Abstract
Objectives. We evaluated the effect of neighborhood disadvantage (ND) on older adults’ prevalence, awareness, treatment, and control of hypertension.
Methods. Data were from the University of Alabama at Birmingham Study of Aging, an observational study of 1000 community-dwelling Black and White Alabamians aged 65 years and older, in 1999 to 2001. We assessed hypertension prevalence, awareness, treatment, and control with blood pressure measurements and self-report data. We assessed ND with US Census data corresponding with participants’ census tracts, created tertiles of ND, and fit models with generalized estimating equations via a logit link function with a binomial distribution. Adjusted models included variables assessing personal advantage and disadvantage, place-based factors, sociodemographics, comorbidities, and health behaviors.
Results. Living in mid-ND (adjusted odds ratio [AOR] = 1.6; 95% confidence interval [CI] = 1.2, 2.1) and high-ND tertiles (AOR = 1.8; 95% CI = 1.3, 2.3) was associated with higher hypertension prevalence, and living in high-ND tertiles was associated with lower odds of controlled hypertension (AOR = 0.6; 95% CI = 0.4, 0.6). In adjusted models, ND was not associated with hypertension awareness or treatment.
Conclusions. These findings show that neighborhood environmental factors matter for hypertension outcomes and suggest the importance of ND for hypertension management in older adults.
The characteristics of the geographic spaces or neighborhoods where people live influence their health throughout the life course.1–9 The mechanisms whereby neighborhood characteristics affect individuals’ health include psychosocial and material resources in those geographic spaces. Specifically, neighborhoods have the potential to be a source of social capital, providing support to persons in need; to have physical capital, offering parks and recreation resources for physical activity; and to have human capital, generating economic output. Any of these resources can contribute to the overall well-being of individuals living there.10 Alternatively, stress caused by high crime, low social support, limited economic resources, or a lack of material resources such as health services6 may ultimately negatively affect the health of individuals living in a neighborhood. Furthermore, limited community-based assistance programs, as well as limited access to healthful foods or adequate shopping opportunities and recreational facilities11 in disadvantaged neighborhoods may also have adverse effects on health. The daily stress of living in such disadvantaged neighborhoods may place a high burden on individuals’ physiological systems, a burden which is sometimes called allostatic load.12,13
These risks and benefits of neighborhood contexts may accrue over a long period of time and may affect people either right away or for many years in the future14 and lead to conditions such as hypertension. In fact, neighborhood-level psychosocial and material deprivations are particularly problematic for individuals’ cardiovascular health and for management of cardiovascular risk factors. In 2004, Diez Roux et al.15 demonstrated an association between negative environments and both cardiovascular and noncardiovascular mortality. Other researchers have found similar effects, including Mujahid et al.16 who showed that walkability, access to healthy food, greater safety, and greater social cohesion were associated with a lower likelihood of hypertension.
Although these findings are useful for gaining insights into the general population, work is needed to assess the effects of neighborhood characteristics on specific, unique subpopulations. To that end, there has been a growing interest in the effects of neighborhood context on older adults because of their potentially greater sensitivity (than the general population) to the effects of their neighborhood contexts on health.8,17–22 This is particularly important, as Lawton and Simon purported in the environmental docility hypothesis,23 because, as persons age and become more ill, losing control of their ability to perform activities of daily living, they may become more sensitive to characteristics of their environments, including the neighborhoods where they live. Specifically, then, older adults’ inability to navigate through disadvantaged neighborhoods may put them at higher risk for hypertension because of more concentrated exposure to psychosocial stressors. In addition, deprivation of health services including access to physicians and pharmacies in disadvantaged neighborhoods may cause adverse outcomes. Finally, older adults’ negative perception of their neighborhood environment may have a negative impact on their likelihood of being mobile and active, even when, in reality, theirs is not an unsafe or disadvantaged neighborhood.
Although there is a burgeoning literature on the relationship between neighborhood characteristics and cardiovascular outcomes and a growing interest in neighborhood effects on older adults, no work known to these authors has examined neighborhood effects on hypertension specifically among older adults. Therefore, we aimed to assess if an association exists between neighborhood disadvantage (ND), measured by a validated ND index (NDI),24 and hypertension prevalence, awareness, treatment, and control in a cohort of community-dwelling older adults.
METHODS
We used data from the baseline assessment of the University of Alabama at Birmingham Study of Aging, an observational, longitudinal study of 1000 Medicare beneficiaries. At baseline in 1999 to 2001, participants were community-dwelling persons aged 65 years and older living in 5 rural and urban counties in central Alabama. The sample was balanced in terms of race, gender, and rural and urban residence so that the final sample was 50% Black, 50% female, and 51% rural. University of Alabama at Birmingham Study of Aging investigators collected data by using standardized questionnaires designed to assess mobility, social and demographic information, medical history, and health services utilization at baseline in the home and in subsequent telephone follow-up interviews conducted every 6 months for up to 8.5 years.25,26 Investigators followed participants until they died, were admitted to a nursing home, refused further participation, or were unreachable. Data for this cross-sectional study were limited to the baseline assessment because direct measures of blood pressure, necessary for this study methodology, were not collected at 6-month follow-up assessments. In addition, we geocoded participants’ addresses and linked the census tract characteristics associated with their place of residence from the 2000 US Census summary files 1 and 3.27,28 Participants resided in 178 unique census tracts. We could not geocode 3 participants’ addresses, so we used the characteristics of their zip codes as proxies, accounting for 2 unique zip codes and resulting in a total of 180 unique census tracts or zip codes.
