Abstract
Background
Although depressive symptoms during pregnancy have been related to negative maternal and child health outcomes such as preterm birth, low birthweight infants, postpartum depression and maladaptive mother-infant interactions, studies on the impact of neighborhood environment on depressive symptoms in pregnant women are limited. Pregnant women residing in disadvantaged neighborhoods reported higher levels of depressive symptoms and lower levels of social support. No researchers have examined the relationship between neighborhood environment and avoidance coping in pregnant women. Guided by the Ecological model and Lazarus and Folkman’s transactional model of stress and coping, we examined whether social support and avoidance coping mediated associations between the neighborhood environment and depressive symptoms in pregnant African American women.
Methods
Pregnant African American women (N = 95) from a medical center in Chicago completed the instruments twice during pregnancy between 15-25 weeks and 25-37 weeks. The self-administered instruments measured perceived neighborhood environment, social support, avoidance coping, and depressive symptoms using items from existing scales. Objective measures of the neighborhood environment were derived using geographic information systems.
Findings
Perceived neighborhood environment, social support, avoidance coping and depressive symptoms were significantly correlated in the expected directions. Objective physical disorder and crime were negatively related to social support. Social support at time one (20 ± 2.6 weeks) mediated associations between the perceived neighborhood environment at time one and depressive symptoms at time two (29 ± 2.7 weeks). An increase in avoidance coping between time one and time two also mediated the effects of perceived neighborhood environment at time one on depressive symptoms at time two.
Conclusion
Pregnant African American women’s negative perceptions of their neighborhoods in the second trimester were related to higher levels of depressive symptoms in the third trimester. If these results are replicable in prospective studies with larger sample sizes, intervention strategies could be implemented at the individual level to support pregnant women in their ability to cope with adverse neighborhood conditions and ultimately improve their mental health.
Depressive symptoms are a common occurrence during pregnancy, ranging from 6% to 38% in individual studies (Field, 2011; Ko, Farr, Dietz, & Robbins, 2012; Meltzer-Brody et al., 2013; Records & Rice, 2007). In a meta-analysis, Gavin and associates (Gavin et al., 2005) found that the prevalence of depression is 11.0% in the first trimester and 8.5% in the second and third trimesters. Compared with pregnant non-Hispanic White women, pregnant African American women have higher rates of depressive symptoms (Holzman et al., 2006; Mustillo et al., 2004). Importantly, pregnant women with high levels of depressive symptoms have a higher risk of negative birth outcomes such as preterm birth and low birthweight infants, postpartum depression, and maladaptive mother-infant interactions (Davalos, Yadon, & Tregellas, 2012; Dunkel Schetter, 2011; Dunkel Schetter & Tanner, 2012; Field, 2011; Field et al., 2004; Meltzer-Brody et al., 2013; Witt et al., 2011). A recent meta-analysis found that women with depression were more likely to have preterm birth (RR=1.24, 95%CI: 1.04-1.47) and low birthweight infants (RR=1.34, 95%CI: 1.10-1.64) (Grote et al., 2010). The risk factors for experiencing depressive symptoms during pregnancy include young maternal age, low socioeconomic status, history of infertility, and complicated pregnancies (Field, 2011; Holzman et al., 2006; Ko et al., 2012; Monti, Agostini, Fagandini, La Sala, & Blickstein, 2009; Toffol, Koponen, & Partonen, 2013). However, depressive symptoms experienced during pregnancy may not be solely attributable to these individual-level risk factors.
Little is known about the impact of neighborhood characteristics on depressive symptoms in pregnant women. Neighborhood disorder, defined as “visible cues indicating a lack of order and social control” (Ross & Mirowsky, 2001, p. 413) in the community, can be both physical (e.g., vacant housing, vandalism) and social (e.g., drug dealing, prostitution) (Ross & Mirowsky, 2001; Skogan, 1990). Pregnant women living in neighborhoods with more property damage and higher vacancy rates (Messer, Maxson, & Miranda, 2012), and reporting higher levels of neighborhood violence (Patterson, Seravalli, Hanlon, & Nelson, 2012) also had higher levels of depressive symptoms. Compared with pregnant non-Hispanic White women, pregnant African American women are more likely to live in neighborhoods with vacant buildings and violent crime (Laraia et al., 2006; Messer, Kaufman, Dole, Herring, & Laraia, 2006). Therefore, neighborhood disorder and violent crime may increase the risk of African American women experiencing depressive symptoms during pregnancy. We did not find any published study that examined the effects of both “objective”, using administrative data, and perceived measures of the neighborhood disorder or crime on depressive symptoms in pregnant women. Also, none of the studies examined the effects of neighborhood disorder or crime early in pregnancy on depressive symptoms that occur later in pregnancy.
The pathways by which the disadvantaged neighborhood environment affects depressive symptoms in pregnant women are not known. Yet, this understanding is important in order to identify additional potential targets for intervention. One potential pathway is through effects of social support and avoidance coping. Pregnant women residing in neighborhoods with more property damage, vacant housing, and violent crime also reported lower levels of social support (Messer et al., 2012). No researchers have examined the relationship between neighborhood environment and avoidance coping in pregnant women. Lack of social support and use of avoidance coping have been related to higher levels of depressive symptoms in a study of pregnant minority women (Rudnicki, Graham, Habboushe, & Ross, 2001). The potential role of social support and avoidance coping as mediators of the effects of neighborhood disorder or crime on depressive symptoms in pregnant women has not been examined.
