Abstract
The purpose of the present study was to apply Berg and Upchurch’s (2007) developmental-conceptual model to understand better how couples cope with cancer. Specifically, we hypothesized a dyadic appraisal model in which proximal factors (relational quality), dyadic appraisal (prognosis uncertainty), and dyadic coping (communication efficacy) predicted adjustment (cancer management). The study was cross-sectional and included 83 dyads in which one partner had been diagnosed with and/or treated for cancer. For both patients and partners, multilevel analyses using the actor-partner interdependence model (APIM) indicated that proximal contextual factors predicted dyadic appraisal and dyadic coping. Dyadic appraisal predicted dyadic coping, which then predicted dyadic adjustment. Patients’ confidence in their ability to talk about the cancer predicted their own cancer management. Partners’ confidence predicted their own and the patient’s ability to cope with cancer, which then predicted patients’ perceptions of their general health. Implications and future research are discussed.
Keywords: Cancer, Couples, Communication, Dyadic Coping, Efficacy, Chronic Illness
The American Cancer Society estimates that more than 1.2 million Americans will be diagnosed with cancer this year alone, resulting in at least one half million deaths (ACS, 2012). Men have an approximate 50% and women a 33% lifetime risk of being diagnosed with cancer, and more than 50% of all types of cancer cannot be cured. If incidence rates remain stable, the total number of cancer cases is expected to double by 2050. Significant advances in cancer care allow for long-term cancer management and survivorship, both of which translate to individuals and partners managing illness for extended periods. Due to this protracted management period, in part, many health-care practitioners consider some cancer patients to be living with a chronic rather than acute condition (National Comprehensive Cancer Network [NCCI], 2013). The Centers for Disease Control (CDC) (2013a, 2013b) describes chronic illnesses as prolonged in duration, not resolving spontaneously, and rarely cured completely. The chronic nature of cancer management affects not only patients but also partners and families (Acitelli & Badr, 2005; Bodenmann, 2005). Living with cancer additionally affects communication patterns between patients and close others (Goldsmith, Miller, & Caughlin, 2007). The developmental-contextual model (DCM: Berg & Upchurch, 2007) presents one approach for considering the effect of patients’ and partners’ perceptions about communication and illness uncertainty on cancer management. Berg and Upchurch’s (2007) DCM describes how contextual factors, dyadic appraisal, and dyadic coping affect patient and partner adjustment to chronic illness. This manuscript uses the DCM to explore how patients’ and partners’ perceptions of relational quality, illness uncertainty, and communication efficacy affect cancer management.
Couples’ Cancer Management
An important supposition of this manuscript is that cancer is managed (or “coped with”) dyadically. Different from individual coping, various terms such as dyadic coping (e.g., Revenson, Kayser, & Bodenmann, 2005), relational-focused coping (e.g., Coyne & Smith, 1991; O’Brien & DeLongis, 1997), communal coping (e.g., Afifi et al.,2006), collaborative coping (e.g., Berg et al., 2008), and a “we” orientation are used to refer to the notion of two people (e.g., patient and partner) together managing one partner’s chronic illness. Although we use the term dyadic (Berg & Upchurch, 2007), the other terms are used interchangeably in literature. An assumption of dyadic management of chronic illnesses such as cancer is that both partners should be motivated to help one another, manage stressful situations, and to engage in a joint effort to manage those stressors (Bodenmann, 2005).
Managing a chronic illness such as cancer affects both individuals and their partners (Berg & Upchurch, 2007), and cancer management both affects and is affected by communication between partners (Kuijer et al., 2000; Manne et al., 2006,2007). A sizable body of research exists on how couples cope with the stresses associated with managing a chronic illness (Revenson et al., 2005), including literature specifically related to coping with cancer (Goldsmith et al., 2007). For example, both cancer patients and their partners report experiencing anxiety and depression (Lambert, Jones, Girgis, Lecathelinais, & DESS de Mathematicques Appliquees, 2012), fear (Lyons, Jacobson, Prescott, & Oswalt, 2002), and feelings of vulnerability (McWilliam, Brown, & Stewart, 2000). Although much research isdevoted to the experiences of cancer patients, in some cases the psychological burden is greater for partners than patients (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008). These stressors are some of the cancer management-related aspects that affect and are affected by couples’ communication.
Dyadic cancer management is complicated by differential illness experience. That is, couples experience the effects of one partner’s illness differently in their relationships (Berg et al., 2008; Checton, Greene, Magsamen-Conrad, & Venetis,2012; Fagundes, Berg, & Wiebe, 2012; Merz et al., 2011). Differential illness experiences between patients and partners are worth exploring to develop strategies for supporting couples, especially with respect to variables over which they have control (e.g., communication perceptions, patterns, and practices) in comparison to those they cannot control (e.g., the chronic illness itself). The DCM (Berg & Upchurch, 2007) is a useful framework for understanding how dyadic coping may vary across different illness contexts (described below). Communication performs a central function in adaptation, negotiation, and management in the context of couples’ dyadic illness management (e.g., information management; see Checton et al., 2012; Checton & Greene, 2012; Steuber & Solomon, 2011, 2012). The purpose of the present study was to apply the DCM framework to couples’ perceptions about cancer communication and management.
DCM
The DCM (Berg & Upchurch, 2007) is a theoretical explanation of how contextual factors, dyadic appraisal, and dyadic coping affect patient and partner adjustment to chronic illness, which we apply to the cancer context. The DCM incorporates a range of developmental features such as how dyadic illness-related coping differs across the lifespan (e.g., young, middle-age, late adulthood), during specific historical times (set expectations for relationships), and throughout the different stages of chronic illness (e.g., initial cancer diagnosis, treatment such as chemotherapy, and daily management). Because disease management, relationships, and individuals change across time, models of disease experiences must take these multiple factors into account, such as by using samples with variability in a range of relationship and disease developmental features (e.g., age, length of disease management, relationship length). Consistent with prior literature, the DCM views chronic illness as affecting not only patients but also partners, “as they are mutually involved in each other’s stressors” (Berg & Upchurch, 2007, p. 933), therefore requiring both patients’ and partners’ assessments of appraisal, coping, and adjustment. Further, the DCM suggests that patients’ and partners’ assessments of contextual characteristics, appraisal, and coping and adjustment are correlated. The following sections focus on these factors.
Contextual characteristics
The DCM (Berg & Upchurch, 2007) suggests that couples who experience chronic illness are affected by sociocultural and proximal contextual factors. Sociocultural contextual factors relate to culture, socioeconomic issues, age, and sex. Previous research indicates that sex may influence cancerpatients’ preferences concerning health care (Wessels et al., 2010), communication about cancer (Goldsmith et al., 2007), distress in coping with cancer (Hagedoorn et al., 2008), and management of chronic illnesses (including cancer) at work (Munir, Pryce, Haslam, Leka, & Griffiths, 2006). Therefore, we ask about the effect of sex on proximal contextual, appraisal, coping, and management factors.
Proximal contextual factors such as relationship quality and illness condition (e.g., length diagnosed) are correlated between partners and influence dyadic appraisal, coping, and adjustment. Previous research indicates that the quality of couples’ relationships plays an important role in helping people maintain their physical and psychological well-being (Uchino, 2004). Recent studies of disclosing information indicate that relational quality is a significant predictor of perceived ability to share the information with others (Afifi & Steuber, 2009; Checton & Greene, 2012; Greene et al., 2012). Further, the transactional nature of the DCM (Berg & Upchurch, 2007) suggests that relational quality can increase the likelihood of positive dyadic appraisal and dyadic coping and be further enhanced by such coping processes (p. 933; see also Berg et al., 2008). Therefore, we suggest that couples’ perceptions of relational quality may serve as an indicator of proximal contextual factors, and that relational quality positively predicts couples’ dyadic appraisal and dyadic coping.
