Abstract
Objective: To test whether the use of a wireless electroceutical dressing (WED) (Procellera®) in conjunction with a 5-day negative pressure wound therapy (NPWT) may reduce the number of dressing changes required per week with this therapy.
Approach: At the Ohio State University Comprehensive Wound Center, chronic wound patients (n=30) undergoing NPWT were randomized into two arms following consent as approved by the institutional review board. The control arm received standard of care NPWT, where the dressing change was performed thrice a week. The test arm received the same care except that the WED was added as an interface layer and dressing change was limited to twice a week.
Results: A reduced cost of care was achieved using the WED in conjunction with NPWT. Despite fewer dressing changes in wounds dressed with the WED, closure outcomes were comparable with no overt signs of any wound complication, including infection. The cost of NPWT care during the week was significantly lower (from $2918 to $2346) in the WED-treated group compared with patients in the control arm.
Innovation: This work introduces a novel technology platform involving a WED, which may be used in conjunction with NPWT. If used as such, NPWT is effective in decreasing the frequency of dressing change and lowering the cost of care.
Conclusion: This work points toward the benefit of using the WED combined with NPWT. A larger clinical trial investigating the cost-effectiveness of WED in wound care is warranted.

Piya Das Ghatak, MS
Introduction
Negative pressure wound therapy (NPWT) has been used to treat wounds since the 1940s.1,2 As an adjunct to surgical procedures to facilitate mass transport of liquids from the body, closed-suction drainage systems have been widely used. In the early 1990s, NPWT assumed a more standardized configuration, which was commercialized as Vacuum-Assisted Closure (VAC®) by Kinetic Concepts, Inc. (KCI, San Antonio, TX). When Medicare first started reimbursing pumps in 2001, the VAC was the only pump that was covered. Starting in 2005, Medicare expanded its coverage to include several new pump models that are manufactured by other companies.
Supported by a growing body of scientific evidence, NPWT is being increasingly used to treat a broader spectrum of chronic wounds.3–6 The use of NPWT under the right conditions is likely to provide improved outcomes and result in overall cost savings. In 1999, it was estimated that an average 22.2-cm2 wound takes 247 days to heal at a cost of $23,465. NPWT could bring down the healing time to 97 days at a cost of $14,546.7 The use of NPWT could lower the overall cost of wound care.8–10 A review of the National Health Service agenda concluded that the use of NPWT may cut costs of chronic wound care as long as it is being used for the right types of wounds.11 However, it also remains a fact that the cost of using NPWT is high and therefore a barrier to wider adoption especially in an environment of shrinking reimbursement.6,12–14 Between 2001 and 2007, Medicare payments for NPWT pumps increased 583%, from $24 to $164 million. The Office of the Inspector General of the Department of Health and Human Services in the United States investigated reimbursements and reported that suppliers paid an average of $3,604 for the new pump models compared to Medicare's purchase price of $17,165.15 NPWT, although effective to treat several wound types, is an expensive treatment. While low-cost negative pressure systems have come to the market,16,17 their effectiveness remains to be proven through appropriate clinical trials.17 Until then, the goal would be to try to utilize the established systems with measures to minimize the cost.
In NPWT, a vacuum or controlled suction force is applied to a wound bed employing a closed drainage system. During such therapy, the wound is filled with gauze or foam as a filler to evenly distribute pressure to the wound bed. Next, the wound is sealed using an adhesive plastic drape, and the drain is connected to a vacuum pump. Using this setup, wound fluid is actively drained and collected in a canister. According to current standards, dressing changes are made thrice a week to avoid infection and other complications. This work is based on our previous observations demonstrating improved reepithelialization and antibiofilm properties of a wireless electroceutical dressing (WED).18,19 In this work, we tested the hypothesis that the use of the bioelectric dressing in conjunction with NPWT would allow us to reduce the dressing change frequency from three to two per week resulting in a lower cost of care without any increased incidence of complication.
Clinical Problem Addressed
NPWT is efficacious but cost-prohibitive in many cases. This work aimed at lowering the cost of NPWT wound care employing a low-cost WED technology with known prohealing and antibiofilm properties.18,19
Materials and Methods
Human subjects
Human studies were approved by the Ohio State University (OSU) Institutional Review Board (IRB 2013H0028). The Declaration of Helsinki protocols was followed, and the patients gave their written informed consent. Subjects (n=30) participating in the study were patients who had undergone a surgery through the abdominal wall at the Ohio State University Comprehensive Wound Center clinics and assigned to NPWT as part of standard postoperative clinical care. Inclusion criteria were patients undergoing surgery through abdominal wall and those aged 18 years or older. Patients suffering from uncontrolled bleeding were excluded. Subject demographics are presented in Table 1.
Table 1.
