often the frontline for prescribing medications in academic institutions. Our proposed objective is to use an ongoing educational program to decrease unwarranted inpatient PPI prescriptions, and in turn decrease inappropriate continuation of PPI prescriptions after discharge, thereby decreasing both the total cost of inpatient hospitalizations and the secondary risk factors associated with PPI usage among VA patients. This research should extend improved outcomes through repeated educational sessions and emphasis on medicine reconciliation, potential side effects, and cost.
SETTING AND PARTICIPANTS: All Medicine admissions to the Washington, D.C. VAMC between September 2012 and February 2013 who received a PPI, were randomized for retrospective chart review for pre-intervention data. The Internal Medicine residents, medical students, and attendings rotating monthly through the Washington, D.C. VA Medical Center (VAMC) general medicine wards, between September 2013 and February 2014, receive the educational intervention. Admission data from this time period will be analyzed for post-intervention retrospective analysis.
DESCRIPTION: The educational intervention includes the definition of “stress ulcer prophylaxis,” stress ulcer pathophysiology, ASHP-approved indications for PPIs, outpatient indications for PPIs, PPI side effects and drug interactions, ways to decrease inappropriate prescribing, including admission and discharge medicine reconciliation, and discontinuation of inpatient PPIs once risk factors resolve. All participants receive an index pocket-card with this information.
EVALUATION: Completed a retrospective chart review of 185 pre-intervention patients who received PPIs during their admission to the Washington, D.C. VAMC between September 2012 and February 2013. Charts were evaluated for PPI appropriateness criteria based on the ASHP guidelines and the 2010 Pharmacist Letter guidelines. Pre-intervention data results include: 69 % of patients were already on PPI at time of admission and 40 % of these PPIs continued without indication. Sixty percent of all PPIs prescribed at the time of admission lacked a documented indication, and 33 % of these prescriptions were continued on discharge. Our plan is to continue with monthly intervention of house staff teaching until February 2014 and use T-tests compare pre- and post-intervention data, and cost analysis.
DISCUSSION/REFLECTION/LESSONS LEARNED: Unfounded cultural habits within medicine, including defensive medicine, can have a negative impact on cost and patient care. Targeted educational initiatives and physician awareness can greatly improve outcomes and lower health care costs. By reducing the number of inappropriate PPI prescriptions we expect to lower costs in medication prescriptions and potentially decrease side effects (C. difficile infections, pneumonia) and medication interactions. Future directions of our project consist in incorporating teaching into a year-long monthly curriculum, and include electronic prompts in the electronic medical record when prescribing PPIs to improve compliance. Due to the unexpectedly high rate of outpatient PPI prescriptions, we plan to extend the teaching sessions to the outpatient VA physicians. Will complete a cost analysis with post-intervention data to evaluate VAMC and patient cost reduction.
ONLINE RESOURCE URL (OPTIONAL): ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. http://www.ncbi.nlm.nih.gov/pubmed/10690219 PHARMACIST’S LETTER/PRESCRIBER’S LETTER July 2010, Volume 26, Number 260705. http://pharmacistsletter.therapeuticresearch.com/pl/detaildocuments/270401-3206.pdf?cs=&s=PL
IMPROVING HOUSE STAFF CONTINUITY ON INPATIENT CARDIOLOGY SERVICES INCREASES PHYSICIAN AND NURSING PERCEIVED QUALITY OF CAREMelissa Dattalo1,2; Ryan E. Childers1,3; Colleen Christmas1. 1Johns Hopkins Bayview Medical Center, Baltimore, MD; 2University of Wisconsin, Madison, WI; 3Oregon Health & Science University, Portland, OR. (Tracking ID #1939061)
NEEDS AND OBJECTIVES: Many medical educators believe that the 2011 Accreditation Council for Graduate Medical Education (AGCME) duty hour restrictions fragment the continuity afforded by traditional overnight call schedules and subsequently reduce quality of care. We restructured our institution’s house staff rotations in the cardiology intensive care unit (CICU) and cardiology progressive care unit (PCU) with two simultaneous objectives: 1) Maximize daily continuity between house officers and cardiology patients, and 2) Comply with ACGME duty hour regulations.
SETTING AND PARTICIPANTS: House officers were surveyed (n = 17) about their experiences on the cardiology rotation at Johns Hopkins Bayview Medical Center (originally a combined CICU and PCU experience) at baseline in July 2012. A newly structured rotation involving separate teams working in the CICU or PCU was piloted from August 2012–January 2013. A follow-up survey about the pilot rotation experience was administered to house officers (n = 25), cardiology nursing staff (n = 19), and cardiology faculty (n = 7) in January 2013.
DESCRIPTION: At baseline, two cardiology house staff teams of 4 house officers plus a cardiology float resident and a physician assistant (PA) were responsible for all cardiology patients in the CICU and PCU. The pilot intervention assigned 6 house officers dedicated to CICU patients, assigned 3 house officers dedicated to PCU patients, and eliminated the need for house staff “cross-coverage” of PA patients overnight. The total number of cardiology house officers and the total number of cardiology beds did not change.
EVALUATION: On a scale from −5 (worst) to +5 (best), the pilot intervention improved house officer-perceived impact of patient continuity on quality of care from −2.9 to 3.1 (p = 0.00) for CICU interns, from −0.4 to 2.0 (p = 0.01) for CICU residents, from −1.6 to 2.6 (p = 0.00) for PCU interns, and from −0.04 to 2.1 (p = 0.00) for PCU residents. Seventy-three percent of house officers, 75 % of PCU nurses, and 60 % of faculty surveyed reported the intervention improved quality of patient care in the PCU. Sixty-seven percent of house officers, 80 % of CICU nurses, and 67 % of faculty surveyed reported the intervention improved quality patient care in the CICU. Eighty-one percent of house officers, 85 % of PCU nurses, and 80 % of CICU nurses stated the intervention enhanced interdisciplinary teamwork. The 30 day readmission rate in the PCU decreased from 18.41 % at baseline to 16.38 % during the intervention period. Average length of stay in the PCU decreased from 5.59 days at baseline to 5.05 days during the pilot intervention and readmission length of stay decreased from 6.50 days to 5.35 days.
DISCUSSION/REFLECTION/LESSONS LEARNED: The new 2011 ACGME duty hour regulations offered our institution an opportunity to restructure the house staff cardiology rotation to increase continuity of care between house officers and patients. Changes aimed at maximizing continuity of care also improved interdisciplinary teamwork, discharge planning, and overall quality of patient care as perceived by house staff, nurses, and faculty.
INNOVATIVE INTERPROFESSIONAL GERIATRIC EDUCATION FOR MEDICAL AND NURSING STUDENTS: FOCUS ON TRANSITIONS IN CARESeki A. Balogun1; Karen Rose2; Shannon Thomas2. 1University of Virginia Health System, Charlottesville, VA; 2University of Virginia Health System, Charlottesville, VA. (Tracking ID #1927010)
NEEDS AND OBJECTIVES: Interprofessional education (IPE) is increasingly essential for all health care professions and is crucial in fostering effective team based patient care, which in turn improves the quality of care and patient outcomes (1). This is especially important in caring for older adults whose needs are often not recognized or met in very complex healthcare delivery systems and are particularly vulnerable to adverse effects across the continuum of care (2). Transitioning care of the elderly, especially those with cognitive or functional deficits, is a very complex process, involving several disciplines and requires careful coordination of care. Inappropriate transition of geriatric care can lead to increased hospital readmissions and adverse drug effects including medication errors, all of which adversely affect patient outcomes. In addition, it leads to increased cost of health care through duplication of services (3–5). Several studies show that comprehensive interdisciplinary assessments can greatly improve outcomes in transitions of geriatric care (6,7). Utilizing IPE experiences in training health care professionals can foster effective collaboration across these professions and greatly improve transitions of care in the elderly. As part of the University of Virginia Health System’s initiative on IPE, we developed and implemented an interprofessional geriatric education workshop for nursing and medical students with a focus on transitions in geriatric care.
SETTING AND PARTICIPANTS: A total of 192 students (107 medical students and 85 nursing students) participated in a 90-minute, interactive, case-based workshop.
DESCRIPTION: The monthly workshops were conducted with groups of an average of 12 medical and 9 nursing students over 1 year. These were facilitated by nursing and medical faculty. Self-perceived competencies in necessary IPE skills and attitudes toward interprofessional teamwork were measured through surveys. Data were analyzed using descriptive and nonparametric statistics.
EVALUATION: Over 90 % of students were better able to describe the necessary interprofessional communication needed to develop a patient-centered care plan in transitioning patients between clinical sites. Four out of five students reported an enhanced appreciation of interprofessional teamwork and stated that the learning experience was valuable. They were also able to identify legal, financial and social implications in transitions of care (77 %). Interestingly, nursing students consistently rated the workshop more highly than medical students across most domains (P < .05).
DISCUSSION/REFLECTION/LESSONS LEARNED: Students improved and demonstrated their knowledge of interprofessional communications skills and strategies required in transitions of geriatric care. Their teamwork skills were also enhanced. Introducing these concepts in medical and nursing training fosters effective interprofessional communication and collaboration. References 1. WHO (World Health Organization) 2010. Framework for Action on Interprofessional Education & Collaborative Practice. Geneva: WHO/HRH/HPN/10.3. 2. Naylor, MD, Hirschman, KB, Bowles, KH, Bixby, MD, Konick-McMahan, J, and Stephens, C. Care coordinator for cognitively impaired older adults and their caregivers. Home Health Care Services Quarterly 26(4), 57–78, 2007. 3. Jack BW, Chetty VK, Anthony D, et al. Ann Intern Med 3;150(3):178–87, 2009. 4. Boockvar KS, Carlson LaCorte H, Giambanco V et al. Am J Geriatr Pharm 4(3):236–43, 2006. 5. American Medical Directors Association. Transitions of Care in the Long -Term Care Continuum. Clinical Practice Guideline. Columbia, MD: AMDA 2010. 6. Berwick, AD, Rees, K, Dieppe, p, et al. Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet 371(9614):725–735, 2008. 7. McCusker, J, and Verdon, J. Do geriatric interventions reduce emergency department visits? A systematic review. Journals of Gerontology: Series A: Biological Sciences and Medical Sciences 61A(1):53–62, 2006.
INTERDISCIPLINARY EVIDENCE-BASED MEDICINE COURSE DESIGN FOR NAS MILESTONE ASSESSMENT THROUGH ONLINE ADAPTIVE LEARNING STRATEGIESRavi Gupta1; Kell Julliard2; Juan Barrientos2. 1Lutheran Medical Center, Brooklyn, NY; 2Lutheran Medical Center, Brooklyn, NY. (Tracking ID #1940936)
NEEDS AND OBJECTIVES: ACGME’s Next Accreditation System (NAS) measures competency in essential tasks of clinical practice, including the ability to find and evaluate clinical research to improve care. Journal Clubs are our primary teaching venue for evidence-based medicine (EBM), but we were unable to fully assess all participants understanding of the concepts presented. Moreover, residents leading journal clubs had variable prior knowledge of EBM, resulting in similarly variable learning experiences for the audience. On the wards, attending physicians evaluated residents’ integration of EBM with clinical care as opportunities arose, leading to inconsistent assessment. The Association of Professors of Medicine reported that although 59 % of online courses reviewed had some type of assessment, none monitored resident learning or objectively reported on milestones (2012). The study called for development of e-Learning courses perceived by students as “providing an advantage over traditional curriculum.” Thus, our specific project goals were to: ● Develop clear EBM learning objectives related to milestones and national guidelines ● Bring teaching of EBM in line with recent developments in learning theory ● Take advantage of new learning technologies ● Enhance resident learning and clinical application of EBM The project team reflected the three essential areas of expertise: a physician provided clinical relevance and accuracy; an EBM expert led content development; and an instructional designer created a pedagogically sound course design informed by learning theory.
SETTING AND PARTICIPANTS: Internal Medicine residents and faculty at an inner city community teaching hospital
DESCRIPTION: The EBM Curriculum comprises the following modules: Introduction to EBM, Randomized Controlled Trials, Cohort and Case-control Studies, Diagnostic Tests, and Meta-Analyses. The course is SCORM compliant and adaptable to any Learning Management System. Modules are optimized for mobile platforms on Android and iOS. Modules cover the basic principles of each EBM study type and integration of research findings with clinical care through the use of four primary modalities: video, animation, simulation, and text. The curriculum emphasizes user-driven adaptability of course content (adaptive learning): the sequence of the course is dependent on user responses to continuous, embedded assessment. Users are remediated only as necessary. Data document each user’s proficiency. Two modules are complete: Introduction to EBM and Randomized Controlled Trials. The third will be complete by the date of the conference. Each assessment item is mapped to specific curricular NAS milestones. User responses including applicable milestone, correctness of responses, number of attempts, and need for remediation are routed to departments for reporting to ACGME.
EVALUATION: 97 % of residents were either satisfied or very satisfied with the course. Ninety-seven percent believed that the modules would improve their clinical skills and practice.
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents participated willingly in taking the modules, and the great majority perceived them as directly benefiting clinical practice. In module testing, residents’ individual learning preferences became apparent, which will guide development of future modules. Making explicit the evidence grading system for online EBM repositories was perceived by residents and faculty as having great clinical relevance. Significantly more time was needed to develop modules than originally anticipated.
ONLINE RESOURCE URL (OPTIONAL): Two modules are available for review at http://lmcmc.certpointsystems.com. Login names are SGIM1, SGIM2, SGIM3, SGIM4, SGIM5; password is password.
INTERNAL MEDICINE RESIDENTS’ ATTITUDES AND BELIEFS OF ACHIEVING THEIR CLINICAL COMPETENCY MILESTONES DURING THEIR NIGHT FLOAT ROTATIONBrian E. Foster; Maryann T. Ally. Walter Reed National Military Medical Center, Bethesda, MD. (Tracking ID #1937176)
NEEDS AND OBJECTIVES: We created standardized presentations for the internal medicine residents on their two-week night float rotation, but it is not known how this impacts their learning experience. At our medical center, most attending physicians supervise cross-cover issues of night float residents during one 2-week period per academic year, leading to a varied learning experience. Our PowerPoint presentations encompass common, cross-cover issues, including atrial fibrillation with rapid ventricular response, bowel management, chest pain, delirium, hypotension, hypertension, mechanical falls, neutropenic fever, pain management, post-operative complications, and stroke. The presentations were disseminated on our password-protected internal medicine website for easy access. The resident on the night float team was instructed to lead a discussion with the interns using these presentations. We developed a survey to assess internal medicine residents’ attitudes and beliefs of achieving their clinical competency milestones after the implementation of these standardized presentations.
SETTING AND PARTICIPANTS: Internal medicine residents in a single-site, academic medical center.
DESCRIPTION: A voluntary and anonymous 9-question survey was distributed electronically to our internal medicine residents during a two-week period in December 2013.
EVALUATION: Of the total 70 internal medicine residents, 23 residents responded to the survey, including 10 PGY-1, 9 PGY-2, and 4 PGY-3. Of the survey respondents, 12 had completed the night float rotation, and 11 had used the night float standardized presentations as outlined above. 84.6 % had used between 1 and 3 lectures on average per week while 15.4 % used an average of 4–6 lectures per week. The majority (77 %) spent an average of 5–15 min per presentation. 45.5 % felt the presentations allowed them to become better teachers, 18.2 % referred to the presentations during the night float rotation when encountering a clinical problem, and 9.1 % referred to the presentations after the night float rotation was completed when encountering a clinical problem. Over half (54.5 %) felt the night float presentations improved their overall clinical knowledge and 1 respondent (9.1 %) stated the presentations improved development of a comprehensive management plan. 27.3 % noted improvement in their effective communication of diagnostic and treatment plans to patients and caregivers after utilizing these presentations. One respondent (9.1 %) felt clinical questions to consultants were better framed as a result of these presentations.
DISCUSSION/REFLECTION/LESSONS LEARNED: Using a brief survey, we assessed the attitudes and beliefs of our internal medicine residents regarding their clinical competency milestones during their night float rotation. In developing and implementing standardized presentations on commonly encountered cross-cover issues, we aimed to enhance the learning experience of our residents and to encourage our residents to become better teachers, communicators, and, ultimately, independent practitioners. This survey identified areas of resident improvement, including developing more comprehensive management plans and communicating more clearly with patients and consultants. We will address these needs by strengthening our curriculum and developing more quality improvement initiatives with our residents.
LONGITUDINAL PATIENT SATISFACTION DATA AFTER INSTITUTING A 4 + 2 PRACTICE MODEL IN RESIDENT CONTINUITY CLINICJulie Oyler; Lisa M. Vinci; Wei Wei Lee; Eileen Wang; Vineet Arora. University of Chicago, Chicago, IL. (Tracking ID #1938913)
NEEDS AND OBJECTIVES: Many internal medicine programs have recently instituted a block scheduling model such as the 4 + 2 model for ambulatory training. As opposed to traditional training models where residents leave inpatient responsibilities for one half day a week to take care of continuity clinic patients, the 4 + 2 model of training separates inpatient and outpatient responsibilities. Little research has been done on the impact of this training model on patient satisfaction.
SETTING AND PARTICIPANTS: On July 1, 2013, an academic internal medicine training program transitioned to a 4 + 2 model in which residents spend 4 weeks on inpatient rotations followed by 2 weeks of outpatient clinic. During the 2 weeks on outpatient, residents participate in 8 half day continuity clinics, 4–6 half day subspecialty clinics, 4 half day teaching sessions and 2–4 administrative sessions per 2 week block. During the 4 weeks on inpatient, residents’ continuity clinic patients are covered by another resident.
DESCRIPTION: Since 2010, American Board of Internal Medicine (ABIM) Cancer Screening Practice Improvement Module (PIM) paper surveys have been administered annually from July to November to patients in the resident continuity clinic. PGY2 residents hand anonymous paper surveys to patients, these surveys are then entered into the ABIM PIM website by staff. This annual patient survey data was used to evaluate patient demographics, satisfaction and access to the resident practice before and after the 4 + 2 curricular change.
EVALUATION: From 2010 to 2012 (pre data) 273 patient surveys and in 2013 (post data) 90 were completed. The majority of patients were female (pre 188/273, 68 %, post 68/90, 76 %) and over the age of 50 (pre 209/273, 76 %, post 76/90, 84 %). About one third of patients rated their health “fair to poor” (pre 88/273, 32 %, post 30/90, 33 %) and another third rated their health “very good to excellent” (pre 64/273, 23 %, post 31/90, 34 %). Patients responded that “the practice was excellent at encouraging question and answering them clearly” (pre 144/273, 53 %, post 51/90, 57 %) and that they would “recommend this practice to others” (pre 253/273, 93 %, post 80/90, 89 %). When evaluating access to the resident practice, patients reported no problems with scheduling appointments (pre 167/269, 62 %, post 65/90, 72 %), reaching someone with a question (pre 175/262, 67 %, post 66/88, 75 %), obtaining prescription refills (pre 196/258, 76 %, post 60/87, 69 %), obtaining test results (pre 212/258, 82 %, post 75/84, 89 %), and obtaining referrals (pre 191/241, 79 %, post 65/84, 77 %).
DISCUSSION/REFLECTION/LESSONS LEARNED: The 4 + 2 schedule more closely matches the responsibilities of a general internist. However, there are periods of 4–8 weeks at a time when the resident is not available and covered by a fellow resident. Interestingly, patients were more satisfied with scheduling appointments but less satisfied with obtaining prescription refills. Despite this curricular change there was no significant change in most areas of patient satisfaction or access to the resident practice.
LONGITUDINAL RESIDENT-STUDENT PATIENT CARE COLLABORATION IN PRIMARY CAREAmy Pasternack1,2; Katherine Lupton1,2. 1Cambridge Health Alliance, Cambridge, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1939424)
NEEDS AND OBJECTIVES: Although the majority of patient care in internal medicine occurs in the ambulatory domain, the bulk of residency training has traditionally taken place in the inpatient setting. Consistent with this, residents receive little exposure to and training in teaching medical students outpatient medicine. Our near-peer educational exchange between PGY-2 and -3 residents and third year medical students will build residents’ skills in outpatient teaching, improve continuity of care for complex patients, and increase the number of complex adult primary care patients that medical students follow longitudinally.
SETTING AND PARTICIPANTS: Cambridge Health Alliance (CHA) is well known for pioneering a longitudinal integrated clerkship for third year Harvard medical students, the Cambridge Integrated Clerkship (CIC). Most of the student teaching in this program is done by attending physicians in the ambulatory setting; as a result, CHA internal medicine residents have fewer opportunities to teach medical students than do residents at many other medicine training programs. The CHA internal medicine residency follows a 2 + 4 immersion model in which two-week ambulatory blocks with concentrated time in primary care clinic alternate with four-week inpatient or elective rotations when residents are out of continuity clinic entirely; during inpatient blocks it can be challenging for residents to maintain close follow up with their more complex patients. This project is being piloted at the Windsor Street Health Center, a safety-net community health center that is the ambulatory medicine training site for six internal medicine residents and four CIC students.
DESCRIPTION: We are currently piloting a collaborative patient care experience in which CIC students pair with PGY-2 and -3 primary care providers to longitudinally co-follow complex medical patients. The student and resident see their collaborative patients together: the student is primarily responsible for running the patient visits while the resident directly observes and helps guide the encounter. The student then presents to the resident—who acts as preceptor for the visit—in the presence of an experienced faculty preceptor who ensures the quality of patient care while observing and later providing feedback on the resident’s teaching skills. The students follow their collaborative patients over the course of the clerkship year, benefiting from frequent direct observation and feedback while learning principles of ambulatory medicine and serving as a point of continuity with patients while residents are out of clinic. The residents, who also complete an ambulatory resident-as-teacher curriculum, gain mentored experience teaching students outpatient medicine. Further work is needed to build the resident-as-teacher curriculum, generate guidelines for patient selection, and establish administrative processes to facilitate the complex schedules involved.
EVALUATION: We are in the early stages of piloting this project. An initial pilot by one resident and two medical students has shown the project to be feasible within the resident and medical student clinic schedules, and other residents and medical students have expressed interest in participating. Residents and students will complete mid-year and year-end surveys assessing their comfort with ambulatory teaching and primary care medicine, respectively, and residents’ teaching skills will be periodically assessed by students and faculty.
