Abstract
Sputum samples from new tuberculosis (TB) cases were collected over 2 years as part of a prospective study in the northeastern part of Lima, Peru. To measure the contribution of recent transmission to the high rates of multidrug resistance (MDR) in this area, Mycobacterium tuberculosis complex (MTBc) isolates were tested for drug susceptibility to first-line drugs and were genotyped by spoligotyping and 15-locus mycobacterial interspersed repetitive-unit (MIRU-15)-variable-number tandem repeat (VNTR) analysis. MDR was found in 6.8% of 844 isolates, of which 593 (70.3%) were identified as belonging to a known MTBc lineage, whereas 198 isolates (23.5%) could not be assigned to these lineages and 12 (1.4%) represented mixed infections. Lineage 4 accounted for 54.9% (n = 463) of the isolates, most of which belonged to the Haarlem family (n = 279). MIRU-15 analysis grouped 551/791 isolates (69.7%) in 102 clusters, with sizes ranging from 2 to 46 strains. The overall high clustering rate suggests a high level of recent transmission in this population, especially among younger patients (odds ratio [OR], 1.6; P = 0.01). Haarlem strains were more prone to cluster, compared to the other families taken together (OR, 2.0; P < 0.0001), while Beijing (OR, 0.6; P = 0.006) and LAM (OR, 0.7; P = 0.07) strains clustered less. Whereas streptomycin-resistant strains were more commonly found in clusters (OR, 1.8; P = 0.03), clustering rates did not differ between MDR and non-MDR strains (OR, 1.8; P = 0.1). Furthermore, only 16/51 MDR strains clustered with other MDR strains, suggesting that patients with primary MDR infections acquired the infections mostly from index cases outside the study population, such as retreated cases.
INTRODUCTION
Tuberculosis (TB) is among the top 10 causes of death in the global ranking (1). Although Peru accounts for only 3% of the population of the Americas, it has 9.5% of the region's TB cases. According to the World Health Organization (WHO), 21,916 new cases of pulmonary TB were reported in Peru between January and November 2013 (2). Urban areas are more affected, with 59% of all Peruvian TB cases, 82% of multidrug-resistant (MDR) TB cases, and 93% of extensively drug-resistant (XDR) TB cases occurring in Lima. Within the capital area, TB cases are heterogeneously distributed. The most affected districts are located in the northeast and together represent 86% of the reported cases in the capital (3, 4). San Juan de Lurigancho is the most populated district in this area, with 1,004,339 inhabitants (5), and reports a pulmonary TB incidence rate of 193 cases per 100,000 inhabitants, a smear-positive TB incidence rate of 126 cases per 100,000 inhabitants (6), and an overall MDR prevalence of 7% (7), exceeding the national averages for the three indicators of 103 cases per 100,000 inhabitants, 62 cases per 100,000 inhabitants, and 5.3%, respectively (8). The HIV prevalence among TB patients in this setting is similar to the national prevalence, which in 2008 was 2.6% (9).
Peru has been considered a good example of the beneficial effects of implementing directly observed therapy short course (DOTS) in a country's health system (10). Nevertheless, national surveys from 1996 and 2006 have shown increases in MDR rates from 2.4% to 5.3% among new cases and from 15.7% to 23.6% among previously treated cases (11). This paradox of improved TB management and worsening resistance prevalence has been explained by increases in the notified cases, i.e., in case detection, although treatment outcomes remain poor (12). Basically, the observed increases in MDR-TB rates may result from two factors, i.e., transmission of MDR-TB and acquired resistance due to ineffective TB treatment selecting for spontaneous mutations in specific genes associated with drug resistance (13, 14).
Molecular strain typing (genotyping) has significantly contributed worldwide to the understanding of TB epidemiology and transmission dynamics (15, 16), by confirming outbreaks (17) and identifying the clonal spread of successful strains, including MDR strains (18, 19). Furthermore, molecular typing has shown that the Mycobacterium tuberculosis complex (MTBc) has a diverse population structure, being composed of seven lineages of human importance, subdivided into families (20, 21) that differ not only in their geographical occurrence but also in their drug resistance profiles (19, 22). Epidemiological data on TB in Peru have so far consisted largely of reports of the number of cases detected, demographic data for the cases, and drug susceptibility profiles of M. tuberculosis isolates. Despite the increased number of recent studies on genetic diversity (23–25), data on the molecular epidemiology of TB in this country are limited; the SpolDB4.0 spoligotyping database includes only 96 Peruvian strains among the 39,609 published entries (26).
To gain more insights regarding the extent of ongoing transmission and its contribution to the high prevalence of MDR-TB, we aimed to describe the circulating MTBc genotypes among new pulmonary TB cases. We used a combination of 15-locus myocobacterial interspersed repetitive-unit (MIRU-15)-variable-number tandem repeat (VNTR) analysis and spoligotyping to define the TB population structure and to perform a cluster analysis to measure the level of recent transmission and its possible association with drug resistance.
MATERIALS AND METHODS
Study setting and population.
This study was embedded in a prospective cohort study of new cases of sputum smear-positive pulmonary TB to assess the contributions of reinfection versus reactivation to recurrent episodes in San Juan de Lurigancho, a semiurban district in the northeastern part of Lima. Patient recruitment was conducted between March 2010 and December 2011 in all 34 public health care facilities (one hospital and 33 first-level health care facilities) in the district. All of these health care facilities provide TB diagnosis and treatment free of charge to patients. For this study, sputum samples were collected from previously untreated pulmonary TB subjects >18 years of age.
Culture and drug susceptibility testing.
Sputum samples were transported to the microbiology laboratory at the Institute of Tropical Medicine Alexander von Humboldt (Lima, Peru) within 6 h after being produced. Samples were cultured on the day they arrived or were kept at 4°C if they arrived late in the afternoon or during the weekend. Quality control assessments were performed for all sputum samples, to determine the presence of blood, mucus, or saliva. Smear microscopy was performed by following the Ziehl-Neelsen method, and samples were cultured on two slopes of Löwenstein-Jensen (LJ) medium after decontamination with the N-acetyl-l-cysteine (NalC)-sodium hydroxide method (27). The MTBc isolates were subjected to drug susceptibility testing (DST) using the 7H10 agar proportion method (28), with the following drug concentrations: 0.2 μg/ml and 1 μg/ml isoniazid, 1 μg/ml rifampin, 2 μg/ml streptomycin, and 6 μg/ml ethambutol. Quality assurance activities included regular checking of the reagents used in test procedures (including expiration dates) and regular maintenance and calibration of equipment.
Data collection methods.
Clinical, bacteriological (smear microscopy results during treatment, DST results, and treatment outcomes), and sociodemographic (name, sex, and age) data were retrieved from patients' files and treatment charts.
DNA isolation.
To obtain genomic DNA for spoligotyping and MIRU-15 typing, mycobacterial colonies grown on LJ medium were resuspended in 500 μl of 1× Tris-EDTA buffer (10 mM Tris-HCl, 1 mM EDTA disodium [pH 8.0]) and heat inactivated at 95°C for 20 min. The suspension was centrifuged at 14,000 rpm for 15 min to pellet cell debris. The supernatant, containing DNA, was stored at −20°C and used in PCRs.
Spoligotyping.
Spoligotyping was performed using primers DRa and DRb, corresponding to the direct repeat (DR) region of the MTBc genome, according to the procedure described by Kamerbeek et al. (29). Amplification and hybridization were performed using a membrane prepared in-house. Detection of hybridized DNA was achieved by using enhanced chemiluminescence (ECL) detection liquid (Amersham Biosciences) followed by exposure to X-ray film (Hyperfilm ECL; Amersham Biosciences), in accordance with the instructions of the manufacturer. Results were read manually to obtain a complete pattern of the presence or absence of the respective spacers.
MIRU-VNTR analysis.
