Abstract
Background
A laparoscopic approach has been proposed to reduce the high morbidity and mortality associated with the Hartmann's procedure for the emergency treatment of diverticulitis.
Objective
The objective of our study was to determine whether a laparoscopic Hartmann's procedure reduces early morbidity or mortality for patients undergoing an emergency operation for diverticulitis.
Design
This is a comparative effectiveness study. A subset of the entire American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) patient sample matched on propensity for undergoing their procedure with the laparoscopic approach were used to compare postoperative outcomes between laparoscopic and open groups.
Setting
This study uses data from the ACS NSQIP Participant User Files from 2005 through 2009.
Patients
All patients who underwent an emergency laparoscopic or open partial colectomy with end colostomy for colonic diverticulitis were reviewed.
Main Outcome Measures
The main outcome measures were 30-day mortality and morbidity.
Results
1,186 patients undergoing emergency partial colectomy with end colostomy for diverticulitis were included in the analysis. Among the entire cohort, the laparoscopic group had fewer overall complications (26% vs. 41.7%, p=0.008) and shorter mean length of hospitalization (8.9 vs. 11.6 days, p=0.0008). Operative times were not significantly different between groups. When controlling for potential confounders, a laparoscopic approach was not associated with a decrease in morbidity or mortality. As compared to a propensity-match cohort, the laparoscopic approach did not reduce postoperative morbidity or mortality.
Limitations
This study is limited by its retrospective nature and the absence of pertinent variables such as postoperative pain indices, time for return of bowel function, and rates of readmission.
Conclusions
A laparoscopic approach to the Hartmann's procedure for the emergency treatment of complicated diverticulitis does not significantly decrease postoperative morbidity or mortality as compared to the open technique.
Introduction
The traditional strategy for treating complicated diverticulitis in the emergency setting has been a two-stage approach comprised of an initial sigmoid resection and end colostomy (Hartmann's procedure) followed by a second surgery to restore intestinal continuity.1 Due to the high complication and mortality rates associated with this approach,2-6 the addition of laparoscopy to the Hartmann's procedure has been proposed to reduce the incidence of postoperative complications and expedite recovery.7,8
During elective surgery for diverticulitis, a laparoscopic approach has been shown in multiple studies to have several perioperative advantages over open surgery including shorter length of hospitalization, quicker return of bowel function, fewer infectious complications, and decreased postoperative pain.9-25 Whether these advantages observed after elective laparoscopic surgery for diverticulitis will extend to emergency surgery for patients with complicated diverticulitis is currently unknown. The objective of this study was to test whether a laparoscopic approach to the Hartmann's procedure was associated with decreased postoperative morbidity and mortality by performing a propensity-matched comparative analysis of laparoscopic and open approaches using data from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP).
Methods
The American College of Surgeons National Surgical Quality Improvement Program Participant User Files for 2005 through 2009 were used for this analysis. Patients were included for analysis if they met all three of the following criteria: (1) primary Current Procedure Terminology code for laparoscopic or open partial colectomy with end colostomy (CPT 44206 or 44143), (2) emergency procedure, and (3) postoperative diagnosis of colonic diverticulitis with or without mention of hemorrhage (International Classification of Diseases 9th Edition codes 562.11 or 562.13).
The primary predictor variable for our analysis was surgical approach for the index procedure (laparoscopic or open). Definitions of other predictor variables definitions are given in the NSQIP participant user guide.26 The primary outcome variables were 30-day postoperative mortality and overall 30-day postoperative morbidity. Specific definitions of secondary outcome variables are also given in the NSQIP participant user guide.26 Three variables had missing data (BMI - 116 patients, Resident Participation - 10 patients, and ASA Classification - 1 patient). Since there was not a significant difference in the percentage of laparoscopic patients (85.7%) versus open patients (90.9%, p=0.15) that had missing data for BMI, we assumed patients were missing BMI data at random and therefore excluded these patients from our multivariate regression models.
Comparisons of preoperative and intraoperative variables for patients undergoing laparoscopic versus open surgery were made using Pearson's chi square tests for categorical variables and Mann-Whitney rank sum tests for continuous variables. Comparisons of the primary and secondary outcomes for the two groups were made in the same manner. For each primary outcome variable, (30-day postoperative mortality and morbidity), all potential preoperative and intraoperative variables were then considered for inclusion in a forward stepwise multivariate logistic regression model, using a p value of < 0.01 as the entry criterion. As the primary predictor of interest, surgical approach (open versus laparoscopic) was forced as a variable into both of these regression models.
In recognition that there was likely a non-random selection bias for treating patients with complicated diverticulitis using an open versus laparoscopic approach, we also conducted a separate analysis using of a subset of the entire NSQIP patient sample matched on propensity for undergoing their procedure with the laparoscopic approach in order to minimize this selection bias. For this analysis, a nonparsimonious logistic regression model was created in order to estimate the likelihood of undergoing the index colectomy procedure laparoscopically, with all of the aforementioned preoperative and intraoperative variables being included as potential confounders in this model. Intraoperative procedure characteristics were specifically included in the model, even those these variables cannot be known preoperative, because they may reflect in part the technical difficulty of a given procedure. A propensity score for laparoscopic approach ranging from 0 to 1 was then calculated for each patient using the logit coefficients for the predictors of laparoscopic approach from the above multivariate logistic regression model. These propensity scores were then used to create two groups of patients matched on their propensity for having undergone laparoscopic surgery using a caliper matching algorithm with a caliper distance of 0.005 and controls being used only once in the matching procedure. Comparison of the preoperative and intraoperative characteristics of the matched cohort of patients was then performed using McNemar's chi-square tests for categorical variables and Wilcoxon signed rank tests for continuous variables. Primary and secondary outcome measures between the matched cohorts were compared in a similar manner. All statistical tests were two tailed with a significance level considered to be p<0.05. All statistical analyses were performed using Stata Version 11.0 (College Station, TX). The statistical methods are summarized in Figure 1.
FIGURE 1.
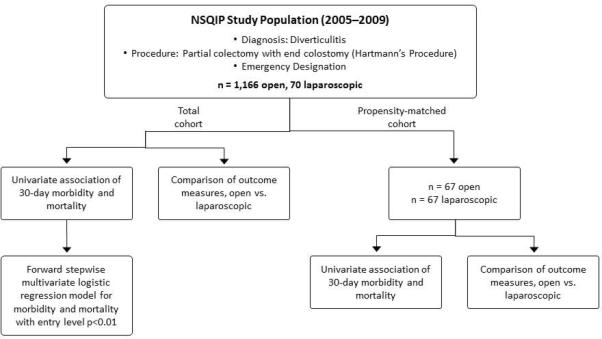
Summary of statistical methods. NSQIP = National Surgical Quality Improvement Program.
Results
A total of 1,186 patients undergoing emergency partial colectomy with end colostomy for diverticulitis were included in the analysis, with 1,116 (94%) and 70 (6%) patients treated with an open and laparoscopic approach respectively. The pre- and intraoperative characteristics of patients included for analysis are summarized in Table 1. As compared to patients treated with open surgery, patients treated laparoscopically had an overall lower operative risk as demonstrated by lower American Society of Anesthesia (ASA) physical status classification (54.3% vs. 66.9% having ASA ≥ 3, p=0.03). Fewer patients in laparoscopic cohort presented with systemic inflammatory response syndrome (SIRS), sepsis, or shock (58.6% vs. 69.5%), although this difference did not reach statistical significance (p=0.06). While operative time did not differ between procedures (132 ± 65 vs. 124 ± 52 minutes, p=0.72), a laparoscopic approach to the Hartmann's procedure were associated with fewer dirty wounds (68.6% vs. 80.6%, p=0.02) and had less resident participation (47.1% vs. 64.2%, p=0.004). Univariate associations of preoperative and intraoperative variables with 30-day postoperative mortality and morbidity are given in Table 2.