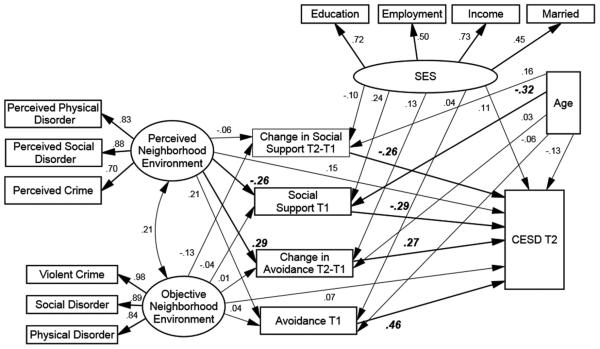
This study was guided by an integration of the Ecological model (Bronfenbrenner, 1986) and Lazarus and Folkman’s transactional model of stress and coping (Lazarus & Folkman, 1984). According to the Ecological model, health outcomes are influenced by personal and environmental factors. We postulate that pregnant women’s depressive symptoms are influenced by personal factors such as social support and avoidance coping, and environmental factors such as neighborhood disorder and crime. Lazarus and Folkman’s transactional model of stress and coping (Lazarus & Folkman, 1984) states that psychological stress occurs when the environment is appraised as taxing or exceeding the person’s resources and endangering personal well-being. The environment, or social demands placed on an individual, may act as an antecedent factors, and social support and coping as mediators. In our model, the neighborhood environment is an antecedent factor; social support and avoidance coping are mediators; and depressive symptoms represent the short-term outcome (Figure 1). We postulate that pregnant women residing in disadvantaged neighborhoods have fewer support persons available to them, use avoidance coping more often and, in turn, have higher levels of depressive symptoms. The purpose of this study was to examine whether social support and avoidance coping mediate the effects of the disadvantaged neighborhood environment on depressive symptoms in pregnant African American women in order to identify potential targets for intervention. It was hypothesized that:
Neighborhood disorder and crime have a direct, positive effect on depressive symptoms;
Social support has a direct, negative effect on depressive symptoms while avoidance coping has a direct, positive effect on depressive symptoms; and
Social support and avoidance coping mediate the effects of neighborhood disorder and crime on depressive symptoms.
Figure 1.
Structural equation model results showing standardized path coefficients and factor loadings [χ2(78) = 97.56, p = .07, CFI = .97, RMSEA = .05] . Significant path coefficients (p < .05) are in bold. Change in Avoidance (the difference between T2 and T1) mediated the effect of Perceived Environment on CES-D T2 controlling for socioeconomic status (SES) and age (p = .02). The specific indirect effect involving Social Support T1 was significant at p = .053. Residual error terms and correlations among residuals were excluded from the figure for clarity; CES-D = Center of Epidemiological Studies Depression Scale.
Methods
Design and Sample
This study used a prospective design. Self-identified African American women from a medical center in Chicago were enrolled in the study between 2009 and 2011 if they (a) were at least 18 years of age; (b) had singleton medically low-risk pregnancy; and (c) were in the second trimester of pregnancy. Women were excluded if they had a medical diagnosis (e.g., hypertensive disorders, pre-gestational diabetes) or obstetrical complications (incompetent cervix, fetal abnormality, multiple pregnancies) as these factors may pose as stressors. One hundred and twenty women were approached to participate in the study. Six women declined participation due to time restrains. Of the 114 women who signed an informed consent, six women did not mail the questionnaires or the questionnaires were lost in the mail. One woman refused participation after signing the informed consent. At the first data collection, 107 women completed questionnaires. At the second data collection, three women did not attend prenatal visits, three changed prenatal care from the participating clinical site, two had termination of pregnancy, one declined to participate due to time restraints, and three had already delivered. Thus, 95 women had complete data available for analysis at both data collection points. The latent variable structural equation modeling analyses used the 95 complete cases. There were no differences in age, gestational age at data collection, marital status, education, income, employment or depressive symptoms at the first data collection between women who completed the questionnaires at the second data collection (N=95) and women who did not complete the questionnaires at the second data collection (N=12).
Procedures
The study was approved by the Institutional Review Board at the University of Illinois at Chicago. The principal investigator obtained a waiver to access medical records of women receiving prenatal care at the participating site in order to identify those who fit the inclusion-exclusion criteria. Potential participants were first contacted by the health care provider. The principal investigator or research assistants met face-to-face with women before or after their prenatal visit, explained the study and invited them to participate. Women provided written informed consent prior to participating in the study. The majority of participants completed the packet of questionnaires in a private room in the clinic. Twelve women completed the questionnaires at home and mailed them. Women received $25 reimbursement for each data collection points ($50 total).
Variables and Instruments
Maternal characteristics
Self-reported maternal sociodemographic characteristics included: maternal age, marital status, education, and income. Medical and obstetrical characteristics (e.g., gestational age at time of data collection, medical history) were collected from medical records.
The neighborhood environment
Physical disorder, social disorder, and crime were assessed using objective and perceived measures. For the objective measures, we first obtained participants’ home addresses and used ArcGIS 9.1 (Redlands, CA) to geocode these addresses and obtain the corresponding 2010 census block group. Three women moved during the study; we used the address at the first data collection point to derive their neighborhood measures. Neighborhood was defined as a 0.5-mile circular buffer around the home address.
