Abstract
Background: Knee osteoarthritis (OA) is the most common musculoskeletal disease among old individuals which affects ability for sitting on the chair, standing, walking and climbing stairs. Our objective was to investigate the short and long-term effects of the most simple and the least expensive exercise protocols in combination to conventional conservative therapy for knee OA.
Methods: It was a single blind RCT study with a 12-months follow-up. Totally, 56 patients with knee OA were assigned into 2 random groups. The patients in exercise group received exercise for knee muscles in combination with non-steroid anti-inflammatory drugs (NSAIDs) and 10 sessions acupuncture and physiotherapy modalities. Non-exercise group received similar treatments except exercise program. The changes in patients’ pain and functional status were evaluated by visual analog scale (VAS), knee and osteoarthritis outcome score (KOOS) questionnaire and functional tests (4 steps, 5 sit up, and 6 min walk test) before and after treatment (1 and 3 months after intervention), and 1 year later at the follow-up.
Results: The results showed that the patients with knee OA in exercise group had significant improvement in pain, disability, walking, stair climbing, and sit up speed after treatment at first and second follow-up when compared with their initial status and when compared with non-exercise group. At third follow up (1 year later) there was significant difference between groups in VAS and in three items of KOOS questionnaire in functional status.
Conclusion: Non aerobic exercises for muscles around knee can augment the effect of other therapeutic interventions like medical therapy, acupuncture, and modalities for knee OA.
Keywords: Knee osteoarthritis, Strengthening exercises, Stretching exercises, Acupuncture, Functional status
Introduction
Knee osteoarthritis (OA) is a degenerative and chronic disease of the knee joint resulting from damage to hyaline cartilage and is the most common type of arthritis (1) and the most common musculoskeletal disease among individuals older than 65 years. The knee OA affects the ability for sitting on the chair, standing, walking and climbing stairs (2-3) and influences almost one-third of this age group (4). Knee OA is highly accompanied by morbidity in the community (5).
Puett and Griffin reviewed 15 RCT studies related to non-invasive and protective treatments of hip and knee OA during 1966-1993 and concluded that exercise reduces the pain and improves the function, though they specified no exercise regimen to achieve this goal (6).
Most patients who have knee OA, use a combination of pharmacological and non-pharmacological therapies (7). According to recommendations by American college of Rheumatology (ACR) on hip and knee OA treatment published in 2012, non-pharmacological treatments of knee OA include aerobic and strength exercise, hydrotherapy, and weight loss (8-10)
Based on our experience, physical therapy modalities and acupuncture, and use of supplements are effective in the re-construction of the cartilage. However, it needs continuous training, though feeling pain during aerobic exercises may lead to exercising less. The purpose of this study was to assay the short and long-term effects of the most simple and the least expensive exercise protocols in combination to conventional conservative therapy on knee OA.
Methods
It was a RCT study with a 12-month follow-up carried out during 2010 – 2012 in Tehran. The study protocol was approved in Ethic Committee of Iran University of Medical Sciences and was registered by code: IRCT138904274409N1. Patients older than 40 with knee pain referred to Sports Medicine Clinic in Hazrat Rasoul Hospital were visited and evaluated by two sports medicine specialists. According to American College of Rheumatology (ACR) criteria (explained in Appendix 1) individuals with knee OA were selected and knee radiography was obtained from patellar, lateral, and AP standing views. The eligible Individuals with following conditions were included in the study: having pain in knee for more than 3 months in most days of week; having arthritis grade II, III, IV in knee radiography according to the criteria of Kellegren-Lawrence (Appendix 2); having BMI in 18-30 kg/m2 range; not having any limitations for performing strength exercise (uncontrolled hypertension, uncontrolled metabolic disease, uncontrolled ventricular arrhythmias, uncontrolled heart failure, severe valvular problems). These individuals were included in the study after obtaining their informed consent.
All participants were examined by two sports medicine specialists. Following initial examination, their age, sex, knee pain duration (Table 1) and medical history were recorded.
