Abstract
Objective
Cervical OPLL is a relatively common cause of developing cervical myelopathy or radiculopathy in Asians. Cervical OPLL is sometimes missed in lateral radiography or MRI. In the present study, we analyzed the diagnostic accuracy of cervical OPLL in lateral radiography and MRI compared to CT scan.
Methods
This is a retrospective study of forty-six patients who underwent decompressive surgery anteriorly or posteriorly in our institute. All patients were diagnosed with cervical OPLL by CT scan. The patients were grouped into continuous type, segmental type, mixed type, and localized type. We then evaluated lateral radiographs and MRI compared to CT scans. The diagnostic accuracy and false negative rates in lateral radiograph and MRI were evaluated.
Results
In a total of 46 patients diagnosed with cervical OPLL in CT scans, diagnostic accuracy using lateral radiograph and MRI were 52.2%(24/46) and 58.7%(27/46), respectively. In the continuous type group, diagnostic accuracy using lateral radiograph and MRI were 85.7%(6/7) and 100.0%(7/7). In the segmental type group, diagnostic accuracy using lateral radiograph and MRI were 27.3%(6/22) and 31.8%(7/22). In the mixed type group, diagnostic accuracy was 91.7%(11/12) in lateral radiograph and 83.3%(10/12) in MRI. In the localized group, diagnostic accuracy was 20.0%(1/5) in lateral radiograph and 60.0%(3/5) in MRI.
Conclusion
The diagnostic accuracy of cervical OPLL using lateral radiograph and MRI was less than using CT scan. For the best treatment plan, preoperative CT scan should be performed to detect conditions of ossifications such as cervical OPLL.
Keywords: Cervical ossification of posterior longitudinal ligament, Computed tomography, Diagnostic accuracy, Magnetic resonance imaging, Radiography
INTRODUCTION
Cervical ossification of posterior longitudinal ligament (OPLL) is an uncommon problem which in clinical practice can cause myelopathy with or without radiculopathy. This entity was first reported in 18385) in the Guy's Hospital Reports, with the majority of the reported cases being described in Japanese literature2,4,5,8,9). The prevalence of cervical OPLL is reported to range from 0.6% to 2.2% in the Korean population4,6,7,11). However, cervical OPLL is quite often seen in Korea. Korean spine surgeons are frequently faced with cervical OPLL during treatment of cervical stenosis and disc herniation. Because distinguishing between ossification of the spinal ligament and hypertrophy of the spinal ligament or disc herniation is sometimes difficult with magnetic resonance imaging (MRI)10), the presence or absence of OPLL discovered after computerized tomography (CT) may change the strategy of treatment. This study describes the lateral radiograph, magnetic resonance image (MRI) and computed tomography (CT) findings in 46 Korean patients who presented with cervical myelopathy with or without radiculopathy caused by cervical OPLL.
In the present study, we analyzed the diagnostic accuracy of cervical OPLL in lateral radiograph and MRI compared to CT scan.
MATERIALS AND METHODS
A retrospective study was undertaken at the national health insurance medical center (NHIC) from January 2009 to December 2010. A total of 46 Korean patients who were diagnosed with cervical OPLL by CT scan were included in this study. There were 12 women and 34 men (mean age 59.4 years, age range 39-82 years). The patients presented myelopathy with or without radiculopathy of varying severity consisting of upper extremities pain, progressive lower extremities numbness, paresthesia, and difficulty in walking which was not relieved by conservative treatment.
The patients were divided into four groups which consisted of continuous type (7 cases), segmental type (22 cases), mixed type (12 cases), and localized type (5 cases). We then evaluated lateral radiographs and MRI compared to CT scans. The diagnostic accuracy and false negative rate in lateral radiograph and MRI were evaluated. And we analyzed the causes of misdiagnosis.
All images were reviewed by a certified spine surgeon and a certified radiologist, and the diagnosis was achieved by consensus. All the present studies were done in our institution.
Both axial and sagittal T1WI utilizing conventional spinecho acquisitions and T2WI utilizing turbo spin-echo MR sequences were performed on a 1.5-T Impact unit (Gyroscan Intera, Philips, The Netherlands). Axial and reconstructed sagittal CT (SOMATOM Sensation 64, Siemens, Germany) sections were obtained through the cervical spine in order to correlate the MR findings and confirm the presence of ossification. Each CT scan was reconstructed using a 1-mm slice thickness.
The SPSS for Windows version 13.0K(SPSS, Inc. Chicago IL) was used for analysis. Descriptive statistics were calculated, including frequencies for categorical variables and means and standard deviations for continuous variables.
