Abstract
Reporting of hospital adverse events relies on Patient Safety Indicators (PSIs) using International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes. The US transition to ICD-10-CM in 2015 could result in erroneous comparisons of PSIs. Using the General Equivalent Mappings (GEMs), we compared the accuracy of ICD-9-CM coded PSIs against recommended ICD-10-CM codes from the Centers for Medicaid/Medicare Services (CMS). We further predict their impact in a cohort of 38 644 patients (1 446 581 visits and 399 hospitals). We compared the predicted results to the published PSI related ICD-10-CM diagnosis codes. We provide the first report of substantial hospital safety reporting errors with five direct comparisons from the 23 types of PSIs (transfusion and anesthesia related PSIs). One PSI was excluded from the comparison between code sets due to reorganization, while 15 additional PSIs were inaccurate to a lesser degree due to the complexity of the coding translation. The ICD-10-CM translations proposed by CMS pose impending risks for (1) comparing safety incidents, (2) inflating the number of PSIs, and (3) increasing the variability of calculations attributable to the abundance of coding system translations. Ethical organizations addressing ‘data-, process-, and system-focused’ improvements could be penalized using the new ICD-10-CM Agency for Healthcare Research and Quality PSIs because of apparent increases in PSIs bearing the same PSI identifier and label, yet calculated differently. Here we investigate which PSIs would reliably transition between ICD-9-CM and ICD-10-CM, and those at risk of under-reporting and over-reporting adverse events while the frequency of these adverse events remain unchanged.
Keywords: adverse events, patient safety indicators, ICD-10-cm, network topology, clinical informatics, hospitals
Introduction
The International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes are assigned to every diagnosis and procedure listed on healthcare encounters in the USA.1 These ICD-9-CM codes are also utilized for compulsory reporting of healthcare quality by the Agency for Healthcare Research and Quality (AHRQ) for their Patient Safety Indicators (PSIs).2 Not only are PSIs a set of measures s to evaluate hospital complications and adverse events, they contribute to a hospital's rating based on data from the Centers for Medicaid and Medicare Services’ (CMS) web portals.3 This accounts for 5% of the popular US News and World Reports’ Best Hospitals’ overall score.
In 2015, CMS is mandating a coding change to ICD-10-CM, which raises financial and technological concerns by the American Medical Association.4 Reputable chief information officers and terminology experts question the material improvement of ICD-10-CM over the current system.4 The majority of scholarly communications about the ICD-10-CM transition report roadmaps for immediate software and training needs,5 while overlooking downstream consequences on the healthcare system. However, previous studies have addressed the potential impact of the complexity of the ICD-10-CM transition on payers and health insurance plans.6 Topaz et al. 7 provide an extensive number of scientific reports contributing to the debate surrounding the ICD-10-CM transition, yet none address hospital adverse event reporting or PSIs.
Specific ICD-9-CM and ICD-10-CM codes have reporting requirements to the federal government, which leads to our focus on PSIs. With several hundred electronic health record (EHR) vendors, all developing tools to help hospitals and physicians with the transition to ICD-10-CM, our assessment of the General Equivalence Mappings (GEMs) and the published ICD-10-CM PSIs will assist in evaluating and comparing future tools. However, PSI calculations are highly dependent on their subsumed coding system (see Methods). To our knowledge, we provide the first comprehensive report of substantial PSI measurement changes introduced by the ICD-10-CM coding system without further guidance from AHRQ.
Methods
Datasets
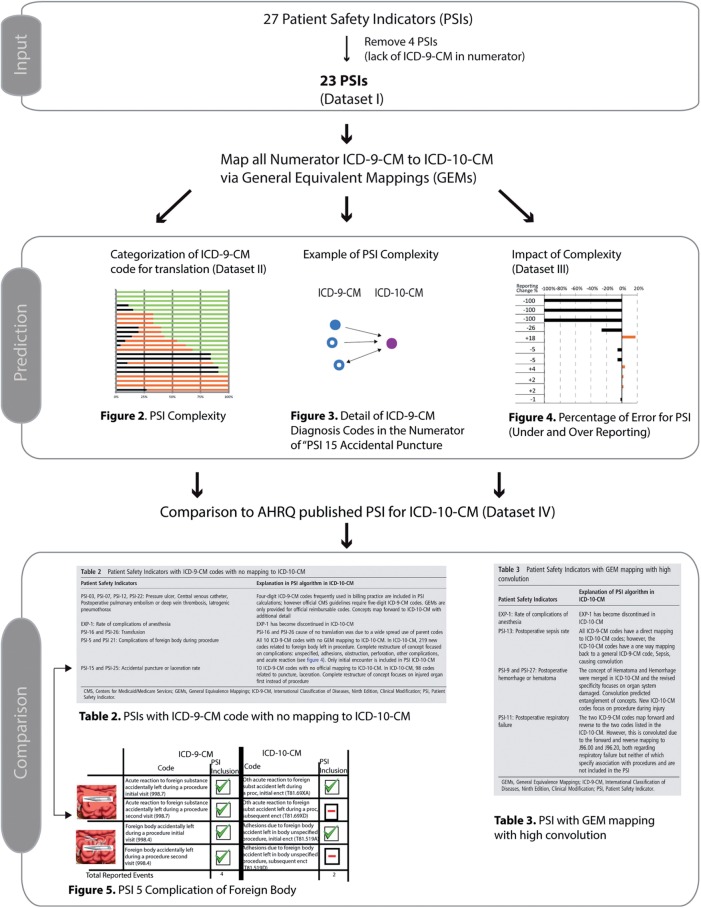
Figure 1 provides an overview of the methodology. Four datasets were used for this study and are described in table 1.2,8,9 Our institution’s review board approved this study (2012–0773).
