Abstract
Objective:
To identify determinants of cigarette smoking initiation, by gender, among schoolchildren in Irbid, Jordan.
Methods:
Between 2008 and 2011, data were collected annually using self-reported questionnaires over 4-years in a prospective cohort of 1,781 students recruited from all 7th grade classes in 19 secondary schools, selected out of a total 60, using probability-proportionate-to-size method. Independent predictors of smoking initiation were identified among the cigarette naïve participants (N = 1,454) with mixed-effect multivariable logistic regression.
Results:
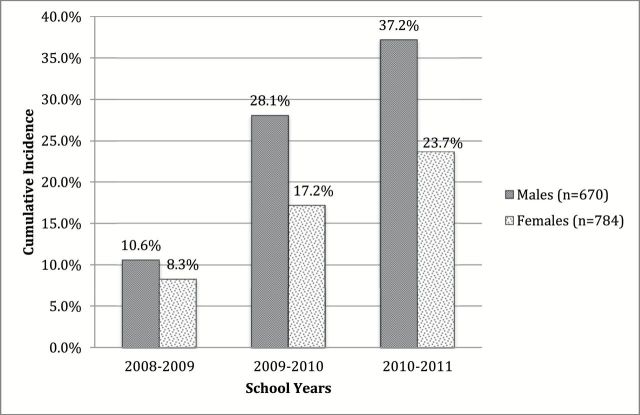
Participants were 12.6 years of age on average at baseline. 29.8% of the 1,454 students (37.2% of boys and 23.7% of girls) initiated cigarette smoking by 10th grade. Of those who initiated (n = 498), 47.2% of boys and 37.2% of girls initiated smoking in the 8th grade. Determinants of cigarette smoking initiation included ever smoking a waterpipe, low cigarette refusal self-efficacy, intention to start smoking cigarettes, and having friends who smoked. For girls, familial smoking was also predictive of cigarette initiation.
Conclusion:
This study shows that many Jordanian youth have an intention to initiate cigarette smoking and are susceptible to cigarette smoking modeled by peers and that girls are influenced as well by familial cigarette smoking. Prevention efforts should be tailored to address culturally relevant gender norms, help strengthen adolescents’ self-efficacy to refuse cigarettes, and foster strong non-smoking social norms.
Introduction
Smoking has been characterized as the most important public health issue of our time.1 Most of the hazards of cigarette smoking are greatest for middle-aged smokers who began smoking as adolescents, but the short-term health consequences for adolescent smokers are serious as well2 and include upper respiratory tract infections, reduced lung growth, reduction in maximum lung function, and poorer self-reported overall health.3–5 Still, in many countries, especially those in the developing world, the prevalence of smoking continues to increase among youth.6,7 While developed countries have the knowledge base and resources to try and reverse these trends, many developing countries like those found in the Eastern Mediterranean Region (EMR), still lack critical information about factors influencing early stages of the smoking habit.8
Therefore, understanding and highlighting some of the salient factors influencing cigarettes smoking initiation among youth in the EMR is of paramount importance to start planning prevention and intervention strategies to reduce smoking.9–13 For instance, over the past decade, waterpipe (WP) smoking has become the most widespread tobacco use method among youth in the EMR.14 Even though WP smoking among adolescents has been shown to be associated with adolescent cigarette smoking in cross-sectional studies, longitudinal evaluation of its importance as a risk factor for youth cigarette uptake in the EMR and elsewhere is very limited.15–19 Additionally, the greater social tolerance of WP smoking for girls in the EMR, as compared to cigarette smoking, may heighten their risk for delayed cigarette initiation, which could pose a unique challenge to prevention efforts in the EMR.16,20–22
Both short-term and long-term health effects of smoking can be influenced by trying to curb initiation and progression during early stages of the smoking habit.5 Such work using a mixture of tobacco control policies and interventions is employed in many developed countries with considerable success.2,23,24 Generally, the establishment of the smoking habit among youth includes shared factors (e.g. addictive nature of nicotine), as well as more specific ones related to the cultural and contextual setting of the environment (e.g. local policy, societal attitude towards smoking).9,25,26
Integrative models applied to study adolescent smoking have positioned potential influences in terms of distance from the individual behavior—that is smoking—ranging from contextual (cultural norms and policies) to immediate social/normative (interpersonal interactions and relationships) to individual (preexisting behaviors, individuals’ characteristics, beliefs, and perceptions).5,27–29 Some of these integrative theories suggest that factors more “distant” from the individual may nonetheless be as powerful, if not more powerful, than individual factors in predicting youth smoking initiation.30,31 Contextual risk factors and those associated with social norms are important in the process of identifying potentially modifiable environmental factors for smoking initiation that are unique to different communities.5,8,9,13,32–41 Guided by these models, we followed a cohort of cigarette naïve school children in Irbid for four years to examine gender-specific predictors of cigarette smoking initiation among Jordanian youth.
