Abstract
Prostate cancer (PCa) is frequently accompanied by osteosclerotic (i.e., excessive bone production) bone metastases. Although bone morphogenetic proteins (BMPs) and Wnts are mediators of PCa-induced osteoblastic activity, the relation between them in PCa bone metastases is unknown. The goal of this study was to define this relationship. Wnt3a and Wnt5a administration or knockdown of (DKK-1), a Wnt inhibitor, induced BMP4 and 6 expression and promoter activation in PCa cells. DKK-1 blocked Wnt activation of the BMP promoters. Transfection of C4-2B cells with axin, an inhibitor of canonical Wnt signaling, blocked Wnt3a, but not Wnt5a induction of the BMP promoters. In contrast, Jnk inhibitor I blocked Wnt5a, but not Wnt3a induction of the BMP promoters. Wnt3a, Wnt5a, and conditioned-media (CM) from C4-2B or LuCaP23.1 cells induced osteoblast differentiation in vitro. The addition of DKK-1 and Noggin, a BMP inhibitor, to CM diminished PCa CM-induced osteoblast differentiation in a synergistic fashion. However, pretreatment of PCa cells with DKK-1 prior to collecting CM blocked osteoblast differentiation; whereas, pretreatment with Noggin only partially reduced osteoblast differentiation and pre-treatment with both DKK-1 and Noggin had no greater effect than pretreatment with DKK-1 alone. Additionally, knockdown of BMP expression in C4-2B cells inhibited Wnt-induced osteoblastic activity. These results demonstrate that PCa promotes osteoblast differentiation through canonical and non-canonical Wnt signaling pathways that stimulate both BMP-dependent and independent osteoblast differentiation. These results demonstrate a clear link between Wnts and BMPs in PCa-induced osteoblast differentiation and provide novel targets, including the non-canonical Wnt pathway, for therapy of PCa.
Keywords: Wnt, bone morphogenetic proteins, prostate cancer, bone metastasis, dickopff-1
Introduction
Prostate cancer (PCa) is the most frequently diagnosed cancer in men and the second leading cause of cancer death among men in the United States (1). The most common site of PCa metastasis is the bone with skeletal metastases identified at autopsy in up to 90% of patients dying from PCa (2). Skeletal metastasis in PCa patients result in significant complications that diminish the quality of life in affected patients. These complications include bone pain, impaired mobility, pathological fracture, spinal cord compression and symptomatic hypercalcemia.
At the metastatic bone site, growth of PCa promotes localized bone remodeling that results in primarily osteosclerotic lesions (also known as osteoblastic lesions characterized by increased production of mineralized bone matrix resulting in increased bone mineral density) with underlying osteolytic lesions (i.e., osteoclast-mediated resorption of mineralized bone matrix resulting in low bone mineral density) (reviewed in 3). Although mechanisms contributing to the osteopenic component of PCa–mediated bone lesions have been elucidated (4, 5), the mechanisms responsible for the osteoblastic component of PCa bone lesions are not well-defined, although a variety of factors such as bone morphogenetic proteins (BMP) (6), endothlin-1 (ET-1) (7), vascular endothelial growth factor (VEGF) (8) and Wnts (9) have been implicated as contributing to osteoblastic metastasis. Understanding the mechanisms that promote PCa-induced osteosclerosis may help identify targets to diminish the progression of these lesions.
BMPs, members of the transforming growth factor (TGF)-β superfamily, were originally discovered because of their ability to induce new bone formation (reviewed in 10). BMPs bind to two different types of serine-threonine kinase transmembrane receptors, type I and type II. BMPs initially bind to BMPR-II, which then phosphorylates BMPR-I, which subsequently phosphorylates SMAD proteins. Target genes of BMPs include osteoblast proteins such as OPG (11) and the osteoblast-specific transcription factor Cbfa-1 (12). Many in vitro studies have demonstrated that BMPs induce osteogenic differentiation (13, 14). A number of studies have demonstrated that BMP expression increases with progression of PCa (15–18) and that BMP-6 induces osteoblastic activity in a murine model of PCa (6) although BMP-7 does not appear to do this (19).
Wnt proteins are soluble glycoproteins that mediate homeostatic and developmental activity (reviewed in 20). The canonical Wnts bind to receptor complexes composed of Lrp5/6 and Frizzled proteins and ultimately induced nuclear translocation of β-catenin. Non-canonical Wnts bind to a variety of receptors, including receptor tyrosine kinases and mediate many different activities, some of which oppose canonical Wnt signaling. Wnt-mediated signaling promotes postnatal bone accrual (21) and is essential for skeletal outgrowth (22). In concordance with Wnts’ role in bone development and growth, PCa-produced Wnts were identified to induce osteoblastic activity in PCa bone metastases (9). However, it is not clear if Wnts mediate this activity through direct action on osteoblasts or through activation of other pro-osteoblastic factors, such as BMPs. As both Wnts and BMPs have been shown to play a role in PCa osteoblastic metastases and Wnts have been shown to promote BMP expression and modulate BMPs’ osteogenic action in the embryo development (23), we tested if BMPs contribute to Wnts’ ability to regulate osteoblastic activity in PCa bone metastases.
MATERIALS AND METHODS
Materials
Wnt-3a and -5a, sFRP-1, DKK-1 and Noggin recombinant proteins were obtained from R&D Systems (Minneapolis, MN). JNK inhibitor I and JNK inhibitor I-Negative Control were obtained from EMD Biosciences (San Diego, CA ). This inhibitor blocks the interaction of JNK and its substrates (24) and were not toxic at doses used in the studies based on dose response proliferation and cell death (trypan blue staining) assays (data not shown).
Cells and cell culture
LNCaP and PC-3 cells were obtained from American Tissue Culture Collection (Bethesda, MD). PC-3 Clone 8 are cells that have been stably transfected with shRNA targeting DKK-1 that resulted in a knockdown of DKK-1 by >80% (9). These PCa cells were maintained in RPMI medium (Life Technologies, Inc., Rockville, MD) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin (Life Technologies, Inc.). The C4-2B cell line, a kind gift from Dr. Leland Chung (Emory University), is an osteogenic derivative cell line of LNCaP cells (25) and was maintained in T medium [80% DMEM (Life Technologies, Inc.), 20% F12 (Irving Scientific, Santa Ana, CA), 3 grams/liter NaCO3, 100 units/liter penicillin G, 100 μg/ml streptomycin, 5 μg/ml insulin, 13.6 pg/ml triiodothyronine, 5 μg/ml transferrin, 0.25 μg/ml biotin, and 25 μg/ml adenine] supplemented with 5% FBS. LuCaP 23.1, kindly provided by Dr. Robert Vessella (University of Washington), is an androgen-sensitive, PSA-producing human prostate cancer xenograph derived from the lymph nodes of a patient that had failed androgen deprivation therapy (26). Single cell suspensions of LuCaP 35 were prepared by resecting the subcutaneous xenografts and cutting them into small pieces in HBSS with 1% FBS as we have previously described (6) then using the Cancer Cell Isolation Kit (Panomics, Freemont, CA) as directed by the manufacturer. Briefly, the small pieces were digested in Tumor Cell Digestion Solution, then the tumor cell suspension was purified by Tumor Cell Purification Solution and the LuCaP 23.1 cells were maintained in RPMI 1640 with 10% FBS. Cell viability was determined by trypan blue counting and only preparations with over 95% viability were used for in vivo injection. The MC3T3-E1 (clone MC-4) (kindly provided by Dr. Renny Franceschi, University of Michigan, Ann Arbor, MI), is a murine preosteoblast cell line that was maintained in -MEM and 10% FBS. All cells are checked for Mycoplasma contamination every 3 months using PCR methods.
For Wnt administration in vitro, recombinant Wnts were added at the indicated doses to culture media. The dose range was designed to encompass the effective dose 50% for these proteins based on previous studies (27, 28) and the manufacturer (R and D Systems). For inhibitor studies using DKK-1 or noggin, the inhibitory compound was added to the media at the same time the culture treatments were initiated. Typically, 50% of the media was replaced every 3 days with fresh conditioned media (CM) containing FBS and treatment compounds at the original concentrations. This was continued until the end of each study as indicated in the figure legends.
