Abstract
This study examined the longitudinal association between fathers’ early involvement in routine care-giving, literacy, play, and responsive caregiving activities at 9 months and maternal depressive symptoms at 4 years. Data for 3,550 children and their biological parents were drawn from the Early Childhood Longitudinal Study-Birth Cohort data set. Analyses in a structural equation modeling framework examined whether the association between father involvement and maternal depressive symptoms differed for families of children with autism spectrum disorder (ASD) and for families of children with other disabilities or delays from families of children who were typically developing. Results indicated that father literacy and responsive caregiving involvement were associated with lower levels of depressive symptoms for mothers of children with ASD. These findings indicate that greater father involvement may benefit families of children with ASD and highlight the need to support and encourage service providers to work with fathers.
Keywords: Depression, Disability related studies, Family and mental illness, Families with disabled members, Fathers level and quality of child-care involvement
Introduction
Over the years, the challenges and benefits to family life of raising children with disabilities or delays have been a topic of interest to researchers [1, 2]. Recent studies have shown that the presence of a child with a disability or delay can affect every family member in both positive and negative ways [2]. A growing body of empirical studies has linked child behavior problems associated with disabilities and developmental delays with maternal anxiety and depressive symptoms [3, 4]. Furthermore, mothers of children with autism spectrum disorder (ASD) may be particularly at risk for experiencing greater levels of stress and depressive symptoms [5, 6].
When experiencing depressive symptoms, mothers of children with disabilities or delays may benefit from a supportive social network, particularly the support of an immediate family member [7–10]. One member of the immediate family that may play a particularly important role in supporting mothers and helping reduce their stress, anxiety, and depressive symptoms is the father. Interest in fathers as active parents has increased dramatically in recent years with considerable attention given to father involvement in direct child-rearing activities [11, 12]. However, the literature on fathers’ influence on child and family well-being has focused primarily on fathering within the context of families of children who are typically developing. This gap in current research is problematic given that families of children with disabilities or delays have been found to experience higher levels of stress and depressive symptoms. Although researchers have begun to explore how fathers contribute to child and maternal well-being in these families [13–15], very few studies have specifically studied how father involvement with children with disabilities may contribute to maternal well-being (for an exception, see [15]). The present study attempts to contribute to this nascent research area by examining this association in a nationally representative sample.
Study Overview
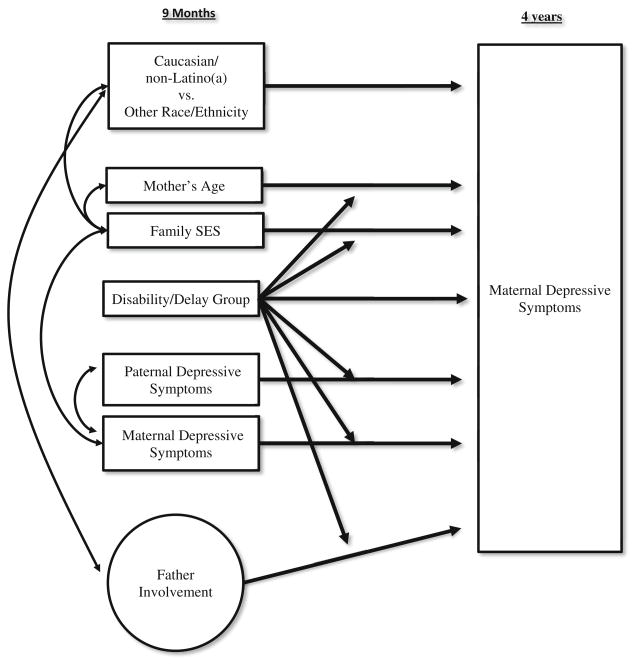
The current study was designed to address gaps in our current understanding of the association between father involvement and maternal depressive symptoms in families of children with disabilities or delays. In examining the association between father involvement and maternal depressive symptoms, our conceptualization of father involvement was guided by Pleck’s [16] revision of the Lamb–Pleck conceptualization [17] focusing on specific types of “positive engagement” available in the data set. Positive engagement is defined as “interaction with the child of the more intensive kind likely to promote development (p. 67)” [16]. We focused on positive engagement because these forms of involvement may be more susceptible to intervention than other forms, such as financial provision, over which practitioners and families may have little control. Four types of father involvement activities were identified: literacy, play, routine caregiving, and responsive caregiving involvement. We classified these activities as positive engagement because they address various developmental needs of children, such as routine physical needs through routine care-giving, physical and cognitive stimulation through play and literacy activities, and less-routine physical needs through responsive caregiving.
