SUMMARY
Early childhood represents a time of developmental changes in both sleep and self-regulation, a construct reflecting the ability to control one’s behavior, attention, and emotion when challenged. Links between sleep and self-regulation processes have been proposed, but experimental evidence with young children is lacking. In the current study, we tested the effects of acute sleep restriction (nap deprivation) on toddlers’ self-regulation. Healthy children (n=12; 4 males; 30–36 months (33.9±1.7) slept on a strict schedule (verified with actigraphy and sleep diaries) for 5 days before each of two afternoon assessments following a Nap and a No-Nap condition (~11-day protocol). Children were videotaped while attempting an unsolvable puzzle, and 10 mutually exclusive self-regulation strategies were later coded. On average, children lost ~90 min of sleep on the No-Nap versus the Nap day. Nap deprivation resulted in moderate-to-large effects on self-regulation strategies, with decreases in skepticism (d=0.77; 7% change), negative self-appraisal (d=0.92; 5% change), and increases in physical self-soothing (d=0.68; 10% change), focus on the puzzle piece that would not fit (perseveration; d=0.50; 9% change), and insistence on completing the unsolvable puzzle (d=0.91; 10% change). Results suggest sleep serves an important role in the way toddlers respond to challenging events in their daily lives. After losing daytime sleep, toddlers were less able to effectively engage in a difficult task and reverted to less mature self-regulation strategies, than when they were well-rested. Over time, chronically missed sleep may impair young children’s self-regulation abilities, resulting in risk for social-emotional, behavioral, and school problems.
Keywords: Sleep, Early Childhood, Children, Behavior, Cognition, Task Performance
INTRODUCTION
In recent years, sleep has become central to integrative, conceptual frameworks of self-regulation (Hagger, 2010). Self-regulation is the ability to control one’s behavior, cognition, attention, and emotion when challenged (Heatherton and Wagner, 2011). Self-regulation strategies include behavioral and cognitive actions that function to maintain or regain such control in an effortful manner (e.g., shifting attention away from a distressing stimulus). Identifying modifiable factors influencing early self-regulation is important, as self-regulation deficits are associated with social-behavioral problems (e.g., externalizing) and school difficulties (e.g., attention problems, poor achievement) (Eisenberg et al., 2010). Sleep plays a key role in the cognitive and affective processes central to self-regulation in school-age children (Sadeh et al., 2002), adolescents (Baum et al., 2013), and adults (Mauss et al., 2012, Pilcher and Huffcutt, 1996). Less is known about younger children.
Understanding how insufficient sleep may affect self-regulation during early childhood is important as this may inform intervention efforts to enhance developmental outcomes by improving sleep. From 2- to 5-years of age, total sleep duration decreases (primarily through dropping naps; Iglowstein et al., 2003), and sleep problems (e.g., bedtime resistance, nighttime awakenings) are prevalent (Owens et al., 2000). Essential self-regulation skills such as persisting at difficult tasks and using distraction and/or cognitive reappraisal to manage emotions also emerge over this period (Blair et al., 2010). Maturing language and increased cognitive self-awareness enable development of such skills (Brownell and Kopp, 2010). Across the toddler-to-preschool transition, children typically move from physical self-regulation strategies (e.g., thumb-sucking) to verbal and cognitively-mediated strategies (e.g., stating how they feel; asking for help; Grolnick et al., 1996, Roben et al., 2012). Children who obtain insufficient sleep may be delayed in such self-regulation milestones and at risk for later problems (Troxel et al., 2013).
Inadequate sleep may reduce self-regulation capacity (Hagger, 2010). Controlled studies of school-age children found that sleep restriction impaired observed (Sadeh et al., 2002) and teacher-reported (Gruber et al., 2012) attention, a cognitive self-regulation skill. Sleep is suggested as critical for the development of executive functioning skills such as working memory, behavioral inhibition, and attention that enable self-regulation (Touchette et al., 2008, Turnbull et al., 2012), but the few extant studies in younger children are correlational and span a wide age range (Bernier et al., 2010, Touchette et al., 2008). Quasi-experimental work examining behavioral self-regulation in 14-month-olds indicated less daytime sleep was related to greater negative affect and less-mature self-regulation strategies (e.g., self-soothing; Ross and Karraker, 1999), and our experimental work with toddlers confirmed that missing one afternoon nap increased negative facial emotion displays (Berger et al., 2012). Well-controlled studies of sleep and self-regulation in young children are scarce, yet critical for a mechanistic understanding of how insufficient sleep may lead to self-regulation difficulties over this unique period when children are transitioning from primarily behavioral and parent-mediated self-regulation to cognitively- and verbally-mediated strategies (Brownell and Kopp, 2010). This study addresses this gap by experimentally examining the effects of acute sleep restriction via nap deprivation on observed behavioral and cognitive self-regulation strategies in 30–36 month-olds, who are developing these skills. We hypothesized that children would show less sophisticated self-regulation (e.g., more ineffective behavioral coping, less cognitive engagement) in a challenge task after missing a nap than after napping.
METHODS
Participants
Details regarding the recruitment and screening of participants have been previously published (Berger et al., 2012). In general, participants were healthy, habitually napping 30- to 36-month-olds with no sleep or behavioral problems. For this analysis, 80 children were screened, 37 met criteria, 17 enrolled, and 12 completed the study. Incomplete assessments were due to children not sleeping during their nap opportunity on the day of the assessment, sickness, or withdrawal from the study. The final sample included 12 toddlers (4 males; 10 Caucasian, 1 African-American, 1 mixed-race) aged 30- to 36-months (33.9±1.7 months). Four attended full-time daycare, 3 had in-home childcare, and 5 were cared for exclusively by their parents.