Hypertension Prevalence, Awareness, Treatment, and Control
Trained interviewers collected blood pressure measurements from participants at baseline in-home visits by using the protocol suggested by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.29 Interviewers were trained by registered nurses and were provided with small, standard, and large adult cuffs, a sphygmomanometer, and stethoscope. Interviewers measured each participant’s blood pressure near the end of the interview, after rapport had been established and the participant had been seated with his or her feet on the floor for more than 5 minutes. Participants were also asked “Have you ever been told by a physician that you have hypertension or high blood pressure” and “Do you currently take antihypertensive medications?”
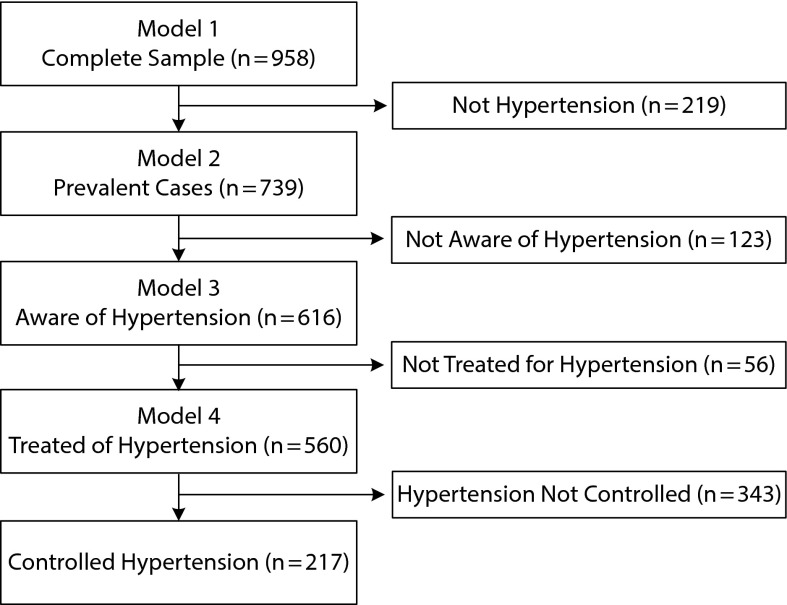
We used these data to assess prevalence, awareness, treatment, and control of hypertension, according to methods published by Hajjar and Kotchen30 and Morenoff et al.7 Specifically, we classified participants as having prevalent hypertension if their systolic blood pressure was 140 millimeters of mercury or higher, their diastolic blood pressure was 90 millimeters of mercury or higher, or if they were taking antihypertensive medication. We assessed participants for awareness if they were a prevalent case (n = 739). We classified them as aware if they answered “yes” to the question “Has a physician ever told you that you had high blood pressure or hypertension?” Participants were eligible to be assessed for treatment if they were aware of their hypertension (n = 616), and we classified them as treated if they were taking antihypertensive medication. Participants were eligible to be assessed for control if they were taking an antihypertensive medication (n = 560); we classified them as controlled if they were taking an antihypertensive medication and had a systolic blood pressure less than 140 millimeters of mercury and diastolic blood pressure of less than 90 millimeters of mercury. The numbers included in each analysis are presented in Figure 1.
FIGURE 1—
Description of analytic sample: The University of Alabama at Birmingham Study of Aging, central Alabama, 1999–2001.
Neighborhood Disadvantage
We measured ND at the census tract level where participants lived. We conceptualized this variable by using the NDI initially published by Ross et al.,24 which has also been used previously with this cohort.17 This index is a composite measure of the prevalence of poverty, determined from the number of households living below the poverty line in the year 2000, and female-headed households, which are households with children younger than 18 years and without a man present, in the census tract. Prevalence rates of poverty in a census tract serve as a marker of economic disadvantage, and prevalence of female-headed or single-mother households serves as a marker of social disadvantage.
In keeping with the methods of Ross et al.,24 we divided the rates of poverty and single-mother households by 10, calculated the mean of these values, and assigned that score to individuals as the NDI. A 1-unit increase in the NDI represents an average 10% increase in the prevalence of poverty or single-mother households at an individual’s census tract level. We stratified the sample into tertiles by level of ND of the 180 neighborhoods where residents lived.17
Covariates
Personal advantage and disadvantage.
To ensure that any detected effects of ND were attributable to the context and not characteristics inherent to the participants’ individual economic or social disadvantage, we controlled for individual-level poverty and perceived social support. We conceptualized poverty based on the 2000 Federal Poverty Guidelines,31 which was $8350 for persons living alone or $11 250 for persons living with someone. In the Study of Aging, we asked participants about their income in categories, including less than $8000 and $8001 to $12 000. We assigned poverty status to persons living alone whose income was less than $8000 and to persons living with someone who had an income $8001 to $12 000. We adjusted for perceived social support, as a marker of individual social disadvantage, by using a modified version of the Arthritis Impact Measurement Scale for Social Support.32 Scores were continuous with higher scores representing lower perceived social support; the range of possible scores was 0 to 16. The questions and methods used for this questionnaire are described elsewhere.17
Place-based factors.