Table 1.
Preoperative and Intraoperative Characteristics of Patients Undergoing Emergent Partial Colectomy and End Ileostomy For Diverticulitis Using Entire NSQIP Sample.
| Preoperative or Intraoperative Variable | All Patients in NSQIP Sample | |||
|---|---|---|---|---|
| Open Procedure | Laparoscopic Procedure | P Value | ||
| Age in years (mean ± SD) | 62.9 ± 14.8 | 59.0 ± 16.4 | 0.04 | |
| Gender | Female (n=621) | 594 (95.7%) | 27 (4.4%) | 0.04 |
| Male (n=615) | 572 (93.0%) | 43 (7.0%) | ||
| Body Mass Index in kg/m2 (mean ± SD) (116 missing values) | 29.3 ± 7.3 | 29.6 ± 5.7 | 0.78 | |
| ASA Class ≥ 3 (1 missing value) | No (n=418) | 386 (92.3%) | 32 (7.7%) | 0.03 |
| Yes (n=817) | 779 (95.4%) | 38 (4.7%) | ||
| Diabetes Mellitus | No (n=1,071) | 1,011 (94.4%) | 60 (5.6%) | 0.81 |
| Yes (n=165) | 155 (93.9%) | 10 (6.1%) | ||
| Tobacco Use | No (n=934) | 877 (93.9%) | 57 (6.1%) | 0.24 |
| Yes (n=302) | 289 (95.7%) | 13 (4.3%) | ||
| Frequent Ethanol Use | No (n=1,160) | 1,094 (94.3%) | 66 (5.7%) | 0.88 |
| Yes (n=76) | 72 (95%) | 4 (5%) | ||
| Dyspnea | No (n=1,047) | 985 (94.1%) | 62 (5.9%) | 0.36 |
| Yes (n=189) | 181 (95.8%) | 8 (4.2%) | ||
| Functional Status | Independent (n=1,173) | 1,105 (94.2%) | 68 (5.8%) | 0.38 |
| Non-Independent (n=63) | 61 (97%) | 2 (3%) | ||
| Preop Ventilator | No (n=1,205) | 1,135 (94.2%) | 70 (5.8%) | 0.17 |
| Yes (n=31) | 31 (100%) | 0 (0%) | ||
| COPD | No (n=1,095) | 1,031 (94.2%) | 64 (5.8%) | 0.44 |
| Yes (n=141) | 135 (95.7%) | 6 (4.3%) | ||
| Preop Pneumonia | No (n=1,217) | 1,147 (94.3%) | 70 (5.7%) | 0.28 |
| Yes (n=19) | 19 (100%) | 0 (0%) | ||
| Ascites | No (n=1,164) | 1,096 (94.2%) | 68 (5.8%) | 0.28 |
| Yes (n=72) | 70 (97%) | 2 (3%) | ||
| Congestive Heart Failure | No (n=1,205) | 1,136 (94.3%) | 69 (5.7%) | 0.55 |
| Yes (n=31) | 30 (97%) | 1 (3%) | ||
| Coronary Artery Disease | No (n=1,064) | 1,000 (94.0%) | 64 (6.0%) | 0.18 |
| Yes (n=172) | 166 (96.5%) | 6 (3.5%) | ||
| Peripheral Vascular Disease | No (n=1,215) | 1,146 (94.3%) | 69 (5.7%) | 0.86 |
| Yes (n=21) | 20 (95%) | 1 (5%) | ||
| Hypertension | No (n=541) | 504 (93.2%) | 37 (6.8%) | 0.12 |
| Yes (n=695) | 662 (95.3%) | 33 (4.8%) | ||
| Renal Disease | No (n=1,183) | 1,113 (94.1%) | 70 (5.9%) | 0.07 |
| Yes (n=53) | 53 (100%) | 0 (0%) | ||
| Neurologic Disorder | No (n=1,092) | 1,028 (94.1%) | 64 (5.9%) | 0.41 |
| Yes (n=144) | 138 (95.8%) | 6 (4.2%) | ||
| Disseminated Cancer | No (n=1,195) | 1,126 (94.2%) | 69 (5.8%) | 0.36 |
| Yes (n=41) | 40 (98%) | 1 (2%) | ||
| Preop Infected Wound | No (n=1,205) | 1,135 (94.2%) | 70 (5.8%) | 0.17 |
| Yes (n=31) | 31 (100%) | 0 (0%) | ||
| Chronic Steroids | No (n=1,031) | 972 (94.3%) | 59 (5.7%) | 0.84 |
| Yes (n=205) | 194 (94.6%) | 11 (5.4%) | ||
| Weight Loss | No (n=1,197) | 1,128 (94.2%) | 69 (5.8%) | 0.4 |
| Yes (n=39) | 38 (97%) | 1 (3%) | ||
| Bleeding Disorder | No (n=1,073) | 1,014 (94.5%) | 59 (5.5%) | 0.52 |
| Yes (n=163) | 152 (93.3%) | 11 (6.8%) | ||
| Preoperative Transfusion | No (n=1,228) | 1,158 (94.3%) | 70 (5.7%) | 0.49 |
| Yes (n=8) | 8 (100%) | 0 (0%) | ||
| Chemotherapy | No (n=1,193) | 1,124 (94.2%) | 69 (5.8%) | 0.34 |
| Yes (n=43) | 42 (98%) | 1 (2%) | ||
| Radiotherapy | No (n=1,215) | 1,146 (94.3%) | 69 (5.7%) | 0.86 |
| Yes (n=21) | 20 (95%) | 1 (5%) | ||
| Preop SIRS, Sepsis, or Septic Shock | No (n=385) | 356 (92.5%) | 29 (7.5%) | 0.06 |
| Yes (n=851) | 810 (95.2%) | 41 (4.8%) | ||
| Dirty/Infected Incisional Wound | No (n=248) | 226 (91.1%) | 22 (8.9%) | 0.02 |
| Yes (n=988) | 940 (95.1%) | 48 (4.9%) | ||
| Operative time in minutes (mean ± SD) | 124 ± 52 | 132 ± 65 | 0.72 | |
| Introperative Transfusion | No (n=1,085) | 1,020 (94.0%) | 65 (6.0%) | 0.18 |
| Yes (n=151) | 146 (96.7%) | 5 (3.3%) | ||
| Resident Participation (10 missing values) | No (n=454) | 417 (91.9%) | 37 (8.2%) | 0.002 |
| Yes (n=772) | 742 (96.1%) | 30 (3.9%) | ||
| Total WRVUs | 37.9 ± 13.7 | 38.0 ± 11.6 | 0.13 | |
Table 2.
