Abstract
Background:
The efficacy of epidural and facet joint injections has been assessed utilizing multiple solutions including saline, local anesthetic, steroids, and others. The responses to these various solutions have been variable and have not been systematically assessed with long-term follow-ups.
Methods:
Randomized trials utilizing a true active control design were included. The primary outcome measure was pain relief and the secondary outcome measure was functional improvement. The quality of each individual article was assessed by Cochrane review criteria, as well as the criteria developed by the American Society of Interventional Pain Physicians (ASIPP) for assessing interventional techniques. An evidence analysis was conducted based on the qualitative level of evidence (Level I to IV).
Results:
A total of 31 trials met the inclusion criteria. There was Level I evidence that local anesthetic with steroids was effective in managing chronic spinal pain based on multiple high-quality randomized controlled trials. The evidence also showed that local anesthetic with steroids and local anesthetic alone were equally effective except in disc herniation, where the superiority of local anesthetic with steroids was demonstrated over local anesthetic alone.
Conclusion:
This systematic review showed equal efficacy for local anesthetic with steroids and local anesthetic alone in multiple spinal conditions except for disc herniation where the superiority of local anesthetic with steroids was seen over local anesthetic alone.
Keywords: Chronic pain, epidural injections, facet joint injections, local anesthetic, spinal pain, steroids, saline
INTRODUCTION
The increasing prevalence of spinal pain and disability, and the explosion of health care costs are major issues for the US and the world.[11,18,28,46,49,72,73,78,101,150,151,163,195,204] Freburger et al.[46] reported a rapid overall increase in low back pain of 162%, rising from 3.9% in 1992 to 10.2% in 2006. A study of US Burden of Disease Collaborators showed spinal pain occupying three of the first five categories of disability.[195] Hoy et al.[72,73] reported various prevalences for spinal pain, with an annual prevalence of 39% in the low back, 26% in the neck, and 13% in the midback or thoracic spine. Leboeuf-Yde et al.[100] reported the prevalence of low back pain to be 43%, neck pain to be 32%, and thoracic pain to be 13%. In addition, the prevalence of persistent pain is high, especially in the elderly and it is closely associated with functional limitations.[14,21,53,201] Overall, chronic persistent low back and neck pain is seen in 25–60% of patients, one year or longer after an initial episode.[39,45,109,157,193]
Martin et al.[150] estimated that treatments for back and neck pain problems accounted for $86 billion in health care expenditures in the US in 2005. This represented an increase in expenditures of 65% and a 49% increase in the number of patients seeking spine-related care from 1997 to 2006. Gaskin and Richard[49] reported annual expenditures of $100 billion for managing moderate and severe pain. Various diagnostic and treatment modalities have been increasingly utilized including surgery, imaging, physical therapy, drugs, and interventional techniques, and have been increasing rapidly.[1,33,34,80,97,108,109,128,129,130,138,149,171,175,186] Consequently, spinal interventional techniques are considered to be one of the major components in the escalation of health care costs among patients with chronic spinal pain, specifically in the US.[1,33,34,45,80,97,108,128,129,130,138,149,171,175,186] Manchikanti et al.[138] analyzed utilization trends and Medicare expenditures from 2000 to 2008 regarding the growth of spinal interventional pain management techniques. They reported that Medicare recipients who received spinal interventional techniques increased 107.8% from 2000 to 2008, with an annual increase of 9.6%. The overall number of spinal interventional techniques performed increased by 186.8%, an annual increase of 14.1% per 100,000 beneficiaries. There was a 240% increase in expenditures for these procedures during the same period.
In another manuscript, Manchikanti et al.[128] reported the overall increase of interventional techniques from 2000 to 2011 to be 228%. In the Medicare population during the same period there was an overall increase of 177% – an annual increase of 11.4%. Abbott et al.,[1] in their analysis of utilization patterns between 2003 and 2007, showed a variable number of procedures performed per patient across all categories during a 12-month inclusion period with high variability among specialties. An increase in interventional techniques along with geographic variability and variability among specialities has been demonstrated.[130] Thus, spinal interventional techniques are increasing exponentially, with their efficacy being scrutinized along with their inappropriate use.[1,9,24,36,43,44,63,80,107,110,113,123,128,130,138,166,170,189]
Epidural injections are used in managing spinal pain secondary to disc herniation, spinal stenosis, postsurgery syndrome, discogenic pain not from facet or sacroiliac joints, and multiple other conditions.[9,24,36,45,63,110,113,123,166,172,189] Facet joint injections are used in managing facet joint pain.[43,44,45,107] Epidural injections are administered by three approaches: caudal in the sacral region; interlaminar in the lumbar, thoracic, and cervical regions; and transforaminal in the lumbar, thoracic, and cervical regions. Facet joint injections are administered by intraarticular injections or facet joint nerve blocks. The efficacy of epidural injections and facet joint injections has been assessed utilizing multiple solutions including saline, local anesthetics, steroids, and other drugs such as clonidine, ketamine, hypertonic sodium chloride solution, and amitriptyline.[12,27,109] Local anesthetic alone or local anesthetic with steroids, or steroids alone or with saline are the most common combinations and most commonly studied, and normal saline is commonly used as a placebo.
The response to epidural injections is variable for various pathologies including disc herniation and/or radiculitis, discogenic pain without disc herniation, spinal stenosis, and postsurgery syndrome. Manchikanti et al.,[109] based on multiple systematic reviews of epidural injections and facet joint injections,[9,36,113,123,166] reported variable evidence for disc herniation with or without radiculitis, spinal stenosis, and discogenic pain. This evidence ranged from good to limited based on the pathology and treatment. The evidence from multiple assessments appears to be similar for local anesthetics alone compared with local anesthetic with steroids.[9,36,43,44,63,107,110,113,123,166] In fact, Bicket et al.[12] performed a systematic review and meta-analysis evaluating “control” injections, utilizing 43 randomized controlled trials, which included 3641 patients, and concluded that epidural nonsteroidal injections were more likely than nonepidural injections to achieve positive outcomes and provide a greater pain score reduction.
Steroids and local anesthetics have multiple mechanisms of action when injected into the epidural space; antiinflammatory effects are predominantly seen with steroids and other effects are seen with local anesthetics.[3,6,19,66,67,99,148,155,158,167,168,181,191] The first reports of caudal epidural injections were with local anesthetics alone.[20,32,40,169,185] Evans[40] and Cyriax[32] published multiple manuscripts indicating the effectiveness of local anesthetic injections without steroid. Bicket et al.[12] combined all control injections rather than separating them into active and inactive solutions, placebo and active control trials, and various solutions such as local anesthetic, amitriptyline, clonidine, hypertonic saline, and normal sodium chloride solution.
