Highlights
-
•
Intussusception is rare in adults.
-
•
Lipoma of the sigmoid colon is rare.
-
•
Colonic lipoma should be considered in the differential diagnosis of adults with intussusception with high index of suspicion for obstruction when lipoma is >2 cm.
-
•
CT scan is an excellent diagnostic modality for adult intussusception.
-
•
Surgical reduction followed by resection leads to excellent results in adults diagnosed with sigmoidorectal intussusception secondary to colonic lipoma.
Keywords: Intussusception, Adult, Sigmoid, Rectal, Lipoma, Colon
Abstract
Introduction
Adult intussusception is rare. Lipoma is the second most common benign tumor of the colon and most common to cause colonic intussusception in adults, but rare.
Presentation of case
A 35-years-old male presented with a history of intermittent abdominal pain and bright red rectal bleeding, with symptoms waxing and waning for one month. On physical examination, the abdomen was distended with tenderness over the periumbilical, suprapubic, and left lower quadrant regions with guarding. CT demonstrated colo-colonic intussusception of the sigmoid colon with a 2.3 cm × 2.6 cm intra-mural lipoma of the rectosigmoid region. The patient underwent an exploratory laparotomy with partial reduction of the intussusception, sigmoid colon resection and end colostomy. Histopathology confirmed a 2.5 cm sub-mucosal lipoma without evidence of malignancy.
Discussion
Sixty–sixty five percent of cases with intussusception of the large bowel in adults are related to a malignant etiology and most cases of sigmoidorectal intussusception reported in the literature are secondary to underlying malignancy. Colo-colic intussusception is the most common type of intussusception in adults. The incidence of lipomas of the large intestine is reported to range from 0.035% to 4.4%. Ninety percent of colonic lipomas are submuscosal and are mostly located in the right hemicolon. Only 25% of patients with colonic lipoma develop symptoms. Colonic lipomas of the rectosigmoid region represent a very rare occurrence and subsequent etiology for sigmoidorectal intussusceptions in adults.
Conclusion
Colonic lipoma should be considered in the differential diagnosis of adults with intussusception, with reduction and resection leading to excellent results.
1. Introduction
Intussusception in adults is rare and accounts for less than 5% of all intussusception cases [1]. Colonic lipoma is rare, and can serve as the lead point for intussusception [2,3].Adult intussusception cases present with nonspecific signs and symptoms and CT scan is the most sensitive diagnostic modality. We report a sigmoidorectal intussusception in an adult in whom an intramural lipoma was identified as the lead point.
2. Presentation of case
A 35-year-old male, with no prior medical or surgical history, presented to the emergency department with a history of progressive abdominal pain and bright red rectal bleeding between and after bowel movements, with symptoms waxing and waning for one month. On presentation, he experienced severe, constant, sharp non-radiating lower abdominal pain described as 10/10 followed by a single episode of greenish emesis.
On physical examination, the patient was in painful distress. Vital signs were normal. The abdomen was distended with tenderness over the periumbilical, suprapubic, and left lower quadrant regions with guarding. There was no nausea, constipation, diarrhea or rectal pain. Bowel sounds were normal. There were no additional signs to suggest peritonitis or acute intestinal obstruction. Three-view plain abdominal x-rays were performed and did not show signs of obstruction or perforation. CT of the abdomen and pelvis demonstrated colo-colonic intussusception of the sigmoid colon with a 2.3 cm × 2.6 cm intra-mural lipoma of the recto-sigmoid region likely to be the lead point and no signs of large bowel obstruction (Figs. 1–4). In the absence of signs suggestive of acute intestinal obstruction and apparent benign nature of the mass on CT, the patient was admitted for initial lower gastrointestinal endoscopy to confirm the lipoma and exclude malignancy. Re-examination on post-admission day one revealed a soft, mildly distended abdomen without guarding and with normal bowel sounds. Vital signs remained within normal. Lower gastrointestinal endoscopy was performed and proctoscopy revealed congested, friable colonic mucosa that completely filled the rectal lumen without evidence of malignancy (Fig. 5). Reduction was not attempted as it did not appear feasible. Exploratory laparotomy was carried and reduction of the intussusception was attempted. Only partial reduction was possible and segmental sigmoidectomy (21 cm) was performed leaving approximately 10 cm of intussusceptum within the intussuscepiens. The condition of the bowel was sub-optimal for primary anastomosis. Both bowel segments after resection were inflamed and edematous, thus end colostomy was performed. The histopathology report confirmed a 2.5 cm sub-mucosal lipoma with no evidence of dysplasia or malignancy. The postoperative period was uneventful and the patient was discharged on the fifth postoperative day. The patient underwent an elective reversal of his colostomy with primary anastomosis after 6 months of follow-up and is doing well.
