Abstract
Treatment of chronic myeloid leukemia (CML) with tyrosine kinase inhibitors has advanced to a stage where many patients achieve very low or undetectable levels of disease. Remarkably, some of these patients remain in sustained remission when treatment is withdrawn, suggesting that they may be at least operationally cured of their disease. Accurate definition of deep molecular responses (MRs) is therefore increasingly important for optimal patient management and comparison of independent data sets. We previously published proposals for broad standardized definitions of MR at different levels of sensitivity. Here we present detailed laboratory recommendations, developed as part of the European Treatment and Outcome Study for CML (EUTOS), to enable testing laboratories to score MR in a reproducible manner for CML patients expressing the most common BCR-ABL1 variants.
Introduction
Molecular monitoring provides important prognostic information for individual chronic myeloid leukemia (CML) patients undergoing therapy, and international treatment recommendations incorporate specific time-dependent molecular milestones to help determine whether a patient is responding optimally or not.1, 2 Molecular measurements are made by reverse transcriptase quantitative PCR (RT-qPCR) to estimate the amount of BCR-ABL1 mRNA relative to an internal reference gene, most commonly ABL1, GUSB or BCR.3, 4 The results are expressed on an International Scale (IS) as a percentage, with 100% BCR-ABLIS corresponding to the International Randomized Study of Interferon and STI571 (IRIS) study standardized baseline and 0.1% BCR-ABLIS being defined as a major molecular response (MMR or MR3; 3 log reduction from the standardized baseline).3 Expression of results on the IS depends on each testing laboratory either having obtained a laboratory-specific conversion factor (CF) by sample exchange with an established reference laboratory or by using kits and reagents that have been calibrated to the World Health Organization International Genetic Reference Panel for quantitation of BCR-ABL1 mRNA.4, 5, 6, 7, 8, 9
Efforts to standardize molecular monitoring to the IS focused initially on detectable residual disease and in particular whether a patient had or had not achieved particular milestones, for example, 10% BCR-ABLIS or 0.1% BCR-ABLIS at various time points. However, with longer follow-up, it became apparent that many patients treated with imatinib achieved deeper levels of response, with BCR-ABL1 becoming undetectable in a minority of cases.10 This, along with the fact that second-generation tyrosine kinase inhibitors produce faster and deeper responses, compared with imatinib,11, 12 prompted the need for robust, standardized definitions of deep MR. Such definitions are particularly important in the context of studies that are enrolling patients with sustained deep responses into treatment-free protocols.13, 14
We previously published proposals for broad standardized definitions of MR at different levels of sensitivity (MR4, MR4.5, and so on; collectively referred to as ‘deep MR'), which were endorsed by the European LeukemiaNet in their most recent recommendations for the treatment of CML patients.1, 15 These broad definitions, however, and clinical studies that have been published to date do not provide the technical details and interpretation to enable laboratories to categorize patients in a standardized manner. As part of the European Treatment and Outcome Study (EUTOS), we have developed laboratory proposals, as detailed below, to enable testing laboratories to define MR in a reproducible manner. These proposals were developed by consensus over several meetings and are described in detail in this paper, along with several examples. The terminology employed is based on the recommendations of the Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines16 and the proposal focuses on qPCR assays for the most common BCR-ABL1 variants (e13a2 and/or e14a2; 97% of CML patients) that use an external plasmid calibrator to estimate numbers of target molecules.
Reference genes other than ABL1
The published definitions of MR focus on the use of ABL1 as a reference gene as this is used by the majority of laboratories worldwide.15 Of the principal alternative reference genes,3 GUSB is used by a significant minority of European laboratories, whereas BCR is used primarily in Australasia and some US laboratories. We have focused here on extending the MR definitions when BCR-ABL1 is undetectable to include GUSB; further work will be required to extend these definitions to include BCR.
To determine the correspondence between ABL1 and GUSB, we collected data from three centers that routinely analyzed the expression of both genes in parallel. We focused on CML samples that were <10% BCR-ABLIS and had >10 000 ABL1 copies. Of 1567 samples, the median ratio of GUSB/ABL1 was 2.4 in the same volume of cDNA and therefore we consider that, for the purpose of defining deep MR, 10 000 ABL1 transcripts are equivalent to 24 000 GUSB transcripts. The previously published15 definitions of MR can therefore be expanded as follows:
MR4 (⩾4-log reduction from IRIS baseline)=either (i) detectable disease ⩽0.01% BCR-ABLIS or (ii) undetectable disease in cDNA with 10 000–31 999 ABL1 transcripts or 24 000–76 999 GUSB transcripts.
