Abstract
Background/Objectives
The number of patients discharged to post-acute care(PAC) facilities after hospitalization increased by 50% nationally between 1996 and 2010. We sought to describe payors and patients most affected by this trend and to identify diagnoses for which PAC facility care may be substituting for continued hospital care.
Design
Retrospective analysis of the National Hospital Discharge Surveyfrom 1996 to 2010.
Setting
Adult discharges from a national sample of non-Federal hospitals.
Participants/Exposures
Adults admitted and discharged to a PAC facilitybetween 1996 and 2010. Our analysis includes 2.99 million sampled discharges, representative of 386million discharges nationally.
Measurements
Patient demographic and hospitalization characteristics, including length of stay(LOS) and diagnoses treated.
Results
More than half (50.7%) of all patients discharged to PAC facilities were 80 years old or older in 2010; 40% of hospitalizations in this age group ended with a PAC stay. Decreases in LOS and increases in PAC facility use were consistent across payors and patient demographics. PAC facilities may be substituting for continued inpatient care for patients with pneumonia, hip fracture, and sepsis as these diagnoses demonstrated the clearest trends of decreasing LOS and increasing discharges to PAC facilities.
Conclusions
The rise in discharges to PAC facilities is occurring in all age groups and payors, though the predominant population is the very old Medicare patient, for whom successful rehabilitation may be most unsure. PAC facility care may be increasingly substituted for prolonged hospitalizations for patients with pneumonia, hip fracture, and sepsis.
Introduction
Medicare’s change from a fee-for-service system to prospective payments for hospitals in 1983 coupled with the rise of managed care in the 1990s resulted in dramatic declines in hospital lengths of stay. This was accompanied by evidence of increased clinical instability of patients being discharged, and perhaps as a result, a significant rise in discharges to post-acute care (PAC) facilities (including skilled nursing and rehabilitation facilities).1–4 The rapid rise in costs associated with PAC facility care were addressed by Medicare through a prospective payment system to home health agencies and PAC facilities, instituted between 1997 and 2002.5,6
However, contemporary data indicate discharges to PAC facilities are increasing rapidly.7 Nearly 50% more patients (1.2 million) were discharged to PAC facilities in the United States in 2010 than 1996, even after adjusting for changes in the US population. The reasons for this increase are unknown, but important to evaluate sincere admissions from PAC facilities exceed those of discharges home and are rising;8 PAC spending is now also the fastest growing area of Medicare costs (> $62 billion in 2012).6,9,10
Since little is known about this important trend, we first sought to describe the extent to which it extends across different payors, patients, and diagnoses in a nationally-representative sample of adult hospital discharges. Since discharges to skilled nursing facilities initially decreased in Medicare patients in response to payment reforms, it is possible that PAC facilities have increasingly attracted other payors to supplement revenue, and this would have important implications for national policy and health care reform. Prior analyses were also limited to Medicare patients with selected diagnoses,5,11 and we sought to extend these analyses by evaluating trends in other age groups and in other diagnostic groups. Nationally-representative trends in patients being discharged to PAC facilities after discharge may also provide normative data to providers and hospital systems for comparison with their local discharge practices.
We also sought to identify the extent to which PAC facility care might be substituting for continued inpatient hospital care. Previous studies demonstrated important shifts in the use of one type of post-acute care (home health, skilled nursing, or inpatient rehabilitation) to another in response to payment reforms, suggesting that for many patients one type of PAC was substituted for another.5,11 However, substitution of skilled nursing or inpatient rehabilitation care for inpatient hospital care has not been examined. We hypothesize that diagnostic groups in which hospital length of stay is decreasing most would be accompanied by the greatest increases in discharges to PAC facilities. These diagnostic groups are important to discover as potentially fruitful targets for future work evaluating the outcomes and appropriateness of this care. To evaluate these trends, we used the National Hospital Discharge Survey, a nationally-representative sample of hospital discharges in the United States, from 1996–2010.
Methods
Study Design and Participants
This was a secondary analysis of the NHDS, an annual national probability sample of discharges from general medical, surgical, and children’s hospitals in all fifty states and the District of Columbia.12 Federal hospitals and hospitals with less than six operating beds are excluded. The NHDS uses a three-stage probability design, identifying 112 primary sampling units across the country, then sampling hospitals from within each primary sampling unit and discharges from each selected hospital, allowing calculation of weighted national averages. Annually, more than 400 hospitals and approximately 200,000 discharges are captured, representing approximately one percent of all hospitalizations nationwide (from 2008–2010, changes in NHDS sampling resulted in sampling approximately 100,000 discharges annually).
We included all hospital discharges of patients aged 18 years or older between 1996 and 2010; patients who died during the hospitalization were excluded. Patients whose admission source was coded as “from the courts or law enforcement” and those who had a payor source of worker’s compensation were excluded (both less than 1% of all discharges), as these may represent distinct populations from the majority of those hospitalized. While the NHDS can contain multiple payor sources, we used the primary payor source only as there was substantial missing data for other payors.The NHDS codes all discharges that are not to hospitals or home as “discharge, transferred to long-term care institution.” This definition encompasses skilled nursing facilities, rehabilitation facilities, and long-term care facilities. Discharges home were coded as “routine discharge/discharge home.” Provision of home health services are not captured by the NHDS. Transfers to other hospitals (4.3% of all discharges), discharges against medical advice (1.0% of all discharges), and discharges without a destination coded were excluded (1.1% of all discharges). Length of stay is reported by NHDS in full days; means are reported in this analysis. Records with hospital lengths of stay of more than 31 days were excluded (these represented less than 1% of our overall data) to avoid the influence of potential outliers. However, a sensitivity analysis including these records was conducted (Supplemental Digital Content 1 reproduces Figures 1, 2, and 3 with these stays included). The NHDS captures only the most proximate source of admission (e.g., emergency department or operating room), thus we were unable to accurately capture prior living situation.