1. Diagnostic Criteria of OPLL
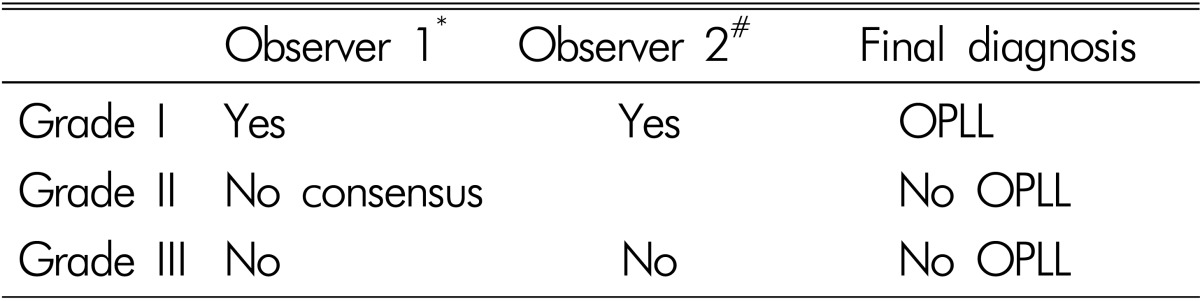
We defined OPLL as a posterior longitudinal ligament (PLL) ossification with a characteristic upside-down T or bowtie PLL configuration on the axial CT image10). OPLL was indicated by the presence of heterotopic ossification in the PLL on the CT scan. In lateral radiography, presence of flowing posterior ossification behind vertebral bodies indicated cervical OPLL10). Because cervical OPLL was often superimposed over facet complex on lateral projection, we designated three grades to diagnose OPLL. Grade I was when two observers agreed on presence of OPLL, and grade II was when two observers could not agree on presence of OPLL due to superimposed facet complex or spondylosis. Grade III was when two observers agreed on absence of OPLL. In MRI, presence of flowing ossification extending over multiple levels on sagittal images and characteristic upside-down T or bowtie configuration on axial images indicated OPLL. All T1- and T2-weighted images showed low signal intensity. If there was significant marrow fat content, MRI showed high signal intensity or marrow signal intensity10). We divided diagnoses on MRI into grade I, II, III according to consensus of the observers. In this study, only grade I was defined as cervical OPLL (Table 1).
Table 1. Diagnostic criteria of OPLL in MRI and radiography.
Radiography: Flowing posterior ossification behind vertebral body
MRI: PLL which shows low signal intensity on T1 and T2 weighted images or significant marrow intensity of PLL
*certified neurosurgeon
#certified radiologist
RESULTS
In a total of 46 patients diagnosed with cervical OPLL in CT scans, overall diagnostic accuracy using lateral radiograph and MRI were 52.2%(24/46) and 58.7%(27/46), respectively. In continuous type group, diagnostic accuracy using lateral radiograph and MRI were 85.7%(6/7) and 100.0%(7/7). In segmental type group, diagnostic accuracy using lateral radiograph and MRI were 27.3%(6/22) and 31.8%(7/22). In mixed type group, diagnostic accuracy was 91.7%(11/12) in lateral radiograph and 83.3%(10/12) in MRI. In the localized group, diagnostic accuracy was 20.0% (1/5) in lateral radiograph and 60.0%(3/5) in MRI (Table 2). There was no significant difference of diagnostic accuracy between lateral radiograph and MRI (p=0.31).
Table 2. Diagnostic accuracy of lateral radiograph vs. MRI.
