Abstract
Importance
To report the clinical and histopathologic findings of ocular adnexal angiolymphoid hyperplasia with eosinophilia (ALHE), an unusual but often misdiagnosed benign disorder.
Observations
The ophthalmologic findings of ALHE with ocular adnexal involvement are variable and include eyelid swelling, ptosis, proptosis, and loss of vision. Imaging studies typically demonstrate a well-circumscribed mass in the orbit. The condition may resemble other diseases involving the orbit and ocular adnexal tissue such as lymphoma, hemangioma, sarcoidosis, and dermoid cyst. The histopathology reveals marked vascular proliferation with an accompanying inflammation composed of numerous eosinophils, lymphocytes, and plasma cells.
Conclusions
ALHE is a rare disease that can affect the ocular adnexal tissue. The clinical presentation is often nonspecific; therefore, histopathologic studies are essential for diagnosis and subsequent management of this benign condition.
Introduction
Angiolymphoid hyperplasia with eosinophilia (ALHE) is a rare benign disorder characterized by marked vascular proliferation and inflammation. The usual sites of involvement are the subcutaneous tissues of the head and neck. Involvement of the ocular adnexa including the orbits has also been reported in the literature.1,2 When ALHE involves the ocular adnexa or orbit, the presenting signs, symptoms, and radiological findings are commonly nonspecific; therefore, histological evaluation is essential in making the diagnosis. We report the clinical and histopathological findings in five cases of ocular adnexal ALHE that presented to us in a twenty-year period. Thirty six cases of ALHE in twenty one reports with orbital and ocular adnexal involvement have been reported previously in the literature. The current report is the largest case series reported in the literature.
Report of cases
There were five patients with ALHE diagnosed at a mean age of 38 years (median 31 years, range 11–86 years) involving 3 male patients and 2 females. The clinical and histopathological characteristics of the patients are summarized in table 1. In all five cases ALHE presented unilaterally, and all patients had eyelid swelling. Four cases had orbital involvement with the imaging studies revealing an intraorbital mass (cases 1, 3, and 4) or enlargement of the lacrimal gland (case 2). All of the patients with orbital involvement presented with ptosis and eyelid swelling. Furthermore, all of the patients with orbital involvement were initially clinically misdiagnosed by the referring ophthalmologist; in two patients lymphoma was suspected and in another two the initial clinical impression was sarcoidosis. The two patients who were suspected of having sarcoidosis were younger and had mildly elevated serum angiotensin-converting-enzyme (ACE). Only one patient was suspected to have ALHE before histopathological evaluation (case 5); this patient had a previous history of multiple scalp lesions consistent with ALHE. All of the patients with orbital involvement underwent incisional biopsy and one case was started on oral steroids (case 1) as well. The case with eyelid involvement underwent total excisional biopsy. The histopathological findings in all cases include proliferation of the small capillaries as well as arterioles and venules. The endothelial cells lining the vessels are histiocyte-like and demonstrate intracytoplasmic vacuolization. Furthermore, all cases show lymphoplasmacytic inflammation with the presence of numerous eosinophils. True lymph follicles with well-differentiated germinal centers were either absent (case 1&4) or were present in very few numbers (case 2, 3, and 5). The patients were followed up for 3 months to 6 years following the initial biopsy. In four out of five cases no recurrence was noted during any of the follow-up visits.
Table 1.