Objective physical disorder was measured using two indicators: (a) proportion of vacant housing based on 2010 Census data and (b) annual number of vandalism incidents based on the Chicago Police Department crime summary data from August 1, 2010 to July 31, 2011 (Chicago Police Department, n.d.). Vacant housing was derived based on the mean of census block groups intersecting the neighborhood. The Chicago Police Department data reflect the annual number of incidents where police responded and completed case reports in the neighborhood. Because these measures are on different scales, z-scores were calculated for the two indicators, and the mean of the z-scores was used in the analysis.
Objective social disorder was measured as the annual number of prostitution- and drug-related incidents in the neighborhood. This was calculated using the Chicago Police Department crime summary data from August 1, 2010 to July 31, 2011 (Chicago Police Department, n.d.).
Objective violent crime was measured as the annual number of incidents of homicide, sexual assault, aggravated assault, and aggravated battery in the neighborhood. We again used Chicago Police Department crime summary data from August 1, 2010 to July 31, 2011 (Chicago Police Department, n.d.) to calculate this. These three objective measures were used to define a latent factor, Objective Neighborhood Environment, for the analysis.
Perceived physical disorder was measured using five items about conditions in the neighborhood (houses generally well maintained – reverse coded, heavy car or truck traffic, a lot of vacant lots or vacant houses, streets and sidewalks kept clean of litter and dumping – reverse coded, a lot of loud noise from cars or neighbors) from the Neighborhood Physical Environment Scale (Israel et al., 2006; Schulz, Zenk, Kannan, Israel, & Stokes, 2012). We omitted two items from the original scale (air pollution, contaminated land) that are not typically used as indicators of disorder (Ross & Mirowsky, 1999) and added one item (vandalism) that is part of the Neighborhood Social Environment Scale (Israel et al., 2006), but which is typically included in physical disorder measures (Ross & Mirowsky, 1999). The six items in the adapted scale were rated on a 5-point scale (strongly agree to strongly disagree) and summed for a potential total score range of 6–30, with higher scores representing higher levels of perceived physical disorder. Supporting the construct validity of the adapted scale, perceived physical disorder was positively associated with perceived social disorder (r=0.69) and perceived crime (r=0.67) in a sample of African American women (Giurgescu et al., 2012). In the current study, Cronbach’s alpha was 0.77.
Perceived social disorder was measured using four items about neighborhood conditions (prostitution, gangs, homeless people, drug use/dealing) from the Neighborhood Problems Scale (Elder, Eccles, Ardelt, & Lord, 1995) and two items (people loitering or hanging around, public drinking) adapted from the Perceived Neighborhood Scale (Martinez, Black, & Starr, 2002). All six items were rated on a 3-point scale (not a problem to a big problem) and summed for a potential total score range of 6-18, with higher scores representing a greater degree of neighborhood problems. Supporting the construct validity of the adapted scale, perceived social disorder was positively associated with perceived physical disorder (r=0.69), perceived crime (r=0.59), and objective social disorder (r=0.25) in a sample of African American women (Giurgescu et al., 2012). The Cronbach’s alpha for the current study was 0.90.
Perceived crime in the neighborhood was measured using six items (e.g., not safe to walk in the neighborhood at night; friends and relatives do not visit me at home because they do not feel safe; people are scared of being robbed in my neighborhood, people are scared of being raped in my neighborhood, people are scared of being mugged in my neighborhood, or people are scared of being murdered in my neighborhood) from the perceived crime subscale of the Perceived Neighborhood Scale (Martinez et al., 2002). Three of the items (troublemakers hanging out, public drinking, open drug use/dealing) were omitted because they were included in our perceived social disorder scale. Each of the six items in the adapted scale was rated on a 5-point scale (strongly agree to strongly disagree) and summed for a potential total score range of 6–30, with higher scores representing higher levels of perceived crime (Martinez, 2000; Martinez et al., 2002). Positive correlations between the adapted scale and perceived physical disorder and perceived social disorder in African American women support construct validity (Giurgescu et al., 2012). In the current study, Cronbach’s alpha was 0.90. These three perceived measures were used to define a latent variable, Perceived Neighborhood Environment, for the analysis.
Social support
Social support was measured by the Medical Outcomes Study (MOS) Social Support Survey (Sherbourne & Stewart, 1991). The instrument contains one question related to information about social networks and 19 items on a 5-point scale related to four functional domains: emotional/informational, tangible, affectionate, and positive social interaction. The sum of the 19 items can range from 19–95 with higher scores representing higher levels of social support. The MOS Social Support Survey has good internal consistency in pregnant and postpartum women (Giurgescu et al., 2013; Giurgescu, Penckofer, Maurer, & Bryant, 2006; Giurgescu et al., 2012). In the current study, Cronbach’s alpha was 0.97. A change in social support score was also computed by subtracting first data collection MOS scores from the second data collection MOS scores.
Avoidance coping
Avoidance coping was measured by a 7-item subscale of the the Prenatal Coping Inventory, (Lobel, Yali, Zhu, DeVinvent, & Meyer, 2002; Yali & Lobel, 2002) with each item rated on a 5-point Likert scale (potential range 0-28). Higher scores represent higher use of avoidance coping. In the current study, Cronbach’s alpha was 0.74. A change in avoidance coping was computed by subtracting first data collection scores from the second data collection scores.
