Abstract
Objectives. We investigated the structural characteristics of a multiplex HIV transmission risk network of drug-using male sex workers and their associates.
Methods. Using a sample of 387 drug-using male sex workers and their male and female associates in Houston, Texas, we estimated an exponential random graph model to examine the venue-mediated relationships between individuals, the structural characteristics of relationships not linked to social venues, and homophily. We collected data in 2003 to 2004. The network comprised social, sexual, and drug-using relationships and affiliations with social venues.
Results. Individuals affiliated with the same social venues, bars, or street intersections were more likely to have nonreciprocated (weak) ties with others. Sex workers were less likely than were other associates to have reciprocated (strong) ties to other sex workers with the same venues. Individuals tended to have reciprocated ties not linked to venues. Partner choice tended to be predicated on homophily.
Conclusions. Social venues may provide a milieu for forming weak ties in HIV transmission risk networks centered on male sex workers, which may foster the efficient diffusion of prevention messages as diverse information is obtained and information redundancy is avoided.
Sex work increases the risk of contracting and transmitting HIV and other sexually transmitted infections through unprotected sexual behaviors or substance use.1 Male sex workers (MSWs) experience high rates of HIV infection, both globally and domestically.2–4 In North America, HIV prevalence among MSWs is estimated to range from 5% to 31%.4 MSWs have high rates of risky sexual behavior and substance use, including drug injection.5–7 However, public health issues related to MSWs have been understudied, and current HIV prevention programs underserve MSWs.4
MSWs are not homogeneous nor are the contexts of male sex work uniform.4,8 Because male sex work takes diverse forms in a variety of contexts,8,9 HIV risks may also vary by context. MSWs who solicit sex on the streets are at high risk for HIV infection, and the context of the street may increase the risk. MSWs working in street venues are more likely to have few financial resources, be undereducated, live in unstable housing or on the streets, be unemployed or disabled, and engage in sex work as a means of survival.8 Numerous MSWs and their clients self-identify as heterosexual.10 Men who have sex with men and women (MSMW) have higher rates of both transactional sex and concurrent illicit drug use and sex than do men who have sex with men only, and, among MSMW, both transactional sex and concurrent illicit drug use predict risky sexual behavior.11
Although sociodemographic characteristics, HIV infection, and risk behaviors of MSWs have been documented,12,13 relatively few studies have provided a relational account of HIV risk within male sex work networks. It is known, for example, that networks of MSWs are connected to networks of other high-risk groups.2,8,10,14,15 Through these network ties, MSWs may bridge with men who have sex with men (MSM), female sex workers, drug users, and other less risky groups.2,16 MSMW are more likely to engage in sex for drugs or money than are other MSM, and MSMW occupy a central position in the network of HIV-infected males.17 However, because of the diversity of male sex work, it may be inappropriate to conceptualize MSWs as a core group.18
Social networks are the structures within which norms are developed and implemented and social support occurs.19,20 Most risk-potential linkages within networks are social,20 and sex ties are often formed through social circles.21 MSWs form unique social networks,9,22 most likely involving risky drug-use and sexual behaviors. The networks are often hierarchical structures in which network leaders control areas for soliciting sex, and the network structure provides mutual support for soliciting sex.9
Rarely do studies on HIV risk networks that involve MSWs regard the network as composed of “persons, places, and the relevant links connecting them.”23(p684) Social venues are an important part of the network structure, forming the setting for MSWs’ social life and facilitating the formation of “sexual affiliation networks.”24 Our previous study25 underscored the duality of people and places26 by focusing on affiliation networks between MSWs and social venues. We found centralized affiliation patterns around a small number of highly interdependent venues. Although interdependent, the venues presented distinct patterns of venue-based clustering.25 These findings, however, were limited because the study focused on venue affiliation. Non–venue-based direct ties also may be important because they are expected to occur within social, drug-using, and sexual relationships. These types of relationships may have different emotional and interpersonal contexts27 that would tend to result in different patterns and types of ties.
We defined a multiplex transmission risk network as composed of multifaceted social contexts that comprise a mix of social, sexual, and drug-using ties and affiliation ties to social venues. The social network perspective informs relational mechanisms of information diffusion and social influence at the entire network and personal network levels. Granovettor’s theory of the strength of weak ties posits, “The weak tie between ego and his acquaintance, therefore, becomes not merely a trivial acquaintance tie but rather a crucial bridge between the two densely knit clumps of close friends.”28(p202) Weak ties avoid information redundancy by enabling individuals to access diverse information and to facilitate the diffusion of information throughout the entire network.29 Although weak ties facilitate information diffusion, they may not be sufficiently powerful to change behavior because of the ties’ transient and passive nature.