MR4.5 (⩾4.5-log reduction from IRIS baseline)=either (i) detectable disease ⩽0.0032% BCR-ABLIS or (ii) undetectable disease in cDNA with 32 000–99 999 ABL1 transcripts or 77 000–239 999 GUSB transcripts.
MR5 (⩾5-log reduction from IRIS baseline)=either (i) detectable disease ⩽0.001% BCR-ABLIS or (ii) undetectable disease in cDNA with ⩾100 000 ABL1 transcripts ⩾240 000 GUSB transcripts.
Although GUSB laboratories may use these definitions, we suggest that they should ideally derive their own correspondence between ABL1 and GUSB (or other reference gene) using at least 50–100 remission (<10% BCR-ABLIS) samples to derive their own cutoffs for different MR levels. Before making this comparison, the amplification conditions should be optimized and in particular the amplification efficiency for the two genes should be the same. This can be achieved easily for ABL1, GUSB and BCR (and BCR-ABL1) using the ERM-AD623 plasmid.17 For laboratory-developed tests, we further recommend that ERM-AD623 is used directly as a qPCR calibrator for routine analysis or indirectly as a calibrator for in-house plasmid dilutions.
Defining detectable and undetectable disease
There are several ways in which testing laboratories differ in how they define disease as detectable or undetectable. For individual amplification reactions and runs, we recommend that the established Europe Against Cancer criteria are used.18 In particular:
The cutoff for positivity should correspond to a quantification cycle (Cq) of intercept +1 (which should generally lead to cutoffs of 41–42 Cq). In other words, samples with a Cq higher than intercept +1 should be considered as undetectable.
The ‘no-template control' wells and reagent blanks should ideally not cross the threshold at any point but should certainly be at least 2 Cq above the intercept Cq for that run. If this is not the case, then the run must be considered as failed.
A major variable between centers is the number of replicate assays that are performed for each sample and the way that those replicates are considered to yield the final result. Typically, both BCR-ABL1 and the reference gene are tested in duplicate, although some centers perform triplicate assays and some only perform single assays. If replicate assays are performed for BCR-ABL1 (as recommended from RNA19, 20 or cDNA21 to help improve the accuracy of results) and any of the individual replicates are positive according to the criteria above, we recommend that the final result is considered as positive, that is, detectable disease. Even when testing in triplicate and two replicates are scored as undetectable and one is scored as detectable, the overall result should be scored as detectable or positive.
The Europe Against Cancer defines assay sensitivity by using normalized copy number and ΔΔCt methods, both of which relate the level of MRD to pretreatment levels for individual patients.22 This is not compatible with the IS in CML, which relates MRD levels to the IRIS standardized baseline, and therefore an alternative approach is required.
Scoring MR when disease is detectable
In general, measurable residual disease23 should be assigned a value on the IS and scored as MR4 if ⩽0.01% BCR-ABLIS, MR4.5 if ⩽0.0032% BCR-ABLIS, and so on, provided that the sample fulfils the minimum quality criteria, that is, ABL1 ⩾10 000 or GUSB ⩾24 000 in each replicate.21 If replicate analyses are performed and the values between replicates are comparable,21 then the number of BCR-ABL1 and reference gene transcripts should be the total value across replicates and the final result expressed on the IS, that is, ((sum of BCR-ABL1 copies)/(sum of reference gene copies)) × CF × 100 (see examples 1–3). As the reference gene in this context is used to estimate the amount of cDNA tested for BCR-ABL1, any difference in the number of replicates performed for BCR-ABL1 and the reference gene will need to be taken into account (see example 4). In addition, we recommend that for scoring MR4.5, the total reference gene number should be 32 000–99 999 ABL1 transcripts or 77 000–239 999 GUSB transcripts regardless of whether the disease is detectable or undetectable. For scoring MR5, the total reference gene number should be ABL1 ⩾100 000 or GUSB ⩾240 000 (Table 1; see example 5).
