Highlights
-
•
Intraosseous meningiomas may be confused with fibrous dysplasia and/or osteoid osteoma.
-
•
Lesions appear either as osteoblastic or osteolytic lesions.
-
•
Usually presents as a painless palpable mass associated with headaches.
-
•
Embryological remnants of neuroectodermal tissue or cellular dedifferentiation seem to justify the lack of dural connections.
-
•
Complete surgical excision is usually curative.
Keywords: Meningioma, Brain tumor, Benign
Abstract
Background
Meningiomas are the most common benign neoplasm of the brain whereas ectopic presentation, although reported, is rare. Among these ectopic tumors, there are a group of purely intraosseous meningiomas, which usually are diagnosed differentially from common primary osseous tumor such as fibrous dysplasia and osteoid osteoma.
Case description
We report a 62-year-old female with a history of headaches and 6 months of progressive right parietal bulging, with no neurological signs. Parietal craniotomy was performed with immediate titanium cranioplasty of the parietal convexity. Histopathology exams revealed an ectopic intradiploic meningioma without invasion of cortical layers, with positive staining for progesterone receptors and epithelial membrane antigen.
Conclusions
Ectopic intraosseous meningiomas remain a rare neoplasm with only a few cases reported. The main theories to justify the unusual topography appear to be embryological remains of neuroectodermal tissue or cellular dedifferentiation. Surgical treatment seems the best curative option.
1. Introduction
Meningioma is the most common type of benign brain tumor [1], whereas ectopic meningioma, although reported, is rare. The head and neck region is the most common ectopic site whereas the scalp, skin, orbit, paranasal sinuses, salivary glands, and intraosseous or intradiploic regions can also be affected [2–5].
In view of their rarity, ectopic meningiomas of the skull are usually not the first preoperative suspicion. The main differential diagnoses are fibrous dysplasia and osteoid osteoma, the most common being benign primary tumors [6]. We report herein the case of a 62-year-old female patient with a pure ectopic intraosseous meningioma without dural invasion.
2. Presentation of case
A 62-year-old female patient presented with a history of classical migraine for the last 30 years. Six month before the diagnosis, her headaches had changed their characteristics to a continuous unilateral (right side) pain of increasing intensity. The patient reported no nausea or vomiting, which usually followed her typical migraines. Also, the patient noted a growing lump on the right parietal side and was referred to our service by her primary care physician. On neurological examination, the patient was alert and oriented, complaining of moderate headache. A hard, slightly painful, elliptical prominence without clearly defined margins was detected on her right parietal bone, which measured approximately 7 × 8 cm.
MRI images showed an osteoblastic lesion in the right parietal bone diploe, with possible involvement of both cortical layers and without dural extension (Fig. 1). The patient was scheduled for elective surgery in the following week. The surgical procedure consisted of a right parietal incision and craniotomy and was completed without intercurrences. The lesion was visible on the outer surface due to bone protrusion. Craniotomy was performed with a clear 1-cm margin and skull convexity was reconstructed with a titanium mesh (Fig. 2).
Fig. 1.
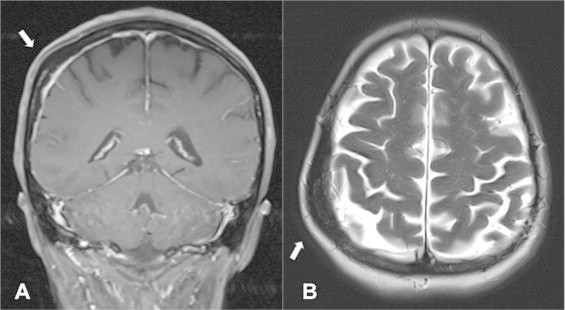
(A) T1-weighted coronal gadolinium-enhanced MRI scan showing an expansive diploic lesion (white arrow) without enhancement or dural invasion. (B) T2-weighted axial scan showing the expansive non-lytic tumor.
Fig. 2.

Intraoperative images. (A) Right parietal arciform incision showing the prominent bone in the center. (B) Bone flap after craniotomy. (C) Cranioplasty with a titanium mesh.
