Highlights
-
•
Incidence, embryological origin and formation of a tailgut cyst.
-
•
Clinical presentation, radiological findings, and diagnosis of a tailgut cyst.
-
•
Description of our patient’s medical course and surgical treatment.
-
•
Surgical indications, pros and cons of different surgical approaches.
Keywords: Tailgut cyst, Kraske surgical approach, Review of the literature
Abstract
Introduction
Tailgut cysts are rare diseases but can be challenging to manage.
Presentation of case
This is a case report of a tailgut cyst, in a 42 year old female. The cyst was incidentally detected on imaging, and treated with Kraske surgical approach.
Discussion
Hereby, we review the relevant information present in the medical literature about the incidence, methods of diagnosis, treatment options and management plans.
Conclusion
Surgical management should be tailored individually for each patient, based on the advantages and disadvantages of each surgical approach.
1. Introduction
The presacral space, also known as retrorectal space, is rich in various elements, that can develop a wide variety of benign and malignant conditions, which most commonly present in the form of masses. These masses can be congenital, inflammatory, embryological remnants, neurogenic, or osseous in nature. They are rare but can be challenging to manage.
The tailgut cyst, being one of the rare congenital malformations which may present in the presacral space, is a remnant of the postnatal part of the hindgut. As the embryo starts to fold inward during the 4th week of gestation to enclose the future gut, the cloacal membrane (made up from the endoderm below the level of Hensen’s node) comes to lie ventral and encloses the caudal portion distal to the eventual hindgut and is called a tailgut. The tailgut normally regresses by the 6th week of gestation. If the mucous-secreting remnants fail to regress, a tailgut cyst is formed.
Tailgut cysts can present at any age, although they usually appear between the ages of 30 and 60. There is a strong predominance in females – the female to male ratio is 5:1. The majority of cysts are asymptomatic, and often missed on digital rectal exam due to low tension in the cyst [1].
In 1984, Bale detected two cases in a series of 363 cases of presacral masses, which makes the incidence among other sacrococcygeal lesions in children to be 0.55% [2]. The largest reported series, constituting 53 cases, was gathered over a period of 35 years by Hjermstad and Helwig from the American Armed Forces Institute of Pathology [3].
2. Case report
We present the case of a 42-year-old female with a medical history of treatment–resistant cycloiriditis. No history of dysuria or difficulties in defecation were reported. As part of the medical investigation to rule out an inflammatory bowel disease, a gastroscopy & colonoscopy were performed. These failed to show a pathological finding, leading to the decision to carry out a MR enterography, which detected a pelvic mass that was further investigated through an abdominopelvic CT. The CT scan showed a left-lying, well-circumscribed, rounded presacral mass at the level of the 4th sacral vertebra, measuring 3.4 × 2.8 cm (red arrow in Fig. 1a and b), with a central liquid component, a peripheral tissue density of 31HE, and a fine calcification at the right rim. No signs of osseous destruction were noted.
Fig. 1.
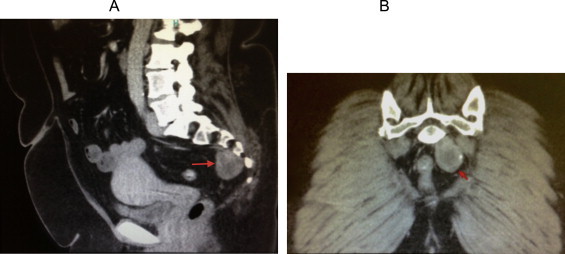
(a) Sagittal section of the abdominopelvic CT scan with the red arrow indicating the tailgut cyst. (b) Axial sections of the abdominopelvic CT scan, showing the tailgut cyst with wall calcification.(For interpretation of the references to color in the text, the reader is referred to the web version of this article).
The physical exam showed an anal sphincter with normal tone, normal flexibility of the perianal soft tissue, and an empty rectal vault with an extrarectal fullness posteriorly that is reachable with the fingertip.