Table 1. Summary of reference gene numbers required for scoring deep molecular response.
| MR4 | MR4.5 | MR5 | |
|---|---|---|---|
| Minimum sum of reference gene transcripts irrespective of whether BCR-ABL1 is detected or nota | 10 000 ABL1 24 000 GUSB | 32 000 ABL1 77 000 GUSB | 100 000 ABL1 240 000 GUSB |
| BCR-ABLIS level for positive samplesb | ⩽0.01% | ⩽0.0032% | ⩽0.001% |
Numbers of reference gene transcripts in same volume of cDNA that is tested for BCR-ABL1. The minimum number in any individual replicate should be 10 000 ABL1 or 24 000 GUSB.
Provided that the minimum reference gene copy numbers in the row above are fulfilled.
Many centres score positive samples with a Cq higher than that of the lowest plasmid standard as ‘low-level positive', positive outside the quantifiable range, ‘<10 BCR-ABL1', if the lowest standard is 10, ‘<4 BCR-ABL1', if the lowest standard is 4, and so on. Indeed, some guidelines specifically recommend that values should not be estimated if they require extrapolation beyond the span of the standard plasmid calibration curve.21 This presents a problem for scoring low levels of disease and means, for example, that a laboratory using 10 as the lowest standard and a CF=1 would need to achieve ABL1 reference gene values of 100 000 or greater to be able to score a sample with low-level detectable disease as MR4 and a value of ⩽320 000 to score a similar sample as MR4.5 (<10 BCR-ABL1/320 000 ABL1=⩽0.0032% BCR-ABL1). Despite the significant errors in quantifying small numbers of target molecules, we suggest that all low level-positive replicates should be assigned a specific number of BCR-ABL1 transcripts by extrapolating below the lowest plasmid standard.
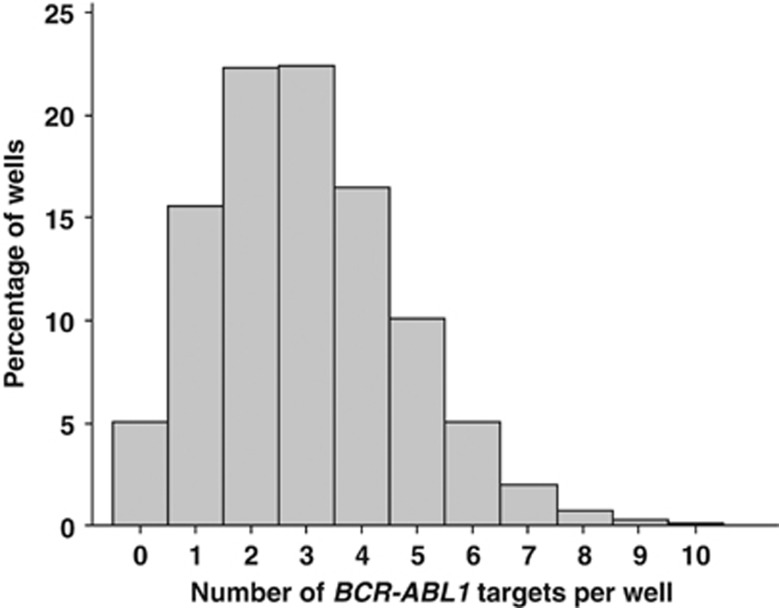
Testing laboratories have generally not rigorously determined their in-house limit of detection (LoD; defined as the lowest concentration of target that can be detected with 95% confidence) for BCR-ABL1 transcripts. One reason for this is that standardized reagents have not been available to perform LoD analysis in a reproducible manner. Now, with the availability of the ERM-AD623 plasmid17 and other calibration reagents,8 we recommend that laboratories specifically measure24 and optimize their BCR-ABL1 LoD. Clearly, the accuracy and precision by which MR can be scored critically depends on the BCR-ABL1 LoD being maximized. A laboratory with a poor LoD may score a sample as undetectable and deep MR, whereas a laboratory with an optimized LoD may detect BCR-ABL1 in the same sample and score it as not deep MR. Several studies have indicated that qPCR can be routinely optimized to detect single target molecules.25, 26, 27 Assuming that a single BCR-ABL1 cDNA target can be detected and that there is no background signal (limit of blank=0), the LoD given by the Poisson distribution as three BCR-ABL1 targets, as for a sample with an average of 3 targets/unit volume, there is a 95% chance that any unit volume will contain at least one target (Figure 1). Thus, we recommend that any replicate scored as positive should be assigned a value of ⩾3 BCR-ABL1 copies, that is, positive replicates with estimated copy numbers of <3 should be scored as 3 (see examples 6–8). Alternative technologies, for example, digital PCR, are likely to be more accurate than qPCR for estimating small numbers of target molecules and may well become the method of choice for more accurate definition of low-level positive disease.28, 29
Figure 1.
