Abstract
Background
Relapse is common in schizophrenia, and seriously impacts patients’ quality of life and social functioning. Many factors have been identified that may potentially increase the risk of relapse. This study was designed to investigate the relapse rate in the year following hospital discharge among Chinese patients with schizophrenia in the naturalistic condition, and to explore possible risk factors related to relapse.
Methods
We conducted a large, multicenter, retrospective, observational study in ten psychiatric hospitals throughout the People’s Republic of China. Nine hundred and ninety-two schizophrenic outpatients aged 18–65 years discharged from these hospitals between September 2011 and February 2012 with recovery/improvement of their condition were included in the study. Information about relapse and correlative factors during the year after discharge was collected by telephone interview using a questionnaire.
Results
Eight hundred and seventy-six of 992 eligible patients completed the telephone survey. Of these patients, 293 (33.4%) had at least one relapse within 1 year after discharge, and 165 (18.8%) were rehospitalized. In respondents’ view, the most important factor contributing to relapse was poor medication adherence (50.7%). Approximately 30% of the respondents had a negative attitude toward medication, with the impression that there was no need to take drugs at all or for a long time. Nonadherent patients (37.9%) had a relapse rate that was 2.5-fold higher than adherent patients (54.5% versus 20.7%, P<0.001). The top five risk factors associated with relapse were nonadherence to medication (odds ratio [OR] 4.602, 95% confidence interval [CI] 3.410–6.211), being without work (OR 3.275, 95% CI 2.291–4.681), poor self-care ability (OR 2.996, 95% CI 2.129–4.214), poor interpersonal skills (OR 2.635, 95% CI 1.951–3.558), and hospitalization on more than three occasions (OR 2.299, 95% CI 1.691–3.126).
Conclusion
The 1-year relapse rate after discharge in patients with schizophrenia was 33.5% in our study. The most important risk factor related to relapse was poor medication adherence, which was mainly due to patients having a negative attitude toward their medication. Lack of psychosocial support and a complicated disease history also increased the risk of relapse.
Keywords: schizophrenia, relapse, medication adherence
Introduction
Schizophrenia is a chronic and disabling mental illness that often presents with a progressive course and multiple relapses. The majority of patients with schizophrenia typically experience acute symptomatic relapses alternating with periods of full or partial remission over a period of many years.1 Frequent relapses are associated with exacerbated psychopathology, a worsened clinical prognosis, and impaired function, which not only seriously impacts on patient quality of life, but also puts a heavy burden on families and society. SOHO, a 3-year prospective observational study evaluating the economic burden of schizophrenia with or without relapse, showed that the costs incurred by patients who ever relapsed were almost double those incurred by patients who never relapsed.2
Relapse prevention is always a critical issue for enhancing the overall treatment outcome in management of schizophrenia. One study3 reported that more than 50% of schizophrenic patients had a relapse within 1 year after hospital discharge. Another study4 that enrolled first-episode schizophrenic patients showed that 21%, 33%, and 40% of patients relapsed in the first, second, and third year, respectively. In a retrospective study,5 conducted in 50 patients who had been followed up for more than 15 years, the relapse rate within 2, 5, 10, and 15 years from remission of the first psychotic episode was 52%, 60%, 86%, and 90%, respectively. Since the first antipsychotic drug, chlorpromazine, was used in the 1950s,6 more than 15 antipsychotic drugs have been approved by the US Food and Drug Administration for the treatment of schizophrenia.7 Antipsychotic agents are recommended as the first-line treatment for schizophrenia. With the advent of antipsychotics, the prognosis of schizophrenia became better and relapse was reduced to some extent, but the high relapse rate is still a great challenge in treatment of the disease.
