Abstract
BACKGROUND
Snacks served in afterschool programs (ASPs, 3–6pm) represent an important opportunity to promote healthy eating. ASP policies suggest a fruit/vegetable is served daily, while sugar-sweetened foods/beverages and artificially-flavored snacks are eliminated. Limited information exists on the types of snacks served in ASPs, if snacks meet existing nutrition policies, whether children eat the snacks, and their cost.
METHODS
Direct observation of snacks served and consumed was collected in 20 ASPs serving over 1,700 elementary-age children. The number of days snacks were served/week was evaluated for compliance with nutrition policies. Costs of snacks were collected via receipts.
RESULTS
Programs served desserts and artificially-flavored salty-snacks on 2.7 and 2.1 days/week. Fruits and vegetables were served 0.6 and 0.1 days/wk, respectively. Sugar-sweetened-beverages were served 1.8 days/wk. Of the children (N=383) observed, 75–100% consumed the snack served, with 95% and 100% of served fruits/vegetables consumed. No ASP served fruit/vegetables daily, 18 served sugar-sweetened foods, 16 served artificially-flavored snacks, and 14 served sugar-sweetened-beverages. Desserts and salty-snacks cost $0.27–$0.32/snack vs. $0.38–$0.40/snack for vegetables/fruits.
CONCLUSIONS
The quality of snacks failed to meet nutrition policies and consists of predominately high-sugar and artificially-flavored options. Strategies to improve snack offerings in ASPs while addressing price barriers are required.
Keywords: Nutrition, Community-based Programs, Children, School, Food
Nationally, afterschool programs (ASPs, 3–6pm) represent one of the largest settings, outside the regular school day, that serve youth (predominately elementary-age children) every school day of the year. As part of their daily routine ASPs serve a snack, in addition to providing time for homework completion or assistance, enrichment (eg, arts-n-crafts), and physical activity. The snack represents an important opportunity to not only provide nourishment between school lunch and dinner in the home, but to promote healthy eating habits.1 Because of this, national and state organizations have developed policies and standards specifically targeting the types of foods and beverages ASPs should serve for snack. In April 2011, the National Afterschool Association (www.naaweb.org) endorsed the first nationally recognized Healthy Eating Standards for ASPs. The Healthy Eating Standards call for ASPs to serve a fruit or vegetable daily, serve water as the primary beverage, not to serve foods with artificial colors or flavors, such as, chips with artificial flavorings, and eliminate sugar-sweetened foods, such as, cookies, and beverages, such as, powdered drink mixes (www.naaweb.org).
Limited information has been gathered on the types of snacks ASPs routinely provide and whether these meet the Healthy Eating Standards. Three studies 2–4 describing snacks served in ASPs indicate the majority of snacks consist of foods high in salt and sugar, with fruits and vegetables almost entirely absent. Major barriers to serving healthier snacks, like fruits and vegetables, are cost and the question of whether children will consume them.5–7 Evidence from school lunch interventions indicates anywhere from 40% to 80% of fruits and vegetables served go uneaten.8–10 If ASPs are to serve healthier snacks, whether these will be consumed or thrown away is important information for both program providers and policy makers. The limited information that does exist on the cost of snacks suggests healthier snacks are more expensive than less healthy snacks.6 However, this is limited to a single study 6 with price information based on 2003–04 market prices, not actual purchase prices. The purpose of this study was to address these gaps by providing information about the types of snacks served, their consumption, cost in a diverse sample of ASPs, and whether ASPs currently meet the Healthy Eating Standards. The information presented here represents baseline data from a multi-year randomized controlled trial.