Figure 1:
Overview of methodology. A total of 27 unique Patient Safety Indicator (PSIs) exist.4 Scores for each PSI are determined by a calculation with a numerator of patients associated with International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes or Vol. 3 ICD-9-CM procedure codes, and a denominator of patients in the surrounding area or volume of procedures for a given area to provide hospital or area level indicators of patient safety.2 The limitation of the dataset and the limitation of hospitals to change the denominators in individual PSI calculations resulted in our focus on the numerator. The four PSIs with procedure codes in their numerators were not interpretable; therefore, we focused on 23 PSIs with specific ICD-9-CM diagnosis codes in their numerators.
Table 1:
Dataset description
| Dataset | I | II | III | IV |
|---|---|---|---|---|
| 23 PSI metrics | Categorization of ICD-9-CM to ICD-10-CM | Illinois Medicaid patient cohort | ICD-10-CM diagnosis codes for PSI reports | |
| Description | 23 diagnosis-related PSI metrics published by AHRQ | The categorization of ICD-9-CM to ICD-10-CM ‘translation complexity’ that we reported (‘no coding’ vs ‘straightforward’ vs ‘convoluted’) by Centers for Medicaid and Medicare Services’ General Equivalency Mappings (GEMs) | A previously identified Illinois Medicaid patient cohort (IL-cohort; 38 644 patients, 1 446 581 visits, 399 hospitals) | The newly published ICD-10-CM diagnosis codes for the new PSI reports |
| Rationale | Standard definition of PSIs (4 were procedure codes and N/A with analysis) | Our prior work derived from official CMS translation tables determining which relationships are straightforward vs convoluted | Our clinical validation cohort | The newly published ICD-10-CM diagnosis codes for the new PSI reports |
| References | ||||
| Authors | Miller MR et al. | Boyd AD et al. | Boyd AD et al. | AHRQ |
| Source | Health Serv Res | J Am Med Inform Assoc | J Am Med Inform Assoc | NA |
AHRQ, Agency for Healthcare Research and Quality; CMS, Centers for Medicaid/Medicare Services; ICD-9-CM, International Classification of Diseases, Ninth Edition, Clinical Modification; PSI, Patient Safety Indicator.
Modeling the complexity of ICD-9-CM transition to ICD-10-CM in PSI
Unique to PSI, individual ICD-9-CM codes are used in the calculations and not the associated Diagnosis Related Groups (DRG) used in Medicare. A PSI calculation requires reporting the number of patients associated with ICD-9-CM codes in the numerator divided by a denominator that consists of a number of patients that may be associated with other ICD-9-CM codes or specific data, such as demographics. For example, the calculation for PSI-17 ‘Birth trauma rate—injury to neonate’ has a numerator that includes the number of patients with discharges associated with ICD-9-CM birth trauma diagnosis codes (767.0, 767.11, 767.3, 767.3, 767.4, 767.5, 767.7, 767.8). It is then divided by the number of all newborns (denominator) with the exclusion of cases associated with the following ICD-9-CM codes:
Preterm infant with birth weight less than 2000 g diagnosis codes (765.00, 765.01, 765.02, 765.03, 765.04, 765.04, 765.05, 765.06, 765.07, 765.11, 765.12, 765.13, 765.14, 765.15, 765.16, 765.17).
Injury to brachial plexus diagnosis code (767.6).
Osteogenesis imperfecta diagnosis code (765.61).
