Abstract
When balance is disturbed, location of the center of pressure (COP) contributes to a person’s ability to recover from a perturbation. This study investigated COP control prior to first step lift-off (FSLO) during lateral perturbations in older non-fallers and fallers. 38 Non-Fallers and 16 Fallers received lateral waist-pulls at 5 different intensities. Crossover stepping responses at the intensity level where the largest number of subjects responded with crossover steps were analyzed. Whole-body center of mass (COM) and COP positions in the medio-lateral (ML) direction with respect to the base of support (BOS), and COP velocity were calculated. An inverted pendulum model was used to define the BOS stability boundary at FSLO, which was also adjusted using the COP position at FSLO (functional boundary). No significant differences were found in the COP velocities between Fallers and Non-Fallers (p>.093). However, the COP positions for Fallers were located significantly more medial at FSLO (p≤.01), resulting in a significantly reduced functional boundary. Although the stability margins, measures of stability based on the BOS, were significantly larger than zero for Fallers (p≤.004), they were not significantly different from zero for the functional boundary, i.e., reaching the functional stability limit. Fallers had reduced functional limits of stability in the ML direction, which would predispose them to more precarious stability conditions than Non-Fallers. This could be a cause for taking more steps than Non-Fallers for balance recovery as we observed. The functional boundary estimation may be a more sensitive marker of balance instability than the BOS boundary.
Keywords: Falls, Balance, Perturbation, Center of pressure, Center of mass
1. Introduction
Falls are the leading cause of serious injuries in older people due to age-related declines in balance control (Nevitt et al., 1989; Tinetti et al., 1988). An impaired ability to control lateral balance is an important aspect of balance problems contributing to falls (Maki and McIlroy, 2006; Rogers and Mille, 2003). A directional vulnerability to falling sideways among older individuals has been supported by a previous prospective study (Hilliard et al., 2008), recent experimental findings on multi-directional protective stepping (Mille et al., 2013), and an observational surveillance study of real-life falls (Robinovitch et al., 2013).
In order to effectively recover balance when standing stability is perturbed, protective steps must be appropriately timed and adjusted to arrest the motion of the whole-body center of mass (COM) (Mille et al., 2013). Older adults are much more likely than younger adults to take multiple balance recovery steps (Luchies et al., 1994; Maki et al., 2000; Mille et al., 2013; Mille et al., 2005), where an inability to recover lateral balance with a single step is predictive of future falls (Hilliard et al., 2008). Moreover, younger adults more often use a side step maneuver with the limb that is passively loaded by the lateral perturbation, whereas older adults more frequently use crossover steps with the passively unloaded limb (Mille et al., 2013; Mille et al., 2005). While crossover stepping with the passively unloaded leg facilitates the onset of stepping, it increases the potential for inter-limb collisions and subsequent falls (Maki et al., 2000; Mille et al., 2005). Thus, balance recovery steps for older adults appear to be less efficient using multiple steps and less effective with more inter-limb collisions using crossover strategies.
While protective stepping parameters after first step lift-off (FSLO), such as step count and step type, could be used as measures of dynamic balance function, they do not fully capture the evolving state of balance stability represented by the COM-base of support (BOS) relationship. For example, the location of the center of pressure (COP) prior to FSLO contributes to a person’s ability to recover balance from a perturbation. When standing balance is disturbed, acceleration (or deceleration) of the COM is directly related to the distance between the COP and COM (Winter et al., 1998). Since the BOS provides a possible area for COP movement, the BOS boundaries have been considered as stability limits within which balance is maintained by rapidly moving the COP to keep the COM from going outside the BOS (Hof et al., 2005; Pai et al., 1998; Winter, 1995). Therefore, how “fast” and how “far” the COP moves with respect to the BOS prior to FSLO is importantly involved with dynamic balance control.
In addition to the COM-BOS relationship, balance would not be maintained if the COM has a sufficiently large horizontal velocity (Brown et al., 1999; McIlroy and Maki, 1996; Pai and Patton, 1997; Pai et al., 1998). Thus, dynamic balance stability has been quantified based on the position-velocity relationship between the COM and BOS (Carty et al., 2011; Hof et al., 2005; Pai and Patton, 1997; Pai et al., 1998), where an analysis applied to the frontal plane showed that older adults used a conservative strategy by stepping well before their stability limit was reached (Patton et al., 2006).
While these models used the BOS boundaries as limits of COP control, it has been shown that the functional limit of the BOS (FBOS), defined as the effectively utilized area for COP movement, is decreased with aging (Fujimoto et al., 2013; King et al., 1994). Such a reduced FBOS would limit an individual’s ability to maintain balance because the COP-COM distance is proportional to the COM acceleration (Winter et al., 1998), which is important for regulating the momentum induced by perturbations as described earlier. A reduced area used for COP movement could predispose older individuals to a precarious condition for maintaining balance stability.