Plasmids and transfections
Flag-tagged human pcDNA3-Axin2 was kindly provided by Dr Eric R. Fearon (Department of Internal Medicine, Human Genetics, and Pathology, University of Michigan, Ann Arbor, MI). The pGL3-BMP4-2443 promoter construct containing 2443 bp of the proximal BMP4 promoter was kindly provided by Dr. L Helvering (Lilly Pharamaceuticals, Indianapolis, IN) (29) and the pGL3-BMP6-1168 promoter that contains 1168BP of the BMP6 promoter was kindly provided by Dr. S. Kitazawa (Kobe University School of Medicine) (30). Cells were transfected using Nucleofection as recommended by the manufacturer (Amaxa Inc, Gaithersburg, MD). Luciferase activity was measured and normalized between transfections using the dual luciferase assay (Promega, Madison, WI). Human BMP4 and BMP6-shRNA and control scrambled shRNA were obtained from Open Biosystems (Huntsville, AL). The shRNAs were provided in a lentiviral expression vector and were packaged in packaging cell line, TLA-HEK293T using the Trans-Lentiviral Packaging System (Open Biosystems). C4-2B cells were then transduced using lentiviral supernatant as directed by the manufacturer. Stably transfected clones were selected using 2μg/mL Puromycin (Invitrogen) selection and used as a polyclonal population.
Obtaining conditioned medium
CM was obtained from cells as previously described (28). Briefly, 5 × 106 cells were plated in 10 cm tissue culture dishes for 12 hours in RPMI 1640 with 10% fetal bovine serum (FBS). Cells were allowed to grow to confluence and then the medium was changed to 10 ml of RPMI plus 0.5% FBS and supernatants were collected 24 hours later. To normalize for differences in cell density due to proliferation during the culture period, cells from each plate were collected and total DNA content/plate was determined (spectrophotometric absorbance at 260 nm). Conditioned medium was then normalized for DNA content between samples by adding RPMI. In some instances, as indicated in the results, cells were pre-treated with either DKK-1 or Noggin or both for 12 hours, followed by replacing the media with fresh media and then collecting CM 24 hours later.
Alkaline phosphatase (ALP )and osteocalcin assay
ALP activity was measured in the cells using a colorimetric assay based on the conversion of P-nitrophenylphosphate as directed by the manufacturer (ALP assay; Sigma). Briefly, MC3T3-E1 cells in 12-well plates were washed with PBS and sonicated in 10 mmol/L of Tris-HCl buffer (pH, 7.5) containing 0.1% Triton X-100. ALP activity in the lysate was assayed by the hydrolysis of p-nitrophenyl phosphate (Sigma) to p-nitrophenol. Absorbance was determined at 405 nm and compared with a p-nitrophenol (Sigma) standard titration curve. ALP activity was normalized to total protein content (Bio Rad Protein Assay). Osteocalcin was measured in supernatants using a mouse-specific ELISA as recommended by the manufacturer (Biomedical Technologies Inc., Stoughton, MA).
Coculture experiments
MC3T3-E1 cells were plated in a twelve-well culture plate at a density of 2×105 cells/well and grown in α-MEM media with 10% FBS for 48 hours (approximately 80% confluent). At the same time, C4-2B cells were plated at a density of 2×105 cells/well in twelve-well culture plates on 10-mm Anopore tissue culture plate inserts (0.2 μm pore size; Nalge Nunc International) and grown in T media plus 10% FBS plus vehicle or recombinant Wnt 3a or Wnt5a at 50ng/ml for 48 hours. At 48 hours post the initiation of cultures, the plates were gently washed with PBS, the culture plate inserts containing C4-2B cells were inserted into the culture plates containing the MC3T3-E1 cells and the media was replaced with fresh α-MEM media plus 10% FBS. The cocultures were maintained for 10 days at which time supernatants were subjected to measurement of ALP and osteoclacin.
Immunoblot analysis
For identification of BMP proteins, whole cell lysates were prepared by incubating cells in ice-cold RIPA lysis buffer (Sigma, St. Louis, MO). Lysates were precleared and the protein concentration was determined by the bicinchoninic acid assay (Pierce Biochemicals, Rockford, IL). For electrophoresis, lysates were supplemented with SDS loading buffer and separated on SDS-12% polyacrylamide gels. Proteins were transferred to nitrocellulose membranes. The blots were incubated in TBS containing 0.1% Tween 20 and 5% nonfat dry milk during the blocking and the antibody incubation steps. Human anti–BMP-4, BMP-6 antibodies (R&D Systems) were used at 1:500 to 1:2,000 dilutions and rabbit anti-actin (Sigma, St. Louis, MO) antibody was used at 1:1,000, and the HRP-conjugated sheep anti-mouse (Amersham International, Buckinghamshire, United Kingdom) and the HRP-conjugated donkey anti-rabbit (Amersham Life Science, Arlington Heights, IL) were used at 1:5,000 dilution. Antibody complexes were detected by enhanced chemiluminescence (Amersham Life Science, Arlington Heights, IL) and exposure to X-Omat film (Kodak, Rochester, NY). Band densities were quantified using NIH Scion Image.
Reverse transcription PCR analysis of BMPs mRNA Expression
Total RNA was extracted using RNeasy kit (Qiagen) and synthesized to cDNA using First Strand cDNA Synthesis Kit (SuperArray Bioscience Co., Frederick, MD). The cDNA was amplified by GeneAmp PCR System 9700(PE Applied Biosystems) using HotStart Sweet PCR master mix (SuperArray) at 95°C for 15min, 95°C for 15 s, 55°C for 30 s, and 72°C for 30 s for 30–40 cycles. β-actin was used as an internal control. The PCR primer set used for BMP4, BMP6 and β-actin were manufactured by SuperArray Bioscience Co., (Frederick, MD). All products were evaluated by electrophoresis on 2% agarose gels.
Real time PCR quantitative analysis of BMP mRNA Expression
Total RNA was extracted using RNeasy kit (Qiagen) and synthesized to cDNA using Reverse Transcription System (Promega, Madison, WI). The cDNA was amplified and quantified by LightCycler (Roche Diagnostics, Indianapolis, IN) using the Real Time SYBR Green PCR master mix (SuperArray Bioscience Co., Frederick, MD) at 95°C for 15min, 95°C for 30 s, 55°C for 30 s, and 72°C for 30 s for 35–55 cycles. β-actin was used as an internal control. The PCR primers used for BMP4, BMP6 and β-actin were manufactured by SuperArray Bioscience Co., (Frederick, MD). The size of the PCR products was confirmed using gel electrophoresis after real-time PCR (data not shown).
Data Analysis
Statistical significance was determined for multivariate comparisons using ANOVA and Fisher’s probable least significant difference for post hoc analysis. Student’s t test was used for bivariate analyses. Statistical significance was determined as P≤0.05. Statistical calculations were performed using Statview software (Abacus Concepts, Berkeley, CA).
RESULTS
Wnt3a and Wnt5a promote BMP4 and BMP6 expression in C4-2B cells
To investigate whether Wnt3a, a canonical Wnt, and Wnt5a, a non-canonical Wnt, regulate the expression of BMP4 and BMP6 in PCa cells, the LNCaP-derivative C4-2B cells (1 × 105 cells/well) were plated in 12-well plates in T medium plus 10% FBS. The cells were treated, respectively, with 0, 25, 50 and 100ng/ml Wnt3a or Wnt5a or vehicle for 8 h, followed by real time RT-PCR to quantify mRNA levels. Wnt3a increased BMP4 mRNA expression but had no effect on BMP6 mRNA expression (Fig. 1A); whereas, Wnt5a increased BMP6 mRNA expression but had no effect on BMP4 mRNA expression in C4-2B cells (Fig. 1B). To determine if protein levels reflected changes in mRNA levels C4-2B cells were treated with Wnt3a (50ng/ml), Wnt5a (50ng/ml) or vehicle for 24 h followed by western blot. Similar to the changes in mRNA levels, Wnt3a increased BMP4 but not BMP6 protein expression; whereas, Wnt5a increased BMP6 but not BMP4 protein expression in C4-2B cells (Fig 1C and quantification shown in Supplemental Fig. 1A). These findings demonstrate that Wnts regulate BMPs expression in C4-2B cells and suggest that BMPs are differentially regulated by canonical versus non-canonical Wnts. To determine if this pathway is also active in a PSA negative, AR negative cell line we used PC-3 cells. We have previously reported that PC-3 cells, which are osteolytic, express high levels of DKK-1 (9). In a previous study to determine the activity of Wnts in PC-3 cells, we had a made PC-3 cell line that was stably transfected with shDKK-1 (PC-3 clone 8) resulting in >80% reduction of DKK-1 protein levels (9). We identified in that study that knockdown of DKK-1 conferred pro-osteoblastic activity on PC-3 cells including the ability of PC-3 cells to promote both AP activity and mineralization of MC-3T3 cells in vitro. To determine if this activity was associated with changes in BMP expression, we measured BMP4 and BMP6 protein and mRNA levels in control-transfected or PC-3 cells stably transfected with shDKK-1 (PC-3 clone 8). Knockdown of DKK-1 induced both BMP-4 and BMP-6 mRNA and protein expression (Figs. 1D and quantification shown in Supplemental Fig. 1B). These data demonstrate that inhibition a Wnt signaling repressor promotes BMP expression indicating that the relation between Wnts and BMP expression is functional in the PSA negative, AR negative PC-3 cell line. This finding also suggests that loss of the osteoblastic activity in the PC-3 cell line may be due to repression of Wnt-mediated BMP expression secondary to DKK-1 repression of Wnt activity.
