Abstract
Objective
Clinicians, advocates, and policy makers have presented mental illnesses as medical diseases in efforts to overcome low service use, poor adherence rates, and stigma. The authors examined the impact of this approach with a 10-year comparison of public endorsement of treatment and prejudice.
Method
The authors analyzed responses to vignettes in the mental health modules of the 1996 and 2006 General Social Survey describing individuals meeting DSM-IV criteria for schizophrenia, major depression, and alcohol dependence to explore whether more of the public 1) embraces neurobiological understandings of mental illness; 2) endorses treatment from providers, including psychiatrists; and 3) reports community acceptance or rejection of people with these disorders. Multivariate analyses examined whether acceptance of neurobiological causes increased treatment support and lessened stigma.
Results
In 2006, 67% of the public attributed major depression to neurobiological causes, compared with 54% in 1996. High proportions of respondents endorsed treatment, with general increases in the proportion endorsing treatment from doctors and specific increases in the proportions endorsing psychiatrists for treatment of alcohol dependence (from 61% in 1996 to 79% in 2006) and major depression (from 75% in 1996 to 85% in 2006). Social distance and perceived danger associated with people with these disorders did not decrease significantly. Holding a neurobiological conception of these disorders increased the likelihood of support for treatment but was generally unrelated to stigma. Where associated, the effect was to increase, not decrease, community rejection.
Conclusions
More of the public embraces a neurobiological understanding of mental illness. This view translates into support for services but not into a decrease in stigma. Reconfiguring stigma reduction strategies may require providers and advocates to shift to an emphasis on competence and inclusion.
The past 20 years have witnessed a resurgence in clinical, policy, and research efforts to reduce stigma attached to mental illness. The White House Conference on Mental Illness and the Surgeon General’s first-ever report on mental health (1), both in 1999, coalesced knowledge and fostered renewed action. These comprehensive assessments applauded the range and efficacy of existing treatments for mental illness brought by advances across the medical and social-behavioral sciences, particularly neuroscience. However, they also documented a “staggeringly low” rate of service use among those in need, a shortage of providers and resources, and continued alarming levels of prejudice and discrimination (1, p. viii; 2).
After reviewing the scientific evidence, the Surgeon General concluded that the stigma attached to mental illness constituted the “primary barrier” to treatment and recovery (1, p. viii). Stigma could be reduced, many believed, if people could be convinced that mental illnesses were “real” brain disorders and not volitional behaviors for which people should be blamed and punished. Many prominent reports emphasized scientific understanding as a way to reduce stigma. For example, the Surgeon General’s report identified scientific research as “a potent weapon against stigma, one that forces skeptics to let go of misconceptions and stereotypes” (1, p. 454). Stigma reduction, based in part on disseminating information on neurobiological causes, became a primary policy recommendation of the President’s New Freedom Commission on Mental Health (3) as well as of international efforts (4). Finally, while not intended specifically as an antistigma effort, commercial advertisements provided information on psychiatric symptoms, brain-based etiologies, and specific psychopharmacological solutions. In fact, direct-to-consumer advertising involved more U.S. resources than all those dedicated to educational campaigns (e.g., over $92 million on Paxil in 2000 [5]).
Deeply embedded in social and cultural norms, stigma includes prejudicial attitudes that discredit individuals, marking them as tainted and devalued (6). For individuals, stigma produces discrimination in employment, housing, medical care, and social relationships (7–9). Individuals with mental illness may be subjected to prejudice and discrimination from others (i.e., received stigma), and they may internalize feelings of devaluation (i.e., self-stigma [10]). On a societal level, stigma has been implicated in low service use, inadequate funding for mental health research and treatment (i.e., institutional stigma), and the “courtesy” stigma attached to families, providers, and mental health treatment systems and research (11–13). Public stigma reflects a larger social and cultural context of negative community-based attitudes, beliefs, and predispositions that shape informal, professional, and institutional responses.
Antistigma efforts in recent years have often been predicated on the assumption that neuroscience offers the most effective tool to reduce prejudice and discrimination. Thus, NAMI’s Campaign to End Discrimination sought to improve public understanding of neurobiological bases of mental illness, facilitating treatment-seeking and lessening stigma. Over the past decade, the American public has been exposed to symptoms, biochemical etiological theories, and the basic argument that mental illnesses are diseases, no different from others amenable to effective medical treatment, control, and recovery (14, 15).
Given projections of the place of mental illness in the global burden of disease in the coming years (for example, depression alone is expected to rank third by 2020 [16]), the unprecedented amount of resources being directed to science-based antistigma campaigns, and the frustration of clinicians, policy makers, and consumers in closing the need-treatment gap, it is crucial that the efficacy and implications of current efforts be evaluated. However, despite reported successes in launching campaigns and disseminating information, few studies have undertaken systematic evaluation of stigma reduction efforts (see references 17 and 18 for exceptions). The critical unanswered question is whether these efforts have changed public understanding and acceptance of persons with mental illness.
In this study, we assessed whether the cumulative impact of efforts over the past decade have produced change in expected directions. Using the mental health modules of nationally representative surveys 10 years apart, we examined whether the public changed during that interval in its embrace of neurobiological understandings of mental illness; its treatment endorsements for a variety of providers, including psychiatrists and general medical doctors; and its reports of community acceptance or rejection of persons described as meeting DSM-IV criteria for schizophrenia, major depression, or alcohol dependence.
Method
Sample
The 2006 National Stigma Study–Replication reproduces the 1996 MacArthur Mental Health Study; both data collections were fielded as modules in the General Social Survey (GSS). The GSS is a biennial stratified multistage area probability sample survey of household clusters in the United States representing noninstitutionalized adults (age 18 and over). Face-to-face interviews were conducted by trained interviewers using pencil and paper in the 1996 survey and a computer-assisted format in the 2006 survey. Mode effects were minimal and were unrelated to the data used here (19). GSS response rates were 76.1% in 1996 and 71.2% in 2006.