Dyadic appraisal
Dyadic appraisal is the second major component of the DCM, and dyadic appraisal parallels between partners. Berg and Upchurch (2007) examine three aspects of dyadic appraisal including illness representations, illness ownership, and specific stressor appraisal. For example, couples’ illness representations address questions such as “Is the illness controllable?” and “What are the consequences of the illness?,” and this parallels prior research that has explored how individuals evaluate their illness experiences (Babrow, 2001, 2007; Mishel & Clayton, 2003) and how they manage uncertainties surrounding illness (Brashers, 2007; Goldsmith, 2009). Less research, however, has focused on the dyadic nature of illness uncertainty (Goldsmith, 2009), such as how one partner’s stressors (e.g., illness uncertainty) affect the other’s stress, how one partner’s coping strategies affect the other’s coping, and in turn how a partner’s coping strategies influence outcomes such as management of one partner’s cancer, as examined in the present study.
Recent studies of people managing chronic illnesses indicate that relational partners experience illness uncertainty differentially. For example, among couples managing one partner’s heart-related condition, the more uncertain partners were about the patient’s prognosis, the more partners perceived that the patient’s illness interfered in their lives (Checton et al., 2012). Further, Checton et al. (2012) found that uncertainty regarding illness symptoms negatively predicted patients’ (but not partners’) perceived ability to talk to their partner about their health condition. Managing the many uncertainties associated with a cancer diagnosis is a day-to-day issue confronting many couples coping with cancer care (Clayton, Mishel, & Belyea,2006). In concordance with the DCM (Berg & Upchurch, 2007), we predict that dyadic appraisal in the form of illness uncertainty predicts dyadic coping such that more uncertainty about the cancer prognosis inhibits dyadic coping.
Dyadic coping
Dyadic coping, the third major component of the DCM, is a developmental process that occurs over time “and sequentially as coping unfolds in more discrete time moments across a conversation or over days” (Berg & Upchurch, 2007, p. 941; see also Bodenmann, 2005). That is, patients’ and partners’ dyadic appraisals of discrete moments and day-to-day discourses that are inherent to coping with cancer are salient in terms of the couple’s adjustment (cancer management). Recent studies have explored dyadic coping appraisals (e.g., collaborative, concordant) and outcomes (e.g., quality of life, psychological distress, management) among patients and partners managing different types of cancers including breast cancer (Feldman & Broussard, 2006; Kayser, Sormanti, & Strainchamps, 1999; Kayser, Watson, & Andrade, 2007), head and neck cancers (Foxwell & Scott, 2011), and prostate cancer (e.g., Berg et al., 2008; Fagundes et al., 2012; Fergus, 2011). For example, among prostate cancer patients and their partners, Merz et al. (2011) found that concordant dyads (i.e., coping appraisal agreement on prostate cancer characteristics) reported better individual health-related quality of life compared to non-concordant dyads (i.e., coping appraisal disagreement).
Appraising the day-to-day issues associated with managing chronic illnesses such as cancer as a “shared problem” may be a starting point for collaborative coping with the issue or may result from such collaborative efforts (Berg & Upchurch, 2007, p. 941; see also Berg et al., 2008). Manne and Badr (2010) suggested that disclosing cancer-related concerns could enhance relationship intimacy and facilitate both partners’ adjustment to head and neck or lung cancers. Among cancer patients and their partners, open communication—that is, greater depth and breadth of cancer-related topics—was associated with lower perceptions of partner burden (Venetis, Magsamen-Conrad, Checton, & Greene, 2014). For patients with gastrointestinal cancers, low levels of disclosure predicted lower relationship functioning and psychological distress (Porter, Keefe, Hurwitz, & Faber, 2005). Overall, research has confirmed the association between disclosure and health benefits (for a review, see Frattaroli, 2006).
The DCM discusses dyadic adjustment in terms of psychosocial adjustment, including psychological, social, and somatic aspects of illness management, which takes into account factors related to both specific (e.g., cancer) and general health management. The ability to share individual worries and concerns within couples may be one way that partners cope with cancer (e.g., to obtain partner’s emotional, informational, and practical support) and facilitate psychosocial, dyadic adjustment. However, even people in supportive, quality relationships may have difficulty sharing certain issues or topics (Goldsmith, 2009; Greene, 2009). Recent studies of people managing chronic illness suggest that perceived ability to share information (e.g., disclosure efficacy, communication efficacy) affects disclosure breadth, depth, and frequency for patients with heart-related conditions (Checton & Greene, 2012) as well as both patients’ and partners’ perceptions about their ability to manage the health condition (Checton et al., 2012). Thus, patients’ and partners’ evaluations of their ability to share cancer concerns may facilitate dyadic coping with the complexities and unpredictability of managing the condition. Therefore, we predictthat communication efficacy, as a facilitator of dyadic coping, predicts dyadic adjustment (cancer management), which then predicts patients’ broader perceptions about their general health. That is, perceived confidence regarding talking about cancer increases patients’ and partners’ perceptions that they can manage the patient’s cancer, which in turn positively affects patient’s feelings of general health.
Proposed model and hypotheses
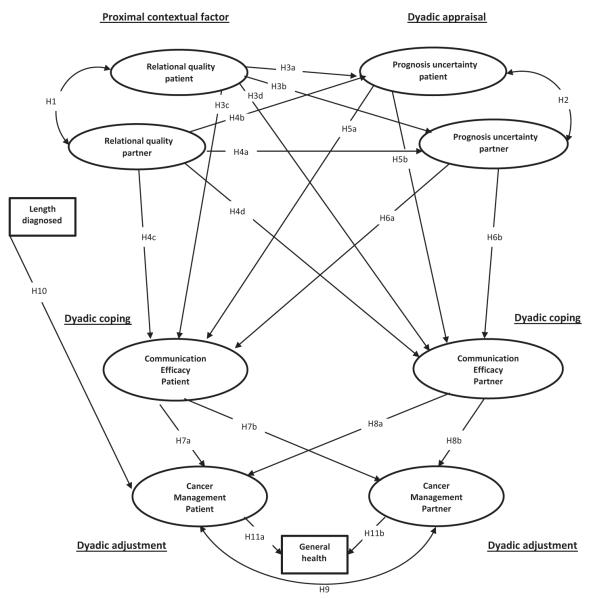
We applied the DCM (Berg & Upchurch, 2007) to dyads in which one partner had been diagnosed with and/or treated for cancer (see Figure 1). First, we hypothesized that patient and partner relational quality (proximal contextual: H1) and patient and partner prognosis uncertainty (dyadic appraisal: H2) are positively correlated. Patient and partner relational quality (proximal context) positively influences patient and partner prognosis uncertainty (dyadic appraisal: H3a, H3b, H4a, H4b) and communication efficacy (dyadic coping: H3c, H3d, H4c, H4d). Prognosis uncertainty (dyadic appraisal) negatively influences patients’ (H5a,H6a) and partners’ communication efficacy (dyadic coping: H5b, H6b). In turn, patients’ and partners’ communication efficacy positively influences patients’ (H7a, H8a) and partners’ (H7b, H8b) cancer management (dyadic adjustment). Patients’ and partners’ cancer management are positively correlated (H9). Length of time since cancer diagnosis (proximal factor) also predicts patients’ cancer management (H10). Finally, both patients’ (H11a) and partners’ (H11b) perceptions about their health-care management predict patients’ perceptions about their general health.
Figure 1.
Hypothesized model.
Method
Participants
The original sample included 95 couples (N = 190 individuals) wherein one partner (n = 95) was diagnosed with cancer. To participate, individuals needed to meet the following inclusion criteria: at least 30 years old; one member of couple diagnosed with cancer (excluding melanoma); in a committed monogamous relationship for at least six months; in this relationship when the patient was diagnosed, or during cancer treatment; completed at least one treatment session (e.g., radiation, chemo-therapy); partner willing to participate; and willing to release phone number for verification callbacks.