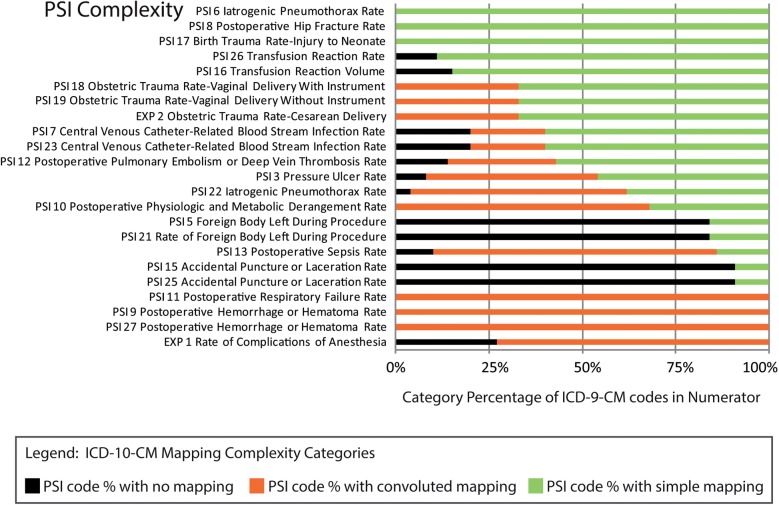
To illustrate the complexity of the ICD-10-CM transition, we assigned a ‘translation complexity’ to each PSI numerator for the coding transition from ICD-9-CM to ICD-10-CM using CMS translation tables (figure 2). By imputing the levels of complexity based on the mapping between the original ICD-9-CM coding and ICD-10-CM coding, we were able to classify the percentage of each PSI numerator's ICD-9-CM codes into three categories: (i) ‘no mapping’, (ii) ‘straightforward translations’, and (iii) ‘convoluted mapping’. ‘No mapping’ occurs when an ICD-9-CM code is deprecated or does not have a corresponding code in ICD-10-CM. ‘Straightforward translations’ comprise ‘identity mapping’, ‘subclass-to-class’, and ‘class-to-subclass’ (in our prior classification8). ‘Convoluted mapping’ corresponds to an ICD-9-CM code that is mapping a number of ICD-10-CM codes that are also recipients of other ICD-9-CM mappings (figure 2 and figure 3). Of note, these calculations are conducted on the numerator of the PSI calculation and represented in figure 2.
Figure 2:
Patient Safety Indicators (PSIs) ranked by increasing risk for possible erroneous and unwarranted reporting associated with complex International Classification of Diseases, Tenth Edition, Clinical Modification (ICD-10-CM) coding. The ICD-9-CM diagnosis codes included in the numerator for each PSI were evaluated to determine which category described the ICD-9-CM transition to ICD-10-CM. The category of each ICD-9-CM diagnosis code was labeled as no mapping (black), convoluted (orange), or simple (green). For each PSI, the number of diagnosis codes in each category were added together and divided by the total number of PSI related ICD-9-CM diagnosis codes to calculate the category percentage. This figure does not show a change in the denominator.
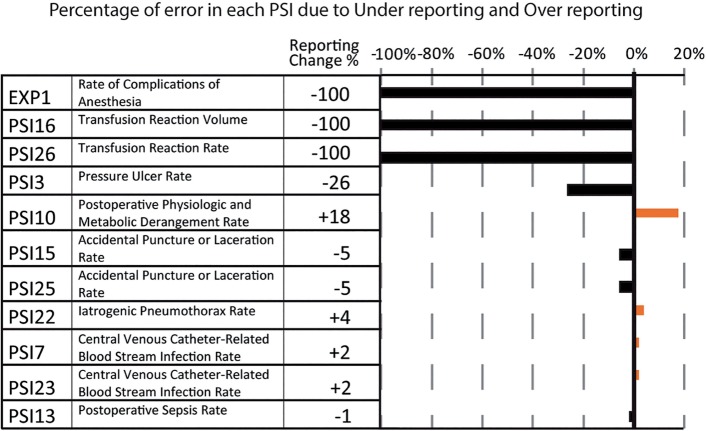
Figure 3:
A convoluted mapping to International Classification of Diseases, Tenth Edition, Clinical Modification (ICD-10-CM) for Patient Safety Indicator (PSI)-15 ‘Accidental puncture’. Healthcare conditions coded as ICD-9-CM ‘998.13’ (Seroma complicating a procedure) and ‘999.99’ (Other and unspecified complications of medical care, not elsewhere classified (NEC)), which are unrelated to the current measurement of PSI-15, regrettably map to the ICD-10-CM codes required for reporting this PSI. Additional mapping of 998.2 to another 22 ICD-10-CM codes are not shown since they relate to the concept of Accidental puncture.
In the first calculation, each of the ICD-9-CM codes utilizing the PSI numerators were assigned a ‘translation complexity’ for the transition to ICD-10-CM and summarized (figure 2). We previously calculated and reported the ‘translational complexity’ of each ICD-9-CM diagnosis code translated to ICD-10-CM using CMS tables.8 Since ICD-9-CM codes are utilized in the calculation of each individual PSI, we imputed the level of complexity of the mapping between the original ICD-9-CM coding and ICD-10-CM. For each PSI numerator, we calculated the percentage of its comprising ICD-9-CM codes that could be classified into each category of translational complexity8: (i) ‘no mapping’, (ii) ‘straightforward translations’, and (iii) ‘convoluted mapping’. We had previously assigned a level of translational complexity to each ICD-9-CM code using CMS tables.7 ‘No mapping’ occurs when an ICD-9-CM code is deprecated or does not have a corresponding code in ICD-10-CM. ‘Straightforward translations’ comprise ‘identity mapping’, ‘subclass-to-class’, and ‘class-to-subclass’ (in our prior classification8). ‘Convoluted mapping’ corresponds to an ICD-9-CM code that is mapping a number of ICD-10-CM codes that are also recipients of other ICD-9-CM mappings (figure 3).