MIRU-VNTR analysis is a PCR-based typing method that determines the copy number of tandem repeats for independent loci (MIRUs) that were found to be polymorphic in the MTBc. For budgetary and logistic reasons, standardized MIRU-15 analyses were performed with the collaboration of the Kobe Institute of Health (Kobe, Japan), the Molecular Mycobacteriology Laboratory (Borstel, Germany), and GenoScreen (Lille, France). Our external collaborators performed the analyses according to the capillary electrophoresis protocol (30–32). Each locus was amplified separately by simplex PCR with the Qiagen Hotstart Taq polymerase kit including Q solution, according to published guidelines (30). Products were analyzed by electrophoresis using 2% agarose (Promega) gels. The H37Rv reference strain was included in each batch of PCRs and gels. To ensure the same level of performance among the participating laboratories, we included blind controls among the samples for each collaborator; no deviations were observed.
MIRU-15 analysis may lack sufficient power of resolution for the classification of Beijing strains (32). Therefore, we randomly selected 62 Beijing strains to be analyzed by MIRU-VNTR typing using 24 loci, and we compared the clustering rates between the 2 methods.
DNA fingerprint analysis.
Basic strain classification in phylogenetic families was performed using the MIRU-VNTRplus server (22, 33). To determine the spoligotype family (26), patterns were compared with those in the international database of spoligotyping patterns (http://www.miru-vntrplus.org/MIRU/index.faces) and the rules for the spoligotype family prototype (16). MIRU-VNTR profiles with double alleles at a single locus were considered to represent heterogeneous populations of the same strain, whereas those with double alleles at 2 or more loci were considered to represent mixed infections or to indicate cross-contamination (34, 35).
For the clustering analysis, we included all samples with complete spoligotyping and MIRU-15 results. A cluster was defined as two or more MTBc isolates sharing identical MIRU-15 and spoligotyping patterns. Heterogenous isolates with double alleles at only one locus were included in the cluster analysis (both patterns were compared). Isolates with no PCR amplicon at only one locus were treated as missing data at the respective locus and also were included, whereas isolates lacking amplicons at two or more loci were excluded from the calculation of clustering rates.
Data management and analysis.
Demographic information (sex and age) and smear, culture, and DST results were entered into a dedicated Access database. Quality control assessment for data entry was performed for 10% of all records and 100% of DST results. For all molecular data (spoligotyping and MIRU-15 analysis), systematic quality control was performed through double data entry.
Spoligotyping patterns in a binary format were entered into an Excel spreadsheet and compared with the spoligotype database SpolDB4 using MIRU-VNTRplus. The chi-square test, or the Fisher exact test when necessary, was applied to evaluate differences in demographic (age and sex), epidemiological (M. tuberculosis families), and microbiological (drug resistance) variables. In order to determine independent risk factors, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by using logistic regression analysis (Epi Info v7). P values of <0.05 were considered significant.
Ethical considerations.
The study was approved by the institutional review board of the Cayetano Heredia University. All enrolled patients provided informed consent. Patients were assigned a unique identifier, and data were managed anonymously. Smear, culture, and DST results were communicated to the health service as soon as they were available.
RESULTS
Patients and samples.
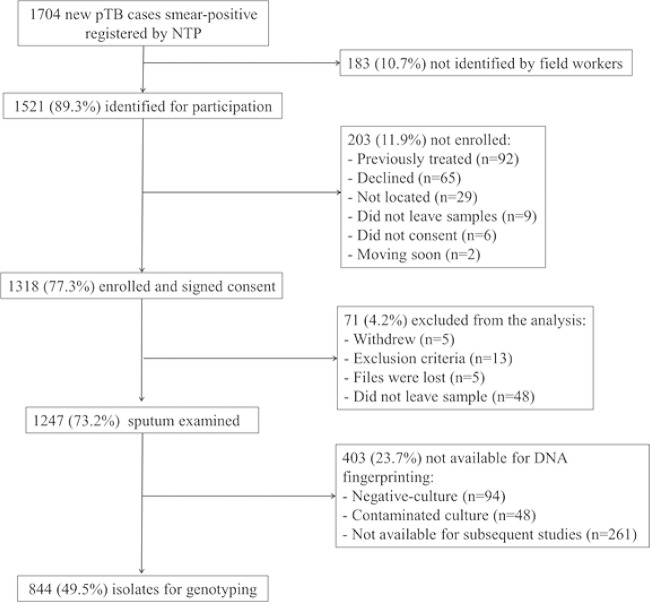
The National TB Program (NTP) registered 1,704 new cases of pulmonary TB in San Juan de Lurigancho between March 2010 and December 2011. A total of 1,521 patients (89.3%) with a first episode of smear-positive pulmonary TB were identified for participation in the cohort study. The remaining cases (10.7%) were not identified by field workers. Of the screened cases, we enrolled 1,318 (77.3%). After thorough questioning, we excluded 71 patients (4.2%) because they withdrew (n = 5), they met the exclusion criteria (n = 13), their files were lost (n = 5), or they did not leave a sputum sample (n = 48). Of the 1,247 sputum samples analyzed, 403 (23.7%) were not available for DNA fingerprinting because the primary culture tested negative (n = 94), was contaminated (n = 48), or was not available for subsequent laboratory analysis (n = 261). Thus, the total number of cultures from different subjects that were available for DNA genotyping was 844, representing 49.5% of the 1,704 new pulmonary TB cases recorded by the NTP (Fig. 1). Age and gender distributions were similar for the total screened population and the enrolled patients with molecular data available (Table 1).
FIG 1.
Patient enrollment flowchart. pTB, pulmonary TB.
TABLE 1.
Demographic characteristics of new pulmonary smear-positive TB cases enrolled versus not enrolled in study cohort
| Patient group | Total no. (%) | Gender |
Age |
||||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) male | No. (%) female | OR (95% CI) | P | No. (%) <40 yr of age | No. (%) ≥40 yr of age | OR (95% CI) | P | ||
| Total screened | 1,521 (100.0) | 912 (60.0) | 609 (40.0) | 1.00 | 1.00 | 1,187 (78.0) | 334 (22.0) | 1.00 | 1.00 |
| Not enrolled | 226 (14.9) | 124 (54.9) | 102 (45.1) | 1.23 (0.9–1.6) | 0.2 | 182 (80.5) | 44 (19.5) | 0.9 (0.6–1.2) | 0.45 |
| Enrolled | 1,295 (85.1) | 788 (60.9) | 507 (39.1) | 0.96 (0.8–1.1) | 0.7 | 1,005 (77.6) | 290 (22.4) | 1.0 (0.9–1.2) | 0.80 |
| Enrolled with molecular data available | 844 (55.49) | 516 (61.3) | 328 (38.9) | 0.95 (0.8–1.1) | 0.6 | 653 (77.4) | 191 (22.6) | 1.0 (0.8–1.3) | 0.74 |
MIRU-15 and spoligotyping analyses were performed for all 844 M. tuberculosis isolates. Of these, 53 isolates (6.3%) were excluded from the final clustering analysis because no PCR amplicon was obtained at two or more MIRU loci for 24 of these isolates, 12 isolates were identified as mixed infections, and 17 isolates showed discrepant results between spoligotyping and MIRU patterns, suggesting a labeling error. Thus, the final data set included 791 isolates with complete sets of spoligotyping and MIRU-15 data, to allow proper cluster analysis.
Drug susceptibility testing.
DST results were available for 754/791 isolates (95.3%). In total, 207 isolates (27.5%) were resistant to at least one drug and 547 (72.5%) were fully susceptible. Fifty-one cases (6.8%) were MDR; 23 (3.1%) were monoresistant to isoniazid, 14 (1.9%) to rifampin, 35 (4.6%) to streptomycin, and 33 (4.4%) to ethambutol (Table 2).
TABLE 2.
Drug resistance patterns of 754 M. tuberculosis complex isolates
| Type of resistancea | No. (%) |
|---|---|
| Monoresistant | 105 (13.9) |
| H | 23 (3.1) |
| R | 14 (1.9) |
| S | 35 (4.6) |
| E | 33 (4.4) |
| Polyresistant (non-MDR) | 51 (6.8) |
| H + S | 15 (2.0) |
| H + E | 7 (0.9) |
| H + S + E | 9 (1.2) |
| R + E | 1 (0.1) |
| R + S | 2 (0.3) |
| S + E | 17 (2.3) |
| MDR | 51 (6.8) |
| H + R | 16 (2.1) |
| H + R + S | 11 (1.5) |
| H + R + E | 10 (1.3) |
| H + R + S + E | 14 (1.9) |
| Any resistance | 207 (27.5) |
| Susceptible to all drugs | 547 (72.5) |
| Total | 754 |
H, isoniazid; R, rifampin; S, streptomycin; E, ethambutol; MDR, multidrug-resistant.