The intraoperative findings showed a well capsulated presacral cyst with a vascular pedicle originating from the sacral periosteum. Complete resection took place through an avascular plane. The surgical specimen was sent for pathological examination that revealed a tailgut cyst (Fig. 2).
Fig. 2.
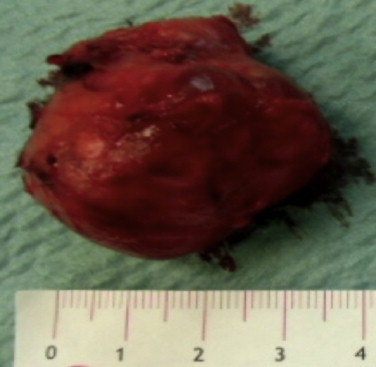
Specimen after in toto surgical excision.
3. Discussion
As the retrorectal region is a potential space surrounded by the rectum anteriorly, the sacrum and coccyx posteriorly, and the peritoneal reflection superiorly, the presence of a space-occupying lesion in that space can lead to different symptoms that can present in a wide variety of clinical pictures.
Their presentation and the subsequent clinical picture can range from an asymptomatic incidental finding on imaging to a prolapsing cyst through the anus; this has been reported in the literature to have been misdiagnosed as hemorrhoids [4,5]. Compression of the nearby organs can cause an array of symptoms, including urological, neurological, and defecation difficulties. Other acute presentations, such as acute urinary retention and obstipation, have been reported with large tailgut cysts [6]. Among reported uncommon presentations is right sciatica [7].
Tailgut cysts when infected can present with signs and symptoms that are similar to perianal or pelvic abscesses. With the natural development of the disease, perianal fistulas may issue and the corresponding faulty treatment has been reported in the literature [8].
The diagnosis can take place as early as a finding on prenatal-screening ultrasonography or as late as a finding in autopsy [9].
Tailgut cyst lining can exhibit different types of epithelium including columnar, transitional and squamous. The presence of some glandular or transitional epithelium differentiates them from epidermoid and dermoid cysts, which can communicate with the skin.
Generally, congenital presacral cysts can be divided into enteric and neurenteric cysts [10]. Rectal duplication cysts, the other differential that forms the enteric division, can be easily differentiated from the tailgut cyst by the presence of smooth muscle cells in the cyst wall.
It is worth mentioning, that in the pediatric population the most common presacral lesion is a teratoma, which is a form of dermoid cyst.
24 cases of malignancy arising from the epithelial lining of the cyst walls have been reported in the literature, including 10 carcinoid tumors as well as adenocarcinoma; thus, a careful histological examination is always required of the extracted surgical specimen [11,12].
3.1. Diagnosis
Imaging modalities such as MRI and CT scans are the cornerstone in discovering presacral masses. Any other investigation modality can only serve to arouse suspicion of the existence of a presacral mass.
On MRI a tailgut cyst typically demonstrates low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, though it may vary according to the content [13].
Although successful attempts of fine needle aspiration under endosonographic guidance have been reported, this procedure is not risk-free, and in case of complication, the subsequent surgical excision would be more difficult [14]. Thus, there is almost a consensus that surgical excision followed by a complete histological examination is the recommended path of treatment, instead of a preoperative biopsy.
3.2. Surgery
Excision of a retrorectal tumor is advised not only as a treatment option for symptomatic patients but also for asymptomatic patients, as those silent masses carry a considerable risk for presenting with serious illnesses when left untreated.
Surgical excision is also advised to rule out the possibility of malignancy or future malignant transformation, infection, defecation difficulties, or potential dystocia in pregnant females. Complete excision for benign lesions promises a life-long disease-free expectancy, and in case of recurrence, the local excision can be safely carried out [15].
A vast range of approaches is described in the literature, varying between transabdominal in means of laparotomy or laparoscopy, trans-sacral, inter-sphincteric, trans-sphincteric parasacrococcygeal, or transanal – whether with endoscopic microsurgery or without.