This systematic review assesses randomized controlled trials of epidural and facet joint injections utilizing saline, local anesthetic, and/or steroids. The objective of this review is to characterize the role of saline and local anesthetic in these procedures and to compare their effects to those of steroids in the long-term.
METHODS
The methodology for this systematic review was derived from evidence-based systematic reviews and meta-analyses of randomized trials.[102] Randomized trials with an active control or placebo control were included. Furthermore, included trials had at least 25 patients in each group or described appropriate sample size calculation, enrolled patients with pain duration of at least 3 months, and followed-up for at least 1 month after treatment.
Only randomized trials utilizing a true active control design with injection of either sodium chloride solution or local anesthetic or steroid into the epidural space, on the nerve root, in the joint, or facet joint nerves were included. True placebo injections, that is, injections of inactive solutions into inactive structures, were not included.
In active control trials, two different procedures or drugs are compared. For this assessment, only the trials comparing sodium chloride solution, local anesthetic, or steroids were utilized. The rationale for assessing only the aforementioned agents is that they are the most clinically relevant medications. Further, trials where a drug was injected outside the epidural space, nerve root, or joint were excluded. This evidence will address the misconception concerning local anesthetic as a placebo or even sodium chloride solution as a pure placebo.
The interventions evaluated were caudal and interlaminar epidural injections in the cervical, thoracic, and lumbar regions; transforaminal epidural injections in the cervical, thoracic, and lumbar regions; and facet joint injections and nerve blocks in the cervical, thoracic, and lumbar regions.
The primary outcome measure was pain relief; the secondary outcome measure was functional improvement. A literature search was performed from various resources including PubMed, the Cochrane Library, the US National Guideline Clearinghouse (NGC), previous systematic reviews, and cross references.
The search period covered from 1966 through March 2014.
The search strategy emphasized chronic neck, thoracic, low back, and upper extremity pain; lower extremity pain; and chest wall pain treated with epidural or facet joint interventions. Search terms were:
(Chronic low back pain or chronic back pain or chronic neck pain or disc herniation or discogenic pain or facet joint pain or herniated lumbar discs or nerve root compression or lumbosciatic pain or postlaminectomy or lumbar surgery syndrome or radicular pain or radiculitis or sciatica or spinal fibrosis or spinal stenosis or zygapophyseal) and (epidural injection or epidural steroid or epidural perineural injection or interlaminar epidural or intraarticular corticosteroid or nerve root blocks or intraarticular injection or periradicular infiltration or saline injection or transforaminal injection or corticosteroid or methylprednisolone or facet joint or medial branch block); Sort by: Publication Date; Filters: Clinical Trial, Controlled Clinical Trial, Evaluation Studies, Multicenter Study, Randomized Controlled Trial, Validation Studies, Comparative Study.
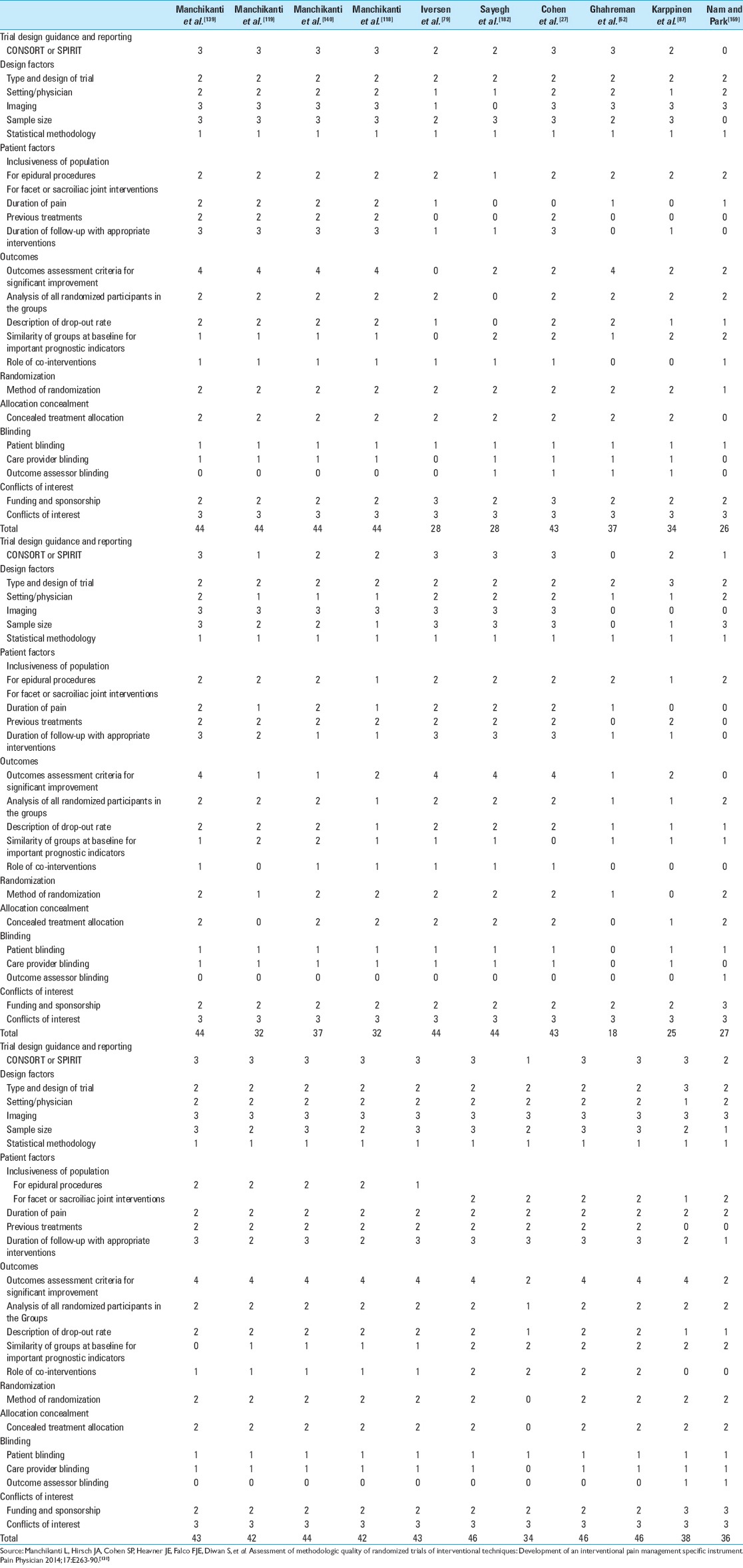
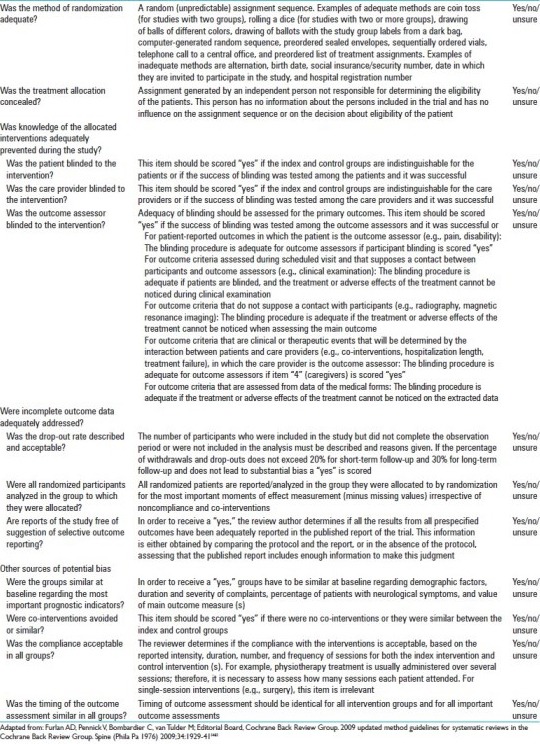
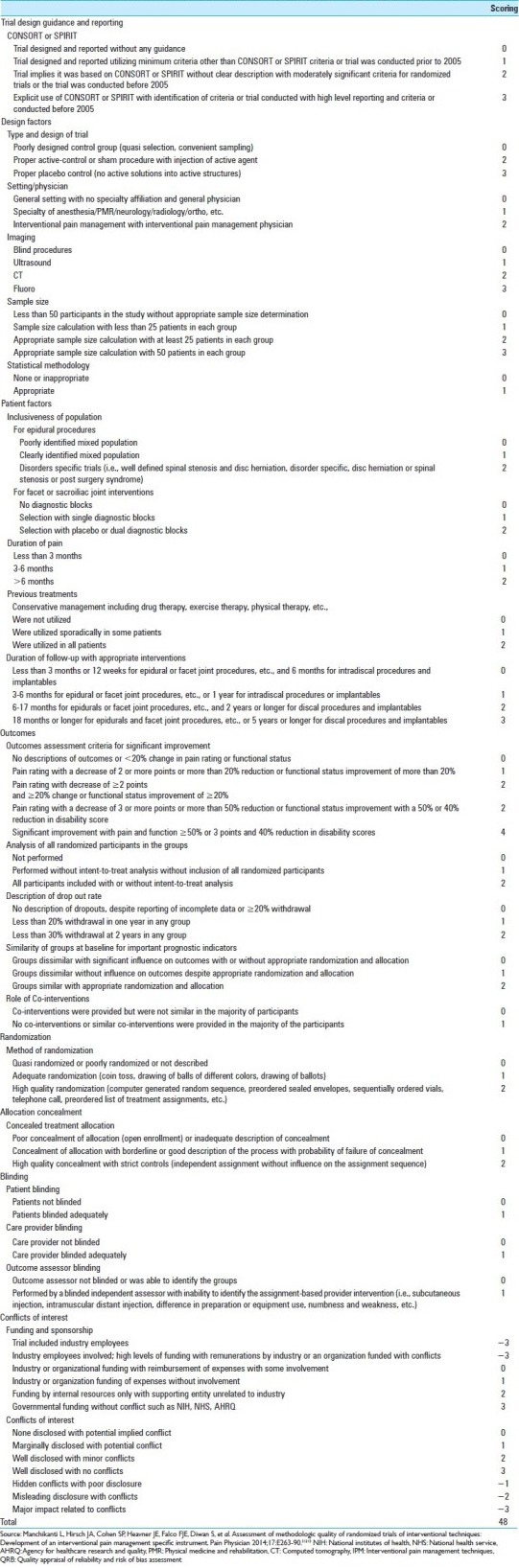
The quality of each individual article was assessed for bias using Cochrane review criteria [Appendix 1][48] and by the American Society of Interventional Pain Physicians (ASIPP) review criteria, titled “Interventional Pain Management Techniques – Quality Appraisal of Reliability and Risk of Bias Assessment (IPM – QRB)” [Appendix 2].[131]
The literature search, selection of trials, and methodological quality assessment were performed by at least two authors for each task. The allocation of trials for methodological quality assessment was distributed among the authors. Any discrepancies were resolved by consensus and the primary (LM) and senior (JH) authors.
Trials scoring 8–12 on Cochrane review criteria or 32–48 on ASIPP criteria were considered high quality, trials scoring 4–7 on Cochrane review criteria or 20–31 on ASIPP criteria were considered moderate quality, and studies scoring less than 4 on Cochrane review criteria or less than 20 on ASIPP criteria were considered low quality.
A meta-analysis was conducted if there were more than two trials that were condition-specific and homogeneous.
Analysis of the evidence was based on the condition, region, and modality (e.g. lumbar disc herniation, cervical spinal stenosis, or thoracic facet joint arthritis) so as to reduce any clinical heterogeneity.
The summary measure for pain was a 50% or more reduction of pain in at least 50% of the patients, or at least a 3-point decrease in pain scores; for disability scores the summary measure was a 50% or more reduction in disability in at least 40% of the patients or at least a 30-point decrease in disability scores measured on a scale of 0–100.
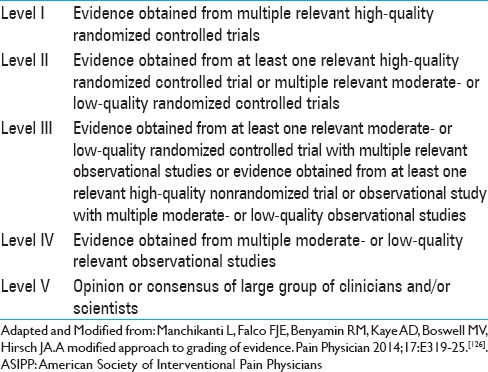
The analysis of evidence was conducted based on the qualitative level of evidence criteria synthesized by ASIPP[126] as shown in Table 1, which was developed from multiple previously utilized grading schemata, most importantly Cochrane reviews and the United States Preventive Services Task Force (USPSTF).[15,62,64,189,196]
Table 1.
Grading of evidence modified by ASIPP
RESULTS
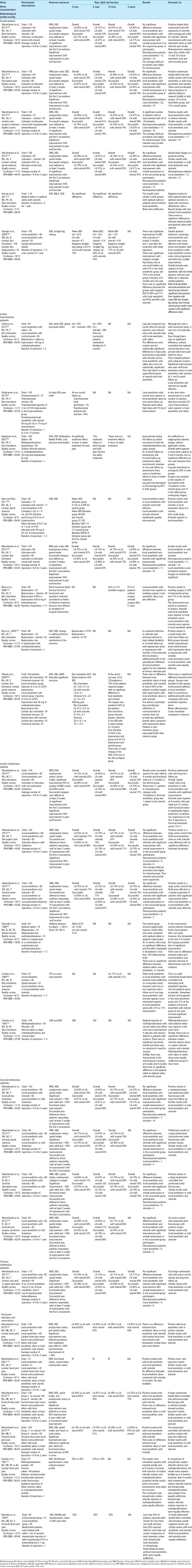
The literature search and study selection is shown in Figure 1 as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).[102] Overall, there were 40 randomized trials for consideration after eliminating duplicate publications.[5,8,16,17,25,27,29,35,47,51,52,79,87,88,94,98,114,115,116,117,118,119,120,121,122,132,133,137,139,140,141,142,143,144,153,159,161,174,177,178,182,188,192,199] Of these, five trials utilized a true placebo design without the ability to assess the role of the drugs injected into the epidural space, facet joints, and over nerves;[5,35,153,174,188] one trial utilized intramuscular steroid injections compared with epidural steroid injections;[199] and another trial[98] utilized intramuscular local anesthetic injections. In another trial,[177] forceful injection was assessed. One facet joint nerve block trial compared two different modalities.[25] Consequently, 31 trials met the inclusion criteria for methodological quality assessment.[8,16,17,27,29,47,52,79,87,114,116,117,118,119,120,121,122,132,133,137,139,140,141,142,143,144,159,161,178,182,192] Each manuscript was independently, in an unblinded, standardized manner, assessed for methodological quality assessment. The primary authors of manuscripts being assessed were not involved in the methodological quality assessment. All disagreements between reviewers were resolved by the primary and senior authors (LM and JH). Methodological quality assessment scores are shown in Tables 2 and 3.
Figure 1.
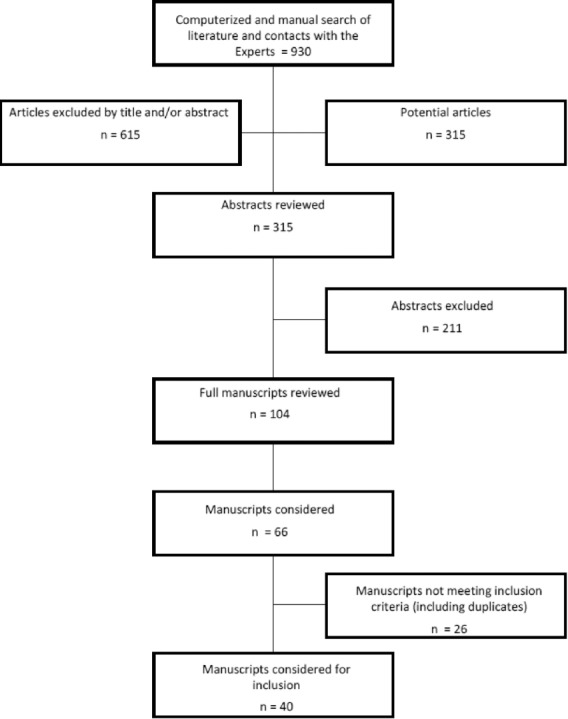
The flow diagram illustrating published literature evaluating various solutions in epidural and facet joint injections
Table 2.
Methodological quality assessment of randomized trials utilizing Cochrane review criteria
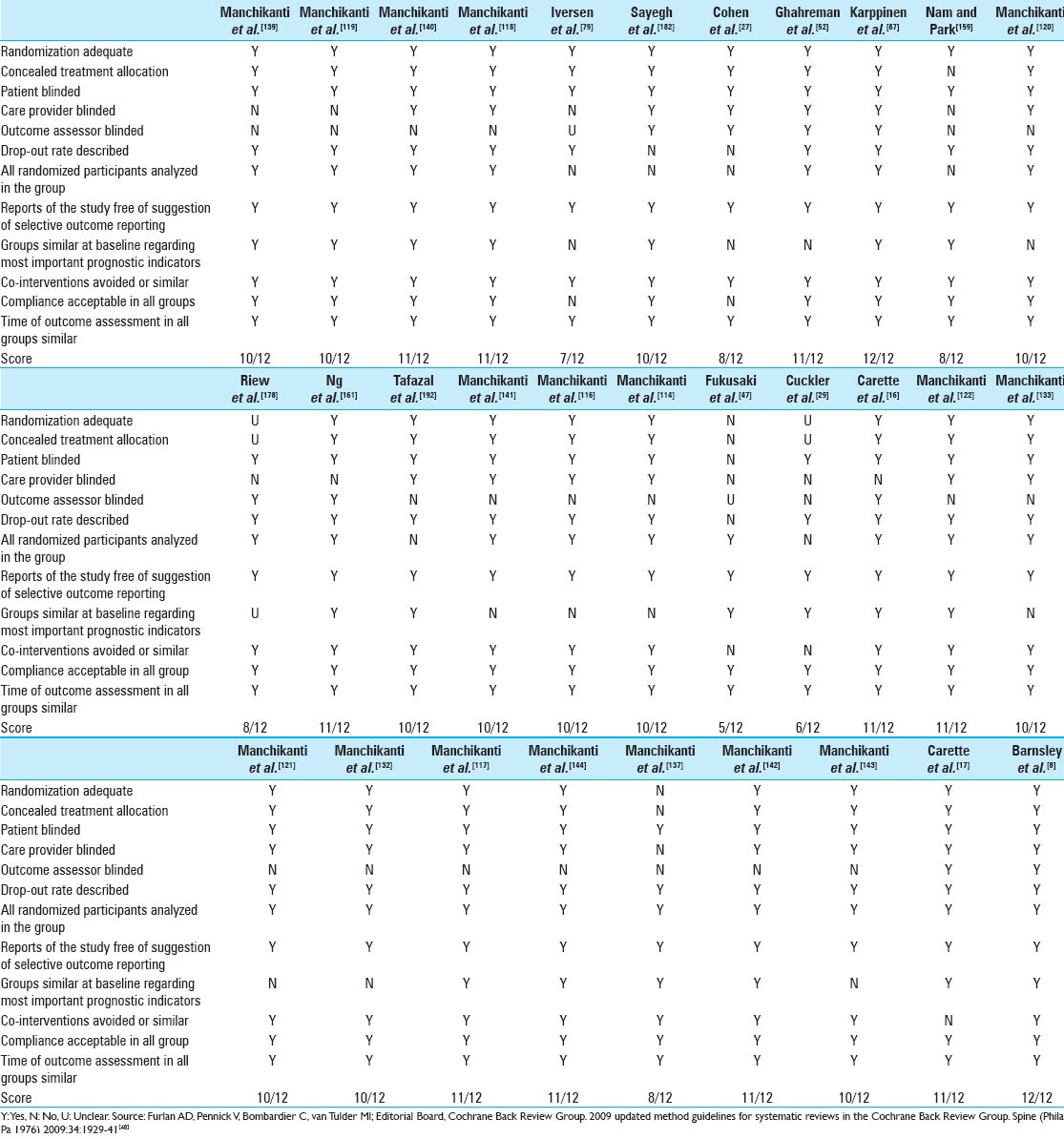
Table 3.