METHODS
Participants
For this study, ASPs were defined as child care programs operating immediately after the school day, every day of the school year for a minimum of 2 hours, serving a minimum of 30 children of elementary age (6–12yrs), operating in a school, community, or faith setting, and providing a snack, homework assistance/completion time, enrichment, and opportunities for physical activity participated in this study.11 Twenty afterschool programs, representing 13 different organizations were randomly selected from an existing registry of 535 ASPs in South Carolina and invited to participate in an intervention targeting healthy eating and physical activity. The information presented herein represents baseline (March–April 2013) snack information collected as part of a larger intervention study. Program eligibility consisted of operating within 1.5hr drive from the university and classification as an ASP as defined above. Across the 20 ASPs, mean enrollment was 88 children (range 30 to 162). No programs received federal or state reimbursement for snack expenditures or self-identified any nutrition policies guiding snack purchasing decisions. The average zip code population poverty status and family in poverty status, based on 2000 US Census data, were 16.8% and 11.7% (range 1.2% to 28.8%), respectively. The ethnic/racial composition of the ASPs was 57% White non-Hispanic and 38% African American.
Snack Classification
The types of foods and beverages served as snack were recorded via direct observation by trained research personnel. Each ASP was visited on 4 non-consecutive unannounced days between March and April 2013. Immediately at the start of snack, the trained observer recorded the brand name(s), size, and packaging, where appropriate, of the foods and beverages served as snack for that day. Foods and beverage items served as snacks were classified according to existing categories for snacks and beverages 1, 4: sugar sweetened beverages, such as soda, powered drink mixed, and sport drinks; dairy food unsweetened, such as string cheese; dairy food sweetened, such as Trix yogurt; milk unsweetened (non-fat, 1%, 2%, and whole); milk sweetened, such as chocolateor strawberry; 100% fruit juice; salty flavored snacks, such as Doritos and Chex Mix, salty unflavored snacks, such as pretzels and plain corn tortilla chips; desserts, such as cookies and pop tarts); candy, such as chocolate and frozen treats; non-fruit fruit, such as fruit roll ups and fruit leather; prepackaged fruit, such as applesauce and fruit in syrup; cereal sugar-sweetened, such as Fruit Loops; cereal unsweetened, such as Cheerios; and fruits and vegetables (fresh, frozen, dried). Water was recorded if programs provided water in cups or bottles during snack time.
Consumption of Snacks
Consumption of snacks was collected using a modified direct observation protocol.12 During snack, children sat in groups of three or more children. At each unannounced site visit, trained research staff randomly selected a group of children. Within this group, no more than five children were randomly selected and observed for the entire duration of the snack time (approximately 15mins). During this time, a single observer recorded what the children were served for snack and indicated whether each child consumed the snack. Consumption was operationalized as observing a child eating 50% or more of an offered snack item. For instance, if children were provided a whole piece of fruit, a child would be classified as consuming the fruit if researchers observed that the child had eaten at least half of the fruit. Where children did not eat any of the snack or only took several bites, consumption was recorded as zero (ie, not consumed). Inter-rater consumption reliability was estimated on 107 children served 217 snacks with a κ= 0.89 and percent agreement 97%.
Costs of Snacks
Costs of the snacks were estimated based on receipts provided by the ASPs from March to June 2013. For each individual snack item cost per snack served was determined using standard serving sizes.1
Statistical Analysis
Descriptive analyses of snacks served, comparison of snacks to the Healthy Eating Standards, and their consumption were conducted summer 2013. The average number of days each food and beverage category was served was calculated and standardized to a 5 day school week across sites. Each ASPs’ snack offerings were evaluated for meeting the Health Eating Standards. The percentage of children consuming the snacks for each snack category, in addition to the average cost per serving for each snack category was estimated. Comparisons in cost per snack among snack categories were made using analysis of variance. All analyses were conducted using STATA (v.12.0, College Station, TX).
RESULTS
A total of 84 days of snack observation were made across the 20 sites (average 4.2 days per ASP, range 4 to 6 days). Two sites had a total of five days and a single site with 6 days of observation each due to cancelation of the program earlier than regularly scheduled (<1hr), although snack was still served at these visits and research protocol for other measures (eg, physical activity – not reported herein) required a return visit in order to observe a complete program day. The average number of times a snack category was observed across a 5 day week, the proportion of children observed consuming 50% of more of the snack items, and the cost per snack are presented in Table 2. On average, ASPs served 1.9 different snack food options per day during snack, with 10 ASPs providing only a single snack item per day, while 2 ASPs offered a choice of a single snack from 4 different snack items. On average, ASPs offered 1.1 beverages per day (range 0 to 3 beverage options per day). Programs not serving a beverage had water fountains available for drinking.
