Abstract
Introduction
Blood pressure is a major cause of cardiovascular disease (CVD) and both may increase as outdoor temperatures fall. However, there are still limited data about seasonal variation in blood pressure and CVD mortality among patients with prior-CVD.
Methods
We analysed data on 23 000 individuals with prior-CVD who were recruited from 10 diverse regions into the China Kadoorie Biobank during 2004–8. After 7 years of follow-up, 1484 CVD deaths were recorded. Baseline survey data were used to assess seasonal variation in systolic blood pressure (SBP) and its association with outdoor temperature. Cox regression was used to examine the association of usual SBP with subsequent CVD mortality, and seasonal variation in CVD mortality was assessed by Poisson regression. All analyses were adjusted for age, sex, and region.
Results
Mean SBP was significantly higher in winter than in summer (145 vs. 136 mmHg, P < 0.001), especially among those without central heating. Above 5°C, each 10°C lower outdoor temperature was associated with 6.2 mmHg higher SBP. Systolic blood pressure predicted subsequent CVD mortality, with each 10 mmHg higher usual SBP associated with 21% (95% confidence interval: 16–27%) increased risk. Cardiovascular disease mortality varied by season, with 41% (21–63%) higher risk in winter compared with summer.
Conclusion
Among adult Chinese with prior-CVD, there is both increased blood pressure and CVD mortality in winter. Careful monitoring and more aggressive blood pressure lowering treatment in the cold months are needed to help reduce the winter excess CVD mortality in high-risk individuals.
Keywords: Blood pressure, Seasonal variation, Cardiovascular disease, Hypertension, Cohort study, China
See page 1152 for the editorial comment on this article (doi:10.1093/eurheartj/ehv024)
Introduction
Cardiovascular disease (CVD) is a leading cause of mortality and morbidity, with an estimated 17 million deaths in 2008.1 Over 80% of CVD deaths now occur in low- and middle-income countries such as China,2 and the burden of disease from CVD is projected to increase further over the next few decades in these countries.3
Increased blood pressure is one of the most important modifiable causes of CVD,4–6 and is known to be associated with lifestyle and environmental factors. There is evidence that outdoor temperature affects blood pressure,7–9 with particularly large effects in China.8 Exposure to cold temperatures can lead to vasoconstriction and tachycardia, both of which contribute to increased blood pressure and cardiac load.10 Excess CVD mortality has been reported during the cold seasons,11–15 part of which may be driven by temperature-related increases in blood pressure. Individuals who are already suffering from CVD may be at, particularly, increased risk when exposed to cold temperatures. However, limited large-scale data exist about seasonal variation in blood pressure and CVD mortality among people with prior-CVD, especially in China where few people have access to central heating in winter and where few people with prior-CVD are properly managed.16
We report data from the China Kadoorie Biobank (CKB) study of over 500 000 adults aged 30–79 years who were recruited from 10 diverse regions in China during 2004–8 and followed up ever since for mortality and morbidity to 31 December 2013. The present study is of 23 000 participants who reported at the baseline visit having a physician diagnosed CVD and aims (a) to examine the association of outdoor temperature with blood pressure measured at recruitment, both overall and in different population subgroups, (b) to investigate the association between usual blood pressure and subsequent CVD mortality, and (c) to assess any seasonal variation in CVD mortality rates and then compare it with predicted risk based on seasonal changes in blood pressure.
Methods
Baseline survey
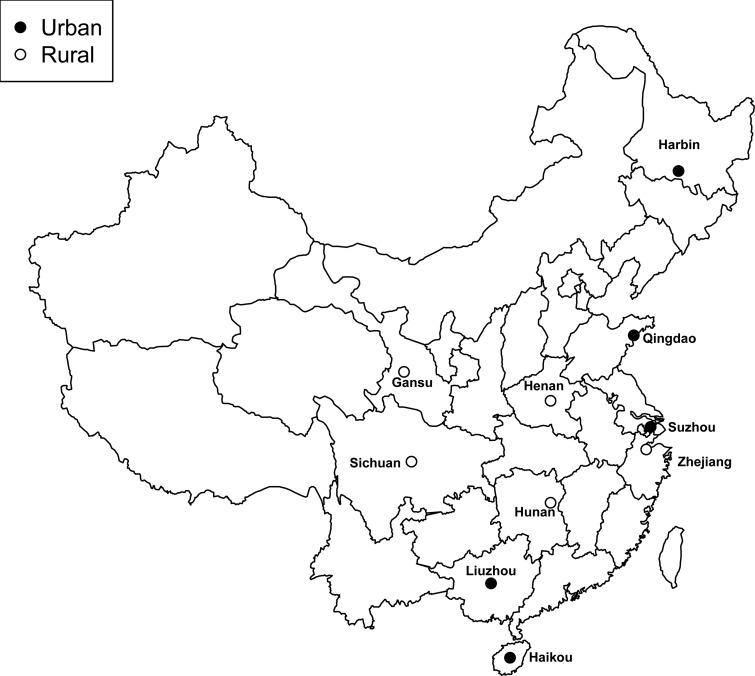
Detailed information about the study design and procedures has been reported previously.8,17 Briefly, the baseline survey took place between 2004 and 2008 in 10 geographically defined areas in China (Figure 1). At the baseline survey, detailed information about general demographic and socio-economic status, dietary and other lifestyle habits (e.g. smoking, alcohol drinking, and physical activity), indoor air pollution, medical history, and current medication were collected using an interviewer-administered laptop-based questionnaire. Participants were asked whether they had ever been diagnosed by a physician with a range of chronic diseases [e.g. diabetes, ischaemic heart disease (IHD), stroke or transient ischaemic attack (TIA), hypertension, chronic obstructive pulmonary disease, cancer, or other common diseases), and if so, the age at first diagnosis and whether they were still on treatment. Participants who had reported having a prior history of IHD, stroke/TIA, diabetes, or hypertension were additionally asked about current usage of specific drugs (aspirin, ACE-I, β-blocker, statins, diuretics, or calcium antagonist).16 A range of physical measurements were undertaken for each participant and a blood sample was collected.