M. tuberculosis population structure.
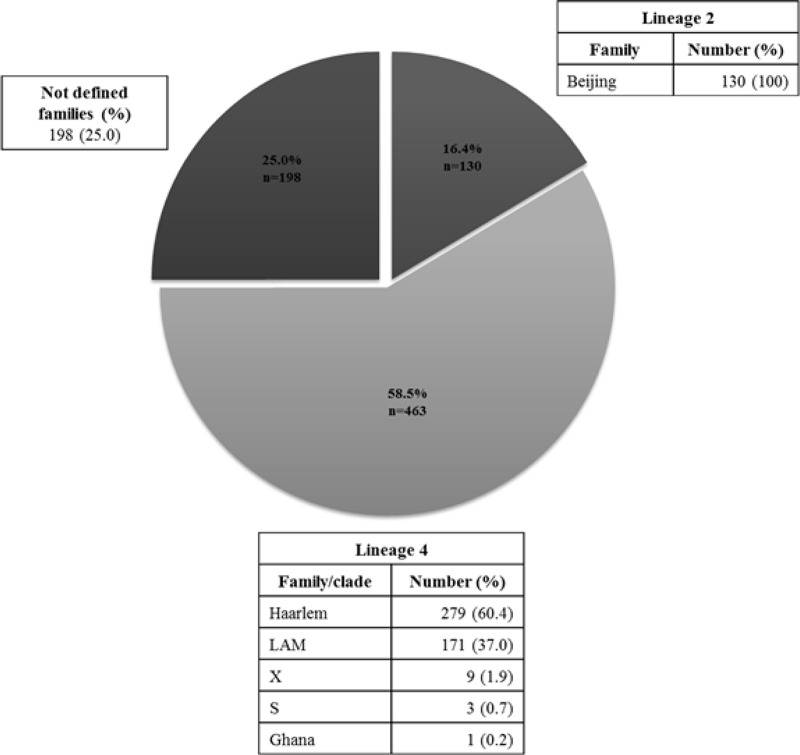
MIRU-15 classified 593/791 isolates (75%) into previously described lineages (21). The largest lineage was lineage 4, which accounted for 58.5% of the isolates, most of which belonged to the Haarlem family (n = 279), followed by the LAM family (n = 171) (Fig. 2). Few isolates belonged to the X (n = 9) and S (n = 3) families. The next most common lineage was lineage 2, represented here by only the Beijing family, which accounted for 16.4% (n = 130) of the total.
FIG 2.
Families based on spoligotyping and MIRU-15 analysis among the 791 isolates of M. tuberculosis.
The remaining 198 isolates (25%) could not be assigned to a recognized lineage or family based on their spoligotyping and/or MIRU-15 profiles and were grouped as nondefined strains (n = 198). A minimum-spanning tree (MST) based on the MIRU-15 data (see Fig. S1 in the supplemental material) confirmed the classification according to unweighted pair group method with arithmetic mean (UPGMA) tree-based analysis.
Stratification of the strains that were resistant to isoniazid and/or rifampin in the different phylogenetic families showed that strains in the most common lineage 4 family (Haarlem) were less prone to be resistant to rifampin (OR, 0.4; P = 0.01) and rifampin plus isoniazid (OR, 0.5; P = 0.05) than were all non-Haarlem strains. In contrast, strains in the LAM family were more prone to be resistant to isoniazid (OR, 1.7; P = 0.03), rifampin (OR, 2.8; P < 0.0001), and isoniazid plus rifampin (OR, 2.3; P = 0.01) than were all non-LAM strains (Table 3).
TABLE 3.
M. tuberculosis families and their association with isoniazid and rifampin resistance (n = 754)
| M. tuberculosis family | Total no.a | Isoniazid |
Rifampin |
MDR |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. resistant | No. sensitive | OR (95% CI) | P | No. resistant | No. sensitive | OR (95% CI) | P | No. with MDR | No. without MDR | OR (95% CI) | P value | ||
| Lineage 2 | 119 | 10 | 109 | 7 | 112 | 7 | 112 | ||||||
| Beijing | 119 | 10 | 109 | 0.6 (0.3–1.3) | 0.08 | 7 | 112 | 0.6 (0.3–1.3) | 0.3 | 7 | 112 | 0.8 (0.4–1.9) | 0.8 |
| Non-Beijing | 635 | 95 | 540 | 61 | 574 | 44 | 591 | ||||||
| Lineage 4 | 444 | 65 | 379 | 45 | 399 | 31 | 413 | ||||||
| Haarlem | 267 | 31 | 236 | 0.7 (0.5–1.2) | 0.2 | 14 | 253 | 0.4 (0.2–0.8) | 0.01 | 11 | 256 | 0.5 (0.2–1.0) | 0.05 |
| Non-Haarlem | 487 | 74 | 413 | 54 | 433 | 40 | 447 | ||||||
| LAM | 165 | 32 | 133 | 1.7 (1.1–2.7) | 0.03 | 28 | 137 | 2.8 (1.7–4.7) | <0.0001 | 19 | 146 | 2.3 (1.3–4.1) | 0.01 |
| Non-LAM | 589 | 73 | 516 | 40 | 549 | 32 | 557 | ||||||
| X clade | 9 | 2 | 7 | NAb | NA | 2 | 7 | NA | NA | 1 | 8 | NA | NA |
| Non-X clade | 745 | 103 | 642 | 66 | 679 | 50 | 695 | ||||||
| S clade | 2 | 0 | 2 | NA | NA | 1 | 1 | NA | NA | 0 | 2 | NA | NA |
| Non-S clade | 752 | 105 | 647 | 67 | 685 | 51 | 701 | ||||||
| Ghana | 1 | 0 | 1 | NA | NA | 0 | 1 | NA | NA | 0 | 1 | NA | NA |
| Non-Ghana | 753 | 105 | 648 | 68 | 685 | 51 | 702 | ||||||
| Nondefined familyc | 190 | 30 | 160 | 1.22 (0.8–1.9) | 0.5 | 16 | 174 | 0.9 (0.5–1.6) | 0.8 | 13 | 177 | 1.0 (0.5–1.9) | 0.9 |
| Defined family | 563 | 75 | 488 | 52 | 511 | 38 | 525 | ||||||
Isolates identified as mixed infections and isolates without complete spoligotyping and MIRU-15 data were excluded from the analysis.
NA, not applicable.
One strain failed the susceptibility test for isoniazid.
Cluster analysis.
MIRU-15 analysis grouped 551/791 isolates (69.7%) in 102 clusters, with sizes ranging from 2 to 46 isolates per cluster. Stratification of clusters in the 2 most common phylogenetic lineages showed a higher probability to cluster for lineage 4 than for lineage 2 (OR, 1.8 [95% CI, 1.2 to 2.8]; P = 0.004). Stratification of clusters in the recognized families showed a higher probability to cluster for the Haarlem family (OR, 2.0; P < 0.0001), while the LAM (OR, 0.7; P = 0.07) and Beijing (OR, 0.6; P < 0.006) families were less prone to cluster, compared to isolates not belonging to those families (Table 4). Additional MIRU-24 typing for 62 of the 130 Beijing isolates supported the observed MIRU-15 clustering for 59 of the isolates and identified 3 isolates as nonclustered, compared to MIRU-15 analysis.
TABLE 4.