Table 2.
Afterschool Program Snacks Served, Consumed, and Cost Estimates
| Snack Food/Beverage Category | Item served (days per week) a | Percent Consumed b | Cost/Snack (US$)c | ||
|---|---|---|---|---|---|
| Foods | M | SD | % | M | SD |
| Dairy - unsweetened (e.g., cheese) | 0.6 | ±0.9 | 96.7 | 0.19 | ±0.10 |
| Dairy - sweetened (e.g., Trix yogurt) | 0.1 | ±0.3 | 100.0 | 0.35 | ±0.04 |
| Dips (e.g., peanut butter, ranch dressing) | 0.5 | ±0.8 | 86.7 | 0.07 | ±0.05 |
| Fruits (e.g., fresh, frozen, dried) | 0.6 | ±1.0 | 95.5 | 0.40 | ±0.19 |
| Vegetables (e.g., baby carrots, celery) | 0.1 | ±0.3 | 100.0 | 0.38 | ±0.18 |
| Pre-packaged vegetables (e.g., pickles) | 0.1 | ±0.4 | 100.0 | --- | --- |
| Salty snacks – flavored (e.g., Doritos, Chex Mix, Cheddar Goldfish) | 2.1 | ±1.7 | 93.6 | 0.32 | ±0.12 |
| Salty snacks – unflavored (e.g., pretzels, crackers, tortilla chips) | 1.3 | ±1.7 | 77.3 | 0.22 | ±0.09 |
| Desserts (e.g., cookies, muffins, snack cakes, cereal bars, pop tarts) | 2.7 | ±1.5 | 92.5 | 0.27 | ±0.11 |
| Cereal – sugar-sweetened (e.g., Fruit Loops) | 0.9 | ±1.3 | 94.7 | 0.34 | ±0.17 |
| Cereal – unsweetened (e.g., Cheerios) | 0.1 | ±0.4 | 100.0 | 0.39 | ±0.04 |
| Non-fruit fruit (e.g., fruit snacks, leather) | 0.1 | ±0.3 | 75.0 | 0.32 | ±0.02 |
| Pre-packaged processed meats (e.g., hot dogs) | 0.2 | ±0.7 | 80.0 | 0.53 | ±0.66 |
| Pre-packaged fruit (e.g., fruit cup) | --- | --- | --- | 0.51 | ±0.19 |
| Candy (e.g., chocolate bars, Twizzlers) | --- | --- | --- | 0.29 | ±0.11 |
| Beverages | |||||
| Sugar-sweetened non-dairy beverages (e.g., non-100% juices, powdered drink mixes, punch) | 1.8 | ±1.8 | 84.5 | 0.24 | ±0.22 |
| Milk – unflavored (e.g., skim, 2%) | 0.7 | ±1.2 | 80.8 | 0.22 | ±0.08 |
| Milk – sugar-sweetened (e.g., chocolate, strawberry) | 0.2 | ±0.6 | 100.0 | --- | --- |
| 100% Fruit Juice | 0.7 | ±1.4 | 78.0 | 0.37 | ±0.09 |
| Water | 1.8 | ±1.7 | 76.6 | --- | --- |
Snack servings per week represent the number of days per a 5 day week a snack was observed, with a minimum value of 0.0 days/wk and maximum value of 5 days/wk. Items with no information were not observed being served or eaten during snack
Consumption based on direct observation of a randomly selected subsample of children (N = 322) during snack time across 84 days (avg. 3.8 children observed per snack time)
Prices based on receipts provided by afterschool programs. All prices reflect Jan–May 2013 prices. Items without prices were not present on receipts
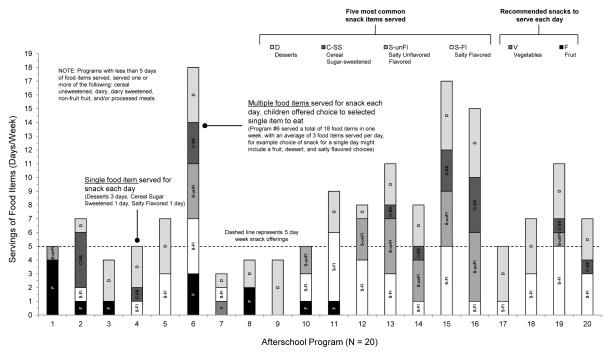