Methodological quality assessment of randomized trials utilizing ASIPP IPM-QRB
Meta-analysis
There was no homogeneity among the 31 trials meeting the inclusion criteria for methodological quality assessment when the region, technique, solutions injected, and use of fluoroscopy were considered. Of the 31 trials, 13 trials by Manchikanti et al. assessing the role of epidural injections were similar in many aspects;[114,116,117,118,119,120,121,122,132,133,139,140,141] they were, however, performed for different pathologies, such as cervical or thoracic or lumbar region involvement, or disc herniation, spinal stenosis, postsurgery syndrome, or discogenic pain. Thus, a meta-analysis was not feasible. Furthermore, the trials were all performed by one group of authors in the same setting with similar protocols. Similarly, four facet joint nerve block manuscripts also had similarities;[137,142,143,144] they were performed in the same setting, but for different regions, by the same group of authors. Consequently, none of them met the criteria for homogeneity so as to be included in a meta-analysis.
Study characteristics
Study characteristics and outcomes are described in Table 4.
Table 4.
Study characteristics and outcomes of randomized epidural and facet joint injection trials
Caudal epidural injections
Among those trials meeting the inclusion criteria, there were six examining the efficacy of caudal epidural injections with multiple solutions.[79,118,119,139,140,182] Of these, four were of high quality utilizing Cochrane and IPM-QRB criteria,[118,119,139,140] one was moderate (IPM-QRB) to high (Cochrane review) quality,[182] and one was of moderate quality utilizing both criteria.[79]
Four of these studies were conducted by Manchikanti et al.[118,119,139,140] Using the same protocol, active controlled trials were conducted assessing the efficacy of epidural injections in a total of 480 patients, either with local anesthetic or local anesthetic with steroids, during a 2-year follow-up in patients with lumbar disc herniation, lumbar discogenic pain without facet joint or sacroiliac joint pain, lumbar central spinal stenosis, and lumbar postsurgery syndrome. These studies were rated as high quality on Cochrane review criteria, with scores ranging from 10 to 11 out of 12 and IPM-QRB scores of 44 out of 48.
All four trials showed similar results for the efficacy of caudal epidural injections with local anesthetic alone or local anesthetic with steroids in 50–80% of the patients. In these trials, success was defined as at least 3 weeks of significant improvement (50% improvement) in pain and function after the first two injections. All patients were grouped into successful (responsive) or nonresponsive categories accordingly. We then calculated the number of patients with disc herniation, discogenic pain, spinal stenosis, or postsurgery syndrome who were nonresponsive to local anesthetic alone or local anesthetic with steroid. We observed no significant differences in the patients who did not respond to either injection for any of the spinal conditions. This suggests that none of the spinal conditions influenced the response to either type of injection.
Table 4 shows the results were superior in the responsive groups in all four diagnostic categories. A limitation of these trials was that none of them included placebo controls. The authors discussed potential pathophysiologic mechanisms for the efficacy of local anesthetic with steroids. Long-term improvement seen with both types of injections and may be attributed to previously described mechanisms of action.[3,6,19,30,58,66,67,68,89,95,96,99,118,119,139,140,148,155,158,167,168,181,185,190,191] In addition, the efficacy of sodium chloride solution injected into joint spaces or the epidural space has also been described.[10,16,17,60,200] All the studies demonstrated the efficacy of local anesthetic with steroids; although the disc herniation group showed higher quality with pain relief improvement at 6 and 12 months. One of the major advantages of these trials was that only patients with chronic pain were enrolled and patient homogeneity was observed by recruiting those with similar diagnoses/conditions instead of lumping all diagnostic groups together and/or including those with acute and subacute pain.
The study by Sayegh et al.[182] is also a moderate (IPM-QRB) to high-quality (Cochrane) randomized controlled trial on the efficacy of local anesthetic alone versus local anesthetic with steroids. This trial showed significant improvement for both local anesthetic, and local anesthetic plus steroids; however, steroids were shown to be superior, in that they provided faster, higher quality, and longer-lasting relief compared with local anesthetic alone. This study included patients with acute and subacute sciatica.
Iversen et al.,[79] in ultrasound-guided caudal epidural injections utilizing either epidural saline or epidural saline plus steroids, showed no significant improvement in either group. The trial was criticized for flaws in its design and conduct.[61,109,111,180,203] The authors did not utilize a local anesthetic, recruited a large proportion of patients with acute pain, and many of the patients had improved before randomization.
In conclusion, there was Level I evidence supported by multiple, relevant high-quality randomized controlled trials[118,119,139,140] and one moderate to high-quality trial[182] reporting the efficacy of local anesthetics with steroids in managing chronic low back and lower extremity pain with a caudal approach.
There was also Level I evidence, based on multiple, relevant high-quality randomized controlled trials,[118,119,140] showing equal effectiveness for local anesthetic alone or local anesthetic with steroids, with one high-quality trial showing that local anesthetic alone or local anesthetic with steroids are equally effective[139] and one moderate to high-quality trial[182] reporting the superiority of local anesthetic with steroids.
Lumbar transforaminal epidural injections
There were eight randomized controlled trials assessing the efficacy of multiple solutions used in lumbar transforaminal administration.[27,52,87,120,159,161,178,192] All of these trials were rated as high-quality, scoring 8–11 out of 12 based on Cochrane review criteria. Utilizing IPM-QRB criteria, however, one trial by Nam and Park[159] was shown to be of moderate-quality with a score of 26 out of 48. The characteristics of these studies were considerably different with varying protocols, multiple injections of solutions, and follow-up periods ranging from 1 month to 2 years.
Cohen et al.,[27] in a 3-month follow-up study, reported that local anesthetic alone and local anesthetic with steroids injections were equally effective, even though they concluded that local anesthetic with steroids may be superior. The study included patients with acute and subacute disc herniations and was rather small, with just 30 patients in the local anesthetic alone group and 28 patients in the local anesthetic with steroids group. This was a high-quality trial based on both Cochrane review criteria (8/12) and IPM-QRB criteria (43/48).
Ghahreman et al.,[52] utilizing multiple groups, assessed the efficacy of bupivacaine alone in 27 patients and in 28 patients who also received steroids. However, the follow-up period was just one month. This trial showed transforaminal epidurals of local anesthetic with steroids to be superior to local anesthetic alone, with a 54% versus 7% improvement. This trial also showed a lack of effectiveness for sodium chloride solution when it was utilized as a true placebo injected away from the nerve root, and a significant effect when sodium chloride solution was injected transforaminally, even though this was still much inferior to local anesthetic with steroids. This was a high-quality trial based on Cochrane review criteria (11/12) as well as IPM-QRB criteria (37/48).
In a large trial, Karppinen et al.[87] studied the efficacy of a single transforaminal injection of sodium chloride solution or methylprednisolone with bupivacaine in patients followed-up at one year. This trial showed rather surprising effects in favor of sodium chloride solution at 3 and 6 months, with no significant difference noted at one year. This was a high-quality trial based on Cochrane review criteria (12/12) as well as IPM-QRB criteria (34/48). In a subgroup analysis, the authors reported the efficacy of transforaminal steroids with local anesthetic compared with sodium chloride solution in disc protrusions.[87,88] These manuscripts also faced significant criticism.[111,145,146,170]
Nam and Park[159] conducted a small study assessing the role of transforaminal epidural injections in lumbar spinal stenosis in 36 patients, with 19 receiving lidocaine and 17 receiving lidocaine with steroids with a short-term follow-up of 3 months. This study showed positive results for local anesthetic with steroids and local anesthetic alone but a superiority for local anesthetic with steroids. This was a high-quality trial based on Cochrane review criteria (8/12) and moderate quality based on IPM-QRB criteria (26/48).
Manchikanti et al.,[120] in an active-controlled trial with a large number of patients and long-term follow-up, showed the efficacy of the local anesthetic lidocaine, as well as lidocaine with steroids. There was significant improvement at the end of 2 years in all parameters in 65% of patients who received local anesthetic alone and 57% of patients who received local anesthetic with steroid. Furthermore, when patients were separated into nonresponsive and responsive categories based on initial relief of at least 3 weeks with two procedures, significant improvement (at least 50% improvement in pain and function) was seen in 80% in the responsive local anesthetic group and 73% in the responsive local anesthetic with steroid group. These patients with disc herniation had improvement in all parameters: Pain intensity, function, and medication reduction. This was a high-quality trial based on Cochrane review criteria (10/12) as well as IPM-QRB criteria (44/48).
Riew et al.,[178] in a study of patients with disc herniation, treated 27 patients with transforaminal epidural injections of bupivacaine alone and 28 patients with bupivacaine with steroids. They reported that 33% of the patients in the local anesthetic group and 71% in the local anesthetic with steroid group avoided surgery. Overall this trial showed both local anesthetic alone and local anesthetic with steroid were effective; however, local anesthetic with steroid was superior. This was a high-quality trial based on Cochrane review criteria (8/12) and IPM-QRB criteria (32/48).
Ng et al.[161] in a trial of 86 patients, with 43 receiving bupivacaine and 43 receiving bupivacaine with steroids, reported efficacy for both treatments at 3 months in 47.5% of the patients in the bupivacaine group and 41.5% in the bupivacaine with steroids group. Consequently, this trial showed equal effectiveness for both, even though it was less than 50% in both groups. This was a high-quality trial based on Cochrane review criteria (11/12) as well as IPM-QRB criteria (37/48).
Tafazal et al.[192] reported the effectiveness of transforaminal local anesthetic with or without steroids in disc herniation and spinal stenosis. They reported superior results for sciatica with similar efficacy for local anesthetic alone or with steroids. This was a high-quality trial based on Cochrane review criteria (10/12) as well as IPM-QRB criteria (32/48).
There was Level I evidence, based on multiple, relevant high-quality randomized controlled trials,[27,120,161,192] that local anesthetic with steroids provides significant improvement in transforaminal epidural injections, and that local anesthetic alone and local anesthetic with steroids are equally effective.
There was Level II evidence, based on one high-quality trial, that local anesthetics with steroids are superior to local anesthetic alone in avoiding surgery (33% vs 71%),[178] with another high-quality trial[192] showing avoidance of surgery in a similar proportion of patients in both the local anesthetic only and local anesthetic with steroids groups, with 82% of the patients able to avoid surgery. There was also Level III evidence that local anesthetic with steroids was superior to local anesthetic alone based on one high-quality randomized trial[52] with short-term follow-up and one moderate- to high-quality randomized trial.[159] There was Level IV evidence that transforaminal injections of sodium chloride solution were equally effective as transforaminal injections of steroids based on one high-quality randomized trial[87] with contradictory results from one high-quality randomized trial.[52]
Lumbar interlaminar epidural injections
There were six randomized controlled trials assessing the efficacy of multiple solutions used in lumbar interlaminar epidurals.[16,29,47,114,116,141] Three of these trials were rated as high quality based on Cochrane review criteria and IPM-QRB criteria.[114,116,141] One trial was high quality based on Cochrane review criteria. Two trials were rated as moderate-quality based on Cochrane review criteria;[29,47] however, utilizing IPM-QRB criteria, Cuckler et al.[29] and Carette et al.[16] were considered moderate-quality and Fukusaki et al.[47] was considered low-quality.
Three of these studies were conducted by Manchikanti et al.[114,116,141] with the same active control design protocol. The studies included a total of 360 patients to assess the efficacy of local anesthetic alone or local anesthetic with steroids in lumbar disc herniation, lumbar discogenic pain without facet joint or sacroiliac joint pain, and lumbar central spinal stenosis. The study period for each was 2 years. These studies were rated as high quality based on Cochrane review criteria, with all of them scoring 10 out of 12. The IPM-QRB for all of them was either 43 or 44 of 48. Similar efficacious results for epidural injections of local anesthetic alone or local anesthetic with steroids were seen in 60–84% of the patients in these studies.
In these manuscripts, the study subcategories were identified as responsive and nonresponsive groups. The responsive groups consisted of patients who received at least 3 weeks of significant improvement (50% improvement) in pain and function with the first two procedures. The number of patients in the nonresponsive category who received interlaminar epidural injections of local anesthetic only included 10 who had disc herniation, five who had discogenic pain, and nine patients who had central stenosis. In the corresponding nonresponsive local anesthetic with steroids category, the number of patients were: One who had disc herniation, six who had discogenic pain, and seven who had central stenosis. Thus, there was a high proportion of patients in the disc herniation group who were nonresponsive to lumbar interlaminar injections of local anesthetic, while there were no differences noted in the central stenosis or the discogenic pain groups compared with the corresponding responsive patients. In addition, in disc herniation, lumbar interlaminar epidural injections have somewhat superior results for pain relief at 6 months, and functional status at 12 months as observed in the local anesthetic with steroid group.[141] Thus, the results indicate that a patient who failed to respond to local anesthetic alone may be treated with the addition of steroids. The results were superior in the successful groups in all four categories. The disadvantage of all four trials has been that there was no inclusion of a placebo group.
