Highlights
-
•
Prostatic utricle is a rare malformation originating from incomplete regression of Mullerian ducts.
-
•
Mini invasive approach is considered the gold standard for surgical treatment.
-
•
Few cases of robot-assisted excision have been reported in the literature.
-
•
We report a case treated with robotic-assisted surgery.
Keywords: Prostatic utricle, Disorders sexual differentiation, Minimally invasive surgery, Robot assisted laparoscopy
Abstract
Introduction
Prostatic utricle is a rare malformation arising from incomplete regression of the Müllerian ducts. Diagnosis is easily made but management may be challenging. The minimally invasive approach has so far been considered the gold standard for surgical treatment. Many endoscopic and surgical procedures have been described for removal, but to date only few cases of robot-assisted procedures have been mentioned in the literature and there are no reports of redos.
Presentation of the case
We report the case of a giant prostatic utricle cyst successfully treated with robotic-assisted surgery two years after an unsuccessful first attempt at laparoscopic excision. No relapse was found at one year follow up.
Discussion
We were able to excise a retro-vescical structure in spite of adhesions caused by the previous surgery and the very large size of the diverticulum thanks to the high magnification and 3-D visualization available in robotic assisted laparoscopy.
Conclusion
Robot assisted laparoscopy should be considered an advantageous technique for the treatment of prostatic utricle.
1. Introduction
The prostatic utricle is a diverticulum of the posterior urethra at the summit of the verumontanum, between and above the two ejaculatory ducts. It arises from incomplete regression of the Müllerian ducts or from inadequate androgen stimulation of the urogenital sinus. The incidence of enlarged prostatic utricle is estimated at between 11 and 14% in association with distal hypospadias or disorder of sexual differentiation (DSD) anomalies and at up to 50% in the presence of perineal hypospadias [1]. Diagnosis is easily made but management can be challenging, and in order to prevent infertility and neoplastic degeneration, treatment is generally reserved to symptomatic cases (urinary tract infections, stones in the pouch, dysuria, back-pressure changes and pseudoincontinence due to secondary trapping of urine in the pouch) [2]. Several surgical and endoscopic techniques have been described, but laparoscopy is considered the gold standard treatment. Robotic-assisted resection of prostatic utricle has rarely been described to date [3–5]. We report the first successful robotic assisted redo-excision of a non-symptomatic, giant prostatic utricle in a 19-year-old boy with DSD.
2. Presentation of case
A 19-year-old boy affected by DSD with chromosome disease (45x-46x-dic(Y)(q 11.2)) was admitted to our department for treatment of a retrovesical mass. A prostatic utricle cyst had been laparoscopically removed two years before in another institution. The patient’s clinical history included right inguinal hernia repair at 4 months of age with excision of an ovotestes (the contralateral intraoperative gonad biopsy detected normal testicular tissue); and urethroplasty for penile hypospadia, performed when the child was 4-year-old.
Clinical examination and blood analysis at admission were normal without any history of urinary infections. Ultrasound (US) revealed a 10 × 6 cm anechoic retrovesical cystic lesion. MRI confirmed a fluid-filled drop-shaped midline cystic mass, tapering to an end behind the hypoplastic prostate, and apparently not communicating with the prostatic urethra (Fig 1). The urethral meatus, on the ventral surface of the glans, was of adequate caliber. Cystoscopy revealed a tortuous distal urethra opening into a utricle at the level of the verumontanum, filled with corpuscolated fluid. At the bottom we identified the stitches from the previous incomplete surgical removal.
Fig. 1.
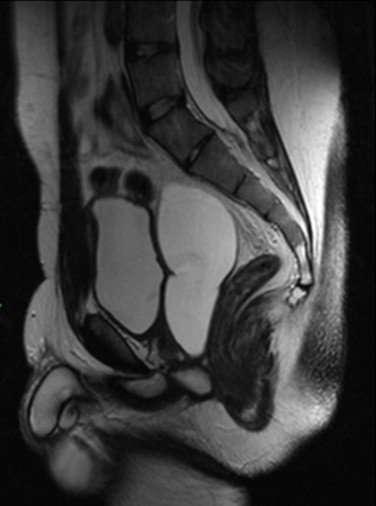
Pre-operative MRI showing a large retrovescical cystic mass.
We approached the lesion by robot-assisted laparoscopy. A uretheral catheter was positioned inside the utricle and a Foley catheter was passed into the bladder. The optical port at the umbilicus was advanced into the peritoneum and two 5-mm working ports were placed on the para-rectal lines. The bladder was suspended to the abdominal wall. The prostatic utricle was easily identified, grasped and carefully dissected free of surrounding tissue to 3 cm from the urethra. Dissection was difficult on the right side because of fibrotic tissue due to the previous intervention. When the prostatic utricle was completely mobilized, we cauterized the utricle mucosa and stapled it, leaving a small stump off the urethra. No significant perioperative complications occurred. Seven days postoperatively the patient was discharged without a urethral catheter. At one-year follow-up US examination showed no relapse and cystourethrography confirmed no significant cyst remnants (Fig 2).