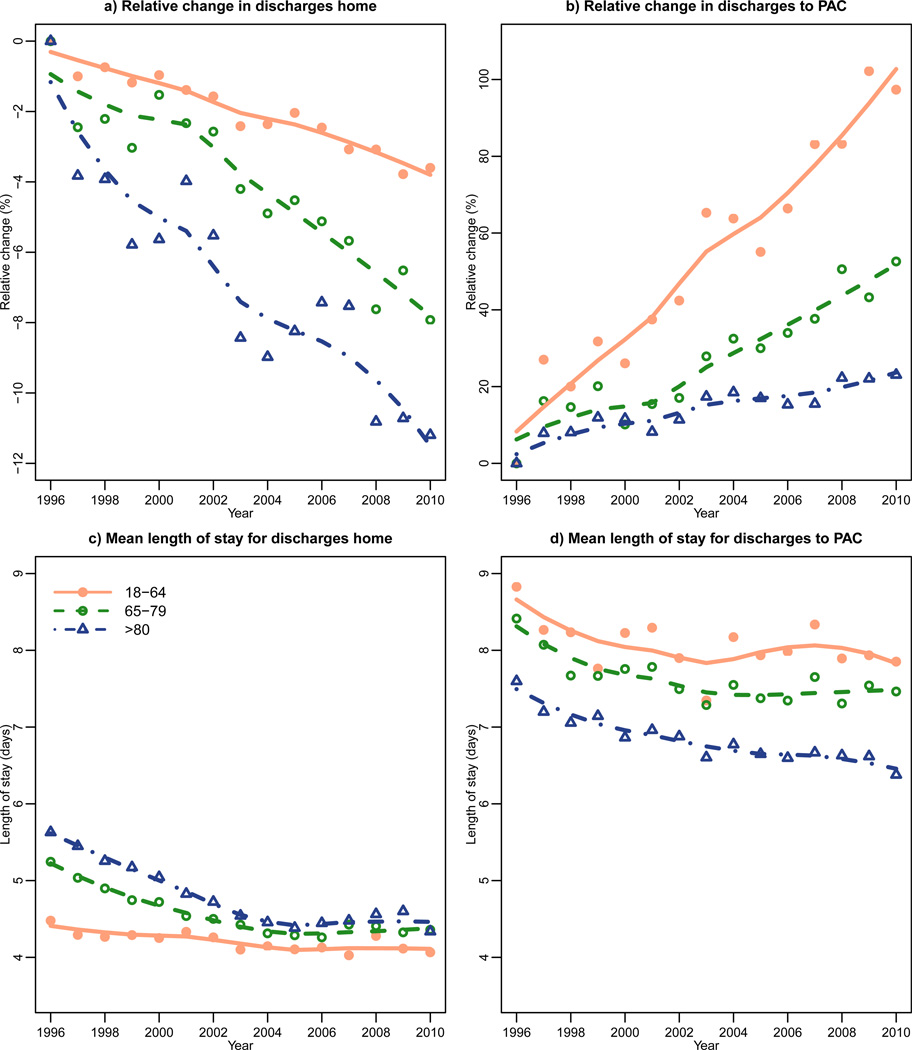
Figure 1. Trends in length of stay and discharges to post-acute care and home, stratified by age group.
Trends in the percentage of patients discharged home or to post-acute care facilities (PAC) are shown using loess smoothing (data points are represented as filled circles, unfilled circles, and unfilled triangles, respectively as age increases with trend lines fit to these data point). Trends are calculated as a relative percent change compared to 1996 levels. Length of stay is reported as mean number of days.For 18–64 year-olds discharged to PAC, slope of line is 6.54 (95% CI 5.64– 7.45) with p-value <0.001. For 65–79 year-olds discharged to PAC, slope is 3.20 (2.58– 3.83) with p-value <0.001. For those 80 and above discharged to PAC, slope is 1.313 (0.99– 1.63) with p-value <0.001.