Methods
Detailed descriptions of the methodology for this study are published elsewhere.16,17,42 Briefly, a school-based prospective cohort of 1,877 seventh grade students (age ≈ 13 at baseline) was recruited in fall 2007 from 5,287 seventh graders in Irbid, Jordan (population ≈ 330,000). A stratified cluster random sample of schools was drawn from all schools (n = 60) in Irbid using probability proportional to size to ensure representativeness. First, the schools were stratified by gender (boys/girls/mixed) and type (public/private) resulting in six strata (boys private, boys public, et cetera). The schools within each strata were then ordered according to size from smallest to largest and assigned blocks of numbers corresponding with the number of 7th graders in that school (for example, if school “A” had 250 students, it was assigned numbers 1–250 and if school “B” had 500 students, it was assigned numbers 251–750 and so forth). Random numbers were then generated and the school in each stratum that contained the number generated was chosen. Nineteen schools were selected (eight all-boy, nine all-girl, and two mixed – six of which were private). All selected schools agreed to participate in the study. Parental consent and student assent was obtained from 95% of the 7th graders in the selected schools (N = 1,781) who comprised the cohort. Self-report questionnaires were administered and collected each school year during class time by trained study personnel from 7th through 10th grade, for a total of four survey cycles.
This study was reviewed and approved by the institutional review boards of Jordan University for Science and Technology, University of Memphis, Syrian Society Against Cancer, and Florida International University.
Survey Instrument
Development of the questionnaire was guided by the international guidelines of the World Health Organization (WHO)43 and other previously used and validated instruments in Arabic.44
Measures
The outcome measure, initiation of cigarette smoking, was defined as the change from “never smoker” (of cigarettes) at baseline to “ever smoker” or “current smoker” (of cigarettes) at any subsequent follow-up surveys. A student was considered a “never smoker” if he/she had never smoked a cigarette, not even a puff or two; an “ever smoker” if he/she reported ever experimenting with smoking; and a “current smoker” if he/she reported smoking within the last 30 days.
Sociodemographic covariates included age, gender, father’s and mother’s education, school type (public/private), daily pocket money, and density index (DI). The DI is calculated by dividing the number of people residing in the house by the number of its rooms (minus kitchen and bathrooms). Income was assessed indirectly using the DI, which is a proxy measure previously used and tested in the Middle East.10,45 Measures of social influences to smoke included: mother, father, sibling, friend, teacher, and movie stars smoking. Attitudes favorable toward cigarette smoking were measured with questions regarding beliefs that smoking is associated with attractiveness and having more friends; perceived ease of quitting smoking; and intention to start smoking. Attitudes considered unfavorable towards cigarette smoking were measured by asking whether smoking is bad for health. Self-efficacy to resist cigarettes was measured by asking whether the participant would smoke a cigarette if offered one by a friend. Exposure to warning labels on cigarette packs was measured by asking participants if they had noticed the health warnings on cigarette packs within the last month. Finally, to assess the perceived relationships participants had with their parent/s, sibling/s, classmates, and teachers, we asked them to rate each relationship as “good,” “normal,” or “not good.”
Statistical Analysis
The cohort for this analysis was derived from cigarette-naïve participants at baseline (N = 1,454). Since differences in smoking behavior and societal perceptions and attitudes towards smoking were shown to be markedly different for males and females in the EMR, we stratified our sample by gender for the analysis of determinants of initiation.2,8,10,12,20,46–52
SAS Proc GLIMMIX was used for the analysis to account for clustering of schools and the repeated measurements during the follow-up. To account for the complex sampling design, weights for each school were calculated by multiplying the number of schools selected from each stratum with the probability of selecting a particular school and taking the inverse of the result. A weight statement was used in the analysis where weight was calculated by dividing the original weight by the mean of the original weight. The proportions reported throughout the manuscript were weighted as described above.
Questions with more than two possible response categories were analyzed first in their original form, and then they were analyzed as binary. For example, multiple levels of education were collapsed from: Cannot read or write; <6 years; 6–12 years; University into: ≤high school versus >high school. We found the associations did not change whether we used multiple categories or binary categories; hence, we used binary categories in this paper for clarity of reporting.53
Baseline characteristics of those students who initiated cigarettes and those who did not were compared using chi-square tests for categorical variables and t test for continuous variables. For all variables measured during the follow-up period, SAS proc GLIMMIX was used for the mixed logistic modeling, stratified by gender (boys and girls). All predictors found to be significant at the p < .20 level in the bivariate analysis were included in the multivariable analysis.54 To assess multicollinearity, correlations among independent variables were examined, as well as checking for extraordinary estimated coefficients and standard errors. Odds ratios (OR) and 95% confidence intervals (CI) are reported. All statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., SAS/STAT 9.3 User’s Guide).
Results
Trends
Of the entire sample (N = 1,781), 327 participants (18.8%) were ever-smokers of cigarettes at baseline. Of the remaining cohort of cigarette naïve students (N = 1,454) the cumulative incidence of cigarette smoking initiation from 7th to 10th grade was 37.2% for boys and 23.7% for girls. At all times, significantly more boys than girls initiated cigarette smoking. Between the 8th and 9th grades the greatest number of boys (n = 128; 47.2%) and girls (n = 72; 37.2%) initiated cigarette smoking (Figure 1).
Figure 1.
Cumulative incidence of cigarette smoking initiation among Jordanian school children age 13 at baseline, Irbid 2008–2011, by gender (N = 1,454)
Baseline Characteristics
Bivariate analysis showed initiators differed from non-initiators on several sociodemographic variables. Initiators were more likely to be males (OR = 1.92; 95% CI = 1.52–2.38), have parents with less than a high school education (fathers: OR = 1.39; CI = 1.10–1.75; mothers: 1.30; 1.01–1.69), and attend public (vs. private) schools (OR = 2.74; CI = 2.05–3.66). Initiators and non-initiators did not differ by age or economic status. Initiators had 1.92 (CI = 1.48–2.49) times increased odds to report ever smoking waterpipe, having at least one parent (OR = 1.66; CI = 1.32–2.09), siblings (OR = 1.55; 1.15–2.08), friends (OR = 1.57; CI = 1.18–2.09), or teachers (OR = 1.99; CI = 1.56–2.52) who smoke. Initiators also had 2.12 (CI = 1.17–3.84) times increased odds to report low cigarette smoking refusal self-efficacy (Table 1).
