Abstract
Objective
This study examined (a) duration of generalized anxiety disorder (GAD) as a moderator of cognitive behavioral therapy (CBT) versus its components (cognitive therapy and self-control desensitization) and (b) increases in dynamic flexibility of anxious symptoms during the course of psychotherapy as a mediator of this moderation. Degree of dynamic flexibility in daily symptoms was quantified as the inverse of spectral power due to daily to intradaily oscillations in four-times-daily diary data (Fisher, Newman, & Molenaar, 2011).
Method
This was a secondary analysis of the data of Borkovec, Newman, Pincus, and Lytle (2002). Seventy-six participants with a principle diagnosis of GAD were assigned randomly to combined CBT (n = 24), cognitive therapy (n = 25), or self-control desensitization (n = 27).
Results
Duration of GAD moderated outcome such that those with longer duration showed greater reliable change from component treatments than they showed from CBT, whereas those with shorter duration fared better in response to CBT. Decreasing predictability in daily and intradaily oscillations of anxiety symptoms during therapy reflected less rigidity and more flexible responding. Increases in flexibility over the course of therapy fully mediated the moderating effect of GAD duration on condition, indicating a mediated moderation process.
Conclusions
Individuals with longer duration of GAD may respond better to more focused treatments, whereas those with shorter duration of GAD may respond better to a treatment that offers more coping strategies. Importantly, the mechanism by which this moderation occurs appears to be the establishment of flexible responding during treatment.
Keywords: moderator, cognitive behavioral therapy, generalized anxiety disorder, mediator, psychotherapy mechanism
It has been several decades since Gordon Paul proposed that psychotherapy researchers determine what works for whom and under what circumstances (Paul, 1967). Nonetheless, in the treatment of generalized anxiety disorder (GAD), little progress has been made. In fact, although there are data on predictors of outcome (Newman, Crits-Christoph, Connelly Gibbons, & Erickson, 2006; Newman, Przeworski, Fisher, & Borkovec, 2010), there are no data on moderators with respect to cognitive behavioral therapy (CBT) and its components. Whereas CBT for GAD is more efficacious than placebo (Borkovec & Costello, 1993), components of CBT are not differentially effective when compared to a combined package of cognitive and behavioral techniques (Borkovec, Newman, Pincus, & Lytle, 2002; Gould, Otto, Pollack, & Yap, 1997). It is possible that some of the null findings in treatment comparison studies have resulted from a failure to examine individual differences that might predict differential outcome. It may therefore be important to reexamine previously published null findings. CBT and its components are not equally effective for everyone, and a substantial number of participants fail to achieve clinically significant change when randomly assigned to treatments (Borkovec & Ruscio, 2001). It seems reasonable to assume that treatment components may work differently for different people and that we should not approach component comparison studies with a “one size fits all” mentality. It is thus crucial to determine individual differences that may predict and moderate differential treatment responses as the first step toward tailoring treatments to individuals (Newman, 2000b). To this end, the current study is a secondary analysis of the data of Borkovec et al. (2002).
In terms of predictors of therapy outcome, a variable that has been examined frequently is duration of GAD symptoms. One might theorize that individuals who have had GAD for a longer duration might be more motivated to change and therefore more responsive to therapy. On the other hand, it is possible that a longer duration of illness would mean that maladaptive behaviors are more habitual and entrenched in nature and therefore more difficult to change. In a trial of cognitive therapy for GAD, longer duration of illness predicted a worse therapeutic outcome (Biswas & Chattopadhyay, 2001). Similarly, longer baseline duration of generalized anxiety and history of previous anxious episodes predicted poor course of the disorder in a 1-year follow-up of medications and/or psychotherapy (van den Brink et al., 2002). Further, having recurrent GAD episodes predicted negative outcome from medications, CBT, or self-help support groups (Seivewright, Tyrer, & Johnson, 1998).
In addition to predicting negative outcome from CBT overall, it is possible that duration of GAD symptoms might serve as a moderator of different types of treatment. For example, longer duration might differentiate those who benefit from more versus fewer CBT techniques, as is the case with combined CBT versus component treatments. Given prior findings that longer duration predicts worse outcome overall, it may be the case that when maladaptive behaviors are more entrenched and habitual, individuals are better able to benefit from treatments in which they are asked to focus more deeply on fewer techniques (e.g., either cognitive or behavioral) compared to treatments that provide a plethora of treatment options. These individuals may need a more focused and intense dose of one particular treatment in order to break the habitual nature of their worrisome thinking and anxiety-oriented behavior. On the other hand, somebody who has had GAD for a shorter time period might be more responsive to a treatment that focused less intensively on one particular set of techniques but that provided more technique options. Perhaps when GAD is less entrenched, and it is less necessary to practice any one technique as intensively, clients can take advantage of sampling a larger number of techniques to figure out which ones work best for them and ultimately settle on the optimal options.
Showing that a particular treatment works better for those with longer duration GAD may provide some information; however, this doesn’t elucidate how and why a particular treatment might work better for these individuals (e.g., Kazdin, 2005, 2007; Kraemer, Wilson, Fairburn, & Agras, 2002). Thus, it also would be important to link symptom duration with a particular mechanism of change.
One promising potential mechanism is the concept of dynamic order in anxious symptoms within individuals. According to dynamic systems theory—a transdisciplinary theory concerned with the behavior of complex systems over time—human systems of cognition, emotion, and behavior experience a tension between stability and flexibility wherein the former gives coherence, structure, and consistency to the system and the latter allows adaptability in response to changing environmental demands. Adaptive degrees of order in such systems likely contain a blend of these elements, as too much stability could be seen as rigidity and too much flexibility as lability. In regard to processes of psychopathology and psychotherapy, dynamic systems theory might predict one of two possibilities regarding degrees of rigidity versus flexibility:
Individuals with clinically severe GAD may exhibit excessively rigid patterns of thought, action, and feeling (e.g., consistent and persistent patterns of reactivity and worry from day to day). Such rigid hypperreactivity might result from habitually biased negative interpretations of ambiguous stimuli and/or conditioned emotional responses to environmental triggers, leaving these individuals less able to respond flexibly. In this case it is the role of CBT to promote more flexible and evidence-based thinking, reduced bodily tension, and reduced automatic emotional and physiological responses to nondangerous external triggers, leading to greater adaptability to the natural environment (e.g., Hayes et al., 2007; Hayes & Strauss, 1998).
Psychopathology is marked by a significant absence of structure and consistency in thought, feeling, and action, leading to inconsistency and unpredictability in emotional and behavioral systems. Here, it would be the role of psychotherapy to provide greater adaptive stability to a highly erratic system via therapeutic interventions aimed at increasing structure, habits, and coherence in response to the environment. Change in rigidity versus flexibility might be a particularly relevant mechanism of response to therapy in individuals who have had GAD for a long duration and who therefore might be expected to begin treatment with particularly entrenched habitual processes underlying patterns of anxious symptoms.
