Abstract
Objectives
To assess use, utility and impact of transition interventions designed to support and empower self-management in youth with chronic health conditions during transition into adult healthcare.
Design
A 4-year mixed-method prospective cohort study.
Setting
2 academic paediatric hospitals (13 clinics) in Canada.
Participants
50 adolescents (42% male; mean age 17.9±0.9 years; 20 underlying diagnoses) with transfer to adult care planned within 1 year.
Interventions
The Youth KIT (an organisational tool that includes goal setting activities); an online transition mentor.
Main outcome measures
Frequency of use, utility and impact of the transition interventions; goal achievement; post-transfer qualitative interviews with youth.
Results
50 participants were enrolled during their last year of paediatric care; 36 (72%) were followed into adult care. All participants had access to the transition interventions from enrolment until the end of the study (exposure time: 12–47 months). Most youth (85%) reported using the medical/health section of the Youth KIT at least once; 20 (40%) participants engaged in chats with the mentor. The overall perceived utility of both interventions was modest; the Youth KIT received the highest ratings for ‘help with goal setting’: (mean (SD): 4.2 (2.3)) on a 7-point Likert scale. 45 (90%) participants set 294 transition goals. Goal achievement performance and satisfaction increased over time (p≤0.001). The qualitative evidence revealed reasons behind the variability in use and utility of the interventions, the interconnectedness of life-course and healthcare transitions, and the need for stronger partnerships between paediatric and adult healthcare systems.
Conclusions
Participants’ perceptions about the utility of the Youth KIT and the online mentor were modest. Transition supports need to be carefully tailored, timed and integrated into healthcare systems. Individualised goal setting may be an important ‘active ingredient’ in optimising transition supports and outcomes. Interventions that focus on youth only are insufficient for empowering self-management.
Keywords: QUALITATIVE RESEARCH, Transition into adult heathcare, Chronic conditions, Disabilities, Longitudinal research
Strengths and limitations of this study.
In total, 50 youth with over 20 different conditions provided information on the use, utility and impact of an organisational tool, and an online transition mentor before and after their actual transfer from a paediatric hospital to an adult healthcare setting.
This longitudinal study captured very realistic challenges associated with sustained youth engagement in patients with neurodevelopmental and other chronic health conditions, from whom previous data on transition interventions has rarely been reported together.
The quantitative evaluation indicated that the two transition interventions are insufficient for empowering youth, while the qualitative evidence revealed reasons behind the variability in their use and utility.
The modest impact observed in transitioning adolescents should be interpreted with caution, as the results may be affected by bias, particularly self-selection at study entry and lack of engagement with adult physicians at follow-up.
Participants were not representative of the transitioning population as a whole as the sample excluded non-English speakers and those who showed full dependence on caregivers in the areas of daily functioning, self-care and communication.
Introduction
For the rapidly growing population of adolescents with chronic health conditions,1 transition to adult healthcare adds a cornerstone challenge to this already complex developmental stage. Evidence suggests that the related healthcare delivery has not been able to keep pace with the multidimensional needs of emerging adults.1–4 For over two decades, professional groups and initiatives have called to improve the process of transitioning care.3 5–8 Nonetheless, youth continue to face adverse health outcomes2 9–12 that compromise with their life-course transitions, health and well-being, as well as increase the burden on healthcare systems.
Regardless of their medical or healthcare condition, emerging adults with chronic illnesses face common barriers in their transition to adult healthcare and require similar supports.13–15 Such supports need to foster medical management while recognising broader developmental aspects of transition into adulthood.16 Accordingly, life-course approaches to health trajectories,17 and approaches promoting gradual self-management and developmentally appropriate autonomy have been recognised as key components of successful transition.18–20
Transition supports can be viewed as complex interventions that consist of multiple components that act independently or interdependently, thus making the ‘active ingredients’ of interventions difficult to specify.21 The challenge is compounded by fragmented approaches to transition. Despite the reported commonalities in transition barriers and supports across different sectors,13–15 much of the literature has focused on single clinics or specific conditions, and evaluated feasibility and effectiveness of transition-enhancing strategies in their respective subspecialty areas.21–25 Broader psychosocial models that can help guide transition processes across various healthcare contexts are lacking.26 For example, a systematic review of transition practices in diabetes found patient education to be a successful strategy while calling for more research to ascertain if this strategy works for other conditions as well.27 Furthermore, research on transition rarely brings together neurodevelopmental and other chronic health conditions, even though evidence suggests that emerging adults in both groups have similar needs and aspirations.28 Not many studies provide longitudinal insights,29 or ask youth directly about their opinions and experiences.30 Increasingly, participants’ perspectives are found to be vital to our understanding of factors that facilitate transition from child-centred to adult-centered healthcare.31
We have taken an innovative approach by providing youth who have various chronic health and neurodevelopmental conditions with a ‘bundle’ of two transition interventions designed to support and empower them during their transition into adult healthcare. The objective of this longitudinal study was to assess the use, utility and impact of the interventions. In doing so, we included the voices of the recipients of the interventions. As youth-focused transition supports are likely to grow in popularity, it is important to know why and how transitioning youth utilise these supports, and what impact such supports may have on their transition experience.
Methods
Study design, setting and participants
This mixed-methods research integrates a longitudinal prospective intervention study, which involves two study visits in paediatric care and up to two visits in the adult healthcare setting (figure 1), with post-transfer qualitative semistructured interviews.
Figure 1.
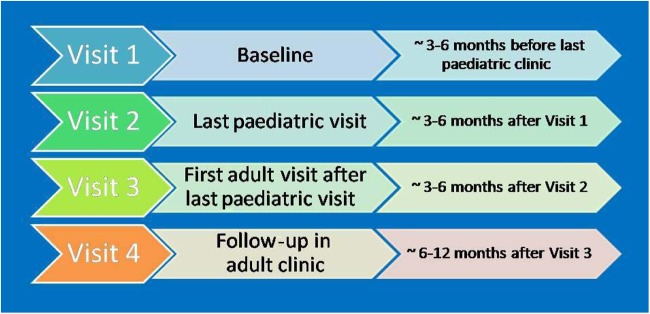
Study visits time frame.
The study spanned from 2009 to 2013, and involved 13 clinics at two major paediatric hospitals in Ontario, Canada. The study protocol received local ethics approvals, and participants provided written informed consent before taking part.
We purposely recruited a convenience sample of youth with a wide range of chronic health conditions and disabilities whose transfer to adult care was planned to occur within 1 year. Since the interventions were meant for use by youth themselves, full dependence on caregivers in the areas of daily functioning, self-care and communication was one exclusion criterion. Additionally, all eligible youth had to be able to utilise the intervention tools and answer assessment questions in English. Candidates with cognitive, verbal and reading impairments were encouraged to seek assistance from a mentor, social worker or family member when using the study supports. The research protocol allowed for extra time and support for completing study assessments as needed.