Among the other trials, Fukusaki et al.[47] studied a small number of patients (53) divided into three groups. The patients were blindly injected with epidural saline (16), bupivacaine (18), or bupivacaine and methylprednisolone (19). There was a lack of effectiveness for any of the solutions at 3 months. Cuckler et al.[29] studied disc herniation and spinal stenosis in 73 patients: 36 with an acute herniated nucleus pulposus and 37 with spinal stenosis. Two injections and a 1-year follow-up showed the superiority of local anesthetic with steroids, however, only 17% in the local anesthetic only group and 31% in the local anesthetic with steroids group responded. This study showed a lack of effectiveness for either local anesthetic alone or local anesthetic with steroids based on the setting of this trial; however, it also showed low level evidence that local anesthetic with steroids may be superior.
Carette et al.,[16] in a widely publicized trial, showed a lack of effectiveness at 3 month follow-up for either normal saline or depomethylprednisolone with normal saline injected epidurally in the lumbar spine. This trial showed initial improvement with steroids; however, subsequent analysis showed no significant improvement. There was significant criticism of this manuscript based on the methodology used and the conclusions reached.[54,147,164,176]
Based on multiple high-quality randomized trials[114,116,141] showing efficacy, with one high-quality randomized trial showing a lack of efficacy for steroids without local anesthetic,[16] and two moderate-quality trials,[29,47] there was Level I evidence for lumbar interlaminar epidural injections in managing low back and/or lower extremity pain with or without local anesthetic with similar efficacy. There was no evidence for the superiority of steroids over local anesthetic with an interlaminar epidural approach, except with local anesthetic with steroids in disc herniation.[141]
Cervical interlaminar epidural injections
Among the trials meeting inclusion criteria, there were four high-quality trials[121,122,132,133] assessing the efficacy of cervical interlaminar epidural injections with multiple solutions.
All studies were conducted by Manchikanti et al.[121,122,132,133] as active control trials, assessing the efficacy of cervical interlaminar epidural injections, either with local anesthetic alone or local anesthetic with steroids, in cervical disc herniation, cervical discogenic pain without facet joint pain, cervical central spinal stenosis, and cervical postsurgery syndrome. Three hundred and fifty-six patients participated. There was a minimum 1-year follow-up for two of the trials and a 2-year follow-up for two of the trials. These studies were rated as high-quality, based on Cochrane review criteria of scores ranging from 10 to 11 of 12 and IPM-QRB criteria, with all of them scoring 42–44 of 48. All four trials showed similar results for the efficacy of epidural injections with local anesthetic alone or with steroids in 64–90% of the patients. In these manuscripts, the study categories were identified as nonresponsive and responsive groups. The responsive group consisted of patients who had at least 3 weeks of significant improvement (50% improvement) in pain and function with the first two procedures. For cervical interlaminar epidural injections in the nonresponsive category with local anesthetic alone, there were seven patients with disc herniation, five patients with discogenic pain, five patients with postsurgery syndrome, and one patient with central stenosis. In the corresponding nonresponsive category of local anesthetic with steroids there were 10, 4, 3, and 4 patients with these pathologies. Thus, there was no significant difference for various conditions in reference to nonresponsive or responsive patient groups. As shown in Table 4, when separate analyses of responsive patients and all patients are conducted, the results were superior in the responsive groups in all four categories. The disadvantage of all four trials was that there was no inclusion of a placebo group.
Based on multiple, high-quality relevant randomized trials,[121,122,132,133] the Level I evidence is equal for the efficacy of cervical epidural injections with local anesthetic alone or local anesthetic with steroids in managing neck and/or upper extremity pain.
Thoracic interlaminar epidural injections
There was only one trial assessing thoracic interlaminar epidural injections. It was conducted by Manchikanti et al.,[117] and of high quality based on Cochrane review criteria and IPM-QRB criteria.
Manchikanti et al.,[117] in a trial with a total of 110 patients, assessed the efficacy of thoracic interlaminar epidural injections with either local anesthetic or local anesthetic with steroids. This was an active control trial with appropriate sample size and a follow-up of 2 years. This trial showed similar efficacy for epidural injections, with improvement in 71% of patients who received local anesthetic alone and in 80% of patients who received local anesthetic with steroids. In this manuscript, the study categories were identified as nonresponsive and responsive groups. The responsive group consisted of at least 3 weeks of significant improvement (50% improvement) in pain and function with the first two procedures. In the nonresponsive category with local anesthetic only, there were four patients, and for local anesthetic with steroids, there were six patients. This study includes not only patients with disc herniation but also those with discogenic pain, central spinal stenosis, and postsurgery syndrome. This is the only study available in the literature studying the efficacy of thoracic interlaminar epidural injections.
There was Level II evidence based on one high-quality randomized trial[117] with positive results and no negative studies for the equal effectiveness of local anesthetic alone or local anesthetic with steroids.
Facet joint interventions
Lumbar, cervical, and thoracic facet joint nerve blocks and cervical and lumbar intraarticular injections have been studied with saline, local anesthetic, and steroids. There were six randomized controlled trials assessing the efficacy of facet joint interventions with multiple solutions.[8,17,137,142,143,144] All of these trials were rated as high-quality based on Cochrane review criteria and IPM-QRB criteria. Among these, four trials assessed the role of facet joint nerve blocks in the cervical, lumbar, and thoracic regions utilizing either local anesthetic alone or local anesthetic with steroids.[137,142,143,144] Two trials studied the role of facet joint intraarticular injections, Carette et al.[17] in the lumbar spine and Barnsley et al.[8] in the cervical spine. The trial by Carette et al.[17] faced significant criticism.[31,57]
Facet joint nerve blocks
Among the trials assessing facet joint nerve blocks, three of them included a 2-year follow-up, active control design, and appropriate outcome parameters.[142,143,144] The fourth one had a 1-year follow-up and was of lesser quality than the other three performed by the same group of authors.[137] All four studies were conducted by Manchikanti et al.[137,142,143,144] Three of them had identical protocols[142,143,144] assessing 330 patients in the cervical, lumbar, and thoracic regions. All three randomized active control trials showed similar results, with improvement sustained after 2 years in 70–92% of the patients. At 1-year follow-up, improvement was seen in 80–92% of the patients. All the studies showed similar results with significant improvement with either local anesthetic alone or local anesthetic with steroids. Thus, there was no significant difference for various regions in reference to the outcomes. The performance of all three studies by one group of authors finding positive results in each study may be considered an advantage or a deficiency. All the trials utilized appropriate outcome parameters and inclusion criteria and followed strict controlled diagnostic blocks with 80% concordant pain relief. The fourth study was performed by the same group of authors;[137] however, the quality parameters were much lower and the improvement was also inferior to the other randomized trials.
Based on the results of this assessment, these four trials, considered to be high-quality based on Cochrane review criteria and IPM-QRB criteria,[137,142,143,144] reported efficacy for facet joint nerve blocks in managing cervical, lumbar, or thoracic facet joint pain. All four trials showed equal effectiveness for local anesthetic with or without steroids, resulting in Level I evidence.
Facet joint injections
There was one randomized controlled trial by Carette et al.[17] assessing intraarticular injections either with isotonic saline or methylprednisolone acetate. Pain improvement was seen in both groups up to 6 months; however, after 6 months, both intraarticular sodium chloride solution and intraarticular methylprednisolone injections were judged to be equally ineffective. The authors concluded that intraarticular sodium chloride injection and methylprednisolone were equally effective after eliminating the confounding variables. Barnsley et al.[8] assessed the role of either local anesthetic intraarticular injection or betamethasone intraarticular injection in cervical facet joint pain and showed a lack of effectiveness for both injections.
Thus, there was Level I evidence for the lack of effectiveness for intraarticular injections based on two high-quality randomized controlled trials.[8,17] There was also Level II evidence based on one high-quality randomized trial that intraarticular steroids or sodium chloride solutions are equally ineffective and local anesthetic or steroids are equally ineffective.[8]
Efficacy of epidural injections in specific spinal conditions
Disc herniation
Disc herniation has been treated with caudal, lumbar interlaminar, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections. There was no identifiable evidence from randomized controlled trials for either cervical transforaminal epidural injections or thoracic transforaminal epidural injections in treating disc herniation.
There were 15 trials assessing the role of epidural injections in disc herniation,[16,27,29,52,79,87,117,120,122,139,141,161,178,182,192]: 3 caudal epidural injection trials,[79,139,182] 7 lumbar transforaminal epidural injection trials,[27,52,87,120,161,178,192] 3 lumbar interlaminar epidural trials,[16,29,141] 1 cervical interlaminar epidural trial,[122] and 1 thoracic interlaminar epidural trial.[117]
Of the three caudal epidural injection trials, one trial[139] was of high-quality based on Cochrane review criteria and IPM-QRB criteria; a second trial was high-quality[182] based on Cochrane review criteria and moderate based on IPM-QRB criteria; and a third trial was of moderate-quality.[79]
All seven randomized controlled trials[27,52,87,120,161,178,192] on the efficacy of transforaminal epidural injections of various drugs in disc herniation were rated as high-quality, scoring above 8 out of 12 on Cochrane review criteria.
Of the three lumbar interlaminar epidural trials,[16,29,141] one trial[141] was rated as high-quality on Cochrane review criteria and IPM-QRB criteria; one trial[16] was rated as high-quality on Cochrane review criteria and moderate-quality on IPM-QRB; and one trial[29] was rated as moderate-quality based on Cochrane review criteria and IPM-QRB criteria. One trial evaluated cervical interlaminar epidural injections[122] and one trial evaluated thoracic interlaminar epidural injections,[117] both of which were high-quality on Cochrane review criteria, as well as IPM-QRB criteria.
There was Level I evidence, based on multiple, relevant high-quality randomized trials,[27,117,122,139,141,161,192] for the efficacy of local anesthetic with steroids and equal efficacy for local anesthetic with or without steroids in managing disc herniation. Two trials of caudal epidural injections, one high-quality[139] and one moderate- to high-quality,[182] and one high-quality trial of lumbar interlaminar epidurals of local anesthetic with steroids compared to local anesthetic alone,[141] showed superiority for local anesthetic with steroids with Level II evidence. There was also Level III evidence, based on one high-quality trial, that local anesthetic with steroids is superior to local anesthetic alone in avoiding surgery.[178] Another high-quality trial[192] reported avoidance of surgery in a similar proportion of patients in both groups, with 82% of the patients avoiding surgery.
In addition to the above, the level of evidence for each vertebral region was variable. There was Level I evidence for caudal, lumbar interlaminar, and lumbar transforaminal injections in managing lumbar disc herniation, with multiple high quality randomized controlled trials. There was also superiority for steroids in managing disc herniation in the lumbosacral region compared with local anesthetic alone in assessments up to one year with caudal and interlaminar epidural injections.
However, there was Level II evidence for managing cervical disc herniation and thoracic disc herniation based on at least one high-quality randomized controlled trial in each category.
Spinal stenosis
Caudal, lumbar interlaminar, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections have been utilized in treating pain from central spinal stenosis. There are no randomized controlled trials assessing the role of cervical or thoracic transforaminal epidural injections in managing pain of central spinal stenosis. There were seven trials assessing the role of epidural injections in central spinal stenosis,[29,47,114,118,133,159,192] one caudal epidural trial,[118] two lumbar transforaminal trials,[159,192] three lumbar interlaminar trials,[29,47,114] and one cervical interlaminar epidural trial.[133]
The caudal epidural injection trial was high quality.[118] Of the two lumbar transforaminal epidural trials, one was high quality based on Cochrane and IPM-QRB criteria[192] and the second one[159] was high quality based on Cochrane review criteria and moderate quality based on IPM-QRB criteria. Among the lumbar interlaminar epidural trials, one was high quality[114] and the other two were moderate quality[29,47] based on Cochrane review criteria, with one being moderate quality[29] and one being low-quality[47] on IPM-QRB criteria. Among cervical interlaminar epidurals, there was only one study which was of high quality.[133] Thus, of the seven trials assessing the role of epidural injections in central spinal stenosis, five were high quality[114,118,133,159,192] and two were moderate quality[29,47] based on Cochrane review criteria and four were high quality,[87,114,118,133] two were moderate quality,[29,159] and one was low quality[47] based on IPM-QRB criteria.
There was Level I evidence, based on relevant high-quality trials,[114,118,133,192] showing positive results, for the equal effectiveness of local anesthetic alone or local anesthetic with steroids. There was Level IV evidence from one moderate-quality trial for the superiority of steroids,[159] and negative evidence from one moderate-quality randomized controlled trial[29] and one low-quality randomized controlled trial[47] with short-term follow-up.
There was Level II evidence in managing lumbar central spinal stenosis based on caudal and lumbar interlaminar trials, whereas there was also Level I evidence in managing cervical central spinal stenosis based on one randomized controlled trial, whereas there was no evidence available in managing thoracic spinal stenosis.
Discogenic pain
Discogenic pain has been treated with caudal, lumbar interlaminar, thoracic interlaminar, and cervical interlaminar epidural injections. There are no studies assessing the role of transforaminal epidural injections for discogenic pain.
There were three trials assessing the role of epidural injections in discogenic pain without disc herniation, radiculitis, or facet joint pain;[116,119,121] one caudal epidural injection trial;[119] one trial of lumbar interlaminar epidural injections;[116] and one trial of cervical interlaminar epidural injections.[121] All the trials were of high-quality and showed positive results with equal effectiveness for local anesthetic alone or local anesthetic with steroids.