Parents signed a Brown University IRB-approved consent form. Compensation to parents was $25 in cash. Children received small gifts (e.g., stickers, trinkets) at each home assessment and a $75 savings bond at the end of the study.
Protocol
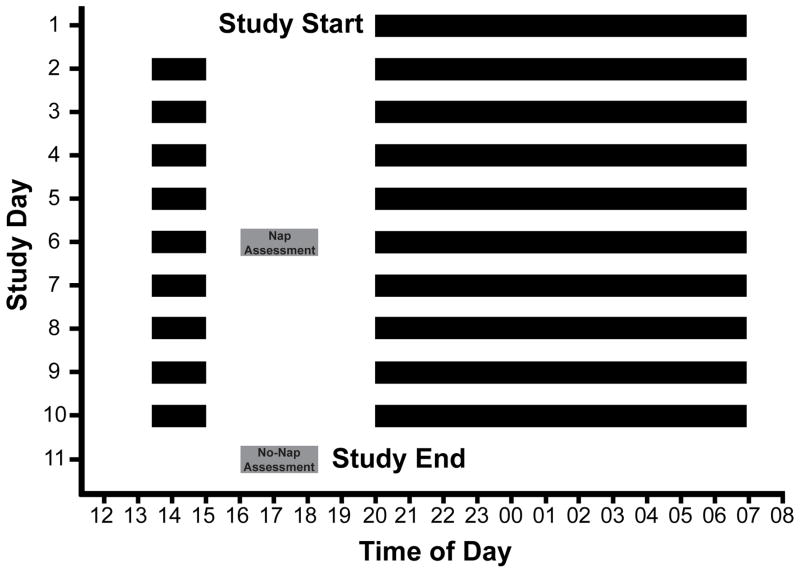
As shown in Figure 1, children followed a strict daytime nap and nighttime sleep schedule for ≥5 days (≥12.5 hours time in bed/24 hour day) before each of two randomly ordered in-home “challenge task” assessments. This individualized bedtime and rise time schedule promotes stabilization of the circadian system and provides needed sleep-wakefulness consistency before the experimental manipulation (Nap versus No-Nap). Daily correspondence with parents via email or telephone was performed to ensure compliance with study procedures. In the case of a protocol violation (i.e., accidental nap (n=1); sleep patterns deviating >15 min from established schedule (n=1); illness (n=1); use of medications affecting sleep and/or alertness; caffeine consumption), challenge task assessments were rescheduled after another 5 days on the sleep schedule. Children were required to have fallen asleep during their nap opportunity ≥50% of days leading up to the challenge assessment. Researchers completed in-home trainings about study procedures (e.g., actigraphy wear and care, completing the sleep diary) with parents prior to the start of the study.
Figure 1.
Sample protocol (11 days) for a child following a strict sleep schedule with a 20:00 bedtime, a 07:00 rise time and a 12:30–14:00 afternoon nap opportunity (12.5 h time in bed/24-h day). Black bars represent time in bed; grey boxes represent the challenge task assessments on Nap and No-Nap days.
Alternate forms of the challenge task were administered on two afternoons following Nap (baseline) and No-Nap (sleep restriction) conditions. In order to reduce the potential influence of sleep inertia on children’s self-regulation strategies, the assessment start time for both conditions was 1-h past individual children’s scheduled nap wake time. Prior to assessment administration, researchers confirmed participant’s compliance with study rules and the sleep schedule by reviewing printed actograms and sleep diary entries. The in-home assessment context was then set-up (i.e., child-sized table and chair, video camera).
Challenge Task
Assessments were designed to present a self-regulation challenge. Children were administered an age-appropriate unsolvable board puzzle. The puzzle included one incorrect piece, which prevented task completion and simulated a frustrating event that toddlers could experience in their day-to-day lives. The challenge task was part of a larger protocol designed to elicit both positive and negative emotion responses (details provided in Berger et al., 2012). We computed the percent time children displayed each of ten distinct self-regulation strategies (described below).
Measures
Parent-Report Screening Questionnaires
Child Behavior Checklist (CBCL 1½–5): The CBCL is a 99-item assessment of early childhood internalizing and externalizing behavior problems. T-scores are defined as within normal limits (T<60), at-risk (T= 60–69), or clinically significant (T≥70). The CBCL has adequate reliability and validity for clinical instruments (Achenbach and Rescorla, 2000).
The Children’s Sleep Habits Questionnaire (CSHQ): The CSHQ is 33-item measure for screening common childhood sleep problems (Owens et al., 2000). Prior findings support the use of the CSHQ as a clinical sleep screener in 2- to 5-year-olds (Goodlin-Jones et al., 2008)
Assessment of Children’s Sleep Schedules
Our standard laboratory procedures for assessing sleep schedule compliance have been described in detail elsewhere (Berger et al., 2012). In short, parents completed a sleep diary and children wore a wrist actigraph for the duration of the study. We used data from actigraphic sleep variables (i.e., lights-out time, rise time, time in bed, sleep start time, sleep end time, sleep period, sleep efficiency) to assess whether children’s sleep opportunity, duration, and quality differed during the 5 days before each challenge task assessment.