Figure 1. Wnts increase BMP mRNA and protein expression in PCa cells.
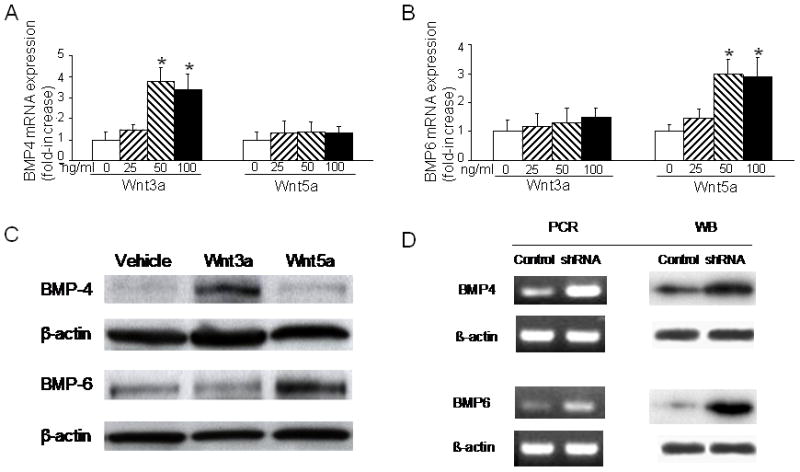
C4-2B cells (1 × 105 cells/well) were plated in 12-well plates in T medium plus 10% FBS. (A and B) The cells were treated with 0, 25, 50 and 100ng/ml of the indicated Wnt3A and Wnt5A for 8 h then total RNA was collected and subjected to real-time RT-PCR for (A) BMP-4 and (B) BMP-6. (C) Cells were treated with Wnt3a (50ng/ml) or Wnt5a (50ng/ml) or vehicle for 24 h. Total protein was collected and subjected to Western blot for BMP4 and BMP6. β-actin was used as loading control. Representative Western blot is shown. (D) Total mRNA or protein from control shRNA-transfected or shDKK-1-transfected PC-3 cells (PC-3 Clone 8) collected and subjected to PCR or Western blot for BMP4, BMP6 and β-actin. Results shown are mean±SD from two to three experiments. *P≤0.05 versus 0ng/ml.
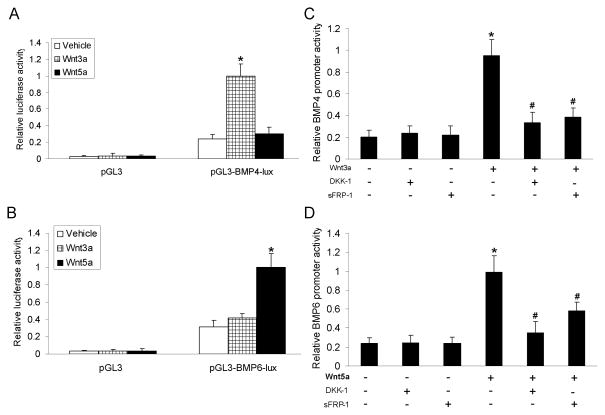
Wnt3a and Wnt5a activate BMP4 and BMP6 promoter activity in C4-2B Cells through Wnt canonical pathway and non-canonical JNK-dependent signaling pathway
The observation that Wnts increased steady-state BMP mRNA and protein expression gave rise to the possibility that Wnts activate BMP promoters. To test this possibility, C4-2B cells were transfected with a luciferase reporter vector driven by the BMP-4 promoter (pGL3-BMP4), the BMP-6 promoter (pGL3-BMP6) or empty control vector (pGL3-basic) and treated with Wnt 3a or Wnt 5a in the absence or presence of two different inhibitors of canonical Wnt signaling: (1) DKK-1(1ug/ml), which inhibits the Wnt receptor LRP-6 and (2) sFRP-1 (5ug/ml), that sequesters Wnts from the membrane-bound Frizzled (FZD) which trimerizes with LRP-6 and Wnt (reviewed in 31). After 8 hours of treatment, cells were harvested, and total cell lysates were subjected to assay for luciferase (lux) levels. Wnt3a induced BMP-4 but not BMP-6 promoter activity; whereas, Wnt5a induced BMP-6 but not BMP-4 promoter activity. (Fig. 2A and B). DKK-1 and sFRP-1, blocked both Wnt3a-induced BMP-4 promoter activity (Fig. 2C), and Wnt5a-induced BMP-6 promoter activity (Fig. 2D). These results indicate that Wnt3a and Wnt5a induce activation of the BMP-4 and BMP-6 promoter, respectively, through a LRP-6-dependent mechanism.
Figure 2. Wnts activate the BMPs promoter in C4-2B cells.
C4-2B cells (1 × 105 cells/well) were plated in 12-well plates in T medium with 10% FBS and after 24 h, the cells were transfected with (A) pGL3-BMP4-2443 promoter-lux or the empty vector pGL3-lux and (B) pGL3-BMP6-1168-promoter-lux or the empty vector pGL3-lux. Twenty four hours after transfection, cells were treated with either vehicle, Wnt3a (50ng/ml) or Wnt5a (50ng/ml). Cells were harvested 8 hours post-treatment and total cell lysates were collected for measurement of luciferase levels. (C and D) C4-2B cells were transfected with (C) pGL-3-BMP4-2443 promoter-lux or (D) pGL-3-BMP6-1168-promoter-lux as described above, then treated with Wnt3a (50ng/ml), Wnt5a (50ng/ml), DKK-1(1ug/ml) and sFRP-1 (5ug/ml). Cells were harvested 8 hours post-treatment and total cell lysates were collected for measurement of luciferase levels. Results shown are mean±SD from three experiments. *P≤0.05 versus vehicle or Control or Vehicle; #P≤0.05 versus Wnt3a or Wnt5a alone.
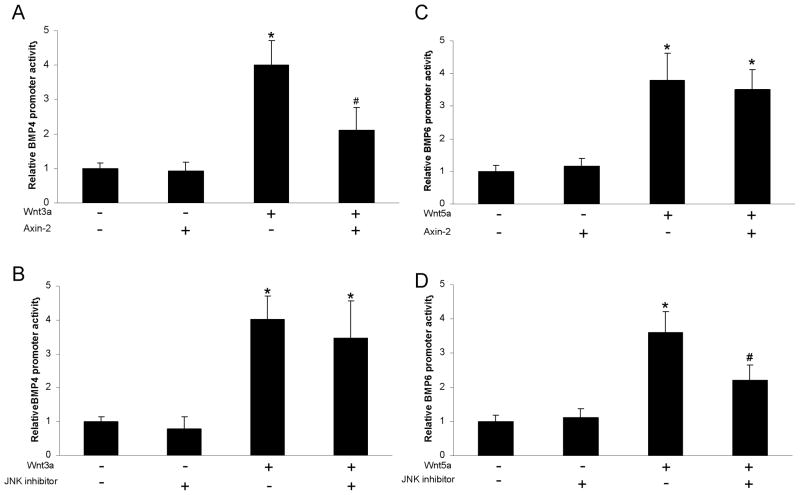
To elucidate further the roles of the Wnt canonical pathway and non-canonical JNK-dependent signaling pathways in Wnt-induced BMP promoter activity, C4-2B cells transfected with either the BMP4 or BMP6 promoter were cotransfected with Axin-2, a negative regulator of the intracellular component of the canonical Wnt pathway, or were pretreated with a cell permeable JNK inhibitor (30uM) (JNK inhibitor I) for 1 h, then cells were treated with either vehicle, Wnt3a (50ng/ml) or Wnt5a (50ng/ml). Eight hours later, cells were harvested, and total cell lysates were assayed for luciferase levels. Axin-2 partially diminished Wnt3a-induced BMP-4 promoter activity (Fig. 3A); whereas, JNK inhibitor I had no effect on the Wnt3a-induced BMP-4 promoter activity (Fig. 3B). In contrast, Axin-2 had no effect on Wnt5a-induced BMP-6 promoter activity (Fig. 3C); whereas, JNK inhibitor I partially diminished Wnt5a-induced BMP-6 promoter activity (Fig. 3D). These results indicate that Wnt3a induces BMP-4 promoter activity through the canonical pathway and Wnt5a activates the BMP-6 promoter activity through a JNK-dependent non-canonical Wnt pathway.