Overall, the most commonly observed snacks items were desserts, salty flavored, salty unflavored, and cereal sugar-sweetened. Across ASPs, less than one fruit or vegetable was served per day. The five most common snack food items observed, as well as fruit or vegetable snacks, for each ASP are illustrated in Figure 1. Several ASPs (eg, ASP #1 and #4) served only a single item for snack each day, while over half of the ASPs (eg, ASP #6, #13, #15, and #16) provided children with a choice of selecting a single snack each day from an option of 2 to 4 food items, such as the choice of either a fruit, or a salty flavored or dessert snack on a given day.
Figure 1.
Daily Snack Food Items Served Across 20 Afterschool Programs
No programs met all the Healthy Eating Standards (see Table 1). No programs met the standard of serving a fruit or vegetable daily, 2 ASPs did not serve sugar-sweetened foods (eg, desserts, dairy sweetened), 2 served water at each snack, 4 did not serve foods with artificial flavors or colors (eg, flavored salty-snacks – cheese puffs; cereal sweetened – Fruit Loops), and 6 did not serve any sugar-sweetened beverages. For consumption, a total of 383 children were observed with 481 foods (avg. 1.3 foods/child) and 271 beverages (avg. 0.7 beverages/child) during snack. Of these, consumption rates ranged from 75% for non-fruit fruit to 100% for sweetened dairy, vegetables, and unsweetened cereal.
Table 1.
National Afterschool Association Healthy Eating Standards
| Standard | Operational Definitiona | Number of ASPs meeting standard |
|---|---|---|
| On a daily basis, the afterschool program… | ||
| Serves a fruit or vegetable | Fruit or vegetable served every day of observation | 0 |
| Offers water at the table and has water accessible at all times | Water served to children during snack | 2 |
| Serves no candy or other foods that are primarily sugar based | No candy or dessert (e.g., cookies, pop tarts) foods served | 2 |
| Serves no beverages that are primarily sugar based | No sugar-sweetened beverages (e.g., powdered drink mixes, non-100% juice, flavored milk – chocolate/strawberry) served | 6 |
| Avoids foods and beverages made with artificial ingredients (sweeteners, flavors, or colors) | Foods with artificial flavors (e.g., sour cream and onion potato chips, cheese crackers) or colors (e.g., Fruit Loops, Trix cereal) are served | 4 |
Definition and evaluation of the Healthy Eating Standards was conducted on mutually exclusive categorization of the snacks served. For instance, artificial sweeteners are present in the “dessert and candy” food categories, but these categories are not included in the assessment of the “avoids foods/beverages made with artificial ingredients” standard but are counted in the “serves no candy or foods that are sugar-based”.