Data were screened for normality and multivariate outliers, and no transformations were needed. Ten couples were eliminated due to missing data. Two couples with extreme scores were eliminated due to age (91-year-old patient) and disease length (22 years). The final sample included 83 participants (male n = 25, 30%; female n = 58, 70%) with the cancer diagnosis (henceforth referred to as “patient”) and their partners. Participants ranged in age from 32 to 86 years (M = 53.62 years, SD = 10.63), identified primarily as Caucasian (85%), and identified as heterosexual (100%), although all couples dating/together more than 6 months were recruited. Participants reported being in a relationship with their partner from less than one year to 58 years (M = 23.77 years, SD = 12.79). Participants reported the following cancer diagnoses: breast (37.5%), hematologic (14.6%), gynecologic (11.5%), male genitourinary (10.4%), throat/neck (9.4%), digestive (5.2%), lung (3%), and other (1%).
Procedure
The researchers utilized a network sampling technique. As one option for the research experience component of a communication research methods course, upper-level undergraduate students recruited couples for the present study. Couples completed surveys at the same time, but individually and privately in their own homes with partners separated. Human-subjects-certified researchers were present during survey completion. Random callbacks included contact with 23% of participants to verify participation and inclusion criteria as well as data collection procedures. All data (n = 6) from any assistant (n = 1) when any callback was not verified were not included in the sample.1
Measures
We measured the following variables for both patients and partners: relational quality, prognosis uncertainty, communication efficacy, and cancer management. We also measured the length of time since patients’ cancer diagnosis and patients’ general health. We used exploratory factor analysis to evaluate the dimensionality of all measures. We created composite scores by averaging responses to individual items and estimated reliability using Cronbach’s alpha. In the next section, sample items are presented from patient surveys, and wording in brackets is from partner surveys. We used identical items for both patient and partner for all composite variables.
Relational quality
We measured relational quality to tap into proximal context. We assessed participants’ perceptions of the quality of their relationships using Rubin’s (1970) Love Scale (see also Solomon & Knobloch, 2004; Theiss & Solomon,2006) with six 7-point Likert-type items. Responses ranged from 1 (strongly disagree) to 7 (strongly agree). Factor analysis using Varimax rotation and scree plot indicated a single factor for patients (eigenvalue = 3.55, 59% var., all items loading above .72) and partners (eigenvalue = 3.34, 56% var., all items loading above .57). A sample item was “It would be hard for me to get along without my partner.” Higher scores indicated perceptions of higher relational quality. Reliability was good for both patients (α = .85, M = 5.70, SD = 1.04) and partners (α = .83, M = 5.84, SD = .98).
Prognosis uncertainty
We measured prognosis uncertainty as a component of patient and partner dyadic (illness) appraisal. Prognosis uncertainty is perceived degree of uncertainty regarding one partner’s cancer prognosis. We measured prognosis uncertainty with five 5-point Likert-type items used in prior research (e.g., Checton et al., 2012; see also Checton & Greene, 2012; Greene, 2009). Responses ranged from 1 (very uncertain) to 5 (very certain). All items were reverse-scored. Factor analysis using Varimax rotation and scree plot indicated a single factor for patients (eigenvalue = 3.56, 71% var., five items loading above .73) and partners (eigenvalue = 3.25, 65% var., five items loading above .72). The instructions began, “These questions ask you about how certain or uncertain you are about the following items. Please complete the following sentence: How certain am I about.” A sample item was “my [my partner’s] future with this cancer.” Higher scores indicated more prognosis uncertainty. Reliability was good for patients (α = .90, M = 2.66, SD = 1.06) and partners (α = .88, M = 2.49, SD = 1.09).
Communication efficacy
We measured communication efficacy to tap into patient and partner dyadic coping. We measured the degree to which patients and partners perceive their ability to share information about the patient’s cancer with each other with six 5-point Likert-type items used in prior research (e.g., Checton et al., 2012; see also Afifi & Steuber, 2009; Caughlin, Afifi, Carpenter-Theune, & Miller, 2005; Greene, 2009). Responses ranged from 1 (strongly disagree) to 5 (strongly agree). Factor analysis using Varimax rotation and scree plot indicated a single factor for patients (eigenvalue = 4.18, 70% var., all items loading above .73) and partners(eigenvalue = 3.25, 65% var., all items loading above .72). A sample item was “I am confident that I can share information about my [my partner’s] cancer with my partner.” Higher scores indicated more communication efficacy. Reliability was good for patients (α = .89, M = 4.44, SD = .63) and partners (α = .84, M = 4.22, SD = .64).
Cancer management
We measured the extent to which patients and partners perceive that they are managing the patient’s cancer with five 5-point Likert-type items used in prior research (e.g., Checton et al., 2012) with responses ranging from 1 (strongly disagree) to 5 (strongly agree). Factor analysis using Varimax rotation and scree plot indicated a single factor for patients (eigenvalue = 2.97, 60% var., all items loading above .57) and partners (eigenvalue = 2.97, 60% var., all items loading above .67). A sample reverse-scored item was “I am not managing my [my partner’s] cancer well.” Higher scores indicated better cancer management. Reliability was good for patients (α = .80, M = 4.20, SD = .62) and partners (α = .81, M = 4.15, SD = .67).
Length diagnosed
We measured the length of time since patients’ cancer diagnosis with a single, open-ended item that asked “How long have you been diagnosed with this cancer? Enter number of years.” Years since diagnosis ranged from less than one year to 20 years (M = 4.73 years, SD = 4.72).
General health
We measured patients’ perceptions of their general health on a scale from 1 (poor) to 5 (excellent) with the 5-point Likert-type item, “In general, I would say my health is:” Higher scores indicated better patient perceptions of their own general health (M = 3.38, SD = 1.00).
Results
This section describes results of the predicted associations. Table 1 presents zero-order bivariate correlations for all variables in the model. First, we conducted independent-samples t-tests to evaluate differences in sociocultural context variables (sex and partners’ perspectives) for study variables. Next, we tested hypotheses using maximum likelihood structural equation modeling (AMOS 18). This strategy accounts for measurement error and makes it possible to assess hypothesized associations. Three goodness-of-fit indices were used to evaluate the models. χ2/df adjusts the χ2 statistic for sample size (Kline, 2011). CFI calculates the ratio of the noncentrality parameter estimate of the hypothesized model to the noncentrality parameter estimate of a baseline model (Bentler, 1990). RMSEA accounts for errors of approximation in the population (Browne & Cudeck, 1993). We determined that the model fit the data if the relative χ2 (χ2/df) was less than 3, CFI was .95 or greater, and RMSEA was less than .08 (Browne & Cudeck, 1993; Kline, 2011; Ullman, 2001). We utilized an actor-partner interdependence model (APIM) as the analytical framework for modeling the dyadic effects predicted by H1–H11 because this approach allows us to account for the interdependence that exists between partners (e.g., Cook & Kenny, 2005; Cook & Snyder, 2005), especially in the context of communication, dyadic appraisal and coping, and adjustment. Our final modelreports the unstandardized path coefficients. This method is favored in studies that compare across groups (i.e., the comparisons made here between patients and partners) because different groups may produce indicators, latent variables, or error terms with different variance (Knobloch & Theiss, 2010).
Table 1.
Bivariate zero-order correlation matrix for study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. RelQuality-Pt | 1.00 | |||||||||
| 2. ProgUncert-Pt | .09 | 1.00 | ||||||||
| 3. Efficacy-Pt | .28* | −.26* | 1.00 | |||||||
| 4. Manage-Pt | .15 | −.42** | .51** | 1.00 | ||||||
| 5. RelQuality-Part | .37** | .23* | −.01 | .03 | 1.00 | |||||
| 6. ProgUncert-Part | .01 | .42** | −.07 | −.17 | .18 | 1.00 | ||||
| 7. Efficacy-Part | .23* | −.16 | .22 | .33* | .37** | −.17 | 1.00 | |||
| 8. Manage -Part | .19 | −.28** | .24 | .42** | .13 | −.14 | .46** | 1.00 | ||
| 9. Length cancer | .01 | .03 | .05 | .27* | −.01 | −.10 | −.01 | .04 | 1.00 | |
| 10. GenHealth-Pat | .11 | .40** | .35** | .51** | .03 | −.34* | .28* | .42** | .26 | 1.00 |
Note: RelQuality-Pt is Patient relational quality; ProgUncert-Pt is patient prognosis uncertainty; Efficacy-Pt is patient communication efficacy; Manage-Pt is patient health condition management; RelQuality-Part is partner relational quality; ProgUncert-Part is partner prognosis uncertainty; Efficacy-Part is partner communication efficacy; Manage-Part is partner health condition management; Length cancer is the length of time since the cancer diagnosis, in years; GenHealth-Pat is patients’ perceptions of their general health.
p < .01,
p < .05, two-tailed.