As a means to measure dynamic systems in psychopathology, Fisher, Newman, and Molenaar (2011) recently introduced a set of innovative quantitative metrics. Using ecological momentary assessment (EMA) data in the form of thrice-daily diary entries, these authors demonstrated that both dynamic factor models (Molenaar, 1985) and spectral analyses of within-individual time series could be used to quantify the structure of anxious experience in time. Dynamic factor modeling uses a structural equation model framework for representing variation in anxiety from measurement to measurement—here, multiple times a day—as a set of regression parameters. Spectral analysis uses a Fourier transformation to decompose a series of observations in time into a set of oscillatory frequencies, and assesses the degree to which each frequency contributes to the overall variability in the data (this is known as the power spectrum).
Both the residual variance of the dynamic factor models as well as the highest frequency band of the power spectrum were proposed to represent the degree of order in day-to-day anxiety. Importantly, these metrics reflect different aspects of symptomatic variability and corresponding dynamic order. The residual variance of the dynamic factor model can be argued to characterize order in the most concrete sense, as it reflects the unpredictable component of the time series (i.e., disorder). In general linear model terms, this relates to symptomatic variation not accounted for within the regression parameters, but in the error. For the spectral analyses, the very-high-frequency band of the power spectrum (VHFP) represents the strength and influence of patterns of anxious symptoms oscillating at a daily to intradaily rate. Greater power in this range reflects more predictable oscillations from day to day and within days and thus significant rigidity and a reduced ability to respond flexibly to daily environmental demands. Reductions in VHFP relate to less consistency, and therefore greater flexibility, in symptomatic variation day to day. Because it cannot be assumed that within- and between-individual variation will be equivalent over time (Fisher et al., 2011; Molenaar, 2004), spectral analyses and dynamic factor models were run independently for each participant. Rank order differences in psychotherapy outcome were then predicted by individual differences across both the residual variance and VHFP parameters. As noted above, adaptive systems exhibit a balance of system stability and organization versus flexibility and responsiveness. Thus, these two metrics provide complementary measures of the functional organization of dynamic systems. While the residual variance reflects the degree of disorder in the system, VHFP indicates the level of flexibility versus rigidity. Consistent with this hypothesis, in Fisher et al. (2011), both measures, derived from data occurring across the course of treatment, equivalently predicted treatment outcome (Cohen’s ds = 0.68 and 0.67, respectively).
The novelty of the methodology introduced by Fisher et al. (2011) is that it is able to model both person-specific and group-level rigidity of symptoms with respect to psychotherapy process and outcome. Nonetheless, measures of rigidity/flexibility in Fisher et al. (2011) were based on a summary of the full course of therapy (Sessions 1–12) and therefore did not account for the timing and extent of change in rigidity. In addition, concurrent relationships between each metric and symptom severity were not examined.
As such, Fisher and Newman (2012) refined this approach by examining the relationship between baseline severity in GAD and symptomatic rigidity, as well as the shape and rate of change in rigidity over three phases of psychotherapy (i.e., early, middle, and late).1 That work and the present study represent important elaborations of the work of Fisher et al. (2011), namely, the examination of changes in rigidity over time and their relation to symptomatology—both initial and outcome. Results of Fisher and Newman (2012) demonstrated that system rigidity (reflected in higher levels of VHFP) was significantly positively correlated with GAD severity at baseline. In addition, within each of the three therapy phases, change in rigidity was linear and always moved unidirectionally from rigidity to flexibility. However, the rate of change varied across phases, with early change in rigidity—from baseline to the fourth session—exhibiting the steepest rate of change. In addition, successful outcome for GAD was predicted by reduced overall levels of anxiety and a more flexible palette of emotional and behavioral responses. Fisher and Newman (2012) laid the foundation for the current study by establishing the character of change in rigidity of emotional responding. The focus of the present study is to examine the mechanistic role of flexibility generation in CBT and its component therapies: self-control desensitization (SCD) and cognitive therapy (CT).
The current study tested two hypotheses. Our first hypothesis was that duration of GAD symptoms would moderate treatment outcome from CBT versus component treatments such that those who had experienced GAD for a longer period of time would benefit more from a treatment that went deeply into either purely cognitive or purely behavioral treatment compared to those who had GAD for a shorter period of time. No prior study has examined moderators of CBT and its components (e.g., CT and SCD) in the treatment of GAD. Our second hypothesis was that change in rigidity from baseline to the fourth session or from the fifth session to the 14th session would be the mechanism by which GAD duration moderated outcome. This is the first study to examine whether change in rigidity serves as a mediator of outcome.
Method
Participants
Four hundred fifty-nine people responded to local newspaper advertisements or referrals from mental health practitioners. Of these, 320 were ruled out by phone screens for not meeting study inclusion criteria, 54 clients were ruled out via an initial structured interview, and 9 clients were ruled out during a second structured interview, leaving 76 participants with primary GAD who entered treatment. However, 7 clients dropped out at early stages of treatment (4 in SCD, 2 in CT, and 1 in CBT), leaving 69 clients who completed treatment. Clients’ average age was 36.62 years (SD = 11.56), and the average duration of the GAD diagnosis was 12.28 years (SD = 11.87). Clients were mostly Caucasian (89.5%) and women (68.4%). Only 2 clients were taking psychotropic medications for anxiety; they agreed to maintain dosage and frequency during therapy. None of these characteristics were significantly different across treatment conditions. All participants consented to the study, and institutional review board approval was attained.
Procedure
Selection and assessor outcome ratings
Admission criteria included consensus between the two diagnostic interviewers on a principal diagnosis of GAD, no diagnosable panic disorder (as recommended by the funding agency’s review committee), a clinician’s severity rating (CSR) for GAD of 4 (moderate) or more, absence of concurrent psychosocial therapy, no history of having received CBT methods in prior therapy, no medical contributions to the anxiety, no antidepressant medication, and absence of severe major depressive disorder, substance abuse, psychosis, and organic brain syndrome. All but two clients (97.1%) concurrently met criteria for GAD according to both the third edition revised and the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–III–R and DSM–IV; American Psychiatric Association, 1987, 1994).
