Abstract
Study Design
A 3D-2D image registration algorithm, “LevelCheck,” was used to automatically label vertebrae in intraoperative mobile radiographs obtained during spine surgery. Accuracy, computation time, and potential failure modes were evaluated in a retrospective study of 20 patients.
Objective
To measurethe performance of the LevelCheck algorithm using clinical images acquired during spine surgery.
Summary of Background Data
In spine surgery, the potential for wrong level surgery is significant due to the difficulty of localizing target vertebrae based solely on visual impression, palpation, and fluoroscopy. To remedy this difficulty and reduce the risk of wrong-level surgery, our team introduced a program (dubbed LevelCheck) to automatically localize target vertebrae in mobile radiographs using robust 3D-2D image registration to preoperative CT.
Methods
Twenty consecutive patients undergoing thoracolumbar spine surgery, for whom both a preoperative CT scan and an intraoperative mobile radiograph were available, were retrospectively analyzed. A board-certified neuroradiologist determined the “true” vertebra levels in each radiograph. Registration of the preoperative CT to the intraoperative radiographwere calculated via LevelCheck, and projection distance errors were analyzed. Five hundred random initializations were performed for eachpatient, andalgorithm settings (viz., the number of robust multi-starts, ranging 50 to 200) were varied to evaluate the tradeoff between registration error and computation time. Failure mode analysis was performed by individually analyzing unsuccessful registrations (>5 mm distance error) observed with 50 multi-starts.
Results
At 200 robust multi-starts (computation time of ∼26 seconds), the registration accuracy was 100% across all 10,000 trials. As the number of multi-starts (and computation time) decreased, the registration remained fairly robust, down to 99.3% registration accuracy at 50 multi-starts (computation time ∼7 seconds).
Conclusion
The LevelCheck algorithm correctly identified target vertebrae in intraoperative mobile radiographs of the thoracolumbar spine, demonstrating acceptable computation time, compatibility with routinely obtained preoperative CT scans, and warranting investigation in prospective studies.
Level of Evidence
N/A
Keywords: automatic, localization, intraoperative, target vertebrae, 3D-2D registration, wrong-site surgery, vertebral labeling, anatomical deformation, LevelCheck, thoracolumbar
Introduction
Wrong-site surgery – and more specifically, wrong-level spine surgery – is a “never-event” occurring at unacceptable frequency and considerable cost to individual health and societal healthcare in general. The reported incidence of wrong-level surgery (subject to variation and possible under-reporting) is estimated to be 1 in every 3,110 spine surgeries [1], implying that approximately 50% of spine surgeons will encounter a wrong-level error at least once in their career, with an approximate monetary cost of $127,000 per case[2]. Costs to the patient include increased morbidity, ineffective therapy, and the need for revision and repeat intervention. Such errors are among the most damaging, costly – and potentially preventable – forms of medical error that have been the focus of publicity and increased awareness in hospital safety over the last decade.
The challenge in spine level localization arises from the difficulty of correctly identifying target vertebrae in the radiographic/fluoroscopic scene and/or by direct visualization. Particularly (but not exclusively) in minimally invasive surgery, even experienced surgeons can be challenged to confidently localize target vertebrae, especially in the mid-thoracic region and in patients exhibiting anatomical variations such as a sixth or transitional lumbar vertebra. Absence of distinct landmarks in the fluoroscopic scene can also inhibit confident localization. The current standard of care for spine level localization in North America includes: 1.) intraoperative localization by “level counting” assisted by fluoroscopy or mobile radiography [3]; and 2.) preoperative placement of radio-opaque markers (e.g., fiduciary markers [4] or bone cement [5]) under real-time CT/fluoroscopy guidance. The intraoperative process is subject to human error in image interpretation and accurate counting (e.g., “up” from the lumbosacral junction or “down” from the occipitocervical junction). The preoperative process adds time, cost, radiation dose, procedure-related risk, and the need for inter-departmental scheduling and logistics. Moreover, despite these preventative measures within the current standard of care, the incidence of wrong-level surgery persists as the second-most common category of wrong-site surgery.