Figure 3. Wnt3a activates the BMP4 promoter and Wnt5a activates the BMP6 promoter through canonical and non-canonical Wnt pathways, respectively.
C4-2B cells were plated in 12-well plates in T medium with 10% FBS, and after 24 h, they were transfected with (A and B) pGL3-BMP4-2443 promoter-lux or the empty vector pGL3-lux or (B and C) pGL3-BMP6-1168-promoter-lux or the empty vector pGL3-lux and then 24 hours later were (A and C) transfected with pcDNA3-Axin2 or empty pcDNA3 vector and allowed to grow for 24 hours or (B and D) treated with vehicle or JNK inhibitor (30uM) for 1h then cells were treated with (A and B) vehicle or Wnt3a (50ng/ml) or (C and D) vehicle or Wnt5a (50ng/ml). Eight hours later, cells were harvested, and total cell lysates were subjected to assay for luciferase levels. Results shown are mean±SD from two experiments. *P≤0.05 versus no Wnt; #P≤0.05 versus (A) Wnt3a plus empty vector or (D) Wnt5a plus vehicle.
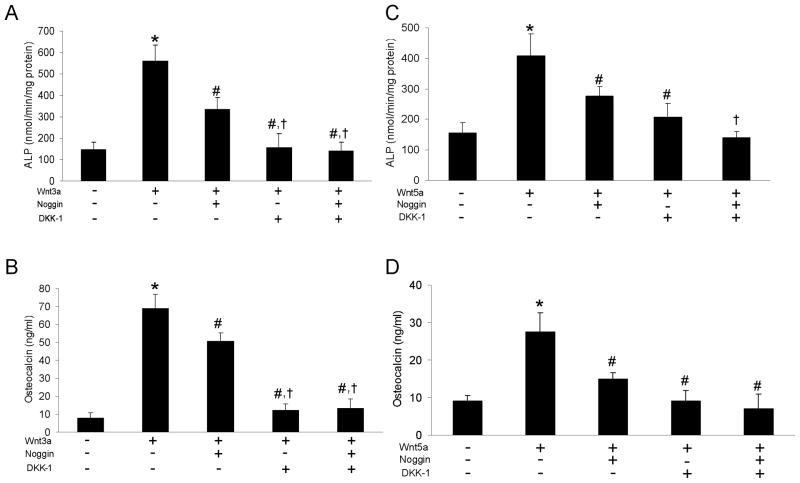
BMPs contribute, in part, to Wnt’s pro-osteoblastic activity
As PCa produces a variety of pro-osteoblastic factors, including Wnts and BMPs, we wanted to define the relationship between Wnt- and BMP-mediated osteoblast activities in our in vitro system. Mouse osteoblast precursor cells, MC3T3-E1 cells, were treated with Wnt3a (50ng/ml), or Wnt5a (50ng/ml) and either Noggin, an inhibitor of BMP activity, or DKK-1 or the combination of both. Noggin is a soluble protein has been shown to inhibit a variety of BMPs including BMP-2, BMP-4 and BMP-6 by binding them and sequestering them from the BMP receptor (32–35). Neither Noggin nor DKK-1 alone or in combination had an effect on basal alkaline phosphatase or osteocalcin levels (not shown). Wnt3a increased alkaline phosphatase activity and osteocalcin levels, indicators of osteoblast maturation, in MC3T3-E1 cells (Fig. 4A and B). Noggin (1 μg/ml) partially blocked Wnt3a-mediated osteoblast activity; whereas, DKK-1 (1 μg/ml) completely blocked Wnt3a-mediated osteoblast activity; and both together did not show further inhibition (Fig 4A and B). Similar to Wnt3a, Wnt5a increased alkaline phosphatase activity and osteocalcin levels (Fig. 4C and D). However, DKK-1 and Noggin only partially blocked Wnt5a-induced alkaline phosphatase activity and together they had an additive effect on alkaline phosphatase inhibition (Fig. 4C and D). Additionally, both DKK-1 and Noggin inhibited Wnt5a-induced osteocalcin activity, without any additional inhibition when added together. The observation that Noggin only partially blocked Wnt3a-induced osteoblast differentiation indicates that Wnt 3a induces osteoblast differentiation both through BMP-dependent and independent paths. However, the observation that DKK-1 completely blocked Wnt3a-induced osteoblast differentiation indicates that Noggin-repressible BMP induced activity is dependent on Wnt3a. In contrast, the observation that Noggin and DKK-1 had an additive inhibitory effect on Wnt5a-induced osteoblast differentiation, yet Noggin alone had no effect on basal levels (not shown) indicates that DKK-1 only partially blocked the Wnt5a induced activity, such that Wnt5a was still able to induce BMP activity in the face of DKK-1.
Figure 4. Wnts increases osteoblast activity, in part, through BMPs.
MC3T3-E1 cells were plated in 12-well plates (1 × 105 cells/well) in α-MEM medium plus 10% FBS. After cells were 80% confluent, they were treated with (A and B) Wnt3a (50ng/ml) or (C and D) Wnt5a (50ng/ml) and Noggin (1 μg/ml) or DKK-1 (1 μg/ml). One half the media was replaced every 3 days with fresh media containing FBS and treatment compounds. At 10 days (24 hours post previous media replacement) supernatants were collected and subjected to assays for alkaline phosphatase (ALP) or osteocalcin. Results shown are mean±SD from three experiments. *P≤0.05 versus no Wnt; #P≤0.05 versus Wnt3a or Wnt5a alone; †P<0.05 versus Wnt plus Noggin.
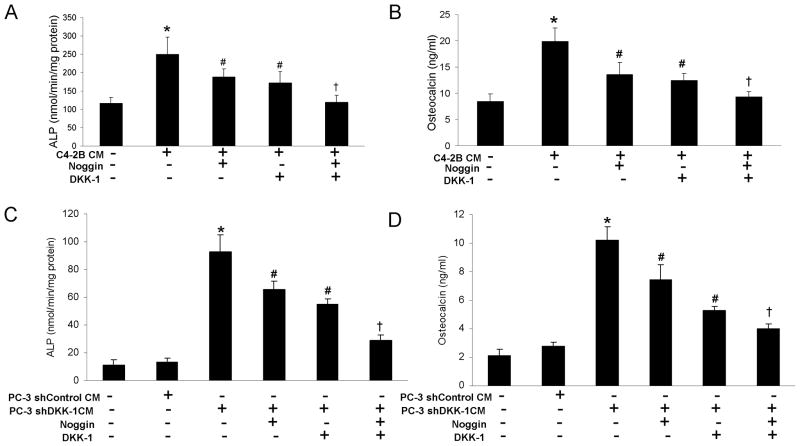
Prostate cancer cells increase osteoblast activity through both Wnt-induced BMPs and BMP-independent paths in MC3T3-E1 cells
We have previously demonstrated that both clinical PCa tissues and PCa cell lines and xenografts produce Wnts and BMPs (6, 8, 9). Thus, it is plausible that PCa can mediate osteoblastic activity through production of Wnts and BMPs similar to the recombinant proteins described above. Thus, to determine the relevance of these observations to PCa-mediated osteoblast activity, it was next examined if secreted proteins from PCa cells mediate osteoblast activity in vitro. MC3T3-E1 pre-osteoblast cells were treated with C4-2B cell or LuCaP23.1 cell conditioned medium (CM). Both C4-2B and LuCaP23.1 CM increased ALP activity and osteocalcin levels (Fig. 5A and B for C4-2B; and Supplemental Fig.2A and B for LuCaP23.1). Both DKK-1 and Noggin partially blocked CM-mediated pro-osteoblast activity and together had an additive inhibitory effect (Fig. 5A and B for C4-2B; and Supplemental Fig.2A and B for LuCaP23.1). These results demonstrate that C4-2B and LuCaP23.1 cells promote an osteoblastic phenotype through both Wnts and BMPs. We previously published that knockdown of DKK-1 in PC-3 cells confers on them pro-osteoblastic ability (9). We also have now described above that knockdown of DKK-1 promotes BMP-4 and BMP-6 expression in PC-3 cell lines (Fig. 1D). To determine if the pro-osteoblastic ability gained by PC-3 cells secondary to knockdown of DKK-1 depends, in part, on BMP expression, we determined if Noggin could inhibit this ability. To evaluate this, MC3T3-E1 cells were incubated with CM from either shControl-transfected PC-3 cells or shDKK-1-transfected cells (PC-3 clone 8) followed by measurement of ALP and osteocalcin levels. The shControl-transfected CM had no effect on either ALP or osteocalcin levels (Fig 5C and D; bars 1 versus 2). In contrast, as previously reported, knockdown of DKK-1 conferred a pro-osteoblastic activity on PC-3 cells (as measured by increased ALP and osteocalcin in the current study) (Figs. 5C and D, compare second and third bars in each figure). Both DKK-1 and Noggin partially blocked PC-3 clone 8 CM-mediated pro-osteoblast activity and together had an additive inhibitory effect (Fig. 5C and D). These results provide evidence that a BMP-dependent component of the pro-osteoblastic pathway is intact in the PSA negative, AR negative PC-3 cell line and that it is inhibited by endogenous DKK-1 in the PC-3 parental cell line. Taken together, with the C4-2B and LuCaP 23.1 results, these data indicate that both Wnts and BMPs contribute to PCa’s pro-osteoblastic activity. However, as we had only obtained CM from the cells, this experiment could not define the dynamic relationship between Wnts and BMPs in PCa cells.