Advanced clinical graduate students trained to reliability in diagnostic interviewing administered 30-min phone screens as well as the Anxiety Disorders Interview Schedule–Revised (ADIS–R; Di Nardo & Barlow, 1988) to determine diagnostic suitability. Those not ruled out by phone screen were administered a modified version of the ADIS–R (Di Nardo & Barlow, 1988), which included the Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959), the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960), CSRs for GAD and comorbid disorders, and additional questions corresponding to two GAD criteria being proposed at the time of study initiation by the DSM–IV (American Psychiatric Association, 1994) subcommittee for GAD (i.e., uncontrollable worrying and three of six associated symptoms). A second ADIS–R was administered within 2 weeks by the therapist who would see the client in therapy to reduce the likelihood of false positive cases. Pretreatment diagnoses, both primary and comorbid, were based on consensus between the independent structured interviewers. A random subsample of 20% of pretreatment audiotapes of ADIS–R interviews conducted by the primary assessor (prior to developing consensus) was reviewed for reliability purposes. For the presence of GAD, kappa agreement was 1. Outcome measures were administered at pre- and posttreatment. The client daily diary was completed 4 times per day during the treatment period.
Outcome measures
Clinician’s severity rating
For each diagnosis, interviewers assigned a 0–8 rating of the degree of distress and interference in functioning associated with the disorder (from 0 = none to 8 = very severely disturbing/disabling). Clients who met criteria for any diagnosis were assigned a CSR of 4 (definitely disturbing/disabling) or higher. If key features of a disorder were present but were not extensive or severe enough to warrant a formal diagnosis (or for disorders in partial remission), a CSR of 1–3 was assigned. When no features of a disorder were present, CSRs of 0 were given. Brown and colleagues (Brown, Di Nardo, Lehman, & Campbell, 2001) demonstrated good to excellent interrater reliability for CSRs for anxiety and mood disorders except dysthymia (r = .36), with correlations ranging from .65 to .84. Diagnostic reliability of CSRs in the current study ranged from an intraclass correlation of .77 to 1, and Finn’s r for GAD, which corrects for a restricted range of CSRs (Whitehurst, 1984), was .74.
State Trait Anxiety Inventory—Trait Version (STAI–T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983)
This 20-item scale is used to measure trait anxiety. Internal consistency reliability is high (in the .80s and .90s; .86 in the current sample), and retest reliability is much higher for the Trait form (high .70s) than the State form (ranging from .27 to .54). Convergent and discriminant validity has also been demonstrated for this questionnaire (Spielberger et al., 1983).
Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959)
This 14-item clinician-administered scale provides a rating of severity of each overarching anxiety symptom cluster on a scale from 0 (not present) to 4 (very severe/incapacitating). Internal consistency ranges from adequate to good (αs = .77 to .81, Moras, di Nardo, & Barlow, 1992; .82 in the current sample). Retest reliability (intraclass correlation coefficient, or ICC) was .86 across 2 days, and interrater reliability ICCs ranged from .74 to .96 (Bruss, Gruenberg, Goldstein, & Barber, 1994).
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is a 16-item self-report measure of pathological worry. Factor analysis indicated that the PSWQ assesses a unidimensional construct with internal consistency of .91 (Meyer et al., 1990; .83 in the current sample). High retest reliability (ranging from .74 to .93) was also demonstrated across periods ranging from 2 to 10 weeks (Molina & Borkovec, 1994). Correlations between the PSWQ and measures of anxiety, depression, and emotional control supported the convergent and discriminant validity of the measure (Brown, Antony, & Barlow, 1992).
Process measures
Client daily diary (CDD)
Using this paper-and-pencil measure, patients recorded their anxiety levels four times a day (upon arising, end of morning, end of afternoon, and end of evening), rating their overall level of anxiety during the preceding time period on a 0–100 scale. Two-week retest reliability was .80 based on baseline data from the current trial. In addition, convergent and discriminant validity were demonstrated by significantly stronger correlations with the HARS and with the Response to Relaxation and Arousal Questionnaire (Heide & Borkovec, 1983) than with the HRSD using pretherapy data from the current study. Clients were asked to complete this measure daily for at least 2 weeks before treatment and throughout the entire treatment period.
Therapy conditions
Fourteen weekly sessions were administered, with one fading/termination session after postassessment. Participants were randomly assigned to receive either SCD (n = 27), CT (n = 25), or combined CBT (n = 24). Therapy manuals were used for each therapy condition. In all conditions, the first four sessions were 2 hr in duration; remaining sessions were 1.5 hr. The first 30 min of each SCD and CT session involved only supportive listening.
Several aspects were common to the three conditions, although their content differed according to assignment: presentation of a model of anxiety and rationale for therapy, self-monitoring and early identification of anxiety cues, homework assignments, and review of homework including results of daily self-monitoring and technique practice and applications. CT entailed logical analysis, examination of evidence and probabilities, labeling of logical errors, decatastrophizing, generation of alternative thoughts and beliefs plus supportive listening. In addition to including supportive listening, SCD entailed progressive relaxation training, cue-controlled and differential relaxation training as described in Bernstein and Borkovec (1973), slowed diaphragmatic breathing, relaxing imagery, meditational relaxation, applied relaxation training, and self-control desensitization as described by Goldfried (1971). CBT contained all of the treatment techniques in CT and SCD but had no supportive listening element included.
Results
Statistical Analyses
Approach to idiographic analyses
Spectral analysis of times series data
Consistent with Fisher et al. (2011), daily diary ratings for each participant were treated as univariate, weakly stationary time series and assessed for oscillatory patterns via spectral analysis (weak stationarity assumes consistency in the mean and variance over time). For each group of analyses (see below) all consecutive observations were contained within a single vector, and the total number of observations was equal to the number of individual diary entries (morning, midday, evening, and night). Daily diary data were divided into eight successive 2-week sections (baseline, Weeks 1 and 2, Weeks 3 and 4, and so forth), each containing 56 total observations, in order to generate estimates of VHFP change across therapy. Thus, references (below) to changes in VHFP over therapy reflect difference scores derived from these 2-week estimates (e.g., Weeks 3 and 4 minus 2-week baseline, and Weeks 13 and 14 minus Weeks 5 and 6). However, in order to produce more intuitive VHFP change scores, directionality of change was inverted such that greater reductions in VHFP yielded higher change scores.
Procedures typically available in standard statistical packages for the spectral analysis of times series assume an even spacing of observations in time. The present data were collected roughly 4, 4, 4, and 8 hr apart each day and thus they do not meet this assumption. Therefore an adapted discrete Fourier transformation which can handle arbitrarily spaced data was applied, yielding a power spectrum and corresponding raw periodogram. This adaptation also accommodates missing data, which can be seen as a variant of unequal spacing in the time series. Details of this Fourier application can be found in Fisher et al. (2011). As noted above, we were interested in the VHFP, that is, the power attributed to variations in anxious symptoms with fixed oscillations of 1 day or less. Such oscillations correspond to patterns of daily and intra-daily structure in each individual’s experience of anxiety. The greater the spectral power in this range, the more prominent and consistent these patterns of occurrence and the more rigid or inflexible the system.