There was Level I evidence, based on multiple high-quality relevant randomized controlled trials,[116,119,121] for the equal efficacy of local anesthetic or local anesthetic with steroids in managing discogenic pain.
There was Level II evidence based on two randomized controlled trials in managing discogenic pain with caudal and lumbar interlaminar epidural injections, with Level II evidence in managing cervical and thoracic discogenic pain, with one high-quality randomized controlled trial in each category.
Postsurgery syndrome
Postsurgery syndrome has been treated with caudal, lumbar transforaminal, thoracic interlaminar, and cervical interlaminar epidural injections. There were no studies assessing the role of lumbar interlaminar or transforaminal epidural injections.
There was only one randomized caudal epidural injection trial[140] and one cervical interlaminar epidural injection trial[132] assessing the role of epidural injections in postsurgery syndrome.
There was Level II evidence, based on the two high-quality, relevant randomized controlled trials,[132,140] for the equal efficacy of caudal and cervical interlaminar epidural injections in managing postsurgery syndrome with local anesthetic alone or local anesthetic with steroids.
There was Level II evidence in managing lumbar postsurgery syndrome with caudal epidural injections and cervical postsurgery syndrome with cervical interlaminar epidural injections, with no evidence available for thoracic postsurgery syndrome.
DISCUSSION
In this assessment of the efficacy of various solutions injected into the spinal epidural space and over the facet joint nerves, there was Level I evidence that local anesthetics with steroids and local anesthetics or steroids administered in combination or separately were equally effective based on multiple, relevant, high-quality randomized controlled trials of spinal pain from various origins. However, for intraarticular injection, the evidence of lack of effectiveness was Level I for injections of sodium chloride solution, local anesthetic, or local anesthetic with steroids. There was also Level II evidence for the superiority of local anesthetic with steroids compared with steroids alone in managing disc herniation and Level IV evidence in spinal stenosis.
In recent years, there has been much debate in reference to interventional techniques in general, and epidural injections of steroids in particular, with catastrophic complications related to transforaminal epidural steroid injections, specifically in the cervical and thoracic spine.[2,7,13,23,42,55,56,69,75,76,81,86,90,91,104,105,106,112,124,125,134,135,136,154,156,183,184,187,194] In fact, recently the Food and Drug Administration (FDA) issued a warning about the risk of serious, though rare, complications, and the lack of effectiveness of epidurally administered steroid injections.[194] However, this advice was issued based on cervical transforaminal epidural particulate steroid injections that resulted in catastrophic complications; only 3% of total epidural injections even involve cervical and thoracic transforaminal epidural injections.[128,130,138] This assessment clearly shows the efficacy of epidural injections of local anesthetic with or without steroids administered caudally, with interlaminar approaches, and with a lumbar transforaminal approach. Facet joint nerve blocks have also been shown to be efficacious. Further, this assessment also determined there was Level II evidence for the superiority of local anesthetic with steroids over local anesthetic alone in managing disc herniation and radiculitis.
The findings of this systematic review, showing the equal effectiveness of local anesthetics alone and local anesthetics with steroid administered into the epidural space, facet joints, or over facet joint nerves, is in contrast to a long-held philosophy and belief in the medical community concerning the effectiveness of steroids in treating spinal pain based on the theory of spinal pain having an inflammatory component. The results of this study are valid as only high-quality, randomized controlled trials were utilized. Further, the grading of the evidence was based on a best-evidence synthesis utilizing a strict approach for methodological quality assessment. The long-term follow-up of one year or longer was utilized in arriving at the conclusions rather than short-term follow-up of 1, 3, 6, or even 12 weeks, etc., In fact, the results are similar to the Bicket et al.[12] study results, which included not only epidural injections, but also nonspinal epidural injections. Even though the Bicket et al.[12] review had some deficiencies,[26,38,127] they concluded that epidural nonsteroid injections may provide greater benefit for spinal pain than nonepidural injections based on the significant but small difference found between the two treatments when examining the positive response outcome. These differences were greater compared with the differences between epidural steroid injections and epidural nonsteroid injections, suggesting that, at least in the short-term, most of the benefit of epidural injections may derive from the solution itself, rather than the steroid.[12] Epidural nonsteroid injections also showed an insignificant trend in Bicket et al.'s[12] evaluation toward greater relief when examining pain score reductions with indirect comparisons. In contrast, in our assessment we utilized long-term assessments with stringent methodological quality criteria; however, we were unable to perform a meta-analysis, which may have not been very accurate by Bicket et al.[12,26,38,127]
The findings of this systematic review may be explained by various mechanisms of steroids and local anesthetics, including the suppression of ectopic discharges from inflamed nerves, enhancing blood flow to ischemic nerve roots, the lysing of iatrogenic and inflammatory adhesions, a washout of proinflammatory cytokines, and reversal of peripheral and central sensitization.[10,30,47,58,60,68,77,89,95,96,179,190,198,200] Bicket et al.[12] hypothesized a placebo effect with epidural injections, especially those administered via the transforaminal approach, often with reproduction of radicular symptoms, which is not observed with soft tissue injections, resulting in high levels of placebo effect and undermining the effectiveness of blinding.[37,85,173] However, Karppinen et al.[87,88] utilized this approach and showed equal results. In contrast, Ghahreman et al.[51,52] essentially showed a better response for an intramuscular injection than a transforaminal sodium chloride solution. The resultant numbness and weakness also may influence blinding as well as the patient's response. However, widespread complex mechanisms and variations in placebo and nocebo response have been well described.[65,70,71,74,84,85,103] And thus far, appropriately designed placebo studies (injecting inactive solutions into inactive structures) have not resulted in a significant placebo effect.[50,51,52]
Noteworthy as well is that investigators may be missing the role of the nocebo effect. The implications of these results may be significant in not only designing clinical trials, but also in managing patients. Further, it is essential to understand the differences between chronic and subacute pain. Many of the studies included subacute or acute patients, leading to erroneous conclusions. In this evaluation, we also included some trials that included subacute patients; however, they were followed long-term.[27,79,182]
Based on this evaluation as well as the Bicket et al.[12] evaluation, it appears that local anesthetic alone epidural injections or facet joint nerve blocks may be a viable option. Using local anesthetic alone may reduce the risk of rare, but potentially fatal, complications such as meningitis[23,81,124,187] and rare, but real, catastrophic consequences, such as paralysis and death, reported from cervical and thoracic transforaminal epidural injections. Further, patients who have undergone previous surgery may also be considered as high risk. The literature shows a lack of superiority for local anesthetic with epidural steroids over local anesthetic alone, even though lumbar interlaminar epidural injections and any type of transforaminal epidural injection have not been studied with appropriate evidence in postsurgery syndrome. In addition, the dose of steroids may be significantly reduced from the traditional doses of 120 mg or higher. In fact, multiple policies have been mandating the use of lower doses of steroids.[22,160,162] There is also support in the literature for a lack of difference in efficacy between high- and low-dose epidural steroid injections and reduction of adverse events with low-dose steroids.[4,41,82,83,92,93,152,165,202] High-risk patients may include not only postsurgery patients, but also the techniques involving transforaminal approaches and patients with diabetes with a risk of hyperglycemia,[41,93,109] plus those at a high risk of osteopenia and osteoporosis,[4,82,92,202] those at risk for avascular necrosis,[59] those with a risk for adverse effects with suppression of the hypothalamic–pituitary–adrenocortical axis scheduled for major surgery,[197] and those with poor wound healing and immunosuppression.
However, these results should be interpreted in the context of their multiple limitations. Based on the results, an abundant amount of steroids is not advised. As explained, there was no meta-analysis performed. The majority of the high-quality, randomized trials included in this analysis were from one group of investigators. Consequently, further trials are essential. At present, this evidence suggests physicians carefully select patients and take the opportunity to discuss with them shared decision-making concerning the equal efficacy of local anesthetic with or without steroids in multiple conditions. Steroids with local anesthetic appear to have some superiority, even though it is derived from a low level of evidence, over local anesthetics alone in managing disc herniation.
CONCLUSION
This systematic review shows a lack of effectiveness for saline and equal effectiveness for local anesthetic alone and local anesthetic with steroids in multiple, high-quality randomized controlled trials for epidural injections for managing spinal pain in various regions for various pathologies and facet joint nerve blocks in managing facet joint pain. The results also showed the superiority of epidural steroid injections with local anesthetic over local anesthetics alone for disc herniation.
ACKNOWLEDGMENTS
The authors wish to thank Vidyasagar Pampati, MSc, for statistical assistance; Tom Prigge, MA, and Laurie Swick, BS, for manuscript review; and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
Appendix 1.
Randomized controlled trials quality rating system
Appendix 2.
Item checklist for assessment of randomized controlled trials of IPM techniques utilizing IPM-QRB
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/5/194/156598
Contributor Information
Laxmaiah Manchikanti, Email: drlm@thepainmd.com.
Devi E. Nampiaparampil, Email: devichechi@gmail.com.
Kavita N. Manchikanti, Email: kavita.manchikanti@gmail.com.
Frank J.E. Falco, Email: cssm01@aol.com.
Vijay Singh, Email: vj@wmpnet.net.
Ramsin M. Benyamin, Email: ramsinbenyamin@yahoo.com.
Alan D. Kaye, Email: alankaye44@hotmail.com.
Nalini Sehgal, Email: Sehgal@rehab.wisc.edu.
Amol Soin, Email: ohiopainclinic@gmail.com.
Thomas T. Simopoulos, Email: tsimopou@bidmc.harvard.edu.
Sanjay Bakshi, Email: drbakshi58@gmail.com.
Christopher G. Gharibo, Email: cgharibo@usa.net.
Christopher J. Gilligan, Email: cgilligan@partners.org.
Joshua A. Hirsch, Email: HIrsch@snisonline.org.
REFERENCES
- 1.Abbott ZI, Nair KV, Allen RR, Akuthota VR. Utilization characteristics of spinal interventions. Spine J. 2012;12:35–43. doi: 10.1016/j.spinee.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Akkaya T, Sayin M. Transforaminal epidural steroid injection and its complications. Agri. 2005;17:27–39. [PubMed] [Google Scholar]
- 3.Alimasi W, Sawaji Y, Endo K, Yorifuji M, Suzuki H, Kosaka T, et al. Regulation of nerve growth factor by anti-inflammatory drugs, a steroid, and a selective cyclooxygenase 2 inhibitor in human intervertebral disc cells stimulated with interleukin-1. Spine (Phila Pa 1976) 2013;38:1466–72. doi: 10.1097/BRS.0b013e318294edb1. [DOI] [PubMed] [Google Scholar]
- 4.Al-Shoha A, Rao DS, Schilling J, Peterson E, Mandel S. Effect of epidural steroid injection on bone mineral density and markers of bone turnover in postmenopausal women. Spine (Phila Pa 1976) 2012;37:E1567–71. doi: 10.1097/BRS.0b013e318270280e. [DOI] [PubMed] [Google Scholar]
- 5.Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study. Rheumatology (Oxford) 2005;44:1399–406. doi: 10.1093/rheumatology/kei028. [DOI] [PubMed] [Google Scholar]
- 6.Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic block. A call for further experimental and systematic clinical studies. Pain. 1990;43:287–97. doi: 10.1016/0304-3959(90)90026-A. [DOI] [PubMed] [Google Scholar]
- 7.Atluri S, Glaser SE, Shah RV, Sudarsha G. Needle position analysis in cases of paralysis from transforaminal epidurals: Consider alternative approaches to traditional techniques. Pain Physician. 2013;16:321–34. [PubMed] [Google Scholar]
- 8.Barnsley L, Lord SM, Wallis BJ, Bogduk N. Lack of effect of intraarticular corticosteroids for chronic pain in the cervical zygapophyseal joints. N Engl J Med. 1994;330:1047–50. doi: 10.1056/NEJM199404143301504. [DOI] [PubMed] [Google Scholar]
- 9.Benyamin RM, Manchikanti L, Parr AT, Diwan SA, Singh V, Falco FJE, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15:E363–404. [PubMed] [Google Scholar]
- 10.Bhatia MT, Parikh LCJ. Epidural saline therapy in lumbo-sciatic syndrome. J Indian Med Assoc. 1966;47:537–42. [PubMed] [Google Scholar]
- 11.Bhushan A, Leigh JP. National trends in occupational injuries before and after 1992 and predictors of workers’ compensation costs. Public Health Rep. 2011;126:625–34. doi: 10.1177/003335491112600504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bicket M, Gupta A, Brown CH, Cohen SP. Epidural injections for spinal pain: A systematic review and meta-analysis evaluating the “control” injections in randomized controlled trials. Anesthesiology. 2013;119:907–31. doi: 10.1097/ALN.0b013e31829c2ddd. [DOI] [PubMed] [Google Scholar]
- 13.Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000;81:1045–50. doi: 10.1053/apmr.2000.7166. [DOI] [PubMed] [Google Scholar]
- 14.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine (Phila Pa 1976) 1999;24:1813–9. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Task Force on Preventive Health Care. Procedure Manual. March 2014. [Last accessed on 2015 Jan 27]. Available from: http://canadiantaskforce.ca/wp-content/uploads/2014/03/Procedure-Manual-2014-v2-0FINAL.pdf/?414ed1 .