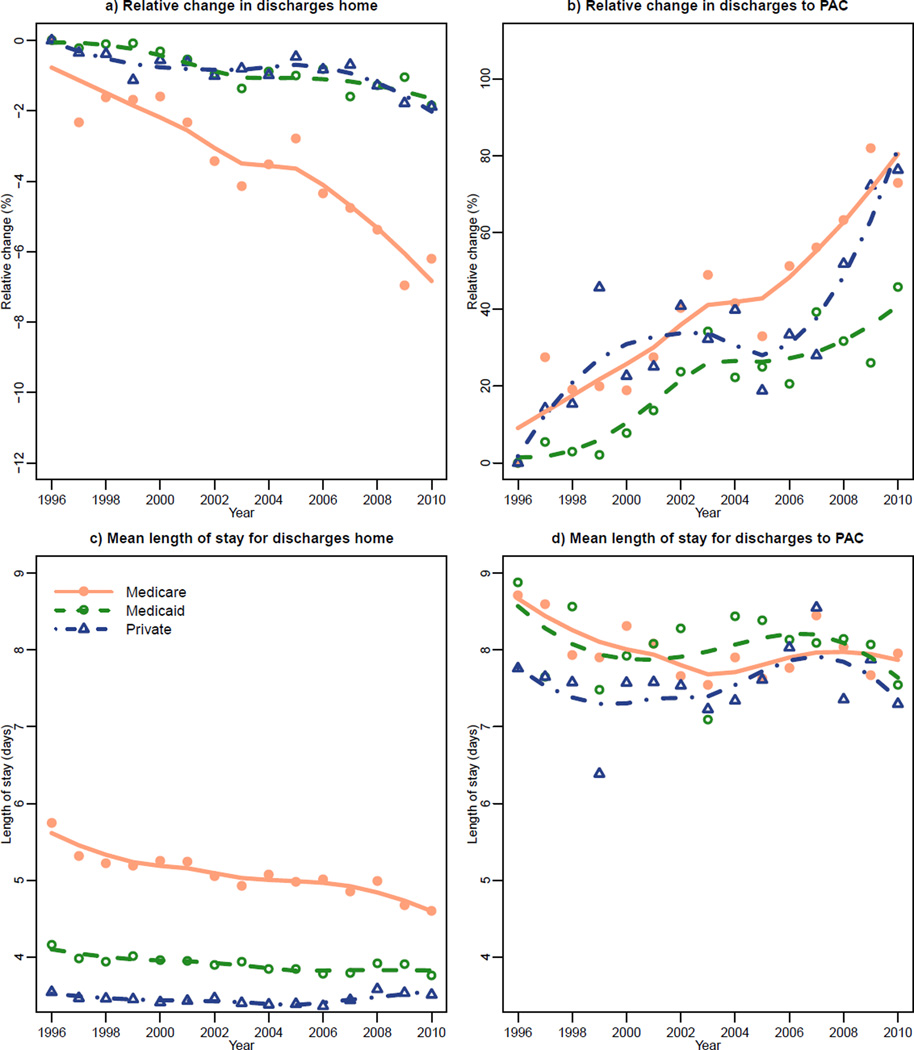
Figure 2. Trends in length of stay and discharges to post-acute care and home, stratified by payor source.
Trends in the percentage of patients discharged home or to post-acute care facilities (PAC) are shown using loess smoothing (data points are represented as filled circles, unfilled circles, and unfilled triangles, respectively). Trends are calculated as a relative percent change compared to 1996 levels. Length of stay is reported as mean number of days. For those discharged to PAC, among Medicare patients slope is 4.69 (95% CI 3.69– 5.69; p-value <0.001), among Medicare patients slope is 2.85 (2.05–3.65; p-value <0.001), and among patients with private insurance slope is 3.617 (1.99–5.24; p-value 0.001).
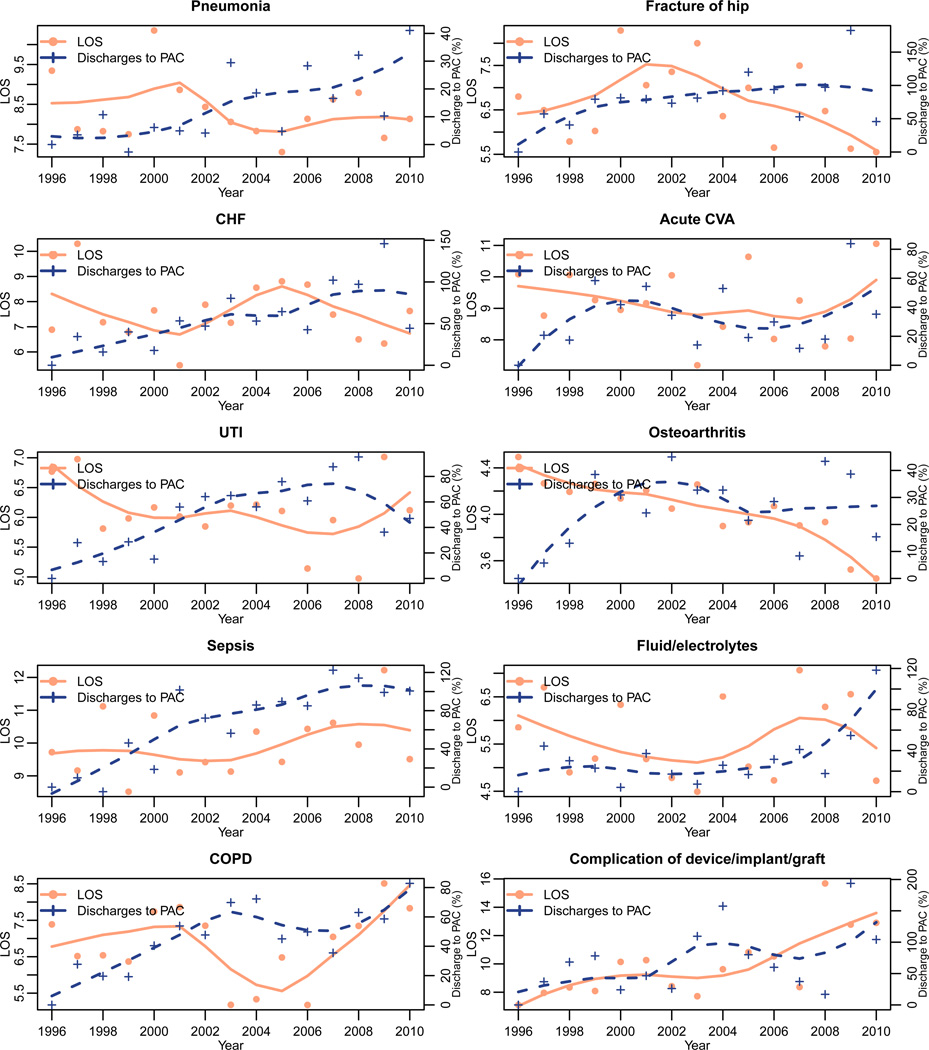
Figure 3. Trends in length of stay and discharges to post-acute care by diagnosis.