To further address these issues, the objective of this study was to investigate the COP control prior to and at FSLO during crossover protective stepping in response to lateral perturbations of standing balance in older non-fallers and fallers. COP velocity prior to FSLO and COP position at FSLO were calculated to assess the COP control. An inverted pendulum model was used to define the BOS lateral stability boundary at FSLO, which was also adjusted using the COP position at FSLO (functional boundary). We hypothesized that fallers would demonstrate a reduced functional boundary with a slower COP velocity than non-fallers.
2. Methods
2.1. Subjects
Thirty-eight healthy, community dwelling older adults [Non-Fallers: 19 men/19 women; age: 74.1 (SD 7.5) years; height: 1.67 (SD 0.09) m; body mass: 76.2 (SD 14.2) kg], and 16 healthy older adults with a history of falls [Fallers: 6 men/10 women; age: 72.9 (SD 4.6) years; height: 1.67 (SD 0.11) m; body mass: 80.0 (SD 19.2) kg] participated in this study. Any individual who fell one or more times in the year prior to testing was categorized as a faller (Lord et al., 1999). A fall was defined as “coming to rest unintentionally on the ground or lower level, not as a result of a major intrinsic event (such as stroke) or overwhelming hazard” (Tinetti et al., 1988). Participants were medically examined by a physician to assess exclusion criteria including: 1) cognitive impairment (Folstein Mini Mental Score < 24); 2) sedative use; 3) non-ambulatory; 4) any clinically significant functional impairment related to musculoskeletal, neurological, cardiopulmonary, metabolic or other general medical problems; 5) participation in any regular vigorous or muscle strengthening exercise regimen; and 6) Centers for Epidemiological Studies Depression Survey score > 16. All participants provided written, informed consent prior to participation, and the study was approved by the Institutional Review Board at the University of Maryland School of Medicine and the Baltimore Veteran’s Administration Medical Center.
2.2. Data collection
Participants received a total of 60 randomly applied, position-controlled, motor-driven waist-pull lateral perturbations at five different intensities (Levels 1–5) in the left and right directions (L and R pulls). The system has been previously described (Pidcoe and Rogers, 1998) and used in prior studies (Hilliard et al., 2008; Mille et al., 2013; Mille et al., 2005; Young et al., 2013; Yungher et al., 2012). Participants wore a waist belt to which cables were attached and through which the perturbations were applied. Six trials were conducted for each intensity and direction (2 directions × 5 intensities × 6 repetitions). The order in which the trials were presented was randomized to minimize anticipation and sequence learning effects. Participants stood in a self-selected, comfortable standing position at the start of each trial with each foot on a separate force platform (AMTI, Newton, MA, USA). The foot locations were traced onto the platform surface to ensure consistent initial foot placement over the trials. Participants were instructed to “relax and react naturally to prevent themselves from falling.”
Whole body motion was captured with a six-camera motion analysis system (Vicon 460, Oxford, UK). 28 reflective markers were placed according to Eames et al. with additional markers on the medial malleoli and 5th metatarsophalangeal (MP) joints (Eames et al., 1999). Three-dimensional marker trajectories were collected at 120 Hz and smoothed using a fourth-order Butterworth filter with a cut-off frequency of 8 Hz. Ground reaction forces (GRFs) were collected by two force platforms located under each foot at 600 Hz and filtered with a 10 Hz cut-off frequency (Hernandez et al., 2012; Maki et al., 1994).
2.3. Data analysis
Since crossover stepping is a common maneuver used by older adults to recover lateral balance (Maki and McIlroy, 2006; Mille et al., 2005), responses to the lateral waist-pulls at intensity Level 4, where the largest number of subjects responded with crossover steps (74% Non-Fallers (28/38) and 44% Fallers (7/16) for L pulls, and 71% Non-Fallers (27/38) and 69% Fallers (11/16) for R pulls), were analyzed. Each set of L and R pulls consisted of 6 repeated trials, and the averages for those trials were used as representative values for each subject.
The whole-body COM was calculated as the weighted sum of 13 body segments, including head and neck, trunk, pelvis, 2 upper arms, 2 forearms with hands, 2 thighs, 2 shanks, and 2 feet (Eames et al., 1999). COM and combined COP positions in the medio-lateral (ML) directions at FSLO were referenced to the medial ankle and normalized to the BOS width. The BOS width was the ML distance between the medial ankle and 5th MP joint of the stance foot determined prior to the perturbation onset (Fig. 1). Peak and average COP velocities prior to FSLO were also calculated both before and after stance width normalization (Maki et al., 1994). FSLO timing was determined as the instant when the vertical GRF dropped to less than 10 N (Brauer et al., 2002). Step onset latency was calculated as the time between the perturbation onset and FSLO. Average COP velocity was the average over the time between the perturbation onset and FSLO.