Univariate Association of Preoperative and Intraoperative Variables With 30-Day Postoperative Mortality and Morbidity.
| Preoperative or Intraoperative Variable | 30-Day Postoperative Outcomes | ||||
|---|---|---|---|---|---|
| Mortality | Morbidity | P Value | |||
| Surgical Approach | Open (n=1,166) | 83 (7.1%) | 0.37 | 486 (41.7%) | 0.008 |
| Laparoscopic (n=70) | 3 (4%) | 18 (26%) | |||
| Age in years (mean ± SD) | 1.08 * | <0.001 | 1.02* | <0.001 | |
| Gender | Female (n=621) | 52 (8.4%) | 0.05 | 257 (41.4%) | 0.66 |
| Male (n=615) | 34 (5.5%) | 247 (40.2%) | |||
| Body Mass Index in kg/m2 (mean ± SD) (116 missing values) | 0.94 | 0.002 | 1.01 | 0.23 | |
| ASA Class ≥ 3 (1 missing value) | No (n=418) | 0 (0%) | <0.001 | 109 (26.1%) | <0.001 |
| Yes (n=817) | 86 (10.5%) | 395 (48.4%) | |||
| Diabetes Mellitus | No (n=1,071) | 67 (6.3%) | 0.01 | 416 (38.8%) | <0.001 |
| Yes (n=165) | 19 (11.5%) | 88 (53.3%) | |||
| Tobacco Use | No (n=934) | 72 (7.7%) | 0.07 | 381 (40.8%) | 0.98 |
| Yes (n=302) | 14 (4.6%) | 123 (40.7%) | |||
| Frequent Ethanol Use | No (n=1,160) | 83 (7.2%) | 0.29 | 468 (40.3%) | 0.23 |
| Yes (n=76) | 3 (4%) | 36 (47%) | |||
| Dyspnea | No (n=1,047) | 44 (4.2%) | <0.001 | 393 (37.5%) | <0.001 |
| Yes (n=189) | 42 (22.2%) | 111 (58.7%) | |||
| Functional Status | Independent (n=1,173) | 68 (5.8%) | <0.001 | 458 (39.1%) | <0.001 |
| Non-Independent (n=63) | 18 (29%) | 46 (73%) | |||
| Preop Ventilator | No (n=1,205) | 74 (6.1%) | <0.001 | 477 (39.6%) | <0.001 |
| Yes (n=31) | 12 (39%) | 27 (87%) | |||
| COPD | No (n=1,095) | 56 (5.1%) | <0.001 | 415 (37.9%) | <0.001 |
| Yes (n=141) | 30 (21.3%) | 89 (63.1%) | |||
| Preop Pneumonia | No (n=1,217) | 79 (6.5%) | <0.001 | 491 (40.4%) | 0.01 |
| Yes (n=19) | 7 (37%) | 13 (68.4%) | |||
| Ascites | No (n=1,164) | 71 (6.1%) | <0.001 | 466 (40.0%) | 0.03 |
| Yes (n=72) | 15 (21%) | 38 (53%) | |||
| Congestive Heart Failure | No (n=1,205) | 76 (6.3%) | <0.001 | 483 (40.1%) | 0.002 |
| Yes (n=31) | 10 (32%) | 21 (68%) | |||
| Coronary Artery Disease | No (n=1,064) | 64 (6.0%) | 0.001 | 415 (39.0%) | 0.002 |
| Yes (n=172) | 22 (12.8%) | 89 (51.7%) | |||
| Peripheral Vascular Disease | No (n=1,215) | 85 (7.0%) | 0.69 | 493 (40.6%) | 0.28 |
| Yes (n=21) | 1 (5%) | 11 (52%) | |||
| Hypertension | No (n=541) | 23 (4.3%) | 0.001 | 182 (33.6%) | <0.001 |
| Yes (n=695) | 63 (9.1%) | 322 (46.3%) | |||
| Renal Disease | No (n=1,183) | 73 (6.2%) | <0.001 | 464 (39.2%) | <0.001 |
| Yes (n=53) | 13 (25%) | 40 (76%) | |||
| Neurologic Disorder | No (n=1,092) | 59 (5.4%) | <0.001 | 424 (38.8%) | <0.001 |
| Yes (n=144) | 27 (18.8%) | 80 (55.6%) | |||
| Disseminated Cancer | No (n=1,195) | 73 (6.1%) | <0.001 | 480 (40.2%) | 0.02 |
| Yes (n=41) | 13 (32%) | 24 (59%) | |||
| Preop Infected Wound | No (n=1,205) | 80 (6.6%) | 0.006 | 483 (40.1%) | 0.002 |
| Yes (n=31) | 6 (19%) | 21 (68%) | |||
| Chronic Steroids | No (n=1,031) | 48 (4.7%) | <0.001 | 394 (38.2%) | <0.001 |
| Yes (n=205) | 38 (18.5%) | 110 (53.7%) | |||
| Weight Loss | No (n=1,197) | 77 (6.4%) | <0.001 | 487 (40.7%) | 0.72 |
| Yes (n=39) | 9 (23.1%) | 17 (44%) | |||
| Bleeding Disorder | No (n=1,073) | 61 (5.7%) | <0.001 | 414 (38.6%) | <0.001 |
| Yes (n=163) | 25 (15.3%) | 90 (55.2%) | |||
| Preoperative Transfusion | No (n=1,228) | 85 (6.9%) | 0.54 | 497 (40.5%) | 0.007 |
| Yes (n=8) | 1 (13%) | 7 (88%) | |||
| Chemotherapy | No (n=1,193) | 77 (6.5%) | <0.001 | 481 (40.3%) | 0.08 |
| Yes (n=43) | 9 (21%) | 23 (53%) | |||
| Radiotherapy | No (n=1,215) | 83 (6.8%) | 0.18 | 493 (40.6%) | 0.28 |
| Yes (n=21) | 3 (14%) | 11 (52%) | |||
| Preop SIRS, Sepsis, or Septic Shock | No (n=385) | 23 (6.0%) | 0.36 | 120 (31.2%) | <0.001 |
| Yes (n=851) | 63 (7.4%) | 384 (45.1%) | |||
| Dirty/Infected Incisional Wound | No (n=248) | 17 (6.9%) | 0.94 | 85 (34.3%) | 0.02 |
| Yes (n=988) | 69 (7.0%) | 419 (42.4%) | |||
| Operative time in minutes (mean ± SD) | 0.99* | 0.99 | 1.002* | 0.02 | |
| Introperative Transfusion | No (n=1,085) | 53 (4.9%) | <0.001 | 403 (37.1%) | <0.001 |
| Yes (n=151) | 33 (21.9%) | 10 (66.9%) | |||
| Resident Participation (10 missing values) | No (n=454) | 34 (7.5%) | 0.56 | 171 (37.7%) | 0.08 |
| Yes (n=772) | 51 (6.6%) | 330 (42.8%) | |||
| Total WRVUs | 1.01* | 0.23 | 1.01* | 0.01 | |
Represents increase in odds of incurring outcome for each unit increase in value of continuous variable.
For all patients in the included NSQIP sample, a laparoscopic approach to partial colectomy and end colostomy was associated with a lower overall complication rate [25.7% (n=18) vs. 41.7% (n=486), p=0.008] and similar postoperative mortality [4.3% (n=3) vs. 7.1% (n=83), p=0.37]. Specifically, laparoscopic procedures had a significantly decreased likelihood of prolonged postoperative ventilation [4.3% (n=3) vs. 15.7% (n=183), p=0.01] and median (25-75%) length of hospitalization [6 (5-11) vs. 8.5 (6-13) days, p=0.0008]. Major cardiovascular complications were similar between groups, as was the rate of organ space infections [4.3% (n=3) vs. 4.9% (n=57), p=0.82] (Table 3).
Table 3.