The 1996 and 2006 GSS modules utilized a vignette strategy to collect data on public knowledge of and response to mental illness. This strategy helps circumvent social desirability bias and allows assessment of public recognition by providing a case description meeting psychiatric diagnostic criteria but no diagnostic label. Respondents were randomly assigned to a single vignette describing a psychiatric disorder meeting DSM-IV criteria for schizophrenia (N=650), major depression (N=676), or alcohol dependence (N=630). The gender, race (white, black, Hispanic), and education (<high school, high school, >high school) of vignette characters were randomly varied.
Because of the adoption in 2004 of a subsampling design to capture nonrespondents, weighting that adjusts for the selection of one adult per household is required for cross-year comparisons (sampling error=±3%). All analyses were conducted in Stata, release 11 (20). Institutional review board approval for the GSS was obtained at the University of Chicago, as well as at Indiana University for secondary data analysis.
Measures
Respondents were read the randomly selected vignette, given a card with the vignette printed on it, and asked questions in three broad areas.
Attributions/causation
Respondents were asked how likely it is that the person in the vignette is experiencing “a mental illness” and/or “the normal ups and downs of life,” as well as how likely the situation might be caused by “a genetic or inherited problem,” “a chemical imbalance in the brain,” “his or her own bad character,” and/or “the way he or she was raised.” Questions were not mutually exclusive, and respondents could endorse multiple attributions. Responses of “very likely” and “somewhat likely” were coded 1; “not very likely,” “not at all likely,” and “do not know” were coded 0. Analyses were run again with responses of “do not know” coded as missing as well as including controls for the vignette character’s race, gender, and education, and substantively similar results were obtained (data available on request from the first author). A neurobiological summary measure was coded 1 if the respondent labeled the problem as mental illness and attributed cause to either a chemical imbalance or a genetic problem; it was coded 0 otherwise.
Treatment endorsement
Respondents were asked whether the person in the vignette should seek consultation with or treatment by “a general medical doctor,” “a psychiatrist,” “a mental hospital,” and/or “prescription medications.” Responses were coded 1 if “yes” and 0 if “no” or “do not know.”
Public stigma
Two sets of measures, for social distance and for perceptions of dangerousness, were used. The first asked respondents how willing they would be to have the person described in the vignette 1) work closely with them on a job; 2) live next door; 3) spend an evening socializing; 4) marry into the family; and 5) as a friend. Responses of “definitely unwilling” and “probably unwilling” were coded 1 (i.e., stigmatizing) and responses of “probably willing,” “definitely willing,” and “do not know” were coded 0. The second measure asked respondents how likely is it that the person in the vignette would “do something violent toward other people” and/or “do something violent toward him/herself.” Responses of “very likely” and “somewhat likely” were coded 1; responses of “not very likely,” “not at all likely,” and “do not know” were coded 0.
Covariates
Respondents’ age (in years), sex (coded 1 for female, 0 for male), education (coded 1 for at least a high school degree, and 0 otherwise), and race (code 1 for white, 0 for other) were included as controls. In 1996, the mean age of respondents was 43 years (SD=16); 51% were female, 31% completed more than a high school degree, and 81% were white. In 2006, the mean age was 45 years (SD=17); 54% were female, 39% completed more than a high school degree, and 75% were white. Profiles are consistent with Census Bureau data. Differences between samples reflect changes in the U.S. population (e.g., significant but small changes in education and race).
Statistical Analysis
We evaluated changes across years in public attributions, endorsement of treatment, and public stigma by comparing unadjusted percentages using a design-based F value, which corrects for survey design with the second-order correction of Rao and Scott (21) and converts the Pearson chi-square statistic into an F statistic (20). To adjust the year effect for demographic shifts across samples, logistic regression models were estimated with controls for respondents’ age, sex, education, and race. While these models control for shifts in demographic composition between the two surveys, traditional tests of the equality of coefficients across groups (in this case, survey year) cannot be used because the estimated logit coefficients confound the magnitude of the effect of a predictor with the degree of unobserved heterogeneity in the model (22). Predicted probabilities are not affected by this problem (J.S. Long, unpublished manuscript, 2009). Accordingly, to illustrate the magnitude of changes over time, we computed the difference in the predicted probabilities for a given outcome (e.g., neuroscience attribution) between 1996 and 2006, calculated with controls held at their means for the combined sample; these are referred to as discrete change coefficients. While these coefficients are not affected by the identification issue that makes it inappropriate to compare regression coefficients between times, the magnitude of the discrete change depends on the level at which the control variables are held. To control for differences in demographic variables between the two survey years, we computed discrete change at the overall mean combining both years. The delta method was used to compute confidence intervals for the changes in probabilities. To be consistent in comparing adjusted and unadjusted predictions, probabilities and discrete changes were multiplied by 100 (e.g., 0.43 becomes 43%).
Results
Attribution/Causation
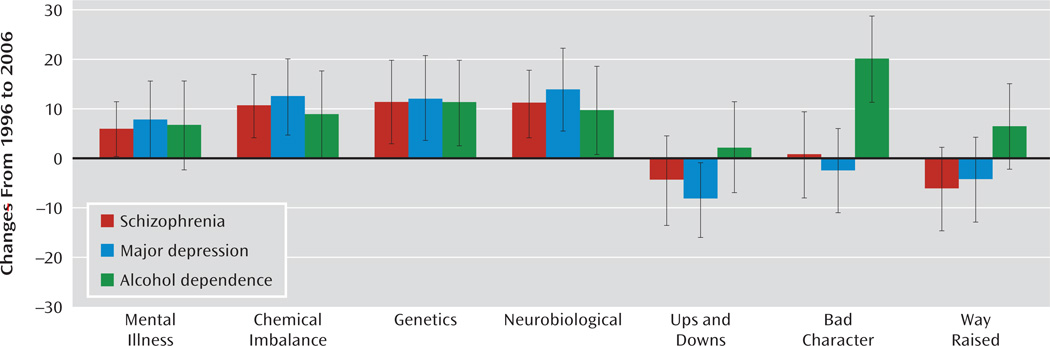
More of the public embraced a neurobiological understanding of mental illness in 2006 than in 1996 (Table 1). A large and statistically significant increase (6 to 13 percentage points) was evident across nearly all indicators and all vignette conditions. The neurobiological summary showed an increase of 10 percentage points for schizophrenia (from 76% to 86%; F=8.00, p=0.01), 13 points for depression (from 54% to 67%; F=9.94, p=0.002) and nine points for alcohol dependence (from 38% to 47%; F=4.06, p=0.04). Social or moral conceptions of mental illness decreased across most indicators, and a significant decrease in labeling the condition as “ups and downs” was observed for depression (from 78% to 67%; F=7.63, p=0.01). However, sociomoral conceptions of alcohol dependence were either largely unchanged or, for attributions of “bad character,” significantly increased (from 49% to 65%; F=13.50, p<0.001). Findings were largely unaffected by the addition of controls for respondents’ age, sex, education, and race (Figure 1). A slight attenuation of the year effect for chemical imbalance for alcohol dependence reduced the effect to nonsignificance. Further analyses (not reported) suggested that this was not due to the addition of any one covariate but to the addition of all covariates simultaneously.