Rarely have network studies focused on the role that affiliation ties play in forming direct ties between individuals. We defined venue-mediated weak or strong ties as 1-mode social, sexual, and drug-using ties formed through jointly affiliating in the same venues. We examined and statistically tested local relational features of venue-mediated weak or strong ties among MSWs and their associates. On the basis of the effect of bar-based social influence interventions led by opinion leaders on HIV risk reduction,30,31 HIV prevention messages disseminated within venues are expected to facilitate the diffusion of information, and, thus, weak ties are more likely than are strong ties to be observed linked to social venues.
In personal networks, reciprocated ties suggest higher levels of trust and intimacy and, in some cases, a strong tendency to engage in risky behaviors.32 The risk of engaging in behaviors that transmit HIV are also heightened during sex for money exchanges, particularly if there is a strong economic incentive for doing so. This suggests that risk is related to the multiple types of ties determined by context. Additionally, homophily affects network ties by influencing the information that people receive, the attitudes formed, and the social interactions experienced.33 We also sought to examine the tendency of reciprocity and the effect of homophily on HIV status and sociodemographic and behavioral factors when forming risk-potential relationships that comprise social, sexual, or drug-using ties but are not linked to social venues. The likelihood of engaging in risk-taking behavior is greater in relationships with a high degree of homophily, as information flows and persuasion tend to be more frequent among like pairs.32 We tested these relational features using a stochastic network modeling approach.
METHODS
We collected data between May 2003 and February 2004 as part of a study of drug-using MSW networks in Houston, Texas. We recruited participants using a combination of sampling methods described in greater detail elsewhere.34,35 To construct the sample, we interviewed key informants and asked them to help contact focal participants. Focal participants were eligible for the study if they were a self-identified male aged at least 17 years, had exchanged sex for money with another man in the past 7 days, and had smoked crack cocaine or injected an illicit substance in the past 48 hours before being screened.
During the interview, we asked focal participants to name men and women with whom they interacted socially or with whom they used drugs or had sex. We listed those names and apportioned them into strata that consisted of sex or drug-use partners, friends, paying sex partners, and other social contacts. We then weighted names to give preference to sex and drug-use contacts. We asked focal participants to contact network members on the list and ask them to participate in the study. We used the same process with network members to create a list of tertiary network members. Network members were eligible if they were aged at least 17 years and linked to the focal or secondary (referring) participants.
Sample
We interviewed a sample of 334 males (84%) and 62 females (16%) to collect sociodemographic, HIV and sexually transmitted infection history, drug use, and risky sexual behavior data. In addition to personal data, we asked respondents about their network contacts’ demographic characteristics, HIV status, risky sexual behaviors, and relationship with the contact. We collected data on venue affiliation by asking respondents the names of places or street intersections where they spent time. We validated intersections using a city map and then geocoding them. We identified 15 bars and 51 intersections, for a total of 66 venues.
We used data to generate an analytic sample consisting of 735 dyads in which contacts were also respondents. This generated 9 isolates who had no ties to other individuals or no affiliation with a venue; we dropped these from the analysis to avoid model divergence. Dyads were composed of 325 (84%) males and 62 (16%) females and included 28% focal respondents, 36% secondary contacts, and 36% tertiary contacts.
Measures
Network data.
We created social network data predicated on a directed 1-mode actor-by-actor adjacency matrix, for which we defined a tie on the basis of any nominations of social, sexual, or drug-use contacts. We defined weak ties as any asymmetric ties between individuals that ran in unidirection only29 and strong ties as ties that ran in both directions. We created affiliation network data grounded on a 2-mode actor-by-venues matrix (row indexes had 387 actors and column indexes had 66 venues), in which we defined a tie as having an affiliation with a specific venue. We combined 1- and 2-mode networks to form the multiplex network data.
HIV status and risk or protective sexual behaviors.
We measured HIV status by respondents’ self-report of HIV testing or status: never tested, negative test, positive test, or indeterminate test. HIV risk sexual behavior measures included ever having traded sex for money, the number of paying sex partners, and the number of nonpaying casual sex partners during the past 30 days (as a continuous scale).
We measured protective sexual behavior as frequency of condom use during anal intercourse with paid or casual sex partners in the past 7 days and defined them as consistent condom use (i.e., always using a condom).
Socioeconomic and demographic variables.
We coded race/ethnicity as Black, White, Hispanic, or other. We coded self-identified homeless as homeless or not homeless. We coded self-identified sexual orientation as gay, straight, or bisexual.
We measured age, years of schooling, number of lifetime arrests, and months of incarceration as continuous scales. To account for the sampling strategy, we created dummy variables representing the recruitment status of the sampling design (seeds, secondary contacts, or tertiary contacts).
Data Analysis
Visualization of multiplex network.