We included a measure of perceived neighborhood disorder by using participants’ affirmative responses to a single question: “Do you limit your activities for fear of being robbed or attacked?” This variable accounts for individuals’ perceptions of their neighborhood safety. We also included rural status; we classified persons living in Bibb, Hale, or Pickens Counties, each of which has fewer than 21 000 individuals per county, as rural. We considered persons living in Jefferson or Tuscaloosa Counties, located in the Standard Metropolitan Statistical Area that encompasses Birmingham and Tuscaloosa, Alabama, as urban.
Sociodemographics.
We included self-reported age in years at baseline, race reported as Black or White, gender, and living alone. Because persons living alone and unmarried (including widowhood) were highly correlated, we did not include marital status. We included education as categorical variable, with less than 7 years as the referent group; other groups were 6th to 12th grade, completed high school, and completed at least some college.
Comorbidities.
To account for health condition–related effects on the hypertension outcomes, we adjusted for 4 comorbidities that may be particularly problematic for hypertension: verified diagnoses of diabetes, stroke, myocardial infarction, and obesity.33 We verified diagnoses of diabetes, stroke, and myocardial infarction with any of the following: (1) self-reported physician diagnosis and taking a medication for the condition (documented at the in-home visit), (2) physician-reported diagnosis on a questionnaire about the participant, or (3) documented diagnosis on hospital discharge records within 3 years of the baseline interview. We defined obesity as body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) of greater than 30, which we assessed with measured height and weight according to the National Heart, Lung, and Blood Institute clinical guidelines.34
Health behavior.
We assessed 2 behavioral and lifestyle factors that may be associated with hypertension-related covariates. First, we measured participation in physical activity with the question: “Have you done any calisthenics, general exercise, or used an exercise bike in past year?” and dichotomized the answers as yes or no. We accounted for smoking status for participants who reported smoking currently or having quit in the past year, with the referent group of having quit more than a year ago or never smoked.
Analytic Sample and Technique
The final analytic sample comprised the 958 participants with complete data. For this cross-sectional analysis, we calculated descriptive statistics for the ND strata and the entire sample and assessed for differences between strata using analysis of variance or the χ2 test. Using generalized estimating equations with a logit link and binomial distribution, we first fit bivariate models with each variable and outcome, and then fit fully adjusted models with all variables included. Generalized estimating equations account for the nesting of cases in a second-level variable such as neighborhood, which may generate nonindependence in responses and otherwise bias the results.35 We used SPSS version 17.0 (SPSS Inc, Chicago, IL) for these analyses.
We conducted sensitivity analyses for 5 possible conditions. First, we included a continuous measure of the length of time participants had lived at their current address as an adjustment for the amount of exposure they had to their neighborhood conditions. Second, we included high alcohol use, defined as drinking more than 3 servings of alcohol per day, as a marker of health behavior. Third, we examined if accounting for poverty at the 150% or 200% level instead of at 100% would affect the outcomes. Fourth, we examined if estimates changed when we used the rural status indicator for individuals by census tract instead of by county. Finally, we assessed for interactions between individual-level income, measured categorically, as described in previous work with this study36 and ND. There were no effects on the primary outcomes of interest in any of these sensitivity analyses, nor were the interaction terms significant, so we did not include them in final models.
RESULTS
We present descriptive statistics in Table 1, both by ND strata and the overall sample. The low-ND (LND) tertile had 326 (34%) participants, the mid-ND tertile (MND) had 315 (33%) participants, and the high-ND (HND) tertile had 317 (33%) participants. Prevalence and awareness of hypertension were greatest among the MND and HND strata; but there were no differences in hypertension treatment and control among ND strata. Participants below poverty, those who reported limiting their activities for fear of being robbed or attacked, Blacks, and those with less education were disproportionately situated in the MND and HND strata. The MND stratum was disproportionately rural compared with the LND and HND strata. Among comorbidity-related covariates, the proportion of people with obesity was highest in the MND and HND strata. Finally, among health behavior covariates, physical activity was greatest in the LND stratum.