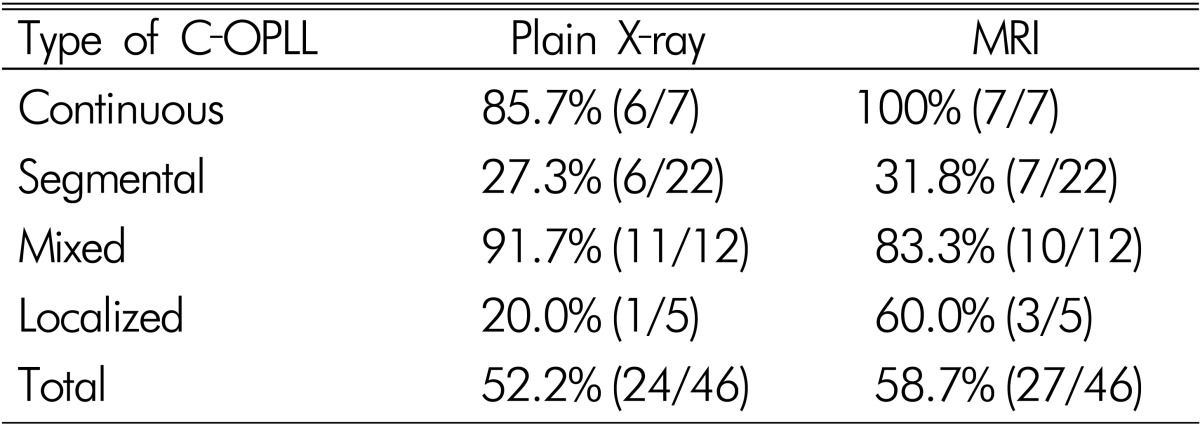
p=0.31
In MRI, patients with cervical OPLL are often incorrectly diagnosed as having PLL hypertrophy. In our study, the overall false negative rate of cervical OPLL in MRI was 41.3%(19/46), with the false negative rate being higher in the segmental type group than in other groups. The main cause of misdiagnosis was posterior longitudinal ligament (PLL) hypertrophy. We misdiagnosed OPLL as PLL hypertrophy (Table 3; Fig. 1).
Table 3. Cause of false negative under MRI.
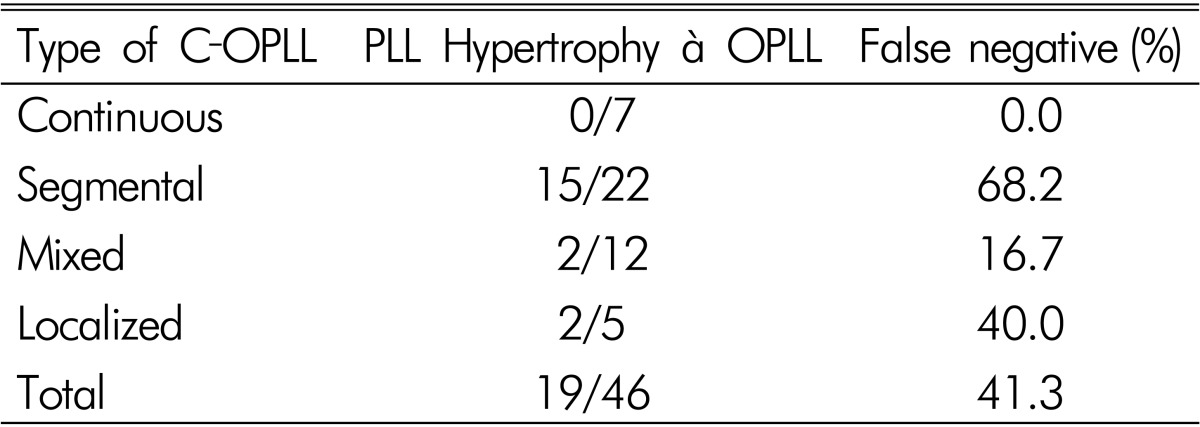
Fig. 1. Posterior longitudinal ligament (PLL) hypertrophy showed low or dark signal intensity in T1WI and T2WI. Occasionally, OPLL showed the same finding such as PLL hypertrophy in MRI. This case was misdiagnosed as PLL hypertrophy in MRI.
In patients diagnosed with OPLL using lateral radiograph, most of the patients showed continuous and mixed type OPLL. In segmental and localized type OPLL, many cases of cervical OPLL were missed on lateral radiograph due to spondylosis, facet joints and pedicles. The overall false negative rate of cervical OPLL in lateral radiograph was 47.8%(22/46). The false negative rate was higher in segmental and localized type groups than in other type groups (Table 4; Fig. 2).
Table 4. Cause of false negative under lateral radiograph.
