Highlights
-
•
It is important to differentiate this rare pathological feature of MD from other entities as the treatment is surgical rather than medical.
-
•
No pathognomonic clinical symptoms indicating MD has been reported.
-
•
Diagnosis usually is by a technetium Tc 99m-pertechnetate scanning.
-
•
The treatment of symptomatic MD is surgical resection (wedge resection of the MD or resection of ileum).
-
•
The heterotopic tissue is: gastric, pancreatic, jejuna, duodenal, colonic or hepatobiliary tissue.
Keywords: Meckel’s diverticulum, Diverticulitis, Intussusception, Hemorrhage, Laparoscopic, Acute abdomen
Abstract
Introduction
Intussusception with the Meckel’s diverticulum (MD) is a rare cause of chonic abdominal pain in the adults. We wish to present this first case of intussusception of MD within its own lumen without small bowel obstruction.
Presentation of case
We report the case of a 27-year-old man who was admitted to the emergency room due to a diffuse abdominal pain. Abdominal CT scan showed invagination of MD. The exploratory laparoscopy revealed the presence of intussusception of MD within its own lumen. Segmental resection of the small intestine was performed. The patient was discharged on the third post-operative day.
Discussion
The prevalence of MD is 1 to 4%. Diagnosis is often difficult and delayed because clinical symptoms are not specific and the diagnosis is performed mainly by imaging studies. Factors pre-disposing these patients to intussusception of MD within its own lumen include a narrow diverticulum, large diverticululm, and associated inflammation of the diverticulum. Intestinal obstruction is a more common complication in adults, whereas in children, bleeding is the more common complication. In our case, the patient had a diffuse abdominal pain without small bowel obstruction because the intussusception of MD was within its own lumen. Laparoscopy may be useful for confirming the presence of intussusception, and demonstrating the underlying organic lesion serving as the lead point.
Conclusion
It is important to differentiate this rare pathological feature of MD from other entities as the treatment is surgical rather than medical. Abdominal surgeons should bear in mind this rare entity.
1. Introduction
Although diverticular disease of the small bowel and colon is frequent, intussusception of the Meckel’s diverticulum (MD) within its own lumen is an uncommon entity. Meckel’s diverticulum is the most common congenital malformation of the gastrointestinal tract (present in 2%–4% of population) due to persistence of the congenital vitello-intestinal duct. Intussusception remains a rare condition in adults, representing 1% –3% of bowel obstructions and it is a different entity in adults than in children. It is a true diverticulum, typically located on anti-mesenteric border, and contains all three coats of intestinal wall with its separate blood supply from the vitelline artery. This case demonstrates the utility of laparacopy in diagnosing an intussusception of the Meckel’s diverticulum. We wish to present this extremely rare case of intussusception of MD within its own lumen, which is the first one that we have encountered in our practise, along with the accompanying diagnostic and therapeutic issues and a review of the literature.
2. Presentation of case
We report the case of a 23-year-old man who was admitted to the emergency room due to a diffuse abdominal pain. He had crampy abdominal pain,without fever. Physical examination revealed a severe diffuse abdominal pain. Laboratory findings showed a white blood cell count of 13,000 per microliter of blood. Abdominal Ultrasound and abdominal CT scan showed invagination of MD (Figs. 1 and 2). The diagnosis was intussuscepted Meckel’s diverticulum. The exploratory laparoscopy revealed the presence of intussusception of the Meckel’s diverticulum within its own lumen (Fig. 3). The laparoscopy was converted to a laparotomy. A midline incision was made. Segmental resection of the small intestine was performed. Microscopic examination disclosed an ectopic gastric and pancreatic mucosa (Fig. 4). The patient tolerated the procedure and the postoperative period was uncomplicated. The patient was discharged on the third post-operative day. Histology showed acute appendicitis without perforation.
Fig. 1.
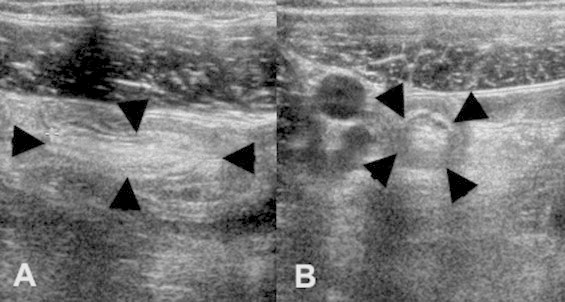
Abdominal Ultrasound showed invagination of MD (arrowhead). A = Longitudinal cut. B = transversal cut.
Fig. 2.
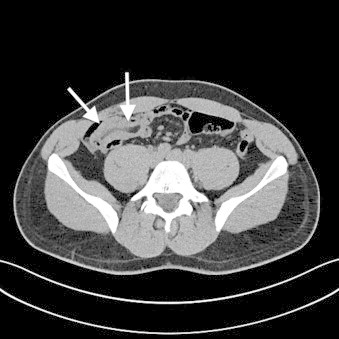
Abdominal CT showed invagination of MD (arrowhead).
Fig. 3.