TABLE 1—
Descriptive Statistics by Level of Neighborhood Disadvantage: The University of Alabama at Birmingham Study of Aging, Central Alabama, 1999–2001
| Variable | Low Disadvantage (n = 326), No. (%) or Mean ±SD | Mid Disadvantage (n = 315), No. (%) or Mean ±SD | High Disadvantage (n = 317), No. (%) or Mean ±SD | Total (n = 958), No. (%) or Mean ±SD |
| Dependent variables | ||||
| Hypertension | ||||
| Prevalence*** (n = 958) | 212 (65) | 253 (80) | 260 (82) | 725 (76) |
| Awareness* (n = 739) | 165 (78) | 208 (82) | 229 (88) | 602 (83) |
| Treatment (n = 616) | 152 (92) | 193 (93) | 215 (94) | 560 (93) |
| Control (n = 560) | 69 (45) | 74 (38) | 74 (34) | 217 (39) |
| Independent variables | ||||
| Personal advantage or disadvantage | ||||
| Persons below poverty*** | 53 (17) | 135 (42) | 131 (41) | 319 (33) |
| Social support | 13.9 ±3.0 | 13.8 ±3.1 | 14.0 ±3.0 | 13.9 ±3.0 |
| Years at address | 26.7 ±17.5 | 27.6 ±18.8 | 28.3 ±18.6 | 27.6 ±18.0 |
| Place-based factors | ||||
| Rural*** | 101 (31) | 207 (66) | 188 (59) | 496 (52) |
| Limit activities—fear of being robbed or attacked*** | 35 (11) | 63 (20) | 66 (21) | 164 (17) |
| Sociodemographics | ||||
| Age, y | 74.9 ±6.4 | 75.4 ±6.5 | 75.3 ±7.3 | 74.3 ±6.7 |
| Black*** | 77 (23) | 171 (54) | 224 (71) | 472 (49) |
| Female | 155 (48) | 161 (51) | 154 (49) | 470 (49) |
| Lives alone | 90 (30) | 106 (35) | 107 (34) | 303 (32) |
| Education | ||||
| < 6th grade*** | 33 (10) | 89 (28) | 73 (23) | 195 (20) |
| 6th–12th grade*** | 72 (22) | 92 (29) | 110 (35) | 274 (29) |
| Completed high school** | 135 (41) | 98 (31) | 97 (31) | 330 (34) |
| Completed some college*** | 86 (26) | 36 (11) | 37 (12) | 159 (17) |
| Comorbidities | ||||
| Diabetes | 68 (29) | 88 (37) | 82 (35) | 238 (25) |
| Stroke | 27 (25) | 38 (36) | 42 (39) | 107 (11) |
| Myocardial infarction | 37 (39) | 34 (35) | 25 (26) | 96 (10) |
| Obesity*** | 68 (21) | 113 (36) | 112 (35) | 293 (31) |
| Health behaviors | ||||
| Physical activity** | 104 (32) | 63 (20) | 84 (27) | 251 (26) |
| High alcohol use | 13 (4) | 12 (4) | 7 (3) | 32 (3) |
| Smoker currently or in past year | 40 (12) | 41 (13) | 40 (13) | 121 (13) |
*P ≤ .05; **P ≤ .01; ***P ≤ .001 (differences by disadvantage tertiles).
We present the results of the generalized estimating equations in Table 2. In model 1, assessing hypertension prevalence, unadjusted odds ratios demonstrated that persons living in mid-disadvantaged and high-disadvantaged neighborhoods had 2.3 greater odds of having hypertension than those living in low-disadvantaged neighborhoods. In adjusted models, the associations remained significant, but the magnitude of the odds ratio was reduced to 1.6 for persons in the MND stratum and 1.8 for those in the HND stratum. In unadjusted analyses in model 2 assessing hypertension treatment, persons in the HND stratum had 2.1 greater odds of being aware of their hypertension than those in the LND stratum; there were no associations in adjusted model 2. In model 3, wherein we examined effects on treatment of hypertension, there were no significant associations. In model 4, assessing neighborhood effects on control of hypertension, in both unadjusted analyses and adjusted analyses, persons in the HND stratum had 40% lower odds of having controlled hypertension.
TABLE 2—
Odds Ratios of Hypertension-Related Outcomes Among Older Adults: University of Alabama at Birmingham Study of Aging, Central Alabama, 1999–2001
| Model 1: Prevalence (n = 958) |
Model 2: Awareness (n = 739) |
Model 3: Treatment (n = 616) |
Model 4: Control (n = 560) |
|||||
| Independent Variables | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) |
| Primary exposure | ||||||||
| Low neighborhood disadvantage (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Mid neighborhood disadvantage | 2.3*** (1.8, 2.9) | 1.6** (1.2, 2.1) | 1.3 (0.8, 2.2) | 0.8 (0.5, 1.3) | 1.0 (0.5, 2.1) | 1.0 (0.4, 2.2) | 0.7 (0.5, 1.0) | 0.7 (0.5, 1.1) |