Figure 1.
Locations of the recruitment centres in China Kadoorie Biobank. The solid circles denote urban areas, and the open circles denote rural areas.
Ethical approval was obtained from the Ethical Review Committee of the Chinese Centre for Disease Control and Prevention, Beijing, China and the Oxford Tropical Research Ethics Committee, University of Oxford, UK. All study participants provided written informed consent.
Blood pressure measurement
Blood pressure was measured at least twice using a UA-779 digital monitor after participants had remained at rest in a seated position for at least 5 min. If the difference between the two measurements was >10 mmHg for SBP, a third measurement was made and the last two measurements were recorded. The procedure for blood pressure measurement was standardized across the 10 study areas, and all measurements were made by trained study personnel. All devices were regularly calibrated to ensure consistency of measurements.8,17
Meteorological data
Daily meteorological measurements for the years 2004–2008 were obtained from China Meteorological Administration local offices at each region. Mean monthly, summer (June, July, August), and winter (December, January, February) outdoor temperatures were calculated as the average of the recorded mean daily outdoor temperatures (the average of four measurements taken at 0200, 0800, 1400, and 2000 h) for all the participants who were surveyed during that month or season.
Follow-up for mortality and morbidity
Since recruitment, participants have been followed up for cause-specific morbidity and mortality through linkage with regional disease and death registers and with the recently established national health insurance (HI) system. Causes of death are sought chiefly from official death certificates supplemented, if necessary, by reviewing medical records or undertaking verbal autopsy, a WHO standard tool to determine probable causes of death for those who died without any medical attention.18 A bespoke IT system developed by the project team for this study is used for entering the data from death and disease registers, with the death certificates or the disease reporting cards scanned. Data linkage with HI agencies is carried out every 6 months in each region, and all hospitalized events occurring in that last half-year are retrieved for matched study participants. So far, ∼98% of the study population is covered by the HI system. To minimize losses to follow-up, active follow-up (i.e. visiting local community or directly contacting participants) is also performed annually.17
The main analyses of the present study only involved individuals who reported having IHD, stroke/TIA at the baseline survey, i.e. defined as ‘prior-CVD participants’. For prospective analyses, only deaths from IHD (ICD-10: I20–I25) or stroke (ICD-10: I60–I61, I63–I64) were considered, henceforth referred to as ‘CVD mortality’.
Statistical methods
Baseline characteristics—mean (SD) for continuous variables, N (%) for categorical variables—were calculated separately for people with or without CVD. All main analyses related to blood pressure and CVD mortality were only for prior-CVD participants. Mean systolic and diastolic blood pressure (SBP, DBP), adjusted for area, age, and sex were calculated separately for each calendar month of the study recruitment period. These blood pressure means were then plotted against the mean day of the year for each month of recruitment, i.e. regardless of the year, with January and February combined to allow for the fall in recruitment over the Chinese New Year. To obtain the estimated change in blood pressure per 10°C lower outdoor temperature, a multiple linear regression analysis was performed of individual SBP on the individual outdoor temperature, adjusted for age and sex. Observations <5°C were omitted from the regression because few participants experienced daily winter temperatures regularly well below that range, with exception of those from Harbin where the winter temperature usually drops well below −10°C and nearly all households have proper central heating from mid-October until March the following year.8 Subgroup analyses by area, sex, age, body mass index (BMI), education, use of anti-hypertensive treatment, medical history of hypertension or diabetes and, for men only, current smoking and alcohol drinking (there were too few female drinkers and smokers for reliable analyses) were performed to assess whether seasonal changes in blood pressure were modified by other known vascular risk factors. To help make allowance for the multiplicity of comparisons when many subgroup analyses are performed, the separate heterogeneity χ2 statistics for each were summed (as were their degrees of freedom) to yield a global test for heterogeneity.19 The individual heterogeneity tests are not shown where trend tests are more appropriate.
