Abstract
Introduction: The ProAct study has shown that a pump switch to the Accu-Chek® Combo system (Roche Diagnostics Deutschland GmbH, Mannheim, Germany) in type 1 diabetes patients results in stable glycemic control with significant improvements in glycated hemoglobin (HbA1c) in patients with unsatisfactory baseline HbA1c and shorter pump usage time.
Patients and Methods: In this post hoc analysis of the ProAct database, we investigated the glycemic control and glycemic variability at baseline by determination of several established parameters and scores (HbA1c, hypoglycemia frequency, J-score, Hypoglycemia and Hyperglycemia Indexes, and Index of Glycemic Control) in participants with different daily bolus and blood glucose measurement frequencies (less than four day, four or five per day, and more than five per day, in both cases). The data were derived from up to 299 patients (172 females, 127 males; age [mean±SD], 39.4±15.2 years; pump treatment duration, 7.0±5.2 years).
Results: Participants with frequent glucose readings had better glycemic control than those with few readings (more than five readings per day vs. less than four readings per day: HbA1c, 7.2±1.1% vs. 8.0±0.9%; mean daily blood glucose, 151±22 mg/dL vs. 176±30 mg/dL; percentage of readings per month >300 mg/dL, 10±4% vs. 14±5%; percentage of readings in target range [80–180 mg/dL], 59% vs. 48% [P<0.05 in all cases]) and had a lower glycemic variability (J-score, 49±13 vs. 71±25 [P<0.05]; Hyperglycemia Index, 0.9±0.5 vs. 1.9±1.2 [P<0.05]; Index of Glycemic Control, 1.9±0.8 vs. 3.1±1.6 [P<0.05]; Hypoglycemia Index, 0.9±0.8 vs. 1.2±1.3 [not significant]). Frequent self-monitoring of blood glucose was associated with a higher number of bolus applications (6.1±2.2 boluses/day vs. 4.5±2.0 boluses/day [P<0.05]). Therefore, a similar but less pronounced effect on glycemic variability in favor of more daily bolus applications was observed (more than five vs. less than four bolues per day: J-score, 57±17 vs. 63±25 [not significant]; Hypoglycemia Index, 1.0±1.0 vs. 1.5±1.4 [P<0.05]; Hyperglycemia Index, 1.3±0.6 vs. 1.6±1.1 [not significant]; Index of Glycemic Control, 2.3±1.1 vs. 3.1±1.7 [P<0.05]).
Conclusions: Pump users who perform frequent daily glucose readings have a better glycemic control with lower glycemic variability.
Introduction
The use of insulin pumps in continuous subcutaneous insulin infusion therapy (CSII) is associated with similar or better glycemic control, lower frequency of hypoglycemic events, higher treatment flexibility, and an increase in treatment satisfaction in comparison with multiple daily injection therapy. It is therefore considered to represent a very efficient way to achieve treatment targets and is preferably used by people with type 1 diabetes (and only occasionally by those with type 2 diabetes).1–6
In the ProAct study, we investigated the course of glycemic control and technology-related aspects of using the Accu-Chek® Combo system (Roche Diagnostics Deutschland GmbH, Mannheim, Germany) in the first 6 months after a switch from previous pump models in a real-world setting (only three visits, no extra study procedures than treatment standard). We observed stable glycemic control with improvements in several observation parameters in several of the analyzed subgroups.7 Participants who benefited most from the switch to the new pump system with respect to glycemic control were those with less CSII experience and patients with high glycated hemoglobin (HbA1c) values at the time of the pump switch. Indicators for an improvement in glycemic control were a decrease in the mean daily blood glucose levels, a decrease in glucose variability, and a decrease in HbA1c level (which reached the level of statistical significance in some subgroups). In consequence, time in the target range blood glucose control increased when using the Accu-Chek Combo system. The results were achieved despite a reduction in the overall number of daily insulin bolus infusions and with a significant increase in the number of daily patient self-monitoring of blood glucose (SMBG) measurements. These findings suggested a more confident diabetes management and a reduced need for correction boluses of the participating type 1 diabetes patients.7
Prior to the study, patients had used different pump models, and data from the previous pump treatment results were also collected prior to the pump switch. This information was still independent from any study effects potentially induced by the ProAct study protocol and the new insulin pump features and is therefore more suitable to provide an understanding of real-world associations among treatment aspects, glucose control, and glycemic variability. The purpose of this post hoc analysis of these baseline data was to explore potential associations between the frequency of daily blood glucose determinations and the number of daily bolus insulin administrations with glucose control and glycemic variability in patients on CSII treatment.