| High neighborhood disadvantage | 2.3*** (1.8, 2.8) | 1.8*** (1.3, 2.3) | 2.1** (1.3, 3.4) | 1.1 (0.7, 1.9) | 1.2 (0.5, 2.7) | 1.1 (0.4, 2.6) | 0.6** (0.4, 0.8) | 0.6** (0.4, 0.8) |
| Personal advantage or disadvantage | ||||||||
| Persons below poverty | 2.1*** (1.5, 3.1) | 1.1 (0.7, 1.9) | 1.7** (1.1, 2.5) | 1.0 (0.6, 1.6) | 0.8 (0.4, 1.6) | 0.5 (0.2, 1.2) | 0.9 (0.6, 1.3) | 0.8 (0.6, 1.3) |
| Social support | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 1.1 (1.0, 1.1) | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) |
| Place-based factors | ||||||||
| Perceived neighborhood disorder | 1.2 (0.8, 1.8) | 0.7 (0.5, 1.1) | 1.7 (0.9, 3.3) | 1.0 (0.5, 2.2) | 1.3 (0.5, 3.3) | 1.5 (0.5, 4.3) | 0.6 (0.4, 1.0) | 0.7 (0.4, 1.2) |
| Rural | 1.3 (0.9, 1.7) | 0.9 (0.7, 1.2) | 1.3 (0.9, 1.9) | 1.2 (0.8, 1.9) | 1.3 (0.7, 2.4) | 1.4 (0.7, 2.9) | 1.0 (0.7, 1.3) | 1.0 (0.7, 1.3) |
| Sociodemographics | ||||||||
| Age | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Black | 2.2*** (1.6, 2.9) | 1.5* (1.1, 2.1) | 2.8*** (1.8, 4.3) | 2.5** (1.4, 4.5) | 1.1 (0.6, 2.0) | 1.7 (0.8, 3.8) | 0.9 (0.6, 1.2) | 1.1 (0.7, 1.7) |
| Female | 1.8*** (1.3, 2.4) | 1.9*** (1.4, 2.5) | 1.2 (0.9, 1.8) | 1.2 (0.8, 1.9) | 1.4 (0.7, 2.6) | 1.9 (0.9, 3.7) | 1.1 (0.8, 1.6) | 1.3 (0.9, 2.0) |
| Lives alone | 1.2 (0.9, 1.8) | 1.2 (0.8, 1.8) | 1.2 (0.8, 1.9) | 1.3 (0.8, 2.1) | 1.0 (0.5, 1.8) | 1.0 (0.5, 2.1) | 0.8 (0.6, 1.1) | 0.8 (0.5, 1.1) |
| Education | ||||||||
| < 6th grade (Ref) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 6th–12th grade | 1.1 (0.8, 1.8) | 1.2 (0.6, 2.2) | 0.8 (0.4, 1.3) | 0.9 (0.5, 1.6) | 1.7 (0.7, 4.1) | 1.9 (0.7, 4.8) | 0.8 (0.5, 1.3) | 0.8 (0.5, 1.3) |
| Completed high school | 0.6* (0.4, 0.9) | 0.7 (0.4, 1.4) | 0.7 (0.4, 1.1) | 0.9 (0.5, 1.8) | 1.1 (0.5, 2.6) | 1.1 (0.4, 3.0) | 0.9 (0.6, 1.5) | 0.8 (0.5, 1.3) |
| Completed some college | 0.5** (0.3, 0.8) | 0.7 (0.4, 1.3) | 0.4* (0.2, 0.7) | 0.5 (0.3, 1.1) | 0.8 (0.3, 2.0) | 0.9 (0.3, 2.5) | 0.5 (0.3, 1.0) | 0.4** (0.2, 0.8) |
| Comorbidities | ||||||||
| Diabetes history | 2.1*** (1.5, 3.0) | 1.7** (1.2, 2.5) | 1.9** (1.2, 3.2) | 1.7* (1.0, 2.8) | 1.2 (0.6, 2.4) | 1.2 (0.5, 2.7) | 0.6** (0.4, 0.9) | 0.6** (0.4, 1.0) |
| Stroke history | 2.5*** (1.6, 4.2) | 2.4*** (1.4, 4.1) | 4.1*** (1.7, 9.5) | 4.8 (2.1, 11.2) | 1.7 (0.6, 4.4) | 1.8 (0.6, 5.0) | 1.8** (1.1, 2.9) | 1.8* (1.1, 3.1) |
| Myocardial infarction history | 1.0 (0.6, 1.8) | 1.2 (0.7, 2.2) | 0.6 (0.3, 1.3) | 0.7 (0.3, 1.3) | 2.1 (0.5, 8.0) | 2.5 (0.6, 10.1) | 0.7 (0.3, 1.3) | 0.7 (0.4, 1.2) |
| Obesity | 2.2*** (1.5, 3.2) | 1.6* (1.1, 2.4) | 2.0** (1.3, 3.0) | 1.3 (0.8, 2.1) | 0.6 (0.3, 1.1) | 0.5 (0.2, 1.0) | 0.7 (0.4, 1.0) | 0.7 (0.4, 1.2) |
| Health behavior | ||||||||
| Physical activity | 1.0 (0.7, 1.5) | 1.1 (0.7, 1.0) | 1.1 (0.8, 1.7) | 1.2 (0.8, 1.8) | 0.8 (0.4, 1.6) | 0.8 (0.4, 1.5) | 1.1 (0.8, 1.6) | 1.1 (0.8, 1.5) |
| Smoker currently or in past year | 1.1 (0.7, 2.9) | 1.1 (0.7, 1.7) | 0.7 (0.4, 1.3) | 0.7 (0.4, 1.2) | 0.8 (0.3, 2.2) | 0.8 (0.3, 2.5) | 0.8 (0.5, 1.4) | 0.8 (0.5, 1.3) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OR = odds ratio (unadjusted).
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
The effects of covariates on hypertension-related outcomes in adjusted models are also shown in Table 2. In model 1, assessing prevalence of hypertension, Blacks and women had higher odds of having hypertension, as did persons with a history of diabetes, stroke, and obesity. In model 2, assessing awareness of hypertension, Blacks and persons with diabetes had higher odds of being aware of their hypertension. In model 3, there were no detected effects on odds of being treated for hypertension. Finally, in model 4, assessing controlled hypertension, persons who had completed some college had lower odds of having controlled hypertension than those with less than sixth-grade education. Persons with a history of stroke had higher odds of having controlled hypertension. Also, persons with diabetes and a previous myocardial infarction had lower odds of having controlled hypertension.
