In this issue of MT, Engeland et al. use an elegant new immunocompetent model to show that measles virus can be the platform for concomitant delivery of direct tumor oncolysis, virus-triggered immune priming, and antitumor immune boosting through T-cell checkpoint inhibition.1 These findings support the concept that oncolytic viruses might just represent the complete package for generation of the dream team combination of local tumor cell cytotoxicity and systemic antitumor immunotherapy.
I recently took my children to see How to Train Your Dragon. As a family outing it was not a great success (lack of serious weaponry for my son and a poor Wi-Fi signal for my daughter's texting ambitions). For me, however, it was inspirational. Despite appearances, it is clear to me that the film was intended as nothing less than a thinly disguised allegory for the trials and tribulations of the development of oncolytic virotherapy. For example, the movie opens by depicting the somewhat tense relationship between the Vikings and the dragons. This clearly speaks to the fear and hostility with which many oncolytic viruses—such as measles, polio, pox, and herpes—were regarded only a couple of decades ago. Nonetheless, with better understanding (and a healthy dose of vision) comes trust.2,3 The Vikings eventually come to see that there is considerably more to dragons than their harsh, fire-breathing image would suggest. Allegorically, we now see that many of those viruses, previously regarded as nothing more than mass serial killers, can be tamed and potentially used to seek and destroy cancers (Figure 1).
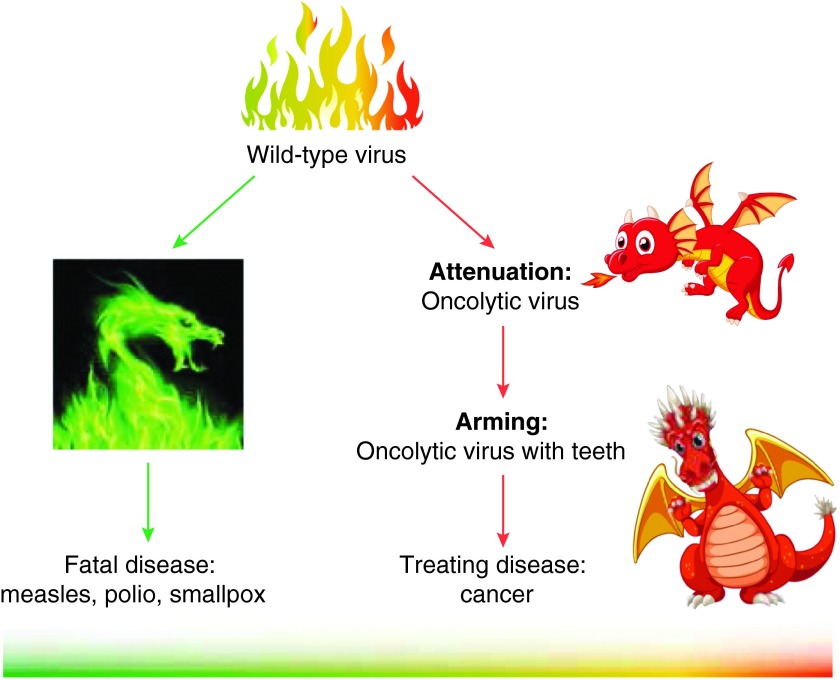
Figure 1.
How to train your oncolytic virus (part 1). Several viruses, which in their natural forms often cause very serious disease, have been adapted for use as oncolytic viruses. The wild-type viruses have been attenuated through culture adaptation, genetic engineering, and re-/de-targeting to generate potentially tumor-selective killers. These attenuating changes inevitably leave the modified virus safer, but less potent, than the wild-type equivalent. Additional therapeutic “teeth” can be provided by adding transgenes, often designed to enhance the immunogenic potency associated with tumor cell killing.
But the analogies work on so many different levels in this film. The lead dragon, Toothless, is initially portrayed as an evil villain, looking only to turn Vikings into toast. But in reality he is soft-hearted and misunderstood, and eventually his fire-breathing skills are put to good use to help the humans. Well, as you can imagine, it didn't take me long to realize the deeper meaning here: Toothless, without a shadow of a doubt, is clearly intended to represent the measles virus.