A variety of risk factors has been reported to be associated with relapse, including medication nonadherence,8 substance abuse,9 criticism, hostility or emotional over-involvement,10 and stressful life events.11 A recent study systematically reviewed and analyzed risk factors for relapse in the early course of psychosis, ie, medication nonadherence, persistent substance use disorder, critical comments from caregivers (but not overall expressed emotion), and poorer premorbid adjustment, and found an increased risk for relapse of 4-fold, 3-fold, 2.3-fold, and 2.2-fold, respectively.12 Among all the associated factors, nonadherence is the strongest predictor of relapse.13,14 Discontinuing antipsychotic drug therapy increases the risk of relapse by almost five times.15 Although ten of eleven guidelines for schizophrenia published after 2000 that refer to discontinuing of antipsychotics in maintenance treatment clearly state that discontinuation of antipsychotics within 5 years is not recommended (American Psychiatric Association, 2004; British Association for Psychopharmacology, 2011; Canadian Journal of Psychiatry, 2005; International Psychopharmacology Algorithm Project, 2004; Leucht et al 2011; Taylor et al 2009; National Institute for Health and Care Excellence, 2009; Schizophrenia Patient Outcomes Research Team, 2009; Texas Medication Algorithm Project, 2008; and World Federation of Societies of Biological Psychiatry, 2006),16 a high discontinuation rate is still observed in clinical practice. CATIE (Clinical Antipsychotic Trials of Intervention Effectiveness) was an 18-month, double-blind trial including 1,493 patients showing that 74% of patients discontinued their medication before 18 months, with a median time to discontinuation was only 4.6 months.17
The data on prevalence and risk factors for schizophrenia relapse is sufficient in many countries, but are scarce in the People’s Republic of China. In this study, we investigated the relapse rate 1 year after hospital discharge in patients with schizophrenia in a naturalistic condition in the People’s Republic of China and explored risk factors related to relapse.
Subjects and methods
Subjects
All patients in our study were selected from ten psychiatric hospitals from seven provinces in the People’s Republic of China. Investigators from each hospital screened eligible patients by reviewing their medical records. Inclusion criteria was age 18–65 years, admission to one of the above ten hospitals with a diagnosis of schizophrenia according to International Classification of Diseases, Tenth Revision criteria, and discharge from hospital with recovery/improvement between September 2011 and February 2012. Exclusion criteria were core symptoms residual at hospital discharge and/or lack of information on therapeutic effects in their medical records. The study protocol was approved by the ethics committee of Peking University Sixth Hospital. Registration of this study was not required.
Methods
This study was conducted as a retrospective observational survey. Information about relapse and related factors of all enrolled patients were investigated by interviewing their caregivers or the patients themselves by telephone 1 year after hospital discharge with a questionnaire designed for the survey. Patients’ caregivers, generally parent(s), spouse, or sibling(s), were preferred for the interviews because they were more likely to provide reliable information in the telephone survey. Patients themselves were accepted for the interview if they lived alone or their caregivers could not be contacted. No interventions were done in the year before the telephone interview. Verbal informed consent was obtained at the beginning of each telephone interview. All investigators were trained licensed psychiatrists working at the above hospitals. A period of 6 months was allowed for the investigation, so we started to enroll eligible patients and made telephone calls from September 2012 to February 2013.
The questionnaire included two parts. The first part collected general demographic data and disease information on the enrolled patients according to medical records. Disease information included duration of schizophrenia, age at onset, lifetime number of hospitalizations, duration of last hospitalization, family history of physical and psychiatric illness, and history of smoking/alcohol abuse history. The second part was a 17-item semistructured questionnaire that was specifically designed for this study to investigate the relapse rate, rehospitalization rate, and the relationship between relapse and potential risk factors and was administered during the telephone interview. Questions included number of hospital visits after discharge, current antipsychotic treatment strategy, medication adherence, relapse and rehospitalization, rehabilitation therapy after discharge, communication with family, self-care ability, interpersonal skills, smoking, drinking, and family economic conditions.
There are currently no established criteria for defining relapse in schizophrenia. In our study, relapse was defined as clinically significant exacerbation of psychotic symptoms evaluated by the investigators during telephone interviews according to self-report or the caregiver’s report. Four operational evaluation criteria were proposed for assessment of exacerbation of symptoms: a change in antipsychotic treatment, more frequent hospital visits, rehospitalization, and closer supervision because of self-harm, aggressive behavior, and/or suicidal or homicidal ideation.18 Patients who met at least one of the above four criteria were considered to have relapsed.