Figure 5. Prostate cancer cells increase osteoblast activity through Wnts and BMPs in MC3T3-E1 cells.
Conditioned media (CM) was obtained from C4-2B cells or the indicated PC-3 cell sublines by plating 5 × 106 cells in 10-cm tissue culture dishes in RPMI and 10% FBS and after cells grew to confluence, the media was changed to RPMI with 0.5% FBS and then supernatants were collected after 24 h. RPMI was added to normalize CM among cell cultures based on cell culture total DNA content. To test effect of CM on osteoblast activity, MC3T3-E1 cells were plated in 12-well plates (1 × 105 cells/well) in α-MEM medium plus 10% FBS. After cells were 80% confluent, they were treated with (A and B) C4-2B CM (80%) or (C and D) PC-3 shControl-transfected or PC-3 shDKK-1-transfected CM (80%) and Noggin (1 μg/ml) or DKK-1 (1 μg/ml). One half the media was replaced every 3 days with fresh CM containing FBS and treatment compounds. At 10 days (24 hours post previous media replacement) supernatants were collected and subjected to assays for alkaline phosphatase (ALP) or osteocalcin. All results shown are mean±SD from three experiments. *P≤0.05 versus no CM or PC-3 shControl CM; #P≤0.05 versus C4-2B CM alone or PC-3 shDKK-1 CM alone; †P<0.05 versus CM plus only Noggin or CM plus only DKK.
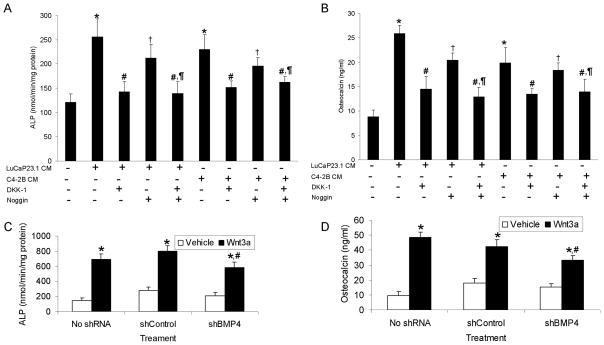
To investigate the relationships between Wnts and BMPs, C4-2B and LuCaP23.1 cells were pre-treated with either DKK-1 alone or Noggin alone or both combined for 12 hours, followed by replacing the media with fresh media and then collecting CM 24 hours later. Pre-treating cells prior to obtaining CM should block production of factors that are dependent on the factor being blocked, although replacing the media with fresh media for 24 hours may diminish this effect. In both cell lines, DKK-1 pre-treatment completely blocked PCa CM-induced ALP and osteocalcin production by MC3T3-E1 cells (Fig. 6A and B). In contrast, pre-treatment of PCa cells with Noggin only partially blocked PCa CM-induced ALP and osteocalcin production (Fig. 6A and B). Pretreatment with the combination of DKK-1 and Noggin had no further inhibition than pre-treatment with DKK-1 alone. These data show that DKK-1 was sufficient to block the CM-induced pro-osteoblastic activity and that inhibition of BMP with Noggin did not provide any additional inhibition of PCa CM-induced osteoblastic activity. In contrast, blocking BMPs with Noggin only had partial reduction of pro-osteoblastic activity, which was further blocked by the addition of DKK-1. Taken together, these results indicate that C4-2B cells and LuCaP23.1 cells increase osteoblast activity through Wnt-mediated BMPs in MC3T3-E1 cells. To explore further if Wnts mediate their effects through BMPs, we performed coculture experiments using MC3T3-E1 cells and C4-2B cells in which BMP4 and or BMP6 expression was decreased through shRNA knockdown. Transduction of C4-2B cells with lentiviral shRNA vectors targeted to BMP4 and BMP6 resulted in greater than 80% decrease of their respective mRNA and protein levels (Supplemental Fig. 3). C4-2B cells were grown on culture inserts and treated with either Wnt3a or Wnt5a for the C4-2B with knockdown of BMP4 or BMP6, respectively, for 48 hours. Then the inserts with the C4-2B cells were transferred to wells containing MC3T3-E1 cells. After 10 days, ALP and osteocalcin expression were then quantified. Wnt3a and Wnt5a induced both ALP and osteocalcin in wildtype (labeled “No shRNA”) and shControl-transduced C4-2B cells (For Wnt3a Fig. 6C and D and for Wnt5a Supplemental Fig.4A and B). Knockdown of BMP-4 and BMP-6, respectively, inhibited Wnt3a and 5a-mediated induction of ALP and osteocalcin (For BMP-4 Fig. 6C and D and for BMP-6 Supplemental Fig. 4A and B). The inhibition was similar to that observed by Noggin-mediated inhibition of Wnt-induced osteoblastic activity. These results indicate that Wnts mediate osteoblastic activity both through BMPs and independently of BMPs.
Figure 6. Prostate cancer cells increase osteoblast activity, in part, through Wnt-induced BMP activity.
(A and B) Single cells suspensions of LuCaP23.1 or C4-2B cells were treated with Noggin (1μg/ml) or DKK-1 (1μg/ml) or both for 12 h follwed by replacement with fresh media and the collection of CM after an additional 24 h. The CM was used to treat MC3T3-E1 cells as described in Figure 5. At 10 days post-treatment of MC3T3 cells (24 hours post previous media replacement) supernatants were collected and subjected to assays for alkaline phosphatase (ALP) or osteocalcin. (C and D) C4-2B cells were transfected with shRNA to BMP4 or scrambled control shRNA. MC3T3-E1 cells were plated in a twelve-well culture plate at a density of 2×105 cells/well and grown in α-MEM media with 10% FBS for 48 hours (approximately 80% confluent). At the same time, C4-2B cells were plated at a density of 2×105 cells/well in twelve-well culture plates on 10-mm Anopore tissue culture plate inserts (0.2 μm pore size; Nalge Nunc International) and grown in T media plus 10% FBS plus vehicle or recombinant Wnt 3a at 50ng/ml for 48 hours. At 48 hours post the initiation of cultures, the plates were gently washed with PBS, the culture plate inserts containing C4-2B cells were inserted into the culture plates containing the MC3T3-E1 cells and the media was replaced with fresh α-MEM media plus 10% FBS. The cocultures were maintained for 10 days at which time supernatants were subjected to measurement of ALP and osteoclacin. All results shown are mean±SD from three experiments. (A and B) *P≤0.05 versus no CM; #P≤0.05 versus C4-2B CM or LuCaP 23.1 CM alone; †P<0.05 versus CM plus DKK-1 alone; ¶P≤0.05 versus CM plus Noggin alone. (C and D) *P<0.05 versus Vehicle; #P<0.05 versus shControl that received Wnt3a.
Discussion
Bone metastases are a frequent complication of advanced PCa. However, the mechanisms through which PCa modulates the bone microenvironment are unclear. A variety of factors have been implicated in the production of osteoblastic lesions in PCa bone metastases including endothelin-1, vascular endothelial growth factor, parathyroid hormone-related protein, BMPs, and Wnts. Most likely no one factor is responsible for these lesions, but rather these factors work in concert to produce the ultimate osteoblastic phenotype. Understanding the interaction between these factors is critical towards defining targets for treatment of bone metastasis. In the current manuscript, we identified that PCa promotes osteoblast activity through both canonical and non-canonical Wnt pathways, which, induce osteoblast activity through both stimulating BMP-dependent and BMP-independent mechanisms. This finding may help lead to identifying targets to modulate PCa-induced metastatic bone lesions.