Observational Coding of Self-Regulation Strategies
Videotapes of children during the challenge task were later coded by trained researchers using The Observer XT software (Noldus Technologies, 2007). Coders were blind to condition and trained on the self-regulation coding categories using standard methods. They consulted with an expert reviewer (AM, a developmental psychologist with observational coding expertise who was also blind to condition) for consensus-coding as needed.
Ten mutually-exclusive self-regulation strategies were coded during the challenge task (described in Table 1). Percent time in each behavior state was calculated and 25% of assessments were double-coded to assess reliability. Inter-rater reliability across codes using intraclass correlation coefficients (ICCs) ranged from .76 to 1.0, with ICCs for all but one code (self-soothing) greater than .90. Self-regulation strategies were based on previous work (Berhenke et al., 2011) and included actions that engaged the examiner (solicit help), verbal comments about the puzzle task (skepticism, cognitive reappraisal, negative self-appraisal, self-talk, insistence on completion), and predominantly non-verbal behaviors that reflected self-regulation and puzzle problem-solving approaches (physical self-soothing, focus on the puzzle piece that would not fit, disruptive behavior, alternate problem solving strategies). In general, we considered physical self-soothing, focusing on the piece that would not fit (“misfit piece”), disruptive behavior, negative self-appraisal, and insistence on completion as less adaptive strategies reflecting a limited capacity to cope with the challenge (listed first in Table 1). We considered skepticism, cognitive reappraisal, self-talk, soliciting help, and alternate problem-solving strategies as more adaptive attempts to actively address the challenge, reflecting cognitive engagement with the task (listed second in Table 1).
Table 1.
Self-Regulation Strategies Coded in Challenge Task
| Behavior | Description |
|---|---|
| Self-Soothing | Child engages in bodily-directed behaviors (often repetitive; e.g., thumb-sucking, hair-twirling, or lip/nail biting) |
| Focus on Misfit Piece | Child visually fixates on the misfit puzzle piece; may ignore other pieces |
| Disruptive Behavior | Child demonstrates aggressive or disruptive behaviors (i.e., yelling, banging, throwing, kicking, hitting) |
| Negative Self-Appraisal | Child attributes trouble completing the task to personal attributes (i.e., “I can’t do this”) |
| Insistence on Completion | Child accepts or ignores that the misfit puzzle piece does not fit – insists puzzle has been completed; |
|
| |
| Skepticism | Child makes comment that indicates that s/he knows that something is wrong with the puzzle (e.g., “this piece doesn’t go in my puzzle”) |
| Cognitive Reappraisal | Child attempts to reframe, and view puzzle situation in more positive manner (e.g., “I never liked puzzles anyway”) |
| Self-Talk | Child talks to him/herself during the task (any type of talking or verbalization) |
| Solicit Help | Child asks experimenter directly for help with puzzle (e.g., “can I have a hint?”) |
| Alternate Strategies | Child uses appropriate problem-solving strategies to attempt to fit the missing piece (e.g., rotating the misfit piece in the space, looking under the table for the “missing” puzzle piece) |
Hypotheses
The overall aim of this study was to examine the effects of acute sleep restriction on toddler’s self-regulation strategies in a challenge context. We hypothesized children would use (a) more strategies reflecting ineffective coping (self-soothing, focus on the misfit piece, disruptive behavior, negative self-appraisal, insistence on completion) and (b) fewer strategies reflecting active cognitive engagement (skepticism, cognitive reappraisal, self-talk, solicit help, alternate problem-solving strategies) in the No-Nap than in the Nap condition.
Analysis
Analyses were performed with the IBM SPSS Statistics Package 21.0 (IBM Corp., Armonk, NY). Repeated measures analyses (Nap versus No-Nap) of continuous data (% time in self-regulation state during challenge task) were performed with paired t-tests. Summary statistics are presented as means and standard deviations (M±SD). The significance level for analyses was set at .05 (one-tailed tests). Effect size in SD units was computed for % time in self-regulation state M comparisons (d = MNo-Nap − MNap/SDpooled). An effect size of 0.25 was considered small, 0.50 considered medium, and ≥0.75 considered large (Cohen, 1988).
RESULTS
Behavioral and Sleep Problem Status
Children scored below clinical cutoffs on the CBCL Internalizing (40.9±7.1) and Externalizing (43.8±7.9) subscales. With regard to reported sleep problems, participants were below the mean of published norms from a sample of preschool children with sleep disturbance on the CSHQ Total (39.0±3.8) and all CSHQ subscales, including Bedtime Resistance (6.6±0.7), Sleep Onset Delay (1.5±0.7), Sleep Duration (3.6±0.7), Sleep Anxiety (4.3±0.6), Night Waking (3.3±0.7), Parasomnias (6.8±0.8), Sleep Disordered Breathing (2.0±0.0), and Daytime Sleepiness (11.0±2.2) (Goodlin-Jones et al., 2008).
Protocol Verification
As shown in Table 2, no differences were found between actigraphic napping and nighttime sleep measures (i.e., lights-out time, rise time, time in bed, sleep start time, sleep end time, sleep period, sleep efficiency) during the 4 days before each challenge task assessment (Nap versus No-Nap conditions). However, nap deprivation resulted in significant changes in children’s sleep period during the 24 hours before each afternoon assessment. Although average bedtime, rise time, sleep start time, sleep end time, and sleep efficiency on the night prior to afternoon assessments was the same, children spent less time in bed (by 113 minutes) and had shorter sleep periods (by 91 minutes) during the 24 hours before No-Nap than Nap assessments (see Table 2).