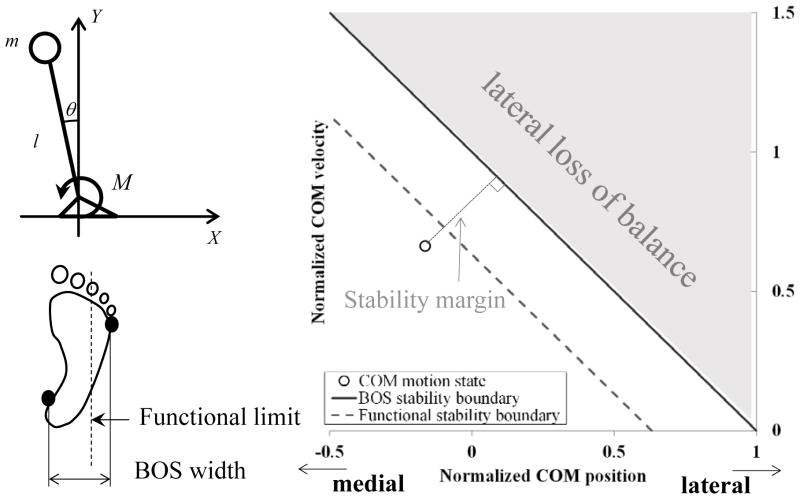
Figure 1.
A single-link-plus-foot inverted pendulum model in the frontal plane and lateral stability boundaries. X indicates the COM position in the medio-lateral direction. m, l and M are whole body mass, pendulum length (distance from the ankle to the COM), and ankle joint moment. The lateral stability boundaries were defined in two ways: one with the BOS width (BOS stability boundary), and the other adjusted with the COP position at FSLO, considering it as a functional limit for COP movement (functional stability boundary). Stability margins were calculated as the shortest distances from the experimental data to those stability boundaries.
A single-link-plus-foot inverted pendulum model was used to define the lateral stability boundary at FSLO, the beginning of the single-limb support phase (Fig. 1), using the following equation (Hof et al., 2005):
where X̃SO and are normalized COM position and velocity at FSLO in the ML direction, defined as X̃SO = (XSO − Xma)/Lw, ( , : Lw: BOS width, Xma: medial ankle, l: pendulum length). In addition, since previous studies have shown that the area functionally used for COP movement is smaller than the BOS (Fujimoto et al., 2013; King et al., 1994), the lateral stability boundary was also determined based on the COP position at FSLO, considering it as a functional limit for COP movement (Fig. 1). Thus, the lateral stability boundaries were defined in two ways: one with the BOS (BOS boundary), and the other adjusted according to the functional limit (functional boundary). In each case, the stability margin was defined as the shortest distance from the experimental data to the respective boundaries (Yang et al., 2009). A larger stability margin indicates that the COM motion state is within the stability limits.
An independent t-test was performed to examine between-group differences in the subject characteristics (age, height, weight, and initial stance width), step count, step onset latency, the ML COP velocities prior to FSLO, the COM position and velocity as well as COP position at FSLO, and the stability margins at FSLO. Since our previous study did not identify any differences in outcome measures between the perturbation directions (Young et al., 2013), no direct comparisons were made between the left and right perturbations. One sample t-tests were also performed to determine if the stability margin was significantly different from zero. Statistical analyses were performed using SPSS (Chicago, IL). Significance level was set at α=.05.
3. Results
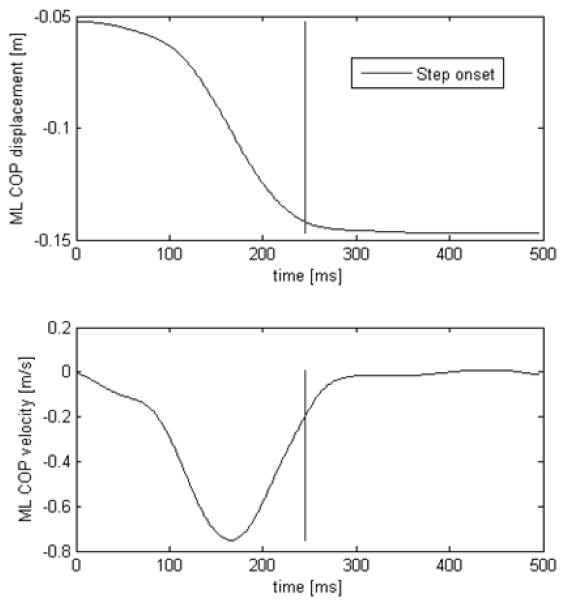
No significant differences were found in the age, height, weight, and initial stance width between Fallers and Non-Fallers (p>.087, Table 1). Fallers took more recovery steps than Non-Fallers (L pull: 1.8 (SD 0.5) vs 2.5 (SD 0.9) steps, p=.007; R pull: 1.7 (SD 0.5) vs 2.9 (SD 1.3) steps, p=.014). Although not significant, Fallers showed longer step onset latency than Non-Fallers (L pull: 333 (SD 102) ms vs. 385 (SD 113) ms, p= .24; R pull: 386 (SD 95) ms vs. 423 (SD 113) ms, p= .32). The COP relative to the medial ankle of the stance foot was initially displaced in the pull direction prior to FSLO and reached a plateau after FSLO (Fig. 2). COP velocity also reached a peak level prior to FSLO. The same trend was observed for Fallers.
