Abstract
Objective
This study evaluated the efficiency of a curved polyetheretherketone (PEEK) cage in comparison with a wedge PEEK cage according to radiologic and clinical outcomes in patients with cervical degenerative disease.
Methods
A total of 37 patients who suffering from cervical disc disease with radiculopathy or myelopathy were reviewed retrospectively. Seventeen patients were underwent anterior cervical discectomy and interbody fusion with a curved shape PEEK cage (curved cage group), and twenty patients with wedge shape PEEK cage (wedge cage group). Clinical assessment was graded using Odom's criteria, NDI score and VAS score. For radiologic analysis, disc height (DH), segmental angle (SA), subsidence were measured at the preoperative and last follow up.
Results
A comparison of the preoperative and postoperative results revealed improvements after the surgery in the DH and SA in both cage groups. The change of postoperative DH between the preoperative and the last follow-up in wedge cage group and curved cage group was 6.85% and 25.5%, respectively. The change of postoperative SA was 1.75° and 0.95°, respectively. There was no statistically significant difference in the DH and SA between the 2 groups. The subsidence rate in the wedge cage group and curved cage group was 20% and 6%, respectively.
Conclusion
The 2 different cage groups showed significant improvements in the disc height, segmental angle and clinical outcomes. However, the shape of PEEK Cage influences the tendency for subsidence. Increasing contact surface area and fitting into two adjacent vertebral body prevent significant subsidence.
Keywords: Cervical, Cage, Discectomy, PEEK
INTRODUCTION
Since the introduction of anterior cervical discectomy and fusion (ACDF), various types of cages, such as titanium and carbon fiber cages4,14), have been used to avoid the complications of iliac bone grafting20). A cervical cage is used to restore disc height and normal spinal alignment. Some studies of titanium and carbon fiber cages, however, reported a high rate of subsidence2,19).
After introduction of a polyetheretherketone (PEEK) cage which has a similar modulus of elasticity to the cortical bone15), ACDF using the PEEK cage has been popular widely in last decade. Currently, different designs of PEEK cages have been established to achieve excellent fusion rates and clinical outcome. To date, however, few studies have examined the clinical and radiological outcomes with ACDF using the different shapes of PEEK cage standalone.
The aim of this study was to compare the clinical and radiological outcomes between patients who underwent ACDF with a different shape of PEEK cage, wedge cage and curved cage.