Phylogenetic families and their association with strain clustering (n = 791)
| M. tuberculosis family | No. of isolatesa | No. of clusters | No. (%) of genotypes |
OR (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Clustered | Unique | |||||
| Lineage 2 | 130 | 7 | 77 (59.2) | 53 (40.8) | ||
| Beijing | 130 | 7 | 77 (59.2) | 53 (40.8) | 0.6 (0.4–0.9) | 0.006 |
| Non-Beijing | 661 | 95 | 474 (71.7) | 187 (28.3) | ||
| Lineage 4 | 463 | 67 | 336 (72.6) | 127 (27.4) | ||
| Haarlem | 279 | 37 | 220 (78.9) | 59 (21.1) | 2.0 (1.5–2.9) | <0.0001 |
| Non-Haarlem | 512 | 65 | 331 (64.7) | 181 (35.3) | ||
| LAM | 171 | 27 | 109 (63.7) | 62 (36.3) | 0.7 (0.5–1.0) | 0.07 |
| Non-LAM | 620 | 75 | 442 (71.3) | 178 (28.7) | ||
| X clade | 9 | 2 | 5 (55.6) | 4 (44.4) | NAb | NA |
| Non-X clade | 782 | 100 | 546 (69.8) | 236 (30.2) | ||
| S clade | 3 | 1 | 2 (66.7) | 1 (33.3) | NA | NA |
| Non-S clade | 788 | 101 | 549 (69.7) | 239 (30.3) | ||
| Ghana | 1 | 0 | 0 (0) | 1 (100) | NA | NA |
| Non-Ghana | 790 | 102 | 551(69.8) | 239 (30.2) | ||
| Nondefined family | 198 | 28 | 142 (71.7) | 56 (28.3) | 1.1 (0.8–1.6) | 0.7 |
| Defined family | 593 | 74 | 413 (69.7) | 180 (30.3) | ||
Isolates identified as mixed infections and isolates without complete spoligotyping and MIRU-15 data were excluded from the analysis.
NA, not applicable.
The ages (mean ± standard deviation) of the study subjects were 31 ± 13.9 years (range, 18 to 83 years), and 61.3% of the patients were male. No correlation was found between being part of a cluster and gender, but younger patients (<40 years of age) were more likely to be part of a cluster than were older patients (OR, 1.6; P = 0.01). To gain insight into the transmission dynamics of resistant strains, the clustering rates were stratified according to drug resistance profiles. Interestingly, despite the high rates of resistance to isoniazid (13.9%) and rifampin (9.0%) and of multidrug resistance (6.8%), none of these patterns was associated with clustering, suggesting widespread (more than one secondary case) recent transmission into this study population. MDR strains were not significantly more prevalent among clustered strains (41/551 isolates [7.4%]) than among nonclustered strains (10/228 isolates [4.1%]) (OR, 1.8; P < 0.1) (Table 5). Clustered MDR strains were distributed over 11 clusters belonging to different lineages and families. Only 14 of 51 MDR strains clustered together with other MDR strains; 3 relatively large clusters, i.e., A, E, and R, included 4, 6, and 4 MDR strains, respectively. We could not document an epidemiological association among patients from these clusters based on the health centers they attended. Strains that were resistant to streptomycin (OR, 2.0; P = 0.01) were more prone to be clustered (Table 6).
TABLE 5.
Characteristics of clusters found in study population
| No. of strains in cluster | No. of clusters | Cluster identification | Lineage(s) | No. of strains showing resistance/susceptibility toa: |
No. of strains with/without MDRb | No. NDc | |||
|---|---|---|---|---|---|---|---|---|---|
| H | R | S | E | ||||||
| 2d | 43 | Multiple | |||||||
| 3d | 22 | Multiple | |||||||
| 4d | 10 | Multiple | |||||||
| 5d | 5 | Multiple | |||||||
| 6 | 1 | A | Beijing | 5/0 | 4/1 | 5/0 | 4/1 | 4/1 | 1 |
| 7 | 1 | B | Haarlem | 2/5 | 1/6 | 2/5 | 2/5 | 1/6 | 0 |
| 8 | 3 | C | Haarlem | 0/8 | 1/7 | 1/7 | 0/8 | 0/8 | 0 |
| D | Haarlem | 0/8 | 0/8 | 2/6 | 1/7 | 0/8 | 0 | ||
| E | Not defined | 4/3 | 4/3 | 1/6 | 4/3 | 4/3 | 1 | ||
| 9 | 4 | F | Haarlem | 4/5 | 0/9 | 3/6 | 0/9 | 0/9 | 0 |
| G | Haarlem | 0/9 | 0/9 | 1/8 | 1/8 | 0/9 | 0 | ||
| H | Not defined | 1/7 | 1/7 | 1/7 | 2/6 | 1/7 | 1 | ||
| I | Not defined | 1/7 | 0/8 | 2/6 | 1/7 | 0/8 | 1 | ||
| 10 | 1 | J | Haarlem | 1/8 | 1/8 | 1/8 | 4/5 | 1/8 | 1 |
| 11 | 1 | K | LAM | 0/10 | 1/9 | 0/10 | 0/10 | 0/10 | 1 |
| 12 | 2 | L | Haarlem | 1/10 | 1/10 | 1/10 | 1/10 | 1/10 | 1 |
| M | Haarlem | 3/9 | 1/11 | 2/10 | 2/10 | 1/11 | 0 | ||
| 15 | 1 | N | Beijing | 1/13 | 1/13 | 2/12 | 1/13 | 1/13 | 1 |
| 16 | 1 | O | LAM | 0/16 | 2/14 | 0/16 | 0/16 | 0/16 | 0 |
| 17 | 2 | P | Not defined | 3/14 | 0/17 | 6/11 | 6/11 | 0/17 | 0 |
| Q | Not defined | 1/16 | 0/17 | 1/16 | 0/17 | 0/17 | 0 | ||
| 20 | 1 | R | LAM | 11/9 | 6/14 | 5/15 | 5/15 | 6/14 | 0 |
| 22 | 1 | S | Not defined | 0/21 | 1/20 | 2/19 | 1/20 | 0/21 | 1 |
| 25 | 1 | T | Haarlem | 1/24 | 1/24 | 4/21 | 2/23 | 0/25 | 0 |
| 38 | 1 | U | Haarlem | 1/35 | 1/35 | 3/33 | 1/35 | 1/35 | 2 |
| 46 | 1 | V | Beijing | 2/41 | 1/42 | 5/38 | 6/37 | 1/42 | 3 |
H, isoniazid; R, rifampin; S, streptomycin; E, ethambutol.
MDR, multidrug-resistant.
ND, susceptibility test was not done.
No details on susceptibility were provided.
TABLE 6.
Demographic characteristics of study subjects, drug resistance patterns, and their association with strain clustering
| Characteristic | Total no. | No (%) with genotyping pattern |
OR (95% CI) | P | |
|---|---|---|---|---|---|
| Clustered | Unique | ||||
| Gender | |||||
| Male | 485 | 346 (71.3) | 139 (28.7) | 1.2 (0.9–1.8) | 0.2 |
| Female | 306 | 205 (67.0) | 101 (33.0) | ||
| Age | |||||
| <40 yr | 610 | 439 (72.0) | 171 (28.0) | 1.6 (1.1–2.2) | 0.01 |
| ≥40 yr | 181 | 112 (61.9) | 69 (38.1) | ||
| Any drug | |||||
| Resistant | 207 | 154 (74.4) | 53 (25.6) | 1.4 (0.9–1.9) | 0.1 |
| Sensitive | 547 | 373 (68.2) | 174 (31.8) | ||
| Isoniazida | |||||
| Resistant | 105 | 82 (78.1) | 23 (21.9) | 1.7 (1.0–2.7) | 0.06 |
| Sensitive | 649 | 444 (68.4) | 205 (31.6) | ||
| Rifampin | |||||
| Resistant | 68 | 52 (76.5) | 16 (23.5) | 1.4 (0.8–2.6) | 0.3 |
| Sensitive | 686 | 475 (69.2) | 211 (30.8) | ||
| Streptomycin | |||||
| Resistant | 103 | 82 (79.6) | 21 (20.4) | 1.8 (1.1–3.0) | 0.03 |
| Sensitive | 651 | 445 (68.4) | 206 (31.6) | ||
| Ethambutol | |||||
| Resistant | 91 | 71 (78.0) | 20 (22.0) | 1.6 (1.0–2.7) | 0.1 |
| Sensitive | 663 | 456 (68.8) | 207 (31.2) | ||
| MDRa | |||||
| Yes | 51 | 41 (80.4) | 10 (19.6) | 1.8 (0.9–3.7) | 0.1 |
| No | 703 | 486 (69.1) | 217 (30.9) | ||
| Resistant to all first-line drugs | |||||
| Yes | 14 | 14 (100) | 0 (0) | NAb | NA |
| No | 740 | 513 (69.3) | 227 (30.7) | ||
One strain failed the susceptibility test for isoniazid.