A transabdominal approach assures visualization of the important structures and thus a better oncological resection for cases with suspected malignancy. While the laparoscopic approaches offer the same benefits with the advantage of being less invasive, the requirement of additional equipment incurs higher costs.
For small, low-lying, non-infected cases, transanal or transrectal approaches can be used, although these result in a theoretically higher risk of pelvic infection as the rectum is used as a portal of entry.
Since primary retrorectal tumors are very rare, the successful treatment of these tumors is dependent on extensive knowledge of pelvic anatomy, and expertise in pelvic surgery is mandatory to avoid serious injuries in an anatomically crowded presacral area.
Choosing the posterior approach for low-lying benign lesions (below S3) that do not involve the rectum offers relatively easy access to the presacral area and avoids entering the peritoneal cavity through the abdomen.
Paul Kraske originally described this approach on 10th December 1884 during the 14th Congress of German Surgeons: it allows exposure of the mid rectum after removal of the coccyx and a portion of the left sacral wing.
Famous surgeons, such as Billroth and Heinecke, who popularized this procedure, have described minor modifications to the original technique [16].
It is advised to avoid this approach for high-lying tumors (above S3), as lack of access to the pelvic vessels in cases of intraoperative bleeding represents a real threat to the patient’s life, keeping in mind that the surgical position of the patient, whether prone or jackknife, would present a drawback for rapid abdominal access. Another potential drawback is the great morbidity that can occur in case of the iatrogenic injury to the lateral pelvic nerves.
As a rule of thumb, if the upper extent of the lesion can be palpated on rectal examination, it is likely to be resectable transsacrally.
In a retrospective analysis carried out between 1985 and 2008 at Mayo Clinic, the author noted that tailgut cyst excisions can be performed safely and effectively using primarily a posterior approach. Routine coccygectomy was not performed, although some authors advocate coccygectomy in order to improve surgical exposure and to eliminate the possibility of recurrence from totipotent cells harbored in the coccyx [15,17,18].
With failure of complete excision, recurrence can occur. For follow up, it has been advised to perform an annual digital exam to assess for recurrence and a baseline CT in the first postoperative year, as well as a control in the fifth [15].
4. Conclusion
A consideration that applies in all fields of surgery remains valid in this case as well: the preferred surgical approach is the one in which the surgeon has the most experience.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Mazen Haydar M.D wrote the full manuscript of this case report and literature review.
Dr. med. Kai Griepentrog provided data, and supervising guidance.
Prof. Dr. med. Wittekind carried out the pathological examination.
Acknowledgment
We are thankful to Prof. Dr. med. Wittekind for providing us with a very detailed pathological report.
Contributor Information
Mazen Haydar, Email: mazen.haydar@hotmail.com.
Kai Griepentrog, Email: k.griepentrog@kkh-stl.de.