Outcomes for Patients Undergoing Emergent Partial Colectomy and End Colostomy For Diverticulitis Using Entire NSQIP Sample.
| Outcome Measure | All Patients in NSQIP Sample | ||
|---|---|---|---|
| Open Procedure (n=1,166) | Laparoscopic Procedure (n=70) | P Value | |
| 30-Day Postoperative Death | 83 (7.1%) | 3 (4%) | 0.37 |
| Overall Complication Rate | 486 (41.7%) | 18 (26%) | 0.008 |
| Specific Complications: | |||
| Superficial Surgical Site Infection | 125 (10.7%) | 3 (5%) | 0.09 |
| Deep Surgical Site Infection | 35 (3.0%) | 1 (1%) | 0.45 |
| Organ/Space Surgical Site Infection | 57 (4.9%) | 3 (4%) | 0.82 |
| Wound Dehiscence | 48 (4.1%) | 0 (0%) | 0.08 |
| Pneumonia | 104 (8.9%) | 3 (4%) | 0.18 |
| Unplanned Reintubation | 78 (6.7%) | 3 (4%) | 0.43 |
| Pulmonary Embolism | 15 (1.3%) | 1 (1%) | 0.92 |
| Prolonged Ventilatory Support | 183 (15.7%) | 3 (4%) | 0.01 |
| Progressive Renal Insufficiency | 13 (1.1%) | 0 (0%) | 0.37 |
| Acute Renal Failure | 21 (1.8%) | 1 (1%) | 0.82 |
| Urinary Tract Infection | 28 (2.4%) | 5 (7%) | 0.02 |
| Stroke | 10 (0.9%) | 1 (1%) | 0.62 |
| Coma > 24 hours | 3 (0.3%) | 0 (0%) | 0.67 |
| Peripheral Nerve Injury61 (9.8%) | 2 (0.2%) | 0 (0%) | 0.73 |
| Cardiac Arrest | 15 (1.3%) | 0 (0%) | 0.34 |
| Myocardial Infarction | 14 (1.2%) | 0 (0%) | 0.36 |
| Bleeding within 72 hours | 10 (0.9%) | 2 (3%) | 0.1 |
| Graft/Prosthetic Failure | 0 (0%) | 0 (0%) | - |
| Deep Venous Thrombosis | 25 (2.1%) | 2 (3%) | 0.69 |
| Sepsis | 76 (6.5%) | 1 (1%) | 0.09 |
| Septic Shock | 105 (9.0%) | 3 (4%) | 0.17 |
| Return to Operating Room | 105 (9.0%) | 9 (13%) | 0.28 |
| Median (IQR) and Mean Length of Postoperative Hopsital Stay | 8.5 (6-13) | 6 (5-11) | 0.0008 |
Stepwise multivariate logistic regression was performed to determine variables associated with 30-day postoperative death and postoperative morbidity, and the results of these analyses are summarized in Tables 4-5. Despite being associated with decreased perioperative morbidity on univariate analysis, a laparoscopic approach to the Hartmann's procedure was not associated overall morbidity or 30-day mortality when controlling for potentially confounding pre- and intra-operative variables.
Table 4.
Preoperative/Intraoperative Variables Significantly Associated with 30-Day Postoperative Death After Emergency Partial Colectomy and End Colostomy for Diverticulitis Using Entire NSQIP Sample.
| Variable | Adjusted Odds Ratio* | 95% Confidence Interval | P Value |
|---|---|---|---|
| Laparoscopic Approach | 0.84 | 0.21-3.23 | 0.79 |
| Dyspnea | 3.60 | 2.09-6.22 | <0.001 |
| Age | 1.08 | 1.05-1.11 | <0.001 |
| Disseminated Cancer | 6.62 | 2.73-16.1 | <0.001 |
| Intraoperative Transfusion | 2.82 | 1.58-5.01 | <0.001 |
| Ascites | 3.81 | 1.75-8.31 | 0.001 |
| Chronic Steroid Use | 2.49 | 1.43-4.35 | 0.001 |
Risk Adjustment using multivariate logistic regression with forward stepwise selection of all available preoperative and intraoperative variables (entry criterion p < 0.01); All patients who died postoperative had an ASA Classification ≥ 3, therefore this variable was dropped from the regression model due to estimability
**Laparoscopic versus Open Approach forced into model because primary predictor variable of interest C-index = 0.85
Table 5.
Preoperative/Intraoperative Variables Significantly Associated with Postoperative Morbidity After Emergency Partial Colectomy and End Colostomy for Diverticulitis Using Entire NSQIP Sample.
| Variable | Adjusted Odds Ratio* | 95% Confidence Interval | P Value |
|---|---|---|---|
| Laparoscopic Approach** | 0.62 | 0.33-1.15 | 0.13 |
| ASA Classification ≥ 3 | 2.03 | 1.53-2.71 | <0.001 |
| Intraoperative Transfusion | 2.53 | 1.69-3.79 | <0.001 |
| Preoperative SIRS/Sepsis/Septic Shock | 1.70 | 1.28-2.25 | <0.001 |
| Preoperative Dyspnea | 1.70 | 1.19-2.44 | 0.004 |
| Preoperative Ventilator | 4.42 | 1.46-13.4 | 0.009 |
Risk Adjustment using multivariate logistic regression with forward stepwise selection of all available preoperative and intraoperative variables (entry criterion p < 0.01)
Laparoscopic versus Open Approach forced into model because primary predictor variable of interest c-index = 0.68
To address potential selection bias in the laparoscopic cohort, a separate analysis using of a subset of the entire NSQIP patient sample matched on propensity for undergoing their procedure with the laparoscopic approach was performed. A final propensity-match subset included 67 patients in both open and laparoscopic groups, with their preoperative and intraoperative characteristics summarized in Table 6. Univariate associations of preoperative and intraoperative variables with 30-day postoperative mortality and morbidity using the propensity matched cohort are given in Table 7. On repeat analysis of outcomes using these propensity matched cohorts, no statistically significant differences between open and laparoscopic groups were demonstrated, including postoperative morbidity and mortality (Table 8).
Table 6.
Preoperative and Intraoperative Characteristics of Patients Undergoing Emergent Partial Colectomy and End Ileostomy For Diverticulitis Using Propensity-Matched Cohorts.