NA, not applicable.
DISCUSSION
Despite the decreases in the national TB incidence since the implementation of DOTS, Peru faces increases in the cases of MDR-TB in the poorest districts of the capital. This study presents an in-depth analysis of the population structure of MTBc strains from new pulmonary TB cases in San Juan de Lurigancho, a setting with high TB and MDR-TB burdens in the northeastern part of Lima, Peru. National surveys from 1996 and 2006 showed an increase in the MDR rate from 2.4% to 5.3% among new cases of pulmonary TB, most of which were detected in Lima (11). The 6.8% MDR-TB rate we observed in our population is in line with these data.
Based on the combination of spoligotyping and MIRU-15 analysis, 75% of the investigated strains were assigned to lineages and families, with lineage 4 being the most prevalent, followed by lineage 2. In contrast to previous reports from Latin America in which LAM was the most common family (11, 36–40), our results demonstrated a predominance of the Haarlem family among new cases in the district of San Juan de Lurigancho.
With the exception of a study on MDR-TB household contacts, in which LAM was most frequent (41), this predominance of the Haarlem genotype has been observed in all Peruvian studies to date (23–25, 42). Despite heterogeneity in the design and size of those studies, the combined data suggest a trend of increasing prevalence of the Haarlem genotype in Lima in the past decade, with an increase from 23.8% to 35.3% (23, 25, 41, 42). Among a selection of MDR-TB and XDR-TB isolates collected in Peru in 2007 to 2009, the prevalence reached 43.6% (24). The widespread occurrence of the genotype in Peru could be due to the stability of the genotype in this population and/or a high rate of recent transmission, as documented by the higher probability of Haarlem strains to be in a cluster in our study. Additionally, our results are in accordance with the finding of LAM as the second most prevalent family in Peru, followed by the Beijing family (23–25), with a seeming increase in Beijing strains in Lima from around 5% in early 2000 (23, 25) to around 15% a decade later (42; this study).
Unlike the situation observed in other South American countries, in which the Beijing family was reported to represent less than 1%, its proportion in Peru was found to be relatively high, i.e., 5.5% (44/794 isolates) for samples obtained between 1999 and 2005 (23), 5.9% (11/185 isolates) in 1999 (43), 9.3% for samples obtained between 2004 and 2006 (25), and 14.1% for samples obtained during 7 months in 2009 (42). This observation was recently explained by Iwamoto et al. (31) as the result of Chinese and Japanese immigrants settling in Peru in the 19th century. The 16.4% prevalence rate observed in this study confirms the trend of increasing prevalence of this family, an expansion due to transmission after a relatively recent introduction. Although Beijing strains overall clustered less in our study population, the largest cluster included 46 Beijing isolates.
In this study, we observed a significant proportion (23.5%) of strains that did not match well-defined lineages but were responsible for large clusters (see Fig. S2 in the supplemental material). Among them, 37% were grouped in the poorly defined T group, and 63% had spoligotyping and/or MIRU patterns that did not match an international type. Future analyses including the additional 9 loci for 24-locus MIRU analysis and/or whole-genome sequencing could help to discriminate better between these strains and to elucidate the real clusters.
Clustering is considered a surrogate marker for strains involved in recent transmission. The efficacy of TB control programs can be assessed by the degree of recent TB transmission in the population (44–46). The validity of molecular epidemiological studies is determined by the resolution of the applied typing method, among other factors. Spoligotyping alone is an unreliable tool for formal phylogenetic analyses, due to the occurrence of independent mutational events in different evolutionary lineages, which may result in identical convergent spoligotyping patterns (47). However, spoligotyping combined with MIRU-15 analysis allows for high-resolution genotyping to study recent transmission (32). We excluded 24 samples lacking data for 2 or more MIRU loci. An occasional lack of PCR amplification of some loci has been reported (32) and might be explained by chromosomal deletions, nucleotide polymorphisms in the sequences complementary to the PCR primers (48), or insufficient DNA quality. MIRU-15 analysis may lack sufficient power of resolution for the classification of Beijing strains (32). However, the comparison between MIRU-15 and MIRU-24 analyses showed similar clusters. Therefore, it is likely that the majority of the remaining strains typed by MIRU-15 analysis would mostly remain clustered if MIRU-VNTR typing was extended to 24 loci (32).
Duration and geographic/population coverage are other important determinants for the validity of molecular epidemiological studies. Due to logistic constraints and human and/or microbiological factors, it is usually not possible to obtain cultures and DNA fingerprints for all eligible cases. In this study, we focused only on new TB cases, which represented approximately 89% of all pulmonary TB cases, and among these we enrolled only smear-positive cases, which represented approximately 65.3% of the new cases (6). Borgdorff et al. confirmed that clustering rates may be underestimated as a result of random sampling in time or in space (49). In settings in which risk factors for clustering may be interpreted as risk factors for recent transmission, these risk factors can be robustly calculated even when sampling is incomplete, i.e., they are also associated with larger cluster sizes. Therefore, odds ratios are generally insensitive to random sampling unless larger clusters are excluded and sampling fractions are small (49). This study analyzed a sampling fraction of almost 50% of the eligible cases, i.e., registered new smear-positive cases of pulmonary TB, and did not exclude any clusters. As a result, the odds ratios of our study are likely robust estimates.
TB is known to cluster in hyperendemic “hot spots,” which often are characterized by social determinants such as crowding, poverty, and HIV infections (50–52). Compared with other infectious diseases, however, for which 20% of the population may generate 80% of transmission, TB transmission appears relatively more homogeneous (53, 54). Previous studies in areas with high TB incidence rates have shown a wide range of transmission rates (clustering rates), ranging from 37 to 72% in settings with TB incidence rates of over 200 cases per 100,000 inhabitants (55–57). In our study population, we observed a relatively high clustering rate of 69.7%, mainly among Haarlem strains.
In agreement with previous national and regional surveillance data (58–60), we found high rates of resistance to isoniazid and/or rifampin in this setting. This high MDR rate does not seem to be attributable primarily to recent transmission among new cases, as our MDR strains were not systematically clustered together. Indeed, they were grouped together with non-MDR strains, mostly resistant to at least isoniazid. Thus, the additional acquisition of rifampin resistance could have occurred in epidemiologically linked retreated cases that were excluded from this study.
MDR-TB strains were underrepresented among clustered strains. There are three possible explanations for the lack of association between clustering and the presence of MDR-TB strains observed among new cases in our setting. First, recent transmission could have occurred from MDR-TB in previously treated patients who were excluded from our study. The fact that MDR strains clustered with strains that were resistant to isoniazid or rifampin supports this hypothesis of acquired MDR in retreated cases, which potentially remained infectious for extended periods if not diagnosed properly and treated appropriately. In Peru, the time to change from the standard schedule to the MDR-TB schedule varies from 28 days for new TB patients with risk factors to 2 months for patients without risk factors (61). Second, transmission could have occurred prior to our sampling period. When we compared our results with those of a previous study conducted in the same district in 2009 (42), however, we found few shared clusters between the two sets of samples; the 2009 study focused on low-MDR-risk patients, who did not represent the entire pool of MDR-TB cases in the area. Moreover, our study covered almost 2 years of sampling, which is considered the minimum time to study recent transmission (62). Third, resistant strains could have been imported from other districts of Lima. According to reports from the Ministry of Health (see Fig. S3 in the supplemental material), however, San Juan de Lurigancho has one of the highest TB incidence rates in the capital. Therefore, export (rather than import) from San Juan de Lurigancho to other districts might be more frequent, as a result of high interdistrict mobility. On the other hand, according to the latest census (performed in 2007), 54.7% of the inhabitants living in San Juan de Lurigancho were born in a different region and 15.7% had moved to the district in the past 5 years (63), which might have caused import of (resistant) strains from those regions. Therefore, infection from previously treated cases, which are at higher risk of being MDR-TB, seems the most plausible explanation for the observed high rates of MDR-TB among new cases.