In addition to father involvement, there are several factors that have been identified as potential influences on maternal depressive symptoms. We controlled for many of these factors in our analyses. Specifically, we controlled for child’s race/ethnicity, maternal age, family SES, and fathers’ depressive symptoms [18, 19].
Finally, we followed past research [6, 7] on families of children with disabilities or delays by examining children with autism spectrum disorder or pervasive developmental disorder (ASD) separately from children diagnosed or receiving services for another disability or delay (CWD). These groups were compared to children who were not known to have a disability or delay and were considered to be typically developing (TYP). In summary, our analyses examined whether fathers’ routine caregiving, literacy, play, and responsive caregiving involvement at 9 months were associated with maternal depressive symptoms at 4 years. Based on past research, we hypothesized that greater levels of early father involvement would be associated with lower levels of maternal depressive symptoms [15]. Furthermore, we explored whether these associations differed for families of children with ASD or families of children with other disabilities or delays than from families of children who were typically developing. Although these group comparisons were exploratory, we anticipated that given the higher levels of stress often experienced by families of children with disabilities or delays [3–6], mothers in these families may benefit more from greater father involvement than families of typically developing children.
Methods
Sample
The data came from the National Center for Education Statistics (NCES) Early Childhood Longitudinal Study-Birth Cohort (ECLS-B) data set. The current study was approved as a project conducting secondary analyses of an already existing dataset by the University of Illinois at Urbana-Champaign’s Institutional Review Board for research involving human subjects. Data on 10,7001 children were gathered when children were approximately 9 months, 2 years, and 4 years of age. To ensure that the same father or mother was the individual who provided information at each time point, it was necessary to restrict the sample to families with biological parents residing with their child across the first 4 years of life. This restriction further ensured that the father continued to be present in the home for the duration of the study and could therefore continue to influence mothers’ depressive symptoms at 4 years. After applying this restriction, the sample consisted of 3,550 children (1,850 male, 1,700 female) and their parents. We applied guidelines outlined by NCES [20] for adjusting standard errors using a Taylor series method in Mplus 7.2 and applying appropriate weights (W3D0 for all analyses) so that findings could be generalized to the US population of children born in 2001 who lived with their biological parents for the first 4 years of life. Weights also accounted for bias introduced by attrition and non-response.
Measures
Disability/Delay Status of the Child
When children were approximately 9 months, 2 years, and 4 years of age, each mother was given a list of disabilities and delays and asked to report whether her child had been diagnosed with the disability or delay or received treatment for a disability or delay. These disabilities/delays included: autism spectrum disorder or pervasive developmental disorder, cerebral palsy, an intellectual disability, spina bifida, blindness, hearing impairment and or deafness, Down syndrome, Turner syndrome, a problem with mobility, another developmental delay, or disabilities or other delays for which the family was receiving early intervention services. Consistent with past research [6, 7], children were placed into three groups: children with autism spectrum disorder or pervasive developmental disorder (ASD; reported at 4 years), children diagnosed or receiving services for another disability or delay (CWD; reported at 9 months, 2 years, and or 4 years), and children who were considered to be typically developing (TYP). There were approximately 50 children in the ASD group, 650 in the CWD group, and 2,900 children in the TYP group with a rounded sample total of 3,550. Two dichotomous indicators, ASD and CWD, were created with the TYP group as the comparison group.
Maternal and Paternal Depressive Symptoms
Mothers and fathers at 9 months and mothers at 4 years completed a 12-item short-form version of the Center for Epidemiological Studies-Depression Scale [21, 22]. The 12 items were summed to form a total depressive symptoms score (Cronbach’s α ranged from 0.78 to 0.93).
Father Involvement
At 9 months, fathers were asked to report how frequently they engaged in several different activities. Response categories ranged from “never” to “more than once a day” and were recoded to represent their approximate weekly occurrence. Conceptual reasoning as well as confirmatory factor analysis (results available upon request) indicated the presence of four types of involvement: literacy, play, routine caregiving, and responsive caregiving. Literacy involvement (three items) refers to fathers’ engagement in reading or other language activities (e.g., read books to the child). Play involvement (two items) refers to play activities fathers engage in with their child (e.g., peek-a-boo). Routine care-giving involvement (six items) refers to activities fathers engage into provide care for their child’s functional needs (e.g., changing diapers, bathing). Responsive caregiving involvement (four items) measures how often fathers were the parent to respond to the less routine caregiving needs of their child. Fathers were asked, “When the following things happen or need to be done, how often are you the one who does them?” regarding such tasks as “taking their child to the doctor” and “soothing their child when upset.” Responsive caregiving differs from the other types of involvement in that it is a measure of father involvement relative to mothers and it measures how often fathers engage in these activities when these activities need to be done. The aforementioned items were used to create latent variables for each type of father involvement as detailed below.