DISCUSSION/REFLECTION/LESSONS LEARNED: This program increases residents’ exposure to medical student teaching in a supervised environment in which they can explore outpatient teaching styles and techniques while receiving feedback and mentoring from experienced educators. Prior to this, ambulatory resident-as-teacher experiences in this residency were limited to resident-run peer didactics. Students benefit from near-peer teaching and direct observation, and are empowered by the opportunity to be an integral member of the healthcare team and serve a key role in maintaining patient continuity over the course of the clerkship year. Defining appropriate patients—who are medically and psychosocially complex enough to require frequent clinic visits and would benefit from continuity with a medical student, but not so complex that the student is overwhelmed and unable to run the visits—has proven to be an early challenge and is a main focus of program development for the remainder of the pilot year.
MEDICAL STUDENTS AS PRIMARY CARE PROVIDERS: AN INTEGRATED MEDICAL STUDENT CLINIC THAT OFFERS A TRUE LONGITUDINAL PRIMARY CARE EXPERIENCESerene I. Chen; Rebecca Liu; Pinar Oray-Schrom. Yale School of Medicine, New Haven, CT. (Tracking ID #1925854)
NEEDS AND OBJECTIVES: Longitudinal clinical care experience is a rarely-met need in medical school education. The Wednesday Evening Clinic (WEC) at the Yale New Haven Hospital adult Primary Care Center (PCC) is a student clinic founded to address this need. It aims to: 1. Provide Yale medical students opportunity for a longitudinal clinical outpatient experience. 2. Offer students the opportunity to care for their own patient cohort and function as primary care providers (PCPs). 3. Provide outstanding medical care for an underserved patient population.
SETTING AND PARTICIPANTS: The WEC is a weekly student-staffed clinic, fully-integrated into the adult PCC of Yale-New Haven Hospital. Annually, 15 medical students beyond their 3rd year participate for at least 1 year.
DESCRIPTION: The WEC was founded in response to medical students’ desire for a longitudinal clinical experience. Modeled after group practice, students are divided into patient care teams, each supervised by a designated faculty attending and rotating volunteer attendings from the Yale and New Haven medical communities. As PCPs, students perform general health maintenance, chronic disease management, age-appropriate screening, counseling and patient-care coordination. Follow-up extends beyond clinic hours. Weekly attendance over 1 year, in conjunction with regular evaluations by faculty, satisfies the primary care clerkship requirement. The WEC is supported jointly by Yale-New Haven Hospital and Yale School of Medicine.
EVALUATION: We surveyed WEC students from 2008 to 2013 on their experience. Throughout this time, over 60 medical students have served as PCPs. Survey results indicate that the WEC provides a unique longitudinal clinical experience not found in the traditional medical school curriculum. Students unanimously report increased comfort in providing ambulatory care after participating in the WEC. In addition, 38 % of WEC graduates pursued residency in primary care specialties versus 33 % among non-WEC graduates. We surveyed patients on their clinic perception and satisfaction. Results indicate that patient flow and wait time are areas for improvement. Prolonged visits and delays are likely due to the requirement for close supervision by attendings.
DISCUSSION/REFLECTION/LESSONS LEARNED: Unlike other free or urgent care student clinics, the WEC is fully integrated into a well-established PCC of a teaching hospital, enabling students to follow results and care over time. The WEC is a unique experience in terms of degree of responsibility, ownership, and longitudinal exposure to patient care, with students functioning as PCPs. It provides insights into disease courses and opportunities for building patient-provider relationships, which are of increasing importance given the rising demand for primary care. The WEC fulfills primary care clerkship requirements, an additional innovation that builds structure for regular feedback and evaluation. The WEC is possible and sustainable by support from Yale School of Medicine, Yale-New Haven Hospital and dedicated volunteer attendings. Billing from encounters contributes to covering facility and staff costs. However, the long-term financial sustainability of the clinic depends on the overall financial health of the Yale-New Haven Health System. While similar opportunities are presently rare, this model can be scaled and implemented elsewhere, especially in light of increasing demand for primary care training.
MOBILE DEVICE APPLICATION BASED EDUCATIONAL TOOL TO IMPROVE COST-CONSCIOUS CARE AMONG INTERNAL MEDICINE RESIDENTSAuras R. Atreya1; Behdad Besharatian1; Stefano Buccy2; Thomas Higgins1,3. 1Baystate Medical Center/Tufts University School of Medicine, Springfield, MA; 2University of Massachusetts, Amherst, MA; 3Baystate Medical Center/Tufts University School of Medicine, Springfield, MA. (Tracking ID #1939067)
NEEDS AND OBJECTIVES: Cost of care in the United States is substantially higher than other nations and health care over-utilization is an area of focus in today’s economic environment. The American Board of Internal Medicine Foundation recently launched the ‘Choosing Wisely’ initiative, aimed at reducing overuse of tests and procedures. Of the major drivers of overuse, one of the proposed physician-related factors is physician culture, which emphasizes thoroughness during medical education and training years. It is possible that this leads to increased test ordering in order to obtain an exhaustive evaluation. However, it has been previously shown that medical residents have poor knowledge of the cost of diagnostic tests. Given that cost-effective care is part of the competencies required by the Accreditation Council for Graduate Medical Education (ACGME), there exists an opportunity to improve awareness of diagnostic tests and facilitate cost-effective care. Our objective was to develop an educational intervention that would raise awareness of medical residents with regard to frequently ordered diagnostic tests.
SETTING AND PARTICIPANTS: Baystate Medical Center is an academic medical center in Springfield, MA that serves as the Western Campus of Tufts University School of Medicine. Educational curriculum for internal medicine residents and medicine-pediatrics residents on the inpatient medicine service includes a half-hour morning report that is based on clinical case-based learning. This is an interactive session where residents hone critical decision-making and are involved in determining appropriate work-up for each particular presentation.
DESCRIPTION: We developed an android OS based application for mobile devices that would display the cost of commonly ordered tests. Cost of tests was based on fee-schedule that was obtained from the Financial Department at Baystate Medical Center. The mobile device can be connected to a projector and the cost of the last ordered test is displayed along with total cost of tests ordered in real-time during morning report. Tests included in the application comprise of serum chemistries, hematological tests, cardiac enzymes, CSF, urine and stool studies. Frequently ordered radiological tests, echocardiography and stress tests were also built into the application.
EVALUATION: Prior to implementing this application in morning report sessions, we conducted a pre-intervention survey where we asked all residents present at an academic half day (protected time to ensure attendance of all internal medicine and medicine-pediatrics residents) to estimate the value of 10 commonly ordered diagnostic tests. We will then educate residents to use the application during morning report. Since only the residents on inpatient medicine service attend morning report, we will have a group of residents exposed to the application in addition to those not exposed to the application. This will then allow us to conduct a post-intervention survey to compare the effect of the educational intervention in those exposed to the application, with the unexposed group serving as a control group.
DISCUSSION/REFLECTION/LESSONS LEARNED: Although educational interventions to encourage cost-effective care among resident physicians have been developed before, this Android application is an innovative tool aimed at incorporating cost-consciousness into the initial work-up of patients admitted to the hospital without compromising thorough medical evaluation. Utilizing this tool during morning report will remain feasible since it does not involve a major change from current practices and it can become part of curriculum for residents on inpatient medicine service. Ultimately, the goal is to extend the use of this application in routine day-to-day patient care on the medicine wards and continue to teach cost-containment to medicine and medicine-pediatrics residents.
MOBILE-CENTERED SPACED LEARNING: A NOVEL APPROACH TO GRADUATE MEDICAL EDUCATION IN THE DIGITAL ERARobert J. Walter; Anantha K. Mallia; Ali Massoumi; Joshua Hartzell. Walter Reed National Military Medical Center, Bethesda, MD. (Tracking ID #1938605)
NEEDS AND OBJECTIVES: Developing an optimal learning environment and curriculum in graduate medical education can be challenging, particularly in light of progressive work hour restrictions limiting the feasibility of traditional academic didactics that compete with patient care duties. Emerging literature has demonstrated the effectiveness of “spaced learning” within medical education as a viable adjunct to conventional pedagogy. This method of learning has been found to improve knowledge acquisition, increase long-term knowledge retention, and improve a learner’s ability to accurately self-assess their knowledge. However, spaced learning shares the same limitations as many other learning models with regard to accessibility, ease of use, and learner acceptance/adoption. Additionally, no studies to date have evaluated the usefulness of a mobile-based spaced learning curriculum within an internal medicine residency program. As such, the goal of our study was to assess the effectiveness and acceptance of a mobile-based spaced learning curriculum within a graduate medical education environment.
SETTING AND PARTICIPANTS: Utilizing a mobile-based application, Qstream, that incorporates an adaptive spaced learning platform, we created an adjunct curriculum to supplement our existing academic didactics for housestaff during their critical care rotation at Walter Reed National Military Medical Center (WRNMMC). The curriculum consisted of 100 high-yield core knowledge questions within the area of critical care medicine. Each learner enrolled in the module received an email and/or RSS feed prompt daily to their mobile device of preference (smartphone, tablet) with 5 questions. Upon answering each question, a brief explanation of clinical reasoning was provided and the learner was anonymously shown their performance in comparison to their cohort. Questions that were answered incorrectly were asked again within 7 days until answered correctly twice, whereas questions initially answered correctly were asked again within 13 days. Questions answered correctly twice in succession (mastery of material) were retired.
DESCRIPTION: We conducted a prospective, randomized, controlled study of 30 interns and residents rotating on the medical and surgical intensive care units at WRNMMC. All participants had their baseline knowledge assessed by a 25 question pre-test based upon the core knowledge topics within our spaced learning module. Sixteen learners were randomized to participate in the spaced learning curriculum (in addition to traditional didactics) and were enrolled within the module. Fourteen learners were randomized to the traditional academic didactics alone. Block randomization was used to minimize cross-communication between learners. All participants completed a 25 question post-test at the conclusion of their 4 week rotation. Learners who were randomized to participate in the spaced learning module answered an additional 10 questions regarding the perceived effectiveness and usability of the module.
EVALUATION: Our cohort consisted of 18 PGY-1’s (60 %), 5 PGY-2’s (17 %), 6 PGY-3’s (20 %), and 1 PGY-4 (3 %). Baseline characteristics (PGY level) were similar between randomized groups. Performance on the pre-test examination was comparable (61 % +/− 18 % vs 68 % +/− 17 %, p = 0.26). Post-test performance was superior within the spaced learning group (86 % +/− 11 % vs 71 % +/− 13 %, p = 0.002) as was the percent improvement from pre-test to post-test (18 % +/− 12 % vs 7 % +/− 13 %, p = 0.03). The spaced learning module received favorable reviews both in terms of overall educational benefit (average rating 4.44 on a 5-point Likert scale) and as an adjunct to traditional didactics and bedside teaching (average rating 3.56 on a 4-point Likert scale). The average time to complete the 5 daily questions was 4.25 min. The overall difficulty and number of questions administered daily were designated as “appropriate” by 81 % and 87 % of learners, respectively.
DISCUSSION/REFLECTION/LESSONS LEARNED: In our cohort, we observed a statistically significant improvement in overall post-test performance within the spaced learning group. Furthermore, acceptance and perceived usefulness of the mobile-based platform was high among learners. This novel approach to traditional didactics may be useful as a means to supplement existing curricula. Additional measurements, such as in-service and ABIM exam scores, gathered from larger, multi-center trials are needed to confirm the overall utility of a spaced learning curriculum as an educational adjunct within graduate medical education.
NOT TOO MUCH, NOT TOO LITTLE, BUT JUST RIGHT: GOLDILOCKS ROUNDS AT THE CAMBRIDGE HEALTH ALLIANCERachael E. Bedard1,2; Alison B. Rapoport1,2; Maren Batalden1,2. 1Cambridge Health Alliance, Cambridge, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1940038)
NEEDS AND OBJECTIVES: The AGCME identifies “Systems-Based Practice” (SBP) as a core competency for internal medicine residents; sub-competencies described in this domain include providing cost-effective care, recognizing system errors and advocating for systems improvement. Through the new Clinical Learning Environment Review program, the ACGME expects training institutions to engage residents in efforts to ensure that their delivery system is providing safe, high quality, evidence-based care to patients. With these mandates, training programs across the country seek to build meaningful curricular opportunities for residents in this domain. The “Goldilocks Rounds” at the Cambridge Health Alliance provides an innovative forum for Internal Medicine residents to discuss cases involving the overuse, underuse and misuse of healthcare resources and to design and implement small tests of change. The objectives of these rounds are as follows: - To provide a forum for honest disclosure and discussion of clinical errors and system failures - To encourage residents to identify examples in their own practice of the overuse or inappropriate use of healthcare resources -To help residents articulate one improvement oriented “action item” from each rounds that residents have the power to implement in real time
SETTING AND PARTICIPANTS: The Cambridge Health Alliance (CHA) is an integrated public healthcare system comprised of two community hospitals and an extensive primary care network. The internal medicine residency has 8 residents in each of the PGY-1, 2 and 3 years; there are an additional 8 psychiatry interns and 7 transitional-year interns who also train on one 32-bed inpatient medicine teaching unit. All residents are invited to monthly Goldilocks Rounds. The two chief medical residents facilitate rounds. Hospitalist teaching faculty are present to offer guidance; an open invitation is extended to nursing staff.
DESCRIPTION: Goldilocks Rounds are scheduled during lunch hour at regular intervals throughout the year. Housestaff come to rounds prepared with recent stories from their own practice that exemplify the overuse or misuse of medical resources, situations in which a clinical error was made, or a system failure occurred. An unnecessary blood draw, a misunderstanding with a nurse: Trainees are encouraged not to accept these issues as byproducts of a complex health system but to identify them as areas for improvement and come up with solutions. During Goldilocks Rounds, participants select 1–2 pressing problems raised in the case discussion, brainstorm potential interventions, and commit to taking some individual or group action. Facilitators help formulate discrete, simple, positive interventions that are within the scope of the residents to enact. When applicable, chief residents lead the group in filing a formal occurrence report to model the importance of reporting errors. Residents are the primary physicians on this dedicated inpatient teaching unit; they interact consistently with the same group of nurses and ancillary staff and can exercise genuine leadership in changing the practice environment. Action items that have resulted from Goldilocks Rounds during this academic year include patient education about how to ask for PRN medications in the hospital and improved end of shift signout protocols between day and night resident teams.
EVALUATION: Prior to the first Goldilocks Rounds all house officers were invited to complete a survey on their attitudes and perceived self-efficacy regarding SBP and quality improvement. Sixty percent of residents responded. The same survey will be administered at the end of this academic year to assess change in attitudes and self-efficacy in these domains. Residents are informally invited to offer feedback on Goldilocks Rounds to the chief residents throughout the year. Finally, the chief medical residents follow up each rounds with a synopsis of issues discussed and proposed interventions. Chief residents audit the implementation and efficacy of those interventions going forward, unless a specific resident champion is identified.
DISCUSSION/REFLECTION/LESSONS LEARNED: Baseline survey results revealed that 43 % of respondents report feeling “very comfortable” discussing a medical error with a fellow housestaff. Only 21 % are “very comfortable” filing a formal occurrence report. Only 22 % currently feel “very comfortable” raising issues about healthcare costs and use of medical resources with their attending physician. Despite this, 72 % of respondents report that they “strongly agree” with the statement “My role as a physician includes a responsibility to improve the system of care in which I practice”. Certainly this enthusiasm for systems-improvement work is evident in the Goldilocks Rounds discussions where trainees are eager to volunteer experiences and generate improvement suggestions. The Goldilocks Rounds are a promising strategy for bringing systems-based practice into the residency curriculum in a practical, relevant way that impacts both resident learning and patient care.
ONLINEMEDED: MOVING MEDICAL KNOWLEDGE OUT OF THE CLASS ROOM AND ONTO THE INTERNETDustyn E. Williams. 1Medical Education Online L3C, New Orleans, LA; 2Tulane University, New Orleans, LA. (Tracking ID #1896418)
NEEDS AND OBJECTIVES: There is much to learn in medical school. The shift in recent years from primarily medical knowledge to promoting a more well-rounded physician has not lessened how much knowledge must be taught, only burdened medical schools and students alike; compressing more into less time. The need, then, is a means by which the medical knowledge component of medical school can be more efficiently delivered to medical students. The goal of this project was three fold. First, it was to consolidate and filter a vast amount of medical knowledge into the medical student level, as defined by the NBME and USMLE. Second, it was to create a method for dissemination that was both cost-effective and immediately scalable. Third, it was to introduce a mode of instruction that could prove fruitful for standardized testing examination as well as clinical practice, but in a completely novel way using the internet.
SETTING AND PARTICIPANTS: Onlinemeded.org is a non-profit website that is available to everyone for free. Anyone is permitted to participate. There is no enrollment, no signup, and no cost. The only barrier is an internet connection that can support online streaming video.
DESCRIPTION: 250 online videos, each approximately 15 min long, are displayed in a one-stop-shop access website. There are 19 categories that span across the core clerkships for the third and fourth years including neurology, psychiatry, medicine, surgery, pediatrics, and the subspecialties. Each page is dedicated to a single video and includes key concepts and errata, a discussion board, and an embedded YouTube Video. Each video is constructed to educate to a medical student, at the medical student level, including the use of advanced organizers, algorithms, and memory tools.
EVALUATION: Google Analytics and YouTube Dashboard Manager were used. Each month over 6,000 unique visitors visit the site and over 24,000 videos are watched. The demographics are equal between men and women, and are primarily from the United States, with centers of use clustering around major cities: New Orleans, New York, and Chicago. Male and female users are equal. Feedback from users has revealed a tremendous amount of anecdotal success from the use of the site. Students comfort level on the wards increases, satisfaction in education increases, and scores on the USMLE Step 2 have shown substantial improvement from their Step 1 scores
DISCUSSION/REFLECTION/LESSONS LEARNED: The demand for a resource like this is overwhelming as shown by the sheer number of users. The cost to maintain such a site is negligible; hosting videos on YouTube is free, and the cost of data for the actual site is minimal. The time cost to develop, film, and edit these videos is the primary barrier. However, once completed, they exist indefinitely until updates are required. This system provides a highly effective way of delivering medical knowledge content to medical students at extremely low cost, that is immediately scalable to every medical student in the world, and in a time-efficient manner, allowing medical schools to focus on the practice of medicine and cultivating future physicians rather than the emphasizing the basics of medical knowledge.
ONLINE RESOURCE URL (OPTIONAL):www.onlinemeded.org
OUTPATIENT MORNING REPORT IN THE EHR ERA: AN OPPORTUNITY TO APPLY ADULT LEARNING THEORY TO THE AMBULATORY CURRICULUMJames O’Keefe. University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1928226)
NEEDS AND OBJECTIVES: The ambulatory curriculum for internal medicine residents is distributed across several venues, of which the Outpatient Morning Report (OMR) provides a unique opportunity to learn from cases from the resident clinics. Our objective was to enhance the learner-centered format of OMR by identifying multiple resident cases organized around a central theme for each session.
SETTING AND PARTICIPANTS: OMR is a 45-minute conference that is attended by 25 residents (PGY2/PGY3) on ambulatory rotations. The conference is led by a chief resident and attended by a faculty preceptor.
DESCRIPTION: The assigned resident chooses a case and notifies the chief resident of the topic. The chief resident performs an EHR search to identify similar cases from the clinics of residents who are attending the conference. Our EHR (Epic Systems) generates “reports,” with search criteria including demographics, diagnoses, medications, tests ordered, vital signs and lab values. Cases are printed and the relevant content is highlighted. During OMR, the assigned resident has 20 min to present their case(s) and lead a group discussion. Next, the chief resident distributes the “surprise cases” to individual residents, who are asked to present the highlighted portions of their cases to the group. The chief resident leads a nonjudgmental discussion of learning points from each case, provides an overview of relevant articles/resources, and allows for commentary by the faculty preceptor. Example: The assigned resident presented three patients for whom advance directives could have been (but were not) discussed in clinic: a 34 year-old with relapsed AML, a 76 year-old with dementia, and a “healthy” 57 year-old. The resident reviewed relevant articles from AFP and JAGS. Next, the chief resident led a discussion of “surprise cases” comprising several patients in which DNR status was documented in clinic but not acknowledged upon subsequent hospital admission. The group focused on potential QI projects to improve code status visibility in the EHR.
EVALUATION: Conference topics are tracked in a spreadsheet to avoid duplication. High-yield topics are identified and repeated across groups of residents.
DISCUSSION/REFLECTION/LESSONS LEARNED: We have applied adult learning theory by using our EHR to identify cases for OMR. We emphasize the relevance of GIM topics by drawing cases from resident clinics; we identify knowledge gaps during the process of chart review; and we direct teaching to the needs of the learners. By splitting conference time between the resident and chief resident, we maintain audience interest and balance topic selection. We are also able to include innovative topics (e.g. cost conscious care or systems-based care) in our curriculum. An unanticipated benefit of the format is near-100 % conference attendance, as residents do not know if one of their patients is chosen as a “surprise case.” The primary challenge is preparation time, which used to search for “surprise cases” (1–2 h) and prepare content (1–2 h). The amount of time has been lessened by asking residents to pick topics within the area of expertise of the guest faculty; this improves faculty engagement and reduces the amount of time for the chief resident to prepare content. A second limitation is that topics must be drawn in the resident practice and our EHR search for certain topics (e.g. refugee health) have yielded insufficient cases for a conference.
PACT ICU - INTERDISCIPLINARY CARE CONFERENCES FOR HIGH RISK PRIMARY CARE PATIENTSWilliam G. Weppner1,2; Janet V. Willis2; Amber Fisher2; Adam Brotman2; Rick Tivis2; Timothy Gordon2; C. Scott Smith1,2. 1University of Washington, Boise, ID; 2Boise VAMC, Boise, ID. (Tracking ID #1938812)
NEEDS AND OBJECTIVES: Workplace interdisciplinary collaboration is recognized as an important part of quality primary care and favorable patient outcomes. However, many health professions training programs provide inadequate opportunities for trainees to develop the knowledge, skills, and attitudes needed for this. Interdisciplinary Case Conferences can address this gap by providing opportunities for participants from multiple professions to learn with, from and about each other through discussion of real patient cases and actionable strategies for care plans.
SETTING AND PARTICIPANTS: The Boise VAMC Centers of Excellence in Primary Care Education developed the “PACT ICU” (Patient Aligned Care Team Interdisciplinary Care Update) to improve care of high risk patients in primary care. Based at our teaching clinic of approximately 32 medical residents and other trainees serving more than 2,000 patients, this offers a conference to develop coordinated, patient-centered care plans and reinforce principles of interdisciplinary collaboration.