- 16.Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634–40. doi: 10.1056/NEJM199706053362303. [DOI] [PubMed] [Google Scholar]
- 17.Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991;325:1002–7. doi: 10.1056/NEJM199110033251405. [DOI] [PubMed] [Google Scholar]
- 18.Cassidy JD, Carroll LJ, Côté P. The Saskatchewan Health and Back Pain Survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23:1860–7. doi: 10.1097/00007632-199809010-00012. [DOI] [PubMed] [Google Scholar]
- 19.Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006;50:265–82. doi: 10.1111/j.1399-6576.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- 20.Cathelin MF. Mode d’action de la cocaine injecte daus l’escape epidural par le procede du canal sacre. Comptes Rendues des Seances de la Societe de Biologie et de ses Filliales (Paris) 1901;43:487. [Google Scholar]
- 21.Cecchi F, Debolini P, Lova RM, Macchi C, Bandinelli S, Bartali B, et al. Epidemiology of back pain in a representative cohort of Italian persons 65 years of age and older: The InCHIANTI study. Spine (Phila Pa 1976) 2006;31:1149–55. doi: 10.1097/01.brs.0000216606.24142.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CGS Administrators, LLC. LCD for Pain Management (L31845) [Revision Effective Date: 01/01/2012]; [Google Scholar]
- 23.Chiller TM, Roy M, Nguyen D, Guh A, Malani AN, Latham R, et al. Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013;4(369):1610–9. doi: 10.1056/NEJMoa1304879. [DOI] [PubMed] [Google Scholar]
- 24.Chou R, Huffman L. Glenview, IL: American Pain Society; 2009. [Last accessed on 2015 Jan 27]. Guideline for the Evaluation and Management of Low Back Pain: Evidence Review. Available from: http://www.americanpainsociety.org/uploads/pdfs/LBPEvidRev.pdf . [Google Scholar]
- 25.Civelek E, Cansever T, Kabatas S, Kircelli A, Yilmaz C, Musluman M, et al. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg. 2012;22:200–6. doi: 10.5137/1019-5149.JTN.5207-11.1. [DOI] [PubMed] [Google Scholar]
- 26.Cohen SP, Bicket MC. In Reply. Anesthesiology. 2014;120:1284–5. doi: 10.1097/ALN.0000000000000199. [DOI] [PubMed] [Google Scholar]
- 27.Cohen SP, White RL, Kurihara C, Larkin TM, Chang A, Griffith SR, et al. Epidural steroids, etanercept, or saline in subacute sciatica: A multicenter, randomized trial. Ann Intern Med. 2012;156:551–9. doi: 10.7326/0003-4819-156-8-201204170-00397. [DOI] [PubMed] [Google Scholar]
- 28.Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23:1689–98. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 29.Cuckler JM, Bernini PA, Wiesel SW, Booth RE, Jr, Rothman RH, Pickens GT. The use of epidural steroid in the treatment of radicular pain. J Bone Joint Surg. 1985;67:63–6. [PubMed] [Google Scholar]
- 30.Cui W, Li Y, Li S, Wang R, Li J. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil based anaesthesia. Eur J Anaesthesiol. 2010;27:41–6. doi: 10.1097/EJA.0b013e32832d5426. [DOI] [PubMed] [Google Scholar]
- 31.Culling RD, Rice JH. Corticosteroid injections for chronic low back pain. N Engl J Med. 1992;326:834. doi: 10.1056/NEJM199203193261213. [DOI] [PubMed] [Google Scholar]
- 32.Cyriax JH. Epidural anesthesia and bedrest in sciatica. Br Med J. 1961;1:20–4. [Google Scholar]
- 33.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441–5. doi: 10.1097/01.brs.0000166503.37969.8a. [DOI] [PubMed] [Google Scholar]
- 34.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–46. doi: 10.1097/01.blo.0000198726.62514.75. [DOI] [PubMed] [Google Scholar]
- 35.Dilke TF, Burry HC, Grahame R. Extradural corticosteroid injection in the management of lumbar nerve root compression. Br Med J. 1973;2:635–7. doi: 10.1136/bmj.2.5867.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diwan SA, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012;15:E405–34. [PubMed] [Google Scholar]
- 37.Dooley JF, McBroom RJ, Taguchi T, Macnab I. Nerve root infiltration in the diagnosis of radicular pain. Spine (Phila Pa 1976) 1988;13:79–83. doi: 10.1097/00007632-198801000-00019. [DOI] [PubMed] [Google Scholar]
- 38.Engel AJ, Kennedy DJ, Macvicar J, Bogduk N. Not all injections are the same. Anesthesiology. 2014;120:1282–3. doi: 10.1097/ALN.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 39.Eriksen J, Ekholm O, Sjøgren P, Rasmussen NK. Development of and recovery from long-term pain. A 6-year follow-up study of a cross-section of the adult Danish population. Pain. 2004;108:154–62. doi: 10.1016/j.pain.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 40.Evans W. Intrasacral epidural injection in the treatment of sciatica. Lancet. 1930;2:1225–9. [Google Scholar]
- 41.Even JL, Crosby CG, Song Y, McGirt MJ, Devin CJ. Effects of epidural steroid injections on blood glucose levels in patients with diabetes mellitus. Spine (Phila Pa 1976) 2012;37:E46–50. doi: 10.1097/BRS.0b013e31821fd21f. [DOI] [PubMed] [Google Scholar]
- 42.Everett CR, Baskin MN, Speech D, Novoseletsky D, Patel R. Flushing as a side effect following lumbar transforaminal epidural steroid injection. Pain Physician. 2004;7:427–9. [PubMed] [Google Scholar]
- 43.Falco FJ, Manchikanti L, Datta S, Sehgal N, Geffert S, Onyewu O, et al. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician. 2012;15:E909–53. [PubMed] [Google Scholar]
- 44.Falco FJ, Manchikanti L, Datta S, Wargo BW, Geffert S, Bryce DA, et al. Systematic review of therapeutic effectiveness of cervical facet joint interventions: An update. Pain Physician. 2012;15:E839–68. [PubMed] [Google Scholar]
- 45.Fernández-de-Las-Peñas C, Alonso-Blanco C, Hernández-Barrera V, Palacios-Ceña D, Jiménez-García R, Carrasco-Garrido P. Has the prevalence of neck pain and low back pain changed over the last 5 years? A population-based national study in Spain. Spine J. 2013;13:1069–76. doi: 10.1016/j.spinee.2013.02.064. [DOI] [PubMed] [Google Scholar]
- 46.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14:148–51. doi: 10.1097/00002508-199806000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Furlan AD, Pennick V, Bombardier C, van Tulder M. Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 49.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–24. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: A randomized double-blind placebo controlled trial. Pain Physician. 2013;16:185–96. [PubMed] [Google Scholar]
- 51.Ghahreman A, Bogduk N. Predictors of a favorable response to transforaminal injection of steroids in patients with lumbar radicular pain due to disc herniation. Pain Med. 2011;12:871–9. doi: 10.1111/j.1526-4637.2011.01116.x. [DOI] [PubMed] [Google Scholar]
- 52.Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010;11:1149–68. doi: 10.1111/j.1526-4637.2010.00908.x. [DOI] [PubMed] [Google Scholar]
- 53.Ghanei I, Rosengren BE, Hasserius R, Nilsson JÅ, Mellström D, Ohlsson C, et al. The prevalence and severity of low back pain and associated symptoms in 3,009 old men. Eur Spine J. 2014;23:814–20. doi: 10.1007/s00586-013-3139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gillies JH, Ward JH, Griesdale DE. Corticosteroid injections for sciatica. N Engl J Med. 1997;337:1242. [PubMed] [Google Scholar]
- 55.Glaser SE, Falco FJ. Paraplegia following a thoracolumbar transforaminal epidural steroid injection. Pain Physician. 2005;8:309–14. [PubMed] [Google Scholar]
- 56.Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: The “unsafe” triangle. Pain Physician. 2010;13:237–44. [PubMed] [Google Scholar]
- 57.Gostine M. Corticosteroid injections for chronic low back pain. N Engl J Med. 1992;326:834–5. [PubMed] [Google Scholar]
- 58.Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012;28:567–72. doi: 10.1097/AJP.0b013e31823b9cc8. [DOI] [PubMed] [Google Scholar]
- 59.Gunal I, Karatosun V. Avascular necrosis of the femoral heads after single corticosteroid injection. CMAJ. 2006;175:31. doi: 10.1503/cmaj.051638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta AK, Mital VK, Azmi RU. Observations of the management of lumbosciatic syndromes (sciatica) by epidural saline. J Indian Med Assoc. 1970;54:194–6. [PubMed] [Google Scholar]
- 61.Gupta S, Ward S, Munglani R, Sharma M. Lversen T, et al., editors. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. Careful patient selection, fluoroscopy and contrast injection are needed for effective spinal injections. Published online 9/26/2011. Author's reply: Published online 9/29/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B, et al. Grading strength of recommendations and quality of evidence in clinical guidelines. Report from an American College of Chest Physicians task force. Chest. 2006;129:174–81. doi: 10.1378/chest.129.1.174. [DOI] [PubMed] [Google Scholar]
- 63.Hansen H, Manchikanti L, Simopoulous TT, Christo PJ, Gupta S, Smith HS, et al. A systematic evaluation of the therapeutic effectiveness of sacroiliac joint interventions. Pain Physician. 2012;15:E247–78. [PubMed] [Google Scholar]
- 64.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the US Preventive Services Task Force. Am J Prevent Med. 2001;20:21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 65.Häuser W, Bartram C, Bartram-Wunn E, Tölle T. Adverse events attributable to nocebo in randomized controlled drug trials in fibromyalgia syndrome and painful diabetic peripheral neuropathy: Systematic review. Clin J Pain. 2012;28:437–51. doi: 10.1097/AJP.0b013e3182321ad8. [DOI] [PubMed] [Google Scholar]
- 66.Hayashi N, Weinstein JN, Meller ST, Lee HM, Spratt KF, Gebhart GF. The effect of epidural injection of betamethasone or bupivacaine in a rat model of lumbar radiculopathy. Spine (Phila Pa 1976) 1998;23:877–85. doi: 10.1097/00007632-199804150-00008. [DOI] [PubMed] [Google Scholar]
- 67.He L, Uçeyler N, Krämer HH, Colaço MN, Lu B, Birklein F, et al. Methylprednisolone prevents nerve injury-induced hyperalgesia in neprilysin knockout mice. Pain. 2014;155:574–80. doi: 10.1016/j.pain.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 68.Hollmann MW, Durieux M. Local anesthetics and the inflammatory response. Anesthesiology. 2000;93:858–75. doi: 10.1097/00000542-200009000-00038. [DOI] [PubMed] [Google Scholar]
- 69.Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: Report of three cases. Spine J. 2002;2:70–5. doi: 10.1016/s1529-9430(01)00159-0. [DOI] [PubMed] [Google Scholar]
- 70.Howick J, Bishop FL, Heneghan C, Wolstenholme J, Stevens S, Hobbs FD, et al. Placebo use in the United Kingdom: Results from a national survey of primary care practitioners. PLOS One. 2013;8:e58247. doi: 10.1371/journal.pone.0058247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Howick J, Friedemann C, Tsakok M, Watson R, Tsakok T, Thomas J, et al. Are treatments more effective than placebos? A systematic review and meta-analysis. PLoS One. 2013;8:e62599. doi: 10.1371/journal.pone.0062599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoy DG, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–37. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 73.Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010;24:783–92. doi: 10.1016/j.berh.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 74.Hróbjartsson A, Gøtzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev. 2010;1:CD003974. doi: 10.1002/14651858.CD003974.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huntoon MA, Martin DP. Paralysis after transforaminal epidural injection and previous spinal surgery. Reg Anesth Pain Med. 2004;29:494–5. doi: 10.1016/j.rapm.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 76.Huston CW, Slipman CW, Garvin C. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehabil. 2005;86:277–83. doi: 10.1016/j.apmr.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 77.Igarashi T, Kikuchi S, Shubayev V, Myers RR. Exogenous tumor necrosis factor-alpha mimics nucleus pulposusinduced neuropathology. Spine. 2000;25:2975–80. doi: 10.1097/00007632-200012010-00003. [DOI] [PubMed] [Google Scholar]
- 78.Washington, DC: The National Academies Press; 2011. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. [PubMed] [Google Scholar]
- 79.Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, et al. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur Spine J. 2011;20:513–22. doi: 10.1007/s00586-010-1603-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kainer MA, Reagan DR, Nguyen DB, Wiese AD, Wise ME, Ward J, et al. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012;367:2194–203. doi: 10.1056/NEJMoa1212972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kang SS, Hwang BM, Son H, Cheong IY, Lee SJ, Chung TY. Changes in bone mineral density in postmenopausal women treated with epidural steroid injections for lower back pain. Pain Physician. 2012;15:229–36. [PubMed] [Google Scholar]
- 83.Kang SS, Hwang BM, Son HJ, Cheong IY, Lee SJ, Lee SH, et al. The dosages of corticosteroid in transforaminal epidural steroid injections for lumbar radicular pain due to a herniated disc. Pain Physician. 2011;14:361–70. [PubMed] [Google Scholar]