Interventions
Study participants had an opportunity to use two related yet distinct transition supports: the Youth KIT and an online transition mentor (described below). At their first visit, participants learned about the interventions and with the help of research coordinators completed the introductory section of the Youth KIT and logged into the online mentor website for the first time. The research coordinators encouraged participants, at all study visits and by email, to work on the Youth KIT at their own pace and in sync with various developments in their life, and to interact with the online mentor. Participants had access to the interventions starting from their first study visit until the end of the study; the exposure time ranged from 12 to 47 months.
Youth KIT organisational tool
The KIT: Keeping It Together for Youth, tool (the ‘Youth KIT’) was designed and developed specifically for youth and for youth with physical and developmental disabilities as a tool to promote organisation, goal setting, and self-management in nine life domains listed in table 3.32 Currently accessible and downloadable at http://www.canchild.ca, the Youth KIT was initially available only in a binder format. The introductory section, Planning for Your Future, allowed participants to reflect on their ability to perform tasks in nine life domains (eg, directing one's personal care; managing medications, appointments, and various information), and introduced them to the process of goal setting (how to set goals, to identify the necessary steps, and to reflect on goal achievement).
Table 3.
Number of participants who used* the Youth KIT pretransfer and post-transfer (n=36)
| Pretransfer paediatric visit | Post-transfer adult visits |
||
|---|---|---|---|
| Visit 2 | Visit 3 | Visit 4 | |
| Youth KIT section | n=21 | n=27 | n=23 |
| Personal information | 16 (76%) | 24 (89%) | 17 (71%)¶ |
| Social information | 15 (71%) | 21 (78%) | 15 (65%) |
| Social activities | 12 (57%) | 20 (74%) | 13 (57%) |
| School information | 13 (62%) | 22 (85%)‡ | 16 (70%) |
| Work information | 13 (62%) | 20 (74%) | 14 (61%) |
| Budget/financial information | 13 (62%) | 20 (77%)‡ | 12 (52%) |
| Personal care and life skills | 12 (57%) | 21 (81%)‡ | 12 (52%) |
| Transportation | 11 (52%) | 16 (62%)‡ | 9 (39%) |
| Medical and health information | 15 (71%) | 23 (85%) | 15 (65%) |
| Obtaining and sharing information | 10 (50%)† | 16 (64%)§ | 11 (48%) |
*“Use” is defined as reading the section or using the section at least once.
Valid numbers are provided if missing data: †n=20; ‡n=26; §n=25 and ¶n=24.
TRACE online transition mentor
The online transition mentor, an occupational therapist with expertise in transition, discussed various transition issues that were of interest to participants. In an effort to put participants at ease, the mentor was given a quirky name (‘TRACE’) and the mentor's identity, age, occupation, and gender were kept anonymous. TRACE was available 4 nights per week through the secure platform of http://www.abilityonline.org, a website designed for youth and young adults with chronic conditions and disabilities. TRACE was available to participants through one-on-one chats, message postings, group chats, and email. Mentor and study coordinators promoted group chats during individual chats, study visits, and email announcements. Group and individual chats were offered in the evening (20:30–22.00).
Measures and data collection
We measured use, utility and impact of the interventions by employing quantitative and qualitative methods at various points in time (table 1).
Table 1.
Overview of outcomes, variables, measures, scales, and assessment points
| Outcome | Variable | Measure | Scale | Assessment points (v) |
|---|---|---|---|---|
| Use | Frequency of interventions’ use: | Scale items: | ||
| Youth KIT's 9 sections and interactions with the online mentor | Youth KIT questionnaires* | Youth KIT: I read this section; I used this section once; I used this section more than once; I did not use this section; This section did not apply to me; Mentor: I used it once; | v2–4 | |
| I used it more than once; I did not use it; it did not apply to me | ||||
| Online activity | Login and chats with the mentor (through the host website) | Not applicable | Throughout the study | |
| Utility | Interventions’ features: | Youth KIT questionnaires, including open-ended responses about likes and suggestions for improvement | 7-point Likert scale: 0=not applicable/did not use it; 1=not at all; 7=very great extent | v2–4 |
| Youth KIT: organised, easy to use; easy to understand; relevant | ||||
| Mentor: easy to use; easy to understand; relevant | ||||
| Impact | Performance and satisfaction with transition goals | Canadian Occupational Performance Measure scoring system† | 10-point Likert scale: 1=lowest; 10=highest | v1–4 |
| Interventions’ helpfulness in self-management areas | Youth KIT questionnaires, including open-ended responses | 7-point Likert scale: 0=not applicable/did not use it; 1=not at all; 7=very great extent | v2–4 | |
| Impact on youth and healthcare providers | Semistructured interviews with youth and healthcare providers about the interventions | Post-transfer | ||
*Use, utility and impact questions for the Youth KIT (and the mentor's) were developed by the team using questionnaires from prior projects involving the Youth KIT.32
†The COPM is an individualised outcome measure designed to detect change in performance and satisfaction with performance in activities identified by the respondent as being important to him/her.33 For this study, we applied the COPM scoring system for performance and satisfaction.
COPM, Canadian Occupational Performance Measure; v, visit.
At the first study visit, participants provided their sociodemographic information. At each subsequent visit, participants indicated their use of the Youth KIT sections, as well as evaluated various aspects of utility (organisation, ease of use, ease of understanding, and relevance) and impact (several domains of self-management) of the Youth KIT and the online mentor using seven-point Likert scales. They also answered open-ended questions about the two interventions. Participants’ use of the online mentor was tracked by web platform software (eg, logins and chats).
Starting from visit 1 in paediatrics, participants had freedom to set goals for a wide range of life domains, often mirroring the nine sections from the Youth KIT. Goal achievement was assessed using the scoring system from the Canadian Occupational Performance Measure (COPM)33 because it is reliable, quick and youth-friendly.34 35 Participants rated each goal for performance and satisfaction using a 10-point Likert scale (1=lowest; 10=highest).
All qualitative interviews were conducted over the phone, audiotaped, and transcribed verbatim. The data collection and analysis of the qualitative interviews was informed by a phenomenological approach, which was suitable given our interest in understanding participants’ lived experience, viewpoints and empowerment.36 The approach allows for a complex and nuanced understanding of a specific phenomenon from multiple perspectives, including temporal, spatial and social perspectives related to participants’ self-awareness, attention, and enabling conditions.37
For all study visits, the research coordinator aimed to meet with participants before or after their clinic appointments. When a face-to-face study visit was not possible, participants completed the measures over the phone or by mail.
Data analysis
Participant demographics and intervention use were analysed descriptively. Means and SDs of Likert scores were calculated for perceived utility and impact of the interventions. Fisher's exact test was used to assess relationships between intervention use and gender or diagnostic group, and to compare the group who completed the follow-up with the group who did not, in terms of their gender and education. An independent Student t test was run to test the differences in participants’ perceptions about helpfulness of the interventions for users compared with non-users, as well as the differences in the age of those who completed the follow-up compared with those who did not. Users were those who reported reading or using the medical and health information section of the Youth KIT at least once, and those who interacted with the mentor at least once.