DESCRIPTION: On a weekly basis, rotating physician and nurse practitioner trainees lead discussion of a high risk patient selected from the top five highest risk patients as predicted by the VA-based Care Assessment Needs registry. A clinic-based registered nurse uses a web-based schedule and guide to facilitate selection and review of patients. The nurse and a physician lead coordinates an hour-long conference with interdisciplinary team members, including medicine residents and attendings, nurse practitioner trainees and supervisors, primary care nurses, pharmacists, psychologists and behavioral health staff, social workers and chaplain service.
EVALUATION: Over the first 8 months of the PACT ICU, 27 trainees have participated, presenting 40 patients with 160 controls. There has been consistent involvement by different disciplines and trainees; surveys of 27 PACT ICU trainee participants suggest effectiveness at teaching PACT principles within a clinic team. The response to the statement “My understanding of all of the elements (biological, social psychological) that must be considered in this patient’s care” increased from 2.8 to 4.6 out of 5 (n = 27, p < 0.001). The response to the statement “My understanding of the roles that each of the team can play in hard to manage patients like this one” increased from 3.0 to 4.5 (p < 0.001). Chart review of consult patterns suggests an increase in referrals to other members within the PACT team, such as pharmacy and behavioral health. Among patients that were presented in the PACT ICU, consults outside the team were 18 % lower than controls and consults to team members (pharmacy, psychology, social work, and RN case manager) increased. This consult pattern is emerging across all patients, suggesting generalizability of interprofessional collaboration. Using case-control methods, data from the first 6 months of this pilot indicates a non-significant trend towards decrease in patient utilization when compared to controls in the PCP’s panel with similar risk scores for ER visits (0.94 vs. 1.20 per patient per year, p = 0.48) and hospitalization (0.34 vs. 0.49 per patient per year, p = 0.38).
DISCUSSION/REFLECTION/LESSONS LEARNED: These findings suggest that PACT ICU has reinforced key patient-centered medical home concepts within an academic primary care setting, improving trainee understanding and referral patterns within the team. Overall, an interdisciplinary care conference such as PACT ICU can be a useful model for (1) teaching interdisciplinary care, (2) facilitating team-based care, and (3) improving patient consult management.
ONLINE RESOURCE URL (OPTIONAL): Online Care Assessment Needs registry (VA-intranet based risk prediction tool) Online Care Management Tool 3.0.0 (VA- intranet based care management tool) Online PACT ICU schedule & tools: http://moodle2.boisevacoe.org
PANEL MANAGEMENT IN ACADEMIC PRACTICES: WHAT IS IT THAT WE REALLY NEED TO TEACH?Kate Dube1; Rachel Willard-Grace1; Janhavi Athavale2; Thomas Bodenheimer1; Reena Gupta3. 1University of California, San Francisco, San Francisco, CA; 2Eastern Virginia Medical School, Norfolk, VA; 3University of California, San Francisco, San Francisco, CA. (Tracking ID #1939756)
NEEDS AND OBJECTIVES: Panel management entails identifying and facilitating needed chronic and preventive care for a population of patients using clinical guidelines. In high-performing primary care practices, panel management is usually conducted by non-clinician members of the team, often medical assistants (MAs) or nurses who work closely with the clinician, relieving some of the routine patient care burden. Little is known about how panel management services are structured in teaching practices, which are charged not only with providing high quality care for patients, but also with teaching their residents requisite clinical and interdisciplinary leadership. We sought to understand how panel management is implemented in teaching practices.
SETTING AND PARTICIPANTS: We conducted site visits at ten primary care residency clinics. Data was collected using a structured site visit guide and semi-structured interviews with clinic leadership, providers, trainees, and clinic staff. Site visit reports were coded and analyzed via matrix by two independent researchers through an iterative process. The research team reviewed these analyses to identify themes.
DESCRIPTION: Two primary panel management models emerged: 1) Residents provide panel management to their assigned patients; or 2) Medical assistants and other allied health professionals provide panel management for the residents’ patients. The first model facilitates learning clinical guidelines, and it provides residents with an understanding of the process of panel management, such that they would understand what their MAs or nurses were doing as they entered the workforce upon completion of their training. On the other hand, the second model reinforces a team-based model of care that is more compatible with many contemporary primary care practices, and it provides an opportunity to build resident skills in leading a team. One site implemented a promising hybrid model that addressed both training residents in clinical skills and in team-based care. In this model, the residents and medical assistants share the panel management responsibility, work together to track patients who are in need of care and conduct outreach calls together.
EVALUATION: Additional research is needed to understand how to define best practices and what patient and resident outcomes are associated with each model.
DISCUSSION/REFLECTION/LESSONS LEARNED: Faced with the dual missions of training residents both in necessary clinical skills and in interdisciplinary team-based care models, teaching clinics have alternately entrusted panel management responsibilities to residents or MAs and nurses. A hybrid model, in which residents work collaborative with MAs or nurses, may provide a useful mode to bridge these models and achieve these dual missions.
PAP EMPHASIS CLINICS: A VENUE TO IMPROVE CANCER SCREENING RATES AND TRAIN RESIDENTS IN WOMEN’S HEALTHMichelle Cleeves; Rebecca Hanratty; Sarah Christensen; Jennifer Adams. Denver Health and Hospital Authority, Denver, CO. (Tracking ID #1938721)
NEEDS AND OBJECTIVES: Needs and Objectives: Though cervical cancer is easily preventable with regular screening, there are roughly 12,000 new cases of advanced cervical cancer annually in the United States. A significant cause of this failure to screen is that women are not offered cervical cancer screening by their primary care doctors, and studies have demonstrated this is especially likely when those care providers are recently graduated from residency. Though the ACGME and ABIM both require training and competency in preventive care counseling and specifically in delivery of pap smears, a deficiency persists in the provision of cervical cancer screening. By creating a “pap emphasis” clinic with specific curriculum and focused patient care for our residents, we aim to increase resident exposure to pelvic exams and cervical cancer screening with the goals of improving both resident education and cervical cancer screening rates in an urban underserved resident training clinic.
SETTING AND PARTICIPANTS: Setting and Participants: PGY1, 2, and 3 internal medicine residents are scheduled to participate in the pap emphasis clinics at their continuity clinic site once during a 6 month intervention period.
DESCRIPTION: Description: 14 patients are scheduled per session and residents perform pelvic exams, pap smears, STI testing, and family planning counseling as indicated. Residents also received a curriculum delivered by a GIM faculty member with expertise in women’s health which includes review of pap screening guidelines, pathophysiology of cervical cancer development, preventive health care screening guidelines, and wet prep microscopy during their pap clinic.
EVALUATION: Evaluation: We are assessing change in attitudes and medical knowledge with a 10-question survey administered to each resident before and after the curriculum is delivered. Topics contained in the survey included cervical cancer screening guidelines, pap smear results interpretation, and slide identification of common wet prep pathology. All 15 residents with continuity clinic at the pilot site will be scheduled to participate in the pap emphasis clinics throughout the study period. The session begins with a brief didactic session followed by direct patient care. We conclude the session with microscopy review of wet preps and a post-test. Although this project is ongoing, we have preliminary analysis demonstrating significant improvement in resident comfort with pelvic exams and medical knowledge in the areas tested. The residents also report high levels of satisfaction with the curriculum. At the same time, the pap rates increased in the pilot clinic sites demonstrating an impact on patient care.
DISCUSSION/REFLECTION/LESSONS LEARNED: Discussion/Reflections/Lessons Learned: Though cervical cancer screening is effective in prevention of invasive cervical cancer, there continue to be gaps in screening rates. Previous studies have demonstrated this is due in part to poor rates of physician implementation, especially among recent residency graduates. By creating a pap emphasis clinic, we were able to increase access to care for our patients and provide targeted teaching of pap smears and other preventive care topics in women’s health, a skill set which will be carried forward into independent clinical practice.
PATIENT SAFETY AT THE MOVIESChaitanya Mandapakala1,2; Diane L. Levine1,3. 1Detroit Medical Center, Detroit, MI; 2John D Dingell VA Medical Center, Detroit, MI; 3Wayne State University, Detroit, MI. (Tracking ID #1938570)
NEEDS AND OBJECTIVES: In the Institute of Medicine landmark report from 2001, “To Err is Human and Crossing the Quality Chasm”, the importance of teaching principles of quality improvement and patient safety throughout the continuum of undergraduate, graduate, and continuing education was emphasized. The Association of American Medical Colleges further recommends integrating these concepts as early as the first year of medical school. Efforts are presently underway to recognize important attributes students should possess at graduation from medical school called “Core Entrustable Professional Activities for Entering Residency” (CEPAER) for all entering residents to perform without direct supervision on day one of residency, regardless of specialty. Among these activities the ability to identify system failure and contribute to a culture of safety and improvement has been deemed as being critical. Wayne State University is the largest single campus medical school in the USA with 300 students per class. Third year medical students are assigned to a 2-month Internal Medicine (IM) clerkship at one of eight clinical sites. This makes teaching patient safety challenging. This year we initiated a patient safety half-day workshop to provide an opportunity for students to learn the principles of quality improvement and patient safety during their IM clerkship. Our medical school was very supportive of this endeavor, but was unable to provide financial support. So we developed a hands-on-experience utilizing low cost easily purchasable episode of a popular television show.
SETTING AND PARTICIPANTS: Students on the clerkship were required to attend a half-day patient safety workshop in the middle of their clinical rotation unless they had their continuity clinic.
DESCRIPTION: A pre-test was administered at the start of the workshop to test 7 basic concepts of quality improvement and patient safety. The session began with a case based presentation (morning report) providing an opportunity to discuss critical and latent medical errors, situations where errors are more probable while emphasizing concepts such as importance of proper transition of care and medication reconciliation. Students were encouraged to participate and identify how these errors could be avoided. Using a variety free resources demonstrating quality improvement from industry and personal stories the curriculum was delivered. Cases were examined to understand how the quality and patient safety department analyzes using various quality improvement techniques to strengthen the system. The high point of the day was the showing of a Grey’s Anatomy episode (cost $2.99) entitled “I saw what I saw”. Popcorn was distributed and lights were dimmed; students enjoyed the episode and participated in making a process map and a root cause analysis based on the events depicted in the episode. Possible solutions and PDSA cycles were described to further understand these principles. A post-test asking the same questions as the pretest was completed at the end of the workshop. Individual pre- post-test scores were analyzed.
EVALUATION: To date three workshops have been conducted. A total of 132 medical students participated. Of the 132 students who attended, 120 (90.9 %) students completed pre and post tests. Analysis of pre-tests showed that 75 % of students were able to give examples of situations where medical errors are more probable. The majority of students (75–99 %) showed knowledge deficits in the remaining concepts tested. All students showed knowledge improvement in all quality improvement and patient safety concepts discussed through this workshop (Swiss Cheese Model of Errors - 97.78 %, Situations where medical errors have higher probability to occur - 100 %, Sentinel Events - 98.75 %, construction of fishbone diagram - 97.48 %, RCA - 95.37 %, PDSA - 86.44 %). Based on feedback received after the first two workshops, the concept of human factors engineering was discussed in more detail during the third workshop with knowledge improvement of 96.42 %. Students also recorded 129 medical errors observed during their first month of clinical clerkship which were then classified into 10 categories. Medication errors (42 %) were the most common type. Interestingly only 1 student reported lack of hand hygiene as a patient safety concern. Finally, at the end of the workshop, 100 % of the students either agreed or strongly agreed to “I am knowledgeable about patient safety”. Qualitative analysis of the student comments indicated that the students found the workshop to be enjoyable and informative.
DISCUSSION/REFLECTION/LESSONS LEARNED: The approach used targeted integrating quality improvement and patient safety thinking into daily workflow. This half day patient safety workshop has proved to be an accessible, feasible, inexpensive and successful way to introduce junior students to the concepts of patient safety and quality improvement.
ONLINE RESOURCE URL (OPTIONAL):http://www.amazon.com/I-Saw-What/dp/B003TTCZNO
PATIENT-CENTERED MEDICAL HOME FOR SICKLE CELL DISEASE: IMPACT ON UTILIZATION OF ACUTE CARE SERVICESTemeia Martin; William P. Moran; Patrick D. Mauldin. Medical University of South Carolina, Charleston, SC. (Tracking ID #1940183)
NEEDS AND OBJECTIVES: Patients with sickle cell disease (SCD) have a life-limiting illness with a chronic relapsing course characterized by painful crises and recurring need for acute care for treatment. We sought to create a SCD outpatient medical home at the Medical University of South Carolina (MUSC) including acute care, individual care plans for each patient including acute treatment protocols and chronic medication regimens, and measure impact on emergency department (ED) visits and hospitalizations.
SETTING AND PARTICIPANTS: University Internal Medicine (UIM) is an NCQA-certified level III PCMH and hospital-based clinic responsible for the care of almost 10,000 medical patients with diverse medical conditions, comorbidities, and behavioral risk factors. Half of the 30,000 annual patient visits occur in the Internal Medicine resident continuity clinic, and half in the contiguous faculty practice with the majority of SCD patients assigned to the resident clinic. We defined our SCD medical home population as a patient seen 2 more times in the UIM practice over the preceding 3 years.
DESCRIPTION: An interdisciplinary team was brought together to provide focused care to SCD patients by way of a patient-centered medical home. Patients were tiered according to their patterns of utilization for enrollment in the SCD medical home. We sent letters asking them if they would like to transfer their care from the UIM practice to the SCD medical home and a follow-up phone call was made. Patients who consented attended a 1 h intake appointment and were scheduled for monthly visits thereafter. Follow-up visits were used to address issues related to SCD, co-existing chronic medical conditions, and health care maintenance. Patients were also given access to acute daily treatment of their pain with intravenous narcotics and hydration. We developed a referral process for medical home patients who presented to the ED. Plans of care for treatment of acute and chronic pain were individualized. A pharmacy clinic was developed for management and monitoring of Hydroxyurea usage in the patient population. We developed a transition plan with pediatrics to support matriculation to adult care. The population included in the SC medical home increased from a pilot of 10 patients to 78 over the first 20 months. The interdisciplinary team met weekly to coordinate ongoing development strategies for the clinic.
EVALUATION: Baseline data demonstrated that SCD accounted for 1 % of the UIM practice and accounted for 15 % of ED visits, 10 % of hospital admissions, and 33 % of re-hospitalizations. Measures of success were utilization of ED and hospital, Hydoxyurea prescribing, and patient satisfaction. Three patients died before the program started and 2 have died since its initiation. Interrupted time series (ITS) pre-post comparison design was used to assess change in utilization and data were limited to MUSC system. Statistically significant decreases in ED utilization (p < 0.0001) were achieved for the top 40 utilizers within the UIM PCMH Sickle Cell clinic following implementation of the clinic. Because of the small sample size, large fluctuations did not allow for significance to be determined for hospitalizations or re-hospitalizations. To determine where the effect on ED utilization of the sickle cell clinic was the strongest, subgroup analyses were performed: top 7 utilizers, next 16 utilizers, and then the remainder of the top 40. Significant decreases in ED utilization were achieved for the top 7 utilizers (p = 0.0006), with the most significant decreases within the “next 16” utilizers (p < 0.0001). There was no increase in Hydroxyurea prescriptions from baseline although there was an improvement in monitoring for toxicity and dose adjustments to target goals. Patient satisfaction data is gathered through qualitative and quantitative mechanisms including surveys and focus groups.
DISCUSSION/REFLECTION/LESSONS LEARNED: Implementation of a patient centered model in SCD appears to have a positive impact on disease management. Greater access to acute and longitudinal medical services improves utilization of acute care services. Patterns of utilization correlate with severity of disease underscoring the need for enhanced models of care for SCD.
ONLINE RESOURCE URL (OPTIONAL): NONE
PRE-CLINICAL ELECTIVE TEACHES END-OF-LIFE COMPETENCIES: EFFECTS PERSIST INTO CLINICAL YEARSMelissa S. Keeport; Brian Cruz. Tulane University Health Sciences Center, New Orleans, LA. (Tracking ID #1927107)
NEEDS AND OBJECTIVES: Medical education inadequately addresses end-of-life (EOL) and palliative care. We previously reported that our intervention—a pre-clinical elective—increased students’ self-perception of readiness to discuss EOL-related issues following completion of the course. The first cohort of intervention students to complete a significant clinical year was assessed to determine if their readiness continued 2 years after taking the course. Our aims were: 1) teach medical students basic EOL care competencies with an emphasis on confidence-building for addressing these topics with patients and their families; and 2) measure the impact of this elective from the pre-clinical (MS-1 and MS-2) years to the clinical (MS-3 and MS-4) years.
SETTING AND PARTICIPANTS: We designed an elective open to first-year medical students at Tulane University School of Medicine. We have implemented it for three consecutive years, starting with the Class of 2014 in their MS-1 year. This cohort has now completed its first and main clinical year of medical school. We administered a survey to the entire Class of 2014 upon completion of their MS-1 year and upon completion of their MS-3 year to assess EOL competencies. Course participants’ responses were compared to control students who did not take the elective.
DESCRIPTION: The elective is open to 25 medical students for 10 total course hours. Creative, active-learning modules are combined with published tools and techniques to explore the basics of hospice and palliative medicine. Multiple domains are addressed using a combination of didactics, group discussion, standardized patients, attendance at the hospital ethics committee meetings, and site visits. The elective utilizes student leadership of MS-3 and MS-4 students, expertise of Tulane’s palliative care specialist on faculty, education by internal medicine residents pursuing fellowships in palliative care, and other multidisciplinary specialists.
EVALUATION: Medical students who completed the elective in their MS-1 year said they felt more prepared to speak to patients and/or patient families about EOL issues than their counterparts, with 78 % of elective students responding “prepared” compared to only 32 % of controls; p < 0.001. These responses persisted 2 years later into the “clinical” training years, where 70 % of MS-3 students who had taken the elective responded “prepared” compared to only 36 % of students who had not taken the elective; p < 0.05.
DISCUSSION/REFLECTION/LESSONS LEARNED: The increased comfort and ability to speak about EOL-related issues that students achieved following their participation in the MS-1 elective has persisted into their clinical years. This student-initiated elective exemplifies the usefulness and high impact of teaching clinically-relevant skills early in the pre-clinical curriculum.
ONLINE RESOURCE URL (OPTIONAL):http://tmedweb.tulane.edu/mu/eol/eol-elective/
PREPARING RESIDENTS FOR THE PRIMARY CARE MEDICAL HOME: SELF-DIRECTED, LONGITUDINAL PROJECTS IN QUALITY IMPROVEMENTCarol Sprague2,1; Christine Mullowney1. 1Oregon Health and Science University, Portland, OR; 2Portland Veterans Affairs, Portland, OR. (Tracking ID #1938533)
NEEDS AND OBJECTIVES: A core principle of the primary care medical home is ongoing engagement in quality and safety activities. Resident training needs to prepare young physicians for this work. We therefore designed and implemented projects in quality improvement with the following objectives: 1) To familiarize residents with the concepts and strategies of the patient-centered medical home 2) To foster the development of creative, systems-based solutions to challenges in clinical care 3) To practice use of the electronic health record in capturing population data and supporting the delivery of evidence-based care
SETTING AND PARTICIPANTS: The Internal Medicine residency at the Oregon Health & Science University (OHSU) is a university-based, mid-sized program. The OHSU ambulatory curriculum includes a primary care clinic experience (for which we have three sites) as well as ambulatory based rotations, one of which is the “Chronic Illness Management” or “CIM” rotation. In addition to a team-based clinical experience, the CIM rotation includes a 2 h weekly session to learn the principles of the medical home. Residents are scheduled for 6 of these sessions over a 6 month period; interns are given a 3 month period to work on a QI project.
DESCRIPTION: The initial sessions include interactive lectures on the patient-centered medical home and the PDSA tool. Residents then apply these concepts toward a self-directed quality improvement project. In deciding upon a project topic, residents account for the structure and patient demographics of their primary care site. Residents develop an “aim statement” and think through each step of a PDSA. They use the medical literature for guidance about benchmarks. Residents then obtain the best performance data available within their clinic setting. Clinic teams are involved in the improvements when possible. Project development is achieved through an interactive, iterative experience in which residents return on a monthly basis to reflect on their progress and to receive feedback from peers. At the final session, residents present their quality project to their peers and are asked to reflect on how they might accomplish their goals with a larger patient panel.
EVALUATION: Resident evaluations of the rotation are positive. Residents appreciate applying the QI concepts to their own patient panels and clinic settings, a process that in one resident’s words “helped me realize the potential . . . to make significant changes in my practice.” Developing projects that are appropriate in three different clinical settings is challenging but helps residents learn about different systems of practice. Last academic year, three residents were selected to present their projects at a Medicine department M&M. The flexibility of the project allows residents to develop skills within the context of their interests and in keeping with their stage of development as a physician.
DISCUSSION/REFLECTION/LESSONS LEARNED: The quality improvement project in the “CIM” rotation provides residents with a longitudinal, self-directed learning experience. Quality improvement concepts seem to be learned well when residents are given flexibility in determining a topic that will be meaningful to them. Our current structure is restricted by each clinic’s capacity to incorporate significant quality projects and by our ability to access accurate data in each setting. Ideally, for those residents with a particular interest, we would propose the development of a separate rotation that allows residents to contribute to clinic-wide, interprofessional efforts toward quality improvement.
PROGRESS TESTING: AN INNOVATIVE APPROACH TO ASSESSMENT OF COMPETENCY-BASED MILESTONES IN CLINICAL SKILLSLauren Block; R. Ellen Pearlman; Judith M. Brenner; Alice Fornari; Joseph S. Weiner; Marie Barilla-Labarca. Hofstra North Shore-LIJ School of Medicine, New Hyde Park, NY. (Tracking ID #1933537)
NEEDS AND OBJECTIVES: Growing evidence suggests that medical student assessment should be developmentally sequenced, competency-based, individualized, and integrated across disciplines. Progress testing offers an efficient, individualized, comprehensive assessment across content areas and academic year. We sought to use a single standardized case as a progress test to compare developmentally-based clinical skills competencies among medical students.
SETTING AND PARTICIPANTS: As the culmination of a longitudinal clinical skills curriculum, a single standardized case was administered in a clinical skills center to first and second year students at Hofstra North Shore-LIJ School of Medicine.
DESCRIPTION: Students performed a history and physical examination on a standardized patient as well as a post-encounter exercise to assess competency in domains including communication, patient care, and professionalism. A committee of standardized patients and clinical faculty reviewed student performance based on proposed milestones expected for the student’s year in each domain.
EVALUATION: 58 first year and 33 s year students completed the examination. 81 % (47) of first-year and 85 % (28) of second-year students met developmental expectations in communication, 90 % (52) and 94 % (31) in patient care, and 84 % (49) and 76 % (25) in professionalism. The 23 students who did not meet expectations were offered remediation through individual feedback, videotape review, and a repeat exam. The implications of these data will be discussed.