Our group has developed a novel method providing an independent check on vertebral level localization. From the perspective of safety science, an independent check is among the higher levels of preventative measure against error, and there is currently no such measure in vertebral level localization within the standard of care. Referred to as “LevelCheck,” our method is based on a robust geometric alignment of preoperative 3D images (e.g., a preoperative CT acquired for diagnosis and/or surgical planning) and intraoperative 2D images (e.g., fluoroscopy or mobile radiographs acquired normally during the procedure). The LevelCheck algorithm allows any structure defined in the preoperative image to be accurately localized in intraoperative fluoroscopy. For spine level localization, the process requires only that the target vertebrae are labeled in the preoperative image – e.g., a single point click on the vertebral bodies of interest – and those same labels are in turn automatically localized on intraoperative fluoroscopy. The levels can be labeled by anatomical designation (e.g., T5, T6, etc., as below) or in terms specific to the intervention (e.g., “Target” etc.), and the method is equally applicable to other landmarks of interest (e.g., adjacent critical structures). It operates without any additional tracking or navigation equipment, computes the geometric registration in as little as 1 second[6, 7], and integrates naturally with surgical workflow by rendering labels automatically in each fluoroscopic view as requested by the surgeon. The method leverages recent advances in high-speed computing combined with a novel “3D-2D registration” algorithm that is robust against anatomical deformation and the presence of surgical tools[7].
In previous studies, the method was evaluated in data 50,000 simulated trials in CT images drawn from image archives of the National Cancer Institute, demonstratingregistration accuracy of 0.2 ± 0.2 mm (mean and standard deviation of the projection distance error, PDE) and success rate (success criteria: PDE < 5.0 mm) of 99.998% (49,999 / 50,000) [6]. The one failure observed in this study was attributed to study parameter settings, as opposed to any specific characteristics of the patient images in question. A subsequent study evaluated LevelCheckin a fresh cadaver to validate robustness in the presence of realistic anatomical deformation occurring between the preoperative CT and intraoperative radiograph. A broad range of acquisition scenarios and deformations were examined with a total of 14,400 trials. Registration was successful in >99.99% with a mean PDE < 1.0 mm and registration time < 5 seconds [7].
The system holds major potential as decision support and an independent check against wrong-level surgery, with clinical studies now underway. Here we describe the first use of the LevelCheck algorithm in actual clinical patient images and report on its accuracy, computation time, and potential failure modes.
Methods
The following study was approved by the Johns Hopkins Medicine Institutional Review Board.
Patient Sample
Twenty consecutive patients undergoing thoracolumbar spine surgery were selected for this retrospective study. For each patient, a pre-operative CT scan and intraoperative mobile radiographs were available for retrospective analysis. Thirteen of these patients were undergoing primary operations without prior instrumentation, while seven patients were revision operations with prior instrumentation in place in the preoperative CT. Once the patient cohort was identified, DICOM files of their pre-operative CT and intra-operative radiographs were uploaded to a research server, and patient identifiers were removed in accordance with HIPAA regulations. Table 1 summarizes the pathologies as well as the procedures performed on the patients in this study.
Table 1.
Ages, pre-operative diagnoses, and procedures performed on the 20 patients selected for this study.