Clinical Features of 5 patients with ALHE
| Case/Sex/ Age, y/Race |
Symptoms/Duration/ Side of involvement |
Visual acuity* |
Pertinent ophthalmic exam findings* |
Radiologic/laboratory findings |
Suspected diagnosis |
Intervention (s) | Histopathology findings* |
Follow-up examination |
|---|---|---|---|---|---|---|---|---|
| 1/F/12/H | Upper eyelid ptosis and swelling/Six months/Right | 20/20 | Upper lid ptosis, inferior globe displacement, 5mm proptosis | CT: left lacrimal gland swelling and proptosis Lab: elevated serum ACE levels |
Sarcoidosis | Oral steroids, Incisional biopsy | Fibrovascular tissue infiltrated with eosinophils, lymphocytes and plasma cells | Persistent lesion at 3- month follow- up |
| 2/F/11/H | Intermittent periorbital swelling and redness/One year/Left | 20/25 | 1.5 mm proptosis with normal motility, ptosis, palpable lacrimal gland mass | MRI: diffuse enlargement of the left lacrimal gland Lab: mildly elevated ACE levels but normal pulmonary evaluation |
Sarcoidosis | Incisional biopsy | Fibrovascular tissue with numerous eosinophils and lymphoid follicles surrounding blood vessels-- rare follicles | No recurrence at 1-year follow-up |
| 3/M/31/W | Ptosis/One month/Right | 20/50 | −3 restriction in all fields of gaze, ptosis | CT: well circumscribed extraconal mass measuring 40 × 24 × 23 mm | Lymphoma | Incisional biopsy | Fibrovascular tissue with sporadic lymphoid follicles infiltrated with numerous eosinophils, lymphocytes, and plasma cell--rare follicles | No recurrence at 6-year follow-up |
| 4/M/86/W | Upper lid ptosis/Three years/Left | 20/40 | Upgaze restriction, ptosis, palpable well circumscribed mass | CT: well circumscribed anterior orbital mass | Lymphoma Metastasis Hemangioma Cyst | Incisional biopsy | Proliferation of small and medium blood vessels and foci of inflammatory cells compose of lymphocytes and eosinophils | No recurrence at 5-year follow-up |
| 5/M/50/B | Left upper and lower lid lesions/Six years/left | NA | Upper and lower eyelid lesions, ptosis | Not performed | ALHE | Excisional biopsy | Vascular hyperplasia with plumped endothelial cells and numerous eosinophils, lymphocytes and plasma cells--rare follicles | No recurrence at 1-year follow-up |
The visual acuity and ophthalmic exam finding are reported for the involved side only. The vascular endothelium in all cases demonstrated atypia (histiocytes-like with intracytoplasmic vacuoles)
W: White
H: Hispanic
B: Black
NA: Not available
Comments
ALHE is a benign condition seen more commonly in non-Asian races and there is a female preponderance.2 The clinical presentation is variable and the definitive diagnosis requires histopathological examination. The histology typically demonstrates a well-circumscribed lesion composed of vascular proliferation and inflammation. The vascular component is characterized by proliferation of capillaries, arterioles, and venules; the inflammation is usually lymphoplasmacytic with numerous eosinophils present.2 ALHE is distinguishable from Kimura’s disease (KD), a closely related condition that shares many of the clinical and histological features of the ALHE.2 In ALHE proliferating arterioles and venules in addition to the proliferating capillaries are often seen; furthermore, the vascular endothelium in ALHE frequently demonstrates atypia3 and intracytoplasmic vacuoles.2 This is in contrast to the vascular proliferation in Kimura’s disease where mostly a proliferation of the capillaries is seen and the endothelial cells do not demonstrate atypia. Other histological features of ALHE that help to distinguish it from Kimura’s disease are relative paucity of follicles and fibrosis.2
The exact pathogenesis of ALHE remains unknown; however, it has been proposed that ALHE may represent a benign proliferation of the endothelial cells in response to trauma or inflammation.3 Treatment consists primarily of surgical excision or debulking.1 Other forms of treatment include irradiation, oral and intralesional steroids, and cytotoxic agents.2 Since most lesions regress spontaneously, it is reasonable to observe the lesion waiting for spontaneous regression following an incisional biopsy. This may be the preferred approach in areas where extensive resections may be disfiguring. Recurrence may occur after incomplete excision.3
The cases presented here share the histological features unique to ALHE including proliferation of arterioles and venules, nuclear atypia of the vascular endothelium, and paucity of follicles. The clinical picture was variable. Ptosis was the most common sign and it was seen in four cases. Two of the patients were in their adolescent years; in contrast to the typical presentation in middle-aged patients. Preoperatively, patients were believed to have lymphoma, hemangioma, or lacrimal gland involvement from sarcoidosis. Two of the younger patients in our series had mildly elevated serum ACE levels; one patient had further pulmonary workup, which proved to be normal. On biopsy no histological evidence of granulomatous inflammation suggestive of sarcoidosis was seen in any of the patients and all of the findings were consistent with ALHE. In general elevated serum ACE levels may be present in younger patients even in the absence of granulomatous disease.4 Case 5 was presented as an ophthalmic image in the literature but not discussed in detail.5
In conclusion, ALHE is a rare orbital and ocular adnexal disease that presents with a variety of nonspecific symptoms such as blurred vision, proptosis, diplopia, and lid swelling. A definitive diagnosis of ALHE can only be made by histopathology; therefore, microscopic evaluation of the biopsied specimens is essential for definitive diagnosis and proper management.
Figure 1. Clinical presentation of the 5 patients with ALHE.