Patients and Methods
The uncontrolled, prospective, open-label ProAct study was performed in five European countries (France, Germany, Italy, Spain, and Sweden) and in collaboration with 61 sites. Detailed information regarding study design and results have been published recently.7
At baseline, the following parameters were obtained from medical records and/or the previous device used: HbA1c, weight, height, frequency of hypoglycemia (glucose meter readout of <70 mg/dL) and hyperglycemia (glucose meter readout of >300 mg/dL), mean number of insulin boluses, mean glucose values and their SDs, number of daily blood glucose measurements, and frequency of additional pump technology use, if applicable. This information was retrospectively collected for the last 3 months prior to study entry by device readouts. The different variability scores were only calculated for those patients with sufficient data quality for the respective score calculation. Therefore, the number of subjects may vary by score.
In addition, we stratified the cohort with respect to the number of daily glucose determinations (less than four per day, four or five per day, and more than five per day) and the number of daily insulin boluses (less than four per day, four or five per day, and more than five per day) and computed several measures of quality of glycemic control and glycemic variability: mean daily blood glucose, mean SD, mean coefficient of variation, mean of the median blood glucose concentrations, percentage in target range (percentage of readings 80–180 mg/dL), percentage in low range and hypoglycemia (percentage of readings <80 mg/dL), percentage in hyperglycemia (percentage of readings >180 mg/dL), Average Daily Risk Range,8 Low Blood Glucose Index (LBGI),8–10 High Blood Glucose Index (HBGI),9–11 Glycemic Risk Assessment Diabetes Equation (GRADE140),12 J-score,13 and Hypoglycemia and Hyperglycemia Indexes and Index of Glycemic Control14,15 in those patients for whom the appropriate information for calculation of the respective index was available.
The statistical analysis, the generation of tables, and patient data listings were performed using the software packages STATA version 12 (StataCorp, College Station, TX) for correlation analysis and R 2.15.0 (R Development Core Team, 2012). The population reported here consisted of the patients who participated in the baseline visit and had detailed information available from the last 4 weeks prior to the visit. Appropriate parametric and nonparametric statistical methods were applied for comparisons between the groups. A value of P<0.05 was considered to be statistically significant. All analyses in this cross-sectional investigation were performed in a descriptive way.