Histopathological examination revealed an ectopic intraosseous meningothelial meningioma, WHO grade 1. Immunohistochemical staining was positive for progesterone receptor and epithelial membrane antigen (Fig. 3). There was no involvement of the cortical layers or pericranium.
Fig. 3.
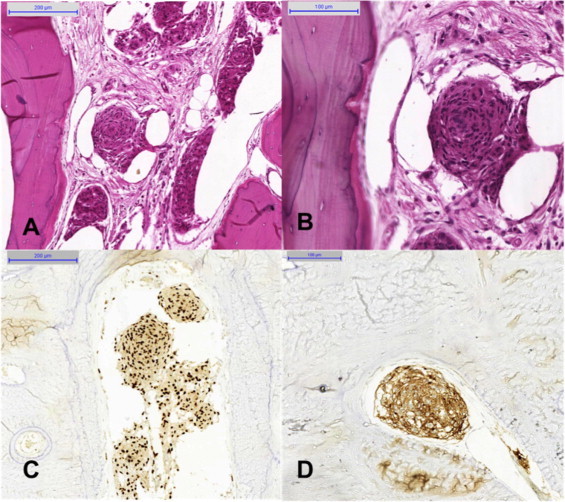
Photomicrographs showing islands of eosinophilic cells arranged in clusters and whorls in the bone fragment. Note the absence of nuclear pleomorphism. H&E, 100× (A) and 200× (B). Positive immunohistochemical staining for progesterone receptor (C, 100×) and epithelial membrane antigen (D, 200×).
The patient was discharged two days after surgery without headaches or other symptoms. Ten months after surgery, the patient remains asymptomatic and shows no signs of recurrence (Fig. 4).
Fig. 4.
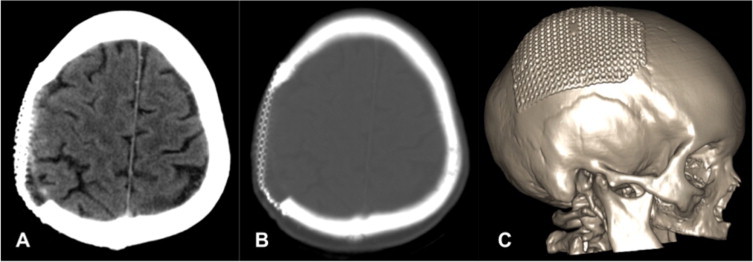
A 10-month postoperative head CT scan showing the right parietal craniotomy with the reconstructive titanium mesh and absence of residual lesions. A: brain window; B: bone window; C: 3D reconstruction.
3. Discussion
A small number of meningiomas without any dural connection has been described. Consequently, any lesions occurring outside the central nervous system are very rare [7]. Ectopic intraosseous meningiomas can also be described as intradiploic or calvarial [8] and may appear as osteoblastic [5,9], osteolytic lesions [4,10–14] or mixed lesions [8] on plain X-rays and computed tomography scans. The present case was a rare intradiploic meningioma. Further investigation by MRI can identify ectopic meningiomas, which do not exhibit the usual paramagnetic contrast enhancement.
The clinical presentation of the present case is similar to that found in previously reported cases of skull tumors, usually headaches and an often painless, palpable mass on the scalp or skull [2,4,10,11,12,15]. Involvement of other ectopic sites such as the paranasal sinuses and orbit usually manifests as pain and proptosis [16], whereas pain and a palpable mass are common when the tumor affects more distant sites. Histologic examination usually presents meningothelial meningiomas, but the microcystic [8] or lipomatous [14] variations are also reported. Immunohistochemical staining is usually positive for progesterone receptor, epithelial membrane antigen as in our described case, and S100 [8,14].