Fig. 1.

Axial view showing the proximal part of the colo-colonic intussusception of the sigmoid colon.
Fig. 2.

Axial view showing a mass (lipoma) filling the distal sigmoid colon that was the lead point.
Fig. 3.

Coronal view.
Fig. 4.

Sagittal view showing mass (lipoma) filling the distal sigmoid.
Fig. 5.
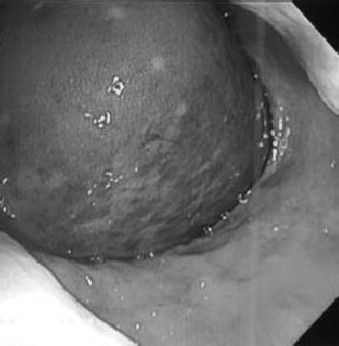
Colonoscopy showing obstruction/intussusception.
3. Discussion
Adult intussusception is a rare clinical condition which constitutes less than 5% of all cases of intussusception and 1–3% of all cases of intestinal obstruction [1]. Intussusception is a process in which a proximal segment of bowel telescopes or invaginates into an adjacent distal segment. The pathophysiology usually involves a lesion in the bowel wall or an irritant in its lumen serving as a lead point that may change the normal peristaltic pattern and initiate the invagination leading to intussusception. Intussusception that occurs in absence of a lead point is classified as primary or idiopathic and is more likely to occur in the small intestines, or as secondary when a lead point is identified [1,4].
Secondary intussusception can be due to benign, malignant, or iatrogenic causes [5]. In adults, intussusception has an identifiable etiology in 90% of cases [6]. In the small intestine, benign lesions represent the majority of lead points, and only 25–30% are malignant lesions [1,7]. Conversely, 60–65% of cases of intussusception occurring in the large bowel have a malignant etiology [1].
Lipomas may occur throughout the intestinal tract with highest incidence in the colon [6]. The reported incidence of lipomas of the large intestine ranges from 0.035% to 4.4% [6,8]. Ninety percent of colonic lipomas are submucosal and mostly located in the right hemicolon [6,8]. Lipomas larger than 4 cm are considered giant, and those larger than 2 cm in diameter can cause bowel obstruction without intussusception [6,9,10]. Over a period of 45 years, only 46 cases of colonic intussusception secondary to colonic lipomas have been reported in the English language literature [6].
Intussusception may be classified into 4 main types depending on its location: (1) entero-enteric – involving the small intestine, (2) colo-colic – involving the large intestine, (3) ileo-colic – involving the terminal ileum and ascending colon, and [4] ileo-cecal – involving the ileo-cecal valve as the lead point. In clinical practice, it is difficult to distinguish between ileo-colic and ileo-cecal [1]. In adults, colo-colic intussusception is the most common type [11]. The colo-colic entity may be further sub-classified into: (1) colo-rectal – colon invaginates through rectal ampulla and (2) recto-rectal – with rectum invaginating into the rectum but with no anal protrusion [1]. Other rare reported locations not included in this classification are gastroduodenal intussusception, and retrograde jejunogastric intussusception following gastro-jejunostomy.