Depressive symptoms
Depressive symptoms were measured by the Center for Epidemiologic Studies Depression Scale (CES-D)(Radloff, 1977). This scale assesses the presence of salient symptoms of depression within the past seven days. A customary cutoff score of 16 or higher is used to identify those with elevated (e.g., clinically relevant) levels of depressive symptoms. The CES-D does not provide a diagnosis of clinical depression, but measures the presence of elevated levels of depressive symptoms. In our analysis we used CES-D as continuous variable. In the current study Cronbach’s alpha was 0.87.
Data Management and Analysis
Data were entered, cleaned, and prepared for analysis on an ongoing basis using SPSS 20 (SPSS Inc., Chicago, IL) and Stata 12 (StataCorp., College Station, Texas). Descriptive statistics (mean, standard deviation, frequency distribution) were used to analyze maternal characteristics. Paired sample t-test was used to examine differences in avoidance coping, social support and depressive symptoms from first to second data collection. Pearson r correlation coefficients were used to examine the relationships among neighborhood environment, social support, avoidance coping, and depressive symptoms at both data collection times. Latent variable structural equation modeling (SEM) was used to estimate the extent to which social support and avoidance coping mediated the effects of neighborhood environment on depressive symptoms.
SEM model formulation
The mediation hypothesis was tested within the context of a causal model. The SEM consisted of two latent exogenous factors, Perceived Neighborhood Environment and Objective Neighborhood Environment. These were each defined by three indicators as described above. Social support and avoidance coping and the change in each were modeled as mediators of the relationship between neighborhood environment at the first data collection and depressive symptoms at the second data collection. Marital status, education, employment, and income defined a latent socioeconomic status exogenous covariate; and age was included as a separate exogenous covariate. The model was recursive, i.e., it had no feedback loops, and was fit to the data using ML estimation. The fit of the final model was evaluated using a strategy recommended by Hu and Benter (Hu & Bentler, 1999). Specifically, Hu and Bentler proposed using the standardized root mean squared residual (SRMR) and one additional measure of fit (Hu & Bentler, 1999). Because the root mean square error of approximation (RMSEA) is generally regarded today as one the most informative of fit indexes we selected it to go with SRMR (Byrne, 2013). The recommended cut-off values for this two-index strategy were SRMR ≤ 0.09, and RMSEA ≤ .06 (Hu & Bentler, 1999). In addition, the chisquare goodness of fit statistic was reported.
Results
Maternal Characteristics
The women’s mean age was 24 years. The mean gestational age at first data collection was 20 weeks and the mean gestational age at the second data collection was 29 weeks. The majority of women were multigravida (69%), were single (83%), and were unemployed (52%); almost half the women had some college (41%) and had an annual household income of less than $10,000 (46%). Women, on average, had high levels of social support; moderate levels of perceived disorder and crime; and low levels of avoidance coping and depressive symptoms. At the first data collection, 28% of women had clinically relevant levels of depressive symptoms (score >16 on CES-D), and 25% similarly surpassed this cutoff at the second data collection (see Table 1). Avoidance coping increased over time (8.43 and 9.30, respectively, t(94)=−2.08, p=.040). There were no differences in social support and depressive symptoms between the first and second data collection points (data not shown).
Table 1.
Descriptive statistics for maternal and neighborhood characteristics (N=95)
| Variable | ||
|---|---|---|
|
Mean
(Standard Deviation) |
Range | |
| Age (in years at T1 a) | 23.97 (5.40) | 18-41 |
| Gestational age at T1 (in weeks) | 19.98 (2.55) | 15-25 |
| Gestational age at T2 (in weeks) | 29.04 (2.67) | 25-37 |
| Number (Frequency) | ||
| Gravida | ||
| Multigravida | 65 (68.7%) | |
| Primigravida | 30 (31.6%) | |
| Marital status | ||
| Single | 79 (83.2%) | |
| Married | 16 (16.8%) | |
| Education | ||
| Less than high school | 13 (13.7%) | |
| Graduated high school | 23 (24.2%) | |
| Some college | 39 (41.1%) | |
| Associate degree | 6 (6.3%) | |
| Bachelor degree | 11 (11.6%) | |
| Graduate program | 3 (3.2%) | |
| Employment | ||
| No | 49 (51.6%) | |
| Yes | 46 (48.4%) | |
| Household income | ||
| Less than $10,000 | 44 (46.2%) | |
| $10,001-20,000 | 13 (13.6%) | |
| $20,001-30,000 | 22 (23.5%) | |
| More than $30,001 | 16 (16.7%) | |
|
Mean
(Standard Deviation) |
Range | |
| Objective physical disorderb | −0.059 (0.90) | −1.80-1.81 |
| Housing vacancy rate (%)c | 15.45 (6.46) | 4.2-30.2 |
| Incidents of vandalismc | 201.60 (79.94) | 48-371 |
| Objective social disorder | 337.09 (384.52) | 0-1,694 |
| Incidents of prostitutionc | 23.04 (49.84) | 0-265 |
| Drug-related incidentsc | 371.04 (372.69) | 16-1,687 |
| Objective violent crime | 181.09 (121.99) | 0-487 |
| Incidents of homicidec | 2.99 (2.46) | 0-11 |
| Incidents of criminal sexual assaultc | 8.95 (5.96) | 0-27 |
| Incidents of aggravated assaultc | 30.11 (18.92) | 0-76 |
| Incidents of aggravated batteryc | 63.39 (43.35) | 0-172 |
| Perceived physical disorder | 13.84 (5.64) | 6-29 |
| Perceived social disorder | 9.71 (3.59) | 6-18 |
| Perceived crime | 11.98 (6.07) | 6-27 |
| Social support at T1 | 83.02 (16.98) | 22-95 |
| Social support at T2 | 81.21 (18.08) | 19-95 |
| Avoidance coping at T1 | 8.43 (4.93) | 0-21 |
| Avoidance coping at T2 | 9.30 (5.11) | 0-22 |
| Depressive symptoms at T1 | 12.12 (9.3) | 0-54 |
| Depressive symptoms at T2 | 12.23 (9.38) Number (Frequency) | 0-53 |
| Number (Frequency) | ||
| Clinically depressive symptoms (CES-D≥16)d at T1 | 27 (28.4) | |
| Clinically depressive symptoms (CES-D≥16) at T2 | 24 (25.3) |
T1=first data collection, T2= second data collection
Calculated as the mean of the standardized scores (z scores)
Presented based on raw numbers within half a mile from address
Center for Epidemiological Studies-Depression
Relationships among Neighborhood Environment, Social Support, Avoidance Coping and Depressive Symptoms
The relationships among variables are presented in Table 2.