For goal achievement, we conducted paired Student t tests to compare mean ratings for performance and satisfaction at the time a goal was identified versus ratings at a subsequent visit when goal achievement was evaluated. Nominal p<0.05 were considered statistically significant; change scores of 2 or greater were considered clinically important.33 IBM SPSS statistics V.22 was used for the quantitative analyses.38
Content analysis was used to arrive at overarching themes for transition goals, as well as to analyse open-ended comments about utility from the Youth KIT and mentor questionnaires, and transcripts from the chats with the online mentor and from the qualitative interviews. To ensure the trustworthiness of the process, three researchers went through several iterations of independently reviewing transcripts, and discussing codes and themes until consensus was reached.39 Once the coding scheme was finalised, the research coordinator completed the analysis of all data.
Results
Participant retention and demographics
Of 140 patients approached by a participating clinic, 107 were eligible and available for further follow-up. Fifty (47%) consented and contributed data for the first study visit. Fifty-seven (53%) declined (often due to reported lack of time, interest, or perceived need and competing priorities).
Of the 50 adolescents who contributed data at their first paediatric visit, 36 (72%) participants completed one or two follow-up study visits in the adult healthcare setting. At baseline, participants’ mean age was 17.9 (SD 0.9), range: 15.8–21.3; 58% were female. Over 20 underlying diagnoses were represented; some participants had more than 1 diagnosis. Most participants were completing secondary education and living in their family's home at the time of enrolment (table 2).
Table 2.
Baseline characteristics
| Variable | Completed 1st paediatric visit (n=50) | Completed at least 1 adult visit (n=36) | Did not complete an adult visit (n=11)*† |
|---|---|---|---|
| Female gender | 29 (58%) | 19 (53%) | 7 (64%) |
| Age, year | 17.9 (0.9) [15.8–21.3] |
18.0 (1.0) [15.8–21.3] |
17.7 (0.5) [16.9–18.8] |
| Health conditions | |||
| Neurodevelopmental‡ | 19 (38%) | 14 (39%) | 5 (46%) |
| Other chronic§ | 31 (62%) | 22 (61%) | 6 (54%) |
| Highest education | |||
| Secondary | 36 (72%) | 25 (69%) | 8 (73%) |
| Postsecondary | 13 (26%) | 10 (28%) | 3 (27%) |
| Literacy course | 1 (2%) | 1 (3%) | 0 |
| Living arrangements | |||
| In family's home | 45 (90%) | 33 (92%) | 9 (82%) |
| On one's own | 1 (2%) | 0 | 1 (9%) |
| On one's own with support from community resources | 3 (6%) | 3 (8%) | 0 |
| Missing | 1 (2%) | 0 | 1 (9%) |
Values are n (%), or mean (SD) [range].
*Not including three individuals who were still waiting for their first adult appointment at the study closeout at the second site.
†There was no difference between the groups (ie, 11 participants who did not complete and 36 participants who completed the follow-up) in terms of gender, education and age (p=0.7; p=1.0 and p=0.06, respectively). The online supplementary file provides further information on the group that did not complete the follow-up.
‡Neurodevelopmental conditions included cerebral palsy, spina bifida, hydrocephalus, acquired brain injury, and epilepsy.
§Other chronic conditions included Crohn's disease, ulcerative colitis, dyslipidemia, hypothyroidism, multiple endocrine neoplasia, adrenal insufficiency, anorexia, Wegener’s granulomatosis, kidney disease (transplant), heart disease (pacemaker), lupus, osteogenesis imperfecta, Klippel-Trenaunay syndrome and tuberous sclerosis.
Forty-four individuals participated in qualitative interviews. These participants included 17 youth who received the interventions (mean age 19.2 (SD 0.8); 50% male) and 7 healthcare providers. Eleven youth who did not receive the interventions provided their perspectives on the transition (these results are not included in this study). Parental perspectives from nine interviewed parents are discussed in detail elsewhere.40
Use and utility of the interventions
Youth KIT: use and utility questionnaires
Use of the Youth KIT peaked around the time leading up to the first adult visit (table 3). The most often used modules were those on personal, school, medical and health, social information, as well as personal care and life skills. Users and non-users of the medical and health information section did not differ significantly in gender or diagnostic group (p=0.07 and p=0.54, respectively).
As table 4 shows, the mean ratings of utility decreased post-transfer, with the lowest ratings for relevance and the highest ratings for organisation of the Youth KIT.
Table 4.
Perceived utility of the Youth KIT and online mentor pretransfer and post-transfer (n=36)
| Pretransfer paediatric visit | Post-transfer adult visits |
||
|---|---|---|---|
| Visit 2 | Visit 3 | Visit 4 | |
| The Youth KIT is… | n=23 | n=29 | n=25 |
| Very well organised | 5.8 (1.6) | 5.3 (2.3) | 5.1 (2.4) |
| Easy to understand | 5.6 (1.8) | 5.5 (2.2) | 4.8 (2.7) |
| Easy to use | 5.8 (1.9) | 5.3 (2.3) | 4.4 (2.8) |
| Relevant for me | 4.2 (2.1) | 3.9 (1.8) | 2.4 (2.2) |
| The online mentor is… | n=22 | n=28 | n=25 |
| Easy to understand | 4.5 (2.6) | 4.4 (2.5) | 3.1 (3.0) |
| Easy to use | 4.2 (2.7) | 4.2 (2.4) | 3.2 (2.9) |
| Relevant for me | 4.1 (2.7) | 3.5 (2.2) | 2.1 (2.4) |
Mean (SD) for 7-point Likert scale: 0=not applicable/didn't use it; 7=very great extent.
The open-ended comments offered important insights on reasons why the Youth KIT was not used or used minimally. Participants often reported competing demands related to school, social life, and sometimes more pressing health needs. Interestingly, one youth reported that his parents used the tool more often than he did. Some found the comprehensive nature of the Youth KIT to be somewhat daunting and perceived the tool as ‘extra work’, not specific to their circumstance; a good idea, but not needed:
Amount of paper is mind-boggling. It would help to incorporate parts of the KIT into clinics.
I didn't use the Youth KIT much. I felt that the information in the binder would be useful if/when I needed it, if I had any questions but I didn't. Knowing that it was available was helpful.
Despite being busy, several participants reported a short, yet meaningful, use of the Youth KIT:
I just went through it quickly but it made me think about stuff though.
Although I don't use it anymore, it helped organise the information I gathered relating to [name of the health condition], keep track of foods to eat etc.
Online transition mentor
A combination of web-based analytics and youth-reported data revealed the following patterns of use of the online transition mentor ‘TRACE’.