Calculation of the cohort study of PSI reported in ICD-10-CM using GEMs
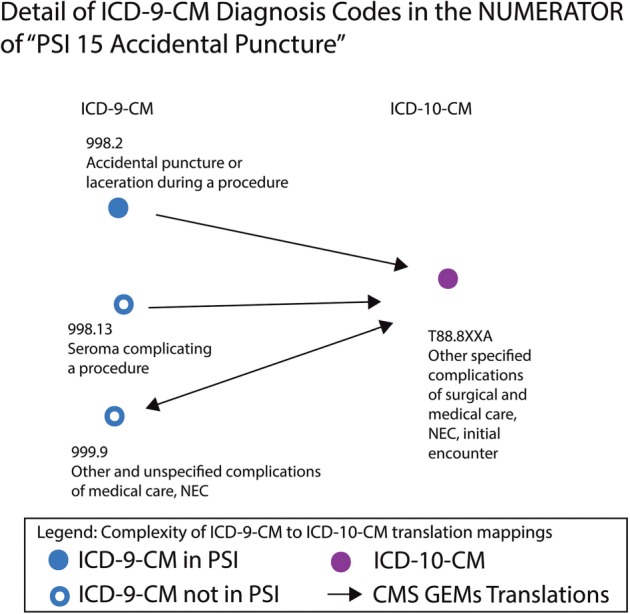
Individual patient visits from the Illinois Medicaid patient cohort (IL-cohort) of 1 446 581 Medicaid visits were mapped to all ICD-10-CM codes using GEMs to predict impact and future evaluation. The ambiguity of a single diagnosis code mapping to multiple mappings was represented as being mapped to all ICD-10-CM diagnosis codes. This enables the highest chance of one ICD-10-CM code being included in the new ICD-10-CM PSI. To calculate the percentages of under- and over-reporting, we first established the Gold Standard of PSI visits in the dataset of the IL-cohort of Medicaid visits using the ICD-9-CM diagnosis codes. Second, we measured the number of visits after the CMS translations in ICD-10-CM of the represented PSIs. Correctly reported PSI visits by ICD-10-CM were by definition also found using the Gold Standard (ICD-9-CM calculation). Under-reported visits are not mapped by the ICD-10-CM calculations, but were originally found by the ICD-9-CM calculation. Over-reported visits were found only with the new ICD-10-CM calculations. The under- and over-reporting are respectively attributed to (i) the number of Medicaid cases that would not be reported in ICD-10-CM due to ‘no mapping’, and (ii) the ‘convoluted’ mapping to the PSI in ICD-10-CM from cases not originally ascribed to it in ICD-9-CM (figure 4).
Figure 4:
Cohort study of Patient Safety Indicators (PSIs) reported in International Classification of Diseases, Tenth Edition, Clinical Modification (ICD-10-CM) using General Equivalency Mappings (GEMs). Under- and over-reporting rates (false negative and false positive errors). The under- and over-reporting (see Methods) are respectively attributed to (i) the number of Medicaid cases that would not be reported in ICD-10-CM due to ‘no mapping’, and (ii) the ‘convoluted’ mapping to the PSI in ICD-10-CM from cases not originally ascribed to it in ICD-9-CM as a prediction for future ICD-10-CM PSI challenges. EXP-1, PSI-16, and PSI-26 had all of the visits identified by ICD-9-CM not mapped forward to ICD-10-CM for an under-reporting of 100%. PSI-10 had an over-reporting of 18%, due to a number of visits associated with other ICD-9-CM codes mapping forward to codes related to PSI related to the mapping forward of ICD-9-CM codes.
Using GEMs as predictions through convolution and under-reporting, we evaluated the complex and erroneous PSIs with their recently published ICD-10-CM algorithms for further analysis of codes with no mapping or convoluted mapping (tables 2 and 3). These PSIs’ official calculation in ICD-10-CM, reported by AHRQ, were compared with the translation using GEMs to analyze any complexities caused by changes in ICD-10-CM and the rules around when to use specific codes in ICD-10-CM. Such changes could cause hospitals to mistakenly under- or over-report incidents.
