Highlights
-
•
64-year-old man complicated with left obstructive pneumonia.
-
•
CT scan showed total atelectasis of the left lung due to obstructive endobronchial tumor.
-
•
Endobronchial tumor resection was performed prior to wedge bronchoplastic lobectomy.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging
Keywords: Lung cancer, Endobronchial electrocautery, Snare, Wedge bronchoplastic lobectomy, Steroid medication
Abstract
Introduction
Occasionally, it is difficult to design an appropriate treatment plan for central-type lung cancer. We present the usefulness of combined treatment with a bronchoscopic electrocautery wire snare prior to wedge bronchoplastic lobectomy for patients with central-type lung cancer.
Presentation of case
A 64-year-old man, who was a long-term corticosteroid user, complicated with left obstructive pneumonia. Chest CT scan showed total atelectasis of the left lung due to obstruction of the left main bronchus by an endobronchial tumor, which protruded from the left lower lobe. He was diagnosed with squamous cell carcinoma of c-T3N0M0 Stage IIB. Endobronchial tumor resection of the left main bronchus was initially performed, which resulted in an improvement of the patient’s symptoms; the patient’s pulmonary function was evaluated and bronchial extension of the tumor was also observed. He subsequently underwent elective bronchoplastic left lower lobectomy and lymphadenectomy, with no recurrence 2 years after surgery.
Discussion
A variety of therapeutic bronchoscopic intervention are available for the treatment of advanced central-type lung cancer. The effectiveness of endobronchial electrocautery using the snare wire has been reported for the treatment of respiratory tract tumors, which allowed planning of the following treatment procedure.
Conclusion
The combination of a bronchoscopic electrocautery wire snare and bronchoplastic surgical procedure was useful for the treatment of central-type lung cancer such as in our case.
1. Introduction
The development of computed tomography (CT) imaging and spreading of health screening programs has facilitated in detecting the lung cancer at a relatively early stage in Japan. In these cases, the incidence of peripheral-type lung cancer is the most common. In contrast to peripheral-type lung cancer, the early detection of central-type lung cancer is difficult because these overlap with the pulmonary hilar and cardiovascular shadow. Occasionally, detection of central-type lung cancer is conducted at later stage, and it is difficult to design an appropriate treatment plan for these cases. In this report, we present the usefulness of combined treatment with bronchoscopic electrocautery wire snare of endobronchial tumor prior to wedge bronchoplastic lobectomy for patients with central-type lung cancer with obstructive pneumonia who were treated with corticosteroid for a long period of time.
2. Presentation of case
A 64-year-old male developed persistent cough that was diagnosed as bronchial asthma, and bronchodilator and inhaled corticosteroids were prescribed at a private clinic. However, his symptom did not improve, and he was referred to our hospital for further examination. His medical history was as follows. Two years prior to consultation, the patient was diagnosed as eosinophilic myositis and was administered 5–30 mg/day of prednisolone for the next 2 years. Physical examination revealed fine resonant wheezing was audible at the left side of the chest. Chest X-ray showed a reticular shadow in the left lung hilum (Fig. 1A). Chest CT imaging showed segmental atelectasis of the left lower lobe and a round tumor shadow at the orifice of the left lower bronchus that protruded into the left main bronchus (Fig. 1B). Despite professional advice to undergo further examination including bronchoscopy, the patient did not comply.
Fig. 1.

(A) Chest X-ray at patient’s first visit, showing a reticular shadow in the left lung hilum. (B) Chest CT scan showing segmental atelectasis of the left lower lobe, and a round tumor shadow at the orifice of the left lower bronchus, which protruded into the left main bronchus.
One month after his first visit to our hospital, the patient again consulted our facility with a chief complaint of febrile dyspnea. Physical examination showed that following vital signs: temperature was 38.8 °C, tachypnea (32 breaths/min), and tachycardia (102 beats/min). There were rough rhonchi and crackles throughout inspiration and expiration on auscultation of the left chest. SpO2 decreased to 80% under room air, therefore, indicating a need for oxygen inhalation. Chest X-ray showed total atelectasis of the left lung field (Fig. 2A). Chest CT scan showed total atelectasis of the left lung due to obstruction of left main bronchus by the endobronchial tumor in the left main bronchus (Fig. 2B). The patient was diagnosed with obstructive pneumonia by endobronchial tumor and an antibiotic was administered.