We visualized a multiplex HIV transmission risk network consisting of a 1-mode network and a 2-mode venue affiliation network to describe the overall structural pattern in relation to self-reported HIV status, sex work status, and venue types.
We used NetworkX (GitHub)36 for visualization.
Exponential random graph models.
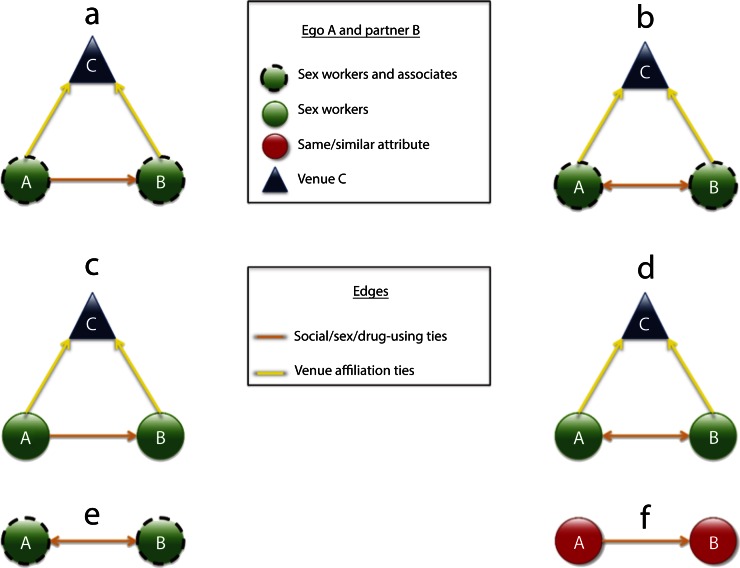
We used exponential random graph models (ERGMs) to model the observed network endogenous structure by taking into account the dependencies among network ties37 as well as the dependencies between network ties and exogenous covariates.38,39 We modeled a 1-mode network39 with the 2-mode network and various attributes and measures of the behavior as covariates. We used results to test how individuals’ self-reported HIV status, risk and protective behavior and attributes, and affiliated venues affect their partners’ social, sexual, and drug-use relationships. We examined our study objectives by statistically testing whether the graph configurations of a venue-mediated weak tie effect (Figure 1a) by sex workers (Figure 1c), venue-mediated strong tie effect (Figure 1b) by sex workers (Figure 1d), 1-mode reciprocated tie effect (Figure 1e), and homophily effect (Figure 1f) are more likely to be observed than expected by chance. We generated the modeling results using MPNet.40
FIGURE 1—
Graph configurations among actors A and B and venue C of (a) venue-mediated weak tie effect, (b) venue-mediated strong tie effect, (c) venue-mediated weak tie effect between sex workers, (d) venue-mediated strong tie effect between sex workers, (e) 1-mode reciprocated tie effect, and (f) 1-mode relational homophily effect: Houston, TX; May 2003–February 2004.
Reviews and detailed descriptions of the ERGMs that we applied (model specification, graph configurations, mathematical expressions, and interpretations) are available as a supplement to the online version of this article at http://www.ajph.org.
RESULTS
The demographic and behavioral characteristics of the 387 MSWs and their associates are shown in Table 1. Among the 735 dyads, 40% of the social ties overlapped with the sex ties, 80% of the social ties overlapped with the drug-using ties, and 33% of the social ties overlapped with both the sex and drug-using ties. On average, the sample was affiliated with 1 venue (SD = 0.90; min = 0; max = 4).
TABLE 1—
Descriptive Statistics of Drug-Using Male Sex Worker (n = 387) Networks: Houston, TX; May 2003–February 2004
| Variable | % (No.) or Mean (SD; Min, Max) |
| HIV status | |
| Positive | 20 (79) |
| Negative | 64 (247) |
| Unknown (including indeterminate) | 16 (61) |
| Gender | |
| Male | 84 (325) |
| Female | 16 (62) |
| Age, y | |
| 16–29 | 40 (155) |
| 30–39 | 36 (138) |
| ≥ 40 | 24 (93) |
| Race/ethnicity | |
| White | 47 (183) |
| Black | 43 (168) |
| Hispanic | 8 (31) |
| Homelessness | 49 (188) |
| Sexual orientation | |
| Gay | 32 (122) |
| Straight | 25 (95) |
| Bisexual | 44 (170) |
| Years of schooling | 11.24 (2.15; 4, 19) |
| Number of cumulative arrests | 10.71 (13.72; 0, 90) |
| Months of incarceration | 48.39 (56.02; 0, 300) |
| Recruitment status | |
| Seeds | 28 (107) |
| Secondary contacts | 36 (140) |
| Tertiary contacts | 36 (140) |
| Ever experienced sex work | 75 (292) |
| Never experienced sex work | 25 (95) |
| No. of paid sex partners | 29.22 (38.83; 0, 150) |
| No. of casual sex partners | 6.92 (19.43; 0, 150) |
| Protective sex | |
| Consistent condom use | 21 (80) |
| Nonconsistent condom use | 40 (155) |
Note. Number of sex partners refers to the past 30 days; the upper limit was set to 150 to minimize recollection problems. There were 39% missing cases for the protective sex variable, and 1% for the others category for the race/ethnicity variable.