BMPs are widely recognized as mediators of bone production. Thus, many investigators have examined for their expression in PCa. Using Northern analysis, Harris et al. (15) examined for BMP-2, 3, 4 and 6 mRNA expression in human normal prostate and CaP cell lines. They found that normal human prostate predominantly expressed BMP-4. The androgen-dependent non-metastatic LNCaP human PCa cell line produced very low to undetectable levels of BMPs. Whereas, the aggressive androgen-independent PC-3 cell line expressed very high levels of BMP-3 and slightly lower levels of BMP-2, -4, and –6 compared to normal cells, but much higher than LNCaP cells. In support of these results, Weber et al. (36), using PCR analysis, identified 16 (73%) of 22 PCa samples were positive for BMP-7 mRNA compared to eight (57%) of 14 normal prostate tissue samples. In another PCR based analysis, Bentley et al. (37), found that several BMPs were expressed in both benign and malignant prostate tissue and in the PC3 and DU145 PCa cell lines. BMP- 6 expression was detected in the prostate tissue of over 50% of patients with clinically defined metastatic PCa, but was not detected in non-metastatic or benign prostate samples. In another study focused on BMP-6 mRNA and protein expression, Barnes et al. (16) observed that BMP-6 was produced by normal and neoplastic human prostate (radical prostatectomy specimens and human carcinoma cell lines DU145 and PC3). However, BMP-6 mRNA and protein expression was higher in PCa as compared with adjacent normal prostate, with higher-grade tumors (Gleason score of 6 or more) having greater BMP-6 immunostaining than the lower-grade tumors (Gleason score of 4 or less). These results were consistent with a later study by Hamdy et al. (17), who reported that BMP-6 mRNA expression was detected exclusively in malignant epithelial cells in 20 of 21 patients (95%) with metastases, in 2 of 11 patients (18%) with localized cancer, and undetectable in 8 benign samples. We identified on tissue microarrays of clinical samples that BMP-6 expression increased with progression in PCa (6). These studies not only suggest that BMP may play a functional role in progressive PCa, but also implicate the potential utility of BMP expression as a biomarker for PCa prognosis or diagnosis. However, to determine if this is useful, controlled prospective studies must be performed.
In addition to the observation that BMP expression increases as PCa progress, it appears that the levels of BMPs produced by PCa cells are similar to those that have been shown to induce osteoblast differentiation in vitro. For example, BMP-6 has been shown to induce osteoblast differentiation at 25 ng/ml (38) and we have measured that a variety of PCa cell lines produce BMP-6 in range of 10–60 ng/ml (6). Thus, the levels produced by PCa cells are in the functional range. Taken together, these observations demonstrate that PCa cells produce increasing levels of BMPs as they progress to a more aggressive phenotype and that they are functional levels; however, the mechanisms that regulate BMP expression in PCa have not been clearly identified. Our results suggest that Wnt expression may contribute to induction of BMP expression in PCa. Additionally, the observation that reduction of DKK-1 in the osteolytic PC-3 PCa cell line promoted BMP expression, suggests that DKK-1-mediated inhibition of Wnt in this cell line confers an osteolytic phenotype through inhibiting BMP, in addition to other Wnt-mediated BMP-independent pro-osteoblastic activity.
In the current study, we demonstrated that Wnts regulate BMP expression in a pathway-specific manner through activation of the BMP promoters. This is the first demonstration of Wnt-mediated regulation of BMP in PCa. To the authors’ knowledge there is only one previous report on the regulation of BMP expression in prostate tissues. In that report, BMP-7 mRNA levels was significantly decreased following orchiectomy and increased by testosterone and dihydrotestosterone (DHT) in the murine ventral and dorsal prostate (39). Consistent with our results, it has been shown Wnt-4 induces BMP-4 expression in developing renal stroma (40) and Wnts induce BMP expression in embryonic stem cells (41). Furthermore, activation of β-catenin was shown to be required for BMP-4 expression in cancer cells (42) and LiCl, an inducer of Wnts, was shown to induce BMP-7 in renal tissue (43). Additionally, our results are consistent with the observation that BMPs induced ALP expression in pre-osteoblast cells through Wnt-mediated activity (44). Although there is little known about BMP regulation in prostate, several studies have demonstrated that many factors regulate BMP mRNA expression including estradiol (45), 1,25(OH)2D3 (46), retinoic acid (47), and even BMPs (39) in non-prostate tissues.
In the current study, we demonstrated that Wnts regulate BMP mRNA expression through promoter activation. The BMP-2, -4, –6 and -7 promoters have been cloned (29, 30, 48–50) and early reports suggested that there were multiple transcription start sites for the human BMP-2 and -4 promoters (48, 51). However, it was recently reported that these promoters were found to have a single transcript initiation site that is conserved across species (29). Retinoic acid compounds and the phorbol ester, PMA, were found to stimulate several BMP promoters (29). Our study indicates that both Wnt-stimulated β-catenin and a Jnk-dependent pathway also activate BMP promoters. Although the current study demonstrates that Wnts induce BMP promoter activation, it does not rule out that post-transcriptional mRNA regulation, such as altered mRNA degradation rate, also occurs.
The mechanisms through which PCa induces osteoblastic lesions are not well defined. In addition to ET-1 (52), FGF (53), and VEGF (8), both Wnts and BMPs have been implicated as potential mediators of PCa-induced osteoblastic activity (6, 9). The observation in the current study that inhibition of Wnt activity, using DKK-1, in PCa CM significantly diminished PCa CM-induced osteoblastic activity in vitro suggests that Wnts are a major component of this activity. Similarly, that inhibition of BMP activity, using Noggin, in PCa CM partially diminished PCa CM-induced osteoblastic activity in vitro suggests that BMPs also contribute to the osteoblastic activity. The current study provides several lines of evidence that indicate a large component of BMP activity is dependent on Wnts. Specifically, (1) Wnts upregulated BMP expression in PCa cells and (2) when PCa cells were pre-treated with DKK-1 prior to collection of CM, both Wnt and BMP pro-osteoblastic activity were lost (indicating that BMP activity was dependent on Wnt activity); whereas, pre-treatment of PCa cells with Noggin resulted in only loss of BMP, but not Wnt activity (indicating that Wnt activity was independent of BMP activity). Previous studies have shown that the relationship between Wnts and BMP are very cell context specific. While Wnts and BMPs have been shown to synergize to promote osteoblast differentiation (54); in some cases, Wnts have been shown to regulate BMP activity (40); whereas, in other instances BMPs have been shown to regulate Wnt activity (55). For example, Wnt 3A was shown to induce BMP-4 expression in osteoblasts (56) and β-catenin signaling has been shown to be required for BMP-2-mediated induction of osteogenesis (57). Additionally, Sclerostin, an osteocyte-derived negative regulator of bone formation, inhibits BMP-stimulated bone formation through antagonizing Wnt signaling in osteoblastic cells (58). Thus, the current study is consistent with these previous reports in other systems as Wnts were shown to regulate BMP activity as a component of the mechanism through which PCa induces osteoblast activity.
In summary, the current study demonstrates that PCa mediates pro-osteoblast activity through both canonical and non-canonical Wnts, which in turn contribute to osteoblast activity through BMP-dependent and -independent pathways. These results indicate that further exploration of these pathways should lead to further refinement of the mechanism through which PCa induced osteoblastic activity. These studies also suggest, that targeting both canonical and non-canonical Wnts and their signaling pathways may be necessary in order to impact PCa-induced bone remodeling.
Supplementary Material
Acknowledgments
We thank Dr. L. Chung for C4-2B cells, Dr. R. Vessella for the LuCaP 23.1 xenograft; Dr. R. Franceschi for MC3T3 cells, Dr. L. Helvering for the BMP-4 promoter; Dr. S. Kitazawa for the BMP-6 promoter; Dr. E. Fearon for the Axin construct.
Supported in part by National Cancer Institute Grant P01 CA093900.