TABLE 1.
Unadjusted Survey Year Differences in Attributions of Mental Illness, Treatment Endorsement, and Stigma, by Vignette Condition, 1996 and 2006a
| Schizophreniab | Major Depressionc | Alcohol Dependenced | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | 1996 (%) | 2006 (%) | Differencee | Ff | p | 1996 (%) | 2006 (%) | Differencee | Ff | p | 1996 (%) | 2006 (%) | Differencee | Ff | p |
| Neurobiological attributions | |||||||||||||||
| Mental illness | 85 | 91 | 6 | 4.42 | 0.04 | 65 | 72 | 8 | 3.68 | 0.06 | 44 | 50 | 6 | 1.82 | 0.18 |
| Chemical imbalance | 78 | 87 | 9 | 6.77 | 0.01 | 67 | 80 | 13 | 11.23 | 0.001 | 59 | 68 | 9 | 3.91 | 0.05 |
| Genetic problem | 61 | 71 | 11 | 6.12 | 0.01 | 51 | 64 | 12 | 8.38 | 0.004 | 58 | 68 | 10 | 5.14 | 0.02 |
| Neurobiological summaryg | 76 | 86 | 10 | 8.00 | 0.01 | 54 | 67 | 13 | 9.94 | 0.002 | 38 | 47 | 9 | 4.06 | 0.04 |
| Sociomoral attributions | |||||||||||||||
| Ups and downs | 40 | 37 | –3 | 0.48 | 0.49 | 78 | 67 | –11 | 7.63 | 0.01 | 60 | 61 | 1 | 0.09 | 0.76 |
| Bad character | 31 | 31 | 0 | 0.01 | 0.91 | 38 | 32 | –6 | 1.83 | 0.18 | 49 | 65 | 16 | 13.50 | <0.001 |
| Way raised | 40 | 33 | –7 | 2.75 | 0.10 | 45 | 41 | –5 | 1.14 | 0.29 | 64 | 69 | 5 | 1.56 | 0.21 |
| Treatment endorsement | |||||||||||||||
| Physician | 72 | 87 | 15 | 14.86 | <0.001 | 78 | 91 | 13 | 20.25 | <0.001 | 74 | 89 | 15 | 19.55 | <0.001 |
| Psychiatrist | 90 | 92 | 2 | 0.50 | 0.48 | 75 | 85 | 10 | 9.27 | 0.002 | 61 | 79 | 18 | 17.78 | <0.001 |
| Mental hospital | 53 | 66 | 13 | 8.97 | 0.003 | 25 | 27 | 2 | 0.31 | 0.58 | 25 | 26 | 1 | 0.10 | 0.75 |
| Prescription medicine | 76 | 86 | 11 | 7.59 | 0.01 | 71 | 79 | 9 | 5.14 | 0.02 | 40 | 53 | 13 | 7.78 | 0.01 |
| Stigma | |||||||||||||||
| Social distance: unwilling to | |||||||||||||||
| Work closely with | 56 | 62 | 6 | 1.97 | 0.16 | 46 | 47 | 0 | 0.01 | 0.95 | 72 | 74 | 2 | 0.15 | 0.69 |
| Have as a neighbor | 34 | 45 | 11 | 6.31 | 0.01 | 23 | 20 | –4 | 1.00 | 0.32 | 44 | 39 | –5 | 1.30 | 0.25 |
| Socialize with | 46 | 52 | 6 | 1.74 | 0.19 | 35 | 30 | –5 | 1.35 | 0.25 | 56 | 54 | –1 | 0.05 | 0.82 |
| Make friends with | 30 | 35 | 5 | 1.27 | 0.26 | 23 | 21 | –2 | 0.36 | 0.55 | 35 | 36 | 2 | 0.13 | 0.72 |
| Have marry into family | 65 | 69 | 4 | 0.88 | 0.35 | 57 | 53 | –5 | 1.19 | 0.28 | 70 | 79 | 8 | 4.01 | 0.05 |
| Dangerousness | |||||||||||||||
| Violent toward self | 81 | 84 | 4 | 1.14 | 0.29 | 73 | 70 | –4 | 0.82 | 0.37 | 78 | 79 | 1 | 0.16 | 0.69 |
| Violent toward others | 54 | 60 | 6 | 1.74 | 0.19 | 33 | 32 | –2 | 0.17 | 0.68 | 65 | 67 | 1 | 0.11 | 0.74 |
Data are from the 1996 and 2006 mental health modules of the General Social Survey and are weighted.
Sample size ranges from 633 to 639 because of missing data.
Sample size ranges from 666 to 671 because of missing data.
Sample size ranges from 617 to 623 because of missing data.
Because of rounding, the year difference does not always equal the 2006 percentage minus the 1996 percentage.
A design-based F test for weighted data tests the equality of the 1996 and 2006 percentages.
Coded 1 if the respondent labeled the problem as mental illness and attributed cause to a chemical imbalance or a genetic problem, coded 0 otherwise.
Figure 1.
Adjusted Survey Year Differences in Attributions of Mental Illness, by Vignette Condition, 1996 and 2006a
aGraphs indicate the discrete change coefficient in the predicted probability for a given outcome with respect to year (multiplied by 100) adjusted for respondents’ age, sex, education, and race. Predicted probabilities calculated with controls held at their means for the combined sample. Data are from the mental health modules of the 1996 and 2006 General Social Surveys and are weighted. Tic marks indicate 95% confidence intervals.