Results
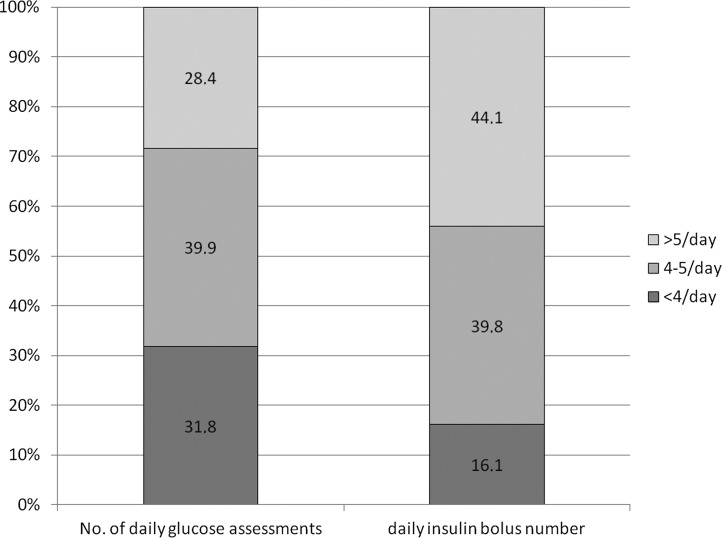
The data from up to 299 participants with type 1 diabetes on CSII treatment collected at baseline of the ProAct study7 could be included into this post hoc cross-sectional analysis (172 females, 127 males; age [mean±SD], 39.4±15.2 years; duration of CSII treatment, 7.0±5.2 years; HbA1c, 7.8±1.1%; total daily insulin dose, 45±23 IU). They were using insulin pumps from different manufacturers (88.6% Roche, 8.4% Medtronic [Northridge, CA], 2.0% Animas [West Chester, PA], and 1.0% Smith Medical Industries [St. Paul, MN]) and different short-acting insulins (64.3% insulin lispro, 26.4% insulin aspart, 5.3% insulin glulisine, and 3.7% regular human insulin). The distribution of the participants into the three glucose testing groups and the three insulin bolus groups is provided in Figure 1. There were no differences among the stratification groups with respect to demographic parameters, such as age, gender, CSII duration, or diabetes duration.
FIG. 1.
Distribution according to the frequency of daily glucose measurements and mean daily insulin bolus.
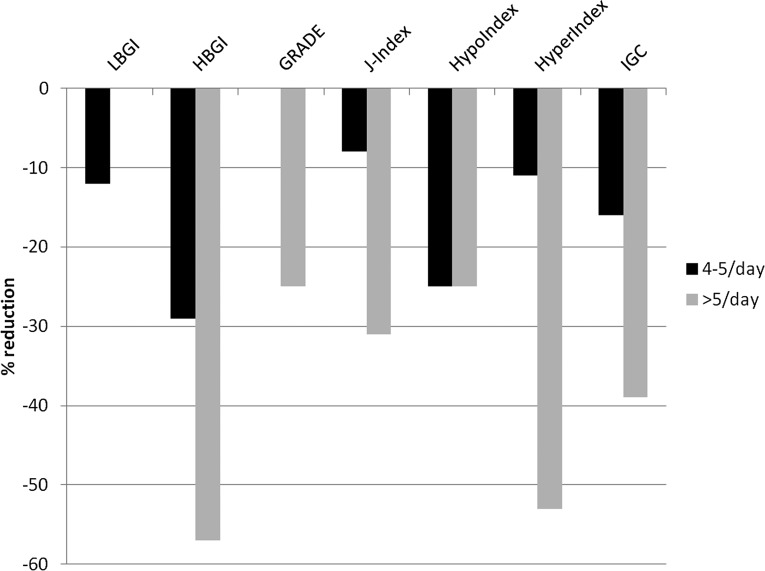
The results obtained for the observation parameters of glycemic control and daily glucose variability after stratification of the cohort according to the number of blood glucose tests per day are provided in Table 1. It can be clearly seen that patients with a higher testing frequency had a significant better long-term control and lower mean daily blood glucose values or median blood glucose values than patients with low testing frequency. Although the absolute number of readings in the low or hypoglycemic range (<80 mg/dL) was obviously higher in the frequent testers because of the larger number of tests, the percentage of hypoglycemic readings was about 10% and similar in all three groups. The percentage of hyperglycemic readings (>180 mg/dL) was significantly lower (30% vs. 41%/42%) and the percentage of readings in target range (80–180 mg/dL) was significantly higher (59% vs. 48/49%) in frequently testing patients in comparison with the two other groups. With respect to glycemic variability assessment scores, the frequently testing patients had lower values for the SD and better values for the majority of the calculated indices, including GRADE, LBGI, HBGI, J-score, Hyperglycemia Index, Hypoglycemia Index, and total Index of Glycemic Control (Table 1). The percentage reduction of glycemic variability by more frequent glucose tests versus the low-frequency test group is shown in Figure 2.