Preliminary Analyses
First, we conducted independent-sample t-tests to evaluate differences in socio-cultural contextual factors such as sex (selecting for only patients and only partners) and illness perspectives (patient vs. partner) for study variables (relational quality, prognosis uncertainty, efficacy, and cancer management, length diagnosed, and patient general health [Tables 2 and 3]). There were no significant differences by sex. However, results revealed one significant difference (t = 2.18, p = .03) between patients and partners on their perceptions of communication efficacy (see Table 4), such that patients, who in our sample were predominantly female (M = 4.41, SD = .64), reported higher efficacy than did partners (M = 4.21, SD = .66). We thoroughly explored potential differences between sex and role (patient/partner) and possible interactions. On every test where we found associations, the role (patient vs. partner) explains differences in study variables (and not sex nor the interaction between sex and role). Thus, we excluded sex from the model for the sake of parsimony.
Table 2.
Preliminary analyses (sociocultural factors): summary table of independentsample t-tests between males and females, patients only.
| Independent-sample t-test (two-tailed) |
Men M, SD | Women M, SD | |
|---|---|---|---|
| Study variables | |||
| Relational quality | t = −.78 | M = 5.58, SD = 1.00 | M = 5.76, SD = 1.04 |
| Prognosis uncertainty | t = −.04 | M = 2.71, SD = 1.04 | M = 2.72, SD = 1.09 |
| Efficacy | t = −1.59 | M = 4.25, SD = .70 | M = 4.43, SD = .63 |
| Cancer management | t = −.44 | M = 4.16, SD = .58 | M = 4.23, SD = .66 |
| Length diagnosed | t = .48 | M = 60.56, SD = 13.04 | M = 53.93, SD = 53.94 |
| General health | t = −.03 | M = 3.40, SD = .22 | M = 3.41, SD = .12 |
Table 3.
Preliminary analyses (sociocultural factors): summary table of independent-sample t-tests between males and females, partners only.
| Independent-sample t-test (two-tailed) |
Men M, SD | Women M, SD | |
|---|---|---|---|
| Study variables | |||
| Relational quality | t = −.51 | M = 5.82, SD = 1.01 | M = 5.92, SD = .94 |
| Prognosis uncertainty | t = −.02 | M = 2.50, SD = .98 | M = 2.51, SD = 1.20 |
| Efficacy | t = −.40 | M = 4.20, SD = .65 | M = 4.26, SD = .71 |
| Cancer management | t = .22 | M = 4.14, SD = .66 | M = 4.12, SD = .71 |
| Length diagnosed | t = .48 | M = 60.56, SD = 13.04 | M = 53.93, SD = 53.94 |
| General health | t = −.03 | M = 3.40, SD = .22 | M = 3.41, SD = .12 |
Table 4.
Preliminary analyses: summary table of independent-sample t-tests between patients and partners.
| Independent-sample t-test (two-tailed) |
Patient M, SD | Partner M, SD | |
|---|---|---|---|
| Study variables | |||
| Relational quality | t = −1.00 | M = 5.70, SD = 1.03 | M = 5.85, SD = .98 |
| Prognosis uncertainty | t = 1.05 | M = 2.70, SD = 1.07 | M = 2.53, SD = 1.06 |
| Efficacy | t = 2.18* | M = 4.41, SD = .64 | M = 4.21, SD = .66 |
| Cancer management | t = .98 | M = 4.22, SD = .62 | M = 4.12, SD = .67 |
| Length diagnosed | t = −.25 | M = 5.11, SD = .52 | M = 5.30, SD = .52 |
| General health (patient) | t = .00 | M = 3.33, SD = 1.00 | M = 3.33, SD = 1.01 |
p < .05.
Next, we explored a number of other variables related to developmental and proximal context factors. For example, we explored possible differences by (or associations with) length diagnosed, age, under care currently (yes/no), taking medication currently (yes/no), and attend support groups (yes/no). The only significant differences for variables in the model were for length diagnosed for patients, which is included in the APIM model.
APIM Analyses
First, we calculated the error variance (1-α) (σ2) for each latent variable in the model to account for measurement error (Bollen, 1989; Stephenson & Holbert, 2003). Results of the SEM revealed that the predicted model (see Figure 1) provided a good fit for the data, χ2(24) = 33.09, relative χ2 = 1.38, p = .10, CFI = 0.94, RMSEA = 0.07. As predicted, patient and partner relational quality and patient and partner prognosis uncertainty were positively correlated, supporting H1 and H2. Partners’ perceptions of relational quality positively predicted patients’ prognosis uncertainty, thus H4b was supported. H3a, H3b, and H4a were not supported. Relational quality positively influenced patients’ and partners’ communication efficacy, with one exception: Partners’ perceptions of the quality of their relationships did not significantly predict patients’ feelings of confidence in talking about their cancer. Thus, H3c, H3d, and H4d were supported, but H4c was not supported. Prognosis uncertainty negatively predicted patients’ and partners’ communication efficacy with one exception: Partners’ certainty about the patients’ cancer prognosis did not significantly predict patients’ feelings of confidence in talking about their cancer. Thus, H5a, H5b, and H6b were supported, but H6a was not supported. Next, patients’ and partners’ communication efficacy positively predicted patients’ and partners’ cancer management with one exception: Patients’ perceptions of being confident in their ability to discuss their cancer with their partners did not significantly predict partners’ cancermanagement. Thus, H7a, H8a, and H8b were supported, but H7b was not supported. Patients’ and partners’ cancer management were positively correlated and H9 was supported. Length diagnosed (proximal factor) predicted patients’ cancer management (H10). Finally, both patients’ (H11a) and partners’ (H11b) perceptions about their health-care management predicted patients’ perceptions about their general health.
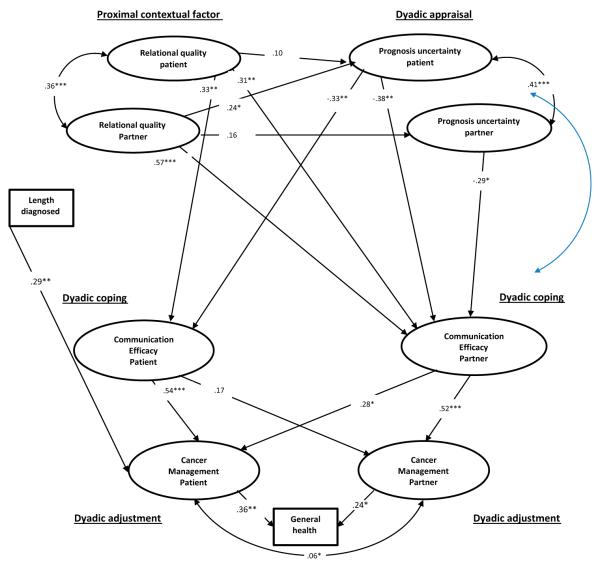
The model was a good fit to the data as hypothesized, but because this is one of the first known tests of the DCM with cancer patients, we wanted to explore the possibility of creating a more parsimonious model by removing nonsignificant paths. We removed nonsignificant paths one at a time starting with the smallest path. First, we removed the path from patients’ perceptions of relational quality to partners’ perceptions of prognosis uncertainty (H3b). Removing this path improved model fit χ2(25) = 33.09, relative χ2 = 1.32, p = .13, CFI = 0.95, RMSEA = 0.06. Second, we removed the path from partners’ perceptions of relational quality to patients’ perceptions of efficacy (H4b). Removing this path improved model fit χ2(26) = 33.72, relative χ2 = 1.30, p = .14, CFI = 0.95, RMSEA = 0.06. Third, we removed the path from partners’ perceptions of prognosis uncertainty to patients’ perceptions of efficacy (H6b). Removing this path improved model fit χ2(27) = 34.15, relative χ2 = 1.27, p = .16, CFI = 0.95, RMSEA = 0.06. Fourth, we removed the path from patients’ perceptions of relational quality to patients’ perceptions of prognosis uncertainty (H3c). Removing this path did not improve model fit and therefore was retained in the final model. Thus, the second model is nested within the first model (Kline, 2011, see also, Gilbar, Weinberg, & Gil, 2012; see Figure 2) and has three fewer paths, improving model parsimony.