Fig. 2.

Post-operative cystography (1 year), showing no significant cyst remnants.
3. Discussion
Surgical excision of the prostatic utricle is usually reserved for symptomatic cases. We describe redo surgery in an asymptomatic patient with giant utricle, with indication for prevention of the risk of malignancy and to preserve function and fertility of the residual testis since almost 12% of enlarged prostatic utricles in adults are associated with subfertility [6]. In 1992, Hendry and Pryor reported 26 cases of male subfertility caused by prostatic utricle, with semen quality improving in 38.5% of patients after surgical treatment [1]. In addition, some reports describe an incidence of malignancy of 3% [7].
Surgical management is challenging due to the rarity of the disorder and the proximity to the ejaculatory ducts, pelvic nerves, rectum, vas deferens and ureters. Several endoscopic techniques have been reported, such as transurethral cyst catheterization and aspiration, cyst orifice dilatation, utricle incision, transurethral deroofing and trans-vesical excision, all with high recurrence rates [2,8]. Open surgery seems to give better results, but the approach to the lesion is too high for a perineal approach and too low for abdominal surgery. Moreover, all the described techniques, although requiring extensive dissection, result in poor exposure and high risk of injury to adjacent structures [9–12]. The minimally invasive approach has been recommended in several reports [4,13–15] because of the clearer view of the deep pelvic structures. In our case, the original laparoscopic surgery had not allowed removal of the entire lesion, and we opted for robotic-assisted laparoscopy in the redo procedure in order to combine the advantages of laparoscopy with the improved three-dimensional (3D) visualization and high instruments dexterity. The 15-fold magnification of the surgical field given by the 3D camera has been reported to translate into enhanced intraoperative and postoperative outcomes [16–17]. Nevertheless, few cases of robot-assisted excision of retrovesical structures have appeared in the literature to date [3–5].
We found that the excellent visualization of the retrovesical structures made this technique safe, lowering the risk of injury to the vas deferens, ureters, rectum and bladder neck. Together with the excellent magnification, the wristed instruments allow for improved dexterity in the small confines of the pelvis. The three-dimensional camera compensates for the lack of tactile feedback to the retrovesical structures. Optimal port placement with a wide angle avoids collision of the robotic arms and can be instrumental in performing more precise surgery [18–20].
4. Conclusions
Robotic-assisted surgery allowed complete removal of a large utricle already submitted to previous unsuccessful laparoscopic resection. We found minimally invasive robotic procedure to be advantageous because of its greater magnification, 3-D visualization and high dexterity wristed instruments. These features allowed us to avoid injury to other structures in the retrovescical space, in spite of the presence of adhesions from the first attempt to treat the utricle. Robot assisted laparoscopy should be considered in redo utricle procedures, and as a valid alternative to laparoscopy for the primary treatment of prostatic utricle.
Conflicts of interest
There are not conflicts of interest.
Funding
Sponsors had no involvement in the drafting of the paper.
Ethical Approval
Ethical approval has been given by Ethics Commission of Fondazione IRCCS San Matteo, Pavia, Italy.
Author contribution
Ilaria Goruppi: Concept and writing the paper.
Luigi Avolio: Concept, writing and review of the paper, surgical intervention.
Piero Romano: Collecting data, surgical intervention.
Alessandro Raffaele: Writing the paper, review of the literature.
Gloria Pelizzo: Review of the paper, surgical intervention.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Ilaria Goruppi.
Luigi Avolio.
