Abstract
This study evaluates the prevalence of mental/emotional distress and its specific correlates among people living with HIV/AIDS (PLWHA) in 20 jail systems across the United States. Of the 878 PLWHA jail detainees, 52% had high levels of mental/emotional distress, defined by the composite Addiction Severity Index score. High mental/emotional distress was found to be associated with the inmate living in a city with lower income inequality, lower health ranking, and higher degree of danger. Proximate variables included being female, bisexual orientation, poorer physical health, and increased severity of substance abuse. Inmates in jails with accredited health services and those satisfied with family support had lower mental/emotional distress scores. These findings indicate the need for expanded mental health assessment of PLWHAs entering jail.
Keywords: HIV, jails, mental/emotional distress, case management
Introduction
There are mutually reinforcing relationships among HIV infection, mental illness, and incarceration. People living with HIV/AIDS (PLWHA) are at a 3.5-fold increased risk of having mental illness and are 2.5 times more likely to be incarcerated (Hammond & Treisman, 2007; Maruschak & Beavers, 2009; McClelland, Teplin, Abram, & Jacobs, 2002; Scheyett et al., 2010). Annually, one in six PLWHAs passes through the criminal justice system (CJS), with 95% of releasees coming out of jails (Spaulding et al., 2009). As a result, any period of incarceration is an important opportunity to address disease education, prevention, and treatment, including delivery of and linkage to care for HIV, mental illness, and substance use (Draine et al., 2011; Flanigan et al., 2010; McClelland et al., 2002; Spaulding et al., 2009; Springer & Altice, 2005; Springer, Azar, & Altice, 2011; Springer, Spaulding, Meyer, & Altice, 2011; Wohl et al., 2011).
The trans-institutionalization (from public psychiatric hospital to jail or prison) of those with mental illness starting in the late 1960s led the CJS to be a repository of care and treatment of the mentally ill. Indeed, one in five people in the CJS qualify for a major psychiatric disorder (James & Glaze, 2006). Rates of mental illness among inmates vary between urban and rural populations (Powell, Holt, & Fondacaro, 1997), jails and prisons (Brink, 2005), men and women (Brink, 2005; James & Glaze, 2006), and those housed and homeless prior to incarceration (Michaels, Zoloth, Alcabes, Braslow, & Safyer, 1992; Steadman, Osher, Robbins, Case, & Samuels, 2009). Studies document a rise in the number of incarcerated individuals suffering from mental illness since the late 1980s (Fellner, 2006; James & Glaze, 2006; Powell et al., 1997), in part because of better screening efforts, advent of trans-institutionalization, lack of community mental health services, and proscriptive criminal justice policies (Baillargeon et al., 2009; Powell et al., 1997).
While researchers have explored links between incarceration and mental illness, less is known about inmates with HIV who have psychiatric illness. Chart reviews of 336,668 inmates in the Texas Department of Criminal Justice (includes prison, jails, and locked substance abuse units) over a 2-year period found 16% of PLWHAs qualified for major depression or other mood and/or psychotic disorders, a rate 3 times greater than noninfected inmates (Baillargeon et al., 2003). A much smaller exploratory study reported that 45% of 101 PLWHAs in North Carolina prisons met criteria for depression (Scheyett et al., 2010). The picture for incarcerated individuals who are HIV+ and mentally ill is complicated and incomplete and may be explained by administrative, political, and economic differences in study populations, disparate and divergent research methods, and underdeveloped assessment protocols (Brink, 2005).
Mental/emotional distress has been linked to risky behaviors (both before and after HIV infection), HIV disease progression, lack of treatment follow-up, and medication non-adherence (Scheyett et al., 2010; Seal, 2005; Sullivan et al., 1999). Treatment of PLWHAs with diagnosed mental illness during incarceration is generally inadequate, and these individuals are consequently at elevated risk of non-adherence with medical appointments and reincarceration (Springer, Spaulding, et al., 2011). The specific aim of this article is to determine the prevalence of mental/emotional distress and associated factors among PLWHAs in jail settings within the United States. These data are critical, as jails differ from prisons in important ways. Jails are more porous facilities engaged in dynamic interactions with the surrounding communities through rapid turnover, with a greater prevalence of recently active substance users, homelessness, and mental illness. As a result, jails provide a unique opportunity to provide rapid assessment and treatment of medical and psychiatric conditions (Draine et al., 2011). However, jail-based interventions and linkage to care after release require a more sophisticated understanding and awareness of the prevalence of mental/emotional distress in these settings.
Methods
Participants
This study examined baseline data from EnhanceLink, a 5-year Health Resources and Services Administration initiative designed to implement and evaluate models for enhanced linkages to health care for people with HIV leaving jail (Draine et al., 2011). This longitudinal, nonrandomized study included 10 sites, representing 20 jail systems in nine states (MA, RI, CT, NY, PA, OH, IL, SC, and GA)—the largest sample of PLWHAs transitioning through jail to date. Participants were recruited into the study if they were 18 years or older, English- or Spanish-speaking, HIV-infected, and able to give informed consent. Two sites (NY and GA) excluded subjects with existent case management for serious mental illness and one site (IL) excluded men. Trained staff conducted baseline interviews and performed chart reviews to extract data from jail and community medical records. Each site had an institutional review board (IRB)-approved protocol, meaning that all protocols were subject to approval from the Office for Human Research Protections.