Demographic Control Variables
Child race/ethnicity was recorded from the child’s birth certificate and five groups were identified: Caucasian, African American, Asian, Latino (a); and Other. Because some groups had very low representation in the ASD group, race/ethnicity was collapsed into a dichotomous variable (1 = Caucasian, non-latino(a), 0 = other race/ethnicity). Additional demographic controls included mother’s age and family socioeconomic status quintile.
Missing Data
Missing data were limited in this sample (<9 % for maternal depressive symptoms at 9 months and <5 % for all other variables). Missing data were addressed using full information maximum-likelihood (FIML) in the Mplus 7.2 program. FIML is a preferred approach to other common methods [23].
Analytic Strategy
Weighted means, standard deviations, and correlations for study variables are reported in Table 1. Analyses were performed within a structural equation modeling framework using Mplus 7.2. Because the distributions of depressive symptoms scores were skewed, the robust maximum likelihood estimator (MLR), which is robust to non-normal data, was used.
Table 1.
Descriptive statistics and group mean differences of study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mothers’ depressive symptoms 4 years | – | |||||||||
| 2. Mothers’ depressive symptoms 9 mo | .42* | – | ||||||||
| 3. Fathers’ depressive symptoms 9 mo | .16* | .23* | – | |||||||
| 4. Fathers’ literacy inv. 9 mo | −.02 | −.04* | −.06* | – | ||||||
| 5. Fathers’ play inv. 9 mo | .00 | −.03 | −.06* | .75* | – | |||||
| 6. Fathers’ routine care. inv. 9 mo | .05* | .05* | −.01 | .27* | .42* | – | ||||
| 7. Fathers’ responsive care. inv. 9 mo | .03 | .03 | −.04* | .29* | .37* | .52* | – | |||
| 8. SES quintile 9 mo | −.15* | −.13* | −.09* | .02 | −.05* | −.04* | −.11* | – | ||
| 9. Mothers’ age | −.05* | −.07* | −.06* | −.02 | −.06* | −.03* | −.04* | .39* | – | |
| 10. Child is caucasian, non-latino (a) | −.04* | −.05* | −.03 | .00 | −.03 | .00 | −.20* | .19* | .08* | – |
| TYP M | 4.31 | 4.07 | 3.10 | 0.00 | 0.00 | 0.00 | 0.00 | 3.39 | 29.1 | 61 % |
| TYP SD | 4.96 | 4.58 | 3.76 | 1.04 | 1.20 | 3.67 | 1.79 | 1.34 | 5.48 | |
| CWD M | 4.42 | 4.42 | 3.69 | −0.03 | 0.00 | −0.35 | −0.21 | 3.52 | 28.8 | 75 % |
| CWD SD | 5.60 | 5.34 | 5.09 | 1.25 | 1.22 | 4.04 | 1.81 | 1.47 | 6.56 | |
| ASD M | 5.49 | 5.84 | 7.05 | 0.12 | 0.00 | 0.04 | 0.90 | 3.62 | 31.8 | 60 % |
| ASD SD | 3.87 | 6.37 | 8.41 | 0.98 | 1.75 | 3.89 | 2.24 | 1.22 | 4.81 | |
| CWD M versus TYP M | > * | a | < † | > * | ||||||
| ASD M versus TYP M | > † | a | > * | |||||||
| ASD M versus CWD M | a | > † | > * |
p <.10
p <.05
Because only weak measurement invariance was achieved for play involvement, it was not appropriate to analyze mean comparisons
The same analytic strategy was used for each type of father involvement: routine caregiving, literacy, play, and responsive caregiving as follows. First, we examined measurement invariance [24] of the latent variables for each type of father involvement across groups following Meredith’s outline of testing for configural, weak, strong, and strict factorial invariance [25]. Conceptually, measurement invariance refers to whether items represent the same underlying latent variable for different groups (ASD, CWD, and TYP). “Strong” or “strict” measurement invariance is a necessary assumption for making direct comparisons between groups [24, 26]. Strict factorial invariance held for literacy, routine caregiving, and responsive caregiving involvement across groups. Thus, fathers appeared to think about their involvement in the aforementioned activities in the same way regardless of their child’s disability/delay status. Weak factorial invariance held for play involvement.