MATERIALS AND METHODS
1. Patient population
We retrospectively assessed clinical and radiological outcomes in 37 patients who underwent single-level ACDF with a PEEK cage. All patients showed upper-extremity radiculopathy and/or myelopathy with symptomatic single- level disc herniation. Patients with cervical instability, acute infection, and multiple spondylosis were excluded.
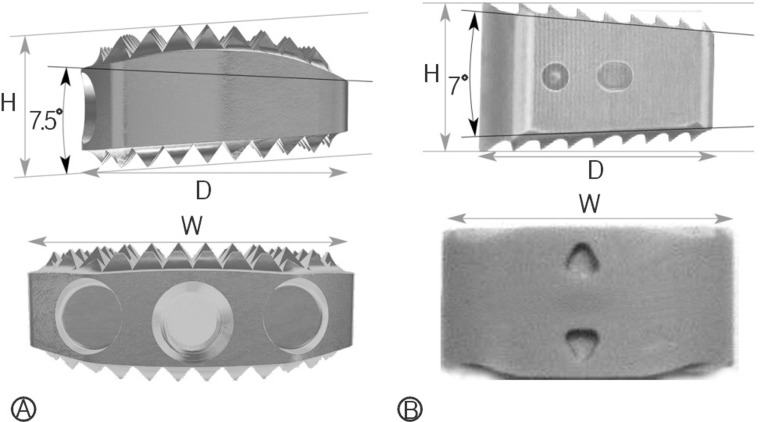
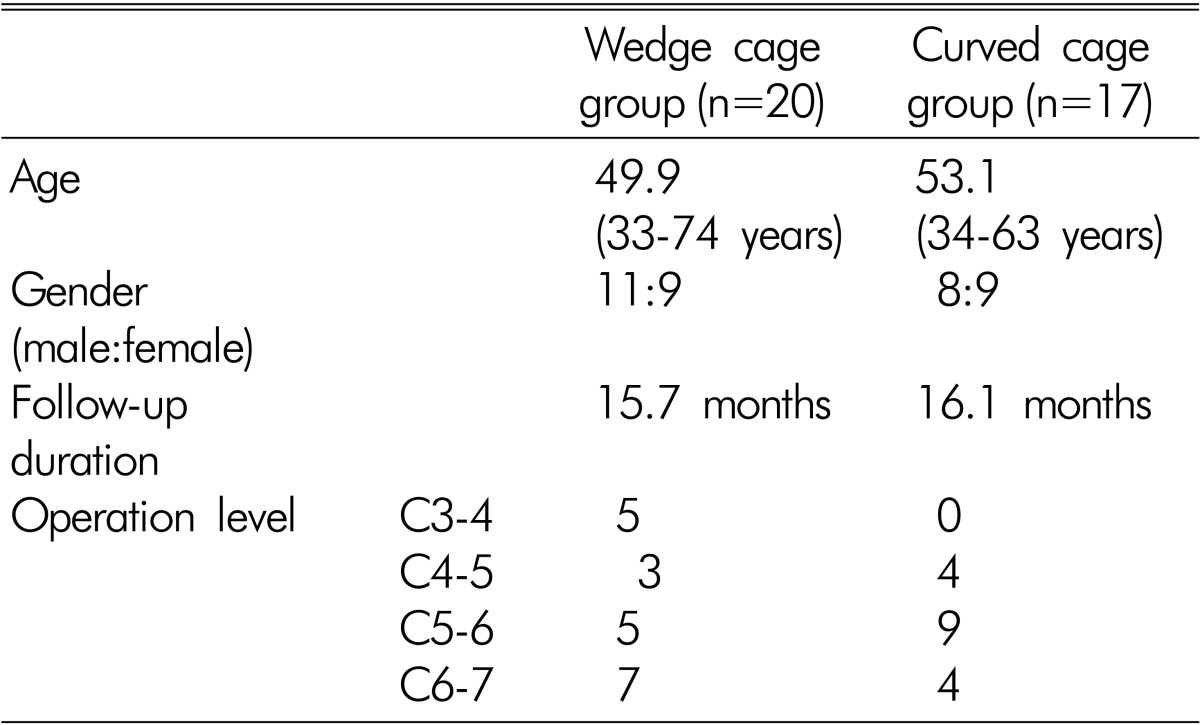
The curved cage group included 17 patients who underwent surgery in which a curved PEEK cage (Cervios; Synthes, Zuchwil, Switzerland) was used from March 2009 to February 2010, and the wedge cage group comprised 20 patients who were operated on and received a wedge PEEK cage (Cornerstone; Medtronic Sofamor-Danek, Memphis, TN, USA) from June 2006 to June 2010 (Fig. 1). The mean follow-up duration in the curved and wedge cage group was 16.1 months and 15.7 months, respectively (Table 1).
Fig. 1. Anatomical shape of the curved PEEK cage with its upper convex part in the frontal and sagittal planes. The cage is curved in two planes on the superior surface to match the normal end-plate and transfers stresses to the strong peripheral bone (A: Curved shape cage; W: 15mm, D: 12.5mm, H: 5-10mm, B: Wedge shape cage, W: 14 mm, D: 11 mm, H: 5-10 mm).
Table 1. Demographic data of patients who received 2 different types of PEEK cage.
2. Surgical managements
All patients were treated using a standard anterior approach to the cervical spine. The basic technique was the same as Robinson and Smith's21). Discectomy and decompression were performed under an operating microscope in all cases. High-speed drill was avoided so as not to destroy the end plates.
A microscopic discectomy was performed with the removal of cartilage on the end plates by using curettes. The wedge cage was filled with demineralized bone matrix (Osteofil; Medtronic Sofamor-Danek, Memphis, TN, USA) and the curved cage was filled with β-tricalcium phosphate (Chronos; Synthes, Zuchwil, Switzerland) before being inserted into the disc space. After PEEK cage insertion, fluoroscopy was done to confirm the anterior and lateral position of the cage.
All patients started ambulation after 1 day of immobilization. A cervical brace (Philadelphia collar) was applied for 8 weeks.
3. Clinical outcome
The clinical outcomes were analyzed using modified Odom's criteria18) at 8 months after the surgery, which categorized as excellent, good, fair, or poor. Physical functions and cervical pain were assessed using the Neck Disability Index (NDI) and the Visual Analog Scale (VAS) pre- and postoperatively.
