Abstract
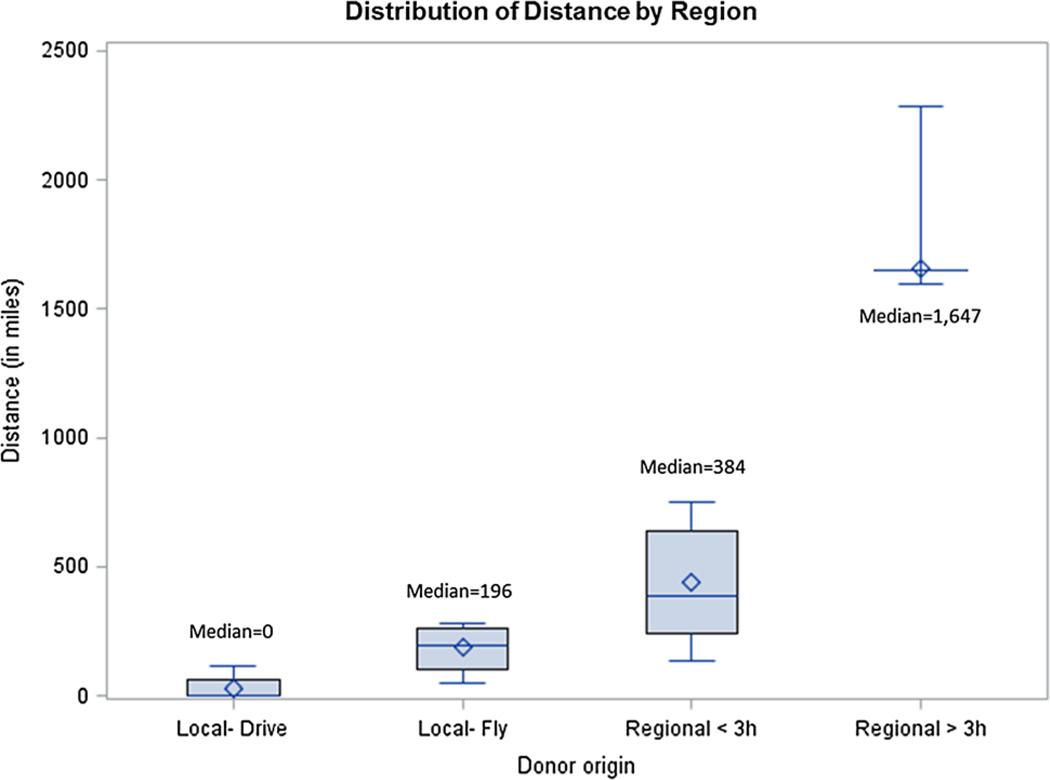
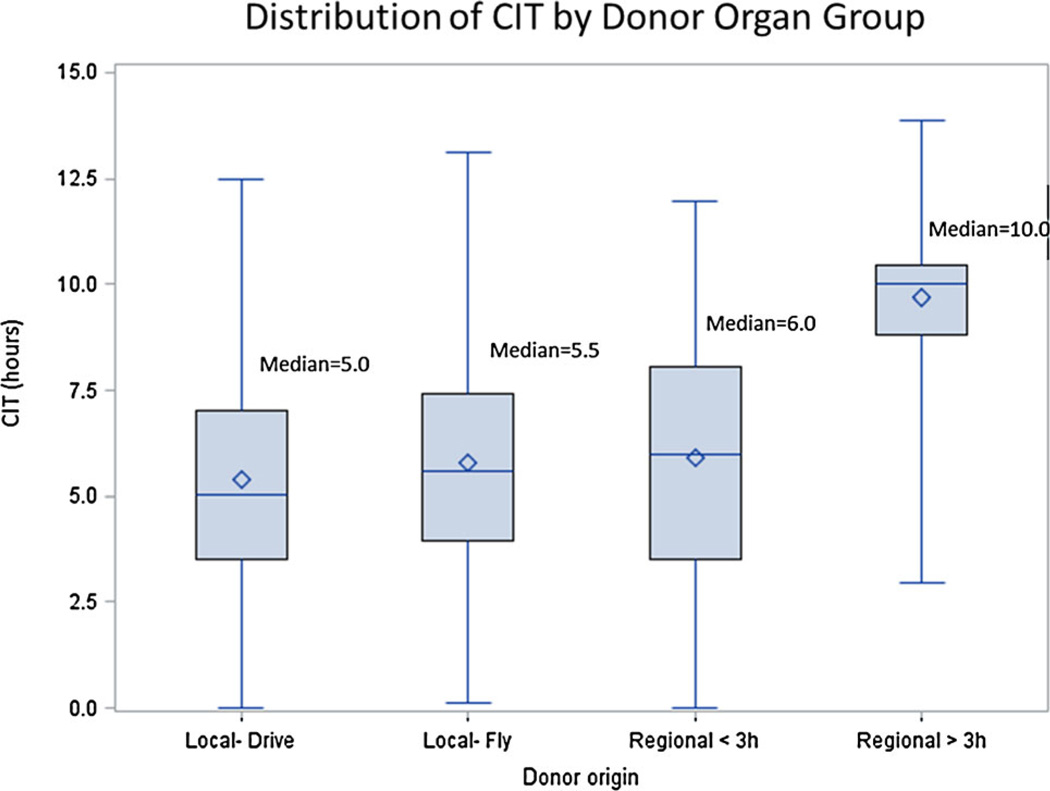
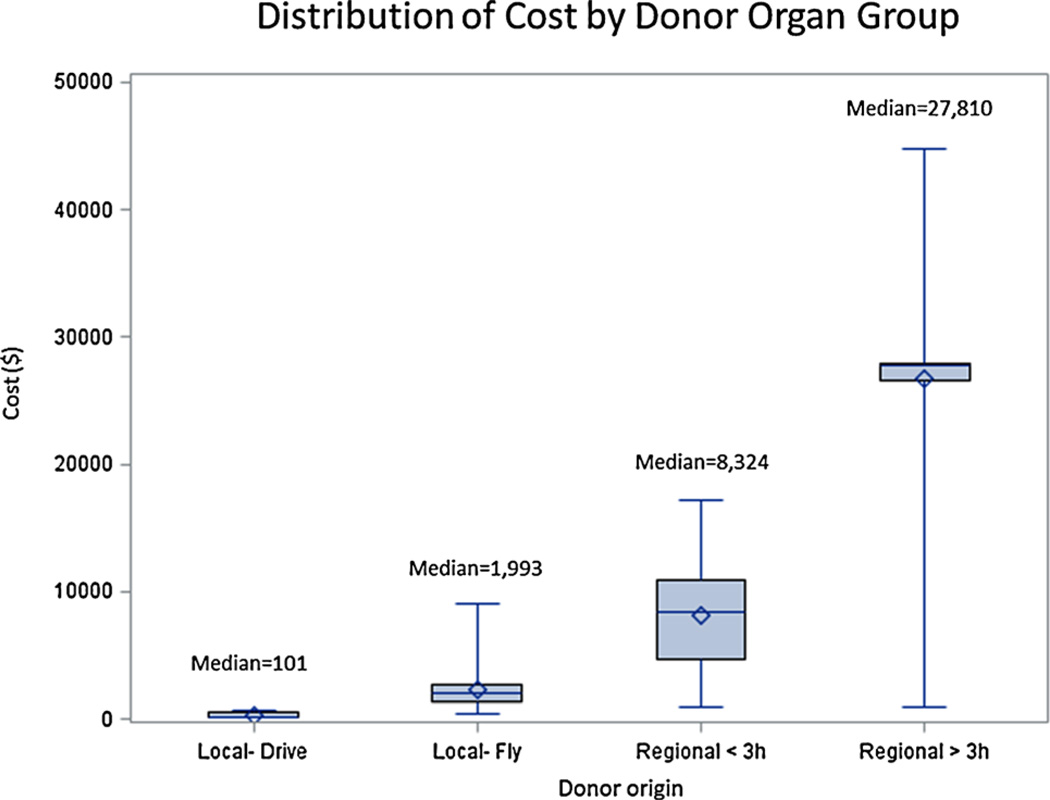
Changes to the liver allocation system have been proposed to decrease regional variation in access to liver transplant. It is unclear what impact these changes will have on cold ischemia times (CITs) and donor transportation costs. Therefore, we performed a retrospective single center study (2008–2012) measuring liver procurement CIT and transportation costs. Four groups were defined: Local-within driving distance (Local-D, n = 262), Local-flight (Local-F, n = 105), Regional-flight <3 h (Regional <3h, n = 61) and Regional-Flight >3 h (Regional >3h, n = 53). The median travel distance increased in each group, varying from zero miles (Local-D), 196 miles (Local-F), 384 miles (Regional <3 h), to 1647 miles (Regional >3 h). Increasing travel distances did not significantly increase CIT until the flight time was >3 h. The average CIT ranged from 5.0 to 6.0 h for Local-D, Local-F and Regional <3h, but increased to 10 h for Regional >3h (p < 0.0001). Transportation costs increased with greater distance traveled: Local-D $101, Local-F $1993, Regional <3h $8324 and Regional >3 h $27 810 (p < 0.0001). With proposed redistricting, local financial modeling suggests that the average liver donor procurement transportation variable direct costs will increase from $2415 to $7547/liver donor, an increase of 313%. These findings suggest that further discussion among transplant centers and insurance providers is needed prior to policy implementation.