Medication adherence is defined as “the extent to which the patient’s behavior (in terms of taking medications, following diets, or executing other lifestyle changes) matches medical recommendations jointly agreed between patient and prescriber”.19 In this study, adherence was assessed based on the medication-taking behavior reported by respondents. Discontinuation of drugs was regarded as extreme nonadherence behavior. According to the timing of nonadherence with regard to the prescription or duration of discontinued medication after discharge, adherence was graded on three levels: adherent (adherent to prescription most of the time, nonadherence time less than 2 months or medication discontinued for less than 2 weeks); moderately nonadherent (adherent to prescription half of the time, nonadherence time more than 2 months but less than 6 months, or medication discontinued for more than 2 weeks but less than 2 months); or severely nonadherent (almost not adherent to prescription, nonadherence time more than 6 months, or medication discontinued for more than 2 months).9,14,20
Statistical analysis
After each hospital completed their surveys, all questionnaires were sent to the study initiator (Peking University Sixth Hospital) for data input and statistical analysis. Statistical Package for the Social Sciences version 16.0 software (SPSS Inc, Chicago, IL, USA) was used for the statistical analysis. Differences between individuals with relapse and those without relapse were calculated in relation to demographic factors, disease characteristics, and the possible risk factors collected by telephone interview. We used t-tests to analyze differences between groups and chi-square tests to determine the relationship between variables and relapse. For all statistical analyses, a P-value less than 0.05 was considered to be statistically significant.
Results
Patient characteristics
Of 992 eligible patients enrolled in the study, 876 (88.3%) responded and completed the telephone survey. Nonresponders (n=116, 11.7%) who were lost to follow-up or refused to participate in the survey were not included in the statistical analysis. The mean age of the responders was 36.1±11.7 years and 44.1% were males. Nearly three-quarters (74.6%) had less than 12 years of education; 38.7% were married, while 48.1% were single and 13.1% were divorced or widowed. Almost half (47.3%) were unemployed or retired (Table 1).
Table 1.
Demographic data of respondent patients (n=876)
| Sex, n (%)a | |
| Male | 386 (44.1) |
| Female | 489 (55.8) |
| Age, mean years | 36.1±11.7 years |
| Age distribution, n (%) | |
| 18–30 years | 335 (38.2) |
| 31–44 years | 311 (35.5) |
| 45–65 years | 230 (26.3) |
| Education level, n (%)b | |
| ≤Middle school | 368 (42.0) |
| High school | 286 (32.6) |
| ≥College | 216 (24.7) |
| Marital status, n (%)c | |
| Married | 339 (38.7) |
| Single | 421 (48.1) |
| Divorced | 105 (12.0) |
| Widowed | 10 (1.1) |
| Employment, n (%)d | |
| Employed | 460 (52.5) |
| Unemployed or retired | 414 (47.3) |
Notes:
One respondent (0.1%) did not provide this information.
Six respondents (0.7%) did not provide this information.
One respondent (0.1%) did not provide this information.
Two respondents (0.2%) did not provide this information.
The mean duration of schizophrenia was 9.7±8.8 years. More than half of the patients developed the illness in their early youth (56.5% at the age of 18–30 years). The mean lifetime number of hospitalizations was 3.0±2.5. Only 28.4% of the patients had had their first hospitalization when they enrolled in the study, and 43.8% had been hospitalized at least three times. The majority of the patients were not fully recovered at discharge (74.1%, Table 2).
Table 2.
Clinical characteristics of respondent patients (n=876)
| Mean duration of schizophrenia | 9.7±8.8 years |
| Distribution of illness duration, n (%) | |
| ≤2 years | 200 (22.8) |
| >2 years, ≤5 years | 160 (18.3) |
| >5 years, ≤10 years | 207 (23.6) |
| >10 years | 309 (35.3) |
| Age at disease onset, n (%)a | |
| <18 years | 141 (16.1) |
| 18–30 years | 495 (56.5) |
| 31–44 years | 188 (21.5) |
| ≥45 years | 51 (5.8) |
| Mean number of hospitalizationsb | 3.0±2.5 times |
| Distribution of numbers of hospitalization, n (%)b | |
| 1 | 249 (28.4) |
| 2 | 222 (25.3) |
| ≥3 | 384 (43.8) |
| Therapeutic effect, n (%) | |
| Recovery | 227 (25.9) |
| Improvement | 649 (74.1) |
Notes:
One respondent (0.1%) did not provide this information.