Table 1.
Results of the Observation Parameters After Stratification into the Different Blood Glucose Assessment Groups
| Number of daily glucose tests | |||
|---|---|---|---|
| Parameter | Low (<4/day) | Intermediate (4–5/day) | High (>5/day) |
| HbA1c (%) | 8.0±0.9 | 7.9±0.9 | 7.2±1.0a |
| Mean daily blood glucose (mg/dL) | 176±30 | 172±27 | 151±22a |
| Mean SD (mg/dL) | 86±20 | 80±14 | 68±12a |
| Mean coefficient of variation (mg/dL) | 49±9 | 47±6 | 45±7 |
| Mean glucose medians (mg/dL) | 164±32 | 163±31 | 141±21 |
| Percentage in | |||
| Low range or hypoglycemia (<80 mg/dL) | 11±8 | 9±5 | 11±7 |
| Hyperglycemia (>180 mg/dL) | 42±14 | 41±14 | 30±12a |
| Target range (80–180 mg/dL) | 48±14 | 49±12 | 59±10a |
| Average Daily Risk Range | 22±7 | 22±6 | 23±6 |
| LBGI | 2.5±2.0 | 2.2±1.4 | 2.5±1.5 |
| HBGI | 5.6±2.6 | 4.0±2.0 | 2.4±1.2a |
| GRADE | 12±3 | 12±3 | 9±2a |
| J-Index | 71±25 | 65±19 | 49±13a |
| Hypoglycemia Index | 1.2±1.3 | 0.9±0.8 | 0.9±0.8 |
| Hyperglycemia Index | 1.9±1.2 | 1.7±0.9 | 0.9±0.5a |
| Index of Glycemic Control | 3.1±1.6 | 2.6±1.0 | 1.9±0.8a |
P<0.05 versus group with low testing frequency.
GRADE, Glycemic Risk Assessment Diabetes Equation; HbA1c, glycated hemoglobin; HBGI, High Blood Glucose Index; LBGI, Low Blood Glucose Index.
FIG. 2.
Reduction of glycemic variability by more frequent glucose tests versus the low frequency test group: Low Blood Glucose Index (LBGI), High Blood Glucose Index (HBGI), Glycemic Risk Assessment Diabetes Equation (GRADE), Hypoglycemia Index (HypoIndex), Hyperglycemia Index (HyperIndex), and Index of Glycemic Control (IGC). Results are normalized to 100% for the low frequency test group.
Frequent testing was associated with a higher number of bolus applications (6.1±2.2 boluses/day vs. 4.5±2.0 boluses/day [P<0.05]). Therefore, a similar but less pronounced effect on glycemic control and parameters of glycemic variability in favor of more daily bolus applications was observed. The results of this analysis are provided in Table 2. In general, pump users with more than five bolus administrations seem to have better glycemic control, but only few of the observation parameters were shown to be of significant difference in favor of frequent bolus applications per day (Hypoglycemia Index and Index of Glycemic Control).
Table 2.