Introduction
There is momentum to change the liver allocation system to decrease regional variation in access to liver transplantation in the United States (1,2). However, there is great debate among the transplant community regarding the appropriate magnitude of “sharing.” Proposed allocation models are based upon the ethical principle of equity (from the perspective of a listed liver transplant recipient). These equity models are balanced with pragmatic concerns about cold ischemia time (CIT) and organ transport. CIT is a weighted variable in the liver donor risk index (DRI) with prolonged CIT associated with decreased graft survival and increased postliver transplant hospital expenses (3,4).
Although it is clear that increasing CIT affects graft outcome (3), it is not clear how travel distance affects CIT, or whether there is a “threshold” travel distance above which CIT becomes unacceptable. Current proposed liver allocation models have been criticized because they use estimated transportation time as a surrogate marker of CIT. These models do not consider other contributors to CIT such as donor hospital practices after cross-clamping, transport time from donor hospital to airport, transport time from airport to recipient hospital, time required for documentation by recipient organ procurement organization (OPO) and recipient hospital practices. These factors can result in significant delays, and as such, prolong CITs.
Although there is an appreciation that donor liver transportation costs will increase with proposed redistricting, these transportation costs are difficult to model because granular cost data is not available on a national level. Donor transportation costs are included in the organ acquisition fees that ultimately are passed on to the liver transplant recipient. Increased sharing undoubtedly will increase donor transportation costs, raising organ acquisition fees, and the cost of liver transplantation. Interestingly, to our knowledge, there is no discussion among private insurance carriers or the Federal Government to increase reimbursement for liver transplantation in concert with changes in the liver allocation system.
The purpose of this study is to leverage data from a high volume liver transplant center that captures detailed variable direct transportation costs as well as recipient outcomes. The goals were to (1) measure liver donor transportation costs as a function of distance traveled, (2) measure liver donor CIT as a function of distance traveled, (3) measure the correlation between donor organ transport distance and recipient hospital length of stay, and (4) measure the relationship between donor organ transport distance and posttransplant survival.
Methods
We carried out a retrospective cohort study examining donor CIT, transportation costs and recipient outcomes related to deceased liver donor procurement practices over a 5-year study period (fiscal years 2008–2013). The University of Alabama at Birmingham (UAB) Institutional Review Board reviewed and approved the study.
Study population
UAB Hospital is an academic medical center located in Birmingham, Alabama. UAB is the 18th largest hospital in the United States, with 1136 inpatient beds (5). UAB transplant center serves the state of Alabama consisting of 4.8 million person population (70% Caucasian, 27% African American, and 19% of population below federal poverty level) (6). The transplant center has been in operation since 1983 and currently includes four liver transplant surgeons that perform approximately 100 transplants per year. UAB is the only liver transplant center in the Alabama Organ Center Donor Service Area. Alabama Organ Center resides in Region 3, which includes Arkansas, Louisiana, Mississippi, Alabama, Georgia, Florida, and Puerto Rico (7). All donor livers assessed that generated transportation costs were included for analysis. There were no liver transplants performed from donation after cardiac death donors during this study period. Liver transplant recipient outcomes include those from a primary or re-transplant, and a single-organ or multi-organ transplant.
Variables of interest
The local procurement team utilizes ground transportation for up to 2.5 h one-way trip for nonthoracic organ procurement. For liver procurement that includes the co-procurement of thoracic organs, the procurement team utilized ground transportation up to 1 h one-way trip, and otherwise utilized a charter flight. All regional donor livers were transported via charter flight. Many regional flights are within 3 h length. One common exception is liver donors from Puerto Rico or the Virgin Islands, which is a 4.5 h one-way flight from Birmingham (defined as group 4 above).
Four mutually exclusive transplant patient groups receiving livers from deceased donors were defined based on donor location and local procurement team practices: (1) Local-Driving, that is ground transportation no greater than 2.5 h; (2) Local-Flight, that is within state charter flight; (3) Regional Fight <3 h, that is all flights outside of Alabama with one-way flight time less than 3 h; and (4) Regional Flight >3 h, that is all flights outside of Alabama with one-way flight time greater than 3 h.
