Highlights
-
•
We report a rare case of cancer arising within fistulae in a Crohn’s disease patient.
-
•
A deterioration of the fistulous disease may conceal a cancer development.
-
•
Examination under anaesthesia with biopsies or curettage of the fistulae is crucial.
-
•
Patients with fistulising Crohn’s disease should be kept under regular surveillance.
Abbreviations: CD, Crohn’s disease; MRI, magnetic resonance imaging
Keywords: Crohn’s disease, Perianal fistula, Adenocarcinoma
Abstract
Introduction
Colorectal adenocarcinoma and Crohn’s disease are known to be associated entities. However, a carcinoma arising within a chronic perianal fistulous tract in a patient with Crohn’s disease is a rare complication.
Presentation of case
We present a case of a 40-year-old male patient with a long-standing perianal Crohn’s disease who developed an anal mucinous adenocarcinoma within the fistulous tracts.
Discussion
Although, Crohn’s disease and colorectal carcinoma association is well established, few cases have been reported where the cancer has originated within a perianal fistula. Constant mucosal regeneration occurring within a fistula seems to be the predominant pathogenetic mechanism, while immunosuppressants and anti-TNF agents may also contribute to the malignant transformation. Unfortunately, the lack of suspicion and the inadequate physical examination or colonoscopy due to exacerbation of the perianal symptoms could lead to delayed diagnosis; and thus, a poor prognosis.
Conclusion
Albeit a rare complication, clinicians should maintain a high degree of vigilance about the possible development of adenocarcinoma in patients with long-standing perianal Crohn’s disease. Thus, these patients should be kept under regular surveillance with examination under anaesthesia and biopsies or curettage of the tracts.
1. Introduction
The association between Crohn’s disease (CD) and colorectal cancer is well established. However, carcinoma associated with chronic fistulous CD is a rare complication. We report a case of a 40-year-old CD patient who developed an anal adenocarcinoma within a long-standing perianal fistulous tract and review the available literature.
2. Presentation of case
A 40-year-old male patient with ileocolonic CD and perianal fistulising lesions, diagnosed 23 years ago, was referred to our institution for a new finding of soft tissue within a perianal fistula. His past medical history included loop sigmoidostomy and seton insertion 3 years ago for control of his perianal disease. Three months later, due to ileus caused by terminal ileitis, he underwent emergency right colectomy. At the same time, the loop sigmoidostomy was converted to end colostomy with closure of the peripheral stump; since, the perianal disease was still uncontrollable. At this time, taking into account the benign nature of the disease, as well as patient’s age, it was decided to give to the patient a second chance to keep his sphincter mechanism rather than to perform an abdominoperineal resection. The patient had received in the past, either in conjunction or consequently, corticosteroids, antibiotics (metronidazole, ciprofloxacin), immunosuppressants (azathioprine, methotrexate) and anti-TNF agents (infliximab) for the control of the frequent flare-ups. On referral, he was on adalimumab and mercaptopurine. Physical examination revealed mild perianal inflammation with muco-purulent discharge from two sore-like fistulous orifices, located at 7 and 11 o’clock in supine position (Fig. 1). Pelvic magnetic resonance imaging (MRI) demonstrated pathological tissue development within one fistulous tract (Fig. 2) suggesting a mucinous cancer arising within the fistula. The rectosigmoidoscopy depicted mild lesions compatible with moderately active CD, without any other sign of obvious malignancy. Mucosal biopsies were obtained from the lesions and the underlying fistulous tracts; granulomatous tissue infiltrated by mucus-producing adenocarcinoma was found on pathology. Staging with computed tomography did not reveal any metastatic disease. Thus, the patient underwent abdominoperineal resection, where a 37 cm segment of colon with the mesorectum, anal canal of 7 cm and the corresponding overlying soft tissue of the perineum was resected. On histopathology, a T4N1 moderately/poorly differentiated mucinous adenocarcinoma was detected (Fig. 3). According to the referrer, his last physical examination, six months prior to admission, was unremarkable. Unfortunately, three months postoperatively the patient developed multiple bone metastases and he is currently receiving chemotherapy.
Fig. 1.