Cox proportional hazards models were used to calculate hazard ratios (HRs), with blood pressure as the exposure variable and CVD mortality as the outcome, and stratified by sex, region (10 groups), age at risk (10 groups), and anti-hypertensive treatment status, and further adjusted for smoking, alcohol drinking, BMI, and education. The 95% confidence interval (CI) for each log HR was estimated using the ‘floating absolute risk’ method, which facilitates many different comparisons and tests for trend between different categories, rather than just pair-wise comparisons between one arbitrarily chosen reference group and each of the other categories.20 To correct for regression dilution bias,4,21 HRs in the groups determined at baseline were plotted against the usual blood pressure, i.e. the mean value of systolic blood pressure in that group at the subsequent resurvey, on average 2.6 years after the baseline survey.
Finally, the number of CVD deaths and person-years for each calendar month were calculated and summed into groups by calendar month regardless of year. Poisson regression, adjusted for age, sex, and area, was used to calculate CVD mortality rates in each of the groups. Analyses were performed using SAS version 9.3 and R version 3.0.1.
Results
A total of 506 673 people (99% of all participants) had data on both blood pressure and outdoor temperature on the day of baseline survey. Table 1 compares the baseline characteristics and the number of deaths from CVD during follow-up between individuals with and without prior-CVD. Overall, 23 040 (4.5%) participants reported having prior-CVD with mean years since diagnosis of 7.2 years. About one-third of those with prior-CVD was from Harbin, which is located in the far northeast of China (Tables 1 and 2). Those with prior-CVD tended to be older (mean age of 61 vs. 51 years) and more likely to have higher mean SBP (141 vs. 131 mmHg) and BMI (24.9 vs. 23.6 kg/m2). At any given age, men with prior-CVD were less likely to be current regular smokers or weekly alcohol drinkers, but more likely to be ex-smokers or ex-drinkers than men without prior-CVD. The lower proportions of current regular smokers or drinkers among men with prior-CVD were probably due to increased rates of quitting because of illness. People with prior-CVD were also more likely to report a prior diagnosis of hypertension (48 vs. 10%) or diabetes (12 vs. 3%), and to be taking anti-hypertensive treatment (31 vs. 4%). During an average of 7.1 (SD 1.3) years of follow-up, a total of 1484 CVD deaths were recorded among those with prior-CVD (748 from IHD and 736 from stroke) (Table 1).
Table 1.
Baseline characteristics of study participants and number of cardiovascular disease-related deaths by self-reported hospital diagnosis of prior-cardiovascular disease
| Overall | With prior-CVD | No prior-CVD | |
|---|---|---|---|
| Number of participants | 506 673 | 23 040 | 483 633 |
| Age (SD, years) | 52 (11) | 61 (9) | 51 (11) |
| SBP (SD, mmHg) | 131 (21) | 141 (23) | 131 (21) |
| DBP (SD, mmHg) | 78 (11) | 80 (12) | 78 (11) |
| BMI (SD, kg/m2) | 23.7 (3.4) | 24.9 (3.6) | 23.6 (3.4) |
| Years since diagnosis (SD, years) | 7.2 (7.1) | – | |
| Men (%) | 41.0 | 43.5 | 40.9 |
| Current smokers (%) | 61.0 | 43.0 | 61.9 |
| Ex-smokers (%) | 13.3 | 29.1 | 12.5 |
| Weekly drinkers (%) | 32.9 | 21.0 | 33.6 |
| Ex-drinkers (%) | 3.7 | 11.8 | 3.3 |
| With central heating (%) | 12.3 | 33.0 | 11.3 |
| Self-reported hypertension (%) | 11.7 | 48.2 | 10.0 |
| Treated for hypertension (%) | 4.8 | 30.6 | 3.6 |
| Self-reported diabetes (%) | 3.2 | 12.3 | 2.7 |
| Number of IHD/stroke deathsa | 7144 | 1484 | 5660 |
aIHD (ICD-10: I20–I25), stroke (ICD-10: I60–I61, I63–I64), follow-up duration: baseline to 31 December 2013.
Table 2.
Mean temperature (°C) and systolic blood pressure (mmHg) in summer and winter, by area, among participants with prior-cardiovascular disease
| Area | Latitude (°N) | % with central heating | Number with prior-CVDs | Summer (June–August) |
Winter (December–February) |
Difference (Summer vs. Winter) |
Change (SE) in SBP per 10°C lower temperatureb (≥5°C only) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Temp (°C) | SBPa | Temp (°C) | SBPa | Temp (°C) | SBPa | |||||
| Harbin | 46 | 94 | 7672 | 22.7 | 131 | −14.1 | 138 | 36.8 | −7 | 5.9 (0.52) |
| Qingdao | 36 | 15 | 2009 | 23.9 | 138 | 1.7 | 146 | 22.1 | −9 | 8.3 (0.81) |
| Henan | 35 | 0 | 3000 | 26.9 | 139 | 1.5 | 150 | 25.4 | −12 | 5.4 (0.62) |
| Gansu | 35 | 1 | 1342 | 22.3 | 139 | −0.1 | 151 | 22.4 | −12 | 9.0 (1.14) |
| Zhejiang | 31 | 0 | 817 | 28.1 | 138 | 6.0 | 153 | 22.2 | −15 | 6.9 (1.05) |
| Suzhou | 31 | 2 | 1017 | 28.0 | 137 | 5.9 | 146 | 22.1 | −9 | 5.8 (0.93) |
| Sichuan | 31 | 0 | 476 | 25.7 | 137 | 6.5 | 144 | 19.2 | −7 | 4.3 (1.55) |
| Hunan | 28 | 1 | 2623 | 27.9 | 143 | 6.9 | 152 | 21.0 | −9 | 4.8 (0.58) |
| Liuzhou | 24 | 0 | 3423 | 28.7 | 133 | 12.1 | 144 | 16.5 | −11 | 7.1 (0.59) |
| Haikou | 20 | 0 | 661 | 28.6 | 129 | 18.5 | 140 | 10.2 | −11 | 7.4 (1.87) |
| Overall | 29 | 23 040 | 25.5 | 136 | 3.8 | 145 | 21.7 | −9 | 6.2 (0.24) | |
aSBP, systolic blood pressure; adjusted for age, sex, and area (where appropriate).