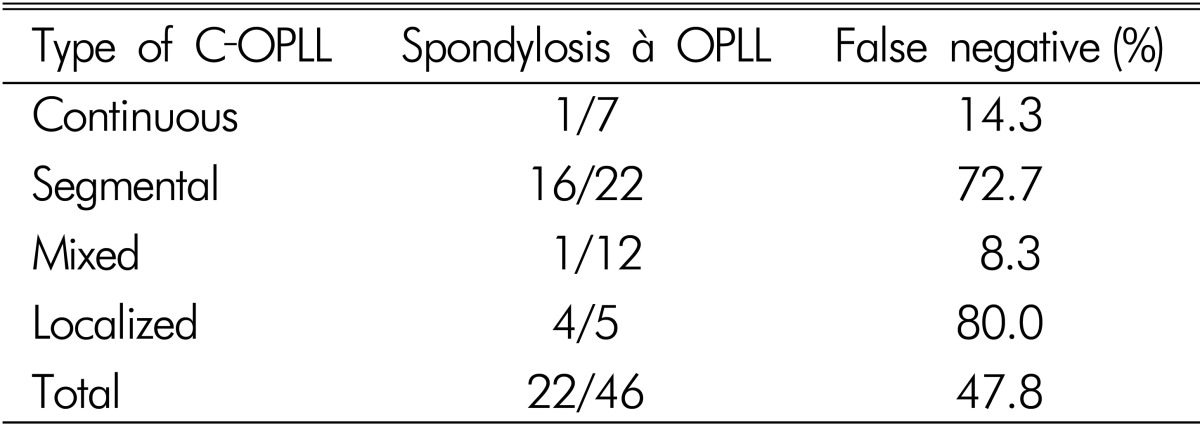
Fig. 2. In lateral radiography, OPLL was obscured because of spondylosis, facet, and pedicle shadow.
An OPLL smaller than 3mm was an important cause of missing OPLL on lateral radiograph. Average thickness of detectable OPLL on lateral radiograph was 3.83mm, range was from 2.99 mm to 4.71mm and standard deviation was 0.56mm(Fig. 3).
Fig. 3. (A) Small OPLL is hard to detect in lateral radiograph. (B) and (C) can be detected in CT scan, but not detected in lateral radiograph.
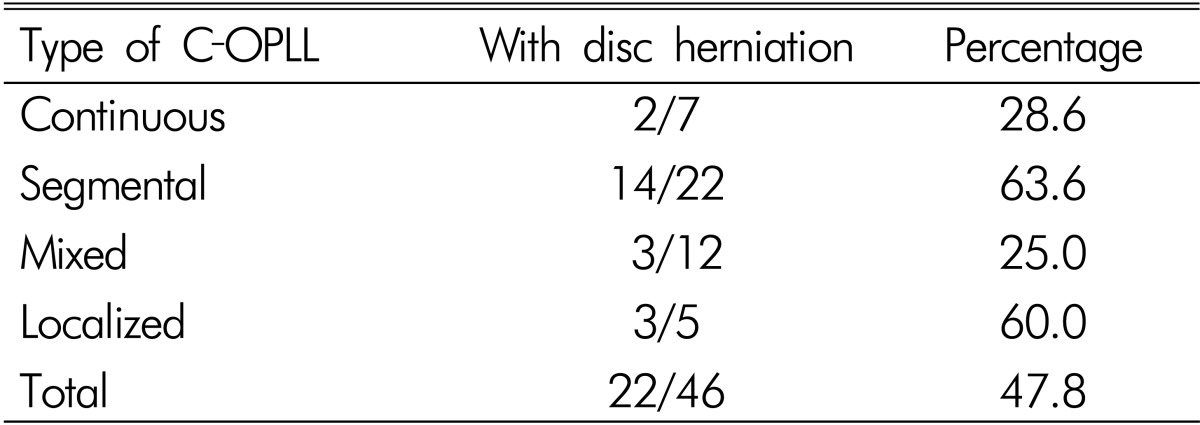
In our study, cervical OPLL concurred with cervical disc herniation in many cases. A total of 47.8%(22/46) of cervical OPLL patients developed disc herniation. Coefficients of coincidence were 63.6%(14/22) and 60.0%(3/5) in segmental type and localized type groups, respectively (Table 5).
Table 5. OPLL with disc herniation.
DISCUSSION
Acquired spinal stenosis caused by OPLL is more often seen in the cervical spine and among Asian populations4,6,7,11). Radiologic examinations play an important role in the diagnosis and evaluation of OPLL. On lateral conventional radiography, OPLL appears as continuous or segmental bony densities projecting into the central spinal canal10). However, cervical OPLL tends to misdiagnosis with plain X-ray or MRI; therefore, cervical CT scan is an essential early step for the proper treatment of cervical disease. In our study, diagnostic accuracy of radiography and MRI was about half of that of CT.
If the thickness of the OPLL was less than 3mm, we had difficulty finding it in a lateral radiograph. Severe spondylosis, facet joints and pedicle shadows hindered the detection of OPLL in the lateral radiograph. CT can detect small OPLLs or OLFs that are not visible on plain Xrays due to facet joint and bone overlapping effects. Therefore, other studies using plain Xrays have reported that continuous-type OPLL is the most common7,11). This may be because the continuous type could be easily detected using Xrays. In our study, segmental-type OPLL was the most frequent type. We propose that the segmental and localized type of OPLL are missed by plain X-rays but can be detected via CT scan. CT is the best diagnostic method for diagnosing ossified disease1,2,10). All previous cervical OPLL prevalence reports have used simple radiography; however, spinal ligament ossification cannot be correctly assessed based on simple radiographic findings4,6,7,11). The actual prevalence of cervical OPLL may be twice as high as found in previous studies.