Second, for routine caregiving, responsive caregiving, and literacy and play involvement, we fit a multiple group measurement model in which the 9-month father involvement latent variables were estimated for each group (ASD, CWD, TYP) according to the results of measurement invariance analyses. Model fit for all father involvement types was adequate (RMSEA was less than 0.026 and CFI was >0.982 for all three models). Latent variables were saved as factor scores for analysis of the path model shown in Fig. 1.
Fig. 1.
Conceptual model
Third, our model building consisted of the following steps: First, maternal depressive symptoms at 4 years were predicted from demographic (child’s race/ethnicity, family SES, mother’s age) and other (mother and father 9-month depressive symptoms) control variables. Next, the main effects of father involvement, ASD diagnosis, and other disability/delay diagnosis (CWD) were added to see if father involvement was associated with later maternal depressive symptoms for the entire sample, controlling for disability/delay status. We then tested for interactions between disability/delay status (ASD, CWD) and mother’s age and family SES and between disability/delay status and mother’s and father’s 9-month depressive symptoms. We did this to check whether these control variables were associated with mothers’ 4-year depressive symptoms differently for each group before testing for group difference related to father involvement. Finally, to explore whether the association between father involvement and mothers’ depressive symptoms varied by group, we tested for interactions between disability/delay status (ASD, CWD) and father involvement. Change in model fit indices (Δχ2 and RMSEA and CFI) were examined at each step and significant interactions were retained. This model building strategy was followed separately for literacy, routine caregiving, and responsive caregiving involvement. Because only weak invariance held across groups for play involvement and thus play involvement represented a different construct for each group, analyses of group differences related to play involvement would be inappropriate and were not conducted.
Results
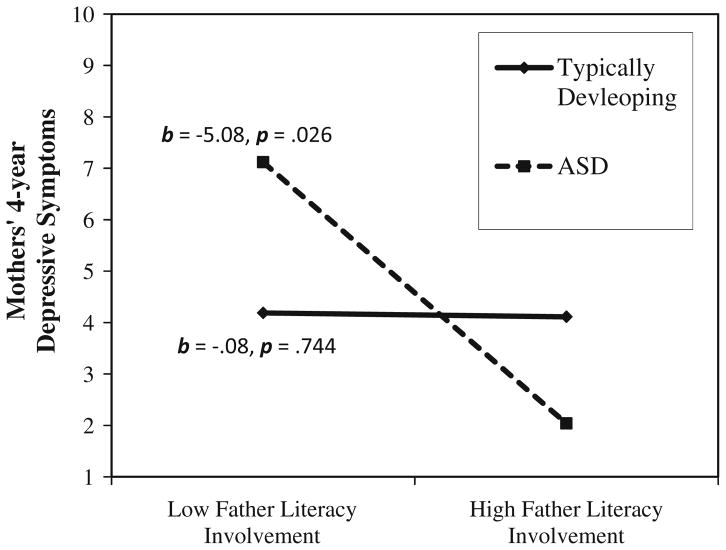
Results from analyses examining mean differences in study variables are reported at the bottom of Table 1. Final models with retained significant interactions are presented in Table 2. Because of space restrictions, covariances between 9 month variables (see Fig. 1) could not be included in Table 2. These are available from the first author upon request. However, bivariate correlations are reported in Table 1. There were no direct associations between father involvement and maternal depressive symptoms for literacy, routine caregiving, or responsive caregiving. Furthermore, there were no significant interactions between disability/delay status (CWD, ASD) and any other study variable except for literacy and responsive caregiving involvement. The interaction between ASD and father literacy involvement was significant and contributed to model fit (Δχ2 = 12.79, p < .001; CFI: 1.00, RMSEA: 0.00). Follow-up tests were conducted using procedures outlined by Aiken and West [27] for post hoc investigation of interactions. The slope of the line representing families of typically developing children was not significantly different from zero. However, the slope of the line representing children with ASD was significantly different from zero indicating that mothers in these families reported fewer depressive symptoms at 4 years when fathers engaged in more literacy involvement at 9 months (see Fig. 2).
Table 2.