Fig. 2.
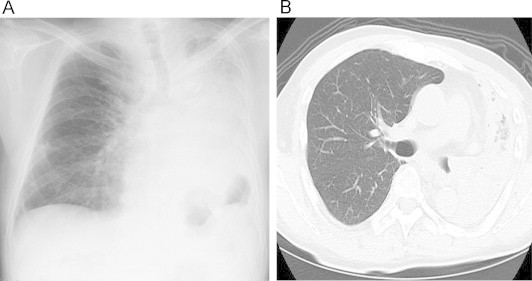
(A) Chest X-ray at 1 month after patient’s first visit to our hospital, showing total atelectasis of the left lung field. (B) Chest CT scan showing total atelectasis of the left lung due to obstruction of left main bronchus by endobronchial tumor in the left main bronchus.
Bronchoscopic examination revealed a pedunculated endobronchial tumor covered with a yellow surface obstructing the distal portion of the left main bronchus (Fig. 3). Pathologic examination of the tumor biopsies confirmed the diagnosis of squamous cell carcinoma. Evaluation for distant metastases, brain MRI, chest and abdominal CT imaging, and bone scintigraphy showed no metastases: therefore, the patient was diagnosed as clinical T3N0M0 stage IIB.
Fig. 3.

Bronchoscopy reveals an endobronchial tumor covered with a yellowish surface obstructing the distal portion of the left main bronchus.
Bronchoscopic tumor resection was performed using electrocautery wire snare under general anesthesia. A wire snare was passed through the bronchoscope biopsy channel. The wire loop was passed over the endobronchial tumor in the left main bronchus. A blended electrocautery current was applied, and the obstructing tumor was successfully resected with minimal bleeding. After the endobronchial resection of the tumor, a significant improvement of symptoms was observed. The chest X-rays showed re-expansion of the left upper lobe (Fig. 4). Respiratory function studies after the re-expansion of the left lung showed an FEV1.0 of 2.770 L and an FEV1.0% of 71.4%. Arterial blood gas was within normal range (pH of 7.44, pCO2 of 36 mm Hg, and pO2 of 94 mm Hg), which indicated that the patient did not require any further administration of oxygen gas.
Fig. 4.

Chest X-rays after the endobronchial resection of the tumor showing re-expansion of the left lung.
One week after the bronchoscopic electrocautery wire snare resection of endobronchial tumor at the left main bronchus, the surgery was accomplished under general anesthesia. At the interlobular space, the tumor was close to the A3a pulmonary artery; therefore, pulmonary artery was ligated and cut at a distal site from A3a. The lingular branch (A4 + 5) of the pulmonary artery descended between the bronchus and upper pulmonary vein, thus facilitating its preservation. After lymph node dissection around the left main bronchus, the underside of the left main bronchus was opened, and wedge-shaped incision was made on the main bronchial wall while confirming the tumor in the lumen, and the left lower lobe including the orifice of the left lower bronchus was removed. The bronchus stump was then assessed as cancer free by rapid pathological examination and then closed with an interrupted suture using 3-0 PDSII. An anastomotic line was reinforced with a pedicled intercostal muscle flap.
The pathological diagnosis of the patient was squamous cell carcinoma, pT2N2(#7)M0 Stage IIIA, and negative for surgical margins. Although the patient’s postoperative condition was uneventful, bronchoscopy performed at 2 weeks after surgery showed bronchial kinking and small ulcer formation at the opposite site of the anastomosis line (Fig. 5A). However, this ulcer spontaneously healed 1 month later (Fig. 5B). Despite our recommend to undergo adjuvant chemotherapy, the patient did not comply. The patient has been carefully followed at our outpatient clinic using CT imaging and bronchofiberscopy, and left bronchial luminal patency was good without recurrence or stenosis 2 years after surgery (Fig. 5C).
Fig. 5.