Figure 2.
Dyadic cancer communication model.
Note: *p < .05, **p < .01, ***p < .001; χ2(27) = 34.15, relative χ2 = 1.27, p = .16, CFI = 0.95, RMSEA = 0.06.
Discussion
The results of this study support an explanation of how patient and partner management of chronic illness (in this case, cancer) is facilitated by communication processes. Although one person “has” cancer, individuals in relationships manage the illness itself (e.g., Arora, Street, Epstein, & Butow, 2009; Kreps & Bonaguro, 2009; Kreps & Sivaram, 2008). The present study makes two important contributions to the literature. First, this study successfully uses the DCM (Berg & Upchurch, 2007) to predict how proximal contextual factors, dyadic appraisal, and dyadic coping relate to dyadic adjustment in a cancer management context. Second, this study illustrates how communication efficacy acts as a facilitator of both patients’ and partners’ ability to cope with one partner’s cancer.
Communication Efficacy in Dyadic Cancer Management
The primary facilitator of dyadic coping we investigated was patients’ and partners’ confidence in their ability to talk about cancer-related information. Couples managing cancer are frequently advised to engage in open, direct communication with their partner, including expressing needs and emotions (ACS, 2011). The ACS(2011) purports “sharing can be helpful both to you and those close to you.” The Susan G. Komen website (2011) similarly advises individuals not to fear talking about their feelings, admonishing that withholding thoughts, fears, and worries can “create a wall between you and actually cause you to grow apart.” However, we must also be aware that frequency and depth of communication are not a panacea for chronic illness management. Indeed, some research suggests that communication avoidance sometimes serves a valuable function depending on the subject matter (Afifi & Guerrero, 1998; Afifi & Caughlin, 2006; Goldsmith et al., 2007; Parks, 2007). Perhaps more relevant for couples managing cancer is having the confidence to talk about an issue if one or the other partner so desires. To this end, we focused on communication efficacy as a facilitator of couples’ cancer management.
Communication efficacy emerged as a salient predictor of both patient and partner cancer management. Partners’ perceived confidence in their ability to talk about thecancer with the patient predicted both their own and patients’ perceptions of their ability to manage cancer, which then predicted patients’ perceptions of general health. However, patients’ communication efficacy predicted their own cancer management but not their partners’ management. These finding are consistent with prior research on the associations between communication efficacy and couples managing a nonvisible health condition (other than cancer, see Checton et al., 2012). Although the path from patients’ communication efficacy to partner’s cancer management was not significant, when the path was removed, the model fit statistics diminished. Therefore, it is likely that although the association between patients’ communication efficacy and partners’ cancer management is not statistically significant, it does account for some variance in the model.
Engaging in open communication requires that partners feel confident in their ability to share information, including the ability to initiate dialog as well as knowing what to say. Beyond that, some topics are more difficult for individuals to discuss than others, for example, discussing burdens and inequalities (Goldsmith & Miller,2014). The ability to communicate with partners about personal and private information (e.g., communication or disclosure efficacy) is important to new disclosures as well as ongoing information sharing (Afifi & Steuber, 2009; Checton & Greene, 2012; Greene et al., 2012). Cancer management among families and partners requires communication about emotions (e.g., fear of death; see Venetis, Greene, Checton, Magsamen-Conrad, in press) as well as about different types of decision-making related to cancer management (instrumental, see Epstein, Bishop, & Baldwin,1982; affective, economic, and technical, see Noller & Fitzpatrick, 1993; Sparks, 2008). Our study illustrates how communication efficacy operates in different ways for patients and partners, and this finding should be investigated further in future research.
One trend in our results is different phenomenon can be used to explain patient and partner efficacy. Patient efficacy is predicted by patient perceptions of relational quality and prognosis uncertainty, specifically as increased relational quality and decreased uncertainty are associated with increased efficacy. Alternatively, both partner and patient perceptions of relational quality and prognosis uncertainty predict partner efficacy. As such, the partner balances not only his/her concerns but also considers the patient’s experiences when determining if s/he is able to communicate about a cancer-related topic. The concept of information “ownership” may explain this finding (see Communication Privacy Management Theory, CPM, Petronio, 2002). According to CPM, once an individual shares information with another the two become co-owners of the information. Perceptions of relational quality may have a diminished effect on patients’ communication efficacy because as owners of the information, patients are already more confident (as was demonstrated by the primary analyses).
CPM (Petronio, 2002) may also explain why partner perceptions of efficacy predicted both patients’ and partners’ cancer management, but patient efficacy predicted their cancer management (but not partners’ management). In the case of illness-related information sharing, some patients may feel more ownership of the information (i.e., they have the chronic condition) and view themselves as“gatekeepers” of information. Partners may desire more breadth or frequency of cancer-related communication but feel it is not their place to initiate discussion. That is, partners are more constrained than patients in regard to efficacy. Partners contend with their own and patients’ perceptions. Patients may not have these same constraints as they are the owners of the information and therefore can serve as gatekeepers determining how, when, and to what degree cancer-related information may be shared. The notion of information ownership highlights the importance of communication efficacy (e.g., feeling confident in the ability to communicate needs) as a form of coping with cancer, especially within the context of co-managed information (Petronio, 2002).
Information management literature may also shed light on the lack of significant predictions between proximal contextual factors of relationship quality and prognosis uncertainty as indicators of dyadic appraisal. In our model, the only significant association among these variables was the positive association between partners’ perceptions of relationship quality and patients’ prognosis uncertainty. As such, those with increased relational quality reported greater prognosis uncertainty. We speculate that other, unmeasured variables may explain this relationship. However, one possible explanation stems from information management literature about reasons for and against disclosure (Derlega, Winstead, Greene, Serovich, & Elwood,2004). In the case of cancer communication, some dyads prefer to avoid discussing cancer, particularly fear of the unknown or potential death (Venetis et al., in press); this avoidance my occur in part to protect the self, other, or relationship from strain or worry or to create normalcy or sustain hope (Goldsmith et al., 2007; Parks, 2007). We suspect that closer dyads may strive to maintain relational quality by avoiding talk of cancer fears and future outcomes; and by avoiding these specific conversations, couples may also foster prognosis uncertainty.