A total of 1,270 inmates consented to participate in the study across all sites. Of these, 392 were missing data on the variables examined, leaving 878 with complete data who were retained for the analyses. Missing data were generally due to failure of the participant to answer certain questions (e.g., income), and, in some cases, data could not be accessed by the site or simply did not exist (e.g., the score on viral load). Most of the covariates were missing fewer than 5% of the observations. Three of the potential correlates were missing for more than 5% (but fewer than 10%) of observations (n > 63): access to HIV treatment (n = 81), income (n = 101), and education (n = 118). Comparisons between those with missing data and those without were made using analysis of variance (for continuous variables) and χ2 tests (for dichotomous variables) at p < .05. Those with missing data were more psychiatrically distressed, from areas with higher poverty and lower income gaps, less likely to be insured, less likely to have accessed HIV treatment, more likely to have accessed medical treatment, less likely to have accessed substance abuse treatment, more likely to have received material support from family, more likely to have been employed, younger, more likely to be female, less likely to have received job training, and less likely to be African American, and had less education and more severe medical conditions. There were no significant differences in city health, jail accreditation, danger, homelessness, committed relationship, family support satisfaction, income, bisexuality, homosexuality, perceived health, Latino, birthplace, Spanish speaking, severity of substance abuse, or viral load.
Table 1 presents demographic data on all study participants in the analysis (N = 878). The overall sample had a mean age of 45 years and was predominantly male (71%) and African American (68%).
Table 1.
Demographics of Jail-detained PLWHAs.
| Mean (SD) or N (%) | |
|---|---|
| Age (range 20-70) | 44.8 (8.6) |
| Gender: Female | 252/29 (28.7) |
| Sexual Orientation: Homosexual | 95/11 (10.8) |
| Bisexual | 81/9 (9.2) |
| Education (years of school completed; range 2-16) | 11.3 (2.0) |
| Race: African-American | 601/68 (68.5) |
| Ethnicity: Latino | 211/24 (24.0) |
| Acculturation: Birthplace (non-US) | 133/15 (15.1) |
| Primary Language (Spanish) | 76/9 (8.7) |
Note. N = 878. PLWHA = people living with HIV/AIDS.
Outcome Measures
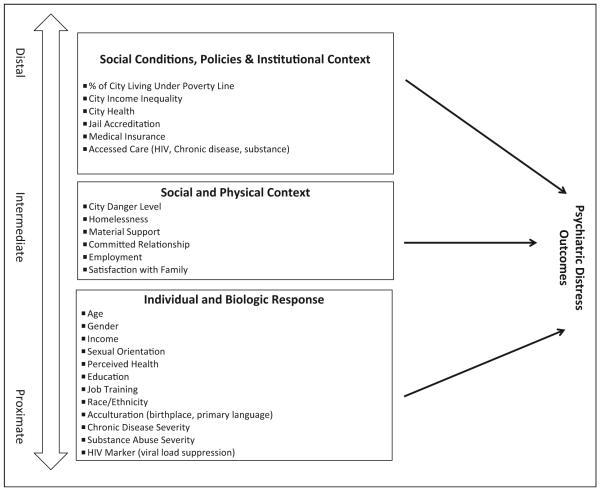
Participants completed the Addiction Severity Index (ASI) and reported on their criminal justice history, health service utilization, and HIV status. Lab results for CD4 count (cells/mm3) and HIV RNA viral load were collected from jail and community clinic charts for any point between 6 months pre-incarceration to incarceration. The Model of Population Health and Health Disparities provides a multilevel framework for understanding health disparities that combines population, clinical, and basic sciences and provides an opportunity to look at data from multiple communities and to include more macro forces that affect the lives of jail inmates (Warnecke et al., 2008). We used this framework to organize our analysis into distal, intermediate, and proximate determinants of health inequities. Distal factors are rooted in the social conditions and policies that underlie them, such as the legal system and organized religion; intermediate determinants of health disparities include the physical and social relationships among individuals; and proximate risk determinants represent individual characteristics that influence health and coping.
ASI
The ASI is a semistructured interview designed to address seven potential problem areas in substance-abusing patients: medical status, employment and support, drug use, alcohol use, legal status, family/social status, and psychiatric status (Cacciola, Pecoraro, & Alterman, 2008; McGafan, Griffith, Parente, & McLellan, 1986; McLellan, Cacciola, Alterman, Rikoon, & Carise, 2006; Rikoon, Cacciola, Carise, Alterman, & McLellan, 2006). Mental/emotional distress was calculated using the ASI psychiatric composite score. The psychiatric composite score is based on self-reported symptoms of depression, anxiety, inability to concentrate, patterns of violent behavior, hallucinations, suicide thoughts and attempts, psychotropic medications, perceptions of severity and duration, and the importance of getting treatment (McGafan et al., 1986). The psychiatric problems section of the ASI-5 is likely the most reliable and validated of any ASI domain (McLellan et al., 2006). The ASI is correlated with multiple scales of psychiatric symptoms and function (Cacciola et al., 2008), and high scores on the ASI psychiatric summary scales predict poor outcomes and need for mental health services (Cacciola et al., 2008). We could not rely on jail medical charts for psychiatric diagnosis as jails differ widely in their ability to screen for and diagnose these conditions during the varying lengths of detention.
Distal factors
Indicators of poverty in the inmate’s city were calculated using U.S. census data as follows: (1) the percentage of individuals living below the poverty line (18.7% to 35%; U.S. Census Bureau, 2012) and (2) the gap between rich and poor by city ranking (1 to 51), with 1 indicating the largest gap (Weinberg, 2011). Indicators of health were derived from the Gallup-Healthways’ WellBeing Index that scores cities on six domains: (1) life evaluation; (2) emotional health; (3) physical health; (4) healthy behavior; (5) work environment; and (6) basic access to money for health care, shelter, and so on. We assigned participants a score based on Gallup-Healthways’ index ranking of the 188 healthiest cities (43 to 167; Gallup-Healthways, 2008), with lower scores indicating greater well-being. Indicators of the jail environment were captured according to whether jails were accredited by the National Commission on Correctional Health Care (NCCHC) in 2011 (1 = Yes;0 = No). Along with the American Correctional Association, NCCHC is one of the two main accreditation organizations for correctional health care. If a site worked in more than one jail, the participant was given a score that reflected the number of jails with accreditation. For example, if four of the five jails at a site had NCCHC accreditation, the participant was given a score of 0.8. Indicators of access to medical insurance, and whether care was received for HIV, substance abuse, or medical needs in the preceding 30 days were scored (1 = Yes; 0 = No).