Primary outcomes of interest included: (1) donor organ transportation distance, (2) CIT, (3) variable direct donor transportation costs, and (4) posttransplant recipient survival. Transportation distance from donor hospital to the transplant center was estimated using a cross-referencing program used to impute addresses into Google Directions API (8), which calculated the driving travel distance in miles. The Scientific Registry of Transplant Recipients provided CIT and survival data. Any donor liver for which transportation costs were generated was considered for analysis as previously described (9). These include costs associated with some donor livers not transplanted such as donor livers procured and discarded, donor livers assessed and turned down in the procurement operating room, and donor livers evaluated and turned down (costs associated with donor blood transport to the reference laboratory for evaluation). Multi-organ transplants (n = 12) were not included in the cost analysis. Direct variable transportation costs, that is no overhead costs, were calculated for both on the ground and in flight modalities. Flight costs were verified from the vendor billing records used to coordinate all procurement flights. All cost data were standardized to 2013 dollars using an inflation factor from the consumer price index (10).
Secondary outcomes included liver transplant basic demographics and recipient outcomes, including basic demographics, that is patient age, gender, race, BMI, and patient disease characteristics including Model for End-Stage Liver Disease (MELD) score, and known hepatocellular carcinoma (HCC) status prior to transplantation.
Statistical analysis
Exploratory data analyses included examination of measures of central tendency (sample mean and median) as well as measures of dispersion (variance, standard deviations). Most data were not normally distributed, thus sample medians and interquartile ranges (IQRs) were reported throughout. A modified DRI score that excludes CIT and donor location (local/regional/national) was generated to solely reflect donor organ quality. Group comparisons of average liver donor transportation costs were compared between groups using analysis of variance as well as the nonparametric Kruskal–Wallis test. The relationships between continuous variables CIT, cost, and distance traveled were examined using Spearman’s correlation and simple linear regression using regression splines in the case of nonlinearity. Patient survival was estimated using Kaplan–Meier survival estimates and compared using log-rank and Cox proportional hazards models. Models were adjusted for DRI (3), MELD score at time of transplant, recipient BMI, race, gender, and HCC status. Proportionality of covariates was tested using Schoenfeld residuals, and variables found to violate the assumption of proportionality were included in the model as time-dependent covariates. All analyses were conducted using SAS 9.3 (SAS, Cary, NC), and statistical significance was defined as a p-value ≤ 0.05.
Supplemental analysis
A supplemental analysis was carried out projecting the potential impact changes in liver allocation may have on transportation costs due to accompanying changes in the distribution of local and district organs. Donor liver transportation cost estimates derived from the present study were used to model potential scenarios using both simple probability and liver simulation allocation model (LSAM) (11) predictions. The rationale for simple probability is based upon the principle that all liver transplant candidates within newly defined districts will have equal access to donor organs. In this case, the projection is that 10% of our center’s transplants will come from local donors and 90% from district donors. This probability is based on historic trends showing that the Alabama Organ Center annually contributes approximately 100 donor livers and the aggregate liver donor volumes from the proposed district that contains Alabama is in excess of 1000 (map of 8 total districts with 3 h transportation distance favored at a recent United Network for Organ Sharing [UNOS] meeting (11)). Thus, 100 liver donors from Alabama among a total of 1000 liver donors with the newly formed district results in an estimate of ~10%. In addition, a variety of other potential changes to the distribution of local and district donors were estimated.
Results
Recipient demographics
Outcomes among 481 adult liver transplant recipients where analyzed. Table 1 illustrates recipient outcomes stratified by donor organ group. Seventy-six percent (367/ 481) of recipients received livers from local donors, and 24% (114/481) from regional donors. There were no recipient differences in age, gender, race or diagnosis of HCC between donor organ groups. Transplant recipient BMI was statistically different between donor organ groups, but the magnitude was not clinically relevant. The MELD scores were 2–4 points higher in recipients of regional donors compared to recipients of local donors (p = 0.0001). The DRI and calculated modified DRI were similar between local donors and regional donors with flight times <3 h, but significantly increased in the regional donors with flight times >3 h (DRI: 1.5 vs. 2.2, p < 0.0001; modified DRI 1.4 vs. 1.8, p < 0.0001).
Table 1.