Table 2.
Relationships among neighborhood environment, social support, avoidance coping, and depressive symptoms (N=95)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Objective physical disorder | — | ||||||||||
| 2. Objective social disorder | .681** | — | |||||||||
| 3. Objective violent crime | .839** | .878** | — | ||||||||
| 4. Perceived physical disorder | .222* | .146 | .227 | — | |||||||
| 5. Perceived social disorder | .179 | .148 | .143 | .717** | — | ||||||
| 6. Perceived crime | .187 | .038 | .120 | .557** | .654** | — | |||||
| 7. Social support T1 a | −.109 | −.095 | −.128 | −.321** | −.288** | −.164 | — | ||||
| 8. Social support T2 | −.242* | −.155 | −.223* | −.389** | −.284** | −.206* | .665** | — | |||
| 9. Avoidance coping T1 | .020 | −.043 | .084 | .133 | .167 | .269** | −.495** | −.416** | — | ||
| 10. Avoidance coping T2 | .060 | .042 | .103 | .314** | .321** | .307** | −.510** | −.494** | .673** | — | |
| 11. Depressive symptoms T1 | .116 | .156 | .175 | .254* | .268** | .282** | −.610** | −.510** | .588** | .616** | — |
| 12. Depressive symptoms T2 | .166 | .171 | .196 | .380** | .324** | .280** | −.464** | −.585** | .526** | .643** | .728** |
p<.05 two-tailed;
p<.01 two-tailed
T1= first data collection; T2= second data collection
Objective and perceived neighborhood environment and depressive symptoms
Perceived physical disorder, perceived social disorder, and perceived crime were positively related to depressive symptoms at both time points. Objective neighborhood environment measures were not related to depressive symptoms.
Social support, avoidance coping and depressive symptoms
Social support was negatively related to depressive symptoms, and avoidance coping was positively related to depressive symptoms at both time points.
Objective and perceived neighborhood environment, social support and avoidance coping
Perceived physical and social disorder were negatively related to social support at both time points and positively related to avoidance coping at the second time point. Perceived crime was negatively related to social support at the second data point and positively related to avoidance coping at both time points. In addition, at the second data collection, objective physical disorder and violent crime were negatively related to social support.
Mediating Effects of Social Support and Avoidance Coping
The model fit well [χ2 (df = 78) = 97.56, p = .07; SRMR = .05; RMSEA =.05], but included several non-significant paths. The fitted model is shown in Figure 1. All paths from the latent factor, Objective Neighborhood Environment, were not significant. In contrast, the Perceived Neighborhood Environment factor had significant direct effects on social support at the first data collection and change in avoidance coping between first and second data collection. The coefficient of determination of the estimated model explained 55.0% of the variation of depressive symptoms.
Social support at the first data collection, and an increase in avoidance coping between the first and second data collection, appeared to mediate the effect of perceived neighborhood environment at the first data collection on depressive symptoms at the second data collection while controlling for socioeconomic status and age. The effect of perceived neighborhood environment on depressive symptoms through social support was 0.07 (= −.26*−.29); the effect of perceived neighborhood environment on depressive symptoms through change in avoidance coping was 0.08 (= .27*.29). Bootstrapped p values for these effects were .053, and .02, respectively. Moreover, the test of joint significance (Mallinckrodt, Abraham, Wei, & Russell, 2006), which uses the simple criteria of significant paths to identify statistically significant mediation, holds here. Thus higher perceived neighborhood environment scores at the first data collection were associated with higher CES-D scores at second data collection and this effect was due to the mediating role of social support at the first data collection and an increase in avoidance coping between first and second data collection. Avoidance coping at first data collection had a direct positive relationship to depressive symptoms at second data collection. An increase in social support between first and data collection had a direct negative relationship to depressive symptoms at the second data collection.
Discussion
Approximately 30% of pregnant African American women in our sample had elevated depressive symptoms. Social support at the first data collection mediated the effects of perceived neighborhood environment at the first data collection on depressive symptoms at the second data collection. Women who had negative perceptions of their neighborhood and lower levels of social support in the second trimester also had higher levels of depressive symptoms in the third trimester. Women who perceive their neighborhoods as disadvantaged may not have the social support necessary to buffer the negative aspects of their neighborhoods (Menjivar, 2000), which could result in higher levels of depressive symptoms. Indeed, lack of social support was associated with higher levels of stress and depressive symptoms for pregnant women (Giurgescu et al., 2006; Rudnicki et al., 2001). We also found that changes in social support between first and second data collection had a direct effect on depressive symptoms for these women. Thus, an increase in social support between second and third trimester of pregnancy resulted in lower levels of depressive symptoms. Offering support during pregnancy by providing the opportunity to talk about their neighborhoods (e.g., perceived neighborhood disorder and crime) might buffer the effects of their perceptions on depressive symptoms and may have a positive effect on their mental health. To our knowledge, this is the first study to examine the importance of social support on mediating the effects of pregnant women’s perceptions of their neighborhoods on depressive symptoms.