Table 1.
Subjects’ age, height, weight and stance width. Data are presented as mean (SD). Stance width was calculated as the mean distance between the left and right lateral ankles and 5th MP joints in the ML direction prior to the onset of perturbation. No significant differences were found between Non-Fallers and Fallers (p≥.087).
| COP velocities | L pull
|
R pull
|
||||
|---|---|---|---|---|---|---|
| Non-Fallers | Fallers | p | Non-Fallers | Fallers | p | |
| # of subjects | 15men/13women | 1man/6women | 16men/11women | 4men/7women | ||
| Age[years] | 72.8 (7.1) | 71.7 (4.9) | .635 | 74.1 (7.3) | 72.6 (4.6) | .450 |
| Height[m] | 1.67 (0.08) | 1.62 (0.04) | .087 | 1.68 (0.08) | 1.69 (0.12) | .807 |
| Weight[kg] | 76.6 (14.2) | 73.9 (15.8) | .653 | 77.6 (14.2) | 82.7 (20.9) | .388 |
| Stance width[cm] | 33.6 (4.5) | 35.0 (3.4) | .460 | 34.2 (4.4) | 36.4 (3.5) | .160 |
Figure 2.
Representative time-history plot of COP displacement relative to the medial ankle of the stance foot (Left) for L pull for Non-Fallers group. Negative is to the left. The same trend was seen in the Faller group.
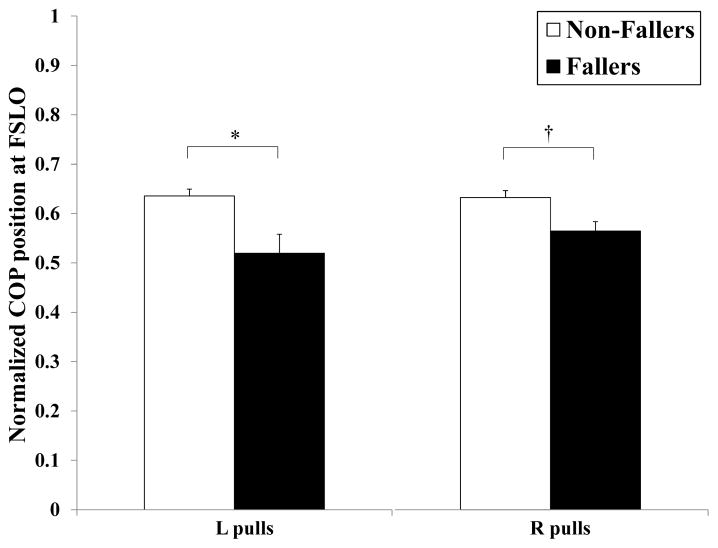
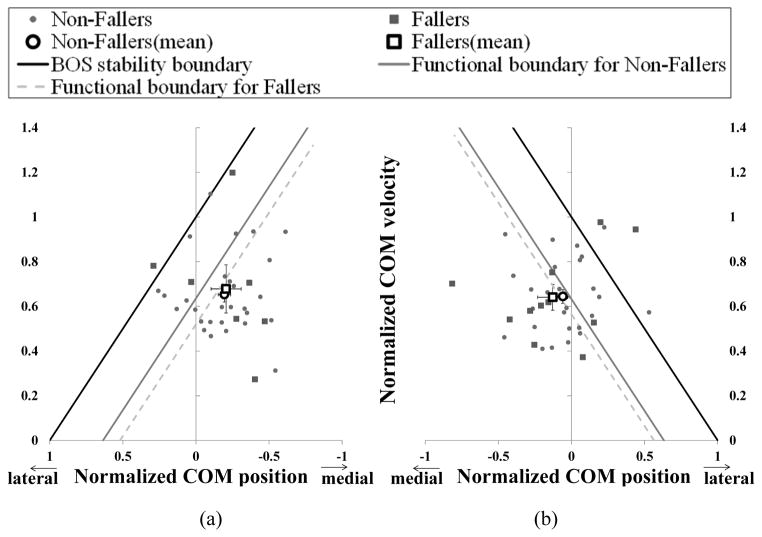
No significant differences were found in the peak or average COP velocities between the groups, regardless of the pull directions (p>.093, Table 2). However, the values of the COP positions at FSLO for Fallers were up to 18% smaller than those for Non-Fallers for both pull directions (L pull: 0.64 (SD 0.07) vs 0.52 (SD 0.10), p=.002; R pull: 0.63 (SD 0.07) vs 0.56 (SD 0.06), p=.01, Fig. 3). This indicates that COP positions with respect to the stance side BOS for Fallers were more medially located compared to Non-Fallers, which resulted in more medially located functional boundaries for Fallers (Fig. 4). No significant differences were found for the COM positions and velocities at FSLO (p>.457, Fig. 4).