Treatment Endorsement
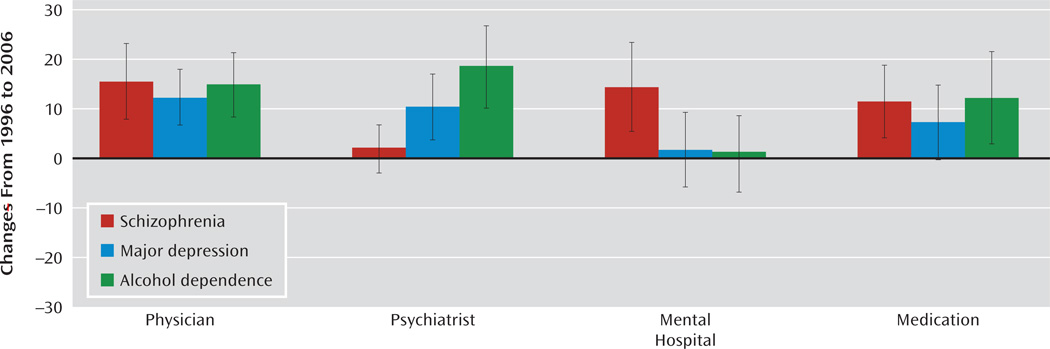
An across-the-board increase in public endorsement of medical treatment was reported (Table 1). In 2006, a large majority supported both general and specialty care for individuals with mental illness. Over 85% indicated that the major depression vignette character should go to a psychiatrist (from 75% in 1996; F=9.27, p=0.002), and 79% recommended psychiatric treatment for alcohol dependence (from 61% in 1996; F=17.78, p<0.001). A significant increase in endorsement of prescription medicine was reported across all vignette conditions. Only treatment at a mental hospital remained unsupported by a majority of respondents for depression or alcohol dependence (27% and 26%, respectively). However, for schizophrenia, not only was hospitalization endorsed by a majority, but support for hospitalization significantly increased (from 53% to 66%; F=8.97, p=0.003). Findings were largely unaffected by the addition of controls for respondents’ age, sex, education, and race. The slight attenuation of the year effect in the endorsement of prescription medication for depression reduced the effect to nonsignificance (Figure 2).
Figure 2.
Adjusted Survey Year Differences in Treatment Endorsement, by Vignette Condition, 1996 and 2006a
aGraphs indicate the discrete change coefficient in the predicted probability for a given outcome with respect to year (multiplied by 100) adjusted for respondents’ age, sex, education, and race. Predicted probabilities calculated with controls held at their means for the combined sample. Data are from the mental health modules of the 1996 and 2006 General Social Surveys and are weighted. Tic marks indicate 95% confidence intervals.
Public Stigma
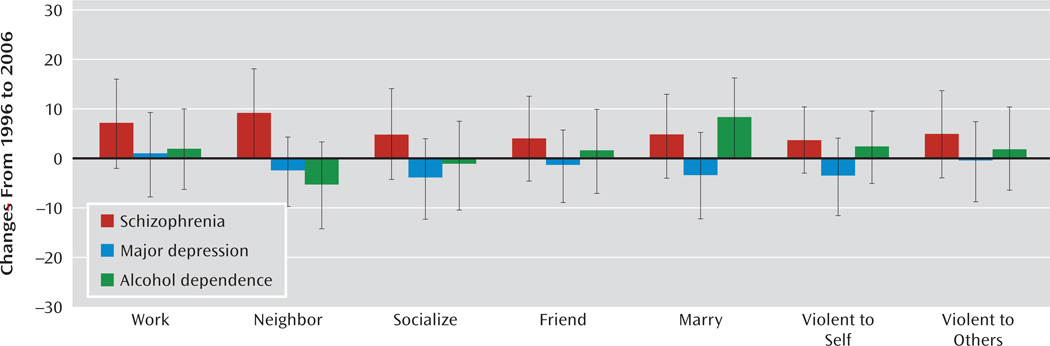
No significant decrease was reported in any indicator of stigma, and levels remained high (Table 1). A majority of the public continued to express an unwillingness to work closely with the person in the vignette (62% for schizophrenia, 74% for alcohol dependence), socialize with the person (52% for schizophrenia, 54% for alcohol dependence), or have the person marry into their family (69% for schizophrenia, 79% for alcohol dependence). In fact, significantly more respondents in the 2006 survey than the 1996 survey reported an unwillingness to have someone with schizophrenia as a neighbor (from 34% to 45%; F=6.31, p=0.01) or to have someone with alcohol dependence marry into their family (from 70% to 79%; F=4.01, p=0.05). Furthermore, a majority again reported that the vignette character with schizophrenia or alcohol dependence would likely be violent toward others. While stigmatizing reactions did not significantly decrease for the depression vignette, levels remained comparatively lower. Findings were unaffected by controls (Figure 3).
Figure 3.
Adjusted Survey Year Differences in Stigma, by Vignette Condition, 1996 and 2006a
aGraphs indicate the discrete change coefficient in the predicted probability for a given outcome with respect to year (multiplied by 100) adjusted for respondents’ age, sex, education, and race. Predicted probabilities are calculated with controls held at their means for the combined sample. Data are from the mental health modules of the 1996 and 2006 General Social Surveys and are weighted. Tic marks indicate 95% confidence intervals.
Association of Neurobiological Attribution With Treatment Endorsement and Stigma
In both survey years and across all conditions, holding a neurobiological conception of mental illness tended to increase the odds of endorsing treatment (e.g., for schizophrenia, from 1996 to 2006, the odds of endorsing a psychiatrist increased by a factor of 7.61; 95% CI=2.43–23.77, p<0.001; see Table 2). However, in both years and across all conditions, holding a neurobiological conception of mental illness either was unrelated to stigma or increased the odds of a stigmatizing reaction. In 2006, holding a neurobiological conception of schizophrenia increased the odds of preferring social distance at work by a factor of 2.20 (95% CI=1.02–4.76, p=0.05), and for depression it increased the odds of perceiving dangerousness to others by a factor of 2.70 (95% CI=1.53=4.78, p<0.001). In no instance was a neurobiological attribution associated with significantly lower odds of stigma. Furthermore, for all but three indicators, the difference in the predicted probability between those who held a neurobiological conception and those who did not was larger in 2006 than 1996. For the depression vignette, a neurobiological attribution increased the predicted probability of perceived dangerousness to self by 20 points in 1996 and by 35 points in 2006, for a difference of 15 points (marginally significant, 95% CI=−1 to 31, p=0.07).