Table 1.
Baseline Characteristics of School Children (i = 1,454) Aged 13 at Baseline, Irbid, Jordan, 2008–2011. Cigarette-Smoking Initiators Versus Noninitiators
| Potential Determinants of Initiation | Total N (%) | Initiators (n = 495), n (%)* | Noninitiators (n = 959), n (%)* | p value** | |
|---|---|---|---|---|---|
| Sociodemographics | Males (vs. females) | 670 (45.3) | 292 (37.2) | 378 (62.8) | .00 |
| Public school (vs. private) | 1216 (71.7) | 445 (84.4) | 771 (66.4) | .00 | |
| Age, M (SD)a | 12.7 (0.6) | 12.8 (0.5) | 12.7 (0.6) | .22 | |
| Density Index, M (SD) | 1.7 (1.0) | 1.7 (1.0) | 1.6 (1.0) | .77 | |
| Father’s education (> High school) | 520 (39.9) | 160 (34.5) | 360 (42.2) | .01 | |
| Mother’s education (>High school) | 356 (26.9) | 105 (23.3) | 251 (28.4) | .05 | |
| Daily pocket money (≥0.50 JOD)b | 261 (21.1) | 83 (19.9) | 178 (21.5) | .48 | |
| Ever-smoke waterpipe | 298 (22.2) | 142 (30.6) | 156 (18.6) | .00 | |
| Participate in sports | 1038 (75.0) | 371 (78.9) | 667 (73.2) | .03 | |
| Social influences | Seen ads promoting smoking last 30 days | 670 (45.4) | 249 (51.5) | 421 (42.9) | .01 |
| Seen ads against smoking last 30 days | 1141 (79.7) | 383 (77.8) | 758 (80.5) | .23 | |
| Seen cigarette package warnings | 1275 (87.4) | 442 (88.8) | 833 (86.8) | .30 | |
| Family warned about dangers of cigarettes | 1121 (76.5) | 374 (76.6) | 747 (76.4) | .91 | |
| Family knows smoke waterpipe | 166 (57.2) | 77 (55.0) | 89 (58.8) | .50 | |
| Father and/or mother smoke cigarettes | 733 (49.7) | 281 (58.6) | 452 (46.0) | .00 | |
| Sibling(s) smoke cigarettes | 237 (16.1) | 103 (20.4) | 134 (14.2) | .01 | |
| Friends smoke cigarettes | 247 (17.1) | 114 (21.9) | 133 (15.1) | .01 | |
| Seen actors smoking in media | 1245 (87.1) | 418 (85.2) | 827 (87.9) | .17 | |
| Teachers smoke around students | 492 (30.0) | 209 (40.6) | 283 (25.6) | .00 | |
| Attitudes | Believe cigarettes are bad for health | 1351 (93.6) | 456 (92.2) | 895 (94.2) | .16 |
| Believe students who smoke have more friends | 318 (39.8) | 120 (39.7) | 198 (39.8) | .98 | |
| Believe students who smoke cigarettes are more attractive | 503 (48.3) | 191 (54.7) | 312 (45.3) | .01 | |
| Believe cigarettes effect weight (lose weight) | 840 (57.5) | 283 (56.4) | 557 (58.0) | .56 | |
| Believe it is easy to stop smoking cigarettes after year or so | 425 (29.8) | 149 (29.3) | 276 (30.1) | .77 | |
| Relations | Relationship with parents (not good) | 39 (2.8) | 14 (2.8) | 25 (2.8) | .95 |
| Relationship with siblings (not good) | 47 (3.1) | 15 (3.3) | 32 (3.0) | .70 | |
| Relationship with classmates (not good) | 56 (3.9) | 17 (3.7) | 39 (4.0) | .08 | |
| Relationship with teachers (not good) | 75 (5.49) | 31 (7.2) | 44 (4.8) | .06 | |
| Would accept cigarette from friends | 41 (3.5) | 23 (5.5) | 18 (2.7) | .01 | |
| Intention to start smoking cigarettes next year | 120 (9.5) | 48 (11.0) | 72 (8.8) | .25 | |
aFor continuous variables, the OR approximates the risk change for every 1 year increase in age or one unit increase in the DI.
bIn Jordanian Dinars (JOD) (1JOD = 1.41USD).
*Standardized proportions are reported to account for complex sampling design.
**Chi-square test for equality of proportions p value reported.
Determinants of Cigarette Smoking Initiation
After controlling for sociodemographic covariates (gender, type of school [public/private], age, DI, father/mother education, and daily pocket money) waterpipe smoking, low refusal self-efficacy, intention to smoke cigarettes next year, and having friends who smoked cigarettes were predictive of cigarette smoking initiation for both boys and girls. Additionally, parental and sibling smoking were predictive of initiation of cigarette smoking among girls only (Table 2). While not having good relationships with family and teachers, as well as having positive attitudes towards cigarette smoking, were risk factors for initiation in the bivariate analysis, these associations were not significant in the multivariable model. Finally, there was no association between smoking initiation and noticing health warnings on cigarette packs.