DISCUSSION/REFLECTION/LESSONS LEARNED: A single standardized case served as a developmental progress test to identify students attaining milestones in clinical skills and highlight areas for feedback and remediation. Standardized patients and faculty cooperated to identify areas of weakness and offer individualized feedback to learners. As developmental milestones are proposed in medical education, it is critical to evaluate whether students meet the recommended competencies. We designed a single case to serve as an integrated clinical skills progress test. Future work will include prospective development of a competency-based instrument for longitudinal assessment in clinical skills.
REACHING CONSENSUS AMONGST PHYSICIANS IN BUILDING AN EVALUATION TOOL TO IMPROVE DISCHARGE SUMMARIES AND OPTIMIZE TRANSITIONS OF CAREKarim Taha; David W. Frost. University Health Network (UHN), Toronto, ON, Canada. (Tracking ID #1936760)
NEEDS AND OBJECTIVES: The discharge summary is an essential communication tool between hospitalists and primary care physicians. Despite advances in electronic transfer of discharge summaries as well as electronic templates, there remain challenges around optimization and standardization of its content. This study aimed to reach consensus amongst family physicians (or general practitioners, GP’s) on the relative importance of various components of the discharge summary, and to determine the best areas to focus educational efforts. Based on these results, an evaluation tool for discharge summaries was developed for both educational and quality assurance purposes.
SETTING AND PARTICIPANTS: Twenty-five family physicians (both academic and community-based) participated in our study employing the Delphi methodology of consensus building based on iterative surveying. This initiative was a partnership between the General Internal Medicine Division of the University Health Network in Toronto and family physicians in Toronto, Ontario and surrounding regions.
DESCRIPTION: Three rounds of surveys regarding discharge summaries were completed. The first round allowed for family physicians to express open-ended opinions about the most salient aspects of discharge summaries. The second round asked participants to rank all opinions generated from the previous round in terms of importance and agreeability to their preferences. Finally, the last round addressed any outlier responses in the overall rankings. The culmination of these rounds served to establish a refined average in each discharge summary category. Findings: Specific instructions for the family physician in the follow-up section and a well-outlined discharge plan were areas of highest relevance to participants. These sections were also noted as least clearly filled out currently. Commonly reported areas requiring improvement included the need for a thorough medication reconciliation section, a concise overall report, and provision of specialist referral information. Participants expressed preference for inclusion of relevant lab results from the entire hospital stay duration, and suggestions were made on appropriate educational interventions to maximize discharge summary quality.
EVALUATION: The tool developed will be subjected to an assessment of intended outcome (improved discharge summary quality), implementation and uptake levels, and determination of perceived value to educators and learners. Feedback generated will guide further revisions and dissemination decisions.
DISCUSSION/REFLECTION/LESSONS LEARNED: Family physicians, as experts in the evaluation of discharge summary quality, purposely engaged with general internal medicine physicians in the successful development of an educational and quality improvement tool using rigorous consensus-building methodology. Deployment of the tool is currently under way in paper and electronic form. Evaluation of its utility in improving discharge summary quality is planned in the near future. With an almost 100 % response rate throughout three rounds of surveys, our ranked results are highly reflective of the collective opinions of partnering family physicians.
RESIDENT AS PRECEPTOR: DEVELOPING SENIOR RESIDENTS’ AMBULATORY TEACHING SKILLS AS PART OF A RESIDENT AS TEACHER CURRICULUMElena Lebduska1; Sudha Dubey2; Darlene LeFrancois1; Sheira Schlair1. 1Montefiore Medical Center, Bronx, NY; 2Beth Israel Medical Center, New York, NY. (Tracking ID #1937669)
NEEDS AND OBJECTIVES: Fostering residents’ teaching skills can complement clinical skill development for internal medicine residents. While there are many opportunities for inpatient resident teaching skill development, opportunities to expand teaching skills may be underutilized in ambulatory settings. Our aim was to teach residents effective precepting skills in the ambulatory setting by providing a “Resident as Preceptor” curriculum followed by supervised precepting sessions with junior residents.
SETTING AND PARTICIPANTS: Third year internal medicine residents on a “Resident as Teacher” elective, first and second year internal medicine residents, and attending internal medicine physicians in three ambulatory internal medicine sites at Montefiore Medical Center (Bronx, NY).
DESCRIPTION: The “Resident as Teacher” elective is an intensive 2 week rotation focused on resident teaching skill development in which residents receive formal teaching skill instruction and are observed and given feedback in diverse teaching encounters. The “Resident as Preceptor” curriculum is a major focus of our “Resident as Teacher” elective. A two-hour learner-centered, multimedia curriculum focuses on adult learning theory, socratic method, the “one-minute preceptor” model, and RIME scheme. Following the didactic session, residents then precept for 1–2 half days. During these sessions the resident precepts a junior (PGY1 or PGY2) resident while an attending physician silently observes. All participants complete evaluation forms and give immediate feedback on the resident preceptor’s precepting skills.
EVALUATION: Resident preceptors, junior residents and attending physicians are surveyed immediately following each precepting session to assess overall precepting effectiveness. Survey instrument outcomes are based on principles of the “one-minute preceptor” model and the RIME scheme with all questions scored on a 1–4 Likert scale (1 = strongly agree to 4 = strongly disagree) or open-ended questions. To date, 13 senior residents, 15 junior residents and 7 attending physicians have participated with the goal of 25 senior residents, 30 junior residents and 10 attending physicians having participated by Spring 2014. Of the initial participants, 66 % of residents and 62 % of attending physicians “strongly agreed” that the resident preceptors effectively elicited the junior residents’ reasoning, assessment, and plan. Seventy percent of residents “strongly agreed” that they were comfortable in their role as preceptor, and 80 % “strongly agreed” that the experience added educational value to their residency. Seventy-five percent of junior residents “strongly agreed” that they received behaviorally specific feedback.
DISCUSSION/REFLECTION/LESSONS LEARNED: Interim analysis of survey and program evaluation data suggests that a learner centered curriculum focused on feedback and precepting skills, and observed precepting experience with immediate feedback on teaching skills, can add educational value to the residency experience. In addition, initial cohorts of resident preceptors seem to have been effective at applying lessons learned in the didactic portion of the curriculum, including principles of adult learning theory and learner assessment. Resident preceptors found it to be an overall rewarding experience. Incorporating resident precepting skill development into a “Resident as Teacher” curriculum can expand educational and assessment opportunities to the ambulatory setting.
RESIDENTS JOIN THE HUDDLE: RESIDENT PARTICIPATION IN A QUALITY IMPROVEMENT PROJECT ON RN-MD COMMUNICATION DEVELOPS SEVERAL ACGME RESIDENT COMPETENCIESRachel Hathaway1; Maren Batalden1; Priyank Jain1; Kathleen M. Clark2. 1Cambridge Health Alliance, Cambridge, MA; 2Cambridge Health Alliance, Cambridge, MA. (Tracking ID #1930039)
NEEDS AND OBJECTIVES: Increased attention to developing resident proficiency in quality improvement has led to the inclusion of competency in quality improvement as an ACGME milestone. Quality improvement efforts emphasize interdisciplinary collaboration in clinical work; the capacity to work in teams is a competency required for the 21st century physician. This project involves residents helping to design and implement a structured, daily nurse-physician “huddle” on an inpatient teaching service to proactively communicate patient care plans at the start of each day. Resident leaders will be instrumental in structuring and evaluating the impact of this intervention. We intend to show that the active participation of Internal Medicine residents at Cambridge Hospital in a quality improvement project allows residents to meet the ACGME milestone of systematically analyzing their practice and engaging in practice improvement. Additionally, several other secondary competencies are strengthened through participating in this project.
SETTING AND PARTICIPANTS: This pilot project will take place on a busy inpatient teaching service at Cambridge Hospital, a university-affiliated, community hospital in an urban, diverse, and largely underserved setting. The service is resident-run and exclusively geographically located on one floor of the hospital, allowing for consistent interactions between residents and a defined cohort of nurses. Participants in the nurse-physician huddle include 2nd and 3rd year residents, all floor nurses, the nurse manager, and the unit secretary.
DESCRIPTION: Currently, MD’s and RN’s primarily communicate with one another via ad-hoc interactions. We intend to institute a daily, structured, and brief “huddle” between residents and nurses at the beginning of the day shift. The intent of this resident-led huddle is to address early in the shift any nursing or patient concerns, potential discharge complications, and to clearly communicate the patient care plan for the day to all relevant providers. Any patients identified as being sick or complex will prompt inclusion of the nurse on MD work rounds to ensure a cohesive team approach. All participants will be encouraged to be engaged and proactive in their roles. Summaries of each patient will be high-yield and concise. Real-time feedback will be solicited from both residents and nurses in order to rapidly improve care and anticipate problems. Objectives of the huddle include improved communication between residents and nurses, improved patient care, better teamwork, and improvement in both RN and MD satisfaction with their work environment.
EVALUATION: There will be several tiers of evaluation. Residents will be quantitatively surveyed regarding their perceived growth in various ACGME competencies including quality improvement. Additionally, we will assess the value residents place on quality improvement and other related competencies as a result of participating in the project. Both residents and nurses will be evaluated regarding any perceived improvement in nurse-physician communication, teamwork, quality of patient care, and work environment satisfaction. Patient satisfaction will be surveyed via changes in Press Ganey scores.
DISCUSSION/REFLECTION/LESSONS LEARNED: Finding meaningful ways for residents to develop competency in the realm of quality improvement is a priority. This is reflected in the current ACGME milestones. This quality improvement pilot project seeks to actively engage Internal Medicine residents at Cambridge Hospital in improving nurse-physician communication on a busy inpatient ward. Nurse-physician communication is improved by means of a structured, daily morning “huddle” to address active, patient-centered concerns. This resident-led initiative provides opportunity to develop and demonstrate competency in several ACGME milestones, including acting as patient advocates, striving for excellence in patient care, successfully participating in interprofessional teams, and practicing effective communication. Residents not only observe the inner workings of a quality improvement initiative but are critical players in the process. Residents will be encouraged to reflect on the impact that their work has had on their own development as leaders, on the culture of the unit in which we work and on patient care.
RESTORING EMPHASIS ON AMBULATORY INTERNAL MEDICINE TRAINING - “THE 3:1 MODEL.”Joshua W. Harrison; Peter Cronkright; Astha Ramaiya. Upstate Medical University, Syracuse, NY. (Tracking ID #1910892)
NEEDS AND OBJECTIVES: Inadequate ambulatory training in internal medicine (IM) residency programs may be partially responsible for the current shortage of primary care physicians. Without an adequate ambulatory care experience, IM residents fail to observe the rewarding nature of developing continuity relationships with their patients and do not gain the confidence and experience to be effective outpatient practitioners. With work hour demands and multiple reports citing concerns regarding ambulatory IM training, reform in this arena is necessary.
SETTING AND PARTICIPANTS: A relatively novel 3:1 scheduling system that creates week long ambulatory blocks every fourth week was instituted for PGY-2/3 residents at our program. During this week residents participate in morning continuity clinic and afternoon subspecialty clinic training. Residents begin ambulatory days learning practice management issues, reviewing an ambulatory medicine article, covering a pharmacy topic, or reviewing a physical exam skill. Each quarter residents participate in a half day “Teaching Activity” allowing faculty to directly observe residents communicate with simulated patients, role play clinical teaching scenarios, or run simulated codes.
DESCRIPTION: We hypothesized that this model would provide a more structured ambulatory educational atmosphere, better continuity of care, more exposure to subspecialty outpatient medicine, and eliminate conflict with inpatient duties. We hoped this would enhance resident satisfaction with ambulatory medicine and achieve our main goal of improving the ambulatory educational experience.
EVALUATION: Surveys were created utilizing a Likert scale and distributed 9 months into this experience. Responses from PGY-1’s maintained on a traditional ½ day per week clinic schedule were compared to PGY-2/3 responses using a t-test. The PGY-2/3 group also retrospectively evaluated their experience in the 3:1 model compared to the prior year’s traditional schedule. These results were analyzed descriptively. Residents reported the 3:1 model had positively affected their satisfaction with residency training in general, their satisfaction with outpatient/primary care training, and their outpatient/clinic educational experience. Residents perceived improvements in continuity of care with patients and in the quality of care they provided for patients. Their experience in ambulatory sub-specialty training was positive. PGY-1 s who remained on a traditional ½ day per week clinic schedule were significantly less satisfied than PGY2/3 s with their ambulatory/primary care training (mean = 3.48 vs. 4.08, p = 0.01). Compared to PGY-2/3 s, PGY-1 s also perceived less continuity of care with their patients (mean = 3.91 vs. 4.38, p = 0.03), less adequate exposure to sub-specialty outpatient medicine (mean = 3.0 vs. 4.58, p ≤ 0.01), and were more distracted or worried about inpatient duties while at clinic (mean = 2.39 vs. 4.92, p ≤ 0.01).
DISCUSSION/REFLECTION/LESSONS LEARNED: We present positive results following the institution of a relatively novel 3:1 scheduling model. This system effectively eliminates the concurrent demands of inpatient and outpatient duties, provides increased time for educational sessions, has improved resident satisfaction in several arenas, likely promotes continuity of care, and provides important exposure to subspecialty outpatient medicine. We believe these changes enhance our residents’ ambulatory educational experience. Given the resoundingly positive results the 3:1 model has since been instituted for all categorical residents at our program.
SEALS: A PROCESS AND INTERMEDIATE OUTCOME EVALUATION OF AN INNOVATIVE PIPELINE CURRICULUMCassandra D. Fritz; Monica Vela. University of Chicago, Chicago, IL. (Tracking ID #1936651)
NEEDS AND OBJECTIVES: Pipeline programs are one proposed method to increase the number of under-represented minority (URM) students matriculating to medical school. Although pipeline programs have demonstrated success in increasing matriculation of URM students, a review conducted by the Department of Health and Human Services in 2003 notes the lack of appropriate evaluation measures for pipeline curriculum. Therefore, our goals were to 1) develop an evaluation mechanism using process and intermediate outcome measures for pipeline programs and 2) apply the evaluation to a novel pilot pipeline program.
SETTING AND PARTICIPANTS: The SEALS summer pipeline program is a novel curriculum established to promote 5 competencies among minority medical students including: Socialization and Professionalism, Education in science learning tools, Acquiring finance literacy, Leveraging Mentorship and Networks, and Social expectations and resilience. Local academically successful URM and/or underserved rising first and second year college students were recruited to apply through the web. IRB approved pre/post program surveys included short answer, likert scale responses, and personal statement writing and were administered to the 13 SEALS students. In addition, this survey was administered to a cohort of ten students in a comparable, research-based pipeline program at our institution during the same summer session. This cohort served as a control.
DESCRIPTION: The pre and post survey instrument included qualitative and quantitative measures designed to assess students’ knowledge, skills, attitudes, and quantify hours of programmatic activities. Students’ knowledge of (1) the medical school admissions process, (2) requirements for medical school, (3) AMCAS application service, (4) Health Care Disparities, and (5) Anatomy and Physiology of systems related to greatest health threats to underserved populations was assessed. Skills of how to (1) shadow a physician effectively, (2) seek out research opportunities, (3) engage and reflect upon service opportunities, (4) develop a personal statement of interest in medicine, (5) interview and communicate, and (6) effectively complete of a financial aid form were also assessed. The survey gauged the students’ attitudes toward the following: (1) service, (2) research, (3) medicine as a profession, and (4) commitment to medicine as a career. Finally, the total number of hours spent on each activity and student’s assessment of the quality of the activities was obtained.
EVALUATION: Our evaluation consisted of process and intermediate outcome measures. Process measures included who participated, quantity of activities, and quality of those activities. Intermediate outcome measures quantified students’ change in knowledge, skills, and attitudes. The evaluation was also administered to the control cohort, who did not differ significantly in any demographic when compared to the SEALS cohort. Process Outcomes. One hundred percent of students agreed/strongly agreed that the Meet the Professor series, Health Care Disparities series, and Pre-Med 101 workshops were instrumental in motivating students to purse their passion for medicine (11 of 11). Furthermore, these curriculum components inspired students to advocate for minority health issues. Intermediate Outcomes. The pre-SEALS to pre-control analysis did not reveal any important statistically significant difference between the two cohorts. A comparison of pre-SEALS to post-SEALS found statistically significant changes favoring post- SEALS: knowledge of MCAT components (p = 0.007), ability to ask for letter of recommendation (p = 0.04), attitudes toward research being an important determinant of success (p = 0.02) and appearing confident during an interview (p = 0.04). The post-SEALS to post-control did uncover a number of statistically significant values including, but not limited to ability to communicate with patients (p = 0.046), understanding of health disparities (p = 0.04), understanding of major disease entities (p < 0.01), and students’ resolve to become a physician (p < 0.01). Pre and post- SEALS personal statements were compared to the control group’s AMCAS personal statement using a 5-point scale. The SEALS cohort average score increased by nearly 1 point. (pre = 2.09 to post = 2.95). These averages were then compared to the control cohort average, which was determined to be 2.40.
DISCUSSION/REFLECTION/LESSONS LEARNED: Two major lessons about pipeline curriculum emerge. First, defining best practices in pipeline curriculum requires process and intermediate outcome measures. Outlining process and intermediate outcome measures of pipeline programs will allow for systematic improvement of program practices and dissemination of successful pipeline practices. Second, use of a control group revealed a gap in professional development training for URM students participating in research-based pipeline programs.
SHARED DECISION MAKING IN CHRONIC CONDITIONS: A CURRICULUM IN USING DECISION AIDS FOR INTERNAL MEDICINE RESIDENTSLeigh H. Simmons1,2; Lauren Leavitt2,1; Alaka Ray1; Blair W. Fosburgh1; Karen R. Sepucha2,1. 1Massachusetts General Hospital, Boston, MA; 2Massachusetts General Hospital, Boston, MA. (Tracking ID #1936903)
NEEDS AND OBJECTIVES: In the current medical environment, there is heightened attention to training physicians in communication skills that will enhance patient understanding of treatment recommendations and reduce “preference misdiagnosis.” The aim of this study was to develop and implement an educational workshop for residents to promote shared decision making (SDM) with their patients during clinical interactions, with a specific focus on decision making for four chronic conditions (diabetes, depression, hypertension, and hyperlipidemia).
SETTING AND PARTICIPANTS: We conducted our study in a large academic internal medicine residency; 120 residents (from all years of training) participated during their ambulatory rotation.
DESCRIPTION: We used a mixed methods approach to understanding our residents’ perspectives on SDM, improving resident knowledge about SDM, and implementing a novel paper decision aid for resident training. We ran focus groups with residents to elicit challenges of decision making with patients for chronic conditions and to get feedback on a new tool, the Choice Report. The Choice Report is a single-page print decision aid that highlights six steps of shared decision making, including FAQs about treatment options. Using the focus group insights, we developed a workshop curriculum including the following: a didactic presentation about risk communication, introduction of the Choice Report to guide conversations about chronic conditions, and role-playing exercises for a chronic condition using the Choice Report. Participants were shown how to download the Choice Reports from the hospital’s primary care-focused intranet (accessible by all clinicians). Participants completed surveys after the session and we tracked the number of times that Choice Reports were downloaded.
EVALUATION: 120 residents attended the workshops over a 4-month period. The interns rated the workshop higher than the residents (81 % very useful content & 62 % excellent overall rating vs. Forty-six percent very useful content & 41 % excellent overall rating). This trend has been observed in our previous workshops, in which interns have generally found the content of shared decision making discussions more useful and rated them more highly than the 2nd and 3rd year residents. The Choice Reports on diabetes, depression, hyperlipidemia, and hypertension were downloaded 1500 times in the 8 months following their introduction.
DISCUSSION/REFLECTION/LESSONS LEARNED: The workshop introduced residents to a SDM communication strategy for routine clinical encounters, with a focus on decision making for chronic conditions. This curriculum was novel in that it introduced a SDM tool to clinical topics not previously recognized as candidates for a “shared decision making” approach. The Choice Reports also generated significant interest from our general medicine clinicians and have continued to be used regularly in the course of routine primary care. We had initially planned to include a component of direct observation, with preceptors completing a mini-CEX of a visit using a Choice Report. However, we found that coordinating direct observations of eligible encounters was prohibitively difficult. Because this tool has been accepted and used by our staff and resident clinicians, we are developing new Choice Reports, to include cancer screening decisions, additional chronic conditions, and multiple language translations.
SIGUIENDO ADELANTE: A MEDICAL SPANISH CURRICULUM FOR RESIDENTSAvik Chatterjee1; Li Qin2; Jaideep S. Talwalkar3. 1Harvard Pilgrim Health Care Institute/Department of Population Medicine at Harvard Medical School, Cambridge, MA; 2Yale School of Public Health, New Haven, CT; 3Yale Univsersity, New Haven, CT. (Tracking ID #1931760)
NEEDS AND OBJECTIVES: Spanish speakers with limited English proficiency (LEP) represent a large and growing part of the population in the United States, with 80 % of hospitals providing care to LEP patients regularly. Having a language-concordant provider is associated with improved patient satisfaction and improved processes of care. Previously described medical Spanish curricula have improved language skills among students and practicing physicians, but these curricula are incompatible with resident schedules. In 2009, a needs assessment at our institution showed that residents saw Spanish-speaking patients regularly and wanted a medical Spanish curriculum designed for residents. Objective: 1) Demonstrate improvement in medical Spanish for a diverse group of residents 2) Improve cultural competency
SETTING AND PARTICIPANTS: Our institution is a 1,541 bed tertiary-care hospital with over 500 resident physicians, in a city of 129,585 people, of whom 27.4 % self-identify as Hispanic. In 2010–2011, we created a pilot curriculum with 20 participants from internal medicine, pediatrics, and combined med-peds programs. The curriculum was well received, so in 2011–2012 we expanded our learner-base, offering the curriculum to residents in their second year or above from all programs at our institution. Participants also were required to have at least a conversational level of Spanish. We had 63 participants, 33 (52 %) of whom were from procedural specialties.
DESCRIPTION: The year-long, self-directed curriculum contains nine month-long modules, with 3 months that residents can take off during particularly demanding clinical rotations. The curriculum includes practice with a variety of skills including grammar, vocabulary, reading, writing, listening comprehension, speaking and cultural competency, in keeping with the principles of adult second-language learning, which suggests that incorporating multiple learning modalities is most effective. Each month-long, systems-based module includes: a grammar/vocabulary activity; a health-related DVD program; patient cases with a Spanish-speaking tutor; and community practice sessions. The community practice sessions involve having participants prepare health education talks on various to practice with English as a Second Language (ESL) students at a local non-profit, getting the chance to practice vocabulary, speaking and listening comprehension skills, while improving understanding of cultural concerns that would arise from the patient population that our residents serve.