In 1960, Hoye et al. [17] reviewed the latest case reports and proposed the classification of ectopic meningiomas into four types: (1) intracranial tumors with extracranial extension; (2) meningiomas originating in cranial nerve sheaths; (3) extracranial tumors without any connection to cranial nerve foramina; (4) intracranial benign lesions with extracranial metastases. In 2000, Lang et al. [18] described a similar, but simpler classification: type 1, purely extracalvarial tumors; type 2, purely calvarial tumors, and type 3, calvarial tumors with extracalvarial extension. Each type is further divided according to location into skull base (S) or calvarial (C) lesions. Our case is classified as type 3 in Hoye’s classification and type 2 in Lang’s classification, since the lesion was restricted to the skull (inner and outer tables), showing no dural invasion on histopathological examination, supporting the hypothesis that the tumor originated in the diploe layer.
Some theories have been offered to explain how a meningioma can appear distant from the usual arachnoid cap cells (meningocytes) [19,20]. One theory suggests that embryological remains of neuroectodermal tissue, which should develop into cap cells, can expand [21] or erroneously migrate to other tissues [4,20]. Other theories that could account for some cases are the spreading of these remnant cells due to trauma, dural lesions, or cells entrapped in cranial sutures and cranial nerve sheaths [22,23]. Some authors proposed the occurrence of dedifferentiation of cells in extracranial tissues, which develop into neoplastic meningocytes [2,24]. None of these theories could be confirmed in the present case, but a probable intradiploic origin is suggested.
Overall, most meningiomas, including ectopic tumors, are benign; therefore, their complete surgical excision should be the rule [2,8,9,21]. Partial resection of residual lesions can be monitored radiologically, while adjuvant therapies such as radiation may provide an alternative for symptomatic and surgically difficult cases [5].
4. Conclusions
Ectopic meningiomas are uncommon, whereas intraosseous meningiomas are even rarer. These tumors are usually benign, without a fully elucidated natural history. Surgical resection remains the only curative option.
Conflict of interest
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this Journal.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author’s contributions
RBV: drafted and designed the manuscript and participated in surgery; PTHF: drafted and coordinated the manuscript; RLL: participated in surgery and reviewed the Literature for previous cases; VZM and FOL: analyzed the pathological and histological materials; FRR: coordinated surgery and grammatical review. MAZ: performed the final review. All authors read and approved the final manuscript.
Contributor Information
Roberto Bezerra Vital, Email: Roberto_vital@hotmail.com.
Pedro Tadao Hamamoto Filho, Email: pthamamotof@hotmail.com.
Renan Luiz Lapate, Email: relapate@gmail.com.
Vinícius Zanin Martins, Email: viniciuszanin@gmail.com.
Flávio de Oliveira Lima, Email: Flavioolima@fmb.unesp.br.
Flávio Ramalho Romero, Email: frromero@ig.com.br.
Marco Antônio Zanini, Email: mzanini@fmb.unesp.br.
References
- 1.Wong R.H., Wong A.K., Vick N. Natural history of multiple meningiomas. Surg. Neurol. Int. 2013;4:71. doi: 10.4103/2152-7806.112617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cirak B., Guven M.B., Ugras S. Fronto-orbitonasal intradiploic meningioma in a child. Pediatr. Neurosurg. 2000;32(1):48–51. doi: 10.1159/000028897. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi S., Kyoshima K., Nakagawa F. Diploic meningioma of the orbital roof. Surg. Neurol. 1980;13(4):277–281. [PubMed] [Google Scholar]
- 4.Kuzeyli K., Duru S., Baykal S. Primary intraosseous meningioma of the temporal bone in an infant. A case report. Neurosurg. Rev. 1996;19(3):197–199. doi: 10.1007/BF00512053. [DOI] [PubMed] [Google Scholar]
