Abstract
Background:
Cervical C5 nerve root palsies may occur in between 0% and 30% of routine anterior or posterior cervical spine operations. They are largely attributed to traction injuries/increased cord migration following anterior/posterior decompressions. Of interest, almost all studies cite spontaneous resolution of these deficits without surgery with 3–24 postoperative months.
Methods:
Different studies cite various frequencies for C5 root palsies following anterior or posterior cervical spine surgery. In their combined anterior/posterior series involving C4-C5 level decompressions, Libelski et al. cited up to a 12% incidence of C5 palsies. In Gu et al. series, C5 root palsies occurred in 3.1% of double-door laminoplasty, 4.5% of open-door laminoplasty, and 11.3% of laminectomy. Miller et al. observed an intermediate 6.9% frequency of C5 palsies followed by posterior cervical decompressions and fusions (PCDF).
Results:
Gu et al. also identified multiple risk factors for developing C5 palsies following posterior surgery; male gender, ossification of the posterior longitudinal ligament (OPLL), narrower foramina, laminectomy, and marked dorsal spinal cord drift. Miller et al. also identified an average $1918 increased cost for physical/occupational therapy for patients with C5 palsies.
Conclusions:
The incidence of C5 root deficits for anterior/posterior cervical surgery at C4-C5 was 12% in one series, and ranged up to 11.3% for laminectomies, while others cited 0–30%. Although identification of preoperative risk factors for C5 root deficits may help educate patients regarding these risks, there is no clear method for their avoidance at this time.
Keywords: Anterior surgery, cervical, C5 root palsies, C4-C5 surgery, factors, posterior surgery, risk
INTRODUCTION
The risk of C5 palsies occurring following anterior, posterior, or circumferential spine surgery varies from 0% to 30%.[3] Although there are multiple theories as to the etiology of these injuries, cord migration with resultant traction injury to the C5 nerve roots, particularly following surgery at the C4-C5 level, predominates. Despite the increased availability of multiple treatment strategies, if postoperative magnetic resonance (MR) studies show no new focal lesion (e.g. hematomas/other), most would recommend nonoperative management as the majority of deficits spontaneously resolve over 3–24 postoperative months. Below we explore the relative frequencies, surgical etiologies, and risk factors leading to postoperative C5 palsies following cervical spine surgery.
RISK OF C5 PALSY WITH ANTERIOR CERVICAL DECOMPRESSION
C5 palsy in 32 patients undergoing extremely wide/asymmetric anterior decompression
Of 459 patients having anterior decompression/fusion at the C4-C5 level for cervical spondylotic myelopathy (CSM), Odate et al. found that 32 (7%) experienced postoperative C5 palsies [Tables 1 and 2].[18] They were divided into two groups (palsy side [n = 35] and nonpalsy side [n = 29]), and their clinical/radiographic studies were compared with 66 consecutive other patients who had the same procedures without C5 root deficits. They found that those with C5 palsies had smaller preoperative C4-C5 foramina, underwent more extensive/wider/asymmetric unilateral decompressions, and exhibited less anterior spinal cord shift.
Table 1.
Frequency of reported C5 palsies following cervical surgery
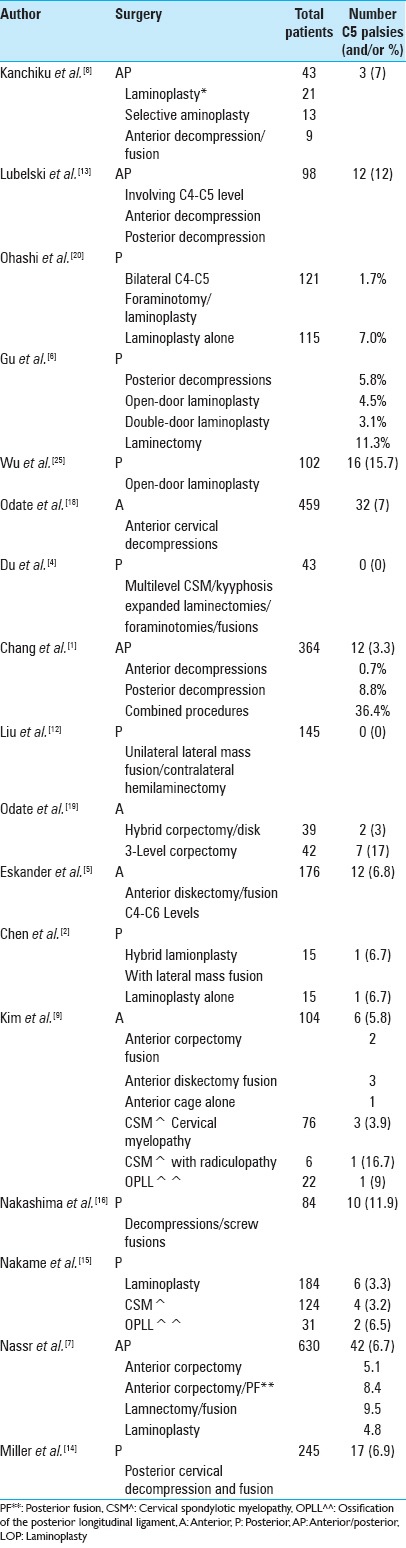
Table 2.