Changes in avoidance coping between first and second data collection mediated the effects of perceived neighborhood environment at the first data collection on depressive symptoms at the second data collection. Women who had negative perceptions of their neighborhood in the second trimester and used more avoidance coping between second and third trimester of pregnancy also had higher levels of depressive symptoms in the third trimester. In addition, avoidance coping in the second trimester had a direct effect on depressive symptoms in the third trimester. Women who have negative perceptions of their neighborhoods may use avoidance or denial to cope with their disadvantaged neighborhoods, which could result in higher levels of depressive symptoms. Indeed, avoidance coping has been related to psychological distress and depressive symptoms in other samples of pregnant women (Faisal-Cury, Savoia, & Menezes, 2012; Giurgescu et al., 2006). This is the first study to examine the relationship between neighborhood environment and avoidance coping in pregnant women. The findings point to the role of early identification of ways women cope with living in disadvantaged neighborhoods since use of avoidance coping in the second trimester had a direct effect on risk of depressive symptoms later in pregnancy. Furthermore, offering support to women from disadvantaged neighborhoods may not only decrease their levels of depressive symptoms, but may also decrease the use of avoidance coping during the pregnancy as the findings of the current study and other researchers suggest (Giurgescu et al., 2006).
Perceived physical disorder, perceived social disorder, and perceived crime were positively related to depressive symptoms. This is in line with Patterson and colleagues (2012) who found that pregnant African American women reporting higher levels of neighborhood violence had higher levels of depressive symptoms. Messer and colleagues (2012) found that pregnant women living in neighborhoods with high physical disorder and vacancy rates reported higher levels of depressive symptoms. While perceptions of physical disorder, social disorder, and crime all significantly related to depressive symptoms, objective measures of these same factors did not. Women’s perceptions of neighborhood environment may not correspond with these objective indicators because of discrepancies between how women define their neighborhood and administrative boundaries for which objective data are available. Assessing neighborhood stressors through both administrative data (e.g., census) and woman’s perceptions is a more thorough approach for examining the impact of neighborhood environment on depressive symptoms.
Low income pregnant African American women in our sample had elevated levels of depressive symptoms. These results are supported by other researchers who found that pregnant African American women have scores that are considered clinically relevant for depressive symptoms (Orr, Blazer, & James, 2006). Even in a study of pregnant African American women in which the majority were married (58%), college educated (62%), employed (81%) and had household incomes of more than $51,000 per year (41%), researchers still found that 23% of participants had depressive symptoms (Jackson, Rowley, & Curry Owens, 2012). Together these results suggest that pregnant African American women have higher levels of depressive symptoms regardless of socioeconomic status. Depressive symptoms have been related to negative birth outcomes such as preterm birth and low birthweight infants (Davalos et al., 2012; Dunkel Schetter, 2011), and African American women have higher rates of each (Hamilton, Martin, & Ventura, 2012). Higher levels of depressive symptoms in African American women may be one of the pathways leading to health disparities (i.e., negative birth outcomes) for this population.
Implications for Practice and/or Policy
The women who perceive their neighborhoods as dangerous or disorderly appear to have an elevated risk for depressive symptoms during pregnancy. If these results are replicable in prospective studies with larger sample sizes, intervention strategies could be implemented at the individual level to support women in their ability to cope with adverse neighborhood conditions and ultimately improve their mental health. Improving the mental health of pregnant women by early detection and treatment of depressive symptoms may improve birth outcomes, bolster the psychological well-being of postpartum women, and ultimately enhance infants’ health and development. We found that social support mediated the effects of perceived neighborhood environment on depressive symptoms for women in our sample. Assessing the social support available to pregnant women and developing supportive interventions during their pregnancies may improve women’s mental health. Our finding that women who used more avoidance coping between second and third trimester of pregnancy had higher levels of depressive symptoms in the third trimester suggests that women might benefit from counseling to assist them with identifying and utilizing more effective coping strategies. More resources may be allocated to allow for each prenatal visit to include a thorough assessment for women living in neighborhoods with high disorder and crime. These expanded screening services would require adequate social services and access to mental health treatment to accommodate the number of women who will be identified from these programs.
Data are limited on the relationships between neighborhood environment and depressive symptoms in pregnant women. More research is needed to examine why perceived neighborhood environment appears to be more closely related to depressive symptoms pregnant women experience than objective neighborhood environment. Mixed methods studies should also be employed to explore women’s perceptions of other aspects of their neighborhoods that may increase their levels of depressive symptoms. Community based participatory research is needed to develop interventions that better support individual women during their pregnancies and address neighborhood conditions that can adversely affect their mental health.
Neighborhood effects on health, specifically, pregnancy outcome, have implications for health policy. On a broader scale, health care providers, such as physicians, nurses, and allied health professionals should collaborate with groups to advocate for public policies targeted at improving neighborhood conditions. Collaborations should extend beyond policy makers to include urban planning, public health, sociologists, economic development, and community partners, such as local businesses, churches, and law enforcement agencies.