In some ways, our results are consistent with prior research on the associations between relationship quality and communication or disclosure efficacy (e.g., Afifi & Steuber, 2009; Checton & Greene, 2012; Steuber & Solomon, 2011, 2012; see also Greene, Carpenter, Catona, & Magsamen-Conrad, 2013), and uncertainty and communication efficacy (e.g., Checton & Greene, 2012; Jang & Tian, 2012; Mccurry, Schrodt, & Ledbetter, 2012). However, our study is unique because it investigates effects in couples, analyzing both partners’ perceptions simultaneously. Similar kinds of studies include several studies of self-efficacy that also demonstrated variation in both effects on and of efficacy between actors and partners (see Knoll, Burkert, Luszczynska, Roigas, & Gralla, 2011; Molero, Shaver, Ferrer, Cuadrado, & Alonso-Arbiol, 2011). Consistent findings of differential effects reinforce the need for a study design that successfully incorporates perceptions of each member of a dyad. As Checton et al. (2012) discovered, patients and partners experience illness differently and this may be especially true as it pertains to illness uncertainty and information management. In contrast to the current study, Checton et al. (2012) found that for couples managing a chronic illness (i.e., other than cancer), patients’ (but not partners’) symptom uncertainty significantly influenced their communication efficacy. Other studies have investigated communication efficacy in a health-relatedinformation-sharing context (e.g., infertility disclosure) incorporating both partners perspectives; however, those studies predicted communication with individuals outside of the couple as opposed to couple’s communication practices with each other (Steuber & Solomon, 2011). Future research should continue to investigate the effect of relational quality and illness uncertainty on communication efficacy and illness management while incorporating dyadic perspectives. Further, future research should continue to explore potential confounding variables in addition to those tested in the current study (length disease, currently under care, etc.), such as severity of cancer diagnosis.
Limitations and Future Research
This study provides an initial test of the DCM (Berg & Upchurch, 2007) in the context of cancer communication and coping. We utilized gender, patient perspective, relationship quality, and communication efficacy to investigate model components. Future research may include potential alternatives for sociocultural contextual factors, proximal contextual factors, dyadic appraisal, dyadic coping, and dyadic adjustment that were not measured in the current study (e.g., time since diagnosis). There are multiple ways to assess how individuals are coping with cancer, and Berg and Upchurch (2007) describe a “host of variables” that may moderate the general patterns of relationships between dyadic coping and adjustment (p. 933). Further, alternative models exist such as those with reserve causal paths (however, model fit diminished in the present study when paths were reversed but future research should explore these associations longitudinally). Further, relational communication is ongoing and this model only captures communication at one point in time.
Another limitation is that our study includes multiple types of cancer, although our sample is not representative of the entire range of cancer diagnoses, nor of patients at different points in their cancer management. These limitations on range of cancer diagnoses lead us to carefully explore control variables for our sample to inform analyses and provide alternative explanations for effects. Future research should consider focusing on one type of cancer or on individuals in similar stages. This strategy might also help protect against potential selection effects within a sample that is currently living with cancer and therefore might have a more positive prognosis. However, the DCM (Berg & Upchurch, 2007) does account for these multiple stages in the second developmental aspect of the model, the temporal process of dyadic coping. Further, the model was originally designed to explain coping in chronic illness, which is much broader than cancer. Finally, our sample is different from typical college student samples and includes a community sample of committed couples that co-managed the chronic illness and their relationship during extended cancer treatment trajectories.
In this study we focus not on communication practices (e.g., “open communication” itself), but on the perceptions of confidence that individuals have in their ability to communicate, should they desire, as a communication-related facilitator of coping. Scholars and practitioners should exercise caution advocating for opencommunication without qualifications because open communication is not always good for management (Goldsmith & Miller, 2014; Parks, 2007), and some topics more frequently end in arguments or are otherwise unproductive. Indeed, knowing what information, experiences, and feelings to share; discerning strategies for how to share information and emotions; and recognizing when not to share may enable better cancer management than the broad recommendation of “being open.” The feeling that “I can share if I want to” may be a more salient aspect of coping than the frequency, breadth, or depth of sharing. Scholars should continue to investigate the role of communication in the process of managing cancer and other chronic illnesses, especially as it pertains to information management and topic avoidance. We should continue research to help provide strategies that practitioners can use to improve communication efficacy for couples managing cancer. This study illustrates that (in addition to the effects of gender, perspective, relationship quality, and illness appraisal) we should focus on efficacy building as a potential strategy for cancer management.
Acknowledgments
Funding This research was supported in part by the Center for Family and Demographic Research, Bowling Green State University, which has core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development [R24HD050959].
Note
As part of a research method course requirement, all students received IRB certification and received training on human subjects generally. Students chose from four different data collection alternatives. Thirty of the 200 enrolled students selected the present dyadic cancer communication study. Study researchers trained the 30 students on the data collection protocol and provided the students with research packets to initiate data collection. Students recruited and collected data from dyads in their personal networks. Participant inclusion criteria were that both partners were at least 30 years old, had been in a committed relationship for at least six months, had been in the relationship at the time of the cancer diagnosis, only one partner had a cancer diagnosis, willing to provide phone number, and the cancer treatment involved more than one treatment session. All forms of skin cancer were excluded from the sample.
Contributor Information
Kate Magsamen-Conrad, Department of Communication, Bowling Green State University..
Maria G. Checton, Department of Health Care Management, College of Saint Elizabeth..
Maria K. Venetis, Brian Lamb School of Communication, Purdue University..
Kathryn Greene, Department of Communication, Rutgers University..
References
- Acitelli LK, Badr H. My illness or our illness? Attending to the relationship when one partner is ill. In: Revenson TA, Kayser K, Bodenmann G, editors. Emerging perspectives on couples’ coping with stress. American Psychological Association; Washington, DC: 2005. pp. 121–136. doi:10.1037/11031.006. [Google Scholar]
- Afifi WA, Caughlin JP. A close look at revealing secrets and some consequences that follow. Communication Research. 1998;33:467–488. doi:10.1177/0093650206293250. [Google Scholar]
- Afifi WA, Guerrero LK. Some things are better left unsaid II: Topic avoidance in friendships. Communication Quarterly. 2009;46:231–249. doi:10.1080/01463379809370099. [Google Scholar]
- Afifi WA, Morgan SE, Stephenson MT, Morse C, Harrison T, Reichert T, Long SD. Examining the decision to talk with family about organ donation: Applying the theory of motivated information management. Communication Monographs. 2006;73:188–215. doi:10.1080/03637750600690700. [Google Scholar]
- Afifi T, Steuber K. The Revelation Risk Model (RRM): Factors that predict the revelation of secrets and the strategies used to reveal them. Communication Monographs. 2009;76(2):144–176. doi:10.1080/03637750902828412. [Google Scholar]
- American Cancer Society (ACS) [Retrieved September 23, 2014];How do I talk to people about my diagnosis? 2011 from http://www.cancer.org/treatment/understandingyourdiagnosis/afterdiagnosis/after-diagnosis-talking-to-others-about-diagnosis.
- American Cancer Society (ACS) [Retrieved September 23, 2014];New report tracks growing population of cancer survivors in the US. 2012 from http://www.cancer.org/cancer/news/news/new-report-tracks-growing-population-of-cancer-survivors-in-the-us.
- Arora NK, Street RL, Epstein RM, Butow PN. Facilitating patient-centered cancer communication: A road map. Patient Education & Counseling. 2009;77:319–321. doi: 10.1016/j.pec.2009.11.003. doi:10.1016/j.pec.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Babrow AS. Uncertainty, value, communication, and problematic integration. Journal of Communication. 2001;51:553–573. doi:10.1111/j.1460-2466.2001.tb02896.x. [Google Scholar]
- Babrow AS. Problematic integration theory. In: Whaley BB, Samter W, editors. Explaining communication: Contemporary theories and exemplars. Lawrence Erlbaum Associates; Mahwah, NJ: 2007. pp. 181–200. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural equation models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. doi:10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult lifespan. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. doi:10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J, Bloor L, Bradstreet C, Upchurch R, Patton G. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychology & Aging. 2008;23:505–516. doi: 10.1037/a0012687. doi:10.1037/a0012687. [DOI] [PubMed] [Google Scholar]
- Bodenmann G. Dyadic coping and its significance for marital functioning. In: Revenson TA, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. American Psychological Association; Washington, DC: 2005. pp. 33–49. [Google Scholar]
- Bollen KA. Structural equations with latent variables. Wiley; New York, NY: 1989. [Google Scholar]
- Brashers DE. A theory of communication and uncertainty management. In: Whaley BB, Samter W, editors. Explaining communication: Contemporary theories and exemplars. Lawrence Erlbaum Associates; Mahwah, NJ: 2007. pp. 201–218. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Caughlin JP, Afifi WA, Carpenter-Theune KE, Miller LE. Reasons for, and consequences of, revealing personal secrets in close relationships: A longitudinal study. Personal Relationships. 2005;12(1):43–59. doi:10.1111/j.1350-4126.2005.00101.x. [Google Scholar]
- Centers for Disease Control and Prevention: Chronic disease prevention and health promotion [Retrieved September 23, 2014];Chronic diseases and health promotion. 2013a from http://www.cdc.gov/chronicdisease/overview/index.htm.