Results of the Observation Parameters After Stratification According to the Mean Daily Insulin Bolus Frequency
| Number of daily glucose tests | |||
|---|---|---|---|
| Parameter | Low (<4/day) | Intermediate (4–5/day) | High (>5/day) |
| HbA1c (%) | 7.8±0.9 | 7.9±1.0 | 7.6±0.9 |
| Mean daily blood glucose (mg/dL) | 165±31 | 168±31 | 161±28 |
| Mean SD (mg/dL) | 81±22 | 77±16 | 74±14 |
| Mean coefficient of variation (mg/dL) | 49±10 | 46±7 | 46±7 |
| Mean glucose medians (mg/dL) | 154±33 | 158±34 | 151±29 |
| Percentage in | |||
| Low range or hypoglycemia (<80 mg/dL) | 13±8 | 10±6 | 10±7 |
| Hyperglycemia (>180 mg/dL) | 38±15 | 38±16 | 35±14 |
| Target range (80–180 mg/dL) | 49±14 | 52±12 | 55±12 |
| Average Daily Risk Range | 25±8 | 21±6 | 23±6 |
| LBGI | 3.2±2.0 | 2.2±1.4 | 2.4±1.6 |
| HBGI | 3.8±2.5 | 3.7±2.3 | 3.2±1.9 |
| GRADE | 12±3 | 11±3 | 11±3 |
| J-Index | 63±25 | 62±22 | 57±18 |
| Hypoglycemia Index | 1.5±1.4 | 0.8±0.8a | 1.0±1.0a |
| Hyperglycemia Index | 1.6±1.1 | 1.5±1.0 | 1.3±0.8 |
| Index of Glycemic Control | 3.1±1.7 | 2.3±1.1a | 2.3±1.1a |
P<0.05 versus group with low testing frequency.
GRADE, Glycemic Risk Assessment Diabetes Equation; HbA1c, glycated hemoglobin; HBGI, High Blood Glucose Index; LBGI, Low Blood Glucose Index.
Discussion
In our cross-sectional post hoc analysis of baseline data collected from participants of the ProAct study,7 we saw a direct correlation between the number of daily blood glucose readings in CSII users with type 1 diabetes and the quality of glycemic control and glycemic variability. Frequent testers (more than five readings per day) had a better glycemic control (as shown by HbA1c and mean and median blood glucose levels) and had a lower glycemic variability (as shown by several glycemic variability indices) than patients with low glucose testing frequency. This effect was predominantly driven by fewer readings in the hyperglycemic range and a significant higher percentage in euglycemia. No difference was detected in the hypoglycemic range. These findings may be explained by a stronger tendency of frequent testers to react to high glucose levels by applying a correction bolus, whereas low glucose levels may only result in a reaction of, for example, glucose uptake, if patients realize the symptoms of hypoglycemia. It can be speculated that a group of people with hypoglycemia unawareness might also benefit from frequent testing similar to the reduction in hyperglycemic readings in our population; however, this hypothesis has to be confirmed in a specifically designed study (e.g., by using devices for continuous glucose monitoring).
Unfortunately, only a few reports exist about studies investigating the correlation of the frequency of patient SMBG with glycemic control and glucose variability. Our results are in line with the study published by Schütt et al.16 in 2006, which found a direct correlation between the SMBG frequency and metabolic control in 19,491 insulin-treated patients with type 1 diabetes. They also reported that HbA1c reduction with higher frequency of SMBG was more pronounced in patients on intensified (four or more daily injections or CSII) therapy (HbA1c reduction of 0.32% for one additional SMBG per day) compared with patients on conventional (one to three daily injections) therapy (HbA1c reduction of 0.16% for one additional SMBG per day).16
Ziegler et al.17 analyzed data from 26,723 children and adolescents 0–18 years of age with type 1 diabetes recorded during 1995–2006 in Germany. After adjustment for age, gender, diabetes duration, year of treatment, insulin regimen, insulin dose, body mass index SDs, and center difference, SMBG frequency was significantly associated with better metabolic control with a drop of HbA1c of 0.20% for one additional SMBG per day (P<0.001).17