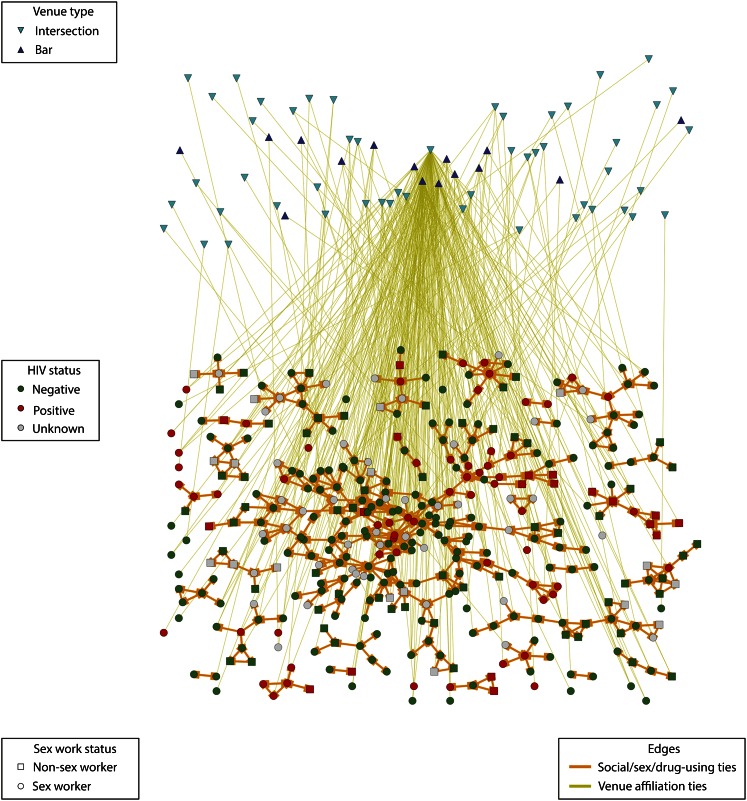
Figure 2 illustrates the multiplex HIV transmission risk network in relation to HIV status, sex work status, and venue types. Although these graphs represent overall structural patterns of the multiplex risk network, they are limited in their ability to identify some distinctive features of the observed network, which we examined by estimating ERGMs.
FIGURE 2—
Multiplex HIV transmission risk network among 387 men who have sex with women and their associates in relation to HIV status, sex work status, and affiliation with social venues: Houston, TX; May 2003–February 2004.
Table 2 shows the results of ERGM parameter estimates and SEs for the network effects of the 1-mode network with the 2-mode network and actor attributes and behavior as exogenous covariates.
TABLE 2—
Exponential Random Graph Model (ERGM) for the Multiplex 1-Mode and 2-Mode HIV Transmission Risk Network: Houston, TX; May 2003–February 2004
| ERGM Components and Structural Effects | b (SE) |
| 1-mode structure | |
| Arc density | –7.391* (0.421) |
| Reciprocity | 7.614* (0.249) |
| No receiver | –3.065* (0.414) |
| Isolate | –2.094* (0.400) |
| Alternating in star | 1.395* (0.235) |
| Alternating out star | –0.977* (0.188) |
| Alternating triangle | 1.007* (0.054) |
| Alternating 2 path | –0.132* (0.033) |
| Sender attributes and behavior | |
| HIV positive | –0.615* (0.212) |
| Race/ethnicity is White | –0.982* (0.275) |
| Race/ethnicity is Black | –0.426 (0.289) |
| Homeless | –0.619* (0.159) |
| Bisexual | –0.056 (0.170) |
| Sex work | –0.059 (0.209) |
| Consistent condom use | –0.341 (0.180) |
| Receiver attributes and behavior | |
| HIV positive | 0.158 (0.168) |
| Race/ethnicity is Black | –0.855* (0.266) |
| Race/ethnicity is White | –0.299 (0.243) |
| Homeless | 0.168 (0.133) |
| Bisexual | –0.346* (0.149) |
| Sex work | –0.647* (0.185) |
| Consistent condom use | 0.297* (0.141) |
| Homophily on binary attributes and behavior | |
| HIV positive | 0.740* (0.141) |
| Race/ethnicity is White | 0.507* (0.190) |
| Race/ethnicity is Black | 1.648* (0.218) |
| Homeless | 0.415* (0.114) |
| Bisexual | 0.375* (0.105) |
| Sex work | 0.524* (0.130) |
| Consistent condom use | 0.278* (0.128) |
| Homophily on continuous attributes and behavior | |
| Age | –0.037* (0.005) |
| Years of schooling | 0.011 (0.016) |
| No. of cumulative arrests | –0.001 (0.002) |
| Months of incarceration | 0.001 (0.001) |
| No. of paid sex partners | 0.001 (0.001) |
| No. of casual sex partners | –0.004* (0.002) |
| Venue-mediated ties | |
| Weak tie | 0.899* (0.310) |
| Strong tie | –1.039 (0.645) |
| Venue-mediated ties among sex workers | |
| Weak tie | 0.494 (0.318) |
| Strong tie | –1.301* (0.668) |
Note. The Hispanic race/ethnicity variable did not have significant effects.