Summary of sections
The frequency of C5 root palsies utilizing different anterior cervical operations for csm; risk of C5 palsy lower with multilevel diskectomies
Shamjii et al. compared the safety/efficacy of multiple anterior cervical approaches (decompressions/fusions) addressing CSM (e.g. excluding ossification of the posterior longitudinal ligament [OPLL], single level CSM) [Tables 1 and 2].[23] Utilizing 10 studies from MEDLINE and the Cochrane Collaboration Library (through 2012) that met inclusion criteria (at least 10 cases each), they compared: “Multiple discectomies with single or multiple corpectomy, multiple discectomies with discectomy-corpectomy hybrid, and multiple corpectomies with discectomy-corpectomy hybrid.” Patients having any of these three procedures improved (based upon the Japanese Orthopedic Association [JOA], Visual Analog Scale [VAS] scales), and experienced few complications. Moderate evidence favored multiple discectomies with single or multiple corpectomy (e.g. better outcomes and improved sagittal alignment), with a lower risk of C5 palsy). Furthermore, discectomy-corpectomy hybrid procedures were preferable to multiple corpectomies.
Hybrid decompression/fusion vs. Plated three-level corpectomy for 4-segment CSM
In 81 patients with 4-level CSM/kyphosis followed for at least 2 years, Odate et al. explored the efficacy/morbidity of hybrid decompressions/fusions (39 patients) vs. plated 3-level anterior corpectomy/fusion (ACF) (42 patients) [Tables 1 and 2].[19] The hybrid procedures included a plated two-vertebra ACF and single-level discectomy performed with stand-alone cage fixation. Halo braces were utilized in 9 (21%) of 42 patients undergoing plated 3-level ACF vs. none in the hybrid group. Advantages of the hybrid procedure included: Fewer construct failures (0% vs. 10%; e.g. graft/plate extrusions/pseudarthrosis), and fewer C5 palsies (3% vs. 17%, respectively). Notably, postoperative C5 palsies occurred in: 25% of C3-C5 ACF, 19% of C4- C6 ACF, but only 11% of C4-C5 ACF/C6-7 discectomy.
Correlation between preoperative spinal cord rotation and postoperative C5 palsy for anterior cervical discectomy/fusion between the c4-c6 levels
In 176 patients undergoing anterior cervical discectomy/fusion (ACDF) between the C4-C6 levels, Eskander et al. correlated the degree of rotation of the cervical cord on MR scans with the 6.8% incidence of postoperative C5 palsies [Tables 1 and 2].[5] They found a significant relationship between the incidence of postoperative C5 palsies and greater degrees of rotation; 0° to 5° (mild Type I: 0 palsies in 159), 6° to 10° (moderate Type 2; 8 palsies of 13), and ≥11° (severe Type 3; 4 palsies of 4).
Analysis of C5 palsies after anterior cervical surgery
In Kim et al. series of 104 patients with CSM, cervical spondylotic myeloradiculopathy (CSM/R), and/or OPLL (vs. another 30 with radiculopathy only), 6 (5.8%) developed C5 palsies [Tables 1 and 2].[9] C5 palsies occurred in 3 of 76 (3.95%) patients with CSM, 1 of 6 (16.7%) with CSM/R, and 2 of 22 (9%) with OPLL, and followed 2 ACF, 3 ACDF, and 1 cage placement/no plate. For the four patients treated conservatively, three fully and one nearly completely resolved, while only one of the two patients undergoing additional foraminal decompression improved; in short, conservative treatment yielded better outcomes. Of interest, their postoperative X-rays showed increased lordosis at the surgical levels (average 6°), and an average increase of 8.2° in sagittal alignment (C3-C7).