EVALUATION: We conducted pre-intervention and final assessments of language skills and cultural competency using previously validated self-report questions. We also collected open-ended feedback from participants and tutors. Of 63 participants, 13 (21 %) responded to the final survey. Of those, nine (71 %) were satisfied or very satisfied with the curriculum, but only five (38 %) completed a majority of the modules. Every respondent cited time as a barrier. There were correlations between number of modules completed and self-reported fluency scores (p = 0.025), change in self-reported receptive language ability (p = 0.025), and self-reported understanding of the health-related cultural beliefs of Spanish speaking patients (p = 0.047). Residents in cognitive specialties were more likely than residents in procedural specialties to complete the post-course evaluation (p = 0.03).
DISCUSSION/REFLECTION/LESSONS LEARNED: We developed and implemented a novel medical Spanish curriculum for residents in order to address the prevalent health disparities issue of communication with Spanish-speaking LEP patients. Residents at our institution recognized the need for specific training to improve language concordance and expressed a desire for a medical Spanish curriculum that fit their schedules. Our institution, recognizing the need, supported our intervention. Our study demonstrated that residents who completed more of the curriculum had better self-reported fluency scores and cultural competency skills. The majority of residents who provided feedback were satisfied with the YRSI and several were able to complete significant parts of the curriculum. However, while residents from multiple specialties were initially enthusiastic about the availability of the curriculum, they ultimately found it difficult to participate, primarily citing time constraints. For future participants, we plan greater clarity about time required, more documentation of completion of curricular materials, frequent reminders, and large-group events to encourage a sense of team. We will also include more surgery-specific activities. Ultimately, measurement of the curriculum’s impact on patient outcomes will also be important. While curricular revision is necessary, we believe that the implementation of a flexible, self-directed curriculum is a feasible way to incorporate Spanish language education into a traditional residency schedule, at our institution and others.
ONLINE RESOURCE URL (OPTIONAL):http://www.yalepediatrics.org/education/residency/spanish/index.aspx
STORY TELLING: MY MOST MEMORABLE PATIENT - LESSONS IN HUMANISM, REFLECTION, AND THE DEVELOPMENT OF EXPERTISEPriya Radhakrishnan1,2; Patti Thorn2,1. 1St Joseph’s Hospital & Medical Center, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ. (Tracking ID #1937664)
NEEDS AND OBJECTIVES: Needs : Humanism in medicine is heavily stressed in undergraduate medical education, particularly within the first and second years of medical school. Yet, when residency begins, there is a gradual erosion of cognitive attention to humanism and the values that initially attracted physicians in training to the profession of medicine are set aside in favor of acquisition of knowledge, patient management, and efficiency. The reduction in duty hours, opportunities for continuity of care, and a relatively young faculty mentor group only accentuate the erosion of attention to humanism and lived expression of meaningful values. In addition, there is a need for physicians in training to be challenged to progress in clinical problem solving abilities along a continuum toward expertise, and, learning to tap into episodic memories of actual patients has been demonstrated to serve this progression. Objectives- 1. To revitalize the humanistic aspect of medicine within Internal Medicine residents 2. To encourage deep reflection and meaningful attention and focus on the primary values of medicine, which when lived frequently, translate to increased career fulfillment 3. To encourage the practice of episodic memory formation which is utilized in advanced clinical problem solving
SETTING AND PARTICIPANTS: Setting & Participants The curriculum has been instituted in the St Josephs Internal Medicine residency program since 2010. It is a series of 3–4 conferences at the end of the academic year. Each third year resident actively participates in the storytelling
DESCRIPTION: All residents anticipate and plan to present a patient or patients that touched them during their training experience. The patients they present are framed as “those that will never be forgotten for the teaching and learning they inspired.” Residents receive a list of learning objectives and a bulleted list of reflection prompts to aid their reflection process. The presentation format is left entirely up to the residents-they may use a Powerpoint or engage in narrative-story telling (the latter is encouraged). The audience includes multi-disciplinary teams from both the inpatient and outpatient care settings, hospital staff, administrators, educators, nurses, hospital leadership and medical students. Following the residents’ shared reflections and narrative, the audience is encouraged to comment and share their thoughts about the impact the story telling had, memories and learning recalled, and similar patient care experiences. These sessions are highly anticipated as a culmination/capstone to the residency training program. Resident participants as well as the audience engage in collective humanism and discussion of the value that form the core of medical professionalism. Residents also reflect on how the learning from their patient has shaped their decision-making and how they anticipate the memory will become significant in their careers as physicians.
EVALUATION: The sessions are evaluated on the response that it generates in the residents and the audience. Both groups are asked to share in writing the value(s) that were evoked by the capstone presentation. Several of the essays have been published by residents in different venues. Audience comments and the narratives are collected and we plan to publish a collection of the best essays in reflection. We also plan to start a Story-Corp collection of the narratives to archive these collections.
DISCUSSION/REFLECTION/LESSONS LEARNED: As the practice of medicine and residency training is transforming in response to the societies’ call for decreased duty hours, there is great danger of the loss of humanism among physicians in training due to the toll of rapid cycle change. In addition, amongst junior and even seasoned faculty, we are observing disillusionment and burnout leading to career attrition. This capstone curriculum is designed to re-invoke the humanism in medicine and bring together team members who may not see the patient but are invested in the success of the enterprise: leaders as well as physicians and the multi-disciplinary team
STORYTELLING WITH INPATIENTSKatherine C. Chretien1,2; Rebecca Swenson3; Bona Yoon1; Ricklie Julian4; Jonathan Keenan2; Raya Kheirbek1,2. 1Washington DC VAMC, Washington, DC; 2George Washington University, Washington, DC; 3Dartmouth-Hitchcock Medical Center, Lebanon, NH; 4Montefiore Medical Center, Bronx, NY. (Tracking ID #1938337)
NEEDS AND OBJECTIVES: Empathy is an essential component of patient-centered care and improves patient outcomes. A recent systematic review of interventions to teach empathy to medical trainees identified a need for future interventions to be built upon a foundation of relationship-centered care. Narrative competence can be defined as “the ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” There are few published educational interventions that address empathy while involving actual patient-provider interactions, and/or address narrative competence. We sought to incorporate a brief experiential narrative medicine curriculum within the third-year medicine clerkship with the goals of developing narrative competence, practicing attentive listening, and stimulating reflection while providing patient-centered care for hospitalized patients.
SETTING AND PARTICIPANTS: Single institution with third-year basic medicine clerkship students on a 4 week rotation and inpatients on the acute (non-ICU) medicine wards.
DESCRIPTION: The narrative medicine curriculum consisted of 1) Introductory session where students were introduced to narrative medicine and practiced attentive listening to storytelling in pairs; 2) Patient activity where students elicited illness narratives from patients, attentively listened, wrote their version of the story, and then read these back to patients. Students also asked patients to select a piece of art to help tell their story, chosen from a digital collection stored on an iPad. 3) Debriefing/reflection session where students wrote reflectively and participated in a facilitated discussion about their experiences with the activity.
EVALUATION: To evaluate and help assess acceptability and feasibility of the curriculum, five focus groups were held between July 2011 and March 2012. Thirty-one students participated. Transcripts were qualitatively analyzed for themes by two independent researchers; disagreements were resolved through discussion. Students discussed their patients’ reactions to the narrative medicine activity, students’ own experiences, the student-patient dynamic, and challenges. They also identified what they felt they learned, including seeing the patient as human, being open, and clinically relevant insights. Students felt that the activity improved the student-patient relationship and, in some cases, powerfully so. Response to the art component was mixed; for some student-patient pairs, the art the patient chose brought new insights into patient understanding. For other pairs, the technology and/or image library created barriers. Interviews with patients revealed generally positive response, although some patients did not recall the activity. Several patients asked their students to be their primary care provider. Comparison of audiotaped patient stories to the corresponding written narratives penned by students is ongoing to assess students’ narrative competence.
DISCUSSION/REFLECTION/LESSONS LEARNED: A brief, experiential narrative medicine curriculum was feasible and acceptable to students and patients. From a time and resource perspective, the curriculum took 2 h of faculty time per month. Both patients and students appear to have yielded benefits - for patients, being attended to and being heard; for students, gaining deeper appreciation of the human side of medicine, of knowing patients better. The impact on the student-patient relationship was often positive, at times powerfully so. Ongoing focus groups helped to make continual improvements to the curriculum, including the retirement of the iPad art component and refinement of how the patient activity was structured to maximize comfort of both students and patients.
TEACHING INTERPROFESSIONAL TRAINEES TO WORK IN CLINICAL CARE TEAMS: THE SAN FRANCISCO VA CENTER OF EXCELLENCE IN PRIMARY CARE EDUCATIONRebecca L. Shunk1,3; Bridget O’Brien1; Maya H. Dulay1,3; Terry Keene2,4; Denise L. Davis1,3; Shalini Patel1,3; Melissa Bachhuber1,3; Calvin L. Chou1,3; Kristen Weaver2,4; Christina Kim2,4; Lynn O’Brien2,4. 1UCSF, San Francisco, CA; 2UCSF, San Francisco, CA; 3San Francisco VA Medical Center, San Francsco, CA; 4San Francisco VA Medical Center, San Francisco, CA. (Tracking ID #1936850)
NEEDS AND OBJECTIVES: Primary care clinics at the San Francisco VA (SFVA) transitioned to an interprofessional team-based model of patient care called Patient Aligned Care Teams (PACTs) in 2010. In 2011 the SFVA was awarded a Center of Excellence to develop and implement an innovative model of patient-centered, interprofessional education in a team-based ambulatory clinic. The core educational domains addressed in our center include sustained relationships, performance improvement, patient-centered communication, and interprofessional collaboration.
SETTING AND PARTICIPANTS: In July 2011, we added trainee squads (2 s-year internal medicine residents and 1 s-year nurse practitioner student) to each of 8 pre-existing “teamlets” (1 registered nurse, 1 clinical associate, 1 clerical associate) in three SFVA primary care clinics. Each trainee acts as primary provider for a personal panel of patients but performs cross-coverage for squad members. Teamlets and squad members discuss team patients in daily huddles or brief meetings along with other interprofessional trainees.
DESCRIPTION: Curricular design for the core domains includes didactics, workplace reinforcement and reflection. For example, we set the foundation for interprofessional collaboration through interactive seminars on team members’ roles, conflict negotiation and huddling, then reinforce these skills in the workplace through daily huddles and interprofessional clinical practice. Team-building retreats provide opportunities to learn and practice skills together; to learn about each other both professionally and personally; and to reflect on teamwork, all requirements of high-functioning teams.
EVALUATION: To assess interprofessional collaboration, members of all trainee teams were asked to complete the Team Development Measure (TDM). The TDM is a tool created by Peace Health and used by the VA for PACT evaluation nationally scored on 0–100 scale. Team members evaluate how their team is functioning in terms of cohesiveness, communication, role clarity and goals and means clarity. Team members complete the TDM early and again later in the academic year and have an opportunity to review and discuss their results during a facilitated session. Scores improved from early year to late year (Year 1–59.4 early/64.6 late) and they started and ended up slightly higher in year 2 compared to year 1. (Year 2–62.4/70.4 late) In June 2013 the first cohort of internal medicine residents graduated and were asked to rate their experience on a 5 point Likert scale with 5 being strongly agree. They rated “effectiveness of working with trainees from other health professions (i.e. pharmacy, psychology, social work, nutrition) to provide quality patient care” 4.5 and “the educational value of opportunities to work with trainees from other health professions” 4.19. Patient surveys indicate a high level of satisfaction equivalent to other VA providers locally and nationally. When asked “using any number from 0 to 10, where 0 is the worst provider possible and 10 is the best provider possible, what number would you use to rate this provider?” 73 % and 76 % of residents’ and NP students’ patients respectively rated their provider either a 9 or 10.
DISCUSSION/REFLECTION/LESSONS LEARNED: Trainee clinical care teams can learn about and improve team functioning through a curriculum involving didactics, workplace reinforcement and reflection. Interprofessional trainees can successfully work and learn together to deliver team-based care creating positive experiences for trainees and patients alike.
TEACHING PATIENT-CENTERED ELECTRONIC MEDICAL RECORD (EMR) USE TO MILLENNIAL LEARNERS: ARE WE PREACHING TO THE CHOIR?Wei Wei Lee; Lollita Alkureishi; Jeanne M. Farnan; Vineet Arora. University of Chicago, Chicago, IL. (Tracking ID #1937618)
NEEDS AND OBJECTIVES: Studies demonstrate that Electronic Medical Record (EMR) use in exam rooms can prevent providers from focusing on patients and be detrimental to patient-doctor communication. Despite rapid EMR adoption, few curricula address how to teach patient-centered EMR use to ‘tech-savvy’ millennial learners. In 2013, we implemented a ‘Patient-Centered EMR Use’ curriculum for second-year medical students (MS2s), which consisted of a lecture and Observed Structured Clinical Exam (OSCE). We aim to assess the impact of our curriculum. Our objectives are to: 1) Compare OSCE performance of MS2s, who received the lecture, to third-year medical students (MS3s), who did not receive training on this topic. 2) Compare MS2 and MS3 post-OSCE survey scores on self-assessed knowledge, attitude and skills.
SETTING AND PARTICIPANTS: We implemented a ‘Patient-Centered EMR use’ curriculum for MS2s which consisted of a 1 h lecture and an OSCE to allow for skills practice. MS3 students served as historical controls; they did not receive the lecture but did participate in the OSCE as part of a required year-end multi-station OSCE exercise.
DESCRIPTION: The MS2 lecture was integrated into a required Clinical Skills course. The OSCE required students to: 1) log into the EMR and review relevant records; 2) address the patient’s chief complaint and; 3) use the EMR to counsel the patient on obesity. MS2s participated in a group OSCE (1 student interacted with the Standardized Patient (SP), 3 students observed). MS3s participated in individual OSCEs, where each student directly interacted with the SP. An ‘SP evaluation tool’ was developed to assess OSCE performance. The SP evaluated every student he directly interacted with during the OSCE. Post-OSCE self-assessment surveys were distributed to all students. MS2s’ performance on the OSCE and self-reported knowledge, attitude and skills was compared to the historical control group of MS3s who did not receive training.
EVALUATION: 45 MS2s attended the lecture, 88 participated in the group OSCE (n = 20 students who directly interacted with the SP; n = 68 student observers), and 80/88 (91 %) post-OSCE surveys were analyzed. Ninety-six MS3s participated in the OSCE and 88/96 (92 %) post-OSCE surveys were analyzed. 96 % (77/80) of MS2s and 85 % (75/88) of MS3s agreed (≥3 on 5 point scale) that the topic was at least moderately ‘important to their current training.’ 55 % (44/80) of MS2s rated their knowledge as good or excellent compared to 19 % (17/88) of MS3s. 39 % (31/80) of MS2s rated their training as good or excellent compared with 14 % (12/88) of MS3s. 87 % (70/80) of MS2s reported moderate confidence (≥3 on 5 point scale) compared with 73 % (64/88) of MS3s. Overall, 85 % (68/80) of MS2s and 70 % (62/88) of MS3s agreed or strongly agreed that ‘training should be required for all students.’ The ‘SP evaluation tool’ consisted of a 16-item checklist (score range: 15–80 points). The SP ratings were significantly higher for MS2s (n = 20) than for MS3s (n = 96) [70.8 (SD = 4.3) v. 58.1 (SD = 13.1), p < 0.001]. Overall, 95 % (19/20) of MS2s were rated as good or excellent in their ability to ‘use the EMR to enhance communication’ compared with only 53 % (51/96) of MS3s.
DISCUSSION/REFLECTION/LESSONS LEARNED: Medical educators may assume that millennial learners are inherently tech-savvy and adept at integrating the EMR into clinical care. Interestingly, we found that MS2s who received a short lecture on patient-centered EMR use performed significantly better on an OSCE than MS3s who received no training on this topic. Our study shows that at baseline, millennial learners may not have the skills necessary to integrate the EMR in a patient-centered manner and should be taught patient-centered EMR use.
TEACHING QUALITY IMPROVEMENT USING A CASE-BASED LEARNING FORMATGeorgia N. McIntosh; Nathan Schwartz; Steven Bishop; Michelle N. Brooks; Bennett Lee. Virginia Commonweallth University, Richmond, VA. (Tracking ID #1933579)
NEEDS AND OBJECTIVES: Despite years of innovation in business, and aviation, the field of QI with regards to medicine is relatively new. As such, there has been little research into the most effective teaching method. The purpose of this project is to pilot a case-based learning format for delivering QI knowledge. This interactive format lends itself to discussion and brainstorming different solutions to problems, the essential piece of developing a QI project. Through this format we aimed to teach residents the components o QI: develop a process map, define change items, create an aims statement and measures and implement and interpret data from a PDSA cycle.
SETTING AND PARTICIPANTS: This educational model is geared towards internal medicine residents but can be used for residents in any field, medical students or faculty members new to quality improvement.
DESCRIPTION: Our case-based learning format occurred over two 2-hour sessions. For the first session, participants first completed a pre-test self- assessment rating their comfort level in different aspects of QI. Residents were divided into groups of 6–7, for a total of 6 small groups. Participants were introduced to a case- a trend of intern duty hour violations during a specific rotation. After a brief overview of QI principles in healthcare, the groups were tasked with creating their own aim statements based on the given case. Using the gallery walk concept where groups post their work on the wall and each group is allowed to view and comment on each proposal, the large group then critiqued and voted on which aim statement to implement. Next, residents were given a brief review of process improvement tools (process mapping, mind maps, Ishikawa diagrams), and were tasked with mapping out a typical day for the rotation in question. After a brief review of the concept of change items and measures development, groups developed their own change items based on their aim statements. The large group again used the gallery walk concept and voted on the change items to implement. In the second session, groups were reminded of the aim statement and change items that were voted on during the previous session. They were tasked with developing their measurement items in their small group work and again voted in the large group format. Participants were then given simulated data based on the intervention they voted on. From this, the concepts of run sheets and variations in data (common cause variation, special cause variation) were introduced. Based on their analysis of this data, groups developed next action items in their PDSA cycles and voted on these.
EVALUATION: Forty-four residents completed the pre-test and 20 completed the post-test survey. To the question “how comfortable are you in your current skills with the following aspects of quality assessment and improvement”, participants answered 12 questions with the following choices: 1) not at all, 2) slightly, 3) moderately or 4) extremely.” We dichotomized the responses into either 1 and 2 or 3 and 4. For all questions, using Fischer’s exact test, respondents reported improved comfort in their quality improvement skills, most notably with using measurement to improve their skills (38 % to 85 %, p = 0.003), identifying whether a change leads to an improvement (37 % to 70 %, p = 0.03), and in using the PDSA model as a systematic framework for trial and learning (10 % to 55 %, 0.004.)
DISCUSSION/REFLECTION/LESSONS LEARNED: Case-based learning is an engaging learning technique that can easily be applied to teaching QI. Because case-based teaching is discussion-based, it lends itself well to the ability to brainstorm different scenarios that are essential to crafting a project. With our format, we were able to effectively introduce the concepts of quality improvement in an active and engaging learning platform, as evidenced by improved self- reporting of their comfort levels. One obvious caveat to our study was the reduction in post-test survey responses, partly due to variability in conference attendance due to clinical duties as well as a lack of perceived importance of residents. We also recognize that this reports comfort level, not actual knowledge or skill. Next steps would include a means to assess knowledge of QI and the subsequent skill of performing a true project. This educational model has the potential to be used for practitioner new to quality improvement regardless of level of training.
TEACHING RESIDENTS SCREENING, BRIEF INTERVENTION AND REFERRAL TO TREATMENT SKILLS FOR ALCOHOL USE: USING CHART-STIMULATED RECALL TO ASSESS CURRICULAR IMPACTMaria A. Wamsley1; Nathaniel Gleason1; Michelle Guy1; Katherine Julian1; Patricia S. O’Sullivan2,1; Scott Steiger1; Jason Satterfield1. 1University of California, San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA. (Tracking ID #1937193)
NEEDS AND OBJECTIVES: It is widely recognized that there is a critical need for more screening, brief intervention and referral to treatment (SBIRT) for alcohol use disorders (AUDs) in primary care settings. Barriers include inadequate provider skills and confidence as well as systems-related factors such as time pressures in the clinical setting and lack of referral resources. The optimal format for curricular interventions to address physician-related barriers remains unclear. One potential solution to systems-related issues is to better support SBIRT for alcohol use disorders using tools in the electronic health record (EHR). We implemented a 3-hour curriculum to instruct primary care internal medicine (IM) residents in SBIRT skills. We also developed a set of tools in the EHR to serve as a scaffold for the SBIRT curricular content, facilitate documentation of alcohol use, and to provide patients with tailored resources.
SETTING AND PARTICIPANTS: This study took place at an academic primary care residency program. Twenty PGY2 and PGY3 primary care IM residents participated in the curriculum and 16 participated in the evaluation.
DESCRIPTION: The curriculum consisted of two 1.5-hour sessions. We developed charting tools for the EHR (EPIC) to prompt residents to consider curricular content and to facilitate appropriate and efficient documentation of alcohol use. These included alcohol use history (HPI) and assessment and plan (A/P) charting tools and patient information resources (PI) with a list of referral resources. We introduced charting tools to learners after SBIRT curriculum completion.
EVALUATION: We evaluated the SBIRT curricular intervention utilizing chart review and chart-stimulated recall (CSR). Six months after curriculum completion, we provided residents a list of their patients seen in the preceding 12 months who were drinking at or above the recommended drinking limits and asked the residents to select up to 3 patients for review with a faculty member. Faculty reviewed charts to determine whether patients were seen in the 6-month period after curriculum completion and used a 25-item checklist to assess resident use of SBIRT skills and charting tools. Faculty met with residents individually, performed a CSR for each patient using a structured interview form and provided feedback to the residents. Residents subsequently evaluated the CSR process.