Table 2:
Patient Safety Indicators with ICD-9-CM codes with no mapping to ICD-10-CM
| Patient Safety Indicators | Explanation in PSI algorithm in ICD-10-CM |
|---|---|
| PSI-03, PSI-07, PSI-12, PSI-22: Pressure ulcer, Central venous catheter, Postoperative pulmonary embolism or deep vein thrombosis, Iatrogenic pneumothorax | Four-digit ICD-9-CM codes frequently used in billing practice are included in PSI calculations; however official CMS guidelines require five-digit ICD-9-CM codes. GEMs are only provided for official reimbursable codes. Concepts map forward to ICD-10-CM with additional detail |
| EXP-1: Rate of complications of anesthesia | EXP-1 has become discontinued in ICD-10-CM |
| PSI-16 and PSI-26: Transfusion | PSI-16 and PSI-26 cause of no translation was due to a wide spread use of parent codes |
| PSI-5 and PSI 21: Complications of foreign body during procedure | All 10 ICD-9-CM codes with no GEM mapping to ICD-10-CM. In ICD-10-CM, 219 new codes related to foreign body left in procedure. Complete restructure of concept focused on complications: unspecified, adhesions, obstruction, perforation, other complications, and acute reaction (see figure 4). Only initial encounter is included in PSI ICD-10-CM |
| PSI-15 and PSI-25: Accidental puncture or laceration rate | 10 ICD-9-CM codes with no official mapping to ICD-10-CM. In ICD-10-CM, 98 codes related to puncture, laceration. Complete restructure of concept focuses on injured organ first instead of procedure |
CMS, Centers for Medicaid/Medicare Services; GEMs, General Equivalence Mappings; ICD-9-CM, International Classification of Diseases, Ninth Edition, Clinical Modification; PSI, Patient Safety Indicator.
Table 3:
Patient Safety Indicators with GEM mapping with high convolution
| Patient Safety Indicators | Explanation of PSI algorithm in ICD-10-CM |
|---|---|
| EXP-1: Rate of complications of anesthesia | EXP-1 has become discontinued in ICD-10-CM |
| PSI-13: Postoperative sepsis rate | All ICD-9-CM codes have a direct mapping to ICD-10-CM codes; however, the ICD-10-CM codes have a one way mapping back to a general ICD-9-CM code, Sepsis, causing convolution |
| PSI-9 and PSI-27: Postoperative hemorrhage or hematoma | The concept of Hematoma and Hemorrhage were merged in ICD-10-CM and the revised specificity focuses on organ system damaged. Convolution predicted entanglement of concepts. New ICD-10-CM codes focus on procedure during injury |
| PSI-11: Postoperative respiratory failure | The two ICD-9-CM codes map forward and reverse to the two codes listed in the ICD-10-CM. However, this is convoluted due to the forward and reverse mapping to J96.00 and J96.20, both regarding respiratory failure but neither of which specify association with procedures and are not included in the PSI |
GEMs, General Equivalence Mappings; ICD-9-CM, International Classification of Diseases, Ninth Edition, Clinical Modification; PSI, Patient Safety Indicator.
Results
Three PSIs had ‘straightforward’ ICD-10-CM equivalence, while 15 demonstrated ‘convoluted’ mappings (figure 2). The complexity of the translation to the ICD-10-CM coding system of a PSI numerator is illustrated (figure 3).
The analysis of ICD-9-CM codes in PSI calculations with no mapping is categorized (see table 2). Some four-digit ICD-9-CM codes have no mapping to ICD-10-CM, where related five-digit ICD-9-CM codes do have mappings to ICD-10-CM (See table 2). Five PSIs have no official mapping to ICD-10-CM through GEMs for billable diagnosis codes; the changed structure of ICD-10-CM limits a direct comparison between ICD-9-CM and ICD-10-CM using GEMs (EXP-1, PSI-5, PSI-15, PSI-21, PSI-25). PSI-9, PSI-11, PSI-13, and PSI-27 had more than 75% of codes with convolution during the translation from ICD-9-CM to ICD-10-CM, predicting challenges in ICD-10-CM (figure 2).
The under- and over- reporting for the PSIs were graphed (figure 4). Because of the absence of translation to ICD-10-CM for their respective ICD-9-CM numerators, three metrics could not have predictions in ICD-10-CM (100% false negative; figure 4): ‘Complications of anesthesia EXP-1’, ‘Transfusion reaction rate PSI-26’, and ‘Transfusion reaction volume PSI-16’. ‘Pressure ulcer rate PSI-3’ has a convoluted translation to ICD-10-CM, which inflates the false negative rate (sensitivity = 0.74; figure 4).
Discussion
In summary, the new ICD-10-CM coding system poses impending risks for: (1) under-reporting safety incidents as previously reported via ICD-9-CM, (2) unwarranted inflation of PSIs due to the increased specification of ICD-10-CM, and (3) increased variability of calculations attributable to abundant alternate ICD-9-CM to ICD-10-CM translations highly susceptible to different interpretations by hospital coding practices (figure 3).
A common reason for no mapping of four-digit ICD-9-CM codes that are paid and used in PSI but are not mapped (table 2) is due to CMS's desired specificity of five-digit ICD-9-CM codes. The more detailed codes have mappings to ICD-10-CM.
Several PSIs illustrate this potential impact of the transition to ICD-10-CM. For the PSIs associated with no mappings and high convolution (figures 2–4), we predicted EXP-1 to be challenging with both no mapping and high convolution. It is not surprising that this PSI has been discontinued. The GEMs and convolutions provide insight into the changes in ICD-10-CM before the PSI ICD-10-CM was published. We predicted foreign body, hematoma, and laceration to be complex based on predictions from GEMs and the final PSI ICD-10-CM diagnosis codes.