Complications with three alternative anterior decompression/fusion techniques for CSM
When Liu et al. evaluated multilevel ACDF vs. hybrid construct vs. long corpectomy performed in 286 patients (166 M/120 F; average age 53.8 (range 33–74) years), 61% exhibited perioperative complications; graft migration/collapse/dislodgement, hoarseness, dysphagia, cerebrospinal fluid (CSF) fistulas, wound infections, and C5 palsies [Tables 1 and 2].[11] As anticipated, long corpectomy constructs yielded the highest complication rates, multilevel ACDF had the highest fusion rates, while cephalad C2-C4 procedures had the highest rates of hoarseness/dysphagia.
RISKS OF C5 PALSY WITH ANTERIOR VS. POSTERIOR CERVICAL SURGERY
C5 root injuries with anterior and posterior surgery in CSM patients averaging 79 years of age
Kanchiku et al. reviewed the frequency of C5 root injuries in 43 consecutive patients averaging 79 years of age undergoing cervical spine surgery for CSM [Tables 1 and 2].[8] Surgical procedures included: 21 laminoplasties (from C3 to C7), 13 selective laminoplasties (1 above/1 below the maximally compressed level), and 9 anterior decompressions/fusions; JOA recovery rates were comparable for all 3 groups. Postoperatively, they observed one wound infection, and three C5 palsies.
Comparing risks of C5 palsy in anterior ‘skip’ corpectomy vs. Posterior surgery for spondylotic myelopathy
Qian et al. compared the efficacy of multilevel anterior “skip” corpectomy vs. posterior cervical decompressions for 3 level CSM [Table 2].[21] For anterior vs. posterior procedures, average surgical times (2.5 and 2.1 h), and mean blood loss (250 and 380 cc) were, respectively, recorded. Postoperative complications following anterior procedures included 5 axial neck pain, 2 hoarseness, 2 mesh subsidence, and 2 plate/screw dislocations, while posterior morbidity included 15 with axial neck pain, 3 CSF leaks, and 2 C5 root palsies. Since JOA scores showed significantly higher recovery rates for anterior surgery, the authors concluded that “skip” corpectomy was more safe/effective vs. posterior surgery for CSM.
Comparable rates of C5 palsy with anterior vs. Posterior cervical surgery
Lawrence et al. evaluated the pros and cons of anterior vs. posterior cervical surgical alternatives to address CSM involving more than 2 levels [Tables 1 and 2].[10] Upon reviewing the literature and other databases (e.g., GRADE [Grading of Recommendation Assessment, Development and Evaluation]/AHRQ [Agency for Healthcare Research and Quality through 9/2012]), they found that only 8 of 135 studies met inclusion criteria. These studies revealed comparable improvement in JOA scores for anterior or posterior surgery, and comparable rates of C5 palsies. Of interest, overall greater canal enlargement correlated with posterior operations. The concluded that there were no unique advantages to anterior vs. posterior cervical surgery for 2-level CSM.
Quantitative measures and frequency of c5 palsy with anterior vs. posterior cervical surgery: Assessment of risk factors and correlation with quality of life measures
Chang et al. assessed the relative risk/frequency of C5 palsy following 364 anterior vs. posterior cervical surgery, and related this to the quality of life [Tables 1 and 2].[1] Twelve (3.3%) had postoperative C5 palsies; 0.7% followed anterior procedures (n = 2), 8.8% followed posterior procedures (n = 6), and 36.4% followed combined anterior/posterior procedures (n = 4). Significant differences observed for the 12 patients with C5 palsies included the manual muscle test (MMT), the action research arm test (ARAT), the Jebsen test of hand function (JTHF), and the European quality of life-5 dimensions (EQ-5D). C5 deficits also highly correlated with: Advanced age, type of cervical lesion, and surgery involving the C4-C5 level.