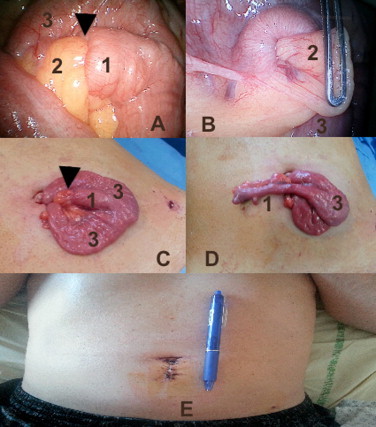
The intra-operative finding of an intussusception (arrowhead) of the Meckel’s diverticulum within its own lumen (1 = MD, 2 = meso, 3 = ileum). A and B = laparoscopic view. C = intussusception of the MD. D = intussusception reduction. E = A midline incision.
Fig. 4.
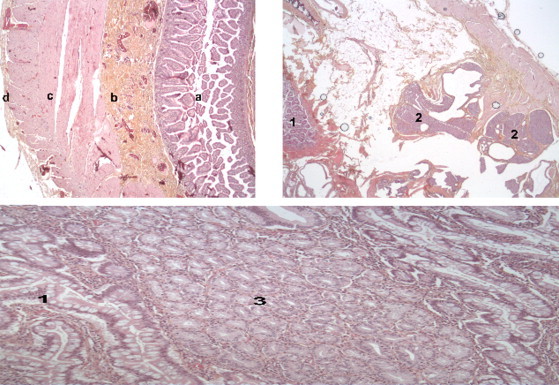
Histology of the fragments of MD (1). In the upper right (HES × 25): ectopic pancreatic tissue (2) was present. In the upper left (HES × 25): MD contains the all three intestinal layers (a = mucosa, b = submucosa, c = muscular, d = serous). Down (HES × 100): ectopic gastric tissue (3) was present.
3. Discussion
This case report presents the unusual case of intussusception of the Meckel’s diverticulum (MD) within its own lumen. By reviewing the literature, we aim to identify the management of this variant.
MD is an intestinal diverticulum that results from incomplete obliteration of the most proximal portion of the vitelline or omphalo-mesenteric duct during the fifth week of fetal development [1]. The failure of closure of the duct can result in an umbilical fecal fistula, umbilical sinus, fibrous cord, enterocystoma, mesodiverticular band or MD (distal ductal closure) [2]. MD contains all the three intestinal layers. It contains heterotopic tissue in 50% cases. The heterotopic tissue is: gastric, pancreatic, jejuna, duodenal, colonic or hepatobiliary tissue [3,4]. It may remain clinically silent and incidentally be identified at autopsy or surgery, or it may mimic disorders such as peptic ulcer disease, appendicitis and Crohn’s disease. Adult intussusception represents only 1%–3% of intestinal obstructions in adults and it is a different entity in adults than in children [5]. The main causes of intussusception in adults are: carcinomas, polyps, strictures, benign tumors and idiopathic, MD and colonic diverticulum. MD is a congenital diverticulum. The most common age at presentation is 2 years. Our patient was 27 years. It is therefore the most common congenital abnormality of the gastrointestinal tract. MD was first described by Fabricus Heldanus in 1650 [6], then Levator in 1671 [7] and then Ruysch in 1730 [8]. However, the diverticulum bears the name of Johann Friedrich Meckel who described the embryology of a small bowel diverticulum in 1809 [9].
In comparison with previous reports on MD in the literature, it was quite unusual that MD exhibited an intussusception within its own lumen. In our case, factors pre-disposing to intussusception of the Meckel’s diverticulum within its own lumen include a narrow diverticulum, large diverticululm, and associated inflammation of the diverticulum.
No pathognomonic clinical symptoms indicating MD had been reported. In our case, the patient had a diffuse abdominal pain with hyperleukocytosis, without small bowel obstruction because the intussusception of MD was within its own lumen. In children, intussusception of MD is frequent and usually presents with a classic triad of symptoms: acute abdominal pain, vomiting and a bloody mucoid stool. However, in adult, intussusception of MD is rare and usually reveals itself with chonic abdominal pain. The clinical presentations are vague and diverse: chronic nonspecific symptoms like intermittent abdominal pain, constipation, diarrhea, dyspepsia and malnutrition and sometimes with acute presentation like gastrointestinal obstruction, diverticulitis (with or without associated hemorrhage), intra-abdominal abscess and perforation (covered or not). In adult, intussusception of MD may present with episodes of intermittent lower bleeding without any abdominal pain. Hemorrhage may be caused by the secretion of gastric acid or alkaline pancreatic juice from the ectopic mucosa (ectopic gastric or pancreatic). Harkines performed a large study (162 cases) of MD-related intussusception. In this study, vomiting and chronic abdominal pain were the leading clinical presentations. Intestinal obstruction is more common complication in adults, whereas in childhood, bleeding is the more common complication.