Adult liver transplant recipients from 2008 to 2012 baseline characteristics
| Local-drive | Local-flight | Regional <3 h | Regional >3 h | Significance (p-value) | |
|---|---|---|---|---|---|
| Population | 262 (54%) | 105 (22%) | 61 (13%) | 53 (11%) | na |
| Age1 | 57 (51–61) | 57 (51–62) | 58 (50–63) | 56 (49–60) | 0.67 |
| Male | 172 (66%) | 66 (63%) | 35 (57%) | 29 (55%) | 0.37 |
| Race | 0.64 | ||||
| White | 219 (84%) | 89 (85%) | 53 (87%) | 43 (81%) | |
| Black | 32 (12%) | 12 (11%) | 8 (13%) | 9(17%) | |
| HCC | 79 (30%) | 23 (22%) | 12 (20%) | 11 (21%) | 0.15 |
| BMI1 | 28 (25–33) | 28 (25–32) | 31 (26–36) | 29 (25–34) | 0.01 |
| MELD1 | 22 (22–25) | 22 (21–24) | 26 (22–32) | 24 (22–30) | 0.0001 |
| DRI1 | 1.5 (1.5–1.7) | 1.4 (1.2–1.7) | 1.6 (1.4–2.0) | 2.2 (1.7–2.5) | <0.0001 |
| Modified DRI1,2 | 1.4 (1.2–1.6) | 1.3 (1.2–1.6) | 1.4 (1.2–1.7) | 1.8 (1.4–2.0) | <0.0001 |
| Cost ($)1 | 101 (101–548) | 1993 (1400–2738) | 8324 (4689–10 913) | 27 810 (26 653–27 943) | <0.0001 |
| Distance (miles)1 | 0 (0–58) | 196 (102–257) | 384 (237–637) | 1647 (1647–1647) | <0.0001 |
| CIT (hours)1 | 5.0 (3.5–7.0) | 5.5 (4.0–7.4) | 6.0 (3.5–8.1) | 10.0 (8.8–10.4) | <0.0001 |
CIT, cold ischemia time; DRI, donor risk index; HCC, hepatocellular carcinoma; MELD, Model for End-Stage Liver Disease.
Data presented as median (interquartile range).
Modified DRI excludes the contributions of CIT and donor location (local/regional/national).
Cold ischemia times
The median travel distance increased in each group, varying from zero miles local-drive, 196 miles local-flight, 384 miles regional <3 h flight, to 1647 miles regional >3 h flight (Figure 1). Increasing travel distances did not significantly increase CITs until the flight time was in excess of 3 h (Figure 2). Median flight time among regional donors <3 h was 85 min (IQR 73–111). The median CIT ranged from 5.0 to 6.0 h for all local donors and regional flights within 3 h, but increased to 10 h for the regional >3 h group. A subgroup analysis was performed of the regional donors <3 h flight measuring CIT in donors that were procured by local surgeons (n = 18) and donors that were procured by the recipient surgical team (n = 43). The CIT was significantly longer in donors procured by local surgeons compared to donors procured by the recipient surgical team (8.8 h [IQR 7.7–10.4] vs. 4.1 h [IQR 3.3–6.4], p < 0.0001). Graft survival was not significantly associated with CIT (p = 0.36). There was a weak linear correlation between increasing travel distance and CIT (Rho = 0.47, p < 0.0001).
Figure 1.
Donor liver transportation distance stratified by donor organ group.
Figure 2.
Cold ischemia times stratified by donor organ group.
Transportation costs
Liver procurement transportation costs increased with mode of transportation and distance traveled (Figure 3). The median transportation cost of a local donor within driving distance was only $101 while the median transportation cost of a local donor requiring air travel was $1993. The composite median cost of a local donor (including all local driving and local flying transportation episodes) was $548. Median liver procurement transportation costs increased significantly for regional flight travel, ranging from $8324 for flights less than 3 h to $27 810 for flights longer than 3 h. There was a strong linear correlation between increasing travel distance and liver procurement transportation costs (Rho = 0.97, p < 0.0001).
Figure 3.
Procurement variable direct cost stratified by donor organ group.
Donor liver transportation cost estimates, based upon local modeling, were generated for a range of local/regional distributions (Table 2). The percentage of local donors for UAB transplants has been predicted to decrease from the present rate of 76% to 10% with redistricting. The median distance traveled for a local donor was 58 miles and for a regional donor with <3 h flight time was 384 miles. Thus, the average distance traveled increased from 136 miles/donor (76% local/24% regional) to 351 miles/donor (10% local/90% district). The median transportation variable direct cost of a local donor was $548 and for a regional donor with <3 h flight time was $8324. Thus, the average transportation cost increased from $2415/donor (76% local/ 24% regional) to $7547/donor (10% local/90% regional).
Table 2.