In the specific case of the Beijing family, worldwide concern has been raised about its frequent association with outbreaks of MDR variants (48, 64, 65); however, this was contested by Glynn et al. (66), who found regional differences in the Beijing family's association with drug resistance, with Colombia and Cuba lacking this association. Our results agree with this observation and previous Peruvian studies in which the Beijing family was present in relatively high proportions but was not associated with multidrug resistance (23, 25, 41, 42). The prevailing Beijing isolates in Lima are associated with the modern subfamily coming from China, consistent with the worldwide trend except in the cases of Japan and Korea, where the ancient subfamily predominates. One particular clone, the PCT001 genotype, has been circulating in Lima since at least 1999 and might have gained a selective advantage allowing for enhanced spreading in the past decade. Indeed, our largest Beijing cluster (n = 46) displayed the typical PCT001 profile, whereas the second cluster (n = 15) had the PCT002 pattern (31).
Our study has some limitations. First, since this was a passive surveillance study, only patients attending health care facilities in the public sector were included. In Peru, however, most cases of TB are treated within this sector (67). Second, this study was embedded in a prospective cohort study of new cases of sputum smear-positive pulmonary TB; therefore, only new TB cases that were smear positive were enrolled. Third, the sampling period covers almost 2 years, which is less than the 4-year window that yielded maximum clustering in a study conducted in Malawi (62).
In conclusion, our study confirms a diverse population structure of M. tuberculosis in the San Juan de Lurigancho district. The predominant family was the Haarlem family and, although the strains of this family showed the greatest probability to cluster, they were less prone to be resistant to isoniazid and rifampin. The high rate of clustering indicates active recent transmission of M. tuberculosis among new cases but was not associated with drug resistance in this study population. Our results suggest that the high MDR-TB rate among new TB cases in Lima is primarily due not to recent transmission among new cases but rather to treatment failure in previous TB infections, which causes the selection of spontaneous mutations in specific genes associated with drug resistance. Future prospective community-based studies, including new and previously treated patients, should aim to study the transmission of drug-resistant strains in the general population, to confirm this hypothesis. Meanwhile, rapid diagnosis and effective treatment of TB remain crucial for interrupting the chains of transmission, with an emphasis on retreated cases for MDR-TB.
Supplementary Material
ACKNOWLEDGMENTS
We thank the field workers for data collection and the staff from the health care facilities.
This study was funded by the Belgian Directorate-General for Development Cooperation through an institutional collaboration between the Institute of Tropical Medicine (Antwerp, Belgium) and the Institute of Tropical Medicine Alexander von Humboldt (Lima, Peru), by Health Science Research grant H26-SHINKO-IPPAN-011 from the Ministry of Health, Labor, and Welfare of Japan, and by MEXT/JSPS KAKENHI grant 24590845.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JCM.03585-14.
REFERENCES
- 1.Mathers CD, Boerma T, Ma Fat D. 2009. Global and regional causes of death. Br Med Bull 92:7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. 2014. Global tuberculosis report. WHO/HTM/TB/2014.08 World Health Organization, Geneva, Switzerland. [Google Scholar]
- 3.Bonilla CA, Crossa A, Jave HO, Mitnick CD, Jamanca RB, Herrera C, Asencios L, Mendoza A, Bayona J, Zignol M, Jaramillo E. 2008. Management of extensively drug-resistant tuberculosis in Peru: cure is possible. PLoS One 3:e2957. doi: 10.1371/journal.pone.0002957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministerio de Salud. 2013. Informe operacional MINSA: otras instituciones. 2013/AMHE/JECC Ministerio de Salud, Lima, Peru. [Google Scholar]
- 5.Instituto Nacional de Estadística e Informática. 2012. Estimaciones y proyecciones de población por sexo, según departamento, provincia y distrito, 2000–2015. Instituto Nacional de Estadística e Informática, Lima, Peru. [Google Scholar]
- 6.Ministerio de Salud. 2011. Análisis de la situación de salud 2011 de la Dirección de Salud IV Lima Este. Ministerio de Salud, Lima, Peru. [Google Scholar]
- 7.Ministerio de Salud. 2010. Dirección de Salud IV Lima Este plan operativo institucional ejercicio fiscal 2010. Ministerio de Salud, Lima, Peru. [Google Scholar]
- 8.World Health Organization. 2013. Global tuberculosis report. WHO/HTM/TB/2013.11 World Health Organization, Geneva, Switzerland. [Google Scholar]
- 9.Ministerio de Salud. 2010. Estrategia sanitaria nacional para la prevención y control de la tuberculosis: informe operacional 2010. Ministerio de Salud, Lima, Peru. [Google Scholar]
- 10.Health Communication Partnership. 2004. The role of communication in Peru's fight against tuberculosis. Health Communication Partnership, Baltimore, MD. [Google Scholar]
- 11.Asencios L, Quispe N, Mendoza-Ticona A, Leo E, Vásquez L, Jave O, Bonilla CA. 2009. Vigilancia nacional de la resistencia a medicamentos antituberculosos, Peru 2005–2006. Rev Peru Med Exp Salud Publica 26:278–287. [Google Scholar]
- 12.World Health Organization. 2012. Global tuberculosis report 2012. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 13.David HL. 1970. Probability distribution of drug-resistant mutants in unselected populations of Mycobacterium tuberculosis. Appl Microbiol 20:810–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banerjee A, Dubnau E, Quemard A, Balasubramanian V, Um KS, Wilson T, Collins D, de Lisle G, Jacobs WR Jr. 1994. inhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science 263:227–230. doi: 10.1126/science.8284673. [DOI] [PubMed] [Google Scholar]
- 15.Garcia de Viedma D, Mokrousov I, Rastogi N. 2011. Innovations in the molecular epidemiology of tuberculosis. Enferm Infecc Microbiol Clin 29(Suppl 1):S8–S13. doi: 10.1016/S0213-005X(11)70012-X. [DOI] [PubMed] [Google Scholar]
- 16.Kato-Maeda M, Metcalfe JZ, Flores L. 2011. Genotyping of Mycobacterium tuberculosis: application in epidemiologic studies. Future Microbiol 6:203–216. doi: 10.2217/fmb.10.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paranjothy S, Eisenhut M, Lilley M, Bracebridge S, Abubakar I, Mulla R, Lack K, Chalkley D, Howard J, Thomas S, McEvoy M. 2008. Extensive transmission of Mycobacterium tuberculosis from 9 year old child with pulmonary tuberculosis and negative sputum smear. BMJ 337:a1184. doi: 10.1136/bmj.a1184. [DOI] [PubMed] [Google Scholar]