| ID | Age | Sex | Pre-operative Diagnosis | Procedure |
| 1 | 44 | F | Reccurent right L5-S1 disk herniation | Revision right L5-S1 microdiskectomy |
| 2 | 52 | M | Metastatic melanoma | Left L1 transpedicular resection of epidural tumor, anterior reconstruction from T12-L2 with Steinman pins and methylmethacrylate, T11-L3 pedicle screw fixation and fusion |
| 3 | 66 | F | Multilevel degeneration with lumbar stenosis, kyphoscoliosis | Smith-Petersen osteotomies at L1 -2, L2-L3, L3-L4, and L4-L5 with decompression and foraminotomies, T11 to sacrum and pelvis fixation and fusion with correction of kyphoscoliotic deformity, cement augmentation of T10 and T11 |
| 4 | 62 | F | Instrumentation failure status post L4-L5 spondylectomy | Revision L2 to sacrum and pelvis fixation and fusion |
| 5 | 56 | M | Pseudoarthrosis at L3-L4, adjacent level disease at L2-L3 | L2-L3 Smith-Petersen osteotomy with decompression and foraminotomies, revision L2-S1 pedicle screw fixation and fusion |
| 6 | 62 | F | Lumbar kyphoscoliosis | L5-S1 anterior diskectomy, interbody arthrodesis and fusion |
| 7 | 60 | F | Epidural mass causing right SI radiculopathy | Right L5 hemilaminotomy, partial L5-S1 medial facetectomy, S1 laminectomy and foraminotomy, resection of extradural mass |
| 8 | 55 | M | Grade 3 L5-S1 spondylolisthesis | L5 laminectomy with resection of Gill body, bilateral L5-S1 diskectomy, reduction of spondylolisthesis, L5-S1 posterior lumbar interbody fusion, L4-S1 pedicle screw fixation and fusion |
| 9 | 79 | M | Grade 1 L5-S1 spondylolisthesis | L5 laminectomy with resection of Gill body, bilateral L5-S1 diskectomy, L5-S1 transforaminal lumbar interbody arthrodesis, L5-S1 pedicle screw fixation and fusion |
| 10 | 68 | M | L5-S1 pseudoarthrosis | L5-S1 Smith-Petersen osteotomy with decompression and foraminotomies, revision L3 to pelvis fixation |
| 11 | 68 | M | Multilevel degeneration, left-sided lumbar scoliotic curvature | L2-3, L3-4, L4-5, L5-S1 Smith-Petersen osteotomies with decompression and foraminotomies, right L3-4 diskectomy, L2 to pelvis fixation, cement augmentation of L2 |
| 12 | 73 | M | T10-T11 disk herniation | T9 and T10 laminectomies, partial medal left T9-T10 and T10-T11 and complete right T9-T10 and T10-T11 facetectomies, transpedicular diskectomy of herniated disk at T10-T11, T9-T11 pedicle screw fixation and fusion |
| 13 | 66 | F | Type 2 split cord malformation, lumbar stenosis | T11 and T12 laminoplasty, untethering of diplomyelia at the T11 -12 segment, L5 and partial S1 laminectomies |
| 14 | 71 | F | L3-L4 pseudoarthrosis | L3-4 Smith-Petersen osteotomies with decompression and foraminotomies, L3-L4 diskectomy, L3-L4 transforaminal lumbar interbody arthrodesis, L2-S1 pedicle screw fixation and fusion |
| 15 | 48 | F | T12 intradural-extramedullary mass | T11 and T12 laminoplasty, resection of intradural-extramedullary mass |
| 16 | 56 | F | L5-S1 pseudoarthrosis | Anterior L5-S1 diskectomy, anterior lumbar interbody fusion |
| 17 | 61 | M | L3-4, L4-5, L5-S1 pseudoarthrosis | Stage 1: anterior L4-L5 and L5-S1 diskectomies, anterior lumbar interbody fusion; Stage 2: revision and replacement of L2 and L4 pedicle screws |
| 18 | 57 | F | L3-L4 lumbar stenosis | L3-4 Smith-Petersen osteotomy with decompression and foraminotomies, bilateral L3-4 diskectomy, L3-4 transforaminal lumbar interbody fusion, L3-S1 pedicle screw fixation and fusion |
| 19 | 77 | M | Broad-based L3-4 disk herniation | Bilateral L3-4 partial laminectomies, medial facetectomies, foraminotomies, and diskectomies |
| 20 | 59 | M | T10-T11 disk herniation | Right-sided T10-T11 hemilaminectomy, complete facetectomy, transpedicular approach for diskectomy, T10-T12 pedicle screw fixation and fusion |
3D-2D Image Registration
3D-2D registration computes a geometric transformation that properly aligns a simulated projection of a 3D image (commonly referred to as a digitally reconstructed radiograph, DRR) with a 2D X-ray projection image. While a variety of 3D-2D registration methods have been reported [8], the LevelCheck method involves three key advances that make it particularly well suited to surgery: 1) a similarity metric that is robust against deformation and mismatch in image content, 2) an optimization strategy that is robust against false local optima; and 3) a high-speed implementation providing orders-of-magnitude acceleration in computation time (Figure 1).