The path to redemption for measles virus started with the somewhat unexpected proposal that it could be used to treat human cancer, based on a preferential ability to replicate in tumor cells over normal cells.4,5 The availability of the adapted, nonpathogenic vaccine strain of the virus made the prospect of an oncolytic measles virochemotherapy rather more palatable, and within a decade measles entered clinical trials6 (Figure 1). The remarkable rehabilitation of the virus recently received a major boost when a patient with multiple myeloma, treated systemically with the virus at the highest dose, underwent a complete durable remission of her disease.7
Several other viruses, many associated with fearsome natural diseases, have also entered clinical trials as oncolytics6,8,9 (Figure 1). However, the taming of these dragons has not been without controversy. One major concern has been how the innate and adaptive components of the immune system would negatively affect viral replication, spread, and oncolysis.10 Happily, there is now increasing optimism that the immune reaction to viral infection of cancer cells has multiple benefits.11 These include initiation of a potent innate reaction at the site of tumor infection, leading to extensive immune-mediated tumor cell killing; the priming of effective adaptive T-cell responses against tumor antigens, released as a result of oncolysis and innate immune killing;12 and even the possibility that neutralizing antibodies may help to carry viruses to tumors as part of immune complexes tethered to circulating immune cells.13
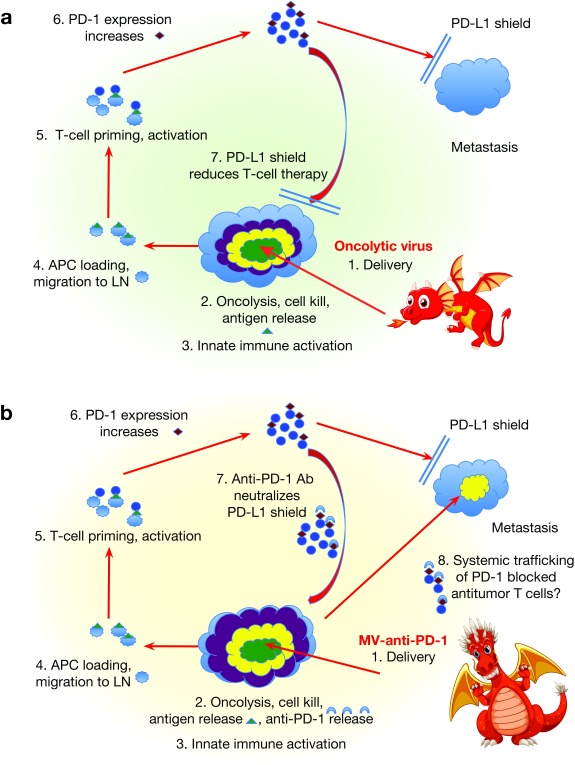
Therefore, although these viruses can breathe an oncolytic fire into a tumor, the presence of the immune system presents both a need, and an opportunity, to sharpen their therapeutic “teeth”11 (Figure 2a) (and the metaphorical significance of training Toothless the dragon will surely not be lost on anyone here). One way in which teeth have been added to oncolytic viruses has been to incorporate additional genes that complement the immunogenic potential of viral replication14 (Figure 1). In particular, oncolytics expressing granulocyte–macrophage colony-stimulating factor, a strong immune modulator that recruits both additional innate killers and antigen-presenting cells, have shown real signs of success in the clinic.15,16 As a result of positive preclinical and clinical results with such immune-armed viruses, oncolytic viruses have become increasingly viewed as, at least in part, immunotherapies17 (Figure 2a).
Figure 2.
How to train your oncolytic virus (the immunological sequel). (a) An oncolytic virus delivered into a tumor leads to direct oncolysis and tumor cell killing (green zone). This activates an innate immune response, which further accentuates tumor cell killing (yellow zone). The immune- and viral-mediated cell death leads to tumor antigen release and carriage to lymph nodes by antigen-presenting cells (APCs), resulting in presentation to T cells. T-cell responses to the tumor antigens are raised, but, with time, T-cell checkpoint inhibitory molecules, such as PD-1, are expressed on the T cells to dampen the T-cell response. Expression of the coinhibitory ligands on tumor cells, such as PD-L1, significantly reduces the T-cell activity and limits the T cell–mediated killing of the tumor (purple zone). (b) When the oncolytic virus carries in a checkpoint inhibitor antibody (such as anti-PD-1), immune-mediated tumor cell killing can be greatly increased—both by de-suppressing innate immune effectors responding to the viral infection (yellow zone) and by removing the brakes from the activated T-cell response against tumor antigens (purple zone). It is still unclear how local expression of the checkpoint inhibitor antibody will affect T-cell responses against distant tumor where the antibody is not present. Ab, antibody; LN, lymph node; MV, measles virus.