*P < .05.
Structural Effects of the 1-Mode Network
The social ties in this multiplex 1-mode network were highly reciprocal, meaning that individuals tended to exhibit mutual ties running in both directions. These networks are characterized by a small number of frequently nominated individuals in the center of a network who received many more nominations than would have been expected if it were at random. Four of the 387 individuals received more than 10 nominations, whereas 240 received 1 or 2 nominations. There also was a tendency for all network members to receive similar numbers of partner nominations. Individuals tended to form closed, but hierarchically structured ties; so frequently nominated individuals tended to be located at the top of a triangle configuration. These individuals also tended not to share multiple sexual, social, or drug partners unless they were connected to each other. There are fewer individuals that were isolated or did not receive any nominations in the 1-mode network.
Individuals who were HIV positive, Black, and homeless nominated fewer others, suggesting that they were less active in the network. Those who were Black, identified as bisexual, or were sex workers were nominated less frequently than were others in the network. Individuals who consistently used condoms were nominated more frequently than were others.
Homophily Effects
HIV-positive individuals, Whites, Blacks, homeless individuals, bisexuals, sex workers, and individuals who consistently use condoms had a tendency to choose sexual, social, and drug partners with the same attributes and behaviors as themselves. There also was a tendency to choose others of similar age or number of casual sex partners.
For continuous attributes, a negative homophily parameter estimate suggests that there was a tendency for individuals to nominate others with similar attribute or behavior measures, as the statistic that represents homophily is defined on the basis of the differences in attribute values of pairs of individuals.
By treating unidirectional ties as weak ties and bidirectional ties as strong ties, individuals affiliated with the same venue were more likely to have weak ties. Results also showed that sex workers were less likely to have reciprocated ties to other sex workers. Results of the recruitment status effect of sampling design and goodness-of-fit tests are available as a supplement to the online version of this article at http://www.ajph.org.
DISCUSSION
We took a social network approach to investigate the structural features that characterize a multifaceted HIV transmission risk network of drug-using MSWs and their associates in the context of social venues and personal network not linked to venues. We found that the 1-mode risk network was characterized by reciprocated relationships, that is, individuals mutually nominated their social, sexual, or drug-use partners, which is indicative of close relationships. Because of this general structural tendency, individuals were more likely to choose their sexual, social, or drug partners on the basis of homophily in HIV-positive status, age, race/ethnicity, homelessness, bisexual orientation, the number of casual sex partners, and protective sex behavior. In combination with venue affiliation, individuals had weak ties with those from the same venue. Conversely, there was an absence of reciprocated, or strong, ties associated with the same venues. This tendency was especially notable for sex workers affiliated with the same venues.
One of the distinguishing features of our study was that we examined venues as part of the risk network. Findings suggest that the venues named by drug-using MSWs and their associates, mostly bars and street corners, facilitate the formation of weak, but not strong, ties. The tendency to form weak ties may be greater, perhaps in part because the venues where MSWs gather are the same as those where they solicit paying sex partners. Our findings also suggest that individuals form strong ties in their personal networks outside social venues and choose their social, sexual, or drug-use partners on the basis of homophily of ties as determined by disease status and risk or protective behaviors and characteristics. For example, HIV-positive men were more likely to have HIV-positive social, sexual, or drug-use partners. Men who self-identified as bisexual were more likely to have bisexual sexual, social, or drug-use partners.
The finding of homophily of ties supports the Centers for Disease Control and Prevention’s supposition that social network strategies for HIV testing, prevention, and engagement in care are important.41,42 Our findings extend this supposition by suggesting that the ties within the network of at-risk groups also are important. For example, peers should not be considered on the basis of a single identifying characteristic, such as male sex work. Multiple characteristics, rather than a single factor such as race/ethnicity, may identify an individual as a peer. Developing more sophisticated models of peers could enhance the utility of a network-level HIV intervention by resulting in significant breadth when targeting the commercial sexual and drug networks. Interventions within personal networks should consider targeting clusters of like individuals while considering numerous identifying factors.