Limitations
The sample consisted largely of young, single, unemployed African American women. These results cannot be generalized to older African American pregnant women from higher socio-economic status or pregnant women from other racial groups. Every effort was made to contact women for their second data collection. Some women failed to attend prenatal visits or changed their healthcare provider, and we were not able to contact them. Therefore, not all women completed both data collection points. However, there were no significant differences in maternal characteristics between women who did not complete the second data collection and women who completed the second data collection Objective neighborhood measures were collected between 8/1/2010-7/31/2011 and do not cover the pregnancy period for some of the women. Due to the nature of the census and administrative data we were not able to match the objective neighborhood measures exactly to the period of pregnancy of individual women. Women were enrolled from one medical center in Chicago, limiting the variability of the objective neighborhood measures in our study. However, women lived in neighborhoods with similar vacancy rates as Chicago data (14.7% and 15.6%, respectively) which indicates that our sample is likely to be representative of the Chicago population. Even though the sample size is relatively small, the strength of this study is in its prospective design. The results of this study need to be replicated with a larger sample.
Conclusion
The perceived environments of pregnant women have a profound effect on depressive symptoms. Health care providers need to assess women’s perception of their neighborhoods and their influence on women’s mental health and provide strategies to deal with depressive symptoms. Health care providers need to advocate for public policies that improve African American women’s living conditions. By incorporating assessment of perceived neighborhood environment during prenatal care and developing relevant interventions, health care providers may improve the health of women and their infants.
Acknowledgement
The study was funded by the National Institutes of Health, National Institute of Nursing Research R03NR010608. We thank the women who participated in the study. I, Carmen Giurgescu, the Principal Investigator, attest that I have had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carmen Giurgescu, College of Nursing, Wayne State University, Detroit, MI.
Shannon N. Zenk, College of Nursing, University of Illinois at Chicago, Chicago, IL.
Thomas Templin, College of Nursing, Wayne State University, Detroit, MI.
Christopher G. Engeland, Department of Biobehavioral Health and College of Nursing, Pennsylvania State University, University Park, PA.
Barbara L. Dancy, College of Nursing, University of Illinois at Chicago, Chicago, IL.
Chang Park, College of Nursing, University of Illinois at Chicago, Chicago, IL.
Karen Kavanaugh, College of Nursing and Children's Hospital of Michigan, Wayne State University, Detroit, MI.
William Dieber, Director Great Cities Urban Data Visualization Program Lab, College of Urban Planning and Public Affairs, University of Illinois at Chicago, Chicago, IL.
Dawn Misra, Associate Chair for Research, Department of Family Medicine and Public Health Sciences, School of Medicine, Wayne State University, Detroit, MI.
References
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications and programing. Routledge; 2013. [Google Scholar]
- Chicago Police Department. (n.d.) CLEARMAP: Citizen law enforcement analysis and reporting. Retrieved from www.gis.chicagopolice.org. [Google Scholar]
- Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health. 2012;15(1):1–14. doi: 10.1007/s00737-011-0251-1. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder GH, Eccles JS, Ardelt M, Lord S. Inner-city parents under economic pressure - Perspectives on the strategies of parenting. Journal of Marriage and the Family. 1995;57(3):771–784. [Google Scholar]
- Faisal-Cury A, Savoia MG, Menezes PR. Coping style and depressive symptomatology during pregnancy in a private setting sample. Spanish Journal of Psychology. 2012;15(1):295–305. doi: 10.5209/rev_sjop.2012.v15.n1.37336. [DOI] [PubMed] [Google Scholar]
- Field T. Prenatal depression effects on early development: A review. Infant Behavior and Development. 2011;34(1):1–14. doi: 10.1016/j.infbeh.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, Bendell D. Prenatal depression effects on the fetus and the newborn. Infant Behavior and Development. 2004;27:216–229. [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. 5 Pt 1. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Giurgescu C, Kavanaugh K, Norr KF, Dancy BL, Twigg N, McFarlin BL, White-Traut RC. Stressors, resources, and stress responses in pregnant African American women: A mixed-methods pilot study. Journal of Perinatal and Neonatal Nursing. 2013;27(1):81–96. doi: 10.1097/JPN.0b013e31828363c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giurgescu C, Penckofer S, Maurer MC, Bryant FB. Impact of uncertainty, social support, and prenatal coping on the psychological well-being of high-risk pregnant women. Nursing Research. 2006;55(5):356–365. doi: 10.1097/00006199-200609000-00008. [DOI] [PubMed] [Google Scholar]
- Giurgescu C, Zenk SN, Dancy BL, Park CG, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in african american women. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2012;41(6):E51–E61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2011 National Vital Statistics Reports. Vol. 61. National Center for Health Statistics; Hyattsville, MD: 2012. [PubMed] [Google Scholar]