The frequency of C5 palsy after multilevel anterior or posterior cervical surgery
Nassr et al. cited a 0–30% incidence of C5 palsies reported in the literature, but found 42 (6.7%) instances of C5 palsies following 630 (292 females/338 males; average age 58 years) consecutive multilevel ACF with/without posterior fusions vs. laminectomy/fusion or laminoplasty in their own series [Tables 1 and 2].[17] Their different frequencies of C5 deficits were not statistically significant and included laminectomy/fusion (9.5%), ACF/posterior fusion (8.4%), ACF alone (5.1%), and laminoplasty (4.8%). They also cited various etiologies for C5 palsies: Spontaneous dorsal cord shift/root tethering, ischemia/reperfusion injury, and direct operative trauma.
FREQUENCY OF C5 PALSIES WITH POSTERIOR CERVICAL SURGERY
C-5 palsy following posterior cervical decompressions/pedicle screw fusions
Nakashima et al. evaluated the unique radiographic risk factors (e.g. utilizing X-ray, MRI, computed tomography [CT]) for 10 (11.9%) of 84 (average age 60.1 years) patients who developed C5 palsies after undergoing posterior cervical decompressions/pedicle screw fusions [Tables 1 and 2].[16] Radiographic risk factors for C5 palsies included: Significant preoperative C4-C5 kyphosis, significantly smaller preoperative C4-C5 foramina (e.g. 2.2–2.3 mm on the palsy side), the presence of OPLL, and the extent of postoperative posterior cord shift at the C4-C5 level. Note that with conservative therapy, seven fully recovered.
C-5 palsy following posterior cervical decompressions/vertex rod-eyelet spinous process fusion (without lateral mass screws)
In Epstein's series (in preparation), 3 (3.3%) of 92 patients undergoing 1-3 level laminectomies (mean 2.5)/and 5-9 level posterior instrumented fusions (average 7.6 level vertex rod/eyelet/braided cable/spinous process fusions) for CSM/OPLL developed delayed postoperative C5 palsies [Tables 1 and 2]. Of interest, the two bilateral and one unilateral C5 palsies occurred in a delayed fashion on days 2, 3, and 5, and all involved C4-C5 laminectomies (e.g. laminectomy C4-C5 (1 patient), laminectomy C4, C5, C6 (2 patients).
C5 palsy with open-door vs. French-door laminoplasty for CSM
Wang et al. compared the relative efficacy/risks/complications of performing open-door laminoplasty (ODL) vs. French-door laminoplasty (FDL) for treating CSM. Four comparative trials were studied [Table 2].[24] Although the postoperative JOA scores were higher for ODL vs. FDL, the following variables were comparable; operative time, intraoperative blood loss, total complication rate, postoperative cervical lordosis, range of motion, and postoperative palsy.
C5 root palsy following expansile open-door laminoplasty forCSM
Wu et al. retrospectively analyzed the risk factors resulting in the development of C5 palsies following open-door laminoplasties for CSM [Tables 1 and 2]. Of 102 patients, 16 (15.7%) had C5 palsies (13 men and 3 women, average age 62.8 years) vs. 86 without palsies (63 men and 23 women, average age 57.8 years) [Tables 1 and 2].[25] Factors predisposing to C5 palsies included; more narrowed width of the intervertebral foramen (WIF), anterior protrusion of the superior articular process (APSAP), a high-signal intensity zone C3-C5 (HIZ: C3-C5), and OPLL; of interest, both groups demonstrated comparable posterior shift of the spinal cord (PSSC).
More C5 root palsies following laminectomy and fusion for csm vs. Modified plate-only open-door laminoplasty for CSM
Yang et al. evaluated the extent of decompression and avoidance of complications (including C5 root palsies) for 141 CSM patients undergoing modified plate-only laminoplasty vs. laminectomy and fusion [Tables 1 and 2].[26] For both groups, postoperative T2-weighted MR scans at the three most compromised levels revealed significant expansion of the dural cross-sectional area, and dorsal spinal cord drift (but laminectomies resulted in more extensive decompressions). Although patients from both groups exhibited comparable postoperative JOA scores, the plate-only laminoplasty patients showed more improvement on the Neck Dysfunction/Disability Index (NDI)/VAS, demonstrated greater preservation of cervical mobility, and exhibited fewer postoperative C5 palsies.