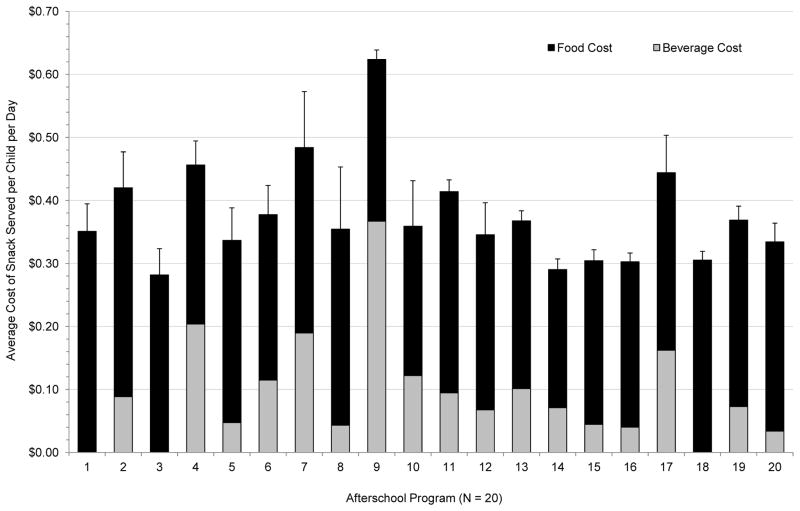
A total of 490 individual food and beverage items, with a median of 10 items per snack category (range 1 for non-100% fruit juice to 149 desserts) were represented in the receipts and used to estimate cost per snack. Prices for beverage items ranged from $0.22 for unflavored milk to $0.37 for 100% juice. The prices per serving for food items ranged from $0.19 for unsweetened dairy and $0.22 for salty unflavored snacks to $0.51 for prepackaged fruit and $0.53 for processed meats. The average snack cost per child per day is presented in Figure 2. On average, ASPs were spending $0.38 per snack per child per day (range $0.28 to $0.62). Fruit and vegetable cost per snack were significantly higher than desserts ($0.12 to $0.14 higher), and salty flavored and salty unflavored ($0.10 to $0.13 higher) snacks. Based on these cost estimates, an ASP serving a fruit or vegetable daily vs. serving a dessert or salty flavored or unflavored snack choice each day to 100 children over a standard 180 day school year would spend $7,244 compared to $4,877 in total snack expenditures.
Figure 2.
Average snack cost per child per day across 20 afterschool programs
DISCUSSION
This is the first study to provide comprehensive information on the types of snacks ASPs serve, their associated cost, and whether children consume them. An important component of this study is the evaluation of the alignment of the snacks currently served with nationally endorsed Healthy Eating Standards. In the 20 participating ASPs, we found that no ASPs met all the standards, only two did not serve foods that were sugar-based, such as pop tarts and cookies, only two served water daily, only four did not serve artificially flavored or colored foods, such as Chex Mix, and only six did not serve a sugar sweetened beverage (eg, Kool Aid). No ASP served fruits or vegetables daily. These findings clearly indicate the types of foods and beverages routinely served in ASPs fail to meet existing nationally recognized nutrition standards.
Failure of any ASP to meet all of the Healthy Eating Standards suggests greater efforts need to be made to assist program leaders in planning and purchasing foods and beverages that promote healthy eating. While meeting the Healthy Eating Standards are voluntary and not required by state or national licensing agencies, such standards do represent an important step towards creating health promoting ASPs.1, 13 Previous studies,2, 4 using either policy or standards to guide snack purchasing decisions have demonstrated increases in fruits and vegetables servings, along with reductions in sugar-based foods and beverages. While these studies indicate the importance of adopting a policy or standards, they failed to address price barriers to purchasing healthier snacks.5 We found that both fruits and vegetables were substantially more expensive per snack than both salty flavored or unflavored snacks and desserts. This is consistent with price differences among snack categories from a previous study.6 Because of the added cost of serving snacks that meet the Healthy Eating Standards, ASPs require additional support to purchase foods at a reduced price. Potential solutions are buying co-ops or partnerships with local grocery stores.13, 14 While, such strategies are in their infancy,14, 15 they represent creative ways to address price barriers. Another strategy to reduce cost is to eliminate flavored beverages from the snack offering. Based on our cost estimates, programs serving a snack (eg, cheese, chips, or cookies) plus a flavored drink (eg, 100% juice, milk, or sugar-sweetened beverage) spent approximately twice as much ($0.27 vs. $0.54/snack) compared to serving the snack with water. Thus, simply eliminating the purchased beverage can provide a substantial cost saving that can be redistributed to purchasing fruits or vegetables. Of note, none of the ASPs in this study budgeted for snack expenditures or were tracking snack expenses. While this might be limited to this sample of ASPs, it suggests ASPs may be unaware of how much they actually spend on snacks, which presents an issue when attempting to design a “healthier” snack menu that conforms to their allocated snack budget.