9-Month father involvement predicting 4-year mothers’ CES-D
| 4 year mothers’ CES-D | Routine caregiving
|
Literacy
|
Responsive caregiving
|
|||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Child’s race/ethnicity | 0.03 | .293 | 0.03 | .283 | 0.02 | .424 |
| Mother’s age | 0.05 | .051 | 0.05 | .049 | 0.05 | .057 |
| 9Mo SES | −0.09 | .002 | −0.09 | .002 | −0.10 | .002 |
| ASD | 0.00 | .904 | 0.01 | .561 | 0.02 | .178 |
| CWD | 0.00 | .821 | −0.01 | .798 | −0.01 | .791 |
| 9Mo mothers’ CES-D | 0.42 | .000 | 0.42 | .000 | 0.42 | .000 |
| 9Mo fathers’ CES-D | 0.05 | .122 | 0.05 | .121 | 0.04 | .148 |
| 9Mo fathers’ routine caregiving | 0.01 | .601 | — | — | — | — |
| 9Mo fathers’ literacy involvement | — | — | −.01 | .744 | — | — |
| 9Mo literacy involvement X ASD | — | — | −.04 | .029 | — | — |
| 9Mo fathers’ responsive caregiving | — | — | — | — | −0.03 | .210 |
| 9Mo responsive caregiving X ASD | — | — | — | — | −0.04 | .027 |
| R2 for mothers’ 4-year CES-D | 19.5 % | 19.7 % | 19.9 % | |||
Not shown are covariances between 9-month variables
Fig. 2.
Interaction between ASD and father literacy involvement in predicting mothers’ depressive symptoms
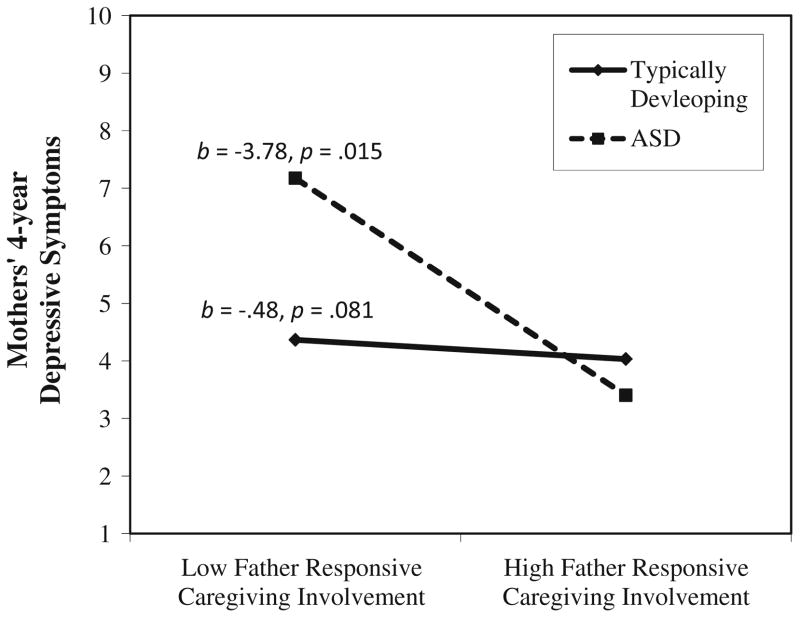
The interaction between CWD and father responsive caregiving involvement was significant and contributed to model fit (Δχ2 = 6.33, p = .012; CFI: 0.970, RMSEA: 0.026). However, follow-up tests indicated that neither the slope of the line representing CWD or of the line representing TYP was significantly different from zero. The interaction between ASD and father responsive caregiving involvement was also significant and contributed to model fit (Δχ2 = 13.86, p <.001; CFI: 0.956, RMSEA: .028). Follow-up analyses indicated that the slope of the line representing TYP was not significantly different from zero. However, the slope of the line representing families of children with ASD was significantly different from zero indicating that mothers in these families reported fewer depressive symptoms at 4 years when fathers engaged in more responsive caregiving involvement at 9 months (see Fig. 3).
Fig. 3.