DISCUSSION
The primary aim of this research was to determine if there was a relationship between ND and the prevalence, awareness, treatment, and control of hypertension among older adults. We found that ND was associated with both prevalence and control of hypertension, and that there was no association of ND with awareness or treatment of hypertension. Specifically, we demonstrated that older adults living in mid- and high-disadvantaged neighborhoods had 60% and 80% greater odds of having hypertension (respectively), after we adjusted for other personal advantage or advantage, place-based factors, sociodemographics, comorbidities, and health behavior covariates. We also found that older adults with hypertension living in high-disadvantaged neighborhoods had 40% lower odds of having controlled hypertension than those in the lowest tertile of ND.
These findings are particularly relevant to the literature on the importance of neighborhood environments for older adults’ health. As older adults lose their mobility, they are increasingly vulnerable to being confined to the geographic spaces where they live. Being unable to escape economically and socially toxic environments, then, may be what is driving the association between ND and hypertension prevalence and control. These findings support Lawton’s environmental docility hypothesis.19,20,37,38 Furthermore, other work examining the association between ND or disorder and hypertension has drawn from the allostatic load hypothesis, namely that individuals exert a physiological response to stressful situations such as disadvantaged neighborhood environments.12,13 This work supports the idea that older adults living in disadvantaged, stressful neighborhood environments are susceptible to greater likelihood of hypertension and less control over their living conditions, a key marker of allostatic load.
We noted in the introduction that there is burgeoning evidence that older adults may be more sensitive to the effects of ND than the general population. Previous work with the aging population has demonstrated that socioeconomic position has been associated with changes in blood pressure39 and that older adults who had access to amenities such as a convenience store and recreational facility in their communities had lower odds of having hypertension.11 Also, in a more age-diverse cohort, ND has been associated with a host of cumulative biological risks, including blood pressure, resting heart rate, hemoglobin A1c, C-reactive protein, waist size, and cholesterol.40
To attempt to understand if it is true that older adults are more sensitive to the effects of ND than the general population, particularly as it relates to hypertension, we contrasted our findings with those of Morenoff et al.7 Their study included participants aged 18 years and older from the Chicago Community Adult Health Study and showed that ND was associated only with treatment of hypertension and not with prevalence, awareness, or control. Although we are unable to make definitive assertions about these differing outcomes because the models are constructed slightly differently and because the samples are from different geographic regions and use different analytic techniques, the differences in the results do provide tentative evidence to support the hypothesis that older adults may, in fact, be more sensitive to disadvantaged neighborhood characteristics than those in the younger population. Specifically, it may be that the stress of living among poverty and in environments with low levels of social support contributes to higher odds of having hypertension and lower odds of being able to control or manage it.
Strengths and Limitations
Our study has several strengths, including the examination of the association of ND on hypertension-related outcomes in a heterogeneous population of community-dwelling older adults drawn from 180 unique neighborhoods. This study has detailed data at the individual level on socioeconomic status, social support, and psychological outcomes, as well as important health-related factors that are both self-reported and confirmed by health care providers and participants’ hospital discharge records. These data are robust and help ensure the validity of our findings.
Also of note, this sample had slightly higher prevalence rates of hypertension (76%) than in a population-based assessment conducted among community-dwelling older adults in Alabama just 1 year later, in 2002–2003 (67%).41 These differences may be attributable to our assessment of hypertension with actual blood pressure measurements and medication use for hypertension compared with the other study, which relied on self-report of “ever having been told by a physician” that the participant had hypertension. In addition, these higher rates of hypertension may be attributable to the Study of Aging’s oversampling of Blacks to achieve a balanced sample. Regardless, the study comprises people who tend to have higher cardiovascular risk factors as ascertained by direct measurement of blood pressure.
While our study has great strengths, it also has limitations. First, we used cross-sectional data that cannot account for changes over time, thus not allowing us to assess if neighborhood characteristics affect individuals’ risk of developing hypertension. Furthermore, the data set is limited to adults aged 65 years and older, precluding us from stratifying by age to determine if neighborhood affects individual outcomes differently for older or younger adults. In addition, the sample is from a single region in the Deep South, limiting generalizability to other regions of the country.
Also, to adequately detect the effects of the neighborhood, a minimum of 5 to 10 cases are needed in a neighborhood, with a minimum of 50 neighborhoods represented.42,43 Few of the participants were nested in specific neighborhoods making hierarchical modeling not appropriate; this precludes us from being able to partition out the variance in hypertension outcomes attributable the neighborhood level, a limitation further described elsewhere.17 Furthermore, using census tracts as a measure of neighborhoods is limited by the fact that residents may not recognize those boundaries as the true boundaries of their neighborhood.8 However, this level of measurement is accepted as an adequate tool for assessing neighborhood characteristics44 and has been shown to detect socioeconomic gradients and neighborhood differences in the general population including populations of older adults.45 Finally, the study is limited by data on study participants during their older adult years; no data are available on life course transitions and exposure to other neighborhoods that may have affected their hypertension-related outcomes.