DISCUSSION/REFLECTION/LESSONS LEARNED: Sixteen residents participated in the chart review; 39 charts met criteria for our study. Residents did reasonably well at documenting alcohol use in the medical record (79 %) including quantity and frequency of use (64 %) and documenting their recommendation for patients to reduce their alcohol use (59 %). Residents correctly diagnosed the patient, documented an appropriate follow-up and plan only about half of the time. Resident reported barriers included time, resident discomfort, competing issues in the visit (medical/mental health), and perceived willingness of the patient to engage. Only 3 charts (8 %) included the use of the electronic HPI tool, 1 chart used the A/P tool, and 3 (8 %) used the PI tool. Resident reported barriers to EHR tool use included lack of awareness of the tools and lack of use of electronic charting tools in their normal workflow. Overall satisfaction with the CSR process was high; residents felt that the CSR reinforced SBIRT curriculum and provided valuable feedback and planned to make changes in their clinical practice. A more intensive curriculum with opportunities to practice skills and receive feedback over time may be required to improve skills. For EHR tools to be useful, additional reinforcement including simulation to practice integration of the tools into the visit workflow is essential.
TEACHING SAFE TRANSITIONS: A POST-DISCHARGE FOLLOW-UP PILOT FOR THIRD-YEAR MEDICAL STUDENTSKara Bischoff; Hemali Patel; Larissa Thomas; Karen E. Hauer; Cindy Lai. University of California, San Francisco, San Francisco, CA. (Tracking ID #1934559)
NEEDS AND OBJECTIVES: Adverse events are common during transitions of care (TOC), including discharge from the hospital. About 20 % of patients experience adverse events after discharge and nearly 20 % of Medicare fee-for-service patients are readmitted within 30 days. Acknowledging the critical role that the healthcare system plays in determining quality of care, medical school curricula are focusing increasingly on systems-based practice. By engaging medical students in analyzing their patients’ transitions out of the hospital, we aimed to develop students’ awareness and skills regarding TOC.
SETTING AND PARTICIPANTS: All third year medical students during their core medicine clerkship at University of California, San Francisco.
DESCRIPTION: Students attended a one-hour, interactive didactic session about TOC. We emphasized common adverse events that occur during TOC, risk factors for these adverse events, and evidence-based strategies to prevent them. Students reviewed the electronic medical record and called at least one patient whom they discharged from the hospital. Students used a templated note to record any common risk factors for adverse events around the time of discharge and whether the patient experienced any adverse events, including inability to obtain medications, inability to adhere to recommendations, uncontrolled symptoms, lack of intended follow-up, emergency visits, or readmissions. Students used a semi-structured phone call format using the Teach-Back Method to assess patients’ comprehension of their medical conditions and treatment plan, as well as their adherence to the plan. Students reinforced healthy behaviors and communicated with primary care providers (PCPs) about any adverse events identified. Students completed a structured, written reflection about ways they will change their clinical practice based on this exercise. They identified systems issues in need of improvement. They shared their work with their inpatient team and sent a summary e-mail to PCPs. Students received quantitative and qualitative feedback from an evaluation committee, which was intended to be constructive and did not contribute to their clerkship grade.
EVALUATION: Students completed surveys before and after this curriculum. So far, 32 students have completed the curriculum. Preliminary results from 32 students who completed the pre-survey and 14 students who completed the post-survey show that the percentage of students who feel knowledgeable about how TOC occur at the time of hospital discharge increased from 31 % before the curriculum to 86 % after. The percentage of students who feel confident in their ability to identify risk factors for adverse events during TOC increased from 38 to 93 %. The percentage of students who feel confident in their ability to prevent or mitigate adverse events during TOC increased from 6 to 64 %. Eighty-six percent of students feel that this exercise fills an educational gap, and 86 % recommend continuing the exercise. The most common criticism, cited by three students, is the time required to complete this exercise. The rate of successful completion of two multiple choice questions that tested students’ ability to identify and mitigate adverse events during TOC increased from 16 % and 94 % prior to the exercise to 36 % and 100 % after the exercise, respectively.
DISCUSSION/REFLECTION/LESSONS LEARNED: This pilot demonstrates that a didactic and experiential curriculum can fill an educational gap and improve students’ knowledge and confidence regarding TOC.
TEACHING SHARED DECISION MAKING: IMPROVING RESIDENT COMMUNICATION THROUGH CURRICULAR INNOVATION AND OBSERVED VISITSMaryann K. Overland1,2; Linda Pyke1; Anne P. Poppe1; Joyce E. Wipf1,2. 1VA Puget Sound Health Care System, Seattle, WA; 2University of Washington, Seattle, WA. (Tracking ID #1927018)
NEEDS AND OBJECTIVES: Communication skills are foundational for primary care physicians and central to patient-centered care. The literature is rich with evidence that shared decision making (SDM) is underutilized among primary care physicians, and there are no best practices for how to teach it. To strengthen the ability of medicine residents and students to engage patients in their care plan, our VA Center of Excellence in Primary Care Education (COEPCE) designed a curriculum to improve mastery of SDM. Our curriculum consisted of direct observation and brief didactics, production and review of several videos of expert clinicians, and standardized patient (SP) encounters.
SETTING AND PARTICIPANTS: In the spring of 2013, our VA COEPCE developed and implemented a half-day seminar on SDM for an interprofessional mix of trainees consisting of internal medicine residents and doctorate-level nurse practitioner students (DNPs). The session was preceded and followed by observed clinical encounters with direct feedback from continuity clinic mentors using a validated SDM tool.
DESCRIPTION: First, faculty mentors were trained to use the OPTION tool and observed trainees during a clinic visit to assess the trainees’ baseline skill in SDM. Then, trainees participated in a half-day seminar that included the following: 1. Didactic on the spirit and skills of SDM 2. Review of videos of unscripted encounters featuring local expert clinical faculty and SPs engaging in SDM. 3. A brief review of clinical guidelines and provision of fact sheets on six cases: diabetes, hypertension, breast cancer screening, depression, atrial fibrillation, and goals-of-care in terminal cancer. 4. SP encounters to practice SDM around the six cases. 5. Wrap up and feedback To maximize participants’ comfort, practice time, and clinical knowledge acquisition, we created three stations where SPs alternated between two unique roles. Medicine residents and DNP students rotated through each station in pairs, practicing and observing each other. The observer and SPs provided immediate and direct feedback. After the seminar, faculty mentors again observed resident clinical encounters to evaluate SDM skill acquisition.
EVALUATION: Faculty observers reported improved use of SDM during patient encounters after the seminar. Trainees reported a meaningful increase in confidence in their ability to use SDM (per visual analog scale) and a high likelihood to use the skills acquired during this seminar (4.5/5 on a 5-point Likert Scale). They were very enthusiastic about the standardized patients and working in pairs (4.7/5 on a 5-point Likert Scale). Trainees highly valued the video demonstrations of brief encounters by experienced clinicians.
DISCUSSION/REFLECTION/LESSONS LEARNED: SDM is an important part of every primary care visit, but is a skill that is difficult to teach, often taking a lifetime to master. In this seminar, we achieved our dual-mission of providing a safe setting for practicing challenging communication skills and embedding it within clinical knowledge attainment. The design of this seminar successfully minimized knowledge differences among interprofessional learners. This innovative curriculum utilizing standardized patient encounters and real-life clinical scenarios allowed primary care physicians to strengthen communication skills around engaging patients in shared decision making.
TEACHING TEAM-BASED CARE: THE USE OF INTERDISCIPLINARY TEAM MEETINGS IN THE AMBULATORY INTERNAL MEDICINE RESIDENCY CURRICULUMJonathan Arend1; Stefani Russo1; Eva Waite1; Deborah Korenstein3; Lauren Peccoralo1; Aparna Sarin1; Alex Federman1; Linda Pagan2; Theresa Soriano1. 1Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3American College of Physicians, Philadelphia, PA. (Tracking ID #1939032)
NEEDS AND OBJECTIVES: Amid increasing enthusiasm for team-based models of patient care, incorporation of team-based care into residency curriculum is starting to emerge. As academic primary care practices embrace the Patient-Centered Medical Home (PCMH) model and residency programs seek ways to satisfy Next Accreditation System (NAS) milestones related to team-based care, educators must develop methods for teaching the skills needed to operate effectively in interdisciplinary care teams. As part of a comprehensive PCMH curriculum, we instituted an outpatient interdisciplinary team meeting structure to support team-based care and team-based quality improvement. We sought to determine the feasibility of team meetings and assess resident satisfaction with interdisciplinary care before and after institution of the meetings.
SETTING AND PARTICIPANTS: In our academic primary care practice at the Icahn School of Medicine at Mount Sinai in New York, NY, internal medicine residents are assigned to 1 of 3 firms, in which they provide patient care and work with firm-based attending physicians, medical assistants, registered nurses, nurse practitioners, social workers, care coordinators, patient navigators, and front desk registration staff. In July 2013, we implemented weekly team meetings in each firm, attended by members of each of the above disciplines. All residents attended their respective team meeting during ambulatory blocks.
DESCRIPTION: We developed the format of the team meetings based on literature review, collaboration with other academic medical centers, and local priorities. Prior to initiating the firm-based meetings, we held several “all-staff” meetings, in which residents, general internal medicine faculty, and clinic staff were trained in principles of teamwork, effective meeting skills, and quality improvement methodology. We redesigned the resident schedule and clinic staffing to provide 1 h per week of protected time for the meetings. The meetings were co-led by a registered nurse and an attending physician and focused on team communication, clinical workflows, practice initiatives, and quality improvement.
EVALUATION: Before implementing the meetings, we surveyed all residents to assess their satisfaction with interdisciplinary care at the practice. Sixty-six surveys were returned (51.5 % response rate). When asked about the practice’s team-based functioning, 8 % of the residents were very satisfied, 42 % were somewhat satisfied, 42 % were somewhat dissatisfied, and 8 % were very dissatisfied. Levels of satisfaction (somewhat satisfied) for components of team-based care, such as co-management of patients’ medical conditions, communication about patient care, shared responsibility of patient care, and personal support from team members, ranged from 37 to 48 %. Six-month follow-up survey results are pending. The regular meeting schedule was maintained without disruption of clinical care, losses in productivity, or significant use of additional funding sources.
DISCUSSION/REFLECTION/LESSONS LEARNED: Weekly interdisciplinary team meetings are a feasible method of introducing internal medicine residents to team-based care in an ambulatory setting. Ongoing evaluation will determine whether participation in such meetings alters attitudes toward team-based care. The role of team meetings in influencing ACGME core competencies or other performance metrics requires further study.
TEACHING THE PATIENT-CENTERED MEDICAL HOMEElisha L. Brownfield; Benjamin Clyburn; Kimberly S. Davis; William P. Moran; Patrick D. Mauldin. MUSC, Charleston, SC. (Tracking ID #1936971)
NEEDS AND OBJECTIVES: The consensus report from the Alliance for Academic Internal Medicine Education Redesign Task Force calls for transformative ambulatory training for Internal Medicine. This would include the training of residents in highly functional ambulatory care settings and allowing residents to take on leadership roles within multidisciplinary clinical care teams while minimizing the conflict between outpatient and inpatient responsibilities. To date, there are few published educational models for Internal Medicine residency programs. In July 2012, our Internal Medicine (IM) residency program redesigned ambulatory training. Our objectives included: 1) improvement of care continuity, 2) increased exposure to common outpatient clinical problems and non-Internal Medicine specialties, 3) expansion of the ambulatory curriculum, 4) separation of inpatient and outpatient responsibilities, and 4) improved resident satisfaction of the clinic experience.
SETTING AND PARTICIPANTS: The University Internal Medicine (UIM) is a hospital-based, General Internal Medicine teaching clinic with approximately 11,000 patients and an NCQA-certified Level 3 Patient Centered Medical Home. Since July 2012, a total of 92 categorical Internal Medicine and combined (Med-Peds and Med-Psych) PGY 2–3 residents have rotated through the new ambulatory curriculum. The UIM is staffed by 15 Internal Medicine faculty members and a complement of registered and licensed practical nurses, certified medical assistants, PharmD/certified diabetes educators, social worker, and administrative support staff.
DESCRIPTION: In July 2012, the IM program transitioned all of its PGY 2–3 categorical residents from a weekly half-day clinic schedule into a monthly clinic block occurring every 4th month throughout the year. During these blocks, residents have no ward responsibilities and spend 6–7 half days per week in the UIM clinic while the remainder of the week rotate through a variety of other experiences including gynecology, dermatology, orthopedics, otolaryngology, allergy and sleep medicine. Each resident also has an assigned academic half day during the week. Residents are grouped into teams of approximately 15 residents all sharing the same nurse case manager. Significant curriculum changes include enhanced didactic conferences and required completion of an online curriculum and mini-CEX evaluations. A weekly interdisciplinary meeting focusing on systems-based care of resident panel patients was introduced and most recently centers on patients with poorly controlled diabetes and hypertension.
EVALUATION: Cumulative resident evaluation scores for the UIM rotation were comparable between pre-intervention and post-intervention time periods (1207 responses: 3.47, 102 responses: 3.50 Likert scale 1–4). In a May 2013 survey of 28 residents, the majority felt the interdisciplinary meeting lead to improvements in clinic operations (57.1 % “strongly agree/agree”). These residents were less sure of their own roles within the PCMH (46.4 % “strongly agree/agree”; 39.3 % “disagree/strongly disagree”) or the roles of team members (32.1 % “strongly agree/agree”, 57.1 % “disagree/strongly disagree”). Follow-up surveys are pending. Resident continuity rates for 6788 visits (Oct 2012–Jan 2013) were 45 % for individual Primary Care Physician and 88–89 % for patient care teams. No pre-intervention comparison is available, and published rates are rare, but generally are below 50 %. Although not an explicit goal of the curricular change, there is an upward trend ambulatory medicine career choice (average 2004–2013:4, 2014:6).
DISCUSSION/REFLECTION/LESSONS LEARNED: Our categorical Internal Medicine residents now experience complete separation of inpatient and outpatient responsibilities and an enhanced PCMH curriculum. Patient panel audits are provided to each resident, and the completion of an online curriculum and mini-CEX requirements are ensured. As our program transitions to ACGME milestone reporting, the ambulatory rotation provided early experience with this new requirement. Patient continuity within resident teams is high, but remains <50 % per individual resident. Overall, resident satisfaction with their outpatient experience is high. Strengths of the new program include: the ability to train residents within a certified PCMH, resident reflection of a patient-care data audit involving an interdisciplinary team, experience with other related specialties, and an excellent opportunity to evaluate residents over time. Our greatest challenges continue to be an increase in the administrative and teaching burden for faculty and staff, clinic staff shortages and turnover, cultural shift changes for all working in the PCMH, patient care continuity in the resident panels, and data management needs for our population management.
THE (ELECTRONIC) CHART WAR: RESIDENT AND FACULTY PERCEPTIONS AND PRACTICES IN OUTPATIENT DOCUMENTATION AND CHART MANAGEMENTSarah A. Tilstra; Peggy Hasley; Anu Munshi; Brian S. Heist; Shanta M. Zimmer; Jaishree Hariharan. University of Pittsburgh Medical Center, Pittsburgh, PA. (Tracking ID #1939144)
NEEDS AND OBJECTIVES: The electronic health record (EHR) has simplified communication among providers and improved clinical decision support while creating complexity in documentation for medical trainees to master. There is no consensus on how to best teach outpatient documentation and chart management to residents. Last year, we reported on current resident practices in outpatient documentation which confirmed that residents excel in documentation within the progress note but routinely fail to update the overall EHR portal. This can impact quality, medical errors, communication with providers, efficiency, and reimbursement. Thus, an ideal resident curriculum should not just focus on the appropriate components of a progress note but also on how to best navigate, update, and utilize the online patient portal. We set out to define residents’ and faculty opinions regarding outpatient chart management by surveying our current residents and teaching faculty. Our objectives are: 1. Determine the perceived efficiency and accuracy of outpatient clinical documentation 2. Describe the barriers to effective documentation 3. Identify curricular needs for an outpatient resident documentation/chart management
SETTING AND PARTICIPANTS: Two faculty/resident clinic sites at the University of Pittsburgh Medical Center where 72 categorical residents and precepting faculty hold their weekly continuity clinic. Both practices have a fully integrated EHR (EpicCare).
DESCRIPTION: Individual surveys for teaching faculty and residents were designed by the curricular team. Twenty-one questions were exactly the same, but appropriately worded for residents or faculty. Two additional questions were included in the faculty survey. Surveys were vetted for clarity and appropriateness by the residency program administration and faculty leadership prior to distribution in May 2013 via Survey Monkey.
EVALUATION: Overall, 39/72 (54 %) residents and 14/19 (74 %) eligible teaching faculty completed surveys. Only 39 % percent of residents report satisfaction with their training in outpatient documentation and chart management, 21 % received formal training in medical school, while 57 % of faculty received training during their career. When compared to faculty, residents have a harder time completing outpatient notes within 24 h (100 % vs. 87 %), are less confident knowing the required documentation elements for a given clinical encounter (86 % vs. 56 %), are less comfortable determining the appropriate billing for a patient encounter (100 % vs. 44 %), are less likely to know how their “quality of care” is measured (93 % vs. 61 %), are more likely to cut-and-paste from their last note (7 % vs. 13 %), and less likely to use templates for documentation (67 % vs. 54 %). Sixty-two percent of residents, compared to 7 % of faculty, report spending >20 min on documentation per patient encounter, with 50 % of these encounters taking more than 25 min per patient. Faculty and residents are equally comfortable using the electronic “tabs” within the EHR, but faculty more often update the tabs to reflect appropriate clinical information. Eighty-six percent of faculty members have received feedback on documentation whereas only 54 % of residents routinely receive feedback. Preceptors routinely give residents feedback 43 % of the time, but do review and make changes to the documentation without giving direct feedback 79 % of the time. Residents mostly “struggle” with completing documentation on time. Knowing what to include in a note for specific patient encounters was second, followed by identifying appropriate billing and updating the tabs in the electronic chart. Nearly 50 % of residents identified “more training” in the electronic chart with “frequent refreshers” as a mandatory step in moving forward, with a subset of residents asking for “easier to use templates” to streamline documentation. Faculty also reported that “time” was a major struggle in completing outpatient documentation and that better templates could make this easier. Training in “billing requirements” and “electronic-portal maintenance” should be vital components in the outpatient curriculum
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents are not well trained in outpatient documentation and electronic chart management, and struggle with efficiency, navigating/updating the electronic portal, identifying needed components for documentation and billing, and do not receive adequate feedback. Going forward, we plan to develop a longitudinal outpatient documentation and chart management curriculum using “minimum standards” that are tailored to each PGY level, develop easy-to-use templates, construct an objective chart evaluation tool, and outline regular feedback intervals for residents.
THE EFFECT OF GENDER ON ATTITUDES TOWARD THE HOMELESS AMONG PRIMARY CARE INTERNAL MEDICINE RESIDENTSFrances Norlock; Laura Sadowski; Meghan Kapolnek. Stroger Hospital of Cook County, Chicago, IL. (Tracking ID #1938650)
NEEDS AND OBJECTIVES: The prevalence of homelessness is increasing. Few resident programs offer formal training in how to provide care for the homeless. Educators implemented a homeless medicine rotation to decrease residents’ stigma associated with homelessness and improve the clinical care they provide to homeless patients. Investigators hypothesized that resident gender would affect one’s attitude toward the homeless in that female residents would have lower stigma than their male counterparts prior to the educational intervention, and in turn, male residents would have greater improvement of their stigma scores than female residents by the end of the rotation.
SETTING AND PARTICIPANTS: PCIM residents (n = 12) participated in a 2 week homeless medicine rotation based at an urban, public hospital focused on collaborating with partners in the community. Residents participated in group seminars on campus, engaged in tours and clinical experiences in the community including working with patients in shelters, clinics and residential housing programs.
DESCRIPTION: Curriculum consisted of small group seminars on the epidemiology, chronic disease management, health outcomes, and lifestyle issues affecting morbidity and mortality in this population. Residents worked in community-based clinics that served the homeless including those with addictions and the recently incarcerated. Learners were assigned evening shifts to care for those in shelters with medical issues as well as residential facilities which cared for women and children. Residents also heard life stories from homeless individuals in small group settings. Residents’ attitudes were assessed before and after the course through an 11 item Attitudes Toward Homelessness Inventory (ATHI) consisting of 4 subscales which attribute homelessness to societal cause; personal cause; having a willingness to affiliate with the homeless; and belief that homelessness is a solvable problem. A higher summation score of the 4 subscales equates to a lower stigmatizing attitude of homelessness. A meaningful difference score of 5.5 was set a priori.
EVALUATION: Results from the ATHI showed that women did have lower levels of stigma toward the homeless at the onset of the rotation with a higher total summation score of 45.5 compared to the male summation score of 38.5 (p-value 0.14) consistent with a meaningful difference in gender prior to the rotation. The improvement in total scores overall was 1.75 among women and 7.6 points among men consistent with a meaningful change in scores between men and women (5.85 points), and a meaningful change in score for male residents (7.6 points) post-rotation. The greatest mean change in score between men and women was an improvement of 2.6 points in the personal cause subscale. Lastly, women had lower stigma scores for all 4 subscales pre- and post-rotation with the greatest improvement of 2.5 points in the societal cause score.
DISCUSSION/REFLECTION/LESSONS LEARNED: Educators showed higher stigmatizing attitudes toward the homeless associated with gender, but with a dedicated homeless medicine rotation male residents did have a meaningful improvement in their attitudes by the end of the rotation with the greatest improvement in the personal cause subscale. Findings suggest the need for residents to be trained in caring for the homeless to improve attitudes and lower stigma when caring for this vulnerable population.
THE NEW KID ON THE BLOCK: TEAM BASED LEARNING CURRICULUM IN AMBULATORY EDUCATION, A PROMISING ALTERNATIVERaghav Sharma; Sandy Balwan; Alice Fornari; Tomoko Ouchi. North Shore LIJ Health System, Great Neck, NY. (Tracking ID #1938778)
NEEDS AND OBJECTIVES: Team Based Learning (TBL) was developed to promote active learning, problem solving, and concept application in college classrooms and is a key strategy in undergraduate medical education. Compared to didactic teaching, TBL provides an active learning strategy that strongly engages participants in the learning process. There is little data however, on the use of TBL in Graduate Medical Education (GME). In 2012, we replaced our didactic based ambulatory medicine curriculum with a TBL curriculum. We hypothesized that residents would report better engagement and that faculty would report more resident involvement. We also hypothesized that residents’ medical knowledge would improve based on their in-training exam scores.
SETTING AND PARTICIPANTS: All ambulatory clinic sites of a large urban internal medicine residency program participated. Each site hosted 12 residents for 35 weeks. A total of 258 Resident surveys and 34 faculty surveys were reviewed.