Interaction between ASD and father responsive caregiving involvement in predicting mothers’ depressive symptoms
Discussion
In the present study, we explored how fathers’ routine caregiving, literacy, and responsive caregiving involvement at 9 months were associated with maternal depressive symptoms at 4 years in families of children who were typically developing, of children who had been diagnosed with ASD, and of children who had other disabilities and or delays. For families of children with ASD, greater father literacy and responsive caregiving involvement at 9 months were associated with lower levels of maternal depressive symptoms at 4 years as hypothesized. In contrast, for families of children with disabilities or delays other than ASD or families of children who were typically developing, father involvement was not associated with later maternal depressive symptoms. Given the considerable variability of disabilities and delays represented in the CWD group and variation in circumstances of the families in the TYP group, we are hesitant to speculate about exactly why involvement as measured in this study was not associated with mothers’ depressive symptoms for these groups. This is an important question for future research.
An important question raised by this study’s findings is why men’s responsive caregiving was associated with lower levels of maternal depressive symptoms in families of children with ASD. Fathers’ responsive caregiving consists of responding to the needs of their children (e.g., soothing a child when he or she is upset). The items measuring responsive caregiving assess how often fathers are the ones to respond and thus indicate fathers’ involvement relative to mothers. Previous research has found that behaviors specific to ASD, such as difficulties with self-regulation skills appearing in the first year of life [28, 29] may contribute to greater levels of maternal stress and depression. Our findings suggest that if fathers are responsive to the needs of their children with ASD when they are exhibiting self-regulation difficulties and if fathers are more frequently the parent that responds to the need of their children, then they may reduce the burden that falls on mothers and the resulting stress and depression. This would suggest that early intervention personnel may want to help fathers of children at risk for ASD become more aware of and responsive to the behavioral problems exhibited by their children early on. Mothers may benefit as fathers are encouraged to more frequently be the parent that responds to their child’s pressing needs early on in their child’s life.
In addition to the benefits derived from greater levels of father responsive caregiving involvement, this study’s findings indicate that fathers’ participation in literacy activities was also associated with lower levels of maternal depressive symptoms in families of children with ASD. Given that communication deficits commonly exhibited by children with ASD may contribute to maternal depression [30], it is not surprising that when fathers engage early on in parenting activities that are directly related to children’s communication skills (e.g., singing songs or reading a story to the child), they may be playing an important role in addressing and or potentially minimizing communication problems that contribute to maternal depressive symptoms. Recent studies indicated that children later diagnosed with ASD exhibited communication difficulties within the first year of life [28, 31]. Thus fathers may have engaged in early literacy involvement in response to these difficulties. These findings indicate that early intervention personnel may be able to support mothers of children at risk for ASD who are experiencing depressive symptoms by encouraging fathers to engage in literacy forms of involvement and thereby address communication problems exhibited by their children.
Finally, the finding that early father involvement with children with ASD appears to promote maternal well-being may be particularly encouraging for families of children with ASD. This finding reflects the reality that even when faced with challenges and stressors associated with ASD, many families adapt, cope, and thrive. Additional research is needed to explore other ways in which father involvement can promote child, mother, family, and even father well-being.
The findings of this study have important implications for policy makers and early intervention service providers. That greater father involvement was associated with better outcomes for maternal well-being underscores the need to develop focused programs to encourage fathers to be involved with their children with disabilities or delays, specifically children with ASD. Furthermore, service providers can be encouraged to engage fathers while providing early intervention services. Service providers can be supported in engaging fathers by being provided with training opportunities and other resources they need to work with fathers. Promoting father involvement is one way that practitioners and policy makers may promote maternal well-being and positive family outcomes through encouraging fathers to be more involved in effective ways.
Limitations
Although results from this exploratory study are encouraging when considering the association between father involvement and maternal depressive symptoms in families of children with ASD, caution must be used when drawing conclusions from specific findings. First, a wide range of disabilities and delays are represented in the CWD group (e.g., cerebral palsy, spina bifida, hearing impairment) used in the analyses. Although other researchers have previously used the approach of separating out ASD from other disability/delay classifications [6, 7], it is important to acknowledge that both the antecedents and consequences of father involvement might differ across the various disability and delays represented in our CWD group. Second, we recognize that our study does not address all possible factors that influence maternal depressive symptoms. While we attempted to address some of these factors, there are other family processes likely at work. Future studies examining the association between father involvement and maternal depressive symptoms will need to consider additional influences on maternal depressive symptoms. Two important influences that should be considered are children’s symptoms associated with ASD or another disability/delay and the diagnosis itself of ASD or another disability/delay. Because symptoms often precede diagnosis, future research should consider how father involvement might moderate the association between both of these influences and maternal well-being. Third, although not a target outcome of this study, it is possible that maternal depressive symptoms influenced father involvement in that fathers adjusted their levels of involvement in response to mothers’ depressive symptoms. Although maternal depressive symptoms were not significantly associated with father involvement at 9 months for families of children with ASD, it is possible that these fathers may have changed their involvement afterward in response to mothers’ depressive symptoms. We did control for prior levels of depressive symptoms in our analyses which removed an important confound, increasing confidence in the direction of effects. However, future research should consider the bidirectional influences of father involvement and maternal depressive symptoms on one another to better understand the role of fathers in these families. Finally, although our sample excluded several important parenting contexts for children with disabilities or delays (e.g., non-residential fathers, father figures, etc.), the findings are still generalizable, with the aforementioned caveat, to all families of children born in 2001 who resided with their biological parents for the first 4 years of life.