References
- 1.Parker SL, Tong T, Bolden S, Wingo PA. Cancer statistics, 1997. CA Cancer J Clin. 1997;47:5–27. doi: 10.3322/canjclin.47.1.5. [DOI] [PubMed] [Google Scholar]
- 2.Bubendorf L, Schopfer A, Wagner U, et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 2000;31:578–83. doi: 10.1053/hp.2000.6698. [DOI] [PubMed] [Google Scholar]
- 3.Keller ET, Brown J. Prostate cancer bone metastases promote both osteolytic and osteoblastic activity. J Cell Biochem. 2004;91:718–29. doi: 10.1002/jcb.10662. [DOI] [PubMed] [Google Scholar]
- 4.Keller ET. The role of osteoclastic activity in prostate cancer skeletal metastases. Drugs Today (Barc) 2002;38:91–102. doi: 10.1358/dot.2002.38.2.820105. [DOI] [PubMed] [Google Scholar]
- 5.Reddi AH, Roodman D, Freeman C, Mohla S. Mechanisms of tumor metastasis to the bone: challenges and opportunities. J Bone Miner Res. 2003;18:190–4. doi: 10.1359/jbmr.2003.18.2.190. [DOI] [PubMed] [Google Scholar]
- 6.Dai J, Keller J, Zhang J, Lu Y, Yao Z, Keller ET. Bone morphogenetic protein-6 promotes osteoblastic prostate cancer bone metastases through a dual mechanism. Cancer Res. 2005;65:8274–85. doi: 10.1158/0008-5472.CAN-05-1891. [DOI] [PubMed] [Google Scholar]
- 7.Nelson JB, Nguyen SH, Wu-Wong JR, et al. New bone formation in an osteoblastic tumor model is increased by endothelin-1 overexpression and decreased by endothelin A receptor blockade. Urology. 1999;53:1063–9. doi: 10.1016/s0090-4295(98)00658-x. [DOI] [PubMed] [Google Scholar]
- 8.Dai J, Kitagawa Y, Zhang J, et al. Vascular endothelial growth factor contributes to the prostate cancer-induced osteoblast differentiation mediated by bone morphogenetic protein. Cancer Res. 2004;64:994–9. doi: 10.1158/0008-5472.can-03-1382. [DOI] [PubMed] [Google Scholar]
- 9.Hall CL, Bafico A, Dai J, Aaronson SA, Keller ET. Prostate cancer cells promote osteoblastic bone metastases through Wnts. Cancer Res. 2005;65:7554–60. doi: 10.1158/0008-5472.CAN-05-1317. [DOI] [PubMed] [Google Scholar]
- 10.Reddi AH. Bone morphogenetic proteins: an unconventional approach to isolation of first mammalian morphogens. Cytokine & growth factor reviews. 1997;8:11–20. doi: 10.1016/s1359-6101(96)00049-4. [DOI] [PubMed] [Google Scholar]
- 11.Wan M, Shi X, Feng X, Cao X. Transcriptional Mechanisms of Bone Morphogenetic Protein-induced Osteoprotegrin Gene Expression. J Biol Chem. 2001;276:10119–25. doi: 10.1074/jbc.M006918200. [DOI] [PubMed] [Google Scholar]
- 12.Gori F, Thomas T, Hicok KC, Spelsberg TC, Riggs BL. Differentiation of human marrow stromal precursor cells: bone morphogenetic protein-2 increases OSF2/CBFA1, enhances osteoblast commitment, and inhibits late adipocyte maturation. J Bone Miner Res. 1999;14:1522–35. doi: 10.1359/jbmr.1999.14.9.1522. [DOI] [PubMed] [Google Scholar]
- 13.Li IW, Cheifetz S, McCulloch CA, Sampath KT, Sodek J. Effects of osteogenic protein-1 (OP-1, BMP-7) on bone matrix protein expression by fetal rat calvarial cells are differentiation stage specific. J Cell Physiol. 1996;169:115–25. doi: 10.1002/(SICI)1097-4652(199610)169:1<115::AID-JCP12>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 14.Maliakal JC, Asahina I, Hauschka PV, Sampath TK. Osteogenic protein-1 (BMP-7) inhibits cell proliferation and stimulates the expression of markers characteristic of osteoblast phenotype in rat osteosarcoma (17/2. 8) cells. Growth Factors. 1994;11:227–34. doi: 10.3109/08977199409046920. [DOI] [PubMed] [Google Scholar]
- 15.Harris SE, Harris MA, Mahy P, Wozney J, Feng JQ, Mundy GR. Expression of bone morphogenetic protein messenger RNAs by normal rat and human prostate and prostate cancer cells. Prostate. 1994;24:204–11. doi: 10.1002/pros.2990240406. [DOI] [PubMed] [Google Scholar]
- 16.Barnes J, Anthony CT, Wall N, Steiner MS. Bone morphogenetic protein-6 expression in normal and malignant prostate. World J Urol. 1995;13:337–43. doi: 10.1007/BF00191214. [DOI] [PubMed] [Google Scholar]
- 17.Hamdy FC, Autzen P, Robinson MC, Horne CH, Neal DE, Robson CN. Immunolocalization and messenger RNA expression of bone morphogenetic protein-6 in human benign and malignant prostatic tissue. Cancer Res. 1997;57:4427–31. [PubMed] [Google Scholar]
- 18.Doak SH, Jenkins SA, Hurle RA, et al. Bone morphogenic factor gene dosage abnormalities in prostatic intraepithelial neoplasia and prostate cancer. Cancer Genet Cytogenet. 2007;176:161–5. doi: 10.1016/j.cancergencyto.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 19.Buijs JT, Rentsch CA, van der Horst G, et al. BMP7, a putative regulator of epithelial homeostasis in the human prostate, is a potent inhibitor of prostate cancer bone metastasis in vivo. Am J Pathol. 2007;171:1047–57. doi: 10.2353/ajpath.2007.070168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon MD, Nusse R. Wnt signaling: multiple pathways, multiple receptors, and multiple transcription factors. J Biol Chem. 2006;281:22429–33. doi: 10.1074/jbc.R600015200. [DOI] [PubMed] [Google Scholar]
- 21.Westendorf JJ, Kahler RA, Schroeder TM. Wnt signaling in osteoblasts and bone diseases. Gene. 2004;341:19–39. doi: 10.1016/j.gene.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 22.Barrow JR, Thomas KR, Boussadia-Zahui O, et al. Ectodermal Wnt3/beta-catenin signaling is required for the establishment and maintenance of the apical ectodermal ridge. Genes Dev. 2003;17:394–409. doi: 10.1101/gad.1044903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakashima A, Katagiri T, Tamura M. Cross-talk between Wnt and bone morphogenetic protein 2 (BMP-2) signaling in differentiation pathway of C2C12 myoblasts. J Biol Chem. 2005;280:37660–8. doi: 10.1074/jbc.M504612200. [DOI] [PubMed] [Google Scholar]
- 24.Bonny C, Oberson A, Negri S, Sauser C, Schorderet DF. Cell-permeable peptide inhibitors of JNK: novel blockers of beta-cell death. Diabetes. 2001;50:77–82. doi: 10.2337/diabetes.50.1.77. [DOI] [PubMed] [Google Scholar]
- 25.Thalmann GN, Anezinis PE, Chang SM, et al. Androgen-independent cancer progression and bone metastasis in the LNCaP model of human prostate cancer. Cancer Res. 1994;54:2577–81. [PubMed] [Google Scholar]
- 26.Corey E, Quinn JE, Bladou F, et al. Establishment and characterization of osseous prostate cancer models: intra-tibial injection of human prostate cancer cells. Prostate. 2002;52:20–33. doi: 10.1002/pros.10091. [DOI] [PubMed] [Google Scholar]
- 27.Almeida M, Han L, Bellido T, Manolagas SC, Kousteni S. Wnt proteins prevent apoptosis of both uncommitted osteoblast progenitors and differentiated osteoblasts by beta-catenin-dependent and -independent signaling cascades involving Src/ERK and phosphatidylinositol 3-kinase/AKT. J Biol Chem. 2005;280:41342–51. doi: 10.1074/jbc.M502168200. [DOI] [PubMed] [Google Scholar]
- 28.Mikels AJ, Nusse R. Purified Wnt5a protein activates or inhibits beta-catenin-TCF signaling depending on receptor context. PLoS biology. 2006;4:e115. doi: 10.1371/journal.pbio.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Helvering LM, Sharp RL, Ou X, Geiser AG. Regulation of the promoters for the human bone morphogenetic protein 2 and 4 genes. Gene. 2000;256:123–38. doi: 10.1016/s0378-1119(00)00364-4. [DOI] [PubMed] [Google Scholar]