Additional impacted PSIs are PSI-15 and PSI-25 ‘Accidental puncture or laceration’ with significant challenges (table 2). The structural change between ICD-9-CM codes and ICD-10-CM codes was so complex that the vast majority of the PSI codes did not have GEMs mappings. The completely new organ focus of ICD-10-CM is different from the procedure focus of the ICD-9-CM puncture or laceration, which could lead to under-reporting as there would be an additional need to read the operative report for the specific location of the puncture or laceration. Similarly, ICD-10-CM PSI-5 and PSI-21 complications of foreign body during the procedure are likely to be under-reported due to this restructure. Each foreign body has additional details such as adhesions, obstruction, perforation, acute reaction, and other complications, as well as details about initial and subsequent encounter, and sequelae. An increase or decrease in foreign body reports could result as over 219 diagnosis codes exist and there is augmented fidelity (see figure 5) due to the number and type of visits associated with the diagnosis. For example, a challenge with the new coding system is a normal pathophysiology response to a foreign body migrating from acute to adhesions that can lead to confusion. The second dimension (A, D, S, for initial encounter, subsequent encounter, and sequelae) of a code can lead to under-counting due to the nature of body healing creating new initial encounters. Since only the initial encounter is included in the new PSI, under-counting can occur (see figure 5 for one example of a patient). The redefinitions of PSI-5 and PSI-21 are likely to cause confusion without a meticulous level of detail to coding in multiple settings.
Figure 5:
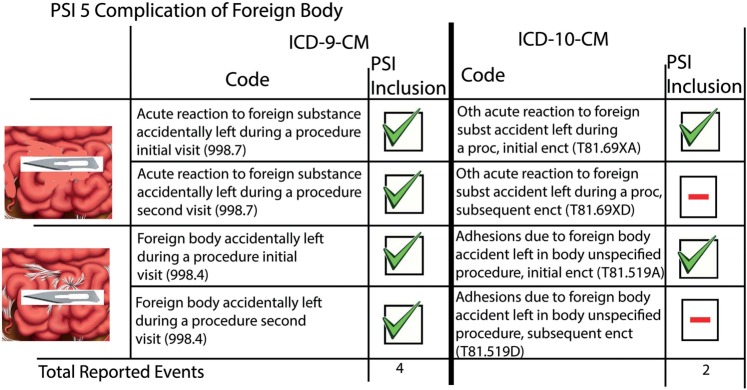
Pathophysiology of Foreign Body and coding in International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) and ICD-10-CM. A small representation of the evolution of the Patient Safety Indicator (PSI) representing a foreign body through coding in ICD-9-CM and ICD-10-CM. A possible decrease of reporting events could occur as the foreign body evolves to adhesions decreasing the reported incidents due to the second visit not counting towards the PSI in ICD-10-CM (see count of total reported events at the bottom of ICD-9-CM and ICD-10-CM columns). Of note, the mappings shown in this figure were conducted using our previously published networks approach using General Equivalence Mappings tables (Methods).
An illustrative example: pressure ulcer rates have been reported to be as high as 15.7% in intensive care units; however, the Joint Commission's goal is zero.10 The utility of ‘Pressure ulcer rate PSI-3’ is substantially impaired as the translation to ICD-10-CM can inflate the false negative rate. Further, its incorporation in the AHRQ PSI Hospital Composite Index magnifies the likelihood of unwarranted improved scores for hospitals and health systems. Finally, ‘Postoperative respiratory failure PSI-11’ could have a reduction in the number of reports due to forward GEMs mapping to both procedure and non-procedure ICD-10-CM codes (table 2). Current coding software for clinicians or coders includes all mappings for an old ICD-9-CM code, leading to a possible erroneous selection and a decrease in PSI-11.
Improved coding guidelines for reporting PSI using ICD-10-CM codes are required to help hospitals and healthcare systems use ICD-10-CM more efficiently for improved patient care and prevention of patient harm. The prior published work with ICD-10-CA (Canadian modification) is helpful but the complexity of ICD-10-CM is many-fold greater in magnitude of codes.11 The widely reported improvement in quality in patient care through ICD-10-CM/Procedure Coding System (PCS) led to this comparison of PSIs before and after the transition.12
The GEMs transition files are not intended to be a direct replacement of one code for another but rather provide a common framework for comparison purposes, even though it is the industry standard for the conversion.13 A number of different discussions about GEMs have been published.14–16 For instance, the Health Information Management Systems Society (HIMSS) has published critical risk mitigation strategies.17 Prior analysis of the GEMs accuracy has evaluated the mappings at 0.2–5%8 and 3%.18 Additional publications have mentioned ICD-10-CM in research with GEM.19 Even with identical terminology between ICD-9-CM and ICD-10-CM, the definitions of terms may have changed.19 Individual payers’ experience with GEMs has also been detailed, including use of the codes for reporting prognostications, pricing, and tracking outcomes.13 GEMs were used as the basis for training, translating business rules with additional resources developed to refine the initial mapping.13 GEMs is the initial starting discussion for all ICD-10-CM transitions as the analysis of PSIs through the initial lens of GEM allows hospitals and providers to see the limitations and compare this analysis with similar tools provided by all EHR companies.