Table 1 . Basic characteristics of two groups .
| No exercise group | Exercise group | p | |
| Age(mean ,SD) | 60±9.87 | 62.32±8.42 | 0.414 |
| Sex(male/female) | 9.13 | 11.17 | 0/24 |
| BMI(mean ,SD) | 29.98±4.29 | 28.21±3.62 | 0.163 |
Participants were divided into two groups randomly. For assigning groups, small pieces of paper were prepared in the same number of the participants. The name of treatment methods was written on the pieces of paper, and then they were put into a bag and were kept by someone who was blind to them. Then participants were asked to take one paper from the bag and thus the treatment type for each person was specified.
About one week after study initiation in without exercise therapy group, individuals received acupuncture during 10 sessions, twice per week by a sports medicine specialist. Every session lasted 15 min, and heading, knee eyes, BL57, LR3, LR9, ST33, ST36, and SP9 points were acupunctured. They were treated by physical modalities during 10 sessions, three times per week. Modalities included trans-electrical nerve stimulation (TENS), ultra sound (US) and infrared (IR). Two electrodes placed medial and lateral to the joint for taking 100 Hz symmetrical TENS (10 minutes in every pad).US and IR were applied to all knee joints for 5 minutes.
In addition, patients used diclofenac 100 mg tablets once daily if they had pain (VAS > 5). All individuals were recommended to use 1500 milligrams glucosamine and 800 milligrams chondroitin.
The patients in exercise therapy group took anaerobic exercises in combination took anaerobic exercises in combination with acupuncture and physical modalities (Figs. 1-6 of Appendix 3). Exercise protocol included 3 stretching exercises and 3 strengthening exercises for muscles around the knee (hamstrings, quadriceps and calf muscles). Individuals were asked to perform the stretching exercises daily and keep doing each exercise for a minimum of 15 seconds in stretching form and repeat them 4 times.(Figs. 1,3,4 of Appendix 3). Strengthening exercises were performed daily and each time every exercise was repeated 10 times in three sets. There was 1-3 min rest between sets.(Figs. 2,5,6 of Appendix 3) The weight of cuff weights tied to the patient's ankle (shown in fig. 5 and 6 of appendix 3) was selected according to the tolerance of patient and his/her basic status. The weight of cuff was added 250 grams each 2 weeks and finally it reached to 2 kilograms.
Fig.1 .
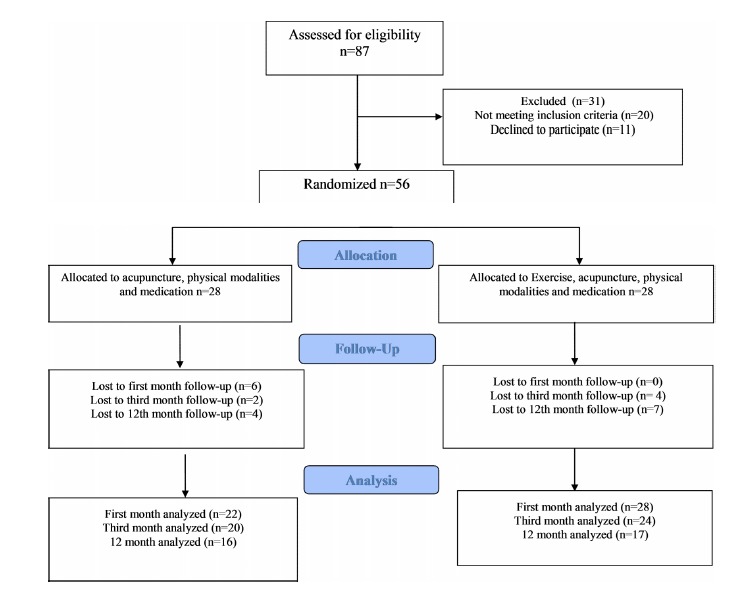
Outline of treatment pathway of patient recruitment, intervention and withdrawal through the trial
During 3 months, the patients in non-exercise group were contacted by researcher weekly on phone and exercise group patients were visited each 2 weeks. They were asked not to perform any aerobic program and use no weight loss treatments up until 3 months. The patients were insured for any possible damage.