Trends in mean length of stay (left Y-axis, filled circles) and relative percent change in discharge to PAC compared to 1996 levels (right Y-axis, + signs) are displayed over time within each of the ten most common diagnoses associated with discharge to PAC; trend lines are fit using loess smoothing. Trends are adjusted for age and for payor type.
Discharge records were abstracted for patient demographic information (age, gender, race, and marital status), primary payor source (Medicare, Medicaid, private, self-pay, other) hospital information (ownership, size, geographic location), dates of hospital admission and discharge, details regarding urgency of admission and disposition at discharge, and primary discharge diagnosis (from ICD-9-CM). Hispanic ethnicity is not captured by the NHDS. Variables with missing data were coded as a separate “Not Reported” category. Variables without a “Not Reported” category (ie., age, sex) did not have any missing data as they are imputed in the NHDS by the hot deck method for missing values that maintains the known age and sex distributions of the ICD-9 primary diagnosis codes.12 We chose not to pursue a multiple imputation method for missing values since there would be few other variables from which to predict the missing values if they were assumed to be missing at random.
Data Analysis
Graphics and the loess smoothing method were implemented in R using the loess function;13 the rest of the analyses were conducted in SAS software (version 9.3, SAS Institute Inc, Cary, NC, USA), using procedures surveyfreq, surveymeans, and surveylogistic. The survey weights included in the NHDS dataset were used to produce nationally representative estimates in all analyses. Survey weights included in the NHDS take into account the specific design and the nonresponse rate. The weight can be understood as the number of discharges that a sampled hospitalization represents.12
We first evaluated differences between patients discharged to PAC facilities and those discharged home, grouping all fifteen years of data using the variables above. Differences of ≥10% were considered clinically meaningful; p-values were not used to assess differences given the large sample size. To assess other temporal trends that may affect discharge destination, we plotted concurrent trends in age, length of stay, and payor source, all dichotomized by discharge destination. All trends were age-adjusted by the US Census population in 2003, the midpoint of our analysis. We calculated relative percent changes for each year using 1996 rates as a baseline. In evaluating changes in payor subgroups, we restricted our analysis to Medicare, Medicaid, and private payors as these accounted for the majority (91.5%) of hospitalizations in our analysis and simplified presentation of payor trends.
To evaluate the trends stratified by the different factors of interest, we considered two modeling approaches: 1) a linear regression on the rates or mean LOS with year as the independent variable for each level of the stratification variable, for example, in evaluating changes in payor there was a linear regression for Medicaid, Medicare and private payor, and 2) a smoothing approach that would allow us to assess changes beyond random variation. The slopes of the linear regression per level in the stratification variable are reported in Table 1 of Supplementary Digital Content 2.
To assess the temporal trends we evaluated the raw trends as well as their local regression (loess) smoothing trends with a span of 0.75 and of degree 2 of a Gaussian family.14 The loess smoothing method consists in finding the best fit of the data where a local regression of a specific degree is fitted using data from the neighbors at each given point. The span controls the amount of neighboring points that are used to fit the regression at each given point and the degree the polynomial degree that is fit in the local regression; the Gaussian family translates into fitting the local regression using least squares. We considered other parameters in the loess smoothing such as a span of 0.5 and degree of 1, which provided similar smoothing curves as the chosen settings (Figure 1, Supplementary Digital Content 2).
We calculated the ten most common primary discharge diagnoses associated with transfer to a PAC facility, comparing the mean percent of patients discharged with that primary diagnosis over the 1996–97 period to the mean percent in 2009–10 to evaluate trends. We used the Agency for Healthcare Research and Quality’s Clinical Classification Software categories15 to aggregate ICD-9 codes into clinically relevant groups. We excluded obstetric diagnoses (such as uncomplicated delivery, representing 14.3% of all discharges) for the purposes of this analysis, as well as diagnoses with less than a one percent overall prevalence. We chose to use two years of data for the beginning and end dates of this analysis to ensure stability of estimates and to reduce possible temporal influences on a single year of data. Then, we calculated absolute numbers of patients discharged with each diagnosis, subtracting the observed percentage discharged with each diagnosis in 2009–2010 by the expected if 1996–97 rates were applied to 2009–10. In this way, we adjust for the larger number of overall discharges in 2009–10 compared to 1996–97. This comparison is not adjusted for age or payor. We also evaluated temporal trends in rates of discharge to PAC facilities and LOS within each of the ten most common diagnoses associated with discharge to PAC facilities to evaluate for a “substitution effect” of PAC facility care for continued inpatient hospital care in an age- and payor-adjusted analysis.
Finally, we conducted multiple logistic regression to analyze the effect of age, payor source, length of stay, and year on the dependent variable of discharge to PAC facility versus home. This analysis was conducted on the visit data, so each record on the dataset corresponds to a hospitalization recorded in the NHDS survey. The variables included in the model were chosen as those that were 1) most different between those discharged home and to PAC facilities; 2) were most expected clinically to affect discharge destination; and 3) were captured by the NHDS. Year was treated as a categorical variable to allow for nonlinear changes in the logit of the probability of discharge to PAC facilities over time.The study received approval as an exempt study by the Colorado Multiple Institutional Review Board (COMIRB).