A few studies have examined the prevalence of spinal ligament ossification based on MRI3). However, MRI has some difficulties in distinguishing ossifications from ligament hypertrophy10). In MRI, OPLL shows two different types. One is bone marrow signal intensity in T1WI and T2WI and the other is dark signal intensity in T1WI and T2WI10). The latter presents some difficulties in distinguishing from ligament hyper trophy. In case of dark signal intensity in T1WI and T2WI, we are not always able to diagnose OPLL. In many cases, there is not OPLL but hypertrophy. We can only suspect OPLL until confirming ossification with CT10).
Koyanagi et al.8) wrote that associated disc protrusion was found to be present at the maximum compression level in 60% of the patients, with the highest incidence of disc protrusion (81%) found in patients with segmental OPLL. In our study, half of cervical OPLL patients showed concurrent disc herniation, while the higher incidence of disc protrusion was found in patients with segmental and localized OPLL.
CONCLUSION
In segmental type and localized type especially, diagnostic accuracy of cervical OPLL using lateral radiograph and MRI was much lower than using CT scan. The thickness of OPLL was an important factor to detecting OPLL in a lateral radiograph. Also, MRI had some difficulties in distinguishing OPLL with ligament hypertrophy. For the best treatment plan in case of cervical disease, preoperative CT scan should be performed to detect conditions of ossifications such as cervical OPLL.
References
- 1.Chiba K, Kato Y, Tsuzuki N, Nagata K, Toyama Y, Iwasaki M, et al. Computer-assisted measurement of the size of ossification in patients with ossification of the posterior longitudinal ligament in the cervical spine. J Orthop Sci. 2005;10:451–456. doi: 10.1007/s00776-005-0925-5. [DOI] [PubMed] [Google Scholar]
- 2.Firooznia H, Rafii M, Golimbu C, Tyler I, Benjamin VM, Pinto RS. Computed tomography of calcification and ossification of posterior longitudinal ligament of the spine. J Comput Tomogr. 1984;8:317–324. doi: 10.1016/0149-936x(84)90082-1. [DOI] [PubMed] [Google Scholar]
- 3.Guo JJ, Luk KD, Karppinen J, Yang H, Cheung KM. Prevalence, distribution, and morphology of ossification of the ligamentum-flavum: a population study of one thousand seven hundred thirty-six magnetic resonance imaging scans. Spine (Phila Pa 1976) 2010;35:51–56. doi: 10.1097/BRS.0b013e3181b3f779. [DOI] [PubMed] [Google Scholar]
- 4.Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery. 2006;58:1027–1039. doi: 10.1227/01.NEU.0000215867.87770.73. [DOI] [PubMed] [Google Scholar]
- 5.Isobe Y, Hara T. A case report of paraplegia combined with ossification of yellow ligament and dural membrane. Nihon Seikeigeka Gakkai Zasshi. 1953;27:339. [Google Scholar]
- 6.Jin BH, Kim YS. Ossification of spinal ligaments. J Korean Neurosurg Soc. 1991;20:875–884. [Google Scholar]
- 7.Kim TJ, Bae KW, Uhm WS, Kim TH, Joo KB, Jun JB. Prevalence of ossification of the posterior longitudinal ligament of the cervical spine. Joint Bone Spine. 2008;75:471–474. doi: 10.1016/j.jbspin.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 8.Koyanagi I, Iwasaki Y, Hida K, Imamura H, Abe H. Magnetic resonance imaging findings in ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg. 1998;88:247–254. doi: 10.3171/jns.1998.88.2.0247. [DOI] [PubMed] [Google Scholar]
- 9.Liu KC. [Epidemiological study on ossification of the posterior longitudinal ligament (opll) in the cervical spine--comparison of the prevalence between Japanese and Taiwanese] Nihon Seikeigeka Gakkai Zasshi. 1990;64:401–408. [PubMed] [Google Scholar]
- 10.Ross JS. Diagnostic imaging spine. Salt Lake City: Amirsys; 2004. pp. II276–II288. [Google Scholar]
- 11.Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984;184:71–84. [PubMed] [Google Scholar]