Future Work
In future analyses we hope to explore neighborhood effects on prospective hypertension outcomes in both the University of Alabama at Birmingham Study of Aging and in larger databases that allow for hierarchical models and that include data collected over time to allow for assessment of ND effects on incident hypertension. We would also like to replicate these findings in a sample that includes both younger and older adults so that we may stratify the sample by age to determine if the adverse neighborhood effects are disproportionately oriented toward older adults. In the long term, as more evidence of neighborhood effects for health-related outcomes emerges, we will consider policy implications. Some responses might include neighborhood-level interventions that focus on changing the dynamics and resources of disadvantaged neighborhood spaces. While a wide range of programs are taking place around many diverse communities within the United States, including through the Centers for Disease Control and Prevention Investments in Community Health, Racial and Ethnic Approaches to Community Health Project,46 we hypothesize that programs and services tailored specifically to individuals based on known characteristics of where they live might be effective. For instance, if older adults with conditions such as hypertension are known to live in a disadvantaged neighborhood, perhaps tailoring a health services or lifestyle intervention to improve control based on those characteristics could increase the intervention’s efficacy.
Finally, more work is needed to identify what neighborhood characteristics should guide both individual and community-level interventions. For example, low cost and dependable transportation services to health care providers and pharmacies and neighborhood walking groups may be appropriate interventions for residents of these neighborhoods. To that end, in future analyses, we hope to include a wider panel of neighborhood-level variables, including other sociodemographic and health services factors in participants’ communities that determine if these or other factors may need to be intervened upon to reduce cardiovascular disease.
Conclusions
We found that community-dwelling older adults living in disadvantaged neighborhoods had higher odds of having hypertension and lower odds of having it under control, independent of other known risk factors. These findings are consistent with other work demonstrating that neighborhood characteristics may have an impact on health-related outcomes, and it strengthens the body of work that shows an association between neighborhood characteristics and health, in particular for older adults. Further exploration should be conducted to explore if this relationship is causal and to begin to consider relevant interventions that account for neighborhood characteristics at both the neighborhood and individual levels.
Acknowledgments
D. R. Buys’ work was supported in part by T32 HS013852 to the University of Alabama at Birmingham’s Center for Outcomes and Effectiveness Research and Education (K. Saag, principal investigator). The University of Alabama at Birmingham Study of Aging was funded in part by grants R01-AG015062, P30AG031054, and 5UL1 RR025777 from the National Institute on Aging to R. M. Allman (principal investigator) and P. Sawyer (co–principal investigator).
Note. The content is solely the responsibility of the authors and does not necessarily reflect the policy of the National Institute on Aging or the National Institutes of Health.
Human Participant Protection
The University of Alabama at Birmingham institutional review board reviewed and approved this project, and all participants provided informed consent.
References
- 1.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155(6):507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 2.Fitzpatrick KM, LaGory ME. “Placing” health in an urban sociology: cities as mosaics of risk and protection. City Community. 2003;2(1):33–46. [Google Scholar]
- 3.Freedman VA, Grafova IB, Schoeni RF, Rogowski J. Neighborhoods and disability in later life. Soc Sci Med. 2008;66(11):2253–2267. doi: 10.1016/j.socscimed.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glass TA, Balfour JL. Neighborhoods, aging, and functional limitations. In: Kawachi I, Berkman LF, editors. Neighborhoods and Health. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 5.Kawachi I, Berkman LF. Neighborhoods and Health. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 6.Kirby JB, Kaneda T. Neighborhood socioeconomic disadvantage and access to health care. J Health Soc Behav. 2005;46(1):15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- 7.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65(9):1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pruchno RA, Wilson-Genderson M, Cartwright FP. The texture of neighborhoods and disability among older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67B(1):89–98. doi: 10.1093/geronb/gbr131. [DOI] [PubMed] [Google Scholar]
- 9.Sampson RJ. The neighborhood context of well-being. Perspect Biol Med. 2003;46(3, suppl):S53–S64. [PubMed] [Google Scholar]
- 10.Fitzpatrick KM, LaGory ME. Unhealthy Cities: Poverty, Race, and Place in America. New York, NY: Routledge; 2010. [Google Scholar]
- 11.Isaac L, LaVeist T. Neighborhood assets and hypertension in disadvantaged communities. Am J Epidemiol. 2010;171(suppl 11):S1–S157. [Google Scholar]
- 12.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896(1):30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 13.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—allostatic load and its health consequences: Macarthur studies of successful aging. Arch Intern Med. 1997;157(19):2259–2268. [PubMed] [Google Scholar]