Figure 1.

Overview of the LevelCheck system. Green circles on Preoperative CT Labeling indicate discrete vertebral levels labeled by the clinician. Yellow plus signs on the Automatically Labeled Radiograph indicate LevelCheck-generated vertebral levels based on the Preoperative CT Spine Labeling. CT indicates computed tomography.
Truth Definition
A board-certified neuroradiologist reviewed all pre-operative CT scans as well as the intraoperative mobile radiographs to assign the “true” vertebral levels in each. Mean projection distance errors (mPDE, the distance between two points in the domain of the projection radiograph) were calculated by comparing the position of these manually selected “true” vertebral level locations to those computed by LevelCheck.
Analysis
To simulate realistic variations in how the mobile radiograph was obtained, the initialization point for the registration process was randomly perturbed from the target level by 30 mm along the anterior-posterior (AP) axis (3σ) and 90 mm along the craniocaudal (CC) axis (3σ) according to a normal distribution. Five hundred such random initializations were performed for each patient for a total of 10,000 trials. To assess tradeoffs between registration accuracy and computation time, each trial was registered with parameter settings of variable multi-starts, a measure of the number of computation steps used during localization, shown previously to provide increased robustness against anatomical deformation[7]. The computation time for 50, 100, 150, and 200 multi-starts was 7.1, 13.1, 17.8, and 25.7 seconds on a desktop PC (Windows 7 64-bit, Intel Xeon 2 processor (2.4 GHz), and GeForce TITAN GPU (nVidia, Santa Clara CA)). “Text” annotations that were introduced to the mobile radiograph were masked (i.e., cropped and ignored in the registration) along with gross external objects (e.g., retractors) introduced to the surgical field intra-operatively. Pre-existing instrumentation for (7) patients undergoing revision operations were not masked. For this study, a successful registration was defined as one yielding mPDE< 5 mm, which was considered to be within the margin of acceptable error for correct labeling of a vertebral body.
Potential failure modes in which LevelCheck were also investigated by examining trials yielding a registration result with mPDE> 5 mm. As detailed in the Results, there were 70 such instances among the 10,000 trials performed at a computation time of 7.1 seconds (50 multi-starts). Each was individually inspected in terms of the nature of misregistration, quality of the DRR, strength of gradient correlation, quality of the radiograph, and other potential confounding influences.
To quantify how well the DRR generated from the pre-operative CT correlated with the intra-operative mobile radiographs, we analyzed the similarity metric (gradient correlation (GC)) for each trial [9]. Overlapping edges between the DRR and radiograph indicate a consistent gradient and give higher GC. The trial resulting in the best fit between the DRR and the radiograph (and thus the highest GC value) was labeled as GC*. For each trial, we analyzed the difference between the GC for that trial and GC*, to quantitatively assess registration accuracy.
Results
The success rate of the LevelCheck algorithm in correctly labeling the intra-operative mobile radiograph spinal levels (mPDE< 5 mm) was calculated as a function of the number of multi-starts and computation time (Figure 2A). The success rate was 100% at 26 seconds (200 multi-starts), 99.97% at 18 seconds (150 multi-starts), 99.86% at 13 seconds (100 multi-starts), and 99.3% at 7 seconds (50 multi-starts). There was no difference in the rate of successful registration between patients undergoing primary operations and those with prior instrumentation undergoing revision surgery. The mPDE for each individual trial is plotted as a function the number of multi-starts in Figure 2B. For 50 and 100 multi-starts (7 and 13 second runtime, respectively), some trials exhibited clear misregistration with PDE > over 100 mm, and overall accuracy was 99.30% and 99.86%, respectively. For 150 multi-starts (18 second runtime), there were a few errors over 40 mm, and overall accuracy was 99.97%. For 200 multi-starts (26 seconds runtime), all 10,000 trials were successful (100% accuracy) in registering vertebral labels with mPDE< 5 mm in comparison to “ground truth.” Example cases of successful LevelCheck registration for a variety of unique instances of anatomical and implant configurations are shown in Figure 3.
Figure 2.