LoD of BCR-ABL1 detection. The graph shows the Poisson distribution with a mean of 3 BCR-ABL1 targets per well. The percentage of wells with 0–10 targets per well is indicated (20 000 computer-generated random datapoints; Minitab version 16, Coventry, UK) and shows that 95% of wells has at least one BCR-ABL1 target. As the LoD is defined as the lowest concentration of target that can be detected with 95% confidence, the maximal theoretical LOD is 3 copies.
Scoring MR when disease is undetectable
Analysis of multiple replicates can increase the sensitivity of detection simply by increasing the amount of sample that is tested. This approach has been used to design very sensitive assays to detect BCR-ABL1 by qRT-PCR in healthy individuals,30 for genomic DNA-based tests for BCR-ABL1 in CML,31, 32, 33 for detection of minimal residual disease in lymphoid disorders25 and for other applications such as noninvasive prenatal testing.34 When BCR-ABL1 is undetectable in all replicates from the same sample, we recommend that the final result is given as (undetectable BCR-ABL1)/(sum of reference gene in all the replicates). We suggest that for routine analysis, a maximum of two or three replicates are performed (examples 9–11), although for specific studies it may be desirable to perform more replicates. Stringent quality criteria are essential, specifically replicates with <10 000 ABL1 or <24 000 GUSB transcripts should be considered as inevaluable for determining deep MR (examples 12 and 13), and laboratories should maximize their LoD for BCR-ABL1 to avoid false-negative results. As above, any difference in the number of replicates performed for BCR-ABL1 and the reference gene should be taken into account (example 14).
Examples
BCR-ABL1 detected in at least one replicate
Example 1 (Lab CF=0.8):
– BCR-ABL1 replicate 1: detectable in 2 μl cDNA, estimated 7 copies.
– BCR-ABL1 replicate 2: detectable in 2 μl cDNA, estimated 3 copies.
– ABL1 replicate 1: 24 000 copies in 2 μl cDNA.
– ABL1 replicate 2: 28 000 copies in 2 μl cDNA.
Result=(sum BCR-ABL1=10)/(sum ABL1=52 000) × 0.8 × 100=0.015%=MMR but not MR4.
Example 2 (Lab CF=1.8):
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: detectable in 5 μl cDNA, estimated 3 copies.
– GUSB replicate 1: 43 000 copies in 5 μl cDNA.
– GUSB replicate 2: 49 000 copies in 5 μl cDNA.
Result=(sum BCR-ABL1=3)/(sum GUSB=92 000) × 1.8 × 100=0.0059%=MR4.
Comment: Testing laboratories use different amounts of RNA to make cDNA, make different volumes of cDNA and use different volumes of cDNA for individual qPCR assays. The number of reference gene transcripts should be estimated in the same volume of cDNA used to test for BCR-ABL1. The use of other reference genes, for example, BCR, is possible, but the number of transcripts required to define different levels of MR remain to be determined.
Example 3 (Lab CF=0.5):
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: detectable in 5 μl cDNA, estimated 3 copies.
– ABL1 replicate 1: 9000 copies in 5 μl cDNA.
– ABL1 replicate 2: 8000 copies in 5 μl cDNA.
Result=inevaluable for MR.
Comment: Although the ((sum of BCR-ABL1)/(sum of reference gene)) × CF × 100 is <0.01%, the sample should be considered as inevaluable for the assessment of MR as the ABL1 copy number in each replicate is <10 000.
Example 4 (Lab CF=0.8):
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 3: detectable in 5 μl cDNA, estimated 4 copies.
– ABL1 replicate 1: 14 000 copies in 5 μl cDNA.
– ABL1 replicate 2: 15 000 copies in 5 μl cDNA.
Result=(sum BCR-ABL1=4)/(sum ABL1=29 000 × 1.5) × 0.8 × 100=0.0074%=MR4.