| Preoperative or Intraoperative Variable | All Patients in NSQIP Sample | |||
|---|---|---|---|---|
| Open Procedure | Laparoscopic Procedure | P Value | ||
| Age in years (mean ± SD) | 59.4 ± 13.5 | 58.5 ± 16.3 | 0.63 | |
| Gender | Female (n=53) | 27 (51%) | 26 (49%) | 1.0 |
| Male (n=81) | 40 (49%) | 41 (51%) | ||
| Body Mass Index in kg/m2 (mean ± SD) | 26.7 ± 6.5 | 27.6 ± 7.8 | 0.56 | |
| ASA Class ≥ 3 | No (n=59) | 27 (46%) | 32 (54%) | 0.47 |
| Yes (n=75) | 40 (53%) | 35 (47%) | ||
| Diabetes Mellitus | No (n=113) | 56 (49.6%) | 57 (50.4%) | 1.0 |
| Yes (n=21) | 11 (52%) | 10 (48%) | ||
| Tobacco Use | No (n=109) | 55 (50%) | 54 (50%) | 1.0 |
| Yes (n=25) | 12 (48%) | 13 (52%) | ||
| Frequent Ethanol Use | No (n=127) | 64 (50.4%) | 63 (49.6%) | 1.0 |
| Yes (n=7) | 3 (43%) | 4 (57%) | ||
| Dyspnea | No (n=117) | 57 (48.7%) | 60 (51.3%) | 0.61 |
| Yes (n=17) | 10 (59%) | 7 (41%) | ||
| Functional Status | Independent (n=131) | 65 (49.6%) | 66 (50.4%) | 1.0 |
| Non-Independent (n=3) | 2 (67%) | 1 (33%) | ||
| Preop Ventilator | No (n=134) | 67 (50%) | 67 (50%) | 1.0 |
| Yes (n=0) | 0 (0%) | 0 (0%) | ||
| COPD | No (n=122) | 60 (49.2%) | 62 (50.8%) | 0.77 |
| Yes (n=12) | 7 (58%) | 5 (42%) | ||
| Preop Pneumonia | No (n=133) | 66 (49.6%) | 67 (50.4%) | 1.0 |
| Yes (n=1) | 1 (100%) | 0 (0%) | ||
| Ascites | No (n=130) | 65 (50.0%) | 65 (50.0%) | 1.0 |
| Yes (n=4) | 2 (50%) | 2 (50%) | ||
| Congestive Heart Failure | No (n=132) | 66 (50.0%) | 66 (50.0%) | 1.0 |
| Yes (n=2) | 1 (50%) | 1 (50%) | ||
| Coronary Artery Disease | No (n=121) | 59 (48.8%) | 62 (51.2%) | 0.58 |
| Yes (n=13) | 8 (62%) | 5 (38%) | ||
| Peripheral Vascular Disease | No (n=131) | 65 (49.6%) | 66 (50.4%) | 1.0 |
| Yes (n=3) | 2 (67%) | 1 (33%) | ||
| Hypertension | No (n=74) | 37 (50.0%) | 37 (50.0%) | 1.0 |
| Yes (n=60) | 30 (50%) | 30 (50%) | ||
| Renal Disease | No (n=134) | 67 (50.0%) | 67 (50.0%) | 1.0 |
| Yes (n=0) | 0 (0%) | 0 (0%) | ||
| Neurologic Disorder | No (n=124) | 62 (50.0%) | 62 (50.0%) | 1.0 |
| Yes (n=10) | 5 (50%) | 5 (50%) | ||
| Disseminated Cancer | No (n=132) | 66 (50.0%) | 66 (50.0%) | 1.0 |
| Yes (n=2) | 1 (50%) | 1 (50%) | ||
| Preop Infected Wound | No (n=134) | 67 (50%) | 67 (50%) | 1.0 |
| Yes (n=0) | 0 (0%) | 0 (0%) | ||
| Chronic Steroids | No (n=115) | 58 (50.4%) | 57 (49.6%) | 1.0 |
| Yes (n=19) | 9 (47%) | 10 (53%) | ||
| Weight Loss | No (n=131) | 65 (49.6%) | 66 (50.4%) | 1.0 |
| Yes (n=3) | 2 (67%) | 1 (33%) | ||
| Bleeding Disorder | No (n=112) | 55 (49.1%) | 57 (50.9%) | 0.81 |
| Yes (n=22) | 12 (55%) | 10 (45%) | ||
| Preoperative Transfusion | No (n=134) | 67 (50.0%) | 67 (50.0%) | 1.0 |
| Yes (n=0) | 0 (0%) | 0 (0%) | ||
| Chemotherapy | No (n=133) | 67 (50.4%) | 66 (49.6%) | 1.0 |
| Yes (n=1) | 0 (0%) | 1 (100%) | ||
| Radiotherapy | No (n=132) | 66 (50.0%) | 66 (50.0%) | 1.0 |
| Yes (n=2) | 1 (50%) | 1 (50%) | ||
| Preop SIRS, Sepsis, or Septic Shock | No (n=54) | 27 (50%) | 27 (50%) | 1.0 |
| Yes (n=80) | 40 (50%) | 40 (50%) | ||
| Dirty/Infected Incisional Wound | No (n=38) | 38 (47%) | 20 (53%) | 0.83 |
| Yes (n=96) | 49 (51%) | 47 (49%) | ||
| Operative time in minutes (mean ± SD) | 138 ± 62 | 132 ± 64 | 0.63 | |
| Introperative Transfusion | No (n=124) | 61 (49.2%) | 63 (50.8%) | 0.75 |
| Yes (n=10) | 6 (60%) | 4 (40%) | ||
| Resident Participation (10 missing values) | No (n=64) | 30 (47%) | 34 (53%) | 0.57 |
| Yes (n=67) | 37 (55%) | 30 (45%) | ||
| Total WRVUs | 38.5 ± 14.9 | 38.1 ± 11.8 | 0.99 | |
Table 7.
Univariate Association of Preoperative and Intraoperative Variables With 30-Day Posteroperative Mortality and Morbidity Using Propensity-Matched Cohorts.
| Preoperative or Intraoperative Variable | 30-Day Postoperative Outcomes | ||||
|---|---|---|---|---|---|
| Mortality | Morbidity | P Value | |||
| Surgical Approach | Open (n=67) | 3 (4%) | 0.65 | 20 (30%) | 0.56 |
| Laparoscopic (n=67) | 2 (3%) | 17 (25%) | |||
| Age in years (mean ± SD) | 1.08 * | 0.05 | 1.02* | 0.12 | |
| Gender | Male (n=81) | 3 (4%) | 0.98 | 23 (28%) | 0.80 |
| Female (n=53) | 2 (4%) | 14 (26%) | |||
| Body Mass Index in kg/m2 (mean ± SD) | 0.85 | 0.10 | 1.01 | 0.84 | |
| ASA Class ≥ 3 | No (n=59) | 0 (0%) | 0.04 | 13 (22%) | 0.20 |
| Yes (n=75) | 6 (7%) | 24 (32%) | |||
| Diabetes Mellitus | No (n=113) | 2 (1.8%) | 0.005 | 29 (25.7%) | 0.24 |
| Yes (n=21) | 3 (14%) | 8 (38%) | |||
| Tobacco Use | No (n=109) | 4 (4%) | 0.94 | 30 (27.5%) | 0.96 |
| Yes (n=25) | 1 (4%) | 7 (28%) | |||
| Frequent Ethanol Use | No (n=127) | 5 (3.9%) | 0.59 | 34 (26.8%) | 0.35 |
| Yes (n=7) | 0 (0%) | 3 (43%) | |||
| Dyspnea | No (n=117) | 0 (0%) | <0.001 | 31 (26.5%) | 0.45 |
| Yes (n=17) | 5 (29%) | 6 (35%) | |||
| Functional Status | Independent (n=131) | 5 (3.8%) | 0.73 | 37 (28.2%) | 0.28 |
| Non-Independent (n=3) | 0 (0%) | 0 (0%) | |||
| Preop Ventilator | No (n=134) | 5 (3.7%) | - | 37 (27.6%) | - |
| Yes (n=0) | - | - | |||
| COPD | No (n=122) | 2 (1.6%) | <0.001 | 33 (27.1%) | 0.64 |
| Yes (n=12) | 3 (25%) | 4 (33%) | |||