The knee pain was measured in resting state by VAS. Persian version of KOOS questionnaire (11) which examines pain and function by 5 items, was filled by the sports medicine specialist beside the patient. There was a 9-questions item in the questionnaire which measured the patient's amount of pain based on a 0-100 scale. The higher scale points represented better situation of the patient.
Individuals function was evaluated using 4 items in KOOS questionnaire which included symptoms, activities of everyday life (ADL), sports activities and quality of life (QOL). Each item had scores between 0-100 with 0 denoting bad situation and 100 denoting good situation.
Three tests including 4 steps, 5 sit ups and 6- MWTs were used before and after intervention to evaluate function and ability of individuals. In 6- MWT test, the patient was asked to walk with normal pace for 6 minutes, and the passed distance was recorded in meter. In 5 sit up test, individual was asked to sit and stand the chair consecutively for 5 times and the duration was recorded in seconds. In 4 step test, the patient was asked to climb up and down the steps (20 cm step) consecutively 4 times and the duration for this test was recorded.
All parameters related to outcome were measured once before intervention, once 1 month after intervention and then 3 months after intervention. One year after treatment initiation, patients were evaluated in terms of all these parameters. During the first 3 months, throughout 10 sessions of acupuncture, participants were constantly in contact with the sports medicine specialist. After completion of acupuncture sessions until the end of third month, the specialist was in contact with these participants by phone, emphasizing performing exercise programs. If there was any problem, the patient was asked to refer to the sports medicine clinic and take face-to-face consulting. There was no further contact with the participants during the 3rd to 12th month in which patients were allowed to use any kind of interventions for treatment.
Of 56 participants included in the study, 28 were assigned to exercise therapy and 28 to without exercise therapy group. Of 56 participants, 50 were evaluated in first follow-up because 6 patients of non exercise group were excluded in first two weeks (5 patients could not take acupuncture more than one or two times a week and one patient went to an unknown physiotherapy clinic with a different therapeutic protocol). In the second follow-up (3 months after treatment initiation) 6 subjects were excluded, one due to 7 kg weight loss and others because of unwillingness. In the 12th month of follow-up, from without exercise therapy group one was not evaluable due to intra-articular injection of corticosteroids, and another one was eliminated due to PRP injection in the joint, and from the exercise therapy group, 3 were not accessible due to changed address and phone number.
Data analysis was performed by SPSS v. 16.0. Results were reported as mean (± SD) when normally distributed and percentages in qualitative variables. Independent student t-test was used for comparison of quantitative variables between the two groups. Also Mann Whitney U test was used as alternative when t-test was not permitted. Paired sample t-test and repeated measured analysis of variances were used for multiple comparisons.
We used Chi Square test in determining the difference between groups' qualitative differences. P< 0.05 was considered statistically significant.
Results
In this study, 87 patients with knee OA were evaluated, 69 of whom were eligible for inclusion in the study. Of 69 participants, 6 disagreed not to use weight loss methods and others were afraid of acupuncture and 3 preferred to use pool during the study, thus all of them were excluded.
In the pre-treatment stage, there was no significant difference between average of variables in both control and intervention groups (p < 0.05).
Results in Table 2 indicate that there was significant difference in all variables between exercise therapy group and without exercise therapy group in three consecutive measurements after 3 months. The results of 12th month follow-up are shown in Table 3. They suggest a significant difference only in everyday life activities, sports activities and pain items from KOOS questionnaire between the two groups. A significant difference was observed regarding VAS between intervention and control groups, too.
