Highlights
-
•
Sclerosing mediastinitis, also known as fibrosing mediastinitis, is a rare disease.
-
•
We experienced a case of sclerosing mediastinitis without IgG4-related disease.
-
•
This case did not fit the criteria for IgG4-related disease, and it was therefore unclear whether steroid therapy should be used for this case.
-
•
We will continue to carefully follow up this patient’s residual lesion, and there have been no changes in the lesion at present.
Abbreviations: CT, computed tomography; IgG4-RD, IgG4-related disease
Keywords: Sclerosing mediastinitis, Fibrosing mediastinitis, IgG4-related disease
Abstract
Introduction
We herein describe a rare case of a sclerosing mediastinitis without IgG4-related disease. This case was clearly excluded from IgG4-related disease, because this patient’s serum IgG4 level was not elevated. Specifically, this patient’s serum IgG4 level was 7.9 mg/dl (4.8–105).
Presentation of case
A 61-year-old Japanese female presented at our hospital due to an abnormal chest X-ray that showed a growing shadow in the mediastinum. Chest computed tomography (CT) showed an 80 × 75 × 75 mm tumor, which located in the anterior mediastinum. This large tumor surrounded the thoracic aorta, left brachiocephalic vein and superior vena cava. It was difficult to obtain a definitive diagnosis. We tried to perform three biopsies, and eventually performed a partial resection of the tumor.
Discussion
This case did not fit the criteria for IgG4-related disease, and it was therefore unclear whether steroid therapy should be used for this case. We will continue to carefully follow up this patient’s residual lesion, and there have been no changes in the lesion at present.
Conclusion
Sclerosing mediastinitis and IgG4-related disease should be included in the differential diagnosis of patients presenting with a mediastinal tumor. However, sclerosing mediastinitis is difficult to diagnose, and it is important to obtain a sufficient amount of tissue to ensure an accurate diagnosis.
1. Introduction
Sclerosing mediastinitis was first described by Oulmont in 1855, and was believed to be secondary to syphilis or tuberculosis until 1925, when an association with fungal infections was proposed by Knox [4]. Sclerosing mediastinitis, also called fibrosing mediastinitis, is a rare syndrome characterized by an aggressive fibroinflammatory process within the mediastinum [1,2]. Progressive fibrosis caused by the proliferation of invasive fibrous tissue within the mediastinum frequently results in compression and functional compromise of vital mediastinal structures [2,3].
The precise etiology and pathogenesis of sclerosing mediastinitis remain unknown, despite extensive research. There has been a suggested link to Histoplasma capsulatum (H. capsulatum) infection in many North American cases. Because histopathological confirmation is lacking in many cases, it has been proposed that the link between H. capsulatum and sclerosing mediastinitis involves an abnormal hypersensitivity reaction to H. capsulatum antigens, rather than direct infection of the mediastinum [5]. Other etiologies have also been cited, including other infections as well as autoimmune and idiopathic fibroinflammatory causes [5,6]. Recently, It is said that sclerosing mediastinitis may be related to IgG4-related disease (IgG4-RD). Some cases were reported to be examples of IgG4-RD. By definition, IgG4-RD is currently considered to be an idiopathic fibroinflammatory disorder, which is characterized by the expansion of IgG4-producing plasma cells. The triggers and pathogenesis of IgG4-RD remain undefined [9–13].
We experienced a case of sclerosing mediastinitis. This case had diffuse noncalcified involvement of the mediastinum, but this patient did not have autoimmune or fibroinflammatory disease and infection disease. Furthermore, this patient’s serum IgG4 level was not elevated. Specifically, this patient’s serum IgG4 level was 7.9 mg/dl (4.8–105). Therefore, this case did not have IgG4-related disease and was not related to any of the infections previously suggested to cause the condition. Consequently, this case may reveal a new origin of sclerosing mediastinitis.
2. Presentation of Case
A 61-year-old Japanese female presented at our hospital due to an abnormal chest X-ray that showed a growing shadow in the mediastinum (Fig. 1A and B). Chest computed tomography (CT) showed an 80 × 75 × 75 mm tumor, which located in the anterior mediastinum (Fig. 2A and B). This large tumor surrounded the thoracic aorta, left brachiocephalic vein and superior vena cava. The patient had only a minor cough and had no remarkable past medical history. Her tumor marker levels were not elevated. Laboratory tests, including a panel of antibodies for autoimmune processes, an immunohistochemical analysis for lymphoma, fungal serology, sputum smears and cultures for acid-fast bacilli, were all negative.
Fig. 1.

(A) and (B): Chest X-rays showing the growing mediastinal shadow from 2010(A) to 2012 years(B).
Fig. 2.