Subject Demographics
| Total recruitment (n) | 30 | |
|---|---|---|
| Completed study (n) | 27 | |
| NPWT | NPWT+WED | |
| Recruitment (n) | 15 | 15 |
| Completed study (n) | 13 | 14 |
| Age (years) | 58.3±12 | 54.7±10 |
| Gender | ||
| Males | 6 | 7 |
| Females | 7 | 7 |
| Ethnicity | ||
| White | 12 | 8 |
| Black | 1 | 6 |
| Weight (lb) | 202.1±85.1 | 215.5±66.2 |
| Diabetic | 4 | 6 |
NPWT, negative pressure wound therapy; WED, wireless electroceutical dressing.
NPWT involves four major components: (i) a filler material (usually a sponge) placed on the wound; (ii) a semipermeable dressing to isolate the wound environment and allow the vacuum system to transmit subatmospheric pressure onto the wound surface; (iii) a connecting tube; and (iv) a vacuum system. A fluid-collecting canister is also incorporated with the device. When the canister is full, an alarm sounds and alerts the clinicians to potential bleeding problems.20 WED is a bioelectric wound care dressing. It is a polyester cloth printed with silver and zinc dots and is applied on the dressing surface in a dot matrix pattern, creating multiple microbatteries. In the presence of moisture, low-level microcurrents are generated at the device surface.18
Study design
In this randomized trial, patients were divided into two groups: (i) the control group received the standard of care NPWT and (ii) the test group received NPWT with standard of care where the WED was used as an interface layer to the wound care protocol. The following wound outcomes were assessed: wound area and pain medications used were also recorded during each dressing change. Dressing change was performed thrice during the 5-day NPWT according to the standard of care for the control group. For the test group, dressing change included the use of WED and was limited to twice during the 5-day NPWT. The surgical follow-up was performed by a surgeon, as indicated in the photographs. All but patient no. 28 received VAC (KCI) as NPWT, whereas patient no. 28 received Galaxy® NPWT.
Wound volume measurements
The wound volume, in cm3, was calculated from the wound surface area, and the depth was recorded using the standard clinical practice.21
Cost of care
It has been recommended that when determining wound healing strategies, cost decisions should be based on the total cost and not on the individual product cost when using an advanced technology as part of the overall treatment plan.22 The following costs are taken into account for calculating the total cost: pain medication (provided by the clinic pharmacy), NPWT rental and supplies (Canister and sponge), nursing time, and the cost of WED where applicable (test group).
Wound culture
Wound cultures were done at the Ohio State University Wexner Medical Center clinical microbiology laboratory using standard culture procedures. In brief, wound specimens were plated on selective media for culture and examinations.23
Statistics
Data are reported as mean±SEM (n=15). The data were first checked for normality, and the comparison between the control and test groups was done using the Student's t-test (two-tailed). The significance level for this study was set at 0.05.
Results
Among a total of 30 wound subjects undergoing the NPWT treatment, 27 subjects completed the study as shown in Table 1. The age and weight of subjects were comparable in the control and test arms. The test arm had 50% higher number of diabetics and sixfold African American subjects than the control arm. Subject distribution in the two arms was based on randomization.
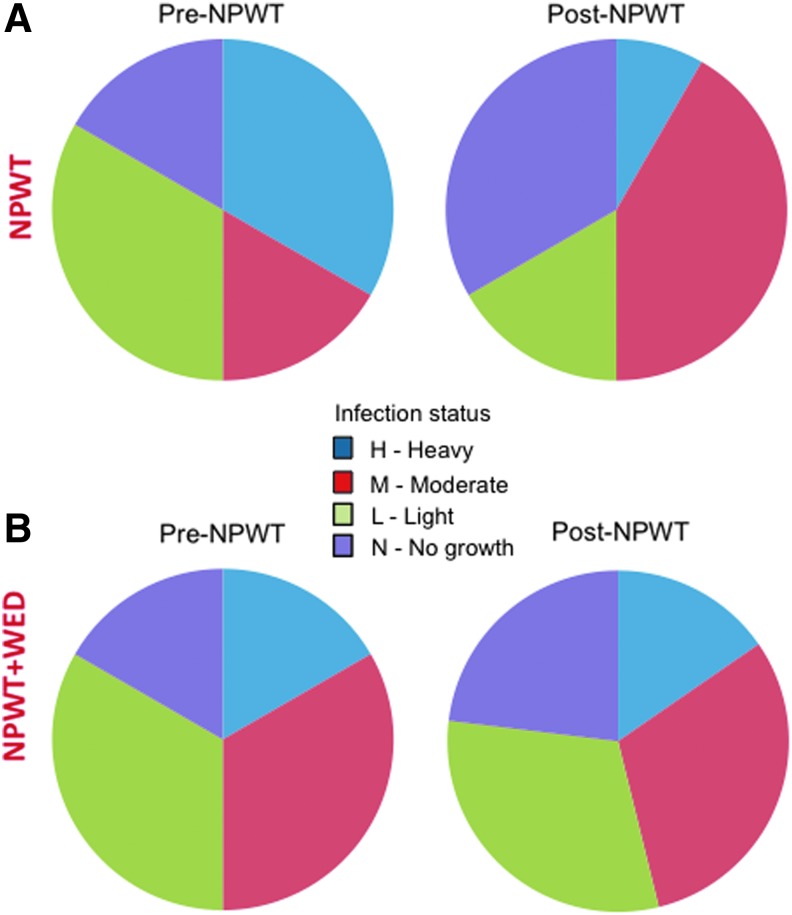
Figure 1 demonstrates the wound appearance of all available wounds in the control arm. In the test arm, subjects were treated exactly as in the control arm, with the addition of the WED as an interface layer, and the dressing change was reduced from thrice to twice a week (Fig. 3A). The progression of wounds in the test arm is depicted in Figure 2. Fewer dressing changes did not compromise the wound closure (Fig. 3B, C). While follow-up visits varied from patient to patient based on scheduling, the number of days from the end of NPWT treatment to the follow-up was comparable in both arms (Fig. 3D). Wound infection status before and after NPWT as recorded clinically are shown in Figure 4.