Intermediate factors
Indicators of physical space were determined by (1) Federal Bureau of Investigation and U.S. Justice Department rankings of dangerousness of the inmate’s city (NeighborhoodScout, 2014), using published city rankings of 1 to 100, with 1 being the most dangerous (cities not ranked were scored 101 and were kept in the analysis); and (2) whether the participant considered himself to be homeless at least part of the time over the 30 days prior to incarceration (1 = Yes;0 = No). Indicators of social relationships were determined by (1) whether the participant received any material support from family (1 = Yes;0 = No); (2) whether the inmate was in a committed relationship (1 = Yes; 0 = No); and (3) whether the inmate worked in the preceding 30 days prior to incarceration (1 = Yes; 0 = No). To measure an institution of the family, we included the degree to which participants were satisfied with the support they receive from family members (1 = very dissatisfied to 5 = very satisfied).
Proximate factors
Indicators include age, gender, income (0 = under $2,000; 1 = over $2,000 in 30 days prior to incarceration), sexual orientation, education and job training (1 = Yes; 0 = No), perceived health (1 = excellent; 5 = poor), race and ethnicity, degree of acculturation using birthplace outside the United States (1 = Yes; 0 = No) and primary language spoken (English; non-English) as proxies, severity of medical condition (number of days out of 30 experiencing the condition), severity of alcohol and/or drug use (number of days out of 30 experiencing alcohol problems plus number of days out of 30 experiencing drug problems. Range extends to 60), and HIV viral load (1 = Yes; 0 = No as suppressed ≤ 400 copies/ml).
Data Analysis
The specific aim of this study was to determine the prevalence of mental/emotional distress among a cohort of PLWHAs incarcerated in jail settings and to identify factors associated with this distress. Multiple regression analysis was used to examine potential correlates of baseline mental/emotional distress (Cohen, Cohen, West, & Aiken, 2002). The ASI psychiatric composite score was analyzed as a continuous variable. To reduce the number of predictors, bivariate analyses were conducted between individual covariates and the ASI psychiatric composite score. Covariates that were correlated at the p < .20 level on bivariate analyses were included in the multiple regression analysis. To create a more parsimonious model, the least significant predictors were trimmed. Model trimming entailed goodness-of-fit comparison tests, performed in an iterative fashion, between the full model and the model less the least statistically significant covariate. To account for limitations in the precision of the data, 99% confidence intervals (CIs) were constructed around β coefficient estimates.
Results
Psychiatric Indicators
Table 2 presents data on psychiatric indicators that were collected. Fifty-two percent of the sample was found to have mental/emotional distress scores above the 0.22 threshold on the ASI. Also notable is the very high rate of inmates with ASI substance abuse composite scores for alcohol (39%) and drug use (66%) reported for the 30 days preceding incarceration.
Table 2.
Jailed-detained PLWHAs: Psychiatric Indicators.
| # (%) | |
|---|---|
| ASI psychiatric score threshold > .22 | 458 (52.2) |
| Reports receiving psychiatric pension | 83 (9.5) |
| Jail chart indicates major mental illness | 220 (25.0) |
| Has been prescribed psychotropic medication at some point in life | 388 (44.2) |
| ASI alcohol use threshold > .15a | 386 (39.0) |
| ASI drug use threshold > .12 a | 579 (66.0) |
Note. N = 878. PLWHA = people living with HIV/AIDS.
AASI composite scores for alcohol and drugs in the 30 days prior to incarceration, using established cutoffs for indicating substance problems
Distal, Intermediate, and Proximate Indicators
Table 3 presents descriptive statistics and univariate correlations with the ASI psychiatric score.
Table 3.
Descriptive Statistics on Jail-Detained PLWHAs.
| Range | Mean (SD) or N (%) | Correlation With ASI | |
|---|---|---|---|
| ASI Psychiatric Distress | .04–1.00 | 0.30 (.26) | |
| Distal | |||
| % of Inmate’s City Living Under Poverty Line | 18.70–35.00 | 22.71 (5.12) | .36*** |
| City Income Inequality Ranking | 1–51 | 16.08 (18.54) | .35*** |
| (lower = higher inequality) | |||
| City Health Ranking (higher = less healthy) | 43–167 | 105.58 (34.38) | .26*** |
| Jail Accreditation: % with NCCHC | .00–1.00 | 0.33 (.44) | .31*** |
| Medical Insurance | 673 (76.7) | −.01 | |
| Accessed Substance Use Care | 180 (20.5) | −.06a | |
| Accessed Chronic Disease Care | 244 (27.8) | −.01 | |
| Accessed HIV Care | 671 (76.4) | .02 | |
| Intermediate | |||
| City Danger Level Ranking | 2–101 | 82.09 (28.88) | −.26*** |
| (lower = more dangerous) | |||
| Homeless | 316 (36.0) | .18*** | |
| Received Material Support from Family | 405 (46.1) | .19*** | |
| Committed Relationship | 267 (30.4) | .03 | |
| Employed | 157 (17.9) | .12** | |
| Satisfaction with Family | 1–5 | 3.52 (1.40) | −.24** |
| % of Lifetime Spent Incarcerated | .00–.17 | .07 (.04) | −.03 |
| Proximate | |||
| Age | 20–70 | 44.75 (8.64) | −.12** |
| Gender: Female | 252 (28.7) | .16*** | |
| Income (above $2,000 monthly) | 90 (10.3) | .09* | |
| Sexual Orientation: Homosexual | 95 (10.8) | .01 | |
| Bisexual | 81 (9.2) | .13*** | |
| Perceived Health (1 = excellent) | 1–5 | 3.23 (1.12) | .13*** |
| Education (years of school completed) | 2–16 | 11.29 (1.95) | −.09** |
| Job Training | 350 (39.9) | .02 | |
| Race: African-American | 601 (68.5) | −.12*** | |
| Ethnicity: Latino | 211 (24.0) | −.06a | |
| Acculturation: Birthplace (non-US) | 133 (15.1) | −.02a | |
| Primary Language (Spanish) | 76 (8.7) | .05 | |
| Chronic Disease Severity, # of days out of 30 | 0–30 | 6.04 (10.64) | .32*** |
| Substance Abuse Severity, # of days out of 30 | 0–60b | 17.20 (18.02) | .22*** |
| HIV Marker (viral load ≤ 400) | 257 (29.3) | .05a |
Note. N = 878. PLWHA = people living with HIV/AIDS; ASI = Addiction Severity Index.