The structural features of a network may be integral to successfully disseminating prevention messages and delivering social influence interventions. The utility of prevention interventions predicated on venue has been demonstrated by Kelly et al.’s bar-based opinion leader intervention among gay men31 and among groups of MSWs.22 However, no study of the diffusion mechanism of prevention messages through the opinion leaders inside venues has been undertaken. Further, although the potential utilities of HIV prevention and intervention on the basis of venue have been suggested in the literature,24,25,43–46 why and how they would be used is unclear and often unspecified.
In regard to network-level interventions employed in public health,47 the weak ties derived from joint venue affiliations suggest that venues could be promising settings for strategically diffusing behavior change messages. Nevertheless, weak ties are not sufficiently powerful for behavior change, only for information diffusion. However, if peers are considered role models, this modeling may have a positive impact on both perceived norms and behavior. Our results suggest that relying on weak ties as a mechanism for the efficient diffusion of intervention messages may be more beneficial for some groups than is focusing on popular opinion leaders.
Limitations
The study has certain limitations. We recruited the sample of drug-using MSWs from street or bar settings. Considering the diversity of sex workers, our results may not be generalizable to MSWs in different work circumstances; MSWs in differing policing, history, or norms; or MSWs who work in different geographical locations.4 Furthermore, we collected the data from 2003 to 2004. However, it is very unlikely that the organization of street- or bar-based sex work may have changed since we collected the data. It is more likely that the expansion of digital media has led to the expansion of sex work venues. However, many drug-using men who solicit sex in street and bar settings are unlikely to have the financial wherewithal to consistently access digital media. Nonetheless, our results should be interpreted with caution as applied to digital opportunities for sex work.
Methodologically, although ERGM analysis of this study controls for recruitment status to minimize the effect of sampling design on structural features, the analysis was still subject to potential bias or artifacts of the sampling strategy. We conceptualized the multiplex 1-mode risk network as a mixture of social, sexual, and drug-using relationships and operationalized these as the types of ties investigated. Consequently, we were limited in our ability to explore the relative contributions of the multiple types of relationships to structuring homophily. Homophily of ties may have been stronger than the results suggest if we had investigated more overlapping ties.33
Finally, we did not consider HIV protective venue affiliation, such as HIV health center or education centers that provide HIV prevention.46 Future research should examine whether our findings apply to these different types of venues.
Conclusions
Despite these limitations, our findings provide a structural account of the dynamics of HIV transmission risk. Because of the occupational hazards of HIV and other infections that MSWs encounter as part of their day-to-day activities, the paucity of HIV prevention interventions and treatment services that have been developed for MSWs,4 and the risks posed to associates, structuring interventions to account for the social- and venue-based affiliation network structure of male sex work is more likely to be effective than are 1-size-fits-all off-the-shelf interventions.
Acknowledgments
This study was supported by the National Institutes of Health ([NIH]; grant NIMH 1R01MH100021) and used data collected by a social network project funded by the NIH (grant NIDA R01DA015025).
We acknowledge the insightful comments of the anonymous reviewers who contributed significantly to improving earlier versions of this article. We also acknowledge Ju Yeong Kim for assistance in the validation of the data and for technical assistance and Dennis Li and Kimberly Cook for assistance in the relevant literature search.
Human Participant Protection
The University of Texas Health Science Center, Houston’s institutional review board approved this study.
References
- 1.Centers for Disease Control and Prevention. HIV risk among adult sex workers in the United States. Available at: http://www.cdc.gov/hiv/pdf/library_factsheet_HIV_among_sex_workers.pdf. Accessed October 28, 2014.