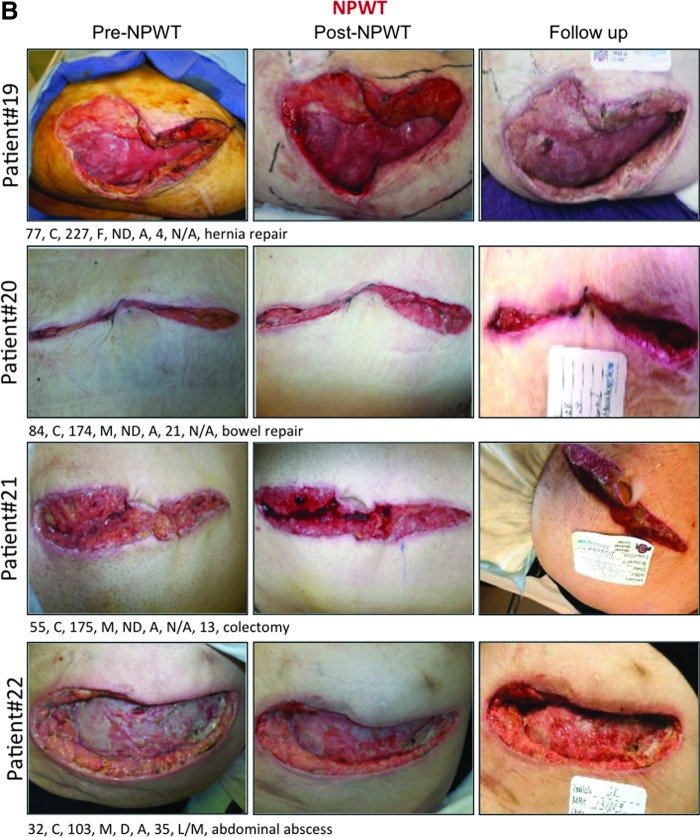
Figure 1.
Wound photographs of patients treated with NPWT per standard of care with three dressing changes per week are shown in four sections A-D. Markings below each photo represent the following in this order: age in years, race, weight in lb, gender, diabetic status, wound position, days from NPWT removal to follow-up, and wound type. A, abdomen; B, Black; C, Caucasian; D, diabetic; F, female; M, male; ND, nondiabetic; VAC, vacuum-assisted closure; NPWT, negative pressure wound therapy. Note that patient no. 28 received Galaxy® NPWT in lieu of VAC® (KCI) NPWT.