While Access to Substance Use Care, Latino, Spanish Speaker, and Viral Load were not significantly correlated with Psychiatric Distress at p < .05, they were at p < .20, the cutoff for inclusion in the multivariate model.
Substance Abuse Severity is the total number of days in which alcohol was judged to be a problem plus the number of days that other substances were judged to be a problem, so the range extends up to 60.
p < .001.
p < .01.
p < .05.
Distal indicators
Three inmate city indicators correlated with higher ASI psychiatric composite scores: cities with a larger proportion living in poverty, those with lower income inequality, and those with a lower health ranking (p < .001). A higher ASI score correlated with jails having NCCHC accreditation (p < .001).
Intermediate indicators
Inmates living in more dangerous cities and who reported being homeless had higher ASI scores (p < .001). Inmates who received material support from family also had higher ASI scores (p < .001).
Proximate indicators
Being female or bisexual was positively correlated with the ASI score (p < .001). Being African American was negatively correlated with the ASI score (p < .001). Inmates perceiving their health to be poorer had higher ASI scores (p < .001) as did those with more severe chronic disease or substance abuse (p < .001).
Table 4 presents a multiple regression analysis of factors that were found to be significant at a p value of < .20 in the bivariate analysis in predicting the ASI psychiatric composite score.
Table 4.
Multivariate Analyses of Correlates of Psychiatric Distress in Jail-detained PLWHAs.
| β | 99% CI | Standardized β | |
|---|---|---|---|
| Distal | |||
| City Income Inequality Ranking (lower = higher inequality) | .004 | [.002, .005] | .27*** |
| City Health Ranking (higher = less healthy) | .002 | [.002, .003] | .32*** |
| Jail Accreditation: % with NCCHC | −.194 | [−.302, −.085] | −.33*** |
| Intermediate | |||
| City Danger Level Ranking (lower = more dangerous) | −.004 | [−.005, −.002] | −.40*** |
| Received Material Support from Family | .036 | [−.003, .075] | .07 |
| Satisfaction with Family | −.028 | [−.041, −.0I4] | −.15*** |
| Proximate | |||
| Gender: Female | .056 | [.014, .098] | .10*** |
| Sexual Orientation: Bisexual | .089 | [.025, .153] | .10*** |
| Education (years of school completed) | −.008 | [−.017, .002] | −.06 |
| Chronic Disease Severity, # of days out of 30 | .004 | [.003, .006] | .18*** |
| Substance Abuse Severity, # of days out of 30 | .002 | [.001, .003] | .16*** |
| HIV Marker (viral load ≤ 400) | .034 | [−.007, .075] | .06 |
Note. N = 878. PLWHA = people living with HIV/AIDS; CI = confidence interval.
p < .001.
**p < .01. The table does not indicate p < .05 as p < .01 was used as the cutoff for analysis, in order to account for the number of statistical tests.
Distal variables
Lower income inequalities in the jail’s location (B = .004, 99% CI [.002, .0056]) and a lower city health ranking (B = .002, 99% CI [.002, .003]) predicted higher mental/emotional distress scores in participants. Jail accreditation was significantly negatively associated (B = −.194, 99% CI [−.302, −.085]) with psychiatric distress.
Intermediate variables
Less danger in the jail’s city predicted lower mental/emotional distress (B = −.004, 99% CI [−.005, −.002]). Greater satisfaction with family support also predicted less mental/emotional distress (B = −.028, 99% CI [−.041, −.014]). None of the other intermediate variables were statistically significantly associated (material support, committed relationship, and employment).
Proximate variables
A number of proximate variables were associated with psychiatric distress. Being female (B = .056, 99% CI [.014, .098]), bisexual orientation (B = .089, 99% CI [.025, .153]), chronic disease severity (B = .004, 99% CI [.003, .006]), and increased severity of substance use (B = .002, 99% CI [.001, .003]) predicted higher distress.
Characteristics of the city and jail (income disparity, city health ranking, city dangerousness, and jail accreditation) alone accounted for 22.2% of the variance in psychiatric distress. Adding the remaining variables into the model accounted for an additional 13.6% of the variance. The final model with all of the variables included accounted for 35.8% of the variance in psychiatric distress.