References
- 1.Hendry W.F., Pryor J.P. Müllerian duct (prostatic utricle) cyst: diagnosis and treatment in subfertile males. Br. J. Urol. 1992;69(1):79–82. doi: 10.1111/j.1464-410x.1992.tb15464.x. [DOI] [PubMed] [Google Scholar]
- 2.Meisheri I.V., Motiwale S.S., Sawant V.V. Surgical management of enlarged prostatic utricle. Pediatr. Surg. Int. 2000;16:199–203. doi: 10.1007/s003830050722. [DOI] [PubMed] [Google Scholar]
- 3.Passerotti C., Cendron M., Gargollo P., Diamond D.A., Borer J.G., Cilento B., Bauers S., Retik A.B., Peters C.A., Nguyen H.T. Minimally invasive surgical approaches to retrovescical structures. Int. J. Med. Rob. Comp. Ass. Surg. 2007;3:307–311. doi: 10.1002/rcs.164. [DOI] [PubMed] [Google Scholar]
- 4.Estrada C.R., Passerotti C.C. Robotic surgery in pediatric urology. Arch. Esp. Urol. 2007;60:471–479. doi: 10.4321/s0004-06142007000400017. [DOI] [PubMed] [Google Scholar]
- 5.Onal B., Diamond D.A., Retik A.B., Cendron M., Nguyen H.T. Robot-assisted laparoscopic excision of symptomatic retrovesical cysts in boys and young adults. J. Urol. 2011;186:2372–2378. doi: 10.1016/j.juro.2011.07.113. [DOI] [PubMed] [Google Scholar]
- 6.Desautel M.G., Stock J., Hanna M.K. Müllerian duct remnants: surgical management and fertility issues. J. Urol. 1999;162:1008–1013. doi: 10.1016/S0022-5347(01)68050-9. [DOI] [PubMed] [Google Scholar]
- 7.Gualco G., Ortega V., Ardao G., Cravioto F. Clear cell adenocarcinoma of the prostatic utricle in an adolescent. Ann. Diagn. Pathol. 2005;9:153–156. doi: 10.1016/j.anndiagpath.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Husmann D.A., Allen T.D. Endoscopic management of infected enlarged prostatic utricles and remnants of rectourethral fistula tracts of high imperforate anus. J. Urol. 1997;157:1902–1906. [PubMed] [Google Scholar]
- 9.Ikoma F., Shima H., Yabumoto H., Mori Y. Surgical treatment for enlarged utricle and vagina masculina in patients with hypospadias. Br. J. Urol. 1986;58:423–428. doi: 10.1111/j.1464-410x.1986.tb09097.x. [DOI] [PubMed] [Google Scholar]
- 10.Keramidas D.C., Kapouleas G.P., Papandreou E. The posterior sagittal approach for the excision of a prostatic utricle cyst. Br. J. Urol. 1995;76:397–398. doi: 10.1111/j.1464-410x.1995.tb07723.x. [DOI] [PubMed] [Google Scholar]
- 11.Krstic Z.D., Smoljanic Z., Micovic Z., Vukadinović V., Sretenović A., Varinac D. Surgical treatment of the Müllerian duct remnants. J. Pediatr. Surg. 2001;36:870–876. doi: 10.1053/jpsu.2001.23958. [DOI] [PubMed] [Google Scholar]
- 12.Monfort G., Guys J.M. Trans vescical approach to surgery on the prostatic utricle. Chir. Pediatr. 1981;22:279–284. [PubMed] [Google Scholar]
- 13.Willetts I.E., Roberts J.P., MacKinnon A.E. Laparoscopic excision of a prostatic utricle in a child. Pediatr. Surg. Int. 2003;19:557–558. doi: 10.1007/s00383-003-0993-6. [DOI] [PubMed] [Google Scholar]
- 14.Barrena S., Aguilar R., Olivares P., Lobato R., López Pereira P., Martínez Urrutia M.J., Jaureguizar E. Laparoscopic resection of the prostatic utricle in children. Chir. Pediatr. 2010;23:15–18. [PubMed] [Google Scholar]
- 15.Yeung C.K., Sihoe J.D., Tam Y.H., Lee K.H. Laparoscopic excision of prostatic utricles in children. BJU Int. 2001;87:505–508. doi: 10.1046/j.1464-410x.2001.00132.x. [DOI] [PubMed] [Google Scholar]
- 16.Menon M. Robot-assisted radical prostatectomy: is the dust settling? Eur. Urol. 2011;59(1):7–9. doi: 10.1016/j.eururo.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 17.Meehan J.J., Sandler A. Pediatric robotic surgery: a single-institutional review of the first 100 consecutive cases. Surg. Endosc. 2008;22(1):177–182. doi: 10.1007/s00464-007-9418-2. [DOI] [PubMed] [Google Scholar]
- 18.Pelizzo G., Nakib G., Romano P., Avolio L., Mencherini S., Zambaiti E., Raffaele A., Stoll T., Mineo N., C.Alcaterra V. Five millimetre-intruments in paediatric robotic surgery: advantages and shortcomings. Minim. Invasive Ther. Allied Technol. 2014;3:1–6. doi: 10.3109/13645706.2014.975135. [DOI] [PubMed] [Google Scholar]
- 19.Pelizzo G., Nakib G., Goruppi I., Avolio L., Romano P., Raffaele A., Scorletti F., Mencherini S., Calcaterra V. Pediatric robotic pyeloplasty in patients weighing less than 10 kg initial experience. Surg. Laparosc. Endosc. Percutan. Tech. 2014;24:29–31. doi: 10.1097/SLE.0b013e31828e3f18. [DOI] [PubMed] [Google Scholar]
- 20.Nakib G., Calcaterra V., Scorletti F., RomanoP. Goruppi I., Mencherini S., Avolio L., Pelizzo G. Robotic assisted surgery in pediatric gynecology: promising innovation in mini invasive surgical procedures. J. Pediatr. Adolesc. Gynecol. 2013;26:5–7. doi: 10.1016/j.jpag.2012.09.009. [DOI] [PubMed] [Google Scholar]