- 18.Mathema B, Kurepina NE, Bifani PJ, Kreiswirth BN. 2006. Molecular epidemiology of tuberculosis: current insights. Clin Microbiol Rev 19:658–685. doi: 10.1128/CMR.00061-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niemann S, Diel R, Khechinashvili G, Gegia M, Mdivani N, Tang YW. 2010. Mycobacterium tuberculosis Beijing lineage favors the spread of multidrug-resistant tuberculosis in the Republic of Georgia. J Clin Microbiol 48:3544–3550. doi: 10.1128/JCM.00715-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Comas I, Coscolla M, Luo T, Borrell S, Holt KE, Kato-Maeda M, Parkhill J, Malla B, Berg S, Thwaites G, Yeboah-Manu D, Bothamley G, Mei J, Wei L, Bentley S, Harris SR, Niemann S, Diel R, Aseffa A, Gao Q, Young D, Gagneux S. 2013. Out-of-Africa migration and Neolithic coexpansion of Mycobacterium tuberculosis with modern humans. Nat Genet 45:1176–1182. doi: 10.1038/ng.2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wirth T, Hildebrand F, Allix-Beguec C, Wolbeling F, Kubica T, Kremer K, van Soolingen D, Rüsch-Gerdes S, Locht C, Brisse S, Meyer A, Supply P, Niemann S. 2008. Origin, spread and demography of the Mycobacterium tuberculosis complex. PLoS Pathog 4:e1000160. doi: 10.1371/journal.ppat.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allix C, Walravens K, Saegerman C, Godfroid J, Supply P, Fauville-Dufaux M. 2006. Evaluation of the epidemiological relevance of variable-number tandem-repeat genotyping of Mycobacterium bovis and comparison of the method with IS6110 restriction fragment length polymorphism analysis and spoligotyping. J Clin Microbiol 44:1951–1962. doi: 10.1128/JCM.01775-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheen P, Couvin D, Grandjean L, Zimic M, Dominguez M, Luna G, Gilman RH, Rastogi N, Moore DA. 2013. Genetic diversity of Mycobacterium tuberculosis in Peru and exploration of phylogenetic associations with drug resistance. PLoS One 8:e65873. doi: 10.1371/journal.pone.0065873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caceres O, Rastogi N, Bartra C, Couvin D, Galarza M, Asencios L, Mendoza-Ticona A. 2014. Characterization of the genetic diversity of extensively-drug resistant Mycobacterium tuberculosis clinical isolates from pulmonary tuberculosis patients in Peru. PLoS One 9:e112789. doi: 10.1371/journal.pone.0112789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taype CA, Agapito JC, Accinelli RA, Espinoza JR, Godreuil S, Goodman SJ, Bañuls AL, Shaw MA. 2012. Genetic diversity, population structure and drug resistance of Mycobacterium tuberculosis in Peru. Infect Genet Evol 12:577–585. doi: 10.1016/j.meegid.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Brudey K, Driscoll JR, Rigouts L, Prodinger WM, Gori A, Al-Hajoj SA, Allix C, Aristimuño L, Arora J, Baumanis V, Binder L, Cafrune P, Cataldi A, Cheong S, Diel R, Ellermeier C, Evans JT, Fauville-Dufaux M, Ferdinand S, Garcia de Viedma D, Garzelli C, Gazzola L, Gomes HM, Guttierez MC, Hawkey PM, van Helden PD, Kadival GV, Kreiswirth BN, Kremer K, Kubin M, Kulkarni SP, Liens B, Lillebaek T, Ho ML, Martin C, Martin C, Mokrousov I, Narvskaïa O, Ngeow YF, Naumann L, Niemann S, Parwati I, Rahim Z, Rasolofo-Razanamparany V, Rasolonavalona T, Rossetti ML, Rüsch-Gerdes S, Sajduda A, Samper S, Shemyakin IG, Singh UB, Somoskovi A, Skuce RA, van Soolingen D, Streicher EM, Suffys PN, Tortoli E, Tracevska T, Vincent V, Victor TC, Warren RM, Yap SF, Zaman K, Portaels F, Rastogi N, Sola C. 2006. Mycobacterium tuberculosis complex genetic diversity: mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol 6:23. doi: 10.1186/1471-2180-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricaldi JN, Guerra H. 2008. A simple and improved method for diagnosis of tuberculosis using hypertonic saline and sodium hydroxide to concentrate and decontaminate sputum. Trop Doct 38:97–99. doi: 10.1258/td.2007.070024. [DOI] [PubMed] [Google Scholar]
- 28.Sirgel F, Wiid I, van Helden P. 2009. Measuring minimum inhibitory concentrations in mycobacteria. Methods Mol Biol 465:173–186. doi: 10.1007/978-1-59745-207-6_11. [DOI] [PubMed] [Google Scholar]
- 29.Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, Bunschoten A, Molhuizen H, Shaw R, Goyal M, van Embden J. 1997. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol 35:907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Supply P. 2005. Multilocus variable number tandem repeat genotyping of Mycobacterium tuberculosis: technical guide. INSERM U629, Institut de Biologie/Institut Pasteur de Lille, Lille, France. [Google Scholar]
- 31.Iwamoto T, Grandjean L, Arikawa K, Nakanishi N, Caviedes L, Coronel J, Sheen P, Wada T, Taype CA, Shaw MA, Moore DA, Gilman RH. 2012. Genetic diversity and transmission characteristics of Beijing family strains of Mycobacterium tuberculosis in Peru. PLoS One 7:e49651. doi: 10.1371/journal.pone.0049651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Supply P, Allix C, Lesjean S, Cardoso-Oelemann M, Rusch-Gerdes S, Willery E, Savine E, de Haas P, van Deutekom H, Roring S, Bifani P, Kurepina N, Kreiswirth B, Sola C, Rastogi N, Vatin V, Gutierrez MC, Fauville M, Niemann S, Skuce R, Kremer K, Locht C, van Soolingen D. 2006. Proposal for standardization of optimized mycobacterial interspersed repetitive unit-variable-number tandem repeat typing of Mycobacterium tuberculosis. J Clin Microbiol 44:4498–4510. doi: 10.1128/JCM.01392-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weniger TKJ, Supply P, Niemann S, Harmsen D. 2010. MIRU-VNTRplus: a web tool for polyphasic genotyping of Mycobacterium tuberculosis complex bacteria. Nucleic Acids Res 38:W326–W331. doi: 10.1093/nar/gkq351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shamputa IC, Rigouts L, Eyongeta LA, El Aila NA, van Deun A, Salim AH, Willery E, Locht C, Supply P, Portaels F. 2004. Genotypic and phenotypic heterogeneity among Mycobacterium tuberculosis isolates from pulmonary tuberculosis patients. J Clin Microbiol 42:5528–5536. doi: 10.1128/JCM.42.12.5528-5536.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shamputa IC, Jugheli L, Sadradze N, Willery E, Portaels F, Supply P, Rigouts L. 2006. Mixed infection and clonal representativeness of a single sputum sample in tuberculosis patients from a penitentiary hospital in Georgia. Respir Res 7:99. doi: 10.1186/1465-9921-7-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gagneux S, DeRiemer K, Van T, Kato-Maeda M, de Jong BC, Narayanan S, Nicol M, Niemann S, Kremer K, Gutierrez MC, Hilty M, Hopewell PC, Small PM. 2006. Variable host-pathogen compatibility in Mycobacterium tuberculosis. Proc Natl Acad Sci U S A 103:2869–2873. doi: 10.1073/pnas.0511240103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Candia N, Lopez B, Zozio T, Carrivale M, Diaz C, Russomando G, de Romero NJ, Jara JC, Barrera L, Rastogi N, Ritacco V. 2007. First insight into Mycobacterium tuberculosis genetic diversity in Paraguay. BMC Microbiol 7:75. doi: 10.1186/1471-2180-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abadia E, Sequera M, Ortega D, Mendez MV, Escalona A, Da Mata O, Izarra E, Rojas Y, Jaspe R, Motiwala AS, Alland D, de Waard J, Takiff HE. 2009. Mycobacterium tuberculosis ecology in Venezuela: epidemiologic correlates of common spoligotypes and a large clonal cluster defined by MIRU-VNTR-24. BMC Infect Dis 9:122. doi: 10.1186/1471-2334-9-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perizzolo PF, Dalla Costa ER, Ribeiro AW, Spies FS, Ribeiro MO, Dias CF, Unis G, Almeida da Silva P, Gomes HM, Suffys PN, Rossetti ML. 2012. Characteristics of multidrug-resistant Mycobacterium tuberculosis in southern Brazil. Tuberculosis 92:56–59. doi: 10.1016/j.tube.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 40.Cerezo I, Jimenez Y, Hernandez J, Zozio T, Murcia MI, Rastogi N. 2012. A first insight on the population structure of Mycobacterium tuberculosis complex as studied by spoligotyping and MIRU-VNTRs in Bogota, Colombia. Infect Genet Evol 12:657–663. doi: 10.1016/j.meegid.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 41.Cohen T, Murray M, Abubakar I, Zhang Z, Sloutsky A, Arteaga F, Chalco K, Franke MF, Becerra MC. 2011. Multiple introductions of multidrug-resistant tuberculosis into households, Lima, Peru. Emerg Infect Dis 17:969–975. doi: 10.3201/eid1706.101471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barletta F, Otero L, Collantes J, Asto B, de Jong BC, Seas C, Rigouts L. 2013. Genetic variability of Mycobacterium tuberculosis complex in patients with no known risk factors for MDR-TB in the North-Eastern part of Lima, Peru. BMC Infect Dis 13:397. doi: 10.1186/1471-2334-13-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ritacco V, Lopez B, Cafrune PI, Ferrazoli L, Suffys PN, Candia N, Vásquez L, Realpe T, Fernández J, Lima KV, Zurita J, Robledo J, Rossetti ML, Kritski AL, Telles MA, Palomino JC, Heersma H, van Soolingen D, Kremer K, Barrera L. 2008. Mycobacterium tuberculosis strains of the Beijing genotype are rarely observed in tuberculosis patients in South America. Mem Inst Oswaldo Cruz 103:489–492. [DOI] [PubMed] [Google Scholar]