Web-based analytics
Forty-one (82%) participants—26 (82%) females and 15 (18%) males—logged into the website to connect with the online mentor pretransfer at least once. Over the course of the study, 20 (40%) participants engaged in 85 one-on-one chats with TRACE: median 2; range 1–11; average chat length 67 min. In addition, three outliers—two male and one female—participated in a total of 65 chats (average chat length 72 min). There were also four intersite group chats (average chat length 87 min). Users and non-users of the online mentor did not differ in gender or diagnostic group (p=0.07 and p=0.52, respectively).
The content analysis of chat transcripts and emails revealed a wide range of topics that participants chose to discuss with the online mentor. The major themes included those pertinent to relationships with peers and parents, school/university, and challenges with developing autonomy and various life-course transitions.
Use and utility questionnaires
Nineteen of the 27 (70%) participants who responded to the questionnaire indicated that they had chatted with TRACE post-transfer at least once. Participants rated one-on-one chats as more helpful than group chats—mean (SD): 3.3 (2.7) and 1.6 (2.5), respectively—on a seven-point Likert scale, with the highest ratings at pretransfer or visit 2.
In terms of utility, this online intervention received the highest mean ratings for its ease of understanding, especially around the transfer point (visits 2 and 3), and the lowest ratings for its relevance, especially at the last study visit (table 4).
In the open-ended comments, participants expressed their appreciation for ‘the supportive environment’ that TRACE created and the opportunities to interact with ‘a medical professional’ and ‘peers who may have the same problems’. For example:
The mentor offered help and different ideas I wouldn’t have thought of.
I used TRACE to talk about things in general (hobbies, interests, classes, etc) more so than just to talk about my healthcare.
I loved talking to TRACE and found that TRACE was extremely supportive and encouraging. I hope to continue to use this service during my transition.
Among the reasons for not using the intervention were a few reports of technical challenges (eg, accessibility issues of the host platform; lost passwords; being grounded from the computer) and personal preference. Examples of the latter included:
I would rather talk to people I know and trust for support and not strangers.
I am not yet comfortable talking to other teens about myself.
Qualitative interviews with youth: interventions’ use
The post-transfer qualitative interviews offered further insights on the use of the Youth KIT and the mentor. The use of both interventions was reportedly influenced by participants’ busy lives and their perceived need for transition supports in general. Some interviewed participants felt that both transition supports would have been more relevant to other individuals—who were younger or with a more severe medical condition or without any supports in place. Some participants said they would have used the Youth KIT more regularly if physicians asked for it when they attended their medical appointments. Notably, several interviewees reported that they felt they were very well supported by their current paediatric healthcare team, the study coordinator and their family.
I would say to personalise [Youth KIT] to each person.
This book [Youth KIT] is, like, totally for people that have, um, large problems.
I didn't use the online mentor much as I was very busy in high school, working at my part-time job and then preparing to go off to university.
At that time [prior to the transfer] I didn't need [the mentor] because of the support from the [paediatric] doctor and the study coordinator.
Mostly I've had a great amount of family support, with going to the doctors and going [through] transition.
Impact
Three data sources helped to understand the impact of the interventions and the study itself: questionnaire items about the interventions’ helpfulness, goal achievement ratings, and individual interviews with youth and healthcare providers.
Interventions’ helpfulness
Participants regarded both interventions to be most helpful pretransfer (visit 2). Both interventions received the highest ratings for help in the area of setting and working towards one's own goals; the Youth KIT also received relatively high ratings for help in taking charge of one's own healthcare. The lowest ratings were given for help in developing supportive and respectful relationships with healthcare workers post-transfer (table 5).
Table 5.
Helpfulness of the Youth KIT and the mentor in domains of self-management (n=36)
| Pretransfer paediatric visit | Post-transfer adult visits |
||
|---|---|---|---|
| Visit 2 | Visit 3 | Visit 4 | |
| n=26* | n=30† | n=26‡ | |
| Developing supportive and respectful relationships with healthcare workers | |||
| KIT | 2.7 (2.6) | 2.1 (2.3)§ | 1.9 (2.3) |
| Mentor | 2.2 (2.6) | 2.2 (2.7) | 0.8 (1.7) |
| Sharing information and communicating about your healthcare | |||
| KIT | 3.1 (2.5) | 2.4 (2.5) | 2.5 (2.6) |
| Mentor | 2.9 (2.8) | 1.9 (2.5)§ | 0.8 (1.8) |
| Taking charge of your own healthcare | |||
| KIT | 3.5 (2.5) | 2.5 (2.5) | 2.8 (2.4) |
| Mentor | 2.8 (2.7) | 1.9 (2.5) | 0.9 (1.8) |
| Setting and working towards your own goals | |||
| KIT | 4.2 (2.3) | 2.9 (2.8) | 2.9 (2.4) |
| Mentor | 3.5 (2.8) | 2.4 (2.8)§ | 1.3 (2.0) |
Mean (SD) for 7-point Likert scale: 0=not applicable/didn't use it; 1=not at all; 7=very great extent.
Including “0=not applicable/didn't use it” responses: *13–40%, †42–52%, ‡25–71% chose 0 response.
§The intervention users had higher ratings than non-users (p≤0.05); users of the Youth KIT are defined as those who reported reading or using the medical and health information section at least once; users of the online mentor are defined as those who interacted with the mentor at least once.
Furthermore, the summarised open-ended responses suggest that youth felt supported and empowered in the following areas: (i) planning and getting organised in various transition aspects that included healthcare self-management, preparation for school/university, and obtaining a driving license; (ii) learning to prioritise by ‘putting certain things aside’; (iii) becoming ‘more mature’; better understanding oneself and ones capabilities and (iv) learning to be more responsible for their health ‘rather than relying on parents for everything’. The goal-related aspects of the interventions were reported to be particularly empowering:
The Youth KIT has been very helpful because it has really put things into perspective for me. It has really helped make me see what I want in my life and how I can achieve it. I have also found through this how, though I am having a difficult time right now with my illness, it doesn’t affect me as much as I thought.
The Youth KIT was very helpful because it has made me reach my goals which I would not have normally done.
TRACE gave me confidence to look forward and follow life to achieve goals … and … to get through personal problems, connect with peers, and get peers’ opinions.
Goal achievement
The goal achievement analysis revealed additional important insights on impact. Forty-five (90%) participants set a total of 294 transition goals. In the process of content analysis of the nominal data (the goals as worded by the participant), two broad categories for transition goals emerged. Healthcare goals were related to healthcare self-management, education, overall well-being and healthy lifestyle, whereas life-course goals were related to social relationships, school, work, and independent life skills.
A total of 150 goals were set and rated by participants for performance and satisfaction. Fifty-nine pairs of healthcare-related goals were identified by 29 (58%) participants and 91 pairs of life-course goals were identified by 27 (54%) participants. The time between setting and rating a baseline goal and its subsequent evaluation by the participant ranged from 4 to 24 months. The mean scores for performance and satisfaction increased for health-related and life-course goals (p≤0.001). The mean changes for the healthcare-related goals increased by an amount that was considered a priori to be clinically important (>2.0; table 6).
Table 6.