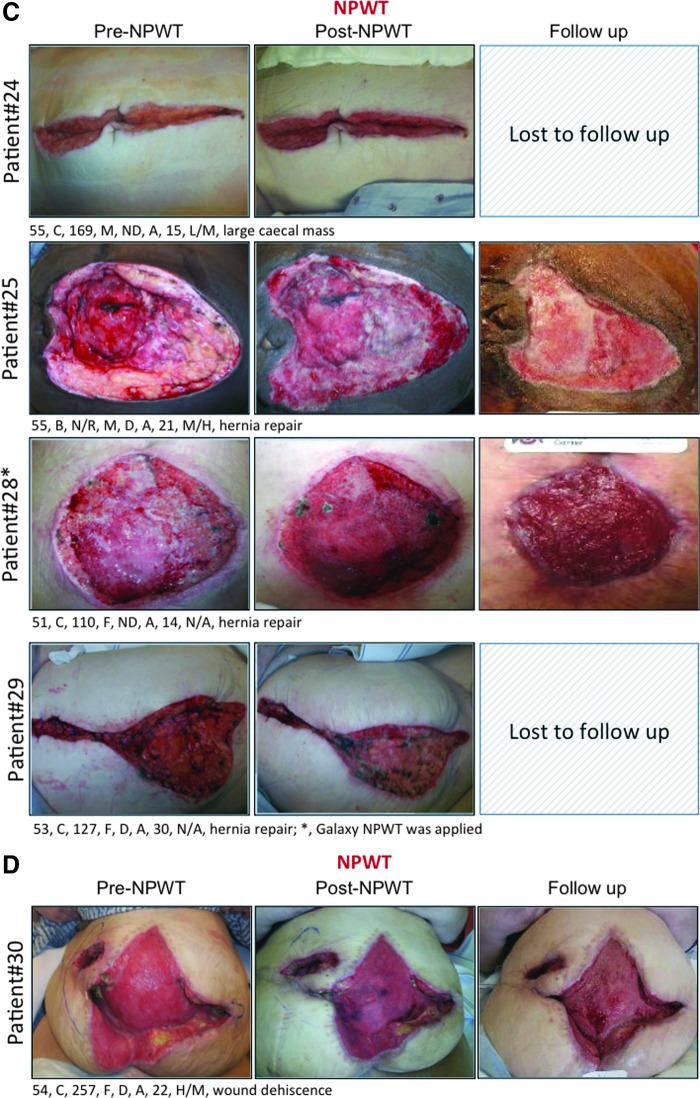
Figure 3.
The WED-treated group received lower number of dressing change during the week of NPWT. Number of dressings changed (A), wound closure (B, C), and number of days from the end of NPWT to follow-up (D) were comparable between the two groups. WED, Procellera® dressing; ns, not significant; NPWT, negative pressure wound therapy.
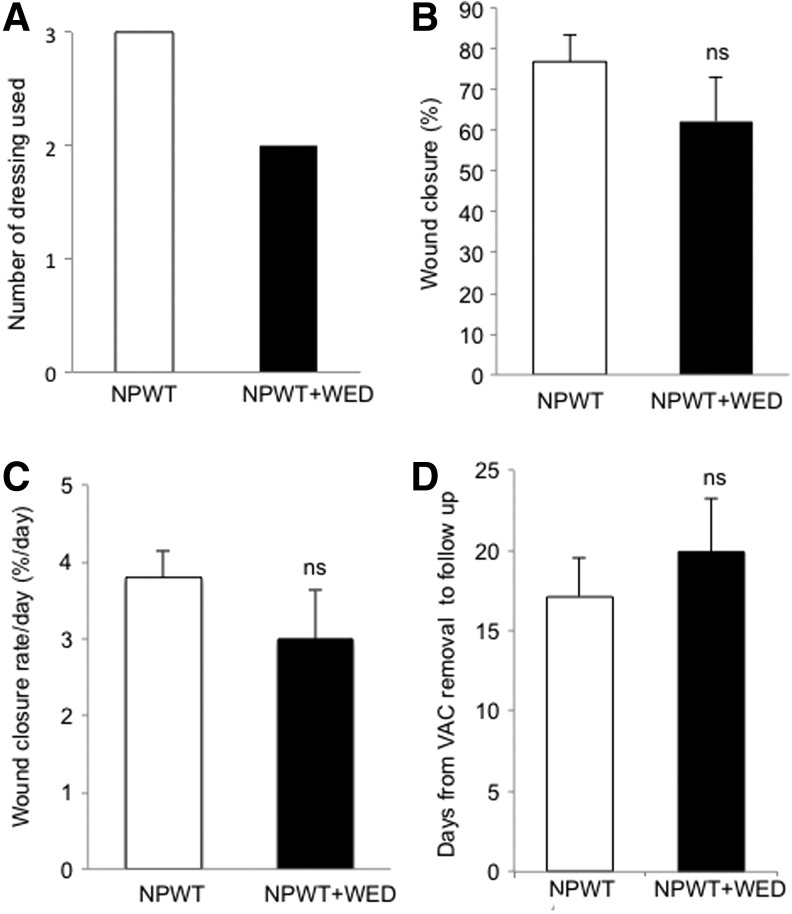
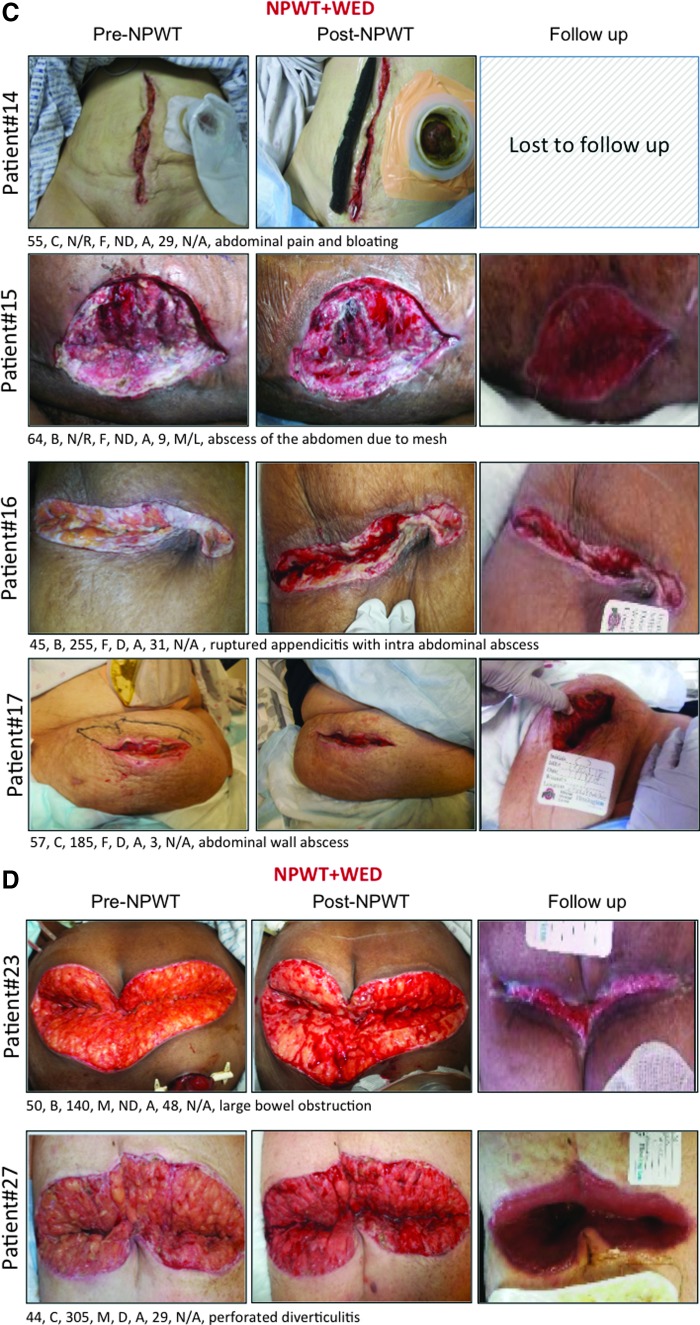
Figure 2.
Wound photographs of patients treated with NPWT per standard of care, where WED was added as an interface layer and dressing change was limited to twice per week are shown in four sections A-D. Markings below each photo represent the following in this order: age in years, race, weight in lb, gender, diabetic status, wound position, days from NPWT removal to follow-up, and wound type. WED, wireless electroceutical dressing.
Figure 4.
Wound infection status before and after NPWT as recorded clinically. (A) Control group; (B) test group. Infection rating: H, heavy; M, moderate; L, light; and N, no growth.
It is well known that patients may experience discomfort and pain during the treatment or dressing changes.24 In such cases, patients received an adequate opioid analgesia. As a measure of pain and discomfort experienced by patients in the two arms, the use of pain medication was recorded. The use of WED in conjunction with NPWT did not influence the consumption of pain medication (Fig. 5). The mean consumption of morphine equivalent for the control and treated groups was 178.8 and 139 mg, respectively. Based on the trend of the scatter plot obtained (Fig. 5), a larger trial may be powered sufficiently to test the hypothesis that WED decreases NPWT-associated consumption of pain medication. Importantly, the use of WED in conjunction with NPWT not only required fewer dressing changes but also led to significant cost savings lowering the cost per patient from $2952 to $2345 (Fig. 6).
Figure 5.