Another important finding was the number of different food categories provided across a week in several of the ASPs (see Figure 1). This may be due, in part, to the Healthy Eating Standards recommending ASPs “on a daily basis, offer choice…” The idea of providing choice is a foundation of youth development professional core competencies, that call for environments to be structured to offer choices that engage and empower children.a In the current study, choice as it relates to the snacks offered, appears to have been translated into serving a healthy snack (ie, fruit) alongside less healthy snacks (eg, desserts and/or salty flavored snacks) – see ASP #6 in Figure 1. Whether children, when faced with choosing a sweet or salty snack versus a fruit will select the fruit is unknown. However, it stands to reason that in this instance children will choose the less healthy salty or sweet option. Based on our consumption data in ASPs that offered a fruit with one or more other snack choices each day (total of 3 days), we observed that approximately 45% of the children (4 of 9 kids) selected and 100% consumed the fruit. These results should be interpreted with caution since fruit served alongside another snack item was observed on only 3 of the 84 observation days. Nevertheless, when ASPs design a snack schedule to include more fruits or vegetables, offering a variety of choices of healthy items (eg, apple, banana, or orange) rather than an apple or chips, can fulfill the need for ASPs to provide choices, and still ensure that all choices promote the health of children in attendance.
The strengths of this study were the use of direct observation of the snacks served and of children’s consumption of those snacks. Additionally, snack cost was determined via receipts provided by the ASPs. Previous studies 2, 4, 6 have relied on snack menus to classify foods/beverages served. In the current sample, we found that on over half of the site visit days snacks served did not align with the snack menu. On these days either none or some of the snacks listed on the menu were provided. The use of direct observation, therefore provides an accurate representation of the types of snacks served. This is among the first studies14 to provide information on child consumption of snacks in the ASP setting. Although limited to a random subsample of children, we observed over 380 children and whether they ate at least half of the provided snack. This should provide representative data on snack consumption at these ASPs. Finally, previous snack cost estimates have been based on 2003–04 market prices and not expenses directly accrued from the ASPs.6 Thus, the cost estimates represent the most accurate cost per snack to date. Unfortunately, snack waste was not collected, thus it is unclear how much food waste was generated from uneaten snacks.
In conclusion, this study demonstrated that ASPs largely fail to meet existing Healthy Eating Standards and serve foods and beverages that are predominately high in sugar and salt. These snacks, in turn, are less expensive than snacks promoted in the standards, and this along with a stable shelf-life (ie, they will not spoil like fresh fruits or vegetables) likely account for their popularity. However, we also demonstrate that when children are provided healthier snack options, the vast majority consume them. Thus, this study provides evidence that children will eat fruits and vegetables when they are served in the ASP setting. Future studies are needed to develop innovative strategies to assist ASPs in overcoming price barriers.
IMPLICATIONS FOR SCHOOL HEALTH
Based on these findings, ASP providers need to carefully evaluate the types of foods and beverages served as snack and determine whether they promote the healthy eating of the children enrolled. In cases where improvements are required and price barriers preclude purchasing healthier foods, programs will need to develop innovative partnerships with foods sellers to lower food prices. Pooling together purchasing power among programs can serve as buying leverage to decreasing prices on items that promote healthy eating, such as fruits and vegetables. Thus, while the majority of snack policies for ASPs are voluntary (they are not mandated, but are recommendations or guidelines), providers need to ask themselves whether promoting healthy eating is important, and if so, what creative strategies can be employed to help achieve this.