Distance and cost estimates based upon local and district distribution of liver donors
| Distribution | Estimates | ||
|---|---|---|---|
| Local (%) | District (%) | Mean distance per donor (miles) |
Mean cost per donor ($) |
| 76 | 24 | 136 | 2415 |
| 10 | 90 | 351 | 7547 |
| 20 | 80 | 319 | 6769 |
| 30 | 70 | 286 | 5991 |
| 40 | 60 | 254 | 5213 |
| 50 | 50 | 221 | 4436 |
| 60 | 40 | 188 | 3659 |
| 70 | 30 | 156 | 2881 |
The current distribution of donors for Alabama is 76% local/24% regional, resulting in a mean distance traveled of 136 miles and mean cost of $2415 per liver donor. With proposed allocation redistricting, the percentage of local donors is expected to significantly decline. Estimates for the mean distance and cost per donor are provided for a range of local/district distributions. Shaded area represents current distribution of local and regional donors.
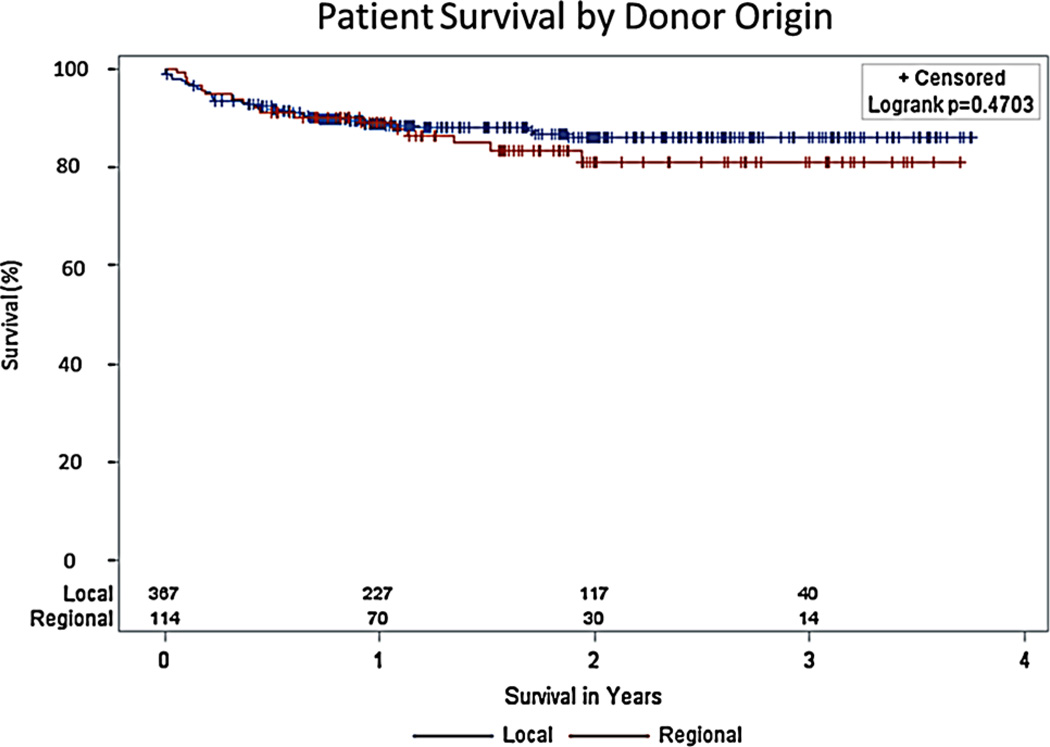
Recipient outcomes
There were no differences in overall transplant recipient survival between local and regional donors from the time of transplantation (Figure 4, p = 0.47). The survival curves cross several times in the first 12 months then separate. Modeled from 12 months posttransplant, unadjusted patient survival in local donors was superior to regional donors (p = 0.05). In an adjusted model, survival did not differ significantly by donor origin (p = 0.93).
Figure 4.
Kaplan–Meier survival estimates in liver transplant recipients of local versus regional donors.
Overall survival was not statistically different (p = 0.47). However, modeled from 12 months posttransplant, unadjusted patient survival in local donors was superior to regional donors (p = 0.05). In an adjusted model, survival did not differ significantly by donor origin (p = 0.93).
Discussion
Our data demonstrates that CITs are relatively unaffected by donor location until the transportation exceeds 3 h flight time. Regional donors with a flight time >3 h originated from Puerto Rico or the Virgin Islands, which has a flight time of 4.5 h and median CIT of 10 h. Our data suggest that 5.5 h of CIT were accrued at the donor hospital, ground transportation, and the recipient hospital (in addition to the 4.5 h of flight CIT) for donor livers with >3 h of flight transport. We believe the primary reason for the long 10 h CIT for regional donors with flights >3 h is because local donor surgeons performed the recoveries and UAB recipient surgeons were unwilling to start the transplant until the graft was transported and available for inspection. However, concerns remain for long-distance procurements, including (1) greater expense for a two-way compared to a one-way flight (as much as $44 800 was paid for a two-way charter flight for 4.5 h each way), (2) pilots“time-out” after 12 h of work (12) and a separate set of pilots may be required for the return flight, and (3) head winds commonly require refueling which adds 1–2 h to the flight times.