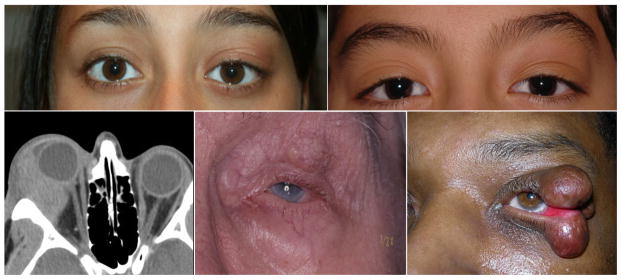
The clinical photographs and radiologic finding in patients with orbital ALHE are demonstrated. The photographs show anterior orbital mass involving the left side with mild swelling and ptosis in case 1(A), case 2(B), case 4(D), and case 5 (E). The computed tomography scan in case 3(C) shows an extraconal mass in the right orbit. In case 5(E) there is marked involvement of the upper and lower eyelids.
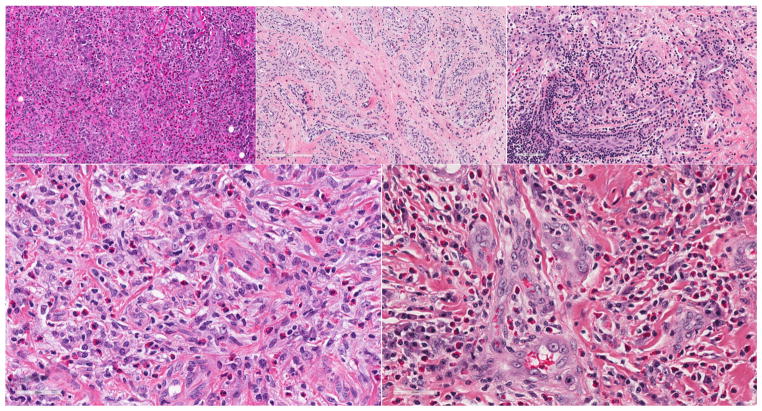
Figure 2. Histopathological studies of ALHE cases.
Histological examination with hematoxylin and eosin stain demonstrates vascular proliferation involving the capillaries, arterioles, and venules in cases 1–5(A–E). The endothelial cells lining the vessels are histiocyte-like and contain intracytoplasmic vacuoles which are depicted with arrows in Case 4(D) and Case 5(E), but were present in all cases. There is an accompanying inflammation marked by large number of eosinophils admixed with lymphocytes and plasma cells in all cases (A–E).
Acknowledgments
We thank Vicky Rogness for her assistance with this project. Amir A. Azari and Mozhgan R. Kanavi had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This work was supported by the National Institutes of Health grant P30-EY016665 (Core Grant for Vision Research) and an unrestricted department award from the Research to Prevent Blindness.
References
- 1.Cunniffe G, Alonso T, Dinares C, Medina FJ, Medel R. Angiolymphoid hyperplasia with eosinophilia of the eyelid and orbit: the Western cousin of Kimura’s disease? Int Ophthalmol. 2013 Mar 5; doi: 10.1007/s10792-013-9741-7. [DOI] [PubMed] [Google Scholar]
- 2.Buggage RR, Spraul CW, Wojno TH, Grossniklaus HE. Kimura disease of the orbit and ocular adnexa. Survey of ophthalmology. 1999 Jul-Aug;44(1):79–91. doi: 10.1016/s0039-6257(99)00064-8. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez-Acosta A, Moreno-Arredondo D, Rubio-Solornio RI, Rodriguez-Martinez HA, Rodriguez-Reyes AA. Angiolymphoid hyperplasia with eosinophilia of the lacrimal gland: a case report. Orbit. 2008;27(3):195–198. doi: 10.1080/01676830701804099. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez GE, Shin BC, Abernathy RS, Kendig EL., Jr Serum angiotensin-converting enzyme activity in normal children and in those with sarcoidosis. The Journal of pediatrics. 1981 Jul;99(1):68–72. doi: 10.1016/s0022-3476(81)80959-6. [DOI] [PubMed] [Google Scholar]
- 5.Thompson MJ, Whitehead J, Gunkel JL, Kulkarni AD. Angiolymphoid hyperplasia with eosinophilia affecting the eyelids. Archives of ophthalmology. 2007 Jul;125(7):987. doi: 10.1001/archopht.125.7.987. [DOI] [PubMed] [Google Scholar]