HUMAN SUBECTS’ APPROVAL
Statement regarding IRB approval required here.
Acknowledgments
None
Funding: Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R01HL112787.
Footnotes
Potential conflicts of interest: None
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Beets MW, Tilley F, Kim Y, Webster C. Nutritional policies and standards for snacks served in after-school programmes: a review. Public Health Nutr. 2011:1–9. doi: 10.1017/S1368980011001145. [DOI] [PubMed] [Google Scholar]
- 2.Cassady D, Vogt R, Oto-Kent D, Mosley R, Lincoln R. The power of policy: a case study of healthy eating among children. Am J Public Health. 2006;96(9):1570–1571. doi: 10.2105/AJPH.2005.072124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coleman KJ, Geller KS, Rosenkranz RR, Dzewaltowski DA. Physical activity and healthy eating in the after-school environment. J Sch Health. 2008;78(12):633–640. doi: 10.1111/j.1746-1561.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 4.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an organizational intervention designed to improve snack and beverage quality in YMCA after-school programs. Am J Public Health. 2009 doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine. [Accessed on April 20, 2012];Child and Adult Care Food Program: aligning dietary guidance for all. 2010 Available at: http://www.iom.edu/Reports/2010/Child-and-Adult-Care-Food-Program-Aligning-Dietary-Guidance-for-All.aspx.
- 6.Mozaffarian RS, Andry A, Lee RM, Wiecha JL, Gortmaker SL. Price and healthfulness of snacks in 32 YMCA after-school programs in 4 US metropolitan areas, 2006–2008. Prev Chronic Dis. 2012;9:E38. doi: 10.5888/pcd9.110097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nanney MS, Glatt C. Exploring implementation of the 2010 Institute of Medicine’s Child and Adult Food Care Program recommendations for after-school snacks. Public Health Nutr. 2011:1–7. doi: 10.1017/S1368980011002722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen JFW, Smit LA, Parker E, Austin SB, Frazier AL, Economos CD, et al. Long-term impact of a chef on school lunch consumption: findings from a 2-Year pilot study in Boston middle schools. J Acad Nutr Diet. 2012;112(6):927–933. doi: 10.1016/j.jand.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Nicklas TA, Liu Y, Stuff JE, Fisher JO, Mendoza JA, O’Neil CE. Characterizing lunch meals served and consumed by pre-school children in Head Start. Public Health Nutr. 2013:1–9. doi: 10.1017/S1368980013001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen JFW, Richardson S, Austin SB, Economos CD, Rimm EB. School lunch waste among middle school students nutrients consumed and costs. Am J Prev Med. 2013;44(2):114–121. doi: 10.1016/j.amepre.2012.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beets MW. Enhancing the translation of physical activity interventions in afterschool programs. Am J Lifestyle Med. 2012;6(4):328–341. [Google Scholar]
- 12.Sweitzer SJ, Briley ME, Roberts-Gray C, Hoelscher DM, Harrist RB, Staskel DM, et al. Lunch is in the bag: increasing fruits, vegetables, and whole grains in sack lunches of preschool-aged children. J Am Diet Assoc. 2010;110(7):1058–1064. doi: 10.1016/j.jada.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beets MW, Webster C, Saunders R, Huberty JL. Translating policies into practice: a framework for addressing childhood obesity in afterschool programs. Health Promot Pract. 2013;14(2):228–237. doi: 10.1177/1524839912446320. [DOI] [PubMed] [Google Scholar]
- 14.Beets MW, Tilley F, Weaver RG, Turner-McGrievy G, Moore JB, Webster C. From policy to practice: Addressing snack quality, consumption, and price in afterschool programs. J Nutr Educ Behav. doi: 10.1016/j.jneb.2013.10.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beets MW, Tilley F, Turner-McGrievy G, Weaver RG, Jones SJ. Community partnership to address snack quality and cost in afterschool programs. J Sch Health. doi: 10.1111/josh.12175. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]