Another limitation of the GEMs files is the complete restructuring of ICD-10-CM codes, as mapping parent codes across the transition is challenging. AHRQ does not report this; however, a simple solution includes adding more details. Two progress reports were provided by the AHRQ to revise PSI indicators using the new ICD-10-CM (July 201320 and a final report in December 20139). While these reports provide a roadmap to the transition of PSI in the ICD-10-CM coding, they overlook in-depth analyses on how the new metrics differ from the previous ones. Our methodology provides an otherwise unavailable metric of complexity showing 14 PSIs being convoluted and complex (as shown in figures 1 and 2).
The major changes for the transition from ICD-9-CM to ICD-10-CM correspond more to a terminology ‘mapping’ or ‘migration’ problem than a translation between minor version management of an unadulterated, foundational terminology. There is extensive literature describing the complexity of clinical terminology mapping and distortion of meaning as one changes terminologies.21,22,23 Specifically, the PSI transition has not evolved gracefully as outlined by the desiderata for controlled terminologies,24 in which terminologies must be stated through ‘clear and detailed descriptions of what changes occur and why’.24 To ensure graceful evolution, concept orientation, the focus on non-vagueness, non-ambiguity, and non-redundancy, needs to be preserved.24 Therefore, redundancy, code reuse, and changed codes should have been avoided. All of the PSIs in ICD-10-CM have non-vagueness since they refer to at least one meaning, but ambiguity occurs with the reuse of PSI labels. PSI-5, -15, -21, and -25’s concepts were restructured, but the names remain the same. Even though the PSI measures are non-redundant (each measure corresponds to no more than one term), ICD-10-CM diagnosis codes include much redundancy, as the codes associated with PSIs as the modifier ‘Unspecified’ are included in a number of the PSI metrics. PSIs have not evolved gracefully, which is a cause for concern for such PSI reports.
Conclusion
The transition to ICD-10-CM has a potentially large impact on PSIs due to the complete change in structure and individual diagnosis codes included in the specific PSI calculations. Changing the definitions in the numerator while the denominator remains the same will result in new results reflecting the change from ICD-9-CM and ICD-10-CM and not improving or worsening of care at an individual hospital. The AHRQ has published new PSI algorithms with the new ICD-10-CM diagnosis codes.5 However, the concepts of the ICD-10-CM diagnosis codes were not designed to mimic the previous PSIs. Using the GEMs, a conceptual understanding of the changes in PSIs through the change from ICD-9-CM to ICD-10-CM can be approached and appreciated.
This analysis of the AHRQ PSIs demonstrates the challenges in the transition to the ICD-10-CM coding system in regard to patient safety. Convolution helped predict the five PSIs with significant reorganization in ICD-10-CM. While the names will remain, the same comparison between the two coding systems is not warranted. Adequate translation of the PSIs should include unambiguous strategies for transition of all ICD-9-CM codes and their hierarchical parents or the redaction or reconstruction of related but new PSIs. The burden to the healthcare system is the neglect to address transition complexity. The transition could incent unethical ‘numbers-focused’ translations to improve adverse events statistics, while observed events may be unchanged or worsened. PSI results published on public reporting sites, such as Hospital Compare, could be non-representative of a safe hospital environment, which is a burden to patients. Publically listing the new and removed PSIs early will help to inform the public about the changes and use of national hospital comparison data for patient safety. Finally, ethical organizations addressing ‘data-, process-, and system-focused’ improvements could be penalized using the new ICD-10-CM AHRQ PSIs because of apparent increases in PSIs bearing the same PSI identifier and label, yet calculated differently.
Acknowledgments
We thank Ms Ikbel Achour, PhD and Mr Don Saner, MS for their editorial contributions.
Contributors
ADB and YAL had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. YMY, JL, and MDB completed the analyses. CK and BB contributed to the interpretation of the results and the manuscript redaction.
Funding
ADB and YAL are supported in part by the Center for Clinical and Translational Sciences of the University of Illinois (NIH 1UL1RR029879-01, NIH/NCATS UL1TR000050), the Institute for Translational Health Informatics of the University of Illinois at Chicago, the Office of the Vice-President for Health Affairs of the University of Illinois Hospital and Health Science System, the Office of the Vice-President for Health Sciences of the University of Arizona, the Arizona Health Sciences Center, the BIO5 Institute, the National Library of Medicine (K22 LM008308-04), and the University of Arizona Cancer Center (P30CA023074).
Competing interests
None.
Ethics approval
University of Illinois IRB study 2012-0773.
Provenance and peer review
Not commissioned; externally peer reviewed.
Data sharing statement
The tables are fully informative and the data inputs are already available online from previous publications and Federal USA agencies.