Results
After inclusion and exclusion criteria were applied, 2.99 million sampled patient discharges were included in the analysis, representing approximately386 million discharges nationally during the 15-year study period. Patients discharged to PAC facilities tended to be older; 50.7% of patients discharged to PAC facilities were age ≥80years (Table 1), and by 2010 40.0% of hospitalizations in this age group ended with a PAC stay. Patients discharged to PAC facilities also tended to be emergently admitted, have Medicare as a payor source (82.3% of all patients discharged to PAC facilities used Medicare benefits for their preceding hospitalization), and have a longer length of stay (>90% had a stay of 3 days or more). Differences between patients discharged home and those discharged to PAC facilities were minimal for other categories, including gender, race/ethnicity, or any hospital characteristics (size, region, ownership including for-profit status, data not shown).
Table 1.
Characteristics of patients discharged to post-acute care facilities (PAC) and home from 1996 to 2010
| Characteristic | Discharged to PAC N=2,644,657 (88.4%) |
Discharged home N=345,367 (11.6%) |
PAC - home difference |
|---|---|---|---|
| % (95%CI) | % (95%CI) | Δ (95% CI) | |
| Age (median, yrs) | 76.6 (76.5–76.7) | 52.9 (52.8–52.9) | 23.7 (23.6 to 23.8) |
| 18–44 | 3.3 (3.2–3.4) | 38.3 (38.2–38.4) | −35.0 (−34.9 to –35.2) |
| 45–64 | 12.5 (12.3–12.8) | 27.5 (27.4–27.6) | −14.9 (−14.7 to −15.2) |
| 65–79 | 33.5 (33.2–33.8) | 22.8 (22.7–22.9) | 10.6 (10.3 to 10.9) |
| ≥80 | 50.7 (50.4–51.0) | 11.4 (11.3–11.4) | 39.3 (39.0 to 39.6) |
| Male gender | 37.0 (36.7–37.3) | 37.2 (37.1–37.3) | −0.2 (−0.1 to −0.6) |
| Race | |||
| White | 66.6 (66.4–66.9) | 61.6 (61.5–61.7) | 5.1 (4.8 to 5.4) |
| Black or African-American | 9.0 (8.8–9.1) | 12.3 (12.2–12.3) | −3.3 (−3.1 to −3.5) |
| Amer. Indian/Alaska Native | 0.3 (0.2–0.3) | 0.5 (0.4–0.5) | −0.2 (−0.2 to −0.2) |
| Asian, N. Hawaiian, or OPI | 0.8 (0.7–0.8) | 1.7 (1.7–1.8) | −1.0 (−0.9 to −1.0) |
| Multiple races | 0.4 (0.3–0.4) | 0.8 (0.8–0.8) | −0.4 (−0.4 to −0.5) |
| Not reported | 22.0 (21.7–22.2) | 21.5 (21.4–21.6) | 0.5 (0.2 to 0.7) |
| Marital status | |||
| Married | 17.1 (16.9–17.4) | 32.9 (32.8–33.0) | −15.8 (−15.5 to −16.0) |
| Non-married | 36.8 (36.5–37.1) | 28.3 (28.2–28.4) | 8.5 (8.2 to 8.8) |
| Not reported | 46.1 (45.7–36.4) | 38.8 (38.7–38.9) | 7.2 (6.9 to7.6) |
| Type of admission | |||
| Non-elective | 75.7 (75.4–76.0) | 62.4 (62.3–62.5) | 13.3 (12.9 to 13.6) |
| Elective | 16.0 (15.7–16.3) | 26.2 (26.1–26.4) | −10.3 (−10.0 to −10.6) |
| Not reported | 8.4 (8.2–8.6) | 11.4 (11.3–11.5) | −3.0 (−2.8 to −3.2) |
| Length of stay | |||
| Same-day discharge | 0.4 (0.3–0.4) | 1.7 (1.6–1.7) | −1.3 (−1.3 to −1.4) |
| 1–2 days | 9.1 (8.9–9.3) | 42.0 (41.9–42.1) | −32.9 (−32.7 to −33.2) |
| 3–7 days | 55.8 (55.5–56.1) | 44.4 (44.3–44.5) | 11.4 (11.1 to 11.7) |
| >7 days | 34.8 (34.5–35.1) | 11.9 (11.9–12.0) | 22.8 (22.5 to 23.1) |
| Source of payment | |||
| Medicare | 82.3 (82.0–82.5) | 36.1 (36.1–36.3) | 46.1 (45.8 to 46.4) |
| Medicaid | 4.9 (4.8–5.1) | 15.3 (15.2–15.4) | −10.4 (−10.2 to −10.5) |
| Private insurance | 10.7 (10.5–10.9) | 39.2 (39.1–39.3) | −28.5 (−28.3 to −28.7) |
| Self-pay | 0.8 (0.7–0.8) | 5.5 (5.5–5.6) | −4.7 (−4.7 to −4.8) |
| Other | 0.6 (0.6–0.6) | 2.2 (2.2–2.2) | −1.6 (−1.5 to −1.6) |
| Not reported | 0.7 (0.7–0.8) | 1.7 (1.6–1.7) | −0.9 (−0.9 to −1.0) |
Number of patients in each group and corresponding percentage are reported in raw (unweighted) form. There was no difference of more than 10% in geographic region of hospital, hospital size, and hospital ownership so they are not presented here. Also not shown is source of admission, as patients from locations other than home were often coded as coming from the Emergency Department. Nonelective admissions refer to those coded as urgent or emergent. N. Hawaiian = native Hawaiian; OPI = other Pacific Islander. Bold signifies a difference between groups of ≥10%, which we deemed a clinically important difference.