RISK FACTORS, EARLY DETECTION, PREDICTION AND PREVENTION OF C5 PALSIES
Risk factors for C5 palsy; cervical laminectomy/fusion width and extent of dorsal cord migration
Radcliff et al. evaluated 17 patients with CSM/OPLL who developed C5 palsies following cervical laminectomy/fusion (CLF) accompanied by wide MR-documented laminectomy troughs [Tables 1 and 2].[22] Patients were compared with eight CSM/OPLL controls also undergoing CLF, but with normal troughs and without C5 palsies. Unique postoperative MR findings for those with C5 palsies included on average, greater dorsal cord drift at the C3-C6 levels (C3 [4.2 vs. 2.2 mm], C4 [4.6 vs. 2.8 mm], C5 [5.1 vs. 2.4 mm], and C6 [5.2 vs. 2.4 mm]), wider C5 laminectomy troughs (17.9 vs. 15.2 mm), but comparable sagittal alignment.
Predicting C5 palsy using preoperative anatomic measurements
Lubelski et al. evaluated whether the incidence of C5 root palsies could be predicted utilizing preoperative anterior posterior canal diameters (APD), foraminal diameters (FD), and/or cord-lamina angles (CLA) [Tables 1 and 2].[13] They correlated these parameters with the 12% frequency of C5 palsies seen in 98 CSM patients undergoing anterior or posterior decompressive procedures involving the C4-C5 level. They found “For every 1-mm increase in APD and FD, the odds of developing palsy decreased 69% (P < 0.0001) and decrease 98% (P < 0.0003), respectively.” In contrast, for every 1-degree increase in CLA, the odds of developing palsy increased by 43% (P < 0.0001). The authors concluded they could use these measures to help predict the onset of postoperative C5 palsy.
Detection and prevention of C5 nerve root palsies after cervical spine decompressions
Utilizing the PubMed, Embase, and Medline databases, Guzman et al. found 60 articles that cited C5 palsies occurring after cervical spine surgery [Tables 1 and 2].[7] They found, however, no clear evidence that intraoperative neural monitoring (IONM) or other measures could accurately predict/detect whether these injuries would occur. Furthermore, the overwhelming recommendation was to treat these deficits conservatively, as “most patients make a full recovery within two years.”
RISK FACTORS AND SURGICAL MEASURES TO AVOID C5 ROOT PALSIES
Posterior cervical surgery; incidence/risk factors correlating with C5 palsy
Gu et al. systematically utilized the PubMed, Embase, Web of Science, and Cochrane CENTRAL databases to evaluate the incidence/risk factors contributing to C5 palsy following posterior cervical decompressive surgery [Tables 1 and 2].[6] Identifying 25 out of 589 studies, they calculated a 5.8% incidence (95%CI: 4.4–7.2%) of C5 palsies following posterior cervical decompressions. The frequency for “open-door laminoplasty, double-door laminoplasty, and laminectomy were 4.5%, 3.1%, and 11.3%, respectively.” Risk factors contributing to C5 palsies included OPLL, narrower preoperative foramina, laminectomy, excessive spinal cord drift (SMD), and male gender.
Efficacy of prophylactic c4-C5 foraminotomy to avoid c5 root injuries following open-door cervical laminoplasty
Over a 2-year period, Ohashi et al. prospectively determined that C5 root injuries could be minimized by prophylactically performing bilateral C4-C5 foraminotomies during open-door cervical laminoplasties [Tables 1 and 2].[20] They compared the frequency of C5 deficits for 121 (85.8%) patients undergoing laminoplasties with bilateral foraminotomies (group F) vs. 115 (81.5%) having lamnoplasties without foraminotomies (group NF); C5 palsies, respectively, occurred in 1.7% vs. 7.0%. Furthermore, bilateral foraminotomies did not significantly increase postoperative instability, range of motion, hinge fractures or nonunions, and resulted in comparable outcomes (e.g. VAS, JOA scores).
Enlarged laminectomy with lateral mass screw fixation eliminated C5 palsy for multilevel csm with kyphosis
For 43 patients (28 M/15 F; average age 59.6 years) with multilevel CSM/kyphosis, Du et al. found performing multilevel expanded laminectomies/foraminal decompressions (average 3.97 levels) with lateral mass screw fixation reduced the incidence of instrumentation failures and C5 palsies and to zero [Tables 1 and 2].[4] X-rays documented fusion an average of 3 months postoperatively. Additionally, MR studies revealed an average 4.72 ± 1.10 mm (range, 0–6.71 mm) of dorsal cord shift. For patients followed an average of 2.8 years, JOA scores in all but two patients (4.7%) completely recovered, and only four (9.3%) having residual axial pain.