- 5.Crawford T.S., Kleinschmidt-DeMasters B.K., Lillehei K.O. Primary intraosseous meningioma. Case report. J. Neurosurg. 1995;83(5):912–915. doi: 10.3171/jns.1995.83.5.0912. [DOI] [PubMed] [Google Scholar]
- 6.Selva D., White V.A., O’Connell J.X. Primary bone tumors of the orbit. Surv. Ophthalmol. 2004;49(3):328–342. doi: 10.1016/j.survophthal.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Farr H.W., Gray G.F., Jr., Vrana M. Extracranial meningioma. J. Surg. Oncol. 1973;5(5):411–420. doi: 10.1002/jso.2930050503. [DOI] [PubMed] [Google Scholar]
- 8.Velazquez Vega J.E., Rosenberg A.E. Microcystic meningioma of the calvarium: a series of 9 cases and review of the Literature. Am. J. Surg. Pathol. 2014 doi: 10.1097/PAS.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 9.Budhdeo S., Ibrahim R.A., Hofer M. Primary intraosseous osteoblastic meningioma. JRSM Short Rep. 2011;2(6):52. doi: 10.1258/shorts.2011.011066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muthukumar N. Primary calvarial meningiomas. Br. J. Neurosurg. 1997;11(5):388–392. doi: 10.1080/02688699745862. [DOI] [PubMed] [Google Scholar]
- 11.Tokgoz N., Oner Y.A., Kaymaz M. Primary intraosseous meningioma: CT and MRI appearance. AJNR Am. J. Neuroradiol. 2005;26(8):2053–2056. [PMC free article] [PubMed] [Google Scholar]
- 12.Agrawal V., Ludwig N., Agrawal A. Intraosseous intracranial meningioma. AJNR Am. J. Neuroradiol. 2007;28(2):314–315. [PMC free article] [PubMed] [Google Scholar]
- 13.Tang V., Lam M., Lai A. Intraosseous meningioma mimicking a metastasis. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-207633. http://www.hindawi.com/journals/crinm/2015/482140/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim L., Huang C., Morey A.L. Intraosseous lipomatous meningioma. Case Rep. Neurol. Med. 2015;2015:482140. doi: 10.1155/2015/482140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akhaddar A., Ennouali H. Intraosseous extradural meningioma of the frontal bone. Pan Afr. Med. J. 2014;17:69. doi: 10.11604/pamj.2014.17.69.3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daffner R.H., Yakulis R., Maroon J.C. Intraosseous meningioma. Skeletal Radiol. 1998;27(2):108–111. doi: 10.1007/s002560050347. [DOI] [PubMed] [Google Scholar]
- 17.Hoye S.J., Hoar C.S., Jr., Murray J.E. Extracranial meningioma presenting as a tumor of the neck. Am. J. Surg. 1960;100:486–489. doi: 10.1016/0002-9610(60)90394-9. [DOI] [PubMed] [Google Scholar]
- 18.Lang F.F., Macdonald O.K., Fuller G.N. Primary extradural meningiomas: a report on nine cases and review of the literature from the era of computerized tomography scanning. J. Neurosurg. 2000;93(6):940–950. doi: 10.3171/jns.2000.93.6.0940. [DOI] [PubMed] [Google Scholar]
- 19.Marta G.N., Correa S.F., Meningioma Teixeira M.J. review of the literature with emphasis on the approach to radiotherapy. Expert Rev. Anticancer Ther. 2011;11(11):1749–1758. doi: 10.1586/era.11.162. [DOI] [PubMed] [Google Scholar]
- 20.Altinors N., Cetin A., Pak I. Scalp meningioma: case report. Neurosurgery. 1985;16(3):379–380. doi: 10.1227/00006123-198503000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Elder J.B., Atkinson R., Zee C.S. Primary intraosseous meningioma. Neurosurg. Focus. 2007;23(4):E13. doi: 10.3171/FOC-07/10/E13. [DOI] [PubMed] [Google Scholar]
- 22.Kaneko F., Takase K., Nishiyama K. Report of a case of intraosseous meningioma. No Shinkei Geka. 1988;16(2):197–202. [PubMed] [Google Scholar]
- 23.Azar Kia B., Sarwar M., Marc J.A. Intraosseous meningioma. Neuroradiology. 1974;6(5):246–253. doi: 10.1007/BF00345784. [DOI] [PubMed] [Google Scholar]
- 24.Shuangshoti S., Netsky M.G., Fitz-Hugh G.S. Parapharyngeal meningioma with special reference to cell of origin. Ann. Otol. Rhinol. Laryngol. 1971;80(3):464–473. doi: 10.1177/000348947108000327. [DOI] [PubMed] [Google Scholar]