Comment: The sum of the reference gene copy number is multiplied by 1.5 (equivalent to multiplying the mean copy number × 3) because only two replicates were performed for the reference gene, whereas three replicates were performed for BCR-ABL1. In general, we consider that it is better to perform the same number of replicates for BCR-ABL1 and the reference gene.
Example 5 (Lab CF=0.25):
– BCR-ABL1 replicate 1: undetectable in 2 μl cDNA.
– BCR-ABL1 replicate 2: detectable in 2 μl cDNA, estimated 3 copies.
– ABL1 replicate 1: 12 000 copies in 2 μl cDNA.
– ABL1 replicate 2: 14 000 copies in 2 μl cDNA.
Result=(sum BCR-ABL1=3)/(sum ABL1=26 000) × 0.25 × 100 =0.0029% sum of ABL1 <32 000=MR4.
Comment: Although the ((sum of BCR-ABL1)/(sum of reference gene)) × CF × 100 is <0.0032%, the total ABL1 value is <32 000 and should thus be considered as MR4. Considering the extreme examples of 31 999 ABL1 transcripts and either 0 or 3 BCR-ABL1 transcripts, it is apparent that this discrepancy only arises if the CF is <0.35 if using ABL1 as a reference gene (or <0.82 if using GUSB).
Example 6 (Lab CF=0.8):
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: detectable in 5 μl cDNA, estimated 2 copies.
– ABL1 replicate 1: 18 000 copies in 5 μl cDNA.
– ABL1 replicate 2: 16 500 copies in 5 μl cDNA.
Result=(sum BCR-ABL1=3)/(sum ABL1=34 500) × 0.8 × 100=0.007%=MR4.
Comment: Each positive replicate should be assigned a value of ⩾3 copies and therefore the second BCR-ABL1 replicate is scored as 3 copies.
Example 7 (Lab CF=0.8):
– BCR-ABL1 replicate 1: detectable in 5 μl cDNA, estimated 2 copies.
– BCR-ABL1 replicate 2: detectable in 5 μl cDNA, estimated 1 copy.
– ABL1 replicate 1: 18 000 copies in 5 μl cDNA.
– ABL1 replicate 2: 16 500 copies in 5 μl cDNA.
Result=(sum BCR-ABL1=6)/(sum ABL1=34 500) × 0.8 × 100=0.014%=MMR but not MR4.
Comment: Each positive replicate should be assigned a value of ⩾3 copies and therefore each BCR-ABL1 replicate is scored as 3 copies.
Example 8 (Lab CF=0.8):
– BCR-ABL1 replicate 1: detectable in 5 μl cDNA, estimated 2 copies.
– BCR-ABL1 replicate 2: detectable in 5 μl cDNA, estimated 5 copies.
– BCR-ABL1 replicate 3: detectable in 5 μl cDNA, estimated 7 copies.
– ABL1 replicate 1: 34 000 copies in 5 μl cDNA.
– ABL1 replicate 2: 38 500 copies in 5 μl cDNA.
– ABL1 replicate 3: 32 500 copies in 5 μl cDNA.
Result=(sum BCR-ABL1=15)/(sum ABL1=105 000) × 0.8 × 100=0.011%=MMR but not MR4.
Comment: Each positive replicate should be assigned a value of ⩾3 copies.
BCR-ABL1 undetected in all replicates
Example 9:
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: undetectable in 5 μl cDNA.
– ABL1 replicate 1: 16 500 copies in 5 μl cDNA.
– ABL1 replicate 2: 18 000 copies in 5 μl cDNA.
Result=undetectable BCR-ABL1 in 34 500 ABL1=MR4.5.
Example 10:
– BCR-ABL1 single analysis: undetectable in 5 μl cDNA.
– ABL1 single analysis: 45 000 copies in 5 μl cDNA.
Result=undetectable BCR-ABL1 in 45 000 ABL1=MR4.5.
Comment: Although single analyses are performed by some centers, replicate assays from RNA or cDNA improves the accuracy of results.19, 20, 21
Example 11:
– BCR-ABL1 replicate 1: undetectable in 2 μl cDNA.
– BCR-ABL1 replicate 2: undetectable in 2 μl cDNA.
– BCR-ABL1 replicate 3: undetectable in 2 μl cDNA.
– ABL1 replicate 1: 24 000 copies in 2 μl cDNA.
– ABL1 replicate 2: 22 500 copies in 2 μl cDNA.
– ABL1 replicate 3: 24 000 copies in 2 μl cDNA.