Table 2 . Comparison of changes in average of variables related to pain and function in control and intervention groups in three consecutive measurements .
|
Before intervention (Mean) |
After 1 month (Mean) |
After 3 months (Mean) |
p | ||||
| Exercise | Control | Exercise | Control | Exercise | Control | ||
| VAS | 8 | 8.82 | 5.96 | 6.64 | 4.75 | 6.14 | .005 |
| KOOS(pain) | 46.96 | 36.92 | 58.43 | 42.73 | 63.39 | 46.65 | .002 |
| KOOS(symptom) | 44.76 | 39.75 | 54.92 | 47.06 | 57.98 | 50.72 | 0.09 |
| KOOS(ADL) | 49.96 | 41.24 | 60.22 | 52.09 | 64.99 | 50.81 | <0.0001 |
| KOOS(Sport) | 18.34 | 6.6 | 23.90 | 13.11 | 29.51 | 16.28 | 0.035 |
| KOOS(QOL) | 28.52 | 23.06 | 33.78 | 33.09 | 39.40 | 35.74 | .000 |
| 5 sit up | 21.90 | 24.81 | 19.42 | 21.39 | 18.73 | 20.88 | .000 |
| 4 step | 21.27 | 25.59 | 19.92 | 23.42 | 17.49 | 22.19 | .000 |
| 6MWT | 29.61 | 24.96 | 31.62 | 26.02 | 33.65 | 27.61 | <0.0001 |
Table 3 . The difference of variables related to pain and knee function in control and intervention groups after 12 months.
| Control | Exercise | p | |
| VAS | 7.22 | 6.09 | 0.029 |
| KOOS(pain) | 49.03 | 48.07 | 0.043 |
| KOOS(symptom) | 54.41 | 47.87 | 0.115 |
| KOOS(ADL) | 58.88 | 46.98 | 0.033 |
| KOOS(Sport) | 26.18 | 11.98 | 0.043 |
| KOOS(QOL) | 38.21 | 30.26 | 0.118 |
| 5 sit up | 20.12 | 20.57 | 0.632 |
| 4 steps | 20.33 | 23.38 | 0.255 |
| 6MWT | 29.61 | 31.16 | 0.843 |
Concerning functional tests, results of 5 sit ups, 4 steps and 6 min walk test did not show any significant difference in both groups.
Compliance
In the first 3 months of treatment, when the patients were administered by telephone or in-person visits once a week, compliance of sports treatment in exercise therapy group was 67.73%. Of 28 participants in this group, 19 performed the sports exercises completely based on the trained pattern. Also 25 received acupuncture and 26 received physical modalities completely, and their compliance percentage was 89.28 and 92.85, respectively. In without exercise therapy group, the compliance rate was 90.9% and of 22 patients, 20 performed suggested treatment. During 3-12 months, when there was no supervision on recommended treatment methods in exercise therapy group, compliance of patients from sports exercises was 14.2%. During this time that any exercise was allowed for the without exercise therapy group, only two individuals irregularly received hydrotherapy in pool.
Discussion
We found that adding the anaerobic exercise protocol (6 exercises, stretching and strengthening the muscles around the knee) to other non-invasive techniques on knee OA relieves the pain and improves the function of the knee in short-term (3 months).The results showed no difference in the first month of treatment in both groups, and improvement in both groups were equal.
In the follow up, particularly in the third month, the strengthening effect of exercises was significant. It should be considered because the exercises were continued during the first to third month while methods were no longer available. Also in the last follow up we observed that the effect of exercises lasted for a year. This finding differs from the results of Bruce study (12) who showed that lasting effect of 6 weeks strength training and electrical stimulation of the quadriceps are same after 14 weeks.
In our study, there was a significant statistical difference in both groups in terms of all consistency with our results in short term. The positive effect of quadriceps and hamstring muscles strengthening exercises to improve symptoms in short-term in patients with knee OA was in agreement to other studies (e.g. 13-17). According to Carvalho trial (14), the treatment effects lasted for 2 years, but there has been no lasting effects from exercise in 5 years.
Considering the fact that only 14.2% of the participants in the exercise group of this trial performed recommended exercises during 3-12 months, the significant differences between the two groups can be attributed to the long acting effect of the exercise protocol up to one year.