Table 2.
Actigraphic sleep measures during the 4 days, as well as 24 hours before each challenge task assessment. One-tailed paired t-tests were performed between nap and no-nap conditions.
| 4 days Before Assessments | Nap | No-Nap | Statistics | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | t | d | P | |
|
|
|
|
|
||||
| Daytime Sleep (Nap) | |||||||
| Days Napping (fell asleep) | 3.3 | 0.89 | 3.3 | 0.87 | −.43 | .00 | .67 |
| Lights-Out Time | 13:23 | 0:45 | 13:22 | 0:49 | .04 | .02 | .97 |
| Rise Time | 15:13 | 0:33 | 15:16 | 0:40 | −.23 | .08 | .82 |
| Time in Bed (minutes) | 110.3 | 19.6 | 113.9 | 15.2 | −1.05 | .21 | .31 |
| Sleep Start Time | 13:49 | 0:57 | 13:55 | 0:59 | −.35 | .10 | .73 |
| Sleep End Time | 15:12 | 0:51 | 15:14 | 0:52 | −.45 | .04 | .66 |
| Sleep Period (minutes) | 84.00 | 20.5 | 78.6 | 11.8 | −.49 | .32 | .63 |
| Sleep Efficiency (%) | 93.4 | 4.9 | 94.1 | 2.8 | −.99 | .18 | .35 |
| Nighttime Sleep | |||||||
| Lights-Out Time | 19:59 | 0:28 | 20:03 | 0:28 | −.80 | .14 | .44 |
| Rise Time | 6:51 | 0:27 | 6:53 | 0:25 | −.56 | .08 | .58 |
| Time in Bed (minutes) | 651.4 | 40.4 | 650.4 | 39.7 | .20 | .02 | .84 |
| Sleep Start Time | 20:40 | 0:33 | 20:41 | 0:35 | −.56 | .03 | .59 |
| Sleep End Time | 6:40 | 0:28 | 6:44 | 0:24 | −.70 | .15 | .50 |
| Sleep Period (minutes) | 599.5 | 41.9 | 602.9 | 39.3 | −.48 | .08 | .64 |
| Sleep Efficiency (%) | 85.2 | 3.8 | 83.4 | 5.0 | 1.93 | .41 | .08 |
| Total 24 h Sleep | |||||||
| Time in Bed (minutes) | 761.7 | 39.7 | 764.4 | 37.5 | −.45 | .07 | .66 |
| Sleep Period (minutes) | 682.3 | 40.2 | 681.5 | 33.6 | −.75 | .02 | .46 |
|
| |||||||
| 24 h Before Assessments | M | SD | M | SD | t | D | P |
|
|
|
|
|
||||
| Daytime Sleep (Nap) | |||||||
| Lights-Out Time | 13:16 | 0:41 | - | - | - | - | - |
| Rise Time | 15:06 | 0:53 | - | - | - | - | - |
| Time in Bed (minutes) | 110.3 | 20.4 | - | - | - | - | - |
| Sleep Start Time | 13:37 | 0:48 | - | - | - | - | - |
| Sleep End Time | 14:58 | 0:55 | - | - | - | - | - |
| Sleep Period (minutes) | 81.6 | 16.6 | - | - | - | - | - |
| Sleep Efficiency (%) | 94.6 | 3.0 | - | - | - | - | - |
| Nighttime Sleep | |||||||
| Lights-Out Time | 19:55 | 0:30 | 20:00 | 0:24 | −1.09 | .18 | .29 |
| Rise Time | 7:00 | 0:26 | 7:03 | 0:23 | −.29 | .12 | .77 |
| Time in Bed (minutes) | 665.3 | 44.3 | 662.6 | 33.8 | −1.1 | .07 | .31 |
| Sleep Start Time | 20:33 | 0:47 | 20:31 | 0:30 | −.42 | .05 | .69 |
| Sleep End Time | 6:51 | 0:30 | 6:54 | 0:31 | .59 | .10 | .57 |
| Sleep Period (minutes) | 617.7 | 53.7 | 623.2 | 39.3 | −.49 | .12 | .63 |
| Sleep Efficiency (%) | 87.4 | 5.6 | 84.0 | 7.8 | 1.27 | .50 | .24 |
| Total 24 h Sleep | |||||||
| Time in Bed (minutes) | 761.7 | 39.7 | 662.6 | 33.8 | 11.3 | 2.7 | .001 |
| Sleep Period (minutes) | 682.3 | 40.2 | 623.2 | 39.3 | 7.6 | 1.5 | .001 |
Napping Patterns
About 15% of daytime naps occurred at daycare or preschool, with sleep timing and duration the same as those taken at home. On average, toddlers napped the same number of days leading up to the nap and no-nap challenge assessments (3.3 days; Table 2). Furthermore, the number of days napping in both conditions was similar within individuals: 75% (n=7) had no difference between conditions, 16% (n=2) napped one less day in the nap than the no-nap condition, and 25% (n=3) napped one more day in the nap than the no-nap condition. The average difference in napping (nap − no-nap) between conditions was 0.08±0.67. Thus, we considered our participants “habitual” nappers meeting part of their regular sleep need via daytime naps.