While the proportion of hospital discharges to PAC facilities increased most rapidly in the 18–64 year-old age group (a 100% relative increase from 3.6 to 7.2 percent), this was eclipsed in terms of absolute numbers by 65–79 year-olds (13.1 to 20.0%; relative increase 52.6%) and those 80 years and up (32.7 to 40.0%; relative increase 22.3%, Figure 1).The oldest age group (≥80 years) had the largest decrease in hospital length of stay before discharge to a PAC facility, from 7.2 to 6.4 days, though LOS decreased for all age groups and payors.
All payors exhibited large relative increases in the number of admissions they covered resulting in a PAC facility stay; private payors had similar increases to Medicare and Medicaid (Figure 2). Elective and nonelective admissions exhibited similar relative increases in discharges to PAC facilities (Figure 2 of Supplemental Digital Content 2), though nonelective admissions were much more commonly discharged to PAC facilities overall. In multivariable analysis, the odds of discharge to a PAC facility in 2010 compared to 1996 was still significant after adjustment for changes in payor type, age, and length of stay (OR 1.78, 95% CI 1.69–1.87).
Eight of the ten most common conditions treated in the hospital that ended with a PAC facility stay were also those with the largest absolute changes in prevalence over the time period, with acute kidney injury (increase) and coronary artery disease (decrease) the other two most changed diagnoses during the study period (Table 2). Nearly all (>90%) “osteoarthritis” admissions were elective, suggesting they primarily represented elective joint surgery. Sepsis was the discharge diagnosis increasing most in absolute terms over time in those discharged to PAC facilities; pneumonia and acute cerebrovascular accidents were most decreased in absolute terms in those discharged to PAC facilities over the time period before adjustment for age or payor. Sepsis increased most in frequency among younger patients, with a relative increase of 110% in 2010 compared to 1996 in the youngest cohort (18–64 year-olds), 33% in 65–79 year-olds, and 17% in those 80 or older.
Table 2.
Most common and most changed discharge diagnoses for patients discharged to PAC from 1996 to 2010
| Discharge diagnosis | % (95% CI) | N (thousands) |
Change in prevalence, % (95% CI) |
N (thousands) |
|---|---|---|---|---|
| 1) Pneumonia | 6.5 (6.4–6.7) | 2911.6 | −3.0 (−3.6 to −2.4) | −820.0 |
| 2) Fracture of hip | 5.4 (5.3–5.5) | 2408.0 | −2.2 (−2.8 to −1.7) | −617.8 |
| 3) CHF | 4.9 (4.8–5.0) | 2191.1 | 0.2 (−0.3 to +0.7) | 59.5 |
| 4) Osteoarthritis | 4.7 (4.6–4.8) | 2096.0 | 1.9 (1.4 to 2.4) | 529.8 |
| 5)Acute CVA | 4.3 (4.2–4.5) | 1938.5 | −2.6 (−3.2 to −2.0) | −713.6 |
| 6) UTI | 4.1 (4.0–4.2) | 1834.9 | 0.8 (0.3 to 1.3) | 220.2 |
| 7) Sepsis | 4.0 (3.9–4.1) | 1775.4 | 1.9 (1.3 to 2.4) | 536.5 |
| 8) Fluid/electrolytes | 3.1 (3.0–3.2) | 1390.6 | −1.1 (−1.5 to −0.7) | −297.4 |
| 9) COPD | 2.6 (2.5–2.6) | 1139.7 | 0.1 (−0.3 to +0.5) | −16.3 |
| 10) Complication of device/implant/graft | 2.3 (2.2–2.4) | 1038.4 | 1.2 (0.8 to 1.5) | 319.6 |
The ten most prevalent discharge diagnoses aggregated over the entire study period are presented, using AHRQ CCS categories derived from discharge ICD-9 codes. Percent changes in prevalence were computed by comparing the mean prevalence of these diagnoses in 1996 and 1997, compared to the mean prevalence in 2009 and 2010. The change in prevalence was calculated by subtracting the actual number of discharges in 2009–10 from the expected number if 1996–97 rates had applied in 2010. All N’s are weighted. CHF = Congestive heart Failure, Acute CVA = Acute cerebrovascular accident, UTI = Urinary tract infection, COPD = Chronic obstructive pulmonary disease, N = number of discharged patients, PAC = Post-acute care.
Three diagnoses (pneumonia, hip fracture/osteoarthritis, and sepsis) were most associated with decreasing LOS and increasing discharges to PAC facilities, though the relationship between these trends varied over time (Figure 3). Adjusting for payor and age resulted in a trend towards increased discharges to PAC facilities for pneumonia, in contrast to our overall findings in Table 2.Trends in LOS and discharges to PAC facilities within each diagnosis, displayed within each payor type, is illustrated in Figure 3 of Supplemental Digital Content 2.
Discussion
This nationally-representative initial description of patients being discharged to PAC facilities revealed that the increase in discharges to these facilities and decreases in hospital LOS extends across payors, patient demographics, and several diagnosis groups with important implications for policy makers and hospital/PAC leadership. Several important facets of these trends are worth noting: first, those 80 years old and older represent more than half of all PAC facility discharges, and more than 40% of hospitalizations in this age group end with a PAC facility stay. Second, patients treated for pneumonia, hip fracture, and sepsis may be experiencing “substitution” of PAC facility care for a prolonged inpatient stay, as their hospital length of stay decreases or is constant and discharges to PAC facilities increase. Third, adjusting for changes in age, payor source, and length of stay did not eliminate the significantly increased odds of discharge to PAC facilities in 2010 compared to 1996, pointing out that unexamined variables likely contribute to this trend.