Conclusions
Despite these limitations, the results of this study provide encouraging insight on how early intervention personnel can offer support for families of children with ASD through efforts that target fathers. Trivette et al. [32] have outlined a family-systems model that may be useful in intervention practices when working with families raising young children with ASD, particularly given the presence of higher levels of maternal depressive symptoms experienced by mothers in these families. Building upon this framework, results from the current study suggest that fathers should be an integral part of this “family systems” approach to working with families, and that when men are encouraged to assume more active parental roles, they may play a critical part in addressing maternal depressive symptoms.
Acknowledgments
This research was supported by a grant from the Institute for Education Sciences of the U.S. Department of Education to B. McBride, R. Santos, S. Hong, and W. J. Dyer (R324A120174). This research was also supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Numbers T32HD007489 and P30HD003352. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Institute for Education Sciences or the National Institutes of Health.
Footnotes
Per NCES requirements when using ECLS-B data, all N’s in this article were rounded to the nearest 50.
Contributor Information
Daniel J. Laxman, Email: dlaxman@Waisman.Wisc.edu, Waisman Center, University of Wisconsin-Madison, Madison, WI, USA
Brent A. McBride, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA
Laurie M. Jeans, St. Ambrose University, Davenport, IA, USA
W. Justin Dyer, Brigham Young University, Provo, UT, USA.
Rosa M. Santos, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA
Justin L. Kern, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA
Niwako Sugimura, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA.
Sarah L. Curtiss, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA
Jenna M. Weglarz-Ward, University of Illinois at Urbana–Champaign, 1105 W. Nevada, Urbana, IL 61801, USA
References
- 1.Risdal D, Singer GHS. Marital adjustment in parents of children with disabilities: A historical review and meta-analysis. Research and Practice for Persons with Severe Disabilities. 2004;29(2):95–103. [Google Scholar]
- 2.Seligman M, Darling RB. Ordinary families, special children: A systems approach to childhood disability. 3. New York: Guilford Press; 2007. [Google Scholar]
- 3.Hastings R, Kovshoff H, Ward N, Espinosa F, Brown T, Remington B. Systems analysis of stress and positive perceptions in mothers and fathers of pre-school children with autism. Journal of Autism and Developmental Disorders. 2005;35(5):635–644. doi: 10.1007/s10803-005-0007-8. [DOI] [PubMed] [Google Scholar]
- 4.Herring S, Gray K, Taffe J, Tonge B, Sweeney D, Einfeld S. Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. Journal of Intellectual Disability Research. 2006;50(Pt 12):874–882. doi: 10.1111/j.1365-2788.2006.00904.x. [DOI] [PubMed] [Google Scholar]
- 5.Jeans LM, Santos RM, Laxman DJ, McBride BA, Dyer WJ. Examining ECLS-B: Maternal stress and depressive symptoms when raising children with ASD. Topics in Early Childhood Special Education. 2013;33(3):162–171. [Google Scholar]
- 6.Estes A, Munson J, Dawson G, Koehler E, Zhou XH, Abbott R. Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism. 2009;13(4):375–387. doi: 10.1177/1362361309105658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olsson MB, Hwang CP. Depression in mothers and fathers of children with intellectual disability. Journal of Intellectual Disability Research. 2001;45(Pt 6):535–543. doi: 10.1046/j.1365-2788.2001.00372.x. [DOI] [PubMed] [Google Scholar]
- 8.Boyd BA. Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities. 2002;17(4):208–215. [Google Scholar]
- 9.Feldman M, McDonald L, Serbin L, Stack D, Secco ML, Yu CT. Predictors of depressive symptoms in primary caregivers of young children with or at risk for developmental delay. Journal of Intellectual Disability Research. 2007;51(Pt 8):606–619. doi: 10.1111/j.1365-2788.2006.00941.x. [DOI] [PubMed] [Google Scholar]