DESCRIPTION: Residents were divided into two groups prior to initiating TBL sessions. Ambulatory faculty members prepared 7 distinct TBL modules: Diabetes, hypertension, hyperlipidemia, perioperative evaluation, asthma, dizziness, and GERD. TBL sessions were held for 1 h, 3 days per week. At the beginning of the TBL sessions, residents underwent a closed book quiz on a previously emailed article, followed by a group quiz, and concluded with a group discussion of the answers. During the second session residents received a clinical vignette on which they self assigned learning objectives (LO), which were discussed in a round table fashion at the close of the week’s TBL session. At the conclusion of the TBL sessions residents were given anonymous peer evaluations and separate surveys assessing peer performance, self-engagement, and faculty member facilitation. The faculty and residents received 10 and 12 survey questions respectively. Responses were measured on a 5-point Likert scale. The results account for the mean of the numeric value of each question. The assessment of medical knowledge of the residents is ongoing, pending the results of the in-service exam scores.
EVALUATION: Most residents and faculty agreed to strongly agreed that co-residents and themselves were actively involved in the TBL session and contributed meaningfully to the discussion. Residents and faculty further responded that residents were paying attention most of the time to the TBL session and residents were active learners during discussions. Residents agreed that they would like more TBL sessions and found the faculty members to be effective facilitators. Residents neither agreed nor disagreed whether the facilitator assumed a lecture model.
DISCUSSION/REFLECTION/LESSONS LEARNED: The Integration of TBL into ambulatory residency curriculum fosters proactive resident engagement and personal accountability of the learner, leading to a more dynamic learning environment and enhanced retention. However, mild barriers remain as facilitators may default to traditional teaching styles while adjusting to a TBL based curriculum. Overall, if appropriately implemented in an ambulatory setting, TBL would help enrich the teaching and learning climate in residency programs throughout the country.
THE RESIDENT AS TEACHER: IMPLEMENTATION OF AN EVIDENCE-BASED, BEST-PRACTICES APPROACH TO CLINICAL EDUCATION THROUGH A TEACHING ELECTIVE FOR RESIDENTSBret Simon1; Christopher Moreland1,2; Kanapa Kornsawad1,2. 1Univ Texas Health Science Center San Antonio, San Antonio, TX; 2South Texas Veterans Health Care System, San Antonio, TX. (Tracking ID #1940759)
NEEDS AND OBJECTIVES: Residents make essential contributions to medical education through their work with fellow residents and medical students. However, like many faculty, residents typically have little to no formal training in educational principles and practices. The “clinical-educator” is typically more clinician than educator. In an effort to improve educational practices generally, and to introduce trainees to current research and practice in clinical teaching, we designed and implemented a one-month elective rotation on “The Resident as Teacher.”
SETTING AND PARTICIPANTS: The course is open to R2 and R3 residents at a large teaching hospital in the south central US. Offered all months except December, and open to no more than two residents per rotation.
DESCRIPTION: The rotation is founded on core tenets of adult learning theory (Knowles) and stresses autonomy, self-identification of learning goals, collaboration in identifying methods of achieving self-identified learning goals, and self-evaluation of progress toward those goals. Reflective writing is a major component of the rotation, as residents are asked to respond in writing to 12–15 current readings from the professional literature. We believe that this practice of “writing to learn” is underutilized in medical education and represents a significant source of learning in this course. Residents also participate in facilitated or guided activity during the rotation through teaching activity, shadowing teams during rounds, giving feedback to students, and observing other educational practices. Readings are selected to parallel resident goals, and reflections are a way to integrate knowledge and direct experience in the teaching activities. A critical component of the course is weekly meetings between residents and course directors. These loosely structured, collegial discussions are a way of promoting critical thinking and self-insight in learners.
EVALUATION: One of the novel aspects of this course is the use of concept mapping as a method of learner evaluation. Residents are provided with resources and examples at the beginning of the rotation and told they will be asked to illustrate the process of clinical teaching via a concept map by the end of the course. Residents share their current concepts and connections during weekly meetings and share their current concept map with course directors. This process encourages deep-learning and the integration of principles and practices. It requires analysis and synthesis—higher order cognitive processes—and helps assure long-term retention and use of content.
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents come to this rotation with a variety of teaching experiences, but the content and methods in this course are clearly new to all residents to date. The course is scholarly in nature, relying heavily on the professional literature and not simply a “how-to” approach to clinical teaching. This practice mirrors the evidence-based approach to medicine advocated in clinical practice, as one of our goals is to help learners recognize that there is body of evidence relevant to teaching as well. We have been somewhat surprised at the learning goals identified by residents, as the same goals are frequently reported: feedback skills, motivating learners, teaching styles, and being a better presenter. The utility of the concept map as a method of self-assessment and summative evaluation has been less clear. We find that some residents enjoy the activity, but many are also perplexed by it. By limiting ourselves to this visual form of organization and synthesis, we may fail to recognize the range of learning approaches residents may take. Thus, we are currently considering other synthetic activities—narrative, checklists—as alternative demonstrations of competence.
THE USE OF SOCIAL MEDIA TO SUPPLEMENT RESIDENT MEDICAL EDUCATIONPanagis Galiatsatos; Fernanda Porto Carreiro; Jennifer Hayashi; Sammy Zakaria; Colleen Christmas. Johns Hopkins Bayview Medical Center, Baltimore, MD. (Tracking ID #1928160)
NEEDS AND OBJECTIVES: Since residents work at variable times, new approaches to asynchronous learning are needed to ensure all residents receive a comprehensive education. The use of social media tools may be useful, because they can be accessed at a time convenient to the learner. The objective of this study is to assess if the use of Twitter for medical education impacts the attitude and behavior of physicians-in-training towards using social media for medical education.
SETTING AND PARTICIPANTS: Pre-intervention and post-intervention surveys. Internal medicine resident physicians were surveyed before the launching of the “Hopkins Bayview IM” Twitter page on August 1, 2013, and again 135 days later, to determine their use of the twitter application, web page, and social media for medical education in general. Participants included residents at an internal medicine urban academic training program.
DESCRIPTION: All residents within our training program were administered web-based surveys, immediately before and then 135 days after creating a Twitter page devoted to medical education. The surveys assessed views and frequency of use of social media for medical education purposes, and consisted of ten Likert scale questions. Each answer consisted of a data-point on a 1–5 scale (1 = not useful, 3 = useful, 5 = very useful). The final question was open ended, and asked for general comments.
EVALUATION: Thirty-five of 50 residents (70 %) completed the pre-survey and 37 (74 %) participated in the post-survey. At baseline, 34 out of 35 residents used social media and 9 used Twitter specifically. However, only 22 (63 %) used social media for medical education, and 3 specifically used Twitter. After the establishment of the Twitter page, the percentage of residents using social media for educational purposes increased (31 of 37 residents, 84 %), 22 specifically used Twitter (p = 0.03 for the change), and their frequency of using the application at least once a week increased from 11.5 to 56.8 % (p < 0.05). Almost all residents (35 of 37) felt that social media could be useful as a medical education tool, which numerically increased from 29 out of 35 in the pre-intervention survey, but these percentages were not statistically significant (p = 0.37).
DISCUSSION/REFLECTION/LESSONS LEARNED: Residents believe social media could be used for medical education. After we launched a Twitter page for medical education, there was a significant increase in the use and frequency of Twitter for resident medical education. Further research should be performed to see if social media can impact overall medical knowledge and patient care.
USING A WEB LOG TO ENHANCE COMPETENCY IN MEDICAL KNOWLEDGE AND PRACTICE BASED LEARNING AND IMPROVEMENTMatthew Hollon. Sacred Heart Medical Center, Spokane, WA. (Tracking ID #1940872)
NEEDS AND OBJECTIVES: Literature suggests that role modeling is a nuanced, deliberate learning strategy. We postulated that faculty transparency in how we learn from uncertainty in our everyday clinical work would lead residents to embrace and incorporate the core principles of the competency of “Practice Based Learning and Improvement” (PBLI) into their professional development. The faculty sought to model the steps of PBLI on a weekly basis through the use of a web log or “blog” by posting a clinical scenario where we were faced with uncertainty about the best way to proceed then translated that into a clinical question and pursued an answer. Simultaneously, we sought to share our acquired medical knowledge with our whole program through the blog.
SETTING AND PARTICIPANTS: A community-based, university-affiliated internal medicine residency program with a total of 21 residents and 8 core faculty.
DESCRIPTION: Prior to the start of the project, we surveyed residents about actions consistent with the fundamental steps of PBLI. Specifically we asked residents the frequency that they felt uncertain in clinical situations over the last month, how often they searched for answers when faced with uncertainty, and how often they successfully found answers. Subsequently, once each week for a period of 24 weeks, 1 of 8 core faculty members wrote a summary of a situation where he or she faced clinical uncertainty, a description of how he or she went about finding an answer, and a discussion of the medical knowledge learned. Prior to the summary being posted to the blog and accessible to everyone in the program, we distributed electronically a single pre-test question to assess baseline knowledge in the area covered by the summary. One week following distribution of the pre-test, we closed access to the question then posted the written summary. Approximately 1 month after the end of this 6 month project, we distributed a final survey. This survey reassessed medical knowledge of topics covered in the faculty posts using the same 24 single pretest questions. The survey also re-evaluated actions consistent with the PBLI steps.
EVALUATION: All residents completed both the initial and final survey and completed, on average, 77 % of the single pretest knowledge questions. The frequency that residents encountered clinical situations where they felt uncertain declined over the course of the 24 weeks from a mean frequency of uncertainty of 36 % to 28 % (p = 0.008). The frequency with which residents sought answers when faced with uncertainty prior to the project was high at mean of 81 % and had not changed significantly 24 weeks later remaining at a mean of 78 %. The range of the frequency of answer seeking when faced with uncertainty was between 30 % and 100 % with a total of 3 residents reporting on the final survey that they sought answers less than half the time when faced with uncertainty while 15 residents sought answers at least 80 % of the time. Success in finding an answer to questions generated by clinical uncertainty did not change significantly from before to after the project, remaining at a mean of approximately 75 %. Medical knowledge improved significantly (p = 0.001) with the use of faculty posts to the blog. Prior to posting answers to clinical questions, residents got a mean of 52 % of knowledge questions correct. When reassessed 1 month after the end of the 6 month period, residents got a mean of 65 % of questions these correct. Lastly, 95 % of residents felt that faculty should continue to post general clinical content to the blog.
DISCUSSION/REFLECTION/LESSONS LEARNED: We noticed a slight decline in clinical uncertainty over the course of 6 months consistent with expectations. However, we failed to show improvement in frequency of searching for answers when faced with uncertainty. Notably, this is already happening at high level for most, which is reassuring, making it difficult to show large improvement. We did note that some residents were less engaged in the fundamentals of PLBLI. It may be that efforts to encourage self-reflection, recognition of clinical uncertainty, and answer seeking are best targeted to this group. Interestingly, strategies for finding answers did not seem to change substantially. Despite faculty role modeling using primary data found through PubMed searches, residents continued to most frequently use general resources when seeking answers to clinical questions. We did demonstrate that faculty posting to a blog led to modest improvements in medical knowledge. This was particularly noteworthy given that retest occurred up to 7 months after the initial posts of answers. Finally, residents truly appreciated this intervention. As the blog became increasingly valued as a resource for clinical information, it even inspired some residents to do their own posting of medical knowledge content. In summary, faculty role modeling of PBLI through a blog was valued by residents and led to modest improvements in medical knowledge but did not alter behavior that was already taking place frequently.
USING COLLABORATIVE EVALUATION TO IDENTIFY CRITERIA FOR THE ASSESSMENT OF ATTENDING PHYSICIANS IN HOSPITAL MEDICINEBret Simon1; Luci Leykum1,2; Jane E. O’Rorke1,2; Megan Freeman1. 1Univ Texas Health Science Center San Antonio, San Antonio, TX; 2South Texas Veterans Health Care System, San Antonio, TX. (Tracking ID #1940677)
NEEDS AND OBJECTIVES: Various approaches to the assessment of attending physicians have been reported in the literature. Externally determined criteria (e.g., ACGME, ABIM) are often used to ensure that measures required for accreditation are addressed. Such tools are useful for making comparisons across institutions, but they may fail to identify institution-specific needs. These measures may be particularly inadequate in cases where rapid curricular changes are being implemented or professional development activity results in extensive and significant changes in the way attendings and residents interact. Nominal Group Technique can be used as a means of identifying institution-, program-, or specialty-specific evaluation issues that are particularly salient or newly emergent. We sought to use NGT as a method for obtaining stakeholder input on attending performance in the inpatient general medicine setting.
SETTING AND PARTICIPANTS: Two teaching hospitals (community and Veteran’s Administration) serving as primary training sites for a large medical school in the south central US. Participants included three categories of stakeholders whose roles were principally in medical education in the inpatient setting. The three groups included hospitalist faculty, administrators (departmental, hospital, and graduate medical education), and residents representing all 3 years of training. A total of 24 individuals participated.
DESCRIPTION: The Nominal Group Technique is designed to solicit input around a particular problem, issue, or concern from a range of stakeholders. The process is transparent—a feature particularly important when participants represent a range of organizational levels (dean, faculty, resident). Participants offer their input as short phrases or words in response to a central question, written on white-boards so they are viewable by all participants. In this case, “What criteria should be used by housestaff to assess attending performance?” The method is a three-step process: 1) solicitation of input from participants in an unedited, round-robin fashion until all views are expressed, 2) group review of the content to consider consolidation or elimination of content that is duplicative, 3) individual ranking of the final list of words or phrases. The ranking process can vary, but in this case participants were asked to identify their top five items. Points were assigned according to rank, with five points assigned to the top rank and one point assigned to the lowest rank. The final product is a list of rank-ordered items, produced by all stakeholders, to address the question posed.
EVALUATION: Participants identified nearly 90 items related to the evaluation of attending performance. After some consolidation, 12 items were eliminated. Despite the large number of items, when they were summed and ranked, only 11 were scored high enough, or were selected by enough participants, to achieve a score of more than 10 points. These items served as the core content for a review and modification of the existing attending evaluation form. Items included: professionalism; clinical knowledge; organized approach to teaching; provides useful, timely, formative and summative, written and oral feedback; clear expectations of all team members; communication skills; ability to convey thought process; ability to provide proper autonomy and supervision; interpersonal skills with learners, patients, and families; quality of teaching; and promotes critical thinking.
DISCUSSION/REFLECTION/LESSONS LEARNED: We found that many of the items identified as important criteria for the assessment of attending performance were already, to some degree, part of the existing evaluation form. Nonetheless, we have been able to utilize the input of our stakeholders to help clarify and operationalize behaviors associated with broad concepts like professionalism and communication skills. Our intent is to continue to use the nominal group technique on a semi-annual basis to assure that our attending evaluation process is adequately representing the needs and concerns of stakeholders.
USING HUDDLES TO INTEGRATE MEDICAL RESIDENTS INTO AMBULATORY TEAMSJoshua M. Liao; Andrew J. Van Wieren; Brigid M. Dolan. Brigham & Women’s Hospital/Harvard Medical School, Boston, MA. (Tracking ID #1927565)
NEEDS AND OBJECTIVES: Harvard Medical School’s Center for Primary Care recently launched the Academic Innovations Collaborative to catalyze widespread innovation and transformation at affiliated primary care clinics. While the initiative requires participating sites to focus on team-based care and incorporate trainees into them, many sites have found it difficult to integrate medical residents - frontline physicians and large portions of the clinical workforce - into care teams.
SETTING AND PARTICIPANTS: Recognizing the importance of resident involvement in team-based care, we selected an affiliated community health center in Southern Jamaica Plan staffed by practicing primary care providers, a cohort of full-time MAs, and resident physicians from the Brigham & Women’s Hospital Internal Medicine Residency. We chose the site because of strong leadership support for this work, low turnover rate among its MAs, and the presence of large proportions of full-time providers with prior experience in huddling with MAs.
DESCRIPTION: We framed our project within the period when residents were physically at their half-day continuity clinic sessions. We incorporated Lean principles to study existing processes and root causes by observing in-clinic communication between physicians - both full-time and resident physicians - and medical assistants (MAs). Based on our mapping and analysis, we used an impact/effort matrix to evaluate and prioritize potential ideas, ultimately deciding on resident-MA huddles as a high yield intervention. We utilized a Plan-Do-Study-Act approach to implement pre- and post-clinic resident-MA huddles. These were initially done under the supervision and guidance of experienced physician preceptors, but eventually residents and MAs ran independent huddles. We collected pre- and post-intervention surveys from practicing physician preceptors, residents and MAs assessing their perceptions of resident integration into care teams.
EVALUATION: Using verbal feedback and written post-intervention surveys, we gathered data on process measures (adherence to huddles) and outcome measures (effect on perceptions of resident integration into care teams). The frequency of both pre- and post-clinic huddles increased over our study period. Our work revealed that while pre-clinic huddles were relatively easy to adopt, post-clinic huddles were considerably more difficult to organize. Interestingly, resident physicians and physician preceptors perceived residents as becoming more integrated into care teams over the study period. In contrast, MAs felt that resident integration did not change significantly. This was in part due to their perception that despite huddles, residents still spent very limited time in the clinic. Another important issue was that MAs felt that while full-time clinic physicians were able to communicate plans iteratively with staff, there was frequently no formal communication plan established between residents and MAs.
DISCUSSION/REFLECTION/LESSONS LEARNED: This project taught us several important lessons. First, it supported the idea that huddles can be used effectively to increase perceptions of resident integration into clinic teams. However, it also revealed that these perceptions can vary based on an individual’s role on the clinical team. These two findings underscore the reality that teamness is based on more than just the execution of pre- and post-clinic communication. Perhaps not surprisingly, they show that the content and format of communication is important. They reveal that how and when information is communicated may be more crucial for building a sense of team than the act and consistency of communication. Our data also suggests that to clinic staff, the activities that occur outside of clinic sessions may also contribute significantly to perceptions of resident integration. The ability for staff to interact with full-time physicians iteratively throughout full workdays may be important for clarifying plans, improving communication, building relationships, and contributing to a sense of team integration. Because in contrast, huddles only add an additional few minutes to a resident’s total time in clinic, staff may perceive them to be less integrated even despite huddles. Going forward, educational changes such as the ambulatory “burst” model will likely increase the amount of contiguous clinic time, and thereby increase the chance that residents can interact iteratively and naturally with MAs like full-time practitioners frequently do. Regardless, huddles will still play important roles in sustaining communication between resident physicians and clinic staff. We plan to maximize adherence to and impact of resident-MA huddles by adjusting our huddle format, ensuring that individuals convey content that is important to team workflow, and developing this into even more of a joint effort among all clinic staff via dashboards in staff meetings and reports of current huddle rates and resident integration scores. We are also exploring expansion of this project to other clinic sites.
UTHSCSA SAFE SPACE: BECOMING AN ALLY TO THE LGBTQ COMMUNITIESChristopher A. Alonzo. UTHSCSA, San Antonio, TX. (Tracking ID #1937061)
NEEDS AND OBJECTIVES: Healthy People 2020 acknowledges a need to address the health disparities endured by many lesbian, gay, bisexual, transgender, and queer/questioning (LGBTQ) individuals. Such disparities are rooted in discrimination, violence, civil rights inequalities, and poor access to health care. Sequeira et al. (2013) noted: “The Institute of Medicine recognizes that few practicing physicians are knowledgeable about and sensitive to the needs of LGBT patients. A recent survey of medical school deans found that medical school curricula devote a median of 5 h covering LGBT-related content across the 4-year curriculum. The same group indicated that improving access to curricular material would be the best way to increase the amount of content presented on this subject.” The need for increased LGBTQ knowledge is clear, and it is necessary that individuals in an academic medical setting learn about health disparities endured by many lesbian, gay, bisexual, transgender, and queer/questioning (LGBTQ) individuals. The Safe Space program aims to correct this lack of knowledge as well as aims to identify the LGBTQ population and their perceptions of the healthcare communities’ knowledge base. This interactive presentation will provide an educational resource for colleagues and future healthcare professionals about this important topic and methods to evaluate its effectiveness. Objectives 1. Discuss how the UTHSCSA Safe Space is educating students, faculty, staff, and clinicians about social, environmental, and physical factors that influence the health of lesbian, gay, bisexual, transgender, and queer (LGBTQ) individuals. 2. Describe Safe Space outcomes to date 3. Discuss Survey model for identifying LGBTQ community demographics and opinions.
SETTING AND PARTICIPANTS: The UT Health Science Center Safe Space program is designed to raise cultural competency and professionalism of all students, faculty, and staff at the Health Science Center to include more knowledge of the LGBTQ population.
DESCRIPTION: Participants in the program undergo one lecture workshop approximately 90 min in length. The lecture and discussions provide information on the following topics:knowledge of LGBT terminology, stereotypes, the coming out process, suicide risk, knowledge of bias, LGBTQ education, LGBTQ resources, Suicide prevention resources, and preparedness for dealing with LGBTQ issues or scenarios. Workshops include opportunities for participants to open a dialogue on topics such as conflict management, employment regulations, adoption practices locally and nationally, substance abuse, suicide, depression and transitions between genders, all concerning LGBTQ persons. Safe Space participants are required to complete a pre and post-training survey that assesses baseline knowledge of LGBTQ terminology, the coming out experience, and suicide resources The LGBT Access to healthcare survey will provide information about the Rio Grande Valleys LGBTQ communities and their access to healthcare in the valley. The survey aims to sample a population of the LGBTQ population in the Rio Grande Valley, the presence of supportive populations, the level of comfort when accessing healthcare in the Rio Grande Valley, the perception of bias from healthcare personal in providing treatment, and the perception of the LGBTQ population on the education status of healthcare workers on LGBT topics. The survey will be anonymous. A copy of the LGBTQ community surveys will also be distributed to the attendees for their review and comments.
EVALUATION: Analysis following a two tailed T-test showed significant improvements in knowledge of LGBT and Suicide resources, the coming out process, suicide risk assessment and most importantly feeling prepared with dealing with LGBT issues.
DISCUSSION/REFLECTION/LESSONS LEARNED: The UT Health Science Center Safe Space Program met with a great amount of success during its initial implementation between 2012 and 2013. The data showed significance in increasing the fund of knowledge of students faculty and in regards to certain topics discussed. Some major feedback that is provided is that participants would like longer sessions to increase discussion times, as well as have more members of the LGBTQ community present to aid in the presentation. The topic is a rapidly developing field and would do well to establish itself as a permanent area of medical education.