Discussion
It is well known that incarcerated PLWHAs with comorbid mental illness in prison settings are at high risk for significantly negative HIV health outcomes as well as greater rates of recidivism (Baillargeon, Binswanger, Penn, Williams, & Murray, 2009; Springer, Spaulding, et al., 2011). The jail setting, however, has not been as well studied. The median length of stay of jails varies depending on the state and the source of data. It has been reported that mean length of stays for jail detainees range from hours to days. Similarly, prison length of stays used to be in the duration of years, but given recent state economic demise, the length of stay of prisons has decreased to months (Draine, Blank Wilson, Metraux, Hadley, & Evans, 2010; Spaulding et al., 2009). The ability to identify and treat mental illness is thus more difficult in jail settings, where there is a higher turnover, as compared to prison settings, where persons are housed for much longer periods. Findings across these 10 sites in the United States indicate high rates of mental/emotional distress (52%), underscoring the need for improved identification of Diagnostic and Statistical Manual of Mental Disorders (DSM) mental disorders and evidence-based psychiatric interventions (American Psychiatric Association, 2013).
The multisite, multi-community nature of the cohort, in a population with known health disparities, presented an opportunity to use the Model of Population Health and Health Disparities to guide our analysis, and contextualize individual-level factors that put people at risk for psychiatric distress. Based on this model, we organize the discussion of our findings based on distal, intermediate, and proximate factors.
Distal Factors
A number of distal factors were linked to mental/emotional distress among PLWHA inmates. The finding that lower income inequality is associated with higher mental/emotional distress is counter-intuitive. This may be accounted for by the fact that many of the cities in our study (with the exception of New York City and Atlanta) could be characterized as uniformly poorer cities, like Chester, PA, in which few higher income individuals live (Weinberg, 2011). A related finding is the significant correlation between the poorer health of the city in which the inmate is incarcerated (another marker of the inmate’s home community) and higher psychiatric distress. Cities with poorer health are less able to meet the needs of their residents and create an environment that is less tolerant of ethnic and sexual differences (Bryner, 2009).
The association between jail health services accreditation and less mental/emotional distress is intriguing, as it suggests a modifiable variable with direct policy implications. Only about 500 correctional facilities across the country are accredited by NCCHC. NCCHC standards include a number of recommendations for managing the delivery of medical and mental health care in correctional settings that improve the health of their inmates and the communities to which they return. These results support the policies advocated by NCCHC and argue in favor of requiring these standards nationwide. This correlation may seem surprising, as the psychiatric index targeted the 30 days prior to incarceration; however, 93% of the group had a prior incarceration, having spent on average 6.7% of their lives locked up.
Intermediate Factors
Several intermediate factors were related to mental/emotional distress among PLWHA inmates. Consistent with earlier research (Stokols, 1992), this study indicated that the social and physical context of the environment is of consequence to psychiatric health. The city dangerousness ranking, a marker of the inmate’s home community, was significantly associated with distress. Physically dangerous environments affect the criminal justice-involved/mentally ill/PLWHAs at multiple levels (Lane et al., 2004). There is an increased prevalence of victimization over a lifetime in correctional populations, including childhood exposure to domestic and community violence, and the increased likelihood of sexual and physical trauma (Wolff & Shi, 2010). In short, violence correlates with poverty (Draine et al., 2010; Ewart & Suchday, 2002). Experience of trauma is associated with poorer physical and mental health in correctional (Wolff & Shi, 2010), HIV (Whetten, Reif, Whetten, & Murphy-McMillan, 2008) and general populations (Margolin, Vickerman, Oliver, & Gordis, 2010), including the presence of post-traumatic stress disorder and depression (Margolin et al., 2010; Whetten et al., 2008; Wolff & Shi, 2010).
Greater satisfaction with family support was linked to lower psychiatric distress. These findings are consistent with previous research linking more perceived support to less mental/emotional distress (Ibarra-Rovillard & Kuiper, 2011; Moak & Agrawal, 2010), including greater family support (Clara, Cox, Enns, Murray, & Torgrudc, 2003), and including those of individuals with HIV (McDowell & Serovich, 2007). The stress-buffering hypothesis suggests that social support mitigates the negative impact of stress; facilitates effective coping; and enhances self-esteem, self-confidence, and self-efficacy (Nezlek, Kowalski, Leary, Blevins, & Holgate, 1997), factors associated with fewer mental health problems. These data underscore the importance of family support in reducing mental health problems for this population and suggest that involving family in treatment efforts may lead to better outcomes postrelease.
Proximate Factors
There was a significant association between mental/emotional distress and being female. Bloom and Covington’s (2008) review of the literature notes that women in jail are 6 times more likely than women in the general population and close to 20% more likely than men in jail to report symptoms of mental illness. Incarcerated women suffer disproportionately from childhood sexual and physical abuse. The authors argue that the effects of this abuse (e.g., post-traumatic stress disorder) leads women into poverty and criminal activity, such as prostitution, and that lack of treatment in the community and in jails is to blame for the continuing imbalance found in the criminal justice system.
Inmates who self-report as bisexual are also linked to higher levels of psychiatric distress. Bisexual as opposed to homosexual individuals have been found to suffer greater stress in intimate relationships, to have more difficulty accessing appropriate medical and community supports, and to suffer from discrimination from both straight and gay communities (Boon, 2008).