Twenty-one respondents (2.4%) did not provide this information.
Results of telephone interview
Relapse
In the year after discharge, 33.4% of patients had at least one relapse and more than 50% of patients experienced their first relapse within 6 months. The mean duration to first relapse was 6.381±3.509 months, and 18.8% required hospitalization (Table 3). There were no demographic differences between the patients who relapsed and controls who did not relapse with regard to age, sex, educational level, or residence. In the view of the respondents, risk factors leading to relapse were poor medication adherence (50.7%), poor family support (18.0%), poor interpersonal relationships (8.9%), stressful life events (8.9%), and seasonal factors (5.3%, Figure 1).
Table 3.
Relapse and readmission of respondents in first year after discharge
| Number | Proportion | |
|---|---|---|
| Relapse or nota | ||
| Yes | 293 | 33.4% |
| No | 581 | 66.3% |
| Mean duration to first relapseb (286/7) | 6.381±3.509 months | |
| Duration to first relapse, monthsb | ||
| <1 | 25 | 8.5% |
| 1–2 | 14 | 4.8% |
| 3–6 | 116 | 39.6% |
| 7–13 | 131 | 44.7% |
| Readmissionc (874/2) | ||
| Yes | 165 | 18.8% |
| No | 709 | 80.9% |
| Number of readmissionsd (163/2) | ||
| 1 | 134 | 81.2% |
| 2 | 23 | 13.9% |
| >2 | 6 | 3.6% |
Notes:
Two respondents (0.2%) did not provide this information.
Seven respondents (2.4%) did not provide this information.
Two respondents (0.2%) did not provide this information.
Two respondents (1.2%) did not provide this information.
Figure 1.
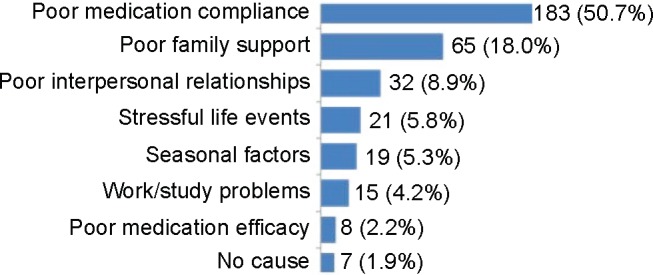
Constituent ratio of possible factors associated with relapse in the respondents’ view.
Adherence
In our study, 542 patients (61.9%) were adherent to antipsychotic treatment, 152 (17.4%) were moderately nonadherent, and 180 (20.5%) were severely nonadherent. In the respondents’ view regarding antipsychotic treatment, 70.4% agreed that antipsychotics were critical in the treatment of schizophrenia and needed to be taken for long-term maintenance. Nonadherent respondents mentioned that the three main reasons for nonadherence were “no need to take prescriptions at all” (28.1%), “drugs could be discontinued after psychotic symptoms disappeared” (24.2%), and “intolerance to adverse events” (14.3%). After discharge, only one third of patients regularly visited a doctor every month, 21.1% never visited a doctor after discharge, and 11.9% discontinued antipsychotic drugs within the first year.
Risk factors of relapse
In our study, medication nonadherence was the main factor predicting relapse. During the year after discharge, 20.7% of adherent patients relapsed, 53.9% of moderately nonadherent patients relapsed, and 55.0% of severely nonadherent patients relapsed. Nonadherent patients (37.9%) had a relapse rate that was 2.5-fold higher than that of adherent patients (P<0.001, Table 4). Nonadherence to medication significantly increased the risk of relapse (odds ratio [OR] 4.602, 95% confidence interval [CI] 3.410–6.211). A further 14 factors were also found to increase the risk of relapse. The top four factors were being without work (OR 3.275, 95% CI 2.291–4.681), poor self-care ability (OR 2.996, 95% CI 2.129–4.214), poor interpersonal skills (OR 2.635, 95% CI 1.951–3.558), and need for hospitalization on more than three occasions (OR 2.299, 95% CI 1.691–3.126). Sample sizes and ORs for significant risk factors were given in Table 5.