Jekinson's trial result is contrary to most studies that have confirmed the effect of weight loss on reduced knee pain and increased function and slowing progression of OA (19-21). In Jekinson's trial (22) on 289 obese participants with knee OA, it was found that the diet and weight loss of approximately 3 kg has no effect on level of pain and function of subjects. In our study, participants were asked not to use any exercise and diet for weight loss during first 3 months of treatment, but after 3 months they were allowed. Because of stability of weight in participants (except for 1 who was excluded for this reason), reduced pain and improved functioning can be attributed to knee muscles exercises. On the other hand, although participants were allowed to use any method for weight loss, no significant weight loss was observed after one year of follow-up.
In a study by Durmus in Turkey (23), it was found that using glucosamine – chondroitin compared to exercise therapy had no impact on delay in radiological progress of knee OA. In our study we found that adding exercise to glucosamine – chondroitin can relieve pain and symptoms and improve functional tests like step climbing, sits up and walking time.
According to some studies (24-25), adding acupuncture to exercise therapy was much more effective in treatment of knee OA symptoms. In a 2010 systematic review (26), RCTs investigating acupuncture impact with placebo in pain control and function in patients with knee OA in short time, found improved function and reduced pain, but the difference in 6-month follow-up was not significant. We found that exercise therapy in combination to acupuncture can boost the positive effects.
According to Brakke at el (27) and Schencking et al (28) studies impacts of TENS modality on reducing pain and improving function in patients with knee OA was trivial compared with strengthening exercises and hydrotherapy. Our results were totally consistent with this study and knee muscles exercises had extra effect over Heat, US, and TENS modalities.
Evaluation of patients at one year follow-up showed that pain at rest (VAS) and pain during the movement of knee (pain items in KOOS questionnaire) in patients who performed exercises were less than other group, and their ability to perform daily activities such as walking and bathing were also better. Nonetheless, the patient's symptoms, such as the ability to do flexion and extension, knee stiffness and quality of life did not differ. However, with gradual decrease of pain, resuming the ability to perform daily activities and sports activities their status will be better in the long term.
Another possible reason corresponding to unimprovement of quality of life (QOL) in long-term may be related to the validity of questions about QOL in the KOOS questionnaire. It is recommended to investigate the QOL score with a stronger questionnaire. It can be considered as a limitation of our study.
According to Campbell study (29), it was observed that there is direct relationship between compliance level and supervision of patients. Our results also showed that as long as people are in relation with a therapist and are observed regularly, their compliance for the exercise is very high. But if there is no observation, reminder or emphasis by the therapist, the compliance reduces significantly from 67.73 % in 3rd month to 14.2% in 12th month. Thus, it can be said that if people were periodically observed during 12 months, better results would be obtained for effect of exercise.
In the 12th month of follow-up, patients were asked about the lack of continuing training. They responded that they had no enough time to do exercises and some others also stated that they forgot that they need exercises. Due to the fact that approximately 65% of the subjects in this study were housewives or retired and performing this exercise protocol takes approximately 30 to 40 minutes a day, we can propose that they did not have enough motivation. Therefore, further studies on the effects of motivation on performing exercise and exercise continuous supervision by the therapist are recommended.
Conclusion
In our study it was found that adding exercise to other noninvasive methods that routinely are used for knee OA have boosting effect in relieving pain and improving knee function. According to this trial, a combination therapy has the most effect on the knee OA. Exercise therapy can be recommended for patients with even severe arthritis as an effective method combined to other palliative methods in knee OA.