TABLE 2.
Neurobiological Attribution of Mental Illness as Predictor of Treatment Endorsement and Stigma in 1996 and 2006, by Vignette Conditiona
| 1996 | 2006 | Discrete Change With Respect to Neurobiological Attributionc |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Odds Ratiob | 95% CI | p | N | Odds Ratiob | 95% CI | p | N | 1996 | 2006 | Differenced | 95% CI | p |
| Schizophrenia | |||||||||||||
| Treatment endorsement | |||||||||||||
| Physician | 1.12 | 0.58 to 2.17 | 0.73 | 290 | 2.73 | 0.93 to 7.97 | 0.07 | 341 | 2 | 14 | 11 | −11 to 34 | 0.33 |
| Psychiatrist | 2.17 | 1.03 to 4.59 | 0.04 | 291 | 7.61 | 2.43 to 23.77 | <0.001 | 341 | 7 | 22 | 15 | −5 to 35 | 0.13 |
| Mental hospital | 3.01 | 1.57 to 5.78 | 0.001 | 288 | 1.84 | 0.77 to 4.35 | 0.16 | 341 | 27 | 14 | −12 | −38 to 13 | 0.34 |
| Prescription medicine | 5.19 | 2.66 to 10.14 | <0.001 | 289 | 9.61 | 3.65 to 25.30 | <0.001 | 341 | 34 | 37 | 3 | −22 to 27 | 0.84 |
| Stigma | |||||||||||||
| Social distance: unwilling to | |||||||||||||
| Work closely with | 1.73 | 0.95 to 3.15 | 0.07 | 292 | 2.20 | 1.02 to 4.76 | 0.05 | 341 | 14 | 19 | 6 | −18 to 30 | 0.65 |
| Have as a neighbor | 1.71 | 0.87 to 3.36 | 0.12 | 292 | 2.39 | 1.07 to 5.37 | 0.03 | 341 | 12 | 20 | 8 | −13 to 30 | 0.45 |
| Socialize with | 1.23 | 0.67 to 2.26 | 0.50 | 292 | 1.83 | 0.85 to 3.94 | 0.12 | 341 | 5 | 15 | 10 | −14 to 33 | 0.42 |
| Make friends with | 1.31 | 0.68 to 2.52 | 0.43 | 292 | 1.79 | 0.77 to 4.17 | 0.17 | 341 | 6 | 12 | 7 | −14 to 27 | 0.53 |
| Have marry into family | 2.39 | 1.27 to 4.48 | 0.01 | 291 | 2.09 | 0.93 to 4.70 | 0.08 | 340 | 21 | 17 | −4 | −28 to 21 | 0.76 |
| Dangerousness | |||||||||||||
| Violent toward self | 2.51 | 1.23 to 5.14 | 0.01 | 293 | 4.62 | 1.99 to 10.73 | <0.001 | 341 | 16 | 26 | 11 | −12 to 33 | 0.36 |
| Violent toward others | 2.23 | 1.20 to 4.13 | 0.01 | 292 | 2.41 | 1.13 to 5.16 | 0.02 | 341 | 20 | 22 | 2 | −22 to 25 | 0.88 |
| Major depression | |||||||||||||
| Treatment endorsement | |||||||||||||
| Physician | 0.84 | 0.46 to 1.53 | 0.57 | 293 | 2.48 | 1.13 to 5.41 | 0.02 | 374 | –3 | 8 | 11 | −2 to 23 | 0.09 |
| Psychiatrist | 2.17 | 1.21 to 3.89 | 0.01 | 290 | 5.77 | 2.92 to 11.43 | <0.001 | 374 | 14 | 23 | 9 | −6 to 23 | 0.23 |
| Mental hospital | 1.87 | 1.01 to 3.46 | 0.05 | 291 | 3.52 | 1.82 to 6.84 | <0.001 | 374 | 11 | 21 | 10 | −4 to 24 | 0.17 |
| Prescription medicine | 2.08 | 1.20 to 3.61 | 0.01 | 290 | 5.62 | 2.95 to 10.72 | <0.001 | 374 | 15 | 30 | 15 | −1 to 31 | 0.06 |
| Stigma | |||||||||||||
| Social distance: unwilling to | |||||||||||||
| Work closely with | 1.01 | 0.61 to 1.67 | 0.97 | 294 | 1.52 | 0.90 to 2.59 | 0.12 | 374 | 0 | 10 | 10 | −8 to 28 | 0.27 |
| Have as a neighbor | 1.03 | 0.56 to 1.90 | 0.91 | 293 | 1.99 | 0.98 to 4.05 | 0.06 | 374 | 1 | 10 | 9 | −5 to 23 | 0.21 |
| Socialize with | 0.76 | 0.45 to 1.28 | 0.30 | 294 | 0.89 | 0.50 to 1.58 | 0.67 | 374 | –6 | −3 | 4 | −13 to 21 | 0.67 |
| Make friends with | 0.90 | 0.47 to 1.70 | 0.74 | 293 | 1.05 | 0.53 to 2.10 | 0.88 | 374 | –2 | 1 | 3 | −13 to 19 | 0.73 |
| Have marry into family | 1.03 | 0.62 to 1.70 | 0.91 | 294 | 1.20 | 0.72 to 2.01 | 0.48 | 374 | 1 | 5 | 4 | −14 to 22 | 0.67 |
| Dangerousness | |||||||||||||
| Violent toward self | 2.85 | 1.61 to 5.04 | <0.001 | 295 | 5.04 | 2.84 to 8.95 | <0.001 | 374 | 20 | 35 | 15 | −1 to 31 | 0.07 |
| Violent toward others | 1.38 | 0.79 to 2.41 | 0.25 | 294 | 2.70 | 1.53 to 4.78 | <0.001 | 374 | 7 | 19 | 12 | −3 to 28 | 0.12 |
| Alcohol dependence | |||||||||||||
| Treatment endorsement | |||||||||||||
| Physician | 1.40 | 0.76 to 2.58 | 0.29 | 274 | 1.65 | 0.77 to 3.53 | 0.20 | 346 | 6 | 5 | −2 | −15 to 11 | 0.80 |
| Psychiatrist | 3.04 | 1.69 to 5.50 | <0.001 | 270 | 2.99 | 1.53 to 5.84 | 0.001 | 346 | 25 | 17 | −8 | −24 to 7 | 0.29 |
| Mental hospital | 3.18 | 1.74 to 5.82 | <0.001 | 273 | 2.04 | 1.15 to 3.64 | 0.02 | 346 | 22 | 14 | −9 | −24 to 7 | 0.28 |
| Prescription medicine | 2.25 | 1.29 to 3.92 | 0.004 | 274 | 1.64 | 0.97 to 2.80 | 0.07 | 346 | 19 | 12 | −7 | −26 to 11 | 0.46 |
| Stigma | |||||||||||||
| Social distance: unwilling to | |||||||||||||
| Work closely with | 0.76 | 0.42 to 1.36 | 0.36 | 273 | 1.30 | 0.72 to 2.34 | 0.38 | 346 | –5 | 5 | 10 | −6 to 26 | 0.20 |
| Have as a neighbor | 1.80 | 1.05 to 3.09 | 0.03 | 273 | 1.23 | 0.73 to 2.08 | 0.43 | 346 | 15 | 5 | −10 | −28 to 8 | 0.29 |
| Socialize with | 1.09 | 0.64 to 1.86 | 0.74 | 273 | 0.75 | 0.45 to 1.26 | 0.28 | 346 | 2 | −7 | −9 | −27 to 9 | 0.32 |
| Make friends with | 0.91 | 0.52 to 1.58 | 0.74 | 273 | 0.70 | 0.42 to 1.18 | 0.18 | 345 | –2 | −8 | −6 | −23 to 11 | 0.50 |
| Have marry into family | 1.06 | 0.57 to 1.95 | 0.86 | 270 | 0.97 | 0.53 to 1.77 | 0.93 | 346 | 1 | 0 | −2 | −17 to 14 | 0.85 |
| Dangerousness | |||||||||||||
| Violent toward self | 2.19 | 1.11 to 4.30 | 0.02 | 275 | 1.17 | 0.62 to 2.21 | 0.62 | 346 | 12 | 2 | −10 | −24 to 4 | 0.16 |