Table 2.
Determinants of Cigarette Smoking Initiation, by Gender, Among a Cohort of Schoolchildren Aged 13 at Baseline, Irbid, Jordan, 2008–2011 (N = 1,454)
| Boys (n = 670) | Girls (n = 784) | |||
|---|---|---|---|---|
| Determinants | OR (95% CI) | AOR* (95% CI) | OR (95% CI) | AOR* (95% CI) |
| Smoke waterpipe | 6.12 (4.30–8.70) | 3.43 (2.06–5.69) | 9.13 (6.28–13.27) | 5.38 (3.43–8.42) |
| Parents smoke cigarettes | 1.33 (0.99–1.79) | 1.15 (0.71–1.85) | 2.48 (1.73–3.55) | 1.90 (1.20–3.00) |
| Sibling(s) smoke cigarettes | 1.55 (1.11–2.18) | 0.91 (0.53–1.55) | 2.48 (1.75–3.51) | 1.75 (1.11–2.75) |
| Friends smoke cigarettes | 5.29 (3.71–7.54) | 2.34 (1.40–3.91) | 5.00 (3.53–7.07) | 2.00 (1.22–3.28) |
| Accept cigarettes from friend | 23.32 (15.91–34.17) | 10.67 (6.14–18.56) | 12.74 (8.48–19.14) | 4.95 (2.70–9.08) |
| Intend to start smoking cigarettes next year | 7.15 (5.14–9.94) | 3.07 (1.77–5.32) | 4.43 (2.90–6.78) | 2.07 (1.09–3.94) |
Note. AOR = adjusted odds ratio; CI = confidence interval.
*Odds ratios adjusted for all variables in the model. Variables with p > 0.20 in bivariate analysis were excluded from the final model.
Discussion
This is the first longitudinal study of smoking initiation among adolescents in the EMR, and one of the very few to be conducted in the developing world. In this prospective cohort of 1,781 Jordanian schoolchildren, we found that nearly one-fifth of adolescents were already smoking cigarettes at baseline (mean age 12.7 years). Of the cigarette naïve students, almost one-third (29.8%) began smoking cigarettes by 10th grade (mean age 14.6 years); with boys slightly more likely to initiate cigarette smoking compared to girls. Cross-sectional analysis among this cohort revealed that WP smoking was more prevalent than cigarette smoking at every time point (2008–2011) in both sexes while cigarette smoking showed a steeper increase over the same time period. Generally, girls had lower levels of smoking than boys for both cigarettes and waterpipe. For girls, overall smoking initiation was about 2 years behind that of boys, with cigarette initiation delayed about 2 years compared to waterpipe.16 For all participants, we found that a mixture of individual (e.g., ever smoked WP, poor refusal skills, intention to smoke) and social (e.g. friends smoking) factors were the most important determinants of smoking initiation. Additionally, solely for girls, familial (e.g. parents/siblings) smoking was a strong predictor of cigarette smoking initiation. These results provide valuable insights to understand smoking initiation among youth, as well as targets for efforts to reduce smoking in this population.
One of the unique features related to cigarette initiation in Jordan and the EMR, is its relation to WP smoking, which is becoming more popular than cigarettes in this region. For example, ever WP smoking was a risk factor for cigarette initiation in our study, more so for girls than boys. Interestingly, WP smoking by girls does not face the same social taboo as cigarette smoking in the EMR. Our results therefore, can signify WP smoking as being a “gateway” to cigarettes, especially among girls. The waterpipe delivers adequate amounts of nicotine to smokers, but it is considerably less accessible than cigarettes (e.g. requires a long time to setup and smoke and is much less portable). Those who become dependent on nicotine through the waterpipe may resort to easily accessible cigarettes to satisfy their urge.55–60 Additionally, many cafés and restaurants in the EMR cater to WP smokers, providing an environment where pro-smoking norms are pervasive, and perhaps conducive to tobacco use by adolescents.61–63 Intervention planning in Jordan and other places in the EMR where WP is commonplace would need to address the WP and its harmful and addictive properties, and involve strong policy provisions such as clean indoor air policies.64,65
Poor refusal self-efficacy and intention to smoke have frequently been identified as strong predictors of adolescent cigarette initiation in developed countries.66–68 They have also been found to be indicative of “late-stage” smoking acquisition, where the adolescent has a clear intention to begin smoking.69 These factors were also strong predictors of cigarette smoking initiation in our population. This shows that patterns of initiation in different parts of the world and cultures do have some shared patterns as well as specific ones such as the WP in this case. Therefore, successful interventions focusing on strengthening refusal skills and self-efficacy may be adaptable to the EMR.70,71 In fact, a clinical trial found that peer-led education increased smoking refusal self-efficacy among Jordanian high-school students with asthma (but not among students free from asthma).72
The influence of friends’ smoking on both boys and girls in our sample is in line with theories emphasizing the power of peer modeling in the development of health behaviors among youth.10,32,40,49,73–79 One of the interesting findings in our study was that family smoking was strongly predictive of cigarette initiation for girls but not for boys. An interpretation could be that in the EMR, where there is greater societal disapproval and less tolerance for girls’ cigarette smoking, smoking among family members may signify more tolerance towards the habit, and perhaps provide girls with more private access to experimentation with it.12,52 Boys on the other hand, would not be subjected to the same social taboo or “bad publicity,” which seems to define a different contextual environment for initiation that is dominated by friends’ smoking.10,49 Just as peer/family influence can be a risk for smoking initiation, their influence can be part of the solution as well. For example, the Truth Campaign of the American Legacy Foundation has utilized peers to promote healthy behaviors among adolescents, and helped reduce adolescent cigarette uptake.80 Our results suggest that gender- and tobacco use method-specific approaches are perhaps needed to limit smoking initiation among adolescents in Jordan, as well as other countries in the EMR, who share much of the cultural attitudes and taboos about smoking. Family and peer involvement in such programs appear to be of major importance, given their potentially salient role in smoking initiation among adolescents.