Table 2.
Peak and average COP velocities prior to FSLO before and after normalization (Norm) by stance width. Data are presented as mean (SD). Pull direction is positive. No significant differences were found between Non-Fallers and Fallers (p>.093).
| COP velocities | L pull
|
R pull
|
||||
|---|---|---|---|---|---|---|
| Non-Fallers | Fallers | p | Non-Fallers | Fallers | p | |
| Peak [m/s] | 0.99 (0.20) | 0.97 (0.33) | .873 | 0.86 (0.19) | 0.89 (0.18) | .608 |
| Norm Peak [/s] | 2.95 (0.53) | 2.75 (0.79) | .437 | 2.51 (0.45) | 2.46 (0.49) | .782 |
| Average [m/s] | 0.42 (0.11) | 0.37 (0.12) | .268 | 0.39 (0.10) | 0.37 (0.11) | .685 |
| Norm Average [/s] | 1.28 (0.31) | 1.06 (0.28) | .093 | 1.15 (0.28) | 1.04 (0.33) | .289 |
Figure 3.
Normalized COP positions at FSLO for Non-Fallers and Fallers. Values and error bars are mean and SEM. (*p=.002, †p=.01.)
Figure 4.
Normalized COM velocity vs. normalized COM position at FSLO in the ML direction for Non-Fallers (◆) and Fallers (■) for (a) L pull and (b) R pull. Mean for each group (◇ and □) are also indicated. Error bars are SEM. The solid line indicates the BOS stability boundary. The two dashed lines indicate the functional stability boundaries for Non-Fallers and Fallers. Since the functional boundaries vary between subjects, the average for all subjects within the group was shown here.
Although not statistically significant, Fallers demonstrated a similar or larger stability margin than Non-fallers based on their BOS boundary (L pull: 0.38 (SD 0.19) vs 0.37 (SD 0.32), p=0.917; R pull: 0.29 (SD 0.20) vs 0.34 (SD 0.31), p=.543), while the stability margins of Fallers became smaller or similar to those of Non-fallers when the functional boundary was used (L pull: 0.13 (SD 0.17) vs 0.03 (SD 0.29), p=.288; R pull: 0.03 (SD 0.18) vs 0.04 (SD 0.28), p=.964) (Fig. 5). In addition, while the functional stability margin was significantly different from zero for L pulls for Non-Fallers (0.13 (SD 0.17), p=.001), it was not significantly different from zero for R pulls for Non-Fallers (0.03 (SD 0.18), p=.37), or for both L and R pulls for Fallers (0.03 (SD 0.29) and 0.04 (SD 0.28), p>.68).
Figure 5.
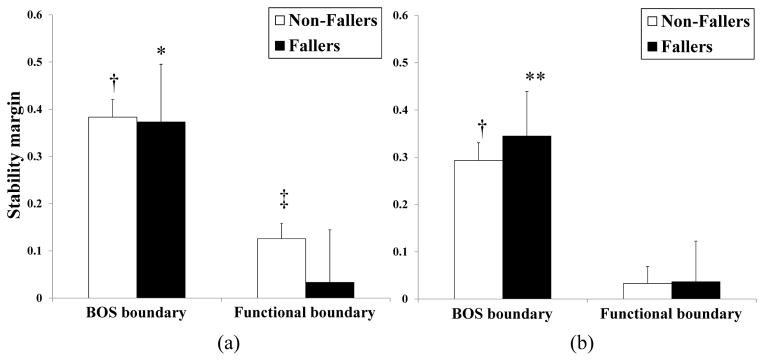
Stability margins based on the BOS and functional stability boundaries for (a) L pull and (b) R pull. Values and error bars are mean and SEM. *, **, †, and ‡ indicate that the stability margin is significantly different from zero (*p<.001, **p=.004, †p=.011, ‡p=.042).
4. Discussion
The objective of this study was to investigate COP control during medio-lateral crossover stepping in older non-fallers and fallers. No significant differences were found in the COP velocities between the groups prior to FSLO. However, the COP positions for Fallers were located significantly more medial at FSLO, suggesting that the area functionally used for COP movement was significantly reduced for Fallers as was hypothesized. These results suggested that Fallers might be predisposed to more precarious stability conditions than Non-Fallers because such a reduced area for COP movement would diminish the limits of lateral stability for COM control.
Fallers took more recovery steps than Non-Fallers, which is consistent with previous findings (Mille et al., 2013) and corroborated the use of multiple steps as a predictor of fall risk (Hilliard et al., 2008). Neither the peak nor average COP velocities differed between the groups, in agreement with a previous report of COP speed during induced ML sway (Maki et al., 1994). The COP velocity may reflect the amount of balancing activity that is needed to maintain a stable upright posture (Maki et al., 1994). Crossover stepping takes advantage of the passive unloading beneath the stepping limb in initiating the response unlike lateral side stepping that requires active unloading of the passively loaded leg (Mille et al., 2005). Such a reduction of active postural movement for crossover steps might have contributed to the lack of difference in COP velocities between the groups.