| Violent toward others | 1.62 | 0.90 to 2.89 | 0.11 | 272 | 1.01 | 0.59 to 1.73 | 0.96 | 346 | 11 | 0 | –10 | −27 to 7 | 0.24 |
Data are from the 1996 and 2006 mental health modules of the General Social Survey and are weighted.
Reports the factor change in the odds of treatment endorsement or stigma for a unit-based increase in endorsing (coded 1, 0 otherwise) neurobiological conception adjusted for respondent’s age, sex, education, and race. Odds ratios >1 indicate that holding a neurobiological conception increases the odds of treatment endorsement or stigma.
Odds ratios indicate the discrete change in the predicted probability for a given outcome with respect to neurobiological attribution multiplied by 100. Predicted probabilities are calculated with controls held at their means for the combined sample.
Reports the year difference in the discrete change multiplied by 100. Because of rounding, this column will not always equal the 2006 discrete change minus the 1996 discrete change.
Discussion
Public attitudes matter. They fuel “the myth that mental illness is lifelong, hopeless, and deserving of revulsion” (14, p. xiv). Public attitudes set the context in which individuals in the community respond to the onset of mental health problems, clinicians respond to individuals who come for treatment, and public policy is crafted. Attitudes can translate directly into fear or understanding, rejection or acceptance, delayed service use or early medical attention. Discrimination in treatment, low funding resources for mental health research, treatment, and practice, and limited rights of citizenship also arise from misinformation and stereotyping. Attitudes help shape legislative and scientific leaders’ responses to issues such as parity, better treatment systems, and dedicated mental illness research funds (23). Assumptions about these attitudes and beliefs have defined most messages of stigma reduction efforts (14, 15).
With House Joint Resolution 174, the U.S. Congress designated the 1990s as the “Decade of the Brain,” premised on the assumption that the advancement of neuroscience was the key to continued progress on debilitating neural diseases and conditions, including mental illness. An explicit goal of the bipartisan measure was to enhance public awareness of the benefits to be derived from brain research. One of these benefits was to come in the area of stigma, and the Decade of the Brain “helped to reduce the stigma attached” to conditions, including “mind disorders” (24). With a neurobiological understanding of mental illness, people would see that symptoms denote real illness and not volitionally driven deviant behaviors. As a consequence, people with mental disorders would be understood and treated rather than blamed and punished. This view found resonance in the Surgeon General’s optimism for the stigma-reducing potential of neurobiological and molecular genetic discoveries (15, 25). Similar optimistic statements have been common in medical journals (26–28).
From a scientific perspective, claims that stigma was dissipating were optimistic and speculative, based on narrow, anecdotal, or unsystematic observation. Whether or not there has been a decrease in stigma is subject to empirical social science evaluation. Mental illness occurs in communities where “the public” is defined beyond political representatives, advocacy groups, and scientific organizations (29).
Our analyses of data from the GSS, the premier, longest-running monitor of American public opinion, reveal that intensive efforts through the 1990s to 2006, mounted on the promise of neuroscience, have been rewarded with significant and widespread increases in public acceptance of neurobiological theories and public support for treatment, including psychiatry, but no reduction in public stigma. Furthermore, in surveys from both 1996 and 2006 and across all vignette conditions, holding a neurobiological conception of mental illness either was unrelated to stigma or tended to increase the odds of a stigmatizing reaction. Our most striking finding is that stigma among the American public appears to be surprisingly fixed, even in the face of anticipated advances in public knowledge.
The patterns reported here are bolstered by a growing body of similar international studies reporting mixed findings (30–32). In a trend analysis in eastern Germany, Angermeyer and Matschinger (30) documented an identical pattern of increases over time in public mental health literacy and the endorsement of neurobiological causation coupled with either no change or an increase in public stigma of mental illness. In Turkey (33), Germany, Russia, and Mongolia (34), the endorsement of neurobiological attributions was also associated with a desire for social distance, although it had no effect on social distance in Australia (35) and in Austria (36).