| Preop Pneumonia | No (n=133) | 5 (3.8%) | 0.84 | 36 (27.1%) | 0.10 |
| Yes (n=1) | 0 (0%) | 1 (100%) | |||
| Ascites | No (n=130) | 5 (3.9%) | 0.69 | 37 (28.5%) | 0.21 |
| No (n=4) | 0 (0%) | 0 (0%) | |||
| Congestive Heart Failure | No (n=132) | 4 (3.0%) | 0.001 | 36 (27.3%) | 0.48 |
| Yes (n=2) | 1 (50%) | 1 (50%) | |||
| Coronary Artery Disease | No (n=121) | 5 (4.1%) | 0.46 | 35 (28.9%) | 0.30 |
| Yes (n=13) | 0 (0%) | 2 (15%) | |||
| Peripheral Vascular Disease | No (n=131) | 5 (3.8%) | 0.73 | 36 (27.5%) | 0.82 |
| Yes (n=3) | 0 (0%) | 1 (33%) | |||
| Hypertension | No (n=74) | 2 (3%) | 0.49 | 17 (23%) | 0.18 |
| Yes (n=60) | 3 (5%) | 20 (33%) | |||
| Renal Disease | No (n=134) | 5 (3.7%) | - | 37 (27.6%) | - |
| Yes (n=0) | - | - | |||
| Neurologic Disorder | No (n=124) | 4 (3.2%) | 0.28 | 32 (25.8%) | 0.10 |
| Yes (n=10) | 1 (10%) | 5 (50%) | |||
| Disseminated Cancer | No (n=132) | 5 (3.8%) | 0.78 | 37 (28.0%) | 0.38 |
| No (n=2) | 0 (0%) | 0 (0%) | |||
| Preop Infected Wound | No (n=134) | 5 (3.7%) | - | 37 (27.6%) | - |
| Yes (n=0) | - | - | |||
| Chronic Steroids | No (n=115) | 2 (1.7%) | 0.003 | 29 (25.2%) | 0.13 |
| Yes (n=19) | 3 (16%) | 8 (42%) | |||
| Weight Loss | No (n=131) | 3 (2.3%) | <0.001 | 37 (28.2%) | 0.28 |
| Yes (n=3) | 2 (67%) | 0 (0%) | |||
| Bleeding Disorder | No (n=112) | 2 (1.8%) | 0.007 | 29 (25.9%) | 0.32 |
| Yes (n=22) | 3 (14%) | 8 (37%) | |||
| Preoperative Transfusion | No (n=134) | 5 (3.7%) | - | 37 (27.6%) | - |
| Yes (n=0) | - | - | |||
| Chemotherapy | No (n=133) | 4 (3.0%) | <0.001 | 36 (27.1%) | 0.10 |
| Yes (n=1) | 1 (100%) | 1 (100%) | |||
| Radiotherapy | No (n=132) | 5 (3.8%) | 0.78 | 35 (26.5%) | 0.02 |
| Yes (n=2) | 0 (0%) | 2 (100%) | |||
| Preop SIRS, Sepsis, or Septic Shock | No (n=54) | 2 (4%) | 0.99 | 16 (30%) | 0.67 |
| Yes (n=80) | 3 (4%) | 21 (26%) | |||
| Dirty/Infected Incisional Wound | No (n=38) | 2 (5%) | 0.56 | 11 (29%) | 0.83 |
| Yes (n=96) | 3 (3%) | 26 (27%) | |||
| Operative time in minutes (mean ± SD) | 1.00* | 0.50 | 1.00* | 0.47 | |
| Introperative Transfusion | No (n=124) | 3 (2.4%) | 0.005 | 33 (26.6%) | 0.36 |
| Yes (n=10) | 2 (20%) | 4 (40%) | |||
| Resident Participation | No (n=64) | 2 (3%) | 0.69 | 17 (27%) | 0.68 |
| Yes (n=67) | 3 (4%) | 20 (30%) | |||
| Total WRVUs | 1.00* | 0.90 | 1.01* | 0.65 | |
Represents increase in odds of incurring outcome for each unit increase in value of continuous variable.
Table 8.
Outcomes for Patients Undergoing Emergent Partial Colectomy and End Colostomy For Diverticulitis Using Propensity-Matched Cohorts.
| Outcome Measure | All Patients in NSQIP Sample | ||
|---|---|---|---|
| Open Procedure (n = 67) | Laparoscopic Procedure (n = 67) | P Value | |
| 30-Day Postoperative Death | 3 (4.5%) | 2 (3.0%) | 1.0 |
| Overall Complication Rate | 20 (30.0%) | 17 (25.4%) | 0.68 |
| Specific Complications: | |||
| Superficial Surgical Site Infection | 11 (16.4%) | 3 (4.5%) | 0.06 |
| Deep Surgical Site Infection | 1 (1.5%) | 1 (1.5%) | 1.0 |
| Organ/Space Surgical Site Infection | 2 (3.0%) | 3 (4.5%) | 1.0 |
| Wound Dehiscence | 2 (3.0%) | 0 (0%) | 0.5 |
| Pneumonia | 0 (0%) | 3 (4.5%) | 0.25 |
| Unplanned Reintubation | 1 (1.5%) | 3 (4.5%) | 0.63 |
| Pulmonary Embolism | 0 (0%) | 1 (1.5%) | 1.0 |
| Prolonged Ventilatory Support | 4 (6.0%) | 2 (3.0%) | 0.69 |
| Progressive Renal Insufficiency | 2 (3.0%) | 0 (0%) | 0.5 |
| Acute Renal Failure | 0 (0%) | 1 (1.5%) | 1.0 |
| Urinary Tract Infection | 2 (3.0%) | 4 (6.0%) | 0.69 |
| Stroke | 1 (1.5%) | 1 (1.5%) | 1.0 |
| Coma > 24 hours | 0 (0%) | 0 (0%) | 1.0 |
| Peripheral Nerve Injury | 0 (0%) | 0 (0%) | 1.0 |
| Cardiac Arrest | 0 (0%) | 0 (0%) | 1.0 |
| Myocardial Infarction | 0 (0%) | 0 (0%) | 1.0 |
| Bleeding within 72 hours | 0 (0%) | 1 (1.5%) | 1.0 |
| Graft/Prosthetic Failure | 0 (0%) | 0 (0%) | 1.0 |
| Deep Venous Thrombosis | 0 (0%) | 2 (3.0%) | 0.5 |
| Sepsis | 4 (6.0%) | 1 (1.5%) | 0.38 |
| Septic Shock | 4 (6.0%) | 3 (4.5%) | 1.0 |
| Return to Operating Room | 3 (4.5%) | 8 (11.9%) | 0.18 |
| Median (IQR) and Mean Length of Postoperative Hopsital Stay | 8 (6-11) | 6 (5-11) | 0.53 |
Discussion
In hopes of decreasing the morbidity of the Hartmann's procedure itself and temper its criticism, a laparoscopic approach to the procedure has emerged but has yet to be validated against the standard open approach.7,8 The primary objective of this study was to determine whether the addition of laparoscopy to the Hartmann's procedure would decrease postoperative morbidity and mortality for treatment of complicated diverticulitis. On univariate analyses of the entire study cohort, the laparoscopic group had a significantly decreased overall complication rate and a shorter hospitalization, which was consistent with previous studies comparing laparoscopic and open approaches in elective surgery for diverticulitis.9-25 However, on both multivariate and case-controlled analyses, the laparoscopic group was not associated with a decrease in either postoperative morbidity or mortality.