References
- 1.Hood D.L., Petras R.E., Grundfest-Broniatowski S., Jagelman D.G. Retrorectal cystic hamartoma: report of five cases with carcinoid tumor arising in two. Am. J. Clin. Pathol. 1988;89:433. [Google Scholar]
- 2.Bale P.M. Sacrococcygeal developmental abnormalities and tumors in children. Perspect. Pediatr. Pathol. 1984;8:48–56. [PubMed] [Google Scholar]
- 3.Hjermstad B.M., Helwig E.B. Tailgut cysts. Report of 53 cases. Am. J. Clin. Pathol. 1988;89(February (2)):139–147. doi: 10.1093/ajcp/89.2.139. [DOI] [PubMed] [Google Scholar]
- 4.Hansen N.H., Qvist N. Tailgut cyst prolapsing through the anus. Eur. J. Pediatr. Surg. 2013;23(June (3)):e3–e4. doi: 10.1055/s-0032-1315814. [DOI] [PubMed] [Google Scholar]
- 5.Leo J.M., O’Connor K.M., Pezim M., Nagy A., Schaeffer D.F. Benign tailgut cyst masquerading as a hemorrhoid. Can. J. Gastroenterol. Hepatol. 2014;28(April (4)):183. doi: 10.1155/2014/757965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abraham V.J., Peacock M., Mammen K.J. Acute urinary retention and obstipation: a rare cause. Indian J. Surg. 2013;75(February (1)):71–72. doi: 10.1007/s12262-012-0421-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yakan S., Ilhan E., Cengiz F., Üstüner M.A., Tanriverdi H.O. Retrorectal cyst presenting with right sciatica. Eur. J. Surg. Sci. 2012;3(2):59–61. [Google Scholar]
- 8.Johnson K.N., Young-Fadok T.M., Carpentieri D., Acosta J.M., Notrica D.M. Case report: misdiagnosis of tailgut cyst presenting as recurrent perianal fistula with pelvic abscess. J. Pediatr. Surg. 2013;48(February (2)):e33–e36. doi: 10.1016/j.jpedsurg.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Chung K.Y., Lee N.M., Choi E.S., Yoo B.H., Kim G.J., Cha S.J., Kim G.H., Kim M.K. A tailgut cyst-cystic mass diagnosed by prenatal ultrasonography. AJP Rep. 2013;3(May (1)):17–20. doi: 10.1055/s-0032-1329681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahan H., Arrivé L., Wendum D., Docou le Pointe H., Djouhri H., Tubiana J.M. Retrorectal developmental cysts in adults: clinical and radiologic-histopathologic review differential diagnosis, and treatment. Radiographics. 2001;21(May–June (3)):575–584. doi: 10.1148/radiographics.21.3.g01ma13575. [DOI] [PubMed] [Google Scholar]
- 11.Mathieu A., Chamlou R., Le Moine F., Maris C., Van de Stadt J., Salmon I. Tailgut cyst associated with a carcinoid tumor: case report and review of the literature. Histol. Histopathol. 2005;20(4):1065–1069. doi: 10.14670/HH-20.1065. [DOI] [PubMed] [Google Scholar]
- 12.Graadt van Roggen J.F., Welvaart K., de Roos A., Offerhaus G.J.A., Hogendoorn P.C.W. Adenocarcinoma arising within a tailgut cyst: clinicopathological description and follow up of an unusual case. J. Clin. Pathol. 1999;52(4):310–312. doi: 10.1136/jcp.52.4.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aflalo-Hazan V., Rousset P., Mourra N., Lewin M., Azizi L., Hoeffel C. Tailgut cysts: MRI findings. Eur. Radiol. 2008;18(November (11)):2586–2593. doi: 10.1007/s00330-008-1028-4. [DOI] [PubMed] [Google Scholar]
- 14.Hall D.A., Pu R.T., Pang Y. Diagnosis of foregut and tailgut cysts by endosonographically guided fine-needle aspiration. Diagn. Cytopathol. 2007;35(January (1)):43–46. doi: 10.1002/dc.20573. [DOI] [PubMed] [Google Scholar]
- 15.Mathis K.L., Dozois E.J., Grewal M.S., Metzger P., Larson P.D.W., Devine R.M. Malignant risk and surgical outcomes of presacral tailgut cysts. Br. J. Surg. 2010;97(April (4)):575–579. doi: 10.1002/bjs.6915. [DOI] [PubMed] [Google Scholar]
- 16.O’Brien P.H. Kraske’s posterior approach to the rectum. Surg. Gynecol. Obstet. 1976;142(March (3)):412–414. [PubMed] [Google Scholar]
- 17.Izant R.J., Jr., Filston H.C. Sacrococcygeal teratomas: analysis of forty-three cases. Am. J. Surg. 1975;130:617–621. doi: 10.1016/0002-9610(75)90523-1. [DOI] [PubMed] [Google Scholar]
- 18.Miles R.M., Stewart G.S., Jr. Sacrococcygeal teratomasin adults. Ann. Surg. 1974;179(May (5)):676–683. doi: 10.1097/00000658-197405000-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]