4. Radiographic assessment
Simple radiographs in the including anteroposterior, lateral, and lateral flexion/extension views were taken before the surgery and again at 1 day and 1, 3, and 8 months after the surgery and last follow-up. The disc height (DH) was measured as the distance from the midpoint between the inferior end plate of the upper vertebra and the superior end plate of the lower vertebra in fusion level. The segmental angle (SA) was calculated as the Cobb's angle between the superior margin of the upper vertebra and the inferior margin of the lower vertebra. The significant subsidence was defined as a change in DH >3mm between the immediate postoperative and follow-up DH.
Fusion was defined according to the following criteria: (1) the lack of visible motion on flexion-extension radiographs, (2) the lack of dark halo around the cage on both AP and lateral radiographs, (3) visible bridging trabecular bone around the cage on anterior or posterior. In addition, in cases where bone fusion was questionable, CT scans using sagittal and coronal plane reconstructions was checked.
5. Statistical analysis
Descriptive data are represented as mean±standard deviation. For comparison of nonparametric data, Wilcoxon signed rank test and repeated measures ANOVA were used. The level of significance was a probability value of less than 0.05. All analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
1. Clinical results
An analysis of the clinical outcomes was performed 8 months after the surgery using Odom's criteria. An excellent and good outcome was achieved in 6 (35%) and 8 (47%) patients, respectively, in the curved cage group, and in 5 (25%) and 10 (50%) patients, respectively, in the wedge cage group.
Cervical pain and physical functions were assessed using the Neck Disability Index (NDI) and the Visual Analog Scale (VAS) both pre- and postoperatively. The mean pre- and post-operative NDI scores were 60.5% and 39.0%, respectively in the wedge cage group, and 62.5% and 36.2% in the curved cage group. There was a significant improvement of physical functions after the surgery in both groups. The mean pre- and post-operative VAS scores were 7.45 and 2.55, respectively in the wedge cage group, and 7.71 and 2.65 in the curved cage group. There was a significant relief of cervical pain after the surgery in both groups. However, there was no significant difference in the Odom's criteria, NDI score and VAS score between the two groups (Table 2).
Table 2. Comparison of clinical outcome between the 2 groups.

2. Radiographic results
1) Disc height
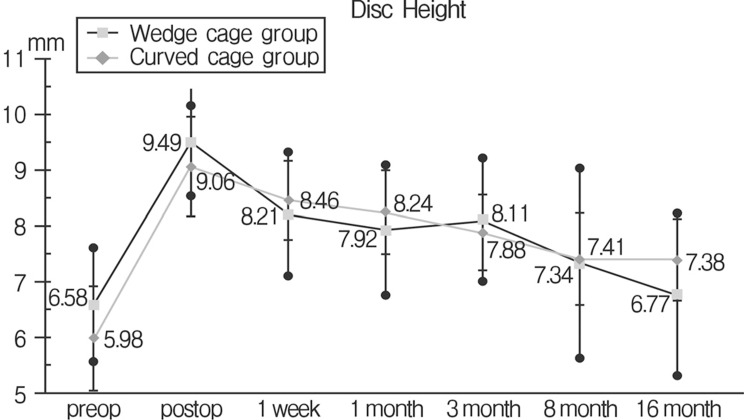
The mean DH in the wedge cage group before the surgery and at the last follow-up was 6.58±1.02mm and 6.65±1.48 mm, respectively. In the curved cage group, the mean DH before the surgery and at the last follow-up was 5.98±0.94 mm and 7.38±0.74mm, respectively. The change of postoperative DH between the preoperative DH and the last follow-up in wedge cage group and curved cage group was 6.85% and 25.5%, respectively. Both groups showed significant improvement in the DH(p<0.05), but there was no significant difference between them(repeated measures ANOVA, p=0.24) (Fig. 2).
Fig. 2. Comparison of mean disc height between the 2 cage group.