Sleep Restriction Effects on Self-Regulation Strategies
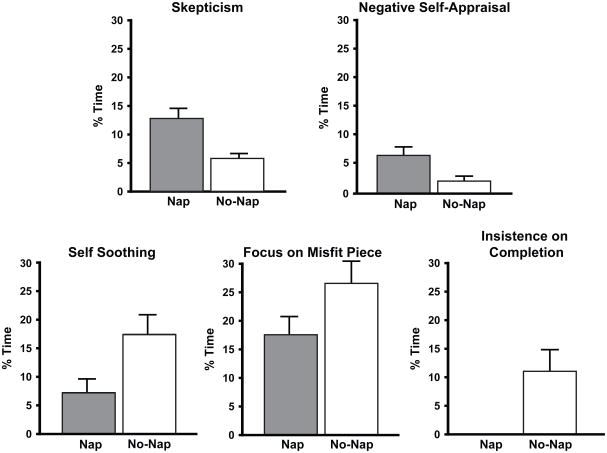
Parametric and non-parametric repeated-measures tests were used given the small sample size; however, results showed identical outcomes. Thus, we present findings from the parametric tests for ease of interpretation. Acute sleep restriction had moderate-to-strong effects on some but not all self-regulation strategies children employed during the challenge task (Table 3 & Figure 2). As hypothesized, toddlers showed a decrease in skepticism in the No-Nap than the Nap condition (7%). Missing an afternoon nap also resulted in a 10% increase in self-soothing, a 9% increase in focus on the misfit piece, and a 10% increase in insistence on completion, in comparison to after napping. Contrary to our expectation, we found a 4% decrease in negative self-appraisal for children in the no-nap as compared to the nap condition. As shown in Table 3, the percent time that children employed different strategies varied within the Nap and No-Nap conditions. For example, while focusing on the misfit piece was the most common strategy observed in both conditions, toddlers rarely demonstrated cognitive reappraisal or disruptive behavior during the task.
Table 3.
Percent time toddlers exhibited self-regulation strategies during the unsolvable puzzle (challenge) task (n=12).
| Nap | No-Nap | Statistics | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | t | d | p | |
| Self-Soothing | 7.3 | 12.1 | 17.5 | 17.2 | −2.41 | 0.68 | 0.017 |
| Focus on Misfit Piece | 17.5 | 15.6 | 26.5 | 20.4 | −1.66 | 0.50 | 0.046 |
| Disruptive Behavior | 0.0 | 0.0 | 0.3 | 0.7 | −1.41 | 0.59 | 0.092 |
| Negative Self-Appraisal | 6.7 | 8.5 | 2.4 | 5.1 | 2.54 | 0.93 | 0.014 |
| Insistence on Completion | 0.7 | 1.4 | 11.2 | 16.2 | −2.15 | 0.91 | 0.028 |
|
| |||||||
| Skepticism | 12.9 | 11.4 | 5.8 | 6.2 | 2.32 | 0.77 | 0.020 |
| Cognitive Reappraisal | 0.2 | 0.7 | 0.6 | 1.2 | −0.62 | 0.13 | 0.270 |
| Self-Talk | 7.0 | 9.2 | 5.6 | 7.1 | 0.54 | 0.17 | 0.300 |
| Solicit Help | 2.6 | 4.0 | 1.16 | 2.0 | 1.04 | 0.44 | 0.161 |
| Alternate strategies | 7.8 | 7.1 | 8.5 | 11.6 | −0.18 | 0.07 | 0.427 |
Figure 2.
Differences in children’s mean self-regulation responses (percent time exhibiting the self-regulation behavior) between Nap and No-Nap conditions. One-tailed paired t-tests (P<0.05).
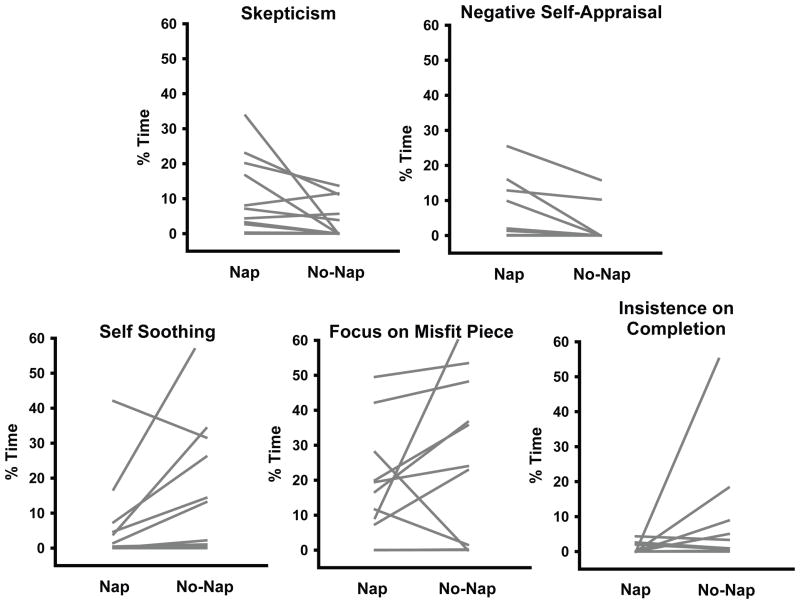
Figure 3 shows individual variability in children’s self-regulatory responses to nap deprivation. In the Nap condition, we observed moderate variation (0–35%) in the percent time that children engaged in verbal strategies (e.g., skepticism, negative self-appraisal). In the No-Nap condition, about half the sample showed a decrease in both of these strategies. Individual variability in self-soothing and focus on the misfit piece was considerable (0%–60%), with some children showing dramatic changes and others exhibiting no change or the opposite effect. Finally, when well-rested, we observed little-to-no variability (<5%) in children’s insistence on completion; however, after missing a nap, one participant had a dramatic increase (this same child showed the greatest decrease in focusing on the misfit piece with nap deprivation), three showed small-to-moderate increases, while the majority exhibited no change between conditions.