Table 4.
Relapse rate in adherent and nonadherent patients
| Relapse (n=293) | Nonrelapse (n=581) | Percentage of relapse | P-value | |
|---|---|---|---|---|
| Medication adherence | 9.98E-24 | |||
| Adherent (n=542) | 112 (38.2%) | 430 (74.0%) | 20.7% | |
| Moderately nonadherent (n=152) | 82 (28.0%) | 70 (12.1%) | 53.9% | |
| Severely nonadherent (n=180) | 99 (33.8%) | 81 (13.9%) | 55.0% |
Note: Two respondents did not provide adherence information and two respondents did not provide relapse information.
Table 5.
Odds ratios for disease information, adherence, and psychosocial support in patients with and without relapse
| Variable | Relapse (n=293)
|
Nonrelapse (n=581)
|
OR | 95% CI |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Nonadherent | 181 (61.8) | 151 (26.0) | 4.602 | 3.410–6.211 |
| Without work | 242 (82.6) | 355 (61.1) | 3.275 | 2.291–4.681 |
| Poor self-care ability | 94 (32.1) | 79 (13.6) | 2.996 | 2.129–4.214 |
| Poor interpersonal skills | 202 (69.0) | 267 (46.0) | 2.635 | 1.951–3.558 |
| More than three hospitalizations | 115 (39.2) | 131 (22.5) | 2.299 | 1.691–3.126 |
| Having medical insurance | 247 (84.3) | 409 (70.4) | 2.255 | 1.565–3.248 |
| Poor family conversation | 47 (16.0) | 52 (9.0) | 1.930 | 1.265–2.945 |
| Living alone | 22 (7.5) | 24 (4.1) | 1.867 | 1.028–3.391 |
| Disease course >2 years | 245 (83.6) | 429 (73.8) | 1.808 | 1.261–2.593 |
| Duration of last hospitalization >1 month | 222 (75.8) | 381 (65.6) | 1.641 | 1.195–2.254 |
| No recovery when discharged | 233 (79.5) | 414 (71.3) | 1.566 | 1.120–2.192 |
| Family income <5,000 RMB | 220 (75.1) | 395 (68.0) | 1.559 | 1.100–2.211 |
| No return visit after discharge | 75 (25.6) | 108 (18.6) | 1.504 | 1.075–2.104 |
| Secondary hospital | 85 (29.0) | 128 (22.0) | 1.446 | 1.051–1.991 |
| Unmarried | 195 (66.6) | 340 (58.5) | 1.425 | 1.062–1.912 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Discussion
Schizophrenia is a chronic cycling disorder with multiple relapses. In this study, we investigated relapse of schizophrenia in the year after discharge and possible risk factors for relapse in the People’s Republic of China as reported by patients and their caregivers. The results showed about one third of schizophrenic patients relapsed within 1 year after discharge and 18.8% were rehospitalized. A previous study in Turkey21 similarly reported that 33% of patients with schizophrenia relapsed and that 12.1% were rehospitalized during 1 year of follow-up. Another study in Germany22 found that 32.5% of patients suffered an exacerbation in the year following discharge. The results of our study and previous studies by others suggest that the challenge of managing relapse in patients with schizophrenia is similar between the People’s Republic of China and Western countries.
Although relapse is defined as re-emergence of symptoms after a various period of remission in most medical conditions, the absence of a widely accepted consensus definition of relapse in schizophrenia is still noteworthy. In previous observational studies, the 1-year relapse rates in patients with schizophrenia varied from 15.1%23 to 52%23 because of the different criteria used in related studies, such as change in Brief Psychiatric Rating Scale, Positive and Negative Syndrome Scale, and Clinical Global Impression Rating24,25 scores, hospitalization for psychopathology,3,26,25 exacerbation of symptoms,3 deliberate self-injury, aggressive behavior, suicidal/homicidal ideation,26 and withdrawal from study.24 A review27 comparing the potential of various antipsychotics to prevent relapse noted that eleven different criteria were used in 17 studies. A recent review28 conducted a systematic literature search to determine specific criteria used to define relapse, and found 19 different criteria were used in 150 publications and guidelines. The most frequently used criteria were hospitalization (62%), the Positive and Negative Syndrome Scale (20%), and the Clinical Global Impression Rating Scale (18%). The lack of a consensus definition or generally accepted criteria for relapse made related research results less reliable, making it difficult to compare the studies further.