- 84.Kaptchuk TJ, Friedlander E, Kelley JM, Sanchez MN, Kokkotou E, Singer JP, et al. Placebos without deception: A randomized controlled trial in irritable bowel syndrome. PLoS ONE. 2010;5:e15591. doi: 10.1371/journal.pone.0015591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kaptchuk TJ, Stason WB, Davis RB, Legedza AR, Schnyer RN, Kerr CE, et al. Sham device v inert pill: Randomised controlled trial of two placebo treatments. BMJ. 2006;332:391–7. doi: 10.1136/bmj.38726.603310.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Karaman H, Kavak GO, Tüfek A, Yldrm ZB. The complications of transforaminal lumbar epidural steroid injections. Spine (Phila Pa 1976) 2011;36:E819–24. doi: 10.1097/BRS.0b013e3181f32bae. [DOI] [PubMed] [Google Scholar]
- 87.Karppinen J, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, Nieminen P, et al. Periradicular infiltration for sciatica: A randomized controlled trial. Spine (Phila Pa 1976) 2001;26:1059–67. doi: 10.1097/00007632-200105010-00015. [DOI] [PubMed] [Google Scholar]
- 88.Karppinen J, Ohinmaa A, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, et al. Cost effectiveness of periradicular infiltration for sciatica: Subgroup analysis of a randomized controlled trial. Spine (Phila Pa 1976) 2001;26:2587–95. doi: 10.1097/00007632-200112010-00013. [DOI] [PubMed] [Google Scholar]
- 89.Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E, et al. Experimental incision induced pain in human skin: Effects of systemic lidocaine on flare formation and hyperalgesia. Pain. 2002;100:77–89. doi: 10.1016/s0304-3959(02)00233-6. [DOI] [PubMed] [Google Scholar]
- 90.Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: Two case reports. Pain Med. 2009;10:1389–94. doi: 10.1111/j.1526-4637.2009.00728.x. [DOI] [PubMed] [Google Scholar]
- 91.Khan S, Pioro EP. Cervical epidural injection complicated by syrinx formation: A case report. Spine (Phila Pa 1976) 2010;35:E614–6. doi: 10.1097/BRS.0b013e3181cf7621. [DOI] [PubMed] [Google Scholar]
- 92.Kim S, Hwang B. Relationship between bone mineral density and the frequent administration of epidural steroid injections in postmenopausal women with low back pain. Pain Res Manag. 2014;19:30–4. doi: 10.1155/2014/870145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kim WH, Sim WS, Shin BS, Lee CJ, Jin HS, Lee JY, et al. Effects of two different doses of epidural steroid on blood glucose levels and pain control in patients with diabetes mellitus. Pain Physician. 2013;16:557–68. [PubMed] [Google Scholar]
- 94.Klenerman L, Greenwood R, Davenport HT, White DC, Peskett S. Lumbar epidural injections in the treatment of sciatica. Br J Rheumatol. 1984;23:35–8. doi: 10.1093/rheumatology/23.1.35. [DOI] [PubMed] [Google Scholar]
- 95.Koppert W, Ostermaier N, Sittl R, Weidner C, Schmelz M. Low dose lidocaine reduces secondary hyperalgesia by a central mode of action. Pain. 2000;85:217–24. doi: 10.1016/s0304-3959(99)00268-7. [DOI] [PubMed] [Google Scholar]
- 96.Koppert W, Zeck S, Sittl R. Low dose lidocaine suppresses experimentally induced hyperalgesia in humans. Anesthesiology. 1998;89:1345–53. doi: 10.1097/00000542-199812000-00011. [DOI] [PubMed] [Google Scholar]
- 97.Kovacs FM, Urrútia G, Alarcón JD. Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: A systematic review of randomized controlled trials. Spine (Phila Pa 1976) 2011;36:E1335–51. doi: 10.1097/BRS.0b013e31820c97b1. [DOI] [PubMed] [Google Scholar]
- 98.Kraemer J, Ludwig J, Bickert U, Owczarek V, Traupe M. Lumbar epidural perineural injection: A new technique. Eur Spine J. 1997;6:357–61. doi: 10.1007/BF01142687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lavoie PA, Khazen T, Filion PR. Mechanisms of the inhibition of fast axonal transport by local anesthetics. Neuropharmacology. 1989;28:175–81. doi: 10.1016/0028-3908(89)90054-3. [DOI] [PubMed] [Google Scholar]
- 100.Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: Do age and gender matter? A population-based study of 34,902 Danish twins 20-71 years of age. BMC Musculoskelet Disord. 2009;10:39. doi: 10.1186/1471-2474-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011;89:728–72. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009;151:W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 103.Lyby PS, Forsberg JT, Asli O, Flaten MA. Induced fear reduces the effectiveness of a placebo intervention on pain. Pain. 2012;153:1114–21. doi: 10.1016/j.pain.2012.02.042. [DOI] [PubMed] [Google Scholar]
- 104.Lyders EM, Morris PP. A case of spinal cord infarction following lumbar transforaminal epidural steroid injection: MR imaging and angiographic findings. AJNR Am J Neuroradiol. 2009;30:1691–3. doi: 10.3174/ajnr.A1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.MacMahon PJ, Crosbie I, Kavanagh EC. Reducing the risk of spinal cord infarction during transforaminal steroid injections. AJNR Am J Neuroradiol. 2010;31:E32. doi: 10.3174/ajnr.A1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Malhotra G, Abbasi A, Rhee M. Complications of transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976) 2009;34:731–9. doi: 10.1097/BRS.0b013e318194e247. [DOI] [PubMed] [Google Scholar]
- 107.Manchikanti KN, Atluri S, Singh V, Geffert S, Sehgal N, Falco FJ. An update of evaluation of therapeutic thoracic facet joint interventions. Pain Physician. 2012;15:E463–81. [PubMed] [Google Scholar]
- 108.Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2 – Guidance. Pain Physician. 2012;15:S67–116. [PubMed] [Google Scholar]
- 109.Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence. based guidelines for interventional techniques of chronic spinal pain: Part II: Guidance and recommendations. Pain Physician. 2013;16:S49–283. [PubMed] [Google Scholar]
- 110.Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res. 2014 Feb 11; doi: 10.1007/s11999-014-3490-4. Epub ahead of print. DOI: 10.1007/s11999-014-3490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Manchikanti L, Benyamin RM, Falco FJE, Caraway DL, Datta S, Hirsch JA. Guidelines warfare over interventional techniques: Is there a lack of discourse or straw man? Pain Physician. 2012;15:E1–26. [PubMed] [Google Scholar]
- 112.Manchikanti L, Benyamin RM, Swicegood JR, Falco FJE, Datta S, Pampati V, et al. Assessment of practice patterns of perioperative management of antiplatelet and anticoagulant therapy in interventional pain management. Pain Physician. 2012;15:E955–68. [PubMed] [Google Scholar]
- 113.Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15:E199–245. [PubMed] [Google Scholar]
- 114.Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. A randomized, double-blind controlled trial of lumbar interlaminar epidural injections in central spinal stenosis: 2-year follow-up. Pain Physician. 2015;18:79–92. [PubMed] [Google Scholar]
- 115.Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. Lumbar interlaminar epidural injections in central spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:51–63. [PubMed] [Google Scholar]
- 116.Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back pain: Results of a 2-year follow-up. Pain Physician. 2013;16:E491–504. [PubMed] [Google Scholar]
- 117.Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. Assessment of thoracic interlaminar epidural injections in managing chronic thoracic pain: A randomized, double-blind, controlled trial with a 2-year follow-up. Pain Physician. 2014;17:E327–38. [PubMed] [Google Scholar]
- 118.Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012;5:371–84. [PubMed] [Google Scholar]
- 119.Manchikanti L, Cash KA, McManus CD, Pampati V. Fluoroscopic caudal epidural injections in managing chronic axial low back pain without disc herniation, radiculitis or facet joint pain. J Pain Res. 2012;5:381–90. doi: 10.2147/JPR.S35924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Manchikanti L, Cash KA, Pampati V, Falco FJ. Transforaminal epidural injections in chronic lumbar disc herniation: A randomized, double-blind, active-control trial. Pain Physician. 2014;17:E489–501. [PubMed] [Google Scholar]
- 121.Manchikanti L, Cash KA, Pampati V, Malla Y. Two-year follow-up results of fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain: A randomized, double-blind, controlled trial. Int J Med Sci. 2014;11:309–20. doi: 10.7150/ijms.8069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. A randomized, double-blind, active control trial of fluoroscopic cervical interlaminar epidural injections in chronic pain of cervical disc herniation: Results of a 2-year follow-up. Pain Physician. 2013;16:465–78. [PubMed] [Google Scholar]
- 123.Manchikanti L, Falco FJ, Diwan S, Hirsch JA, Smith HS. Cervical radicular pain: The role of interlaminar and transforaminal epidural injections. Curr Pain Headache Rep. 2014;18:389. doi: 10.1007/s11916-013-0389-9. [DOI] [PubMed] [Google Scholar]
- 124.Manchikanti L, Falco FJE, Benyamin RM, Caraway DL, Helm S, II, Wargo BW, et al. Assessment of infection control practices for interventional techniques: A best evidence synthesis of safe injection practices and use of single-dose medication vials. Pain Physician. 2012;15:E573–614. [PubMed] [Google Scholar]
- 125.Manchikanti L, Falco FJ, Benyamin RM, Caraway DL, Kaye AD, Helm S, II, et al. Assessment of bleeding risk of interventional techniques: A best evidence synthesis of practice patterns and perioperative management of anticoagulant and antithrombotic therapy. Pain Physician. 2013;16:SE261–318. [PubMed] [Google Scholar]
- 126.Manchikanti L, Falco FJE, Benyamin RM, Kaye AD, Boswell MV, Hirsch JA. A modified approach to grading of evidence. Pain Physician. 2014;17:E319–25. [PubMed] [Google Scholar]
- 127.Manchikanti L, Falco FJ, Hirsch JA. Bicket M, Gupta A, Brown CH, Cohen SP, editors. Epidural injections for spinal pain: A systematic review and meta-analysis evaluating the “control” injections in randomized controlled trials. Anesthesiology. 2013;119:907–31. doi: 10.1097/ALN.0b013e31829c2ddd. [DOI] [PubMed] [Google Scholar]
- 128.Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, et al. Utilization of interventional techniques in managing chronic pain in the Medicare population: Analysis of growth patterns from 2000 to 2011. Pain Physician. 2012;15:E969–82. [PubMed] [Google Scholar]
- 129.Manchikanti L, Helm S, II, Fellows B, Janata JW, Pampati V, Grider JS, et al. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9–38. [PubMed] [Google Scholar]
- 130.Manchikanti L, Helm S, II, Singh V, Hirsch JA. Accountable interventional pain management: A collaboration among practitioners, patients, payers, and government. Pain Physician. 2013;16:E635–70. [PubMed] [Google Scholar]
- 131.Manchikanti L, Hirsch JA, Cohen SP, Heavner JE, Falco FJ, Diwan S, et al. Assessment of methodologic quality of randomized trials of interventional techniques: Development of an interventional pain management specific instrument. Pain Physician. 2014;17:E263–90. [PubMed] [Google Scholar]
- 132.Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical post-surgery syndrome: Preliminary results of a randomized, double-blind active control trial. Pain Physician. 2012;15:13–26. [PubMed] [Google Scholar]
- 133.Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic epidural injections in cervical spinal stenosis: Preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:E59–70. [PubMed] [Google Scholar]
- 134.Manchikanti L, Malla Y, Wargo BW, Cash KA, McManus CD, Damron KS, et al. A prospective evaluation of bleeding risk of interventional techniques in chronic pain. Pain Physician. 2011;14:317–29. [PubMed] [Google Scholar]
- 135.Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012;15:131–40. [PubMed] [Google Scholar]
- 136.Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: A prospective evaluation of 7,500 episodes with 43,000 nerve blocks. Pain Physician. 2012;15:E143–50. [PubMed] [Google Scholar]
- 137.Manchikanti L, Pampati V, Bakhit C, Rivera J, Beyer C, Damron K, et al. Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: A randomized clinical trial. Pain Physician. 2001;4:101–17. [PubMed] [Google Scholar]
- 138.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: Analysis of utilization trends and medicare expenditures 2000 to 2008. Spine (Phila Pa 1976) 2013;38:157–68. doi: 10.1097/BRS.0b013e318267f463. [DOI] [PubMed] [Google Scholar]
- 139.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: A randomized, controlled, double blind trial with a two-year follow-up. Pain Physician. 2012;15:273–86. [PubMed] [Google Scholar]
- 140.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: Two-year results of a randomized, double-blind, active-control trial. Int J Med Sci. 2012;9:582–91. doi: 10.7150/ijms.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. A randomized, double-blind, active-control trial of the effectiveness of lumbar interlaminar epidural injections in disc herniation. Pain Physician. 2014;17:E61–74. [PubMed] [Google Scholar]
- 142.Manchikanti L, Singh V, Falco FJ, Cash KA, Fellows B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: A randomized, double. blind controlled trial. Pain Physician. 2010;13:437–50. [PubMed] [Google Scholar]