Figure 3.
Individual differences in children’s self-regulation strategies in the Nap and No-Nap conditions.
DISCUSSION
Self-regulation has been conceptualized as a limited resource that requires energy, similar to a muscle (Heatherton and Wagner, 2011). Sleep may be critical for the development of self-regulation skills and their effective use. As proposed by Hagger (2010), prolonged wakefulness may reduce the capacity for self-regulation, which can then be restored through sleep (Hagger, 2010). In this study, we employed a well-controlled experimental design to examine the effects of acute sleep restriction on young children’s self-regulation strategies in a challenge context. We found support for our hypothesis that removing one daytime nap would lead to changes in observed self-regulation strategies related to cognitive engagement with the task, and in the skills needed to cope with challenge. Specifically, in our sample of healthy, good-sleeping 30- to 36-month-olds, eliminating one afternoon nap caused decreases in skepticism, negative self-appraisal, and increases in physical self-soothing, focus on the misfit piece, and insistence that the child had completed an impossible puzzle. Findings suggest that inadequate sleep promotes children using less active cognitive engagement and more immature coping strategies when presented with a challenging task. Results are discussed with regard to the role of sleep for self-regulation of cognitive, behavioral, and emotion processes associated with adaptation and school readiness in early childhood.
Cognitive Engagement Decreases with Sleep-Restriction
Self-regulated learning involves cognitive, motivational, and self-evaluative components (Pintrich and De Groot, 1990). Evaluating one’s strengths and weaknesses is an important metacognitive strategy appearing as early as age 3 years (Whitebread et al., 2009). We found that nap deprivation resulted in less skepticism, a behavior indicating that children were cognitively engaged enough to realize something was wrong with the puzzle and comment to the examiner. Although we hypothesized that negative self-appraisal statements would increase with sleep restriction, we found the opposite. Considering negative self-appraisal as a realistic self-evaluation of performance, however, this finding makes sense. Although toddlers are not yet capable of engaging in high-level metacognitive reflections, they have the rudimentary ability to appropriately evaluate the situation and their own performance. Studies of preschoolers suggest that such task-relevant “private speech” during challenging tasks reflects externally-displayed metacognitive processes, and predicts better academic achievement (Manning et al., 1994, Winsler et al., 2011), and classroom adjustment (Winsler et al., 2011). Here, when children had not napped, they were less likely to state that the puzzle was “faulty” (skepticism) or to realistically evaluate their own abilities (negative self-appraisal). These findings suggest that even missing one nap had a negative effect on these important metacognitive self-regulation processes.
Consistent with prior findings in older children and adolescents (Fallone et al., 2001, Randazzo et al., 1998), sleep restriction did not cause changes in all observed toddler selfregulation behaviors, perhaps suggesting differential effects on higher- versus lower-order cognitive skills (Gomez et al., 2011). Our findings suggest that sleep restriction reduced children’s higher-level metacognitive abilities to appropriately evaluate the puzzle task as too difficult but may not have interfered as much with their propensity to simply keep working on the task (i.e., problem solving) or to talk about it (i.e., self-talk, reappraisal). The level of sophistication in problem-solving and self-talk increases dramatically from 2- to 3-years of age, so the effects of missing sleep on such behaviors may become more pronounced with development. Of note, many of the self-regulation behaviors we assessed likely also reflect children’s underlying executive functioning capabilities such as attention and working memory, which have been shown to be impaired under poor sleep conditions in older children (Sadeh et al., 2002; Steenari et al., 2003). Sleep is increasingly suggested as critical for executive functioning skills even in very young children (Gomez et al., 2011, Kopasz et al., 2010; Turnbull et al., 2012). Although we did not assess memory or other executive functioning domains, such skills may be an important mechanism underlying the association of sleep deprivation and poor observed self-regulation as we saw in the current study; future work in this area is warranted.
More Use of Immature Coping Strategies with Sleep Restriction
Prior experimental studies indicate that sleep restriction increases negative mood in children (Berger et al., 2012) and adolescents (Baum et al., 2013) and that sleep deprivation can increase perceived stress (Minkel et al., 2012). Furthermore, adults reporting poorer sleep quality are less likely to use cognitive reappraisal strategies in response to an emotional challenge (Mauss et al., 2012). We extend these findings by showing that missing one daytime nap increased physical self-soothing, a less mature strategy than verbally-mediated responses in toddlers (Grolnick et al., 1996). Verbal skills are foundational for effective self-regulation; children who can verbalize their feelings may manage challenging situations more effectively (Roben et al., 2012). We also found that when sleep-restricted, compared to well-rested, toddlers tended to maintain a perseverative focus on the misfit puzzle piece and insist that the puzzle had been completed even though it had not been. Most definitions of adaptive self-regulation emphasize shifting strategies to suit the context or situation at hand (e.g., (McClelland and Cameron, 2012, Wrosch et al., 2003) while appropriately ignoring irrelevant stimuli (MacCoon et al., 2004, Posner and Rothbart, 2000); perseveration thus represents a less adaptive strategy. Over time, persistent use of ineffective strategies, coupled with not verbalizing for help from peers or caregivers, may increase children’s risk for academic and social-behavioral difficulties.