Because of the nature of our telephone interviews with caregivers/patients, it was not possible to undertake a detailed scale-based interview using the Positive and Negative Syndrome Scale, Clinical Global Impression Rating Scale, or Brief Psychiatric Rating Scale to evaluate relapse, so we searched previous studies and screened for other criteria that could be easily implemented for telephone interviewing. Although the most common relapse criterion was hospitalization in most studies, using this alone may underestimate the real relapse rate in the People’s Republic of China due to some patients being unwilling to visit hospital even if their psychotic symptoms become exacerbated. Hence, three further criteria, including change of medication, more frequent hospital visits, and strengthened supervision because of self-harm, aggressive behavior, and/or suicidal or homicidal ideation, were added in our study as proxies for relapse.
In the opinion of the patients and their caregivers, the most important factor for relapse was poor medication adherence. Our results show that nonadherent patients had a relapse rate approximately 2.5-fold higher than in adherent patients. Nonadherence increased the risk of relapse by 4.602 times the rate seen in adherent patients. This result is similar to previous studies15,29 in which nonadherence greatly increased the risk of exacerbation and rehospitalization. Further, we found another 14 risk factors associating with relapse, which mainly focused on psychosocial aspects and medical history. Lack of psychosocial support, such as being unemployed, having a poor family environment, being socially isolated, and poor self-care ability, a complicated disease history, such as more episodes and longer durations of hospitalization, a course of schizophrenia lasting more than 2 years, and not recovered at discharge also increased the risk of relapse. Unlike the results of some previous studies,12,30,31 we did not find a smoking/drinking history to be associated with relapse.
Nonadherence is prevalent in patients with schizophrenia. One report32 suggested that 20%–56% of patients with schizophrenia were not adherent to their prescriptions. In our study, the nonadherence rate was 37.9%, and another study showed that only a minority of patients with schizophrenia adhere to their medication in the first 2 months after discharge from first hospitalization in Finland.33 Because neither Finland nor the People’s Republic of China have compulsory outpatient treatment, all patients discharged from hospital were prescribed antipsychotic medication with the assumption that they and their caregivers would treat the disease appropriately. However, adherence is not necessarily better in patients with caregivers because family members may oppose treatment with medication.34 Poor adherence can result from multiple factors, encompassing the illness, medication, services, clinicians, patients, and caregivers these six domains.35 A negative attitude toward medication, poor insight, substance abuse, poor family and social support, and adverse effects have an impact on adherence.36 In our study, almost 30% of respondents had a negative attitude toward their medication, which was the most important reason for nonadherence. More than 50% of nonadherent patients thought that there was no need to take drugs at all or for a long time. Therefore, it is necessary to strengthen the education available for patients and families to improve adherence.
This was a large retrospective observational study evaluating relapse and related risk factors in Chinese patients with schizophrenia. Most of the previous related studies in the People’s Republic of China were single-center and small sized. Our study contributes further information in this field, but some limitations are acknowledged. We interviewed enrolled subjects by telephone. A degree of memory bias is possible since we asked subjects to remember events dating a year back. False information that respondents provided in a perfunctory manner, and missing information when respondents refused to answer certain questions are inevitable when using a telephone interview and may cause information bias. Furthermore, our findings regarding relapse, adherence, and other factors were less reliable because they were assessed based on respondents’ subjective reports rather than using an objective measurement tool.
In conclusion, there is a high relapse rate in the Chinese outpatient population with schizophrenia. The strongest factor associated with relapse is poor medication adherence, which is mainly due to a negative attitude toward medication. Lack of psychosocial support and a complicated disease history also increase the risk of relapse.