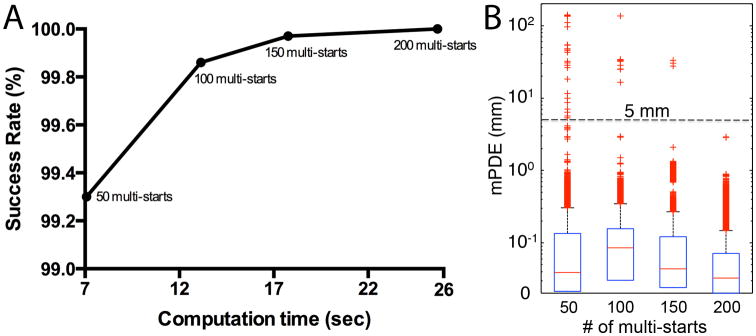
Registration accuracy. A, Registration success rate plotted as a function of computation time (with registration success defined as mPDE< 5 mm).B, Box and whisker plots of mPDE as a function of the number of multi-starts. Boxes denote the first/third quartiles, whiskers denote min/max values providing 99.3% coverage, themedian is marked by the horizontal line within each box, and and outliers (> 2.7σ) are marked by crosses. mPDE indicates mean projection distance error.
Figure 3.
Example registrations with LevelCheck-labeled intra-operative mobile radiographs on left and gradient maps on right. Denser white outlines on the gradient map indicate better overlap between the DRR and intra-operative radiograph: A, Anatomical variant in which the patient had 13 pairs of ribs and four lumbar vertebrae, with T13 being a level of surgical interest. B, Successful registration despite interval T11 vertebroplasty from pre-operative CT to intra-operative radiograph.C, LevelCheck performance in a revision operation with pre-existing implants. D, Variant anatomy with four lumbar vertebrae. DRR indicates digitally reconstructed radiograph; CT, computed tomography.
Analysis of potential failure modes was conducted based on the trials yielding mPDE> 5 mm for the case of 50 multi-starts (7 second runtime) for which there 70 / 10,000 such trials. The observed modes of failure could generally be categorized into four categories: first, primarily an in-plane error resulting in a registration shift by an entire vertebral body level (Figure 4A); second, an out-of-plane error that causes the registration to be less accurate, though not to the extent of being off by an entire vertebral body level (Figure 4B); third, an error in registration due to addition or removal of implants on the intra-operative radiograph causing mismatch of the implants from the radiograph and the DRR (Figure 4C); finally, error stemming from poor quality of the intra-operative radiograph (e.g., low contrast) (Figure 4D). Thirty-one of the 70 failed instances were primarily in-plane errors, 15 were primarily out-of-plane failures, 8 were due to implant mismatch, and 16 were due to poor contrast of the intra-operative mobile radiograph. The LevelCheck algorithm did not appear to favor in-plane versus out-of-plane failures in the 70 trials evaluated.
Figure 4.
Representative instances of potential failure modes with intra-operative mobile radiographs on left and gradient maps on right. Yellow crosses denote LevelCheck-generated labels, and blue crosses indicate the true vertebral body levels. Weaker white outlines on the gradient map (compared to Figure 4) indicate reduced quality of overlap between the DRR and intra-operative radiograph. Potential failure modes include: A, In-plane error. B, Out-of-plane error.C, Implant error.D, low image quality error. DRR indicates digitally reconstructed radiograph; |GC–GC*|, quantitative measure of the degree of overlap between the DRR and the intra-operative radiograph, with higher values indicating poor overlap and vice versa; mPDE, mean projection distance error.
In quantifying the degree of overlap between the DRR and the intra-operative radiograph, the similarity metric difference between the GC for that trial and GC* for the best possible registration was analyzed (|GC–GC*|). Results are shown in Figure 5A. As the computation time and number of multi-start increases, there is a greater degree of overlapping edges (i.e., consistent gradients) between the DRR and the radiograph such that at 26 seconds (200 multi-starts), the difference between GC and the most reliable registration of GC* is essentially zero. There appears to be a correlation between high |GC–GC*| values and high mPDE values and a correspondence to instances of registration failure owing to poor overlap between the DRR and the radiograph as shown in Figure 5B. In particular, all registration failures (for all multi-start settings tested) occurred when |GC–GC*| was greater than 0.1.