The COP position for Fallers was more medially located than that for Non-Fallers. This indicated that the area functionally used for COP movement in the ML direction was significantly reduced in Fallers, which resulted in a significant reduction in the functional stability boundary. Although the BOS is the area within which the COP can possibly move, the area effectively used for COP movement, i.e., FBOS, to control the COM was limited. Age-related decreases in the FBOS have been previously reported in the AP direction (Fujimoto et al., 2013; King et al., 1994). The present results further indicated that the area used for COP movement can also be limited in the ML direction and reduced in older adults at greater risk for falls, thus constricting the limits of lateral stability. Since the range of the COP excursion needs to be greater than that of the COM to effectively reduce the momentum induced by perturbations, such a reduced area for COP movement would limit one’s ability to maintain balance.
Because of this functional limitation, larger stability margins based on the BOS might not always mean that they are well within the stability limits as suggested previously for forward and lateral induced stepping (Pai et al., 1998; Patton et al., 2006; Rogers and Mille, 2003). In fact, although the stability margins for Fallers were significantly different from zero for the BOS boundaries, they were not significantly different for the functional boundaries, i.e., reaching the functional stability limit. These results suggested that even when the COM motion state for Fallers is located farther from the BOS boundary than for Non-Fallers, it is possible that they have approached their functional limit. Therefore, the functional boundary estimation may be a more sensitive marker of balance instability than the BOS boundary. In this regard, a previous study of lateral balance recovery reported that older fallers stepped well before they reached their stability limit during crossover steps (Patton et al., 2006). It is plausible that older adults at greater risk for falls adopt a more conservative strategy by preserving greater BOS stability margins. However, our results indicated that Fallers might actually be predisposed to more precarious stability conditions than those estimated by the BOS boundaries because of the reduction in their functional limit for COP movement.
What caused such a reduction in the functional limit in Fallers? An earlier step initiation time due to safety concerns has been previously reported in older adults and fallers (Mille et al., 2013; Rogers et al., 2001). Such an earlier step initiation due to anxiety about falling could limit the COP movement before FSLO. However, in this study, the Fallers showed a tendency to have a later step onset time than Non-Fallers. Therefore, it is unlikely that a later step onset contributed to the more medially located COP in Fallers since a later step onset would result in a more laterally located COP imposed by the perturbation. From a motor control perspective, the reduced area for COP movement could be related to ankle or hip muscle performance capacity. Ankle invertor-evertor and hip abductor-adductor muscle torques contribute to the lateral COP movement (Rietdyk et al., 1999). A reduction in muscle strength or power related to the risk of falls could therefore have contributed to the functional stability differences between the groups. Furthermore, deterioration in foot plantar mechanoreception might also have contributed to the reduced area for COP movement. Previous studies have indicated an influential role for cutaneous sensation from the plantar surface of the foot in the control of balance, where impaired cutaneous sensation has been associated with impaired postural control and increased risk of falling (Lin et al., 2010; Lord et al., 1994; Maki et al., 1999; Perry, 2006; Perry et al., 2000; Perry et al., 2008). Diminished sensation could play a role in detecting the proximity of the COM to the stability boundaries of the BOS to maintain balance (Maki et al., 1999). Further investigation is needed to determine the relationship between neuromuscular and sensorimotor functions and COP control during lateral balance recovery responses.
Among the limitations of the study is the smaller number of subjects classified as Fallers. However, the significant findings pertaining to a medially located COP position at FSLO for Fallers would only likely be further strengthened with a larger sample size and increased statistical power. Another limitation is that we did not control for the number of recovery steps used by participants which could have influenced the results obtained by using combined single and multiple stepping trials. However, even when the same analyses involved only the multiple stepping trials it did not affect the findings, where the COP positions for Fallers were located significantly more medial (Non-Fallers vs. Fallers: 0.63 (SD 0.08) vs. 0.52 (SD 0.10), p=.005 (L pulls); 0.63 (SD 0.08) vs. 0.56 (SD 0.06), p=.015 (R pulls)). It should also be noted that the functional stability margin for Non-Fallers was significantly different from zero for L pulls, although it was not significantly different for R pulls, indicating asymmetries in dynamic balance stability. Although such asymmetries in stability margins were not seen in Fallers, the causes remain to be determined.