The differential diagnosis includes neoplasms (with or without perforation), foreign body perforation, traumatic hematoma, medication-induced ulceration (non-steroidal anti-inflammatory drug), and Crohn’s disease. The neoplasms of the small bowel are: adenocarcinoma, carcinoids, gastrointestinal stromal tumors (GIST), lymphoma, and metastases. Diagnosis is often difficult and delayed because clinical symptoms are not specific and the diagnosis is performed mainly by imaging studies. In our case, the exploratory laparoscopy revealed the presence of intussusception of the Meckel’s diverticulum within its own lumen. In the present case, the laparoscopic approach was useful for diagnosis and treatment.
The small intestine is difficult to examine using the endoscopic methods; therefore, the radiographic diagnosis of these diverticula is the diagnostic tool of choice even if difficult to establish. Diagnosis is usually done using a technetium Tc 99m-pertechnetate scanning. Abdominal CT is the diagnostic tool of choice even if it Is not possible to identify all small bowel diverticula and is currently considered the most sensitive radiological method for confirming intussusception. However, on an abdominal CT, Intussusception might be misinterpreted as another lesion, such as a polyp or hematoma. In our patient, the unusual presentation of the abdominal pain prompted us to do a diagnostic laparoscopy first. This report illustrates the use of laparoscopy to diagnose the intussusception of MD. Laparoscopy, especially by an experienced surgeon, may be useful for confirming the presence of intussusception, localizing the disease, and demonstrating the underlying organic lesion serving as the lead point. Tae Hee Lee et al. concluded that the colonoscopy can help to confirm the presence of intussusception of MD and can potentially eliminate unnecessary surgery [10].
Compared with open interventions, the advantages of laparoscopic treatment like the shorter hospital stay and earlier return to work have been extensively studied [11]. The resection of asymptomatic Meckel’s diverticulum remains controversial. As for symptomatic MD, surgical resection is the treatment of choice. It can be achieved either by the diverticulectomy or by the segmental bowel resection and anastomosis, especially when there is palpable ectopic tissue at the diverticular-intestinal junction, intestinal ischemia or perforation. In our case, segmental resection of the small intestine was performed.
According to the well-known statement of Charles Mayo, ‘MD is frequently suspected, often looked for and seldom found’. Although intussusception of the Meckel’s diverticulum within its own lumen is extremely rare, general surgeons should be aware of the possibility of this presentation.
Conflict of interest
No.
Sources of funding
No sources of funding for our research.
Consent
“Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”
Authors contribution
Radwan Kassir: writing.
Sylviane Baccot and Tarek Debs: conceptualized and designed the paper.
Violaine Yvorel and Claire Boutet: data collections.
Joelle Dubois and Alexia Boueil: reviewed the paper.
Olivier Tiffet: conceptualized, designed the paper, reviewed and revised the paper.
References
- 1.Limas C., Seretis K., Soultanidis C., Anagnostoulis S. Axial torsion and gangrene of a giant Meckel’s diverticulum. J. Gastrointestin. Liver Dis. 2006;15:67–68. [PubMed] [Google Scholar]
- 2.Moore G.P., Burkle F.M., Jr. Isolated axial volvulus of a Meckel’s diverticulum. Am. J. Emerg. Med. 1988;6:137–142. doi: 10.1016/0735-6757(88)90052-6. [DOI] [PubMed] [Google Scholar]
- 3.Khan N.A., Chandramohan M., McDonald S. Meckel divertculum. Radiol. Pediatr. 2008;110:205–210. [Google Scholar]
- 4.Malik A.A., Wani K.A., Khaja A.R. Meckel’s diverticulum: revisited Saudi. J. Gastroenterol. 2010;16:3–7. doi: 10.4103/1319-3767.58760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewardson R.H., Bombeck C.T., Nyhus L.M. Critical operative management of small bowel obstruction. Ann. Surg. 1978;187:189–193. doi: 10.1097/00000658-197802000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]; Azar T., Berger D.L. Adult intussusception. Ann. Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaudhuri T.K., Christie J.H. False positive Meckel’s diverticulum scan. Surgery. 1972;71:313. [PubMed] [Google Scholar]
- 7.Dalinka M.K., Wunder J.F. Meckel’s diverticulum and its complications, with emphasis on roentgenologic demonstration. Radiology. 1973;106:295–298. doi: 10.1148/106.2.295. [DOI] [PubMed] [Google Scholar]
- 8.Duszynski D.O. Radionuclide imaging of gastrointestinal disorders. Semin. Nucl. Med. 1972;11:383. doi: 10.1016/s0001-2998(72)80028-x. [DOI] [PubMed] [Google Scholar]
- 9.Guss D.A., Hoyt D.B. Axial volvulus of Meckel’s diverticulum: a rare cause of acute abdominal pain. Ann. Emerg. Med. 1987;16:811–812. doi: 10.1016/s0196-0644(87)80583-8. [DOI] [PubMed] [Google Scholar]
- 10.Hee T., Jin-Oh L., Jae K., Kim J., Sook S., So H., Jin Y., Gun H., Joo K., Cho Y., Seong Lee J. A case of intussuscepted Meckel’s diverticulum. World J. Gastroenterol. 2009;15(Oct 28 40):5109–5111. doi: 10.3748/wjg.15.5109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kassir R., Bourbon M. Management of the Aymand’s hernia in laparoscopy. J. Curr. Surg. 2013;3(2):92–94. [Google Scholar]