- 10.Raina P, O’Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):e626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- 11.Brown GL, McBride BA, Shin N, Bost KK. Parenting predictors of father-child attachment security: Interactive effects of father involvement and fathering quality. Fathering. 2007;5(3):197–219. [Google Scholar]
- 12.McBride B, Schoppe-Sullivan SJ, Ho M-H. The mediating role of fathers’ school involvement on student achievement. Journal of Applied Developmental Psychology. 2005;26(2):201–216. [Google Scholar]
- 13.Dyson LL. Fathers and mothers of school-age children with developmental disabilities: Parental stress, family functioning, and social support. American Journal on Mental Retardation. 1997;102(3):267–279. doi: 10.1352/0895-8017(1997)102<0267:FAMOSC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Saloviita T, Italinna M, Leinonen E. Explaining the parental stress of fathers and mothers caring for a child with intellectual disability: A double ABCX model. Journal of Intellectual Disability Research. 2003;47(4–5):300–312. doi: 10.1046/j.1365-2788.2003.00492.x. [DOI] [PubMed] [Google Scholar]
- 15.Simmerman S, Blacher J, Baker BL. Fathers’ and mothers’ perceptions of father involvement in families with young children with a disability. Journal of Intellectual and Developmental Disability. 2001;26(4):325–338. [Google Scholar]
- 16.Pleck JH. Paternal involvement: Revised conceptualization and theoretical linkages with child outcomes. In: Lamb ME, editor. The role of the father in child development. 5. Hoboken: Wiley; 2010. pp. 58–93. [Google Scholar]
- 17.Lamb M, Pleck J, Charnov E, Levine J. Paternal behavior in humans. American Zoologist. 1985;25(3):883–894. [Google Scholar]
- 18.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal of Obstetrics and Gynecology. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paulson JF, Bazemore SD. Prenatal and post-partum depression in fathers and its association with maternal depression: A meta-analysis. JAMA. 2010;303(19):1961–1969. doi: 10.1001/jama.2010.605. [DOI] [PubMed] [Google Scholar]
- 20.Snow K, Derecho A, Wheeless S, Lennon J, Rosen J, Rogers J, et al. Early childhood longitudinal study, birth cohort (ECLS-B), kindergarten 2006 and 2007 data file user’s manual (2010–010) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2009. [Google Scholar]
- 21.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 22.Poulin C, Hand D, Boudreau B. Validity of a 12-item version of the CES-D used in the national longitudinal study of children and youth. Chronic Diseases in Canada. 2005;26(2–3):65–72. [PubMed] [Google Scholar]
- 23.Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67(4):1012–1028. [Google Scholar]
- 24.Vandenberg RJ, Lance CE. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods. 2000;3(1):4–70. doi: 10.1177/109442810031002. [DOI] [Google Scholar]
- 25.Meredith W. Measurement invariance, factor analysis and factorial invariance. Psychometrika. 1993;58(4):525–543. doi: 10.1007/BF02294825. [DOI] [Google Scholar]
- 26.Widaman KF, Reise SP. Exploring the measurement invariance of psychological instruments: Applications in the substance abuse domain. In: Bryant KJ, editor. Alcohol and substance use research. Washington, DC: American Psychological Association; 1997. pp. 281–324. [Google Scholar]
- 27.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage; 1991. [Google Scholar]
- 28.Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. International Journal of Developmental Neuroscience. 2005;23(2–3):143–152. doi: 10.1016/j.ijdevneu.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders. 2008;38(7):1278–1291. doi: 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
- 30.Bebko JM, Konstantareas MM, Springer J. Parent and professional evaluations of family stress associated with characteristics of autism. Journal of Autism and Developmental Disorders. 1987;17(4):565–576. doi: 10.1007/BF01486971. [DOI] [PubMed] [Google Scholar]
- 31.Jeans LM, Santos RM, Laxman DJ, McBride BA, Dyer WJ. Early identifiers of autism spectrum disorders in young children using a nationally representative dataset. Journal of Early Intervention. 2013;35(4):303–331. [Google Scholar]
- 32.Trivette CM, Dunst CJ, Hamby DW. Influences of family-systems intervention practices on parent-child interactions and child development. Topics in Early Childhood Special Education. 2010;30(1):3–19. doi: 10.1177/0271121410364250. [DOI] [Google Scholar]