bAdjusted for age, sex, and area (where appropriate).
A seasonal cycle of mean blood pressure, especially SBP, was observed in people with prior-CVD, with highest levels in winter and lowest levels in summer in both men and women (Figure 2). Overall, SBP varied from 145 mmHg in winter to 136 mmHg in summer (P < 0.001), but the magnitude of this variation differed between regions (Table 2). Indeed, in Harbin, although the mean outdoor temperature was on average 36°C colder in winter than in summer, the mean SBP only differed by 7 mmHg between winter and summer seasons, with a small fall, rather than increase, in SBP in winter when the central heating was turned on (Figure 3).
Figure 2.
Monthly variation in blood pressure and outdoor temperature in people with prior-cardiovascular disease in (A) men and (B) women. The horizontal placement of each month combined over the full 4 years of recruitment represents the mean number of days since the first participant was recruited for participants recruited in average over years for that month. J/F = January and February combined (recruitment dropped in January and February due to the Chinese New Year). For both blood pressure and temperature, the mean monthly values are the mean for all participants whose baseline survey happened during that month (regardless of the year). Means of blood pressure were adjusted for sex and age. The winter months are placed centrally to display the winter peak in blood pressure.
Figure 3.
Monthly variation in systolic blood pressure and outdoor temperature among people with prior-cardiovascular disease, Other regions together vs. Harbin. Conventions as in Figure 1.
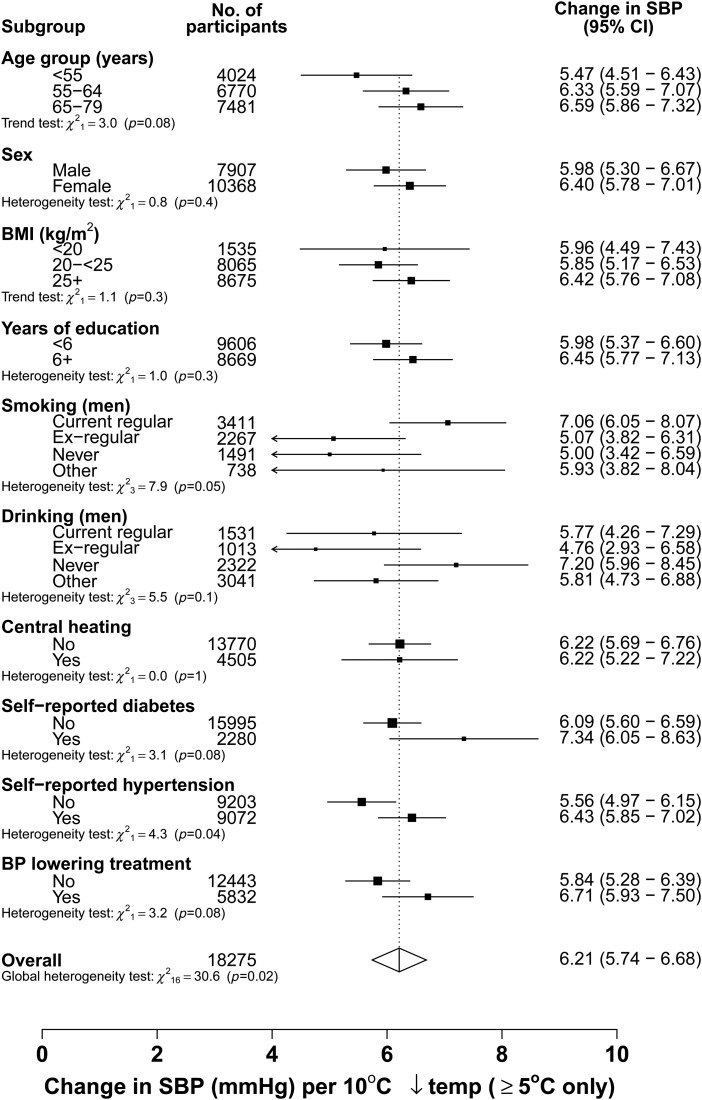
There was an approximately linear inverse association between SBP and temperature >5°C, with a mean increase of 6.2 (SE 0.24) mmHg in SBP for each 10°C decrease in outdoor temperature. There was a 2-fold difference in the strength of this relationship between areas (phet = 0.003), ranging from 4.3 mmHg in Sichuan to 9.0 mmHg in Gansu (Table 2, Supplementary material online, eFigure S1). However, the association was largely consistent between most other subgroups studied (P for global test of heterogeneity = 0.02) (Figure 4).