Result=undetectable BCR-ABL1 in 70 500 ABL1=MR4.5.
Example 12:
– BCR-ABL1 replicate 1: undetectable in 5 μl .
– BCR-ABL1 replicate 2: undetectable in 5 μl cDNA.
– ABL1 replicate 1: 7000 copies in 5 μl cDNA.
– ABL1 replicate 2: 8000 copies in 5 μl cDNA.
Result=inevaluable for MR as ABL1 <10 000 in each replicate.
Example 13:
– BCR-ABL1 replicate 1: undetectable in 5 μl cDNA.
– BCR-ABL1 replicate 2: undetectable in 5 μl cDNA.
– ABL1 replicate 1: 6000 copies in 5 μl cDNA.
– ABL1 replicate 2: 14 000 copies in 5 μl cDNA.
Result=inevaluable for MR.
Comment: One replicate is <10 000 ABL1 and hence the sample should be considered as inevaluable for MR. As the two ABL1 replicates are discordant, the reference gene qPCR could be repeated.
Example 14:
– BCR-ABL1 replicate 1: undetectable in 2 μl cDNA.
– BCR-ABL1 replicate 2: undetectable in 2 μl cDNA.
– BCR-ABL1 replicate 3: undetectable in 2 μl cDNA.
– ABL1 replicate 1: 16 500 copies in 2 μl cDNA.
– ABL1 replicate 2: 18 000 copies in 2 μl cDNA.
Result=undetectable BCR-ABL1 in (34 500 × 1.5=51 750 ABL1)=MR4.5.
Comment: The sum of the reference gene copy number is multiplied by 1.5 because only two replicates were performed for the reference gene, whereas three replicates were performed for BCR-ABL1.
Concluding remarks
The remarkable progress in the treatment of CML has demanded definitions of deep MR that are stretching the technology of molecular monitoring to its limit. The recommendations described here are an attempt to develop standardized laboratory approaches that strike a reasonable balance between scientific accuracy and clinical reality. It should be recognized that there is considerable inherent uncertainty in defining very low levels of disease and that it will be important to continue to look at trends over time to recognize sustained MR. Furthermore, the reproducible application of the recommendations depends critically on the ability of testing laboratories to measure absolute numbers of reference gene transcripts in a comparable manner, as well as their ability to maximize the LoD for BCR-ABL1 and minimize interassay variability. It is obvious that future methodological improvements that increase the amount of sample tested (as determined by the number of reference gene transcripts) will increase the precision and accuracy of scoring MR4 or MR,4.5 as well as enabling even deeper levels of MR to be determined.
We recognize that these recommendations may need to be adapted to local requirements and changing technologies. We also recognize that laboratory recommendations in isolation are meaningless and that the critical question is the clinical significance of achieving deep levels of MR. We anticipate that the standardized definitions described here will help to progress clinical studies that aim ultimately to cure CML as well as providing a common framework for reporting routine results.
Acknowledgments
We thank all the European Treatment and Outcome Study laboratory members and other individuals who have contributed to the discussions that have led to the development of these recommendations. GM was supported by NGS-PTL FP7 European Project, and ER regional project. This work was supported by the European LeukemiaNet via the ‘European Treatment and Outcome Study' for CML. EUTOS is funded by Novartis, but the recommendations described in this paper were developed, finalized and written entirely by the authors.
The authors declare no conflict of interest.