Although the Hartmann's procedure has for many years been considered the traditional conservative treatment for such complications,1 it is associated with significant perioperative morbidity (up to 50%) and mortality (15-25%).2-6 Such perioperative morbidity and mortality is likely multifactorial and associated with other patient variables such as patient physiologic status, surgeon experience, and patient comorbidities. To account for patient variables thought to be associated with poor outcomes not available in the NSQIP database and to minimize selection bias, we also performed a propensity-matched analysis. No statistically significant advantages of laparoscopic over open technique including mortality, overall morbidity, and length of hospital stay were demonstrated between propensity-match cohorts.
The results of this study seem to imply whatever advantages garnered from a minimally invasive approach to the Hartmann's procedure may be abrogated by the end results (i.e. systemic toxicity) of the disease process itself. Thus, in the acute setting of perforated diverticulitis when purulent and or feculent peritonitis may be present, a laparoscopic sigmoid resection with end colostomy may not provide any appreciable advantage over the open approach in terms of postoperative morbidity or mortality. These results are in contrast to those of previous studies which have reported laparoscopic sigmoid resection for the elective treatment of complicated diverticulitis to decrease postoperative morbidity and length of hospitalization.9-25 Given that a laparoscopic approach seems to only provide a benefit to the patient in the elective setting, the optimal emergency treatment for perforated or complicated diverticulitis may be one that could temporize the resultant peritonitis and systemic toxicity until a sigmoid resection could be performed electively. One such strategy may be to treat acute perforations of diverticulitis with a laparoscopic peritoneal lavage and drainage procedure. 27 Advocates of this approach report laparoscopic peritoneal lavage and drainage combined with intravenous antibiotics can effectively treat the acute peritonitis and systemic toxicity of perforated diverticulitis such that a later sigmoid resection and primary anastomosis can be performed on an elective basis. Thus, with this approach, patients might be spared the high morbidity and requisite temporary ostomy of the classic two-stage approach.28-32 Whether such an approach is an effective alternative to primary sigmoid resection with or without colostomy for perforated diverticulitis is currently under investigation in an ongoing randomized, prospective trial.2
As it is comprised of a large national dataset encompassing a contemporary time frame (2005-2009), NSQIP provides a unique and powerful tool for evaluating 30-day outcomes after major surgical procedures. However, the NSQIP database has several inherent limitations which should be taken into consideration when interpreting studies using its data.33 First of all, it is reliant on CPT coding for describing procedure type, which can be variable among providers. In the case of this study, CPT coding did not allow us to discriminate potential confounding variations of either the open or laparoscopic Hartmann's procedure. Specifically, it is unclear whether a patients in this study could have been started laparoscopically but converted to open, were explored using a lower midline or full laparotomy incision, or required a splenic flexure mobilization. Second, NSQIP does not provide pertinent information regarding the extent or severity of diverticular disease (i.e. Hinchey classification) or complexity of the specific Hartmann's procedure. However, we used the total work relative value units associated with the index operation (which is comprised of the individual WRVUs associated with each CPT code) in attempt to account for procedure complexity.34-36 Third, we do not know the exact indication for the emergency operation in the patients included in our analysis (for example, free perforation vs. contained perforation vs. obstruction). Despite the lack of information regarding the specific indication for surgery, some of the covariates in our analysis should allow adjustment for the end result of these specific indications (e.g. signs of septic shock or dirty/contaminated incisional wound classification). Fourth, laparoscopic surgery in other settings has demonstrated other advantages over open surgery that could not be detected using NSQIP data.9-25 For instance, pertinent variables for this study not recorded in the NSQIP database include postoperative pain indices, time for return of bowel function, and rates of readmission. Therefore, we are unable to say with authority that the laparoscopic approach does not reduce rates of postoperative morbidity and mortality. However, the results of the propensity-matched analysis would suggest that if there were undetected benefits, they are likely not as pronounced as for elective surgery. Finally, while this study constitutes the largest comparison to date; the relatively small number of patients does subject our analysis to type II error.
Despite these limitations, we conclude from our analysis that the laparoscopic Hartmann's procedure offers no clear advantages over the open technique for the management of complicated diverticulitis in the emergency setting. As the realm of minimally-invasive surgery continues to grow, it will become important to identify which procedures are truly enhanced with such techniques. Using a prospective database encompassing more than 250 participating hospitals, we found that laparoscopic partial colectomy with end colostomy for emergency treatment of diverticulitis can be performed efficiently with similar operative times as standard open techniques. However, when compared to a propensity-matched cohort, laparoscopic Hartmann's procedure did not confer any advantages over open surgery in terms of mortality, overall morbidity, or length of hospitalization.
Acknowledgments
Funding: NIH Grant 5T32CA093245 and NIH Loan Repayment Program (RST).
Footnotes
Conflicts of Interest: None
Podium Presentation at the ASCRS Annual Meeting (GSF-4), San Antonio, TX, June 2-6, 2012
Authorship Contribution: All authors met the following criteria as outlined by DCR: (a). Made substantial contributions to the conception and design, or acquisition of data, or analysis and interpretation of data; (b). Drafting the article or revising it critically for important intellectual content; (c). Final approval of the version to be published.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References Cited
- 1.Vermeulen J, Lange JF. Treatment of perforated diverticulitis with generalized peritonitis: past, present, and future. World J Surg. 2010;34:587–593. doi: 10.1007/s00268-009-0372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swank HA, Vermeulen J, Lange JF, et al. The ladies trial: laparoscopic peritoneal lavage or resection for purulent peritonitis and Hartmann's procedure or resection with primary anastomosis for purulent or faecal peritonitis in perforated diverticulitis (NTR2037). BMC Surg. 2010;10:29. doi: 10.1186/1471-2482-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Constantinides VA, Tekkis PP, Senapati A. Prospective multicentre evaluation of adverse outcomes following treatment for complicated diverticular disease. Br J Surg. 2006;93:1503–1513. doi: 10.1002/bjs.5402. [DOI] [PubMed] [Google Scholar]