2) Segmental angle
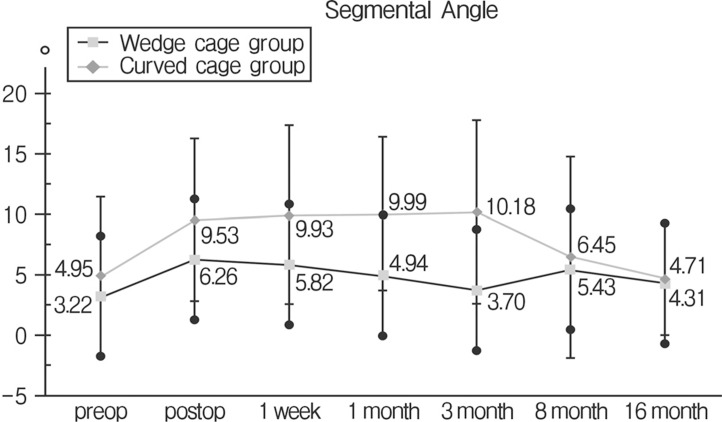
The mean SA was -3.22±5.80° before surgery and -4.31±4.92° at the last follow-up in the wedge cage group. The mean SA was -4.95±6.54° before the surgery and -4.71±4.74° at the last follow-up in the curved cage group. SA was increased in both groups. The change of postoperative SA between the preoperative SA and the last follow-up in wedge cage group and curved cage group was 1.75° and 0.95°, respectively. A statistical significance was found between the preoperative and postoperative data of each group (p<0.05). However, there was no statistical significance in the comparison of postoperative data between the 2 groups (Fig. 3).
Fig. 3. Comparison of segmental angle between the 2 cage group.
3) Bone fusion and Subsidence
The results of follow-up X-ray showed that fusion was achieved in 33 patients at the last follow up. CT scans were obtained in 4 questionable cases. But, four patients had no evidence of non-union and successful fusion was achieved.
Significant subsidence was found in 1 patient (6%) at 1 month follow-up in the curved cage group, and in 4 patients (20%) at 1 month and the last follow up in the wedge cage group. The mean degree of subsidence was 2.43mm in the wedge cage group, 1.68mm in the curved cage group. This difference reached statistical significance (p=0.036) (Table 3).
Table 3. Comparison of Subsidence rate between the 2 groups.

DISCUSSION
Cervical alignment is most dependent on disc height and shape. Disc degeneration occurs with aging and leads to a loss of intervertebral disc height, which contributes to a loss of cervical alignment and causes cervical neurological symptoms16).
Among the various surgical procedures for cervical degenerative disease, ACDF is widely considered to be a standard surgical treatment. For a long time, the techniques of Cloward and Robinson were the gold standard for ACDF. The primary purpose of the treatment is the decompression of the affected nerve root and restoration of cervical alignment. Although traditional cervical interbody fusion by using the iliac bone can maintain the patency of the neural foramen and ensure solid fusion, graft collapse, nonunion, dislodgement, and donor site complications remain problematic6). After Bagby et al.1) introduced an interbody fusion cage in 1988, a range of fusion materials have been developed to accommodate the structural stability and fusion rate and restore intervertebral disc height.
Different types of cages are available to perform ACDF, including cylindrical titanium, rectangular carbon, and polyetheretherketone (PEEK) cages. Titanium cage can provide mechanical support and disc height maintenance; however, unfavorable outcomes resulting in disc height collapse and kyphotic deformity were reported in some studies6,17). Carbon cage can be safe and effective, and can lead to restore cervical lordosis and solid fusion; however, high level of subsidence have been reported2). PEEK cage is a non-resorbable semicrystalline aromatic polymer that has a similar modulus of elasticity to cortical bone3,15) and reduces the possibility of subsidence of the graft into the vertebral body5). In addition, PEEK cages are radiolucent and do not produce artifacts on radiographs or CT scans, which allows for precise radiological evaluation of bony union. Some authors reported the efficiency of a PEEK cage in providing solid fusion and increasing cervical lordosis and disc height9).