Minder et al.18 reported recently about an evaluation of HbA1c values and preceding SMBG frequencies over a period of 12 months in 150 patients with type 1 diabetes on intensified insulin treatment. The authors concluded that optimal diabetes control can be achieved in routine diabetes care with flexible intensified insulin therapy based on continuing patients' education and with a minimum of four SMBGs per day.18
Miller et al.19 analyzed data from 20,555 participants in the T1D Exchange Clinic Registry with type 1 diabetes for ≥1 year and not using a continuous glucose monitoring system. A higher number of SMBG measurements per day was strongly associated with a lower HbA1c level (adjusted P<0.001), with the association being present in all age groups and in both insulin pump and injection users. The authors concluded that it is important for insurers to consider that reducing restrictions on the number of test strips provided per month may lead to improved glycemic control for some people with type 1 diabetes.19
All the above referenced results are in line with our findings, and we were not able to identify a contradictory study report during our literature research. However, our study has several limitations that need to be addressed. Next to the nature of the data collection with standardized questionnaires under real-world conditions, a major weakness of this post hoc analysis is the distribution of the pump models used by the patients at baseline. In the ProAct study, participants were included who switched to the Accu-Chek Combo system during routine treatment. By nature, many of these subjects (88%) were already using previous pump models from Roche and wanted to switch to the next-generation model. In addition, some of the explored indices for glycemic variability have been developed for interpretation of data from continuous glucose monitoring systems and may be less useful for interpretation of SMBG assessments. This disadvantage may have been counterbalanced by the large amount of data points derived from the large cohort in this post hoc analysis. In any case, these limitations have to be considered when trying to transfer our results and conclusions to all pump users.
In conclusion, this post hoc analysis of a cross-sectional data pool from CSII users with type 1 diabetes shows that frequent daily glucose testing is associated with better glycemic control and a lower glycemic variability compared with a low glucose testing frequency. Because of the observed association between frequent glucose testing and frequent bolus applications, a comparable post hoc analysis on the number of daily insulin bolus applications resulted in a similar, but less pronounced, effect in favor of more frequent bolus administrations.
Acknowledgments
Funding for the ProAct study and this post hoc analysis was provided by Roche Diagnostics Deutschland GmbH, Mannheim, Germany. The statistical analysis was performed by ClinLogix Europe GmbH, Mainz, Germany. The authors are very grateful to the patients and study sites for their committed participation in the study.
Author Disclosure Statement
J.W. and N.W. are employed by Roche Diagnostics Deutschland GmbH. A.P. and R.Z. participate in advisory boards and as a consultant for Roche. S.M. and E.D. declare no competing financial interests exist.
All authors contributed to analysis and interpretation of data, drafting the article, and revising it critically for important intellectual content and gave final approval of the version to be published.
References
- 1.Pickup JC: Insulin-pump therapy for type 1 diabetes mellitus. N Engl J Med 2012;366:1616–1624 [DOI] [PubMed] [Google Scholar]
- 2.Boland EA, Grey M, Oesterle A, Fredrickson L, Tamborlane WV: Continuous subcutaneous insulin infusion. A new way to lower risk of severe hypoglycemia, improve metabolic control, and enhance coping in adolescents with type 1 diabetes. Diabetes Care 1999;22:1779–1784 [DOI] [PubMed] [Google Scholar]
- 3.Paul N, Kohno T, Klonoff DC: A review of the security of insulin pump infusion systems. J Diabetes Sci Technol 2011;5:1557–1562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Didangelos T, Iliadis F: Insulin pump therapy in adults. Diabetes Res Clin Pract 2011;93(Suppl 1):S109–S113 [DOI] [PubMed] [Google Scholar]