Changes in patient, provider, and payor factors may all have influenced the trends we discovered. In terms of patient-level factors, the changing epidemiology of diagnoses treated preceding a PAC facility stay may influence PAC facility discharges. For example, hospitalizations for sepsis are increasing nationally.16 These patients have both physical and cognitive deficits after critical illness that often are difficult to address in the home setting and may persist for years, resulting in significant post-discharge care utilization.17–19 In pneumonia, significant work has been conducted using severity scores to support treating many patients with community-acquired pneumonia in the community safely, potentially resulting in a higher threshold for admission.20,21 Once admitted, treatment of this population of potentially sicker patients may also focus on decreasing LOS, with unintended consequences.22
The rise of hospitalist care in the United States, which coincides with these trends,23 may be the most significant provider-level factor influencing these results. Hospitalists decrease length of stay and costs in the acute setting, but there is evidence of cost-shifting to the post-acute environment, including increased discharges to PAC facilities.24 This may in part be due to the limited training25 or feedback on the use of PAC facilities hospitalists receive, leaving significant uncertainly about the role of PAC for individual patients.26
Payor influences may be most significant. Medicare’s payment reforms -- incenting shorter hospital stays -- may also have influenced other payors resulting in more discharges to PAC facilities in younger cohorts.27 The “quicker and sicker” high-throughput culture of many U.S. hospitals could then result in care shifting to the PAC facility setting, at significant cost to the U.S. health care system as a whole. Currently, hospitals are not penalized for readmissions from PAC facilities, but are penalized by Medicare for high risk-adjusted 30-day readmission rates for patients with pneumonia, for example, which may drive discharges to PAC facilities.
The implications of these findings are far-reaching and require further exploration. The advanced age of the majority of patients discharged to PAC facilities mandates research to determine which patients benefit most from a PAC facility stay,26 and how best to rehabilitate them. In the United States currently, only 28% of Medicare patients return to the community from a PAC facility within 100 days of their index hospital admission.28 Little evidence exists to guide therapy for increasingly common conditions discharged to PAC facilities (eg, sepsis), nor how much of these patients’ post-discharge health care utilization and functional impairment is modifiable.29,30 National data demonstrates significant geographic variability in spending on PAC and outcomes of PAC; the link between these is not well-established.8,31 New payment reforms, such as penalties for 30-day readmissions from PAC facilities,32 or for Accountable Care Organizations who will now be responsible for the costs and outcomes of discharging patients in an unprecedented way, may offer substantial impetus to advance the science.
Our large, nationally-representative sample is a key strength of this study. However, we are unable to audit the data. Thus, errors in ICD-9 coding, for example, may have biased our results. Previous investigators have found the data reliable when compared to outside samples.16,33 Our results do not apply to Federal hospitals (not included in NHDS), and children were excluded from this analysis. Our analysis is descriptive; we report associations but were unable to assess to what extent changes in patient characteristics caused the increased use of PAC facilities in the United States.
Important concurrent trends in other factors (changes in use of home health care, supply of PAC facility beds, PAC facility affiliations with hospitals, geographic trends in the proportion of elderly patients or managed care penetration, hospital readmissions) likely also influence the use of PAC facilities but we could not evaluate these in this analysis. In particular, there is clear evidence of regional variation in use of PAC among Medicare patients, the drivers of which are unknown and unable to be explored using this dataset. Geographic region of discharging hospital was captured as four regions in the NHDS, which prevented similar analysis to the Dartmouth Atlas; this may be why differences between patients discharged to home and to PAC facilities did not differ significantly by region. The drivers of high and low use of PAC facilities on a regional level would be important to identify in a subsequent analysis. The NHDS does not collect data on patient comorbidities, functional status, or social support, all of which could be expected to affect discharge destination. The NHDS also does not separate long-term care from short-term skilled nursing care and it is likely that some proportion of facility discharges in our analysis represent long-term care. However, we believe the contribution of discharges to long-term care to the trend we have observed is likely to be minimal because both the number of nursing homes and number of long-term nursing home residents has been steadily declining nationally since 2003.34 While the data presented documents discharges to PAC facilities, the outcomes of this care after hospital discharge are not captured.
Increasing numbers of hospitalized patients are being discharged to PAC facilities; this increase presents substantial challenges to clinicians to ensure the safety and cost-effectiveness of this care. Further research is needed to identify which patients are most likely to benefit as well as structures and processes of hospital and post-hospital care that maximize patient-centered outcomes and reduce costs.
Supplementary Material
Acknowledgments
Funding sources: Drs. Burke, Juarez-Colunga, Prochazka, and Ginde were supported by the Colorado Clinical Translational Science Institute (NIH UL1 TR001082) and Drs. Burke, Levy, and Prochazka by the VA HSR&D Center for Innovation: Value-Centered and Value-Driven Care. Dr. Ginde was supported by NIH grant K23AG040708. These sponsors had no role in the design, conduct, analysis, interpretation, or presentation of the study.