In conclusion, COP position with respect to the BOS at FSLO for Fallers was found to be located more medial to that for Non-Fallers, indicating reduced functional limits of dynamic stability. This implies that even when Fallers seem to use a more conservative strategy than Non-Fallers, ensuring a greater stability margin in relation to their BOS, the stability margin relative to the functional limit for COP movement could still be smaller. The functional limit might therefore provide more sensitive estimation of lateral stability. The reduced functional limits of stability for Fallers would predispose them to more precarious stability conditions than Non-Fallers by limiting their ability to regulate COM momentum induced by perturbations. Consequently, this could be a biomechanical cause for lateral instability requiring older fallers to take more steps than Non-Fallers for balance recovery.
Acknowledgments
This study was supported by NIH grant RO1 AG029510, the University of Maryland Claude D Pepper - Older Americans Independence Center Grant (OAIC) NIH/NIA grant P30 AG028747, the University of Maryland Advanced Neuromotor Rehabilitation Research Training (UMANRRT) Program, supported by the National Institute on Disability and Rehabilitation Research grant H133P100014, and the Baltimore VA Medical Center, Geriatric Research, Education and Clinical Center (GRECC).
Footnotes
Conflict of interest
The authors have no conflicts of interest in relation to the work reported here.
References
- Brauer SG, Woollacott M, Shumway-Cook A. The influence of a concurrent cognitive task on the compensatory stepping response to a perturbation in balance-impaired and healthy elders. Gait & posture. 2002;15:83–93. doi: 10.1016/s0966-6362(01)00163-1. [DOI] [PubMed] [Google Scholar]
- Brown LA, Shumway-Cook A, Woollacott MH. Attentional demands and postural recovery: the effects of aging. J Gerontol A Biol Sci Med Sci. 1999;54:M165–171. doi: 10.1093/gerona/54.4.m165. [DOI] [PubMed] [Google Scholar]
- Carty CP, Mills P, Barrett R. Recovery from forward loss of balance in young and older adults using the stepping strategy. Gait & posture. 2011;33:261–267. doi: 10.1016/j.gaitpost.2010.11.017. [DOI] [PubMed] [Google Scholar]
- Eames MHA, Cosgrove A, Baker R. Comparing methods of estimating the total body centre of mass in three-dimensions in normal and pathological gaits. Human Movement Science. 1999;18:637–646. [Google Scholar]
- Fujimoto M, Hsu WL, Woollacott MH, Chou LS. Ankle dorsiflexor strength relates to the ability to restore balance during a backward support surface translation. Gait & posture. 2013;38:812–817. doi: 10.1016/j.gaitpost.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez ME, Ashton-Miller JA, Alexander NB. Age-related changes in speed and accuracy during rapid targeted center of pressure movements near the posterior limit of the base of support. Clinical biomechanics (Bristol, Avon) 2012;27:910–916. doi: 10.1016/j.clinbiomech.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard MJ, Martinez KM, Janssen I, Edwards B, Mille ML, Zhang Y, Rogers MW. Lateral balance factors predict future falls in community-living older adults. Archives of physical medicine and rehabilitation. 2008;89:1708–1713. doi: 10.1016/j.apmr.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hof AL, Gazendam MG, Sinke WE. The condition for dynamic stability. J Biomech. 2005;38:1–8. doi: 10.1016/j.jbiomech.2004.03.025. [DOI] [PubMed] [Google Scholar]
- King MB, Judge JO, Wolfson L. Functional base of support decreases with age. Journal of gerontology. 1994;49:M258–263. doi: 10.1093/geronj/49.6.m258. [DOI] [PubMed] [Google Scholar]
- Lin SI, Chen YR, Liao CF, Chou CW. Association between sensorimotor function and forward reach in patients with diabetes. Gait & posture. 2010;32:581–585. doi: 10.1016/j.gaitpost.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Lord SR, Rogers MW, Howland A, Fitzpatrick R. Lateral stability, sensorimotor function and falls in older people. Journal of the American Geriatrics Society. 1999;47:1077–1081. doi: 10.1111/j.1532-5415.1999.tb05230.x. [DOI] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. Journal of the American Geriatrics Society. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- Luchies CW, Alexander NB, Schultz AB, Ashton-Miller J. Stepping responses of young and old adults to postural disturbances: kinematics. Journal of the American Geriatrics Society. 1994;42:506–512. doi: 10.1111/j.1532-5415.1994.tb04972.x. [DOI] [PubMed] [Google Scholar]
- Maki BE, Edmondstone MA, McIlroy WE. Age-related differences in laterally directed compensatory stepping behavior. J Gerontol A Biol Sci Med Sci. 2000;55:M270–277. doi: 10.1093/gerona/55.5.m270. [DOI] [PubMed] [Google Scholar]
- Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. Journal of gerontology. 1994;49:M72–84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age and ageing. 2006;35(Suppl 2):ii12–ii18. doi: 10.1093/ageing/afl078. [DOI] [PubMed] [Google Scholar]