- 2.Morse EV, Simon PM, Osofsky HJ, Balson PM, Gaumer HR. The male street prostitute: a vector for transmission of HIV infection into the heterosexual world. Soc Sci Med. 1991;32(5):535–539. doi: 10.1016/0277-9536(91)90287-m. [DOI] [PubMed] [Google Scholar]
- 3.Elifson KW, Boles J, Sweat M. Risk factors associated with HIV infection among male prostitutes. Am J Public Health. 1993;83(1):79–83. doi: 10.2105/ajph.83.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baral SD, Friedman RM, Geibel S et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2014 doi: 10.1016/S0140-6736(14)60801-1. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams ML, Timpson S, Klovdahl A, Bowen A, Ross M, Keel K. HIV risk among a sample of male sex workers. AIDS. 2003;17(9):1402–1404. doi: 10.1097/00002030-200306130-00020. [DOI] [PubMed] [Google Scholar]
- 6.Rietmeijer CA, Wolitski RJ, Fishbein M, Corby NH, Cohn DL. Sex hustling, injection drug use, and nongay identification by men who have sex with men. Associations with high-risk sexual behaviors and condom use. Sex Transm Dis. 1998;25(7):353–360. doi: 10.1097/00007435-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Reisner SL, Mimiaga MJ, Mayer KH, Tinsley JP, Safren SA. Tricks of the trade: sexual health behaviors, the context of HIV risk, and potential prevention intervention strategies for male sex workers. J LGBT Health Res. 2008;4(4):195–209. doi: 10.1080/15574090903114739. [DOI] [PubMed] [Google Scholar]
- 8.Minichiello V, Scott J, Callander D. New pleasures and old dangers: reinventing male sex work. J Sex Res. 2013;50(3–4):263–275. doi: 10.1080/00224499.2012.760189. [DOI] [PubMed] [Google Scholar]
- 9.Boles J, Elifson KW. The social organization of transvestite prostitution and AIDS. Soc Sci Med. 1994;39(1):85–93. doi: 10.1016/0277-9536(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 10.Scott J, Minichiello V. Reframing male sex work. In: Scott J, Minichiello SJ, editors. Male Sex Work and Society. New York, NY: Harrington Park Press; 2014. pp. xii–xxvii. [Google Scholar]
- 11.Friedman MR, Kurtz SP, Buttram ME, Wei C, Silvestre AJ, Stall R. HIV risk among substance-using men who have sex with men and women (MSMW): findings from South Florida. AIDS Behav. 2014;18(1):111–119. doi: 10.1007/s10461-013-0495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belza MJ, Llácer A, Mora R, Morales M, Castilla J, de la Fuente L. Sociodemographic characteristics and HIV risk behaviour patterns of male sex workers in Madrid, Spain. AIDS Care. 2001;13(5):677–682. doi: 10.1080/09540120120063296. [DOI] [PubMed] [Google Scholar]
- 13.Timpson SC, Ross MW, Williams ML, Atkinson J. Characteristics, drug use, and sex partners of a sample of male sex workers. Am J Drug Alcohol Abuse. 2007;33(1):63–69. doi: 10.1080/00952990601082670. [DOI] [PubMed] [Google Scholar]
- 14.Logan TD. Personal characteristics, sexual behaviors, and male sex work: a quantitative approach. Am Sociol Rev. 2010;75(5):679–704. [Google Scholar]
- 15.Mimiaga MJ, Reisner SL, Tinsley JP, Mayer KH, Safren SA. Street workers and Internet escorts: contextual and psychosocial factors surrounding HIV risk behavior among men who engage in sex work with other men. J Urban Health. 2009;86(1):54–66. doi: 10.1007/s11524-008-9316-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams ML, Bowen AM, Timpson S, Keel BK. Drug injection and sexual mixing patterns of drug-using male sex workers. Sex Transm Dis. 2003;30(7):571–574. doi: 10.1097/00007435-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Hightow LB, Leone PA, MacDonald DM, McCoy SI, Sampson LA, Kaplan AH. Men who have sex with men and women: a unique risk group for HIV transmission on North Carolina college campuses. Sex Transm Dis. 2006;33(10):585–593. doi: 10.1097/01.olq.0000216031.93089.68. [DOI] [PubMed] [Google Scholar]
- 18.Parker M. Core groups and the transmission of HIV: learning from male sex workers. J Biosoc Sci. 2006;38(1):117–131. doi: 10.1017/S0021932005001136. [DOI] [PubMed] [Google Scholar]
- 19.Schneider JA, Cornwell B, Ostrow D et al. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among Black men who have sex with men. Am J Public Health. 2013;103(1):e28–e36. doi: 10.2105/AJPH.2012.301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman SR, Aral S. Social networks, risk-potential networks, health, and disease. J Urban Health. 2001;78(3):411–418. doi: 10.1093/jurban/78.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dragowski EA, Halkitis PN, Moeller RW, Siconolfi DE. Social and sexual contexts explain sexual risk taking in young gay, bisexual, and other young men who have sex with men, ages 13–29 years. J HIV AIDS Soc Serv. 2013;12(2):236–255. [Google Scholar]
- 22.Miller RL, Klotz D, Eckholdt HM. HIV prevention with male prostitutes and patrons of hustler bars: replication of an HIV preventive intervention. Am J Community Psychol. 1998;26(1):97–131. doi: 10.1023/a:1021886208524. [DOI] [PubMed] [Google Scholar]