Early diagnosis of adult intussusception is a challenging task because most cases present with non-specific signs and symptoms and have a chronic or sub-acute course. Abdominal pain is the most common presenting symptom before intussusception. Colonic lipomas are usually asymptomatic but may rarely cause bleeding, obstruction and intussusception. The four cardinal symptoms of bowel obstruction are pain, vomiting, obstipation/absolute constipation, and distention. Obstipation, change in bowel habits, complete constipation, and abdominal distention are the predominant symptoms in large bowel obstruction [12]. Only 25% of patients with colonic lipoma develop symptoms [6]. Symptom duration before intussusception may vary from 1 day to 7 years, and the size of the lipoma is a predictor of symptomatology [6]. After intussusception, symptoms are specific to the intussusception rather than the lipoma. Only about 10% of adult intussusception present with the typical triad of abdominal pain, palpable mass and bloody stool, with abdominal pain being the most common symptom followed by nausea and vomiting, and bleeding per rectum [7,13]. Symptom duration is usually longer in benign as compared with malignant lesions, and in enteric as compared with colonic lesions [14]. This variable presentation along with the chronic indolent course of the disease contributes to the fact that most cases are diagnosed at emergent laparotomy when bowel ischemia supervenes. Preoperative diagnosis has been reported at rates as low as 40.7% and 50% [1].
Abdominal CT is the most sensitive diagnostic modality with reported accuracy ranging from 58% to 100% [1]. The characteristic ‘target’ sign or the ‘sausage-shaped’ soft tissue mass with a layering effect is a classical finding. Mesenteric vessels within the bowel lumen are also typically described. The CT can often differentiate between lead point and non-lead point intussusceptions. In patients presenting with sub-acute or chronic large bowel obstruction, flexible lower gastrointestinal endoscopy is helpful in confirming the diagnosis of intussusception, detecting its location, diagnosing the underlying lesion (lead point), and may represent a treatment option.
Adult intussusception is almost always treated surgically. There is debate on whether reduction of the intussusception should be attempted before resection. Reducing the intussusception before resection caries the risk of disseminating malignant cells when an underlying malignancy is suspected. On the other hand, the advantage of reduction, especially in the small bowel, is preservation of considerable lengths of the bowel to prevent development of short bowel syndrome. Several authors have suggested surgical resection without reduction (en bloc resection) when the bowel is inflamed, ischemic or friable, or when the risk of malignancy is high [4,15,16]. Azar et al. suggested that surgical resection without reduction is generally the preferred treatment in adults, as almost 50% of both colonic and enteric intussusceptions are associated with malignancy [4,14]. However, reduction is acceptable in post-traumatic, idiopathic, and benign lead point intussusceptions. While intussusception itself has good prognosis, the main prognostic factor affecting the course of the disease is the nature of the causative lesion. Mortality for adult intussusception increases from 8.7% for the benign lesions to 52.4% for the malignant variety [7].
4. Conclusion
Sigmoidorectal intussusception in adults secondary to intramural lipoma is rare. Colonic lipoma may result in complete obstruction despite the absence of some cardinal features of acute intestinal obstruction. Colonic lipoma should be considered in the differential diagnosis of adults with intussusception and high index of suspicion for obstruction should be maintained especially when the lipoma is >2 cm. Surgical reduction followed by sigmoid resection represents an excellent treatment modality in intussusception secondary to colonic lipoma.
Conflicts of interest
None.
Sources of funding
None.
Ethical Approval
Hurley Medical Center Scientific Review Committee was contacted and verified that IRB approval was not required for this case report.
Author contribution
All authors were involved in the preparation of this manuscript. Mohamed Mohamed designed and performed all aspects of the operation. Karim Elghawy assisted in data collection and drafting the manuscript. Donald Scholten, Kenneth Wilson and Michael McCann made substantial edits and revisions to the drafted manuscript. Michael McCann contributed to the design and provided overall supervision of the paper. All authors read and approved this article.