This impressive public relations coup in changing the perception of these viruses—from serial killers to immunoviral cancer assassins—could not have come at a better time. Cancer immunotherapy has recently received rave reviews from the critics because of impressive responses in patients treated with checkpoint inhibitor antibodies.18,19,20,21 T cells, once activated, must ultimately be suppressed to prevent uncontrolled proliferation and killing of nontarget tissues. This suppression is achieved through inhibition of proliferation at certain critical checkpoints of T-cell activation. It is mediated by negative regulatory molecules on the surface of previously activated T cells, which bind ligands on other T cells, or antigen-presenting cells (such as PD-1/PD-L1; CTLA-4/CD28) (Figure 2a). Effective blocking antibodies have been raised against many of these negative T-cell regulatory pathways. By supplying these blocking antibodies systemically, T-cell activity—especially against tumor-associated antigens—can be sustained and increased, leading to tumor rejection.18,19,20,21
With almost unlimited enthusiasm for checkpoint inhibition at the moment, the hunt is on for ways to trigger highly specific, tumor antigen–associated T-cell responses, which can then be amplified (nonspecifically) by checkpoint inhibition. Enter stage right: the dragons. Oncolytic viruses offer a very attractive mechanism by which tumor cells can be killed in a highly immunogenic manner,12 leading to priming of T-cell responses against tumor antigens.17 With the subsequent addition of checkpoint inhibitor antibodies, oncolytic virus–induced, tumor-specific T-cell responses could be unleashed to act throughout the body.22,23 Engeland et al. take this burgeoning alliance between oncolytic viruses and checkpoint inhibitor immunotherapy to an exciting new level.1
One problem with development of measles virus as an oncolytic immunovirotherapy has been a lack of immunocompetent models—partly because murine cells do not replicate the virus as they lack receptors for virus entry. Engeland et al. bypassed this problem by generating B16 melanoma cells transfected with CD20 and then using a measles virus expressing a single-chain variable domain, allowing it to be retargeted to CD20-expressing cells. These modifications allowed virus entry into the B16-CD20 cells, enabling limited replication. Critically, this allowed therapy experiments to be carried out against subcutaneous B16 melanomas growing in the context of a fully functional immune system.
The second major advance was the construction of the negative-strand RNA measles virus–expressing (checkpoint inhibitor) antibodies (anti-CTLA-4 or anti-PD-L1). The authors confirmed that the recombinant viruses expressed functional antibodies and behaved as oncolytic viruses against human—and, to a lesser extent, B16-CD20 murine—tumor cells.
The stage was therefore now set for the investigators to demonstrate a clear therapeutic benefit of adding vector-delivered checkpoint inhibition to intratumoral oncolytic measles virotherapy (Figure 2a,b). Whereas MV-anti-CTLA-4 delayed progression of tumors, MV-anti-PD-L1 increased median overall survival and induced tumor remissions in some mice. Therapeutic gains were associated with predicted immune consequences of checkpoint inhibition, including enhanced cytotoxic T-cell and reduced regulatory T-cell infiltration into tumors. These new antibody-expressing viruses also retained oncolytic efficacy against human tumor xenografts and replicated well in primary human melanoma tumor tissue.
Naturally enough, several important issues remain to be resolved. These studies implied that the particular choice of checkpoint inhibition could be important. In addition to the CTLA-4 and PD-1 pathways, other costimulatory and coinhibitory interactions exist between T cells and tumor cells or professional antigen-presenting cells, all of which have different kinetics of action.24 For example, CTLA-4 T-cell inhibition acts early in generation of the T-cell response, whereas PD-1/PD-L1 inhibition mediates the later, effector phase of T-cell activation.20 If the checkpoint inhibitor is carried by the virus, as opposed to being introduced systemically, kinetics of its expression will need to correlate with the phase of T-cell activation/suppression that is being targeted. Therefore, viral clearance rates, which are inexorably linked to inhibitor antibody expression, must be matched closely to the waxing and waning of checkpoint molecule expression on T cells. In addition to timing, location of expression of the checkpoint inhibitors is likely to be critical. Tumor-delivered oncolytic virus will produce high levels of inhibitor antibodies at the tumor site. This is ideal for blockade of tumor-expressed negative regulators of T-cell activation, such as PD-L1 (Figure 2). However, a blanket blockade of negative regulators may require that the checkpoint inhibitor be expressed elsewhere—such as in lymphoid tissues, in the periphery, or even in tumors not targeted by the virus (Figure 2b). Thus, future experiments will concentrate on the nature, timing, and location of virus-delivered checkpoint inhibitors as well as the relative benefits of virus expression, compared with systemic injection, of antibodies.