ONLINE RESOURCE URL (OPTIONAL): 1. “Lesbian, Gay, Bisexual, and Transgender Health.” Healthy People 2020. 22 Mar 2012. http://healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=25. 2. “LGBT (Lesbian, Gay, Bisexual, Transgender) Safe Space Training.” Office of Diversity, Northwestern University Feinberg School of Medicine. 6 Mar 2012. http://www.feinberg.northwestern.edu/diversity/programs/safe-space/index.html. 3. Gina M. Sequeira, Chayan Chakraborti, Brandy A. Panunti. “Integrating Lesbian, Gay, Bisexual, and Transgender (LGBT) Content Into Undergraduate Medical School Curricula: A Qualitative Study.” Ochsner J. 2012 Winter; 12(4): 379–382. PMCID: PMC3527869
VHA’S COMPREHENSIVE WOMEN’S HEALTH SCAN-ECHO PROGRAM: LESSONS LEARNEDKristina M. Cordasco1,3; Jessica Zuchowski1; Alison B. Hamilton1,4; Herschel Knapp2; Joann O. Saavedra2; Donna L. Washington1,3. 1VA Greater Los Angeles Healthcare System, North Hills, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA; 3The University of California, Los Angeles, Los Angeles, CA; 4The University of California, Los Angeles, Los Angeles, CA. (Tracking ID #1939313)
NEEDS AND OBJECTIVES: Although women are among the fasting growing segment of the Veterans’ Health Administration (VHA) patient population, many VHA primary care providers’ (PCPs) have relatively small female caseloads, making it challenging for them to build and maintain their women’s health knowledge and skills. Therefore, as part of VA’s SCAN-ECHO (Specialty Care Access Network - Extension for Community Healthcare Outcomes) program, we implemented a Comprehensive Women’s Health SCAN-ECHO program with the objective of building and maintaining VHA women’s health PCPs’ knowledge in the evaluation and management of conditions specific to, more common in, or with special considerations relevant to women (e.g., gynecology, breast issues, depression, osteoporosis).
SETTING AND PARTICIPANTS: Our participants included women’s health PCPs across three VHA healthcare systems.
DESCRIPTION: The program consisted of monthly group PCP-specialist clinical tele-videoconferencing sessions in which PCPs obtained virtual specialist consultation on their cases and received serial patient-based education. Prior to each session, PCPs submitted consultation requests on patients for whom they wanted diagnostic and/or therapeutic management advice. During sessions, the specialist at a “hub” facility and PCPs at multiple “spoke” sites engaged in real-time group discussions about the cases. In addition to giving recommendations, the specialist discussed the underlying evidence or rationale. Content also included patient communication strategies (e.g., explaining contraceptive options). The PCP who submitted the consult, as well as other PCPs participating in the session, interacted with the specialist and with each other, asking clarifying questions. The specialist also provided a brief didactic relevant to the cases. Continuing Medical Education credit was provided. Each session was held at the noon hour in the hosting site’s time zone.
EVALUATION: We used participation logs, participant surveys, semi-structured interviews, and field notes from key stakeholder meetings to evaluate our program. We conducted 14 sessions over 16 months. Overall, 65 PCPs in three VHA health care systems participated in one or more sessions, with an average of 11 participants per session. Participation rates were much higher in the one healthcare system where providers were provided with time protected from their clinic responsibilities (rather than meeting over lunch). Attempts to expand to two additional VHA healthcare systems, where the session would have been in the lunch hour, were not successful secondary to conflicting meetings or educational programming. Of the 58 post-session surveys received, in 45 (78 %) the participant strongly agreed, and in 7 (12 %) the participant agreed, that the information provided in the session would influence their patient care. Of these 52, 74 % indicated that the information would change their ordering of diagnostic studies; 83 % their treatment plans; 58 % their prescription of medications; and 68 % their overall interactions with patients. Among the 10 PCP interviewees, all reported that they found SCAN-ECHO to be useful for building and maintaining their knowledge on women’s health topics. However, all interviewees also reported that the session being conducted during their lunch hour was a limiting factor for consistent participation, with morning clinics often running late and participants having competing clinical, administrative, educational and personal priorities for that time. Interviewees and discussions with key stakeholders revealed that the rotating specialists and topics across the breadth of women’s health, although appealing in its comprehensiveness, also limited submission of cases as PCPs were unlikely to have active case-based questions coincident with the monthly specialist’s area of expertise.
DISCUSSION/REFLECTION/LESSONS LEARNED: VA’s SCAN-ECHO program is a promising modality for building and maintaining PCP knowledge on women’s health topics, with attendees indicating that it influences their patient care. However, PCPs receiving time protected from clinical responsibilities is essential for robust and consistent participation. Further, narrowing in on a consistent women’s health area, such as gynecology, although sacrificing the program’s comprehensiveness, may facilitate PCPs having active cased-based questions for the sessions.
ONLINE RESOURCE URL (OPTIONAL):http://vaww.portal.gla.med.va.gov/sites/PAC/SCAN/Shared%20Documents/Gynecology.aspx
VIDEOTAPING HOME VISITS—FIRST-YEAR MEDICAL STUDENTS BRING PATIENTS’ WORLDS TO THE CLINICAL TEAMBarbara Ogur1,2; Marie-Louise Jean-Baptiste1; Jeremy Keller1; Nancy Blum1; Andreas Mitchell1; Margaret Fallon1; Elorm Avakame1; Ethan Balgley1; Betty Erfe1; Grace Chao1; Jose O. Gutierrez1. 1Harvard Medical School, Boston, MA; 2Harvard Medical School, Boston, MA. (Tracking ID #1934147)
NEEDS AND OBJECTIVES: Early exposure to patients is recognized as very valuable in providing students with opportunities to ground their scientific studies in clinical practice. According to learning theory and corroborated by observation, students learn more and feel motivated to learn more deeply when their learning is directly connected to real patients’ experiences. Many programs begin clinical exposure in the first year, through a course in interviewing patients. These courses are highly valued by students. We describe a pilot to extend these curricula using the hypothesis that students will learn even more powerfully if their learning experiences provide them an opportunity to not just learn from patients but to actually contribute to their patient’s care.
SETTING AND PARTICIPANTS: At Harvard Medical School, first year students have a year-long course in interviewing, Patient-Doctor 1, which emphasizes human connection and the understanding of patients’ experiences of illness by providing students opportunities to interview patients and to reflect on their experiences in small groups with experienced clinician preceptors.
DESCRIPTION: We planned and implemented a pilot program to explore ways for first-year students to both learn from patients and also contribute meaningfully to patients’ care. In one section of the course, as part of a required home visit, we asked one group of students, with written consent of their patients, to videotape the home environment. Students then provided their video and the written report of their home visit, including what special insights they learned about the patient from being in the home, to their patient’s ambulatory clinical care team.
EVALUATION: We surveyed students, preceptors, and the clinical team caring for the patient to determine their feelings about this exercise. Samples of the videos will be available for review. Students reported that these home visits provided them with an expanded sense of the patient as a person with important connections to family and friends, with a role in the community, and with a coherent set of beliefs about health and diet perhaps not totally aligned with the beliefs of the medical world. Students found experiencing the physical adaptations for patients with mobility constraints very informative and directly witnessed possible environmental triggers for a patient with asthma. Clinical team members learned new information about patients’ belief systems, adaptations, and social supports.
DISCUSSION/REFLECTION/LESSONS LEARNED: We piloted a small innovation of a medical school interviewing course that both provided students with a powerful learning experience in contextualizing patients’ illnesses through the lens of patients’ lives in their homes and communities and also through the lens of performing a valued function of bringing this broader view of the patient back to the clinical team. We believe this exercise warrants a trial with a larger cohort. We learned that students, preceptors, and clinical teams found the exercise useful and inspiring. We believe that first-year students can bring a valuable, humanizing perspective on the patient to over-stretched clinical teams as they also learn to be caring physicians attuned to their patients’ real experiences.
VISUAL THINKING STRATEGIES: AN ARTS-BASED INTERVENTION TO TEACH TEAMWORK TO SENIOR MEDICAL STUDENTSElizabeth Karwowski1,2; Alexa R. Miller3; Suzanne Sarfaty1. 1Boston University Medical Center, Boston, MA; 2Boston VA Healthcare System, Boston, MA; 3Brandeis University, Waltham, MA. (Tracking ID #1939008)
NEEDS AND OBJECTIVES: In recent years, Boston University School of Medicine (BUSM) recognized a local need to develop a formal curriculum to teach teamwork. The BUSM curriculum committee simultaneously advocated for increased exposure to the arts and humanities throughout medical school training. In order to meet these needs, the BUSM fourth year Advanced Internal Medicine clerkship developed a new curriculum using Visual Thinking Strategies (VTS) to facilitate teaching teamwork skills. VTS has been shown to successfully teach observation skills but has been studied infrequently outside of teaching observation. Objectives of the curriculum include: *Identify characteristics of a highly functioning team *Listen actively and encourage ideas/opinions of other team members *Practice respectful dialogue and expressing differences in opinion *Explore conflict resolution skills in a group setting *Integrate viewpoints of all team members
SETTING AND PARTICIPANTS: The VTS and Teamwork curriculum was developed for the BUSM Advanced Internal Medicine clerkship, a mandatory four-week clerkship completed during the final year of medical school. The clerkship includes 1 day of classroom-based didactic teaching per week with a focus on teaching advanced communication skills. The VTS and Teamwork curriculum was inserted into these didactic sessions.
DESCRIPTION: Development of the VTS and Teamwork curriculum has been an iterative process with changes in response to student feedback. The curriculum was first implemented in June 2013, evolved over the next several blocks, and finalized in December 2013. The curriculum is divided into three distinct workshops: 1) Introduction to VTS and Teamwork: Speak up, 2) Listening as a Team Member, and 3) Listening as a Leader. VTS is a well-described process that involves the facilitated discussion of artwork to build skills in observation, communication, and listening. During a VTS session a trained facilitator guides learner discussion of a work of art using three questions: what is happening here? What do you see that makes you say that? What more can we find? Each workshop includes at least one VTS session. Additionally, two of the workshops include modified VTS type activities. The second workshop incorporates a small group activity to enhance listening skills. The third workshop uses a separate small group activity to allow students to practice the role of group facilitator. In addition, students also receive formal teaching on teamwork. The curriculum uses the model described by Amy Edmondson called ‘Teaming on the Fly’, which describes five attributes of highly functioning teams: speaking up, listening intensely, integrating different facts and points of view, experimenting iteratively, reflecting on your own ideas on actions.
EVALUATION: There are two methods of curriculum evaluation. First, the students complete a pre and post survey. Both surveys include the TeamSTEPPS - Teamwork Attitudes Questionnaire, a validated survey developed by the Agency for Healthcare Research and Quality to study self-rated attitudes towards teamwork. The change in score after completion of the curriculum will be analyzed. The post survey includes an additional set of questions to determine student perceptions of the curriculum. Second, the students take part in a focus group at the completion of the clerkship to further explore their attitudes towards the curriculum. The BUSM Institutional Review Board approved this study. Data collection began in late fall 2013.
DISCUSSION/REFLECTION/LESSONS LEARNED: Preliminary data reveal that students largely value the addition of VTS to their curriculum as a novel method of medical education. At times they struggle to link VTS with learning teamwork skills and continue to seek an explicit set of techniques to improve their teamwork skill set. A subgroup of students express striking discontent with the curriculum. A subgroup analysis is planned to attempt to determine unique attributes of students dissatisfied with the curriculum. Thus far it seems that using an art-based intervention to teach skills beyond observation alone is generally well received and valued by students. Future attempts to develop novel arts-based curricular interventions need to focus on an explicit connection between the activity and the clinical skill to be learned.
WELCOME TO THE NEIGHBORHOOD: TEACHING THE SOCIAL DETERMINANTS OF HEALTHJada C. Bussey-Jones; Maura George; Stacie Schmidt; Jennifer E. Bracey; Mehul Tejani; Schuyler D. Livingston. Emory University, Atlanta, GA. (Tracking ID #1934052)
NEEDS AND OBJECTIVES: New physicians require broad medical knowledge and a practiced set of procedural skills. Training in these areas would suffice in decreasing disease burden if medical care were the only factor relevant to patient health outcomes. Research suggests, however, that multiple complex social determinants (e.g. neighborhood characteristics, social policies, and available resources) play a significant role in producing or mitigating health outcomes and racial/ethnic disparities. Studies suggest that fourth year students were no more knowledgeable about health care access than first-year students, and that students’ attitudes toward the underserved become more negative throughout medical school. Further, most current educational environments do not prepare learners for engagement with broader health issues. This course was designed to 1) describe the complexity and impact of community and other social determinants of health on patient health outcomes, and 2) state ways, to connect community/public service and advocacy with learners clinical and academic work.
SETTING AND PARTICIPANTS: Emory University School of Medicine month long elective course available to interprofessional learners (nursing, medical, PA students) at Emory and Morehouse Schools of Medicine, as well as visiting students from outside institutions.
DESCRIPTION: Our curriculum uses a combination of didactic lectures, readings, experiential learning, direct service activities and personal reflection to equip future physicians to practice medicine in a socially complex world. We help students better understand and cooperatively address the problems facing patients and communities. Examples of student activities include assessment of community resources such as green space, fresh vegetables, pharmacy supply, safety, tobacco, alcohol stores/billboards. Learners also participate in simulation experiences (e.g. navigate public hospital as a patient - assessing wait times, barriers, etc.). Participants engage with community partners’ sites using an asset model approach to collaborate and participate in health related interventions. Our students also engage several essential community resources that provide context for the health of many of their patients including, homeless shelters, nursing homes, and prison medical facilities. Finally, they are trained asked to complete advocacy tasks such as visiting the state capital, meeting with legislators, writing letters to the editor or position papers. This course also utilizes several means of reflection including small group discussions, journaling, photo journaling.
EVALUATION: The course was evaluated in several ways 1. Learners’ attitudes were compared to controls through use of Medical Student Attitudes toward the Underserved questionnaire (MSATU), a validated survey instrument administered at 0, 1 and 12 months. Our preliminary results reveal a significant difference in MSATU scores between controls and course participants at -month 0. However, there was no significant change in scores when comparing 0 to 1 month survey results within social med participants or controls. This suggests that there may baseline attitudes among self-selected participants that led them to this course. 2. Semi-structured interviews were completed at the end of the elective to characterize the learners and identify best received components of the elective. The curriculum was very well received, and we had a marked increase in the number of requested participants in the course over the 2 years of implementation. 3. Ongoing analysis is underway, including an electronic database for longitudinal analysis of elective participants.
DISCUSSION/REFLECTION/LESSONS LEARNED: This presentation will highlight the development and implementation of the Social Determinants of Health curriculum at Emory University School of Medicine. We will describe the core components of our curriculum, share tools, and discuss challenges. We will also specifically discuss strategies to forge relationships with community partners, collaborate with educational leadership to broaden our curricular impact, increase core faculty knowledge and expertise, and evaluate and modify curriculum. This elective seems to attract a selected group of individuals with positive baseline attitudes about caring for the underserved. Qualitative interviews suggest these positive attitudes were bolstered through service learning. Learners in our course expressed a desire for more social medicine concepts and didactics to occur earlier in undergraduate medical education. An increased number of learners and ongoing evaluation efforts will direct future course development and improve our understanding of the personal characteristics, qualities, and experiences that lead to positive attitudes about care of underservedand careers in community engagement, service, and health advocacy.
WORK-PLACE BASED ASSESSMENTS: LEVERAGING CLOUD-BASED MOBILE TECHNOLOGY FOR CAPTURING NARRATIVE COMMENTSChurlson Han; Gary S. Ferenchick; David Solomon. Michigan State University, East Lansing, MI. (Tracking ID #1939243)
NEEDS AND OBJECTIVES: Direct observation and feedback are essential components of medical education. Immediate, specific feedback can be vital to learner development. Valued feedback is frequent, relevant to observed behavior, specific, and timely. The purpose of this exploratory study was to calculate the percentage of work-place based assessments, completed with a Cloud-based mobile just-in-time evaluation system (i.e. JIT, described below), that included any written comments (i.e. comment-enhanced evaluation); and to calculate the percentage of comments that were general, specific, or specific with detail, regarding students’ clinical performance; and to describe evaluator variables affecting comment specificity.
SETTING AND PARTICIPANTS: Between July 2012 and September 2013, 256 students at Michigan State University’s College of Human Medicine were required to obtain ten directly observed evaluations. Using JIT, all evaluator comments were electronically captured in a permanent, cloud-based record, and were subsequently coded on three levels: general (“Good physical exam skills” or “Practice more”), specific (“Excellent neuro exam” or “Better organization”), or specific with detail (“Listened to axilla for radiation” or “Percuss lung fields & compare sides”). Evaluators were not provided any training on providing narrative comments. Three raters independently coded all narrative comments after establishing inter-rater reliability.
DESCRIPTION: We developed, implemented and assessed a Cloud-based clinical evaluation application (i.e. Just In Time Medicine or JIT) for internet-enabled devices including smart phones, which displays customized competency checklists for 17 CDIM training problems for evaluators to use when implementing work-place based assessments of students’ clinical skills in authentic clinical settings. JIT includes discretionary sections for evaluators to provide narrative written comments pertaining to: 1) “one area the student did well” and 2) “one area the student can improve upon”.
EVALUATION: 2658 CEX assessments were completed among the 256 students, with 227 students (88.7 %) having at least one comment-enhanced evaluation. The range of comment-enhanced evaluations per student was 0–11, with an average of 4.9. Out of a total of 1285 comments, 288 included only “well done” comments, 44 included only “needs improvement” comments. Nine hundred fifty-five included comments for both. For “well done” feedback, 17.2 % were general, 57.2 % specific, and 22.7 % specific with detail. For “needs improvement” feedback, 14.8 % were general, 53.4 % specific, and 31.8 % specific with detail. Resident feedback was compared to faculty. For “well done” comments, faculty feedback was 28.0 % general, 56.0 % specific, and 16.0 % specific with feedback, while resident feedback was 18.2 %, 58.4 %, and 23.4 % respectively. For “needs improvement” comments, faculty feedback was 11.5 %, 50.3 %, and 38.2 %, while resident feedback was 16.4 %, 55.3 %, and 28.3 % respectively.
DISCUSSION/REFLECTION/LESSONS LEARNED: When directly observing and assessing learner performance in authentic clinical settings, we determined that written comments accompany a high percentage of evaluations using Cloud-based technology delivered via mobile devices. These comments provide a high level of specificity. Evaluators displayed more detailed feedback for “needs improvement” items. We did not observe any variance in “well done” comments between faculty and residents, but faculty provided more specific with detail feedback on “needs improvement” items. This use of technology to capture narrative comments can provide specific and relevant student feedback.
ONLINE RESOURCE URL (OPTIONAL):www.justintimemedicine.com/mobile UN: testuser@msu.edu PW: testuser
WORKING TOWARDS MEANINGFUL RESIDENT INVOLVEMENT IN QUALITY IMPROVEMENT AT TWO UNIVERSITY CONTINUITY CLINICSDanielle F. Loeb; Susan M. Nikels; Rachel Swigris; Suzanne Brandenburg. University of Colorado Denver, Aurora, CO. (Tracking ID #1938666)
NEEDS AND OBJECTIVES: The ACGME requires that “residents are integrated and actively participate in interdisciplinary clinical quality improvement (QI) and patient safety programs.” In 2012 we initially introduced a QI curriculum in the ambulatory setting for all interns. Summative assessment by QI faculty and leadership revealed that lack of faculty exposure to QI principles and a non standardized approach to project organization led to high variability in project quality and resident involvement. The objective of this project was to improve integration of interns into QI projects in their continuity clinic settings.
SETTING AND PARTICIPANTS: This educational innovation took place in two resident ambulatory internal medicine clinics associated with one university hospital. It included 19 interns in the two clinics.
DESCRIPTION: Drawing on our prior experience and a literature review of best practices, we developed a combined didactic and experiential curriculum (Figure 1). The primary improvements include: 1) IHI (Institute for Health Care Improvement) QI curriculum required for interns and QI faculty 2) Each intern developed a personal QI project to practice fundamental QI skills 3) Interns integrated into designated clinic team QI projects 4) Dedicated FTE for QI faculty to lead clinic team QI projects 5) Personal QI projects will be reviewed with a standardized evaluation including: SMART aim statement, outcome measures, systematic data collection, PDSA cycle completion, presentation of data, and completion of IHI curriculum. 6) Each intern will submit summary of team QI project including: SMART aim statement, literature review, fishbone diagram or process maps, outcome measures, and PDSA cycle completion. Figure 1. Quality Improvement Curriculum by Calendar Month July ■ IHI Open School (IHI OS) QI 101–103 completed through GME August ■ IHI OS QI 105: The Human Side of QI ■ Completion of QIKAT Pre-test September ■ Create Personal Improvement project ■ Conduct Personal PDSA cycle October ■ Review concepts from IHI OS QI 101 ■ Begin to compile list of possible QI projects November ■ IHI Open School QI 102 and 103 ■ Choose QI projects (determine teams, etc.) December ■ IHI Open School QI 104 ■ Start project charter ■ Determine clinical team dedicated to mentor project January ■ Review project charter with faculty, revise PRN ■ Create Aim Statement February ■ Review Aim statement with faculty, revise PRN ■ Determine sources of data ■ Start SIPOC analysis March ■ Revise SIPOC analysis ■ Start drafting Fishbone or Process map April ■ Define metrics ■ Propose PDSA cycles May ■ Conduct PDSA cycles (if possible) June ■ Submit QI H&P and Reflection summary to MedHub ■ Create “Next Steps” Summary ■ Present to Clinic
EVALUATION: To date, 10 of 19 interns have presented personal QI projects with satisfactory review. These will be completed by February 2014. Of those who have presented personal project, all have satisfactorily completed their SMART Aim statement, balancing measures, systematic data collection, graphed results, PDSA cycle completion for their personal QI projects. Interns have completed 88 % of their assigned IHI modules. The interns will start integration into clinical teams in February with completion of team QI summary report in June 2014.
DISCUSSION/REFLECTION/LESSONS LEARNED: The primary lessons learned include: The didactic curriculum should be offered in conjunction temporally with the experiential curriculum (personal QI project) ● Supervising faculty for QI projects need adequate education in QI ● Residents should be integrated into projects that align with clinic goals to ensure dedicated QI faculty time and other support needed for success ● Flexibility and willingness to adapt on the fly are important approaches to implementing new curricular elements in clinical settings In conclusion, involving residents in QI continuity clinic projects offers important opportunities to integrate them into their clinics while providing them with essential QI skills. Steps toward achieving meaningful integration include providing faculty and resident didactics, offering an experiential curriculum and securing support for key faculty supervisors.