Consent
Permission to release information, photographs or video tapes was obtained from the patient for the purpose of publication of this case report. The consent form number *001142* was signed by the patient and the corresponding author, and is available for review by the Editor-in-Chief of this journal upon request.
Guarantor
Mohamed Mohamed, MD.Michael McCann, DO.
References
- 1.Ongom P.A., Kijjambu S.C. Adult intussusception: a continuously unveiling clinical complex illustrating both acute (emergency) and chronic disease management. OA Emergency Med. 2013;1(August 01 (1)):3. [Google Scholar]
- 2.Babu K.V., Chowhan A.K., Yootla M., Reddy M.K. Submucous lipoma of sigmoid colon: a rare entity. J. Lab Phys. 2009;1(July (2)):82–83. doi: 10.4103/0974-2727.59706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrei L.S., Andrei A.C., Usurelu D.L., Puscasu L.I., Dima C., Preda E., Lupescu I., Herlea V., Popescu I. Chirurgia (Bucur) 2014;109(Janurary–Februay (1)):142–147. [PubMed] [Google Scholar]
- 4.Yalarmathi S., Smith R.C. Adult intussusception: case reports and review of literature. Postgrad. Med. J. 2005;81:174–177. doi: 10.1136/pgmj.2004.022749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishii M., Teramoto S., Yakabe M. Small intestinal intussusceptions caused by percutaneous endoscopic jejunostomy tube placement. J. Am. Geriatr. Soc. 2007;55(December (12)):2093–2094. doi: 10.1111/j.1532-5415.2007.01439.x. [DOI] [PubMed] [Google Scholar]
- 6.Paskauskas S., Latkauskas T., Valeikaite G., Parseliunas A., Svagzdys S., Saladzinkas Z. Colonic intussusception caused by colonic lipoma: a case report. Medicina (Kaunas) 2010;46(7):477–481. [PubMed] [Google Scholar]
- 7.Soni S., Moss P., Jaiganesh T. Idiopathic adult intussusception. Int. J. Emergency Med. 2011;4:8. doi: 10.1186/1865-1380-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nallamothu G., Adler D.G. Review large colonic lipoma. Gastroenterol. Hepatol. 2011;7(7):490–492. [PMC free article] [PubMed] [Google Scholar]
- 9.Chiba T., Suzuki S., Sato M. A case of a lipoma in the colon complicated by intussusception. Eur. J. Gastroenterol. Hepatol. 2002;14:701–702. doi: 10.1097/00042737-200206000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Bahadursingh A.M., Robbins P.L., Longo W.E. Giant submucosal sigmoid colon lipoma. Am. J. Surg. 2003;186:81–82. doi: 10.1016/s0002-9610(03)00111-9. [DOI] [PubMed] [Google Scholar]
- 11.Olakolu S., Lloyd C., Day G., Wellington P. Adult intussusception: managed by reduction–resection; a case report. Internet J. Third World Med. 2012;10(1) [Google Scholar]
- 12.M.N. Kulaylat, R.J. Doer, Small bowel obstruction. In: R.G. Holzheimer, J.A. Mannick, (Eds). Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt, (2001). Available from: <http://www.ncbi.nlm.nih.gov/books/NBK6873/>. [PubMed]
- 13.Allos Z., Zhubandykova D. Large benign submucosal lipoma presented with descending colonic intussusception in an adult. Am. J. Case Rep. 2013;14:245–249. doi: 10.12659/AJCR.883975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azar T., Berger D.L. Adult intussusception. Ann. Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Begos D.G., Sandor A., Modlin I.M. The diagnosis and management of adult intussusception. Am. J. Surg. 1997;73:88–94. doi: 10.1016/S0002-9610(96)00419-9. [DOI] [PubMed] [Google Scholar]
- 16.Khan M.N., Agrawal A., Strauss P. Intussusception–a rare cause of acute intestinal obstruction in adults: case report and literature review. World J. Emerg. Surg. 2008;3(26) doi: 10.1186/1749-7922-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]