Variability in Sleep Restriction Effects
We found notable variation among individuals in behaviors reflecting cognitive engagement (skepticism, negative self-appraisal) in the well-rested condition; that is, children ranged in their levels of these behaviors in this condition. We found less variability between children in the no-nap condition; most children decreased in these behaviors when sleep-restricted. The opposite pattern emerged for coping behaviors (self-soothing, focus on misfit piece, insistence on completion), with greater variability in the no-nap condition. These differences in patterns of variability in response to the manipulation are intriguing and suggest it may be important in future work with larger samples to consider not only overall response to insufficient sleep, but also individual characteristics of children (e.g., temperament; Troxel, 2013) that may determine their sensitivity to insufficient sleep.
Implications
Our experimental findings have important implications for understanding links between insufficient sleep, self-regulation, social-emotional functioning, and learning. When toddlers skipped just one afternoon nap of ~95 minutes and were asked to complete an unsolvable puzzle, we observed decreased metacognitive comments and increased immature strategies. Little is known about how poor sleep may affect the development of self-regulation over time (Bernier et al., 2010). Our puzzle task approximates situations that children may encounter at school; it is worth considering whether children who obtain chronically inadequate (daytime and/or nighttime) sleep also demonstrate self-regulation difficulties in real-world contexts. Sleep restriction appears to affect the very skills children need to succeed at school. Children who cannot remain cognitively engaged or realistically evaluate their own performance, or become upset and frustrated when challenged, are less likely to learn effectively in busy classroom settings with many distractions (McClelland and Cameron, 2012). If chronically missing sleep, children may also struggle to initially acquire or retain the information to which they are exposed (Gomez et al., 2011, Kopasz et al., 2010). These are at least two specific pathways through which chronic sleep deprivation may result in poor self-regulation, impaired learning skills and ultimately lower academic achievement. More research on sleep and the specific mechanisms and brain circuitry associated with self-regulation of cognition, behavior, and emotion, would better elucidate these processes.
Limitations and Future Directions
As with all research, the current study had limitations. First, although our puzzle task appeared to challenge our participants, it was conducted in a lab-type format in the home, and thus was not highly naturalistic. It would be valuable to examine how sleep restriction affects child behavior in real-world settings, which may pose greater self-regulation challenges. Second, our overall design precluded the ability to balance the Nap and No-Nap conditions for this study (7 of 12 children in the final analysis received the Nap condition first). We found no order effects on any outcomes, but the study is likely underpowered to detect such effects. Additionally, our sample size was small. Although the experimental design is a strength and large nap-dependent effects on self-regulation were observed, future studies using larger samples are needed to confirm our results and to understand individual sensitivity to sleep loss in early childhood. Finally, findings may not be widely generalizable, as our sample consisted of good sleepers with few behavior problems, which was necessary given protocol demands, but may not be the norm for very young children (Owens et al., 2000). We only examined napping, and it is important to consider whether other forms of sleep restriction would have similar effects. Examining how acute sleep restriction affects self-regulation among children with chronic sleep difficulties and determining the longitudinal impact of early sleep restriction on developmental outcomes are important areas of future research.
Acknowledgments
Funding: This research was supported by grants from the National Institute of Mental Health (K01-MH74643 and R01-MH086566 to M. K. LeBourgeois; K01-MH066139 to A. L. Miller). Mary A. Carskadon, Ph.D. and Oskar Jenni, M.D. gave valuable advice in designing the study. We are very grateful to the children and families for their time and effort in making this study possible.
Footnotes
Financial/Conflict of Interest Disclosure: The authors have nothing to declare.
Author Contributions:
Alison Miller conceptualized and designed the study, drafted the initial manuscript, interpreted the results, reviewed and revised the manuscript drafts, and approved the final manuscript.
Ronald Seifer conceptualized and designed the study, provided data analytic support, reviewed and revised the manuscript drafts, and approved the final manuscript.
Rebecca Crossin coded the data for the study, and approved the final manuscript.