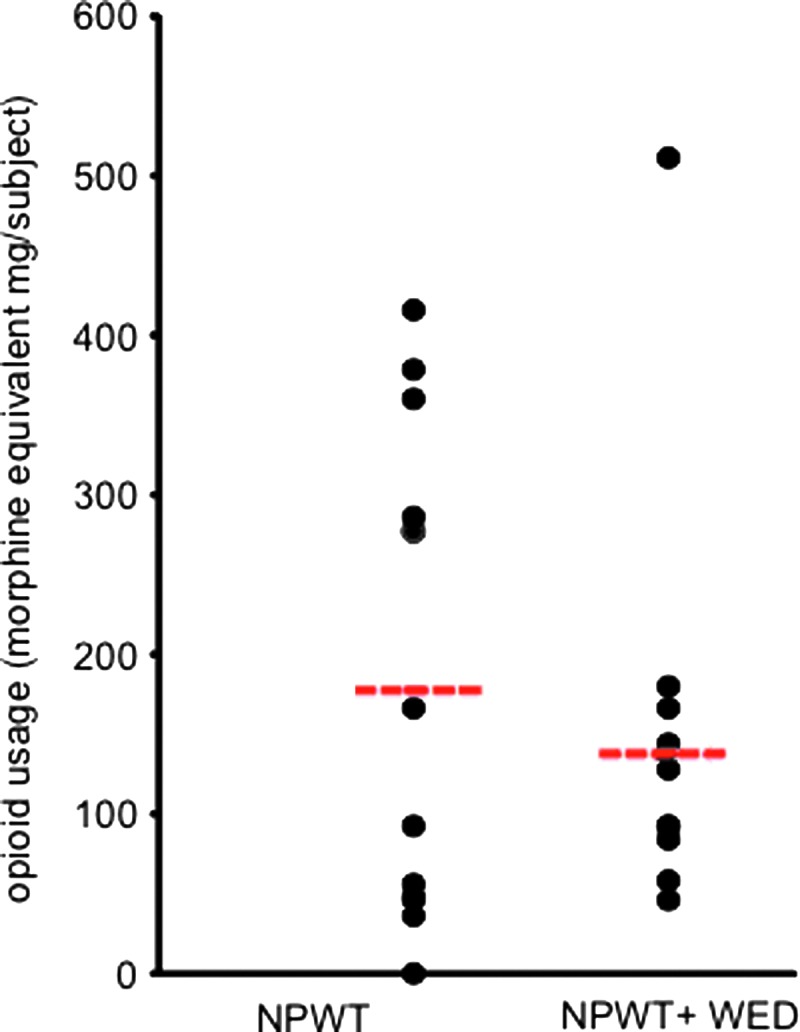
Use of WED in conjunction with NPWT tended to decrease the consumption of opioid analgesic pain medication. Data are shown as scatter plot where the dashed line represents the mean value of each group.
Figure 6.
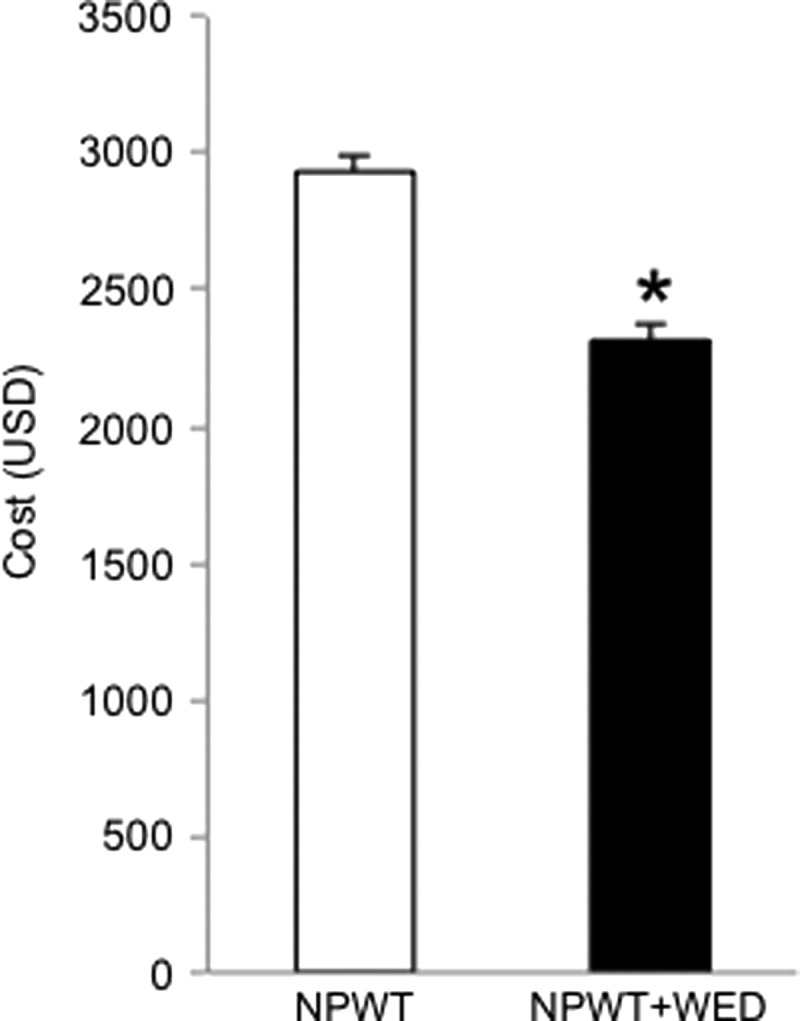
Use of WED significantly reduced the cost of NPWT care. Data are shown as mean±SEM. n=15, *p<0.05.