Figure 4.
Seasonal variation in systolic blood pressure and outdoor temperature among people with prior-cardiovascular disease by various subgroups, with the temperature range at least >5°C. The analysis was adjusted for age, sex, and area (where appropriate). Each closed square represents a change in systolic blood pressure per 10°C lower outdoor temperatures. The dotted vertical line indicates the overall change in systolic blood pressure; the open diamond indicates it and its 95% CI.
A positive association was observed between usual SBP and CVD mortality, with 21% (95% CI: 16–27%) higher risk of CVD mortality for each 10 mmHg higher usual SBP (Figure 5). The excess risk was similar between people treated with blood pressure lowering agents and those without (HR (95% CI) = 1.25 (1.18–1.33) vs. 1.18 (1.08–1.28), P for heterogeneity = 0.28). Overall, the adjusted CVD mortality rate was 2.35 per 1000 person-years, but fluctuated over the course of the year, with a winter peak observed (2.78 in winter vs. 1.98 per 1000 person-years in summer) (Figure 6). Among people with prior-CVD, both absolute-CVD mortality rates and the relative seasonal changes were weaker in Harbin than in the other regions (Harbin: 1.96 vs. 1.61 per 1000 person-years, rate ratio (95% CI) = 1.22 (1.07–1.39); all other combined: 4.10 vs. 2.73 per 1000 person-years, rate ratio = 1.50 (1.39–1.61)).
Figure 5.
Hazard ratios for cardiovascular disease mortality vs. usual blood pressure among people with prior-cardiovascular disease. Analyses were stratified by region, age, gender, and blood pressure lowering treatment status, and adjusted for education, smoking, alcohol drinking, and body mass index. The hazard ratios are plotted on a floating absolute scale. Each square has an area inversely proportional to the standard error of the log risk. Vertical lines indicate the corresponding 95% confidence intervals. Numbers above confidence intervals are of hazard ratios and those below are the numbers of cardiovascular disease deaths.
Figure 6.
Seasonal variation in cardiovascular disease mortality rates among people with prior-cardiovascular disease, between 2004 and 2013. Deaths and person-days at risk for a given months are totalled across the follow-up period. The analysis is adjusted for age group, study site, and sex, but not for year of follow-up. To make the curve smoother, two calendar months are combined and winter months are again placed centrally, as in Figure 1. Vertical lines indicate the corresponding 95% confidence intervals. Numbers above confidence intervals are of mortality rates (per 1000 person-years) and those below are the numbers of deaths.
Discussion
In this large study of over 23 000 individuals with prior-CVD who were recruited from the general communities in 10 diverse regions of China, we observed substantial seasonal variation of blood pressure, especially, in areas where there is little use of central heating in the cold months. Overall, the mean SBP was 9 mmHg higher in winter than in summer, and, >5°C in outdoor temperature, SBP was 6.2 mmHg higher for each 10°C decrease in temperature. Among people with prior-CVD, blood pressure is a strong independent predictor of subsequent CVD mortality, with each 10 mmHg higher usual SBP associated with ∼21% higher risk of CVD death. Mirroring the seasonal variation of blood pressure, there was a 41% increase in CVD mortality during winter.
Several studies have provided evidence about seasonal variation of blood pressure, but most of them were in general populations, with only a few involving high-risk populations such as people in old age,7,22–24 those with low BMI,7,25 hypertension,7,24,26 or end-stage renal disease.27 The present large study in China provides large-scale evidence about climate-related changes in blood pressure in people with prior-CVD. In this Chinese population, the seasonal variation in blood pressure was generally more extreme than that observed in western populations, and was abolished by the use of home central heating. The large variation in blood pressure between seasons observed in the present study has strong implications for detection and clinical management of hypertension. People maybe more likely to be diagnosed with hypertension if examined in winter than in summer, and hypertensive patients may suffer even higher blood pressure in the cold season due to inadequate blood pressure control. In a prospective study of 184 elderly Israeli patients with essential hypertension, supplementary anti-hypertensive treatment was required during winter in 38% of them.28 We were not able to assess seasonal changes within individuals since it is not practicable to monitor changes in participants' blood pressure and treatment during follow-up among 0.5 million participants. In our study, the mean blood pressure was much higher in winter than in summer among both those taking and those not taking blood pressure lowering treatment. Blood pressure, especially SBP, is an independent predictor of CVD risk not only in general population but also in those with prior vascular diseases.4,29 The beneficial effects of blood pressure lowering treatments on the risks of major CVD diseases are well established.30 In this study population with prior-CVD, the strength of the association – i.e. 21% higher CVD mortality per 10 mmHg higher usual SBP—was weaker than previous estimates from general populations (both Chinese and Western), that have estimated ∼40% higher stroke mortality and 30% higher IHD death.4 This may be explained by the fact that a high proportion of the individuals with prior-CVD in the present study were on anti-hypertensive treatment that may well attenuate the effects of blood pressure on subsequent CVD risk.