REFERENCES
- 1.Winter A, Haux R. Strategic information management in hospitals. Health information systems: architectures and strategies. 2nd edn London: Springer, 2011. [Google Scholar]
- 2.Miller MR, Elixhauser A, Zhan C, et al. Patient Safety Indicators: using administrative data to identify potential patient safety concerns. Health Serv Res 2001;36:110–32. [PMC free article] [PubMed] [Google Scholar]
- 3.CMS. Hospital Compare 2013. http://www.medicare.gov/hospitalcompare/ (accessed 24 Apr 2013).
- 4.Chute CG, Huff SM, Ferguson JA, et al. There are important reasons for delaying implementation of the new ICD-10 coding system. Health Aff (Millwood) 2012;31:836–42. [DOI] [PubMed] [Google Scholar]
- 5.Sanders TB, Bowens FM, Pierce W, et al. The road to ICD-10-CM/PCS implementation: forecasting the transition for providers, payers, and other healthcare organizations. Perspect Health Inf Manag 2012;9:1f. [PMC free article] [PubMed] [Google Scholar]
- 6.Meyer H. Coding complexity: US Health Care gets ready for the coming of ICD-10. Health Aff (Millwood) 2011;30:968–74. [DOI] [PubMed] [Google Scholar]
- 7.Topaz M, Shafran-Topaz L, Bowles KH. ICD-9 to ICD-10: evolution, revolution, and current debates in the United States. Perspect Health Inf Manag 2013;10:1d. [PMC free article] [PubMed] [Google Scholar]
- 8.Boyd AD, Burton MD, Li J, et al. The discriminatory cost of ICD-10-CM transition between clinical specialties: metrics, case study, and mitigating tools. J Am Med Inform Assoc 2013;20:708–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agency for HealthCare Research and Quality. Review of Proposed Changes with ICD-10-CM/PCS Conversion of AHRQ Quality Indicators 2013. http://www.qualityindicators.ahrq.gov/icd10/ (accessed 15 Jan 2014). [DOI] [PubMed]
- 10.Duncan KD. Preventing pressure ulcers: the goal is zero. Jt Comm J Qual Patient Saf 2007;33:605–10. [DOI] [PubMed] [Google Scholar]
- 11.Quan H, Eastwood C, Cunningham CT, et al. Validity of AHRQ patient safety indicators derived from ICD-10 hospital discharge abstract data (chart review study). BMJ Open 2013;3:e003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark JS. The facts about ICD-10-CM/PCS implementation. Implementation will improve the quality of patient care. J AHIMA 2012;83:42–3. [PubMed] [Google Scholar]
- 13.Ross-Davis SV. Preparing for ICD-10-CM/PCS: one payer's experience with general equivalence mappings (GEMs). Perspect Health Inf Manag 2012;9:1e. [PMC free article] [PubMed] [Google Scholar]
- 14.Bowie MJ, Schaffer RM. Understanding ICD-10-CM and ICD-10-PCS: a worktext. 2nd edn Cengage Learning, 2013:736 ISBN-13: 9781133961031. [Google Scholar]
- 15.Buehler MS, Mock L. ICD-10 Transition—Ready or Not, Here it Comes. Health Data Mgmt, March 17, 2014. http://www.healthdatamanagement.com/blogs/icd-10-ready-or-not-here-it-comes-47462-1.html.
- 16.Butler R. The ICD-10 General Equivalence Mappings. Bridging the translation gap from ICD-9. J AHIMA 2007;78:84–5. [PubMed] [Google Scholar]
- 17.Healthcare Information and Management Systems Society. ICD-10 Transformation: Five Critical Risk-Mitigation Strategies 2013. http://himss.files.cms-plus.com/HIMSSorg/content/files/icd10/G7AdvisoryReport_ICD10%20Version12.pdf (accessed 12 Dec 2013).
- 18.Caskey R, Zaman J, Nam H, et al. The transition to ICD-10-CM: potential challenges for pediatric practice. Pediatrics 2014;134:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riordan R. PS3–11: Beyond General Equivalency Mappings (GEMs): understanding the implications of ICD 10 in research. Clin Med Res 2013;11:177. [Google Scholar]
- 20.Cox G. AHRQ ICD-10-CM/PCS Conversion Project 2013. http://www.qualityindicators.ahrq.gov/Downloads/Resources/Publications/2013/ICD-10%20Report%2007-15-2013.pdf (accessed 3 Nov 2013), HHSA290201200001C.
- 21.Nadkarmi PM, Darer JA. Migrating existing clinical content from ICD-9 to SNOMED. J Am Med Inform Assoc 2010;17:602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCray AT, Miller RA. Making the conceptual connections: the UMLS after a decade of research and development. J Am Med Inform Assoc 1998;5:129–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bales ME, Lussier YA, Johnson SB. Research paper: topological analysis of large-scale biomedical terminology structures. J Am Med Inform Assoc 2007;14:788–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med 1998;37:394–403. [PMC free article] [PubMed] [Google Scholar]