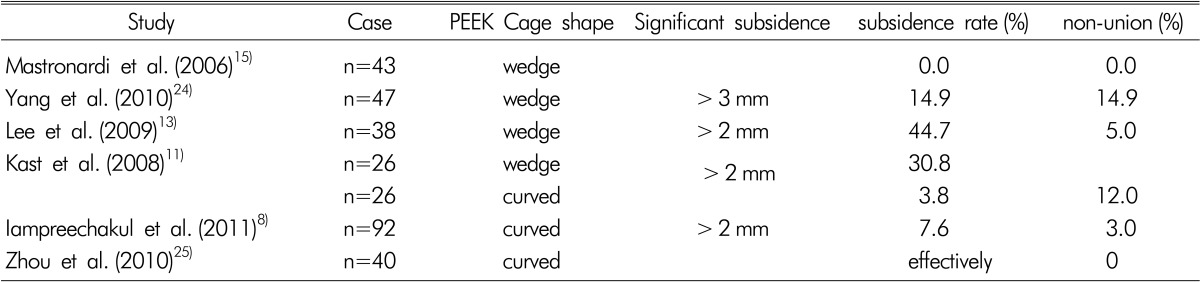
To date, various shapes of PEEK cages are available to perform ACDF, and various degrees of subsidence have been reported after ACDF using stand-alone various PEEK cages (Table 4). In the present study, 37 patients underwent ACDF using 2 different types of PEEK cage. Both groups had improvement of postoperative clinical and radiological outcomes. Disc height was increased and segmental angle was improved in both groups; however, there are no significant differences in both parameters between the 2 groups. Intervetebral fusion was achieved in all patients at the last follow up and the significant subsidence rate in the curved cage and the wedge cage group was 6% and 20%, respectively. Mean degree of subsidence were 2.43mm in the wedge cage group, 1.68mm in the curved cage group.
Table 4. Summary of studies about significant subsidence and non-union using PEEK cages.
Cervios, an anatomically, curved shape cage, is designed for an optimal fit into the natural concavity and have a convex superior aspect to match the anatomy of the end plates of the cervical vertebra (Fig. 1). Owing to its anatomical shape, the curved cage offers a wide grafting space and allows close contact between the end-plate bone and the implant, thus enhancing the load-bearing ability of the graft or bone substitute and facilitating arthrodesis. The upper and lower surfaces of the curved cage are retaining surfaces that limit the risks of implant displacement and subsidence.
Subsidence may be influenced by many factors, including disce ctomy, postoperative cervical motion, cage design, endplate preparation, and bone mineral density12,23). Fujibayashi et al.7) divide subsidence after ACDF with stand alone cage into two types. The first type, transient cage subsidence, is related to stabilization of the cage by the bony endplate subsequent to the interlocking of the cage spikes with the bone, and occurred early in the postoperative period. The second type, progressive cage subsidence, led to nonunion. So, they suggest that for reducing cage subsidence, curved shape cage was usually selected for simple disc herniation, a wedge shape cage was selected for disc herniation combined with spondylosis.
In addition, the contact area at the implant-bone interface and the endplate geometry also contribute to subsidence10). To insert the wedge shape cage into disc space, partial resection of the vertebral endplate for removal the posterior osteophyte was often required, it might reduce initial stability, which relates to cage subsidence. This study focused on the cage design and disc geometry. In the present study, the curved cage group showed a lower subsidence rate, owing to the larger contact surface of the curved cage compared with the wedge cage and appropriate endplate preparation.
Fujibayashi et al.7) reported that significant subsidence occurred with the wedge cage but not with the curved cage. It is important for the cage to have a contact surface that is as similar as possible to the anatomical curvature of the involved end plates. Van der Haven et al.22) found that an oversized cage is associated with a high rate of subsidence. In the present study, use of curved PEEK cages resulted in subsidence in only 1 patient, without producing progressive symptoms after followup; however, subsidence occurred in 4 patients who received wedge cages.
This study has the limitation of a small number of cases and a short-term follow-up. Therefore, further study will be needed.
CONCLUSION
The 2 different cage groups showed significant improvements in the disc height, segmental angle and clinical outcomes. But the shape of PEEK cage influences the tendency for subsidence. For endplate shape variance, selection of optimal cage in ACDF using PEEK cage is important. And increasing contact surface area and fitting into two adjacent vertebral body can prevent significant subsidence.