Footnotes
Meeting: none
References
- 1.Halm EA, Fine MJ, Kapoor WN, Singer DE, Marrie TJ, Siu AL. Instability on hospital discharge and the risk of adverse outcomes in patients with pneumonia. Arch Intern Med. 2002;162(11):1278–1284. doi: 10.1001/archinte.162.11.1278. [DOI] [PubMed] [Google Scholar]
- 2.Halm EA, Magaziner J, Hannan EL, et al. Frequency and impact of active clinical issues and new impairments on hospital discharge in patients with hip fracture. Arch Intern Med. 2003;163(1):108–113. doi: 10.1001/archinte.163.1.107. [DOI] [PubMed] [Google Scholar]
- 3.Kosecoff J, Kahn KL, Rogers WH, et al. Prospective payment system and impairment at discharge. The “quicker-and-sicker” story revisited. JAMA. 1990;264(15):1980–1983. [PubMed] [Google Scholar]
- 4.Qian X, Russell LB, Valiyeva E, Miller JE. “Quicker and sicker” under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63(1):1–27. doi: 10.1111/j.1467-8586.2010.00369.x. [DOI] [PubMed] [Google Scholar]
- 5.Buntin MB, Colla CH, Escarce JJ. Effects of payment changes on trends in post-acute care. Health Serv Res. 2009;44(4):1188–1210. doi: 10.1111/j.1475-6773.2009.00968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ackerly DC, Grabowski DC. Post-acute care reform--beyond the ACA. N Engl J Med. 2014;370(8):689–691. doi: 10.1056/NEJMp1315350. [DOI] [PubMed] [Google Scholar]
- 7.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Rise of Post-Acute Care Facilities as a Discharge Destination of US Hospitalizations. JAMA Intern Med. 2015;175(2):295–296. doi: 10.1001/jamainternmed.2014.6383. [DOI] [PubMed] [Google Scholar]
- 8.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff Proj Hope. 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff Proj Hope. 2013;32(5):864–872. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mechanic R. Post-acute care--the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692–694. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 11.Lin W-C, Kane RL, Mehr DR, Madsen RW, Petroski GF. Changes in the use of postacute care during the initial Medicare payment reforms. Health Serv Res. 2006;41(4 Pt 1):1338–1356. doi: 10.1111/j.1475-6773.2006.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat. 2000;(39):1–42. [PubMed] [Google Scholar]
- 13.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; http://www.R-project.org/. [Google Scholar]
- 14.Cleveland W. Visualizing Data. Lafayette, IN: Hobart Press; 1993. [Google Scholar]
- 15.Cowen ME, Dusseau DJ, Toth BG, Guisinger C, Zodet MW, Shyr Y. Casemix adjustment of managed care claims data using the clinical classification for health policy research method. Med Care. 1998;36(7):1108–1113. doi: 10.1097/00005650-199807000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 17.Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J RespirCrit Care Med. 2014;190(1):62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc. 2012;60(6):1070–1077. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yealy DM, Auble TE, Stone RA, et al. Effect of increasing the intensity of implementing pneumonia guidelines: a randomized, controlled trial. Ann Intern Med. 2005;143(12):881–894. doi: 10.7326/0003-4819-143-12-200512200-00006. [DOI] [PubMed] [Google Scholar]
- 21.Marrie TJ, Lau CY, Wheeler SL, Wong CJ, Vandervoort MK, Feagan BG. A controlled trial of a critical pathway for treatment of community-acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin. JAMA. 2000;283(6):749–755. doi: 10.1001/jama.283.6.749. [DOI] [PubMed] [Google Scholar]
- 22.Carratalà J, Garcia-Vidal C, Ortega L, et al. Effect of a 3-step critical pathway to reduce duration of intravenous antibiotic therapy and length of stay in community-acquired pneumonia: a randomized controlled trial. Arch Intern Med. 2012;172(12):922–928. doi: 10.1001/archinternmed.2012.1690. [DOI] [PubMed] [Google Scholar]
- 23.Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3):152–159. doi: 10.1059/0003-4819-155-3-201108020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ward KT, Eslami MS, Garcia MB, McCreath HE. Do Internal Medicine Residents Know Enough About Skilled Nursing Facilities To Orchestrate a Good Care Transition? J Am Med Dir Assoc. 2014 doi: 10.1016/j.jamda.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kane RL. Finding the right level of posthospital care: “We didn’t realize there was any other option for him”. JAMA. 2011;305(3):284–293. doi: 10.1001/jama.2010.2015. [DOI] [PubMed] [Google Scholar]
- 27.Carter GM, Jacobson PD, Kominski GF, Perry MJ. Use of diagnosis-related groups by non-Medicare payers. Health Care Financ Rev. 1994;16(2):127–158. [PMC free article] [PubMed] [Google Scholar]
- 28.Kramer A, Fish R, Min S. Community Discharge and Rehospitalization Outcome Measures. Washington (D.C.): Medicare Payment Advisory Commission; 2013. Apr, [Accessed March 24, 2014]. http://medpac.gov/documents/Apr13_CommunityDischarge_CONTRACTOR.pdf. [Google Scholar]
- 29.Mehlhorn J, Freytag A, Schmidt K, et al. Rehabilitation interventions for postintensive care syndrome: a systematic review. Crit Care Med. 2014;42(5):1263–1271. doi: 10.1097/CCM.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 30.Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev. 2013;2:CD004294. doi: 10.1002/14651858.CD004294.pub3. [DOI] [PubMed] [Google Scholar]
- 31.Newhouse JP, Garber AM. Geographic variation in health care spending in the United States: insights from an Institute of Medicine report. JAMA. 2013;310(12):1227–1228. doi: 10.1001/jama.2013.278139. [DOI] [PubMed] [Google Scholar]
- 32.House Committee on Ways and Means. [Accessed March 5, 2014];PAC Reform Fact Sheet. 2013 Jun; http://waysandmeans.house.gov/uploadedfiles/pac_reform_fact_sheet.pdf.
- 33.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005;294(21):2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 34.Nursing Home Compendium. Washington (D.C.): Center for Medicare and Medicaid Services; 2013. [Accessed September 16, 2014]. http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/nursinghomedatacompendium_508.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.