These concerns were pertinent to long-distance procurements and not observed in regional <3 h flights, where donor organ procurement by the recipient surgical team was preferred. Having the recipient surgical team perform the procurement lowered the CIT by 4.7 h in regional donors with a flight time <3 h. Our clinical approach with a regional donor procured by (our) recipient team is to have the patient in the room about 2 h prior and start the transplant about 1 h prior to the anticipated arrival with the donor liver (assuming the visual inspection is acceptable). We do not use this approach when a local surgeon procures the liver because we previously have been left in a difficult position starting a liver transplant and delivered an unusable organ. When a local surgeon procures the liver, our approach is to examine the liver, performing much of the back table operation, prior to bringing the patient into the room. The timing of transplant start likely accounts for around 3 h of additional CIT. The remaining 1.7 h of CIT, in our experience, is mainly due to transportation delays and from poor communications. Organ transport from the procurement hospital to the airport occurs much faster when the recipient team performs the recovery. To avoid these delays, it has been proposed to have the recipient team procure donor livers. However, all procurement transportation raises safety concerns given documented procurement team deaths during flight transport (13).
Liver transportation costs increased in a stepwise fashion with distance from transplant center and mode of transport. Not surprisingly, flights were substantially more expensive than ground transportation. Redistricting proposals would increase overall flight transport of donor liver allographs, although it is unclear how the distribution of local versus district donors would change. There was enthusiasm for the 8 district 3 h average transport time model at the November 2013 Liver and Intestine committee meeting (11). The LSAM predicted 40% local and 58% district for the 8 district model (11). However, the LSAM model may have overestimated the percentage of local donors. By definition, all recipients in a district would have equal access to donors and no preference is given to the local center for a local donor. Thus, it may be argued that simple probability would be a better predictor of the local/district distribution. For example, the most recent 8 district 3 h transport time model had Alabama in a district with Florida, Mississippi, Louisiana, and Texas. Collectively, OPOs in these states generated 1038 liver donors in 2012 of which 100 were from Alabama (14). The likelihood of a local Alabama donor liver staying in Alabama was 100/1038 or ~10%. Without local preference, it is a statistical improbability that 40% of Alabama donors would stay locally.
Using simple probability modeling with the 8 district 3 h transport proposal, the percentage of local liver donors decreased from the present rate of 76% to ~10%. The average liver donor distance traveled increased from 136 miles to 351 miles, and the median donor variable direct costs increased from $2415 to $7547, or a 313% increase. UAB performs approximately 100 transplants per year, thus the increased donor liver procurement transportation costs would be an annual increase of $513 000. It is important to note that this value is only direct variable cost, and the actual billed charges once indirect expenses are included would be substantially higher. The average liver organ acquisition fee for the Alabama Organ Center in fiscal year 2013 was $32 200, for which transportation costs account for 8%. Increased donor organ transportation costs with redistricting would account for 24% of the total organ acquisition fee (if not increased). Proposed redistricting models predicted that nationally 62 lives would be saved annually (11) out of ~6500 annual liver transplants performed (14). Based upon this financial modeling, the additional donor liver procurement transportation variable direct cost per life saved is $538 000. Based upon theLSAM predictions of local/district donors, the additional transportation variable direct cost per life saved is $293 000.
This study has several limitations. This is a single center/single OPO study limited by sample size out of necessity because most of the data analyzed is not available via large registry databases. The regional flight >3 h was a unique group because the donor organs had a higher DRI (and modified DRI scores) than in the other organ donor groups, and the organ procurement and transport were complicated by several factors that exacerbated the logistics and finances of these donors. The modeling is based upon a single geographic version of the 8 district 3 h transport limit proposal, a model bound to change substantially with further data and input from the transplant community. The trends found in this analysis, however, are generalizable since all centers will see a significant increase in regional sharing of livers. In fact, the transportation costs reported in this study may underestimate increases seen in centers near the coast, northeast or in larger cities where charter flights are more expensive. Furthermore, some centers with the largest disparity (greatest donor need), have the geographically largest proposed districts (such as California), thus longer flights will be the most likely scenario further increasing transportation costs. A 4 district plan is also being considered (Liver and Intestine Committee, April 1, 2014 meeting O’Hare Chicago, IL—personal communication) for which the donor transportation costs reported in this report would significantly underestimate the costs from substantially larger districts in the 4 district plan compared to the 8 district plan model.