Appendix
Appendix 1
Diagnostic criteria of ACR (American college of rheumatology) for knee OA (1986)
-knee pain + 5 of 9
1- Age >50 6- bony enlargement
2- Stiffness< 30 min 7- ESR < 40 mmol/hour
3- Crepitus 8- RF <1/40
4- Bony tenderness 9- synovial fluid signs of osteoarthritis
5- No palpable warmth
Appendix 2
Kellgren Lawrence scale:
Grade I: normal, Grade II: uncertain joint space, possible osteophyte, Grade III: Decreased certain joint space, mild sclerosis, certain osteophyte, Grade III: Significant reduction in joint space, moderate sclerosis, moderate osteophyte, possible cysts, possible deformity, Grade IV :Total reduction in joint space, severe sclerosis, great osteophyte, certain deformity
Appendix 3
Figures of exercises according to knee pamphlet
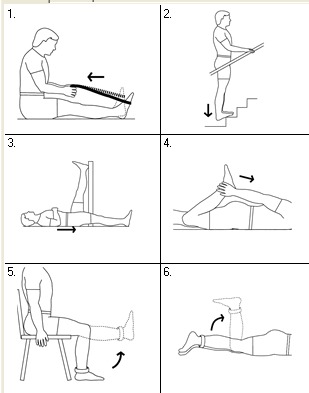
Figures of exercises according to knee pamphlet
Cite this article as: Nejati P, Farzinmehr A, Moradi-Lakeh M. The effect of exercise therapy on knee osteoarthritis: a random-ized clinical trial. Med J Islam Repub Iran 2015 (25 February). Vol. 29:186.
References
- 1.Maurer BT, Stern AG, Kinossian B, Cook KD, Schumacher HR Jr. Osteoarthritis of the knee: isokinetic quadriceps exercise versus an educational intervention. Archives of physical medicine and rehabilitation. 1999;80(10):1293–1299. doi: 10.1016/s0003-9993(99)90032-1. [DOI] [PubMed] [Google Scholar]
- 2. Felson D.T. Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The epidemiology of knee osteoarthritis: results from the Framingham Osteoarthritis Study. In Seminars in arthritis and rheumatism. 1990: Elsevier.
- 3.Felson D T, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly The Framingham Osteoarthritis Study. Arthritis & Rheumatism. 2005;30(8):914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 4.Ringdahl E, S S. Treatment of knee osteoarthritis. American Pandit Family Physician. 2011;83(11):1287. [PubMed] [Google Scholar]
- 5.Badley E, Tennant A. Disablement associated with rheumatic disorders in a British population: problems with activities of daily living and level of support. Rheumatology. 1993;32(7):601–608. doi: 10.1093/rheumatology/32.7.601. [DOI] [PubMed] [Google Scholar]
- 6.Puett D. W and Griffin MR Published trials of nonmedicinal and noninvasive therapies for hip and knee osteoarthritis. Ann Intern Med. 1994;121(2):133–40. doi: 10.7326/0003-4819-121-2-199407150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Hochberg M C, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J. et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research. 2012;64(4):465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 8. Kolen A P.A. Evidence based Rehabilitation in knee artherosis Z Dokazi Podprta Rehabilitacija.
- 9.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N. et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18(4):476–99. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Thomson Jr R, Oegema T Jr, and Lewis J. Osteoarthritic changes after acute transarticular load. J Bone Joint Surg Am. 1991;73:990–1001. [PubMed] [Google Scholar]
- 11.Salavati M, Mazaheri M, Negahban H, Sohani SM, Ebrahimian MR, Ebrahimi I. et al. Validation of a Persianversion of Knee injury and Osteoarthritis Outcome Score (KOOS) in Iranians with knee injuries. Osteoarthritis and Cartilage. 2008;16(10):1178–1182. doi: 10.1016/j.joca.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Bruce-Brand R A, Walls R J, Ong J C, Emerson B nS, O’Byrneand J M, Moyna N M. et al. Effects of homebased resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial. BMC Musculoskeletal Disorders. 2012;13(1):118. doi: 10.1186/1471-2474-13-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iwamoto J, Takeda T, and Sato Y. Effect of muscle strengthening exercises on the muscle strength in patients with osteoarthritis of the knee. The Knee. 2007;14(3):224. doi: 10.1016/j.knee.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 14. Carvalho, N.A.d. A. , Simoni Teixeira B, Flávia R, Souza P, Mônica F, Robson Roberto S. , Manual for guided home exercises for osteoarthritis of the knee. Clinics. 2010;65(8):775–780. doi: 10.1590/S1807-59322010000800007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shakoor N, Furmanov S, Nelson DE, Li Y, Block JA. Pain and its relationship with muscle strength and proprioception in knee OA: results of an 8-week home exercise pilot study. J Musculoskelet Neuronal Interact. 2008;8(1):35–42. [PubMed] [Google Scholar]