- Centers for Disease Control and Prevention: Chronic disease prevention and health promotion [Retrieved September 23, 2014];Chronic diseases. 2013b from http://www.cdc.gov/chronicdisease/resources/publications/AAG/chronic.htm.
- Checton MG, Greene K. Beyond initial disclosure: The role of prognosis and symptom uncertainty in patterns of disclosure in relationships. Health Communication. 2012;27(2):145–157. doi: 10.1080/10410236.2011.571755. doi:10.1080/10410236.2011.571755. [DOI] [PubMed] [Google Scholar]
- Checton MG, Greene K, Magsamen-Conrad K, Venetis MK. Patients’ and partners’ perspectives of chronic illness and its management. Families, Systems, & Health: The Journal of Collaborative Family Healthcare. 2012;30(2):114–129. doi: 10.1037/a0028598. doi:10.1037/a0028598. [DOI] [PubMed] [Google Scholar]
- Clayton MF, Mishel MH, Belyea M. Testing a model of symptoms, communication, uncertainty, and well-being, in older breast cancer survivors. Research in Nursing & Health. 2006;29:18–39. doi: 10.1002/nur.20108. doi:10.1002/nur.20108. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. The actor-partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 2005;29(2):101–109. doi:10.1080/01650250444000405. [Google Scholar]
- Cook WL, Snyder DK. Analyzing nonindependent outcomes in couple therapy using the actor-partner interdependence model. Journal of Family Psychology. 2005;19(1):133–141. doi: 10.1037/0893-3200.19.1.133. doi:10.1037/0893-3200.19.1.133. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Smith DA. Couples coping with a myocardial infarction: A contextual perspective on wives’ distress. Journal of Personality and Social Psychology. 1991;61:404–412. doi: 10.1037//0022-3514.61.3.404. doi:10.1037/0022-3514.61.3.404. [DOI] [PubMed] [Google Scholar]
- Derlega VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Reasons for HIV disclosure/nondisclosure in close relationships: Testing a model of HIV–disclosure decision making. Journal of Social and Clinical Psychology. 2004;23:747–767. doi:10.1521/jscp.23.6.747.54804. [Google Scholar]
- Epstein NB, Bishop DS, Baldwin LM. McMaster model of family functioning. In: Walsh F, editor. Normal family processes. Guilford Press; New York, NY: 1982. pp. 115–141. [Google Scholar]
- Fagundes CP, Berg CA, Wiebe DJ. Intrusion, avoidance, and daily negative affect among couples coping with prostate cancer: A dyadic investigation. Journal of Family Psychology. 2012;26:246–253. doi: 10.1037/a0027332. doi:10.1037/a0027332. [DOI] [PubMed] [Google Scholar]
- Feldman BN, Broussard CA. Men’s adjustment to their partners’ breast cancer: A dyadic coping perspective. Health & Social Work. 2006;31:117–127. doi: 10.1093/hsw/31.2.117. doi:10.1093/hsw/31.2.117. [DOI] [PubMed] [Google Scholar]
- Fergus KD. The rupture and repair of the couple’s communal body with prostate cancer. Families, Systems & Health: The Journal of Collaborative Family Healthcare. 2011;29(2):95–113. doi: 10.1037/a0023413. doi:10.1037/a0023413. [DOI] [PubMed] [Google Scholar]
- Foxwell KR, Scott SE. Coping together and apart: Exploring how patients and their caregivers manage terminal head and neck cancer. Journal of Psychosocial Oncology. 2011;29:308–326. doi: 10.1080/07347332.2011.563343. doi:10.1080/07347332.2011.563343. [DOI] [PubMed] [Google Scholar]
- Frattaroli J. Experimental disclosure and its moderators: A meta-analysis. Psychological Bulletin. 2006;132:823–865. doi: 10.1037/0033-2909.132.6.823. doi:10.1037/0033-2909.132.6.823. [DOI] [PubMed] [Google Scholar]
- Gilbar O, Weinberg M, Gil S. The effects of coping strategies on PTSD in victims of a terror attack and their spouses: Testing dyadic dynamics using an actor-partner interdependence model. Journal of Social and Personal Relationships. 2012;29:246–261. doi:10.1177/0265407511426939. [Google Scholar]
- Goldsmith DJ. Uncertainty and communication in couples coping with serious illness. In: Afifi TD, Afifi WA, editors. Uncertainty and information regulation in interpersonal contexts: Theories and applications. Routledge; New York, NY: 2009. pp. 204–225. [Google Scholar]
- Goldsmith DJ, Miller GA. Conceptualizing how couples talk about cancer. Health Communication. 2014;29(1):51–63. doi: 10.1080/10410236.2012.717215. doi:10.1080/10410236.2012.717215. [DOI] [PubMed] [Google Scholar]
- Goldsmith DJ, Miller LE, Caughlin J. Openness and avoidance in couples communicating about cancer. In: Beck C, editor. Communication yearbook. Vol. 31. Blackwell; Malden, MA: 2007. pp. 62–117. [Google Scholar]
- Greene K. An integrated model of health disclosure decision-making. In: Afifi TD, Afifi WA, editors. Uncertainty and information regulation in interpersonal contexts: Theories and applications. Routledge; New York, NY: 2009. pp. 226–253. [Google Scholar]
- Greene K, Carpenter A, Catona D, Magsamen-Conrad K. The Brief Disclosure Intervention (BDI): Facilitating African Americans’ disclosure of HIV. Journal of Communication. 2013;63(1):138–158. doi:10.1111/jcom.12010. [Google Scholar]
- Greene K, Magsamen-Conrad K, Venetis MK, Checton MG, Bagdasarov Z, Banerjee SC. Assessing health diagnosis disclosure decisions in relationships: Testing the disclosure decision-making model. Health Communication. 2012;27:356–368. doi: 10.1080/10410236.2011.586988. doi:10.1080/10410236.2011.586988. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134(1):1–30. doi: 10.1037/0033-2909.134.1.1. doi:10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Jang SA, Tian Y. The effects of communication efficacy on information-seeking following events that increase uncertainty: A cross-lagged panel analysis. Communication Quarterly. 2012;60:234–254. doi:10.1080/01463373.2012.669325. [Google Scholar]
- Kayser K, Sormanti M, Strainchamps E. Women coping with cancer: The influence of relationship factors on psychological adjustment. Psychology of Women Quarterly. 1999;23:725–739. doi:10.1111/j.1471-6402.1999.tb00394.x. [Google Scholar]
- Kayser K, Watson LE, Andrade JT. Cancer as a “We-Disease”: Examining the process of coping from a relational perspective. Families, Systems & Health: The Journal of Collaborative Family Healthcare. 2007;25:404–418. doi:10.1037/1091-7527.25.4.404. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3rd ed Guilford; New York, NY: 2011. [Google Scholar]
- Knobloch LK, Theiss JA. An actor-partner interdependence model of relational turbulence: Cognitions and emotions. Journal of Social and Personal Relationships. 2010;27:597–619. doi:10.1177/0265407510368967. [Google Scholar]
- Knoll N, Burkert S, Luszczynska A, Roigas J, Gralla O. Predictors of support provision: A study with couples adapting to incontinence following radical prostatectomy. British Journal of Health Psychology. 2011;16:472–487. doi: 10.1348/135910710X522860. doi:10.1348/135910710X522860. [DOI] [PubMed] [Google Scholar]
- Kreps GL, Bonaguro EW. Health communication as applied communication inquiry. In: Frey L, Cissna K, editors. The handbook of applied communication research. Lawrence Erlbaum Associates; Hillsdale, NJ: 2009. pp. 970–993. [Google Scholar]