Tobacco control policies, such as banning advertisement and enforcing graphic warning labels have been shown to influence adolescents’ cigarette uptake in developed countries.81–84 In Jordan, and perhaps other EMR countries, the situation seems to be different. For example, Jordan has a graphic warning policy in place that requires covering 30% of the front and rear sides of the cigarette package. In our study, noticing such warnings was widespread among students, yet it was not associated with smoking initiation. It is possible that in the absence of comprehensive tobacco control policy environment, single measures will not lead to changing the social norms, and thus will have lesser impact on smoking.30,81,82,85
Strengths and Limitations
A weakness of this study could be that all responses were self-reported and due to the social undesirability of cigarette smoking among females in Jordan, there may be a higher level of underreporting of smoking by girls. However, research has shown strong agreement between self-reported smoking rates among adolescents and those verified with biochemical measures.86 Additionally, our previous research among adolescents in the EMR has found them willing to share honestly about their smoking experience when confidentiality is assured.87
Conclusions
Our results suggest that multiple levels of influence are involved in the onset of cigarette smoking among adolescents in Jordan, and that both individual level and social (family-friend) level factors are important in this regard. Some of these risk factors have also been identified among adolescents in developed countries and have been successfully addressed with multiple strategies including public health policy, clean indoor air laws, supportive school environment, and personal skills development.85 Components of these interventions therefore, can perhaps be adopted for use among youth in Jordan and the EMR, but they are unlikely to be effective unless they are dealt with within a comprehensive tobacco control package. Other factors, such as the effect of WP smoking on cigarette initiation, especially among girls, need to be addressed based on local evidence. Taken together, these findings could help form the basis for effective tobacco control interventions and policies in Jordan and provide a starting point for other similarly situated countries in their fight against youth tobacco use.
Supplementary Material
Supplementary material can be found online at http://www.ntr.oxfordjournals.org
Funding
This work is supported by the National Institute on Drug Abuse Grants (R01 DA024876 and R01 DA035160).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The corresponding author hereby affirms that all who made significant contributions to this work have been listed. The funder had no role in the study design, conduct, collection, management, analysis or interpretation of the data or preparation, review or approval of the manuscript.
References
- 1. Williams CL, Hayman LL, Daniels SR, et al. Cardiovascular health in childhood: a statement for health professionals from the committee on atherosclerosis, hypertension, and obesity in the young (AHOY) of the council on cardiovascular disease in the young, American Heart Association. Circulation. 2002;106:143–160. [DOI] [PubMed] [Google Scholar]
- 2. Thun M, Peto R, Boreham J, Lopez AD. Stages of the cigarette epidemic on entering its second century. Tob Control. 2012;21:96–101. [DOI] [PubMed] [Google Scholar]
- 3. Flouris AD, Faught BE, Klentrou P. Cardiovascular disease risk in adolescent smokers: Evidence of a ‘smoker lifestyle’. J Child Health Care. 2008;12:221–231. [DOI] [PubMed] [Google Scholar]
- 4. Holmen TL, Barrett-Connor E, Holmen J, Bjermer L. Health problems in teenage daily smokers versus nonsmokers, Norway, 1995–1997: the Nord-Trondelag health study. Am J Epidemiol. 2000;151:148–155. [DOI] [PubMed] [Google Scholar]
- 5. US Department of Health and Human Services. Preventing tobacco use among youth and young adults: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/. Accessed September 2, 2014. [Google Scholar]
- 6. Mackay J, Eriksen M, Shafey O. The Tobacco Atlas. 2nd Atlanta, GA: American Cancer Society; 2006. [Google Scholar]
- 7. Warren CW. The Global Youth Tobacco Survey Collaborative Group. Tobacco use among youth: a cross country comparison. Tob Control. 2002;11:52–70. [Google Scholar]
- 8. Global Youth Tobacco Survey Collaborating Group. Differences in worldwide tobacco use by gender: findings from the Global Youth Tobacco Survey (Special report). J School Health. 2003;73:207–215 http://go.galegroup.com/ps/i.do?id=GALE%7CA106142966&v=2.1&u=miam11506&it=r&p=AIM&sw=w&asid=e27938faf8db3688e25789c9ce7fe323. Accessed September 2, 2014. [DOI] [PubMed] [Google Scholar]
- 9. Kong G, Singh N, Krishnan-Sarin S. A review of culturally targeted/tailored tobacco prevention and cessation interventions for minority adolescents. Nicotine Tob Res. 2012;14:1394–1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maziak W, Rastam S, Eissenberg T, et al. Gender and smoking status-based analysis of views regarding waterpipe and cigarette smoking in Aleppo, Syria. Prev Med. 2004;38:479–484. [DOI] [PubMed] [Google Scholar]