Figure 5.

Similarity measure: A, Box and whisker plots of |GC–GC*| based on the number of multi-starts. Boxes denote the first/third quartiles, whiskers denote min/max values providing 99.3% coverage, the median is marked by the horizontal line, and outliers (> 2.7σ) are marked by crosses. B, Scatterplot of all trials plotted as a function of mPDE versus |GC–GC*|. All failed registrations are bounded by |GC–GC*| > 0.1 and mPDE> 5 mm (the right upper quadrant of the plot). |GC–GC*| indicates a quantitative measure of the degree of overlap between the digitally reconstructed radiograph and the intra-operative radiograph, with higher values indicating poor overlap; mPDE, mean projection distance error.
Discussion
Despite improved imaging and technological advances in recent decades, localization of specific vertebrae during spine surgery remains uniquely challenging. This technical challenge has resulted in an appreciable rate of wrong-level surgery, contributing to patient morbidity and increased hospital costs. In current practice, spine surgeons generally rely on the presence of conspicuous local pathology, use of fiduciary markers, or sequential intraoperative imaging and vertebral level counting to determine the level of interest. Even with these techniques, the rate of wrong-level surgery is 0.03%, a truly unacceptable rate.
Using the LevelCheck algorithm, all target vertebrae were correctly identified within 5 mm when using 200 multi-starts in approximately 26 seconds of computation time. This was despite initialization errors as large as 90 mm (equal to one to two vertebral bodies from the actual level of interest)and the presence of radiopaque instruments in the surgical field. Additionally, success was achieved even when there were anomalous anatomical variations, including either fewer or extra lumbar or thoracic vertebrae, as well as presence of surgical instruments or foreign objects within the intra-operative radiograph. Although this is a clear improvement over historical subjective data suggesting a nonzero error rate, it is in line with error rates reported using other novel strategies, including vertebroplasty and preoperative percutaneous fiducial screw placement, both of which have been demonstrated to have 100% accuracy. However, LevelCheck improves on both of these techniques by significantly reducing costs, working within the natural workflow of surgery, and reducing patient morbidity (c.f., an additional preoperative procedure for cement injection). The LevelCheck algorithm entails one-time cost associated with the software and hardware acquisition and does not compound with increasing patient application. In contrast, both vertebroplasty and preoperative fiducial screw placement require sedation and additional procedures, increasing both monetary and time costs and patient morbidity.
When reducing computation time by a factor of almost four (from 27 second runtime for 200 multi-starts to 7 seconds for 50 multi-starts), accuracy was 99.3%. Instances of potential failure from this series are instructive in demonstrating some of the limitations of the algorithm. Failures could be generally categorized as: out-of-plane, in-plane, implant mismatch, or poor quality imaging. Regardless of failure mode, all failures appeared to be correlated with the strength of gradient correlation between the DRR and intraoperative radiograph. In this study, we were able to compare each image registration with the image registration that resulted in the greatest degree of overlap, allowing an internal check on the results. Such analysis demonstrated that a GC difference greater than 0.1 suggested misregistration by greater than 5 mm. These results suggest that the gradient correlation parameter may offer a quantitative scale by which each registration can be assessed in terms of the probability of correct vertebral body localization in a clinical setting. This could allow for an added confidence check of internal validity when running the LevelCheck algorithm. In cases where the confidence metric (e.g., gradient correlation difference) is beyond a certain threshold, spine surgeons could ideally develop a higher index of suspicion, preventing already rare localization errors associated with the LevelCheck algorithm. Further elucidation of the ideal gradient correlation threshold that could be used clinically to judge success is the subject of future experimentation.
Although an accuracy of 99.3% with 50 multi-starts may be acceptable in a purely theoretical research setting, when considering clinical application and the devastating consequence of wrong-level surgery, this would not be ideal. As such, future clinical studies will use a parameter setting of 200 multi-starts, as this resulted in a 100% success rate.