In conclusion, this study measured liver donor procurement CITs and transportation variable direct costs. CITs are not significantly different between local donors and regional donors with <3 h flight transportation. The median transportation costs increased with greater distance traveled. Financial modeling suggests that donor transportation costs would significantly increase with proposed redistricting models, which likely would manifest in increased liver organ acquisition fees. These findings suggest that further discussion among transplant centers, OPOs, and insurance providers is needed prior to policy implementation.
Acknowledgments
Special thanks to Walt Montgomery and Melissa Wallace from the Alabama Organ Center for donor data retrieval, and to Chris Matkin from Platinum Air Services, LLC for flight data retrieval. This research was funded by National Institutes of Health grant number 1 K23 DK091514-01A1 (DAD). The University of Alabama at Birmingham Comprehensive Transplant Institute Outcomes Research Center provided methodological and statistical support.
Abbreviations
- ANOVA
analysis of variance
- BMI
body mass index
- DRI
donor risk index
- HCC
hepatocellular carcinoma
- LSAM
liver simulation allocation model
- MELD
Model for End-Stage Liver Disease
- OPO
organ procurement organization
- UAB
University of Alabama Birmingham
- UNOS
United Network for Organ Sharing
Footnotes
Portions of this data were presented at the Emory/UAB Symposium for Southeast Transplant Centers; Atlanta, GA; March 2014.
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
References
- 1.Gentry SE, Massie AB, Cheek SW, et al. Addressing geographic disparities in liver transplantation through redistricting. Am J Transplant. 2013;13:2052–2058. doi: 10.1111/ajt.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymous. Proposal to create regional distribution of livers for MELD/PELD candidates. [Accessed March 24, 2014];2014 Available at: http://optn.transplant.hrsa.gov/PublicComment/pubcommentPropSub_239.pdf.
- 3.Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: The concept of a donor risk index. Am J Transplant. 2006;6:783–790. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 4.Axelrod DA, Schnitzler M, Salvalaggio PR, Swindle J, Abecassis MM. The economic impact of the utilization of liver allografts with high donor risk index. Am J Transplant. 2007;7:990–997. doi: 10.1111/j.1600-6143.2006.01724.x. [DOI] [PubMed] [Google Scholar]
- 5.Oh J. Becker’s hospital review: 50 largest hospitals in America. [Accessed April 2014];2010 Available at: http://www.beckershospitalreview.com/lists/50-largest-hospitals-in-america.html. [Google Scholar]
- 6.Bishaw A. Poverty 2000–2012: American community survey briefs. [Accessed May 22, 2014];2013 Available at: http://www.census.gov/prod/2013pubs/acsbr12-01.pdf.
- 7.Anonymous. OPTN US geographic regions. [Accessed March 24, 2014];2014 Available at: http://optn.transplant.hrsa.gov/members/regions.asp.
- 8.Anonymous. Google maps API web services. [Accessed February 3, 2014];2014 Available at: https://developers.google.com/maps/documentation/webservices/. [Google Scholar]
- 9.Dubay DA, Redden DT, Bryant MK, et al. Resource utilization associated with procurement of transplantable organs from donors that do not meet OPTN eligible death criteria. Transplantation. 2014;97:1043–1048. doi: 10.1097/01.TP.0000441093.32217.cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anonymous. U.S. Bureau of Labor Statistics, Division of Consumer Prices and Price Indexes. [Accessed February 19, 2014];2014 Available at: http://www.bls.gov/cpi/tables.htm.
- 11.Anonymous. OPTN/UNOS Liver and Intestinal Organ Transplantation Committee Report to the Board of Directors November 11–12, 2013, Atlanta, GA. [Accessed March 24, 2014];2013 Available at: http://optn.transplant.hrsa.gov/CommitteeReports/board_main_Liver&IntestinalOrgan-TransplantationCommittee_11_13_2013_16_49.pdf.
- 12.Anonymous. Final Rule, Flightcrew Member Duty and Rest Requirements–Department of Transportation Federal Aviation Administration. [Accessed January 15, 2014];2011 Available at: http://www.faa.gov/regulations_policies/rulemaking/recently_published/media/2120-AJ58-FinalRule.pdf.
- 13.Englesbe MJ, Merion RM. The riskiest job in medicine: Transplant surgeons and organ procurement travel. Am J Transplant. 2009;9:2406–2415. doi: 10.1111/j.1600-6143.2009.02774.x. [DOI] [PubMed] [Google Scholar]
- 14.Anonymous. Organ Procurement and Transplantation Network. [Accessed April 7, 2014];2014 Available at: http://optn.transplant.hrsa.gov/latestData/rptData.asp.