A winter peak in CVD mortality has been consistently reported among general populations in many studies.11,12,31–35 However, only one previous study has simultaneously examined seasonal changes in blood pressure and mortality in people with prior-CVD.15 In that study of 19 000 male British civil servants aged 40–69 years with 25-year follow-up , the seasonal effect on all-cause mortality was more extreme among 3284 men with prevalent IHD than those without (rate ratio for winter vs. summer of 1.38 and 1.18, respectively, P = 0.03). Among those with prior-IHD participants, the rate ratios were 1.31 for IHD mortality and 1.48 for stroke.15 In our study, where mean SBP differed by ∼10 mmHg between winter and summer, we observed 41% higher CVD mortality in winter compared with summer, which is somewhat greater than predicted from our prospective analysis of prognostic effect of blood pressure on CVD mortality, although it is comparable with the risk estimates for a prolonged 10 mmHg SBP difference reported from the general population.4 It is unlikely that all the epidemiologically expected risk would be observed by the short- to medium-term rise in blood pressure during winter and it is likely that there are additional factors that contributed to the winter rise in mortality. Nevertheless, some of the observed winter peak in CVD mortality may well be driven by rises in blood pressure due to the cold temperature.
There are some limitations to our study. Although it was explicit that all reported prior disease history should be based on physician diagnosis, it was not possible with such a large cohort to adjudicate all the self-reported cases retrospectively. However, there is an evidence from other studies of similar nature in China that self-reported history of CVD showed a good consistency with hospital records.36 Moreover, in a separate analysis when comparing the CVD mortality rates observed in our prior-CVD population with rates in those without, a 3-fold higher risk was consistently appeared in each month [overall HR = 2.98 (95% CI: 2.80–3.18)] (Supplementary material online, eFigure S2). This provides indirect evidence that self-reports of prior-CVD in our study were generally reliable. Occlusive and haemorrhagic CVD may involve different pathophysiological mechanisms.37 Although the present study included a sufficiently large number of CVD deaths to assess the overall effect of season on CVD mortality, the statistical power to separately examine the seasonal patterns of subtype of CVD mortality is rather limited. The isolated clinic BP measurements used in our study are unable to provide as reliable an assessment of blood pressure as ambulatory blood pressure monitoring, and may lead us to underestimate any patterns or associations. However, the high comparability of baseline characteristics between participants enrolled at different seasons or months, as reported previously,8 suggests that seasonal variation in blood pressure is likely to be driven primarily by changes in outdoor temperature rather than by other lifestyle factors.
Our study findings suggest that seasonal variation in CVD mortality rates in people with prior-CVD result, at least partly, from seasonal variation of blood pressure. Given the high prevalence of CVD in the Chinese population, especially of stroke, even moderate increases in CVD mortality rates during the winter months, as shown in this study, must account for large excess numbers of CVD deaths. The results from the present analyses suggest that seasonal changes in blood pressure should be taken into account in the diagnosis and treatment of hypertension and CVD. For patients with prior-CVD or other high-risk individuals, more intensive anti-hypertensive treatment and more frequent blood pressure monitoring may be required in winter to achieve the same blood pressure control as in other seasons. Longer follow-up of this large cohort study and the use of well-characterized non-fatal CVD events may allow for more detailed analyses of seasonal variation separately in the main components of CVD, namely IHD, ischaemic, and haemorrhagic stroke.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The baseline survey and the first re-survey were supported by a research grant from the Kadoorie Charitable Foundation in Hong Kong. The long-term continuation of the project during 2009–2014 is supported by program grants from the Wellcome Trust in the UK (088158/Z/09/Z) and the Chinese Ministry of Science and Technology. The UK Medical Research Council, the British Heart Foundation and Cancer Research UK also provide core funding to the Clinical Trial Service Unit and Epidemiological Studies Unit at Oxford University for the project. Funding to pay the Open Access publication charges for this article was provided by Welcome Trust.
Conflict of interest: none declared.
Appendix
Members of the China Kadoorie Biobank collaborative group
(a) International steering committee
Liming Li (PI), Junshi Chen, Rory Collins, Richard Peto, Zhengming Chen (PI).
(b) Study Coordinating Centres
International Co-ordinating Centre, Oxford: Zhengming Chen, Garry Lancaster, Xiaoming Yang, Alex Williams, Margaret Smith, Ling Yang, Yumei Chang, Iona Millwood, Yiping Chen, Sarah Lewington.
National Co-ordinating Centre, Beijing: Yu Guo, Zheng Bian, Can Hou, Yunlong Tan, Huiyan Zhou.
Regional Co-ordinating Centres, 10 areas in China:
Qingdao
Qingdao CDC: Zengchang Pang, Shaojie Wang, Yun Zhang, Kui Zhang.
Licang CDC: Silu Liu, Wei Hou.
Heilongjiang
Provincial CDC: Zhonghou Zhao, Shumei Liu, Zhigang Pang. Nangang CDC: Weijia Feng, Shuling Wu, Liqiu Yang, Huili Han, Hui He, Bo Yu.
Hainan
Provincial CDC: Xianhai Pan, Shanqing Wang, Hongmei Wang. Meilan CDC: Xinhua Hao, Chunxing Chen, Shuxiong Lin, Xiangyang Zheng.