A big potential plus of local expression of these antibodies is that it may reduce the toxicity seen with systemic delivery in patients.19,21,24,25 Further studies looking at both acute (inflammatory) and chronic (largely autoimmune) side effects will be required to test this hypothesis. It will also be fascinating to compare the effects of checkpoint inhibition on the balance between antitumor and antivirus T-cell immunity. The current working model is that taking the brakes off antitumor T-cell activation will be highly therapeutic, with the caveat of possible autoimmune sequelae. What, however, will be the overall effects of further desuppressing the activity of antiviral T cells? This could be good for safety by preventing virus spread through the body. It may also boost antitumor efficacy, by increasing antiviral T-cell responses against virally infected tumor cells. Alternatively, an increased antiviral T-cell response may clear the oncolytic infection in tumor more rapidly, thereby decreasing viral spread/oncolysis and/or virus-mediated immune activation.
It will also be interesting to monitor expression of molecules such as PD1, CTLA-4, and others,24 on innate immune effectors (e.g., natural killer cells) to investigate whether increased antitumor therapy results in part from enhancing their local antitumor killing activity (which will also lead to faster clearance of the virus—which may not be such a good thing). As is frequently the case when considering the pros and cons of the immune system in oncolytic immunovirotherapy, the answers to these questions are likely to involve a great deal of “On the one hand…and on the other…”
In summary, Engeland et al. have made a significant step forward in showing that oncolytic immunovirotherapy can be combined effectively with checkpoint inhibition–mediated immunotherapy. Oncolytic viruses have already shown tantalizing potential in clinical trials. The current studies add credibility to the belief that it will be possible to add further, significant firepower to these dragons-turned-knights in shining armor. At the end of How to Train Your Dragon, all prejudices, fears, and grudges are put aside as the war between the Vikings and the dragons ends in harmonious friendship. The analogy is surely clear for all to see: a set of viruses, which we were previously intent on eradicating, may now offer new hope for the future of cancer therapy. By giving oncolytic viruses additional immune-activating teeth, a new era in this partnership is about to begin. That being said, I am not completely convinced that my children were quite as sensitive to the deep symbolic significance of Toothless and his dragon friends as I would have hoped.
References
- Engeland CE, Grossardt C, Veinalde R, Bossow S, Lutz D, Kaufmann JK.et al. (2014CTLA-4 and PD-L1 checkpoint blockade enhances oncolytic measles virus therapy Mol Ther 221949–1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly E, Russell SJ. History of oncolytic viruses: genesis to genetic engineering. Mol Ther. 2007;15:651–659. doi: 10.1038/sj.mt.6300108. [DOI] [PubMed] [Google Scholar]
- Russell SJ, Peng KW, Bell JC. Oncolytic virotherapy. Nat Biotechnol. 2012;30:658–670. doi: 10.1038/nbt.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura T, Russell SJ. Oncolytic measles viruses for cancer therapy. Expert Opin Biol Ther. 2004;4:1685–1692. doi: 10.1517/14712598.4.10.1685. [DOI] [PubMed] [Google Scholar]
- Russell SJ. Review: RNA viruses as virotherapy agents. Cancer Gene Ther. 2002;9:961–966. doi: 10.1038/sj.cgt.7700535. [DOI] [PubMed] [Google Scholar]