- Kreps GL, Sivaram R. Strategic health communication across the continuum of breast cancer care in limited-resource countries. Cancer. 2008;113:2331–2337. doi: 10.1002/cncr.23832. doi:10.1002/cncr.23832. [DOI] [PubMed] [Google Scholar]
- Kuijer RG, Ybema JF, Buunk BP, De Jong GM, Thijsboer F, Sanderman R. Active engagement, protective buffering, and overprotection: Three ways of giving support by intimate partners of patients with cancer. Journal of Social and Clinical Psychology. 2000;19:256–275. doi:10.1521/jscp.2000.19.2.256. [Google Scholar]
- Lambert SD, Jones BL, Girgis A, Lecathelinais C, DESS de Mathematicques Appliquees Distressed partners and caregivers do not recover easily: Adjustment trajectories among partners and caregivers of cancer survivors. Annals of Behavioral Medicine. 2012;44:225–235. doi: 10.1007/s12160-012-9385-2. doi:10.1007/s12160-012-9385-2. [DOI] [PubMed] [Google Scholar]
- Lyons MA, Jacobson SS, Prescott B, Oswalt D. Women’s experiences during the first year following diagnosis of breast cancer. Southern Online Journal of Nursing Research. 2002;1(3):1–26. [Google Scholar]
- Manne S, Badr H. Intimacy processes and psychological distress among couples coping with head and neck or lung cancers. Psycho-Oncology. 2010;19:941–954. doi: 10.1002/pon.1645. doi:10.1002/pon.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Norton TR, Ostroff JS, Winkel G, Fox K, Grana G. Protective buffering and psychological distress among couples coping with breast cancer: The moderating role of relationship satisfaction. Journal of Family Psychology. 2007;21:380–388. doi: 10.1037/0893-3200.21.3.380. doi:10.1037/0893-3200.21.3.380. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho-Oncology. 2006;15:234–247. doi: 10.1002/pon.941. doi:10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- Mccurry AL, Schrodt P, Ledbetter AM. Relational uncertainty and communication efficacy as predictors of religious conversations in romantic relationships. Journal of Social & Personal Relationships. 2012;29:1085–1108. doi:10.1177/0265407512449402. [Google Scholar]
- McWilliam CL, Brown JB, Stewart M. Breast cancer patients’ experiences of patient–doctor communication: A working relationship. Patient Education & Counseling. 2000;39:191–204. doi: 10.1016/s0738-3991(99)00040-3. doi:10.1016/S0738-3991(99)00040-3. [DOI] [PubMed] [Google Scholar]
- Merz EL, Malcarne VL, Ko CM, Sadler M, Kwack L, Varni JW, Sadler GR. Dyadic concordance among prostate cancer patients and their partners and health-related quality of life: Does it matter? Psychology & Health. 2011;26:651–666. doi: 10.1080/08870441003721251. doi:10.1080/08870441003721251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishel MH, Clayton MF. Theories of uncertainty. In: Smith MJ, Liehr PR, editors. Middle range theory for nursing. Springer; New York, NY: 2003. pp. 25–48. [Google Scholar]
- Molero F, Shaver PR, Ferrer E, Cuadrado I, Alonso-Arbiol I. Attachment insecurities and interpersonal processes in Spanish couples: A dyadic approach. Personal Relationships. 2011;18:617–629. doi:10.1111/j.1475-6811.2010.01325.x. [Google Scholar]
- Munir F, Pryce J, Haslam C, Leka S, Griffiths A. Gender differences in managing chronic illness at work: Exploring predictors for disclosure. Journal of Vocational Rehabilitation. 2006;25:173–180. [Google Scholar]
- National Comprehensive Cancer Network (NCCI) [Retrieved September 23, 2014];Managing cancer as a chronic condition. 2013 from http://www.nccn.org/patients/resources/life_after_cancer/
- Noller P, Fitzpatrick MA. Communication in family relationships. Prentice Hall; Englewood Cliffs, CA: 1993. [Google Scholar]
- O’Brien TB, DeLongis A. Coping with chronic stress: An interpersonal perspective. In: Gottlieb B, editor. Coping with chronic stress. Plenum Press; New York, NY: 1997. pp. 161–190. [Google Scholar]
- Parks MR. Personal relationships and personal networks. Lawrence Erlbaum Associates; Mahwah, NJ: 2007. [Google Scholar]
- Petronio S. Boundaries of privacy: Dialectics of disclosure. State University of New York Press; Albany, NY: 2002. [Google Scholar]
- Porter LS, Keefe FJ, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psycho-Oncology. 2005;14:1030–1042. doi: 10.1002/pon.915. doi:10.1002/pon.915. [DOI] [PubMed] [Google Scholar]
- Revenson TA, Kayser K, Bodenman G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. American Psychological Association; Washington, DC: 2005. [Google Scholar]
- Rubin Z. Measurement of romantic love. Journal of Personality and Social Psychology. 1970;16:265–273. doi: 10.1037/h0029841. doi:10.1037/h0029841. [DOI] [PubMed] [Google Scholar]
- Solomon DH, Knobloch LK. A model of relational turbulence: The role of intimacy, relational uncertainty, and interference from partners in appraisals of irritations. Journal of Social and Personal Relationships. 2004;21:795–816. doi:10.1177/0265407504047838. [Google Scholar]
- Sparks L. Family decision-making. In: Donsbach W, editor. The international encyclopedia of communication. Vol. 4. Wiley-Blackwell; Oxford: 2008. pp. 1729–1733. [Google Scholar]
- Stephenson MT, Holbert RL. A Monte Carlo simulation of observable-versus latent-variable structural equation modeling techniques. Communication Research. 2003;30(3):332–354. doi:10.1177/0093650203030003004. [Google Scholar]
- Steuber KR, Solomon DH. Factors that predict married partners’ disclosures about infertility to social network members. Journal of Applied Communication Research. 2011;39(3):250–270. doi:10.1080/00909882.2011.585401. [Google Scholar]
- Steuber KR, Solomon DH. Relational uncertainty, partner interference, and privacy boundary turbulence: Explaining spousal discrepancies in infertility disclosures. Journal of Social and Personal Relationships. 2012;29(1):3–27. doi:10.1177/0265407511406896. [Google Scholar]
- Susan G, Komen for the Cure . Facts for life: Talking with your partner. [Retrieved September 23, 2014]. 2011. from http://ww5.komen.org/uploadedfiles/Content_Binaries/806-401.pdf. [Google Scholar]
- Theiss JA, Solomon DH. A relational turbulence model of communication about irritations in romantic relationships. Communication Research. 2006;33:391–418. doi:10.1177/0093650206291482. [Google Scholar]
- Uchino BN. Social support and physical health. Yale University Press; New Haven, CT: 2004. [Google Scholar]
- Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, editors. Using multivariate statistics. Allyn & Bacon; Needham Heights, MA: 2001. pp. 653–771. [Google Scholar]
- Venetis MK, Greene K, Checton MG, Magsamen-Conrad K. Decision making in cancer-related topic avoidance. Journal of Health Communication. doi: 10.1080/10810730.2014.965364. (in press) [DOI] [PubMed] [Google Scholar]
- Venetis MK, Magsamen-Conrad K, Checton MG, Greene K. Cancer communication and partner burden: An exploratory study. Journal of Communication. 2014;64(1):82–102. doi:10.1111/jcom.12069. [Google Scholar]
- Wessels H, de Graeff A, Wynia K, de Heus M, Kruitwagen CLJJ, Woltjeroest GTGJ, Voest EE. Gender-related needs and preferences in cancer care indicate the need for an individualized approach to cancer patients. The Oncologist. 2010;15:648–655. doi: 10.1634/theoncologist.2009-0337. doi:10.1634/theoncologist.2009-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]