Transition goal achievement (n=45)
| Goals | Rating when goal set | Rating when goal evaluated | Change |
|---|---|---|---|
| Healthcare-related 59 goals set by 29 participants | |||
| Performance | 4.3 (2.4) | 6.5 (2.3) | 2.2 (3.0)** |
| Satisfaction | 4.3 (2.5) | 6.4 (2.6) | 2.1 (2.8)** |
| Life-course 91 goals set by 27 participants | |||
| Performance | 5.2 (2.6) | 6.7 (2.6) | 1.5 (3.1)* |
| Satisfaction | 5.1(2.8) | 6.7 (2.6) | 1.6 (3.5)* |
Mean (SD) for 10-point Likert scale: 1=lowest, 10=highest.
*Statistically significant (p≤0.001); **both statistically significant and clinically important; clinical importance defined as >2.0 improvement.32
Qualitative interviews
In addition to the study's impact in the areas of goal achievement, planning and self-awareness discussed earlier, the interviewed youth reported to have become more prepared, organised and independent during their transition:
I feel that I am prepared for [the next adult appointment] because I keep everything I get from the hospital in a folder.
The mentor and the youth KIT helped me be more independent.
For the year that I've been on my own [waiting for an adult appointment], the study helped in the area of goal setting, diet, and self-management. I liked the study because of the freedom to discuss a variety of topics and because it was open-ended.
For some participants, the interventions increased their confidence and provided a safety net. Multiple chats with the mentor enabled one youth to comfortably talk to other people about her health condition; she was encouraged to share about her disorder with her new roommate and in a writing contest. Another participant summarised the impact of the study this way: “I never felt forgotten in the transition.”
The interviews with healthcare providers resulted in three major themes that are summarised in table 7.
Table 7.
Healthcare providers’ perspectives: qualitative interviews themes
| Theme | Related quotes |
|---|---|
| Practice changes as a result of participating in the study: eg, formalising the process; starting transitioning planning earlier; adjusting communication styles towards emerging adults | I think the project has made me more conscientious of the process of transition. (Physician)
When we had to identify youth who were eligible for the study, it made us aware that we didn’t actually have a system in place to identify clients who will be turning 18 and transitioning. (Physician) With increased awareness, we shifted the average age at the transition clinic to 14–15 [from 16–18]. (Physician) Generally when [caregivers] are in the room, I address myself to the youth trying to promote that concept that this is your body, your health, your responsibility. (Nurse) Sometimes people describe the transition experience as that they are falling off a cliff. [The study interventions] are something that we offer young people almost as a bit of a safety net, as a service that is available after they are “discharged” so that if they have questions they can direct them back to the online mentor. One of the most positive things has been being able to offer that as an option. (Occupational therapist) |
| Ways to optimise Youth KIT use | The Youth KIT was designed … to be self-directed…. Clinicians don’t get a copy of the Youth KIT. The KIT is put into the youth’s hands. …Going to a binder about planning isn’t something that most kids that I work with will do. So what we’ve done we incorporated parts of the Youth KIT into our summer sessions of the teen independence program. (Occupational therapist) So even if it was more of a protocol amongst all physicians who said, at every appointment, please have your Youth KIT… that might encourage the use… If we want to make it a success it has to be integrated, not something outside clinic. (Physician) |
| Need to bridge the divide between paediatric and adult healthcare systems and to improve continuation of comprehensive care, particularly in the area of developmental disabilities | Once we have raised awareness, parents became very proactive and started asking us questions that we cannot answer. The biggest challenge for me is to find a similar model to our multidisciplinary spina bifida clinic or spasticity clinic to transfer to (as there is no adult counterpart)…. It then falls back to the family doctor who is not always familiar with the issues. (Physician) The adult world is not as trained to handle patients with developmental disabilities. Having a joint meeting or conference to engage adult healthcare providers …may help. (Physician) At age 18… we “let the children go”, and there are a lot of unknowns after that… There is a strong need for some sort of continuity… We need to bridge the divide. (Physician) |
Discussion
The quantitative and qualitative study findings taken together suggest variable use of the Youth KIT and the online transition mentor; modest perceptions about their utility especially post-transfer; and meaningful impact on some youth and healthcare providers. Participants reported that the interventions were most helpful for setting and working towards goals. Goal setting is clearly an important aspect of transition as 90% of the participants set transition goals, and the change scores for healthcare and life-course goals were statistically significant, with the change scores for the former clinically important as well.
The findings of the study support the ABC notion of the transition process41 that consists of Awareness, Building capacity and Collaboration among all stakeholders: youth, families, and healthcare systems (paediatric and adult). One of the most meaningful impacts of the study is this heightened awareness of transition as a multifaceted process that requires planning and collaboration among youth, families, and healthcare providers (paediatric and adult). A failure to recognise the importance of transition has been cited as a primary barrier that can result in being lost in transition.20 42 Participants explicitly told us that it was not a case only for them as participation in the study did increase awareness among transitioning youth (and their families), as well as their healthcare providers.
Not many studies take on the challenge of investigating the complex concept of youth empowerment or the related patterns of utilisation of youth-focused resources that have the potential to reduce the burden on the healthcare system. In the process of this study, it became evident that we should be asking questions of how to empower transitioning youth meaningfully, and whether putting transition tools and supports in their hands will suffice. Indeed, it has been recognised that “the hurdles of transition medicine lie as much with healthcare teams as with the patients and their families… The relationship between the pediatric and adult health clinics is central to success.”43 A metasynthesis of 18 qualitative studies reports critical challenges that transitioning young adults experience with the changing relationships with their healthcare providers.44 In our study, the predominant focus on youth may partly account for the finding that the interventions were perceived as least helpful in the domain of ‘developing supportive and respectful relationships with healthcare workers’ post-transfer. The modest levels of use and perceived utility of the interventions may be a function of the target user, as much as they are a function of the specific interventions chosen. Despite our intentional focus on youth, the study results remind us that healthcare providers play a crucial role in the uptake of the interventions, in promoting gradual self-management, and in enabling empowerment during the transition process. It is important to consider youths’ level of self-management in the planning of health services and related interventions, including concurrent parental interventions, as it is an essential element in the promotion of health and adaptability.2 18 40
The transition interventions in this study were deliberately broad and holistic in their scope. For similar transition supports to be more relevant, their generic aspects need to be balanced with condition specific ones. Participants showed most interest in the medical and health section of the Youth KIT whereas other popular sections were those about personal and school information. It was also clear that some participants appreciated the wide range of topics that they could discuss with the online mentor and thus, were prompted to think about the relationships between their healthcare transition and other transitions in their life. The patterns of the Youth KIT use, as well as the wide array of topics and goals participants chose to focus on, reinforce the need to consider healthcare transition in the context of multiple equally important life-course transitions.44–47 These other transitions often compete for attention and time of youth, thus relegating their healthcare and healthcare transition to a lower priority and further increasing the importance for engaging parents and healthcare professionals in the process.40
The study findings may inform the design, timing and assessment of similar interventions. The perceived utility of the interventions was greatest pretransfer. The highest use and perceptions of helpfulness were reported post-transfer (after the 1st adult clinic visit), which is likely when some participants realised the differences between adult and child-based services. The formats and media of the youth-based interventions need to consider variable and changing preferences of youth. We transformed the print-based Youth KIT into an online format at the early request of some of our participants, whereas other participants indicated their preference for the hard copy. Similarly, we expected the online mentor to be popular with a wide range of participants while the emerging evidence suggests that when interacting online, youth prefer not to identify themselves with their health status or disability,48 and texting has become a more appealing option.49 More female participants accessed the online resource, which is consistent with other research.50 The variability in use of the interventions at the individual level (including 2 male outliers who used the online mentor most extensively) underscores the importance of individualised, tailored approaches to design and assessment. The individualised goal setting aspect of the study turned out to be the most helpful for participants, amounting to an effective intervention itself. Participants set and worked towards goals that were most meaningful to them, thus suggesting that there may be an important active ingredient of youth engagement and empowerment within the goal setting process.