- 44.Small PM, Hopewell PC, Singh SP, Paz A, Parsonnet J, Ruston DC, Schecter GF, Daley CL, Schoolnik GK. 1994. The epidemiology of tuberculosis in San Francisco: a population-based study using conventional and molecular methods. N Engl J Med 330:1703–1709. doi: 10.1056/NEJM199406163302402. [DOI] [PubMed] [Google Scholar]
- 45.Barnes PF, Yang Z, Preston-Martin S, Pogoda JM, Jones BE, Otaya M, Eisenach KD, Knowles L, Harvey S, Cave MD. 1997. Patterns of tuberculosis transmission in Central Los Angeles. JAMA 278:1159–1163. doi: 10.1001/jama.1997.03550140051039. [DOI] [PubMed] [Google Scholar]
- 46.Niemann S, Rusch-Gerdes S, Richter E, Thielen H, Heykes-Uden H, Diel R. 2000. Stability of IS6110 restriction fragment length polymorphism patterns of Mycobacterium tuberculosis strains in actual chains of transmission. J Clin Microbiol 38:2563–2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Comas I, Homolka S, Niemann S, Gagneux S. 2009. Genotyping of genetically monomorphic bacteria: DNA sequencing in Mycobacterium tuberculosis highlights the limitations of current methodologies. PLoS One 4:e7815. doi: 10.1371/journal.pone.0007815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Affolabi D, Faihun F, Sanoussi N, Anyo G, Shamputa IC, Rigouts L, Kestens L, Anagonou S, Portaels F. 2009. Possible outbreak of streptomycin-resistant Mycobacterium tuberculosis Beijing in Benin. Emerg Infect Dis 15:1123–1125. doi: 10.3201/eid1507.080697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Borgdorff MW, van den Hof S, Kalisvaart N, Kremer K, van Soolingen D. 2011. Influence of sampling on clustering and associations with risk factors in the molecular epidemiology of tuberculosis. Am J Epidemiol 174:243–251. doi: 10.1093/aje/kwr061. [DOI] [PubMed] [Google Scholar]
- 50.Gilks CF, Godfrey-Faussett P, Batchelor BI, Ojoo JC, Ojoo SJ, Brindle RJ, Paul J, Kimari J, Bruce MC, Bwayo J, Plummer FA, Warrell DA. 1997. Recent transmission of tuberculosis in a cohort of HIV-1-infected female sex workers in Nairobi, Kenya. AIDS 11:911–918. doi: 10.1097/00002030-199707000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Horsburgh CR Jr, O'Donnell M, Chamblee S, Moreland JL, Johnson J, Marsh BJ, Narita M, Johnson LS, von Reyn CF. 2010. Revisiting rates of reactivation tuberculosis: a population-based approach. Am J Respir Crit Care Med 182:420–425. doi: 10.1164/rccm.200909-1355OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.World Health Organization. 2011. Global tuberculosis control. WHO/HTM/TB/2011.16 World Health Organization, Geneva, Switzerland. [Google Scholar]
- 53.Sutherland I, Svandova E, Radhakrishna S. 1982. The development of clinical tuberculosis following infection with tubercle bacilli. 1. A theoretical model for the development of clinical tuberculosis following infection, linking from data on the risk of tuberculous infection and the incidence of clinical tuberculosis in the Netherlands. Tubercle 63:255–268. doi: 10.1016/S0041-3879(82)80013-5. [DOI] [PubMed] [Google Scholar]
- 54.Golub JE, Saraceni V, Cavalcante SC, Pacheco AG, Moulton LH, King BS, Efron A, Moore RD, Chaisson RE, Durovni B. 2007. The impact of antiretroviral therapy and isoniazid preventive therapy on tuberculosis incidence in HIV-infected patients in Rio de Janeiro, Brazil. AIDS 21:1441–1448. doi: 10.1097/QAD.0b013e328216f441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Verver S, Warren RM, Munch Z, Vynnycky E, van Helden PD, Richardson M, van der Spuy GD, Enarson DA, Borgdorff MW, Behr MA, Beyers N. 2004. Transmission of tuberculosis in a high incidence urban community in South Africa. Int J Epidemiol 33:351–357. doi: 10.1093/ije/dyh021. [DOI] [PubMed] [Google Scholar]
- 56.Mulenga C, Shamputa IC, Mwakazanga D, Kapata N, Portaels F, Rigouts L. 2010. Diversity of Mycobacterium tuberculosis genotypes circulating in Ndola, Zambia. BMC Infect Dis 10:177. doi: 10.1186/1471-2334-10-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tessema B, Beer J, Merker M, Emmrich F, Sack U, Rodloff AC, Niemann S. 2013. Molecular epidemiology and transmission dynamics of Mycobacterium tuberculosis in Northwest Ethiopia: new phylogenetic lineages found in Northwest Ethiopia. BMC Infect Dis 13:131. doi: 10.1186/1471-2334-13-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Velasquez GE, Yagui M, Cegielski JP, Asencios L, Bayona J, Bonilla C, Jave HO, Yale G, Suárez C, Atwood S, Contreras CC, Shin SS. 2011. Targeted drug-resistance testing strategy for multidrug-resistant tuberculosis detection, Lima, Peru, 2005–2008. Emerg Infect Dis 17:432–440. doi: 10.3201/eid1703.101553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reference deleted.
- 60.Roetzer A, Diel R, Kohl TA, Rückert C, Nübel U, Blom J, Wirth T, Jaenicke S, Schuback S, Rüsch-Gerdes S, Supply P, Kalinowski J, Niemann S. 2013. Whole genome sequencing versus traditional genotyping for investigation of a Mycobacterium tuberculosis outbreak: a longitudinal molecular epidemiological study. PLoS Med 10:e1001387. doi: 10.1371/journal.pmed.1001387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Otero L, De Orbegoso A, Navarro AF, Rios J, Parraga T, Gotuzzo E, Seas C, Van der Stuyft P. 2015. Time to initiation of multidrug resistant tuberculosis treatment and its relation with outcome in a high incidence district in Lima, Peru. Trop Med Int Health 20:322–325. doi: 10.1111/tmi.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Glynn JR, Crampin AC, Yates MD, Traore H, Mwaungulu FD, Ngwira BM, Ndlovu R, Drobniewski F, Fine PE. 2005. The importance of recent infection with Mycobacterium tuberculosis in an area with high HIV prevalence: a long-term molecular epidemiological study in Northern Malawi. J Infect Dis 192:480–487. doi: 10.1086/431517. [DOI] [PubMed] [Google Scholar]
- 63.Instituto Nacional de Estadística e Informática. 2007. Censos nacionales 2007: XI de población y VI de vivienda. Instituto Nacional de Estadística e Informática, Lima, Peru. [Google Scholar]
- 64.Bifani PJ, Mathema B, Kurepina NE, Kreiswirth BN. 2002. Global dissemination of the Mycobacterium tuberculosis W-Beijing family strains. Trends Microbiol 10:45–52. doi: 10.1016/S0966-842X(01)02277-6. [DOI] [PubMed] [Google Scholar]
- 65.Devaux I, Kremer K, Heersma H, Van Soolingen D. 2009. Clusters of multidrug-resistant Mycobacterium tuberculosis cases, Europe. Emerg Infect Dis 15:1052–1060. doi: 10.3201/eid1507.080994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Glynn JR, Whiteley J, Bifani PJ, Kremer K, van Soolingen D. 2002. Worldwide occurrence of Beijing/W strains of Mycobacterium tuberculosis: a systematic review. Emerg Infect Dis 8:843–849. doi: 10.3201/eid0805.020002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ministerio de Salud. 2006. Estrategia sanitaria nacional para la prevención y control de la tuberculosis: norma técnica de salud para el control de la tuberculosis. Ministerio de Salud, Lima, Peru. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.