This study has a variety of limitations. Firstly, the study was retrospective in nature and not a statistically powered prospective trial. Furthermore, clinical images in this study were from patients with pathologies that did not severely deform the spinal axis such as adolescent idiopathic scoliosis. If patients with significant deformity, trauma, or tumor growth that prevented clear delineation of vertebral structures were included, it is possible that the reported accuracy could have decreased. Thirdly, the method requires adequate quality pre-operative imaging in the form of a CT scan that encompasses the region proximal and/or distal to the surgical site with appropriate spatial resolution (ideally isotropic ∼1 mm slices). One final limitation is that LevelCheck was not tested in the AP plane due to the lack of radiographs taken in this plane as our case series focused on the thoracolumbar spine and institutional practice generally involves use of only lateral radiographs in this anatomical distribution. Although these limitations are present, the results overall are promising and warrant future prospective clinical studies. Future work also includes using a pre-operative MRI as an alternative to CT, usage of AP radiographs, determining the appropriate GC threshold as a reliable internal check on registration accuracy, further acceleration of runtime, comparison to surgeon clinical judgment, and evaluation of intraoperative workflow.
Conclusion
The LevelCheck algorithm was able to accurately identify target vertebrae with an acceptable computation time in intraoperative mobile radiographs of the thoracolumbar spine based on routinely obtained preoperative CT scans. The method could provide a useful assistant to the surgeon in reducing localization errors and improving workflow. Further prospective clinical studies are necessary to validate its benefit as a reliable independent check.
Acknowledgments
The National Institutes of Health (R01 EB017226) and academic-industry partnership with Siemens Healthcare (XP Division, Erlangen Germany) grantfunds were received in support of this work.
Relevant financial activities outside the submitted work: consultancy, grants, employment, expert testimony, payment for lectures, stocks, travel/accommodations/meeting expenses.
Footnotes
The device(s)/drug(s) that is/are the subject of this manuscript is/are not FDA-approved for this indication and is/are not commercially available in the United States.
References
- 1.Mody MG, Nourbakhsh A, Stahl DL, et al. The prevalence of wrong level surgery among spine surgeons. Spine. 2008;33:194–198. doi: 10.1097/BRS.0b013e31816043d1. [DOI] [PubMed] [Google Scholar]
- 2.Mehtsun WT, Ibrahim AM, Diener-West M, et al. Surgical never events in the United States. Surgery. 2013;153:465–472. doi: 10.1016/j.surg.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Hsiang J. Wrong-level surgery: A unique problem in spine surgery. Surg Neurol Int. 2011;2:47. doi: 10.4103/2152-7806.79769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Upadhyaya CD, Wu JC, Chin CT, et al. Avoidance of wrong-level thoracic spine surgery: intraoperative localization with preoperative percutaneous fiducial screw placement. J Neurosurg Spine. 2012;16:280–284. doi: 10.3171/2011.3.SPINE10445. [DOI] [PubMed] [Google Scholar]
- 5.Hsu W, Sciubba DM, Sasson AD, et al. Intraoperative localization of thoracic spine level with preoperative percutaneous placement of intravertebral polymethylmethacrylate. J Spinal Disord Tech. 2008;21:72–75. doi: 10.1097/BSD.0b013e3181493194. [DOI] [PubMed] [Google Scholar]
- 6.Otake Y, Schafer S, Stayman JW, et al. Automatic localization of vertebral levels in x-ray fluoroscopy using 3D-2D registration: a tool to reduce wrong-site surgery. Phys Med Biol. 2012;57:5485–5508. doi: 10.1088/0031-9155/57/17/5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Otake Y, Wang AS, Webster Stayman J, et al. Robust 3D-2D image registration: application to spine interventions and vertebral labeling in the presence of anatomical deformation. Phys Med Biol. 2013;58:8535–8553. doi: 10.1088/0031-9155/58/23/8535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markelj P, Tomaževič D, Likar B, Pernuš F. A review of 3D/2D registration methods for image-guided interventions. Med Image Anal. 2012;16:642–661. doi: 10.1016/j.media.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 9.Penney GP, Weese J, Little JA, et al. A comparison of similarity measures for use in 2-D-3-D medical image registration. IEEE Trans Med Imaging. 1998;17:586–595. doi: 10.1109/42.730403. [DOI] [PubMed] [Google Scholar]