Our effort is not without limitations. First, vignette approaches can be sensitive to large and small changes in core descriptions (10, 37). How the public would react to individuals at different places along the diagnostic spectrum remains unanswered. Our “cases” met DSM-IV diagnostic criteria and simulated what individuals in the community encounter—a person with “problem” behaviors but no medical labels or history. This vignette strategy allowed us to explore the association of a neurobiological understanding of current or active “problem” behaviors with stigmatizing responses. However, the assumption underlying many antistigma interventions is that embracing a neurobiological understanding of mental illness will increase support for help-seeking behavior and subsequently lead to treatment that can mitigate symptoms. This in turn would reduce others’ stigmatizing responses. Testing this idea of recovery and stigma reduction would require a different set of vignette circumstances than ours. It stands as an important hypothesis for future research. Second, attitudes are not behaviors, and predispositions may or may not closely track discrimination (38). Both classic and recent studies suggest that attitudes reveal more negative tendencies than individuals are willing to act upon in real situations (39, 40). While important, these limitations are unlikely to have affected our observed results.
Clinical, Research, and Policy Implications
What appears to have been mistaken is the assumption that global change in neuroscientific beliefs would translate into global reductions in stigma. Our analyses suggest that even if the embrace of neuroscience had been more pronounced, a significant and widespread reduction in stigma would not have followed. We are not the first to suggest that there may be unintended consequences or a backlash effect of genetic explanations of mental illness (41). Even in 1999, the Surgeon General’s report cautioned against a simplistic approach, noting that most recent studies suggested that increased knowledge among the public did not appear to translate into lower levels of stigma.
The critical question centers on future directions. As an alternative to our focus on neuroscience, we also considered another approach that pervades public debates. Given the efforts of the Treatment Advocacy Center to link violence in mental illness to policy changes necessary to improve the mental health system, we did a post hoc analysis that looked at the associations among public perceptions of dangerousness, social distance, and public support for increased funding. As Torrey (42) has argued, people who recognize the potential dangerousness of untreated mental illness will support the infusion of more resources to the mental health system. Americans’ assessments of dangerousness are high and, as in previous research, significantly related to social distance (43). However, a measure of public support for federally funded services is not significantly associated with public perceptions of danger. Far from providing the public support needed to improve the mental health system, such fear only appears to have a detrimental effect on community acceptance.
We stand at a critical juncture. Neuroscientific advances are fundamentally transforming the landscape of mental illness and psychiatry. Given expectations surrounding the Decade of the Brain and the blame that pervaded earlier etiological theories of individual moral weakness and family deficits, it is hardly surprising that antistigma efforts relied on neuroscience. The “disease like any other” tagline has taken clinical and policy efforts far but is not without problems. It is our contention that future stigma reduction efforts need to be reconfigured or at least supplemented. An overreliance on the neurobiological causes of mental illness and substance use disorders is at best ineffective and at worst potentially stigmatizing.
Historians, looking to instances in the past where stigma decreased, suggest that continued advances in neuroscience that will prevent, cure, or control mental illnesses are critical to developing treatments that will render them less disabling (44). In fact, the past decade has witnessed major policy and clinical progress, including the passage of the Mental Health Parity and Addiction Equity Act in 2008 and inroads into the genetics of schizophrenia (45). However, clinicians need to be aware that focusing on genetics or brain dysfunction in order to decrease feelings of blame in the clinical encounter may have the unintended effect of increasing client and family feelings of hopelessness and permanence.
Antistigma campaigns will require new visions, new directions for change, and a rethinking of what motivates stigma and what may reduce it, a conclusion reached at a 2009 meeting of stigma experts at the Carter Center. While new research will be needed, current stigma research suggests that a focus on the abilities, competencies, and community integration of persons with mental illness and substance use disorders may offer a promising direction to address public stigma (46).
Footnotes
All authors report no financial relationships with commercial interests.
References
- 1.US Department of Health and Human Services: Mental Health: A Report of the Surgeon General. Bethesda, Md: US Department of Health and Human Services; 1999. [Google Scholar]
- 2.US Department of Health and Human Services: Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: US Department of Health and Human Services; 2001. [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services: Achieving the Promise: Transforming Mental Health Care in America: The President’s New Freedom Commission on Mental Health Report. Bethesda, Md: US Department of Health and Human Services; 2003. [Google Scholar]
- 4.Sartorius N. Fighting schizophrenia and its stigma: a new World Psychiatric Association educational programme. Br J Psychiatry. 1997;170:297. doi: 10.1192/bjp.170.4.297. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal MB, Berndt ER, Frank RG, Donohue JM, Epstein AM. Promotion of prescription drugs to consumers. N Engl J Med. 2002;346:498–505. doi: 10.1056/NEJMsa012075. [DOI] [PubMed] [Google Scholar]
- 6.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- 7.Link BG, Cullen FT, Struening EL, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 8.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 9.Rosenfeld S, Wenzel S. Social networks and chronic mental illness: a test of four perspectives. Social Problems. 1997;44:200–216. [Google Scholar]