The strengths of the study largely stem from its approach and design. First, the study captured the breadth of over 20 underlying diagnoses and engaged 13 clinics at two sites. The healthcare communities at both sites built on earlier transition initiatives with widely variable transitional care planning across clinics. For example, some clinics provided transitioning youth with an information package, joint visits, counsellor and transition clinics. This variability may have had an impact on youth perceptions about the need for additional transition supports. Nonetheless, the findings support the across-condition approach and are consistent with other evidence in favour of generic transition programming.13 22 44 The results highlight the universality of transition themes and challenges. At the same time, the findings underscore the importance for generic transition supports to be carefully tailored to needs, goals and abilities of individual youth (and families) and integrated into paediatric and adult healthcare systems. Second, the study's focus on preparation for and the actual landing in the adult healthcare system is not very common as most studies tend to limit their focus on transfer points.29 The longitudinal aspects resulted in a more nuanced understanding of the interventions’ use and utility, as well as changing perceptions of youth at different stages of the transition. Third, the mixed-methods design, which is often promoted but rarely carried out,21 offered important insights on what worked in the transition interventions, what did not, and why it did not. While the quantitative data indicated the decreasing trend in the interventions’ use and modest perceptions of the interventions’ utility, the qualitative data provided insights, for example, that some participants felt well supported and more confident, and thus were less likely to seek out supports. This latter example may have been one of the reasons why the utilisation decreased over time. For those participants who reported becoming more mature, organised and independent, the interventions may have lost their relevance. Overall, we can argue that the strength of the study lies in capturing very realistic challenges associated with sustained youth engagement.
The study had several limitations. First, sample-wise, the mean age of the participants (18 years) may account, at least in part, for the modest ratings on relevance of the transition supports or their inconsistent use, which underlines the need for transition preparation as early as age 12. Some eligible youth viewed the study interventions as not very applicable or necessary at the time we approached them, and decided against participating. While any transitioning youth would benefit from transition supports designed to empower them by making them more self-aware and transition aware, risk assessment may be helpful in identifying youth in need for similar transition supports. Further, despite our efforts to include youth with neurodevelopmental disabilities, our sample is not representative of those with low (verbal) IQ or those with limitations in social communication such as autism spectrum disorder (ASD). Similarly, the sample did not include chronic conditions, such as juvenile rheumatoid arthritis, cystic fibrosis, and diabetes, with well-documented poor health outcomes in transition. Second, poor health outcomes were initial drivers of this study, but are not addressed in this paper as it stays close to the outcomes afforded by transition supports’ use and utility. Long-term health outcomes, such as improved well-being, increased health surveillance, and decreased unexpected complications or emergencies, remain the impetus for quality improvement. Transition interventions may be best measured using the ‘Triple Aim’ framework of experience of care, population health, and cost of care.51 Finally, we made efforts to engage with adult healthcare providers, initially and throughout the study, whenever possible. Our research team included some healthcare providers who work with paediatric and adult population. Nonetheless, we were not able to follow about a quarter of participants into adult healthcare; the group that was followed, however, did not differ significantly from the initial cohort.
As recommended by a recent knowledge synthesis on transition care for children with special care needs, more research on self-management is necessary.52 Particularly, more research is needed in the area of meaningful empowerment of transitioning youth, including those with more complex care needs and neurodevelopmental conditions that tend to be excluded from studies. One way to address the unrealistic demands on self-management of any transitioning adolescent may lie in the shared management model that involves a planned systematic process of a gradual shift in responsibilities from the healthcare provider and parents to the young person, as developmentally appropriate.14 53 Such model supports graded opportunities for self-management throughout the healthcare systems,53 and recognises that brain development and the related executive function extend to beyond the age of 20 years.22 44 54 Goal setting and evaluation of goal achievement, as our study shows, may be important ingredients in this gradual self-management process. These warrant further research and can be studied in conjunction with validated self-management tools for transitioning youth (age 12–18 years).55 Armed with the results of this study, the team is now embarking on a larger province-wide comparative study that will involve six healthcare centres to prevent negative transition outcomes in youth with chronic health conditions.
In conclusion, participants’ perceptions about the utility of the transition interventions were modest. Interventions that focus on youth only are insufficient for empowering transitioning youth. Transition supports need to be carefully tailored, timed and integrated into healthcare systems. Various ingredients, including goal setting, can optimise transition supports, patient engagement, and healthcare across conditions and systems.
Acknowledgments
The authors thank the participating clinic staff members at both sites: Anita Allen, Laura Bainbridge, Sharon Bobzener, Karen Frost, Nancy Goldie, Liz Helden, Robert Issenman, Keith Lau, Brandon Meaney, Ronit Mesterman, Chris Radoja, Rajesh Ramachandran Nair, Laurian Roche, Gabriel Ronen, Adrian Smith, Sandi Spree, John van der Meulen, Cheryl Webb, Laurie Willie and Marc Woodbury-Smith, who also offered his insights to this manuscript. They are particularly indebted to the participating youth and their families and healthcare providers who shared their time and perspectives on transition process.
Footnotes
Twitter: Follow Jan Willem Gorter (TranstionDoctor) at @Dr_Gorter
Collaborators: TRACE Study group: The following are members of TRACE (Transition into Adulthood with Cyberguide Evaluation) study at the McMaster University and Hamilton Health Sciences site: Jan Willem Gorter and Zubin Punthakee (co-principal investigators); Steve Arora, Herbert Brill, John Cairney, Andrew Don-Wauchope, Christina Grant, Andrea Morrison, Kim Nagel, Deb Stewart and Peter Rosenbaum (co-investigators); and Tram Nguyen, Hee-Jin Kim, Barb Galuppi and Oksana Hlyva (research and project staff members). The members of TRACE study at the Hospital for Sick Kids in Toronto included Eyal Cohen (collaborating co-investigator), Khush Amaria, Ashley Lacombe-Duncan and Natalie Weiser.