- 11. Maziak W, Nakkash R, Bahelah R, Husseini A, Fanous N, Eissenberg T. Tobacco in the Arab world: old and new epidemics amidst policy paralysis. Health Policy Plan. 2014;29:784–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Okoli C, Greaves L, Fagyas V. Sex differences in smoking initiation among children and adolescents. Public Health. 2013;127:3–10. [DOI] [PubMed] [Google Scholar]
- 13. Wade B, Lariscy JT, Hummer RA. Racial/ethnic and nativity patterns of U.S. adolescent and young adult smoking. Population Research and Policy Review. 2013;32:353–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maziak W. The waterpipe: a new global threat to CV health? Glob Heart. 2012;7:179–181. [DOI] [PubMed] [Google Scholar]
- 15. Kelishadi R, Mokhtari M, Tavasoli A, et al. Determinants of tobacco use among youths in Isfahan, Iran. Int J Pub Health. 2007;52:173–179. [DOI] [PubMed] [Google Scholar]
- 16. McKelvey KL, Wilcox ML, Madhivanan P, Mzayek F, Khader Y, Maziak W. Time trends of cigarette and waterpipe smoking among a cohort of school children in Irbid, Jordan, 2008–11. Eur J Public Health. 2013;23:862–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mzayek F, Khader Y, Eissenberg T, Al Ali R, Ward K, Maziak W. Patterns of water-pipe and cigarette smoking initiation in schoolchildren: Irbid longitudinal smoking study. Nicotine Tob Res. 2012;14:448–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nasim A, Khader Y, Blank MD, Cobb CO, Eissenberg T. Trends in alternative tobacco use among light, moderate, and heavy smokers in adolescence, 1999–2009. Addict Behav. 2012;37:866–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parna K, Usin J, Ringmets I. Cigarette and waterpipe smoking among adolescents in Estonia: HBSC survey results, 1994–2006. BMC Public Health. 2008;8:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Amos A, Greaves L, Nichter M, Bloch M. Women and tobacco: A call for including gender in tobacco control research, policy and practice. Tob Control. 2012;21:236–243. [DOI] [PubMed] [Google Scholar]
- 21. Prokhorov AV, Winickoff JP, Ahluwalia JS, et al. ; Tobacco Consortium, American Academy of Pediatrics Center for Child Health Research. Youth tobacco use: a global perspective for child health care clinicians. Pediatrics. 2006;118:e890–e903. [DOI] [PubMed] [Google Scholar]
- 22. Warren CW, Riley L, Asma S, et al. Tobacco use by youth: a surveillance report from the global youth tobacco survey project. Bull World Health Organ. 2000;78:868–876. [PMC free article] [PubMed] [Google Scholar]
- 23. Derzon JH, Lipsey MW. Predicting tobacco use to age 18: a synthesis of longitudinal research. Addiction. 1999;94:995–1006. [DOI] [PubMed] [Google Scholar]
- 24. Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control. 1994;3:242–247. [Google Scholar]
- 25. Fernander A, Resnicow K, Viswanath K, Pérez-Stable EJ. Cigarette smoking interventions among diverse populations. Am J Health Promot. 2011;25(S5):S1–S4. [DOI] [PubMed] [Google Scholar]
- 26. Maziak W, Eissenberg T, Klesges RC, Keil U, Ward K. Adapting smoking cessation interventions for developing countries: a model for the Middle East. Int J Tuberc Lung Dis. 2004;8:403–413 http://www.ingentaconnect.com/content/iuatld/ijtld/2004/00000008/00000004/art00003. Accessed September 2, 2014. [PubMed] [Google Scholar]
- 27. Petraitis J, Flay BR, Miller TQ. Reviewing theories of adolescent substance use: organizing pieces in the puzzle. Psychol Bull. 1995;117:67–86. [DOI] [PubMed] [Google Scholar]
- 28. Sussman S, Skara S, Ames SL. Substance abuse among adolescents. Subst Use Misuse. 2008;43:1802–1828. [DOI] [PubMed] [Google Scholar]
- 29. Turner L, Mermelstein R, Flay B. Individual and contextual influences on adolescent smoking. Ann N Y Acad Sci. 2004;1021:175–197. [DOI] [PubMed] [Google Scholar]
- 30. Ennett ST, Foshee VA, Bauman KE, et al. A social contextual analysis of youth cigarette smoking development. Nicotine Tob Res. 2010;12:950–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wilcox P. An ecological approach to understanding youth smoking trajectories: problems and prospects. Addiction. 2003;98:57–77. [DOI] [PubMed] [Google Scholar]
- 32. Chang F, Lee C, Lai H, Chiang J, Lee P, Chen W. Social influences and self-efficacy as predictors of youth smoking initiation and cessation: a 3-year longitudinal study of vocational high school students in Taiwan. Addiction. 2006;101:1645–1655. [DOI] [PubMed] [Google Scholar]
- 33. de Vries H, Backbier E, Kok G, Dijkstra M. The impact of social influences in the context of attitude, self-efficacy, intention, and previous behavior as predictors of smoking onset. J Appl Soc Psychol. 1995;25:237–257. [Google Scholar]
- 34. Grucza RA, Plunk AD, Hipp PR, et al. Long-term effects of laws governing youth access to tobacco. Am J Public Health. 2013;103:1493–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoving C, Reubsaet A, de Vries H. Predictors of smoking stage transitions for adolescent boys and girls. Prev Med. 2007;44:485–489. [DOI] [PubMed] [Google Scholar]