- Maki BE, Perry SD, Norrie RG, McIlroy WE. Effect of facilitation of sensation from plantar foot-surface boundaries on postural stabilization in young and older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M281–287. doi: 10.1093/gerona/54.6.m281. [DOI] [PubMed] [Google Scholar]
- McIlroy WE, Maki BE. Age-related changes in compensatory stepping in response to unpredictable perturbations. J Gerontol A Biol Sci Med Sci. 1996;51:M289–296. doi: 10.1093/gerona/51a.6.m289. [DOI] [PubMed] [Google Scholar]
- Mille ML, Johnson-Hilliard M, Martinez KM, Zhang Y, Edwards BJ, Rogers MW. One step, two steps, three steps more … Directional vulnerability to falls in community-dwelling older people. J Gerontol A Biol Sci Med Sci. 2013;68:1540–1548. doi: 10.1093/gerona/glt062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mille ML, Johnson ME, Martinez KM, Rogers MW. Age-dependent differences in lateral balance recovery through protective stepping. Clinical biomechanics (Bristol, Avon) 2005;20:607–616. doi: 10.1016/j.clinbiomech.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. Jama. 1989;261:2663–2668. [PubMed] [Google Scholar]
- Pai YC, Patton J. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30:347–354. doi: 10.1016/s0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- Pai YC, Rogers MW, Patton J, Cain TD, Hanke TA. Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults. J Biomech. 1998;31:1111–1118. doi: 10.1016/s0021-9290(98)00124-9. [DOI] [PubMed] [Google Scholar]
- Patton JL, Hilliard MJ, Martinez K, Mille ML, Rogers MW. A simple model of stability limits applied to sidestepping in young, elderly and elderly fallers. Conf Proc IEEE Eng Med Biol Soc. 2006;1:3305–3308. doi: 10.1109/IEMBS.2006.260199. [DOI] [PubMed] [Google Scholar]
- Perry SD. Evaluation of age-related plantar-surface insensitivity and onset age of advanced insensitivity in older adults using vibratory and touch sensation tests. Neuroscience letters. 2006;392:62–67. doi: 10.1016/j.neulet.2005.08.060. [DOI] [PubMed] [Google Scholar]
- Perry SD, McIlroy WE, Maki BE. The role of plantar cutaneous mechanoreceptors in the control of compensatory stepping reactions evoked by unpredictable, multi-directional perturbation. Brain research. 2000;877:401–406. doi: 10.1016/s0006-8993(00)02712-8. [DOI] [PubMed] [Google Scholar]
- Perry SD, Radtke A, McIlroy WE, Fernie GR, Maki BE. Efficacy and effectiveness of a balance-enhancing insole. J Gerontol A Biol Sci Med Sci. 2008;63:595–602. doi: 10.1093/gerona/63.6.595. [DOI] [PubMed] [Google Scholar]
- Pidcoe PE, Rogers MW. A closed-loop stepper motor waist-pull system for inducing protective stepping in humans. J Biomech. 1998;31:377–381. doi: 10.1016/s0021-9290(98)00017-7. [DOI] [PubMed] [Google Scholar]
- Rietdyk S, Patla AE, Winter DA, Ishac MG, Little CE. NACOB presentation CSB New Investigator Award. Balance recovery from medio-lateral perturbations of the upper body during standing. North American Congress on Biomechanics. J Biomech. 1999;32:1149–1158. doi: 10.1016/s0021-9290(99)00116-5. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, Loughin M. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013;381:47–54. doi: 10.1016/S0140-6736(12)61263-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MW, Hedman LD, Johnson ME, Cain TD, Hanke TA. Lateral stability during forward-induced stepping for dynamic balance recovery in young and older adults. J Gerontol A Biol Sci Med Sci. 2001;56:M589–594. doi: 10.1093/gerona/56.9.m589. [DOI] [PubMed] [Google Scholar]
- Rogers MW, Mille ML. Lateral stability and falls in older people. Exercise and sport sciences reviews. 2003;31:182–187. doi: 10.1097/00003677-200310000-00005. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Winter DA. ABC of Balance during Standing and Walking. Waterloo Biomechanics; Waterloo: 1995. [Google Scholar]
- Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K. Stiffness control of balance in quiet standing. J Neurophysiol. 1998;80:1211–1221. doi: 10.1152/jn.1998.80.3.1211. [DOI] [PubMed] [Google Scholar]
- Yang F, Espy D, Pai YC. Feasible stability region in the frontal plane during human gait. Ann Biomed Eng. 2009;37:2606–2614. doi: 10.1007/s10439-009-9798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young PM, Whitall J, Bair WN, Rogers MW. Leg preference associated with protective stepping responses in older adults. Clinical biomechanics (Bristol, Avon) 2013;28:927–932. doi: 10.1016/j.clinbiomech.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yungher DA, Morgia J, Bair WN, Inacio M, Beamer BA, Prettyman MG, Rogers MW. Short-term changes in protective stepping for lateral balance recovery in older adults. Clinical biomechanics (Bristol, Avon) 2012;27:151–157. doi: 10.1016/j.clinbiomech.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]