Hemilaminectomy/unilateral lateral mass fusion limits C5 root injury in cervical OPLL surgery
In theory, following typical cervical laminectomy or laminoplasty, excessive dorsal cord migration contributes to C5 palsies. Liu et al., therefore, performed unilateral hemilaminectomy with contralateral lateral mass fusion in 146 myelopathic OPLL patients to decompress the cord/maintain stability, and reduce the extent of dorsal cord migration, yielding a 0% incidence of C5 palsies [Tables 1 and 2].[12] The mean JOA score improved from 10 to 14 postoperatively, and the cervical lordosis was unchanged (8.7° preoperatively to 9.1° postoperatively).
Use of posterior hybrid technique for treatment of segmental instability in cervical opll failed to limit C5 palsies
Chen et al. compared outcomes for 15 cervical OPLL patients with segmental instability (SI) and frequent MR-documented high-signal intensity zones (HIZ; typically at SI levels) managed with laminoplasty/lateral mass screw fixation (hybrid model) vs. 15 OPLL patients without SI treated with laminoplasty alone [Tables 1 and 2].[2] Postoperatively (e.g. 3–4 years), the hybrid technique resulted in better maintenance of lordosis, greater postoperative JOA scores, and no progression of kyphosis/OPLL. Alternatively, laminoplasty patients demonstrated increased kyphosis (26.7%), progression of OPLL (13.3%), and three instances of delayed neurological deterioration. Notably, each group exhibited a single C5 palsy.
USE OF INTRAOPERATIVE NEURAL MONITORING TO DETECT C5 PALSIES
C5 palsy using ionm transcranial motor evoked potentials
Nakame et al. correlated postoperative C5 root palsies with intraoperative changes in transcranial motor evoked potentials (MEP; deltoid, biceps, and triceps muscles bilaterally) occurring during 184 laminoplasties [Tables 1 and 2].[15] C5 palsies occurred in 6 (3.3%) patients (5 M/1F); 4 (3.2%) of 124 with CSM, and 2 (6.5%) of 31 with OPLL. Notably, none exhibited MEP changes.
C5 palsies in cervical spine surgery despite intraoperative monitoring
Currier reviewed the “etiology, risk factors, prevention, and treatment of C5 palsy” occurring during cervical surgery despite the use of IONM [Table 2].[3] He noted the 3 of 1000 frequency of major deficits (severe motor weakness involving 2 or more extremities in 12 h of surgery) associated with spinal surgery, but the much higher up to 30% incidence of C5 palsies attributed to cervical surgery; fortunately for latter, 70% recover completely with conservative treatment (e.g., no surgery) over an average of 4–5 postoperative months. Furthermore, no treatment strategy (surgery vs. nonsurgical measures) has to reduce the duration, frequency, or degree of resolution of these C5 root deficits. Although evidence supports the role of IONM in detecting/avoiding major neurological injury, there was such evidence documenting the efficacy of IONM in avoiding C5 palsies.
COST AND QUALITY OF LIFE WITH C5 PALSY AFTER POSTERIOR SURGERY
Incidence, cost, and quality of life with C5 palsy after posterior cervical decompression and fusion
Miller et al. looked at the quality-of-life/costs of C5 palsy following posterior cervical decompression and fusion (PCDF).[14] They performed a 2:1 matched retrospective cohort study at a single tertiary-care institution (2007 and 2012) that included all patients undergoing PCDF [Tables 1 and 2]. They studied self-reported “Euroqol-5 Dimensions quality-of-life survey,” physiological parameters (e.g. deltoid and biceps strength – manual testing), functional costs of treatment, and missed workdays. Of 245 patients having PCDF, 17 had C5 palsies (6.9%). Of interest, the costs of physical/occupational therapy for the C5 group was significantly higher (average of $2078) as were their overall costs ($1918 higher) vs. those without C5 palsies. Nevertheless, when matched with 34 controls, there were no significant differences in demographic/operative characteristics, cost of hospital stay, surgery, or other direct/indirect costs.