Contributors: JWG is the guarantor. JWG, DS, EC, AM, BG, KA and ZP contributed in the study conception and design. OH, BG, TN, Ashley Lacombe-Duncan, Natalie Weiser (research coordinators at the Toronto site or at the Hospital for Sick Children) and Hee-Jin Kim (Master's student at the Hamilton site or at McMaster University) were involved in the acquisition of data. JWG, OH and ZP contributed in the drafting of the manuscript. DS, KA, BG, EC and AM were involved in the critical revision. All the authors were involved in the analysis and interpretation of the data; and gave their final approval.
Funding: This study was funded by an unrestricted grant received from Hamilton Academic Health Sciences Organisation (HAHSO); grant number (09-124).
Competing interests: JWG and ZP have received research grants from Hamilton Academic Health Sciences Organisation (HAHSO); grant number (09-124). JWG holds the Scotiabank Chair in Child Health Research (2013–2017). DS was involved in development of the Youth KIT that is available online, free of charge. OH, BG and TN were paid for collecting and analysing the data as research staff members. AM was paid in part for her work as an online transition mentor.
Ethics approval: The study obtained ethics approvals from the Hamilton Health Sciences/McMaster Health Research Ethics Board (09-124) and the Hospital for Sick Children's Research Ethics Board (09-104).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
Contributor Information
Collaborators: Steve Arora, Herbert Brill, John Cairney, Andrew Don-Wauchope, Christina Grant, Kim Nagel, Peter Rosenbaum, Hee-Jin Kim, Ashley Lacombe-Duncan, and Natalie Weiser
References
- 1.Goodman DM, Hall M, Levin A et al. Adults with chronic health conditions originating in childhood: inpatient experience in children's hospitals. Pediatrics 2011;128:5–13. 10.1542/peds.2010-2037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gorter JW, Stewart D, Woodbury-Smith M. Youth in transition: care, health and development. Child Care Health Dev 2011;37:757–63. 10.1111/j.1365-2214.2011.01336.x [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2011;128:182–200. 10.1542/peds.2011-0969 [DOI] [PubMed] [Google Scholar]
- 4.Blomquist KB. Health, education, work, and independence of young adults with disabilities. Orthop Nurs 2006;25:168–87. 10.1097/00006416-200605000-00005 [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics 2002;110(6 pt 2):1304–6. [PubMed] [Google Scholar]
- 6.Department of Health/Child Health and Maternity Services Branch. Transition: getting it right for young people: Improving the transition of young people with long term conditions from children's to adult health services. London: Department of Health, 2006. [Google Scholar]
- 7.Baltzer F, Elliott A, Katzman DK et al. Transition to adult care for youth with special health care needs. Paediatr Child Health 2007;12:785–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics. Department of Research. Survey: transition services lacking for teens with special needs. AAP News 2009;30:12. [Google Scholar]
- 9.Watson P. Non-compliance and transfer from pediatric to adult transplant unit. Pediatr Nephrol 2000;14:469–72. 10.1007/s004670050794 [DOI] [PubMed] [Google Scholar]
- 10.Bleyer A. Young adult oncology: the patients and their survival challenges. CA Cancer J Clin 2007;57:242–55. 10.3322/canjclin.57.4.242 [DOI] [PubMed] [Google Scholar]
- 11.Kipps S, Bahu T, Ong K et al. Current methods of transfer of young people with Type 1 diabetes to adult services. Diabet Med 2002;19:649–54. 10.1046/j.1464-5491.2002.00757.x [DOI] [PubMed] [Google Scholar]
- 12.Binks JA, Barden WS, Burke TA et al. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil 2007;88:1064–73. 10.1016/j.apmr.2007.04.018 [DOI] [PubMed] [Google Scholar]
- 13.Nagra A. Transition in practice: “Ready, Steady, Go”. BMJ 2012. http://www.bmj.com/content/344/bmj.e3718/rr/596733 [Google Scholar]
- 14.Gorter JW, Roebroeck M. Transition to adulthood: enhancing health and quality of life for emerging adults with neurological and developmental conditions. In: Ronen G, Rosenbaum P, eds. Life quality outcomes in children and young people with neurological and developmental conditions: concepts, evidence and practice. London: MacKeith Press, 2013:306–17. [Google Scholar]
- 15.Roebroeck ME, Jahnsen R, Carona C et al. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol 2009;51:670–8. 10.1111/j.1469-8749.2009.03322.x [DOI] [PubMed] [Google Scholar]
- 16.Sattoe JN, Hilberink SR, Peeters MA et al. ‘Skills for growing up’: supporting autonomy in young people with kidney disease. J Ren Care 2014;40:131–9. 10.1002/jorc.12046 [DOI] [PubMed] [Google Scholar]
- 17.Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q 2002;80:433–79. 10.1111/1468-0009.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huber M, Knottnerus JA, Green L et al. How should we define health? BMJ 2011;343:d4163 10.1136/bmj.d4163 [DOI] [PubMed] [Google Scholar]
- 19.Reiss J. Health care transition for emerging adults with chronic health conditions and disabilities. Pediatr Ann 2012;41:429–35. 10.3928/00904481-20120924-16 [DOI] [PubMed] [Google Scholar]
- 20.Kennedy A, Sloman F, Douglass JA et al. Young people with chronic illness: the approach to transition. Intern Med J 2007;37:555–60. 10.1111/j.1445-5994.2007.01440.x [DOI] [PubMed] [Google Scholar]
- 21.Hilderson D, Westhovens R, Wouters C et al. Rationale, design and baseline data of a mixed methods study examining the clinical impact of a brief transition programme for young people with juvenile idiopathic arthritis: the DON'T RETARD project. BMJ Open 2013;3:e003591 10.1136/bmjopen-2013-003591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harden PN, Walsh G, Bandler N et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ 2012;344:e3718 10.1136/bmj.e3718 [DOI] [PubMed] [Google Scholar]
- 23.Chaturvedi S, Jones C, Walker RG et al. The transition of kidney transplant recipients: a work in progress. Pediatr Nephrol 2009;24:1055–60. 10.1007/s00467-009-1124-y [DOI] [PubMed] [Google Scholar]
- 24.Craig SL Towns S, Bibby H. Moving on from paediatric to adult health care: an initial evaluation of a transition program for young people with cystic fibrosis. Int J Adolesc Med Health 2007;19:333–43. 10.1515/IJAMH.2007.19.3.333 [DOI] [PubMed] [Google Scholar]
- 25.McDonagh JE, Southwood TR, Shaw KL. British Society of Paediatric and Adolescent Rheumatology. The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatology (Oxford) 2007;46:161–8. 10.1093/rheumatology/kel198 [DOI] [PubMed] [Google Scholar]