Discussion
According to the manufacturer's recommendation, the dressing for NPWT should be changed once every 48–72 h, but not less than thrice a week. It is also recommended that for infected wounds, dressings may need to be changed more often.25 Based on these recommendations, at the Ohio State University Comprehensive Wound Center, dressing change for NPWT is performed thrice a week as part of standard of care. One of the key goals of the dressing change is to minimize bacterial load in the wound.25,26 Cleansing and irrigating the wound and periwound areas primarily address this. The bacterial burden in postoperative wounds is a major concern because it may necessitate repeated surgical interventions, longer hospital stay, and higher healthcare cost.23 The use of a silver-coated polyurethane dressing (VAC GranuFoam® Silver Dressing; KCI) during NPWT is aimed at infection control. However, it is reported that such a dressing is not effective in delivering silver ions to the wound and most silver is removed by the suction force and found in the wound exudate.27 In case of using WED, the wound maintains a direct contact with the dressing and receives the benefit of continuous microcurrent generated by WED. Recent work in our laboratory shows that WED disrupts Pseudomonas aeruginosa PAO1 biofilm by a redox-sensitive pathway.18,19
This work provides the first evidence demonstrating that the use of WED during NPWT may lower the cost of NPWT-assisted wound care. Larger randomized studies, testing this hypothesis, addressing a longer duration of wound care are warranted.
KEY FINDINGS.
• Use of WED in conjunction with NPWT decreases the need for dressing change from thrice to twice a week in the population studied.
• WED is effective in lowering the cost of NPWT care.
Limitations
This is a pilot study with a small patient population over a short period. Studies addressing a longer duration of wound care are needed to effectively evaluate the outcomes with respect to wound healing and the total cost of treatment toward healing. These limitations recognized that this work provides the first evidence toward an interesting direction, which has the clear potential to lower the cost of NPWT in wound care.
Innovation
This work introduces a novel technology platform involving a WED, which may be used in conjunction with NPWT. If used as such, WED is effective in lowering the cost of NPWT.
Abbreviations and Acronyms
- NPWT
negative pressure wound therapy
- VAC
vacuum-assisted closure
- WED
wireless electroceutical dressing
Acknowledgment and Funding Sources
This work was supported, in part, by a research contract sponsored by Vomaris, Inc., the manufacturer of Procellera. The company had no control over the conduct or reporting of this work.
Author Disclosure and Ghostwriting
No competing financial interests exist. No ghostwriters were involved in the writing of this work.
About the Authors
Piya Das Ghatak, MS is a member of the research staff in the Department of Surgery at the Ohio State University Wexner Medical Center. She holds a Master of Science degree in Biotechnology. Sashwati Roy, PhD is an Associate Professor of Surgery and Director of Research at the Ohio State University Comprehensive Wound Center. Dr. Roy's research interests include wound inflammation, mechanisms of resolution of diabetic wound inflammation, and the role of miRNA in tissue repair processes. Richard Schlanger, MD, specializes in wound care and hyperbarics at the Ohio State University Comprehensive Wound Center. Kasturi Ganesh, MD is a research associate in the Department of Surgery at the Ohio State University Wexner Medical Center. Lynn Lambert, BS, CWS is a certified clinician with a long-term experience in wound care. Gayle Gordillo, MD, is an Associate Professor of Plastic Surgery and Medical Director of the Comprehensive Wound Center at the Ohio State University Wexner Medical Center. Patsy Martinsek, BSN is a patient care coordinator for Wound and Ostomy Service at the Comprehensive Wound Center of the Ohio State University Wexner Medical Center.