Acknowledgments
This study was supported by grant from the Beijing Municipal Commission of Science and Technology Clinical Application Special Fund (Z121107001012039). We acknowledge the substantial contribution and cooperation of the other nine hospitals involved in this study. Many thanks to Ligang Zhang, Xiaozhi Wang, Fengchun Wu, Yongqiao Liu, Zhanmin Wang, Wenbin Ma, Ying Qiao, Hesheng Wang, and Junyan Zhu, who were the principal investigators at these hospitals.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.de Sena EP, Santos-Jesus R, Miranda-Scippa A, et al. Relapse in patients with schizophrenia: a comparison between risperidone and haloperidol. Rev Bras Psiquiatr. 2003;25(4):220–223. doi: 10.1590/s1516-44462003000400007. [DOI] [PubMed] [Google Scholar]
- 2.Hong J, Windmeijer F, Novick D, Haro JM, Brown J. The cost of relapse in patients with schizophrenia in the European SOHO (Schizophrenia Outpatient Health Outcomes) study. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(5):835–841. doi: 10.1016/j.pnpbp.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Schennach R, Obermeier M, Meyer S, et al. Predictors of relapse in the year after hospital discharge among patients with schizophrenia. Psychiatr Serv. 2012;63(1):87–90. doi: 10.1176/appi.ps.201100084. [DOI] [PubMed] [Google Scholar]
- 4.Chen EY, Hui CL, Dunn EL, et al. A prospective 3-year longitudinal study of cognitive predictors of relapse in first-episode schizophrenic patients. Schizophr Res. 2005;77(1):99–104. doi: 10.1016/j.schres.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 5.Ohmori T, Ito K, Abekawa T, Koyama T. Psychotic relapse and maintenance therapy in paranoid schizophrenia: a 15 year follow up. Eur Arch Psychiatry Clin Neurosci. 1999;249(2):73–78. doi: 10.1007/s004060050069. [DOI] [PubMed] [Google Scholar]
- 6.Kapur S, Mamo D. Half a century of antipsychotics and still a central role for dopamine D2 receptors. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(7):1081–1090. doi: 10.1016/j.pnpbp.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–962. doi: 10.1016/S0140-6736(13)60733-3. [DOI] [PubMed] [Google Scholar]
- 8.Ayuso-Gutiérrez JL, del Río Vega JM. Factors influencing relapse in the long-term course of schizophrenia. Schizophr Res. 1997;28(2–3):199–206. doi: 10.1016/s0920-9964(97)00131-x. [DOI] [PubMed] [Google Scholar]
- 9.Hunt GE, Bergen J, Bashir M. Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophr Res. 2002;54(3):253–264. doi: 10.1016/s0920-9964(01)00261-4. [DOI] [PubMed] [Google Scholar]
- 10.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998;55(6):547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- 11.Chabungbam G, Avasthi A, Sharan P. Sociodemographic and clinical factors associated with relapse in schizophrenia. Psychiatry Clin Neurosci. 2007;61(6):587–593. doi: 10.1111/j.1440-1819.2007.01722.x. [DOI] [PubMed] [Google Scholar]
- 12.Alvarez-Jimenez M, Priede A, Hetrick SE, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012;139(1–3):116–128. doi: 10.1016/j.schres.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67(3):453–460. doi: 10.4088/jcp.v67n0317. [DOI] [PubMed] [Google Scholar]
- 14.Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2–3):109–113. doi: 10.1016/j.psychres.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Robinson D, Woerner MG, Alvir JM, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56(3):241–247. doi: 10.1001/archpsyc.56.3.241. [DOI] [PubMed] [Google Scholar]
- 16.Takeuchi H, Suzuki T, Uchida H, Watanabe K, Mimura M. Antipsychotic treatment for schizophrenia in the maintenance phase: a systematic review of the guidelines and algorithms. Schizophr Res. 2012;134(2–3):219–225. doi: 10.1016/j.schres.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 17.Naber D, Lambert M. The CATIE and CUtLASS studies in schizophrenia: results and implications for clinicians. CNS Drugs. 2009;23(8):649–659. doi: 10.2165/00023210-200923080-00002. [DOI] [PubMed] [Google Scholar]