References
- Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122:872–884. doi: 10.1182/blood-2013-05-501569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien S, Radich JP, Abboud CN, Akhtari M, Altman JK, Berman E, et al. Chronic myelogenous leukemia, version 1.2015. J Natl Compr Canc Netw. 2014;12:1590–1610. doi: 10.6004/jnccn.2014.0159. [DOI] [PubMed] [Google Scholar]
- Hughes T, Deininger M, Hochhaus A, Branford S, Radich J, Kaeda J, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37. doi: 10.1182/blood-2006-01-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross NC. Standardisation of molecular monitoring for chronic myeloid leukaemia. Best Pract Res Clin Haematol. 2009;22:355–365. doi: 10.1016/j.beha.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Branford S, Cross NC, Hochhaus A, Radich J, Saglio G, Kaeda J, et al. Rationale for the recommendations for harmonizing current methodology for detecting BCR-ABL transcripts in patients with chronic myeloid leukaemia. Leukemia. 2006;20:1925–1930. doi: 10.1038/sj.leu.2404388. [DOI] [PubMed] [Google Scholar]
- Branford S, Fletcher L, Cross NC, Muller MC, Hochhaus A, Kim DW, et al. Desirable performance characteristics for BCR-ABL measurement on an international reporting scale to allow consistent interpretation of individual patient response and comparison of response rates between clinical trials. Blood. 2008;112:3330–3338. doi: 10.1182/blood-2008-04-150680. [DOI] [PubMed] [Google Scholar]
- White HE, Matejtschuk P, Rigsby P, Gabert J, Lin F, Lynn Wang Y, et al. Establishment of the first World Health Organization International Genetic Reference Panel for quantitation of BCR-ABL mRNA. Blood. 2010;116:e111–e117. doi: 10.1182/blood-2010-06-291641. [DOI] [PubMed] [Google Scholar]
- White HE, Hedges J, Bendit I, Branford S, Colomer D, Hochhaus A, et al. Establishment and validation of analytical reference panels for the standardization of quantitative BCR-ABL1 measurements on the international scale. Clin Chem. 2013;59:938–948. doi: 10.1373/clinchem.2012.196477. [DOI] [PubMed] [Google Scholar]
- Maute C, Nibourel O, Rea D, Coiteux V, Grardel N, Preudhomme C, et al. Calibration of BCR-ABL1 mRNA quantification methods using genetic reference materials is a valid strategy to report results on the international scale. Clin Biochem. 2014;47:1333–1336. doi: 10.1016/j.clinbiochem.2014.05.067. [DOI] [PubMed] [Google Scholar]
- Hehlmann R, Grimwade D, Simonsson B, Apperley J, Baccarani M, Barbui T, et al. The European LeukemiaNet: achievements and perspectives. Haematologica. 2011;96:156–162. doi: 10.3324/haematol.2010.032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362:2251–2259. doi: 10.1056/NEJMoa0912614. [DOI] [PubMed] [Google Scholar]
- Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2010;362:2260–2270. doi: 10.1056/NEJMoa1002315. [DOI] [PubMed] [Google Scholar]
- Mahon FX, Rea D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–1035. doi: 10.1016/S1470-2045(10)70233-3. [DOI] [PubMed] [Google Scholar]
- Rousselot P, Charbonnier A, Cony-Makhoul P, Agape P, Nicolini FE, Varet B, et al. Loss of major molecular response as a trigger for restarting tyrosine kinase inhibitor therapy in patients with chronic-phase chronic myelogenous leukemia who have stopped imatinib after durable undetectable disease. J Clin Oncol. 2014;32:424–430. doi: 10.1200/JCO.2012.48.5797. [DOI] [PubMed] [Google Scholar]
- Cross NC, White HE, Muller MC, Saglio G, Hochhaus A. Standardized definitions of molecular response in chronic myeloid leukemia. Leukemia. 2012;26:2172–2175. doi: 10.1038/leu.2012.104. [DOI] [PubMed] [Google Scholar]
- Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem. 2009;55:611–622. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- White H, Deprez L, Corbisier P, Hall V, Lin F, Mazoua S, et al. A certified plasmid reference material for the standardisation of BCR-ABL1 mRNA quantification by eal time quantitative PCR. Leukemia. 2014;29:369–376. doi: 10.1038/leu.2014.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabert J, Beillard E, van der Velden VH, Bi W, Grimwade D, Pallisgaard N, et al. Standardization and quality control studies of 'real-time' quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia—a Europe Against Cancer program. Leukemia. 2003;17:2318–2357. doi: 10.1038/sj.leu.2403135. [DOI] [PubMed] [Google Scholar]