Fistulous orifices at 7 and 11 o’clock.
Fig. 2.
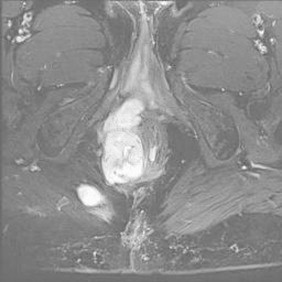
MRI of adenocarcinoma developing within fistulous tracts (high signal intensity on T2-weighted image).
Fig. 3.
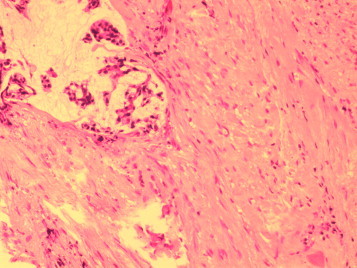
Histological section of perianal fistulous tract infiltrated by moderately–poorly differentiated mucus – producing adenocarcinoma (haematoxylin − eosin × 100).
3. Discussion
Up to 43% of CD patients will develop perianal fistulising disease [1]. The development of carcinoma within a chronic perianal fistula is a rare complication of CD, first reported by Lightdale et al. in 1975 [2]. Iesalnieks et al. has reported 65 cases with anorectal cancer associated with perianal fistulae in patients with CD [3] with an estimated incidence of 0.3–0.7% [4].
The pathogenesis has not yet been fully elucidated; Traube at al. suggested that the environment of constant mucosal regeneration occurring within a fistula may cause dysplastic changes, which may ultimately lead to adenocarcinoma [5]. On the contrary, Church et al. supported that a fistula formation may be a result of the cancer itself [6]. In the present case, the pre-existence of long-standing fistulae renders the latter improbable. It has been suggested that immunosuppressants and anti-TNF agents may contribute to the malignant transformation [7]. In a recent article, Osterman et al. supported that patients treated with combination of adalimumab and immunomodulators were more likely to develop cancer compared both to general population and patients with adalimumab monotherapy [8]. This plausible pathogenetic mechanism may hold true in the present case, where the patient had been treated with anti-TNF and immunomodulators for approximately ten years prior to the diagnosis of cancer.
Patients with long-standing CD, diagnosed before thirty years of age and with faecal diversion are at greater risk for the development of carcinoma arising in association with a perianal fistula [9]. Unfortunately, the majority of these patients have poor prognosis due to the advanced disease stage at diagnosis. Similarities between benign deterioration of the perianal symptoms and de novo development of cancer, as well as the lack of a high degree of suspicion for this rare complication may be responsible for the delay of diagnosis. Furthermore, the exacerbation of the symptoms makes physical examination or colonoscopy cumbersome to occur. A complex, long-standing fistula requires thorough examination of the rectum and the perianal area under anaesthesia followed by biopsies and/or curettage of the fistulous tracts. It follows, those patients with chronic perianal fistulising CD should be kept under a regular and careful surveillance. Ogawa et al. have suggested that a patient should undergo surveillance for carcinoma after seven years of perianal disease [4].
The gold standard treatment of fistulae-associated anal adenocarcinoma in patients with CD is abdominoperineal resection. In a recent article, Gaertner et al. reported that all patients with perianal adenocarcinoma who had undergone neoadjuvant chemoradiation therapy followed by abdominoperineal resection had a complete response [10]. The potential benefits of this kind of therapy have not yet been established; and therefore, in our patient we proceeded only to surgical treatment.
4. Conclusion
Clinicians who manage patients with long-standing perianal CD should maintain high level of suspicion for adenocarcinoma development on the setting of perianal fistulising CD. A chronic, complex fistulous disease may conceal a tumour and the examination under anaesthesia with biopsies and/or curettage of the fistulous tracts may be warranted. Therefore, all patients suffering from chronic perianal CD should be kept under regular surveillance.
Conflict of interest
All authors declare that there is no financial arrangement or other relationship that could be construed as a conflict of interest.
Funding
There was not involvement of study sponsors in this work.
Authors contribution
Papaconstantinou I. conceived of the study, carried out its design and the critical revision for important intellectual content and had the overall responsibility of the manuscript.