(A) and (B): Chest computed tomography (CT) scans of the thorax showed an ill-defined and inhomogenously enhanced infiltration at the anterior mediastinum.
We initially tried to perform a core needle biopsy in the anterior mediastinum. However, we could not obtain a definite diagnosis based on this specimen. We next tried an open thoracic biopsy which was performed from the left second intercostal space. At this time, we got a specimen (ϕ15 × 15 × 15 mm). However, no definite diagnosis was possible from this specimen because this specimen was inflammatory change. Finally, we performed a median sternotomy and tried to extirpate the tumor, but could not resect the entire tumor because of its invasion into the superior vena cava and right atrium. Therefore, we resected the left side of the tumor and left brachiocephalic vein, which was replaced with an artificial vessel (The 8 mm diameter Gore-Tex expanded polytetrafluoroethylene graft).
The pathological diagnosis was sclerosing mediastinitis. The ill-defined tumorous lesion was composed of an overgrowth of sclerosing hyalinized fibrocollagenous bundles displaying irregular fascicle or whorl-like structures with a predominant lymphoplasmacytic infiltrate, admixed with a small number of eosinophils, neutrophils and histiocytes, involving the adipose tissue and medium-sized to large arteries in the anterior mediastinum. In the peripheral areas, vasculitis with fibrinoid necrosis and organizing thrombosis was seen in the medium-sized vessels. In the immunohistochemical findings, there were very few IgG4-positive plasma cells (Fig. 3A and B).
Fig. 3.
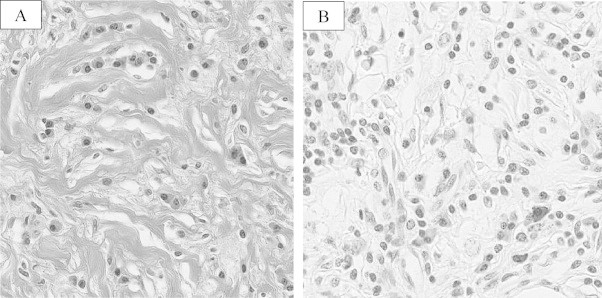
(A) The ill-defined tumorous lesions were composed of an overgrowth of sclerosing hyalinized fibrocollagenous bundles displaying irregular fascicular or whorl-like structures, with a predominant lymphoplasmacytic infiltrate, admixed with a small number of eosinophils, neutrophils and histiocytes, involving the adipose tissue and medium-sized to large arteries in the anterior mediastinum. (B) In the immunohistochemical study, there were only a few IgG4-positive plasma cells, ruling out a diagnosis of IgG4-RD.
3. Discussion
It is difficult to obtain a definitive diagnosis of sclerosing mediastinitis. It is indispensable to exclude other diseases, particularly malignant disease, in cases with sclerosing mediastinitis. Therefore, it is very important to obtain a sufficient quantity of tumor tissue.
In the present case, we first tried to do a core needle biopsy, but could not diagnose the tumor. Then, we tried an open thoracic biopsy, which was performed from the left second intercostal space, but were still unable to obtain a definite diagnosis. Third, we performed a median sternotomy and tried to extirpate the tumor, but could not resect the entire tumor because it had invaded the superior vena cava and right atrium. However, we were finally able to obtain a definite diagnosis.
Fibrous diseases similar to sclerosing mediastinitis occur in the pancreas, peritoneum, salivary gland, etc. [7–9]. Some cases were reported to be examples of IgG4-related disease (IgG4-RD). By definition, IgG4-RD is currently considered to be an idiopathic fibroinflammatory disorder, which is characterized by the expansion of IgG4-producing plasma cells. The triggers and pathogenesis of IgG4-RD remain undefined. However, the disease is typically responsive to glucocorticoid therapy [9–13]. Inoue et al. suggested that the serum IgG4 level is a good selective indicator for steroid therapy in patients with sclerosing mediastinitis [14]. Steroid therapy may also be able to cure patients with sclerosing mediastinitis with IgG4-RD.
However, the present case did not fit the criteria for IgG4-related disease, and the cause remains unknown. Therefore, it is unknown whether steroid therapy should be used for this case. We will continue to carefully follow up this patient’s symptoms and will regularly examine the tumor for changes. When a physician is confronted with a patient who has a mediastinal tumor, it is necessary to include sclerosing mediastinitis and IgG4-RD as potential diagnoses.
4 Conclusion
Sclerosing mediastinitis and IgG4-RD should be included in the differential diagnosis of patients presenting with a mediastinal tumor. However, sclerosing mediastinitis is difficult to diagnose, and it is important to obtain a sufficient amount of tissue to ensure an accurate diagnosis.
Conflict of interest
We have no conflict of interest.
Sources of funding
We have no sources of funding for our research.