- 10.Link BG, Yang L, Phelan JC, Collins P. Measuring mental illness stigma. Schizophr Bull. 2004;30:511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- 11.Estroff SE. Making It Crazy: An Ethnography of Psychiatric Clients in an American Community. Berkeley: University of California Press; 1981. [Google Scholar]
- 12.Markowitz FE. Modeling processes in recovery from mental illness: relationships between symptoms, life satisfaction, and self-concept. J Health Soc Behav. 2001;42:64–79. [PubMed] [Google Scholar]
- 13.Wahl OF. Mental health consumers’ experience of stigma. Schizophr Bull. 1999;25:467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- 14.Hinshaw SP. The Mark of Shame: Stigma of Mental Illness and an Agenda for Change. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 15.Shostak S, Conrad P, Horwitz AV. Sequencing and its consequences: path dependence and the relationships between genetics and medicalization. Am J Sociol. 2008;114(suppl):S287–S316. doi: 10.1086/595570. [DOI] [PubMed] [Google Scholar]
- 16.Murray CJL, Lopez AD. Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass: Harvard School of Public Health; 1996. [Google Scholar]
- 17.Dumesnil H, Verger P. Public awareness campaigns about depression and suicide: a review. Psychiatr Serv. 2009;60:1203–1213. doi: 10.1176/ps.2009.60.9.1203. [DOI] [PubMed] [Google Scholar]
- 18.Pilgrim D, Rogers AE. Psychiatrists as social engineers: a study of an anti-stigma campaign. Soc Sci Med. 2005;61:2546–2556. doi: 10.1016/j.socscimed.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 19.Smith TW, Kim S. GSS Methodological Report. Chicago: National Opinion Research Center; 2003. A Review of CAPI Effects on the 2002. [Google Scholar]
- 20.StataCorp: Survey Data Reference Manual. College Station, Tex: Stata Press; 2009. [Google Scholar]
- 21.Rao JNK, Scott AJ. On chi-squared tests for multi-way tables with cell proportions estimated from survey data. Ann Stat. 1984;12:46–60. [Google Scholar]
- 22.Allison PD. Comparing logit and probit coefficients across groups. Sociol Methods Res. 1999;28:186–208. [Google Scholar]
- 23.Burstein P. Should sociologists consider the impact of public opinion on public policy? Soc Forces. 1998;77:27–62. [Google Scholar]
- 24.Jones EG, Mendell LM. Assessing the decade of the brain. Science. 1999;284:739. doi: 10.1126/science.284.5415.739. [DOI] [PubMed] [Google Scholar]
- 25.Blazer DG. The Age of Melancholy: Major Depression and Its Social Origins. New York: Routledge; 2005. [Google Scholar]
- 26.Baxter WE. American psychiatry celebrates 150 years of caring. Psychiatr Clin North Am. 1994;17:683–693. [PubMed] [Google Scholar]
- 27.Editorial: Reducing the stigma of mental illness. Lancet. 2001;357:1055. [PubMed] [Google Scholar]
- 28.Goin MK. Presidential address. Am J Psychiatry. 2004;161:1768–1771. [Google Scholar]
- 29.Pescosolido BA, Martin JK, Lang A, Olafsdottir S. Rethinking theoretical approaches to stigma: a framework integrating normative influences on stigma (FINIS) Soc Sci Med. 2008;67:431–440. doi: 10.1016/j.socscimed.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Angermeyer MC, Matschinger H. Causal beliefs and attitudes to people with schizophrenia: trend analysis based on data from two population surveys in Germany. Br J Psychiatry. 2005;186:331–334. doi: 10.1192/bjp.186.4.331. [DOI] [PubMed] [Google Scholar]
- 31.Blumner KH, Marcus SC. Changing perceptions of depression: ten-year trends from the General Social Survey. Psychiatr Serv. 2009;60:306–312. doi: 10.1176/ps.2009.60.3.306. [DOI] [PubMed] [Google Scholar]
- 32.Mehta N, Kassam A, Leese M, Butler G, Thornicroft G. Public attitudes towards people with mental illness in England and Scotland, 1994–2003. Br J Psychiatry. 2009;194:278–284. doi: 10.1192/bjp.bp.108.052654. [DOI] [PubMed] [Google Scholar]
- 33.Bag B, Yilmaz S, Kirpinar I. Factors influencing social distance from people with schizophrenia. Int J Clin Pract. 2006;60:289–294. doi: 10.1111/j.1368-5031.2006.00743.x. [DOI] [PubMed] [Google Scholar]
- 34.Dietrich S, Beck M, Bujantugs B, Kenzine D, Matschinger H, Angermeyer M. The relationship between public causal beliefs and social distance toward mentally ill people. Aust NZ J Psychiatry. 2004;38:348–354. doi: 10.1080/j.1440-1614.2004.01363.x. [DOI] [PubMed] [Google Scholar]
- 35.Jorm AF, Griffiths KM. The public’s stigmatizing attitudes towards people with mental disorders: how important are biomedical conceptualizations? Acta Psychiatr Scand. 2008;118:315–321. doi: 10.1111/j.1600-0447.2008.01251.x. [DOI] [PubMed] [Google Scholar]
- 36.Grausgruber A, Meise U, Katsching H, Schony W, Fleischhaker WW. Patterns of social distance towards people suffering from schizophrenia in Austria: a comparison between the general public, relatives, and mental health staff. Acta Psychiatr Scand. 2006;115:310–319. doi: 10.1111/j.1600-0447.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- 37.Finch J. The vignette technique in survey research. Sociology. 1987;21:105–114. [Google Scholar]
- 38.Asch S. The Legacy of Solomon Asch: Essays in Cognition and Social Psychology. Hillsdale, NJ: Laurence Erlbaum Associates; 1990. [Google Scholar]
- 39.LaPiere RT. Attitudes vs actions. Soc Forces. 1934;13:230–237. [Google Scholar]
- 40.Smith ER, Mackie DM. Surprising emotions. Science. 2009;323:215–216. doi: 10.1126/science.1168650. [DOI] [PubMed] [Google Scholar]
- 41.Phelan JC. Geneticization of deviant behavior and consequences for stigma: the case of mental illness. J Health Soc Behav. 2005;46:307–322. doi: 10.1177/002214650504600401. [DOI] [PubMed] [Google Scholar]
- 42.Torrey EF. The Insanity Offense: How America’s Failure to Treat the Seriously Mentally Ill Endangers Its Citizens. New York: WW Norton; 2008. [Google Scholar]
- 43.Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public’s view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health. 1999;89:1339–1345. doi: 10.2105/ajph.89.9.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grob GN. From Asylum to Community: Mental Health Policy in Modern America. Princeton, NJ: Princeton University Press; 1991. [Google Scholar]
- 45.Torkamani A, Dean B, Schork NJ, Thomas EA. Coexpression network analysis of neural tissue reveals perturbations in developmental processes in schizophrenia. Genome Res. 2010;20:403–412. doi: 10.1101/gr.101956.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ware NC, Hopper K, Tugenbert T, Dickey B, Fisher D. Connectedness and citizenship: redefining social integration. Psychiatr Serv. 2007;58:469–474. doi: 10.1176/ps.2007.58.4.469. [DOI] [PubMed] [Google Scholar]