- Branford S, Hughes T. Diagnosis and monitoring of chronic myeloid leukemia by qualitative and quantitative RT-PCR. Methods Mol Med. 2006;125:69–92. doi: 10.1385/1-59745-017-0:69. [DOI] [PubMed] [Google Scholar]
- Jennings LJ, Smith FA, Halling KC, Persons DL, Kamel-Reid S, Molecular Oncology Resource Committee of the College of American P Design and analytic validation of BCR-ABL1 quantitative reverse transcription polymerase chain reaction assay for monitoring minimal residual disease. Arch Pathol Lab Med. 2012;136:33–40. doi: 10.5858/arpa.2011-0136-OA. [DOI] [PubMed] [Google Scholar]
- Foroni L, Wilson G, Gerrard G, Mason J, Grimwade D, White HE, et al. Guidelines for the measurement of BCR-ABL1 transcripts in chronic myeloid leukaemia. Br J Haematol. 2011;153:179–190. doi: 10.1111/j.1365-2141.2011.08603.x. [DOI] [PubMed] [Google Scholar]
- Beillard E, Pallisgaard N, van der Velden VH, Bi W, Dee R, van der Schoot E, et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using 'real-time' quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR)—a Europe against cancer program. Leukemia. 2003;17:2474–2486. doi: 10.1038/sj.leu.2403136. [DOI] [PubMed] [Google Scholar]
- Goldman JM, Gale RP. What does MRD in leukemia really mean. Leukemia. 2014;28:1131. doi: 10.1038/leu.2013.318. [DOI] [PubMed] [Google Scholar]
- CLSI Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures; Approved Guideline2nd edn. (EP17-A2)Clinical and Laboratory Standards Institute: Wayne, PA, USA; 2012 [Google Scholar]
- Morley AA, Latham S, Brisco MJ, Sykes PJ, Sutton R, Hughes E, et al. Sensitive and specific measurement of minimal residual disease in acute lymphoblastic leukemia. J Mol Diagn. 2009;11:201–210. doi: 10.2353/jmoldx.2009.080048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladetto M, Lobetti-Bodoni C, Mantoan B, Ceccarelli M, Boccomini C, Genuardi E, et al. Persistence of minimal residual disease in bone marrow predicts outcome in follicular lymphomas treated with a rituximab-intensive program. Blood. 2013;122:3759–3766. doi: 10.1182/blood-2013-06-507319. [DOI] [PubMed] [Google Scholar]
- Morley AA. Digital PCR: a brief history. Biomol Detect Quantif. 2014;1:1–2. doi: 10.1016/j.bdq.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh HG, Lin M, Fukushima T, Saglio G, Kim D, Choi SY, et al. Sensitive quantitation of minimal residual disease in chronic myeloid leukemia using nanofluidic digital polymerase chain reaction assay. Leuk Lymphoma. 2011;52:896–904. doi: 10.3109/10428194.2011.555569. [DOI] [PubMed] [Google Scholar]
- Jennings LJ, George D, Czech J, Yu M, Joseph L. Detection and quantification of BCR-ABL1 fusion transcripts by droplet digital PCR. J Mol Diagn. 2014;16:174–179. doi: 10.1016/j.jmoldx.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Bose S, Deininger M, Gora-Tybor J, Goldman JM, Melo JV. The presence of typical and atypical BCR-ABL fusion genes in leukocytes of normal individuals: biologic significance and implications for the assessment of minimal residual disease. Blood. 1998;92:3362–3367. [PubMed] [Google Scholar]
- Sobrinho-Simoes M, Wilczek V, Score J, Cross NC, Apperley JF, Melo JV. In search of the original leukemic clone in chronic myeloid leukemia patients in complete molecular remission after stem cell transplantation or imatinib. Blood. 2010;116:1329–1335. doi: 10.1182/blood-2009-11-255109. [DOI] [PubMed] [Google Scholar]
- Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Bartley PA, et al. Patients with chronic myeloid leukemia who maintain a complete molecular response after stopping imatinib treatment have evidence of persistent leukemia by DNA PCR. Leukemia. 2010;24:1719–1724. doi: 10.1038/leu.2010.185. [DOI] [PubMed] [Google Scholar]
- Bartley PA, Ross DM, Latham S, Martin-Harris MH, Budgen B, Wilczek V, et al. Sensitive detection and quantification of minimal residual disease in chronic myeloid leukaemia using nested quantitative PCR for BCR-ABL DNA. Int J Lab Hematol. 2010;32:e222–e228. doi: 10.1111/j.1751-553X.2010.01236.x. [DOI] [PubMed] [Google Scholar]
- Hromadnikova I, Houbova B, Hridelova D, Voslarova S, Kofer J, Komrska V, et al. Replicate real-time PCR testing of DNA in maternal plasma increases the sensitivity of non-invasive fetal sex determination. Prenat Diagn. 2003;23:235–238. doi: 10.1002/pd.556. [DOI] [PubMed] [Google Scholar]