- 143.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. The role of thoracic medial branch blocks in managing chronic mid and upper back pain: A randomized, double-blind, active-control trial with a 2-year follow-up. Anesthesiol Res Pract 2012. 2012 doi: 10.1155/2012/585806. 585806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: A randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010;7:124–35. doi: 10.7150/ijms.7.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Manchikanti L, Singh V. Periradicular infiltration for sciatica. Spine (Phila Pa 1976) 2002;27:215–7. doi: 10.1097/00007632-200201150-00022. [DOI] [PubMed] [Google Scholar]
- 146.Manchikanti L, Singh V. Periradicular infiltration for sciatica. Spine (Phila Pa 1976) 2002;27:335–6. doi: 10.1097/00007632-200202010-00037. [DOI] [PubMed] [Google Scholar]
- 147.Manning DC, Hopwood MB. Corticosteroid injections for sciatica. N Engl J Med. 1997;337:1242. [PubMed] [Google Scholar]
- 148.Mao J, Chen LL. Systemic lidocaine for neuropathic pain relief. Pain. 2000;87:7–17. doi: 10.1016/S0304-3959(00)00229-3. [DOI] [PubMed] [Google Scholar]
- 149.Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: A national database analysis between 2002 and 2011. Spine (Phila Pa 1976) 2014;39:476–81. doi: 10.1097/BRS.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 150.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299:656–64. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 151.Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine (Phila Pa 1976) 2009;34:2077–84. doi: 10.1097/BRS.0b013e3181b1fad1. [DOI] [PubMed] [Google Scholar]
- 152.McCahon RA, Ravenscroft A, Hodgkinson V, Evley R, Hardman J. A pilot study of the dose-response of caudal methylprednisolone with levobupivacaine in chronic lower back pain. Anaesthesia. 2011;66:595–603. doi: 10.1111/j.1365-2044.2011.06764.x. [DOI] [PubMed] [Google Scholar]
- 153.Meadeb J, Rozenberg S, Duquesnoy B, Kuntz JL, Le Loët X, Sebert JL, et al. Forceful sacrococcygeal injections in the treatment of postdiscectomy sciatica. A controlled study versus glucocorticoid injections. Joint Bone Spine. 2001;68:43–9. doi: 10.1016/s1297-319x(00)00234-7. [DOI] [PubMed] [Google Scholar]
- 154.Mehta S, Khalil AA, Alshekhlee A. Air myelopathy following a cervical epidural injection. Pain Med. 2010;11:1678–9. doi: 10.1111/j.1526-4637.2010.00971.x. [DOI] [PubMed] [Google Scholar]
- 155.Melzack R, Coderre TJ, Katz J, Vaccarino AL. Central neuroplasticity and pathological pain. Ann N Y Acad Sci. 2001;933:157–74. doi: 10.1111/j.1749-6632.2001.tb05822.x. [DOI] [PubMed] [Google Scholar]
- 156.Mendelson J, Muppidi S, Silberstein S. Multiple intracerebral hemorrhages after cervical epidural injections. Neurology. 2008;70:2415–6. doi: 10.1212/01.wnl.0000314692.58259.e3. [DOI] [PubMed] [Google Scholar]
- 157.Miedema HS, Chorus AM, Wevers CW, van der Linden S. Chronicity of back problems during working life. Spine. 1998;23:2021–8. doi: 10.1097/00007632-199809150-00020. [DOI] [PubMed] [Google Scholar]
- 158.Minamide A, Tamaki T, Hashizume H, Yoshida M, Kawakami M, Hayashi N. Effects of steroids and lipopolysaccharide on spontaneous resorption of herniated intervertebral discs: An experimental study in the rabbit. Spine (Phila Pa 1976) 1998;23:870–6. doi: 10.1097/00007632-199804150-00007. [DOI] [PubMed] [Google Scholar]
- 159.Nam HS, Park YB. Effects of transforaminal injection for degenerative lumbar scoliosis combined with spinal stenosis. Ann Rehabil Med. 2011;35:514–23. doi: 10.5535/arm.2011.35.4.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.National Government Services, Inc. LCD for Pain Management (L28529). Effective Date 01/01/2009 [Google Scholar]
- 161.Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain. A randomized, double-blind, controlled trial. Spine (Phila Pa 1976) 2005;30:857–62. doi: 10.1097/01.brs.0000158878.93445.a0. [DOI] [PubMed] [Google Scholar]
- 162.Noridian Healthcare Solutions, LLC. Local Coverage Determination (LCD). Lumbar Epidural Injections L33836. [Revision effective Date: 2/26/2014]; [Google Scholar]
- 163.Ohayon MM, Stingl JC. Prevalence and comorbidity of chronic pain in the German general population. J Psychiatr Res. 2012;46:444–50. doi: 10.1016/j.jpsychires.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 164.Orlando MP, Sherman MO. Corticosteroid injections for sciatica. N Engl J Med. 1997;337:1242. [PubMed] [Google Scholar]
- 165.Owlia MB, Salimzadeh A, Alishiri G, Haghighi A. Comparison of two doses of corticosteroid in epidural steroid injection for lumbar radicular pain. Singapore Med J. 2007;48:241–5. [PubMed] [Google Scholar]
- 166.Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM, et al. Caudal epidural injections in the management of chronic low back pain: A systematic appraisal of the literature. Pain Physician. 2012;15:E159–98. [PubMed] [Google Scholar]
- 167.Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F, et al. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: Single injection versus continuous infusion. Clin J Pain. 2007;23:551–7. doi: 10.1097/AJP.0b013e318074c95c. [DOI] [PubMed] [Google Scholar]
- 168.Pasqualucci A. Experimental and clinical studies about the preemptive analgesia with local anesthetics. Possible reasons of the failure. Minerva Anestesiol. 1998;64:445–57. [PubMed] [Google Scholar]
- 169.Pasquier MM, Leri D. Injection intra-et extradurales de cocaine a dose minime daus le traitments dela sciatique. Bull Gen Ther. 1901;142:196. [Google Scholar]
- 170.Patel N, Karppinen J, et al. Periradicular infiltration for sciatica. A randomized controlled trial. Spine 26, 1059-1067:2001. Spine (Phila Pa 1976) 2002;27:1588–9. doi: 10.1097/00007632-200207150-00025. [DOI] [PubMed] [Google Scholar]
- 171.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–8. [PubMed] [Google Scholar]
- 172.Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, et al. Epidural corticosteroid injections in the management of sciatica: A systematic review and meta-analysis. Ann Intern Med. 2012;157:865–77. doi: 10.7326/0003-4819-157-12-201212180-00564. [DOI] [PubMed] [Google Scholar]
- 173.Plastaras CT, Heller DS, Sorosky BS, Houle TT. Pain reproduction during lumbosacral transforaminal epidural steroid injection does not affect outcome. J Back Musculoskeletal Rehab. 2006;19:57–60. [Google Scholar]
- 174.Price C, Arden N, Coglan L, Rogers P. Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess. 2005;9:1–58. doi: 10.3310/hta9330. iii. [DOI] [PubMed] [Google Scholar]
- 175.Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67–76. doi: 10.1097/BRS.0b013e31820cccfb. [DOI] [PubMed] [Google Scholar]
- 176.Raza K. Corticosteroid injections for sciatica. N Engl J Med. 1997;337:1241. [PubMed] [Google Scholar]
- 177.Revel M, Auleley GR, Alaoui S, Nguyen M, Duruoz T, Eck-Michaud S, et al. Forceful epidural injections for the treatment of lumbosciatic pain with post-operative lumbar spinal fibrosis. Rev Rhum Engl Ed. 1996;63:270–7. [PubMed] [Google Scholar]
- 178.Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000;82-A:1589–93. doi: 10.2106/00004623-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 179.Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of lumbosacral transforaminal epidural steroid injections: A systematic review. PM R. 2009;1:657–68. doi: 10.1016/j.pmrj.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 180.Saripanidis S. Lversen T, et al., editors. Re: Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. Gate control pain modulation theory invalidates the control group used in this research. Published online 10/8/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sato C, Sakai A, Ikeda Y, Suzuki H, Sakamoto A. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg. 2008;106:313–20. doi: 10.1213/01.ane.0000296460.91012.51. [DOI] [PubMed] [Google Scholar]
- 182.Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: A prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976) 2009;34:1441–7. doi: 10.1097/BRS.0b013e3181a4804a. [DOI] [PubMed] [Google Scholar]
- 183.Shah RV. Paraplegia following thoracic and lumbar transforaminal epidural steroid injections: How relevant are particulate steroids? Pain Pract. 2014;14:297–300. doi: 10.1111/papr.12110. [DOI] [PubMed] [Google Scholar]
- 184.Shah RV. Paraplegia following thoracic and lumbar transforaminal epidural steroid injections: How relevant is physician negligence? J Neurointerv Surg. 2014;6:166–8. doi: 10.1136/neurintsurg-2013-010903. [DOI] [PubMed] [Google Scholar]
- 185.Sicard MA. Les injections medicamenteuse extradurales par voie saracoccygiene. Comptes Renues des Seances de la Societe de Biologie et de ses Filliales (Paris) 1901;53:452–3. [Google Scholar]
- 186.Singh K, Nandyala SV, Marquez-Lara A, Fineberg SJ. Epidemiological trends in the utilization of bone morphogenetic protein in spinal fusions from 2002 to 2011. Spine (Phila Pa 1976) 2014;39:491–6. doi: 10.1097/BRS.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 187.Smith RM, Schaefer MK, Kainer MA, Wise M, Finks J, Duwve J, et al. Fungal infections associated with contaminated methylprednisolone injections. N Engl J Med. 2013;369:1598–609. doi: 10.1056/NEJMoa1213978. [DOI] [PubMed] [Google Scholar]
- 188.Snoek W, Weber H, Jørgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977;48:635–41. doi: 10.3109/17453677708994810. [DOI] [PubMed] [Google Scholar]
- 189.Staal JB, de Bie RA, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: An updated Cochrane review. Spine (Phila Pa 1976) 2009;34:49–59. doi: 10.1097/BRS.0b013e3181909558. [DOI] [PubMed] [Google Scholar]
- 190.Sugimoto M, Uchida I, Mashimoto T. Local anaesthetics have different mechanisms and sites of action at the recombinant NMDA receptors. Br J Pharmacol. 2003;138:876–82. doi: 10.1038/sj.bjp.0705107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation. Spine (Phila Pa 1976) 2008;33:743–7. doi: 10.1097/BRS.0b013e3181696132. [DOI] [PubMed] [Google Scholar]
- 192.Tafazal S, Ng L, Chaudhary N, Sell P. Corticosteroids in peri-radicular infiltration for radicular pain: A randomised double blind controlled trial. One year results and subgroup analysis. Eur Spine J. 2009;18:1220–5. doi: 10.1007/s00586-009-1000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Thelin A, Holmberg S, Thelin N. Functioning in neck and low back pain from a 12-year perspective: A prospective population-based study. J Rehabil Med. 2008;40:555–61. doi: 10.2340/16501977-0205. [DOI] [PubMed] [Google Scholar]
- 194.U. S. Food and Drug Administration. Drug Safety Communications. FDA Drug Safety Communication: FDA requires label changes to warn of rare but serious neurologic problems after epidural corticosteroid injections for pain. [Last accessed on 2015 Jan 27]. Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM394286.pdf .
- 195.US Burden of Disease Collaborators. The state of US health, 1999-2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.van Tulder MW, Suttorp M, Morton S, Bouter LM, Shekelle P. Empirical evidence of an association between internal validity and effect size in randomized controlled trials of low-back pain. Spine (Phila Pa 1976) 2009;34:1685–92. doi: 10.1097/BRS.0b013e3181ab6a78. [DOI] [PubMed] [Google Scholar]
- 197.Ward A, Watson J, Wood P, Dunne C, Kerr D. Glucocorticoid epidural for sciatica: Metabolic and endocrine sequelae. Rheumatology (Oxford) 2002;41:68–71. doi: 10.1093/rheumatology/41.1.68. [DOI] [PubMed] [Google Scholar]
- 198.Wilkinson IM, Cohen SP. Epidural steroid injections. Curr Pain Headache Rep. 2012;16:50–9. doi: 10.1007/s11916-011-0236-9. [DOI] [PubMed] [Google Scholar]
- 199.Wilson-MacDonald J, Burt G, Griffin D, Glynn C. Epidural steroid injection for nerve root compression: A randomized, controlled trial. J Bone Joint Surg Br. 2005;87-B:352–5. doi: 10.1302/0301-620x.87b3.15338. [DOI] [PubMed] [Google Scholar]
- 200.Wittenberg RH, Greskötter KR, Steffen R, Schoenfeld BL. Is epidural injection treatment with hypertonic saline solution in intervertebral disk displacement useful? (The effect of NaCl solution on intervertebral disk tissue) Z Orthop Ihre Grenzgeb. 1990;128:223–6. doi: 10.1055/s-2008-1039504. [DOI] [PubMed] [Google Scholar]
- 201.Yamashita T, Takahashi K, Yonenobu K, Kikuchi S. Prevalence of neuropathic pain in cases with chronic pain related to spinal disorders. J Orthop Sci. 2014;19:15–21. doi: 10.1007/s00776-013-0496-9. [DOI] [PubMed] [Google Scholar]
- 202.Yi Y, Hwang B, Son H, Cheong I. Low bone mineral density, but not epidural steroid injection, is associated with fracture in postmenopausal women with low back pain. Pain Physician. 2012;15:441–9. [PubMed] [Google Scholar]
- 203.Yland MJ, Iversen T, et al. Re: Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: Multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. Published online 11/19/2011. Author's reply: Published online 9/29/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zhang Y, Baik SH, Fendrick AM, Baicker K. Comparing local and regional variation in health care spending. N Engl J Med. 2012;367:1724–31. doi: 10.1056/NEJMsa1203980. [DOI] [PMC free article] [PubMed] [Google Scholar]