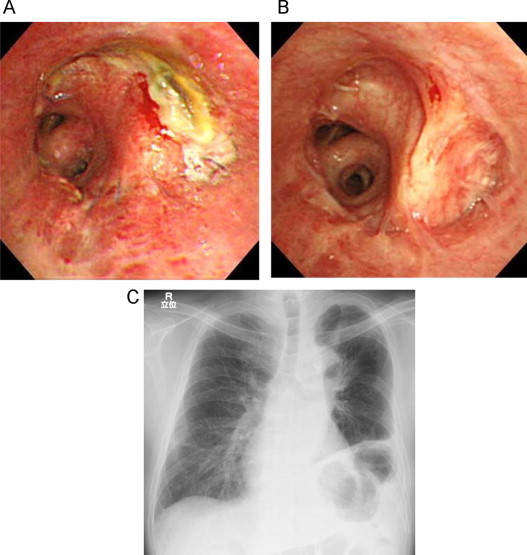
(A) Bronchoscopy performed at 2 weeks after surgery showed bronchial kinking, and the formation of an ulcer at the opposite site of the anastomosis line, (B) which spontaneously healed after 1 month. (C) Chest X-ray at 2 year after surgery.
3. Discussion
Central-type lung cancer is strongly associated with two major clinical problems: the difficulty in detecting a tumor shadow due to its overlap with the pulmonary hilar and the cardiovascular shadow, and rapid deterioration of the patient’s condition due to the obstruction of blood vessels and bronchi. A variety of therapeutic bronchoscopic intervention are available for the treatment of advanced central-type lung cancer such as tumor resection with forceps, laser, electrocautery, and bronchodilators using a stent placed under the rigid or flexible bronchoscope. The treatment used for each case is determined by the actual condition of the patient [1,2]. The effectiveness and safety of endobronchial electrocautery using the snare wire or laser have been reported for the treatment of respiratory tract tumor [3–5]. Wahidi et al. [5] described the treatment of 117 cases using endobronchial electrocautery wire snare. The rate of endoscopic improvement was 94%, symptom relief was 71%, radiological improvement was 78%, and severe complications was 0.8%. In the present case, it was not possible to assess lung function because the patient had dyspnea at admission. Based on this condition, surgical procedures could not be designed for this patient. In this case, CT imaging was conducted 1 month prior to hospitalization, which detected a tumor that protruded to the left main bronchus. Therefore, based on the clinical and radiological course of disease, left total atelectasis was due to obstruction of the left main bronchus by a tumor that protruded from the left lower lobe, which may have occurred several days prior. A treatment regimen was then designed, initially consisting of the resecting the endobronchial tumor of the left main bronchus by endobronchial electrocautery wire snare to assess the degree invasion to the bronchial wall of the left upper lobe, the presence or absence of re-expansion of the left upper lobe, and improvement of clinical symptoms and lung function. After these evaluations, a surgical treatment was then selected, i.e., left lower lobectomy with bronchoplasty or left pneumonectomy.
Pneumonectomy is often necessary in cases of lung cancer involving hilum invasion such as that described in our case. However, after pneumonectomy, postoperative pulmonary function and performance status decreased, which in turn resulted in restricted postoperative chemotherapy and therapeutic methods. When we consider pneumonectomy as a treatment approach, the choice of the chemoradiation therapy should also be considered [6]. Bronchoplastic lobectomy, i.e., sleeve or wedge bronchoplastic lobectomy is generally performed in patients with impaired pulmonary function in whom pneumonectomy may difficulty. It is also performed in cases that can tolerate pneumonectomy, and the postoperative performance status is better than pneumonectomy [7–10]. In our case, we were concerned about anastomosis failure after bronchoplastic lobectomy, particularly sleeve lobectomy, because patient is often treated with corticosteroids for 2 years for eosinophilic myelitis. Therefore, we performed left lower lobectomy with bronchial wedge resection. Bronchoscopic examination 2 weeks after the operation showed bronchial kinking; the distal bronchial anastomosis area was slightly folded into proximal bronchial lumen due to the difference in bronchial diameter and formation of an ulcer at the opposite side of the anastomotic line, however, the ulcer spontaneously healed and no perforation and stenosis was observed 2 years after surgery.