Jiangsu
Provincial CDC: Xiaoshu Hu, Minghao Zhou, Ming Wu, Ran Tao. Suzhou CDC: Yeyuan Wang, Yihe Hu, Liangcai Ma, Renxian Zhou, Guanqun Xu, Yan Lu.
Guangxi
Provincial CDC: Baiqing Dong, Naying Chen, Ying Huang. Liuzhou CDC: Mingqiang Li, Jinhuai Meng, Zhigao Gan, Jiujiu Xu, Yun Liu, Jingxin Qing.
Sichuan
Provincial CDC: Xianping Wu, Yali Gao, Ningmei Zhang Pengzhou CDC: Guojin Luo, Xiangsan Que, Xiaofang Chen.
Gansu
Provincial CDC: Pengfei Ge, Jian He, Xiaolan Ren. Maiji CDC: Hui Zhang, Enke Mao, Guanzhong Li, Zhongxiao Li, Jun He, Yulong Lei, Xiaoping Wang.
Henan
Provincial CDC: Guohua Liu, Baoyu Zhu, Gang Zhou, Shixian Feng. Huixian CDC: Yulian Gao, Tianyou He, Li Jiang, Jianhua Qin, Huarong Sun.
Zhejiang
Provincial CDC: Liqun Liu, Min Yu, Yaping Chen, Ruying Hu. Tongxiang CDC: Zhixiang Hu, Jianjin Hu, Yijian Qian, Zhiying Wu, Chunmei Wang, Lingli Chen.
Hunan
Provincial CDC: Wen Liu, Guangchun Li, Huilin Liu. Liuyang CDC: Xiangquan Long, Xin Xu, Youping Xiong, Zhongwen Tan, Xuqiu Xie, Yunfang Peng, Weifang Jia.
Contributor Information
Collaborators: On Behalf of the China Kadoorie Biobank Study Collaboration, Liming Li, Junshi Chen, Rory Collins, Richard Peto, Zhengming Chen, Zhengming Chen, Garry Lancaster, Xiaoming Yang, Alex Williams, Margaret Smith, Ling Yang, Yumei Chang, Iona Millwood, Yiping Chen, Sarah Lewington, Yu Guo, Zheng Bian, Can Hou, Yunlong Tan, Huiyan Zhou, Zengchang Pang, Shaojie Wang, Yun Zhang, Kui Zhang, Silu Liu, Wei Hou, Zhonghou Zhao, Shumei Liu, Zhigang Pang, Weijia Feng, Shuling Wu, Liqiu Yang, Huili Han, Hui He, Bo Yu, Xianhai Pan, Shanqing Wang, Hongmei Wang, Xinhua Hao, Chunxing Chen, Shuxiong Lin, Xiangyang Zheng, Xiaoshu Hu, Minghao Zhou, Ming Wu, Ran Tao, Yeyuan Wang, Yihe Hu, Liangcai Ma, Renxian Zhou, Guanqun Xu, Yan Lu, Baiqing Dong, Naying Chen, Ying Huang, Mingqiang Li, Jinhuai Meng, Zhigao Gan, Jiujiu Xu, Yun Liu, Jingxin Qing, Xianping Wu, Yali Gao, Guojin Luo, Xiangsan Que, Xiaofang Chen, Pengfei Ge, Jian He, Xiaolan Ren, Hui Zhang, Enke Mao, Guanzhong Li, Zhongxiao Li, Jun He, Yulong Lei, Xiaoping Wang, Guohua Liu, Baoyu Zhu, Gang Zhou, Shixian Feng, Yulian Gao, Tianyou He, Li Jiang, Jianhua Qin, Huarong Sun, Liqun Liu, Min Yu, Yaping Chen, Ruying Hu, Zhixiang Hu, Jianjin Hu, Yijian Qian, Zhiying Wu, Chunmei Wang, Lingli Chen, Wen Liu, Guangchun Li, Huilin Liu, Xiangquan Long, Xin Xu, Youping Xiong, Zhongwen Tan, Xuqiu Xie, Yunfang Peng, and Weifang Jia
References
- 1.WHO. Cardiovascular diseases (CVDS) http://www.Who.Int/mediacentre/factsheets/fs317/en/ 2013.