- 16.Doi T, Akai M, Fujino K, Iwaya T, Kurosawa H, Hayashi K. et al. Effect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal ant iinflammatory drugs: a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation. 2008;87(4):258–269. doi: 10.1097/PHM.0b013e318168c02d. [DOI] [PubMed] [Google Scholar]
- 17.Schilke J M, Johnson GO, Housh TJ, O'Dell JR. Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nursing research. 1996;45(2):68–72. doi: 10.1097/00006199-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Vincent K R, Vincent H K. Resistance Exercise for Knee Osteoarthritis. PM & R. 2012;4(5):S45–S52. doi: 10.1016/j.pmrj.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wluka A E, Lombard C B, Cicuttini F M. Tackling obesity in knee osteoarthritis. Nature Reviews Rheumatology. 2012 doi: 10.1038/nrrheum.2012.224. [DOI] [PubMed] [Google Scholar]
- 20.Messier S P. Diet and exercise for obeseadults with knee osteoarthritis. Clinics in Geriatricmedicine. 2010;26(3):461. doi: 10.1016/j.cger.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Messier S P, Legault C, Loeser RF, Van Arsdale SJ, Davis C, Ettinger WH. et al. Does high weight loss in older adults with knee osteoarthritis affect bone-onbone joint loads and muscle forces during walking? Osteoarthritis and Cartilage. 2011;19(3):272–280. doi: 10.1016/j.joca.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jenkinson C.M, Doherty M, Anthony J, Read A, Moira A, Tracey H. et al. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ. 2009;339:b3170. doi: 10.1136/bmj.b3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Durmus D, Alayli G, Bayrak IK, Canturk F. et al. Assessment of the effect of glucosamine sulfate and exercise on knee cartilage using magnetic resonance imaging in patients with knee osteoarthritis: A randomized controlled clinical trial. Journal of back and musculoskeletal rehabilitation. 2012;25(4):275–284. doi: 10.3233/BMR-2012-0336. [DOI] [PubMed] [Google Scholar]
- 24.Whitehurst D G, Bryan S, Hay EM, Thomas E, Young J, Foster NE. Cost-effectiveness of acupuncture care as an adjunct to exercise-based physical therapy for osteoarthritis of the knee. Physical therapy. 2011;91(5):630–641. doi: 10.2522/ptj.20100239. [DOI] [PubMed] [Google Scholar]
- 25.Hurley M V, Walsh N E. Effectiveness and clinical applicability of integrated rehabilitation programs for knee osteoarthritis. Current opinion in rheumatology. 2009;21(2):171–176. doi: 10.1097/BOR.0b013e3283244422. [DOI] [PubMed] [Google Scholar]
- 26.Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S. et al. Acupuncture for peripheral joint osteoarthritis. The Cochrane Library. 2010 doi: 10.1002/14651858.CD001977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brakke R, Singh J, and Sullivan W. Physical Therapy in Persons with Osteoarthritis. PM & R. 2012;4(5):S53–S58. doi: 10.1016/j.pmrj.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 28.Schencking M, Wilm S, Redaelli M. A comparison of Kneipp hydrotherapy with conventional physiotherapy in the treatment of osteoarthritis of the hip or knee: protocol of a prospective randomised controlled clinical trial. BMC Musculoskeletal Disorders. 2009;10(1):104. doi: 10.1186/1471-2474-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell R, Evans M, Tucker M, Quilty B, Dieppe P, Donovan JL. Why don't patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. Journal of epidemiology and community health. 2001;55(2):132–138. doi: 10.1136/jech.55.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]