References
- 1.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11(6):931–934. doi: 10.3928/0147-7447-19880601-13. [DOI] [PubMed] [Google Scholar]
- 2.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58(3):502–508. doi: 10.1227/01.NEU.0000197258.30821.50. [DOI] [PubMed] [Google Scholar]
- 3.Boakye M, Mummaneni PV, Garrett M, Rodts G, Haid R. Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. J Neurosurg Spine. 2005;2(5):521–525. doi: 10.3171/spi.2005.2.5.0521. [DOI] [PubMed] [Google Scholar]
- 4.Brooke NS, Rorke AW, King AT, Gullan RW. Preliminary experience of carbon fibre cage prostheses for treatment of cervical spine disorders. Br J Neurosurg. 1997;11(3):221–227. doi: 10.1080/02688699746285. [DOI] [PubMed] [Google Scholar]
- 5.Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (peek) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51(6):1343–1349. [PubMed] [Google Scholar]
- 6.Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, et al. Efficacy of anterior cervical fusion: Comparison of titanium cages, polyetheretherketone (peek) cages and autogenous bone grafts. J Clin Neurosci. 2008;15(11):1240–1245. doi: 10.1016/j.jocn.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: Sequential changes in cage subsidence. J Clin Neurosci. 2008;15(9):1017–1022. doi: 10.1016/j.jocn.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Iampreechakul P, Srisawat C, Tirakotai W. Stand-alone cervical polyetheretherketone (peek) cage (cervios) for single to two-level degenerative disc disease. J Med Assoc Thai. 2011;94(2):185–192. [PubMed] [Google Scholar]
- 9.Jung YT, Paeng SH, Pyo SY, Kim MS, Jeong YG. Comparison between carbon fiber composite frame and peek (polyetheretherketone) cages in the efficiency of interbody fusion for surgical treatment of cervical disc diseases. Korean J Spine. 2010;7(1):10–16. [Google Scholar]
- 10.Kandziora F, Pflugmacher R, Schäfer J, Born C, Duda G, Haas NP, et al. Biomechanical comparison of cervical spine interbody fusion cages. Spine (Phila Pa 1976) 2001;26(17):1850–1857. doi: 10.1097/00007632-200109010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 2009;32(2):207–214. doi: 10.1007/s10143-008-0168-y. [DOI] [PubMed] [Google Scholar]
- 12.Kettler A, Wilke HJ, Claes L. Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg. 2001;94(1):97–107. doi: 10.3171/spi.2001.94.1.0097. [DOI] [PubMed] [Google Scholar]
- 13.Lee SH, Suk KS, Kim KT, Lee JH, Seo EM, Im YS. Outcome analysis of single level anterior cervical fusion using interbody peek cage with autologous iliac bone graft. J Korean Orthop Assoc. 2009;44(1):93–101. [Google Scholar]
- 14.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24(15):1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 15.Mastronardi L, Ducati A, Ferrante L. Anterior cervical fusion with polyetheretherketone (peek) cages in the treatment of degenerative disc disease. Preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir (Wien) 2006;148(3):307–312. doi: 10.1007/s00701-005-0657-5. [DOI] [PubMed] [Google Scholar]
- 16.Morishita Y, Hida S, Miyazaki M, Hong SW, Zou J, Wei F, et al. The effects of the degenerative changes in the functional spinal unit on the kinematics of the cervical spine. Spine (Phila Pa 1976) 2008;33(6):E178–E182. doi: 10.1097/BRS.0b013e318166f059. [DOI] [PubMed] [Google Scholar]
- 17.Niu CC, Chen LH, Lai PL, Fu TS, Chen WJ. Trapezoidal titanium cage in anterior cervical interbody fusion: a clinical experience. Chang Gung Med J. 2005;28(4):212–221. [PubMed] [Google Scholar]
- 18.Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166(1):23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 19.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 20.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2003;28(2):134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 21.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40(3):607–624. [PubMed] [Google Scholar]
- 22.Van der Haven I, Van Loon PJ, Bartels RH, van Susante JL. Anterior cervical interbody fusion with radiolucent carbon fiber cages: Clinical and radiological results. Acta Orthop Belg. 2005;71(5):604–609. [PubMed] [Google Scholar]
- 23.Wilke HJ, Kettler A, Goetz C, Claes L. Subsidence resulting from simulated postoperative neck movements: an in vitro investigation with a new cervical fusion cage. Spine (Phila Pa 1976) 2000;25(21):2762–2770. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]
- 24.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (peek) cage. Clin Orthop Surg. 2011;3(1):16–23. doi: 10.4055/cios.2011.3.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou J, Xia Q, Dong J, Li X, Zhou X, Fang T, et al. Comparison of stand-alone polyetheretherketone cages and iliac crest autografts for the treatment of cervical degenerative disc diseases. Acta Neurochir (Wien) 2011;153(1):115–122. doi: 10.1007/s00701-010-0821-4. [DOI] [PubMed] [Google Scholar]