References
- 1.Fox JWT, Golden GT. The use of drains in subcutaneous surgical procedures. Am J Surg 1976;132:673–674 [DOI] [PubMed] [Google Scholar]
- 2.Fay MF. Drainage systems. Their role in wound healing. AORN J 1987;46:442–455 [DOI] [PubMed] [Google Scholar]
- 3.Dumville JC, et al. Negative pressure wound therapy for treating foot wounds in people with diabetes mellitus. Cochrane Database Syst Rev 2013;10:CD010318. [DOI] [PubMed] [Google Scholar]
- 4.Dumville JC, Munson C. Negative pressure wound therapy for partial-thickness burns. Cochrane Database Syst Rev 2012;12:CD006215. [DOI] [PubMed] [Google Scholar]
- 5.Webster J, et al. Negative pressure wound therapy for skin grafts and surgical wounds healing by primary intention. Cochrane Database Syst Rev 2012;4:CD009261. [DOI] [PubMed] [Google Scholar]
- 6.Webster J, et al. Negative pressure wound therapy for skin grafts and surgical wounds healing by primary intention. Cochrane Database Syst Rev 2014;10:CD009261. [DOI] [PubMed] [Google Scholar]
- 7.Philbeck TE Jr., et al. The clinical and cost effectiveness of externally applied negative pressure wound therapy in the treatment of wounds in home healthcare Medicare patients. Ostomy Wound Manag 1999;45:41–50 [PubMed] [Google Scholar]
- 8.Mokhtari A, et al. The cost of vacuum-assisted closure therapy in treatment of deep sternal wound infection. Scand Cardiovasc J 2008;42:85–89 [DOI] [PubMed] [Google Scholar]
- 9.Kaplan M, Daly D, Stemkowski S. Early intervention of negative pressure wound therapy using vacuum-assisted closure in trauma patients: impact on hospital length of stay and cost. Adv Skin Wound Care 2009;22:128–132 [DOI] [PubMed] [Google Scholar]
- 10.Le Franc B, et al. Cost-effectiveness analysis of vacuum-assisted closure in the surgical wound bed preparation of soft tissue injuries. Ann Chir Plast Esthet 2010;55:195–203 [DOI] [PubMed] [Google Scholar]
- 11.Othman D. Negative pressure wound therapy literature review of efficacy, cost effectiveness, and impact on patients' quality of life in chronic wound management and its implementation in the United kingdom. Plast Surg Int 2012;2012:374398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karr JC, et al. Wound healing and cost-saving benefits of combining negative-pressure wound therapy with silver. Adv Skin Wound Care 2013;26:562–565 [DOI] [PubMed] [Google Scholar]
- 13.Neubauer G, Ujlaky R. The cost-effectiveness of topical negative pressure versus other wound-healing therapies. J Wound Care 2003;12:392–393 [DOI] [PubMed] [Google Scholar]
- 14.Baharestani MM. Negative pressure wound therapy: an examination of cost-effectiveness. Ostomy Wound Manag 2004;50 (11A Suppl):29S–33S [PubMed] [Google Scholar]
- 15.Levinson DR. Comparison of Prices for Negative Pressure Wound Therapy Pumps: Report of the Office of Inspector General, Department of Health & Human Services. Department of Health and Human Services, USA, 2009, 1–23 [Google Scholar]
- 16.Lerman B, et al. Evaluation of chronic wound treatment with the SNaP wound care system versus modern dressing protocols. Plast Reconstr Surg 2010;126:1253–1261 [DOI] [PubMed] [Google Scholar]
- 17.Gnanaraj J. Low-cost topical negative pressure wound dressing system. Trop Doct 2010;40:208–209 [DOI] [PubMed] [Google Scholar]
- 18.Banerjee J, et al. Improvement of human keratinocyte migration by a redox active bioelectric dressing. PLoS One 2014;9:e89239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banerjee J, et al. Electroceutical wound dressing disrupts biofilm. PLoS One 2014 (submitted) [Epub ahead of print]; DOI: 10.1371/journal.pone.0119531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang C, et al. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 2014;51:301–331 [DOI] [PubMed] [Google Scholar]
- 21.Gordillo GM, et al. Topical oxygen therapy induces vascular endothelial growth factor expression and improves closure of clinically presented chronic wounds. Clin Exp Pharmacol Physiol 2008;35:957–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Leon JM, et al. Cost-effectiveness of negative pressure wound therapy for postsurgical patients in long-term acute care. Adv Skin Wound Care 2009;22:122–127 [DOI] [PubMed] [Google Scholar]
- 23.Elgharably H, et al. First evidence of sternal wound biofilm following cardiac surgery. PLoS One 2013;8:e70360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malmsjo M, et al. Negative pressure wound therapy-associated tissue trauma and pain: a controlled in vivo study comparing foam and gauze dressing removal by immunohistochemistry for substance P and calcitonin gene-related peptide in the wound edge. Ostomy Wound Manag 2011;57:30–35 [PubMed] [Google Scholar]
- 25.KCI. VAC Therapy: Dressing Change Reference Guide. http://kci-medical.com/cs/Satellite?blobcol=urldata&blobheadername1=Content-type&blobheadername2=Content-disposition&blobheadername3=MDT-Type&blobheadervalue1=application%2Fpdf&blobheadervalue2=inline%3B+filename%3D961%252F357%252FVAC_Therapy_Dressing_Change_Ref_Guide_KCI_AU_102_updated_May_2010.pdf&blobheadervalue3=abinary%3B+charset%3DUTF-8&blobkey=id&blobtable=MungoBlobs&blobwhere=1226640717148&ssbinary=true (2010)
- 26.KCI. VAC Therapy: Clinical Guidelines—Reference Source for Clinicians. http://kci1.com/cs/Satellite?blobcol=urldata&blobheader=application%2Fpdf&blobkey=id&blobtable=MungoBlobs&blobwhere=1226689404554&ssbinary=true (2014)
- 27.Abarca-Buis RF, et al. Silver from polyurethane dressing is delivered by gradient to exudate, tissue, and serum of patients undergoing negative-pressure wound treatment. Adv Skin Wound Care 2014;27:156–162 [DOI] [PubMed] [Google Scholar]