Examining change in rigidity
In assessing change from pretherapy baseline to the conclusion of treatment, Fisher and Newman (2012; using the same data as the current study) found that the direction of change was linear, with flexibility increasing from baseline to the end of therapy. However, using piecewise models of time, these authors demonstrated that the rate of change differed across the treatment period, with the steepest slope occurring from baseline through the 4th week of treatment.
In the present study we assessed the percentage of change in rigidity generated first from baseline through the fourth session and then from the fifth session to the 14th session (end of treatment) and found that change from baseline to the 4th week of treatment accounted for ~50% of change (compared to change during the last 10 weeks). Given two apparently critical periods of change, we explored the mechanistic function of change in rigidity within each of these two periods. Thus, we created two change scores: the difference in rigidity (VHFP) from baseline to Week 4 of therapy, and the difference in rigidity between Week 5 and Week 14 of therapy. Consistent with Fisher and Newman (2012), all point estimates of VHFP were log-transformed to adjust for right-skewed distributions. These transformations were performed before changes in order were calculated. As noted above, change scores were inverted for analyses so that a higher change score reflected greater reductions in VHFP.
Missing data
Of the 69 participants, one had insufficient data for calculating spectral power across baseline—requisite for subsequent calculations of change in order—and four presented with enough missing data to preclude calculation of spectral power in a given 2-week within-therapy period. These participants exhibited 230, 211, 244, 280, and 335 missing observations (48%, 44%, 51%, 59%, and 70% missingness, respectively). These participants were removed from analyses as a function of listwise deletion. For the remaining 64 participants the average number of missing observations was 60.31 (12.6%), with a standard deviation of 47.69. However, the distribution of missingness was strongly right-skewed, and thus the median of 48 missing observations (10%) may better represent the central tendency of the data. The minimum number of missing observations was 0 (0%), and the maximum was 194 (41%).
Nomothetic Analyses
Similar to other treatment studies (Clark et al., 1999; Newman et al., 2011), we created a single continuous variable to represent GAD severity. A single composite is considered more valid than any one measure of symptoms. A composite not only provides a more valid measure of the construct of interest but also provides one means of reducing experiment-wise error rate, since it replaces four sets of analyses with a single, more powerful one (Horowitz, Inouye, & Siegelman, 1979). The four measures used for the composite were significantly correlated with one another (ranging from .62 to .84). Raw scores for the PSWQ, HARS, CSRs for GAD, and STAI–T were converted to standardized z scores and averaged for each participant. We also created a GAD-change measure by calculating the average reliable change index (RCI; Jacobson & Truax, 1991) across the four GAD outcome measures. RCI reflects the degree of change that occurred beyond the fluctuations of an imprecise measure (McGlinchey, Atkins, & Jacobson, 2002), with higher numbers indicating greater reliable change. RCI is favored over the use of categorical classifications because of its greater statistical power as a continuous variable (Steketee & Chambless, 1992). The following values were used in the RCI formulae in the present study: GAD CSR, SD = 0.91, reliability = .72; STAI–T, SD = 7.66, reliability = .84; PSWQ, SD = 8.09, reliability = .91; HARS, SD = 6.90, reliability = .80. Standard deviations represent the standard deviation of the pooled sample at pretherapy assessment, and the reliability estimates represent reported retest reliability coefficients for each measure (Bruss et al., 1994; Meyer et al., 1990; Newman et al., 2010; Spielberger et al., 1983). Mean RCIs were calculated for change immediately after treatment relative to pretherapy assessment.
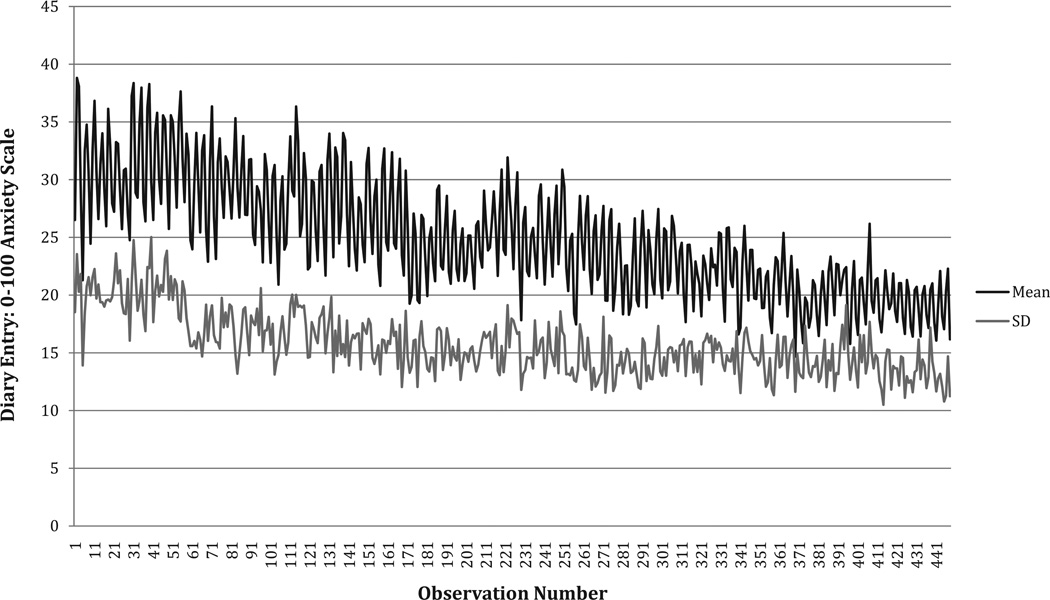
There were no differences between the therapy conditions on any pretherapy assessment and no differences in duration of GAD symptoms, F(2, 68) = 0.024, p = .976, across conditions. Also, at baseline there was neither a relationship between clinician-rated GAD severity and GAD duration (r = −.11, p = .36) nor a relationship between average diary anxiety and GAD duration (r = −.007, p = .95). Moreover, there were no significant differences between conditions in treatment efficacy, and all three treatments led to significant improvements at posttreatment that were maintained over a 2-year follow-up period. Figure 1 depicts the average (across all participants) overall pattern of change in four-times-daily diary entries from baseline to Week 14 of the therapy period.
Figure 1.
Means and standard deviations for client daily diary—by observation— over study period.
Approach to mediation analysis
A given variable or process serves as a mediator when (a) the independent variable, X, has a direct and significant effect on the dependent variable, Y; (b) the mediator, M, has a direct and significant effect on Y when controlling for X; and (c) the direct effect of X on Y is reduced or negated when allowing an indirect effect of X on Y via M, that is, when M mediates the relationship between X and Y (Baron & Kenny, 1986; Cole & Maxwell, 2003; Kenny, Kashy, & Bolger, 1998). A negation of the direct effect of X on Y is a full mediation, whereas a significant reduction is a partial mediation. However, Cole and Maxwell (2003) noted that additional concern must be given to the temporal nature of the data. Mediators are assumed to be mechanisms by which X exerts its effect on Y. Therefore, X must cause M, and M, in turn, must cause Y. In order to satisfy these causal requirements, X must precede M, and M must precede Y, in time (Cole & Maxwell, 2003; Holland, 1986). Finally, Kraemer, Wilson, Fairburn, and Agras (2002) set three criteria for the definition and evaluation of mediators within randomized controlled trials: They must occur during treatment, they must correlate with treatment condition, and they must have a main or interactive effect on treatment outcome. The mediational analyses to follow meet each of the above-mentioned criteria.