- 4.Constantinides VA, Tekkis PP, Athanasiou T, et al. Primary resection with anastomosis vs. Hartmann's procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Diseases of the colon and rectum. 2006;49:966–981. doi: 10.1007/s10350-006-0547-9. [DOI] [PubMed] [Google Scholar]
- 5.Abbas S. Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis. 2007;22:351–357. doi: 10.1007/s00384-005-0059-4. [DOI] [PubMed] [Google Scholar]
- 6.Salem L, Flum DR. Primary anastomosis or Hartmann's procedure for patients with diverticular peritonitis? A systematic review. Diseases of the colon and rectum. 2004;47:1953–1964. doi: 10.1007/s10350-004-0701-1. [DOI] [PubMed] [Google Scholar]
- 7.Agaba EA, Zaidi RM, Ramzy P, et al. Laparoscopic Hartmann's procedure: a viable option for treatment of acutely perforated diverticultis. Surg Endosc. 2009;23:1483–1486. doi: 10.1007/s00464-009-0380-z. [DOI] [PubMed] [Google Scholar]
- 8.Albrecht R, Bochmann C. [Is it possible to perform a laparoscopic assisted Hartmann's procedure and a subsequent laparoscopically assisted reversal in complicated diverticulitis?]. Zentralbl Chir. 2011;136:61–65. doi: 10.1055/s-0030-1262683. [DOI] [PubMed] [Google Scholar]
- 9.Bruce CJ, Coller JA, Murray JJ, Schoetz DJ, Jr, Roberts PL, Rusin LC. Laparoscopic resection for diverticular disease. Dis Colon Rectum. 1996;39(10 Suppl):S1–6. doi: 10.1007/BF02053798. [DOI] [PubMed] [Google Scholar]
- 10.Dwivedi A, Chahin F, Agrawal S, et al. Laparoscopic colectomy vs. open colectomy for sigmoid diverticular disease. Dis Colon Rectum. 2002;45:1309–1315. doi: 10.1007/s10350-004-6415-6. [DOI] [PubMed] [Google Scholar]
- 11.Faynsod M, Stamos MJ, Arnell T, Borden C, Udani S, Vargas H. A case-control study of laparoscopic versus open sigmoid colectomy for diverticulitis. Am Surg. 2000;66:841–843. [PubMed] [Google Scholar]
- 12.Gonzalez R, Smith CD, Mattar SG, et al. Laparoscopic vs open resection for the treatment of diverticular disease. Surg Endosc. 2004;18:276–280. doi: 10.1007/s00464-003-8809-2. [DOI] [PubMed] [Google Scholar]
- 13.Guller U, Jain N, Hervey S, Purves H, Pietrobon R. Laparoscopic vs open colectomy: outcomes comparison based on large nationwide databases. Arch Surg. 2003;138:1179–1186. doi: 10.1001/archsurg.138.11.1179. [DOI] [PubMed] [Google Scholar]
- 14.Kohler L, Rixen D, Troidl H. Laparoscopic colorectal resection for diverticulitis. Int J Colorectal Dis. 1998;13:43–47. doi: 10.1007/s003840050130. [DOI] [PubMed] [Google Scholar]
- 15.Lawrence DM, Pasquale MD, Wasser TE. Laparoscopic versus open sigmoid colectomy for diverticulitis. Am Surg. 2003;69:499–503. [PubMed] [Google Scholar]
- 16.Liberman MA, Phillips EH, Carroll BJ, Fallas M, Rosenthal R. Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc. 1996;10:15–18. doi: 10.1007/s004649910002. [DOI] [PubMed] [Google Scholar]
- 17.Lopez F, Soto G, Tapia G, et al. [Elective laparoscopic surgery in diverticular disease. A comparative study with conventional operative surgery ]. Rev Med Chil. 2003;131:719–726. [PubMed] [Google Scholar]
- 18.Senagore AJ, Duepree HJ, Delaney CP, Dissanaike S, Brady KM, Fazio VW. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45:485–490. doi: 10.1007/s10350-004-6225-x. [DOI] [PubMed] [Google Scholar]
- 19.Thaler K, Baig MK, Berho M, et al. Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum. 2003;46:385–388. doi: 10.1007/s10350-004-6560-y. [DOI] [PubMed] [Google Scholar]
- 20.Tuech JJ, Pessaux P, Rouge C, Regenet N, Bergamaschi R, Arnaud JP. Laparoscopic vs open colectomy for sigmoid diverticulitis: a prospective comparative study in the elderly. Surg Endosc. 2000;14:1031–1033. doi: 10.1007/s004640000267. [DOI] [PubMed] [Google Scholar]
- 21.Levack M, Berger D, Sylla P, Rattner D, Bordeianou L. Laparoscopy decreases anastomotic leak rate in sigmoid colectomy for diverticulitis. Arch Surg. 2011;146:207–210. doi: 10.1001/archsurg.2010.325. [DOI] [PubMed] [Google Scholar]
- 22.Lu CT, Ho YH. Elective laparoscopic surgical management of recurrent and complicated sigmoid diverticulitis. Tech Coloproctol. 2008;12:201–206. doi: 10.1007/s10151-008-0421-y. [DOI] [PubMed] [Google Scholar]
- 23.Anderson J, Luchtefeld M, Dujovny N, Hoedema R, Kim D, Butcher J. A comparison of laparoscopic, hand-assist and open sigmoid resection in the treatment of diverticular disease. Am J Surg. 2007;193:400–403. doi: 10.1016/j.amjsurg.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Simon T, Orangio GR, Ambroze WL, et al. Factors associated with complications of open versus laparoscopic sigmoid resection for diverticulitis. JSLS. 2005;9:63–67. [PMC free article] [PubMed] [Google Scholar]
- 25.Klarenbeek BR, Veenhof AA, Bergamaschi R, et al. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Annals of surgery. 2009;249:39–44. doi: 10.1097/SLA.0b013e31818e416a. [DOI] [PubMed] [Google Scholar]
- 26.User Guide for the 2009 Participant Use Data File. American College of Surgeons National Surgical Quality Improvement Program. 2010 [Google Scholar]
- 27.Afshar S, Kurer MA. Laparoscopic Peritoneal Lavage for Perforated Sigmoid Diverticulitis. Colorect Dis. 2011 Mar 17; doi: 10.1111/j.1463-1318.2011.02606.x. [DOI] [PubMed] [Google Scholar]
- 28.Karoui M, Champault A, Pautrat K, Valleur P, Cherqui D, Champault G. Laparoscopic peritoneal lavage or primary anastomosis with defunctioning stoma for Hinchey 3 complicated diverticulitis: results of a comparative study. Dis Colon Rectum. 2009;52:609–615. doi: 10.1007/DCR.0b013e3181a0a674. [DOI] [PubMed] [Google Scholar]
- 29.O'Sullivan GC, Murphy D, O'Brien MG, Ireland A. Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg. 1996;171:432–434. doi: 10.1016/S0002-9610(97)89625-0. [DOI] [PubMed] [Google Scholar]
- 30.Franklin ME, Jr., Portillo G, Trevino JM, Gonzalez JJ, Glass JL. Long-term experience with the laparoscopic approach to perforated diverticulitis plus generalized peritonitis. World J Surg. 2008;32:1507–1511. doi: 10.1007/s00268-007-9463-y. [DOI] [PubMed] [Google Scholar]
- 31.Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis. 2006;8:501–505. doi: 10.1111/j.1463-1318.2006.01011.x. [DOI] [PubMed] [Google Scholar]
- 32.Ringley C, Lee YK, Iqbal A, et al. Comparison of conventional laparoscopic and hand-assisted oncologic segmental colonic resection. Surg Endosc. 2007;21:2137–2141. doi: 10.1007/s00464-007-9401-y. [DOI] [PubMed] [Google Scholar]
- 33.Lidsky M, Thacker J, Lagoo S, Scarborough J. Advance Age is an Independent Predictor for Increased Morbidity and Mortality After Emergent Surgery for Diverticulitis. Surgery. 2012 doi: 10.1016/j.surg.2012.06.038. In Press. [DOI] [PubMed] [Google Scholar]
- 34.Davenport DL, Henderson WG, Khuri SF, Mentzer RM., Jr Preoperative risk factors and surgical complexity are more predictive of costs than postoperative complications: a case study using the National Surgical Quality Improvement Program (NSQIP) database. Ann Surg. 2005 Oct;242(4):463–468. doi: 10.1097/01.sla.0000183348.15117.ab. discussion 468-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Physician CfMaMSCN, File. FSRV. Centers for Medicare and Medicaid Services (CMS). National Physician Fee Schedule Relative Value File. 2002 Oct; 2002 Available at: http://www.cms.hhs.gov/physicians/pfs/RVU02_a.zip.
- 36.Kirchhoff P, Dincler S, Buchmann P. A multivariate analysis of potential risk factors for intra- and postoperative complications in 1316 elective laparoscopic colorectal procedures. Ann Surg. 2008 Aug;248(2):259–265. doi: 10.1097/SLA.0b013e31817bbe3a. [DOI] [PubMed] [Google Scholar]