- 36. Lando HA, Hipple BJ, Muramoto M, et al. Tobacco control and children: an international perspective. Pediatr Allergy Immunol Pulmonol. 2010;23:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lando HA, Borrelli B, Klein LC, et al. The landscape in global tobacco control research: a guide to gaining a foothold. Am J Public Health. 2005;95:939–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Latimer W, Zur J. Epidemiologic trends of adolescent use of alcohol, tobacco, and other drugs. Child Adolesc Psychiatr Clin N Am. 2010;19:451–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lee G, Lee J, Lee S. Risk factors of future smoking among Thai youth: a secondary analysis of the Thai Global Youth Tobacco Survey [published online ahead of print May 10, 2013]. Asia Pac J Public Health. 10.1177/1010539513487015. [DOI] [PubMed] [Google Scholar]
- 40. Ma H, Unger JB, Chou C, et al. Risk factors for adolescent smoking in urban and rural China: findings from the China seven cities study. Addict Behav. 2008;33:1081–1085. [DOI] [PubMed] [Google Scholar]
- 41. Mamudu HM, Veeranki SP, John RM. Tobacco use among school-going adolescents (11–17 years) in Ghana. Nicotine Tob Res. 2013;15:1355–1364. [DOI] [PubMed] [Google Scholar]
- 42. Mzayek F, Khader Y, Eissenberg T, Ward K, Maziak W. Design, baseline results of Irbid longitudinal, school-based smoking study. Am J Health Behav. 2011;35:746–755. [PMC free article] [PubMed] [Google Scholar]
- 43. World Health Organization. Guidelines for controlling and monitoring the tobacco epidemic. Geneva: WHO, 2000; 1998. apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan= 1&codcol=15&codcch=468. Accessed September 2, 2014. [Google Scholar]
- 44. Maziak W, Ward K, Afifi Soweid RA, Eissenberg T. Standardizing questionnaire items for the assessment of waterpipe tobacco use in epidemiological studies. Public Health. 2005;119:400–404. [DOI] [PubMed] [Google Scholar]
- 45. Maziak W, Asfar T. Physical abuse in low-income women in Aleppo, Syria. Health Care Women Int. 2003;24:313–326. [DOI] [PubMed] [Google Scholar]
- 46. Austin SB, Gortmaker SL. Dieting and smoking initiation in early adolescent girls and boys: a prospective study. Am J Public Health. 2001;91:446–450 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446587/pdf/11236412.pdf. Accessed September 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Babar AA, Stigler MH, Perry CL, Arora M, Shrivastav R, Reddy KS. Tobacco-use psychosocial risk profiles of girls and boys in urban India: implications for gender-specific tobacco intervention development. Nicotine Tob Res. 2010;12:29–36. [DOI] [PubMed] [Google Scholar]
- 48. Greaves L. Gender, equity and tobacco control. Health Sociol Rev. 2007;16:115–129. [Google Scholar]
- 49. Nichter M. Smoking: what does culture have to do with it? Addiction. 2003;98(S1):139–145. [DOI] [PubMed] [Google Scholar]
- 50. Rice VH, Weglicki LS, Templin TN, Jamil H, Hammad A. Intervention effects on tobacco use in Arab and non-Arab American adolescents. Addict Behav. 2010;35:46–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Trudeau L, Spoth R, Randall GK, Azevedo K. Longitudinal effects of a universal family-focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: gender comparisons. J Youth Adolesc. 2007;36:725–740. [Google Scholar]
- 52. Zhu BP, Liu M, Shelton D, Liu S, Giovino GA. Cigarette smoking and its risk factors among elementary school students in Beijing. Am J Public Health. 1996;86:368–375 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1380518/pdf/amjph00514-0082.pdf. Accessed September 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. DeCoster J, Iselin AR, Gallucci M. A conceptual and empirical examination of justifications for dichotomization. Psychol Methods. 2009;14:349. [DOI] [PubMed] [Google Scholar]
- 54. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed New York, NY: John Wiley and Sons, Inc.; 2000. [Google Scholar]
- 55. Kassim S, Al-Bakri A, al’Absi M, Croucher R. Waterpipe tobacco dependence in U.K. male adult residents: a cross-sectional study. Nicotine Tob Res. 2014;16:316–325. [DOI] [PubMed] [Google Scholar]
- 56. Maziak W. The waterpipe: a new way of hooking youth on tobacco. Am J Addict. 2013;23:103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rastam S, Eissenberg T, Ibrahim I, Ward K, Khalil R, Maziak W. Comparative analysis of waterpipe and cigarette suppression of abstinence and craving symptoms. Addict Behav. 2011;36:555–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rice VH, Weglicki LS, Templin T, Hammad A, Jamil H, Kulwicki A. Predictors of Arab American adolescent tobacco use. Merrill Palmer Q (Wayne State Univ Press). 2006;52:327–342 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1533871/. Accessed September 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Roskin J, Aveyard P. Canadian and English students’ beliefs about waterpipe smoking: a qualitative study. BMC Public Health. 