Monique LeBourgeois conceptualized and designed the study, analyzed the data, interpreted the results, reviewed and revised the manuscript drafts, and approved the final manuscript.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1-to 5-year-old children. Sleep. 2005;28:1568–1577. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA Preschool Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2000. [Google Scholar]
- Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psyc. 2013 doi: 10.1111/jcpp.12125. (article published online July 30, 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. J Sleep Res. 2012;21:235–246. doi: 10.1111/j.1365-2869.2011.00962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berhenke A, Miller AL, Brown E, Seifer R, Dickstein S. Observed emotional and behavioral indicators of motivation predict school readiness in Head Start graduates. Early Child Res Q. 2011;26:430–441. doi: 10.1016/j.ecresq.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier A, Carlson SM, Bordeleau S, Carrier J. Relations between physiological and cognitive regulatory systems: infant sleep regulation and subsequent executive functioning. Child Dev. 2010;81:1739–1752. doi: 10.1111/j.1467-8624.2010.01507.x. [DOI] [PubMed] [Google Scholar]
- Blair C, Calkins S, Kopp L. Self-regulation as the interface of emotional and cognitive development. In: Hoyle RH, editor. Handbook of Personality and Self-Regulation. Wiley-Blackwell; Oxford, UK: 2010. pp. 64–90. [Google Scholar]
- Brownell CA, Kopp CB. Socioemotional development in the toddler years: Transitions and transformations. Guilford Press; New York, NY: 2010. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Eisenberg N, Valiente C, Eggum ND. Self-regulation and school readiness. Early Educ Dev. 2010;21:681–698. doi: 10.1080/10409289.2010.497451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallone G, Acebo C, Arnedt JT, Seifer R, Carskadon MA. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Motor Skill. 2001;93:213–229. doi: 10.2466/pms.2001.93.1.213. [DOI] [PubMed] [Google Scholar]
- Gomez RL, Newman-Smith KC, Breslin JH, Bootzin RR. Learning, memory, and sleep in children. Sleep Med Clin. 2011;6:45–57. [Google Scholar]
- Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. JDBP. 2008;29:82–88. doi: 10.1097/dbp.0b013e318163c39a. [DOI] [PubMed] [Google Scholar]
- Grolnick WS, Bridges LJ, Connell JP. Emotion regulation in two-year-olds: strategies and emotional expression in four contexts. Child Dev. 1996;67:928–941. [PubMed] [Google Scholar]
- Gruber R, Michaelsen S, Bergmame L, et al. Short sleep duration is associated with teacher-reported inattention and cognitive problems in healthy school-aged children. Nat Sci Sleep. 2012;4:33–40. doi: 10.2147/NSS.S24607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger MS. Sleep, self-regulation, self-control and health. Stress Health. 2010;26:181–185. [Google Scholar]
- Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends Cogn Sci. 2011;15:132–139. doi: 10.1016/j.tics.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- Kopasz M, Loessl B, Hornyak M, et al. Sleep and memory in healthy children and adolescents–a critical review. Sleep Med Rev. 2010;14:167–177. doi: 10.1016/j.smrv.2009.10.006. [DOI] [PubMed] [Google Scholar]
- MacCoon DG, Wallace JF, Newman JP. Self-regulation: context-appropriate balanced attention. In: Baumeister RF, Vohs KD, editors. Handbook of Self-Regulation: Research, Theory, and Applications. Guilford Press; New York, NY: 2004. pp. 422–444. [Google Scholar]
- Manning BH, White CS, Daugherty M. Young children’s private speech as a precursor to metacognitive strategy use during task engagement. Discourse Processes. 1994;17:191–211. [Google Scholar]
- Mauss IB, Troy AS, LeBourgeois MK. Poorer sleep quality is associated with lower emotion-regulation ability in a laboratory paradigm. Cogn Emot. 2012;27:567–76. doi: 10.1080/02699931.2012.727783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland MM, Cameron CE. Self-regulation in early childhood: improving conceptual clarity and developing ecologically valid measures. Child Dev Perspectives. 2012;6:136–142. [Google Scholar]
- Minkel JD, Banks S, Htaik O, et al. Sleep deprivation and stressors: evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. 2012;12:1015–1020. doi: 10.1037/a0026871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. JDBP. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Huffcutt AJ. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19:318–326. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- Pintrich PR, De Groot EV. Motivational and self-regulated learning components of classroom academic performance. J Educ Psychol. 1990;82:33–40. [Google Scholar]
- Posner MI, Rothbart MK. Developing mechanisms of self-regulation. Dev Psychopathol. 2000;12:427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- Randazzo AC, Muehlbach MJ, Schweitzer PK, Walsh JK. Cognitive function following acute sleep restriction in children ages 10–14. Sleep. 1998;21:861–868. [PubMed] [Google Scholar]
- Roben CK, Cole PM, Armstrong LM. Longitudinal relations among language skills, anger expression, and regulatory strategies in early childhood. Child Dev. 2012;84:891–905. doi: 10.1111/cdev.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CN, Karraker KH. Effects of fatigue on infant emotional reactivity and regulation. Inf Mental Hlth J. 1999;20:410–428. [Google Scholar]
- Sadeh A, Gruber R, Raviv A. Sleep, Neurobehavioral functioning, and behavior problems in school-age children. Child Dev. 2002;73:405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31:395–401. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenari MR, Vuontela V, Paavonen EJ, Carlson S, Fjällberg M, Aronen ET. Working memory and sleep in 6-to 13-year-old schoolchildren. J Am Acad Child Adolesc Psychiatry. 2003;42:85–92. doi: 10.1097/00004583-200301000-00014. [DOI] [PubMed] [Google Scholar]
- Touchette E, Mongrain V, Petit D, Tremblay RE, Montplaisir JY. Development of sleep-wake schedules during childhood and relationship with sleep duration. Arch Pediat Adol Med. 2008;162:343–349. doi: 10.1001/archpedi.162.4.343. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Trentacosta CJ, Forbes EE, Campbell SB. Negative emotionality moderates associations among attachment, toddler sleep, and later problem behaviors. Jnl Fam Psych. 2013;27:127–136. doi: 10.1037/a0031149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull K, Reid GJ, Morton JB. Behavioral sleep problems and their potential impact on developing executive function in children. Sleep. 2012;36:1077–1084. doi: 10.5665/sleep.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitebread D, Coltman P, Pasternak DP, et al. The development of two observational tools for assessing metacognition and self-regulated learning in young children. Metacognition and Learning. 2009;4:63–85. [Google Scholar]
- Winsler A, Ducenne L, Koury A. Singing one’s way to self-regulation: the role of early music and movement curricula and private speech. Early Educ Dev. 2011;22:274–304. [Google Scholar]
- Wrosch C, Scheier MF, Carver CS, Schulz R. The importance of goal disengagement in adaptive self-regulation: when giving up is beneficial. Self Identity. 2003;2:1–20. [Google Scholar]