CONCLUSION
The frequency of C5 palsies reportedly varies from 0% to 30%, with many focusing on a risk of 3.1–12%. The presence of preoperative MR-documented HIZ: C3-C5 in the cord opposite the C4-C5 level, surgery (e.g. either anterior or posterior) at the C4-C5 level, and dorsal cord migration all constitute significant risk factors for developing postoperative C5 palsies. Although this review discusses the frequency of C5 root palsies, there appears to be no clear-cut method for avoiding these injuries. Fortunately, the majorities resolve within 3–24 postoperative months without conservative treatment alone.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/5/154/156556
Contributor Information
Nancy E. Epstein, Email: nancy.epsteinmd@gmail.com.
Renee Hollingsworth, Email: rhollingsworth@winthrop.org.
REFERENCES
- 1.Chang PY, Chan RC, Tsai YA, Huang WC, Cheng H, Wang JC, et al. Quantitative measures of functional outcomes and quality of life in patients with C5 palsy. J Chin Med Assoc. 2013;76:378–84. doi: 10.1016/j.jcma.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y, Chen D, Wang X, Yang H, Liu X, Miao J, et al. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique. Arch Orthop Trauma Surg. 2013;133:171–7. doi: 10.1007/s00402-012-1658-5. [DOI] [PubMed] [Google Scholar]
- 3.Currier BL. Neurological complications of cervical spine surgery: C5 palsy and intraoperative monitoring. Spine (Phila Pa 1976) 2012;37:E328–34. doi: 10.1097/BRS.0b013e3182417276. [DOI] [PubMed] [Google Scholar]
- 4.Du W, Zhang P, Shen Y, Zhang YZ, Ding WY, Ren LX. Enlarged laminectomy and lateral mass screw fixation for multilevel cervical degenerative myelopathy associated with kyphosis. Spine J. 2014;14:57–64. doi: 10.1016/j.spinee.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Eskander MS, Balsis SM, Balinger C, Howard CM, Lewing NW, Eskander JP, et al. The association between preoperative spinal cord rotation and postoperative C5 nerve palsy. J Bone Joint Surg Am. 2012;94:1605–9. doi: 10.2106/JBJS.K.00664. [DOI] [PubMed] [Google Scholar]
- 6.Gu Y, Cao P, Gao R, Tian Y, Liang L, Wang C, et al. Incidence and risk factors of C5 palsy following posterior cervical decompression: A systematic review. PLoS One. 2014;9:e101933. doi: 10.1371/journal.pone.0101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guzman JZ, Baird EO, Fields AC, McAnany SJ, Qureshi SA, Hecht AC, et al. C5 nerve root palsy following decompression of the cervical spine: A systematic evaluation of the literature. Bone Joint J. 2014;96-B:950–5. doi: 10.1302/0301-620X.96B7.33665. [DOI] [PubMed] [Google Scholar]
- 8.Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Nishida N, Taguchi T. Results of surgical treatment of cervical spondylotic myelopathy in patients aged 75 years or more: A comparative study of operative methods. Arch Orthop Trauma Surg. 2014;134:1045–50. doi: 10.1007/s00402-014-2017-5. [DOI] [PubMed] [Google Scholar]
- 9.Kim S, Lee SH, Kim ES, Eoh W. Clinical and radiographic analysis of c5 palsy after anterior cervical decompression and fusion for cervical degenerative disease. J Spinal Disord Tech. 2014;27:436–41. doi: 10.1097/BSD.0b013e31826a10b0. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: A systematic review. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S173–82. doi: 10.1097/BRS.0b013e3182a7eaaf. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Qi M, Chen H, Yang L, Wang X, Shi G, et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J. 2012;21:2428–35. doi: 10.1007/s00586-012-2323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu K, Shi J, Jia L, Yuan W. Surgical technique: Hemilaminectomy and unilateral lateral mass fixation for cervical ossification of the posterior longitudinal ligament. Clin Orthop Relat Res. 2013;471:2219–24. doi: 10.1007/s11999-013-2889-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lubelski D, Derakhshan A, Nowacki AS, Wang JC, Steinmetz MP, Benzel EC, et al. Predicting C5 palsy via the use of preoperative anatomic measurements. Spine J. 2014;14:1895–901. doi: 10.1016/j.spinee.2013.10.038. [DOI] [PubMed] [Google Scholar]