- 2.Chen Z. The third national retrospective sampling mortality survey report. Beijing: China Union Medical University Publishing House; 2008. [Google Scholar]
- 3.Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, Koplan JP. Emergence of chronic non-communicable diseases in China. Lancet 2008;372:1697–1705. [DOI] [PubMed] [Google Scholar]
- 4.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 5.He J, Gu D, Chen J, Wu X, Kelly TN, Huang JF, Chen JC, Chen CS, Bazzano LA, Reynolds K, Whelton PK, Klag MJ. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009;374:1765–1772. [DOI] [PubMed] [Google Scholar]
- 6.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, Abbott R, Godwin J, Dyer A, Stamler J. Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990;335:765–774. [DOI] [PubMed] [Google Scholar]
- 7.Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J 1982;285:919–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, Whitlock G, Yang L, Collins R, Chen J, Wu X, Wang S, Hu Y, Jiang L, Lacey B, Peto R, Chen Z. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012;30:1383–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose G. Seasonal variation in blood pressure in man. Nature 1961;189:235. [DOI] [PubMed] [Google Scholar]
- 10.Cuspidi C, Ochoa JE, Parati G. Seasonal variations in blood pressure: a complex phenomenon. J Hypertens 2012;30(7):1315–1320. [DOI] [PubMed] [Google Scholar]
- 11.Group TE. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The eurowinter group. Lancet 1997;349:1341–1346. [PubMed] [Google Scholar]
- 12.Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, Kirchmayer U, Ballester F, Cadum E, Goodman PG, Hojs A, Sunyer J, Tiittanen P, Michelozzi P. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol 2008;168:1397–1408. [DOI] [PubMed] [Google Scholar]
- 13.Danet S, Richard F, Montaye M, Beauchant S, Lemaire B, Graux C, Cottel D, Marecaux N, Amouyel P. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths. A 10-year survey: the Lille-World Health Organization MONICA project (monitoring trends and determinants in cardiovascular disease). Circulation 1999;100:E1–E7. [DOI] [PubMed] [Google Scholar]
- 14.Mercer JB. Cold – an underrated risk factor for health. Environ Res 2003;92:8–13. [DOI] [PubMed] [Google Scholar]
- 15.van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG. Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first whitehall study. Int J Epidemiol 2001;30:1109–1116. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Li L, Zhang Q, Clarke R, Chen J, Guo Y, Bian Z, Pan X, Peto R, Tao R, Shi K, Collins R, Ma L, Sun H, Chen Z. Use of drug treatment for secondary prevention of cardiovascular disease in urban and rural communities of China: China Kadoorie Biobank study of 0.5 million people. Int J Cardiol 2014;172:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, Li L. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol 2011;40:1652–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO. Verbal autopsy standards: ascertaining and attributing causes of death http://www.Who.Int/healthinfo/statistics/verbalautopsystandards/en/ (15 September 2014).
- 19.Group EBCTC. Treatment of early breast cancer. Volume 1: worldwide evidence 1985–1990. Oxford: Oxford University Press; 1990. [Google Scholar]
- 20.Plummer M. Improved estimates of floating absolute risk. Stat Med 2004;23:93–104. [DOI] [PubMed] [Google Scholar]
- 21.Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol 1999;150:341–353. [DOI] [PubMed] [Google Scholar]
- 22.Kunes J, Tremblay J, Bellavance F, Hamet P. Influence of environmental temperature on the blood pressure of hypertensive patients in montreal. Am J Hypertens 1991;4:422–426. [DOI] [PubMed] [Google Scholar]
- 23.Alperovitch A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetiere P, Tzourio C. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the three-city study. Arch Intern Med 2009;169:75–80. [DOI] [PubMed] [Google Scholar]
- 24.Postolache T, Gautier S, Laloux B, Safar M, Benetos A. Positive correlation between the blood pressure and heart rate response to the cold pressor test and the environmental temperature in older hypertensives. Am J Hypertens 1993;6:376–381. [DOI] [PubMed] [Google Scholar]
- 25.Kristal-Boneh E, Harari G, Green MS, Ribak J. Body mass index is associated with differential seasonal change in ambulatory blood pressure levels. Am J Hypertens 1996;9:1179–1185. [DOI] [PubMed] [Google Scholar]
- 26.Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessi-Fulgheri P, Sarzani R. Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J Hypertens 2012;30:1392–1398. [DOI] [PubMed] [Google Scholar]
- 27.Argiles A, Mourad G, Mion C. Seasonal changes in blood pressure in patients with end-stage renal disease treated with hemodialysis. N Engl J Med 1998;339:1364–1370. [DOI] [PubMed] [Google Scholar]
- 28.Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology 2004;50:315–321. [DOI] [PubMed] [Google Scholar]
- 29.Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlof B, Sever PS, Poulter NR. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905. [DOI] [PubMed] [Google Scholar]
- 30.Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 31.Barnett AG, de Looper M, Fraser JF. The seasonality in heart failure deaths and total cardiovascular deaths. Aust N Z J Public Health 2008;32:408–413. [DOI] [PubMed] [Google Scholar]
- 32.Guo Y, Barnett AG, Pan X, Yu W, Tong S. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect 2011;119:1719–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kan HD, Jia J, Chen BH. Temperature and daily mortality in shanghai: a time-series study. Biomed Environ Sci 2003;16:133–139. [PubMed] [Google Scholar]
- 34.Sheth T, Nair C, Muller J, Yusuf S. Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol 1999;33:1916–1919. [DOI] [PubMed] [Google Scholar]
- 35.Tian Z, Li S, Zhang J, Jaakkola JJ, Guo Y. Ambient temperature and coronary heart disease mortality in Beijing, China: a time series study. Environ Health 2012;11:11–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, Kruger A, Kutty R, Lanas F, Lisheng L, Wei L, Lopez-Jaramillo P, Oguz A, Rahman O, Swidan H, Yusoff K, Zatonski W, Rosengren A, Teo KK. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the pure study): a prospective epidemiological survey. Lancet 2011;378:1231–1243. [DOI] [PubMed] [Google Scholar]
- 37.Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 1995;345:353–355. [DOI] [PubMed] [Google Scholar]