Consent
We had informed consent from this patient for writing this paper.
Authors contribution
Soichi Oka: study design, writing.
Hidetaka Uramoto: study design, writing.
Sohsuke Yamada: others.
Fumihiro Tanaka: others.
References
- 1.Flieder D.B., Suster S., Moran C.A. Idiopathic fibroiflammatory (Fibrosing/Sclerosing) lesion of the mediastinum: a study of 30 cases with emphasis on morphologic heterogeneity. Mod. Pathol. 1999;12:257–264. [PubMed] [Google Scholar]
- 2.Peikert T., Colby T.V., Midthun D.E. Fibrosing mediastinitis: clinical presentation, therapeutic outcomes, and adaptive immune response. Medicine. 2011;90:412–423. doi: 10.1097/MD.0b013e318237c8e6. [DOI] [PubMed] [Google Scholar]
- 3.Rossi S.E., McAdams H.P., Rosado-de-Christenson M.L., Franks T.J., Galvin J.R. From the archives of the AFIP: fibrosing mediastinitis. Radiograhics. 2001;21:737–757. doi: 10.1148/radiographics.21.3.g01ma17737. [DOI] [PubMed] [Google Scholar]
- 4.Guerrero A., Hoffer E.K., Hudson L., Schuler P., Karmy-Jones R. Treatment of pulmonary artery compression due to fibrous mediastinitis with endovascular stent placement. Chest. 2001;119:966–968. doi: 10.1378/chest.119.3.966. [DOI] [PubMed] [Google Scholar]
- 5.Rossi S.E., McAdams H.P., Rosado-de-Christenson M.L., Franks T.J., Galvin J.R. Fibrosing mediastinitis. Radiograhics. 2001;21:737–757. doi: 10.1148/radiographics.21.3.g01ma17737. [DOI] [PubMed] [Google Scholar]
- 6.Kandzari D.E., Warner J.J., O'Laughlin M.P., Harrison J.K. Percutaneous stenting of right pulmonary artery stenosis in fibrosing mediastinitis. Catheter. Cardiovasc. Interv. 2000;49:321–324. doi: 10.1002/(sici)1522-726x(200003)49:3<321::aid-ccd20>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 7.Hamano H., Kawa S., Horiuchi A. High serum IgG4 concentrations in patients with sclerosing mediastinitis. N. Engl. J. Med. 2001;344:732–738. doi: 10.1056/NEJM200103083441005. [DOI] [PubMed] [Google Scholar]
- 8.Kitagawa S., Zen Y., Harada K. Abundant IgG4-positive plasma cell infiltration characterizes chronic sclerosing sialadenitis (Kuttner’s Tumor) Am. J. Surg. Pathol. 2005;29:783–791. doi: 10.1097/01.pas.0000164031.59940.fc. [DOI] [PubMed] [Google Scholar]
- 9.Zen Y., Harada K., Sasaki M. IgG4-related scletosing cholangitis with and without hepatic infilammatory pseudotumor, and sclerosing pancreatitis associated sclerosing cholangitis: do they belong to a spectrum of sclerosing pancreatitis. Am. J. Surg. Pathol. 2004;28:1193–1203. doi: 10.1097/01.pas.0000136449.37936.6c. [DOI] [PubMed] [Google Scholar]
- 10.Cheuk W., Chen J.K.C. IgG4-related sclerosing disease a critical appraisal of an evolving clinicopathologic entity. Adv. Anat. Pathol. 2010;17:303–332. doi: 10.1097/PAP.0b013e3181ee63ce. [DOI] [PubMed] [Google Scholar]
- 11.Kamisawa T., Okamoto A. IgG4-related sclerosing disease. World J. Gastroenterol. 2008;14:3948–3955. doi: 10.3748/wjg.14.3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carrutheres M.N., Stone J.H., Khostoshahi A. The latest on IgG4-RD: a rapidly emerging disease. Curr. Opin. Rhumatol. 2012;24:60–69. doi: 10.1097/BOR.0b013e32834ddb4a. [DOI] [PubMed] [Google Scholar]
- 13.Khosroshahi V., Deshpande J. The clinical and pathological features of IgG4-related sisease. Curr. Pheumatol. Reports. 2011;13:473–481. doi: 10.1007/s11926-011-0213-7. [DOI] [PubMed] [Google Scholar]
- 14.Inoue M., Nose N., Nishikawa H., Takahashi M., Zen Y., Kawaguchi M. Successful treatment of sclerosing mediastinitis with a high serum IgG4 leve. Gen. Thorac. Cardiovasc. Surg. 2007;55:431–433. doi: 10.1007/s11748-007-0154-2. [DOI] [PubMed] [Google Scholar]