- Holzman C, Eyster J, Tiedje LB, Roman LA, Seagull E, Rahbar MH. A life course perspective on depressive symptoms in mid-pregnancy. Maternal and Child Health Journal. 2006;10(2):127–138. doi: 10.1007/s10995-005-0044-0. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Israel BA, Schulz AJ, Estrada-Martinez L, Zenk SN, Viruell-Fuentes E, Villarruel AM, Stokes C. Engaging urban residents in assessing neighborhood environments and their implications for health. Journal of Urban Health. 2006;83(3):523–539. doi: 10.1007/s11524-006-9053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson FM, Rowley DL, Curry Owens T. Contextualized Stress, Global Stress, and Depression in Well-Educated, Pregnant, African-American Women. Women's Health Issues. 2012;22(3):e329–e336. doi: 10.1016/j.whi.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005-2009. Journal of Women's Health. 2012;21(8):830–836. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia BA, Messer L, Kaufman JS, Dole N, Caughy M, O'Campo P, Savitz DA. Direct observation of neighborhood attributes in an urban area of the US south: Characterizing the social context of pregnancy. International Journal of Health Geography. 2006;5:11. doi: 10.1186/1476-072X-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal and coping. Springer; New York: 1984. [Google Scholar]
- Lobel M, Yali AM, Zhu W, DeVinvent CJ, Meyer BA. Beneficial association between optimistic disposition and emotional distress in high-risk pregnancy. Psychology and Health. 2002;17(1):77–95. [Google Scholar]
- Mallinckrodt B, Abraham WT, Wei M, Russell DW. Advances in testing the statistical significance of mediation effects. Journal of Counseling Psychology. 2006;53(3):372–378. [Google Scholar]
- Martinez ML. Neighborhood context and the development of African American children. Garland Publishing, Inc.; New York: 2000. [Google Scholar]
- Martinez ML, Black M, Starr RH. Factorial structure of the Perceived Neighborhood Scale (PNS): A test of longitudinal invariance. Journal of Community Psychology. 2002;30(1):23–43. [Google Scholar]
- Meltzer-Brody S, Bledsoe-Mansori SE, Johnson N, Killian C, Hamer RM, Jackson C, Thorp J. A prospective study of perinatal depression and trauma history in pregnant minority adolescents. American Journal of Obstetrics and Gynecology. 2013;208(3):211e211–211e217. doi: 10.1016/j.ajog.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menjivar C. Fragmented Ties: Salvadoran Immigrant Networks in America. Berkeley, CA: 2000. [Google Scholar]
- Messer LC, Kaufman JS, Dole N, Herring A, Laraia BA. Violent crime exposure classification and adverse birth outcomes: A geographically-defined cohort study. International Journal of Health Geography. 2006;5:22. doi: 10.1186/1476-072X-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Maxson P, Miranda ML. The urban built environment and associations with women's psychosocial health. Journal of Urban Health. 2012;90(5):857–871. doi: 10.1007/s11524-012-9743-1. doi: 10.1007/s11524-012-9743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti F, Agostini F, Fagandini P, La Sala GB, Blickstein I. Depressive symptoms during late pregnancy and early parenthood following assisted reproductive technology. Fertility and Sterility. 2009;91(3):851–857. doi: 10.1016/j.fertnstert.2008.01.021. [DOI] [PubMed] [Google Scholar]
- Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: The CARDIA Study. American Journal of Public Health. 2004;94(12):2125–2131. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr ST, Blazer DG, James SA. Racial disparities in elevated prenatal depressive symptoms among black and white women in eastern North Carolina. Annals of Epidemiology. 2006;16(6):463–468. doi: 10.1016/j.annepidem.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Patterson F, Seravalli L, Hanlon A, Nelson DB. Neighborhood safety as a correlate of tobacco use in a sample of urban, pregnant women. Addict Behav. 2012;37(10):1132–1137. doi: 10.1016/j.addbeh.2012.05.011. doi: 10.1016/j.addbeh.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Records K, Rice M. Psychosocial correlates of depression symptoms during the third trimester of pregnancy. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2007;36(3):231–242. doi: 10.1111/j.1552-6909.2007.00140.x. [DOI] [PubMed] [Google Scholar]
- Ross C, Mirowsky J. Disorder and decay: The concept and measurement of perceived neighborhood disorder. Urban Affairs Review. 1999;34(3):412–432. [Google Scholar]
- Ross C, Mirowsky J. Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior. 2001;42:258–276. [PubMed] [Google Scholar]
- Rudnicki SR, Graham JL, Habboushe DF, Ross RD. Social support and avoidant coping: Correlates of depressed mood during pregnancy in minority women. Women and Health. 2001;34(3):19–34. doi: 10.1300/J013v34n03_02. [DOI] [PubMed] [Google Scholar]
- Schulz A, Zenk S, Kannan S, Israel B, Stokes C. Israel B, Schulz A, Parker E, editors. Community-based participation in survey design and implementation. Methods for conducting community-based participatory research for health. (2nd) 2012:197–224. [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social Support Survey. Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Skogan W. Disorder and decline: Crime and the spiral of decay in American neighbourhoods. The Free Press; New York: 1990. [Google Scholar]
- Toffol E, Koponen P, Partonen T. Miscarriage and mental health: Results of two population-based studies. Psychiatry Research. 2013;205(1-2):151–158. doi: 10.1016/j.psychres.2012.08.029. [DOI] [PubMed] [Google Scholar]
- Witt WP, Wisk LE, Cheng ER, Hampton JM, Creswell PD, Hagen EW, DeLeire T. Poor Prepregnancy and Antepartum Mental Health Predicts Postpartum Mental Health Problems among US Women: A Nationally Representative Population-Based Study. Women's Health Issues. 2011;21(4):304–313. doi: 10.1016/j.whi.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yali AM, Lobel M. Stress-resistance resources and coping in pregnancy. Anxiety, Stress, and Coping. 2002;15(3):289–309. [Google Scholar]