- 23.Klovdahl AS, Graviss EA, Yaganehdoost A et al. Networks and tuberculosis: an undetected community outbreak involving public places. Soc Sci Med. 2001;52(5):681–694. doi: 10.1016/s0277-9536(00)00170-2. [DOI] [PubMed] [Google Scholar]
- 24.Frost SDW. Using sexual affiliation networks to describe the sexual structure of a population. Sex Transm Infect. 2007;83(suppl 1):i37–i42. doi: 10.1136/sti.2006.023580. [DOI] [PubMed] [Google Scholar]
- 25.Fujimoto K, Williams ML, Ross MW. Venue-based affiliation network and HIV risk behavior among male sex workers. Sex Transm Dis. 2013;40(6):453–458. doi: 10.1097/OLQ.0b013e31829186e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breiger RL. Duality of persons and groups. Soc Forces. 1974;53(2):181–190. [Google Scholar]
- 27.Fujimoto K, Williams ML, Ross MW. A network analysis of relationship dynamics in sexual dyads as correlates of HIV risk misperceptions among high-risk MSM. Sex Transm Infect. 2014 doi: 10.1136/sextrans-2014-051742. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Granovetter MS. The strength of weak ties: a network theory revisited. Sociol Theory. 1983;1:201–233. [Google Scholar]
- 29.Granovetter MS. The strength of weak ties. Am J Sociol. 1973;78(6):1360–1380. [Google Scholar]
- 30.Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–150. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- 31.Kelly JA, St. Lawrence JS, Diaz YE et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valente TW. Social Networks and Health: Models, Methods, and Applications. New York, NY: Oxford University Press; 2010. [Google Scholar]
- 33.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol. 2001;27:415–444. [Google Scholar]
- 34.Williams ML, Atkinson J, Klovdahl AS, Ross MW, Timson S. Spatial bridging in a network of drug-using male sex workers. J Urban Health. 2005;82(suppl 1):i35–i42. doi: 10.1093/jurban/jti022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams ML, Ross MW, Atkinson JA, Bowen A, Klovdahl A, Timpson SC. An investigation of concurrent sex partnering in two samples having large numbers of sex partners. Int J STD AIDS. 2006;17(5):309–314. doi: 10.1258/095646206776790123. [DOI] [PubMed] [Google Scholar]
- 36.Hagberg AA, Schult DA, Swart PJ. Exploring network structure, dynamics, and function using NetworkX. In: Varoquaux G, Vaught T, Millman J, editors. Proceedings of the 7th Python in Science Conference (SciPy2008) Pasadena, CA: 2008. pp. 11–15. [Google Scholar]
- 37.Pattison PE, Snijders TAB. Modeling social networks: next steps. In: Lusher D, Koskinen J, Robins G, editors. Exponential Random Graph Models for Social Networks: Theories, Methods and Applications. New York, NY: Cambridge University Press; 2013. pp. 287–301. [Google Scholar]
- 38.Robins G, Elliott P, Pattison PE. Network models for social selection processes. Soc Networks. 2001;23:1–30. [Google Scholar]
- 39.Wang P, Robins G, Pattison P, Lazega E. Exponential random graph models for multilevel networks. Soc Networks. 2013;35(1):96–115. [Google Scholar]
- 40.Wang P, Robins G, Pattison P. PNet: A Program for the Simulation and Estimation of Exponential Random Graph Models. Melbourne, Australia: University of Melbourne; 2009. [Google Scholar]
- 41.Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: the social networks demonstration project. Am J Public Health. 2009;99(6):1093–1099. doi: 10.2105/AJPH.2008.139329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCree DH, Millett G, Baytop C et al. Lessons learned from use of social network strategy in HIV testing programs targeting African American men who have sex with men. Am J Public Health. 2013;103(10):1851–1856. doi: 10.2105/AJPH.2013.301260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holloway IW, Rice E, Kipke MD. Venue-based network analysis to inform HIV prevention efforts among young gay, bisexual, and other men who have sex with men. Prev Sci. 2014;15(3):419–427. doi: 10.1007/s11121-014-0462-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee SS, Tam DK, Tan Y et al. An exploratory study on the social and genotypic clustering of HIV infection in men having sex with men. AIDS. 2009;23(13):1755–1764. doi: 10.1097/QAD.0b013e32832dc025. [DOI] [PubMed] [Google Scholar]
- 45.Schneider JA. Sociostructural 2-mode network analysis: critical connections for HIV transmission elimination. Sex Transm Dis. 2013;40(6):459–461. doi: 10.1097/01.olq.0000430672.69321.0a. [DOI] [PubMed] [Google Scholar]
- 46.Schneider JA, Walsh T, Cornwell B, Ostrow D, Michaels S, Laumann EO. HIV health center affiliation networks of Black men who have sex with men: disentangling fragmented patterns of HIV prevention. Sex Transm Dis. 2012;39(8):598–604. doi: 10.1097/OLQ.0b013e3182515cee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Valente TW. Network interventions: a taxonomy of behavior change interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]