All regression analyses and path models were conducted with Mplus, Version 5.1, using maximum-likelihood estimation with robust standard errors (i.e., Satorra–Bentler correction). The Cohen’s d statistic was used to reflect effect size. Effect sizes were calculated via the algorithm d = t(2/n)1/2 (Dunlap, Cortina, Vaslow, & Burke, 1996).
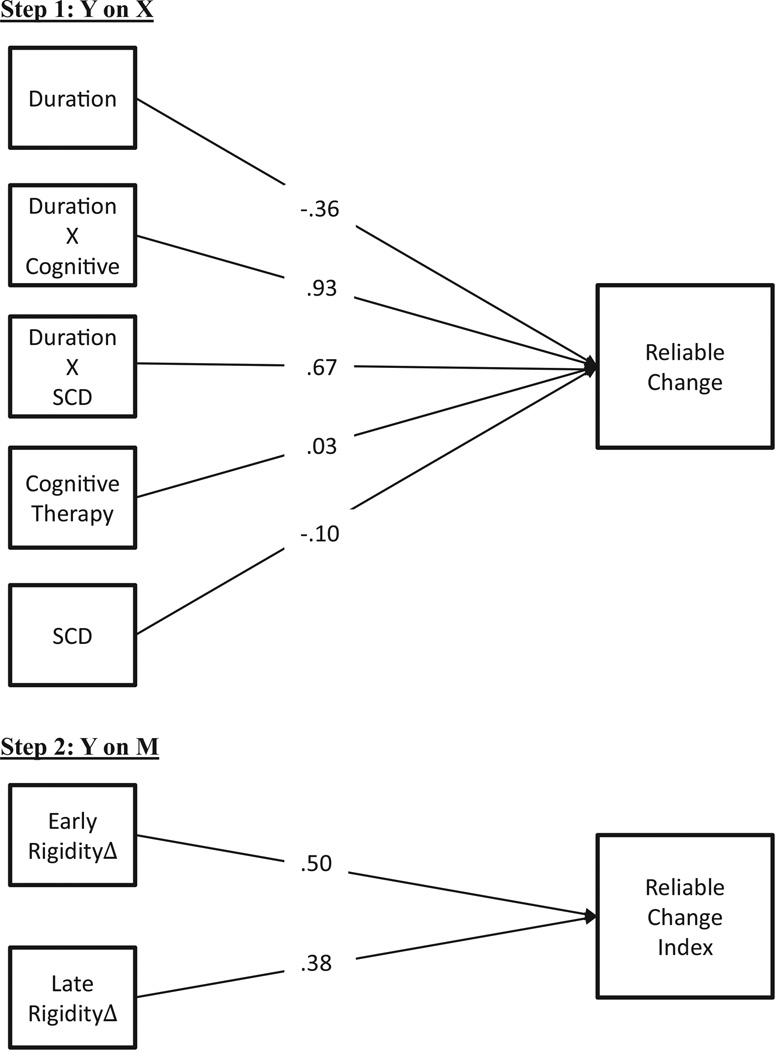
Step 1: Y on X
Table 1 contains the parameter estimates for the regression of reliable change at posttreatment on GAD duration, CT, SCD, and the interaction terms for CT × Duration and SCD × Duration (df = 62). Main effects for condition (CT and SCD) were nonsignificant, whereas the main effect for duration exhibited a significant negative effect on the RCI. Both the CT × Duration and the SCD × Duration interaction effects were positive and significant. Thus, for individuals in the CT and SCD conditions, the degree of reliable change at posttreatment was dependent on the duration of GAD pathology such that those individuals with greater GAD duration fared better at posttreatment in these conditions. In contrast, for individuals in the CBT condition, greater GAD duration predicted poorer outcome at posttreatment. Figure 2 depicts the relationship between main and moderating baseline effects and posttreatment reliable change.
Table 1.
Parameter Estimates for Step 1, Y on X
| Predictor | β | SE | t | p | d |
|---|---|---|---|---|---|
| Reliable change on | |||||
| CT | 0.074 | 0.668 | 0.110 | .912 | 0.03 |
| SCD | −0.240 | 0.724 | −0.331 | .740 | −0.10 |
| Duration | −0.095 | 0.045 | −2.108 | .035 | −0.36 |
| CT × Duration | 0.175 | 0.056 | 3.137 | .002 | 0.93 |
| SCD × Duration | 0.129 | 0.057 | 2.272 | .020 | 0.67 |
Note. CT = cognitive therapy; SCD = self-control desensitization.
Figure 2.
Steps 1 and 2, Y on X and Y on M (paths reported as Cohen’s d). Δ = change. Reliable Change Index is a composite measure of the Penn State Worry Questionnaire, the Hamilton Anxiety Rating Scale, Clinician’s Severity Ratings for generalized anxiety disorder, and the Trait version of the State Trait Anxiety Inventory using the formula from Jacobson and Truax (1991). SCD = self-control desensitization.
Step 2: Y on M
The effects of the proposed mediators—change in rigidity as a function of increases or decreases in rigidity from baseline to Week 4 and change from Week 5 to Week 14—on reliable change at posttreatment were tested and found to be significant: df = 61, β= .84, SE = 0.29, t = 2.90, p = .004, d = 0.50 and β = .78, SE = 0.35, t = 2.23, p = .02, d = 0.38, respectively. Thus, greater change from rigidity to flexibility predicted greater reliable change at posttreatment. Figure 2 depicts the relationship between change in rigidity and posttreatment reliable change.