- 26.Kreindler JL, Miller VA. Cystic fibrosis: addressing the transition from pediatric to adult-oriented health care. Patient Prefer Adherence 2013;7:1221–6. 10.2147/PPA.S37710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowley R, Wolfe I, Lock K et al. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548–53. 10.1136/adc.2010.202473 [DOI] [PubMed] [Google Scholar]
- 28.Stewart D, Law M, Young N et al. Complexities during transitions to adulthood for youth with disabilities: person-environment interactions. Disabil Rehabil 2014;36:1998–2004. 10.3109/09638288.2014.885994 [DOI] [PubMed] [Google Scholar]
- 29.Gorter JW, Stewart D, Smith MW et al. Pathways toward positive psychosocial outcomes and mental health for youth with disabilities: a knowledge synthesis of developmental trajectories. Can J Commun Ment Health 2014;33:45–61. 10.7870/cjcmh-2014-005 [DOI] [Google Scholar]
- 30.Vander Laenen F. ‘I don't trust you, you are going to tell’, adolescents with emotional and behavioural disorders participating in qualitative research. Child Care Health Dev 2009;35:323–9. 10.1111/j.1365-2214.2009.00936.x [DOI] [PubMed] [Google Scholar]
- 31.Lugasi T, Achille M, Stevenson M. Patients’ perspective on factors that facilitate transition from child-centred to adult-centred health care: a theory integrated metasummary of quantitative and qualitative studies. J Adol Health 2011;48:429–40. 10.1016/j.jadohealth.2010.10.016 [DOI] [PubMed] [Google Scholar]
- 32.Freeman M. Development and evaluation of the Youth KIT: Keeping It Together™ for Youth (the ‘Youth KIT’) to assist youth with disabilities in managing information. Child Care Health Dev 2015;41:222–9. 10.1111/cch.12199 [DOI] [PubMed] [Google Scholar]
- 33.Law M, Baptiste S, Carswell A et al. Canadian Occupational Performance Measure. 4th edn. Ottawa, ON: CAOT Publications ACE, 2005. [Google Scholar]
- 34.McColl MA, Carswell A, Law M et al. Research on the Canadian Occupational Performance Measure: an annotated resource. Ottawa, ON: CAOT Publications ACE, 2006. [Google Scholar]
- 35.Carswell A, McColl MA, Baptiste S et al. The Canadian Occupational Performance Measure: a research and clinical literature review. Canadian J Occup Ther 2004;71:210–22. 10.1177/000841740407100406 [DOI] [PubMed] [Google Scholar]
- 36.Biggerstaff DL, Thompson AR. Interpretative phenomenological analysis (IPA): a qualitative methodology of choice in healthcare research. Qual Res Psychol 2008;5:214–24. 10.1080/14780880802314304 [DOI] [Google Scholar]
- 37.Smith DW. Phenomenology. In: Zalta EN, ed. The Stanford Encyclopedia of Philosophy. Winter 2013 Edition. http://plato.stanford.edu/entries/phenomenology/ (accessed Sep 2014). [Google Scholar]
- 38.IBM Corp. IBM SPSS statistics for Windows, Version 22.0 Armonk, NY: IBM Corp, 2013. [Google Scholar]
- 39.Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 40.Nguyen T, Stewart D, Hlyva O et al. An interdependent dance in transition to adulthood: perspectives of youth, parents, and healthcare providers. European Academy of Childhood Disability (EACD) Conference October 2013 (Poster Presentation). Gateshead, UK (with the authors’ permission). [Google Scholar]
- 41.Gorter JW. Editorial. Making links across the lifespan in neurology. Can J Neurol Sci 2012;39:1–2. 10.1017/S0317167100012580 [DOI] [PubMed] [Google Scholar]
- 42.Moola FJ, Norman ME. ‘Down the rabbit hole’: enhancing the transition process for youth with cystic fibrosis and congenital heart disease by re-imagining the future and time. Child Care Health Dev 2011;37:841–51. 10.1111/j.1365-2214.2011.01317.x [DOI] [PubMed] [Google Scholar]
- 43.Fraser S. Transition of care in children with chronic disease: healthcare teams need to adapt to change as much as patients and their families. BMJ 2007;334:1231 10.1136/bmj.39255.292627.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fegran L, Hall EO, Uhrenfeldt L et al. Adolescents’ and young adults’ transition experiences when transferring from paediatric to adult care. Int J Nurs Stud 2014;51:123–35. 10.1016/j.ijnurstu.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 45.Kraus de Camargo O. Systems of care: transition from the bio-psycho-social perspective of the International Classification of Functioning, Disability and Health. Child Care Health Dev 2011;37:792–9. 10.1111/j.1365-2214.2011.01323.x [DOI] [PubMed] [Google Scholar]
- 46.Nguyen T, Gorter JW. Use of the international classification of functioning, disability and health as a framework for transition from paediatric to adult healthcare. Child Care Health Dev 2014;40:759–61. 10.1111/cch.12125 [DOI] [PubMed] [Google Scholar]
- 47.Nguyen T, Stewart D, Hlyva O et al. The use, utility and impact of the Youth KIT, a tool to aid transitioning youth: lessons learned from a longitudinal study. American Academy for Cerebral Palsy and Developmental Medicine (AACPDM) Conference September 2014 (Poster Presentation) San Diego, CA. [Google Scholar]
- 48.van der Velden M, El Emam K. “Not all my friends need to know”: a qualitative study of teenage patients, privacy, and social media. J Am Med Inform Assoc 2013;20:16–24. 10.1136/amiajnl-2012-000949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miloh T, Annunziato R, Arnon R et al. Improved adherence and outcomes for pediatric liver transplant recipients by using text messaging. Pediatrics 2009;124:844–50. 10.1542/peds.2009-0415 [DOI] [PubMed] [Google Scholar]
- 50.Suris JC, Akre C, Berchtold A et al. Chronically connected? Internet use among adolescents with chronic conditions. J Adol Health 2010;46:200–2. 10.1016/j.jadohealth.2009.07.008 [DOI] [PubMed] [Google Scholar]
- 51.Prior M, McManus M, White P et al. Measuring the “triple aim” in transition care: a systematic review. Pediatrics 2014;134:e1648–61. 10.1542/peds.2014-1704 [DOI] [PubMed] [Google Scholar]
- 52.Davis A, Brown R, Lounds Taylor J et al. Transition care for children with special health care needs. Pediatrics 2014;134:900–8. 10.1542/peds.2014-1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gall C, Kingsnorth S, Healy H. Growing up ready: a shared management approach. Phys Occup Ther Pediatr 2006;26:47–62. [PubMed] [Google Scholar]
- 54.Colver A, Longwell S. New understanding of adolescent brain development: relevance to transitional healthcare for young people with long-term conditions. Arch Dis Child 2013;98:902–7. 10.1136/archdischild-2013-303945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Klassen A, Grant C, Barr R et al. Development and validation of a generic scale for use in transition programs to measure self-management skills in adolescents with chronic health conditions: The TRANSITION-Q. Child Care Health Dev 2014. Published Online First 28 Oct 2014. doi:10.1111/cch.12207 10.1111/cch.12207 [DOI] [PubMed] [Google Scholar]