2009;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Weglicki LS, Templin TN, Rice VH, Jamil H, Hammad A. Comparison of cigarette and water-pipe smoking by Arab and Non–Arab-American youth. Am J Prev Med. 2008;35:334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Maziak W, Ward K, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tob Control. 2004;13:327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Maziak W. The waterpipe: time for action. Addiction. 2008;103:1763–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Backinger CL, Fagan P, Matthews E, Grana R. Adolescent and young adult tobacco prevention and cessation: current status and future directions. Tob Control. 2003;12(S4):IV46–53 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1766138/pdf/v012p0iv46.pdf. Accessed September 2, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Mitschke DB, Matsunaga DS, Loebl K, Tatafu E, Robinett H. Multi-ethnic adolescents’ attitudes toward smoking: a focus group analysis. Am J Health Promot. 2008;22:393–399. [DOI] [PubMed] [Google Scholar]
- 66. Skara S, Sussman S, Dent CW. Predicting regular cigarette use among continuation high school students. Am J Health Behav. 2001;25:147–156 http://dx.doi.org/10.5993/AJHB.25.2.7. Accessed September 2, 2014. [DOI] [PubMed] [Google Scholar]
- 67. Stanton WR, Barnett AG, Silva PA. Adolescents’ intentions to smoke as a predictor of smoking. Prev Med. 2005;40:221–226. [DOI] [PubMed] [Google Scholar]
- 68. Vitória PD, Salgueiro MF, Silva SA, de Vries H. Social influence, intention to smoke, and adolescent smoking behaviour longitudinal relations. Br J Health Psychol. 2011;16:779–798. [DOI] [PubMed] [Google Scholar]
- 69. Hill AJ, Boudreau F, Amyot É, Déry D, Godin G. Predicting the stages of smoking acquisition according to the Theory of Planned Behavior. J Adolescent Health. 1997;21:107–115. [DOI] [PubMed] [Google Scholar]
- 70. Moyer VA. Primary care interventions to prevent tobacco use in children and adolescents: U.S. preventive services task force recommendation statement. Pediatrics. 2013;132:560–565. [DOI] [PubMed] [Google Scholar]
- 71. Sims TH, Committee on Substance Abuse. From the American Academy of Pediatrics: technical report--tobacco as a substance of abuse. Pediatrics. 2009;124:e1045–53. [DOI] [PubMed] [Google Scholar]
- 72. Al-sheyab N, Gallagher R, Crisp J, Shah S. Peer-led education for adolescents with asthma in Jordan: a cluster-randomized controlled trial. Pediatrics. 2012;129:e106–e112. [DOI] [PubMed] [Google Scholar]
- 73. Bidstrup PE, Frederiksen K, Siersma V, et al. Social-cognitive and school factors in initiation of smoking among adolescents: a prospective cohort study. Cancer Epidemiol Biomarkers Prevent. 2009;18:384–392. [DOI] [PubMed] [Google Scholar]
- 74. Hiemstra M, Otten R, de Leeuw RNH, van Schayck OCP, Engels R. The changing role of self-efficacy in adolescent smoking initiation. J Adolescent Health. 2011;48:597–603. [DOI] [PubMed] [Google Scholar]
- 75. Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug Alcohol Depend. 2000;59:61–81. [DOI] [PubMed] [Google Scholar]
- 76. O’Loughlin JL, Karp I, Koulis T, Paradis G, DiFranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am J Epidemiol. 2009;170:585–597. [DOI] [PubMed] [Google Scholar]
- 77. Piko BF, Luszczynska A, Gibbons FX, Teközel M. A culture-based study of personal and social influences of adolescent smoking. Eur J Public Health. 2005;15:393–398. [DOI] [PubMed] [Google Scholar]
- 78. Scal P, Ireland M, Borowsky I. Smoking among American adolescents: a risk and protective factor analysis. J Community Health. 2003;28:79–97. [DOI] [PubMed] [Google Scholar]
- 79. Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7:409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Brechwald WA, Prinstein MJ. Beyond homophily: a decade of advances in understanding peer influence processes. J Res Adolescence. 2011;21:166–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Biener L, Ji M, Gilpin EA, Albers AB. The impact of emotional tone, message, and broadcast parameters in youth anti-smoking advertisements. J Health Commun. 2004;9:259–274. [DOI] [PubMed] [Google Scholar]
- 82. Terry-McElrath Y, Wakefield M, Ruel E, et al. The effect of antismoking advertisement executional characteristics on youth comprehension, appraisal, recall, and engagement. J Health Commun. 2005;10:127–143. [DOI] [PubMed] [Google Scholar]
- 83. Wakefield M, Flay B, Nichter M, Giovino G. Role of the media in influencing trajectories of youth smoking. Addiction. 2003;98(S1):79–103. [DOI] [PubMed] [Google Scholar]
- 84. White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours? Addiction. 2008;103:1562–1571. [DOI] [PubMed] [Google Scholar]
- 85. Jackson SF, Perkins F, Khandor E, Cordwell L, Hamann S, Buasai S. Integrated health promotion strategies: a contribution to tackling current and future health challenges. Health Promot Int. 2006;21(S1):75–83. [DOI] [PubMed] [Google Scholar]
- 86. Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolescent Health. 2003;33:436–457. [DOI] [PubMed] [Google Scholar]
- 87. Maziak W, Mzayek F. Characterization of the smoking habit among high school students in Syria. Eur J Epidemiol. 2000;16:1169–1176. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.