- Miest TS, Cattaneo R. New viruses for cancer therapy: meeting clinical needs. Nat Rev Microbiol. 2014;12:23–34. doi: 10.1038/nrmicro3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell SJ, Federspiel MJ, Peng KW, Tong C, Dingli D, Morice WG.et al. (2014Remission of disseminated cancer after systemic oncolytic virotherapy Mayo Clin Proc 89926–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly O, Harrington K, Melcher A, Pandha H. Live viruses to treat cancer. J R Soc Med. 2013;106:310–314. doi: 10.1177/0141076813494196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly OG, Errington-Mais F, Prestwich R, Harrington K, Pandha H, Vile R.et al. (2012Recent clinical experience with oncolytic viruses Curr Pharm Biotechnol 131834–1841. [DOI] [PubMed] [Google Scholar]
- Prestwich RJ, Errington F, Diaz RM, Pandha HS, Harrington KJ, Melcher AA.et al. (2009The case of oncolytic viruses versus the immune system: waiting on the judgment of Solomon Hum Gene Ther 201119–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melcher A, Parato K, Rooney CM, Bell JC. Thunder and lightning: immunotherapy and oncolytic viruses collide. Mol Ther. 2011;19:1008–1016. doi: 10.1038/mt.2011.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo ZS, Liu Z, Bartlett DL. Oncolytic immunotherapy: dying the right way is a key to eliciting potent antitumor immunity. Front Oncol. 2014;4:74. doi: 10.3389/fonc.2014.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilett E, Kottke T, Donnelly O, Thompson J, Willmon C, Diaz R.et al. (2014Cytokine conditioning enhances systemic delivery and therapy of an oncolytic virus Mol Ther 221851–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo R, Miest T, Shashkova EV, Barry MA. Reprogrammed viruses as cancer therapeutics: targeted, armed and shielded. Nat Rev Microbiol. 2008;6:529–540. doi: 10.1038/nrmicro1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbach CJ, Burke J, Jonker D, Stephenson J, Haas AR, Chow LQM.et al. (2011Intravenous delivery of a multi-mechanistic cancer-targeted oncolytic poxvirus in humans Nature 47799–102. [DOI] [PubMed] [Google Scholar]
- Senzer NN, Kaufman HL, Amatruda T, Nemunaitis M, Reid T, Daniels G.et al. (2009Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor–encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma J Clin Oncol 275763–5771. [DOI] [PubMed] [Google Scholar]
- Lichty BD, Breitbach CJ, Stojdl DF, Bell JC. Going viral with cancer immunotherapy. Nat Rev Cancer. 2014;14:559–567. doi: 10.1038/nrc3770. [DOI] [PubMed] [Google Scholar]
- Quezada SA, Peggs KS. Exploiting CTLA-4, PD-1 and PD-L1 to reactivate the host immune response against cancer. Br J Cancer. 2013;108:1560–1565. doi: 10.1038/bjc.2013.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB.et al. (2010Improved survival with ipilimumab in patients with metastatic melanoma N Engl J Med 363711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott PA, Hodi FS, Robert C. CTLA-4 and PD-1/PD-L1 blockade: new immunotherapeutic modalities with durable clinical benefit in melanoma patients. Clin Cancer Res. 2013;19:5300–5309. doi: 10.1158/1078-0432.CCR-13-0143. [DOI] [PubMed] [Google Scholar]
- Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH.et al. (2014Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab J Clin Oncol 321020–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias JD, Hemminki O, Diaconu I, Hirvinen M, Bonetti A, Guse K.et al. (2012Targeted cancer immunotherapy with oncolytic adenovirus coding for a fully human monoclonal antibody specific for CTLA-4 Gene Ther 19988–998. [DOI] [PubMed] [Google Scholar]
- Zamarin D, Holmgaard RB, Subudhi SK, Park JS, Mansour M, Palese P.et al. (2014Localized oncolytic virotherapy overcomes systemic tumor resistance to immune checkpoint blockade immunotherapy Sci Transl Med 6226ra232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melero I, Grimaldi AM, Perez-Gracia JL, Ascierto PA. Clinical development of immunostimulatory monoclonal antibodies and opportunities for combination. Clin Cancer Res. 2013;19:997–1008. doi: 10.1158/1078-0432.CCR-12-2214. [DOI] [PubMed] [Google Scholar]
- Kong YC, Flynn JC. Opportunistic autoimmune disorders potentiated by immune-checkpoint inhibitors Anti-CTLA-4 and Anti-PD-1. Front Immunol. 2014;5:206. doi: 10.3389/fimmu.2014.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]