Mantzos S.D. carried out the design, the collection, analysis and interpretation of the data and drafted the manuscript.
Kondi-Pafiti A. provided some of the data and participated in the critical revision.
Koutroubakis I. conceived of the study, participated in the design and carried out the critical revision.
All authors read and approved the final manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgements
We would like to express our very great appreciation to Mr Mylonas S.N. MD, of the Vascular Unit of Aretaieion Hospital, as well as Mr Elissaios Kontis MD and Mr Spyropoulos B.G. MD of the 2nd Department of Surgery of Aretaieion Hospital, for their valuable advice regarding to the final form of this manuscript.
Contributor Information
Ioannis Papaconstantinou, Email: johnpapacon@hotmail.com.
Dionysios S. Mantzos, Email: dionmantzos1@yahoo.gr.
Agathi Kondi-Pafiti, Email: akondi@med.uoa.gr.
Ioannis E. Koutroubakis, Email: ikoutroubakis@gmail.com.
References
- 1.Loftus E.V., Jr, Cima R.R. Inflammatory bowel disease. In: Yeo C.J., Matthews J.B., Mc Fadden D.W., Pemberton J.H., Peters J.H., editors. Shackelford’s Surgery of the Alimentary Tract. 7th edition. Philadelphia: Elsevier; 2013. pp. 1966–1968. [Google Scholar]
- 2.Lightdale C.J., Sternberg S.S., Posner G., Sherlock P. Carcinoma complicating Crohn’s disease. Report of seven cases and review of the literature. Am. J. Med. 1975;59:262–268. doi: 10.1016/0002-9343(75)90361-7. [DOI] [PubMed] [Google Scholar]
- 3.Iesalnieks I., Gaertner W.B., Glass H., Strauch U., Hipp M., Agha A. Fistula-associated anal adenocarcinoma in Crohn’s disease. Inflamm. Bowel Dis. 2010;16:1643–1648. doi: 10.1002/ibd.21228. [DOI] [PubMed] [Google Scholar]
- 4.Ogawa H., Haneda S., Shibata C., Miura K., Nagao M., Ohnuma S. Adenocarcinoma associated with perianal fistulas in Crohn’s disease. Anticancer Res. 2013;33:685–689. [PubMed] [Google Scholar]
- 5.Traube J., Simpson S., Riddell R.H., Levin B., Kirsner J.B. Crohn’s disease and adenocarcinoma of the bowel. Digest. Dis. Sci. 1980;25:939–944. doi: 10.1007/BF01308045. [DOI] [PubMed] [Google Scholar]
- 6.Church J.M., Weakley F.L., Fazio V.W., Sebek B.A., Achkar E., Carwell M. The relationship between fistulas in Crohn’s disease and associated carcinoma: report of four cases and a review of the literature. Dis. Colon Rectum. 1985;28:361–366. doi: 10.1007/BF02560444. [DOI] [PubMed] [Google Scholar]
- 7.Ball C.S., Wujanto R., Haboubi N.Y., Schofield P.F. Carcinoma in anal Crohn’s disease: discussion paper. J. R. Soc. Med. 1988;81:217–219. doi: 10.1177/014107688808100411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterman M.T., Sandborn W.J., Colombel J.F., Robinson A.M., Lau W., Huang B. Increased risk of malignancy with adalimumab combination therapy, compared with monotherapy, for Crohn’s disease. Gastroenterology. 2014;146:941–949. doi: 10.1053/j.gastro.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 9.Tokunaga Y., Sasaki H., Saito T. Carcinoma in anorectal fistulas of Crohn’s Disease with seton drainage case report and review of the literature. Digestion. 2008;77:20–21. doi: 10.1159/000114964. [DOI] [PubMed] [Google Scholar]
- 10.Gaertner W.B., Hagerman G.F., Finne C.O., Alavi K., Jessurun J., Rothenberger D.A. Fistula-associated anal adenocarcinoma: good results with aggressive therapy. Dis. Colon Rectum. 2008;51:1061–1067. doi: 10.1007/s10350-008-9294-4. [DOI] [PubMed] [Google Scholar]