- 14.Clarke P, Morenoff J, Debbink M, Golberstein E, Elliott MR, Lantz PM. Cumulative exposure to neighborhood context: consequences for health transitions over the adult life course. Res Aging. 2013;36(1):115–142. doi: 10.1177/0164027512470702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diez Roux AV, Borrell LN, Haan M, Jackson SA, Schultz R. Neighbourhood environments and mortality in an elderly cohort: results from the cardiovascular health study. J Epidemiol Community Health. 2004;58(11):917–923. doi: 10.1136/jech.2003.019596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mujahid MS, Roux AVD, Shen M et al. Relation between neighborhood environments and obesity in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167(11):1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 17.Buys DR, Borch C, Drentea P et al. Physical impairment is associated with nursing home admission for older adults in disadvantaged but not other neighborhoods: results from the UAB Study of Aging. Gerontologist. 2013;53(4):641–653. doi: 10.1093/geront/gns118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawton MP. Environment and other determinants of well-being in older people. Gerontologist. 1983;23(4):349–357. doi: 10.1093/geront/23.4.349. [DOI] [PubMed] [Google Scholar]
- 19.Lawton MP. Social ecology and the health of older people. Am J Public Health. 1974;64(3):257–260. doi: 10.2105/ajph.64.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawton MP. Environment and Aging. Belmont, CA: Brooks/Cole; 1986. [Google Scholar]
- 21.Wahl H-W, Iwarsson S, Oswald F. Aging well and the environment: toward an integrative model and research agenda for the future. Gerontologist. 2012;52(3):306–316. doi: 10.1093/geront/gnr154. [DOI] [PubMed] [Google Scholar]
- 22.Greenfield EA. Using ecological frameworks to advance a field of research, practice, and policy on aging-in-place initiatives. Gerontologist. 2012;52(1):1–12. doi: 10.1093/geront/gnr108. [DOI] [PubMed] [Google Scholar]
- 23.Lawton MP, Simon B. The ecology of social relationships in housing for the elderly. Gerontologist. 1968;8(2):108–115. doi: 10.1093/geront/8.2.108. [DOI] [PubMed] [Google Scholar]
- 24.Ross CE, Mirowsky J, Pribesh S. Powerlessness and the amplification of threat: neighborhood disadvantage, disorder, and mistrust. Am Sociol Rev. 2001;66(4):568–591. [Google Scholar]
- 25.Allman RM, Sawyer P, Roseman JM. The UAB Study of Aging: background and insights into life–space mobility among older Americans in rural and urban settings. Aging Health. 2006;2(3):417–429. [Google Scholar]
- 26.Peel C, Baker PS, Roth DL, Brown CJ, Bodner EV, Allman RM. Assessing mobility in older adults: the UAB Study of Aging life–space assessment. Phys Ther. 2005;85(10):1008–1019. [PubMed] [Google Scholar]
- 27.US Census 2000, Summary File 1. Washington, DC: US Census Bureau; 2001. Available at: https://www.census.gov/census2000/sumfile1.html. Accessed June 26, 2014. [Google Scholar]
- 28.US Census 2000, Summary File 3. Washington, DC: US Census Bureau, US Department of Commerce; 2001. Available at: https://www.census.gov/census2000/sumfile3.html. Accessed June 26, 2014. [Google Scholar]
- 29.The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, MD: National Heart Lung and Blood Institute; 1997. [Google Scholar]
- 30.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 31. The 2000 HHS Poverty Guidelines. 2000. Available at: http://aspe.hhs.gov/poverty/00poverty.htm. Accessed June 26, 2014.
- 32.Meenan RF, Mason JH, Anderson JJ, Guccione AA, Kazis LE. AIMS2. The content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis Rheum. 1992;35(1):1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- 33.Howard G, Prineas R, Moy C et al. Racial and geographic differences in awareness, treatment, and control of hypertension: the Reasons for Geographic and Racial Differences in Stroke Study. Stroke. 2006;37(5):1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 34. National Institutes of Health, National Heart, Lung, and Blood Institute in cooperation with National Institute of Diabetes, Digestive, and Kidney Diseases. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. 1998. NIH publication no. 98-4083. Available at: http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. Accessed March 1, 2011.
- 35.Hubbard AE, Ahern J, Fleischer NL et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- 36.Locher JL, Ritchie CS, Roth DL, Baker PS, Bodner EV, Allman RM. Social isolation, support, and capital and nutritional risk in an older sample: ethnic and gender differences. Soc Sci Med. 2005;60(4):747–761. doi: 10.1016/j.socscimed.2004.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lawton MP, Moss M, Moles E. The suprapersonal neighborhood context of older people. Environ Behav. 1984;16(1):89–109. [Google Scholar]
- 38.Lawton MP, Nahemow L. Ecology and the aging process. In: Eisendorfer C, Lawton MP, editors. The Psychology of Adult Development and Aging. Washington, DC: American Psychological Association; 1973. p. 619. [Google Scholar]
- 39.Diez Roux AV, Chambless L, Merkin SS et al. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002;106(6):703–710. doi: 10.1161/01.cir.0000025402.84600.cd. [DOI] [PubMed] [Google Scholar]
- 40.King KE, Morenoff JD, House JS. Neighborhood context and social disparities in cumulative biological risk factors. Psychosom Med. 2011;73(7):572–579. doi: 10.1097/PSY.0b013e318227b062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baker PS, Allman RM. Charting the Course: Alabama Long Term Needs Assessment. Birmingham, AL: University of Alabama at Birmingham and Alabama Division of Medicaid; 2004. [Google Scholar]
- 42.Hox JJ. Multilevel Analysis: Techniques and Applications. New York, NY: Routledge; 2010. [Google Scholar]
- 43.Kreft IGG. Are Multilevel Techniques Necessary? An Overview, Including Simulation Studies. Los Angeles, CA: California State University; 1996. [Google Scholar]
- 44.Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL, Karlamangla AS, Seeman TE. Urban neighborhoods and depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2007;62(1):S52–S59. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- 45.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—The Public Health Disparities Geocoding Project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. Investments in community health: Racial and Ethnic Approaches to Community Health (REACH) 2013. Available at: http://www.cdc.gov/nccdphp/dch/programs/reach. Accessed March 30, 2014.