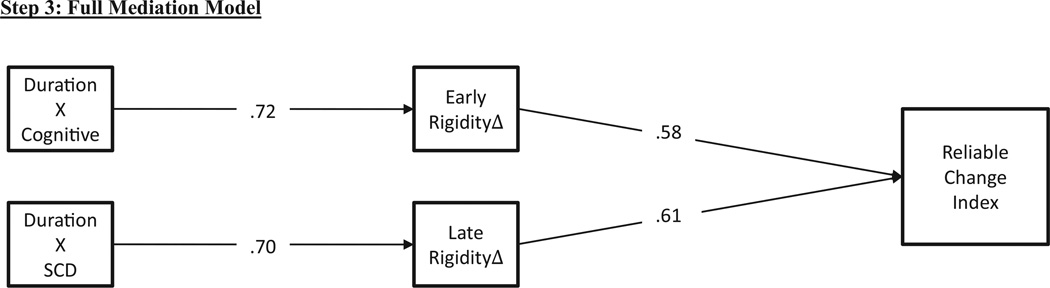
Step 3: Full mediation model
Table 2 contains the parameter estimates for the mediated moderation model (df = 61). The two change variables were entered as mediators of the CT × Duration and SCD × Duration moderation effects. Paths were allowed from baseline main and interaction terms to early and late change in rigidity, and from change in rigidity to RCI at posttreatment. This model provided an excellent fit to the data, χ2 (1) = 1.485, p = .57, comparative fit index (CFI) = .99, standardized root mean residual (SRMR) = .016. Figure 3 presents the final path diagram. All baseline effects were fully mediated by change in rigidity. Of note, the CT × Duration effect was mediated by early change in rigidity, whereas the SCD × Duration effect was mediated by late change in rigidity. Thus, the degree to which clients with longer GAD duration fared better in CT or SCD was a function of the degree to which therapy effectively reduced rigidity in symptomatic organization and increased flexibility during the treatment period; however, these conditions appeared to be mediated by differential periods of treatment. Nevertheless, for individuals in both the CT and SCD conditions, greater GAD duration predicted greater flexibility generation during treatment, which in turn predicted greater reliable change at posttreatment. The opposite was true for individuals in the CBT condition. For these individuals, greater GAD duration predicted less generation of flexibility in symptoms, which in turn predicted less reliable change at posttreatment.
Table 2.
Parameter Estimates for Mediated Moderation Model
| Predictor | β | SE | t | p | d |
|---|---|---|---|---|---|
| Reliable change on | |||||
| CT | −0.720 | 1.142 | −0.630 | .529 | −0.19 |
| SCD | −0.347 | 1.142 | −0.303 | .762 | −0.09 |
| Duration | −0.302 | 0.351 | −0.861 | .389 | −0.16 |
| CT × Duration | 0.815 | 0.506 | 1.609 | .108 | 0.47 |
| SCD × Duration | −0.081 | 0.542 | −0.149 | .882 | 0.04 |
| Change 1 | 0.981 | 0.305 | 3.221 | .001 | −0.58 |
| Change 2 | 0.898 | 0.265 | 3.393 | .001 | −0.61 |
| Change 1 on | |||||
| CT | −1.465 | 0.338 | 4.337 | <.001 | 1.28 |
| SCD | −0.338 | 0.423 | 0.800 | .424 | 0.24 |
| Duration | −0.211 | 0.124 | 1.706 | .088 | 0.31 |
| CT × Duration | 0.385 | 0.158 | −2.433 | .015 | −0.72 |
| SCD × Duration | 0.169 | 0.218 | −0.775 | .438 | −0.23 |
| Change 2 on | |||||
| CT | 0.020 | 0.611 | −0.033 | .974 | 0.01 |
| SCD | −1.144 | 0.586 | 1.951 | .051 | 0.58 |
| Duration | −0.293 | 0.198 | 1.476 | .140 | 0.27 |
| CT × Duration | −0.070 | 0.248 | 0.284 | .777 | −0.08 |
| SCD × Duration | 0.519 | 0.218 | −2.384 | .020 | −0.70 |
Note. CT = cognitive therapy; SCD = self-control desensitization; Change 1 = change in very-high-frequency power from baseline to Session 4; Change 2 = change in very-high-frequency power from Session 5 to Session 14 (end of therapy).
Figure 3.
Step 3, full mediated moderation model (paths reported as Cohen’s d). Nonsignificant parameters and paths are not depicted, χ2 (1) = 1.49, p = .22, comparative fit index = .99, standardized root mean residual = .016. Δ = change. Reliable Change Index is a composite measure of the Penn State Worry Questionnaire, the Hamilton Anxiety Rating Scale, clinician’s severity ratings for generalized anxiety disorder, and the Trait version of the State Trait Anxiety Inventory using the formula from Jacobson and Truax (1991). Early rigidity change = change in very-high-frequency power from baseline to Session 4 of therapy. Late rigidity change = change in very-high-frequency power from Session 5 to Session 14 of therapy. SCD = self-control desensitization.
Discussion
The goals of this study were to examine duration as a moderator of CBT for GAD and its components (CT or SCD) and to determine whether the degree of increased flexibility in anxious symptoms established during therapy served to mediate the proposed moderation effect. As predicted, individuals with longer duration GAD showed more reliable change from component treatments than from combined CBT, with no significant differences between components. In contrast, shorter duration GAD predicted better outcome from CBT than from SCD or CT alone. In addition, consistent with our prediction, for individuals receiving CT or SCD, longer duration GAD predicted greater increases in flexibility during treatment, which in turn predicted more reliable change at posttreatment. The opposite was true for individuals with longer duration GAD in the CBT condition. For these individuals, longer duration predicted less change in rigidity of symptomatic organization during the course of therapy, which in turn predicted less reliable change at posttreatment.
The symptoms of GAD are thought to result from habitual interactions between cognitive, imaginal, and physiological responses to perceived threat (Borkovec & Newman, 1998; Newman, 2000a), causing a spiraling, intensification of anxiety. According to Fisher and Newman (2012), this results in a rigid and inflexible symptom picture, wherein those with GAD have developed a pattern of habitual fluctuations in anxiety of large amplitude (habitual worry cycles) while at the same time maintaining a chronically higher level of overall anxiety (see Figure 1) than is the case following treatment. Such inflexible patterns are consistent with evidence that people with GAD are hyperreactive, are less present-moment focused, and tend to process new information with a negatively biased perspective (Newman, Llera, Erickson, Przeworski, & Castonguay, in press). As a result, they are less able to respond flexibly.
CBT provides clients with a series of techniques meant to target each of the cognitive, imaginal, and physiological response systems. These interventions are aimed at giving clients numerous coping skills, with the expectation that these skills might help them develop more adaptive and flexible habitual processes as a substitute for maladaptive rigid processes (Borkovec & Newman, 1998; Newman & Borkovec, 2002). Clients are asked to identify early triggers for worry and to intervene immediately with a coping response. Each time a coping response occurs, it is theorized to have three important effects. First, the client’s body and mind acquire a new association with an anxiety cue; instead of being a conditioned stimulus for mounting anxiety and worry, the anxiety cue will become associated with using a coping strategy. Second, cutting the spiral off early precludes the reinforcement of anxious responses and meanings, thus weakening these associations in memory. Third, a new sequence is stored in memory and is strengthened (i.e., cue leads to immediate coping). The hope is that anxiety cues, instead of growing as they do with regular worry, will actually shrink in number and strength. As the coping responses become more practiced and stronger, they lead to a greater present-moment focus and a more flexible ability to gauge and match one’s response realistically to the changing natural environment. Thus, this process is likely to result in fewer habitual anxiety spikes in response to triggers, and lessened chronic anxiety, leading to greater adaptive flexibility of anxious symptomatology (flexible lower levels of anxiety, spiking less frequently, with lower amplitude, and only in response to true threat).