- 30.Tamada H, Kitazawa R, Gohji K, Kamidono S, Maeda S, Kitazawa S. Molecular cloning and analysis of the 5′-flanking region of the human bone morphogenetic protein-6 (BMP-6) Biochim Biophys Acta. 1998;1395:247–51. doi: 10.1016/s0167-4781(97)00191-7. [DOI] [PubMed] [Google Scholar]
- 31.Hall CL, Kang S, MacDougald OA, Keller ET. Role of Wnts in prostate cancer bone metastases. J Cell Biochem. 2006;97:661–72. doi: 10.1002/jcb.20735. [DOI] [PubMed] [Google Scholar]
- 32.Canalis E, Economides AN, Gazzerro E. Bone morphogenetic proteins, their antagonists, and the skeleton. Endocrine reviews. 2003;24:218–35. doi: 10.1210/er.2002-0023. [DOI] [PubMed] [Google Scholar]
- 33.Gazzerro E, Canalis E. Bone morphogenetic proteins and their antagonists. Rev Endocr Metab Disord. 2006;7:51–65. doi: 10.1007/s11154-006-9000-6. [DOI] [PubMed] [Google Scholar]
- 34.Rosen V. BMP and BMP inhibitors in bone. Annals of the New York Academy of Sciences. 2006;1068:19–25. doi: 10.1196/annals.1346.005. [DOI] [PubMed] [Google Scholar]
- 35.Yanagita M. BMP antagonists: their roles in development and involvement in pathophysiology. Cytokine & growth factor reviews. 2005;16:309–17. doi: 10.1016/j.cytogfr.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 36.Weber KL, Bolander ME, Rock MG, Pritchard D, Sarkar G. Evidence for the upregulation of osteogenic protein-1 mRNA expression in musculoskeletal neoplasms. J Orthop Res. 1998;16:8–14. doi: 10.1002/jor.1100160103. [DOI] [PubMed] [Google Scholar]
- 37.Bentley H, Hamdy FC, Hart KA, et al. Expression of bone morphogenetic proteins in human prostatic adenocarcinoma and benign prostatic hyperplasia. Br J Cancer. 1992;66:1159–63. doi: 10.1038/bjc.1992.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hughes FJ, Collyer J, Stanfield M, Goodman SA. The effects of bone morphogenetic protein-2, -4, and -6 on differentiation of rat osteoblast cells in vitro. Endocrinology. 1995;136:2671–7. doi: 10.1210/endo.136.6.7750491. [DOI] [PubMed] [Google Scholar]
- 39.Thomas R, Anderson WA, Raman V, Reddi AH. Androgen-dependent gene expression of bone morphogenetic protein 7 in mouse prostate. Prostate. 1998;37:236–45. doi: 10.1002/(sici)1097-0045(19981201)37:4<236::aid-pros5>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 40.Itaranta P, Chi L, Seppanen T, et al. Wnt-4 signaling is involved in the control of smooth muscle cell fate via Bmp-4 in the medullary stroma of the developing kidney. Dev Biol. 2006;293:473–83. doi: 10.1016/j.ydbio.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 41.Haegele L, Ingold B, Naumann H, Tabatabai G, Ledermann B, Brandner S. Wnt signalling inhibits neural differentiation of embryonic stem cells by controlling bone morphogenetic protein expression. Mol Cell Neurosci. 2003;24:696–708. doi: 10.1016/s1044-7431(03)00232-x. [DOI] [PubMed] [Google Scholar]
- 42.Kim JS, Crooks H, Dracheva T, et al. Oncogenic beta-catenin is required for bone morphogenetic protein 4 expression in human cancer cells. Cancer Res. 2002;62:2744–8. [PubMed] [Google Scholar]
- 43.Godin RE, Takaesu NT, Robertson EJ, Dudley AT. Regulation of BMP7 expression during kidney development. Development. 1998;125:3473–82. doi: 10.1242/dev.125.17.3473. [DOI] [PubMed] [Google Scholar]
- 44.Rawadi G, Vayssiere B, Dunn F, Baron R, Roman-Roman S. BMP-2 controls alkaline phosphatase expression and osteoblast mineralization by a Wnt autocrine loop. J Bone Miner Res. 2003;18:1842–53. doi: 10.1359/jbmr.2003.18.10.1842. [DOI] [PubMed] [Google Scholar]
- 45.Ozkaynak E, Jin DF, Jelic M, Vukicevic S, Oppermann H. Osteogenic protein-1 mRNA in the uterine endometrium. Biochem Biophys Res Commun. 1997;234:242–6. doi: 10.1006/bbrc.1997.6624. [DOI] [PubMed] [Google Scholar]
- 46.Faucheux C, Bareille R, Amedee J, Triffitt JT. Effect of 1,25(OH)2D3 on bone morphogenetic protein-3 mRNA expression. J Cell Biochem. 1999;73:11–9. doi: 10.1002/(sici)1097-4644(19990401)73:1<11::aid-jcb2>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 47.Grimsrud CD, Rosier RN, Puzas JE, et al. Bone morphogenetic protein-7 in growth-plate chondrocytes: regulation by retinoic acid is dependent on the stage of chondrocyte maturation. J Orthop Res. 1998;16:247–55. doi: 10.1002/jor.1100160212. [DOI] [PubMed] [Google Scholar]
- 48.Feng JQ, Chen D, Cooney AJ, et al. The mouse bone morphogenetic protein-4 gene. Analysis of promoter utilization in fetal rat calvarial osteoblasts and regulation by COUP- TFI orphan receptor. J Biol Chem. 1995;270:28364–73. doi: 10.1074/jbc.270.47.28364. [DOI] [PubMed] [Google Scholar]
- 49.Kawai S, Sugiura T. Characterization of human bone morphogenetic protein (BMP)-4 and -7 gene promoters: activation of BMP promoters by Gli, a sonic hedgehog mediator. Bone. 2001;29:54–61. doi: 10.1016/s8756-3282(01)00470-7. [DOI] [PubMed] [Google Scholar]
- 50.Paralkar VM, Grasser WA, Mansolf AL, et al. Regulation of BMP-7 expression by retinoic acid and prostaglandin E(2) J Cell Physiol. 2002;190:207–17. doi: 10.1002/jcp.10048. [DOI] [PubMed] [Google Scholar]
- 51.Feng JQ, Harris MA, Ghosh-Choudhury N, Feng M, Mundy GR, Harris SE. Structure and sequence of mouse bone morphogenetic protein-2 gene (BMP- 2): comparison of the structures and promoter regions of BMP-2 and BMP- 4 genes. Biochim Biophys Acta. 1994;1218:221–4. doi: 10.1016/0167-4781(94)90017-5. [DOI] [PubMed] [Google Scholar]
- 52.Mohammad KS, Guise TA. Mechanisms of osteoblastic metastases: role of endothelin-1. Clin Orthop. 2003:S67–74. doi: 10.1097/01.blo.0000093047.96273.4e. [DOI] [PubMed] [Google Scholar]
- 53.Tenta R, Tiblalexi D, Sotiriou E, Lembessis P, Manoussakis M, Koutsilieris M. Bone microenvironment-related growth factors modulate differentially the anticancer actions of zoledronic acid and doxorubicin on PC-3 prostate cancer cells. Prostate. 2004;59:120–31. doi: 10.1002/pros.10363. [DOI] [PubMed] [Google Scholar]
- 54.Mbalaviele G, Sheikh S, Stains JP, et al. Beta-catenin and BMP-2 synergize to promote osteoblast differentiation and new bone formation. J Cell Biochem. 2005;94:403–18. doi: 10.1002/jcb.20253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang L, Yamasaki K, Shirakata Y, et al. Bone morphogenetic protein-2 modulates Wnt and frizzled expression and enhances the canonical pathway of Wnt signaling in normal keratinocytes. J Dermatol Sci. 2006;42:111–9. doi: 10.1016/j.jdermsci.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 56.Winkler DG, Sutherland MS, Ojala E, et al. Sclerostin inhibition of Wnt-3a-induced C3H10T1/2 cell differentiation is indirect and mediated by bone morphogenetic proteins. J Biol Chem. 2005;280:2498–502. doi: 10.1074/jbc.M400524200. [DOI] [PubMed] [Google Scholar]
- 57.Chen Y, Whetstone HC, Youn A, et al. Beta-catenin signaling pathway is crucial for bone morphogenetic protein 2 to induce new bone formation. J Biol Chem. 2007;282:526–33. doi: 10.1074/jbc.M602700200. [DOI] [PubMed] [Google Scholar]
- 58.van Bezooijen RL, Svensson JP, Eefting D, et al. Wnt but not BMP signaling is involved in the inhibitory action of sclerostin on BMP-stimulated bone formation. J Bone Miner Res. 2007;22:19–28. doi: 10.1359/jbmr.061002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.