- 5.Hoogma RP, Hammond PJ, Gomis R, Kerr D, Bruttomesso D, Bouter KP, Wiefels KJ, de la Calle H, Schweitzer DH, Pfohl M, Torlone E, Krinelke LG, Bolli GB; 5-Nations Study Group: Comparison of the effects of continuous subcutaneous insulin infusion (CSII) and NPH-based multiple daily insulin injections (MDI) on glycaemic control and quality of life: results of the 5-Nations Trial. Diabet Med 2006;23:141–147 [DOI] [PubMed] [Google Scholar]
- 6.Pickup JC, Sutton AJ: Severe hypoglycemia and glycemic control in Type 1 patients: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med 2008;25:765–774 [DOI] [PubMed] [Google Scholar]
- 7.Ziegler R, Tubili C, Chico A, Guerci B, Lundberg E, Borchert M, Löffler A, Bloethner S, Weissmann J, Pfützner A: ProAct Study: new features of insulin pumps improve diabetes management and glycemic control in patients after transition of continuous subcutaneous insulin infusion systems. Diabetes Technol Ther 2013;15:738–743 [DOI] [PubMed] [Google Scholar]
- 8.Kovatchev BP, Otto E, Cox D, Gonder-Frederick L, Clarke W: Evaluation of a new measure of blood glucose variability in diabetes. Diabetes Care 2006;29:2433–2438 [DOI] [PubMed] [Google Scholar]
- 9.Kovatchev BP, Clarke WL, Breton M, Brayman K, McCall A: Quantifying temporal glucose variability in diabetes via continuous glucose monitoring: mathematical methods and clinical applications. Diabetes Technol Ther 2005;7:849–862 [DOI] [PubMed] [Google Scholar]
- 10.Kovatchev BP, Straume M, Cox DJ, Gonder-Frederick LA, Clarke WL: Algorithmic evaluation of metabolic control and risk of severe hypoglycemia in Type 1 and Type 2 diabetes using self-monitoring blood glucose data. Diabetes Technol Ther 2003;5:817–828 [DOI] [PubMed] [Google Scholar]
- 11.Kovatchev BP, Straume M, Cox DJ, Farhi LS: Risk analysis of blood glucose data: a quantitative approach to optimizing the control of insulin dependent diabetes. J Theor Med 2001;3:1–10 [Google Scholar]
- 12.Hill NR, Hindmarsh PC, Stevens RJ, Stratton IM, Levy JC, Matthews DR: A method for assessing quality of control from glucose profiles. Diabet Med 2003;24:753–758 [DOI] [PubMed] [Google Scholar]
- 13.Wojcicki J: “J”-index: A new proposition of the assessment of current glucose control in diabetic patients. Horm Metab Res 1995;27:41–42 [DOI] [PubMed] [Google Scholar]
- 14.Rodbard D: Interpretation of continuous glucose monitoring data: glycemic variability and quality of control. Diabetes Technol Ther 2009;11(Suppl 1):S-55–S-67 [DOI] [PubMed] [Google Scholar]
- 15.Rodbard D: New and improved methods to characterize glycemic variability and quality of control. Diabetes Technol Ther 2009;11:551–565 [DOI] [PubMed] [Google Scholar]
- 16.Schütt M, Kern W, Krause U, Busch P, Dapp A, Grziwotz R, Mayer I, Rosenbauer J, Wagner C, Zimmermann A, Kerner W, Holl RW; DPV Initiative: Is the frequency of self-monitoring of blood glucose related to long-term metabolic control? Multicenter analysis including 24,500 patients from 191 centers in Germany and Austria. Exp Clin Endocrinol Diabetes 2006;114:384–388 [DOI] [PubMed] [Google Scholar]
- 17.Ziegler R, Heidtmann B, Hilgard D, Hofer S, Rosenbauer J, Holl R; DPV-Wiss-Initiative: Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes 2011;12:11–17 [DOI] [PubMed] [Google Scholar]
- 18.Minder AE, Albrecht D, Schäfer J, Zulewski H: Frequency of blood glucose testing in well educated patients with diabetes mellitus type 1: how often is enough? Diabetes Res Clin Pract 2013;101:57–61 [DOI] [PubMed] [Google Scholar]
- 19.Miller KM, Beck RW, Bergenstal RM, Goland RS, Haller MJ, McGill JB, Rodriguez H, Simmons JH, Hirsch IB; T1D Exchange Clinic Network: Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D Exchange Clinic Registry participants. Diabetes Care 2013;36:2009–2014 [DOI] [PMC free article] [PubMed] [Google Scholar]