- 18.Gleeson JF, Alvarez-Jimenez M, Cotton SM, Parker AG, Hetrick S. A systematic review of relapse measurement in randomized controlled trials of relapse prevention in first-episode psychosis. Schizophr Res. 2010;119(1–3):79–88. doi: 10.1016/j.schres.2010.02.1073. [DOI] [PubMed] [Google Scholar]
- 19.Acosta FJ, Hernandez JL, Pereira J, Herrera J, Rodríguez CJ. Medication adherence in schizophrenia. World J Psychiatry. 2012;2(5):74–82. doi: 10.5498/wjp.v2.i5.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi: 10.1186/1471-244X-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uçok A, Polat A, Cakir S, Genç A. One year outcome in first episode schizophrenia. predictors of relapse. Eur Arch Psychiatry Clin Neurosci. 2006;256(1):37–43. doi: 10.1007/s00406-005-0598-2. [DOI] [PubMed] [Google Scholar]
- 22.Bachmann S, Bottmer C, Schroder J. One-year outcome and its prediction in first-episode schizophrenia – a naturalistic study. Psychopathology. 2008;41(2):115–123. doi: 10.1159/000112027. [DOI] [PubMed] [Google Scholar]
- 23.Ciudad A, San L, Bernardo M, et al. Relapse and therapeutic interventions in a 1-year observational cohort study of nonadherent outpatients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2012;36(2):245–250. doi: 10.1016/j.pnpbp.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 24.Arato M, O’Connor R, Meltzer HY, ZEUS Study Group A 1-year, double-blind, placebo-controlled trial of ziprasidone 40, 80 and 160 mg/day in chronic schizophrenia: the Ziprasidone Extended Use in Schizophrenia (ZEUS) study. Int Clin Psychopharmacol. 2002;17(5):207–215. doi: 10.1097/00004850-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Crespo-Facorro B, Perez-Iglesias R, Mata I, et al. Relapse prevention and remission attainment in first-episode non-affective psychosis. A randomized, controlled 1-year follow-up comparison of haloperidol, risperidone and olanzapine. J Psychiatr Res. 2011;45(6):763–769. doi: 10.1016/j.jpsychires.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. doi: 10.1016/j.schres.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 27.Leucht S, Barnes TR, Kissling W, Engel RR, Correll C, Kane JM. Relapse prevention in schizophrenia with new-generation antipsychotics: a systematic review and exploratory meta-analysis of randomized, controlled trials. Am J Psychiatry. 2003;160(7):1209–1222. doi: 10.1176/appi.ajp.160.7.1209. [DOI] [PubMed] [Google Scholar]
- 28.Olivares JM, Sermon J, Hemels M, Schreiner A. Definitions and drivers of relapse in patients with schizophrenia: a systematic literature review. Ann Gen Psychiatry. 2013;12(1):32. doi: 10.1186/1744-859X-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert PL, Harris MJ, McAdams LA, Jeste DV. Neuroleptic withdrawal in schizophrenic patients. A review of the literature. Arch Gen Psychiatry. 1995;52(3):173–188. doi: 10.1001/archpsyc.1995.03950150005001. [DOI] [PubMed] [Google Scholar]
- 30.Sariah AE, Outwater AH, Malima KI. Risk and protective factors for relapse among individuals with schizophrenia: a qualitative study in Dar es Salaam, Tanzania. BMC Psychiatry. 2014;14:240. doi: 10.1186/s12888-014-0240-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.San L, Bernardo M, Gómez A, Peña M. Factors associated with relapse in patients with schizophrenia. Int J Psychiatry Clin Pract. 2013;17(1):2–9. doi: 10.3109/13651501.2012.687452. [DOI] [PubMed] [Google Scholar]
- 32.Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. doi: 10.4088/jcp.v63n1007. [DOI] [PubMed] [Google Scholar]
- 33.Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–609. doi: 10.1176/appi.ajp.2011.10081224. [DOI] [PubMed] [Google Scholar]
- 34.Shuler KM. Approaches to improve adherence to pharmacotherapy in patients with schizophrenia. Patient Prefer Adherence. 2014;8:701–714. doi: 10.2147/PPA.S59371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62. doi: 10.2147/PROM.S42735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Haan L, van Amelsvoort T, Dingemans P, Linszen D. Risk factors for medication non-adherence in patients with first episode schizophrenia and related disorders; a prospective five year follow-up. Pharmacopsychiatry. 2007;40(6):264–268. doi: 10.1055/s-2007-992141. [DOI] [PubMed] [Google Scholar]