One key difference between combined CBT and component treatments is that CBT involves more regular introduction to new strategies and new foci of homework practice throughout treatment than do CT or SCD. What is viewed as the potential benefit of providing a larger menu of options within combined CBT is that clients are more likely to hit upon strategies that work for them and that clients are targeting both cognitive and behavioral maladaptive processes simultaneously. However, one explanation for the current study results is that, whereas the strategy of providing more options to choose from and targeting more systems may work exactly as intended for those with shorter duration GAD, this strategy is not optimal for clients who have had GAD for a longer period of time. Those with longer duration GAD may benefit from a more focused treatment containing either purely cognitive or purely behavioral techniques. Such treatment may be better suited to break longer standing habits and patterns of anxious symptomatology within those with longer duration GAD, perhaps by more intense focus on fewer strategies, more repetition and homework practice of any one strategy, and a treatment dedicated to going more deeply within one system (i.e., cognitive or behavioral). This more intense focus may have led to greater establishment of flexibility in anxiety symptoms during treatment, which in turn led to better outcome for these individuals. In contrast, perhaps introducing many more potentially new strategies within combined CBT for those with longer duration GAD led to less establishment of flexible responding because for these individuals, too many techniques may have over-whelmed their ability to reduce rigidity without the intense practice needed to break longstanding habitual processes.
An alternative explanation for our moderation findings may be that SCD and CT contained a supportive listening segment, whereas CBT did not. Supportive listening was included in the component treatments as a placebo factor to ensure that these treatments were equal to CBT in amount of overall therapist contact time. Although supportive listening was viewed as a placebo therapy, and therefore was not predicted to be the reason for any differences found, it could indeed have played a role in the moderation effect of duration of GAD symptoms. Perhaps providing unstructured time to talk about topics and foci of clients’ choosing may be crucial in the development of a therapeutic alliance with those who have had GAD for a longer duration. It is also possible that having pathological worry for a longer time period increased the likelihood that clients would develop difficulties beyond their GAD symptomatology. As a result, these clients may have a greater need for unstructured therapy time to address such added difficulties than those with shorter duration GAD.
Our finding that GAD duration predicts a differential response to CBT versus component treatments contrasts with the original results of Borkovec et al. (2002), which showed no significant differences between CBT and its components. Moreover, the current study findings are relevant to the notion of the “dodo bird verdict” (Luborsky, Singer, & Luborsky, 1975) and point to the importance of examining individual differences as moderators before drawing conclusions that there are no differences between different treatments. The current finding of duration as a moderator also highlights the importance of the recent emphasis on personalized interventions. In particular, our data point to the need to tailor CBT to individuals depending on the duration of their GAD symptomatology. Thus, using duration of symptoms as a means to assign participants to either component treatments or combined CBT may be warranted.
The current study also provides a theoretical mechanism for the impact of duration using a dynamic systems theory framework. This mechanism of change appears to be to decrease maladaptive rigidity in symptomatic phenomenology and increase adaptive flexibility in clients’ anxious experience. To wit, the differential impact of duration on CBT and its components was fully mediated by the extent to which flexibility was established within these treatments, suggesting that the degree of adaptive flexibility generated during psychotherapy is a potentially crucial mechanism of change. Importantly, the present study represents the first time that either rigidity/flexibility or decreasing rigidity have been tested as mediators of treatment outcome. An additional finding was that for those with longer duration GAD in the CT condition, flexibility generated from baseline to the fourth session of therapy (the first 8 hr of therapy) mediated outcome, whereas for those with longer duration GAD in the SCD condition, flexibility generated during the last 10 sessions (15 hr of therapy) mediated outcome. This points to the possibility that the crucial time period for establishing adaptive flexibility may vary across therapeutic approaches. In CT, the first four sessions are used to present the therapy rationale and to teach clients how to identify early anxiety triggers and dysfunctional thoughts. Perhaps such a process of helping longer duration GAD clients understand their maladaptive patterns may be the important mechanism of establishing flexibility and achieving reliable change in CT. For SCD, the important mechanism of establishing flexibility and achieving change may occur in the last two thirds of the therapy sessions, when clients begin to achieve mastery over the SCD and relaxation techniques and experience the lessened reactivity to triggers that occurs with practice.
The findings of this study highlight the relevance of including intensive repeated measurements throughout the therapy period and analyzing these data using methodologies that reflect individual differences in symptomatic rigidity. These data also provide further support for the quantitative technique developed by Fisher et al. (2011) to model nomothetic relationships between idiographic structures. This two-step process first models within-individual variation in diary data, isolating predictable variation due to daily and intradaily oscillations (VHFP). Individual differences in VHFP are then used to determine group-level differences in outcome. However, the Fisher et al. study used static rigidity/flexibility metrics (of both VHFP and residual variance in dynamic factor models), whereas the present study followed Fisher and Newman (2012) in modeling changes in rigidity generated during therapy. Given that greater flexibility generation appears to be a powerful, global predictor of outcome, it is imperative to continue to examine ways in which greater flexibility is generated to facilitate more effective interventions. This might be done by collecting intensive repeated measures of symptomatology during the course of therapy using diary methods or momentary assessment devices. Future research might also examine whether dynamic processes are specific mediators within active treatments in comparison to placebos.
This study has several limitations. The sample was predominantly White, and therefore our results may not generalize to more diverse samples. Similarly, given our exclusion of clients diagnosed with clinical levels of panic disorder or with very severe major depressive disorder, our findings may not generalize to these groups. In addition, the study was restricted to individuals with generalized anxiety disorder treated with CBT, and thus the results may not generalize to other diagnostic groups or other psychotherapy approaches. Further, we cannot rule out the possibility that supportive listening contained within the CT and SCD treatment components was what contributed to the moderation effect for those with longer duration GAD. There is also the possibility that monitoring of anxiety levels across 16 weeks four times each day led to reactivity to the daily diary and influenced our findings in some systematic way unrelated to the psychotherapy. Nonetheless, it is unlikely that such a relationship would systematically differ across treatment conditions and duration of GAD.
Acknowledgments
This research was supported in part by National Institute of Mental Health Research Grant R01 MH-309172-01.