Of the proximate factors, one of the strongest associations was between mental/emotional distress and substance use severity. This strong association and the importance of addressing substance use disorders (SUDs) concomitantly in HIV care has been described elsewhere (Altice, Kamarulzaman, Soriano, Schechter, & Friedland, 2010; Springer, Azar, et al., 2011). Addiction treatment has been the focus in several studies in CJS populations, including randomized controlled trials, and is associated with reduced substance use and recidivism (Chandler, Fletcher, & Volkow, 2009; Mitchell, Wilson, & MacKenzie, 2007; Springer, Spaulding, et al., 2011). Unfortunately, very few incarceration settings offer addiction treatment in the form of pharmacotherapy (Chandler et al., 2009; Springer, Azar, et al., 2011; Nunn et al., 2009), despite its documented benefit on decreased relapse (Kinlock, Gordon, Schwartz, Fitzgerald, & O’Grady, 2009; Springer, Chen, & Altice, 2010) and on improved HIV treatment outcomes after release to the community (Springer et al., 2010). Identification and treatment of SUDs during incarceration in jail could likely improve linkages to care upon release and improve adherence to antiretroviral therapy (ART) and HIV treatment outcomes as has been demonstrated in prison release interventions (Magura et al., 2009; Springer et al., 2010; Tomasino, Swanson, Nolan, & Shuman, 2001) and Project Bridge (Rich et al., 2001).
In other analyses of this cohort, higher mental/emotional distress was independently associated with a higher likelihood of having an HIV care provider and receiving ART prior to incarceration (Chitsaz et al., 2013) and with viral suppression at 6 months postrelease (Spaulding et al., 2012). Being engaged in one form of treatment (HIV or not) appears to promote engagement into other forms of treatment (Chitsaz et al., 2013).
Limitations
Several study limitations warrant careful consideration of the results. First, the ASI is a self-report instrument that does not provide psychiatric diagnoses. However, previous research suggests that the ASI is a reasonable correlate of multiple types of psychiatric symptoms and functioning (Cacciola et al., 2008) and in a jail population, the ASI psychiatric score did correlate with the presence of DSM-III Axis I disorders as determined by the Diagnostic Interview Schedule (Amoureus, Van den Hurk, Breteler, & Schippers, 1994). Second, the ASI was completed during a time of distress (jail incarceration) and covers other issues that may not be necessarily related to mental illness (e.g., violent behavior, inability to concentrate), which are more common in jail populations. Third, the timing between the interview and intake varied across sites, introducing possible recall variation and bias. Fourth, only 878 individuals had complete data on all of the predictors, leading to a significantly reduced sample size and possibly less external validity. Fifth, individuals were not independent but grouped by site (and there were many differences in the programs at each site). This may have affected the standard errors and hypotheses tests, as the small number of sites prohibited the use of a multilevel modeling approach to correct for this. In addition, certain measures (e.g., indicators of poverty, city health and danger rankings) were assessed at the level of the site, which conflates the variable being assessed with other characteristics of the site. Sixth, New York City and Atlanta excluded inmates with severe mental illness, and participants with greater psychiatric distress were more likely to have missing data and to not be included in many analyses. Thus, the finding of 52% of jail inmates having mental/emotional distress should be considered a conservative estimate.
Conclusion
Mental/emotional distress was prevalent among 52% of PLWHAs entering jail and associated with community, institutional, and individual factors. The correctional system offers an important public health opportunity to identify mental illness and deliver interventions to improve health outcomes while incarcerated and upon release. Inmates entering jails that meet the standards for NCCHC accreditation exhibited less psychiatric distress, another indicator that the availability of better treatment in jail matters. In addition, this study identified factors that may improve specific health interventions, such as targeting women, those identifying as bisexual, and those with chronic illness or SUDs, or involving families, or offering treatment at the time of incarceration and upon release in concert with mental illness diagnosis and treatment. This study also provides a better understanding of the social conditions that underlie psychiatric distress. Further research regarding accurate mental illness diagnosis and linkage with treatment, in addition to the results of this study, will help in the development of interventions to improve health for HIV-infected released jail detainees.
Figure 1.
Analytical framework. Adapted from the model for analysis of population health and health disparities (Warnecke et al., 2008).
Acknowledgments
The authors would like to thank the frontline staff at participating sites and the detainees who shared their lives with us.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was made possible by grant # H97HA08537A0 from the U.S. Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of HHS.
Footnotes
Declaration of Conflicting Interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Author Altice has received speaker fees from Bristol-Myers Squibb, Merck & Co., and Gilead Sciences, and research grant support from Gilead Sciences. For information about JCHC’s disclosure policy, please see the Self-Study Exam.
References
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: 2013. Author. [Google Scholar]
- Amoureus MPSR, Van den Hurk AA, Breteler MHM, Schippers GM. The addiction severity index in penitentiaries. International Journal of Offender Therapy and Comparative Criminology. 1994;38:309–318. doi:10.1177/0306624x9403800404. [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ. Psychiatric disorders and repeat incarcerations: The revolving prison door. American Journal of Psychiatry. 2009;166:103–109. doi: 10.1176/appi.ajp.2008.08030416. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Ducate S, Pulvino J, Bradshaw P, Murray O, Olvera R. The association of psychiatric disorders and HIV infection in the correctional setting. Annals of Epidemiology. 2003;13:606–612. doi: 10.1016/S1047-2797(03)00061-9. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Williams BA, Mellow J, Harzke AJ, Hoge SK, Baillargeon G, Greifinger RB. Parole revocation among prison inmates with psychiatric and substance use disorders. Psychiatric Services. 2009;60:1516–1521. doi: 10.1176/appi.ps.60.11.1516. doi:10.1176/appi.ps.60.11.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom BE, Covington SS. Addressing the mental health needs of women offenders. In: Gido RL, Dalley L, editors. Women’s mental health issues across the criminal justice system. Prentice Hall; Columbus, OH: 2008. pp. 160–176. [Google Scholar]
- Boon M. Bisexuals face prejudice from straight and queer communities, lack bi-specific services. Daily Xtra. 2008 Retrieved from http://www.xtra.ca/public/National/Study_explores_link_between_bisexuality_poormental_health-5693.aspx.