- 14.Miller JA, Lubelski D, Alvin MD, Benzel EC, Mroz TE. C5 palsy after posterior cervical decompression and fusion: Cost and quality-of-life implications. Spine J. 2014;14:2854–60. doi: 10.1016/j.spinee.2014.03.038. [DOI] [PubMed] [Google Scholar]
- 15.Nakamae T, Tanaka N, Nakanishi K, Kamei N, Izumi B, Fujioka Y, et al. Investigation of segmental motor paralysis after cervical laminoplasty using intraoperative spinal cord monitoring with transcranial electric motor-evoked potentials. J Spinal Disord Tech. 2012;25:92–8. doi: 10.1097/BSD.0b013e318211fc4e. [DOI] [PubMed] [Google Scholar]
- 16.Nakashima H, Imagama S, Yukawa Y, Kanemura T, Kamiya M, Yanase M, et al. Multivariate analysis of C-5 palsy incidence after cervical posterior fusion with instrumentation. J Neurosurg Spine. 2012;17:103–10. doi: 10.3171/2012.4.SPINE11255. [DOI] [PubMed] [Google Scholar]
- 17.Nassr A, Eck JC, Ponnappan RK, Zanoun RR, Donaldson WF, 3rd, Kang JD. The incidence of C5 palsy after multilevel cervical decompression procedures: A review of 750 consecutive cases. Spine (Phila Pa 1976) 2012;37:174–8. doi: 10.1097/BRS.0b013e318219cfe9. [DOI] [PubMed] [Google Scholar]
- 18.Odate S, Shikata J, Yamamura S, Soeda T. Extremely wide and asymmetric anterior decompression causes postoperative C5 palsy: An analysis of 32 patients with postoperative C5 palsy after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 2013;38:2184–9. doi: 10.1097/BRS.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 19.Odate S, Shikata J, Kimura H, Soeda T. Hybrid decompression and fixation technique versus plated three-vertebra corpectomy for four-segment cervical myelopathy: Analysis of 81 cases with a minimum 2-year follow-up. J Spinal Disord Tech. 2013 Nov 8; doi: 10.1097/BSD.0b013e31827ada34. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Ohashi M, Yamazaki A, Watanabe K, Katsumi K, Shoji H. Two-year clinical and radiological outcomes of open-door cervical laminoplasty with prophylactic bilateral C4-C5 foraminotomy in a prospective study. Spine (Phila Pa 1976) 2014;39:721–7. doi: 10.1097/BRS.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 21.Qian L, Shao J, Liu Z, Cheng L, Zeng Z, Jia Y, et al. Comparison of the safety and efficacy of anterior ‘skip’ corpectomy versus posterior decompression in the treatment of cervical spondylotic myelopathy. J Orthop Surg Res. 2014;9:63. doi: 10.1186/s13018-014-0063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radcliff KE, Limthongkul W, Kepler CK, Sidhu GD, Anderson DG, Rihn JA, et al. Cervical laminectomy width and spinal cord drift are risk factors for postoperative C5 palsy. J Spinal Disord Tech. 2014;27:86–92. doi: 10.1097/BSD.0b013e31824e53af. [DOI] [PubMed] [Google Scholar]
- 23.Shamji MF, Massicotte EM, Traynelis VC, Norvell DC, Hermsmeyer JT, Fehlings MG. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: A systematic review. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S195–209. doi: 10.1097/BRS.0b013e3182a7eb27. [DOI] [PubMed] [Google Scholar]
- 24.Wang L, Wang Y, Yu B, Li Z, Liu X. Open-door versus French-door laminoplasty for the treatment of cervical multilevel compressive myelopathy. J Clin Neurosci. 2015;22:450–5. doi: 10.1016/j.jocn.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 25.Wu FL, Sun Y, Pan SF, Zhang L, Liu ZJ. Risk factors associated with upper extremity palsy after expansive open-door laminoplasty for cervical myelopathy. Spine J. 2014;14:909–15. doi: 10.1016/j.spinee.2013.07.445. [DOI] [PubMed] [Google Scholar]
- 26.Yang L, Gu Y, Shi J, Gao R, Liu Y, Li J, et al. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy. Orthopedics. 2013;36:e79–87. doi: 10.3928/01477447-20121217-23. [DOI] [PubMed] [Google Scholar]