Footnotes
Given constraints related to statistical power, this study was limited to the spectral analysis of therapy phases and necessarily excluded dynamic factor modeling and the extraction of residual variance. Thus we henceforth focus specifically on the degree of rigidity versus flexibility.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: Author; 1987. rev.). [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bernstein DA, Borkovec TD. Progressive relaxation training: A manual for the helping professions. Champaign, IL: Research Press; 1973. [Google Scholar]
- Biswas A, Chattopadhyay PK. Predicting psychotherapeutic outcomes in patients with generalised anxiety disorder. Journal of Personality and Clinical Studies. 2001;17:27–32. [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG. Worry and generalized anxiety disorder. In: Bellack AS, Hersen M, editors. Comprehensive clinical psychology: Vol. 6. Adults: Clinical formulation and treatment. Oxford, England: Pergamon Press; 1998. pp. 439–459. (Series Ed.) [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Borkovec TD, Ruscio AM. Psychotherapy for generalized anxiety disorder. Journal of Clinical Psychiatry. 2001;62:37–42. [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview Guide: Joint interview and test–retest methods for interrater reliability. Psychiatry Research. 1994;53:191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 1999;67:583–589. doi: 10.1037//0022-006x.67.4.583. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule—Revised (ADIS–R) Albany, NY: Center for Stress and Anxiety Disorders; 1988. [DOI] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Fisher AJ, Newman MG. Reductions in complexity and high-frequency variability of daily symptoms during therapy predict greater change at post-treatment in CBT for GAD. 2013 Manuscript submitted for publication. [Google Scholar]
- Fisher AJ, Newman MG, Molenaar PC. A quantitative method for the analysis of nomothetic relationships between idiographic structures: Dynamic patterns create attractor states for sustained posttreatment change. Journal of Consulting and Clinical Psychology. 2011;79:552–563. doi: 10.1037/a0024069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfried MR. Systematic desensitization as training in self-control. Journal of Consulting and Clinical Psychology. 1971;37:228–234. doi: 10.1037/h0031974. [DOI] [PubMed] [Google Scholar]
- Gould RA, Otto MW, Pollack MH, Yap L. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder: A preliminary meta-analysis. Behavior Therapy. 1997;28:285–305. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Feldman GC, Beevers CG, Laurenceau JP, Cardaciotto L, Lewis-Smith J. Discontinuities and cognitive changes in an exposure-based cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 2007;75:409–421. doi: 10.1037/0022-006X.75.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Strauss JL. Dynamic systems theory as a paradigm for the study of change in psychotherapy: An application of cognitive therqapy for depression. Journal of Consulting and Clinical Psychology. 1998;66:939–947. doi: 10.1037//0022-006x.66.6.939. [DOI] [PubMed] [Google Scholar]
- Heide FJ, Borkovec TD. Relaxation-induced anxiety: Paradoxical anxiety enhancement due to relaxation training. Journal of Consulting and Clinical Psychology. 1983;51:171–182. doi: 10.1037//0022-006x.51.2.171. [DOI] [PubMed] [Google Scholar]
- Holland PW. Statistics and causal inference. Journal of the American Statistical Association. 1986;81:945–960. [Google Scholar]
- Horowitz LM, Inouye D, Siegelman EY. On averaging judges’ ratings to increase their correlation with an external criterion. Journal of Consulting and Clinical Psychology. 1979;47:453–458. doi: 10.1037//0022-006x.47.3.453. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Treatment outcomes, common factors, and continued neglect of mechanisms of change. Clinical Psychology: Science and Practice. 2005;12:184–188. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. 4th ed. 1 and 2. New York, NY: McGraw-Hill; 1998. pp. 233–265. [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Singer B, Luborsky L. Comparative studies of psychotherapies. Is it true that “everyone has won and all must have prizes”? Archives of General Psychiatry. 1975;32:995–1008. doi: 10.1001/archpsyc.1975.01760260059004. [DOI] [PubMed] [Google Scholar]
- McGlinchey JB, Atkins DC, Jacobson NS. Clinical significance methods: Which one to use and how useful are they? Behavior Therapy. 2002;33:529–550. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Molenaar PCM. A dynamic factor model for the analysis of multivariate time series. Psychometrika. 1985;50:181–202. [Google Scholar]
- Molenaar PCM. A manifesto on psychology as idiographic science: Bringing the person back into scientific psychology, this time forever. Measurement: Interdisciplinary Research and Perspectives. 2004;2:201–218. [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: Wiley; 1994. pp. 265–283. [Google Scholar]
- Moras K, di Nardo PA, Barlow DH. Distinguishing anxiety and depression: Reexamination of the reconstructed Hamilton scales. Psychological Assessment. 1992;4:224–227. [Google Scholar]
- Newman MG. Generalized anxiety disorder. In: Hersen M, Biaggio M, editors. Effective brief therapies: A clinician’s guide. San Diego, CA: Academic Press; 2000a. pp. 157–178. [Google Scholar]
- Newman MG. Recommendations for a cost-offset model of psychotherapy allocation using generalized anxiety disorder as an example. Journal of Consulting and Clinical Psychology. 2000b;68:549–555. [PubMed] [Google Scholar]
- Newman MG, Borkovec TD. Cognitive behavioral therapy for worry and generalized anxiety disorder. In: Simos G, editor. Cognitive behaviour therapy: A guide for the practising clinician. New York, NY: Taylor & Francis; 2002. pp. 150–172. [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell J, Szkodny LE, Nordberg SS. A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology. 2011;79:171–181. doi: 10.1037/a0022489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Crits-Christoph P, Connelly Gibbons MB, Erickson TM. Participant factors in treating anxiety disorders. In: Castonguay LG, Beutler LE, editors. Principles of therapeutic change that work. New York, NY: Oxford University Press; 2006. pp. 121–154. [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: A review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annual Review of Clinical Psychology. doi: 10.1146/annurev-clinpsy-050212-185544. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, Borkovec TD. Diagnostic comorbidity in adults with generalized anxiety disorder: Impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy. 2010;41:59–72. doi: 10.1016/j.beth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul GL. Strategy of outcome research in psychotherapy. Journal of Consulting Psychology. 1967;31:109–118. doi: 10.1037/h0024436. [DOI] [PubMed] [Google Scholar]
- Seivewright H, Tyrer P, Johnson T. Prediction of outcome in neurotic disorder: A 5-year prospective study. Psychological Medicine. 1998;28:1149–1157. doi: 10.1017/s0033291798007119. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory STAI (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- Steketee G, Chambless DL. Methodological issues in prediction of treatment outcome. Clinical Psychology Review. 1992;12:387–400. [Google Scholar]
- van den Brink RHS, Ormel J, Tiemens BG, Smit A, Jenner JA, van der Meer K, van Os TWDP. Predictability of the one-year course of depression and generalized anxiety in primary care. General Hospital Psychiatry. 2002;24:156–163. doi: 10.1016/s0163-8343(02)00183-4. [DOI] [PubMed] [Google Scholar]
- Whitehurst GJ. Interrater agreement for journal manuscript reviews. American Psychologist. 1984;39:22–28. [Google Scholar]