- Brink J. Epidemiology of mental illness in a correctional system. Current Opinions in Psychiatry. 2005;18:536–541. doi: 10.1097/01.yco.0000179493.15688.78. doi:10.1097/01.yco.0000179493.15688.78. [DOI] [PubMed] [Google Scholar]
- Bryner J. Happiest states are wealthy and tolerant. LiveScience. 2009 Retrieved from http://www.livescience.com/7960-happiest-states-wealthy-tolerant.html.
- Cacciola JS, Pecoraro A, Alterman AI. Development of ASI psychiatric severity cut-off scores to identify co-occurring psychiatric disorders. International Journal of Mental Health and Addiction. 2008;6:77–92. doi:10.1007/s11469-007-9103-7. [Google Scholar]
- Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. Journal of the American Medical Association. 2009;301:183–190. doi: 10.1001/jama.2008.976. doi:10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chitsaz E, Meyer JP, Krishnan A, Springer SA, Marcus R, Zaller N, Altice FL. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS and Behavior. 2013;17:S118–S127. doi: 10.1007/s10461-013-0506-0. doi:10.1007/s10461-013-0506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clara IP, Cox BJ, Enns MW, Murray LT, Torgrudc LJ. Confirmatory factor analysis of the multidimensional scale of perceived social support in clinically distressed and student samples. Journal of Personality Assessment. 2003;81:265–270. doi: 10.1207/S15327752JPA8103_09. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd Lawrence Erlbaum; Mahwah, NJ: 2002. [Google Scholar]
- Draine J, Ahuja D, Altice FL, Arriola KJ, Avery AK, Beckwith CG, Tinsley MJ. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011;23:366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- Draine J, Blank Wilson A, Metraux S, Hadley T, Evans AC. The impact of mental illness status on the length of jail detention and the legal mechanism of jail release. Psychiatric Services. 2010;61:458–462. doi: 10.1176/ps.2010.61.5.458. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: Development and validation of a neighborhood stress index. Health Psychology. 2002;21:254–262. doi: 10.1037//0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- Fellner JA. Corrections quandary: Mental illness and prison rules. Harvard Civil Rights-Civil Liberties Review. 2006;41:391–412. [Google Scholar]
- Flanigan TP, Zaller N, Beckwith CG, Bazerman LB, Rana A, Gardner A, Altice FL. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: Still a missed opportunity for public health and HIV prevention. Journal of Acquired Immune Deficiency Syndrome. 2010;55:S78–S83. doi: 10.1097/QAI.0b013e3181fbc94f. [DOI] [PubMed] [Google Scholar]
- Gallup-Healthways Gallup-healthways well-being index. 2008 Retrieved from http://info.healthways.com/wellbeingindex.
- Hammond E, Treisman G. Psychiatric Times. 2007. HIV and psychiatric illness; p. 24. Retrieved from http://www.psychiatrictimes.com/display/article/10168/54466. [Google Scholar]
- Ibarra-Rovillard MS, Kuiper NA. Social support and social negativity findings in depression: Perceived responsiveness to basic psychological needs. Clinical Psychology Review. 2011;31:342–352. doi: 10.1016/j.cpr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- James DJ, Glaze LE. Mental health problems of prison and jail inmates (NCJ 213600) 2006 Retrieved from http://www.bjs.gov/index.cfm?ty=pbdetail&iid=789.
- Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: Results at 12 months postrelease. Journal of Substance Abuse Treatment. 2009;37:277–285. doi: 10.1016/j.jsat.2009.03.002. doi:10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SD, Rubinstein RA, Keefe RH, Webster N, Cibula DA, Rosenthal A, Dowdell J. Structural violence and racial disparity in HIV transmission. Journal of Health Care for the Poor and Underserved. 2004;15:319–335. doi: 10.1353/hpu.2004.0043. [DOI] [PubMed] [Google Scholar]
- Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: A randomized clinical trial. Drug and Alcohol Dependence. 2009;99:222–230. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolin G, Vickerman KA, Oliver PH, Gordis EB. Violence exposure in multiple interpersonal domains: Cumulative and differential effects. Journal of Adolescent Health. 2010;47:198–205. doi: 10.1016/j.jadohealth.2010.01.020. doi:10. 1016/j.jadohealth.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruschak L, Beavers R. HIV in prisons, 2007–2008 (NCJ 228307) Bureau of Justice Statistics. 2009 Retrieved from http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1747.