4. Conclusion
We report a case of central-type lung cancer with obstructive pneumonia who was treated with corticosteroid for a long period of time which was initially treated with endobronchial tumor resection using the bronchoscopic electrocautery wire snare. After bronchoscopic intervention, we could assess the degree of bronchial invasion and patient’s pulmonary function, and this allowed planning of the treatment regimen and surgical procedure.
Conflicts of interest
None.
Funding
None.
Ethical approval
Ethical approval not required.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
This manuscript has not been published and is not under consideration for publication elsewhere.
All the authors have read the manuscript and have approved this submission.
The authors will transfer copyright to the publisher upon acceptance of the manuscript.
Authors contribution
All authors were involved in patient care, writing and critical review of the manuscript.
Guarantor
All authors are guarantor.
References
- 1.Cavalieri S., Venuta F., Foccoli P., Toninelli C., Face B. Endoscopic treatment of malignant airway obstructions in 2008 patients. Chest. 1996;110:1536–1542. doi: 10.1378/chest.110.6.1536. [DOI] [PubMed] [Google Scholar]
- 2.Morris C.D., Budde J.M., Godette K.D., Kerwin T.L., Miller J.I., Jr. Palliative management of malignant airway obstruction. Ann. Thorac. Surg. 2002;74:1928–1932. doi: 10.1016/s0003-4975(02)04085-7. [DOI] [PubMed] [Google Scholar]
- 3.Hooper R.G., Jackson F.N. Endobronchial electrocautery. Chest. 1988;94:595–598. doi: 10.1378/chest.94.3.595. [DOI] [PubMed] [Google Scholar]
- 4.Kawasaki H., Ishikawa K., Kawabata T., Ohta M., Kuniyoshi M., Genka K. Endobronchial leiomyoma successfully treated by endobronchial electrocautery. J. Bronchol. 2000;7:240–243. [Google Scholar]
- 5.Wahidi M.M., Unroe M.A., Adlakha N., Beyea M., Shofer S.L. The use of electrocautery as the primary ablation modality for malignant and benign airway obstruction. J. Thorac. Oncol. 2011;6:1516–1520. doi: 10.1097/JTO.0b013e3182242142. [DOI] [PubMed] [Google Scholar]
- 6.Albain K.S., Swann R.S., Rusch V.W., Turrisi A.T., 3rd., Shepherd F.A., Smith C. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet. 2009;374:379–386. doi: 10.1016/S0140-6736(09)60737-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Massard G., Kessler R., Gasser B., Ducrocq X., Elia S., Gouzou S. Local control of disease and survival following bronchoplastic lobectomy for non-small cell lung cancer. Eur. J. CardioThorac. Surg. 1999;16:276–282. doi: 10.1016/s1010-7940(99)00233-x. [DOI] [PubMed] [Google Scholar]
- 8.Okada M., Yamagishi H., Satake S., Matsuoka H., Miyamoto Y., Yoshimura M. Survival related to lymph node involvement in lung cancer after sleeve lobectomy compared with pneumonectomy. J. Thorac. Cardiovasc. Surg. 2000;119:814–819. doi: 10.1016/S0022-5223(00)70018-3. [DOI] [PubMed] [Google Scholar]
- 9.Deslauriers J., Grégoire J., Jacques L.F., Piraux M., Guojin L., Lacasse Y. Sleeve lobectomy versus pneumonectomy for lung cancer: a comparative analysis of survival and sites or recurrences. Ann. Thorac. Surg. 2004;77:1152–1156. doi: 10.1016/j.athoracsur.2003.07.040. [DOI] [PubMed] [Google Scholar]
- 10.Park S.Y., Lee H.S., Jang H.J., Joo J., Kim M.S., Lee J.M. Wedge bronchoplastic lobectomy for non-small cell lung cancer as an alternative to sleeve lobectomy. J. Thorac. Cardiovasc. Surg. 2012;143:825–831. doi: 10.1016/j.jtcvs.2011.10.057. [DOI] [PubMed] [Google Scholar]