- McClelland GM, Teplin LA, Abram KM, Jacobs N. HIV and AIDS risk behaviors among female jail detainees: Implications for public health policy. American Journal of Public Health. 2002;92:818–825. doi: 10.2105/ajph.92.5.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19:1223–1229. doi: 10.1080/09540120701402830. doi:10.1080/09540120701402830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGafan P, Griffith J, Parente R, McLellan AT. Addiction severity index composite scores manual. University of Pennsylvania/Veterans Administration Center for Studies of Addiction/Treatment Research Institute; Philadelphia: 1986. [Google Scholar]
- McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The addiction severity index at 25: Origins, contributions and transitions. American Journal on Addictions. 2006;15:113–124. doi: 10.1080/10550490500528316. doi:10. 1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- Michaels D, Zoloth SR, Alcabes P, Braslow CA, Safyer S. Homelessness and indicators of mental illness among inmates in New York City’s correctional system. Hospital and Community Psychiatry. 1992;43:150–155. doi: 10.1176/ps.43.2.150. [DOI] [PubMed] [Google Scholar]
- Mitchell O, Wilson DB, MacKenzie DL. Does incarceration-based drug treatment reduce recidivism? A meta-analytic synthesis of the research. Journal of Experimental Criminology. 2007;3:353–375. doi:10.1007/s11292-007-9040-2. [Google Scholar]
- Moak ZB, Agrawal A. The association between perceived interpersonal social support and physical and mental health: Results from the national epidemiological survey on alcohol and related conditions. American Journal of Public Health. 2010;32:191–201. doi: 10.1093/pubmed/fdp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NeighborhoodScout . NeighborhoodScout’s top 100 most dangerous cities in the U.S. 2014. Retrieved from http://www.neighborhoodscout.com/neighborhoods/crime-rates/top100dangerous/ [Google Scholar]
- Nezlek JB, Kowalski RM, Leary MR, Blevins T, Holgate S. Personality moderators of reactions to interpersonal rejection: Depression and trait self-esteem. Personality and Social Psychology Bulletin. 1997;23:1235–1244. [Google Scholar]
- Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in U.S. prison systems: Results from a nationwide survey. Drug and Alcohol Dependence. 2009;105:83–88. doi: 10.1016/j.drugalcdep.2009.06.015. doi:10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell TA, Holt JC, Fondacaro KM. The prevalence of mental illness among inmates in a rural state. Law and Human Behavior. 1997;21:427–438. doi: 10.1023/a:1024811303834. [DOI] [PubMed] [Google Scholar]
- Rich JD, Holmes L, Salas C, Macalino G, Davis D, Ryczek J, Flanigan T. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. Journal of Urban Health. 2001;78:279–289. doi: 10.1093/jurban/78.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from addiction severity index composite scores. Journal of Substance Abuse Treatment. 2006;31:17–24. doi: 10.1016/j.jsat.2006.03.003. doi:10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Scheyett A, Parker S, Golin C, White B, Davis CP, Wohl D. HIV-infected prison inmates: Depression and implications for release back to communities. AIDS and Behavior. 2010;14:300–307. doi: 10.1007/s10461-008-9443-8. doi:10. 1007/s10461-008-9443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal DW. HIV-related issues and concerns for imprisoned persons throughout the world. Current Opinion in Psychiatry. 2005;18:530–535. doi: 10.1097/01.yco.0000179492.08064.de. [DOI] [PubMed] [Google Scholar]
- Spaulding AC, Messina LC, Kim BI, Chung K, Lincoln T, Teixeira P, Flanigan TP. Planning for success predicts virus suppressed: Results of a non-controlled-observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS and Behavior. 2012;17:S203–S211. doi: 10.1007/s10461-012-0341-8. doi:10.1007/s10461-012-0341-8. [DOI] [PubMed] [Google Scholar]
- Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from U.S. correctional facilities, 2006: Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4:e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Altice FL. Managing HIV/AIDS in correctional settings. Current HIV/AIDS Report. 2005;2:165–170. doi: 10.1007/s11904-005-0011-9. [DOI] [PubMed] [Google Scholar]
- Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: A review and call for evidence-based treatment for released prisoners. American Journal of Drug and Alcohol Abuse. 2011;37:12–21. doi: 10.3109/00952990.2010.540280. doi:10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Chen S, Altice FL. Improved HIV and substance abuse treatment outcomes for released HIV-infected prisoners: The impact of buprenorphine treatment. Journal of Urban Health. 2010;87:592–602. doi: 10.1007/s11524-010-9438-4. doi:10.1007/s11524-010-9438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: Five essential components. Clinical Infectious Diseases. 2011;53:469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatric Services. 2009;60:761–765. doi: 10.1176/ps.2009.60.6.761. [DOI] [PubMed] [Google Scholar]
- Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. American Psychologist. 1992;47:6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- Sullivan G, Koegel P, Kanouse DE, Cournos F, McKinnon K, Young AS, Bean D. HIV and people with serious mental illness: The public sector’s role in reducing HIV risk and improving care. Psychiatric Services. 1999;50:648–652. doi: 10.1176/ps.50.5.648. [DOI] [PubMed] [Google Scholar]
- Tomasino V, Swanson AJ, Nolan J, Shuman HI. The Key Extended Entry Program (KEEP): A methadone treatment program for opiate-dependent inmates. Mt Sinai Journal of Medicine. 2001;68:14–20. [PubMed] [Google Scholar]
- U.S. Census Bureau . Income, expenditures, poverty, and wealth. 2012. Retrieved from http://www.census.gov/compendia/statab/cats/income_expenditures_poverty_wealth.html. [Google Scholar]
- Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, Hiatt RA. Approaching health disparities from a population perspective: The national institutes of health centers for population health and health disparities. American Journal of Public Health. 2008;98:1608–1615. doi: 10.2105/AJPH.2006.102525. doi:10.2105/AJPH. 2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg D. U.S. neighborhood income inequality in the 2005–2009 period. American Community Survey Reports, ACS-16. 2011 Retrieved from http://www.census.gov/prod/2011pubs/acs-16.pdf.
- Whetten K, Reif S, Whetten R, Murphy-McMillan LK. Trauma, mental health, distrust, and stigma among HIV-positive persons: Implications for effective care. Psychosomatic Medicine. 2008;70:531–538. doi: 10.1097/PSY.0b013e31817749dc. doi:10.1097/PSY.0b013e31817749dc. [DOI] [PubMed] [Google Scholar]
- Wohl DA, Scheyett A, Golin CE, White B, Matuszewski J, Bowling M, Earp J. Intensive case management before and after prison release is no more effective than comprehensive pre-release discharge planning in linking HIV-infected prisoners to care: A randomized trial. AIDS and Behavior. 2011;15:356–364. doi: 10.1007/s10461-010-9843-4. doi:10.1007/s10461-010-9843-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff NL, Shi J. Trauma and incarcerated persons. In: Scott CL, editor. Handbook of correctional mental health. 2nd American Psychiatric Publishing; Washington DC: 2010. pp. 277–320. [Google Scholar]